User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Urticaria: An elusive disorder with ‘a high unmet need for treatment’
In the clinical experience of Adam Friedman, MD, when patients present with acute urticaria, the culprit is usually food, a drug, or a bug.
But in some cases, the trigger remains elusive. “We don’t always find the source, but don’t beat yourself up about it,” Dr. Friedman, professor and chair of dermatology at George Washington University, Washington, said at the ODAC Dermatology, Aesthetic, and Surgical Conference. “The basic rule is to treat patients to clearance and keep them clear.”
Chronic urticaria is characterized by plaques with a burning/itch sensation that often “move” to different locations on the body over minutes to hours, and they typically last for less than 24 hours. The plaques are often oval, round, or irregular in shape and they typically leave no postinflammatory pigmentary alteration or scarring other than from scratching.
Urticaria affects an estimated 20% of the population, Dr. Friedman said, and is more common in females than males. More than two-thirds of cases are self-limiting but 10% can persist longer than 5 years. Acute episodes are more likely to have an identifiable trigger, while chronic episodes, which last more than six weeks, typically do not. The longer the duration, the lower the chance of identifying the root cause. The foods/food products most commonly affecting children with acute urticaria include milk, egg, peanut, wheat, and soy, while the common culprits in adults are tree nuts, peanuts, and shellfish. Other triggers include the yellow food dye annatto, the red food dye carmine, contact with raw fruits or vegetables, animal saliva, and certain detergents or perfume.
“When you have no idea what the cause is for acute urticaria, I think about viral or bacterial infections, especially in children,” Dr. Friedman said, particularly mycoplasma, adenovirus, enterovirus, rotavirus, respiratory syncytial virus, Epstein-Barr virus, and cytomegalovirus. COVID-19 has also been a new etiologic source for a recent rise in acute urticaria cases.
Other causes include certain medications such as antibiotics, opiates, muscle relaxants, salicylates, and NSAIDs; stinging insects; and exposure to latex products, which can cross react with passion fruit, banana, avocado, chestnut, and kiwi. Alcohol consumption can also trigger urticaria.
“Ask patients if they have joint discomfort or pain,” Dr. Friedman advised, referring to urticaria arthritis syndrome that is typically seen more often in women than in men. “It’s rare but important, because that may distinguish for you what is needed to get those patients under control.”
which spontaneously occurs after an exposure to an external force. “The distinguishing feature here is that it doesn’t last long – 30 minutes or so – and is typically unresponsive to corticosteroids,” Dr. Friedman said. “It comes on quickly but disappears quickly whereas with chronic spontaneous urticaria, someone might be getting those wheals of flare for hours and hours.”
The most common form of physical urticaria is dermatographism, while other examples include physical urticaria resulting from exposure to cholinergic agents, heat, exercise, cold, water, sunlight, and pressure on the skin.
About half of patients with chronic urticaria are disease free within 1 year, but 20% continue to experience episodes for more than 10 years. One study found that patients with chronic spontaneous urticaria who were diagnosed at a younger age trended toward a longer disease course, and rates were higher in women, compared with men. “Perceived stress can make this worse,” Dr. Friedman added.
According to Dr. Friedman, it’s more important to ask patients targeted questions during office visits than it is to do a full workup. “I ask patients to keep a diary, which can help them identify triggers if there are any,” he said. “I also ask them to take a picture of the papules with their smartphone. There can be a genetic association, so it’s important to ask if anyone else in the family has urticaria. No routine lab tests are required unless there’s something in the history that suggests it’s worthwhile. Let the patient guide the diagnostic workup; don’t just order a million tests.”
That said, known comorbidities associated with urticaria include autoimmune disease, atopy, infections, metabolic conditions, and neoplastic disorders. “Biopsies are typically useless because this is an invisible dermatosis,” he said. “They’re useful when it’s urticarial, not urticaria, when you’re trying to figure out what it is.”
According to recently published international guidelines on urticaria, published in September 2021, the recommended first line of treatment for urticaria is with second-generation nonsedating antihistamines such as cetirizine and loratadine, up to four times the recommended dose.
Second-generation derivatives include desloratadine, levocetirizine, and fexofenadine. “I like using fexofenadine in the morning for folks who don’t tolerate cetirizine, then I’ll recommend something a little more sedating at night,” Dr. Friedman said. “We max out [the dose] by week 4. If it works, great. If not, we move on to something else.”
In late 2021, the British Association of Dermatologists also published guidelines on the treatment of chronic urticaria.
As for markers of treatment success, a study of 240 children with chronic spontaneous urticaria found that risk factors for a poor response included longer duration of disease, higher treatment step until initial disease control, and food sensitization.
Vitamin D supplementation may also add some benefit. One study of 42 adults with urticaria found that low and high doses of vitamin D added to antihistamine therapy can boost effectiveness. “This may be because vitamin D could be a marker of severity,” Dr. Friedman said. “The reality is, however, that a lot of patients don’t do well.”
Data from the large, prospective study known as AWARE (A World-Wide Antihistamine-Refractory Chronic Urticaria Patient Evaluation) found that 23% patients treated with nonsedating H1-antihistamines and 42% patients treated with up-dosed nonsedating H1-antihistamines had uncontrolled chronic spontaneous urticaria at month 24.
A second-line treatment option for patients aged 6 and older is the anti-IgE antibody omalizumab, 150-300 mg by subcutaneous injection every 4 weeks. Dr. Friedman typically uses only the 300-mg dose. “You do not need to take pretreatment serum IgE levels,” he said. “The most significant adverse event is anaphylaxis, which only affects 0.2% of patients.”
A third-line option is cyclosporine A. A dose of 3-5mg/kg per day appears to benefit about two-thirds of patients with antihistamine recalcitrant chronic urticaria. “It works fast but you can’t keep patients on it for very long,” he said.
Another third-line option is mycophenolate mofetil, which may work by inhibiting the production of autoantibodies to the high-affinity IgE receptor and/or IgE. “It does work well, especially in conjunction with antihistamines; it’s kind of a softer immunosuppressant,” he said. Methotrexate can also be used as an add-on therapy to H1 antihistamine therapy in difficult-to-treat cases.
“It’s great we have [a Food and Drug Administration]–approved biologic therapy in omalizumab and access to over-the-counter antihistamines, but there is a high unmet need for treatment,” and a need for new therapies, Dr. Friedman said. “Only about 39% achieve symptomatic control with conventional dosing of antihistamines, and 63% of nonresponders achieve symptom control with a fourfold increased dosing of antihistamines.” In addition, about 20% of patients will not respond to either standard or increased doses of antihistamines and are eligible for treatment with omalizumab. However, more than 50% of such patients experience a delay or lack of response to omalizumab. “We need innovation; we need to understand the disease better,” he said.
Dr. Friedman disclosed that he serves as a consultant and/or adviser for Loreal, La Roche Posay, Cerave, Galderma, Aveeno, Microcures, Pfizer, Novartis, Dermira, Brickell Biotech, Incyte, UCB, Janssen, Pfizer, Bristol-Myers Squibb, Almirall, Zylo Therapeutics, Hoth Therapeutics, Corbus, Greenway Therapeutics, TruPotency, and Dermavant. He is a speaker for Regeneron/Sanofi, AbbVie, Janssen, Brickell Biotech, and Incyte, and has received grants from Pfizer, the Dermatology Foundation, Incyte, and Galderma.
In the clinical experience of Adam Friedman, MD, when patients present with acute urticaria, the culprit is usually food, a drug, or a bug.
But in some cases, the trigger remains elusive. “We don’t always find the source, but don’t beat yourself up about it,” Dr. Friedman, professor and chair of dermatology at George Washington University, Washington, said at the ODAC Dermatology, Aesthetic, and Surgical Conference. “The basic rule is to treat patients to clearance and keep them clear.”
Chronic urticaria is characterized by plaques with a burning/itch sensation that often “move” to different locations on the body over minutes to hours, and they typically last for less than 24 hours. The plaques are often oval, round, or irregular in shape and they typically leave no postinflammatory pigmentary alteration or scarring other than from scratching.
Urticaria affects an estimated 20% of the population, Dr. Friedman said, and is more common in females than males. More than two-thirds of cases are self-limiting but 10% can persist longer than 5 years. Acute episodes are more likely to have an identifiable trigger, while chronic episodes, which last more than six weeks, typically do not. The longer the duration, the lower the chance of identifying the root cause. The foods/food products most commonly affecting children with acute urticaria include milk, egg, peanut, wheat, and soy, while the common culprits in adults are tree nuts, peanuts, and shellfish. Other triggers include the yellow food dye annatto, the red food dye carmine, contact with raw fruits or vegetables, animal saliva, and certain detergents or perfume.
“When you have no idea what the cause is for acute urticaria, I think about viral or bacterial infections, especially in children,” Dr. Friedman said, particularly mycoplasma, adenovirus, enterovirus, rotavirus, respiratory syncytial virus, Epstein-Barr virus, and cytomegalovirus. COVID-19 has also been a new etiologic source for a recent rise in acute urticaria cases.
Other causes include certain medications such as antibiotics, opiates, muscle relaxants, salicylates, and NSAIDs; stinging insects; and exposure to latex products, which can cross react with passion fruit, banana, avocado, chestnut, and kiwi. Alcohol consumption can also trigger urticaria.
“Ask patients if they have joint discomfort or pain,” Dr. Friedman advised, referring to urticaria arthritis syndrome that is typically seen more often in women than in men. “It’s rare but important, because that may distinguish for you what is needed to get those patients under control.”
which spontaneously occurs after an exposure to an external force. “The distinguishing feature here is that it doesn’t last long – 30 minutes or so – and is typically unresponsive to corticosteroids,” Dr. Friedman said. “It comes on quickly but disappears quickly whereas with chronic spontaneous urticaria, someone might be getting those wheals of flare for hours and hours.”
The most common form of physical urticaria is dermatographism, while other examples include physical urticaria resulting from exposure to cholinergic agents, heat, exercise, cold, water, sunlight, and pressure on the skin.
About half of patients with chronic urticaria are disease free within 1 year, but 20% continue to experience episodes for more than 10 years. One study found that patients with chronic spontaneous urticaria who were diagnosed at a younger age trended toward a longer disease course, and rates were higher in women, compared with men. “Perceived stress can make this worse,” Dr. Friedman added.
According to Dr. Friedman, it’s more important to ask patients targeted questions during office visits than it is to do a full workup. “I ask patients to keep a diary, which can help them identify triggers if there are any,” he said. “I also ask them to take a picture of the papules with their smartphone. There can be a genetic association, so it’s important to ask if anyone else in the family has urticaria. No routine lab tests are required unless there’s something in the history that suggests it’s worthwhile. Let the patient guide the diagnostic workup; don’t just order a million tests.”
That said, known comorbidities associated with urticaria include autoimmune disease, atopy, infections, metabolic conditions, and neoplastic disorders. “Biopsies are typically useless because this is an invisible dermatosis,” he said. “They’re useful when it’s urticarial, not urticaria, when you’re trying to figure out what it is.”
According to recently published international guidelines on urticaria, published in September 2021, the recommended first line of treatment for urticaria is with second-generation nonsedating antihistamines such as cetirizine and loratadine, up to four times the recommended dose.
Second-generation derivatives include desloratadine, levocetirizine, and fexofenadine. “I like using fexofenadine in the morning for folks who don’t tolerate cetirizine, then I’ll recommend something a little more sedating at night,” Dr. Friedman said. “We max out [the dose] by week 4. If it works, great. If not, we move on to something else.”
In late 2021, the British Association of Dermatologists also published guidelines on the treatment of chronic urticaria.
As for markers of treatment success, a study of 240 children with chronic spontaneous urticaria found that risk factors for a poor response included longer duration of disease, higher treatment step until initial disease control, and food sensitization.
Vitamin D supplementation may also add some benefit. One study of 42 adults with urticaria found that low and high doses of vitamin D added to antihistamine therapy can boost effectiveness. “This may be because vitamin D could be a marker of severity,” Dr. Friedman said. “The reality is, however, that a lot of patients don’t do well.”
Data from the large, prospective study known as AWARE (A World-Wide Antihistamine-Refractory Chronic Urticaria Patient Evaluation) found that 23% patients treated with nonsedating H1-antihistamines and 42% patients treated with up-dosed nonsedating H1-antihistamines had uncontrolled chronic spontaneous urticaria at month 24.
A second-line treatment option for patients aged 6 and older is the anti-IgE antibody omalizumab, 150-300 mg by subcutaneous injection every 4 weeks. Dr. Friedman typically uses only the 300-mg dose. “You do not need to take pretreatment serum IgE levels,” he said. “The most significant adverse event is anaphylaxis, which only affects 0.2% of patients.”
A third-line option is cyclosporine A. A dose of 3-5mg/kg per day appears to benefit about two-thirds of patients with antihistamine recalcitrant chronic urticaria. “It works fast but you can’t keep patients on it for very long,” he said.
Another third-line option is mycophenolate mofetil, which may work by inhibiting the production of autoantibodies to the high-affinity IgE receptor and/or IgE. “It does work well, especially in conjunction with antihistamines; it’s kind of a softer immunosuppressant,” he said. Methotrexate can also be used as an add-on therapy to H1 antihistamine therapy in difficult-to-treat cases.
“It’s great we have [a Food and Drug Administration]–approved biologic therapy in omalizumab and access to over-the-counter antihistamines, but there is a high unmet need for treatment,” and a need for new therapies, Dr. Friedman said. “Only about 39% achieve symptomatic control with conventional dosing of antihistamines, and 63% of nonresponders achieve symptom control with a fourfold increased dosing of antihistamines.” In addition, about 20% of patients will not respond to either standard or increased doses of antihistamines and are eligible for treatment with omalizumab. However, more than 50% of such patients experience a delay or lack of response to omalizumab. “We need innovation; we need to understand the disease better,” he said.
Dr. Friedman disclosed that he serves as a consultant and/or adviser for Loreal, La Roche Posay, Cerave, Galderma, Aveeno, Microcures, Pfizer, Novartis, Dermira, Brickell Biotech, Incyte, UCB, Janssen, Pfizer, Bristol-Myers Squibb, Almirall, Zylo Therapeutics, Hoth Therapeutics, Corbus, Greenway Therapeutics, TruPotency, and Dermavant. He is a speaker for Regeneron/Sanofi, AbbVie, Janssen, Brickell Biotech, and Incyte, and has received grants from Pfizer, the Dermatology Foundation, Incyte, and Galderma.
In the clinical experience of Adam Friedman, MD, when patients present with acute urticaria, the culprit is usually food, a drug, or a bug.
But in some cases, the trigger remains elusive. “We don’t always find the source, but don’t beat yourself up about it,” Dr. Friedman, professor and chair of dermatology at George Washington University, Washington, said at the ODAC Dermatology, Aesthetic, and Surgical Conference. “The basic rule is to treat patients to clearance and keep them clear.”
Chronic urticaria is characterized by plaques with a burning/itch sensation that often “move” to different locations on the body over minutes to hours, and they typically last for less than 24 hours. The plaques are often oval, round, or irregular in shape and they typically leave no postinflammatory pigmentary alteration or scarring other than from scratching.
Urticaria affects an estimated 20% of the population, Dr. Friedman said, and is more common in females than males. More than two-thirds of cases are self-limiting but 10% can persist longer than 5 years. Acute episodes are more likely to have an identifiable trigger, while chronic episodes, which last more than six weeks, typically do not. The longer the duration, the lower the chance of identifying the root cause. The foods/food products most commonly affecting children with acute urticaria include milk, egg, peanut, wheat, and soy, while the common culprits in adults are tree nuts, peanuts, and shellfish. Other triggers include the yellow food dye annatto, the red food dye carmine, contact with raw fruits or vegetables, animal saliva, and certain detergents or perfume.
“When you have no idea what the cause is for acute urticaria, I think about viral or bacterial infections, especially in children,” Dr. Friedman said, particularly mycoplasma, adenovirus, enterovirus, rotavirus, respiratory syncytial virus, Epstein-Barr virus, and cytomegalovirus. COVID-19 has also been a new etiologic source for a recent rise in acute urticaria cases.
Other causes include certain medications such as antibiotics, opiates, muscle relaxants, salicylates, and NSAIDs; stinging insects; and exposure to latex products, which can cross react with passion fruit, banana, avocado, chestnut, and kiwi. Alcohol consumption can also trigger urticaria.
“Ask patients if they have joint discomfort or pain,” Dr. Friedman advised, referring to urticaria arthritis syndrome that is typically seen more often in women than in men. “It’s rare but important, because that may distinguish for you what is needed to get those patients under control.”
which spontaneously occurs after an exposure to an external force. “The distinguishing feature here is that it doesn’t last long – 30 minutes or so – and is typically unresponsive to corticosteroids,” Dr. Friedman said. “It comes on quickly but disappears quickly whereas with chronic spontaneous urticaria, someone might be getting those wheals of flare for hours and hours.”
The most common form of physical urticaria is dermatographism, while other examples include physical urticaria resulting from exposure to cholinergic agents, heat, exercise, cold, water, sunlight, and pressure on the skin.
About half of patients with chronic urticaria are disease free within 1 year, but 20% continue to experience episodes for more than 10 years. One study found that patients with chronic spontaneous urticaria who were diagnosed at a younger age trended toward a longer disease course, and rates were higher in women, compared with men. “Perceived stress can make this worse,” Dr. Friedman added.
According to Dr. Friedman, it’s more important to ask patients targeted questions during office visits than it is to do a full workup. “I ask patients to keep a diary, which can help them identify triggers if there are any,” he said. “I also ask them to take a picture of the papules with their smartphone. There can be a genetic association, so it’s important to ask if anyone else in the family has urticaria. No routine lab tests are required unless there’s something in the history that suggests it’s worthwhile. Let the patient guide the diagnostic workup; don’t just order a million tests.”
That said, known comorbidities associated with urticaria include autoimmune disease, atopy, infections, metabolic conditions, and neoplastic disorders. “Biopsies are typically useless because this is an invisible dermatosis,” he said. “They’re useful when it’s urticarial, not urticaria, when you’re trying to figure out what it is.”
According to recently published international guidelines on urticaria, published in September 2021, the recommended first line of treatment for urticaria is with second-generation nonsedating antihistamines such as cetirizine and loratadine, up to four times the recommended dose.
Second-generation derivatives include desloratadine, levocetirizine, and fexofenadine. “I like using fexofenadine in the morning for folks who don’t tolerate cetirizine, then I’ll recommend something a little more sedating at night,” Dr. Friedman said. “We max out [the dose] by week 4. If it works, great. If not, we move on to something else.”
In late 2021, the British Association of Dermatologists also published guidelines on the treatment of chronic urticaria.
As for markers of treatment success, a study of 240 children with chronic spontaneous urticaria found that risk factors for a poor response included longer duration of disease, higher treatment step until initial disease control, and food sensitization.
Vitamin D supplementation may also add some benefit. One study of 42 adults with urticaria found that low and high doses of vitamin D added to antihistamine therapy can boost effectiveness. “This may be because vitamin D could be a marker of severity,” Dr. Friedman said. “The reality is, however, that a lot of patients don’t do well.”
Data from the large, prospective study known as AWARE (A World-Wide Antihistamine-Refractory Chronic Urticaria Patient Evaluation) found that 23% patients treated with nonsedating H1-antihistamines and 42% patients treated with up-dosed nonsedating H1-antihistamines had uncontrolled chronic spontaneous urticaria at month 24.
A second-line treatment option for patients aged 6 and older is the anti-IgE antibody omalizumab, 150-300 mg by subcutaneous injection every 4 weeks. Dr. Friedman typically uses only the 300-mg dose. “You do not need to take pretreatment serum IgE levels,” he said. “The most significant adverse event is anaphylaxis, which only affects 0.2% of patients.”
A third-line option is cyclosporine A. A dose of 3-5mg/kg per day appears to benefit about two-thirds of patients with antihistamine recalcitrant chronic urticaria. “It works fast but you can’t keep patients on it for very long,” he said.
Another third-line option is mycophenolate mofetil, which may work by inhibiting the production of autoantibodies to the high-affinity IgE receptor and/or IgE. “It does work well, especially in conjunction with antihistamines; it’s kind of a softer immunosuppressant,” he said. Methotrexate can also be used as an add-on therapy to H1 antihistamine therapy in difficult-to-treat cases.
