User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Not your ordinary neuropathy
She has had a diagnosis of type 2 diabetes for the past 4 years. She initially presented with polyuria/polydipsia and a hemoglobin A1c level of 9.5. She has previously not tolerated metformin, and did not want to take any subsequent medications. She was seen 4 months ago and at that time had an A1c level of 12.5. She decided she wanted to really treat her diabetes as well as she could. She started consuming a low carbohydrate diet, restarted metformin and began using a continuous glucose monitor. She also started taking nighttime glargine insulin, and mealtime insulin apart. She reports she lost 20 pounds over the past 4 months, her blood sugars now run between 100-120 fasting, and up to 180 before meals. She has had a severe, sharp pain in both of her feet over the past month that is interfering with sleep and makes walking painful for her. An exam reveals hyperesthesia of both feet, and her A1c level is 7.5. What is the most likely cause of her neuropathic symptoms?
A. Vitamin B12 deficiency
B. Diabetic neuropathy
C. Insulin neuritis
D. Charcot-Marie-Tooth disease
The most likely cause
In this case, certainly considering vitamin B12 deficiency is reasonable. It is highly unlikely though, given the rapidity of onset of symptoms, and that the patient has been on metformin for a very short period of time. Chronic metformin use is associated with low B12 levels, and the American Diabetes Association has advised that regular monitoring of vitamin B12 levels should be done on patients who are on long-term metformin.1
Diabetic neuropathy is also unlikely, given the rapidity of symptoms in this patient. What is most likely in this patient is treatment-induced neuropathy (TIN), first described with the name “insulin neuritis”.
Research on TIN
Gibbons and colleagues evaluated 16 patients with diabetes with recent marked, rapid improvement in glycemic control who developed a sudden, painful neuropathy.2 All developed symptoms within 8 weeks of intensive glucose control, with 69% having autonomic dysfunction as well, and all developing worsening retinopathy.
Gibbons and Freeman did a retrospective study of patients referred to a diabetic neuropathy clinic over a 5-year period to try to understand how prevalent TIN is.3
A total of 954 patients were evaluated for diabetic neuropathy. Treatment induced neuropathy was defined as a painful neuropathy and/or autonomic dysfunction occurring within 8 weeks of intensified treatment and a drop of the A1c level greater than 2 over a 3-month period.
A total of 104 patients (10.9%) met the criteria for treatment induced neuropathy. Patients who had a decrease in A1c had a much greater chance of developing a painful or autonomic neuropathy than patients who had no change in A1c (P < .0001). The same patients had a much higher risk of developing retinopathy (P < .001). The greater the reduction in A1c, the greater the risk. Patients whose A1c decreased by 2%-3% over 3 months had an absolute risk of 20%, whereas those with a A1c decease of greater than 4% had an 80% absolute risk.
Siddique and colleagues reported on three cases with very different clinical presentations of TIN.4 One patient had an acute third nerve palsy, another patient had a lumbosacral radiculoplexus neuropathy, and the third patient presented with a diffuse painful sensory neuropathy and postural hypotension.
Most patients improve over time from their neuropathic symptoms, with better recovery in patients with type 1 diabetes.2
Pearl
Strongly consider treatment induced neuropathy in your patients with diabetes who present with acute painful neuropathy and/or autonomic dysfunction in the setting of rapid improvement of glucose control.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. American Diabetes Association. Diabetes Care. 2019 Jan;42(Suppl 1):S90-102.
2. Gibbons CH and Freeman R. Ann Neurol 2010; 67:534–41.
3. Gibbons CH and Freeman R. Brain. 2015;138:43-52.
4. Siddique N et al. Endocrinol Diabetes Metab Case Rep. 2020 Feb 26;2020:19-0140.
She has had a diagnosis of type 2 diabetes for the past 4 years. She initially presented with polyuria/polydipsia and a hemoglobin A1c level of 9.5. She has previously not tolerated metformin, and did not want to take any subsequent medications. She was seen 4 months ago and at that time had an A1c level of 12.5. She decided she wanted to really treat her diabetes as well as she could. She started consuming a low carbohydrate diet, restarted metformin and began using a continuous glucose monitor. She also started taking nighttime glargine insulin, and mealtime insulin apart. She reports she lost 20 pounds over the past 4 months, her blood sugars now run between 100-120 fasting, and up to 180 before meals. She has had a severe, sharp pain in both of her feet over the past month that is interfering with sleep and makes walking painful for her. An exam reveals hyperesthesia of both feet, and her A1c level is 7.5. What is the most likely cause of her neuropathic symptoms?
A. Vitamin B12 deficiency
B. Diabetic neuropathy
C. Insulin neuritis
D. Charcot-Marie-Tooth disease
The most likely cause
In this case, certainly considering vitamin B12 deficiency is reasonable. It is highly unlikely though, given the rapidity of onset of symptoms, and that the patient has been on metformin for a very short period of time. Chronic metformin use is associated with low B12 levels, and the American Diabetes Association has advised that regular monitoring of vitamin B12 levels should be done on patients who are on long-term metformin.1
Diabetic neuropathy is also unlikely, given the rapidity of symptoms in this patient. What is most likely in this patient is treatment-induced neuropathy (TIN), first described with the name “insulin neuritis”.
Research on TIN
Gibbons and colleagues evaluated 16 patients with diabetes with recent marked, rapid improvement in glycemic control who developed a sudden, painful neuropathy.2 All developed symptoms within 8 weeks of intensive glucose control, with 69% having autonomic dysfunction as well, and all developing worsening retinopathy.
Gibbons and Freeman did a retrospective study of patients referred to a diabetic neuropathy clinic over a 5-year period to try to understand how prevalent TIN is.3
A total of 954 patients were evaluated for diabetic neuropathy. Treatment induced neuropathy was defined as a painful neuropathy and/or autonomic dysfunction occurring within 8 weeks of intensified treatment and a drop of the A1c level greater than 2 over a 3-month period.
A total of 104 patients (10.9%) met the criteria for treatment induced neuropathy. Patients who had a decrease in A1c had a much greater chance of developing a painful or autonomic neuropathy than patients who had no change in A1c (P < .0001). The same patients had a much higher risk of developing retinopathy (P < .001). The greater the reduction in A1c, the greater the risk. Patients whose A1c decreased by 2%-3% over 3 months had an absolute risk of 20%, whereas those with a A1c decease of greater than 4% had an 80% absolute risk.
Siddique and colleagues reported on three cases with very different clinical presentations of TIN.4 One patient had an acute third nerve palsy, another patient had a lumbosacral radiculoplexus neuropathy, and the third patient presented with a diffuse painful sensory neuropathy and postural hypotension.
Most patients improve over time from their neuropathic symptoms, with better recovery in patients with type 1 diabetes.2
Pearl
Strongly consider treatment induced neuropathy in your patients with diabetes who present with acute painful neuropathy and/or autonomic dysfunction in the setting of rapid improvement of glucose control.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. American Diabetes Association. Diabetes Care. 2019 Jan;42(Suppl 1):S90-102.
2. Gibbons CH and Freeman R. Ann Neurol 2010; 67:534–41.
3. Gibbons CH and Freeman R. Brain. 2015;138:43-52.
4. Siddique N et al. Endocrinol Diabetes Metab Case Rep. 2020 Feb 26;2020:19-0140.
She has had a diagnosis of type 2 diabetes for the past 4 years. She initially presented with polyuria/polydipsia and a hemoglobin A1c level of 9.5. She has previously not tolerated metformin, and did not want to take any subsequent medications. She was seen 4 months ago and at that time had an A1c level of 12.5. She decided she wanted to really treat her diabetes as well as she could. She started consuming a low carbohydrate diet, restarted metformin and began using a continuous glucose monitor. She also started taking nighttime glargine insulin, and mealtime insulin apart. She reports she lost 20 pounds over the past 4 months, her blood sugars now run between 100-120 fasting, and up to 180 before meals. She has had a severe, sharp pain in both of her feet over the past month that is interfering with sleep and makes walking painful for her. An exam reveals hyperesthesia of both feet, and her A1c level is 7.5. What is the most likely cause of her neuropathic symptoms?
A. Vitamin B12 deficiency
B. Diabetic neuropathy
C. Insulin neuritis
D. Charcot-Marie-Tooth disease
The most likely cause
In this case, certainly considering vitamin B12 deficiency is reasonable. It is highly unlikely though, given the rapidity of onset of symptoms, and that the patient has been on metformin for a very short period of time. Chronic metformin use is associated with low B12 levels, and the American Diabetes Association has advised that regular monitoring of vitamin B12 levels should be done on patients who are on long-term metformin.1
Diabetic neuropathy is also unlikely, given the rapidity of symptoms in this patient. What is most likely in this patient is treatment-induced neuropathy (TIN), first described with the name “insulin neuritis”.
Research on TIN
Gibbons and colleagues evaluated 16 patients with diabetes with recent marked, rapid improvement in glycemic control who developed a sudden, painful neuropathy.2 All developed symptoms within 8 weeks of intensive glucose control, with 69% having autonomic dysfunction as well, and all developing worsening retinopathy.
Gibbons and Freeman did a retrospective study of patients referred to a diabetic neuropathy clinic over a 5-year period to try to understand how prevalent TIN is.3
A total of 954 patients were evaluated for diabetic neuropathy. Treatment induced neuropathy was defined as a painful neuropathy and/or autonomic dysfunction occurring within 8 weeks of intensified treatment and a drop of the A1c level greater than 2 over a 3-month period.
A total of 104 patients (10.9%) met the criteria for treatment induced neuropathy. Patients who had a decrease in A1c had a much greater chance of developing a painful or autonomic neuropathy than patients who had no change in A1c (P < .0001). The same patients had a much higher risk of developing retinopathy (P < .001). The greater the reduction in A1c, the greater the risk. Patients whose A1c decreased by 2%-3% over 3 months had an absolute risk of 20%, whereas those with a A1c decease of greater than 4% had an 80% absolute risk.
Siddique and colleagues reported on three cases with very different clinical presentations of TIN.4 One patient had an acute third nerve palsy, another patient had a lumbosacral radiculoplexus neuropathy, and the third patient presented with a diffuse painful sensory neuropathy and postural hypotension.
Most patients improve over time from their neuropathic symptoms, with better recovery in patients with type 1 diabetes.2
Pearl
Strongly consider treatment induced neuropathy in your patients with diabetes who present with acute painful neuropathy and/or autonomic dysfunction in the setting of rapid improvement of glucose control.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. American Diabetes Association. Diabetes Care. 2019 Jan;42(Suppl 1):S90-102.
2. Gibbons CH and Freeman R. Ann Neurol 2010; 67:534–41.
3. Gibbons CH and Freeman R. Brain. 2015;138:43-52.
4. Siddique N et al. Endocrinol Diabetes Metab Case Rep. 2020 Feb 26;2020:19-0140.
Medical licensing questions continue to violate ADA
With the COVID-19 pandemic, already high rates of suicide, depression, and burnout among physicians became even more acute. Yet, 3 years after the Federation of State Medical Boards issued recommendations on what questions about mental health status license applications should – or mostly should not – include, only North Carolina fully complies with all four recommendations, and most states comply with two or fewer, a study of state medical board applications has found (JAMA. 2021 May 18;325[19];2017-8).
Questions about mental health history or “its hypothetical effect on competency,” violate the Americans with Disabilities Act, the study authors stated. In a research letter to JAMA, the authors also reported that five state boards do not comply with any of the FSMB recommendations. Twenty-four states comply with three of the four recommendations.
Overall, the mean consistency score was 2.1, which means state medical licensing applications typically run afoul of the Americans With Disabilities Act when it comes to mental health history of applicants.
“No one should ever wonder, ‘Will I lose my job, or should I get help?’ ” said co–senior author Jessica A. Gold, MD, MS, a psychiatrist at Washington University in St. Louis. “This should absolutely never be a question on someone’s mind. And the fact that it is, in medicine, is a problem that needs to be solved. I hope that people are beginning to see that, and we can make a change to get people the help they need before it is too late.”
High rates of depression, suicide
She noted that before COVID-19, physicians already had higher rates of depression, burnout, and suicide than the general population. “Over COVID-19, it has become clear that the mental health of physicians has become additionally compounded,” Dr. Gold said.
One study found that physicians had a 44% higher rate of suicide (PLoS One. 2019 Dec;14[12]:e0226361), but they’re notoriously reluctant to seek out mental health care. A 2017 study reported that 40% of physicians would be reluctant to seek mental health care because of concerns about their licensure (Mayo Clin Proc. 2017;92[10]:1486-93).
As the pandemic went on, Dr. Gold and her colleagues decided to study whether state boards had improved their compliance with the FSMB recommendations issued in 2018. Those recommendations include these four limitations regarding questions about mental health conditions on license applications:
- Include only when they result in impairment.
- Include only when the mental health conditions are current – that is, when they’ve occurred within the past 2 years.
- Provide safe haven nonreporting – that is, allow physicians to not report previously diagnosed and treated mental health conditions if they’re being monitored and are in good standing with a physician health program.
- Include supportive or nonjudgmental language about seeking mental health care.
The study considered board applications that had questions about mental health status as consistent with the first three recommendations. Seventeen states complied.
Thirty-nine state boards complied with the first recommendation regarding impairment; 41 with the second recommendation about near-term history; 25 with safe-haven nonreporting. Only eight states were consistent with the recommendation on supportive language.
The ADA limits inquiries about an applicant’s impairment to only current conditions. In a 2017 study, only 21 state boards had limited questions to current impairment. “This is a significant improvement, but this still means the rest of the states are violating an actual law,” Dr. Gold said. “Another plus is that 17 states asked no questions at all that could require mental health disclosure. This, too is significant because it highlights change in thinking.”
But still, the fact that five states didn’t comply with any recommendation and only one followed all of them is “utterly unacceptable,” Dr. Gold said. “Instead, we should have universal adoption of FSMB recommendations.”
Time to remove stigma
Michael F. Myers, MD, a clinical psychiatrist at the State University of New York, Brooklyn, said removing the stigma of seeking help for mental health conditions is especially important for physicians. He’s written several books about physician mental health, including his latest, “Becoming a Doctor’s Doctor: A Memoir.”
