User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'medstat-accordion-set article-series')]
Can we get to ‘COVID zero’? Experts predict the next 8 months
COVID-19 is likely to follow a seasonal pattern – similar to some other respiratory viruses – with fewer cases come summer 2021 followed by a jump next winter, experts predicted in a Thursday briefing.
If that pattern holds, it could mean a need to reinforce the mask-wearing message as the weather gets colder and people once again congregate indoors.
“Right now, we are projecting the United States all the way to Aug. 1 [will have] 619,000 deaths from COVID-19, with 4.7 million globally,” said Ali H. Mokdad, PhD, professor of health metrics sciences at the Institute for Health Metrics and Evaluation at the University of Washington, Seattle, during today’s media briefing sponsored by the Infectious Diseases Society of America and IHME.
The encouraging news is the vaccines appear to be working, and more Americans are getting them. “If you look at the data for these vaccines, they are extremely safe, they are extremely efficacious, and they make you basically impervious – for the most part – to getting serious disease, hospitalization, or death,” said Amesh Adalja, MD, senior scholar at Johns Hopkins University Center for Health Security in Baltimore.
“These vaccines do what they were meant to do: defang this virus,” said Dr. Adalja, who is an IDSA Fellow and adjunct assistant professor at Johns Hopkins Bloomberg School of Public Health. Emerging data out of Israel and other countries suggest a vaccinated person is less likely to transmit the virus as well, he added.
Still aiming for herd immunity
Furthermore, the U.S. Food and Drug Administration is likely to approve emergency use authorization (EUA) among teenagers 12-15 years old “imminently,” thereby expanding the pool of people potentially protected by vaccines.
Such authorization could help with overall public health efforts. “That’s simply a mathematical formula,” Dr. Adalja said. “The more people that are vaccinated, including children, the quicker we’ll get to herd immunity.”
In addition, with lower case numbers expected this summer, herd immunity might become more achievable, said Dr. Mokdad, who is also chief strategy officer for population health at the University of Washington.
As important as herd immunity is, so-called decoupling is “more important to me,” Dr. Adalja said. Decoupling refers to separating infections from the more severe outcomes, so people who get COVID-19 are less likely to need hospitalization or die from it.
Vaccines get the credit here, he added, including with the variants. “Even if you get a breakthrough infection with a variant, it’s not likely to land you in the hospital or cause serious disease or death,” Dr. Adalja said.
Masks and the uncommon cold
Wearing a mask until we reach herd immunity is important because it’s not possible to tell who is vaccinated and who isn’t, Dr. Mokdad said. “Remember, as many people are waiting to get a vaccine, all of us have access to a mask,” he said.
Dr. Adalja agreed, adding that public health guidance on masks will likely stay in place until we cross that herd immunity threshold and community circulation of the virus goes down.
“People are probably going to want to continue wearing masks, at least some proportion, because they see the benefit for other respiratory viruses,” Dr. Adalja said. “How many of you had a common cold this year?”
Variants: Some good news?
Experts are monitoring the spread of variants of concern in the United States and abroad. On a positive note, the B.1.1.7 variant first identified in the United Kingdom appears to be dominant in the United States at this time, which is potentially good for two reasons. One is that the available COVID-19 vaccines show sufficient efficacy against the strain, Dr. Mokdad said.
Second, a predominance of B.1.1.7 makes it more difficult for other emerging variants of concern like P1 [Brazil] or B.1.351 [South Africa] to gain control, Dr. Adalja said.
“B.1.1.7 is such an efficient transmitter,” he said. “That’s kind of an advantage … because the more B.1.1.7, you have the less opportunity B.1.351 and P1 have to set up shop.”
Hesitancy from misinformation
Vaccine hesitancy remains a concern, particularly at a time when some predict a drop in the number of Americans seeking vaccination. Although needle phobia plays a role in dissuading some from vaccination, the bigger issue is vaccine misinformation, Dr. Adalja said.
“Some people are just terrified when they see the needle. That’s a small part of the proportion of people who don’t want to get vaccinated,” Dr. Adalja said. In contrast, he attributed most hesitancy to misinformation about the vaccine, including reports that the vaccines are fake.
Even celebrities are getting drawn into the misinformation.
“I just had to answer something about Mariah Carey’s vaccination,” he said. Someone believed “that it was done with a retractable needle that didn’t really go into her arm.”
Vaccine hesitancy is more about people not understanding the risk-benefit analysis, taking side effects out of out of context if there are side effects, or being influenced by “arbitrary statements about microchips, infertility, or whatever it might be,” Dr. Adalja said.
The future is subject to change
“We’re expecting another rise in cases and more mortality in our winter season here in the United States,” Dr. Mokdad said, adding that the efficacy of the vaccines is likely to attenuate the mortality rate in particular.
However, as the epidemiology of the pandemic evolves, so too will the long-term predictions. Factors that could influence future numbers include the expansion of vaccination to teens 12-15 years old and (eventually) younger children, a need for booster vaccines, emerging variants, and the changing proportion of the population who are fully vaccinated or were previously infected.
Again, getting people to adhere to mask wearing come winter could be challenging if the scenario over the summer is “close to normal with less than 200 deaths a day in the United States,” he added. Asking people to wear masks again will be like “swimming upstream.”
“I think it’s a mistake to think that we’re going to get to ‘COVID zero,’ ” Dr. Adalja said. “This is not an eradicable disease. There’s only been one human infectious disease eradicated from the planet, and that’s smallpox, and it had very different characteristics.”
A version of this article first appeared on Medscape.com.
COVID-19 is likely to follow a seasonal pattern – similar to some other respiratory viruses – with fewer cases come summer 2021 followed by a jump next winter, experts predicted in a Thursday briefing.
If that pattern holds, it could mean a need to reinforce the mask-wearing message as the weather gets colder and people once again congregate indoors.
“Right now, we are projecting the United States all the way to Aug. 1 [will have] 619,000 deaths from COVID-19, with 4.7 million globally,” said Ali H. Mokdad, PhD, professor of health metrics sciences at the Institute for Health Metrics and Evaluation at the University of Washington, Seattle, during today’s media briefing sponsored by the Infectious Diseases Society of America and IHME.
The encouraging news is the vaccines appear to be working, and more Americans are getting them. “If you look at the data for these vaccines, they are extremely safe, they are extremely efficacious, and they make you basically impervious – for the most part – to getting serious disease, hospitalization, or death,” said Amesh Adalja, MD, senior scholar at Johns Hopkins University Center for Health Security in Baltimore.
“These vaccines do what they were meant to do: defang this virus,” said Dr. Adalja, who is an IDSA Fellow and adjunct assistant professor at Johns Hopkins Bloomberg School of Public Health. Emerging data out of Israel and other countries suggest a vaccinated person is less likely to transmit the virus as well, he added.
Still aiming for herd immunity
Furthermore, the U.S. Food and Drug Administration is likely to approve emergency use authorization (EUA) among teenagers 12-15 years old “imminently,” thereby expanding the pool of people potentially protected by vaccines.
Such authorization could help with overall public health efforts. “That’s simply a mathematical formula,” Dr. Adalja said. “The more people that are vaccinated, including children, the quicker we’ll get to herd immunity.”
In addition, with lower case numbers expected this summer, herd immunity might become more achievable, said Dr. Mokdad, who is also chief strategy officer for population health at the University of Washington.
As important as herd immunity is, so-called decoupling is “more important to me,” Dr. Adalja said. Decoupling refers to separating infections from the more severe outcomes, so people who get COVID-19 are less likely to need hospitalization or die from it.
Vaccines get the credit here, he added, including with the variants. “Even if you get a breakthrough infection with a variant, it’s not likely to land you in the hospital or cause serious disease or death,” Dr. Adalja said.
Masks and the uncommon cold
Wearing a mask until we reach herd immunity is important because it’s not possible to tell who is vaccinated and who isn’t, Dr. Mokdad said. “Remember, as many people are waiting to get a vaccine, all of us have access to a mask,” he said.
Dr. Adalja agreed, adding that public health guidance on masks will likely stay in place until we cross that herd immunity threshold and community circulation of the virus goes down.
“People are probably going to want to continue wearing masks, at least some proportion, because they see the benefit for other respiratory viruses,” Dr. Adalja said. “How many of you had a common cold this year?”
Variants: Some good news?
Experts are monitoring the spread of variants of concern in the United States and abroad. On a positive note, the B.1.1.7 variant first identified in the United Kingdom appears to be dominant in the United States at this time, which is potentially good for two reasons. One is that the available COVID-19 vaccines show sufficient efficacy against the strain, Dr. Mokdad said.
Second, a predominance of B.1.1.7 makes it more difficult for other emerging variants of concern like P1 [Brazil] or B.1.351 [South Africa] to gain control, Dr. Adalja said.
“B.1.1.7 is such an efficient transmitter,” he said. “That’s kind of an advantage … because the more B.1.1.7, you have the less opportunity B.1.351 and P1 have to set up shop.”
Hesitancy from misinformation
Vaccine hesitancy remains a concern, particularly at a time when some predict a drop in the number of Americans seeking vaccination. Although needle phobia plays a role in dissuading some from vaccination, the bigger issue is vaccine misinformation, Dr. Adalja said.
“Some people are just terrified when they see the needle. That’s a small part of the proportion of people who don’t want to get vaccinated,” Dr. Adalja said. In contrast, he attributed most hesitancy to misinformation about the vaccine, including reports that the vaccines are fake.
Even celebrities are getting drawn into the misinformation.
“I just had to answer something about Mariah Carey’s vaccination,” he said. Someone believed “that it was done with a retractable needle that didn’t really go into her arm.”
Vaccine hesitancy is more about people not understanding the risk-benefit analysis, taking side effects out of out of context if there are side effects, or being influenced by “arbitrary statements about microchips, infertility, or whatever it might be,” Dr. Adalja said.
The future is subject to change
“We’re expecting another rise in cases and more mortality in our winter season here in the United States,” Dr. Mokdad said, adding that the efficacy of the vaccines is likely to attenuate the mortality rate in particular.
However, as the epidemiology of the pandemic evolves, so too will the long-term predictions. Factors that could influence future numbers include the expansion of vaccination to teens 12-15 years old and (eventually) younger children, a need for booster vaccines, emerging variants, and the changing proportion of the population who are fully vaccinated or were previously infected.
Again, getting people to adhere to mask wearing come winter could be challenging if the scenario over the summer is “close to normal with less than 200 deaths a day in the United States,” he added. Asking people to wear masks again will be like “swimming upstream.”
“I think it’s a mistake to think that we’re going to get to ‘COVID zero,’ ” Dr. Adalja said. “This is not an eradicable disease. There’s only been one human infectious disease eradicated from the planet, and that’s smallpox, and it had very different characteristics.”
A version of this article first appeared on Medscape.com.
COVID-19 is likely to follow a seasonal pattern – similar to some other respiratory viruses – with fewer cases come summer 2021 followed by a jump next winter, experts predicted in a Thursday briefing.
If that pattern holds, it could mean a need to reinforce the mask-wearing message as the weather gets colder and people once again congregate indoors.
“Right now, we are projecting the United States all the way to Aug. 1 [will have] 619,000 deaths from COVID-19, with 4.7 million globally,” said Ali H. Mokdad, PhD, professor of health metrics sciences at the Institute for Health Metrics and Evaluation at the University of Washington, Seattle, during today’s media briefing sponsored by the Infectious Diseases Society of America and IHME.
The encouraging news is the vaccines appear to be working, and more Americans are getting them. “If you look at the data for these vaccines, they are extremely safe, they are extremely efficacious, and they make you basically impervious – for the most part – to getting serious disease, hospitalization, or death,” said Amesh Adalja, MD, senior scholar at Johns Hopkins University Center for Health Security in Baltimore.
“These vaccines do what they were meant to do: defang this virus,” said Dr. Adalja, who is an IDSA Fellow and adjunct assistant professor at Johns Hopkins Bloomberg School of Public Health. Emerging data out of Israel and other countries suggest a vaccinated person is less likely to transmit the virus as well, he added.
Still aiming for herd immunity
Furthermore, the U.S. Food and Drug Administration is likely to approve emergency use authorization (EUA) among teenagers 12-15 years old “imminently,” thereby expanding the pool of people potentially protected by vaccines.
Such authorization could help with overall public health efforts. “That’s simply a mathematical formula,” Dr. Adalja said. “The more people that are vaccinated, including children, the quicker we’ll get to herd immunity.”
In addition, with lower case numbers expected this summer, herd immunity might become more achievable, said Dr. Mokdad, who is also chief strategy officer for population health at the University of Washington.
As important as herd immunity is, so-called decoupling is “more important to me,” Dr. Adalja said. Decoupling refers to separating infections from the more severe outcomes, so people who get COVID-19 are less likely to need hospitalization or die from it.
Vaccines get the credit here, he added, including with the variants. “Even if you get a breakthrough infection with a variant, it’s not likely to land you in the hospital or cause serious disease or death,” Dr. Adalja said.
Masks and the uncommon cold
Wearing a mask until we reach herd immunity is important because it’s not possible to tell who is vaccinated and who isn’t, Dr. Mokdad said. “Remember, as many people are waiting to get a vaccine, all of us have access to a mask,” he said.
Dr. Adalja agreed, adding that public health guidance on masks will likely stay in place until we cross that herd immunity threshold and community circulation of the virus goes down.
“People are probably going to want to continue wearing masks, at least some proportion, because they see the benefit for other respiratory viruses,” Dr. Adalja said. “How many of you had a common cold this year?”
Variants: Some good news?
Experts are monitoring the spread of variants of concern in the United States and abroad. On a positive note, the B.1.1.7 variant first identified in the United Kingdom appears to be dominant in the United States at this time, which is potentially good for two reasons. One is that the available COVID-19 vaccines show sufficient efficacy against the strain, Dr. Mokdad said.
Second, a predominance of B.1.1.7 makes it more difficult for other emerging variants of concern like P1 [Brazil] or B.1.351 [South Africa] to gain control, Dr. Adalja said.
“B.1.1.7 is such an efficient transmitter,” he said. “That’s kind of an advantage … because the more B.1.1.7, you have the less opportunity B.1.351 and P1 have to set up shop.”
Hesitancy from misinformation
Vaccine hesitancy remains a concern, particularly at a time when some predict a drop in the number of Americans seeking vaccination. Although needle phobia plays a role in dissuading some from vaccination, the bigger issue is vaccine misinformation, Dr. Adalja said.
“Some people are just terrified when they see the needle. That’s a small part of the proportion of people who don’t want to get vaccinated,” Dr. Adalja said. In contrast, he attributed most hesitancy to misinformation about the vaccine, including reports that the vaccines are fake.
Even celebrities are getting drawn into the misinformation.
“I just had to answer something about Mariah Carey’s vaccination,” he said. Someone believed “that it was done with a retractable needle that didn’t really go into her arm.”
Vaccine hesitancy is more about people not understanding the risk-benefit analysis, taking side effects out of out of context if there are side effects, or being influenced by “arbitrary statements about microchips, infertility, or whatever it might be,” Dr. Adalja said.
The future is subject to change
“We’re expecting another rise in cases and more mortality in our winter season here in the United States,” Dr. Mokdad said, adding that the efficacy of the vaccines is likely to attenuate the mortality rate in particular.
However, as the epidemiology of the pandemic evolves, so too will the long-term predictions. Factors that could influence future numbers include the expansion of vaccination to teens 12-15 years old and (eventually) younger children, a need for booster vaccines, emerging variants, and the changing proportion of the population who are fully vaccinated or were previously infected.
Again, getting people to adhere to mask wearing come winter could be challenging if the scenario over the summer is “close to normal with less than 200 deaths a day in the United States,” he added. Asking people to wear masks again will be like “swimming upstream.”
“I think it’s a mistake to think that we’re going to get to ‘COVID zero,’ ” Dr. Adalja said. “This is not an eradicable disease. There’s only been one human infectious disease eradicated from the planet, and that’s smallpox, and it had very different characteristics.”
A version of this article first appeared on Medscape.com.
Small clinics, practices key to COVID-19 vaccine success: State officials
Primary care physicians and providers in small offices and clinics are going to be key to ensuring that the remaining half of the nation receives a COVID-19 vaccination, state health officials said Wednesday, and the federal government will soon start shipping smaller packages of the Pfizer/BioNTech vaccine that can be more readily used by individual doctors.
According to the Centers for Disease Control and Prevention, as of April 21, more than 215 million doses have been administered. About 40% – 134 million Americans – have had at least one dose of a vaccine.
Among those who still haven’t received a shot are people who don’t have the time, may be homebound, or who have questions about the vaccine, or might say they will never be vaccinated, said Nirav Shah, MD, JD, president of the Association of State and Territorial Health Officials and director of the Maine Center for Disease Control and Prevention, on a call with reporters.
Especially for those who fall into the “not-ever” category, state officials “are working to find trusted messengers like doctors” who can connect with these individuals and give them information, he said.
Primary care physicians’ offices and other small practice settings are “where we are most likely to reach many of the remaining 50%,” Steven Stack, MD, MBA, FACEP, commissioner of the Kentucky Department for Public Health, said on the briefing.
State officials also “need to support all people to consult their personal physicians in whom they have confidence and trust to be informed of the benefits of COVID vaccination and the safety of this vaccination,” he said, adding that “this is the way we put this pandemic in the rearview mirror and move on with our lives.”
Dr. Stack said the federal government is starting by working with Pfizer to slim down its packages from 1,170 doses to 450 doses. That should happen before June, said Dr. Stack, adding that state health officials will be able to distribute the smaller packages “more widely and to smaller settings.”
Ideally, packaging for all vaccines will get down to single-dose, pre-filled syringes, he said. But that is a “journey” that the federal government has just begun, said Dr. Stack.
The White House had not responded to a request from this news organization for comment by press time.
Having vaccines onsite in a physician’s office is important, Dr. Stack said, adding that doctors “need to reach people in their persuadable moment.”
Bringing pediatricians on board
Illinois state health officials have begun a process that will let pediatricians have weekly vaccination clinics and also have vaccine on hand to meet patients in the moment, said Ngozi Ezike, MD, director of the Illinois Department of Public Health, on the briefing.
She said the distribution can start even before the Pfizer vaccine is shipped in smaller packages – and as soon as the Food and Drug Administration authorizes the vaccine for adolescents. Pfizer applied for emergency use approval for children aged 12-15 on April 9.
Local health departments will store the vaccine in their ultra-cold freezers. Pediatricians will identify how many people they hope to vaccinate each week and receive the doses on Monday, with the understanding that they must use the vaccine within 5 days, said Dr. Ezike.
The aim is to support vaccination clinics but also to ensure doctors have “doses on hand,” so that a parent or adolescent could opt for vaccination during a visit.
Although estimating the number of doses required will be difficult and likely involve some waste, Dr. Ezike said it’s important to be able to offer a vaccine in the office instead of having to refer someone elsewhere.
A version of this article first appeared on Medscape.com.
Primary care physicians and providers in small offices and clinics are going to be key to ensuring that the remaining half of the nation receives a COVID-19 vaccination, state health officials said Wednesday, and the federal government will soon start shipping smaller packages of the Pfizer/BioNTech vaccine that can be more readily used by individual doctors.
According to the Centers for Disease Control and Prevention, as of April 21, more than 215 million doses have been administered. About 40% – 134 million Americans – have had at least one dose of a vaccine.
Among those who still haven’t received a shot are people who don’t have the time, may be homebound, or who have questions about the vaccine, or might say they will never be vaccinated, said Nirav Shah, MD, JD, president of the Association of State and Territorial Health Officials and director of the Maine Center for Disease Control and Prevention, on a call with reporters.
Especially for those who fall into the “not-ever” category, state officials “are working to find trusted messengers like doctors” who can connect with these individuals and give them information, he said.
Primary care physicians’ offices and other small practice settings are “where we are most likely to reach many of the remaining 50%,” Steven Stack, MD, MBA, FACEP, commissioner of the Kentucky Department for Public Health, said on the briefing.
State officials also “need to support all people to consult their personal physicians in whom they have confidence and trust to be informed of the benefits of COVID vaccination and the safety of this vaccination,” he said, adding that “this is the way we put this pandemic in the rearview mirror and move on with our lives.”
Dr. Stack said the federal government is starting by working with Pfizer to slim down its packages from 1,170 doses to 450 doses. That should happen before June, said Dr. Stack, adding that state health officials will be able to distribute the smaller packages “more widely and to smaller settings.”
Ideally, packaging for all vaccines will get down to single-dose, pre-filled syringes, he said. But that is a “journey” that the federal government has just begun, said Dr. Stack.
The White House had not responded to a request from this news organization for comment by press time.
Having vaccines onsite in a physician’s office is important, Dr. Stack said, adding that doctors “need to reach people in their persuadable moment.”
Bringing pediatricians on board
Illinois state health officials have begun a process that will let pediatricians have weekly vaccination clinics and also have vaccine on hand to meet patients in the moment, said Ngozi Ezike, MD, director of the Illinois Department of Public Health, on the briefing.
She said the distribution can start even before the Pfizer vaccine is shipped in smaller packages – and as soon as the Food and Drug Administration authorizes the vaccine for adolescents. Pfizer applied for emergency use approval for children aged 12-15 on April 9.
Local health departments will store the vaccine in their ultra-cold freezers. Pediatricians will identify how many people they hope to vaccinate each week and receive the doses on Monday, with the understanding that they must use the vaccine within 5 days, said Dr. Ezike.