“It’s great we have [a Food and Drug Administration]–approved biologic therapy in omalizumab and access to over-the-counter antihistamines, but there is a high unmet need for treatment,” and a need for new therapies, Dr. Friedman said. “Only about 39% achieve symptomatic control with conventional dosing of antihistamines, and 63% of nonresponders achieve symptom control with a fourfold increased dosing of antihistamines.” In addition, about 20% of patients will not respond to either standard or increased doses of antihistamines and are eligible for treatment with omalizumab. However, more than 50% of such patients experience a delay or lack of response to omalizumab. “We need innovation; we need to understand the disease better,” he said.
Dr. Friedman disclosed that he serves as a consultant and/or adviser for Loreal, La Roche Posay, Cerave, Galderma, Aveeno, Microcures, Pfizer, Novartis, Dermira, Brickell Biotech, Incyte, UCB, Janssen, Pfizer, Bristol-Myers Squibb, Almirall, Zylo Therapeutics, Hoth Therapeutics, Corbus, Greenway Therapeutics, TruPotency, and Dermavant. He is a speaker for Regeneron/Sanofi, AbbVie, Janssen, Brickell Biotech, and Incyte, and has received grants from Pfizer, the Dermatology Foundation, Incyte, and Galderma.
FROM ODAC 2022
Long COVID is real and consists of these conditions – or does it?
Loss of smell. Fatigue. Mental health challenges. Difficulty breathing and other lower respiratory diseases. Fluid and electrolyte disorders. Cardiac dysrhythmia and other nonspecific chest pains. Trouble with urination. Diabetes?
Statistically, . The data, presented at the Conference on Retroviruses and Opportunistic Infections, can be used to guide diagnoses of long COVID, and may be the guide soon at Kaiser Permanente offices, Michael Horberg, MD, executive director of research, community benefit, and Medicaid strategy at the Mid-Atlantic Permanente Research Institute, said in an interview.
“There are some real conditions you could ask about” if you were evaluating a patient who believes they have PASC, Dr. Horberg said. “And there are real conditions that are symptoms patients have but they don’t fit the PASC diagnosis.”
That list is likely to evolve as specific symptoms emerge with new variants, he said. And there’s also the nationwide Researching COVID to Enhance Recovery (RECOVER) trial being conducted by the National Institutes of Health (NIH). Dr. Horberg is withholding judgment on diabetes, though, until more data come in.
During the global pandemic, Dr. Horberg, an HIV physician by training, found himself writing policies and guidelines for Kaiser’s Mid-Atlantic States (KPMAS) COVID response. Not long after that, the reports of symptoms that have come to be called long COVID started to come in. But they were “a mishmash of things” – everything from binge eating to the skin condition vitiligo to cranial nerve impairment, along with the more common complaints like fever, insomnia, and shortness of breath.
So Dr. Horberg looked back through KPMAS patient charts and found 28,118 members who had received a positive SARS-CoV-2 PCR test result in 2020. Then he matched them 3:1 with 70,293 members who didn’t have a positive PCR. The majority were women, nearly half were younger than 50, more than 40% were Black, and 24.5% were Latinx. The majority met clinical definitions of overweight or obese and many had other chronic illnesses, including diabetes (18.7% in the COVID-positive group), chronic kidney disease (3%) and cancer (2.6%). Rates of chronic illnesses were similar between arms.
Then they went back to 4 years before each positive PCR test and looked for all the illnesses before COVID, all those that emerged within 30 days of COVID diagnosis and those illnesses that emerged between 1 and 3 months after diagnosis.
From that search, they found 15 symptoms that were more common among people who’d had COVID. In addition to the symptoms listed above, those included abdominal pain, other nervous system disorders, dizziness or vertigo, and nausea and vomiting. Then they looked at whether each patient had experienced those symptoms in the 4 years before COVID to see if they were, in fact, new diagnoses.
More than 1 in 10
About one in four people who’d had COVID reported symptoms they thought might be long COVID, but through the analysis, they found that only 13% actually developed new conditions that could be categorized as long COVID.
“When you start controlling for all those chronic conditions, a lot of symptoms fall out,” Dr. Horberg told this news organization. “Plus, when you start comparing to the COVID-negative population, especially in the first 30 days of your positive diagnosis, actually, the COVID-negative patients have essentially almost the same amount, sometimes more.”
For instance, in the first month after diagnosis, though people with COVID reported anxiety symptoms after their diagnoses, people who’d never had COVID were coming in even more often with that symptom. And although gastrointestinal disorders were common in people who’d had COVID, they were just as likely in people who had not. Nausea and vomiting were actually 19% more common in people without COVID than in those with it. And people without COVID were nearly twice as likely to develop nutritional and endocrine disorders.
In the longer run, people who’d had COVID were 25% more likely to develop dysrhythmias, 20% more likely to develop diabetes, 60% more likely to develop fatigue, 21% more likely to develop genitourinary conditions, 39% more likely to develop chest pains, and a full 3.88 times more likely to develop trouble with olfaction.
And although people who’d had COVID were numerically 5% more likely to develop both abdominal pain and vertigo, 4% more likely to develop nervous system disorders, and 1% more likely to develop anxiety disorders longer term, none of those reached statistical significance.
The only diagnosis that doesn’t make sense to Dr. Horberg is diabetes.
“At this point I don’t think it’s been fully explained,” Dr. Horberg said. “I don’t think COVID is affecting the pancreas. But I do think that these are people who probably sought medical care, who hadn’t been seeking medical care and that the findings of diabetes were incidental diagnoses.”
Still, Dr. Horberg isn’t saying never on that. “As they say, more research is needed,” he added.
Ready to define long COVID?
As an intensive care unit physician and pulmonologist, Michael Risbano, MD, assistant professor of medicine at the University of Pittsburgh, has seen a lot of COVID. As the co-manager of the medical system’s post-COVID clinic, he’s also seen a lot of people coming in for help with what could be long COVID. When he saw the data from Dr. Horberg’s presentation, at first it seemed to confirm what he’d already known. But then he looked further.
“Well, this is actually making sense,” Dr. Risbano thought. At his clinic, it’s been an ongoing challenge to tease out what symptoms existed before COVID. Unlike Kaiser, the University of Pittsburgh Medical Center is not a closed system.
“We know some people who tend to get sick [with COVID] have some underlying medical issues already,” Dr. Risbano said in an interview. “But we don’t always have a good baseline as to what they were like beforehand, so we don’t always know what’s changed.”
He said the study design here, though retrospective and based on chart review rather than prospective observation, starts to put symptoms into the larger context of a patient’s life. And the diabetes association really stood out to him. He recalled one patient who, when she was admitted to the ICU, had a hemoglobin A1c that was totally normal. But when that patient returned a few months later, her blood sugar had skyrocketed.
“It was sky-high, like 13, and she was in diabetic ketoacidosis,” he said. “I know that’s an N of 1, but my wife is a dietitian and a case manager, and she’s having a lot of people coming in with a new diagnosis of diabetes.”
Still, he said he’s not sure that the conditions the study identified should be the basis for a definition of long COVID.
“I don’t know if you can come up with a definition out of this,” he said. “But I think this is at least helpful in telling us what disease states are different pre- and post-COVID, and what sorts of diagnoses clinicians should look for when a patient comes in after having a COVID diagnosis.”
Dr. Horberg and Dr. Risbano have disclosed no relevant financial relationships. The study was funded by the National Institute of Allergy and Infectious Diseases at the National Institutes of Health.
A version of this article first appeared on Medscape.com.
Loss of smell. Fatigue. Mental health challenges. Difficulty breathing and other lower respiratory diseases. Fluid and electrolyte disorders. Cardiac dysrhythmia and other nonspecific chest pains. Trouble with urination. Diabetes?
Statistically, . The data, presented at the Conference on Retroviruses and Opportunistic Infections, can be used to guide diagnoses of long COVID, and may be the guide soon at Kaiser Permanente offices, Michael Horberg, MD, executive director of research, community benefit, and Medicaid strategy at the Mid-Atlantic Permanente Research Institute, said in an interview.
“There are some real conditions you could ask about” if you were evaluating a patient who believes they have PASC, Dr. Horberg said. “And there are real conditions that are symptoms patients have but they don’t fit the PASC diagnosis.”
That list is likely to evolve as specific symptoms emerge with new variants, he said. And there’s also the nationwide Researching COVID to Enhance Recovery (RECOVER) trial being conducted by the National Institutes of Health (NIH). Dr. Horberg is withholding judgment on diabetes, though, until more data come in.
During the global pandemic, Dr. Horberg, an HIV physician by training, found himself writing policies and guidelines for Kaiser’s Mid-Atlantic States (KPMAS) COVID response. Not long after that, the reports of symptoms that have come to be called long COVID started to come in. But they were “a mishmash of things” – everything from binge eating to the skin condition vitiligo to cranial nerve impairment, along with the more common complaints like fever, insomnia, and shortness of breath.
So Dr. Horberg looked back through KPMAS patient charts and found 28,118 members who had received a positive SARS-CoV-2 PCR test result in 2020. Then he matched them 3:1 with 70,293 members who didn’t have a positive PCR. The majority were women, nearly half were younger than 50, more than 40% were Black, and 24.5% were Latinx. The majority met clinical definitions of overweight or obese and many had other chronic illnesses, including diabetes (18.7% in the COVID-positive group), chronic kidney disease (3%) and cancer (2.6%). Rates of chronic illnesses were similar between arms.
Then they went back to 4 years before each positive PCR test and looked for all the illnesses before COVID, all those that emerged within 30 days of COVID diagnosis and those illnesses that emerged between 1 and 3 months after diagnosis.
From that search, they found 15 symptoms that were more common among people who’d had COVID. In addition to the symptoms listed above, those included abdominal pain, other nervous system disorders, dizziness or vertigo, and nausea and vomiting. Then they looked at whether each patient had experienced those symptoms in the 4 years before COVID to see if they were, in fact, new diagnoses.
More than 1 in 10
About one in four people who’d had COVID reported symptoms they thought might be long COVID, but through the analysis, they found that only 13% actually developed new conditions that could be categorized as long COVID.
“When you start controlling for all those chronic conditions, a lot of symptoms fall out,” Dr. Horberg told this news organization. “Plus, when you start comparing to the COVID-negative population, especially in the first 30 days of your positive diagnosis, actually, the COVID-negative patients have essentially almost the same amount, sometimes more.”
For instance, in the first month after diagnosis, though people with COVID reported anxiety symptoms after their diagnoses, people who’d never had COVID were coming in even more often with that symptom. And although gastrointestinal disorders were common in people who’d had COVID, they were just as likely in people who had not. Nausea and vomiting were actually 19% more common in people without COVID than in those with it. And people without COVID were nearly twice as likely to develop nutritional and endocrine disorders.
In the longer run, people who’d had COVID were 25% more likely to develop dysrhythmias, 20% more likely to develop diabetes, 60% more likely to develop fatigue, 21% more likely to develop genitourinary conditions, 39% more likely to develop chest pains, and a full 3.88 times more likely to develop trouble with olfaction.
And although people who’d had COVID were numerically 5% more likely to develop both abdominal pain and vertigo, 4% more likely to develop nervous system disorders, and 1% more likely to develop anxiety disorders longer term, none of those reached statistical significance.
The only diagnosis that doesn’t make sense to Dr. Horberg is diabetes.
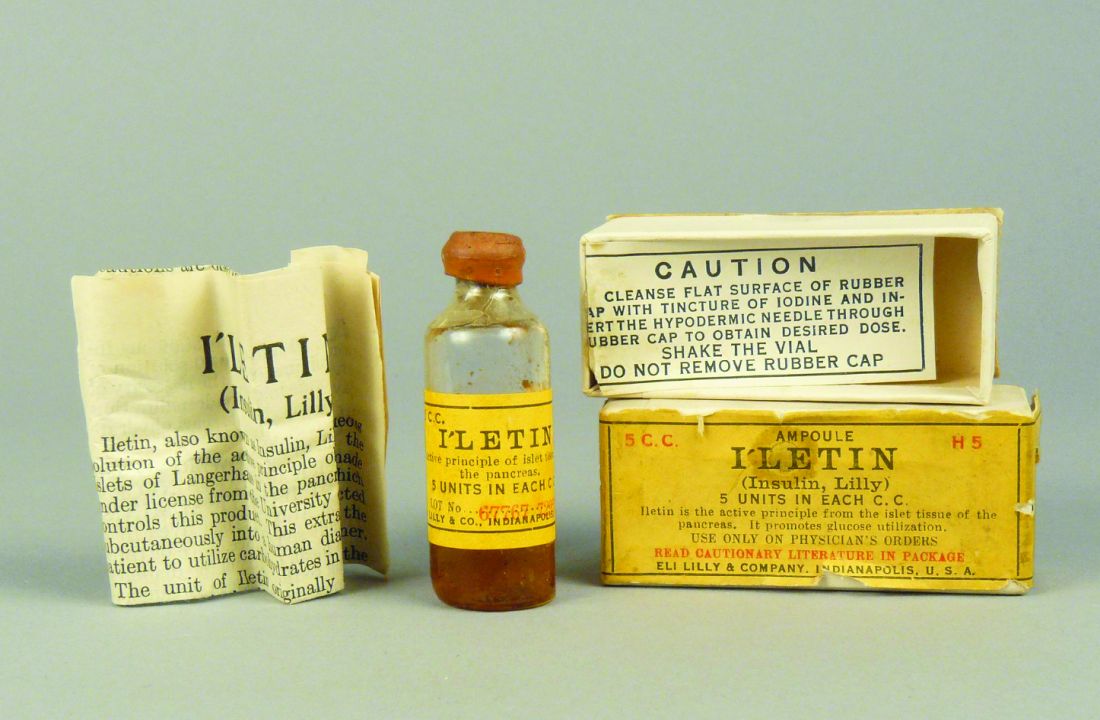
“At this point I don’t think it’s been fully explained,” Dr. Horberg said. “I don’t think COVID is affecting the pancreas. But I do think that these are people who probably sought medical care, who hadn’t been seeking medical care and that the findings of diabetes were incidental diagnoses.”
Still, Dr. Horberg isn’t saying never on that. “As they say, more research is needed,” he added.
Ready to define long COVID?
As an intensive care unit physician and pulmonologist, Michael Risbano, MD, assistant professor of medicine at the University of Pittsburgh, has seen a lot of COVID. As the co-manager of the medical system’s post-COVID clinic, he’s also seen a lot of people coming in for help with what could be long COVID. When he saw the data from Dr. Horberg’s presentation, at first it seemed to confirm what he’d already known. But then he looked further.
“Well, this is actually making sense,” Dr. Risbano thought. At his clinic, it’s been an ongoing challenge to tease out what symptoms existed before COVID. Unlike Kaiser, the University of Pittsburgh Medical Center is not a closed system.
“We know some people who tend to get sick [with COVID] have some underlying medical issues already,” Dr. Risbano said in an interview. “But we don’t always have a good baseline as to what they were like beforehand, so we don’t always know what’s changed.”
He said the study design here, though retrospective and based on chart review rather than prospective observation, starts to put symptoms into the larger context of a patient’s life. And the diabetes association really stood out to him. He recalled one patient who, when she was admitted to the ICU, had a hemoglobin A1c that was totally normal. But when that patient returned a few months later, her blood sugar had skyrocketed.
“It was sky-high, like 13, and she was in diabetic ketoacidosis,” he said. “I know that’s an N of 1, but my wife is a dietitian and a case manager, and she’s having a lot of people coming in with a new diagnosis of diabetes.”
Still, he said he’s not sure that the conditions the study identified should be the basis for a definition of long COVID.
“I don’t know if you can come up with a definition out of this,” he said. “But I think this is at least helpful in telling us what disease states are different pre- and post-COVID, and what sorts of diagnoses clinicians should look for when a patient comes in after having a COVID diagnosis.”
Dr. Horberg and Dr. Risbano have disclosed no relevant financial relationships. The study was funded by the National Institute of Allergy and Infectious Diseases at the National Institutes of Health.
A version of this article first appeared on Medscape.com.
Loss of smell. Fatigue. Mental health challenges. Difficulty breathing and other lower respiratory diseases. Fluid and electrolyte disorders. Cardiac dysrhythmia and other nonspecific chest pains. Trouble with urination. Diabetes?
Statistically, . The data, presented at the Conference on Retroviruses and Opportunistic Infections, can be used to guide diagnoses of long COVID, and may be the guide soon at Kaiser Permanente offices, Michael Horberg, MD, executive director of research, community benefit, and Medicaid strategy at the Mid-Atlantic Permanente Research Institute, said in an interview.
“There are some real conditions you could ask about” if you were evaluating a patient who believes they have PASC, Dr. Horberg said. “And there are real conditions that are symptoms patients have but they don’t fit the PASC diagnosis.”
That list is likely to evolve as specific symptoms emerge with new variants, he said. And there’s also the nationwide Researching COVID to Enhance Recovery (RECOVER) trial being conducted by the National Institutes of Health (NIH). Dr. Horberg is withholding judgment on diabetes, though, until more data come in.
During the global pandemic, Dr. Horberg, an HIV physician by training, found himself writing policies and guidelines for Kaiser’s Mid-Atlantic States (KPMAS) COVID response. Not long after that, the reports of symptoms that have come to be called long COVID started to come in. But they were “a mishmash of things” – everything from binge eating to the skin condition vitiligo to cranial nerve impairment, along with the more common complaints like fever, insomnia, and shortness of breath.
So Dr. Horberg looked back through KPMAS patient charts and found 28,118 members who had received a positive SARS-CoV-2 PCR test result in 2020. Then he matched them 3:1 with 70,293 members who didn’t have a positive PCR. The majority were women, nearly half were younger than 50, more than 40% were Black, and 24.5% were Latinx. The majority met clinical definitions of overweight or obese and many had other chronic illnesses, including diabetes (18.7% in the COVID-positive group), chronic kidney disease (3%) and cancer (2.6%). Rates of chronic illnesses were similar between arms.
Then they went back to 4 years before each positive PCR test and looked for all the illnesses before COVID, all those that emerged within 30 days of COVID diagnosis and those illnesses that emerged between 1 and 3 months after diagnosis.
From that search, they found 15 symptoms that were more common among people who’d had COVID. In addition to the symptoms listed above, those included abdominal pain, other nervous system disorders, dizziness or vertigo, and nausea and vomiting. Then they looked at whether each patient had experienced those symptoms in the 4 years before COVID to see if they were, in fact, new diagnoses.
More than 1 in 10
About one in four people who’d had COVID reported symptoms they thought might be long COVID, but through the analysis, they found that only 13% actually developed new conditions that could be categorized as long COVID.
“When you start controlling for all those chronic conditions, a lot of symptoms fall out,” Dr. Horberg told this news organization. “Plus, when you start comparing to the COVID-negative population, especially in the first 30 days of your positive diagnosis, actually, the COVID-negative patients have essentially almost the same amount, sometimes more.”
For instance, in the first month after diagnosis, though people with COVID reported anxiety symptoms after their diagnoses, people who’d never had COVID were coming in even more often with that symptom. And although gastrointestinal disorders were common in people who’d had COVID, they were just as likely in people who had not. Nausea and vomiting were actually 19% more common in people without COVID than in those with it. And people without COVID were nearly twice as likely to develop nutritional and endocrine disorders.
In the longer run, people who’d had COVID were 25% more likely to develop dysrhythmias, 20% more likely to develop diabetes, 60% more likely to develop fatigue, 21% more likely to develop genitourinary conditions, 39% more likely to develop chest pains, and a full 3.88 times more likely to develop trouble with olfaction.
And although people who’d had COVID were numerically 5% more likely to develop both abdominal pain and vertigo, 4% more likely to develop nervous system disorders, and 1% more likely to develop anxiety disorders longer term, none of those reached statistical significance.
The only diagnosis that doesn’t make sense to Dr. Horberg is diabetes.
“At this point I don’t think it’s been fully explained,” Dr. Horberg said. “I don’t think COVID is affecting the pancreas. But I do think that these are people who probably sought medical care, who hadn’t been seeking medical care and that the findings of diabetes were incidental diagnoses.”
Still, Dr. Horberg isn’t saying never on that. “As they say, more research is needed,” he added.
Ready to define long COVID?
As an intensive care unit physician and pulmonologist, Michael Risbano, MD, assistant professor of medicine at the University of Pittsburgh, has seen a lot of COVID. As the co-manager of the medical system’s post-COVID clinic, he’s also seen a lot of people coming in for help with what could be long COVID. When he saw the data from Dr. Horberg’s presentation, at first it seemed to confirm what he’d already known. But then he looked further.
“Well, this is actually making sense,” Dr. Risbano thought. At his clinic, it’s been an ongoing challenge to tease out what symptoms existed before COVID. Unlike Kaiser, the University of Pittsburgh Medical Center is not a closed system.
