User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
The pandemic changed smokers, but farming didn’t change humans
Pandemic smoking: More or less?
The COVID-19 pandemic has changed a lot of habits in people, for better or worse. Some people may have turned to food and alcohol for comfort, while others started on health kicks to emerge from the ordeal as new people. Well, the same can be said about smokers.
New evidence comes from a survey conducted from May to July 2020 of 694 current and former smokers with an average age of 53 years. All had been hospitalized prior to the pandemic and had previously participated in clinical trials to for smoking cessation in Boston, Nashville, and Pittsburgh hospitals.
Researchers found that 32% of participants smoked more, 37% smoked less, and 31% made no change in their smoking habits. By the time of the survey, 28% of former smokers had relapsed. Although 68% of the participants believed smoking increased the risk of getting COVID-19, that still didn’t stop some people from smoking more. Why?
Respondents “might have increased their smoking due to stress and boredom. On the other hand, the fear of catching COVID might have led them to cut down or quit smoking,” said lead author Nancy A. Rigotti, MD. “Even before the pandemic, tobacco smoking was the leading preventable cause of death in the United States. COVID-19 has given smokers yet another good reason to stop smoking.”
This creates an opportunity for physicians to preach the gospel to smokers about their vulnerability to respiratory disease in hopes of getting them to quit for good. We just wish the same could be said for all of our excessive pandemic online shopping.
3,000 years and just one pair of genomes to wear
Men and women are different. We’ll give you a moment to pick your jaw off the ground.
It makes sense though, the sexes being different, especially when you look at the broader animal kingdom. The males and females of many species are slightly different when it comes to size and shape, but there’s a big question that literally only anthropologists have asked: Were human males and females more different in the past than they are today?
To be more specific, some scientists believe that males and females grew more similar when humans shifted from a hunter-gatherer lifestyle to a farming-based lifestyle, as agriculture encouraged a more equitable division of labor. Others believe that the differences come down to random chance.
Researchers from Penn State University analyzed genomic data from over 350,000 males and females stored in the UK Biobank and looked at the recent (within the last ~3,000 years; post-agriculture adoption in Britain) evolutionary histories of these loci. Height, body mass, hip circumference, body fat percentage, and waist circumference were analyzed, and while there were thousands of differences in the genomes, only one trait occurred more frequently during that time period: Females gained a significantly higher body fat content than males.
It’s a sad day then for the millions of people who were big fans of the “farming caused men and women to become more similar” theory. Count the LOTME crew among them. Be honest: Wouldn’t life be so much simpler if men and women were exactly the same? Just think about it, no more arguments about leaving the toilet seat up. It’d be worth it just for that.
Proteins don’t lie
Research published in Open Biology shows that the human brain contains 14,315 different proteins. The team conducting that study wanted to find out which organ was the most similar to the old brain box, so they did protein counts for the 32 other major tissue types, including heart, salivary gland, lung, spleen, and endometrium.
The tissue with the most proteins in common with the center of human intelligence? You’re thinking it has to be colon at this point, right? We were sure it was going to be colon, but it’s not.
The winner, with 13,442 shared proteins, is the testes. The testes have 15,687 proteins, of which 85.7% are shared with the brain. The researchers, sadly, did not provide protein counts for the other tissue types, but we bet colon was a close second.
Dreaming about COVID?
We thought we were the only ones who have been having crazy dreams lately. Each one seems crazier and more vivid than the one before. Have you been having weird dreams lately?
This is likely your brain’s coping mechanism to handle your pandemic stress, according to Dr. Erik Hoel of Tufts University. Dreams that are crazy and scary might make real life seem lighter and simpler. He calls it the “overfitted brain hypothesis.”
“It is their very strangeness that gives them their biological function,” Dr. Hoel said. It literally makes you feel like COVID-19 and lockdowns aren’t as scary as they seem.
We always knew our minds were powerful things. Apparently, your brain gets tired of everyday familiarity just like you do, and it creates crazy dreams to keep things interesting.
Just remember: That recurring dream that you’re back in college and missing 10 assignments is there to help you, not scare you! Even though it is pretty scary.
Pandemic smoking: More or less?
The COVID-19 pandemic has changed a lot of habits in people, for better or worse. Some people may have turned to food and alcohol for comfort, while others started on health kicks to emerge from the ordeal as new people. Well, the same can be said about smokers.
New evidence comes from a survey conducted from May to July 2020 of 694 current and former smokers with an average age of 53 years. All had been hospitalized prior to the pandemic and had previously participated in clinical trials to for smoking cessation in Boston, Nashville, and Pittsburgh hospitals.
Researchers found that 32% of participants smoked more, 37% smoked less, and 31% made no change in their smoking habits. By the time of the survey, 28% of former smokers had relapsed. Although 68% of the participants believed smoking increased the risk of getting COVID-19, that still didn’t stop some people from smoking more. Why?
Respondents “might have increased their smoking due to stress and boredom. On the other hand, the fear of catching COVID might have led them to cut down or quit smoking,” said lead author Nancy A. Rigotti, MD. “Even before the pandemic, tobacco smoking was the leading preventable cause of death in the United States. COVID-19 has given smokers yet another good reason to stop smoking.”
This creates an opportunity for physicians to preach the gospel to smokers about their vulnerability to respiratory disease in hopes of getting them to quit for good. We just wish the same could be said for all of our excessive pandemic online shopping.
3,000 years and just one pair of genomes to wear
Men and women are different. We’ll give you a moment to pick your jaw off the ground.
It makes sense though, the sexes being different, especially when you look at the broader animal kingdom. The males and females of many species are slightly different when it comes to size and shape, but there’s a big question that literally only anthropologists have asked: Were human males and females more different in the past than they are today?
To be more specific, some scientists believe that males and females grew more similar when humans shifted from a hunter-gatherer lifestyle to a farming-based lifestyle, as agriculture encouraged a more equitable division of labor. Others believe that the differences come down to random chance.
Researchers from Penn State University analyzed genomic data from over 350,000 males and females stored in the UK Biobank and looked at the recent (within the last ~3,000 years; post-agriculture adoption in Britain) evolutionary histories of these loci. Height, body mass, hip circumference, body fat percentage, and waist circumference were analyzed, and while there were thousands of differences in the genomes, only one trait occurred more frequently during that time period: Females gained a significantly higher body fat content than males.
It’s a sad day then for the millions of people who were big fans of the “farming caused men and women to become more similar” theory. Count the LOTME crew among them. Be honest: Wouldn’t life be so much simpler if men and women were exactly the same? Just think about it, no more arguments about leaving the toilet seat up. It’d be worth it just for that.
Proteins don’t lie
Research published in Open Biology shows that the human brain contains 14,315 different proteins. The team conducting that study wanted to find out which organ was the most similar to the old brain box, so they did protein counts for the 32 other major tissue types, including heart, salivary gland, lung, spleen, and endometrium.
The tissue with the most proteins in common with the center of human intelligence? You’re thinking it has to be colon at this point, right? We were sure it was going to be colon, but it’s not.
The winner, with 13,442 shared proteins, is the testes. The testes have 15,687 proteins, of which 85.7% are shared with the brain. The researchers, sadly, did not provide protein counts for the other tissue types, but we bet colon was a close second.
Dreaming about COVID?
We thought we were the only ones who have been having crazy dreams lately. Each one seems crazier and more vivid than the one before. Have you been having weird dreams lately?
This is likely your brain’s coping mechanism to handle your pandemic stress, according to Dr. Erik Hoel of Tufts University. Dreams that are crazy and scary might make real life seem lighter and simpler. He calls it the “overfitted brain hypothesis.”
“It is their very strangeness that gives them their biological function,” Dr. Hoel said. It literally makes you feel like COVID-19 and lockdowns aren’t as scary as they seem.
We always knew our minds were powerful things. Apparently, your brain gets tired of everyday familiarity just like you do, and it creates crazy dreams to keep things interesting.
Just remember: That recurring dream that you’re back in college and missing 10 assignments is there to help you, not scare you! Even though it is pretty scary.
Pandemic smoking: More or less?
The COVID-19 pandemic has changed a lot of habits in people, for better or worse. Some people may have turned to food and alcohol for comfort, while others started on health kicks to emerge from the ordeal as new people. Well, the same can be said about smokers.
New evidence comes from a survey conducted from May to July 2020 of 694 current and former smokers with an average age of 53 years. All had been hospitalized prior to the pandemic and had previously participated in clinical trials to for smoking cessation in Boston, Nashville, and Pittsburgh hospitals.
Researchers found that 32% of participants smoked more, 37% smoked less, and 31% made no change in their smoking habits. By the time of the survey, 28% of former smokers had relapsed. Although 68% of the participants believed smoking increased the risk of getting COVID-19, that still didn’t stop some people from smoking more. Why?
Respondents “might have increased their smoking due to stress and boredom. On the other hand, the fear of catching COVID might have led them to cut down or quit smoking,” said lead author Nancy A. Rigotti, MD. “Even before the pandemic, tobacco smoking was the leading preventable cause of death in the United States. COVID-19 has given smokers yet another good reason to stop smoking.”
This creates an opportunity for physicians to preach the gospel to smokers about their vulnerability to respiratory disease in hopes of getting them to quit for good. We just wish the same could be said for all of our excessive pandemic online shopping.
3,000 years and just one pair of genomes to wear
Men and women are different. We’ll give you a moment to pick your jaw off the ground.
It makes sense though, the sexes being different, especially when you look at the broader animal kingdom. The males and females of many species are slightly different when it comes to size and shape, but there’s a big question that literally only anthropologists have asked: Were human males and females more different in the past than they are today?
To be more specific, some scientists believe that males and females grew more similar when humans shifted from a hunter-gatherer lifestyle to a farming-based lifestyle, as agriculture encouraged a more equitable division of labor. Others believe that the differences come down to random chance.
Researchers from Penn State University analyzed genomic data from over 350,000 males and females stored in the UK Biobank and looked at the recent (within the last ~3,000 years; post-agriculture adoption in Britain) evolutionary histories of these loci. Height, body mass, hip circumference, body fat percentage, and waist circumference were analyzed, and while there were thousands of differences in the genomes, only one trait occurred more frequently during that time period: Females gained a significantly higher body fat content than males.
It’s a sad day then for the millions of people who were big fans of the “farming caused men and women to become more similar” theory. Count the LOTME crew among them. Be honest: Wouldn’t life be so much simpler if men and women were exactly the same? Just think about it, no more arguments about leaving the toilet seat up. It’d be worth it just for that.
Proteins don’t lie
Research published in Open Biology shows that the human brain contains 14,315 different proteins. The team conducting that study wanted to find out which organ was the most similar to the old brain box, so they did protein counts for the 32 other major tissue types, including heart, salivary gland, lung, spleen, and endometrium.
The tissue with the most proteins in common with the center of human intelligence? You’re thinking it has to be colon at this point, right? We were sure it was going to be colon, but it’s not.
The winner, with 13,442 shared proteins, is the testes. The testes have 15,687 proteins, of which 85.7% are shared with the brain. The researchers, sadly, did not provide protein counts for the other tissue types, but we bet colon was a close second.
Dreaming about COVID?
We thought we were the only ones who have been having crazy dreams lately. Each one seems crazier and more vivid than the one before. Have you been having weird dreams lately?
This is likely your brain’s coping mechanism to handle your pandemic stress, according to Dr. Erik Hoel of Tufts University. Dreams that are crazy and scary might make real life seem lighter and simpler. He calls it the “overfitted brain hypothesis.”
“It is their very strangeness that gives them their biological function,” Dr. Hoel said. It literally makes you feel like COVID-19 and lockdowns aren’t as scary as they seem.
We always knew our minds were powerful things. Apparently, your brain gets tired of everyday familiarity just like you do, and it creates crazy dreams to keep things interesting.
Just remember: That recurring dream that you’re back in college and missing 10 assignments is there to help you, not scare you! Even though it is pretty scary.
By the numbers: Children and COVID-19 prevention
Over 6.3 million doses of COVID-19 vaccine have been administered to children aged 12-17 years as of June 7, according to data from the Centers for Disease Control and Prevention.
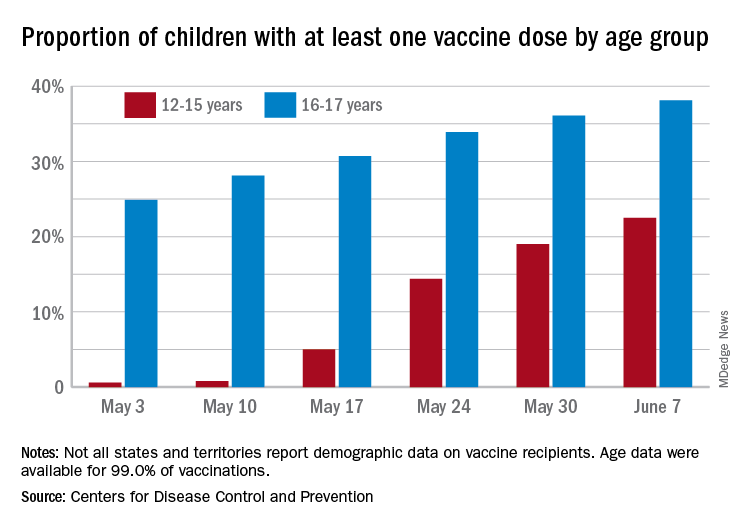
The latest results from the CDC’s COVID Data Tracker show that , with the corresponding figures for vaccine completion coming in at 4.1% and 26.4%. Compared with a week earlier, those numbers are up by 15.4% (one dose) and 486% (completion) for the younger group and by 4.7% and 8.6%, respectively, for the older children.
Children aged 12-15 represented 17.9% of all persons who initiated vaccination in the last 14 days up to June 7, while children aged 16-17 made up 4.8% of vaccine initiation over that period. The 25- to 39-year-olds, at 23.7% of all vaccine initiators, were the only group ahead of those aged 12-15, and the 50- to 64-year-olds were just behind at 17.7%, the CDC data show.
Both groups of children were on the low side, however, when it came to vaccine completion in the last 14 days, with those aged 12-15 at 6.7% of the total and those aged 16-17 years at 4.3%. The only age groups lower than that were ≥75 at 3.5% and <12 at 0.2%, and the highest share of vaccine completion was 26.0% for those aged 25-39, which also happens to be the group with the largest share of the U.S. population (20.5%), the CDC said.
People considered fully vaccinated are those who have received the second dose of a two-dose series or one dose of a single-shot vaccine, but children under age 18 years are eligible only for the Pfizer-BioNTech version, the CDC noted.
Meanwhile, back on the incidence side of the COVID-19 pandemic, the number of new cases in U.S. children for the week ending June 3 was at its lowest point (16,281) since mid-June of 2020, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
Cases among children now total 3.99 million, which represents 14.1% of cases among all ages, a proportion that hasn’t increased since mid-May, which hasn’t happened since the two groups started keeping track in mid-April of 2020 in the 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam that report such data by age.
Less encouraging was the CDC’s report that “COVID-19-associated hospitalization rates among adolescents ages 12-17 years increased during March and April, following declines in January and February 2021.”
Children have been experiencing much lower rates of severe disease than those of adults throughout the pandemic, the CDC pointed out, but “recent increases in COVID-19-associated hospitalization rates and the potential for severe disease in adolescents reinforce the importance of continued prevention strategies, including vaccination and the correct and consistent use of masks in those who are not yet fully vaccinated.”