The aim is to support vaccination clinics but also to ensure doctors have “doses on hand,” so that a parent or adolescent could opt for vaccination during a visit.
Although estimating the number of doses required will be difficult and likely involve some waste, Dr. Ezike said it’s important to be able to offer a vaccine in the office instead of having to refer someone elsewhere.
A version of this article first appeared on Medscape.com.
Primary care physicians and providers in small offices and clinics are going to be key to ensuring that the remaining half of the nation receives a COVID-19 vaccination, state health officials said Wednesday, and the federal government will soon start shipping smaller packages of the Pfizer/BioNTech vaccine that can be more readily used by individual doctors.
According to the Centers for Disease Control and Prevention, as of April 21, more than 215 million doses have been administered. About 40% – 134 million Americans – have had at least one dose of a vaccine.
Among those who still haven’t received a shot are people who don’t have the time, may be homebound, or who have questions about the vaccine, or might say they will never be vaccinated, said Nirav Shah, MD, JD, president of the Association of State and Territorial Health Officials and director of the Maine Center for Disease Control and Prevention, on a call with reporters.
Especially for those who fall into the “not-ever” category, state officials “are working to find trusted messengers like doctors” who can connect with these individuals and give them information, he said.
Primary care physicians’ offices and other small practice settings are “where we are most likely to reach many of the remaining 50%,” Steven Stack, MD, MBA, FACEP, commissioner of the Kentucky Department for Public Health, said on the briefing.
State officials also “need to support all people to consult their personal physicians in whom they have confidence and trust to be informed of the benefits of COVID vaccination and the safety of this vaccination,” he said, adding that “this is the way we put this pandemic in the rearview mirror and move on with our lives.”
Dr. Stack said the federal government is starting by working with Pfizer to slim down its packages from 1,170 doses to 450 doses. That should happen before June, said Dr. Stack, adding that state health officials will be able to distribute the smaller packages “more widely and to smaller settings.”
Ideally, packaging for all vaccines will get down to single-dose, pre-filled syringes, he said. But that is a “journey” that the federal government has just begun, said Dr. Stack.
The White House had not responded to a request from this news organization for comment by press time.
Having vaccines onsite in a physician’s office is important, Dr. Stack said, adding that doctors “need to reach people in their persuadable moment.”
Bringing pediatricians on board
Illinois state health officials have begun a process that will let pediatricians have weekly vaccination clinics and also have vaccine on hand to meet patients in the moment, said Ngozi Ezike, MD, director of the Illinois Department of Public Health, on the briefing.
She said the distribution can start even before the Pfizer vaccine is shipped in smaller packages – and as soon as the Food and Drug Administration authorizes the vaccine for adolescents. Pfizer applied for emergency use approval for children aged 12-15 on April 9.
Local health departments will store the vaccine in their ultra-cold freezers. Pediatricians will identify how many people they hope to vaccinate each week and receive the doses on Monday, with the understanding that they must use the vaccine within 5 days, said Dr. Ezike.
The aim is to support vaccination clinics but also to ensure doctors have “doses on hand,” so that a parent or adolescent could opt for vaccination during a visit.
Although estimating the number of doses required will be difficult and likely involve some waste, Dr. Ezike said it’s important to be able to offer a vaccine in the office instead of having to refer someone elsewhere.
A version of this article first appeared on Medscape.com.
Percentage of doctors who are Black barely changed in 120 years
according to a new study.
In 1900, 1.3% of physicians were Black. In 1940, 2.8% of physicians were Black, and by 2018 – when almost 13% of the population was Black – 5.4% of doctors were Black, reports Dan Ly, MD, PhD, MPP, an assistant professor of medicine at the University of California, Los Angeles, in a study published online April 19, 2021, in the Journal of General Internal Medicine.
The proportion of male Black physicians was 2.7% in 1940 and 2.6% in 2018.
Dr. Ly also found a significant wage gap. The median income earned by White doctors was $50,000 more than the median income of Black physicians in 2018. Dr. Ly based his findings on the U.S. Census Decennial Census long form, accessed via IPUMS, a free database funded by the National Institutes of Health and other organizations.
“If we care about the health of the population, particularly the health of Black patients, we should care about how small the proportion of our physicians who are Black is and the extremely slow progress we have made as a medical system in increasing that proportion,” Dr. Ly said in an interview.
Dr. Ly said he took on this research in part because previous studies have shown that Black patients are more likely to seek preventive care from Black doctors. Thus, increasing the numbers of Black physicians could narrow gaps in life expectancy between Whites and Blacks.
He also wanted to see whether progress had been made as a result of various medical organizations and the Association of American Medical Colleges undertaking initiatives to increase workforce diversity. There has been “very, very little” progress, he said.
Norma Poll-Hunter, PhD, the AAMC’s senior director of workforce diversity, said Dr. Ly’s report “was not surprising at all.”
The AAMC reported in 2014 that the number of Black men who apply to and matriculate into medical schools has been declining since 1978. That year, there were 1,410 Black male applicants and 542 Black enrollees. In 2014, there were 1,337 applicants and 515 enrollees.
Since 2014, Black male enrollment has increased slightly, rising from 2.4% in the 2014-2015 school year to 2.9% in the 2019-2020 year, the AAMC reported last year.
In addition, among other historically underrepresented minorities, “we really have seen very small progress” despite the increase in the number of medical schools, Dr. Poll-Hunter said in an interview.
The AAMC and the National Medical Association consider the lack of Black male applicants and matriculants to be a national crisis. The two groups started an alliance in 2020 aimed at finding ways to amplify and support Black men’s interest in medicine and the biomedical sciences and to “develop systems-based solutions to address exclusionary practices that create barriers for Black men and prevent them from having equitable opportunities to successfully enroll in medical school.”
Solutions include requiring medical school admissions committees and application screeners to undergo implicit bias awareness and mitigation training, adopting holistic admissions reviews, and incentivizing institutions of higher learning to partner with Black communities in urban and rural school systems to establish K-12 health sciences academies, said NMA President Leon McDougle, MD, MPH.
“There are the systems factors, and racism is a big one that we have to tackle,” said Dr. Poll-Hunter.
Diversity isn’t just about numbers, said Dr. McDougle, a professor of family medicine and associate dean for diversity and inclusion at Ohio State University, Columbus. “We know that medical school graduates who are African American or Black, Hispanic or Latinx, or American Indian or Alaskan Native are more likely to serve those communities as practicing physicians.
“The COVID-19 pandemic highlighted the urgent need for more African American or Black, Hispanic or Latinx, or American Indian or Alaskan Native physicians,” he said. “Inadequate access to culturally competent care has exacerbated existing health disparities, resulting in death and hospitalization rates up to three to four times the rates of European American or White people.”
Dr. Poll-Hunter also said that studies have shown that diversity in the classroom creates a more enriched learning environment and increases civic mindedness and cognitive complexity, “as well as helps us understand people who are different than ourselves.”
The diversity goal “is not about quotas, it’s about excellence,” she said. “We know that there’s talent that exists, and we want to make sure that everyone has an opportunity to be successful.”
Dr. Ly has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new study.
In 1900, 1.3% of physicians were Black. In 1940, 2.8% of physicians were Black, and by 2018 – when almost 13% of the population was Black – 5.4% of doctors were Black, reports Dan Ly, MD, PhD, MPP, an assistant professor of medicine at the University of California, Los Angeles, in a study published online April 19, 2021, in the Journal of General Internal Medicine.
The proportion of male Black physicians was 2.7% in 1940 and 2.6% in 2018.
Dr. Ly also found a significant wage gap. The median income earned by White doctors was $50,000 more than the median income of Black physicians in 2018. Dr. Ly based his findings on the U.S. Census Decennial Census long form, accessed via IPUMS, a free database funded by the National Institutes of Health and other organizations.
“If we care about the health of the population, particularly the health of Black patients, we should care about how small the proportion of our physicians who are Black is and the extremely slow progress we have made as a medical system in increasing that proportion,” Dr. Ly said in an interview.
Dr. Ly said he took on this research in part because previous studies have shown that Black patients are more likely to seek preventive care from Black doctors. Thus, increasing the numbers of Black physicians could narrow gaps in life expectancy between Whites and Blacks.
He also wanted to see whether progress had been made as a result of various medical organizations and the Association of American Medical Colleges undertaking initiatives to increase workforce diversity. There has been “very, very little” progress, he said.
Norma Poll-Hunter, PhD, the AAMC’s senior director of workforce diversity, said Dr. Ly’s report “was not surprising at all.”
The AAMC reported in 2014 that the number of Black men who apply to and matriculate into medical schools has been declining since 1978. That year, there were 1,410 Black male applicants and 542 Black enrollees. In 2014, there were 1,337 applicants and 515 enrollees.
Since 2014, Black male enrollment has increased slightly, rising from 2.4% in the 2014-2015 school year to 2.9% in the 2019-2020 year, the AAMC reported last year.
In addition, among other historically underrepresented minorities, “we really have seen very small progress” despite the increase in the number of medical schools, Dr. Poll-Hunter said in an interview.
The AAMC and the National Medical Association consider the lack of Black male applicants and matriculants to be a national crisis. The two groups started an alliance in 2020 aimed at finding ways to amplify and support Black men’s interest in medicine and the biomedical sciences and to “develop systems-based solutions to address exclusionary practices that create barriers for Black men and prevent them from having equitable opportunities to successfully enroll in medical school.”
Solutions include requiring medical school admissions committees and application screeners to undergo implicit bias awareness and mitigation training, adopting holistic admissions reviews, and incentivizing institutions of higher learning to partner with Black communities in urban and rural school systems to establish K-12 health sciences academies, said NMA President Leon McDougle, MD, MPH.
“There are the systems factors, and racism is a big one that we have to tackle,” said Dr. Poll-Hunter.
Diversity isn’t just about numbers, said Dr. McDougle, a professor of family medicine and associate dean for diversity and inclusion at Ohio State University, Columbus. “We know that medical school graduates who are African American or Black, Hispanic or Latinx, or American Indian or Alaskan Native are more likely to serve those communities as practicing physicians.
“The COVID-19 pandemic highlighted the urgent need for more African American or Black, Hispanic or Latinx, or American Indian or Alaskan Native physicians,” he said. “Inadequate access to culturally competent care has exacerbated existing health disparities, resulting in death and hospitalization rates up to three to four times the rates of European American or White people.”
Dr. Poll-Hunter also said that studies have shown that diversity in the classroom creates a more enriched learning environment and increases civic mindedness and cognitive complexity, “as well as helps us understand people who are different than ourselves.”
The diversity goal “is not about quotas, it’s about excellence,” she said. “We know that there’s talent that exists, and we want to make sure that everyone has an opportunity to be successful.”
Dr. Ly has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new study.
In 1900, 1.3% of physicians were Black. In 1940, 2.8% of physicians were Black, and by 2018 – when almost 13% of the population was Black – 5.4% of doctors were Black, reports Dan Ly, MD, PhD, MPP, an assistant professor of medicine at the University of California, Los Angeles, in a study published online April 19, 2021, in the Journal of General Internal Medicine.
The proportion of male Black physicians was 2.7% in 1940 and 2.6% in 2018.
Dr. Ly also found a significant wage gap. The median income earned by White doctors was $50,000 more than the median income of Black physicians in 2018. Dr. Ly based his findings on the U.S. Census Decennial Census long form, accessed via IPUMS, a free database funded by the National Institutes of Health and other organizations.
“If we care about the health of the population, particularly the health of Black patients, we should care about how small the proportion of our physicians who are Black is and the extremely slow progress we have made as a medical system in increasing that proportion,” Dr. Ly said in an interview.
Dr. Ly said he took on this research in part because previous studies have shown that Black patients are more likely to seek preventive care from Black doctors. Thus, increasing the numbers of Black physicians could narrow gaps in life expectancy between Whites and Blacks.
He also wanted to see whether progress had been made as a result of various medical organizations and the Association of American Medical Colleges undertaking initiatives to increase workforce diversity. There has been “very, very little” progress, he said.
Norma Poll-Hunter, PhD, the AAMC’s senior director of workforce diversity, said Dr. Ly’s report “was not surprising at all.”
The AAMC reported in 2014 that the number of Black men who apply to and matriculate into medical schools has been declining since 1978. That year, there were 1,410 Black male applicants and 542 Black enrollees. In 2014, there were 1,337 applicants and 515 enrollees.
Since 2014, Black male enrollment has increased slightly, rising from 2.4% in the 2014-2015 school year to 2.9% in the 2019-2020 year, the AAMC reported last year.
In addition, among other historically underrepresented minorities, “we really have seen very small progress” despite the increase in the number of medical schools, Dr. Poll-Hunter said in an interview.
The AAMC and the National Medical Association consider the lack of Black male applicants and matriculants to be a national crisis. The two groups started an alliance in 2020 aimed at finding ways to amplify and support Black men’s interest in medicine and the biomedical sciences and to “develop systems-based solutions to address exclusionary practices that create barriers for Black men and prevent them from having equitable opportunities to successfully enroll in medical school.”
Solutions include requiring medical school admissions committees and application screeners to undergo implicit bias awareness and mitigation training, adopting holistic admissions reviews, and incentivizing institutions of higher learning to partner with Black communities in urban and rural school systems to establish K-12 health sciences academies, said NMA President Leon McDougle, MD, MPH.
“There are the systems factors, and racism is a big one that we have to tackle,” said Dr. Poll-Hunter.
Diversity isn’t just about numbers, said Dr. McDougle, a professor of family medicine and associate dean for diversity and inclusion at Ohio State University, Columbus. “We know that medical school graduates who are African American or Black, Hispanic or Latinx, or American Indian or Alaskan Native are more likely to serve those communities as practicing physicians.
“The COVID-19 pandemic highlighted the urgent need for more African American or Black, Hispanic or Latinx, or American Indian or Alaskan Native physicians,” he said. “Inadequate access to culturally competent care has exacerbated existing health disparities, resulting in death and hospitalization rates up to three to four times the rates of European American or White people.”
Dr. Poll-Hunter also said that studies have shown that diversity in the classroom creates a more enriched learning environment and increases civic mindedness and cognitive complexity, “as well as helps us understand people who are different than ourselves.”
The diversity goal “is not about quotas, it’s about excellence,” she said. “We know that there’s talent that exists, and we want to make sure that everyone has an opportunity to be successful.”
Dr. Ly has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Vaccinating homebound patients is an uphill battle

There are about 2 million to 4 million homebound patients in the United States, according to a webinar from The Trust for America’s Health, which was broadcast in March. But many of these individuals have not been vaccinated yet because of logistical challenges.
Some homebound COVID-19 immunization programs are administering Moderna and Pfizer vaccines to their patients, but many state, city, and local programs administered the Johnson & Johnson vaccine after it was cleared for use by the Food and Drug Administration in February 2021. The efficacy of the one-shot vaccine, as well as it being easier to store and ship than the Moderna and Pfizer vaccines, makes getting it to homebound patients less challenging.
“With Pfizer and Moderna, transportation is a challenge because the temperature demands and the fragility of [messenger] RNA–based vaccines,” Brent Feorene, executive director of the American Academy of Home Care Medicine, said in an interview. That’s why [the Johnson & Johnson] vaccine held such promise – it’s less fragile, [can be stored in] higher temperatures, and was a one shot.”
Other hurdles to getting homebound patients vaccinated had already been in place prior to the 10-day-pause on using the J&J vaccine that occurred for federal agencies to consider possible serious side effects linked to it.
Many roadblocks to vaccination
Although many homebound patients can’t readily go out into the community and be exposed to the COVID-19 virus themselves, they are dependent on caregivers and family members who do go out into the community.
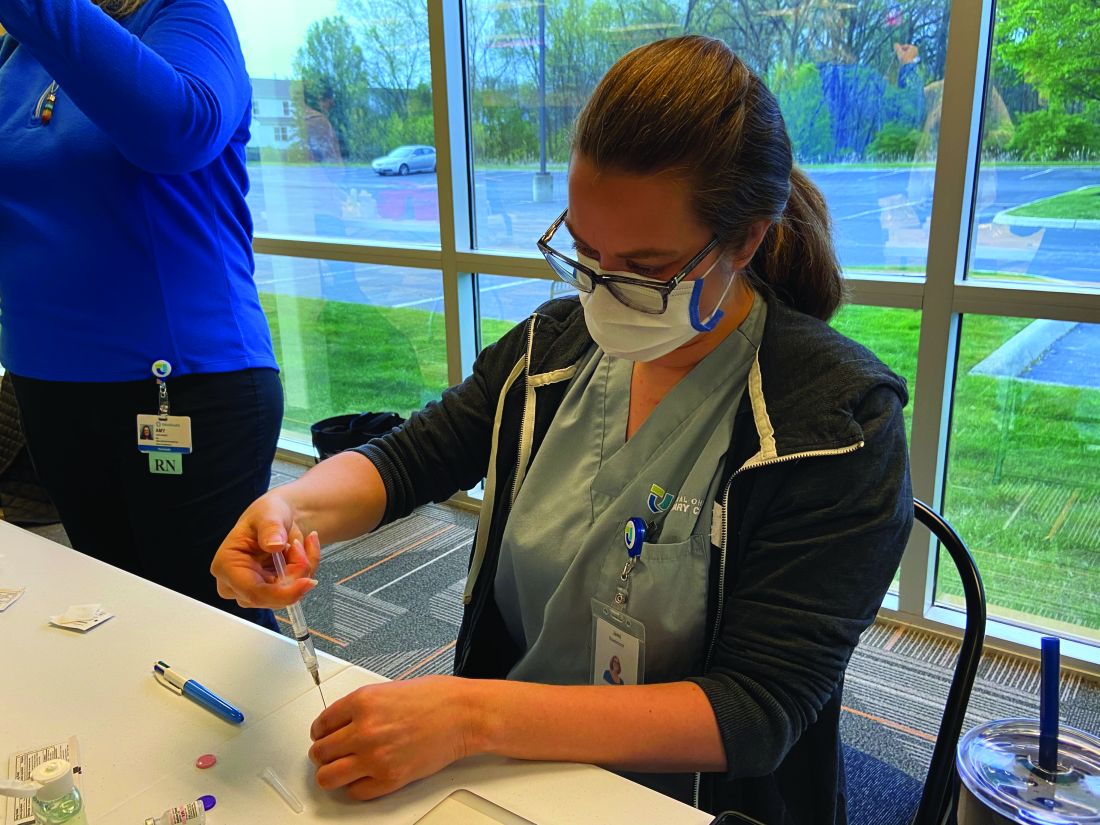
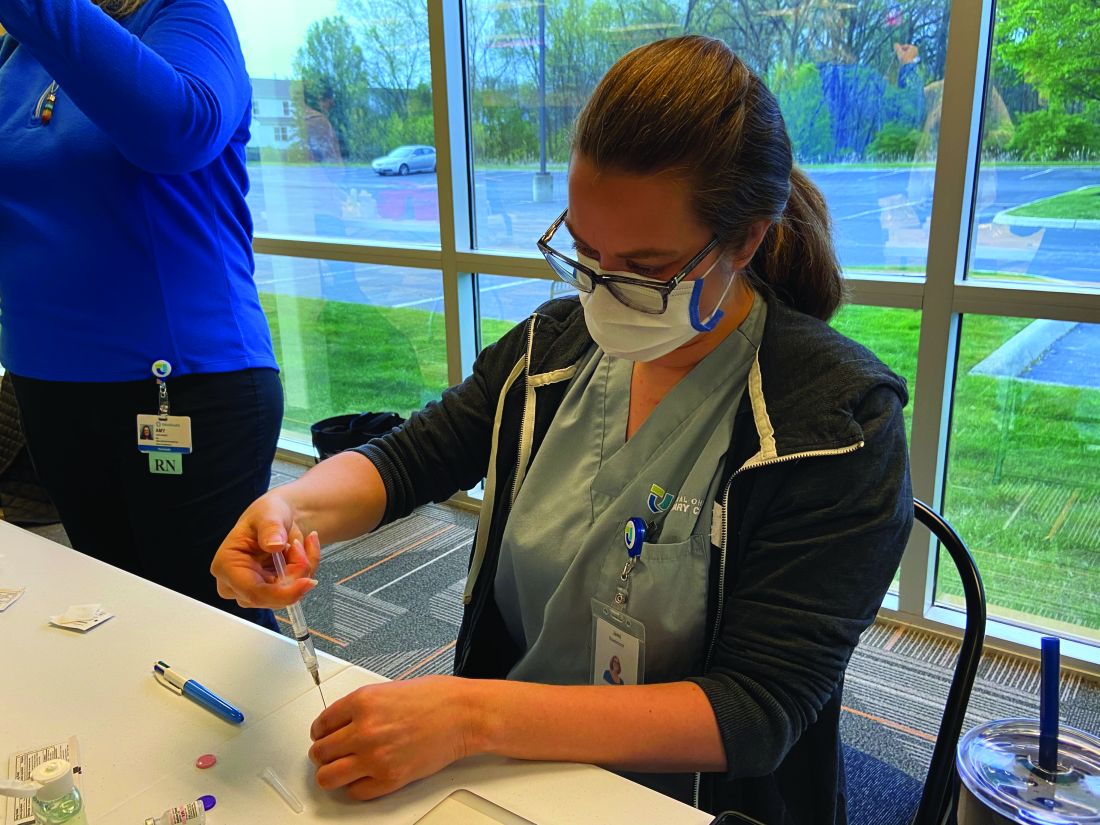
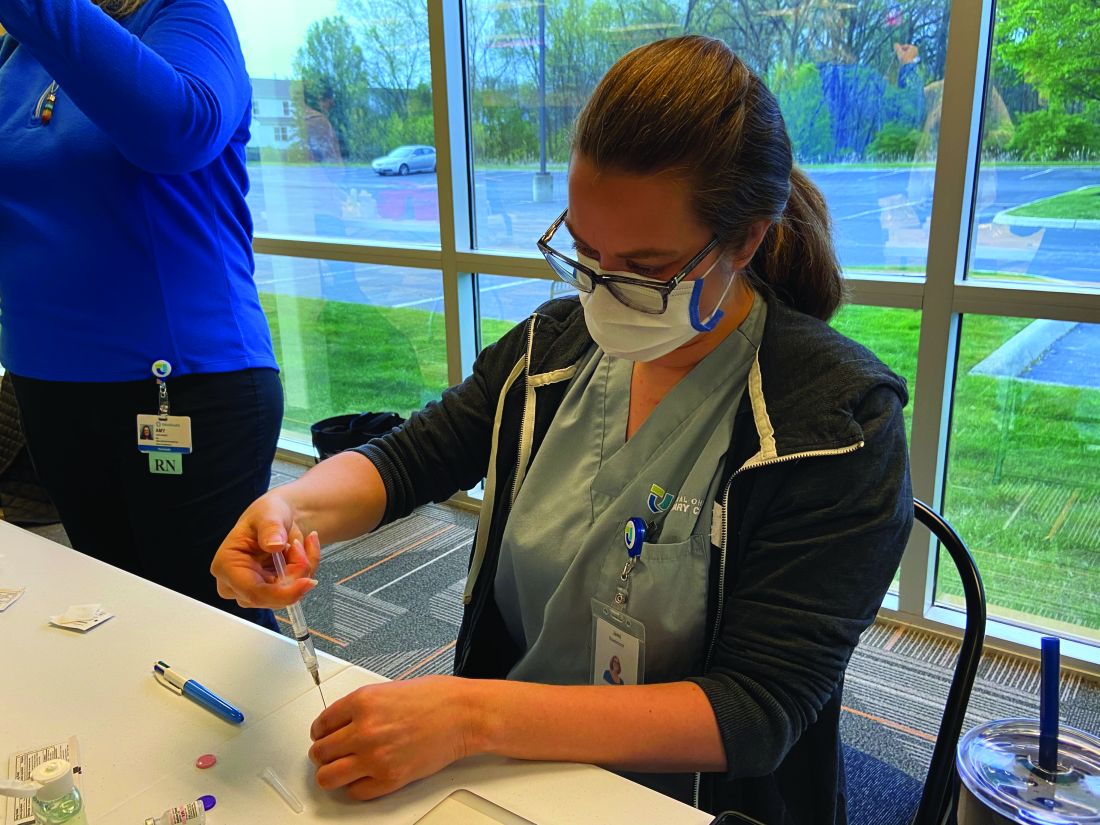
“Their friends, family, neighbors, home health aides, and other kinds of health care workers come into the home,” said Shawn Amer, clinical program director at Central Ohio Primary Care in Columbus.
