User login
PHS Message to Military Health Providers: Join Us
NATIONAL HARBOR, MD—As the Military Health System is undergoing significant structural and eventually manpower changes, ADM Brett P. Giroir, MD, the Assistant Secretary for Health in the US Department of Health and Human Services (HHS) and the US Food and Drug Administration acting commissioner, had one message: Come and join us. “Recruitment and retention are our top priorities,” ADM Giroir told the largely military health care provider audience, “If there is downsizing of any of the military health [system], we want you. If you touch health in any way…we need great people who are committed to our national goals in the Commissioned Corps.”
Not long ago, the US Public Health Service (PHS) was facing its own pressures to either reduce its workforce or to eliminate the PHS Commissioned Corps altogether. “The Corps’ mission assignments and functions have not evolved in step with the public health needs of the nation,” argued the fiscal year 2019 Office of Management and Budget, Budget of The U.S. Government. “It is time for that to change. HHS is committed to providing the best public health services and emergency response at the lowest cost and is undertaking a comprehensive look at how the Corps is structured.”
In response, PHS has undertaken a top-to-bottom audit and reevaluation of its mission, ADM Giroir noted, with the goal of defining the role for the PHS in the 21st century and beyond. As a result, the PHS recently completed the development of a modernization plan. The plan entails specifically managing the force to meet mission requirements, developing and training a Ready Reserve force, enhancing training and professional development for the Commissioned Corps, and updating and improving PHS systems and processes.
As a part of the modernization plan, ADM Giroir outlined projected growth plans for the Corps: an increase from the 6,400 regular Corps officers in FY 2018 to 7,725 by FY 2024 with an additional 2,500 Ready Reserve officers, to “minimally meet the mission requirements as we understand it,” ADM Giroir noted.
According to ADM Giroir, the goals for the Ready Reserve are an essential component in the PHS mission to meet any regional, national, or global public health emergency. The Ready Reserve would be a well-trained public health force that would be ready to deploy quickly. Whereas in the past, PHS officer deployments and specialties were tailored to the needs of the agencies in which they are embedded, this force would be more aligned with the needs for a rapid public health emergency response and would include specialized providers. In that context health care providers with military rapid response training would be highly valued.
Although the PHS has outlined its modernization plan, no budget has been allocated for it. Moreover, as ADM Giroir, has noted, PHS still remains dependent on the budgets of the embedding agencies to pay for the Commissioned Corps. “Right now our force structure is really determined by what federal agencies need,” he noted.
Currently, there are bills pending in both the House of Representatives and the Senate to codify the modernization effort.
NATIONAL HARBOR, MD—As the Military Health System is undergoing significant structural and eventually manpower changes, ADM Brett P. Giroir, MD, the Assistant Secretary for Health in the US Department of Health and Human Services (HHS) and the US Food and Drug Administration acting commissioner, had one message: Come and join us. “Recruitment and retention are our top priorities,” ADM Giroir told the largely military health care provider audience, “If there is downsizing of any of the military health [system], we want you. If you touch health in any way…we need great people who are committed to our national goals in the Commissioned Corps.”
Not long ago, the US Public Health Service (PHS) was facing its own pressures to either reduce its workforce or to eliminate the PHS Commissioned Corps altogether. “The Corps’ mission assignments and functions have not evolved in step with the public health needs of the nation,” argued the fiscal year 2019 Office of Management and Budget, Budget of The U.S. Government. “It is time for that to change. HHS is committed to providing the best public health services and emergency response at the lowest cost and is undertaking a comprehensive look at how the Corps is structured.”
In response, PHS has undertaken a top-to-bottom audit and reevaluation of its mission, ADM Giroir noted, with the goal of defining the role for the PHS in the 21st century and beyond. As a result, the PHS recently completed the development of a modernization plan. The plan entails specifically managing the force to meet mission requirements, developing and training a Ready Reserve force, enhancing training and professional development for the Commissioned Corps, and updating and improving PHS systems and processes.
As a part of the modernization plan, ADM Giroir outlined projected growth plans for the Corps: an increase from the 6,400 regular Corps officers in FY 2018 to 7,725 by FY 2024 with an additional 2,500 Ready Reserve officers, to “minimally meet the mission requirements as we understand it,” ADM Giroir noted.
According to ADM Giroir, the goals for the Ready Reserve are an essential component in the PHS mission to meet any regional, national, or global public health emergency. The Ready Reserve would be a well-trained public health force that would be ready to deploy quickly. Whereas in the past, PHS officer deployments and specialties were tailored to the needs of the agencies in which they are embedded, this force would be more aligned with the needs for a rapid public health emergency response and would include specialized providers. In that context health care providers with military rapid response training would be highly valued.
Although the PHS has outlined its modernization plan, no budget has been allocated for it. Moreover, as ADM Giroir, has noted, PHS still remains dependent on the budgets of the embedding agencies to pay for the Commissioned Corps. “Right now our force structure is really determined by what federal agencies need,” he noted.
Currently, there are bills pending in both the House of Representatives and the Senate to codify the modernization effort.
NATIONAL HARBOR, MD—As the Military Health System is undergoing significant structural and eventually manpower changes, ADM Brett P. Giroir, MD, the Assistant Secretary for Health in the US Department of Health and Human Services (HHS) and the US Food and Drug Administration acting commissioner, had one message: Come and join us. “Recruitment and retention are our top priorities,” ADM Giroir told the largely military health care provider audience, “If there is downsizing of any of the military health [system], we want you. If you touch health in any way…we need great people who are committed to our national goals in the Commissioned Corps.”
Not long ago, the US Public Health Service (PHS) was facing its own pressures to either reduce its workforce or to eliminate the PHS Commissioned Corps altogether. “The Corps’ mission assignments and functions have not evolved in step with the public health needs of the nation,” argued the fiscal year 2019 Office of Management and Budget, Budget of The U.S. Government. “It is time for that to change. HHS is committed to providing the best public health services and emergency response at the lowest cost and is undertaking a comprehensive look at how the Corps is structured.”
In response, PHS has undertaken a top-to-bottom audit and reevaluation of its mission, ADM Giroir noted, with the goal of defining the role for the PHS in the 21st century and beyond. As a result, the PHS recently completed the development of a modernization plan. The plan entails specifically managing the force to meet mission requirements, developing and training a Ready Reserve force, enhancing training and professional development for the Commissioned Corps, and updating and improving PHS systems and processes.
As a part of the modernization plan, ADM Giroir outlined projected growth plans for the Corps: an increase from the 6,400 regular Corps officers in FY 2018 to 7,725 by FY 2024 with an additional 2,500 Ready Reserve officers, to “minimally meet the mission requirements as we understand it,” ADM Giroir noted.
According to ADM Giroir, the goals for the Ready Reserve are an essential component in the PHS mission to meet any regional, national, or global public health emergency. The Ready Reserve would be a well-trained public health force that would be ready to deploy quickly. Whereas in the past, PHS officer deployments and specialties were tailored to the needs of the agencies in which they are embedded, this force would be more aligned with the needs for a rapid public health emergency response and would include specialized providers. In that context health care providers with military rapid response training would be highly valued.
Although the PHS has outlined its modernization plan, no budget has been allocated for it. Moreover, as ADM Giroir, has noted, PHS still remains dependent on the budgets of the embedding agencies to pay for the Commissioned Corps. “Right now our force structure is really determined by what federal agencies need,” he noted.
Currently, there are bills pending in both the House of Representatives and the Senate to codify the modernization effort.
The Worst and the Best of 2019
Readers may recall that at the end of each calendar as opposed to fiscal year—I know it is hard to believe time exists outside the Federal system—Federal Practitioner publishes my ethics-focused version of the familiar year-end roundup. This year I am reversing the typical order of most annual rankings by putting the worst first for 2 morally salient reasons.
The first is that, sadly, it is almost always easier to identify multiple incidents that compete ignominiously for the “worst” of federal health care. Even more disappointing, it is comparatively difficult to find stories for the “best” that are of the same scale and scope as the bad news. This is not to say that every day there are not individual narratives of courage and compassion reported in US Department of Defense, US Public Health Service, and US Department of Veterans Affairs (VA), and hundreds more unsung heroes.
The second reason is that as human beings our psychology is such that we gravitate toward the worst things more powerfully and persistently than we do the best. This is in part why it is more difficult to find uplifting stories and why the demoralizing ones affect us so strongly. In an exhaustive review of the subject, psychologists Roy Baumeister and colleagues conclude that,
When equal measures of good and bad are present, however, the psychological effects of bad ones outweigh those of the good ones. This may in fact be a general principle or law of psychological phenomena, possibly reflecting the innate predispositions of the psyche or at least reflecting the almost inevitable adaptation of each individual to the exigencies of daily life.2
I am thus saving the best for last in the hope that it will be more memorable and impactful than the worst.
Unique to this year’s look-back, both the negative and the positive accounts come from the domain of end-of-life care. And unlike prior reviews where the lack of administrative vigilance and professional competence affected hundreds of patients, families, and staff, each of this year’s incidents involve a single patient.
An incident that occurred in September 2019 at a VA Community Living Center (CLC) in Georgia stood out in infamy apart from all others. It was the report of a veteran in a VA nursing home who had been bitten more than 100 times by ants crawling all over his room. He died shortly afterward. In a scene out of a horror movie tapping into the most primeval human fears, his daughter Laquana Ross described her father, a Vietnam Air Force veteran with cancer, to media and VA officials in graphic terms. “I understand mistakes happen,” she said. “I’ve had ants. But he was bit by ants two days in a row. They feasted on him.”3
In this new era of holding its senior executive service accountable, the outraged chair of the Senate Veterans Affairs Committee demanded that heads roll, and the VA acted rapidly to comply.4 The VA Central Office placed the network director on administrative leave, reassigned the chief medical officer, and initiated quality and safety reviews as well as an administrative investigative board to scrutinize how the parent Atlanta VA medical center managed the situation. In total, 9 officials connected to the incident were placed on leave. The VA apologized, with VA Secretary Robert Wilke zeroing in on the core values involved in the tragedy, “This is about basic humanity and dignity,” he said. “I don’t care what steps were taken to address the issues. We did not treat a vet with the dignity that he and his family deserved.”5 Yet it was the veteran’s daughter, with unbelievable charity, who asked the most crucial question that must be answered within the framework of a just culture if similar tragedies are not to occur in the future, “I know the staff, without a shadow of doubt, respected my dad and even loved him,” Ross said. “But what’s their ability to assess situations and fix things?”3
To begin to give Ms. Ross the answer she deserves, we must understand that the antithesis of love is not hate but indifference; of compassion, it is not cruelty but coldness. A true just culture reserves individual blame for those who have ill-will and adopts a systems perspective of organizational improvement toward most other types of errors.6 This means that the deplorable conditions in the CLC cannot be charged to the failure of a single staff member to fulfil their obligations but to collective collapse at many levels of the organization. Just culture is ethically laudable and far superior to the history in federal service of capricious punishment or institutional apathy that far too often were the default reactions to media exposures or congressional ire. Justice, though necessary, is not sufficient to achieve virtue. Those who work in health care also must be inspired to offer mercy, kindness, and compassion, especially in our most sacred privilege to provide care of the dying.
The best of 2019 illustrates this distinction movingly. This account also involves a Vietnam veteran, this time a Marine also dying of cancer, which happened just about a month after the earlier report. To be transparent it occurred at my home VA medical center in New Mexico. I was peripherally involved in the case as a consultant but had no role in the wondrous things that transpired. The last wish of a patient dying in the hospice unit on campus was to see his beloved dog who had been taken to the local city animal shelter when he was hospitalized because he had no friends or family to look after the companion animal. A social worker on the palliative care team called the animal shelter and explained the patient did not have much time left but wanted to see his dog before he died. Working together with support from facility leadership, shelter workers brought the dog to visit with the patient for an entire day while hospice staff cried with joy and sadness.7
As the epigraph for this editorial from Dame Cicely Saunders, the founder of the modern hospice movement, says, the difference between unspeakable pain and meaningful suffering can be measured in the depth of compassion caregivers show to the dying. It is this quality of mercy that in one case condemns, and in the other praises, us all as health care and administrative professionals in the service of our country. Baumeister and colleagues suggest that the human tendency to magnify the bad and minimize the good in everyday myopia may in a wider vision actually be a reason for hope:
It may be that humans and animals show heightened awareness of and responded more quickly to negative information because it signals a need for change. Hence, the adaptiveness of self-regulation partly lies in the organism’s ability to detect when response modifications are necessary and when they are unnecessary. Moreover, the lessons learned from bad events should ideally be retained permanently so that the same dangers or costs are not encountered repeatedly. Meanwhile, good events (such as those that provide a feeling of satisfaction and contentment) should ideally wear off so that the organism is motivated to continue searching for more and better outcomes.2
Let us all take this lesson into our work in 2020 so that when it comes time to write this column next year in the chilling cold of late autumn there will be more stories of light than darkness from which to choose.
1. Saunders C. The management of patients in the terminal stage. In: Raven R, ed. Cancer, Vol. 6. London: Butterworth and Company; 1960:403-417.
2. Baumeister RF, Bratslavasky E, Finkenauer C, Vohs KD. Bad is stronger than good. Rev General Psychol. 2001;5(4);323-370.
3. Knowles H. ‘They feasted on him’: Ants at VA nursing home bite a veteran 100 times before his death, daughter says. Washington Post. September 17, 2019. https://www.washingtonpost.com/health/2019/09/13/they-feasted-him-ants-va-nursing-home-bit-veteran-times-before-his-death-daughter-says. Accessed November 25, 2019.
4. Axelrod T. GOP senator presses VA after veteran reportedly bitten by ants in nursing home. https://thehill.com/homenews/senate/461196-gop-senator-presses-va-after-veteran-reportedly-bitten-by-ants-at-nursing. Published September 12, 2019. Accessed November 25, 2019.
5. Kime P. Nine VA leaders, staff placed on leave amid anti-bite scandal. https://www.military.com/daily-news/2019/09/17/nine-va-leaders-staff-placed-leave-amid-ant-bite-scandal.html. Published September 17, 2019. Accessed November 22, 2019.
6. Sculli GL, Hemphill R. Culture of safety and just culture. https://www.patientsafety.va.gov/docs/joe/just_culture_2013_tagged.pdf. Accessed November 22, 2019.
7. Hughes M. A Vietnam veteran in hospice care got to see his beloved dog one last time. https://www.cnn.com/2019/10/21/us/veteran-dying-wish-dog-trnd/index.html. Published October 21, 2019. Accessed November 22, 2019.
