User login
VRE Bacteremia Treatment With Linezolid or Daptomycin
Enterococci have been identified as a causative organism in approximately 10% of all nosocomial bloodstream infections (BSIs).1, 2 In 2006, the Infectious Diseases Society of America identified vancomycin‐ resistant Enterococcus faecium (VRE) as 1 of 6 microbes considered to be among the most dangerous due to high rates of resistance and a limited number of effective antimicrobials.3 E. faecium has exhibited high rates of glycopeptide resistance with as many as 60% of isolates from BSIs being resistant to vancomycin.2, 4 Due to increasing resistance to glycopeptides, vancomycin has become obsolete in the treatment of E. faecium infections.5
A limited number of antimicrobials are available for the treatment of infections due to VRE. Agents active in vitro are quinupristin‐dalfopristin, tigecycline, linezolid, and daptomycin. Quinupristin‐dalfopristin was one of the first agents approved for use in VRE infections; however, treatment with this agent has been limited because of mediocre clinical response rates, undesirable adverse effects, high cost, and insufficient E. faecalis activity.6, 7 Tigecycline is not an optimal antibiotic for the treatment of VRE bacteremia, because serum concentrations achieved after administration are inadequate to treat BSIs.7 In contrast, linezolid and daptomycin have evinced efficacy against VRE bacteremia, with reported microbiologic response rates of 85% and 80%, respectively.7, 8 One inherent difference between these antibiotics that may theoretically affect their use in immunocompromised patients is that linezolid is bacteriostatic, whereas daptomycin is bactericidal. It has been postulated that by using a bactericidal antibiotic such as daptomycin in the immunocompromised host, one may achieve superior clinical and microbiologic response rates.3, 7, 9, 10
Since the introduction of the oxazolidinone linezolid in 2000, widespread use has led to reports of linezolid‐resistant VRE as well as nosocomial transmission of linezolid‐resistant VRE in hospitals.4, 1114 Despite linezolid being a key antibiotic for the treatment of VRE infections over the last 10 years, development of resistance along with potential hematologic and neurologic toxicity during long‐term use remains a concern.7, 8 Although daptomycin is active against several resistant organisms, including VRE, the evidence supporting use of daptomycin for VRE BSI is limited to case reports or small case series.7, 9 Moreover, daptomycin has not received US Food and Drug Administration approval for the treatment of VRE infections,15 and emerging data regarding daptomycin‐nonsusceptible enterococci (Minimum Inhibitory Concentration, MIC >4 mg/L) highlight a new problem for this multidrug‐resistant pathogen.16, 17 Few studies in recent years have compared these 2 antibiotics in the treatment of VRE BSIs.4, 18, 19 Due to the high rates of vancomycin resistance reported at our institution and the ubiquitous use of linezolid and daptomycin in the treatment of VRE bacteremia, we chose to evaluate response rates for these antibiotics in an effort to add to previously published literature on this topic.
MATERIALS AND METHODS
Patient Selection
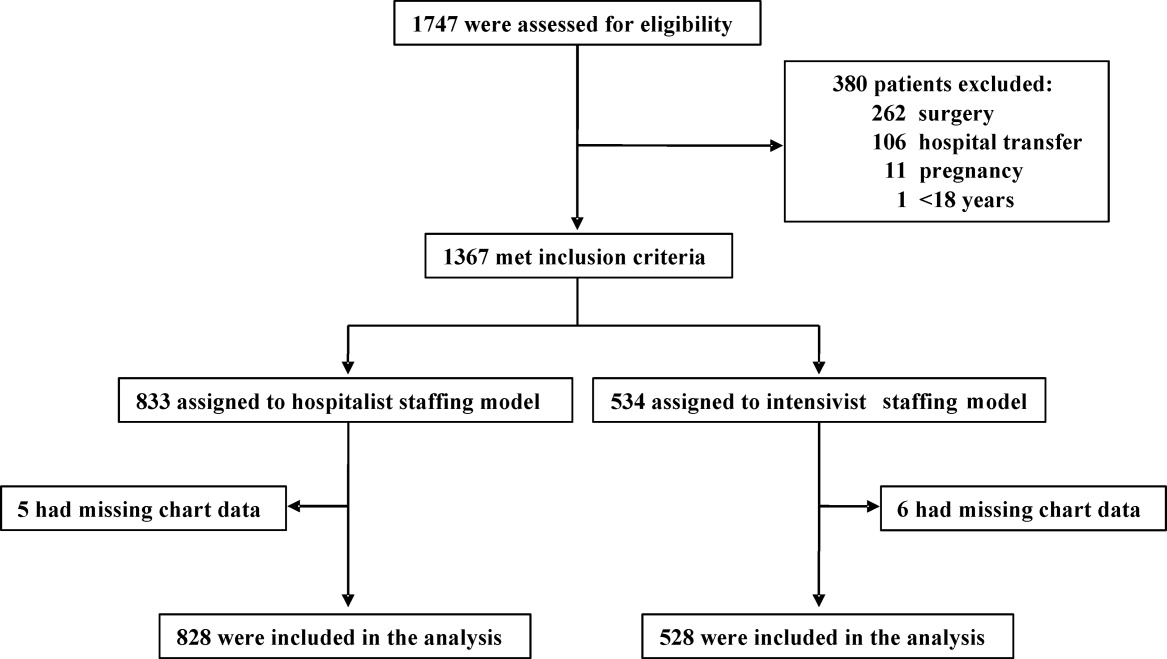
Methodist University Hospital (MUH) in Memphis, Tennessee, is part of a 7‐hospital system with 697 licensed beds. MUH is a tertiary teaching hospital with centers of excellence in neuroscience and transplantation. Patients admitted to MUH diagnosed with VRE bacteremia between January 1, 2004, and July 31, 2009, were identified by the microbiology laboratory. All patients who were 18 years of age, had 1 documented positive VRE blood culture, and received linezolid or daptomycin for 5 days were eligible. Patients were excluded if they were treated simultaneously with more than 1 agent active against VRE. This study was approved by the MUH Institutional Review Board. Of note, use of linezolid or daptomycin at MUH is restricted to an infectious disease physician or pulmonologist. Currently, there are no protocols at our institution for treating VRE infections.
Data Collection and Definitions
Cerner Millennium was used to collect all pertinent patient information. Patient records were reviewed to determine demographic data, comorbid illnesses, laboratory data (from admission to discharge), medications, and discharge status (home, long‐term care facility, or death). Comorbid illnesses evaluated included: chronic obstructive pulmonary disease, diabetes mellitus, malignancy (solid or hematologic), transplant (liver or kidney), end‐stage renal disease (ESRD) (hemodialysis or nonhemodialysis), cirrhosis, and endocarditis. ESRD and endocarditis were defined per chart diagnosis. Laboratory data collected included serum creatinine, creatine phosphokinase, absolute neutrophil count (neutropenia defined as absolute neutrophil count <1000), and number and site (intravenous line or peripheral blood draw) of positive VRE blood cultures. Other data collected were (1) time elapsed to adequate antibiotic coverage, which was defined as microbiologic documentation of an infection that was being effectively treated at the time of its identification, and (2) time to appropriate antibiotic coverage, which was defined as antimicrobial treatment selected for efficacy based on presumptive identification of the causative pathogen, the antimicrobial agent's spectrum of activity, and local microbial resistance patterns.20 Doses of daptomycin and linezolid used in patients with VRE bacteremia were also documented.
Clinical cure was defined as a resolution of signs and/or symptoms of infection (white blood cell count <10,000/mm3, bands <5%, heart rate <90 beats per minute, respiratory rate <20 breaths per minute, and maximum oral temperature <38C) after gram‐positive therapy was discontinued. The definition of microbiologic cure was lack of positive blood cultures for VRE at least 14 days after cessation of gram‐positive therapy. Microbiologic failure was defined as positive VRE blood cultures obtained on gram‐positive therapy necessitating a change in treatment. Recurrence was defined as VRE bacteremia within 30 days after discontinuation of gram‐positive therapy. Reinfection was defined as VRE bacteremia that appeared 30 days after completion of primary gram‐positive therapy.
All isolates were tested for susceptibility to linezolid using the MicroScan system, whereas daptomycin susceptibility patterns were obtained by either the Etest or MicroScan system. Of importance, our laboratory did not routinely report isolate susceptibility for daptomycin until 2008. Clinical Laboratory Standards Institute breakpoint guidelines were used to delineate minimum inhibitory concentrations for linezolid and daptomycin.
Outcomes
The primary objective was to determine the cure rate, both clinical and microbiologic, of VRE bacteremia with the use of linezolid and daptomycin. Secondary outcomes were rates of recurrence and reinfection as well as 30‐day mortality. Clinical and microbiologic response rates for subsets of the patient population that were deemed immunocompromised or at an increased risk for VRE infections (neutropenic, transplant, malignancy, and ESRD on hemodialysis) were also evaluated.
Statistical Analysis
Data were analyzed using SAS version 9.2 (SAS Inc, Cary, NC). Patients with categorical characteristics were compared using a chi‐square test or Fisher's exact test. Continuous data were analyzed using a Student t test and are expressed as the mean standard deviation. The mean duration of initial antibiotics, time to appropriate antibiotics, time to adequate antibiotic therapy, and LOS were all calculated for the linezolid and daptomycin group with a Student t test used to compare the differences. Multivariate logistic regression was used for the following outcomes: clinical cure, microbiologic cure, mortality, reinfection, and recurrence. For the interval variable, LOS, stepwise multiple regression was used to choose significant independent variables. P < 0.05 was considered statistically significant.
RESULTS
Patient Characteristics
Of the 361 patients identified with a positive VRE blood culture, 201 were included in the study. The remaining 160 patients were excluded for one of the following reasons: <5 days of therapy (n = 87), no documented gram‐positive therapy (n = 49), simultaneous gram‐positive therapy (n = 10), or insufficient data to evaluate response rates (n = 14). For the treatment of VRE bacteremia, 138 patients received linezolid and 63 patients received daptomycin. Demographics, comorbid illnesses, and patient characteristics are shown in Table 1. There was a statistically significant difference in the average age, with the linezolid group consisting of older patients. The daptomycin group had more patients with hematologic malignancies than the linezolid group (33% vs 14%; P = 0.0021) and more patients who received liver transplants (13% vs 4%; P = 0.0264).
| Linezolid (n = 138) | Daptomycin (n = 63) | P Value | |
|---|---|---|---|
| |||
| Average age, years, mean SD | 60 16 | 5315 | 0.0028 |
| Male, No. (%) | 59 (43) | 36 (57) | 0.0682 |
| Race, No. (%) | |||
| Caucasian | 34 (25) | 23 (37) | 0.1043 |
| African American | 103 (75) | 39 (62) | |
| Other | 1 (1) | 1 (2) | |
| COPD, No. (%) | 8 (6) | 2 (3) | 0.7277 |
| Diabetes mellitus, No. (%) | 61 (44) | 21 (33) | 0.1655 |
| Hemodialysis, No. (%) | 35 (25) | 17 (27) | 0.8627 |
| Malignancy, No. (%) | |||
| Solid organ | 26 (19) | 16 (25) | 0.3499 |
| Hematologic | 19 (14) | 21 (33) | 0.0021 |
| Transplant, No. (%) | |||
| Liver | 5 (4) | 8 (13) | 0.0264 |
| Kidney | 3 (2) | 0 | 0.5533 |
| Endocarditis,* No. (%) | 4 (3) | 3 (5) | 0.6801 |
| Species of VRE (%) | |||
| Enterococcus faecalis | 33 (24) | 10 (16) | 0.2658 |
| Enterococcus faecium | 105 (76) | 53 (84) | 0.2658 |
| Time to appropriate abx therapy, hours, mean SD | 12.4 26.9 | 818.8 | 0.1851 |
| Time to adequate abx therapy, days, mean SD | 2.3 1.8 | 1.81.5 | 0.0554 |
| Duration of initial abx, days, mean SD | 11.1 6.0 | 14.114.6 | 0.0401 |
| Abx before initial therapy, No. (%) | 85 (62) | 34 (54) | 0.3541 |
| Average dose, mg/kg, mean SD | NA | 6.11.5 | NA |
| Mortality, No. (%) | 25 (18) | 15 (24) | 0.3481 |
| LOS (days) | 37.527.7 | 40.827.9 | 0.4336 |
From the microbiology laboratory report of initial blood cultures, 78.6% of the isolates were noted as being E. faecium, with the remainder being E. faecalis (21.4%). One patient was classified as having linezolid‐resistant E. faecium (MIC >4 mg/L) upon repeat blood culture. Daptomycin MICs were obtained for 44 isolates using the Etest or MicroScan system; all isolates were susceptible with MICs ranging from 0.254 mg/L. As mentioned previously, our laboratory did not routinely report isolate susceptibility to daptomycin until 2008.
There were no statistically significant differences between the treatment groups with regard to time to appropriate or adequate antibiotic therapy (Table 1). However, there was a statistically significant difference in the mean duration of initial antibiotics between linezolid and daptomycin (11.1 days vs 14.1 days; P = 0.0401). Dosing strategies used in these patients were also evaluated. All linezolid patients received a dose of 600 mg every 12 hours by mouth or intravenously. The average dose of daptomycin was 6.1 mg/kg (range, 3.410.4 mg/kg; median, 6 mg/kg). The average LOS was 37 days for linezolid vs 40 days for daptomycin, which did not confer statistical significance. Overall mortality was 20%, occurring in 25 linezolid patients versus 15 daptomycin patients (P = 0.3481). The stepwise multiple regression analysis did not identify any statistically significant variables in patients treated with linezolid or daptomycin that affected any of the outcomes.
Outcomes and Analysis
As shown in Table 2, there were no statistically significant differences in clinical or microbiologic cure between the linezolid and daptomycin groups (74% vs 75% and 94% vs 94%, respectively). However, the linezolid group compared with the daptomycin group had fewer patients that developed a positive blood culture while on their initial antibiotic therapy (8% vs 22%; P = 0.0097). Follow‐up cultures were required to determine rates of recurrence and reinfection. Only 107/138 patients in the linezolid group and 51/63 patients in the daptomycin group had follow‐up cultures collected. Recurrence was documented in 3% of linezolid patients vs 12% of daptomycin patients (P = 0.0321). The odds ratio for developing a recurrent infection with daptomycin versus linezolid was 5.51 (95% confidence interval, 1.2524.28). Out of 6 patients that developed a recurrent VRE infection in the daptomycin group, 2 were prescribed doses <4 mg/kg with no reported MICs, and 2 patients received 6 mg/kg with reported MICs of 4 mg/L. No statistically significant difference existed for the rate of reinfection between linezolid and daptomycin (1% vs 6%; P = 0.0992).
| Linezolid (n = 138) | Daptomycin (n = 63) | P Value | |
|---|---|---|---|
| |||
| Patients with positive culture on G+ therapy | 11 (8) | 14 (22) | 0.0097 |
| Clinical cure | 102 (74) | 47 (75) | 1 |
| Microbiologic cure | 130 (94) | 59 (94) | 1 |
| Recurrence* | 3 (3) | 6 (12) | 0.0321 |
| Reinfection* | 1 (1) | 3 (6) | 0.0992 |
Table 3 provides information on subsets of the patient population deemed high‐risk for VRE infection or immunocompromised. There was no statistically significant difference between the 2 antibiotic groups in clinical or microbiologic cure. In the subsets of immunocompromised patients, there was no difference in recurrence or reinfection between the linezolid and daptomycin patients. Furthermore, all groups had similar LOS regardless of the antibiotic used to treat the VRE BSI. Moreover, there were no statistically significant differences in 30‐day mortality in these subsets of the population with regard to initial antibiotic choice. No significant independent variables were found between linezolid or daptomycin that affected any of the outcomes listed in Table 3.
| Neutropenia (%) | Hematologic Malignancy (%) | ESRD on Hemodialysis (%) | Liver Transplant (%) | |||||
|---|---|---|---|---|---|---|---|---|
| LZD (n = 16) | Dapto (n = 5) | LZD (n = 19) | Dapto (n = 21) | LZD (n = 35) | Dapto (n = 17) | LZD (n = 5) | Dapto (n = 8) | |
| ||||||||
| Clinical cure, No. (%) | 12 (75) | 5 (100) | 18 (95) | 17 (81) | 24 (69) | 12 (71) | 4 (80) | 3 (38) |
| Microbiologic cure,* No. (%) | 13 (81) | 5 (100) | 18 (95) | 20 (95) | 33 (94) | 16 (94) | 5 (100) | 8 (100) |
| Recurrence,* No. (%) | 2 (13) | 1 (20) | 1 (6) | 2 (11) | 0 | 2 (15) | 0 | 1 (14) |
| Reinfection,* No. (%) | 0 | 0 | 0 | 0 | 1 (4) | 2 (15) | 0 | 1 (14) |
| Mortality, No. (%) | 3 (19) | 1 (20) | 4 (21) | 3 (14) | 7 (20) | 4 (24) | 1 (20) | 4 (50) |
| LOS, days, meanSD | 57.422 | 39.412.4 | 47.626.2 | 4127.1 | 38.833.8 | 39.640.4 | 5034.5 | 73.338.8 |
DISCUSSION
Vergis et al21 reported that infections with VRE compared with vancomycin‐sensitive infections were associated with a higher rate of mortality and that the chosen antimicrobial therapy may play a pivotal role in the risk of death. Our retrospective study suggests that linezolid and daptomycin appear to be equally efficacious for the treatment of VRE BSIs. The results from our study for clinical and microbiologic cure rates for linezolid and daptomycin are similar to previously published data.7, 8 In accordance with previous studies,4 our data demonstrate that there is a higher rate of recurrence in patients treated with daptomycin. This finding may be explained by the fact that the daptomycin group was comprised of more complex patients with a greater disease burden versus the linezolid group; therefore, they were more susceptible to a recurrent VRE infection. In our study, patients who were treated with daptomycin were 5.5 times more likely to have a recurrent infection than linezolid‐treated patients. However, this finding must be scrutinized, because over half of the patients with recurrence either received an inappropriate dose or had high MICs to daptomycin.
Despite there being few clinical and microbiologic outcome data with daptomycin, our study proposes that a bactericidal antibiotic and a bacteriostatic antibiotic have comparable efficacy in the treatment of VRE BSIs. Previous literature has mainly comprised case studies or series that have evaluated clinical outcomes with daptomycin in the treatment of VRE BSIs. Gallagher et al7 reported the results of a retrospective case series of 30 patients with VRE bacteremia who were treated with daptomycin. In this study, microbiologic cure was achieved in 80% of patients, with clinical success in 59% of the patients. In 2009, Mave et al4 compared clinical outcomes between daptomycin and linezolid in the treatment of VRE bacteremia. Reported results demonstrated a microbiologic cure rate of 90% for daptomycin versus 88% for linezolid.4 Moreover, there were no differences in mortality between the groups in our study. In 2010, Crank et al18 reported no differences in mortality (in‐hospital) for hospitalized patients with VRE BSIs treated with linezolid or daptomycin. Our results seem to be consistent with what has been published previously concerning clinical outcomes associated with linezolid or daptomycin in the treatment of VRE BSI.
The average daptomycin dose received in our patients was 6.1 mg/kg with doses ranging from 3.410.4 mg/kg. The underdosing as well as higher MICs to daptomycin may have contributed to a higher rate of recurrence. Previous reports state that Enterococcus species may have higher MICs to daptomycin than Staphylococcus or Streptococcus species; consequently, higher doses may be needed to adequately treat enterococcal infections.7 In the aforementioned study by Gallagher et al,7 doses of daptomycin 6 mg/kg were associated with a positive clinical outcome in 81% of patients compared with 31% if the dose used was <6 mg/kg. Linezolid is dosed 600 mg every 12 hours by mouth or intravenously, with no variations. There have been no studies comparing the uniform dosing of linezolid to the weight‐based dosing of daptomycin and their effects on outcomes.
Patients particularly susceptible to VRE infections include those with neutropenia and/or cancer, patients receiving long‐term hemodialysis, and liver transplant recipients.3, 22, 23 Upon review of this immunocompromised population, we noted no statistically significant differences in overall outcomes. A study by Kraft et al.24 supports the findings in our study that both drugs appear useful in the treatment of VRE bacteremia in patients with hematologic malignancy. We did identify a difference, albeit nonsignificant, in LOS for daptomycin versus linezolid in patients with a history of liver transplantation. Again, the level of care that these patients needed compared with the general population may explain this difference. As mentioned previously, another pertinent factor would be the dose of daptomycin used in these patients, because the dose can affect clinical success. Because all of the other patients had a similar LOS, we cannot determine that the increased LOS seen in liver transplant patients treated with daptomycin was solely due to daptomycin use. The reason for the increased LOS seems to be multifactorial. In the neutropenic population, a difference in LOS was also recognized, but follow‐up complete blood count values were not collected for these patients to determine whether linezolid contributed to further bone marrow suppression leading to an increase in LOS. For both of these patient populations, the number of patients included is very small (n = 21 for neutropenia total, n = 13 for liver transplant total), which can lead to a high degree of variance.
This study has several limitations. This was a retrospective review; therefore, we had no control over the selection of therapy. This may be reflected in an apparent preferential use of daptomycin in immunocompromised patients. Furthermore, 62% of linezolid patients and 54% of daptomycin patients received an antibiotic before initial therapy that could have potentially altered response rates. Due to the paucity of documentation surrounding initial site of infection, some of the positive cultures may represent potential contamination, because VRE may contaminate skin.25 Contamination seems implausible, however, because patients were seen by an infectious disease physician and had at least 1 documented positive VRE blood culture. We chose arbitrary definitions for clinical cure, microbiologic cure, microbiologic failure, recurrence, and reinfection. Previous studies have used their own definitions leading to discrepancies in reporting. Another limitation was that follow‐up cultures were not obtained on all of the patients, which was needed to determine rates of recurrence, reinfection, and microbiologic cure. MICs to daptomycin were not reported in 30% of our patients, potentially altering the recurrence rate seen in the daptomycin‐treated patients. Because clinical cure was not documented in the chart, it was inferred from the laboratory values and vital sign information. One investigator analyzed all of the values and made the determination of clinical cure, allowing for a consistent approach to data review.
In the face of the imposing threat of a highly resistant organism such as VRE with a limited number of efficacious antibiotics, antimicrobial selection becomes increasingly important and is requisite to clinical and microbiological success. To our knowledge, this is one of the largest studies to date comparing the efficacy of linezolid with that of daptomycin in the treatment of VRE bacteremia. Both of these agents are effective for the treatment of VRE BSIs. Nevertheless, specific factors related to the medication (eg, dose, route of administration) as well as the patient (eg, comorbid conditions, acuity of illness) should be taken into consideration when selecting an initial antimicrobial agent. Because the treatment of VRE BSIs continues to be a challenge, larger prospective randomized controlled trials are needed to corroborate our results and determine the optimal therapy for this serious infection.
Acknowledgements
Disclosures: Michael S. Gelfand is on the speaker's bureau for Cubist and Pfizer.
- ,,,,,.Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study.Clin Infect Dis.2004;39:309–317.
- ,,, et al.Clinical practice guidelines for the management of intravascular catheter‐related infection: 2009 update by the Infectious Diseases Society of America.Clin Infect Dis.2009;49:1–45.
- ,,,,,.Bad bugs need drugs: an update on the development pipeline from the antimicrobial availability task force of the infectious diseases society of America.Clin Infect Dis.2006;42:657–668.
- ,,,.Vancomycin‐resistant enterococcal bacteraemia: is daptomycin as effective as linezolid?J Antimicrob Chemother.2009;64:175–180.
- ,,.Management of multidrug‐resistant enterococcal Infections.Clin Microbiol Infect.2010;16:555–562.
- ,,, et al.Treatment of vancomycin‐resistant Enterococcus faecium infections with quinupristin/dalfopristin.Clin Infect Dis.2001;33:1816–1823.
- ,,, et al.Daptomycin for vancomycin‐resistant enterococcol bacteremia: a retrospective case series of 30 patients.Pharmacotherapy.2009;29:792–799.
- ,,, et al.Safety, efficacy and pharmacokinetics of linezolid for treatment of resistant gram positive infections in cancer patients with neutropenia.Ann Oncol.2003;14:795–801.
- ,,,,.Daptomycin for the treatment of vancomycin resistant Enterococcus faecium bacteremia.Scand J Infect Dis.2003;38:290–292.
- ,.New antimicrobial agents for the treatment of gram positive bacterial infections.Clin Microbiol Infec.2008;14:411–420.
- ,.Emergence and management of drug‐resistant enterococcal infections.Expert Rev Anti Infect Ther.2008;6:637–655.
- ,,.Nosocomial spread of linezolid‐resistant, Vancomycin resistant Enterococcus faecium.N Engl J Med.2002;346:867–869.
- ,, et al.Nosocomial superinfections due to linezolid‐resitant Enterococcus faecalis: evidence for a gene dosage effect of linezolid MICs.Diagn Microbiol Infect Dis.2003;47:511–513.
- .Quinupristin‐dalfopristin and linezolid: evidence and opinion.Clin Infect Dis.2003;36:473–481.
- Cubicin (Daptomycin for injection) [package insert].Lexington, MA:Cubist Pharmaceuticals;2010.
- ,,,.Daptomycin nonsusceptible Enterococci: an emerging challenge for clinicians.Clin Infect Dis.2011;52:228–234.
- ,,,.A potential role for daptomycin in enterococcal infections: what is the evidence?J Antimicrob Chemother.2010;65:1126–1136.
- ,,, et al.Comparison of outcomes from daptomycin or linezolid for vancomycin‐resistant enterococcal bloodstream infection: a retrospective, multicenter, cohort study.Clin Ther.2010;32:1713–1719.
- ,,,,,.Observational study of the epidemiology and outcomes of vancomycin‐resistant Enterococcus bacteraemia treated with newer antimicrobial agents.Epidemiol Infect.2010;15:1–9.
- .Inadequate antimicrobial treatment: an important determinant of outcome for hospitalized patients.Clin Infect Dis.2000;31:S131–S138.
- ,,, et al.Determinants of vancomycin resistance and mortality rates in enterococcal bacteremia: a prospective multicenter study.Ann Intern Med.2001;135:484–492.
- ,,,,,.Vancomycin resistant enterococci among chronic hemodialysis patients: a prospective study of acquisition.Clin Infect Dis.2001;32:23–29.
- ,,, et al.A nationwide, multicenter, case control study comparing risk factors, treatment, and outcome for vancomycin resistant andsusceptible enterococcal bacteremia.Diagn Microbiol Infect Dis.2000;36:145–158.
- ,,,,.Outcomes of therapy: vancomycin‐resistant enterococcal bacteremia in hematology and bone marrow transplant patients [published online ahead of print November 26, 2010].Support Care Cancer. doi: 10.1007/s00520–010‐1038‐z.
- ,,, et al.Skin colonization with vancomycin‐resistant enterococci among hospitalized patients with bacteremia.Clin Infect Dis.1997;24:704–706.
Enterococci have been identified as a causative organism in approximately 10% of all nosocomial bloodstream infections (BSIs).1, 2 In 2006, the Infectious Diseases Society of America identified vancomycin‐ resistant Enterococcus faecium (VRE) as 1 of 6 microbes considered to be among the most dangerous due to high rates of resistance and a limited number of effective antimicrobials.3 E. faecium has exhibited high rates of glycopeptide resistance with as many as 60% of isolates from BSIs being resistant to vancomycin.2, 4 Due to increasing resistance to glycopeptides, vancomycin has become obsolete in the treatment of E. faecium infections.5
A limited number of antimicrobials are available for the treatment of infections due to VRE. Agents active in vitro are quinupristin‐dalfopristin, tigecycline, linezolid, and daptomycin. Quinupristin‐dalfopristin was one of the first agents approved for use in VRE infections; however, treatment with this agent has been limited because of mediocre clinical response rates, undesirable adverse effects, high cost, and insufficient E. faecalis activity.6, 7 Tigecycline is not an optimal antibiotic for the treatment of VRE bacteremia, because serum concentrations achieved after administration are inadequate to treat BSIs.7 In contrast, linezolid and daptomycin have evinced efficacy against VRE bacteremia, with reported microbiologic response rates of 85% and 80%, respectively.7, 8 One inherent difference between these antibiotics that may theoretically affect their use in immunocompromised patients is that linezolid is bacteriostatic, whereas daptomycin is bactericidal. It has been postulated that by using a bactericidal antibiotic such as daptomycin in the immunocompromised host, one may achieve superior clinical and microbiologic response rates.3, 7, 9, 10
Since the introduction of the oxazolidinone linezolid in 2000, widespread use has led to reports of linezolid‐resistant VRE as well as nosocomial transmission of linezolid‐resistant VRE in hospitals.4, 1114 Despite linezolid being a key antibiotic for the treatment of VRE infections over the last 10 years, development of resistance along with potential hematologic and neurologic toxicity during long‐term use remains a concern.7, 8 Although daptomycin is active against several resistant organisms, including VRE, the evidence supporting use of daptomycin for VRE BSI is limited to case reports or small case series.7, 9 Moreover, daptomycin has not received US Food and Drug Administration approval for the treatment of VRE infections,15 and emerging data regarding daptomycin‐nonsusceptible enterococci (Minimum Inhibitory Concentration, MIC >4 mg/L) highlight a new problem for this multidrug‐resistant pathogen.16, 17 Few studies in recent years have compared these 2 antibiotics in the treatment of VRE BSIs.4, 18, 19 Due to the high rates of vancomycin resistance reported at our institution and the ubiquitous use of linezolid and daptomycin in the treatment of VRE bacteremia, we chose to evaluate response rates for these antibiotics in an effort to add to previously published literature on this topic.
MATERIALS AND METHODS
Patient Selection
Methodist University Hospital (MUH) in Memphis, Tennessee, is part of a 7‐hospital system with 697 licensed beds. MUH is a tertiary teaching hospital with centers of excellence in neuroscience and transplantation. Patients admitted to MUH diagnosed with VRE bacteremia between January 1, 2004, and July 31, 2009, were identified by the microbiology laboratory. All patients who were 18 years of age, had 1 documented positive VRE blood culture, and received linezolid or daptomycin for 5 days were eligible. Patients were excluded if they were treated simultaneously with more than 1 agent active against VRE. This study was approved by the MUH Institutional Review Board. Of note, use of linezolid or daptomycin at MUH is restricted to an infectious disease physician or pulmonologist. Currently, there are no protocols at our institution for treating VRE infections.
Data Collection and Definitions
Cerner Millennium was used to collect all pertinent patient information. Patient records were reviewed to determine demographic data, comorbid illnesses, laboratory data (from admission to discharge), medications, and discharge status (home, long‐term care facility, or death). Comorbid illnesses evaluated included: chronic obstructive pulmonary disease, diabetes mellitus, malignancy (solid or hematologic), transplant (liver or kidney), end‐stage renal disease (ESRD) (hemodialysis or nonhemodialysis), cirrhosis, and endocarditis. ESRD and endocarditis were defined per chart diagnosis. Laboratory data collected included serum creatinine, creatine phosphokinase, absolute neutrophil count (neutropenia defined as absolute neutrophil count <1000), and number and site (intravenous line or peripheral blood draw) of positive VRE blood cultures. Other data collected were (1) time elapsed to adequate antibiotic coverage, which was defined as microbiologic documentation of an infection that was being effectively treated at the time of its identification, and (2) time to appropriate antibiotic coverage, which was defined as antimicrobial treatment selected for efficacy based on presumptive identification of the causative pathogen, the antimicrobial agent's spectrum of activity, and local microbial resistance patterns.20 Doses of daptomycin and linezolid used in patients with VRE bacteremia were also documented.
Clinical cure was defined as a resolution of signs and/or symptoms of infection (white blood cell count <10,000/mm3, bands <5%, heart rate <90 beats per minute, respiratory rate <20 breaths per minute, and maximum oral temperature <38C) after gram‐positive therapy was discontinued. The definition of microbiologic cure was lack of positive blood cultures for VRE at least 14 days after cessation of gram‐positive therapy. Microbiologic failure was defined as positive VRE blood cultures obtained on gram‐positive therapy necessitating a change in treatment. Recurrence was defined as VRE bacteremia within 30 days after discontinuation of gram‐positive therapy. Reinfection was defined as VRE bacteremia that appeared 30 days after completion of primary gram‐positive therapy.
All isolates were tested for susceptibility to linezolid using the MicroScan system, whereas daptomycin susceptibility patterns were obtained by either the Etest or MicroScan system. Of importance, our laboratory did not routinely report isolate susceptibility for daptomycin until 2008. Clinical Laboratory Standards Institute breakpoint guidelines were used to delineate minimum inhibitory concentrations for linezolid and daptomycin.
Outcomes
The primary objective was to determine the cure rate, both clinical and microbiologic, of VRE bacteremia with the use of linezolid and daptomycin. Secondary outcomes were rates of recurrence and reinfection as well as 30‐day mortality. Clinical and microbiologic response rates for subsets of the patient population that were deemed immunocompromised or at an increased risk for VRE infections (neutropenic, transplant, malignancy, and ESRD on hemodialysis) were also evaluated.
Statistical Analysis
Data were analyzed using SAS version 9.2 (SAS Inc, Cary, NC). Patients with categorical characteristics were compared using a chi‐square test or Fisher's exact test. Continuous data were analyzed using a Student t test and are expressed as the mean standard deviation. The mean duration of initial antibiotics, time to appropriate antibiotics, time to adequate antibiotic therapy, and LOS were all calculated for the linezolid and daptomycin group with a Student t test used to compare the differences. Multivariate logistic regression was used for the following outcomes: clinical cure, microbiologic cure, mortality, reinfection, and recurrence. For the interval variable, LOS, stepwise multiple regression was used to choose significant independent variables. P < 0.05 was considered statistically significant.
RESULTS
Patient Characteristics
Of the 361 patients identified with a positive VRE blood culture, 201 were included in the study. The remaining 160 patients were excluded for one of the following reasons: <5 days of therapy (n = 87), no documented gram‐positive therapy (n = 49), simultaneous gram‐positive therapy (n = 10), or insufficient data to evaluate response rates (n = 14). For the treatment of VRE bacteremia, 138 patients received linezolid and 63 patients received daptomycin. Demographics, comorbid illnesses, and patient characteristics are shown in Table 1. There was a statistically significant difference in the average age, with the linezolid group consisting of older patients. The daptomycin group had more patients with hematologic malignancies than the linezolid group (33% vs 14%; P = 0.0021) and more patients who received liver transplants (13% vs 4%; P = 0.0264).
| Linezolid (n = 138) | Daptomycin (n = 63) | P Value | |
|---|---|---|---|
| |||
| Average age, years, mean SD | 60 16 | 5315 | 0.0028 |
| Male, No. (%) | 59 (43) | 36 (57) | 0.0682 |
| Race, No. (%) | |||
| Caucasian | 34 (25) | 23 (37) | 0.1043 |
| African American | 103 (75) | 39 (62) | |
| Other | 1 (1) | 1 (2) | |
| COPD, No. (%) | 8 (6) | 2 (3) | 0.7277 |
| Diabetes mellitus, No. (%) | 61 (44) | 21 (33) | 0.1655 |
| Hemodialysis, No. (%) | 35 (25) | 17 (27) | 0.8627 |
| Malignancy, No. (%) | |||
| Solid organ | 26 (19) | 16 (25) | 0.3499 |
| Hematologic | 19 (14) | 21 (33) | 0.0021 |
| Transplant, No. (%) | |||
| Liver | 5 (4) | 8 (13) | 0.0264 |
| Kidney | 3 (2) | 0 | 0.5533 |
| Endocarditis,* No. (%) | 4 (3) | 3 (5) | 0.6801 |
| Species of VRE (%) | |||
| Enterococcus faecalis | 33 (24) | 10 (16) | 0.2658 |
| Enterococcus faecium | 105 (76) | 53 (84) | 0.2658 |
| Time to appropriate abx therapy, hours, mean SD | 12.4 26.9 | 818.8 | 0.1851 |
| Time to adequate abx therapy, days, mean SD | 2.3 1.8 | 1.81.5 | 0.0554 |
| Duration of initial abx, days, mean SD | 11.1 6.0 | 14.114.6 | 0.0401 |
| Abx before initial therapy, No. (%) | 85 (62) | 34 (54) | 0.3541 |
| Average dose, mg/kg, mean SD | NA | 6.11.5 | NA |
| Mortality, No. (%) | 25 (18) | 15 (24) | 0.3481 |
| LOS (days) | 37.527.7 | 40.827.9 | 0.4336 |
From the microbiology laboratory report of initial blood cultures, 78.6% of the isolates were noted as being E. faecium, with the remainder being E. faecalis (21.4%). One patient was classified as having linezolid‐resistant E. faecium (MIC >4 mg/L) upon repeat blood culture. Daptomycin MICs were obtained for 44 isolates using the Etest or MicroScan system; all isolates were susceptible with MICs ranging from 0.254 mg/L. As mentioned previously, our laboratory did not routinely report isolate susceptibility to daptomycin until 2008.
There were no statistically significant differences between the treatment groups with regard to time to appropriate or adequate antibiotic therapy (Table 1). However, there was a statistically significant difference in the mean duration of initial antibiotics between linezolid and daptomycin (11.1 days vs 14.1 days; P = 0.0401). Dosing strategies used in these patients were also evaluated. All linezolid patients received a dose of 600 mg every 12 hours by mouth or intravenously. The average dose of daptomycin was 6.1 mg/kg (range, 3.410.4 mg/kg; median, 6 mg/kg). The average LOS was 37 days for linezolid vs 40 days for daptomycin, which did not confer statistical significance. Overall mortality was 20%, occurring in 25 linezolid patients versus 15 daptomycin patients (P = 0.3481). The stepwise multiple regression analysis did not identify any statistically significant variables in patients treated with linezolid or daptomycin that affected any of the outcomes.
