User login
Surprise patients with the truth about pain and aging
Healthcare Quality Accounting Metrics Need Improvement

—Gregg Meyer, MD, MSc, chief clinical officer and executive vice president for population health for the Dartmouth-Hitchcock Health System in Lebanon, N.H.
As healthcare quality reporting continues to evolve in this era of value-based purchasing (VBP), players on both the giving and receiving ends of performance incentives agree on the need to improve the accountability metrics with which providers are measured, ranked, rewarded, and penalized. Many of the measures currently in use—e.g., Centers for Medicare & Medicaid Services’ (CMS) core process measures and patient satisfaction ratings, the gross outcome metrics of mortality, infection, and readmission rates—are blunt instruments in need of refinement.
Entities such as the National Quality Forum (NQF), the American Medical Association’s Physician Consortium for Performance Improvement (PCPI), and the National Quality Measures Clearinghouse (NQMC) recognize the need to develop and endorse more timely, credible, and patient-centered outcome metrics. Largely missing from the current crop of outcome measure sets is a meaningful account of the patient’s perspective.
Enter patient-reported outcomes (PROs), defined as “any report of the status of a patient’s health condition that comes directly from the patient, without interpretation of the patient’s response by a clinician or anyone else.”1 PRO tools “measure what patients are able to do and how they feel by asking questions” (see “Types of Patient-Reported Outcomes [PROs],” p. 19).
If successfully adapted for public reporting on a wide scale, PROs could become the next evolutionary step in healthcare quality reporting, integrating health status and patient experience data into outcome metrics that truly matter to patients. They could enable a richer understanding of their clinical experiences and responses to therapy, and help providers target necessary improvements with greater precision.
“As a provider, I care about my patients not developing infections, getting the right medications, and not being readmitted. Patients, however, have a different set of priorities around issues like ‘How quickly will I be able to return to work? When will I be able to chase my grandkids around the yard? How much is this care going to cost me out of pocket?’” says healthcare quality expert Gregg Meyer, MD, MSc, chief clinical officer and executive vice president for population health for the Dartmouth-Hitchcock Health System in Lebanon, N.H. “This next generation of accountability will allow us to move from being provider- and payor-centered to becoming truly patient-centered, and will serve as a key reminder that patients are no longer passive participants. They are key partners, in both the delivery of care and the measurement of that care.”
The idea of PROs is one whose “time has finally arrived,” according to medical outcomes researcher David Cella, PhD, professor and chair of the Department of Medical Social Sciences at Northwestern University Feinberg School of Medicine in Chicago.
“The case for inclusion of outcomes that matter most to patients, like the effect of treatment upon their symptoms, function, and overall well-being, has always been compelling as an ideal to strive toward,” Cella adds. “PROs can and should be considered as true treatment outcome measures, and their ability to capture quality information efficiently make them well-suited for this role.”
The FDA even permits PROs (i.e. pain, anxiety, depression, sleep, and physical and social functioning) to be used as experimental endpoints for clinical trials to support claims in medical product labeling.2
The Patient Voice
The Department Health and Human Services (HHS) is searching for ways to fill current gaps in outcome measures, and has funded a patient outcomes project by the NQF to help ramp up patient-focused measure development activities within the federal government. In a recent report stemming from that project, the NQF states: “The patient’s voice is not readily captured in traditional health records and data systems, yet the beneficiary of healthcare services is often in the best position to evaluate the effectiveness of those services.”3
The NQF also is conducting foundational work to evaluate the most promising and viable PROs for quality measurement use and methodological issues involved in collecting and aggregating PRO data for provider performance assessment, says Helen Burstin, MD, MPH, NQF’s senior vice president for performance measures.
“PROs provide the opportunity to hear about the outcome of a clinician’s intervention directly from the patient—for example, visual improvement after cataract surgery, relief from nausea after chemotherapy, and mobility enhancement and pain relief after a hip or knee replacement,” she says. “The goal is to develop reliable and valid PRO performance measures that are applicable across multiple settings of care and/or multiple conditions, which the NQF can endorse for accountability and quality-improvement purposes.”
Specific NQF recommendations regarding PROs and performance measurement are expected to be available for review and comment this month, with a 30-day public and member comment period.
A wide variety of patient-level instruments to measure PROs have been used for clinical research purposes, many of which have been evaluated and catalogued within a system of assessment tools known as the National Institutes of Health’s (NIH) Patient-Reported Outcome Measurement Information System (PROMIS), Dr. Burstin says. PROMIS questionnaires prompt patients to measure such outcomes as how much difficulty they experience when walking a block on flat ground, getting in and out of bed, or doing strenuous activities, such as bicycling or jogging. NIH-funded studies using PROMIS tools are taking place at 12 sites across the country (http://nihpromis.org/default).
“PROMIS provides two distinct advantages to the PRO performance metric landscape,” argues Cella, who is principal investigator of the Statistical Center for PROMIS. “It has a computerized adaptive testing option, so efficient and accurate assessment is now possible at the individual patient level, with just a few questions per area. It also standardizes its scoring and reporting, such that many other similar measures can be used and their scores reported on a common, PROMIS metric.”
HM Applications
“The voice of the clinician is also needed during this PRO development process,” Dr. Burstin says. “We welcome hospitalists to engage in our projects and weigh in about the most meaningful and actionable patient outcomes that are relevant to their practice.”
“Taking PROs and applying them to hospital medicine is really doable if you take into account the lessons learned from providers who have already used PROs successfully in clinical settings,” says Pat Courneya, MD, medical director for HealthPartners Health Plan in Minnesota.
HealthPartners recently began using PROs in a quality measurement and reward program, offering financial bonuses to physical therapists who achieve a high PRO score relative to resource use (number of PT sessions required). “Having objective PRO measurements allows clinicians to create benchmarks for their patients regarding how much functional improvement they expect to achieve, and how many PT sessions are required to achieve that degree of improvement,” Dr. Courneya says. Using an interactive, Web-based PRO assessment tool, the program has helped tailor care to the expectations of patients while also significantly reducing the overall number of PT visits, especially by medically complex, post-operative patients.
HealthPartners has successfully used PROs as part of an innovative care model for managing patients with depression. At the outset of treatment, patients are administered the PHQ-9, a nine-item patient health questionnaire designed to assess depression symptoms and functional impairment, and derive a severity score. Patients receive care by a team composed of a primary-care physician, a care manager, and a consulting psychiatrist, after which their degree of symptom improvement is again measured. With this program, HealthPartners has achieved significantly more patients with depression into remission by six months compared with typical primary-care treatment, Dr. Courneya says. This model of care has since garnered a CMS Innovation Grant, managed by the HealthPartners Institute for Education and Research and directed by Minnesota’s Institute for Clinical Systems Improvement, aimed at spreading the model to five other states.
“PROs are potentially as useful for hospital medicine as for any other type of medical practice,” says Shaun Frost, MD, SFHM, SHM president and associate medical director of care delivery systems for HealthPartners Health Plan. “There is a big opportunity for hospitalists to incorporate shared decision-making to learn patients’ preferences, such as expectations of when they will be discharged, and understanding of therapeutic options.”
Peri-surgical care is a particularly important opportunity for hospitalists to demonstrate their value by leveraging PROs, according to Dr. Frost. “Patients sometimes come to the table with unrealistic prior expectations that physicians can make pain go away completely. We need to clarify their expectations preoperatively, when we meet them for the very first time, so that they establish a realistic baseline,” he says. “We then need to have a diligent conversation with them immediately after their operation to discuss their pain-management goals, a realistic physical therapy schedule, and post-discharge expectations.”
By clearly understanding patient objectives, hospitalists can “adjust the therapy they’re getting to their expectations, maximizing its effectiveness while minimizing delays in care and transitions to other care settings,” Dr. Frost says.
Chris Guadagnino is a freelance medical writer in Philadelphia.
References
- National Quality Forum. Patient-reported outcomes. National Quality Forum website. Available at: http://www.qualityforum.org/Projects/n-r/Patient-Reported_Outcomes/Patient-Reported_Outcomes.aspx. Accessed Oct. 2, 2012.
- U.S. Food and Drug Administration. The Patient-Reported Outcomes Consortium. U.S. Food and Drug Administration website. Available at: http://www.fda.gov/AboutFDA/PartnershipsCollaborations/PublicPrivatePartnershipProgram/ucm231129.htm. Accessed Oct. 2, 2012.
- National Quality Forum. National voluntary consensus standards for patient outcomes 2009.National Quality Forum website. Available at: http://www.qualityforum.org/Publications/2011/07/National_Voluntary_Consensus_Standards_for_Patient_Outcomes_2009.aspx. Accessed Oct. 2, 2012.

—Gregg Meyer, MD, MSc, chief clinical officer and executive vice president for population health for the Dartmouth-Hitchcock Health System in Lebanon, N.H.
As healthcare quality reporting continues to evolve in this era of value-based purchasing (VBP), players on both the giving and receiving ends of performance incentives agree on the need to improve the accountability metrics with which providers are measured, ranked, rewarded, and penalized. Many of the measures currently in use—e.g., Centers for Medicare & Medicaid Services’ (CMS) core process measures and patient satisfaction ratings, the gross outcome metrics of mortality, infection, and readmission rates—are blunt instruments in need of refinement.
Entities such as the National Quality Forum (NQF), the American Medical Association’s Physician Consortium for Performance Improvement (PCPI), and the National Quality Measures Clearinghouse (NQMC) recognize the need to develop and endorse more timely, credible, and patient-centered outcome metrics. Largely missing from the current crop of outcome measure sets is a meaningful account of the patient’s perspective.
Enter patient-reported outcomes (PROs), defined as “any report of the status of a patient’s health condition that comes directly from the patient, without interpretation of the patient’s response by a clinician or anyone else.”1 PRO tools “measure what patients are able to do and how they feel by asking questions” (see “Types of Patient-Reported Outcomes [PROs],” p. 19).
If successfully adapted for public reporting on a wide scale, PROs could become the next evolutionary step in healthcare quality reporting, integrating health status and patient experience data into outcome metrics that truly matter to patients. They could enable a richer understanding of their clinical experiences and responses to therapy, and help providers target necessary improvements with greater precision.
“As a provider, I care about my patients not developing infections, getting the right medications, and not being readmitted. Patients, however, have a different set of priorities around issues like ‘How quickly will I be able to return to work? When will I be able to chase my grandkids around the yard? How much is this care going to cost me out of pocket?’” says healthcare quality expert Gregg Meyer, MD, MSc, chief clinical officer and executive vice president for population health for the Dartmouth-Hitchcock Health System in Lebanon, N.H. “This next generation of accountability will allow us to move from being provider- and payor-centered to becoming truly patient-centered, and will serve as a key reminder that patients are no longer passive participants. They are key partners, in both the delivery of care and the measurement of that care.”
The idea of PROs is one whose “time has finally arrived,” according to medical outcomes researcher David Cella, PhD, professor and chair of the Department of Medical Social Sciences at Northwestern University Feinberg School of Medicine in Chicago.
“The case for inclusion of outcomes that matter most to patients, like the effect of treatment upon their symptoms, function, and overall well-being, has always been compelling as an ideal to strive toward,” Cella adds. “PROs can and should be considered as true treatment outcome measures, and their ability to capture quality information efficiently make them well-suited for this role.”
The FDA even permits PROs (i.e. pain, anxiety, depression, sleep, and physical and social functioning) to be used as experimental endpoints for clinical trials to support claims in medical product labeling.2
The Patient Voice
The Department Health and Human Services (HHS) is searching for ways to fill current gaps in outcome measures, and has funded a patient outcomes project by the NQF to help ramp up patient-focused measure development activities within the federal government. In a recent report stemming from that project, the NQF states: “The patient’s voice is not readily captured in traditional health records and data systems, yet the beneficiary of healthcare services is often in the best position to evaluate the effectiveness of those services.”3
The NQF also is conducting foundational work to evaluate the most promising and viable PROs for quality measurement use and methodological issues involved in collecting and aggregating PRO data for provider performance assessment, says Helen Burstin, MD, MPH, NQF’s senior vice president for performance measures.
“PROs provide the opportunity to hear about the outcome of a clinician’s intervention directly from the patient—for example, visual improvement after cataract surgery, relief from nausea after chemotherapy, and mobility enhancement and pain relief after a hip or knee replacement,” she says. “The goal is to develop reliable and valid PRO performance measures that are applicable across multiple settings of care and/or multiple conditions, which the NQF can endorse for accountability and quality-improvement purposes.”
Specific NQF recommendations regarding PROs and performance measurement are expected to be available for review and comment this month, with a 30-day public and member comment period.
A wide variety of patient-level instruments to measure PROs have been used for clinical research purposes, many of which have been evaluated and catalogued within a system of assessment tools known as the National Institutes of Health’s (NIH) Patient-Reported Outcome Measurement Information System (PROMIS), Dr. Burstin says. PROMIS questionnaires prompt patients to measure such outcomes as how much difficulty they experience when walking a block on flat ground, getting in and out of bed, or doing strenuous activities, such as bicycling or jogging. NIH-funded studies using PROMIS tools are taking place at 12 sites across the country (http://nihpromis.org/default).
“PROMIS provides two distinct advantages to the PRO performance metric landscape,” argues Cella, who is principal investigator of the Statistical Center for PROMIS. “It has a computerized adaptive testing option, so efficient and accurate assessment is now possible at the individual patient level, with just a few questions per area. It also standardizes its scoring and reporting, such that many other similar measures can be used and their scores reported on a common, PROMIS metric.”
HM Applications
“The voice of the clinician is also needed during this PRO development process,” Dr. Burstin says. “We welcome hospitalists to engage in our projects and weigh in about the most meaningful and actionable patient outcomes that are relevant to their practice.”
“Taking PROs and applying them to hospital medicine is really doable if you take into account the lessons learned from providers who have already used PROs successfully in clinical settings,” says Pat Courneya, MD, medical director for HealthPartners Health Plan in Minnesota.
HealthPartners recently began using PROs in a quality measurement and reward program, offering financial bonuses to physical therapists who achieve a high PRO score relative to resource use (number of PT sessions required). “Having objective PRO measurements allows clinicians to create benchmarks for their patients regarding how much functional improvement they expect to achieve, and how many PT sessions are required to achieve that degree of improvement,” Dr. Courneya says. Using an interactive, Web-based PRO assessment tool, the program has helped tailor care to the expectations of patients while also significantly reducing the overall number of PT visits, especially by medically complex, post-operative patients.
HealthPartners has successfully used PROs as part of an innovative care model for managing patients with depression. At the outset of treatment, patients are administered the PHQ-9, a nine-item patient health questionnaire designed to assess depression symptoms and functional impairment, and derive a severity score. Patients receive care by a team composed of a primary-care physician, a care manager, and a consulting psychiatrist, after which their degree of symptom improvement is again measured. With this program, HealthPartners has achieved significantly more patients with depression into remission by six months compared with typical primary-care treatment, Dr. Courneya says. This model of care has since garnered a CMS Innovation Grant, managed by the HealthPartners Institute for Education and Research and directed by Minnesota’s Institute for Clinical Systems Improvement, aimed at spreading the model to five other states.
“PROs are potentially as useful for hospital medicine as for any other type of medical practice,” says Shaun Frost, MD, SFHM, SHM president and associate medical director of care delivery systems for HealthPartners Health Plan. “There is a big opportunity for hospitalists to incorporate shared decision-making to learn patients’ preferences, such as expectations of when they will be discharged, and understanding of therapeutic options.”
Peri-surgical care is a particularly important opportunity for hospitalists to demonstrate their value by leveraging PROs, according to Dr. Frost. “Patients sometimes come to the table with unrealistic prior expectations that physicians can make pain go away completely. We need to clarify their expectations preoperatively, when we meet them for the very first time, so that they establish a realistic baseline,” he says. “We then need to have a diligent conversation with them immediately after their operation to discuss their pain-management goals, a realistic physical therapy schedule, and post-discharge expectations.”
By clearly understanding patient objectives, hospitalists can “adjust the therapy they’re getting to their expectations, maximizing its effectiveness while minimizing delays in care and transitions to other care settings,” Dr. Frost says.
Chris Guadagnino is a freelance medical writer in Philadelphia.
References
- National Quality Forum. Patient-reported outcomes. National Quality Forum website. Available at: http://www.qualityforum.org/Projects/n-r/Patient-Reported_Outcomes/Patient-Reported_Outcomes.aspx. Accessed Oct. 2, 2012.