“I would say at least 15% of the families that I interviewed who lost a physician loved one to suicide have said the doctor was petrified of going for professional help because of fears of what this could do to their medical license,” he said. “It is extremely important that those licensing questions will be either brought up to speed, or – the ones that are clearly violating the ADA – that they be removed.”
Applications for hospital privileges can also run afoul of the same ADA standard, Dr. Myers added. “Physicians have told me that when they go to get medical privileges at a medical center, they get asked all kinds of questions that are outdated, that are intrusive, that violate the ADA,” he said.
Credentialing is another area that Dr. Gold and her colleagues are interested in studying, she said. “Sometimes the licensing applications can be fine, but then the hospital someone is applying to work at can ask the same illegal questions anyway,” she said. “So it doesn’t matter that the state fixed the problem because the hospital asked them anyway. You feel your job is at risk in the same way, so you still don’t get help.”
Dr. Gold and Dr. Myers have no relevant financial relationships to disclose.
With the COVID-19 pandemic, already high rates of suicide, depression, and burnout among physicians became even more acute. Yet, 3 years after the Federation of State Medical Boards issued recommendations on what questions about mental health status license applications should – or mostly should not – include, only North Carolina fully complies with all four recommendations, and most states comply with two or fewer, a study of state medical board applications has found (JAMA. 2021 May 18;325[19];2017-8).
Questions about mental health history or “its hypothetical effect on competency,” violate the Americans with Disabilities Act, the study authors stated. In a research letter to JAMA, the authors also reported that five state boards do not comply with any of the FSMB recommendations. Twenty-four states comply with three of the four recommendations.
Overall, the mean consistency score was 2.1, which means state medical licensing applications typically run afoul of the Americans With Disabilities Act when it comes to mental health history of applicants.
“No one should ever wonder, ‘Will I lose my job, or should I get help?’ ” said co–senior author Jessica A. Gold, MD, MS, a psychiatrist at Washington University in St. Louis. “This should absolutely never be a question on someone’s mind. And the fact that it is, in medicine, is a problem that needs to be solved. I hope that people are beginning to see that, and we can make a change to get people the help they need before it is too late.”
High rates of depression, suicide
She noted that before COVID-19, physicians already had higher rates of depression, burnout, and suicide than the general population. “Over COVID-19, it has become clear that the mental health of physicians has become additionally compounded,” Dr. Gold said.
One study found that physicians had a 44% higher rate of suicide (PLoS One. 2019 Dec;14[12]:e0226361), but they’re notoriously reluctant to seek out mental health care. A 2017 study reported that 40% of physicians would be reluctant to seek mental health care because of concerns about their licensure (Mayo Clin Proc. 2017;92[10]:1486-93).
As the pandemic went on, Dr. Gold and her colleagues decided to study whether state boards had improved their compliance with the FSMB recommendations issued in 2018. Those recommendations include these four limitations regarding questions about mental health conditions on license applications:
- Include only when they result in impairment.
- Include only when the mental health conditions are current – that is, when they’ve occurred within the past 2 years.
- Provide safe haven nonreporting – that is, allow physicians to not report previously diagnosed and treated mental health conditions if they’re being monitored and are in good standing with a physician health program.
- Include supportive or nonjudgmental language about seeking mental health care.
The study considered board applications that had questions about mental health status as consistent with the first three recommendations. Seventeen states complied.
Thirty-nine state boards complied with the first recommendation regarding impairment; 41 with the second recommendation about near-term history; 25 with safe-haven nonreporting. Only eight states were consistent with the recommendation on supportive language.
The ADA limits inquiries about an applicant’s impairment to only current conditions. In a 2017 study, only 21 state boards had limited questions to current impairment. “This is a significant improvement, but this still means the rest of the states are violating an actual law,” Dr. Gold said. “Another plus is that 17 states asked no questions at all that could require mental health disclosure. This, too is significant because it highlights change in thinking.”
But still, the fact that five states didn’t comply with any recommendation and only one followed all of them is “utterly unacceptable,” Dr. Gold said. “Instead, we should have universal adoption of FSMB recommendations.”
Time to remove stigma
Michael F. Myers, MD, a clinical psychiatrist at the State University of New York, Brooklyn, said removing the stigma of seeking help for mental health conditions is especially important for physicians. He’s written several books about physician mental health, including his latest, “Becoming a Doctor’s Doctor: A Memoir.”
“I would say at least 15% of the families that I interviewed who lost a physician loved one to suicide have said the doctor was petrified of going for professional help because of fears of what this could do to their medical license,” he said. “It is extremely important that those licensing questions will be either brought up to speed, or – the ones that are clearly violating the ADA – that they be removed.”
Applications for hospital privileges can also run afoul of the same ADA standard, Dr. Myers added. “Physicians have told me that when they go to get medical privileges at a medical center, they get asked all kinds of questions that are outdated, that are intrusive, that violate the ADA,” he said.
Credentialing is another area that Dr. Gold and her colleagues are interested in studying, she said. “Sometimes the licensing applications can be fine, but then the hospital someone is applying to work at can ask the same illegal questions anyway,” she said. “So it doesn’t matter that the state fixed the problem because the hospital asked them anyway. You feel your job is at risk in the same way, so you still don’t get help.”
Dr. Gold and Dr. Myers have no relevant financial relationships to disclose.
With the COVID-19 pandemic, already high rates of suicide, depression, and burnout among physicians became even more acute. Yet, 3 years after the Federation of State Medical Boards issued recommendations on what questions about mental health status license applications should – or mostly should not – include, only North Carolina fully complies with all four recommendations, and most states comply with two or fewer, a study of state medical board applications has found (JAMA. 2021 May 18;325[19];2017-8).
Questions about mental health history or “its hypothetical effect on competency,” violate the Americans with Disabilities Act, the study authors stated. In a research letter to JAMA, the authors also reported that five state boards do not comply with any of the FSMB recommendations. Twenty-four states comply with three of the four recommendations.
Overall, the mean consistency score was 2.1, which means state medical licensing applications typically run afoul of the Americans With Disabilities Act when it comes to mental health history of applicants.
“No one should ever wonder, ‘Will I lose my job, or should I get help?’ ” said co–senior author Jessica A. Gold, MD, MS, a psychiatrist at Washington University in St. Louis. “This should absolutely never be a question on someone’s mind. And the fact that it is, in medicine, is a problem that needs to be solved. I hope that people are beginning to see that, and we can make a change to get people the help they need before it is too late.”
High rates of depression, suicide
She noted that before COVID-19, physicians already had higher rates of depression, burnout, and suicide than the general population. “Over COVID-19, it has become clear that the mental health of physicians has become additionally compounded,” Dr. Gold said.
One study found that physicians had a 44% higher rate of suicide (PLoS One. 2019 Dec;14[12]:e0226361), but they’re notoriously reluctant to seek out mental health care. A 2017 study reported that 40% of physicians would be reluctant to seek mental health care because of concerns about their licensure (Mayo Clin Proc. 2017;92[10]:1486-93).
As the pandemic went on, Dr. Gold and her colleagues decided to study whether state boards had improved their compliance with the FSMB recommendations issued in 2018. Those recommendations include these four limitations regarding questions about mental health conditions on license applications:
- Include only when they result in impairment.
- Include only when the mental health conditions are current – that is, when they’ve occurred within the past 2 years.
- Provide safe haven nonreporting – that is, allow physicians to not report previously diagnosed and treated mental health conditions if they’re being monitored and are in good standing with a physician health program.
- Include supportive or nonjudgmental language about seeking mental health care.
The study considered board applications that had questions about mental health status as consistent with the first three recommendations. Seventeen states complied.
Thirty-nine state boards complied with the first recommendation regarding impairment; 41 with the second recommendation about near-term history; 25 with safe-haven nonreporting. Only eight states were consistent with the recommendation on supportive language.
The ADA limits inquiries about an applicant’s impairment to only current conditions. In a 2017 study, only 21 state boards had limited questions to current impairment. “This is a significant improvement, but this still means the rest of the states are violating an actual law,” Dr. Gold said. “Another plus is that 17 states asked no questions at all that could require mental health disclosure. This, too is significant because it highlights change in thinking.”
But still, the fact that five states didn’t comply with any recommendation and only one followed all of them is “utterly unacceptable,” Dr. Gold said. “Instead, we should have universal adoption of FSMB recommendations.”
Time to remove stigma
Michael F. Myers, MD, a clinical psychiatrist at the State University of New York, Brooklyn, said removing the stigma of seeking help for mental health conditions is especially important for physicians. He’s written several books about physician mental health, including his latest, “Becoming a Doctor’s Doctor: A Memoir.”
“I would say at least 15% of the families that I interviewed who lost a physician loved one to suicide have said the doctor was petrified of going for professional help because of fears of what this could do to their medical license,” he said. “It is extremely important that those licensing questions will be either brought up to speed, or – the ones that are clearly violating the ADA – that they be removed.”
Applications for hospital privileges can also run afoul of the same ADA standard, Dr. Myers added. “Physicians have told me that when they go to get medical privileges at a medical center, they get asked all kinds of questions that are outdated, that are intrusive, that violate the ADA,” he said.
Credentialing is another area that Dr. Gold and her colleagues are interested in studying, she said. “Sometimes the licensing applications can be fine, but then the hospital someone is applying to work at can ask the same illegal questions anyway,” she said. “So it doesn’t matter that the state fixed the problem because the hospital asked them anyway. You feel your job is at risk in the same way, so you still don’t get help.”
Dr. Gold and Dr. Myers have no relevant financial relationships to disclose.
FROM JAMA
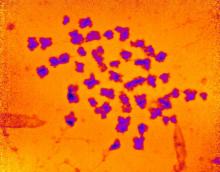
Mortality trends in childhood after infant bacterial meningitis
Among infants younger than 1 year of age, bacterial meningitis is associated with worse long-term mortality, even after recovery from the initial infection. Heightened mortality risk stretched out to 10 years, and was highest in the wake of infection from Streptococcus agalactiae, according to a retrospective analysis of children in the Netherlands.
“The adjusted hazard rates were high for the whole group of bacterial meningitis, especially within the first year after onset. (Staphylococcus agalactiae) meningitis has the highest mortality risk within one year of disease onset,” Linde Snoek said during her presentation of the study (abstract 913) at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. Ms. Snoek is a PhD student at Amsterdam University Medical Center.
Over longer time periods, the mortality associations were different. “The adjusted hazard rates were highest for pneumococcal meningitis compared to the other pathogens. And this was the case for 1 year, 5 years, and 10 years after disease onset,” said Ms. Snoek.
The study appears to be the first to look at extended mortality following bacterial meningitis in this age group, according to Marie Rohr, MD, who comoderated the session where the research was presented.
“In a quick review of the literature I did not find any [equivalent] study concerning short- and long-term mortality after bacterial meningitis in under 1 year of age,” said Dr. Rohr, a fellow in pediatric infectious diseases at University Hospitals of Geneva. But the message to physicians is clear. “Children with history of bacterial meningitis have a higher long-term mortality than children without a history of bacterial meningitis,” said Dr. Rohr.
The study did have a key limitation: For matched controls, it relied on anonymous data from the Municipal Personal Records Database in Statistics Netherlands. “Important information like cause of death is lacking,” said Dr. Rohr.
Bacterial meningitis is associated with significant mortality and morbidity. Pathogens behind the infections vary with age group and geographic location, as well as immunization status.
To examine long-term mortality after bacterial meningitis, the researchers collected 1,646 records from an exposed cohort, with a date range of 1995 to 2018, from the Netherlands Reference Laboratory for Bacterial Meningitis. Included patients had a positive culture diagnosis of bacterial meningitis during the first year of life. Each exposed subject was compared to 10 controls matched by birth month, birth year, and sex, who had no exposure to bacterial meningitis.
Staphylococcus pneumoniae accounted for the most cases, at 32.0% (median age of onset, 180 days), followed by Neisseria meningitidis at 29.0% (median age of onset, 203 days). Other pathogens included S. agalactiae (19.7%, 10 days), Escherichia coli (8.8%, 13 days), and Haemophilus influenzae (5.4%, 231 days).
The mortality risk within 1 year of disease onset was higher for all pathogens (6.2% vs. 0.2% unexposed). The highest mortality risk was seen for S. agalactiae (8.7%), followed by E. coli (6.4%), N. meningitidis (4.9%), and H. influenzae (3.4%).
Hazard ratios (HR) for mortality were also higher, particularly in the first year after disease onset. For all pathogens, mortality rates were higher within 1 year (HR, 39.2), 5 years (HR, 28.7), and 10 years (HR, 24.1). The consistently highest mortality rates were associated with S. pneumoniae over 1-year, 5-year, and 10-year follow-up (HR, 42.8; HR, 45.6; HR, 40.6, respectively). Within 1 year, the highest mortality rate was associated with N. meningitidis (HR, 58.4).
Ms. Snoek and Dr. Rohr have no relevant financial disclosures.
Among infants younger than 1 year of age, bacterial meningitis is associated with worse long-term mortality, even after recovery from the initial infection. Heightened mortality risk stretched out to 10 years, and was highest in the wake of infection from Streptococcus agalactiae, according to a retrospective analysis of children in the Netherlands.
“The adjusted hazard rates were high for the whole group of bacterial meningitis, especially within the first year after onset. (Staphylococcus agalactiae) meningitis has the highest mortality risk within one year of disease onset,” Linde Snoek said during her presentation of the study (abstract 913) at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. Ms. Snoek is a PhD student at Amsterdam University Medical Center.
Over longer time periods, the mortality associations were different. “The adjusted hazard rates were highest for pneumococcal meningitis compared to the other pathogens. And this was the case for 1 year, 5 years, and 10 years after disease onset,” said Ms. Snoek.
The study appears to be the first to look at extended mortality following bacterial meningitis in this age group, according to Marie Rohr, MD, who comoderated the session where the research was presented.
“In a quick review of the literature I did not find any [equivalent] study concerning short- and long-term mortality after bacterial meningitis in under 1 year of age,” said Dr. Rohr, a fellow in pediatric infectious diseases at University Hospitals of Geneva. But the message to physicians is clear. “Children with history of bacterial meningitis have a higher long-term mortality than children without a history of bacterial meningitis,” said Dr. Rohr.
The study did have a key limitation: For matched controls, it relied on anonymous data from the Municipal Personal Records Database in Statistics Netherlands. “Important information like cause of death is lacking,” said Dr. Rohr.