Readers may recall that at the end of each calendar as opposed to fiscal year—I know it is hard to believe time exists outside the Federal system—Federal Practitioner publishes my ethics-focused version of the familiar year-end roundup. This year I am reversing the typical order of most annual rankings by putting the worst first for 2 morally salient reasons.
The first is that, sadly, it is almost always easier to identify multiple incidents that compete ignominiously for the “worst” of federal health care. Even more disappointing, it is comparatively difficult to find stories for the “best” that are of the same scale and scope as the bad news. This is not to say that every day there are not individual narratives of courage and compassion reported in US Department of Defense, US Public Health Service, and US Department of Veterans Affairs (VA), and hundreds more unsung heroes.
The second reason is that as human beings our psychology is such that we gravitate toward the worst things more powerfully and persistently than we do the best. This is in part why it is more difficult to find uplifting stories and why the demoralizing ones affect us so strongly. In an exhaustive review of the subject, psychologists Roy Baumeister and colleagues conclude that,
When equal measures of good and bad are present, however, the psychological effects of bad ones outweigh those of the good ones. This may in fact be a general principle or law of psychological phenomena, possibly reflecting the innate predispositions of the psyche or at least reflecting the almost inevitable adaptation of each individual to the exigencies of daily life.2
I am thus saving the best for last in the hope that it will be more memorable and impactful than the worst.
Unique to this year’s look-back, both the negative and the positive accounts come from the domain of end-of-life care. And unlike prior reviews where the lack of administrative vigilance and professional competence affected hundreds of patients, families, and staff, each of this year’s incidents involve a single patient.
An incident that occurred in September 2019 at a VA Community Living Center (CLC) in Georgia stood out in infamy apart from all others. It was the report of a veteran in a VA nursing home who had been bitten more than 100 times by ants crawling all over his room. He died shortly afterward. In a scene out of a horror movie tapping into the most primeval human fears, his daughter Laquana Ross described her father, a Vietnam Air Force veteran with cancer, to media and VA officials in graphic terms. “I understand mistakes happen,” she said. “I’ve had ants. But he was bit by ants two days in a row. They feasted on him.”3
In this new era of holding its senior executive service accountable, the outraged chair of the Senate Veterans Affairs Committee demanded that heads roll, and the VA acted rapidly to comply.4 The VA Central Office placed the network director on administrative leave, reassigned the chief medical officer, and initiated quality and safety reviews as well as an administrative investigative board to scrutinize how the parent Atlanta VA medical center managed the situation. In total, 9 officials connected to the incident were placed on leave. The VA apologized, with VA Secretary Robert Wilke zeroing in on the core values involved in the tragedy, “This is about basic humanity and dignity,” he said. “I don’t care what steps were taken to address the issues. We did not treat a vet with the dignity that he and his family deserved.”5 Yet it was the veteran’s daughter, with unbelievable charity, who asked the most crucial question that must be answered within the framework of a just culture if similar tragedies are not to occur in the future, “I know the staff, without a shadow of doubt, respected my dad and even loved him,” Ross said. “But what’s their ability to assess situations and fix things?”3
To begin to give Ms. Ross the answer she deserves, we must understand that the antithesis of love is not hate but indifference; of compassion, it is not cruelty but coldness. A true just culture reserves individual blame for those who have ill-will and adopts a systems perspective of organizational improvement toward most other types of errors.6 This means that the deplorable conditions in the CLC cannot be charged to the failure of a single staff member to fulfil their obligations but to collective collapse at many levels of the organization. Just culture is ethically laudable and far superior to the history in federal service of capricious punishment or institutional apathy that far too often were the default reactions to media exposures or congressional ire. Justice, though necessary, is not sufficient to achieve virtue. Those who work in health care also must be inspired to offer mercy, kindness, and compassion, especially in our most sacred privilege to provide care of the dying.
The best of 2019 illustrates this distinction movingly. This account also involves a Vietnam veteran, this time a Marine also dying of cancer, which happened just about a month after the earlier report. To be transparent it occurred at my home VA medical center in New Mexico. I was peripherally involved in the case as a consultant but had no role in the wondrous things that transpired. The last wish of a patient dying in the hospice unit on campus was to see his beloved dog who had been taken to the local city animal shelter when he was hospitalized because he had no friends or family to look after the companion animal. A social worker on the palliative care team called the animal shelter and explained the patient did not have much time left but wanted to see his dog before he died. Working together with support from facility leadership, shelter workers brought the dog to visit with the patient for an entire day while hospice staff cried with joy and sadness.7
As the epigraph for this editorial from Dame Cicely Saunders, the founder of the modern hospice movement, says, the difference between unspeakable pain and meaningful suffering can be measured in the depth of compassion caregivers show to the dying. It is this quality of mercy that in one case condemns, and in the other praises, us all as health care and administrative professionals in the service of our country. Baumeister and colleagues suggest that the human tendency to magnify the bad and minimize the good in everyday myopia may in a wider vision actually be a reason for hope:
It may be that humans and animals show heightened awareness of and responded more quickly to negative information because it signals a need for change. Hence, the adaptiveness of self-regulation partly lies in the organism’s ability to detect when response modifications are necessary and when they are unnecessary. Moreover, the lessons learned from bad events should ideally be retained permanently so that the same dangers or costs are not encountered repeatedly. Meanwhile, good events (such as those that provide a feeling of satisfaction and contentment) should ideally wear off so that the organism is motivated to continue searching for more and better outcomes.2
Let us all take this lesson into our work in 2020 so that when it comes time to write this column next year in the chilling cold of late autumn there will be more stories of light than darkness from which to choose.
Readers may recall that at the end of each calendar as opposed to fiscal year—I know it is hard to believe time exists outside the Federal system—Federal Practitioner publishes my ethics-focused version of the familiar year-end roundup. This year I am reversing the typical order of most annual rankings by putting the worst first for 2 morally salient reasons.
The first is that, sadly, it is almost always easier to identify multiple incidents that compete ignominiously for the “worst” of federal health care. Even more disappointing, it is comparatively difficult to find stories for the “best” that are of the same scale and scope as the bad news. This is not to say that every day there are not individual narratives of courage and compassion reported in US Department of Defense, US Public Health Service, and US Department of Veterans Affairs (VA), and hundreds more unsung heroes.
The second reason is that as human beings our psychology is such that we gravitate toward the worst things more powerfully and persistently than we do the best. This is in part why it is more difficult to find uplifting stories and why the demoralizing ones affect us so strongly. In an exhaustive review of the subject, psychologists Roy Baumeister and colleagues conclude that,
When equal measures of good and bad are present, however, the psychological effects of bad ones outweigh those of the good ones. This may in fact be a general principle or law of psychological phenomena, possibly reflecting the innate predispositions of the psyche or at least reflecting the almost inevitable adaptation of each individual to the exigencies of daily life.2
I am thus saving the best for last in the hope that it will be more memorable and impactful than the worst.
Unique to this year’s look-back, both the negative and the positive accounts come from the domain of end-of-life care. And unlike prior reviews where the lack of administrative vigilance and professional competence affected hundreds of patients, families, and staff, each of this year’s incidents involve a single patient.
An incident that occurred in September 2019 at a VA Community Living Center (CLC) in Georgia stood out in infamy apart from all others. It was the report of a veteran in a VA nursing home who had been bitten more than 100 times by ants crawling all over his room. He died shortly afterward. In a scene out of a horror movie tapping into the most primeval human fears, his daughter Laquana Ross described her father, a Vietnam Air Force veteran with cancer, to media and VA officials in graphic terms. “I understand mistakes happen,” she said. “I’ve had ants. But he was bit by ants two days in a row. They feasted on him.”3
In this new era of holding its senior executive service accountable, the outraged chair of the Senate Veterans Affairs Committee demanded that heads roll, and the VA acted rapidly to comply.4 The VA Central Office placed the network director on administrative leave, reassigned the chief medical officer, and initiated quality and safety reviews as well as an administrative investigative board to scrutinize how the parent Atlanta VA medical center managed the situation. In total, 9 officials connected to the incident were placed on leave. The VA apologized, with VA Secretary Robert Wilke zeroing in on the core values involved in the tragedy, “This is about basic humanity and dignity,” he said. “I don’t care what steps were taken to address the issues. We did not treat a vet with the dignity that he and his family deserved.”5 Yet it was the veteran’s daughter, with unbelievable charity, who asked the most crucial question that must be answered within the framework of a just culture if similar tragedies are not to occur in the future, “I know the staff, without a shadow of doubt, respected my dad and even loved him,” Ross said. “But what’s their ability to assess situations and fix things?”3
To begin to give Ms. Ross the answer she deserves, we must understand that the antithesis of love is not hate but indifference; of compassion, it is not cruelty but coldness. A true just culture reserves individual blame for those who have ill-will and adopts a systems perspective of organizational improvement toward most other types of errors.6 This means that the deplorable conditions in the CLC cannot be charged to the failure of a single staff member to fulfil their obligations but to collective collapse at many levels of the organization. Just culture is ethically laudable and far superior to the history in federal service of capricious punishment or institutional apathy that far too often were the default reactions to media exposures or congressional ire. Justice, though necessary, is not sufficient to achieve virtue. Those who work in health care also must be inspired to offer mercy, kindness, and compassion, especially in our most sacred privilege to provide care of the dying.
The best of 2019 illustrates this distinction movingly. This account also involves a Vietnam veteran, this time a Marine also dying of cancer, which happened just about a month after the earlier report. To be transparent it occurred at my home VA medical center in New Mexico. I was peripherally involved in the case as a consultant but had no role in the wondrous things that transpired. The last wish of a patient dying in the hospice unit on campus was to see his beloved dog who had been taken to the local city animal shelter when he was hospitalized because he had no friends or family to look after the companion animal. A social worker on the palliative care team called the animal shelter and explained the patient did not have much time left but wanted to see his dog before he died. Working together with support from facility leadership, shelter workers brought the dog to visit with the patient for an entire day while hospice staff cried with joy and sadness.7
As the epigraph for this editorial from Dame Cicely Saunders, the founder of the modern hospice movement, says, the difference between unspeakable pain and meaningful suffering can be measured in the depth of compassion caregivers show to the dying. It is this quality of mercy that in one case condemns, and in the other praises, us all as health care and administrative professionals in the service of our country. Baumeister and colleagues suggest that the human tendency to magnify the bad and minimize the good in everyday myopia may in a wider vision actually be a reason for hope:
It may be that humans and animals show heightened awareness of and responded more quickly to negative information because it signals a need for change. Hence, the adaptiveness of self-regulation partly lies in the organism’s ability to detect when response modifications are necessary and when they are unnecessary. Moreover, the lessons learned from bad events should ideally be retained permanently so that the same dangers or costs are not encountered repeatedly. Meanwhile, good events (such as those that provide a feeling of satisfaction and contentment) should ideally wear off so that the organism is motivated to continue searching for more and better outcomes.2
Let us all take this lesson into our work in 2020 so that when it comes time to write this column next year in the chilling cold of late autumn there will be more stories of light than darkness from which to choose.
1. Saunders C. The management of patients in the terminal stage. In: Raven R, ed. Cancer, Vol. 6. London: Butterworth and Company; 1960:403-417.
2. Baumeister RF, Bratslavasky E, Finkenauer C, Vohs KD. Bad is stronger than good. Rev General Psychol. 2001;5(4);323-370.
3. Knowles H. ‘They feasted on him’: Ants at VA nursing home bite a veteran 100 times before his death, daughter says. Washington Post. September 17, 2019. https://www.washingtonpost.com/health/2019/09/13/they-feasted-him-ants-va-nursing-home-bit-veteran-times-before-his-death-daughter-says. Accessed November 25, 2019.
4. Axelrod T. GOP senator presses VA after veteran reportedly bitten by ants in nursing home. https://thehill.com/homenews/senate/461196-gop-senator-presses-va-after-veteran-reportedly-bitten-by-ants-at-nursing. Published September 12, 2019. Accessed November 25, 2019.
5. Kime P. Nine VA leaders, staff placed on leave amid anti-bite scandal. https://www.military.com/daily-news/2019/09/17/nine-va-leaders-staff-placed-leave-amid-ant-bite-scandal.html. Published September 17, 2019. Accessed November 22, 2019.
6. Sculli GL, Hemphill R. Culture of safety and just culture. https://www.patientsafety.va.gov/docs/joe/just_culture_2013_tagged.pdf. Accessed November 22, 2019.
7. Hughes M. A Vietnam veteran in hospice care got to see his beloved dog one last time. https://www.cnn.com/2019/10/21/us/veteran-dying-wish-dog-trnd/index.html. Published October 21, 2019. Accessed November 22, 2019.
1. Saunders C. The management of patients in the terminal stage. In: Raven R, ed. Cancer, Vol. 6. London: Butterworth and Company; 1960:403-417.
2. Baumeister RF, Bratslavasky E, Finkenauer C, Vohs KD. Bad is stronger than good. Rev General Psychol. 2001;5(4);323-370.
3. Knowles H. ‘They feasted on him’: Ants at VA nursing home bite a veteran 100 times before his death, daughter says. Washington Post. September 17, 2019. https://www.washingtonpost.com/health/2019/09/13/they-feasted-him-ants-va-nursing-home-bit-veteran-times-before-his-death-daughter-says. Accessed November 25, 2019.
4. Axelrod T. GOP senator presses VA after veteran reportedly bitten by ants in nursing home. https://thehill.com/homenews/senate/461196-gop-senator-presses-va-after-veteran-reportedly-bitten-by-ants-at-nursing. Published September 12, 2019. Accessed November 25, 2019.
5. Kime P. Nine VA leaders, staff placed on leave amid anti-bite scandal. https://www.military.com/daily-news/2019/09/17/nine-va-leaders-staff-placed-leave-amid-ant-bite-scandal.html. Published September 17, 2019. Accessed November 22, 2019.
6. Sculli GL, Hemphill R. Culture of safety and just culture. https://www.patientsafety.va.gov/docs/joe/just_culture_2013_tagged.pdf. Accessed November 22, 2019.
7. Hughes M. A Vietnam veteran in hospice care got to see his beloved dog one last time. https://www.cnn.com/2019/10/21/us/veteran-dying-wish-dog-trnd/index.html. Published October 21, 2019. Accessed November 22, 2019.