Over 6.3 million doses of COVID-19 vaccine have been administered to children aged 12-17 years as of June 7, according to data from the Centers for Disease Control and Prevention.
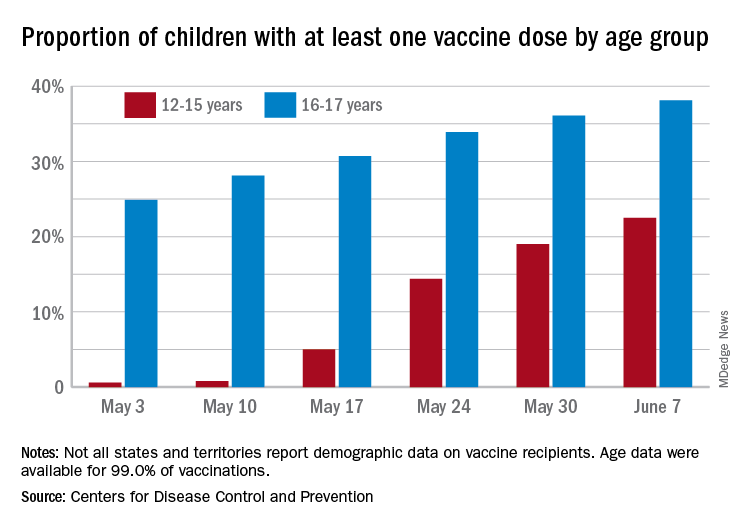
The latest results from the CDC’s COVID Data Tracker show that , with the corresponding figures for vaccine completion coming in at 4.1% and 26.4%. Compared with a week earlier, those numbers are up by 15.4% (one dose) and 486% (completion) for the younger group and by 4.7% and 8.6%, respectively, for the older children.
Children aged 12-15 represented 17.9% of all persons who initiated vaccination in the last 14 days up to June 7, while children aged 16-17 made up 4.8% of vaccine initiation over that period. The 25- to 39-year-olds, at 23.7% of all vaccine initiators, were the only group ahead of those aged 12-15, and the 50- to 64-year-olds were just behind at 17.7%, the CDC data show.
Both groups of children were on the low side, however, when it came to vaccine completion in the last 14 days, with those aged 12-15 at 6.7% of the total and those aged 16-17 years at 4.3%. The only age groups lower than that were ≥75 at 3.5% and <12 at 0.2%, and the highest share of vaccine completion was 26.0% for those aged 25-39, which also happens to be the group with the largest share of the U.S. population (20.5%), the CDC said.
People considered fully vaccinated are those who have received the second dose of a two-dose series or one dose of a single-shot vaccine, but children under age 18 years are eligible only for the Pfizer-BioNTech version, the CDC noted.
Meanwhile, back on the incidence side of the COVID-19 pandemic, the number of new cases in U.S. children for the week ending June 3 was at its lowest point (16,281) since mid-June of 2020, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
Cases among children now total 3.99 million, which represents 14.1% of cases among all ages, a proportion that hasn’t increased since mid-May, which hasn’t happened since the two groups started keeping track in mid-April of 2020 in the 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam that report such data by age.
Less encouraging was the CDC’s report that “COVID-19-associated hospitalization rates among adolescents ages 12-17 years increased during March and April, following declines in January and February 2021.”
Children have been experiencing much lower rates of severe disease than those of adults throughout the pandemic, the CDC pointed out, but “recent increases in COVID-19-associated hospitalization rates and the potential for severe disease in adolescents reinforce the importance of continued prevention strategies, including vaccination and the correct and consistent use of masks in those who are not yet fully vaccinated.”
Over 6.3 million doses of COVID-19 vaccine have been administered to children aged 12-17 years as of June 7, according to data from the Centers for Disease Control and Prevention.
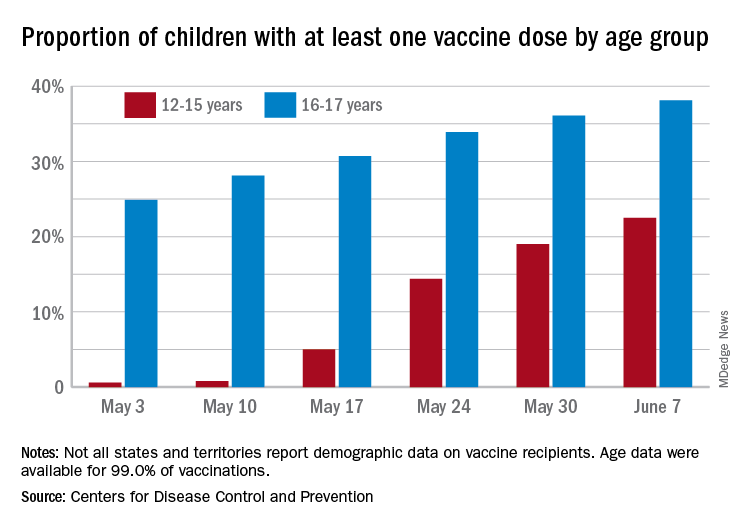
The latest results from the CDC’s COVID Data Tracker show that , with the corresponding figures for vaccine completion coming in at 4.1% and 26.4%. Compared with a week earlier, those numbers are up by 15.4% (one dose) and 486% (completion) for the younger group and by 4.7% and 8.6%, respectively, for the older children.
Children aged 12-15 represented 17.9% of all persons who initiated vaccination in the last 14 days up to June 7, while children aged 16-17 made up 4.8% of vaccine initiation over that period. The 25- to 39-year-olds, at 23.7% of all vaccine initiators, were the only group ahead of those aged 12-15, and the 50- to 64-year-olds were just behind at 17.7%, the CDC data show.
Both groups of children were on the low side, however, when it came to vaccine completion in the last 14 days, with those aged 12-15 at 6.7% of the total and those aged 16-17 years at 4.3%. The only age groups lower than that were ≥75 at 3.5% and <12 at 0.2%, and the highest share of vaccine completion was 26.0% for those aged 25-39, which also happens to be the group with the largest share of the U.S. population (20.5%), the CDC said.
People considered fully vaccinated are those who have received the second dose of a two-dose series or one dose of a single-shot vaccine, but children under age 18 years are eligible only for the Pfizer-BioNTech version, the CDC noted.
Meanwhile, back on the incidence side of the COVID-19 pandemic, the number of new cases in U.S. children for the week ending June 3 was at its lowest point (16,281) since mid-June of 2020, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
Cases among children now total 3.99 million, which represents 14.1% of cases among all ages, a proportion that hasn’t increased since mid-May, which hasn’t happened since the two groups started keeping track in mid-April of 2020 in the 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam that report such data by age.
Less encouraging was the CDC’s report that “COVID-19-associated hospitalization rates among adolescents ages 12-17 years increased during March and April, following declines in January and February 2021.”
Children have been experiencing much lower rates of severe disease than those of adults throughout the pandemic, the CDC pointed out, but “recent increases in COVID-19-associated hospitalization rates and the potential for severe disease in adolescents reinforce the importance of continued prevention strategies, including vaccination and the correct and consistent use of masks in those who are not yet fully vaccinated.”
First year of life sees initial bleeding episodes in children with von Willebrand disease
To remedy a lack of data on infants and toddlers with von Willebrand disease (VWD), researchers examined data on patients collected from the U.S. Hemophilia Treatment Center Network. They examined birth characteristics, bleeding episodes, and complications experienced by 105 patients with VWD who were younger than 2 years of age.
For these patients, the mean age of diagnosis was 7 months, with little variation by sex. Patients with type 2 VWD were diagnosed earlier than those with types 1 or 3 (P = .04), and those with a family history of VWD were diagnosed approximately 4 months earlier than those with none (P < .001), according to the report by Brandi Dupervil, DHSC, of the National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention, Atlanta, and colleagues.
Approximately 14% of the patients were born preterm and 13% had low birth weight, proportions that were higher than national preterm birth rates (approximately 12% and 8%, respectively). There was no way of knowing from the data whether this was due to the presence of VWD or other factors, according to the report (Blood Adv. 2021;5[8]:2079-86).
Specialized care
The study found that initial bleeding episodes were most commonly oropharyngeal, related to circumcision, or intracranial or extracranial, and that most initial bleeding episodes occurred within the first year of life, according to the researchers.
Overall, there were 274 bleeding episodes among 73 children, including oral/nasal episodes (38 patients experienced 166 episodes), soft tissue hematomas (15 patients experienced 57 episodes), and head injuries, including skull fractures (13 patients experienced 19 episodes), according to the report.
In terms of treatment, among the two-thirds of the patients who had intervention to prevent or treat bleeding, most received either plasma-derived VW factor/factor VIII concentrates or antifibrinolytics.
Overall, the researchers advocated a team approach to treating these children “including genetic counselors throughout the prepartum period who work to increase expectant mothers’ understanding of the risks associated with having a child with VWD.”
They also recommended the input of “adult and pediatric hematologists, obstetrician gynecologists, genetic counselors, nurses, and social workers throughout the pre- and postpartum period who seek to optimize outcomes and disease management.”
The authors reported that they had no competing interests.
To remedy a lack of data on infants and toddlers with von Willebrand disease (VWD), researchers examined data on patients collected from the U.S. Hemophilia Treatment Center Network. They examined birth characteristics, bleeding episodes, and complications experienced by 105 patients with VWD who were younger than 2 years of age.
For these patients, the mean age of diagnosis was 7 months, with little variation by sex. Patients with type 2 VWD were diagnosed earlier than those with types 1 or 3 (P = .04), and those with a family history of VWD were diagnosed approximately 4 months earlier than those with none (P < .001), according to the report by Brandi Dupervil, DHSC, of the National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention, Atlanta, and colleagues.
Approximately 14% of the patients were born preterm and 13% had low birth weight, proportions that were higher than national preterm birth rates (approximately 12% and 8%, respectively). There was no way of knowing from the data whether this was due to the presence of VWD or other factors, according to the report (Blood Adv. 2021;5[8]:2079-86).
Specialized care
The study found that initial bleeding episodes were most commonly oropharyngeal, related to circumcision, or intracranial or extracranial, and that most initial bleeding episodes occurred within the first year of life, according to the researchers.
Overall, there were 274 bleeding episodes among 73 children, including oral/nasal episodes (38 patients experienced 166 episodes), soft tissue hematomas (15 patients experienced 57 episodes), and head injuries, including skull fractures (13 patients experienced 19 episodes), according to the report.
In terms of treatment, among the two-thirds of the patients who had intervention to prevent or treat bleeding, most received either plasma-derived VW factor/factor VIII concentrates or antifibrinolytics.
Overall, the researchers advocated a team approach to treating these children “including genetic counselors throughout the prepartum period who work to increase expectant mothers’ understanding of the risks associated with having a child with VWD.”
They also recommended the input of “adult and pediatric hematologists, obstetrician gynecologists, genetic counselors, nurses, and social workers throughout the pre- and postpartum period who seek to optimize outcomes and disease management.”
The authors reported that they had no competing interests.
To remedy a lack of data on infants and toddlers with von Willebrand disease (VWD), researchers examined data on patients collected from the U.S. Hemophilia Treatment Center Network. They examined birth characteristics, bleeding episodes, and complications experienced by 105 patients with VWD who were younger than 2 years of age.
For these patients, the mean age of diagnosis was 7 months, with little variation by sex. Patients with type 2 VWD were diagnosed earlier than those with types 1 or 3 (P = .04), and those with a family history of VWD were diagnosed approximately 4 months earlier than those with none (P < .001), according to the report by Brandi Dupervil, DHSC, of the National Center on Birth Defects and Developmental Disabilities, Centers for Disease Control and Prevention, Atlanta, and colleagues.
Approximately 14% of the patients were born preterm and 13% had low birth weight, proportions that were higher than national preterm birth rates (approximately 12% and 8%, respectively). There was no way of knowing from the data whether this was due to the presence of VWD or other factors, according to the report (Blood Adv. 2021;5[8]:2079-86).
Specialized care
The study found that initial bleeding episodes were most commonly oropharyngeal, related to circumcision, or intracranial or extracranial, and that most initial bleeding episodes occurred within the first year of life, according to the researchers.
Overall, there were 274 bleeding episodes among 73 children, including oral/nasal episodes (38 patients experienced 166 episodes), soft tissue hematomas (15 patients experienced 57 episodes), and head injuries, including skull fractures (13 patients experienced 19 episodes), according to the report.
In terms of treatment, among the two-thirds of the patients who had intervention to prevent or treat bleeding, most received either plasma-derived VW factor/factor VIII concentrates or antifibrinolytics.
Overall, the researchers advocated a team approach to treating these children “including genetic counselors throughout the prepartum period who work to increase expectant mothers’ understanding of the risks associated with having a child with VWD.”
They also recommended the input of “adult and pediatric hematologists, obstetrician gynecologists, genetic counselors, nurses, and social workers throughout the pre- and postpartum period who seek to optimize outcomes and disease management.”
The authors reported that they had no competing interests.
FROM BLOOD ADVANCES
Improving emergency care for children living outside of urban areas
A new physician workforce study documents that almost all clinically active pediatric emergency physicians in the United States – 99% of them – work in urban areas, and that those who do practice in rural areas are significantly older and closer to retirement age.
The portrait of approximately 2,400 self-identified pediatric emergency medicine (EM) physicians may be unsurprising given the overall propensity of physicians – including board-certified general emergency physicians – to practice in urban areas. Even so, it underscores a decades-long concern that many children do not have access to optimal pediatric emergency care.
And the findings highlight the need, the authors say, to keep pressing to improve emergency care for a population of children with “a mortality rate that is already higher than that of its suburban and urban peers (JAMA Network Open 2021;4[5]:e2110084).”
Emergent care of pediatric patients is well within the scope of practice for physicians with training and board certification in general EM, but children and adolescents have different clinical needs and “there are high-stakes scenarios [in children] that we [as emergency physicians] don’t get exposed to as often because we’re not in a children’s hospital or we just don’t have that additional level of training,” said Christopher L. Bennett, MD, MA, of the department of emergency medicine at Stanford University and lead author of the study.
Researchers have documented that some emergency physicians have some discomfort in caring for very ill pediatric patients, he and his coauthors wrote.
Children account for more than 20% of annual ED visits, and most children who seek emergency care in the United States – upwards of 80% – present to general emergency departments. Yet the vast majority of these EDs care for fewer than 14-15 children a day.
With such low pediatric volume, “there will never be pediatric emergency medicine physicians in the rural hospitals in [our] health care system,” said Kathleen M. Brown, MD, medical director for quality and safety of the Emergency Medicine and Trauma Center at Children’s National Medical Center in Washington.
Redistribution “is not a practical solution, and we’ve known that for a long time,” said Dr. Brown, past chairperson of the American College of Emergency Physicians’ pediatric emergency medicine committee. “That’s why national efforts have focused on better preparing the general emergency department and making sure the hospital workforce is ready to take care of children ... to manage and stabilize [them] and recognize when they need more definitive care.”