Bacterial meningitis is associated with significant mortality and morbidity. Pathogens behind the infections vary with age group and geographic location, as well as immunization status.
To examine long-term mortality after bacterial meningitis, the researchers collected 1,646 records from an exposed cohort, with a date range of 1995 to 2018, from the Netherlands Reference Laboratory for Bacterial Meningitis. Included patients had a positive culture diagnosis of bacterial meningitis during the first year of life. Each exposed subject was compared to 10 controls matched by birth month, birth year, and sex, who had no exposure to bacterial meningitis.
Staphylococcus pneumoniae accounted for the most cases, at 32.0% (median age of onset, 180 days), followed by Neisseria meningitidis at 29.0% (median age of onset, 203 days). Other pathogens included S. agalactiae (19.7%, 10 days), Escherichia coli (8.8%, 13 days), and Haemophilus influenzae (5.4%, 231 days).
The mortality risk within 1 year of disease onset was higher for all pathogens (6.2% vs. 0.2% unexposed). The highest mortality risk was seen for S. agalactiae (8.7%), followed by E. coli (6.4%), N. meningitidis (4.9%), and H. influenzae (3.4%).
Hazard ratios (HR) for mortality were also higher, particularly in the first year after disease onset. For all pathogens, mortality rates were higher within 1 year (HR, 39.2), 5 years (HR, 28.7), and 10 years (HR, 24.1). The consistently highest mortality rates were associated with S. pneumoniae over 1-year, 5-year, and 10-year follow-up (HR, 42.8; HR, 45.6; HR, 40.6, respectively). Within 1 year, the highest mortality rate was associated with N. meningitidis (HR, 58.4).
Ms. Snoek and Dr. Rohr have no relevant financial disclosures.
Among infants younger than 1 year of age, bacterial meningitis is associated with worse long-term mortality, even after recovery from the initial infection. Heightened mortality risk stretched out to 10 years, and was highest in the wake of infection from Streptococcus agalactiae, according to a retrospective analysis of children in the Netherlands.
“The adjusted hazard rates were high for the whole group of bacterial meningitis, especially within the first year after onset. (Staphylococcus agalactiae) meningitis has the highest mortality risk within one year of disease onset,” Linde Snoek said during her presentation of the study (abstract 913) at the annual meeting of the European Society for Paediatric Infectious Diseases, held virtually this year. Ms. Snoek is a PhD student at Amsterdam University Medical Center.
Over longer time periods, the mortality associations were different. “The adjusted hazard rates were highest for pneumococcal meningitis compared to the other pathogens. And this was the case for 1 year, 5 years, and 10 years after disease onset,” said Ms. Snoek.
The study appears to be the first to look at extended mortality following bacterial meningitis in this age group, according to Marie Rohr, MD, who comoderated the session where the research was presented.
“In a quick review of the literature I did not find any [equivalent] study concerning short- and long-term mortality after bacterial meningitis in under 1 year of age,” said Dr. Rohr, a fellow in pediatric infectious diseases at University Hospitals of Geneva. But the message to physicians is clear. “Children with history of bacterial meningitis have a higher long-term mortality than children without a history of bacterial meningitis,” said Dr. Rohr.
The study did have a key limitation: For matched controls, it relied on anonymous data from the Municipal Personal Records Database in Statistics Netherlands. “Important information like cause of death is lacking,” said Dr. Rohr.
Bacterial meningitis is associated with significant mortality and morbidity. Pathogens behind the infections vary with age group and geographic location, as well as immunization status.
To examine long-term mortality after bacterial meningitis, the researchers collected 1,646 records from an exposed cohort, with a date range of 1995 to 2018, from the Netherlands Reference Laboratory for Bacterial Meningitis. Included patients had a positive culture diagnosis of bacterial meningitis during the first year of life. Each exposed subject was compared to 10 controls matched by birth month, birth year, and sex, who had no exposure to bacterial meningitis.
Staphylococcus pneumoniae accounted for the most cases, at 32.0% (median age of onset, 180 days), followed by Neisseria meningitidis at 29.0% (median age of onset, 203 days). Other pathogens included S. agalactiae (19.7%, 10 days), Escherichia coli (8.8%, 13 days), and Haemophilus influenzae (5.4%, 231 days).
The mortality risk within 1 year of disease onset was higher for all pathogens (6.2% vs. 0.2% unexposed). The highest mortality risk was seen for S. agalactiae (8.7%), followed by E. coli (6.4%), N. meningitidis (4.9%), and H. influenzae (3.4%).
Hazard ratios (HR) for mortality were also higher, particularly in the first year after disease onset. For all pathogens, mortality rates were higher within 1 year (HR, 39.2), 5 years (HR, 28.7), and 10 years (HR, 24.1). The consistently highest mortality rates were associated with S. pneumoniae over 1-year, 5-year, and 10-year follow-up (HR, 42.8; HR, 45.6; HR, 40.6, respectively). Within 1 year, the highest mortality rate was associated with N. meningitidis (HR, 58.4).
Ms. Snoek and Dr. Rohr have no relevant financial disclosures.
FROM ESPID 2021
Novel text-messaging program boosts ADHD treatment adherence
An innovative text-messaging program that reminds patients with attention-deficit/hyperactivity disorder to take their medication and warns them about the hazards of noncompliance significantly increases treatment adherence in children and adults, new research suggests.
In a pediatric study, 85% of participants who received a text message had their prescriptions refilled in a timely manner, compared with 62% of those who received treatment as usual and no text messaging. In a second study of adults, 81% of the group that received a text message refilled their prescriptions, versus 36% of those in the usual-treatment group.
“Patients are not going to be fully compliant if they do not understand what the implications are if they do not take their pills,” lead author Joseph Biederman, MD, chief of clinical and research programs in pediatric psychopharmacology and adult ADHD at the Massachusetts General Hospital and professor of psychiatry at Harvard Medical School, Boston, told this news organization.
He noted that the text-messaging program also provides information, support, encouragement, and guidance.
“We remind them to get in touch with their prescriber as renewals come due, and if they tell us no, we tell them how important it is” to do so, Dr. Biederman said.
The findings were presented at the virtual American Society of Clinical Psychopharmacology 2021 annual meeting.
Poor adherence
“Adherence to medications for ADHD is extremely poor, among the worst in medicine, despite the fact that ADHD is very morbid and we have excellent treatments people can take,” Dr. Biederman noted. “That’s the first tragedy, and it is totally unappreciated.”
He added that when patients require multiple prescriptions, he said.
Another contributor to medication nonadherence is the ongoing prejudice or stigma associated with ADHD, said Dr. Biederman.
“There is bad press about ADHD. There are no good comments, only disaster, doom and gloom, catastrophe, and so on. All people read in the available media are bad things about ADHD, and that only adds to stigma and misinformation,” he noted.
To combat these factors, Dr. Biederman and his team conducted two studies on the effectiveness of a novel ADHD-centric intervention based on text messaging.
One study included 87 children aged 6-12 years, and the other included 117 adults aged 18-55 years. Both groups were from primary care settings and were prescribed a stimulant medication for the treatment of ADHD.
As comparators, the researchers used age- and sex-matched pediatric patients and age-, race-, and sex-matched adult patients from the same primary care settings. They had also been prescribed stimulants but had not received the text messaging intervention.
Timely reminders
Results showed that 85% of the children who received text messages refilled their prescriptions vs. 65% of those who did not get the intervention (odds ratio, 3.46; 95% confidence interval, 1.82-6.58; P < .001).
Among adults, 81% of the intervention group refilled their prescriptions vs. 36% of the comparator group (OR, 7.54; 95% CI, 4.46-12.77; P < .001).
“In the number-needed-to-treat analysis, for every five pediatric patients who receive text messaging, we can keep one adherent with stimulant medication. In adults, that is one in every three who receive the text-messaging intervention,” Dr. Biederman said.
Text messaging reminds patients with ADHD to take their medications as prescribed, and it also reminds them of the consequences of not taking their medications, he added.
In another study presented at the ASCP meeting, Dr. Biederman introduced a new tool to help clinicians determine whether a patient with ADHD also has deficient emotional self-regulation (DESR).
ADHD has been associated with low frustration tolerance, impatience, and quickness to anger, he noted.
Emotional dysregulation, however, “is not a mood disorder,” said Dr. Biederman. “Some people use the term ‘hot tempered.’ These are people who overreact to things, and this is associated with a wide range of difficulties.”
Clinical guidance
The investigators operationalized DESR using the eight-item Emotional Dysregulation (ED) subscale of the Barkley Current Behavior Scale. They then used receiver operating characteristic curves to identify the optimal cutoff on the Barkley ED Scale that would categorize patients as having high- vs. low-level DESR.
“We wanted to give some guidance to clinicians, using a very simple rating scale that was developed by Dr. Barkley. It is one we think configures this syndrome of emotional dysregulation and emotional impulsivity,” Dr. Biederman said.
The study included 441 newly referred 18- to 55-year-old men and women who met DSM-5 diagnostic criteria for ADHD.
Using a cutoff score of 8 to represent high levels of DESR, the researchers identified 191 adults as having high-level DESR and the rest as having low-level DESR.
Those with high-level DESR had significantly more severe symptoms of ADHD, executive dysfunction, autistic traits, levels of psychopathology, and worse quality of life, compared with those with low-level DESR.
The problem of emotional dysregulation in ADHD is widespread and affects many people, Dr. Biederman noted.
“If you take 5% of adults at a minimum and 10% of children with ADHD [and] if 50% of those have emotional dysregulation, we’re talking about millions of people. And it is very morbid,” he said. “Having emotional dysregulation problems will get you in hot water.”
Promising results
Commenting on the findings for this news organization, Ira D. Glick, MD, professor emeritus of psychiatry and behavioral sciences, Stanford (Calif.) University, said the new studies are important.
He noted that, although ADHD has become more accepted as a “disease of the brain” over the past 20 years, patients with the disorder and their families often are not accepting of the diagnosis.
“Instead, they try to downplay it. They say this is just a ploy by psychiatrists to get business or this is just normal boys’ behavior, [and] they don’t need medicines,” said Dr. Glick, who was not involved in the current research.
“Biederman is trying to make clear that ADHD is a brain disease, and DESR symptoms are cardinal signs of a brain illness,” he said.
Dr. Glick also agreed that text messaging could be very useful for these patients.
“Text messaging might be helpful, especially in this population which can often be disorganized or forgetful. The results of that study were very promising,” he said.
Dr. Biederman is in the process of commercializing the text program used in the study. Dr. Glick reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An innovative text-messaging program that reminds patients with attention-deficit/hyperactivity disorder to take their medication and warns them about the hazards of noncompliance significantly increases treatment adherence in children and adults, new research suggests.
In a pediatric study, 85% of participants who received a text message had their prescriptions refilled in a timely manner, compared with 62% of those who received treatment as usual and no text messaging. In a second study of adults, 81% of the group that received a text message refilled their prescriptions, versus 36% of those in the usual-treatment group.
“Patients are not going to be fully compliant if they do not understand what the implications are if they do not take their pills,” lead author Joseph Biederman, MD, chief of clinical and research programs in pediatric psychopharmacology and adult ADHD at the Massachusetts General Hospital and professor of psychiatry at Harvard Medical School, Boston, told this news organization.
He noted that the text-messaging program also provides information, support, encouragement, and guidance.
“We remind them to get in touch with their prescriber as renewals come due, and if they tell us no, we tell them how important it is” to do so, Dr. Biederman said.
The findings were presented at the virtual American Society of Clinical Psychopharmacology 2021 annual meeting.
Poor adherence
“Adherence to medications for ADHD is extremely poor, among the worst in medicine, despite the fact that ADHD is very morbid and we have excellent treatments people can take,” Dr. Biederman noted. “That’s the first tragedy, and it is totally unappreciated.”
He added that when patients require multiple prescriptions, he said.
Another contributor to medication nonadherence is the ongoing prejudice or stigma associated with ADHD, said Dr. Biederman.
“There is bad press about ADHD. There are no good comments, only disaster, doom and gloom, catastrophe, and so on. All people read in the available media are bad things about ADHD, and that only adds to stigma and misinformation,” he noted.
To combat these factors, Dr. Biederman and his team conducted two studies on the effectiveness of a novel ADHD-centric intervention based on text messaging.
One study included 87 children aged 6-12 years, and the other included 117 adults aged 18-55 years. Both groups were from primary care settings and were prescribed a stimulant medication for the treatment of ADHD.
As comparators, the researchers used age- and sex-matched pediatric patients and age-, race-, and sex-matched adult patients from the same primary care settings. They had also been prescribed stimulants but had not received the text messaging intervention.
Timely reminders
Results showed that 85% of the children who received text messages refilled their prescriptions vs. 65% of those who did not get the intervention (odds ratio, 3.46; 95% confidence interval, 1.82-6.58; P < .001).
Among adults, 81% of the intervention group refilled their prescriptions vs. 36% of the comparator group (OR, 7.54; 95% CI, 4.46-12.77; P < .001).
“In the number-needed-to-treat analysis, for every five pediatric patients who receive text messaging, we can keep one adherent with stimulant medication. In adults, that is one in every three who receive the text-messaging intervention,” Dr. Biederman said.
Text messaging reminds patients with ADHD to take their medications as prescribed, and it also reminds them of the consequences of not taking their medications, he added.
In another study presented at the ASCP meeting, Dr. Biederman introduced a new tool to help clinicians determine whether a patient with ADHD also has deficient emotional self-regulation (DESR).
ADHD has been associated with low frustration tolerance, impatience, and quickness to anger, he noted.
Emotional dysregulation, however, “is not a mood disorder,” said Dr. Biederman. “Some people use the term ‘hot tempered.’ These are people who overreact to things, and this is associated with a wide range of difficulties.”
Clinical guidance
The investigators operationalized DESR using the eight-item Emotional Dysregulation (ED) subscale of the Barkley Current Behavior Scale. They then used receiver operating characteristic curves to identify the optimal cutoff on the Barkley ED Scale that would categorize patients as having high- vs. low-level DESR.
“We wanted to give some guidance to clinicians, using a very simple rating scale that was developed by Dr. Barkley. It is one we think configures this syndrome of emotional dysregulation and emotional impulsivity,” Dr. Biederman said.
The study included 441 newly referred 18- to 55-year-old men and women who met DSM-5 diagnostic criteria for ADHD.
