User login
Case of the Month
A 56-year-old Hispanic female with a past medical history significant for basal cell carcinoma presented with a history of itchy, erythematous papules on her right cheek. Four days prior, she presented for suture removal after reconstruction with an island pedicle flap following Mohs micrographic surgery. She experienced a similar rash on her forearm following another surgery in the past.
a) Cellulitis
b) Contact dermatitis
c) Herpes simplex virus
Diagnosis: Contact dermatitis secondary to Mastisol and Steri-Strips
Contact dermatitis is a localized, pruritic, erythematous rash that occurs after contact with a certain allergen or irritant. The disorder is typically classified as either allergic contact dermatitis or irritant contact dermatitis.
Allergic contact dermatitis is a T cell–mediated, type-IV, delayed-type hypersensitivity reaction that requires prior sensitization with the causative agent before the patient becomes allergic to it. The typical rash of pruritus, erythema, edema, and vesicle formation occurs with further exposures.
The mechanism of immune response to a particular allergen requires that the antigen be of low molecular weight (less than 500 d) in order to penetrate the stratum corneum and gain access to the immunologic system. CD4, CD8, T regulatory cells, and natural killer T cells have all been implicated.
The process is composed of an afferent (sensitization) phase and an efferent (elicitation) phase.
Common haptens or immunogenic agents include nickel, urushiol from poison ivy resin, ultraviolet light, dyes, and fragrances.
This patient revealed a history of a similar reaction to the one presented in this case following wound dressing on her forearm with two products: Steri-Strips and Mastisol liquid adhesive. Unfortunately, she did not reveal this history until she had experienced the reaction a second time. The patient was instructed to apply hydrocortisone 1% cream twice daily to the red areas only and to follow up with a clinic visit in 4-5 days. Documentation of her allergy was included in her medical record.
This case was submitted by Dr. Keyvan Nouri; Dr. Katlein Franca; Jennifer Ledon; and Jessica Savas of the University of Miami.
–Donna Bilu Martin, M.D.
A 56-year-old Hispanic female with a past medical history significant for basal cell carcinoma presented with a history of itchy, erythematous papules on her right cheek. Four days prior, she presented for suture removal after reconstruction with an island pedicle flap following Mohs micrographic surgery. She experienced a similar rash on her forearm following another surgery in the past.
a) Cellulitis
b) Contact dermatitis
c) Herpes simplex virus
Diagnosis: Contact dermatitis secondary to Mastisol and Steri-Strips
Contact dermatitis is a localized, pruritic, erythematous rash that occurs after contact with a certain allergen or irritant. The disorder is typically classified as either allergic contact dermatitis or irritant contact dermatitis.
Allergic contact dermatitis is a T cell–mediated, type-IV, delayed-type hypersensitivity reaction that requires prior sensitization with the causative agent before the patient becomes allergic to it. The typical rash of pruritus, erythema, edema, and vesicle formation occurs with further exposures.
The mechanism of immune response to a particular allergen requires that the antigen be of low molecular weight (less than 500 d) in order to penetrate the stratum corneum and gain access to the immunologic system. CD4, CD8, T regulatory cells, and natural killer T cells have all been implicated.
The process is composed of an afferent (sensitization) phase and an efferent (elicitation) phase.
Common haptens or immunogenic agents include nickel, urushiol from poison ivy resin, ultraviolet light, dyes, and fragrances.
This patient revealed a history of a similar reaction to the one presented in this case following wound dressing on her forearm with two products: Steri-Strips and Mastisol liquid adhesive. Unfortunately, she did not reveal this history until she had experienced the reaction a second time. The patient was instructed to apply hydrocortisone 1% cream twice daily to the red areas only and to follow up with a clinic visit in 4-5 days. Documentation of her allergy was included in her medical record.
This case was submitted by Dr. Keyvan Nouri; Dr. Katlein Franca; Jennifer Ledon; and Jessica Savas of the University of Miami.
–Donna Bilu Martin, M.D.
A 56-year-old Hispanic female with a past medical history significant for basal cell carcinoma presented with a history of itchy, erythematous papules on her right cheek. Four days prior, she presented for suture removal after reconstruction with an island pedicle flap following Mohs micrographic surgery. She experienced a similar rash on her forearm following another surgery in the past.
a) Cellulitis
b) Contact dermatitis
c) Herpes simplex virus
Diagnosis: Contact dermatitis secondary to Mastisol and Steri-Strips
Contact dermatitis is a localized, pruritic, erythematous rash that occurs after contact with a certain allergen or irritant. The disorder is typically classified as either allergic contact dermatitis or irritant contact dermatitis.
Allergic contact dermatitis is a T cell–mediated, type-IV, delayed-type hypersensitivity reaction that requires prior sensitization with the causative agent before the patient becomes allergic to it. The typical rash of pruritus, erythema, edema, and vesicle formation occurs with further exposures.
The mechanism of immune response to a particular allergen requires that the antigen be of low molecular weight (less than 500 d) in order to penetrate the stratum corneum and gain access to the immunologic system. CD4, CD8, T regulatory cells, and natural killer T cells have all been implicated.
The process is composed of an afferent (sensitization) phase and an efferent (elicitation) phase.
Common haptens or immunogenic agents include nickel, urushiol from poison ivy resin, ultraviolet light, dyes, and fragrances.
This patient revealed a history of a similar reaction to the one presented in this case following wound dressing on her forearm with two products: Steri-Strips and Mastisol liquid adhesive. Unfortunately, she did not reveal this history until she had experienced the reaction a second time. The patient was instructed to apply hydrocortisone 1% cream twice daily to the red areas only and to follow up with a clinic visit in 4-5 days. Documentation of her allergy was included in her medical record.
This case was submitted by Dr. Keyvan Nouri; Dr. Katlein Franca; Jennifer Ledon; and Jessica Savas of the University of Miami.
–Donna Bilu Martin, M.D.
FDA approves plasma product

The FDA has approved a pooled plasma blood product (Octaplas) that can be used to replace coagulation factors in patients with certain medical conditions.
The product is a sterile, frozen solution of human plasma from several donors that has been treated with a solvent detergent process to minimize the risk of serious virus transmission.
The plasma used to manufacture Octaplas is collected from US donors who have been screened and tested for diseases transmitted by blood.
“For patients suffering with clotting disorders, this product provides a viable alternative to single-donor fresh-frozen plasma [FFP] and provides a reduced risk of certain viral transmissions,” said Karen Midthun, MD, director of the FDA’s Center for Biologics Evaluation and Research.
Indications and administration
Octaplas is indicated for the replacement of multiple coagulation factors in patients with acquired deficiencies due to liver disease or undergoing cardiac surgery or liver transplant. Octaplas can also be
used for plasma exchange in patients with thrombotic thrombocytopenic purpura (TTP).
Like FFP, Octaplas should be matched to the recipient’s blood group to help avoid transfusion reactions. Each lot of Octaplas is tested for composition of key clotting factors and is only released if the levels are within acceptable ranges.
The product is administered by intravenous infusion after thawing, using an infusion set with a filter. An aseptic technique must be used throughout the infusion.
The dosage depends upon the clinical situation and the underlying disorder. But 12-15 mL/kg of body weight is a generally accepted starting dose, and it should increase the patient’s plasma coagulation factor levels by about 25%.
It is important to monitor patient response, both clinically and with measurement of prothrombin time, partial thromboplastin time, and/or specific coagulation factor assays.
Prior experience with Octaplas
The FDA’s approval of Octaplas was primarily based on studies conducted in patients with liver disease, liver transplant, heart surgery, and TTP. The most common adverse reactions observed in these trials were shortness of breath, dizziness, chest discomfort, pruritis/rash, headache, and paresthesia.
Additional data supporting the safe use of Octaplas for the US market came from prior use of the product in Europe and other approved markets, where it has been used extensively.
A previous generation of Octaplas was first marketed in 1992, and the current version has been marketed since 2006. In total, more than 2 million patients outside the US have been treated with more than 7 million doses of Octaplas.
The product is manufactured by Octapharma, located in Vienna, Austria. For more information on Octaplas, visit the Octapharma website. ![]()

The FDA has approved a pooled plasma blood product (Octaplas) that can be used to replace coagulation factors in patients with certain medical conditions.
The product is a sterile, frozen solution of human plasma from several donors that has been treated with a solvent detergent process to minimize the risk of serious virus transmission.
The plasma used to manufacture Octaplas is collected from US donors who have been screened and tested for diseases transmitted by blood.
“For patients suffering with clotting disorders, this product provides a viable alternative to single-donor fresh-frozen plasma [FFP] and provides a reduced risk of certain viral transmissions,” said Karen Midthun, MD, director of the FDA’s Center for Biologics Evaluation and Research.
Indications and administration
Octaplas is indicated for the replacement of multiple coagulation factors in patients with acquired deficiencies due to liver disease or undergoing cardiac surgery or liver transplant. Octaplas can also be
used for plasma exchange in patients with thrombotic thrombocytopenic purpura (TTP).
Like FFP, Octaplas should be matched to the recipient’s blood group to help avoid transfusion reactions. Each lot of Octaplas is tested for composition of key clotting factors and is only released if the levels are within acceptable ranges.
The product is administered by intravenous infusion after thawing, using an infusion set with a filter. An aseptic technique must be used throughout the infusion.
The dosage depends upon the clinical situation and the underlying disorder. But 12-15 mL/kg of body weight is a generally accepted starting dose, and it should increase the patient’s plasma coagulation factor levels by about 25%.
It is important to monitor patient response, both clinically and with measurement of prothrombin time, partial thromboplastin time, and/or specific coagulation factor assays.
Prior experience with Octaplas
The FDA’s approval of Octaplas was primarily based on studies conducted in patients with liver disease, liver transplant, heart surgery, and TTP. The most common adverse reactions observed in these trials were shortness of breath, dizziness, chest discomfort, pruritis/rash, headache, and paresthesia.
Additional data supporting the safe use of Octaplas for the US market came from prior use of the product in Europe and other approved markets, where it has been used extensively.
A previous generation of Octaplas was first marketed in 1992, and the current version has been marketed since 2006. In total, more than 2 million patients outside the US have been treated with more than 7 million doses of Octaplas.
The product is manufactured by Octapharma, located in Vienna, Austria. For more information on Octaplas, visit the Octapharma website. ![]()

The FDA has approved a pooled plasma blood product (Octaplas) that can be used to replace coagulation factors in patients with certain medical conditions.
The product is a sterile, frozen solution of human plasma from several donors that has been treated with a solvent detergent process to minimize the risk of serious virus transmission.
The plasma used to manufacture Octaplas is collected from US donors who have been screened and tested for diseases transmitted by blood.
“For patients suffering with clotting disorders, this product provides a viable alternative to single-donor fresh-frozen plasma [FFP] and provides a reduced risk of certain viral transmissions,” said Karen Midthun, MD, director of the FDA’s Center for Biologics Evaluation and Research.
Indications and administration
Octaplas is indicated for the replacement of multiple coagulation factors in patients with acquired deficiencies due to liver disease or undergoing cardiac surgery or liver transplant. Octaplas can also be
used for plasma exchange in patients with thrombotic thrombocytopenic purpura (TTP).
Like FFP, Octaplas should be matched to the recipient’s blood group to help avoid transfusion reactions. Each lot of Octaplas is tested for composition of key clotting factors and is only released if the levels are within acceptable ranges.
The product is administered by intravenous infusion after thawing, using an infusion set with a filter. An aseptic technique must be used throughout the infusion.
The dosage depends upon the clinical situation and the underlying disorder. But 12-15 mL/kg of body weight is a generally accepted starting dose, and it should increase the patient’s plasma coagulation factor levels by about 25%.
It is important to monitor patient response, both clinically and with measurement of prothrombin time, partial thromboplastin time, and/or specific coagulation factor assays.
Prior experience with Octaplas
The FDA’s approval of Octaplas was primarily based on studies conducted in patients with liver disease, liver transplant, heart surgery, and TTP. The most common adverse reactions observed in these trials were shortness of breath, dizziness, chest discomfort, pruritis/rash, headache, and paresthesia.
Additional data supporting the safe use of Octaplas for the US market came from prior use of the product in Europe and other approved markets, where it has been used extensively.
A previous generation of Octaplas was first marketed in 1992, and the current version has been marketed since 2006. In total, more than 2 million patients outside the US have been treated with more than 7 million doses of Octaplas.
The product is manufactured by Octapharma, located in Vienna, Austria. For more information on Octaplas, visit the Octapharma website. ![]()
Academic Hospitalist Balanced Scorecard
The field of hospital medicine, now the fastest growing specialty in medical history,[1] was born out of pressure to improve the efficiency and quality of clinical care in US hospitals.[2] Delivering safe and high‐value clinical care is a central goal of the field and has been an essential component of its growth and success.
The clinical demands on academic hospitalists have grown recently, fueled by the need to staff services previously covered by housestaff, whose hours are now restricted. Despite these new demands, expectations have grown in other arenas as well. Academic hospitalist groups (AHGs) are often expected to make significant contributions in quality improvement, patient safety, education, research, and administration. With broad expectations beyond clinical care, AHGs face unique challenges. Groups that focus mainly on providing coverage and improving clinical performance may find that they are unable to fully contribute in these other domains. To be successful, AHGs must develop strategies that balance their energies, resources, and performance.
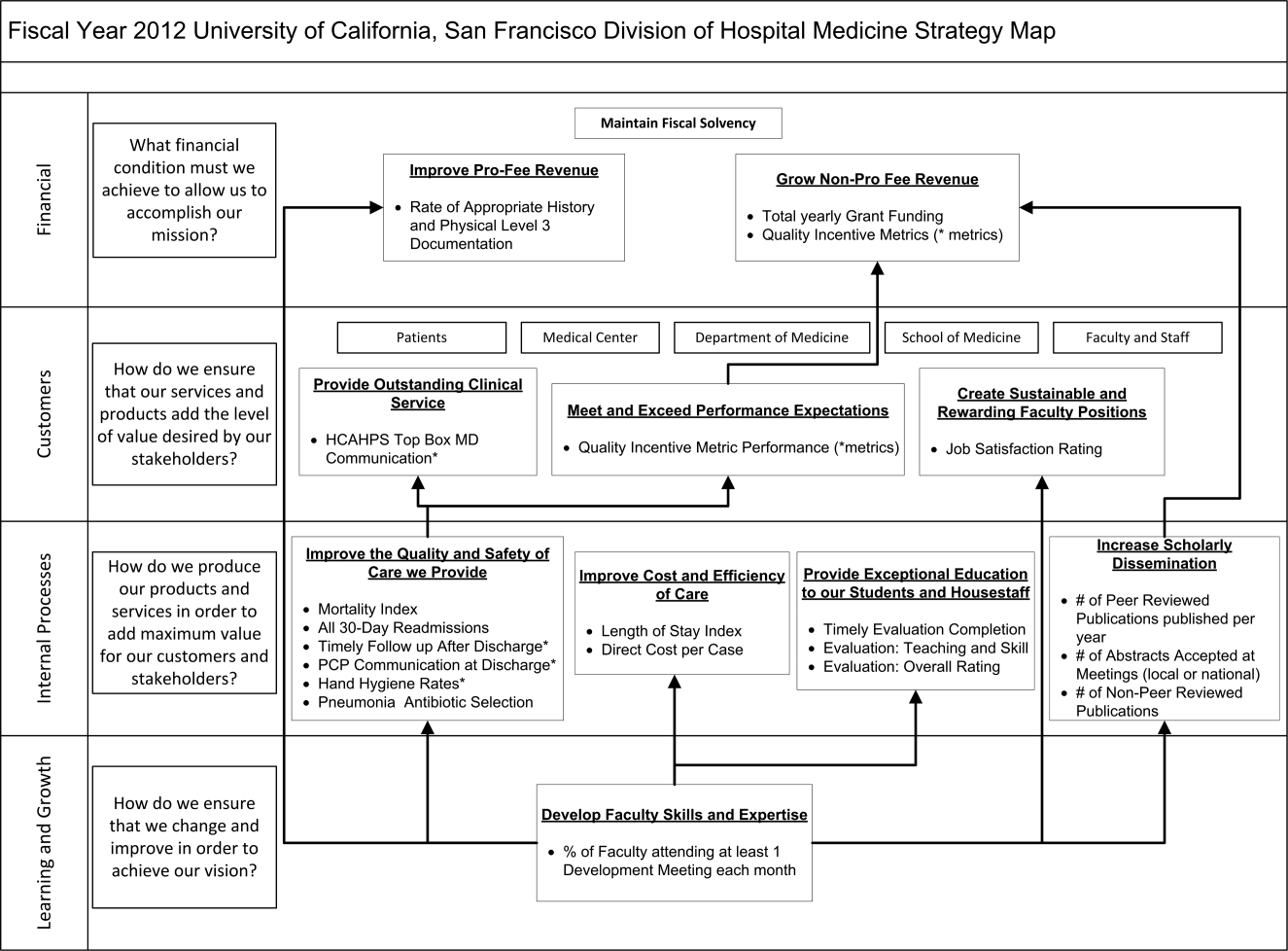
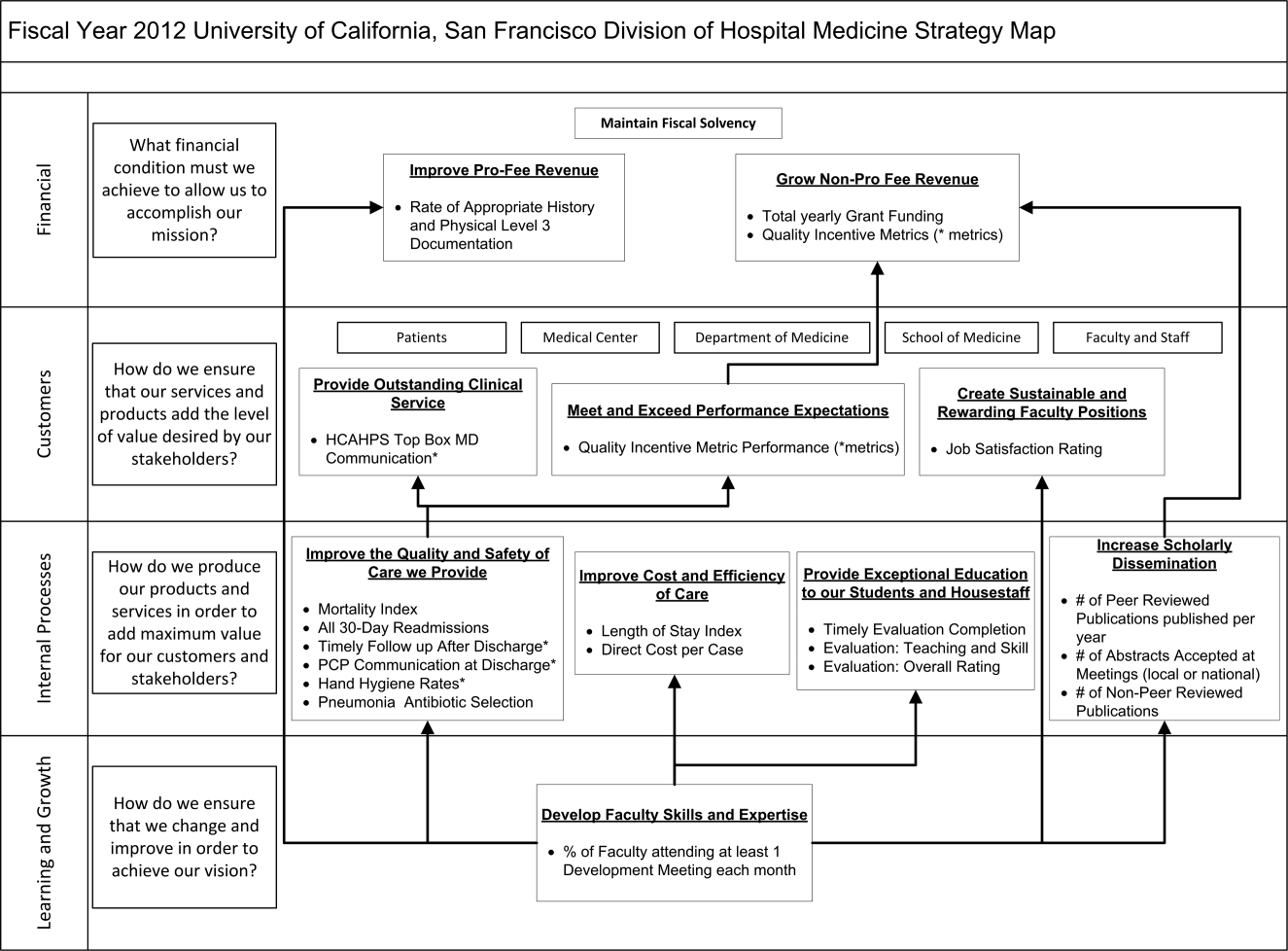
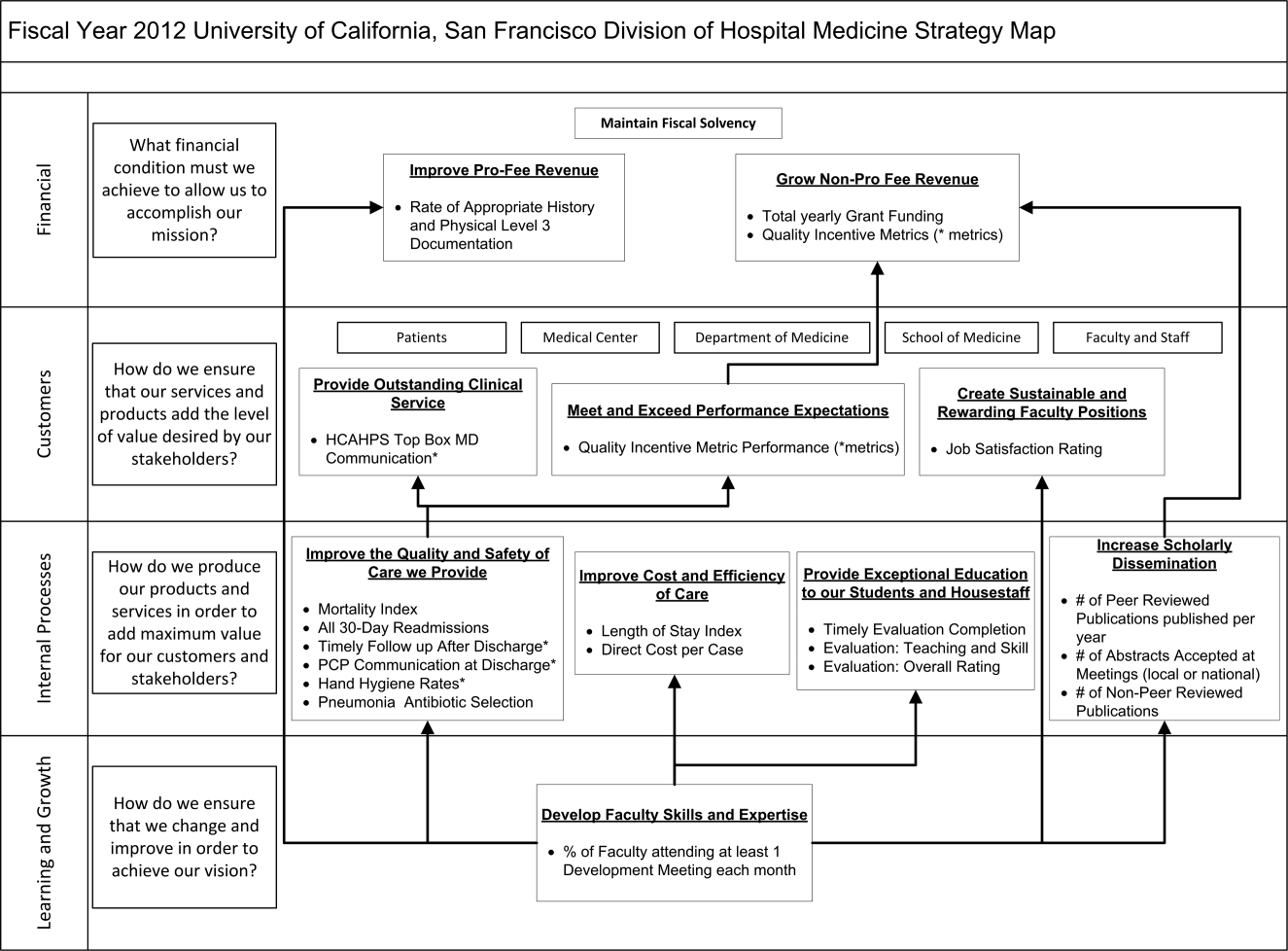
The balanced scorecard (BSC) was introduced by Kaplan and Norton in 1992 to allow corporations to view their performance broadly, rather than narrowly focusing on financial measures. The BSC requires organizations to develop a balanced portfolio of performance metrics across 4 key perspectives: financial, customers, internal processes, and learning and growth. Metrics within these perspectives should help answer fundamental questions about the organization (Table 1).[3] Over time, the BSC evolved from a performance measurement tool to a strategic management system.[4] Successful organizations translate their mission and vision to specific strategic objectives in each of the 4 perspectives, delineate how these objectives will help the organization reach its vision with a strategy map,[5] and then utilize the BSC to track and monitor performance to ensure that the vision is achieved.[6]
| BSC Perspective | Traditional Questions[3] | Questions Revised for AHCs |
|---|---|---|
| ||
| Financial | How do we look to our shareholders? | What financial condition must we be in to allow us to accomplish our mission? |
| Customers | How do customers see us? | How do we ensure that our services and products add the level of value desired by our stakeholders? |
| Internal processes | What must we excel at? | How do we produce our products and services to add maximum value for our customers and stakeholders? |
| Learning and growth | How can we continue to improve and create value? | How do we ensure that we change and improve in order to achieve our vision? |
Although originally conceived for businesses, the BSC has found its way into the healthcare industry, with reports of successful implementation in organizations ranging from individual departments to research collaboratives[7] to national healthcare systems.[8] However, there are few reports of BSC implementation in academic health centers.[9, 10] Because most academic centers are not‐for‐profit, Zelman suggests that the 4 BSC perspectives be modified to better fit their unique characteristics (Table 1).[11] To the best of our knowledge, there is no literature describing the development of a BSC in an academic hospitalist group. In this article, we describe the development of, and early experiences with, an academic hospital medicine BSC developed as part of a strategic planning initiative.
METHODS
The University of California, San Francisco (UCSF) Division of Hospital Medicine (DHM) was established in 2005. Currently, there are more than 50 faculty members, having doubled in the last 4 years. In addition to staffing several housestaff and nonhousestaff clinical services, faculty are involved in a wide variety of nonclinical endeavors at local and national levels. They participate and lead initiatives in education, faculty development, patient safety, care efficiency, quality improvement, information technology, and global health. There is an active research enterprise that generates nearly $5 million in grant funding annually.
Needs Assessment
During a division retreat in 2009, faculty identified several areas in need of improvement, including: clinical care processes, educational promotion, faculty development, and work‐life balance. Based on these needs, divisional mission and vision statements were created (Table 2).
|
| Our mission: to provide the highest quality clinical care, education, research, and innovation in academic hospital medicine. |
| Our vision: to be the best division of hospital medicine by promoting excellence, integrity, innovation, and professional satisfaction among our faculty, trainees, and staff. |
Division leadership made it a priority to create a strategic plan to address these wide‐ranging issues. To accomplish this, we recognized the need to develop a formal way of translating our vision into specific and measurable objectives, establish systems of performance measurement, improve accountability, and effectively communicate these strategic goals to the group. Based on these needs, we set out to develop a divisional BSC.
Development
At the time of BSC development, the DHM was organized into 4 functional areas: quality and safety, education, faculty development, and academics and research. A task force was formed, comprised of 8 senior faculty representing these key areas. The mission and vision statements were used as the foundation for the development of division goals and objectives. The group was careful to choose objectives within each of the 4 BSC perspectives for academic centers, as defined by Zelman (Table 1). The taskforce then brainstormed specific metrics that would track performance within the 4 functional areas. The only stipulation during this process was that the metrics had to meet the following criteria:
- Important to the division and to the individual faculty members
- Measurable through either current or developed processes
- Data are valid and their validity trusted by the faculty members
- Amenable to improvement by faculty (ie, through their individual action they could impact the metric)
From the subsequent list of metrics, we used a modified Delphi method to rank‐order them by importance to arrive at our final set of metrics. Kaplan and Norton noted that focusing on a manageable number of metrics (ie, a handful in each BSC perspective) is important for an achievable strategic vision.[6] With the metrics chosen, we identified data sources or developed new systems to collect data for which there was no current source. We assigned individuals responsible for collecting and analyzing the data, identified local or national benchmarks, if available, and established performance targets for the coming year, when possible.
The BSC is updated quarterly, and results are presented to the division during a noon meeting and posted on the division website. Metrics are re‐evaluated on a yearly basis. They are continued, modified, or discarded depending on performance and/or changes in strategic priorities.
The initial BSC focused on division‐wide metrics and performance. Early efforts to develop the scorecard were framed as experimental, with no clear decision taken regarding how metrics might ultimately be used to improve performance (ie, how public to make both individual and group results, whether to tie bonus payments to performance).