- U.S. Food and Drug Administration. The Patient-Reported Outcomes Consortium. U.S. Food and Drug Administration website. Available at: http://www.fda.gov/AboutFDA/PartnershipsCollaborations/PublicPrivatePartnershipProgram/ucm231129.htm. Accessed Oct. 2, 2012.
- National Quality Forum. National voluntary consensus standards for patient outcomes 2009.National Quality Forum website. Available at: http://www.qualityforum.org/Publications/2011/07/National_Voluntary_Consensus_Standards_for_Patient_Outcomes_2009.aspx. Accessed Oct. 2, 2012.

—Gregg Meyer, MD, MSc, chief clinical officer and executive vice president for population health for the Dartmouth-Hitchcock Health System in Lebanon, N.H.
As healthcare quality reporting continues to evolve in this era of value-based purchasing (VBP), players on both the giving and receiving ends of performance incentives agree on the need to improve the accountability metrics with which providers are measured, ranked, rewarded, and penalized. Many of the measures currently in use—e.g., Centers for Medicare & Medicaid Services’ (CMS) core process measures and patient satisfaction ratings, the gross outcome metrics of mortality, infection, and readmission rates—are blunt instruments in need of refinement.
Entities such as the National Quality Forum (NQF), the American Medical Association’s Physician Consortium for Performance Improvement (PCPI), and the National Quality Measures Clearinghouse (NQMC) recognize the need to develop and endorse more timely, credible, and patient-centered outcome metrics. Largely missing from the current crop of outcome measure sets is a meaningful account of the patient’s perspective.
Enter patient-reported outcomes (PROs), defined as “any report of the status of a patient’s health condition that comes directly from the patient, without interpretation of the patient’s response by a clinician or anyone else.”1 PRO tools “measure what patients are able to do and how they feel by asking questions” (see “Types of Patient-Reported Outcomes [PROs],” p. 19).
If successfully adapted for public reporting on a wide scale, PROs could become the next evolutionary step in healthcare quality reporting, integrating health status and patient experience data into outcome metrics that truly matter to patients. They could enable a richer understanding of their clinical experiences and responses to therapy, and help providers target necessary improvements with greater precision.
“As a provider, I care about my patients not developing infections, getting the right medications, and not being readmitted. Patients, however, have a different set of priorities around issues like ‘How quickly will I be able to return to work? When will I be able to chase my grandkids around the yard? How much is this care going to cost me out of pocket?’” says healthcare quality expert Gregg Meyer, MD, MSc, chief clinical officer and executive vice president for population health for the Dartmouth-Hitchcock Health System in Lebanon, N.H. “This next generation of accountability will allow us to move from being provider- and payor-centered to becoming truly patient-centered, and will serve as a key reminder that patients are no longer passive participants. They are key partners, in both the delivery of care and the measurement of that care.”
The idea of PROs is one whose “time has finally arrived,” according to medical outcomes researcher David Cella, PhD, professor and chair of the Department of Medical Social Sciences at Northwestern University Feinberg School of Medicine in Chicago.
“The case for inclusion of outcomes that matter most to patients, like the effect of treatment upon their symptoms, function, and overall well-being, has always been compelling as an ideal to strive toward,” Cella adds. “PROs can and should be considered as true treatment outcome measures, and their ability to capture quality information efficiently make them well-suited for this role.”
The FDA even permits PROs (i.e. pain, anxiety, depression, sleep, and physical and social functioning) to be used as experimental endpoints for clinical trials to support claims in medical product labeling.2
The Patient Voice
The Department Health and Human Services (HHS) is searching for ways to fill current gaps in outcome measures, and has funded a patient outcomes project by the NQF to help ramp up patient-focused measure development activities within the federal government. In a recent report stemming from that project, the NQF states: “The patient’s voice is not readily captured in traditional health records and data systems, yet the beneficiary of healthcare services is often in the best position to evaluate the effectiveness of those services.”3
The NQF also is conducting foundational work to evaluate the most promising and viable PROs for quality measurement use and methodological issues involved in collecting and aggregating PRO data for provider performance assessment, says Helen Burstin, MD, MPH, NQF’s senior vice president for performance measures.
“PROs provide the opportunity to hear about the outcome of a clinician’s intervention directly from the patient—for example, visual improvement after cataract surgery, relief from nausea after chemotherapy, and mobility enhancement and pain relief after a hip or knee replacement,” she says. “The goal is to develop reliable and valid PRO performance measures that are applicable across multiple settings of care and/or multiple conditions, which the NQF can endorse for accountability and quality-improvement purposes.”
Specific NQF recommendations regarding PROs and performance measurement are expected to be available for review and comment this month, with a 30-day public and member comment period.
A wide variety of patient-level instruments to measure PROs have been used for clinical research purposes, many of which have been evaluated and catalogued within a system of assessment tools known as the National Institutes of Health’s (NIH) Patient-Reported Outcome Measurement Information System (PROMIS), Dr. Burstin says. PROMIS questionnaires prompt patients to measure such outcomes as how much difficulty they experience when walking a block on flat ground, getting in and out of bed, or doing strenuous activities, such as bicycling or jogging. NIH-funded studies using PROMIS tools are taking place at 12 sites across the country (http://nihpromis.org/default).
“PROMIS provides two distinct advantages to the PRO performance metric landscape,” argues Cella, who is principal investigator of the Statistical Center for PROMIS. “It has a computerized adaptive testing option, so efficient and accurate assessment is now possible at the individual patient level, with just a few questions per area. It also standardizes its scoring and reporting, such that many other similar measures can be used and their scores reported on a common, PROMIS metric.”
HM Applications
“The voice of the clinician is also needed during this PRO development process,” Dr. Burstin says. “We welcome hospitalists to engage in our projects and weigh in about the most meaningful and actionable patient outcomes that are relevant to their practice.”
“Taking PROs and applying them to hospital medicine is really doable if you take into account the lessons learned from providers who have already used PROs successfully in clinical settings,” says Pat Courneya, MD, medical director for HealthPartners Health Plan in Minnesota.
HealthPartners recently began using PROs in a quality measurement and reward program, offering financial bonuses to physical therapists who achieve a high PRO score relative to resource use (number of PT sessions required). “Having objective PRO measurements allows clinicians to create benchmarks for their patients regarding how much functional improvement they expect to achieve, and how many PT sessions are required to achieve that degree of improvement,” Dr. Courneya says. Using an interactive, Web-based PRO assessment tool, the program has helped tailor care to the expectations of patients while also significantly reducing the overall number of PT visits, especially by medically complex, post-operative patients.
HealthPartners has successfully used PROs as part of an innovative care model for managing patients with depression. At the outset of treatment, patients are administered the PHQ-9, a nine-item patient health questionnaire designed to assess depression symptoms and functional impairment, and derive a severity score. Patients receive care by a team composed of a primary-care physician, a care manager, and a consulting psychiatrist, after which their degree of symptom improvement is again measured. With this program, HealthPartners has achieved significantly more patients with depression into remission by six months compared with typical primary-care treatment, Dr. Courneya says. This model of care has since garnered a CMS Innovation Grant, managed by the HealthPartners Institute for Education and Research and directed by Minnesota’s Institute for Clinical Systems Improvement, aimed at spreading the model to five other states.
“PROs are potentially as useful for hospital medicine as for any other type of medical practice,” says Shaun Frost, MD, SFHM, SHM president and associate medical director of care delivery systems for HealthPartners Health Plan. “There is a big opportunity for hospitalists to incorporate shared decision-making to learn patients’ preferences, such as expectations of when they will be discharged, and understanding of therapeutic options.”
Peri-surgical care is a particularly important opportunity for hospitalists to demonstrate their value by leveraging PROs, according to Dr. Frost. “Patients sometimes come to the table with unrealistic prior expectations that physicians can make pain go away completely. We need to clarify their expectations preoperatively, when we meet them for the very first time, so that they establish a realistic baseline,” he says. “We then need to have a diligent conversation with them immediately after their operation to discuss their pain-management goals, a realistic physical therapy schedule, and post-discharge expectations.”
By clearly understanding patient objectives, hospitalists can “adjust the therapy they’re getting to their expectations, maximizing its effectiveness while minimizing delays in care and transitions to other care settings,” Dr. Frost says.
Chris Guadagnino is a freelance medical writer in Philadelphia.
References
- National Quality Forum. Patient-reported outcomes. National Quality Forum website. Available at: http://www.qualityforum.org/Projects/n-r/Patient-Reported_Outcomes/Patient-Reported_Outcomes.aspx. Accessed Oct. 2, 2012.
- U.S. Food and Drug Administration. The Patient-Reported Outcomes Consortium. U.S. Food and Drug Administration website. Available at: http://www.fda.gov/AboutFDA/PartnershipsCollaborations/PublicPrivatePartnershipProgram/ucm231129.htm. Accessed Oct. 2, 2012.
- National Quality Forum. National voluntary consensus standards for patient outcomes 2009.National Quality Forum website. Available at: http://www.qualityforum.org/Publications/2011/07/National_Voluntary_Consensus_Standards_for_Patient_Outcomes_2009.aspx. Accessed Oct. 2, 2012.
Medical Coding: Hospice Care vs. Palliative Care
Hospice care” and “palliative care” are not synonymous terms. Hospice care is defined as a comprehensive set of services (see “Hospice Coverage,” below) identified and coordinated by an interdisciplinary group to provide for the physical, psychosocial, spiritual, and emotional needs of a terminally ill patient and/or family members, as delineated in a specific patient plan of care.1 Palliative care is defined as patient- and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering. Palliative care throughout the continuum of illness involves addressing physical, intellectual, emotional, social, and spiritual needs, and facilitates patient autonomy, access to information, and choice.1
As an approach, hospice care of terminally ill individuals involves palliative care (relief of pain and uncomfortable symptoms), and emphasizes maintaining the patient at home with family and friends as long as possible. Hospice services can be provided in a home, center, skilled-nursing facility, or hospital setting. In contrast, palliative-care services can be provided during hospice care, or coincide with care that is focused on a cure.
Many hospitalists provide both hospice care and palliative-care services to their patients. Different factors affect how to report these services. These programs can be quite costly, as they involve several team members and a substantial amount of time delivering these services. Capturing services appropriately and obtaining reimbursement to help continue program initiatives are significant issues.
Hospice Care
When a patient enrolls in hospice, all rights to Medicare Part B payments are waived during the benefit period involving professional services related to the treatment and management of the terminal illness. Payment is made through the Part A benefit for the associated costs of daily care and the services provided by the hospice-employed physician. An exception occurs for professional services of an independent attending physician who is not an employee of the designated hospice and does not receive compensation from the hospice for those services. The “attending physician” for hospice services must be an individual who is a doctor of medicine or osteopathy, or a nurse practitioner identified by the individual, at the time they elect hospice coverage, as having the most significant role in the determination and delivery of their medical care.2
Patients often receive hospice in the hospital setting, where the hospitalist manages the patient’s daily care. If the hospitalist is designated as the “attending physician” for hospice services, the visits should be reported to Medicare Part B with modifier GV (e.g. 99232-GV).3 This will allow for separate payment to the hospitalist (the independent attending physician), while the hospice agency maintains its daily-care rate. Reporting services absent this modifier will result in denial.
In some cases, the hospitalist is not identified as the “attending physician” for hospice services but occasionally provides care related to the terminal illness. This situation proves most difficult. Although the hospitalist might be the most accessible physician to the staff and is putting the patient’s needs first, reimbursement is unlikely. Regulations stipulate that patients must not see independent physicians other than their “attending physician” for care related to their terminal illness unless the hospice arranges it. When the service is related to the hospice patient’s terminal illness but was furnished by someone other than the designated “attending physician,” this “other physician” must look to the hospice for payment.3
Nonhospice Palliative Care
Members of the palliative-care team often are called to provide management options to assist in reducing pain and suffering. When the palliative-care specialist is asked to provide opinions or advice, the initial service may qualify as a consultation for those payors that still recognize these codes. However, all of the requirements4 must be met in order to report the service as an inpatient consultation (99251-99255):3
- There must be a written request from a qualified healthcare provider who is involved in the patient’s care (e.g. physician, resident, nurse practitioner); this may be documented as a physician order or in the assessment/plan of the requesting provider’s progress note. Standing orders for consultation are not permitted.
- The requesting provider should clearly and accurately identify the reason for consult request to support the medical necessity of the service.
- The palliative-care physician renders and documents the service.
- The palliative-care physician reports his or her findings to the requesting physician via written communication; because the requesting physician and the consultant share a common inpatient medical record, the consultant’s inpatient progress note satisfies the “written report” requirement.
Consider the nature of the request when reporting a consultation. If the request demonstrates the need for opinions or advice from the palliative-care specialist, the service can be reported as a consultation. If the indication cites “medical management” or “palliative management,” payors are less likely to consider the service as a consultation because the physician is not seeking opinions or advice from the consultant to incorporate into his or her own plan of care for the patient and would rather the consultant just take over that portion of patient care. When consultations do not meet the requirements, subsequent hospital care services should be reported (99231-99233).3
The requesting physician can be in the same or a different provider group as the consultant. The consultant must possess expertise in an area that is beyond that of the requesting provider. Because most hospitalists carry a specialty designation of internal medicine (physician specialty code 11), hospitalists providing palliative-care services can distinguish themselves by their own code (physician specialty code 17, hospice and palliative care).5 Payor concerns arise when physicians of the same designated specialty submit a claim for the same patient on the same date. The payor is likely to pay the first claim received and deny the second claim received pending review of documentation. If this occurs, submit a copy of both progress notes for the date in question to distinguish the services provided. The payor may still require that both encounters be reported as one cumulative service under one physician.
Consultations are not an option for Medicare beneficiaries. Hospitalists providing palliative care can report initial hospital care codes (99221-99223) for their first encounter with the patient.3 This is only acceptable when no other hospitalist from the group has reported initial hospital care during the patient stay, unless the palliative-care hospitalist carries the corresponding designation (i.e. enrolled with Medicare as physician specialty code 17). Without this separate designation, the palliative-care hospitalist can only report subsequent hospital care codes (99231-99233) as the patient was seen previously by a hospitalist in the same group.3
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- U.S. Government Printing Office. Electronic Code of Federal Regulations: Title 42: Public Health, Part 418: Hospice Care, §418.3. June 2012. U.S. Government Printing Office website. Available at: http://ecfr.gpoaccess.gov/cgi/t/text/text-idx?c=ecfr&sid=818258235647b14d2961ad30fa3e68e6&rgn=div5&view=text&node=42:3.0.1.1.5&idno=42#42:3.0.1.1.5.1.3.3. Accessed June 23, 2012.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 11: processing hospice claims. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c11.pdf. Accessed June 23, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- American Medical Association. Consultation services and transfer of care. American Medical Association website. Available at: http://www.ama-assn.org/resources/doc/cpt/cpt-consultation-services.pdf. Accessed June 23, 2012.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 26: completing and processing form CMS-1500 data set. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c26.pdf. Accessed June 23, 2012. Department of Health and Human Services.
- Hospice Payment System: payment system fact sheet series. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/hospice_pay_sys_fs.pdf. Accessed June 23, 2012.
Hospice care” and “palliative care” are not synonymous terms. Hospice care is defined as a comprehensive set of services (see “Hospice Coverage,” below) identified and coordinated by an interdisciplinary group to provide for the physical, psychosocial, spiritual, and emotional needs of a terminally ill patient and/or family members, as delineated in a specific patient plan of care.1 Palliative care is defined as patient- and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering. Palliative care throughout the continuum of illness involves addressing physical, intellectual, emotional, social, and spiritual needs, and facilitates patient autonomy, access to information, and choice.1
As an approach, hospice care of terminally ill individuals involves palliative care (relief of pain and uncomfortable symptoms), and emphasizes maintaining the patient at home with family and friends as long as possible. Hospice services can be provided in a home, center, skilled-nursing facility, or hospital setting. In contrast, palliative-care services can be provided during hospice care, or coincide with care that is focused on a cure.
Many hospitalists provide both hospice care and palliative-care services to their patients. Different factors affect how to report these services. These programs can be quite costly, as they involve several team members and a substantial amount of time delivering these services. Capturing services appropriately and obtaining reimbursement to help continue program initiatives are significant issues.
