User login
News and Views that Matter to Pediatricians
The leading independent newspaper covering news and commentary in pediatrics.
Even COVID-19 can’t stop a true optimist
Squeezing a little lemonade out of COVID-19
We like to think of ourselves as optimists here at LOTME. A glass is half full, the sky is partly sunny, and our motto is “Always look on the bright side of insanity.” Then again, our motto before that was “LOTME: Where science meets stupid,” so what do we know?
Anyway, it’s that upbeat, can-do attitude that allows us to say something positive – two somethings, actually – about the insanity that is COVID-19.
Our journey to the bright side begins, oddly enough, in the courtroom. Seems that our old friend, the face mask, is something of a lie-detector aid for juries. The authors of a recent literature review of studies on deception “found that facial expressions and other forms of nonverbal behaviour are an unreliable indicator of deceit,” according to a statement from the University of Portsmouth, where the analysis was conducted.
The one study that directly examined the role of face coverings in court proceedings showed that, “by taking away the distraction of nonverbal behaviours, observers had to rely on speech content, which turned out to be better for detecting lies,” the university said.
The second stage of our positivity trek brings us to the National Trends in Disability Employment monthly update, where we see a fourth consecutive month of gains for people with disabilities despite the larger trend of declines among those without disabilities.
Here are some numbers from the Kessler Foundation and the University of New Hampshire’s Institute on Disability to tell the story: From October to November, the employment-to-population ratio increased 4.2% for working-age people with disabilities, compared with 0.4% for people without disabilities. At the same time, the labor force participation rate rose 2.4% for working-age people with disabilities and just 0.1% for working-age people without disabilities.
Both indicators surpassed their historic highs, Andrew Houtenville, PhD, director of the Institute on Disability, said in the update. “These gains suggest that the restructuring resulting from the pandemic may be benefiting people with disabilities. Ironically, it may have taken a pandemic to shake the labor market loose for people with disabilities.”
And that is how a world-class optimist turns one gigantic lemon into lemonade.
Cut the cheese for better sleep
So, we’ve already talked about the TikTok lettuce tea hack that’s supposed to help us sleep better. Well, there’s another food that could have the opposite effect.
According to an article from the BBC, cheese has something of a reputation. Ever since the 1960s, when a researcher noted that one patient’s nightmares stopped after he quit eating an ounce or two of cheddar each night, there’s been speculation that cheese gives you weird dreams. Another study in 2005 suggested certain types of cheese cause certain types of dreams. Blue cheese for vivid dreams and cheddar cheese for celebrity cameos.
But is there any truth to it at all?
Regardless of what we eat, going to bed hungry could cause vivid dreams, according to research by Tore Nielsen, director of the University of Montreal’s dream and nightmare lab. The 2015 study showed that high lactose could have an effect on dreams.
In that study, 17% of participants said their dreams were influenced by what they ate, but the kicker was that dairy products were the foods most reported as causing the weird dreams, the BBC noted.
“It’s likely an indirect effect in that lactose produces symptoms like gas, bloating and diarrhoea and influences dreams, as dreams draw on somatic sources like this. And if you have certain kinds of intolerances, you still may be likely to eat those foods sometimes,” Mr. Nielsen told the BBC.
There’s also the theory that it’s all in the timing of consumption. Are you the type of person to sneak a slice of cheese from the fridge late at night? (Nods.) Same.
“One reason cheese and nightmares come about is that eating later before bed is more likely to disrupt sleep, and cheese can be hard to digest,” said Charlotte Gupta, a research fellow at Central Queensland University in Australia and a coauthor of a 2020 review on how diet affects our sleep.
So as tempting as it is, maybe skip sprinkling Parmesan cheese shreds into your mouth at the open fridge before bed.
Teeing up against Parkinson’s
For the nearly 1 million people in the United States with Parkinson’s disease, tai chi is one of the best ways to alleviate the symptoms. The average Parkinson’s patient, however, is going to be on the older side and more likely to view the martial art as some sort of communist plot. And would you participate in a communist plot? We don’t think so.
One group of researchers saw that patients weren’t keeping up with their therapy and decided to try a different activity, something that older people would be more likely to stick with. Something a bit more stereotypical. No, not shuffleboard. They tried golf.
“Golf is popular – the most popular sport for people over the age of 55 – which might encourage people to try it and stick with it,” study author Anne-Marie A. Wills, MD, of Massachusetts General Hospital, Boston, said in a Study Finds report.
In a small study, the investigators had a group of patients with Parkinson’s regularly go to a driving range for 10 weeks to hit golf balls (all expenses paid too, and that’s a big deal for golf), while another group continued with their tai chi.
At the end of the study, the 8 patients who went to the driving range had significantly better results in a Parkinson’s mobility test than those of the 12 patients in the tai chi group. In addition, the golf-group participants said they were more likely to continue with their therapy than were those who did tai chi.
Despite the small size of the study, the research team said the results certainly warrant further research. After all, the best sort of therapy is the kind that actually gets done. And golf just gets in your head. The eternal quest to add distance, to straighten out that annoying slice, to stop thinning half your chips, to make those annoying 4-footers. ... Maybe that’s just us.
Squeezing a little lemonade out of COVID-19
We like to think of ourselves as optimists here at LOTME. A glass is half full, the sky is partly sunny, and our motto is “Always look on the bright side of insanity.” Then again, our motto before that was “LOTME: Where science meets stupid,” so what do we know?
Anyway, it’s that upbeat, can-do attitude that allows us to say something positive – two somethings, actually – about the insanity that is COVID-19.
Our journey to the bright side begins, oddly enough, in the courtroom. Seems that our old friend, the face mask, is something of a lie-detector aid for juries. The authors of a recent literature review of studies on deception “found that facial expressions and other forms of nonverbal behaviour are an unreliable indicator of deceit,” according to a statement from the University of Portsmouth, where the analysis was conducted.
The one study that directly examined the role of face coverings in court proceedings showed that, “by taking away the distraction of nonverbal behaviours, observers had to rely on speech content, which turned out to be better for detecting lies,” the university said.
The second stage of our positivity trek brings us to the National Trends in Disability Employment monthly update, where we see a fourth consecutive month of gains for people with disabilities despite the larger trend of declines among those without disabilities.
Here are some numbers from the Kessler Foundation and the University of New Hampshire’s Institute on Disability to tell the story: From October to November, the employment-to-population ratio increased 4.2% for working-age people with disabilities, compared with 0.4% for people without disabilities. At the same time, the labor force participation rate rose 2.4% for working-age people with disabilities and just 0.1% for working-age people without disabilities.
Both indicators surpassed their historic highs, Andrew Houtenville, PhD, director of the Institute on Disability, said in the update. “These gains suggest that the restructuring resulting from the pandemic may be benefiting people with disabilities. Ironically, it may have taken a pandemic to shake the labor market loose for people with disabilities.”
And that is how a world-class optimist turns one gigantic lemon into lemonade.
Cut the cheese for better sleep
So, we’ve already talked about the TikTok lettuce tea hack that’s supposed to help us sleep better. Well, there’s another food that could have the opposite effect.
According to an article from the BBC, cheese has something of a reputation. Ever since the 1960s, when a researcher noted that one patient’s nightmares stopped after he quit eating an ounce or two of cheddar each night, there’s been speculation that cheese gives you weird dreams. Another study in 2005 suggested certain types of cheese cause certain types of dreams. Blue cheese for vivid dreams and cheddar cheese for celebrity cameos.
But is there any truth to it at all?
Regardless of what we eat, going to bed hungry could cause vivid dreams, according to research by Tore Nielsen, director of the University of Montreal’s dream and nightmare lab. The 2015 study showed that high lactose could have an effect on dreams.
In that study, 17% of participants said their dreams were influenced by what they ate, but the kicker was that dairy products were the foods most reported as causing the weird dreams, the BBC noted.
“It’s likely an indirect effect in that lactose produces symptoms like gas, bloating and diarrhoea and influences dreams, as dreams draw on somatic sources like this. And if you have certain kinds of intolerances, you still may be likely to eat those foods sometimes,” Mr. Nielsen told the BBC.
There’s also the theory that it’s all in the timing of consumption. Are you the type of person to sneak a slice of cheese from the fridge late at night? (Nods.) Same.
“One reason cheese and nightmares come about is that eating later before bed is more likely to disrupt sleep, and cheese can be hard to digest,” said Charlotte Gupta, a research fellow at Central Queensland University in Australia and a coauthor of a 2020 review on how diet affects our sleep.
So as tempting as it is, maybe skip sprinkling Parmesan cheese shreds into your mouth at the open fridge before bed.
Teeing up against Parkinson’s
For the nearly 1 million people in the United States with Parkinson’s disease, tai chi is one of the best ways to alleviate the symptoms. The average Parkinson’s patient, however, is going to be on the older side and more likely to view the martial art as some sort of communist plot. And would you participate in a communist plot? We don’t think so.
One group of researchers saw that patients weren’t keeping up with their therapy and decided to try a different activity, something that older people would be more likely to stick with. Something a bit more stereotypical. No, not shuffleboard. They tried golf.
“Golf is popular – the most popular sport for people over the age of 55 – which might encourage people to try it and stick with it,” study author Anne-Marie A. Wills, MD, of Massachusetts General Hospital, Boston, said in a Study Finds report.
In a small study, the investigators had a group of patients with Parkinson’s regularly go to a driving range for 10 weeks to hit golf balls (all expenses paid too, and that’s a big deal for golf), while another group continued with their tai chi.
At the end of the study, the 8 patients who went to the driving range had significantly better results in a Parkinson’s mobility test than those of the 12 patients in the tai chi group. In addition, the golf-group participants said they were more likely to continue with their therapy than were those who did tai chi.
Despite the small size of the study, the research team said the results certainly warrant further research. After all, the best sort of therapy is the kind that actually gets done. And golf just gets in your head. The eternal quest to add distance, to straighten out that annoying slice, to stop thinning half your chips, to make those annoying 4-footers. ... Maybe that’s just us.
Squeezing a little lemonade out of COVID-19
We like to think of ourselves as optimists here at LOTME. A glass is half full, the sky is partly sunny, and our motto is “Always look on the bright side of insanity.” Then again, our motto before that was “LOTME: Where science meets stupid,” so what do we know?
Anyway, it’s that upbeat, can-do attitude that allows us to say something positive – two somethings, actually – about the insanity that is COVID-19.
Our journey to the bright side begins, oddly enough, in the courtroom. Seems that our old friend, the face mask, is something of a lie-detector aid for juries. The authors of a recent literature review of studies on deception “found that facial expressions and other forms of nonverbal behaviour are an unreliable indicator of deceit,” according to a statement from the University of Portsmouth, where the analysis was conducted.
The one study that directly examined the role of face coverings in court proceedings showed that, “by taking away the distraction of nonverbal behaviours, observers had to rely on speech content, which turned out to be better for detecting lies,” the university said.
The second stage of our positivity trek brings us to the National Trends in Disability Employment monthly update, where we see a fourth consecutive month of gains for people with disabilities despite the larger trend of declines among those without disabilities.
Here are some numbers from the Kessler Foundation and the University of New Hampshire’s Institute on Disability to tell the story: From October to November, the employment-to-population ratio increased 4.2% for working-age people with disabilities, compared with 0.4% for people without disabilities. At the same time, the labor force participation rate rose 2.4% for working-age people with disabilities and just 0.1% for working-age people without disabilities.
Both indicators surpassed their historic highs, Andrew Houtenville, PhD, director of the Institute on Disability, said in the update. “These gains suggest that the restructuring resulting from the pandemic may be benefiting people with disabilities. Ironically, it may have taken a pandemic to shake the labor market loose for people with disabilities.”
And that is how a world-class optimist turns one gigantic lemon into lemonade.
Cut the cheese for better sleep
So, we’ve already talked about the TikTok lettuce tea hack that’s supposed to help us sleep better. Well, there’s another food that could have the opposite effect.
According to an article from the BBC, cheese has something of a reputation. Ever since the 1960s, when a researcher noted that one patient’s nightmares stopped after he quit eating an ounce or two of cheddar each night, there’s been speculation that cheese gives you weird dreams. Another study in 2005 suggested certain types of cheese cause certain types of dreams. Blue cheese for vivid dreams and cheddar cheese for celebrity cameos.
But is there any truth to it at all?
Regardless of what we eat, going to bed hungry could cause vivid dreams, according to research by Tore Nielsen, director of the University of Montreal’s dream and nightmare lab. The 2015 study showed that high lactose could have an effect on dreams.
In that study, 17% of participants said their dreams were influenced by what they ate, but the kicker was that dairy products were the foods most reported as causing the weird dreams, the BBC noted.
“It’s likely an indirect effect in that lactose produces symptoms like gas, bloating and diarrhoea and influences dreams, as dreams draw on somatic sources like this. And if you have certain kinds of intolerances, you still may be likely to eat those foods sometimes,” Mr. Nielsen told the BBC.
There’s also the theory that it’s all in the timing of consumption. Are you the type of person to sneak a slice of cheese from the fridge late at night? (Nods.) Same.
“One reason cheese and nightmares come about is that eating later before bed is more likely to disrupt sleep, and cheese can be hard to digest,” said Charlotte Gupta, a research fellow at Central Queensland University in Australia and a coauthor of a 2020 review on how diet affects our sleep.
So as tempting as it is, maybe skip sprinkling Parmesan cheese shreds into your mouth at the open fridge before bed.
Teeing up against Parkinson’s
For the nearly 1 million people in the United States with Parkinson’s disease, tai chi is one of the best ways to alleviate the symptoms. The average Parkinson’s patient, however, is going to be on the older side and more likely to view the martial art as some sort of communist plot. And would you participate in a communist plot? We don’t think so.
One group of researchers saw that patients weren’t keeping up with their therapy and decided to try a different activity, something that older people would be more likely to stick with. Something a bit more stereotypical. No, not shuffleboard. They tried golf.
“Golf is popular – the most popular sport for people over the age of 55 – which might encourage people to try it and stick with it,” study author Anne-Marie A. Wills, MD, of Massachusetts General Hospital, Boston, said in a Study Finds report.
In a small study, the investigators had a group of patients with Parkinson’s regularly go to a driving range for 10 weeks to hit golf balls (all expenses paid too, and that’s a big deal for golf), while another group continued with their tai chi.
At the end of the study, the 8 patients who went to the driving range had significantly better results in a Parkinson’s mobility test than those of the 12 patients in the tai chi group. In addition, the golf-group participants said they were more likely to continue with their therapy than were those who did tai chi.
Despite the small size of the study, the research team said the results certainly warrant further research. After all, the best sort of therapy is the kind that actually gets done. And golf just gets in your head. The eternal quest to add distance, to straighten out that annoying slice, to stop thinning half your chips, to make those annoying 4-footers. ... Maybe that’s just us.
How does atopic dermatitis present in skin of color?