RESULTS
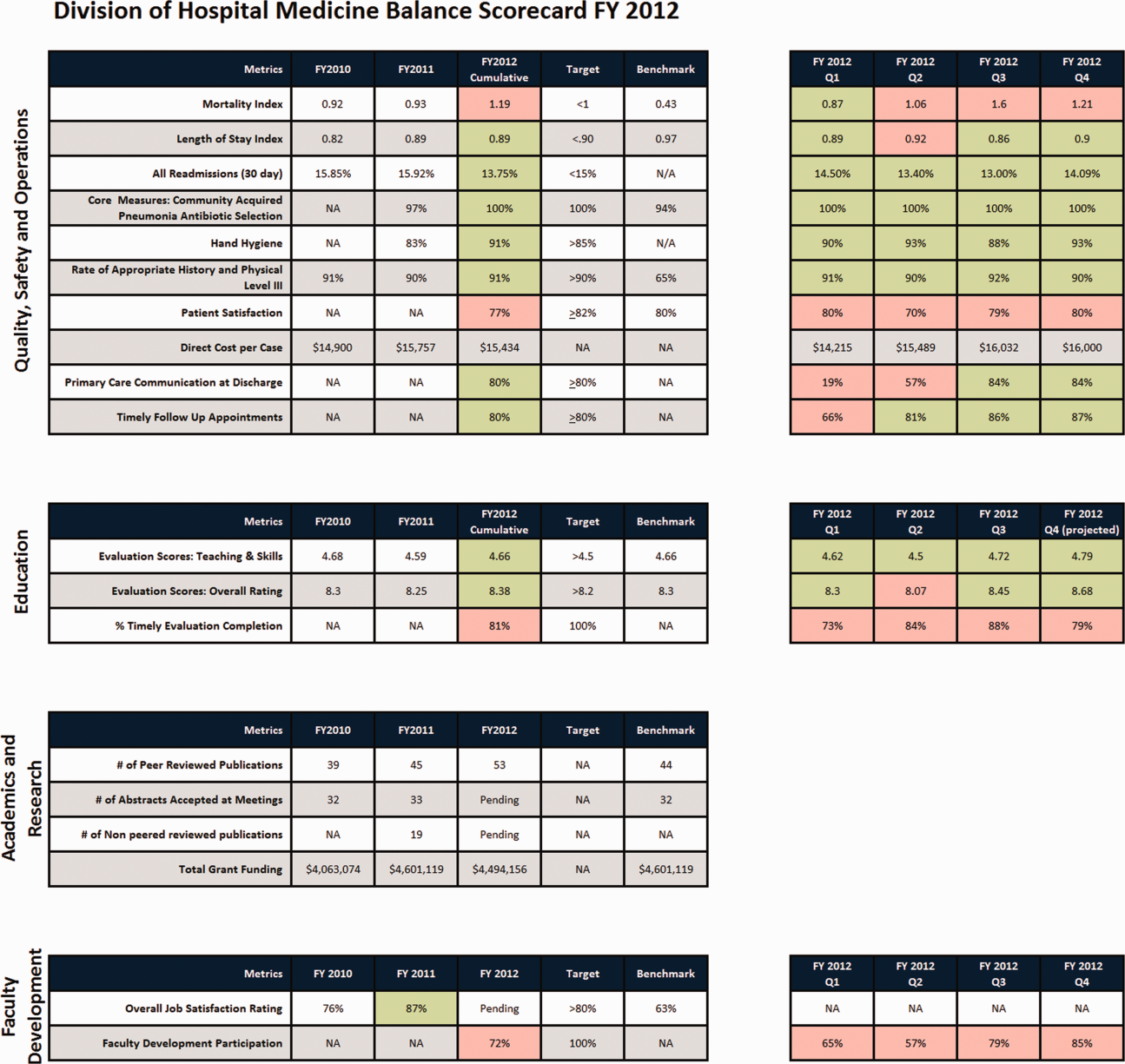
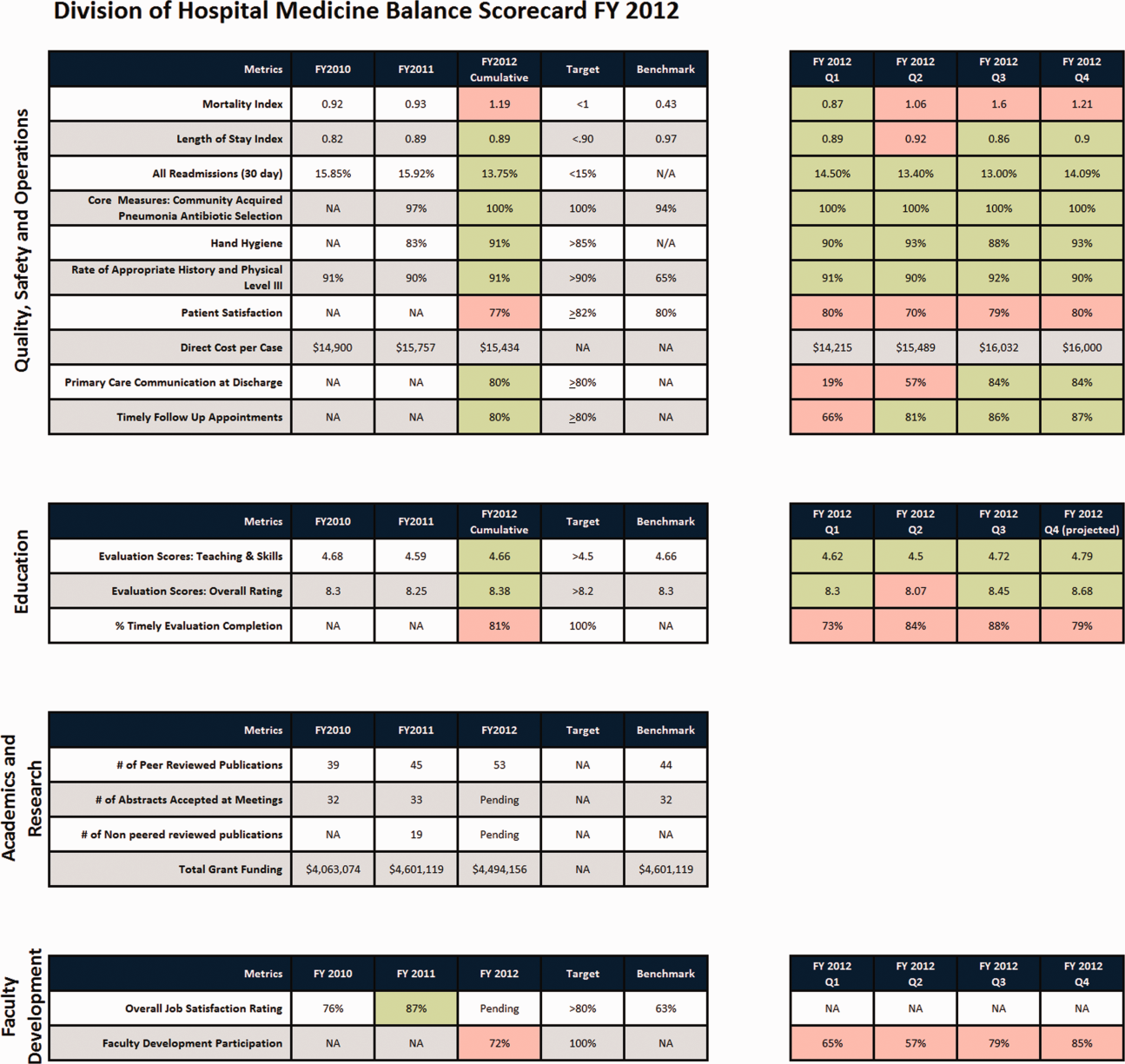
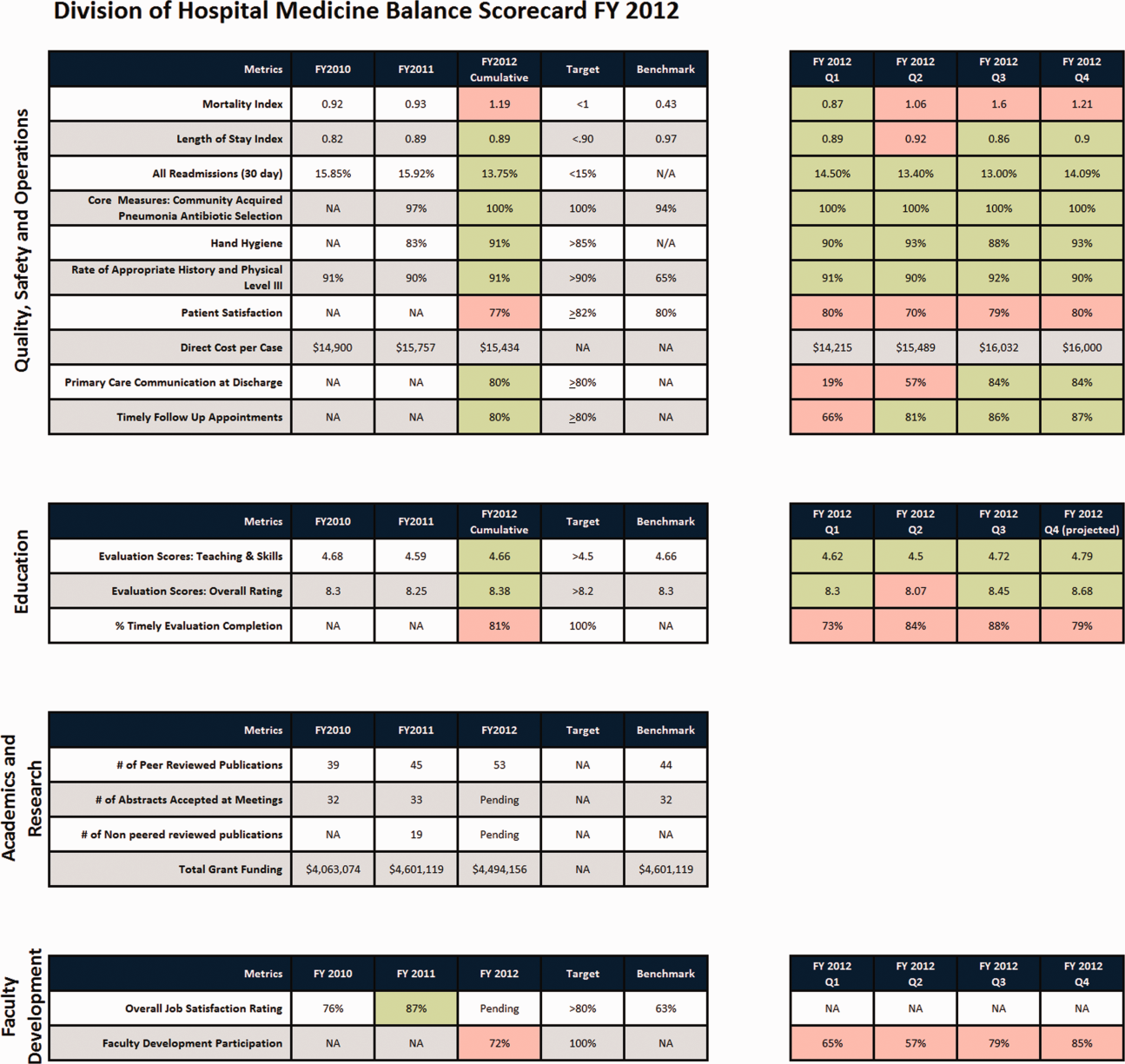
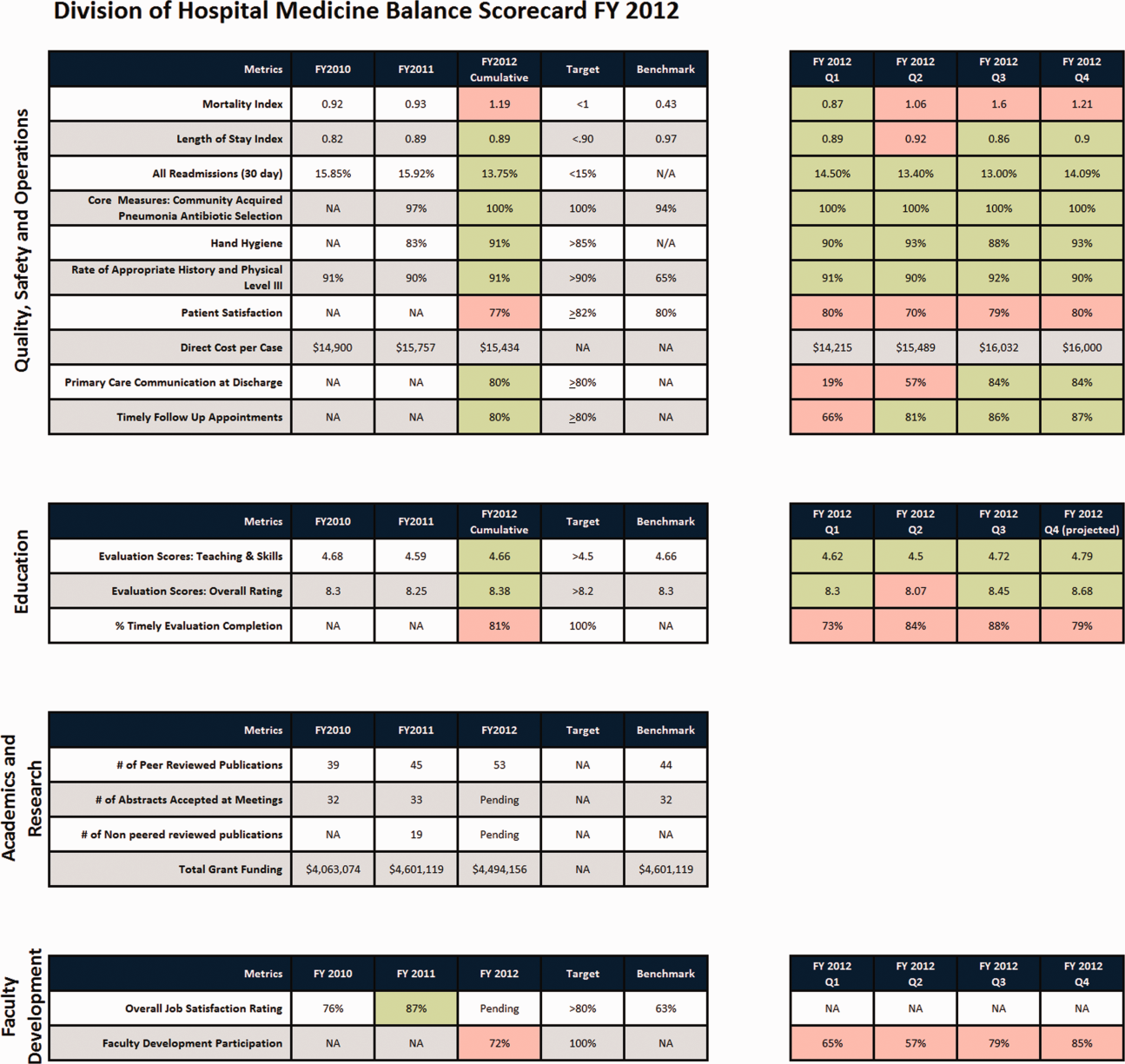
There were 41 initial metrics considered by the division BSC task force (Table 3). Of these, 16 were chosen for the initial BSC through the modified Delphi method. Over the past 2 years, these initial metrics have been modified to reflect current strategic goals and objectives. Figure 1 illustrates the BSC for fiscal year (FY) 2012. An online version of this, complete with graphical representations of the data and metric definitions, can be found at
| Quality, Safety, and Operations | Education | Academics and Research | Faculty Development |
|---|---|---|---|
| |||
| Appropriate level of care | CME courses taught | Abstracts accepted | Attendance and participation |
| Billing and documentation | Curriculum development | Academic reputation | Being an agent of change |
| Clinical efficiency | Student/housestaff feedback | Grant funding | Division citizenship |
| Clinical professionalism | Mentoring | Mentorship | Job satisfaction |
| Communication | Quality of teaching rounds | Papers published | Mentorship |
| Core measures performance | Participation in national organizations | Committees and task forces | |
| Practice evidence‐based medicine | |||
| Fund of knowledge | |||
| Guideline adherence | |||
| Unplanned transfers to ICU | |||
| Implementation and initiation of projects | |||
| Length of stay | |||
| Medical errors | |||
| Mortality | |||
| Multidisciplinary approach to patient care | |||
| Multisource feedback evaluations | |||
| Never events | |||
| Patient‐centered care | |||
| Patient satisfaction | |||
| Practice‐based learning | |||
| Procedures | |||
| Readmissions | |||
| Reputation and expertise | |||
| Seeing patient on the day of admission | |||
| Quality of transfers of care | |||
DISCUSSION
Like many hospitalist groups, our division has experienced tremendous growth, both in our numbers and the breadth of roles that we fill. With this growth has come increasing expectations in multiple domains, competing priorities, and limited resources. We successfully developed a BSC as a tool to help our division reach its vision: balancing high quality clinical care, education, academics, and faculty development while maintaining a strong sense of community. We have found that the BSC has helped us meet several key goals.
The first goal was to allow for a broad view of our performance. This is the BSC's most basic function, and we saw immediate and tangible benefits. The scorecard provided a broad snapshot of our performance in a single place. For example, in the clinical domain, we saw that our direct cost per case was increasing despite our adjusted average length of stay remaining stable from FY2010‐FY2011. In academics and research, we saw that the number of abstracts accepted at national meetings increased by almost 30% in FY2011 (Figure 1).
The second goal was to create transparency and accountability. By measuring performance and displaying it on the division Web site, the BSC has promoted transparency. If performance does not meet our targets, the division as a whole becomes accountable. Leadership must understand why performance fell short and initiate changes to improve it. For instance, the rising direct cost per case has spurred the development of a high‐value care committee tasked with finding ways of reducing cost while providing high‐quality care.[12]
The third goal was to communicate goals and engage our faculty. As our division has grown, ensuring a shared vision among our entire faculty became an increasing challenge. The BSC functions as a communication platform between leadership and faculty, and yielded multiple benefits. As the metrics were born out of our mission and vision, the BSC has become a tangible representation of our core values. Moreover, individual faculty can see that they are part of a greater, high‐performing organization and realize they can impact the group's performance through their individual effort. For example, this has helped promote receptivity to carefully disseminated individual performance measures for billing and documentation, and patient satisfaction, in conjunction with faculty development in these areas.
The fourth goal was to ensure that we use data to guide strategic decisions. We felt that strategic decisions needed to be based on objective, rather than perceived or anecdotal, information. This meant translating our vision into measurable objectives that would drive performance improvement. For example, before the BSC, we were committed to the dissemination of our research and innovations. Yet, we quickly realized that we did not have a system to collect even basic data on academic performancea deficit we filled by leveraging information gathered from online databases and faculty curricula vitae. These data allowed us, for the first time, to objectively reflect on this as a strategic goal and to have an ongoing mechanism to monitor academic productivity.
Lessons Learned/Keys to Success
With our initial experience, we have gained insight that may be helpful to other AHGs considering implementing a BSC. First, and most importantly, AHGs should take the necessary time to build consensus and buy‐in. Particularly in areas where data are analyzed for the first time, faculty are often wary about the validity of the data or the purpose and utility of performance measurement. Faculty may be concerned about how collection of performance data could affect promotion or create a hostile and competitive work environment.
This concern grows when one moves from division‐wide to individual data. It is inevitable that the collection and dissemination of performance data will create some level of discomfort among faculty members, which can be a force for improvement or for angst. These issues should be anticipated, discussed, and actively managed. It is critical to be transparent with how data will be used. We have made clear that the transition from group to individual performance data, and from simple transparency to incentives, will be done thoughtfully and with tremendous input from our faculty. This tension can also be mitigated by choosing metrics that are internally driven, rather than determined by external groups (ie, following the principle that the measures should be important to the division and individual faculty members).
Next, the process of developing a mature BSC takes time. Much of our first year was spent developing systems for measurement, collecting data, and determining appropriate comparators and targets. The data in the first BSC functioned mainly as a baseline marker of performance. Some metrics, particularly in education and academics, had no national or local benchmarks. In these cases we identified comparable groups (such as other medical teaching services or other well‐established AHGs) or merely used our prior year's performance as a benchmark. Also, some of our metrics did not initially have performance targets. In most instances, this was because this was the first time that we looked at these data, and it was unclear what an appropriate target would be until more data became available.
Moving into our third year, we are seeing a natural evolution in the BSC's use. Some metrics that were initially chosen have been replaced or modified to reflect changing goals and priorities. Functional directors participate in choosing and developing performance metrics in their area. Previously, there was no formal structure for these groups to develop and measure strategic objectives and be accountable for performance improvement. They are now expected to define goals with measurable outcomes, to report progress to division leadership, and to develop their own scorecard to track performance. Each group chooses 2 to 4 metrics within their domain that are the most important for the division to improve on, which are then included in the division BSC.
We have also made efforts to build synergy between our BSC and performance goals set by external groups. Although continuing to favor metrics that are internally driven and meaningful to our faculty, we recognize that our goals must also reflect the needs and interests of broader stakeholders. For example, hand hygiene rates and patient satisfaction scores are UCSF medical center and divisional priorities (the former includes them in a financial incentive system for managers, staff, and many physicians) and are incorporated into the BSC as division‐wide incentive metrics.
Limitations
Our project has several limitations. It was conducted at a single institution, and our metrics may not be generalizable to other groups. However, the main goal of this article was not to focus on specific metrics but the process that we undertook to choose and develop them. Other institutions will likely identify different metrics based on their specific strategic objectives. We are also early in our experience with the BSC, and it is still not clear what effect it will have on the desired outcomes for our objectives. However, Henriksen recently reported that implementing a BSC at a large academic health center, in parallel with other performance improvement initiatives, resulted in substantial improvement in their chosen performance metrics.[13]
Despite the several years of development, we still view this as an early version of a BSC. To fully realize its benefits, an organization must choose metrics that will not simply measure performance but drive it. Our current BSC relies primarily on lagging measures, which show what our performance has been, and includes few leading metrics, which can predict trends in performance. As explained by Kaplan and Norton, this type of BSC risks skewing toward controlling rather than driving performance.[14] A mature BSC will include a mix of leading and lagging indicators, the combination illustrating a logical progression from measurement to performance. For instance, we measure total grant funding per year, which is a lagging indicator. However, to be most effective we could measure the percent of faculty who have attended grant‐writing workshops, the number of new grant sources identified, or the number of grant proposals submitted each quarter. These leading indicators would allow us to see performance trends that could be improved before the final outcome, total grant funding, is realized.
Finally, the issues surrounding the acceptability of this overall strategy will likely hinge on how we implement the more complex steps that relate to transparency, individual attribution, and perhaps ultimately incentives. Success in this area depends as much on culture as on strategy.
Next Steps
The next major step in the evolution of the BSC, and part of a broader faculty development program, will be the development of individual BSCs. They will be created using a similar methodology and allow faculty to reflect on their performance compared to peers and recognized benchmarks. Ideally, this will allow hospitalists in our group to establish personal strategic plans and monitor their performance over time. Individualizing these BSCs will be critical; although a research‐oriented faculty member might be striving for more than 5 publications and a large grant in a year, a clinician‐educator may seek outstanding teaching reviews and completion of a key quality improvement project. Both efforts need to be highly valued, and the divisional BSC should roll up these varied individual goals into a balanced whole.
In conclusion, we successfully developed and implemented a BSC to aid in strategic planning. The BSC ensures that we make strategic decisions using data, identify internally driven objectives, develop systems of performance measurement, and increase transparency and accountability. Our hope is that this description of the development of our BSC will be useful to other groups considering a similar endeavor.
Acknowledgments
The authors thank Noori Dhillon, Sadaf Akbaryar, Katie Quinn, Gerri Berg, and Maria Novelero for data collection and analysis. The authors also thank the faculty and staff who participated in the development process of the BSC.
Disclosure
Nothing to report.
- . The hospitalist field turns 15: new opportunities and challenges. J Hosp Med. 2011;6(4):E1–E4.
- , . The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335(7):514–517.
- , . The balanced scorecard—measures that drive performance. Harv Bus Rev. 1992;70(1):71–79.
- , . Using the balanced scorecard as a strategic management system. Harv Bus Rev. 1996;74(1):75–85.
- , . Having trouble with your strategy? Then map it. Harv Bus Rev. 2000;78:167–176, 202.
- , . Putting the balanced scorecard to work. Harv Bus Rev. 1993;71:134–147.
- , , , et al. Development and implementation of a performance measure tool in an academic pediatric research network. Contemp Clin Trials. 2010;31(5):429–437.
- , . Lives in the balance: an analysis of the balanced scorecard (BSC) in healthcare organizations. Int J Prod Perform Manag. 2007;57(1):6–21.
- , . The “Balanced Scorecard”: development and implementation in an academic clinical department. Acad Med. 1999;74(2):114–122.
- . Introducing a balanced scorecard management system in a university anesthesiology department. Anesth Analg. 2002;95(6):1731–1738, table of contents.
- , , , , . Issues for academic health centers to consider before implementing a balanced‐scorecard effort. Acad Med. 1999;74(12):1269–1277.
- , . Cents and sensitivity—teaching physicians to think about costs. N Engl J Med. 2012;367(2):99–101.
- , , , et al. 10‐year experience integrating strategic performance improvement initiatives: can the balanced scorecard, Six Sigma, and team training all thrive in a single hospital? In: Henriksen K, Battles JB, Keyes MA, Grady ML, eds. Advances in Patient Safety: New Directions and Alternative Approaches. Vol 3. Performance and Tools. Rockville, MD: Agency for Healthcare Research and Quality; 2008. Available at: http://www.ncbi.nlm.nih.gov/books/NBK43660. Accessed 15 June 2011.
- , . Linking the balanced scorecard to strategy. Calif Manage Rev. 1996;39(1):53–79.
The field of hospital medicine, now the fastest growing specialty in medical history,[1] was born out of pressure to improve the efficiency and quality of clinical care in US hospitals.[2] Delivering safe and high‐value clinical care is a central goal of the field and has been an essential component of its growth and success.
The clinical demands on academic hospitalists have grown recently, fueled by the need to staff services previously covered by housestaff, whose hours are now restricted. Despite these new demands, expectations have grown in other arenas as well. Academic hospitalist groups (AHGs) are often expected to make significant contributions in quality improvement, patient safety, education, research, and administration. With broad expectations beyond clinical care, AHGs face unique challenges. Groups that focus mainly on providing coverage and improving clinical performance may find that they are unable to fully contribute in these other domains. To be successful, AHGs must develop strategies that balance their energies, resources, and performance.
The balanced scorecard (BSC) was introduced by Kaplan and Norton in 1992 to allow corporations to view their performance broadly, rather than narrowly focusing on financial measures. The BSC requires organizations to develop a balanced portfolio of performance metrics across 4 key perspectives: financial, customers, internal processes, and learning and growth. Metrics within these perspectives should help answer fundamental questions about the organization (Table 1).[3] Over time, the BSC evolved from a performance measurement tool to a strategic management system.[4] Successful organizations translate their mission and vision to specific strategic objectives in each of the 4 perspectives, delineate how these objectives will help the organization reach its vision with a strategy map,[5] and then utilize the BSC to track and monitor performance to ensure that the vision is achieved.[6]
| BSC Perspective | Traditional Questions[3] | Questions Revised for AHCs |
|---|---|---|
| ||
| Financial | How do we look to our shareholders? | What financial condition must we be in to allow us to accomplish our mission? |
| Customers | How do customers see us? | How do we ensure that our services and products add the level of value desired by our stakeholders? |
| Internal processes | What must we excel at? | How do we produce our products and services to add maximum value for our customers and stakeholders? |
| Learning and growth | How can we continue to improve and create value? | How do we ensure that we change and improve in order to achieve our vision? |
Although originally conceived for businesses, the BSC has found its way into the healthcare industry, with reports of successful implementation in organizations ranging from individual departments to research collaboratives[7] to national healthcare systems.[8] However, there are few reports of BSC implementation in academic health centers.[9, 10] Because most academic centers are not‐for‐profit, Zelman suggests that the 4 BSC perspectives be modified to better fit their unique characteristics (Table 1).[11] To the best of our knowledge, there is no literature describing the development of a BSC in an academic hospitalist group. In this article, we describe the development of, and early experiences with, an academic hospital medicine BSC developed as part of a strategic planning initiative.
METHODS
The University of California, San Francisco (UCSF) Division of Hospital Medicine (DHM) was established in 2005. Currently, there are more than 50 faculty members, having doubled in the last 4 years. In addition to staffing several housestaff and nonhousestaff clinical services, faculty are involved in a wide variety of nonclinical endeavors at local and national levels. They participate and lead initiatives in education, faculty development, patient safety, care efficiency, quality improvement, information technology, and global health. There is an active research enterprise that generates nearly $5 million in grant funding annually.
Needs Assessment
During a division retreat in 2009, faculty identified several areas in need of improvement, including: clinical care processes, educational promotion, faculty development, and work‐life balance. Based on these needs, divisional mission and vision statements were created (Table 2).
|
| Our mission: to provide the highest quality clinical care, education, research, and innovation in academic hospital medicine. |
| Our vision: to be the best division of hospital medicine by promoting excellence, integrity, innovation, and professional satisfaction among our faculty, trainees, and staff. |
Division leadership made it a priority to create a strategic plan to address these wide‐ranging issues. To accomplish this, we recognized the need to develop a formal way of translating our vision into specific and measurable objectives, establish systems of performance measurement, improve accountability, and effectively communicate these strategic goals to the group. Based on these needs, we set out to develop a divisional BSC.