Nurses from Ms. Amer’s practice vaccinated approximately ten homebound patients with the J&J vaccine through a pilot program in March. Then on April 24, nurses from Central Ohio Primary Care vaccinated just under 40 homebound patients and about a handful of their caregivers who were not able to get their vaccines elsewhere, according to Ms. Amer. This time they used the Pfizer vaccine and will be returning to these patients’ homes on May 15 to administer the second dose.
“Any time you are getting in the car and adding miles, it adds complexity,” Ms. Amer said.
“We called patients 24 to 36 hours before coming to their homes to make sure they were ready, but we learned that just because the healthcare power of attorney agrees to a patient getting vaccinated does not mean that patient will be willing to get the vaccine when the nurse shows up," she noted.
Ms. Amer elaborated that three patients with dementia refused the vaccine when nurses arrived at their home on April 24.
“We had to pivot and find other people,” Ms. Amer. Her practice ended up having to waste one shot.
Expenses are greater
The higher costs of getting homebound patients vaccinated is an additional hurdle to getting these vulnerable individuals protected by COVID-19 shots.
Vaccinating patients in their homes “doesn’t require a lot of technology, but it does require a lot of time” and the staffing expense becomes part of the challenge, Ms. Amer noted.
For each of the two days that Central Ohio Primary Care provides the Pfizer vaccine to homebound patients, the practice needs to pay seven nurses to administer the vaccine, Ms. Amer explained.
There have also been reports of organizations that administer the vaccines – which are free for patients because the federal government is paying for them – not being paid enough by Medicare to cover staff time and efforts to vaccinate patients in their homes, Kaiser Health News reported. According to the Centers for Medicare & Medicaid Services, they pay $40 for the administration of a single-dose COVID-19 vaccine and, for COVID-19 vaccines requiring multiple doses, Medicare pays approximately $40 for each dose in the series. These rates were implemented after March 15. Before that date, the rates were even lower, with the Medicare reimbursement rates for initial doses of COVID-19 vaccines being $16.94 and final doses being $28.39.
William Dombi, president of the National Association for Home Care & Hospice, told Kaiser Health News that the actual cost of these homebound visits are closer to $150 or $160.
“The reimbursement for the injection is pretty minimal,” Mr. Feorene said. “So unless you’re a larger organization and able to have staff to deploy some of your smaller practices, just couldn’t afford to do it.”
Many homebound patients have also been unable to get the lifesaving shots because of logistical roadblocks and many practices not being able to do home visits.
“I think that initially when the [Centers for Disease Control and Prevention] came out with vaccine guidance for medical providers, they offered no guidance for in-home medical providers and we had to go back and ask for that, which they did produce,” Mr. Feorene said. “And we’re grateful for that. But I think just this general understanding that there is a population of folks that are [limited to their home], that they do receive medical care and other care in the home, and that we have to remember that the medical providers who provide care in the home are also primary care providers.”
Furthermore, trying to navigate or find programs delivering vaccines to the homebound can be difficult depending on where a patient lives.
While some programs have been launched on the country or city level – the New York Fire Department launched a pilot program to bring the Johnson & Johnson vaccine to homebound seniors – other programs have been spearheaded by hospital networks like Northwell and Mount Sinai. However, many of these hospital networks only reach out to people who already have a relationship with the hospital.
Ms Amer said identifying homebound patients and reaching out to them can be tough and can contribute to the logistics and time involved in setting patients up for the vaccine.
“Reaching some of these patients is difficult,” Ms. Amer noted. “Sometimes the best way to reach them or get a hold of them is through their caregiver. And so do you have the right phone number? Do you have the right name?”
Overcoming the challenges
With the absence of a national plan targeting homebound patients, many local initiatives were launched to help these individuals get vaccinated. Local fire department paramedics have gone door to door to administer the COVID-19 vaccine in cities like Chicago, New York, and Miami. The suspension of the Johnson & Johnson vaccine resulted in the suspension of in-home vaccinations for some people in New York City. However, the program resumed after the FDA and CDC lifted the pause on April 24.

Health systems like Mount Sinai vaccinated approximately 530 people through the Mount Sinai Visiting Doctors Program, including patients and their caregivers, according to Peter Gliatto, MD, associate director of the Mount Sinai Visiting Doctors Program.
“In different cities, townships, and jurisdictions, different health departments and different provider groups are approaching [the distribution of the COVID-19 vaccine] slightly differently,” Ms. Amer said. So a lot of the decisions surrounding the distribution of shots are local or dependent on local resourcing.
People who live in rural areas present a unique challenge, but Mr. Feorene said reaching out to local emergency medical services or the local health departments can provide some insight on what their town is doing to vaccinate homebound patients.
“I think understanding what a [public health department] is doing would be the very first place to start,” Mr. Feorene said in an interview.
If a patient is bedridden and is mobile enough to sit in a car, Mr. Feorene also recommends finding out if there are vaccine fairs “within a reasonable driving distance.”
Ms. Amer said continuing this mission of getting homebound patients vaccinated is necessary for public health.
“Even if it’s going to take longer to vaccinate these homebound patients, we still have to make an effort. So much of the country’s vaccine efforts have been focused on getting as many shots in as many arms as quickly as possible. And that is definitely super important,” she said.
Ms. Amer is working with her practice’s primary care physicians to try to identify all of those patients who are functionally debilitated or unable to leave their home to get vaccinated and that Central Ohio Primary Care will vaccinate more homebound patients, she added.
The experts interviewed in this article have no conflicts.
Katie Lennon contributed to this report.
This article was updated 4/29/21.

There are about 2 million to 4 million homebound patients in the United States, according to a webinar from The Trust for America’s Health, which was broadcast in March. But many of these individuals have not been vaccinated yet because of logistical challenges.
Some homebound COVID-19 immunization programs are administering Moderna and Pfizer vaccines to their patients, but many state, city, and local programs administered the Johnson & Johnson vaccine after it was cleared for use by the Food and Drug Administration in February 2021. The efficacy of the one-shot vaccine, as well as it being easier to store and ship than the Moderna and Pfizer vaccines, makes getting it to homebound patients less challenging.
“With Pfizer and Moderna, transportation is a challenge because the temperature demands and the fragility of [messenger] RNA–based vaccines,” Brent Feorene, executive director of the American Academy of Home Care Medicine, said in an interview. That’s why [the Johnson & Johnson] vaccine held such promise – it’s less fragile, [can be stored in] higher temperatures, and was a one shot.”
Other hurdles to getting homebound patients vaccinated had already been in place prior to the 10-day-pause on using the J&J vaccine that occurred for federal agencies to consider possible serious side effects linked to it.
Many roadblocks to vaccination
Although many homebound patients can’t readily go out into the community and be exposed to the COVID-19 virus themselves, they are dependent on caregivers and family members who do go out into the community.
“Their friends, family, neighbors, home health aides, and other kinds of health care workers come into the home,” said Shawn Amer, clinical program director at Central Ohio Primary Care in Columbus.
Nurses from Ms. Amer’s practice vaccinated approximately ten homebound patients with the J&J vaccine through a pilot program in March. Then on April 24, nurses from Central Ohio Primary Care vaccinated just under 40 homebound patients and about a handful of their caregivers who were not able to get their vaccines elsewhere, according to Ms. Amer. This time they used the Pfizer vaccine and will be returning to these patients’ homes on May 15 to administer the second dose.
“Any time you are getting in the car and adding miles, it adds complexity,” Ms. Amer said.
“We called patients 24 to 36 hours before coming to their homes to make sure they were ready, but we learned that just because the healthcare power of attorney agrees to a patient getting vaccinated does not mean that patient will be willing to get the vaccine when the nurse shows up," she noted.
Ms. Amer elaborated that three patients with dementia refused the vaccine when nurses arrived at their home on April 24.
“We had to pivot and find other people,” Ms. Amer. Her practice ended up having to waste one shot.
Expenses are greater
The higher costs of getting homebound patients vaccinated is an additional hurdle to getting these vulnerable individuals protected by COVID-19 shots.
Vaccinating patients in their homes “doesn’t require a lot of technology, but it does require a lot of time” and the staffing expense becomes part of the challenge, Ms. Amer noted.
For each of the two days that Central Ohio Primary Care provides the Pfizer vaccine to homebound patients, the practice needs to pay seven nurses to administer the vaccine, Ms. Amer explained.
There have also been reports of organizations that administer the vaccines – which are free for patients because the federal government is paying for them – not being paid enough by Medicare to cover staff time and efforts to vaccinate patients in their homes, Kaiser Health News reported. According to the Centers for Medicare & Medicaid Services, they pay $40 for the administration of a single-dose COVID-19 vaccine and, for COVID-19 vaccines requiring multiple doses, Medicare pays approximately $40 for each dose in the series. These rates were implemented after March 15. Before that date, the rates were even lower, with the Medicare reimbursement rates for initial doses of COVID-19 vaccines being $16.94 and final doses being $28.39.
William Dombi, president of the National Association for Home Care & Hospice, told Kaiser Health News that the actual cost of these homebound visits are closer to $150 or $160.
“The reimbursement for the injection is pretty minimal,” Mr. Feorene said. “So unless you’re a larger organization and able to have staff to deploy some of your smaller practices, just couldn’t afford to do it.”
Many homebound patients have also been unable to get the lifesaving shots because of logistical roadblocks and many practices not being able to do home visits.
“I think that initially when the [Centers for Disease Control and Prevention] came out with vaccine guidance for medical providers, they offered no guidance for in-home medical providers and we had to go back and ask for that, which they did produce,” Mr. Feorene said. “And we’re grateful for that. But I think just this general understanding that there is a population of folks that are [limited to their home], that they do receive medical care and other care in the home, and that we have to remember that the medical providers who provide care in the home are also primary care providers.”
Furthermore, trying to navigate or find programs delivering vaccines to the homebound can be difficult depending on where a patient lives.
While some programs have been launched on the country or city level – the New York Fire Department launched a pilot program to bring the Johnson & Johnson vaccine to homebound seniors – other programs have been spearheaded by hospital networks like Northwell and Mount Sinai. However, many of these hospital networks only reach out to people who already have a relationship with the hospital.
Ms Amer said identifying homebound patients and reaching out to them can be tough and can contribute to the logistics and time involved in setting patients up for the vaccine.
“Reaching some of these patients is difficult,” Ms. Amer noted. “Sometimes the best way to reach them or get a hold of them is through their caregiver. And so do you have the right phone number? Do you have the right name?”
Overcoming the challenges
With the absence of a national plan targeting homebound patients, many local initiatives were launched to help these individuals get vaccinated. Local fire department paramedics have gone door to door to administer the COVID-19 vaccine in cities like Chicago, New York, and Miami. The suspension of the Johnson & Johnson vaccine resulted in the suspension of in-home vaccinations for some people in New York City. However, the program resumed after the FDA and CDC lifted the pause on April 24.

Health systems like Mount Sinai vaccinated approximately 530 people through the Mount Sinai Visiting Doctors Program, including patients and their caregivers, according to Peter Gliatto, MD, associate director of the Mount Sinai Visiting Doctors Program.
“In different cities, townships, and jurisdictions, different health departments and different provider groups are approaching [the distribution of the COVID-19 vaccine] slightly differently,” Ms. Amer said. So a lot of the decisions surrounding the distribution of shots are local or dependent on local resourcing.
People who live in rural areas present a unique challenge, but Mr. Feorene said reaching out to local emergency medical services or the local health departments can provide some insight on what their town is doing to vaccinate homebound patients.
“I think understanding what a [public health department] is doing would be the very first place to start,” Mr. Feorene said in an interview.
If a patient is bedridden and is mobile enough to sit in a car, Mr. Feorene also recommends finding out if there are vaccine fairs “within a reasonable driving distance.”
Ms. Amer said continuing this mission of getting homebound patients vaccinated is necessary for public health.
“Even if it’s going to take longer to vaccinate these homebound patients, we still have to make an effort. So much of the country’s vaccine efforts have been focused on getting as many shots in as many arms as quickly as possible. And that is definitely super important,” she said.
Ms. Amer is working with her practice’s primary care physicians to try to identify all of those patients who are functionally debilitated or unable to leave their home to get vaccinated and that Central Ohio Primary Care will vaccinate more homebound patients, she added.
The experts interviewed in this article have no conflicts.
Katie Lennon contributed to this report.
This article was updated 4/29/21.

There are about 2 million to 4 million homebound patients in the United States, according to a webinar from The Trust for America’s Health, which was broadcast in March. But many of these individuals have not been vaccinated yet because of logistical challenges.
Some homebound COVID-19 immunization programs are administering Moderna and Pfizer vaccines to their patients, but many state, city, and local programs administered the Johnson & Johnson vaccine after it was cleared for use by the Food and Drug Administration in February 2021. The efficacy of the one-shot vaccine, as well as it being easier to store and ship than the Moderna and Pfizer vaccines, makes getting it to homebound patients less challenging.
“With Pfizer and Moderna, transportation is a challenge because the temperature demands and the fragility of [messenger] RNA–based vaccines,” Brent Feorene, executive director of the American Academy of Home Care Medicine, said in an interview. That’s why [the Johnson & Johnson] vaccine held such promise – it’s less fragile, [can be stored in] higher temperatures, and was a one shot.”
Other hurdles to getting homebound patients vaccinated had already been in place prior to the 10-day-pause on using the J&J vaccine that occurred for federal agencies to consider possible serious side effects linked to it.
Many roadblocks to vaccination
Although many homebound patients can’t readily go out into the community and be exposed to the COVID-19 virus themselves, they are dependent on caregivers and family members who do go out into the community.
“Their friends, family, neighbors, home health aides, and other kinds of health care workers come into the home,” said Shawn Amer, clinical program director at Central Ohio Primary Care in Columbus.
Nurses from Ms. Amer’s practice vaccinated approximately ten homebound patients with the J&J vaccine through a pilot program in March. Then on April 24, nurses from Central Ohio Primary Care vaccinated just under 40 homebound patients and about a handful of their caregivers who were not able to get their vaccines elsewhere, according to Ms. Amer. This time they used the Pfizer vaccine and will be returning to these patients’ homes on May 15 to administer the second dose.
“Any time you are getting in the car and adding miles, it adds complexity,” Ms. Amer said.
“We called patients 24 to 36 hours before coming to their homes to make sure they were ready, but we learned that just because the healthcare power of attorney agrees to a patient getting vaccinated does not mean that patient will be willing to get the vaccine when the nurse shows up," she noted.
Ms. Amer elaborated that three patients with dementia refused the vaccine when nurses arrived at their home on April 24.
“We had to pivot and find other people,” Ms. Amer. Her practice ended up having to waste one shot.
Expenses are greater
The higher costs of getting homebound patients vaccinated is an additional hurdle to getting these vulnerable individuals protected by COVID-19 shots.
Vaccinating patients in their homes “doesn’t require a lot of technology, but it does require a lot of time” and the staffing expense becomes part of the challenge, Ms. Amer noted.
For each of the two days that Central Ohio Primary Care provides the Pfizer vaccine to homebound patients, the practice needs to pay seven nurses to administer the vaccine, Ms. Amer explained.
There have also been reports of organizations that administer the vaccines – which are free for patients because the federal government is paying for them – not being paid enough by Medicare to cover staff time and efforts to vaccinate patients in their homes, Kaiser Health News reported. According to the Centers for Medicare & Medicaid Services, they pay $40 for the administration of a single-dose COVID-19 vaccine and, for COVID-19 vaccines requiring multiple doses, Medicare pays approximately $40 for each dose in the series. These rates were implemented after March 15. Before that date, the rates were even lower, with the Medicare reimbursement rates for initial doses of COVID-19 vaccines being $16.94 and final doses being $28.39.
William Dombi, president of the National Association for Home Care & Hospice, told Kaiser Health News that the actual cost of these homebound visits are closer to $150 or $160.
“The reimbursement for the injection is pretty minimal,” Mr. Feorene said. “So unless you’re a larger organization and able to have staff to deploy some of your smaller practices, just couldn’t afford to do it.”
Many homebound patients have also been unable to get the lifesaving shots because of logistical roadblocks and many practices not being able to do home visits.
“I think that initially when the [Centers for Disease Control and Prevention] came out with vaccine guidance for medical providers, they offered no guidance for in-home medical providers and we had to go back and ask for that, which they did produce,” Mr. Feorene said. “And we’re grateful for that. But I think just this general understanding that there is a population of folks that are [limited to their home], that they do receive medical care and other care in the home, and that we have to remember that the medical providers who provide care in the home are also primary care providers.”
Furthermore, trying to navigate or find programs delivering vaccines to the homebound can be difficult depending on where a patient lives.
While some programs have been launched on the country or city level – the New York Fire Department launched a pilot program to bring the Johnson & Johnson vaccine to homebound seniors – other programs have been spearheaded by hospital networks like Northwell and Mount Sinai. However, many of these hospital networks only reach out to people who already have a relationship with the hospital.
Ms Amer said identifying homebound patients and reaching out to them can be tough and can contribute to the logistics and time involved in setting patients up for the vaccine.
“Reaching some of these patients is difficult,” Ms. Amer noted. “Sometimes the best way to reach them or get a hold of them is through their caregiver. And so do you have the right phone number? Do you have the right name?”
Overcoming the challenges
With the absence of a national plan targeting homebound patients, many local initiatives were launched to help these individuals get vaccinated. Local fire department paramedics have gone door to door to administer the COVID-19 vaccine in cities like Chicago, New York, and Miami. The suspension of the Johnson & Johnson vaccine resulted in the suspension of in-home vaccinations for some people in New York City. However, the program resumed after the FDA and CDC lifted the pause on April 24.

Health systems like Mount Sinai vaccinated approximately 530 people through the Mount Sinai Visiting Doctors Program, including patients and their caregivers, according to Peter Gliatto, MD, associate director of the Mount Sinai Visiting Doctors Program.
“In different cities, townships, and jurisdictions, different health departments and different provider groups are approaching [the distribution of the COVID-19 vaccine] slightly differently,” Ms. Amer said. So a lot of the decisions surrounding the distribution of shots are local or dependent on local resourcing.
People who live in rural areas present a unique challenge, but Mr. Feorene said reaching out to local emergency medical services or the local health departments can provide some insight on what their town is doing to vaccinate homebound patients.