Outcomes and Analysis
As shown in Table 2, there were no statistically significant differences in clinical or microbiologic cure between the linezolid and daptomycin groups (74% vs 75% and 94% vs 94%, respectively). However, the linezolid group compared with the daptomycin group had fewer patients that developed a positive blood culture while on their initial antibiotic therapy (8% vs 22%; P = 0.0097). Follow‐up cultures were required to determine rates of recurrence and reinfection. Only 107/138 patients in the linezolid group and 51/63 patients in the daptomycin group had follow‐up cultures collected. Recurrence was documented in 3% of linezolid patients vs 12% of daptomycin patients (P = 0.0321). The odds ratio for developing a recurrent infection with daptomycin versus linezolid was 5.51 (95% confidence interval, 1.2524.28). Out of 6 patients that developed a recurrent VRE infection in the daptomycin group, 2 were prescribed doses <4 mg/kg with no reported MICs, and 2 patients received 6 mg/kg with reported MICs of 4 mg/L. No statistically significant difference existed for the rate of reinfection between linezolid and daptomycin (1% vs 6%; P = 0.0992).
| Linezolid (n = 138) | Daptomycin (n = 63) | P Value | |
|---|---|---|---|
| |||
| Patients with positive culture on G+ therapy | 11 (8) | 14 (22) | 0.0097 |
| Clinical cure | 102 (74) | 47 (75) | 1 |
| Microbiologic cure | 130 (94) | 59 (94) | 1 |
| Recurrence* | 3 (3) | 6 (12) | 0.0321 |
| Reinfection* | 1 (1) | 3 (6) | 0.0992 |
Table 3 provides information on subsets of the patient population deemed high‐risk for VRE infection or immunocompromised. There was no statistically significant difference between the 2 antibiotic groups in clinical or microbiologic cure. In the subsets of immunocompromised patients, there was no difference in recurrence or reinfection between the linezolid and daptomycin patients. Furthermore, all groups had similar LOS regardless of the antibiotic used to treat the VRE BSI. Moreover, there were no statistically significant differences in 30‐day mortality in these subsets of the population with regard to initial antibiotic choice. No significant independent variables were found between linezolid or daptomycin that affected any of the outcomes listed in Table 3.
| Neutropenia (%) | Hematologic Malignancy (%) | ESRD on Hemodialysis (%) | Liver Transplant (%) | |||||
|---|---|---|---|---|---|---|---|---|
| LZD (n = 16) | Dapto (n = 5) | LZD (n = 19) | Dapto (n = 21) | LZD (n = 35) | Dapto (n = 17) | LZD (n = 5) | Dapto (n = 8) | |
| ||||||||
| Clinical cure, No. (%) | 12 (75) | 5 (100) | 18 (95) | 17 (81) | 24 (69) | 12 (71) | 4 (80) | 3 (38) |
| Microbiologic cure,* No. (%) | 13 (81) | 5 (100) | 18 (95) | 20 (95) | 33 (94) | 16 (94) | 5 (100) | 8 (100) |
| Recurrence,* No. (%) | 2 (13) | 1 (20) | 1 (6) | 2 (11) | 0 | 2 (15) | 0 | 1 (14) |
| Reinfection,* No. (%) | 0 | 0 | 0 | 0 | 1 (4) | 2 (15) | 0 | 1 (14) |
| Mortality, No. (%) | 3 (19) | 1 (20) | 4 (21) | 3 (14) | 7 (20) | 4 (24) | 1 (20) | 4 (50) |
| LOS, days, meanSD | 57.422 | 39.412.4 | 47.626.2 | 4127.1 | 38.833.8 | 39.640.4 | 5034.5 | 73.338.8 |
DISCUSSION
Vergis et al21 reported that infections with VRE compared with vancomycin‐sensitive infections were associated with a higher rate of mortality and that the chosen antimicrobial therapy may play a pivotal role in the risk of death. Our retrospective study suggests that linezolid and daptomycin appear to be equally efficacious for the treatment of VRE BSIs. The results from our study for clinical and microbiologic cure rates for linezolid and daptomycin are similar to previously published data.7, 8 In accordance with previous studies,4 our data demonstrate that there is a higher rate of recurrence in patients treated with daptomycin. This finding may be explained by the fact that the daptomycin group was comprised of more complex patients with a greater disease burden versus the linezolid group; therefore, they were more susceptible to a recurrent VRE infection. In our study, patients who were treated with daptomycin were 5.5 times more likely to have a recurrent infection than linezolid‐treated patients. However, this finding must be scrutinized, because over half of the patients with recurrence either received an inappropriate dose or had high MICs to daptomycin.
Despite there being few clinical and microbiologic outcome data with daptomycin, our study proposes that a bactericidal antibiotic and a bacteriostatic antibiotic have comparable efficacy in the treatment of VRE BSIs. Previous literature has mainly comprised case studies or series that have evaluated clinical outcomes with daptomycin in the treatment of VRE BSIs. Gallagher et al7 reported the results of a retrospective case series of 30 patients with VRE bacteremia who were treated with daptomycin. In this study, microbiologic cure was achieved in 80% of patients, with clinical success in 59% of the patients. In 2009, Mave et al4 compared clinical outcomes between daptomycin and linezolid in the treatment of VRE bacteremia. Reported results demonstrated a microbiologic cure rate of 90% for daptomycin versus 88% for linezolid.4 Moreover, there were no differences in mortality between the groups in our study. In 2010, Crank et al18 reported no differences in mortality (in‐hospital) for hospitalized patients with VRE BSIs treated with linezolid or daptomycin. Our results seem to be consistent with what has been published previously concerning clinical outcomes associated with linezolid or daptomycin in the treatment of VRE BSI.
The average daptomycin dose received in our patients was 6.1 mg/kg with doses ranging from 3.410.4 mg/kg. The underdosing as well as higher MICs to daptomycin may have contributed to a higher rate of recurrence. Previous reports state that Enterococcus species may have higher MICs to daptomycin than Staphylococcus or Streptococcus species; consequently, higher doses may be needed to adequately treat enterococcal infections.7 In the aforementioned study by Gallagher et al,7 doses of daptomycin 6 mg/kg were associated with a positive clinical outcome in 81% of patients compared with 31% if the dose used was <6 mg/kg. Linezolid is dosed 600 mg every 12 hours by mouth or intravenously, with no variations. There have been no studies comparing the uniform dosing of linezolid to the weight‐based dosing of daptomycin and their effects on outcomes.
Patients particularly susceptible to VRE infections include those with neutropenia and/or cancer, patients receiving long‐term hemodialysis, and liver transplant recipients.3, 22, 23 Upon review of this immunocompromised population, we noted no statistically significant differences in overall outcomes. A study by Kraft et al.24 supports the findings in our study that both drugs appear useful in the treatment of VRE bacteremia in patients with hematologic malignancy. We did identify a difference, albeit nonsignificant, in LOS for daptomycin versus linezolid in patients with a history of liver transplantation. Again, the level of care that these patients needed compared with the general population may explain this difference. As mentioned previously, another pertinent factor would be the dose of daptomycin used in these patients, because the dose can affect clinical success. Because all of the other patients had a similar LOS, we cannot determine that the increased LOS seen in liver transplant patients treated with daptomycin was solely due to daptomycin use. The reason for the increased LOS seems to be multifactorial. In the neutropenic population, a difference in LOS was also recognized, but follow‐up complete blood count values were not collected for these patients to determine whether linezolid contributed to further bone marrow suppression leading to an increase in LOS. For both of these patient populations, the number of patients included is very small (n = 21 for neutropenia total, n = 13 for liver transplant total), which can lead to a high degree of variance.
This study has several limitations. This was a retrospective review; therefore, we had no control over the selection of therapy. This may be reflected in an apparent preferential use of daptomycin in immunocompromised patients. Furthermore, 62% of linezolid patients and 54% of daptomycin patients received an antibiotic before initial therapy that could have potentially altered response rates. Due to the paucity of documentation surrounding initial site of infection, some of the positive cultures may represent potential contamination, because VRE may contaminate skin.25 Contamination seems implausible, however, because patients were seen by an infectious disease physician and had at least 1 documented positive VRE blood culture. We chose arbitrary definitions for clinical cure, microbiologic cure, microbiologic failure, recurrence, and reinfection. Previous studies have used their own definitions leading to discrepancies in reporting. Another limitation was that follow‐up cultures were not obtained on all of the patients, which was needed to determine rates of recurrence, reinfection, and microbiologic cure. MICs to daptomycin were not reported in 30% of our patients, potentially altering the recurrence rate seen in the daptomycin‐treated patients. Because clinical cure was not documented in the chart, it was inferred from the laboratory values and vital sign information. One investigator analyzed all of the values and made the determination of clinical cure, allowing for a consistent approach to data review.
In the face of the imposing threat of a highly resistant organism such as VRE with a limited number of efficacious antibiotics, antimicrobial selection becomes increasingly important and is requisite to clinical and microbiological success. To our knowledge, this is one of the largest studies to date comparing the efficacy of linezolid with that of daptomycin in the treatment of VRE bacteremia. Both of these agents are effective for the treatment of VRE BSIs. Nevertheless, specific factors related to the medication (eg, dose, route of administration) as well as the patient (eg, comorbid conditions, acuity of illness) should be taken into consideration when selecting an initial antimicrobial agent. Because the treatment of VRE BSIs continues to be a challenge, larger prospective randomized controlled trials are needed to corroborate our results and determine the optimal therapy for this serious infection.
Acknowledgements
Disclosures: Michael S. Gelfand is on the speaker's bureau for Cubist and Pfizer.
Enterococci have been identified as a causative organism in approximately 10% of all nosocomial bloodstream infections (BSIs).1, 2 In 2006, the Infectious Diseases Society of America identified vancomycin‐ resistant Enterococcus faecium (VRE) as 1 of 6 microbes considered to be among the most dangerous due to high rates of resistance and a limited number of effective antimicrobials.3 E. faecium has exhibited high rates of glycopeptide resistance with as many as 60% of isolates from BSIs being resistant to vancomycin.2, 4 Due to increasing resistance to glycopeptides, vancomycin has become obsolete in the treatment of E. faecium infections.5
A limited number of antimicrobials are available for the treatment of infections due to VRE. Agents active in vitro are quinupristin‐dalfopristin, tigecycline, linezolid, and daptomycin. Quinupristin‐dalfopristin was one of the first agents approved for use in VRE infections; however, treatment with this agent has been limited because of mediocre clinical response rates, undesirable adverse effects, high cost, and insufficient E. faecalis activity.6, 7 Tigecycline is not an optimal antibiotic for the treatment of VRE bacteremia, because serum concentrations achieved after administration are inadequate to treat BSIs.7 In contrast, linezolid and daptomycin have evinced efficacy against VRE bacteremia, with reported microbiologic response rates of 85% and 80%, respectively.7, 8 One inherent difference between these antibiotics that may theoretically affect their use in immunocompromised patients is that linezolid is bacteriostatic, whereas daptomycin is bactericidal. It has been postulated that by using a bactericidal antibiotic such as daptomycin in the immunocompromised host, one may achieve superior clinical and microbiologic response rates.3, 7, 9, 10
Since the introduction of the oxazolidinone linezolid in 2000, widespread use has led to reports of linezolid‐resistant VRE as well as nosocomial transmission of linezolid‐resistant VRE in hospitals.4, 1114 Despite linezolid being a key antibiotic for the treatment of VRE infections over the last 10 years, development of resistance along with potential hematologic and neurologic toxicity during long‐term use remains a concern.7, 8 Although daptomycin is active against several resistant organisms, including VRE, the evidence supporting use of daptomycin for VRE BSI is limited to case reports or small case series.7, 9 Moreover, daptomycin has not received US Food and Drug Administration approval for the treatment of VRE infections,15 and emerging data regarding daptomycin‐nonsusceptible enterococci (Minimum Inhibitory Concentration, MIC >4 mg/L) highlight a new problem for this multidrug‐resistant pathogen.16, 17 Few studies in recent years have compared these 2 antibiotics in the treatment of VRE BSIs.4, 18, 19 Due to the high rates of vancomycin resistance reported at our institution and the ubiquitous use of linezolid and daptomycin in the treatment of VRE bacteremia, we chose to evaluate response rates for these antibiotics in an effort to add to previously published literature on this topic.
MATERIALS AND METHODS
Patient Selection
Methodist University Hospital (MUH) in Memphis, Tennessee, is part of a 7‐hospital system with 697 licensed beds. MUH is a tertiary teaching hospital with centers of excellence in neuroscience and transplantation. Patients admitted to MUH diagnosed with VRE bacteremia between January 1, 2004, and July 31, 2009, were identified by the microbiology laboratory. All patients who were 18 years of age, had 1 documented positive VRE blood culture, and received linezolid or daptomycin for 5 days were eligible. Patients were excluded if they were treated simultaneously with more than 1 agent active against VRE. This study was approved by the MUH Institutional Review Board. Of note, use of linezolid or daptomycin at MUH is restricted to an infectious disease physician or pulmonologist. Currently, there are no protocols at our institution for treating VRE infections.
Data Collection and Definitions
Cerner Millennium was used to collect all pertinent patient information. Patient records were reviewed to determine demographic data, comorbid illnesses, laboratory data (from admission to discharge), medications, and discharge status (home, long‐term care facility, or death). Comorbid illnesses evaluated included: chronic obstructive pulmonary disease, diabetes mellitus, malignancy (solid or hematologic), transplant (liver or kidney), end‐stage renal disease (ESRD) (hemodialysis or nonhemodialysis), cirrhosis, and endocarditis. ESRD and endocarditis were defined per chart diagnosis. Laboratory data collected included serum creatinine, creatine phosphokinase, absolute neutrophil count (neutropenia defined as absolute neutrophil count <1000), and number and site (intravenous line or peripheral blood draw) of positive VRE blood cultures. Other data collected were (1) time elapsed to adequate antibiotic coverage, which was defined as microbiologic documentation of an infection that was being effectively treated at the time of its identification, and (2) time to appropriate antibiotic coverage, which was defined as antimicrobial treatment selected for efficacy based on presumptive identification of the causative pathogen, the antimicrobial agent's spectrum of activity, and local microbial resistance patterns.20 Doses of daptomycin and linezolid used in patients with VRE bacteremia were also documented.
Clinical cure was defined as a resolution of signs and/or symptoms of infection (white blood cell count <10,000/mm3, bands <5%, heart rate <90 beats per minute, respiratory rate <20 breaths per minute, and maximum oral temperature <38C) after gram‐positive therapy was discontinued. The definition of microbiologic cure was lack of positive blood cultures for VRE at least 14 days after cessation of gram‐positive therapy. Microbiologic failure was defined as positive VRE blood cultures obtained on gram‐positive therapy necessitating a change in treatment. Recurrence was defined as VRE bacteremia within 30 days after discontinuation of gram‐positive therapy. Reinfection was defined as VRE bacteremia that appeared 30 days after completion of primary gram‐positive therapy.
All isolates were tested for susceptibility to linezolid using the MicroScan system, whereas daptomycin susceptibility patterns were obtained by either the Etest or MicroScan system. Of importance, our laboratory did not routinely report isolate susceptibility for daptomycin until 2008. Clinical Laboratory Standards Institute breakpoint guidelines were used to delineate minimum inhibitory concentrations for linezolid and daptomycin.
Outcomes
The primary objective was to determine the cure rate, both clinical and microbiologic, of VRE bacteremia with the use of linezolid and daptomycin. Secondary outcomes were rates of recurrence and reinfection as well as 30‐day mortality. Clinical and microbiologic response rates for subsets of the patient population that were deemed immunocompromised or at an increased risk for VRE infections (neutropenic, transplant, malignancy, and ESRD on hemodialysis) were also evaluated.
Statistical Analysis
Data were analyzed using SAS version 9.2 (SAS Inc, Cary, NC). Patients with categorical characteristics were compared using a chi‐square test or Fisher's exact test. Continuous data were analyzed using a Student t test and are expressed as the mean standard deviation. The mean duration of initial antibiotics, time to appropriate antibiotics, time to adequate antibiotic therapy, and LOS were all calculated for the linezolid and daptomycin group with a Student t test used to compare the differences. Multivariate logistic regression was used for the following outcomes: clinical cure, microbiologic cure, mortality, reinfection, and recurrence. For the interval variable, LOS, stepwise multiple regression was used to choose significant independent variables. P < 0.05 was considered statistically significant.
RESULTS
Patient Characteristics
Of the 361 patients identified with a positive VRE blood culture, 201 were included in the study. The remaining 160 patients were excluded for one of the following reasons: <5 days of therapy (n = 87), no documented gram‐positive therapy (n = 49), simultaneous gram‐positive therapy (n = 10), or insufficient data to evaluate response rates (n = 14). For the treatment of VRE bacteremia, 138 patients received linezolid and 63 patients received daptomycin. Demographics, comorbid illnesses, and patient characteristics are shown in Table 1. There was a statistically significant difference in the average age, with the linezolid group consisting of older patients. The daptomycin group had more patients with hematologic malignancies than the linezolid group (33% vs 14%; P = 0.0021) and more patients who received liver transplants (13% vs 4%; P = 0.0264).
| Linezolid (n = 138) | Daptomycin (n = 63) | P Value | |
|---|---|---|---|
| |||
| Average age, years, mean SD | 60 16 | 5315 | 0.0028 |
| Male, No. (%) | 59 (43) | 36 (57) | 0.0682 |
| Race, No. (%) | |||
| Caucasian | 34 (25) | 23 (37) | 0.1043 |
| African American | 103 (75) | 39 (62) | |
| Other | 1 (1) | 1 (2) | |
| COPD, No. (%) | 8 (6) | 2 (3) | 0.7277 |
| Diabetes mellitus, No. (%) | 61 (44) | 21 (33) | 0.1655 |
| Hemodialysis, No. (%) | 35 (25) | 17 (27) | 0.8627 |
| Malignancy, No. (%) | |||
| Solid organ | 26 (19) | 16 (25) | 0.3499 |
| Hematologic | 19 (14) | 21 (33) | 0.0021 |
| Transplant, No. (%) | |||
| Liver | 5 (4) | 8 (13) | 0.0264 |
| Kidney | 3 (2) | 0 | 0.5533 |
| Endocarditis,* No. (%) | 4 (3) | 3 (5) | 0.6801 |
| Species of VRE (%) | |||
| Enterococcus faecalis | 33 (24) | 10 (16) | 0.2658 |
| Enterococcus faecium | 105 (76) | 53 (84) | 0.2658 |
| Time to appropriate abx therapy, hours, mean SD | 12.4 26.9 | 818.8 | 0.1851 |
| Time to adequate abx therapy, days, mean SD | 2.3 1.8 | 1.81.5 | 0.0554 |
| Duration of initial abx, days, mean SD | 11.1 6.0 | 14.114.6 | 0.0401 |
| Abx before initial therapy, No. (%) | 85 (62) | 34 (54) | 0.3541 |
| Average dose, mg/kg, mean SD | NA | 6.11.5 | NA |
| Mortality, No. (%) | 25 (18) | 15 (24) | 0.3481 |
| LOS (days) | 37.527.7 | 40.827.9 | 0.4336 |
From the microbiology laboratory report of initial blood cultures, 78.6% of the isolates were noted as being E. faecium, with the remainder being E. faecalis (21.4%). One patient was classified as having linezolid‐resistant E. faecium (MIC >4 mg/L) upon repeat blood culture. Daptomycin MICs were obtained for 44 isolates using the Etest or MicroScan system; all isolates were susceptible with MICs ranging from 0.254 mg/L. As mentioned previously, our laboratory did not routinely report isolate susceptibility to daptomycin until 2008.
There were no statistically significant differences between the treatment groups with regard to time to appropriate or adequate antibiotic therapy (Table 1). However, there was a statistically significant difference in the mean duration of initial antibiotics between linezolid and daptomycin (11.1 days vs 14.1 days; P = 0.0401). Dosing strategies used in these patients were also evaluated. All linezolid patients received a dose of 600 mg every 12 hours by mouth or intravenously. The average dose of daptomycin was 6.1 mg/kg (range, 3.410.4 mg/kg; median, 6 mg/kg). The average LOS was 37 days for linezolid vs 40 days for daptomycin, which did not confer statistical significance. Overall mortality was 20%, occurring in 25 linezolid patients versus 15 daptomycin patients (P = 0.3481). The stepwise multiple regression analysis did not identify any statistically significant variables in patients treated with linezolid or daptomycin that affected any of the outcomes.
Outcomes and Analysis
As shown in Table 2, there were no statistically significant differences in clinical or microbiologic cure between the linezolid and daptomycin groups (74% vs 75% and 94% vs 94%, respectively). However, the linezolid group compared with the daptomycin group had fewer patients that developed a positive blood culture while on their initial antibiotic therapy (8% vs 22%; P = 0.0097). Follow‐up cultures were required to determine rates of recurrence and reinfection. Only 107/138 patients in the linezolid group and 51/63 patients in the daptomycin group had follow‐up cultures collected. Recurrence was documented in 3% of linezolid patients vs 12% of daptomycin patients (P = 0.0321). The odds ratio for developing a recurrent infection with daptomycin versus linezolid was 5.51 (95% confidence interval, 1.2524.28). Out of 6 patients that developed a recurrent VRE infection in the daptomycin group, 2 were prescribed doses <4 mg/kg with no reported MICs, and 2 patients received 6 mg/kg with reported MICs of 4 mg/L. No statistically significant difference existed for the rate of reinfection between linezolid and daptomycin (1% vs 6%; P = 0.0992).
| Linezolid (n = 138) | Daptomycin (n = 63) | P Value | |
|---|---|---|---|
| |||
| Patients with positive culture on G+ therapy | 11 (8) | 14 (22) | 0.0097 |
| Clinical cure | 102 (74) | 47 (75) | 1 |
| Microbiologic cure | 130 (94) | 59 (94) | 1 |
| Recurrence* | 3 (3) | 6 (12) | 0.0321 |
| Reinfection* | 1 (1) | 3 (6) | 0.0992 |
Table 3 provides information on subsets of the patient population deemed high‐risk for VRE infection or immunocompromised. There was no statistically significant difference between the 2 antibiotic groups in clinical or microbiologic cure. In the subsets of immunocompromised patients, there was no difference in recurrence or reinfection between the linezolid and daptomycin patients. Furthermore, all groups had similar LOS regardless of the antibiotic used to treat the VRE BSI. Moreover, there were no statistically significant differences in 30‐day mortality in these subsets of the population with regard to initial antibiotic choice. No significant independent variables were found between linezolid or daptomycin that affected any of the outcomes listed in Table 3.
| Neutropenia (%) | Hematologic Malignancy (%) | ESRD on Hemodialysis (%) | Liver Transplant (%) | |||||
|---|---|---|---|---|---|---|---|---|
| LZD (n = 16) | Dapto (n = 5) | LZD (n = 19) | Dapto (n = 21) | LZD (n = 35) | Dapto (n = 17) | LZD (n = 5) | Dapto (n = 8) | |
| ||||||||
| Clinical cure, No. (%) | 12 (75) | 5 (100) | 18 (95) | 17 (81) | 24 (69) | 12 (71) | 4 (80) | 3 (38) |
| Microbiologic cure,* No. (%) | 13 (81) | 5 (100) | 18 (95) | 20 (95) | 33 (94) | 16 (94) | 5 (100) | 8 (100) |
| Recurrence,* No. (%) | 2 (13) | 1 (20) | 1 (6) | 2 (11) | 0 | 2 (15) | 0 | 1 (14) |
| Reinfection,* No. (%) | 0 | 0 | 0 | 0 | 1 (4) | 2 (15) | 0 | 1 (14) |
| Mortality, No. (%) | 3 (19) | 1 (20) | 4 (21) | 3 (14) | 7 (20) | 4 (24) | 1 (20) | 4 (50) |
| LOS, days, meanSD | 57.422 | 39.412.4 | 47.626.2 | 4127.1 | 38.833.8 | 39.640.4 | 5034.5 | 73.338.8 |
DISCUSSION
Vergis et al21 reported that infections with VRE compared with vancomycin‐sensitive infections were associated with a higher rate of mortality and that the chosen antimicrobial therapy may play a pivotal role in the risk of death. Our retrospective study suggests that linezolid and daptomycin appear to be equally efficacious for the treatment of VRE BSIs. The results from our study for clinical and microbiologic cure rates for linezolid and daptomycin are similar to previously published data.7, 8 In accordance with previous studies,4 our data demonstrate that there is a higher rate of recurrence in patients treated with daptomycin. This finding may be explained by the fact that the daptomycin group was comprised of more complex patients with a greater disease burden versus the linezolid group; therefore, they were more susceptible to a recurrent VRE infection. In our study, patients who were treated with daptomycin were 5.5 times more likely to have a recurrent infection than linezolid‐treated patients. However, this finding must be scrutinized, because over half of the patients with recurrence either received an inappropriate dose or had high MICs to daptomycin.
Despite there being few clinical and microbiologic outcome data with daptomycin, our study proposes that a bactericidal antibiotic and a bacteriostatic antibiotic have comparable efficacy in the treatment of VRE BSIs. Previous literature has mainly comprised case studies or series that have evaluated clinical outcomes with daptomycin in the treatment of VRE BSIs. Gallagher et al7 reported the results of a retrospective case series of 30 patients with VRE bacteremia who were treated with daptomycin. In this study, microbiologic cure was achieved in 80% of patients, with clinical success in 59% of the patients. In 2009, Mave et al4 compared clinical outcomes between daptomycin and linezolid in the treatment of VRE bacteremia. Reported results demonstrated a microbiologic cure rate of 90% for daptomycin versus 88% for linezolid.4 Moreover, there were no differences in mortality between the groups in our study. In 2010, Crank et al18 reported no differences in mortality (in‐hospital) for hospitalized patients with VRE BSIs treated with linezolid or daptomycin. Our results seem to be consistent with what has been published previously concerning clinical outcomes associated with linezolid or daptomycin in the treatment of VRE BSI.
The average daptomycin dose received in our patients was 6.1 mg/kg with doses ranging from 3.410.4 mg/kg. The underdosing as well as higher MICs to daptomycin may have contributed to a higher rate of recurrence. Previous reports state that Enterococcus species may have higher MICs to daptomycin than Staphylococcus or Streptococcus species; consequently, higher doses may be needed to adequately treat enterococcal infections.7 In the aforementioned study by Gallagher et al,7 doses of daptomycin 6 mg/kg were associated with a positive clinical outcome in 81% of patients compared with 31% if the dose used was <6 mg/kg. Linezolid is dosed 600 mg every 12 hours by mouth or intravenously, with no variations. There have been no studies comparing the uniform dosing of linezolid to the weight‐based dosing of daptomycin and their effects on outcomes.
Patients particularly susceptible to VRE infections include those with neutropenia and/or cancer, patients receiving long‐term hemodialysis, and liver transplant recipients.3, 22, 23 Upon review of this immunocompromised population, we noted no statistically significant differences in overall outcomes. A study by Kraft et al.24 supports the findings in our study that both drugs appear useful in the treatment of VRE bacteremia in patients with hematologic malignancy. We did identify a difference, albeit nonsignificant, in LOS for daptomycin versus linezolid in patients with a history of liver transplantation. Again, the level of care that these patients needed compared with the general population may explain this difference. As mentioned previously, another pertinent factor would be the dose of daptomycin used in these patients, because the dose can affect clinical success. Because all of the other patients had a similar LOS, we cannot determine that the increased LOS seen in liver transplant patients treated with daptomycin was solely due to daptomycin use. The reason for the increased LOS seems to be multifactorial. In the neutropenic population, a difference in LOS was also recognized, but follow‐up complete blood count values were not collected for these patients to determine whether linezolid contributed to further bone marrow suppression leading to an increase in LOS. For both of these patient populations, the number of patients included is very small (n = 21 for neutropenia total, n = 13 for liver transplant total), which can lead to a high degree of variance.
This study has several limitations. This was a retrospective review; therefore, we had no control over the selection of therapy. This may be reflected in an apparent preferential use of daptomycin in immunocompromised patients. Furthermore, 62% of linezolid patients and 54% of daptomycin patients received an antibiotic before initial therapy that could have potentially altered response rates. Due to the paucity of documentation surrounding initial site of infection, some of the positive cultures may represent potential contamination, because VRE may contaminate skin.25 Contamination seems implausible, however, because patients were seen by an infectious disease physician and had at least 1 documented positive VRE blood culture. We chose arbitrary definitions for clinical cure, microbiologic cure, microbiologic failure, recurrence, and reinfection. Previous studies have used their own definitions leading to discrepancies in reporting. Another limitation was that follow‐up cultures were not obtained on all of the patients, which was needed to determine rates of recurrence, reinfection, and microbiologic cure. MICs to daptomycin were not reported in 30% of our patients, potentially altering the recurrence rate seen in the daptomycin‐treated patients. Because clinical cure was not documented in the chart, it was inferred from the laboratory values and vital sign information. One investigator analyzed all of the values and made the determination of clinical cure, allowing for a consistent approach to data review.
In the face of the imposing threat of a highly resistant organism such as VRE with a limited number of efficacious antibiotics, antimicrobial selection becomes increasingly important and is requisite to clinical and microbiological success. To our knowledge, this is one of the largest studies to date comparing the efficacy of linezolid with that of daptomycin in the treatment of VRE bacteremia. Both of these agents are effective for the treatment of VRE BSIs. Nevertheless, specific factors related to the medication (eg, dose, route of administration) as well as the patient (eg, comorbid conditions, acuity of illness) should be taken into consideration when selecting an initial antimicrobial agent. Because the treatment of VRE BSIs continues to be a challenge, larger prospective randomized controlled trials are needed to corroborate our results and determine the optimal therapy for this serious infection.
Acknowledgements
Disclosures: Michael S. Gelfand is on the speaker's bureau for Cubist and Pfizer.
- ,,,,,.Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study.Clin Infect Dis.2004;39:309–317.
- ,,, et al.Clinical practice guidelines for the management of intravascular catheter‐related infection: 2009 update by the Infectious Diseases Society of America.Clin Infect Dis.2009;49:1–45.
- ,,,,,.Bad bugs need drugs: an update on the development pipeline from the antimicrobial availability task force of the infectious diseases society of America.Clin Infect Dis.2006;42:657–668.
- ,,,.Vancomycin‐resistant enterococcal bacteraemia: is daptomycin as effective as linezolid?J Antimicrob Chemother.2009;64:175–180.
- ,,.Management of multidrug‐resistant enterococcal Infections.Clin Microbiol Infect.2010;16:555–562.
- ,,, et al.Treatment of vancomycin‐resistant Enterococcus faecium infections with quinupristin/dalfopristin.Clin Infect Dis.2001;33:1816–1823.
- ,,, et al.Daptomycin for vancomycin‐resistant enterococcol bacteremia: a retrospective case series of 30 patients.Pharmacotherapy.2009;29:792–799.
- ,,, et al.Safety, efficacy and pharmacokinetics of linezolid for treatment of resistant gram positive infections in cancer patients with neutropenia.Ann Oncol.2003;14:795–801.
- ,,,,.Daptomycin for the treatment of vancomycin resistant Enterococcus faecium bacteremia.Scand J Infect Dis.2003;38:290–292.
- ,.New antimicrobial agents for the treatment of gram positive bacterial infections.Clin Microbiol Infec.2008;14:411–420.
- ,.Emergence and management of drug‐resistant enterococcal infections.Expert Rev Anti Infect Ther.2008;6:637–655.
- ,,.Nosocomial spread of linezolid‐resistant, Vancomycin resistant Enterococcus faecium.N Engl J Med.2002;346:867–869.
- ,, et al.Nosocomial superinfections due to linezolid‐resitant Enterococcus faecalis: evidence for a gene dosage effect of linezolid MICs.Diagn Microbiol Infect Dis.2003;47:511–513.
- .Quinupristin‐dalfopristin and linezolid: evidence and opinion.Clin Infect Dis.2003;36:473–481.
- Cubicin (Daptomycin for injection) [package insert].Lexington, MA:Cubist Pharmaceuticals;2010.
- ,,,.Daptomycin nonsusceptible Enterococci: an emerging challenge for clinicians.Clin Infect Dis.2011;52:228–234.
- ,,,.A potential role for daptomycin in enterococcal infections: what is the evidence?J Antimicrob Chemother.2010;65:1126–1136.
- ,,, et al.Comparison of outcomes from daptomycin or linezolid for vancomycin‐resistant enterococcal bloodstream infection: a retrospective, multicenter, cohort study.Clin Ther.2010;32:1713–1719.
- ,,,,,.Observational study of the epidemiology and outcomes of vancomycin‐resistant Enterococcus bacteraemia treated with newer antimicrobial agents.Epidemiol Infect.2010;15:1–9.
- .Inadequate antimicrobial treatment: an important determinant of outcome for hospitalized patients.Clin Infect Dis.2000;31:S131–S138.
- ,,, et al.Determinants of vancomycin resistance and mortality rates in enterococcal bacteremia: a prospective multicenter study.Ann Intern Med.2001;135:484–492.
- ,,,,,.Vancomycin resistant enterococci among chronic hemodialysis patients: a prospective study of acquisition.Clin Infect Dis.2001;32:23–29.
- ,,, et al.A nationwide, multicenter, case control study comparing risk factors, treatment, and outcome for vancomycin resistant andsusceptible enterococcal bacteremia.Diagn Microbiol Infect Dis.2000;36:145–158.
- ,,,,.Outcomes of therapy: vancomycin‐resistant enterococcal bacteremia in hematology and bone marrow transplant patients [published online ahead of print November 26, 2010].Support Care Cancer. doi: 10.1007/s00520–010‐1038‐z.
- ,,, et al.Skin colonization with vancomycin‐resistant enterococci among hospitalized patients with bacteremia.Clin Infect Dis.1997;24:704–706.
- ,,,,,.Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study.Clin Infect Dis.2004;39:309–317.
- ,,, et al.Clinical practice guidelines for the management of intravascular catheter‐related infection: 2009 update by the Infectious Diseases Society of America.Clin Infect Dis.2009;49:1–45.
- ,,,,,.Bad bugs need drugs: an update on the development pipeline from the antimicrobial availability task force of the infectious diseases society of America.Clin Infect Dis.2006;42:657–668.
- ,,,.Vancomycin‐resistant enterococcal bacteraemia: is daptomycin as effective as linezolid?J Antimicrob Chemother.2009;64:175–180.
- ,,.Management of multidrug‐resistant enterococcal Infections.Clin Microbiol Infect.2010;16:555–562.
- ,,, et al.Treatment of vancomycin‐resistant Enterococcus faecium infections with quinupristin/dalfopristin.Clin Infect Dis.2001;33:1816–1823.
- ,,, et al.Daptomycin for vancomycin‐resistant enterococcol bacteremia: a retrospective case series of 30 patients.Pharmacotherapy.2009;29:792–799.
- ,,, et al.Safety, efficacy and pharmacokinetics of linezolid for treatment of resistant gram positive infections in cancer patients with neutropenia.Ann Oncol.2003;14:795–801.
- ,,,,.Daptomycin for the treatment of vancomycin resistant Enterococcus faecium bacteremia.Scand J Infect Dis.2003;38:290–292.
- ,.New antimicrobial agents for the treatment of gram positive bacterial infections.Clin Microbiol Infec.2008;14:411–420.
- ,.Emergence and management of drug‐resistant enterococcal infections.Expert Rev Anti Infect Ther.2008;6:637–655.
- ,,.Nosocomial spread of linezolid‐resistant, Vancomycin resistant Enterococcus faecium.N Engl J Med.2002;346:867–869.
- ,, et al.Nosocomial superinfections due to linezolid‐resitant Enterococcus faecalis: evidence for a gene dosage effect of linezolid MICs.Diagn Microbiol Infect Dis.2003;47:511–513.
- .Quinupristin‐dalfopristin and linezolid: evidence and opinion.Clin Infect Dis.2003;36:473–481.
- Cubicin (Daptomycin for injection) [package insert].Lexington, MA:Cubist Pharmaceuticals;2010.
- ,,,.Daptomycin nonsusceptible Enterococci: an emerging challenge for clinicians.Clin Infect Dis.2011;52:228–234.
- ,,,.A potential role for daptomycin in enterococcal infections: what is the evidence?J Antimicrob Chemother.2010;65:1126–1136.
- ,,, et al.Comparison of outcomes from daptomycin or linezolid for vancomycin‐resistant enterococcal bloodstream infection: a retrospective, multicenter, cohort study.Clin Ther.2010;32:1713–1719.
- ,,,,,.Observational study of the epidemiology and outcomes of vancomycin‐resistant Enterococcus bacteraemia treated with newer antimicrobial agents.Epidemiol Infect.2010;15:1–9.
- .Inadequate antimicrobial treatment: an important determinant of outcome for hospitalized patients.Clin Infect Dis.2000;31:S131–S138.
- ,,, et al.Determinants of vancomycin resistance and mortality rates in enterococcal bacteremia: a prospective multicenter study.Ann Intern Med.2001;135:484–492.
- ,,,,,.Vancomycin resistant enterococci among chronic hemodialysis patients: a prospective study of acquisition.Clin Infect Dis.2001;32:23–29.
- ,,, et al.A nationwide, multicenter, case control study comparing risk factors, treatment, and outcome for vancomycin resistant andsusceptible enterococcal bacteremia.Diagn Microbiol Infect Dis.2000;36:145–158.
- ,,,,.Outcomes of therapy: vancomycin‐resistant enterococcal bacteremia in hematology and bone marrow transplant patients [published online ahead of print November 26, 2010].Support Care Cancer. doi: 10.1007/s00520–010‐1038‐z.
- ,,, et al.Skin colonization with vancomycin‐resistant enterococci among hospitalized patients with bacteremia.Clin Infect Dis.1997;24:704–706.
Copyright © 2011 Society of Hospital Medicine
Report Finds U.S. Health Quality Stagnant
A recent report (PDF) from The Commonwealth Fund that suggests the quality and efficacy of the U.S. healthcare system has remained relatively static in the past three years has bright spots for HM, an academic hospitalist says.
Kedar Mate, MD, assistant professor of medicine with the division of hospital medicine at Weill Cornell Medical School in New York City, says the report, which was compiled before any of the facets of the Affordable Care Act were implemented, helps argue why hospitalists are poised to take the reins of those needed quality reforms.
"They're the natural leaders of this work moving forward from the physician perspective," says Dr. Mate, a faculty member at the Institute for Healthcare Improvement in Cambridge, Mass. "They have a strong role to play in shepherding and championing and really being the arms and legs of the quality and safety movement, in many ways. Not only leading it, but actually executing it."
The report released last month, "Why Not the Best? Results from the National Scorecard on U.S. Health System Performance, 2011," measures 42 indicators of healthcare quality, access, efficiency, equity, and healthy lives. In overall terms, the U.S. score has varied only slightly in the third national scorecard. And while the report cautions that year-to-year analyses of quality measures are not directly comparable because of changing categories, Dr. Mate notes there have been significant improvements in areas that HM and health system improvement efforts have targeted.
The study, for example, reports half of adults with high blood pressure had the condition under control in 2007-2008, up from 31% in 1999-2000. The data also show that the rate of controlled blood sugar levels in adults with diabetes ticked up to 86% in 2007-2008 from 79% in 1999-2000.
"Where we turn our attention, particularly with focused quality initiatives, we're seeing some measurable change," Dr. Mate says. "There's absolutely value in identifying and knowing where we are seeing benefits, because those ought to be built upon."
A recent report (PDF) from The Commonwealth Fund that suggests the quality and efficacy of the U.S. healthcare system has remained relatively static in the past three years has bright spots for HM, an academic hospitalist says.
Kedar Mate, MD, assistant professor of medicine with the division of hospital medicine at Weill Cornell Medical School in New York City, says the report, which was compiled before any of the facets of the Affordable Care Act were implemented, helps argue why hospitalists are poised to take the reins of those needed quality reforms.
"They're the natural leaders of this work moving forward from the physician perspective," says Dr. Mate, a faculty member at the Institute for Healthcare Improvement in Cambridge, Mass. "They have a strong role to play in shepherding and championing and really being the arms and legs of the quality and safety movement, in many ways. Not only leading it, but actually executing it."