DoD Explores Virtual Health for Traumatic Brain Injury
NATIONAL HARBOR, MD – As it moves to expand the use of virtual health offerings, the US Department of Defense (DoD) Regional Health Command Europe piloted a virtual health (telehealth) program to treat service members with traumatic brain injury (TBI). Ronald Keen, FNP-C, and Steve Cain, PA, reported on the DoD use of virtual health at the 2019 AMSUS annual meeting in Maryland.
The study, conducted between October 2016 and May 2018, included 15 patients stationed in 4 countries, including Poland, Turkey, and Egypt and 67 total health care encounters. Patients were limited to service members in the direct care system or those who were in remote areas where gaps in care existed in the Tricare Network. The virtual health program was centered at Landstuhl Regional Medical Center in Germany and sought to determine whether virtual health was feasible to treat TBI and whether it would increase patient satisfaction. The multidisciplinary program brought together specialists in 7 different disciplines, including sleep medicine, optometry, behavioral health, and occupational therapy.
According to Keen, the results of the 15-patient pilot were promising. He conservatively estimated a savings of $3,700, and more important, the program saved 322 hours of on-duty time. Health care providers used the program an average 2.8 times, and patients used the system 1.6 times on average. Currently the DoD is requiring active permission from patients to receive a telehealth visit.
NATIONAL HARBOR, MD – As it moves to expand the use of virtual health offerings, the US Department of Defense (DoD) Regional Health Command Europe piloted a virtual health (telehealth) program to treat service members with traumatic brain injury (TBI). Ronald Keen, FNP-C, and Steve Cain, PA, reported on the DoD use of virtual health at the 2019 AMSUS annual meeting in Maryland.
The study, conducted between October 2016 and May 2018, included 15 patients stationed in 4 countries, including Poland, Turkey, and Egypt and 67 total health care encounters. Patients were limited to service members in the direct care system or those who were in remote areas where gaps in care existed in the Tricare Network. The virtual health program was centered at Landstuhl Regional Medical Center in Germany and sought to determine whether virtual health was feasible to treat TBI and whether it would increase patient satisfaction. The multidisciplinary program brought together specialists in 7 different disciplines, including sleep medicine, optometry, behavioral health, and occupational therapy.
According to Keen, the results of the 15-patient pilot were promising. He conservatively estimated a savings of $3,700, and more important, the program saved 322 hours of on-duty time. Health care providers used the program an average 2.8 times, and patients used the system 1.6 times on average. Currently the DoD is requiring active permission from patients to receive a telehealth visit.
NATIONAL HARBOR, MD – As it moves to expand the use of virtual health offerings, the US Department of Defense (DoD) Regional Health Command Europe piloted a virtual health (telehealth) program to treat service members with traumatic brain injury (TBI). Ronald Keen, FNP-C, and Steve Cain, PA, reported on the DoD use of virtual health at the 2019 AMSUS annual meeting in Maryland.
The study, conducted between October 2016 and May 2018, included 15 patients stationed in 4 countries, including Poland, Turkey, and Egypt and 67 total health care encounters. Patients were limited to service members in the direct care system or those who were in remote areas where gaps in care existed in the Tricare Network. The virtual health program was centered at Landstuhl Regional Medical Center in Germany and sought to determine whether virtual health was feasible to treat TBI and whether it would increase patient satisfaction. The multidisciplinary program brought together specialists in 7 different disciplines, including sleep medicine, optometry, behavioral health, and occupational therapy.
According to Keen, the results of the 15-patient pilot were promising. He conservatively estimated a savings of $3,700, and more important, the program saved 322 hours of on-duty time. Health care providers used the program an average 2.8 times, and patients used the system 1.6 times on average. Currently the DoD is requiring active permission from patients to receive a telehealth visit.
Improving Veteran Care With the Mission Act
NATIONAL HARBOR, MD–The US Department of Veterans Affairs (VA) is in the midst of a significant change in the way it will deliver care to veterans. Agency officials remain optimistic that the change will be for the better, and early indications are positive.
The change is being driven by the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (Mission) Act of 2018, a bill that opens health services options for veterans and integrates VA-administered care and care from community-based providers.
“This is change that is enhancing their experience in the system, and this is enhancing their options and the quality of the options in the system,” Jennifer MacDonald, MD, chief consultant to the principal deputy undersecretary for health at the VA, said during a December 3 session at the AMSUS 2019 annual meeting. “We need also for our workforce to understand how important they are to us across this degree of change.”
Dr. MacDonald highlighted integration with community-based care, including a community urgent care provision that allows veterans to access urgent care facilities and receive care without the need for prior authorization.
“The important piece about that is that we are also looking at the way this care has been accessed,” she said. “By and large, what we have seen from the data is that veterans are indeed seeking community urgent care at a site close to home. This may be CVS or Walgreens. It may be a stand-alone urgent care with a bit more functionality than those Minute Clinics tend to have. We are seeing veterans typically access care through those sites for those minor concerns and illnesses.”
However, she noted that this type of access does not alter the role the VA plays in administration of health care services.
“We are seeing them come back to VA for the majority of their care and for their core care–when there are serious issues, when insulin needs to be adjusted for diabetes, when there are heart disease medications that need to be refilled–we are seeing veterans not seek out urgent care, but come to us, and that is exactly what we want,” she said. “We want the continuity of care to continue and we want to help guide people to the right care, right place, right time.”
Dr. MacDonald also highlighted the expansion of a program that provides a stipend to caregivers that allows veterans to avoid institutionalization and remain within the community under that caregiver’s (a family or friend) supervision. This will expand by year’s end to Vietnam War-era veterans and within 2 years, to veterans that fall between the Vietnam War-era and the September 11, 2001, terrorist attacks.
“We wanted to do this equitably across all eras of veterans,” she said. “This now gives us that opportunity.”
Telehealth also plays a key role.
“For the first time ever, VA now has what we term ‘anywhere-to-anywhere’ telehealth under the Mission Act, an enormous opportunity for us,” she said. “Since we stretch … from New York City to Guam, we need the opportunity to provide care where it may be difficult to recruit and retain providers wherever veterans choose to live,” she said. “We believe that we should be able to meet people where they are regardless of where they choose to live. That’s an aspirational vision, but it is one we believe is exceptionally important and indeed we are moving toward that.”
These are just the beginning; the full implementation of the act goes out to 2034.
According to Dr. MacDonald, the agency is working hard to engage both veterans and the workforce to keep tabs on how the implementation is going.
“It’s a fundamental change in the day-to-day business that they’ve been doing, sometimes for years, and so extremely important across this change is that we have set up processes and now a joint operations center and a number of forums to hear directly from our front line and make sure that their issues are our issues in central office, in DC here, and that they feel heard and that they know that when they have needs, those needs are actioned,” she said.
The VA, under the Mission Act, is also working hard to engage health care providers in the community, including making VA training to community partners, including training on opioid use, suicide prevent and military culture.
However, all these change are for naught if the veterans are not on board. But so far, Dr. MacDonald said the early feedback is very positive.
She cited a VFW survey that asked a question about the Mission Act changes so far and whether they would recommend the VA to other veterans. Ninety percent of the respondents answered they would.
“That’s our marker that we are getting somewhere with these changes and the way we do business,” she said. “That is what we want to see continue to increase.”
NATIONAL HARBOR, MD–The US Department of Veterans Affairs (VA) is in the midst of a significant change in the way it will deliver care to veterans. Agency officials remain optimistic that the change will be for the better, and early indications are positive.
The change is being driven by the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (Mission) Act of 2018, a bill that opens health services options for veterans and integrates VA-administered care and care from community-based providers.
“This is change that is enhancing their experience in the system, and this is enhancing their options and the quality of the options in the system,” Jennifer MacDonald, MD, chief consultant to the principal deputy undersecretary for health at the VA, said during a December 3 session at the AMSUS 2019 annual meeting. “We need also for our workforce to understand how important they are to us across this degree of change.”
Dr. MacDonald highlighted integration with community-based care, including a community urgent care provision that allows veterans to access urgent care facilities and receive care without the need for prior authorization.
“The important piece about that is that we are also looking at the way this care has been accessed,” she said. “By and large, what we have seen from the data is that veterans are indeed seeking community urgent care at a site close to home. This may be CVS or Walgreens. It may be a stand-alone urgent care with a bit more functionality than those Minute Clinics tend to have. We are seeing veterans typically access care through those sites for those minor concerns and illnesses.”
However, she noted that this type of access does not alter the role the VA plays in administration of health care services.
“We are seeing them come back to VA for the majority of their care and for their core care–when there are serious issues, when insulin needs to be adjusted for diabetes, when there are heart disease medications that need to be refilled–we are seeing veterans not seek out urgent care, but come to us, and that is exactly what we want,” she said. “We want the continuity of care to continue and we want to help guide people to the right care, right place, right time.”
Dr. MacDonald also highlighted the expansion of a program that provides a stipend to caregivers that allows veterans to avoid institutionalization and remain within the community under that caregiver’s (a family or friend) supervision. This will expand by year’s end to Vietnam War-era veterans and within 2 years, to veterans that fall between the Vietnam War-era and the September 11, 2001, terrorist attacks.
“We wanted to do this equitably across all eras of veterans,” she said. “This now gives us that opportunity.”
Telehealth also plays a key role.
“For the first time ever, VA now has what we term ‘anywhere-to-anywhere’ telehealth under the Mission Act, an enormous opportunity for us,” she said. “Since we stretch … from New York City to Guam, we need the opportunity to provide care where it may be difficult to recruit and retain providers wherever veterans choose to live,” she said. “We believe that we should be able to meet people where they are regardless of where they choose to live. That’s an aspirational vision, but it is one we believe is exceptionally important and indeed we are moving toward that.”
These are just the beginning; the full implementation of the act goes out to 2034.
According to Dr. MacDonald, the agency is working hard to engage both veterans and the workforce to keep tabs on how the implementation is going.
“It’s a fundamental change in the day-to-day business that they’ve been doing, sometimes for years, and so extremely important across this change is that we have set up processes and now a joint operations center and a number of forums to hear directly from our front line and make sure that their issues are our issues in central office, in DC here, and that they feel heard and that they know that when they have needs, those needs are actioned,” she said.
The VA, under the Mission Act, is also working hard to engage health care providers in the community, including making VA training to community partners, including training on opioid use, suicide prevent and military culture.
However, all these change are for naught if the veterans are not on board. But so far, Dr. MacDonald said the early feedback is very positive.
She cited a VFW survey that asked a question about the Mission Act changes so far and whether they would recommend the VA to other veterans. Ninety percent of the respondents answered they would.
“That’s our marker that we are getting somewhere with these changes and the way we do business,” she said. “That is what we want to see continue to increase.”
NATIONAL HARBOR, MD–The US Department of Veterans Affairs (VA) is in the midst of a significant change in the way it will deliver care to veterans. Agency officials remain optimistic that the change will be for the better, and early indications are positive.
The change is being driven by the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (Mission) Act of 2018, a bill that opens health services options for veterans and integrates VA-administered care and care from community-based providers.
“This is change that is enhancing their experience in the system, and this is enhancing their options and the quality of the options in the system,” Jennifer MacDonald, MD, chief consultant to the principal deputy undersecretary for health at the VA, said during a December 3 session at the AMSUS 2019 annual meeting. “We need also for our workforce to understand how important they are to us across this degree of change.”
Dr. MacDonald highlighted integration with community-based care, including a community urgent care provision that allows veterans to access urgent care facilities and receive care without the need for prior authorization.
“The important piece about that is that we are also looking at the way this care has been accessed,” she said. “By and large, what we have seen from the data is that veterans are indeed seeking community urgent care at a site close to home. This may be CVS or Walgreens. It may be a stand-alone urgent care with a bit more functionality than those Minute Clinics tend to have. We are seeing veterans typically access care through those sites for those minor concerns and illnesses.”
However, she noted that this type of access does not alter the role the VA plays in administration of health care services.
“We are seeing them come back to VA for the majority of their care and for their core care–when there are serious issues, when insulin needs to be adjusted for diabetes, when there are heart disease medications that need to be refilled–we are seeing veterans not seek out urgent care, but come to us, and that is exactly what we want,” she said. “We want the continuity of care to continue and we want to help guide people to the right care, right place, right time.”
Dr. MacDonald also highlighted the expansion of a program that provides a stipend to caregivers that allows veterans to avoid institutionalization and remain within the community under that caregiver’s (a family or friend) supervision. This will expand by year’s end to Vietnam War-era veterans and within 2 years, to veterans that fall between the Vietnam War-era and the September 11, 2001, terrorist attacks.
“We wanted to do this equitably across all eras of veterans,” she said. “This now gives us that opportunity.”
Telehealth also plays a key role.
“For the first time ever, VA now has what we term ‘anywhere-to-anywhere’ telehealth under the Mission Act, an enormous opportunity for us,” she said. “Since we stretch … from New York City to Guam, we need the opportunity to provide care where it may be difficult to recruit and retain providers wherever veterans choose to live,” she said. “We believe that we should be able to meet people where they are regardless of where they choose to live. That’s an aspirational vision, but it is one we believe is exceptionally important and indeed we are moving toward that.”
These are just the beginning; the full implementation of the act goes out to 2034.
According to Dr. MacDonald, the agency is working hard to engage both veterans and the workforce to keep tabs on how the implementation is going.
“It’s a fundamental change in the day-to-day business that they’ve been doing, sometimes for years, and so extremely important across this change is that we have set up processes and now a joint operations center and a number of forums to hear directly from our front line and make sure that their issues are our issues in central office, in DC here, and that they feel heard and that they know that when they have needs, those needs are actioned,” she said.
The VA, under the Mission Act, is also working hard to engage health care providers in the community, including making VA training to community partners, including training on opioid use, suicide prevent and military culture.
However, all these change are for naught if the veterans are not on board. But so far, Dr. MacDonald said the early feedback is very positive.
She cited a VFW survey that asked a question about the Mission Act changes so far and whether they would recommend the VA to other veterans. Ninety percent of the respondents answered they would.
“That’s our marker that we are getting somewhere with these changes and the way we do business,” she said. “That is what we want to see continue to increase.”
Better Planning Needed to Help Veterans During, After Service
NATIONAL HARBOR, MD – More work and planning is needed for veterans after they serve in the Armed Forces, Rep. Brad Wenstrup, MD (R-Ohio), told attendees of the 2019 AMSUS annual meeting.
Rep. Wenstrup, in his December 3 keynote address, suggested that in addition to recruiters asking about what enlistees want to do in the military, they also should be asking what they want to do after military service.
“Let’s plan for that right now because it’s so much better, it’s so much healthier when you have a plan,” he said, noting that many military members struggle when integrating back into civilian life: They don’t have a plan, and they don’t feel “essential” and part of a team the way they did while serving. He pointed to graduating college students who have made plans for their next steps.