“I think understanding what a [public health department] is doing would be the very first place to start,” Mr. Feorene said in an interview.
If a patient is bedridden and is mobile enough to sit in a car, Mr. Feorene also recommends finding out if there are vaccine fairs “within a reasonable driving distance.”
Ms. Amer said continuing this mission of getting homebound patients vaccinated is necessary for public health.
“Even if it’s going to take longer to vaccinate these homebound patients, we still have to make an effort. So much of the country’s vaccine efforts have been focused on getting as many shots in as many arms as quickly as possible. And that is definitely super important,” she said.
Ms. Amer is working with her practice’s primary care physicians to try to identify all of those patients who are functionally debilitated or unable to leave their home to get vaccinated and that Central Ohio Primary Care will vaccinate more homebound patients, she added.
The experts interviewed in this article have no conflicts.
Katie Lennon contributed to this report.
This article was updated 4/29/21.
Helpful giant rodents and our old friend, the hookworm
Rat-ting out coronavirus
Did you know there is a possibility that giant rodents could rat out coronavirus? Not many people are keen on the presence of a 3-foot-long African giant pouched rat, but they have already been trained to sniff out diseases that are dangerous to humans, such as brucellosis and tuberculosis, according to researchers at the University of Glasgow.
Professor Dan Haydon and his associates believe there is a good possibility that the rats can be trained to sniff out COVID-19. Dogs have been helpful in sniffing for COVID-19 at airports and are being trained to detect it through armpit sweat, making detection of the virus easier for travelers and staff. Even robots have gotten into the COVID-19 detecting act.
Since African giant pouched rats can grow to be the size of a small dog and “are easily tamed as companion animals,” it seems likely that they have the potential to do the same. That is, sniffing for COVID-19, not appearing at your local airport. That’s still gross.
Stay healthy, get a parasite bestie
The key to health could actually be swimming around in your gut. Researchers from University College London have found that a parasitic worm could be the answer to longevity and avoidance of chronic diseases.
The seeming immunity from inflammatory diseases such as arthritis, diabetes, and multiple sclerosis may come from helminth parasites, or hookworms – parasites that have been coexisting harmlessly with the human body for thousands of years. The investigators went so far as to call them “old friends,” but the kind that you rarely see at reunions or call up for a favor.
As a result of modern sanitation and improved hygiene, humans and hookworms are seeing much less of each other, which may be a factor in the rise of “aging-associated inflammation” such as COVID-19 symptoms, they suggested. So is there a way to get these old friends back?
“Restorative hookworm treatments” could help with heart disease or dementia, according to the investigators, but maybe you’re not totally on board with getting an actual parasite in your system. We get it. There are helminth-derived proteins that have already been tested to get the job done.
Maybe old friends really do make the best friends.
I love the smell of microbe-infected aerosols in the morning
Have you gone into a public restroom and just stood around for a while appreciating the fine aromas? No? You haven’t? You do your business and get out? Well, it’s a good thing you act like a normal person, because the aerosols released when toilets flush can contain all sorts of nasty bacteria and viruses.
The authors of a new study published in Physics of Fluids came to this groundbreaking conclusion by going to a public bathroom, sticking particle counters above a urinal and a toilet, and letting them sit for a while. After 3 hours and 100 flushes, the ambient level of particles 0.3-3 mcm in diameter had increased dramatically, with particles sized 0.5-1 mcm particularly prone to lingering. For those particles, the level from baseline increased by over 200%.
This is a major concern, the researchers said, because the sort of microbes that are expelled through feces, urine, and vomit can include some pretty nasty things. Ebola, noroviruses that can cause food poisoning, and even good old SARS-CoV-2 can be expelled from the body but remain viable for a time in these aerosols. The researchers recommended improving the ventilation systems in restrooms so that aerosols don’t hang around for hours at a time. Plus, it might make the place not smell like a, uh, public restroom.
Not to question the research and the people behind it, but we’re not sure how necessary it was to give people another reason not to hang out in a place where hundreds, if not thousands, of people come to relieve themselves. There’s a reason we’re supposed to “stop and smell the roses” and not “stop and smell the public bathroom.”
World ends not with a bang but with a cheeseburger
Speaking of old sayings, one of our favorites, “You are what you eat,” may offer a culinary explanation for those who do enjoy the ambiance of a fine, aerosol-infested public restroom.
That explanation involves the high-calorie, high-fat smorgasbord known as the Western diet and some mice who were forced to consume it. Those mice, it turns out, were more anxious and less cognitively advanced than their counterparts who were not eating “highly palatable, energy dense foods (e.g., high saturated fat, high sugar) that are commonly consumed by humans,” according to the authors of a recent literature review.
“Consumption of a Western diet is related to poorer cognitive performance across the lifespan,” the investigators said, adding that consumption of a Western diet “during critical early life stages of development has negative consequences on various cognitive abilities later in adulthood.”
To show their appreciation for the sacrifices these brave test subjects had made in the name of science, the scientists released the Western diet–addled rodents from captivity. Not only did they survive and thrive in the wilds of darkest suburbia, but within 6 months almost half of them were running for Congress.
Rat-ting out coronavirus
Did you know there is a possibility that giant rodents could rat out coronavirus? Not many people are keen on the presence of a 3-foot-long African giant pouched rat, but they have already been trained to sniff out diseases that are dangerous to humans, such as brucellosis and tuberculosis, according to researchers at the University of Glasgow.
Professor Dan Haydon and his associates believe there is a good possibility that the rats can be trained to sniff out COVID-19. Dogs have been helpful in sniffing for COVID-19 at airports and are being trained to detect it through armpit sweat, making detection of the virus easier for travelers and staff. Even robots have gotten into the COVID-19 detecting act.
Since African giant pouched rats can grow to be the size of a small dog and “are easily tamed as companion animals,” it seems likely that they have the potential to do the same. That is, sniffing for COVID-19, not appearing at your local airport. That’s still gross.
Stay healthy, get a parasite bestie
The key to health could actually be swimming around in your gut. Researchers from University College London have found that a parasitic worm could be the answer to longevity and avoidance of chronic diseases.
The seeming immunity from inflammatory diseases such as arthritis, diabetes, and multiple sclerosis may come from helminth parasites, or hookworms – parasites that have been coexisting harmlessly with the human body for thousands of years. The investigators went so far as to call them “old friends,” but the kind that you rarely see at reunions or call up for a favor.
As a result of modern sanitation and improved hygiene, humans and hookworms are seeing much less of each other, which may be a factor in the rise of “aging-associated inflammation” such as COVID-19 symptoms, they suggested. So is there a way to get these old friends back?
“Restorative hookworm treatments” could help with heart disease or dementia, according to the investigators, but maybe you’re not totally on board with getting an actual parasite in your system. We get it. There are helminth-derived proteins that have already been tested to get the job done.
Maybe old friends really do make the best friends.
I love the smell of microbe-infected aerosols in the morning
Have you gone into a public restroom and just stood around for a while appreciating the fine aromas? No? You haven’t? You do your business and get out? Well, it’s a good thing you act like a normal person, because the aerosols released when toilets flush can contain all sorts of nasty bacteria and viruses.
The authors of a new study published in Physics of Fluids came to this groundbreaking conclusion by going to a public bathroom, sticking particle counters above a urinal and a toilet, and letting them sit for a while. After 3 hours and 100 flushes, the ambient level of particles 0.3-3 mcm in diameter had increased dramatically, with particles sized 0.5-1 mcm particularly prone to lingering. For those particles, the level from baseline increased by over 200%.
This is a major concern, the researchers said, because the sort of microbes that are expelled through feces, urine, and vomit can include some pretty nasty things. Ebola, noroviruses that can cause food poisoning, and even good old SARS-CoV-2 can be expelled from the body but remain viable for a time in these aerosols. The researchers recommended improving the ventilation systems in restrooms so that aerosols don’t hang around for hours at a time. Plus, it might make the place not smell like a, uh, public restroom.
Not to question the research and the people behind it, but we’re not sure how necessary it was to give people another reason not to hang out in a place where hundreds, if not thousands, of people come to relieve themselves. There’s a reason we’re supposed to “stop and smell the roses” and not “stop and smell the public bathroom.”
World ends not with a bang but with a cheeseburger
Speaking of old sayings, one of our favorites, “You are what you eat,” may offer a culinary explanation for those who do enjoy the ambiance of a fine, aerosol-infested public restroom.
That explanation involves the high-calorie, high-fat smorgasbord known as the Western diet and some mice who were forced to consume it. Those mice, it turns out, were more anxious and less cognitively advanced than their counterparts who were not eating “highly palatable, energy dense foods (e.g., high saturated fat, high sugar) that are commonly consumed by humans,” according to the authors of a recent literature review.
“Consumption of a Western diet is related to poorer cognitive performance across the lifespan,” the investigators said, adding that consumption of a Western diet “during critical early life stages of development has negative consequences on various cognitive abilities later in adulthood.”
To show their appreciation for the sacrifices these brave test subjects had made in the name of science, the scientists released the Western diet–addled rodents from captivity. Not only did they survive and thrive in the wilds of darkest suburbia, but within 6 months almost half of them were running for Congress.
Rat-ting out coronavirus
Did you know there is a possibility that giant rodents could rat out coronavirus? Not many people are keen on the presence of a 3-foot-long African giant pouched rat, but they have already been trained to sniff out diseases that are dangerous to humans, such as brucellosis and tuberculosis, according to researchers at the University of Glasgow.
Professor Dan Haydon and his associates believe there is a good possibility that the rats can be trained to sniff out COVID-19. Dogs have been helpful in sniffing for COVID-19 at airports and are being trained to detect it through armpit sweat, making detection of the virus easier for travelers and staff. Even robots have gotten into the COVID-19 detecting act.
Since African giant pouched rats can grow to be the size of a small dog and “are easily tamed as companion animals,” it seems likely that they have the potential to do the same. That is, sniffing for COVID-19, not appearing at your local airport. That’s still gross.
Stay healthy, get a parasite bestie
The key to health could actually be swimming around in your gut. Researchers from University College London have found that a parasitic worm could be the answer to longevity and avoidance of chronic diseases.
The seeming immunity from inflammatory diseases such as arthritis, diabetes, and multiple sclerosis may come from helminth parasites, or hookworms – parasites that have been coexisting harmlessly with the human body for thousands of years. The investigators went so far as to call them “old friends,” but the kind that you rarely see at reunions or call up for a favor.
As a result of modern sanitation and improved hygiene, humans and hookworms are seeing much less of each other, which may be a factor in the rise of “aging-associated inflammation” such as COVID-19 symptoms, they suggested. So is there a way to get these old friends back?
“Restorative hookworm treatments” could help with heart disease or dementia, according to the investigators, but maybe you’re not totally on board with getting an actual parasite in your system. We get it. There are helminth-derived proteins that have already been tested to get the job done.
Maybe old friends really do make the best friends.
I love the smell of microbe-infected aerosols in the morning
Have you gone into a public restroom and just stood around for a while appreciating the fine aromas? No? You haven’t? You do your business and get out? Well, it’s a good thing you act like a normal person, because the aerosols released when toilets flush can contain all sorts of nasty bacteria and viruses.
The authors of a new study published in Physics of Fluids came to this groundbreaking conclusion by going to a public bathroom, sticking particle counters above a urinal and a toilet, and letting them sit for a while. After 3 hours and 100 flushes, the ambient level of particles 0.3-3 mcm in diameter had increased dramatically, with particles sized 0.5-1 mcm particularly prone to lingering. For those particles, the level from baseline increased by over 200%.
This is a major concern, the researchers said, because the sort of microbes that are expelled through feces, urine, and vomit can include some pretty nasty things. Ebola, noroviruses that can cause food poisoning, and even good old SARS-CoV-2 can be expelled from the body but remain viable for a time in these aerosols. The researchers recommended improving the ventilation systems in restrooms so that aerosols don’t hang around for hours at a time. Plus, it might make the place not smell like a, uh, public restroom.
Not to question the research and the people behind it, but we’re not sure how necessary it was to give people another reason not to hang out in a place where hundreds, if not thousands, of people come to relieve themselves. There’s a reason we’re supposed to “stop and smell the roses” and not “stop and smell the public bathroom.”
World ends not with a bang but with a cheeseburger
Speaking of old sayings, one of our favorites, “You are what you eat,” may offer a culinary explanation for those who do enjoy the ambiance of a fine, aerosol-infested public restroom.
That explanation involves the high-calorie, high-fat smorgasbord known as the Western diet and some mice who were forced to consume it. Those mice, it turns out, were more anxious and less cognitively advanced than their counterparts who were not eating “highly palatable, energy dense foods (e.g., high saturated fat, high sugar) that are commonly consumed by humans,” according to the authors of a recent literature review.
“Consumption of a Western diet is related to poorer cognitive performance across the lifespan,” the investigators said, adding that consumption of a Western diet “during critical early life stages of development has negative consequences on various cognitive abilities later in adulthood.”
To show their appreciation for the sacrifices these brave test subjects had made in the name of science, the scientists released the Western diet–addled rodents from captivity. Not only did they survive and thrive in the wilds of darkest suburbia, but within 6 months almost half of them were running for Congress.
The neurology of long-haul COVID-19
Long-haul neurologic symptoms of COVID-19 seem to be distinct from neurologic conditions found in acute disease. Much work remains to be done to understand the biological mechanisms behind these problems, but inflammation and autoimmune responses may play a role in some cases.
Those were some of the takeaways from a talk by Serena Spudich, MD, who presented her research at the 2021 annual meeting of the American Academy of Neurology. Dr. Spudich is the division chief of neurologic infections and global neurology and codirector of the Center for Neuroepidemiology and Clinical Neurological Research at Yale University, New Haven, Conn.
Examining the nervous system’s involvement in COVID-19
Even early on in the pandemic, it became clear that there were lingering complaints of neuromuscular problems, cognitive dysfunction, and mood and psychiatric issues. Breathing and heart rate problems also can arise. “There seems to be a preponderance of syndromes that reflect involvement of the nervous system,” said Dr. Spudich.
To try to understand the etiology of these persistent problems, Dr. Spudich said it’s important to examine the nervous system’s involvement in acute COVID-19. She has been involved in these efforts since early in the pandemic, when she ran an inpatient consult service at Yale dedicated to neurologic effects of acute COVID-19. She witnessed complications including stroke, encephalopathy, and seizures, among others.
Stroke during acute COVID-19 seemed to be associated with inflammation and endothelial activation or endotheliopathy. SARS-CoV-2 has been undetectable in the cerebrospinal fluid (CSF) of patients with acute COVID-19 and neurologic symptoms, but inflammatory cytokines can be present along with increased frequency of B cells. Anti–SARS-CoV-2 antibodies have also been found in CSF, some of which were auto reactive to brain tissue. The immune response was altered, compared with healthy controls, and in the CNS, compared with in the blood, “raising the question of whether inflammation and autoimmunity may be underlying causes of these syndromes,” said Dr. Spudich.
She also pointed to an MRI study of autopsied brain tissue of patients with COVID-19 and neurologic complications, which showed indications of both hemorrhagic and ischemic microvascular injury. “It’s just a reminder that, during acute COVID-19, there may be inflammation in the brain, there may be autoimmune reactions, and there may be vascular changes that underlie some of the neurologic syndromes that are seen,” said Dr. Spudich.
A panoply of different syndromes
In October, Yale set up a post-COVID neurologic clinic that brought together pulmonary, cardiology, and psychiatric specialists, many of whom saw the same patients, about 60% of whom had cognitive impairment, more than 40% had neuromuscular problems, and over 30% headache. “There’s not a single entity of a post-COVID neurologic syndrome. There’s a panoply of different syndromes that may have similar or distinct etiologies,” said Dr. Spudich.
Most patients were in their 30s, 40s, or 50s. That doesn’t necessarily mean this is the most common age range for these issues, though. There could be some bias if these individuals are seeking specialty care because they expected to recover from COVID-19 quickly. But it could be that there is something biologically unique among this age group that predisposes them to complications. Regardless, two out of three patients were never hospitalized, “suggesting that even mild COVID-19 can lead to some long-term sequelae,” said Dr. Spudich.
One potential explanation for long-term neurologic syndromes is that they are an extension of the inflammation, autoimmunity, and immune perturbation occurring during acute disease. One study looked at 18 cancer patients who had neurologic complications with COVID-19. Two months after onset, they had elevated markers of neuroinflammation and neuronal injury in the cerebral spinal fluid compared to cancer patients with no history of COVID-19.
Looking for biologic markers
An Italian study looked at patients who were evaluated during acute hospitalization and again 3 months later, and found that some markers of inflation in the blood were associated with later cognitive impairment. The patients were more severely ill, so it’s not clear what the findings mean for patients who present with neurologic symptoms after milder illness.
A PET scan study of 35 patients with persistent neurologic symptoms found patterns of reduced fluorodeoxyglucose uptake in some regions of the brain that are believed to be associated with some symptoms. Lower values were associated with greater severity for symptoms like memory dysfunction, and anosmia. “Why there might be hypometabolism in these regions I think needs to be assessed and used as a biomarker to associate hypometabolism with other kinds of processes in blood and spinal fluid,” said Dr. Spudich.
Along with colleagues at Yale, Dr. Spudich is conducting the MIND study, which is using PET and MRI imaging along with blood and CSF biomarkers to track the progress of patients after COVID-19. There are few results to discuss since only 20 patients have been recruited so far, except that brain imaging and blood values are generally normal despite neurologic complaints. Most were not hospitalized for COVID-19. Dr. Spudich highlighted one man in his 30s who developed new-onset psychosis, despite no previous history. Although clinical tests were all negative, a novel autoantibody detection method revealed a previously unknown autoreactive antibody in his spinal fluid. “This may suggest that there is autoantibody production in some individuals with post–COVID-19 psychosis, and potentially other syndromes,” said Dr. Spudich.
The research task ahead
The case illustrates the task ahead for neurology. “There’s a real research mandate to understand the biological substrates of these diverse disorders, not only to address the emergent public health concern and reduce the stigma in our patients, but to develop targeted therapeutic interventions,” said Dr. Spudich.
Anna Cervantes-Arslanian, MD, an associate professor of neurology at Boston University who also treats and studies patients with post-COVID neurologic symptoms, agreed with that assessment. “It’s not like every patient that has muscle aches and fatigue also has brain fog. It’s really hard to parse them out into specific phenotypes that are pretty classic. Some people will have all of those things, some will have very few of them,” said Dr. Cervantes-Arslanian. “We need to be able to identify them sand see if there is clustering of symptoms so we can better look into what the biological underpinnings are. That’s the first step to thinking about a therapeutic target.”
Dr. Spudich and Dr. Cervantes-Arslanian had no relevant financial disclosures.
Long-haul neurologic symptoms of COVID-19 seem to be distinct from neurologic conditions found in acute disease. Much work remains to be done to understand the biological mechanisms behind these problems, but inflammation and autoimmune responses may play a role in some cases.
Those were some of the takeaways from a talk by Serena Spudich, MD, who presented her research at the 2021 annual meeting of the American Academy of Neurology. Dr. Spudich is the division chief of neurologic infections and global neurology and codirector of the Center for Neuroepidemiology and Clinical Neurological Research at Yale University, New Haven, Conn.
Examining the nervous system’s involvement in COVID-19
Even early on in the pandemic, it became clear that there were lingering complaints of neuromuscular problems, cognitive dysfunction, and mood and psychiatric issues. Breathing and heart rate problems also can arise. “There seems to be a preponderance of syndromes that reflect involvement of the nervous system,” said Dr. Spudich.
To try to understand the etiology of these persistent problems, Dr. Spudich said it’s important to examine the nervous system’s involvement in acute COVID-19. She has been involved in these efforts since early in the pandemic, when she ran an inpatient consult service at Yale dedicated to neurologic effects of acute COVID-19. She witnessed complications including stroke, encephalopathy, and seizures, among others.
Stroke during acute COVID-19 seemed to be associated with inflammation and endothelial activation or endotheliopathy. SARS-CoV-2 has been undetectable in the cerebrospinal fluid (CSF) of patients with acute COVID-19 and neurologic symptoms, but inflammatory cytokines can be present along with increased frequency of B cells. Anti–SARS-CoV-2 antibodies have also been found in CSF, some of which were auto reactive to brain tissue. The immune response was altered, compared with healthy controls, and in the CNS, compared with in the blood, “raising the question of whether inflammation and autoimmunity may be underlying causes of these syndromes,” said Dr. Spudich.
She also pointed to an MRI study of autopsied brain tissue of patients with COVID-19 and neurologic complications, which showed indications of both hemorrhagic and ischemic microvascular injury. “It’s just a reminder that, during acute COVID-19, there may be inflammation in the brain, there may be autoimmune reactions, and there may be vascular changes that underlie some of the neurologic syndromes that are seen,” said Dr. Spudich.
A panoply of different syndromes
In October, Yale set up a post-COVID neurologic clinic that brought together pulmonary, cardiology, and psychiatric specialists, many of whom saw the same patients, about 60% of whom had cognitive impairment, more than 40% had neuromuscular problems, and over 30% headache. “There’s not a single entity of a post-COVID neurologic syndrome. There’s a panoply of different syndromes that may have similar or distinct etiologies,” said Dr. Spudich.