Hospice Care
When a patient enrolls in hospice, all rights to Medicare Part B payments are waived during the benefit period involving professional services related to the treatment and management of the terminal illness. Payment is made through the Part A benefit for the associated costs of daily care and the services provided by the hospice-employed physician. An exception occurs for professional services of an independent attending physician who is not an employee of the designated hospice and does not receive compensation from the hospice for those services. The “attending physician” for hospice services must be an individual who is a doctor of medicine or osteopathy, or a nurse practitioner identified by the individual, at the time they elect hospice coverage, as having the most significant role in the determination and delivery of their medical care.2
Patients often receive hospice in the hospital setting, where the hospitalist manages the patient’s daily care. If the hospitalist is designated as the “attending physician” for hospice services, the visits should be reported to Medicare Part B with modifier GV (e.g. 99232-GV).3 This will allow for separate payment to the hospitalist (the independent attending physician), while the hospice agency maintains its daily-care rate. Reporting services absent this modifier will result in denial.
In some cases, the hospitalist is not identified as the “attending physician” for hospice services but occasionally provides care related to the terminal illness. This situation proves most difficult. Although the hospitalist might be the most accessible physician to the staff and is putting the patient’s needs first, reimbursement is unlikely. Regulations stipulate that patients must not see independent physicians other than their “attending physician” for care related to their terminal illness unless the hospice arranges it. When the service is related to the hospice patient’s terminal illness but was furnished by someone other than the designated “attending physician,” this “other physician” must look to the hospice for payment.3
Nonhospice Palliative Care
Members of the palliative-care team often are called to provide management options to assist in reducing pain and suffering. When the palliative-care specialist is asked to provide opinions or advice, the initial service may qualify as a consultation for those payors that still recognize these codes. However, all of the requirements4 must be met in order to report the service as an inpatient consultation (99251-99255):3
- There must be a written request from a qualified healthcare provider who is involved in the patient’s care (e.g. physician, resident, nurse practitioner); this may be documented as a physician order or in the assessment/plan of the requesting provider’s progress note. Standing orders for consultation are not permitted.
- The requesting provider should clearly and accurately identify the reason for consult request to support the medical necessity of the service.
- The palliative-care physician renders and documents the service.
- The palliative-care physician reports his or her findings to the requesting physician via written communication; because the requesting physician and the consultant share a common inpatient medical record, the consultant’s inpatient progress note satisfies the “written report” requirement.
Consider the nature of the request when reporting a consultation. If the request demonstrates the need for opinions or advice from the palliative-care specialist, the service can be reported as a consultation. If the indication cites “medical management” or “palliative management,” payors are less likely to consider the service as a consultation because the physician is not seeking opinions or advice from the consultant to incorporate into his or her own plan of care for the patient and would rather the consultant just take over that portion of patient care. When consultations do not meet the requirements, subsequent hospital care services should be reported (99231-99233).3
The requesting physician can be in the same or a different provider group as the consultant. The consultant must possess expertise in an area that is beyond that of the requesting provider. Because most hospitalists carry a specialty designation of internal medicine (physician specialty code 11), hospitalists providing palliative-care services can distinguish themselves by their own code (physician specialty code 17, hospice and palliative care).5 Payor concerns arise when physicians of the same designated specialty submit a claim for the same patient on the same date. The payor is likely to pay the first claim received and deny the second claim received pending review of documentation. If this occurs, submit a copy of both progress notes for the date in question to distinguish the services provided. The payor may still require that both encounters be reported as one cumulative service under one physician.
Consultations are not an option for Medicare beneficiaries. Hospitalists providing palliative care can report initial hospital care codes (99221-99223) for their first encounter with the patient.3 This is only acceptable when no other hospitalist from the group has reported initial hospital care during the patient stay, unless the palliative-care hospitalist carries the corresponding designation (i.e. enrolled with Medicare as physician specialty code 17). Without this separate designation, the palliative-care hospitalist can only report subsequent hospital care codes (99231-99233) as the patient was seen previously by a hospitalist in the same group.3
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- U.S. Government Printing Office. Electronic Code of Federal Regulations: Title 42: Public Health, Part 418: Hospice Care, §418.3. June 2012. U.S. Government Printing Office website. Available at: http://ecfr.gpoaccess.gov/cgi/t/text/text-idx?c=ecfr&sid=818258235647b14d2961ad30fa3e68e6&rgn=div5&view=text&node=42:3.0.1.1.5&idno=42#42:3.0.1.1.5.1.3.3. Accessed June 23, 2012.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 11: processing hospice claims. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c11.pdf. Accessed June 23, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- American Medical Association. Consultation services and transfer of care. American Medical Association website. Available at: http://www.ama-assn.org/resources/doc/cpt/cpt-consultation-services.pdf. Accessed June 23, 2012.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 26: completing and processing form CMS-1500 data set. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c26.pdf. Accessed June 23, 2012. Department of Health and Human Services.
- Hospice Payment System: payment system fact sheet series. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/hospice_pay_sys_fs.pdf. Accessed June 23, 2012.
Hospice care” and “palliative care” are not synonymous terms. Hospice care is defined as a comprehensive set of services (see “Hospice Coverage,” below) identified and coordinated by an interdisciplinary group to provide for the physical, psychosocial, spiritual, and emotional needs of a terminally ill patient and/or family members, as delineated in a specific patient plan of care.1 Palliative care is defined as patient- and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering. Palliative care throughout the continuum of illness involves addressing physical, intellectual, emotional, social, and spiritual needs, and facilitates patient autonomy, access to information, and choice.1
As an approach, hospice care of terminally ill individuals involves palliative care (relief of pain and uncomfortable symptoms), and emphasizes maintaining the patient at home with family and friends as long as possible. Hospice services can be provided in a home, center, skilled-nursing facility, or hospital setting. In contrast, palliative-care services can be provided during hospice care, or coincide with care that is focused on a cure.
Many hospitalists provide both hospice care and palliative-care services to their patients. Different factors affect how to report these services. These programs can be quite costly, as they involve several team members and a substantial amount of time delivering these services. Capturing services appropriately and obtaining reimbursement to help continue program initiatives are significant issues.
Hospice Care
When a patient enrolls in hospice, all rights to Medicare Part B payments are waived during the benefit period involving professional services related to the treatment and management of the terminal illness. Payment is made through the Part A benefit for the associated costs of daily care and the services provided by the hospice-employed physician. An exception occurs for professional services of an independent attending physician who is not an employee of the designated hospice and does not receive compensation from the hospice for those services. The “attending physician” for hospice services must be an individual who is a doctor of medicine or osteopathy, or a nurse practitioner identified by the individual, at the time they elect hospice coverage, as having the most significant role in the determination and delivery of their medical care.2
Patients often receive hospice in the hospital setting, where the hospitalist manages the patient’s daily care. If the hospitalist is designated as the “attending physician” for hospice services, the visits should be reported to Medicare Part B with modifier GV (e.g. 99232-GV).3 This will allow for separate payment to the hospitalist (the independent attending physician), while the hospice agency maintains its daily-care rate. Reporting services absent this modifier will result in denial.
In some cases, the hospitalist is not identified as the “attending physician” for hospice services but occasionally provides care related to the terminal illness. This situation proves most difficult. Although the hospitalist might be the most accessible physician to the staff and is putting the patient’s needs first, reimbursement is unlikely. Regulations stipulate that patients must not see independent physicians other than their “attending physician” for care related to their terminal illness unless the hospice arranges it. When the service is related to the hospice patient’s terminal illness but was furnished by someone other than the designated “attending physician,” this “other physician” must look to the hospice for payment.3
Nonhospice Palliative Care
Members of the palliative-care team often are called to provide management options to assist in reducing pain and suffering. When the palliative-care specialist is asked to provide opinions or advice, the initial service may qualify as a consultation for those payors that still recognize these codes. However, all of the requirements4 must be met in order to report the service as an inpatient consultation (99251-99255):3
- There must be a written request from a qualified healthcare provider who is involved in the patient’s care (e.g. physician, resident, nurse practitioner); this may be documented as a physician order or in the assessment/plan of the requesting provider’s progress note. Standing orders for consultation are not permitted.
- The requesting provider should clearly and accurately identify the reason for consult request to support the medical necessity of the service.
- The palliative-care physician renders and documents the service.
- The palliative-care physician reports his or her findings to the requesting physician via written communication; because the requesting physician and the consultant share a common inpatient medical record, the consultant’s inpatient progress note satisfies the “written report” requirement.
Consider the nature of the request when reporting a consultation. If the request demonstrates the need for opinions or advice from the palliative-care specialist, the service can be reported as a consultation. If the indication cites “medical management” or “palliative management,” payors are less likely to consider the service as a consultation because the physician is not seeking opinions or advice from the consultant to incorporate into his or her own plan of care for the patient and would rather the consultant just take over that portion of patient care. When consultations do not meet the requirements, subsequent hospital care services should be reported (99231-99233).3
The requesting physician can be in the same or a different provider group as the consultant. The consultant must possess expertise in an area that is beyond that of the requesting provider. Because most hospitalists carry a specialty designation of internal medicine (physician specialty code 11), hospitalists providing palliative-care services can distinguish themselves by their own code (physician specialty code 17, hospice and palliative care).5 Payor concerns arise when physicians of the same designated specialty submit a claim for the same patient on the same date. The payor is likely to pay the first claim received and deny the second claim received pending review of documentation. If this occurs, submit a copy of both progress notes for the date in question to distinguish the services provided. The payor may still require that both encounters be reported as one cumulative service under one physician.
Consultations are not an option for Medicare beneficiaries. Hospitalists providing palliative care can report initial hospital care codes (99221-99223) for their first encounter with the patient.3 This is only acceptable when no other hospitalist from the group has reported initial hospital care during the patient stay, unless the palliative-care hospitalist carries the corresponding designation (i.e. enrolled with Medicare as physician specialty code 17). Without this separate designation, the palliative-care hospitalist can only report subsequent hospital care codes (99231-99233) as the patient was seen previously by a hospitalist in the same group.3
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
References
- U.S. Government Printing Office. Electronic Code of Federal Regulations: Title 42: Public Health, Part 418: Hospice Care, §418.3. June 2012. U.S. Government Printing Office website. Available at: http://ecfr.gpoaccess.gov/cgi/t/text/text-idx?c=ecfr&sid=818258235647b14d2961ad30fa3e68e6&rgn=div5&view=text&node=42:3.0.1.1.5&idno=42#42:3.0.1.1.5.1.3.3. Accessed June 23, 2012.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 11: processing hospice claims. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Downloads/clm104c11.pdf. Accessed June 23, 2012.
- Abraham M, Ahlman J, Anderson C, Boudreau A, Connelly J. Current Procedural Terminology 2012 Professional Edition. Chicago: American Medical Association Press; 2011.
- American Medical Association. Consultation services and transfer of care. American Medical Association website. Available at: http://www.ama-assn.org/resources/doc/cpt/cpt-consultation-services.pdf. Accessed June 23, 2012.
- Centers for Medicare & Medicaid Services. Medicare Claims Processing Manual: Chapter 26: completing and processing form CMS-1500 data set. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c26.pdf. Accessed June 23, 2012. Department of Health and Human Services.
- Hospice Payment System: payment system fact sheet series. Centers for Medicare & Medicaid Services website. Available at: http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/hospice_pay_sys_fs.pdf. Accessed June 23, 2012.
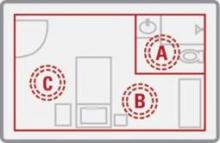
UV Light Beat Bleach for C. difficile Decontamination
SAN FRANCISCO – The M.D. Anderson Cancer Center is abandoning bleach for cleaning hospital rooms exposed to Clostridium difficile in favor of a new machine that kills the organism using ultraviolet light.
The machine reduced C. difficile counts as much as, or more than, bleach cleaning in a preliminary prospective trial in 30 hospital rooms previously occupied by patients infected with C. difficile. The machine is a bit more expensive than bleach at a cost of approximately $82,000 (or $3,000-$4,000 per month to lease), but it avoids damage to materials and the toxic environment for workers caused by the use of bleach or other corrosive chemicals, Dr. Shashank S. Ghantoji said in an interview at a poster presentation at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Bleach treatment reduced the average number of colony-forming units of C. difficile from 2.39 before cleaning to 0.71, a 70% reduction in the contamination level. Treatment with the Pulsed Xenon UV machine (PX-UV) reduced the average number of colony-forming units from 22.97 to 1.10, a 95% reduction.
The postcleaning contamination levels were not statistically different between the bleach and PX-UV rooms, Dr. Ghantoji and his associates found. However, PX-UV decontamination is faster than using bleach, Dr. Ghantoji said. "It takes at least 45 minutes to clean a room with bleach, and it’s not good for the patients or the health care professionals," plus admissions staff usually are clamoring for the room to be ready as soon as possible, he said. Cleaning a room using the PX-UV method takes perhaps 15 minutes.
The PX-UV machine has been available for some time, but its adoption depends on how proactive hospital infection control teams are, he added. He said he is aware of at least two medical centers beyond M.D. Anderson that are also using the machine.
In the study, 298 samples were taken before and after cleaning from high-touch surfaces – the bathroom handrail, the bed control panel, the bed rail, the top of the bedside table, and the IV pole control panel or other equipment control panel – and analyzed for C. difficile endospores. Fifteen rooms were cleaned by the conventional method using a 1:10 solution of sodium hypochlorite (bleach), and 15 underwent a visual, nonbleach cleaning of surfaces followed by 15 minutes of treatment with the PX-UV.
With the PX-UV method, housekeeping workers clean the bathroom and place the remote-operated PX-UV in the bathroom with the door shut while they finish cleaning the rest of the room. Then the machine is placed on each side of the bed for 4 minutes of operation with workers gone. Sensors stop the machine if any movement is detected.
It works by emitting ultraviolet C light, which kills C. difficile. And here’s a bonus – it also kills vancomycin-resistant enterococci and methicillin-resistant Staphylococcus aureus, Dr. Ghantoji of M.D. Anderson, Houston, said at the meeting, sponsored by the American Society for Microbiology.
"The PX-UV method may be a promising alternative to the current standard of decontamination, bleach," he said. Future studies should look at whether the PX-UV method decreases not just endospore counts but transmission of C. difficile, he added.
C. difficile causes more than 300,000 health care–associated infections each year in the United States, incurring $2,500-$3,500 in costs per infection aside from any surgical costs, he estimated. Current guidelines recommend that rooms previously occupied by patients infected with C. difficile be cleaned with a disinfectant registered with the Environmental Protection Agency as effective against the organism.
Xenex Healthcare Services, which markets the PX-UV machine, funded the study, and two of the investigators are employees of the company. Dr. Ghantoji reported having no other relevant financial disclosures.
SAN FRANCISCO – The M.D. Anderson Cancer Center is abandoning bleach for cleaning hospital rooms exposed to Clostridium difficile in favor of a new machine that kills the organism using ultraviolet light.
The machine reduced C. difficile counts as much as, or more than, bleach cleaning in a preliminary prospective trial in 30 hospital rooms previously occupied by patients infected with C. difficile. The machine is a bit more expensive than bleach at a cost of approximately $82,000 (or $3,000-$4,000 per month to lease), but it avoids damage to materials and the toxic environment for workers caused by the use of bleach or other corrosive chemicals, Dr. Shashank S. Ghantoji said in an interview at a poster presentation at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Bleach treatment reduced the average number of colony-forming units of C. difficile from 2.39 before cleaning to 0.71, a 70% reduction in the contamination level. Treatment with the Pulsed Xenon UV machine (PX-UV) reduced the average number of colony-forming units from 22.97 to 1.10, a 95% reduction.
The postcleaning contamination levels were not statistically different between the bleach and PX-UV rooms, Dr. Ghantoji and his associates found. However, PX-UV decontamination is faster than using bleach, Dr. Ghantoji said. "It takes at least 45 minutes to clean a room with bleach, and it’s not good for the patients or the health care professionals," plus admissions staff usually are clamoring for the room to be ready as soon as possible, he said. Cleaning a room using the PX-UV method takes perhaps 15 minutes.
The PX-UV machine has been available for some time, but its adoption depends on how proactive hospital infection control teams are, he added. He said he is aware of at least two medical centers beyond M.D. Anderson that are also using the machine.
In the study, 298 samples were taken before and after cleaning from high-touch surfaces – the bathroom handrail, the bed control panel, the bed rail, the top of the bedside table, and the IV pole control panel or other equipment control panel – and analyzed for C. difficile endospores. Fifteen rooms were cleaned by the conventional method using a 1:10 solution of sodium hypochlorite (bleach), and 15 underwent a visual, nonbleach cleaning of surfaces followed by 15 minutes of treatment with the PX-UV.
With the PX-UV method, housekeeping workers clean the bathroom and place the remote-operated PX-UV in the bathroom with the door shut while they finish cleaning the rest of the room. Then the machine is placed on each side of the bed for 4 minutes of operation with workers gone. Sensors stop the machine if any movement is detected.