“We need to do the same thing for our troops who serve us [and] prepare them for what is next,” he said.
In addition to ensuring the health and well-being of service members when they come home, Rep. Wenstrup also discussed the need to ensure that medical staff are prepared for emergencies, identifying it as one of the challenges of military medicine right now.
“It’s a challenge for a lot in the active component when we are not at war … to sustain those skills, and it is very frustrating to the providers all the way around,” Rep. Wenstrup said. He noted that a lot of military medical staff help keep and refine those skills by working in the trauma department of major city hospitals.
“We are working together to try and bring our military assets, our civilian assets, DEA, whatever we can, together so that we make sure that we can provide and be ready,” he said. “And the importance of building these bridges is key to the future of medicine,” especially in a time of domestic crisis, so that all medical personnel, civilian and military, can work together for the common good of providing that service. “These are bridges we have to build.”
Rep. Wenstrup also talked about the need to do more to ensure a healthier population.
“The key is how do we live healthier, longer, because that is the real savings. A healthy nation is a stronger nation,” he said.
When comparing the amounts paid to providers for surgery with those paid for health and wellness, he contended that high payments for surgeons are due to the high skill set required for difficult procedures. However, health and wellness providers are paid poorly, as is payment for the management of chronic illness. “We don’t pay very well to the doctor who works with the patient and prevents the need to do open heart surgery,” he said. “Let’s start looking at that. Let’s start keeping people healthier longer.”
NATIONAL HARBOR, MD – More work and planning is needed for veterans after they serve in the Armed Forces, Rep. Brad Wenstrup, MD (R-Ohio), told attendees of the 2019 AMSUS annual meeting.
Rep. Wenstrup, in his December 3 keynote address, suggested that in addition to recruiters asking about what enlistees want to do in the military, they also should be asking what they want to do after military service.
“Let’s plan for that right now because it’s so much better, it’s so much healthier when you have a plan,” he said, noting that many military members struggle when integrating back into civilian life: They don’t have a plan, and they don’t feel “essential” and part of a team the way they did while serving. He pointed to graduating college students who have made plans for their next steps.
“We need to do the same thing for our troops who serve us [and] prepare them for what is next,” he said.
In addition to ensuring the health and well-being of service members when they come home, Rep. Wenstrup also discussed the need to ensure that medical staff are prepared for emergencies, identifying it as one of the challenges of military medicine right now.
“It’s a challenge for a lot in the active component when we are not at war … to sustain those skills, and it is very frustrating to the providers all the way around,” Rep. Wenstrup said. He noted that a lot of military medical staff help keep and refine those skills by working in the trauma department of major city hospitals.
“We are working together to try and bring our military assets, our civilian assets, DEA, whatever we can, together so that we make sure that we can provide and be ready,” he said. “And the importance of building these bridges is key to the future of medicine,” especially in a time of domestic crisis, so that all medical personnel, civilian and military, can work together for the common good of providing that service. “These are bridges we have to build.”
Rep. Wenstrup also talked about the need to do more to ensure a healthier population.
“The key is how do we live healthier, longer, because that is the real savings. A healthy nation is a stronger nation,” he said.
When comparing the amounts paid to providers for surgery with those paid for health and wellness, he contended that high payments for surgeons are due to the high skill set required for difficult procedures. However, health and wellness providers are paid poorly, as is payment for the management of chronic illness. “We don’t pay very well to the doctor who works with the patient and prevents the need to do open heart surgery,” he said. “Let’s start looking at that. Let’s start keeping people healthier longer.”
NATIONAL HARBOR, MD – More work and planning is needed for veterans after they serve in the Armed Forces, Rep. Brad Wenstrup, MD (R-Ohio), told attendees of the 2019 AMSUS annual meeting.
Rep. Wenstrup, in his December 3 keynote address, suggested that in addition to recruiters asking about what enlistees want to do in the military, they also should be asking what they want to do after military service.
“Let’s plan for that right now because it’s so much better, it’s so much healthier when you have a plan,” he said, noting that many military members struggle when integrating back into civilian life: They don’t have a plan, and they don’t feel “essential” and part of a team the way they did while serving. He pointed to graduating college students who have made plans for their next steps.
“We need to do the same thing for our troops who serve us [and] prepare them for what is next,” he said.
In addition to ensuring the health and well-being of service members when they come home, Rep. Wenstrup also discussed the need to ensure that medical staff are prepared for emergencies, identifying it as one of the challenges of military medicine right now.
“It’s a challenge for a lot in the active component when we are not at war … to sustain those skills, and it is very frustrating to the providers all the way around,” Rep. Wenstrup said. He noted that a lot of military medical staff help keep and refine those skills by working in the trauma department of major city hospitals.
“We are working together to try and bring our military assets, our civilian assets, DEA, whatever we can, together so that we make sure that we can provide and be ready,” he said. “And the importance of building these bridges is key to the future of medicine,” especially in a time of domestic crisis, so that all medical personnel, civilian and military, can work together for the common good of providing that service. “These are bridges we have to build.”
Rep. Wenstrup also talked about the need to do more to ensure a healthier population.
“The key is how do we live healthier, longer, because that is the real savings. A healthy nation is a stronger nation,” he said.
When comparing the amounts paid to providers for surgery with those paid for health and wellness, he contended that high payments for surgeons are due to the high skill set required for difficult procedures. However, health and wellness providers are paid poorly, as is payment for the management of chronic illness. “We don’t pay very well to the doctor who works with the patient and prevents the need to do open heart surgery,” he said. “Let’s start looking at that. Let’s start keeping people healthier longer.”
CDC finds that efforts to reduce new HIV infections have stalled
, according to a Vital Signs report published by the Centers for Disease Control and Prevention based upon a simultaneous MMWR Early Release. The report indicates that many Americans with HIV are not aware of their status or are not receiving effective treatment. Furthermore, the data suggest that few Americans who could benefit from preexposure prophylaxis (PrEP), a daily pill that prevents HIV, are receiving it.
The report “shows that HIV testing, treatment, and prevention have not reached enough Americans, and it emphasizes the continued urgent need to increase these interventions,” said Jay C. Butler, MD, deputy director for infectious diseases at the CDC, at a press conference. “We made a lot of progress in the late ’90s and into the early part of the 21st century in reducing the number of new cases of HIV. But HIV prevention progress has stalled in America since 2013. This stalling underscores the need to increase resources, deploy new technologies, and build expertise, particularly in areas where they’re needed most.”
To achieve these objectives, the CDC has proposed a federal initiative called Ending the HIV Epidemic: A Plan for America. The goal of the initiative is to reduce new HIV infections by 90% by 2030, in part by expanding access to PrEP medications.
Data suggest shortcomings in diagnosis, treatment, and prevention
In its review of data on HIV testing and treatment in 2017, the Vital Signs report found that approximately 154,000 people with HIV (that is, 14% of the total population with HIV) were unaware that they had the virus. These patients consequently could not take advantage of HIV treatment to maintain health, control the virus, and prevent HIV transmission. Young people aged 13-24 years were less likely to know their HIV status than did those aged 25 years and older, according to the report.
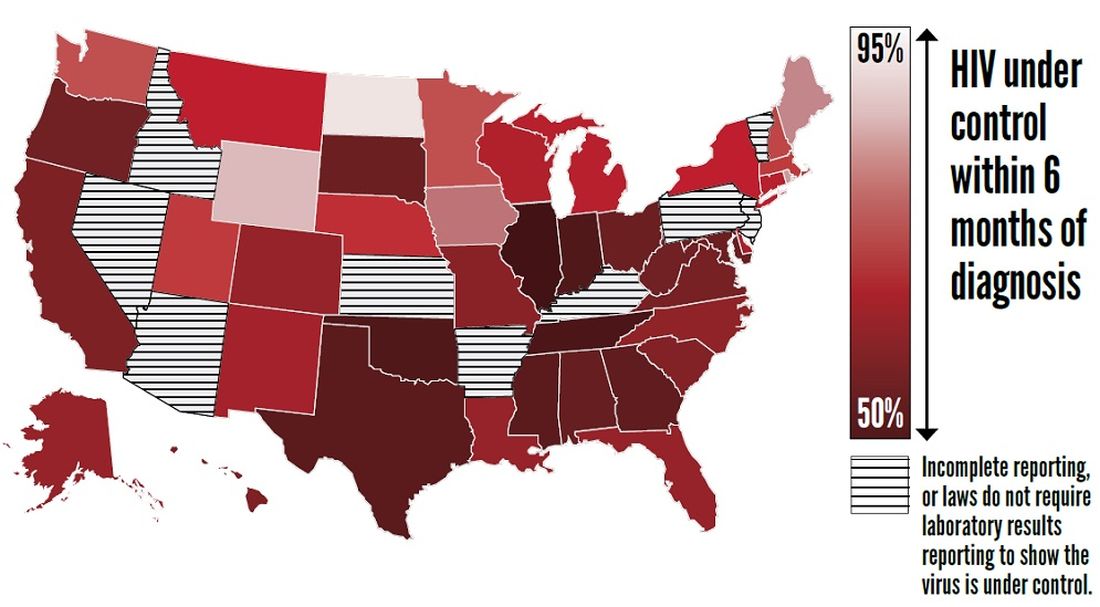
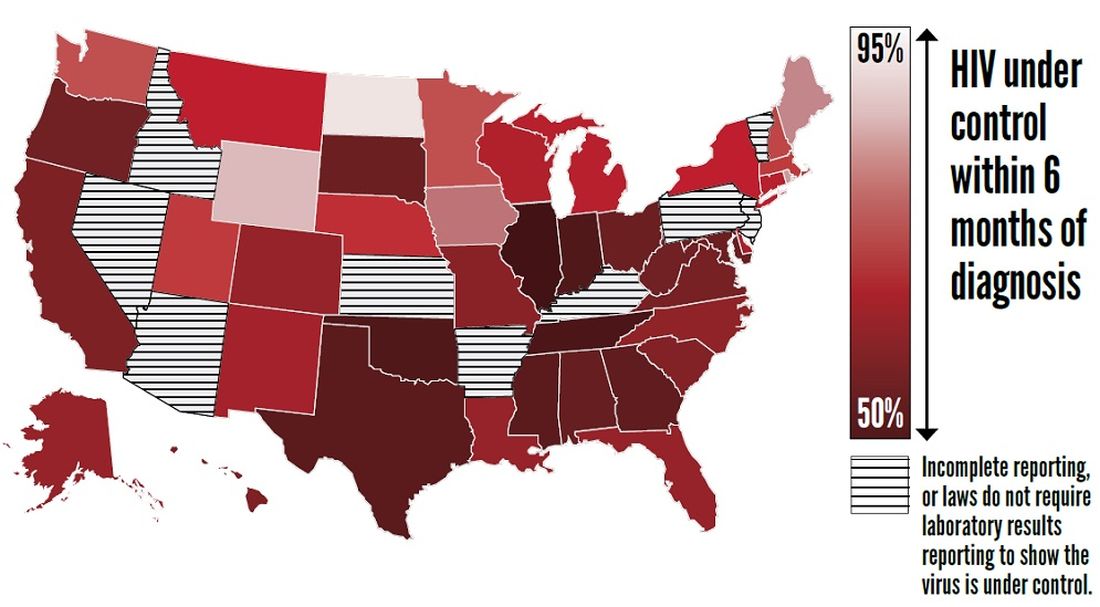
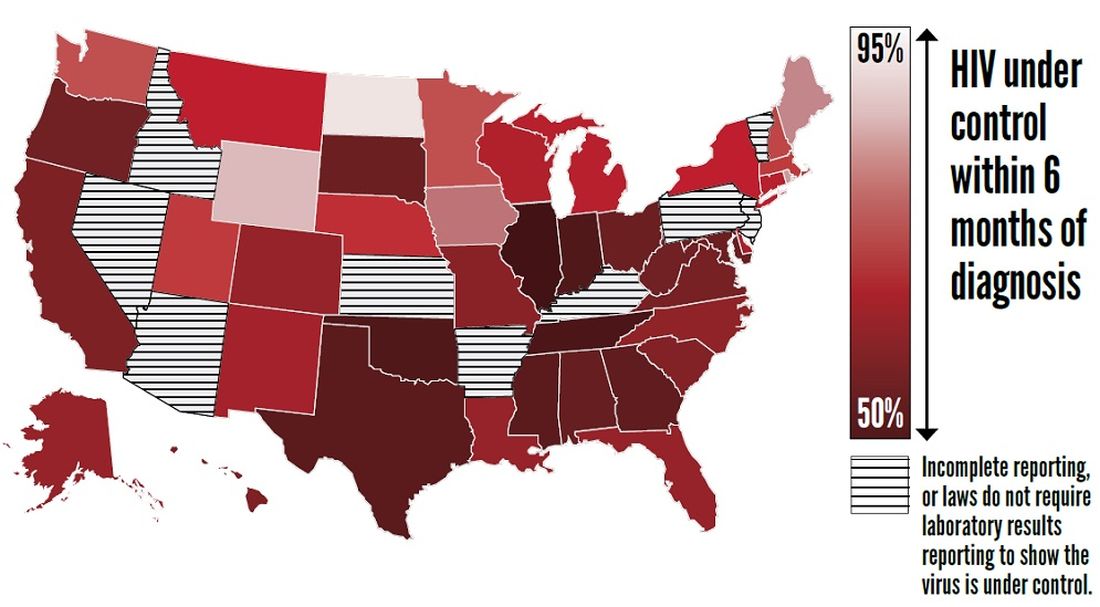
Furthermore, approximately two-thirds (63%) of patients who knew that they had HIV had the virus under control through effective treatment. Young people and African Americans were least likely to have the virus under control, according to the report.
The report also examines data about treatment with PrEP in 2018. About 1.2 million Americans could benefit from PrEP, but only 219,700 (18%) of them had received a prescription for the drug. The eligible groups with the lowest rates of coverage were young people, African Americans, and Latinos.
The report presents a conservative estimate of PrEP coverage, however. Researchers examined data from 92% of prescriptions from retail pharmacies in the United States but did not include prescriptions from closed health care systems such as managed care organizations and military health plans. PrEP coverage in 2018 likely was higher than these estimates indicate, according to the CDC.
“There has been a rapid increase in the number of people taking PrEP over the past 3 years, but there is no doubt that PrEP uptake is too low,” said Eugene McCray, MD, director of CDC’s division of HIV/AIDS prevention. “We are working hard to increase access to PrEP, especially among gay and bisexual men, women, transgender people, young people, African Americans, and Latinos.”
