User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Keep antibiotics unchanged in breakthrough UTIs
Changing the continuous antibiotic prophylactic agent had no significant effect on the risk of a second infection in children with breakthrough urinary tract infections (UTIs), based on data from 62 children treated at a single center.
Continuous antibiotic prophylaxis (CAP) is often used for UTI prevention in children with febrile UTIs or anomalies that predispose them to UTIs, such as vesicoureteral reflux (VUR) or bladder and bowel dysfunction, said Lane M. Shish, MPH, of the University of Washington, Bothell, and colleagues in a poster (#1245) presented at the Pediatric Academic Societies annual meeting.
CAP, once initiated, is used until a planned endpoint or a breakthrough UTI, at which point alternative treatments usually include surgical intervention or a CAP agent change, the researchers said. However, changing the CAP agent is based on consensus without evidence of benefit, they noted.
To evaluate the potential effect of switching or maintaining CAP in cases of breakthrough UTIs, the researchers conducted a retrospective cohort study of all patients younger than 18 years on CAP for UTI prevention enrolled in a pediatric urology registry between January 2013 and August 2020.
All patients experienced a breakthrough UTI while on CAP; CAP was changed for 24 patients and left unchanged for 38 patients.
The primary outcome of second-breakthrough infections occurred in 12 of the changed CAP group and 22 of the unchanged group, with a relative risk of 0.86. The percentage of second breakthrough UTIs resistant to the current CAP was not significantly different between the changed and unchanged CAP groups (75% vs. 77%; P = 0.88).
The researchers also identified a rate ratio of 0.67 for a second breakthrough UTI in the changed CAP group, and found that approximately one-third of these patients (33.3%) developed antibiotic resistance to their initial antibiotic agent and the changed antibiotic agent.
The study findings were limited by several factors, including the retrospective design and small sample size, the researchers noted.
However, the results suggest that changing the CAP after an initial breakthrough UTI in children did not increase the risk of a second breakthrough UTI, and that CAP changing did introduce a risk of developing a second UTI with increased CAP resistance, the researchers noted. The results support leaving a child’s CAP unchanged after an initial breakthrough UTI, although additional research is needed to verify the findings, including studies involving a larger cohort with a multi-institutional prospective evaluation, they concluded.
Manage UTIs to reduce recurrence and resistance
“As we know, avoiding recurrent UTIs is important in preserving renal function in pediatric patients,” said Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice, in an interview.
“Avoiding recurrent UTIs is also important to avoid the development and spread of multidrug-resistant organisms,” he said.
Dr. Joos said he was surprised by some of the study findings. “I was surprised that, over the course of this 7-year retrospective review, overall only approximately 50% of patients with a first breakthrough UTI on CAP developed a second breakthrough UTI,” he noted. “Also, the relative risk of a second UTI was not significantly affected by whether the CAP antibiotic was changed after the first infection,” he said. “It would be interesting to see whether these results hold up in a randomized, prospective study,” he added.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose, but serves as a member of the Pediatric News Editorial Advisory Board.
Changing the continuous antibiotic prophylactic agent had no significant effect on the risk of a second infection in children with breakthrough urinary tract infections (UTIs), based on data from 62 children treated at a single center.
Continuous antibiotic prophylaxis (CAP) is often used for UTI prevention in children with febrile UTIs or anomalies that predispose them to UTIs, such as vesicoureteral reflux (VUR) or bladder and bowel dysfunction, said Lane M. Shish, MPH, of the University of Washington, Bothell, and colleagues in a poster (#1245) presented at the Pediatric Academic Societies annual meeting.
CAP, once initiated, is used until a planned endpoint or a breakthrough UTI, at which point alternative treatments usually include surgical intervention or a CAP agent change, the researchers said. However, changing the CAP agent is based on consensus without evidence of benefit, they noted.
To evaluate the potential effect of switching or maintaining CAP in cases of breakthrough UTIs, the researchers conducted a retrospective cohort study of all patients younger than 18 years on CAP for UTI prevention enrolled in a pediatric urology registry between January 2013 and August 2020.
All patients experienced a breakthrough UTI while on CAP; CAP was changed for 24 patients and left unchanged for 38 patients.
The primary outcome of second-breakthrough infections occurred in 12 of the changed CAP group and 22 of the unchanged group, with a relative risk of 0.86. The percentage of second breakthrough UTIs resistant to the current CAP was not significantly different between the changed and unchanged CAP groups (75% vs. 77%; P = 0.88).
The researchers also identified a rate ratio of 0.67 for a second breakthrough UTI in the changed CAP group, and found that approximately one-third of these patients (33.3%) developed antibiotic resistance to their initial antibiotic agent and the changed antibiotic agent.
The study findings were limited by several factors, including the retrospective design and small sample size, the researchers noted.
However, the results suggest that changing the CAP after an initial breakthrough UTI in children did not increase the risk of a second breakthrough UTI, and that CAP changing did introduce a risk of developing a second UTI with increased CAP resistance, the researchers noted. The results support leaving a child’s CAP unchanged after an initial breakthrough UTI, although additional research is needed to verify the findings, including studies involving a larger cohort with a multi-institutional prospective evaluation, they concluded.
Manage UTIs to reduce recurrence and resistance
“As we know, avoiding recurrent UTIs is important in preserving renal function in pediatric patients,” said Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice, in an interview.
“Avoiding recurrent UTIs is also important to avoid the development and spread of multidrug-resistant organisms,” he said.
Dr. Joos said he was surprised by some of the study findings. “I was surprised that, over the course of this 7-year retrospective review, overall only approximately 50% of patients with a first breakthrough UTI on CAP developed a second breakthrough UTI,” he noted. “Also, the relative risk of a second UTI was not significantly affected by whether the CAP antibiotic was changed after the first infection,” he said. “It would be interesting to see whether these results hold up in a randomized, prospective study,” he added.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose, but serves as a member of the Pediatric News Editorial Advisory Board.
Changing the continuous antibiotic prophylactic agent had no significant effect on the risk of a second infection in children with breakthrough urinary tract infections (UTIs), based on data from 62 children treated at a single center.
Continuous antibiotic prophylaxis (CAP) is often used for UTI prevention in children with febrile UTIs or anomalies that predispose them to UTIs, such as vesicoureteral reflux (VUR) or bladder and bowel dysfunction, said Lane M. Shish, MPH, of the University of Washington, Bothell, and colleagues in a poster (#1245) presented at the Pediatric Academic Societies annual meeting.
CAP, once initiated, is used until a planned endpoint or a breakthrough UTI, at which point alternative treatments usually include surgical intervention or a CAP agent change, the researchers said. However, changing the CAP agent is based on consensus without evidence of benefit, they noted.
To evaluate the potential effect of switching or maintaining CAP in cases of breakthrough UTIs, the researchers conducted a retrospective cohort study of all patients younger than 18 years on CAP for UTI prevention enrolled in a pediatric urology registry between January 2013 and August 2020.
All patients experienced a breakthrough UTI while on CAP; CAP was changed for 24 patients and left unchanged for 38 patients.
The primary outcome of second-breakthrough infections occurred in 12 of the changed CAP group and 22 of the unchanged group, with a relative risk of 0.86. The percentage of second breakthrough UTIs resistant to the current CAP was not significantly different between the changed and unchanged CAP groups (75% vs. 77%; P = 0.88).
The researchers also identified a rate ratio of 0.67 for a second breakthrough UTI in the changed CAP group, and found that approximately one-third of these patients (33.3%) developed antibiotic resistance to their initial antibiotic agent and the changed antibiotic agent.
The study findings were limited by several factors, including the retrospective design and small sample size, the researchers noted.
However, the results suggest that changing the CAP after an initial breakthrough UTI in children did not increase the risk of a second breakthrough UTI, and that CAP changing did introduce a risk of developing a second UTI with increased CAP resistance, the researchers noted. The results support leaving a child’s CAP unchanged after an initial breakthrough UTI, although additional research is needed to verify the findings, including studies involving a larger cohort with a multi-institutional prospective evaluation, they concluded.
Manage UTIs to reduce recurrence and resistance
“As we know, avoiding recurrent UTIs is important in preserving renal function in pediatric patients,” said Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice, in an interview.
“Avoiding recurrent UTIs is also important to avoid the development and spread of multidrug-resistant organisms,” he said.
Dr. Joos said he was surprised by some of the study findings. “I was surprised that, over the course of this 7-year retrospective review, overall only approximately 50% of patients with a first breakthrough UTI on CAP developed a second breakthrough UTI,” he noted. “Also, the relative risk of a second UTI was not significantly affected by whether the CAP antibiotic was changed after the first infection,” he said. “It would be interesting to see whether these results hold up in a randomized, prospective study,” he added.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose, but serves as a member of the Pediatric News Editorial Advisory Board.
FROM PAS 2021
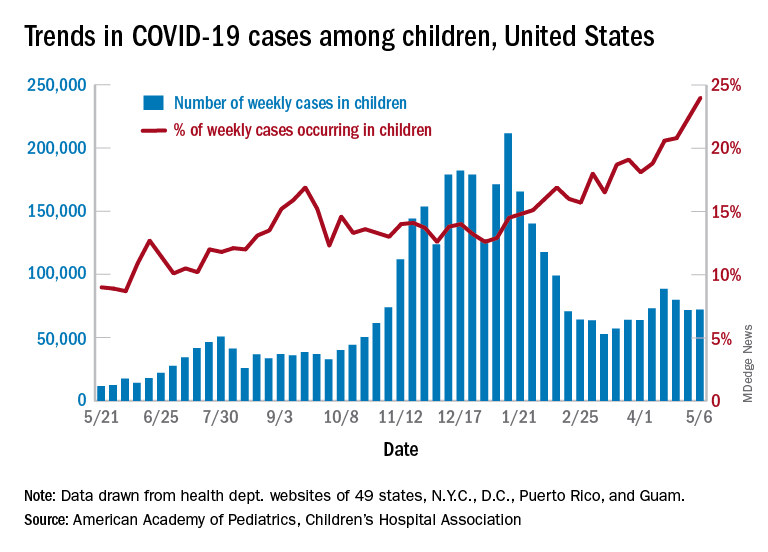
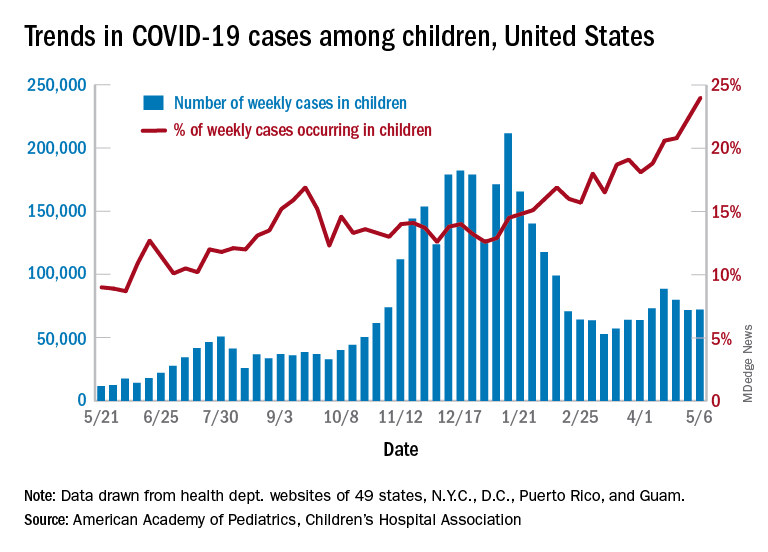
Small increase seen in new COVID-19 cases among children
After 2 consecutive weeks of declines, the number of new COVID-19 cases in children rose slightly, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
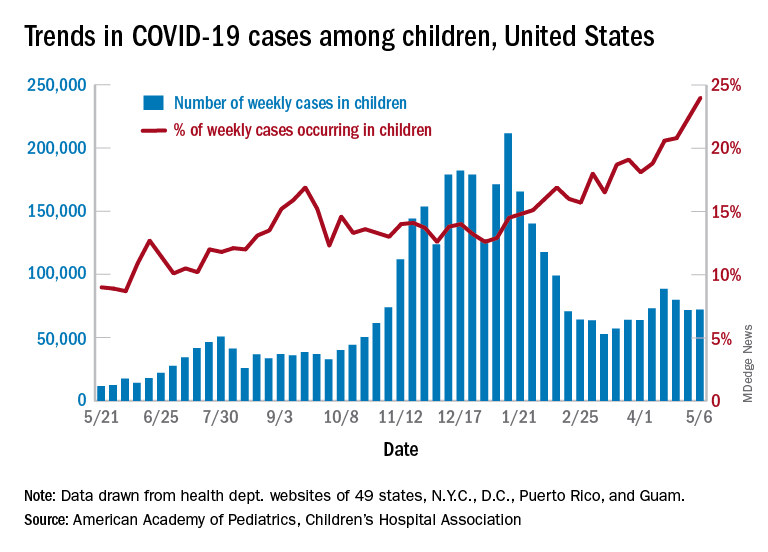
higher than at any other time during the pandemic, the AAP and CHA data show.
It is worth noting, however, that Rhode Island experienced a 30% increase in the last week, adding about 4,900 cases because of data revision and a lag in reporting, the AAP and CHA said in their weekly COVID-19 report.
All the new cases bring the total national count to just over 3.54 million in children, which represents 14.0% of all cases in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. The cumulative case rate as of May 6 was 5,122 per 100,000 children, the two organizations said.
All the new cases that were added to Rhode Island’s total give it the highest cumulative rate in the country: 9,614 cases per 100,000 children. North Dakota is right behind with 9,526 per 100,000, followed by Tennessee (8,898), Connecticut (8,281), and South Carolina (8,274). Vermont has the highest proportion of cases in children at 22.4%, with Alaska next at 20.3% and South Carolina third at 18.7%, according to the AAP and CHA.
Hawaii just reported its first COVID-19–related death in a child, which drops the number of states with zero deaths in children from 10 to 9. Two other new deaths in children from April 30 to May 6 bring the total number to 306 in the 43 states, along with New York City, Puerto Rico, and Guam, that are reporting the age distribution of deaths.
In a separate statement, AAP president Lee Savio Beers acknowledged the Food and Drug Administration’s authorization of the Pfizer-BioNTech vaccine for children aged 12-15 years as “a critically important step in bringing lifesaving vaccines to children and adolescents. ... We look forward to the discussion by the Advisory Committee on Immunization Practices of the CDC, which will make recommendations about the use of this vaccine in adolescents.”
After 2 consecutive weeks of declines, the number of new COVID-19 cases in children rose slightly, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
higher than at any other time during the pandemic, the AAP and CHA data show.
It is worth noting, however, that Rhode Island experienced a 30% increase in the last week, adding about 4,900 cases because of data revision and a lag in reporting, the AAP and CHA said in their weekly COVID-19 report.