Continuing efforts to increase “pediatric readiness” in general EDs is one of the recommendations issued by the American Academy of Pediatrics, ACEP, and Emergency Nurses Association in its most recent joint policy statement on emergency care for children, published in May (Pediatrics 2021;147[5]:e2021050787). A 2018 joint policy statement detailed the resources – medications, equipment, policies, and education – necessary for EDs to provide effective pediatric care (Pediatrics 2018;142[5]:e20182459).
There is some evidence that pediatric readiness has improved and that EDs with higher readiness scores may have better pediatric outcomes and lower mortality, said Dr. Brown, a coauthor of both policy statements. (One study cited in the 2018 policy statement, for example, found that children with extremity immobilization and a pain score of 5 or greater had faster management of their pain and decreased exposure to radiation when they were treated in a better-prepared facility than in a facility with less readiness.)
Yet many hospitals still do not have designated pediatric emergency care coordinators (PECCs) – roles that are widely believed to be central to pediatric readiness. PECCs (physicians and nurses) were recommended in 2006 by the then-Institute of Medicine and have been advocated by the AAP, ACEP, and other organizations.
According to 2013 data from the National Pediatric Readiness Project (NPRP), launched that year by the AAP, ACEP, ENA, and the federal Emergency Medical Services for Children program of the Health Resources and Services Administration, at least 15% of EDs lacked at least 1 piece of recommended equipment, and 81% reported barriers to pediatric emergency care guidelines. The NPRP is currently conducting an updated assessment, Dr. Brown said.
Some experts have proposed a different kind of solution – one in which American Board of Pediatrics–certified pediatric EM physicians would care for selective adult patients with common disease patterns who present to rural EDs, in addition to children. They might provide direct patient care across several hospitals in a region, while also addressing quality improvement and assisting EPs and other providers in the region on pediatric care issues.
The proposal, published in May 2020, comes from the 13-member special subcommittee of the ACEP committee on PEM that was tasked with exploring strategies to improve access to emergency pediatric expertise and disaster preparedness in all settings. The proposal was endorsed by the ACEP board of directors, said Jim Homme, MD, a coauthor of the paper (JACEP Open 2020;1:1520-6.)
“We’re saying, look at the ped-trained pediatric emergency provider more broadly. They can actually successfully care for a broader patient population and make it financially feasible ... [for that physician] to be a part of the system,” said Dr. Homme, program director of the emergency medicine residency at the Mayo Clinic College of Medicine and Science in Rochester, Minn.
“The benefit would be not only having the expertise to see children, but to train up other individuals in the institution, and be advocates for the care of children,” he said.
“We’re not saying we want a pediatrics-trained EM physician in every site so that every child would be seen by one – that’s not the goal,” Dr. Homme said. “The goal is to distribute them more broadly than they currently are, and in doing so, make available the other benefits besides direct patient care.”
Most of the physicians in the United States who identify as pediatric EM physicians have completed either a pediatrics or EM residency, followed by a pediatric EM fellowship. It is much more common to have primary training in pediatrics than in EM, said Dr. Homme and Dr. Bennett. A small number of physicians, like Dr. Homme, are dually trained in pediatrics and EM through the completion of two residencies. Dr. Bennett’s workforce study used the American Medical Association Physician Masterfile database and identified 2,403 clinically active pediatric EPs – 5% of all clinically active emergency physicians. Those practicing in rural areas had a median age of 59, compared with a median age of 46 in urban areas. More than half of the pediatric EPs – 68% – reported having pediatric EM board certification.
Three states – Montana, South Dakota, and Wyoming – had no pediatric EMs at all, Dr. Bennett noted.
Readiness in rural Oregon, New England
Torree McGowan, MD, an emergency physician with the St. Charles Health System in Oregon, works in small critical access hospitals in the rural towns of Madras and Prineville, each several hours by ground to the nearest pediatric hospital. She said she feels well equipped to care for children through her training (a rotation in a pediatric ICU and several months working in pediatric EDs) and through her ongoing work with pediatric patients. Children and adolescents comprise about 20%-30% of her volume.
She sees more pediatric illness – children with respiratory syncytial virus who need respiratory support, for instance, and children with severe asthma or diabetic ketoacidosis – than pediatric trauma. When she faces questions, uncertainties, or wants confirmation of a decision, she consults by phone with pediatric subspecialists.
“I don’t take care of kids on vasopressor drips on a regular basis [for instance],” said Dr. McGowan, who sits on ACEP’s disaster preparedness committee and is an Air Force veteran. “But I know the basics and can phone a colleague to be sure I’m doing it correctly. The ability to outreach is there.”
Telemedicine is valuable, she said, but there may also be value in working alongside a pediatric EM physician. One of her EP colleagues is fellowship-trained in ultrasonography and “leads us in training and quality control,” Dr. McGowan said. “And if she’s on shift with you she’ll teach you all about ultrasound. There’s probably utility in having a pediatric EP who does that as well. But incentivizing that and taking them away from the pediatric hospital is a paradigm shift.”
Either way, she said, “being able to bring that expertise out of urban centers, whether it’s to a hospital group like ours or whether it’s by telemedicine, is really, really helpful.”
Her group does not have official PECCs, but the joint policy statements by AAP/ACEP/ENA on pediatric readiness and the “whole pediatric readiness effort’ have been valuable in “driving conversations” with administrators about needs such as purchasing pediatric-sized video laryngoscope blades and other equipment needed for pediatric emergencies, however infrequently they may occur, Dr. McGowan said.
In New England, researchers leading a grassroots regional intervention to establish a PECC in every ED in the region have reported an increased prevalence of “pediatric champions” from less than 30% 5 years ago to greater than 90% in 2019, investigators have reported (Pediatr Emerg Care. 2021. doi: 10.1097/PEC.0000000000002456).
The initiative involved individual outreach to leaders of each ED – largely through phone and e-mail appeals – and collaboration among the State Emergency Medical Services for Children agencies and ACEP and ENA state chapters. The researchers are currently investigating the direct impact of PECCs on patient outcomes.
More on regionalization of ped-trained EPs
Dr. Bennett sees telemedicine as a primary part of improving pediatric emergency care. “I think that’s where things are going to go in pediatric emergency medicine,” he said, especially in the wake of COVID-19: “I don’t see how it’s not going to become much more common.”
Dr. Homme maintains that a broader integration of ABP-certified pediatric EM physicians into underserved regions would advance ED preparedness in a way that telemedicine, or even the appointment of PECCs, does not, said Dr. Homme.
Institutions would need to acknowledge that many of the current restrictions on pediatric EM physicians’ scope of practice are based on arbitrary age cut-offs, and their leaders would need to expand hospital-defined privileges to better align with training and capabilities, he said. Local credentialing provisions and other policies would also need to be adjusted.
Pediatric EM physicians spend at least 4 months of their graduate EM training in an adult ED, and there is significant overlap in the core competencies and the procedures considered essential for practice between pediatric EM fellowship programs and EM programs, Dr. Homme and his coauthors wrote in their proposal. “The pandemic really reinforced this concept,” Dr. Homme said. “As the number of patients in pediatric EDs plummeted, many of the ped-trained providers had to pivot and help care for adults. ... It worked great.”
The broader integration of pediatrics-trained pediatric EM physicians fits well, he believes, with current workforce dynamics. “There aren’t enough individuals coming out of an EM background and doing that subspecialty training to have any hope that they’d be able to cover these underserved areas,” he said. “And the academic pediatric workforce is getting kind of saturated. So having additional employment opportunities would be great.”
Dr. Homme pursued an EM residency after pediatrics training (rather than a pediatric EM fellowship) because he did not want to be limited geographically and because, while he wanted to focus on children, he also “wanted to be available to a larger population.”
He believes that some pediatrics-trained pediatric EM physicians would choose rural practice options, and hopes that the proposal will gain traction. Some EPs will be opposed, he said, and some pediatrics-trained EPs will not interested, “but if we can find people open to the idea on both sides, I think we can really move the needle in the direction we’re trying to, which is to disseminate an area of expertise into areas that just don’t have it.”
A new physician workforce study documents that almost all clinically active pediatric emergency physicians in the United States – 99% of them – work in urban areas, and that those who do practice in rural areas are significantly older and closer to retirement age.
The portrait of approximately 2,400 self-identified pediatric emergency medicine (EM) physicians may be unsurprising given the overall propensity of physicians – including board-certified general emergency physicians – to practice in urban areas. Even so, it underscores a decades-long concern that many children do not have access to optimal pediatric emergency care.
And the findings highlight the need, the authors say, to keep pressing to improve emergency care for a population of children with “a mortality rate that is already higher than that of its suburban and urban peers (JAMA Network Open 2021;4[5]:e2110084).”
Emergent care of pediatric patients is well within the scope of practice for physicians with training and board certification in general EM, but children and adolescents have different clinical needs and “there are high-stakes scenarios [in children] that we [as emergency physicians] don’t get exposed to as often because we’re not in a children’s hospital or we just don’t have that additional level of training,” said Christopher L. Bennett, MD, MA, of the department of emergency medicine at Stanford University and lead author of the study.
Researchers have documented that some emergency physicians have some discomfort in caring for very ill pediatric patients, he and his coauthors wrote.
Children account for more than 20% of annual ED visits, and most children who seek emergency care in the United States – upwards of 80% – present to general emergency departments. Yet the vast majority of these EDs care for fewer than 14-15 children a day.
With such low pediatric volume, “there will never be pediatric emergency medicine physicians in the rural hospitals in [our] health care system,” said Kathleen M. Brown, MD, medical director for quality and safety of the Emergency Medicine and Trauma Center at Children’s National Medical Center in Washington.
Redistribution “is not a practical solution, and we’ve known that for a long time,” said Dr. Brown, past chairperson of the American College of Emergency Physicians’ pediatric emergency medicine committee. “That’s why national efforts have focused on better preparing the general emergency department and making sure the hospital workforce is ready to take care of children ... to manage and stabilize [them] and recognize when they need more definitive care.”
Continuing efforts to increase “pediatric readiness” in general EDs is one of the recommendations issued by the American Academy of Pediatrics, ACEP, and Emergency Nurses Association in its most recent joint policy statement on emergency care for children, published in May (Pediatrics 2021;147[5]:e2021050787). A 2018 joint policy statement detailed the resources – medications, equipment, policies, and education – necessary for EDs to provide effective pediatric care (Pediatrics 2018;142[5]:e20182459).
There is some evidence that pediatric readiness has improved and that EDs with higher readiness scores may have better pediatric outcomes and lower mortality, said Dr. Brown, a coauthor of both policy statements. (One study cited in the 2018 policy statement, for example, found that children with extremity immobilization and a pain score of 5 or greater had faster management of their pain and decreased exposure to radiation when they were treated in a better-prepared facility than in a facility with less readiness.)
Yet many hospitals still do not have designated pediatric emergency care coordinators (PECCs) – roles that are widely believed to be central to pediatric readiness. PECCs (physicians and nurses) were recommended in 2006 by the then-Institute of Medicine and have been advocated by the AAP, ACEP, and other organizations.
According to 2013 data from the National Pediatric Readiness Project (NPRP), launched that year by the AAP, ACEP, ENA, and the federal Emergency Medical Services for Children program of the Health Resources and Services Administration, at least 15% of EDs lacked at least 1 piece of recommended equipment, and 81% reported barriers to pediatric emergency care guidelines. The NPRP is currently conducting an updated assessment, Dr. Brown said.
Some experts have proposed a different kind of solution – one in which American Board of Pediatrics–certified pediatric EM physicians would care for selective adult patients with common disease patterns who present to rural EDs, in addition to children. They might provide direct patient care across several hospitals in a region, while also addressing quality improvement and assisting EPs and other providers in the region on pediatric care issues.
The proposal, published in May 2020, comes from the 13-member special subcommittee of the ACEP committee on PEM that was tasked with exploring strategies to improve access to emergency pediatric expertise and disaster preparedness in all settings. The proposal was endorsed by the ACEP board of directors, said Jim Homme, MD, a coauthor of the paper (JACEP Open 2020;1:1520-6.)
“We’re saying, look at the ped-trained pediatric emergency provider more broadly. They can actually successfully care for a broader patient population and make it financially feasible ... [for that physician] to be a part of the system,” said Dr. Homme, program director of the emergency medicine residency at the Mayo Clinic College of Medicine and Science in Rochester, Minn.
“The benefit would be not only having the expertise to see children, but to train up other individuals in the institution, and be advocates for the care of children,” he said.
“We’re not saying we want a pediatrics-trained EM physician in every site so that every child would be seen by one – that’s not the goal,” Dr. Homme said. “The goal is to distribute them more broadly than they currently are, and in doing so, make available the other benefits besides direct patient care.”
Most of the physicians in the United States who identify as pediatric EM physicians have completed either a pediatrics or EM residency, followed by a pediatric EM fellowship. It is much more common to have primary training in pediatrics than in EM, said Dr. Homme and Dr. Bennett. A small number of physicians, like Dr. Homme, are dually trained in pediatrics and EM through the completion of two residencies. Dr. Bennett’s workforce study used the American Medical Association Physician Masterfile database and identified 2,403 clinically active pediatric EPs – 5% of all clinically active emergency physicians. Those practicing in rural areas had a median age of 59, compared with a median age of 46 in urban areas. More than half of the pediatric EPs – 68% – reported having pediatric EM board certification.
Three states – Montana, South Dakota, and Wyoming – had no pediatric EMs at all, Dr. Bennett noted.
Readiness in rural Oregon, New England
Torree McGowan, MD, an emergency physician with the St. Charles Health System in Oregon, works in small critical access hospitals in the rural towns of Madras and Prineville, each several hours by ground to the nearest pediatric hospital. She said she feels well equipped to care for children through her training (a rotation in a pediatric ICU and several months working in pediatric EDs) and through her ongoing work with pediatric patients. Children and adolescents comprise about 20%-30% of her volume.
She sees more pediatric illness – children with respiratory syncytial virus who need respiratory support, for instance, and children with severe asthma or diabetic ketoacidosis – than pediatric trauma. When she faces questions, uncertainties, or wants confirmation of a decision, she consults by phone with pediatric subspecialists.
“I don’t take care of kids on vasopressor drips on a regular basis [for instance],” said Dr. McGowan, who sits on ACEP’s disaster preparedness committee and is an Air Force veteran. “But I know the basics and can phone a colleague to be sure I’m doing it correctly. The ability to outreach is there.”
Telemedicine is valuable, she said, but there may also be value in working alongside a pediatric EM physician. One of her EP colleagues is fellowship-trained in ultrasonography and “leads us in training and quality control,” Dr. McGowan said. “And if she’s on shift with you she’ll teach you all about ultrasound. There’s probably utility in having a pediatric EP who does that as well. But incentivizing that and taking them away from the pediatric hospital is a paradigm shift.”
Either way, she said, “being able to bring that expertise out of urban centers, whether it’s to a hospital group like ours or whether it’s by telemedicine, is really, really helpful.”
Her group does not have official PECCs, but the joint policy statements by AAP/ACEP/ENA on pediatric readiness and the “whole pediatric readiness effort’ have been valuable in “driving conversations” with administrators about needs such as purchasing pediatric-sized video laryngoscope blades and other equipment needed for pediatric emergencies, however infrequently they may occur, Dr. McGowan said.
In New England, researchers leading a grassroots regional intervention to establish a PECC in every ED in the region have reported an increased prevalence of “pediatric champions” from less than 30% 5 years ago to greater than 90% in 2019, investigators have reported (Pediatr Emerg Care. 2021. doi: 10.1097/PEC.0000000000002456).