The rate of new HIV infections has not decreased, but remained stable, according to the report. The CDC estimates that there were about 38,000 new infections per year from 2013 to 2017.
Proposed initiative focuses on areas of greatest need
The proposed Ending the HIV Epidemic initiative, if it is funded, will target the locations of greatest need throughout the country. Its initial focus will be on 50 areas that account for more than half of new HIV diagnoses, including 48 counties; San Juan, Puerto Rico; and Washington, D.C. It also will direct resources to seven states with high rates of infection in rural areas. In a second phase, the initiative will expand nationwide, provided that additional resources are made available.
The proposed initiative relies on four science-based strategies. First, it will aim to diagnose all Americans with HIV (at least 95% of HIV infections) as early as possible. Second, the initiative will enable people with HIV to receive treatment rapidly and effectively. The CDC’s target is to achieve viral suppression in at least 95% of people with diagnosed HIV. Third, the initiative will use proven interventions such as PrEP and syringe services programs to prevent new HIV transmissions. One related goal is for at least 50% of people who could benefit from PrEP to receive a prescription. Finally, the initiative is intended to respond quickly to potential HIV outbreaks and provide prevention and treatment to those who need them.
The U.S. Department of Health & Human Services already has taken steps to enable the initiative to be implemented quickly if it is funded in 2020. The department has provided funding to Baltimore City, Md.; DeKalb County, Ga.; and East Baton Rouge Parish, La. to begin pursuing parts of the initiative. These communities are encouraged to share the lessons of their experiences with other communities. HHS also has supported local efforts to develop plans under the initiative in all priority geographic areas. These plans draw upon recommendations from the community, HIV-planning bodies, and health care providers.
“Ending the HIV epidemic would be one of the greatest public health triumphs in our nation’s history,” said Dr. McCray.
SOURCES: Centers for Disease Control and Prevention. CDC Vital Signs. 2019 Dec 3. and Harris NS et al. MMWR Morb Mortal Wkly Rep. 2019 Dec 3.
, according to a Vital Signs report published by the Centers for Disease Control and Prevention based upon a simultaneous MMWR Early Release. The report indicates that many Americans with HIV are not aware of their status or are not receiving effective treatment. Furthermore, the data suggest that few Americans who could benefit from preexposure prophylaxis (PrEP), a daily pill that prevents HIV, are receiving it.
The report “shows that HIV testing, treatment, and prevention have not reached enough Americans, and it emphasizes the continued urgent need to increase these interventions,” said Jay C. Butler, MD, deputy director for infectious diseases at the CDC, at a press conference. “We made a lot of progress in the late ’90s and into the early part of the 21st century in reducing the number of new cases of HIV. But HIV prevention progress has stalled in America since 2013. This stalling underscores the need to increase resources, deploy new technologies, and build expertise, particularly in areas where they’re needed most.”
To achieve these objectives, the CDC has proposed a federal initiative called Ending the HIV Epidemic: A Plan for America. The goal of the initiative is to reduce new HIV infections by 90% by 2030, in part by expanding access to PrEP medications.
Data suggest shortcomings in diagnosis, treatment, and prevention
In its review of data on HIV testing and treatment in 2017, the Vital Signs report found that approximately 154,000 people with HIV (that is, 14% of the total population with HIV) were unaware that they had the virus. These patients consequently could not take advantage of HIV treatment to maintain health, control the virus, and prevent HIV transmission. Young people aged 13-24 years were less likely to know their HIV status than did those aged 25 years and older, according to the report.
Furthermore, approximately two-thirds (63%) of patients who knew that they had HIV had the virus under control through effective treatment. Young people and African Americans were least likely to have the virus under control, according to the report.
The report also examines data about treatment with PrEP in 2018. About 1.2 million Americans could benefit from PrEP, but only 219,700 (18%) of them had received a prescription for the drug. The eligible groups with the lowest rates of coverage were young people, African Americans, and Latinos.
The report presents a conservative estimate of PrEP coverage, however. Researchers examined data from 92% of prescriptions from retail pharmacies in the United States but did not include prescriptions from closed health care systems such as managed care organizations and military health plans. PrEP coverage in 2018 likely was higher than these estimates indicate, according to the CDC.
“There has been a rapid increase in the number of people taking PrEP over the past 3 years, but there is no doubt that PrEP uptake is too low,” said Eugene McCray, MD, director of CDC’s division of HIV/AIDS prevention. “We are working hard to increase access to PrEP, especially among gay and bisexual men, women, transgender people, young people, African Americans, and Latinos.”
The rate of new HIV infections has not decreased, but remained stable, according to the report. The CDC estimates that there were about 38,000 new infections per year from 2013 to 2017.
Proposed initiative focuses on areas of greatest need
The proposed Ending the HIV Epidemic initiative, if it is funded, will target the locations of greatest need throughout the country. Its initial focus will be on 50 areas that account for more than half of new HIV diagnoses, including 48 counties; San Juan, Puerto Rico; and Washington, D.C. It also will direct resources to seven states with high rates of infection in rural areas. In a second phase, the initiative will expand nationwide, provided that additional resources are made available.
The proposed initiative relies on four science-based strategies. First, it will aim to diagnose all Americans with HIV (at least 95% of HIV infections) as early as possible. Second, the initiative will enable people with HIV to receive treatment rapidly and effectively. The CDC’s target is to achieve viral suppression in at least 95% of people with diagnosed HIV. Third, the initiative will use proven interventions such as PrEP and syringe services programs to prevent new HIV transmissions. One related goal is for at least 50% of people who could benefit from PrEP to receive a prescription. Finally, the initiative is intended to respond quickly to potential HIV outbreaks and provide prevention and treatment to those who need them.
The U.S. Department of Health & Human Services already has taken steps to enable the initiative to be implemented quickly if it is funded in 2020. The department has provided funding to Baltimore City, Md.; DeKalb County, Ga.; and East Baton Rouge Parish, La. to begin pursuing parts of the initiative. These communities are encouraged to share the lessons of their experiences with other communities. HHS also has supported local efforts to develop plans under the initiative in all priority geographic areas. These plans draw upon recommendations from the community, HIV-planning bodies, and health care providers.
“Ending the HIV epidemic would be one of the greatest public health triumphs in our nation’s history,” said Dr. McCray.
SOURCES: Centers for Disease Control and Prevention. CDC Vital Signs. 2019 Dec 3. and Harris NS et al. MMWR Morb Mortal Wkly Rep. 2019 Dec 3.
, according to a Vital Signs report published by the Centers for Disease Control and Prevention based upon a simultaneous MMWR Early Release. The report indicates that many Americans with HIV are not aware of their status or are not receiving effective treatment. Furthermore, the data suggest that few Americans who could benefit from preexposure prophylaxis (PrEP), a daily pill that prevents HIV, are receiving it.
The report “shows that HIV testing, treatment, and prevention have not reached enough Americans, and it emphasizes the continued urgent need to increase these interventions,” said Jay C. Butler, MD, deputy director for infectious diseases at the CDC, at a press conference. “We made a lot of progress in the late ’90s and into the early part of the 21st century in reducing the number of new cases of HIV. But HIV prevention progress has stalled in America since 2013. This stalling underscores the need to increase resources, deploy new technologies, and build expertise, particularly in areas where they’re needed most.”
To achieve these objectives, the CDC has proposed a federal initiative called Ending the HIV Epidemic: A Plan for America. The goal of the initiative is to reduce new HIV infections by 90% by 2030, in part by expanding access to PrEP medications.
Data suggest shortcomings in diagnosis, treatment, and prevention
In its review of data on HIV testing and treatment in 2017, the Vital Signs report found that approximately 154,000 people with HIV (that is, 14% of the total population with HIV) were unaware that they had the virus. These patients consequently could not take advantage of HIV treatment to maintain health, control the virus, and prevent HIV transmission. Young people aged 13-24 years were less likely to know their HIV status than did those aged 25 years and older, according to the report.
Furthermore, approximately two-thirds (63%) of patients who knew that they had HIV had the virus under control through effective treatment. Young people and African Americans were least likely to have the virus under control, according to the report.
The report also examines data about treatment with PrEP in 2018. About 1.2 million Americans could benefit from PrEP, but only 219,700 (18%) of them had received a prescription for the drug. The eligible groups with the lowest rates of coverage were young people, African Americans, and Latinos.
The report presents a conservative estimate of PrEP coverage, however. Researchers examined data from 92% of prescriptions from retail pharmacies in the United States but did not include prescriptions from closed health care systems such as managed care organizations and military health plans. PrEP coverage in 2018 likely was higher than these estimates indicate, according to the CDC.
“There has been a rapid increase in the number of people taking PrEP over the past 3 years, but there is no doubt that PrEP uptake is too low,” said Eugene McCray, MD, director of CDC’s division of HIV/AIDS prevention. “We are working hard to increase access to PrEP, especially among gay and bisexual men, women, transgender people, young people, African Americans, and Latinos.”
The rate of new HIV infections has not decreased, but remained stable, according to the report. The CDC estimates that there were about 38,000 new infections per year from 2013 to 2017.
Proposed initiative focuses on areas of greatest need
The proposed Ending the HIV Epidemic initiative, if it is funded, will target the locations of greatest need throughout the country. Its initial focus will be on 50 areas that account for more than half of new HIV diagnoses, including 48 counties; San Juan, Puerto Rico; and Washington, D.C. It also will direct resources to seven states with high rates of infection in rural areas. In a second phase, the initiative will expand nationwide, provided that additional resources are made available.
The proposed initiative relies on four science-based strategies. First, it will aim to diagnose all Americans with HIV (at least 95% of HIV infections) as early as possible. Second, the initiative will enable people with HIV to receive treatment rapidly and effectively. The CDC’s target is to achieve viral suppression in at least 95% of people with diagnosed HIV. Third, the initiative will use proven interventions such as PrEP and syringe services programs to prevent new HIV transmissions. One related goal is for at least 50% of people who could benefit from PrEP to receive a prescription. Finally, the initiative is intended to respond quickly to potential HIV outbreaks and provide prevention and treatment to those who need them.
The U.S. Department of Health & Human Services already has taken steps to enable the initiative to be implemented quickly if it is funded in 2020. The department has provided funding to Baltimore City, Md.; DeKalb County, Ga.; and East Baton Rouge Parish, La. to begin pursuing parts of the initiative. These communities are encouraged to share the lessons of their experiences with other communities. HHS also has supported local efforts to develop plans under the initiative in all priority geographic areas. These plans draw upon recommendations from the community, HIV-planning bodies, and health care providers.
“Ending the HIV epidemic would be one of the greatest public health triumphs in our nation’s history,” said Dr. McCray.
SOURCES: Centers for Disease Control and Prevention. CDC Vital Signs. 2019 Dec 3. and Harris NS et al. MMWR Morb Mortal Wkly Rep. 2019 Dec 3.
FROM THE CDC
Vaping front and center at Hahn’s first FDA confirmation hearing
Stephen Hahn, MD, President Trump’s pick to head the Food and Drug Administration, faced questions from both sides of the aisle on youth vaping, but came up short when asked to commit to taking action, particularly on banning flavored vaping products.
Speaking at a Nov. 20 confirmation hearing before the Senate Health, Education, Labor, and Pensions Committee, Dr. Hahn said that youth vaping and e-cigarette use is “an important, urgent crisis in this country. I do not want to see another generation of Americans become addicted to tobacco and nicotine and I believe that we need to take aggressive to stop that.”
Sen. Patty Murray (D-Wash), the committee’s ranking member, asked Dr. Hahn whether he would work to finalize a ban flavored e-cigarette products, first proposed but then backed away from, by the president in September.
“I understand that the final compliance policy is under consideration by the administration, and I look forward to their decision,” Dr. Hahn said. “I am not privy to those decision-making processes, but I very much agree and support that aggressive action needs to be taken to protect our children.”
When pressed by Sen. Murray as to whether he told President Trump that he disagrees with the decision to back away the proposed ban, Dr. Hahn revealed that he has “not had a conversation with the president.”
Dr. Hahn, a radiation oncologist who currently serves as chief medical executive at MD Anderson Cancer Center, Houston, held firm to just coming up short of making that commitment when questioned by senators from both parties.
Sen. Mitt Romney (R-Utah) warned Dr. Hahn that the playing of politics would be unlike anything he has seen and is already being played out in the lobbying of the administration to change its stance on flavored e-cigarette products, which can run counter to the science about the harmful effects of these products.
“The question is how you will balance those things in which you put forward,” Sen. Romney asked. “How you will deal with this issue is a pretty good test case for how you would deal with this issue on an ongoing basis on matters not just related to vaping.”
He also brought up President Trump’s September announcement on a flavor ban and the administration’s signaling they are moving away from a flavor ban. “Is the FDA, under your leadership, able and willing to take action which will protect our kids, whether or not the White House wants you to take that action?”
Dr. Hahn cited his pledge as a doctor to always put the patient first and reiterated that “I take that pledge very seriously and I think if you ask anyone who has worked with me, they will tell you that I have upheld that pledge.”
But he fell short of saying that he would take actions that would oppose the White House, saying only that “patients need to come first and the decisions that we make need to be guided by science and data, congruent with the law.”
When asked by Sen. Romney if he saw any reason for holding off on a flavor ban, given the evidence that suggests flavored e-cigarette products are the gateway to youths nicotine addiction, Dr. Hahn said that he has seen the same evidence and that it requires “bold action,” but did not commit to a flavor ban. “I will use science and data to guide the decisions if I am fortunate enough to be confirmed, and I won’t back away from that.”
Sen. Doug Jones (D-Ala.) expressed concern about Dr. Hahn’s answers.
“I was less than happy with many of the answers you gave to members of this committee with regard to vaping and the potential ban on flavored e-cigarettes,” Sen. Jones said. “I think you can tell from the questions of so many senators that is one of the biggest issues that the United States Senate and Congress is facing right now. It is with this committee.”
Outside of vaping, much of the senators’ questioning was nonconfrontational, with questions spanning a gamut of issues facing the FDA.
Dr. Hahn offered his commitment to working with Congress to address drug shortages, noting nonspecifically that, “there are things that we can do to help.”
He also pledged to work with Congress on addressing patent reform to get more biosimilars to market in an effort to help drive down drug prices.
Regarding opioids, Dr. Hahn was asked about balancing the needs of those who legitimately need access to opioids against abuse and diversion.