It works by emitting ultraviolet C light, which kills C. difficile. And here’s a bonus – it also kills vancomycin-resistant enterococci and methicillin-resistant Staphylococcus aureus, Dr. Ghantoji of M.D. Anderson, Houston, said at the meeting, sponsored by the American Society for Microbiology.
"The PX-UV method may be a promising alternative to the current standard of decontamination, bleach," he said. Future studies should look at whether the PX-UV method decreases not just endospore counts but transmission of C. difficile, he added.
C. difficile causes more than 300,000 health care–associated infections each year in the United States, incurring $2,500-$3,500 in costs per infection aside from any surgical costs, he estimated. Current guidelines recommend that rooms previously occupied by patients infected with C. difficile be cleaned with a disinfectant registered with the Environmental Protection Agency as effective against the organism.
Xenex Healthcare Services, which markets the PX-UV machine, funded the study, and two of the investigators are employees of the company. Dr. Ghantoji reported having no other relevant financial disclosures.
SAN FRANCISCO – The M.D. Anderson Cancer Center is abandoning bleach for cleaning hospital rooms exposed to Clostridium difficile in favor of a new machine that kills the organism using ultraviolet light.
The machine reduced C. difficile counts as much as, or more than, bleach cleaning in a preliminary prospective trial in 30 hospital rooms previously occupied by patients infected with C. difficile. The machine is a bit more expensive than bleach at a cost of approximately $82,000 (or $3,000-$4,000 per month to lease), but it avoids damage to materials and the toxic environment for workers caused by the use of bleach or other corrosive chemicals, Dr. Shashank S. Ghantoji said in an interview at a poster presentation at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy.
Bleach treatment reduced the average number of colony-forming units of C. difficile from 2.39 before cleaning to 0.71, a 70% reduction in the contamination level. Treatment with the Pulsed Xenon UV machine (PX-UV) reduced the average number of colony-forming units from 22.97 to 1.10, a 95% reduction.
The postcleaning contamination levels were not statistically different between the bleach and PX-UV rooms, Dr. Ghantoji and his associates found. However, PX-UV decontamination is faster than using bleach, Dr. Ghantoji said. "It takes at least 45 minutes to clean a room with bleach, and it’s not good for the patients or the health care professionals," plus admissions staff usually are clamoring for the room to be ready as soon as possible, he said. Cleaning a room using the PX-UV method takes perhaps 15 minutes.
The PX-UV machine has been available for some time, but its adoption depends on how proactive hospital infection control teams are, he added. He said he is aware of at least two medical centers beyond M.D. Anderson that are also using the machine.
In the study, 298 samples were taken before and after cleaning from high-touch surfaces – the bathroom handrail, the bed control panel, the bed rail, the top of the bedside table, and the IV pole control panel or other equipment control panel – and analyzed for C. difficile endospores. Fifteen rooms were cleaned by the conventional method using a 1:10 solution of sodium hypochlorite (bleach), and 15 underwent a visual, nonbleach cleaning of surfaces followed by 15 minutes of treatment with the PX-UV.
With the PX-UV method, housekeeping workers clean the bathroom and place the remote-operated PX-UV in the bathroom with the door shut while they finish cleaning the rest of the room. Then the machine is placed on each side of the bed for 4 minutes of operation with workers gone. Sensors stop the machine if any movement is detected.
It works by emitting ultraviolet C light, which kills C. difficile. And here’s a bonus – it also kills vancomycin-resistant enterococci and methicillin-resistant Staphylococcus aureus, Dr. Ghantoji of M.D. Anderson, Houston, said at the meeting, sponsored by the American Society for Microbiology.
"The PX-UV method may be a promising alternative to the current standard of decontamination, bleach," he said. Future studies should look at whether the PX-UV method decreases not just endospore counts but transmission of C. difficile, he added.
C. difficile causes more than 300,000 health care–associated infections each year in the United States, incurring $2,500-$3,500 in costs per infection aside from any surgical costs, he estimated. Current guidelines recommend that rooms previously occupied by patients infected with C. difficile be cleaned with a disinfectant registered with the Environmental Protection Agency as effective against the organism.
Xenex Healthcare Services, which markets the PX-UV machine, funded the study, and two of the investigators are employees of the company. Dr. Ghantoji reported having no other relevant financial disclosures.
Major Finding: Bleach killed 70% of C. difficile spores in hospital rooms compared with 95% decontamination using nonbleach cleaning plus UV light treatment. The difference between groups was not statistically significant.
Data Source: A prospective comparison was performed of the two cleaning methods in 30 rooms after discharge of patients infected with C. difficile.
Disclosures: Xenex Healthcare Services, which markets the PX-UV machine, funded the study, and two of the investigators are employees of the company. Dr. Ghantoji reported having no other relevant financial disclosures.
UV-C Light Blasts 'Bad Bugs' in Hospital Rooms
SAN DIEGO – A portable device that emits ultraviolet C light destroyed vancomycin-resistant enterococci, Acinetobacter, and Clostridium difficile from hospital rooms where patients infected with those bacteria had been housed, results from a small study demonstrated.
"There is growing evidence that the environment can be a source for acquisition of bad bugs," lead study investigator Dr. Deverick J. Anderson said in an interview prior to IDWeek 2012, where the research was presented during a poster session.
"Our study further strengthens the data that no-touch systems like UV-C light kill important bacteria and can potentially help with current cleaning strategies. While several groups have demonstrated that UV-C light work in experimental conditions we are demonstrating that it works in a real-world hospital environment."
Dr. Anderson of the department of medicine in the division of infectious diseases at Duke University, Durham, N.C., and his associates analyzed 39 rooms at two tertiary care hospitals that had just housed a patient with one of the different bad bugs: vancomycin-resistant enterococci (VRE), Acinetobacter, and C. difficile. After the patient was discharged but prior to the regular cleaning, the investigators obtained 15 or more cultures from several different locations in the hospital rooms, including bed rails, remote controls, and toilets. Then they wheeled in the TRU-D, an automated mobile disinfection system manufactured by Lumalier that is about 6 feet tall and is equipped with 8 sensors and 16 bulbs that emit UV-C light.
"Each room was irradiated between 25 and 45 minutes in order to eradicate both bacteria and bacterial spores," Dr. Anderson explained during a premeeting telephone press conference. "We then went back into the rooms and cultured the environment from the same locations."
After comparing the number of colony-forming units (CFUs) before and after irradiation "we were able to demonstrate that we could achieve well over 90% reduction in each of those three bad bugs after using the UV light," said Dr. Anderson, who also chairs the antimicrobial stewardship and evaluation team at Duke University Medical Center. "This occurred in all locations sampled, in both direct and indirect light."
Specifically, the UV-C irradiation reduced CFUs of VRE by 98%, C. difficile by 93%, and Acinetobacter by 98%.
"Based on these results we came to the conclusion that UV-C light is indeed effective in killing VRE, C. difficile, and Acinetobacter from the real-world hospital environment," Dr. Anderson said during the telephone press conference. "The idea behind achieving bacterial irradiation in shadow is actually taking advantage of the reflective properties of UV light. It literally bounces around the room and ends up hitting areas in shadow. That’s how bacterial reduction occurs."
He acknowledged certain limitations of the study, including the fact that the researchers were able to evaluate onlytwo hospital rooms with Acinetobacter "because of how infrequently this organism causes infections. Regardless, we reduced the amount of Acinetobacter in both of those rooms."
The study was sponsored by the Centers for Disease Control and Prevention. Lumalier donated the machines used in the study but had no role in the trial design or in review of the data. Dr. Anderson said that he had no relevant financial conflicts to disclose.
IDWeek 2012 is the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
SAN DIEGO – A portable device that emits ultraviolet C light destroyed vancomycin-resistant enterococci, Acinetobacter, and Clostridium difficile from hospital rooms where patients infected with those bacteria had been housed, results from a small study demonstrated.
"There is growing evidence that the environment can be a source for acquisition of bad bugs," lead study investigator Dr. Deverick J. Anderson said in an interview prior to IDWeek 2012, where the research was presented during a poster session.
"Our study further strengthens the data that no-touch systems like UV-C light kill important bacteria and can potentially help with current cleaning strategies. While several groups have demonstrated that UV-C light work in experimental conditions we are demonstrating that it works in a real-world hospital environment."
Dr. Anderson of the department of medicine in the division of infectious diseases at Duke University, Durham, N.C., and his associates analyzed 39 rooms at two tertiary care hospitals that had just housed a patient with one of the different bad bugs: vancomycin-resistant enterococci (VRE), Acinetobacter, and C. difficile. After the patient was discharged but prior to the regular cleaning, the investigators obtained 15 or more cultures from several different locations in the hospital rooms, including bed rails, remote controls, and toilets. Then they wheeled in the TRU-D, an automated mobile disinfection system manufactured by Lumalier that is about 6 feet tall and is equipped with 8 sensors and 16 bulbs that emit UV-C light.
"Each room was irradiated between 25 and 45 minutes in order to eradicate both bacteria and bacterial spores," Dr. Anderson explained during a premeeting telephone press conference. "We then went back into the rooms and cultured the environment from the same locations."
After comparing the number of colony-forming units (CFUs) before and after irradiation "we were able to demonstrate that we could achieve well over 90% reduction in each of those three bad bugs after using the UV light," said Dr. Anderson, who also chairs the antimicrobial stewardship and evaluation team at Duke University Medical Center. "This occurred in all locations sampled, in both direct and indirect light."
Specifically, the UV-C irradiation reduced CFUs of VRE by 98%, C. difficile by 93%, and Acinetobacter by 98%.
"Based on these results we came to the conclusion that UV-C light is indeed effective in killing VRE, C. difficile, and Acinetobacter from the real-world hospital environment," Dr. Anderson said during the telephone press conference. "The idea behind achieving bacterial irradiation in shadow is actually taking advantage of the reflective properties of UV light. It literally bounces around the room and ends up hitting areas in shadow. That’s how bacterial reduction occurs."
He acknowledged certain limitations of the study, including the fact that the researchers were able to evaluate onlytwo hospital rooms with Acinetobacter "because of how infrequently this organism causes infections. Regardless, we reduced the amount of Acinetobacter in both of those rooms."
The study was sponsored by the Centers for Disease Control and Prevention. Lumalier donated the machines used in the study but had no role in the trial design or in review of the data. Dr. Anderson said that he had no relevant financial conflicts to disclose.
IDWeek 2012 is the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
SAN DIEGO – A portable device that emits ultraviolet C light destroyed vancomycin-resistant enterococci, Acinetobacter, and Clostridium difficile from hospital rooms where patients infected with those bacteria had been housed, results from a small study demonstrated.
"There is growing evidence that the environment can be a source for acquisition of bad bugs," lead study investigator Dr. Deverick J. Anderson said in an interview prior to IDWeek 2012, where the research was presented during a poster session.
"Our study further strengthens the data that no-touch systems like UV-C light kill important bacteria and can potentially help with current cleaning strategies. While several groups have demonstrated that UV-C light work in experimental conditions we are demonstrating that it works in a real-world hospital environment."
Dr. Anderson of the department of medicine in the division of infectious diseases at Duke University, Durham, N.C., and his associates analyzed 39 rooms at two tertiary care hospitals that had just housed a patient with one of the different bad bugs: vancomycin-resistant enterococci (VRE), Acinetobacter, and C. difficile. After the patient was discharged but prior to the regular cleaning, the investigators obtained 15 or more cultures from several different locations in the hospital rooms, including bed rails, remote controls, and toilets. Then they wheeled in the TRU-D, an automated mobile disinfection system manufactured by Lumalier that is about 6 feet tall and is equipped with 8 sensors and 16 bulbs that emit UV-C light.
"Each room was irradiated between 25 and 45 minutes in order to eradicate both bacteria and bacterial spores," Dr. Anderson explained during a premeeting telephone press conference. "We then went back into the rooms and cultured the environment from the same locations."
After comparing the number of colony-forming units (CFUs) before and after irradiation "we were able to demonstrate that we could achieve well over 90% reduction in each of those three bad bugs after using the UV light," said Dr. Anderson, who also chairs the antimicrobial stewardship and evaluation team at Duke University Medical Center. "This occurred in all locations sampled, in both direct and indirect light."
Specifically, the UV-C irradiation reduced CFUs of VRE by 98%, C. difficile by 93%, and Acinetobacter by 98%.
"Based on these results we came to the conclusion that UV-C light is indeed effective in killing VRE, C. difficile, and Acinetobacter from the real-world hospital environment," Dr. Anderson said during the telephone press conference. "The idea behind achieving bacterial irradiation in shadow is actually taking advantage of the reflective properties of UV light. It literally bounces around the room and ends up hitting areas in shadow. That’s how bacterial reduction occurs."
He acknowledged certain limitations of the study, including the fact that the researchers were able to evaluate onlytwo hospital rooms with Acinetobacter "because of how infrequently this organism causes infections. Regardless, we reduced the amount of Acinetobacter in both of those rooms."
The study was sponsored by the Centers for Disease Control and Prevention. Lumalier donated the machines used in the study but had no role in the trial design or in review of the data. Dr. Anderson said that he had no relevant financial conflicts to disclose.
IDWeek 2012 is the combined annual meetings of the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, the HIV Medicine Association, and the Pediatric Infectious Diseases Society.
Major Finding: UV-C irradiation of hospital rooms with a portable disinfection system reduced colony-forming units of vancomycin-resistant enterococci by 98%, C. difficile by 93%, and Acinetobacter by 98%.
Data Source: Results were taken from a study conducted in 39 hospital rooms at two tertiary medical centers.
Disclosures: The study was sponsored by the Centers for Disease Control and Prevention. Lumalier donated the machines used in the study but had no role in the trial design or in review of the data. Dr. Anderson said that he had no relevant financial conflicts to disclose.
Pharmacologic and nonpharmacologic treatment options for panic disorder
Promising C. difficile Antibiotic in Pipeline
SAN FRANCISCO – Those desperate for new treatments for Clostridium difficile infection may want to keep an eye on the experimental oral antibiotic cadazolid, which looked promising in an early-phase trial, according to Daniela Baldoni, Pharm.D.
Cadazolid is in the oxazolidinone class of antibiotics. Its mechanism of action consists mainly of bacterial protein-synthesis inhibition.
Cadazolid produced low systemic exposure with high concentrations at the desired site – the colon – and was well tolerated in 64 healthy men who received up to 3,000 mg b.i.d. for 10 days, she reported in a poster presentation at the conference. Dr. Baldoni is employed by Actelion Pharmaceuticals, the company that is developing cadazolid.
The study randomized nonsmoking men aged 45-60 years and a body mass index of 18-32 kg/m2 to single or multiple doses of cadazolid or placebo.
In the single-dose group, 30 fasting subjects received a single dose of 30, 100, 300, 1,000, or 3,000 mg cadazolid and 10 subjects received matching placebo. After a wash-out period of 8-15 days, the six subjects who had taken 300 mg received a second dose of 300 mg after eating instead of after fasting. In the multiple-dose group, 18 subjects took 300, 1,000, or 3,000 mg of cadazolid twice a day and 6 received matching placebo for 10 days.
Taking cadazolid with food appeared to increase the rate and extent of drug absorption by two- to fivefold. Blood samples showed low systemic exposure after single or multiple doses, with a minor, twofold increase in cadazolid in plasma after 10 days for all doses in the twice-a-day group, Dr. Baldoni reported at the meeting, sponsored by the American Society for Microbiology.
The dose or duration of treatment did not seem to affect the number of adverse events (none of which were serious). They occurred in 27%-39% of cadazolid-treated subjects and in 17%-40% taking placebo and were mostly headache or diarrhea.
All subjects completed the study except one man in the 100-mg single-dose subgroup who withdrew consent for reasons unrelated to adverse events.
SAN FRANCISCO – Those desperate for new treatments for Clostridium difficile infection may want to keep an eye on the experimental oral antibiotic cadazolid, which looked promising in an early-phase trial, according to Daniela Baldoni, Pharm.D.
Cadazolid is in the oxazolidinone class of antibiotics. Its mechanism of action consists mainly of bacterial protein-synthesis inhibition.
Cadazolid produced low systemic exposure with high concentrations at the desired site – the colon – and was well tolerated in 64 healthy men who received up to 3,000 mg b.i.d. for 10 days, she reported in a poster presentation at the conference. Dr. Baldoni is employed by Actelion Pharmaceuticals, the company that is developing cadazolid.
The study randomized nonsmoking men aged 45-60 years and a body mass index of 18-32 kg/m2 to single or multiple doses of cadazolid or placebo.
