User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
Powered by CHEST Physician, Clinician Reviews, MDedge Family Medicine, Internal Medicine News, and The Journal of Clinical Outcomes Management.
Increase brings flu activity back to seasonal high
for the week ending Jan. 21, compared with three states the week before, according to the Centers for Disease Control and Prevention.
Alabama, Kansas, New Jersey, Oklahoma, and South Carolina were at level 10 on the CDC’s 1-10 scale of ILI activity, with Oklahoma reaching that level for the third consecutive week. Georgia (level 9) and Louisiana, Minnesota, Missouri, and Tennessee (level 8) were also in the “high” range, the CDC reported.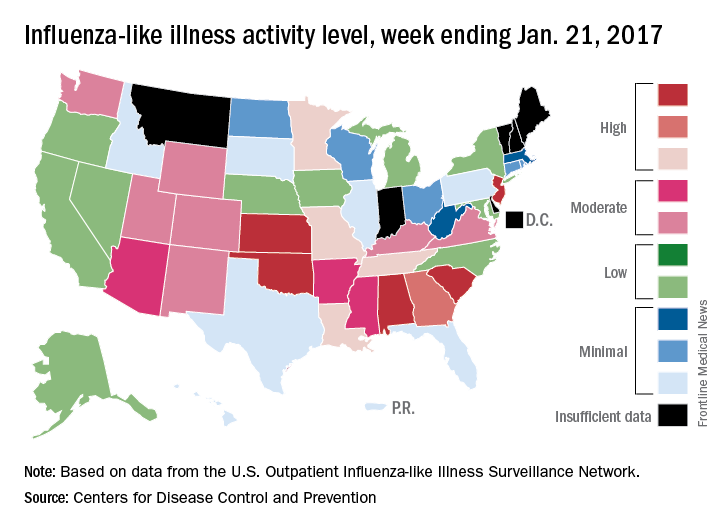
Three flu-related pediatric deaths were reported for the week, although two occurred during the week ending Jan. 14. The two earlier deaths were associated with an influenza A (H3) virus, and the more recent death was associated with an influenza B virus. For the 2016-2017 season so far, there have been a total of eight pediatric deaths, the CDC said.
for the week ending Jan. 21, compared with three states the week before, according to the Centers for Disease Control and Prevention.
Alabama, Kansas, New Jersey, Oklahoma, and South Carolina were at level 10 on the CDC’s 1-10 scale of ILI activity, with Oklahoma reaching that level for the third consecutive week. Georgia (level 9) and Louisiana, Minnesota, Missouri, and Tennessee (level 8) were also in the “high” range, the CDC reported.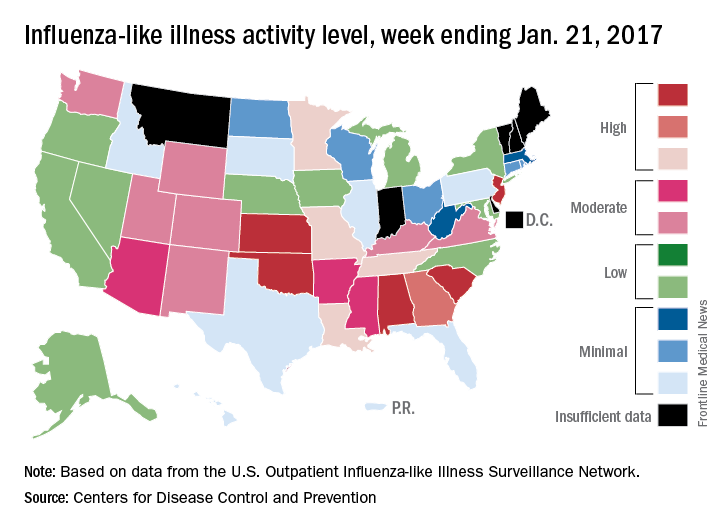
Three flu-related pediatric deaths were reported for the week, although two occurred during the week ending Jan. 14. The two earlier deaths were associated with an influenza A (H3) virus, and the more recent death was associated with an influenza B virus. For the 2016-2017 season so far, there have been a total of eight pediatric deaths, the CDC said.
for the week ending Jan. 21, compared with three states the week before, according to the Centers for Disease Control and Prevention.
Alabama, Kansas, New Jersey, Oklahoma, and South Carolina were at level 10 on the CDC’s 1-10 scale of ILI activity, with Oklahoma reaching that level for the third consecutive week. Georgia (level 9) and Louisiana, Minnesota, Missouri, and Tennessee (level 8) were also in the “high” range, the CDC reported.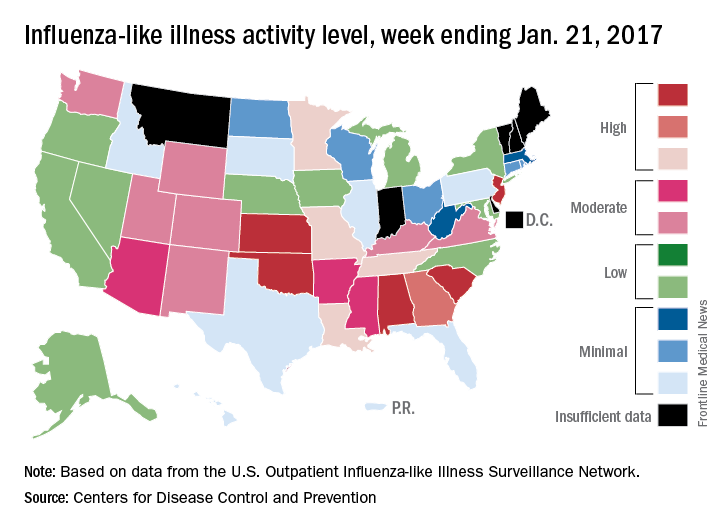
Three flu-related pediatric deaths were reported for the week, although two occurred during the week ending Jan. 14. The two earlier deaths were associated with an influenza A (H3) virus, and the more recent death was associated with an influenza B virus. For the 2016-2017 season so far, there have been a total of eight pediatric deaths, the CDC said.
Lung cancer screening a challenge to implement
A comprehensive lung cancer screening program carried out at Veterans Health Administration hospitals was taxing to implement and revealed a large number of patients with results requiring follow-up, though only 1.5% had cancers.
Investigators at eight VHA hospitals, led by Linda S. Kinsinger, MD, of the VHA’s National Center for Health Promotion and Disease Prevention in Durham, N.C., looked at records from about 93,000 primary care patients and identified 4,246 eligible for screening, based on age, medical history, and smoking history (JAMA Intern Med. 2017 Jan 30. doi: 10.1001/jamainternmed.2016.9022).
Approximately 58% of the eligible patients consented, and 2,106 underwent screening with low-dose computed tomography (LDCT). The mean age of patients was 65 years, and 96% of patients were male.
Nearly 60% of patients screened (1,257) had nodules, 1,184 patients (56.2%) required tracking, and 31 patients (1.5%) had lung cancer.
The pilot study was developed in response to a 2013 recommendation from the U.S. Preventive Services Task Force favoring annual screening with LDCT in current or former heavy smokers between 55 and 80 years old.
The recommendation sparked concerns about the practicability of implementing large-scale lung cancer screening, which Dr. Kinsinger and her colleagues’ study seemed to underscore. For example, “creating electronic tools to capture the necessary clinical data in real time … proved to be difficult, even with the VHA’s highly regarded electronic medical record,” the investigators wrote. A key measure used in the screening program – cigarette pack-years – was “not fully captured” in the system’s EMR.
The investigators also noted that if the eligibility criteria used in the pilot program were applied to the VHA nationwide, about 900,000 patients would be eligible for LDCT screening, and that fewer than 60% of patients in this study had consented. That meant that “accurately identifying these patients and discussing with them the benefits and harms of [screening] will take significant effort for primary care teams,” the researchers noted.
In addition, the required follow-up “may stress the capacity” of radiology and pulmonology services, the study authors cautioned.
Finally, “primary care will need to be involved in deciding which incidental findings need further evaluation,” they wrote. “These clinical efforts will require coordination and communication among clinical services and between patients and staff, and dedicated coordinators will need to be hired.”
The investigators noted that their findings might not be generalizable to non-VHA health care systems. The experience of the VHA, “owing to its central organizational structure, may represent a best-case scenario,” they wrote.
The Veterans Health Administration funded the study. Two of its coauthors reported commercial conflicts of interest; one of those disclosed a grant application to the Bristol-Myers Squibb Foundation related to lung cancer screening.
A comprehensive lung cancer screening program carried out at Veterans Health Administration hospitals was taxing to implement and revealed a large number of patients with results requiring follow-up, though only 1.5% had cancers.
Investigators at eight VHA hospitals, led by Linda S. Kinsinger, MD, of the VHA’s National Center for Health Promotion and Disease Prevention in Durham, N.C., looked at records from about 93,000 primary care patients and identified 4,246 eligible for screening, based on age, medical history, and smoking history (JAMA Intern Med. 2017 Jan 30. doi: 10.1001/jamainternmed.2016.9022).
Approximately 58% of the eligible patients consented, and 2,106 underwent screening with low-dose computed tomography (LDCT). The mean age of patients was 65 years, and 96% of patients were male.
Nearly 60% of patients screened (1,257) had nodules, 1,184 patients (56.2%) required tracking, and 31 patients (1.5%) had lung cancer.
The pilot study was developed in response to a 2013 recommendation from the U.S. Preventive Services Task Force favoring annual screening with LDCT in current or former heavy smokers between 55 and 80 years old.
The recommendation sparked concerns about the practicability of implementing large-scale lung cancer screening, which Dr. Kinsinger and her colleagues’ study seemed to underscore. For example, “creating electronic tools to capture the necessary clinical data in real time … proved to be difficult, even with the VHA’s highly regarded electronic medical record,” the investigators wrote. A key measure used in the screening program – cigarette pack-years – was “not fully captured” in the system’s EMR.
The investigators also noted that if the eligibility criteria used in the pilot program were applied to the VHA nationwide, about 900,000 patients would be eligible for LDCT screening, and that fewer than 60% of patients in this study had consented. That meant that “accurately identifying these patients and discussing with them the benefits and harms of [screening] will take significant effort for primary care teams,” the researchers noted.
In addition, the required follow-up “may stress the capacity” of radiology and pulmonology services, the study authors cautioned.
Finally, “primary care will need to be involved in deciding which incidental findings need further evaluation,” they wrote. “These clinical efforts will require coordination and communication among clinical services and between patients and staff, and dedicated coordinators will need to be hired.”
The investigators noted that their findings might not be generalizable to non-VHA health care systems. The experience of the VHA, “owing to its central organizational structure, may represent a best-case scenario,” they wrote.
The Veterans Health Administration funded the study. Two of its coauthors reported commercial conflicts of interest; one of those disclosed a grant application to the Bristol-Myers Squibb Foundation related to lung cancer screening.
A comprehensive lung cancer screening program carried out at Veterans Health Administration hospitals was taxing to implement and revealed a large number of patients with results requiring follow-up, though only 1.5% had cancers.
Investigators at eight VHA hospitals, led by Linda S. Kinsinger, MD, of the VHA’s National Center for Health Promotion and Disease Prevention in Durham, N.C., looked at records from about 93,000 primary care patients and identified 4,246 eligible for screening, based on age, medical history, and smoking history (JAMA Intern Med. 2017 Jan 30. doi: 10.1001/jamainternmed.2016.9022).
Approximately 58% of the eligible patients consented, and 2,106 underwent screening with low-dose computed tomography (LDCT). The mean age of patients was 65 years, and 96% of patients were male.
Nearly 60% of patients screened (1,257) had nodules, 1,184 patients (56.2%) required tracking, and 31 patients (1.5%) had lung cancer.
The pilot study was developed in response to a 2013 recommendation from the U.S. Preventive Services Task Force favoring annual screening with LDCT in current or former heavy smokers between 55 and 80 years old.
The recommendation sparked concerns about the practicability of implementing large-scale lung cancer screening, which Dr. Kinsinger and her colleagues’ study seemed to underscore. For example, “creating electronic tools to capture the necessary clinical data in real time … proved to be difficult, even with the VHA’s highly regarded electronic medical record,” the investigators wrote. A key measure used in the screening program – cigarette pack-years – was “not fully captured” in the system’s EMR.
The investigators also noted that if the eligibility criteria used in the pilot program were applied to the VHA nationwide, about 900,000 patients would be eligible for LDCT screening, and that fewer than 60% of patients in this study had consented. That meant that “accurately identifying these patients and discussing with them the benefits and harms of [screening] will take significant effort for primary care teams,” the researchers noted.
In addition, the required follow-up “may stress the capacity” of radiology and pulmonology services, the study authors cautioned.