Development
At the time of BSC development, the DHM was organized into 4 functional areas: quality and safety, education, faculty development, and academics and research. A task force was formed, comprised of 8 senior faculty representing these key areas. The mission and vision statements were used as the foundation for the development of division goals and objectives. The group was careful to choose objectives within each of the 4 BSC perspectives for academic centers, as defined by Zelman (Table 1). The taskforce then brainstormed specific metrics that would track performance within the 4 functional areas. The only stipulation during this process was that the metrics had to meet the following criteria:
- Important to the division and to the individual faculty members
- Measurable through either current or developed processes
- Data are valid and their validity trusted by the faculty members
- Amenable to improvement by faculty (ie, through their individual action they could impact the metric)
From the subsequent list of metrics, we used a modified Delphi method to rank‐order them by importance to arrive at our final set of metrics. Kaplan and Norton noted that focusing on a manageable number of metrics (ie, a handful in each BSC perspective) is important for an achievable strategic vision.[6] With the metrics chosen, we identified data sources or developed new systems to collect data for which there was no current source. We assigned individuals responsible for collecting and analyzing the data, identified local or national benchmarks, if available, and established performance targets for the coming year, when possible.
The BSC is updated quarterly, and results are presented to the division during a noon meeting and posted on the division website. Metrics are re‐evaluated on a yearly basis. They are continued, modified, or discarded depending on performance and/or changes in strategic priorities.
The initial BSC focused on division‐wide metrics and performance. Early efforts to develop the scorecard were framed as experimental, with no clear decision taken regarding how metrics might ultimately be used to improve performance (ie, how public to make both individual and group results, whether to tie bonus payments to performance).
RESULTS
There were 41 initial metrics considered by the division BSC task force (Table 3). Of these, 16 were chosen for the initial BSC through the modified Delphi method. Over the past 2 years, these initial metrics have been modified to reflect current strategic goals and objectives. Figure 1 illustrates the BSC for fiscal year (FY) 2012. An online version of this, complete with graphical representations of the data and metric definitions, can be found at
| Quality, Safety, and Operations | Education | Academics and Research | Faculty Development |
|---|---|---|---|
| |||
| Appropriate level of care | CME courses taught | Abstracts accepted | Attendance and participation |
| Billing and documentation | Curriculum development | Academic reputation | Being an agent of change |
| Clinical efficiency | Student/housestaff feedback | Grant funding | Division citizenship |
| Clinical professionalism | Mentoring | Mentorship | Job satisfaction |
| Communication | Quality of teaching rounds | Papers published | Mentorship |
| Core measures performance | Participation in national organizations | Committees and task forces | |
| Practice evidence‐based medicine | |||
| Fund of knowledge | |||
| Guideline adherence | |||
| Unplanned transfers to ICU | |||
| Implementation and initiation of projects | |||
| Length of stay | |||
| Medical errors | |||
| Mortality | |||
| Multidisciplinary approach to patient care | |||
| Multisource feedback evaluations | |||
| Never events | |||
| Patient‐centered care | |||
| Patient satisfaction | |||
| Practice‐based learning | |||
| Procedures | |||
| Readmissions | |||
| Reputation and expertise | |||
| Seeing patient on the day of admission | |||
| Quality of transfers of care | |||
DISCUSSION
Like many hospitalist groups, our division has experienced tremendous growth, both in our numbers and the breadth of roles that we fill. With this growth has come increasing expectations in multiple domains, competing priorities, and limited resources. We successfully developed a BSC as a tool to help our division reach its vision: balancing high quality clinical care, education, academics, and faculty development while maintaining a strong sense of community. We have found that the BSC has helped us meet several key goals.
The first goal was to allow for a broad view of our performance. This is the BSC's most basic function, and we saw immediate and tangible benefits. The scorecard provided a broad snapshot of our performance in a single place. For example, in the clinical domain, we saw that our direct cost per case was increasing despite our adjusted average length of stay remaining stable from FY2010‐FY2011. In academics and research, we saw that the number of abstracts accepted at national meetings increased by almost 30% in FY2011 (Figure 1).
The second goal was to create transparency and accountability. By measuring performance and displaying it on the division Web site, the BSC has promoted transparency. If performance does not meet our targets, the division as a whole becomes accountable. Leadership must understand why performance fell short and initiate changes to improve it. For instance, the rising direct cost per case has spurred the development of a high‐value care committee tasked with finding ways of reducing cost while providing high‐quality care.[12]
The third goal was to communicate goals and engage our faculty. As our division has grown, ensuring a shared vision among our entire faculty became an increasing challenge. The BSC functions as a communication platform between leadership and faculty, and yielded multiple benefits. As the metrics were born out of our mission and vision, the BSC has become a tangible representation of our core values. Moreover, individual faculty can see that they are part of a greater, high‐performing organization and realize they can impact the group's performance through their individual effort. For example, this has helped promote receptivity to carefully disseminated individual performance measures for billing and documentation, and patient satisfaction, in conjunction with faculty development in these areas.
The fourth goal was to ensure that we use data to guide strategic decisions. We felt that strategic decisions needed to be based on objective, rather than perceived or anecdotal, information. This meant translating our vision into measurable objectives that would drive performance improvement. For example, before the BSC, we were committed to the dissemination of our research and innovations. Yet, we quickly realized that we did not have a system to collect even basic data on academic performancea deficit we filled by leveraging information gathered from online databases and faculty curricula vitae. These data allowed us, for the first time, to objectively reflect on this as a strategic goal and to have an ongoing mechanism to monitor academic productivity.
Lessons Learned/Keys to Success
With our initial experience, we have gained insight that may be helpful to other AHGs considering implementing a BSC. First, and most importantly, AHGs should take the necessary time to build consensus and buy‐in. Particularly in areas where data are analyzed for the first time, faculty are often wary about the validity of the data or the purpose and utility of performance measurement. Faculty may be concerned about how collection of performance data could affect promotion or create a hostile and competitive work environment.
This concern grows when one moves from division‐wide to individual data. It is inevitable that the collection and dissemination of performance data will create some level of discomfort among faculty members, which can be a force for improvement or for angst. These issues should be anticipated, discussed, and actively managed. It is critical to be transparent with how data will be used. We have made clear that the transition from group to individual performance data, and from simple transparency to incentives, will be done thoughtfully and with tremendous input from our faculty. This tension can also be mitigated by choosing metrics that are internally driven, rather than determined by external groups (ie, following the principle that the measures should be important to the division and individual faculty members).
Next, the process of developing a mature BSC takes time. Much of our first year was spent developing systems for measurement, collecting data, and determining appropriate comparators and targets. The data in the first BSC functioned mainly as a baseline marker of performance. Some metrics, particularly in education and academics, had no national or local benchmarks. In these cases we identified comparable groups (such as other medical teaching services or other well‐established AHGs) or merely used our prior year's performance as a benchmark. Also, some of our metrics did not initially have performance targets. In most instances, this was because this was the first time that we looked at these data, and it was unclear what an appropriate target would be until more data became available.
Moving into our third year, we are seeing a natural evolution in the BSC's use. Some metrics that were initially chosen have been replaced or modified to reflect changing goals and priorities. Functional directors participate in choosing and developing performance metrics in their area. Previously, there was no formal structure for these groups to develop and measure strategic objectives and be accountable for performance improvement. They are now expected to define goals with measurable outcomes, to report progress to division leadership, and to develop their own scorecard to track performance. Each group chooses 2 to 4 metrics within their domain that are the most important for the division to improve on, which are then included in the division BSC.
We have also made efforts to build synergy between our BSC and performance goals set by external groups. Although continuing to favor metrics that are internally driven and meaningful to our faculty, we recognize that our goals must also reflect the needs and interests of broader stakeholders. For example, hand hygiene rates and patient satisfaction scores are UCSF medical center and divisional priorities (the former includes them in a financial incentive system for managers, staff, and many physicians) and are incorporated into the BSC as division‐wide incentive metrics.
Limitations
Our project has several limitations. It was conducted at a single institution, and our metrics may not be generalizable to other groups. However, the main goal of this article was not to focus on specific metrics but the process that we undertook to choose and develop them. Other institutions will likely identify different metrics based on their specific strategic objectives. We are also early in our experience with the BSC, and it is still not clear what effect it will have on the desired outcomes for our objectives. However, Henriksen recently reported that implementing a BSC at a large academic health center, in parallel with other performance improvement initiatives, resulted in substantial improvement in their chosen performance metrics.[13]
Despite the several years of development, we still view this as an early version of a BSC. To fully realize its benefits, an organization must choose metrics that will not simply measure performance but drive it. Our current BSC relies primarily on lagging measures, which show what our performance has been, and includes few leading metrics, which can predict trends in performance. As explained by Kaplan and Norton, this type of BSC risks skewing toward controlling rather than driving performance.[14] A mature BSC will include a mix of leading and lagging indicators, the combination illustrating a logical progression from measurement to performance. For instance, we measure total grant funding per year, which is a lagging indicator. However, to be most effective we could measure the percent of faculty who have attended grant‐writing workshops, the number of new grant sources identified, or the number of grant proposals submitted each quarter. These leading indicators would allow us to see performance trends that could be improved before the final outcome, total grant funding, is realized.
Finally, the issues surrounding the acceptability of this overall strategy will likely hinge on how we implement the more complex steps that relate to transparency, individual attribution, and perhaps ultimately incentives. Success in this area depends as much on culture as on strategy.
Next Steps
The next major step in the evolution of the BSC, and part of a broader faculty development program, will be the development of individual BSCs. They will be created using a similar methodology and allow faculty to reflect on their performance compared to peers and recognized benchmarks. Ideally, this will allow hospitalists in our group to establish personal strategic plans and monitor their performance over time. Individualizing these BSCs will be critical; although a research‐oriented faculty member might be striving for more than 5 publications and a large grant in a year, a clinician‐educator may seek outstanding teaching reviews and completion of a key quality improvement project. Both efforts need to be highly valued, and the divisional BSC should roll up these varied individual goals into a balanced whole.
In conclusion, we successfully developed and implemented a BSC to aid in strategic planning. The BSC ensures that we make strategic decisions using data, identify internally driven objectives, develop systems of performance measurement, and increase transparency and accountability. Our hope is that this description of the development of our BSC will be useful to other groups considering a similar endeavor.
Acknowledgments
The authors thank Noori Dhillon, Sadaf Akbaryar, Katie Quinn, Gerri Berg, and Maria Novelero for data collection and analysis. The authors also thank the faculty and staff who participated in the development process of the BSC.
Disclosure
Nothing to report.
The field of hospital medicine, now the fastest growing specialty in medical history,[1] was born out of pressure to improve the efficiency and quality of clinical care in US hospitals.[2] Delivering safe and high‐value clinical care is a central goal of the field and has been an essential component of its growth and success.
The clinical demands on academic hospitalists have grown recently, fueled by the need to staff services previously covered by housestaff, whose hours are now restricted. Despite these new demands, expectations have grown in other arenas as well. Academic hospitalist groups (AHGs) are often expected to make significant contributions in quality improvement, patient safety, education, research, and administration. With broad expectations beyond clinical care, AHGs face unique challenges. Groups that focus mainly on providing coverage and improving clinical performance may find that they are unable to fully contribute in these other domains. To be successful, AHGs must develop strategies that balance their energies, resources, and performance.
The balanced scorecard (BSC) was introduced by Kaplan and Norton in 1992 to allow corporations to view their performance broadly, rather than narrowly focusing on financial measures. The BSC requires organizations to develop a balanced portfolio of performance metrics across 4 key perspectives: financial, customers, internal processes, and learning and growth. Metrics within these perspectives should help answer fundamental questions about the organization (Table 1).[3] Over time, the BSC evolved from a performance measurement tool to a strategic management system.[4] Successful organizations translate their mission and vision to specific strategic objectives in each of the 4 perspectives, delineate how these objectives will help the organization reach its vision with a strategy map,[5] and then utilize the BSC to track and monitor performance to ensure that the vision is achieved.[6]
| BSC Perspective | Traditional Questions[3] | Questions Revised for AHCs |
|---|---|---|
| ||
| Financial | How do we look to our shareholders? | What financial condition must we be in to allow us to accomplish our mission? |
| Customers | How do customers see us? | How do we ensure that our services and products add the level of value desired by our stakeholders? |
| Internal processes | What must we excel at? | How do we produce our products and services to add maximum value for our customers and stakeholders? |
| Learning and growth | How can we continue to improve and create value? | How do we ensure that we change and improve in order to achieve our vision? |
Although originally conceived for businesses, the BSC has found its way into the healthcare industry, with reports of successful implementation in organizations ranging from individual departments to research collaboratives[7] to national healthcare systems.[8] However, there are few reports of BSC implementation in academic health centers.[9, 10] Because most academic centers are not‐for‐profit, Zelman suggests that the 4 BSC perspectives be modified to better fit their unique characteristics (Table 1).[11] To the best of our knowledge, there is no literature describing the development of a BSC in an academic hospitalist group. In this article, we describe the development of, and early experiences with, an academic hospital medicine BSC developed as part of a strategic planning initiative.
METHODS
The University of California, San Francisco (UCSF) Division of Hospital Medicine (DHM) was established in 2005. Currently, there are more than 50 faculty members, having doubled in the last 4 years. In addition to staffing several housestaff and nonhousestaff clinical services, faculty are involved in a wide variety of nonclinical endeavors at local and national levels. They participate and lead initiatives in education, faculty development, patient safety, care efficiency, quality improvement, information technology, and global health. There is an active research enterprise that generates nearly $5 million in grant funding annually.
Needs Assessment
During a division retreat in 2009, faculty identified several areas in need of improvement, including: clinical care processes, educational promotion, faculty development, and work‐life balance. Based on these needs, divisional mission and vision statements were created (Table 2).
|
| Our mission: to provide the highest quality clinical care, education, research, and innovation in academic hospital medicine. |
| Our vision: to be the best division of hospital medicine by promoting excellence, integrity, innovation, and professional satisfaction among our faculty, trainees, and staff. |
Division leadership made it a priority to create a strategic plan to address these wide‐ranging issues. To accomplish this, we recognized the need to develop a formal way of translating our vision into specific and measurable objectives, establish systems of performance measurement, improve accountability, and effectively communicate these strategic goals to the group. Based on these needs, we set out to develop a divisional BSC.
Development
At the time of BSC development, the DHM was organized into 4 functional areas: quality and safety, education, faculty development, and academics and research. A task force was formed, comprised of 8 senior faculty representing these key areas. The mission and vision statements were used as the foundation for the development of division goals and objectives. The group was careful to choose objectives within each of the 4 BSC perspectives for academic centers, as defined by Zelman (Table 1). The taskforce then brainstormed specific metrics that would track performance within the 4 functional areas. The only stipulation during this process was that the metrics had to meet the following criteria:
- Important to the division and to the individual faculty members
- Measurable through either current or developed processes
- Data are valid and their validity trusted by the faculty members
- Amenable to improvement by faculty (ie, through their individual action they could impact the metric)
From the subsequent list of metrics, we used a modified Delphi method to rank‐order them by importance to arrive at our final set of metrics. Kaplan and Norton noted that focusing on a manageable number of metrics (ie, a handful in each BSC perspective) is important for an achievable strategic vision.[6] With the metrics chosen, we identified data sources or developed new systems to collect data for which there was no current source. We assigned individuals responsible for collecting and analyzing the data, identified local or national benchmarks, if available, and established performance targets for the coming year, when possible.
The BSC is updated quarterly, and results are presented to the division during a noon meeting and posted on the division website. Metrics are re‐evaluated on a yearly basis. They are continued, modified, or discarded depending on performance and/or changes in strategic priorities.
The initial BSC focused on division‐wide metrics and performance. Early efforts to develop the scorecard were framed as experimental, with no clear decision taken regarding how metrics might ultimately be used to improve performance (ie, how public to make both individual and group results, whether to tie bonus payments to performance).
RESULTS
There were 41 initial metrics considered by the division BSC task force (Table 3). Of these, 16 were chosen for the initial BSC through the modified Delphi method. Over the past 2 years, these initial metrics have been modified to reflect current strategic goals and objectives. Figure 1 illustrates the BSC for fiscal year (FY) 2012. An online version of this, complete with graphical representations of the data and metric definitions, can be found at
| Quality, Safety, and Operations | Education | Academics and Research | Faculty Development |
|---|---|---|---|
| |||
| Appropriate level of care | CME courses taught | Abstracts accepted | Attendance and participation |
| Billing and documentation | Curriculum development | Academic reputation | Being an agent of change |
| Clinical efficiency | Student/housestaff feedback | Grant funding | Division citizenship |
| Clinical professionalism | Mentoring | Mentorship | Job satisfaction |
| Communication | Quality of teaching rounds | Papers published | Mentorship |
| Core measures performance | Participation in national organizations | Committees and task forces | |
| Practice evidence‐based medicine | |||
| Fund of knowledge | |||
| Guideline adherence | |||
| Unplanned transfers to ICU | |||
| Implementation and initiation of projects | |||
| Length of stay | |||
| Medical errors | |||
| Mortality | |||
| Multidisciplinary approach to patient care | |||
| Multisource feedback evaluations | |||
| Never events | |||
| Patient‐centered care | |||
| Patient satisfaction | |||
| Practice‐based learning | |||
| Procedures | |||
| Readmissions | |||
| Reputation and expertise | |||
| Seeing patient on the day of admission | |||
| Quality of transfers of care | |||
DISCUSSION
Like many hospitalist groups, our division has experienced tremendous growth, both in our numbers and the breadth of roles that we fill. With this growth has come increasing expectations in multiple domains, competing priorities, and limited resources. We successfully developed a BSC as a tool to help our division reach its vision: balancing high quality clinical care, education, academics, and faculty development while maintaining a strong sense of community. We have found that the BSC has helped us meet several key goals.
The first goal was to allow for a broad view of our performance. This is the BSC's most basic function, and we saw immediate and tangible benefits. The scorecard provided a broad snapshot of our performance in a single place. For example, in the clinical domain, we saw that our direct cost per case was increasing despite our adjusted average length of stay remaining stable from FY2010‐FY2011. In academics and research, we saw that the number of abstracts accepted at national meetings increased by almost 30% in FY2011 (Figure 1).
The second goal was to create transparency and accountability. By measuring performance and displaying it on the division Web site, the BSC has promoted transparency. If performance does not meet our targets, the division as a whole becomes accountable. Leadership must understand why performance fell short and initiate changes to improve it. For instance, the rising direct cost per case has spurred the development of a high‐value care committee tasked with finding ways of reducing cost while providing high‐quality care.[12]
The third goal was to communicate goals and engage our faculty. As our division has grown, ensuring a shared vision among our entire faculty became an increasing challenge. The BSC functions as a communication platform between leadership and faculty, and yielded multiple benefits. As the metrics were born out of our mission and vision, the BSC has become a tangible representation of our core values. Moreover, individual faculty can see that they are part of a greater, high‐performing organization and realize they can impact the group's performance through their individual effort. For example, this has helped promote receptivity to carefully disseminated individual performance measures for billing and documentation, and patient satisfaction, in conjunction with faculty development in these areas.
The fourth goal was to ensure that we use data to guide strategic decisions. We felt that strategic decisions needed to be based on objective, rather than perceived or anecdotal, information. This meant translating our vision into measurable objectives that would drive performance improvement. For example, before the BSC, we were committed to the dissemination of our research and innovations. Yet, we quickly realized that we did not have a system to collect even basic data on academic performancea deficit we filled by leveraging information gathered from online databases and faculty curricula vitae. These data allowed us, for the first time, to objectively reflect on this as a strategic goal and to have an ongoing mechanism to monitor academic productivity.
Lessons Learned/Keys to Success
With our initial experience, we have gained insight that may be helpful to other AHGs considering implementing a BSC. First, and most importantly, AHGs should take the necessary time to build consensus and buy‐in. Particularly in areas where data are analyzed for the first time, faculty are often wary about the validity of the data or the purpose and utility of performance measurement. Faculty may be concerned about how collection of performance data could affect promotion or create a hostile and competitive work environment.
This concern grows when one moves from division‐wide to individual data. It is inevitable that the collection and dissemination of performance data will create some level of discomfort among faculty members, which can be a force for improvement or for angst. These issues should be anticipated, discussed, and actively managed. It is critical to be transparent with how data will be used. We have made clear that the transition from group to individual performance data, and from simple transparency to incentives, will be done thoughtfully and with tremendous input from our faculty. This tension can also be mitigated by choosing metrics that are internally driven, rather than determined by external groups (ie, following the principle that the measures should be important to the division and individual faculty members).
Next, the process of developing a mature BSC takes time. Much of our first year was spent developing systems for measurement, collecting data, and determining appropriate comparators and targets. The data in the first BSC functioned mainly as a baseline marker of performance. Some metrics, particularly in education and academics, had no national or local benchmarks. In these cases we identified comparable groups (such as other medical teaching services or other well‐established AHGs) or merely used our prior year's performance as a benchmark. Also, some of our metrics did not initially have performance targets. In most instances, this was because this was the first time that we looked at these data, and it was unclear what an appropriate target would be until more data became available.
Moving into our third year, we are seeing a natural evolution in the BSC's use. Some metrics that were initially chosen have been replaced or modified to reflect changing goals and priorities. Functional directors participate in choosing and developing performance metrics in their area. Previously, there was no formal structure for these groups to develop and measure strategic objectives and be accountable for performance improvement. They are now expected to define goals with measurable outcomes, to report progress to division leadership, and to develop their own scorecard to track performance. Each group chooses 2 to 4 metrics within their domain that are the most important for the division to improve on, which are then included in the division BSC.
We have also made efforts to build synergy between our BSC and performance goals set by external groups. Although continuing to favor metrics that are internally driven and meaningful to our faculty, we recognize that our goals must also reflect the needs and interests of broader stakeholders. For example, hand hygiene rates and patient satisfaction scores are UCSF medical center and divisional priorities (the former includes them in a financial incentive system for managers, staff, and many physicians) and are incorporated into the BSC as division‐wide incentive metrics.
Limitations
Our project has several limitations. It was conducted at a single institution, and our metrics may not be generalizable to other groups. However, the main goal of this article was not to focus on specific metrics but the process that we undertook to choose and develop them. Other institutions will likely identify different metrics based on their specific strategic objectives. We are also early in our experience with the BSC, and it is still not clear what effect it will have on the desired outcomes for our objectives. However, Henriksen recently reported that implementing a BSC at a large academic health center, in parallel with other performance improvement initiatives, resulted in substantial improvement in their chosen performance metrics.[13]
Despite the several years of development, we still view this as an early version of a BSC. To fully realize its benefits, an organization must choose metrics that will not simply measure performance but drive it. Our current BSC relies primarily on lagging measures, which show what our performance has been, and includes few leading metrics, which can predict trends in performance. As explained by Kaplan and Norton, this type of BSC risks skewing toward controlling rather than driving performance.[14] A mature BSC will include a mix of leading and lagging indicators, the combination illustrating a logical progression from measurement to performance. For instance, we measure total grant funding per year, which is a lagging indicator. However, to be most effective we could measure the percent of faculty who have attended grant‐writing workshops, the number of new grant sources identified, or the number of grant proposals submitted each quarter. These leading indicators would allow us to see performance trends that could be improved before the final outcome, total grant funding, is realized.
Finally, the issues surrounding the acceptability of this overall strategy will likely hinge on how we implement the more complex steps that relate to transparency, individual attribution, and perhaps ultimately incentives. Success in this area depends as much on culture as on strategy.
Next Steps
The next major step in the evolution of the BSC, and part of a broader faculty development program, will be the development of individual BSCs. They will be created using a similar methodology and allow faculty to reflect on their performance compared to peers and recognized benchmarks. Ideally, this will allow hospitalists in our group to establish personal strategic plans and monitor their performance over time. Individualizing these BSCs will be critical; although a research‐oriented faculty member might be striving for more than 5 publications and a large grant in a year, a clinician‐educator may seek outstanding teaching reviews and completion of a key quality improvement project. Both efforts need to be highly valued, and the divisional BSC should roll up these varied individual goals into a balanced whole.
In conclusion, we successfully developed and implemented a BSC to aid in strategic planning. The BSC ensures that we make strategic decisions using data, identify internally driven objectives, develop systems of performance measurement, and increase transparency and accountability. Our hope is that this description of the development of our BSC will be useful to other groups considering a similar endeavor.
Acknowledgments
The authors thank Noori Dhillon, Sadaf Akbaryar, Katie Quinn, Gerri Berg, and Maria Novelero for data collection and analysis. The authors also thank the faculty and staff who participated in the development process of the BSC.
Disclosure
Nothing to report.
- . The hospitalist field turns 15: new opportunities and challenges. J Hosp Med. 2011;6(4):E1–E4.
- , . The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335(7):514–517.
- , . The balanced scorecard—measures that drive performance. Harv Bus Rev. 1992;70(1):71–79.
- , . Using the balanced scorecard as a strategic management system. Harv Bus Rev. 1996;74(1):75–85.
- , . Having trouble with your strategy? Then map it. Harv Bus Rev. 2000;78:167–176, 202.
- , . Putting the balanced scorecard to work. Harv Bus Rev. 1993;71:134–147.
- , , , et al. Development and implementation of a performance measure tool in an academic pediatric research network. Contemp Clin Trials. 2010;31(5):429–437.
- , . Lives in the balance: an analysis of the balanced scorecard (BSC) in healthcare organizations. Int J Prod Perform Manag. 2007;57(1):6–21.
- , . The “Balanced Scorecard”: development and implementation in an academic clinical department. Acad Med. 1999;74(2):114–122.
- . Introducing a balanced scorecard management system in a university anesthesiology department. Anesth Analg. 2002;95(6):1731–1738, table of contents.
- , , , , . Issues for academic health centers to consider before implementing a balanced‐scorecard effort. Acad Med. 1999;74(12):1269–1277.
- , . Cents and sensitivity—teaching physicians to think about costs. N Engl J Med. 2012;367(2):99–101.
- , , , et al. 10‐year experience integrating strategic performance improvement initiatives: can the balanced scorecard, Six Sigma, and team training all thrive in a single hospital? In: Henriksen K, Battles JB, Keyes MA, Grady ML, eds. Advances in Patient Safety: New Directions and Alternative Approaches. Vol 3. Performance and Tools. Rockville, MD: Agency for Healthcare Research and Quality; 2008. Available at: http://www.ncbi.nlm.nih.gov/books/NBK43660. Accessed 15 June 2011.
- , . Linking the balanced scorecard to strategy. Calif Manage Rev. 1996;39(1):53–79.
- . The hospitalist field turns 15: new opportunities and challenges. J Hosp Med. 2011;6(4):E1–E4.
- , . The emerging role of “hospitalists” in the American health care system. N Engl J Med. 1996;335(7):514–517.
- , . The balanced scorecard—measures that drive performance. Harv Bus Rev. 1992;70(1):71–79.
- , . Using the balanced scorecard as a strategic management system. Harv Bus Rev. 1996;74(1):75–85.
- , . Having trouble with your strategy? Then map it. Harv Bus Rev. 2000;78:167–176, 202.
- , . Putting the balanced scorecard to work. Harv Bus Rev. 1993;71:134–147.
- , , , et al. Development and implementation of a performance measure tool in an academic pediatric research network. Contemp Clin Trials. 2010;31(5):429–437.
- , . Lives in the balance: an analysis of the balanced scorecard (BSC) in healthcare organizations. Int J Prod Perform Manag. 2007;57(1):6–21.
- , . The “Balanced Scorecard”: development and implementation in an academic clinical department. Acad Med. 1999;74(2):114–122.
- . Introducing a balanced scorecard management system in a university anesthesiology department. Anesth Analg. 2002;95(6):1731–1738, table of contents.
- , , , , . Issues for academic health centers to consider before implementing a balanced‐scorecard effort. Acad Med. 1999;74(12):1269–1277.
- , . Cents and sensitivity—teaching physicians to think about costs. N Engl J Med. 2012;367(2):99–101.
- , , , et al. 10‐year experience integrating strategic performance improvement initiatives: can the balanced scorecard, Six Sigma, and team training all thrive in a single hospital? In: Henriksen K, Battles JB, Keyes MA, Grady ML, eds. Advances in Patient Safety: New Directions and Alternative Approaches. Vol 3. Performance and Tools. Rockville, MD: Agency for Healthcare Research and Quality; 2008. Available at: http://www.ncbi.nlm.nih.gov/books/NBK43660. Accessed 15 June 2011.
- , . Linking the balanced scorecard to strategy. Calif Manage Rev. 1996;39(1):53–79.
It's Not About Pager Replacement
Clinical communication among healthcare providers to coordinate patient care is important, accounting for the majority of information exchanges in healthcare.[1, 2] Breakdowns in communication have therefore been identified as the major contributor to medical errors.[3, 4, 5]
There is a growing literature related to asynchronous clinical communication practices, or communication that does not occur at the same time in hospitals, and the limitations of using the traditional numeric pager. These include the inability to indicate the urgency of the message, frequent interruptions, contacting the wrong physician, and inefficiencies coordinating care across multiple disciplines and specialties.[6, 7, 8, 9, 10, 11, 12]
Hospitals have implemented a variety of health information technology (HIT) solutions to replace the numeric pager and address these clinical communication issues, including the use of alphanumeric pagers, smartphone devices, and Web‐based applications that allow clinicians to triage the urgency of issues.[13, 14, 15, 16] Although these solutions have resolved some of the deficiencies previously identified, issues relating to the impact on the interprofessional nature of healthcare remain unaddressed.[17] In some cases, the implementation of HIT has created unintended consequences that have an impact on effective communication.
One of the widely cited examples of HIT creating unintended consequences is the implementation of computerized physician order entry systems.[18, 19, 20] Other studies looking more broadly at patient information systems have identified problems caused by poor user interfaces that promoted errors in entry and retrieval of data, inflexible features forcing clinician workarounds, and technology designs that impeded clinical workflow.[21, 22, 23]
These observations suggest that although many of the issues with clinical communication stem from the reliance on numeric paging, simply replacing pagers with newer technology may not solve the problems and can in fact create other unintended consequences. These include unintended consequences resulting from the sociotechnical aspects of HIT, which is the interplay of technology with existing clinical workflow, culture, and social interactions.[21] Our institution recently implemented a Web‐based messaging system to replace the use of numeric pagers. We aimed to evaluate the unintended consequences resulting from the implementation of this system and to describe their impact on the delivery of clinical care on a general internal medicine (GIM) service.