In the single-dose group, 30 fasting subjects received a single dose of 30, 100, 300, 1,000, or 3,000 mg cadazolid and 10 subjects received matching placebo. After a wash-out period of 8-15 days, the six subjects who had taken 300 mg received a second dose of 300 mg after eating instead of after fasting. In the multiple-dose group, 18 subjects took 300, 1,000, or 3,000 mg of cadazolid twice a day and 6 received matching placebo for 10 days.
Taking cadazolid with food appeared to increase the rate and extent of drug absorption by two- to fivefold. Blood samples showed low systemic exposure after single or multiple doses, with a minor, twofold increase in cadazolid in plasma after 10 days for all doses in the twice-a-day group, Dr. Baldoni reported at the meeting, sponsored by the American Society for Microbiology.
The dose or duration of treatment did not seem to affect the number of adverse events (none of which were serious). They occurred in 27%-39% of cadazolid-treated subjects and in 17%-40% taking placebo and were mostly headache or diarrhea.
All subjects completed the study except one man in the 100-mg single-dose subgroup who withdrew consent for reasons unrelated to adverse events.
SAN FRANCISCO – Those desperate for new treatments for Clostridium difficile infection may want to keep an eye on the experimental oral antibiotic cadazolid, which looked promising in an early-phase trial, according to Daniela Baldoni, Pharm.D.
Cadazolid is in the oxazolidinone class of antibiotics. Its mechanism of action consists mainly of bacterial protein-synthesis inhibition.
Cadazolid produced low systemic exposure with high concentrations at the desired site – the colon – and was well tolerated in 64 healthy men who received up to 3,000 mg b.i.d. for 10 days, she reported in a poster presentation at the conference. Dr. Baldoni is employed by Actelion Pharmaceuticals, the company that is developing cadazolid.
The study randomized nonsmoking men aged 45-60 years and a body mass index of 18-32 kg/m2 to single or multiple doses of cadazolid or placebo.
In the single-dose group, 30 fasting subjects received a single dose of 30, 100, 300, 1,000, or 3,000 mg cadazolid and 10 subjects received matching placebo. After a wash-out period of 8-15 days, the six subjects who had taken 300 mg received a second dose of 300 mg after eating instead of after fasting. In the multiple-dose group, 18 subjects took 300, 1,000, or 3,000 mg of cadazolid twice a day and 6 received matching placebo for 10 days.
Taking cadazolid with food appeared to increase the rate and extent of drug absorption by two- to fivefold. Blood samples showed low systemic exposure after single or multiple doses, with a minor, twofold increase in cadazolid in plasma after 10 days for all doses in the twice-a-day group, Dr. Baldoni reported at the meeting, sponsored by the American Society for Microbiology.
The dose or duration of treatment did not seem to affect the number of adverse events (none of which were serious). They occurred in 27%-39% of cadazolid-treated subjects and in 17%-40% taking placebo and were mostly headache or diarrhea.
All subjects completed the study except one man in the 100-mg single-dose subgroup who withdrew consent for reasons unrelated to adverse events.
Major Finding: The experimental antibiotic cadazolid concentrated in feces with low systemic exposure and few side effects after single doses or twice-a-day dosing for 10 days.
Data Source: Data are from a randomized, placebo-controlled study in 64 healthy, nonsmoking men.
Disclosures: Dr. Baldoni and most of her coinvestigators are employees of Actelion Pharmaceuticals, which funded the study.
Higher Dose for Severe C. difficile Speeds Response
SAN FRANCISCO – Two small studies suggest that treating severe Clostridium difficile infection with a higher initial dose of vancomycin may work better than the recommended dose of 125 mg every 6 hours.
The most recent study, presented in a poster at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy, surprised the investigators.
"Pharmacodynamically, the concentrations in stool of the standard dose of 125 mg are about 500-1,000 times greater than the MIC [minimum inhibitory concentration]," Yleana T. Garcia, Pharm.D., said in an interview. "So, we have enough concentration in the stool. We wanted to see that we have similar outcomes with patients who are treated with standard doses as with higher doses."
Instead, the retrospective review of 62 patients with severe diarrhea who received oral vancomycin for at least 3 days found that symptoms resolved significantly quicker in 19 patients who got 250 mg every 6 hours compared with 43 patients who got 125 mg every 6 hours, she and her associates reported.
Symptoms resolved by day 3 in nine patients (47%) on the high dose and six patients (15%) on the conventional dose, said Dr. Garcia, a palliative care fellow at the James J. Peters Veterans Affairs Medical Center, Bronx, N.Y.
There also were statistically nonsignificant trends toward a higher likelihood of clinical cure, shorter length of stay, and reduced risk of recurrence in patients with the higher dose. An increased death rate in the higher-dose group also was not statistically significant, and might be due to greater severity of illness at baseline in patients who got the higher dose of vancomycin, she said at the meeting, sponsored by the American Society for Microbiology.
The findings support those of a small prospective study that analyzed levels of vancomycin in feces collected from 15 patients with presumed or confirmed C. difficile infection. Drug concentrations were high in patients who got 250 or 500 mg q.i.d. but were inadequate in at least one patient on the first day of treatment with 125 mg q.i.d. (BMC Infect. Dis. 2010;10:363).<< http://www.biomedcentral.com/1471-2334/10/363 >>
"Higher doses like 250-500 mg may be warranted to reach adequate concentrations in the stool in the first 24-48 hours," Dr. Garcia said. "I’m not saying to use 250 for the whole treatment course, but there may be a role for a loading dose of 250 mg q6 for the first 24-48 hours, and then switching to 125 mg q6 for the remainder of the treatment course. We know that 125 does have adequate fecal concentration; it just may not be adequate on day 1."
The 2010 update to clinical practice guidelines for C. difficile infection in adults recommends treating severe C. difficile infection with oral vancomycin 125 mg every 6 hours or using 500 mg every 6 hours for patients with severe disease complicated by ileus, megacolon, or hypotension (Infect. Control Hosp. Epidemiol. 2010;31:431-55).
Severe C. difficile infection generally is defined as the presence of the organism plus leukocytosis with a white blood cell count of 15,000 cells/microL or greater, or a serum creatinine level at least 1.5 times baseline. The study reviewed records of patients who received vancomycin for these indications or hypotension, shock, ileus, megacolon, or evidence of colitis. The study excluded patients who were treated with any other medication besides metronidazole.
The study is continuing in order to increase the number of patients reviewed and the power of the findings.
Dr. Garcia reported having no financial disclosures.
SAN FRANCISCO – Two small studies suggest that treating severe Clostridium difficile infection with a higher initial dose of vancomycin may work better than the recommended dose of 125 mg every 6 hours.
The most recent study, presented in a poster at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy, surprised the investigators.
"Pharmacodynamically, the concentrations in stool of the standard dose of 125 mg are about 500-1,000 times greater than the MIC [minimum inhibitory concentration]," Yleana T. Garcia, Pharm.D., said in an interview. "So, we have enough concentration in the stool. We wanted to see that we have similar outcomes with patients who are treated with standard doses as with higher doses."
Instead, the retrospective review of 62 patients with severe diarrhea who received oral vancomycin for at least 3 days found that symptoms resolved significantly quicker in 19 patients who got 250 mg every 6 hours compared with 43 patients who got 125 mg every 6 hours, she and her associates reported.
Symptoms resolved by day 3 in nine patients (47%) on the high dose and six patients (15%) on the conventional dose, said Dr. Garcia, a palliative care fellow at the James J. Peters Veterans Affairs Medical Center, Bronx, N.Y.
There also were statistically nonsignificant trends toward a higher likelihood of clinical cure, shorter length of stay, and reduced risk of recurrence in patients with the higher dose. An increased death rate in the higher-dose group also was not statistically significant, and might be due to greater severity of illness at baseline in patients who got the higher dose of vancomycin, she said at the meeting, sponsored by the American Society for Microbiology.
The findings support those of a small prospective study that analyzed levels of vancomycin in feces collected from 15 patients with presumed or confirmed C. difficile infection. Drug concentrations were high in patients who got 250 or 500 mg q.i.d. but were inadequate in at least one patient on the first day of treatment with 125 mg q.i.d. (BMC Infect. Dis. 2010;10:363).<< http://www.biomedcentral.com/1471-2334/10/363 >>
"Higher doses like 250-500 mg may be warranted to reach adequate concentrations in the stool in the first 24-48 hours," Dr. Garcia said. "I’m not saying to use 250 for the whole treatment course, but there may be a role for a loading dose of 250 mg q6 for the first 24-48 hours, and then switching to 125 mg q6 for the remainder of the treatment course. We know that 125 does have adequate fecal concentration; it just may not be adequate on day 1."
The 2010 update to clinical practice guidelines for C. difficile infection in adults recommends treating severe C. difficile infection with oral vancomycin 125 mg every 6 hours or using 500 mg every 6 hours for patients with severe disease complicated by ileus, megacolon, or hypotension (Infect. Control Hosp. Epidemiol. 2010;31:431-55).
Severe C. difficile infection generally is defined as the presence of the organism plus leukocytosis with a white blood cell count of 15,000 cells/microL or greater, or a serum creatinine level at least 1.5 times baseline. The study reviewed records of patients who received vancomycin for these indications or hypotension, shock, ileus, megacolon, or evidence of colitis. The study excluded patients who were treated with any other medication besides metronidazole.
The study is continuing in order to increase the number of patients reviewed and the power of the findings.
Dr. Garcia reported having no financial disclosures.
SAN FRANCISCO – Two small studies suggest that treating severe Clostridium difficile infection with a higher initial dose of vancomycin may work better than the recommended dose of 125 mg every 6 hours.
The most recent study, presented in a poster at the annual Interscience Conference on Antimicrobial Agents and Chemotherapy, surprised the investigators.
"Pharmacodynamically, the concentrations in stool of the standard dose of 125 mg are about 500-1,000 times greater than the MIC [minimum inhibitory concentration]," Yleana T. Garcia, Pharm.D., said in an interview. "So, we have enough concentration in the stool. We wanted to see that we have similar outcomes with patients who are treated with standard doses as with higher doses."
Instead, the retrospective review of 62 patients with severe diarrhea who received oral vancomycin for at least 3 days found that symptoms resolved significantly quicker in 19 patients who got 250 mg every 6 hours compared with 43 patients who got 125 mg every 6 hours, she and her associates reported.
Symptoms resolved by day 3 in nine patients (47%) on the high dose and six patients (15%) on the conventional dose, said Dr. Garcia, a palliative care fellow at the James J. Peters Veterans Affairs Medical Center, Bronx, N.Y.
There also were statistically nonsignificant trends toward a higher likelihood of clinical cure, shorter length of stay, and reduced risk of recurrence in patients with the higher dose. An increased death rate in the higher-dose group also was not statistically significant, and might be due to greater severity of illness at baseline in patients who got the higher dose of vancomycin, she said at the meeting, sponsored by the American Society for Microbiology.
The findings support those of a small prospective study that analyzed levels of vancomycin in feces collected from 15 patients with presumed or confirmed C. difficile infection. Drug concentrations were high in patients who got 250 or 500 mg q.i.d. but were inadequate in at least one patient on the first day of treatment with 125 mg q.i.d. (BMC Infect. Dis. 2010;10:363).<< http://www.biomedcentral.com/1471-2334/10/363 >>
"Higher doses like 250-500 mg may be warranted to reach adequate concentrations in the stool in the first 24-48 hours," Dr. Garcia said. "I’m not saying to use 250 for the whole treatment course, but there may be a role for a loading dose of 250 mg q6 for the first 24-48 hours, and then switching to 125 mg q6 for the remainder of the treatment course. We know that 125 does have adequate fecal concentration; it just may not be adequate on day 1."
The 2010 update to clinical practice guidelines for C. difficile infection in adults recommends treating severe C. difficile infection with oral vancomycin 125 mg every 6 hours or using 500 mg every 6 hours for patients with severe disease complicated by ileus, megacolon, or hypotension (Infect. Control Hosp. Epidemiol. 2010;31:431-55).
Severe C. difficile infection generally is defined as the presence of the organism plus leukocytosis with a white blood cell count of 15,000 cells/microL or greater, or a serum creatinine level at least 1.5 times baseline. The study reviewed records of patients who received vancomycin for these indications or hypotension, shock, ileus, megacolon, or evidence of colitis. The study excluded patients who were treated with any other medication besides metronidazole.
The study is continuing in order to increase the number of patients reviewed and the power of the findings.
Dr. Garcia reported having no financial disclosures.
Major Finding: Symptoms of severe C. difficile infection resolved by day 3 of oral vancomycin treatment in 9 of 19 patients treated with 250 mg every 6 hours (47%) compared with 6 of 43 patients on 125 mg every 6 hours (15%).
Data Source: Retrospective review of records on 62 adults at one institution treated for at least 3 days with oral vancomycin for severe C. difficile infection.
Disclosures: Dr. Garcia reported having no financial disclosures.
New Directions in Small-Vessel Vasculitis: ANCA, Target Organs, Treatment, and Beyond
Supplement Editor:
Carol Langford, MD, MHS
Associate Editors:
Leonard Calabrese, DO, and Gary Hoffman, MD
Contents
Diagnosis, ANCA testing, and disease activity
Clinical features and diagnosis of small-vessel vasculitis
Carol Langford, MD, MHS
Controversies in ANCA testing
Ulrich Specks, MD
Defining disease activity and damage in patients with small-vessel vasculitis
Peter A. Merkel, MD, MPH
Impact on individual organs
Upper airway manifestations of granulomatosis with polyangiitis
Daniel S. Alam, MD; Rahul Seth, MD; Raj Sindwani, MD; Erika A. Woodson, MD; and Karthik Rajasekaran, MD
Renal disease in small-vessel vasculitis
Kirsten de Groot, MD
Pulmonary disease in small-vessel vasculitis
Thomas R. Gildea, MD, MS
Ocular manifestations of small-vessel vasculitis
James A. Garrity, MD
Monitoring and safety
Monitoring patients with vasculitis
Alexandra Villa-Forte, MD, MPH
Safety issues in vasculitis: Infections and immunizations in the immunosuppressed host
Carlos M. Isada, MD, FCCP
Treatment considerations
Treating vasculitis with conventional immunosuppressive agents
David Jayne, MD, FRCP
Biologic agents in the treatment of granulomatosis with polyangiitis
Ulrich Specks, MD
Historical perspective
History of vasculitis: The life and work of Adolf Kussmaul
Eric L. Matteson, MD, MPH
Supplement Editor:
Carol Langford, MD, MHS
Associate Editors:
Leonard Calabrese, DO, and Gary Hoffman, MD
Contents
Diagnosis, ANCA testing, and disease activity
Clinical features and diagnosis of small-vessel vasculitis
Carol Langford, MD, MHS
Controversies in ANCA testing
Ulrich Specks, MD
Defining disease activity and damage in patients with small-vessel vasculitis
Peter A. Merkel, MD, MPH
Impact on individual organs
Upper airway manifestations of granulomatosis with polyangiitis
Daniel S. Alam, MD; Rahul Seth, MD; Raj Sindwani, MD; Erika A. Woodson, MD; and Karthik Rajasekaran, MD
Renal disease in small-vessel vasculitis
Kirsten de Groot, MD
Pulmonary disease in small-vessel vasculitis
Thomas R. Gildea, MD, MS
Ocular manifestations of small-vessel vasculitis
James A. Garrity, MD
Monitoring and safety
Monitoring patients with vasculitis
Alexandra Villa-Forte, MD, MPH
Safety issues in vasculitis: Infections and immunizations in the immunosuppressed host
Carlos M. Isada, MD, FCCP
Treatment considerations
Treating vasculitis with conventional immunosuppressive agents
David Jayne, MD, FRCP
Biologic agents in the treatment of granulomatosis with polyangiitis
Ulrich Specks, MD
Historical perspective
History of vasculitis: The life and work of Adolf Kussmaul
Eric L. Matteson, MD, MPH
Supplement Editor:
Carol Langford, MD, MHS
Associate Editors:
Leonard Calabrese, DO, and Gary Hoffman, MD
Contents
Diagnosis, ANCA testing, and disease activity
Clinical features and diagnosis of small-vessel vasculitis
Carol Langford, MD, MHS
Controversies in ANCA testing
Ulrich Specks, MD
Defining disease activity and damage in patients with small-vessel vasculitis
Peter A. Merkel, MD, MPH
Impact on individual organs
Upper airway manifestations of granulomatosis with polyangiitis
Daniel S. Alam, MD; Rahul Seth, MD; Raj Sindwani, MD; Erika A. Woodson, MD; and Karthik Rajasekaran, MD
Renal disease in small-vessel vasculitis
Kirsten de Groot, MD
Pulmonary disease in small-vessel vasculitis
Thomas R. Gildea, MD, MS
Ocular manifestations of small-vessel vasculitis
James A. Garrity, MD
Monitoring and safety
Monitoring patients with vasculitis
Alexandra Villa-Forte, MD, MPH
Safety issues in vasculitis: Infections and immunizations in the immunosuppressed host
Carlos M. Isada, MD, FCCP
Treatment considerations
Treating vasculitis with conventional immunosuppressive agents
David Jayne, MD, FRCP
Biologic agents in the treatment of granulomatosis with polyangiitis
Ulrich Specks, MD
Historical perspective
History of vasculitis: The life and work of Adolf Kussmaul
Eric L. Matteson, MD, MPH
Clinical features and diagnosis of small-vessel vasculitis
Vasculitis refers to inflammation of the blood vessel. This inflammation can cause vessel wall thickening that compromises or occludes the vessel lumen, ultimately resulting in organ ischemia. It also can cause vessel wall attenuation that predisposes to aneurysm formation or breach of the vessel integrity with resultant hemorrhage into the tissue.