“We see very heterogenous and broad clinical presentations across the diverse patient populations that we see,” Andrew F. Alexis, MD, MPH, said at the Revolutionizing Atopic Dermatitis symposium. “Some of these differences might be related to population variations in skin barrier function, immunologic factors, genetic factors, and environmental factors, which all interplay to produce variations in the clinical presentation and overall impact of AD. Many nongenetic factors also contribute to differences that we see, including some socioeconomic and other factors that feed into health disparities.”
Dr. Alexis, professor of clinical dermatology at Weill Cornell Medicine, New York, discussed four main clinical features of AD in skin of color.
Erythema is less visible because it is masked by pigment
“There can be some masking of the redness and alteration of that color such that it doesn’t look bright red as it would in the background of lightly pigmented skin,” Dr. Alexis said. “Instead, the [AD lesions] have shades of grayish-red or grayish-brown or reddish-brown. It’s important to recognize this clinical presentation and look carefully and assess the patient – not just visually but with palpation and take into consideration symptomatology so that you don’t fall into the trap of calling an AD lesion postinflammatory hyperpigmentation. It’s also helpful to isolate the islands of normal or nonlesional skin and contrast that with the areas of lesional skin, to get a sense of how active and inflamed the areas are. Palpation really helps to appreciate the elevation of the lesions that are involved.”
Follicular accentuation
Morphological variants common in skin of color include the follicular variant or micropapular variant of AD. “You might just see a collection of papules that are 1-2 mm in size and pruritic and in typical sites of predilection [for] eczema,” he said. Prurigo nodularis–like lesions or prurigo nodularis in association with AD are also seen more frequently in skin of color.
Lichenification
The lichenoid variant of AD is characterized by a violaceous hue and other features that resemble lichen planus and has been reported to be more common in individuals of African descent. A prospective study of about 1,000 patients with AD seen over 2 years at a dermatology clinic in southeastern Nigeria found that 54% of patients had papular lichenoid lesions. In addition, 51% had elevated blood eosinophil counts, especially those with severe disease.
Dr. Alexis added that psoriasiform features have been reported in studies of East Asian populations with AD. These plaques may be more well demarcated and have clinical and histologic features that resemble psoriasis.
Dyspigmentation
One common feature across the spectrum of patients with skin of color “is the risk of longstanding pigmentary sequelae in the form of hyperpigmentation or hypopigmentation,” said Dr. Alexis, who is also vice chair for diversity and inclusion for the department of dermatology at Weill Cornell Medicine. “In very severe longstanding areas with chronic excoriation to the point of breaking of the skin, eroding of the skin, causing permanent damage to the melanocytes, dyspigmentation that resembles vitiligo can be seen. We can also see hypopigmentation as a consequence of topical corticosteroids, particularly those that are class I or class II and are used for prolonged periods of time.”
Dr. Alexis noted that delays in treatment and undertreatment can contribute to a higher risk of pigmentary and other long-term sequelae. “New therapies show promise in improving outcomes in AD patients with skin of color. When it comes to therapeutic responses, there are some post hoc studies that have investigated potential differences in safety and efficacy of the agents that have been recently approved. We clearly need more data to better understand if there are potential racial or ethnic differences.”
Dr. Alexis reported no relevant financial relationships.
Commentary by Lawrence F. Eichenfield, MD
Atopic dermatitis (AD) is highly heterogenous, with tremendous variations in extent, qualities of eczema, symptom complex, and physical presentation. Prior studies have reported disparities of care delivered to racial and ethnic minorities in the United States, as well as higher susceptibility to AD and odds of persistent disease into adulthood from child-onset AD. Recognizing some differences in presentation of AD in patients with skin of color is important as we select our therapeutic interventions, including assessing new treatments being added to our armamentarium. Erythema may be harder to notice in darker skin, but attempting to blanch the skin with pressure can help to assess the color and inflammation. Appreciating lichenoid changes, including papular and “micropapular” AD, and psoriasiform-like thickening in certain patients (reportedly more common in East Asian populations) are important as well. And dyspigmentation is an important aspect of the disease presentation and patient and parental concern, given both hypopigmentaton and hyperpigmentation commonly seen over the course of AD.
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children's Hospital-San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. He disclosed that he has served as an investigator and/or consultant to AbbVie, Lilly, Pfizer, Regeneron, Sanofi-Genzyme, and Verrica.
A version of this article first appeared on Medscape.com.
This article was updated 6/18/22.
“We see very heterogenous and broad clinical presentations across the diverse patient populations that we see,” Andrew F. Alexis, MD, MPH, said at the Revolutionizing Atopic Dermatitis symposium. “Some of these differences might be related to population variations in skin barrier function, immunologic factors, genetic factors, and environmental factors, which all interplay to produce variations in the clinical presentation and overall impact of AD. Many nongenetic factors also contribute to differences that we see, including some socioeconomic and other factors that feed into health disparities.”
Dr. Alexis, professor of clinical dermatology at Weill Cornell Medicine, New York, discussed four main clinical features of AD in skin of color.
Erythema is less visible because it is masked by pigment
“There can be some masking of the redness and alteration of that color such that it doesn’t look bright red as it would in the background of lightly pigmented skin,” Dr. Alexis said. “Instead, the [AD lesions] have shades of grayish-red or grayish-brown or reddish-brown. It’s important to recognize this clinical presentation and look carefully and assess the patient – not just visually but with palpation and take into consideration symptomatology so that you don’t fall into the trap of calling an AD lesion postinflammatory hyperpigmentation. It’s also helpful to isolate the islands of normal or nonlesional skin and contrast that with the areas of lesional skin, to get a sense of how active and inflamed the areas are. Palpation really helps to appreciate the elevation of the lesions that are involved.”
Follicular accentuation
Morphological variants common in skin of color include the follicular variant or micropapular variant of AD. “You might just see a collection of papules that are 1-2 mm in size and pruritic and in typical sites of predilection [for] eczema,” he said. Prurigo nodularis–like lesions or prurigo nodularis in association with AD are also seen more frequently in skin of color.
Lichenification
The lichenoid variant of AD is characterized by a violaceous hue and other features that resemble lichen planus and has been reported to be more common in individuals of African descent. A prospective study of about 1,000 patients with AD seen over 2 years at a dermatology clinic in southeastern Nigeria found that 54% of patients had papular lichenoid lesions. In addition, 51% had elevated blood eosinophil counts, especially those with severe disease.
Dr. Alexis added that psoriasiform features have been reported in studies of East Asian populations with AD. These plaques may be more well demarcated and have clinical and histologic features that resemble psoriasis.
Dyspigmentation
One common feature across the spectrum of patients with skin of color “is the risk of longstanding pigmentary sequelae in the form of hyperpigmentation or hypopigmentation,” said Dr. Alexis, who is also vice chair for diversity and inclusion for the department of dermatology at Weill Cornell Medicine. “In very severe longstanding areas with chronic excoriation to the point of breaking of the skin, eroding of the skin, causing permanent damage to the melanocytes, dyspigmentation that resembles vitiligo can be seen. We can also see hypopigmentation as a consequence of topical corticosteroids, particularly those that are class I or class II and are used for prolonged periods of time.”
Dr. Alexis noted that delays in treatment and undertreatment can contribute to a higher risk of pigmentary and other long-term sequelae. “New therapies show promise in improving outcomes in AD patients with skin of color. When it comes to therapeutic responses, there are some post hoc studies that have investigated potential differences in safety and efficacy of the agents that have been recently approved. We clearly need more data to better understand if there are potential racial or ethnic differences.”
Dr. Alexis reported no relevant financial relationships.
Commentary by Lawrence F. Eichenfield, MD
Atopic dermatitis (AD) is highly heterogenous, with tremendous variations in extent, qualities of eczema, symptom complex, and physical presentation. Prior studies have reported disparities of care delivered to racial and ethnic minorities in the United States, as well as higher susceptibility to AD and odds of persistent disease into adulthood from child-onset AD. Recognizing some differences in presentation of AD in patients with skin of color is important as we select our therapeutic interventions, including assessing new treatments being added to our armamentarium. Erythema may be harder to notice in darker skin, but attempting to blanch the skin with pressure can help to assess the color and inflammation. Appreciating lichenoid changes, including papular and “micropapular” AD, and psoriasiform-like thickening in certain patients (reportedly more common in East Asian populations) are important as well. And dyspigmentation is an important aspect of the disease presentation and patient and parental concern, given both hypopigmentaton and hyperpigmentation commonly seen over the course of AD.
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children's Hospital-San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. He disclosed that he has served as an investigator and/or consultant to AbbVie, Lilly, Pfizer, Regeneron, Sanofi-Genzyme, and Verrica.
A version of this article first appeared on Medscape.com.
This article was updated 6/18/22.
“We see very heterogenous and broad clinical presentations across the diverse patient populations that we see,” Andrew F. Alexis, MD, MPH, said at the Revolutionizing Atopic Dermatitis symposium. “Some of these differences might be related to population variations in skin barrier function, immunologic factors, genetic factors, and environmental factors, which all interplay to produce variations in the clinical presentation and overall impact of AD. Many nongenetic factors also contribute to differences that we see, including some socioeconomic and other factors that feed into health disparities.”
Dr. Alexis, professor of clinical dermatology at Weill Cornell Medicine, New York, discussed four main clinical features of AD in skin of color.
Erythema is less visible because it is masked by pigment
“There can be some masking of the redness and alteration of that color such that it doesn’t look bright red as it would in the background of lightly pigmented skin,” Dr. Alexis said. “Instead, the [AD lesions] have shades of grayish-red or grayish-brown or reddish-brown. It’s important to recognize this clinical presentation and look carefully and assess the patient – not just visually but with palpation and take into consideration symptomatology so that you don’t fall into the trap of calling an AD lesion postinflammatory hyperpigmentation. It’s also helpful to isolate the islands of normal or nonlesional skin and contrast that with the areas of lesional skin, to get a sense of how active and inflamed the areas are. Palpation really helps to appreciate the elevation of the lesions that are involved.”
Follicular accentuation
Morphological variants common in skin of color include the follicular variant or micropapular variant of AD. “You might just see a collection of papules that are 1-2 mm in size and pruritic and in typical sites of predilection [for] eczema,” he said. Prurigo nodularis–like lesions or prurigo nodularis in association with AD are also seen more frequently in skin of color.
Lichenification
The lichenoid variant of AD is characterized by a violaceous hue and other features that resemble lichen planus and has been reported to be more common in individuals of African descent. A prospective study of about 1,000 patients with AD seen over 2 years at a dermatology clinic in southeastern Nigeria found that 54% of patients had papular lichenoid lesions. In addition, 51% had elevated blood eosinophil counts, especially those with severe disease.
Dr. Alexis added that psoriasiform features have been reported in studies of East Asian populations with AD. These plaques may be more well demarcated and have clinical and histologic features that resemble psoriasis.
Dyspigmentation
One common feature across the spectrum of patients with skin of color “is the risk of longstanding pigmentary sequelae in the form of hyperpigmentation or hypopigmentation,” said Dr. Alexis, who is also vice chair for diversity and inclusion for the department of dermatology at Weill Cornell Medicine. “In very severe longstanding areas with chronic excoriation to the point of breaking of the skin, eroding of the skin, causing permanent damage to the melanocytes, dyspigmentation that resembles vitiligo can be seen. We can also see hypopigmentation as a consequence of topical corticosteroids, particularly those that are class I or class II and are used for prolonged periods of time.”
Dr. Alexis noted that delays in treatment and undertreatment can contribute to a higher risk of pigmentary and other long-term sequelae. “New therapies show promise in improving outcomes in AD patients with skin of color. When it comes to therapeutic responses, there are some post hoc studies that have investigated potential differences in safety and efficacy of the agents that have been recently approved. We clearly need more data to better understand if there are potential racial or ethnic differences.”
Dr. Alexis reported no relevant financial relationships.
Commentary by Lawrence F. Eichenfield, MD
Atopic dermatitis (AD) is highly heterogenous, with tremendous variations in extent, qualities of eczema, symptom complex, and physical presentation. Prior studies have reported disparities of care delivered to racial and ethnic minorities in the United States, as well as higher susceptibility to AD and odds of persistent disease into adulthood from child-onset AD. Recognizing some differences in presentation of AD in patients with skin of color is important as we select our therapeutic interventions, including assessing new treatments being added to our armamentarium. Erythema may be harder to notice in darker skin, but attempting to blanch the skin with pressure can help to assess the color and inflammation. Appreciating lichenoid changes, including papular and “micropapular” AD, and psoriasiform-like thickening in certain patients (reportedly more common in East Asian populations) are important as well. And dyspigmentation is an important aspect of the disease presentation and patient and parental concern, given both hypopigmentaton and hyperpigmentation commonly seen over the course of AD.
Dr. Eichenfield is chief of pediatric and adolescent dermatology at Rady Children's Hospital-San Diego. He is vice chair of the department of dermatology and professor of dermatology and pediatrics at the University of California, San Diego. He disclosed that he has served as an investigator and/or consultant to AbbVie, Lilly, Pfizer, Regeneron, Sanofi-Genzyme, and Verrica.
A version of this article first appeared on Medscape.com.
This article was updated 6/18/22.
FROM REVOLUTIONIZING AD 2021
Delayed umbilical cord clamping improves outcomes in very preterm infants
Delayed umbilical cord clamping for at least 60 seconds after birth significantly reduced death or disability in infants of less than 30 weeks’ gestation, according to data from nearly 1,500 infants.
The burden of disability and mortality for babies born before 30 weeks’ gestation remains high, especially in low- and middle-income countries, wrote Kristy P. Robledo, PhD, of the University of Sydney, Australia, and colleagues. Delayed clamping of the umbilical cord is a simple procedure that may improve mortality in this population, but more research is needed; recommended times to delayed clamping range from 30 seconds to 3 minutes, they noted.
In a study published in The Lancet Child & Adolescent Health, the researchers randomized 767 very preterm infants to delayed clamping at least 60 seconds after birth and 764 to immediate clamping. Of these, 384 were multiple births (who were individually randomized), 862 were male, and 505 were born before 27 weeks’ gestation. The primary outcome was death or disability at 2 years of age. Major disability was defined as cerebral palsy, severe visual loss, deafness requiring a hearing aid or cochlear implants, major language or speech problems, or cognitive delay at 2 years corrected age. The median time to clamping was 60 seconds in the delayed group and 5 seconds in the immediate group.
Primary outcome data were available for 1,419 infants. Death or major disability occurred in 29% of infants assigned to delayed clamping compared to 34% of those assigned to immediate clamping (relative risk 0.83, P = .010). The infants were part of the APTS Childhood Follow-Up Study, an open-label superiority trial conducted in Australia and New Zealand.
By age 2 years, 8% of infants in the delayed group and 11% of those in the immediate group had died; 23% and 26%, respectively, met criteria for major disability. The impact of delayed clamping translates to a 30% reduction in relative risk of mortality at 2 years of age, but no significant impact on major disability, the researchers wrote.