“We know some people who tend to get sick [with COVID] have some underlying medical issues already,” Dr. Risbano said in an interview. “But we don’t always have a good baseline as to what they were like beforehand, so we don’t always know what’s changed.”
He said the study design here, though retrospective and based on chart review rather than prospective observation, starts to put symptoms into the larger context of a patient’s life. And the diabetes association really stood out to him. He recalled one patient who, when she was admitted to the ICU, had a hemoglobin A1c that was totally normal. But when that patient returned a few months later, her blood sugar had skyrocketed.
“It was sky-high, like 13, and she was in diabetic ketoacidosis,” he said. “I know that’s an N of 1, but my wife is a dietitian and a case manager, and she’s having a lot of people coming in with a new diagnosis of diabetes.”
Still, he said he’s not sure that the conditions the study identified should be the basis for a definition of long COVID.
“I don’t know if you can come up with a definition out of this,” he said. “But I think this is at least helpful in telling us what disease states are different pre- and post-COVID, and what sorts of diagnoses clinicians should look for when a patient comes in after having a COVID diagnosis.”
Dr. Horberg and Dr. Risbano have disclosed no relevant financial relationships. The study was funded by the National Institute of Allergy and Infectious Diseases at the National Institutes of Health.
A version of this article first appeared on Medscape.com.
FROM CROI 2022
When your medical error harmed a patient and you’re wracked with guilt
Peter Schwartz, MD, was chair of the department of obstetrics and gynecology at a hospital in Reading, Pa., in the mid-1990s when a young physician sought him out. The doctor, whom Dr. Schwartz regarded as talented and empathetic, was visibly shaken. The expectant mother they were caring for had just lost her unborn child.
“The doctor came into my office within an hour of the event and asked me to look at the case,” Dr. Schwartz recalled. “I could see that they had failed to recognize ominous changes in the fetal heart rate, and I faced the pain of having to tell them, ‘I think this could have been handled much better.’” Dr. Schwartz delivered the news as compassionately as he could, but a subsequent review confirmed his suspicion: The doctor had made a serious error.
“The doctor was devastated,” he said. “She got counseling and took time off, but in the end, she quit practicing medicine. She said, ‘If I keep practicing, something like that could happen again, and I don’t think I could handle it.’”
To err may be human, but in a health care setting, the harm can be catastrophic. that their feelings of guilt, shame, and self-doubt can lead to depression, anxiety, post-traumatic stress disorder, and even suicidal ideation. The trauma can be so profound that, in a now famous 2000 editorial in the British Medical Journal, Albert Wu, MD, gave the phenomenon a name: “second victim syndrome.”
Today, as quality improvement organizations and health systems work to address medical errors in a just and transparent way, they’re realizing that finding ways to help traumatized clinicians is integral to their efforts.
Are doctors really ‘second victims?’
Although the medical field is moving away from the term “second victim,” which patient advocates argue lacks a ring of accountability, the emotional trauma doctors and other clinicians endure is garnering increased attention. In the 2 decades since Dr. Wu wrote his editorial, research has shown that many types of adverse health care events can evoke traumatic responses. In fact, studies indicate that from 10.4% to 43.3% of health care workers may experience negative symptoms following an adverse event.
But for doctors – who have sworn an oath to do no harm – the emotional toll of having committed a serious medical error can be particularly burdensome and lingering. In a Dutch study involving more than 4,300 doctors and nurses, respondents who were involved in a patient safety incident that resulted in harm were nine times more likely to have negative symptoms lasting longer than 6 months than those who were involved in a near-miss experience.
“There’s a feeling of wanting to erase yourself,” says Danielle Ofri, MD, a New York internist and author of “When We Do Harm: A Doctor Confronts Medical Error.”
That emotional response can have a profound impact on the way medical errors are disclosed, investigated, and ultimately resolved, said Thomas Gallagher, MD, an internist and executive director of the Collaborative for Accountability and Improvement, a patient safety program at the University of Washington.
“When something goes wrong, as physicians, we don’t know what to do,” Dr. Gallagher says. “We feel awful, and often our human reflexes lead us astray. The doctor’s own emotions become barriers to addressing the situation.” For example, guilt and shame may lead doctors to try to hide or diminish their mistakes. Some doctors might try to shift blame, while others may feel so guilty they assume they were responsible for an outcome that was beyond their control.
Recognizing that clinicians’ responses to medical errors are inextricably tangled with how those events are addressed, a growing number of health systems are making clinician support a key element when dealing with medical errors.
Emotional first aid
Although it’s typical for physicians to feel isolated in the wake of errors, these experiences are far from unique. Research conducted by University of Missouri Health Care nurse scientist Susan Scott, RN, PhD, shows that just as most individuals experiencing grief pass through several distinct emotional stages, health care professionals who make errors go through emotional stages that may occur sequentially or concurrently.
An initial period of chaos is often followed by intrusive reflections, haunting re-enactments, and feelings of inadequacy. The doctor’s thinking moves from “How did that happen?” to “What did I miss?” to “What will people think about me?” As the error comes under scrutiny by quality improvement organizations, licensing boards, and/or lawyers, the doctor feels besieged. The doctor may want to reach out but is afraid to. According to Dr. Scott, only 15% of care providers ask for help.
Recognizing that physicians and other care providers rarely ask for support – or may not realize they need it – a growing number of health systems are implementing Communication and Resolution Programs (CRPs). Rather than respond to medical errors with a deny-and-defend mentality, CRPs emphasize transparency and accountability.
This approach, which the Agency for Healthcare Research and Quality has embraced and codified with its Communication and Optimal Resolution (CANDOR) toolkit, focuses on prompt incident reporting; communication with and support for patients, family members, and caregivers affected by the event; event analysis; quality improvement; and just resolution of the event, including apologies and financial compensation where appropriate.
The CANDOR toolkit, which includes a module entitled Care for the Caregiver, directs health systems to identify individuals and establish teams, led by representatives from patient safety and/or risk management, who can respond promptly to an event. After ensuring the patient is clinically stable and safe, the CANDOR process provides for immediate and ongoing emotional support to the patient, the family, and the caregiver.
“A lot of what CRPs are about is creating structures and processes that normalize an open and compassionate response to harm events in medicine,” says Dr. Gallagher, who estimates that between 400 and 500 health systems now have CRPs in place.
Wisdom through adversity
While clinicians experience many difficult and negative emotions in the wake of medical errors, how they move forward after the event varies markedly. Some, unable to come to terms with the trauma, may move to another institution or leave medicine entirely. Others, while occasionally reliving the trauma, learn to cope. For the most fortunate, enduring the trauma of a medical error can lead to growth, insight, and wisdom.
In an article published in the journal Academic Medicine, researchers asked 61 physicians who had made serious medical errors, “What helped you to cope positively?” Some of the most common responses – talking about their feelings with a peer, disclosing and apologizing for a mistake, and developing system changes to prevent additional errors – are baked into some health systems’ CRP programs. Other respondents said they dedicated themselves to learning from the mistake, becoming experts in a given field, or sharing what they learned from the experience through teaching.
Dr. Ofri said that after she made an error decades ago while managing a patient with diabetic ketoacidosis, her senior resident publicly berated her for it. The incident taught her a clinical lesson: Never remove an insulin drip without administering long-acting insulin. More importantly, the resident’s verbal thumping taught her about the corrosive effects of shame. Today, Dr. Ofri, who works in a teaching hospital, says that when meeting a new medical team, she begins by recounting her five biggest medical errors.
“I want them to come to me if they make a mistake,” she says. “I want to first make sure the patient is okay. But then I want to make sure the doctor is okay. I also want to know: What was it about the system that contributed to the error, and what can we do to prevent similar errors in the future?”
Acceptance and compassion
Time, experience, supportive peers, an understanding partner or spouse: all of these can help a doctor recover from the trauma of a mistake. “But they’re not an eraser,” Dr. Schwartz said.
Sometimes, doctors say, the path forward starts with acceptance.
Jan Bonhoeffer, MD, author of “Dare to Care: How to Survive and Thrive in Today’s Medical World,” tells a story about a mistake that transformed his life. In 2004, he was working in a busy London emergency department when an adolescent girl arrived complaining of breathing trouble. Dr. Bonhoeffer diagnosed her with asthma and discharged her with an inhaler. The next day, the girl was back in the hospital – this time in the ICU, intubated, and on a ventilator. Because he had failed to take an x-ray, Dr. Bonhoeffer missed the tumor growing in the girl’s chest.
Dr. Bonhoeffer was shattered by his error. “After that experience, I knew I wanted to make learning from my mistakes part of my daily practice,” he says. Now, at the end of each workday, Dr. Bonhoeffer takes an inventory of the day and reflects on all his actions, large and small, clinical and not. “I take a few minutes and think about everything I did and what I should have done differently,” he said. The daily practice can be humbling because it forces him to confront his errors, but it is also empowering, he said, “because the next day I get to make a different choice.”
Dr. Bonhoeffer added, “Doctors are fallible, and you have to be compassionate with yourself. Compassion isn’t sweet. It’s not motherhood and honey pies. It’s coming to terms with reality. It’s not a cure, but it’s healing.”
A version of this article first appeared on Medscape.com.
Peter Schwartz, MD, was chair of the department of obstetrics and gynecology at a hospital in Reading, Pa., in the mid-1990s when a young physician sought him out. The doctor, whom Dr. Schwartz regarded as talented and empathetic, was visibly shaken. The expectant mother they were caring for had just lost her unborn child.
“The doctor came into my office within an hour of the event and asked me to look at the case,” Dr. Schwartz recalled. “I could see that they had failed to recognize ominous changes in the fetal heart rate, and I faced the pain of having to tell them, ‘I think this could have been handled much better.’” Dr. Schwartz delivered the news as compassionately as he could, but a subsequent review confirmed his suspicion: The doctor had made a serious error.
“The doctor was devastated,” he said. “She got counseling and took time off, but in the end, she quit practicing medicine. She said, ‘If I keep practicing, something like that could happen again, and I don’t think I could handle it.’”
To err may be human, but in a health care setting, the harm can be catastrophic. that their feelings of guilt, shame, and self-doubt can lead to depression, anxiety, post-traumatic stress disorder, and even suicidal ideation. The trauma can be so profound that, in a now famous 2000 editorial in the British Medical Journal, Albert Wu, MD, gave the phenomenon a name: “second victim syndrome.”
Today, as quality improvement organizations and health systems work to address medical errors in a just and transparent way, they’re realizing that finding ways to help traumatized clinicians is integral to their efforts.
Are doctors really ‘second victims?’
Although the medical field is moving away from the term “second victim,” which patient advocates argue lacks a ring of accountability, the emotional trauma doctors and other clinicians endure is garnering increased attention. In the 2 decades since Dr. Wu wrote his editorial, research has shown that many types of adverse health care events can evoke traumatic responses. In fact, studies indicate that from 10.4% to 43.3% of health care workers may experience negative symptoms following an adverse event.
But for doctors – who have sworn an oath to do no harm – the emotional toll of having committed a serious medical error can be particularly burdensome and lingering. In a Dutch study involving more than 4,300 doctors and nurses, respondents who were involved in a patient safety incident that resulted in harm were nine times more likely to have negative symptoms lasting longer than 6 months than those who were involved in a near-miss experience.
“There’s a feeling of wanting to erase yourself,” says Danielle Ofri, MD, a New York internist and author of “When We Do Harm: A Doctor Confronts Medical Error.”
That emotional response can have a profound impact on the way medical errors are disclosed, investigated, and ultimately resolved, said Thomas Gallagher, MD, an internist and executive director of the Collaborative for Accountability and Improvement, a patient safety program at the University of Washington.
“When something goes wrong, as physicians, we don’t know what to do,” Dr. Gallagher says. “We feel awful, and often our human reflexes lead us astray. The doctor’s own emotions become barriers to addressing the situation.” For example, guilt and shame may lead doctors to try to hide or diminish their mistakes. Some doctors might try to shift blame, while others may feel so guilty they assume they were responsible for an outcome that was beyond their control.
Recognizing that clinicians’ responses to medical errors are inextricably tangled with how those events are addressed, a growing number of health systems are making clinician support a key element when dealing with medical errors.
Emotional first aid
Although it’s typical for physicians to feel isolated in the wake of errors, these experiences are far from unique. Research conducted by University of Missouri Health Care nurse scientist Susan Scott, RN, PhD, shows that just as most individuals experiencing grief pass through several distinct emotional stages, health care professionals who make errors go through emotional stages that may occur sequentially or concurrently.
An initial period of chaos is often followed by intrusive reflections, haunting re-enactments, and feelings of inadequacy. The doctor’s thinking moves from “How did that happen?” to “What did I miss?” to “What will people think about me?” As the error comes under scrutiny by quality improvement organizations, licensing boards, and/or lawyers, the doctor feels besieged. The doctor may want to reach out but is afraid to. According to Dr. Scott, only 15% of care providers ask for help.
Recognizing that physicians and other care providers rarely ask for support – or may not realize they need it – a growing number of health systems are implementing Communication and Resolution Programs (CRPs). Rather than respond to medical errors with a deny-and-defend mentality, CRPs emphasize transparency and accountability.
This approach, which the Agency for Healthcare Research and Quality has embraced and codified with its Communication and Optimal Resolution (CANDOR) toolkit, focuses on prompt incident reporting; communication with and support for patients, family members, and caregivers affected by the event; event analysis; quality improvement; and just resolution of the event, including apologies and financial compensation where appropriate.
The CANDOR toolkit, which includes a module entitled Care for the Caregiver, directs health systems to identify individuals and establish teams, led by representatives from patient safety and/or risk management, who can respond promptly to an event. After ensuring the patient is clinically stable and safe, the CANDOR process provides for immediate and ongoing emotional support to the patient, the family, and the caregiver.
“A lot of what CRPs are about is creating structures and processes that normalize an open and compassionate response to harm events in medicine,” says Dr. Gallagher, who estimates that between 400 and 500 health systems now have CRPs in place.
Wisdom through adversity
While clinicians experience many difficult and negative emotions in the wake of medical errors, how they move forward after the event varies markedly. Some, unable to come to terms with the trauma, may move to another institution or leave medicine entirely. Others, while occasionally reliving the trauma, learn to cope. For the most fortunate, enduring the trauma of a medical error can lead to growth, insight, and wisdom.
In an article published in the journal Academic Medicine, researchers asked 61 physicians who had made serious medical errors, “What helped you to cope positively?” Some of the most common responses – talking about their feelings with a peer, disclosing and apologizing for a mistake, and developing system changes to prevent additional errors – are baked into some health systems’ CRP programs. Other respondents said they dedicated themselves to learning from the mistake, becoming experts in a given field, or sharing what they learned from the experience through teaching.
Dr. Ofri said that after she made an error decades ago while managing a patient with diabetic ketoacidosis, her senior resident publicly berated her for it. The incident taught her a clinical lesson: Never remove an insulin drip without administering long-acting insulin. More importantly, the resident’s verbal thumping taught her about the corrosive effects of shame. Today, Dr. Ofri, who works in a teaching hospital, says that when meeting a new medical team, she begins by recounting her five biggest medical errors.
“I want them to come to me if they make a mistake,” she says. “I want to first make sure the patient is okay. But then I want to make sure the doctor is okay. I also want to know: What was it about the system that contributed to the error, and what can we do to prevent similar errors in the future?”
Acceptance and compassion
Time, experience, supportive peers, an understanding partner or spouse: all of these can help a doctor recover from the trauma of a mistake. “But they’re not an eraser,” Dr. Schwartz said.
Sometimes, doctors say, the path forward starts with acceptance.
Jan Bonhoeffer, MD, author of “Dare to Care: How to Survive and Thrive in Today’s Medical World,” tells a story about a mistake that transformed his life. In 2004, he was working in a busy London emergency department when an adolescent girl arrived complaining of breathing trouble. Dr. Bonhoeffer diagnosed her with asthma and discharged her with an inhaler. The next day, the girl was back in the hospital – this time in the ICU, intubated, and on a ventilator. Because he had failed to take an x-ray, Dr. Bonhoeffer missed the tumor growing in the girl’s chest.
Dr. Bonhoeffer was shattered by his error. “After that experience, I knew I wanted to make learning from my mistakes part of my daily practice,” he says. Now, at the end of each workday, Dr. Bonhoeffer takes an inventory of the day and reflects on all his actions, large and small, clinical and not. “I take a few minutes and think about everything I did and what I should have done differently,” he said. The daily practice can be humbling because it forces him to confront his errors, but it is also empowering, he said, “because the next day I get to make a different choice.”
Dr. Bonhoeffer added, “Doctors are fallible, and you have to be compassionate with yourself. Compassion isn’t sweet. It’s not motherhood and honey pies. It’s coming to terms with reality. It’s not a cure, but it’s healing.”
A version of this article first appeared on Medscape.com.
Peter Schwartz, MD, was chair of the department of obstetrics and gynecology at a hospital in Reading, Pa., in the mid-1990s when a young physician sought him out. The doctor, whom Dr. Schwartz regarded as talented and empathetic, was visibly shaken. The expectant mother they were caring for had just lost her unborn child.
“The doctor came into my office within an hour of the event and asked me to look at the case,” Dr. Schwartz recalled. “I could see that they had failed to recognize ominous changes in the fetal heart rate, and I faced the pain of having to tell them, ‘I think this could have been handled much better.’” Dr. Schwartz delivered the news as compassionately as he could, but a subsequent review confirmed his suspicion: The doctor had made a serious error.
“The doctor was devastated,” he said. “She got counseling and took time off, but in the end, she quit practicing medicine. She said, ‘If I keep practicing, something like that could happen again, and I don’t think I could handle it.’”
To err may be human, but in a health care setting, the harm can be catastrophic. that their feelings of guilt, shame, and self-doubt can lead to depression, anxiety, post-traumatic stress disorder, and even suicidal ideation. The trauma can be so profound that, in a now famous 2000 editorial in the British Medical Journal, Albert Wu, MD, gave the phenomenon a name: “second victim syndrome.”
Today, as quality improvement organizations and health systems work to address medical errors in a just and transparent way, they’re realizing that finding ways to help traumatized clinicians is integral to their efforts.
Are doctors really ‘second victims?’
Although the medical field is moving away from the term “second victim,” which patient advocates argue lacks a ring of accountability, the emotional trauma doctors and other clinicians endure is garnering increased attention. In the 2 decades since Dr. Wu wrote his editorial, research has shown that many types of adverse health care events can evoke traumatic responses. In fact, studies indicate that from 10.4% to 43.3% of health care workers may experience negative symptoms following an adverse event.
But for doctors – who have sworn an oath to do no harm – the emotional toll of having committed a serious medical error can be particularly burdensome and lingering. In a Dutch study involving more than 4,300 doctors and nurses, respondents who were involved in a patient safety incident that resulted in harm were nine times more likely to have negative symptoms lasting longer than 6 months than those who were involved in a near-miss experience.
“There’s a feeling of wanting to erase yourself,” says Danielle Ofri, MD, a New York internist and author of “When We Do Harm: A Doctor Confronts Medical Error.”
That emotional response can have a profound impact on the way medical errors are disclosed, investigated, and ultimately resolved, said Thomas Gallagher, MD, an internist and executive director of the Collaborative for Accountability and Improvement, a patient safety program at the University of Washington.
“When something goes wrong, as physicians, we don’t know what to do,” Dr. Gallagher says. “We feel awful, and often our human reflexes lead us astray. The doctor’s own emotions become barriers to addressing the situation.” For example, guilt and shame may lead doctors to try to hide or diminish their mistakes. Some doctors might try to shift blame, while others may feel so guilty they assume they were responsible for an outcome that was beyond their control.
Recognizing that clinicians’ responses to medical errors are inextricably tangled with how those events are addressed, a growing number of health systems are making clinician support a key element when dealing with medical errors.
Emotional first aid
Although it’s typical for physicians to feel isolated in the wake of errors, these experiences are far from unique. Research conducted by University of Missouri Health Care nurse scientist Susan Scott, RN, PhD, shows that just as most individuals experiencing grief pass through several distinct emotional stages, health care professionals who make errors go through emotional stages that may occur sequentially or concurrently.
An initial period of chaos is often followed by intrusive reflections, haunting re-enactments, and feelings of inadequacy. The doctor’s thinking moves from “How did that happen?” to “What did I miss?” to “What will people think about me?” As the error comes under scrutiny by quality improvement organizations, licensing boards, and/or lawyers, the doctor feels besieged. The doctor may want to reach out but is afraid to. According to Dr. Scott, only 15% of care providers ask for help.