Vasculitis can be thought of as a primary or secondary process. Primary vasculitides are unique disease entities without a currently identified underlying cause in which vasculitis forms the pathologic basis of tissue injury. Vasculitis can occur secondary to medication exposure or an underlying illness, including infections, malignancy, cryoglobulinemia, and rheumatic diseases (such as systemic lupus erythematosus, rheumatoid arthritis, Sjögren syndrome, or myositis).
Primary vasculitides may differ in epidemiology, such as the age at which they occur and the gender most likely to be affected, their clinical manifestations (including signs, symptoms, and patterns of organ involvement), the diagnostic approach (biopsy, arteriography, and laboratory investigation), treatment (supportive care, glucocorticoids alone, or in combination with other immunosuppressants), and the size of the vessels predominantly affected (large, medium, or small).
Small-vessel vasculitis affects the arteriole, capillary, and venule. An excellent example of small-vessel vasculitis and the one most commonly encountered in clinical practice is cutaneous vasculitis, in which extravasation of erythrocytes from disrupted small vessels is observed histologically, with the clinical sequelae of palpable purpura. Although categorization based on the predominant vessel size that is affected is a helpful way to view these diseases, this is not absolute and each disease has the potential to affect a diverse range of vessels.
This article explores the clinical features and diagnosis of three forms of vasculitis that predominantly affect the small vessels: granulomatosis with polyangiitis (GPA [Wegener’s granulomatosis]), microscopic polyangiitis (MPA), and eosinophilic GPA (Churg-Strauss syndrome, EGPA).
GRANULOMATOSIS WITH POLYANGIITIS
Granulomatosis with polyangiitis is characterized by granulomatous inflammation involving the respiratory tract and by vasculitis affecting small- to medium-sized vessels in which necrotizing glomerulonephritis is common.
Wide range of presentations, manifestations
Approximately 90% of patients with GPA have upper or lower airway involvement or both.1 Upper airway or ear symptoms affect 73% of patients initially and 92% overall.1 Direct inspection of the nasal membranes shows a cobblestoned or ulcerated appearance, and computed tomography reveals mucosal thickening of the sinuses. In some instances, sinus disease can compromise blood supply to the cartilaginous portion of the nasal septum, leading to nasal septum perforations or collapse of the nasal bridge. Another manifestation of upper airway disease and GPA is subglottic stenosis, a narrowing in the subglottic region located just below the vocal cords. The narrowing typically spans about 1 cm and rarely extends or involves the remainder of the trachea.
The lungs are involved in 85% of patients.1 Radiographic abnormalities can be diverse and include bilateral pulmonary nodular infiltrates, single or multiple cavities, and bilateral ground glass infiltrates as can be seen in pulmonary hemorrhage (Figure). Bronchoscopy may reveal endobronchial stenosis, and pleural disease can occur rarely.
Approximately 20% of patients with GPA may have glomerulonephritis when they first present for medical attention, but it eventually develops in nearly 80% of patients during the disease course.1 Despite its potential for rapid progression, glomerulonephritis presents a diagnostic challenge because it is asymptomatic. It is detected by evidence of proteinuria and an active urine sediment with dysmorphic red blood cells and red blood cell casts.
Ocular involvement occurs eventually in 52% of patients with GPA.1 Any ocular structure can be affected and ocular involvement can be visually threatening. The more prominent ocular manifestations include scleritis/episcleritis or orbital disease.
Cutaneous manifestations, observed in 46% of patients, include verrucous-appearing lesions on the elbow and infarctions in the skin and nail folds.1 Other rare manifestations can occur, such as pericarditis and cerebral vasculitis.
Although nearly all patients present with upper or lower airway symptoms, the multisystem nature of GPA explains the wide range of presentations and the varying degrees of disease severity.
Differential diagnosis
The differential diagnosis in GPA is varied. Particularly in the setting of isolated lung or sinus disease, infection is foremost in the differential diagnosis. Even in the nonimmunosuppressed host, unusual infections such as mycobacteria, histoplasmosis, and other fungal infections should be considered. Lymphadenopathy, rarely seen in GPA, should raise concern for other causes of disease. Lymphoproliferative processes and other neoplasms, other rheumatic diseases, granulomatous disease (ie, sarcoidosis), and other causes of glomerulonephritis (when present) also merit consideration. Differentiation of these entities from GPA is essential because the treatment differs in many instances.
The differential diagnosis for patients who present with midline destructive lesions must include other causes of collapse of the nasal bridge, nasal septum perforation, and possibly palate destruction. Erosions of the hard palate in particular should raise an immediate red flag for entities other than GPA, such as lymphoproliferative diseases; rare infections, particularly if the patient has studied or worked abroad; and cocaine exposure.
Diagnostic evaluation
A diagnosis of GPA is typically based on the presence of histologic features in a clinically compatible setting. Diagnostic features include necrosis, granulomatous inflammation, vasculitis, and special stains and cultures negative for microorganisms.
Biopsy sites are determined by evidence of clinical disease affecting a target organ and the likelihood of obtaining diagnostically meaningful findings from that site. One challenge is that biopsies are not always diagnostic. The changes tend to be patchy and the likelihood of a positive yield is associated with the amount of tissue that can be obtained. Tissues from the ear, nose, and throat have a yield of about 20%, depending upon the site and the biopsy size. The highest yield comes from radiographically abnormal pulmonary parenchyma. Although transbronchial biopsies are attractive because they are less invasive than open lung biopsy, they are also far less diagnostic, with fewer than 10% having a positive yield. Because cutaneous vasculitis is observed in many settings, its presence is usually insufficient evidence for diagnosis. The renal histologic appearance is a focal, segmental, crescentic, and necrotizing glomerulonephritis that has few to no immune complexes (pauciimmune glomerulonephritis).1–3
Chest imaging should be performed in any patient in whom GPA is part of the differential diagnosis, since up to one-third of patients may be asymptomatic yet have pulmonary radiographic findings.
Laboratory assessment should include serum chemistries to evaluate renal and hepatic function, complete blood count, erythrocyte sedimentation rate, measurement of C-reactive protein, and urinalysis. If the urinalysis is positive for blood, microscopy should be performed on fresh urine to look for casts. In the setting of pulmonary-renal manifestations, testing for other causes, such as antiglomerular basement antibodies and antinuclear antibodies, should be considered.
Serologic testing for antineutrophil cytoplasmic antibodies (ANCA) has provided a useful tool in suggesting the diagnosis of GPA. Two forms of ANCA have been identified in patients with vasculitis: ANCA directed against the neutrophil serine protease proteinase-3 (PR3), which results in a cytoplasmic immunofluorescence (cANCA) pattern; and ANCA directed against the neutrophil enzyme myeloperoxidase (MPO), which causes a perinuclear immunofluorescence (pANCA) pattern.4 Approximately 80% to 95% of ANCA found in patients with active severe GPA are detectable PR3-cANCA, while 5% to 20% are MPO-pANCA.5 The predictive value of ANCA for the diagnosis depends on the spectrum of clinical features. As ANCA can be seen in other settings, ANCA as the basis for diagnosis in place of tissue biopsy should be used with caution and only in selected instances where their predictive value would equal that of biopsy. The presence of ANCA is not necessary to establish the diagnosis, as up to 20% of patients with GPA may be ANCA-negative.6
MICROSCOPIC POLYANGIITIS
The history of MPA dates to 1866, with the description of periarteritis nodosa.7 The term “microscopic polyarteritis” was introduced in 1948, when glomerular disease was recognized in some patients.8 In 1994, the Chapel Hill Consensus Conference defined MPA as a necrotizing vasculitis with few or no immune deposits that affects small vessels (ie, capillaries, venules, or arterioles). Necrotizing arteritis of small- and medium-sized arteries may be present. Necrotizing glomerulonephritis and pulmonary capillaritis commonly occur.9 MPA shares many clinical features with GPA and is currently said to be distinguished by the absence of granulomatous inflammation.9
Presentations and manifestations
In one assessment of organ system involvement in 85 patients with MPA, investigators observed glomerular syndrome in 82% of patients.10 They also found a high predilection for involvement of the skin, joints, and lungs. Pulmonary hemorrhage is a particularly important manifestation of MPA because it can be immediately life-threatening.
Differential diagnosis
The differential diagnosis for MPA is similar to GPA in the inclusion of other causes of classic pulmonary-renal syndromes, such as antiglomerular basement membrane disease and systemic lupus erythematosus. Poststreptococcal glomerulonephritis should be considered when the kidney is the predominant organ involved in the absence of lung disease. In the setting of pulmonary infiltrates, infections and neoplasms remain significant in the differential diagnosis.
Diagnostic evaluation
The diagnosis of MPA is based on consistent clinical features and compatible histologic findings. The histologic renal lesion is identical to that seen in GPA. Pulmonary disease typically includes capillaritis and is notable for the absence of evidence of immune deposition, in contrast to antiglomerular basement membrane disease.
Chest imaging is indicated when MPA is part of the differential diagnosis. Computed tomography is the preferred technique, as early alveolar hemorrhage that can occur in MPA may not be visualized on a chest radiograph.
Laboratory assessment should include serum chemistries, complete blood count, erythrocyte sedimentation rate, measurement of C-reactive protein, and urinalysis. Additional testing should be pursued for other diseases as indicated by the clinical features.
Approximately 40% to 80% of patients with MPA have MPO-pANCA.5 Approximately 15% of patients are MPO-pANCA positive,6 and 0% to 20% are ANCA-negative. As with GPA, ANCA is useful to suggest—but not diagnose—disease in many instances. The absence of ANCA does not rule out MPA.
EOSINOPHILIC GPA
Eosinophilic GPA is a unique entity characterized by eosinophil-rich and granulomatous inflammation involving the respiratory tract and necrotizing vasculitis of small- to medium-size vessels. It is also associated with asthma and eosinophilia.
Different disease phases
Eosinophilic GPA is often thought of as having three phases: prodromal, eosinophilic, and vasculitic.11,12 Although helpful conceptually, these phases may not always be present and may not occur in sequence.
The prodromal phase is characterized by asthma associated with allergic rhinitis with or without polyposis. The eosinophilic phase is characterized by the presence of eosinophilia in the blood and tissue. Eosinophilia is a prominent feature, although accurate detection and assessment can be challenging in the setting of glucocorticoid use for asthma as this normalizes the eosinophil count.
The vasculitic phase distinguishes EGPA from other eosinophilic disorders. Features of vasculitis may occur in multiple organ sites, including the nerves, lungs, heart, gastrointestinal tract, and kidneys. In one series of 96 patients, nearly 100% had asthma, and peripheral nervous system involvement in the form of mononeuritis multiplex was present in 72%.12 Cardiac involvement is of particular importance as it is a prominent cause of disease-related mortality. Cardiac manifestations include myocarditis, pericarditis, endocarditis, valvulitis, and coronary vasculitis.
Differential diagnosis
The differential diagnosis of EGPA shares similarities with GPA and MPA, but also includes eosino philic disorders such as hypereosinophilic syndrome, eosinophilic leukemia, and parasitic diseases.
Diagnostic evaluation
Diagnosis is often based on the presence of asthma, a finding of peripheral eosinophilia (> 1,500 cells/mm3), and the presence of systemic vasculitis involving, ideally, two or more extrapulmonary organs. While histologic confirmation remains ideal, demonstration of characteristic findings on biopsy can be difficult. Glomerular involvement is far less common than in GPA and MPA, but, when present, the renal lesion is identical. Pulmonary histologic findings can be diverse and include the classic “allergic-granuloma” as originally described by Churg and Strauss, as well as isolated granulomatous inflammation, eosinophilic inflammation, or small-vessel vasculitis. Tissue eosinophilia is a prominent finding that typically is seen on biopsies of skin, nerve, and gastrointestinal tissues.
Chest imaging should be performed when EGPA is part of the differential diagnosis. Because of the potential for cardiac involvement, a baseline echocardiogram should be obtained. Pulmonary function tests may be useful, particularly in patients who have a strong asthmatic component.
Similar to GPA and MPA, laboratory assessment includes serum chemistries, complete blood count with differential to determine the eosinophil count, erythrocyte sedimentation rate, measurement of C-reactive protein, and urinalysis. With the allergic and asthmatic components, immunoglobulin E levels are frequently elevated. Additional testing for other eosinophilic diseases should be pursued as indicated by the clinical features.
Only about 40% of patients are ANCA-positive.13 Most of these are MPO-pANCA, with PR3-cANCA occurring less commonly. Although some reports have suggested differing clinical patterns of EGPA based on ANCA positivity, the presence or absence of ANCA is less helpful in the diagnosis.13
DIFFERENTIATION
A key histologic difference between GPA and MPA is the presence of granulomatous inflammation in GPA and its absence in MPA under the current nomenclature system.9 Granulomatous inflammation can be seen in EGPA, but it is usually accompanied by eosinophils, which are less likely to be present in GPA and MPA.
The predominance of the ANCA immunofluorescence pattern and target antigen differs between GPA and MPA, with ANCA positivity occurring in 38% of patients with EGPA.13
SUMMARY
Conceptualizing vasculitic disease based on vessel size can be useful, but it is not an absolute definition. Although GPA, MPA, and EGPA predominantly affect small- to medium-sized vessels, these disease entities are phenotypically unique, with both shared features and differences. Common to all three entities is the potential for organ- and life-threatening manifestations, particularly involving the lungs, kidneys, nerves, gastrointestinal tract, and heart. All three entities need aggressive immuno suppression for severe disease. Recognition of these entities and the distinctions among them can guide the approach to diagnosis, treatment, and future outcomes.
- Hoffman GS, Kerr GS, Leavitt RY, et al Wegener granulomatosis: an analysis of 158 patients. Ann Intern Med 1992; 116:488–498.
- Travis WD, Hoffman GS, Leavitt RY, Pass HI, Fauci AS. Surgical pathology of the lung in Wegener’s granulomatosis: review of 87 open lung biopsies from 67 patients. Am J Surg Pathol 1991; 15:315–333.
- Devaney KO, Travis WD, Hoffman G, Leavitt R, Lebovics R, Fauci AS. Interpretation of head and neck biopsies in Wegener’s granulomatosis: a pathologic study of 126 biopsies in 70 patients. Am J Surg Pathol 1990; 14:555–564.
- Bosch X, Guilabert A, Font J. Antineutrophil cytoplasmic antibodies. Lancet 2006; 368:404–418.
- Hoffman GS, Specks U. Antineutrophil cytoplasmic antibodies. Arthritis Rheum 1998;1521–1537.
- Wiik A. What you should know about PR3-ANCA. An introduction. Arthritis Res 2000; 2:252–254.
- Kussmaul A, Maier R. Über eine bisher nicht beschriebene eigenthümliche Arterienerkrankung (Periarteritis nodosa), die mit Morbus Brightii und rapid fortschreitender allgemeiner Muskellähmung einhergeht. Dtsch Arch Klin Med 1866; 1:484–518.
- Davson J, Ball J, Platt R. The kidney in periarteritis nodosa. Q J Med 1948; 17:175–202.
- Jennette C, Falk RJ, Andrassy K, et al Nomenclature of systemic vasculitides: proposal of an international consensus conference. Arthritis Rheum 1994; 37:187–192.
- Guillevin L, Durand-Gasselin B, Cevallos R, et al Microscopic polyangiitis: clinical and laboratory findings in eighty-five patients. Arthritis Rheum 1999; 42:421–430.