The findings were limited by several factors including the unblinded study design, lack of data on heart rate or time to first breath, and the clamping prior to 60 seconds in 26% of infants in the delayed group based on clinical concerns for these specific infants, the researchers noted.
However, the results were strengthened by the large size, low risk of bias, and specific primary outcome, they said. The data support findings from recent systematic reviews and highlight the need for further trials to evaluate delayed clamping at different time points, with larger populations, inclusion of time to first breath and heart rate, and improved measures of disability, the researchers added.
In clinical practice, “Given that aiming to delay cord clamping for 60 seconds or more improved 2-year outcomes and short-term hematological measures with no evidence of significant harm, it seems reasonable to conclude that delayed clamping is appropriate as standard care in very preterm infants,” they concluded.
Accepting simple intervention could have great impact
This study is important in light of the overwhelming burden of preterm birth on the health care system and society as a whole, Lisette D. Tanner, MD, of Emory University, Atlanta, said in an interview.
“Preterm birth is associated with billions in health care costs each year, and a large portion of that money is directed to the complications associated with preterm birth, such as early intervention services, educational support, and ongoing medical care,” Dr. Tanner said. “This study is particularly timely, as we are quickly approaching 2030, the deadline for achieving the United Nations Sustainable Development Goal of ending preventable deaths of newborns and children under 5 years of age,” she said. The goal involves “all countries aiming to reduce neonatal mortality to at least as low as 12 per 1,000 live births and under-5 mortality to at least as low as 25 per 1,000 live births. Effective treatments to reduce infant and child mortality would make strong inroads toward this goal,” she explained.
Dr. Tanner said she was not surprised by the findings because previous studies have shown similar results. “However, the large, multicenter nature of this study provides additional weight to recommendations to delay cord clamping as standard practice,” she said.
“The findings of this study support the recommendations of a number of large organizations,” said Dr. Tanner. “The World Health Organization recommends that the umbilical cord not be clamped earlier than 1 minute after birth in term or preterm infants who do not require positive pressure ventilation. The American College of Obstetricians and Gynecologists and the American Academy of Pediatrics now recommend a delay in umbilical cord clamping in vigorous term and preterm infants for at least 30–60 seconds after birth,” she said. “The Royal College of Obstetricians and Gynaecologists also recommends deferring umbilical cord clamping for healthy term and preterm infants for at least 2 minutes after birth,” she added.
However, “the delay in adoption of this guidelines in practice appears to be related to some concerns regarding universal adoption of this approach,” Dr. Tanner noted. “Some clinicians have suggested that delayed cord clamping could delay vital neonatal resuscitative efforts, leading to worse neonatal outcomes, but this concern has not been borne out in the data, as all guidelines specifically state that this intervention is for vigorous newborns,” she said. “In fact, in preterm infants, delayed cord clamping is associated with improved transitional circulation, decreased need for blood transfusion, and lower incidence of necrotizing enterocolitis and intraventricular hemorrhage,” Dr. Tanner emphasized. “Additionally, concerns persist that delayed cord clamping could lead to excessive transfusion with resultant polycythemia. Again, no data have supported this claim to date,” she said.
“Finally, some clinicians are concerned that delayed clamping could lead to delay in addressing maternal complications of birth such as hemorrhage, but studies have shown the opposite; delayed umbilical cord clamping has not been associated with an increased risk of postpartum hemorrhage or increased blood loss at delivery, nor has it been with a difference in the need for blood transfusion,” said Dr. Tanner.
Ideally, practitioners will become more comfortable in delaying cord clamping as a routine practice as more data demonstrating the safety and benefit of this easy intervention are disseminated, she said.
Additional research delineating which gestational ages benefit most from delayed cord clamping would help direct education efforts to implement this intervention, Dr. Tanner noted.
The study was funded by the Australian National Health and Medical Research Council. The researchers and Dr. Tanner had no financial conflicts to disclose.
Delayed umbilical cord clamping for at least 60 seconds after birth significantly reduced death or disability in infants of less than 30 weeks’ gestation, according to data from nearly 1,500 infants.
The burden of disability and mortality for babies born before 30 weeks’ gestation remains high, especially in low- and middle-income countries, wrote Kristy P. Robledo, PhD, of the University of Sydney, Australia, and colleagues. Delayed clamping of the umbilical cord is a simple procedure that may improve mortality in this population, but more research is needed; recommended times to delayed clamping range from 30 seconds to 3 minutes, they noted.
In a study published in The Lancet Child & Adolescent Health, the researchers randomized 767 very preterm infants to delayed clamping at least 60 seconds after birth and 764 to immediate clamping. Of these, 384 were multiple births (who were individually randomized), 862 were male, and 505 were born before 27 weeks’ gestation. The primary outcome was death or disability at 2 years of age. Major disability was defined as cerebral palsy, severe visual loss, deafness requiring a hearing aid or cochlear implants, major language or speech problems, or cognitive delay at 2 years corrected age. The median time to clamping was 60 seconds in the delayed group and 5 seconds in the immediate group.
Primary outcome data were available for 1,419 infants. Death or major disability occurred in 29% of infants assigned to delayed clamping compared to 34% of those assigned to immediate clamping (relative risk 0.83, P = .010). The infants were part of the APTS Childhood Follow-Up Study, an open-label superiority trial conducted in Australia and New Zealand.
By age 2 years, 8% of infants in the delayed group and 11% of those in the immediate group had died; 23% and 26%, respectively, met criteria for major disability. The impact of delayed clamping translates to a 30% reduction in relative risk of mortality at 2 years of age, but no significant impact on major disability, the researchers wrote.
The findings were limited by several factors including the unblinded study design, lack of data on heart rate or time to first breath, and the clamping prior to 60 seconds in 26% of infants in the delayed group based on clinical concerns for these specific infants, the researchers noted.
However, the results were strengthened by the large size, low risk of bias, and specific primary outcome, they said. The data support findings from recent systematic reviews and highlight the need for further trials to evaluate delayed clamping at different time points, with larger populations, inclusion of time to first breath and heart rate, and improved measures of disability, the researchers added.
In clinical practice, “Given that aiming to delay cord clamping for 60 seconds or more improved 2-year outcomes and short-term hematological measures with no evidence of significant harm, it seems reasonable to conclude that delayed clamping is appropriate as standard care in very preterm infants,” they concluded.
Accepting simple intervention could have great impact
This study is important in light of the overwhelming burden of preterm birth on the health care system and society as a whole, Lisette D. Tanner, MD, of Emory University, Atlanta, said in an interview.
“Preterm birth is associated with billions in health care costs each year, and a large portion of that money is directed to the complications associated with preterm birth, such as early intervention services, educational support, and ongoing medical care,” Dr. Tanner said. “This study is particularly timely, as we are quickly approaching 2030, the deadline for achieving the United Nations Sustainable Development Goal of ending preventable deaths of newborns and children under 5 years of age,” she said. The goal involves “all countries aiming to reduce neonatal mortality to at least as low as 12 per 1,000 live births and under-5 mortality to at least as low as 25 per 1,000 live births. Effective treatments to reduce infant and child mortality would make strong inroads toward this goal,” she explained.
Dr. Tanner said she was not surprised by the findings because previous studies have shown similar results. “However, the large, multicenter nature of this study provides additional weight to recommendations to delay cord clamping as standard practice,” she said.
“The findings of this study support the recommendations of a number of large organizations,” said Dr. Tanner. “The World Health Organization recommends that the umbilical cord not be clamped earlier than 1 minute after birth in term or preterm infants who do not require positive pressure ventilation. The American College of Obstetricians and Gynecologists and the American Academy of Pediatrics now recommend a delay in umbilical cord clamping in vigorous term and preterm infants for at least 30–60 seconds after birth,” she said. “The Royal College of Obstetricians and Gynaecologists also recommends deferring umbilical cord clamping for healthy term and preterm infants for at least 2 minutes after birth,” she added.
However, “the delay in adoption of this guidelines in practice appears to be related to some concerns regarding universal adoption of this approach,” Dr. Tanner noted. “Some clinicians have suggested that delayed cord clamping could delay vital neonatal resuscitative efforts, leading to worse neonatal outcomes, but this concern has not been borne out in the data, as all guidelines specifically state that this intervention is for vigorous newborns,” she said. “In fact, in preterm infants, delayed cord clamping is associated with improved transitional circulation, decreased need for blood transfusion, and lower incidence of necrotizing enterocolitis and intraventricular hemorrhage,” Dr. Tanner emphasized. “Additionally, concerns persist that delayed cord clamping could lead to excessive transfusion with resultant polycythemia. Again, no data have supported this claim to date,” she said.
“Finally, some clinicians are concerned that delayed clamping could lead to delay in addressing maternal complications of birth such as hemorrhage, but studies have shown the opposite; delayed umbilical cord clamping has not been associated with an increased risk of postpartum hemorrhage or increased blood loss at delivery, nor has it been with a difference in the need for blood transfusion,” said Dr. Tanner.
Ideally, practitioners will become more comfortable in delaying cord clamping as a routine practice as more data demonstrating the safety and benefit of this easy intervention are disseminated, she said.
Additional research delineating which gestational ages benefit most from delayed cord clamping would help direct education efforts to implement this intervention, Dr. Tanner noted.
The study was funded by the Australian National Health and Medical Research Council. The researchers and Dr. Tanner had no financial conflicts to disclose.
Delayed umbilical cord clamping for at least 60 seconds after birth significantly reduced death or disability in infants of less than 30 weeks’ gestation, according to data from nearly 1,500 infants.
The burden of disability and mortality for babies born before 30 weeks’ gestation remains high, especially in low- and middle-income countries, wrote Kristy P. Robledo, PhD, of the University of Sydney, Australia, and colleagues. Delayed clamping of the umbilical cord is a simple procedure that may improve mortality in this population, but more research is needed; recommended times to delayed clamping range from 30 seconds to 3 minutes, they noted.
In a study published in The Lancet Child & Adolescent Health, the researchers randomized 767 very preterm infants to delayed clamping at least 60 seconds after birth and 764 to immediate clamping. Of these, 384 were multiple births (who were individually randomized), 862 were male, and 505 were born before 27 weeks’ gestation. The primary outcome was death or disability at 2 years of age. Major disability was defined as cerebral palsy, severe visual loss, deafness requiring a hearing aid or cochlear implants, major language or speech problems, or cognitive delay at 2 years corrected age. The median time to clamping was 60 seconds in the delayed group and 5 seconds in the immediate group.
Primary outcome data were available for 1,419 infants. Death or major disability occurred in 29% of infants assigned to delayed clamping compared to 34% of those assigned to immediate clamping (relative risk 0.83, P = .010). The infants were part of the APTS Childhood Follow-Up Study, an open-label superiority trial conducted in Australia and New Zealand.
By age 2 years, 8% of infants in the delayed group and 11% of those in the immediate group had died; 23% and 26%, respectively, met criteria for major disability. The impact of delayed clamping translates to a 30% reduction in relative risk of mortality at 2 years of age, but no significant impact on major disability, the researchers wrote.
The findings were limited by several factors including the unblinded study design, lack of data on heart rate or time to first breath, and the clamping prior to 60 seconds in 26% of infants in the delayed group based on clinical concerns for these specific infants, the researchers noted.
However, the results were strengthened by the large size, low risk of bias, and specific primary outcome, they said. The data support findings from recent systematic reviews and highlight the need for further trials to evaluate delayed clamping at different time points, with larger populations, inclusion of time to first breath and heart rate, and improved measures of disability, the researchers added.
In clinical practice, “Given that aiming to delay cord clamping for 60 seconds or more improved 2-year outcomes and short-term hematological measures with no evidence of significant harm, it seems reasonable to conclude that delayed clamping is appropriate as standard care in very preterm infants,” they concluded.
Accepting simple intervention could have great impact
This study is important in light of the overwhelming burden of preterm birth on the health care system and society as a whole, Lisette D. Tanner, MD, of Emory University, Atlanta, said in an interview.
“Preterm birth is associated with billions in health care costs each year, and a large portion of that money is directed to the complications associated with preterm birth, such as early intervention services, educational support, and ongoing medical care,” Dr. Tanner said. “This study is particularly timely, as we are quickly approaching 2030, the deadline for achieving the United Nations Sustainable Development Goal of ending preventable deaths of newborns and children under 5 years of age,” she said. The goal involves “all countries aiming to reduce neonatal mortality to at least as low as 12 per 1,000 live births and under-5 mortality to at least as low as 25 per 1,000 live births. Effective treatments to reduce infant and child mortality would make strong inroads toward this goal,” she explained.
Dr. Tanner said she was not surprised by the findings because previous studies have shown similar results. “However, the large, multicenter nature of this study provides additional weight to recommendations to delay cord clamping as standard practice,” she said.
“The findings of this study support the recommendations of a number of large organizations,” said Dr. Tanner. “The World Health Organization recommends that the umbilical cord not be clamped earlier than 1 minute after birth in term or preterm infants who do not require positive pressure ventilation. The American College of Obstetricians and Gynecologists and the American Academy of Pediatrics now recommend a delay in umbilical cord clamping in vigorous term and preterm infants for at least 30–60 seconds after birth,” she said. “The Royal College of Obstetricians and Gynaecologists also recommends deferring umbilical cord clamping for healthy term and preterm infants for at least 2 minutes after birth,” she added.
However, “the delay in adoption of this guidelines in practice appears to be related to some concerns regarding universal adoption of this approach,” Dr. Tanner noted. “Some clinicians have suggested that delayed cord clamping could delay vital neonatal resuscitative efforts, leading to worse neonatal outcomes, but this concern has not been borne out in the data, as all guidelines specifically state that this intervention is for vigorous newborns,” she said. “In fact, in preterm infants, delayed cord clamping is associated with improved transitional circulation, decreased need for blood transfusion, and lower incidence of necrotizing enterocolitis and intraventricular hemorrhage,” Dr. Tanner emphasized. “Additionally, concerns persist that delayed cord clamping could lead to excessive transfusion with resultant polycythemia. Again, no data have supported this claim to date,” she said.
“Finally, some clinicians are concerned that delayed clamping could lead to delay in addressing maternal complications of birth such as hemorrhage, but studies have shown the opposite; delayed umbilical cord clamping has not been associated with an increased risk of postpartum hemorrhage or increased blood loss at delivery, nor has it been with a difference in the need for blood transfusion,” said Dr. Tanner.
Ideally, practitioners will become more comfortable in delaying cord clamping as a routine practice as more data demonstrating the safety and benefit of this easy intervention are disseminated, she said.
Additional research delineating which gestational ages benefit most from delayed cord clamping would help direct education efforts to implement this intervention, Dr. Tanner noted.
The study was funded by the Australian National Health and Medical Research Council. The researchers and Dr. Tanner had no financial conflicts to disclose.