The initiative involved individual outreach to leaders of each ED – largely through phone and e-mail appeals – and collaboration among the State Emergency Medical Services for Children agencies and ACEP and ENA state chapters. The researchers are currently investigating the direct impact of PECCs on patient outcomes.
More on regionalization of ped-trained EPs
Dr. Bennett sees telemedicine as a primary part of improving pediatric emergency care. “I think that’s where things are going to go in pediatric emergency medicine,” he said, especially in the wake of COVID-19: “I don’t see how it’s not going to become much more common.”
Dr. Homme maintains that a broader integration of ABP-certified pediatric EM physicians into underserved regions would advance ED preparedness in a way that telemedicine, or even the appointment of PECCs, does not, said Dr. Homme.
Institutions would need to acknowledge that many of the current restrictions on pediatric EM physicians’ scope of practice are based on arbitrary age cut-offs, and their leaders would need to expand hospital-defined privileges to better align with training and capabilities, he said. Local credentialing provisions and other policies would also need to be adjusted.
Pediatric EM physicians spend at least 4 months of their graduate EM training in an adult ED, and there is significant overlap in the core competencies and the procedures considered essential for practice between pediatric EM fellowship programs and EM programs, Dr. Homme and his coauthors wrote in their proposal. “The pandemic really reinforced this concept,” Dr. Homme said. “As the number of patients in pediatric EDs plummeted, many of the ped-trained providers had to pivot and help care for adults. ... It worked great.”
The broader integration of pediatrics-trained pediatric EM physicians fits well, he believes, with current workforce dynamics. “There aren’t enough individuals coming out of an EM background and doing that subspecialty training to have any hope that they’d be able to cover these underserved areas,” he said. “And the academic pediatric workforce is getting kind of saturated. So having additional employment opportunities would be great.”
Dr. Homme pursued an EM residency after pediatrics training (rather than a pediatric EM fellowship) because he did not want to be limited geographically and because, while he wanted to focus on children, he also “wanted to be available to a larger population.”
He believes that some pediatrics-trained pediatric EM physicians would choose rural practice options, and hopes that the proposal will gain traction. Some EPs will be opposed, he said, and some pediatrics-trained EPs will not interested, “but if we can find people open to the idea on both sides, I think we can really move the needle in the direction we’re trying to, which is to disseminate an area of expertise into areas that just don’t have it.”
A new physician workforce study documents that almost all clinically active pediatric emergency physicians in the United States – 99% of them – work in urban areas, and that those who do practice in rural areas are significantly older and closer to retirement age.
The portrait of approximately 2,400 self-identified pediatric emergency medicine (EM) physicians may be unsurprising given the overall propensity of physicians – including board-certified general emergency physicians – to practice in urban areas. Even so, it underscores a decades-long concern that many children do not have access to optimal pediatric emergency care.
And the findings highlight the need, the authors say, to keep pressing to improve emergency care for a population of children with “a mortality rate that is already higher than that of its suburban and urban peers (JAMA Network Open 2021;4[5]:e2110084).”
Emergent care of pediatric patients is well within the scope of practice for physicians with training and board certification in general EM, but children and adolescents have different clinical needs and “there are high-stakes scenarios [in children] that we [as emergency physicians] don’t get exposed to as often because we’re not in a children’s hospital or we just don’t have that additional level of training,” said Christopher L. Bennett, MD, MA, of the department of emergency medicine at Stanford University and lead author of the study.
Researchers have documented that some emergency physicians have some discomfort in caring for very ill pediatric patients, he and his coauthors wrote.
Children account for more than 20% of annual ED visits, and most children who seek emergency care in the United States – upwards of 80% – present to general emergency departments. Yet the vast majority of these EDs care for fewer than 14-15 children a day.
With such low pediatric volume, “there will never be pediatric emergency medicine physicians in the rural hospitals in [our] health care system,” said Kathleen M. Brown, MD, medical director for quality and safety of the Emergency Medicine and Trauma Center at Children’s National Medical Center in Washington.
Redistribution “is not a practical solution, and we’ve known that for a long time,” said Dr. Brown, past chairperson of the American College of Emergency Physicians’ pediatric emergency medicine committee. “That’s why national efforts have focused on better preparing the general emergency department and making sure the hospital workforce is ready to take care of children ... to manage and stabilize [them] and recognize when they need more definitive care.”
Continuing efforts to increase “pediatric readiness” in general EDs is one of the recommendations issued by the American Academy of Pediatrics, ACEP, and Emergency Nurses Association in its most recent joint policy statement on emergency care for children, published in May (Pediatrics 2021;147[5]:e2021050787). A 2018 joint policy statement detailed the resources – medications, equipment, policies, and education – necessary for EDs to provide effective pediatric care (Pediatrics 2018;142[5]:e20182459).
There is some evidence that pediatric readiness has improved and that EDs with higher readiness scores may have better pediatric outcomes and lower mortality, said Dr. Brown, a coauthor of both policy statements. (One study cited in the 2018 policy statement, for example, found that children with extremity immobilization and a pain score of 5 or greater had faster management of their pain and decreased exposure to radiation when they were treated in a better-prepared facility than in a facility with less readiness.)
Yet many hospitals still do not have designated pediatric emergency care coordinators (PECCs) – roles that are widely believed to be central to pediatric readiness. PECCs (physicians and nurses) were recommended in 2006 by the then-Institute of Medicine and have been advocated by the AAP, ACEP, and other organizations.
According to 2013 data from the National Pediatric Readiness Project (NPRP), launched that year by the AAP, ACEP, ENA, and the federal Emergency Medical Services for Children program of the Health Resources and Services Administration, at least 15% of EDs lacked at least 1 piece of recommended equipment, and 81% reported barriers to pediatric emergency care guidelines. The NPRP is currently conducting an updated assessment, Dr. Brown said.
Some experts have proposed a different kind of solution – one in which American Board of Pediatrics–certified pediatric EM physicians would care for selective adult patients with common disease patterns who present to rural EDs, in addition to children. They might provide direct patient care across several hospitals in a region, while also addressing quality improvement and assisting EPs and other providers in the region on pediatric care issues.
The proposal, published in May 2020, comes from the 13-member special subcommittee of the ACEP committee on PEM that was tasked with exploring strategies to improve access to emergency pediatric expertise and disaster preparedness in all settings. The proposal was endorsed by the ACEP board of directors, said Jim Homme, MD, a coauthor of the paper (JACEP Open 2020;1:1520-6.)
“We’re saying, look at the ped-trained pediatric emergency provider more broadly. They can actually successfully care for a broader patient population and make it financially feasible ... [for that physician] to be a part of the system,” said Dr. Homme, program director of the emergency medicine residency at the Mayo Clinic College of Medicine and Science in Rochester, Minn.
“The benefit would be not only having the expertise to see children, but to train up other individuals in the institution, and be advocates for the care of children,” he said.
“We’re not saying we want a pediatrics-trained EM physician in every site so that every child would be seen by one – that’s not the goal,” Dr. Homme said. “The goal is to distribute them more broadly than they currently are, and in doing so, make available the other benefits besides direct patient care.”
Most of the physicians in the United States who identify as pediatric EM physicians have completed either a pediatrics or EM residency, followed by a pediatric EM fellowship. It is much more common to have primary training in pediatrics than in EM, said Dr. Homme and Dr. Bennett. A small number of physicians, like Dr. Homme, are dually trained in pediatrics and EM through the completion of two residencies. Dr. Bennett’s workforce study used the American Medical Association Physician Masterfile database and identified 2,403 clinically active pediatric EPs – 5% of all clinically active emergency physicians. Those practicing in rural areas had a median age of 59, compared with a median age of 46 in urban areas. More than half of the pediatric EPs – 68% – reported having pediatric EM board certification.
Three states – Montana, South Dakota, and Wyoming – had no pediatric EMs at all, Dr. Bennett noted.
Readiness in rural Oregon, New England
Torree McGowan, MD, an emergency physician with the St. Charles Health System in Oregon, works in small critical access hospitals in the rural towns of Madras and Prineville, each several hours by ground to the nearest pediatric hospital. She said she feels well equipped to care for children through her training (a rotation in a pediatric ICU and several months working in pediatric EDs) and through her ongoing work with pediatric patients. Children and adolescents comprise about 20%-30% of her volume.
She sees more pediatric illness – children with respiratory syncytial virus who need respiratory support, for instance, and children with severe asthma or diabetic ketoacidosis – than pediatric trauma. When she faces questions, uncertainties, or wants confirmation of a decision, she consults by phone with pediatric subspecialists.
“I don’t take care of kids on vasopressor drips on a regular basis [for instance],” said Dr. McGowan, who sits on ACEP’s disaster preparedness committee and is an Air Force veteran. “But I know the basics and can phone a colleague to be sure I’m doing it correctly. The ability to outreach is there.”
Telemedicine is valuable, she said, but there may also be value in working alongside a pediatric EM physician. One of her EP colleagues is fellowship-trained in ultrasonography and “leads us in training and quality control,” Dr. McGowan said. “And if she’s on shift with you she’ll teach you all about ultrasound. There’s probably utility in having a pediatric EP who does that as well. But incentivizing that and taking them away from the pediatric hospital is a paradigm shift.”
Either way, she said, “being able to bring that expertise out of urban centers, whether it’s to a hospital group like ours or whether it’s by telemedicine, is really, really helpful.”
Her group does not have official PECCs, but the joint policy statements by AAP/ACEP/ENA on pediatric readiness and the “whole pediatric readiness effort’ have been valuable in “driving conversations” with administrators about needs such as purchasing pediatric-sized video laryngoscope blades and other equipment needed for pediatric emergencies, however infrequently they may occur, Dr. McGowan said.
In New England, researchers leading a grassroots regional intervention to establish a PECC in every ED in the region have reported an increased prevalence of “pediatric champions” from less than 30% 5 years ago to greater than 90% in 2019, investigators have reported (Pediatr Emerg Care. 2021. doi: 10.1097/PEC.0000000000002456).
The initiative involved individual outreach to leaders of each ED – largely through phone and e-mail appeals – and collaboration among the State Emergency Medical Services for Children agencies and ACEP and ENA state chapters. The researchers are currently investigating the direct impact of PECCs on patient outcomes.
More on regionalization of ped-trained EPs
Dr. Bennett sees telemedicine as a primary part of improving pediatric emergency care. “I think that’s where things are going to go in pediatric emergency medicine,” he said, especially in the wake of COVID-19: “I don’t see how it’s not going to become much more common.”
Dr. Homme maintains that a broader integration of ABP-certified pediatric EM physicians into underserved regions would advance ED preparedness in a way that telemedicine, or even the appointment of PECCs, does not, said Dr. Homme.
Institutions would need to acknowledge that many of the current restrictions on pediatric EM physicians’ scope of practice are based on arbitrary age cut-offs, and their leaders would need to expand hospital-defined privileges to better align with training and capabilities, he said. Local credentialing provisions and other policies would also need to be adjusted.
Pediatric EM physicians spend at least 4 months of their graduate EM training in an adult ED, and there is significant overlap in the core competencies and the procedures considered essential for practice between pediatric EM fellowship programs and EM programs, Dr. Homme and his coauthors wrote in their proposal. “The pandemic really reinforced this concept,” Dr. Homme said. “As the number of patients in pediatric EDs plummeted, many of the ped-trained providers had to pivot and help care for adults. ... It worked great.”
The broader integration of pediatrics-trained pediatric EM physicians fits well, he believes, with current workforce dynamics. “There aren’t enough individuals coming out of an EM background and doing that subspecialty training to have any hope that they’d be able to cover these underserved areas,” he said. “And the academic pediatric workforce is getting kind of saturated. So having additional employment opportunities would be great.”
Dr. Homme pursued an EM residency after pediatrics training (rather than a pediatric EM fellowship) because he did not want to be limited geographically and because, while he wanted to focus on children, he also “wanted to be available to a larger population.”
He believes that some pediatrics-trained pediatric EM physicians would choose rural practice options, and hopes that the proposal will gain traction. Some EPs will be opposed, he said, and some pediatrics-trained EPs will not interested, “but if we can find people open to the idea on both sides, I think we can really move the needle in the direction we’re trying to, which is to disseminate an area of expertise into areas that just don’t have it.”
Cortical thinning in adolescence ‘definitively’ tied to subsequent psychosis
Subtle differences in brain morphometric features present in adolescence were associated with the subsequent development of psychosis in what is believed to be the largest neuroimaging investigation to date involving people at clinical high risk (CHR).
Investigators found widespread lower cortical thickness (CT) in individuals at CHR, consistent with previously reported CT differences in individuals with an established psychotic disorder.
“This is the first study to definitively show that there are subtle, widespread structural brain differences in high-risk youth before they develop psychosis,” study investigator Maria Jalbrzikowski, PhD, assistant professor of psychiatry, University of Pittsburgh, said in an interview.
The findings also suggest that there are developmental periods during which certain brain abnormalities may be more apparent, “highlighting the need to consider developmental period when developing objective, biological risk factors for early intervention in psychosis,” Dr. Jalbrzikowski said.
The study was published online May 5 in JAMA Psychiatry.
‘Sobering’ results
The findings are based on pooled structural MRI scans from 3,169 individuals recruited at 31 international sites participating in the Enhancing Neuro Imaging Genetics Through Meta-Analysis (ENIGMA) Clinical High Risk for Psychosis Working Group.
Forty-five percent of the participants were female; the mean age was 21 years (range, 9.5 to 39.9 years).
The cohort included 1,792 individuals at CHR for psychosis and 1,377 healthy control persons. Using longitudinal clinical information, the researchers identified 253 individuals at CHR who went on to develop a psychotic disorder (CHR-PS+) and 1,234 at CHR who did not develop a psychotic disorder (CHR-PS-). For the remaining 305 individuals at CHR, follow-up data were unavailable.
Compared with healthy control persons, individuals at CHR had widespread lower CT measures but not lower surface area or subcortical volume. Lower CT measures in the fusiform, superior temporal, and paracentral regions were associated with conversion to psychosis.
The pattern of differences in cortical thickness in those in the CHR-PS+ group mirrored patterns seen in people with schizophrenia and in people with 22q11.2 microdeletion syndrome who developed a psychotic disorder.
The researchers note that although all individuals experience cortical thinning as they move into adulthood, in their study, cortical thinning was already present in participants aged 12 to 16 years who developed psychosis.
“We don’t yet know exactly what this means, but adolescence is a critical time in a child’s life – it’s a time of opportunity to take risks and explore, but also a period of vulnerability,” Dr. Jalbrzikowski said in a news release.
“We could be seeing the result of something that happened even earlier in brain development but only begins to influence behavior during this developmental stage,” she noted.
This analysis represents the largest-ever pooling of brain scans in children and young adults who were determined by psychiatric assessment to be at high risk of developing psychosis.
“These results were, in a sense, sobering. On the one hand, our dataset includes 600% more high-risk youth who developed psychosis than any existing study, allowing us to see statistically significant results in brain structure.”
“But the variance between whether or not a high-risk youth develops psychosis is so small that it would be impossible to see a difference at the individual level,” Dr. Jalbrzikowski said.
More work is needed in order for the findings to be translated into clinical care, she added.