The report released last month, "Why Not the Best? Results from the National Scorecard on U.S. Health System Performance, 2011," measures 42 indicators of healthcare quality, access, efficiency, equity, and healthy lives. In overall terms, the U.S. score has varied only slightly in the third national scorecard. And while the report cautions that year-to-year analyses of quality measures are not directly comparable because of changing categories, Dr. Mate notes there have been significant improvements in areas that HM and health system improvement efforts have targeted.
The study, for example, reports half of adults with high blood pressure had the condition under control in 2007-2008, up from 31% in 1999-2000. The data also show that the rate of controlled blood sugar levels in adults with diabetes ticked up to 86% in 2007-2008 from 79% in 1999-2000.
"Where we turn our attention, particularly with focused quality initiatives, we're seeing some measurable change," Dr. Mate says. "There's absolutely value in identifying and knowing where we are seeing benefits, because those ought to be built upon."
A recent report (PDF) from The Commonwealth Fund that suggests the quality and efficacy of the U.S. healthcare system has remained relatively static in the past three years has bright spots for HM, an academic hospitalist says.
Kedar Mate, MD, assistant professor of medicine with the division of hospital medicine at Weill Cornell Medical School in New York City, says the report, which was compiled before any of the facets of the Affordable Care Act were implemented, helps argue why hospitalists are poised to take the reins of those needed quality reforms.
"They're the natural leaders of this work moving forward from the physician perspective," says Dr. Mate, a faculty member at the Institute for Healthcare Improvement in Cambridge, Mass. "They have a strong role to play in shepherding and championing and really being the arms and legs of the quality and safety movement, in many ways. Not only leading it, but actually executing it."
The report released last month, "Why Not the Best? Results from the National Scorecard on U.S. Health System Performance, 2011," measures 42 indicators of healthcare quality, access, efficiency, equity, and healthy lives. In overall terms, the U.S. score has varied only slightly in the third national scorecard. And while the report cautions that year-to-year analyses of quality measures are not directly comparable because of changing categories, Dr. Mate notes there have been significant improvements in areas that HM and health system improvement efforts have targeted.
The study, for example, reports half of adults with high blood pressure had the condition under control in 2007-2008, up from 31% in 1999-2000. The data also show that the rate of controlled blood sugar levels in adults with diabetes ticked up to 86% in 2007-2008 from 79% in 1999-2000.
"Where we turn our attention, particularly with focused quality initiatives, we're seeing some measurable change," Dr. Mate says. "There's absolutely value in identifying and knowing where we are seeing benefits, because those ought to be built upon."
Church Coalition Helps Prevent Readmissions
A partnership with nearly 400 local churches is helping the seven-hospital Methodist Le Bonheur Healthcare System, based in Memphis, Tenn., return hospitalized patients to their communities with the support they need to manage such chronic conditions as congestive heart failure.
Preliminary research into the Congregational Health Network shows a 20% decrease in readmissions by participating patients, compared with matched controls, says Teresa Cutts, PhD, director of research for innovation for Methodist's Center of Excellence in Faith & Health.
But the program is more than just "outreach" from the health system to the churches, she adds. It also is "in-reach" from community partners to the health system and a true collaboration. "The clergy have a covenant; they have deep ownership of this network," she says.
Trained volunteer liaisons at each participating church are the bridge to the health system. Patients who are members of the network and who opt in at admission are connected to liaisons or other church volunteers, who then visit patients in the hospital and at their homes following discharge. Hospital-employed community care workers (called navigators) help coordinate these connections, supported by Methodist's electronic health record (EHR).
The network has 12,000 registered members. Approximately 1,100 volunteers have received training in such subjects as hospital visitation, hands-on aftercare, and mental health first aid. Larger goals, Dr. Cutts says, include pushing this support further upstream into preventive care, documenting outcomes, and incorporating more clinical issues into the volunteer training.
"We think it's time, and will really empower people," she says.
In September, health system representatives visited the White House to share the coalition's success story. For more information, contact Cutts at [email protected].
A partnership with nearly 400 local churches is helping the seven-hospital Methodist Le Bonheur Healthcare System, based in Memphis, Tenn., return hospitalized patients to their communities with the support they need to manage such chronic conditions as congestive heart failure.
Preliminary research into the Congregational Health Network shows a 20% decrease in readmissions by participating patients, compared with matched controls, says Teresa Cutts, PhD, director of research for innovation for Methodist's Center of Excellence in Faith & Health.
But the program is more than just "outreach" from the health system to the churches, she adds. It also is "in-reach" from community partners to the health system and a true collaboration. "The clergy have a covenant; they have deep ownership of this network," she says.
Trained volunteer liaisons at each participating church are the bridge to the health system. Patients who are members of the network and who opt in at admission are connected to liaisons or other church volunteers, who then visit patients in the hospital and at their homes following discharge. Hospital-employed community care workers (called navigators) help coordinate these connections, supported by Methodist's electronic health record (EHR).
The network has 12,000 registered members. Approximately 1,100 volunteers have received training in such subjects as hospital visitation, hands-on aftercare, and mental health first aid. Larger goals, Dr. Cutts says, include pushing this support further upstream into preventive care, documenting outcomes, and incorporating more clinical issues into the volunteer training.
"We think it's time, and will really empower people," she says.
In September, health system representatives visited the White House to share the coalition's success story. For more information, contact Cutts at [email protected].
A partnership with nearly 400 local churches is helping the seven-hospital Methodist Le Bonheur Healthcare System, based in Memphis, Tenn., return hospitalized patients to their communities with the support they need to manage such chronic conditions as congestive heart failure.
Preliminary research into the Congregational Health Network shows a 20% decrease in readmissions by participating patients, compared with matched controls, says Teresa Cutts, PhD, director of research for innovation for Methodist's Center of Excellence in Faith & Health.
But the program is more than just "outreach" from the health system to the churches, she adds. It also is "in-reach" from community partners to the health system and a true collaboration. "The clergy have a covenant; they have deep ownership of this network," she says.
Trained volunteer liaisons at each participating church are the bridge to the health system. Patients who are members of the network and who opt in at admission are connected to liaisons or other church volunteers, who then visit patients in the hospital and at their homes following discharge. Hospital-employed community care workers (called navigators) help coordinate these connections, supported by Methodist's electronic health record (EHR).
The network has 12,000 registered members. Approximately 1,100 volunteers have received training in such subjects as hospital visitation, hands-on aftercare, and mental health first aid. Larger goals, Dr. Cutts says, include pushing this support further upstream into preventive care, documenting outcomes, and incorporating more clinical issues into the volunteer training.
"We think it's time, and will really empower people," she says.
In September, health system representatives visited the White House to share the coalition's success story. For more information, contact Cutts at [email protected].
FDA: Trilipix May Not Cut Heart Attack Risk
Treatment with fenofibric acid "may not" lower the risk of myocardial infarction or stroke in patients treated with the cholesterol-lowering medication, information that is being added to the drug’s label, the Food and Drug Administration announced on Nov. 9.
The FDA statement and decision to make the labeling change are based on the agency’s review of the ACCORD (Action to Control Cardiovascular Risk in Diabetes) lipid trial, which showed no significant differences in the risk of major adverse cardiac events between patients treated with fenofibrate and simvastatin and those treated with simvastatin alone.
Data from the ACCORD lipid trial have been added to the drug label’s "Important Limitations of Use" and "Warnings and Precautions" sections, and to the medication guide given to patients with each prescription.
"Health care professionals should consider the benefits and risks of Trilipix when deciding to prescribe the drug to patients," the FDA cautioned in its statement, and physicians should encourage their patients to read the medication guide.
At a meeting of the FDA’s Endocrinologic and Metabolic Drugs Advisory Committee earlier this year, the panel was divided over how the ACCORD lipid results should affect the drugs labeling and the approved indication for use with a statin. Of the 13 panel members, 6 agreed that the main findings of ACCORD should be added to the drug’s label, while 4 said that the co-administration indication should be withdrawn. The remaining three panelists said that marketing should continue with no label changes.
Fenofibric acid, a peroxisome proliferator receptor-alpha activator marketed as Trilipix by Abbott Laboratories, was approved in 2008, for use with a statin to reduce triglycerides and increase HDL cholesterol in patients with mixed dyslipidemia and coronary heart disease or a CHD risk equivalent who are on optimal statin therapy to achieve their LDL cholesterol goal. It is also indicated as monotherapy to reduce triglycerides in patients with severe hypertriglyceridemia; as monotherapy to reduce elevated LDL cholesterol levels, total-C cholesterol, triglycerides, and apolipoprotein-B, and to increase HDL cholesterol levels in patients with primary hyperlipidemia or mixed dyslipidemia.
In the ACCORD lipid study, patients were treated with simvastatin for 4 weeks and were then randomized to continue treatment with simvastatin and placebo (2,753 patients) or simvastatin and fenofibrate (2,765 patients).
Over a mean follow-up of 4.7 years, the risk of major adverse cardiovascular events (nonfatal MI, nonfatal stroke, and death from cardiovascular disease) was 8% lower among patients on the combination, but the difference was not statistically significant. Among men, the risk was reduced by 18% among those on the combination, compared with those on simvastatin alone.
Among women, however, the risk of major adverse cardiovascular events was 38% greater among those on the combination, compared with those on placebo.
That gender effect was not seen in another large randomized controlled clinical trial comparing fenofibrate to placebo, so "the clinical significance of this subgroup finding is unclear," the FDA statement noted.
But "the study results also raised the hypothesis that a subgroup of patients with high triglycerides and low high-density lipoprotein cholesterol may experience some reduction in the risk of MACE [major adverse cardiovascular events] from the combination therapy vs. simvastatin monotherapy," the agency noted.
The FDA will require Abbott to conduct a randomized, double-blind, placebo-controlled clinical trial to evaluate whether combination treatment with fenofibrate plus a statin significantly reduces the rate of MACE in men and women who are at their LDL cholesterol goal on statin therapy but have residually high triglycerides and low HDL cholesterol.
Serious adverse events associated with Trilipix should be reported to the FDA’s MedWatch program online or at 800-332-1088.
Treatment with fenofibric acid "may not" lower the risk of myocardial infarction or stroke in patients treated with the cholesterol-lowering medication, information that is being added to the drug’s label, the Food and Drug Administration announced on Nov. 9.
The FDA statement and decision to make the labeling change are based on the agency’s review of the ACCORD (Action to Control Cardiovascular Risk in Diabetes) lipid trial, which showed no significant differences in the risk of major adverse cardiac events between patients treated with fenofibrate and simvastatin and those treated with simvastatin alone.
Data from the ACCORD lipid trial have been added to the drug label’s "Important Limitations of Use" and "Warnings and Precautions" sections, and to the medication guide given to patients with each prescription.
"Health care professionals should consider the benefits and risks of Trilipix when deciding to prescribe the drug to patients," the FDA cautioned in its statement, and physicians should encourage their patients to read the medication guide.
At a meeting of the FDA’s Endocrinologic and Metabolic Drugs Advisory Committee earlier this year, the panel was divided over how the ACCORD lipid results should affect the drugs labeling and the approved indication for use with a statin. Of the 13 panel members, 6 agreed that the main findings of ACCORD should be added to the drug’s label, while 4 said that the co-administration indication should be withdrawn. The remaining three panelists said that marketing should continue with no label changes.
Fenofibric acid, a peroxisome proliferator receptor-alpha activator marketed as Trilipix by Abbott Laboratories, was approved in 2008, for use with a statin to reduce triglycerides and increase HDL cholesterol in patients with mixed dyslipidemia and coronary heart disease or a CHD risk equivalent who are on optimal statin therapy to achieve their LDL cholesterol goal. It is also indicated as monotherapy to reduce triglycerides in patients with severe hypertriglyceridemia; as monotherapy to reduce elevated LDL cholesterol levels, total-C cholesterol, triglycerides, and apolipoprotein-B, and to increase HDL cholesterol levels in patients with primary hyperlipidemia or mixed dyslipidemia.
In the ACCORD lipid study, patients were treated with simvastatin for 4 weeks and were then randomized to continue treatment with simvastatin and placebo (2,753 patients) or simvastatin and fenofibrate (2,765 patients).
Over a mean follow-up of 4.7 years, the risk of major adverse cardiovascular events (nonfatal MI, nonfatal stroke, and death from cardiovascular disease) was 8% lower among patients on the combination, but the difference was not statistically significant. Among men, the risk was reduced by 18% among those on the combination, compared with those on simvastatin alone.
Among women, however, the risk of major adverse cardiovascular events was 38% greater among those on the combination, compared with those on placebo.
That gender effect was not seen in another large randomized controlled clinical trial comparing fenofibrate to placebo, so "the clinical significance of this subgroup finding is unclear," the FDA statement noted.
But "the study results also raised the hypothesis that a subgroup of patients with high triglycerides and low high-density lipoprotein cholesterol may experience some reduction in the risk of MACE [major adverse cardiovascular events] from the combination therapy vs. simvastatin monotherapy," the agency noted.
The FDA will require Abbott to conduct a randomized, double-blind, placebo-controlled clinical trial to evaluate whether combination treatment with fenofibrate plus a statin significantly reduces the rate of MACE in men and women who are at their LDL cholesterol goal on statin therapy but have residually high triglycerides and low HDL cholesterol.
Serious adverse events associated with Trilipix should be reported to the FDA’s MedWatch program online or at 800-332-1088.
Treatment with fenofibric acid "may not" lower the risk of myocardial infarction or stroke in patients treated with the cholesterol-lowering medication, information that is being added to the drug’s label, the Food and Drug Administration announced on Nov. 9.
The FDA statement and decision to make the labeling change are based on the agency’s review of the ACCORD (Action to Control Cardiovascular Risk in Diabetes) lipid trial, which showed no significant differences in the risk of major adverse cardiac events between patients treated with fenofibrate and simvastatin and those treated with simvastatin alone.
Data from the ACCORD lipid trial have been added to the drug label’s "Important Limitations of Use" and "Warnings and Precautions" sections, and to the medication guide given to patients with each prescription.
"Health care professionals should consider the benefits and risks of Trilipix when deciding to prescribe the drug to patients," the FDA cautioned in its statement, and physicians should encourage their patients to read the medication guide.
At a meeting of the FDA’s Endocrinologic and Metabolic Drugs Advisory Committee earlier this year, the panel was divided over how the ACCORD lipid results should affect the drugs labeling and the approved indication for use with a statin. Of the 13 panel members, 6 agreed that the main findings of ACCORD should be added to the drug’s label, while 4 said that the co-administration indication should be withdrawn. The remaining three panelists said that marketing should continue with no label changes.
Fenofibric acid, a peroxisome proliferator receptor-alpha activator marketed as Trilipix by Abbott Laboratories, was approved in 2008, for use with a statin to reduce triglycerides and increase HDL cholesterol in patients with mixed dyslipidemia and coronary heart disease or a CHD risk equivalent who are on optimal statin therapy to achieve their LDL cholesterol goal. It is also indicated as monotherapy to reduce triglycerides in patients with severe hypertriglyceridemia; as monotherapy to reduce elevated LDL cholesterol levels, total-C cholesterol, triglycerides, and apolipoprotein-B, and to increase HDL cholesterol levels in patients with primary hyperlipidemia or mixed dyslipidemia.
In the ACCORD lipid study, patients were treated with simvastatin for 4 weeks and were then randomized to continue treatment with simvastatin and placebo (2,753 patients) or simvastatin and fenofibrate (2,765 patients).
Over a mean follow-up of 4.7 years, the risk of major adverse cardiovascular events (nonfatal MI, nonfatal stroke, and death from cardiovascular disease) was 8% lower among patients on the combination, but the difference was not statistically significant. Among men, the risk was reduced by 18% among those on the combination, compared with those on simvastatin alone.
Among women, however, the risk of major adverse cardiovascular events was 38% greater among those on the combination, compared with those on placebo.
That gender effect was not seen in another large randomized controlled clinical trial comparing fenofibrate to placebo, so "the clinical significance of this subgroup finding is unclear," the FDA statement noted.
But "the study results also raised the hypothesis that a subgroup of patients with high triglycerides and low high-density lipoprotein cholesterol may experience some reduction in the risk of MACE [major adverse cardiovascular events] from the combination therapy vs. simvastatin monotherapy," the agency noted.
The FDA will require Abbott to conduct a randomized, double-blind, placebo-controlled clinical trial to evaluate whether combination treatment with fenofibrate plus a statin significantly reduces the rate of MACE in men and women who are at their LDL cholesterol goal on statin therapy but have residually high triglycerides and low HDL cholesterol.
Serious adverse events associated with Trilipix should be reported to the FDA’s MedWatch program online or at 800-332-1088.
FROM THE FOOD AND DRUG ADMINISTRATION
New Tool Improves Outcome Assessment in Pediatric Vasculitis
Overuse injuries are very common in children and teenagers, especially among kids who play sports throughout the year.
Although rare, primary systemic vasculitis in children is associated with significant mortality and morbidity when not properly treated. Optimal management of the group of multiorgan inflammatory conditions is hampered by the lack of evidence-based therapies. This shortage of data has been attributed, in part, to the absence of a standardized outcome measure for use in clinical trials, according to Dr. Pavla Dolezalova.
"Until recently, no standardized vasculitis activity assessment tool has been available for children, so some pediatric studies apply adult measures, such as the Birmingham Vasculitis Activity Score [BVAS]," she said. Further, although nonspecific inflammatory markers such as erythrocyte sedimentation rate or C-reactive protein can reflect systemic vasculitis disease activity, they do not distinguish it from infectious complications. Use of the global assessment of disease activity by the treating physician using the visual analog scale is of limited utility in clinical trials, she noted.
In an effort to facilitate more informative clinical trials of primary systemic vasculitis in children, Dr. Dolezalova of Charles University and General University Hospital in Prague, Czech Republic, and her colleagues have developed a quantitative clinical index of manifestations of active disease, called the Pediatric Vasculitis Activity Score (PVAS), which has been preliminarily validated as a useful clinical measure with good interobserver reliability (Pediatr. Rheumatol. Online J. 2011 [doi:10.1186/1546-0096-9-S1-P92]).
In this column, Dr. Dolezalova describes the need for the assessment tool as well as some of the development challenges.
Question: Why are outcome assessment tools used for adults with systemic vasculitis not ideal for measuring disease activity in children?
Dr. Dolezalova: Tools used in adults are not fully applicable in children for multiple reasons. Disease presentations and outcome of primary systemic vasculitides appear to be different in children. Among the most obvious differences between adult and pediatric variants of the disease are the developmental and growth aspects; differences in functional, educational, and social impacts of longstanding disease; different drug pharmacokinetics and toxicity profiles; and the absence of comorbidities in children.
Question: What specific features have been incorporated into the PVAS?
Dr. Dolezalova: The development of the pediatric-specific tool has been a result of an international collaborative effort of pediatric rheumatologists from the vasculitis working groups of PReS (Pediatric Rheumatology European Society) and CARRA (North American Childhood Arthritis & Rheumatology Research Alliance), with the help of the European Vasculitis Study Group (EUVAS). We adapted the Birmingham Vasculitis Activity Score (BVAS 2003), the most commonly used tool in adult vasculitis patients, into PVAS. It is a systematic clinical scoring system that identifies selected features of active vasculitis in nine organ systems. Based on the analysis of the most common systemic vasculitis presentations in children reported to the PReS/PRINTO (Pediatric Rheumatology International Trials Organization) vasculitis registry, eight pediatric-relevant items and their definitions were added to the original BVAS 2003 in the cutaneous, cardiovascular, and abdominal systems. Additionally, by consensus, the maximum score for each organ system was to remain unchanged to facilitate longitudinal congruity with the BVAS. Among the 56 BVAS 2003 items, we redefined 22 for pediatric use.
Question: What were some of the challenges involved in the development of this tool?
Dr. Dolezalova: At the beginning of the process, we had to decide which principal way to follow: whether to start developing a brand new, originally pediatric tool, or to explore the applicability of existing measures and rely on the expertise of our adult rheumatology colleagues. Having gone for the second option meant that we had to accept existing adult concepts of vasculitis activity and damage assessments. The next challenge we had to overcome was that of modifying definitions of individual disease signs and symptoms from the BVAS glossary to be appropriate for pediatric patients. We wanted them to remain compatible with their adult counterparts but also to reflect pediatric reality. Learning the training process of vasculitis activity assessment and undergoing it according to the principles set up by EUVAS had been a true challenge for all pediatricians involved in the PVAS development.
Question: How is the PVAS tool being validated?
Dr. Dolezalova: The PVAS validation has been a multistep process that is now in its final stage. During consensus meetings, content and face validity were established, resulting in minor modifications to the PVAS and its glossary. Scoring of the pediatric paper cases during the training process provided information on the tool’s feasibility. Prospective real-patient assessment, including duplicate assessments by two trained researchers and follow-up evaluation in newly diagnosed or relapsing patients, provided data on the tool’s reliability, responsiveness, and discriminative ability. Currently, analysis of the prospective multicenter data on the larger patient cohort is ongoing.
Interview by Diana Mahoney
Dr. Dolezalova is the national co-coordinator of PRINTO and chairperson of the PReS clinical affairs committee. She had no relevant financial disclosures.
Overuse injuries are very common in children and teenagers, especially among kids who play sports throughout the year.
Although rare, primary systemic vasculitis in children is associated with significant mortality and morbidity when not properly treated. Optimal management of the group of multiorgan inflammatory conditions is hampered by the lack of evidence-based therapies. This shortage of data has been attributed, in part, to the absence of a standardized outcome measure for use in clinical trials, according to Dr. Pavla Dolezalova.
"Until recently, no standardized vasculitis activity assessment tool has been available for children, so some pediatric studies apply adult measures, such as the Birmingham Vasculitis Activity Score [BVAS]," she said. Further, although nonspecific inflammatory markers such as erythrocyte sedimentation rate or C-reactive protein can reflect systemic vasculitis disease activity, they do not distinguish it from infectious complications. Use of the global assessment of disease activity by the treating physician using the visual analog scale is of limited utility in clinical trials, she noted.
In an effort to facilitate more informative clinical trials of primary systemic vasculitis in children, Dr. Dolezalova of Charles University and General University Hospital in Prague, Czech Republic, and her colleagues have developed a quantitative clinical index of manifestations of active disease, called the Pediatric Vasculitis Activity Score (PVAS), which has been preliminarily validated as a useful clinical measure with good interobserver reliability (Pediatr. Rheumatol. Online J. 2011 [doi:10.1186/1546-0096-9-S1-P92]).
In this column, Dr. Dolezalova describes the need for the assessment tool as well as some of the development challenges.
Question: Why are outcome assessment tools used for adults with systemic vasculitis not ideal for measuring disease activity in children?
Dr. Dolezalova: Tools used in adults are not fully applicable in children for multiple reasons. Disease presentations and outcome of primary systemic vasculitides appear to be different in children. Among the most obvious differences between adult and pediatric variants of the disease are the developmental and growth aspects; differences in functional, educational, and social impacts of longstanding disease; different drug pharmacokinetics and toxicity profiles; and the absence of comorbidities in children.
Question: What specific features have been incorporated into the PVAS?
Dr. Dolezalova: The development of the pediatric-specific tool has been a result of an international collaborative effort of pediatric rheumatologists from the vasculitis working groups of PReS (Pediatric Rheumatology European Society) and CARRA (North American Childhood Arthritis & Rheumatology Research Alliance), with the help of the European Vasculitis Study Group (EUVAS). We adapted the Birmingham Vasculitis Activity Score (BVAS 2003), the most commonly used tool in adult vasculitis patients, into PVAS. It is a systematic clinical scoring system that identifies selected features of active vasculitis in nine organ systems. Based on the analysis of the most common systemic vasculitis presentations in children reported to the PReS/PRINTO (Pediatric Rheumatology International Trials Organization) vasculitis registry, eight pediatric-relevant items and their definitions were added to the original BVAS 2003 in the cutaneous, cardiovascular, and abdominal systems. Additionally, by consensus, the maximum score for each organ system was to remain unchanged to facilitate longitudinal congruity with the BVAS. Among the 56 BVAS 2003 items, we redefined 22 for pediatric use.
Question: What were some of the challenges involved in the development of this tool?
Dr. Dolezalova: At the beginning of the process, we had to decide which principal way to follow: whether to start developing a brand new, originally pediatric tool, or to explore the applicability of existing measures and rely on the expertise of our adult rheumatology colleagues. Having gone for the second option meant that we had to accept existing adult concepts of vasculitis activity and damage assessments. The next challenge we had to overcome was that of modifying definitions of individual disease signs and symptoms from the BVAS glossary to be appropriate for pediatric patients. We wanted them to remain compatible with their adult counterparts but also to reflect pediatric reality. Learning the training process of vasculitis activity assessment and undergoing it according to the principles set up by EUVAS had been a true challenge for all pediatricians involved in the PVAS development.
Question: How is the PVAS tool being validated?
Dr. Dolezalova: The PVAS validation has been a multistep process that is now in its final stage. During consensus meetings, content and face validity were established, resulting in minor modifications to the PVAS and its glossary. Scoring of the pediatric paper cases during the training process provided information on the tool’s feasibility. Prospective real-patient assessment, including duplicate assessments by two trained researchers and follow-up evaluation in newly diagnosed or relapsing patients, provided data on the tool’s reliability, responsiveness, and discriminative ability. Currently, analysis of the prospective multicenter data on the larger patient cohort is ongoing.
Interview by Diana Mahoney
Dr. Dolezalova is the national co-coordinator of PRINTO and chairperson of the PReS clinical affairs committee. She had no relevant financial disclosures.
Overuse injuries are very common in children and teenagers, especially among kids who play sports throughout the year.
Although rare, primary systemic vasculitis in children is associated with significant mortality and morbidity when not properly treated. Optimal management of the group of multiorgan inflammatory conditions is hampered by the lack of evidence-based therapies. This shortage of data has been attributed, in part, to the absence of a standardized outcome measure for use in clinical trials, according to Dr. Pavla Dolezalova.
"Until recently, no standardized vasculitis activity assessment tool has been available for children, so some pediatric studies apply adult measures, such as the Birmingham Vasculitis Activity Score [BVAS]," she said. Further, although nonspecific inflammatory markers such as erythrocyte sedimentation rate or C-reactive protein can reflect systemic vasculitis disease activity, they do not distinguish it from infectious complications. Use of the global assessment of disease activity by the treating physician using the visual analog scale is of limited utility in clinical trials, she noted.
In an effort to facilitate more informative clinical trials of primary systemic vasculitis in children, Dr. Dolezalova of Charles University and General University Hospital in Prague, Czech Republic, and her colleagues have developed a quantitative clinical index of manifestations of active disease, called the Pediatric Vasculitis Activity Score (PVAS), which has been preliminarily validated as a useful clinical measure with good interobserver reliability (Pediatr. Rheumatol. Online J. 2011 [doi:10.1186/1546-0096-9-S1-P92]).
In this column, Dr. Dolezalova describes the need for the assessment tool as well as some of the development challenges.
Question: Why are outcome assessment tools used for adults with systemic vasculitis not ideal for measuring disease activity in children?
Dr. Dolezalova: Tools used in adults are not fully applicable in children for multiple reasons. Disease presentations and outcome of primary systemic vasculitides appear to be different in children. Among the most obvious differences between adult and pediatric variants of the disease are the developmental and growth aspects; differences in functional, educational, and social impacts of longstanding disease; different drug pharmacokinetics and toxicity profiles; and the absence of comorbidities in children.
Question: What specific features have been incorporated into the PVAS?
Dr. Dolezalova: The development of the pediatric-specific tool has been a result of an international collaborative effort of pediatric rheumatologists from the vasculitis working groups of PReS (Pediatric Rheumatology European Society) and CARRA (North American Childhood Arthritis & Rheumatology Research Alliance), with the help of the European Vasculitis Study Group (EUVAS). We adapted the Birmingham Vasculitis Activity Score (BVAS 2003), the most commonly used tool in adult vasculitis patients, into PVAS. It is a systematic clinical scoring system that identifies selected features of active vasculitis in nine organ systems. Based on the analysis of the most common systemic vasculitis presentations in children reported to the PReS/PRINTO (Pediatric Rheumatology International Trials Organization) vasculitis registry, eight pediatric-relevant items and their definitions were added to the original BVAS 2003 in the cutaneous, cardiovascular, and abdominal systems. Additionally, by consensus, the maximum score for each organ system was to remain unchanged to facilitate longitudinal congruity with the BVAS. Among the 56 BVAS 2003 items, we redefined 22 for pediatric use.
Question: What were some of the challenges involved in the development of this tool?
Dr. Dolezalova: At the beginning of the process, we had to decide which principal way to follow: whether to start developing a brand new, originally pediatric tool, or to explore the applicability of existing measures and rely on the expertise of our adult rheumatology colleagues. Having gone for the second option meant that we had to accept existing adult concepts of vasculitis activity and damage assessments. The next challenge we had to overcome was that of modifying definitions of individual disease signs and symptoms from the BVAS glossary to be appropriate for pediatric patients. We wanted them to remain compatible with their adult counterparts but also to reflect pediatric reality. Learning the training process of vasculitis activity assessment and undergoing it according to the principles set up by EUVAS had been a true challenge for all pediatricians involved in the PVAS development.
Question: How is the PVAS tool being validated?
Dr. Dolezalova: The PVAS validation has been a multistep process that is now in its final stage. During consensus meetings, content and face validity were established, resulting in minor modifications to the PVAS and its glossary. Scoring of the pediatric paper cases during the training process provided information on the tool’s feasibility. Prospective real-patient assessment, including duplicate assessments by two trained researchers and follow-up evaluation in newly diagnosed or relapsing patients, provided data on the tool’s reliability, responsiveness, and discriminative ability. Currently, analysis of the prospective multicenter data on the larger patient cohort is ongoing.
Interview by Diana Mahoney
Dr. Dolezalova is the national co-coordinator of PRINTO and chairperson of the PReS clinical affairs committee. She had no relevant financial disclosures.
Hospitalists and Intensivists in the ICU
Observational studies suggest intensive care unit (ICU) patients have decreased mortality and length of stay (LOS) when cared for by intensivists.111 This prior literature relies on many small, single‐center studies with retrospective designs or historical controls, and compares intensivists to non‐intensivists with concurrent inpatient and outpatient responsibilities.113 These findings are the foundation for patient safety initiatives advocating intensivist involvement with all critically ill patients in urban ICUs.14
Critical care workforce evaluations predict a widening disparity between the United States supply and demand for intensivists,1516 raising concern that national ICU staffing with these specialists is not feasible. The most current data suggests that intensivists care for only one‐third of ICU patients due to a nationwide shortage.15 As a result, other specialists and generalistsincluding 75% of hospitalistsprovide critical care management.17
Despite prevalent hospitalist practice in ICUs,17 no studies evaluate their adult ICU patient outcomes, with or without intensivist consultation. Our primary aim was to compare the mortality and LOS of medical ICU patients cared for by a hospitalist team with those of an intensivist‐led team. While baseline differences were expected between each teams' patients, we hypothesized that the adjusted patient outcomes would not be different.
METHODS AND PATIENTS
Design Overview
We used a prospective observational design to measure patient mortality and LOS within 2 medical ICU staffing paradigms. This was a collaborative study between the Division of Hospital Medicine and the Division of Pulmonary and Critical Care Medicine, with approval from Emory University's Institutional Review Board.
The hospitalist ICU model was staffed by a board certified internal medicine attending, with clinical responsibilities limited to the ICU. An intensivist‐led consult team (members distinct from the intensivist‐led ICU team) was staffed by a board certified pulmonary critical care attending and non‐physician providers. This consult team comanaged mechanically ventilated patients and was available for additional critical care consultation at the hospitalists' discretion. The intensivist‐led ICU model was staffed by a board certified pulmonary critical care attending, a pulmonary critical care fellow (postgraduate years 46) and 4 internal medicine residents (postgraduate years 23).
For their respective patients, the hospitalist and intensivist‐led teams participated in similar multidisciplinary ICU rounds with the charge nurse, respiratory therapist, and pharmacist. Both teams used the same evidence‐based ICU protocols and order sets. The hospitalists and intensivists were aware of the ongoing study.
Setting and Participants
Our study was conducted in an urban, community teaching hospital that is affiliated with a major regional academic university and has 400 medical‐surgical beds, including 56 ICU beds. All medical ICU patients receiving primary medical care from the hospitalist or intensivist‐led team were assessed for inclusion between October 2007 and September 2008. Predetermined exclusion criteria included surgery under general anesthesia, outside hospital transfers, pregnancy, and age under 18.
Selection of the admitting ICU team followed existing institutional referral patterns. For emergency department (ED) patients, the ED physicians made the decision to admit to the ICU and contacted an ICU team based on the respiratory support needs of the patient, not the admitting diagnosis. ED patients with respiratory failure who required invasive ventilatory support were admitted to the intensivist‐led ICU team. Those without invasive ventilatory support were admitted to the hospitalist ICU team, including ones with respiratory failure requiring noninvasive ventilation. Patients transferred from a hospital floor bed to the ICU by non‐hospitalist physicians were assigned to the intensivist‐led ICU team, while those transferred by hospitalist floor teams were assigned to the hospitalist ICU team, regardless of diagnosis or respiratory support needs. Patient assignments deviated from these patterns, however, based on ICU teams' census. The intensivist‐led ICU team had a strict limit of 20 patients, established by the residency program, and the hospitalist ICU team had a preferred limit of 12 patients.
Measurement of Outcomes and Follow‐Up
Study endpoints were in‐hospital and ICU mortality, as well as hospital and ICU LOS. Patient characteristics and outcome data were collected prospectively from medical records and hospital databases by 2 trained research nurses according to study protocol. For data collection training, 1 investigator (K.R.W.) reviewed sample data from 108 patients to ensure consistency and accuracy of data abstraction. Patients with several ICU admissions during 1 hospitalization had ICU data collected only from the first ICU entry, consistent with other trials' methodology.1, 4, 10, 1820 Additional ICU entries did not change ICU LOS derived only from the initial entry, but did contribute to hospital LOS. Data from patients with multiple ICU entries was analyzed with the original team assignment. All patients were followed until death or hospital discharge.
Statistical Analysis
Sample size was determined a priori using an expected inpatient mortality of 10% from historical data, power of 80%, and 2‐sided alpha of 0.05 to demonstrate no difference in outcomes, defined as a mortality difference of <5% between teams. This mortality difference used for the power calculation is consistent with other trial designs.2125 The required sample size was 1306 patients calculated using PASS software (version 2008, NCSS, Kaysville, UT), accounting for an expected 3:2 admission rate to the hospitalists. The statistician was blinded to team assignments.
Clinical characteristics of the groups were compared with the Student t test. The outcome and predictor variable distributions were examined with univariate analyses. Bivariate analyses were calculated for each predictor and endpoint. Multiple logistic and linear regression analyses were performed. Propensity scores were used and defined as the conditional probability of admission to the hospitalist versus intensivist‐led ICU team given a patient's covariates. It included all predictors in Table 1 and was calculated using logistic regression. Outcome measures were excluded from the regression.
| Hospitalist No. Patients (%) | Intensivist No. Patients (%) | P Value | |
|---|---|---|---|
| |||
| Gendermale | 399 (48.2) | 256 (48.5) | 0.92 |
| Agemean (SD) | 61.3 (17.9) | 60.5 (16.3) | 0.40 |
| Race* | 0.70 | ||
| Black | 678 (81.9) | 426 (80.7) | |
| White | 141 (17.0) | 94 (17.8) | |
| Cardiovascular disease | 660 (79.7) | 432 (81.8) | 0.34 |
| Diabetes mellitus | 318 (38.4) | 212 (40.2) | 0.52 |
| Renal disease | 288 (34.8) | 189 (35.8) | 0.70 |
| Pulmonary disease | 232 (28.0) | 179 (33.9) | 0.02 |
| Neurological disorders | 219 (26.5) | 137 (26.0) | 0.84 |
| GI disease | 138 (16.7) | 90 (17.1) | 0.86 |
| Cancer | 72 (8.7) | 63 (11.9) | 0.05 |
| Morbid obesity (BMI 40) | 72 (8.7) | 28 (5.3) | 0.02 |
| HIV/AIDS | 55 (6.6) | 33 (6.3) | 0.78 |
| Immunological disorders | 26 (3.1) | 31 (5.9) | 0.01 |
| SAPS IImean (SD) | 37.4 (14.5) | 45.1 (16.9) | <0.001 |
| Noninvasive ventilation | 148 (17.9) | 136 (25.8) | <0.001 |
| Mechanical ventilation | 91 (11.0) | 274 (51.9) | <0.001 |
| Central venous catheters | 241 (29.1) | 268 (50.8) | <0.001 |
A generalized linear model (GENMOD), using a binomial distribution and an identity link function,26 assessed the in‐hospital and ICU mortality rate differences between teams while controlling for major risk factors identified. GENMOD, however, does not accommodate several covariates, as it often fails for lack of convergence. Hence, logistic regression models with adjusted odds ratios (aOR) are reported as well.
The initial logistic regression model for in‐hospital and ICU mortality included all 20 independent variables from patient demographics, comorbidities, simplified acute physiology score (SAPS) II,27 respiratory support, central venous catheter (CVC) utilization, which included peripherally placed central catheters, and all terms for 2‐way interactions with team assignment. To determine the best model, a hierarchical backward elimination was executed while assessing for interactions, confounding, and estimate precision. Before removing a regression term, a likelihood ratio test was applied to each coefficient followed by Wald's chi square test.28 Collinearity diagnostic for nonlinear models was applied to look for multicollinearity. To exclude variables or regression terms, a condition index of 30 and variance decomposition proportion of 0.5 were used. The final model was evaluated for goodness‐of‐fit using the Hosmer and Lemeshow test.
LOS was analyzed with linear regression using the same covariates and backward elimination as the logistic model. Goodness‐of‐fit was evaluated using coefficient of determination (r2). A variance inflation factor of 10 was used to assess for collinearity. Two‐sided P values 0.05 were considered statistically significant. All analyses were performed with SAS software (version 9.1, SAS Institute, Cary, NC).
RESULTS
Patients
A total of 1747 patients received critical care from the hospitalist or intensivist‐led teams (Figure 1). Of the 1367 patients who met inclusion criteria, complete data was available for 1356 patients. The ED was the ICU admission source for 68.8% of hospitalist and 69.9% of intensivist patients. Baseline patient demographics were similar (Table 1). Among preexisting comorbidities, morbid obesity was more prevalent in hospitalist patients, whereas cancer and pulmonary and immunological diseases were more prevalent in intensivist patients (Table 1).