FROM THE LANCET CHILD & ADOLESCENT HEALTH
More Americans skipping medical care because of cost, survey says
That’s the highest reported number since the pandemic began and a tripling from March to October.
Even 20% of the country’s highest-income households – earning more than $120,000 per year – said they’ve also skipped care. That’s an increase of about seven times for higher-income families since March.
“Americans tend to think there is a group of lower-income people, and they have worse health care than the rest of us, and the rest of us, we’re okay,” Tim Lash, chief strategy officer for West Health, a nonprofit focused on lowering health care costs, told CBS News.
“What we are seeing now in this survey is this group of people who are identifying themselves as struggling with health care costs is growing,” he said.
As part of the 2021 Healthcare in America Report, researchers surveyed more than 6,000 people in September and October about their concerns and experiences with affording health care and treatment. About half of respondents said health care in America has gotten worse because of the pandemic, and more than half said they’re more worried about medical costs than before.
What’s more, many Americans put off routine doctor visits at the beginning of the pandemic, and now that they’re beginning to schedule appointments again, they’re facing major costs, the survey found. Some expenses have increased in the past year, including prescription medications.
The rising costs have led many people to skip care or treatment, which can have major consequences. About 1 in 20 adults said they know a friend or family member who died during the past year because they couldn’t afford medical care, the survey found. And about 20% of adults said they or someone in their household had a health issue that grew worse after postponing care because of price.
About 23% of survey respondents said that paying for health care represents a major financial burden, which increases to a third of respondents who earn less than $48,000 per year. Out-of-pocket costs such as deductibles and insurance premiums have increased, which have taken up larger portions of people’s budgets.
“We often overlook the side effect of costs, and it’s quite toxic – there is a financial toxicity that exists in health care,” Mr. Lash said. “We know when you skip treatment, that can have an impact on mortality.”
A version of this article first appeared on WebMD.com.
That’s the highest reported number since the pandemic began and a tripling from March to October.
Even 20% of the country’s highest-income households – earning more than $120,000 per year – said they’ve also skipped care. That’s an increase of about seven times for higher-income families since March.
“Americans tend to think there is a group of lower-income people, and they have worse health care than the rest of us, and the rest of us, we’re okay,” Tim Lash, chief strategy officer for West Health, a nonprofit focused on lowering health care costs, told CBS News.
“What we are seeing now in this survey is this group of people who are identifying themselves as struggling with health care costs is growing,” he said.
As part of the 2021 Healthcare in America Report, researchers surveyed more than 6,000 people in September and October about their concerns and experiences with affording health care and treatment. About half of respondents said health care in America has gotten worse because of the pandemic, and more than half said they’re more worried about medical costs than before.
What’s more, many Americans put off routine doctor visits at the beginning of the pandemic, and now that they’re beginning to schedule appointments again, they’re facing major costs, the survey found. Some expenses have increased in the past year, including prescription medications.
The rising costs have led many people to skip care or treatment, which can have major consequences. About 1 in 20 adults said they know a friend or family member who died during the past year because they couldn’t afford medical care, the survey found. And about 20% of adults said they or someone in their household had a health issue that grew worse after postponing care because of price.
About 23% of survey respondents said that paying for health care represents a major financial burden, which increases to a third of respondents who earn less than $48,000 per year. Out-of-pocket costs such as deductibles and insurance premiums have increased, which have taken up larger portions of people’s budgets.
“We often overlook the side effect of costs, and it’s quite toxic – there is a financial toxicity that exists in health care,” Mr. Lash said. “We know when you skip treatment, that can have an impact on mortality.”
A version of this article first appeared on WebMD.com.
That’s the highest reported number since the pandemic began and a tripling from March to October.
Even 20% of the country’s highest-income households – earning more than $120,000 per year – said they’ve also skipped care. That’s an increase of about seven times for higher-income families since March.
“Americans tend to think there is a group of lower-income people, and they have worse health care than the rest of us, and the rest of us, we’re okay,” Tim Lash, chief strategy officer for West Health, a nonprofit focused on lowering health care costs, told CBS News.
“What we are seeing now in this survey is this group of people who are identifying themselves as struggling with health care costs is growing,” he said.
As part of the 2021 Healthcare in America Report, researchers surveyed more than 6,000 people in September and October about their concerns and experiences with affording health care and treatment. About half of respondents said health care in America has gotten worse because of the pandemic, and more than half said they’re more worried about medical costs than before.
What’s more, many Americans put off routine doctor visits at the beginning of the pandemic, and now that they’re beginning to schedule appointments again, they’re facing major costs, the survey found. Some expenses have increased in the past year, including prescription medications.
The rising costs have led many people to skip care or treatment, which can have major consequences. About 1 in 20 adults said they know a friend or family member who died during the past year because they couldn’t afford medical care, the survey found. And about 20% of adults said they or someone in their household had a health issue that grew worse after postponing care because of price.
About 23% of survey respondents said that paying for health care represents a major financial burden, which increases to a third of respondents who earn less than $48,000 per year. Out-of-pocket costs such as deductibles and insurance premiums have increased, which have taken up larger portions of people’s budgets.
“We often overlook the side effect of costs, and it’s quite toxic – there is a financial toxicity that exists in health care,” Mr. Lash said. “We know when you skip treatment, that can have an impact on mortality.”
A version of this article first appeared on WebMD.com.
COVID-19 asymptomatic infection rate remains high
Based on data from a meta-analysis of 95 studies that included nearly 30,000,000 individuals, the pooled percentage of asymptomatic COVID-19 infections was 0.25% in the tested population and 40.5% among confirmed cases.
, wrote Qiuyue Ma, PhD, and colleagues of Peking University, Beijing.
In a study published in JAMA Network Open the researchers identified 44 cross-sectional studies, 41 cohort studies, seven case series, and three case series on transmission studies. A total of 74 studies were conducted in developed countries, including those in Europe, North America, and Asia. Approximately one-third (37) of the studies were conducted among health care workers or in-hospital patients, 17 among nursing home staff or residents, and 14 among community residents. In addition, 13 studies involved pregnant women, eight involved air or cruise ship travelers, and six involved close contacts of individuals with confirmed infections.
The meta-analysis included 29,776,306 tested individuals; 11,516 of them had asymptomatic infections.
Overall, the pooled percentage of asymptomatic infections among the tested population was 0.25%. In an analysis of different study populations, the percentage was higher in nursing home residents or staff (4.52%), air or cruise ship travelers (2.02%), and pregnant women (2.34%), compared against the pooled percentage.
The pooled percentage of asymptomatic infections among the confirmed population was 40.50%, and this percentage was higher in pregnant women (54.11%), air or cruise ship travelers (52.91%), and nursing home residents or staff (47.53%).
The pooled percentage in the tested population was higher than the overall percentage when the mean age of the study population was 60 years or older (3.69%). By contrast, in the confirmed population, the pooled percentage was higher than the overall percentage when the study population was younger than 20 years (60.2%) or aged 20 to 39 years (49.5%).
The researchers noted in their discussion that the varying percentage of asymptomatic individuals according to community prevalence might impact the heterogeneity of the included studies. They also noted the high number of studies conducted in nursing home populations, groups in which asymptomatic individuals were more likely to be tested.
The study findings were limited by several factors, including the potential for missed studies that were not published at the time of the meta-analysis, as well as the exclusion of studies written in Chinese, the researchers noted. Other limitations included lack of follow-up on presymptomatic and covert infections, and the focus on specific populations, factors that may limit the degree to which the results can be generalized.
However, the results highlight the need to screen for asymptomatic infections, especially in countries where COVID-19 has been better controlled, the researchers said. Management strategies for asymptomatic infections, when identified, should include isolation and contact tracing similar to strategies used with confirmed cases, they added.
More testing needed to catch cases early
“During the initial phase of [the] COVID-19 pandemic, testing was not widely available in the United States or the rest of the world,” Setu Patolia, MD, of Saint Louis University School of Medicine, Missouri, said in an interview. Much of the world still lacks access to COVID-19 testing, and early in the pandemic only severely symptomatic patients were tested, he said. “With new variants, particularly the Omicron variant, which may have mild or minimally symptomatic disease, asymptomatic carriers play an important role in propagation of the pandemic,” he explained. “It is important to know the asymptomatic carrier rate among the general population for the future control of [the] pandemic,” he added.
Dr. Patolia said he was surprised by the study finding that one in 400 people in the general population could be asymptomatic carriers of COVID-19.
“Also, nursing home patients are more at risk of complications of COVID, and I expected that they would have a higher rate of symptomatic disease as compared to [the] general population,” said Dr. Patolia. He was also surprised by the high rate of asymptomatic infections in travelers.
“Physicians should be more aware about the asymptomatic carrier rate, particularly in travelers and nursing home patients,” he noted. “Travelers carry high risk of transferring infection from one region to another region of the world, and physicians should advise them to get tested despite the absence of symptoms,” Dr. Patolia emphasized. “Similarly, once any nursing home patient has been diagnosed with COVID-19, physicians should be more careful with the rest of the nursing home patients and test them despite the absence of the symptoms,” he added.
Dr. Patolia also recommended that pregnant women wear masks to help prevent disease transmission when visiting a doctor’s office or labor unit.
Looking ahead, there is a need for cheaper at-home testing kits so that all vulnerable populations can be tested fast and frequently, Dr. Patolia said.
The study was supported by the National Natural Science Foundation of China. The researchers had no financial conflicts to disclose. Dr. Patolia has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Based on data from a meta-analysis of 95 studies that included nearly 30,000,000 individuals, the pooled percentage of asymptomatic COVID-19 infections was 0.25% in the tested population and 40.5% among confirmed cases.
, wrote Qiuyue Ma, PhD, and colleagues of Peking University, Beijing.
In a study published in JAMA Network Open the researchers identified 44 cross-sectional studies, 41 cohort studies, seven case series, and three case series on transmission studies. A total of 74 studies were conducted in developed countries, including those in Europe, North America, and Asia. Approximately one-third (37) of the studies were conducted among health care workers or in-hospital patients, 17 among nursing home staff or residents, and 14 among community residents. In addition, 13 studies involved pregnant women, eight involved air or cruise ship travelers, and six involved close contacts of individuals with confirmed infections.
The meta-analysis included 29,776,306 tested individuals; 11,516 of them had asymptomatic infections.
Overall, the pooled percentage of asymptomatic infections among the tested population was 0.25%. In an analysis of different study populations, the percentage was higher in nursing home residents or staff (4.52%), air or cruise ship travelers (2.02%), and pregnant women (2.34%), compared against the pooled percentage.
The pooled percentage of asymptomatic infections among the confirmed population was 40.50%, and this percentage was higher in pregnant women (54.11%), air or cruise ship travelers (52.91%), and nursing home residents or staff (47.53%).
The pooled percentage in the tested population was higher than the overall percentage when the mean age of the study population was 60 years or older (3.69%). By contrast, in the confirmed population, the pooled percentage was higher than the overall percentage when the study population was younger than 20 years (60.2%) or aged 20 to 39 years (49.5%).
The researchers noted in their discussion that the varying percentage of asymptomatic individuals according to community prevalence might impact the heterogeneity of the included studies. They also noted the high number of studies conducted in nursing home populations, groups in which asymptomatic individuals were more likely to be tested.
The study findings were limited by several factors, including the potential for missed studies that were not published at the time of the meta-analysis, as well as the exclusion of studies written in Chinese, the researchers noted. Other limitations included lack of follow-up on presymptomatic and covert infections, and the focus on specific populations, factors that may limit the degree to which the results can be generalized.
However, the results highlight the need to screen for asymptomatic infections, especially in countries where COVID-19 has been better controlled, the researchers said. Management strategies for asymptomatic infections, when identified, should include isolation and contact tracing similar to strategies used with confirmed cases, they added.
More testing needed to catch cases early
“During the initial phase of [the] COVID-19 pandemic, testing was not widely available in the United States or the rest of the world,” Setu Patolia, MD, of Saint Louis University School of Medicine, Missouri, said in an interview. Much of the world still lacks access to COVID-19 testing, and early in the pandemic only severely symptomatic patients were tested, he said. “With new variants, particularly the Omicron variant, which may have mild or minimally symptomatic disease, asymptomatic carriers play an important role in propagation of the pandemic,” he explained. “It is important to know the asymptomatic carrier rate among the general population for the future control of [the] pandemic,” he added.
Dr. Patolia said he was surprised by the study finding that one in 400 people in the general population could be asymptomatic carriers of COVID-19.
“Also, nursing home patients are more at risk of complications of COVID, and I expected that they would have a higher rate of symptomatic disease as compared to [the] general population,” said Dr. Patolia. He was also surprised by the high rate of asymptomatic infections in travelers.
“Physicians should be more aware about the asymptomatic carrier rate, particularly in travelers and nursing home patients,” he noted. “Travelers carry high risk of transferring infection from one region to another region of the world, and physicians should advise them to get tested despite the absence of symptoms,” Dr. Patolia emphasized. “Similarly, once any nursing home patient has been diagnosed with COVID-19, physicians should be more careful with the rest of the nursing home patients and test them despite the absence of the symptoms,” he added.
Dr. Patolia also recommended that pregnant women wear masks to help prevent disease transmission when visiting a doctor’s office or labor unit.
Looking ahead, there is a need for cheaper at-home testing kits so that all vulnerable populations can be tested fast and frequently, Dr. Patolia said.
The study was supported by the National Natural Science Foundation of China. The researchers had no financial conflicts to disclose. Dr. Patolia has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Based on data from a meta-analysis of 95 studies that included nearly 30,000,000 individuals, the pooled percentage of asymptomatic COVID-19 infections was 0.25% in the tested population and 40.5% among confirmed cases.
, wrote Qiuyue Ma, PhD, and colleagues of Peking University, Beijing.
In a study published in JAMA Network Open the researchers identified 44 cross-sectional studies, 41 cohort studies, seven case series, and three case series on transmission studies. A total of 74 studies were conducted in developed countries, including those in Europe, North America, and Asia. Approximately one-third (37) of the studies were conducted among health care workers or in-hospital patients, 17 among nursing home staff or residents, and 14 among community residents. In addition, 13 studies involved pregnant women, eight involved air or cruise ship travelers, and six involved close contacts of individuals with confirmed infections.
The meta-analysis included 29,776,306 tested individuals; 11,516 of them had asymptomatic infections.
Overall, the pooled percentage of asymptomatic infections among the tested population was 0.25%. In an analysis of different study populations, the percentage was higher in nursing home residents or staff (4.52%), air or cruise ship travelers (2.02%), and pregnant women (2.34%), compared against the pooled percentage.
The pooled percentage of asymptomatic infections among the confirmed population was 40.50%, and this percentage was higher in pregnant women (54.11%), air or cruise ship travelers (52.91%), and nursing home residents or staff (47.53%).