Recognizing that physicians and other care providers rarely ask for support – or may not realize they need it – a growing number of health systems are implementing Communication and Resolution Programs (CRPs). Rather than respond to medical errors with a deny-and-defend mentality, CRPs emphasize transparency and accountability.
This approach, which the Agency for Healthcare Research and Quality has embraced and codified with its Communication and Optimal Resolution (CANDOR) toolkit, focuses on prompt incident reporting; communication with and support for patients, family members, and caregivers affected by the event; event analysis; quality improvement; and just resolution of the event, including apologies and financial compensation where appropriate.
The CANDOR toolkit, which includes a module entitled Care for the Caregiver, directs health systems to identify individuals and establish teams, led by representatives from patient safety and/or risk management, who can respond promptly to an event. After ensuring the patient is clinically stable and safe, the CANDOR process provides for immediate and ongoing emotional support to the patient, the family, and the caregiver.
“A lot of what CRPs are about is creating structures and processes that normalize an open and compassionate response to harm events in medicine,” says Dr. Gallagher, who estimates that between 400 and 500 health systems now have CRPs in place.
Wisdom through adversity
While clinicians experience many difficult and negative emotions in the wake of medical errors, how they move forward after the event varies markedly. Some, unable to come to terms with the trauma, may move to another institution or leave medicine entirely. Others, while occasionally reliving the trauma, learn to cope. For the most fortunate, enduring the trauma of a medical error can lead to growth, insight, and wisdom.
In an article published in the journal Academic Medicine, researchers asked 61 physicians who had made serious medical errors, “What helped you to cope positively?” Some of the most common responses – talking about their feelings with a peer, disclosing and apologizing for a mistake, and developing system changes to prevent additional errors – are baked into some health systems’ CRP programs. Other respondents said they dedicated themselves to learning from the mistake, becoming experts in a given field, or sharing what they learned from the experience through teaching.
Dr. Ofri said that after she made an error decades ago while managing a patient with diabetic ketoacidosis, her senior resident publicly berated her for it. The incident taught her a clinical lesson: Never remove an insulin drip without administering long-acting insulin. More importantly, the resident’s verbal thumping taught her about the corrosive effects of shame. Today, Dr. Ofri, who works in a teaching hospital, says that when meeting a new medical team, she begins by recounting her five biggest medical errors.
“I want them to come to me if they make a mistake,” she says. “I want to first make sure the patient is okay. But then I want to make sure the doctor is okay. I also want to know: What was it about the system that contributed to the error, and what can we do to prevent similar errors in the future?”
Acceptance and compassion
Time, experience, supportive peers, an understanding partner or spouse: all of these can help a doctor recover from the trauma of a mistake. “But they’re not an eraser,” Dr. Schwartz said.
Sometimes, doctors say, the path forward starts with acceptance.
Jan Bonhoeffer, MD, author of “Dare to Care: How to Survive and Thrive in Today’s Medical World,” tells a story about a mistake that transformed his life. In 2004, he was working in a busy London emergency department when an adolescent girl arrived complaining of breathing trouble. Dr. Bonhoeffer diagnosed her with asthma and discharged her with an inhaler. The next day, the girl was back in the hospital – this time in the ICU, intubated, and on a ventilator. Because he had failed to take an x-ray, Dr. Bonhoeffer missed the tumor growing in the girl’s chest.
Dr. Bonhoeffer was shattered by his error. “After that experience, I knew I wanted to make learning from my mistakes part of my daily practice,” he says. Now, at the end of each workday, Dr. Bonhoeffer takes an inventory of the day and reflects on all his actions, large and small, clinical and not. “I take a few minutes and think about everything I did and what I should have done differently,” he said. The daily practice can be humbling because it forces him to confront his errors, but it is also empowering, he said, “because the next day I get to make a different choice.”
Dr. Bonhoeffer added, “Doctors are fallible, and you have to be compassionate with yourself. Compassion isn’t sweet. It’s not motherhood and honey pies. It’s coming to terms with reality. It’s not a cure, but it’s healing.”
A version of this article first appeared on Medscape.com.
AAP approves CDC’s child/adolescent vax schedule for 2022
In a policy statement published online Feb. 17 in Pediatrics, the AAP said the updated recommendations differ little from those released last year by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention.
“The only significant change this year was to add the dengue vaccine to the schedule,” Sean T. O’Leary, MD, MPH, vice chair of the AAP’s 2021-2022 Committee on Infectious Diseases and a coauthor of the statement, told this news organization. “But that is really only relevant for children living in endemic areas, primarily Puerto Rico but some other smaller U.S .territories as well.”
Dengue fever also is endemic in American Samoa and the U.S. Virgin Islands.
Notably, a new section has been added on routine recommendations for use of the Dengvaxia vaccine.
The 2022 policy statement addresses regular immunization of children from birth to 18 years and catch-up vaccination for those aged 4 months to 18 years. In addition to the AAP, multiple complementary physician and nurse organizations have approved the updates. The ACIP schedule is revised annually to reflect current recommendations on vaccines licensed by the U.S. Food and Drug Administration.
Most of the other changes this year involve minor updates to clarify language or improve usability. “CDC and AAP are always working to make the schedule as user-friendly as possible, with improvements made every year,” Dr. O’Leary, professor of pediatric infectious diseases at the University of Colorado at Denver, Aurora, said.
In terms of physician acceptance, he added, “I don’t think any of the changes would be considered controversial.”
Among other updates and clarifications:
- For Haemophilus influenzae type b (Hib) vaccination, the text now includes recommendations for the hexavalent Vaxelis vaccine (diphtheria, tetanus, pertussis, polio, Hib, and hepatitis B) for both routine and catch-up vaccination.
- For hepatitis A, the relevant note has been updated to clarify the age for routine vaccination.
- For human papillomavirus (HPV), the note now clarifies when an HPV series is complete with no additional dose recommended.
- The special situations section has been amended to specify which persons with immunocompromising conditions such as HIV should receive three doses of HPV vaccine regardless of age at initial vaccination.
- For measles, mumps, and rubella, routine vaccination now includes recommendations on the combination measles, mumps, rubella, and varicella vaccine.
- For meningococcal serogroup A, C, W, and Y vaccines, the augmented text explains when these can be simultaneously administered with serogroup B meningococcal vaccines, preferably at different anatomic sites. The language for the dosing schedule for Menveo vaccination in infants also has been clarified.
- In the catch-up immunization schedule for late-starting children aged 4 months to 18 years, the text on Hib has been changed so that the minimum interval between dose two and dose three now refers to Vaxelis, while reference to the discontinued Comvax (Hib-Hep B) vaccine has been removed.
As in other years, graphic changes have been made to table coloration and layout to improve accessibility. And as before, the 2022 childhood and adolescent immunization schedule has been updated to ensure consistency between its format and that of the 2022 adult immunization schedules.
The AAP committee stressed that clinically significant adverse events after immunization should be reported to the Vaccine Adverse Event Reporting System.
The full 2022 schedule can be found on the CDC’s website.
A version of this article first appeared on Medscape.com.
In a policy statement published online Feb. 17 in Pediatrics, the AAP said the updated recommendations differ little from those released last year by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention.
“The only significant change this year was to add the dengue vaccine to the schedule,” Sean T. O’Leary, MD, MPH, vice chair of the AAP’s 2021-2022 Committee on Infectious Diseases and a coauthor of the statement, told this news organization. “But that is really only relevant for children living in endemic areas, primarily Puerto Rico but some other smaller U.S .territories as well.”
Dengue fever also is endemic in American Samoa and the U.S. Virgin Islands.
Notably, a new section has been added on routine recommendations for use of the Dengvaxia vaccine.
The 2022 policy statement addresses regular immunization of children from birth to 18 years and catch-up vaccination for those aged 4 months to 18 years. In addition to the AAP, multiple complementary physician and nurse organizations have approved the updates. The ACIP schedule is revised annually to reflect current recommendations on vaccines licensed by the U.S. Food and Drug Administration.
Most of the other changes this year involve minor updates to clarify language or improve usability. “CDC and AAP are always working to make the schedule as user-friendly as possible, with improvements made every year,” Dr. O’Leary, professor of pediatric infectious diseases at the University of Colorado at Denver, Aurora, said.
In terms of physician acceptance, he added, “I don’t think any of the changes would be considered controversial.”
Among other updates and clarifications:
- For Haemophilus influenzae type b (Hib) vaccination, the text now includes recommendations for the hexavalent Vaxelis vaccine (diphtheria, tetanus, pertussis, polio, Hib, and hepatitis B) for both routine and catch-up vaccination.
- For hepatitis A, the relevant note has been updated to clarify the age for routine vaccination.
- For human papillomavirus (HPV), the note now clarifies when an HPV series is complete with no additional dose recommended.
- The special situations section has been amended to specify which persons with immunocompromising conditions such as HIV should receive three doses of HPV vaccine regardless of age at initial vaccination.
- For measles, mumps, and rubella, routine vaccination now includes recommendations on the combination measles, mumps, rubella, and varicella vaccine.
- For meningococcal serogroup A, C, W, and Y vaccines, the augmented text explains when these can be simultaneously administered with serogroup B meningococcal vaccines, preferably at different anatomic sites. The language for the dosing schedule for Menveo vaccination in infants also has been clarified.
- In the catch-up immunization schedule for late-starting children aged 4 months to 18 years, the text on Hib has been changed so that the minimum interval between dose two and dose three now refers to Vaxelis, while reference to the discontinued Comvax (Hib-Hep B) vaccine has been removed.
As in other years, graphic changes have been made to table coloration and layout to improve accessibility. And as before, the 2022 childhood and adolescent immunization schedule has been updated to ensure consistency between its format and that of the 2022 adult immunization schedules.
The AAP committee stressed that clinically significant adverse events after immunization should be reported to the Vaccine Adverse Event Reporting System.
The full 2022 schedule can be found on the CDC’s website.
A version of this article first appeared on Medscape.com.
In a policy statement published online Feb. 17 in Pediatrics, the AAP said the updated recommendations differ little from those released last year by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention.
“The only significant change this year was to add the dengue vaccine to the schedule,” Sean T. O’Leary, MD, MPH, vice chair of the AAP’s 2021-2022 Committee on Infectious Diseases and a coauthor of the statement, told this news organization. “But that is really only relevant for children living in endemic areas, primarily Puerto Rico but some other smaller U.S .territories as well.”
Dengue fever also is endemic in American Samoa and the U.S. Virgin Islands.
Notably, a new section has been added on routine recommendations for use of the Dengvaxia vaccine.
The 2022 policy statement addresses regular immunization of children from birth to 18 years and catch-up vaccination for those aged 4 months to 18 years. In addition to the AAP, multiple complementary physician and nurse organizations have approved the updates. The ACIP schedule is revised annually to reflect current recommendations on vaccines licensed by the U.S. Food and Drug Administration.
Most of the other changes this year involve minor updates to clarify language or improve usability. “CDC and AAP are always working to make the schedule as user-friendly as possible, with improvements made every year,” Dr. O’Leary, professor of pediatric infectious diseases at the University of Colorado at Denver, Aurora, said.
In terms of physician acceptance, he added, “I don’t think any of the changes would be considered controversial.”
Among other updates and clarifications:
- For Haemophilus influenzae type b (Hib) vaccination, the text now includes recommendations for the hexavalent Vaxelis vaccine (diphtheria, tetanus, pertussis, polio, Hib, and hepatitis B) for both routine and catch-up vaccination.
- For hepatitis A, the relevant note has been updated to clarify the age for routine vaccination.
- For human papillomavirus (HPV), the note now clarifies when an HPV series is complete with no additional dose recommended.
- The special situations section has been amended to specify which persons with immunocompromising conditions such as HIV should receive three doses of HPV vaccine regardless of age at initial vaccination.
- For measles, mumps, and rubella, routine vaccination now includes recommendations on the combination measles, mumps, rubella, and varicella vaccine.
- For meningococcal serogroup A, C, W, and Y vaccines, the augmented text explains when these can be simultaneously administered with serogroup B meningococcal vaccines, preferably at different anatomic sites. The language for the dosing schedule for Menveo vaccination in infants also has been clarified.
- In the catch-up immunization schedule for late-starting children aged 4 months to 18 years, the text on Hib has been changed so that the minimum interval between dose two and dose three now refers to Vaxelis, while reference to the discontinued Comvax (Hib-Hep B) vaccine has been removed.
As in other years, graphic changes have been made to table coloration and layout to improve accessibility. And as before, the 2022 childhood and adolescent immunization schedule has been updated to ensure consistency between its format and that of the 2022 adult immunization schedules.
The AAP committee stressed that clinically significant adverse events after immunization should be reported to the Vaccine Adverse Event Reporting System.
The full 2022 schedule can be found on the CDC’s website.
A version of this article first appeared on Medscape.com.
Thirty-seven percent of COVID-19 patients lose sense of taste, study says
, according to a new study.
Many COVID-19 patients report losing their sense of taste as well as their sense of smell, but scientists have been skeptical because the two senses are closely related and it was relatively rare for people to lose their taste sense before the COVID pandemic, says the Monell Chemical Senses Center, a nonprofit research institute in Philadelphia.
But a new Monell Center analysis found that 37% – or about four in every 10 -- of COVID-19 patients actually did lose their sense of taste and that “reports of taste loss are in fact genuine and distinguishable from smell loss.”
Taste dysfunction can be total taste loss, partial taste loss, and taste distortion. It’s an “underrated” symptom that could help doctors better treat COVID patients, the Monell Center said in a news release.
“It is time to turn to the tongue” to learn why taste is affected and to start on how to reverse or repair the loss, said Mackenzie Hannum, PhD, an author of the report and a postdoctoral fellow in the lab of Danielle Reed, PhD.
Researchers looked at data regarding 138,785 COVID patients from 241 studies that assessed taste loss and were published between May 15, 2020, and June 1, 2021. Of those patients, 32,918 said they had some form of taste loss. Further, female patients were more likely than males to lose their sense of taste, and people 36-50 years old had the highest rate of taste loss.
The information came from self-reports and direct reports.
“Self-reports are more subjective and can be in the form of questionnaires, interviews, health records, for example,” Dr. Hannum said. “On the other hand, direct measures of taste are more objective. They are conducted using testing kits that contain various sweet, salty, and sometimes bitter and sour solutions given to participants via drops, strips, or sprays.”
Though self-reports were subjective, they proved just as good as direct reports at detecting taste loss, the study said.
“Here self-reports are backed up by direct measures, proving that loss of taste is a real, distinct symptom of COVID-19 that is not to be confused with smell loss,” said study co-author Vicente Ramirez, a visiting scientist at Monell and a doctoral student at the University of California, Merced.
A version of this article first appeared on WebMD.com.
, according to a new study.
Many COVID-19 patients report losing their sense of taste as well as their sense of smell, but scientists have been skeptical because the two senses are closely related and it was relatively rare for people to lose their taste sense before the COVID pandemic, says the Monell Chemical Senses Center, a nonprofit research institute in Philadelphia.
But a new Monell Center analysis found that 37% – or about four in every 10 -- of COVID-19 patients actually did lose their sense of taste and that “reports of taste loss are in fact genuine and distinguishable from smell loss.”
Taste dysfunction can be total taste loss, partial taste loss, and taste distortion. It’s an “underrated” symptom that could help doctors better treat COVID patients, the Monell Center said in a news release.
“It is time to turn to the tongue” to learn why taste is affected and to start on how to reverse or repair the loss, said Mackenzie Hannum, PhD, an author of the report and a postdoctoral fellow in the lab of Danielle Reed, PhD.
Researchers looked at data regarding 138,785 COVID patients from 241 studies that assessed taste loss and were published between May 15, 2020, and June 1, 2021. Of those patients, 32,918 said they had some form of taste loss. Further, female patients were more likely than males to lose their sense of taste, and people 36-50 years old had the highest rate of taste loss.
The information came from self-reports and direct reports.
“Self-reports are more subjective and can be in the form of questionnaires, interviews, health records, for example,” Dr. Hannum said. “On the other hand, direct measures of taste are more objective. They are conducted using testing kits that contain various sweet, salty, and sometimes bitter and sour solutions given to participants via drops, strips, or sprays.”
Though self-reports were subjective, they proved just as good as direct reports at detecting taste loss, the study said.
“Here self-reports are backed up by direct measures, proving that loss of taste is a real, distinct symptom of COVID-19 that is not to be confused with smell loss,” said study co-author Vicente Ramirez, a visiting scientist at Monell and a doctoral student at the University of California, Merced.
A version of this article first appeared on WebMD.com.
, according to a new study.
Many COVID-19 patients report losing their sense of taste as well as their sense of smell, but scientists have been skeptical because the two senses are closely related and it was relatively rare for people to lose their taste sense before the COVID pandemic, says the Monell Chemical Senses Center, a nonprofit research institute in Philadelphia.
But a new Monell Center analysis found that 37% – or about four in every 10 -- of COVID-19 patients actually did lose their sense of taste and that “reports of taste loss are in fact genuine and distinguishable from smell loss.”
Taste dysfunction can be total taste loss, partial taste loss, and taste distortion. It’s an “underrated” symptom that could help doctors better treat COVID patients, the Monell Center said in a news release.
“It is time to turn to the tongue” to learn why taste is affected and to start on how to reverse or repair the loss, said Mackenzie Hannum, PhD, an author of the report and a postdoctoral fellow in the lab of Danielle Reed, PhD.
Researchers looked at data regarding 138,785 COVID patients from 241 studies that assessed taste loss and were published between May 15, 2020, and June 1, 2021. Of those patients, 32,918 said they had some form of taste loss. Further, female patients were more likely than males to lose their sense of taste, and people 36-50 years old had the highest rate of taste loss.
The information came from self-reports and direct reports.
“Self-reports are more subjective and can be in the form of questionnaires, interviews, health records, for example,” Dr. Hannum said. “On the other hand, direct measures of taste are more objective. They are conducted using testing kits that contain various sweet, salty, and sometimes bitter and sour solutions given to participants via drops, strips, or sprays.”
Though self-reports were subjective, they proved just as good as direct reports at detecting taste loss, the study said.
“Here self-reports are backed up by direct measures, proving that loss of taste is a real, distinct symptom of COVID-19 that is not to be confused with smell loss,” said study co-author Vicente Ramirez, a visiting scientist at Monell and a doctoral student at the University of California, Merced.
A version of this article first appeared on WebMD.com.
FROM CHEMICAL SENSES
Why is vitamin D hype so impervious to evidence?
The vitamin D story exudes teaching points: It offers a master class in critical appraisal, connecting the concepts of biologic plausibility, flawed surrogate markers, confounded observational studies, and slews of randomized controlled trials (RCTs) showing no benefits on health outcomes.
Yet despite the utter lack of benefit seen in trials, the hype continues. And the pandemic has only enhanced this hype as an onslaught of papers have reported the association of low vitamin D levels and COVID-19 disease.
My questions are simple: Why doesn’t the evidence persuade people? How many nonsignificant trials do we need before researchers stop studying vitamin D, doctors stop (routinely) measuring levels, and patients stop wasting money on the unhelpful supplement? What are the implications for this lack of persuasion?
Before exploring these questions, I want to set out that symptomatic vitamin deficiencies of any sort ought to be corrected.
Biologic plausibility and the pull of observational studies
It has long been known that vitamin D is crucial for bone health and that it can be produced in the skin with sun exposure. In the last decade, however, experts note that nearly every tissue and cell in our body has a vitamin D receptor. It then follows that if this many cells in the body can activate vitamin D, it must be vital for cardiovascular health, immune function, cancer prevention: basically, everything health related.
Oodles of observational studies have found that low serum levels of vitamin D correlate with higher mortality from all causes, cancer, cardiovascular disease, and now even COVID-19. Yet no matter the amount of statistical adjustment in these studies, we cannot know whether these associations are due to true causality.
The major issue is confounding: That is, people with low vitamin D levels have other conditions or diseases that lead to higher rates of ill health. Consider a patient with obesity, arthritis, and cognitive decline; this person is unlikely to do much exercise in the sun and may have low vitamin D levels. The low vitamin D level is simply a marker of overall poor health.
The randomized controlled trials tell a clear story
There are hundreds of vitamin D RCTs. The results simplify into one sentence: Vitamin D supplements do not improve health outcomes.
Here is a short summary of some recent studies.