Definitive findings
Commenting on the findings for an interview, Russell Margolis, MD, clinical director, Johns Hopkins Schizophrenia Center, said that “it’s not so much that the findings are novel but rather that they’re fairly definitive in that this is by far the largest study of its kind looking at this particular question, and that gives it power. The problem with imaging studies has often been inconsistent results from study to study because of small sample size.”
“In order to see these differences in a robust way, you need a large sample size, meaning that for any one individual, this kind of structural imaging is not going to add much to the prediction of whether someone will eventually develop a schizophrenia-like illness,” said Dr. Margolis, professor of psychiatry and behavioral sciences, Johns Hopkins University, Baltimore.
From a clinical standpoint,
“The predominant hypothesis in the field is that early developmental abnormalities are the root cause of schizophrenia and related disorders, and this study is consistent with that, particularly the age-related differences, which are suggestive of neurodevelopmental abnormalities preceding the development of overt symptoms, which many other findings have also suggested,” Dr. Margolis said.
“Abnormalities in cortical thickness could be from a number of different neurobiological processes, and research into those processes are worth investigating,” he added.
The researchers received support from numerous funders, all of which are listed in the original article, along with author disclosures for ENIGMA working group members. Dr. Margolis has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Subtle differences in brain morphometric features present in adolescence were associated with the subsequent development of psychosis in what is believed to be the largest neuroimaging investigation to date involving people at clinical high risk (CHR).
Investigators found widespread lower cortical thickness (CT) in individuals at CHR, consistent with previously reported CT differences in individuals with an established psychotic disorder.
“This is the first study to definitively show that there are subtle, widespread structural brain differences in high-risk youth before they develop psychosis,” study investigator Maria Jalbrzikowski, PhD, assistant professor of psychiatry, University of Pittsburgh, said in an interview.
The findings also suggest that there are developmental periods during which certain brain abnormalities may be more apparent, “highlighting the need to consider developmental period when developing objective, biological risk factors for early intervention in psychosis,” Dr. Jalbrzikowski said.
The study was published online May 5 in JAMA Psychiatry.
‘Sobering’ results
The findings are based on pooled structural MRI scans from 3,169 individuals recruited at 31 international sites participating in the Enhancing Neuro Imaging Genetics Through Meta-Analysis (ENIGMA) Clinical High Risk for Psychosis Working Group.
Forty-five percent of the participants were female; the mean age was 21 years (range, 9.5 to 39.9 years).
The cohort included 1,792 individuals at CHR for psychosis and 1,377 healthy control persons. Using longitudinal clinical information, the researchers identified 253 individuals at CHR who went on to develop a psychotic disorder (CHR-PS+) and 1,234 at CHR who did not develop a psychotic disorder (CHR-PS-). For the remaining 305 individuals at CHR, follow-up data were unavailable.
Compared with healthy control persons, individuals at CHR had widespread lower CT measures but not lower surface area or subcortical volume. Lower CT measures in the fusiform, superior temporal, and paracentral regions were associated with conversion to psychosis.
The pattern of differences in cortical thickness in those in the CHR-PS+ group mirrored patterns seen in people with schizophrenia and in people with 22q11.2 microdeletion syndrome who developed a psychotic disorder.
The researchers note that although all individuals experience cortical thinning as they move into adulthood, in their study, cortical thinning was already present in participants aged 12 to 16 years who developed psychosis.
“We don’t yet know exactly what this means, but adolescence is a critical time in a child’s life – it’s a time of opportunity to take risks and explore, but also a period of vulnerability,” Dr. Jalbrzikowski said in a news release.
“We could be seeing the result of something that happened even earlier in brain development but only begins to influence behavior during this developmental stage,” she noted.
This analysis represents the largest-ever pooling of brain scans in children and young adults who were determined by psychiatric assessment to be at high risk of developing psychosis.
“These results were, in a sense, sobering. On the one hand, our dataset includes 600% more high-risk youth who developed psychosis than any existing study, allowing us to see statistically significant results in brain structure.”
“But the variance between whether or not a high-risk youth develops psychosis is so small that it would be impossible to see a difference at the individual level,” Dr. Jalbrzikowski said.
More work is needed in order for the findings to be translated into clinical care, she added.
Definitive findings
Commenting on the findings for an interview, Russell Margolis, MD, clinical director, Johns Hopkins Schizophrenia Center, said that “it’s not so much that the findings are novel but rather that they’re fairly definitive in that this is by far the largest study of its kind looking at this particular question, and that gives it power. The problem with imaging studies has often been inconsistent results from study to study because of small sample size.”
“In order to see these differences in a robust way, you need a large sample size, meaning that for any one individual, this kind of structural imaging is not going to add much to the prediction of whether someone will eventually develop a schizophrenia-like illness,” said Dr. Margolis, professor of psychiatry and behavioral sciences, Johns Hopkins University, Baltimore.
From a clinical standpoint,
“The predominant hypothesis in the field is that early developmental abnormalities are the root cause of schizophrenia and related disorders, and this study is consistent with that, particularly the age-related differences, which are suggestive of neurodevelopmental abnormalities preceding the development of overt symptoms, which many other findings have also suggested,” Dr. Margolis said.
“Abnormalities in cortical thickness could be from a number of different neurobiological processes, and research into those processes are worth investigating,” he added.
The researchers received support from numerous funders, all of which are listed in the original article, along with author disclosures for ENIGMA working group members. Dr. Margolis has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Subtle differences in brain morphometric features present in adolescence were associated with the subsequent development of psychosis in what is believed to be the largest neuroimaging investigation to date involving people at clinical high risk (CHR).
Investigators found widespread lower cortical thickness (CT) in individuals at CHR, consistent with previously reported CT differences in individuals with an established psychotic disorder.
“This is the first study to definitively show that there are subtle, widespread structural brain differences in high-risk youth before they develop psychosis,” study investigator Maria Jalbrzikowski, PhD, assistant professor of psychiatry, University of Pittsburgh, said in an interview.
The findings also suggest that there are developmental periods during which certain brain abnormalities may be more apparent, “highlighting the need to consider developmental period when developing objective, biological risk factors for early intervention in psychosis,” Dr. Jalbrzikowski said.
The study was published online May 5 in JAMA Psychiatry.
‘Sobering’ results
The findings are based on pooled structural MRI scans from 3,169 individuals recruited at 31 international sites participating in the Enhancing Neuro Imaging Genetics Through Meta-Analysis (ENIGMA) Clinical High Risk for Psychosis Working Group.
Forty-five percent of the participants were female; the mean age was 21 years (range, 9.5 to 39.9 years).
The cohort included 1,792 individuals at CHR for psychosis and 1,377 healthy control persons. Using longitudinal clinical information, the researchers identified 253 individuals at CHR who went on to develop a psychotic disorder (CHR-PS+) and 1,234 at CHR who did not develop a psychotic disorder (CHR-PS-). For the remaining 305 individuals at CHR, follow-up data were unavailable.
Compared with healthy control persons, individuals at CHR had widespread lower CT measures but not lower surface area or subcortical volume. Lower CT measures in the fusiform, superior temporal, and paracentral regions were associated with conversion to psychosis.
The pattern of differences in cortical thickness in those in the CHR-PS+ group mirrored patterns seen in people with schizophrenia and in people with 22q11.2 microdeletion syndrome who developed a psychotic disorder.
The researchers note that although all individuals experience cortical thinning as they move into adulthood, in their study, cortical thinning was already present in participants aged 12 to 16 years who developed psychosis.
“We don’t yet know exactly what this means, but adolescence is a critical time in a child’s life – it’s a time of opportunity to take risks and explore, but also a period of vulnerability,” Dr. Jalbrzikowski said in a news release.
“We could be seeing the result of something that happened even earlier in brain development but only begins to influence behavior during this developmental stage,” she noted.
This analysis represents the largest-ever pooling of brain scans in children and young adults who were determined by psychiatric assessment to be at high risk of developing psychosis.
“These results were, in a sense, sobering. On the one hand, our dataset includes 600% more high-risk youth who developed psychosis than any existing study, allowing us to see statistically significant results in brain structure.”
“But the variance between whether or not a high-risk youth develops psychosis is so small that it would be impossible to see a difference at the individual level,” Dr. Jalbrzikowski said.
More work is needed in order for the findings to be translated into clinical care, she added.
Definitive findings
Commenting on the findings for an interview, Russell Margolis, MD, clinical director, Johns Hopkins Schizophrenia Center, said that “it’s not so much that the findings are novel but rather that they’re fairly definitive in that this is by far the largest study of its kind looking at this particular question, and that gives it power. The problem with imaging studies has often been inconsistent results from study to study because of small sample size.”
“In order to see these differences in a robust way, you need a large sample size, meaning that for any one individual, this kind of structural imaging is not going to add much to the prediction of whether someone will eventually develop a schizophrenia-like illness,” said Dr. Margolis, professor of psychiatry and behavioral sciences, Johns Hopkins University, Baltimore.
From a clinical standpoint,
“The predominant hypothesis in the field is that early developmental abnormalities are the root cause of schizophrenia and related disorders, and this study is consistent with that, particularly the age-related differences, which are suggestive of neurodevelopmental abnormalities preceding the development of overt symptoms, which many other findings have also suggested,” Dr. Margolis said.
“Abnormalities in cortical thickness could be from a number of different neurobiological processes, and research into those processes are worth investigating,” he added.
The researchers received support from numerous funders, all of which are listed in the original article, along with author disclosures for ENIGMA working group members. Dr. Margolis has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CDC director cites rise in hospitalizations in urging teen vaccinations
“I am deeply concerned by the numbers of hospitalized adolescents and saddened to see the number of adolescents who required treatment in intensive care units or mechanical ventilation,” CDC Director Rochelle Walensky, MD, said in a statement.
While urging teenagers to wear masks and take precautions around others, she asked “parents, relatives, and close friends to join me and talk with teens about the importance of these prevention strategies and to encourage them to get vaccinated.”
Dr. Walensky referred to the CDC’s Morbidity and Mortality Weekly Report that showed adolescent hospitalizations peaked at 2.1 per 100,000 in early January 2021, then dropped to 0.6 per 100,000 in mid-March.
Alarmingly, hospitalizations rose to 1.3 per 100,000 in April, and a number of teens required serious interventions.
“Among hospitalized adolescents, nearly one-third required intensive care unit admission, and 5% required invasive mechanical ventilation,” the report said. No deaths occurred.
The study looked at 376 adolescents aged 12-17 who were hospitalized and tested positive for coronavirus. Of that group, 204 were hospitalized for COVID-19 and the other 172 were hospitalized for reasons not directly related to COVID-19.
Of the 204 hospitalized for COVID-19, 70.6% had an underlying medical condition such as obesity or chronic lung disease.
The study noted that children and teenagers have lower hospitalization rates and generally show less severe symptoms than do older people.
Possible causes for the rise in adolescent COVID-19 hospitalizations include the arrival of variants, the growing number of children returning to in-person education, and the changes in mask-wearing and other safety precautions, the study said.
The American Academy of Pediatrics said that as of May 27, 4 million children have tested positive for COVID-19 since the pandemic began, with about 34,500 new child cases reported for the week ending May 27.
The AAP said children have represented 14.1% of total cases since the pandemic began, but for the week ending May 27, children represented 24.3% of new reported weekly COVID-19 cases.
On May 10, the FDA granted emergency use authorization for the Pfizer coronavirus vaccine to be given to children aged 12-15 years. Previously, the FDA had authorized the Pfizer vaccine for people aged 16 years and up, whereas the Moderna and Johnson & Johnson vaccines are authorized for people aged 18 years and up.
“Vaccination is our way out of this pandemic,” Dr. Walensky said in her statement. “I continue to see promising signs in CDC data that we are nearing the end of this pandemic in this country; however, we all have to do our part and get vaccinated to cross the finish line.”
A version of this article was first published on WebMD.com.
“I am deeply concerned by the numbers of hospitalized adolescents and saddened to see the number of adolescents who required treatment in intensive care units or mechanical ventilation,” CDC Director Rochelle Walensky, MD, said in a statement.
While urging teenagers to wear masks and take precautions around others, she asked “parents, relatives, and close friends to join me and talk with teens about the importance of these prevention strategies and to encourage them to get vaccinated.”
Dr. Walensky referred to the CDC’s Morbidity and Mortality Weekly Report that showed adolescent hospitalizations peaked at 2.1 per 100,000 in early January 2021, then dropped to 0.6 per 100,000 in mid-March.
Alarmingly, hospitalizations rose to 1.3 per 100,000 in April, and a number of teens required serious interventions.
“Among hospitalized adolescents, nearly one-third required intensive care unit admission, and 5% required invasive mechanical ventilation,” the report said. No deaths occurred.
The study looked at 376 adolescents aged 12-17 who were hospitalized and tested positive for coronavirus. Of that group, 204 were hospitalized for COVID-19 and the other 172 were hospitalized for reasons not directly related to COVID-19.
Of the 204 hospitalized for COVID-19, 70.6% had an underlying medical condition such as obesity or chronic lung disease.
The study noted that children and teenagers have lower hospitalization rates and generally show less severe symptoms than do older people.
Possible causes for the rise in adolescent COVID-19 hospitalizations include the arrival of variants, the growing number of children returning to in-person education, and the changes in mask-wearing and other safety precautions, the study said.
The American Academy of Pediatrics said that as of May 27, 4 million children have tested positive for COVID-19 since the pandemic began, with about 34,500 new child cases reported for the week ending May 27.
The AAP said children have represented 14.1% of total cases since the pandemic began, but for the week ending May 27, children represented 24.3% of new reported weekly COVID-19 cases.
On May 10, the FDA granted emergency use authorization for the Pfizer coronavirus vaccine to be given to children aged 12-15 years. Previously, the FDA had authorized the Pfizer vaccine for people aged 16 years and up, whereas the Moderna and Johnson & Johnson vaccines are authorized for people aged 18 years and up.
“Vaccination is our way out of this pandemic,” Dr. Walensky said in her statement. “I continue to see promising signs in CDC data that we are nearing the end of this pandemic in this country; however, we all have to do our part and get vaccinated to cross the finish line.”
A version of this article was first published on WebMD.com.
“I am deeply concerned by the numbers of hospitalized adolescents and saddened to see the number of adolescents who required treatment in intensive care units or mechanical ventilation,” CDC Director Rochelle Walensky, MD, said in a statement.
While urging teenagers to wear masks and take precautions around others, she asked “parents, relatives, and close friends to join me and talk with teens about the importance of these prevention strategies and to encourage them to get vaccinated.”
Dr. Walensky referred to the CDC’s Morbidity and Mortality Weekly Report that showed adolescent hospitalizations peaked at 2.1 per 100,000 in early January 2021, then dropped to 0.6 per 100,000 in mid-March.
Alarmingly, hospitalizations rose to 1.3 per 100,000 in April, and a number of teens required serious interventions.
“Among hospitalized adolescents, nearly one-third required intensive care unit admission, and 5% required invasive mechanical ventilation,” the report said. No deaths occurred.
The study looked at 376 adolescents aged 12-17 who were hospitalized and tested positive for coronavirus. Of that group, 204 were hospitalized for COVID-19 and the other 172 were hospitalized for reasons not directly related to COVID-19.
Of the 204 hospitalized for COVID-19, 70.6% had an underlying medical condition such as obesity or chronic lung disease.