Finally, “primary care will need to be involved in deciding which incidental findings need further evaluation,” they wrote. “These clinical efforts will require coordination and communication among clinical services and between patients and staff, and dedicated coordinators will need to be hired.”
The investigators noted that their findings might not be generalizable to non-VHA health care systems. The experience of the VHA, “owing to its central organizational structure, may represent a best-case scenario,” they wrote.
The Veterans Health Administration funded the study. Two of its coauthors reported commercial conflicts of interest; one of those disclosed a grant application to the Bristol-Myers Squibb Foundation related to lung cancer screening.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Comprehensive lung cancer screening is complex to implement in hospital primary care settings and may trigger resource-intensive follow-up.
Major finding: Of more than 2,000 patients screened, nearly 60% were positive for nodules, though only 1.5% had cancer.
Data source: A pilot study in 4,246 eligible primary care patients at eight Veterans Health Administration hospitals; 2,106 were screened using low-dose computed tomography.
Disclosures: The Veterans Health Administration funded the study. Two of its coauthors reported commercial conflicts of interest; one of those disclosed a grant application to the Bristol-Myers Squibb Foundation related to lung cancer screening.
Carbapenem-resistant K. pneumoniae occurs in 25% of long-term acute care hospital cultures
Nearly one-quarter of Klebsiella pneumoniae cultures in a network of U.S. long-term acute care hospitals are resistant to carbapenem, according to Jennifer H. Han, MD, and her associates.
From a sample of 3,846 K. pneumoniae cultures taken from 64 long-term acute care hospitals in 16 states, 946, or 24.6%, of the cultures were carbapenem-resistant, and were taken from 821 patients. Just under 54% of CRKP isolates were taken from a respiratory source, with 37% coming from urine and the remaining 9.4% coming from blood. Nearly all CRKP isolates were resistant to fluoroquinolones, and 59.2% were resistant to amikacin.
Of the 16 states where cultures were taken from, California had the highest rate of carbapenem resistance, with 45.5% of K. pneumoniae cultures showing resistance. Other states with high rates of CRKP included South Carolina, Kentucky, and Indiana.
“Given the chronically, critically ill population, with convergence of at-risk patients from multiple facilities, future studies of optimal infection prevention strategies are urgently needed for this setting. In addition, expansion of national surveillance efforts and improved communication between [long-term acute care hospitals] and acute care hospitals will be critical for reducing the continued emergence and dissemination of CRKP across the health care continuum,” Dr. Han and her associates concluded.
Find the full study in Clinical Infectious Diseases (doi: 10.1 LTACHs 093/cid/ciw856)
Nearly one-quarter of Klebsiella pneumoniae cultures in a network of U.S. long-term acute care hospitals are resistant to carbapenem, according to Jennifer H. Han, MD, and her associates.
From a sample of 3,846 K. pneumoniae cultures taken from 64 long-term acute care hospitals in 16 states, 946, or 24.6%, of the cultures were carbapenem-resistant, and were taken from 821 patients. Just under 54% of CRKP isolates were taken from a respiratory source, with 37% coming from urine and the remaining 9.4% coming from blood. Nearly all CRKP isolates were resistant to fluoroquinolones, and 59.2% were resistant to amikacin.
Of the 16 states where cultures were taken from, California had the highest rate of carbapenem resistance, with 45.5% of K. pneumoniae cultures showing resistance. Other states with high rates of CRKP included South Carolina, Kentucky, and Indiana.
“Given the chronically, critically ill population, with convergence of at-risk patients from multiple facilities, future studies of optimal infection prevention strategies are urgently needed for this setting. In addition, expansion of national surveillance efforts and improved communication between [long-term acute care hospitals] and acute care hospitals will be critical for reducing the continued emergence and dissemination of CRKP across the health care continuum,” Dr. Han and her associates concluded.
Find the full study in Clinical Infectious Diseases (doi: 10.1 LTACHs 093/cid/ciw856)
Nearly one-quarter of Klebsiella pneumoniae cultures in a network of U.S. long-term acute care hospitals are resistant to carbapenem, according to Jennifer H. Han, MD, and her associates.
From a sample of 3,846 K. pneumoniae cultures taken from 64 long-term acute care hospitals in 16 states, 946, or 24.6%, of the cultures were carbapenem-resistant, and were taken from 821 patients. Just under 54% of CRKP isolates were taken from a respiratory source, with 37% coming from urine and the remaining 9.4% coming from blood. Nearly all CRKP isolates were resistant to fluoroquinolones, and 59.2% were resistant to amikacin.
Of the 16 states where cultures were taken from, California had the highest rate of carbapenem resistance, with 45.5% of K. pneumoniae cultures showing resistance. Other states with high rates of CRKP included South Carolina, Kentucky, and Indiana.
“Given the chronically, critically ill population, with convergence of at-risk patients from multiple facilities, future studies of optimal infection prevention strategies are urgently needed for this setting. In addition, expansion of national surveillance efforts and improved communication between [long-term acute care hospitals] and acute care hospitals will be critical for reducing the continued emergence and dissemination of CRKP across the health care continuum,” Dr. Han and her associates concluded.
Find the full study in Clinical Infectious Diseases (doi: 10.1 LTACHs 093/cid/ciw856)
FROM CLINICAL INFECTIOUS DISEASES
Sleep apnea may induce distinct form of atrial fibrillation
ORLANDO – Patients with atrial fibrillation (AF) should be screened for obstructive sleep apnea (OSA), because this information may be useful in guiding ablation strategies, according to results of a prospective study.
The study, which associated OSA in AF with a high relative rate of non–pulmonary vein (PV) triggers, has contributed to the “growing body of evidence implicating sleep apnea in atrial remodeling and promotion of the AF substrate,” Elad Anter, MD, associate director of the clinical electrophysiology laboratory at Beth Israel Deaconess Medical Center, Boston, reported at the annual International AF Symposium.
Despite the close association between OSA and AF, it has been unclear whether OSA is a causative factor. Dr. Anter suggested that mechanistic association is strengthening, however.
It has been hypothesized that OSA generates AF substrate through negative intrathoracic pressure changes and autonomic nervous system activation. But Dr. Anter reported that there is more recent and compelling evidence that the repetitive occlusions produced by OSA result in remodeling of the atria, producing scar tissue that slows conduction and produces susceptibility to reentry AF.
A newly completed prospective multicenter study adds support to this latter hypothesis. In the protocol, patients with paroxysmal AF scheduled for ablation were required to undergo a sleep study, an AF mapping study, and follow-up for at least 12 months. A known history of OSA was an exclusion criterion. To isolate the effect of OSA, there were exclusions for other major etiologies for AF, such as heart failure or coronary artery disease.
The AF mapping was conducted when patients were in sinus rhythm “to evaluate the baseline atrial substrate and avoid measurements related to acute electrical remodeling,” Dr. Anter explained.
Of 172 patients initially enrolled, 133 completed the sleep study, 118 completed the mapping study, and 110 completed both and were followed for at least 12 months. Of these, 43 patients without OSA were compared with 43 patients with OSA defined as an apnea-hypopnea index (AHI) of at least 15. Patients in the two groups did not differ significantly for relevant characteristics, such as body mass index (BMI), age, presence of hypertension, or duration of AF; but the left atrial (LA) volume was significantly greater (P = .01) in those with OSA than those without.
Even though the prevalence of voltage abnormalities was higher in the OSA group for the right (P = .01) and left atria (P = .0001) before ablation, the prevalence of PV triggers (63% vs. 65%), non-PV triggers (19% vs. 12%) and noninducible triggers (19% vs. 23%) were similar.
After ablation, PV triggers were no longer inducible in either group, but there was a striking difference in inducible non-PV triggers. While only 11.6% remained inducible in the non-OSA group, 41.8% (P = .003) remained inducible in the OSA patients.
“AF triggers in OSA were most commonly located at the LA septum, at the zone of low voltage and abnormal electrograms, as determined during sinus rhythm,” Dr. Anter reported. “Ablation of these triggers at the zone of tissue abnormality in the OSA patients resulted in termination of AF in 9 (64.2%) of the 14 patients.”
Overall, at the end of 12 months, 79% of those without OSA remained in arrhythmia-free survival, versus 65.1% of the group with OSA that were treated with PV isolation alone.
The lower rate of success in the OSA group shows the importance of specifically directing ablation to the areas of low voltage and slow conduction in the left anterior septum that Dr. Anter indicated otherwise would be missed.
“These zones are a common source of extra-PV triggers and localized circuits or rotors of AF in OSA patients,” he reported. “Ablation of these low voltage zones is associated with improved clinical outcome in OSA patients with paroxysmal AF.”
The data, which Dr. Anter said are consistent with a growing body of work regarding the relationship of OSA and AF, provided the basis for suggesting that AF patients undergo routine screening for OSA.
In patients with OSA, ablation of PV triggers alone even in paroxysmal PAF “may not be sufficient,” he cautioned. “Evaluation of non-PV triggers should also be performed.”
Dr. Anter reported financial relationships with Biosense Webster and Boston Scientific.
Atrial fibrillation (AF) is the most common cardiac arrhythmia encountered in clinical practice and is associated with increased morbidity and mortality due to thromboembolism, stroke, and worsening of pre-existing heart failure. Both its incidence and prevalence are increasing as AF risk increases with advancing age.1 While the strategies of heart rate control and anticoagulation to lower stroke risk and rhythm control have been found comparable with regard to survival, many patients remain highly symptomatic because of palpitations and reduced cardiac output.1
Structural abnormalities of the atria, including fibrosis and dilation, accompanied by conduction abnormalities, provide the underlying substrate for AF. It is well established that AF episodes perpetuate atrial remodeling leading to more frequent and prolonged AF episodes. Hence, there is the long-standing notion that “AF begets AF.” While a variety of antiarrhythmic drugs have been employed over the years to prevent AF recurrences and to maintain sinus rhythm, their use has decreased over the past 2 decades due to their major side effects and their potential of proarrhythmia.
Since AF patients represent a heterogeneous group of patients with CV diseases of varying type and severity as well as comorbidities, it stands to reason that the pulmonary venous–left atrial junction may not be the sole culprit region of all cases of AF and that other anatomical locations might serve as triggers for AF.
In support of this notion are the results of the prospective multicenter study presented by Dr. Elad Anter at the annual International AF Symposium. This important study is consistent with and expands upon prior studies that have suggested that sites within the atria remote from the pulmonary veins may serve as triggers for AF, rather than lower technical success of pulmonary vein ablation.5 It further highlights the importance of fibrosis and associated electrical dispersion to the pathogenesis of AF.6 However, the recommendation that patients with AF be screened for OSA is not new, as nearly half of patients with AF also have OSA.7 While AF and OSA share common risk factors/comorbidities such as male gender, obesity, hypertension, coronary artery disease, and congestive heart failure, OSA has been found to be an independent risk factor for AF development.
It is important to know whether OSA was treated, as the presence of OSA raises the risk of AF recurrence and OSA treatment decreases AF recurrence after ablation.8,9 Conversely, in the setting of OSA, AF is more resistive to rhythm control. Enhanced vagal activation, elevated sympathetic tone, and oxidative stresses due to oxygen desaturation and left atrial distension have all been implicated in the pathogenesis linking OSA to the development of AF. Repeated increases in upper airway resistance during airway obstruction have been shown to lead to atrial stretch, dilation, and fibrosis.10 Since patients with heart failure, coronary artery disease, and other underlying causes for AF were excluded from the onset, the results may not be applicable to a large segment of AF patients. Exclusion of underlying cardiac conditions potentially raised the yield of patients found to have OSA and the potential value of OSA screening. Of note: Less than half of patients that were enrolled had complete data for analysis, which may further limit applicability of the study findings. All patients had paroxysmal AF and were in sinus rhythm while the mapping procedure was performed, leaving questions as to how to approach patients presenting acutely with persistent or long standing AF, or those recently treated with antiarrhythmic therapy. Also, since arrhythmia-free survival decreases from 1 to 5 years after AF ablation, and short-time success rates do not predict longer success rates, the present study results should be interpreted with cautious optimism.11
However, these limitations should not detract from the major implications of the study. In the setting of AF, OSA should be clinically suspected not only because of the frequent coexistence of the two disorders but because the presence of OSA should prompt electrophysiologists to consider non–pulmonary vein triggers of AF prior to ablation attempts. The consideration of alternative ablation sites might help to explain the lack of ablation procedure endpoints to predict long-term success of ablation and holds promise for increasing technical success rates. Given that airway obstruction may occur in other clinical settings such as seizure-induced laryngospasm and that seizures may induce arrhythmias and sudden death, there is potential for non–pulmonary vein sites to trigger AF and other arrhythmias in settings other than OSA as well.12 Whether other disease states are associated with a higher likelihood of non-pulmonary veins trigger sites also merits further study. Moreover, this study underscores the notion that with regard to AF ablation, “no one site fits all” and “clinical mapping” may serve as a valuable adjunct to anatomical mapping. It also serves as a reminder of the multidisciplinary nature of Chest Medicine and the need of a team oriented approach..