METHODS
This was a pre‐post mixed‐methods study utilizing both quantitative and qualitative measures. We integrated these 2 data‐collection methods to improve the quality of the results. The study was conducted on the GIM service at the University Health Network Toronto Western Hospital site, a tertiary‐care academic teaching center fully affiliated with the University of Toronto (Toronto, Canada). The GIM service at Toronto Western Hospital consists of 4 clinical teams, each staffed by an attending physician, 3 to 4 residents, and 2 to 3 medical students.
Prior to this study, nonface‐to‐face communication on the wards was facilitated through numeric paging, where nurses, pharmacists, and social workers on the GIM wards would page residents to a hospital phone and wait for them to call back. Figures 1, 2, and 3 visualize the Web‐based messaging system we implemented at the University Health Network in May 2010. All residents on the service were provided smartphones that they used for communication. In addition to these, there was a dedicated team smartphone that acted as a central point of contact for the team 24 hours a day, 7 days a week and was carried by the physician covering the team at the time. The system allowed nurses, pharmacists, and social workers to triage the urgency of messages and include details providing context to the issue. Issues flagged as urgent were immediately sent to the team smartphone by e‐mail to alert the physician, who could respond from the smartphone. These messages could be forwarded to a team member, often the physician most familiar with the patient, to address. Issues flagged as nonurgent were posted to the system's message board, which the physicians accessed by logging into the Web‐based messaging system on a regular basis. The message board was designed to allow physicians to respond to multiple non‐urgent issues at once. To close the loop on communication, logic was developed so that if a physician did not respond to a non‐urgent message within the specified timeframe, the message was escalated and sent as an alerting e‐mail to the team smartphone every 15 minutes until it was addressed. The timeframes for responding varied from 1 hour to not needing a response until the next morning.
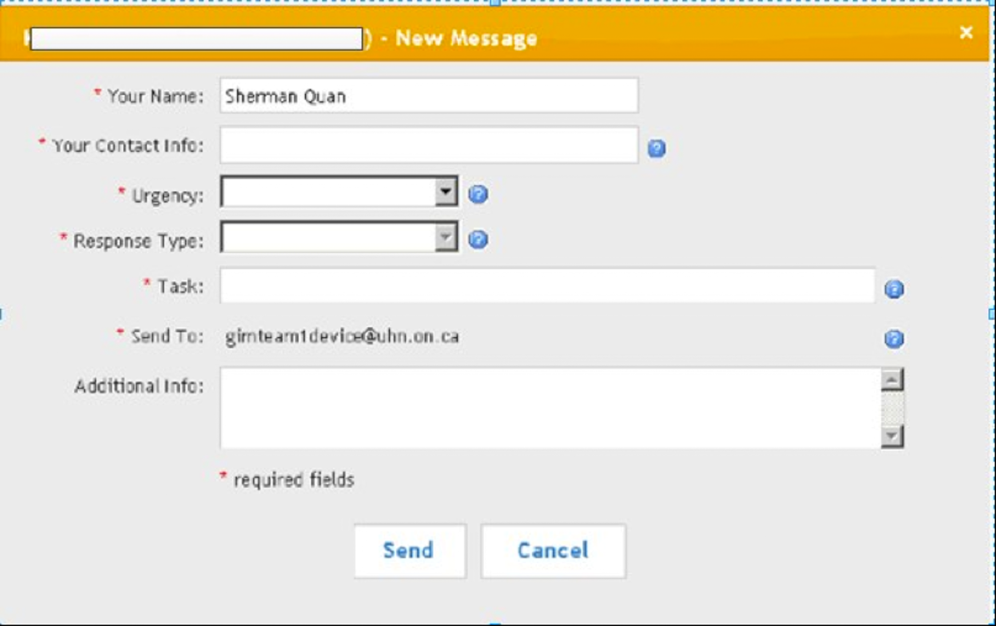
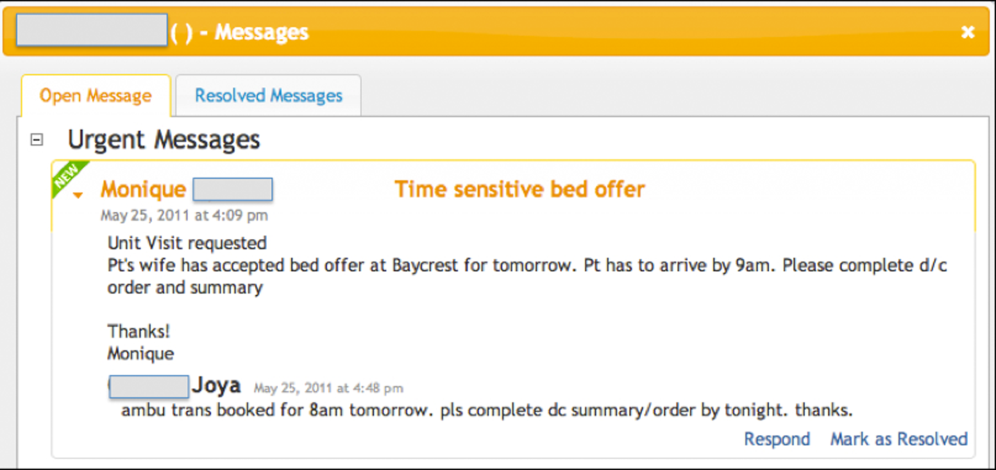
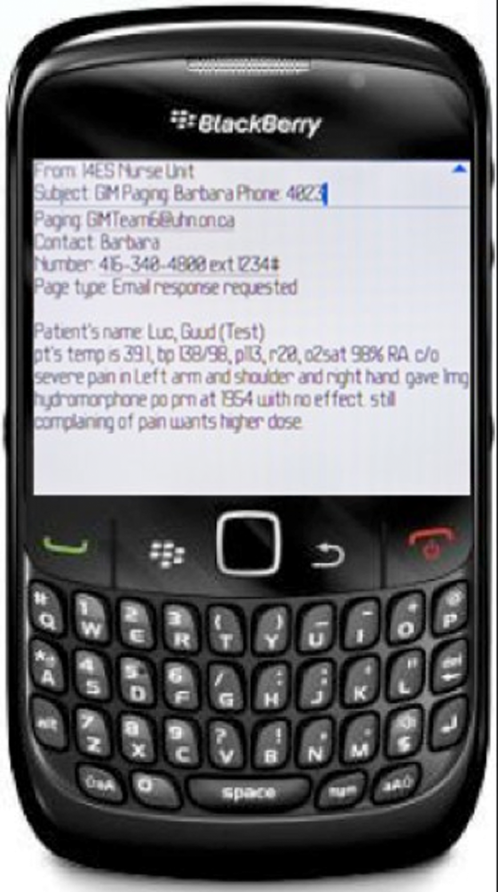
Ongoing training on the use of the system was built into the clinical orientation for the physician and nursing staff, as turnover in an academic teaching hospital is quite high. The orientation included instructions on how to use the features of the Web‐based messaging system but also provided guidelines on general etiquette with using the system to ensure sustainability of the communication process. For example, physicians were asked to check the system regularly, as the process worked only if they responded to messages. Nurses were asked not to send messages during scheduled educational sessions unless necessary and to limit messages they flagged as urgent to ones that were in fact urgent.
Our quantitative evaluation compared interruptions, which we define as communication that caused a medical resident to stop current activity to address, before and after the implementation of the Web‐based messaging system to assess the volume and time distribution of messages, and compared these results with our qualitative evaluation. For the pre‐implementation phase, interruptions were all numeric pages sent to all residents during the period of July 1427, 2008. For the post‐implementation phase, interruptions were the e‐mails sent directly to the team smartphones from the Web‐based messaging system to all residents during the period of October 1124, 2010. We excluded messages from the postimplementation phase if the same message was sent >10 times, typically indicating technical issues such as a malfunction of the smartphone causing the escalation process to continue.
Our qualitative evaluation consisted of semistructured interviews that were conducted after implementation. A research coordinator sent e‐mails to potential physician participants during a 1‐month rotation (n=16), and nurses (N=50), pharmacists (N=4), and social workers (N=4) from a representative ward inviting them to be part of this study. A set of open‐ended questions (see Supporting Information, Appendix A, in the online version of this article) developed based on informal feedback regarding the system provided by physicians, nurses, pharmacists, and social workers served as a guide to highlight key themes of interest. Based on the participants' responses, further questions were asked to drill down into more detail. Interviews were transcribed verbatim and anonymized.
The interview data were analyzed using thematic analysis to generate categories and overarching themes.[24, 25] Once the coding structure was developed, the transcripts were imported into qualitative analysis software (NVivo 9, QSR International) and then coded and analyzed, pulling the key themes that emerged from the text to be used in interpreting the data.
RESULTS
Our quantitative before‐after comparison of clinical messages sent to physicians revealed an increase in interruptions. We compared these results to the results of our interviews to understand why this might have occurred. Several key themes emerged from the analysis of the interviews, including increase in interruptions, accountability, and tactics to improve personal productivity. We interviewed 5 physicians, 8 nurses, 2 pharmacists, and 2 social workers.
Pre‐Post System Usage Data: Quantitative Assessment
Table 1 outlines the number of numeric pages sent during the pre‐implementation phase of July 1427, 2008. All pages sent immediately alerted the resident and so were all considered interruptions. Table 1 also outlines the number of urgent and escalation messages sent via e‐mail to the residents during the post‐implementation phase of October 1124, 2010. All messages were sent immediately to the team smartphone alerting the resident and so were all considered interruptions. During both timeframes, there were 15 resident physicians on service. During the pre‐implementation phase, 117 patients were admitted to the GIM service, and 162 patients were admitted during the post‐implementation phase.
| Numeric Paging (Predata) | Advance Communication System (Postdata) | ||
|---|---|---|---|
| Pages sent | 710 | Urgent | 951 |
| Interruptions | 710 | Escalations | 1245 |
| Interruptions per resident per day | 3 | Interruptions | 2196 |
| Interruptions per resident per day | 10 | ||
Table 1 shows that the number of interruptions in the pre‐implementation phase was 710 (3 per resident per day) compared with 2196 (10 per resident per day) in the post‐implementation phase, a 233% increase in interruptions. Because admissions were higher in the post‐implementation phase, it is possible that higher patient volumes could have contributed to the increase in interruptions.
Semi‐Structured Interviews: Qualitative Assessment
Increase in Interruptions
The intent of the web‐based messaging system was to reduce interruptions by triaging clinical messages and allowing healthcare professionals to respond to multiple non‐urgent issues at once. The unexpected result, however, was that the frequency at which physicians were interrupted actually increased following implementation.
I feel like I'm constantly bombarded with things Just psychologically I feel like it's harassing me a lot more than the pager used to. [MD02, physician]
Yes. Definitely, I'm paging them more frequently in general than I would have previously. [RN02, nurse]
Increased interruptions occurred in part because traditional barriers to paging, like having to wait by a phone for a response, were eliminated by the new system. Sending a message was easy, and with the reliability introduced through team‐based paging, there was greater temptation to send separate messages for singular issues.
I think [that] before, things were saved up and then paged and given all at once. And now it's, like, there's a temptation just to send things all the time, like, small issues. [AH01, pharmacist]
Communication also increased due to the impersonal nature of the electronic system. With many of the barriers to communicating removed, such as receiving immediate feedback regarding the appropriateness of a message, staff no longer hesitated when sending messages regarding less‐important issues.
So some stuff that you may have not wanted to call for before 'cause it's kind of silly, you can just send it information‐only. So they're aware 'cause the thing about with using electronics it's a lot more impersonal and indirect. [RN03, nurse]
At the same time, nurses, pharmacists, and social workers acknowledged that receiving all of this additional, sometimes unnecessary, information could be frustrating for the physicians. This recognition alone, however, was not sufficient to modify their behavior.
So I find that I can imagine for them it may be a little frustrating 'cause they're getting all these tidbits of information. [RN03, nurse]
I'm sure they get overwhelmed and I've had the feedback from the team They were saying that they were getting constantly paged, not by me, just by me, but by everybody. [AH01, pharmacist]
Accountability
As part of their professional practice, nurses described a medico‐legal obligation to inform physicians about relevant patient issues such as abnormal laboratory values. A culture of accountability, therefore, underpinned many of the actions taken by the nurses, reinforced because the electronic messages sent through the system were permanent and retrievable. The physicians also used the system as an electronic record of discussions that occurred.
Because it's just, like, this thing about accountability in terms of letting them know, that they are aware. [RN03, nurse]
And I think everything you do is recorded, like, you can go back and check, so there's that legal piece, which I guess covers you, in terms of time you called, those things which are critical, what you are calling for. [RN09, nurse]
'Cause I use it now as a reference. So even if I have a phone conversation with a nurse, based on a message that we've had, I will record what we said and send it. [MD03, physician]
Some of the more junior nurses periodically felt unsure or uncomfortable with clinical situations and would send a message to the physician to share their concerns. The messaging reassured the nurses and made them feel like they were fulfilling their professional responsibilities.
So a senior nurse could probably take a look at some situation and they can acknowledge whether the issue is urgent or nonurgent But from a novice perspective, as you're still learning it kind of gives you peace of mind and feels like you're filling your responsibility and accountability, that you're passing on the messages. [RN03, nurse]
Whereas nurses felt they were fulfilling their professional obligations, some physicians felt that nurses were using the system to absolve themselves of their clinical responsibilities.
Some just feel the need to send everything on there and maybe they feel that by sending it on here they absolve themselves of responsibility. [MD05, physician]
Other clinicians felt that the system created more of a responsibility or obligation for the physicians to respond. They believed the escalation feature of the system helped ensure the physicians responded in some fashion to close the loop.
[T]hey have the responsibility to answer it if it's an urgent message and because it keeps coming on to remind them. [AH02, social worker]
Interestingly, there were physicians that identified the opposite and felt the system created less of a responsibility or obligation for them to respond. By knowing the context of the message, it gave them the ability to prioritize or ignore the message if they knew it was not life threatening.
[T]here's less of a responsibility or an obligation They get a message and then they can actually delay the process So in a way it actually allows us to kind of get away with some things and that happens because, you know, we're prioritizing something that we're doing as being more important to us. [MD01, physician]
Tactics to Improve Personal Productivity
The web‐based messaging system's triaging feature allows the sender of the message to indicate whether an issue is urgent or non‐urgent. Urgent issues result in an immediate e‐mail that is intended to elicit an immediate response. Some of the nurses, pharmacists, and social workers exploited features of the system to elicit immediate responses from the physicians for non‐urgent issues, including using their knowledge of the urgent and non‐urgent features of the system to interrupt the physicians.
I kind of cheat and don't use the system properly. So every message I send I always send it as urgent because I want it go to the smartphone. [AH01, pharmacist]
I like that if you know how to use the urgent and nonurgent features effectively it generally works quite well in getting a response in a timely fashion. [RN02, nurse]
One tactic that physicians perceived the nurses were using to elicit a response from them was to exaggerate the severity or urgency of the issue in their message.
Some details will be sort of cherry picked to make the issue sound very dire I'll give you a classic, like, high blood pressure and patient has a headache. So initially, you know, I have to think, does this patient have a hypertensive emergency? So by putting sort of history together in this way, that sort of suggestive way, then yeah. [MD03, physician]
The nurses, pharmacists. and social workers frequently exaggerated the urgency of their clinical messages at the end of their shifts in an effort to resolve outstanding issues immediately in order to avoid transferring tasks to another colleague or delaying them until the next day.
But in terms of a shift change, for example, I need a response now 'cause that is a lot of times where it is that although it's not clinically urgent it's time sensitive. So it is urgent. [RN02, nurse]
I do also notice that around changeover time, issues that have been sort of chronically or have preexisting, become urgent issues. [MD01, physician]
Messages were also sent inappropriately as urgent as a strategy to ensure the physician dealt with the issue promptly and did not forget to complete the requested task associated with the issue.
Everybody puts urgent because we want the response immediately. Otherwise, if you put nonurgent, the doctors will just drag and drag and will forget to respond to the issue. [RN09, nurse]
However, because physicians received context clarifying the urgency of the message, they were able to prioritize their tasks and defer less‐important issues without compromising patient safety or quality of care, allowing them to use their time more productively. This, however, did not always align with the sender's request.
I think the key thing is that the information coming to us is text and it describes the issue. So we can, at our end, then we can make a call as to what the priority is. [MD03, physician]
DISCUSSION
The purpose of this study was to evaluate a Web‐based messaging system and identify the unintended consequences observed with implementing HIT to improve clinical communication. This is an important study because healthcare organizations are beginning to develop strategies for improving clinical communication but believe the solution involves simply replacing pager technology. Support for this approach is seen with larger vendors in the smartphone and communication industry, who promote their products as pager‐replacement solutions and even help customers develop pager‐replacement strategies.[26, 27, 28] Simply replacing pagers with smartphones and sending text messages will have only a limited impact on improving clinical communication and will likely result in unintended negative consequences, as seen in this study.
Whereas the Web‐based messaging system was designed to reduce interruptions from clinical messaging, interruptions actually increased, although the mental burden of each interruption was likely lower because responding to a text message is less interruptive than finding a telephone to answer a page. A key contributor to this effect was a culture of accountability among nurses, pharmacists, and social workers who felt it was their professional obligation to notify physicians about all issues of concern. This belief and related behavior is aligned with the standards promoted by professional regulatory bodies that identify accountability as a vital practice expectation.[29] Nurses and nursing staff take responsibility for the care they provide and answer for their own judgments and actions.[30] The system eliminated many of the previous barriers to paging and provided a less‐personal form of communication. The cumulative and unexpected outcome was an increase of interruptions for physicians and the adoption of workarounds by all healthcare professionals to improve personal productivity. Although the system was built in an iterative fashion with frontline clinicians, it is likely that oversights in the design of the system also contributed to these problems, which speaks to the complexity of clinical communication. Centralizing communication to the team smartphone could have overburdened the physicians covering it at the time, causing them to ignore messages because they were too busy to address them.
There were limitations to this study. One limitation was that this study examined only a cross‐section of messaging activity at a given point in time, and therefore it may not be representative of the behaviors of the physicians, nurses, pharmacists, and social workers over time as the culture of the environment evolves and they adjust to the new technology. The pre‐implementation data were collected 2 years prior to the post‐implementation data, but it was necessary to use data this old because other interventions were implemented prior to the Web‐based messaging system, so baseline paging data were no longer available. Whereas most clinical disciplines were represented in the interviews, the sample included only 17 participants from 1 clinical service, so generalizability of the results may be limited.
Although the reliance on numeric paging technology was previously identified as a primary source of problems with communication, the real issues are much more complex. This study highlighted that many of the underlying obstacles relate to existing social interactions and habits of multiple professions working together. Failures in collaboration among healthcare professionals have a negative impact on health outcomes and routinely stem from the lack of explicit definitions of roles, the absence of clear leadership, insufficient time for team‐building, the us‐and‐them effects created by professional socialization, and frustration created by power and status differentials of each discipline.[31, 32, 33] Therefore, it is critical that healthcare organizations focus on the people and clinical processes when implementing technology to solve issues with clinical communication. These observations are consistent with other studies examining the unintended consequences caused by the sociotechnical aspects of HIT implementation, where workarounds to game the system were also employed.[21]
In summary, improving clinical communication cannot be achieved simply by replacing pagers with newer technology; it requires a fundamental shift in how healthcare professionals interact, with a focus on the sociotechnical aspects of HIT. As patient volumes and the complexity of care continue to increase, more effective methods for facilitating interprofessional communication and collaboration must be developed.
Acknowledgements
Disclosures: This study was funded in part by a Frederick Banting and Charles Best Canada Graduate Scholarship from the Canadian Institutes of Health Research. The authors report no conflicts of interest.
- . When conversation is better than computation. J Am Med Inform Assoc. 2000;7(3):277–286.
- , , , et al. Synchronous communication facilitates interruptive workflow for attending physicians and nurses in clinical settings. Int J Med Inform. 2009;78(9):629–637.
- , , , et al. The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324(6):377–384.
- , , . Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186–194.
- The Joint Commission. Improving America's Hospitals: The Joint Commission's Annual Report on Quality and Safety. Oakbrook Terrace, IL: The Joint Commission; 2007. Available at: http://www.jointcommission.org/assets/1/6/2007_Annual_Report.pdf. Accessed on April 16, 2012.
- , . Residents' suggestions for reducing errors in teaching hospitals. N Engl J Med. 2003;348(9):851–855.
- , . Interruptions in healthcare: theoretical views. Int J Med Inform. 2009;78(5):293–307.
- , , , et al. Frequency and clinical importance of pages sent to the wrong physician. Arch Intern Med. 2009;169(11):1072–1073.
- , , , , . Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care. 2005;14(6):401–407.
- , , , , , . Towards safer interprofessional communication: Constructing a model of “utility” from preoperative team briefings. J Interprof Care. 2006;20(5):471–483.
- , , . Interprofessional collaboration: effects of practice‐based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009(3):CD000072.
- , . The effects of hands free communication devices on clinical communication: balancing communication access needs with user control. AMIA Annu Symp Proc. 2008;621–625.
- , , , , . Beyond paging: building a web‐based communication tool for nurses and physicians. J Gen Intern Med. 2009;24(1):105–110.
- , , , et al. The use of smartphones for clinical communication on internal medicine wards. J Hosp Med. 2010;5(9):553–559.
- , , , . Implementation and evaluation of an alpha‐numeric paging system on a resident inpatient teaching service. J Hosp Med. 2009;4(8):E34–E40.
- , , , et al. Effects of clinical communication interventions in hospitals: a systematic review of information and communication technology adoptions for improved communication between clinicians. Int J Med Inform. 2012;81(11):723–732.
- , , , et al. An evaluation of the use of smartphones to communicate between clinicians: a mixed‐methods study. J Med Internet Res. 2011;13(3):e59.
- , , . Computerized physician order entry in the critical care environment: a review of current literature. J Intensive Care Med. 2011;26(3):165–171.
- , , , et al. Factors contributing to an increase in duplicate medication order errors after CPOE implementation. J Am Med Inform Assoc. 2011;18(6):774–782.
- , , , et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293(10):1197–1203.
- , , . Unintended consequences of information technologies in health care—an interactive sociotechnical analysis. J Am Med Inform Assoc. 2007;14(5):542–549.
- . Why did that happen? Exploring the proliferation of barely usable software in healthcare systems. Qual Saf Health Care. 2006;(15 suppl 1):i76–i81.
- , , . Some unintended consequences of information technology in health care: the nature of patient care information system‐related errors. J Am Med Inform Assoc. 2004;11(2):104–112.
- , , . An overview of three different approaches to the interpretation of qualitative data. Part 1: Theoretical issues. Nurse Res. 2002;10(1):30–42.
- , . Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288.
- Research in Motion, Amcom Software. Six things hospitals need to know about replacing pagers with smartphones. Available at: http://us.blackberry.com/business/industry/healthcare/6ThingstoKnow_ReplacingHospitalPagers_WhitePaper.pdf. Accessed on April 16, 2012.
- Vocera, Wallace Wireless. The Longstreet Clinic: replacing pagers, supercharging communication with WIC pager. Available at: http://www.vocera.com/assets/pdf/case_studies/cs_longstreetclinic_0910_v1.pdf. Accessed on April 16, 2012.
- Amcom Software reports strong momentum with its new smartphone messaging and pager replacement solution [press release]. Minneapolis, MN: Amcom Software; September 29, 2010. Available at: http://www.amcomsoftware.com/News/09‐29‐10.aspx. Accessed on April 16, 2012.
- College of Nurses of Ontario. 2011 standards and guidelines. Availableat: http://www.cno.org/en/learn‐about‐standards‐guidelines/publications‐list/standards‐and‐guidelines. Accessed on April 16, 2012.
- , , . Accountability and responsibility: principle of nursing practice B. Nurs Stand. 2011;25(29):35–36.
- , , , , . The association between interdisciplinary collaboration and patient outcomes in a medical intensive care unit. Heart Lung. 1992;21(1):18–24.
- . Professionalization and socialization in interprofessional collaboration. In: Casto RM, Julia MC, eds. Interprofessional Care and Collaborative Practice. 1st ed. Independence, KY: Cengage Learning; 1994:23–31.
- , . Knowledge translation and interprofessional collaboration: where the rubber of evidence‐based care hits the road of teamwork. J Contin Educ Health Prof. 2006;26(1):46–54.
Clinical communication among healthcare providers to coordinate patient care is important, accounting for the majority of information exchanges in healthcare.[1, 2] Breakdowns in communication have therefore been identified as the major contributor to medical errors.[3, 4, 5]
There is a growing literature related to asynchronous clinical communication practices, or communication that does not occur at the same time in hospitals, and the limitations of using the traditional numeric pager. These include the inability to indicate the urgency of the message, frequent interruptions, contacting the wrong physician, and inefficiencies coordinating care across multiple disciplines and specialties.[6, 7, 8, 9, 10, 11, 12]
Hospitals have implemented a variety of health information technology (HIT) solutions to replace the numeric pager and address these clinical communication issues, including the use of alphanumeric pagers, smartphone devices, and Web‐based applications that allow clinicians to triage the urgency of issues.[13, 14, 15, 16] Although these solutions have resolved some of the deficiencies previously identified, issues relating to the impact on the interprofessional nature of healthcare remain unaddressed.[17] In some cases, the implementation of HIT has created unintended consequences that have an impact on effective communication.
One of the widely cited examples of HIT creating unintended consequences is the implementation of computerized physician order entry systems.[18, 19, 20] Other studies looking more broadly at patient information systems have identified problems caused by poor user interfaces that promoted errors in entry and retrieval of data, inflexible features forcing clinician workarounds, and technology designs that impeded clinical workflow.[21, 22, 23]
These observations suggest that although many of the issues with clinical communication stem from the reliance on numeric paging, simply replacing pagers with newer technology may not solve the problems and can in fact create other unintended consequences. These include unintended consequences resulting from the sociotechnical aspects of HIT, which is the interplay of technology with existing clinical workflow, culture, and social interactions.[21] Our institution recently implemented a Web‐based messaging system to replace the use of numeric pagers. We aimed to evaluate the unintended consequences resulting from the implementation of this system and to describe their impact on the delivery of clinical care on a general internal medicine (GIM) service.
METHODS
This was a pre‐post mixed‐methods study utilizing both quantitative and qualitative measures. We integrated these 2 data‐collection methods to improve the quality of the results. The study was conducted on the GIM service at the University Health Network Toronto Western Hospital site, a tertiary‐care academic teaching center fully affiliated with the University of Toronto (Toronto, Canada). The GIM service at Toronto Western Hospital consists of 4 clinical teams, each staffed by an attending physician, 3 to 4 residents, and 2 to 3 medical students.
Prior to this study, nonface‐to‐face communication on the wards was facilitated through numeric paging, where nurses, pharmacists, and social workers on the GIM wards would page residents to a hospital phone and wait for them to call back. Figures 1, 2, and 3 visualize the Web‐based messaging system we implemented at the University Health Network in May 2010. All residents on the service were provided smartphones that they used for communication. In addition to these, there was a dedicated team smartphone that acted as a central point of contact for the team 24 hours a day, 7 days a week and was carried by the physician covering the team at the time. The system allowed nurses, pharmacists, and social workers to triage the urgency of messages and include details providing context to the issue. Issues flagged as urgent were immediately sent to the team smartphone by e‐mail to alert the physician, who could respond from the smartphone. These messages could be forwarded to a team member, often the physician most familiar with the patient, to address. Issues flagged as nonurgent were posted to the system's message board, which the physicians accessed by logging into the Web‐based messaging system on a regular basis. The message board was designed to allow physicians to respond to multiple non‐urgent issues at once. To close the loop on communication, logic was developed so that if a physician did not respond to a non‐urgent message within the specified timeframe, the message was escalated and sent as an alerting e‐mail to the team smartphone every 15 minutes until it was addressed. The timeframes for responding varied from 1 hour to not needing a response until the next morning.