VITAL, a massive (N > 25,000) RCT with 5 years of follow-up, compared vitamin D supplements to placebo and found no differences in the primary endpoints of cancer or cardiac events. Rates of death from any cause were nearly identical. Crucially, in subgroup analyses, the effects did not vary according to vitamin D levels at baseline.
The D-Health investigators randomly assigned more than 21,000 adults to vitamin D or placebo and after 5.7 years of follow-up reported no differences in the primary endpoint of overall mortality. There also were no differences in cardiovascular disease mortality.
Then you have the Mendelian randomized studies, which some have called nature’s RCT. These studies take advantage of the fact that some people are born with gene variations that predispose to low vitamin D levels. More than 60 Mendelian randomization studies have evaluated the consequences of lifelong genetically lowered vitamin D levels on various outcomes; most of these have found null effects.
Then there are the meta-analyses and systematic reviews. I loved the conclusion of this review of systematic reviews from the BMJ (emphasis mine):
“Despite a few hundred systematic reviews and meta-analyses, highly convincing evidence of a clear role of vitamin D does not exist for any outcome, but associations with a selection of outcomes are probable.”
The failure to persuade
My original plan was to emphasize the power of the RCT. Despite strong associations of low vitamin D levels with poor outcomes, the trials show no benefit to treatment. This strongly suggests (or nearly proves) that low vitamin D levels are akin to premature ventricular complexes after myocardial infarction: a marker for risk but not a target for therapy.
But I now see the more important issue as why scientists, funders, clinicians, and patients are not persuaded by clear evidence. Every day in clinic I see patients on vitamin D supplements; the journals keep publishing vitamin D studies. The proponents of vitamin D remain positive. And lately there is outsized attention and hope that vitamin D will mitigate SARS-CoV2 infection – based only on observational data.
You might argue against this point by saying vitamin D is natural and relatively innocuous, so who cares?
I offer three rebuttals to that point: Opportunity costs, distraction, and the insidious danger of poor critical appraisal skills. If you are burning money on vitamin D research, there is less available to study other important issues. If a patient is distracted by low vitamin D levels, she may pay less attention to her high body mass index or hypertension. And on the matter of critical appraisal, trust in medicine requires clinicians to be competent in critical appraisal. And these days, what could be more important than trust in medical professionals?
One major reason for the failure of persuasion of evidence is spin – or language that distracts from the primary endpoint. Here are two (of many) examples:
A meta-analysis of 50 vitamin D trials set out to study mortality. The authors found no significant difference in that primary endpoint. But the second sentence in their conclusion was that vitamin D supplements reduced the risk for cancer deaths by 15%. That’s a secondary endpoint in a study with nonsignificance in the primary endpoint. That is spin. This meta-analysis was completed before the Australian D-Health trial found that cancer deaths were 15% higher in the vitamin D arm, a difference that did not reach statistical significance.
The following example is worse: The authors of the VITAL trial, which found that vitamin D supplements had no effect on the primary endpoint of invasive cancer or cardiovascular disease, published a secondary analysis of the trial looking at a different endpoint: A composite incidence of metastatic and fatal invasive total cancer. They reported a 0.4% lower rate for the vitamin D group, a difference that barely made statistical significance at a P value of .04.
But everyone knows the dangers of reanalyzing data with a new endpoint after you have seen the data. What’s more, even if this were a reasonable post hoc analysis, the results are neither clinically meaningful nor statistically robust. Yet the fatally flawed paper has been viewed 60,000 times and picked up by 48 news outlets.
Another way to distract from nonsignificant primary outcomes is to nitpick the trials. The vitamin D dose wasn’t high enough, for instance. This might persuade me if there were one or two vitamin D trials, but there are hundreds of trials and meta-analyses, and their results are consistently null.
Conclusion: No, it is not hopeless
A nihilist would argue that fighting spin is futile. They would say you can’t fight incentives and business models. The incentive structure to publish is strong, and the journals and media know vitamin D studies garner attention – which is their currency.
I am not a nihilist and believe strongly that we must continue to teach critical appraisal and numerical literacy.
In fact, I would speculate that decades of poor critical appraisal by the medical profession have fostered outsized hope and created erroneous norms.
Imagine a counter-factual world in which clinicians have taught society that the human body is unlike an engine that can be repaired by fixing one part (i.e., the vitamin D level), that magic bullets (insulin) are rare, that most treatments fail, or that you can’t rely on association studies to prove efficacy.
In this world, people would be immune from spin and hype.
The norm would be that pills, supplements, and procedures are not what delivers good health. What delivers health is an amalgam of good luck, healthy habits, and lots of time spent outside playing in the sun.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky., and is a writer and podcaster for Medscape. He espouses a conservative approach to medical practice. He participates in clinical research and writes often about the state of medical evidence. He has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
The vitamin D story exudes teaching points: It offers a master class in critical appraisal, connecting the concepts of biologic plausibility, flawed surrogate markers, confounded observational studies, and slews of randomized controlled trials (RCTs) showing no benefits on health outcomes.
Yet despite the utter lack of benefit seen in trials, the hype continues. And the pandemic has only enhanced this hype as an onslaught of papers have reported the association of low vitamin D levels and COVID-19 disease.
My questions are simple: Why doesn’t the evidence persuade people? How many nonsignificant trials do we need before researchers stop studying vitamin D, doctors stop (routinely) measuring levels, and patients stop wasting money on the unhelpful supplement? What are the implications for this lack of persuasion?
Before exploring these questions, I want to set out that symptomatic vitamin deficiencies of any sort ought to be corrected.
Biologic plausibility and the pull of observational studies
It has long been known that vitamin D is crucial for bone health and that it can be produced in the skin with sun exposure. In the last decade, however, experts note that nearly every tissue and cell in our body has a vitamin D receptor. It then follows that if this many cells in the body can activate vitamin D, it must be vital for cardiovascular health, immune function, cancer prevention: basically, everything health related.
Oodles of observational studies have found that low serum levels of vitamin D correlate with higher mortality from all causes, cancer, cardiovascular disease, and now even COVID-19. Yet no matter the amount of statistical adjustment in these studies, we cannot know whether these associations are due to true causality.
The major issue is confounding: That is, people with low vitamin D levels have other conditions or diseases that lead to higher rates of ill health. Consider a patient with obesity, arthritis, and cognitive decline; this person is unlikely to do much exercise in the sun and may have low vitamin D levels. The low vitamin D level is simply a marker of overall poor health.
The randomized controlled trials tell a clear story
There are hundreds of vitamin D RCTs. The results simplify into one sentence: Vitamin D supplements do not improve health outcomes.
Here is a short summary of some recent studies.
VITAL, a massive (N > 25,000) RCT with 5 years of follow-up, compared vitamin D supplements to placebo and found no differences in the primary endpoints of cancer or cardiac events. Rates of death from any cause were nearly identical. Crucially, in subgroup analyses, the effects did not vary according to vitamin D levels at baseline.
The D-Health investigators randomly assigned more than 21,000 adults to vitamin D or placebo and after 5.7 years of follow-up reported no differences in the primary endpoint of overall mortality. There also were no differences in cardiovascular disease mortality.
Then you have the Mendelian randomized studies, which some have called nature’s RCT. These studies take advantage of the fact that some people are born with gene variations that predispose to low vitamin D levels. More than 60 Mendelian randomization studies have evaluated the consequences of lifelong genetically lowered vitamin D levels on various outcomes; most of these have found null effects.
Then there are the meta-analyses and systematic reviews. I loved the conclusion of this review of systematic reviews from the BMJ (emphasis mine):
“Despite a few hundred systematic reviews and meta-analyses, highly convincing evidence of a clear role of vitamin D does not exist for any outcome, but associations with a selection of outcomes are probable.”
The failure to persuade
My original plan was to emphasize the power of the RCT. Despite strong associations of low vitamin D levels with poor outcomes, the trials show no benefit to treatment. This strongly suggests (or nearly proves) that low vitamin D levels are akin to premature ventricular complexes after myocardial infarction: a marker for risk but not a target for therapy.
But I now see the more important issue as why scientists, funders, clinicians, and patients are not persuaded by clear evidence. Every day in clinic I see patients on vitamin D supplements; the journals keep publishing vitamin D studies. The proponents of vitamin D remain positive. And lately there is outsized attention and hope that vitamin D will mitigate SARS-CoV2 infection – based only on observational data.
You might argue against this point by saying vitamin D is natural and relatively innocuous, so who cares?
I offer three rebuttals to that point: Opportunity costs, distraction, and the insidious danger of poor critical appraisal skills. If you are burning money on vitamin D research, there is less available to study other important issues. If a patient is distracted by low vitamin D levels, she may pay less attention to her high body mass index or hypertension. And on the matter of critical appraisal, trust in medicine requires clinicians to be competent in critical appraisal. And these days, what could be more important than trust in medical professionals?
One major reason for the failure of persuasion of evidence is spin – or language that distracts from the primary endpoint. Here are two (of many) examples:
A meta-analysis of 50 vitamin D trials set out to study mortality. The authors found no significant difference in that primary endpoint. But the second sentence in their conclusion was that vitamin D supplements reduced the risk for cancer deaths by 15%. That’s a secondary endpoint in a study with nonsignificance in the primary endpoint. That is spin. This meta-analysis was completed before the Australian D-Health trial found that cancer deaths were 15% higher in the vitamin D arm, a difference that did not reach statistical significance.
The following example is worse: The authors of the VITAL trial, which found that vitamin D supplements had no effect on the primary endpoint of invasive cancer or cardiovascular disease, published a secondary analysis of the trial looking at a different endpoint: A composite incidence of metastatic and fatal invasive total cancer. They reported a 0.4% lower rate for the vitamin D group, a difference that barely made statistical significance at a P value of .04.
But everyone knows the dangers of reanalyzing data with a new endpoint after you have seen the data. What’s more, even if this were a reasonable post hoc analysis, the results are neither clinically meaningful nor statistically robust. Yet the fatally flawed paper has been viewed 60,000 times and picked up by 48 news outlets.
Another way to distract from nonsignificant primary outcomes is to nitpick the trials. The vitamin D dose wasn’t high enough, for instance. This might persuade me if there were one or two vitamin D trials, but there are hundreds of trials and meta-analyses, and their results are consistently null.
Conclusion: No, it is not hopeless
A nihilist would argue that fighting spin is futile. They would say you can’t fight incentives and business models. The incentive structure to publish is strong, and the journals and media know vitamin D studies garner attention – which is their currency.
I am not a nihilist and believe strongly that we must continue to teach critical appraisal and numerical literacy.
In fact, I would speculate that decades of poor critical appraisal by the medical profession have fostered outsized hope and created erroneous norms.
Imagine a counter-factual world in which clinicians have taught society that the human body is unlike an engine that can be repaired by fixing one part (i.e., the vitamin D level), that magic bullets (insulin) are rare, that most treatments fail, or that you can’t rely on association studies to prove efficacy.
In this world, people would be immune from spin and hype.
The norm would be that pills, supplements, and procedures are not what delivers good health. What delivers health is an amalgam of good luck, healthy habits, and lots of time spent outside playing in the sun.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky., and is a writer and podcaster for Medscape. He espouses a conservative approach to medical practice. He participates in clinical research and writes often about the state of medical evidence. He has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
The vitamin D story exudes teaching points: It offers a master class in critical appraisal, connecting the concepts of biologic plausibility, flawed surrogate markers, confounded observational studies, and slews of randomized controlled trials (RCTs) showing no benefits on health outcomes.
Yet despite the utter lack of benefit seen in trials, the hype continues. And the pandemic has only enhanced this hype as an onslaught of papers have reported the association of low vitamin D levels and COVID-19 disease.
My questions are simple: Why doesn’t the evidence persuade people? How many nonsignificant trials do we need before researchers stop studying vitamin D, doctors stop (routinely) measuring levels, and patients stop wasting money on the unhelpful supplement? What are the implications for this lack of persuasion?
Before exploring these questions, I want to set out that symptomatic vitamin deficiencies of any sort ought to be corrected.
Biologic plausibility and the pull of observational studies
It has long been known that vitamin D is crucial for bone health and that it can be produced in the skin with sun exposure. In the last decade, however, experts note that nearly every tissue and cell in our body has a vitamin D receptor. It then follows that if this many cells in the body can activate vitamin D, it must be vital for cardiovascular health, immune function, cancer prevention: basically, everything health related.
Oodles of observational studies have found that low serum levels of vitamin D correlate with higher mortality from all causes, cancer, cardiovascular disease, and now even COVID-19. Yet no matter the amount of statistical adjustment in these studies, we cannot know whether these associations are due to true causality.
The major issue is confounding: That is, people with low vitamin D levels have other conditions or diseases that lead to higher rates of ill health. Consider a patient with obesity, arthritis, and cognitive decline; this person is unlikely to do much exercise in the sun and may have low vitamin D levels. The low vitamin D level is simply a marker of overall poor health.
The randomized controlled trials tell a clear story
There are hundreds of vitamin D RCTs. The results simplify into one sentence: Vitamin D supplements do not improve health outcomes.
Here is a short summary of some recent studies.
VITAL, a massive (N > 25,000) RCT with 5 years of follow-up, compared vitamin D supplements to placebo and found no differences in the primary endpoints of cancer or cardiac events. Rates of death from any cause were nearly identical. Crucially, in subgroup analyses, the effects did not vary according to vitamin D levels at baseline.
The D-Health investigators randomly assigned more than 21,000 adults to vitamin D or placebo and after 5.7 years of follow-up reported no differences in the primary endpoint of overall mortality. There also were no differences in cardiovascular disease mortality.
Then you have the Mendelian randomized studies, which some have called nature’s RCT. These studies take advantage of the fact that some people are born with gene variations that predispose to low vitamin D levels. More than 60 Mendelian randomization studies have evaluated the consequences of lifelong genetically lowered vitamin D levels on various outcomes; most of these have found null effects.
Then there are the meta-analyses and systematic reviews. I loved the conclusion of this review of systematic reviews from the BMJ (emphasis mine):
“Despite a few hundred systematic reviews and meta-analyses, highly convincing evidence of a clear role of vitamin D does not exist for any outcome, but associations with a selection of outcomes are probable.”
The failure to persuade
My original plan was to emphasize the power of the RCT. Despite strong associations of low vitamin D levels with poor outcomes, the trials show no benefit to treatment. This strongly suggests (or nearly proves) that low vitamin D levels are akin to premature ventricular complexes after myocardial infarction: a marker for risk but not a target for therapy.
But I now see the more important issue as why scientists, funders, clinicians, and patients are not persuaded by clear evidence. Every day in clinic I see patients on vitamin D supplements; the journals keep publishing vitamin D studies. The proponents of vitamin D remain positive. And lately there is outsized attention and hope that vitamin D will mitigate SARS-CoV2 infection – based only on observational data.
You might argue against this point by saying vitamin D is natural and relatively innocuous, so who cares?
I offer three rebuttals to that point: Opportunity costs, distraction, and the insidious danger of poor critical appraisal skills. If you are burning money on vitamin D research, there is less available to study other important issues. If a patient is distracted by low vitamin D levels, she may pay less attention to her high body mass index or hypertension. And on the matter of critical appraisal, trust in medicine requires clinicians to be competent in critical appraisal. And these days, what could be more important than trust in medical professionals?
One major reason for the failure of persuasion of evidence is spin – or language that distracts from the primary endpoint. Here are two (of many) examples:
A meta-analysis of 50 vitamin D trials set out to study mortality. The authors found no significant difference in that primary endpoint. But the second sentence in their conclusion was that vitamin D supplements reduced the risk for cancer deaths by 15%. That’s a secondary endpoint in a study with nonsignificance in the primary endpoint. That is spin. This meta-analysis was completed before the Australian D-Health trial found that cancer deaths were 15% higher in the vitamin D arm, a difference that did not reach statistical significance.
The following example is worse: The authors of the VITAL trial, which found that vitamin D supplements had no effect on the primary endpoint of invasive cancer or cardiovascular disease, published a secondary analysis of the trial looking at a different endpoint: A composite incidence of metastatic and fatal invasive total cancer. They reported a 0.4% lower rate for the vitamin D group, a difference that barely made statistical significance at a P value of .04.
But everyone knows the dangers of reanalyzing data with a new endpoint after you have seen the data. What’s more, even if this were a reasonable post hoc analysis, the results are neither clinically meaningful nor statistically robust. Yet the fatally flawed paper has been viewed 60,000 times and picked up by 48 news outlets.
Another way to distract from nonsignificant primary outcomes is to nitpick the trials. The vitamin D dose wasn’t high enough, for instance. This might persuade me if there were one or two vitamin D trials, but there are hundreds of trials and meta-analyses, and their results are consistently null.
Conclusion: No, it is not hopeless
A nihilist would argue that fighting spin is futile. They would say you can’t fight incentives and business models. The incentive structure to publish is strong, and the journals and media know vitamin D studies garner attention – which is their currency.
I am not a nihilist and believe strongly that we must continue to teach critical appraisal and numerical literacy.
In fact, I would speculate that decades of poor critical appraisal by the medical profession have fostered outsized hope and created erroneous norms.
Imagine a counter-factual world in which clinicians have taught society that the human body is unlike an engine that can be repaired by fixing one part (i.e., the vitamin D level), that magic bullets (insulin) are rare, that most treatments fail, or that you can’t rely on association studies to prove efficacy.
In this world, people would be immune from spin and hype.
The norm would be that pills, supplements, and procedures are not what delivers good health. What delivers health is an amalgam of good luck, healthy habits, and lots of time spent outside playing in the sun.
Dr. Mandrola practices cardiac electrophysiology in Louisville, Ky., and is a writer and podcaster for Medscape. He espouses a conservative approach to medical practice. He participates in clinical research and writes often about the state of medical evidence. He has disclosed no relevant financial relationships. A version of this article first appeared on Medscape.com.
CDC preparing to update mask guidance
, CDC Director Rochelle P. Walensky, MD, said on Feb. 16.
“As we consider future metrics, which will be updated soon, we recognize the importance of not just cases … but critically, medically severe disease that leads to hospitalizations,” Dr. Walensky said at a White House news briefing. “We must consider hospital capacity as an additional important barometer.”
She later added, “We are looking at an overview of much of our guidance, and masking in all settings will be a part of that.”
Coronavirus cases continue to drop nationwide. This week’s 7-day daily average of cases is 147,000, a decrease of 40%. Hospitalizations have dropped 28% to 9,500, and daily deaths are 2,200, a decrease of 9%.
“Omicron cases are declining, and we are all cautiously optimistic about the trajectory we’re on,” Dr. Walensky said. “Things are moving in the right direction, but we want to remain vigilant to do all we can so this trajectory continues.”
Dr. Walensky said public masking remains especially important if someone is symptomatic or not feeling well, or if there has been a COVID-19 exposure. Those who are within 10 days of being diagnosed with the virus should also remain masked in public.
“We all share the same goal: to get to a point where COVID-19 is no longer disrupting our daily lives. A time when it won’t be a constant crisis,” Dr. Walensky said. “Moving from this pandemic will be a process led by science and epidemiological trends, and one that relies on the powerful tools we already have.”
A version of this article first appeared on WebMD.com.
, CDC Director Rochelle P. Walensky, MD, said on Feb. 16.
“As we consider future metrics, which will be updated soon, we recognize the importance of not just cases … but critically, medically severe disease that leads to hospitalizations,” Dr. Walensky said at a White House news briefing. “We must consider hospital capacity as an additional important barometer.”
She later added, “We are looking at an overview of much of our guidance, and masking in all settings will be a part of that.”
Coronavirus cases continue to drop nationwide. This week’s 7-day daily average of cases is 147,000, a decrease of 40%. Hospitalizations have dropped 28% to 9,500, and daily deaths are 2,200, a decrease of 9%.
“Omicron cases are declining, and we are all cautiously optimistic about the trajectory we’re on,” Dr. Walensky said. “Things are moving in the right direction, but we want to remain vigilant to do all we can so this trajectory continues.”
Dr. Walensky said public masking remains especially important if someone is symptomatic or not feeling well, or if there has been a COVID-19 exposure. Those who are within 10 days of being diagnosed with the virus should also remain masked in public.
“We all share the same goal: to get to a point where COVID-19 is no longer disrupting our daily lives. A time when it won’t be a constant crisis,” Dr. Walensky said. “Moving from this pandemic will be a process led by science and epidemiological trends, and one that relies on the powerful tools we already have.”
A version of this article first appeared on WebMD.com.
, CDC Director Rochelle P. Walensky, MD, said on Feb. 16.