References
1. Iwasaki YK, Nishida K, Kato T, Nattel S. Atrial fibrillation pathophysiology: implications for management. Circulation. 2011;124:2264-74.
2. Verma A, Jiang CY, Betts TR, et al. Approaches to catheter ablation for persistent atrial fibrillation. N Engl J Med. 2015;372:1812-22.
3. Kuck KH, Brugada J, Fürnkranz A, et al. Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med. 2016;374:2235-45.
4. Calkins H, Reynolds MR, Spector P, et al. Treatment of atrial fibrillation with antiarrhythmic drugs or radiofrequency ablation: two systematic literature reviews and meta-analyses. Circ Arrhythm Electrophysiol. 2009;2:349-61.
5. Narayan SM, Krummen DE, Shivkumar K, et al. Treatment of atrial fibrillation by the ablation of localized sources: CONFIRM (Conventional Ablation for Atrial Fibrillation With or Without Focal Impulse and Rotor Modulation) trial. J Am Coll Cardiol. 2012;60:628-36.
6. Kottkamp H, Berg J, Bender R, et al. Box Isolation of Fibrotic Areas (BIFA): a patient-tailored substrate modified application approach for ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2016;27:22-30.
7. Stevenson IH, Teichtahl H, Cunnington D, et al. Prevalence of sleep disordered breathing in paroxysmal and persistent atrial fibrillation patients with normal left ventricular function. Eur Heart J. 2008;29:1662-9.
8. Fein AS, Shvilkin A, Shah D, et al. Treatment of obstructive sleep apnea reduces the risk of atrial fibrillation recurrence after catheter ablation. J Am Coll Cardiol. 2013;62:300-5.
9. Naruse Y, Tada H, Satoh M, et al. Concomitant obstructive sleep apnea increases the recurrence of atrial fibrillation following radiofrequency catheter ablation of atrial fibrillation: clinical impact of continuous positive airway pressure therapy. Heart Rhythm. 2013;10:331-7.
10. Otto M, Belohlavek M, Romero-Corral A, et al. Comparison of cardiac structural and functional changes in obese otherwise healthy adults with versus without obstructive sleep apnea. Am J Cardiol. 2007;99:1298-302.
11. Kis Z, Muka T, Franco OH, et al. The short and long-term efficacy of pulmonary vein isolation as a sole treatment strategy for paroxysmal atrial fibrillation: a systematic review and meta-analysis. Curr Cardiol Rev. 2017 Jan 17. [Epub ahead of print].
12. Nakase K, Kollmar R, Lazar J, et al. Laryngospasm, central and obstructive apnea during seizures: defining pathophysiology for sudden death in a rat model. Epilepsy Res. 2016;128:126-39.
Atrial fibrillation (AF) is the most common cardiac arrhythmia encountered in clinical practice and is associated with increased morbidity and mortality due to thromboembolism, stroke, and worsening of pre-existing heart failure. Both its incidence and prevalence are increasing as AF risk increases with advancing age.1 While the strategies of heart rate control and anticoagulation to lower stroke risk and rhythm control have been found comparable with regard to survival, many patients remain highly symptomatic because of palpitations and reduced cardiac output.1
Structural abnormalities of the atria, including fibrosis and dilation, accompanied by conduction abnormalities, provide the underlying substrate for AF. It is well established that AF episodes perpetuate atrial remodeling leading to more frequent and prolonged AF episodes. Hence, there is the long-standing notion that “AF begets AF.” While a variety of antiarrhythmic drugs have been employed over the years to prevent AF recurrences and to maintain sinus rhythm, their use has decreased over the past 2 decades due to their major side effects and their potential of proarrhythmia.
Since AF patients represent a heterogeneous group of patients with CV diseases of varying type and severity as well as comorbidities, it stands to reason that the pulmonary venous–left atrial junction may not be the sole culprit region of all cases of AF and that other anatomical locations might serve as triggers for AF.
In support of this notion are the results of the prospective multicenter study presented by Dr. Elad Anter at the annual International AF Symposium. This important study is consistent with and expands upon prior studies that have suggested that sites within the atria remote from the pulmonary veins may serve as triggers for AF, rather than lower technical success of pulmonary vein ablation.5 It further highlights the importance of fibrosis and associated electrical dispersion to the pathogenesis of AF.6 However, the recommendation that patients with AF be screened for OSA is not new, as nearly half of patients with AF also have OSA.7 While AF and OSA share common risk factors/comorbidities such as male gender, obesity, hypertension, coronary artery disease, and congestive heart failure, OSA has been found to be an independent risk factor for AF development.
It is important to know whether OSA was treated, as the presence of OSA raises the risk of AF recurrence and OSA treatment decreases AF recurrence after ablation.8,9 Conversely, in the setting of OSA, AF is more resistive to rhythm control. Enhanced vagal activation, elevated sympathetic tone, and oxidative stresses due to oxygen desaturation and left atrial distension have all been implicated in the pathogenesis linking OSA to the development of AF. Repeated increases in upper airway resistance during airway obstruction have been shown to lead to atrial stretch, dilation, and fibrosis.10 Since patients with heart failure, coronary artery disease, and other underlying causes for AF were excluded from the onset, the results may not be applicable to a large segment of AF patients. Exclusion of underlying cardiac conditions potentially raised the yield of patients found to have OSA and the potential value of OSA screening. Of note: Less than half of patients that were enrolled had complete data for analysis, which may further limit applicability of the study findings. All patients had paroxysmal AF and were in sinus rhythm while the mapping procedure was performed, leaving questions as to how to approach patients presenting acutely with persistent or long standing AF, or those recently treated with antiarrhythmic therapy. Also, since arrhythmia-free survival decreases from 1 to 5 years after AF ablation, and short-time success rates do not predict longer success rates, the present study results should be interpreted with cautious optimism.11
However, these limitations should not detract from the major implications of the study. In the setting of AF, OSA should be clinically suspected not only because of the frequent coexistence of the two disorders but because the presence of OSA should prompt electrophysiologists to consider non–pulmonary vein triggers of AF prior to ablation attempts. The consideration of alternative ablation sites might help to explain the lack of ablation procedure endpoints to predict long-term success of ablation and holds promise for increasing technical success rates. Given that airway obstruction may occur in other clinical settings such as seizure-induced laryngospasm and that seizures may induce arrhythmias and sudden death, there is potential for non–pulmonary vein sites to trigger AF and other arrhythmias in settings other than OSA as well.12 Whether other disease states are associated with a higher likelihood of non-pulmonary veins trigger sites also merits further study. Moreover, this study underscores the notion that with regard to AF ablation, “no one site fits all” and “clinical mapping” may serve as a valuable adjunct to anatomical mapping. It also serves as a reminder of the multidisciplinary nature of Chest Medicine and the need of a team oriented approach..
References
1. Iwasaki YK, Nishida K, Kato T, Nattel S. Atrial fibrillation pathophysiology: implications for management. Circulation. 2011;124:2264-74.
2. Verma A, Jiang CY, Betts TR, et al. Approaches to catheter ablation for persistent atrial fibrillation. N Engl J Med. 2015;372:1812-22.
3. Kuck KH, Brugada J, Fürnkranz A, et al. Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med. 2016;374:2235-45.
4. Calkins H, Reynolds MR, Spector P, et al. Treatment of atrial fibrillation with antiarrhythmic drugs or radiofrequency ablation: two systematic literature reviews and meta-analyses. Circ Arrhythm Electrophysiol. 2009;2:349-61.
5. Narayan SM, Krummen DE, Shivkumar K, et al. Treatment of atrial fibrillation by the ablation of localized sources: CONFIRM (Conventional Ablation for Atrial Fibrillation With or Without Focal Impulse and Rotor Modulation) trial. J Am Coll Cardiol. 2012;60:628-36.
6. Kottkamp H, Berg J, Bender R, et al. Box Isolation of Fibrotic Areas (BIFA): a patient-tailored substrate modified application approach for ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2016;27:22-30.
7. Stevenson IH, Teichtahl H, Cunnington D, et al. Prevalence of sleep disordered breathing in paroxysmal and persistent atrial fibrillation patients with normal left ventricular function. Eur Heart J. 2008;29:1662-9.
8. Fein AS, Shvilkin A, Shah D, et al. Treatment of obstructive sleep apnea reduces the risk of atrial fibrillation recurrence after catheter ablation. J Am Coll Cardiol. 2013;62:300-5.
9. Naruse Y, Tada H, Satoh M, et al. Concomitant obstructive sleep apnea increases the recurrence of atrial fibrillation following radiofrequency catheter ablation of atrial fibrillation: clinical impact of continuous positive airway pressure therapy. Heart Rhythm. 2013;10:331-7.
10. Otto M, Belohlavek M, Romero-Corral A, et al. Comparison of cardiac structural and functional changes in obese otherwise healthy adults with versus without obstructive sleep apnea. Am J Cardiol. 2007;99:1298-302.
11. Kis Z, Muka T, Franco OH, et al. The short and long-term efficacy of pulmonary vein isolation as a sole treatment strategy for paroxysmal atrial fibrillation: a systematic review and meta-analysis. Curr Cardiol Rev. 2017 Jan 17. [Epub ahead of print].
12. Nakase K, Kollmar R, Lazar J, et al. Laryngospasm, central and obstructive apnea during seizures: defining pathophysiology for sudden death in a rat model. Epilepsy Res. 2016;128:126-39.
Atrial fibrillation (AF) is the most common cardiac arrhythmia encountered in clinical practice and is associated with increased morbidity and mortality due to thromboembolism, stroke, and worsening of pre-existing heart failure. Both its incidence and prevalence are increasing as AF risk increases with advancing age.1 While the strategies of heart rate control and anticoagulation to lower stroke risk and rhythm control have been found comparable with regard to survival, many patients remain highly symptomatic because of palpitations and reduced cardiac output.1
Structural abnormalities of the atria, including fibrosis and dilation, accompanied by conduction abnormalities, provide the underlying substrate for AF. It is well established that AF episodes perpetuate atrial remodeling leading to more frequent and prolonged AF episodes. Hence, there is the long-standing notion that “AF begets AF.” While a variety of antiarrhythmic drugs have been employed over the years to prevent AF recurrences and to maintain sinus rhythm, their use has decreased over the past 2 decades due to their major side effects and their potential of proarrhythmia.
Since AF patients represent a heterogeneous group of patients with CV diseases of varying type and severity as well as comorbidities, it stands to reason that the pulmonary venous–left atrial junction may not be the sole culprit region of all cases of AF and that other anatomical locations might serve as triggers for AF.
In support of this notion are the results of the prospective multicenter study presented by Dr. Elad Anter at the annual International AF Symposium. This important study is consistent with and expands upon prior studies that have suggested that sites within the atria remote from the pulmonary veins may serve as triggers for AF, rather than lower technical success of pulmonary vein ablation.5 It further highlights the importance of fibrosis and associated electrical dispersion to the pathogenesis of AF.6 However, the recommendation that patients with AF be screened for OSA is not new, as nearly half of patients with AF also have OSA.7 While AF and OSA share common risk factors/comorbidities such as male gender, obesity, hypertension, coronary artery disease, and congestive heart failure, OSA has been found to be an independent risk factor for AF development.
It is important to know whether OSA was treated, as the presence of OSA raises the risk of AF recurrence and OSA treatment decreases AF recurrence after ablation.8,9 Conversely, in the setting of OSA, AF is more resistive to rhythm control. Enhanced vagal activation, elevated sympathetic tone, and oxidative stresses due to oxygen desaturation and left atrial distension have all been implicated in the pathogenesis linking OSA to the development of AF. Repeated increases in upper airway resistance during airway obstruction have been shown to lead to atrial stretch, dilation, and fibrosis.10 Since patients with heart failure, coronary artery disease, and other underlying causes for AF were excluded from the onset, the results may not be applicable to a large segment of AF patients. Exclusion of underlying cardiac conditions potentially raised the yield of patients found to have OSA and the potential value of OSA screening. Of note: Less than half of patients that were enrolled had complete data for analysis, which may further limit applicability of the study findings. All patients had paroxysmal AF and were in sinus rhythm while the mapping procedure was performed, leaving questions as to how to approach patients presenting acutely with persistent or long standing AF, or those recently treated with antiarrhythmic therapy. Also, since arrhythmia-free survival decreases from 1 to 5 years after AF ablation, and short-time success rates do not predict longer success rates, the present study results should be interpreted with cautious optimism.11
However, these limitations should not detract from the major implications of the study. In the setting of AF, OSA should be clinically suspected not only because of the frequent coexistence of the two disorders but because the presence of OSA should prompt electrophysiologists to consider non–pulmonary vein triggers of AF prior to ablation attempts. The consideration of alternative ablation sites might help to explain the lack of ablation procedure endpoints to predict long-term success of ablation and holds promise for increasing technical success rates. Given that airway obstruction may occur in other clinical settings such as seizure-induced laryngospasm and that seizures may induce arrhythmias and sudden death, there is potential for non–pulmonary vein sites to trigger AF and other arrhythmias in settings other than OSA as well.12 Whether other disease states are associated with a higher likelihood of non-pulmonary veins trigger sites also merits further study. Moreover, this study underscores the notion that with regard to AF ablation, “no one site fits all” and “clinical mapping” may serve as a valuable adjunct to anatomical mapping. It also serves as a reminder of the multidisciplinary nature of Chest Medicine and the need of a team oriented approach..