The study noted that children and teenagers have lower hospitalization rates and generally show less severe symptoms than do older people.
Possible causes for the rise in adolescent COVID-19 hospitalizations include the arrival of variants, the growing number of children returning to in-person education, and the changes in mask-wearing and other safety precautions, the study said.
The American Academy of Pediatrics said that as of May 27, 4 million children have tested positive for COVID-19 since the pandemic began, with about 34,500 new child cases reported for the week ending May 27.
The AAP said children have represented 14.1% of total cases since the pandemic began, but for the week ending May 27, children represented 24.3% of new reported weekly COVID-19 cases.
On May 10, the FDA granted emergency use authorization for the Pfizer coronavirus vaccine to be given to children aged 12-15 years. Previously, the FDA had authorized the Pfizer vaccine for people aged 16 years and up, whereas the Moderna and Johnson & Johnson vaccines are authorized for people aged 18 years and up.
“Vaccination is our way out of this pandemic,” Dr. Walensky said in her statement. “I continue to see promising signs in CDC data that we are nearing the end of this pandemic in this country; however, we all have to do our part and get vaccinated to cross the finish line.”
A version of this article was first published on WebMD.com.
Sleep Medicine A Special Report
Sleep Medicine A Special Report
- MOBILE PHONE RELIANCE
How it’s linked to young adults’ sleep problems in two studies - OBSTRUCTIVE SLEEP APNEA
New research validates phenotypes in Latinos - DEMENTIA
Papers show associations between disease and sleep therapies
Sleep Medicine A Special Report
- MOBILE PHONE RELIANCE
How it’s linked to young adults’ sleep problems in two studies - OBSTRUCTIVE SLEEP APNEA
New research validates phenotypes in Latinos - DEMENTIA
Papers show associations between disease and sleep therapies
Sleep Medicine A Special Report
- MOBILE PHONE RELIANCE
How it’s linked to young adults’ sleep problems in two studies - OBSTRUCTIVE SLEEP APNEA
New research validates phenotypes in Latinos - DEMENTIA
Papers show associations between disease and sleep therapies
Texas hospital workers sue over vaccine mandates
objecting to its policy of requiring employees and contractors to be vaccinated against COVID-19 or risk losing their jobs.
Plaintiffs include Jennifer Bridges, RN, a medical-surgical nurse at the hospital who has become the public face and voice of health care workers who object to mandatory vaccination, as well as Bob Nevens, the hospital’s director of corporate risk.
Mr. Nevens said the hospital was requiring him to be vaccinated even though he doesn’t treat patients and has been working from home for most of the past year.
“My civil rights and liberties have been trampled on,” he said in comments posted on an online petition. “My right to protect myself from unknown side effects of these vaccines has been placed below the optics of ‘leading medicine,’ “ he said.
Mr. Nevens says in his comments that he was fired on April 15, although the lawsuit says he is currently employed by the hospital’s corporate office.
The Texas attorney who filed the lawsuit, Jared Woodfill, is known to champion conservative causes. In March 2020, he challenged Harris County’s stay-at-home order, charging that it violated religious liberty. He was chairman of the Harris County Republican Party for more than a decade. His website says he is a frequent guest on the local Fox News affiliate.
The lawsuit hinges on a section of the federal law that authorizes emergency use of medical products – US Code 360bbb-3.
That law says that individuals to whom the product is administered should be informed “of the option to accept or refuse administration of the product, of the consequence, if any, of refusing administration of the product, and of the alternatives to the product that are available and of their benefits and risks.”
Legal experts are split as to what the provision means for vaccination mandates. Courts have not yet weighed in with their interpretations of the law.
The petition also repeats a popular antivaccination argument that likens requiring a vaccine approved for emergency use to the kind of medical experimentation performed by Nazi doctors on Jewish prisoners in concentration camps. It says forcing people to choose between an experimental vaccine and a job is a violation of the Nuremberg Code, which says that people must voluntarily and knowingly consent to participating in research.
The vaccines have already been tested in clinical trials. People who are getting them now are not part of those studies, though vaccine manufacturers, regulators, and safety experts are still watching closely for any sign of problems tied to the new shots.
It is true, however, that the emergency use authorization granted by the U.S. Food and Drug Administraiton sped up the process of getting the vaccines onto market. Vaccine manufacturers are currently completing the process of submitting documentation required for a full biologics license application, the mechanism the FDA uses for full approval.
Houston Methodist sent an email to employees in April notifying them that they had until June 7 to start the vaccination process or apply for a medical or religious exemption. Those who decide not to will be terminated.
Marc Boom, MD, the health care system’s president and CEO, has explained that the policy is in place to protect patients and that it was the first hospital in the United States to require it. Since then, other hospitals, including the University of Pennsylvania Health System, have required COVID vaccines.
A version of this article first appeared on Medscape.com.
objecting to its policy of requiring employees and contractors to be vaccinated against COVID-19 or risk losing their jobs.
Plaintiffs include Jennifer Bridges, RN, a medical-surgical nurse at the hospital who has become the public face and voice of health care workers who object to mandatory vaccination, as well as Bob Nevens, the hospital’s director of corporate risk.
Mr. Nevens said the hospital was requiring him to be vaccinated even though he doesn’t treat patients and has been working from home for most of the past year.
“My civil rights and liberties have been trampled on,” he said in comments posted on an online petition. “My right to protect myself from unknown side effects of these vaccines has been placed below the optics of ‘leading medicine,’ “ he said.
Mr. Nevens says in his comments that he was fired on April 15, although the lawsuit says he is currently employed by the hospital’s corporate office.
The Texas attorney who filed the lawsuit, Jared Woodfill, is known to champion conservative causes. In March 2020, he challenged Harris County’s stay-at-home order, charging that it violated religious liberty. He was chairman of the Harris County Republican Party for more than a decade. His website says he is a frequent guest on the local Fox News affiliate.
The lawsuit hinges on a section of the federal law that authorizes emergency use of medical products – US Code 360bbb-3.
That law says that individuals to whom the product is administered should be informed “of the option to accept or refuse administration of the product, of the consequence, if any, of refusing administration of the product, and of the alternatives to the product that are available and of their benefits and risks.”
Legal experts are split as to what the provision means for vaccination mandates. Courts have not yet weighed in with their interpretations of the law.
The petition also repeats a popular antivaccination argument that likens requiring a vaccine approved for emergency use to the kind of medical experimentation performed by Nazi doctors on Jewish prisoners in concentration camps. It says forcing people to choose between an experimental vaccine and a job is a violation of the Nuremberg Code, which says that people must voluntarily and knowingly consent to participating in research.
The vaccines have already been tested in clinical trials. People who are getting them now are not part of those studies, though vaccine manufacturers, regulators, and safety experts are still watching closely for any sign of problems tied to the new shots.
It is true, however, that the emergency use authorization granted by the U.S. Food and Drug Administraiton sped up the process of getting the vaccines onto market. Vaccine manufacturers are currently completing the process of submitting documentation required for a full biologics license application, the mechanism the FDA uses for full approval.
Houston Methodist sent an email to employees in April notifying them that they had until June 7 to start the vaccination process or apply for a medical or religious exemption. Those who decide not to will be terminated.
Marc Boom, MD, the health care system’s president and CEO, has explained that the policy is in place to protect patients and that it was the first hospital in the United States to require it. Since then, other hospitals, including the University of Pennsylvania Health System, have required COVID vaccines.
A version of this article first appeared on Medscape.com.
objecting to its policy of requiring employees and contractors to be vaccinated against COVID-19 or risk losing their jobs.
Plaintiffs include Jennifer Bridges, RN, a medical-surgical nurse at the hospital who has become the public face and voice of health care workers who object to mandatory vaccination, as well as Bob Nevens, the hospital’s director of corporate risk.
Mr. Nevens said the hospital was requiring him to be vaccinated even though he doesn’t treat patients and has been working from home for most of the past year.
“My civil rights and liberties have been trampled on,” he said in comments posted on an online petition. “My right to protect myself from unknown side effects of these vaccines has been placed below the optics of ‘leading medicine,’ “ he said.
Mr. Nevens says in his comments that he was fired on April 15, although the lawsuit says he is currently employed by the hospital’s corporate office.
The Texas attorney who filed the lawsuit, Jared Woodfill, is known to champion conservative causes. In March 2020, he challenged Harris County’s stay-at-home order, charging that it violated religious liberty. He was chairman of the Harris County Republican Party for more than a decade. His website says he is a frequent guest on the local Fox News affiliate.
The lawsuit hinges on a section of the federal law that authorizes emergency use of medical products – US Code 360bbb-3.
That law says that individuals to whom the product is administered should be informed “of the option to accept or refuse administration of the product, of the consequence, if any, of refusing administration of the product, and of the alternatives to the product that are available and of their benefits and risks.”
Legal experts are split as to what the provision means for vaccination mandates. Courts have not yet weighed in with their interpretations of the law.
The petition also repeats a popular antivaccination argument that likens requiring a vaccine approved for emergency use to the kind of medical experimentation performed by Nazi doctors on Jewish prisoners in concentration camps. It says forcing people to choose between an experimental vaccine and a job is a violation of the Nuremberg Code, which says that people must voluntarily and knowingly consent to participating in research.
The vaccines have already been tested in clinical trials. People who are getting them now are not part of those studies, though vaccine manufacturers, regulators, and safety experts are still watching closely for any sign of problems tied to the new shots.
It is true, however, that the emergency use authorization granted by the U.S. Food and Drug Administraiton sped up the process of getting the vaccines onto market. Vaccine manufacturers are currently completing the process of submitting documentation required for a full biologics license application, the mechanism the FDA uses for full approval.
Houston Methodist sent an email to employees in April notifying them that they had until June 7 to start the vaccination process or apply for a medical or religious exemption. Those who decide not to will be terminated.
Marc Boom, MD, the health care system’s president and CEO, has explained that the policy is in place to protect patients and that it was the first hospital in the United States to require it. Since then, other hospitals, including the University of Pennsylvania Health System, have required COVID vaccines.
A version of this article first appeared on Medscape.com.
EULAR, ACR present preliminary recommendations for rare genetic autoinflammatory diseases
As researchers learn more about the genetic etiology of immunopathology, they have been able to more clearly understand rare but debilitating autoinflammatory conditions in ways that have improved identification and management of these diseases. At this year’s European Congress of Rheumatology, two researchers outlined new recommendations from the European Alliance of Associations for Rheumatology (EULAR) and the American College of Rheumatology (ACR) for the management of two groups of such autoinflammatory diseases: interleukin-1-mediated and Type-I interferonopathies, and suspected macrophage activation syndrome and hemophagocytic lymphohistiocytosis.
These are the first recommendations from EULAR for these diseases, according to Loreto Carmona, MD, PhD, chair of the EULAR scientific program committee and scientific director of the Institute for Musculoskeletal Health in Madrid.
“They are rare diseases and there is a great need to standardize diagnosis and care for the safety and outcome of the patients,” Dr. Carmona said in an interview. “These diseases need deep expertise and so the experts are trying, they are still preliminary, to add clarity to their management.” Dr. Carmona was not involved with the development of the guidelines and moderated the session during which they were presented.
“The rapidly emerging knowledge of the genetic causes of novel systemic autoinflammatory diseases, which present typically in early childhood with severe and chronic systemic and organ-specific inflammation, linked the disease pathogenesis to the pathologic production of major proinflammatory cytokines,” presenter Raphaela Goldbach-Mansky, MD, a senior investigator and chief of the translational autoinflammatory disease studies unit of the U.S. National Institute of Allergy and Infectious Diseases, told congress attendees. This greater understanding led to the “targeted and anticytokine treatments that have changed patients’ lives,” she said.
The guidelines relied on the products of three working groups for each disease type. After meeting to come up with clinical questions, the groups each conducted systematic literature reviews through EMBASE, PubMed, and the Cochrane Library for publications dated from 1970 to August 2020 that excluded non-English-language studies, case reports, and animal model or basic science studies. They then met again to develop final consensus statements.
The interferonopathy and interleukin (IL)-1-mediated systemic autoinflammatory diseases (SAIDs) working groups met throughout 2020, and the hemophagocytic lymphohistiocytosis (HLH)/ macrophage activation syndrome (MAS) working group met in March and April of 2021.
“One needs a lot of experience with these diseases to even think about them,” Dr. Carmona said. “We haven’t been presented yet with all the details of the recommendations, but we hope they are clear because they are much needed.”
She noted that these preliminary recommendations are based on the best available evidence to date along with expertise from multidisciplinary panels.
“We need to be acquainted with these recommendations, as the majority of us, either if we are pediatric or adult rheumatologists, will face some problem with these diseases at some point,” Dr. Carmona said.
IL-1-mediated SAIDs
Recommendations for IL-1-mediated SAIDs focused on mevalonate kinase deficiency (MKD), tumor necrosis factor receptor-associated periodic syndrome (TRAPS), cryopyrinopathies (CAPS), and deficiency of the IL-1 receptor antagonist (DIRA). Presentation of these conditions involves chronic or intermittent flares of systemic and organ inflammation that can cause progressive organ damage, morbidity, and increased mortality if not treated. Diagnosis requires a multidisciplinary team whose evaluation should include disease-related complications and long-term care plans.
Diagnostic workup should include genetic testing using next-generation sequencing as this “facilitates initiation of targeted treatments, genetic counseling, and informs prognosis” for patients with CAPS, TRAPS, MKD, and DIRA, Erkan Demirkaya, MD, a scientist at the Children’s Health Research Institute and professor of pediatric rheumatology at the University of Western Ontario in London, Canada, told attendees. Evaluation should also include clinical workup that focuses on the extent of inflammatory organ involvement, and screening for disease- and treatment-related comorbidities.
“The goal of therapy is to control clinical signs and symptoms and normalize laboratory biomarkers of systemic inflammation,” Dr. Demirkaya said. Long-term monitoring goals should focus on the following:
- “Adequate treatment adjusted to the needs of the growing child and prevention of systemic and organ-specific inflammatory manifestations;
- Fostering of self-management skills and medical decision-making;
- Initiating a transition program to adult specialist care in adolescent patients.”
Type-1 interferonopathies
The recommendations for this disease group focused on chronic atypical neutrophilic dermatosis with lipodystrophy and elevated temperatures (CANDLE)/proteasome-associated autoinflammatory syndromes (PRAAS), STING-associated vasculopathy with onset in infancy (SAVI), and Aicardi-Goutières syndrome (AGS).
These patients similarly present with chronic and organ-specific inflammation that leads to progressive organ damage, morbidity, and higher mortality risk when not managed. Each of these diseases requires a confirmed genetic diagnosis so that treatments can be targeted and the patient receives appropriate genetic counseling, screening for complications, and information on prognosis, Dr. Goldbach-Mansky said.
Treatment goals for type-1 interferonopathies are to “reduce systematic and organ inflammation to prevent or limit the development of progression of organ injury or damage and to improve quality of life,” Dr. Goldbach-Mansky told attendees.
Each patient requires a multidisciplinary care provider team that conducts long-term monitoring of disease activity, damage to specific organs, and any treatment-related complications.