“As we consider future metrics, which will be updated soon, we recognize the importance of not just cases … but critically, medically severe disease that leads to hospitalizations,” Dr. Walensky said at a White House news briefing. “We must consider hospital capacity as an additional important barometer.”
She later added, “We are looking at an overview of much of our guidance, and masking in all settings will be a part of that.”
Coronavirus cases continue to drop nationwide. This week’s 7-day daily average of cases is 147,000, a decrease of 40%. Hospitalizations have dropped 28% to 9,500, and daily deaths are 2,200, a decrease of 9%.
“Omicron cases are declining, and we are all cautiously optimistic about the trajectory we’re on,” Dr. Walensky said. “Things are moving in the right direction, but we want to remain vigilant to do all we can so this trajectory continues.”
Dr. Walensky said public masking remains especially important if someone is symptomatic or not feeling well, or if there has been a COVID-19 exposure. Those who are within 10 days of being diagnosed with the virus should also remain masked in public.
“We all share the same goal: to get to a point where COVID-19 is no longer disrupting our daily lives. A time when it won’t be a constant crisis,” Dr. Walensky said. “Moving from this pandemic will be a process led by science and epidemiological trends, and one that relies on the powerful tools we already have.”
A version of this article first appeared on WebMD.com.
Tiny hitchhikers like to ride in the trunk
Junk (germs) in the trunk
It’s been a long drive, and you’ve got a long way to go. You pull into a rest stop to use the bathroom and get some food. Quick, which order do you do those things in?
If you’re not a crazy person, you’d use the bathroom and then get your food. Who would bring food into a dirty bathroom? That’s kind of gross. Most people would take care of business, grab food, then get back in the car, eating along the way. Unfortunately, if you’re searching for a sanitary eating environment, your car may not actually be much better than that bathroom, according to new research from Aston University in Birmingham, England.
Let’s start off with the good news. The steering wheels of the five used cars that were swabbed for bacteria were pretty clean. Definitely cleaner than either of the toilet seats analyzed, likely thanks to increased usage of sanitizer, courtesy of the current pandemic. It’s easy to wipe down the steering wheel. Things break down, though, once we look elsewhere. The interiors of the five cars all contained just as much, if not more, bacteria than the toilet seats, with fecal matter commonly appearing on the driver’s seat.
The car interiors were less than sanitary, but they paled in comparison with the real winner here: the trunk. In each of the five cars, bacteria levels there far exceeded those in the toilets, and included everyone’s favorites – Escherichia coli and Staphylococcus aureus.
So, snacking on a bag of chips as you drive along is probably okay, but the food that popped out of its bag and spent the last 5 minutes rolling around the back? Perhaps less okay. You may want to wash it. Or burn it. Or torch the entire car for good measure like we’re about to do. Next time we’ll buy a car without poop in it.
Shut the lid when you flush
Maybe you’ve never thought about this, but it’s actually extremely important to shut the toilet lid when you flush. Just think of all those germs flying around from the force of the flush. Is your toothbrush anywhere near the toilet? Ew. Those pesky little bacteria and viruses are everywhere, and we know we can’t really escape them, but we should really do our best once we’re made aware of where to find them.
It seems like a no-brainer these days since we’ve all been really focused on cleanliness during the pandemic, but according to a poll in the United Kingdom, 55% of the 2,000 participants said they don’t put the lid down while flushing.
The OnePoll survey commissioned by Harpic, a company that makes toilet-cleaning products, also advised that toilet water isn’t even completely clean after flushed several times and can still be contaminated with many germs. Company researchers took specialized pictures of flushing toilets and they looked like tiny little Fourth of July fireworks shows, minus the sparklers. The pictures proved that droplets can go all over the place, including on bathroom users.
“There has never been a more important time to take extra care around our homes, although the risks associated with germ spread in unhygienic bathrooms are high, the solution to keeping them clean is simple,” a Harpic researcher said. Since other studies have shown that coronavirus can be found in feces, it’s become increasingly important to keep ourselves and others safe. Fireworks are pretty, but not when they come out of your toilet.
The latest in MRI fashion
Do you see that photo just below? Looks like something you could buy at the Lego store, right? Well, it’s not. Nor is it the proverbial thinking cap come to life.
(Did someone just say “come to life”? That reminds us of our favorite scene from Frosty the Snowman.)
Anywaaay, about the photo. That funny-looking chapeau is what we in the science business call a metamaterial.
Nope, metamaterials have nothing to do with Facebook parent company Meta. We checked. According to a statement from Boston University, they are engineered structures “created from small unit cells that might be unspectacular alone, but when grouped together in a precise way, get new superpowers not found in nature.”
Superpowers, eh? Who doesn’t want superpowers? Even if they come with a funny hat.
The unit cells, known as resonators, are just plastic tubes wrapped in copper wiring, but when they are grouped in an array and precisely arranged into a helmet, they can channel the magnetic field of the MRI machine during a scan. In theory, that would create “crisper images that can be captured at twice the normal speed,” Xin Zhang, PhD, and her team at BU’s Photonics Center explained in the university statement.
In the future, the metamaterial device could “be used in conjunction with cheaper low-field MRI machines to make the technology more widely available, particularly in the developing world,” they suggested. Or, like so many other superpowers, it could fall into the wrong hands. Like those of Lex Luthor. Or Mark Zuckerberg. Or Frosty the Snowman.
The highway of the mind
How fast can you think on your feet? Well, according to a recently published study, it could be a legitimate measure of intelligence. Here’s the science.
Researchers from the University of Würzburg in Germany and Indiana University have suggested that a person’s intelligence score measures the ability, based on certain neuronal networks and their communication structures, to switch between resting state and different task states.
The investigators set up a study to observe almost 800 people while they completed seven tasks. By monitoring brain activity with functional magnetic resonance imaging, the teams found that subjects who had higher intelligence scores required “less adjustment when switching between different cognitive states,” they said in a separate statement.
It comes down to the network architecture of their brains.
Kirsten Hilger, PhD, head of the German group, described it in terms of highways. The resting state of the brain is normal traffic. It’s always moving. Holiday traffic is the task. The ability to handle the increased flow of commuters is a function of the highway infrastructure. The better the infrastructure, the higher the intelligence.
So the next time you’re stuck in traffic, think how efficient your brain would be with such a task. The quicker, the better.
Junk (germs) in the trunk
It’s been a long drive, and you’ve got a long way to go. You pull into a rest stop to use the bathroom and get some food. Quick, which order do you do those things in?
If you’re not a crazy person, you’d use the bathroom and then get your food. Who would bring food into a dirty bathroom? That’s kind of gross. Most people would take care of business, grab food, then get back in the car, eating along the way. Unfortunately, if you’re searching for a sanitary eating environment, your car may not actually be much better than that bathroom, according to new research from Aston University in Birmingham, England.
Let’s start off with the good news. The steering wheels of the five used cars that were swabbed for bacteria were pretty clean. Definitely cleaner than either of the toilet seats analyzed, likely thanks to increased usage of sanitizer, courtesy of the current pandemic. It’s easy to wipe down the steering wheel. Things break down, though, once we look elsewhere. The interiors of the five cars all contained just as much, if not more, bacteria than the toilet seats, with fecal matter commonly appearing on the driver’s seat.
The car interiors were less than sanitary, but they paled in comparison with the real winner here: the trunk. In each of the five cars, bacteria levels there far exceeded those in the toilets, and included everyone’s favorites – Escherichia coli and Staphylococcus aureus.
So, snacking on a bag of chips as you drive along is probably okay, but the food that popped out of its bag and spent the last 5 minutes rolling around the back? Perhaps less okay. You may want to wash it. Or burn it. Or torch the entire car for good measure like we’re about to do. Next time we’ll buy a car without poop in it.
Shut the lid when you flush
Maybe you’ve never thought about this, but it’s actually extremely important to shut the toilet lid when you flush. Just think of all those germs flying around from the force of the flush. Is your toothbrush anywhere near the toilet? Ew. Those pesky little bacteria and viruses are everywhere, and we know we can’t really escape them, but we should really do our best once we’re made aware of where to find them.
It seems like a no-brainer these days since we’ve all been really focused on cleanliness during the pandemic, but according to a poll in the United Kingdom, 55% of the 2,000 participants said they don’t put the lid down while flushing.
The OnePoll survey commissioned by Harpic, a company that makes toilet-cleaning products, also advised that toilet water isn’t even completely clean after flushed several times and can still be contaminated with many germs. Company researchers took specialized pictures of flushing toilets and they looked like tiny little Fourth of July fireworks shows, minus the sparklers. The pictures proved that droplets can go all over the place, including on bathroom users.
“There has never been a more important time to take extra care around our homes, although the risks associated with germ spread in unhygienic bathrooms are high, the solution to keeping them clean is simple,” a Harpic researcher said. Since other studies have shown that coronavirus can be found in feces, it’s become increasingly important to keep ourselves and others safe. Fireworks are pretty, but not when they come out of your toilet.
The latest in MRI fashion
Do you see that photo just below? Looks like something you could buy at the Lego store, right? Well, it’s not. Nor is it the proverbial thinking cap come to life.
(Did someone just say “come to life”? That reminds us of our favorite scene from Frosty the Snowman.)
Anywaaay, about the photo. That funny-looking chapeau is what we in the science business call a metamaterial.
Nope, metamaterials have nothing to do with Facebook parent company Meta. We checked. According to a statement from Boston University, they are engineered structures “created from small unit cells that might be unspectacular alone, but when grouped together in a precise way, get new superpowers not found in nature.”
Superpowers, eh? Who doesn’t want superpowers? Even if they come with a funny hat.
The unit cells, known as resonators, are just plastic tubes wrapped in copper wiring, but when they are grouped in an array and precisely arranged into a helmet, they can channel the magnetic field of the MRI machine during a scan. In theory, that would create “crisper images that can be captured at twice the normal speed,” Xin Zhang, PhD, and her team at BU’s Photonics Center explained in the university statement.
In the future, the metamaterial device could “be used in conjunction with cheaper low-field MRI machines to make the technology more widely available, particularly in the developing world,” they suggested. Or, like so many other superpowers, it could fall into the wrong hands. Like those of Lex Luthor. Or Mark Zuckerberg. Or Frosty the Snowman.
The highway of the mind
How fast can you think on your feet? Well, according to a recently published study, it could be a legitimate measure of intelligence. Here’s the science.
Researchers from the University of Würzburg in Germany and Indiana University have suggested that a person’s intelligence score measures the ability, based on certain neuronal networks and their communication structures, to switch between resting state and different task states.
The investigators set up a study to observe almost 800 people while they completed seven tasks. By monitoring brain activity with functional magnetic resonance imaging, the teams found that subjects who had higher intelligence scores required “less adjustment when switching between different cognitive states,” they said in a separate statement.
It comes down to the network architecture of their brains.
Kirsten Hilger, PhD, head of the German group, described it in terms of highways. The resting state of the brain is normal traffic. It’s always moving. Holiday traffic is the task. The ability to handle the increased flow of commuters is a function of the highway infrastructure. The better the infrastructure, the higher the intelligence.
So the next time you’re stuck in traffic, think how efficient your brain would be with such a task. The quicker, the better.
Junk (germs) in the trunk
It’s been a long drive, and you’ve got a long way to go. You pull into a rest stop to use the bathroom and get some food. Quick, which order do you do those things in?
If you’re not a crazy person, you’d use the bathroom and then get your food. Who would bring food into a dirty bathroom? That’s kind of gross. Most people would take care of business, grab food, then get back in the car, eating along the way. Unfortunately, if you’re searching for a sanitary eating environment, your car may not actually be much better than that bathroom, according to new research from Aston University in Birmingham, England.
Let’s start off with the good news. The steering wheels of the five used cars that were swabbed for bacteria were pretty clean. Definitely cleaner than either of the toilet seats analyzed, likely thanks to increased usage of sanitizer, courtesy of the current pandemic. It’s easy to wipe down the steering wheel. Things break down, though, once we look elsewhere. The interiors of the five cars all contained just as much, if not more, bacteria than the toilet seats, with fecal matter commonly appearing on the driver’s seat.
The car interiors were less than sanitary, but they paled in comparison with the real winner here: the trunk. In each of the five cars, bacteria levels there far exceeded those in the toilets, and included everyone’s favorites – Escherichia coli and Staphylococcus aureus.
So, snacking on a bag of chips as you drive along is probably okay, but the food that popped out of its bag and spent the last 5 minutes rolling around the back? Perhaps less okay. You may want to wash it. Or burn it. Or torch the entire car for good measure like we’re about to do. Next time we’ll buy a car without poop in it.
Shut the lid when you flush
Maybe you’ve never thought about this, but it’s actually extremely important to shut the toilet lid when you flush. Just think of all those germs flying around from the force of the flush. Is your toothbrush anywhere near the toilet? Ew. Those pesky little bacteria and viruses are everywhere, and we know we can’t really escape them, but we should really do our best once we’re made aware of where to find them.
It seems like a no-brainer these days since we’ve all been really focused on cleanliness during the pandemic, but according to a poll in the United Kingdom, 55% of the 2,000 participants said they don’t put the lid down while flushing.
The OnePoll survey commissioned by Harpic, a company that makes toilet-cleaning products, also advised that toilet water isn’t even completely clean after flushed several times and can still be contaminated with many germs. Company researchers took specialized pictures of flushing toilets and they looked like tiny little Fourth of July fireworks shows, minus the sparklers. The pictures proved that droplets can go all over the place, including on bathroom users.
“There has never been a more important time to take extra care around our homes, although the risks associated with germ spread in unhygienic bathrooms are high, the solution to keeping them clean is simple,” a Harpic researcher said. Since other studies have shown that coronavirus can be found in feces, it’s become increasingly important to keep ourselves and others safe. Fireworks are pretty, but not when they come out of your toilet.
The latest in MRI fashion
Do you see that photo just below? Looks like something you could buy at the Lego store, right? Well, it’s not. Nor is it the proverbial thinking cap come to life.
(Did someone just say “come to life”? That reminds us of our favorite scene from Frosty the Snowman.)
Anywaaay, about the photo. That funny-looking chapeau is what we in the science business call a metamaterial.
Nope, metamaterials have nothing to do with Facebook parent company Meta. We checked. According to a statement from Boston University, they are engineered structures “created from small unit cells that might be unspectacular alone, but when grouped together in a precise way, get new superpowers not found in nature.”
Superpowers, eh? Who doesn’t want superpowers? Even if they come with a funny hat.
The unit cells, known as resonators, are just plastic tubes wrapped in copper wiring, but when they are grouped in an array and precisely arranged into a helmet, they can channel the magnetic field of the MRI machine during a scan. In theory, that would create “crisper images that can be captured at twice the normal speed,” Xin Zhang, PhD, and her team at BU’s Photonics Center explained in the university statement.
In the future, the metamaterial device could “be used in conjunction with cheaper low-field MRI machines to make the technology more widely available, particularly in the developing world,” they suggested. Or, like so many other superpowers, it could fall into the wrong hands. Like those of Lex Luthor. Or Mark Zuckerberg. Or Frosty the Snowman.
The highway of the mind
How fast can you think on your feet? Well, according to a recently published study, it could be a legitimate measure of intelligence. Here’s the science.
Researchers from the University of Würzburg in Germany and Indiana University have suggested that a person’s intelligence score measures the ability, based on certain neuronal networks and their communication structures, to switch between resting state and different task states.
The investigators set up a study to observe almost 800 people while they completed seven tasks. By monitoring brain activity with functional magnetic resonance imaging, the teams found that subjects who had higher intelligence scores required “less adjustment when switching between different cognitive states,” they said in a separate statement.
It comes down to the network architecture of their brains.
Kirsten Hilger, PhD, head of the German group, described it in terms of highways. The resting state of the brain is normal traffic. It’s always moving. Holiday traffic is the task. The ability to handle the increased flow of commuters is a function of the highway infrastructure. The better the infrastructure, the higher the intelligence.
So the next time you’re stuck in traffic, think how efficient your brain would be with such a task. The quicker, the better.
Stroke risk is highest right after COVID infection
, new research shows.
The study among Medicare beneficiaries with COVID-19 also showed that stroke risk is higher for relatively young older adults, those aged 65 to 74 years, and those without a history of stroke.
The study highlights the impact COVID-19 has on the cardiovascular system, said study author Quanhe Yang, PhD, senior scientist, Division for Heart Disease and Stroke Prevention, Centers for Disease Control and Prevention, Atlanta.
“Clinicians and patients should understand that stroke might be one of the very important clinical consequences of COVID-19.”
The study was presented during the hybrid International Stroke Conference held in New Orleans and online. The meeting was presented by the American Stroke Association, a division of the American Heart Association.
Stroke is the fifth leading cause of death in the U.S. As an increasing number of people become infected with COVID-19, “it’s important to determine if there’s a relationship between COVID and the risk of stroke,” said Dr. Yang.
Findings from prior research examining the link between stroke and COVID-19 have been inconsistent, he noted. Some studies found an association while others did not, and in still others, the association was not as strong as expected.
Many factors may contribute to these inconsistent findings, said Dr. Yang, including differences in study design, inclusion criteria, comparison groups, sample sizes, and countries where the research was carried out. Dr. Yang pointed out that many of these studies were done in the early stages of the pandemic or didn’t include older adults, the population most at risk for stroke.
The current study included 19,553 Medicare beneficiaries aged 65 years and older diagnosed with COVID-19 and hospitalized with acute ischemic stroke. The median age at diagnosis of COVID-19 was 80.5 years, 57.5% were women, and more than 75% were non-Hispanic Whites.
To ensure the stroke occurred after a COVID infection, researchers used a self-controlled case series study design, a “within person” comparison between the risk period and the control period.
They divided the study period (Jan. 1, 2019 to Feb. 28, 2021) into the exposure or stroke risk periods after the COVID diagnosis (0-3 days; 4-7 days; 8-15 days; and 15-28 days) and control periods.
Strokes that occurred 7 days before or 28 days after a COVID diagnosis served as a control period. “Any stroke that occurred outside the risk window is in the control period,” explained Dr. Yang.
He added that the control period provides a baseline. “Without COVID-19, this is what I would expect” in terms of the number of strokes.
To estimate the incidence rate ratio (IRR), investigators compared the incidence of acute ischemic stroke in the various risk periods with control periods.
The IRR was 10.97 (95% confidence interval, 10.30-11.68) at 0-3 days. The risk then quickly declined but stayed higher than the control period. The IRRs were: 1.59 (95% CI, 1.35-1.87) at 4-7 days; 1.23 (95% CI, 1.07-1.41) at 8-14 days; and 1.06 (95% CI, 0.95-1.18) at 15-28 days.
The temporary increase in stroke risk early after an infection isn’t novel; the pattern has been observed with influenza, respiratory infections, and shingles, said Dr. Yang. “But COVID-19 appears to be particularly risky.”
Although the mechanism driving the early increased stroke risk isn’t fully understood, it’s likely tied to an “exaggerated inflammatory response,” said Dr. Yang. This can trigger the cascade of events setting the stage for a stroke – a hypercoagulation state leading to the formation of blood clots that then block arteries to the brain, he said.
It’s also possible the infection directly affects endothelial cells, leading to rupture of plaque, again blocking arteries and raising stroke risks, added Dr. Yang.
The association was stronger among younger beneficiaries, aged 65 to 74 years, compared with those 85 years and older, a finding Dr. Yang said was somewhat surprising. But he noted other studies have found stroke patients with COVID are younger than stroke patients without COVID – by some 5 to 6 years.
“If COVID-19 disproportionately affects younger patients, that may explain the stronger association,” said Dr. Yang. “Stroke risk increases tremendously with age, so if you’re a younger age, your baseline stroke risk is lower.”
The association was also stronger among beneficiaries without a history of stroke. Again, this could be related to the stronger association among younger patients who are less likely to have suffered a stroke. The association was largely consistent across sex and race/ethnicities.
Dr. Yang stressed that the findings need to be confirmed with further studies.
The study was carried out before widespread use of vaccinations in the U.S. Once those data are available, Dr. Yang and his colleagues plan to determine if vaccinations modify the association between COVID-19 and stroke risk.
The new results contribute to the mounting evidence that a COVID-19 infection “can actually affect multiple human organs structurally or functionally in addition to the impact on [the] respiratory system,” said Dr. Yang.
Some dates of COVID-19 diagnoses may be incorrect due to limited test availability, particularly early in the pandemic. Another limitation of the study was possible misclassification from the use of Medicare real-time preliminary claims.