References
1. Iwasaki YK, Nishida K, Kato T, Nattel S. Atrial fibrillation pathophysiology: implications for management. Circulation. 2011;124:2264-74.
2. Verma A, Jiang CY, Betts TR, et al. Approaches to catheter ablation for persistent atrial fibrillation. N Engl J Med. 2015;372:1812-22.
3. Kuck KH, Brugada J, Fürnkranz A, et al. Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med. 2016;374:2235-45.
4. Calkins H, Reynolds MR, Spector P, et al. Treatment of atrial fibrillation with antiarrhythmic drugs or radiofrequency ablation: two systematic literature reviews and meta-analyses. Circ Arrhythm Electrophysiol. 2009;2:349-61.
5. Narayan SM, Krummen DE, Shivkumar K, et al. Treatment of atrial fibrillation by the ablation of localized sources: CONFIRM (Conventional Ablation for Atrial Fibrillation With or Without Focal Impulse and Rotor Modulation) trial. J Am Coll Cardiol. 2012;60:628-36.
6. Kottkamp H, Berg J, Bender R, et al. Box Isolation of Fibrotic Areas (BIFA): a patient-tailored substrate modified application approach for ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2016;27:22-30.
7. Stevenson IH, Teichtahl H, Cunnington D, et al. Prevalence of sleep disordered breathing in paroxysmal and persistent atrial fibrillation patients with normal left ventricular function. Eur Heart J. 2008;29:1662-9.
8. Fein AS, Shvilkin A, Shah D, et al. Treatment of obstructive sleep apnea reduces the risk of atrial fibrillation recurrence after catheter ablation. J Am Coll Cardiol. 2013;62:300-5.
9. Naruse Y, Tada H, Satoh M, et al. Concomitant obstructive sleep apnea increases the recurrence of atrial fibrillation following radiofrequency catheter ablation of atrial fibrillation: clinical impact of continuous positive airway pressure therapy. Heart Rhythm. 2013;10:331-7.
10. Otto M, Belohlavek M, Romero-Corral A, et al. Comparison of cardiac structural and functional changes in obese otherwise healthy adults with versus without obstructive sleep apnea. Am J Cardiol. 2007;99:1298-302.
11. Kis Z, Muka T, Franco OH, et al. The short and long-term efficacy of pulmonary vein isolation as a sole treatment strategy for paroxysmal atrial fibrillation: a systematic review and meta-analysis. Curr Cardiol Rev. 2017 Jan 17. [Epub ahead of print].
12. Nakase K, Kollmar R, Lazar J, et al. Laryngospasm, central and obstructive apnea during seizures: defining pathophysiology for sudden death in a rat model. Epilepsy Res. 2016;128:126-39.
ORLANDO – Patients with atrial fibrillation (AF) should be screened for obstructive sleep apnea (OSA), because this information may be useful in guiding ablation strategies, according to results of a prospective study.
The study, which associated OSA in AF with a high relative rate of non–pulmonary vein (PV) triggers, has contributed to the “growing body of evidence implicating sleep apnea in atrial remodeling and promotion of the AF substrate,” Elad Anter, MD, associate director of the clinical electrophysiology laboratory at Beth Israel Deaconess Medical Center, Boston, reported at the annual International AF Symposium.
Despite the close association between OSA and AF, it has been unclear whether OSA is a causative factor. Dr. Anter suggested that mechanistic association is strengthening, however.
It has been hypothesized that OSA generates AF substrate through negative intrathoracic pressure changes and autonomic nervous system activation. But Dr. Anter reported that there is more recent and compelling evidence that the repetitive occlusions produced by OSA result in remodeling of the atria, producing scar tissue that slows conduction and produces susceptibility to reentry AF.
A newly completed prospective multicenter study adds support to this latter hypothesis. In the protocol, patients with paroxysmal AF scheduled for ablation were required to undergo a sleep study, an AF mapping study, and follow-up for at least 12 months. A known history of OSA was an exclusion criterion. To isolate the effect of OSA, there were exclusions for other major etiologies for AF, such as heart failure or coronary artery disease.
The AF mapping was conducted when patients were in sinus rhythm “to evaluate the baseline atrial substrate and avoid measurements related to acute electrical remodeling,” Dr. Anter explained.
Of 172 patients initially enrolled, 133 completed the sleep study, 118 completed the mapping study, and 110 completed both and were followed for at least 12 months. Of these, 43 patients without OSA were compared with 43 patients with OSA defined as an apnea-hypopnea index (AHI) of at least 15. Patients in the two groups did not differ significantly for relevant characteristics, such as body mass index (BMI), age, presence of hypertension, or duration of AF; but the left atrial (LA) volume was significantly greater (P = .01) in those with OSA than those without.
Even though the prevalence of voltage abnormalities was higher in the OSA group for the right (P = .01) and left atria (P = .0001) before ablation, the prevalence of PV triggers (63% vs. 65%), non-PV triggers (19% vs. 12%) and noninducible triggers (19% vs. 23%) were similar.
After ablation, PV triggers were no longer inducible in either group, but there was a striking difference in inducible non-PV triggers. While only 11.6% remained inducible in the non-OSA group, 41.8% (P = .003) remained inducible in the OSA patients.
“AF triggers in OSA were most commonly located at the LA septum, at the zone of low voltage and abnormal electrograms, as determined during sinus rhythm,” Dr. Anter reported. “Ablation of these triggers at the zone of tissue abnormality in the OSA patients resulted in termination of AF in 9 (64.2%) of the 14 patients.”
Overall, at the end of 12 months, 79% of those without OSA remained in arrhythmia-free survival, versus 65.1% of the group with OSA that were treated with PV isolation alone.
The lower rate of success in the OSA group shows the importance of specifically directing ablation to the areas of low voltage and slow conduction in the left anterior septum that Dr. Anter indicated otherwise would be missed.
“These zones are a common source of extra-PV triggers and localized circuits or rotors of AF in OSA patients,” he reported. “Ablation of these low voltage zones is associated with improved clinical outcome in OSA patients with paroxysmal AF.”
The data, which Dr. Anter said are consistent with a growing body of work regarding the relationship of OSA and AF, provided the basis for suggesting that AF patients undergo routine screening for OSA.
In patients with OSA, ablation of PV triggers alone even in paroxysmal PAF “may not be sufficient,” he cautioned. “Evaluation of non-PV triggers should also be performed.”
Dr. Anter reported financial relationships with Biosense Webster and Boston Scientific.
ORLANDO – Patients with atrial fibrillation (AF) should be screened for obstructive sleep apnea (OSA), because this information may be useful in guiding ablation strategies, according to results of a prospective study.
The study, which associated OSA in AF with a high relative rate of non–pulmonary vein (PV) triggers, has contributed to the “growing body of evidence implicating sleep apnea in atrial remodeling and promotion of the AF substrate,” Elad Anter, MD, associate director of the clinical electrophysiology laboratory at Beth Israel Deaconess Medical Center, Boston, reported at the annual International AF Symposium.
Despite the close association between OSA and AF, it has been unclear whether OSA is a causative factor. Dr. Anter suggested that mechanistic association is strengthening, however.
It has been hypothesized that OSA generates AF substrate through negative intrathoracic pressure changes and autonomic nervous system activation. But Dr. Anter reported that there is more recent and compelling evidence that the repetitive occlusions produced by OSA result in remodeling of the atria, producing scar tissue that slows conduction and produces susceptibility to reentry AF.
A newly completed prospective multicenter study adds support to this latter hypothesis. In the protocol, patients with paroxysmal AF scheduled for ablation were required to undergo a sleep study, an AF mapping study, and follow-up for at least 12 months. A known history of OSA was an exclusion criterion. To isolate the effect of OSA, there were exclusions for other major etiologies for AF, such as heart failure or coronary artery disease.
The AF mapping was conducted when patients were in sinus rhythm “to evaluate the baseline atrial substrate and avoid measurements related to acute electrical remodeling,” Dr. Anter explained.
Of 172 patients initially enrolled, 133 completed the sleep study, 118 completed the mapping study, and 110 completed both and were followed for at least 12 months. Of these, 43 patients without OSA were compared with 43 patients with OSA defined as an apnea-hypopnea index (AHI) of at least 15. Patients in the two groups did not differ significantly for relevant characteristics, such as body mass index (BMI), age, presence of hypertension, or duration of AF; but the left atrial (LA) volume was significantly greater (P = .01) in those with OSA than those without.
Even though the prevalence of voltage abnormalities was higher in the OSA group for the right (P = .01) and left atria (P = .0001) before ablation, the prevalence of PV triggers (63% vs. 65%), non-PV triggers (19% vs. 12%) and noninducible triggers (19% vs. 23%) were similar.
After ablation, PV triggers were no longer inducible in either group, but there was a striking difference in inducible non-PV triggers. While only 11.6% remained inducible in the non-OSA group, 41.8% (P = .003) remained inducible in the OSA patients.
“AF triggers in OSA were most commonly located at the LA septum, at the zone of low voltage and abnormal electrograms, as determined during sinus rhythm,” Dr. Anter reported. “Ablation of these triggers at the zone of tissue abnormality in the OSA patients resulted in termination of AF in 9 (64.2%) of the 14 patients.”
Overall, at the end of 12 months, 79% of those without OSA remained in arrhythmia-free survival, versus 65.1% of the group with OSA that were treated with PV isolation alone.
The lower rate of success in the OSA group shows the importance of specifically directing ablation to the areas of low voltage and slow conduction in the left anterior septum that Dr. Anter indicated otherwise would be missed.
“These zones are a common source of extra-PV triggers and localized circuits or rotors of AF in OSA patients,” he reported. “Ablation of these low voltage zones is associated with improved clinical outcome in OSA patients with paroxysmal AF.”
The data, which Dr. Anter said are consistent with a growing body of work regarding the relationship of OSA and AF, provided the basis for suggesting that AF patients undergo routine screening for OSA.
In patients with OSA, ablation of PV triggers alone even in paroxysmal PAF “may not be sufficient,” he cautioned. “Evaluation of non-PV triggers should also be performed.”
Dr. Anter reported financial relationships with Biosense Webster and Boston Scientific.
Key clinical point: Atrial fibrillation associated with sleep apnea appears to have features that should be addressed specifically for sustained rhythm control.
Major finding: AF patients with sleep apnea have more non–pulmonary vein triggers after ablation than do those without sleep apnea (41.8% vs. 11.6%).
Data source: A prospective multicenter observational study.
Disclosures: Dr. Anter reported financial relationships with Biosense Webster and Boston Scientific.
Flu activity up slightly, but still down from seasonal peak
After rising to a high point for the season in the last week of 2016, influenza activity dropped a bit in the first week of the new year but then rose again in the second week, according to the Centers for Disease Control and Prevention.
As measured by outpatient visits for influenza-like illness (ILI), activity slipped from 3.4% at the end of 2016 to 3.2% for the week ending Jan. 7 but then ticked up to 3.3% for the week ending Jan. 14, the CDC reported. The national baseline level of outpatient visits is 2.2% for ILI, which is defined as fever (temperature of 100° F or greater) and cough and/or sore throat.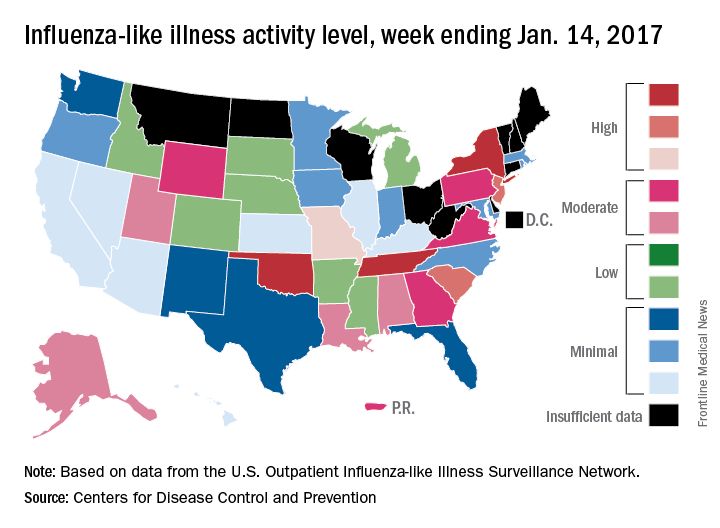
Two influenza-related pediatric deaths were reported for the week ending Jan. 14, although both occurred in earlier weeks: one during the week ending Dec. 10 and one during the week ending Jan. 7. So far for the 2016-2017 season, a total of five flu-related pediatric deaths have been reported, according to the CDC.