Using a cutoff score of 8 to represent high levels of DESR, the researchers identified 191 adults as having high-level DESR and the rest as having low-level DESR.
Those with high-level DESR had significantly more severe symptoms of ADHD, executive dysfunction, autistic traits, levels of psychopathology, and worse quality of life, compared with those with low-level DESR.
The problem of emotional dysregulation in ADHD is widespread and affects many people, Dr. Biederman noted.
“If you take 5% of adults at a minimum and 10% of children with ADHD [and] if 50% of those have emotional dysregulation, we’re talking about millions of people. And it is very morbid,” he said. “Having emotional dysregulation problems will get you in hot water.”
Promising results
Commenting on the findings for this news organization, Ira D. Glick, MD, professor emeritus of psychiatry and behavioral sciences, Stanford (Calif.) University, said the new studies are important.
He noted that, although ADHD has become more accepted as a “disease of the brain” over the past 20 years, patients with the disorder and their families often are not accepting of the diagnosis.
“Instead, they try to downplay it. They say this is just a ploy by psychiatrists to get business or this is just normal boys’ behavior, [and] they don’t need medicines,” said Dr. Glick, who was not involved in the current research.
“Biederman is trying to make clear that ADHD is a brain disease, and DESR symptoms are cardinal signs of a brain illness,” he said.
Dr. Glick also agreed that text messaging could be very useful for these patients.
“Text messaging might be helpful, especially in this population which can often be disorganized or forgetful. The results of that study were very promising,” he said.
Dr. Biederman is in the process of commercializing the text program used in the study. Dr. Glick reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An innovative text-messaging program that reminds patients with attention-deficit/hyperactivity disorder to take their medication and warns them about the hazards of noncompliance significantly increases treatment adherence in children and adults, new research suggests.
In a pediatric study, 85% of participants who received a text message had their prescriptions refilled in a timely manner, compared with 62% of those who received treatment as usual and no text messaging. In a second study of adults, 81% of the group that received a text message refilled their prescriptions, versus 36% of those in the usual-treatment group.
“Patients are not going to be fully compliant if they do not understand what the implications are if they do not take their pills,” lead author Joseph Biederman, MD, chief of clinical and research programs in pediatric psychopharmacology and adult ADHD at the Massachusetts General Hospital and professor of psychiatry at Harvard Medical School, Boston, told this news organization.
He noted that the text-messaging program also provides information, support, encouragement, and guidance.
“We remind them to get in touch with their prescriber as renewals come due, and if they tell us no, we tell them how important it is” to do so, Dr. Biederman said.
The findings were presented at the virtual American Society of Clinical Psychopharmacology 2021 annual meeting.
Poor adherence
“Adherence to medications for ADHD is extremely poor, among the worst in medicine, despite the fact that ADHD is very morbid and we have excellent treatments people can take,” Dr. Biederman noted. “That’s the first tragedy, and it is totally unappreciated.”
He added that when patients require multiple prescriptions, he said.
Another contributor to medication nonadherence is the ongoing prejudice or stigma associated with ADHD, said Dr. Biederman.
“There is bad press about ADHD. There are no good comments, only disaster, doom and gloom, catastrophe, and so on. All people read in the available media are bad things about ADHD, and that only adds to stigma and misinformation,” he noted.
To combat these factors, Dr. Biederman and his team conducted two studies on the effectiveness of a novel ADHD-centric intervention based on text messaging.
One study included 87 children aged 6-12 years, and the other included 117 adults aged 18-55 years. Both groups were from primary care settings and were prescribed a stimulant medication for the treatment of ADHD.
As comparators, the researchers used age- and sex-matched pediatric patients and age-, race-, and sex-matched adult patients from the same primary care settings. They had also been prescribed stimulants but had not received the text messaging intervention.
Timely reminders
Results showed that 85% of the children who received text messages refilled their prescriptions vs. 65% of those who did not get the intervention (odds ratio, 3.46; 95% confidence interval, 1.82-6.58; P < .001).
Among adults, 81% of the intervention group refilled their prescriptions vs. 36% of the comparator group (OR, 7.54; 95% CI, 4.46-12.77; P < .001).
“In the number-needed-to-treat analysis, for every five pediatric patients who receive text messaging, we can keep one adherent with stimulant medication. In adults, that is one in every three who receive the text-messaging intervention,” Dr. Biederman said.
Text messaging reminds patients with ADHD to take their medications as prescribed, and it also reminds them of the consequences of not taking their medications, he added.
In another study presented at the ASCP meeting, Dr. Biederman introduced a new tool to help clinicians determine whether a patient with ADHD also has deficient emotional self-regulation (DESR).
ADHD has been associated with low frustration tolerance, impatience, and quickness to anger, he noted.
Emotional dysregulation, however, “is not a mood disorder,” said Dr. Biederman. “Some people use the term ‘hot tempered.’ These are people who overreact to things, and this is associated with a wide range of difficulties.”
Clinical guidance
The investigators operationalized DESR using the eight-item Emotional Dysregulation (ED) subscale of the Barkley Current Behavior Scale. They then used receiver operating characteristic curves to identify the optimal cutoff on the Barkley ED Scale that would categorize patients as having high- vs. low-level DESR.
“We wanted to give some guidance to clinicians, using a very simple rating scale that was developed by Dr. Barkley. It is one we think configures this syndrome of emotional dysregulation and emotional impulsivity,” Dr. Biederman said.
The study included 441 newly referred 18- to 55-year-old men and women who met DSM-5 diagnostic criteria for ADHD.
Using a cutoff score of 8 to represent high levels of DESR, the researchers identified 191 adults as having high-level DESR and the rest as having low-level DESR.
Those with high-level DESR had significantly more severe symptoms of ADHD, executive dysfunction, autistic traits, levels of psychopathology, and worse quality of life, compared with those with low-level DESR.
The problem of emotional dysregulation in ADHD is widespread and affects many people, Dr. Biederman noted.
“If you take 5% of adults at a minimum and 10% of children with ADHD [and] if 50% of those have emotional dysregulation, we’re talking about millions of people. And it is very morbid,” he said. “Having emotional dysregulation problems will get you in hot water.”
Promising results
Commenting on the findings for this news organization, Ira D. Glick, MD, professor emeritus of psychiatry and behavioral sciences, Stanford (Calif.) University, said the new studies are important.
He noted that, although ADHD has become more accepted as a “disease of the brain” over the past 20 years, patients with the disorder and their families often are not accepting of the diagnosis.
“Instead, they try to downplay it. They say this is just a ploy by psychiatrists to get business or this is just normal boys’ behavior, [and] they don’t need medicines,” said Dr. Glick, who was not involved in the current research.
“Biederman is trying to make clear that ADHD is a brain disease, and DESR symptoms are cardinal signs of a brain illness,” he said.
Dr. Glick also agreed that text messaging could be very useful for these patients.
“Text messaging might be helpful, especially in this population which can often be disorganized or forgetful. The results of that study were very promising,” he said.
Dr. Biederman is in the process of commercializing the text program used in the study. Dr. Glick reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FDA approves secukinumab in psoriasis patients age six and older
The who are candidates for systemic therapy or phototherapy. The expanded indication marks the first time the drug has been available for a pediatric population in the United States.
Children with plaque psoriasis are often undertreated because of fear of side effects of therapies, according to Kelly M. Cordoro, MD, professor of dermatology and pediatrics at the University of California, San Francisco. “Now, more and more medicines are being tested for safety and efficacy in children, and we no longer have to rely on adult studies to inform treatment choices for children,” Dr. Cordoro told this news organization.
The FDA approval of secukinumab for children aged 6 and older with moderate to severe psoriasis “is a welcome addition to the therapeutic toolbox for pediatric psoriasis,” she said. “We’ve entered an era where severe pediatric psoriasis has become a condition that can be adequately controlled with minimal risk and with the convenience of intermittent injections. This has changed the playing field for these children and their families completely. Given the potential short- and long-term negative impact of chronic inflammation on the body of a growing child, we now have approved treatments that can safely offset the risks of undertreated severe psoriasis on the functional and psychological health of the child.”
The approved pediatric dosing for secukinumab is 75 mg or 150 mg depending on the child’s weight at the time of dosing, and it is administered by subcutaneous injection every 4 weeks after an initial loading regimen. According to a press release from Novartis, the FDA approval came on the heels of two phase 3 studies that evaluated the use of secukinumab in children aged 6 to younger than 18 years with plaque psoriasis. The first was a 52-week, randomized, double-blind, placebo- and active-controlled study which included 162 children 6 years of age and older with severe plaque psoriasis. The doses evaluated were 75 mg for children who weighed less than 50 kg and 150 mg for those 50 kg or greater.
At week 12, the Psoriasis Area Severity Index (PASI)-75 response was 55% among children in the 75-mg dosing group vs. 10% in the placebo group and 86% in the 150-mg dosing group vs. 19% in the placebo group.
Meanwhile, the Investigator’s Global Assessment modified 2011 (IGA) “clear” response was achieved in 32% of children in the 75-mg dosing group vs. 5% in the placebo group and in 81% of children in the 150-mg dosing group vs. 5% in the placebo group. An IGA “almost clear” skin response was achieved in 81% of children in the 75-mg dosing group vs. 5% in the placebo group.
The second phase 3 study was a randomized open-label, 208-week trial of 84 subjects 6 years of age and older with moderate to severe plaque psoriasis. According to the Novartis press release, the safety profile reported in both trials was consistent with the safety profile reported in adult plaque psoriasis trials and no new safety signals were observed. The updated prescribing information for secukinumab can be found here.
“When considering treatment with a systemic agent such as a biologic, it is important to consider objective measures of severity, such as extent of disease and involvement of joints but also subjective indicators of severity such as impact beyond the skin on psychological well-being,” Dr. Cordoro said in the interview. “Kids with psoriasis in visible locations may socially isolate themselves due to embarrassment or bullying. Therefore, the impact of moderate to severe psoriasis not only on overall health but on self-esteem and identity formation can be significant, and therefore adequately treating children of all ages to prevent the downstream negative consequences of childhood psoriasis is critical.”
Dr. Cordoro reported having no financial disclosures.
The who are candidates for systemic therapy or phototherapy. The expanded indication marks the first time the drug has been available for a pediatric population in the United States.
Children with plaque psoriasis are often undertreated because of fear of side effects of therapies, according to Kelly M. Cordoro, MD, professor of dermatology and pediatrics at the University of California, San Francisco. “Now, more and more medicines are being tested for safety and efficacy in children, and we no longer have to rely on adult studies to inform treatment choices for children,” Dr. Cordoro told this news organization.
The FDA approval of secukinumab for children aged 6 and older with moderate to severe psoriasis “is a welcome addition to the therapeutic toolbox for pediatric psoriasis,” she said. “We’ve entered an era where severe pediatric psoriasis has become a condition that can be adequately controlled with minimal risk and with the convenience of intermittent injections. This has changed the playing field for these children and their families completely. Given the potential short- and long-term negative impact of chronic inflammation on the body of a growing child, we now have approved treatments that can safely offset the risks of undertreated severe psoriasis on the functional and psychological health of the child.”
The approved pediatric dosing for secukinumab is 75 mg or 150 mg depending on the child’s weight at the time of dosing, and it is administered by subcutaneous injection every 4 weeks after an initial loading regimen. According to a press release from Novartis, the FDA approval came on the heels of two phase 3 studies that evaluated the use of secukinumab in children aged 6 to younger than 18 years with plaque psoriasis. The first was a 52-week, randomized, double-blind, placebo- and active-controlled study which included 162 children 6 years of age and older with severe plaque psoriasis. The doses evaluated were 75 mg for children who weighed less than 50 kg and 150 mg for those 50 kg or greater.
At week 12, the Psoriasis Area Severity Index (PASI)-75 response was 55% among children in the 75-mg dosing group vs. 10% in the placebo group and 86% in the 150-mg dosing group vs. 19% in the placebo group.
Meanwhile, the Investigator’s Global Assessment modified 2011 (IGA) “clear” response was achieved in 32% of children in the 75-mg dosing group vs. 5% in the placebo group and in 81% of children in the 150-mg dosing group vs. 5% in the placebo group. An IGA “almost clear” skin response was achieved in 81% of children in the 75-mg dosing group vs. 5% in the placebo group.
The second phase 3 study was a randomized open-label, 208-week trial of 84 subjects 6 years of age and older with moderate to severe plaque psoriasis. According to the Novartis press release, the safety profile reported in both trials was consistent with the safety profile reported in adult plaque psoriasis trials and no new safety signals were observed. The updated prescribing information for secukinumab can be found here.
“When considering treatment with a systemic agent such as a biologic, it is important to consider objective measures of severity, such as extent of disease and involvement of joints but also subjective indicators of severity such as impact beyond the skin on psychological well-being,” Dr. Cordoro said in the interview. “Kids with psoriasis in visible locations may socially isolate themselves due to embarrassment or bullying. Therefore, the impact of moderate to severe psoriasis not only on overall health but on self-esteem and identity formation can be significant, and therefore adequately treating children of all ages to prevent the downstream negative consequences of childhood psoriasis is critical.”
Dr. Cordoro reported having no financial disclosures.
The who are candidates for systemic therapy or phototherapy. The expanded indication marks the first time the drug has been available for a pediatric population in the United States.
Children with plaque psoriasis are often undertreated because of fear of side effects of therapies, according to Kelly M. Cordoro, MD, professor of dermatology and pediatrics at the University of California, San Francisco. “Now, more and more medicines are being tested for safety and efficacy in children, and we no longer have to rely on adult studies to inform treatment choices for children,” Dr. Cordoro told this news organization.
The FDA approval of secukinumab for children aged 6 and older with moderate to severe psoriasis “is a welcome addition to the therapeutic toolbox for pediatric psoriasis,” she said. “We’ve entered an era where severe pediatric psoriasis has become a condition that can be adequately controlled with minimal risk and with the convenience of intermittent injections. This has changed the playing field for these children and their families completely. Given the potential short- and long-term negative impact of chronic inflammation on the body of a growing child, we now have approved treatments that can safely offset the risks of undertreated severe psoriasis on the functional and psychological health of the child.”