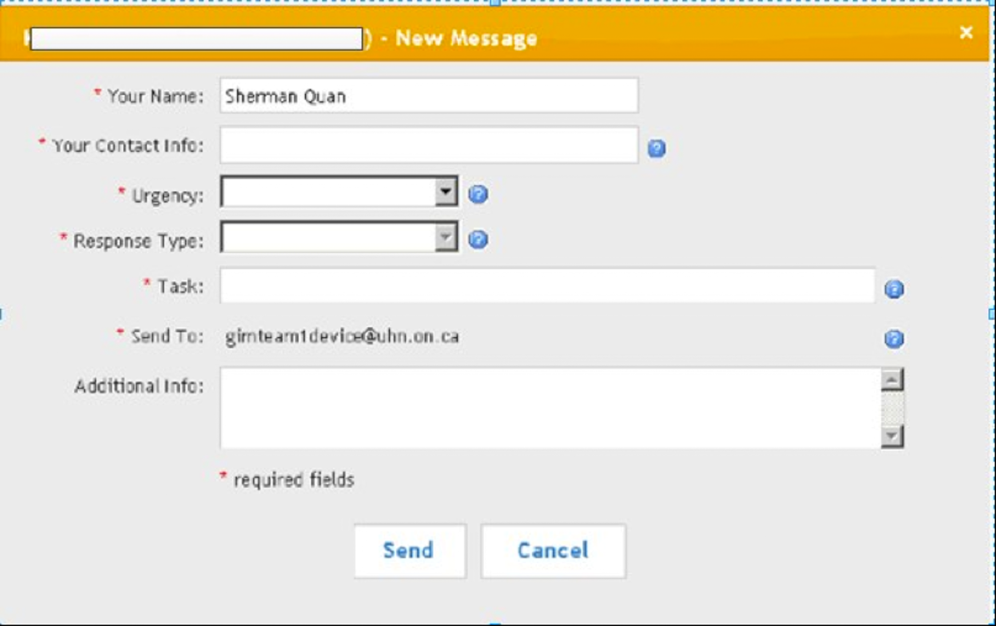
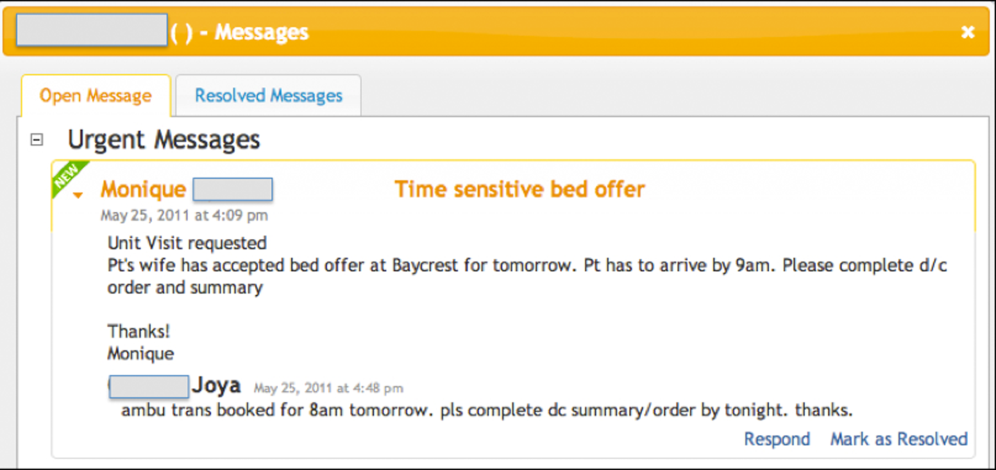
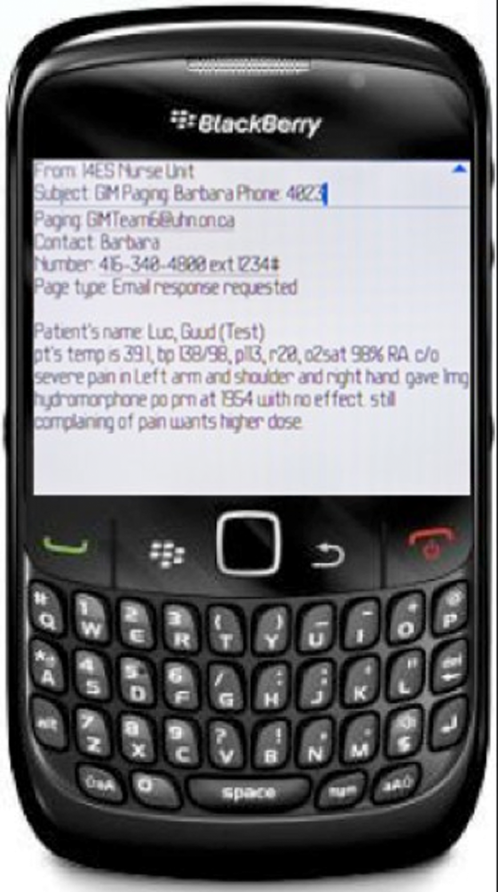
Ongoing training on the use of the system was built into the clinical orientation for the physician and nursing staff, as turnover in an academic teaching hospital is quite high. The orientation included instructions on how to use the features of the Web‐based messaging system but also provided guidelines on general etiquette with using the system to ensure sustainability of the communication process. For example, physicians were asked to check the system regularly, as the process worked only if they responded to messages. Nurses were asked not to send messages during scheduled educational sessions unless necessary and to limit messages they flagged as urgent to ones that were in fact urgent.
Our quantitative evaluation compared interruptions, which we define as communication that caused a medical resident to stop current activity to address, before and after the implementation of the Web‐based messaging system to assess the volume and time distribution of messages, and compared these results with our qualitative evaluation. For the pre‐implementation phase, interruptions were all numeric pages sent to all residents during the period of July 1427, 2008. For the post‐implementation phase, interruptions were the e‐mails sent directly to the team smartphones from the Web‐based messaging system to all residents during the period of October 1124, 2010. We excluded messages from the postimplementation phase if the same message was sent >10 times, typically indicating technical issues such as a malfunction of the smartphone causing the escalation process to continue.
Our qualitative evaluation consisted of semistructured interviews that were conducted after implementation. A research coordinator sent e‐mails to potential physician participants during a 1‐month rotation (n=16), and nurses (N=50), pharmacists (N=4), and social workers (N=4) from a representative ward inviting them to be part of this study. A set of open‐ended questions (see Supporting Information, Appendix A, in the online version of this article) developed based on informal feedback regarding the system provided by physicians, nurses, pharmacists, and social workers served as a guide to highlight key themes of interest. Based on the participants' responses, further questions were asked to drill down into more detail. Interviews were transcribed verbatim and anonymized.
The interview data were analyzed using thematic analysis to generate categories and overarching themes.[24, 25] Once the coding structure was developed, the transcripts were imported into qualitative analysis software (NVivo 9, QSR International) and then coded and analyzed, pulling the key themes that emerged from the text to be used in interpreting the data.
RESULTS
Our quantitative before‐after comparison of clinical messages sent to physicians revealed an increase in interruptions. We compared these results to the results of our interviews to understand why this might have occurred. Several key themes emerged from the analysis of the interviews, including increase in interruptions, accountability, and tactics to improve personal productivity. We interviewed 5 physicians, 8 nurses, 2 pharmacists, and 2 social workers.
Pre‐Post System Usage Data: Quantitative Assessment
Table 1 outlines the number of numeric pages sent during the pre‐implementation phase of July 1427, 2008. All pages sent immediately alerted the resident and so were all considered interruptions. Table 1 also outlines the number of urgent and escalation messages sent via e‐mail to the residents during the post‐implementation phase of October 1124, 2010. All messages were sent immediately to the team smartphone alerting the resident and so were all considered interruptions. During both timeframes, there were 15 resident physicians on service. During the pre‐implementation phase, 117 patients were admitted to the GIM service, and 162 patients were admitted during the post‐implementation phase.
| Numeric Paging (Predata) | Advance Communication System (Postdata) | ||
|---|---|---|---|
| Pages sent | 710 | Urgent | 951 |
| Interruptions | 710 | Escalations | 1245 |
| Interruptions per resident per day | 3 | Interruptions | 2196 |
| Interruptions per resident per day | 10 | ||
Table 1 shows that the number of interruptions in the pre‐implementation phase was 710 (3 per resident per day) compared with 2196 (10 per resident per day) in the post‐implementation phase, a 233% increase in interruptions. Because admissions were higher in the post‐implementation phase, it is possible that higher patient volumes could have contributed to the increase in interruptions.
Semi‐Structured Interviews: Qualitative Assessment
Increase in Interruptions
The intent of the web‐based messaging system was to reduce interruptions by triaging clinical messages and allowing healthcare professionals to respond to multiple non‐urgent issues at once. The unexpected result, however, was that the frequency at which physicians were interrupted actually increased following implementation.
I feel like I'm constantly bombarded with things Just psychologically I feel like it's harassing me a lot more than the pager used to. [MD02, physician]
Yes. Definitely, I'm paging them more frequently in general than I would have previously. [RN02, nurse]
Increased interruptions occurred in part because traditional barriers to paging, like having to wait by a phone for a response, were eliminated by the new system. Sending a message was easy, and with the reliability introduced through team‐based paging, there was greater temptation to send separate messages for singular issues.
I think [that] before, things were saved up and then paged and given all at once. And now it's, like, there's a temptation just to send things all the time, like, small issues. [AH01, pharmacist]
Communication also increased due to the impersonal nature of the electronic system. With many of the barriers to communicating removed, such as receiving immediate feedback regarding the appropriateness of a message, staff no longer hesitated when sending messages regarding less‐important issues.
So some stuff that you may have not wanted to call for before 'cause it's kind of silly, you can just send it information‐only. So they're aware 'cause the thing about with using electronics it's a lot more impersonal and indirect. [RN03, nurse]
At the same time, nurses, pharmacists, and social workers acknowledged that receiving all of this additional, sometimes unnecessary, information could be frustrating for the physicians. This recognition alone, however, was not sufficient to modify their behavior.
So I find that I can imagine for them it may be a little frustrating 'cause they're getting all these tidbits of information. [RN03, nurse]
I'm sure they get overwhelmed and I've had the feedback from the team They were saying that they were getting constantly paged, not by me, just by me, but by everybody. [AH01, pharmacist]
Accountability
As part of their professional practice, nurses described a medico‐legal obligation to inform physicians about relevant patient issues such as abnormal laboratory values. A culture of accountability, therefore, underpinned many of the actions taken by the nurses, reinforced because the electronic messages sent through the system were permanent and retrievable. The physicians also used the system as an electronic record of discussions that occurred.
Because it's just, like, this thing about accountability in terms of letting them know, that they are aware. [RN03, nurse]
And I think everything you do is recorded, like, you can go back and check, so there's that legal piece, which I guess covers you, in terms of time you called, those things which are critical, what you are calling for. [RN09, nurse]
'Cause I use it now as a reference. So even if I have a phone conversation with a nurse, based on a message that we've had, I will record what we said and send it. [MD03, physician]
Some of the more junior nurses periodically felt unsure or uncomfortable with clinical situations and would send a message to the physician to share their concerns. The messaging reassured the nurses and made them feel like they were fulfilling their professional responsibilities.
So a senior nurse could probably take a look at some situation and they can acknowledge whether the issue is urgent or nonurgent But from a novice perspective, as you're still learning it kind of gives you peace of mind and feels like you're filling your responsibility and accountability, that you're passing on the messages. [RN03, nurse]
Whereas nurses felt they were fulfilling their professional obligations, some physicians felt that nurses were using the system to absolve themselves of their clinical responsibilities.
Some just feel the need to send everything on there and maybe they feel that by sending it on here they absolve themselves of responsibility. [MD05, physician]
Other clinicians felt that the system created more of a responsibility or obligation for the physicians to respond. They believed the escalation feature of the system helped ensure the physicians responded in some fashion to close the loop.
[T]hey have the responsibility to answer it if it's an urgent message and because it keeps coming on to remind them. [AH02, social worker]
Interestingly, there were physicians that identified the opposite and felt the system created less of a responsibility or obligation for them to respond. By knowing the context of the message, it gave them the ability to prioritize or ignore the message if they knew it was not life threatening.
[T]here's less of a responsibility or an obligation They get a message and then they can actually delay the process So in a way it actually allows us to kind of get away with some things and that happens because, you know, we're prioritizing something that we're doing as being more important to us. [MD01, physician]
Tactics to Improve Personal Productivity
The web‐based messaging system's triaging feature allows the sender of the message to indicate whether an issue is urgent or non‐urgent. Urgent issues result in an immediate e‐mail that is intended to elicit an immediate response. Some of the nurses, pharmacists, and social workers exploited features of the system to elicit immediate responses from the physicians for non‐urgent issues, including using their knowledge of the urgent and non‐urgent features of the system to interrupt the physicians.
I kind of cheat and don't use the system properly. So every message I send I always send it as urgent because I want it go to the smartphone. [AH01, pharmacist]
I like that if you know how to use the urgent and nonurgent features effectively it generally works quite well in getting a response in a timely fashion. [RN02, nurse]
One tactic that physicians perceived the nurses were using to elicit a response from them was to exaggerate the severity or urgency of the issue in their message.
Some details will be sort of cherry picked to make the issue sound very dire I'll give you a classic, like, high blood pressure and patient has a headache. So initially, you know, I have to think, does this patient have a hypertensive emergency? So by putting sort of history together in this way, that sort of suggestive way, then yeah. [MD03, physician]
The nurses, pharmacists. and social workers frequently exaggerated the urgency of their clinical messages at the end of their shifts in an effort to resolve outstanding issues immediately in order to avoid transferring tasks to another colleague or delaying them until the next day.
But in terms of a shift change, for example, I need a response now 'cause that is a lot of times where it is that although it's not clinically urgent it's time sensitive. So it is urgent. [RN02, nurse]
I do also notice that around changeover time, issues that have been sort of chronically or have preexisting, become urgent issues. [MD01, physician]
Messages were also sent inappropriately as urgent as a strategy to ensure the physician dealt with the issue promptly and did not forget to complete the requested task associated with the issue.
Everybody puts urgent because we want the response immediately. Otherwise, if you put nonurgent, the doctors will just drag and drag and will forget to respond to the issue. [RN09, nurse]
However, because physicians received context clarifying the urgency of the message, they were able to prioritize their tasks and defer less‐important issues without compromising patient safety or quality of care, allowing them to use their time more productively. This, however, did not always align with the sender's request.
I think the key thing is that the information coming to us is text and it describes the issue. So we can, at our end, then we can make a call as to what the priority is. [MD03, physician]
DISCUSSION
The purpose of this study was to evaluate a Web‐based messaging system and identify the unintended consequences observed with implementing HIT to improve clinical communication. This is an important study because healthcare organizations are beginning to develop strategies for improving clinical communication but believe the solution involves simply replacing pager technology. Support for this approach is seen with larger vendors in the smartphone and communication industry, who promote their products as pager‐replacement solutions and even help customers develop pager‐replacement strategies.[26, 27, 28] Simply replacing pagers with smartphones and sending text messages will have only a limited impact on improving clinical communication and will likely result in unintended negative consequences, as seen in this study.
Whereas the Web‐based messaging system was designed to reduce interruptions from clinical messaging, interruptions actually increased, although the mental burden of each interruption was likely lower because responding to a text message is less interruptive than finding a telephone to answer a page. A key contributor to this effect was a culture of accountability among nurses, pharmacists, and social workers who felt it was their professional obligation to notify physicians about all issues of concern. This belief and related behavior is aligned with the standards promoted by professional regulatory bodies that identify accountability as a vital practice expectation.[29] Nurses and nursing staff take responsibility for the care they provide and answer for their own judgments and actions.[30] The system eliminated many of the previous barriers to paging and provided a less‐personal form of communication. The cumulative and unexpected outcome was an increase of interruptions for physicians and the adoption of workarounds by all healthcare professionals to improve personal productivity. Although the system was built in an iterative fashion with frontline clinicians, it is likely that oversights in the design of the system also contributed to these problems, which speaks to the complexity of clinical communication. Centralizing communication to the team smartphone could have overburdened the physicians covering it at the time, causing them to ignore messages because they were too busy to address them.
There were limitations to this study. One limitation was that this study examined only a cross‐section of messaging activity at a given point in time, and therefore it may not be representative of the behaviors of the physicians, nurses, pharmacists, and social workers over time as the culture of the environment evolves and they adjust to the new technology. The pre‐implementation data were collected 2 years prior to the post‐implementation data, but it was necessary to use data this old because other interventions were implemented prior to the Web‐based messaging system, so baseline paging data were no longer available. Whereas most clinical disciplines were represented in the interviews, the sample included only 17 participants from 1 clinical service, so generalizability of the results may be limited.
Although the reliance on numeric paging technology was previously identified as a primary source of problems with communication, the real issues are much more complex. This study highlighted that many of the underlying obstacles relate to existing social interactions and habits of multiple professions working together. Failures in collaboration among healthcare professionals have a negative impact on health outcomes and routinely stem from the lack of explicit definitions of roles, the absence of clear leadership, insufficient time for team‐building, the us‐and‐them effects created by professional socialization, and frustration created by power and status differentials of each discipline.[31, 32, 33] Therefore, it is critical that healthcare organizations focus on the people and clinical processes when implementing technology to solve issues with clinical communication. These observations are consistent with other studies examining the unintended consequences caused by the sociotechnical aspects of HIT implementation, where workarounds to game the system were also employed.[21]
In summary, improving clinical communication cannot be achieved simply by replacing pagers with newer technology; it requires a fundamental shift in how healthcare professionals interact, with a focus on the sociotechnical aspects of HIT. As patient volumes and the complexity of care continue to increase, more effective methods for facilitating interprofessional communication and collaboration must be developed.
Acknowledgements
Disclosures: This study was funded in part by a Frederick Banting and Charles Best Canada Graduate Scholarship from the Canadian Institutes of Health Research. The authors report no conflicts of interest.
Clinical communication among healthcare providers to coordinate patient care is important, accounting for the majority of information exchanges in healthcare.[1, 2] Breakdowns in communication have therefore been identified as the major contributor to medical errors.[3, 4, 5]
There is a growing literature related to asynchronous clinical communication practices, or communication that does not occur at the same time in hospitals, and the limitations of using the traditional numeric pager. These include the inability to indicate the urgency of the message, frequent interruptions, contacting the wrong physician, and inefficiencies coordinating care across multiple disciplines and specialties.[6, 7, 8, 9, 10, 11, 12]
Hospitals have implemented a variety of health information technology (HIT) solutions to replace the numeric pager and address these clinical communication issues, including the use of alphanumeric pagers, smartphone devices, and Web‐based applications that allow clinicians to triage the urgency of issues.[13, 14, 15, 16] Although these solutions have resolved some of the deficiencies previously identified, issues relating to the impact on the interprofessional nature of healthcare remain unaddressed.[17] In some cases, the implementation of HIT has created unintended consequences that have an impact on effective communication.
One of the widely cited examples of HIT creating unintended consequences is the implementation of computerized physician order entry systems.[18, 19, 20] Other studies looking more broadly at patient information systems have identified problems caused by poor user interfaces that promoted errors in entry and retrieval of data, inflexible features forcing clinician workarounds, and technology designs that impeded clinical workflow.[21, 22, 23]
These observations suggest that although many of the issues with clinical communication stem from the reliance on numeric paging, simply replacing pagers with newer technology may not solve the problems and can in fact create other unintended consequences. These include unintended consequences resulting from the sociotechnical aspects of HIT, which is the interplay of technology with existing clinical workflow, culture, and social interactions.[21] Our institution recently implemented a Web‐based messaging system to replace the use of numeric pagers. We aimed to evaluate the unintended consequences resulting from the implementation of this system and to describe their impact on the delivery of clinical care on a general internal medicine (GIM) service.
METHODS
This was a pre‐post mixed‐methods study utilizing both quantitative and qualitative measures. We integrated these 2 data‐collection methods to improve the quality of the results. The study was conducted on the GIM service at the University Health Network Toronto Western Hospital site, a tertiary‐care academic teaching center fully affiliated with the University of Toronto (Toronto, Canada). The GIM service at Toronto Western Hospital consists of 4 clinical teams, each staffed by an attending physician, 3 to 4 residents, and 2 to 3 medical students.
Prior to this study, nonface‐to‐face communication on the wards was facilitated through numeric paging, where nurses, pharmacists, and social workers on the GIM wards would page residents to a hospital phone and wait for them to call back. Figures 1, 2, and 3 visualize the Web‐based messaging system we implemented at the University Health Network in May 2010. All residents on the service were provided smartphones that they used for communication. In addition to these, there was a dedicated team smartphone that acted as a central point of contact for the team 24 hours a day, 7 days a week and was carried by the physician covering the team at the time. The system allowed nurses, pharmacists, and social workers to triage the urgency of messages and include details providing context to the issue. Issues flagged as urgent were immediately sent to the team smartphone by e‐mail to alert the physician, who could respond from the smartphone. These messages could be forwarded to a team member, often the physician most familiar with the patient, to address. Issues flagged as nonurgent were posted to the system's message board, which the physicians accessed by logging into the Web‐based messaging system on a regular basis. The message board was designed to allow physicians to respond to multiple non‐urgent issues at once. To close the loop on communication, logic was developed so that if a physician did not respond to a non‐urgent message within the specified timeframe, the message was escalated and sent as an alerting e‐mail to the team smartphone every 15 minutes until it was addressed. The timeframes for responding varied from 1 hour to not needing a response until the next morning.
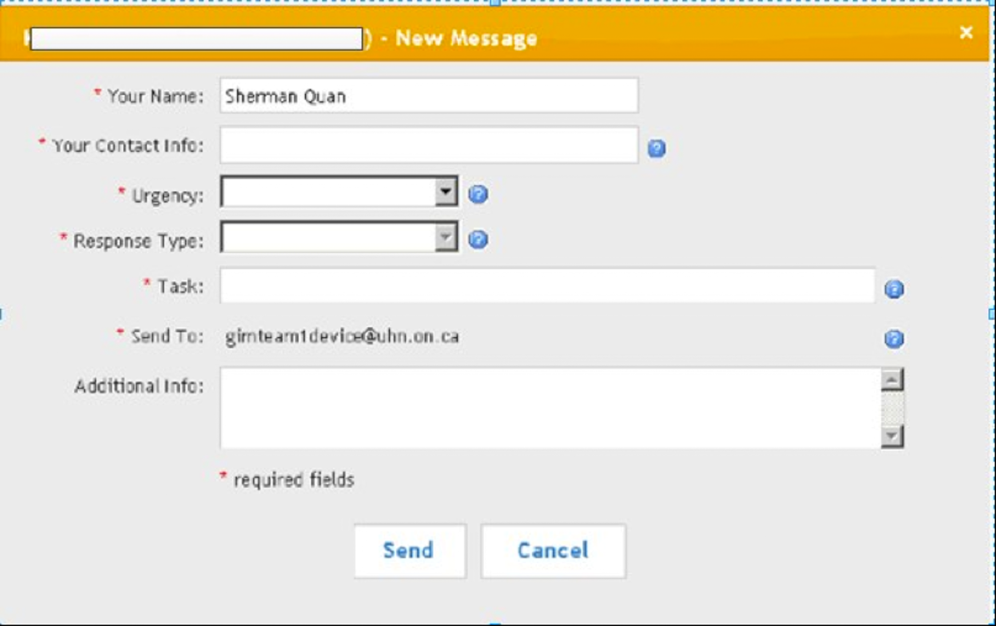
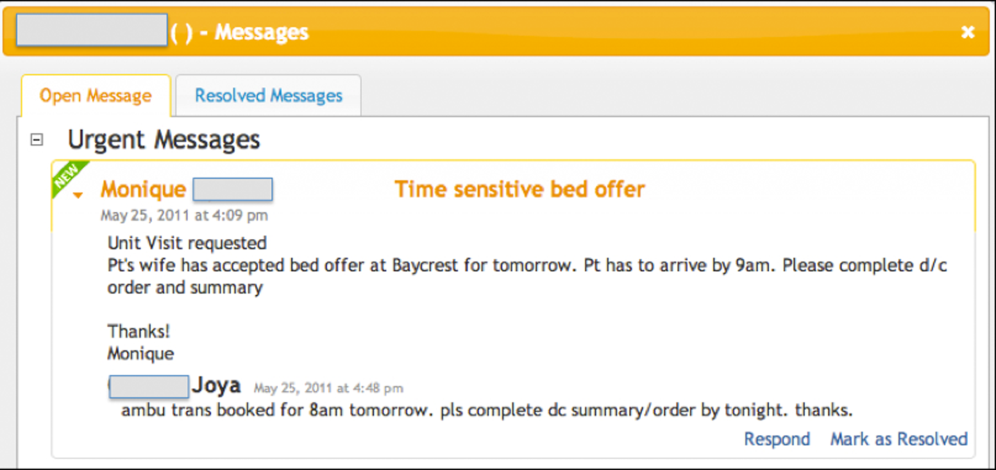
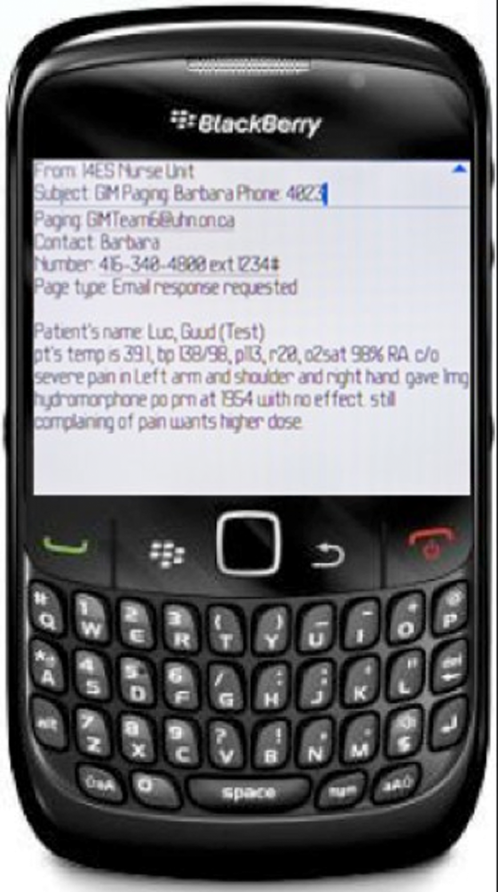
Ongoing training on the use of the system was built into the clinical orientation for the physician and nursing staff, as turnover in an academic teaching hospital is quite high. The orientation included instructions on how to use the features of the Web‐based messaging system but also provided guidelines on general etiquette with using the system to ensure sustainability of the communication process. For example, physicians were asked to check the system regularly, as the process worked only if they responded to messages. Nurses were asked not to send messages during scheduled educational sessions unless necessary and to limit messages they flagged as urgent to ones that were in fact urgent.
Our quantitative evaluation compared interruptions, which we define as communication that caused a medical resident to stop current activity to address, before and after the implementation of the Web‐based messaging system to assess the volume and time distribution of messages, and compared these results with our qualitative evaluation. For the pre‐implementation phase, interruptions were all numeric pages sent to all residents during the period of July 1427, 2008. For the post‐implementation phase, interruptions were the e‐mails sent directly to the team smartphones from the Web‐based messaging system to all residents during the period of October 1124, 2010. We excluded messages from the postimplementation phase if the same message was sent >10 times, typically indicating technical issues such as a malfunction of the smartphone causing the escalation process to continue.
Our qualitative evaluation consisted of semistructured interviews that were conducted after implementation. A research coordinator sent e‐mails to potential physician participants during a 1‐month rotation (n=16), and nurses (N=50), pharmacists (N=4), and social workers (N=4) from a representative ward inviting them to be part of this study. A set of open‐ended questions (see Supporting Information, Appendix A, in the online version of this article) developed based on informal feedback regarding the system provided by physicians, nurses, pharmacists, and social workers served as a guide to highlight key themes of interest. Based on the participants' responses, further questions were asked to drill down into more detail. Interviews were transcribed verbatim and anonymized.
The interview data were analyzed using thematic analysis to generate categories and overarching themes.[24, 25] Once the coding structure was developed, the transcripts were imported into qualitative analysis software (NVivo 9, QSR International) and then coded and analyzed, pulling the key themes that emerged from the text to be used in interpreting the data.
RESULTS
Our quantitative before‐after comparison of clinical messages sent to physicians revealed an increase in interruptions. We compared these results to the results of our interviews to understand why this might have occurred. Several key themes emerged from the analysis of the interviews, including increase in interruptions, accountability, and tactics to improve personal productivity. We interviewed 5 physicians, 8 nurses, 2 pharmacists, and 2 social workers.
Pre‐Post System Usage Data: Quantitative Assessment
Table 1 outlines the number of numeric pages sent during the pre‐implementation phase of July 1427, 2008. All pages sent immediately alerted the resident and so were all considered interruptions. Table 1 also outlines the number of urgent and escalation messages sent via e‐mail to the residents during the post‐implementation phase of October 1124, 2010. All messages were sent immediately to the team smartphone alerting the resident and so were all considered interruptions. During both timeframes, there were 15 resident physicians on service. During the pre‐implementation phase, 117 patients were admitted to the GIM service, and 162 patients were admitted during the post‐implementation phase.
| Numeric Paging (Predata) | Advance Communication System (Postdata) | ||
|---|---|---|---|
| Pages sent | 710 | Urgent | 951 |
| Interruptions | 710 | Escalations | 1245 |
| Interruptions per resident per day | 3 | Interruptions | 2196 |
| Interruptions per resident per day | 10 | ||
Table 1 shows that the number of interruptions in the pre‐implementation phase was 710 (3 per resident per day) compared with 2196 (10 per resident per day) in the post‐implementation phase, a 233% increase in interruptions. Because admissions were higher in the post‐implementation phase, it is possible that higher patient volumes could have contributed to the increase in interruptions.
Semi‐Structured Interviews: Qualitative Assessment
Increase in Interruptions
The intent of the web‐based messaging system was to reduce interruptions by triaging clinical messages and allowing healthcare professionals to respond to multiple non‐urgent issues at once. The unexpected result, however, was that the frequency at which physicians were interrupted actually increased following implementation.
I feel like I'm constantly bombarded with things Just psychologically I feel like it's harassing me a lot more than the pager used to. [MD02, physician]
Yes. Definitely, I'm paging them more frequently in general than I would have previously. [RN02, nurse]
Increased interruptions occurred in part because traditional barriers to paging, like having to wait by a phone for a response, were eliminated by the new system. Sending a message was easy, and with the reliability introduced through team‐based paging, there was greater temptation to send separate messages for singular issues.
I think [that] before, things were saved up and then paged and given all at once. And now it's, like, there's a temptation just to send things all the time, like, small issues. [AH01, pharmacist]
Communication also increased due to the impersonal nature of the electronic system. With many of the barriers to communicating removed, such as receiving immediate feedback regarding the appropriateness of a message, staff no longer hesitated when sending messages regarding less‐important issues.