All the new cases bring the total national count to just over 3.54 million in children, which represents 14.0% of all cases in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. The cumulative case rate as of May 6 was 5,122 per 100,000 children, the two organizations said.
All the new cases that were added to Rhode Island’s total give it the highest cumulative rate in the country: 9,614 cases per 100,000 children. North Dakota is right behind with 9,526 per 100,000, followed by Tennessee (8,898), Connecticut (8,281), and South Carolina (8,274). Vermont has the highest proportion of cases in children at 22.4%, with Alaska next at 20.3% and South Carolina third at 18.7%, according to the AAP and CHA.
Hawaii just reported its first COVID-19–related death in a child, which drops the number of states with zero deaths in children from 10 to 9. Two other new deaths in children from April 30 to May 6 bring the total number to 306 in the 43 states, along with New York City, Puerto Rico, and Guam, that are reporting the age distribution of deaths.
In a separate statement, AAP president Lee Savio Beers acknowledged the Food and Drug Administration’s authorization of the Pfizer-BioNTech vaccine for children aged 12-15 years as “a critically important step in bringing lifesaving vaccines to children and adolescents. ... We look forward to the discussion by the Advisory Committee on Immunization Practices of the CDC, which will make recommendations about the use of this vaccine in adolescents.”
After 2 consecutive weeks of declines, the number of new COVID-19 cases in children rose slightly, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
higher than at any other time during the pandemic, the AAP and CHA data show.
It is worth noting, however, that Rhode Island experienced a 30% increase in the last week, adding about 4,900 cases because of data revision and a lag in reporting, the AAP and CHA said in their weekly COVID-19 report.
All the new cases bring the total national count to just over 3.54 million in children, which represents 14.0% of all cases in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. The cumulative case rate as of May 6 was 5,122 per 100,000 children, the two organizations said.
All the new cases that were added to Rhode Island’s total give it the highest cumulative rate in the country: 9,614 cases per 100,000 children. North Dakota is right behind with 9,526 per 100,000, followed by Tennessee (8,898), Connecticut (8,281), and South Carolina (8,274). Vermont has the highest proportion of cases in children at 22.4%, with Alaska next at 20.3% and South Carolina third at 18.7%, according to the AAP and CHA.
Hawaii just reported its first COVID-19–related death in a child, which drops the number of states with zero deaths in children from 10 to 9. Two other new deaths in children from April 30 to May 6 bring the total number to 306 in the 43 states, along with New York City, Puerto Rico, and Guam, that are reporting the age distribution of deaths.
In a separate statement, AAP president Lee Savio Beers acknowledged the Food and Drug Administration’s authorization of the Pfizer-BioNTech vaccine for children aged 12-15 years as “a critically important step in bringing lifesaving vaccines to children and adolescents. ... We look forward to the discussion by the Advisory Committee on Immunization Practices of the CDC, which will make recommendations about the use of this vaccine in adolescents.”
Dr. Fauci: Feds may ease indoor mask mandates soon
Federal guidance on indoor mask use may change soon, Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said on May 9.
He was asked whether it’s time to start relaxing indoor mask requirements.
“I think so, and I think you’re going to probably be seeing that as we go along and as more people get vaccinated,” Dr. Fauci said on ABC News’s This Week.Nearly 150 million adults in the United States – or about 58% of the adult population – have received at least one COVID-19 vaccine dose, according to the latest CDC tally. About 113 million adults, or 44%, are considered fully vaccinated.
“The CDC will be, you know, almost in real time … updating their recommendations and their guidelines,” Dr. Fauci said.
In April, the CDC relaxed its guidance for those who have been vaccinated against COVID-19. Those who have gotten a shot don’t need to wear a mask outdoors or in small indoor gatherings with other vaccinated people, but both vaccinated and unvaccinated people are still advised to wear masks in indoor public spaces.
“We do need to start being more liberal as we get more people vaccinated,” Dr. Fauci said. “As you get more people vaccinated, the number of cases per day will absolutely go down.”
The United States is averaging about 43,000 cases per day, he said, adding that the cases need to be “much, much lower.” When the case numbers drop and vaccination numbers increase, the risk of infection will fall dramatically indoors and outdoors, he said.
Even after the pandemic, though, wearing masks could become a seasonal habit, Dr. Fauci said May 9 on NBC News’s Meet the Press.“I think people have gotten used to the fact that wearing masks, clearly if you look at the data, it diminishes respiratory diseases. We’ve had practically a nonexistent flu season this year,” he said.
“So it is conceivable that as we go on, a year or 2 or more from now, that during certain seasonal periods when you have respiratory-borne viruses like the flu, people might actually elect to wear masks to diminish the likelihood that you’ll spread these respiratory-borne diseases,” he said.
Dr. Fauci was asked about indoor mask guidelines on May 9 after former FDA Commissioner Scott Gottlieb, MD, said face mask requirements should be relaxed.
“Certainly outdoors, we shouldn’t be putting limits on gatherings anymore,” Dr. Gottlieb said on CBS News’s Face the Nation.“The states where prevalence is low, vaccination rates are high, we have good testing in place, and we’re identifying infections, I think we could start lifting these restrictions indoors as well, on a broad basis,” he said.
Lifting pandemic-related restrictions in areas where they’re no longer necessary could also encourage people to implement them again if cases increase during future surges, such as this fall or winter, Dr. Gottlieb said.
At the same time, Americans should continue to follow CDC guidance and wait for new guidelines before changing their indoor mask use, Jeffrey Zients, the White House COVID-19 response coordinator, said on CNN’s State of the Union on May 9.
“We all want to get back to a normal lifestyle,” he said. “I think we’re on the path to do that, but stay disciplined, and let’s take advantage of the new privilege of being vaccinated and not wearing masks outdoors, for example, unless you’re in a crowded place.”
Mr. Zients pointed to President Joe Biden’s goal for 70% of adults to receive at least one vaccine dose by July 4.
“As we all move toward that 70% goal, there will be more and more advantages to being vaccinated,” he said. “And if you’re not vaccinated, you’re not protected.”
A version of this article first appeared on WebMD.com.
Federal guidance on indoor mask use may change soon, Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said on May 9.
He was asked whether it’s time to start relaxing indoor mask requirements.
“I think so, and I think you’re going to probably be seeing that as we go along and as more people get vaccinated,” Dr. Fauci said on ABC News’s This Week.Nearly 150 million adults in the United States – or about 58% of the adult population – have received at least one COVID-19 vaccine dose, according to the latest CDC tally. About 113 million adults, or 44%, are considered fully vaccinated.
“The CDC will be, you know, almost in real time … updating their recommendations and their guidelines,” Dr. Fauci said.
In April, the CDC relaxed its guidance for those who have been vaccinated against COVID-19. Those who have gotten a shot don’t need to wear a mask outdoors or in small indoor gatherings with other vaccinated people, but both vaccinated and unvaccinated people are still advised to wear masks in indoor public spaces.
“We do need to start being more liberal as we get more people vaccinated,” Dr. Fauci said. “As you get more people vaccinated, the number of cases per day will absolutely go down.”
The United States is averaging about 43,000 cases per day, he said, adding that the cases need to be “much, much lower.” When the case numbers drop and vaccination numbers increase, the risk of infection will fall dramatically indoors and outdoors, he said.
Even after the pandemic, though, wearing masks could become a seasonal habit, Dr. Fauci said May 9 on NBC News’s Meet the Press.“I think people have gotten used to the fact that wearing masks, clearly if you look at the data, it diminishes respiratory diseases. We’ve had practically a nonexistent flu season this year,” he said.
“So it is conceivable that as we go on, a year or 2 or more from now, that during certain seasonal periods when you have respiratory-borne viruses like the flu, people might actually elect to wear masks to diminish the likelihood that you’ll spread these respiratory-borne diseases,” he said.
Dr. Fauci was asked about indoor mask guidelines on May 9 after former FDA Commissioner Scott Gottlieb, MD, said face mask requirements should be relaxed.
“Certainly outdoors, we shouldn’t be putting limits on gatherings anymore,” Dr. Gottlieb said on CBS News’s Face the Nation.“The states where prevalence is low, vaccination rates are high, we have good testing in place, and we’re identifying infections, I think we could start lifting these restrictions indoors as well, on a broad basis,” he said.
Lifting pandemic-related restrictions in areas where they’re no longer necessary could also encourage people to implement them again if cases increase during future surges, such as this fall or winter, Dr. Gottlieb said.
At the same time, Americans should continue to follow CDC guidance and wait for new guidelines before changing their indoor mask use, Jeffrey Zients, the White House COVID-19 response coordinator, said on CNN’s State of the Union on May 9.
“We all want to get back to a normal lifestyle,” he said. “I think we’re on the path to do that, but stay disciplined, and let’s take advantage of the new privilege of being vaccinated and not wearing masks outdoors, for example, unless you’re in a crowded place.”
Mr. Zients pointed to President Joe Biden’s goal for 70% of adults to receive at least one vaccine dose by July 4.
“As we all move toward that 70% goal, there will be more and more advantages to being vaccinated,” he said. “And if you’re not vaccinated, you’re not protected.”
A version of this article first appeared on WebMD.com.
Federal guidance on indoor mask use may change soon, Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, said on May 9.
He was asked whether it’s time to start relaxing indoor mask requirements.
“I think so, and I think you’re going to probably be seeing that as we go along and as more people get vaccinated,” Dr. Fauci said on ABC News’s This Week.Nearly 150 million adults in the United States – or about 58% of the adult population – have received at least one COVID-19 vaccine dose, according to the latest CDC tally. About 113 million adults, or 44%, are considered fully vaccinated.
“The CDC will be, you know, almost in real time … updating their recommendations and their guidelines,” Dr. Fauci said.
In April, the CDC relaxed its guidance for those who have been vaccinated against COVID-19. Those who have gotten a shot don’t need to wear a mask outdoors or in small indoor gatherings with other vaccinated people, but both vaccinated and unvaccinated people are still advised to wear masks in indoor public spaces.
“We do need to start being more liberal as we get more people vaccinated,” Dr. Fauci said. “As you get more people vaccinated, the number of cases per day will absolutely go down.”
The United States is averaging about 43,000 cases per day, he said, adding that the cases need to be “much, much lower.” When the case numbers drop and vaccination numbers increase, the risk of infection will fall dramatically indoors and outdoors, he said.
Even after the pandemic, though, wearing masks could become a seasonal habit, Dr. Fauci said May 9 on NBC News’s Meet the Press.“I think people have gotten used to the fact that wearing masks, clearly if you look at the data, it diminishes respiratory diseases. We’ve had practically a nonexistent flu season this year,” he said.
“So it is conceivable that as we go on, a year or 2 or more from now, that during certain seasonal periods when you have respiratory-borne viruses like the flu, people might actually elect to wear masks to diminish the likelihood that you’ll spread these respiratory-borne diseases,” he said.
Dr. Fauci was asked about indoor mask guidelines on May 9 after former FDA Commissioner Scott Gottlieb, MD, said face mask requirements should be relaxed.
“Certainly outdoors, we shouldn’t be putting limits on gatherings anymore,” Dr. Gottlieb said on CBS News’s Face the Nation.“The states where prevalence is low, vaccination rates are high, we have good testing in place, and we’re identifying infections, I think we could start lifting these restrictions indoors as well, on a broad basis,” he said.
Lifting pandemic-related restrictions in areas where they’re no longer necessary could also encourage people to implement them again if cases increase during future surges, such as this fall or winter, Dr. Gottlieb said.
At the same time, Americans should continue to follow CDC guidance and wait for new guidelines before changing their indoor mask use, Jeffrey Zients, the White House COVID-19 response coordinator, said on CNN’s State of the Union on May 9.
“We all want to get back to a normal lifestyle,” he said. “I think we’re on the path to do that, but stay disciplined, and let’s take advantage of the new privilege of being vaccinated and not wearing masks outdoors, for example, unless you’re in a crowded place.”
Mr. Zients pointed to President Joe Biden’s goal for 70% of adults to receive at least one vaccine dose by July 4.
“As we all move toward that 70% goal, there will be more and more advantages to being vaccinated,” he said. “And if you’re not vaccinated, you’re not protected.”
A version of this article first appeared on WebMD.com.
FDA authorizes Pfizer COVID vaccine for teens 12-15
The Food and Drug Administration on May 10 granted emergency use authorization (EUA) for the Pfizer coronavirus vaccine to be given to children 12-15 years old.
The much-expected decision increases the likelihood that schools in the United States will fully reopen in the fall – a goal of both the Biden and Trump administrations.
Acting FDA Commissioner Janet Woodcock, MD, called the decision “a significant step” in “returning to a sense of normalcy.”
“Today’s action allows for a younger population to be protected from COVID-19, bringing us closer to returning to a sense of normalcy and to ending the pandemic,” she said in a statement. “Parents and guardians can rest assured that the agency undertook a rigorous and thorough review of all available data, as we have with all of our COVID-19 vaccine emergency use authorizations.”
The Pfizer adolescent vaccine is not yet a done deal, though.
Next, the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices will decide on May 12 whether to recommend use of the vaccine in this age group. After that, CDC Director Rochelle Walensky, MD, will decide whether to give the green light for the vaccine to be administered to that age group.
The FDA action on May 10 amends the Dec. 11, 2020, emergency use authorization that allowed the Pfizer vaccine to be given to people 16 and older. Pfizer was the first company to receive an EUA for its adult vaccine and is the first to receive authorization for its adolescent vaccine. Pfizer is conducting clinical trials on much younger children, too.
The Moderna and Johnson & Johnson vaccines are authorized for people 18 and up. Moderna also has launched clinical trials in children.
Most health experts have said the United States needs to vaccinate children before the COVID-19 pandemic can truly be brought under control. The 12- to 15-year-old group represents 17 million people, about 5% of the population. Thus far, 58% of U.S. adults have had at least one dose of a vaccine and 34.8% of all Americans are fully vaccinated.
American Academy of Pediatrics President Lee Savio Beers, MD, praised the agency’s decision, calling it a “critically important step in bringing life-saving vaccines to children and adolescents. Our youngest generations have shouldered heavy burdens over the past year, and the vaccine is a hopeful sign that they will be able to begin to experience all the activities that are so important for their health and development.”
President Joe Biden recently announced a new strategy for expanding vaccinations in which vaccinating 12- to 15-year-olds was a key component. He said the administration was ready to ship the adolescent vaccine directly to pharmacies and pediatricians to speed up the vaccination rate.
In March, Anthony S. Fauci, MD, told a Senate committee, “We don’t really know what that magical point of herd immunity is, but we do know that if we get the overwhelming population vaccinated, we’re going to be in good shape. … We ultimately would like to get and have to get children into that mix.”
Pfizer submitted data to the FDA in late March showing its mRNA vaccine was 100% effective at preventing COVID-19 infection in children ages 12-15 in clinical trials.