“When I first went to medical school and started taking care of cancer patients, the teaching was that cancer patients should be treated liberally with opioids and that they don’t become addicted to pain medications,” he said. “We found out that wasn’t the case – and in some instances – with tragic consequences.”
He noted that pain therapy has evolved and that his institution now takes a multidisciplinary approach employing both opioid and nonopioid medications.
“I am very much a supporter of the multidisciplinary approach to treating pain,” he said. “I think it is something that we need to more of and if I am fortunate enough to be confirmed as commissioner of [FDA], I look forward to furthering the education efforts for providers and patients.”
Other areas he committed to included helping to improve clinical trial design for psychiatric medications and improving development of therapies for rare diseases.
Committee Chairman Lamar Alexander (R-Tenn.) said he plans to schedule a Dec. 3 vote to advance Dr. Hahn’s nomination to the full Senate for its consideration.
Stephen Hahn, MD, President Trump’s pick to head the Food and Drug Administration, faced questions from both sides of the aisle on youth vaping, but came up short when asked to commit to taking action, particularly on banning flavored vaping products.
Speaking at a Nov. 20 confirmation hearing before the Senate Health, Education, Labor, and Pensions Committee, Dr. Hahn said that youth vaping and e-cigarette use is “an important, urgent crisis in this country. I do not want to see another generation of Americans become addicted to tobacco and nicotine and I believe that we need to take aggressive to stop that.”
Sen. Patty Murray (D-Wash), the committee’s ranking member, asked Dr. Hahn whether he would work to finalize a ban flavored e-cigarette products, first proposed but then backed away from, by the president in September.
“I understand that the final compliance policy is under consideration by the administration, and I look forward to their decision,” Dr. Hahn said. “I am not privy to those decision-making processes, but I very much agree and support that aggressive action needs to be taken to protect our children.”
When pressed by Sen. Murray as to whether he told President Trump that he disagrees with the decision to back away the proposed ban, Dr. Hahn revealed that he has “not had a conversation with the president.”
Dr. Hahn, a radiation oncologist who currently serves as chief medical executive at MD Anderson Cancer Center, Houston, held firm to just coming up short of making that commitment when questioned by senators from both parties.
Sen. Mitt Romney (R-Utah) warned Dr. Hahn that the playing of politics would be unlike anything he has seen and is already being played out in the lobbying of the administration to change its stance on flavored e-cigarette products, which can run counter to the science about the harmful effects of these products.
“The question is how you will balance those things in which you put forward,” Sen. Romney asked. “How you will deal with this issue is a pretty good test case for how you would deal with this issue on an ongoing basis on matters not just related to vaping.”
He also brought up President Trump’s September announcement on a flavor ban and the administration’s signaling they are moving away from a flavor ban. “Is the FDA, under your leadership, able and willing to take action which will protect our kids, whether or not the White House wants you to take that action?”
Dr. Hahn cited his pledge as a doctor to always put the patient first and reiterated that “I take that pledge very seriously and I think if you ask anyone who has worked with me, they will tell you that I have upheld that pledge.”
But he fell short of saying that he would take actions that would oppose the White House, saying only that “patients need to come first and the decisions that we make need to be guided by science and data, congruent with the law.”
When asked by Sen. Romney if he saw any reason for holding off on a flavor ban, given the evidence that suggests flavored e-cigarette products are the gateway to youths nicotine addiction, Dr. Hahn said that he has seen the same evidence and that it requires “bold action,” but did not commit to a flavor ban. “I will use science and data to guide the decisions if I am fortunate enough to be confirmed, and I won’t back away from that.”
Sen. Doug Jones (D-Ala.) expressed concern about Dr. Hahn’s answers.
“I was less than happy with many of the answers you gave to members of this committee with regard to vaping and the potential ban on flavored e-cigarettes,” Sen. Jones said. “I think you can tell from the questions of so many senators that is one of the biggest issues that the United States Senate and Congress is facing right now. It is with this committee.”
Outside of vaping, much of the senators’ questioning was nonconfrontational, with questions spanning a gamut of issues facing the FDA.
Dr. Hahn offered his commitment to working with Congress to address drug shortages, noting nonspecifically that, “there are things that we can do to help.”
He also pledged to work with Congress on addressing patent reform to get more biosimilars to market in an effort to help drive down drug prices.
Regarding opioids, Dr. Hahn was asked about balancing the needs of those who legitimately need access to opioids against abuse and diversion.
“When I first went to medical school and started taking care of cancer patients, the teaching was that cancer patients should be treated liberally with opioids and that they don’t become addicted to pain medications,” he said. “We found out that wasn’t the case – and in some instances – with tragic consequences.”
He noted that pain therapy has evolved and that his institution now takes a multidisciplinary approach employing both opioid and nonopioid medications.
“I am very much a supporter of the multidisciplinary approach to treating pain,” he said. “I think it is something that we need to more of and if I am fortunate enough to be confirmed as commissioner of [FDA], I look forward to furthering the education efforts for providers and patients.”
Other areas he committed to included helping to improve clinical trial design for psychiatric medications and improving development of therapies for rare diseases.
Committee Chairman Lamar Alexander (R-Tenn.) said he plans to schedule a Dec. 3 vote to advance Dr. Hahn’s nomination to the full Senate for its consideration.
Stephen Hahn, MD, President Trump’s pick to head the Food and Drug Administration, faced questions from both sides of the aisle on youth vaping, but came up short when asked to commit to taking action, particularly on banning flavored vaping products.
Speaking at a Nov. 20 confirmation hearing before the Senate Health, Education, Labor, and Pensions Committee, Dr. Hahn said that youth vaping and e-cigarette use is “an important, urgent crisis in this country. I do not want to see another generation of Americans become addicted to tobacco and nicotine and I believe that we need to take aggressive to stop that.”
Sen. Patty Murray (D-Wash), the committee’s ranking member, asked Dr. Hahn whether he would work to finalize a ban flavored e-cigarette products, first proposed but then backed away from, by the president in September.
“I understand that the final compliance policy is under consideration by the administration, and I look forward to their decision,” Dr. Hahn said. “I am not privy to those decision-making processes, but I very much agree and support that aggressive action needs to be taken to protect our children.”
When pressed by Sen. Murray as to whether he told President Trump that he disagrees with the decision to back away the proposed ban, Dr. Hahn revealed that he has “not had a conversation with the president.”
Dr. Hahn, a radiation oncologist who currently serves as chief medical executive at MD Anderson Cancer Center, Houston, held firm to just coming up short of making that commitment when questioned by senators from both parties.
Sen. Mitt Romney (R-Utah) warned Dr. Hahn that the playing of politics would be unlike anything he has seen and is already being played out in the lobbying of the administration to change its stance on flavored e-cigarette products, which can run counter to the science about the harmful effects of these products.
“The question is how you will balance those things in which you put forward,” Sen. Romney asked. “How you will deal with this issue is a pretty good test case for how you would deal with this issue on an ongoing basis on matters not just related to vaping.”
He also brought up President Trump’s September announcement on a flavor ban and the administration’s signaling they are moving away from a flavor ban. “Is the FDA, under your leadership, able and willing to take action which will protect our kids, whether or not the White House wants you to take that action?”
Dr. Hahn cited his pledge as a doctor to always put the patient first and reiterated that “I take that pledge very seriously and I think if you ask anyone who has worked with me, they will tell you that I have upheld that pledge.”
But he fell short of saying that he would take actions that would oppose the White House, saying only that “patients need to come first and the decisions that we make need to be guided by science and data, congruent with the law.”
When asked by Sen. Romney if he saw any reason for holding off on a flavor ban, given the evidence that suggests flavored e-cigarette products are the gateway to youths nicotine addiction, Dr. Hahn said that he has seen the same evidence and that it requires “bold action,” but did not commit to a flavor ban. “I will use science and data to guide the decisions if I am fortunate enough to be confirmed, and I won’t back away from that.”
Sen. Doug Jones (D-Ala.) expressed concern about Dr. Hahn’s answers.
“I was less than happy with many of the answers you gave to members of this committee with regard to vaping and the potential ban on flavored e-cigarettes,” Sen. Jones said. “I think you can tell from the questions of so many senators that is one of the biggest issues that the United States Senate and Congress is facing right now. It is with this committee.”
Outside of vaping, much of the senators’ questioning was nonconfrontational, with questions spanning a gamut of issues facing the FDA.
Dr. Hahn offered his commitment to working with Congress to address drug shortages, noting nonspecifically that, “there are things that we can do to help.”
He also pledged to work with Congress on addressing patent reform to get more biosimilars to market in an effort to help drive down drug prices.
Regarding opioids, Dr. Hahn was asked about balancing the needs of those who legitimately need access to opioids against abuse and diversion.
“When I first went to medical school and started taking care of cancer patients, the teaching was that cancer patients should be treated liberally with opioids and that they don’t become addicted to pain medications,” he said. “We found out that wasn’t the case – and in some instances – with tragic consequences.”
He noted that pain therapy has evolved and that his institution now takes a multidisciplinary approach employing both opioid and nonopioid medications.
“I am very much a supporter of the multidisciplinary approach to treating pain,” he said. “I think it is something that we need to more of and if I am fortunate enough to be confirmed as commissioner of [FDA], I look forward to furthering the education efforts for providers and patients.”
Other areas he committed to included helping to improve clinical trial design for psychiatric medications and improving development of therapies for rare diseases.
Committee Chairman Lamar Alexander (R-Tenn.) said he plans to schedule a Dec. 3 vote to advance Dr. Hahn’s nomination to the full Senate for its consideration.
REPORTING FROM A SENATE SUBCOMMITTEE HEARING
Feds propose new price transparency rules in health care
Three federal agencies have jointly issued a price transparency proposal that would require most employer-based health plans and health insurance issuers to disclose price and cost-sharing information up front.
The goal behind the proposal is to give consumers accurate estimates about the out-of-pocket costs they may incur for medical services, giving them the opportunity to shop around for medical treatment.
“Under the status quo, health care prices are about as clear as mud to patients,” Seema Verma, administrator of the Centers for Medicare & Medicaid Services said in a statement, adding that “we are throwing open the shutters and bringing to light the price of care for American consumers. Kept secret, these prices are simply dollar amounts on a ledger; disclosed, they deliver fuel to the engines of competition among hospitals and insurers.”
The “Transparency in Coverage” proposed rule, was released online on Nov. 15 jointly by the Department of Health & Human Services, the Department of Labor, and the Department of the Treasury. If finalized, it would give consumers “real-time, personalized access to cost-sharing information, including an estimate of their cost-sharing liability for all covered health care items and services through an online tool that most group health plans and health insurance issuers would be required to make available to all of their members, and in paper form, at the consumer’s request,” a fact sheet outlining the features of the proposed rule states.
Health plans would also “be required to disclose on a public website their negotiated rates for in-network providers and allowed amounts paid for out-of-network providers,” the fact sheet continues.
The proposal comes as the CMS finalized transparency-related rules in the 2020 update to the hospital outpatient prospective payment system (OPPS). The price transparency portion of the OPPS is scheduled to go into effect on Jan. 1, 2021.
A fact sheet on the OPPS states that each hospital in the United States will be required to “establish (and update) and make public a yearly list of the hospital’s standard charges for items and services provided by the hospital.”
That list must include all standard charges, including gross charges, discounted cash prices, payer-specific negotiated charges, and deidentified minimum and maximum negotiated charges for all hospital items and services, as well as cash prices, payer-specific negotiated charges, and deidentified minimum and maximum negotiated charges for 300 shoppable services (70 identified by CMS and 230 selected by the hospital). A shoppable service is a service that can be scheduled in advance.
“This final rule and the proposed rule will bring forward the transparency we need to finally begin reducing the overall health care costs,” Ms. Verma said. “Today’s rules usher in a new era that upends the status quo to empower patients and put them first.”
America’s Health Insurance Plans said in a statement that it is evaluating the proposal and the final OPPS rule through a lens of three core principles: that consumers deserve transparency about out-of-pocket costs to help them make informed decisions; that transparency should be achieved in a way that encourages, not undermines, competitive negotiations to lower costs; and that public programs and the free market work together to deliver on our commitments to affordable, quality, and value.
“Neither of these rules, together or separately, satisfies these principles,” AHIP stated.
The Federation of American Hospitals is already anticipating a legal challenge to the rules.
“Patients should have readily available and easy-to-understand cost-sharing information when they need to make health care decisions,” FAH President and CEO Chip Kahn said in a statement. “Health care pricing transparency ought to be defined by the right information at the right time. This final regulation on hospital transparency fails to meet the definition of price transparency useful for patients. Instead, it will only result in patient overload of useless information while distorting the competitive market for purchasing hospital care.”
Mr. Kahn said FAH plans “on joining with hospitals to file a legal challenge,” asserting that CMS has exceeded it’s authority with these rules.
Three federal agencies have jointly issued a price transparency proposal that would require most employer-based health plans and health insurance issuers to disclose price and cost-sharing information up front.
The goal behind the proposal is to give consumers accurate estimates about the out-of-pocket costs they may incur for medical services, giving them the opportunity to shop around for medical treatment.
“Under the status quo, health care prices are about as clear as mud to patients,” Seema Verma, administrator of the Centers for Medicare & Medicaid Services said in a statement, adding that “we are throwing open the shutters and bringing to light the price of care for American consumers. Kept secret, these prices are simply dollar amounts on a ledger; disclosed, they deliver fuel to the engines of competition among hospitals and insurers.”
The “Transparency in Coverage” proposed rule, was released online on Nov. 15 jointly by the Department of Health & Human Services, the Department of Labor, and the Department of the Treasury. If finalized, it would give consumers “real-time, personalized access to cost-sharing information, including an estimate of their cost-sharing liability for all covered health care items and services through an online tool that most group health plans and health insurance issuers would be required to make available to all of their members, and in paper form, at the consumer’s request,” a fact sheet outlining the features of the proposed rule states.
Health plans would also “be required to disclose on a public website their negotiated rates for in-network providers and allowed amounts paid for out-of-network providers,” the fact sheet continues.
The proposal comes as the CMS finalized transparency-related rules in the 2020 update to the hospital outpatient prospective payment system (OPPS). The price transparency portion of the OPPS is scheduled to go into effect on Jan. 1, 2021.
A fact sheet on the OPPS states that each hospital in the United States will be required to “establish (and update) and make public a yearly list of the hospital’s standard charges for items and services provided by the hospital.”