Most patients were in their 30s, 40s, or 50s. That doesn’t necessarily mean this is the most common age range for these issues, though. There could be some bias if these individuals are seeking specialty care because they expected to recover from COVID-19 quickly. But it could be that there is something biologically unique among this age group that predisposes them to complications. Regardless, two out of three patients were never hospitalized, “suggesting that even mild COVID-19 can lead to some long-term sequelae,” said Dr. Spudich.
One potential explanation for long-term neurologic syndromes is that they are an extension of the inflammation, autoimmunity, and immune perturbation occurring during acute disease. One study looked at 18 cancer patients who had neurologic complications with COVID-19. Two months after onset, they had elevated markers of neuroinflammation and neuronal injury in the cerebral spinal fluid compared to cancer patients with no history of COVID-19.
Looking for biologic markers
An Italian study looked at patients who were evaluated during acute hospitalization and again 3 months later, and found that some markers of inflation in the blood were associated with later cognitive impairment. The patients were more severely ill, so it’s not clear what the findings mean for patients who present with neurologic symptoms after milder illness.
A PET scan study of 35 patients with persistent neurologic symptoms found patterns of reduced fluorodeoxyglucose uptake in some regions of the brain that are believed to be associated with some symptoms. Lower values were associated with greater severity for symptoms like memory dysfunction, and anosmia. “Why there might be hypometabolism in these regions I think needs to be assessed and used as a biomarker to associate hypometabolism with other kinds of processes in blood and spinal fluid,” said Dr. Spudich.
Along with colleagues at Yale, Dr. Spudich is conducting the MIND study, which is using PET and MRI imaging along with blood and CSF biomarkers to track the progress of patients after COVID-19. There are few results to discuss since only 20 patients have been recruited so far, except that brain imaging and blood values are generally normal despite neurologic complaints. Most were not hospitalized for COVID-19. Dr. Spudich highlighted one man in his 30s who developed new-onset psychosis, despite no previous history. Although clinical tests were all negative, a novel autoantibody detection method revealed a previously unknown autoreactive antibody in his spinal fluid. “This may suggest that there is autoantibody production in some individuals with post–COVID-19 psychosis, and potentially other syndromes,” said Dr. Spudich.
The research task ahead
The case illustrates the task ahead for neurology. “There’s a real research mandate to understand the biological substrates of these diverse disorders, not only to address the emergent public health concern and reduce the stigma in our patients, but to develop targeted therapeutic interventions,” said Dr. Spudich.
Anna Cervantes-Arslanian, MD, an associate professor of neurology at Boston University who also treats and studies patients with post-COVID neurologic symptoms, agreed with that assessment. “It’s not like every patient that has muscle aches and fatigue also has brain fog. It’s really hard to parse them out into specific phenotypes that are pretty classic. Some people will have all of those things, some will have very few of them,” said Dr. Cervantes-Arslanian. “We need to be able to identify them sand see if there is clustering of symptoms so we can better look into what the biological underpinnings are. That’s the first step to thinking about a therapeutic target.”
Dr. Spudich and Dr. Cervantes-Arslanian had no relevant financial disclosures.
Long-haul neurologic symptoms of COVID-19 seem to be distinct from neurologic conditions found in acute disease. Much work remains to be done to understand the biological mechanisms behind these problems, but inflammation and autoimmune responses may play a role in some cases.
Those were some of the takeaways from a talk by Serena Spudich, MD, who presented her research at the 2021 annual meeting of the American Academy of Neurology. Dr. Spudich is the division chief of neurologic infections and global neurology and codirector of the Center for Neuroepidemiology and Clinical Neurological Research at Yale University, New Haven, Conn.
Examining the nervous system’s involvement in COVID-19
Even early on in the pandemic, it became clear that there were lingering complaints of neuromuscular problems, cognitive dysfunction, and mood and psychiatric issues. Breathing and heart rate problems also can arise. “There seems to be a preponderance of syndromes that reflect involvement of the nervous system,” said Dr. Spudich.
To try to understand the etiology of these persistent problems, Dr. Spudich said it’s important to examine the nervous system’s involvement in acute COVID-19. She has been involved in these efforts since early in the pandemic, when she ran an inpatient consult service at Yale dedicated to neurologic effects of acute COVID-19. She witnessed complications including stroke, encephalopathy, and seizures, among others.
Stroke during acute COVID-19 seemed to be associated with inflammation and endothelial activation or endotheliopathy. SARS-CoV-2 has been undetectable in the cerebrospinal fluid (CSF) of patients with acute COVID-19 and neurologic symptoms, but inflammatory cytokines can be present along with increased frequency of B cells. Anti–SARS-CoV-2 antibodies have also been found in CSF, some of which were auto reactive to brain tissue. The immune response was altered, compared with healthy controls, and in the CNS, compared with in the blood, “raising the question of whether inflammation and autoimmunity may be underlying causes of these syndromes,” said Dr. Spudich.
She also pointed to an MRI study of autopsied brain tissue of patients with COVID-19 and neurologic complications, which showed indications of both hemorrhagic and ischemic microvascular injury. “It’s just a reminder that, during acute COVID-19, there may be inflammation in the brain, there may be autoimmune reactions, and there may be vascular changes that underlie some of the neurologic syndromes that are seen,” said Dr. Spudich.
A panoply of different syndromes
In October, Yale set up a post-COVID neurologic clinic that brought together pulmonary, cardiology, and psychiatric specialists, many of whom saw the same patients, about 60% of whom had cognitive impairment, more than 40% had neuromuscular problems, and over 30% headache. “There’s not a single entity of a post-COVID neurologic syndrome. There’s a panoply of different syndromes that may have similar or distinct etiologies,” said Dr. Spudich.
Most patients were in their 30s, 40s, or 50s. That doesn’t necessarily mean this is the most common age range for these issues, though. There could be some bias if these individuals are seeking specialty care because they expected to recover from COVID-19 quickly. But it could be that there is something biologically unique among this age group that predisposes them to complications. Regardless, two out of three patients were never hospitalized, “suggesting that even mild COVID-19 can lead to some long-term sequelae,” said Dr. Spudich.
One potential explanation for long-term neurologic syndromes is that they are an extension of the inflammation, autoimmunity, and immune perturbation occurring during acute disease. One study looked at 18 cancer patients who had neurologic complications with COVID-19. Two months after onset, they had elevated markers of neuroinflammation and neuronal injury in the cerebral spinal fluid compared to cancer patients with no history of COVID-19.
Looking for biologic markers
An Italian study looked at patients who were evaluated during acute hospitalization and again 3 months later, and found that some markers of inflation in the blood were associated with later cognitive impairment. The patients were more severely ill, so it’s not clear what the findings mean for patients who present with neurologic symptoms after milder illness.
A PET scan study of 35 patients with persistent neurologic symptoms found patterns of reduced fluorodeoxyglucose uptake in some regions of the brain that are believed to be associated with some symptoms. Lower values were associated with greater severity for symptoms like memory dysfunction, and anosmia. “Why there might be hypometabolism in these regions I think needs to be assessed and used as a biomarker to associate hypometabolism with other kinds of processes in blood and spinal fluid,” said Dr. Spudich.
Along with colleagues at Yale, Dr. Spudich is conducting the MIND study, which is using PET and MRI imaging along with blood and CSF biomarkers to track the progress of patients after COVID-19. There are few results to discuss since only 20 patients have been recruited so far, except that brain imaging and blood values are generally normal despite neurologic complaints. Most were not hospitalized for COVID-19. Dr. Spudich highlighted one man in his 30s who developed new-onset psychosis, despite no previous history. Although clinical tests were all negative, a novel autoantibody detection method revealed a previously unknown autoreactive antibody in his spinal fluid. “This may suggest that there is autoantibody production in some individuals with post–COVID-19 psychosis, and potentially other syndromes,” said Dr. Spudich.
The research task ahead
The case illustrates the task ahead for neurology. “There’s a real research mandate to understand the biological substrates of these diverse disorders, not only to address the emergent public health concern and reduce the stigma in our patients, but to develop targeted therapeutic interventions,” said Dr. Spudich.
Anna Cervantes-Arslanian, MD, an associate professor of neurology at Boston University who also treats and studies patients with post-COVID neurologic symptoms, agreed with that assessment. “It’s not like every patient that has muscle aches and fatigue also has brain fog. It’s really hard to parse them out into specific phenotypes that are pretty classic. Some people will have all of those things, some will have very few of them,” said Dr. Cervantes-Arslanian. “We need to be able to identify them sand see if there is clustering of symptoms so we can better look into what the biological underpinnings are. That’s the first step to thinking about a therapeutic target.”
Dr. Spudich and Dr. Cervantes-Arslanian had no relevant financial disclosures.
FROM AAN 2021
Boosting the presence of darker skin in rheumatology education
Studies are flagging racial and ethnic disparities in rheumatology training materials, pointing to a need to boost representation of darker skin tones and better educate physicians in evaluating this cohort.
Not enough is known about these disparities in rheumatology education, despite the fact that minorities make up 40% of the population in the United States.
The problem starts with books and references used in medical schools, Lynn McKinley-Grant, MD, immediate past president of the Skin of Color Society and associate professor of dermatology at Howard University, Washington, said in an interview. “In the medical literature there has been a dearth of images in skin of color in all specialties,” she said. With an increased diversity in the U.S. population, there is a need for health care providers to be able to recognize disease patterns in all skin types.” If a physician is training at an institution where there are not many patients of color in the community, the rheumatologists are even more limited in terms of their clinical experience.
This lack of training in diagnosis of disease has serious clinical repercussions, as seen in COVID cases, Dr. McKinley-Grant noted. “You end up not being able to recognize early erythema, jaundice, anemia, or hypoxemia because those conditions are a different color or pattern in the darker skin types. This can lead to errors in treatment, diagnosis, and medical care, resulting in increased morbidity and mortality.”
Studies point to education gaps
A team of researchers from Washington University in St. Louis called attention to this issue at the American College of Rhematology’s Convergence 2020 conference.
“Patients of color with lupus are especially vulnerable as they often carry a greater disease burden, yet studies show that individuals with darker skin tones are underrepresented in medical educational materials,” Vijay Kannuthurai, MD, and colleagues wrote in their study abstract. The team surveyed 132 providers in St. Louis, Mo., on their confidence in evaluating any rash, and rashes in patients with lupus and varied skin tones.
Participating clinicians, mostly rheumatologists, dermatologists, or internists, had a higher confidence level in diagnosing any rash versus lupus rashes, but were considerably less confident in diagnosing lupus rash on darker skin, compared with those on fair skin. This represents “a disparity between provider confidence and the patient population lupus traditionally affects,” the investigators concluded.
Another recent study found evidence of disparities in clinical education resources. “The lack of dark skin representation among rheumatology educational materials contributes to the implicit bias and structural racism present in medical education by promoting White-only models of disease,” lead author Adrienne Strait, a medical student at the University of California, San Francisco, said in an interview. “Given that rheumatic diseases disproportionately impact racial and ethnic minorities, we felt it was important to examine the representation of these groups within rheumatology training resources.”
She and her colleagues gathered images of rheumatic diseases from four major databases: the American College of Rheumatology’s Image Library, UpToDate, the New England Journal of Medicine Images in Clinical Medicine and Clinical Cases filtered by “Rheumatology,” and the 9th edition of Kelley’s Textbook of Rheumatology. They used Fitzpatrick’s skin phototypes to independently code images depicting skin as “light” (skin types I-IV), “dark” (skin types V-VI), or “indeterminate,” focusing on systemic lupus erythematosus (SLE) and rheumatoid arthritis, two conditions with a known connection to racial and ethnic health disparities.
Taking into account the high incidence of sarcoidosis and SLE in Black patients when compared with White patients, the investigators did a secondary analysis that excluded these cases.
Among 1,043 patient images studied, just 13.4% represented dark skin, compared with 84% that represented light skin. More than 2% represented an indeterminate skin color. Comparing dark-skin representation in the clinical images and SLE images with the representation of Asian, Native American, and Black individuals in the United States and within lupus cases nationally, the investigators found significant underrepresentation of dark skin.
Only 4.2% of RA images had dark-skin representation, making RA one of the diseases with the lowest representation in the study, along with juvenile idiopathic arthritis, the spondyloarthropathies, and Kawasaki disease. “Representation of dark skin in SLE was also lower than the proportion of Black individuals in SLE studies,” the investigators noted. Overall, representation of dark skin in SLE images was just 22.6%. Sarcoidosis comparatively had the largest representation of dark-skin images (69.6%, n = 32).
“Excluding sarcoidosis and SLE images, the overall representation of dark skin was 9.4% (n = 84), which was significantly lower than the proportion of Asian, Native American, and Black individuals within the U.S. Census population,” according to Ms. Strait and her associates. UpToDate contained the largest proportion of images of dark skin respective to other databases, whereas Kelley’s Textbook had the smallest.
Actionable steps
Many physicians are willing to improve upon their skills in identifying conditions on darker skin, as the study by Dr. Kannuthurai and associates suggests. Overall, 93% of the survey’s participants wanted to learn more about rashes in patients of color. “Future educational interventions may help practitioners improve their confidence when diagnosing rashes in lupus patients” with darker skin, they suggested.
Ms. Strait and her colleagues recommended a series of actionable steps to improve diversity and equity of dark skin tone representation in rheumatology curricula.
Editors of educational resources, for example, should make image diversity a priority for those diseases that are most commonly associated with cutaneous manifestations, such as SLE, vasculitis, inflammatory myopathies, systemic sclerosis, sarcoidosis, and psoriasis. They also called for educators in academic rheumatology programs to collaborate to improve diversity in resources used at the undergraduate and graduate medical education level.
Efforts should take place at the local, regional, and national level to publicly discuss and educate clinicians about rheumatic diseases in individuals of color. Speakers at rheumatology conferences should strive to educate learners about presentations of rheumatic diseases in individuals of color. The ACR in the meantime could establish a task force to enhance racial and ethnic diversity in their image library and other published resources.
“These steps may improve provider recognition and diagnosis of rheumatic disease manifestations in skin of color, which may in turn reduce health disparities among racial and ethnic minority groups,” Ms. Strait said.
Beth L. Jonas, MD, chair of the ACR’s Committee on Rheumatology Training and Workforce Issues, called the findings of this study “timely and important.” The researchers highlighted a deficiency in rheumatology training materials that needs addressing, she said in an interview. “I definitely agree that ACR needs to be mindful of this. There’s no doubt that we need to take these recommendations and move along these lines.”
The ACR took a first step in 2020 with the creation of a diversity, equity, and inclusion committee. “We are undergoing a college-wide look at what we do, with an eye toward inclusion. There is a strong interest in addressing health disparities and being an equitable and inclusive community of rheumatology health care professionals,” said Dr. Jonas, chief of the University of North Carolina at Chapel Hill’s division of rheumatology, allergy, and immunology.
The American Academy of Dermatology is also working to improve the image library with images of disease in skin of color. “Everyone’s jumping on this now,” Dr. McKinley-Grant observed. The medical profession can’t afford not to. It’s a life-threatening issue when rheumatoid arthritis and other diseases in people of color aren’t diagnosed early and correctly, she added.
Technologies seek to reduce bias
While many organizations are taking steps to improve representation of darker skin images, VisualDx has taken the lead on this, she said. “They’ve been doing this for years now. There are over 14,000 images of disease in skin of color, including all the rheumatologic diseases. There’s a mobile app and desktop decision support system, and it is very popular. A majority of medical schools have this as a library resource, and hospital systems license it for EHR integration.” Doctors can also get it individually. This enables them to share images and handouts of a diagnosis and select images of patients of color, said Dr. McKinley-Grant, who uses the VisualDx smartphone app DermExpert, which is an app for nondermatologists that features an image library of skin lesions, including darker-skin images.
ProjectIMPACT, powered by VisualDx, is another effort to support reducing health care bias in darker skin. The project is a collaboration between the New England Journal of Medicine Group and the Skin Of Color Society. According to Dr. McKinley-Grant, the organizers are building awareness of the importance of reducing the educational and clinical gaps in diagnosing patients of color and trying to get students and educators to pledge to take meaningful steps and to have real-world impact.
This isn’t just exclusive to dermatology and rheumatology – it involves all medical specialties, she stressed.
ProjectIMPACT isn’t just a resource for physicians, she continued. Librarians can also use it to develop more resources on skin of color.
The Skin Of Color Society and VisualDx have also partnered with the NEJM Group to develop a comprehensive virtual series on the impact of skin color and ethnicity on clinical research. The four-part series addresses structural racism and racial bias in medicine, hair disorders in people of color, pigmentary disorders, keloids, COVID-19 comorbidities, and cutaneous manifestations of systemic diseases in children and adults.
Nuances of recognizing disease
As a medical student, Dr. McKinley-Grant said she was fortunate to attend the Albert Schweitzer Hospital in Lambarene, Gabon, on a fellowship. For 3 months, she gained a wealth of experience examining only African patients with brown skin.
In her other training in medicine, “I’ve been at institutions with diverse populations, in Boston, New York, and Washington,” learning more about all different skin pigments.
This type of training should be more widely available, especially now, with COVID-19 producing new manifestations of skin lesions, she emphasized. Such efforts involve a diversification of images physicians are being trained on so that they can recognize the same disease in a person of color.
“Doctors have to be able to recognize different colors, different shades of brown and shades of white. Not all white skin is the same color,” she noted. In looking at a rash or lesion, “you have to learn how to discern differences in the background color of the skin, which is determined by melanin in the skin (Fitzpatrick skin types I-VI) and by what’s going on in the blood, such as how much oxygen and hemoglobin the patient has in their blood.” Inflammation and infection (erythema) will appear more violaceous in IV-VI skin types, for example.
At the University of North Carolina at Chapel Hill, a group of students and faculty have created a dermatology image library to address the deficiency in the availability of images for teaching purposes. “Our medical students recognized the gap and started this,” Dr. Jonas said. Julie Mervak, MD, assistant professor of dermatology, is spearheading this effort, with students Linnea Westerkam and Anuj Pranav Sanghvi.
“I understand that others around the country are working on similar initiatives,” Dr. Jonas said.
None of the sources for this story had any relevant disclosures.
Studies are flagging racial and ethnic disparities in rheumatology training materials, pointing to a need to boost representation of darker skin tones and better educate physicians in evaluating this cohort.
Not enough is known about these disparities in rheumatology education, despite the fact that minorities make up 40% of the population in the United States.
The problem starts with books and references used in medical schools, Lynn McKinley-Grant, MD, immediate past president of the Skin of Color Society and associate professor of dermatology at Howard University, Washington, said in an interview. “In the medical literature there has been a dearth of images in skin of color in all specialties,” she said. With an increased diversity in the U.S. population, there is a need for health care providers to be able to recognize disease patterns in all skin types.” If a physician is training at an institution where there are not many patients of color in the community, the rheumatologists are even more limited in terms of their clinical experience.
This lack of training in diagnosis of disease has serious clinical repercussions, as seen in COVID cases, Dr. McKinley-Grant noted. “You end up not being able to recognize early erythema, jaundice, anemia, or hypoxemia because those conditions are a different color or pattern in the darker skin types. This can lead to errors in treatment, diagnosis, and medical care, resulting in increased morbidity and mortality.”
Studies point to education gaps
A team of researchers from Washington University in St. Louis called attention to this issue at the American College of Rhematology’s Convergence 2020 conference.
“Patients of color with lupus are especially vulnerable as they often carry a greater disease burden, yet studies show that individuals with darker skin tones are underrepresented in medical educational materials,” Vijay Kannuthurai, MD, and colleagues wrote in their study abstract. The team surveyed 132 providers in St. Louis, Mo., on their confidence in evaluating any rash, and rashes in patients with lupus and varied skin tones.
Participating clinicians, mostly rheumatologists, dermatologists, or internists, had a higher confidence level in diagnosing any rash versus lupus rashes, but were considerably less confident in diagnosing lupus rash on darker skin, compared with those on fair skin. This represents “a disparity between provider confidence and the patient population lupus traditionally affects,” the investigators concluded.
Another recent study found evidence of disparities in clinical education resources. “The lack of dark skin representation among rheumatology educational materials contributes to the implicit bias and structural racism present in medical education by promoting White-only models of disease,” lead author Adrienne Strait, a medical student at the University of California, San Francisco, said in an interview. “Given that rheumatic diseases disproportionately impact racial and ethnic minorities, we felt it was important to examine the representation of these groups within rheumatology training resources.”
She and her colleagues gathered images of rheumatic diseases from four major databases: the American College of Rheumatology’s Image Library, UpToDate, the New England Journal of Medicine Images in Clinical Medicine and Clinical Cases filtered by “Rheumatology,” and the 9th edition of Kelley’s Textbook of Rheumatology. They used Fitzpatrick’s skin phototypes to independently code images depicting skin as “light” (skin types I-IV), “dark” (skin types V-VI), or “indeterminate,” focusing on systemic lupus erythematosus (SLE) and rheumatoid arthritis, two conditions with a known connection to racial and ethnic health disparities.
Taking into account the high incidence of sarcoidosis and SLE in Black patients when compared with White patients, the investigators did a secondary analysis that excluded these cases.
Among 1,043 patient images studied, just 13.4% represented dark skin, compared with 84% that represented light skin. More than 2% represented an indeterminate skin color. Comparing dark-skin representation in the clinical images and SLE images with the representation of Asian, Native American, and Black individuals in the United States and within lupus cases nationally, the investigators found significant underrepresentation of dark skin.