Though most children have milder symptoms when infected with the coronavirus, about 1.5 million cases in children aged 11-17 were reported to the CDC between March 1, 2020, and April 30 of this year, the FDA news release said.
Albert Bourla, CEO of Pfizer, tweeted that “today brings very encouraging news for families and adolescents across the United States.
“While this is a meaningful step forward, we are still in a critical period of combating #COVID19 around the world. In the coming weeks, we hope to continue to receive authorizations from global regulators to support worldwide vaccination efforts,” he said.
“It’s essential for children to be vaccinated against COVID-19. According to data compiled by the AAP and Children’s Hospital Association, more than 3.8 million children have tested positive for COVID-19 in the United States since the start of the pandemic,” said Dr. Savio Beers. “While fewer children than adults have suffered the most severe disease, this is not a benign disease in children. Thousands of children have been hospitalized, and hundreds have died. We will soon have a very safe, highly effective vaccine that can prevent so much suffering. I encourage parents to talk with their pediatricians about how to get the vaccine for their adolescents as soon as they are eligible.”
A version of this article first appeared on Medscape.com.
The Food and Drug Administration on May 10 granted emergency use authorization (EUA) for the Pfizer coronavirus vaccine to be given to children 12-15 years old.
The much-expected decision increases the likelihood that schools in the United States will fully reopen in the fall – a goal of both the Biden and Trump administrations.
Acting FDA Commissioner Janet Woodcock, MD, called the decision “a significant step” in “returning to a sense of normalcy.”
“Today’s action allows for a younger population to be protected from COVID-19, bringing us closer to returning to a sense of normalcy and to ending the pandemic,” she said in a statement. “Parents and guardians can rest assured that the agency undertook a rigorous and thorough review of all available data, as we have with all of our COVID-19 vaccine emergency use authorizations.”
The Pfizer adolescent vaccine is not yet a done deal, though.
Next, the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices will decide on May 12 whether to recommend use of the vaccine in this age group. After that, CDC Director Rochelle Walensky, MD, will decide whether to give the green light for the vaccine to be administered to that age group.
The FDA action on May 10 amends the Dec. 11, 2020, emergency use authorization that allowed the Pfizer vaccine to be given to people 16 and older. Pfizer was the first company to receive an EUA for its adult vaccine and is the first to receive authorization for its adolescent vaccine. Pfizer is conducting clinical trials on much younger children, too.
The Moderna and Johnson & Johnson vaccines are authorized for people 18 and up. Moderna also has launched clinical trials in children.
Most health experts have said the United States needs to vaccinate children before the COVID-19 pandemic can truly be brought under control. The 12- to 15-year-old group represents 17 million people, about 5% of the population. Thus far, 58% of U.S. adults have had at least one dose of a vaccine and 34.8% of all Americans are fully vaccinated.
American Academy of Pediatrics President Lee Savio Beers, MD, praised the agency’s decision, calling it a “critically important step in bringing life-saving vaccines to children and adolescents. Our youngest generations have shouldered heavy burdens over the past year, and the vaccine is a hopeful sign that they will be able to begin to experience all the activities that are so important for their health and development.”
President Joe Biden recently announced a new strategy for expanding vaccinations in which vaccinating 12- to 15-year-olds was a key component. He said the administration was ready to ship the adolescent vaccine directly to pharmacies and pediatricians to speed up the vaccination rate.
In March, Anthony S. Fauci, MD, told a Senate committee, “We don’t really know what that magical point of herd immunity is, but we do know that if we get the overwhelming population vaccinated, we’re going to be in good shape. … We ultimately would like to get and have to get children into that mix.”
Pfizer submitted data to the FDA in late March showing its mRNA vaccine was 100% effective at preventing COVID-19 infection in children ages 12-15 in clinical trials.
Though most children have milder symptoms when infected with the coronavirus, about 1.5 million cases in children aged 11-17 were reported to the CDC between March 1, 2020, and April 30 of this year, the FDA news release said.
Albert Bourla, CEO of Pfizer, tweeted that “today brings very encouraging news for families and adolescents across the United States.
“While this is a meaningful step forward, we are still in a critical period of combating #COVID19 around the world. In the coming weeks, we hope to continue to receive authorizations from global regulators to support worldwide vaccination efforts,” he said.
“It’s essential for children to be vaccinated against COVID-19. According to data compiled by the AAP and Children’s Hospital Association, more than 3.8 million children have tested positive for COVID-19 in the United States since the start of the pandemic,” said Dr. Savio Beers. “While fewer children than adults have suffered the most severe disease, this is not a benign disease in children. Thousands of children have been hospitalized, and hundreds have died. We will soon have a very safe, highly effective vaccine that can prevent so much suffering. I encourage parents to talk with their pediatricians about how to get the vaccine for their adolescents as soon as they are eligible.”
A version of this article first appeared on Medscape.com.
The Food and Drug Administration on May 10 granted emergency use authorization (EUA) for the Pfizer coronavirus vaccine to be given to children 12-15 years old.
The much-expected decision increases the likelihood that schools in the United States will fully reopen in the fall – a goal of both the Biden and Trump administrations.
Acting FDA Commissioner Janet Woodcock, MD, called the decision “a significant step” in “returning to a sense of normalcy.”
“Today’s action allows for a younger population to be protected from COVID-19, bringing us closer to returning to a sense of normalcy and to ending the pandemic,” she said in a statement. “Parents and guardians can rest assured that the agency undertook a rigorous and thorough review of all available data, as we have with all of our COVID-19 vaccine emergency use authorizations.”
The Pfizer adolescent vaccine is not yet a done deal, though.
Next, the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices will decide on May 12 whether to recommend use of the vaccine in this age group. After that, CDC Director Rochelle Walensky, MD, will decide whether to give the green light for the vaccine to be administered to that age group.
The FDA action on May 10 amends the Dec. 11, 2020, emergency use authorization that allowed the Pfizer vaccine to be given to people 16 and older. Pfizer was the first company to receive an EUA for its adult vaccine and is the first to receive authorization for its adolescent vaccine. Pfizer is conducting clinical trials on much younger children, too.
The Moderna and Johnson & Johnson vaccines are authorized for people 18 and up. Moderna also has launched clinical trials in children.
Most health experts have said the United States needs to vaccinate children before the COVID-19 pandemic can truly be brought under control. The 12- to 15-year-old group represents 17 million people, about 5% of the population. Thus far, 58% of U.S. adults have had at least one dose of a vaccine and 34.8% of all Americans are fully vaccinated.
American Academy of Pediatrics President Lee Savio Beers, MD, praised the agency’s decision, calling it a “critically important step in bringing life-saving vaccines to children and adolescents. Our youngest generations have shouldered heavy burdens over the past year, and the vaccine is a hopeful sign that they will be able to begin to experience all the activities that are so important for their health and development.”
President Joe Biden recently announced a new strategy for expanding vaccinations in which vaccinating 12- to 15-year-olds was a key component. He said the administration was ready to ship the adolescent vaccine directly to pharmacies and pediatricians to speed up the vaccination rate.
In March, Anthony S. Fauci, MD, told a Senate committee, “We don’t really know what that magical point of herd immunity is, but we do know that if we get the overwhelming population vaccinated, we’re going to be in good shape. … We ultimately would like to get and have to get children into that mix.”
Pfizer submitted data to the FDA in late March showing its mRNA vaccine was 100% effective at preventing COVID-19 infection in children ages 12-15 in clinical trials.
Though most children have milder symptoms when infected with the coronavirus, about 1.5 million cases in children aged 11-17 were reported to the CDC between March 1, 2020, and April 30 of this year, the FDA news release said.
Albert Bourla, CEO of Pfizer, tweeted that “today brings very encouraging news for families and adolescents across the United States.
“While this is a meaningful step forward, we are still in a critical period of combating #COVID19 around the world. In the coming weeks, we hope to continue to receive authorizations from global regulators to support worldwide vaccination efforts,” he said.
“It’s essential for children to be vaccinated against COVID-19. According to data compiled by the AAP and Children’s Hospital Association, more than 3.8 million children have tested positive for COVID-19 in the United States since the start of the pandemic,” said Dr. Savio Beers. “While fewer children than adults have suffered the most severe disease, this is not a benign disease in children. Thousands of children have been hospitalized, and hundreds have died. We will soon have a very safe, highly effective vaccine that can prevent so much suffering. I encourage parents to talk with their pediatricians about how to get the vaccine for their adolescents as soon as they are eligible.”
A version of this article first appeared on Medscape.com.
Operational changes in primary care linked with improved smoking, blood pressure outcomes
The qualitative analysis, published in Annals of Family Medicine , included smoking and blood pressure as separate outcome measures.
The outcomes were calculated using Clinical Quality Measure improvements, with targets of at least 10-point absolute improvements in the proportion of patients with smoking screening, if relevant, counseling, and in the proportion of hypertensive patients with adequately controlled BP. The results were obtained from practices participating in Evidence-NOW, a multisite cardiovascular disease prevention initiative. Configurational Comparative Methods were used to evaluate the joint effects of multiple factors on outcomes.
The majority of practices in the analysis were clinician owned, small (fewer than six clinicians), and/or in an urban location. The researchers sampled and interviewed practice staff from a subset of 104 primary care practices across 7 Cooperatives and 12 states, ranging from small to medium in size, having 10 or fewer clinicians. The interview data were analyzed to identify operational changes, then transformed into numeric data.
Operational changes led to improvements in specific contexts
In clinician-owned practices, process improvement, documentation, and referral to resources, combined with a moderate level of facilitation support, led to an improvement of at least 10 points in smoking outcomes.
However, the researchers found that these patterns were not observed in system–owned practices or Federally Qualified Health Centers.
In solo practices, training medical assistants to take an accurate blood pressure led to an improvement of at least 10 points in blood pressure outcomes.
Among larger, clinician-owned practices, measurement of blood pressure a second time when the first was elevated, and documentation of this reading in the electronic heath record, also led to a 10-point or greater improvement in BP outcome when combined with a large amount (50 hours or more) of facilitation.
“There was no magic bullet for improving smoking cessation counseling and blood pressure outcomes across the diverse primary care practices studied,” lead author Deborah J. Cohen, PhD, of Oregon Health & Science University, Portland, said in an interview. “Combinations of operational changes among practice sizes and types led to improvements.”
Smaller practices more nimble, experts say
Results of the qualitative data analysis suggest that smaller and clinician-owned practices are more likely to have the capacity for change and improvement compared with larger, hospital/health system–owned practices.
Commenting on the study, Noel Deep, MD, regional medical director at Aspirus Clinics, Ironwood, Mich., said solo or small private practices have a distinct advantage over larger hospital or system-owned practices when implementing new operational changes to improve clinical outcomes.
“A smaller independent practice is nimble, with the physician [or physicians] able to make a quick decision at analyzing the scientific data, planning the changes, implementing them quickly, and doing a rapid cycle review of the results and tweaking the program to attain the targets,” said Dr. Deep, a member of the editorial advisory board of Internal Medicine News.
Kate Rowland, MD, MS, assistant professor in the department of family medicine at Rush Medical College, Chicago, also noted that smaller practices have unique advantages over larger health organizations.
“Larger organizations should replicate the benefits of the smaller office, providing as much local decision-making and autonomy as possible to the site where the changes are happening,” Dr. Rowland explained in an interview.
“The clinicians at these sites are mostly likely to know what is going to be successful for achieving measurable change in the patients they care for,” she added.
The study was funded by the Agency for Healthcare Research and Quality. The authors and other experts interviewed for this piece reported having no conflicts of interest.
The qualitative analysis, published in Annals of Family Medicine , included smoking and blood pressure as separate outcome measures.
The outcomes were calculated using Clinical Quality Measure improvements, with targets of at least 10-point absolute improvements in the proportion of patients with smoking screening, if relevant, counseling, and in the proportion of hypertensive patients with adequately controlled BP. The results were obtained from practices participating in Evidence-NOW, a multisite cardiovascular disease prevention initiative. Configurational Comparative Methods were used to evaluate the joint effects of multiple factors on outcomes.
The majority of practices in the analysis were clinician owned, small (fewer than six clinicians), and/or in an urban location. The researchers sampled and interviewed practice staff from a subset of 104 primary care practices across 7 Cooperatives and 12 states, ranging from small to medium in size, having 10 or fewer clinicians. The interview data were analyzed to identify operational changes, then transformed into numeric data.
Operational changes led to improvements in specific contexts
In clinician-owned practices, process improvement, documentation, and referral to resources, combined with a moderate level of facilitation support, led to an improvement of at least 10 points in smoking outcomes.
However, the researchers found that these patterns were not observed in system–owned practices or Federally Qualified Health Centers.
In solo practices, training medical assistants to take an accurate blood pressure led to an improvement of at least 10 points in blood pressure outcomes.
Among larger, clinician-owned practices, measurement of blood pressure a second time when the first was elevated, and documentation of this reading in the electronic heath record, also led to a 10-point or greater improvement in BP outcome when combined with a large amount (50 hours or more) of facilitation.
“There was no magic bullet for improving smoking cessation counseling and blood pressure outcomes across the diverse primary care practices studied,” lead author Deborah J. Cohen, PhD, of Oregon Health & Science University, Portland, said in an interview. “Combinations of operational changes among practice sizes and types led to improvements.”
Smaller practices more nimble, experts say
Results of the qualitative data analysis suggest that smaller and clinician-owned practices are more likely to have the capacity for change and improvement compared with larger, hospital/health system–owned practices.
Commenting on the study, Noel Deep, MD, regional medical director at Aspirus Clinics, Ironwood, Mich., said solo or small private practices have a distinct advantage over larger hospital or system-owned practices when implementing new operational changes to improve clinical outcomes.
“A smaller independent practice is nimble, with the physician [or physicians] able to make a quick decision at analyzing the scientific data, planning the changes, implementing them quickly, and doing a rapid cycle review of the results and tweaking the program to attain the targets,” said Dr. Deep, a member of the editorial advisory board of Internal Medicine News.
Kate Rowland, MD, MS, assistant professor in the department of family medicine at Rush Medical College, Chicago, also noted that smaller practices have unique advantages over larger health organizations.
“Larger organizations should replicate the benefits of the smaller office, providing as much local decision-making and autonomy as possible to the site where the changes are happening,” Dr. Rowland explained in an interview.
“The clinicians at these sites are mostly likely to know what is going to be successful for achieving measurable change in the patients they care for,” she added.
The study was funded by the Agency for Healthcare Research and Quality. The authors and other experts interviewed for this piece reported having no conflicts of interest.
The qualitative analysis, published in Annals of Family Medicine , included smoking and blood pressure as separate outcome measures.
The outcomes were calculated using Clinical Quality Measure improvements, with targets of at least 10-point absolute improvements in the proportion of patients with smoking screening, if relevant, counseling, and in the proportion of hypertensive patients with adequately controlled BP. The results were obtained from practices participating in Evidence-NOW, a multisite cardiovascular disease prevention initiative. Configurational Comparative Methods were used to evaluate the joint effects of multiple factors on outcomes.