- Keogh KA, Specks U. Churg-Strauss syndrome. Semin Respir Crit Care Med 2006; 27:148–157.
- Guillevin L, Cohen P, Gayraud M, Lhote F, Jarrousse B, Casassus P. Churg-Strauss syndrome: clinical study and long-term follow-up of 96 patients. Medicine 1999; 78:26–37.
- Sablé-Fourtassou R, Cohen P, Mahr A, et al., for the French Vasculitis Study Group. Antineutrophil cytoplasmic antibodies and the Churg-Strauss syndrome. Ann Intern Med 2005; 143:632–638.
Vasculitis refers to inflammation of the blood vessel. This inflammation can cause vessel wall thickening that compromises or occludes the vessel lumen, ultimately resulting in organ ischemia. It also can cause vessel wall attenuation that predisposes to aneurysm formation or breach of the vessel integrity with resultant hemorrhage into the tissue.
Vasculitis can be thought of as a primary or secondary process. Primary vasculitides are unique disease entities without a currently identified underlying cause in which vasculitis forms the pathologic basis of tissue injury. Vasculitis can occur secondary to medication exposure or an underlying illness, including infections, malignancy, cryoglobulinemia, and rheumatic diseases (such as systemic lupus erythematosus, rheumatoid arthritis, Sjögren syndrome, or myositis).
Primary vasculitides may differ in epidemiology, such as the age at which they occur and the gender most likely to be affected, their clinical manifestations (including signs, symptoms, and patterns of organ involvement), the diagnostic approach (biopsy, arteriography, and laboratory investigation), treatment (supportive care, glucocorticoids alone, or in combination with other immunosuppressants), and the size of the vessels predominantly affected (large, medium, or small).
Small-vessel vasculitis affects the arteriole, capillary, and venule. An excellent example of small-vessel vasculitis and the one most commonly encountered in clinical practice is cutaneous vasculitis, in which extravasation of erythrocytes from disrupted small vessels is observed histologically, with the clinical sequelae of palpable purpura. Although categorization based on the predominant vessel size that is affected is a helpful way to view these diseases, this is not absolute and each disease has the potential to affect a diverse range of vessels.
This article explores the clinical features and diagnosis of three forms of vasculitis that predominantly affect the small vessels: granulomatosis with polyangiitis (GPA [Wegener’s granulomatosis]), microscopic polyangiitis (MPA), and eosinophilic GPA (Churg-Strauss syndrome, EGPA).
GRANULOMATOSIS WITH POLYANGIITIS
Granulomatosis with polyangiitis is characterized by granulomatous inflammation involving the respiratory tract and by vasculitis affecting small- to medium-sized vessels in which necrotizing glomerulonephritis is common.
Wide range of presentations, manifestations
Approximately 90% of patients with GPA have upper or lower airway involvement or both.1 Upper airway or ear symptoms affect 73% of patients initially and 92% overall.1 Direct inspection of the nasal membranes shows a cobblestoned or ulcerated appearance, and computed tomography reveals mucosal thickening of the sinuses. In some instances, sinus disease can compromise blood supply to the cartilaginous portion of the nasal septum, leading to nasal septum perforations or collapse of the nasal bridge. Another manifestation of upper airway disease and GPA is subglottic stenosis, a narrowing in the subglottic region located just below the vocal cords. The narrowing typically spans about 1 cm and rarely extends or involves the remainder of the trachea.
The lungs are involved in 85% of patients.1 Radiographic abnormalities can be diverse and include bilateral pulmonary nodular infiltrates, single or multiple cavities, and bilateral ground glass infiltrates as can be seen in pulmonary hemorrhage (Figure). Bronchoscopy may reveal endobronchial stenosis, and pleural disease can occur rarely.
Approximately 20% of patients with GPA may have glomerulonephritis when they first present for medical attention, but it eventually develops in nearly 80% of patients during the disease course.1 Despite its potential for rapid progression, glomerulonephritis presents a diagnostic challenge because it is asymptomatic. It is detected by evidence of proteinuria and an active urine sediment with dysmorphic red blood cells and red blood cell casts.
Ocular involvement occurs eventually in 52% of patients with GPA.1 Any ocular structure can be affected and ocular involvement can be visually threatening. The more prominent ocular manifestations include scleritis/episcleritis or orbital disease.
Cutaneous manifestations, observed in 46% of patients, include verrucous-appearing lesions on the elbow and infarctions in the skin and nail folds.1 Other rare manifestations can occur, such as pericarditis and cerebral vasculitis.
Although nearly all patients present with upper or lower airway symptoms, the multisystem nature of GPA explains the wide range of presentations and the varying degrees of disease severity.
Differential diagnosis
The differential diagnosis in GPA is varied. Particularly in the setting of isolated lung or sinus disease, infection is foremost in the differential diagnosis. Even in the nonimmunosuppressed host, unusual infections such as mycobacteria, histoplasmosis, and other fungal infections should be considered. Lymphadenopathy, rarely seen in GPA, should raise concern for other causes of disease. Lymphoproliferative processes and other neoplasms, other rheumatic diseases, granulomatous disease (ie, sarcoidosis), and other causes of glomerulonephritis (when present) also merit consideration. Differentiation of these entities from GPA is essential because the treatment differs in many instances.
The differential diagnosis for patients who present with midline destructive lesions must include other causes of collapse of the nasal bridge, nasal septum perforation, and possibly palate destruction. Erosions of the hard palate in particular should raise an immediate red flag for entities other than GPA, such as lymphoproliferative diseases; rare infections, particularly if the patient has studied or worked abroad; and cocaine exposure.
Diagnostic evaluation
A diagnosis of GPA is typically based on the presence of histologic features in a clinically compatible setting. Diagnostic features include necrosis, granulomatous inflammation, vasculitis, and special stains and cultures negative for microorganisms.
Biopsy sites are determined by evidence of clinical disease affecting a target organ and the likelihood of obtaining diagnostically meaningful findings from that site. One challenge is that biopsies are not always diagnostic. The changes tend to be patchy and the likelihood of a positive yield is associated with the amount of tissue that can be obtained. Tissues from the ear, nose, and throat have a yield of about 20%, depending upon the site and the biopsy size. The highest yield comes from radiographically abnormal pulmonary parenchyma. Although transbronchial biopsies are attractive because they are less invasive than open lung biopsy, they are also far less diagnostic, with fewer than 10% having a positive yield. Because cutaneous vasculitis is observed in many settings, its presence is usually insufficient evidence for diagnosis. The renal histologic appearance is a focal, segmental, crescentic, and necrotizing glomerulonephritis that has few to no immune complexes (pauciimmune glomerulonephritis).1–3
Chest imaging should be performed in any patient in whom GPA is part of the differential diagnosis, since up to one-third of patients may be asymptomatic yet have pulmonary radiographic findings.
Laboratory assessment should include serum chemistries to evaluate renal and hepatic function, complete blood count, erythrocyte sedimentation rate, measurement of C-reactive protein, and urinalysis. If the urinalysis is positive for blood, microscopy should be performed on fresh urine to look for casts. In the setting of pulmonary-renal manifestations, testing for other causes, such as antiglomerular basement antibodies and antinuclear antibodies, should be considered.
Serologic testing for antineutrophil cytoplasmic antibodies (ANCA) has provided a useful tool in suggesting the diagnosis of GPA. Two forms of ANCA have been identified in patients with vasculitis: ANCA directed against the neutrophil serine protease proteinase-3 (PR3), which results in a cytoplasmic immunofluorescence (cANCA) pattern; and ANCA directed against the neutrophil enzyme myeloperoxidase (MPO), which causes a perinuclear immunofluorescence (pANCA) pattern.4 Approximately 80% to 95% of ANCA found in patients with active severe GPA are detectable PR3-cANCA, while 5% to 20% are MPO-pANCA.5 The predictive value of ANCA for the diagnosis depends on the spectrum of clinical features. As ANCA can be seen in other settings, ANCA as the basis for diagnosis in place of tissue biopsy should be used with caution and only in selected instances where their predictive value would equal that of biopsy. The presence of ANCA is not necessary to establish the diagnosis, as up to 20% of patients with GPA may be ANCA-negative.6
MICROSCOPIC POLYANGIITIS
The history of MPA dates to 1866, with the description of periarteritis nodosa.7 The term “microscopic polyarteritis” was introduced in 1948, when glomerular disease was recognized in some patients.8 In 1994, the Chapel Hill Consensus Conference defined MPA as a necrotizing vasculitis with few or no immune deposits that affects small vessels (ie, capillaries, venules, or arterioles). Necrotizing arteritis of small- and medium-sized arteries may be present. Necrotizing glomerulonephritis and pulmonary capillaritis commonly occur.9 MPA shares many clinical features with GPA and is currently said to be distinguished by the absence of granulomatous inflammation.9
Presentations and manifestations
In one assessment of organ system involvement in 85 patients with MPA, investigators observed glomerular syndrome in 82% of patients.10 They also found a high predilection for involvement of the skin, joints, and lungs. Pulmonary hemorrhage is a particularly important manifestation of MPA because it can be immediately life-threatening.
Differential diagnosis
The differential diagnosis for MPA is similar to GPA in the inclusion of other causes of classic pulmonary-renal syndromes, such as antiglomerular basement membrane disease and systemic lupus erythematosus. Poststreptococcal glomerulonephritis should be considered when the kidney is the predominant organ involved in the absence of lung disease. In the setting of pulmonary infiltrates, infections and neoplasms remain significant in the differential diagnosis.
Diagnostic evaluation
The diagnosis of MPA is based on consistent clinical features and compatible histologic findings. The histologic renal lesion is identical to that seen in GPA. Pulmonary disease typically includes capillaritis and is notable for the absence of evidence of immune deposition, in contrast to antiglomerular basement membrane disease.
Chest imaging is indicated when MPA is part of the differential diagnosis. Computed tomography is the preferred technique, as early alveolar hemorrhage that can occur in MPA may not be visualized on a chest radiograph.
Laboratory assessment should include serum chemistries, complete blood count, erythrocyte sedimentation rate, measurement of C-reactive protein, and urinalysis. Additional testing should be pursued for other diseases as indicated by the clinical features.
Approximately 40% to 80% of patients with MPA have MPO-pANCA.5 Approximately 15% of patients are MPO-pANCA positive,6 and 0% to 20% are ANCA-negative. As with GPA, ANCA is useful to suggest—but not diagnose—disease in many instances. The absence of ANCA does not rule out MPA.
EOSINOPHILIC GPA
Eosinophilic GPA is a unique entity characterized by eosinophil-rich and granulomatous inflammation involving the respiratory tract and necrotizing vasculitis of small- to medium-size vessels. It is also associated with asthma and eosinophilia.
Different disease phases
Eosinophilic GPA is often thought of as having three phases: prodromal, eosinophilic, and vasculitic.11,12 Although helpful conceptually, these phases may not always be present and may not occur in sequence.
The prodromal phase is characterized by asthma associated with allergic rhinitis with or without polyposis. The eosinophilic phase is characterized by the presence of eosinophilia in the blood and tissue. Eosinophilia is a prominent feature, although accurate detection and assessment can be challenging in the setting of glucocorticoid use for asthma as this normalizes the eosinophil count.
The vasculitic phase distinguishes EGPA from other eosinophilic disorders. Features of vasculitis may occur in multiple organ sites, including the nerves, lungs, heart, gastrointestinal tract, and kidneys. In one series of 96 patients, nearly 100% had asthma, and peripheral nervous system involvement in the form of mononeuritis multiplex was present in 72%.12 Cardiac involvement is of particular importance as it is a prominent cause of disease-related mortality. Cardiac manifestations include myocarditis, pericarditis, endocarditis, valvulitis, and coronary vasculitis.
Differential diagnosis
The differential diagnosis of EGPA shares similarities with GPA and MPA, but also includes eosino philic disorders such as hypereosinophilic syndrome, eosinophilic leukemia, and parasitic diseases.
Diagnostic evaluation
Diagnosis is often based on the presence of asthma, a finding of peripheral eosinophilia (> 1,500 cells/mm3), and the presence of systemic vasculitis involving, ideally, two or more extrapulmonary organs. While histologic confirmation remains ideal, demonstration of characteristic findings on biopsy can be difficult. Glomerular involvement is far less common than in GPA and MPA, but, when present, the renal lesion is identical. Pulmonary histologic findings can be diverse and include the classic “allergic-granuloma” as originally described by Churg and Strauss, as well as isolated granulomatous inflammation, eosinophilic inflammation, or small-vessel vasculitis. Tissue eosinophilia is a prominent finding that typically is seen on biopsies of skin, nerve, and gastrointestinal tissues.
Chest imaging should be performed when EGPA is part of the differential diagnosis. Because of the potential for cardiac involvement, a baseline echocardiogram should be obtained. Pulmonary function tests may be useful, particularly in patients who have a strong asthmatic component.
Similar to GPA and MPA, laboratory assessment includes serum chemistries, complete blood count with differential to determine the eosinophil count, erythrocyte sedimentation rate, measurement of C-reactive protein, and urinalysis. With the allergic and asthmatic components, immunoglobulin E levels are frequently elevated. Additional testing for other eosinophilic diseases should be pursued as indicated by the clinical features.
Only about 40% of patients are ANCA-positive.13 Most of these are MPO-pANCA, with PR3-cANCA occurring less commonly. Although some reports have suggested differing clinical patterns of EGPA based on ANCA positivity, the presence or absence of ANCA is less helpful in the diagnosis.13
DIFFERENTIATION
A key histologic difference between GPA and MPA is the presence of granulomatous inflammation in GPA and its absence in MPA under the current nomenclature system.9 Granulomatous inflammation can be seen in EGPA, but it is usually accompanied by eosinophils, which are less likely to be present in GPA and MPA.
The predominance of the ANCA immunofluorescence pattern and target antigen differs between GPA and MPA, with ANCA positivity occurring in 38% of patients with EGPA.13
SUMMARY
Conceptualizing vasculitic disease based on vessel size can be useful, but it is not an absolute definition. Although GPA, MPA, and EGPA predominantly affect small- to medium-sized vessels, these disease entities are phenotypically unique, with both shared features and differences. Common to all three entities is the potential for organ- and life-threatening manifestations, particularly involving the lungs, kidneys, nerves, gastrointestinal tract, and heart. All three entities need aggressive immuno suppression for severe disease. Recognition of these entities and the distinctions among them can guide the approach to diagnosis, treatment, and future outcomes.
Vasculitis refers to inflammation of the blood vessel. This inflammation can cause vessel wall thickening that compromises or occludes the vessel lumen, ultimately resulting in organ ischemia. It also can cause vessel wall attenuation that predisposes to aneurysm formation or breach of the vessel integrity with resultant hemorrhage into the tissue.
Vasculitis can be thought of as a primary or secondary process. Primary vasculitides are unique disease entities without a currently identified underlying cause in which vasculitis forms the pathologic basis of tissue injury. Vasculitis can occur secondary to medication exposure or an underlying illness, including infections, malignancy, cryoglobulinemia, and rheumatic diseases (such as systemic lupus erythematosus, rheumatoid arthritis, Sjögren syndrome, or myositis).
Primary vasculitides may differ in epidemiology, such as the age at which they occur and the gender most likely to be affected, their clinical manifestations (including signs, symptoms, and patterns of organ involvement), the diagnostic approach (biopsy, arteriography, and laboratory investigation), treatment (supportive care, glucocorticoids alone, or in combination with other immunosuppressants), and the size of the vessels predominantly affected (large, medium, or small).
Small-vessel vasculitis affects the arteriole, capillary, and venule. An excellent example of small-vessel vasculitis and the one most commonly encountered in clinical practice is cutaneous vasculitis, in which extravasation of erythrocytes from disrupted small vessels is observed histologically, with the clinical sequelae of palpable purpura. Although categorization based on the predominant vessel size that is affected is a helpful way to view these diseases, this is not absolute and each disease has the potential to affect a diverse range of vessels.
This article explores the clinical features and diagnosis of three forms of vasculitis that predominantly affect the small vessels: granulomatosis with polyangiitis (GPA [Wegener’s granulomatosis]), microscopic polyangiitis (MPA), and eosinophilic GPA (Churg-Strauss syndrome, EGPA).
GRANULOMATOSIS WITH POLYANGIITIS
Granulomatosis with polyangiitis is characterized by granulomatous inflammation involving the respiratory tract and by vasculitis affecting small- to medium-sized vessels in which necrotizing glomerulonephritis is common.