Only 4.2% of RA images had dark-skin representation, making RA one of the diseases with the lowest representation in the study, along with juvenile idiopathic arthritis, the spondyloarthropathies, and Kawasaki disease. “Representation of dark skin in SLE was also lower than the proportion of Black individuals in SLE studies,” the investigators noted. Overall, representation of dark skin in SLE images was just 22.6%. Sarcoidosis comparatively had the largest representation of dark-skin images (69.6%, n = 32).
“Excluding sarcoidosis and SLE images, the overall representation of dark skin was 9.4% (n = 84), which was significantly lower than the proportion of Asian, Native American, and Black individuals within the U.S. Census population,” according to Ms. Strait and her associates. UpToDate contained the largest proportion of images of dark skin respective to other databases, whereas Kelley’s Textbook had the smallest.
Actionable steps
Many physicians are willing to improve upon their skills in identifying conditions on darker skin, as the study by Dr. Kannuthurai and associates suggests. Overall, 93% of the survey’s participants wanted to learn more about rashes in patients of color. “Future educational interventions may help practitioners improve their confidence when diagnosing rashes in lupus patients” with darker skin, they suggested.
Ms. Strait and her colleagues recommended a series of actionable steps to improve diversity and equity of dark skin tone representation in rheumatology curricula.
Editors of educational resources, for example, should make image diversity a priority for those diseases that are most commonly associated with cutaneous manifestations, such as SLE, vasculitis, inflammatory myopathies, systemic sclerosis, sarcoidosis, and psoriasis. They also called for educators in academic rheumatology programs to collaborate to improve diversity in resources used at the undergraduate and graduate medical education level.
Efforts should take place at the local, regional, and national level to publicly discuss and educate clinicians about rheumatic diseases in individuals of color. Speakers at rheumatology conferences should strive to educate learners about presentations of rheumatic diseases in individuals of color. The ACR in the meantime could establish a task force to enhance racial and ethnic diversity in their image library and other published resources.
“These steps may improve provider recognition and diagnosis of rheumatic disease manifestations in skin of color, which may in turn reduce health disparities among racial and ethnic minority groups,” Ms. Strait said.
Beth L. Jonas, MD, chair of the ACR’s Committee on Rheumatology Training and Workforce Issues, called the findings of this study “timely and important.” The researchers highlighted a deficiency in rheumatology training materials that needs addressing, she said in an interview. “I definitely agree that ACR needs to be mindful of this. There’s no doubt that we need to take these recommendations and move along these lines.”
The ACR took a first step in 2020 with the creation of a diversity, equity, and inclusion committee. “We are undergoing a college-wide look at what we do, with an eye toward inclusion. There is a strong interest in addressing health disparities and being an equitable and inclusive community of rheumatology health care professionals,” said Dr. Jonas, chief of the University of North Carolina at Chapel Hill’s division of rheumatology, allergy, and immunology.
The American Academy of Dermatology is also working to improve the image library with images of disease in skin of color. “Everyone’s jumping on this now,” Dr. McKinley-Grant observed. The medical profession can’t afford not to. It’s a life-threatening issue when rheumatoid arthritis and other diseases in people of color aren’t diagnosed early and correctly, she added.
Technologies seek to reduce bias
While many organizations are taking steps to improve representation of darker skin images, VisualDx has taken the lead on this, she said. “They’ve been doing this for years now. There are over 14,000 images of disease in skin of color, including all the rheumatologic diseases. There’s a mobile app and desktop decision support system, and it is very popular. A majority of medical schools have this as a library resource, and hospital systems license it for EHR integration.” Doctors can also get it individually. This enables them to share images and handouts of a diagnosis and select images of patients of color, said Dr. McKinley-Grant, who uses the VisualDx smartphone app DermExpert, which is an app for nondermatologists that features an image library of skin lesions, including darker-skin images.
ProjectIMPACT, powered by VisualDx, is another effort to support reducing health care bias in darker skin. The project is a collaboration between the New England Journal of Medicine Group and the Skin Of Color Society. According to Dr. McKinley-Grant, the organizers are building awareness of the importance of reducing the educational and clinical gaps in diagnosing patients of color and trying to get students and educators to pledge to take meaningful steps and to have real-world impact.
This isn’t just exclusive to dermatology and rheumatology – it involves all medical specialties, she stressed.
ProjectIMPACT isn’t just a resource for physicians, she continued. Librarians can also use it to develop more resources on skin of color.
The Skin Of Color Society and VisualDx have also partnered with the NEJM Group to develop a comprehensive virtual series on the impact of skin color and ethnicity on clinical research. The four-part series addresses structural racism and racial bias in medicine, hair disorders in people of color, pigmentary disorders, keloids, COVID-19 comorbidities, and cutaneous manifestations of systemic diseases in children and adults.
Nuances of recognizing disease
As a medical student, Dr. McKinley-Grant said she was fortunate to attend the Albert Schweitzer Hospital in Lambarene, Gabon, on a fellowship. For 3 months, she gained a wealth of experience examining only African patients with brown skin.
In her other training in medicine, “I’ve been at institutions with diverse populations, in Boston, New York, and Washington,” learning more about all different skin pigments.
This type of training should be more widely available, especially now, with COVID-19 producing new manifestations of skin lesions, she emphasized. Such efforts involve a diversification of images physicians are being trained on so that they can recognize the same disease in a person of color.
“Doctors have to be able to recognize different colors, different shades of brown and shades of white. Not all white skin is the same color,” she noted. In looking at a rash or lesion, “you have to learn how to discern differences in the background color of the skin, which is determined by melanin in the skin (Fitzpatrick skin types I-VI) and by what’s going on in the blood, such as how much oxygen and hemoglobin the patient has in their blood.” Inflammation and infection (erythema) will appear more violaceous in IV-VI skin types, for example.
At the University of North Carolina at Chapel Hill, a group of students and faculty have created a dermatology image library to address the deficiency in the availability of images for teaching purposes. “Our medical students recognized the gap and started this,” Dr. Jonas said. Julie Mervak, MD, assistant professor of dermatology, is spearheading this effort, with students Linnea Westerkam and Anuj Pranav Sanghvi.
“I understand that others around the country are working on similar initiatives,” Dr. Jonas said.
None of the sources for this story had any relevant disclosures.
Studies are flagging racial and ethnic disparities in rheumatology training materials, pointing to a need to boost representation of darker skin tones and better educate physicians in evaluating this cohort.
Not enough is known about these disparities in rheumatology education, despite the fact that minorities make up 40% of the population in the United States.
The problem starts with books and references used in medical schools, Lynn McKinley-Grant, MD, immediate past president of the Skin of Color Society and associate professor of dermatology at Howard University, Washington, said in an interview. “In the medical literature there has been a dearth of images in skin of color in all specialties,” she said. With an increased diversity in the U.S. population, there is a need for health care providers to be able to recognize disease patterns in all skin types.” If a physician is training at an institution where there are not many patients of color in the community, the rheumatologists are even more limited in terms of their clinical experience.
This lack of training in diagnosis of disease has serious clinical repercussions, as seen in COVID cases, Dr. McKinley-Grant noted. “You end up not being able to recognize early erythema, jaundice, anemia, or hypoxemia because those conditions are a different color or pattern in the darker skin types. This can lead to errors in treatment, diagnosis, and medical care, resulting in increased morbidity and mortality.”
Studies point to education gaps
A team of researchers from Washington University in St. Louis called attention to this issue at the American College of Rhematology’s Convergence 2020 conference.
“Patients of color with lupus are especially vulnerable as they often carry a greater disease burden, yet studies show that individuals with darker skin tones are underrepresented in medical educational materials,” Vijay Kannuthurai, MD, and colleagues wrote in their study abstract. The team surveyed 132 providers in St. Louis, Mo., on their confidence in evaluating any rash, and rashes in patients with lupus and varied skin tones.
Participating clinicians, mostly rheumatologists, dermatologists, or internists, had a higher confidence level in diagnosing any rash versus lupus rashes, but were considerably less confident in diagnosing lupus rash on darker skin, compared with those on fair skin. This represents “a disparity between provider confidence and the patient population lupus traditionally affects,” the investigators concluded.
Another recent study found evidence of disparities in clinical education resources. “The lack of dark skin representation among rheumatology educational materials contributes to the implicit bias and structural racism present in medical education by promoting White-only models of disease,” lead author Adrienne Strait, a medical student at the University of California, San Francisco, said in an interview. “Given that rheumatic diseases disproportionately impact racial and ethnic minorities, we felt it was important to examine the representation of these groups within rheumatology training resources.”
She and her colleagues gathered images of rheumatic diseases from four major databases: the American College of Rheumatology’s Image Library, UpToDate, the New England Journal of Medicine Images in Clinical Medicine and Clinical Cases filtered by “Rheumatology,” and the 9th edition of Kelley’s Textbook of Rheumatology. They used Fitzpatrick’s skin phototypes to independently code images depicting skin as “light” (skin types I-IV), “dark” (skin types V-VI), or “indeterminate,” focusing on systemic lupus erythematosus (SLE) and rheumatoid arthritis, two conditions with a known connection to racial and ethnic health disparities.
Taking into account the high incidence of sarcoidosis and SLE in Black patients when compared with White patients, the investigators did a secondary analysis that excluded these cases.
Among 1,043 patient images studied, just 13.4% represented dark skin, compared with 84% that represented light skin. More than 2% represented an indeterminate skin color. Comparing dark-skin representation in the clinical images and SLE images with the representation of Asian, Native American, and Black individuals in the United States and within lupus cases nationally, the investigators found significant underrepresentation of dark skin.
Only 4.2% of RA images had dark-skin representation, making RA one of the diseases with the lowest representation in the study, along with juvenile idiopathic arthritis, the spondyloarthropathies, and Kawasaki disease. “Representation of dark skin in SLE was also lower than the proportion of Black individuals in SLE studies,” the investigators noted. Overall, representation of dark skin in SLE images was just 22.6%. Sarcoidosis comparatively had the largest representation of dark-skin images (69.6%, n = 32).
“Excluding sarcoidosis and SLE images, the overall representation of dark skin was 9.4% (n = 84), which was significantly lower than the proportion of Asian, Native American, and Black individuals within the U.S. Census population,” according to Ms. Strait and her associates. UpToDate contained the largest proportion of images of dark skin respective to other databases, whereas Kelley’s Textbook had the smallest.
Actionable steps
Many physicians are willing to improve upon their skills in identifying conditions on darker skin, as the study by Dr. Kannuthurai and associates suggests. Overall, 93% of the survey’s participants wanted to learn more about rashes in patients of color. “Future educational interventions may help practitioners improve their confidence when diagnosing rashes in lupus patients” with darker skin, they suggested.
Ms. Strait and her colleagues recommended a series of actionable steps to improve diversity and equity of dark skin tone representation in rheumatology curricula.
Editors of educational resources, for example, should make image diversity a priority for those diseases that are most commonly associated with cutaneous manifestations, such as SLE, vasculitis, inflammatory myopathies, systemic sclerosis, sarcoidosis, and psoriasis. They also called for educators in academic rheumatology programs to collaborate to improve diversity in resources used at the undergraduate and graduate medical education level.
Efforts should take place at the local, regional, and national level to publicly discuss and educate clinicians about rheumatic diseases in individuals of color. Speakers at rheumatology conferences should strive to educate learners about presentations of rheumatic diseases in individuals of color. The ACR in the meantime could establish a task force to enhance racial and ethnic diversity in their image library and other published resources.
“These steps may improve provider recognition and diagnosis of rheumatic disease manifestations in skin of color, which may in turn reduce health disparities among racial and ethnic minority groups,” Ms. Strait said.
Beth L. Jonas, MD, chair of the ACR’s Committee on Rheumatology Training and Workforce Issues, called the findings of this study “timely and important.” The researchers highlighted a deficiency in rheumatology training materials that needs addressing, she said in an interview. “I definitely agree that ACR needs to be mindful of this. There’s no doubt that we need to take these recommendations and move along these lines.”
The ACR took a first step in 2020 with the creation of a diversity, equity, and inclusion committee. “We are undergoing a college-wide look at what we do, with an eye toward inclusion. There is a strong interest in addressing health disparities and being an equitable and inclusive community of rheumatology health care professionals,” said Dr. Jonas, chief of the University of North Carolina at Chapel Hill’s division of rheumatology, allergy, and immunology.
The American Academy of Dermatology is also working to improve the image library with images of disease in skin of color. “Everyone’s jumping on this now,” Dr. McKinley-Grant observed. The medical profession can’t afford not to. It’s a life-threatening issue when rheumatoid arthritis and other diseases in people of color aren’t diagnosed early and correctly, she added.
Technologies seek to reduce bias
While many organizations are taking steps to improve representation of darker skin images, VisualDx has taken the lead on this, she said. “They’ve been doing this for years now. There are over 14,000 images of disease in skin of color, including all the rheumatologic diseases. There’s a mobile app and desktop decision support system, and it is very popular. A majority of medical schools have this as a library resource, and hospital systems license it for EHR integration.” Doctors can also get it individually. This enables them to share images and handouts of a diagnosis and select images of patients of color, said Dr. McKinley-Grant, who uses the VisualDx smartphone app DermExpert, which is an app for nondermatologists that features an image library of skin lesions, including darker-skin images.
ProjectIMPACT, powered by VisualDx, is another effort to support reducing health care bias in darker skin. The project is a collaboration between the New England Journal of Medicine Group and the Skin Of Color Society. According to Dr. McKinley-Grant, the organizers are building awareness of the importance of reducing the educational and clinical gaps in diagnosing patients of color and trying to get students and educators to pledge to take meaningful steps and to have real-world impact.
This isn’t just exclusive to dermatology and rheumatology – it involves all medical specialties, she stressed.
ProjectIMPACT isn’t just a resource for physicians, she continued. Librarians can also use it to develop more resources on skin of color.
The Skin Of Color Society and VisualDx have also partnered with the NEJM Group to develop a comprehensive virtual series on the impact of skin color and ethnicity on clinical research. The four-part series addresses structural racism and racial bias in medicine, hair disorders in people of color, pigmentary disorders, keloids, COVID-19 comorbidities, and cutaneous manifestations of systemic diseases in children and adults.
Nuances of recognizing disease
As a medical student, Dr. McKinley-Grant said she was fortunate to attend the Albert Schweitzer Hospital in Lambarene, Gabon, on a fellowship. For 3 months, she gained a wealth of experience examining only African patients with brown skin.
In her other training in medicine, “I’ve been at institutions with diverse populations, in Boston, New York, and Washington,” learning more about all different skin pigments.
This type of training should be more widely available, especially now, with COVID-19 producing new manifestations of skin lesions, she emphasized. Such efforts involve a diversification of images physicians are being trained on so that they can recognize the same disease in a person of color.
“Doctors have to be able to recognize different colors, different shades of brown and shades of white. Not all white skin is the same color,” she noted. In looking at a rash or lesion, “you have to learn how to discern differences in the background color of the skin, which is determined by melanin in the skin (Fitzpatrick skin types I-VI) and by what’s going on in the blood, such as how much oxygen and hemoglobin the patient has in their blood.” Inflammation and infection (erythema) will appear more violaceous in IV-VI skin types, for example.
At the University of North Carolina at Chapel Hill, a group of students and faculty have created a dermatology image library to address the deficiency in the availability of images for teaching purposes. “Our medical students recognized the gap and started this,” Dr. Jonas said. Julie Mervak, MD, assistant professor of dermatology, is spearheading this effort, with students Linnea Westerkam and Anuj Pranav Sanghvi.
“I understand that others around the country are working on similar initiatives,” Dr. Jonas said.
None of the sources for this story had any relevant disclosures.
Early pediatric rheumatology residency exposure key to solving workforce shortages
The biggest factors that attract medical students to enter pediatric rheumatology are interest in disease pathology, the patient-physician relationship, and clinical exposure in residency, according to preliminary research shared at the annual scientific meeting of the Childhood Arthritis and Rheumatology Research Alliance.
A shortage in pediatric rheumatology already exists and is expected to worsen to 61% by 2030, noted the authors. About one-third (32%) of current pediatric rheumatologists will retire in the next decade, and less than two-thirds of fellowship slots have filled in the past 5 years.
Katherine Schultz, MD, a clinical fellow in the division of rheumatology at Cincinnati Children’s Medical Center, led the study and said she was surprised that medical school exposure did not play a bigger role in attracting people to the field, but perhaps that’s because too few people received that early exposure.
“If we had earlier exposure, maybe that wouldn’t be definitive for saying, ‘yes, I want to do this subspecialty of pediatric rheumatology,’ but it would open the door, so when you hit residency, you can explore it further,” Dr. Schultz said in an interview.
Dr. Schultz and her colleagues conducted a survey using the CARRA registry during September-December 2020. Respondents included pediatric rheumatology clinical fellows, early-career pediatric rheumatology faculty with less than 7 years practice experience, and mid- to late-career pediatric rheumatology faculty – those with more than 7 years of practice. They are currently in the process of analyzing additional qualitative data.
Of the 428 clinicians recruited to complete the study, 92 did so, for a response rate of 21%. Most respondents were female and non-Hispanic White. A total of 40% were clinical fellows, 41% were early-career faculty, and 18% were mid- to late-career faculty.
Positive factors for choosing the field
More than 80% of respondents across all three experience levels cited disease pathology as a positive attribute of pediatric rheumatology, something that Dr. Schultz mentioned as well.
“The rewarding part of pediatric rheumatology is we take these complex diseases and we help give kids their life back,” she said.
Nearly all the clinical fellows who responded said the patient-physician relationship was important, which early- and mid- and late-career faculty mentioned as well, although to a slightly lesser extent.
Other factors following closely behind disease pathology, patient-physician relationship, and clinical exposure in residency were having a role model in the field – cited by more than three-quarters of clinical fellows and early-career faculty – and having mentorship during residency.
“One of the strengths of our field and one of the things I love about pediatric rheumatology is our community is so close-knit, so kind, and so welcoming,” Dr. Schultz said. “If students can have that exposure and they can see the kind of people who are in this field, that’s our greatest power to draw people to our field.”
Low compensation is a deterrent
The least frequently mentioned positive factors were research opportunities and income. In fact, income was by far the most commonly cited negative attribute of pediatric rheumatology, reported by nearly half of clinical fellows and more than a quarter of early- and mid- and late-career faculty.
“We are one of the lowest paid specialties in pediatrics. We often make [income] comparable to or less than a general pediatrician,” Dr. Schultz said. One reason for that is the difficulty of doing pediatric rheumatology in private practice. Most positions are at academic institutions, which will nearly always involve lower pay scales, she said. The field is also not a procedure-based one, which makes billing more difficult to quantify.
“If I spend an hour thinking about a patient’s diagnosis and interpreting their labs, how do we quantify that?” she asked. “Our field is so cognitive that it makes it hard to bill in the same manner” as fields who bill more procedures, she said.
Colleen Correll, MD, MPH, an assistant professor of pediatric rheumatology at the University of Minnesota in Minneapolis, was also not surprised to see salary listed as the biggest deterrent to the field.
“Unfortunately, compared to other specialties, our compensation is lower, and this can be a real barrier for people who have large medical student loans to repay and for those providing for their families,” Dr. Correll said in an interview. She and Dr. Schultz both said that workforce advocacy groups are working on ways to compensate for that difference, including loan repayment programs.
The other specialties that respondents considered before choosing pediatric rheumatology varied by generation, but allergy and immunology and endocrinology were among the most cited by early-, mid-, and late-career faculty. Clinical fellows’ responses were more evenly distributed across a range of different subspecialties.
Early exposure is key
A large proportion of all three groups, including almost 90% of early-career faculty and clinical fellows, said they received exposure to pediatric rheumatology during residency. However, only a little more than two-thirds of clinical fellows had exposure to the field in medical school, and fewer than that reported medical school exposure among both faculty groups.
Both Dr. Correll and Dr. Schultz said that early exposure to pediatric rheumatology was key to bringing more people into the workforce.
“I believe that once a medical student or resident has an opportunity to work with a pediatric rheumatologist, they are able to see the many reasons for which this is a great career choice,” Dr. Correll said. “Pediatric rheumatologists are seen as positive role models. We love what we do, we have great patient-physician relationships, and we see interesting disease pathophysiology on a regular basis.”
Although earlier exposure to the field is primarily an institutional issue, clinicians can play a role as well.
“For the individual practitioners, the biggest way they can make an impact is to make themselves visible,” Dr. Schultz said. Although the subspecialty is stretched thin, she encouraged pediatric rheumatologists to do med school and resident lectures, volunteer to do feedback sessions, offer residents opportunities to rotate with them, and generally make themselves more visible. “It’s going to take the community to really make the change we need,” she said.
She and Dr. Correll both cited the American College of Rheumatology and CARRA pediatric residency programs as helpful, but there’s more to do. Other ways to increase exposure to the field include creating medical student rotations in pediatric rheumatology, working on case reports or small research projects with new learners, and requesting that pediatric rheumatology be a mandatory rotation in pediatrics training, Dr. Correll said.
“We absolutely have a responsibility to promote our field because if we don’t, the workforce supply issue will continue to worsen,” Dr. Correll said. “We already have a workforce shortage, and models show this shortage will only worsen if we don’t improve recruitment into the field, especially with many pediatric rheumatologists coming up on retirement. Once we are able to expose medical students and residents to the field, I think they easily see our passion and our love for the field, and it’s easy to recruit them.”
The research was funded by CARRA, which receives funding from the Arthritis Foundation. Dr. Schultz and Dr. Correll had no disclosures.