The approved pediatric dosing for secukinumab is 75 mg or 150 mg depending on the child’s weight at the time of dosing, and it is administered by subcutaneous injection every 4 weeks after an initial loading regimen. According to a press release from Novartis, the FDA approval came on the heels of two phase 3 studies that evaluated the use of secukinumab in children aged 6 to younger than 18 years with plaque psoriasis. The first was a 52-week, randomized, double-blind, placebo- and active-controlled study which included 162 children 6 years of age and older with severe plaque psoriasis. The doses evaluated were 75 mg for children who weighed less than 50 kg and 150 mg for those 50 kg or greater.
At week 12, the Psoriasis Area Severity Index (PASI)-75 response was 55% among children in the 75-mg dosing group vs. 10% in the placebo group and 86% in the 150-mg dosing group vs. 19% in the placebo group.
Meanwhile, the Investigator’s Global Assessment modified 2011 (IGA) “clear” response was achieved in 32% of children in the 75-mg dosing group vs. 5% in the placebo group and in 81% of children in the 150-mg dosing group vs. 5% in the placebo group. An IGA “almost clear” skin response was achieved in 81% of children in the 75-mg dosing group vs. 5% in the placebo group.
The second phase 3 study was a randomized open-label, 208-week trial of 84 subjects 6 years of age and older with moderate to severe plaque psoriasis. According to the Novartis press release, the safety profile reported in both trials was consistent with the safety profile reported in adult plaque psoriasis trials and no new safety signals were observed. The updated prescribing information for secukinumab can be found here.
“When considering treatment with a systemic agent such as a biologic, it is important to consider objective measures of severity, such as extent of disease and involvement of joints but also subjective indicators of severity such as impact beyond the skin on psychological well-being,” Dr. Cordoro said in the interview. “Kids with psoriasis in visible locations may socially isolate themselves due to embarrassment or bullying. Therefore, the impact of moderate to severe psoriasis not only on overall health but on self-esteem and identity formation can be significant, and therefore adequately treating children of all ages to prevent the downstream negative consequences of childhood psoriasis is critical.”
Dr. Cordoro reported having no financial disclosures.
FDA approves diagnostic device for autism spectrum disorder
The Food and Drug Administration has approved marketing for a device that will help diagnose autism spectrum disorder (ASD) in children between the ages of 18 months and 5 years old who exhibit potential symptoms.
Cognoa ASD Diagnosis Aid is a machine learning–based software program that receives information from parents or caregivers, video analysts, and health care providers to assist physicians in evaluating whether a child is at risk of having autism.
Autism is a developmental disorder that can cause social, communication, and behavioral challenges, according to the Centers for Disease Control and Prevention. The disorder affects about 1 in 54 children. The disorder is difficult to diagnose because there isn’t a medical test to diagnose the it. Instead, physicians have to look at a child’s developmental history and behavior to make a diagnosis.
Many children are not diagnosed with ASD until later in childhood, which in some cases delays treatment and early intervention. ASD may be detected as early as 18 months, but the average age of diagnosis for ASD is 4.3 years, according to the FDA.
“[ASD] can delay a child’s physical, cognitive, and social development, including motor skill development, learning, communication, and interacting with others. The earlier ASD can be diagnosed, the more quickly intervention strategies and appropriate therapies can begin,” Jeff Shuren, MD, JD, director of the FDA’s Center for Devices and Radiological Health, said in a statement. “Today’s marketing authorization provides a new tool for helping diagnose children with ASD.”
The safety and efficacy of the Cognoa ASD Diagnosis Aid was assessed in a study of 425 patients between the ages of 18 months and 5 years old. For the study, researchers compared the diagnostic assessments made by the device to those made by a panel of clinical experts who used the current standard ASD diagnostic process. The device diagnosed 32% of the children with either a “Positive for ASD” or a “Negative for ASD” result. Researchers found that the device matched the panel’s conclusions for 81% of the patients who received a positive diagnosis. For those who received a negative diagnosis, the device matched the panel’s conclusions for 98% of the patients. In addition, the device made an accurate ASD determination in 98.4% of patients with the condition and in 78.9% of patients without the condition.
Cognoa ASD Diagnosis Aid has three main components. One component includes a mobile app for caregivers to answer questions about the child’s behavioral problems and to upload videos of the child. The next component is a video analysis portal for specialists to view and analyze uploaded videos of patients. Another component is a portal for health care providers that allows them to enter answers to preloaded questions about behavior problems, track the information provided by parents, and review a report of the results.
After the machine learning–based device processes the information provided by parents and health care providers, it reports either a positive or a negative diagnosis. If there is insufficient information to make either a positive or a negative diagnosis, the ASD Diagnostic AID will report that no result can be generated.
Some of the risks associated with this device include misdiagnosis and delayed diagnosis of ASD because of a false-positive or false-negative result, or when no result is generated. Researchers said a false-positive result occurred in 15 out of 303 study subjects without ASD and a false-negative result occurred in 1 out of 122 study subjects with ASD.
The FDA emphasized that the device is indicated to aid physicians in the process of diagnosing ASD in children. This means it shouldn’t be treated as a standalone diagnostic device, but as an adjunct to the diagnostic process.
The Food and Drug Administration has approved marketing for a device that will help diagnose autism spectrum disorder (ASD) in children between the ages of 18 months and 5 years old who exhibit potential symptoms.
Cognoa ASD Diagnosis Aid is a machine learning–based software program that receives information from parents or caregivers, video analysts, and health care providers to assist physicians in evaluating whether a child is at risk of having autism.
Autism is a developmental disorder that can cause social, communication, and behavioral challenges, according to the Centers for Disease Control and Prevention. The disorder affects about 1 in 54 children. The disorder is difficult to diagnose because there isn’t a medical test to diagnose the it. Instead, physicians have to look at a child’s developmental history and behavior to make a diagnosis.
Many children are not diagnosed with ASD until later in childhood, which in some cases delays treatment and early intervention. ASD may be detected as early as 18 months, but the average age of diagnosis for ASD is 4.3 years, according to the FDA.
“[ASD] can delay a child’s physical, cognitive, and social development, including motor skill development, learning, communication, and interacting with others. The earlier ASD can be diagnosed, the more quickly intervention strategies and appropriate therapies can begin,” Jeff Shuren, MD, JD, director of the FDA’s Center for Devices and Radiological Health, said in a statement. “Today’s marketing authorization provides a new tool for helping diagnose children with ASD.”
The safety and efficacy of the Cognoa ASD Diagnosis Aid was assessed in a study of 425 patients between the ages of 18 months and 5 years old. For the study, researchers compared the diagnostic assessments made by the device to those made by a panel of clinical experts who used the current standard ASD diagnostic process. The device diagnosed 32% of the children with either a “Positive for ASD” or a “Negative for ASD” result. Researchers found that the device matched the panel’s conclusions for 81% of the patients who received a positive diagnosis. For those who received a negative diagnosis, the device matched the panel’s conclusions for 98% of the patients. In addition, the device made an accurate ASD determination in 98.4% of patients with the condition and in 78.9% of patients without the condition.
Cognoa ASD Diagnosis Aid has three main components. One component includes a mobile app for caregivers to answer questions about the child’s behavioral problems and to upload videos of the child. The next component is a video analysis portal for specialists to view and analyze uploaded videos of patients. Another component is a portal for health care providers that allows them to enter answers to preloaded questions about behavior problems, track the information provided by parents, and review a report of the results.
After the machine learning–based device processes the information provided by parents and health care providers, it reports either a positive or a negative diagnosis. If there is insufficient information to make either a positive or a negative diagnosis, the ASD Diagnostic AID will report that no result can be generated.
Some of the risks associated with this device include misdiagnosis and delayed diagnosis of ASD because of a false-positive or false-negative result, or when no result is generated. Researchers said a false-positive result occurred in 15 out of 303 study subjects without ASD and a false-negative result occurred in 1 out of 122 study subjects with ASD.
The FDA emphasized that the device is indicated to aid physicians in the process of diagnosing ASD in children. This means it shouldn’t be treated as a standalone diagnostic device, but as an adjunct to the diagnostic process.
The Food and Drug Administration has approved marketing for a device that will help diagnose autism spectrum disorder (ASD) in children between the ages of 18 months and 5 years old who exhibit potential symptoms.
Cognoa ASD Diagnosis Aid is a machine learning–based software program that receives information from parents or caregivers, video analysts, and health care providers to assist physicians in evaluating whether a child is at risk of having autism.
Autism is a developmental disorder that can cause social, communication, and behavioral challenges, according to the Centers for Disease Control and Prevention. The disorder affects about 1 in 54 children. The disorder is difficult to diagnose because there isn’t a medical test to diagnose the it. Instead, physicians have to look at a child’s developmental history and behavior to make a diagnosis.
Many children are not diagnosed with ASD until later in childhood, which in some cases delays treatment and early intervention. ASD may be detected as early as 18 months, but the average age of diagnosis for ASD is 4.3 years, according to the FDA.
“[ASD] can delay a child’s physical, cognitive, and social development, including motor skill development, learning, communication, and interacting with others. The earlier ASD can be diagnosed, the more quickly intervention strategies and appropriate therapies can begin,” Jeff Shuren, MD, JD, director of the FDA’s Center for Devices and Radiological Health, said in a statement. “Today’s marketing authorization provides a new tool for helping diagnose children with ASD.”
The safety and efficacy of the Cognoa ASD Diagnosis Aid was assessed in a study of 425 patients between the ages of 18 months and 5 years old. For the study, researchers compared the diagnostic assessments made by the device to those made by a panel of clinical experts who used the current standard ASD diagnostic process. The device diagnosed 32% of the children with either a “Positive for ASD” or a “Negative for ASD” result. Researchers found that the device matched the panel’s conclusions for 81% of the patients who received a positive diagnosis. For those who received a negative diagnosis, the device matched the panel’s conclusions for 98% of the patients. In addition, the device made an accurate ASD determination in 98.4% of patients with the condition and in 78.9% of patients without the condition.
Cognoa ASD Diagnosis Aid has three main components. One component includes a mobile app for caregivers to answer questions about the child’s behavioral problems and to upload videos of the child. The next component is a video analysis portal for specialists to view and analyze uploaded videos of patients. Another component is a portal for health care providers that allows them to enter answers to preloaded questions about behavior problems, track the information provided by parents, and review a report of the results.
After the machine learning–based device processes the information provided by parents and health care providers, it reports either a positive or a negative diagnosis. If there is insufficient information to make either a positive or a negative diagnosis, the ASD Diagnostic AID will report that no result can be generated.
Some of the risks associated with this device include misdiagnosis and delayed diagnosis of ASD because of a false-positive or false-negative result, or when no result is generated. Researchers said a false-positive result occurred in 15 out of 303 study subjects without ASD and a false-negative result occurred in 1 out of 122 study subjects with ASD.
The FDA emphasized that the device is indicated to aid physicians in the process of diagnosing ASD in children. This means it shouldn’t be treated as a standalone diagnostic device, but as an adjunct to the diagnostic process.
Noses can be electronic, and toilets can be smart
Cancer loses … by a nose
Since the human nose is unpredictable at best, we’ve learned to rely on animals for our detailed nozzle needs. But researchers have found the next best thing to man’s best friend to accurately identify cancers.
A team at the University of Pennsylvania has developed an electronic olfaction, or “e-nose,” that has a 95% accuracy rate in distinguishing benign and malignant pancreatic and ovarian cancer cells from a single blood sample. How?
The e-nose system is equipped with nanosensors that are able to detect the volatile organic compounds (VOCs) emitted by cells in a blood sample. Not only does this create an opportunity for an easier, noninvasive screening practice, but it’s fast. The e-nose can distinguish VOCs from healthy to cancerous blood cells in 20 minutes or less and is just as effective in picking up on early- and late-stage cancers.
The investigators hope that this innovative technology can pave the way for similar devices with other uses. Thanks to the e-nose, a handheld device is in development that may be able to sniff out the signature odor of people with COVID-19.
That’s one smart schnoz.
Do you think this is a (food) game?
Dieting and eating healthy is tough, even during the best of times, and it has not been the best of times. With all respect to Charles Dickens, it’s been the worst of times, full stop. Millions of people have spent the past year sitting around their homes doing nothing, and it’s only natural that many would let their discipline slide.
Naturally, the solution to unhealthy eating habits is to sit down and play with your phone. No, that’s not the joke, the Food Trainer app, available on all cellular devices near you, is designed to encourage healthy eating by turning it into a game of sorts. When users open the app, they’re presented with images of food, and they’re trained to tap on images of healthy food and pass on images of unhealthy ones. The process takes less than 5 minutes.
It sounds really simple, but in a study of more than 1,000 people, consumption of junk food fell by 1 point on an 8-point scale (ranging from four times per day to zero to one time per month), participants lost about half a kilogram (a little over one pound), and more healthy food was eaten. Those who used the app more regularly, along the lines of 10 times per month or more, saw greater benefits.
The authors did acknowledge that those who used the app more may have been more motivated to lose weight anyway, which perhaps limits the overall benefit, but reviews on Google Play were overall quite positive, and if there’s one great truth in this world, it’s that Internet reviewers are almost impossible to please. So perhaps this app is worth looking into if you’re like the LOTME staff and you’re up at the top end of that 8-point scale. What, pizza is delicious, who wouldn’t eat it four times a day? And you can also get it from your phone!
It’s time for a little mass kickin’
The universe, scientists tell us, is a big place. Really big. Chromosomes, scientists tell us, are small. Really small. But despite this very fundamental difference, the universe and chromosomes share a deep, dark secret: unexplained mass.
This being a medical publication, we’ll start with chromosomes. A group of researchers measured their mass with x-rays for the first time and found that “the 46 chromosomes in each of our cells weigh 242 picograms (trillionths of a gram). This is heavier than we would expect, and, if replicated, points to unexplained excess mass in chromosomes,” Ian K. Robinson, PhD, said in a written statement.
We’re not just talking about a bit of a beer belly here. “The chromosomes were about 20 times heavier than the DNA they contained,” according to the investigators.
Now to the universe. Here’s what CERN, the European Council for Nuclear Research, has to say about the mass of the universe: “Galaxies in our universe … are rotating with such speed that the gravity generated by their observable matter could not possibly hold them together. … which leads scientists to believe that something we cannot see is at work. They think something we have yet to detect directly is giving these galaxies extra mass.”
But wait, there’s more! “The matter we know and that makes up all stars and galaxies only accounts for 5% of the content of the universe!”