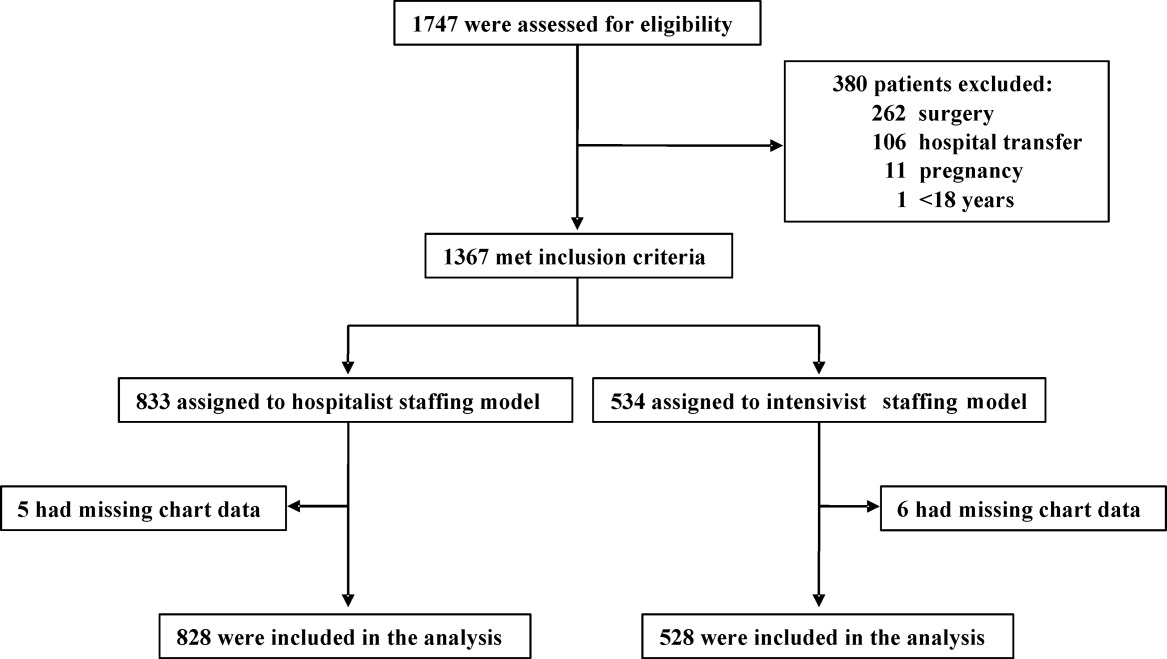
Hospitalist patients, compared to intensivist patients, had a lower mean SAPS II (37.4 vs 45.1, P < 0.001), less noninvasive (17.9% vs 25.8%, P < 0.001) and mechanical (11.0% vs 51.9%, P < 0.001) ventilation utilization, and fewer CVCs (29.1% vs 50.8%, P < 0.001) (Table 1). The intensivist‐led consult team comanaged 18.4% of the hospitalist patients. These 152 patients had a mean SAPS II of 41, and 19.7% required noninvasive ventilation while 44.1% required mechanical ventilation. For mechanically ventilated hospitalist patients, 80.2% were comanaged by the intensivist‐led consult team, 5.5% had palliative care for end‐of‐life management, 6.6% died imminently, and 7.7% received short‐term ventilation managed by the hospitalist. Hospitalist and intensivist‐led teams' ICU readmission rates were similar (7.0% vs 5.9%, P = 0.41).
Outcomes
Of the 1356 patients, there were 168 (12.4%) deaths and 135 (10.0%) occurred in the ICU. The overall mean ICU LOS was 4.0 days (SD 5.9), and mean hospital LOS was 9.1 days (SD 9.0). The mean hospital LOS for survivors was 9.0 days (SD 8.8).
Bivariate Outcomes
Patients were stratified for bivariate analysis into 3 tiers based on SAPS II to reflect low (33), intermediate (34‐51), and high (52) disease acuity corresponding to a predicted mortality of <15%, between 15 and 50%, and >50% (Table 2). Those with intermediate severity only showed an ICU LOS difference that was shorter for hospitalist patients. All remaining strata demonstrated lower mortality and LOS among the hospitalist patients (Table 2).
| Hospitalist % (No. Died) | Intensivist% (No. Died) | Mortality Rate Difference* 95% CI | P Value | |
|---|---|---|---|---|
| Hospitalist Days (No. Patients) | Intensivist Days (No. Patients) | LOS Difference 95% CI | P Value | |
| ||||
| In‐hospital mortality | ||||
| SAPS 33 | 1.4 (5) | 4.4 (6) | 3.0 (0.09, 5.80) | 0.04 |
| SAPS 34‐51 | 7.9 (16) | 10.7 (24) | 2.8 (2.10, 7.70) | 0.26 |
| SAPS 52 | 29.6 (40) | 40.6 (67) | 11.0 (0.07, 21.88) | 0.05 |
| ICU mortality | ||||
| SAPS 33 | 0.6 (2) | 3.6 (5) | 3.1 (0.80, 5.40) | 0.01 |
| SAPS 34‐51 | 6.1 (20) | 9.3 (21) | 3.3 (1.17, 7.70) | 0.15 |
| SAPS 52 | 22.2 (30) | 34.6 (57) | 12.3 (2.02, 22.63) | 0.02 |
| Hospital LOS | ||||
| SAPS 33 | 6.0 (363) | 8.2 (138) | 2.2 (0.81, 3.60) | 0.002 |
| SAPS 34‐51 | 9.8 (330) | 9.2 (225) | 0.6 (2.01, 0.77) | 0.38 |
| SAPS 52 | 10.9 (135) | 13.4 (165) | 2.5 (0.15, 5.15) | 0.06 |
| ICU LOS | ||||
| SAPS 33 | 2.2 (363) | 3.8 (138) | 1.6 (0.89, 2.27) | <0.001 |
| SAPS 34‐51 | 3.5 (330) | 4.9 (225) | 1.4 (0.44, 2.31) | 0.004 |
| SAPS 52 | 4.7 (135) | 7.4 (165) | 2.7 (0.84, 5.60) | 0.005 |
Adjusted Outcomes
The logistic and linear regression models include covariates detailed in the Table 3 legend and are referent to the hospitalist team. Logistic regression models demonstrated no difference in adjusted in‐hospital mortality (aOR 0.8 [95% confidence interval (CI): 0.49, 1.18], P = 0.23) and adjusted ICU mortality (aOR 0.8 [95% CI: 0.51, 1.32], P = 0.41) between the 2 ICU staffing models (Table 3). Linear regression models also demonstrated no difference in adjusted hospital LOS difference (0.9 days [95% CI: 1.88, 0.12], P = 0.98) and adjusted ICU LOS (0.3 days [95% CI: 0.92, 0.30], P = 0.32) (Table 3). Outcomes were re‐analyzed using propensity scores within the regression models, yielding similar results that did not change the estimate or improve precision. The overall results also remained comparable when calculations were repeated, excluding patient outliers (SAPS II >75 or hospital LOS >30days).
| Adjusted Mortality Difference [%] (95% CI) | P Value | Adjusted Mortality OR (95% CI) | P Value | Mean LOS Difference [days] (95% CI) | P Value | |
|---|---|---|---|---|---|---|
| ||||||
| All patients* (n = 1356) | ||||||
| In‐hospital | 0.3 (1.83, 1.19) | 0.68 | 0.8 (0.49, 1.18) | 0.22 | 0.9 (1.88, 0.12) | 0.98 |
| ICU | 0.2 (1.19, 1.57) | 0.79 | 0.8 (0.51, 1.32) | 0.41 | 0.3 (0.92, 0.30) | 0.32 |
| Without MV (n = 991) | ||||||
| In‐hospital | 0.2 (1.97, 1.57) | 0.82 | 0.8 (0.38, 1.56) | 0.47 | 0.2 (1.12, 0.78) | 0.72 |
| ICU | 0.4 (1.29, 2.12) | 0.63 | 1.0 (0.44, 2.27) | 0.99 | 0.03 (0.39, 0.34) | 0.89 |
| With MV (n = 365) | ||||||
| In‐hospital | 2.7 (13.69, 8.22) | 0.62 | 0.8 (0.45, 1.45) | 0.48 | 2.0 (4.74, 0.66) | 0.14 |
| ICU | 5.2 (16.10, 5.69) | 0.35 | 0.7 (0.38, 1.25) | 0.26 | 0.2 (2.18, 1.74) | 0.82 |
Subgroup Analysis
Since each team's respiratory support utilization differed greatly and was a significant variable in the logistic and linear regression models, we performed subgroup analysis of mechanically ventilated patients (Table 4). Without mechanical ventilation, no significant outcome differences were detected between the intensivist and hospitalist groups when stratified by disease severity (Table 4).
| Without Mechanical Ventilation | With Mechanical Ventilation | |||||
|---|---|---|---|---|---|---|
| Hospitalist % (No. Died) | Intensivist % (No. Died) | P Value | Hospitalist % (No. Died) | Intensivist % (No. Died) | P Value | |
| Hospitalist Days (Patients) | Intensivist Days (Patients) | P Value | Hospitalist Days (Patients) | Intensivist Days (Patients) | P Value | |
| ||||||
| In‐hospital mortality | ||||||
| SAPS 33 | 1.4 (5) | 2.2 (2) | 0.63 | 0.0 (0) | 8.9 (4) | 0.22 |
| SAPS 3451 | 5.2 (15) | 4.3 (5) | 0.72 | 27.5 (11) | 17.4 (19) | 0.18 |
| SAPS 52 | 20.0 (20) | 15.6 (7) | 0.53 | 57.1 (20) | 50.0 (60) | 0.46 |
| ICU mortality | ||||||
| SAPS 33 | 0.6 (2) | 1.1 (1) | 0.60 | 0.0 (0) | 8.9 (4) | 0.22 |
| SAPS 3451 | 3.1 (9) | 3.5 (4) | 0.86 | 27.5 (11) | 15.6 (17) | 0.10 |
| SAPS 52 | 11.0 (11) | 11.1 (5) | 0.98 | 54.3 (19) | 43.3 (52) | 0.26 |
| Hospital LOS | ||||||
| SAPS 33 | 5.6 (347) | 6.5 (93) | 0.25 | 13.8 (16) | 11.8 (45) | 0.50 |
| SAPS 3451 | 8.7 (290) | 7.9 (116) | 0.28 | 17.8 (40) | 10.6 (109) | <0.001 |
| SAPS 52 | 10.2 (100) | 11.0 (45) | 0.62 | 12.7 (35) | 14.3 (120) | 0.56 |
| ICU LOS (days) | ||||||
| SAPS 33 | 1.9 (347) | 2.2 (93) | 0.30 | 8.0 (16) | 7.0 (45) | 0.67 |
| SAPS 3451 | 2.6 (290) | 2.8 (116) | 0.52 | 10.6 (40) | 7.2 (109) | 0.02 |
| SAPS 52 | 3.5 (100) | 2.8 (45) | 0.17 | 8.1 (35) | 9.2 (120) | 0.61 |
With mechanical ventilation, patients with intermediate illness severity had a significantly shorter hospital LOS (10.6 vs 17.8 days, P < 0.001) and ICU LOS (7.2 vs 10.6 days, P = 0.02) when managed by the intensivist‐led team (Table 4). When the calculations were repeated for only the patients who survived hospitalization, the shorter ICU LOS (6.5 vs 10.9 days, P = 0.01) remained significant but not the hospital LOS (10.3 vs 19.3 days, P = 0.10). The patients with intermediate acuity also showed a trend toward a decreased ICU mortality (15.6% vs 27.5%, P = 0.10) when managed by the intensivist‐led team (Table 4).
Adjusting for relevant risk factors, no statistically significant mortality rate difference was demonstrated between the hospitalist and intensivist‐led teams when evaluating all patients or patients without mechanical ventilation. The result, however, was inconclusive for patients with mechanical ventilation and did not allow refutation of the null hypothesis because the confidence interval for the mortality rate difference crossed the prespecified mortality difference threshold for clinical significance (Figure 2).
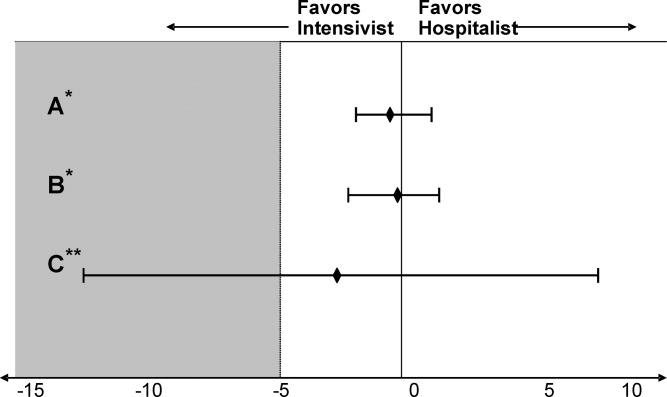
DISCUSSION
We present the first prospective evaluation of adult patient outcomes comparing intensivist‐led and hospitalist ICU staffing models. This study was powered to demonstrate no difference in hospital and ICU mortality between these ICU staffing models at a single university‐affiliated community hospital, though subgroups were not accounted for in these calculations. Consistent with our observational design, we did not influence or change established triage systems. This led to expected significant differences in baseline patient severity of illness and mechanical ventilation use. We adjusted for these and other potential confounders by stratifying patients with SAPS II, examining mechanically ventilated patients separately, and using logistic and linear regression models and propensity scores, recognizing that unmeasured differences in illness severity may remain.29
Our initial adjustment for baseline patient disparities between teams used bivariate analysis with SAPS II to stratify patients into 3 tiers to reflect low (33), intermediate (34‐51), and high (52) disease acuity. Hospitalist patients with intermediate acuity comprised the only tier without decreased in‐hospital and ICU mortality when compared to the intensivist intermediate patients (Table 2). We suspect these mortality differences are related to the intensivist patients' increased mechanical ventilation utilization seen at all acuity levels. Hospitalist patients had a significantly shorter hospital LOS for low‐acuity patients and significantly shorter ICU LOS for all severity groups (Table 2). This lower LOS may stem from greater efficiency of hospitalist ICU attendings managing transitions from the ICU in conjunction with other hospitalist colleagues. It also may reflect other unmeasured factors that affected illness severity in the intensivist patients.
When patients were stratified by both SAPS II and mechanical ventilation status, the lower mortality and LOS findings previously seen with hospitalist patients were no longer apparent (Table 4). Interestingly, patients with intermediate or high SAPS II requiring mechanical ventilation had lower mortality (10% absolute difference) in the intensivist‐led teamalbeit none reached statistical significance, probably due to small subgroup sizes (Table 4). Intensivist patients requiring mechanical ventilation also had a statistically significant shorter hospital LOS in the intermediate acuity patients (Table 4). These results contradict the controversial findings by Levy et al. which suggested that ICU patients with intermediate disease acuity have increased hospital mortality when cared for by intensivists versus non‐intensivists.18 We postulate these demonstrated differences likely reflect intensivist training and experience in caring for mechanically ventilated, higher acuity patients. Surprisingly, the presence of an intensivist‐led consult team did not mitigate the mortality and LOS differences seen for mechanically ventilated patients on the hospitalist team. Perhaps intensivist expertise was underutilized when they served in the consultant role.
The adjusted outcomes using multivariable analysis with logistic and linear regression models did not find a statistically significant difference in mortality or LOS, regardless of mechanical ventilation status (Table 3). These statistical models used 20 patient variables and identified key variables with the greatest impactSAPS II, mechanical ventilation, and CVC presence. We next examined mortality differences adjusting only for these 3 variables and were unable to detect a statistically significant mortality difference between the teams (Figure 2). We suspect that a CVC is not an independent risk factor but instead a surrogate marker of illness severity and likely of vasopressor use.
Study Limitations
Our study has several obvious limitations. It uses an observational design within a single hospital. However, this is seen in prior comparisons of intensivists to non‐intensivists.15, 810 Our study is unique with its prospective design and sample‐size calculation to demonstrate no difference in outcomes. Because our data is from a single center, it eliminates practice differences encountered when comparing multiple institutions, but it may also limit its generalizability.
Another major limitation in our comparison of an intensivist‐led ICU team to a hospitalist ICU team is their composition. Instead of 2 multidisciplinary teams, we compared a hospitalist's performance to that of a group of physicians at various levels of training. Similar comparisons have been seen in prior studies. For example, in the large study by Levy et al., half of the intensivists studied were in academic centers affiliated with teaching teams.18 Housestaff involvement, however, may have confounded the intensivist‐led team's patient outcomes. Tenner et al. demonstrated improved survival and decreased LOS in a pediatric ICU when hospitalists provided after‐hours coverage instead of residents.30 Furthermore, the patient census varied between the ICU teams, potentially impacting outcomes. While each service had only 1 attending, the hospitalist team had 1 clinician caring for patients whereas the intensivist‐led team had 5 to 6 clinicians. This study's implications may be more relevant to academic centers. A similar study of hospitalists and intensivists conducted in a nonteaching institution may yield different results.
Our 2 patient groups had substantial differences in illness severity and mechanical ventilation. Despite statistical techniques to address potential confounders in observational trials including stratification, multivariable adjustment, and propensity scores,29 residual confounders may still remain that influence the results and thus our conclusions. SAPS II is a validated method to objectively quantify disease severity and provide predictive mortality,27 however, it has known deficiencies. The use of propensity scores may not fully account for selection biases in team assignments introduced by the ED physicians. Biases may stem from the ICU teams' awareness of the ongoing study, and each team may have tried to maintain improved outcomes.
Additionally, the mortality outcomes represent in‐hospital mortality, not 30‐day mortality. This may be a less‐useful indicator of ICU performance because of post‐ICU transitions to extended care facilities and emphasis on end‐of‐life care. The majority of patients from both ICU models, however, did transfer to inpatient medical units under the care of non‐ICU hospitalist teams. Furthermore, this study did not capture important outcomes reported in other investigations, such as discharge disposition or quality of life after discharge.3132 Finally, the adjusted odds ratio for the intensivist‐led team's in‐hospital mortality (aOR 0.8, P = 0.23), referent to the hospitalist, does not eliminate the possibility that an intensivist‐led model may reduce mortality risk.
Our study suggests that intermediate‐ and high‐acuity, mechanically ventilated patients may benefit from care by intensivists rather than hospitalists. The results from this initial study could be used to design and estimate sample size for future studies of hospitalists and intensivists to elucidate risk reduction. Randomized and multicenter trials are needed to provide more robust data, because our subgroups were small and not accounted for in the sample size calculation. Considering the severe intensivist shortage, 1 strategy to provide effective and efficient coverage of the growing American ICU population may be to ask hospitalists to care independently for lower acuity ICU patientsespecially nonventilated patientswhile encouraging or requiring intensivist care for higher acuity patients, especially once mechanically ventilated.
Conclusion
We anticipate this initial study of hospitalist and intensivist‐led ICU teams will validate a hospitalist ICU staffing model for further investigation. We propose that hospitalists can provide quality care for lower acuity critical care patients. This may improve intensivist availability to higher acuity critically ill patients and allow for judicious utilization of the limited intensivist supply. Future studies may better delineate specific subgroups of critically ill patients who benefit most from intensivist primary involvement. Additional research may also help generate evidence‐based triage standards to appropriate critical care teams and foster guideline development. Hospitalists may be instrumental in the critical care staffing shortage, however, identification of their ideal role requires further study.
Acknowledgements
The authors thank Ralph Bailey, RN; Daniel S. Budnitz, MD, MPH; Kirk Easley, MPH; Michael Heisler, MD, MPH; Joan Lopez, RN; Jason Stein, MD; and David Tong MD, MPH for their support and contributions.
- ,,,,,.On‐site physician staffing in a community hospital intensivist care unit.JAMA.1984;252(15):2023–2027.
- ,,,.Impact of critical care physician staffing on patients with septic shock in a university hospital medical intensive care unit.JAMA.1988;260(23):3446–3450.
- ,.Effect on ICU mortality of a full‐time critical care specialist.Chest.1989;96(1):127–129.
- ,,, et al.Effects of organizational change in the medical intensive care unit of a teaching hospital.JAMA.1996;276(4):322–328.
- ,,, et al.Effects of a medical intensivist on patient care in a community teaching hospital.Mayo Clin Proc.1997;72(5):391–399.
- ,,, et al.A ‘closed’ medical intensive care unit (MICU) improves resource utilization when compared with an ‘open’ MICU.Am J Respir Crit Care Med.1998;157(5):1468–1473.
- ,,, et al.Organizational characteristics of intensive care units related to outcomes of abdominal aortic surgery.JAMA.1999;281(14):1310–1312.
- ,,, et al.Effects of an organized critical care service on outcomes and resource utilization: a cohort study.Crit Care Med.1999;27(2):270–274.
- ,.Out‐of‐hours consultant cover and case‐mix adjusted mortality in intensive care.Lancet.2000;356:735–736.
- ,,.The impact of organizational changes on outcomes in an intensive care unit in the United Kingdom.Intensive Care Med.2001;27:865–872.
- ,,.Do intensivists in ICU improve outcome?Best Pract Res Clin Anaesthesiol.2005;19(1):125–135.
- ,,, et al.Physician staffing patterns and clinical outcomes in critically ill patients: a systemic review.JAMA.2002;288(17):2151–2162.
- ,.Potential reduction in mortality rates using an intensivist model to manage intensive care units.Eff Clin Pract.2000;3(6):284–289.
- The Leapfrog Group Fact Sheet. ICU Physician Staffing Fact Sheet. Available at: http://www.leapfroggroup.org/media/file/Leapfrog _ICU_Physician_Staffing_Fact_Sheet.pdf and http://www.leapfroggroup.org/media/file/Fact_Sheet_Leapfrog_Group.pdf. Accessed November 8,2009.
- ,,,,.Committee on Manpower for Pulmonary and Critical Care Societies (COMPACCS). Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population?JAMA.2000;284(21):2762–2770.
- US Department of Health and Human Services, Health Resources and Services Administration (HRSA).Report to Congress: the critical care workforce; a study of the supply and demand for critical care physicians. Senate Report 108–181.Rockville, MD:HRSA; May2006.
- ,.2007–2008 Survey: The Authoritative Source on the State of the Hospital Medicine Movement.Philadelphia, PA:Society of Hospital Medicine;2008.
- ,,,,,.Association between critical care physician management and patient mortality in the intensive care unit.Ann Intern Med.2008;148(11):801–809.
- ,,,.Variations in mortality and length of stay in intensive care units.Ann Intern Med.1993;118(10):753–761.
- ,,,.Hospital mortality in relation to staff workload: a 4‐year study in an adult intensive‐care unit.Lancet.2000;356:185–189.
- ,,, et al.A comparison of albumin and saline for fluid resuscitation in the intensive care unit.N Engl J Med.2004;350(22):2247–2256.
- ,,, et al.A multicenter, randomized controlled clinical trial of transfusion requirements in critical care.N Engl J Med.1999;340(6):409–417.
- ,,, et al.Early goal‐directed therapy in the treatment of severe sepsis and septic shock.N Engl J Med.2001;345(19):1368–1377.
- ,,, et al.Intensive insulin therapy in critically ill patients.N Engl J Med.2001;345(19):1359–1367.
- ,,, et al.Pulmonary‐artery versus central venous catheter to guide treatment of acute lung injury.N Engl J Med.2006;354(21):2213–2224.
- ,.Easy SAS calculations for risk or prevalence ratios and differences.Am J Epidemiol.2005;162(3):199–200.
- ,,.A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study.JAMA.1993;270(24):2957–2963.
- .Epidemiologic methods: the “art” in the state of the art.J Clin Epidemiol.2002;55(12):1196–1200.
- ,,.Methods to adjust for bias and confounding in critical care health services research involving observational data.J Crit Care.2006;21:1–7.
- ,,.Improved survival with hospitalists in a pediatric intensive care unit.Crit Care Med.2003;31(3):847–852.
- ,.ABC of intensive care: outcome data and scoring systems.BMJ.1999;319:241–244.
- ,,.Survival, morbidity, and quality of life after discharge from intensive care.Crit Care Med.2000;28(7):2293–2299.
Observational studies suggest intensive care unit (ICU) patients have decreased mortality and length of stay (LOS) when cared for by intensivists.111 This prior literature relies on many small, single‐center studies with retrospective designs or historical controls, and compares intensivists to non‐intensivists with concurrent inpatient and outpatient responsibilities.113 These findings are the foundation for patient safety initiatives advocating intensivist involvement with all critically ill patients in urban ICUs.14
Critical care workforce evaluations predict a widening disparity between the United States supply and demand for intensivists,1516 raising concern that national ICU staffing with these specialists is not feasible. The most current data suggests that intensivists care for only one‐third of ICU patients due to a nationwide shortage.15 As a result, other specialists and generalistsincluding 75% of hospitalistsprovide critical care management.17
Despite prevalent hospitalist practice in ICUs,17 no studies evaluate their adult ICU patient outcomes, with or without intensivist consultation. Our primary aim was to compare the mortality and LOS of medical ICU patients cared for by a hospitalist team with those of an intensivist‐led team. While baseline differences were expected between each teams' patients, we hypothesized that the adjusted patient outcomes would not be different.
METHODS AND PATIENTS
Design Overview
We used a prospective observational design to measure patient mortality and LOS within 2 medical ICU staffing paradigms. This was a collaborative study between the Division of Hospital Medicine and the Division of Pulmonary and Critical Care Medicine, with approval from Emory University's Institutional Review Board.
The hospitalist ICU model was staffed by a board certified internal medicine attending, with clinical responsibilities limited to the ICU. An intensivist‐led consult team (members distinct from the intensivist‐led ICU team) was staffed by a board certified pulmonary critical care attending and non‐physician providers. This consult team comanaged mechanically ventilated patients and was available for additional critical care consultation at the hospitalists' discretion. The intensivist‐led ICU model was staffed by a board certified pulmonary critical care attending, a pulmonary critical care fellow (postgraduate years 46) and 4 internal medicine residents (postgraduate years 23).
For their respective patients, the hospitalist and intensivist‐led teams participated in similar multidisciplinary ICU rounds with the charge nurse, respiratory therapist, and pharmacist. Both teams used the same evidence‐based ICU protocols and order sets. The hospitalists and intensivists were aware of the ongoing study.
Setting and Participants
Our study was conducted in an urban, community teaching hospital that is affiliated with a major regional academic university and has 400 medical‐surgical beds, including 56 ICU beds. All medical ICU patients receiving primary medical care from the hospitalist or intensivist‐led team were assessed for inclusion between October 2007 and September 2008. Predetermined exclusion criteria included surgery under general anesthesia, outside hospital transfers, pregnancy, and age under 18.
Selection of the admitting ICU team followed existing institutional referral patterns. For emergency department (ED) patients, the ED physicians made the decision to admit to the ICU and contacted an ICU team based on the respiratory support needs of the patient, not the admitting diagnosis. ED patients with respiratory failure who required invasive ventilatory support were admitted to the intensivist‐led ICU team. Those without invasive ventilatory support were admitted to the hospitalist ICU team, including ones with respiratory failure requiring noninvasive ventilation. Patients transferred from a hospital floor bed to the ICU by non‐hospitalist physicians were assigned to the intensivist‐led ICU team, while those transferred by hospitalist floor teams were assigned to the hospitalist ICU team, regardless of diagnosis or respiratory support needs. Patient assignments deviated from these patterns, however, based on ICU teams' census. The intensivist‐led ICU team had a strict limit of 20 patients, established by the residency program, and the hospitalist ICU team had a preferred limit of 12 patients.
Measurement of Outcomes and Follow‐Up
Study endpoints were in‐hospital and ICU mortality, as well as hospital and ICU LOS. Patient characteristics and outcome data were collected prospectively from medical records and hospital databases by 2 trained research nurses according to study protocol. For data collection training, 1 investigator (K.R.W.) reviewed sample data from 108 patients to ensure consistency and accuracy of data abstraction. Patients with several ICU admissions during 1 hospitalization had ICU data collected only from the first ICU entry, consistent with other trials' methodology.1, 4, 10, 1820 Additional ICU entries did not change ICU LOS derived only from the initial entry, but did contribute to hospital LOS. Data from patients with multiple ICU entries was analyzed with the original team assignment. All patients were followed until death or hospital discharge.
Statistical Analysis
Sample size was determined a priori using an expected inpatient mortality of 10% from historical data, power of 80%, and 2‐sided alpha of 0.05 to demonstrate no difference in outcomes, defined as a mortality difference of <5% between teams. This mortality difference used for the power calculation is consistent with other trial designs.2125 The required sample size was 1306 patients calculated using PASS software (version 2008, NCSS, Kaysville, UT), accounting for an expected 3:2 admission rate to the hospitalists. The statistician was blinded to team assignments.
Clinical characteristics of the groups were compared with the Student t test. The outcome and predictor variable distributions were examined with univariate analyses. Bivariate analyses were calculated for each predictor and endpoint. Multiple logistic and linear regression analyses were performed. Propensity scores were used and defined as the conditional probability of admission to the hospitalist versus intensivist‐led ICU team given a patient's covariates. It included all predictors in Table 1 and was calculated using logistic regression. Outcome measures were excluded from the regression.
| Hospitalist No. Patients (%) | Intensivist No. Patients (%) | P Value | |
|---|---|---|---|
| |||
| Gendermale | 399 (48.2) | 256 (48.5) | 0.92 |
| Agemean (SD) | 61.3 (17.9) | 60.5 (16.3) | 0.40 |
| Race* | 0.70 | ||
| Black | 678 (81.9) | 426 (80.7) | |
| White | 141 (17.0) | 94 (17.8) | |
| Cardiovascular disease | 660 (79.7) | 432 (81.8) | 0.34 |
| Diabetes mellitus | 318 (38.4) | 212 (40.2) | 0.52 |
| Renal disease | 288 (34.8) | 189 (35.8) | 0.70 |
| Pulmonary disease | 232 (28.0) | 179 (33.9) | 0.02 |
| Neurological disorders | 219 (26.5) | 137 (26.0) | 0.84 |
| GI disease | 138 (16.7) | 90 (17.1) | 0.86 |
| Cancer | 72 (8.7) | 63 (11.9) | 0.05 |
| Morbid obesity (BMI 40) | 72 (8.7) | 28 (5.3) | 0.02 |
| HIV/AIDS | 55 (6.6) | 33 (6.3) | 0.78 |
| Immunological disorders | 26 (3.1) | 31 (5.9) | 0.01 |
| SAPS IImean (SD) | 37.4 (14.5) | 45.1 (16.9) | <0.001 |
| Noninvasive ventilation | 148 (17.9) | 136 (25.8) | <0.001 |
| Mechanical ventilation | 91 (11.0) | 274 (51.9) | <0.001 |
| Central venous catheters | 241 (29.1) | 268 (50.8) | <0.001 |
A generalized linear model (GENMOD), using a binomial distribution and an identity link function,26 assessed the in‐hospital and ICU mortality rate differences between teams while controlling for major risk factors identified. GENMOD, however, does not accommodate several covariates, as it often fails for lack of convergence. Hence, logistic regression models with adjusted odds ratios (aOR) are reported as well.
The initial logistic regression model for in‐hospital and ICU mortality included all 20 independent variables from patient demographics, comorbidities, simplified acute physiology score (SAPS) II,27 respiratory support, central venous catheter (CVC) utilization, which included peripherally placed central catheters, and all terms for 2‐way interactions with team assignment. To determine the best model, a hierarchical backward elimination was executed while assessing for interactions, confounding, and estimate precision. Before removing a regression term, a likelihood ratio test was applied to each coefficient followed by Wald's chi square test.28 Collinearity diagnostic for nonlinear models was applied to look for multicollinearity. To exclude variables or regression terms, a condition index of 30 and variance decomposition proportion of 0.5 were used. The final model was evaluated for goodness‐of‐fit using the Hosmer and Lemeshow test.
LOS was analyzed with linear regression using the same covariates and backward elimination as the logistic model. Goodness‐of‐fit was evaluated using coefficient of determination (r2). A variance inflation factor of 10 was used to assess for collinearity. Two‐sided P values 0.05 were considered statistically significant. All analyses were performed with SAS software (version 9.1, SAS Institute, Cary, NC).
RESULTS
Patients
A total of 1747 patients received critical care from the hospitalist or intensivist‐led teams (Figure 1). Of the 1367 patients who met inclusion criteria, complete data was available for 1356 patients. The ED was the ICU admission source for 68.8% of hospitalist and 69.9% of intensivist patients. Baseline patient demographics were similar (Table 1). Among preexisting comorbidities, morbid obesity was more prevalent in hospitalist patients, whereas cancer and pulmonary and immunological diseases were more prevalent in intensivist patients (Table 1).
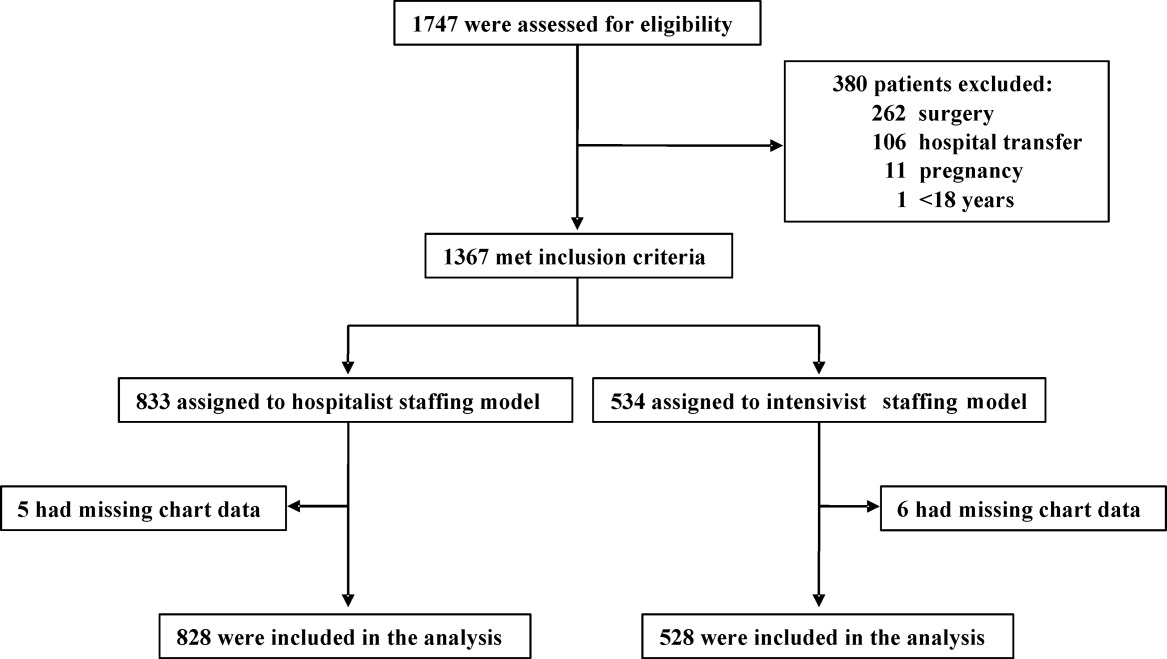
Hospitalist patients, compared to intensivist patients, had a lower mean SAPS II (37.4 vs 45.1, P < 0.001), less noninvasive (17.9% vs 25.8%, P < 0.001) and mechanical (11.0% vs 51.9%, P < 0.001) ventilation utilization, and fewer CVCs (29.1% vs 50.8%, P < 0.001) (Table 1). The intensivist‐led consult team comanaged 18.4% of the hospitalist patients. These 152 patients had a mean SAPS II of 41, and 19.7% required noninvasive ventilation while 44.1% required mechanical ventilation. For mechanically ventilated hospitalist patients, 80.2% were comanaged by the intensivist‐led consult team, 5.5% had palliative care for end‐of‐life management, 6.6% died imminently, and 7.7% received short‐term ventilation managed by the hospitalist. Hospitalist and intensivist‐led teams' ICU readmission rates were similar (7.0% vs 5.9%, P = 0.41).
Outcomes
Of the 1356 patients, there were 168 (12.4%) deaths and 135 (10.0%) occurred in the ICU. The overall mean ICU LOS was 4.0 days (SD 5.9), and mean hospital LOS was 9.1 days (SD 9.0). The mean hospital LOS for survivors was 9.0 days (SD 8.8).