The majority of practices in the analysis were clinician owned, small (fewer than six clinicians), and/or in an urban location. The researchers sampled and interviewed practice staff from a subset of 104 primary care practices across 7 Cooperatives and 12 states, ranging from small to medium in size, having 10 or fewer clinicians. The interview data were analyzed to identify operational changes, then transformed into numeric data.
Operational changes led to improvements in specific contexts
In clinician-owned practices, process improvement, documentation, and referral to resources, combined with a moderate level of facilitation support, led to an improvement of at least 10 points in smoking outcomes.
However, the researchers found that these patterns were not observed in system–owned practices or Federally Qualified Health Centers.
In solo practices, training medical assistants to take an accurate blood pressure led to an improvement of at least 10 points in blood pressure outcomes.
Among larger, clinician-owned practices, measurement of blood pressure a second time when the first was elevated, and documentation of this reading in the electronic heath record, also led to a 10-point or greater improvement in BP outcome when combined with a large amount (50 hours or more) of facilitation.
“There was no magic bullet for improving smoking cessation counseling and blood pressure outcomes across the diverse primary care practices studied,” lead author Deborah J. Cohen, PhD, of Oregon Health & Science University, Portland, said in an interview. “Combinations of operational changes among practice sizes and types led to improvements.”
Smaller practices more nimble, experts say
Results of the qualitative data analysis suggest that smaller and clinician-owned practices are more likely to have the capacity for change and improvement compared with larger, hospital/health system–owned practices.
Commenting on the study, Noel Deep, MD, regional medical director at Aspirus Clinics, Ironwood, Mich., said solo or small private practices have a distinct advantage over larger hospital or system-owned practices when implementing new operational changes to improve clinical outcomes.
“A smaller independent practice is nimble, with the physician [or physicians] able to make a quick decision at analyzing the scientific data, planning the changes, implementing them quickly, and doing a rapid cycle review of the results and tweaking the program to attain the targets,” said Dr. Deep, a member of the editorial advisory board of Internal Medicine News.
Kate Rowland, MD, MS, assistant professor in the department of family medicine at Rush Medical College, Chicago, also noted that smaller practices have unique advantages over larger health organizations.
“Larger organizations should replicate the benefits of the smaller office, providing as much local decision-making and autonomy as possible to the site where the changes are happening,” Dr. Rowland explained in an interview.
“The clinicians at these sites are mostly likely to know what is going to be successful for achieving measurable change in the patients they care for,” she added.
The study was funded by the Agency for Healthcare Research and Quality. The authors and other experts interviewed for this piece reported having no conflicts of interest.
FROM ANNALS OF FAMILY MEDICINE
NSAIDs don’t make COVID-19 worse in hospitalized patients
NSAIDs don’t boost the risk of more severe disease or death in hospitalized patients with COVID-19, a new study finds.
“To our knowledge, our prospective study includes the largest number of patients admitted to hospital with COVID-19 to date, and adds to the literature on the safety of NSAIDs and in-hospital outcomes. NSAIDs do not appear to increase the risk of worse in-hospital outcomes ...” the study authors wrote. “NSAIDs are an important analgesic modality and have a vital opioid-sparing role in pain management. Patients and clinicians should be reassured by these findings that NSAIDs are safe in the context of the pandemic.”
The report was published online May 7 in The Lancet Rheumatology and led by clinical research fellow Thomas M. Drake, MBChB, of the University of Edinburgh’s Usher Institute.
For more than a year, researchers worldwide have debated about whether NSAIDs spell trouble for people at risk of COVID-19. In March 2020, French health officials announced that use of the painkillers such as NSAIDs may increase the severity of the disease, and they recommended that patients take acetaminophen instead. The National Health Service in the United Kingdom made a similar recommendation. But other agencies didn’t believe there was enough evidence to support ditching NSAIDs, and recent research studies published in Annals of the Rheumatic Diseases and PLoS Medicine suggested they may be right.
For the new study, researchers identified 72,179 patients who were treated for COVID-19 in British hospitals during January-August 2020. About 56% were men, 74% were White, and 6% took NSAIDs on a regular basis before they entered the hospital. The average age was 70.
The researchers examined whether the patients in either group were more or less likely to die in the hospital, be admitted into a critical care unit, need oxygen treatment, need a ventilator, or suffer kidney injury.
In terms of outcomes, there weren’t any major gaps between the groups overall. The differences in most comparisons were statistically insignificant. For example, 31% of those who didn’t take NSAIDs died vs. 30% of those who did (P = .227). In both groups, 14% required critical care admission (P = .476).
The researchers then focused on two matched groups of 4,205 patients: One group used NSAIDs regularly, and the other group didn’t. The difference in risk of death in those who took NSAIDs vs. those who didn’t was statistically insignificant (odds ratio, 0.95; 95% confidence interval, 0.84-1.07; P = .35). Other comparisons were also statistically insignificant.
The findings offer insight into whether the use of NSAIDs might actually be helpful for patients who develop COVID-19. Scientists believe that COVID-19 is linked to inflammation in the body, and NSAIDs, of course, reduce inflammation. But the researchers didn’t turn up any sign of a benefit.
The new study has some weaknesses: It doesn’t say anything about whether NSAIDs have an impact on whether people get COVID-19 in the first place. Researchers don’t know if high use of NSAIDs may affect the severity of the disease. And it doesn’t examine the potential effect of acetaminophen, although other research suggests the drug also may not cause harm in patients with COVID-19.
Still, the researchers say the study is the largest of its kind to look at the use of NSAIDs by patients who are admitted to the hospital with COVID-19. “Considering all the evidence, if there was an extreme effect of NSAIDs on COVID-19 outcomes or severity, this would have been observed in one or more of the studies that have been done, including the present study,” they wrote.
In a commentary that accompanied the study, three physicians from hospitals in Denmark, led by Kristian Kragholm, MD, of Aalborg University Hospital, praised the research and wrote that it adds to “a growing body of evidence” that NSAIDs don’t make things worse for patients with COVID-19.
The study was funded by the U.K. National Institute for Health Research and the U.K. Medical Research Council. The study and commentary authors reported no relevant disclosures.
NSAIDs don’t boost the risk of more severe disease or death in hospitalized patients with COVID-19, a new study finds.
“To our knowledge, our prospective study includes the largest number of patients admitted to hospital with COVID-19 to date, and adds to the literature on the safety of NSAIDs and in-hospital outcomes. NSAIDs do not appear to increase the risk of worse in-hospital outcomes ...” the study authors wrote. “NSAIDs are an important analgesic modality and have a vital opioid-sparing role in pain management. Patients and clinicians should be reassured by these findings that NSAIDs are safe in the context of the pandemic.”
The report was published online May 7 in The Lancet Rheumatology and led by clinical research fellow Thomas M. Drake, MBChB, of the University of Edinburgh’s Usher Institute.
For more than a year, researchers worldwide have debated about whether NSAIDs spell trouble for people at risk of COVID-19. In March 2020, French health officials announced that use of the painkillers such as NSAIDs may increase the severity of the disease, and they recommended that patients take acetaminophen instead. The National Health Service in the United Kingdom made a similar recommendation. But other agencies didn’t believe there was enough evidence to support ditching NSAIDs, and recent research studies published in Annals of the Rheumatic Diseases and PLoS Medicine suggested they may be right.
For the new study, researchers identified 72,179 patients who were treated for COVID-19 in British hospitals during January-August 2020. About 56% were men, 74% were White, and 6% took NSAIDs on a regular basis before they entered the hospital. The average age was 70.
The researchers examined whether the patients in either group were more or less likely to die in the hospital, be admitted into a critical care unit, need oxygen treatment, need a ventilator, or suffer kidney injury.
In terms of outcomes, there weren’t any major gaps between the groups overall. The differences in most comparisons were statistically insignificant. For example, 31% of those who didn’t take NSAIDs died vs. 30% of those who did (P = .227). In both groups, 14% required critical care admission (P = .476).
The researchers then focused on two matched groups of 4,205 patients: One group used NSAIDs regularly, and the other group didn’t. The difference in risk of death in those who took NSAIDs vs. those who didn’t was statistically insignificant (odds ratio, 0.95; 95% confidence interval, 0.84-1.07; P = .35). Other comparisons were also statistically insignificant.
The findings offer insight into whether the use of NSAIDs might actually be helpful for patients who develop COVID-19. Scientists believe that COVID-19 is linked to inflammation in the body, and NSAIDs, of course, reduce inflammation. But the researchers didn’t turn up any sign of a benefit.
The new study has some weaknesses: It doesn’t say anything about whether NSAIDs have an impact on whether people get COVID-19 in the first place. Researchers don’t know if high use of NSAIDs may affect the severity of the disease. And it doesn’t examine the potential effect of acetaminophen, although other research suggests the drug also may not cause harm in patients with COVID-19.
Still, the researchers say the study is the largest of its kind to look at the use of NSAIDs by patients who are admitted to the hospital with COVID-19. “Considering all the evidence, if there was an extreme effect of NSAIDs on COVID-19 outcomes or severity, this would have been observed in one or more of the studies that have been done, including the present study,” they wrote.
In a commentary that accompanied the study, three physicians from hospitals in Denmark, led by Kristian Kragholm, MD, of Aalborg University Hospital, praised the research and wrote that it adds to “a growing body of evidence” that NSAIDs don’t make things worse for patients with COVID-19.
The study was funded by the U.K. National Institute for Health Research and the U.K. Medical Research Council. The study and commentary authors reported no relevant disclosures.
NSAIDs don’t boost the risk of more severe disease or death in hospitalized patients with COVID-19, a new study finds.
“To our knowledge, our prospective study includes the largest number of patients admitted to hospital with COVID-19 to date, and adds to the literature on the safety of NSAIDs and in-hospital outcomes. NSAIDs do not appear to increase the risk of worse in-hospital outcomes ...” the study authors wrote. “NSAIDs are an important analgesic modality and have a vital opioid-sparing role in pain management. Patients and clinicians should be reassured by these findings that NSAIDs are safe in the context of the pandemic.”
The report was published online May 7 in The Lancet Rheumatology and led by clinical research fellow Thomas M. Drake, MBChB, of the University of Edinburgh’s Usher Institute.
For more than a year, researchers worldwide have debated about whether NSAIDs spell trouble for people at risk of COVID-19. In March 2020, French health officials announced that use of the painkillers such as NSAIDs may increase the severity of the disease, and they recommended that patients take acetaminophen instead. The National Health Service in the United Kingdom made a similar recommendation. But other agencies didn’t believe there was enough evidence to support ditching NSAIDs, and recent research studies published in Annals of the Rheumatic Diseases and PLoS Medicine suggested they may be right.
For the new study, researchers identified 72,179 patients who were treated for COVID-19 in British hospitals during January-August 2020. About 56% were men, 74% were White, and 6% took NSAIDs on a regular basis before they entered the hospital. The average age was 70.
The researchers examined whether the patients in either group were more or less likely to die in the hospital, be admitted into a critical care unit, need oxygen treatment, need a ventilator, or suffer kidney injury.
In terms of outcomes, there weren’t any major gaps between the groups overall. The differences in most comparisons were statistically insignificant. For example, 31% of those who didn’t take NSAIDs died vs. 30% of those who did (P = .227). In both groups, 14% required critical care admission (P = .476).
The researchers then focused on two matched groups of 4,205 patients: One group used NSAIDs regularly, and the other group didn’t. The difference in risk of death in those who took NSAIDs vs. those who didn’t was statistically insignificant (odds ratio, 0.95; 95% confidence interval, 0.84-1.07; P = .35). Other comparisons were also statistically insignificant.
The findings offer insight into whether the use of NSAIDs might actually be helpful for patients who develop COVID-19. Scientists believe that COVID-19 is linked to inflammation in the body, and NSAIDs, of course, reduce inflammation. But the researchers didn’t turn up any sign of a benefit.
The new study has some weaknesses: It doesn’t say anything about whether NSAIDs have an impact on whether people get COVID-19 in the first place. Researchers don’t know if high use of NSAIDs may affect the severity of the disease. And it doesn’t examine the potential effect of acetaminophen, although other research suggests the drug also may not cause harm in patients with COVID-19.
Still, the researchers say the study is the largest of its kind to look at the use of NSAIDs by patients who are admitted to the hospital with COVID-19. “Considering all the evidence, if there was an extreme effect of NSAIDs on COVID-19 outcomes or severity, this would have been observed in one or more of the studies that have been done, including the present study,” they wrote.
In a commentary that accompanied the study, three physicians from hospitals in Denmark, led by Kristian Kragholm, MD, of Aalborg University Hospital, praised the research and wrote that it adds to “a growing body of evidence” that NSAIDs don’t make things worse for patients with COVID-19.
The study was funded by the U.K. National Institute for Health Research and the U.K. Medical Research Council. The study and commentary authors reported no relevant disclosures.
FROM THE LANCET RHEUMATOLOGY
Two treatments show early promise for hypothalamic obesity
Two different agents showed potential for safely treating patients with hypothalamic obesity in two pilot studies with small numbers of patients.
One study prospectively randomized 21 adults with acquired hypothalamic obesity to treatment with placebo or Tesomet, a compound that combines the novel monoamine reuptake inhibitor tesofensine with metoprolol, a beta-blocker added to protect against adverse effects from tesofensine on heart rate and cardiac contractility. After 24 weeks of treatment, people on tesofensine/metoprolol had significant weight loss, compared with controls, while showing good tolerance with no significant effects on heart rate, blood pressure, or heart rhythm, Ulla Feldt-Rasmussen, MD, DMSc, reported at the annual meeting of the Endocrine Society.
The second report reviewed 18 children and adolescents with either acquired or genetic hypothalamic obesity who received open-label treatment with dextroamphetamine for an average of 20 months, and overall patients safely lost an average of 0.43 in their body mass index (BMI) standard deviation score, reported Jiska van Schaik, MD, in a separate talk at the meeting.
‘A supplement for lost satiety’
Patients with hypothalamic obesity face a dual problem from hypothalamic dysfunction that’s addressed by tesofensine, the weight-loss agent in Tesomet that increases hypothalamic levels of dopamine, serotonin, and noradrenaline by blocking reuptake, and thereby dulls appetite and food craving while also increasing fat metabolism, explained Dr. Feldt-Rasmussen, a professor of medical endocrinology at the University of Denmark and Rigshospitalet in Copenhagen. No treatment currently has regulatory approval for treating any form of hypothalamic obesity.
Tesofensine works as “a supplement for lost satiety, and satiety is what is lost” in patients with hypothalamic obesity as well in patients as Prader-Willi syndrome, the two disorders for which tesofensine/metoprolol is currently undergoing testing. “That’s the rationale, and it seems to work,” she declared during her talk. The formulation contains 0.5 mg tesofensine and 50 mg metoprolol administered orally once daily.