The pooled percentage in the tested population was higher than the overall percentage when the mean age of the study population was 60 years or older (3.69%). By contrast, in the confirmed population, the pooled percentage was higher than the overall percentage when the study population was younger than 20 years (60.2%) or aged 20 to 39 years (49.5%).
The researchers noted in their discussion that the varying percentage of asymptomatic individuals according to community prevalence might impact the heterogeneity of the included studies. They also noted the high number of studies conducted in nursing home populations, groups in which asymptomatic individuals were more likely to be tested.
The study findings were limited by several factors, including the potential for missed studies that were not published at the time of the meta-analysis, as well as the exclusion of studies written in Chinese, the researchers noted. Other limitations included lack of follow-up on presymptomatic and covert infections, and the focus on specific populations, factors that may limit the degree to which the results can be generalized.
However, the results highlight the need to screen for asymptomatic infections, especially in countries where COVID-19 has been better controlled, the researchers said. Management strategies for asymptomatic infections, when identified, should include isolation and contact tracing similar to strategies used with confirmed cases, they added.
More testing needed to catch cases early
“During the initial phase of [the] COVID-19 pandemic, testing was not widely available in the United States or the rest of the world,” Setu Patolia, MD, of Saint Louis University School of Medicine, Missouri, said in an interview. Much of the world still lacks access to COVID-19 testing, and early in the pandemic only severely symptomatic patients were tested, he said. “With new variants, particularly the Omicron variant, which may have mild or minimally symptomatic disease, asymptomatic carriers play an important role in propagation of the pandemic,” he explained. “It is important to know the asymptomatic carrier rate among the general population for the future control of [the] pandemic,” he added.
Dr. Patolia said he was surprised by the study finding that one in 400 people in the general population could be asymptomatic carriers of COVID-19.
“Also, nursing home patients are more at risk of complications of COVID, and I expected that they would have a higher rate of symptomatic disease as compared to [the] general population,” said Dr. Patolia. He was also surprised by the high rate of asymptomatic infections in travelers.
“Physicians should be more aware about the asymptomatic carrier rate, particularly in travelers and nursing home patients,” he noted. “Travelers carry high risk of transferring infection from one region to another region of the world, and physicians should advise them to get tested despite the absence of symptoms,” Dr. Patolia emphasized. “Similarly, once any nursing home patient has been diagnosed with COVID-19, physicians should be more careful with the rest of the nursing home patients and test them despite the absence of the symptoms,” he added.
Dr. Patolia also recommended that pregnant women wear masks to help prevent disease transmission when visiting a doctor’s office or labor unit.
Looking ahead, there is a need for cheaper at-home testing kits so that all vulnerable populations can be tested fast and frequently, Dr. Patolia said.
The study was supported by the National Natural Science Foundation of China. The researchers had no financial conflicts to disclose. Dr. Patolia has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Spice in breast milk could shape taste preferences later
They say you are what you eat, but scientists have long wondered whether breastfeeding babies are what their mothers eat, too. Their question: How much of a nursing mother’s diet eventually plays a role in a child’s food preferences later in life?
The aroma, taste, and makeup of breast milk change from day to day, based mostly on the mother’s diet. But previous research has already shown that the foods a mother eats do not directly translate into the same smells and tastes of that food in breast milk. Some substances from the mother’s diet enter her breast milk, some don’t, and even ones that do may have a different scent or flavor than what the mother experiences.
But a new study suggests that the active ingredient in black pepper makes its way into breast milk and may help the infant develop a tolerance to pepper later. The researchers published their findings in the journal Molecular Nutrition & Food Research.
Pinch of pepper
The study authors thought that maybe some food preferences could result from sensory programming that occurs through breast milk in the first few months of life. Though past studies have looked at which odor-producing substances transfer into breast milk, not many have explored specific substances that give food its distinctive flavor, or even what makes up the taste of breast milk. So they decided to investigate what happens when a mother consumes a meal containing three specific compounds: those that give pepper, chili, and ginger their particularly pungent flavors.
The researchers recruited 18 healthy, nonsmoking, nursing mothers who were producing more than enough milk for their baby’s needs. Their breastfeeding children ranged in age from 8 weeks to 1 year old. The women all ate a curry dish after having spent 2 days avoiding onion, garlic, and the spices in the curry. Then they provided pumped breast milk samples at 1, 2, and 3 hours after eating the curry.
Within an hour of the women eating the curry, the scientists were able to detect piperine, the compound that gives black pepper its bite, in the mothers’ breast milk. They did not find the compounds from ginger, chili, or curcumin – the main active ingredient in turmeric – in the breast milk. The piperine remained there for several hours, but there wasn’t enough for an adult to be able to taste it. It wasn’t possible to reliably tell whether the infants could consciously detect the flavor, but the researchers don’t think it’s likely they did.
But the scientists do suggest it’s possible that the piperine in breast milk could regularly activate a protein that detects pungent or potentially harmful substances. This is the same protein that produces the sensation of heat when eating a spicy food. If the piperine frequently activates that protein in a nursing baby at levels too low for the baby to notice, it may increase the baby’s tolerance for similar spicy substances later in life.
Ultimately, the findings suggest that .
A version of this story first appeared on WebMD.com.
They say you are what you eat, but scientists have long wondered whether breastfeeding babies are what their mothers eat, too. Their question: How much of a nursing mother’s diet eventually plays a role in a child’s food preferences later in life?
The aroma, taste, and makeup of breast milk change from day to day, based mostly on the mother’s diet. But previous research has already shown that the foods a mother eats do not directly translate into the same smells and tastes of that food in breast milk. Some substances from the mother’s diet enter her breast milk, some don’t, and even ones that do may have a different scent or flavor than what the mother experiences.
But a new study suggests that the active ingredient in black pepper makes its way into breast milk and may help the infant develop a tolerance to pepper later. The researchers published their findings in the journal Molecular Nutrition & Food Research.
Pinch of pepper
The study authors thought that maybe some food preferences could result from sensory programming that occurs through breast milk in the first few months of life. Though past studies have looked at which odor-producing substances transfer into breast milk, not many have explored specific substances that give food its distinctive flavor, or even what makes up the taste of breast milk. So they decided to investigate what happens when a mother consumes a meal containing three specific compounds: those that give pepper, chili, and ginger their particularly pungent flavors.
The researchers recruited 18 healthy, nonsmoking, nursing mothers who were producing more than enough milk for their baby’s needs. Their breastfeeding children ranged in age from 8 weeks to 1 year old. The women all ate a curry dish after having spent 2 days avoiding onion, garlic, and the spices in the curry. Then they provided pumped breast milk samples at 1, 2, and 3 hours after eating the curry.
Within an hour of the women eating the curry, the scientists were able to detect piperine, the compound that gives black pepper its bite, in the mothers’ breast milk. They did not find the compounds from ginger, chili, or curcumin – the main active ingredient in turmeric – in the breast milk. The piperine remained there for several hours, but there wasn’t enough for an adult to be able to taste it. It wasn’t possible to reliably tell whether the infants could consciously detect the flavor, but the researchers don’t think it’s likely they did.
But the scientists do suggest it’s possible that the piperine in breast milk could regularly activate a protein that detects pungent or potentially harmful substances. This is the same protein that produces the sensation of heat when eating a spicy food. If the piperine frequently activates that protein in a nursing baby at levels too low for the baby to notice, it may increase the baby’s tolerance for similar spicy substances later in life.
Ultimately, the findings suggest that .
A version of this story first appeared on WebMD.com.
They say you are what you eat, but scientists have long wondered whether breastfeeding babies are what their mothers eat, too. Their question: How much of a nursing mother’s diet eventually plays a role in a child’s food preferences later in life?
The aroma, taste, and makeup of breast milk change from day to day, based mostly on the mother’s diet. But previous research has already shown that the foods a mother eats do not directly translate into the same smells and tastes of that food in breast milk. Some substances from the mother’s diet enter her breast milk, some don’t, and even ones that do may have a different scent or flavor than what the mother experiences.
But a new study suggests that the active ingredient in black pepper makes its way into breast milk and may help the infant develop a tolerance to pepper later. The researchers published their findings in the journal Molecular Nutrition & Food Research.
Pinch of pepper
The study authors thought that maybe some food preferences could result from sensory programming that occurs through breast milk in the first few months of life. Though past studies have looked at which odor-producing substances transfer into breast milk, not many have explored specific substances that give food its distinctive flavor, or even what makes up the taste of breast milk. So they decided to investigate what happens when a mother consumes a meal containing three specific compounds: those that give pepper, chili, and ginger their particularly pungent flavors.
The researchers recruited 18 healthy, nonsmoking, nursing mothers who were producing more than enough milk for their baby’s needs. Their breastfeeding children ranged in age from 8 weeks to 1 year old. The women all ate a curry dish after having spent 2 days avoiding onion, garlic, and the spices in the curry. Then they provided pumped breast milk samples at 1, 2, and 3 hours after eating the curry.
Within an hour of the women eating the curry, the scientists were able to detect piperine, the compound that gives black pepper its bite, in the mothers’ breast milk. They did not find the compounds from ginger, chili, or curcumin – the main active ingredient in turmeric – in the breast milk. The piperine remained there for several hours, but there wasn’t enough for an adult to be able to taste it. It wasn’t possible to reliably tell whether the infants could consciously detect the flavor, but the researchers don’t think it’s likely they did.
But the scientists do suggest it’s possible that the piperine in breast milk could regularly activate a protein that detects pungent or potentially harmful substances. This is the same protein that produces the sensation of heat when eating a spicy food. If the piperine frequently activates that protein in a nursing baby at levels too low for the baby to notice, it may increase the baby’s tolerance for similar spicy substances later in life.
Ultimately, the findings suggest that .
A version of this story first appeared on WebMD.com.
FROM MOLECULAR NUTRITION & FOOD RESEARCH
Children and COVID: Weekly cases resume their climb
After a brief lull in activity, weekly COVID-19 cases in children returned to the upward trend that began in early November, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
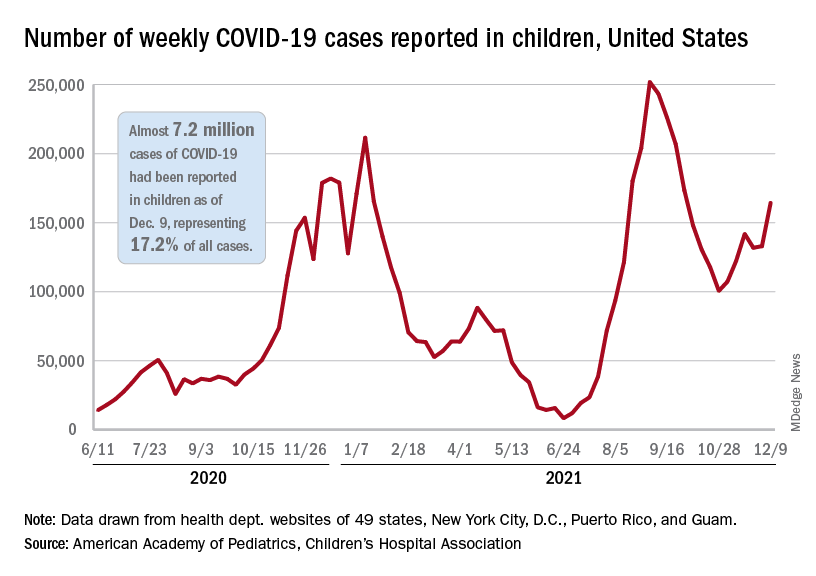
according to the Centers for Disease Control and Prevention.
New COVID-19 cases were up by 23.5% for the week of Dec. 3-9, after a 2-week period that saw a drop and then just a slight increase, the AAP and CHA said in their latest weekly COVID report. There were 164,000 new cases from Dec. 3 to Dec. 9 in 46 states (Alabama, Nebraska, and Texas stopped reporting over the summer of 2021 and New York has never reported by age), the District of Columbia, New York City, Puerto Rico, and Guam.
The increase occurred across all four regions of the country, but the largest share came in the Midwest, with over 65,000 new cases, followed by the West (just over 35,000), the Northeast (just under 35,000), and the South (close to 28,000), the AAP/CHA data show.
The 7.2 million cumulative cases in children as of Dec. 9 represent 17.2% of all cases reported in the United States since the start of the pandemic, with available state reports showing that proportion ranges from 12.3% in Florida to 26.1% in Vermont. Alaska has the highest incidence of COVID at 19,000 cases per 100,000 children, and Hawaii has the lowest (5,300 per 100,000) among the states currently reporting, the AAP and CHA said.
State reporting on vaccinations shows that 37% of children aged 5-11 years in Massachusetts have received at least one dose, the highest of any state, while West Virginia is lowest at just 4%. The highest vaccination rate for children aged 12-17 goes to Massachusetts at 84%, with Wyoming lowest at 37%, the AAP said in a separate report.
Nationally, new vaccinations fell by a third during the week of Dec. 7-13, compared with the previous week, with the largest decline (34.7%) coming from the 5- to 11-year-olds, who still represented the majority (almost 84%) of the 430,000 new child vaccinations received, according to the CDC’s COVID Data Tracker. Corresponding declines for the last week were 27.5% for 12- to 15-year-olds and 22.7% for those aged 16-17.
Altogether, 21.2 million children aged 5-17 had received at least one dose and 16.0 million were fully vaccinated as of Dec. 13. By age group, 19.2% of children aged 5-11 years have gotten at least one dose and 9.6% are fully vaccinated, compared with 62.1% and 52.3%, respectively, among children aged 12-17, the CDC said.
After a brief lull in activity, weekly COVID-19 cases in children returned to the upward trend that began in early November, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
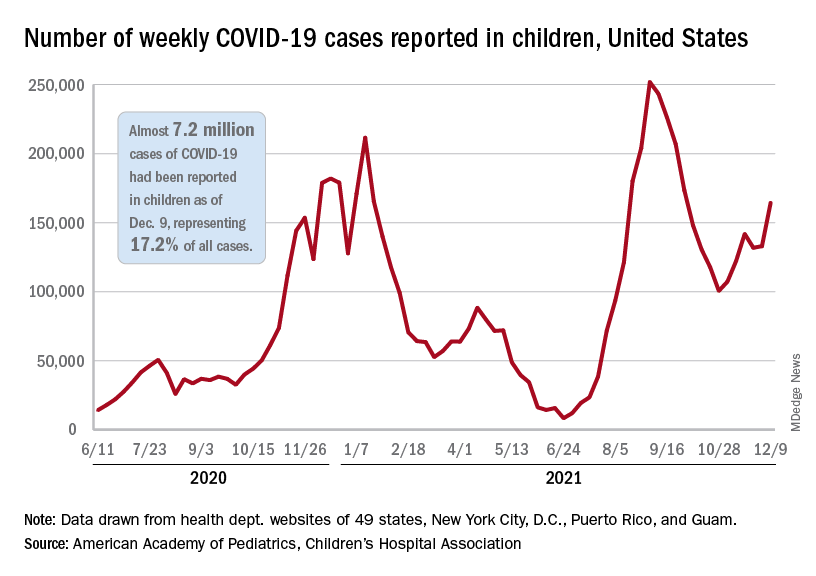
according to the Centers for Disease Control and Prevention.