So some stuff that you may have not wanted to call for before 'cause it's kind of silly, you can just send it information‐only. So they're aware 'cause the thing about with using electronics it's a lot more impersonal and indirect. [RN03, nurse]
At the same time, nurses, pharmacists, and social workers acknowledged that receiving all of this additional, sometimes unnecessary, information could be frustrating for the physicians. This recognition alone, however, was not sufficient to modify their behavior.
So I find that I can imagine for them it may be a little frustrating 'cause they're getting all these tidbits of information. [RN03, nurse]
I'm sure they get overwhelmed and I've had the feedback from the team They were saying that they were getting constantly paged, not by me, just by me, but by everybody. [AH01, pharmacist]
Accountability
As part of their professional practice, nurses described a medico‐legal obligation to inform physicians about relevant patient issues such as abnormal laboratory values. A culture of accountability, therefore, underpinned many of the actions taken by the nurses, reinforced because the electronic messages sent through the system were permanent and retrievable. The physicians also used the system as an electronic record of discussions that occurred.
Because it's just, like, this thing about accountability in terms of letting them know, that they are aware. [RN03, nurse]
And I think everything you do is recorded, like, you can go back and check, so there's that legal piece, which I guess covers you, in terms of time you called, those things which are critical, what you are calling for. [RN09, nurse]
'Cause I use it now as a reference. So even if I have a phone conversation with a nurse, based on a message that we've had, I will record what we said and send it. [MD03, physician]
Some of the more junior nurses periodically felt unsure or uncomfortable with clinical situations and would send a message to the physician to share their concerns. The messaging reassured the nurses and made them feel like they were fulfilling their professional responsibilities.
So a senior nurse could probably take a look at some situation and they can acknowledge whether the issue is urgent or nonurgent But from a novice perspective, as you're still learning it kind of gives you peace of mind and feels like you're filling your responsibility and accountability, that you're passing on the messages. [RN03, nurse]
Whereas nurses felt they were fulfilling their professional obligations, some physicians felt that nurses were using the system to absolve themselves of their clinical responsibilities.
Some just feel the need to send everything on there and maybe they feel that by sending it on here they absolve themselves of responsibility. [MD05, physician]
Other clinicians felt that the system created more of a responsibility or obligation for the physicians to respond. They believed the escalation feature of the system helped ensure the physicians responded in some fashion to close the loop.
[T]hey have the responsibility to answer it if it's an urgent message and because it keeps coming on to remind them. [AH02, social worker]
Interestingly, there were physicians that identified the opposite and felt the system created less of a responsibility or obligation for them to respond. By knowing the context of the message, it gave them the ability to prioritize or ignore the message if they knew it was not life threatening.
[T]here's less of a responsibility or an obligation They get a message and then they can actually delay the process So in a way it actually allows us to kind of get away with some things and that happens because, you know, we're prioritizing something that we're doing as being more important to us. [MD01, physician]
Tactics to Improve Personal Productivity
The web‐based messaging system's triaging feature allows the sender of the message to indicate whether an issue is urgent or non‐urgent. Urgent issues result in an immediate e‐mail that is intended to elicit an immediate response. Some of the nurses, pharmacists, and social workers exploited features of the system to elicit immediate responses from the physicians for non‐urgent issues, including using their knowledge of the urgent and non‐urgent features of the system to interrupt the physicians.
I kind of cheat and don't use the system properly. So every message I send I always send it as urgent because I want it go to the smartphone. [AH01, pharmacist]
I like that if you know how to use the urgent and nonurgent features effectively it generally works quite well in getting a response in a timely fashion. [RN02, nurse]
One tactic that physicians perceived the nurses were using to elicit a response from them was to exaggerate the severity or urgency of the issue in their message.
Some details will be sort of cherry picked to make the issue sound very dire I'll give you a classic, like, high blood pressure and patient has a headache. So initially, you know, I have to think, does this patient have a hypertensive emergency? So by putting sort of history together in this way, that sort of suggestive way, then yeah. [MD03, physician]
The nurses, pharmacists. and social workers frequently exaggerated the urgency of their clinical messages at the end of their shifts in an effort to resolve outstanding issues immediately in order to avoid transferring tasks to another colleague or delaying them until the next day.
But in terms of a shift change, for example, I need a response now 'cause that is a lot of times where it is that although it's not clinically urgent it's time sensitive. So it is urgent. [RN02, nurse]
I do also notice that around changeover time, issues that have been sort of chronically or have preexisting, become urgent issues. [MD01, physician]
Messages were also sent inappropriately as urgent as a strategy to ensure the physician dealt with the issue promptly and did not forget to complete the requested task associated with the issue.
Everybody puts urgent because we want the response immediately. Otherwise, if you put nonurgent, the doctors will just drag and drag and will forget to respond to the issue. [RN09, nurse]
However, because physicians received context clarifying the urgency of the message, they were able to prioritize their tasks and defer less‐important issues without compromising patient safety or quality of care, allowing them to use their time more productively. This, however, did not always align with the sender's request.
I think the key thing is that the information coming to us is text and it describes the issue. So we can, at our end, then we can make a call as to what the priority is. [MD03, physician]
DISCUSSION
The purpose of this study was to evaluate a Web‐based messaging system and identify the unintended consequences observed with implementing HIT to improve clinical communication. This is an important study because healthcare organizations are beginning to develop strategies for improving clinical communication but believe the solution involves simply replacing pager technology. Support for this approach is seen with larger vendors in the smartphone and communication industry, who promote their products as pager‐replacement solutions and even help customers develop pager‐replacement strategies.[26, 27, 28] Simply replacing pagers with smartphones and sending text messages will have only a limited impact on improving clinical communication and will likely result in unintended negative consequences, as seen in this study.
Whereas the Web‐based messaging system was designed to reduce interruptions from clinical messaging, interruptions actually increased, although the mental burden of each interruption was likely lower because responding to a text message is less interruptive than finding a telephone to answer a page. A key contributor to this effect was a culture of accountability among nurses, pharmacists, and social workers who felt it was their professional obligation to notify physicians about all issues of concern. This belief and related behavior is aligned with the standards promoted by professional regulatory bodies that identify accountability as a vital practice expectation.[29] Nurses and nursing staff take responsibility for the care they provide and answer for their own judgments and actions.[30] The system eliminated many of the previous barriers to paging and provided a less‐personal form of communication. The cumulative and unexpected outcome was an increase of interruptions for physicians and the adoption of workarounds by all healthcare professionals to improve personal productivity. Although the system was built in an iterative fashion with frontline clinicians, it is likely that oversights in the design of the system also contributed to these problems, which speaks to the complexity of clinical communication. Centralizing communication to the team smartphone could have overburdened the physicians covering it at the time, causing them to ignore messages because they were too busy to address them.
There were limitations to this study. One limitation was that this study examined only a cross‐section of messaging activity at a given point in time, and therefore it may not be representative of the behaviors of the physicians, nurses, pharmacists, and social workers over time as the culture of the environment evolves and they adjust to the new technology. The pre‐implementation data were collected 2 years prior to the post‐implementation data, but it was necessary to use data this old because other interventions were implemented prior to the Web‐based messaging system, so baseline paging data were no longer available. Whereas most clinical disciplines were represented in the interviews, the sample included only 17 participants from 1 clinical service, so generalizability of the results may be limited.
Although the reliance on numeric paging technology was previously identified as a primary source of problems with communication, the real issues are much more complex. This study highlighted that many of the underlying obstacles relate to existing social interactions and habits of multiple professions working together. Failures in collaboration among healthcare professionals have a negative impact on health outcomes and routinely stem from the lack of explicit definitions of roles, the absence of clear leadership, insufficient time for team‐building, the us‐and‐them effects created by professional socialization, and frustration created by power and status differentials of each discipline.[31, 32, 33] Therefore, it is critical that healthcare organizations focus on the people and clinical processes when implementing technology to solve issues with clinical communication. These observations are consistent with other studies examining the unintended consequences caused by the sociotechnical aspects of HIT implementation, where workarounds to game the system were also employed.[21]
In summary, improving clinical communication cannot be achieved simply by replacing pagers with newer technology; it requires a fundamental shift in how healthcare professionals interact, with a focus on the sociotechnical aspects of HIT. As patient volumes and the complexity of care continue to increase, more effective methods for facilitating interprofessional communication and collaboration must be developed.
Acknowledgements
Disclosures: This study was funded in part by a Frederick Banting and Charles Best Canada Graduate Scholarship from the Canadian Institutes of Health Research. The authors report no conflicts of interest.
- . When conversation is better than computation. J Am Med Inform Assoc. 2000;7(3):277–286.
- , , , et al. Synchronous communication facilitates interruptive workflow for attending physicians and nurses in clinical settings. Int J Med Inform. 2009;78(9):629–637.
- , , , et al. The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324(6):377–384.
- , , . Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186–194.
- The Joint Commission. Improving America's Hospitals: The Joint Commission's Annual Report on Quality and Safety. Oakbrook Terrace, IL: The Joint Commission; 2007. Available at: http://www.jointcommission.org/assets/1/6/2007_Annual_Report.pdf. Accessed on April 16, 2012.
- , . Residents' suggestions for reducing errors in teaching hospitals. N Engl J Med. 2003;348(9):851–855.
- , . Interruptions in healthcare: theoretical views. Int J Med Inform. 2009;78(5):293–307.
- , , , et al. Frequency and clinical importance of pages sent to the wrong physician. Arch Intern Med. 2009;169(11):1072–1073.
- , , , , . Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care. 2005;14(6):401–407.
- , , , , , . Towards safer interprofessional communication: Constructing a model of “utility” from preoperative team briefings. J Interprof Care. 2006;20(5):471–483.
- , , . Interprofessional collaboration: effects of practice‐based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009(3):CD000072.
- , . The effects of hands free communication devices on clinical communication: balancing communication access needs with user control. AMIA Annu Symp Proc. 2008;621–625.
- , , , , . Beyond paging: building a web‐based communication tool for nurses and physicians. J Gen Intern Med. 2009;24(1):105–110.
- , , , et al. The use of smartphones for clinical communication on internal medicine wards. J Hosp Med. 2010;5(9):553–559.
- , , , . Implementation and evaluation of an alpha‐numeric paging system on a resident inpatient teaching service. J Hosp Med. 2009;4(8):E34–E40.
- , , , et al. Effects of clinical communication interventions in hospitals: a systematic review of information and communication technology adoptions for improved communication between clinicians. Int J Med Inform. 2012;81(11):723–732.
- , , , et al. An evaluation of the use of smartphones to communicate between clinicians: a mixed‐methods study. J Med Internet Res. 2011;13(3):e59.
- , , . Computerized physician order entry in the critical care environment: a review of current literature. J Intensive Care Med. 2011;26(3):165–171.
- , , , et al. Factors contributing to an increase in duplicate medication order errors after CPOE implementation. J Am Med Inform Assoc. 2011;18(6):774–782.
- , , , et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293(10):1197–1203.
- , , . Unintended consequences of information technologies in health care—an interactive sociotechnical analysis. J Am Med Inform Assoc. 2007;14(5):542–549.
- . Why did that happen? Exploring the proliferation of barely usable software in healthcare systems. Qual Saf Health Care. 2006;(15 suppl 1):i76–i81.
- , , . Some unintended consequences of information technology in health care: the nature of patient care information system‐related errors. J Am Med Inform Assoc. 2004;11(2):104–112.
- , , . An overview of three different approaches to the interpretation of qualitative data. Part 1: Theoretical issues. Nurse Res. 2002;10(1):30–42.
- , . Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288.
- Research in Motion, Amcom Software. Six things hospitals need to know about replacing pagers with smartphones. Available at: http://us.blackberry.com/business/industry/healthcare/6ThingstoKnow_ReplacingHospitalPagers_WhitePaper.pdf. Accessed on April 16, 2012.
- Vocera, Wallace Wireless. The Longstreet Clinic: replacing pagers, supercharging communication with WIC pager. Available at: http://www.vocera.com/assets/pdf/case_studies/cs_longstreetclinic_0910_v1.pdf. Accessed on April 16, 2012.
- Amcom Software reports strong momentum with its new smartphone messaging and pager replacement solution [press release]. Minneapolis, MN: Amcom Software; September 29, 2010. Available at: http://www.amcomsoftware.com/News/09‐29‐10.aspx. Accessed on April 16, 2012.
- College of Nurses of Ontario. 2011 standards and guidelines. Availableat: http://www.cno.org/en/learn‐about‐standards‐guidelines/publications‐list/standards‐and‐guidelines. Accessed on April 16, 2012.
- , , . Accountability and responsibility: principle of nursing practice B. Nurs Stand. 2011;25(29):35–36.
- , , , , . The association between interdisciplinary collaboration and patient outcomes in a medical intensive care unit. Heart Lung. 1992;21(1):18–24.
- . Professionalization and socialization in interprofessional collaboration. In: Casto RM, Julia MC, eds. Interprofessional Care and Collaborative Practice. 1st ed. Independence, KY: Cengage Learning; 1994:23–31.
- , . Knowledge translation and interprofessional collaboration: where the rubber of evidence‐based care hits the road of teamwork. J Contin Educ Health Prof. 2006;26(1):46–54.
- . When conversation is better than computation. J Am Med Inform Assoc. 2000;7(3):277–286.
- , , , et al. Synchronous communication facilitates interruptive workflow for attending physicians and nurses in clinical settings. Int J Med Inform. 2009;78(9):629–637.
- , , , et al. The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324(6):377–384.
- , , . Communication failures: an insidious contributor to medical mishaps. Acad Med. 2004;79(2):186–194.
- The Joint Commission. Improving America's Hospitals: The Joint Commission's Annual Report on Quality and Safety. Oakbrook Terrace, IL: The Joint Commission; 2007. Available at: http://www.jointcommission.org/assets/1/6/2007_Annual_Report.pdf. Accessed on April 16, 2012.
- , . Residents' suggestions for reducing errors in teaching hospitals. N Engl J Med. 2003;348(9):851–855.
- , . Interruptions in healthcare: theoretical views. Int J Med Inform. 2009;78(5):293–307.
- , , , et al. Frequency and clinical importance of pages sent to the wrong physician. Arch Intern Med. 2009;169(11):1072–1073.
- , , , , . Communication failures in patient sign‐out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care. 2005;14(6):401–407.
- , , , , , . Towards safer interprofessional communication: Constructing a model of “utility” from preoperative team briefings. J Interprof Care. 2006;20(5):471–483.
- , , . Interprofessional collaboration: effects of practice‐based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2009(3):CD000072.
- , . The effects of hands free communication devices on clinical communication: balancing communication access needs with user control. AMIA Annu Symp Proc. 2008;621–625.
- , , , , . Beyond paging: building a web‐based communication tool for nurses and physicians. J Gen Intern Med. 2009;24(1):105–110.
- , , , et al. The use of smartphones for clinical communication on internal medicine wards. J Hosp Med. 2010;5(9):553–559.
- , , , . Implementation and evaluation of an alpha‐numeric paging system on a resident inpatient teaching service. J Hosp Med. 2009;4(8):E34–E40.
- , , , et al. Effects of clinical communication interventions in hospitals: a systematic review of information and communication technology adoptions for improved communication between clinicians. Int J Med Inform. 2012;81(11):723–732.
- , , , et al. An evaluation of the use of smartphones to communicate between clinicians: a mixed‐methods study. J Med Internet Res. 2011;13(3):e59.
- , , . Computerized physician order entry in the critical care environment: a review of current literature. J Intensive Care Med. 2011;26(3):165–171.
- , , , et al. Factors contributing to an increase in duplicate medication order errors after CPOE implementation. J Am Med Inform Assoc. 2011;18(6):774–782.
- , , , et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293(10):1197–1203.
- , , . Unintended consequences of information technologies in health care—an interactive sociotechnical analysis. J Am Med Inform Assoc. 2007;14(5):542–549.
- . Why did that happen? Exploring the proliferation of barely usable software in healthcare systems. Qual Saf Health Care. 2006;(15 suppl 1):i76–i81.
- , , . Some unintended consequences of information technology in health care: the nature of patient care information system‐related errors. J Am Med Inform Assoc. 2004;11(2):104–112.
- , , . An overview of three different approaches to the interpretation of qualitative data. Part 1: Theoretical issues. Nurse Res. 2002;10(1):30–42.
- , . Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288.
- Research in Motion, Amcom Software. Six things hospitals need to know about replacing pagers with smartphones. Available at: http://us.blackberry.com/business/industry/healthcare/6ThingstoKnow_ReplacingHospitalPagers_WhitePaper.pdf. Accessed on April 16, 2012.
- Vocera, Wallace Wireless. The Longstreet Clinic: replacing pagers, supercharging communication with WIC pager. Available at: http://www.vocera.com/assets/pdf/case_studies/cs_longstreetclinic_0910_v1.pdf. Accessed on April 16, 2012.
- Amcom Software reports strong momentum with its new smartphone messaging and pager replacement solution [press release]. Minneapolis, MN: Amcom Software; September 29, 2010. Available at: http://www.amcomsoftware.com/News/09‐29‐10.aspx. Accessed on April 16, 2012.
- College of Nurses of Ontario. 2011 standards and guidelines. Availableat: http://www.cno.org/en/learn‐about‐standards‐guidelines/publications‐list/standards‐and‐guidelines. Accessed on April 16, 2012.
- , , . Accountability and responsibility: principle of nursing practice B. Nurs Stand. 2011;25(29):35–36.
- , , , , . The association between interdisciplinary collaboration and patient outcomes in a medical intensive care unit. Heart Lung. 1992;21(1):18–24.
- . Professionalization and socialization in interprofessional collaboration. In: Casto RM, Julia MC, eds. Interprofessional Care and Collaborative Practice. 1st ed. Independence, KY: Cengage Learning; 1994:23–31.
- , . Knowledge translation and interprofessional collaboration: where the rubber of evidence‐based care hits the road of teamwork. J Contin Educ Health Prof. 2006;26(1):46–54.
Copyright © 2013 Society of Hospital Medicine
Acute Respiratory Failure Epidemiology
Acute respiratory failure (ARF), a common and serious complication in hospitalized patients, may be caused by several conditions including pneumonia, chronic obstructive pulmonary disease (COPD), adult respiratory distress syndrome (ARDS), and congestive heart failure (CHF). Although ARF is conventionally defined by an arterial oxygen tension of <60 mm Hg, an arterial carbon dioxide tension of >45 mm Hg, or both, these thresholds serve as a guide to be used in combination with history and clinical assessment of the patient.[1, 2] Supplemental oxygen and treatment of the underlying cause is the mainstay of therapy for ARF, but in severe cases patients are treated with invasive mechanical ventilation (IMV) or noninvasive ventilation (NIV). ARF is the most frequent reason for admission to the intensive care unit (ICU)[3, 4] and has an in‐hospital mortality rate of 33% to 37% among those who require IMV.[5, 6] The majority of epidemiologic studies of ARF have been limited to patients requiring mechanical ventilation or those admitted to the ICU, and information about the characteristics and outcomes of patients across the full spectrum of severity is much more limited.[5, 7, 8, 9, 10, 11] General improvements in the management of underlying conditions, implementation of more effective ventilation strategies,[12, 13] and increasing use of NIV[14, 15] may have led to better outcomes for patients with ARF, yet empirical evidence of a change in the adjusted mortality rate over time is lacking.
The objective of this study was to provide a broad characterization of the epidemiology of ARF among adults hospitalized in the United States using a large nationally representative database. We sought to evaluate whether incidence, mortality, cost, or ventilation practice associated with ARF in the United States changed over the period of 2001 to 2009.
METHODS
Data Source
We utilized data from the Nationwide Inpatient Sample (NIS) of the Health Care Cost and Utilization Project,[16] which is a 20% stratified probability sample of all US acute‐care hospitals each year. These data are drawn from a sampling frame that contains close to 95% of all discharges in the United States, with the hospital discharge record as the unit of analysis. The NIS has been used to study trends in many different diagnoses.[17, 18, 19] The database contains demographic information, payer information, principal and secondary diagnoses, cost, discharge disposition, and death during hospitalization. It also contains information on hospital characteristics including ownership, size, teaching status, and geographic region.
Definitions
We included patients 18 years old discharged between 2001 and 2009 with a primary or secondary diagnosis of ARF. We identified cases of ARF using diagnostic codes (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD‐9‐CM]) previously used in studies of acute organ dysfunction in sepsis (518.81, 518.82, 518.84, 518.4, 799.1, 786.09).[17, 20, 21] To define ARDS we relied on ICD‐9‐CM codes (518.4, 518.82, 518.5, 786.09) used in prior studies that showed good sensitivity and specificity.[22, 23] The use of ventilatory support was identified using the ICD‐9‐CM procedure codes[24] (93.90, 93.70, 93.71, 93.76). Comorbidities were classified using the Agency for Healthcare Research and Quality's (Rockville, MD) Healthcare Cost and Utilization Project's (HCUP) Comorbidity Software version 3.103.5.[25]
Outcomes
The primary outcomes included the annual number of hospitalizations, population incidence, hospital mortality, and costs of care. Secondary outcomes included length of stay, most common diagnoses associated with ARF, disposition at discharge, and use and type of ventilatory support.
Analysis
We estimated the number of hospitalizations with a diagnosis of ARF/year, and we calculated the weighted frequencies following HCUP‐NIS recommendations using SAS/STAT survey procedures. Using population estimates for the years 2001 to 2009 from the US Census Bureau, we employed direct standardization to calculate age‐, gender‐, and race‐adjusted population incidence and mortality rates of ARF per 100,000 population. Hospital mortality was defined as the ratio of ARF hospitalizations ending in death divided by total number of ARF hospitalizations. Mechanical ventilation rates and rates of selected comorbidities were similarly defined.
We employed indirect standardization to adjust hospital mortality rates for age, sex, race/ethnicity, comorbidities, and hospital characteristics using logistic regression models from 2001 to predict hospital mortality for 2002 to 2009. We used linear regression models to test whether the slope of year was significant for trends in outcomes overtime. Costs were calculated using hospital‐specific cost‐to‐charge ratios when available and a weighted group average at the state level for remaining hospitals. We converted all costs to 2009 US dollars using the Consumer Price Index. Costs and lengths of stay were not normally distributed, so we calculated weighted geometric means (the average of all logarithmic values), then converted back to a base‐10 number. Using a Taylor series expansion, we then calculated standard errors. All analyses were performed using SAS version 9.2 (SAS Institute, Inc., Cary, NC).
The Baystate Medical Center institutional review board determined that the project did not constitute human subjects research.
RESULTS
Hospitalization Trends
The number of hospitalizations with an ARF diagnosis code increased at an average annual rate of 11.3% from 1,007,549 (standard deviation [SD] = 19,268) in 2001 to 1,917,910 (SD = 47,558) in 2009. More than two‐thirds of ARF admissions were associated with medical, rather than surgical, conditions (69.5% in 2001 and 71.2% in 2009). The median age, racial make‐up, and gender did not change significantly. Over the study period we observed an increase in ARF‐related hospitalizations in large, urban, teaching hospitals and in hospitals located in the Midwest (Table 1).
| 2001 | 2003 | 2005 | 2007 | 2009 | |
|---|---|---|---|---|---|
| |||||
| Patient characteristics | |||||
| All, N (SD) | 1,007,549 (19,268) | 1,184,928 (25,542) | 1,288,594 (30,493) | 1,480,270 (32,002) | 1,917,910 (47,558) |
| Age, mean (SE), y | 66.6 (0.2) | 66.0 (0.2) | 66.1 (0.2) | 65.8 (0.2) | 65.8 (0.2) |
| Age group, % | |||||
| 1844 | 11.5 | 12.0 | 11.5 | 11.6 | 10.9 |
| 4564* | 26.7 | 28.9 | 29.6 | 30.7 | 31.7 |
| 6584* | 50.2 | 47.8 | 47.0 | 45.7 | 45.3 |
| 85+ | 11.5 | 11.4 | 11.9 | 12.0 | 12.1 |
| Male* | 48.1 | 48.2 | 48.6 | 49.3 | 49.2 |
| Race | |||||
| White | 75.8 | 71.9 | 76.5 | 71.8 | 73.4 |
| Black | 12.7 | 13.6 | 11.2 | 14.2 | 12.5 |
| Hispanic | 7.2 | 9.8 | 7.7 | 8.5 | 7.8 |
| Other | 4.2 | 4.7 | 4.7 | 5.5 | 6.3 |
| Primary ARF | 20.7 | 20.9 | 25.9 | 26.1 | 19.9 |
| Secondary ARF | 79.3 | 79.1 | 74.1 | 73.9 | 80.1 |
| Medical* | 69.5 | 69.1 | 69.9 | 70.2 | 71.2 |
| Surgical* | 30.5 | 30.8 | 30.1 | 29.8 | 28.8 |
| Hospital characteristics, % | |||||
| Number of beds | |||||
| Small | 10.0 | 10.1 | 10.5 | 10.8 | 11.3 |
| Medium | 25.2 | 25.3 | 24.6 | 24.0 | 22.7 |
| Large | 64.7 | 64.6 | 64.9 | 65.2 | 66.0 |
| Region | |||||
| South* | 18.5 | 18.5 | 17.6 | 17.0 | 16.3 |
| Midwest | 21.4 | 22.0 | 23.6 | 23.2 | 23.5 |
| Northeast | 42.6 | 41.7 | 41.4 | 42.2 | 42.1 |
| West* | 17.5 | 17.8 | 17.3 | 17.6 | 18.1 |
| Hospital type | |||||
| Rural | 13.6 | 13.0 | 11.8 | 11.0 | 10.8 |
| Urban nonteaching | 45.5 | 44.5 | 50.1 | 45.3 | 45.7 |
| Urban teaching | 40.9 | 42.5 | 38.1 | 43.7 | 43.6 |
| Patient outcomes | |||||
| Ventilation strategy | |||||
| IMV* | 48.5 | 48.4 | 47.5 | 46.5 | 42.1 |
| NIV* | 3.8 | 5.3 | 6.9 | 9.4 | 10.1 |
| IMV or NIV | 50.9 | 51.7 | 52.1 | 52.9 | 49.7 |
| Disposition | |||||
| Home/home healthcare* | 42.1 | 43.8 | 42.8 | 43.4 | 45.7 |
| Transfer to acute care | 5.2 | 4.7 | 4.6 | 4.6 | 4.4 |
| Nursing facility* | 24.4 | 24.9 | 27.4 | 28.6 | 29.0 |
| Other | 0.7 | 0.8 | 0.9 | 0.9 | 1.0 |
| Adjusted mortality, % (SE)* | 27.6 (0.3) | 26.4 (0.4) | 24.9 (0.4) | 22.7 (0.4) | 20.6 (0.3) |
| Adjusted mean, LOS/case, d (SE)* | 7.8 (0.1) | 7.9 (0.1) | 7.7 (0.1) | 7.5 (0.1) | 7.1 (0.1) |
| Adjusted mean cost/case, 2009 US$, (SE) | 15,818 (251) | 16,981 (419) | 17,236 (411) | 16,941 (436) | 15,987 (402) |
After adjusting for age and sex, the population incidence of ARF increased from 502 (standard error [SE] = 10) cases per 100,000 in 2001 to 784 (SE = 19) cases per 100,000 in 2009 (a 56% increase, P < 0.0001). Hispanics had the lowest rates of ARF, with both black and white groups having similar rates (Table 2).
| 2001 | 2003 | 2005 | 2007 | 2009 | |
|---|---|---|---|---|---|
| |||||
| All* | 502 (10) | 569 (12) | 595 (14) | 627 (14) | 784 (19) |
| Age group | |||||
| 1844* | 107 (3) | 130 (4) | 137 (4) | 153 (5) | 189 (6) |
| 4564* | 422 (9) | 500 (12) | 521 (13) | 580 (14) | 739 (19) |
| 6584* | 1697 (35) | 1863 (42) | 1950 (50) | 2066 (46) | 2578 (69) |
| 85+ | 3449 (86) | 3792 (106) | 3981 (120) | 3429 (97) | 4163 (123) |
| Sex | |||||
| Male* | 491 (10) | 553 (13) | 582 (14) | 629 (14) | 782 (20) |
| Female* | 512 (10) | 583 (12) | 607 (15) | 625 (13) | 786 (19) |
| Race/ethnicity | |||||
| White* | 398 (11) | 427 (12) | 466 (16) | 450 (13) | 699 (21) |
| Black* | 423 (27) | 513 (33) | 432 (26) | 574 (38) | 738 (37) |
| Hispanic* | 247 (24) | 381 (42) | 307 (27) | 353 (34) | 478 (42) |
| Other* | 268 (20) | 342 (29) | 347 (26) | 424 (29) | 713 (77) |
| In‐hospital mortality | 140 (3) | 148 (3) | 146 (3) | 140 (3) | 154 (4) |
The most common etiologies of ARF among medical patients were pneumonia, CHF, ARDS, COPD exacerbation, and sepsis. Over the 9‐year study, the proportion of cases secondary to pneumonia and sepsis rose significantly: from 39% to 46% and 13% to 21%, respectively (Figure 1).