After rising to a high point for the season in the last week of 2016, influenza activity dropped a bit in the first week of the new year but then rose again in the second week, according to the Centers for Disease Control and Prevention.
As measured by outpatient visits for influenza-like illness (ILI), activity slipped from 3.4% at the end of 2016 to 3.2% for the week ending Jan. 7 but then ticked up to 3.3% for the week ending Jan. 14, the CDC reported. The national baseline level of outpatient visits is 2.2% for ILI, which is defined as fever (temperature of 100° F or greater) and cough and/or sore throat.
Two influenza-related pediatric deaths were reported for the week ending Jan. 14, although both occurred in earlier weeks: one during the week ending Dec. 10 and one during the week ending Jan. 7. So far for the 2016-2017 season, a total of five flu-related pediatric deaths have been reported, according to the CDC.
After rising to a high point for the season in the last week of 2016, influenza activity dropped a bit in the first week of the new year but then rose again in the second week, according to the Centers for Disease Control and Prevention.
As measured by outpatient visits for influenza-like illness (ILI), activity slipped from 3.4% at the end of 2016 to 3.2% for the week ending Jan. 7 but then ticked up to 3.3% for the week ending Jan. 14, the CDC reported. The national baseline level of outpatient visits is 2.2% for ILI, which is defined as fever (temperature of 100° F or greater) and cough and/or sore throat.
Two influenza-related pediatric deaths were reported for the week ending Jan. 14, although both occurred in earlier weeks: one during the week ending Dec. 10 and one during the week ending Jan. 7. So far for the 2016-2017 season, a total of five flu-related pediatric deaths have been reported, according to the CDC.
Survey finds link between e-cigarette use and high-risk behaviors
High school students who use electronic vapor products (EVPs), whether alone or in combination with cigarette smoking, are more likely to engage in violence, substance abuse, and other high-risk behaviors, compared with nonusers, according to the results of a national survey.
“Given that EVPs are relatively new to the U.S. marketplace, little is known about the use of these products in the context of other health behaviors, which can persist throughout life and contribute to significant morbidity and mortality during adolescence and adulthood,” Zewditu Demissie, PhD, and her associates wrote in a study published online in the Jan. 23, 2017, issue of Pediatrics. They went on to note that to date, “studies on the association between EVPs and health-risk behaviors among adolescents and young adults has been limited to examining the associations between e-cigarette and substance use. These studies have found that use of e-cigarettes was associated with alcohol use, binge drinking, and marijuana use.”
Of the 15,624 respondents, 74% reported that they did not smoke cigarettes or use EVPs, while 3% smoked cigarettes only, 16% used EVPs only, and 8% used both cigarettes and EVPs.
Compared with nonusers, cigarette-only smokers, EVP-only users, and dual users were significantly more likely to:
• Engage in a physical fight (prevalence ratio range, 1.7-2.9).
• Attempt suicide (PR range, 1.9-4.0).
• Currently drink alcohol (PR range, 2.6-3.3).
• Currently use marijuana (PR range, 3.5-5.2).
• Report nonmedical use of prescription drugs (PR range, 2.3-4.1).
• Be currently sexually active (PR range, 1.9-2.3).
“Engaging in health-risk behaviors did not generally differ between EVP-only users and cigarette-only smokers,” the researchers wrote. “However, cigarette-only smokers were significantly more likely than EVP-only users to attempt suicide, ever use synthetic marijuana, have four or more lifetime sexual partners, drink soda three or more times/day, and be physically active less than 7 days in the 7 days before the survey.”
Dr. Demissie and her associates concluded that the findings “underscore the importance of comprehensive efforts to address health-risk behaviors among adolescents, including prevention strategies focused on all forms of tobacco use, including EVPs. Additionally, educational and counseling efforts focusing on the harms associated with adolescent tobacco use, including EVPs, are critical.”
They acknowledged certain limitations of the study, including its observational design and the fact that Youth Risk Behavior Survey data are self-reported.
The investigators reported having no relevant financial disclosures.
“Recent longitudinal research has provided an unpleasant surprise: Among initial nonsmokers, those who use e-cigarettes are more likely to start smoking combustible cigarettes. This puts a somewhat different light on the situation. If e-cigarettes are without risk, it does not matter much if they attract new users. Being related to smoking onset, however, puts a behavioral risk into the picture. The finding of associations with other health-risk behaviors augments concern because, as the authors note, the odds of experiencing poor health increase with the addition of each unhealthy behavior. And importantly, Demissie et al. show that among adolescent smokers, those who use e-cigarettes actually smoke more frequently, an effect that is contrary to the hopes of harm reduction advocates and has now been found internationally.
“Are e-cigarettes going to replace traditional cigarettes, or are they operating to recruit a new audience of adolescents to tobacco products? Our wish is for the former. But at present the empirical evidence looks more like the latter. We need surveillance and mechanism research to understand what e-cigarettes will mean for youth risk status. However, there is enough evidence now to advocate programs for educating teenagers about e-cigarettes.”
Thomas A. Wills, PhD., is with the Cancer Prevention and Control Program at the University of Hawaii Cancer Center, Honolulu. His views are excerpted from a commentary published online in response to the study by Dr. Demissie et al. (Pediatrics. 2017 Jan 23. doi: 10.1542/peds.2016-3736). This work was supported by grants from the National Cancer Institute. Dr. Wills reported having no relevant financial disclosures.
“Recent longitudinal research has provided an unpleasant surprise: Among initial nonsmokers, those who use e-cigarettes are more likely to start smoking combustible cigarettes. This puts a somewhat different light on the situation. If e-cigarettes are without risk, it does not matter much if they attract new users. Being related to smoking onset, however, puts a behavioral risk into the picture. The finding of associations with other health-risk behaviors augments concern because, as the authors note, the odds of experiencing poor health increase with the addition of each unhealthy behavior. And importantly, Demissie et al. show that among adolescent smokers, those who use e-cigarettes actually smoke more frequently, an effect that is contrary to the hopes of harm reduction advocates and has now been found internationally.
“Are e-cigarettes going to replace traditional cigarettes, or are they operating to recruit a new audience of adolescents to tobacco products? Our wish is for the former. But at present the empirical evidence looks more like the latter. We need surveillance and mechanism research to understand what e-cigarettes will mean for youth risk status. However, there is enough evidence now to advocate programs for educating teenagers about e-cigarettes.”
Thomas A. Wills, PhD., is with the Cancer Prevention and Control Program at the University of Hawaii Cancer Center, Honolulu. His views are excerpted from a commentary published online in response to the study by Dr. Demissie et al. (Pediatrics. 2017 Jan 23. doi: 10.1542/peds.2016-3736). This work was supported by grants from the National Cancer Institute. Dr. Wills reported having no relevant financial disclosures.
“Recent longitudinal research has provided an unpleasant surprise: Among initial nonsmokers, those who use e-cigarettes are more likely to start smoking combustible cigarettes. This puts a somewhat different light on the situation. If e-cigarettes are without risk, it does not matter much if they attract new users. Being related to smoking onset, however, puts a behavioral risk into the picture. The finding of associations with other health-risk behaviors augments concern because, as the authors note, the odds of experiencing poor health increase with the addition of each unhealthy behavior. And importantly, Demissie et al. show that among adolescent smokers, those who use e-cigarettes actually smoke more frequently, an effect that is contrary to the hopes of harm reduction advocates and has now been found internationally.
“Are e-cigarettes going to replace traditional cigarettes, or are they operating to recruit a new audience of adolescents to tobacco products? Our wish is for the former. But at present the empirical evidence looks more like the latter. We need surveillance and mechanism research to understand what e-cigarettes will mean for youth risk status. However, there is enough evidence now to advocate programs for educating teenagers about e-cigarettes.”
Thomas A. Wills, PhD., is with the Cancer Prevention and Control Program at the University of Hawaii Cancer Center, Honolulu. His views are excerpted from a commentary published online in response to the study by Dr. Demissie et al. (Pediatrics. 2017 Jan 23. doi: 10.1542/peds.2016-3736). This work was supported by grants from the National Cancer Institute. Dr. Wills reported having no relevant financial disclosures.
High school students who use electronic vapor products (EVPs), whether alone or in combination with cigarette smoking, are more likely to engage in violence, substance abuse, and other high-risk behaviors, compared with nonusers, according to the results of a national survey.
“Given that EVPs are relatively new to the U.S. marketplace, little is known about the use of these products in the context of other health behaviors, which can persist throughout life and contribute to significant morbidity and mortality during adolescence and adulthood,” Zewditu Demissie, PhD, and her associates wrote in a study published online in the Jan. 23, 2017, issue of Pediatrics. They went on to note that to date, “studies on the association between EVPs and health-risk behaviors among adolescents and young adults has been limited to examining the associations between e-cigarette and substance use. These studies have found that use of e-cigarettes was associated with alcohol use, binge drinking, and marijuana use.”
Of the 15,624 respondents, 74% reported that they did not smoke cigarettes or use EVPs, while 3% smoked cigarettes only, 16% used EVPs only, and 8% used both cigarettes and EVPs.
Compared with nonusers, cigarette-only smokers, EVP-only users, and dual users were significantly more likely to:
• Engage in a physical fight (prevalence ratio range, 1.7-2.9).
• Attempt suicide (PR range, 1.9-4.0).
• Currently drink alcohol (PR range, 2.6-3.3).
• Currently use marijuana (PR range, 3.5-5.2).
• Report nonmedical use of prescription drugs (PR range, 2.3-4.1).
• Be currently sexually active (PR range, 1.9-2.3).
“Engaging in health-risk behaviors did not generally differ between EVP-only users and cigarette-only smokers,” the researchers wrote. “However, cigarette-only smokers were significantly more likely than EVP-only users to attempt suicide, ever use synthetic marijuana, have four or more lifetime sexual partners, drink soda three or more times/day, and be physically active less than 7 days in the 7 days before the survey.”
Dr. Demissie and her associates concluded that the findings “underscore the importance of comprehensive efforts to address health-risk behaviors among adolescents, including prevention strategies focused on all forms of tobacco use, including EVPs. Additionally, educational and counseling efforts focusing on the harms associated with adolescent tobacco use, including EVPs, are critical.”
They acknowledged certain limitations of the study, including its observational design and the fact that Youth Risk Behavior Survey data are self-reported.
The investigators reported having no relevant financial disclosures.
High school students who use electronic vapor products (EVPs), whether alone or in combination with cigarette smoking, are more likely to engage in violence, substance abuse, and other high-risk behaviors, compared with nonusers, according to the results of a national survey.
“Given that EVPs are relatively new to the U.S. marketplace, little is known about the use of these products in the context of other health behaviors, which can persist throughout life and contribute to significant morbidity and mortality during adolescence and adulthood,” Zewditu Demissie, PhD, and her associates wrote in a study published online in the Jan. 23, 2017, issue of Pediatrics. They went on to note that to date, “studies on the association between EVPs and health-risk behaviors among adolescents and young adults has been limited to examining the associations between e-cigarette and substance use. These studies have found that use of e-cigarettes was associated with alcohol use, binge drinking, and marijuana use.”
Of the 15,624 respondents, 74% reported that they did not smoke cigarettes or use EVPs, while 3% smoked cigarettes only, 16% used EVPs only, and 8% used both cigarettes and EVPs.
Compared with nonusers, cigarette-only smokers, EVP-only users, and dual users were significantly more likely to:
• Engage in a physical fight (prevalence ratio range, 1.7-2.9).
• Attempt suicide (PR range, 1.9-4.0).
• Currently drink alcohol (PR range, 2.6-3.3).
• Currently use marijuana (PR range, 3.5-5.2).
• Report nonmedical use of prescription drugs (PR range, 2.3-4.1).
• Be currently sexually active (PR range, 1.9-2.3).
“Engaging in health-risk behaviors did not generally differ between EVP-only users and cigarette-only smokers,” the researchers wrote. “However, cigarette-only smokers were significantly more likely than EVP-only users to attempt suicide, ever use synthetic marijuana, have four or more lifetime sexual partners, drink soda three or more times/day, and be physically active less than 7 days in the 7 days before the survey.”