Bivariate Outcomes
Patients were stratified for bivariate analysis into 3 tiers based on SAPS II to reflect low (33), intermediate (34‐51), and high (52) disease acuity corresponding to a predicted mortality of <15%, between 15 and 50%, and >50% (Table 2). Those with intermediate severity only showed an ICU LOS difference that was shorter for hospitalist patients. All remaining strata demonstrated lower mortality and LOS among the hospitalist patients (Table 2).
| Hospitalist % (No. Died) | Intensivist% (No. Died) | Mortality Rate Difference* 95% CI | P Value | |
|---|---|---|---|---|
| Hospitalist Days (No. Patients) | Intensivist Days (No. Patients) | LOS Difference 95% CI | P Value | |
| ||||
| In‐hospital mortality | ||||
| SAPS 33 | 1.4 (5) | 4.4 (6) | 3.0 (0.09, 5.80) | 0.04 |
| SAPS 34‐51 | 7.9 (16) | 10.7 (24) | 2.8 (2.10, 7.70) | 0.26 |
| SAPS 52 | 29.6 (40) | 40.6 (67) | 11.0 (0.07, 21.88) | 0.05 |
| ICU mortality | ||||
| SAPS 33 | 0.6 (2) | 3.6 (5) | 3.1 (0.80, 5.40) | 0.01 |
| SAPS 34‐51 | 6.1 (20) | 9.3 (21) | 3.3 (1.17, 7.70) | 0.15 |
| SAPS 52 | 22.2 (30) | 34.6 (57) | 12.3 (2.02, 22.63) | 0.02 |
| Hospital LOS | ||||
| SAPS 33 | 6.0 (363) | 8.2 (138) | 2.2 (0.81, 3.60) | 0.002 |
| SAPS 34‐51 | 9.8 (330) | 9.2 (225) | 0.6 (2.01, 0.77) | 0.38 |
| SAPS 52 | 10.9 (135) | 13.4 (165) | 2.5 (0.15, 5.15) | 0.06 |
| ICU LOS | ||||
| SAPS 33 | 2.2 (363) | 3.8 (138) | 1.6 (0.89, 2.27) | <0.001 |
| SAPS 34‐51 | 3.5 (330) | 4.9 (225) | 1.4 (0.44, 2.31) | 0.004 |
| SAPS 52 | 4.7 (135) | 7.4 (165) | 2.7 (0.84, 5.60) | 0.005 |
Adjusted Outcomes
The logistic and linear regression models include covariates detailed in the Table 3 legend and are referent to the hospitalist team. Logistic regression models demonstrated no difference in adjusted in‐hospital mortality (aOR 0.8 [95% confidence interval (CI): 0.49, 1.18], P = 0.23) and adjusted ICU mortality (aOR 0.8 [95% CI: 0.51, 1.32], P = 0.41) between the 2 ICU staffing models (Table 3). Linear regression models also demonstrated no difference in adjusted hospital LOS difference (0.9 days [95% CI: 1.88, 0.12], P = 0.98) and adjusted ICU LOS (0.3 days [95% CI: 0.92, 0.30], P = 0.32) (Table 3). Outcomes were re‐analyzed using propensity scores within the regression models, yielding similar results that did not change the estimate or improve precision. The overall results also remained comparable when calculations were repeated, excluding patient outliers (SAPS II >75 or hospital LOS >30days).
| Adjusted Mortality Difference [%] (95% CI) | P Value | Adjusted Mortality OR (95% CI) | P Value | Mean LOS Difference [days] (95% CI) | P Value | |
|---|---|---|---|---|---|---|
| ||||||
| All patients* (n = 1356) | ||||||
| In‐hospital | 0.3 (1.83, 1.19) | 0.68 | 0.8 (0.49, 1.18) | 0.22 | 0.9 (1.88, 0.12) | 0.98 |
| ICU | 0.2 (1.19, 1.57) | 0.79 | 0.8 (0.51, 1.32) | 0.41 | 0.3 (0.92, 0.30) | 0.32 |
| Without MV (n = 991) | ||||||
| In‐hospital | 0.2 (1.97, 1.57) | 0.82 | 0.8 (0.38, 1.56) | 0.47 | 0.2 (1.12, 0.78) | 0.72 |
| ICU | 0.4 (1.29, 2.12) | 0.63 | 1.0 (0.44, 2.27) | 0.99 | 0.03 (0.39, 0.34) | 0.89 |
| With MV (n = 365) | ||||||
| In‐hospital | 2.7 (13.69, 8.22) | 0.62 | 0.8 (0.45, 1.45) | 0.48 | 2.0 (4.74, 0.66) | 0.14 |
| ICU | 5.2 (16.10, 5.69) | 0.35 | 0.7 (0.38, 1.25) | 0.26 | 0.2 (2.18, 1.74) | 0.82 |
Subgroup Analysis
Since each team's respiratory support utilization differed greatly and was a significant variable in the logistic and linear regression models, we performed subgroup analysis of mechanically ventilated patients (Table 4). Without mechanical ventilation, no significant outcome differences were detected between the intensivist and hospitalist groups when stratified by disease severity (Table 4).
| Without Mechanical Ventilation | With Mechanical Ventilation | |||||
|---|---|---|---|---|---|---|
| Hospitalist % (No. Died) | Intensivist % (No. Died) | P Value | Hospitalist % (No. Died) | Intensivist % (No. Died) | P Value | |
| Hospitalist Days (Patients) | Intensivist Days (Patients) | P Value | Hospitalist Days (Patients) | Intensivist Days (Patients) | P Value | |
| ||||||
| In‐hospital mortality | ||||||
| SAPS 33 | 1.4 (5) | 2.2 (2) | 0.63 | 0.0 (0) | 8.9 (4) | 0.22 |
| SAPS 3451 | 5.2 (15) | 4.3 (5) | 0.72 | 27.5 (11) | 17.4 (19) | 0.18 |
| SAPS 52 | 20.0 (20) | 15.6 (7) | 0.53 | 57.1 (20) | 50.0 (60) | 0.46 |
| ICU mortality | ||||||
| SAPS 33 | 0.6 (2) | 1.1 (1) | 0.60 | 0.0 (0) | 8.9 (4) | 0.22 |
| SAPS 3451 | 3.1 (9) | 3.5 (4) | 0.86 | 27.5 (11) | 15.6 (17) | 0.10 |
| SAPS 52 | 11.0 (11) | 11.1 (5) | 0.98 | 54.3 (19) | 43.3 (52) | 0.26 |
| Hospital LOS | ||||||
| SAPS 33 | 5.6 (347) | 6.5 (93) | 0.25 | 13.8 (16) | 11.8 (45) | 0.50 |
| SAPS 3451 | 8.7 (290) | 7.9 (116) | 0.28 | 17.8 (40) | 10.6 (109) | <0.001 |
| SAPS 52 | 10.2 (100) | 11.0 (45) | 0.62 | 12.7 (35) | 14.3 (120) | 0.56 |
| ICU LOS (days) | ||||||
| SAPS 33 | 1.9 (347) | 2.2 (93) | 0.30 | 8.0 (16) | 7.0 (45) | 0.67 |
| SAPS 3451 | 2.6 (290) | 2.8 (116) | 0.52 | 10.6 (40) | 7.2 (109) | 0.02 |
| SAPS 52 | 3.5 (100) | 2.8 (45) | 0.17 | 8.1 (35) | 9.2 (120) | 0.61 |
With mechanical ventilation, patients with intermediate illness severity had a significantly shorter hospital LOS (10.6 vs 17.8 days, P < 0.001) and ICU LOS (7.2 vs 10.6 days, P = 0.02) when managed by the intensivist‐led team (Table 4). When the calculations were repeated for only the patients who survived hospitalization, the shorter ICU LOS (6.5 vs 10.9 days, P = 0.01) remained significant but not the hospital LOS (10.3 vs 19.3 days, P = 0.10). The patients with intermediate acuity also showed a trend toward a decreased ICU mortality (15.6% vs 27.5%, P = 0.10) when managed by the intensivist‐led team (Table 4).
Adjusting for relevant risk factors, no statistically significant mortality rate difference was demonstrated between the hospitalist and intensivist‐led teams when evaluating all patients or patients without mechanical ventilation. The result, however, was inconclusive for patients with mechanical ventilation and did not allow refutation of the null hypothesis because the confidence interval for the mortality rate difference crossed the prespecified mortality difference threshold for clinical significance (Figure 2).
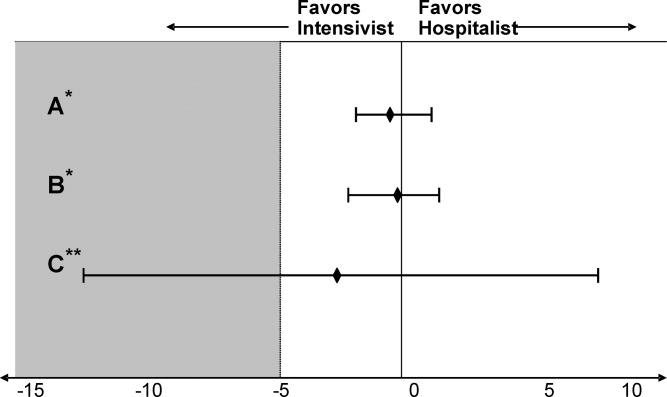
DISCUSSION
We present the first prospective evaluation of adult patient outcomes comparing intensivist‐led and hospitalist ICU staffing models. This study was powered to demonstrate no difference in hospital and ICU mortality between these ICU staffing models at a single university‐affiliated community hospital, though subgroups were not accounted for in these calculations. Consistent with our observational design, we did not influence or change established triage systems. This led to expected significant differences in baseline patient severity of illness and mechanical ventilation use. We adjusted for these and other potential confounders by stratifying patients with SAPS II, examining mechanically ventilated patients separately, and using logistic and linear regression models and propensity scores, recognizing that unmeasured differences in illness severity may remain.29
Our initial adjustment for baseline patient disparities between teams used bivariate analysis with SAPS II to stratify patients into 3 tiers to reflect low (33), intermediate (34‐51), and high (52) disease acuity. Hospitalist patients with intermediate acuity comprised the only tier without decreased in‐hospital and ICU mortality when compared to the intensivist intermediate patients (Table 2). We suspect these mortality differences are related to the intensivist patients' increased mechanical ventilation utilization seen at all acuity levels. Hospitalist patients had a significantly shorter hospital LOS for low‐acuity patients and significantly shorter ICU LOS for all severity groups (Table 2). This lower LOS may stem from greater efficiency of hospitalist ICU attendings managing transitions from the ICU in conjunction with other hospitalist colleagues. It also may reflect other unmeasured factors that affected illness severity in the intensivist patients.
When patients were stratified by both SAPS II and mechanical ventilation status, the lower mortality and LOS findings previously seen with hospitalist patients were no longer apparent (Table 4). Interestingly, patients with intermediate or high SAPS II requiring mechanical ventilation had lower mortality (10% absolute difference) in the intensivist‐led teamalbeit none reached statistical significance, probably due to small subgroup sizes (Table 4). Intensivist patients requiring mechanical ventilation also had a statistically significant shorter hospital LOS in the intermediate acuity patients (Table 4). These results contradict the controversial findings by Levy et al. which suggested that ICU patients with intermediate disease acuity have increased hospital mortality when cared for by intensivists versus non‐intensivists.18 We postulate these demonstrated differences likely reflect intensivist training and experience in caring for mechanically ventilated, higher acuity patients. Surprisingly, the presence of an intensivist‐led consult team did not mitigate the mortality and LOS differences seen for mechanically ventilated patients on the hospitalist team. Perhaps intensivist expertise was underutilized when they served in the consultant role.
The adjusted outcomes using multivariable analysis with logistic and linear regression models did not find a statistically significant difference in mortality or LOS, regardless of mechanical ventilation status (Table 3). These statistical models used 20 patient variables and identified key variables with the greatest impactSAPS II, mechanical ventilation, and CVC presence. We next examined mortality differences adjusting only for these 3 variables and were unable to detect a statistically significant mortality difference between the teams (Figure 2). We suspect that a CVC is not an independent risk factor but instead a surrogate marker of illness severity and likely of vasopressor use.
Study Limitations
Our study has several obvious limitations. It uses an observational design within a single hospital. However, this is seen in prior comparisons of intensivists to non‐intensivists.15, 810 Our study is unique with its prospective design and sample‐size calculation to demonstrate no difference in outcomes. Because our data is from a single center, it eliminates practice differences encountered when comparing multiple institutions, but it may also limit its generalizability.
Another major limitation in our comparison of an intensivist‐led ICU team to a hospitalist ICU team is their composition. Instead of 2 multidisciplinary teams, we compared a hospitalist's performance to that of a group of physicians at various levels of training. Similar comparisons have been seen in prior studies. For example, in the large study by Levy et al., half of the intensivists studied were in academic centers affiliated with teaching teams.18 Housestaff involvement, however, may have confounded the intensivist‐led team's patient outcomes. Tenner et al. demonstrated improved survival and decreased LOS in a pediatric ICU when hospitalists provided after‐hours coverage instead of residents.30 Furthermore, the patient census varied between the ICU teams, potentially impacting outcomes. While each service had only 1 attending, the hospitalist team had 1 clinician caring for patients whereas the intensivist‐led team had 5 to 6 clinicians. This study's implications may be more relevant to academic centers. A similar study of hospitalists and intensivists conducted in a nonteaching institution may yield different results.
Our 2 patient groups had substantial differences in illness severity and mechanical ventilation. Despite statistical techniques to address potential confounders in observational trials including stratification, multivariable adjustment, and propensity scores,29 residual confounders may still remain that influence the results and thus our conclusions. SAPS II is a validated method to objectively quantify disease severity and provide predictive mortality,27 however, it has known deficiencies. The use of propensity scores may not fully account for selection biases in team assignments introduced by the ED physicians. Biases may stem from the ICU teams' awareness of the ongoing study, and each team may have tried to maintain improved outcomes.
Additionally, the mortality outcomes represent in‐hospital mortality, not 30‐day mortality. This may be a less‐useful indicator of ICU performance because of post‐ICU transitions to extended care facilities and emphasis on end‐of‐life care. The majority of patients from both ICU models, however, did transfer to inpatient medical units under the care of non‐ICU hospitalist teams. Furthermore, this study did not capture important outcomes reported in other investigations, such as discharge disposition or quality of life after discharge.3132 Finally, the adjusted odds ratio for the intensivist‐led team's in‐hospital mortality (aOR 0.8, P = 0.23), referent to the hospitalist, does not eliminate the possibility that an intensivist‐led model may reduce mortality risk.
Our study suggests that intermediate‐ and high‐acuity, mechanically ventilated patients may benefit from care by intensivists rather than hospitalists. The results from this initial study could be used to design and estimate sample size for future studies of hospitalists and intensivists to elucidate risk reduction. Randomized and multicenter trials are needed to provide more robust data, because our subgroups were small and not accounted for in the sample size calculation. Considering the severe intensivist shortage, 1 strategy to provide effective and efficient coverage of the growing American ICU population may be to ask hospitalists to care independently for lower acuity ICU patientsespecially nonventilated patientswhile encouraging or requiring intensivist care for higher acuity patients, especially once mechanically ventilated.
Conclusion
We anticipate this initial study of hospitalist and intensivist‐led ICU teams will validate a hospitalist ICU staffing model for further investigation. We propose that hospitalists can provide quality care for lower acuity critical care patients. This may improve intensivist availability to higher acuity critically ill patients and allow for judicious utilization of the limited intensivist supply. Future studies may better delineate specific subgroups of critically ill patients who benefit most from intensivist primary involvement. Additional research may also help generate evidence‐based triage standards to appropriate critical care teams and foster guideline development. Hospitalists may be instrumental in the critical care staffing shortage, however, identification of their ideal role requires further study.
Acknowledgements
The authors thank Ralph Bailey, RN; Daniel S. Budnitz, MD, MPH; Kirk Easley, MPH; Michael Heisler, MD, MPH; Joan Lopez, RN; Jason Stein, MD; and David Tong MD, MPH for their support and contributions.
Observational studies suggest intensive care unit (ICU) patients have decreased mortality and length of stay (LOS) when cared for by intensivists.111 This prior literature relies on many small, single‐center studies with retrospective designs or historical controls, and compares intensivists to non‐intensivists with concurrent inpatient and outpatient responsibilities.113 These findings are the foundation for patient safety initiatives advocating intensivist involvement with all critically ill patients in urban ICUs.14
Critical care workforce evaluations predict a widening disparity between the United States supply and demand for intensivists,1516 raising concern that national ICU staffing with these specialists is not feasible. The most current data suggests that intensivists care for only one‐third of ICU patients due to a nationwide shortage.15 As a result, other specialists and generalistsincluding 75% of hospitalistsprovide critical care management.17
Despite prevalent hospitalist practice in ICUs,17 no studies evaluate their adult ICU patient outcomes, with or without intensivist consultation. Our primary aim was to compare the mortality and LOS of medical ICU patients cared for by a hospitalist team with those of an intensivist‐led team. While baseline differences were expected between each teams' patients, we hypothesized that the adjusted patient outcomes would not be different.
METHODS AND PATIENTS
Design Overview
We used a prospective observational design to measure patient mortality and LOS within 2 medical ICU staffing paradigms. This was a collaborative study between the Division of Hospital Medicine and the Division of Pulmonary and Critical Care Medicine, with approval from Emory University's Institutional Review Board.
The hospitalist ICU model was staffed by a board certified internal medicine attending, with clinical responsibilities limited to the ICU. An intensivist‐led consult team (members distinct from the intensivist‐led ICU team) was staffed by a board certified pulmonary critical care attending and non‐physician providers. This consult team comanaged mechanically ventilated patients and was available for additional critical care consultation at the hospitalists' discretion. The intensivist‐led ICU model was staffed by a board certified pulmonary critical care attending, a pulmonary critical care fellow (postgraduate years 46) and 4 internal medicine residents (postgraduate years 23).
For their respective patients, the hospitalist and intensivist‐led teams participated in similar multidisciplinary ICU rounds with the charge nurse, respiratory therapist, and pharmacist. Both teams used the same evidence‐based ICU protocols and order sets. The hospitalists and intensivists were aware of the ongoing study.
Setting and Participants
Our study was conducted in an urban, community teaching hospital that is affiliated with a major regional academic university and has 400 medical‐surgical beds, including 56 ICU beds. All medical ICU patients receiving primary medical care from the hospitalist or intensivist‐led team were assessed for inclusion between October 2007 and September 2008. Predetermined exclusion criteria included surgery under general anesthesia, outside hospital transfers, pregnancy, and age under 18.
Selection of the admitting ICU team followed existing institutional referral patterns. For emergency department (ED) patients, the ED physicians made the decision to admit to the ICU and contacted an ICU team based on the respiratory support needs of the patient, not the admitting diagnosis. ED patients with respiratory failure who required invasive ventilatory support were admitted to the intensivist‐led ICU team. Those without invasive ventilatory support were admitted to the hospitalist ICU team, including ones with respiratory failure requiring noninvasive ventilation. Patients transferred from a hospital floor bed to the ICU by non‐hospitalist physicians were assigned to the intensivist‐led ICU team, while those transferred by hospitalist floor teams were assigned to the hospitalist ICU team, regardless of diagnosis or respiratory support needs. Patient assignments deviated from these patterns, however, based on ICU teams' census. The intensivist‐led ICU team had a strict limit of 20 patients, established by the residency program, and the hospitalist ICU team had a preferred limit of 12 patients.
Measurement of Outcomes and Follow‐Up
Study endpoints were in‐hospital and ICU mortality, as well as hospital and ICU LOS. Patient characteristics and outcome data were collected prospectively from medical records and hospital databases by 2 trained research nurses according to study protocol. For data collection training, 1 investigator (K.R.W.) reviewed sample data from 108 patients to ensure consistency and accuracy of data abstraction. Patients with several ICU admissions during 1 hospitalization had ICU data collected only from the first ICU entry, consistent with other trials' methodology.1, 4, 10, 1820 Additional ICU entries did not change ICU LOS derived only from the initial entry, but did contribute to hospital LOS. Data from patients with multiple ICU entries was analyzed with the original team assignment. All patients were followed until death or hospital discharge.
Statistical Analysis
Sample size was determined a priori using an expected inpatient mortality of 10% from historical data, power of 80%, and 2‐sided alpha of 0.05 to demonstrate no difference in outcomes, defined as a mortality difference of <5% between teams. This mortality difference used for the power calculation is consistent with other trial designs.2125 The required sample size was 1306 patients calculated using PASS software (version 2008, NCSS, Kaysville, UT), accounting for an expected 3:2 admission rate to the hospitalists. The statistician was blinded to team assignments.
Clinical characteristics of the groups were compared with the Student t test. The outcome and predictor variable distributions were examined with univariate analyses. Bivariate analyses were calculated for each predictor and endpoint. Multiple logistic and linear regression analyses were performed. Propensity scores were used and defined as the conditional probability of admission to the hospitalist versus intensivist‐led ICU team given a patient's covariates. It included all predictors in Table 1 and was calculated using logistic regression. Outcome measures were excluded from the regression.
| Hospitalist No. Patients (%) | Intensivist No. Patients (%) | P Value | |
|---|---|---|---|
| |||
| Gendermale | 399 (48.2) | 256 (48.5) | 0.92 |
| Agemean (SD) | 61.3 (17.9) | 60.5 (16.3) | 0.40 |
| Race* | 0.70 | ||
| Black | 678 (81.9) | 426 (80.7) | |
| White | 141 (17.0) | 94 (17.8) | |
| Cardiovascular disease | 660 (79.7) | 432 (81.8) | 0.34 |
| Diabetes mellitus | 318 (38.4) | 212 (40.2) | 0.52 |
| Renal disease | 288 (34.8) | 189 (35.8) | 0.70 |
| Pulmonary disease | 232 (28.0) | 179 (33.9) | 0.02 |
| Neurological disorders | 219 (26.5) | 137 (26.0) | 0.84 |
| GI disease | 138 (16.7) | 90 (17.1) | 0.86 |
| Cancer | 72 (8.7) | 63 (11.9) | 0.05 |
| Morbid obesity (BMI 40) | 72 (8.7) | 28 (5.3) | 0.02 |
| HIV/AIDS | 55 (6.6) | 33 (6.3) | 0.78 |
| Immunological disorders | 26 (3.1) | 31 (5.9) | 0.01 |
| SAPS IImean (SD) | 37.4 (14.5) | 45.1 (16.9) | <0.001 |
| Noninvasive ventilation | 148 (17.9) | 136 (25.8) | <0.001 |
| Mechanical ventilation | 91 (11.0) | 274 (51.9) | <0.001 |
| Central venous catheters | 241 (29.1) | 268 (50.8) | <0.001 |
A generalized linear model (GENMOD), using a binomial distribution and an identity link function,26 assessed the in‐hospital and ICU mortality rate differences between teams while controlling for major risk factors identified. GENMOD, however, does not accommodate several covariates, as it often fails for lack of convergence. Hence, logistic regression models with adjusted odds ratios (aOR) are reported as well.
The initial logistic regression model for in‐hospital and ICU mortality included all 20 independent variables from patient demographics, comorbidities, simplified acute physiology score (SAPS) II,27 respiratory support, central venous catheter (CVC) utilization, which included peripherally placed central catheters, and all terms for 2‐way interactions with team assignment. To determine the best model, a hierarchical backward elimination was executed while assessing for interactions, confounding, and estimate precision. Before removing a regression term, a likelihood ratio test was applied to each coefficient followed by Wald's chi square test.28 Collinearity diagnostic for nonlinear models was applied to look for multicollinearity. To exclude variables or regression terms, a condition index of 30 and variance decomposition proportion of 0.5 were used. The final model was evaluated for goodness‐of‐fit using the Hosmer and Lemeshow test.
LOS was analyzed with linear regression using the same covariates and backward elimination as the logistic model. Goodness‐of‐fit was evaluated using coefficient of determination (r2). A variance inflation factor of 10 was used to assess for collinearity. Two‐sided P values 0.05 were considered statistically significant. All analyses were performed with SAS software (version 9.1, SAS Institute, Cary, NC).
RESULTS
Patients
A total of 1747 patients received critical care from the hospitalist or intensivist‐led teams (Figure 1). Of the 1367 patients who met inclusion criteria, complete data was available for 1356 patients. The ED was the ICU admission source for 68.8% of hospitalist and 69.9% of intensivist patients. Baseline patient demographics were similar (Table 1). Among preexisting comorbidities, morbid obesity was more prevalent in hospitalist patients, whereas cancer and pulmonary and immunological diseases were more prevalent in intensivist patients (Table 1).
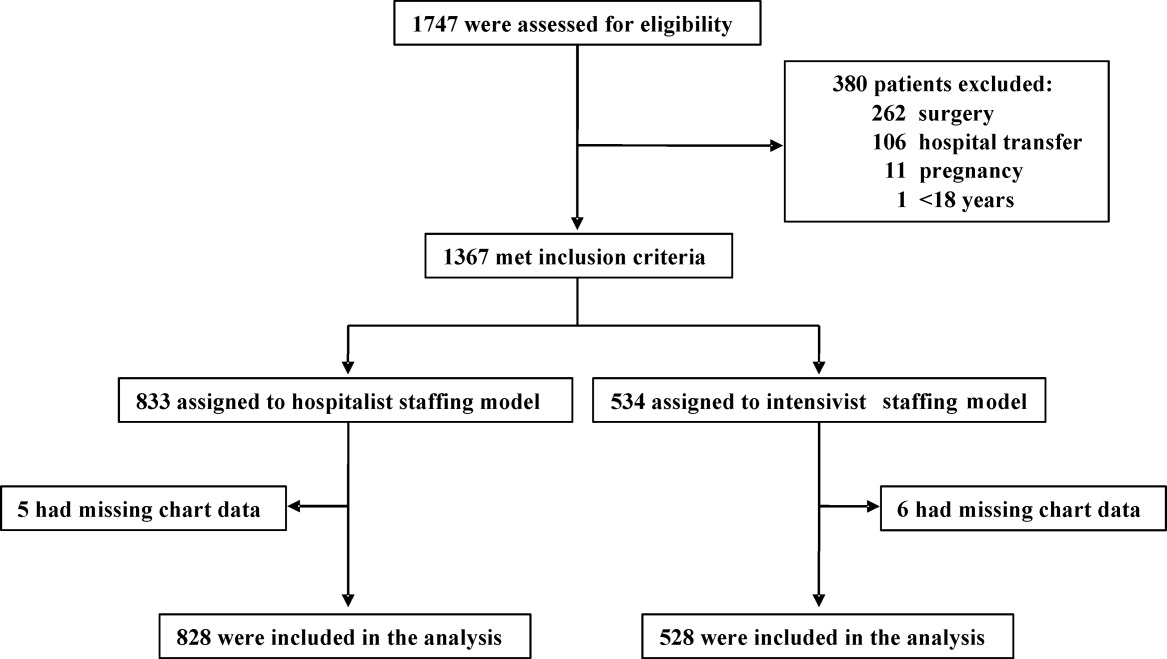
Hospitalist patients, compared to intensivist patients, had a lower mean SAPS II (37.4 vs 45.1, P < 0.001), less noninvasive (17.9% vs 25.8%, P < 0.001) and mechanical (11.0% vs 51.9%, P < 0.001) ventilation utilization, and fewer CVCs (29.1% vs 50.8%, P < 0.001) (Table 1). The intensivist‐led consult team comanaged 18.4% of the hospitalist patients. These 152 patients had a mean SAPS II of 41, and 19.7% required noninvasive ventilation while 44.1% required mechanical ventilation. For mechanically ventilated hospitalist patients, 80.2% were comanaged by the intensivist‐led consult team, 5.5% had palliative care for end‐of‐life management, 6.6% died imminently, and 7.7% received short‐term ventilation managed by the hospitalist. Hospitalist and intensivist‐led teams' ICU readmission rates were similar (7.0% vs 5.9%, P = 0.41).
Outcomes
Of the 1356 patients, there were 168 (12.4%) deaths and 135 (10.0%) occurred in the ICU. The overall mean ICU LOS was 4.0 days (SD 5.9), and mean hospital LOS was 9.1 days (SD 9.0). The mean hospital LOS for survivors was 9.0 days (SD 8.8).
Bivariate Outcomes
Patients were stratified for bivariate analysis into 3 tiers based on SAPS II to reflect low (33), intermediate (34‐51), and high (52) disease acuity corresponding to a predicted mortality of <15%, between 15 and 50%, and >50% (Table 2). Those with intermediate severity only showed an ICU LOS difference that was shorter for hospitalist patients. All remaining strata demonstrated lower mortality and LOS among the hospitalist patients (Table 2).
| Hospitalist % (No. Died) | Intensivist% (No. Died) | Mortality Rate Difference* 95% CI | P Value | |
|---|---|---|---|---|
| Hospitalist Days (No. Patients) | Intensivist Days (No. Patients) | LOS Difference 95% CI | P Value | |
| ||||
| In‐hospital mortality | ||||
| SAPS 33 | 1.4 (5) | 4.4 (6) | 3.0 (0.09, 5.80) | 0.04 |
| SAPS 34‐51 | 7.9 (16) | 10.7 (24) | 2.8 (2.10, 7.70) | 0.26 |
| SAPS 52 | 29.6 (40) | 40.6 (67) | 11.0 (0.07, 21.88) | 0.05 |
| ICU mortality | ||||
| SAPS 33 | 0.6 (2) | 3.6 (5) | 3.1 (0.80, 5.40) | 0.01 |
| SAPS 34‐51 | 6.1 (20) | 9.3 (21) | 3.3 (1.17, 7.70) | 0.15 |
| SAPS 52 | 22.2 (30) | 34.6 (57) | 12.3 (2.02, 22.63) | 0.02 |
| Hospital LOS | ||||
| SAPS 33 | 6.0 (363) | 8.2 (138) | 2.2 (0.81, 3.60) | 0.002 |
| SAPS 34‐51 | 9.8 (330) | 9.2 (225) | 0.6 (2.01, 0.77) | 0.38 |
| SAPS 52 | 10.9 (135) | 13.4 (165) | 2.5 (0.15, 5.15) | 0.06 |
| ICU LOS | ||||
| SAPS 33 | 2.2 (363) | 3.8 (138) | 1.6 (0.89, 2.27) | <0.001 |
| SAPS 34‐51 | 3.5 (330) | 4.9 (225) | 1.4 (0.44, 2.31) | 0.004 |
| SAPS 52 | 4.7 (135) | 7.4 (165) | 2.7 (0.84, 5.60) | 0.005 |
Adjusted Outcomes
The logistic and linear regression models include covariates detailed in the Table 3 legend and are referent to the hospitalist team. Logistic regression models demonstrated no difference in adjusted in‐hospital mortality (aOR 0.8 [95% confidence interval (CI): 0.49, 1.18], P = 0.23) and adjusted ICU mortality (aOR 0.8 [95% CI: 0.51, 1.32], P = 0.41) between the 2 ICU staffing models (Table 3). Linear regression models also demonstrated no difference in adjusted hospital LOS difference (0.9 days [95% CI: 1.88, 0.12], P = 0.98) and adjusted ICU LOS (0.3 days [95% CI: 0.92, 0.30], P = 0.32) (Table 3). Outcomes were re‐analyzed using propensity scores within the regression models, yielding similar results that did not change the estimate or improve precision. The overall results also remained comparable when calculations were repeated, excluding patient outliers (SAPS II >75 or hospital LOS >30days).
| Adjusted Mortality Difference [%] (95% CI) | P Value | Adjusted Mortality OR (95% CI) | P Value | Mean LOS Difference [days] (95% CI) | P Value | |
|---|---|---|---|---|---|---|
| ||||||
| All patients* (n = 1356) | ||||||
| In‐hospital | 0.3 (1.83, 1.19) | 0.68 | 0.8 (0.49, 1.18) | 0.22 | 0.9 (1.88, 0.12) | 0.98 |
| ICU | 0.2 (1.19, 1.57) | 0.79 | 0.8 (0.51, 1.32) | 0.41 | 0.3 (0.92, 0.30) | 0.32 |
| Without MV (n = 991) | ||||||
| In‐hospital | 0.2 (1.97, 1.57) | 0.82 | 0.8 (0.38, 1.56) | 0.47 | 0.2 (1.12, 0.78) | 0.72 |
| ICU | 0.4 (1.29, 2.12) | 0.63 | 1.0 (0.44, 2.27) | 0.99 | 0.03 (0.39, 0.34) | 0.89 |
| With MV (n = 365) | ||||||
| In‐hospital | 2.7 (13.69, 8.22) | 0.62 | 0.8 (0.45, 1.45) | 0.48 | 2.0 (4.74, 0.66) | 0.14 |
| ICU | 5.2 (16.10, 5.69) | 0.35 | 0.7 (0.38, 1.25) | 0.26 | 0.2 (2.18, 1.74) | 0.82 |
Subgroup Analysis
Since each team's respiratory support utilization differed greatly and was a significant variable in the logistic and linear regression models, we performed subgroup analysis of mechanically ventilated patients (Table 4). Without mechanical ventilation, no significant outcome differences were detected between the intensivist and hospitalist groups when stratified by disease severity (Table 4).
| Without Mechanical Ventilation | With Mechanical Ventilation | |||||
|---|---|---|---|---|---|---|
| Hospitalist % (No. Died) | Intensivist % (No. Died) | P Value | Hospitalist % (No. Died) | Intensivist % (No. Died) | P Value | |
| Hospitalist Days (Patients) | Intensivist Days (Patients) | P Value | Hospitalist Days (Patients) | Intensivist Days (Patients) | P Value | |
| ||||||
| In‐hospital mortality | ||||||
| SAPS 33 | 1.4 (5) | 2.2 (2) | 0.63 | 0.0 (0) | 8.9 (4) | 0.22 |
| SAPS 3451 | 5.2 (15) | 4.3 (5) | 0.72 | 27.5 (11) | 17.4 (19) | 0.18 |
| SAPS 52 | 20.0 (20) | 15.6 (7) | 0.53 | 57.1 (20) | 50.0 (60) | 0.46 |
| ICU mortality | ||||||
| SAPS 33 | 0.6 (2) | 1.1 (1) | 0.60 | 0.0 (0) | 8.9 (4) | 0.22 |
| SAPS 3451 | 3.1 (9) | 3.5 (4) | 0.86 | 27.5 (11) | 15.6 (17) | 0.10 |
| SAPS 52 | 11.0 (11) | 11.1 (5) | 0.98 | 54.3 (19) | 43.3 (52) | 0.26 |
| Hospital LOS | ||||||
| SAPS 33 | 5.6 (347) | 6.5 (93) | 0.25 | 13.8 (16) | 11.8 (45) | 0.50 |
| SAPS 3451 | 8.7 (290) | 7.9 (116) | 0.28 | 17.8 (40) | 10.6 (109) | <0.001 |
| SAPS 52 | 10.2 (100) | 11.0 (45) | 0.62 | 12.7 (35) | 14.3 (120) | 0.56 |
| ICU LOS (days) | ||||||
| SAPS 33 | 1.9 (347) | 2.2 (93) | 0.30 | 8.0 (16) | 7.0 (45) | 0.67 |
| SAPS 3451 | 2.6 (290) | 2.8 (116) | 0.52 | 10.6 (40) | 7.2 (109) | 0.02 |
| SAPS 52 | 3.5 (100) | 2.8 (45) | 0.17 | 8.1 (35) | 9.2 (120) | 0.61 |
With mechanical ventilation, patients with intermediate illness severity had a significantly shorter hospital LOS (10.6 vs 17.8 days, P < 0.001) and ICU LOS (7.2 vs 10.6 days, P = 0.02) when managed by the intensivist‐led team (Table 4). When the calculations were repeated for only the patients who survived hospitalization, the shorter ICU LOS (6.5 vs 10.9 days, P = 0.01) remained significant but not the hospital LOS (10.3 vs 19.3 days, P = 0.10). The patients with intermediate acuity also showed a trend toward a decreased ICU mortality (15.6% vs 27.5%, P = 0.10) when managed by the intensivist‐led team (Table 4).
Adjusting for relevant risk factors, no statistically significant mortality rate difference was demonstrated between the hospitalist and intensivist‐led teams when evaluating all patients or patients without mechanical ventilation. The result, however, was inconclusive for patients with mechanical ventilation and did not allow refutation of the null hypothesis because the confidence interval for the mortality rate difference crossed the prespecified mortality difference threshold for clinical significance (Figure 2).
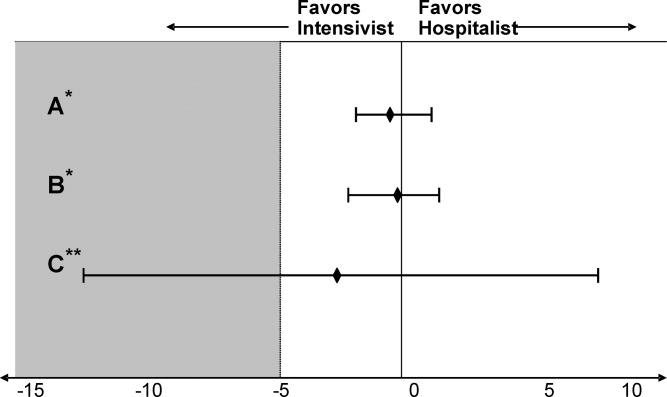
DISCUSSION
We present the first prospective evaluation of adult patient outcomes comparing intensivist‐led and hospitalist ICU staffing models. This study was powered to demonstrate no difference in hospital and ICU mortality between these ICU staffing models at a single university‐affiliated community hospital, though subgroups were not accounted for in these calculations. Consistent with our observational design, we did not influence or change established triage systems. This led to expected significant differences in baseline patient severity of illness and mechanical ventilation use. We adjusted for these and other potential confounders by stratifying patients with SAPS II, examining mechanically ventilated patients separately, and using logistic and linear regression models and propensity scores, recognizing that unmeasured differences in illness severity may remain.29
Our initial adjustment for baseline patient disparities between teams used bivariate analysis with SAPS II to stratify patients into 3 tiers to reflect low (33), intermediate (34‐51), and high (52) disease acuity. Hospitalist patients with intermediate acuity comprised the only tier without decreased in‐hospital and ICU mortality when compared to the intensivist intermediate patients (Table 2). We suspect these mortality differences are related to the intensivist patients' increased mechanical ventilation utilization seen at all acuity levels. Hospitalist patients had a significantly shorter hospital LOS for low‐acuity patients and significantly shorter ICU LOS for all severity groups (Table 2). This lower LOS may stem from greater efficiency of hospitalist ICU attendings managing transitions from the ICU in conjunction with other hospitalist colleagues. It also may reflect other unmeasured factors that affected illness severity in the intensivist patients.
When patients were stratified by both SAPS II and mechanical ventilation status, the lower mortality and LOS findings previously seen with hospitalist patients were no longer apparent (Table 4). Interestingly, patients with intermediate or high SAPS II requiring mechanical ventilation had lower mortality (10% absolute difference) in the intensivist‐led teamalbeit none reached statistical significance, probably due to small subgroup sizes (Table 4). Intensivist patients requiring mechanical ventilation also had a statistically significant shorter hospital LOS in the intermediate acuity patients (Table 4). These results contradict the controversial findings by Levy et al. which suggested that ICU patients with intermediate disease acuity have increased hospital mortality when cared for by intensivists versus non‐intensivists.18 We postulate these demonstrated differences likely reflect intensivist training and experience in caring for mechanically ventilated, higher acuity patients. Surprisingly, the presence of an intensivist‐led consult team did not mitigate the mortality and LOS differences seen for mechanically ventilated patients on the hospitalist team. Perhaps intensivist expertise was underutilized when they served in the consultant role.
The adjusted outcomes using multivariable analysis with logistic and linear regression models did not find a statistically significant difference in mortality or LOS, regardless of mechanical ventilation status (Table 3). These statistical models used 20 patient variables and identified key variables with the greatest impactSAPS II, mechanical ventilation, and CVC presence. We next examined mortality differences adjusting only for these 3 variables and were unable to detect a statistically significant mortality difference between the teams (Figure 2). We suspect that a CVC is not an independent risk factor but instead a surrogate marker of illness severity and likely of vasopressor use.
Study Limitations
Our study has several obvious limitations. It uses an observational design within a single hospital. However, this is seen in prior comparisons of intensivists to non‐intensivists.15, 810 Our study is unique with its prospective design and sample‐size calculation to demonstrate no difference in outcomes. Because our data is from a single center, it eliminates practice differences encountered when comparing multiple institutions, but it may also limit its generalizability.
Another major limitation in our comparison of an intensivist‐led ICU team to a hospitalist ICU team is their composition. Instead of 2 multidisciplinary teams, we compared a hospitalist's performance to that of a group of physicians at various levels of training. Similar comparisons have been seen in prior studies. For example, in the large study by Levy et al., half of the intensivists studied were in academic centers affiliated with teaching teams.18 Housestaff involvement, however, may have confounded the intensivist‐led team's patient outcomes. Tenner et al. demonstrated improved survival and decreased LOS in a pediatric ICU when hospitalists provided after‐hours coverage instead of residents.30 Furthermore, the patient census varied between the ICU teams, potentially impacting outcomes. While each service had only 1 attending, the hospitalist team had 1 clinician caring for patients whereas the intensivist‐led team had 5 to 6 clinicians. This study's implications may be more relevant to academic centers. A similar study of hospitalists and intensivists conducted in a nonteaching institution may yield different results.
Our 2 patient groups had substantial differences in illness severity and mechanical ventilation. Despite statistical techniques to address potential confounders in observational trials including stratification, multivariable adjustment, and propensity scores,29 residual confounders may still remain that influence the results and thus our conclusions. SAPS II is a validated method to objectively quantify disease severity and provide predictive mortality,27 however, it has known deficiencies. The use of propensity scores may not fully account for selection biases in team assignments introduced by the ED physicians. Biases may stem from the ICU teams' awareness of the ongoing study, and each team may have tried to maintain improved outcomes.