The study, run at Rigshospitalet, randomized 21 patients aged 18-75 years and with a BMI of at least 27 kg/m2who all had acquired hypothalamic obesity secondary to hypothalamic damage following cancer treatment. Patients averaged about 45 years of age, three-quarters were women, and their average BMI was about 37, with 90% having a BMI of at least 30.
The study’s design calls for 48-week follow-up; Dr. Feldt-Rasmussen presented the interim results after 24 weeks, with 18 of the 21 enrolled patients remaining in the study through 24 weeks. Three patients dropped out because of adverse events: one in the placebo arm, and two who received tesofensine/metoprolol.
Weight dropped by an average of 6.6 kg from baseline among the 11 patients who completed 24 weeks on tesofensine/metoprolol treatment, compared with no average change from baseline among the seven patients who completed the study on placebo, a significant difference. The researchers measured a validated, composite satiety score every 4 weeks, and found significantly more improvement among patients on tesofensine/metoprolol than in those on placebo during the study’s first half, but subsequently average scores among the actively treated patients fell to the same level of modest improvement as in the placebo patients.
Despite this, average weight loss in the patients on tesofensine/metoprolol steadily increased throughout the full 24 weeks.
Safety measures of diastolic blood pressure, heart rate, and corrected QT interval showed no significant between-group difference. Systolic pressure showed a transient average rise of 4 mm Hg above baseline in the tesofensine/metoprolol group, compared with a small dip in the control patients, but by 24 weeks average systolic blood pressure had reverted closer to baseline levels in both subgroups and showed no significant between-group difference. Two patients on tesofensine/metoprolol developed serious adverse events. In one patient these were not treatment related. The other patient developed anxiety after 8 weeks that was possibly treatment related but remained on treatment. Other adverse effects on tesofensine/metoprolol included dizziness, sleep disorder, and dry mouth, but all of these were mild and patients were willing to tolerate them to achieve their weight loss, Dr. Feldt-Rasmussen said.
Repurposing an ADHD treatment
Dextroamphetamine increases satiety and boosts resting energy expenditure, and is a common treatment for attention deficit hyperactivity disorder. Dr. van Schaik and coauthors reviewed 13 children and adolescents with acquired hypothalamic obesity and 5 with genetic hypothalamic obesity who received the treatment at either of two Dutch hospitals during 2014-2020. All 18 patients went on dextroamphetamine after other interventions had failed to produce improvement, said Dr. van Schaik, a researcher at University Medical Center and Wilhelmina Children’s Hospital in Utrecht, the Netherlands. The patients averaged about 13 years of age.
In addition to an overall effect on weight across all 18 subjects, the researchers found they could subdivide the full cohort into 10 responders (56%), 4 (22%) with weight stabilization on treatment, and 4 nonresponders (22%) who continued to gain weight despite treatment. The 10 responding patients had an average drop in their BMI standard deviation score of 0.91. All 10 responders had acquired hypothalamic obesity, and they averaged a 12.5 percentage point rise in their resting energy expenditure level, compared with baseline, while on treatment. The four whose weight stabilized on treatment included three patients with genetic hypothalamic obesity. The four nonresponders split into two with acquired hypothalamic obesity and two with the genetic form.
Thirteen patients (72%) had improvements in hyperphagia, energy, and behavior, and no patient had a serious adverse effect. One patient stopped treatment after 1 month because of elevated blood pressure.
“Dextroamphetamine may be promising, especially for acquired hypothalamic obesity,” Dr. van Schaik concluded, adding that prospective, controlled assessments are needed, and that a healthy lifestyle is the foundation of hypothalamic obesity treatment.
The Tesomet study was sponsored by Saniona, the company developing Tesomet. Dr Feldt-Rasmussen is an advisor to Saniona, and some of the coauthors on the study are Saniona employees. Dr. van Schaik had no disclosures.
Two different agents showed potential for safely treating patients with hypothalamic obesity in two pilot studies with small numbers of patients.
One study prospectively randomized 21 adults with acquired hypothalamic obesity to treatment with placebo or Tesomet, a compound that combines the novel monoamine reuptake inhibitor tesofensine with metoprolol, a beta-blocker added to protect against adverse effects from tesofensine on heart rate and cardiac contractility. After 24 weeks of treatment, people on tesofensine/metoprolol had significant weight loss, compared with controls, while showing good tolerance with no significant effects on heart rate, blood pressure, or heart rhythm, Ulla Feldt-Rasmussen, MD, DMSc, reported at the annual meeting of the Endocrine Society.
The second report reviewed 18 children and adolescents with either acquired or genetic hypothalamic obesity who received open-label treatment with dextroamphetamine for an average of 20 months, and overall patients safely lost an average of 0.43 in their body mass index (BMI) standard deviation score, reported Jiska van Schaik, MD, in a separate talk at the meeting.
‘A supplement for lost satiety’
Patients with hypothalamic obesity face a dual problem from hypothalamic dysfunction that’s addressed by tesofensine, the weight-loss agent in Tesomet that increases hypothalamic levels of dopamine, serotonin, and noradrenaline by blocking reuptake, and thereby dulls appetite and food craving while also increasing fat metabolism, explained Dr. Feldt-Rasmussen, a professor of medical endocrinology at the University of Denmark and Rigshospitalet in Copenhagen. No treatment currently has regulatory approval for treating any form of hypothalamic obesity.
Tesofensine works as “a supplement for lost satiety, and satiety is what is lost” in patients with hypothalamic obesity as well in patients as Prader-Willi syndrome, the two disorders for which tesofensine/metoprolol is currently undergoing testing. “That’s the rationale, and it seems to work,” she declared during her talk. The formulation contains 0.5 mg tesofensine and 50 mg metoprolol administered orally once daily.
The study, run at Rigshospitalet, randomized 21 patients aged 18-75 years and with a BMI of at least 27 kg/m2who all had acquired hypothalamic obesity secondary to hypothalamic damage following cancer treatment. Patients averaged about 45 years of age, three-quarters were women, and their average BMI was about 37, with 90% having a BMI of at least 30.
The study’s design calls for 48-week follow-up; Dr. Feldt-Rasmussen presented the interim results after 24 weeks, with 18 of the 21 enrolled patients remaining in the study through 24 weeks. Three patients dropped out because of adverse events: one in the placebo arm, and two who received tesofensine/metoprolol.
Weight dropped by an average of 6.6 kg from baseline among the 11 patients who completed 24 weeks on tesofensine/metoprolol treatment, compared with no average change from baseline among the seven patients who completed the study on placebo, a significant difference. The researchers measured a validated, composite satiety score every 4 weeks, and found significantly more improvement among patients on tesofensine/metoprolol than in those on placebo during the study’s first half, but subsequently average scores among the actively treated patients fell to the same level of modest improvement as in the placebo patients.
Despite this, average weight loss in the patients on tesofensine/metoprolol steadily increased throughout the full 24 weeks.
Safety measures of diastolic blood pressure, heart rate, and corrected QT interval showed no significant between-group difference. Systolic pressure showed a transient average rise of 4 mm Hg above baseline in the tesofensine/metoprolol group, compared with a small dip in the control patients, but by 24 weeks average systolic blood pressure had reverted closer to baseline levels in both subgroups and showed no significant between-group difference. Two patients on tesofensine/metoprolol developed serious adverse events. In one patient these were not treatment related. The other patient developed anxiety after 8 weeks that was possibly treatment related but remained on treatment. Other adverse effects on tesofensine/metoprolol included dizziness, sleep disorder, and dry mouth, but all of these were mild and patients were willing to tolerate them to achieve their weight loss, Dr. Feldt-Rasmussen said.
Repurposing an ADHD treatment
Dextroamphetamine increases satiety and boosts resting energy expenditure, and is a common treatment for attention deficit hyperactivity disorder. Dr. van Schaik and coauthors reviewed 13 children and adolescents with acquired hypothalamic obesity and 5 with genetic hypothalamic obesity who received the treatment at either of two Dutch hospitals during 2014-2020. All 18 patients went on dextroamphetamine after other interventions had failed to produce improvement, said Dr. van Schaik, a researcher at University Medical Center and Wilhelmina Children’s Hospital in Utrecht, the Netherlands. The patients averaged about 13 years of age.
In addition to an overall effect on weight across all 18 subjects, the researchers found they could subdivide the full cohort into 10 responders (56%), 4 (22%) with weight stabilization on treatment, and 4 nonresponders (22%) who continued to gain weight despite treatment. The 10 responding patients had an average drop in their BMI standard deviation score of 0.91. All 10 responders had acquired hypothalamic obesity, and they averaged a 12.5 percentage point rise in their resting energy expenditure level, compared with baseline, while on treatment. The four whose weight stabilized on treatment included three patients with genetic hypothalamic obesity. The four nonresponders split into two with acquired hypothalamic obesity and two with the genetic form.
Thirteen patients (72%) had improvements in hyperphagia, energy, and behavior, and no patient had a serious adverse effect. One patient stopped treatment after 1 month because of elevated blood pressure.
“Dextroamphetamine may be promising, especially for acquired hypothalamic obesity,” Dr. van Schaik concluded, adding that prospective, controlled assessments are needed, and that a healthy lifestyle is the foundation of hypothalamic obesity treatment.
The Tesomet study was sponsored by Saniona, the company developing Tesomet. Dr Feldt-Rasmussen is an advisor to Saniona, and some of the coauthors on the study are Saniona employees. Dr. van Schaik had no disclosures.
Two different agents showed potential for safely treating patients with hypothalamic obesity in two pilot studies with small numbers of patients.
One study prospectively randomized 21 adults with acquired hypothalamic obesity to treatment with placebo or Tesomet, a compound that combines the novel monoamine reuptake inhibitor tesofensine with metoprolol, a beta-blocker added to protect against adverse effects from tesofensine on heart rate and cardiac contractility. After 24 weeks of treatment, people on tesofensine/metoprolol had significant weight loss, compared with controls, while showing good tolerance with no significant effects on heart rate, blood pressure, or heart rhythm, Ulla Feldt-Rasmussen, MD, DMSc, reported at the annual meeting of the Endocrine Society.
The second report reviewed 18 children and adolescents with either acquired or genetic hypothalamic obesity who received open-label treatment with dextroamphetamine for an average of 20 months, and overall patients safely lost an average of 0.43 in their body mass index (BMI) standard deviation score, reported Jiska van Schaik, MD, in a separate talk at the meeting.
‘A supplement for lost satiety’
Patients with hypothalamic obesity face a dual problem from hypothalamic dysfunction that’s addressed by tesofensine, the weight-loss agent in Tesomet that increases hypothalamic levels of dopamine, serotonin, and noradrenaline by blocking reuptake, and thereby dulls appetite and food craving while also increasing fat metabolism, explained Dr. Feldt-Rasmussen, a professor of medical endocrinology at the University of Denmark and Rigshospitalet in Copenhagen. No treatment currently has regulatory approval for treating any form of hypothalamic obesity.
Tesofensine works as “a supplement for lost satiety, and satiety is what is lost” in patients with hypothalamic obesity as well in patients as Prader-Willi syndrome, the two disorders for which tesofensine/metoprolol is currently undergoing testing. “That’s the rationale, and it seems to work,” she declared during her talk. The formulation contains 0.5 mg tesofensine and 50 mg metoprolol administered orally once daily.
The study, run at Rigshospitalet, randomized 21 patients aged 18-75 years and with a BMI of at least 27 kg/m2who all had acquired hypothalamic obesity secondary to hypothalamic damage following cancer treatment. Patients averaged about 45 years of age, three-quarters were women, and their average BMI was about 37, with 90% having a BMI of at least 30.
The study’s design calls for 48-week follow-up; Dr. Feldt-Rasmussen presented the interim results after 24 weeks, with 18 of the 21 enrolled patients remaining in the study through 24 weeks. Three patients dropped out because of adverse events: one in the placebo arm, and two who received tesofensine/metoprolol.
Weight dropped by an average of 6.6 kg from baseline among the 11 patients who completed 24 weeks on tesofensine/metoprolol treatment, compared with no average change from baseline among the seven patients who completed the study on placebo, a significant difference. The researchers measured a validated, composite satiety score every 4 weeks, and found significantly more improvement among patients on tesofensine/metoprolol than in those on placebo during the study’s first half, but subsequently average scores among the actively treated patients fell to the same level of modest improvement as in the placebo patients.
Despite this, average weight loss in the patients on tesofensine/metoprolol steadily increased throughout the full 24 weeks.
Safety measures of diastolic blood pressure, heart rate, and corrected QT interval showed no significant between-group difference. Systolic pressure showed a transient average rise of 4 mm Hg above baseline in the tesofensine/metoprolol group, compared with a small dip in the control patients, but by 24 weeks average systolic blood pressure had reverted closer to baseline levels in both subgroups and showed no significant between-group difference. Two patients on tesofensine/metoprolol developed serious adverse events. In one patient these were not treatment related. The other patient developed anxiety after 8 weeks that was possibly treatment related but remained on treatment. Other adverse effects on tesofensine/metoprolol included dizziness, sleep disorder, and dry mouth, but all of these were mild and patients were willing to tolerate them to achieve their weight loss, Dr. Feldt-Rasmussen said.
Repurposing an ADHD treatment
Dextroamphetamine increases satiety and boosts resting energy expenditure, and is a common treatment for attention deficit hyperactivity disorder. Dr. van Schaik and coauthors reviewed 13 children and adolescents with acquired hypothalamic obesity and 5 with genetic hypothalamic obesity who received the treatment at either of two Dutch hospitals during 2014-2020. All 18 patients went on dextroamphetamine after other interventions had failed to produce improvement, said Dr. van Schaik, a researcher at University Medical Center and Wilhelmina Children’s Hospital in Utrecht, the Netherlands. The patients averaged about 13 years of age.
In addition to an overall effect on weight across all 18 subjects, the researchers found they could subdivide the full cohort into 10 responders (56%), 4 (22%) with weight stabilization on treatment, and 4 nonresponders (22%) who continued to gain weight despite treatment. The 10 responding patients had an average drop in their BMI standard deviation score of 0.91. All 10 responders had acquired hypothalamic obesity, and they averaged a 12.5 percentage point rise in their resting energy expenditure level, compared with baseline, while on treatment. The four whose weight stabilized on treatment included three patients with genetic hypothalamic obesity. The four nonresponders split into two with acquired hypothalamic obesity and two with the genetic form.
Thirteen patients (72%) had improvements in hyperphagia, energy, and behavior, and no patient had a serious adverse effect. One patient stopped treatment after 1 month because of elevated blood pressure.
“Dextroamphetamine may be promising, especially for acquired hypothalamic obesity,” Dr. van Schaik concluded, adding that prospective, controlled assessments are needed, and that a healthy lifestyle is the foundation of hypothalamic obesity treatment.