New COVID-19 cases were up by 23.5% for the week of Dec. 3-9, after a 2-week period that saw a drop and then just a slight increase, the AAP and CHA said in their latest weekly COVID report. There were 164,000 new cases from Dec. 3 to Dec. 9 in 46 states (Alabama, Nebraska, and Texas stopped reporting over the summer of 2021 and New York has never reported by age), the District of Columbia, New York City, Puerto Rico, and Guam.
The increase occurred across all four regions of the country, but the largest share came in the Midwest, with over 65,000 new cases, followed by the West (just over 35,000), the Northeast (just under 35,000), and the South (close to 28,000), the AAP/CHA data show.
The 7.2 million cumulative cases in children as of Dec. 9 represent 17.2% of all cases reported in the United States since the start of the pandemic, with available state reports showing that proportion ranges from 12.3% in Florida to 26.1% in Vermont. Alaska has the highest incidence of COVID at 19,000 cases per 100,000 children, and Hawaii has the lowest (5,300 per 100,000) among the states currently reporting, the AAP and CHA said.
State reporting on vaccinations shows that 37% of children aged 5-11 years in Massachusetts have received at least one dose, the highest of any state, while West Virginia is lowest at just 4%. The highest vaccination rate for children aged 12-17 goes to Massachusetts at 84%, with Wyoming lowest at 37%, the AAP said in a separate report.
Nationally, new vaccinations fell by a third during the week of Dec. 7-13, compared with the previous week, with the largest decline (34.7%) coming from the 5- to 11-year-olds, who still represented the majority (almost 84%) of the 430,000 new child vaccinations received, according to the CDC’s COVID Data Tracker. Corresponding declines for the last week were 27.5% for 12- to 15-year-olds and 22.7% for those aged 16-17.
Altogether, 21.2 million children aged 5-17 had received at least one dose and 16.0 million were fully vaccinated as of Dec. 13. By age group, 19.2% of children aged 5-11 years have gotten at least one dose and 9.6% are fully vaccinated, compared with 62.1% and 52.3%, respectively, among children aged 12-17, the CDC said.
After a brief lull in activity, weekly COVID-19 cases in children returned to the upward trend that began in early November, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
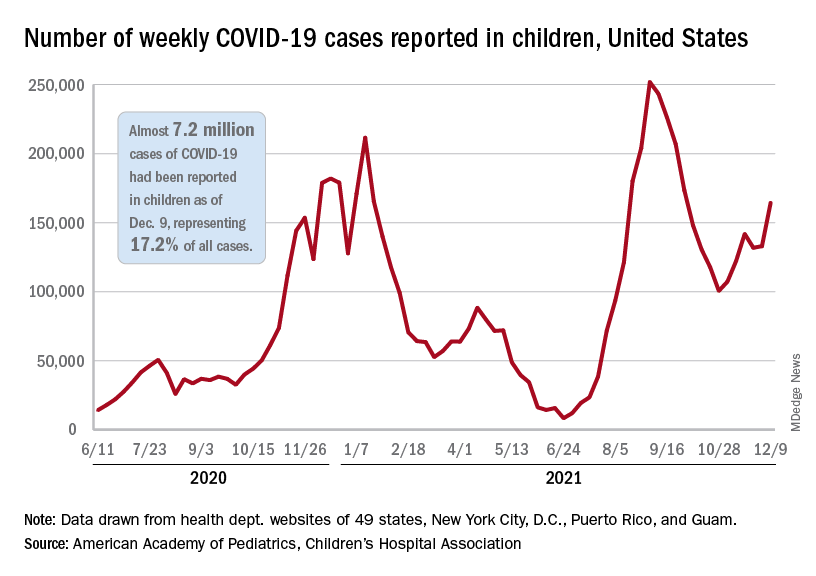
according to the Centers for Disease Control and Prevention.
New COVID-19 cases were up by 23.5% for the week of Dec. 3-9, after a 2-week period that saw a drop and then just a slight increase, the AAP and CHA said in their latest weekly COVID report. There were 164,000 new cases from Dec. 3 to Dec. 9 in 46 states (Alabama, Nebraska, and Texas stopped reporting over the summer of 2021 and New York has never reported by age), the District of Columbia, New York City, Puerto Rico, and Guam.
The increase occurred across all four regions of the country, but the largest share came in the Midwest, with over 65,000 new cases, followed by the West (just over 35,000), the Northeast (just under 35,000), and the South (close to 28,000), the AAP/CHA data show.
The 7.2 million cumulative cases in children as of Dec. 9 represent 17.2% of all cases reported in the United States since the start of the pandemic, with available state reports showing that proportion ranges from 12.3% in Florida to 26.1% in Vermont. Alaska has the highest incidence of COVID at 19,000 cases per 100,000 children, and Hawaii has the lowest (5,300 per 100,000) among the states currently reporting, the AAP and CHA said.
State reporting on vaccinations shows that 37% of children aged 5-11 years in Massachusetts have received at least one dose, the highest of any state, while West Virginia is lowest at just 4%. The highest vaccination rate for children aged 12-17 goes to Massachusetts at 84%, with Wyoming lowest at 37%, the AAP said in a separate report.
Nationally, new vaccinations fell by a third during the week of Dec. 7-13, compared with the previous week, with the largest decline (34.7%) coming from the 5- to 11-year-olds, who still represented the majority (almost 84%) of the 430,000 new child vaccinations received, according to the CDC’s COVID Data Tracker. Corresponding declines for the last week were 27.5% for 12- to 15-year-olds and 22.7% for those aged 16-17.
Altogether, 21.2 million children aged 5-17 had received at least one dose and 16.0 million were fully vaccinated as of Dec. 13. By age group, 19.2% of children aged 5-11 years have gotten at least one dose and 9.6% are fully vaccinated, compared with 62.1% and 52.3%, respectively, among children aged 12-17, the CDC said.
Infant milk allergy guidelines promote overdiagnosis, study says
International guidelines developed to help nonspecialists diagnose cow’s milk allergy (CMA) lead providers to attribute normal infant symptoms to CMA and result in overdiagnosis, say authors of a study published online in Clinical & Experimental Allergy.
Lead author Rosie Vincent, MBChB, with Population Health Sciences at University of Bristol, United Kingdom, told this news organization their study shows that symptoms listed in the international Milk Allergy in Primary Care (iMAP) guidelines as indicative of non-immunoglobulin E (IgE)-mediated milk allergy are very common in a baby’s first year. Examples include vomiting, regurgitating milk, loose or more frequent stools, colic, and irritability.
Findings come from performing a secondary analysis of data from 1,303 infants from the EAT study, a population-based, randomized controlled trial in the U.K. that looked at whether introducing allergenic foods into an infant’s diet reduced the risk of developing an allergy to that food.
In an indication of how common the symptoms in the guidelines (published in 2017 and 2019) are found in all infants, nearly three-fourths (74%) of participants reported at least two mild-to-moderate symptoms, and 9% reported at least two severe symptoms in at least one month between 3 and 12 months of age. Data were not available for younger infants.
However, the prevalence of non–IgE-mediated CMA is thought to be less than 1% in infants in European countries, the study states.
In the study, two or more non-IgE CMA mild-to-moderate symptoms were reported by 25% of families, and 1.4% reported severe symptoms each month between ages 3 and 12 months.
“These symptoms peaked at 38%, with at least two mild-to-moderate symptoms and 4.3% with at least two severe symptoms at 3 months, when participants were not directly consuming cow’s milk,” Ms. Vincent said.
Researchers write that at 6 months there was no significant difference in the proportion of children with at least two symptoms between those consuming and not consuming cow’s milk.
Consequences of misdiagnosis
Overdiagnosing milk allergy can lead to additional costs, unnecessary tests, and less breastfeeding, she said.
Cow’s milk protein is commonly found in standard infant formula or in milk-containing foods.
The authors note that “small levels of lactoglobulin are found in breastmilk; however, the quantities are below the threshold likely to trigger a reaction in more than 99% of infants with IgE-mediated cow’s milk allergy.”
Misdiagnosis is likely to result in increasing prescriptions of unwarranted specialized formula, with increased cost to patients and health care systems, and use of unvalidated allergy tests, Ms. Vincent said.
Ms. Vincent added that even the suggestion that cow’s milk protein delivered through breast milk might be inducing symptoms could lead a mother to stop breastfeeding.
The authors also note that in reviewing recent CMA guidelines, “three of nine CMA guidelines were directly supported by formula manufacturers or marketing consultants, and 81% of all guideline authors reported a conflict of interest with formula manufacturers.”
Heather Cassell, MD, a pediatric allergy and immunology specialist with Banner Health and a clinical associate professor of pediatrics at the University of Arizona College of Medicine in Tucson, told this news organization the conflicts of interest in milk allergy research and guidelines have been a long-standing problem.
She said historically there has been a big push “that people who can afford formula should be paying for formula. That was 100% marketed by the formula companies.”
“We have formula companies bringing us samples to encourage pediatricians to use the formula early if we’re concerned about a milk protein allergy,” Dr. Cassell said.
As for the overdiagnosis of milk allergy, she said reintroduction of cow’s milk later is one way to improve diagnosis to see if the child no longer has a reaction. However, she points out that in this study, only 21% of parents reintroduced cow’s milk.
“Really, it should be closer to 100%, with the exception of the babies who are having severe symptoms,” Dr. Cassell said. “You don’t want to keep a baby from progressing with their diet.”
She said families and providers need to look at several contextual clues before they land on a milk allergy label.
“It’s not just about reflux, it’s not just about a baby spitting up. Happy babies spit up and there’s nothing that needs to be done because they will eventually grow out of it,” Dr. Cassell stressed.
She said significant irritability with blood in the stool might warrant more concern. “I think the [emphasis] needs to be on retrying the food another time,” she suggested.
Ms. Vincent pointed out that there is no quick or easy test to diagnose non–IgE-mediated cow’s milk allergy.
“We need further research to identify what symptoms are much more likely to point to a diagnosis,” she said.
Although the researchers used iMAP guidelines, they write that results are likely to apply to other CMA guidelines, because they list similar symptoms and signs.
The study was funded by the International Society of Atopic Dermatitis. Ms. Vincent reports receiving a 3-month research fellowship award from Pfizer and support from the NIHR School for Primary Care Research. Other authors’ financial disclosures are available with the full text. Dr. Cassell reports that the University of Arizona School of Medicine is a trial site for testing a patch to help with diagnosing milk protein allergy in infants.
A version of this article first appeared on Medscape.com.
International guidelines developed to help nonspecialists diagnose cow’s milk allergy (CMA) lead providers to attribute normal infant symptoms to CMA and result in overdiagnosis, say authors of a study published online in Clinical & Experimental Allergy.
Lead author Rosie Vincent, MBChB, with Population Health Sciences at University of Bristol, United Kingdom, told this news organization their study shows that symptoms listed in the international Milk Allergy in Primary Care (iMAP) guidelines as indicative of non-immunoglobulin E (IgE)-mediated milk allergy are very common in a baby’s first year. Examples include vomiting, regurgitating milk, loose or more frequent stools, colic, and irritability.
Findings come from performing a secondary analysis of data from 1,303 infants from the EAT study, a population-based, randomized controlled trial in the U.K. that looked at whether introducing allergenic foods into an infant’s diet reduced the risk of developing an allergy to that food.
In an indication of how common the symptoms in the guidelines (published in 2017 and 2019) are found in all infants, nearly three-fourths (74%) of participants reported at least two mild-to-moderate symptoms, and 9% reported at least two severe symptoms in at least one month between 3 and 12 months of age. Data were not available for younger infants.
However, the prevalence of non–IgE-mediated CMA is thought to be less than 1% in infants in European countries, the study states.
In the study, two or more non-IgE CMA mild-to-moderate symptoms were reported by 25% of families, and 1.4% reported severe symptoms each month between ages 3 and 12 months.
“These symptoms peaked at 38%, with at least two mild-to-moderate symptoms and 4.3% with at least two severe symptoms at 3 months, when participants were not directly consuming cow’s milk,” Ms. Vincent said.
Researchers write that at 6 months there was no significant difference in the proportion of children with at least two symptoms between those consuming and not consuming cow’s milk.
Consequences of misdiagnosis
Overdiagnosing milk allergy can lead to additional costs, unnecessary tests, and less breastfeeding, she said.
Cow’s milk protein is commonly found in standard infant formula or in milk-containing foods.
The authors note that “small levels of lactoglobulin are found in breastmilk; however, the quantities are below the threshold likely to trigger a reaction in more than 99% of infants with IgE-mediated cow’s milk allergy.”
Misdiagnosis is likely to result in increasing prescriptions of unwarranted specialized formula, with increased cost to patients and health care systems, and use of unvalidated allergy tests, Ms. Vincent said.
Ms. Vincent added that even the suggestion that cow’s milk protein delivered through breast milk might be inducing symptoms could lead a mother to stop breastfeeding.
The authors also note that in reviewing recent CMA guidelines, “three of nine CMA guidelines were directly supported by formula manufacturers or marketing consultants, and 81% of all guideline authors reported a conflict of interest with formula manufacturers.”
Heather Cassell, MD, a pediatric allergy and immunology specialist with Banner Health and a clinical associate professor of pediatrics at the University of Arizona College of Medicine in Tucson, told this news organization the conflicts of interest in milk allergy research and guidelines have been a long-standing problem.
She said historically there has been a big push “that people who can afford formula should be paying for formula. That was 100% marketed by the formula companies.”
“We have formula companies bringing us samples to encourage pediatricians to use the formula early if we’re concerned about a milk protein allergy,” Dr. Cassell said.
As for the overdiagnosis of milk allergy, she said reintroduction of cow’s milk later is one way to improve diagnosis to see if the child no longer has a reaction. However, she points out that in this study, only 21% of parents reintroduced cow’s milk.
“Really, it should be closer to 100%, with the exception of the babies who are having severe symptoms,” Dr. Cassell said. “You don’t want to keep a baby from progressing with their diet.”
She said families and providers need to look at several contextual clues before they land on a milk allergy label.
“It’s not just about reflux, it’s not just about a baby spitting up. Happy babies spit up and there’s nothing that needs to be done because they will eventually grow out of it,” Dr. Cassell stressed.
She said significant irritability with blood in the stool might warrant more concern. “I think the [emphasis] needs to be on retrying the food another time,” she suggested.
Ms. Vincent pointed out that there is no quick or easy test to diagnose non–IgE-mediated cow’s milk allergy.
“We need further research to identify what symptoms are much more likely to point to a diagnosis,” she said.