Additionally, the mortality outcomes represent in‐hospital mortality, not 30‐day mortality. This may be a less‐useful indicator of ICU performance because of post‐ICU transitions to extended care facilities and emphasis on end‐of‐life care. The majority of patients from both ICU models, however, did transfer to inpatient medical units under the care of non‐ICU hospitalist teams. Furthermore, this study did not capture important outcomes reported in other investigations, such as discharge disposition or quality of life after discharge.3132 Finally, the adjusted odds ratio for the intensivist‐led team's in‐hospital mortality (aOR 0.8, P = 0.23), referent to the hospitalist, does not eliminate the possibility that an intensivist‐led model may reduce mortality risk.
Our study suggests that intermediate‐ and high‐acuity, mechanically ventilated patients may benefit from care by intensivists rather than hospitalists. The results from this initial study could be used to design and estimate sample size for future studies of hospitalists and intensivists to elucidate risk reduction. Randomized and multicenter trials are needed to provide more robust data, because our subgroups were small and not accounted for in the sample size calculation. Considering the severe intensivist shortage, 1 strategy to provide effective and efficient coverage of the growing American ICU population may be to ask hospitalists to care independently for lower acuity ICU patientsespecially nonventilated patientswhile encouraging or requiring intensivist care for higher acuity patients, especially once mechanically ventilated.
Conclusion
We anticipate this initial study of hospitalist and intensivist‐led ICU teams will validate a hospitalist ICU staffing model for further investigation. We propose that hospitalists can provide quality care for lower acuity critical care patients. This may improve intensivist availability to higher acuity critically ill patients and allow for judicious utilization of the limited intensivist supply. Future studies may better delineate specific subgroups of critically ill patients who benefit most from intensivist primary involvement. Additional research may also help generate evidence‐based triage standards to appropriate critical care teams and foster guideline development. Hospitalists may be instrumental in the critical care staffing shortage, however, identification of their ideal role requires further study.
Acknowledgements
The authors thank Ralph Bailey, RN; Daniel S. Budnitz, MD, MPH; Kirk Easley, MPH; Michael Heisler, MD, MPH; Joan Lopez, RN; Jason Stein, MD; and David Tong MD, MPH for their support and contributions.
- ,,,,,.On‐site physician staffing in a community hospital intensivist care unit.JAMA.1984;252(15):2023–2027.
- ,,,.Impact of critical care physician staffing on patients with septic shock in a university hospital medical intensive care unit.JAMA.1988;260(23):3446–3450.
- ,.Effect on ICU mortality of a full‐time critical care specialist.Chest.1989;96(1):127–129.
- ,,, et al.Effects of organizational change in the medical intensive care unit of a teaching hospital.JAMA.1996;276(4):322–328.
- ,,, et al.Effects of a medical intensivist on patient care in a community teaching hospital.Mayo Clin Proc.1997;72(5):391–399.
- ,,, et al.A ‘closed’ medical intensive care unit (MICU) improves resource utilization when compared with an ‘open’ MICU.Am J Respir Crit Care Med.1998;157(5):1468–1473.
- ,,, et al.Organizational characteristics of intensive care units related to outcomes of abdominal aortic surgery.JAMA.1999;281(14):1310–1312.
- ,,, et al.Effects of an organized critical care service on outcomes and resource utilization: a cohort study.Crit Care Med.1999;27(2):270–274.
- ,.Out‐of‐hours consultant cover and case‐mix adjusted mortality in intensive care.Lancet.2000;356:735–736.
- ,,.The impact of organizational changes on outcomes in an intensive care unit in the United Kingdom.Intensive Care Med.2001;27:865–872.
- ,,.Do intensivists in ICU improve outcome?Best Pract Res Clin Anaesthesiol.2005;19(1):125–135.
- ,,, et al.Physician staffing patterns and clinical outcomes in critically ill patients: a systemic review.JAMA.2002;288(17):2151–2162.
- ,.Potential reduction in mortality rates using an intensivist model to manage intensive care units.Eff Clin Pract.2000;3(6):284–289.
- The Leapfrog Group Fact Sheet. ICU Physician Staffing Fact Sheet. Available at: http://www.leapfroggroup.org/media/file/Leapfrog _ICU_Physician_Staffing_Fact_Sheet.pdf and http://www.leapfroggroup.org/media/file/Fact_Sheet_Leapfrog_Group.pdf. Accessed November 8,2009.
- ,,,,.Committee on Manpower for Pulmonary and Critical Care Societies (COMPACCS). Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population?JAMA.2000;284(21):2762–2770.
- US Department of Health and Human Services, Health Resources and Services Administration (HRSA).Report to Congress: the critical care workforce; a study of the supply and demand for critical care physicians. Senate Report 108–181.Rockville, MD:HRSA; May2006.
- ,.2007–2008 Survey: The Authoritative Source on the State of the Hospital Medicine Movement.Philadelphia, PA:Society of Hospital Medicine;2008.
- ,,,,,.Association between critical care physician management and patient mortality in the intensive care unit.Ann Intern Med.2008;148(11):801–809.
- ,,,.Variations in mortality and length of stay in intensive care units.Ann Intern Med.1993;118(10):753–761.
- ,,,.Hospital mortality in relation to staff workload: a 4‐year study in an adult intensive‐care unit.Lancet.2000;356:185–189.
- ,,, et al.A comparison of albumin and saline for fluid resuscitation in the intensive care unit.N Engl J Med.2004;350(22):2247–2256.
- ,,, et al.A multicenter, randomized controlled clinical trial of transfusion requirements in critical care.N Engl J Med.1999;340(6):409–417.
- ,,, et al.Early goal‐directed therapy in the treatment of severe sepsis and septic shock.N Engl J Med.2001;345(19):1368–1377.
- ,,, et al.Intensive insulin therapy in critically ill patients.N Engl J Med.2001;345(19):1359–1367.
- ,,, et al.Pulmonary‐artery versus central venous catheter to guide treatment of acute lung injury.N Engl J Med.2006;354(21):2213–2224.
- ,.Easy SAS calculations for risk or prevalence ratios and differences.Am J Epidemiol.2005;162(3):199–200.
- ,,.A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study.JAMA.1993;270(24):2957–2963.
- .Epidemiologic methods: the “art” in the state of the art.J Clin Epidemiol.2002;55(12):1196–1200.
- ,,.Methods to adjust for bias and confounding in critical care health services research involving observational data.J Crit Care.2006;21:1–7.
- ,,.Improved survival with hospitalists in a pediatric intensive care unit.Crit Care Med.2003;31(3):847–852.
- ,.ABC of intensive care: outcome data and scoring systems.BMJ.1999;319:241–244.
- ,,.Survival, morbidity, and quality of life after discharge from intensive care.Crit Care Med.2000;28(7):2293–2299.
- ,,,,,.On‐site physician staffing in a community hospital intensivist care unit.JAMA.1984;252(15):2023–2027.
- ,,,.Impact of critical care physician staffing on patients with septic shock in a university hospital medical intensive care unit.JAMA.1988;260(23):3446–3450.
- ,.Effect on ICU mortality of a full‐time critical care specialist.Chest.1989;96(1):127–129.
- ,,, et al.Effects of organizational change in the medical intensive care unit of a teaching hospital.JAMA.1996;276(4):322–328.
- ,,, et al.Effects of a medical intensivist on patient care in a community teaching hospital.Mayo Clin Proc.1997;72(5):391–399.
- ,,, et al.A ‘closed’ medical intensive care unit (MICU) improves resource utilization when compared with an ‘open’ MICU.Am J Respir Crit Care Med.1998;157(5):1468–1473.
- ,,, et al.Organizational characteristics of intensive care units related to outcomes of abdominal aortic surgery.JAMA.1999;281(14):1310–1312.
- ,,, et al.Effects of an organized critical care service on outcomes and resource utilization: a cohort study.Crit Care Med.1999;27(2):270–274.
- ,.Out‐of‐hours consultant cover and case‐mix adjusted mortality in intensive care.Lancet.2000;356:735–736.
- ,,.The impact of organizational changes on outcomes in an intensive care unit in the United Kingdom.Intensive Care Med.2001;27:865–872.
- ,,.Do intensivists in ICU improve outcome?Best Pract Res Clin Anaesthesiol.2005;19(1):125–135.
- ,,, et al.Physician staffing patterns and clinical outcomes in critically ill patients: a systemic review.JAMA.2002;288(17):2151–2162.
- ,.Potential reduction in mortality rates using an intensivist model to manage intensive care units.Eff Clin Pract.2000;3(6):284–289.
- The Leapfrog Group Fact Sheet. ICU Physician Staffing Fact Sheet. Available at: http://www.leapfroggroup.org/media/file/Leapfrog _ICU_Physician_Staffing_Fact_Sheet.pdf and http://www.leapfroggroup.org/media/file/Fact_Sheet_Leapfrog_Group.pdf. Accessed November 8,2009.
- ,,,,.Committee on Manpower for Pulmonary and Critical Care Societies (COMPACCS). Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population?JAMA.2000;284(21):2762–2770.
- US Department of Health and Human Services, Health Resources and Services Administration (HRSA).Report to Congress: the critical care workforce; a study of the supply and demand for critical care physicians. Senate Report 108–181.Rockville, MD:HRSA; May2006.
- ,.2007–2008 Survey: The Authoritative Source on the State of the Hospital Medicine Movement.Philadelphia, PA:Society of Hospital Medicine;2008.
- ,,,,,.Association between critical care physician management and patient mortality in the intensive care unit.Ann Intern Med.2008;148(11):801–809.
- ,,,.Variations in mortality and length of stay in intensive care units.Ann Intern Med.1993;118(10):753–761.
- ,,,.Hospital mortality in relation to staff workload: a 4‐year study in an adult intensive‐care unit.Lancet.2000;356:185–189.
- ,,, et al.A comparison of albumin and saline for fluid resuscitation in the intensive care unit.N Engl J Med.2004;350(22):2247–2256.
- ,,, et al.A multicenter, randomized controlled clinical trial of transfusion requirements in critical care.N Engl J Med.1999;340(6):409–417.
- ,,, et al.Early goal‐directed therapy in the treatment of severe sepsis and septic shock.N Engl J Med.2001;345(19):1368–1377.
- ,,, et al.Intensive insulin therapy in critically ill patients.N Engl J Med.2001;345(19):1359–1367.
- ,,, et al.Pulmonary‐artery versus central venous catheter to guide treatment of acute lung injury.N Engl J Med.2006;354(21):2213–2224.
- ,.Easy SAS calculations for risk or prevalence ratios and differences.Am J Epidemiol.2005;162(3):199–200.
- ,,.A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study.JAMA.1993;270(24):2957–2963.
- .Epidemiologic methods: the “art” in the state of the art.J Clin Epidemiol.2002;55(12):1196–1200.
- ,,.Methods to adjust for bias and confounding in critical care health services research involving observational data.J Crit Care.2006;21:1–7.
- ,,.Improved survival with hospitalists in a pediatric intensive care unit.Crit Care Med.2003;31(3):847–852.
- ,.ABC of intensive care: outcome data and scoring systems.BMJ.1999;319:241–244.
- ,,.Survival, morbidity, and quality of life after discharge from intensive care.Crit Care Med.2000;28(7):2293–2299.
Copyright © 2011 Society of Hospital Medicine
Seven-Day Schedule Could Improve Hospital Quality, Capacity
A new study evaluating outcomes for hospitals participating in the American Heart Association’s Get with the Guidelines program found no correlation between high performance on adhering to measures and care standards for acute myocardial infarction and for heart failure despite overlap between the sets of care processes (J Am Coll Cardio. 2011;58:637-644).
A total of 400,000 heart patients were studied, and 283 participating hospitals were stratified into thirds based on their adherence to core quality measures for each disease, with the upper third labeled superior in performance. Lead author Tracy Wang, MD, MHS, MSc, of the Duke Clinical Research Institute in Durham, N.C., and colleagues found that superior performance for only one of the two diseases led to such end-result outcomes as in-hospital mortality that were no better than for hospitals that were not high performers for either condition. But hospitals with superior performance for both conditions had lower in-hospital mortality rates.
“Perhaps quality is more than just following checklists,” Dr. Wang says. “There’s something special about these high-performing hospitals across the board, with better QI, perhaps a little more investment in infrastructure for quality.”
This result, Dr. Wang says, should give ammunition for hospitalists and other physicians to go to their hospital administrators to request more investment in quality improvement overall, not just for specific conditions.
A new study evaluating outcomes for hospitals participating in the American Heart Association’s Get with the Guidelines program found no correlation between high performance on adhering to measures and care standards for acute myocardial infarction and for heart failure despite overlap between the sets of care processes (J Am Coll Cardio. 2011;58:637-644).
A total of 400,000 heart patients were studied, and 283 participating hospitals were stratified into thirds based on their adherence to core quality measures for each disease, with the upper third labeled superior in performance. Lead author Tracy Wang, MD, MHS, MSc, of the Duke Clinical Research Institute in Durham, N.C., and colleagues found that superior performance for only one of the two diseases led to such end-result outcomes as in-hospital mortality that were no better than for hospitals that were not high performers for either condition. But hospitals with superior performance for both conditions had lower in-hospital mortality rates.
“Perhaps quality is more than just following checklists,” Dr. Wang says. “There’s something special about these high-performing hospitals across the board, with better QI, perhaps a little more investment in infrastructure for quality.”
This result, Dr. Wang says, should give ammunition for hospitalists and other physicians to go to their hospital administrators to request more investment in quality improvement overall, not just for specific conditions.
A new study evaluating outcomes for hospitals participating in the American Heart Association’s Get with the Guidelines program found no correlation between high performance on adhering to measures and care standards for acute myocardial infarction and for heart failure despite overlap between the sets of care processes (J Am Coll Cardio. 2011;58:637-644).
A total of 400,000 heart patients were studied, and 283 participating hospitals were stratified into thirds based on their adherence to core quality measures for each disease, with the upper third labeled superior in performance. Lead author Tracy Wang, MD, MHS, MSc, of the Duke Clinical Research Institute in Durham, N.C., and colleagues found that superior performance for only one of the two diseases led to such end-result outcomes as in-hospital mortality that were no better than for hospitals that were not high performers for either condition. But hospitals with superior performance for both conditions had lower in-hospital mortality rates.
“Perhaps quality is more than just following checklists,” Dr. Wang says. “There’s something special about these high-performing hospitals across the board, with better QI, perhaps a little more investment in infrastructure for quality.”
This result, Dr. Wang says, should give ammunition for hospitalists and other physicians to go to their hospital administrators to request more investment in quality improvement overall, not just for specific conditions.
Intermountain Risk Score Could Help Heart Failure Cases
A risk measurement model created by the Heart Institute at Intermountain Medical Center in Murray, Utah, may one day be a familiar tool to HM groups.
Known as the Intermountain Risk Score (http://intermountainhealthcare.org/IMRS/), the tool uses 15 parameters culled from complete blood counts (CBC) and the basic metabolic profile (BMP) to determine risk. The model, which is free, was used to stratify mortality risk in heart failure patients receiving an internal cardioverter defibrillator (ICD) in a paper presented in September at the 15th annual scientific meeting of the Heart Failure Society of America.
The report found that mortality at one-year post-ICD was 2.4%, 11.8%, and 28.2% for the low-, moderate-, and high-risk groups, respectively. And while the study was narrow in its topic, Benjamin Horne, PhD, director of cardiovascular and genetic epidemiology at the institute, says its application to a multitude of inpatient settings is a natural evolution for the tool.
“One of the things about the innovation of this risk score is the lab tests are so common already,” Dr. Horne says. “They are so familiar to physicians. They’ve been around for decades. What no one had realized before is they had additional risk information contained within them.”
A risk measurement model created by the Heart Institute at Intermountain Medical Center in Murray, Utah, may one day be a familiar tool to HM groups.
Known as the Intermountain Risk Score (http://intermountainhealthcare.org/IMRS/), the tool uses 15 parameters culled from complete blood counts (CBC) and the basic metabolic profile (BMP) to determine risk. The model, which is free, was used to stratify mortality risk in heart failure patients receiving an internal cardioverter defibrillator (ICD) in a paper presented in September at the 15th annual scientific meeting of the Heart Failure Society of America.
The report found that mortality at one-year post-ICD was 2.4%, 11.8%, and 28.2% for the low-, moderate-, and high-risk groups, respectively. And while the study was narrow in its topic, Benjamin Horne, PhD, director of cardiovascular and genetic epidemiology at the institute, says its application to a multitude of inpatient settings is a natural evolution for the tool.
“One of the things about the innovation of this risk score is the lab tests are so common already,” Dr. Horne says. “They are so familiar to physicians. They’ve been around for decades. What no one had realized before is they had additional risk information contained within them.”
A risk measurement model created by the Heart Institute at Intermountain Medical Center in Murray, Utah, may one day be a familiar tool to HM groups.
Known as the Intermountain Risk Score (http://intermountainhealthcare.org/IMRS/), the tool uses 15 parameters culled from complete blood counts (CBC) and the basic metabolic profile (BMP) to determine risk. The model, which is free, was used to stratify mortality risk in heart failure patients receiving an internal cardioverter defibrillator (ICD) in a paper presented in September at the 15th annual scientific meeting of the Heart Failure Society of America.
The report found that mortality at one-year post-ICD was 2.4%, 11.8%, and 28.2% for the low-, moderate-, and high-risk groups, respectively. And while the study was narrow in its topic, Benjamin Horne, PhD, director of cardiovascular and genetic epidemiology at the institute, says its application to a multitude of inpatient settings is a natural evolution for the tool.
“One of the things about the innovation of this risk score is the lab tests are so common already,” Dr. Horne says. “They are so familiar to physicians. They’ve been around for decades. What no one had realized before is they had additional risk information contained within them.”
Pediatric HM Literature
Clinical question: What is the efficacy of dexamethasone in mechanically ventilated children younger than two years of age with respiratory syncytial virus (RSV) lower respiratory tract infections?
Background: Although RSV typically causes self-limited respiratory tract disease with stable and low mortality rates, a small proportion of infants will have severe lower respiratory tract disease requiring mechanical ventilation. The authors previously found no evidence of a benefit of corticosteroids in these infants, but post-hoc analysis suggested a benefit in infants with mild oxygenation abnormalities.
Study design: International, multicenter, randomized, double-blind, placebo-controlled trial.
Setting: Twelve ICUs in Europe.
Synopsis: All patients <2 years of age with RSV-positive bronchiolitis requiring mechanical ventilation were eligible if they had not received corticosteroids in the previous two weeks. Patients were categorized as having either mild or severe oxygenation abnormalities based on their arterial partial pressure of oxygen/fractional inspired oxygen concentration and/or mean airway pressure. The primary outcome measure was duration of mechanical ventilation, and the trial was stopped after interim analysis of 89 patients in the mild oxygenation abnormalities arm revealed insufficient power to detect a >20% difference between the groups if the planned number of 128 patients were ultimately enrolled.
Fifty-six patients were enrolled in the severe oxygenation abnormalities arm. For both groups, there were no differences in either the duration of mechanical ventilation or secondary outcomes, such as length of stay or duration of supplemental oxygen, between intervention and control patients.
This well-designed study adds to an established body of literature painting a clear picture of the inefficacy of corticosteroids in infants with bronchiolitis, with or without severe disease. Although enrollment was slow and ultimately the trial was prematurely terminated, the randomization resulted in almost perfectly matched groups, which likely strengthens the findings despite the small sample size.
Bottom line: Corticosteroids should not be administered to critically ill children with bronchiolitis.
Citation: Van Woensel JB, Vyas H, et al. Dexamethasone in children mechanically ventilated for lower respiratory tract infection caused by respiratory syncytial virus: a randomized controlled trial. Crit Care Med. 2011;39(7):1779-1783.
Reviewed by Pediatric Editor Mark Shen, MD, FHM, medical director of hospital medicine at Dell Children’s Medical Center, Austin, Texas.
Clinical question: What is the efficacy of dexamethasone in mechanically ventilated children younger than two years of age with respiratory syncytial virus (RSV) lower respiratory tract infections?
Background: Although RSV typically causes self-limited respiratory tract disease with stable and low mortality rates, a small proportion of infants will have severe lower respiratory tract disease requiring mechanical ventilation. The authors previously found no evidence of a benefit of corticosteroids in these infants, but post-hoc analysis suggested a benefit in infants with mild oxygenation abnormalities.
Study design: International, multicenter, randomized, double-blind, placebo-controlled trial.
Setting: Twelve ICUs in Europe.
Synopsis: All patients <2 years of age with RSV-positive bronchiolitis requiring mechanical ventilation were eligible if they had not received corticosteroids in the previous two weeks. Patients were categorized as having either mild or severe oxygenation abnormalities based on their arterial partial pressure of oxygen/fractional inspired oxygen concentration and/or mean airway pressure. The primary outcome measure was duration of mechanical ventilation, and the trial was stopped after interim analysis of 89 patients in the mild oxygenation abnormalities arm revealed insufficient power to detect a >20% difference between the groups if the planned number of 128 patients were ultimately enrolled.
Fifty-six patients were enrolled in the severe oxygenation abnormalities arm. For both groups, there were no differences in either the duration of mechanical ventilation or secondary outcomes, such as length of stay or duration of supplemental oxygen, between intervention and control patients.
This well-designed study adds to an established body of literature painting a clear picture of the inefficacy of corticosteroids in infants with bronchiolitis, with or without severe disease. Although enrollment was slow and ultimately the trial was prematurely terminated, the randomization resulted in almost perfectly matched groups, which likely strengthens the findings despite the small sample size.
Bottom line: Corticosteroids should not be administered to critically ill children with bronchiolitis.
Citation: Van Woensel JB, Vyas H, et al. Dexamethasone in children mechanically ventilated for lower respiratory tract infection caused by respiratory syncytial virus: a randomized controlled trial. Crit Care Med. 2011;39(7):1779-1783.
Reviewed by Pediatric Editor Mark Shen, MD, FHM, medical director of hospital medicine at Dell Children’s Medical Center, Austin, Texas.
Clinical question: What is the efficacy of dexamethasone in mechanically ventilated children younger than two years of age with respiratory syncytial virus (RSV) lower respiratory tract infections?
Background: Although RSV typically causes self-limited respiratory tract disease with stable and low mortality rates, a small proportion of infants will have severe lower respiratory tract disease requiring mechanical ventilation. The authors previously found no evidence of a benefit of corticosteroids in these infants, but post-hoc analysis suggested a benefit in infants with mild oxygenation abnormalities.
Study design: International, multicenter, randomized, double-blind, placebo-controlled trial.
Setting: Twelve ICUs in Europe.
Synopsis: All patients <2 years of age with RSV-positive bronchiolitis requiring mechanical ventilation were eligible if they had not received corticosteroids in the previous two weeks. Patients were categorized as having either mild or severe oxygenation abnormalities based on their arterial partial pressure of oxygen/fractional inspired oxygen concentration and/or mean airway pressure. The primary outcome measure was duration of mechanical ventilation, and the trial was stopped after interim analysis of 89 patients in the mild oxygenation abnormalities arm revealed insufficient power to detect a >20% difference between the groups if the planned number of 128 patients were ultimately enrolled.
Fifty-six patients were enrolled in the severe oxygenation abnormalities arm. For both groups, there were no differences in either the duration of mechanical ventilation or secondary outcomes, such as length of stay or duration of supplemental oxygen, between intervention and control patients.
This well-designed study adds to an established body of literature painting a clear picture of the inefficacy of corticosteroids in infants with bronchiolitis, with or without severe disease. Although enrollment was slow and ultimately the trial was prematurely terminated, the randomization resulted in almost perfectly matched groups, which likely strengthens the findings despite the small sample size.
Bottom line: Corticosteroids should not be administered to critically ill children with bronchiolitis.
Citation: Van Woensel JB, Vyas H, et al. Dexamethasone in children mechanically ventilated for lower respiratory tract infection caused by respiratory syncytial virus: a randomized controlled trial. Crit Care Med. 2011;39(7):1779-1783.
Reviewed by Pediatric Editor Mark Shen, MD, FHM, medical director of hospital medicine at Dell Children’s Medical Center, Austin, Texas.
Workplace Violence at Hospitals
Patients and their relatives exposed to mental stress caused by hospitalization or illness might use violence against healthcare staff. Previous surveys reported that healthcare staff experience more workplace violence than other industry workers.13 Workplace violence by patients or their relatives may cause psychological problems or somatic effects on healthcare staff, such as losing self‐respect, depression, post‐traumatic stress disorder, stomachache, headache, or insomnia. Because those effects might lead to higher than usual turnovers of healthcare staff at a hospital, and interfere with high‐quality healthcare services, workplace violence at healthcare settings became a global concern; a lot of studies investigating those circumstances mainly were conducted in developed countries.415 Those studies revealed that the psychiatric ward, the emergency room, or the long‐term care facilities were the high‐risk areas of workplace violence; the incidence rate of physical aggression in the past year ranged from 3% to 35%; and the incidence rate of verbal abuse in the past year ranged from 26% to 64%. But the overall circumstances are still unclear, because most of the subjects in those studies were limited to nurses or some departments, such as the psychiatric ward or the emergency room. There might be other professions or departments with higher risk of workplace violence.
The aim of this study was to investigate the incidence of workplace violence and the attributes of healthcare staff, such as profession, age, gender, departments, and so on, who are at high risk of experiencing workplace violence.
METHODS
A questionnaire‐based, anonymous, and self‐administered cross‐sectional survey was conducted at 19 hospitals in Japan from January to December 2009. Among the 19 hospitals, 8 hospitals had less than 200 beds, 7 hospitals had 200 to 500 beds for acute care, and 4 hospitals had more than 500 beds for acute care. Thirteen of 19 hospitals were teaching hospitals. Eight out of 19 hospitals were located in urban areas. The characteristics of the 19 hospitals are shown in Table 4 of Supporting Appendix (in the online version of this article). The questionnaires were distributed to all 11,095 healthcare staff with a sealed reply envelope, and were collected anonymously using a collection box at each hospital.
The questionnaire contained questions about workplace violence, the work environment, and other topics. This study classifies workplace violence into physical aggression, verbal abuse, and sexual harassment. The respondents were requested to reply in regard to their experiences with each of these 3 types of workplace violence by patients or their relatives, over the past year. In this article, only those 3 questions and some background information of respondents were used for analysis. The race of patients and medical staff was not investigated because Japan is a racially homogeneous nation, and more than 99% of the population is Asian.
Logistic regression analysis with forced entry of all variables to examine the effect of attributes of healthcare staff to workplace violence was used. In this analysis, random effects of each hospital or area were not taken into account. All analyses were performed using SPSS 18.0 (SPSS, Inc, Chicago, IL), and P < 0.05 was used to determine significance.
In this study, workplace violence was defined as an event that was subjectively recognized by healthcare staff as violence caused by patients or their relatives. The violence among healthcare staff was excluded.
RESULTS
The response rate was 79.1% (8711/11,095). Among the 8771 respondents, 36.4% experienced workplace violence by patients or their relatives over the past year; 15.9% experienced physical aggressions, 29.8% experienced verbal abuse, and 9.9% experienced sexual harassment. Table 1 provides characteristics of the respondents; Table 2 shows the proportion of victims for workplace violence.
| No. of Respondents | |||
|---|---|---|---|
| n | (%)* | ||
| |||
| No. of beds in their hospital | <200 beds | 1298 | (14.8) |
| 200‐500 beds | 3041 | (34.7) | |
| 500 beds or more | 4432 | (50.5) | |
| Section | General ward | 2377 | (27.1) |
| Administration department | 989 | (11.3) | |
| Outpatient department | 675 | (7.7) | |
| Physicians' department | 610 | (7.0) | |
| Dietary department | 435 | (5.0) | |
| Long‐term care ward | 331 | (3.8) | |
| Rehabilitation department | 318 | (3.6) | |
| Critical care center, ICU, or CCU | 306 | (3.5) | |
| Obstetrics and gynecology ward, perinatal ward, or NICU | 287 | (3.3) | |
| Clinical laboratory or physiology department | 266 | (3.0) | |
| Operation department | 264 | (3.0) | |
| Pharmaceutical department | 209 | (2.4) | |
| Pediatric ward | 203 | (2.3) | |
| Radiology department | 197 | (2.2) | |
| Dialysis department | 104 | (1.2) | |
| Psychiatric ward | 56 | (0.6) | |
| Others | 1144 | (13.0) | |
| Profession | Nurse | 4298 | (49.0) |
| Clerk | 1208 | (13.8) | |
| Doctor | 610 | (7.0) | |
| Nursing aide or care worker | 585 | (6.7) | |
| Technician | 547 | (6.2) | |
| Dietician or cook | 435 | (5.0) | |
| Therapist | 313 | (3.6) | |
| Pharmacist | 183 | (2.1) | |
| Others | 592 | (6.7) | |
| Years of experience in their own specialty or profession | <5 yr | 3497 | (39.9) |
| 6‐10 yr | 1618 | (18.4) | |
| 11‐15 yr | 1041 | (11.9) | |
| 16‐20 yr | 761 | (8.7) | |
| 21 yr or more | 1218 | (13.9) | |
| Not reported | 636 | (7.3) | |
| Working hours per week | <20 hr | 640 | (7.3) |
| 20‐40 hr | 1720 | (19.6) | |
| 40‐60 hr | 4638 | (52.9) | |
| 60 hr or more | 655 | (7.5) | |
| Not reported | 1118 | (12.7) | |
| Gender | Male | 1941 | (22.1) |
| Female | 6272 | (71.5) | |
| Not reported | 558 | (6.4) | |
| Direct interaction or contact with patients | Having those contacts | 7227 | (82.4) |
| Not having those contacts | 1001 | (11.4) | |
| Not reported | 543 | (6.2) | |
| Total | 8771 | (100.0) | |
| No. of Respondents | Physical Aggression Experience | Verbal Abuse Experience | Sexual Harassment Experience | Experience of at Least 1 of the 3 Kinds of Violence | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | n | (%)* | n | (%)* | n | (%)* | n | (%)* | ||
| No. of beds in their hospital | <200 beds | 1298 | 244 | (18.8) | 306 | (23.6) | 109 | (8.4) | 413 | (31.8) |
| 200‐500 beds | 3041 | 503 | (16.5) | 971 | (31.9) | 354 | (11.6) | 1173 | (38.6) | |
| 500 beds or more | 4432 | 645 | (14.6) | 1338 | (30.2) | 406 | (9.2) | 1606 | (36.2) | |
| Section | Psychiatric ward | 56 | 33 | (58.9) | 37 | (66.1) | 8 | (14.3) | 42 | (75.0) |
| General ward | 2377 | 852 | (35.8) | 1057 | (44.5) | 536 | (22.5) | 1371 | (57.7) | |
| Dialysis department | 104 | 5 | (4.8) | 44 | (42.3) | 24 | (23.1) | 55 | (52.9) | |
| Critical care center, ICU, or CCU | 306 | 90 | (29.4) | 108 | (35.3) | 41 | (13.4) | 151 | (49.3) | |
| Long‐term care ward | 331 | 108 | (32.6) | 109 | (32.9) | 38 | (11.5) | 157 | (47.4) | |
| Outpatient department | 675 | 47 | (7.0) | 268 | (39.7) | 44 | (6.5) | 292 | (43.3) | |
| Physicians' department | 610 | 33 | (5.4) | 193 | (31.6) | 6 | (1.0) | 203 | (33.3) | |
| Pediatric ward | 203 | 23 | (11.3) | 50 | (24.6) | 13 | (6.4) | 62 | (30.5) | |
| Rehabilitation department | 318 | 53 | (16.7) | 70 | (22.0) | 31 | (9.7) | 96 | (30.2) | |
| Administration department | 989 | 10 | (1.0) | 247 | (25.0) | 16 | (1.6) | 251 | (25.4) | |
| Clinical radiology department | 197 | 11 | (5.6) | 40 | (20.3) | 2 | (1.0) | 48 | (24.4) | |
| Operation department | 264 | 11 | (4.2) | 38 | (14.4) | 9 | (3.4) | 43 | (16.3) | |
| Clinical laboratory or physiology department | 266 | 4 | (1.5) | 37 | (13.9) | 9 | (3.4) | 43 | (16.2) | |
| Obstetrics and gynecology ward, perinatal ward, or NICU | 287 | 3 | (1.0) | 26 | (9.1) | 2 | (0.7) | 28 | (9.8) | |
| Dietary department | 435 | 7 | (1.6) | 39 | (9.0) | 8 | (1.8) | 42 | (9.7) | |
| Pharmaceutical department | 209 | 1 | (0.5) | 15 | (7.2) | 5 | (2.4) | 19 | (9.1) | |
| Others | 1144 | 101 | (8.8) | 237 | (20.7) | 77 | (6.7) | 289 | (25.3) | |
| Profession | Nurse | 4298 | 1150 | (26.8) | 1694 | (39.4) | 729 | (17.0) | 2155 | (50.1) |
| Doctor | 610 | 33 | (5.4) | 193 | (31.6) | 6 | (1.0) | 203 | (33.3) | |
| Nursing aide or care worker | 585 | 104 | (17.8) | 151 | (25.8) | 39 | (6.7) | 191 | (32.6) | |
| Therapist | 313 | 53 | (16.9) | 71 | (22.7) | 31 | (9.9) | 96 | (30.7) | |
| Clerk | 1208 | 15 | (1.2) | 311 | (25.7) | 23 | (1.9) | 314 | (26.0) | |
| Technician | 547 | 15 | (2.7) | 79 | (14.4) | 19 | (3.5) | 97 | (17.7) | |
| Dietician or cook | 435 | 7 | (1.6) | 38 | (8.7) | 8 | (1.8) | 41 | (9.4) | |
| Pharmacist | 183 | 0 | (0.0) | 13 | (7.1) | 5 | (2.7) | 17 | (9.3) | |
| Others | 592 | 15 | (2.5) | 65 | (11.0) | 9 | (1.5) | 78 | (13.2) | |
| Years of experience in their own specialty or profession | <5 yr | 3497 | 527 | (15.1) | 919 | (26.3) | 384 | (11.0) | 1183 | (33.8) |
| 6‐10 yr | 1618 | 316 | (19.5) | 510 | (31.5) | 183 | (11.3) | 636 | (39.3) | |
| 11‐15 yr | 1041 | 210 | (20.2) | 350 | (33.6) | 125 | (12.0) | 421 | (40.4) | |
| 16‐20 yr | 761 | 111 | (14.6) | 253 | (33.2) | 58 | (7.6) | 294 | (38.6) | |
| 21 yr or more | 1218 | 160 | (13.1) | 422 | (34.6) | 85 | (7.0) | 475 | (39.0) | |
| Not reported | 636 | 68 | (10.7) | 161 | (25.3) | 34 | (5.3) | 183 | (28.8) | |
| Working hours per week | <20 hr | 640 | 50 | (7.8) | 148 | (23.1) | 39 | (6.1) | 173 | (27.0) |
| 20‐40 hr | 1720 | 234 | (13.6) | 473 | (27.5) | 157 | (9.1) | 583 | (33.9) | |
| 40‐60 hr | 4638 | 798 | (17.2) | 1424 | (30.7) | 498 | (10.7) | 1726 | (37.2) | |
| 60 hr or more | 655 | 103 | (15.7) | 242 | (36.9) | 50 | (7.6) | 279 | (42.6) | |
| Not reported | 1118 | 207 | (18.5) | 328 | (29.3) | 125 | (11.2) | 431 | (38.6) | |
| Gender | Male | 1941 | 185 | (9.5) | 471 | (24.3) | 77 | (4.0) | 529 | (27.3) |
| Female | 6272 | 1137 | (18.1) | 2004 | (32.0) | 752 | (12.0) | 2494 | (39.8) | |
| Not reported | 558 | 70 | (12.5) | 140 | (25.1) | 40 | (7.2) | 169 | (30.3) | |
| Direct interaction or contact with patients | Having those contacts | 7227 | 1325 | (18.3) | 2395 | (33.1) | 834 | (11.5) | 2945 | (40.7) |
| Not having those contacts | 1001 | 17 | (1.7) | 100 | (10.0) | 7 | (0.7) | 107 | (10.7) | |
| Not reported | 543 | 50 | (9.2) | 120 | (22.1) | 28 | (5.2) | 140 | (25.8) | |
| Total | 8771 | 1392 | (15.9) | 2615 | (29.8) | 869 | (9.9) | 3192 | (36.4) | |
Because of missing values, 6654 out of 8771 (75.9%) replies were used for the logistic regression analysis. Nagelkerke R2 for physical aggression was 0.33, for verbal abuse was 0.16, for sexual harassment was 0.23, and for at least one of the above types of violence was 0.23. The proportions of respondents, who had experienced each type of workplace violence, were not significantly different among the replies with missing data and with the effective data actually used.