The Tesomet study was sponsored by Saniona, the company developing Tesomet. Dr Feldt-Rasmussen is an advisor to Saniona, and some of the coauthors on the study are Saniona employees. Dr. van Schaik had no disclosures.
FROM ENDO 2021
TIPP the scales in managing stress
The past year presented unprecedented challenges for many. In addition, mental health services have also been stretched to capacity. Anecdotally, some hospitals and emergency departments note that more youth have been presenting in mental health crises, and the severity of symptoms has also been higher. Safety planning is important, including working with patients to identify skills they can use in distress. Even those who do not experience suicidal thoughts may struggle with dysregulation or may use coping strategies that may not be the healthiest in the long term.
Within my practice, I see some families who are still waiting for an available therapist, or some may not wish to participate in therapy despite its being recommended. For these families, supporting them in using strategies that they may be willing and able to use in the moment to help them get through the moment of crisis can been helpful:
Case example (identifying details have been changed)
Emily is a 17-year-old girl who has a history of generalized anxiety disorder and obsessive-compulsive disorder. She has had multiple medication trials and a course of cognitive behavioral therapy when younger, with significant improvement in symptoms. She returns to clinic because of increased anxiety related to stressors of the pandemic. She wishes to not return to therapy because of feeling that she received maximal benefit and that further sessions would not be fruitful. However, she struggles with identifying what skills she can use, and her anxiety heightens significantly to near-panic and hyperventilating with even cursory exploration of triggers for her symptoms. Medications are also discussed during this appointment, and it is noted that it may take some time to see therapeutic effect. Of note, she reports no acute safety concerns. She has engaged in skin picking. No reported substance use. As she hyperventilates, she was asked to identify items in the room matching the colors of the rainbow in order. She was able to quickly do this, and then was asked to do it again. Afterward, she noted feeling much less anxious because it distracted her from her thoughts.
Distress tolerance skills can be very helpful to navigate getting through a crisis. When under stress, some may be more likely to engage in behaviors that are not helpful in the long term such as using avoidance; procrastinating; consuming tobacco, alcohol, or other substances; spending too much time on screens; or engaging in self-harm behaviors. While some of these activities may be okay in moderation, others are always harmful. At times, when encouraging patients to use skills with which they may be more familiar, e.g., deep breathing, progressive muscle relaxation, the response may be, “these don’t work!” It can be important to distinguish that the function of these skills is not to make someone feel good or to eliminate the stressor, but to “take some of the edge off” so they are less likely to slide into problematic behaviors. It can be beneficial to have multiple tools at one’s disposal because not all skills will always be effective or available.
TIPP skills (temperature, intense exercise, paced breathing, progressive muscle relaxation) are distress tolerance skills from dialectical behavioral therapy (DBT),1 which was initially developed to treat individuals with borderline personality disorder. More recently, the therapy modality has been applied to individuals who may struggle with emotion regulation for a variety of reasons. TIPP skills work quickly (within seconds to minutes) with the aim to decrease physiological arousal. They do not require a lot of thinking, and many are portable or easy to use. Given the speed of effect, these skills can also be used in lieu of p.r.n. medications or patients can be counseled about trying these instead of turning to substance use. The effect is brief (5-20 minutes), although this may lower the affective temperature sufficiently for someone to get through the intense moment or to be able to then utilize other skills that may require more cognitive reserves.
T – Temperature
Holding one’s breath and placing one’s face in cold water (above 50°) for 10-20 seconds to stimulate the diving response and decrease heart rate. Patients can repeat this up to 3 times. Alternatively, cold compresses or gel eye masks can be used.
I – Intense exercise
Aerobic exercise for 10-20 minutes. This can include running, jumping jacks, dancing to loud music in a way that feels intense. The parasympathetic nervous system (PNS) is activated for approximately 20 minutes after cessation of intense exercise.
P – Paced breathing
Decreasing rate of breathing, with each inhalation/exhalation cycle lasting 10-12 seconds and the exhale being longer than the inhale also activates the PNS.
P – Progressive muscle relaxation (PMR)
Sequentially tensing and relaxing muscles from head to toes. Having at least 5-10 minutes to perform this exercise is preferred.2 Children’s Hospital of Philadelphia offerssample PMR recordings.
Body scans can also be helpful. This practice differs from PMR in that it is a mindfulness practice noting body sensations without trying to change them. The University of Vermont offers some sample exercises.3
These skills were described to Emily. She noted that dunking her face in cold water was effective and it was reassuring knowing she had a tool to help her anxiety. She started to push herself to go outside to exercise. We additionally incorporated other distraction techniques such as identifying items from colors of the rainbow that were around her. She appreciated that she could even do this discreetly while at school. At times she had to do a couple of rounds, but this could help stop her repetitive thoughts so she could use other skills.
Helping patients identify skills that can help in the moment can help them feel supported and gain traction in other areas.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. She has no relevant financial disclosures
References
1. Rathus JH, Miller AL. DBT® Skills manual for adolescents. 2015. Guilford Press.
2. Guided Relaxation Exercises, Children’s Hospital of Philadelphia.
3. Vermont Center for Children, Youth, and Families: Staying Close While Keeping Your Distance.
The past year presented unprecedented challenges for many. In addition, mental health services have also been stretched to capacity. Anecdotally, some hospitals and emergency departments note that more youth have been presenting in mental health crises, and the severity of symptoms has also been higher. Safety planning is important, including working with patients to identify skills they can use in distress. Even those who do not experience suicidal thoughts may struggle with dysregulation or may use coping strategies that may not be the healthiest in the long term.
Within my practice, I see some families who are still waiting for an available therapist, or some may not wish to participate in therapy despite its being recommended. For these families, supporting them in using strategies that they may be willing and able to use in the moment to help them get through the moment of crisis can been helpful:
Case example (identifying details have been changed)
Emily is a 17-year-old girl who has a history of generalized anxiety disorder and obsessive-compulsive disorder. She has had multiple medication trials and a course of cognitive behavioral therapy when younger, with significant improvement in symptoms. She returns to clinic because of increased anxiety related to stressors of the pandemic. She wishes to not return to therapy because of feeling that she received maximal benefit and that further sessions would not be fruitful. However, she struggles with identifying what skills she can use, and her anxiety heightens significantly to near-panic and hyperventilating with even cursory exploration of triggers for her symptoms. Medications are also discussed during this appointment, and it is noted that it may take some time to see therapeutic effect. Of note, she reports no acute safety concerns. She has engaged in skin picking. No reported substance use. As she hyperventilates, she was asked to identify items in the room matching the colors of the rainbow in order. She was able to quickly do this, and then was asked to do it again. Afterward, she noted feeling much less anxious because it distracted her from her thoughts.
Distress tolerance skills can be very helpful to navigate getting through a crisis. When under stress, some may be more likely to engage in behaviors that are not helpful in the long term such as using avoidance; procrastinating; consuming tobacco, alcohol, or other substances; spending too much time on screens; or engaging in self-harm behaviors. While some of these activities may be okay in moderation, others are always harmful. At times, when encouraging patients to use skills with which they may be more familiar, e.g., deep breathing, progressive muscle relaxation, the response may be, “these don’t work!” It can be important to distinguish that the function of these skills is not to make someone feel good or to eliminate the stressor, but to “take some of the edge off” so they are less likely to slide into problematic behaviors. It can be beneficial to have multiple tools at one’s disposal because not all skills will always be effective or available.
TIPP skills (temperature, intense exercise, paced breathing, progressive muscle relaxation) are distress tolerance skills from dialectical behavioral therapy (DBT),1 which was initially developed to treat individuals with borderline personality disorder. More recently, the therapy modality has been applied to individuals who may struggle with emotion regulation for a variety of reasons. TIPP skills work quickly (within seconds to minutes) with the aim to decrease physiological arousal. They do not require a lot of thinking, and many are portable or easy to use. Given the speed of effect, these skills can also be used in lieu of p.r.n. medications or patients can be counseled about trying these instead of turning to substance use. The effect is brief (5-20 minutes), although this may lower the affective temperature sufficiently for someone to get through the intense moment or to be able to then utilize other skills that may require more cognitive reserves.
T – Temperature
Holding one’s breath and placing one’s face in cold water (above 50°) for 10-20 seconds to stimulate the diving response and decrease heart rate. Patients can repeat this up to 3 times. Alternatively, cold compresses or gel eye masks can be used.
I – Intense exercise
Aerobic exercise for 10-20 minutes. This can include running, jumping jacks, dancing to loud music in a way that feels intense. The parasympathetic nervous system (PNS) is activated for approximately 20 minutes after cessation of intense exercise.
P – Paced breathing
Decreasing rate of breathing, with each inhalation/exhalation cycle lasting 10-12 seconds and the exhale being longer than the inhale also activates the PNS.
P – Progressive muscle relaxation (PMR)
Sequentially tensing and relaxing muscles from head to toes. Having at least 5-10 minutes to perform this exercise is preferred.2 Children’s Hospital of Philadelphia offerssample PMR recordings.
Body scans can also be helpful. This practice differs from PMR in that it is a mindfulness practice noting body sensations without trying to change them. The University of Vermont offers some sample exercises.3
These skills were described to Emily. She noted that dunking her face in cold water was effective and it was reassuring knowing she had a tool to help her anxiety. She started to push herself to go outside to exercise. We additionally incorporated other distraction techniques such as identifying items from colors of the rainbow that were around her. She appreciated that she could even do this discreetly while at school. At times she had to do a couple of rounds, but this could help stop her repetitive thoughts so she could use other skills.
Helping patients identify skills that can help in the moment can help them feel supported and gain traction in other areas.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. She has no relevant financial disclosures
References
1. Rathus JH, Miller AL. DBT® Skills manual for adolescents. 2015. Guilford Press.
2. Guided Relaxation Exercises, Children’s Hospital of Philadelphia.
3. Vermont Center for Children, Youth, and Families: Staying Close While Keeping Your Distance.
The past year presented unprecedented challenges for many. In addition, mental health services have also been stretched to capacity. Anecdotally, some hospitals and emergency departments note that more youth have been presenting in mental health crises, and the severity of symptoms has also been higher. Safety planning is important, including working with patients to identify skills they can use in distress. Even those who do not experience suicidal thoughts may struggle with dysregulation or may use coping strategies that may not be the healthiest in the long term.
Within my practice, I see some families who are still waiting for an available therapist, or some may not wish to participate in therapy despite its being recommended. For these families, supporting them in using strategies that they may be willing and able to use in the moment to help them get through the moment of crisis can been helpful:
Case example (identifying details have been changed)
Emily is a 17-year-old girl who has a history of generalized anxiety disorder and obsessive-compulsive disorder. She has had multiple medication trials and a course of cognitive behavioral therapy when younger, with significant improvement in symptoms. She returns to clinic because of increased anxiety related to stressors of the pandemic. She wishes to not return to therapy because of feeling that she received maximal benefit and that further sessions would not be fruitful. However, she struggles with identifying what skills she can use, and her anxiety heightens significantly to near-panic and hyperventilating with even cursory exploration of triggers for her symptoms. Medications are also discussed during this appointment, and it is noted that it may take some time to see therapeutic effect. Of note, she reports no acute safety concerns. She has engaged in skin picking. No reported substance use. As she hyperventilates, she was asked to identify items in the room matching the colors of the rainbow in order. She was able to quickly do this, and then was asked to do it again. Afterward, she noted feeling much less anxious because it distracted her from her thoughts.
Distress tolerance skills can be very helpful to navigate getting through a crisis. When under stress, some may be more likely to engage in behaviors that are not helpful in the long term such as using avoidance; procrastinating; consuming tobacco, alcohol, or other substances; spending too much time on screens; or engaging in self-harm behaviors. While some of these activities may be okay in moderation, others are always harmful. At times, when encouraging patients to use skills with which they may be more familiar, e.g., deep breathing, progressive muscle relaxation, the response may be, “these don’t work!” It can be important to distinguish that the function of these skills is not to make someone feel good or to eliminate the stressor, but to “take some of the edge off” so they are less likely to slide into problematic behaviors. It can be beneficial to have multiple tools at one’s disposal because not all skills will always be effective or available.
TIPP skills (temperature, intense exercise, paced breathing, progressive muscle relaxation) are distress tolerance skills from dialectical behavioral therapy (DBT),1 which was initially developed to treat individuals with borderline personality disorder. More recently, the therapy modality has been applied to individuals who may struggle with emotion regulation for a variety of reasons. TIPP skills work quickly (within seconds to minutes) with the aim to decrease physiological arousal. They do not require a lot of thinking, and many are portable or easy to use. Given the speed of effect, these skills can also be used in lieu of p.r.n. medications or patients can be counseled about trying these instead of turning to substance use. The effect is brief (5-20 minutes), although this may lower the affective temperature sufficiently for someone to get through the intense moment or to be able to then utilize other skills that may require more cognitive reserves.
T – Temperature
Holding one’s breath and placing one’s face in cold water (above 50°) for 10-20 seconds to stimulate the diving response and decrease heart rate. Patients can repeat this up to 3 times. Alternatively, cold compresses or gel eye masks can be used.
I – Intense exercise
Aerobic exercise for 10-20 minutes. This can include running, jumping jacks, dancing to loud music in a way that feels intense. The parasympathetic nervous system (PNS) is activated for approximately 20 minutes after cessation of intense exercise.
P – Paced breathing
Decreasing rate of breathing, with each inhalation/exhalation cycle lasting 10-12 seconds and the exhale being longer than the inhale also activates the PNS.
P – Progressive muscle relaxation (PMR)
Sequentially tensing and relaxing muscles from head to toes. Having at least 5-10 minutes to perform this exercise is preferred.2 Children’s Hospital of Philadelphia offerssample PMR recordings.
Body scans can also be helpful. This practice differs from PMR in that it is a mindfulness practice noting body sensations without trying to change them. The University of Vermont offers some sample exercises.3
These skills were described to Emily. She noted that dunking her face in cold water was effective and it was reassuring knowing she had a tool to help her anxiety. She started to push herself to go outside to exercise. We additionally incorporated other distraction techniques such as identifying items from colors of the rainbow that were around her. She appreciated that she could even do this discreetly while at school. At times she had to do a couple of rounds, but this could help stop her repetitive thoughts so she could use other skills.
Helping patients identify skills that can help in the moment can help them feel supported and gain traction in other areas.
Dr. Strange is an assistant professor in the department of psychiatry at the University of Vermont Medical Center and University of Vermont Robert Larner College of Medicine, both in Burlington. She works with children and adolescents. She has no relevant financial disclosures
References
1. Rathus JH, Miller AL. DBT® Skills manual for adolescents. 2015. Guilford Press.
2. Guided Relaxation Exercises, Children’s Hospital of Philadelphia.
3. Vermont Center for Children, Youth, and Families: Staying Close While Keeping Your Distance.
Focus on youth concerns at well visits
Taking teens’ strengths, values, and dreams, into account through a previsit questionnaire was acceptable to them and may promote discussions with providers, based on data from 91 adolescents.