Although the researchers used iMAP guidelines, they write that results are likely to apply to other CMA guidelines, because they list similar symptoms and signs.
The study was funded by the International Society of Atopic Dermatitis. Ms. Vincent reports receiving a 3-month research fellowship award from Pfizer and support from the NIHR School for Primary Care Research. Other authors’ financial disclosures are available with the full text. Dr. Cassell reports that the University of Arizona School of Medicine is a trial site for testing a patch to help with diagnosing milk protein allergy in infants.
A version of this article first appeared on Medscape.com.
International guidelines developed to help nonspecialists diagnose cow’s milk allergy (CMA) lead providers to attribute normal infant symptoms to CMA and result in overdiagnosis, say authors of a study published online in Clinical & Experimental Allergy.
Lead author Rosie Vincent, MBChB, with Population Health Sciences at University of Bristol, United Kingdom, told this news organization their study shows that symptoms listed in the international Milk Allergy in Primary Care (iMAP) guidelines as indicative of non-immunoglobulin E (IgE)-mediated milk allergy are very common in a baby’s first year. Examples include vomiting, regurgitating milk, loose or more frequent stools, colic, and irritability.
Findings come from performing a secondary analysis of data from 1,303 infants from the EAT study, a population-based, randomized controlled trial in the U.K. that looked at whether introducing allergenic foods into an infant’s diet reduced the risk of developing an allergy to that food.
In an indication of how common the symptoms in the guidelines (published in 2017 and 2019) are found in all infants, nearly three-fourths (74%) of participants reported at least two mild-to-moderate symptoms, and 9% reported at least two severe symptoms in at least one month between 3 and 12 months of age. Data were not available for younger infants.
However, the prevalence of non–IgE-mediated CMA is thought to be less than 1% in infants in European countries, the study states.
In the study, two or more non-IgE CMA mild-to-moderate symptoms were reported by 25% of families, and 1.4% reported severe symptoms each month between ages 3 and 12 months.
“These symptoms peaked at 38%, with at least two mild-to-moderate symptoms and 4.3% with at least two severe symptoms at 3 months, when participants were not directly consuming cow’s milk,” Ms. Vincent said.
Researchers write that at 6 months there was no significant difference in the proportion of children with at least two symptoms between those consuming and not consuming cow’s milk.
Consequences of misdiagnosis
Overdiagnosing milk allergy can lead to additional costs, unnecessary tests, and less breastfeeding, she said.
Cow’s milk protein is commonly found in standard infant formula or in milk-containing foods.
The authors note that “small levels of lactoglobulin are found in breastmilk; however, the quantities are below the threshold likely to trigger a reaction in more than 99% of infants with IgE-mediated cow’s milk allergy.”
Misdiagnosis is likely to result in increasing prescriptions of unwarranted specialized formula, with increased cost to patients and health care systems, and use of unvalidated allergy tests, Ms. Vincent said.
Ms. Vincent added that even the suggestion that cow’s milk protein delivered through breast milk might be inducing symptoms could lead a mother to stop breastfeeding.
The authors also note that in reviewing recent CMA guidelines, “three of nine CMA guidelines were directly supported by formula manufacturers or marketing consultants, and 81% of all guideline authors reported a conflict of interest with formula manufacturers.”
Heather Cassell, MD, a pediatric allergy and immunology specialist with Banner Health and a clinical associate professor of pediatrics at the University of Arizona College of Medicine in Tucson, told this news organization the conflicts of interest in milk allergy research and guidelines have been a long-standing problem.
She said historically there has been a big push “that people who can afford formula should be paying for formula. That was 100% marketed by the formula companies.”
“We have formula companies bringing us samples to encourage pediatricians to use the formula early if we’re concerned about a milk protein allergy,” Dr. Cassell said.
As for the overdiagnosis of milk allergy, she said reintroduction of cow’s milk later is one way to improve diagnosis to see if the child no longer has a reaction. However, she points out that in this study, only 21% of parents reintroduced cow’s milk.
“Really, it should be closer to 100%, with the exception of the babies who are having severe symptoms,” Dr. Cassell said. “You don’t want to keep a baby from progressing with their diet.”
She said families and providers need to look at several contextual clues before they land on a milk allergy label.
“It’s not just about reflux, it’s not just about a baby spitting up. Happy babies spit up and there’s nothing that needs to be done because they will eventually grow out of it,” Dr. Cassell stressed.
She said significant irritability with blood in the stool might warrant more concern. “I think the [emphasis] needs to be on retrying the food another time,” she suggested.
Ms. Vincent pointed out that there is no quick or easy test to diagnose non–IgE-mediated cow’s milk allergy.
“We need further research to identify what symptoms are much more likely to point to a diagnosis,” she said.
Although the researchers used iMAP guidelines, they write that results are likely to apply to other CMA guidelines, because they list similar symptoms and signs.
The study was funded by the International Society of Atopic Dermatitis. Ms. Vincent reports receiving a 3-month research fellowship award from Pfizer and support from the NIHR School for Primary Care Research. Other authors’ financial disclosures are available with the full text. Dr. Cassell reports that the University of Arizona School of Medicine is a trial site for testing a patch to help with diagnosing milk protein allergy in infants.
A version of this article first appeared on Medscape.com.
FROM CLINICAL & EXPERIMENTAL ALLERGY
Physician gender pay gap isn’t news; health inequity is rampant
A recent study examined projected career earnings between the genders in a largely community-based physician population, finding a difference of about $2 million in career earnings. That a gender pay gap exists in medicine is not news – but the manner in which this study was done, the investigators’ ability to control for a number of confounding variables, and the size of the study group (over 80,000) are newsworthy.
Some of the key findings include that gender pay gaps start with your first job, and you never close the gap, even as you gain experience and efficiency. Also, the more highly remunerated your specialty, the larger the gap. The gender pay gap joins a growing list of inequities within health care. Although physician compensation is not the most important, given that nearly all physicians are well-paid, and we have much more significant inequities that lead to direct patient harm, the reasons for this discrepancy warrant further consideration.
When I was first being educated about social inequity as part of work in social determinants of health, I made the error of using “inequality” and “inequity” interchangeably. The subtle yet important difference between the two terms was quickly described to me. Inequality is a gastroenterologist getting paid more money to do a colonoscopy than a family physician. Inequity is a female gastroenterologist getting paid less than a male gastroenterologist. Global Health Europe boldly identifies that “inequity is the result of failure.” In looking at the inequity inherent in the gender pay gap, I consider what failed and why.
I’m currently making a major career change, leaving an executive leadership position to return to full-time clinical practice. There is a significant pay decrease that will accompany this change because I am in a primary care specialty. Beyond that, I am considering two employment contracts from different systems to do a similar clinical role.
One of the questions my husband asked was which will pay more over the long run. This is difficult to discern because the compensation formula each health system uses is different, even though they are based on standard national benchmarking data. It is possible that women, in general, are like I am and look for factors other than compensation to make a job decision – assuming, like I do, that it will be close enough to not matter or is generally fair. In fact, while compensation is most certainly a consideration for me, once I determined that it was likely to be in the same ballpark, I stopped comparing. Even as the sole breadwinner in our family, I take this (probably faulty) approach.
It’s time to reconsider how we pay physicians
Women may be more likely to gloss over compensation details that men evaluate and negotiate carefully. To change this, women must first take responsibility for being an active, informed, and engaged part of compensation negotiations. In addition, employers who value gender pay equity must negotiate in good faith, keeping in mind the well-described vulnerabilities in discussions about pay. Finally, male and female mentors and leaders should actively coach female physicians on how to approach these conversations with confidence and skill.
In primary care, female physicians spend, on average, about 15% more time with their patients during a visit. Despite spending as much time in clinic seeing patients per week, they see fewer patients, thereby generating less revenue. For compensation plans that are based on productivity, the extra time spent costs money. In this case, it costs the female physicians lost compensation.
The way in which women are more likely to practice medicine, which includes the amount of time they spend with patients, may affect clinical outcomes without directly increasing productivity. A 2017 study demonstrated that elderly patients had lower rates of mortality and readmission when cared for by a female rather than a male physician. These findings require health systems to critically evaluate what compensation plans value and to promote an appropriate balance between quality of care, quantity of care, and style of care.
Although I’ve seen gender pay inequity as blatant as two different salaries for physicians doing the same work – one male and one female – I think this is uncommon. Like many forms of inequity, the outputs are often related to a failed system rather than solely a series of individual failures. Making compensation formulas gender-blind is an important step – but it is only the first step, not the last. Recognizing that the structure of a compensation formula may be biased toward a style of medical practice more likely to be espoused by one gender is necessary as well.
The data, including the findings of this recent study, clearly identify the gender pay gap that exists in medicine, as it does in many other fields, and that it is not explainable solely by differences in specialties, work hours, family status, or title.
To address the inequity, it is imperative that women engage with employers and leaders to both understand and develop skills around effective and appropriate compensation negotiation. Recognizing that compensation plans, especially those built on productivity models, may fail to place adequate value on gender-specific practice styles.
Jennifer Frank is a family physician, physician leader, wife, and mother in Northeast Wisconsin.
A version of this article first appeared on Medscape.com.
A recent study examined projected career earnings between the genders in a largely community-based physician population, finding a difference of about $2 million in career earnings. That a gender pay gap exists in medicine is not news – but the manner in which this study was done, the investigators’ ability to control for a number of confounding variables, and the size of the study group (over 80,000) are newsworthy.
Some of the key findings include that gender pay gaps start with your first job, and you never close the gap, even as you gain experience and efficiency. Also, the more highly remunerated your specialty, the larger the gap. The gender pay gap joins a growing list of inequities within health care. Although physician compensation is not the most important, given that nearly all physicians are well-paid, and we have much more significant inequities that lead to direct patient harm, the reasons for this discrepancy warrant further consideration.
When I was first being educated about social inequity as part of work in social determinants of health, I made the error of using “inequality” and “inequity” interchangeably. The subtle yet important difference between the two terms was quickly described to me. Inequality is a gastroenterologist getting paid more money to do a colonoscopy than a family physician. Inequity is a female gastroenterologist getting paid less than a male gastroenterologist. Global Health Europe boldly identifies that “inequity is the result of failure.” In looking at the inequity inherent in the gender pay gap, I consider what failed and why.
I’m currently making a major career change, leaving an executive leadership position to return to full-time clinical practice. There is a significant pay decrease that will accompany this change because I am in a primary care specialty. Beyond that, I am considering two employment contracts from different systems to do a similar clinical role.
One of the questions my husband asked was which will pay more over the long run. This is difficult to discern because the compensation formula each health system uses is different, even though they are based on standard national benchmarking data. It is possible that women, in general, are like I am and look for factors other than compensation to make a job decision – assuming, like I do, that it will be close enough to not matter or is generally fair. In fact, while compensation is most certainly a consideration for me, once I determined that it was likely to be in the same ballpark, I stopped comparing. Even as the sole breadwinner in our family, I take this (probably faulty) approach.
It’s time to reconsider how we pay physicians
Women may be more likely to gloss over compensation details that men evaluate and negotiate carefully. To change this, women must first take responsibility for being an active, informed, and engaged part of compensation negotiations. In addition, employers who value gender pay equity must negotiate in good faith, keeping in mind the well-described vulnerabilities in discussions about pay. Finally, male and female mentors and leaders should actively coach female physicians on how to approach these conversations with confidence and skill.
In primary care, female physicians spend, on average, about 15% more time with their patients during a visit. Despite spending as much time in clinic seeing patients per week, they see fewer patients, thereby generating less revenue. For compensation plans that are based on productivity, the extra time spent costs money. In this case, it costs the female physicians lost compensation.
The way in which women are more likely to practice medicine, which includes the amount of time they spend with patients, may affect clinical outcomes without directly increasing productivity. A 2017 study demonstrated that elderly patients had lower rates of mortality and readmission when cared for by a female rather than a male physician. These findings require health systems to critically evaluate what compensation plans value and to promote an appropriate balance between quality of care, quantity of care, and style of care.
Although I’ve seen gender pay inequity as blatant as two different salaries for physicians doing the same work – one male and one female – I think this is uncommon. Like many forms of inequity, the outputs are often related to a failed system rather than solely a series of individual failures. Making compensation formulas gender-blind is an important step – but it is only the first step, not the last. Recognizing that the structure of a compensation formula may be biased toward a style of medical practice more likely to be espoused by one gender is necessary as well.
The data, including the findings of this recent study, clearly identify the gender pay gap that exists in medicine, as it does in many other fields, and that it is not explainable solely by differences in specialties, work hours, family status, or title.
To address the inequity, it is imperative that women engage with employers and leaders to both understand and develop skills around effective and appropriate compensation negotiation. Recognizing that compensation plans, especially those built on productivity models, may fail to place adequate value on gender-specific practice styles.
Jennifer Frank is a family physician, physician leader, wife, and mother in Northeast Wisconsin.
A version of this article first appeared on Medscape.com.
A recent study examined projected career earnings between the genders in a largely community-based physician population, finding a difference of about $2 million in career earnings. That a gender pay gap exists in medicine is not news – but the manner in which this study was done, the investigators’ ability to control for a number of confounding variables, and the size of the study group (over 80,000) are newsworthy.
Some of the key findings include that gender pay gaps start with your first job, and you never close the gap, even as you gain experience and efficiency. Also, the more highly remunerated your specialty, the larger the gap. The gender pay gap joins a growing list of inequities within health care. Although physician compensation is not the most important, given that nearly all physicians are well-paid, and we have much more significant inequities that lead to direct patient harm, the reasons for this discrepancy warrant further consideration.
When I was first being educated about social inequity as part of work in social determinants of health, I made the error of using “inequality” and “inequity” interchangeably. The subtle yet important difference between the two terms was quickly described to me. Inequality is a gastroenterologist getting paid more money to do a colonoscopy than a family physician. Inequity is a female gastroenterologist getting paid less than a male gastroenterologist. Global Health Europe boldly identifies that “inequity is the result of failure.” In looking at the inequity inherent in the gender pay gap, I consider what failed and why.
I’m currently making a major career change, leaving an executive leadership position to return to full-time clinical practice. There is a significant pay decrease that will accompany this change because I am in a primary care specialty. Beyond that, I am considering two employment contracts from different systems to do a similar clinical role.
One of the questions my husband asked was which will pay more over the long run. This is difficult to discern because the compensation formula each health system uses is different, even though they are based on standard national benchmarking data. It is possible that women, in general, are like I am and look for factors other than compensation to make a job decision – assuming, like I do, that it will be close enough to not matter or is generally fair. In fact, while compensation is most certainly a consideration for me, once I determined that it was likely to be in the same ballpark, I stopped comparing. Even as the sole breadwinner in our family, I take this (probably faulty) approach.