The biggest factors that attract medical students to enter pediatric rheumatology are interest in disease pathology, the patient-physician relationship, and clinical exposure in residency, according to preliminary research shared at the annual scientific meeting of the Childhood Arthritis and Rheumatology Research Alliance.
A shortage in pediatric rheumatology already exists and is expected to worsen to 61% by 2030, noted the authors. About one-third (32%) of current pediatric rheumatologists will retire in the next decade, and less than two-thirds of fellowship slots have filled in the past 5 years.
Katherine Schultz, MD, a clinical fellow in the division of rheumatology at Cincinnati Children’s Medical Center, led the study and said she was surprised that medical school exposure did not play a bigger role in attracting people to the field, but perhaps that’s because too few people received that early exposure.
“If we had earlier exposure, maybe that wouldn’t be definitive for saying, ‘yes, I want to do this subspecialty of pediatric rheumatology,’ but it would open the door, so when you hit residency, you can explore it further,” Dr. Schultz said in an interview.
Dr. Schultz and her colleagues conducted a survey using the CARRA registry during September-December 2020. Respondents included pediatric rheumatology clinical fellows, early-career pediatric rheumatology faculty with less than 7 years practice experience, and mid- to late-career pediatric rheumatology faculty – those with more than 7 years of practice. They are currently in the process of analyzing additional qualitative data.
Of the 428 clinicians recruited to complete the study, 92 did so, for a response rate of 21%. Most respondents were female and non-Hispanic White. A total of 40% were clinical fellows, 41% were early-career faculty, and 18% were mid- to late-career faculty.
Positive factors for choosing the field
More than 80% of respondents across all three experience levels cited disease pathology as a positive attribute of pediatric rheumatology, something that Dr. Schultz mentioned as well.
“The rewarding part of pediatric rheumatology is we take these complex diseases and we help give kids their life back,” she said.
Nearly all the clinical fellows who responded said the patient-physician relationship was important, which early- and mid- and late-career faculty mentioned as well, although to a slightly lesser extent.
Other factors following closely behind disease pathology, patient-physician relationship, and clinical exposure in residency were having a role model in the field – cited by more than three-quarters of clinical fellows and early-career faculty – and having mentorship during residency.
“One of the strengths of our field and one of the things I love about pediatric rheumatology is our community is so close-knit, so kind, and so welcoming,” Dr. Schultz said. “If students can have that exposure and they can see the kind of people who are in this field, that’s our greatest power to draw people to our field.”
Low compensation is a deterrent
The least frequently mentioned positive factors were research opportunities and income. In fact, income was by far the most commonly cited negative attribute of pediatric rheumatology, reported by nearly half of clinical fellows and more than a quarter of early- and mid- and late-career faculty.
“We are one of the lowest paid specialties in pediatrics. We often make [income] comparable to or less than a general pediatrician,” Dr. Schultz said. One reason for that is the difficulty of doing pediatric rheumatology in private practice. Most positions are at academic institutions, which will nearly always involve lower pay scales, she said. The field is also not a procedure-based one, which makes billing more difficult to quantify.
“If I spend an hour thinking about a patient’s diagnosis and interpreting their labs, how do we quantify that?” she asked. “Our field is so cognitive that it makes it hard to bill in the same manner” as fields who bill more procedures, she said.
Colleen Correll, MD, MPH, an assistant professor of pediatric rheumatology at the University of Minnesota in Minneapolis, was also not surprised to see salary listed as the biggest deterrent to the field.
“Unfortunately, compared to other specialties, our compensation is lower, and this can be a real barrier for people who have large medical student loans to repay and for those providing for their families,” Dr. Correll said in an interview. She and Dr. Schultz both said that workforce advocacy groups are working on ways to compensate for that difference, including loan repayment programs.
The other specialties that respondents considered before choosing pediatric rheumatology varied by generation, but allergy and immunology and endocrinology were among the most cited by early-, mid-, and late-career faculty. Clinical fellows’ responses were more evenly distributed across a range of different subspecialties.
Early exposure is key
A large proportion of all three groups, including almost 90% of early-career faculty and clinical fellows, said they received exposure to pediatric rheumatology during residency. However, only a little more than two-thirds of clinical fellows had exposure to the field in medical school, and fewer than that reported medical school exposure among both faculty groups.
Both Dr. Correll and Dr. Schultz said that early exposure to pediatric rheumatology was key to bringing more people into the workforce.
“I believe that once a medical student or resident has an opportunity to work with a pediatric rheumatologist, they are able to see the many reasons for which this is a great career choice,” Dr. Correll said. “Pediatric rheumatologists are seen as positive role models. We love what we do, we have great patient-physician relationships, and we see interesting disease pathophysiology on a regular basis.”
Although earlier exposure to the field is primarily an institutional issue, clinicians can play a role as well.
“For the individual practitioners, the biggest way they can make an impact is to make themselves visible,” Dr. Schultz said. Although the subspecialty is stretched thin, she encouraged pediatric rheumatologists to do med school and resident lectures, volunteer to do feedback sessions, offer residents opportunities to rotate with them, and generally make themselves more visible. “It’s going to take the community to really make the change we need,” she said.
She and Dr. Correll both cited the American College of Rheumatology and CARRA pediatric residency programs as helpful, but there’s more to do. Other ways to increase exposure to the field include creating medical student rotations in pediatric rheumatology, working on case reports or small research projects with new learners, and requesting that pediatric rheumatology be a mandatory rotation in pediatrics training, Dr. Correll said.
“We absolutely have a responsibility to promote our field because if we don’t, the workforce supply issue will continue to worsen,” Dr. Correll said. “We already have a workforce shortage, and models show this shortage will only worsen if we don’t improve recruitment into the field, especially with many pediatric rheumatologists coming up on retirement. Once we are able to expose medical students and residents to the field, I think they easily see our passion and our love for the field, and it’s easy to recruit them.”
The research was funded by CARRA, which receives funding from the Arthritis Foundation. Dr. Schultz and Dr. Correll had no disclosures.
The biggest factors that attract medical students to enter pediatric rheumatology are interest in disease pathology, the patient-physician relationship, and clinical exposure in residency, according to preliminary research shared at the annual scientific meeting of the Childhood Arthritis and Rheumatology Research Alliance.
A shortage in pediatric rheumatology already exists and is expected to worsen to 61% by 2030, noted the authors. About one-third (32%) of current pediatric rheumatologists will retire in the next decade, and less than two-thirds of fellowship slots have filled in the past 5 years.
Katherine Schultz, MD, a clinical fellow in the division of rheumatology at Cincinnati Children’s Medical Center, led the study and said she was surprised that medical school exposure did not play a bigger role in attracting people to the field, but perhaps that’s because too few people received that early exposure.
“If we had earlier exposure, maybe that wouldn’t be definitive for saying, ‘yes, I want to do this subspecialty of pediatric rheumatology,’ but it would open the door, so when you hit residency, you can explore it further,” Dr. Schultz said in an interview.
Dr. Schultz and her colleagues conducted a survey using the CARRA registry during September-December 2020. Respondents included pediatric rheumatology clinical fellows, early-career pediatric rheumatology faculty with less than 7 years practice experience, and mid- to late-career pediatric rheumatology faculty – those with more than 7 years of practice. They are currently in the process of analyzing additional qualitative data.
Of the 428 clinicians recruited to complete the study, 92 did so, for a response rate of 21%. Most respondents were female and non-Hispanic White. A total of 40% were clinical fellows, 41% were early-career faculty, and 18% were mid- to late-career faculty.
Positive factors for choosing the field
More than 80% of respondents across all three experience levels cited disease pathology as a positive attribute of pediatric rheumatology, something that Dr. Schultz mentioned as well.
“The rewarding part of pediatric rheumatology is we take these complex diseases and we help give kids their life back,” she said.
Nearly all the clinical fellows who responded said the patient-physician relationship was important, which early- and mid- and late-career faculty mentioned as well, although to a slightly lesser extent.
Other factors following closely behind disease pathology, patient-physician relationship, and clinical exposure in residency were having a role model in the field – cited by more than three-quarters of clinical fellows and early-career faculty – and having mentorship during residency.
“One of the strengths of our field and one of the things I love about pediatric rheumatology is our community is so close-knit, so kind, and so welcoming,” Dr. Schultz said. “If students can have that exposure and they can see the kind of people who are in this field, that’s our greatest power to draw people to our field.”
Low compensation is a deterrent
The least frequently mentioned positive factors were research opportunities and income. In fact, income was by far the most commonly cited negative attribute of pediatric rheumatology, reported by nearly half of clinical fellows and more than a quarter of early- and mid- and late-career faculty.
“We are one of the lowest paid specialties in pediatrics. We often make [income] comparable to or less than a general pediatrician,” Dr. Schultz said. One reason for that is the difficulty of doing pediatric rheumatology in private practice. Most positions are at academic institutions, which will nearly always involve lower pay scales, she said. The field is also not a procedure-based one, which makes billing more difficult to quantify.
“If I spend an hour thinking about a patient’s diagnosis and interpreting their labs, how do we quantify that?” she asked. “Our field is so cognitive that it makes it hard to bill in the same manner” as fields who bill more procedures, she said.
Colleen Correll, MD, MPH, an assistant professor of pediatric rheumatology at the University of Minnesota in Minneapolis, was also not surprised to see salary listed as the biggest deterrent to the field.
“Unfortunately, compared to other specialties, our compensation is lower, and this can be a real barrier for people who have large medical student loans to repay and for those providing for their families,” Dr. Correll said in an interview. She and Dr. Schultz both said that workforce advocacy groups are working on ways to compensate for that difference, including loan repayment programs.
The other specialties that respondents considered before choosing pediatric rheumatology varied by generation, but allergy and immunology and endocrinology were among the most cited by early-, mid-, and late-career faculty. Clinical fellows’ responses were more evenly distributed across a range of different subspecialties.
Early exposure is key
A large proportion of all three groups, including almost 90% of early-career faculty and clinical fellows, said they received exposure to pediatric rheumatology during residency. However, only a little more than two-thirds of clinical fellows had exposure to the field in medical school, and fewer than that reported medical school exposure among both faculty groups.
Both Dr. Correll and Dr. Schultz said that early exposure to pediatric rheumatology was key to bringing more people into the workforce.
“I believe that once a medical student or resident has an opportunity to work with a pediatric rheumatologist, they are able to see the many reasons for which this is a great career choice,” Dr. Correll said. “Pediatric rheumatologists are seen as positive role models. We love what we do, we have great patient-physician relationships, and we see interesting disease pathophysiology on a regular basis.”
Although earlier exposure to the field is primarily an institutional issue, clinicians can play a role as well.
“For the individual practitioners, the biggest way they can make an impact is to make themselves visible,” Dr. Schultz said. Although the subspecialty is stretched thin, she encouraged pediatric rheumatologists to do med school and resident lectures, volunteer to do feedback sessions, offer residents opportunities to rotate with them, and generally make themselves more visible. “It’s going to take the community to really make the change we need,” she said.
She and Dr. Correll both cited the American College of Rheumatology and CARRA pediatric residency programs as helpful, but there’s more to do. Other ways to increase exposure to the field include creating medical student rotations in pediatric rheumatology, working on case reports or small research projects with new learners, and requesting that pediatric rheumatology be a mandatory rotation in pediatrics training, Dr. Correll said.
“We absolutely have a responsibility to promote our field because if we don’t, the workforce supply issue will continue to worsen,” Dr. Correll said. “We already have a workforce shortage, and models show this shortage will only worsen if we don’t improve recruitment into the field, especially with many pediatric rheumatologists coming up on retirement. Once we are able to expose medical students and residents to the field, I think they easily see our passion and our love for the field, and it’s easy to recruit them.”
The research was funded by CARRA, which receives funding from the Arthritis Foundation. Dr. Schultz and Dr. Correll had no disclosures.
FROM CARRA 2021
Study shows how COVID-19 disrupted RA meds
During the first 3 months of the COVID-19 pandemic last year, about one-third of people with rheumatoid arthritis in the United States made changes in their RA medications, and, before the American College of Rheumatology tweaked its guidelines midway through that period, they were about twice as likely to make medication changes on their own than before the pandemic, according to an analysis of data in FORWARD, the National Databank for Rheumatic Diseases.
The study, published in Arthritis Care & Research, also found that about 10% of RA patients on hydroxychloroquine lost access to the drug at a time it was drawing interest as a treatment for COVID-19. Another finding was that a high percentage of patients on non–tumor necrosis factor biologic disease-modifying antirheumatic drugs (bDMARDs) and Janus kinase (JAK) inhibitors canceled or postponed appointments.
“Our results show that persons with RA who had medication changes in the first 3 months of the COVID-19 pandemic in the U.S. were more likely to have worse disease activity and higher exposure to prior DMARDs, but no statistical difference was found in terms of comorbidities,” first author Kaleb Michaud, PhD, and coauthors wrote. Dr. Michaud is with the National Databank for Rheumatic Diseases, Wichita, Kan., and the University of Nebraska Medical Center, Omaha.
The study evaluated responses from 734 adults who participated in FORWARD, an observational, multidisease registry. They answered online surveys about COVID-19 in May 2020 and had provided data on their medication use before the pandemic. A total of 30% (n = 221) reported medication changes in that period.
Details on medication changes
Medication changers were more likely to use glucocorticoids (GCs) (32.6% vs. 18.1%) and less likely to use nonhydroxychloroquine conventional DMARDs (49.3% vs. 62%) pre-COVID. Changers also reported higher rates of economic hardship during the pandemic (22.6% vs. 14.6%).
In the midst of the study period, the ACR issued a clinical guideline for treatment of rheumatic and musculoskeletal diseases (RMDs), emphasizing the need to maintain DMARD therapy, control disease activity, and reduce prednisone/GC use. The guideline advised continuing hydroxychloroquine and interleukin-6 inhibitor biologics in people with suspected or confirmed COVID-19.
Dr. Michaud and coauthors acknowledged the ongoing lack of knowledge about real-world treatment patterns for RA during the pandemic. They set out with this study to fill those knowledge gaps.
They noted that patients on bDMARDs (17.6%) and JAK inhibitors (17.1%) were more than twice as likely to discontinue medications than were those on conventional DMARDs (8.2%).
Switching to telehealth was the most common pandemic-related behavior change among patients in all DMARD groups, with rates ranging from 31% to 47.1%, followed by canceling or postponing appointments, with rates ranging from 27.9% to 36.4% depending on the DMARD group.
The study also found that RA patients widely adopted the behavior changes that the Centers for Disease Control and Prevention recommended during the pandemic, although the rates of restricting social contacts were significantly lower than the 90% reported in an early Italian study.
Dr. Michaud and coauthors also provided some explanation of why people on GCs and DMARDs were more likely than others to change medication patterns. “This may reflect efforts to reduce the perceived risk of infections due to GCs as well as the likely less-controlled disease activity associated with GC use,” they wrote. While the ACR’s early pandemic guidance followed the 2015 guidelines – that patients should continue on GCs at the “lowest possible dose” and not stop them “abruptly” – most U.S. rheumatologists reported cutting back on GC use during the pandemic.
The researchers acknowledged that evidence linking GC use with hospitalization for COVID-19, which emerged after they had surveyed study participants, was consistent their findings, but that the overall risk of COVID-19 in RA patients still isn’t known.
Pfizer funded the analysis, and a coauthor is an employee of Pfizer.
During the first 3 months of the COVID-19 pandemic last year, about one-third of people with rheumatoid arthritis in the United States made changes in their RA medications, and, before the American College of Rheumatology tweaked its guidelines midway through that period, they were about twice as likely to make medication changes on their own than before the pandemic, according to an analysis of data in FORWARD, the National Databank for Rheumatic Diseases.
The study, published in Arthritis Care & Research, also found that about 10% of RA patients on hydroxychloroquine lost access to the drug at a time it was drawing interest as a treatment for COVID-19. Another finding was that a high percentage of patients on non–tumor necrosis factor biologic disease-modifying antirheumatic drugs (bDMARDs) and Janus kinase (JAK) inhibitors canceled or postponed appointments.
“Our results show that persons with RA who had medication changes in the first 3 months of the COVID-19 pandemic in the U.S. were more likely to have worse disease activity and higher exposure to prior DMARDs, but no statistical difference was found in terms of comorbidities,” first author Kaleb Michaud, PhD, and coauthors wrote. Dr. Michaud is with the National Databank for Rheumatic Diseases, Wichita, Kan., and the University of Nebraska Medical Center, Omaha.
The study evaluated responses from 734 adults who participated in FORWARD, an observational, multidisease registry. They answered online surveys about COVID-19 in May 2020 and had provided data on their medication use before the pandemic. A total of 30% (n = 221) reported medication changes in that period.
Details on medication changes
Medication changers were more likely to use glucocorticoids (GCs) (32.6% vs. 18.1%) and less likely to use nonhydroxychloroquine conventional DMARDs (49.3% vs. 62%) pre-COVID. Changers also reported higher rates of economic hardship during the pandemic (22.6% vs. 14.6%).
In the midst of the study period, the ACR issued a clinical guideline for treatment of rheumatic and musculoskeletal diseases (RMDs), emphasizing the need to maintain DMARD therapy, control disease activity, and reduce prednisone/GC use. The guideline advised continuing hydroxychloroquine and interleukin-6 inhibitor biologics in people with suspected or confirmed COVID-19.
Dr. Michaud and coauthors acknowledged the ongoing lack of knowledge about real-world treatment patterns for RA during the pandemic. They set out with this study to fill those knowledge gaps.
They noted that patients on bDMARDs (17.6%) and JAK inhibitors (17.1%) were more than twice as likely to discontinue medications than were those on conventional DMARDs (8.2%).
Switching to telehealth was the most common pandemic-related behavior change among patients in all DMARD groups, with rates ranging from 31% to 47.1%, followed by canceling or postponing appointments, with rates ranging from 27.9% to 36.4% depending on the DMARD group.
The study also found that RA patients widely adopted the behavior changes that the Centers for Disease Control and Prevention recommended during the pandemic, although the rates of restricting social contacts were significantly lower than the 90% reported in an early Italian study.
Dr. Michaud and coauthors also provided some explanation of why people on GCs and DMARDs were more likely than others to change medication patterns. “This may reflect efforts to reduce the perceived risk of infections due to GCs as well as the likely less-controlled disease activity associated with GC use,” they wrote. While the ACR’s early pandemic guidance followed the 2015 guidelines – that patients should continue on GCs at the “lowest possible dose” and not stop them “abruptly” – most U.S. rheumatologists reported cutting back on GC use during the pandemic.
The researchers acknowledged that evidence linking GC use with hospitalization for COVID-19, which emerged after they had surveyed study participants, was consistent their findings, but that the overall risk of COVID-19 in RA patients still isn’t known.
Pfizer funded the analysis, and a coauthor is an employee of Pfizer.
During the first 3 months of the COVID-19 pandemic last year, about one-third of people with rheumatoid arthritis in the United States made changes in their RA medications, and, before the American College of Rheumatology tweaked its guidelines midway through that period, they were about twice as likely to make medication changes on their own than before the pandemic, according to an analysis of data in FORWARD, the National Databank for Rheumatic Diseases.
The study, published in Arthritis Care & Research, also found that about 10% of RA patients on hydroxychloroquine lost access to the drug at a time it was drawing interest as a treatment for COVID-19. Another finding was that a high percentage of patients on non–tumor necrosis factor biologic disease-modifying antirheumatic drugs (bDMARDs) and Janus kinase (JAK) inhibitors canceled or postponed appointments.
“Our results show that persons with RA who had medication changes in the first 3 months of the COVID-19 pandemic in the U.S. were more likely to have worse disease activity and higher exposure to prior DMARDs, but no statistical difference was found in terms of comorbidities,” first author Kaleb Michaud, PhD, and coauthors wrote. Dr. Michaud is with the National Databank for Rheumatic Diseases, Wichita, Kan., and the University of Nebraska Medical Center, Omaha.
The study evaluated responses from 734 adults who participated in FORWARD, an observational, multidisease registry. They answered online surveys about COVID-19 in May 2020 and had provided data on their medication use before the pandemic. A total of 30% (n = 221) reported medication changes in that period.
Details on medication changes
Medication changers were more likely to use glucocorticoids (GCs) (32.6% vs. 18.1%) and less likely to use nonhydroxychloroquine conventional DMARDs (49.3% vs. 62%) pre-COVID. Changers also reported higher rates of economic hardship during the pandemic (22.6% vs. 14.6%).
In the midst of the study period, the ACR issued a clinical guideline for treatment of rheumatic and musculoskeletal diseases (RMDs), emphasizing the need to maintain DMARD therapy, control disease activity, and reduce prednisone/GC use. The guideline advised continuing hydroxychloroquine and interleukin-6 inhibitor biologics in people with suspected or confirmed COVID-19.
Dr. Michaud and coauthors acknowledged the ongoing lack of knowledge about real-world treatment patterns for RA during the pandemic. They set out with this study to fill those knowledge gaps.
They noted that patients on bDMARDs (17.6%) and JAK inhibitors (17.1%) were more than twice as likely to discontinue medications than were those on conventional DMARDs (8.2%).
Switching to telehealth was the most common pandemic-related behavior change among patients in all DMARD groups, with rates ranging from 31% to 47.1%, followed by canceling or postponing appointments, with rates ranging from 27.9% to 36.4% depending on the DMARD group.