The American Academy of Pediatrics’ Bright Futures initiative recommends the use of a strength-based approach for adolescent well visits, but the extensive positive psychology inventories to identify teen strengths and values are impractical for the clinical visit setting, wrote Yidan Cao, MPH, of the Child Development through Primary Care at the University of Michigan, Ann Arbor, and colleagues. However, 76% of youth participating in focus groups responded that “using a confidential questionnaire about a teen’s strengths and goals before checkup visits would be a good addition to health care for teens,” the researchers said.
In a study presented in a poster session (#515) at the Pediatric Academic Societies annual meeting, the researchers recruited 91 community youth to participate in 13 focus groups related to teen depression and substance use. The age of the focus group participants ranged from 12 to 18 years, with an average of 15 years, 61.5% were female, and 1.1% identified as transgender. The racial breakdown was 51.6% White, 27.5% African American, 8.8% Asian, 2.2% Native American, 3.3% biracial, and 6.6% unknown.
The participants provided information on potential questionnaire items for an online previsit screening for well visits to assess strengths and identify values, goals, dream jobs, and life wishes.
Suggestions from the participants informed changes to the questionnaire, which included five categories: personal/social goals, goals for academics/training, strengths, values, and dream jobs.
The top endorsed personal goal of “to be happy” was chosen by 13.1% of the participants. The top academic goal was “get good grades” (45.5%). The top endorsed strength was “fitness/coordination/sports/physical activity” (22.9%), while the top value was caring and kindness (25.8%), and the top dream job category was health/medical (30.8%).
Key comments made by the youth participants for improving the previsit questionnaire included adding an option for “I can’t decide,” and allowing for multiple responses to avoid feeling pinned down or judged, the researchers noted.
The researchers highlighted one teen comment: “While I understand the purpose of limiting the participants to two answers, it is incredibly difficult to only choose two. Being limited to two very much restricts your understanding of our values. For example, I would’ve also liked to select ‘to do well in school’ and ‘to make a difference,’ but ‘being happy’ and ‘being loving to all those around me’ had to take precedent.”
The study was limited by not being fully generalizable to all teens, as other teens may hold views and beliefs that differ from those of the focus group participants, the researchers noted.
However, the findings support the value of a strength-based previsit questionnaire for adolescents, they said.
“Structured previsit data could facilitate relationship building and be actionable for assigning strength and resiliency building resources,” they noted. “A final strengths and goals questionnaire is now being piloted in computerized form contributing to decision supports for suggested teleprompters and associated resource options,” and future research may show the value of such previsit data for improved clinical process and outcomes of youth well visits, they concluded.
Recognize the uncertainty of adolescence
“Adolescents are at crossroads of identity, trying to figure out who they are, their goals and values,” said Kelly A. Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, in an interview. “Adolescence is also a critical time when teens have more control and choice over behaviors that impact their health, such as diet, exercise, substance use, and sexual activity. In this critical time period, clinicians can intervene on health-related behaviors and shape the trajectory of a teen’s life. However, to promote teen health, pediatricians need to have their patients’ trust, which can be hard to gain,” she emphasized.
“In my practice, I’ve found that teens often just want to be seen and heard,” said Dr. Curran. “Teens often have many adults in their life who focus on the ‘don’ts’ – don’t use drugs, don’t have sex, for example – and few that praise healthy behaviors or strengths, or seek to understand what is important to them. By listening to teens and understanding what’s important to them, we can then use motivational interviewing techniques to help create meaningful change in health-related behaviors. However, this takes time and investment, which is often in conflict with time pressures in the modern medical system.
“This study is useful because it examined the acceptability of a positive psychology questionnaire to be used at well visits when reviewed by youth, that could be used to streamline this important process,” said Dr. Curran.
“From my practice, I know that understanding a teen’s goals, values, and strengths is important – we do this daily in our practice when working with patients – but it was exciting to see that youth found it acceptable to do this via a previsit survey, which can potentially streamline well visits,” she noted.
The questionnaire is being developed as a pilot program, but more research is needed to determine the direct clinical impact, said Dr. Curran. “It will be important in the future to see if implementation of this questionnaire can be helpful in integrating this information into motivational interviewing and rapport building to help improve teens’ health outcomes.”
The study was supported in part by the National Institute on Drug Abuse and the National Institute of Mental Health. Two coauthors have a financial interest in the CHADIS online reporting program used in the study. Dr. Curran had no financial conflicts to disclose.
Taking teens’ strengths, values, and dreams, into account through a previsit questionnaire was acceptable to them and may promote discussions with providers, based on data from 91 adolescents.
The American Academy of Pediatrics’ Bright Futures initiative recommends the use of a strength-based approach for adolescent well visits, but the extensive positive psychology inventories to identify teen strengths and values are impractical for the clinical visit setting, wrote Yidan Cao, MPH, of the Child Development through Primary Care at the University of Michigan, Ann Arbor, and colleagues. However, 76% of youth participating in focus groups responded that “using a confidential questionnaire about a teen’s strengths and goals before checkup visits would be a good addition to health care for teens,” the researchers said.
In a study presented in a poster session (#515) at the Pediatric Academic Societies annual meeting, the researchers recruited 91 community youth to participate in 13 focus groups related to teen depression and substance use. The age of the focus group participants ranged from 12 to 18 years, with an average of 15 years, 61.5% were female, and 1.1% identified as transgender. The racial breakdown was 51.6% White, 27.5% African American, 8.8% Asian, 2.2% Native American, 3.3% biracial, and 6.6% unknown.
The participants provided information on potential questionnaire items for an online previsit screening for well visits to assess strengths and identify values, goals, dream jobs, and life wishes.
Suggestions from the participants informed changes to the questionnaire, which included five categories: personal/social goals, goals for academics/training, strengths, values, and dream jobs.
The top endorsed personal goal of “to be happy” was chosen by 13.1% of the participants. The top academic goal was “get good grades” (45.5%). The top endorsed strength was “fitness/coordination/sports/physical activity” (22.9%), while the top value was caring and kindness (25.8%), and the top dream job category was health/medical (30.8%).
Key comments made by the youth participants for improving the previsit questionnaire included adding an option for “I can’t decide,” and allowing for multiple responses to avoid feeling pinned down or judged, the researchers noted.
The researchers highlighted one teen comment: “While I understand the purpose of limiting the participants to two answers, it is incredibly difficult to only choose two. Being limited to two very much restricts your understanding of our values. For example, I would’ve also liked to select ‘to do well in school’ and ‘to make a difference,’ but ‘being happy’ and ‘being loving to all those around me’ had to take precedent.”
The study was limited by not being fully generalizable to all teens, as other teens may hold views and beliefs that differ from those of the focus group participants, the researchers noted.
However, the findings support the value of a strength-based previsit questionnaire for adolescents, they said.
“Structured previsit data could facilitate relationship building and be actionable for assigning strength and resiliency building resources,” they noted. “A final strengths and goals questionnaire is now being piloted in computerized form contributing to decision supports for suggested teleprompters and associated resource options,” and future research may show the value of such previsit data for improved clinical process and outcomes of youth well visits, they concluded.
Recognize the uncertainty of adolescence
“Adolescents are at crossroads of identity, trying to figure out who they are, their goals and values,” said Kelly A. Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, in an interview. “Adolescence is also a critical time when teens have more control and choice over behaviors that impact their health, such as diet, exercise, substance use, and sexual activity. In this critical time period, clinicians can intervene on health-related behaviors and shape the trajectory of a teen’s life. However, to promote teen health, pediatricians need to have their patients’ trust, which can be hard to gain,” she emphasized.
“In my practice, I’ve found that teens often just want to be seen and heard,” said Dr. Curran. “Teens often have many adults in their life who focus on the ‘don’ts’ – don’t use drugs, don’t have sex, for example – and few that praise healthy behaviors or strengths, or seek to understand what is important to them. By listening to teens and understanding what’s important to them, we can then use motivational interviewing techniques to help create meaningful change in health-related behaviors. However, this takes time and investment, which is often in conflict with time pressures in the modern medical system.
“This study is useful because it examined the acceptability of a positive psychology questionnaire to be used at well visits when reviewed by youth, that could be used to streamline this important process,” said Dr. Curran.
“From my practice, I know that understanding a teen’s goals, values, and strengths is important – we do this daily in our practice when working with patients – but it was exciting to see that youth found it acceptable to do this via a previsit survey, which can potentially streamline well visits,” she noted.
The questionnaire is being developed as a pilot program, but more research is needed to determine the direct clinical impact, said Dr. Curran. “It will be important in the future to see if implementation of this questionnaire can be helpful in integrating this information into motivational interviewing and rapport building to help improve teens’ health outcomes.”
The study was supported in part by the National Institute on Drug Abuse and the National Institute of Mental Health. Two coauthors have a financial interest in the CHADIS online reporting program used in the study. Dr. Curran had no financial conflicts to disclose.
Taking teens’ strengths, values, and dreams, into account through a previsit questionnaire was acceptable to them and may promote discussions with providers, based on data from 91 adolescents.
The American Academy of Pediatrics’ Bright Futures initiative recommends the use of a strength-based approach for adolescent well visits, but the extensive positive psychology inventories to identify teen strengths and values are impractical for the clinical visit setting, wrote Yidan Cao, MPH, of the Child Development through Primary Care at the University of Michigan, Ann Arbor, and colleagues. However, 76% of youth participating in focus groups responded that “using a confidential questionnaire about a teen’s strengths and goals before checkup visits would be a good addition to health care for teens,” the researchers said.
In a study presented in a poster session (#515) at the Pediatric Academic Societies annual meeting, the researchers recruited 91 community youth to participate in 13 focus groups related to teen depression and substance use. The age of the focus group participants ranged from 12 to 18 years, with an average of 15 years, 61.5% were female, and 1.1% identified as transgender. The racial breakdown was 51.6% White, 27.5% African American, 8.8% Asian, 2.2% Native American, 3.3% biracial, and 6.6% unknown.
The participants provided information on potential questionnaire items for an online previsit screening for well visits to assess strengths and identify values, goals, dream jobs, and life wishes.
Suggestions from the participants informed changes to the questionnaire, which included five categories: personal/social goals, goals for academics/training, strengths, values, and dream jobs.
The top endorsed personal goal of “to be happy” was chosen by 13.1% of the participants. The top academic goal was “get good grades” (45.5%). The top endorsed strength was “fitness/coordination/sports/physical activity” (22.9%), while the top value was caring and kindness (25.8%), and the top dream job category was health/medical (30.8%).
Key comments made by the youth participants for improving the previsit questionnaire included adding an option for “I can’t decide,” and allowing for multiple responses to avoid feeling pinned down or judged, the researchers noted.
The researchers highlighted one teen comment: “While I understand the purpose of limiting the participants to two answers, it is incredibly difficult to only choose two. Being limited to two very much restricts your understanding of our values. For example, I would’ve also liked to select ‘to do well in school’ and ‘to make a difference,’ but ‘being happy’ and ‘being loving to all those around me’ had to take precedent.”
The study was limited by not being fully generalizable to all teens, as other teens may hold views and beliefs that differ from those of the focus group participants, the researchers noted.
However, the findings support the value of a strength-based previsit questionnaire for adolescents, they said.
“Structured previsit data could facilitate relationship building and be actionable for assigning strength and resiliency building resources,” they noted. “A final strengths and goals questionnaire is now being piloted in computerized form contributing to decision supports for suggested teleprompters and associated resource options,” and future research may show the value of such previsit data for improved clinical process and outcomes of youth well visits, they concluded.
Recognize the uncertainty of adolescence
“Adolescents are at crossroads of identity, trying to figure out who they are, their goals and values,” said Kelly A. Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, in an interview. “Adolescence is also a critical time when teens have more control and choice over behaviors that impact their health, such as diet, exercise, substance use, and sexual activity. In this critical time period, clinicians can intervene on health-related behaviors and shape the trajectory of a teen’s life. However, to promote teen health, pediatricians need to have their patients’ trust, which can be hard to gain,” she emphasized.
“In my practice, I’ve found that teens often just want to be seen and heard,” said Dr. Curran. “Teens often have many adults in their life who focus on the ‘don’ts’ – don’t use drugs, don’t have sex, for example – and few that praise healthy behaviors or strengths, or seek to understand what is important to them. By listening to teens and understanding what’s important to them, we can then use motivational interviewing techniques to help create meaningful change in health-related behaviors. However, this takes time and investment, which is often in conflict with time pressures in the modern medical system.
“This study is useful because it examined the acceptability of a positive psychology questionnaire to be used at well visits when reviewed by youth, that could be used to streamline this important process,” said Dr. Curran.
“From my practice, I know that understanding a teen’s goals, values, and strengths is important – we do this daily in our practice when working with patients – but it was exciting to see that youth found it acceptable to do this via a previsit survey, which can potentially streamline well visits,” she noted.
The questionnaire is being developed as a pilot program, but more research is needed to determine the direct clinical impact, said Dr. Curran. “It will be important in the future to see if implementation of this questionnaire can be helpful in integrating this information into motivational interviewing and rapport building to help improve teens’ health outcomes.”
The study was supported in part by the National Institute on Drug Abuse and the National Institute of Mental Health. Two coauthors have a financial interest in the CHADIS online reporting program used in the study. Dr. Curran had no financial conflicts to disclose.
FROM PAS 2021
SGIM annual meeting focuses on inclusivity
In her welcome video on the opening day at the annual meeting of the Society of General Internal Medicine, meeting chair Rita Lee, MD, said she hoped that this year’s event, though virtual, will allow attendees an opportunity to “regroup, find inspiration, and celebrate the incredible strengths and diverse voices of our community.”
“We are living in an incredibly polarized world,” Dr. Lee said in an interview. “ as recent events, such as the death of George Floyd and many others, plus the disparities revealed by the COVID-19 pandemic, have brought issues of structural racism and oppression in the United States to the forefront,” she said in the interview.
“Given these circumstances, it is important now, more than ever, for generalists to move our values into action – to effect change at the health system, community, and policy levels – so our patients can achieve optimal health,” Dr. Lee emphasized.
She noted that SGIM’s vision: “A just system of care in which all people can achieve optimal health,” underlies the meeting’s sessions.
Some challenges related to adopting more antiracist training in medical education center on faculty development, Dr. Lee noted. “There are also students who don’t feel that this is part of the role of being a physician. One way to overcome these challenges is by directly linking structural competency to health outcomes for our patients,” she added. “We have evidence that structural racism impacts health and we should make that clear to our educational leaders and faculty to increase buy in. So many of our SGIM members are working on developing curricula for this.”
Two of the meeting’s workshops that addressed racism in medicine and medical education and strategies for change were “Demystifying Structural Competency – How to Develop Antiracist Training in Medical Education,” and “Combating Systemic Racism in the Health Care System – Practical Actions You Can Take Today.” Below are some details about these.