So chromosomes are about 20 times heavier than the DNA they contain, and the universe is about 20 times heavier than the matter that can be seen. Interesting.
We are, of course, happy to share this news with our readers, but there is one catch: Don’t tell Neil deGrasse Tyson. He’ll want to reclassify our genetic solar system into 45 chromosomes and one dwarf chromosome.
A photo finish for the Smart Toilet
We know that poop can tell us a lot about our health, but new research by scientists at Duke University is really on a roll. Their Smart Toilet has been created to help people keep an eye on their bowel health. The device takes pictures of poop after it is flushed and can tell whether the consistency is loose, bloody, or normal.
The Smart Toilet can really help people with issues such as irritable bowel syndrome and inflammatory bowel disease by helping them, and their doctors, keep tabs on their poop. “Typically, gastroenterologists have to rely on patient self-reported information about their stool to help determine the cause of their gastrointestinal health issues, which can be very unreliable,” study lead author Deborah Fisher said.
Not many people look too closely at their poop before it’s flushed, so the fecal photos can make a big difference. The Smart Toilet is installed into the pipes of a toilet and does its thing when the toilet is flushed, so there doesn’t seem to be much work on the patient’s end. Other than the, um, you know, usual work from the patient’s end.
Cancer loses … by a nose
Since the human nose is unpredictable at best, we’ve learned to rely on animals for our detailed nozzle needs. But researchers have found the next best thing to man’s best friend to accurately identify cancers.
A team at the University of Pennsylvania has developed an electronic olfaction, or “e-nose,” that has a 95% accuracy rate in distinguishing benign and malignant pancreatic and ovarian cancer cells from a single blood sample. How?
The e-nose system is equipped with nanosensors that are able to detect the volatile organic compounds (VOCs) emitted by cells in a blood sample. Not only does this create an opportunity for an easier, noninvasive screening practice, but it’s fast. The e-nose can distinguish VOCs from healthy to cancerous blood cells in 20 minutes or less and is just as effective in picking up on early- and late-stage cancers.
The investigators hope that this innovative technology can pave the way for similar devices with other uses. Thanks to the e-nose, a handheld device is in development that may be able to sniff out the signature odor of people with COVID-19.
That’s one smart schnoz.
Do you think this is a (food) game?
Dieting and eating healthy is tough, even during the best of times, and it has not been the best of times. With all respect to Charles Dickens, it’s been the worst of times, full stop. Millions of people have spent the past year sitting around their homes doing nothing, and it’s only natural that many would let their discipline slide.
Naturally, the solution to unhealthy eating habits is to sit down and play with your phone. No, that’s not the joke, the Food Trainer app, available on all cellular devices near you, is designed to encourage healthy eating by turning it into a game of sorts. When users open the app, they’re presented with images of food, and they’re trained to tap on images of healthy food and pass on images of unhealthy ones. The process takes less than 5 minutes.
It sounds really simple, but in a study of more than 1,000 people, consumption of junk food fell by 1 point on an 8-point scale (ranging from four times per day to zero to one time per month), participants lost about half a kilogram (a little over one pound), and more healthy food was eaten. Those who used the app more regularly, along the lines of 10 times per month or more, saw greater benefits.
The authors did acknowledge that those who used the app more may have been more motivated to lose weight anyway, which perhaps limits the overall benefit, but reviews on Google Play were overall quite positive, and if there’s one great truth in this world, it’s that Internet reviewers are almost impossible to please. So perhaps this app is worth looking into if you’re like the LOTME staff and you’re up at the top end of that 8-point scale. What, pizza is delicious, who wouldn’t eat it four times a day? And you can also get it from your phone!
It’s time for a little mass kickin’
The universe, scientists tell us, is a big place. Really big. Chromosomes, scientists tell us, are small. Really small. But despite this very fundamental difference, the universe and chromosomes share a deep, dark secret: unexplained mass.
This being a medical publication, we’ll start with chromosomes. A group of researchers measured their mass with x-rays for the first time and found that “the 46 chromosomes in each of our cells weigh 242 picograms (trillionths of a gram). This is heavier than we would expect, and, if replicated, points to unexplained excess mass in chromosomes,” Ian K. Robinson, PhD, said in a written statement.
We’re not just talking about a bit of a beer belly here. “The chromosomes were about 20 times heavier than the DNA they contained,” according to the investigators.
Now to the universe. Here’s what CERN, the European Council for Nuclear Research, has to say about the mass of the universe: “Galaxies in our universe … are rotating with such speed that the gravity generated by their observable matter could not possibly hold them together. … which leads scientists to believe that something we cannot see is at work. They think something we have yet to detect directly is giving these galaxies extra mass.”
But wait, there’s more! “The matter we know and that makes up all stars and galaxies only accounts for 5% of the content of the universe!”
So chromosomes are about 20 times heavier than the DNA they contain, and the universe is about 20 times heavier than the matter that can be seen. Interesting.
We are, of course, happy to share this news with our readers, but there is one catch: Don’t tell Neil deGrasse Tyson. He’ll want to reclassify our genetic solar system into 45 chromosomes and one dwarf chromosome.
A photo finish for the Smart Toilet
We know that poop can tell us a lot about our health, but new research by scientists at Duke University is really on a roll. Their Smart Toilet has been created to help people keep an eye on their bowel health. The device takes pictures of poop after it is flushed and can tell whether the consistency is loose, bloody, or normal.
The Smart Toilet can really help people with issues such as irritable bowel syndrome and inflammatory bowel disease by helping them, and their doctors, keep tabs on their poop. “Typically, gastroenterologists have to rely on patient self-reported information about their stool to help determine the cause of their gastrointestinal health issues, which can be very unreliable,” study lead author Deborah Fisher said.
Not many people look too closely at their poop before it’s flushed, so the fecal photos can make a big difference. The Smart Toilet is installed into the pipes of a toilet and does its thing when the toilet is flushed, so there doesn’t seem to be much work on the patient’s end. Other than the, um, you know, usual work from the patient’s end.
Cancer loses … by a nose
Since the human nose is unpredictable at best, we’ve learned to rely on animals for our detailed nozzle needs. But researchers have found the next best thing to man’s best friend to accurately identify cancers.
A team at the University of Pennsylvania has developed an electronic olfaction, or “e-nose,” that has a 95% accuracy rate in distinguishing benign and malignant pancreatic and ovarian cancer cells from a single blood sample. How?
The e-nose system is equipped with nanosensors that are able to detect the volatile organic compounds (VOCs) emitted by cells in a blood sample. Not only does this create an opportunity for an easier, noninvasive screening practice, but it’s fast. The e-nose can distinguish VOCs from healthy to cancerous blood cells in 20 minutes or less and is just as effective in picking up on early- and late-stage cancers.
The investigators hope that this innovative technology can pave the way for similar devices with other uses. Thanks to the e-nose, a handheld device is in development that may be able to sniff out the signature odor of people with COVID-19.
That’s one smart schnoz.
Do you think this is a (food) game?
Dieting and eating healthy is tough, even during the best of times, and it has not been the best of times. With all respect to Charles Dickens, it’s been the worst of times, full stop. Millions of people have spent the past year sitting around their homes doing nothing, and it’s only natural that many would let their discipline slide.
Naturally, the solution to unhealthy eating habits is to sit down and play with your phone. No, that’s not the joke, the Food Trainer app, available on all cellular devices near you, is designed to encourage healthy eating by turning it into a game of sorts. When users open the app, they’re presented with images of food, and they’re trained to tap on images of healthy food and pass on images of unhealthy ones. The process takes less than 5 minutes.
It sounds really simple, but in a study of more than 1,000 people, consumption of junk food fell by 1 point on an 8-point scale (ranging from four times per day to zero to one time per month), participants lost about half a kilogram (a little over one pound), and more healthy food was eaten. Those who used the app more regularly, along the lines of 10 times per month or more, saw greater benefits.
The authors did acknowledge that those who used the app more may have been more motivated to lose weight anyway, which perhaps limits the overall benefit, but reviews on Google Play were overall quite positive, and if there’s one great truth in this world, it’s that Internet reviewers are almost impossible to please. So perhaps this app is worth looking into if you’re like the LOTME staff and you’re up at the top end of that 8-point scale. What, pizza is delicious, who wouldn’t eat it four times a day? And you can also get it from your phone!
It’s time for a little mass kickin’
The universe, scientists tell us, is a big place. Really big. Chromosomes, scientists tell us, are small. Really small. But despite this very fundamental difference, the universe and chromosomes share a deep, dark secret: unexplained mass.
This being a medical publication, we’ll start with chromosomes. A group of researchers measured their mass with x-rays for the first time and found that “the 46 chromosomes in each of our cells weigh 242 picograms (trillionths of a gram). This is heavier than we would expect, and, if replicated, points to unexplained excess mass in chromosomes,” Ian K. Robinson, PhD, said in a written statement.
We’re not just talking about a bit of a beer belly here. “The chromosomes were about 20 times heavier than the DNA they contained,” according to the investigators.
Now to the universe. Here’s what CERN, the European Council for Nuclear Research, has to say about the mass of the universe: “Galaxies in our universe … are rotating with such speed that the gravity generated by their observable matter could not possibly hold them together. … which leads scientists to believe that something we cannot see is at work. They think something we have yet to detect directly is giving these galaxies extra mass.”
But wait, there’s more! “The matter we know and that makes up all stars and galaxies only accounts for 5% of the content of the universe!”
So chromosomes are about 20 times heavier than the DNA they contain, and the universe is about 20 times heavier than the matter that can be seen. Interesting.
We are, of course, happy to share this news with our readers, but there is one catch: Don’t tell Neil deGrasse Tyson. He’ll want to reclassify our genetic solar system into 45 chromosomes and one dwarf chromosome.
A photo finish for the Smart Toilet
We know that poop can tell us a lot about our health, but new research by scientists at Duke University is really on a roll. Their Smart Toilet has been created to help people keep an eye on their bowel health. The device takes pictures of poop after it is flushed and can tell whether the consistency is loose, bloody, or normal.
The Smart Toilet can really help people with issues such as irritable bowel syndrome and inflammatory bowel disease by helping them, and their doctors, keep tabs on their poop. “Typically, gastroenterologists have to rely on patient self-reported information about their stool to help determine the cause of their gastrointestinal health issues, which can be very unreliable,” study lead author Deborah Fisher said.
Not many people look too closely at their poop before it’s flushed, so the fecal photos can make a big difference. The Smart Toilet is installed into the pipes of a toilet and does its thing when the toilet is flushed, so there doesn’t seem to be much work on the patient’s end. Other than the, um, you know, usual work from the patient’s end.
Subclinical myocarditis found in some athletes post COVID
Myocarditis is present in a small percentage of competitive athletes after COVID-19 infection, even in those without symptoms, new research suggests.
In a cohort study of 1,597 competitive collegiate athletes undergoing comprehensive cardiovascular testing in the United States, the prevalence of clinical myocarditis based on a symptom-based screening strategy was only 0.31%.
But screening with cardiac MRI increased the prevalence of clinical and subclinical myocarditis by a factor of 7.4, to 2.3%, the authors reported.
The findings are published online May 27, 2021, in JAMA Cardiology.
“It was the largest study to evaluate college athletes who have had COVID with extensive cardiac testing, including MRI, and this gave us a very objective look at the cardiac findings, as they were not purely based upon a subjective evaluation of symptoms,” lead investigator Curt J. Daniels, MD, professor at Ohio State University Wexner Medical Center, Columbus, said in an interview.
“Unfortunately, our study showed that athletes can be asymptomatic, or at least not report symptoms. This is a very subjective feature, and we don’t know if they don’t report symptoms because they didn’t want to get tested. That is why we took a very objective approach,” Dr. Daniels said.
The finding that more than half of the asymptomatic athletes had myocarditis, or as the investigators called it, “subclinical myocarditis,” was a surprise, he acknowledged.
“More than half of the athletes found to have myocarditis reported no symptoms, and yes, that was a surprise, because prior to this study, the protocols that had been published stated that you had to have symptoms to even enter into the protocol for cardiac MRI. But, as our ... paper shows, if we had followed that protocol, we only would have found about 5 cases of myocarditis, as opposed to the total of 37 we found with cardiac MRI,” Dr. Daniels said.
In October 2020, the American College of Cardiology’s Sports and Exercise Council recommended that cardiac MRI be limited to athletes who exhibited symptoms as part of their guide to ensuring a safe return to play.
As reported by this news organization the council recommended a tiered approach to screening based on the presence of symptoms, followed by electrocardiography, injury biomarkers, and echocardiography. Any abnormalities detected were to be further characterized by the selective use of cardiac MRI.
At the time, there were relatively few data to support the recommendations, and all stakeholders called for larger datasets to better drive informed recommendations in the future.
In the current study, Dr. Daniels and associates conducted comprehensive cardiac screening – including ECG, troponin testing, echocardiography, and cardiac MRI – of 1,597 college athlete survivors of COVID-19.
The athletes were part of the Big Ten athletic conference, which consists of 13 major American universities.
Cardiac MRI revealed that 37 (2.3%) of these athletes demonstrated diagnostic criteria for COVID-19 myocarditis; of these, 20 had no cardiovascular symptoms and had normal ECGs, echocardiography, and troponin test results.
“These patients would not have been identified without CMR imaging. If we were going according to the older protocol, we would not have made this discovery. Cardiac MRI is the most sensitive and specific test for myocardial inflammation, there is no argument about that,” Dr. Daniels said.
The catch is, cardiac MRI is expensive and often difficult to access, especially in remote, rural, or other underserviced areas.
“You can’t get an MRI for every person who has had COVID, it’s just not feasible,” Dr. Daniels said. “We are not advocating that everybody get an MRI. But we do hope that our study creates awareness among clinicians and athletes themselves that if you’ve had COVID, even if you’re asymptomatic, there may be some heart changes. So be aware when you start to exercise again, if you have any symptoms, pause and seek medical care.”
Kudos to the sports cardiology community
In an accompanying editorial, James E. Udelson, MD, Ethan J. Rowin, MD, and Barry J. Maron, MD, from the CardioVascular Center at Tufts Medical Center, Boston, applauded the sports cardiology community for its diligence in acquiring and publishing data about the post–COVID-19 prevalence of cardiac abnormalities in competitive athletes.