In a provided statement, Louise D. McCullough, MD, PhD, chair of the ISC 2022 and professor and chair of neurology, McGovern Medical School, University of Texas Health Science Center at Houston, noted that the study focused on older adults because it was examining Medicare beneficiaries.
“But everyone is likely at risk for stroke after COVID,” she said. “Any infection is linked to stroke risk, probably because any infection will cause inflammation, and inflammation can cause clots or thrombus, which is the cause of stroke.”
There was no outside funding for the study. No relevant conflicts of interest were disclosed.
A version of this article first appeared on Medscape.com.
, new research shows.
The study among Medicare beneficiaries with COVID-19 also showed that stroke risk is higher for relatively young older adults, those aged 65 to 74 years, and those without a history of stroke.
The study highlights the impact COVID-19 has on the cardiovascular system, said study author Quanhe Yang, PhD, senior scientist, Division for Heart Disease and Stroke Prevention, Centers for Disease Control and Prevention, Atlanta.
“Clinicians and patients should understand that stroke might be one of the very important clinical consequences of COVID-19.”
The study was presented during the hybrid International Stroke Conference held in New Orleans and online. The meeting was presented by the American Stroke Association, a division of the American Heart Association.
Stroke is the fifth leading cause of death in the U.S. As an increasing number of people become infected with COVID-19, “it’s important to determine if there’s a relationship between COVID and the risk of stroke,” said Dr. Yang.
Findings from prior research examining the link between stroke and COVID-19 have been inconsistent, he noted. Some studies found an association while others did not, and in still others, the association was not as strong as expected.
Many factors may contribute to these inconsistent findings, said Dr. Yang, including differences in study design, inclusion criteria, comparison groups, sample sizes, and countries where the research was carried out. Dr. Yang pointed out that many of these studies were done in the early stages of the pandemic or didn’t include older adults, the population most at risk for stroke.
The current study included 19,553 Medicare beneficiaries aged 65 years and older diagnosed with COVID-19 and hospitalized with acute ischemic stroke. The median age at diagnosis of COVID-19 was 80.5 years, 57.5% were women, and more than 75% were non-Hispanic Whites.
To ensure the stroke occurred after a COVID infection, researchers used a self-controlled case series study design, a “within person” comparison between the risk period and the control period.
They divided the study period (Jan. 1, 2019 to Feb. 28, 2021) into the exposure or stroke risk periods after the COVID diagnosis (0-3 days; 4-7 days; 8-15 days; and 15-28 days) and control periods.
Strokes that occurred 7 days before or 28 days after a COVID diagnosis served as a control period. “Any stroke that occurred outside the risk window is in the control period,” explained Dr. Yang.
He added that the control period provides a baseline. “Without COVID-19, this is what I would expect” in terms of the number of strokes.
To estimate the incidence rate ratio (IRR), investigators compared the incidence of acute ischemic stroke in the various risk periods with control periods.
The IRR was 10.97 (95% confidence interval, 10.30-11.68) at 0-3 days. The risk then quickly declined but stayed higher than the control period. The IRRs were: 1.59 (95% CI, 1.35-1.87) at 4-7 days; 1.23 (95% CI, 1.07-1.41) at 8-14 days; and 1.06 (95% CI, 0.95-1.18) at 15-28 days.
The temporary increase in stroke risk early after an infection isn’t novel; the pattern has been observed with influenza, respiratory infections, and shingles, said Dr. Yang. “But COVID-19 appears to be particularly risky.”
Although the mechanism driving the early increased stroke risk isn’t fully understood, it’s likely tied to an “exaggerated inflammatory response,” said Dr. Yang. This can trigger the cascade of events setting the stage for a stroke – a hypercoagulation state leading to the formation of blood clots that then block arteries to the brain, he said.
It’s also possible the infection directly affects endothelial cells, leading to rupture of plaque, again blocking arteries and raising stroke risks, added Dr. Yang.
The association was stronger among younger beneficiaries, aged 65 to 74 years, compared with those 85 years and older, a finding Dr. Yang said was somewhat surprising. But he noted other studies have found stroke patients with COVID are younger than stroke patients without COVID – by some 5 to 6 years.
“If COVID-19 disproportionately affects younger patients, that may explain the stronger association,” said Dr. Yang. “Stroke risk increases tremendously with age, so if you’re a younger age, your baseline stroke risk is lower.”
The association was also stronger among beneficiaries without a history of stroke. Again, this could be related to the stronger association among younger patients who are less likely to have suffered a stroke. The association was largely consistent across sex and race/ethnicities.
Dr. Yang stressed that the findings need to be confirmed with further studies.
The study was carried out before widespread use of vaccinations in the U.S. Once those data are available, Dr. Yang and his colleagues plan to determine if vaccinations modify the association between COVID-19 and stroke risk.
The new results contribute to the mounting evidence that a COVID-19 infection “can actually affect multiple human organs structurally or functionally in addition to the impact on [the] respiratory system,” said Dr. Yang.
Some dates of COVID-19 diagnoses may be incorrect due to limited test availability, particularly early in the pandemic. Another limitation of the study was possible misclassification from the use of Medicare real-time preliminary claims.
In a provided statement, Louise D. McCullough, MD, PhD, chair of the ISC 2022 and professor and chair of neurology, McGovern Medical School, University of Texas Health Science Center at Houston, noted that the study focused on older adults because it was examining Medicare beneficiaries.
“But everyone is likely at risk for stroke after COVID,” she said. “Any infection is linked to stroke risk, probably because any infection will cause inflammation, and inflammation can cause clots or thrombus, which is the cause of stroke.”
There was no outside funding for the study. No relevant conflicts of interest were disclosed.
A version of this article first appeared on Medscape.com.
, new research shows.
The study among Medicare beneficiaries with COVID-19 also showed that stroke risk is higher for relatively young older adults, those aged 65 to 74 years, and those without a history of stroke.
The study highlights the impact COVID-19 has on the cardiovascular system, said study author Quanhe Yang, PhD, senior scientist, Division for Heart Disease and Stroke Prevention, Centers for Disease Control and Prevention, Atlanta.
“Clinicians and patients should understand that stroke might be one of the very important clinical consequences of COVID-19.”
The study was presented during the hybrid International Stroke Conference held in New Orleans and online. The meeting was presented by the American Stroke Association, a division of the American Heart Association.
Stroke is the fifth leading cause of death in the U.S. As an increasing number of people become infected with COVID-19, “it’s important to determine if there’s a relationship between COVID and the risk of stroke,” said Dr. Yang.
Findings from prior research examining the link between stroke and COVID-19 have been inconsistent, he noted. Some studies found an association while others did not, and in still others, the association was not as strong as expected.
Many factors may contribute to these inconsistent findings, said Dr. Yang, including differences in study design, inclusion criteria, comparison groups, sample sizes, and countries where the research was carried out. Dr. Yang pointed out that many of these studies were done in the early stages of the pandemic or didn’t include older adults, the population most at risk for stroke.
The current study included 19,553 Medicare beneficiaries aged 65 years and older diagnosed with COVID-19 and hospitalized with acute ischemic stroke. The median age at diagnosis of COVID-19 was 80.5 years, 57.5% were women, and more than 75% were non-Hispanic Whites.
To ensure the stroke occurred after a COVID infection, researchers used a self-controlled case series study design, a “within person” comparison between the risk period and the control period.
They divided the study period (Jan. 1, 2019 to Feb. 28, 2021) into the exposure or stroke risk periods after the COVID diagnosis (0-3 days; 4-7 days; 8-15 days; and 15-28 days) and control periods.
Strokes that occurred 7 days before or 28 days after a COVID diagnosis served as a control period. “Any stroke that occurred outside the risk window is in the control period,” explained Dr. Yang.
He added that the control period provides a baseline. “Without COVID-19, this is what I would expect” in terms of the number of strokes.
To estimate the incidence rate ratio (IRR), investigators compared the incidence of acute ischemic stroke in the various risk periods with control periods.
The IRR was 10.97 (95% confidence interval, 10.30-11.68) at 0-3 days. The risk then quickly declined but stayed higher than the control period. The IRRs were: 1.59 (95% CI, 1.35-1.87) at 4-7 days; 1.23 (95% CI, 1.07-1.41) at 8-14 days; and 1.06 (95% CI, 0.95-1.18) at 15-28 days.
The temporary increase in stroke risk early after an infection isn’t novel; the pattern has been observed with influenza, respiratory infections, and shingles, said Dr. Yang. “But COVID-19 appears to be particularly risky.”
Although the mechanism driving the early increased stroke risk isn’t fully understood, it’s likely tied to an “exaggerated inflammatory response,” said Dr. Yang. This can trigger the cascade of events setting the stage for a stroke – a hypercoagulation state leading to the formation of blood clots that then block arteries to the brain, he said.
It’s also possible the infection directly affects endothelial cells, leading to rupture of plaque, again blocking arteries and raising stroke risks, added Dr. Yang.
The association was stronger among younger beneficiaries, aged 65 to 74 years, compared with those 85 years and older, a finding Dr. Yang said was somewhat surprising. But he noted other studies have found stroke patients with COVID are younger than stroke patients without COVID – by some 5 to 6 years.
“If COVID-19 disproportionately affects younger patients, that may explain the stronger association,” said Dr. Yang. “Stroke risk increases tremendously with age, so if you’re a younger age, your baseline stroke risk is lower.”
The association was also stronger among beneficiaries without a history of stroke. Again, this could be related to the stronger association among younger patients who are less likely to have suffered a stroke. The association was largely consistent across sex and race/ethnicities.
Dr. Yang stressed that the findings need to be confirmed with further studies.
The study was carried out before widespread use of vaccinations in the U.S. Once those data are available, Dr. Yang and his colleagues plan to determine if vaccinations modify the association between COVID-19 and stroke risk.
The new results contribute to the mounting evidence that a COVID-19 infection “can actually affect multiple human organs structurally or functionally in addition to the impact on [the] respiratory system,” said Dr. Yang.
Some dates of COVID-19 diagnoses may be incorrect due to limited test availability, particularly early in the pandemic. Another limitation of the study was possible misclassification from the use of Medicare real-time preliminary claims.
In a provided statement, Louise D. McCullough, MD, PhD, chair of the ISC 2022 and professor and chair of neurology, McGovern Medical School, University of Texas Health Science Center at Houston, noted that the study focused on older adults because it was examining Medicare beneficiaries.
“But everyone is likely at risk for stroke after COVID,” she said. “Any infection is linked to stroke risk, probably because any infection will cause inflammation, and inflammation can cause clots or thrombus, which is the cause of stroke.”
There was no outside funding for the study. No relevant conflicts of interest were disclosed.
A version of this article first appeared on Medscape.com.
FROM ISC 2022
The battle of egos behind the life-saving discovery of insulin
Leonard Thompson’s father was so desperate to save his 14-year-old child from certain death due to diabetes that, on Jan. 11, 1922, he took him to Toronto General Hospital to receive what is arguably the first dose of insulin given to a human. From an anticipated life expectancy of weeks – months at best – Thompson lived for an astonishing further 13 years, eventually dying from pneumonia unrelated to diabetes.
By all accounts, the story is a centenary celebration of a remarkable discovery. Insulin has changed what was once a death sentence to a near-normal life expectancy for the millions of people with type 1 diabetes over the past 100 years.
But behind the life-changing success of the discovery – and the Nobel Prize that went with it – lies a tale blighted by disputed claims, twisted truths, and likely injustices between the scientists involved, as they each vied for an honored place in medical history.
Kersten Hall, PhD, honorary fellow, religion and history of science, at the University of Leeds, England, has scoured archives and personal records held at the University of Toronto to uncover the personal stories behind insulin’s discovery.
Despite the wranglings, Dr. Hall asserts: “There’s a distinction between the science and the scientists. Scientists are wonderfully flawed and complex human beings with all their glorious virtues and vices, as we all are. It’s no surprise that they get greedy, jealous, and insecure.”
At death’s door: Diabetes before the 1920s
Prior to insulin’s discovery in 1921, a diagnosis of type 1 diabetes placed someone at death’s door, with nothing but starvation – albeit a slightly slower death – to mitigate a fast-approaching departure from this world. At that time, most diabetes cases would have been type 1 diabetes because, with less obesogenic diets and shorter lifespans, people were much less likely to develop type 2 diabetes.
Nowadays, it is widely recognized that the prevalence of type 2 diabetes is on a steep upward curve, but so too is type 1 diabetes. In the United States alone, there are 1.5 million people diagnosed with type 1 diabetes, a number expected to rise to around 5 million by 2050, according to JDRF, the type 1 diabetes advocacy organization.
Interestingly, 100 years since the first treated patient, life-long insulin remains the only real effective therapy for patients with type 1 diabetes. Once pancreatic beta cells have ceased to function and insulin production has stopped, insulin replacement is the only way to keep blood glucose levels within the recommended range (A1c ≤ 48 mmol/mol [6.5%]), according to the UK National Institute for Health and Care Excellence (NICE), as well as numerous diabetes organizations, including the American Diabetes Association (ADA).
Preliminary clinical trials have looked at stem cell transplantation, prematurely dubbed as a “cure” for type 1 diabetes, as an alternative to insulin therapy. The procedure involves transplanting stem cell–derived cells, which become functional beta cells when infused into humans, but requires immunosuppression, as reported by this news organization.
Today, the life expectancy of people with type 1 diabetes treated with insulin is close to those without the disease, although this is dependent on how tightly blood glucose is controlled. Some studies show life expectancy of those with type 1 diabetes is around 8-12 years lower than the general population but varies depending on where a person lives.
In some lower-income countries, many with type 1 diabetes still die prematurely either because they are undiagnosed or cannot access insulin. The high cost of insulin in the United States is well publicized, as featured in numerous articles by this news organization, and numerous patients in the United States have died because they cannot afford insulin.
Without insulin, young Leonard Thompson would have been lucky to have reached his 15th birthday.
“Such patients were cachectic and thin and would have weighed around 40-50 pounds (18-23 kg), which is very low for an older child. Survival was short and lasted weeks or months usually,” said Elizabeth Stephens, MD, an endocrinologist in Portland, Ore.
“The discovery of insulin was really a miracle because without it diabetes patients were facing certain death. Even nowadays, if people don’t get their insulin because they can’t afford it or for whatever reason, they can still die,” Dr. Stephens stressed.
Antidiabetic effects of pancreatic extract limited
Back in 1869, Paul Langerhans, MD, discovered pancreatic islet cells, or islets of Langerhans, as a medical student. Researchers tried to produce extracts that lowered blood glucose but they were too toxic for patient use.
In 1908, as detailed in his recent book, Insulin – the Crooked Timber, Dr. Hall also refers to the fact that a German researcher, Georg Zuelzer, MD, demonstrated in six patients that pancreatic extracts could reduce urinary levels of glucose and ketones, and that in one case, the treatment woke the patient from a coma. Dr. Zuelzer had purified the extract with alcohol but patients still experienced convulsions and coma; in fact, they were experiencing hypoglycemic shock, but Dr. Zuelzer had not identified it as such.
“He thought his preparation was full of impurities – and that’s the irony. He had in his hands an insulin prep that was so clean and so potent that it sent the test animals into hypoglycemic shock,” Dr. Hall pointed out.
By 1921, two young researchers, Frederick G. Banting, MD, a practicing medical doctor in Toronto, together with a final year physiology student at the University of Toronto, Charles H. Best, MD, DSc, collaborated on the instruction of Dr. Best’s superior, John James Rickard Macleod, MBChB, professor of physiology at the University of Toronto, to make pancreatic extracts, first from dogs and then from cattle.
Over the months prior to treating Thompson, working together in the laboratory, Dr. Banting and Dr. Best prepared the pancreatic extract from cattle and tested it on dogs with diabetes.
Then, in what amounted to a phase 1 trial of its day, with an “n of one,” a frail and close-to-death Thompson was given 15 cc of pancreatic extract at Toronto General Hospital in January 1922. His blood glucose level dropped by 25%, but unfortunately, his body still produced ketones, indicating the antidiabetic effect was limited. He also experienced an adverse reaction at the injection site with an accumulation of abscesses.
So despite success with isolating the extract and administering it to Thompson, the product remained tainted with impurities.
At this point, colleague James Collip, MD, PhD, came to the rescue. He used his skills as a biochemist to purify the pancreatic extract enough to eliminate impurities.
When Thompson was treated 2 weeks later with the purified extract, he experienced a more positive outcome. Gone was the injection site reaction, gone were the high blood glucose levels, and Thompson “became brighter, more active, looked better, and said he felt stronger,” according to a publication describing the treatment.
Dr. Collip also determined that by over-purifying the product, the animals he experimented on could overreact and experience convulsions, coma, and death due to hypoglycemia from too much insulin.
Fighting talk
Recalling an excerpt from Dr. Banting’s diary, Dr. Hall said that Dr. Banting had a mercurial temper and testified to his loss of patience with Dr. Collip when the chemist refused to share his formula of purification. His diary reads: “I grabbed him in one hand by the overcoat ... and almost lifting him I sat him down hard on the chair ... I remember telling him that it was a good job he was so much smaller – otherwise I would ‘knock hell out of him.’ ”
According to Dr. Hall, in 1923, when Dr. Banting and Dr. Macleod were jointly awarded the Nobel Prize for Medicine, Dr. Best resented being excluded, and despite Dr. Banting’s sharing half his prize money with Dr. Best, animosity prevailed.
At one point, before leaving on a plane for a wartime mission to the United Kingdom, Dr. Banting noted that if he didn’t make it back alive, “and they give my [professorial] chair to that son-of-a-bitch Best, I’ll never rest in my grave.” In a cruel twist of fate, Dr. Banting’s plane crashed and all aboard died.
The Nobel Prize had also been a source of rivalry between Dr. Banting and his boss, Dr. Macleod. In late 1921, while presenting the findings from animal models at the American Physiological Society conference, Dr. Banting’s nerves got the better of him and Dr. Macleod took over at the podium to finish the talk. Dr. Banting perceived this as his boss stealing the limelight.
Only a few months later, at the Association of American Physicians annual conference, Dr. Macleod played to an audience for a second time by making the first formal announcement of the discovery to the scientific community. Notably, Dr. Banting was absent.
The Nobel Prize or a poisoned chalice?
Awarded annually for physics, chemistry, medicine/physiology, literature, peace, and economics, Nobel Prizes are usually considered the holy grail of achievement. In 1895, funds for the prizes were bequeathed by Alfred Nobel in his last will and testament, with each prize worth around $40,000 at the time (approximately $1,000,000 in today’s value).
Writing in 2001 in the journal Diabetes Voice, Professor Sir George Alberti, DPhil, BM BCh, former president of the UK Royal College of Physicians, summarized the burden that accompanies the Nobel Prize: “I personally believe that such prizes and awards do more harm than good and should be abolished. Many a scientist has gone to their grave feeling deeply aggrieved because they were not awarded a Nobel Prize.”
Such high stakes surround the prize that, in the case of insulin, the course of its discovery meant courtesies and truth were swept aside in hot pursuit of fame. After Dr. Macleod died in 1935 and Dr. Banting died in 1941, Dr. Best took the opportunity to try to revise history. There was the small obstacle of Dr. Collip, but Dr. Best managed to play down Dr. Collip’s contribution by focusing on the eureka moment as being the first insulin dose administered, despite the fact that a more complete recovery without side effects was later achieved only with Dr. Collip’s help.
Despite exclusion from the Nobel Prize, Dr. Best nevertheless became recognized as the “go-to-guy” for the discovery of insulin, said Dr. Hall. When Dr. Best spoke about the discovery of insulin at the New York Diabetes Association meeting in 1946, he was introduced as a speaker whose reputation was already so great that he did “not require much of an introduction.”
“And when a new research institute was opened in Toronto in 1953, it was named in his honor. The opening address, by Sir Henry Dale of the UK Medical Research Council, sang Best’s praises to the rafters, much to the disgruntlement of Best’s former colleague, James Collip, who was sitting in the audience,” Dr. Hall pointed out.
Both Dr. Hall and Dr. Stephens live with type 1 diabetes and have benefited from the efforts of Dr. Banting, Dr. Best, Dr. Collip, Dr. Zuelzer, and Dr. Macleod.
“The discovery of insulin was a miracle, it has allowed people to survive,” said Dr. Stephens. “Few medicines can reverse a death sentence like insulin can. It’s easy to forget how it was when insulin wasn’t there – and it wasn’t that long ago.”
Dr. Hall reflects that scientific progress and discovery are often portrayed as being the result of towering geniuses standing on each other’s shoulders.