Dr. Demissie and her associates concluded that the findings “underscore the importance of comprehensive efforts to address health-risk behaviors among adolescents, including prevention strategies focused on all forms of tobacco use, including EVPs. Additionally, educational and counseling efforts focusing on the harms associated with adolescent tobacco use, including EVPs, are critical.”
They acknowledged certain limitations of the study, including its observational design and the fact that Youth Risk Behavior Survey data are self-reported.
The investigators reported having no relevant financial disclosures.
FROM PEDIATRICS
Key clinical point:
Major finding: Compared with nonusers, cigarette-only smokers, electronic vapor products–only users, and dual users were significantly more likely to engage in a physical fight (prevalence ratio range, 1.7-2.3), to currently use marijuana (PR range, 3.5-5.2), and to be currently sexually active (PR range, 1.9-2.3).
Data source: An analysis of responses from 15,624 high school students who completed the 2015 national Youth Risk Behavior Survey.
Disclosures: The researchers reported having no relevant financial disclosures.
Childhood PCV program produces overall protection
Childhood pneumococcal conjugate vaccines continue to indirectly produce widespread societal protection against invasive pneumococcal disease, a review and meta-analysis showed.
In fact, the reviewed studies suggest that the use of these vaccines in children can lead to an overall 90% drop in invasive pneumococcal disease within fewer than 10 years.
Herd immunity appears to be at work, the review authors said. The effect is so powerful that the findings raise questions about “the merit of offering [the 13-valent pneumococcal vaccine] in older groups” in places that have a children’s pneumococcal conjugate vaccine (PCV) program, the investigators said.
U.S. guidelines recommend vaccinations for older people, although the recommendations are up for review in 2018.
According to the review, childhood PCVs have had a tremendous impact since a seven-valent version (PCV7) was first released in 2000. “In vaccinated young children, disease due to serotypes included in the vaccines has been reduced to negligible levels,” the authors wrote.
But unvaccinated people, especially the elderly, remain susceptible.
The review authors, led by Tinevimbo Shiri, PhD, of the University of Warwick, Coventry, England, updated a 2013 systemic review (Vaccine. 2013 Dec 17;32[1]:133-45). They focused on studies from 1994 to 2016 that examined the effects of introducing PCV in children.
A total of 242 studies were included in the meta-analysis, published in the January issue of Lancet Global Health (2017 Jan;5[1]:e51-e9), including 70 from the previous review. Of these, only 9 (4%) were performed in poor or middle-income countries, with most of the rest having been done in North America (42%) and Europe (38%).
The researchers found that “[herd] immunity effects continued to accumulate over time and reduced disease due to PCV7 serotypes, for which follow-up data have generally been available for the longest period, with a 90% average reduction after about 9 years.”
Specifically, the review estimated it would take 8.9 years for a 90% reduction in invasive pneumococcal disease for grouped serotypes in the PCV7 and 9.5 years for the extra six grouped serotypes in the 13-valent PCV. The latter vaccine was introduced in 2010.
The researchers found evidence of a similar annual reduction in disease linked to grouped serotypes in the 23-valent pneumococcal polysaccharide vaccine in adults aged 19 and up. They noted that the 11 serotypes contained in PPV23 but not in PCV13 “did not change invasive pneumococcal disease at any age.”
The investigators added: “In countries with mature pediatric PCV programmes such as Canada, Germany, the Netherlands, the U.K., and the U.S.A., invasive pneumococcal disease due to PCV7 serotypes has been nearly eliminated through indirect protection - i.e., the average incidence of PCV7-invasive pneumococcal disease after nearly a decade of PCV7 use is less than 10 per 100,000 people. In these countries, consistent decreases in vaccine-type adult community-acquired pneumonia (CAP) or meningitis, and nonbacteraemic CAP, have been observed, indicating substantial indirect protection effects against noninvasive disease from childhood vaccination.”
The review authors noted that a major “evidence gap” in the effectiveness of childhood PCV programs in low-income countries exists. “Because these countries are increasingly undertaking childhood vaccination programs, research to assess the indirect effects in these settings is particularly relevant,” they wrote.
The review’s limitations include the possibility that the results could be thrown off by variations across nations in areas like diagnostic protocols, surveillance, and outcome measures.
The authors of the review, funded by the Policy Research Program of England’s Department of Health, reported no relevant financial disclosures.
The impact of pneumococcal conjugate vaccines has been hampered by serotypes that they don’t address, said David Goldblatt, PhD, MBChB, of the Great Ormond Street Institute of Child Health and University College London, in a commentary accompanying this review and meta-analysis (Lancet Glob Health. 2017 Jan;5[1]:e6-e7).
“Data from this meta-analysis have shown an overall reduction of invasive pneumococcal disease in all unvaccinated age groups of just 1%. … New extended-valency vaccines will be required to halt this erosion of PCV impact,” he wrote.
Dr. Goldblatt reported receiving grants and personal fees from GlaxoSmithKline, Merck, Sharpe, and Dohme and a publication with Pfizer.
The impact of pneumococcal conjugate vaccines has been hampered by serotypes that they don’t address, said David Goldblatt, PhD, MBChB, of the Great Ormond Street Institute of Child Health and University College London, in a commentary accompanying this review and meta-analysis (Lancet Glob Health. 2017 Jan;5[1]:e6-e7).
“Data from this meta-analysis have shown an overall reduction of invasive pneumococcal disease in all unvaccinated age groups of just 1%. … New extended-valency vaccines will be required to halt this erosion of PCV impact,” he wrote.
Dr. Goldblatt reported receiving grants and personal fees from GlaxoSmithKline, Merck, Sharpe, and Dohme and a publication with Pfizer.
The impact of pneumococcal conjugate vaccines has been hampered by serotypes that they don’t address, said David Goldblatt, PhD, MBChB, of the Great Ormond Street Institute of Child Health and University College London, in a commentary accompanying this review and meta-analysis (Lancet Glob Health. 2017 Jan;5[1]:e6-e7).
“Data from this meta-analysis have shown an overall reduction of invasive pneumococcal disease in all unvaccinated age groups of just 1%. … New extended-valency vaccines will be required to halt this erosion of PCV impact,” he wrote.
Dr. Goldblatt reported receiving grants and personal fees from GlaxoSmithKline, Merck, Sharpe, and Dohme and a publication with Pfizer.
Childhood pneumococcal conjugate vaccines continue to indirectly produce widespread societal protection against invasive pneumococcal disease, a review and meta-analysis showed.
In fact, the reviewed studies suggest that the use of these vaccines in children can lead to an overall 90% drop in invasive pneumococcal disease within fewer than 10 years.
Herd immunity appears to be at work, the review authors said. The effect is so powerful that the findings raise questions about “the merit of offering [the 13-valent pneumococcal vaccine] in older groups” in places that have a children’s pneumococcal conjugate vaccine (PCV) program, the investigators said.
U.S. guidelines recommend vaccinations for older people, although the recommendations are up for review in 2018.
According to the review, childhood PCVs have had a tremendous impact since a seven-valent version (PCV7) was first released in 2000. “In vaccinated young children, disease due to serotypes included in the vaccines has been reduced to negligible levels,” the authors wrote.
But unvaccinated people, especially the elderly, remain susceptible.
The review authors, led by Tinevimbo Shiri, PhD, of the University of Warwick, Coventry, England, updated a 2013 systemic review (Vaccine. 2013 Dec 17;32[1]:133-45). They focused on studies from 1994 to 2016 that examined the effects of introducing PCV in children.
A total of 242 studies were included in the meta-analysis, published in the January issue of Lancet Global Health (2017 Jan;5[1]:e51-e9), including 70 from the previous review. Of these, only 9 (4%) were performed in poor or middle-income countries, with most of the rest having been done in North America (42%) and Europe (38%).
The researchers found that “[herd] immunity effects continued to accumulate over time and reduced disease due to PCV7 serotypes, for which follow-up data have generally been available for the longest period, with a 90% average reduction after about 9 years.”
Specifically, the review estimated it would take 8.9 years for a 90% reduction in invasive pneumococcal disease for grouped serotypes in the PCV7 and 9.5 years for the extra six grouped serotypes in the 13-valent PCV. The latter vaccine was introduced in 2010.
The researchers found evidence of a similar annual reduction in disease linked to grouped serotypes in the 23-valent pneumococcal polysaccharide vaccine in adults aged 19 and up. They noted that the 11 serotypes contained in PPV23 but not in PCV13 “did not change invasive pneumococcal disease at any age.”
The investigators added: “In countries with mature pediatric PCV programmes such as Canada, Germany, the Netherlands, the U.K., and the U.S.A., invasive pneumococcal disease due to PCV7 serotypes has been nearly eliminated through indirect protection - i.e., the average incidence of PCV7-invasive pneumococcal disease after nearly a decade of PCV7 use is less than 10 per 100,000 people. In these countries, consistent decreases in vaccine-type adult community-acquired pneumonia (CAP) or meningitis, and nonbacteraemic CAP, have been observed, indicating substantial indirect protection effects against noninvasive disease from childhood vaccination.”
The review authors noted that a major “evidence gap” in the effectiveness of childhood PCV programs in low-income countries exists. “Because these countries are increasingly undertaking childhood vaccination programs, research to assess the indirect effects in these settings is particularly relevant,” they wrote.
The review’s limitations include the possibility that the results could be thrown off by variations across nations in areas like diagnostic protocols, surveillance, and outcome measures.
The authors of the review, funded by the Policy Research Program of England’s Department of Health, reported no relevant financial disclosures.
Childhood pneumococcal conjugate vaccines continue to indirectly produce widespread societal protection against invasive pneumococcal disease, a review and meta-analysis showed.
In fact, the reviewed studies suggest that the use of these vaccines in children can lead to an overall 90% drop in invasive pneumococcal disease within fewer than 10 years.
Herd immunity appears to be at work, the review authors said. The effect is so powerful that the findings raise questions about “the merit of offering [the 13-valent pneumococcal vaccine] in older groups” in places that have a children’s pneumococcal conjugate vaccine (PCV) program, the investigators said.
U.S. guidelines recommend vaccinations for older people, although the recommendations are up for review in 2018.
According to the review, childhood PCVs have had a tremendous impact since a seven-valent version (PCV7) was first released in 2000. “In vaccinated young children, disease due to serotypes included in the vaccines has been reduced to negligible levels,” the authors wrote.
But unvaccinated people, especially the elderly, remain susceptible.
The review authors, led by Tinevimbo Shiri, PhD, of the University of Warwick, Coventry, England, updated a 2013 systemic review (Vaccine. 2013 Dec 17;32[1]:133-45). They focused on studies from 1994 to 2016 that examined the effects of introducing PCV in children.
A total of 242 studies were included in the meta-analysis, published in the January issue of Lancet Global Health (2017 Jan;5[1]:e51-e9), including 70 from the previous review. Of these, only 9 (4%) were performed in poor or middle-income countries, with most of the rest having been done in North America (42%) and Europe (38%).
The researchers found that “[herd] immunity effects continued to accumulate over time and reduced disease due to PCV7 serotypes, for which follow-up data have generally been available for the longest period, with a 90% average reduction after about 9 years.”
Specifically, the review estimated it would take 8.9 years for a 90% reduction in invasive pneumococcal disease for grouped serotypes in the PCV7 and 9.5 years for the extra six grouped serotypes in the 13-valent PCV. The latter vaccine was introduced in 2010.
The researchers found evidence of a similar annual reduction in disease linked to grouped serotypes in the 23-valent pneumococcal polysaccharide vaccine in adults aged 19 and up. They noted that the 11 serotypes contained in PPV23 but not in PCV13 “did not change invasive pneumococcal disease at any age.”
The investigators added: “In countries with mature pediatric PCV programmes such as Canada, Germany, the Netherlands, the U.K., and the U.S.A., invasive pneumococcal disease due to PCV7 serotypes has been nearly eliminated through indirect protection - i.e., the average incidence of PCV7-invasive pneumococcal disease after nearly a decade of PCV7 use is less than 10 per 100,000 people. In these countries, consistent decreases in vaccine-type adult community-acquired pneumonia (CAP) or meningitis, and nonbacteraemic CAP, have been observed, indicating substantial indirect protection effects against noninvasive disease from childhood vaccination.”
The review authors noted that a major “evidence gap” in the effectiveness of childhood PCV programs in low-income countries exists. “Because these countries are increasingly undertaking childhood vaccination programs, research to assess the indirect effects in these settings is particularly relevant,” they wrote.
The review’s limitations include the possibility that the results could be thrown off by variations across nations in areas like diagnostic protocols, surveillance, and outcome measures.
The authors of the review, funded by the Policy Research Program of England’s Department of Health, reported no relevant financial disclosures.