“It is a real tribute to the sports cardiology community. There has been an amazing growth of information, and they not only gathered this information, they analyzed and published it, starting out with a study of 29 or 30 athletes, and now thousands,” Dr. Udelson said in an interview.
At the start of the pandemic, it appeared that 15%-20% of athletes had myocarditis, and athletic conferences were discussing canceling sports events.
However, with greater numbers comes a more accurate picture of the extent of the problem.
“Once you get thousands of subjects in these studies, you can hone in on what the real number is, so now we understand that if you screen everybody with a cardiac MRI, 1%, 2%, or 3% will have some evidence of what looks like myocarditis,” he said.
Dr. Udelson agreed that doing cardiac imaging in everyone is not feasible.
“This study looked at a very large number of people who all had an MRI, but that doesn’t mean everyone should have them. If you just do an echo, an EKG, and a troponin test, and if everything is normal, which is kind of what current recommendations are, this paper tells us that we are going to miss one or two people out of a hundred, and that might be okay,” he said. “So, if you are at a huge university that has a large medical center and you want to screen all your athletes with MRI, great. But if you’re at a high school in a remote area, you know that the alternative, not having an MRI, isn’t so bad, either.”
A version of this article first appeared on Medscape.com.
Myocarditis is present in a small percentage of competitive athletes after COVID-19 infection, even in those without symptoms, new research suggests.
In a cohort study of 1,597 competitive collegiate athletes undergoing comprehensive cardiovascular testing in the United States, the prevalence of clinical myocarditis based on a symptom-based screening strategy was only 0.31%.
But screening with cardiac MRI increased the prevalence of clinical and subclinical myocarditis by a factor of 7.4, to 2.3%, the authors reported.
The findings are published online May 27, 2021, in JAMA Cardiology.
“It was the largest study to evaluate college athletes who have had COVID with extensive cardiac testing, including MRI, and this gave us a very objective look at the cardiac findings, as they were not purely based upon a subjective evaluation of symptoms,” lead investigator Curt J. Daniels, MD, professor at Ohio State University Wexner Medical Center, Columbus, said in an interview.
“Unfortunately, our study showed that athletes can be asymptomatic, or at least not report symptoms. This is a very subjective feature, and we don’t know if they don’t report symptoms because they didn’t want to get tested. That is why we took a very objective approach,” Dr. Daniels said.
The finding that more than half of the asymptomatic athletes had myocarditis, or as the investigators called it, “subclinical myocarditis,” was a surprise, he acknowledged.
“More than half of the athletes found to have myocarditis reported no symptoms, and yes, that was a surprise, because prior to this study, the protocols that had been published stated that you had to have symptoms to even enter into the protocol for cardiac MRI. But, as our ... paper shows, if we had followed that protocol, we only would have found about 5 cases of myocarditis, as opposed to the total of 37 we found with cardiac MRI,” Dr. Daniels said.
In October 2020, the American College of Cardiology’s Sports and Exercise Council recommended that cardiac MRI be limited to athletes who exhibited symptoms as part of their guide to ensuring a safe return to play.
As reported by this news organization the council recommended a tiered approach to screening based on the presence of symptoms, followed by electrocardiography, injury biomarkers, and echocardiography. Any abnormalities detected were to be further characterized by the selective use of cardiac MRI.
At the time, there were relatively few data to support the recommendations, and all stakeholders called for larger datasets to better drive informed recommendations in the future.
In the current study, Dr. Daniels and associates conducted comprehensive cardiac screening – including ECG, troponin testing, echocardiography, and cardiac MRI – of 1,597 college athlete survivors of COVID-19.
The athletes were part of the Big Ten athletic conference, which consists of 13 major American universities.
Cardiac MRI revealed that 37 (2.3%) of these athletes demonstrated diagnostic criteria for COVID-19 myocarditis; of these, 20 had no cardiovascular symptoms and had normal ECGs, echocardiography, and troponin test results.
“These patients would not have been identified without CMR imaging. If we were going according to the older protocol, we would not have made this discovery. Cardiac MRI is the most sensitive and specific test for myocardial inflammation, there is no argument about that,” Dr. Daniels said.
The catch is, cardiac MRI is expensive and often difficult to access, especially in remote, rural, or other underserviced areas.
“You can’t get an MRI for every person who has had COVID, it’s just not feasible,” Dr. Daniels said. “We are not advocating that everybody get an MRI. But we do hope that our study creates awareness among clinicians and athletes themselves that if you’ve had COVID, even if you’re asymptomatic, there may be some heart changes. So be aware when you start to exercise again, if you have any symptoms, pause and seek medical care.”
Kudos to the sports cardiology community
In an accompanying editorial, James E. Udelson, MD, Ethan J. Rowin, MD, and Barry J. Maron, MD, from the CardioVascular Center at Tufts Medical Center, Boston, applauded the sports cardiology community for its diligence in acquiring and publishing data about the post–COVID-19 prevalence of cardiac abnormalities in competitive athletes.
“It is a real tribute to the sports cardiology community. There has been an amazing growth of information, and they not only gathered this information, they analyzed and published it, starting out with a study of 29 or 30 athletes, and now thousands,” Dr. Udelson said in an interview.
At the start of the pandemic, it appeared that 15%-20% of athletes had myocarditis, and athletic conferences were discussing canceling sports events.
However, with greater numbers comes a more accurate picture of the extent of the problem.
“Once you get thousands of subjects in these studies, you can hone in on what the real number is, so now we understand that if you screen everybody with a cardiac MRI, 1%, 2%, or 3% will have some evidence of what looks like myocarditis,” he said.
Dr. Udelson agreed that doing cardiac imaging in everyone is not feasible.
“This study looked at a very large number of people who all had an MRI, but that doesn’t mean everyone should have them. If you just do an echo, an EKG, and a troponin test, and if everything is normal, which is kind of what current recommendations are, this paper tells us that we are going to miss one or two people out of a hundred, and that might be okay,” he said. “So, if you are at a huge university that has a large medical center and you want to screen all your athletes with MRI, great. But if you’re at a high school in a remote area, you know that the alternative, not having an MRI, isn’t so bad, either.”
A version of this article first appeared on Medscape.com.
Myocarditis is present in a small percentage of competitive athletes after COVID-19 infection, even in those without symptoms, new research suggests.
In a cohort study of 1,597 competitive collegiate athletes undergoing comprehensive cardiovascular testing in the United States, the prevalence of clinical myocarditis based on a symptom-based screening strategy was only 0.31%.
But screening with cardiac MRI increased the prevalence of clinical and subclinical myocarditis by a factor of 7.4, to 2.3%, the authors reported.
The findings are published online May 27, 2021, in JAMA Cardiology.
“It was the largest study to evaluate college athletes who have had COVID with extensive cardiac testing, including MRI, and this gave us a very objective look at the cardiac findings, as they were not purely based upon a subjective evaluation of symptoms,” lead investigator Curt J. Daniels, MD, professor at Ohio State University Wexner Medical Center, Columbus, said in an interview.
“Unfortunately, our study showed that athletes can be asymptomatic, or at least not report symptoms. This is a very subjective feature, and we don’t know if they don’t report symptoms because they didn’t want to get tested. That is why we took a very objective approach,” Dr. Daniels said.
The finding that more than half of the asymptomatic athletes had myocarditis, or as the investigators called it, “subclinical myocarditis,” was a surprise, he acknowledged.
“More than half of the athletes found to have myocarditis reported no symptoms, and yes, that was a surprise, because prior to this study, the protocols that had been published stated that you had to have symptoms to even enter into the protocol for cardiac MRI. But, as our ... paper shows, if we had followed that protocol, we only would have found about 5 cases of myocarditis, as opposed to the total of 37 we found with cardiac MRI,” Dr. Daniels said.
In October 2020, the American College of Cardiology’s Sports and Exercise Council recommended that cardiac MRI be limited to athletes who exhibited symptoms as part of their guide to ensuring a safe return to play.
As reported by this news organization the council recommended a tiered approach to screening based on the presence of symptoms, followed by electrocardiography, injury biomarkers, and echocardiography. Any abnormalities detected were to be further characterized by the selective use of cardiac MRI.
At the time, there were relatively few data to support the recommendations, and all stakeholders called for larger datasets to better drive informed recommendations in the future.
In the current study, Dr. Daniels and associates conducted comprehensive cardiac screening – including ECG, troponin testing, echocardiography, and cardiac MRI – of 1,597 college athlete survivors of COVID-19.
The athletes were part of the Big Ten athletic conference, which consists of 13 major American universities.
Cardiac MRI revealed that 37 (2.3%) of these athletes demonstrated diagnostic criteria for COVID-19 myocarditis; of these, 20 had no cardiovascular symptoms and had normal ECGs, echocardiography, and troponin test results.
“These patients would not have been identified without CMR imaging. If we were going according to the older protocol, we would not have made this discovery. Cardiac MRI is the most sensitive and specific test for myocardial inflammation, there is no argument about that,” Dr. Daniels said.
The catch is, cardiac MRI is expensive and often difficult to access, especially in remote, rural, or other underserviced areas.
“You can’t get an MRI for every person who has had COVID, it’s just not feasible,” Dr. Daniels said. “We are not advocating that everybody get an MRI. But we do hope that our study creates awareness among clinicians and athletes themselves that if you’ve had COVID, even if you’re asymptomatic, there may be some heart changes. So be aware when you start to exercise again, if you have any symptoms, pause and seek medical care.”
Kudos to the sports cardiology community
In an accompanying editorial, James E. Udelson, MD, Ethan J. Rowin, MD, and Barry J. Maron, MD, from the CardioVascular Center at Tufts Medical Center, Boston, applauded the sports cardiology community for its diligence in acquiring and publishing data about the post–COVID-19 prevalence of cardiac abnormalities in competitive athletes.
“It is a real tribute to the sports cardiology community. There has been an amazing growth of information, and they not only gathered this information, they analyzed and published it, starting out with a study of 29 or 30 athletes, and now thousands,” Dr. Udelson said in an interview.
At the start of the pandemic, it appeared that 15%-20% of athletes had myocarditis, and athletic conferences were discussing canceling sports events.
However, with greater numbers comes a more accurate picture of the extent of the problem.
“Once you get thousands of subjects in these studies, you can hone in on what the real number is, so now we understand that if you screen everybody with a cardiac MRI, 1%, 2%, or 3% will have some evidence of what looks like myocarditis,” he said.
Dr. Udelson agreed that doing cardiac imaging in everyone is not feasible.
“This study looked at a very large number of people who all had an MRI, but that doesn’t mean everyone should have them. If you just do an echo, an EKG, and a troponin test, and if everything is normal, which is kind of what current recommendations are, this paper tells us that we are going to miss one or two people out of a hundred, and that might be okay,” he said. “So, if you are at a huge university that has a large medical center and you want to screen all your athletes with MRI, great. But if you’re at a high school in a remote area, you know that the alternative, not having an MRI, isn’t so bad, either.”
A version of this article first appeared on Medscape.com.
DOJ charges 14 with COVID-19–related fraud nearing $150M
The U.S. Department of Justice (DOJ) on May 26 announced charges against 14 defendants across the country who allegedly engaged in health care fraud schemes that exploited the COVID-19 pandemic and resulted in over $143 million in false billings to Medicare.
Among the defendants, a DOJ news release said, were a telemedicine company executive, a physician, marketers, and medical business owners.
In addition, the Centers for Medicare and Medicaid Services separately announced that it had taken “adverse administrative actions” against more than 50 providers for their involvement in fraud schemes related to COVID-19 or the abuse of CMS programs that were designed to encourage access to medical care during the pandemic.
Several of the defendants allegedly offered COVID-19 tests to Medicare beneficiaries in senior living facilities, drive-through COVID-19 testing sites, and medical offices to induce the beneficiaries to provide their personal identifying information and a saliva or a blood sample.
The DOJ charges claim the defendants then misused the information and the samples to submit claims to Medicare for unrelated, medically unnecessary, and far more expensive lab tests, including cancer genetic testing, allergy testing, and respiratory pathogen panel tests.
In some cases, it’s alleged, the lab results were not provided to the individuals in a timely fashion or were not reliable.
Other defendants are charged with exploiting temporary changes in CMS telehealth regulations that were designed to increase access to health care during the pandemic. In these cases, which the DOJ said were the first charges related to the expansion of telehealth under the COVID-19 emergency declaration, the defendants allegedly submitted false and fraudulent claims to Medicare for sham telemedicine encounters that did not occur.
“As part of these cases, medical professionals are alleged to have [been] offered and paid bribes in exchange for the medical professionals’ referral of unnecessary testing,” the DOJ news release said. However, no physicians were identified by the department.
Commenting on this aspect of the law enforcement action, FBI Director Christopher Wray said in the release: “Medical providers have been the unsung heroes for the American public throughout the pandemic. It’s disheartening that some have abused their authorities and committed COVID-19–related fraud against trusting citizens. The FBI, along with our federal law enforcement and private sector partners, are committed to continuing to combat health care fraud and protect the American people.”
The law enforcement action includes the third set of criminal charges related to the misuse of Provider Relief Fund monies, according to the release.
More than 340 individuals were charged in September 2020 with submitting $6 billion in fraudulent claims to federal health care programs and private insurers for telehealth consultations and substance abuse treatment. About $4.5 billion of that was related to telehealth, as reported by this news organization.
The new criminal charges were brought in federal district courts in Arkansas, California, Louisiana, Florida, New Jersey, and New York.
Case summaries
The DOJ provided several case summaries. One defendant, lab owner Billy Joe Taylor of Lavaca, Ark., was charged with participating in a scheme to defraud the government of over $42 million by filing false claims that were billed in combination with COVID-19 testing claims. He also allegedly billed for tests that were not performed.
Petros Hannesyan of Burbank, Calif., the owner of a home health agency, was charged with obtaining over $229,000 from COVID-19 relief programs under false pretenses. His firm allegedly misappropriated funds from the CARES Act Provider Relief Fund and submitted false loan applications and a false loan agreement to the Economic Injury Disaster Loan Program.
Michael Stein and Leonel Palatnik of Palm Beach County, Fla., were charged in a connection with an alleged $73 million conspiracy to defraud the government and to pay and receive health care kickbacks during the pandemic.