Medical education evolves to include structural competency
In the workshop “Demystifying Structural Competency – How to Develop Antiracist Training in Medical Education,” participants used interactive exercises to build structural differentials for patient cases. The workshop was based in part on the experiences of including structural competency in medical education at Albert Einstein College of Medicine, New York, and the University of Pittsburgh.
During the session, participants practiced building a structural differential diagnosis in small groups, and also practiced using a structurally competent version of the 1-minute preceptor to promote structural competency in learners.
“Structural competency represents a shift in medical education towards attention to forces that influence health outcomes at levels above individual clinical interactions and develop a provider’s capacity to recognize and respond to health and illness as downstream effects of social, political and economic structures,” presenter Iman Hassan, MD, of Albert Einstein College of Medicine and Montefiore Health System, both in New York, said in an interview.
“At the same time, structural competency incorporates structural humility, which decentralizes the provider role in addressing structural factors and emphasizes collaboration with patients and communities,” she said in the interview. “Structural competency is a useful antiracism framework because it explicitly engages learners with the broader structural forces that result in health disparities, including structural racism and its downstream effects,” Dr. Hassan explained.
Addressing structural competency is important in medical education because structural and social determinants of health contribute more than half of overall health outcomes, said Dr. Hassan.
A structural competency framework equips learners to identify, discuss, and work with patients to navigate social needs such as lack of health insurance, food, or transportation, that are preventing them from accessing needed health care services, Dr. Hassan noted.
“Importantly, training in structural competency empowers physicians to be agents of change within their clinics, health systems, and communities and to recognize the value of community-led advocacy in promoting health equity,” she said.
Structural competency training also “will also allow them to engage more fully with the body of literature that exists surrounding social determinants of health and health disparities, and the use of approaches such as critical race theory through which to view health care,” she emphasized. “Importantly, understanding of the historical and structural context of medicine allows clinicians to more readily recognize when their own clinical practices, such as use of race-based clinical prediction tools, may perpetuate disparities, and work collectively to eliminate those practices.”
Recalibrating calculators for clinical care
Another workshop, “Combating Systemic Racism in the Health Care System – Practical Actions You Can Take Today,” took on the challenge of inherent bias in clinical care caused by various factors, notably medical calculators such as those used to measure kidney function and pulmonary function.
Lamar K. Johnson, MD, of Christiana Care Hospital Partners/Christiana Care Pediatric Hospitalists in Newark, Del., and Celeste Newby, MD, of Tulane University, New Orleans, discussed the inherent biases in some calculators and how to take those biases into account. A stated goal of the workshop was to increase awareness of the origins of medical calculators in order to enhance equity and improve shared decision-making between patients and providers.
Addressing implicit bias in clinical practice is important because such bias has been shown to negatively affect physician behavior and clinical decision making, Dr. Johnson said in an interview.
“These effects can also negatively affect the doctor-patient relationship and lead to poorer health outcomes due to delays in or avoidance of care or avoidance of the health care system, and mistrust, resulting in nonadherence,” Dr. Johnson noted.
“Implicit bias training helps empower medical students and residents to recognize and address bias and advocate for patients. Such training can potentially be beneficial to faculty, too,” Dr. Johnson emphasized in the interview.
“Race is primarily a social, not a biological, construct, and we must be careful when we use it, as its use in the past has been largely inappropriate and not scientifically sound,” he said.
During the session, one of the presenters said removing specific mentions of race from clinical documentation can reduce racial bias in clinical practice.
The presenters also highlighted the estimated glomerular filtration rate (eGFR) which is used to estimate kidney function.
The eGFR “reports higher eGFR values for Blacks based on a faulty hypothesis that Black people have higher muscle mass. This higher estimated value can delay referral for specialist care or transplantation, leading to worse outcomes,” Dr. Johnson explained in the interview.
In response, “Many major institutions have eliminated the race modifier in eGFR, and a joint task force created by the National Kidney Foundation and American Society of Nephrology has recommended against using a race modifier as of March 2021,” Dr. Johnson said.
The presenters had no relevant financial conflicts to disclose.
In her welcome video on the opening day at the annual meeting of the Society of General Internal Medicine, meeting chair Rita Lee, MD, said she hoped that this year’s event, though virtual, will allow attendees an opportunity to “regroup, find inspiration, and celebrate the incredible strengths and diverse voices of our community.”
“We are living in an incredibly polarized world,” Dr. Lee said in an interview. “ as recent events, such as the death of George Floyd and many others, plus the disparities revealed by the COVID-19 pandemic, have brought issues of structural racism and oppression in the United States to the forefront,” she said in the interview.
“Given these circumstances, it is important now, more than ever, for generalists to move our values into action – to effect change at the health system, community, and policy levels – so our patients can achieve optimal health,” Dr. Lee emphasized.
She noted that SGIM’s vision: “A just system of care in which all people can achieve optimal health,” underlies the meeting’s sessions.
Some challenges related to adopting more antiracist training in medical education center on faculty development, Dr. Lee noted. “There are also students who don’t feel that this is part of the role of being a physician. One way to overcome these challenges is by directly linking structural competency to health outcomes for our patients,” she added. “We have evidence that structural racism impacts health and we should make that clear to our educational leaders and faculty to increase buy in. So many of our SGIM members are working on developing curricula for this.”
Two of the meeting’s workshops that addressed racism in medicine and medical education and strategies for change were “Demystifying Structural Competency – How to Develop Antiracist Training in Medical Education,” and “Combating Systemic Racism in the Health Care System – Practical Actions You Can Take Today.” Below are some details about these.
Medical education evolves to include structural competency
In the workshop “Demystifying Structural Competency – How to Develop Antiracist Training in Medical Education,” participants used interactive exercises to build structural differentials for patient cases. The workshop was based in part on the experiences of including structural competency in medical education at Albert Einstein College of Medicine, New York, and the University of Pittsburgh.
During the session, participants practiced building a structural differential diagnosis in small groups, and also practiced using a structurally competent version of the 1-minute preceptor to promote structural competency in learners.
“Structural competency represents a shift in medical education towards attention to forces that influence health outcomes at levels above individual clinical interactions and develop a provider’s capacity to recognize and respond to health and illness as downstream effects of social, political and economic structures,” presenter Iman Hassan, MD, of Albert Einstein College of Medicine and Montefiore Health System, both in New York, said in an interview.
“At the same time, structural competency incorporates structural humility, which decentralizes the provider role in addressing structural factors and emphasizes collaboration with patients and communities,” she said in the interview. “Structural competency is a useful antiracism framework because it explicitly engages learners with the broader structural forces that result in health disparities, including structural racism and its downstream effects,” Dr. Hassan explained.
Addressing structural competency is important in medical education because structural and social determinants of health contribute more than half of overall health outcomes, said Dr. Hassan.
A structural competency framework equips learners to identify, discuss, and work with patients to navigate social needs such as lack of health insurance, food, or transportation, that are preventing them from accessing needed health care services, Dr. Hassan noted.
“Importantly, training in structural competency empowers physicians to be agents of change within their clinics, health systems, and communities and to recognize the value of community-led advocacy in promoting health equity,” she said.
Structural competency training also “will also allow them to engage more fully with the body of literature that exists surrounding social determinants of health and health disparities, and the use of approaches such as critical race theory through which to view health care,” she emphasized. “Importantly, understanding of the historical and structural context of medicine allows clinicians to more readily recognize when their own clinical practices, such as use of race-based clinical prediction tools, may perpetuate disparities, and work collectively to eliminate those practices.”
Recalibrating calculators for clinical care
Another workshop, “Combating Systemic Racism in the Health Care System – Practical Actions You Can Take Today,” took on the challenge of inherent bias in clinical care caused by various factors, notably medical calculators such as those used to measure kidney function and pulmonary function.
Lamar K. Johnson, MD, of Christiana Care Hospital Partners/Christiana Care Pediatric Hospitalists in Newark, Del., and Celeste Newby, MD, of Tulane University, New Orleans, discussed the inherent biases in some calculators and how to take those biases into account. A stated goal of the workshop was to increase awareness of the origins of medical calculators in order to enhance equity and improve shared decision-making between patients and providers.
Addressing implicit bias in clinical practice is important because such bias has been shown to negatively affect physician behavior and clinical decision making, Dr. Johnson said in an interview.
“These effects can also negatively affect the doctor-patient relationship and lead to poorer health outcomes due to delays in or avoidance of care or avoidance of the health care system, and mistrust, resulting in nonadherence,” Dr. Johnson noted.
“Implicit bias training helps empower medical students and residents to recognize and address bias and advocate for patients. Such training can potentially be beneficial to faculty, too,” Dr. Johnson emphasized in the interview.
“Race is primarily a social, not a biological, construct, and we must be careful when we use it, as its use in the past has been largely inappropriate and not scientifically sound,” he said.
During the session, one of the presenters said removing specific mentions of race from clinical documentation can reduce racial bias in clinical practice.
The presenters also highlighted the estimated glomerular filtration rate (eGFR) which is used to estimate kidney function.
The eGFR “reports higher eGFR values for Blacks based on a faulty hypothesis that Black people have higher muscle mass. This higher estimated value can delay referral for specialist care or transplantation, leading to worse outcomes,” Dr. Johnson explained in the interview.
In response, “Many major institutions have eliminated the race modifier in eGFR, and a joint task force created by the National Kidney Foundation and American Society of Nephrology has recommended against using a race modifier as of March 2021,” Dr. Johnson said.
The presenters had no relevant financial conflicts to disclose.
In her welcome video on the opening day at the annual meeting of the Society of General Internal Medicine, meeting chair Rita Lee, MD, said she hoped that this year’s event, though virtual, will allow attendees an opportunity to “regroup, find inspiration, and celebrate the incredible strengths and diverse voices of our community.”
“We are living in an incredibly polarized world,” Dr. Lee said in an interview. “ as recent events, such as the death of George Floyd and many others, plus the disparities revealed by the COVID-19 pandemic, have brought issues of structural racism and oppression in the United States to the forefront,” she said in the interview.
“Given these circumstances, it is important now, more than ever, for generalists to move our values into action – to effect change at the health system, community, and policy levels – so our patients can achieve optimal health,” Dr. Lee emphasized.
She noted that SGIM’s vision: “A just system of care in which all people can achieve optimal health,” underlies the meeting’s sessions.
Some challenges related to adopting more antiracist training in medical education center on faculty development, Dr. Lee noted. “There are also students who don’t feel that this is part of the role of being a physician. One way to overcome these challenges is by directly linking structural competency to health outcomes for our patients,” she added. “We have evidence that structural racism impacts health and we should make that clear to our educational leaders and faculty to increase buy in. So many of our SGIM members are working on developing curricula for this.”
Two of the meeting’s workshops that addressed racism in medicine and medical education and strategies for change were “Demystifying Structural Competency – How to Develop Antiracist Training in Medical Education,” and “Combating Systemic Racism in the Health Care System – Practical Actions You Can Take Today.” Below are some details about these.
Medical education evolves to include structural competency
In the workshop “Demystifying Structural Competency – How to Develop Antiracist Training in Medical Education,” participants used interactive exercises to build structural differentials for patient cases. The workshop was based in part on the experiences of including structural competency in medical education at Albert Einstein College of Medicine, New York, and the University of Pittsburgh.
During the session, participants practiced building a structural differential diagnosis in small groups, and also practiced using a structurally competent version of the 1-minute preceptor to promote structural competency in learners.
“Structural competency represents a shift in medical education towards attention to forces that influence health outcomes at levels above individual clinical interactions and develop a provider’s capacity to recognize and respond to health and illness as downstream effects of social, political and economic structures,” presenter Iman Hassan, MD, of Albert Einstein College of Medicine and Montefiore Health System, both in New York, said in an interview.
“At the same time, structural competency incorporates structural humility, which decentralizes the provider role in addressing structural factors and emphasizes collaboration with patients and communities,” she said in the interview. “Structural competency is a useful antiracism framework because it explicitly engages learners with the broader structural forces that result in health disparities, including structural racism and its downstream effects,” Dr. Hassan explained.
Addressing structural competency is important in medical education because structural and social determinants of health contribute more than half of overall health outcomes, said Dr. Hassan.
A structural competency framework equips learners to identify, discuss, and work with patients to navigate social needs such as lack of health insurance, food, or transportation, that are preventing them from accessing needed health care services, Dr. Hassan noted.
“Importantly, training in structural competency empowers physicians to be agents of change within their clinics, health systems, and communities and to recognize the value of community-led advocacy in promoting health equity,” she said.
Structural competency training also “will also allow them to engage more fully with the body of literature that exists surrounding social determinants of health and health disparities, and the use of approaches such as critical race theory through which to view health care,” she emphasized. “Importantly, understanding of the historical and structural context of medicine allows clinicians to more readily recognize when their own clinical practices, such as use of race-based clinical prediction tools, may perpetuate disparities, and work collectively to eliminate those practices.”
Recalibrating calculators for clinical care
Another workshop, “Combating Systemic Racism in the Health Care System – Practical Actions You Can Take Today,” took on the challenge of inherent bias in clinical care caused by various factors, notably medical calculators such as those used to measure kidney function and pulmonary function.
Lamar K. Johnson, MD, of Christiana Care Hospital Partners/Christiana Care Pediatric Hospitalists in Newark, Del., and Celeste Newby, MD, of Tulane University, New Orleans, discussed the inherent biases in some calculators and how to take those biases into account. A stated goal of the workshop was to increase awareness of the origins of medical calculators in order to enhance equity and improve shared decision-making between patients and providers.
Addressing implicit bias in clinical practice is important because such bias has been shown to negatively affect physician behavior and clinical decision making, Dr. Johnson said in an interview.
“These effects can also negatively affect the doctor-patient relationship and lead to poorer health outcomes due to delays in or avoidance of care or avoidance of the health care system, and mistrust, resulting in nonadherence,” Dr. Johnson noted.
“Implicit bias training helps empower medical students and residents to recognize and address bias and advocate for patients. Such training can potentially be beneficial to faculty, too,” Dr. Johnson emphasized in the interview.
“Race is primarily a social, not a biological, construct, and we must be careful when we use it, as its use in the past has been largely inappropriate and not scientifically sound,” he said.
During the session, one of the presenters said removing specific mentions of race from clinical documentation can reduce racial bias in clinical practice.
The presenters also highlighted the estimated glomerular filtration rate (eGFR) which is used to estimate kidney function.
The eGFR “reports higher eGFR values for Blacks based on a faulty hypothesis that Black people have higher muscle mass. This higher estimated value can delay referral for specialist care or transplantation, leading to worse outcomes,” Dr. Johnson explained in the interview.
In response, “Many major institutions have eliminated the race modifier in eGFR, and a joint task force created by the National Kidney Foundation and American Society of Nephrology has recommended against using a race modifier as of March 2021,” Dr. Johnson said.
The presenters had no relevant financial conflicts to disclose.
FROM SGIM 2021