FROM THE LANCET GLOBAL HEALTH
Key clinical point: Through apparent herd immunity, childhood pneumococcal conjugate vaccines produce societywide reductions in invasive pneumococcal disease in less than a decade.
Major finding: When a seven-valent PCV is given to children, it would take an estimated 8.9 years for a 90% reduction in invasive pneumococcal disease to be seen among the grouped serotypes. It would take an estimated 9.5 years for an identical reduction in the extra six grouped serotypes in the 13-valent PCV.
Data source: A review and meta-analysis of 242 studies from 1994 to 2016 that examined the effects of introducing PCVs in children.
Disclosures: The review authors reported no relevant financial disclosures.
Ultrashort course antibiotics may be enough in stable VAP
Ultrashort courses of antibiotics led to similar outcomes as longer durations of therapy among adults with suspected ventilator-associated pneumonia but minimal and stable ventilator settings, according to a large retrospective observational study.
The duration of antibiotic therapy did not significantly affect the time to extubation alive (hazard ratio, 1.2; 95% CI, 1.0-1.4), time to hospital discharge (HR, 1.1; 95% CI, 0.9-1.3), rates of ventilator death (HR, 0.8; 95% CI, 0.6-1.2), or rates of hospital death (HR, 1.0; 95% CI, 0.8-1.31).), said Michael Klompas, MD, and his associates at Harvard Medical School in Boston. If confirmed, the findings would support surveillance of serial ventilator settings to “identify candidates for early antibiotic discontinuation,” the investigators reported (Clin Infect Dis. 2016 Dec 29. doi: 10.1093/cid/ciw870).
Suspected respiratory infections account for up to 70% of ICU antibiotic prescriptions, a “substantial fraction” of which may be unnecessary, the researchers said. “The predilection to overprescribe antibiotics for patients with possible ventilator-associated pneumonia (VAP) is not due to poor clinical skills per se, but rather the tension between practice guidelines that encourage early and aggressive prescribing [and] the difficulty [of] accurately diagnosing VAP,” they wrote. While withholding antibiotics in suspected VAP is “unrealistic” and can contribute to mortality, observing clinical trajectories and stopping antibiotics early when appropriate “may be more promising,” they added.
To test that idea, the researchers studied 1,290 cases of suspected VAP treated at Brigham and Women’s Hospital between 2006 and 2014. On the day antibiotics were started and during each of the next 2 days, all patients had a daily minimum positive end-expiratory pressure (PEEP) of no more than 5 cm H2O and a daily minimum fraction of inspired oxygen (FiO2) of no more than 40%.
A total of 259 patients received 1-3 days of antibiotics, while 1,031 patients received more than 3 days of therapy. These two groups were similar demographically, clinically, and in terms of comorbidities. Point estimates tended to favor ultrashort course antibiotics, but no association reached statistical significance in the overall analysis or in subgroups based on confirmed VAP diagnosis, confirmed pathogenic infection, or propensity-matched pairs.
The results suggest “that patients with suspected VAP but minimal and stable ventilator settings can be adequately managed with very short courses of antibiotics,” Dr. Klompas and his associates concluded. “If these findings are confirmed, assessing ventilator settings may prove to be a simple and objective strategy to identify potential candidates for early antibiotic discontinuation.”
The work was supported by the Centers for Disease Control and Prevention’s Prevention Epicenters Program. The investigators had no relevant financial disclosures.
Ultrashort courses of antibiotics led to similar outcomes as longer durations of therapy among adults with suspected ventilator-associated pneumonia but minimal and stable ventilator settings, according to a large retrospective observational study.
The duration of antibiotic therapy did not significantly affect the time to extubation alive (hazard ratio, 1.2; 95% CI, 1.0-1.4), time to hospital discharge (HR, 1.1; 95% CI, 0.9-1.3), rates of ventilator death (HR, 0.8; 95% CI, 0.6-1.2), or rates of hospital death (HR, 1.0; 95% CI, 0.8-1.31).), said Michael Klompas, MD, and his associates at Harvard Medical School in Boston. If confirmed, the findings would support surveillance of serial ventilator settings to “identify candidates for early antibiotic discontinuation,” the investigators reported (Clin Infect Dis. 2016 Dec 29. doi: 10.1093/cid/ciw870).
Suspected respiratory infections account for up to 70% of ICU antibiotic prescriptions, a “substantial fraction” of which may be unnecessary, the researchers said. “The predilection to overprescribe antibiotics for patients with possible ventilator-associated pneumonia (VAP) is not due to poor clinical skills per se, but rather the tension between practice guidelines that encourage early and aggressive prescribing [and] the difficulty [of] accurately diagnosing VAP,” they wrote. While withholding antibiotics in suspected VAP is “unrealistic” and can contribute to mortality, observing clinical trajectories and stopping antibiotics early when appropriate “may be more promising,” they added.
To test that idea, the researchers studied 1,290 cases of suspected VAP treated at Brigham and Women’s Hospital between 2006 and 2014. On the day antibiotics were started and during each of the next 2 days, all patients had a daily minimum positive end-expiratory pressure (PEEP) of no more than 5 cm H2O and a daily minimum fraction of inspired oxygen (FiO2) of no more than 40%.
A total of 259 patients received 1-3 days of antibiotics, while 1,031 patients received more than 3 days of therapy. These two groups were similar demographically, clinically, and in terms of comorbidities. Point estimates tended to favor ultrashort course antibiotics, but no association reached statistical significance in the overall analysis or in subgroups based on confirmed VAP diagnosis, confirmed pathogenic infection, or propensity-matched pairs.
The results suggest “that patients with suspected VAP but minimal and stable ventilator settings can be adequately managed with very short courses of antibiotics,” Dr. Klompas and his associates concluded. “If these findings are confirmed, assessing ventilator settings may prove to be a simple and objective strategy to identify potential candidates for early antibiotic discontinuation.”
The work was supported by the Centers for Disease Control and Prevention’s Prevention Epicenters Program. The investigators had no relevant financial disclosures.
Ultrashort courses of antibiotics led to similar outcomes as longer durations of therapy among adults with suspected ventilator-associated pneumonia but minimal and stable ventilator settings, according to a large retrospective observational study.
The duration of antibiotic therapy did not significantly affect the time to extubation alive (hazard ratio, 1.2; 95% CI, 1.0-1.4), time to hospital discharge (HR, 1.1; 95% CI, 0.9-1.3), rates of ventilator death (HR, 0.8; 95% CI, 0.6-1.2), or rates of hospital death (HR, 1.0; 95% CI, 0.8-1.31).), said Michael Klompas, MD, and his associates at Harvard Medical School in Boston. If confirmed, the findings would support surveillance of serial ventilator settings to “identify candidates for early antibiotic discontinuation,” the investigators reported (Clin Infect Dis. 2016 Dec 29. doi: 10.1093/cid/ciw870).
Suspected respiratory infections account for up to 70% of ICU antibiotic prescriptions, a “substantial fraction” of which may be unnecessary, the researchers said. “The predilection to overprescribe antibiotics for patients with possible ventilator-associated pneumonia (VAP) is not due to poor clinical skills per se, but rather the tension between practice guidelines that encourage early and aggressive prescribing [and] the difficulty [of] accurately diagnosing VAP,” they wrote. While withholding antibiotics in suspected VAP is “unrealistic” and can contribute to mortality, observing clinical trajectories and stopping antibiotics early when appropriate “may be more promising,” they added.
To test that idea, the researchers studied 1,290 cases of suspected VAP treated at Brigham and Women’s Hospital between 2006 and 2014. On the day antibiotics were started and during each of the next 2 days, all patients had a daily minimum positive end-expiratory pressure (PEEP) of no more than 5 cm H2O and a daily minimum fraction of inspired oxygen (FiO2) of no more than 40%.
A total of 259 patients received 1-3 days of antibiotics, while 1,031 patients received more than 3 days of therapy. These two groups were similar demographically, clinically, and in terms of comorbidities. Point estimates tended to favor ultrashort course antibiotics, but no association reached statistical significance in the overall analysis or in subgroups based on confirmed VAP diagnosis, confirmed pathogenic infection, or propensity-matched pairs.
The results suggest “that patients with suspected VAP but minimal and stable ventilator settings can be adequately managed with very short courses of antibiotics,” Dr. Klompas and his associates concluded. “If these findings are confirmed, assessing ventilator settings may prove to be a simple and objective strategy to identify potential candidates for early antibiotic discontinuation.”
The work was supported by the Centers for Disease Control and Prevention’s Prevention Epicenters Program. The investigators had no relevant financial disclosures.
Key clinical point: Ultrashort antibiotic courses yielded outcomes that were similar to those with longer courses in patients with suspected ventilator-associated pneumonia but minimal and stable ventilator settings.
Major finding: The groups did not significantly differ based on time to extubation alive (hazard ratio, 1.2), time to hospital discharge (HR, 1.1; 95% CI, 0.9-1.3), rates of ventilator death (HR, 0.8; 95% CI, 0.6-1.2), or rates of hospital death (HR, 1.0; 95% CI, 0.8-1.31).
Data source: A single-center retrospective observational study of 1,290 patients with suspected ventilator-associated pneumonia.
Disclosures: The work was supported by the Centers for Disease Control and Prevention’s Prevention Epicenters Program. The investigators had no relevant financial disclosures.
High volume of noninvasive ventilation in hospitals doesn’t ensure good outcomes in acute COPD
Hospitals that frequently treat acute COPD exacerbations using noninvasive ventilation – a practice known to reduce mortality, length of stay, and the need for more invasive treatment – did not have better patient outcomes than did hospitals that used noninvasive ventilation less frequently, according to a report published in Annals of the American Thoracic Society.
Acute COPD exacerbations are “one of the few conditions with high-level evidence demonstrating the benefits of noninvasive ventilation in patients with respiratory distress,” and the treatment has been widely adopted for this patient population. However, for noninvasive ventilation to succeed, patients must be carefully selected and closely monitored, and a multidisciplinary team of nurses, respiratory therapists, and physicians must coordinate the treatment, often across multiple hospital settings, said Anuj B. Mehta, MD, of The Pulmonary Center, Boston University, and his associates.
Until now, it was not known whether hospitals with a high volume of noninvasive ventilation develop specialized expertise and thus deliver superior patient outcomes, or whether a high volume results from suboptimal patient selection or otherwise puts a strain on a hospital’s staff and thus produces poor outcomes. To examine this question, Dr. Mehta and his associates analyzed information in a database enrolling adults treated at 252 California hospitals for acute COPD exacerbation. They focused on 37,516 hospitalizations that occurred during a single year.
Overall, 9.3% of these patients received noninvasive ventilation. The median annual case volume of noninvasive ventilation for any indication was 64 per hospital. But rates of noninvasive ventilation varied widely across hospitals, with 40% of facilities significantly deviating from this median rate.
“Contrary to our hypothesis, we did not observe significantly lower COPD mortality” in hospitals with high volumes of noninvasive ventilation. For individual patients, admission to a hospital with a high volume of noninvasive ventilation was associated with significantly higher odds of treatment failure (adjusted OR, 1.95), and such failure was associated with significantly higher odds of death (adjusted OR, 1.81). In addition, at the hospital level, a high volume of noninvasive ventilation was associated with a significantly higher risk of treatment failure, which in turn was associated with higher patient mortality.
“Hospitals with higher total noninvasive ventilation case volume tended to use [it] in patients with more comorbidities and acute organ failures, suggesting potential overuse among patients at higher risk of treatment failure. ... [This] may partially explain why hospitals with high rates of using an evidence-based intervention did not achieve significant mortality benefits,” Dr. Mehta and his associates said (Ann Am Thorac Soc. 2016;13[10]:1752-9).
They added that the wide variation between hospitals in failure rates for noninvasive ventilation were likely attributable to unmeasured hospital factors, speculating that the site of treatment (regular ward vs. ICU); staffing ratios for nurses, respiratory therapists, and physicians; and the intensity of patient monitoring, such as the frequency of blood-gas measurement, may contribute.
“High rates of treatment failure at some hospitals suggest that further work is needed to maximize the real-world effectiveness of noninvasive ventilation, even for an indication [backed by] strong evidence,” the investigators said.
The National Institutes of Health; the National Heart, Lung, and Blood Institute; and Boston University supported the study. The investigators’ financial disclosures are available at www.atsjournals.org.
Eric Gartman, MD, FCCP, comments: It is unclear what conclusions can be drawn from this study given the likely heterogeneity between the included hospitals.
Eric Gartman, MD, FCCP, comments: It is unclear what conclusions can be drawn from this study given the likely heterogeneity between the included hospitals.
Eric Gartman, MD, FCCP, comments: It is unclear what conclusions can be drawn from this study given the likely heterogeneity between the included hospitals.