Management of HLH/MAS
Early recognition and management of HLH and MAS can be challenging because systemic hyperinflammation exists along an immunopathologic continuum with typically nonspecific clinical and laboratory findings, Dr. Goldbach-Mansky said, but holistic, longitudinal consideration of these findings “are recognizable and warrant prompt diagnostic evaluation.” Even if the patient does not meet all specific diagnostic criteria for HLH/MAS, it may be necessary to begin therapies, she said.
One important point to consider is that “systemic hyperinflammation can be associated with hyperferritinemia and can progress to life-threatening HLH/MAS,” Dr. Goldbach-Mansky said. Further, although “systemic hyperinflammation and HLH/MAS can occur in nearly any inflammatory state,” certain common triggers and predisposing conditions can indicate the need to consider these conditions and begin appropriate treatment if needed. Part of effective management of systemic hyperinflammation and HLH/MAS is determining any modifiable factors contributing to the disease and mitigating or treating those.
HLH/MAS requires urgent intervention based on the patient’s degree of inflammation and extent of organ dysfunction, the recommendations state. Treatment goals include preventing or limiting immunopathology, preserving the integrity of the diagnostic workup, and minimizing therapy-related toxicity.
Dr. Carmona, Dr. Goldbach-Mansky, and Dr. Demirkaya have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As researchers learn more about the genetic etiology of immunopathology, they have been able to more clearly understand rare but debilitating autoinflammatory conditions in ways that have improved identification and management of these diseases. At this year’s European Congress of Rheumatology, two researchers outlined new recommendations from the European Alliance of Associations for Rheumatology (EULAR) and the American College of Rheumatology (ACR) for the management of two groups of such autoinflammatory diseases: interleukin-1-mediated and Type-I interferonopathies, and suspected macrophage activation syndrome and hemophagocytic lymphohistiocytosis.
These are the first recommendations from EULAR for these diseases, according to Loreto Carmona, MD, PhD, chair of the EULAR scientific program committee and scientific director of the Institute for Musculoskeletal Health in Madrid.
“They are rare diseases and there is a great need to standardize diagnosis and care for the safety and outcome of the patients,” Dr. Carmona said in an interview. “These diseases need deep expertise and so the experts are trying, they are still preliminary, to add clarity to their management.” Dr. Carmona was not involved with the development of the guidelines and moderated the session during which they were presented.
“The rapidly emerging knowledge of the genetic causes of novel systemic autoinflammatory diseases, which present typically in early childhood with severe and chronic systemic and organ-specific inflammation, linked the disease pathogenesis to the pathologic production of major proinflammatory cytokines,” presenter Raphaela Goldbach-Mansky, MD, a senior investigator and chief of the translational autoinflammatory disease studies unit of the U.S. National Institute of Allergy and Infectious Diseases, told congress attendees. This greater understanding led to the “targeted and anticytokine treatments that have changed patients’ lives,” she said.
The guidelines relied on the products of three working groups for each disease type. After meeting to come up with clinical questions, the groups each conducted systematic literature reviews through EMBASE, PubMed, and the Cochrane Library for publications dated from 1970 to August 2020 that excluded non-English-language studies, case reports, and animal model or basic science studies. They then met again to develop final consensus statements.
The interferonopathy and interleukin (IL)-1-mediated systemic autoinflammatory diseases (SAIDs) working groups met throughout 2020, and the hemophagocytic lymphohistiocytosis (HLH)/ macrophage activation syndrome (MAS) working group met in March and April of 2021.
“One needs a lot of experience with these diseases to even think about them,” Dr. Carmona said. “We haven’t been presented yet with all the details of the recommendations, but we hope they are clear because they are much needed.”
She noted that these preliminary recommendations are based on the best available evidence to date along with expertise from multidisciplinary panels.
“We need to be acquainted with these recommendations, as the majority of us, either if we are pediatric or adult rheumatologists, will face some problem with these diseases at some point,” Dr. Carmona said.
IL-1-mediated SAIDs
Recommendations for IL-1-mediated SAIDs focused on mevalonate kinase deficiency (MKD), tumor necrosis factor receptor-associated periodic syndrome (TRAPS), cryopyrinopathies (CAPS), and deficiency of the IL-1 receptor antagonist (DIRA). Presentation of these conditions involves chronic or intermittent flares of systemic and organ inflammation that can cause progressive organ damage, morbidity, and increased mortality if not treated. Diagnosis requires a multidisciplinary team whose evaluation should include disease-related complications and long-term care plans.
Diagnostic workup should include genetic testing using next-generation sequencing as this “facilitates initiation of targeted treatments, genetic counseling, and informs prognosis” for patients with CAPS, TRAPS, MKD, and DIRA, Erkan Demirkaya, MD, a scientist at the Children’s Health Research Institute and professor of pediatric rheumatology at the University of Western Ontario in London, Canada, told attendees. Evaluation should also include clinical workup that focuses on the extent of inflammatory organ involvement, and screening for disease- and treatment-related comorbidities.
“The goal of therapy is to control clinical signs and symptoms and normalize laboratory biomarkers of systemic inflammation,” Dr. Demirkaya said. Long-term monitoring goals should focus on the following:
- “Adequate treatment adjusted to the needs of the growing child and prevention of systemic and organ-specific inflammatory manifestations;
- Fostering of self-management skills and medical decision-making;
- Initiating a transition program to adult specialist care in adolescent patients.”
Type-1 interferonopathies
The recommendations for this disease group focused on chronic atypical neutrophilic dermatosis with lipodystrophy and elevated temperatures (CANDLE)/proteasome-associated autoinflammatory syndromes (PRAAS), STING-associated vasculopathy with onset in infancy (SAVI), and Aicardi-Goutières syndrome (AGS).
These patients similarly present with chronic and organ-specific inflammation that leads to progressive organ damage, morbidity, and higher mortality risk when not managed. Each of these diseases requires a confirmed genetic diagnosis so that treatments can be targeted and the patient receives appropriate genetic counseling, screening for complications, and information on prognosis, Dr. Goldbach-Mansky said.
Treatment goals for type-1 interferonopathies are to “reduce systematic and organ inflammation to prevent or limit the development of progression of organ injury or damage and to improve quality of life,” Dr. Goldbach-Mansky told attendees.
Each patient requires a multidisciplinary care provider team that conducts long-term monitoring of disease activity, damage to specific organs, and any treatment-related complications.
Management of HLH/MAS
Early recognition and management of HLH and MAS can be challenging because systemic hyperinflammation exists along an immunopathologic continuum with typically nonspecific clinical and laboratory findings, Dr. Goldbach-Mansky said, but holistic, longitudinal consideration of these findings “are recognizable and warrant prompt diagnostic evaluation.” Even if the patient does not meet all specific diagnostic criteria for HLH/MAS, it may be necessary to begin therapies, she said.
One important point to consider is that “systemic hyperinflammation can be associated with hyperferritinemia and can progress to life-threatening HLH/MAS,” Dr. Goldbach-Mansky said. Further, although “systemic hyperinflammation and HLH/MAS can occur in nearly any inflammatory state,” certain common triggers and predisposing conditions can indicate the need to consider these conditions and begin appropriate treatment if needed. Part of effective management of systemic hyperinflammation and HLH/MAS is determining any modifiable factors contributing to the disease and mitigating or treating those.
HLH/MAS requires urgent intervention based on the patient’s degree of inflammation and extent of organ dysfunction, the recommendations state. Treatment goals include preventing or limiting immunopathology, preserving the integrity of the diagnostic workup, and minimizing therapy-related toxicity.
Dr. Carmona, Dr. Goldbach-Mansky, and Dr. Demirkaya have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
As researchers learn more about the genetic etiology of immunopathology, they have been able to more clearly understand rare but debilitating autoinflammatory conditions in ways that have improved identification and management of these diseases. At this year’s European Congress of Rheumatology, two researchers outlined new recommendations from the European Alliance of Associations for Rheumatology (EULAR) and the American College of Rheumatology (ACR) for the management of two groups of such autoinflammatory diseases: interleukin-1-mediated and Type-I interferonopathies, and suspected macrophage activation syndrome and hemophagocytic lymphohistiocytosis.
These are the first recommendations from EULAR for these diseases, according to Loreto Carmona, MD, PhD, chair of the EULAR scientific program committee and scientific director of the Institute for Musculoskeletal Health in Madrid.
“They are rare diseases and there is a great need to standardize diagnosis and care for the safety and outcome of the patients,” Dr. Carmona said in an interview. “These diseases need deep expertise and so the experts are trying, they are still preliminary, to add clarity to their management.” Dr. Carmona was not involved with the development of the guidelines and moderated the session during which they were presented.
“The rapidly emerging knowledge of the genetic causes of novel systemic autoinflammatory diseases, which present typically in early childhood with severe and chronic systemic and organ-specific inflammation, linked the disease pathogenesis to the pathologic production of major proinflammatory cytokines,” presenter Raphaela Goldbach-Mansky, MD, a senior investigator and chief of the translational autoinflammatory disease studies unit of the U.S. National Institute of Allergy and Infectious Diseases, told congress attendees. This greater understanding led to the “targeted and anticytokine treatments that have changed patients’ lives,” she said.
The guidelines relied on the products of three working groups for each disease type. After meeting to come up with clinical questions, the groups each conducted systematic literature reviews through EMBASE, PubMed, and the Cochrane Library for publications dated from 1970 to August 2020 that excluded non-English-language studies, case reports, and animal model or basic science studies. They then met again to develop final consensus statements.
The interferonopathy and interleukin (IL)-1-mediated systemic autoinflammatory diseases (SAIDs) working groups met throughout 2020, and the hemophagocytic lymphohistiocytosis (HLH)/ macrophage activation syndrome (MAS) working group met in March and April of 2021.
“One needs a lot of experience with these diseases to even think about them,” Dr. Carmona said. “We haven’t been presented yet with all the details of the recommendations, but we hope they are clear because they are much needed.”
She noted that these preliminary recommendations are based on the best available evidence to date along with expertise from multidisciplinary panels.
“We need to be acquainted with these recommendations, as the majority of us, either if we are pediatric or adult rheumatologists, will face some problem with these diseases at some point,” Dr. Carmona said.
IL-1-mediated SAIDs
Recommendations for IL-1-mediated SAIDs focused on mevalonate kinase deficiency (MKD), tumor necrosis factor receptor-associated periodic syndrome (TRAPS), cryopyrinopathies (CAPS), and deficiency of the IL-1 receptor antagonist (DIRA). Presentation of these conditions involves chronic or intermittent flares of systemic and organ inflammation that can cause progressive organ damage, morbidity, and increased mortality if not treated. Diagnosis requires a multidisciplinary team whose evaluation should include disease-related complications and long-term care plans.
Diagnostic workup should include genetic testing using next-generation sequencing as this “facilitates initiation of targeted treatments, genetic counseling, and informs prognosis” for patients with CAPS, TRAPS, MKD, and DIRA, Erkan Demirkaya, MD, a scientist at the Children’s Health Research Institute and professor of pediatric rheumatology at the University of Western Ontario in London, Canada, told attendees. Evaluation should also include clinical workup that focuses on the extent of inflammatory organ involvement, and screening for disease- and treatment-related comorbidities.
“The goal of therapy is to control clinical signs and symptoms and normalize laboratory biomarkers of systemic inflammation,” Dr. Demirkaya said. Long-term monitoring goals should focus on the following:
- “Adequate treatment adjusted to the needs of the growing child and prevention of systemic and organ-specific inflammatory manifestations;
- Fostering of self-management skills and medical decision-making;
- Initiating a transition program to adult specialist care in adolescent patients.”
Type-1 interferonopathies
The recommendations for this disease group focused on chronic atypical neutrophilic dermatosis with lipodystrophy and elevated temperatures (CANDLE)/proteasome-associated autoinflammatory syndromes (PRAAS), STING-associated vasculopathy with onset in infancy (SAVI), and Aicardi-Goutières syndrome (AGS).
These patients similarly present with chronic and organ-specific inflammation that leads to progressive organ damage, morbidity, and higher mortality risk when not managed. Each of these diseases requires a confirmed genetic diagnosis so that treatments can be targeted and the patient receives appropriate genetic counseling, screening for complications, and information on prognosis, Dr. Goldbach-Mansky said.
Treatment goals for type-1 interferonopathies are to “reduce systematic and organ inflammation to prevent or limit the development of progression of organ injury or damage and to improve quality of life,” Dr. Goldbach-Mansky told attendees.
Each patient requires a multidisciplinary care provider team that conducts long-term monitoring of disease activity, damage to specific organs, and any treatment-related complications.
Management of HLH/MAS
Early recognition and management of HLH and MAS can be challenging because systemic hyperinflammation exists along an immunopathologic continuum with typically nonspecific clinical and laboratory findings, Dr. Goldbach-Mansky said, but holistic, longitudinal consideration of these findings “are recognizable and warrant prompt diagnostic evaluation.” Even if the patient does not meet all specific diagnostic criteria for HLH/MAS, it may be necessary to begin therapies, she said.
One important point to consider is that “systemic hyperinflammation can be associated with hyperferritinemia and can progress to life-threatening HLH/MAS,” Dr. Goldbach-Mansky said. Further, although “systemic hyperinflammation and HLH/MAS can occur in nearly any inflammatory state,” certain common triggers and predisposing conditions can indicate the need to consider these conditions and begin appropriate treatment if needed. Part of effective management of systemic hyperinflammation and HLH/MAS is determining any modifiable factors contributing to the disease and mitigating or treating those.
HLH/MAS requires urgent intervention based on the patient’s degree of inflammation and extent of organ dysfunction, the recommendations state. Treatment goals include preventing or limiting immunopathology, preserving the integrity of the diagnostic workup, and minimizing therapy-related toxicity.
Dr. Carmona, Dr. Goldbach-Mansky, and Dr. Demirkaya have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE EULAR 2021 CONGRESS
Child suicides drive Colorado hospital to declare state of emergency
On May 25, Jena Hausmann, CEO of Children’s Hospital Colorado, Aurora, declared a state of emergency in youth mental health in response to an astronomical increase in pediatric mental health cases, including suicide, which has overwhelmed the institution.
From April 2019 to April 2021, the demand for pediatric behavioral health treatment at the hospital system increased by 90%. In Colorado, suicide is now the number one cause of death among youth and occurs in children as young as 10 years of age.
“Now we are seeing our pediatric emergency departments and our inpatient units overrun with kids attempting suicide and suffering from other forms of major mental health illness,” Dr. Hausmann said in a press release.
“We had to draw attention to what we’re seeing in our hospital and our community on an everyday basis – an unprecedented number of suicidal children who need acute treatment for behavioral health problems – and when I say ‘unprecedented,’ I’m serious – I’ve been in pediatrics for two decades and have never seen anything like this before,” David Brumbaugh, MD, a pediatric gastroenterologist and chief medical officer for Children’s Colorado, told this news organization.
Christine Crawford, MD, associate medical director of the National Alliance on Mental Illness, stated in an interview that she “commends the CEO of the hospital for making this announcement, because it is outrageous to see what is happening with more and more children with significant psychiatric symptoms who are not getting adequate care.”
Jenna Glover, PhD, child psychologist and director of psychology training at Children’s Hospital, said that during the past decade, there has been a steady increase in depression, anxiety, and suicide among youth in Colorado. Suicide, she added, is now the number one cause of death in youth, “so we were already in a state of crisis.” She added that COVID-19 was “the straw that broke the camel’s back.”