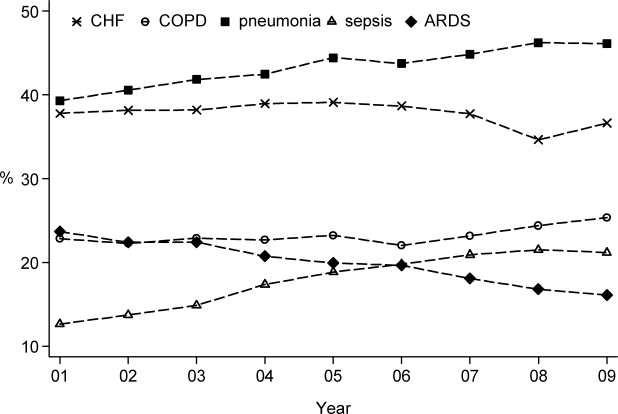
Mortality and Other Outcomes
The number of in‐hospital deaths related to ARF increased from 277,407 deaths in 2001 to 381,155 in 2009 (a 37% increase, P < 0.001). Standardized to the population, deaths increased from 140 in 2001 to 154 cases per 100,000 in 2009 (a 10% increase, P = 0.027). Despite slightly increasing mortality rates at a population level, adjusted in‐hospital mortality improved from 27.6% in 2001 to 20.6% in 2009 (P < 0.001). Mortality declined for both IMV and NIV patients from 35.3% in 2001 to 30.2% in 2009 and from 23.5% to 19%, respectively, but increased for those who required both NIV and IMV (from 26.9% in 2001 to 28% in 2009).
Adjusted hospital length of stay decreased from 7.8 days per patient in 2001 to 7.1 days in 2009 (P < 0.001), with a concomitant increase in discharges to nursing facilities, from 24% in 2001 to 29% in 2009. There was no linear trend in adjusted cost per case, with $15,818 in 2001 and $15,987 in 2009 (in 2009 US dollars) (Table 1).
Ventilation Practices
Overall, 50.9% patients received ventilatory support (NIV or IMV or both) in 2001 and 49.7% in 2009 (P= 0.25). The use of NIV increased from 3.8% to 10.1% (P < 0.001), a 169% increase, whereas the utilization of IMV decreased from 48.5% in 2001 to 42.1% in 2009 (P for trend < 0.0001), a 13% decrease. Uses of both NIV and IMV during hospitalization were seen in 1.4% of cases in 2001 and 2.5% of cases in 2009.
2009 Data Analysis
In 2009 the 1,917,910 hospitalizations with ARF resulted in 381,155 (SD = 8965) deaths and a total inpatient cost of $54 billion. The most common etiologies in patients over 65 years old were pneumonia, CHF, COPD, ARDS, and sepsis. In patients younger than 45 years the most frequent diagnoses were pneumonia, ARDS, sepsis, asthma, drug ingestion, and trauma. Stratified analysis by gender and by age groups showed that mortality rates among men were higher than for women and were highest in patients older than 85 years (Table 3).
| Disease | Total | Age <45 Years | 4565 Years | 6584 Years | 85+ Years | Male | Female |
|---|---|---|---|---|---|---|---|
| |||||||
| Medical | |||||||
| Total, N (%) | 1,364,624 (71.2) | 144,715 (10.6) | 416,922 (30.6) | 615,009 (45.1) | 187,977 (13.8) | 647,894 (47.5) | 716,635 (52.5) |
| Pneumonia, %* | 46.1 | 41.7 | 42.8 | 46.9 | 54.3 | 48.8 | 43.7 |
| CHF, %* | 36.6 | 10.4 | 27.3 | 43.6 | 54.8 | 35.0 | 38.1 |
| ARDS, %* | 16.1 | 22.9 | 16.2 | 14.5 | 15.9 | 15.5 | 16.7 |
| Sepsis, %* | 21.2 | 18.1 | 21.3 | 21.3 | 23.1 | 22.8 | 19.8 |
| COPD, %* | 25.4 | 4.2 | 25.6 | 32.3 | 18.3 | 25.0 | 25.7 |
| AMI, %* | 9.0 | 2.6 | 7.1 | 10.5 | 13.3 | 9.3 | 8.8 |
| Asthma, %* | 9.2 | 18.1 | 11.6 | 6.7 | 5.4 | 6.2 | 12.0 |
| Stroke, %* | 4.8 | 2.3 | 4.1 | 5.5 | 6.0 | 5.0 | 4.7 |
| Trauma or burns, %* | 3.4 | 5.4 | 2.9 | 3.0 | 4.1 | 4.3 | 2.5 |
| Cardiorespiratory arrest, %* | 4.1 | 3.9 | 4.4 | 4.1 | 3.8 | 4.6 | 3.7 |
| Drug, %* | 3.7 | 16.6 | 5.1 | 0.8 | 0.3 | 3.8 | 3.6 |
| IMV, %* | 37.7 | 54.6 | 43.7 | 33.5 | 24.8 | 41.1 | 34.5 |
| NIV, %* | 11.9 | 7.1 | 11.5 | 13.0 | 12.7 | 11.4 | 12.3 |
| In‐hospital mortality (CI) | 22 (21.322.7) | 12.9 (11.913.9) | 18.5 (17.619.4) | 23.9 (23.024.9) | 31.8 (30.633.1) | 24.2 (23.325.1) | 20.9 (20.121.7) |
| Surgical | |||||||
| Total, N (%) | 552971 (28.8) | 64983 (11.8) | 190225 (34.4) | 254336 (46) | 43426 (7.9) | 295660 (53.5) | 257287 (46.5) |
| Pneumonia, %* | 34.9 | 33.0 | 34.0 | 35.0 | 40.5 | 37.1 | 32.2 |
| CHF, %* | 27.2 | 8.9 | 21.7 | 33.3 | 42.6 | 26.7 | 27.7 |
| ARDS, %* | 45.5 | 51.5 | 45.2 | 44.7 | 42.7 | 45.0 | 46.1 |
| Sepsis, %* | 25.1 | 22.8 | 25.4 | 25.2 | 26.1 | 25.4 | 24.7 |
| COPD, %* | 8.2 | 1.1 | 7.4 | 10.8 | 7.5 | 8.3 | 8.1 |
| AMI, %* | 16.9 | 4.9 | 17.0 | 19.8 | 17.9 | 19.1 | 14.4 |
| Asthma, %* | 6.1 | 7.6 | 7.2 | 5.4 | 3.6 | 4.1 | 8.5 |
| Stroke, %* | 8.9 | 6.6 | 9.2 | 9.4 | 7.2 | 8.9 | 8.8 |
| Trauma or burns, %* | 12.2 | 26.5 | 9.6 | 9.2 | 20.3 | 13.8 | 10.4 |
| Cardiorespiratory arrest, %* | 5.5 | 4.4 | 6.0 | 5.4 | 5.2 | 6.1 | 4.7 |
| Drug, %* | 0.5 | 1.3 | 0.7 | 0.2 | 0.2 | 0.4 | 0.6 |
| IMV, %* | 52.9 | 57.1 | 54.3 | 51.3 | 50.0 | 54.5 | 51.0 |
| NIV, %* | 5.8 | 3.5 | 5.5 | 6.4 | 6.4 | 5.6 | 6.0 |
| In‐hospital mortality, % (CI) | 18.6 (17.819.5) | 10.7 (9.312.0) | 15.5 (14.216.8) | 20.8 (19.821.9) | 29.4 (27.831.1) | 19.0 (18.219.8) | 18.3 (17.319.2) |
When we examined ventilation practices among medical patients we found that patients older than 85 years, when compared to patients younger than 45 years, were less likely to be treated with IMV (25% vs 55%) and more likely to be treated with NIV (12.7% vs 7%). At the same time, the average cost per case was lowest among patients 85 years and older, and hospital costs per case fell sharply after age 70 years. Costs were considerably higher for those who did not survive during hospitalization, particularly for patients younger than 45 years (Figure 2).
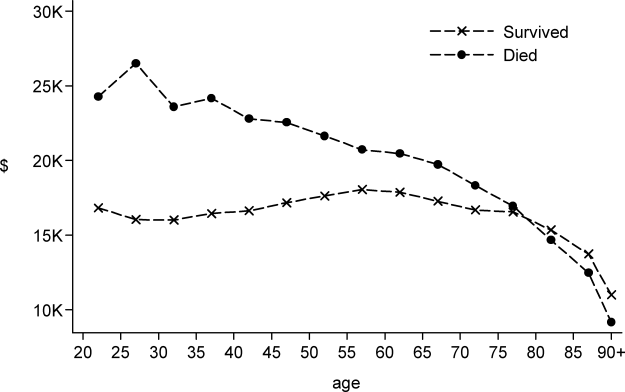
DISCUSSION
In this large population‐based study, we found that the number of hospitalizations associated with a diagnosis of ARF almost doubled over a 9‐year period. In 2009 there were nearly 2 million hospitalizations with ARF in the United States, resulting in approximately 380,000 deaths and inpatient costs of over $54 billion. The population‐adjusted ARF hospitalization rates increased in all age groups, and patients 85 years and older had the highest age‐specific hospitalization rate. Although overall rates of mechanical ventilation (NIV or IMV) remained stable over the 9‐year period, there was an important shift away from IMV (which decreased from 48% in 2001 to 42% in 2009) toward NIV (which increased from 4% in 2001 to 10% in 2009). Overall, there was a significant increase in the number of total deaths despite a decline in adjusted in‐hospital mortality rates. In‐hospital mortality rates decreased for all cases of ARF regardless of ventilation choice.
The findings of this study mirror results of others that have shown that although the incidence of critical care illnesses like sepsis[17, 20, 21, 26] and acute renal failure[27] has increased over the last decade, in‐hospital mortality rates have decreased.[20, 21, 28] Our results also compliment the results of a recent study that looked at hospitalizations for noncardiogenic ARF, which observed a 3.7‐fold increase in the number of cases and a steady decline in case fatality.[11]
Most prior studies addressing the incidence of ARF have included only patients receiving mechanical ventilation. In 1994, the estimated number of cases of ARF requiring IMV was 329,766,[9] which increased to 790,257 in 2005.[10] In our study we found that in 2009, the number of patients with ARF hospitalizations with IMV increased to 806,538. The increase in the overall number of cases with ARF was mainly driven by a surge in cases of sepsis and pneumonia. Our findings are consistent with national trends over time in noncardiogenic ARF[11] and in conditions that predispose patients to ARF such as sepsis[17, 20, 28] and acute renal failure.[27] As the number of claims for ARF doubled and the number of deaths increased, we found that adjusted hospital mortality improved from 27.6% in 2001 to 20.6% in 2009. This decline in hospital mortality was observed among all patients groups, regardless of ventilation choice. The decline in overall case fatality is consistent with prior findings in noncardiogenic ARF,[11] sepsis,[17, 28] and CHF.[29]
There are a number of potential explanations for the reduction in mortality observed over the study period, including improvements in hospital management of the underlying conditions leading to ARF, an increase in the proportion of patients being treated with NIV,[30] and advances in the care of critically ill patients such as the use of low‐tidal volume ventilation.[31, 32] Another contributor may be an increase in the proportion of discharges to nursing facilities, although this change in discharge disposition cannot fully explain our findings. For example, from 2007 to 2009, mortality decreased by 2 percentage points, and nursing home discharges increased by only 0.4 percentage points. Growth and aging of the US population only partially explain the increase we observed in the incidence of ARF, as age‐ and sex‐adjusted population rates increased by 56% from 2001 to 2009. In addition, the NIS captures data on hospital discharges and not individual patients; thus, a patient may have had multiple admissions. Over the last decade adoption of a more intensive practice style has been associated with improved in‐hospital mortality,[33, 34] and although these patients may be living longer they may have multiple readmissions.[35, 36]
We also observed that older patients were less likely to be treated with IMV, had a higher mortality rate, and less expensive care. These results are consistent with other studies and suggest that the intensity of treatment decreases with increasing age, and decisions to withhold or withdraw life‐supporting treatments are more frequent in the elderly.[26, 37] Prior research has shown that severity of illness is more important than age on patients' prognosis,[38, 39] and aggressive treatment strategies are not less cost‐effective when provided to older patients.[40]
Another important finding of this study is the marked increase in the use of NIV paired with a modest reduction in the use of IMV in the treatment of patients with ARF. This finding adds to evidence from other studies, which have similarly reported a dramatic increase in the use of NIV and a decrease in the use of IMV in patients with COPD as well as in ARF of other etiologies.[30, 41]
Our work has several limitations. First, we identified ARF based on ICD‐9‐CM codes and therefore cannot exclude disease misclassification. We did not find any studies in the literature addressing the accuracy and the completeness of ARF coding. However, we employed the same codes used to define ARF as has been used to define organ dysfunction in studies of severe sepsis,[17, 20] and the ICD‐9‐CM codes that we used to identify cases of ARDS have been used in prior studies.[11, 22, 23] Another limitation is that it is not clear to what extent the trends we observed may be due to changes over time in documentation and coding practices. Although this should be considered given the additional reimbursement associated with the diagnosis of ARF, our observation that rates of assisted ventilation have remained almost flat over the 9‐year period of the study suggest that would not wholly account for the rise in ARF. Second, because we did not have access to physiological data such as results of blood gas testing, we could not determine whether the threshold for applying the diagnosis of ARF or for delivering ventilatory support has changed over time. Third, for the purpose of this study we employed a broad definition of ARF, not limiting cases to those requiring mechanical ventilation, and this led to a more heterogeneous cohort including less severe cases of ARF. However, this is not dissimilar to the heterogeneity in disease severity observed among patients who receive a diagnosis of heart failure or acute renal failure. Fourth, survivors of ARF remain at high risk of death in the months after hospitalization,[42] but we assessed only in‐hospital mortality. It is possible that although in‐hospital mortality has improved, 30‐day mortality remained stable. Finally, as the NIS contains only discharge‐level data, we could not distinguish between patients admitted for ARF from those who developed ARF (potentially iatrogenic) after admission.
In summary, over the period of 2001 to 2009, there was a large increase in the number of patients given a diagnosis of ARF and a concomitant reduction in inpatient mortality. Although rates of mechanical ventilation remained relatively constant, there was a significant shift toward greater use of NIV at the expense of IMV.
Disclosures
Dr. Stefan is supported by KM1 CA156726 from the National Cancer Institute (NCI) and by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health (NIH), through grant UL1 RR025752. The work on this study was supported by a Charlton grant from Tufts University School of Medicine. Dr. Lindenauer and Dr. Pekow are supported by 1R18HL108810‐01 from the National Heart, Lung, and Blood Institute (NHLBI). The content of this publication is solely the responsibility of the authors and does not represent the official views of the NIH, NHLBI, or NCI.
All authors have read and approved the manuscript and none of them have any potential conflicts of interest to report.
Dr. Stefan had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Conception and design: Mihaela S. Stefan, Penelope S. Pekow, Michael B. Rothberg, Jay Steingrub, Peter K. Lindenauer; analysis and interpretation: Meng‐Shiou Shieh, Mihaela S. Stefan, Penelope S. Pekow, Michael B. Rothberg, Tara Lagu, Peter K. Lindenauer; drafting the manuscript for important intellectual content: Mihaela S. Stefan, Penelope S. Pekow, Michael B. Rothberg, Jay Steingrub, Tara Lagu, and Peter K. Lindenauer.
- , . Goldman's Cecil Medicine. 24th ed. Amsterdam, the Netherlands: Elsevier Inc.; 2012.
- , . Textbook of Respiratory Medicine. 5th ed. Philadelphia, PA: Saunders; 2010.
- , , . Epidemiology and outcome of acute respiratory failure in intensive care unit patients. Crit Care Med. 2003;31(4 suppl):S296–S299.
- , , , et al. Epidemiology of critical care syndromes, organ failures, and life‐support interventions in a suburban US community. Chest. 2011;140(6):1447–1455.
- , , , , . The changing epidemiology of mechanical ventilation: a population‐based study. J Intensive Care Med. 2006;21(3):173–182.
- , , , , . Mechanical ventilation in Ontario, 1992–2000: incidence, survival, and hospital bed utilization of noncardiac surgery adult patients. Crit Care Med. 2004;32(7):1504–1509.
- . Contributions to the epidemiology of acute respiratory failure. Crit Care. 2003;7(4):288–290.
- , , , et al. Incidence, severity, and mortality of acute respiratory failure in Berlin, Germany. Am J Respir Crit Care Med. 1995;151(4):1121–1125.
- . Acute respiratory failure in the United States: incidence and 31‐day survival. Chest. 2000;118(4):1100–1105.
- , , , , , . The epidemiology of mechanical ventilation use in the United States. Crit Care Med. 2010;38(10):1947–1953.
- , , , . Trends in the incidence of noncardiogenic acute respiratory failure: the role of race. Crit Care Med. 2012;40(5):1532–1538.
- , , , , . Secular trends in nosocomial infections and mortality associated with noninvasive ventilation in patients with exacerbation of COPD and pulmonary edema. JAMA. 2003;290(22):2985–2991.
- , , , et al. Association of noninvasive ventilation with nosocomial infections and survival in critically ill patients. JAMA. 2000;284(18):2361–2367.
- , , , , . Noninvasive versus conventional mechanical ventilation. An epidemiologic survey. Am J Respir Crit Care Med. 2001;163(4):874–880.
- , , , , , . Does noninvasive ventilation reduce the ICU nosocomial infection risk? A prospective clinical survey. Intensive Care Med. 1999;25(6):567–573.
- Heathcare Cost and Utilization Project (HCUP). Overview of the Nationwide Inpatient Sample. Available at: http://www.hcup‐us.ahrq.gov/nisoverview.jsp. Accessed December 6, 2011.
- , , , , , . Hospitalizations, costs, and outcomes of severe sepsis in the United States 2003 to 2007. Crit Care Med. 2011;40(3):754–761.
- , , , , . Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003–2009. JAMA. 2012;307(13):1405–1413.
- , , , , . Little evidence of correlation between growth in health care spending and reduced mortality. Health Aff (Millwood). 2010;29(8):1523–1531.
- , , , . The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–1554.
- , , , . Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003. Crit Care Med. 2007;35(5):1244–1250.
- , , . Risk factors for ARDS in the United States: analysis of the 1993 National Mortality Followback Study. Chest. 2001;119(4):1179–1184.
- , , , , , . Acute respiratory distress syndrome: estimated incidence and mortality rate in a 5 million‐person population base. Crit Care. 1998;2(1):29–34.
- , , . Validity of procedure codes in International Classification of Diseases, 9th Revision, Clinical Modification administrative data. Med Care. 2004;42(8):801–809.
- , , , . Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27.
- , . Epidemiology of sepsis: an update. Crit Care Med. 2001;29(7 suppl):S109–S116.
- , , , , , . Epidemiology and outcomes of acute renal failure in hospitalized patients: a national survey. Clin J Am Soc Nephrol. 2006;1(1):43–51.
- , , , . Facing the challenge: decreasing case fatality rates in severe sepsis despite increasing hospitalizations. Crit Care Med. 2005;33(11):2555–2562.
- , , , . National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries,1998–2008. JAMA. 2011;306(15):1669–1678.
- , , , et al. Outcomes of noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease in the United States, 1998–2008. Am J Respir Crit Care Med. 2011;185(2):152–159.
- , , , et al. A trial of goal‐oriented hemodynamic therapy in critically ill patients. SvO2 Collaborative Group. N Engl J Med. 1995;333(16):1025–1032.
- , . Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury. N Engl J Med. 2000;343(11):813; author reply 813–814.
- , , . Short‐ and long‐term survival of nonsurgical intensive care patients and its relation to diagnosis, severity of disease, age and comorbidities. Curr Aging Sci. 2009;2(3):240–248.
- , , , , , . The impact of COPD on management and outcomes of patients hospitalized with acute myocardial infarction—a ten‐year retrospective observational study. Chest. 2012;141(6):1441–1448.
- . The paradox of health. N Engl J Med. 1988;318(7):414–418.
- , , . Rehospitalizations among patients in the Medicare fee‐for‐service program. N Engl J Med. 2009;360(14):1418–1428.
- , , , et al. Outcomes and cost‐effectiveness of ventilator support and aggressive care for patients with acute respiratory failure due to pneumonia or acute respiratory distress syndrome. Am J Med. 2000;109(8):614–620.
- , , , et al. Older age, aggressiveness of care, and survival for seriously ill, hospitalized adults. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Ann Intern Med. 1999;131(10):721–728.
- , , , et al. Patient age and decisions to withhold life‐sustaining treatments from seriously ill, hospitalized adults. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. Ann Intern Med. 1999;130(2):116–125.
- , , , et al. Are aggressive treatment strategies less cost‐effective for older patients? The case of ventilator support and aggressive care for patients with acute respiratory failure. J Am Geriatr Soc. 2001;49(4):382–390.
- , . Utilization of non‐invasive ventilation in patients with acute respiratory failure from 2000–2009: a population‐based study. Am J Respir Crit Care Med. 2012;185:A6488.
- , , , et al. One‐year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;348(8):683–693.
Acute respiratory failure (ARF), a common and serious complication in hospitalized patients, may be caused by several conditions including pneumonia, chronic obstructive pulmonary disease (COPD), adult respiratory distress syndrome (ARDS), and congestive heart failure (CHF). Although ARF is conventionally defined by an arterial oxygen tension of <60 mm Hg, an arterial carbon dioxide tension of >45 mm Hg, or both, these thresholds serve as a guide to be used in combination with history and clinical assessment of the patient.[1, 2] Supplemental oxygen and treatment of the underlying cause is the mainstay of therapy for ARF, but in severe cases patients are treated with invasive mechanical ventilation (IMV) or noninvasive ventilation (NIV). ARF is the most frequent reason for admission to the intensive care unit (ICU)[3, 4] and has an in‐hospital mortality rate of 33% to 37% among those who require IMV.[5, 6] The majority of epidemiologic studies of ARF have been limited to patients requiring mechanical ventilation or those admitted to the ICU, and information about the characteristics and outcomes of patients across the full spectrum of severity is much more limited.[5, 7, 8, 9, 10, 11] General improvements in the management of underlying conditions, implementation of more effective ventilation strategies,[12, 13] and increasing use of NIV[14, 15] may have led to better outcomes for patients with ARF, yet empirical evidence of a change in the adjusted mortality rate over time is lacking.
The objective of this study was to provide a broad characterization of the epidemiology of ARF among adults hospitalized in the United States using a large nationally representative database. We sought to evaluate whether incidence, mortality, cost, or ventilation practice associated with ARF in the United States changed over the period of 2001 to 2009.
METHODS
Data Source
We utilized data from the Nationwide Inpatient Sample (NIS) of the Health Care Cost and Utilization Project,[16] which is a 20% stratified probability sample of all US acute‐care hospitals each year. These data are drawn from a sampling frame that contains close to 95% of all discharges in the United States, with the hospital discharge record as the unit of analysis. The NIS has been used to study trends in many different diagnoses.[17, 18, 19] The database contains demographic information, payer information, principal and secondary diagnoses, cost, discharge disposition, and death during hospitalization. It also contains information on hospital characteristics including ownership, size, teaching status, and geographic region.
Definitions
We included patients 18 years old discharged between 2001 and 2009 with a primary or secondary diagnosis of ARF. We identified cases of ARF using diagnostic codes (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD‐9‐CM]) previously used in studies of acute organ dysfunction in sepsis (518.81, 518.82, 518.84, 518.4, 799.1, 786.09).[17, 20, 21] To define ARDS we relied on ICD‐9‐CM codes (518.4, 518.82, 518.5, 786.09) used in prior studies that showed good sensitivity and specificity.[22, 23] The use of ventilatory support was identified using the ICD‐9‐CM procedure codes[24] (93.90, 93.70, 93.71, 93.76). Comorbidities were classified using the Agency for Healthcare Research and Quality's (Rockville, MD) Healthcare Cost and Utilization Project's (HCUP) Comorbidity Software version 3.103.5.[25]
Outcomes
The primary outcomes included the annual number of hospitalizations, population incidence, hospital mortality, and costs of care. Secondary outcomes included length of stay, most common diagnoses associated with ARF, disposition at discharge, and use and type of ventilatory support.
Analysis
We estimated the number of hospitalizations with a diagnosis of ARF/year, and we calculated the weighted frequencies following HCUP‐NIS recommendations using SAS/STAT survey procedures. Using population estimates for the years 2001 to 2009 from the US Census Bureau, we employed direct standardization to calculate age‐, gender‐, and race‐adjusted population incidence and mortality rates of ARF per 100,000 population. Hospital mortality was defined as the ratio of ARF hospitalizations ending in death divided by total number of ARF hospitalizations. Mechanical ventilation rates and rates of selected comorbidities were similarly defined.
We employed indirect standardization to adjust hospital mortality rates for age, sex, race/ethnicity, comorbidities, and hospital characteristics using logistic regression models from 2001 to predict hospital mortality for 2002 to 2009. We used linear regression models to test whether the slope of year was significant for trends in outcomes overtime. Costs were calculated using hospital‐specific cost‐to‐charge ratios when available and a weighted group average at the state level for remaining hospitals. We converted all costs to 2009 US dollars using the Consumer Price Index. Costs and lengths of stay were not normally distributed, so we calculated weighted geometric means (the average of all logarithmic values), then converted back to a base‐10 number. Using a Taylor series expansion, we then calculated standard errors. All analyses were performed using SAS version 9.2 (SAS Institute, Inc., Cary, NC).
The Baystate Medical Center institutional review board determined that the project did not constitute human subjects research.
RESULTS
Hospitalization Trends
The number of hospitalizations with an ARF diagnosis code increased at an average annual rate of 11.3% from 1,007,549 (standard deviation [SD] = 19,268) in 2001 to 1,917,910 (SD = 47,558) in 2009. More than two‐thirds of ARF admissions were associated with medical, rather than surgical, conditions (69.5% in 2001 and 71.2% in 2009). The median age, racial make‐up, and gender did not change significantly. Over the study period we observed an increase in ARF‐related hospitalizations in large, urban, teaching hospitals and in hospitals located in the Midwest (Table 1).
| 2001 | 2003 | 2005 | 2007 | 2009 | |
|---|---|---|---|---|---|
| |||||
| Patient characteristics | |||||
| All, N (SD) | 1,007,549 (19,268) | 1,184,928 (25,542) | 1,288,594 (30,493) | 1,480,270 (32,002) | 1,917,910 (47,558) |
| Age, mean (SE), y | 66.6 (0.2) | 66.0 (0.2) | 66.1 (0.2) | 65.8 (0.2) | 65.8 (0.2) |
| Age group, % | |||||
| 1844 | 11.5 | 12.0 | 11.5 | 11.6 | 10.9 |
| 4564* | 26.7 | 28.9 | 29.6 | 30.7 | 31.7 |
| 6584* | 50.2 | 47.8 | 47.0 | 45.7 | 45.3 |
| 85+ | 11.5 | 11.4 | 11.9 | 12.0 | 12.1 |
| Male* | 48.1 | 48.2 | 48.6 | 49.3 | 49.2 |
| Race | |||||
| White | 75.8 | 71.9 | 76.5 | 71.8 | 73.4 |
| Black | 12.7 | 13.6 | 11.2 | 14.2 | 12.5 |
| Hispanic | 7.2 | 9.8 | 7.7 | 8.5 | 7.8 |
| Other | 4.2 | 4.7 | 4.7 | 5.5 | 6.3 |
| Primary ARF | 20.7 | 20.9 | 25.9 | 26.1 | 19.9 |
| Secondary ARF | 79.3 | 79.1 | 74.1 | 73.9 | 80.1 |
| Medical* | 69.5 | 69.1 | 69.9 | 70.2 | 71.2 |
| Surgical* | 30.5 | 30.8 | 30.1 | 29.8 | 28.8 |
| Hospital characteristics, % | |||||
| Number of beds | |||||
| Small | 10.0 | 10.1 | 10.5 | 10.8 | 11.3 |
| Medium | 25.2 | 25.3 | 24.6 | 24.0 | 22.7 |
| Large | 64.7 | 64.6 | 64.9 | 65.2 | 66.0 |
| Region | |||||
| South* | 18.5 | 18.5 | 17.6 | 17.0 | 16.3 |
| Midwest | 21.4 | 22.0 | 23.6 | 23.2 | 23.5 |
| Northeast | 42.6 | 41.7 | 41.4 | 42.2 | 42.1 |
| West* | 17.5 | 17.8 | 17.3 | 17.6 | 18.1 |
| Hospital type | |||||
| Rural | 13.6 | 13.0 | 11.8 | 11.0 | 10.8 |
| Urban nonteaching | 45.5 | 44.5 | 50.1 | 45.3 | 45.7 |
| Urban teaching | 40.9 | 42.5 | 38.1 | 43.7 | 43.6 |
| Patient outcomes | |||||
| Ventilation strategy | |||||
| IMV* | 48.5 | 48.4 | 47.5 | 46.5 | 42.1 |
| NIV* | 3.8 | 5.3 | 6.9 | 9.4 | 10.1 |
| IMV or NIV | 50.9 | 51.7 | 52.1 | 52.9 | 49.7 |
| Disposition | |||||
| Home/home healthcare* | 42.1 | 43.8 | 42.8 | 43.4 | 45.7 |
| Transfer to acute care | 5.2 | 4.7 | 4.6 | 4.6 | 4.4 |
| Nursing facility* | 24.4 | 24.9 | 27.4 | 28.6 | 29.0 |
| Other | 0.7 | 0.8 | 0.9 | 0.9 | 1.0 |
| Adjusted mortality, % (SE)* | 27.6 (0.3) | 26.4 (0.4) | 24.9 (0.4) | 22.7 (0.4) | 20.6 (0.3) |
| Adjusted mean, LOS/case, d (SE)* | 7.8 (0.1) | 7.9 (0.1) | 7.7 (0.1) | 7.5 (0.1) | 7.1 (0.1) |
| Adjusted mean cost/case, 2009 US$, (SE) | 15,818 (251) | 16,981 (419) | 17,236 (411) | 16,941 (436) | 15,987 (402) |
After adjusting for age and sex, the population incidence of ARF increased from 502 (standard error [SE] = 10) cases per 100,000 in 2001 to 784 (SE = 19) cases per 100,000 in 2009 (a 56% increase, P < 0.0001). Hispanics had the lowest rates of ARF, with both black and white groups having similar rates (Table 2).
| 2001 | 2003 | 2005 | 2007 | 2009 | |
|---|---|---|---|---|---|
| |||||
| All* | 502 (10) | 569 (12) | 595 (14) | 627 (14) | 784 (19) |
| Age group | |||||
| 1844* | 107 (3) | 130 (4) | 137 (4) | 153 (5) | 189 (6) |
| 4564* | 422 (9) | 500 (12) | 521 (13) | 580 (14) | 739 (19) |
| 6584* | 1697 (35) | 1863 (42) | 1950 (50) | 2066 (46) | 2578 (69) |
| 85+ | 3449 (86) | 3792 (106) | 3981 (120) | 3429 (97) | 4163 (123) |
| Sex | |||||
| Male* | 491 (10) | 553 (13) | 582 (14) | 629 (14) | 782 (20) |
| Female* | 512 (10) | 583 (12) | 607 (15) | 625 (13) | 786 (19) |
| Race/ethnicity | |||||
| White* | 398 (11) | 427 (12) | 466 (16) | 450 (13) | 699 (21) |
| Black* | 423 (27) | 513 (33) | 432 (26) | 574 (38) | 738 (37) |
| Hispanic* | 247 (24) | 381 (42) | 307 (27) | 353 (34) | 478 (42) |
| Other* | 268 (20) | 342 (29) | 347 (26) | 424 (29) | 713 (77) |
| In‐hospital mortality | 140 (3) | 148 (3) | 146 (3) | 140 (3) | 154 (4) |
The most common etiologies of ARF among medical patients were pneumonia, CHF, ARDS, COPD exacerbation, and sepsis. Over the 9‐year study, the proportion of cases secondary to pneumonia and sepsis rose significantly: from 39% to 46% and 13% to 21%, respectively (Figure 1).