Hospitals that frequently treat acute COPD exacerbations using noninvasive ventilation – a practice known to reduce mortality, length of stay, and the need for more invasive treatment – did not have better patient outcomes than did hospitals that used noninvasive ventilation less frequently, according to a report published in Annals of the American Thoracic Society.
Acute COPD exacerbations are “one of the few conditions with high-level evidence demonstrating the benefits of noninvasive ventilation in patients with respiratory distress,” and the treatment has been widely adopted for this patient population. However, for noninvasive ventilation to succeed, patients must be carefully selected and closely monitored, and a multidisciplinary team of nurses, respiratory therapists, and physicians must coordinate the treatment, often across multiple hospital settings, said Anuj B. Mehta, MD, of The Pulmonary Center, Boston University, and his associates.
Until now, it was not known whether hospitals with a high volume of noninvasive ventilation develop specialized expertise and thus deliver superior patient outcomes, or whether a high volume results from suboptimal patient selection or otherwise puts a strain on a hospital’s staff and thus produces poor outcomes. To examine this question, Dr. Mehta and his associates analyzed information in a database enrolling adults treated at 252 California hospitals for acute COPD exacerbation. They focused on 37,516 hospitalizations that occurred during a single year.
Overall, 9.3% of these patients received noninvasive ventilation. The median annual case volume of noninvasive ventilation for any indication was 64 per hospital. But rates of noninvasive ventilation varied widely across hospitals, with 40% of facilities significantly deviating from this median rate.
“Contrary to our hypothesis, we did not observe significantly lower COPD mortality” in hospitals with high volumes of noninvasive ventilation. For individual patients, admission to a hospital with a high volume of noninvasive ventilation was associated with significantly higher odds of treatment failure (adjusted OR, 1.95), and such failure was associated with significantly higher odds of death (adjusted OR, 1.81). In addition, at the hospital level, a high volume of noninvasive ventilation was associated with a significantly higher risk of treatment failure, which in turn was associated with higher patient mortality.
“Hospitals with higher total noninvasive ventilation case volume tended to use [it] in patients with more comorbidities and acute organ failures, suggesting potential overuse among patients at higher risk of treatment failure. ... [This] may partially explain why hospitals with high rates of using an evidence-based intervention did not achieve significant mortality benefits,” Dr. Mehta and his associates said (Ann Am Thorac Soc. 2016;13[10]:1752-9).
They added that the wide variation between hospitals in failure rates for noninvasive ventilation were likely attributable to unmeasured hospital factors, speculating that the site of treatment (regular ward vs. ICU); staffing ratios for nurses, respiratory therapists, and physicians; and the intensity of patient monitoring, such as the frequency of blood-gas measurement, may contribute.
“High rates of treatment failure at some hospitals suggest that further work is needed to maximize the real-world effectiveness of noninvasive ventilation, even for an indication [backed by] strong evidence,” the investigators said.
The National Institutes of Health; the National Heart, Lung, and Blood Institute; and Boston University supported the study. The investigators’ financial disclosures are available at www.atsjournals.org.
Hospitals that frequently treat acute COPD exacerbations using noninvasive ventilation – a practice known to reduce mortality, length of stay, and the need for more invasive treatment – did not have better patient outcomes than did hospitals that used noninvasive ventilation less frequently, according to a report published in Annals of the American Thoracic Society.
Acute COPD exacerbations are “one of the few conditions with high-level evidence demonstrating the benefits of noninvasive ventilation in patients with respiratory distress,” and the treatment has been widely adopted for this patient population. However, for noninvasive ventilation to succeed, patients must be carefully selected and closely monitored, and a multidisciplinary team of nurses, respiratory therapists, and physicians must coordinate the treatment, often across multiple hospital settings, said Anuj B. Mehta, MD, of The Pulmonary Center, Boston University, and his associates.
Until now, it was not known whether hospitals with a high volume of noninvasive ventilation develop specialized expertise and thus deliver superior patient outcomes, or whether a high volume results from suboptimal patient selection or otherwise puts a strain on a hospital’s staff and thus produces poor outcomes. To examine this question, Dr. Mehta and his associates analyzed information in a database enrolling adults treated at 252 California hospitals for acute COPD exacerbation. They focused on 37,516 hospitalizations that occurred during a single year.
Overall, 9.3% of these patients received noninvasive ventilation. The median annual case volume of noninvasive ventilation for any indication was 64 per hospital. But rates of noninvasive ventilation varied widely across hospitals, with 40% of facilities significantly deviating from this median rate.
“Contrary to our hypothesis, we did not observe significantly lower COPD mortality” in hospitals with high volumes of noninvasive ventilation. For individual patients, admission to a hospital with a high volume of noninvasive ventilation was associated with significantly higher odds of treatment failure (adjusted OR, 1.95), and such failure was associated with significantly higher odds of death (adjusted OR, 1.81). In addition, at the hospital level, a high volume of noninvasive ventilation was associated with a significantly higher risk of treatment failure, which in turn was associated with higher patient mortality.
“Hospitals with higher total noninvasive ventilation case volume tended to use [it] in patients with more comorbidities and acute organ failures, suggesting potential overuse among patients at higher risk of treatment failure. ... [This] may partially explain why hospitals with high rates of using an evidence-based intervention did not achieve significant mortality benefits,” Dr. Mehta and his associates said (Ann Am Thorac Soc. 2016;13[10]:1752-9).
They added that the wide variation between hospitals in failure rates for noninvasive ventilation were likely attributable to unmeasured hospital factors, speculating that the site of treatment (regular ward vs. ICU); staffing ratios for nurses, respiratory therapists, and physicians; and the intensity of patient monitoring, such as the frequency of blood-gas measurement, may contribute.
“High rates of treatment failure at some hospitals suggest that further work is needed to maximize the real-world effectiveness of noninvasive ventilation, even for an indication [backed by] strong evidence,” the investigators said.
The National Institutes of Health; the National Heart, Lung, and Blood Institute; and Boston University supported the study. The investigators’ financial disclosures are available at www.atsjournals.org.
FROM ANNALS OF THE AMERICAN THORACIC SOCIETY
Key clinical point: Outcomes for patients with acute COPD exacerbations were no better at hospitals where noninvasive ventilation was frequently used.
Major finding: For individual patients, admission to a hospital with a high volume of noninvasive ventilation was associated with significantly higher odds of treatment failure (adjusted OR, 1.95), and such failure was associated with significantly higher odds of death (adjusted OR, 1.81).
Data source: A multicenter observational study involving 37,516 hospitalizations for COPD exacerbation at 252 California medical centers during a 1-year period.
Disclosures: The National Institutes of Health; the National Heart, Lung, and Blood Institute; and Boston University supported the study. The investigators’ financial disclosures are available at www.atsjournals.org.
PCV effective against HNIs, pHNIs that require hospitalization in immunized children
Pneumococcal conjugate vaccines (PCV) in immunized children show effectiveness against head and neck infections (HNIs), especially against pneumococcal HNIs (pHNIs) that require hospitalization, according to Tal Marom, MD, of Tel Aviv University, Zerifin, Israel, and associates.
In a retrospective study, researchers identified children aged 0-16 years who were hospitalized with HNIs between Jan. 1, 2007 and Dec. 31, 2014. HNIs accounted for 2.5%-4.7% of admissions to the pediatric department, and there was a downward trend in the incidence in the post-PCV years, compared with previous years. Of the 820 children admitted with HNIs, 11% children were identified with pHNIs, 5% with acute otitis media, 4% with acute mastoiditis, and 2% with meningitis; there were no cases of pneumococcal acute bacterial sinusitis or pneumococcal head and neck abscesses. In 2009-2010 (considered as the “transition years,” in which both PCV7 and PCV13 were implemented in Israel), pHNIs incidence sharply decreased, from 7/1,000 to 1.74/1,000 hospitalized children per year, because of a 55% reduction of pneumococcal acute otitis media episodes. There also was an additional decrease observed in the post-PCV years of 2012-2014 (1.62/1,000 hospitalized children per year).
It was noted that unimmunized children were more likely to suffer from pneumococcal infections than immunized children (P = .001). There were no significant differences in the clinical presentation of these two groups, except for the need for surgery, which was significantly greater in immunized children (P = .042).
“The findings of the current study provide further evidence of PCV effectiveness against HNIs in PCV immunized children, and particularly against pHNI which required hospitalization,” Dr. Marom and associates concluded. “A substantial reduction in the all-cause HNIs incidence, and more specifically in pHNIs, in PCV immunized children who required hospitalization, was evident in the present study. This was also followed by a significant reduction in [acute otitis media] rates and to a much lesser extent, in [acute mastoiditis] and meningitis rates.”
Find the full study in the Pediatric Infectious Disease Journal (2016. doi: 10.1097/INF.0000000000001425).
Pneumococcal conjugate vaccines (PCV) in immunized children show effectiveness against head and neck infections (HNIs), especially against pneumococcal HNIs (pHNIs) that require hospitalization, according to Tal Marom, MD, of Tel Aviv University, Zerifin, Israel, and associates.
In a retrospective study, researchers identified children aged 0-16 years who were hospitalized with HNIs between Jan. 1, 2007 and Dec. 31, 2014. HNIs accounted for 2.5%-4.7% of admissions to the pediatric department, and there was a downward trend in the incidence in the post-PCV years, compared with previous years. Of the 820 children admitted with HNIs, 11% children were identified with pHNIs, 5% with acute otitis media, 4% with acute mastoiditis, and 2% with meningitis; there were no cases of pneumococcal acute bacterial sinusitis or pneumococcal head and neck abscesses. In 2009-2010 (considered as the “transition years,” in which both PCV7 and PCV13 were implemented in Israel), pHNIs incidence sharply decreased, from 7/1,000 to 1.74/1,000 hospitalized children per year, because of a 55% reduction of pneumococcal acute otitis media episodes. There also was an additional decrease observed in the post-PCV years of 2012-2014 (1.62/1,000 hospitalized children per year).
It was noted that unimmunized children were more likely to suffer from pneumococcal infections than immunized children (P = .001). There were no significant differences in the clinical presentation of these two groups, except for the need for surgery, which was significantly greater in immunized children (P = .042).
“The findings of the current study provide further evidence of PCV effectiveness against HNIs in PCV immunized children, and particularly against pHNI which required hospitalization,” Dr. Marom and associates concluded. “A substantial reduction in the all-cause HNIs incidence, and more specifically in pHNIs, in PCV immunized children who required hospitalization, was evident in the present study. This was also followed by a significant reduction in [acute otitis media] rates and to a much lesser extent, in [acute mastoiditis] and meningitis rates.”
Find the full study in the Pediatric Infectious Disease Journal (2016. doi: 10.1097/INF.0000000000001425).
Pneumococcal conjugate vaccines (PCV) in immunized children show effectiveness against head and neck infections (HNIs), especially against pneumococcal HNIs (pHNIs) that require hospitalization, according to Tal Marom, MD, of Tel Aviv University, Zerifin, Israel, and associates.
In a retrospective study, researchers identified children aged 0-16 years who were hospitalized with HNIs between Jan. 1, 2007 and Dec. 31, 2014. HNIs accounted for 2.5%-4.7% of admissions to the pediatric department, and there was a downward trend in the incidence in the post-PCV years, compared with previous years. Of the 820 children admitted with HNIs, 11% children were identified with pHNIs, 5% with acute otitis media, 4% with acute mastoiditis, and 2% with meningitis; there were no cases of pneumococcal acute bacterial sinusitis or pneumococcal head and neck abscesses. In 2009-2010 (considered as the “transition years,” in which both PCV7 and PCV13 were implemented in Israel), pHNIs incidence sharply decreased, from 7/1,000 to 1.74/1,000 hospitalized children per year, because of a 55% reduction of pneumococcal acute otitis media episodes. There also was an additional decrease observed in the post-PCV years of 2012-2014 (1.62/1,000 hospitalized children per year).
It was noted that unimmunized children were more likely to suffer from pneumococcal infections than immunized children (P = .001). There were no significant differences in the clinical presentation of these two groups, except for the need for surgery, which was significantly greater in immunized children (P = .042).
“The findings of the current study provide further evidence of PCV effectiveness against HNIs in PCV immunized children, and particularly against pHNI which required hospitalization,” Dr. Marom and associates concluded. “A substantial reduction in the all-cause HNIs incidence, and more specifically in pHNIs, in PCV immunized children who required hospitalization, was evident in the present study. This was also followed by a significant reduction in [acute otitis media] rates and to a much lesser extent, in [acute mastoiditis] and meningitis rates.”
Find the full study in the Pediatric Infectious Disease Journal (2016. doi: 10.1097/INF.0000000000001425).
FROM THE PEDIATRIC INFECTIOUS DISEASE JOURNAL