“In January to April of this year, behavioral health ED visits to Children’s Hospital were 72% higher than they were 2 years ago at this time,” she said. “Colorado Springs had a 145% increase for ED behavioral health visits during the first 4 months of 2021, compared to the first 4 months of 2020.”
COVID’s impact
Other problems that have been “skyrocketing” in youth are self-harm, substance use, and eating disorders. Younger children are experiencing an increase in behavioral problems, including developmental regression, such as tantrums, and problems with sleeping, toileting, and eating, Dr. Glover noted.
The youth mental health crisis has mushroomed, although social distancing requirements are now beginning to ease and we are in the “home stretch of the pandemic,” Dr. Brumbaugh said.
One possible reason “is that we took kids out of their normal routines, social circles, friendships, etc., for 12 months, and that was the limit of their physiological or mental resistance, and they got to the end of their rope,” he speculated.
Dr. Glover said, “Kids are burned out, and although they’re asking to return to their life, they don’t feel they have the resources. They feel so behind; they don’t know how to catch up.”
Dr. Brumbaugh said that there are not enough child psychiatrists to provide outpatient services or enough inpatient beds for children in crisis.
“This is an unacceptable situation. We would never allow a child with leukemia or appendicitis to go several weeks without treatment,” he said.
Community donors have come forward, enabling an anticipated 50% increase in Children’s Hospital’s mental health outpatient, inpatient, and day services by March 2022.
“On a hospital level, we are continuing to do things to expand access to care, like opening units that provide different levels of care for patients with psychiatric problems, as well as expanding into areas that are more rural,” Dr. Glover said.
However, the “blueprint is not in action yet, and a lot of money still needs to be allocated. A workforce has to be created, because there are not enough clinicians to fill these roles,” she added.
Chronic underfunding
Dr. Brumbaugh said Colorado has always had a “relatively underfunded behavioral health system for kids.” A 2021 report by
However, Dr. Glover noted that Colorado is “not exceptional.” The increased vulnerability to youth mental illness and suicide is characteristic of other mountain states, which have larger rural areas, less access to care, and increased access to guns, she said.
Mass shootings may have amped up stress levels. “For some kids, this is happening in their schools or towns, and they feel traumatized and unsafe,” Dr. Glover added.
Dr. Crawford, who is an assistant professor of psychiatry at Boston University, also pointed out that the mental health crisis in youth is not unique to Colorado.
“Throughout the country, we’ve seen these colliding pandemics – inadequate mental health resources for children and COVID-19, which exacerbated the existing mental health crisis,” she said.
“The pandemic led to an increase in telehealth services, making individual and group psychotherapy available to kids in areas that never had access to these before, which is a ‘silver lining’ of the pandemic,” Dr. Glover said.
Dr. Crawford is “encouraged that we are having more conversations about pediatric mental health, because the pandemic amplified what was already going on and made it impossible to ignore.”
Screening is essential
Screening for mental health problems should be at the top of the mind of pediatricians and other clinicians who work with children, Dr. Glover said.
“Pediatricians are in the best place to catch potentially suicidal kids, because they are more likely to see these kids than therapists,” she noted.
She suggested using a rapid screen for depression, such as the Patient Health Questionnaire-9 (PHQ-9) modified for adolescents. Parents can also fill out a PHQ-9 for younger children and even for themselves.
“Depression, anxiety, and suicidality affect the whole family, so screening for these conditions in adults will benefit the children too,” she said. Teachers should also “be aware of what depression and anxiety symptoms look like in kids, because sometimes they can manifest more as irritability,” Dr. Glover added.
Policymakers and insurers need to prioritize pediatric mental health when determining allocation of health care, said Dr. Crawford.
“Financial incentives should be provided for hospitals to want to reserve beds for psychiatric patients, and in the outpatient setting, we also need to look at the payment structure of psychiatric visits,” she added.
Many psychiatrists do not want to accept insurance because of the increased bureaucracy and low reimbursement rates of insurance companies, and families cannot afford to pay out of pocket, “so we really need to look at the insurance issue at a policy level,” Dr. Crawford said.
Dr. Brumbaugh, Dr. Glover, and Dr. Crawford have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
On May 25, Jena Hausmann, CEO of Children’s Hospital Colorado, Aurora, declared a state of emergency in youth mental health in response to an astronomical increase in pediatric mental health cases, including suicide, which has overwhelmed the institution.
From April 2019 to April 2021, the demand for pediatric behavioral health treatment at the hospital system increased by 90%. In Colorado, suicide is now the number one cause of death among youth and occurs in children as young as 10 years of age.
“Now we are seeing our pediatric emergency departments and our inpatient units overrun with kids attempting suicide and suffering from other forms of major mental health illness,” Dr. Hausmann said in a press release.
“We had to draw attention to what we’re seeing in our hospital and our community on an everyday basis – an unprecedented number of suicidal children who need acute treatment for behavioral health problems – and when I say ‘unprecedented,’ I’m serious – I’ve been in pediatrics for two decades and have never seen anything like this before,” David Brumbaugh, MD, a pediatric gastroenterologist and chief medical officer for Children’s Colorado, told this news organization.
Christine Crawford, MD, associate medical director of the National Alliance on Mental Illness, stated in an interview that she “commends the CEO of the hospital for making this announcement, because it is outrageous to see what is happening with more and more children with significant psychiatric symptoms who are not getting adequate care.”
Jenna Glover, PhD, child psychologist and director of psychology training at Children’s Hospital, said that during the past decade, there has been a steady increase in depression, anxiety, and suicide among youth in Colorado. Suicide, she added, is now the number one cause of death in youth, “so we were already in a state of crisis.” She added that COVID-19 was “the straw that broke the camel’s back.”
“In January to April of this year, behavioral health ED visits to Children’s Hospital were 72% higher than they were 2 years ago at this time,” she said. “Colorado Springs had a 145% increase for ED behavioral health visits during the first 4 months of 2021, compared to the first 4 months of 2020.”
COVID’s impact
Other problems that have been “skyrocketing” in youth are self-harm, substance use, and eating disorders. Younger children are experiencing an increase in behavioral problems, including developmental regression, such as tantrums, and problems with sleeping, toileting, and eating, Dr. Glover noted.
The youth mental health crisis has mushroomed, although social distancing requirements are now beginning to ease and we are in the “home stretch of the pandemic,” Dr. Brumbaugh said.
One possible reason “is that we took kids out of their normal routines, social circles, friendships, etc., for 12 months, and that was the limit of their physiological or mental resistance, and they got to the end of their rope,” he speculated.
Dr. Glover said, “Kids are burned out, and although they’re asking to return to their life, they don’t feel they have the resources. They feel so behind; they don’t know how to catch up.”
Dr. Brumbaugh said that there are not enough child psychiatrists to provide outpatient services or enough inpatient beds for children in crisis.
“This is an unacceptable situation. We would never allow a child with leukemia or appendicitis to go several weeks without treatment,” he said.
Community donors have come forward, enabling an anticipated 50% increase in Children’s Hospital’s mental health outpatient, inpatient, and day services by March 2022.
“On a hospital level, we are continuing to do things to expand access to care, like opening units that provide different levels of care for patients with psychiatric problems, as well as expanding into areas that are more rural,” Dr. Glover said.
However, the “blueprint is not in action yet, and a lot of money still needs to be allocated. A workforce has to be created, because there are not enough clinicians to fill these roles,” she added.
Chronic underfunding
Dr. Brumbaugh said Colorado has always had a “relatively underfunded behavioral health system for kids.” A 2021 report by
However, Dr. Glover noted that Colorado is “not exceptional.” The increased vulnerability to youth mental illness and suicide is characteristic of other mountain states, which have larger rural areas, less access to care, and increased access to guns, she said.
Mass shootings may have amped up stress levels. “For some kids, this is happening in their schools or towns, and they feel traumatized and unsafe,” Dr. Glover added.
Dr. Crawford, who is an assistant professor of psychiatry at Boston University, also pointed out that the mental health crisis in youth is not unique to Colorado.
“Throughout the country, we’ve seen these colliding pandemics – inadequate mental health resources for children and COVID-19, which exacerbated the existing mental health crisis,” she said.
“The pandemic led to an increase in telehealth services, making individual and group psychotherapy available to kids in areas that never had access to these before, which is a ‘silver lining’ of the pandemic,” Dr. Glover said.
Dr. Crawford is “encouraged that we are having more conversations about pediatric mental health, because the pandemic amplified what was already going on and made it impossible to ignore.”
Screening is essential
Screening for mental health problems should be at the top of the mind of pediatricians and other clinicians who work with children, Dr. Glover said.
“Pediatricians are in the best place to catch potentially suicidal kids, because they are more likely to see these kids than therapists,” she noted.
She suggested using a rapid screen for depression, such as the Patient Health Questionnaire-9 (PHQ-9) modified for adolescents. Parents can also fill out a PHQ-9 for younger children and even for themselves.
“Depression, anxiety, and suicidality affect the whole family, so screening for these conditions in adults will benefit the children too,” she said. Teachers should also “be aware of what depression and anxiety symptoms look like in kids, because sometimes they can manifest more as irritability,” Dr. Glover added.
Policymakers and insurers need to prioritize pediatric mental health when determining allocation of health care, said Dr. Crawford.
“Financial incentives should be provided for hospitals to want to reserve beds for psychiatric patients, and in the outpatient setting, we also need to look at the payment structure of psychiatric visits,” she added.
Many psychiatrists do not want to accept insurance because of the increased bureaucracy and low reimbursement rates of insurance companies, and families cannot afford to pay out of pocket, “so we really need to look at the insurance issue at a policy level,” Dr. Crawford said.
Dr. Brumbaugh, Dr. Glover, and Dr. Crawford have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
On May 25, Jena Hausmann, CEO of Children’s Hospital Colorado, Aurora, declared a state of emergency in youth mental health in response to an astronomical increase in pediatric mental health cases, including suicide, which has overwhelmed the institution.
From April 2019 to April 2021, the demand for pediatric behavioral health treatment at the hospital system increased by 90%. In Colorado, suicide is now the number one cause of death among youth and occurs in children as young as 10 years of age.
“Now we are seeing our pediatric emergency departments and our inpatient units overrun with kids attempting suicide and suffering from other forms of major mental health illness,” Dr. Hausmann said in a press release.
“We had to draw attention to what we’re seeing in our hospital and our community on an everyday basis – an unprecedented number of suicidal children who need acute treatment for behavioral health problems – and when I say ‘unprecedented,’ I’m serious – I’ve been in pediatrics for two decades and have never seen anything like this before,” David Brumbaugh, MD, a pediatric gastroenterologist and chief medical officer for Children’s Colorado, told this news organization.
Christine Crawford, MD, associate medical director of the National Alliance on Mental Illness, stated in an interview that she “commends the CEO of the hospital for making this announcement, because it is outrageous to see what is happening with more and more children with significant psychiatric symptoms who are not getting adequate care.”
Jenna Glover, PhD, child psychologist and director of psychology training at Children’s Hospital, said that during the past decade, there has been a steady increase in depression, anxiety, and suicide among youth in Colorado. Suicide, she added, is now the number one cause of death in youth, “so we were already in a state of crisis.” She added that COVID-19 was “the straw that broke the camel’s back.”
“In January to April of this year, behavioral health ED visits to Children’s Hospital were 72% higher than they were 2 years ago at this time,” she said. “Colorado Springs had a 145% increase for ED behavioral health visits during the first 4 months of 2021, compared to the first 4 months of 2020.”
COVID’s impact
Other problems that have been “skyrocketing” in youth are self-harm, substance use, and eating disorders. Younger children are experiencing an increase in behavioral problems, including developmental regression, such as tantrums, and problems with sleeping, toileting, and eating, Dr. Glover noted.
The youth mental health crisis has mushroomed, although social distancing requirements are now beginning to ease and we are in the “home stretch of the pandemic,” Dr. Brumbaugh said.
One possible reason “is that we took kids out of their normal routines, social circles, friendships, etc., for 12 months, and that was the limit of their physiological or mental resistance, and they got to the end of their rope,” he speculated.
Dr. Glover said, “Kids are burned out, and although they’re asking to return to their life, they don’t feel they have the resources. They feel so behind; they don’t know how to catch up.”
Dr. Brumbaugh said that there are not enough child psychiatrists to provide outpatient services or enough inpatient beds for children in crisis.
“This is an unacceptable situation. We would never allow a child with leukemia or appendicitis to go several weeks without treatment,” he said.
Community donors have come forward, enabling an anticipated 50% increase in Children’s Hospital’s mental health outpatient, inpatient, and day services by March 2022.
“On a hospital level, we are continuing to do things to expand access to care, like opening units that provide different levels of care for patients with psychiatric problems, as well as expanding into areas that are more rural,” Dr. Glover said.
However, the “blueprint is not in action yet, and a lot of money still needs to be allocated. A workforce has to be created, because there are not enough clinicians to fill these roles,” she added.
Chronic underfunding
Dr. Brumbaugh said Colorado has always had a “relatively underfunded behavioral health system for kids.” A 2021 report by
However, Dr. Glover noted that Colorado is “not exceptional.” The increased vulnerability to youth mental illness and suicide is characteristic of other mountain states, which have larger rural areas, less access to care, and increased access to guns, she said.
Mass shootings may have amped up stress levels. “For some kids, this is happening in their schools or towns, and they feel traumatized and unsafe,” Dr. Glover added.
Dr. Crawford, who is an assistant professor of psychiatry at Boston University, also pointed out that the mental health crisis in youth is not unique to Colorado.
“Throughout the country, we’ve seen these colliding pandemics – inadequate mental health resources for children and COVID-19, which exacerbated the existing mental health crisis,” she said.
“The pandemic led to an increase in telehealth services, making individual and group psychotherapy available to kids in areas that never had access to these before, which is a ‘silver lining’ of the pandemic,” Dr. Glover said.
Dr. Crawford is “encouraged that we are having more conversations about pediatric mental health, because the pandemic amplified what was already going on and made it impossible to ignore.”
Screening is essential
Screening for mental health problems should be at the top of the mind of pediatricians and other clinicians who work with children, Dr. Glover said.
“Pediatricians are in the best place to catch potentially suicidal kids, because they are more likely to see these kids than therapists,” she noted.
She suggested using a rapid screen for depression, such as the Patient Health Questionnaire-9 (PHQ-9) modified for adolescents. Parents can also fill out a PHQ-9 for younger children and even for themselves.
“Depression, anxiety, and suicidality affect the whole family, so screening for these conditions in adults will benefit the children too,” she said. Teachers should also “be aware of what depression and anxiety symptoms look like in kids, because sometimes they can manifest more as irritability,” Dr. Glover added.
Policymakers and insurers need to prioritize pediatric mental health when determining allocation of health care, said Dr. Crawford.
“Financial incentives should be provided for hospitals to want to reserve beds for psychiatric patients, and in the outpatient setting, we also need to look at the payment structure of psychiatric visits,” she added.
Many psychiatrists do not want to accept insurance because of the increased bureaucracy and low reimbursement rates of insurance companies, and families cannot afford to pay out of pocket, “so we really need to look at the insurance issue at a policy level,” Dr. Crawford said.
Dr. Brumbaugh, Dr. Glover, and Dr. Crawford have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.