That list must include all standard charges, including gross charges, discounted cash prices, payer-specific negotiated charges, and deidentified minimum and maximum negotiated charges for all hospital items and services, as well as cash prices, payer-specific negotiated charges, and deidentified minimum and maximum negotiated charges for 300 shoppable services (70 identified by CMS and 230 selected by the hospital). A shoppable service is a service that can be scheduled in advance.
“This final rule and the proposed rule will bring forward the transparency we need to finally begin reducing the overall health care costs,” Ms. Verma said. “Today’s rules usher in a new era that upends the status quo to empower patients and put them first.”
America’s Health Insurance Plans said in a statement that it is evaluating the proposal and the final OPPS rule through a lens of three core principles: that consumers deserve transparency about out-of-pocket costs to help them make informed decisions; that transparency should be achieved in a way that encourages, not undermines, competitive negotiations to lower costs; and that public programs and the free market work together to deliver on our commitments to affordable, quality, and value.
“Neither of these rules, together or separately, satisfies these principles,” AHIP stated.
The Federation of American Hospitals is already anticipating a legal challenge to the rules.
“Patients should have readily available and easy-to-understand cost-sharing information when they need to make health care decisions,” FAH President and CEO Chip Kahn said in a statement. “Health care pricing transparency ought to be defined by the right information at the right time. This final regulation on hospital transparency fails to meet the definition of price transparency useful for patients. Instead, it will only result in patient overload of useless information while distorting the competitive market for purchasing hospital care.”
Mr. Kahn said FAH plans “on joining with hospitals to file a legal challenge,” asserting that CMS has exceeded it’s authority with these rules.
Three federal agencies have jointly issued a price transparency proposal that would require most employer-based health plans and health insurance issuers to disclose price and cost-sharing information up front.
The goal behind the proposal is to give consumers accurate estimates about the out-of-pocket costs they may incur for medical services, giving them the opportunity to shop around for medical treatment.
“Under the status quo, health care prices are about as clear as mud to patients,” Seema Verma, administrator of the Centers for Medicare & Medicaid Services said in a statement, adding that “we are throwing open the shutters and bringing to light the price of care for American consumers. Kept secret, these prices are simply dollar amounts on a ledger; disclosed, they deliver fuel to the engines of competition among hospitals and insurers.”
The “Transparency in Coverage” proposed rule, was released online on Nov. 15 jointly by the Department of Health & Human Services, the Department of Labor, and the Department of the Treasury. If finalized, it would give consumers “real-time, personalized access to cost-sharing information, including an estimate of their cost-sharing liability for all covered health care items and services through an online tool that most group health plans and health insurance issuers would be required to make available to all of their members, and in paper form, at the consumer’s request,” a fact sheet outlining the features of the proposed rule states.
Health plans would also “be required to disclose on a public website their negotiated rates for in-network providers and allowed amounts paid for out-of-network providers,” the fact sheet continues.
The proposal comes as the CMS finalized transparency-related rules in the 2020 update to the hospital outpatient prospective payment system (OPPS). The price transparency portion of the OPPS is scheduled to go into effect on Jan. 1, 2021.
A fact sheet on the OPPS states that each hospital in the United States will be required to “establish (and update) and make public a yearly list of the hospital’s standard charges for items and services provided by the hospital.”
That list must include all standard charges, including gross charges, discounted cash prices, payer-specific negotiated charges, and deidentified minimum and maximum negotiated charges for all hospital items and services, as well as cash prices, payer-specific negotiated charges, and deidentified minimum and maximum negotiated charges for 300 shoppable services (70 identified by CMS and 230 selected by the hospital). A shoppable service is a service that can be scheduled in advance.
“This final rule and the proposed rule will bring forward the transparency we need to finally begin reducing the overall health care costs,” Ms. Verma said. “Today’s rules usher in a new era that upends the status quo to empower patients and put them first.”
America’s Health Insurance Plans said in a statement that it is evaluating the proposal and the final OPPS rule through a lens of three core principles: that consumers deserve transparency about out-of-pocket costs to help them make informed decisions; that transparency should be achieved in a way that encourages, not undermines, competitive negotiations to lower costs; and that public programs and the free market work together to deliver on our commitments to affordable, quality, and value.
“Neither of these rules, together or separately, satisfies these principles,” AHIP stated.
The Federation of American Hospitals is already anticipating a legal challenge to the rules.
“Patients should have readily available and easy-to-understand cost-sharing information when they need to make health care decisions,” FAH President and CEO Chip Kahn said in a statement. “Health care pricing transparency ought to be defined by the right information at the right time. This final regulation on hospital transparency fails to meet the definition of price transparency useful for patients. Instead, it will only result in patient overload of useless information while distorting the competitive market for purchasing hospital care.”
Mr. Kahn said FAH plans “on joining with hospitals to file a legal challenge,” asserting that CMS has exceeded it’s authority with these rules.
FDA still concerned about biotin affecting troponin tests
The
However, not all troponin tests are affected, according to the update. “Since the FDA’s safety communication on this topic in 2017, some lab test developers have been successful at mitigating the biotin interference of their assays, but others have not yet addressed it,” according to the new communication, issued in early November.
Also known as vitamin B7 and appearing in many dietary supplements, including prenatal multivitamins and supplements for hair, skin, and nail growth, biotin can lead to falsely low results on some troponin tests, especially at high levels. The worry is that biotin interference could therefore lead to missed diagnoses. The FDA has provided a list of those tests that have not taken biotin’s effects into account, titled “Biotin Interference with Troponin Lab Tests – Assays Subject to Biotin Interference.”
The daily recommended allowance for biotin, according to the communication, is about 0.3 mg, but it isn’t always clear how much is actually included in supplements – some can contain 20 mg or even as much as 100 mg per pill of biotin. The communication includes recommendations for patients, health care professionals, laboratory personnel, and lab test manufacturers and developers.
The full safety communication can be found on the FDA website, and problems with tests can be reported via the FDA’s MedWatch Voluntary Reporting Form.
The
However, not all troponin tests are affected, according to the update. “Since the FDA’s safety communication on this topic in 2017, some lab test developers have been successful at mitigating the biotin interference of their assays, but others have not yet addressed it,” according to the new communication, issued in early November.
Also known as vitamin B7 and appearing in many dietary supplements, including prenatal multivitamins and supplements for hair, skin, and nail growth, biotin can lead to falsely low results on some troponin tests, especially at high levels. The worry is that biotin interference could therefore lead to missed diagnoses. The FDA has provided a list of those tests that have not taken biotin’s effects into account, titled “Biotin Interference with Troponin Lab Tests – Assays Subject to Biotin Interference.”
The daily recommended allowance for biotin, according to the communication, is about 0.3 mg, but it isn’t always clear how much is actually included in supplements – some can contain 20 mg or even as much as 100 mg per pill of biotin. The communication includes recommendations for patients, health care professionals, laboratory personnel, and lab test manufacturers and developers.
The full safety communication can be found on the FDA website, and problems with tests can be reported via the FDA’s MedWatch Voluntary Reporting Form.
The
However, not all troponin tests are affected, according to the update. “Since the FDA’s safety communication on this topic in 2017, some lab test developers have been successful at mitigating the biotin interference of their assays, but others have not yet addressed it,” according to the new communication, issued in early November.
Also known as vitamin B7 and appearing in many dietary supplements, including prenatal multivitamins and supplements for hair, skin, and nail growth, biotin can lead to falsely low results on some troponin tests, especially at high levels. The worry is that biotin interference could therefore lead to missed diagnoses. The FDA has provided a list of those tests that have not taken biotin’s effects into account, titled “Biotin Interference with Troponin Lab Tests – Assays Subject to Biotin Interference.”
The daily recommended allowance for biotin, according to the communication, is about 0.3 mg, but it isn’t always clear how much is actually included in supplements – some can contain 20 mg or even as much as 100 mg per pill of biotin. The communication includes recommendations for patients, health care professionals, laboratory personnel, and lab test manufacturers and developers.
The full safety communication can be found on the FDA website, and problems with tests can be reported via the FDA’s MedWatch Voluntary Reporting Form.
The Jewel in the Lotus: A Meditation on Memory for Veterans Day 2019
On the 11th day of the 11th month, we celebrate Veterans Day (no apostrophe because it is not a day that veterans possess or that belongs to any individual veteran).2,3 Interestingly, the US Department of Defense (DoD) and the US Department of Veterans Affairs (VA) have web pages correcting any confusion about the meaning of Memorial Day and Veterans Day so that the public understands the unique purpose of each holiday. Memorial Day commemorates all those who lost their lives in the line of duty to the nation, whereas Veterans Day commemorates all those who have honorably served their country as service members. While Memorial Day is a solemn occasion of remembering and respect for those who have died, Veterans Day is an event of gratitude and appreciation focused on veterans still living. The dual mission of the 2 holidays is to remind the public of the debt of remembrance and reverence we owe all veterans both those who have gone before us and those who remain with us.
Memory is what most intrinsically unites the 2 commemorations. In fact, in Great Britain, Canada, and Australia, November 11 is called Remembrance Day.2 Yet memory is a double-edged sword that can be raised in tribute to service members or can deeply lacerate them. Many of the wounds that cause the most prolonged and deepest suffering are not physical—they are mental. Disturbances of memory are among the criteria for posttraumatic stress disorder (PTSD). Under its section on intrusive cluster, the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM) lists “recurrent, involuntary, and intrusive distressing memories of the traumatic event(s).” The avoidance cluster underscores how the afflicted mind tries to escape itself: “Avoidance of or efforts to avoid distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s).”4
PTSD was first recognized as a psychiatric diagnosis in DSM-III in 1980, and since then VA and DoD have devoted enormous resources to developing effective treatments for the disorder, most notably evidence-based psychotherapies. Sadly ironic, the only psychiatric disorder whose etiology is understood has proved to be the most difficult to treat much less cure. As with most serious mental illnesses, some cases become chronic and refractory to the best of care. These tormented individuals live as if in a twilight zone between the past and the present.
Memory and war have a long history in literature, poetry, and history. Haunting memories of PTSD are found in the ancient epics of Homer. On the long treacherous journey home from sacking Troy, Odysseus and his army arrive in the land of the Lotus-eaters, where native sweet fruit induces a state of timeless forgetfulness in which torment and tragedy dissolve along with motivation and meaning.5 Jonathan Shay, VA psychiatrist and pioneer of the Homer-PTSD connection, suggested the analogy between the land of the Lotus-eaters and addiction: Each is a self-medication of the psychic aftermath of war.6
But what if those devastating memories could be selectively erased or even better blocked before they were formed? Although this solution may seem like science fiction, research into these possibilities is in reality science fact. Over the past decades, the DoD and the VA have sought such a neuroscience jewel in the lotus. Studies in rodents and humans have looked at the ability of a number of medications, most recently β blockers, such as propranolol, to interfere with the consolidation of emotionally traumatic memories (memory erasure) and disrupting their retention once consolidated (memory extinction).7 While researchers cannot yet completely wipe out a selected memory, like in the movie Star Trek, it has been shown that medications at least in study settings do reduce fear and can attenuate the development of PTSD when combined with psychotherapy. Neuroscientists call these more realistic alterations of recall memory dampening. Though these medications are not ready for regular clinical application, the unprecedented pace of neuroscience makes it nearly inevitable that in the not so distant future some significant blunting of traumatic memory will be possible.
Once science answers in the affirmative the question, “Is this intervention something we could conceivably do?” The next question belongs to ethics, “Is this intervention something we should do even if we can?” As early as 2001, the President’s Council on Bioethics answered the latter with “probably not.”
Use of memory-blunters at the time of traumatic events could interfere with the normal psychic work and adaptive value of emotionally charged memory....Thus, by blunting the emotional impact of events, beta-blockers or their successors would concomitantly weaken our recollection of the traumatic events we have just experienced. Yet often it is important in the after of such events that at least someone remember them clearly. For legal reasons, to say nothing of deeper social and personal ones, the wisdom of routinely interfering with the memories of traumatic survivors and witnesses is highly questionable.8
Many neuroscientists and neuroethicists objected to the perspective of the Bioethics Council as being too puritanical and its position overly pessimistic:
Whereas memory dampening has its drawbacks, such may be the price we pay in order to heal immense suffering. In some contexts, there may be steps that ought to be taken to preserve valuable factual or emotional information contained in memory, even when we must delay or otherwise impose limits on access to memory dampening. None of these concerns, however, even if they find empirical support, are strong enough to justify brushed restrictions on memory dampening.9
The proponents of the 2 views propose and oppose the contrarian position on issues both philosophical and practical, such as the function of traumatic experience in personal growth; how the preservation of memory is related to the integrity of the person and authenticity of the life lived; how blunting of memories of especially combat trauma may normalize our reactions to suffering and evil; and most important for this Veterans Day essay, whether remembering is an ethical duty and if so whose is it to discharge, the individual, his family, community, or country.
More pragmatic, there would be a need to refine our understanding of the risk factors for chronic and disabling PTSD; to determine when in the course of the trauma experience to pharmacologically interfere with memory and to what degree and scope; how to protect the autonomy of the service member to consent or to refuse the procedure within the recognized confines of military ethics; and most important for this essay, how to prevent governments, corporations, or any other entity from exploiting neurobiologic discoveries for power or profit.
Elie Wiesel is an important modern prophet of the critical role of memory in the survival of civilization. His prophecy is rooted in the incomprehensible anguish and horror he personally and communally witnessed in the Holocaust. He suggests in this editorial’s epigraph that there are deep and profound issues to be pondered about memory and its inextricable link to suffering. Meditations offer thoughts, not answers, and I encourage readers to spend a few minutes considering the solemn ones presented here this Veterans Day.
1. Wiesel E. Nobel lecture: hope, despair and memory. https://www.nobelprize.org/prizes/peace/1986/wiesel/lecture. Published December 11, 1986. Accessed October 20, 2019.
2. US Department of Veterans Affairs, Office of Public and Intergovernmental Affairs. Veterans Day frequently asked questions. https://www.va.gov/opa/vetsday/vetday_faq.asp. Accessed October 29, 2019.
3. Lange K. Five facts to know about Veterans Day. https://www.defense.gov/explore/story/article/1675470/5-facts-to-know-about-veterans-day. Published November 5, 2019. Accessed October 29, 2019.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Association; 2013.
5. Homer. The Odyssey. Wilson E, trans. New York: Norton; 2018:Bk 9:90 ff.
6. Shay J. Odysseus in America. New York: Scribner’s; 2002:35-41. 7. Giustino TF, Fitzgerald PJ, Maren S. Revisiting propranolol and PTSD: memory erasure or extinction enhancement. Neurobiol Learn Mem. 2016;130:26-33.