“But I think that when German philosopher Immanuel Kant remarked that ‘Out of the crooked timber of humanity, no straight thing can ever be made,’ he offered us a much more accurate picture of how science works. And I think that there’s perhaps no more powerful example of this than the story of insulin,” he said.
A version of this article first appeared on Medscape.com.
Leonard Thompson’s father was so desperate to save his 14-year-old child from certain death due to diabetes that, on Jan. 11, 1922, he took him to Toronto General Hospital to receive what is arguably the first dose of insulin given to a human. From an anticipated life expectancy of weeks – months at best – Thompson lived for an astonishing further 13 years, eventually dying from pneumonia unrelated to diabetes.
By all accounts, the story is a centenary celebration of a remarkable discovery. Insulin has changed what was once a death sentence to a near-normal life expectancy for the millions of people with type 1 diabetes over the past 100 years.
But behind the life-changing success of the discovery – and the Nobel Prize that went with it – lies a tale blighted by disputed claims, twisted truths, and likely injustices between the scientists involved, as they each vied for an honored place in medical history.
Kersten Hall, PhD, honorary fellow, religion and history of science, at the University of Leeds, England, has scoured archives and personal records held at the University of Toronto to uncover the personal stories behind insulin’s discovery.
Despite the wranglings, Dr. Hall asserts: “There’s a distinction between the science and the scientists. Scientists are wonderfully flawed and complex human beings with all their glorious virtues and vices, as we all are. It’s no surprise that they get greedy, jealous, and insecure.”
At death’s door: Diabetes before the 1920s
Prior to insulin’s discovery in 1921, a diagnosis of type 1 diabetes placed someone at death’s door, with nothing but starvation – albeit a slightly slower death – to mitigate a fast-approaching departure from this world. At that time, most diabetes cases would have been type 1 diabetes because, with less obesogenic diets and shorter lifespans, people were much less likely to develop type 2 diabetes.
Nowadays, it is widely recognized that the prevalence of type 2 diabetes is on a steep upward curve, but so too is type 1 diabetes. In the United States alone, there are 1.5 million people diagnosed with type 1 diabetes, a number expected to rise to around 5 million by 2050, according to JDRF, the type 1 diabetes advocacy organization.
Interestingly, 100 years since the first treated patient, life-long insulin remains the only real effective therapy for patients with type 1 diabetes. Once pancreatic beta cells have ceased to function and insulin production has stopped, insulin replacement is the only way to keep blood glucose levels within the recommended range (A1c ≤ 48 mmol/mol [6.5%]), according to the UK National Institute for Health and Care Excellence (NICE), as well as numerous diabetes organizations, including the American Diabetes Association (ADA).
Preliminary clinical trials have looked at stem cell transplantation, prematurely dubbed as a “cure” for type 1 diabetes, as an alternative to insulin therapy. The procedure involves transplanting stem cell–derived cells, which become functional beta cells when infused into humans, but requires immunosuppression, as reported by this news organization.
Today, the life expectancy of people with type 1 diabetes treated with insulin is close to those without the disease, although this is dependent on how tightly blood glucose is controlled. Some studies show life expectancy of those with type 1 diabetes is around 8-12 years lower than the general population but varies depending on where a person lives.
In some lower-income countries, many with type 1 diabetes still die prematurely either because they are undiagnosed or cannot access insulin. The high cost of insulin in the United States is well publicized, as featured in numerous articles by this news organization, and numerous patients in the United States have died because they cannot afford insulin.
Without insulin, young Leonard Thompson would have been lucky to have reached his 15th birthday.
“Such patients were cachectic and thin and would have weighed around 40-50 pounds (18-23 kg), which is very low for an older child. Survival was short and lasted weeks or months usually,” said Elizabeth Stephens, MD, an endocrinologist in Portland, Ore.
“The discovery of insulin was really a miracle because without it diabetes patients were facing certain death. Even nowadays, if people don’t get their insulin because they can’t afford it or for whatever reason, they can still die,” Dr. Stephens stressed.
Antidiabetic effects of pancreatic extract limited
Back in 1869, Paul Langerhans, MD, discovered pancreatic islet cells, or islets of Langerhans, as a medical student. Researchers tried to produce extracts that lowered blood glucose but they were too toxic for patient use.
In 1908, as detailed in his recent book, Insulin – the Crooked Timber, Dr. Hall also refers to the fact that a German researcher, Georg Zuelzer, MD, demonstrated in six patients that pancreatic extracts could reduce urinary levels of glucose and ketones, and that in one case, the treatment woke the patient from a coma. Dr. Zuelzer had purified the extract with alcohol but patients still experienced convulsions and coma; in fact, they were experiencing hypoglycemic shock, but Dr. Zuelzer had not identified it as such.
“He thought his preparation was full of impurities – and that’s the irony. He had in his hands an insulin prep that was so clean and so potent that it sent the test animals into hypoglycemic shock,” Dr. Hall pointed out.
By 1921, two young researchers, Frederick G. Banting, MD, a practicing medical doctor in Toronto, together with a final year physiology student at the University of Toronto, Charles H. Best, MD, DSc, collaborated on the instruction of Dr. Best’s superior, John James Rickard Macleod, MBChB, professor of physiology at the University of Toronto, to make pancreatic extracts, first from dogs and then from cattle.
Over the months prior to treating Thompson, working together in the laboratory, Dr. Banting and Dr. Best prepared the pancreatic extract from cattle and tested it on dogs with diabetes.
Then, in what amounted to a phase 1 trial of its day, with an “n of one,” a frail and close-to-death Thompson was given 15 cc of pancreatic extract at Toronto General Hospital in January 1922. His blood glucose level dropped by 25%, but unfortunately, his body still produced ketones, indicating the antidiabetic effect was limited. He also experienced an adverse reaction at the injection site with an accumulation of abscesses.
So despite success with isolating the extract and administering it to Thompson, the product remained tainted with impurities.
At this point, colleague James Collip, MD, PhD, came to the rescue. He used his skills as a biochemist to purify the pancreatic extract enough to eliminate impurities.
When Thompson was treated 2 weeks later with the purified extract, he experienced a more positive outcome. Gone was the injection site reaction, gone were the high blood glucose levels, and Thompson “became brighter, more active, looked better, and said he felt stronger,” according to a publication describing the treatment.
Dr. Collip also determined that by over-purifying the product, the animals he experimented on could overreact and experience convulsions, coma, and death due to hypoglycemia from too much insulin.
Fighting talk
Recalling an excerpt from Dr. Banting’s diary, Dr. Hall said that Dr. Banting had a mercurial temper and testified to his loss of patience with Dr. Collip when the chemist refused to share his formula of purification. His diary reads: “I grabbed him in one hand by the overcoat ... and almost lifting him I sat him down hard on the chair ... I remember telling him that it was a good job he was so much smaller – otherwise I would ‘knock hell out of him.’ ”
According to Dr. Hall, in 1923, when Dr. Banting and Dr. Macleod were jointly awarded the Nobel Prize for Medicine, Dr. Best resented being excluded, and despite Dr. Banting’s sharing half his prize money with Dr. Best, animosity prevailed.
At one point, before leaving on a plane for a wartime mission to the United Kingdom, Dr. Banting noted that if he didn’t make it back alive, “and they give my [professorial] chair to that son-of-a-bitch Best, I’ll never rest in my grave.” In a cruel twist of fate, Dr. Banting’s plane crashed and all aboard died.
The Nobel Prize had also been a source of rivalry between Dr. Banting and his boss, Dr. Macleod. In late 1921, while presenting the findings from animal models at the American Physiological Society conference, Dr. Banting’s nerves got the better of him and Dr. Macleod took over at the podium to finish the talk. Dr. Banting perceived this as his boss stealing the limelight.
Only a few months later, at the Association of American Physicians annual conference, Dr. Macleod played to an audience for a second time by making the first formal announcement of the discovery to the scientific community. Notably, Dr. Banting was absent.
The Nobel Prize or a poisoned chalice?
Awarded annually for physics, chemistry, medicine/physiology, literature, peace, and economics, Nobel Prizes are usually considered the holy grail of achievement. In 1895, funds for the prizes were bequeathed by Alfred Nobel in his last will and testament, with each prize worth around $40,000 at the time (approximately $1,000,000 in today’s value).
Writing in 2001 in the journal Diabetes Voice, Professor Sir George Alberti, DPhil, BM BCh, former president of the UK Royal College of Physicians, summarized the burden that accompanies the Nobel Prize: “I personally believe that such prizes and awards do more harm than good and should be abolished. Many a scientist has gone to their grave feeling deeply aggrieved because they were not awarded a Nobel Prize.”
Such high stakes surround the prize that, in the case of insulin, the course of its discovery meant courtesies and truth were swept aside in hot pursuit of fame. After Dr. Macleod died in 1935 and Dr. Banting died in 1941, Dr. Best took the opportunity to try to revise history. There was the small obstacle of Dr. Collip, but Dr. Best managed to play down Dr. Collip’s contribution by focusing on the eureka moment as being the first insulin dose administered, despite the fact that a more complete recovery without side effects was later achieved only with Dr. Collip’s help.
Despite exclusion from the Nobel Prize, Dr. Best nevertheless became recognized as the “go-to-guy” for the discovery of insulin, said Dr. Hall. When Dr. Best spoke about the discovery of insulin at the New York Diabetes Association meeting in 1946, he was introduced as a speaker whose reputation was already so great that he did “not require much of an introduction.”
“And when a new research institute was opened in Toronto in 1953, it was named in his honor. The opening address, by Sir Henry Dale of the UK Medical Research Council, sang Best’s praises to the rafters, much to the disgruntlement of Best’s former colleague, James Collip, who was sitting in the audience,” Dr. Hall pointed out.
Both Dr. Hall and Dr. Stephens live with type 1 diabetes and have benefited from the efforts of Dr. Banting, Dr. Best, Dr. Collip, Dr. Zuelzer, and Dr. Macleod.
“The discovery of insulin was a miracle, it has allowed people to survive,” said Dr. Stephens. “Few medicines can reverse a death sentence like insulin can. It’s easy to forget how it was when insulin wasn’t there – and it wasn’t that long ago.”
Dr. Hall reflects that scientific progress and discovery are often portrayed as being the result of towering geniuses standing on each other’s shoulders.
“But I think that when German philosopher Immanuel Kant remarked that ‘Out of the crooked timber of humanity, no straight thing can ever be made,’ he offered us a much more accurate picture of how science works. And I think that there’s perhaps no more powerful example of this than the story of insulin,” he said.
A version of this article first appeared on Medscape.com.
Leonard Thompson’s father was so desperate to save his 14-year-old child from certain death due to diabetes that, on Jan. 11, 1922, he took him to Toronto General Hospital to receive what is arguably the first dose of insulin given to a human. From an anticipated life expectancy of weeks – months at best – Thompson lived for an astonishing further 13 years, eventually dying from pneumonia unrelated to diabetes.
By all accounts, the story is a centenary celebration of a remarkable discovery. Insulin has changed what was once a death sentence to a near-normal life expectancy for the millions of people with type 1 diabetes over the past 100 years.
But behind the life-changing success of the discovery – and the Nobel Prize that went with it – lies a tale blighted by disputed claims, twisted truths, and likely injustices between the scientists involved, as they each vied for an honored place in medical history.
Kersten Hall, PhD, honorary fellow, religion and history of science, at the University of Leeds, England, has scoured archives and personal records held at the University of Toronto to uncover the personal stories behind insulin’s discovery.
Despite the wranglings, Dr. Hall asserts: “There’s a distinction between the science and the scientists. Scientists are wonderfully flawed and complex human beings with all their glorious virtues and vices, as we all are. It’s no surprise that they get greedy, jealous, and insecure.”
At death’s door: Diabetes before the 1920s
Prior to insulin’s discovery in 1921, a diagnosis of type 1 diabetes placed someone at death’s door, with nothing but starvation – albeit a slightly slower death – to mitigate a fast-approaching departure from this world. At that time, most diabetes cases would have been type 1 diabetes because, with less obesogenic diets and shorter lifespans, people were much less likely to develop type 2 diabetes.
Nowadays, it is widely recognized that the prevalence of type 2 diabetes is on a steep upward curve, but so too is type 1 diabetes. In the United States alone, there are 1.5 million people diagnosed with type 1 diabetes, a number expected to rise to around 5 million by 2050, according to JDRF, the type 1 diabetes advocacy organization.
Interestingly, 100 years since the first treated patient, life-long insulin remains the only real effective therapy for patients with type 1 diabetes. Once pancreatic beta cells have ceased to function and insulin production has stopped, insulin replacement is the only way to keep blood glucose levels within the recommended range (A1c ≤ 48 mmol/mol [6.5%]), according to the UK National Institute for Health and Care Excellence (NICE), as well as numerous diabetes organizations, including the American Diabetes Association (ADA).
Preliminary clinical trials have looked at stem cell transplantation, prematurely dubbed as a “cure” for type 1 diabetes, as an alternative to insulin therapy. The procedure involves transplanting stem cell–derived cells, which become functional beta cells when infused into humans, but requires immunosuppression, as reported by this news organization.
Today, the life expectancy of people with type 1 diabetes treated with insulin is close to those without the disease, although this is dependent on how tightly blood glucose is controlled. Some studies show life expectancy of those with type 1 diabetes is around 8-12 years lower than the general population but varies depending on where a person lives.
In some lower-income countries, many with type 1 diabetes still die prematurely either because they are undiagnosed or cannot access insulin. The high cost of insulin in the United States is well publicized, as featured in numerous articles by this news organization, and numerous patients in the United States have died because they cannot afford insulin.
Without insulin, young Leonard Thompson would have been lucky to have reached his 15th birthday.
“Such patients were cachectic and thin and would have weighed around 40-50 pounds (18-23 kg), which is very low for an older child. Survival was short and lasted weeks or months usually,” said Elizabeth Stephens, MD, an endocrinologist in Portland, Ore.
“The discovery of insulin was really a miracle because without it diabetes patients were facing certain death. Even nowadays, if people don’t get their insulin because they can’t afford it or for whatever reason, they can still die,” Dr. Stephens stressed.
Antidiabetic effects of pancreatic extract limited
Back in 1869, Paul Langerhans, MD, discovered pancreatic islet cells, or islets of Langerhans, as a medical student. Researchers tried to produce extracts that lowered blood glucose but they were too toxic for patient use.
In 1908, as detailed in his recent book, Insulin – the Crooked Timber, Dr. Hall also refers to the fact that a German researcher, Georg Zuelzer, MD, demonstrated in six patients that pancreatic extracts could reduce urinary levels of glucose and ketones, and that in one case, the treatment woke the patient from a coma. Dr. Zuelzer had purified the extract with alcohol but patients still experienced convulsions and coma; in fact, they were experiencing hypoglycemic shock, but Dr. Zuelzer had not identified it as such.
“He thought his preparation was full of impurities – and that’s the irony. He had in his hands an insulin prep that was so clean and so potent that it sent the test animals into hypoglycemic shock,” Dr. Hall pointed out.
By 1921, two young researchers, Frederick G. Banting, MD, a practicing medical doctor in Toronto, together with a final year physiology student at the University of Toronto, Charles H. Best, MD, DSc, collaborated on the instruction of Dr. Best’s superior, John James Rickard Macleod, MBChB, professor of physiology at the University of Toronto, to make pancreatic extracts, first from dogs and then from cattle.
Over the months prior to treating Thompson, working together in the laboratory, Dr. Banting and Dr. Best prepared the pancreatic extract from cattle and tested it on dogs with diabetes.
Then, in what amounted to a phase 1 trial of its day, with an “n of one,” a frail and close-to-death Thompson was given 15 cc of pancreatic extract at Toronto General Hospital in January 1922. His blood glucose level dropped by 25%, but unfortunately, his body still produced ketones, indicating the antidiabetic effect was limited. He also experienced an adverse reaction at the injection site with an accumulation of abscesses.
So despite success with isolating the extract and administering it to Thompson, the product remained tainted with impurities.
At this point, colleague James Collip, MD, PhD, came to the rescue. He used his skills as a biochemist to purify the pancreatic extract enough to eliminate impurities.
When Thompson was treated 2 weeks later with the purified extract, he experienced a more positive outcome. Gone was the injection site reaction, gone were the high blood glucose levels, and Thompson “became brighter, more active, looked better, and said he felt stronger,” according to a publication describing the treatment.
Dr. Collip also determined that by over-purifying the product, the animals he experimented on could overreact and experience convulsions, coma, and death due to hypoglycemia from too much insulin.
Fighting talk
Recalling an excerpt from Dr. Banting’s diary, Dr. Hall said that Dr. Banting had a mercurial temper and testified to his loss of patience with Dr. Collip when the chemist refused to share his formula of purification. His diary reads: “I grabbed him in one hand by the overcoat ... and almost lifting him I sat him down hard on the chair ... I remember telling him that it was a good job he was so much smaller – otherwise I would ‘knock hell out of him.’ ”
According to Dr. Hall, in 1923, when Dr. Banting and Dr. Macleod were jointly awarded the Nobel Prize for Medicine, Dr. Best resented being excluded, and despite Dr. Banting’s sharing half his prize money with Dr. Best, animosity prevailed.
At one point, before leaving on a plane for a wartime mission to the United Kingdom, Dr. Banting noted that if he didn’t make it back alive, “and they give my [professorial] chair to that son-of-a-bitch Best, I’ll never rest in my grave.” In a cruel twist of fate, Dr. Banting’s plane crashed and all aboard died.
The Nobel Prize had also been a source of rivalry between Dr. Banting and his boss, Dr. Macleod. In late 1921, while presenting the findings from animal models at the American Physiological Society conference, Dr. Banting’s nerves got the better of him and Dr. Macleod took over at the podium to finish the talk. Dr. Banting perceived this as his boss stealing the limelight.
Only a few months later, at the Association of American Physicians annual conference, Dr. Macleod played to an audience for a second time by making the first formal announcement of the discovery to the scientific community. Notably, Dr. Banting was absent.
The Nobel Prize or a poisoned chalice?
Awarded annually for physics, chemistry, medicine/physiology, literature, peace, and economics, Nobel Prizes are usually considered the holy grail of achievement. In 1895, funds for the prizes were bequeathed by Alfred Nobel in his last will and testament, with each prize worth around $40,000 at the time (approximately $1,000,000 in today’s value).
Writing in 2001 in the journal Diabetes Voice, Professor Sir George Alberti, DPhil, BM BCh, former president of the UK Royal College of Physicians, summarized the burden that accompanies the Nobel Prize: “I personally believe that such prizes and awards do more harm than good and should be abolished. Many a scientist has gone to their grave feeling deeply aggrieved because they were not awarded a Nobel Prize.”
Such high stakes surround the prize that, in the case of insulin, the course of its discovery meant courtesies and truth were swept aside in hot pursuit of fame. After Dr. Macleod died in 1935 and Dr. Banting died in 1941, Dr. Best took the opportunity to try to revise history. There was the small obstacle of Dr. Collip, but Dr. Best managed to play down Dr. Collip’s contribution by focusing on the eureka moment as being the first insulin dose administered, despite the fact that a more complete recovery without side effects was later achieved only with Dr. Collip’s help.
Despite exclusion from the Nobel Prize, Dr. Best nevertheless became recognized as the “go-to-guy” for the discovery of insulin, said Dr. Hall. When Dr. Best spoke about the discovery of insulin at the New York Diabetes Association meeting in 1946, he was introduced as a speaker whose reputation was already so great that he did “not require much of an introduction.”
“And when a new research institute was opened in Toronto in 1953, it was named in his honor. The opening address, by Sir Henry Dale of the UK Medical Research Council, sang Best’s praises to the rafters, much to the disgruntlement of Best’s former colleague, James Collip, who was sitting in the audience,” Dr. Hall pointed out.
Both Dr. Hall and Dr. Stephens live with type 1 diabetes and have benefited from the efforts of Dr. Banting, Dr. Best, Dr. Collip, Dr. Zuelzer, and Dr. Macleod.
“The discovery of insulin was a miracle, it has allowed people to survive,” said Dr. Stephens. “Few medicines can reverse a death sentence like insulin can. It’s easy to forget how it was when insulin wasn’t there – and it wasn’t that long ago.”
Dr. Hall reflects that scientific progress and discovery are often portrayed as being the result of towering geniuses standing on each other’s shoulders.
“But I think that when German philosopher Immanuel Kant remarked that ‘Out of the crooked timber of humanity, no straight thing can ever be made,’ he offered us a much more accurate picture of how science works. And I think that there’s perhaps no more powerful example of this than the story of insulin,” he said.
A version of this article first appeared on Medscape.com.