It’s time to reconsider how we pay physicians
Women may be more likely to gloss over compensation details that men evaluate and negotiate carefully. To change this, women must first take responsibility for being an active, informed, and engaged part of compensation negotiations. In addition, employers who value gender pay equity must negotiate in good faith, keeping in mind the well-described vulnerabilities in discussions about pay. Finally, male and female mentors and leaders should actively coach female physicians on how to approach these conversations with confidence and skill.
In primary care, female physicians spend, on average, about 15% more time with their patients during a visit. Despite spending as much time in clinic seeing patients per week, they see fewer patients, thereby generating less revenue. For compensation plans that are based on productivity, the extra time spent costs money. In this case, it costs the female physicians lost compensation.
The way in which women are more likely to practice medicine, which includes the amount of time they spend with patients, may affect clinical outcomes without directly increasing productivity. A 2017 study demonstrated that elderly patients had lower rates of mortality and readmission when cared for by a female rather than a male physician. These findings require health systems to critically evaluate what compensation plans value and to promote an appropriate balance between quality of care, quantity of care, and style of care.
Although I’ve seen gender pay inequity as blatant as two different salaries for physicians doing the same work – one male and one female – I think this is uncommon. Like many forms of inequity, the outputs are often related to a failed system rather than solely a series of individual failures. Making compensation formulas gender-blind is an important step – but it is only the first step, not the last. Recognizing that the structure of a compensation formula may be biased toward a style of medical practice more likely to be espoused by one gender is necessary as well.
The data, including the findings of this recent study, clearly identify the gender pay gap that exists in medicine, as it does in many other fields, and that it is not explainable solely by differences in specialties, work hours, family status, or title.
To address the inequity, it is imperative that women engage with employers and leaders to both understand and develop skills around effective and appropriate compensation negotiation. Recognizing that compensation plans, especially those built on productivity models, may fail to place adequate value on gender-specific practice styles.
Jennifer Frank is a family physician, physician leader, wife, and mother in Northeast Wisconsin.
A version of this article first appeared on Medscape.com.
Pollutants tied to changes in ratio of boys to girls born
The season of conception does not affect whether more boys than girls are born, nor do temperatures in the environment, a large study reveals. Similarly, researchers found no connection with a location’s violent crime level, unemployment rate, or major events like Hurricane Katrina.
But certain chemical pollutants were related to fewer boys being born compared to girls when researchers looked at data for more than 3 million newborns over 8 years in the U.S. and another 3 million born over 30 years in Sweden.
“With data on births in 150 million people in the U.S. over 8 years and 9 million Swedes over 9 years, this is almost surely the largest study to date on the question of environmental factors and their influence on sex ratio at birth,” says Shanna Swan, PhD, who was not affiliated with the research
Variations in the annual sex birth ratio (SRB) – the number of boys born compared to the total birth rate – are well-accepted. Less clear is what things drive these changes.
Although not the first study to look for connections between major events or pollutants in the air, water, and land and the SRB, it is the first to mine two very large electronic medical record databases for answers, senior study author Andrey Rzhetsky, PhD, a professor of medicine and human genetics at the University of Chicago, tells this news organization.
The findings were published Dec. 2, 2021, in PLOS Computational Biology.
And even though the SRB did not vary significantly after Hurricane Katrina in 2005, it did after the 2007 shooting at Virginia Tech, Dr. Rzhetsky and colleagues found. The SRB was lower than expected 34 weeks after the mass shooting.
Location, location, location
The researchers also found the levels of chemical pollutants “varied remarkably” across different regions of the country. For example, lead in the land was elevated in the Northeast, Southwest, and Mideastern U.S. but not in the South. Also, the highest levels of total mercury in water samples was found mostly in Eastern states, especially in the Northeast.
Dr. Rzhetsky and colleagues mapped these regional differences in many factors, including hydrazine. Hydrazine is a foaming agent used to make pharmaceuticals, agrochemicals, and as a propellant for spacecraft.
“Hydrazine appears to follow capricious, blotch-like shapes in the eastern U.S., each blotch likely centered at a factory emitting this pollutant,” the authors wrote.
To get a more complete picture, the investigators also compared changes in the SRB to data from the U.S. National Oceanic and Atmospheric Administration, U.S. Environmental Protection Agency, Swedish Meteorological and Hydrological Institute, and Statistics Sweden.
They found that aluminium in air, chromium in water, and total mercury levels drove the SRB up. By comparison, lead in soil and areas with a higher renter occupancy were linked to a lower SRB, or a higher proportion of girls being born.
Dr. Rzhetsky and colleagues also add to the evidence for a link between polychlorinated biphenyls (PCBs) and the SRB. Previous findings conflict, the authors noted.
“Since the sample sizes of the studies published thus far were very small, our PCBs result would have substantially larger statistical power,” they said.
Several pollutants had no significant link to SRB in the study, including levels of lead or chromium in the air, arsenic in the soil, and cadmium in the air or water.
Consistent findings
That said, the research had limits.
“The magnitude is new in terms of number of births, and the statistical methods are unusually sophisticated, but the conclusions don’t really differ from much of what has been published,” says Dr. Swan, a professor of environmental medicine and public health at the Icahn School of Medicine at Mount Sinai, New York.
“The takeaway message that many examined exposures are associated with lower – and some with higher – SRBs is not new but consistent with other, smaller studies,” says Dr. Swan, who co-authored a Sept. 2021 study evaluating endocrine-disrupting chemicals and lower birth rates in Asia.
The data on environmental exposures “is, however, quite uneven, and only known at the ecologic and not the individual level,” she says. “We learn, for example, that SRB was significantly reduced ... among families living in areas with the highest septile of lead exposure but also in those among the highest septile of percent renter occupancy.”
“Evaluating these as to mechanism and plausibility is difficult,” Dr. Swan says.
More research warranted
The mechanism remains unknown, but the investigators suggested that female embryo pregnancies may end early in development, driving the SRB up. Also, male embryo deaths are more common in the late second or third trimester, at which point they would drive the SRB down. A third factor, maternal hormone levels around the time of conception, could also alter the SRB.
The associations between individual factors and SRB changes are just that – associations – not intended to be interpreted as “sex-specific selection mechanisms” causing the differences at this point, the authors noted. Further studies to confirm the associations are needed.
The research is a good stepping off point for future studies to look closer at the contribution of pollutants like arsenic, lead, cadmium, and more, Dr. Rzhetsky says.
A version of this article first appeared on WebMD.com.
The season of conception does not affect whether more boys than girls are born, nor do temperatures in the environment, a large study reveals. Similarly, researchers found no connection with a location’s violent crime level, unemployment rate, or major events like Hurricane Katrina.
But certain chemical pollutants were related to fewer boys being born compared to girls when researchers looked at data for more than 3 million newborns over 8 years in the U.S. and another 3 million born over 30 years in Sweden.
“With data on births in 150 million people in the U.S. over 8 years and 9 million Swedes over 9 years, this is almost surely the largest study to date on the question of environmental factors and their influence on sex ratio at birth,” says Shanna Swan, PhD, who was not affiliated with the research
Variations in the annual sex birth ratio (SRB) – the number of boys born compared to the total birth rate – are well-accepted. Less clear is what things drive these changes.
Although not the first study to look for connections between major events or pollutants in the air, water, and land and the SRB, it is the first to mine two very large electronic medical record databases for answers, senior study author Andrey Rzhetsky, PhD, a professor of medicine and human genetics at the University of Chicago, tells this news organization.
The findings were published Dec. 2, 2021, in PLOS Computational Biology.
And even though the SRB did not vary significantly after Hurricane Katrina in 2005, it did after the 2007 shooting at Virginia Tech, Dr. Rzhetsky and colleagues found. The SRB was lower than expected 34 weeks after the mass shooting.
Location, location, location
The researchers also found the levels of chemical pollutants “varied remarkably” across different regions of the country. For example, lead in the land was elevated in the Northeast, Southwest, and Mideastern U.S. but not in the South. Also, the highest levels of total mercury in water samples was found mostly in Eastern states, especially in the Northeast.
Dr. Rzhetsky and colleagues mapped these regional differences in many factors, including hydrazine. Hydrazine is a foaming agent used to make pharmaceuticals, agrochemicals, and as a propellant for spacecraft.
“Hydrazine appears to follow capricious, blotch-like shapes in the eastern U.S., each blotch likely centered at a factory emitting this pollutant,” the authors wrote.
To get a more complete picture, the investigators also compared changes in the SRB to data from the U.S. National Oceanic and Atmospheric Administration, U.S. Environmental Protection Agency, Swedish Meteorological and Hydrological Institute, and Statistics Sweden.
They found that aluminium in air, chromium in water, and total mercury levels drove the SRB up. By comparison, lead in soil and areas with a higher renter occupancy were linked to a lower SRB, or a higher proportion of girls being born.
Dr. Rzhetsky and colleagues also add to the evidence for a link between polychlorinated biphenyls (PCBs) and the SRB. Previous findings conflict, the authors noted.
“Since the sample sizes of the studies published thus far were very small, our PCBs result would have substantially larger statistical power,” they said.
Several pollutants had no significant link to SRB in the study, including levels of lead or chromium in the air, arsenic in the soil, and cadmium in the air or water.
Consistent findings
That said, the research had limits.
“The magnitude is new in terms of number of births, and the statistical methods are unusually sophisticated, but the conclusions don’t really differ from much of what has been published,” says Dr. Swan, a professor of environmental medicine and public health at the Icahn School of Medicine at Mount Sinai, New York.
“The takeaway message that many examined exposures are associated with lower – and some with higher – SRBs is not new but consistent with other, smaller studies,” says Dr. Swan, who co-authored a Sept. 2021 study evaluating endocrine-disrupting chemicals and lower birth rates in Asia.
The data on environmental exposures “is, however, quite uneven, and only known at the ecologic and not the individual level,” she says. “We learn, for example, that SRB was significantly reduced ... among families living in areas with the highest septile of lead exposure but also in those among the highest septile of percent renter occupancy.”
“Evaluating these as to mechanism and plausibility is difficult,” Dr. Swan says.
More research warranted
The mechanism remains unknown, but the investigators suggested that female embryo pregnancies may end early in development, driving the SRB up. Also, male embryo deaths are more common in the late second or third trimester, at which point they would drive the SRB down. A third factor, maternal hormone levels around the time of conception, could also alter the SRB.
The associations between individual factors and SRB changes are just that – associations – not intended to be interpreted as “sex-specific selection mechanisms” causing the differences at this point, the authors noted. Further studies to confirm the associations are needed.
The research is a good stepping off point for future studies to look closer at the contribution of pollutants like arsenic, lead, cadmium, and more, Dr. Rzhetsky says.
A version of this article first appeared on WebMD.com.
The season of conception does not affect whether more boys than girls are born, nor do temperatures in the environment, a large study reveals. Similarly, researchers found no connection with a location’s violent crime level, unemployment rate, or major events like Hurricane Katrina.
But certain chemical pollutants were related to fewer boys being born compared to girls when researchers looked at data for more than 3 million newborns over 8 years in the U.S. and another 3 million born over 30 years in Sweden.
“With data on births in 150 million people in the U.S. over 8 years and 9 million Swedes over 9 years, this is almost surely the largest study to date on the question of environmental factors and their influence on sex ratio at birth,” says Shanna Swan, PhD, who was not affiliated with the research
Variations in the annual sex birth ratio (SRB) – the number of boys born compared to the total birth rate – are well-accepted. Less clear is what things drive these changes.
Although not the first study to look for connections between major events or pollutants in the air, water, and land and the SRB, it is the first to mine two very large electronic medical record databases for answers, senior study author Andrey Rzhetsky, PhD, a professor of medicine and human genetics at the University of Chicago, tells this news organization.
The findings were published Dec. 2, 2021, in PLOS Computational Biology.
And even though the SRB did not vary significantly after Hurricane Katrina in 2005, it did after the 2007 shooting at Virginia Tech, Dr. Rzhetsky and colleagues found. The SRB was lower than expected 34 weeks after the mass shooting.
Location, location, location
The researchers also found the levels of chemical pollutants “varied remarkably” across different regions of the country. For example, lead in the land was elevated in the Northeast, Southwest, and Mideastern U.S. but not in the South. Also, the highest levels of total mercury in water samples was found mostly in Eastern states, especially in the Northeast.
Dr. Rzhetsky and colleagues mapped these regional differences in many factors, including hydrazine. Hydrazine is a foaming agent used to make pharmaceuticals, agrochemicals, and as a propellant for spacecraft.
“Hydrazine appears to follow capricious, blotch-like shapes in the eastern U.S., each blotch likely centered at a factory emitting this pollutant,” the authors wrote.
To get a more complete picture, the investigators also compared changes in the SRB to data from the U.S. National Oceanic and Atmospheric Administration, U.S. Environmental Protection Agency, Swedish Meteorological and Hydrological Institute, and Statistics Sweden.
They found that aluminium in air, chromium in water, and total mercury levels drove the SRB up. By comparison, lead in soil and areas with a higher renter occupancy were linked to a lower SRB, or a higher proportion of girls being born.
Dr. Rzhetsky and colleagues also add to the evidence for a link between polychlorinated biphenyls (PCBs) and the SRB. Previous findings conflict, the authors noted.
“Since the sample sizes of the studies published thus far were very small, our PCBs result would have substantially larger statistical power,” they said.
Several pollutants had no significant link to SRB in the study, including levels of lead or chromium in the air, arsenic in the soil, and cadmium in the air or water.
Consistent findings
That said, the research had limits.
“The magnitude is new in terms of number of births, and the statistical methods are unusually sophisticated, but the conclusions don’t really differ from much of what has been published,” says Dr. Swan, a professor of environmental medicine and public health at the Icahn School of Medicine at Mount Sinai, New York.
“The takeaway message that many examined exposures are associated with lower – and some with higher – SRBs is not new but consistent with other, smaller studies,” says Dr. Swan, who co-authored a Sept. 2021 study evaluating endocrine-disrupting chemicals and lower birth rates in Asia.
The data on environmental exposures “is, however, quite uneven, and only known at the ecologic and not the individual level,” she says. “We learn, for example, that SRB was significantly reduced ... among families living in areas with the highest septile of lead exposure but also in those among the highest septile of percent renter occupancy.”
“Evaluating these as to mechanism and plausibility is difficult,” Dr. Swan says.
More research warranted
The mechanism remains unknown, but the investigators suggested that female embryo pregnancies may end early in development, driving the SRB up. Also, male embryo deaths are more common in the late second or third trimester, at which point they would drive the SRB down. A third factor, maternal hormone levels around the time of conception, could also alter the SRB.
The associations between individual factors and SRB changes are just that – associations – not intended to be interpreted as “sex-specific selection mechanisms” causing the differences at this point, the authors noted. Further studies to confirm the associations are needed.
The research is a good stepping off point for future studies to look closer at the contribution of pollutants like arsenic, lead, cadmium, and more, Dr. Rzhetsky says.
A version of this article first appeared on WebMD.com.