Factors Associated With Higher Risk of Violence
Adjusted odds ratios of physical aggression were significantly high in general wards, psychiatric wards, critical care centers/emntensive care units (ICU)/cardiac care units (CCU), and long‐term care wards; and for nurses, nursing aides/care workers; for longer working hours; and for direct interaction with patients (Table 3).
| Physical Aggression | Verbal Abuse | Sexual Harassment | At Least 1 of the 3 Kinds of Violence | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P | Odds Ratio (95%Cl) | P | Odds Ratio (95%Cl) | P | Odds Ratio (95%Cl) | P | Odds Ratio (95%Cl) | ||||||
| |||||||||||||
| No. of beds in their hospital | <200 beds | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| 200‐500 beds | 0.51 | 0.90 | (0.67‐1.22) | <0.01* | 1.64 | (1.30‐2.07) | 0.19 | 1.27 | (0.89‐1.80) | <0.01* | 1.45 | (1.16‐1.81) | |
| 500 beds or more | 0.02* | 0.69 | (0.51‐0.94) | <0.01* | 1.57 | (1.24‐1.98) | 0.49 | 0.88 | (0.62‐1.26) | 0.01* | 1.32 | (1.06‐1.65) | |
| Section | Physicians' department | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Psychiatric ward | <0.01* | 9.28 | (4.39‐19.62) | <0.01* | 3.33 | (1.65‐6.70) | 0.69 | 0.80 | (0.27‐2.40) | <0.01* | 4.55 | (2.07‐1.02) | |
| Long‐term care ward | <0.01* | 2.48 | (1.55‐3.96) | <0.01* | 1.90 | (1.27‐2.86) | 0.65 | 1.15 | (0.63‐2.09) | <0.01* | 2.20 | (1.50‐3.24) | |
| General ward | <0.01* | 3.00 | (2.18‐4.13) | <0.01* | 1.73 | (1.36‐2.21) | <0.01* | 1.89 | (1.32‐2.69) | <0.01* | 1.98 | (1.57‐2.51) | |
| Dialysis department | 0.02* | 0.32 | (0.12‐0.83) | 0.04* | 1.65 | (1.02‐2.66) | 0.01* | 2.21 | (1.23‐3.97) | 0.02* | 1.81 | (1.12‐2.92) | |
| Critical care center, ICU, or CCU | <0.01* | 2.44 | (1.60‐3.74) | 0.49 | 1.13 | (0.79‐1.61) | 0.56 | 1.17 | (0.70‐1.94) | 0.04* | 1.43 | (1.01‐2.01) | |
| Administration department | 0.22 | 0.55 | (0.21‐1.44) | 0.07 | 1.38 | (0.98‐1.93) | 0.29 | 0.64 | (0.27‐1.48) | 0.07 | 1.37 | (0.98‐1.91) | |
| Clinical radiology department | 0.53 | 1.42 | (0.48‐4.21) | 0.51 | 1.21 | (0.69‐2.12) | 0.02* | 0.17 | (0.04‐0.78) | 0.57 | 1.17 | (0.69‐1.98) | |
| Rehabilitation department | 0.93 | 0.93 | (0.18‐4.77) | 0.88 | 1.08 | (0.42‐2.80) | 0.82 | 1.22 | (0.22‐6.79) | 0.77 | 1.14 | (0.46‐2.85) | |
| Outpatient department | <0.01* | 0.41 | (0.26‐0.65) | 0.03* | 1.35 | (1.02‐1.78) | 0.02* | 0.56 | (0.35‐0.90) | 0.40 | 1.12 | (0.86‐1.47) | |
| Dietary department | 0.33 | 1.94 | (0.51‐7.35) | 0.66 | 1.13 | (0.65‐1.99) | 0.85 | 1.13 | (0.30‐4.26) | 0.84 | 1.06 | (0.61‐1.82) | |
| Clinical laboratory or physiology department | 0.40 | 0.53 | (0.12‐2.34) | 0.85 | 1.06 | (0.59‐1.89) | 0.21 | 0.52 | (0.18‐1.45) | 0.87 | 0.96 | (0.55‐1.65) | |
| Pediatric ward | 0.27 | 0.72 | (0.41‐1.29) | 0.08 | 0.69 | (0.45‐1.05) | 0.02* | 0.43 | (0.21‐0.90) | 0.03* | 0.65 | (0.43‐0.97) | |
| Pharmaceutical department | 0.05 | 0.52 | (0.26‐1.01) | 0.71 | 1.26 | (0.36‐4.38) | 0.14 | 0.63 | (0.34‐1.17) | ||||
| Operation department | <0.01* | 0.24 | (0.12‐0.48) | <0.01* | 0.36 | (0.23‐0.55) | <0.01* | 0.21 | (0.09‐0.48) | <0.01* | 0.27 | (0.18‐0.41) | |
| Obstetrics and gynecology ward, perinatal ward, or NICU | <0.01* | 0.04 | (0.01‐0.18) | <0.01* | 0.19 | (0.12‐0.32) | <0.01* | 0.02 | (0.00‐0.18) | <0.01* | 0.14 | (0.08‐0.22) | |
| Profession | Doctor | 1.00 | 1.00 | 1.00 | <0.01* | 1.00 | |||||||
| Nurse | <0.01* | 4.09 | (2.41‐6.95) | 0.16 | 1.27 | (0.91‐1.76) | <0.01* | 11.64 | (4.38‐30.90) | 1.64 | (1.19‐2.26) | ||
| Therapist | 0.10 | 4.03 | (0.76‐21.28) | 0.83 | 0.90 | (0.34‐2.39) | 0.05* | 7.11 | (1.02‐49.3) | 0.83 | 1.11 | (0.43‐2.83) | |
| Nursing aide or care worker | 0.03* | 1.95 | (1.07‐3.55) | 0.09 | 0.71 | (0.47‐1.05) | <0.01* | 4.66 | (1.63‐13.31) | 0.19 | 0.77 | (0.53‐1.14) | |
| Clerk | 0.03* | 0.36 | (0.14‐0.90) | 0.27 | 0.80 | (0.54‐1.19) | 0.17 | 2.26 | (0.70‐7.27) | 0.09 | 0.72 | (0.49‐1.06) | |
| Technician | 0.27 | 0.55 | (0.19‐1.60) | <0.01* | 0.37 | (0.22‐0.61) | <0.01* | 6.92 | (2.20‐21.76) | <0.01* | 0.46 | (0.28‐0.74) | |
| Others | <0.01* | 0.21 | (0.08‐0.57) | <0.01* | 0.39 | (0.25‐0.60) | 0.24 | 2.14 | (0.60‐7.63) | <0.01* | 0.39 | (0.25‐0.59) | |
| Years of experience in their own specialty or profession | <5 yr | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| 6‐10 yr | <0.01* | 1.42 | (1.17‐1.72) | 0.01* | 1.22 | (1.05‐1.42) | 0.84 | 0.98 | (0.78‐1.22) | 0.01* | 1.22 | (1.05‐1.42) | |
| 11‐15 yr | <0.01* | 1.64 | (1.31‐2.05) | <0.01* | 1.45 | (1.22‐1.73) | 0.30 | 1.14 | (0.89‐1.47) | <0.01* | 1.35 | (1.13‐1.60) | |
| 16‐20 yr | 0.30 | 1.16 | (0.88‐1.52) | <0.01* | 1.47 | (1.21‐1.79) | 0.09 | 0.75 | (0.54‐1.04) | <0.01* | 1.34 | (1.10‐1.63) | |
| 21 yr or more | 0.58 | 1.07 | (0.84‐1.37) | <0.01* | 1.65 | (1.39‐1.96) | <0.01* | 0.63 | (0.47‐0.85) | <0.01* | 1.38 | (1.16‐1.64) | |
| Working hours per week | <20 hr | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| 20‐40 hr | 0.04* | 1.49 | (1.01‐2.19) | 0.52 | 1.08 | (0.85‐1.39) | 0.12 | 1.40 | (0.91‐2.15) | 0.10 | 1.23 | (0.96‐1.56) | |
| 40‐60 hr | <0.01* | 1.80 | (1.25‐2.58) | 0.03* | 1.28 | (1.02‐1.60) | 0.05* | 1.50 | (1.00‐2.24) | <0.01* | 1.39 | (1.11‐1.74) | |
| 60 hr or more | <0.01* | 2.14 | (1.37‐3.34) | <0.01* | 1.62 | (1.21‐2.17) | 0.14 | 1.49 | (0.88‐2.50) | <0.01* | 1.90 | (1.43‐2.54) | |
| Gender | (Female vs male) | 0.69 | 0.95 | (0.76‐1.20) | 0.16 | 1.12 | (0.95‐1.32) | <0.01* | 1.59 | (1.18‐2.12) | 0.01* | 1.22 | (1.05‐1.43) |
| Direct interaction or contact with patients | (Constant and direct interaction with patients vs no interaction) | 0.02* | 2.17 | (1.11‐4.22) | <0.01* | 2.46 | (1.87‐3.24) | <0.01* | 6.80 | (2.43‐19.03) | <0.01* | 2.58 | (1.97‐3.37) |
Adjusted odds ratios of verbal abuse were significantly high in hospital with 200 beds or more, in general wards, psychiatric wards, long‐term care wards, outpatient departments, and dialysis departments; and for longer years of experience in their own specialty; for longer working hours; and for direct interaction with patients.
Adjusted odds ratios of sexual harassment were significantly high in general wards, and dialysis departments; for nurses, nursing aides/care workers, technicians, therapists; for females; and for direct interaction with patients.
Adjusted odds ratios for at least 1 of the 3 kinds of workplace violence were significantly high in hospitals with 200 beds or more, in general wards, psychiatric wards, critical care centers/ICU/CCU, long‐term care wards, and dialysis departments; for nurses; for longer years of experience in their own specialty; for longer working hours; for females; and for direct interaction with patients.
Factors Associated With Lower Risk of Violence
Adjusted odds ratios of physical aggression were significantly low in dialysis departments; outpatient departments; operation departments; obstetrics and gynecology wards, perinatal wards, or neonatal intensive care units (NICU); and for clerks.
Adjusted odds ratios of verbal abuse were significantly low in operation departments; obstetrics and gynecology wards, perinatal wards, or NICU; and for technicians.
Adjusted odds ratios of sexual harassment were significantly low in clinical radiology departments; outpatient departments; pediatric wards; operation departments; obstetrics and gynecology wards, perinatal wards, or NICU; and for longer years of experience in their own specialty.
Adjusted odds ratios for at least 1 of the 3 kinds of workplace violence were significantly low in pediatric wards; operation departments; obstetrics and gynecology wards, perinatal wards, or NICU; and for technicians.
DISCUSSION
Among the healthcare staff, 36.4% experienced workplace violence by patients or their relatives over the past year; 15.9% experienced physical aggressions, 29.8% verbal abuse, and 9.9% sexual harassment. The risk factors of workplace violence identified in the present study were similar to those studies conducted not only in Japan, but also in Western countries. Though the target population was limited to Asians, our results can be applicable to other races, countries, and cultures.
Incidence of Workplace Violence
Most previous studies covered only specific professions at hospitals, such as nurses or critical care center staff, and there are only few multicenter studies covering entire sections and professions like this study.510, 1214 A Spanish study including about 8000 healthcare workers reported that 11% had experienced physical aggression, 64% had experienced threatening behavior, intimidation, or insults in the past year.11 The incidence of physical aggression was similar in both studies, but the incidence of verbal abuse was about twice as high as that of this study. The low response rate in the Spanish study (24%) might have contributed to a higher number of verbal abuse incidents, because those with experience of workplace violence would likely have answered the questionnaire. It is difficult to compare the incidence of workplace violence among different studies because the definitions of workplace violence differ widely. Ethnic culture might also affect the acknowledgement of workplace violence. The European NEXT study including about 30,000 nurses in 8 European countries reported a range of 10.4% incidence of workplace violence in the Netherlands, and 39.1% in France.10
Risk Factors of Physical Aggression
Previous studies reported that the prevalence of physical aggression is high in psychiatric wards, critical care centers, or long‐term care wards.1015 In these departments, patients with mental illness, postoperative delirium, or dementia are likely to be admitted.
Nurses and nursing aides are reported to be likely to experience physical aggression.3, 11, 15 Nurses and nursing aides have longer work hours with direct interaction with patients than other professions, and are considered to be at high risk of physical aggression.
Some studies, which did not examine influences by profession or department, reported that male was a risk factor for physical aggression and verbal abuse.6, 10, 11, 13 In this study though, the male gender was not associated with physical aggression or verbal abuse. Male nurses and nursing aides are likely to be assigned to high‐risk departments or to care for high‐risk patients. Gender may be confounded with variables such as profession or department.15
Longer work hours mean more frequent interaction with patients, and the risk for physical aggression might increase. Constant and direct interaction with patients is a risk factor, not only for physical aggression, but also for verbal abuse and sexual harassment.10
Risk Factors of Verbal Abuse
Previous studies reported that incidents of verbal abuse are high for nurses and nursing aides.15 Although in this study the proportion of verbal abuse was the highest in nurses (39.4%), adjusted odds ratio was not significant. Factors other than nurse profession, such as department and direct interaction with patients relating to the nurse profession, might be the higher risk factors for verbal abuse.
As reported in previous studies, psychiatric wards and long‐term care wards are risk factors of verbal abuse also in this study.10, 13, 15 Long waiting time at outpatient departments might increase the risk of verbal abuse.
Dialysis departments are at high risk of verbal abuse and sexual harassment. Compared to other outpatients, dialysis patients are forced to stay a long time in hospitals and there is, therefore, more interaction with nurses and technicians. The characteristic personality of dialysis patients, such as neuroticism or psychoticism, might also affect verbal abuse or sexual harassment.16
Because longer working hours mean more frequent interaction with patients, the risk of verbal abuse might increase.17 Managers with longer work experience might be at high risk for verbal abuse, because they often assume responsibility and take on the task of dealing with patients and their relevant complaints.11
Risk Factors of Sexual Harassment
Nurses are likely to experience sexual harassment because their public image seems to combine sexuality and maternalism.18 Nursing aides, technicians, and therapists also experience sexual harassment. The common risk factor among those professions is the direct contact with the patient's body during the patient's transfer. A lot of studies reported that female gender is a risk factor of sexual harassment.17, 19
Safety Factors of Workplace Violence
Adjusted odds ratios of operation departments, and obstetrics and gynecology wards, perinatal wards, or NICU were common safety factors for each type of workplace violence. Usually, the patients in operation rooms cannot talk or move a finger carelessly during the surgery. The fact that there are no adult male patients in obstetrics and gynecology wards, perinatal wards, or NICU, might have an influence on lower occurrence of workplace violence in these areas.
Limitations
This study used a questionnaire survey asking about subjective experiences of workplace violence over the 1 year before the study. There is the possibility of recall bias, and the same incident recognized as workplace violence by one person might not have been recognized as such by another person, because sensitivity differs among respondents.
In some categories with fewer respondents, such as the pharmaceutical department, it might be difficult to examine the exact confidence intervals of odds ratio. Further study with increased respondents of those categories is needed to confirm the odds ratios and the confidence intervals.
The rates of victims or risk for workplace violence were considered to vary with the character of the residents of each area or policy of each hospital. Therefore, a further analysis with adjustment for those factors is needed.
CONCLUSIONS
This study reveals that a significant proportion of healthcare staff (36.4%) has experienced workplace violence over the 1 year before the study was conducted and suggests that workplace violence is a serious problem. The attributes of healthcare staff who are at risk of workplace violence could be identified for each type of workplace violence. The mechanisms and the countermeasures for each type of workplace violence at those high‐risk areas should be further investigated. Further studies are necessary to confirm whether these findings are applicable to different races and different countries with different cultures.
- Home Office. Violence at Work: Findings From the 2002/2003 British Crime Survey. Available at: http://www.homeoffice.gov.uk/rds/pdfs2/rdsolr0404.pdf. Accessed November 10,2010.
- ,.Workplace violence in Finland: high‐risk groups and preventive strategies.Am J Ind Med Suppl.1999;1:80–81.
- .Violence in the Workplace 1993–99, National Crime Victimization Survey,Washington, DC:Bureau of Justice Statistics;2001:1–12.
- .International perspectives on workplace bullying among nurses: a review.Int Nurs Rev.2009;56(1):34–40.
- ,,.Scoping workplace aggression in nursing: findings from an Australian study.J Adv Nurs.2006;55(6):778–787.
- ,,, et al.Violence against nurses working in US emergency departments.J Nurs Adm.2009;39(7–8):340–349.
- ,,.Hospital staff responses to workplace violence in a psychiatric hospital in Taiwan.Int J Occup Environ Health.2009;15(2):173–179.
- All Japan Hospital Association. Research on actual conditions of risk management system and workplace violence at hospitals (Japanese). Available at: http://www.ajha.or.jp/voice/pdf/other/080422.pdf. Accessed November 10, 2010.
- ,,, et al.The present situation and the countermeasure for verbal abuse and physical aggression of patients (Japanese).Japan Medical Journal.2007;4354:81–84.
- ,,, et al.Work‐related factors and violence among nursing staff in the European NEXT study: a longitudinal cohort study.Int J Nurs Stud.2008;45(1):35–50.
- ,,, et al.Aggression towards health care workers in Spain: a multi‐facility study to evaluate the distribution of growing violence among professionals, health facilities and departments.Int J Occup Environ Health.2009;15(1):29–35.
- Office of Policy Planning, Japanese Nursing Association.Research on actual conditions of workplace violence at healthcare sector 2003 (Japanese).Survey Report of Japanese Nursing Association.2004;71:7–16.
- ,.Factors related to on‐the‐job abuse of nurses by patients.Health Rep.2009;20(2):7–19.
- ,,, et al.Risk factors for work‐related assaults on nurses.Epidemiology.2005;16(5):704–709.
- ,,, et al.Characterizing violence in health care in British Columbia.J Adv Nurs.2009;65(8):1655–1663.
- ,,, et al.Personality dimensions of haemodialysis patients related to initial renal disease.EDTNA ERCA J.2002;28(1):21–24.
- ,,.Factors associated with workplace violence in paramedics.Prehosp Disaster Med.2009;24(5):417–421.
- .Sexuality. An uninvited guest.Nurs Times.1989;85(5):25–28.
- ,,, et al.Universal problems during residency: abuse and harassment.Med Educ.2009;43(7):628–636.
Patients and their relatives exposed to mental stress caused by hospitalization or illness might use violence against healthcare staff. Previous surveys reported that healthcare staff experience more workplace violence than other industry workers.13 Workplace violence by patients or their relatives may cause psychological problems or somatic effects on healthcare staff, such as losing self‐respect, depression, post‐traumatic stress disorder, stomachache, headache, or insomnia. Because those effects might lead to higher than usual turnovers of healthcare staff at a hospital, and interfere with high‐quality healthcare services, workplace violence at healthcare settings became a global concern; a lot of studies investigating those circumstances mainly were conducted in developed countries.415 Those studies revealed that the psychiatric ward, the emergency room, or the long‐term care facilities were the high‐risk areas of workplace violence; the incidence rate of physical aggression in the past year ranged from 3% to 35%; and the incidence rate of verbal abuse in the past year ranged from 26% to 64%. But the overall circumstances are still unclear, because most of the subjects in those studies were limited to nurses or some departments, such as the psychiatric ward or the emergency room. There might be other professions or departments with higher risk of workplace violence.
The aim of this study was to investigate the incidence of workplace violence and the attributes of healthcare staff, such as profession, age, gender, departments, and so on, who are at high risk of experiencing workplace violence.
METHODS
A questionnaire‐based, anonymous, and self‐administered cross‐sectional survey was conducted at 19 hospitals in Japan from January to December 2009. Among the 19 hospitals, 8 hospitals had less than 200 beds, 7 hospitals had 200 to 500 beds for acute care, and 4 hospitals had more than 500 beds for acute care. Thirteen of 19 hospitals were teaching hospitals. Eight out of 19 hospitals were located in urban areas. The characteristics of the 19 hospitals are shown in Table 4 of Supporting Appendix (in the online version of this article). The questionnaires were distributed to all 11,095 healthcare staff with a sealed reply envelope, and were collected anonymously using a collection box at each hospital.
The questionnaire contained questions about workplace violence, the work environment, and other topics. This study classifies workplace violence into physical aggression, verbal abuse, and sexual harassment. The respondents were requested to reply in regard to their experiences with each of these 3 types of workplace violence by patients or their relatives, over the past year. In this article, only those 3 questions and some background information of respondents were used for analysis. The race of patients and medical staff was not investigated because Japan is a racially homogeneous nation, and more than 99% of the population is Asian.
Logistic regression analysis with forced entry of all variables to examine the effect of attributes of healthcare staff to workplace violence was used. In this analysis, random effects of each hospital or area were not taken into account. All analyses were performed using SPSS 18.0 (SPSS, Inc, Chicago, IL), and P < 0.05 was used to determine significance.
In this study, workplace violence was defined as an event that was subjectively recognized by healthcare staff as violence caused by patients or their relatives. The violence among healthcare staff was excluded.
RESULTS
The response rate was 79.1% (8711/11,095). Among the 8771 respondents, 36.4% experienced workplace violence by patients or their relatives over the past year; 15.9% experienced physical aggressions, 29.8% experienced verbal abuse, and 9.9% experienced sexual harassment. Table 1 provides characteristics of the respondents; Table 2 shows the proportion of victims for workplace violence.
| No. of Respondents | |||
|---|---|---|---|
| n | (%)* | ||
| |||
| No. of beds in their hospital | <200 beds | 1298 | (14.8) |
| 200‐500 beds | 3041 | (34.7) | |
| 500 beds or more | 4432 | (50.5) | |
| Section | General ward | 2377 | (27.1) |
| Administration department | 989 | (11.3) | |
| Outpatient department | 675 | (7.7) | |
| Physicians' department | 610 | (7.0) | |
| Dietary department | 435 | (5.0) | |
| Long‐term care ward | 331 | (3.8) | |
| Rehabilitation department | 318 | (3.6) | |
| Critical care center, ICU, or CCU | 306 | (3.5) | |
| Obstetrics and gynecology ward, perinatal ward, or NICU | 287 | (3.3) | |
| Clinical laboratory or physiology department | 266 | (3.0) | |
| Operation department | 264 | (3.0) | |
| Pharmaceutical department | 209 | (2.4) | |
| Pediatric ward | 203 | (2.3) | |
| Radiology department | 197 | (2.2) | |
| Dialysis department | 104 | (1.2) | |
| Psychiatric ward | 56 | (0.6) | |
| Others | 1144 | (13.0) | |
| Profession | Nurse | 4298 | (49.0) |
| Clerk | 1208 | (13.8) | |
| Doctor | 610 | (7.0) | |
| Nursing aide or care worker | 585 | (6.7) | |
| Technician | 547 | (6.2) | |
| Dietician or cook | 435 | (5.0) | |
| Therapist | 313 | (3.6) | |
| Pharmacist | 183 | (2.1) | |
| Others | 592 | (6.7) | |
| Years of experience in their own specialty or profession | <5 yr | 3497 | (39.9) |
| 6‐10 yr | 1618 | (18.4) | |
| 11‐15 yr | 1041 | (11.9) | |
| 16‐20 yr | 761 | (8.7) | |
| 21 yr or more | 1218 | (13.9) | |
| Not reported | 636 | (7.3) | |
| Working hours per week | <20 hr | 640 | (7.3) |
| 20‐40 hr | 1720 | (19.6) | |
| 40‐60 hr | 4638 | (52.9) | |
| 60 hr or more | 655 | (7.5) | |
| Not reported | 1118 | (12.7) | |
| Gender | Male | 1941 | (22.1) |
| Female | 6272 | (71.5) | |
| Not reported | 558 | (6.4) | |
| Direct interaction or contact with patients | Having those contacts | 7227 | (82.4) |
| Not having those contacts | 1001 | (11.4) | |
| Not reported | 543 | (6.2) | |
| Total | 8771 | (100.0) | |
| No. of Respondents | Physical Aggression Experience | Verbal Abuse Experience | Sexual Harassment Experience | Experience of at Least 1 of the 3 Kinds of Violence | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | n | (%)* | n | (%)* | n | (%)* | n | (%)* | ||
| No. of beds in their hospital | <200 beds | 1298 | 244 | (18.8) | 306 | (23.6) | 109 | (8.4) | 413 | (31.8) |
| 200‐500 beds | 3041 | 503 | (16.5) | 971 | (31.9) | 354 | (11.6) | 1173 | (38.6) | |
| 500 beds or more | 4432 | 645 | (14.6) | 1338 | (30.2) | 406 | (9.2) | 1606 | (36.2) | |
| Section | Psychiatric ward | 56 | 33 | (58.9) | 37 | (66.1) | 8 | (14.3) | 42 | (75.0) |
| General ward | 2377 | 852 | (35.8) | 1057 | (44.5) | 536 | (22.5) | 1371 | (57.7) | |
| Dialysis department | 104 | 5 | (4.8) | 44 | (42.3) | 24 | (23.1) | 55 | (52.9) | |
| Critical care center, ICU, or CCU | 306 | 90 | (29.4) | 108 | (35.3) | 41 | (13.4) | 151 | (49.3) | |
| Long‐term care ward | 331 | 108 | (32.6) | 109 | (32.9) | 38 | (11.5) | 157 | (47.4) | |
| Outpatient department | 675 | 47 | (7.0) | 268 | (39.7) | 44 | (6.5) | 292 | (43.3) | |
| Physicians' department | 610 | 33 | (5.4) | 193 | (31.6) | 6 | (1.0) | 203 | (33.3) | |
| Pediatric ward | 203 | 23 | (11.3) | 50 | (24.6) | 13 | (6.4) | 62 | (30.5) | |
| Rehabilitation department | 318 | 53 | (16.7) | 70 | (22.0) | 31 | (9.7) | 96 | (30.2) | |
| Administration department | 989 | 10 | (1.0) | 247 | (25.0) | 16 | (1.6) | 251 | (25.4) | |
| Clinical radiology department | 197 | 11 | (5.6) | 40 | (20.3) | 2 | (1.0) | 48 | (24.4) | |
| Operation department | 264 | 11 | (4.2) | 38 | (14.4) | 9 | (3.4) | 43 | (16.3) | |
| Clinical laboratory or physiology department | 266 | 4 | (1.5) | 37 | (13.9) | 9 | (3.4) | 43 | (16.2) | |
| Obstetrics and gynecology ward, perinatal ward, or NICU | 287 | 3 | (1.0) | 26 | (9.1) | 2 | (0.7) | 28 | (9.8) | |
| Dietary department | 435 | 7 | (1.6) | 39 | (9.0) | 8 | (1.8) | 42 | (9.7) | |
| Pharmaceutical department | 209 | 1 | (0.5) | 15 | (7.2) | 5 | (2.4) | 19 | (9.1) | |
| Others | 1144 | 101 | (8.8) | 237 | (20.7) | 77 | (6.7) | 289 | (25.3) | |
| Profession | Nurse | 4298 | 1150 | (26.8) | 1694 | (39.4) | 729 | (17.0) | 2155 | (50.1) |
| Doctor | 610 | 33 | (5.4) | 193 | (31.6) | 6 | (1.0) | 203 | (33.3) | |
| Nursing aide or care worker | 585 | 104 | (17.8) | 151 | (25.8) | 39 | (6.7) | 191 | (32.6) | |
| Therapist | 313 | 53 | (16.9) | 71 | (22.7) | 31 | (9.9) | 96 | (30.7) | |
| Clerk | 1208 | 15 | (1.2) | 311 | (25.7) | 23 | (1.9) | 314 | (26.0) | |
| Technician | 547 | 15 | (2.7) | 79 | (14.4) | 19 | (3.5) | 97 | (17.7) | |
| Dietician or cook | 435 | 7 | (1.6) | 38 | (8.7) | 8 | (1.8) | 41 | (9.4) | |
| Pharmacist | 183 | 0 | (0.0) | 13 | (7.1) | 5 | (2.7) | 17 | (9.3) | |
| Others | 592 | 15 | (2.5) | 65 | (11.0) | 9 | (1.5) | 78 | (13.2) | |
| Years of experience in their own specialty or profession | <5 yr | 3497 | 527 | (15.1) | 919 | (26.3) | 384 | (11.0) | 1183 | (33.8) |
| 6‐10 yr | 1618 | 316 | (19.5) | 510 | (31.5) | 183 | (11.3) | 636 | (39.3) | |
| 11‐15 yr | 1041 | 210 | (20.2) | 350 | (33.6) | 125 | (12.0) | 421 | (40.4) | |
| 16‐20 yr | 761 | 111 | (14.6) | 253 | (33.2) | 58 | (7.6) | 294 | (38.6) | |
| 21 yr or more | 1218 | 160 | (13.1) | 422 | (34.6) | 85 | (7.0) | 475 | (39.0) | |
| Not reported | 636 | 68 | (10.7) | 161 | (25.3) | 34 | (5.3) | 183 | (28.8) | |
| Working hours per week | <20 hr | 640 | 50 | (7.8) | 148 | (23.1) | 39 | (6.1) | 173 | (27.0) |
| 20‐40 hr | 1720 | 234 | (13.6) | 473 | (27.5) | 157 | (9.1) | 583 | (33.9) | |
| 40‐60 hr | 4638 | 798 | (17.2) | 1424 | (30.7) | 498 | (10.7) | 1726 | (37.2) | |
| 60 hr or more | 655 | 103 | (15.7) | 242 | (36.9) | 50 | (7.6) | 279 | (42.6) | |
| Not reported | 1118 | 207 | (18.5) | 328 | (29.3) | 125 | (11.2) | 431 | (38.6) | |
| Gender | Male | 1941 | 185 | (9.5) | 471 | (24.3) | 77 | (4.0) | 529 | (27.3) |
| Female | 6272 | 1137 | (18.1) | 2004 | (32.0) | 752 | (12.0) | 2494 | (39.8) | |
| Not reported | 558 | 70 | (12.5) | 140 | (25.1) | 40 | (7.2) | 169 | (30.3) | |
| Direct interaction or contact with patients | Having those contacts | 7227 | 1325 | (18.3) | 2395 | (33.1) | 834 | (11.5) | 2945 | (40.7) |
| Not having those contacts | 1001 | 17 | (1.7) | 100 | (10.0) | 7 | (0.7) | 107 | (10.7) | |
| Not reported | 543 | 50 | (9.2) | 120 | (22.1) | 28 | (5.2) | 140 | (25.8) | |
| Total | 8771 | 1392 | (15.9) | 2615 | (29.8) | 869 | (9.9) | 3192 | (36.4) | |
Because of missing values, 6654 out of 8771 (75.9%) replies were used for the logistic regression analysis. Nagelkerke R2 for physical aggression was 0.33, for verbal abuse was 0.16, for sexual harassment was 0.23, and for at least one of the above types of violence was 0.23. The proportions of respondents, who had experienced each type of workplace violence, were not significantly different among the replies with missing data and with the effective data actually used.
Factors Associated With Higher Risk of Violence
Adjusted odds ratios of physical aggression were significantly high in general wards, psychiatric wards, critical care centers/emntensive care units (ICU)/cardiac care units (CCU), and long‐term care wards; and for nurses, nursing aides/care workers; for longer working hours; and for direct interaction with patients (Table 3).
| Physical Aggression | Verbal Abuse | Sexual Harassment | At Least 1 of the 3 Kinds of Violence | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P | Odds Ratio (95%Cl) | P | Odds Ratio (95%Cl) | P | Odds Ratio (95%Cl) | P | Odds Ratio (95%Cl) | ||||||
| |||||||||||||
| No. of beds in their hospital | <200 beds | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| 200‐500 beds | 0.51 | 0.90 | (0.67‐1.22) | <0.01* | 1.64 | (1.30‐2.07) | 0.19 | 1.27 | (0.89‐1.80) | <0.01* | 1.45 | (1.16‐1.81) | |
| 500 beds or more | 0.02* | 0.69 | (0.51‐0.94) | <0.01* | 1.57 | (1.24‐1.98) | 0.49 | 0.88 | (0.62‐1.26) | 0.01* | 1.32 | (1.06‐1.65) | |
| Section | Physicians' department | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Psychiatric ward | <0.01* | 9.28 | (4.39‐19.62) | <0.01* | 3.33 | (1.65‐6.70) | 0.69 | 0.80 | (0.27‐2.40) | <0.01* | 4.55 | (2.07‐1.02) | |
| Long‐term care ward | <0.01* | 2.48 | (1.55‐3.96) | <0.01* | 1.90 | (1.27‐2.86) | 0.65 | 1.15 | (0.63‐2.09) | <0.01* | 2.20 | (1.50‐3.24) | |
| General ward | <0.01* | 3.00 | (2.18‐4.13) | <0.01* | 1.73 | (1.36‐2.21) | <0.01* | 1.89 | (1.32‐2.69) | <0.01* | 1.98 | (1.57‐2.51) | |
| Dialysis department | 0.02* | 0.32 | (0.12‐0.83) | 0.04* | 1.65 | (1.02‐2.66) | 0.01* | 2.21 | (1.23‐3.97) | 0.02* | 1.81 | (1.12‐2.92) | |
| Critical care center, ICU, or CCU | <0.01* | 2.44 | (1.60‐3.74) | 0.49 | 1.13 | (0.79‐1.61) | 0.56 | 1.17 | (0.70‐1.94) | 0.04* | 1.43 | (1.01‐2.01) | |
| Administration department | 0.22 | 0.55 | (0.21‐1.44) | 0.07 | 1.38 | (0.98‐1.93) | 0.29 | 0.64 | (0.27‐1.48) | 0.07 | 1.37 | (0.98‐1.91) | |
| Clinical radiology department | 0.53 | 1.42 | (0.48‐4.21) | 0.51 | 1.21 | (0.69‐2.12) | 0.02* | 0.17 | (0.04‐0.78) | 0.57 | 1.17 | (0.69‐1.98) | |
| Rehabilitation department | 0.93 | 0.93 | (0.18‐4.77) | 0.88 | 1.08 | (0.42‐2.80) | 0.82 | 1.22 | (0.22‐6.79) | 0.77 | 1.14 | (0.46‐2.85) | |
| Outpatient department | <0.01* | 0.41 | (0.26‐0.65) | 0.03* | 1.35 | (1.02‐1.78) | 0.02* | 0.56 | (0.35‐0.90) | 0.40 | 1.12 | (0.86‐1.47) | |
| Dietary department | 0.33 | 1.94 | (0.51‐7.35) | 0.66 | 1.13 | (0.65‐1.99) | 0.85 | 1.13 | (0.30‐4.26) | 0.84 | 1.06 | (0.61‐1.82) | |
| Clinical laboratory or physiology department | 0.40 | 0.53 | (0.12‐2.34) | 0.85 | 1.06 | (0.59‐1.89) | 0.21 | 0.52 | (0.18‐1.45) | 0.87 | 0.96 | (0.55‐1.65) | |
| Pediatric ward | 0.27 | 0.72 | (0.41‐1.29) | 0.08 | 0.69 | (0.45‐1.05) | 0.02* | 0.43 | (0.21‐0.90) | 0.03* | 0.65 | (0.43‐0.97) | |
| Pharmaceutical department | 0.05 | 0.52 | (0.26‐1.01) | 0.71 | 1.26 | (0.36‐4.38) | 0.14 | 0.63 | (0.34‐1.17) | ||||
| Operation department | <0.01* | 0.24 | (0.12‐0.48) | <0.01* | 0.36 | (0.23‐0.55) | <0.01* | 0.21 | (0.09‐0.48) | <0.01* | 0.27 | (0.18‐0.41) | |
| Obstetrics and gynecology ward, perinatal ward, or NICU | <0.01* | 0.04 | (0.01‐0.18) | <0.01* | 0.19 | (0.12‐0.32) | <0.01* | 0.02 | (0.00‐0.18) | <0.01* | 0.14 | (0.08‐0.22) | |
| Profession | Doctor | 1.00 | 1.00 | 1.00 | <0.01* | 1.00 | |||||||
| Nurse | <0.01* | 4.09 | (2.41‐6.95) | 0.16 | 1.27 | (0.91‐1.76) | <0.01* | 11.64 | (4.38‐30.90) | 1.64 | (1.19‐2.26) | ||
| Therapist | 0.10 | 4.03 | (0.76‐21.28) | 0.83 | 0.90 | (0.34‐2.39) | 0.05* | 7.11 | (1.02‐49.3) | 0.83 | 1.11 | (0.43‐2.83) | |
| Nursing aide or care worker | 0.03* | 1.95 | (1.07‐3.55) | 0.09 | 0.71 | (0.47‐1.05) | <0.01* | 4.66 | (1.63‐13.31) | 0.19 | 0.77 | (0.53‐1.14) | |
| Clerk | 0.03* | 0.36 | (0.14‐0.90) | 0.27 | 0.80 | (0.54‐1.19) | 0.17 | 2.26 | (0.70‐7.27) | 0.09 | 0.72 | (0.49‐1.06) | |
| Technician | 0.27 | 0.55 | (0.19‐1.60) | <0.01* | 0.37 | (0.22‐0.61) | <0.01* | 6.92 | (2.20‐21.76) | <0.01* | 0.46 | (0.28‐0.74) | |
| Others | <0.01* | 0.21 | (0.08‐0.57) | <0.01* | 0.39 | (0.25‐0.60) | 0.24 | 2.14 | (0.60‐7.63) | <0.01* | 0.39 | (0.25‐0.59) | |
| Years of experience in their own specialty or profession | <5 yr | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| 6‐10 yr | <0.01* | 1.42 | (1.17‐1.72) | 0.01* | 1.22 | (1.05‐1.42) | 0.84 | 0.98 | (0.78‐1.22) | 0.01* | 1.22 | (1.05‐1.42) | |
| 11‐15 yr | <0.01* | 1.64 | (1.31‐2.05) | <0.01* | 1.45 | (1.22‐1.73) | 0.30 | 1.14 | (0.89‐1.47) | <0.01* | 1.35 | (1.13‐1.60) | |
| 16‐20 yr | 0.30 | 1.16 | (0.88‐1.52) | <0.01* | 1.47 | (1.21‐1.79) | 0.09 | 0.75 | (0.54‐1.04) | <0.01* | 1.34 | (1.10‐1.63) | |
| 21 yr or more | 0.58 | 1.07 | (0.84‐1.37) | <0.01* | 1.65 | (1.39‐1.96) | <0.01* | 0.63 | (0.47‐0.85) | <0.01* | 1.38 | (1.16‐1.64) | |
| Working hours per week | <20 hr | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| 20‐40 hr | 0.04* | 1.49 | (1.01‐2.19) | 0.52 | 1.08 | (0.85‐1.39) | 0.12 | 1.40 | (0.91‐2.15) | 0.10 | 1.23 | (0.96‐1.56) | |
| 40‐60 hr | <0.01* | 1.80 | (1.25‐2.58) | 0.03* | 1.28 | (1.02‐1.60) | 0.05* | 1.50 | (1.00‐2.24) | <0.01* | 1.39 | (1.11‐1.74) | |
| 60 hr or more | <0.01* | 2.14 | (1.37‐3.34) | <0.01* | 1.62 | (1.21‐2.17) | 0.14 | 1.49 | (0.88‐2.50) | <0.01* | 1.90 | (1.43‐2.54) | |
| Gender | (Female vs male) | 0.69 | 0.95 | (0.76‐1.20) | 0.16 | 1.12 | (0.95‐1.32) | <0.01* | 1.59 | (1.18‐2.12) | 0.01* | 1.22 | (1.05‐1.43) |
| Direct interaction or contact with patients | (Constant and direct interaction with patients vs no interaction) | 0.02* | 2.17 | (1.11‐4.22) | <0.01* | 2.46 | (1.87‐3.24) | <0.01* | 6.80 | (2.43‐19.03) | <0.01* | 2.58 | (1.97‐3.37) |
Adjusted odds ratios of verbal abuse were significantly high in hospital with 200 beds or more, in general wards, psychiatric wards, long‐term care wards, outpatient departments, and dialysis departments; and for longer years of experience in their own specialty; for longer working hours; and for direct interaction with patients.
Adjusted odds ratios of sexual harassment were significantly high in general wards, and dialysis departments; for nurses, nursing aides/care workers, technicians, therapists; for females; and for direct interaction with patients.
Adjusted odds ratios for at least 1 of the 3 kinds of workplace violence were significantly high in hospitals with 200 beds or more, in general wards, psychiatric wards, critical care centers/ICU/CCU, long‐term care wards, and dialysis departments; for nurses; for longer years of experience in their own specialty; for longer working hours; for females; and for direct interaction with patients.
Factors Associated With Lower Risk of Violence
Adjusted odds ratios of physical aggression were significantly low in dialysis departments; outpatient departments; operation departments; obstetrics and gynecology wards, perinatal wards, or neonatal intensive care units (NICU); and for clerks.
Adjusted odds ratios of verbal abuse were significantly low in operation departments; obstetrics and gynecology wards, perinatal wards, or NICU; and for technicians.
Adjusted odds ratios of sexual harassment were significantly low in clinical radiology departments; outpatient departments; pediatric wards; operation departments; obstetrics and gynecology wards, perinatal wards, or NICU; and for longer years of experience in their own specialty.