8. President’s Council on Bioethics. Beyond therapy: biotechnology and the pursuit of happiness. https://bioethicsarchive.georgetown.edu/pcbe/reports/beyondtherapy/fulldoc.html. Published October 15, 2003. Accessed October 30, 2019.
9. Kobler AJ. Ethical implications of memory dampening. In: Farah MJ, ed. Neuroethics: An Introduction with Readings. Cambridge MA: MIT Press; 2010:112.
On the 11th day of the 11th month, we celebrate Veterans Day (no apostrophe because it is not a day that veterans possess or that belongs to any individual veteran).2,3 Interestingly, the US Department of Defense (DoD) and the US Department of Veterans Affairs (VA) have web pages correcting any confusion about the meaning of Memorial Day and Veterans Day so that the public understands the unique purpose of each holiday. Memorial Day commemorates all those who lost their lives in the line of duty to the nation, whereas Veterans Day commemorates all those who have honorably served their country as service members. While Memorial Day is a solemn occasion of remembering and respect for those who have died, Veterans Day is an event of gratitude and appreciation focused on veterans still living. The dual mission of the 2 holidays is to remind the public of the debt of remembrance and reverence we owe all veterans both those who have gone before us and those who remain with us.
Memory is what most intrinsically unites the 2 commemorations. In fact, in Great Britain, Canada, and Australia, November 11 is called Remembrance Day.2 Yet memory is a double-edged sword that can be raised in tribute to service members or can deeply lacerate them. Many of the wounds that cause the most prolonged and deepest suffering are not physical—they are mental. Disturbances of memory are among the criteria for posttraumatic stress disorder (PTSD). Under its section on intrusive cluster, the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM) lists “recurrent, involuntary, and intrusive distressing memories of the traumatic event(s).” The avoidance cluster underscores how the afflicted mind tries to escape itself: “Avoidance of or efforts to avoid distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s).”4
PTSD was first recognized as a psychiatric diagnosis in DSM-III in 1980, and since then VA and DoD have devoted enormous resources to developing effective treatments for the disorder, most notably evidence-based psychotherapies. Sadly ironic, the only psychiatric disorder whose etiology is understood has proved to be the most difficult to treat much less cure. As with most serious mental illnesses, some cases become chronic and refractory to the best of care. These tormented individuals live as if in a twilight zone between the past and the present.
Memory and war have a long history in literature, poetry, and history. Haunting memories of PTSD are found in the ancient epics of Homer. On the long treacherous journey home from sacking Troy, Odysseus and his army arrive in the land of the Lotus-eaters, where native sweet fruit induces a state of timeless forgetfulness in which torment and tragedy dissolve along with motivation and meaning.5 Jonathan Shay, VA psychiatrist and pioneer of the Homer-PTSD connection, suggested the analogy between the land of the Lotus-eaters and addiction: Each is a self-medication of the psychic aftermath of war.6
But what if those devastating memories could be selectively erased or even better blocked before they were formed? Although this solution may seem like science fiction, research into these possibilities is in reality science fact. Over the past decades, the DoD and the VA have sought such a neuroscience jewel in the lotus. Studies in rodents and humans have looked at the ability of a number of medications, most recently β blockers, such as propranolol, to interfere with the consolidation of emotionally traumatic memories (memory erasure) and disrupting their retention once consolidated (memory extinction).7 While researchers cannot yet completely wipe out a selected memory, like in the movie Star Trek, it has been shown that medications at least in study settings do reduce fear and can attenuate the development of PTSD when combined with psychotherapy. Neuroscientists call these more realistic alterations of recall memory dampening. Though these medications are not ready for regular clinical application, the unprecedented pace of neuroscience makes it nearly inevitable that in the not so distant future some significant blunting of traumatic memory will be possible.
Once science answers in the affirmative the question, “Is this intervention something we could conceivably do?” The next question belongs to ethics, “Is this intervention something we should do even if we can?” As early as 2001, the President’s Council on Bioethics answered the latter with “probably not.”
Use of memory-blunters at the time of traumatic events could interfere with the normal psychic work and adaptive value of emotionally charged memory....Thus, by blunting the emotional impact of events, beta-blockers or their successors would concomitantly weaken our recollection of the traumatic events we have just experienced. Yet often it is important in the after of such events that at least someone remember them clearly. For legal reasons, to say nothing of deeper social and personal ones, the wisdom of routinely interfering with the memories of traumatic survivors and witnesses is highly questionable.8
Many neuroscientists and neuroethicists objected to the perspective of the Bioethics Council as being too puritanical and its position overly pessimistic:
Whereas memory dampening has its drawbacks, such may be the price we pay in order to heal immense suffering. In some contexts, there may be steps that ought to be taken to preserve valuable factual or emotional information contained in memory, even when we must delay or otherwise impose limits on access to memory dampening. None of these concerns, however, even if they find empirical support, are strong enough to justify brushed restrictions on memory dampening.9
The proponents of the 2 views propose and oppose the contrarian position on issues both philosophical and practical, such as the function of traumatic experience in personal growth; how the preservation of memory is related to the integrity of the person and authenticity of the life lived; how blunting of memories of especially combat trauma may normalize our reactions to suffering and evil; and most important for this Veterans Day essay, whether remembering is an ethical duty and if so whose is it to discharge, the individual, his family, community, or country.
More pragmatic, there would be a need to refine our understanding of the risk factors for chronic and disabling PTSD; to determine when in the course of the trauma experience to pharmacologically interfere with memory and to what degree and scope; how to protect the autonomy of the service member to consent or to refuse the procedure within the recognized confines of military ethics; and most important for this essay, how to prevent governments, corporations, or any other entity from exploiting neurobiologic discoveries for power or profit.
Elie Wiesel is an important modern prophet of the critical role of memory in the survival of civilization. His prophecy is rooted in the incomprehensible anguish and horror he personally and communally witnessed in the Holocaust. He suggests in this editorial’s epigraph that there are deep and profound issues to be pondered about memory and its inextricable link to suffering. Meditations offer thoughts, not answers, and I encourage readers to spend a few minutes considering the solemn ones presented here this Veterans Day.
On the 11th day of the 11th month, we celebrate Veterans Day (no apostrophe because it is not a day that veterans possess or that belongs to any individual veteran).2,3 Interestingly, the US Department of Defense (DoD) and the US Department of Veterans Affairs (VA) have web pages correcting any confusion about the meaning of Memorial Day and Veterans Day so that the public understands the unique purpose of each holiday. Memorial Day commemorates all those who lost their lives in the line of duty to the nation, whereas Veterans Day commemorates all those who have honorably served their country as service members. While Memorial Day is a solemn occasion of remembering and respect for those who have died, Veterans Day is an event of gratitude and appreciation focused on veterans still living. The dual mission of the 2 holidays is to remind the public of the debt of remembrance and reverence we owe all veterans both those who have gone before us and those who remain with us.
Memory is what most intrinsically unites the 2 commemorations. In fact, in Great Britain, Canada, and Australia, November 11 is called Remembrance Day.2 Yet memory is a double-edged sword that can be raised in tribute to service members or can deeply lacerate them. Many of the wounds that cause the most prolonged and deepest suffering are not physical—they are mental. Disturbances of memory are among the criteria for posttraumatic stress disorder (PTSD). Under its section on intrusive cluster, the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM) lists “recurrent, involuntary, and intrusive distressing memories of the traumatic event(s).” The avoidance cluster underscores how the afflicted mind tries to escape itself: “Avoidance of or efforts to avoid distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s).”4
PTSD was first recognized as a psychiatric diagnosis in DSM-III in 1980, and since then VA and DoD have devoted enormous resources to developing effective treatments for the disorder, most notably evidence-based psychotherapies. Sadly ironic, the only psychiatric disorder whose etiology is understood has proved to be the most difficult to treat much less cure. As with most serious mental illnesses, some cases become chronic and refractory to the best of care. These tormented individuals live as if in a twilight zone between the past and the present.
Memory and war have a long history in literature, poetry, and history. Haunting memories of PTSD are found in the ancient epics of Homer. On the long treacherous journey home from sacking Troy, Odysseus and his army arrive in the land of the Lotus-eaters, where native sweet fruit induces a state of timeless forgetfulness in which torment and tragedy dissolve along with motivation and meaning.5 Jonathan Shay, VA psychiatrist and pioneer of the Homer-PTSD connection, suggested the analogy between the land of the Lotus-eaters and addiction: Each is a self-medication of the psychic aftermath of war.6
But what if those devastating memories could be selectively erased or even better blocked before they were formed? Although this solution may seem like science fiction, research into these possibilities is in reality science fact. Over the past decades, the DoD and the VA have sought such a neuroscience jewel in the lotus. Studies in rodents and humans have looked at the ability of a number of medications, most recently β blockers, such as propranolol, to interfere with the consolidation of emotionally traumatic memories (memory erasure) and disrupting their retention once consolidated (memory extinction).7 While researchers cannot yet completely wipe out a selected memory, like in the movie Star Trek, it has been shown that medications at least in study settings do reduce fear and can attenuate the development of PTSD when combined with psychotherapy. Neuroscientists call these more realistic alterations of recall memory dampening. Though these medications are not ready for regular clinical application, the unprecedented pace of neuroscience makes it nearly inevitable that in the not so distant future some significant blunting of traumatic memory will be possible.
Once science answers in the affirmative the question, “Is this intervention something we could conceivably do?” The next question belongs to ethics, “Is this intervention something we should do even if we can?” As early as 2001, the President’s Council on Bioethics answered the latter with “probably not.”
Use of memory-blunters at the time of traumatic events could interfere with the normal psychic work and adaptive value of emotionally charged memory....Thus, by blunting the emotional impact of events, beta-blockers or their successors would concomitantly weaken our recollection of the traumatic events we have just experienced. Yet often it is important in the after of such events that at least someone remember them clearly. For legal reasons, to say nothing of deeper social and personal ones, the wisdom of routinely interfering with the memories of traumatic survivors and witnesses is highly questionable.8
Many neuroscientists and neuroethicists objected to the perspective of the Bioethics Council as being too puritanical and its position overly pessimistic:
Whereas memory dampening has its drawbacks, such may be the price we pay in order to heal immense suffering. In some contexts, there may be steps that ought to be taken to preserve valuable factual or emotional information contained in memory, even when we must delay or otherwise impose limits on access to memory dampening. None of these concerns, however, even if they find empirical support, are strong enough to justify brushed restrictions on memory dampening.9
The proponents of the 2 views propose and oppose the contrarian position on issues both philosophical and practical, such as the function of traumatic experience in personal growth; how the preservation of memory is related to the integrity of the person and authenticity of the life lived; how blunting of memories of especially combat trauma may normalize our reactions to suffering and evil; and most important for this Veterans Day essay, whether remembering is an ethical duty and if so whose is it to discharge, the individual, his family, community, or country.
More pragmatic, there would be a need to refine our understanding of the risk factors for chronic and disabling PTSD; to determine when in the course of the trauma experience to pharmacologically interfere with memory and to what degree and scope; how to protect the autonomy of the service member to consent or to refuse the procedure within the recognized confines of military ethics; and most important for this essay, how to prevent governments, corporations, or any other entity from exploiting neurobiologic discoveries for power or profit.
Elie Wiesel is an important modern prophet of the critical role of memory in the survival of civilization. His prophecy is rooted in the incomprehensible anguish and horror he personally and communally witnessed in the Holocaust. He suggests in this editorial’s epigraph that there are deep and profound issues to be pondered about memory and its inextricable link to suffering. Meditations offer thoughts, not answers, and I encourage readers to spend a few minutes considering the solemn ones presented here this Veterans Day.
1. Wiesel E. Nobel lecture: hope, despair and memory. https://www.nobelprize.org/prizes/peace/1986/wiesel/lecture. Published December 11, 1986. Accessed October 20, 2019.
2. US Department of Veterans Affairs, Office of Public and Intergovernmental Affairs. Veterans Day frequently asked questions. https://www.va.gov/opa/vetsday/vetday_faq.asp. Accessed October 29, 2019.
3. Lange K. Five facts to know about Veterans Day. https://www.defense.gov/explore/story/article/1675470/5-facts-to-know-about-veterans-day. Published November 5, 2019. Accessed October 29, 2019.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Association; 2013.
5. Homer. The Odyssey. Wilson E, trans. New York: Norton; 2018:Bk 9:90 ff.
6. Shay J. Odysseus in America. New York: Scribner’s; 2002:35-41. 7. Giustino TF, Fitzgerald PJ, Maren S. Revisiting propranolol and PTSD: memory erasure or extinction enhancement. Neurobiol Learn Mem. 2016;130:26-33.
8. President’s Council on Bioethics. Beyond therapy: biotechnology and the pursuit of happiness. https://bioethicsarchive.georgetown.edu/pcbe/reports/beyondtherapy/fulldoc.html. Published October 15, 2003. Accessed October 30, 2019.
9. Kobler AJ. Ethical implications of memory dampening. In: Farah MJ, ed. Neuroethics: An Introduction with Readings. Cambridge MA: MIT Press; 2010:112.
1. Wiesel E. Nobel lecture: hope, despair and memory. https://www.nobelprize.org/prizes/peace/1986/wiesel/lecture. Published December 11, 1986. Accessed October 20, 2019.
2. US Department of Veterans Affairs, Office of Public and Intergovernmental Affairs. Veterans Day frequently asked questions. https://www.va.gov/opa/vetsday/vetday_faq.asp. Accessed October 29, 2019.
3. Lange K. Five facts to know about Veterans Day. https://www.defense.gov/explore/story/article/1675470/5-facts-to-know-about-veterans-day. Published November 5, 2019. Accessed October 29, 2019.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Association; 2013.
5. Homer. The Odyssey. Wilson E, trans. New York: Norton; 2018:Bk 9:90 ff.
6. Shay J. Odysseus in America. New York: Scribner’s; 2002:35-41. 7. Giustino TF, Fitzgerald PJ, Maren S. Revisiting propranolol and PTSD: memory erasure or extinction enhancement. Neurobiol Learn Mem. 2016;130:26-33.
8. President’s Council on Bioethics. Beyond therapy: biotechnology and the pursuit of happiness. https://bioethicsarchive.georgetown.edu/pcbe/reports/beyondtherapy/fulldoc.html. Published October 15, 2003. Accessed October 30, 2019.
9. Kobler AJ. Ethical implications of memory dampening. In: Farah MJ, ed. Neuroethics: An Introduction with Readings. Cambridge MA: MIT Press; 2010:112.