Wide range of presentations, manifestations
Approximately 90% of patients with GPA have upper or lower airway involvement or both.1 Upper airway or ear symptoms affect 73% of patients initially and 92% overall.1 Direct inspection of the nasal membranes shows a cobblestoned or ulcerated appearance, and computed tomography reveals mucosal thickening of the sinuses. In some instances, sinus disease can compromise blood supply to the cartilaginous portion of the nasal septum, leading to nasal septum perforations or collapse of the nasal bridge. Another manifestation of upper airway disease and GPA is subglottic stenosis, a narrowing in the subglottic region located just below the vocal cords. The narrowing typically spans about 1 cm and rarely extends or involves the remainder of the trachea.
The lungs are involved in 85% of patients.1 Radiographic abnormalities can be diverse and include bilateral pulmonary nodular infiltrates, single or multiple cavities, and bilateral ground glass infiltrates as can be seen in pulmonary hemorrhage (Figure). Bronchoscopy may reveal endobronchial stenosis, and pleural disease can occur rarely.
Approximately 20% of patients with GPA may have glomerulonephritis when they first present for medical attention, but it eventually develops in nearly 80% of patients during the disease course.1 Despite its potential for rapid progression, glomerulonephritis presents a diagnostic challenge because it is asymptomatic. It is detected by evidence of proteinuria and an active urine sediment with dysmorphic red blood cells and red blood cell casts.
Ocular involvement occurs eventually in 52% of patients with GPA.1 Any ocular structure can be affected and ocular involvement can be visually threatening. The more prominent ocular manifestations include scleritis/episcleritis or orbital disease.
Cutaneous manifestations, observed in 46% of patients, include verrucous-appearing lesions on the elbow and infarctions in the skin and nail folds.1 Other rare manifestations can occur, such as pericarditis and cerebral vasculitis.
Although nearly all patients present with upper or lower airway symptoms, the multisystem nature of GPA explains the wide range of presentations and the varying degrees of disease severity.
Differential diagnosis
The differential diagnosis in GPA is varied. Particularly in the setting of isolated lung or sinus disease, infection is foremost in the differential diagnosis. Even in the nonimmunosuppressed host, unusual infections such as mycobacteria, histoplasmosis, and other fungal infections should be considered. Lymphadenopathy, rarely seen in GPA, should raise concern for other causes of disease. Lymphoproliferative processes and other neoplasms, other rheumatic diseases, granulomatous disease (ie, sarcoidosis), and other causes of glomerulonephritis (when present) also merit consideration. Differentiation of these entities from GPA is essential because the treatment differs in many instances.
The differential diagnosis for patients who present with midline destructive lesions must include other causes of collapse of the nasal bridge, nasal septum perforation, and possibly palate destruction. Erosions of the hard palate in particular should raise an immediate red flag for entities other than GPA, such as lymphoproliferative diseases; rare infections, particularly if the patient has studied or worked abroad; and cocaine exposure.
Diagnostic evaluation
A diagnosis of GPA is typically based on the presence of histologic features in a clinically compatible setting. Diagnostic features include necrosis, granulomatous inflammation, vasculitis, and special stains and cultures negative for microorganisms.
Biopsy sites are determined by evidence of clinical disease affecting a target organ and the likelihood of obtaining diagnostically meaningful findings from that site. One challenge is that biopsies are not always diagnostic. The changes tend to be patchy and the likelihood of a positive yield is associated with the amount of tissue that can be obtained. Tissues from the ear, nose, and throat have a yield of about 20%, depending upon the site and the biopsy size. The highest yield comes from radiographically abnormal pulmonary parenchyma. Although transbronchial biopsies are attractive because they are less invasive than open lung biopsy, they are also far less diagnostic, with fewer than 10% having a positive yield. Because cutaneous vasculitis is observed in many settings, its presence is usually insufficient evidence for diagnosis. The renal histologic appearance is a focal, segmental, crescentic, and necrotizing glomerulonephritis that has few to no immune complexes (pauciimmune glomerulonephritis).1–3
Chest imaging should be performed in any patient in whom GPA is part of the differential diagnosis, since up to one-third of patients may be asymptomatic yet have pulmonary radiographic findings.
Laboratory assessment should include serum chemistries to evaluate renal and hepatic function, complete blood count, erythrocyte sedimentation rate, measurement of C-reactive protein, and urinalysis. If the urinalysis is positive for blood, microscopy should be performed on fresh urine to look for casts. In the setting of pulmonary-renal manifestations, testing for other causes, such as antiglomerular basement antibodies and antinuclear antibodies, should be considered.
Serologic testing for antineutrophil cytoplasmic antibodies (ANCA) has provided a useful tool in suggesting the diagnosis of GPA. Two forms of ANCA have been identified in patients with vasculitis: ANCA directed against the neutrophil serine protease proteinase-3 (PR3), which results in a cytoplasmic immunofluorescence (cANCA) pattern; and ANCA directed against the neutrophil enzyme myeloperoxidase (MPO), which causes a perinuclear immunofluorescence (pANCA) pattern.4 Approximately 80% to 95% of ANCA found in patients with active severe GPA are detectable PR3-cANCA, while 5% to 20% are MPO-pANCA.5 The predictive value of ANCA for the diagnosis depends on the spectrum of clinical features. As ANCA can be seen in other settings, ANCA as the basis for diagnosis in place of tissue biopsy should be used with caution and only in selected instances where their predictive value would equal that of biopsy. The presence of ANCA is not necessary to establish the diagnosis, as up to 20% of patients with GPA may be ANCA-negative.6
MICROSCOPIC POLYANGIITIS
The history of MPA dates to 1866, with the description of periarteritis nodosa.7 The term “microscopic polyarteritis” was introduced in 1948, when glomerular disease was recognized in some patients.8 In 1994, the Chapel Hill Consensus Conference defined MPA as a necrotizing vasculitis with few or no immune deposits that affects small vessels (ie, capillaries, venules, or arterioles). Necrotizing arteritis of small- and medium-sized arteries may be present. Necrotizing glomerulonephritis and pulmonary capillaritis commonly occur.9 MPA shares many clinical features with GPA and is currently said to be distinguished by the absence of granulomatous inflammation.9
Presentations and manifestations
In one assessment of organ system involvement in 85 patients with MPA, investigators observed glomerular syndrome in 82% of patients.10 They also found a high predilection for involvement of the skin, joints, and lungs. Pulmonary hemorrhage is a particularly important manifestation of MPA because it can be immediately life-threatening.
Differential diagnosis
The differential diagnosis for MPA is similar to GPA in the inclusion of other causes of classic pulmonary-renal syndromes, such as antiglomerular basement membrane disease and systemic lupus erythematosus. Poststreptococcal glomerulonephritis should be considered when the kidney is the predominant organ involved in the absence of lung disease. In the setting of pulmonary infiltrates, infections and neoplasms remain significant in the differential diagnosis.
Diagnostic evaluation
The diagnosis of MPA is based on consistent clinical features and compatible histologic findings. The histologic renal lesion is identical to that seen in GPA. Pulmonary disease typically includes capillaritis and is notable for the absence of evidence of immune deposition, in contrast to antiglomerular basement membrane disease.
Chest imaging is indicated when MPA is part of the differential diagnosis. Computed tomography is the preferred technique, as early alveolar hemorrhage that can occur in MPA may not be visualized on a chest radiograph.
Laboratory assessment should include serum chemistries, complete blood count, erythrocyte sedimentation rate, measurement of C-reactive protein, and urinalysis. Additional testing should be pursued for other diseases as indicated by the clinical features.
Approximately 40% to 80% of patients with MPA have MPO-pANCA.5 Approximately 15% of patients are MPO-pANCA positive,6 and 0% to 20% are ANCA-negative. As with GPA, ANCA is useful to suggest—but not diagnose—disease in many instances. The absence of ANCA does not rule out MPA.
EOSINOPHILIC GPA
Eosinophilic GPA is a unique entity characterized by eosinophil-rich and granulomatous inflammation involving the respiratory tract and necrotizing vasculitis of small- to medium-size vessels. It is also associated with asthma and eosinophilia.
Different disease phases
Eosinophilic GPA is often thought of as having three phases: prodromal, eosinophilic, and vasculitic.11,12 Although helpful conceptually, these phases may not always be present and may not occur in sequence.
The prodromal phase is characterized by asthma associated with allergic rhinitis with or without polyposis. The eosinophilic phase is characterized by the presence of eosinophilia in the blood and tissue. Eosinophilia is a prominent feature, although accurate detection and assessment can be challenging in the setting of glucocorticoid use for asthma as this normalizes the eosinophil count.
The vasculitic phase distinguishes EGPA from other eosinophilic disorders. Features of vasculitis may occur in multiple organ sites, including the nerves, lungs, heart, gastrointestinal tract, and kidneys. In one series of 96 patients, nearly 100% had asthma, and peripheral nervous system involvement in the form of mononeuritis multiplex was present in 72%.12 Cardiac involvement is of particular importance as it is a prominent cause of disease-related mortality. Cardiac manifestations include myocarditis, pericarditis, endocarditis, valvulitis, and coronary vasculitis.
Differential diagnosis
The differential diagnosis of EGPA shares similarities with GPA and MPA, but also includes eosino philic disorders such as hypereosinophilic syndrome, eosinophilic leukemia, and parasitic diseases.
Diagnostic evaluation
Diagnosis is often based on the presence of asthma, a finding of peripheral eosinophilia (> 1,500 cells/mm3), and the presence of systemic vasculitis involving, ideally, two or more extrapulmonary organs. While histologic confirmation remains ideal, demonstration of characteristic findings on biopsy can be difficult. Glomerular involvement is far less common than in GPA and MPA, but, when present, the renal lesion is identical. Pulmonary histologic findings can be diverse and include the classic “allergic-granuloma” as originally described by Churg and Strauss, as well as isolated granulomatous inflammation, eosinophilic inflammation, or small-vessel vasculitis. Tissue eosinophilia is a prominent finding that typically is seen on biopsies of skin, nerve, and gastrointestinal tissues.
Chest imaging should be performed when EGPA is part of the differential diagnosis. Because of the potential for cardiac involvement, a baseline echocardiogram should be obtained. Pulmonary function tests may be useful, particularly in patients who have a strong asthmatic component.
Similar to GPA and MPA, laboratory assessment includes serum chemistries, complete blood count with differential to determine the eosinophil count, erythrocyte sedimentation rate, measurement of C-reactive protein, and urinalysis. With the allergic and asthmatic components, immunoglobulin E levels are frequently elevated. Additional testing for other eosinophilic diseases should be pursued as indicated by the clinical features.
Only about 40% of patients are ANCA-positive.13 Most of these are MPO-pANCA, with PR3-cANCA occurring less commonly. Although some reports have suggested differing clinical patterns of EGPA based on ANCA positivity, the presence or absence of ANCA is less helpful in the diagnosis.13
DIFFERENTIATION
A key histologic difference between GPA and MPA is the presence of granulomatous inflammation in GPA and its absence in MPA under the current nomenclature system.9 Granulomatous inflammation can be seen in EGPA, but it is usually accompanied by eosinophils, which are less likely to be present in GPA and MPA.
The predominance of the ANCA immunofluorescence pattern and target antigen differs between GPA and MPA, with ANCA positivity occurring in 38% of patients with EGPA.13
SUMMARY
Conceptualizing vasculitic disease based on vessel size can be useful, but it is not an absolute definition. Although GPA, MPA, and EGPA predominantly affect small- to medium-sized vessels, these disease entities are phenotypically unique, with both shared features and differences. Common to all three entities is the potential for organ- and life-threatening manifestations, particularly involving the lungs, kidneys, nerves, gastrointestinal tract, and heart. All three entities need aggressive immuno suppression for severe disease. Recognition of these entities and the distinctions among them can guide the approach to diagnosis, treatment, and future outcomes.
- Hoffman GS, Kerr GS, Leavitt RY, et al Wegener granulomatosis: an analysis of 158 patients. Ann Intern Med 1992; 116:488–498.
- Travis WD, Hoffman GS, Leavitt RY, Pass HI, Fauci AS. Surgical pathology of the lung in Wegener’s granulomatosis: review of 87 open lung biopsies from 67 patients. Am J Surg Pathol 1991; 15:315–333.
- Devaney KO, Travis WD, Hoffman G, Leavitt R, Lebovics R, Fauci AS. Interpretation of head and neck biopsies in Wegener’s granulomatosis: a pathologic study of 126 biopsies in 70 patients. Am J Surg Pathol 1990; 14:555–564.
- Bosch X, Guilabert A, Font J. Antineutrophil cytoplasmic antibodies. Lancet 2006; 368:404–418.
- Hoffman GS, Specks U. Antineutrophil cytoplasmic antibodies. Arthritis Rheum 1998;1521–1537.
- Wiik A. What you should know about PR3-ANCA. An introduction. Arthritis Res 2000; 2:252–254.
- Kussmaul A, Maier R. Über eine bisher nicht beschriebene eigenthümliche Arterienerkrankung (Periarteritis nodosa), die mit Morbus Brightii und rapid fortschreitender allgemeiner Muskellähmung einhergeht. Dtsch Arch Klin Med 1866; 1:484–518.
- Davson J, Ball J, Platt R. The kidney in periarteritis nodosa. Q J Med 1948; 17:175–202.
- Jennette C, Falk RJ, Andrassy K, et al Nomenclature of systemic vasculitides: proposal of an international consensus conference. Arthritis Rheum 1994; 37:187–192.
- Guillevin L, Durand-Gasselin B, Cevallos R, et al Microscopic polyangiitis: clinical and laboratory findings in eighty-five patients. Arthritis Rheum 1999; 42:421–430.
- Keogh KA, Specks U. Churg-Strauss syndrome. Semin Respir Crit Care Med 2006; 27:148–157.
- Guillevin L, Cohen P, Gayraud M, Lhote F, Jarrousse B, Casassus P. Churg-Strauss syndrome: clinical study and long-term follow-up of 96 patients. Medicine 1999; 78:26–37.
- Sablé-Fourtassou R, Cohen P, Mahr A, et al., for the French Vasculitis Study Group. Antineutrophil cytoplasmic antibodies and the Churg-Strauss syndrome. Ann Intern Med 2005; 143:632–638.
- Hoffman GS, Kerr GS, Leavitt RY, et al Wegener granulomatosis: an analysis of 158 patients. Ann Intern Med 1992; 116:488–498.
- Travis WD, Hoffman GS, Leavitt RY, Pass HI, Fauci AS. Surgical pathology of the lung in Wegener’s granulomatosis: review of 87 open lung biopsies from 67 patients. Am J Surg Pathol 1991; 15:315–333.
- Devaney KO, Travis WD, Hoffman G, Leavitt R, Lebovics R, Fauci AS. Interpretation of head and neck biopsies in Wegener’s granulomatosis: a pathologic study of 126 biopsies in 70 patients. Am J Surg Pathol 1990; 14:555–564.
- Bosch X, Guilabert A, Font J. Antineutrophil cytoplasmic antibodies. Lancet 2006; 368:404–418.
- Hoffman GS, Specks U. Antineutrophil cytoplasmic antibodies. Arthritis Rheum 1998;1521–1537.
- Wiik A. What you should know about PR3-ANCA. An introduction. Arthritis Res 2000; 2:252–254.
- Kussmaul A, Maier R. Über eine bisher nicht beschriebene eigenthümliche Arterienerkrankung (Periarteritis nodosa), die mit Morbus Brightii und rapid fortschreitender allgemeiner Muskellähmung einhergeht. Dtsch Arch Klin Med 1866; 1:484–518.
- Davson J, Ball J, Platt R. The kidney in periarteritis nodosa. Q J Med 1948; 17:175–202.
- Jennette C, Falk RJ, Andrassy K, et al Nomenclature of systemic vasculitides: proposal of an international consensus conference. Arthritis Rheum 1994; 37:187–192.
- Guillevin L, Durand-Gasselin B, Cevallos R, et al Microscopic polyangiitis: clinical and laboratory findings in eighty-five patients. Arthritis Rheum 1999; 42:421–430.
- Keogh KA, Specks U. Churg-Strauss syndrome. Semin Respir Crit Care Med 2006; 27:148–157.
- Guillevin L, Cohen P, Gayraud M, Lhote F, Jarrousse B, Casassus P. Churg-Strauss syndrome: clinical study and long-term follow-up of 96 patients. Medicine 1999; 78:26–37.
- Sablé-Fourtassou R, Cohen P, Mahr A, et al., for the French Vasculitis Study Group. Antineutrophil cytoplasmic antibodies and the Churg-Strauss syndrome. Ann Intern Med 2005; 143:632–638.