Adjusted odds ratios for at least 1 of the 3 kinds of workplace violence were significantly low in pediatric wards; operation departments; obstetrics and gynecology wards, perinatal wards, or NICU; and for technicians.
DISCUSSION
Among the healthcare staff, 36.4% experienced workplace violence by patients or their relatives over the past year; 15.9% experienced physical aggressions, 29.8% verbal abuse, and 9.9% sexual harassment. The risk factors of workplace violence identified in the present study were similar to those studies conducted not only in Japan, but also in Western countries. Though the target population was limited to Asians, our results can be applicable to other races, countries, and cultures.
Incidence of Workplace Violence
Most previous studies covered only specific professions at hospitals, such as nurses or critical care center staff, and there are only few multicenter studies covering entire sections and professions like this study.510, 1214 A Spanish study including about 8000 healthcare workers reported that 11% had experienced physical aggression, 64% had experienced threatening behavior, intimidation, or insults in the past year.11 The incidence of physical aggression was similar in both studies, but the incidence of verbal abuse was about twice as high as that of this study. The low response rate in the Spanish study (24%) might have contributed to a higher number of verbal abuse incidents, because those with experience of workplace violence would likely have answered the questionnaire. It is difficult to compare the incidence of workplace violence among different studies because the definitions of workplace violence differ widely. Ethnic culture might also affect the acknowledgement of workplace violence. The European NEXT study including about 30,000 nurses in 8 European countries reported a range of 10.4% incidence of workplace violence in the Netherlands, and 39.1% in France.10
Risk Factors of Physical Aggression
Previous studies reported that the prevalence of physical aggression is high in psychiatric wards, critical care centers, or long‐term care wards.1015 In these departments, patients with mental illness, postoperative delirium, or dementia are likely to be admitted.
Nurses and nursing aides are reported to be likely to experience physical aggression.3, 11, 15 Nurses and nursing aides have longer work hours with direct interaction with patients than other professions, and are considered to be at high risk of physical aggression.
Some studies, which did not examine influences by profession or department, reported that male was a risk factor for physical aggression and verbal abuse.6, 10, 11, 13 In this study though, the male gender was not associated with physical aggression or verbal abuse. Male nurses and nursing aides are likely to be assigned to high‐risk departments or to care for high‐risk patients. Gender may be confounded with variables such as profession or department.15
Longer work hours mean more frequent interaction with patients, and the risk for physical aggression might increase. Constant and direct interaction with patients is a risk factor, not only for physical aggression, but also for verbal abuse and sexual harassment.10
Risk Factors of Verbal Abuse
Previous studies reported that incidents of verbal abuse are high for nurses and nursing aides.15 Although in this study the proportion of verbal abuse was the highest in nurses (39.4%), adjusted odds ratio was not significant. Factors other than nurse profession, such as department and direct interaction with patients relating to the nurse profession, might be the higher risk factors for verbal abuse.
As reported in previous studies, psychiatric wards and long‐term care wards are risk factors of verbal abuse also in this study.10, 13, 15 Long waiting time at outpatient departments might increase the risk of verbal abuse.
Dialysis departments are at high risk of verbal abuse and sexual harassment. Compared to other outpatients, dialysis patients are forced to stay a long time in hospitals and there is, therefore, more interaction with nurses and technicians. The characteristic personality of dialysis patients, such as neuroticism or psychoticism, might also affect verbal abuse or sexual harassment.16
Because longer working hours mean more frequent interaction with patients, the risk of verbal abuse might increase.17 Managers with longer work experience might be at high risk for verbal abuse, because they often assume responsibility and take on the task of dealing with patients and their relevant complaints.11
Risk Factors of Sexual Harassment
Nurses are likely to experience sexual harassment because their public image seems to combine sexuality and maternalism.18 Nursing aides, technicians, and therapists also experience sexual harassment. The common risk factor among those professions is the direct contact with the patient's body during the patient's transfer. A lot of studies reported that female gender is a risk factor of sexual harassment.17, 19
Safety Factors of Workplace Violence
Adjusted odds ratios of operation departments, and obstetrics and gynecology wards, perinatal wards, or NICU were common safety factors for each type of workplace violence. Usually, the patients in operation rooms cannot talk or move a finger carelessly during the surgery. The fact that there are no adult male patients in obstetrics and gynecology wards, perinatal wards, or NICU, might have an influence on lower occurrence of workplace violence in these areas.
Limitations
This study used a questionnaire survey asking about subjective experiences of workplace violence over the 1 year before the study. There is the possibility of recall bias, and the same incident recognized as workplace violence by one person might not have been recognized as such by another person, because sensitivity differs among respondents.
In some categories with fewer respondents, such as the pharmaceutical department, it might be difficult to examine the exact confidence intervals of odds ratio. Further study with increased respondents of those categories is needed to confirm the odds ratios and the confidence intervals.
The rates of victims or risk for workplace violence were considered to vary with the character of the residents of each area or policy of each hospital. Therefore, a further analysis with adjustment for those factors is needed.
CONCLUSIONS
This study reveals that a significant proportion of healthcare staff (36.4%) has experienced workplace violence over the 1 year before the study was conducted and suggests that workplace violence is a serious problem. The attributes of healthcare staff who are at risk of workplace violence could be identified for each type of workplace violence. The mechanisms and the countermeasures for each type of workplace violence at those high‐risk areas should be further investigated. Further studies are necessary to confirm whether these findings are applicable to different races and different countries with different cultures.
Patients and their relatives exposed to mental stress caused by hospitalization or illness might use violence against healthcare staff. Previous surveys reported that healthcare staff experience more workplace violence than other industry workers.13 Workplace violence by patients or their relatives may cause psychological problems or somatic effects on healthcare staff, such as losing self‐respect, depression, post‐traumatic stress disorder, stomachache, headache, or insomnia. Because those effects might lead to higher than usual turnovers of healthcare staff at a hospital, and interfere with high‐quality healthcare services, workplace violence at healthcare settings became a global concern; a lot of studies investigating those circumstances mainly were conducted in developed countries.415 Those studies revealed that the psychiatric ward, the emergency room, or the long‐term care facilities were the high‐risk areas of workplace violence; the incidence rate of physical aggression in the past year ranged from 3% to 35%; and the incidence rate of verbal abuse in the past year ranged from 26% to 64%. But the overall circumstances are still unclear, because most of the subjects in those studies were limited to nurses or some departments, such as the psychiatric ward or the emergency room. There might be other professions or departments with higher risk of workplace violence.
The aim of this study was to investigate the incidence of workplace violence and the attributes of healthcare staff, such as profession, age, gender, departments, and so on, who are at high risk of experiencing workplace violence.
METHODS
A questionnaire‐based, anonymous, and self‐administered cross‐sectional survey was conducted at 19 hospitals in Japan from January to December 2009. Among the 19 hospitals, 8 hospitals had less than 200 beds, 7 hospitals had 200 to 500 beds for acute care, and 4 hospitals had more than 500 beds for acute care. Thirteen of 19 hospitals were teaching hospitals. Eight out of 19 hospitals were located in urban areas. The characteristics of the 19 hospitals are shown in Table 4 of Supporting Appendix (in the online version of this article). The questionnaires were distributed to all 11,095 healthcare staff with a sealed reply envelope, and were collected anonymously using a collection box at each hospital.
The questionnaire contained questions about workplace violence, the work environment, and other topics. This study classifies workplace violence into physical aggression, verbal abuse, and sexual harassment. The respondents were requested to reply in regard to their experiences with each of these 3 types of workplace violence by patients or their relatives, over the past year. In this article, only those 3 questions and some background information of respondents were used for analysis. The race of patients and medical staff was not investigated because Japan is a racially homogeneous nation, and more than 99% of the population is Asian.
Logistic regression analysis with forced entry of all variables to examine the effect of attributes of healthcare staff to workplace violence was used. In this analysis, random effects of each hospital or area were not taken into account. All analyses were performed using SPSS 18.0 (SPSS, Inc, Chicago, IL), and P < 0.05 was used to determine significance.
In this study, workplace violence was defined as an event that was subjectively recognized by healthcare staff as violence caused by patients or their relatives. The violence among healthcare staff was excluded.
RESULTS
The response rate was 79.1% (8711/11,095). Among the 8771 respondents, 36.4% experienced workplace violence by patients or their relatives over the past year; 15.9% experienced physical aggressions, 29.8% experienced verbal abuse, and 9.9% experienced sexual harassment. Table 1 provides characteristics of the respondents; Table 2 shows the proportion of victims for workplace violence.
| No. of Respondents | |||
|---|---|---|---|
| n | (%)* | ||
| |||
| No. of beds in their hospital | <200 beds | 1298 | (14.8) |
| 200‐500 beds | 3041 | (34.7) | |
| 500 beds or more | 4432 | (50.5) | |
| Section | General ward | 2377 | (27.1) |
| Administration department | 989 | (11.3) | |
| Outpatient department | 675 | (7.7) | |
| Physicians' department | 610 | (7.0) | |
| Dietary department | 435 | (5.0) | |
| Long‐term care ward | 331 | (3.8) | |
| Rehabilitation department | 318 | (3.6) | |
| Critical care center, ICU, or CCU | 306 | (3.5) | |
| Obstetrics and gynecology ward, perinatal ward, or NICU | 287 | (3.3) | |
| Clinical laboratory or physiology department | 266 | (3.0) | |
| Operation department | 264 | (3.0) | |
| Pharmaceutical department | 209 | (2.4) | |
| Pediatric ward | 203 | (2.3) | |
| Radiology department | 197 | (2.2) | |
| Dialysis department | 104 | (1.2) | |
| Psychiatric ward | 56 | (0.6) | |
| Others | 1144 | (13.0) | |
| Profession | Nurse | 4298 | (49.0) |
| Clerk | 1208 | (13.8) | |
| Doctor | 610 | (7.0) | |
| Nursing aide or care worker | 585 | (6.7) | |
| Technician | 547 | (6.2) | |
| Dietician or cook | 435 | (5.0) | |
| Therapist | 313 | (3.6) | |
| Pharmacist | 183 | (2.1) | |
| Others | 592 | (6.7) | |
| Years of experience in their own specialty or profession | <5 yr | 3497 | (39.9) |
| 6‐10 yr | 1618 | (18.4) | |
| 11‐15 yr | 1041 | (11.9) | |
| 16‐20 yr | 761 | (8.7) | |
| 21 yr or more | 1218 | (13.9) | |
| Not reported | 636 | (7.3) | |
| Working hours per week | <20 hr | 640 | (7.3) |
| 20‐40 hr | 1720 | (19.6) | |
| 40‐60 hr | 4638 | (52.9) | |
| 60 hr or more | 655 | (7.5) | |
| Not reported | 1118 | (12.7) | |
| Gender | Male | 1941 | (22.1) |
| Female | 6272 | (71.5) | |
| Not reported | 558 | (6.4) | |
| Direct interaction or contact with patients | Having those contacts | 7227 | (82.4) |
| Not having those contacts | 1001 | (11.4) | |
| Not reported | 543 | (6.2) | |
| Total | 8771 | (100.0) | |
| No. of Respondents | Physical Aggression Experience | Verbal Abuse Experience | Sexual Harassment Experience | Experience of at Least 1 of the 3 Kinds of Violence | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | n | (%)* | n | (%)* | n | (%)* | n | (%)* | ||
| No. of beds in their hospital | <200 beds | 1298 | 244 | (18.8) | 306 | (23.6) | 109 | (8.4) | 413 | (31.8) |
| 200‐500 beds | 3041 | 503 | (16.5) | 971 | (31.9) | 354 | (11.6) | 1173 | (38.6) | |
| 500 beds or more | 4432 | 645 | (14.6) | 1338 | (30.2) | 406 | (9.2) | 1606 | (36.2) | |
| Section | Psychiatric ward | 56 | 33 | (58.9) | 37 | (66.1) | 8 | (14.3) | 42 | (75.0) |
| General ward | 2377 | 852 | (35.8) | 1057 | (44.5) | 536 | (22.5) | 1371 | (57.7) | |
| Dialysis department | 104 | 5 | (4.8) | 44 | (42.3) | 24 | (23.1) | 55 | (52.9) | |
| Critical care center, ICU, or CCU | 306 | 90 | (29.4) | 108 | (35.3) | 41 | (13.4) | 151 | (49.3) | |
| Long‐term care ward | 331 | 108 | (32.6) | 109 | (32.9) | 38 | (11.5) | 157 | (47.4) | |
| Outpatient department | 675 | 47 | (7.0) | 268 | (39.7) | 44 | (6.5) | 292 | (43.3) | |
| Physicians' department | 610 | 33 | (5.4) | 193 | (31.6) | 6 | (1.0) | 203 | (33.3) | |
| Pediatric ward | 203 | 23 | (11.3) | 50 | (24.6) | 13 | (6.4) | 62 | (30.5) | |
| Rehabilitation department | 318 | 53 | (16.7) | 70 | (22.0) | 31 | (9.7) | 96 | (30.2) | |
| Administration department | 989 | 10 | (1.0) | 247 | (25.0) | 16 | (1.6) | 251 | (25.4) | |
| Clinical radiology department | 197 | 11 | (5.6) | 40 | (20.3) | 2 | (1.0) | 48 | (24.4) | |
| Operation department | 264 | 11 | (4.2) | 38 | (14.4) | 9 | (3.4) | 43 | (16.3) | |
| Clinical laboratory or physiology department | 266 | 4 | (1.5) | 37 | (13.9) | 9 | (3.4) | 43 | (16.2) | |
| Obstetrics and gynecology ward, perinatal ward, or NICU | 287 | 3 | (1.0) | 26 | (9.1) | 2 | (0.7) | 28 | (9.8) | |
| Dietary department | 435 | 7 | (1.6) | 39 | (9.0) | 8 | (1.8) | 42 | (9.7) | |
| Pharmaceutical department | 209 | 1 | (0.5) | 15 | (7.2) | 5 | (2.4) | 19 | (9.1) | |
| Others | 1144 | 101 | (8.8) | 237 | (20.7) | 77 | (6.7) | 289 | (25.3) | |
| Profession | Nurse | 4298 | 1150 | (26.8) | 1694 | (39.4) | 729 | (17.0) | 2155 | (50.1) |
| Doctor | 610 | 33 | (5.4) | 193 | (31.6) | 6 | (1.0) | 203 | (33.3) | |
| Nursing aide or care worker | 585 | 104 | (17.8) | 151 | (25.8) | 39 | (6.7) | 191 | (32.6) | |
| Therapist | 313 | 53 | (16.9) | 71 | (22.7) | 31 | (9.9) | 96 | (30.7) | |
| Clerk | 1208 | 15 | (1.2) | 311 | (25.7) | 23 | (1.9) | 314 | (26.0) | |
| Technician | 547 | 15 | (2.7) | 79 | (14.4) | 19 | (3.5) | 97 | (17.7) | |
| Dietician or cook | 435 | 7 | (1.6) | 38 | (8.7) | 8 | (1.8) | 41 | (9.4) | |
| Pharmacist | 183 | 0 | (0.0) | 13 | (7.1) | 5 | (2.7) | 17 | (9.3) | |
| Others | 592 | 15 | (2.5) | 65 | (11.0) | 9 | (1.5) | 78 | (13.2) | |
| Years of experience in their own specialty or profession | <5 yr | 3497 | 527 | (15.1) | 919 | (26.3) | 384 | (11.0) | 1183 | (33.8) |
| 6‐10 yr | 1618 | 316 | (19.5) | 510 | (31.5) | 183 | (11.3) | 636 | (39.3) | |
| 11‐15 yr | 1041 | 210 | (20.2) | 350 | (33.6) | 125 | (12.0) | 421 | (40.4) | |
| 16‐20 yr | 761 | 111 | (14.6) | 253 | (33.2) | 58 | (7.6) | 294 | (38.6) | |
| 21 yr or more | 1218 | 160 | (13.1) | 422 | (34.6) | 85 | (7.0) | 475 | (39.0) | |
| Not reported | 636 | 68 | (10.7) | 161 | (25.3) | 34 | (5.3) | 183 | (28.8) | |
| Working hours per week | <20 hr | 640 | 50 | (7.8) | 148 | (23.1) | 39 | (6.1) | 173 | (27.0) |
| 20‐40 hr | 1720 | 234 | (13.6) | 473 | (27.5) | 157 | (9.1) | 583 | (33.9) | |
| 40‐60 hr | 4638 | 798 | (17.2) | 1424 | (30.7) | 498 | (10.7) | 1726 | (37.2) | |
| 60 hr or more | 655 | 103 | (15.7) | 242 | (36.9) | 50 | (7.6) | 279 | (42.6) | |
| Not reported | 1118 | 207 | (18.5) | 328 | (29.3) | 125 | (11.2) | 431 | (38.6) | |
| Gender | Male | 1941 | 185 | (9.5) | 471 | (24.3) | 77 | (4.0) | 529 | (27.3) |
| Female | 6272 | 1137 | (18.1) | 2004 | (32.0) | 752 | (12.0) | 2494 | (39.8) | |
| Not reported | 558 | 70 | (12.5) | 140 | (25.1) | 40 | (7.2) | 169 | (30.3) | |
| Direct interaction or contact with patients | Having those contacts | 7227 | 1325 | (18.3) | 2395 | (33.1) | 834 | (11.5) | 2945 | (40.7) |
| Not having those contacts | 1001 | 17 | (1.7) | 100 | (10.0) | 7 | (0.7) | 107 | (10.7) | |
| Not reported | 543 | 50 | (9.2) | 120 | (22.1) | 28 | (5.2) | 140 | (25.8) | |
| Total | 8771 | 1392 | (15.9) | 2615 | (29.8) | 869 | (9.9) | 3192 | (36.4) | |
Because of missing values, 6654 out of 8771 (75.9%) replies were used for the logistic regression analysis. Nagelkerke R2 for physical aggression was 0.33, for verbal abuse was 0.16, for sexual harassment was 0.23, and for at least one of the above types of violence was 0.23. The proportions of respondents, who had experienced each type of workplace violence, were not significantly different among the replies with missing data and with the effective data actually used.
Factors Associated With Higher Risk of Violence
Adjusted odds ratios of physical aggression were significantly high in general wards, psychiatric wards, critical care centers/emntensive care units (ICU)/cardiac care units (CCU), and long‐term care wards; and for nurses, nursing aides/care workers; for longer working hours; and for direct interaction with patients (Table 3).
| Physical Aggression | Verbal Abuse | Sexual Harassment | At Least 1 of the 3 Kinds of Violence | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P | Odds Ratio (95%Cl) | P | Odds Ratio (95%Cl) | P | Odds Ratio (95%Cl) | P | Odds Ratio (95%Cl) | ||||||
| |||||||||||||
| No. of beds in their hospital | <200 beds | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| 200‐500 beds | 0.51 | 0.90 | (0.67‐1.22) | <0.01* | 1.64 | (1.30‐2.07) | 0.19 | 1.27 | (0.89‐1.80) | <0.01* | 1.45 | (1.16‐1.81) | |
| 500 beds or more | 0.02* | 0.69 | (0.51‐0.94) | <0.01* | 1.57 | (1.24‐1.98) | 0.49 | 0.88 | (0.62‐1.26) | 0.01* | 1.32 | (1.06‐1.65) | |
| Section | Physicians' department | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Psychiatric ward | <0.01* | 9.28 | (4.39‐19.62) | <0.01* | 3.33 | (1.65‐6.70) | 0.69 | 0.80 | (0.27‐2.40) | <0.01* | 4.55 | (2.07‐1.02) | |
| Long‐term care ward | <0.01* | 2.48 | (1.55‐3.96) | <0.01* | 1.90 | (1.27‐2.86) | 0.65 | 1.15 | (0.63‐2.09) | <0.01* | 2.20 | (1.50‐3.24) | |
| General ward | <0.01* | 3.00 | (2.18‐4.13) | <0.01* | 1.73 | (1.36‐2.21) | <0.01* | 1.89 | (1.32‐2.69) | <0.01* | 1.98 | (1.57‐2.51) | |
| Dialysis department | 0.02* | 0.32 | (0.12‐0.83) | 0.04* | 1.65 | (1.02‐2.66) | 0.01* | 2.21 | (1.23‐3.97) | 0.02* | 1.81 | (1.12‐2.92) | |
| Critical care center, ICU, or CCU | <0.01* | 2.44 | (1.60‐3.74) | 0.49 | 1.13 | (0.79‐1.61) | 0.56 | 1.17 | (0.70‐1.94) | 0.04* | 1.43 | (1.01‐2.01) | |
| Administration department | 0.22 | 0.55 | (0.21‐1.44) | 0.07 | 1.38 | (0.98‐1.93) | 0.29 | 0.64 | (0.27‐1.48) | 0.07 | 1.37 | (0.98‐1.91) | |
| Clinical radiology department | 0.53 | 1.42 | (0.48‐4.21) | 0.51 | 1.21 | (0.69‐2.12) | 0.02* | 0.17 | (0.04‐0.78) | 0.57 | 1.17 | (0.69‐1.98) | |
| Rehabilitation department | 0.93 | 0.93 | (0.18‐4.77) | 0.88 | 1.08 | (0.42‐2.80) | 0.82 | 1.22 | (0.22‐6.79) | 0.77 | 1.14 | (0.46‐2.85) | |
| Outpatient department | <0.01* | 0.41 | (0.26‐0.65) | 0.03* | 1.35 | (1.02‐1.78) | 0.02* | 0.56 | (0.35‐0.90) | 0.40 | 1.12 | (0.86‐1.47) | |
| Dietary department | 0.33 | 1.94 | (0.51‐7.35) | 0.66 | 1.13 | (0.65‐1.99) | 0.85 | 1.13 | (0.30‐4.26) | 0.84 | 1.06 | (0.61‐1.82) | |
| Clinical laboratory or physiology department | 0.40 | 0.53 | (0.12‐2.34) | 0.85 | 1.06 | (0.59‐1.89) | 0.21 | 0.52 | (0.18‐1.45) | 0.87 | 0.96 | (0.55‐1.65) | |
| Pediatric ward | 0.27 | 0.72 | (0.41‐1.29) | 0.08 | 0.69 | (0.45‐1.05) | 0.02* | 0.43 | (0.21‐0.90) | 0.03* | 0.65 | (0.43‐0.97) | |
| Pharmaceutical department | 0.05 | 0.52 | (0.26‐1.01) | 0.71 | 1.26 | (0.36‐4.38) | 0.14 | 0.63 | (0.34‐1.17) | ||||
| Operation department | <0.01* | 0.24 | (0.12‐0.48) | <0.01* | 0.36 | (0.23‐0.55) | <0.01* | 0.21 | (0.09‐0.48) | <0.01* | 0.27 | (0.18‐0.41) | |
| Obstetrics and gynecology ward, perinatal ward, or NICU | <0.01* | 0.04 | (0.01‐0.18) | <0.01* | 0.19 | (0.12‐0.32) | <0.01* | 0.02 | (0.00‐0.18) | <0.01* | 0.14 | (0.08‐0.22) | |
| Profession | Doctor | 1.00 | 1.00 | 1.00 | <0.01* | 1.00 | |||||||
| Nurse | <0.01* | 4.09 | (2.41‐6.95) | 0.16 | 1.27 | (0.91‐1.76) | <0.01* | 11.64 | (4.38‐30.90) | 1.64 | (1.19‐2.26) | ||
| Therapist | 0.10 | 4.03 | (0.76‐21.28) | 0.83 | 0.90 | (0.34‐2.39) | 0.05* | 7.11 | (1.02‐49.3) | 0.83 | 1.11 | (0.43‐2.83) | |
| Nursing aide or care worker | 0.03* | 1.95 | (1.07‐3.55) | 0.09 | 0.71 | (0.47‐1.05) | <0.01* | 4.66 | (1.63‐13.31) | 0.19 | 0.77 | (0.53‐1.14) | |
| Clerk | 0.03* | 0.36 | (0.14‐0.90) | 0.27 | 0.80 | (0.54‐1.19) | 0.17 | 2.26 | (0.70‐7.27) | 0.09 | 0.72 | (0.49‐1.06) | |
| Technician | 0.27 | 0.55 | (0.19‐1.60) | <0.01* | 0.37 | (0.22‐0.61) | <0.01* | 6.92 | (2.20‐21.76) | <0.01* | 0.46 | (0.28‐0.74) | |
| Others | <0.01* | 0.21 | (0.08‐0.57) | <0.01* | 0.39 | (0.25‐0.60) | 0.24 | 2.14 | (0.60‐7.63) | <0.01* | 0.39 | (0.25‐0.59) | |
| Years of experience in their own specialty or profession | <5 yr | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| 6‐10 yr | <0.01* | 1.42 | (1.17‐1.72) | 0.01* | 1.22 | (1.05‐1.42) | 0.84 | 0.98 | (0.78‐1.22) | 0.01* | 1.22 | (1.05‐1.42) | |
| 11‐15 yr | <0.01* | 1.64 | (1.31‐2.05) | <0.01* | 1.45 | (1.22‐1.73) | 0.30 | 1.14 | (0.89‐1.47) | <0.01* | 1.35 | (1.13‐1.60) | |
| 16‐20 yr | 0.30 | 1.16 | (0.88‐1.52) | <0.01* | 1.47 | (1.21‐1.79) | 0.09 | 0.75 | (0.54‐1.04) | <0.01* | 1.34 | (1.10‐1.63) | |
| 21 yr or more | 0.58 | 1.07 | (0.84‐1.37) | <0.01* | 1.65 | (1.39‐1.96) | <0.01* | 0.63 | (0.47‐0.85) | <0.01* | 1.38 | (1.16‐1.64) | |
| Working hours per week | <20 hr | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| 20‐40 hr | 0.04* | 1.49 | (1.01‐2.19) | 0.52 | 1.08 | (0.85‐1.39) | 0.12 | 1.40 | (0.91‐2.15) | 0.10 | 1.23 | (0.96‐1.56) | |
| 40‐60 hr | <0.01* | 1.80 | (1.25‐2.58) | 0.03* | 1.28 | (1.02‐1.60) | 0.05* | 1.50 | (1.00‐2.24) | <0.01* | 1.39 | (1.11‐1.74) | |
| 60 hr or more | <0.01* | 2.14 | (1.37‐3.34) | <0.01* | 1.62 | (1.21‐2.17) | 0.14 | 1.49 | (0.88‐2.50) | <0.01* | 1.90 | (1.43‐2.54) | |
| Gender | (Female vs male) | 0.69 | 0.95 | (0.76‐1.20) | 0.16 | 1.12 | (0.95‐1.32) | <0.01* | 1.59 | (1.18‐2.12) | 0.01* | 1.22 | (1.05‐1.43) |
| Direct interaction or contact with patients | (Constant and direct interaction with patients vs no interaction) | 0.02* | 2.17 | (1.11‐4.22) | <0.01* | 2.46 | (1.87‐3.24) | <0.01* | 6.80 | (2.43‐19.03) | <0.01* | 2.58 | (1.97‐3.37) |
Adjusted odds ratios of verbal abuse were significantly high in hospital with 200 beds or more, in general wards, psychiatric wards, long‐term care wards, outpatient departments, and dialysis departments; and for longer years of experience in their own specialty; for longer working hours; and for direct interaction with patients.
Adjusted odds ratios of sexual harassment were significantly high in general wards, and dialysis departments; for nurses, nursing aides/care workers, technicians, therapists; for females; and for direct interaction with patients.
Adjusted odds ratios for at least 1 of the 3 kinds of workplace violence were significantly high in hospitals with 200 beds or more, in general wards, psychiatric wards, critical care centers/ICU/CCU, long‐term care wards, and dialysis departments; for nurses; for longer years of experience in their own specialty; for longer working hours; for females; and for direct interaction with patients.
Factors Associated With Lower Risk of Violence
Adjusted odds ratios of physical aggression were significantly low in dialysis departments; outpatient departments; operation departments; obstetrics and gynecology wards, perinatal wards, or neonatal intensive care units (NICU); and for clerks.
Adjusted odds ratios of verbal abuse were significantly low in operation departments; obstetrics and gynecology wards, perinatal wards, or NICU; and for technicians.
Adjusted odds ratios of sexual harassment were significantly low in clinical radiology departments; outpatient departments; pediatric wards; operation departments; obstetrics and gynecology wards, perinatal wards, or NICU; and for longer years of experience in their own specialty.
Adjusted odds ratios for at least 1 of the 3 kinds of workplace violence were significantly low in pediatric wards; operation departments; obstetrics and gynecology wards, perinatal wards, or NICU; and for technicians.
DISCUSSION
Among the healthcare staff, 36.4% experienced workplace violence by patients or their relatives over the past year; 15.9% experienced physical aggressions, 29.8% verbal abuse, and 9.9% sexual harassment. The risk factors of workplace violence identified in the present study were similar to those studies conducted not only in Japan, but also in Western countries. Though the target population was limited to Asians, our results can be applicable to other races, countries, and cultures.
Incidence of Workplace Violence
Most previous studies covered only specific professions at hospitals, such as nurses or critical care center staff, and there are only few multicenter studies covering entire sections and professions like this study.510, 1214 A Spanish study including about 8000 healthcare workers reported that 11% had experienced physical aggression, 64% had experienced threatening behavior, intimidation, or insults in the past year.11 The incidence of physical aggression was similar in both studies, but the incidence of verbal abuse was about twice as high as that of this study. The low response rate in the Spanish study (24%) might have contributed to a higher number of verbal abuse incidents, because those with experience of workplace violence would likely have answered the questionnaire. It is difficult to compare the incidence of workplace violence among different studies because the definitions of workplace violence differ widely. Ethnic culture might also affect the acknowledgement of workplace violence. The European NEXT study including about 30,000 nurses in 8 European countries reported a range of 10.4% incidence of workplace violence in the Netherlands, and 39.1% in France.10
Risk Factors of Physical Aggression
Previous studies reported that the prevalence of physical aggression is high in psychiatric wards, critical care centers, or long‐term care wards.1015 In these departments, patients with mental illness, postoperative delirium, or dementia are likely to be admitted.
Nurses and nursing aides are reported to be likely to experience physical aggression.3, 11, 15 Nurses and nursing aides have longer work hours with direct interaction with patients than other professions, and are considered to be at high risk of physical aggression.
Some studies, which did not examine influences by profession or department, reported that male was a risk factor for physical aggression and verbal abuse.6, 10, 11, 13 In this study though, the male gender was not associated with physical aggression or verbal abuse. Male nurses and nursing aides are likely to be assigned to high‐risk departments or to care for high‐risk patients. Gender may be confounded with variables such as profession or department.15
Longer work hours mean more frequent interaction with patients, and the risk for physical aggression might increase. Constant and direct interaction with patients is a risk factor, not only for physical aggression, but also for verbal abuse and sexual harassment.10
Risk Factors of Verbal Abuse
Previous studies reported that incidents of verbal abuse are high for nurses and nursing aides.15 Although in this study the proportion of verbal abuse was the highest in nurses (39.4%), adjusted odds ratio was not significant. Factors other than nurse profession, such as department and direct interaction with patients relating to the nurse profession, might be the higher risk factors for verbal abuse.
As reported in previous studies, psychiatric wards and long‐term care wards are risk factors of verbal abuse also in this study.10, 13, 15 Long waiting time at outpatient departments might increase the risk of verbal abuse.
Dialysis departments are at high risk of verbal abuse and sexual harassment. Compared to other outpatients, dialysis patients are forced to stay a long time in hospitals and there is, therefore, more interaction with nurses and technicians. The characteristic personality of dialysis patients, such as neuroticism or psychoticism, might also affect verbal abuse or sexual harassment.16
Because longer working hours mean more frequent interaction with patients, the risk of verbal abuse might increase.17 Managers with longer work experience might be at high risk for verbal abuse, because they often assume responsibility and take on the task of dealing with patients and their relevant complaints.11
Risk Factors of Sexual Harassment
Nurses are likely to experience sexual harassment because their public image seems to combine sexuality and maternalism.18 Nursing aides, technicians, and therapists also experience sexual harassment. The common risk factor among those professions is the direct contact with the patient's body during the patient's transfer. A lot of studies reported that female gender is a risk factor of sexual harassment.17, 19
Safety Factors of Workplace Violence
Adjusted odds ratios of operation departments, and obstetrics and gynecology wards, perinatal wards, or NICU were common safety factors for each type of workplace violence. Usually, the patients in operation rooms cannot talk or move a finger carelessly during the surgery. The fact that there are no adult male patients in obstetrics and gynecology wards, perinatal wards, or NICU, might have an influence on lower occurrence of workplace violence in these areas.
Limitations
This study used a questionnaire survey asking about subjective experiences of workplace violence over the 1 year before the study. There is the possibility of recall bias, and the same incident recognized as workplace violence by one person might not have been recognized as such by another person, because sensitivity differs among respondents.
In some categories with fewer respondents, such as the pharmaceutical department, it might be difficult to examine the exact confidence intervals of odds ratio. Further study with increased respondents of those categories is needed to confirm the odds ratios and the confidence intervals.
The rates of victims or risk for workplace violence were considered to vary with the character of the residents of each area or policy of each hospital. Therefore, a further analysis with adjustment for those factors is needed.
CONCLUSIONS
This study reveals that a significant proportion of healthcare staff (36.4%) has experienced workplace violence over the 1 year before the study was conducted and suggests that workplace violence is a serious problem. The attributes of healthcare staff who are at risk of workplace violence could be identified for each type of workplace violence. The mechanisms and the countermeasures for each type of workplace violence at those high‐risk areas should be further investigated. Further studies are necessary to confirm whether these findings are applicable to different races and different countries with different cultures.
- Home Office. Violence at Work: Findings From the 2002/2003 British Crime Survey. Available at: http://www.homeoffice.gov.uk/rds/pdfs2/rdsolr0404.pdf. Accessed November 10,2010.
- ,.Workplace violence in Finland: high‐risk groups and preventive strategies.Am J Ind Med Suppl.1999;1:80–81.
- .Violence in the Workplace 1993–99, National Crime Victimization Survey,Washington, DC:Bureau of Justice Statistics;2001:1–12.
- .International perspectives on workplace bullying among nurses: a review.Int Nurs Rev.2009;56(1):34–40.
- ,,.Scoping workplace aggression in nursing: findings from an Australian study.J Adv Nurs.2006;55(6):778–787.
- ,,, et al.Violence against nurses working in US emergency departments.J Nurs Adm.2009;39(7–8):340–349.
- ,,.Hospital staff responses to workplace violence in a psychiatric hospital in Taiwan.Int J Occup Environ Health.2009;15(2):173–179.
- All Japan Hospital Association. Research on actual conditions of risk management system and workplace violence at hospitals (Japanese). Available at: http://www.ajha.or.jp/voice/pdf/other/080422.pdf. Accessed November 10, 2010.
- ,,, et al.The present situation and the countermeasure for verbal abuse and physical aggression of patients (Japanese).Japan Medical Journal.2007;4354:81–84.
- ,,, et al.Work‐related factors and violence among nursing staff in the European NEXT study: a longitudinal cohort study.Int J Nurs Stud.2008;45(1):35–50.
- ,,, et al.Aggression towards health care workers in Spain: a multi‐facility study to evaluate the distribution of growing violence among professionals, health facilities and departments.Int J Occup Environ Health.2009;15(1):29–35.
- Office of Policy Planning, Japanese Nursing Association.Research on actual conditions of workplace violence at healthcare sector 2003 (Japanese).Survey Report of Japanese Nursing Association.2004;71:7–16.
- ,.Factors related to on‐the‐job abuse of nurses by patients.Health Rep.2009;20(2):7–19.
- ,,, et al.Risk factors for work‐related assaults on nurses.Epidemiology.2005;16(5):704–709.
- ,,, et al.Characterizing violence in health care in British Columbia.J Adv Nurs.2009;65(8):1655–1663.
- ,,, et al.Personality dimensions of haemodialysis patients related to initial renal disease.EDTNA ERCA J.2002;28(1):21–24.
- ,,.Factors associated with workplace violence in paramedics.Prehosp Disaster Med.2009;24(5):417–421.
- .Sexuality. An uninvited guest.Nurs Times.1989;85(5):25–28.
- ,,, et al.Universal problems during residency: abuse and harassment.Med Educ.2009;43(7):628–636.
- Home Office. Violence at Work: Findings From the 2002/2003 British Crime Survey. Available at: http://www.homeoffice.gov.uk/rds/pdfs2/rdsolr0404.pdf. Accessed November 10,2010.
- ,.Workplace violence in Finland: high‐risk groups and preventive strategies.Am J Ind Med Suppl.1999;1:80–81.
- .Violence in the Workplace 1993–99, National Crime Victimization Survey,Washington, DC:Bureau of Justice Statistics;2001:1–12.
- .International perspectives on workplace bullying among nurses: a review.Int Nurs Rev.2009;56(1):34–40.
- ,,.Scoping workplace aggression in nursing: findings from an Australian study.J Adv Nurs.2006;55(6):778–787.
- ,,, et al.Violence against nurses working in US emergency departments.J Nurs Adm.2009;39(7–8):340–349.
- ,,.Hospital staff responses to workplace violence in a psychiatric hospital in Taiwan.Int J Occup Environ Health.2009;15(2):173–179.
- All Japan Hospital Association. Research on actual conditions of risk management system and workplace violence at hospitals (Japanese). Available at: http://www.ajha.or.jp/voice/pdf/other/080422.pdf. Accessed November 10, 2010.
- ,,, et al.The present situation and the countermeasure for verbal abuse and physical aggression of patients (Japanese).Japan Medical Journal.2007;4354:81–84.
- ,,, et al.Work‐related factors and violence among nursing staff in the European NEXT study: a longitudinal cohort study.Int J Nurs Stud.2008;45(1):35–50.
- ,,, et al.Aggression towards health care workers in Spain: a multi‐facility study to evaluate the distribution of growing violence among professionals, health facilities and departments.Int J Occup Environ Health.2009;15(1):29–35.
- Office of Policy Planning, Japanese Nursing Association.Research on actual conditions of workplace violence at healthcare sector 2003 (Japanese).Survey Report of Japanese Nursing Association.2004;71:7–16.
- ,.Factors related to on‐the‐job abuse of nurses by patients.Health Rep.2009;20(2):7–19.
- ,,, et al.Risk factors for work‐related assaults on nurses.Epidemiology.2005;16(5):704–709.
- ,,, et al.Characterizing violence in health care in British Columbia.J Adv Nurs.2009;65(8):1655–1663.
- ,,, et al.Personality dimensions of haemodialysis patients related to initial renal disease.EDTNA ERCA J.2002;28(1):21–24.
- ,,.Factors associated with workplace violence in paramedics.Prehosp Disaster Med.2009;24(5):417–421.
- .Sexuality. An uninvited guest.Nurs Times.1989;85(5):25–28.
- ,,, et al.Universal problems during residency: abuse and harassment.Med Educ.2009;43(7):628–636.
Copyright © 2011 Society of Hospital Medicine