Mr. Stein, who owned a “purported” consulting company, and Mr. Palatnik, who owned testing labs in Texas, allegedly exploited Medicare’s waiver of telehealth restrictions “by offering telehealth providers access to Medicare beneficiaries for whom they could bill consultations. In exchange, these providers agreed to refer beneficiaries to [Mr. Palatnik’s] laboratories for expensive and medically unnecessary cancer and cardiovascular genetic testing.”
A version of this article first appeared on Medscape.com.
The U.S. Department of Justice (DOJ) on May 26 announced charges against 14 defendants across the country who allegedly engaged in health care fraud schemes that exploited the COVID-19 pandemic and resulted in over $143 million in false billings to Medicare.
Among the defendants, a DOJ news release said, were a telemedicine company executive, a physician, marketers, and medical business owners.
In addition, the Centers for Medicare and Medicaid Services separately announced that it had taken “adverse administrative actions” against more than 50 providers for their involvement in fraud schemes related to COVID-19 or the abuse of CMS programs that were designed to encourage access to medical care during the pandemic.
Several of the defendants allegedly offered COVID-19 tests to Medicare beneficiaries in senior living facilities, drive-through COVID-19 testing sites, and medical offices to induce the beneficiaries to provide their personal identifying information and a saliva or a blood sample.
The DOJ charges claim the defendants then misused the information and the samples to submit claims to Medicare for unrelated, medically unnecessary, and far more expensive lab tests, including cancer genetic testing, allergy testing, and respiratory pathogen panel tests.
In some cases, it’s alleged, the lab results were not provided to the individuals in a timely fashion or were not reliable.
Other defendants are charged with exploiting temporary changes in CMS telehealth regulations that were designed to increase access to health care during the pandemic. In these cases, which the DOJ said were the first charges related to the expansion of telehealth under the COVID-19 emergency declaration, the defendants allegedly submitted false and fraudulent claims to Medicare for sham telemedicine encounters that did not occur.
“As part of these cases, medical professionals are alleged to have [been] offered and paid bribes in exchange for the medical professionals’ referral of unnecessary testing,” the DOJ news release said. However, no physicians were identified by the department.
Commenting on this aspect of the law enforcement action, FBI Director Christopher Wray said in the release: “Medical providers have been the unsung heroes for the American public throughout the pandemic. It’s disheartening that some have abused their authorities and committed COVID-19–related fraud against trusting citizens. The FBI, along with our federal law enforcement and private sector partners, are committed to continuing to combat health care fraud and protect the American people.”
The law enforcement action includes the third set of criminal charges related to the misuse of Provider Relief Fund monies, according to the release.
More than 340 individuals were charged in September 2020 with submitting $6 billion in fraudulent claims to federal health care programs and private insurers for telehealth consultations and substance abuse treatment. About $4.5 billion of that was related to telehealth, as reported by this news organization.
The new criminal charges were brought in federal district courts in Arkansas, California, Louisiana, Florida, New Jersey, and New York.
Case summaries
The DOJ provided several case summaries. One defendant, lab owner Billy Joe Taylor of Lavaca, Ark., was charged with participating in a scheme to defraud the government of over $42 million by filing false claims that were billed in combination with COVID-19 testing claims. He also allegedly billed for tests that were not performed.
Petros Hannesyan of Burbank, Calif., the owner of a home health agency, was charged with obtaining over $229,000 from COVID-19 relief programs under false pretenses. His firm allegedly misappropriated funds from the CARES Act Provider Relief Fund and submitted false loan applications and a false loan agreement to the Economic Injury Disaster Loan Program.
Michael Stein and Leonel Palatnik of Palm Beach County, Fla., were charged in a connection with an alleged $73 million conspiracy to defraud the government and to pay and receive health care kickbacks during the pandemic.
Mr. Stein, who owned a “purported” consulting company, and Mr. Palatnik, who owned testing labs in Texas, allegedly exploited Medicare’s waiver of telehealth restrictions “by offering telehealth providers access to Medicare beneficiaries for whom they could bill consultations. In exchange, these providers agreed to refer beneficiaries to [Mr. Palatnik’s] laboratories for expensive and medically unnecessary cancer and cardiovascular genetic testing.”
A version of this article first appeared on Medscape.com.
The U.S. Department of Justice (DOJ) on May 26 announced charges against 14 defendants across the country who allegedly engaged in health care fraud schemes that exploited the COVID-19 pandemic and resulted in over $143 million in false billings to Medicare.
Among the defendants, a DOJ news release said, were a telemedicine company executive, a physician, marketers, and medical business owners.
In addition, the Centers for Medicare and Medicaid Services separately announced that it had taken “adverse administrative actions” against more than 50 providers for their involvement in fraud schemes related to COVID-19 or the abuse of CMS programs that were designed to encourage access to medical care during the pandemic.
Several of the defendants allegedly offered COVID-19 tests to Medicare beneficiaries in senior living facilities, drive-through COVID-19 testing sites, and medical offices to induce the beneficiaries to provide their personal identifying information and a saliva or a blood sample.
The DOJ charges claim the defendants then misused the information and the samples to submit claims to Medicare for unrelated, medically unnecessary, and far more expensive lab tests, including cancer genetic testing, allergy testing, and respiratory pathogen panel tests.
In some cases, it’s alleged, the lab results were not provided to the individuals in a timely fashion or were not reliable.
Other defendants are charged with exploiting temporary changes in CMS telehealth regulations that were designed to increase access to health care during the pandemic. In these cases, which the DOJ said were the first charges related to the expansion of telehealth under the COVID-19 emergency declaration, the defendants allegedly submitted false and fraudulent claims to Medicare for sham telemedicine encounters that did not occur.
“As part of these cases, medical professionals are alleged to have [been] offered and paid bribes in exchange for the medical professionals’ referral of unnecessary testing,” the DOJ news release said. However, no physicians were identified by the department.
Commenting on this aspect of the law enforcement action, FBI Director Christopher Wray said in the release: “Medical providers have been the unsung heroes for the American public throughout the pandemic. It’s disheartening that some have abused their authorities and committed COVID-19–related fraud against trusting citizens. The FBI, along with our federal law enforcement and private sector partners, are committed to continuing to combat health care fraud and protect the American people.”
The law enforcement action includes the third set of criminal charges related to the misuse of Provider Relief Fund monies, according to the release.
More than 340 individuals were charged in September 2020 with submitting $6 billion in fraudulent claims to federal health care programs and private insurers for telehealth consultations and substance abuse treatment. About $4.5 billion of that was related to telehealth, as reported by this news organization.
The new criminal charges were brought in federal district courts in Arkansas, California, Louisiana, Florida, New Jersey, and New York.
Case summaries
The DOJ provided several case summaries. One defendant, lab owner Billy Joe Taylor of Lavaca, Ark., was charged with participating in a scheme to defraud the government of over $42 million by filing false claims that were billed in combination with COVID-19 testing claims. He also allegedly billed for tests that were not performed.
Petros Hannesyan of Burbank, Calif., the owner of a home health agency, was charged with obtaining over $229,000 from COVID-19 relief programs under false pretenses. His firm allegedly misappropriated funds from the CARES Act Provider Relief Fund and submitted false loan applications and a false loan agreement to the Economic Injury Disaster Loan Program.
Michael Stein and Leonel Palatnik of Palm Beach County, Fla., were charged in a connection with an alleged $73 million conspiracy to defraud the government and to pay and receive health care kickbacks during the pandemic.
Mr. Stein, who owned a “purported” consulting company, and Mr. Palatnik, who owned testing labs in Texas, allegedly exploited Medicare’s waiver of telehealth restrictions “by offering telehealth providers access to Medicare beneficiaries for whom they could bill consultations. In exchange, these providers agreed to refer beneficiaries to [Mr. Palatnik’s] laboratories for expensive and medically unnecessary cancer and cardiovascular genetic testing.”
A version of this article first appeared on Medscape.com.
Benzene found in some sunscreen products, online pharmacy says
Valisure, an online pharmacy known for testing every batch of medication it sells, announced that it has
The company tested 294 batches from 69 companies and found benzene in 27% – many in major national brands like Neutrogena and Banana Boat. Some batches contained as much as three times the emergency FDA limit of 2 parts per million.
Long-term exposure to benzene is known to cause cancer in humans.
“This is especially concerning with sunscreen because multiple FDA studies have shown that sunscreen ingredients absorb through the skin and end up in the blood at high levels,” said David Light, CEO of Valisure.
The FDA is seeking more information about the potential risks from common sunscreen ingredients.
“There is not a safe level of benzene that can exist in sunscreen products,” Christopher Bunick, MD, PhD, associate professor of dermatology at Yale University, New Haven, Conn., said in Valisure’s FDA petition. “The total mass of sunscreen required to cover and protect the human body, in single daily application or repeated applications daily, means that even benzene at 0.1 ppm in a sunscreen could expose people to excessively high nanogram amounts of benzene.”
Valisure’s testing previously led to FDA recalls of heartburn medications and hand sanitizers.
Examining sunscreen’s environmental impact
Chemicals in sunscreen may be harmful to other forms of life, too. For years, scientists have been examining whether certain chemicals in sunscreen could be causing damage to marine life, in particular the world’s coral reefs. Specific ingredients, including oxybenzone, benzophenone-1, benzophenone-8, OD-PABA, 4-methylbenzylidene camphor, 3-benzylidene camphor, nano-titanium dioxide, nano-zinc oxide, octinoxate, and octocrylene, have been identified as potential risks.
Earlier this year, the National Academies of Sciences, Engineering, and Medicine created a committee to review the existing science about the potential environmental hazards. Over the next 2 years, they’ll also consider the public health implications if people stopped using sunscreen.
Valisure’s announcement included this message: “It is important to note that not all sunscreen products contain benzene and that uncontaminated products are available, should continue to be used, and are important for protecting against potentially harmful solar radiation.”
Using sunscreen with SPF 15 every day can lower risk of squamous cell carcinoma by around 40% and melanoma by 50%. The American Academy of Dermatology recommends a broad-spectrum, water-resistant sunscreen with an SPF of 30 or higher.
A version of this article first appeared on WebMD.com.
Valisure, an online pharmacy known for testing every batch of medication it sells, announced that it has
The company tested 294 batches from 69 companies and found benzene in 27% – many in major national brands like Neutrogena and Banana Boat. Some batches contained as much as three times the emergency FDA limit of 2 parts per million.
Long-term exposure to benzene is known to cause cancer in humans.
“This is especially concerning with sunscreen because multiple FDA studies have shown that sunscreen ingredients absorb through the skin and end up in the blood at high levels,” said David Light, CEO of Valisure.
The FDA is seeking more information about the potential risks from common sunscreen ingredients.
“There is not a safe level of benzene that can exist in sunscreen products,” Christopher Bunick, MD, PhD, associate professor of dermatology at Yale University, New Haven, Conn., said in Valisure’s FDA petition. “The total mass of sunscreen required to cover and protect the human body, in single daily application or repeated applications daily, means that even benzene at 0.1 ppm in a sunscreen could expose people to excessively high nanogram amounts of benzene.”
Valisure’s testing previously led to FDA recalls of heartburn medications and hand sanitizers.
Examining sunscreen’s environmental impact
Chemicals in sunscreen may be harmful to other forms of life, too. For years, scientists have been examining whether certain chemicals in sunscreen could be causing damage to marine life, in particular the world’s coral reefs. Specific ingredients, including oxybenzone, benzophenone-1, benzophenone-8, OD-PABA, 4-methylbenzylidene camphor, 3-benzylidene camphor, nano-titanium dioxide, nano-zinc oxide, octinoxate, and octocrylene, have been identified as potential risks.
Earlier this year, the National Academies of Sciences, Engineering, and Medicine created a committee to review the existing science about the potential environmental hazards. Over the next 2 years, they’ll also consider the public health implications if people stopped using sunscreen.
Valisure’s announcement included this message: “It is important to note that not all sunscreen products contain benzene and that uncontaminated products are available, should continue to be used, and are important for protecting against potentially harmful solar radiation.”
Using sunscreen with SPF 15 every day can lower risk of squamous cell carcinoma by around 40% and melanoma by 50%. The American Academy of Dermatology recommends a broad-spectrum, water-resistant sunscreen with an SPF of 30 or higher.
A version of this article first appeared on WebMD.com.
Valisure, an online pharmacy known for testing every batch of medication it sells, announced that it has
The company tested 294 batches from 69 companies and found benzene in 27% – many in major national brands like Neutrogena and Banana Boat. Some batches contained as much as three times the emergency FDA limit of 2 parts per million.
Long-term exposure to benzene is known to cause cancer in humans.
“This is especially concerning with sunscreen because multiple FDA studies have shown that sunscreen ingredients absorb through the skin and end up in the blood at high levels,” said David Light, CEO of Valisure.
The FDA is seeking more information about the potential risks from common sunscreen ingredients.
“There is not a safe level of benzene that can exist in sunscreen products,” Christopher Bunick, MD, PhD, associate professor of dermatology at Yale University, New Haven, Conn., said in Valisure’s FDA petition. “The total mass of sunscreen required to cover and protect the human body, in single daily application or repeated applications daily, means that even benzene at 0.1 ppm in a sunscreen could expose people to excessively high nanogram amounts of benzene.”
Valisure’s testing previously led to FDA recalls of heartburn medications and hand sanitizers.
Examining sunscreen’s environmental impact
Chemicals in sunscreen may be harmful to other forms of life, too. For years, scientists have been examining whether certain chemicals in sunscreen could be causing damage to marine life, in particular the world’s coral reefs. Specific ingredients, including oxybenzone, benzophenone-1, benzophenone-8, OD-PABA, 4-methylbenzylidene camphor, 3-benzylidene camphor, nano-titanium dioxide, nano-zinc oxide, octinoxate, and octocrylene, have been identified as potential risks.
Earlier this year, the National Academies of Sciences, Engineering, and Medicine created a committee to review the existing science about the potential environmental hazards. Over the next 2 years, they’ll also consider the public health implications if people stopped using sunscreen.
Valisure’s announcement included this message: “It is important to note that not all sunscreen products contain benzene and that uncontaminated products are available, should continue to be used, and are important for protecting against potentially harmful solar radiation.”
Using sunscreen with SPF 15 every day can lower risk of squamous cell carcinoma by around 40% and melanoma by 50%. The American Academy of Dermatology recommends a broad-spectrum, water-resistant sunscreen with an SPF of 30 or higher.
A version of this article first appeared on WebMD.com.