The study also found that RA patients widely adopted the behavior changes that the Centers for Disease Control and Prevention recommended during the pandemic, although the rates of restricting social contacts were significantly lower than the 90% reported in an early Italian study.
Dr. Michaud and coauthors also provided some explanation of why people on GCs and DMARDs were more likely than others to change medication patterns. “This may reflect efforts to reduce the perceived risk of infections due to GCs as well as the likely less-controlled disease activity associated with GC use,” they wrote. While the ACR’s early pandemic guidance followed the 2015 guidelines – that patients should continue on GCs at the “lowest possible dose” and not stop them “abruptly” – most U.S. rheumatologists reported cutting back on GC use during the pandemic.
The researchers acknowledged that evidence linking GC use with hospitalization for COVID-19, which emerged after they had surveyed study participants, was consistent their findings, but that the overall risk of COVID-19 in RA patients still isn’t known.
Pfizer funded the analysis, and a coauthor is an employee of Pfizer.
FROM ARTHRITIS CARE & RESEARCH
Most patients with chronic inflammatory diseases have sufficient response to COVID-19 vaccination
Glucocorticoids and B-cell–depleting therapies are trouble spots
Although most patients with chronic inflammatory diseases mounted immune responses after two doses of mRNA-based COVID-19 vaccines, glucocorticoids and B-cell–depleting therapies markedly reduced the response, according to a recently published preprint of a new study.
The study, published on MedRxiv and not yet peer reviewed, involved a prospective look at 133 patients with chronic inflammatory disease (CID) and 53 patients with healthy immune systems at Washington University, St. Louis, and the University of California, San Francisco. It is regarded as the largest and most detailed study yet in how vaccines perform in people with immune-mediated inflammatory disease. The patients were enrolled between December 2020 and March 2021, and the most common diseases were inflammatory bowel disease (32%), rheumatoid arthritis (29%), spondyloarthritis (15%), and systemic lupus erythematosus (11%).
A ‘modest’ reduction in antibody response
Senior author Alfred Kim, MD, PhD, of the department of medicine at Washington University, said the overall results so far are encouraging.
“Most patients with an autoimmune disease that are on immunosuppression can mount antibody responses,” he said. “We’re seeing the majority of our subjects respond.”
The immune-healthy controls and most of the patients with CID had a robust immune response against the spike protein, although the CID group had a mean reduction in antibody titers that was three times lower than the controls (P = .0092). The CID group similarly had a 2.7-fold reduction in preventing neutralization, or halting the virus’ ability to infect (P < .0001), researchers reported.
This reduction in response is “modest,” he said.
“Is the level of reduction going to be detrimental for protection? Time will tell,” he said, adding that researchers anticipate that it won’t have a critical effect on protection because responses tended to be within the range of the immunocompetent controls, who themselves had wildly varied antibody titers across a 20-fold range. “ ‘Optimal’ isn’t necessarily the same as ‘sufficient.’ ”
Type of medication has big impact on antibody titers
But there was a wide variety of effects on the immune response depending on the medication. Glucorticoids resulted in a response that was 10 times lower than the immune-healthy controls, as well as fewer circulating plasmablasts after vaccination. Researchers found that 98% of controls were seropositive for antibody, compared with 92% of those with CID who were not taking prednisone, and 65% of CID patients on prednisone (P = .0006 and .0115, respectively). Prevention of neutralization of the virus was similarly reduced in those groups, compared with the controls. Dr. Kim noted this was a small sample size, with about 15 patients. These effects were seen regardless of the dose.
“We would’ve anticipated this would have been dose dependent, so this was a little bit surprising,” Dr. Kim said.
B-cell–depleting therapies, such as rituximab (Rituxan) and ocrelizumab (Ocrevus), reduced antibody titers by 36 times, compared with controls (P < .0001), with a similar reduction in preventing infection (P = .0066), the researchers found. The reduction in antibody titers was the most pronounced among those who had received B-cell–depleting therapies within the previous 6 months. Dr. Kim noted this was a small sample size, with about 10 patients.
CID study subjects taking an antimetabolite, including methotrexate, had an average of a two- to threefold reduction in antibody titers and in neutralization (P = .0006). This reduction was greatest with methotrexate, researchers found (P = .0027).
JAK inhibitors also significantly reduced antibody titers (P = .0066), but the reduction in neutralization of the virus was not significant. In addition, researchers found a reduction in antibody titers, the prevention of viral infection, and circulating plasmablasts among those on tumor necrosis factor (TNF) inhibitors, compared with controls, but these were insignificant statistically except for virus neutralization.
Dr. Kim said he hopes the glucocorticoid data spur physicians to try harder to wean patients off the drugs, when possible, in keeping with recommendations already in place.
“The general culture in rheumatology has been very lax about the need to reduce glucocorticoids,” he said. “This reinvigorates that call.” Questions about possible drug holidays from glucocorticoids remain, regarding how long a holiday would be needed, he said. He noted that many patients on glucocorticoids nonetheless mounted responses.
Those on B-cell–depleting therapies present a “much more difficult” question, he said. Some patients possibly could wait a bit longer than their normal, every-6-month schedule, but it’s an individual decision, he said. Since a booster of influenza vaccine has been found to enhance the response even within the 6-month window among ocrelizumab patients, a booster of COVID-19 vaccine might also help, although this remains to be studied.
The study group has already increased its sample size and is looking at adverse reactions and long-term immune responses, Dr. Kim said.
Encouraging, rather than discouraging, results
Leonard Calabrese, DO, professor of medicine at the Cleveland Clinic in Ohio, said the findings shouldn’t discourage clinicians from encouraging vaccination.
“There’s still a preponderance of people who will develop a robust antibody vaccine response,” he said.
He cautioned that the findings look only at antibodies to the spike protein and at plasmablasts. The reduction in these titers is “of concern,” he said, but “we don’t really know with certainty what are the effects of these drugs, and these data are on the overall biologic protective effect of the vaccine. There’s much more to a vaccine response than anti–spike protein and plasmablasts,” including cell-mediated immune response.
For an individual patient, the findings “mean a lot,” he said.
“I think that people who are on significant prednisone and B-cell–depleting agents, I think you have to share with them that there’s a reasonable chance that you’re not going to be making a response similar to healthy people,” he said. “Thus, even with your vaccine, we’re not going to cut you loose to do things that are violating social distancing and group settings. … Should you be hugging your grandchildren if you’re a rituximab vaccine recipient? I think I would wait until we have a little bit more data.”
Kevin Winthrop, MD, MPH, professor of ophthalmology at Oregon Health & Science University, Portland, where he studies vaccinations in the immunocompromised, said that glucocorticoids tend to have little effect on vaccinations generally at low doses.
When effects are seen they can be difficult to interpret, he said.
“It’s hard to extricate that from the effect of the underlying disease,” he said. The drug can be a proxy for worse disease control.
Although it’s a small study, it’s reassuring that overall the responses were similar to healthy controls.
For B-cell–depleting therapies, his usual guidance is to not give vaccine until a patient is at least 3 months out from their last dose, and not to restart until at least 2 weeks after vaccination.
“It’s not surprising that some of these DMARDs [disease-modifying antirheumatic drugs] do negatively affect vaccine response, particularly B-cell–depletion therapy. We need to do some studies to find a way to overcome that, or optimize delivery of the vaccine.”
Dr. Kim reported participating in consulting, advisory board, or speaker’s bureau for Alexion, Aurinia, Annexon Biosciences, Exagen Diagnostics, and GlaxoSmithKline, and receiving funding under a sponsored research agreement unrelated to the data in the paper from GlaxoSmithKline. Dr. Winthrop reported receiving consulting fees from Pfizer, AbbVie, UCB, Eli Lilly, Galapagos, GlaxoSmithKline, Roche, Gilead, Bristol-Myers Squibb, Regeneron, Sanofi, AstraZeneca, Novartis, and research grants from Bristol-Myers Squibb and Pfizer. Dr. Calabrese reported no relevant disclosures.
Glucocorticoids and B-cell–depleting therapies are trouble spots
Glucocorticoids and B-cell–depleting therapies are trouble spots
Although most patients with chronic inflammatory diseases mounted immune responses after two doses of mRNA-based COVID-19 vaccines, glucocorticoids and B-cell–depleting therapies markedly reduced the response, according to a recently published preprint of a new study.
The study, published on MedRxiv and not yet peer reviewed, involved a prospective look at 133 patients with chronic inflammatory disease (CID) and 53 patients with healthy immune systems at Washington University, St. Louis, and the University of California, San Francisco. It is regarded as the largest and most detailed study yet in how vaccines perform in people with immune-mediated inflammatory disease. The patients were enrolled between December 2020 and March 2021, and the most common diseases were inflammatory bowel disease (32%), rheumatoid arthritis (29%), spondyloarthritis (15%), and systemic lupus erythematosus (11%).
A ‘modest’ reduction in antibody response
Senior author Alfred Kim, MD, PhD, of the department of medicine at Washington University, said the overall results so far are encouraging.
“Most patients with an autoimmune disease that are on immunosuppression can mount antibody responses,” he said. “We’re seeing the majority of our subjects respond.”
The immune-healthy controls and most of the patients with CID had a robust immune response against the spike protein, although the CID group had a mean reduction in antibody titers that was three times lower than the controls (P = .0092). The CID group similarly had a 2.7-fold reduction in preventing neutralization, or halting the virus’ ability to infect (P < .0001), researchers reported.
This reduction in response is “modest,” he said.
“Is the level of reduction going to be detrimental for protection? Time will tell,” he said, adding that researchers anticipate that it won’t have a critical effect on protection because responses tended to be within the range of the immunocompetent controls, who themselves had wildly varied antibody titers across a 20-fold range. “ ‘Optimal’ isn’t necessarily the same as ‘sufficient.’ ”
Type of medication has big impact on antibody titers
But there was a wide variety of effects on the immune response depending on the medication. Glucorticoids resulted in a response that was 10 times lower than the immune-healthy controls, as well as fewer circulating plasmablasts after vaccination. Researchers found that 98% of controls were seropositive for antibody, compared with 92% of those with CID who were not taking prednisone, and 65% of CID patients on prednisone (P = .0006 and .0115, respectively). Prevention of neutralization of the virus was similarly reduced in those groups, compared with the controls. Dr. Kim noted this was a small sample size, with about 15 patients. These effects were seen regardless of the dose.
“We would’ve anticipated this would have been dose dependent, so this was a little bit surprising,” Dr. Kim said.
B-cell–depleting therapies, such as rituximab (Rituxan) and ocrelizumab (Ocrevus), reduced antibody titers by 36 times, compared with controls (P < .0001), with a similar reduction in preventing infection (P = .0066), the researchers found. The reduction in antibody titers was the most pronounced among those who had received B-cell–depleting therapies within the previous 6 months. Dr. Kim noted this was a small sample size, with about 10 patients.
CID study subjects taking an antimetabolite, including methotrexate, had an average of a two- to threefold reduction in antibody titers and in neutralization (P = .0006). This reduction was greatest with methotrexate, researchers found (P = .0027).
JAK inhibitors also significantly reduced antibody titers (P = .0066), but the reduction in neutralization of the virus was not significant. In addition, researchers found a reduction in antibody titers, the prevention of viral infection, and circulating plasmablasts among those on tumor necrosis factor (TNF) inhibitors, compared with controls, but these were insignificant statistically except for virus neutralization.
Dr. Kim said he hopes the glucocorticoid data spur physicians to try harder to wean patients off the drugs, when possible, in keeping with recommendations already in place.
“The general culture in rheumatology has been very lax about the need to reduce glucocorticoids,” he said. “This reinvigorates that call.” Questions about possible drug holidays from glucocorticoids remain, regarding how long a holiday would be needed, he said. He noted that many patients on glucocorticoids nonetheless mounted responses.
Those on B-cell–depleting therapies present a “much more difficult” question, he said. Some patients possibly could wait a bit longer than their normal, every-6-month schedule, but it’s an individual decision, he said. Since a booster of influenza vaccine has been found to enhance the response even within the 6-month window among ocrelizumab patients, a booster of COVID-19 vaccine might also help, although this remains to be studied.
The study group has already increased its sample size and is looking at adverse reactions and long-term immune responses, Dr. Kim said.
Encouraging, rather than discouraging, results
Leonard Calabrese, DO, professor of medicine at the Cleveland Clinic in Ohio, said the findings shouldn’t discourage clinicians from encouraging vaccination.
“There’s still a preponderance of people who will develop a robust antibody vaccine response,” he said.
He cautioned that the findings look only at antibodies to the spike protein and at plasmablasts. The reduction in these titers is “of concern,” he said, but “we don’t really know with certainty what are the effects of these drugs, and these data are on the overall biologic protective effect of the vaccine. There’s much more to a vaccine response than anti–spike protein and plasmablasts,” including cell-mediated immune response.
For an individual patient, the findings “mean a lot,” he said.
“I think that people who are on significant prednisone and B-cell–depleting agents, I think you have to share with them that there’s a reasonable chance that you’re not going to be making a response similar to healthy people,” he said. “Thus, even with your vaccine, we’re not going to cut you loose to do things that are violating social distancing and group settings. … Should you be hugging your grandchildren if you’re a rituximab vaccine recipient? I think I would wait until we have a little bit more data.”
Kevin Winthrop, MD, MPH, professor of ophthalmology at Oregon Health & Science University, Portland, where he studies vaccinations in the immunocompromised, said that glucocorticoids tend to have little effect on vaccinations generally at low doses.
When effects are seen they can be difficult to interpret, he said.
“It’s hard to extricate that from the effect of the underlying disease,” he said. The drug can be a proxy for worse disease control.
Although it’s a small study, it’s reassuring that overall the responses were similar to healthy controls.
For B-cell–depleting therapies, his usual guidance is to not give vaccine until a patient is at least 3 months out from their last dose, and not to restart until at least 2 weeks after vaccination.
“It’s not surprising that some of these DMARDs [disease-modifying antirheumatic drugs] do negatively affect vaccine response, particularly B-cell–depletion therapy. We need to do some studies to find a way to overcome that, or optimize delivery of the vaccine.”
Dr. Kim reported participating in consulting, advisory board, or speaker’s bureau for Alexion, Aurinia, Annexon Biosciences, Exagen Diagnostics, and GlaxoSmithKline, and receiving funding under a sponsored research agreement unrelated to the data in the paper from GlaxoSmithKline. Dr. Winthrop reported receiving consulting fees from Pfizer, AbbVie, UCB, Eli Lilly, Galapagos, GlaxoSmithKline, Roche, Gilead, Bristol-Myers Squibb, Regeneron, Sanofi, AstraZeneca, Novartis, and research grants from Bristol-Myers Squibb and Pfizer. Dr. Calabrese reported no relevant disclosures.
Although most patients with chronic inflammatory diseases mounted immune responses after two doses of mRNA-based COVID-19 vaccines, glucocorticoids and B-cell–depleting therapies markedly reduced the response, according to a recently published preprint of a new study.
The study, published on MedRxiv and not yet peer reviewed, involved a prospective look at 133 patients with chronic inflammatory disease (CID) and 53 patients with healthy immune systems at Washington University, St. Louis, and the University of California, San Francisco. It is regarded as the largest and most detailed study yet in how vaccines perform in people with immune-mediated inflammatory disease. The patients were enrolled between December 2020 and March 2021, and the most common diseases were inflammatory bowel disease (32%), rheumatoid arthritis (29%), spondyloarthritis (15%), and systemic lupus erythematosus (11%).
A ‘modest’ reduction in antibody response
Senior author Alfred Kim, MD, PhD, of the department of medicine at Washington University, said the overall results so far are encouraging.
“Most patients with an autoimmune disease that are on immunosuppression can mount antibody responses,” he said. “We’re seeing the majority of our subjects respond.”
The immune-healthy controls and most of the patients with CID had a robust immune response against the spike protein, although the CID group had a mean reduction in antibody titers that was three times lower than the controls (P = .0092). The CID group similarly had a 2.7-fold reduction in preventing neutralization, or halting the virus’ ability to infect (P < .0001), researchers reported.
This reduction in response is “modest,” he said.
“Is the level of reduction going to be detrimental for protection? Time will tell,” he said, adding that researchers anticipate that it won’t have a critical effect on protection because responses tended to be within the range of the immunocompetent controls, who themselves had wildly varied antibody titers across a 20-fold range. “ ‘Optimal’ isn’t necessarily the same as ‘sufficient.’ ”
Type of medication has big impact on antibody titers
But there was a wide variety of effects on the immune response depending on the medication. Glucorticoids resulted in a response that was 10 times lower than the immune-healthy controls, as well as fewer circulating plasmablasts after vaccination. Researchers found that 98% of controls were seropositive for antibody, compared with 92% of those with CID who were not taking prednisone, and 65% of CID patients on prednisone (P = .0006 and .0115, respectively). Prevention of neutralization of the virus was similarly reduced in those groups, compared with the controls. Dr. Kim noted this was a small sample size, with about 15 patients. These effects were seen regardless of the dose.
“We would’ve anticipated this would have been dose dependent, so this was a little bit surprising,” Dr. Kim said.
B-cell–depleting therapies, such as rituximab (Rituxan) and ocrelizumab (Ocrevus), reduced antibody titers by 36 times, compared with controls (P < .0001), with a similar reduction in preventing infection (P = .0066), the researchers found. The reduction in antibody titers was the most pronounced among those who had received B-cell–depleting therapies within the previous 6 months. Dr. Kim noted this was a small sample size, with about 10 patients.
CID study subjects taking an antimetabolite, including methotrexate, had an average of a two- to threefold reduction in antibody titers and in neutralization (P = .0006). This reduction was greatest with methotrexate, researchers found (P = .0027).
JAK inhibitors also significantly reduced antibody titers (P = .0066), but the reduction in neutralization of the virus was not significant. In addition, researchers found a reduction in antibody titers, the prevention of viral infection, and circulating plasmablasts among those on tumor necrosis factor (TNF) inhibitors, compared with controls, but these were insignificant statistically except for virus neutralization.
Dr. Kim said he hopes the glucocorticoid data spur physicians to try harder to wean patients off the drugs, when possible, in keeping with recommendations already in place.
“The general culture in rheumatology has been very lax about the need to reduce glucocorticoids,” he said. “This reinvigorates that call.” Questions about possible drug holidays from glucocorticoids remain, regarding how long a holiday would be needed, he said. He noted that many patients on glucocorticoids nonetheless mounted responses.
Those on B-cell–depleting therapies present a “much more difficult” question, he said. Some patients possibly could wait a bit longer than their normal, every-6-month schedule, but it’s an individual decision, he said. Since a booster of influenza vaccine has been found to enhance the response even within the 6-month window among ocrelizumab patients, a booster of COVID-19 vaccine might also help, although this remains to be studied.
The study group has already increased its sample size and is looking at adverse reactions and long-term immune responses, Dr. Kim said.
Encouraging, rather than discouraging, results
Leonard Calabrese, DO, professor of medicine at the Cleveland Clinic in Ohio, said the findings shouldn’t discourage clinicians from encouraging vaccination.
“There’s still a preponderance of people who will develop a robust antibody vaccine response,” he said.
He cautioned that the findings look only at antibodies to the spike protein and at plasmablasts. The reduction in these titers is “of concern,” he said, but “we don’t really know with certainty what are the effects of these drugs, and these data are on the overall biologic protective effect of the vaccine. There’s much more to a vaccine response than anti–spike protein and plasmablasts,” including cell-mediated immune response.
For an individual patient, the findings “mean a lot,” he said.
“I think that people who are on significant prednisone and B-cell–depleting agents, I think you have to share with them that there’s a reasonable chance that you’re not going to be making a response similar to healthy people,” he said. “Thus, even with your vaccine, we’re not going to cut you loose to do things that are violating social distancing and group settings. … Should you be hugging your grandchildren if you’re a rituximab vaccine recipient? I think I would wait until we have a little bit more data.”
Kevin Winthrop, MD, MPH, professor of ophthalmology at Oregon Health & Science University, Portland, where he studies vaccinations in the immunocompromised, said that glucocorticoids tend to have little effect on vaccinations generally at low doses.
When effects are seen they can be difficult to interpret, he said.
“It’s hard to extricate that from the effect of the underlying disease,” he said. The drug can be a proxy for worse disease control.
Although it’s a small study, it’s reassuring that overall the responses were similar to healthy controls.
For B-cell–depleting therapies, his usual guidance is to not give vaccine until a patient is at least 3 months out from their last dose, and not to restart until at least 2 weeks after vaccination.
“It’s not surprising that some of these DMARDs [disease-modifying antirheumatic drugs] do negatively affect vaccine response, particularly B-cell–depletion therapy. We need to do some studies to find a way to overcome that, or optimize delivery of the vaccine.”
Dr. Kim reported participating in consulting, advisory board, or speaker’s bureau for Alexion, Aurinia, Annexon Biosciences, Exagen Diagnostics, and GlaxoSmithKline, and receiving funding under a sponsored research agreement unrelated to the data in the paper from GlaxoSmithKline. Dr. Winthrop reported receiving consulting fees from Pfizer, AbbVie, UCB, Eli Lilly, Galapagos, GlaxoSmithKline, Roche, Gilead, Bristol-Myers Squibb, Regeneron, Sanofi, AstraZeneca, Novartis, and research grants from Bristol-Myers Squibb and Pfizer. Dr. Calabrese reported no relevant disclosures.
FROM MEDRXIV





