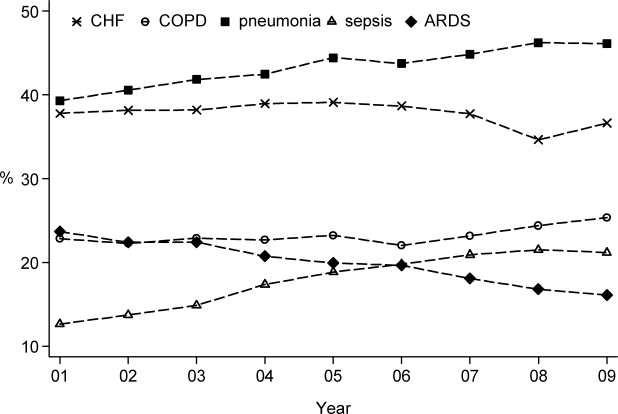
Mortality and Other Outcomes
The number of in‐hospital deaths related to ARF increased from 277,407 deaths in 2001 to 381,155 in 2009 (a 37% increase, P < 0.001). Standardized to the population, deaths increased from 140 in 2001 to 154 cases per 100,000 in 2009 (a 10% increase, P = 0.027). Despite slightly increasing mortality rates at a population level, adjusted in‐hospital mortality improved from 27.6% in 2001 to 20.6% in 2009 (P < 0.001). Mortality declined for both IMV and NIV patients from 35.3% in 2001 to 30.2% in 2009 and from 23.5% to 19%, respectively, but increased for those who required both NIV and IMV (from 26.9% in 2001 to 28% in 2009).
Adjusted hospital length of stay decreased from 7.8 days per patient in 2001 to 7.1 days in 2009 (P < 0.001), with a concomitant increase in discharges to nursing facilities, from 24% in 2001 to 29% in 2009. There was no linear trend in adjusted cost per case, with $15,818 in 2001 and $15,987 in 2009 (in 2009 US dollars) (Table 1).
Ventilation Practices
Overall, 50.9% patients received ventilatory support (NIV or IMV or both) in 2001 and 49.7% in 2009 (P= 0.25). The use of NIV increased from 3.8% to 10.1% (P < 0.001), a 169% increase, whereas the utilization of IMV decreased from 48.5% in 2001 to 42.1% in 2009 (P for trend < 0.0001), a 13% decrease. Uses of both NIV and IMV during hospitalization were seen in 1.4% of cases in 2001 and 2.5% of cases in 2009.
2009 Data Analysis
In 2009 the 1,917,910 hospitalizations with ARF resulted in 381,155 (SD = 8965) deaths and a total inpatient cost of $54 billion. The most common etiologies in patients over 65 years old were pneumonia, CHF, COPD, ARDS, and sepsis. In patients younger than 45 years the most frequent diagnoses were pneumonia, ARDS, sepsis, asthma, drug ingestion, and trauma. Stratified analysis by gender and by age groups showed that mortality rates among men were higher than for women and were highest in patients older than 85 years (Table 3).
| Disease | Total | Age <45 Years | 4565 Years | 6584 Years | 85+ Years | Male | Female |
|---|---|---|---|---|---|---|---|
| |||||||
| Medical | |||||||
| Total, N (%) | 1,364,624 (71.2) | 144,715 (10.6) | 416,922 (30.6) | 615,009 (45.1) | 187,977 (13.8) | 647,894 (47.5) | 716,635 (52.5) |
| Pneumonia, %* | 46.1 | 41.7 | 42.8 | 46.9 | 54.3 | 48.8 | 43.7 |
| CHF, %* | 36.6 | 10.4 | 27.3 | 43.6 | 54.8 | 35.0 | 38.1 |
| ARDS, %* | 16.1 | 22.9 | 16.2 | 14.5 | 15.9 | 15.5 | 16.7 |
| Sepsis, %* | 21.2 | 18.1 | 21.3 | 21.3 | 23.1 | 22.8 | 19.8 |
| COPD, %* | 25.4 | 4.2 | 25.6 | 32.3 | 18.3 | 25.0 | 25.7 |
| AMI, %* | 9.0 | 2.6 | 7.1 | 10.5 | 13.3 | 9.3 | 8.8 |
| Asthma, %* | 9.2 | 18.1 | 11.6 | 6.7 | 5.4 | 6.2 | 12.0 |
| Stroke, %* | 4.8 | 2.3 | 4.1 | 5.5 | 6.0 | 5.0 | 4.7 |
| Trauma or burns, %* | 3.4 | 5.4 | 2.9 | 3.0 | 4.1 | 4.3 | 2.5 |
| Cardiorespiratory arrest, %* | 4.1 | 3.9 | 4.4 | 4.1 | 3.8 | 4.6 | 3.7 |
| Drug, %* | 3.7 | 16.6 | 5.1 | 0.8 | 0.3 | 3.8 | 3.6 |
| IMV, %* | 37.7 | 54.6 | 43.7 | 33.5 | 24.8 | 41.1 | 34.5 |
| NIV, %* | 11.9 | 7.1 | 11.5 | 13.0 | 12.7 | 11.4 | 12.3 |
| In‐hospital mortality (CI) | 22 (21.322.7) | 12.9 (11.913.9) | 18.5 (17.619.4) | 23.9 (23.024.9) | 31.8 (30.633.1) | 24.2 (23.325.1) | 20.9 (20.121.7) |
| Surgical | |||||||
| Total, N (%) | 552971 (28.8) | 64983 (11.8) | 190225 (34.4) | 254336 (46) | 43426 (7.9) | 295660 (53.5) | 257287 (46.5) |
| Pneumonia, %* | 34.9 | 33.0 | 34.0 | 35.0 | 40.5 | 37.1 | 32.2 |
| CHF, %* | 27.2 | 8.9 | 21.7 | 33.3 | 42.6 | 26.7 | 27.7 |
| ARDS, %* | 45.5 | 51.5 | 45.2 | 44.7 | 42.7 | 45.0 | 46.1 |
| Sepsis, %* | 25.1 | 22.8 | 25.4 | 25.2 | 26.1 | 25.4 | 24.7 |
| COPD, %* | 8.2 | 1.1 | 7.4 | 10.8 | 7.5 | 8.3 | 8.1 |
| AMI, %* | 16.9 | 4.9 | 17.0 | 19.8 | 17.9 | 19.1 | 14.4 |
| Asthma, %* | 6.1 | 7.6 | 7.2 | 5.4 | 3.6 | 4.1 | 8.5 |
| Stroke, %* | 8.9 | 6.6 | 9.2 | 9.4 | 7.2 | 8.9 | 8.8 |
| Trauma or burns, %* | 12.2 | 26.5 | 9.6 | 9.2 | 20.3 | 13.8 | 10.4 |
| Cardiorespiratory arrest, %* | 5.5 | 4.4 | 6.0 | 5.4 | 5.2 | 6.1 | 4.7 |
| Drug, %* | 0.5 | 1.3 | 0.7 | 0.2 | 0.2 | 0.4 | 0.6 |
| IMV, %* | 52.9 | 57.1 | 54.3 | 51.3 | 50.0 | 54.5 | 51.0 |
| NIV, %* | 5.8 | 3.5 | 5.5 | 6.4 | 6.4 | 5.6 | 6.0 |
| In‐hospital mortality, % (CI) | 18.6 (17.819.5) | 10.7 (9.312.0) | 15.5 (14.216.8) | 20.8 (19.821.9) | 29.4 (27.831.1) | 19.0 (18.219.8) | 18.3 (17.319.2) |
When we examined ventilation practices among medical patients we found that patients older than 85 years, when compared to patients younger than 45 years, were less likely to be treated with IMV (25% vs 55%) and more likely to be treated with NIV (12.7% vs 7%). At the same time, the average cost per case was lowest among patients 85 years and older, and hospital costs per case fell sharply after age 70 years. Costs were considerably higher for those who did not survive during hospitalization, particularly for patients younger than 45 years (Figure 2).
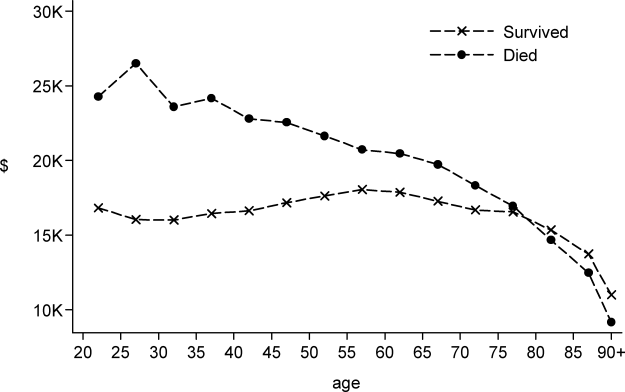
DISCUSSION
In this large population‐based study, we found that the number of hospitalizations associated with a diagnosis of ARF almost doubled over a 9‐year period. In 2009 there were nearly 2 million hospitalizations with ARF in the United States, resulting in approximately 380,000 deaths and inpatient costs of over $54 billion. The population‐adjusted ARF hospitalization rates increased in all age groups, and patients 85 years and older had the highest age‐specific hospitalization rate. Although overall rates of mechanical ventilation (NIV or IMV) remained stable over the 9‐year period, there was an important shift away from IMV (which decreased from 48% in 2001 to 42% in 2009) toward NIV (which increased from 4% in 2001 to 10% in 2009). Overall, there was a significant increase in the number of total deaths despite a decline in adjusted in‐hospital mortality rates. In‐hospital mortality rates decreased for all cases of ARF regardless of ventilation choice.
The findings of this study mirror results of others that have shown that although the incidence of critical care illnesses like sepsis[17, 20, 21, 26] and acute renal failure[27] has increased over the last decade, in‐hospital mortality rates have decreased.[20, 21, 28] Our results also compliment the results of a recent study that looked at hospitalizations for noncardiogenic ARF, which observed a 3.7‐fold increase in the number of cases and a steady decline in case fatality.[11]
Most prior studies addressing the incidence of ARF have included only patients receiving mechanical ventilation. In 1994, the estimated number of cases of ARF requiring IMV was 329,766,[9] which increased to 790,257 in 2005.[10] In our study we found that in 2009, the number of patients with ARF hospitalizations with IMV increased to 806,538. The increase in the overall number of cases with ARF was mainly driven by a surge in cases of sepsis and pneumonia. Our findings are consistent with national trends over time in noncardiogenic ARF[11] and in conditions that predispose patients to ARF such as sepsis[17, 20, 28] and acute renal failure.[27] As the number of claims for ARF doubled and the number of deaths increased, we found that adjusted hospital mortality improved from 27.6% in 2001 to 20.6% in 2009. This decline in hospital mortality was observed among all patients groups, regardless of ventilation choice. The decline in overall case fatality is consistent with prior findings in noncardiogenic ARF,[11] sepsis,[17, 28] and CHF.[29]
There are a number of potential explanations for the reduction in mortality observed over the study period, including improvements in hospital management of the underlying conditions leading to ARF, an increase in the proportion of patients being treated with NIV,[30] and advances in the care of critically ill patients such as the use of low‐tidal volume ventilation.[31, 32] Another contributor may be an increase in the proportion of discharges to nursing facilities, although this change in discharge disposition cannot fully explain our findings. For example, from 2007 to 2009, mortality decreased by 2 percentage points, and nursing home discharges increased by only 0.4 percentage points. Growth and aging of the US population only partially explain the increase we observed in the incidence of ARF, as age‐ and sex‐adjusted population rates increased by 56% from 2001 to 2009. In addition, the NIS captures data on hospital discharges and not individual patients; thus, a patient may have had multiple admissions. Over the last decade adoption of a more intensive practice style has been associated with improved in‐hospital mortality,[33, 34] and although these patients may be living longer they may have multiple readmissions.[35, 36]
We also observed that older patients were less likely to be treated with IMV, had a higher mortality rate, and less expensive care. These results are consistent with other studies and suggest that the intensity of treatment decreases with increasing age, and decisions to withhold or withdraw life‐supporting treatments are more frequent in the elderly.[26, 37] Prior research has shown that severity of illness is more important than age on patients' prognosis,[38, 39] and aggressive treatment strategies are not less cost‐effective when provided to older patients.[40]
Another important finding of this study is the marked increase in the use of NIV paired with a modest reduction in the use of IMV in the treatment of patients with ARF. This finding adds to evidence from other studies, which have similarly reported a dramatic increase in the use of NIV and a decrease in the use of IMV in patients with COPD as well as in ARF of other etiologies.[30, 41]
Our work has several limitations. First, we identified ARF based on ICD‐9‐CM codes and therefore cannot exclude disease misclassification. We did not find any studies in the literature addressing the accuracy and the completeness of ARF coding. However, we employed the same codes used to define ARF as has been used to define organ dysfunction in studies of severe sepsis,[17, 20] and the ICD‐9‐CM codes that we used to identify cases of ARDS have been used in prior studies.[11, 22, 23] Another limitation is that it is not clear to what extent the trends we observed may be due to changes over time in documentation and coding practices. Although this should be considered given the additional reimbursement associated with the diagnosis of ARF, our observation that rates of assisted ventilation have remained almost flat over the 9‐year period of the study suggest that would not wholly account for the rise in ARF. Second, because we did not have access to physiological data such as results of blood gas testing, we could not determine whether the threshold for applying the diagnosis of ARF or for delivering ventilatory support has changed over time. Third, for the purpose of this study we employed a broad definition of ARF, not limiting cases to those requiring mechanical ventilation, and this led to a more heterogeneous cohort including less severe cases of ARF. However, this is not dissimilar to the heterogeneity in disease severity observed among patients who receive a diagnosis of heart failure or acute renal failure. Fourth, survivors of ARF remain at high risk of death in the months after hospitalization,[42] but we assessed only in‐hospital mortality. It is possible that although in‐hospital mortality has improved, 30‐day mortality remained stable. Finally, as the NIS contains only discharge‐level data, we could not distinguish between patients admitted for ARF from those who developed ARF (potentially iatrogenic) after admission.
In summary, over the period of 2001 to 2009, there was a large increase in the number of patients given a diagnosis of ARF and a concomitant reduction in inpatient mortality. Although rates of mechanical ventilation remained relatively constant, there was a significant shift toward greater use of NIV at the expense of IMV.
Disclosures
Dr. Stefan is supported by KM1 CA156726 from the National Cancer Institute (NCI) and by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health (NIH), through grant UL1 RR025752. The work on this study was supported by a Charlton grant from Tufts University School of Medicine. Dr. Lindenauer and Dr. Pekow are supported by 1R18HL108810‐01 from the National Heart, Lung, and Blood Institute (NHLBI). The content of this publication is solely the responsibility of the authors and does not represent the official views of the NIH, NHLBI, or NCI.
All authors have read and approved the manuscript and none of them have any potential conflicts of interest to report.
Dr. Stefan had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Conception and design: Mihaela S. Stefan, Penelope S. Pekow, Michael B. Rothberg, Jay Steingrub, Peter K. Lindenauer; analysis and interpretation: Meng‐Shiou Shieh, Mihaela S. Stefan, Penelope S. Pekow, Michael B. Rothberg, Tara Lagu, Peter K. Lindenauer; drafting the manuscript for important intellectual content: Mihaela S. Stefan, Penelope S. Pekow, Michael B. Rothberg, Jay Steingrub, Tara Lagu, and Peter K. Lindenauer.
Acute respiratory failure (ARF), a common and serious complication in hospitalized patients, may be caused by several conditions including pneumonia, chronic obstructive pulmonary disease (COPD), adult respiratory distress syndrome (ARDS), and congestive heart failure (CHF). Although ARF is conventionally defined by an arterial oxygen tension of <60 mm Hg, an arterial carbon dioxide tension of >45 mm Hg, or both, these thresholds serve as a guide to be used in combination with history and clinical assessment of the patient.[1, 2] Supplemental oxygen and treatment of the underlying cause is the mainstay of therapy for ARF, but in severe cases patients are treated with invasive mechanical ventilation (IMV) or noninvasive ventilation (NIV). ARF is the most frequent reason for admission to the intensive care unit (ICU)[3, 4] and has an in‐hospital mortality rate of 33% to 37% among those who require IMV.[5, 6] The majority of epidemiologic studies of ARF have been limited to patients requiring mechanical ventilation or those admitted to the ICU, and information about the characteristics and outcomes of patients across the full spectrum of severity is much more limited.[5, 7, 8, 9, 10, 11] General improvements in the management of underlying conditions, implementation of more effective ventilation strategies,[12, 13] and increasing use of NIV[14, 15] may have led to better outcomes for patients with ARF, yet empirical evidence of a change in the adjusted mortality rate over time is lacking.
The objective of this study was to provide a broad characterization of the epidemiology of ARF among adults hospitalized in the United States using a large nationally representative database. We sought to evaluate whether incidence, mortality, cost, or ventilation practice associated with ARF in the United States changed over the period of 2001 to 2009.
METHODS
Data Source
We utilized data from the Nationwide Inpatient Sample (NIS) of the Health Care Cost and Utilization Project,[16] which is a 20% stratified probability sample of all US acute‐care hospitals each year. These data are drawn from a sampling frame that contains close to 95% of all discharges in the United States, with the hospital discharge record as the unit of analysis. The NIS has been used to study trends in many different diagnoses.[17, 18, 19] The database contains demographic information, payer information, principal and secondary diagnoses, cost, discharge disposition, and death during hospitalization. It also contains information on hospital characteristics including ownership, size, teaching status, and geographic region.
Definitions
We included patients 18 years old discharged between 2001 and 2009 with a primary or secondary diagnosis of ARF. We identified cases of ARF using diagnostic codes (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD‐9‐CM]) previously used in studies of acute organ dysfunction in sepsis (518.81, 518.82, 518.84, 518.4, 799.1, 786.09).[17, 20, 21] To define ARDS we relied on ICD‐9‐CM codes (518.4, 518.82, 518.5, 786.09) used in prior studies that showed good sensitivity and specificity.[22, 23] The use of ventilatory support was identified using the ICD‐9‐CM procedure codes[24] (93.90, 93.70, 93.71, 93.76). Comorbidities were classified using the Agency for Healthcare Research and Quality's (Rockville, MD) Healthcare Cost and Utilization Project's (HCUP) Comorbidity Software version 3.103.5.[25]
Outcomes
The primary outcomes included the annual number of hospitalizations, population incidence, hospital mortality, and costs of care. Secondary outcomes included length of stay, most common diagnoses associated with ARF, disposition at discharge, and use and type of ventilatory support.
Analysis
We estimated the number of hospitalizations with a diagnosis of ARF/year, and we calculated the weighted frequencies following HCUP‐NIS recommendations using SAS/STAT survey procedures. Using population estimates for the years 2001 to 2009 from the US Census Bureau, we employed direct standardization to calculate age‐, gender‐, and race‐adjusted population incidence and mortality rates of ARF per 100,000 population. Hospital mortality was defined as the ratio of ARF hospitalizations ending in death divided by total number of ARF hospitalizations. Mechanical ventilation rates and rates of selected comorbidities were similarly defined.
We employed indirect standardization to adjust hospital mortality rates for age, sex, race/ethnicity, comorbidities, and hospital characteristics using logistic regression models from 2001 to predict hospital mortality for 2002 to 2009. We used linear regression models to test whether the slope of year was significant for trends in outcomes overtime. Costs were calculated using hospital‐specific cost‐to‐charge ratios when available and a weighted group average at the state level for remaining hospitals. We converted all costs to 2009 US dollars using the Consumer Price Index. Costs and lengths of stay were not normally distributed, so we calculated weighted geometric means (the average of all logarithmic values), then converted back to a base‐10 number. Using a Taylor series expansion, we then calculated standard errors. All analyses were performed using SAS version 9.2 (SAS Institute, Inc., Cary, NC).
The Baystate Medical Center institutional review board determined that the project did not constitute human subjects research.
RESULTS
Hospitalization Trends
The number of hospitalizations with an ARF diagnosis code increased at an average annual rate of 11.3% from 1,007,549 (standard deviation [SD] = 19,268) in 2001 to 1,917,910 (SD = 47,558) in 2009. More than two‐thirds of ARF admissions were associated with medical, rather than surgical, conditions (69.5% in 2001 and 71.2% in 2009). The median age, racial make‐up, and gender did not change significantly. Over the study period we observed an increase in ARF‐related hospitalizations in large, urban, teaching hospitals and in hospitals located in the Midwest (Table 1).
| 2001 | 2003 | 2005 | 2007 | 2009 | |
|---|---|---|---|---|---|
| |||||
| Patient characteristics | |||||
| All, N (SD) | 1,007,549 (19,268) | 1,184,928 (25,542) | 1,288,594 (30,493) | 1,480,270 (32,002) | 1,917,910 (47,558) |
| Age, mean (SE), y | 66.6 (0.2) | 66.0 (0.2) | 66.1 (0.2) | 65.8 (0.2) | 65.8 (0.2) |
| Age group, % | |||||
| 1844 | 11.5 | 12.0 | 11.5 | 11.6 | 10.9 |
| 4564* | 26.7 | 28.9 | 29.6 | 30.7 | 31.7 |
| 6584* | 50.2 | 47.8 | 47.0 | 45.7 | 45.3 |
| 85+ | 11.5 | 11.4 | 11.9 | 12.0 | 12.1 |
| Male* | 48.1 | 48.2 | 48.6 | 49.3 | 49.2 |
| Race | |||||
| White | 75.8 | 71.9 | 76.5 | 71.8 | 73.4 |
| Black | 12.7 | 13.6 | 11.2 | 14.2 | 12.5 |
| Hispanic | 7.2 | 9.8 | 7.7 | 8.5 | 7.8 |
| Other | 4.2 | 4.7 | 4.7 | 5.5 | 6.3 |
| Primary ARF | 20.7 | 20.9 | 25.9 | 26.1 | 19.9 |
| Secondary ARF | 79.3 | 79.1 | 74.1 | 73.9 | 80.1 |
| Medical* | 69.5 | 69.1 | 69.9 | 70.2 | 71.2 |
| Surgical* | 30.5 | 30.8 | 30.1 | 29.8 | 28.8 |
| Hospital characteristics, % | |||||
| Number of beds | |||||
| Small | 10.0 | 10.1 | 10.5 | 10.8 | 11.3 |
| Medium | 25.2 | 25.3 | 24.6 | 24.0 | 22.7 |
| Large | 64.7 | 64.6 | 64.9 | 65.2 | 66.0 |
| Region | |||||
| South* | 18.5 | 18.5 | 17.6 | 17.0 | 16.3 |
| Midwest | 21.4 | 22.0 | 23.6 | 23.2 | 23.5 |
| Northeast | 42.6 | 41.7 | 41.4 | 42.2 | 42.1 |
| West* | 17.5 | 17.8 | 17.3 | 17.6 | 18.1 |
| Hospital type | |||||
| Rural | 13.6 | 13.0 | 11.8 | 11.0 | 10.8 |
| Urban nonteaching | 45.5 | 44.5 | 50.1 | 45.3 | 45.7 |
| Urban teaching | 40.9 | 42.5 | 38.1 | 43.7 | 43.6 |
| Patient outcomes | |||||
| Ventilation strategy | |||||
| IMV* | 48.5 | 48.4 | 47.5 | 46.5 | 42.1 |
| NIV* | 3.8 | 5.3 | 6.9 | 9.4 | 10.1 |
| IMV or NIV | 50.9 | 51.7 | 52.1 | 52.9 | 49.7 |
| Disposition | |||||
| Home/home healthcare* | 42.1 | 43.8 | 42.8 | 43.4 | 45.7 |
| Transfer to acute care | 5.2 | 4.7 | 4.6 | 4.6 | 4.4 |
| Nursing facility* | 24.4 | 24.9 | 27.4 | 28.6 | 29.0 |
| Other | 0.7 | 0.8 | 0.9 | 0.9 | 1.0 |
| Adjusted mortality, % (SE)* | 27.6 (0.3) | 26.4 (0.4) | 24.9 (0.4) | 22.7 (0.4) | 20.6 (0.3) |
| Adjusted mean, LOS/case, d (SE)* | 7.8 (0.1) | 7.9 (0.1) | 7.7 (0.1) | 7.5 (0.1) | 7.1 (0.1) |
| Adjusted mean cost/case, 2009 US$, (SE) | 15,818 (251) | 16,981 (419) | 17,236 (411) | 16,941 (436) | 15,987 (402) |
After adjusting for age and sex, the population incidence of ARF increased from 502 (standard error [SE] = 10) cases per 100,000 in 2001 to 784 (SE = 19) cases per 100,000 in 2009 (a 56% increase, P < 0.0001). Hispanics had the lowest rates of ARF, with both black and white groups having similar rates (Table 2).
| 2001 | 2003 | 2005 | 2007 | 2009 | |
|---|---|---|---|---|---|
| |||||
| All* | 502 (10) | 569 (12) | 595 (14) | 627 (14) | 784 (19) |
| Age group | |||||
| 1844* | 107 (3) | 130 (4) | 137 (4) | 153 (5) | 189 (6) |
| 4564* | 422 (9) | 500 (12) | 521 (13) | 580 (14) | 739 (19) |
| 6584* | 1697 (35) | 1863 (42) | 1950 (50) | 2066 (46) | 2578 (69) |
| 85+ | 3449 (86) | 3792 (106) | 3981 (120) | 3429 (97) | 4163 (123) |
| Sex | |||||
| Male* | 491 (10) | 553 (13) | 582 (14) | 629 (14) | 782 (20) |
| Female* | 512 (10) | 583 (12) | 607 (15) | 625 (13) | 786 (19) |
| Race/ethnicity | |||||
| White* | 398 (11) | 427 (12) | 466 (16) | 450 (13) | 699 (21) |
| Black* | 423 (27) | 513 (33) | 432 (26) | 574 (38) | 738 (37) |
| Hispanic* | 247 (24) | 381 (42) | 307 (27) | 353 (34) | 478 (42) |
| Other* | 268 (20) | 342 (29) | 347 (26) | 424 (29) | 713 (77) |
| In‐hospital mortality | 140 (3) | 148 (3) | 146 (3) | 140 (3) | 154 (4) |
The most common etiologies of ARF among medical patients were pneumonia, CHF, ARDS, COPD exacerbation, and sepsis. Over the 9‐year study, the proportion of cases secondary to pneumonia and sepsis rose significantly: from 39% to 46% and 13% to 21%, respectively (Figure 1).
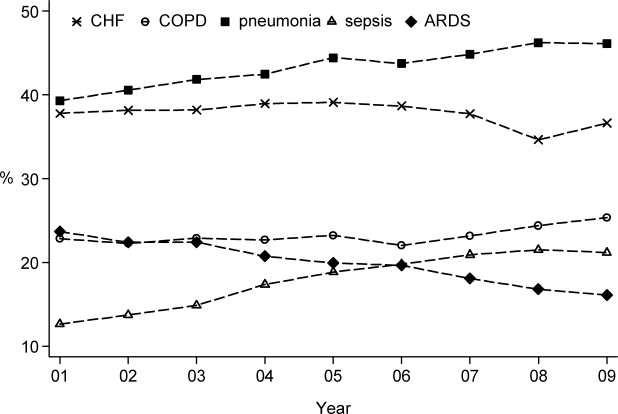
Mortality and Other Outcomes
The number of in‐hospital deaths related to ARF increased from 277,407 deaths in 2001 to 381,155 in 2009 (a 37% increase, P < 0.001). Standardized to the population, deaths increased from 140 in 2001 to 154 cases per 100,000 in 2009 (a 10% increase, P = 0.027). Despite slightly increasing mortality rates at a population level, adjusted in‐hospital mortality improved from 27.6% in 2001 to 20.6% in 2009 (P < 0.001). Mortality declined for both IMV and NIV patients from 35.3% in 2001 to 30.2% in 2009 and from 23.5% to 19%, respectively, but increased for those who required both NIV and IMV (from 26.9% in 2001 to 28% in 2009).
Adjusted hospital length of stay decreased from 7.8 days per patient in 2001 to 7.1 days in 2009 (P < 0.001), with a concomitant increase in discharges to nursing facilities, from 24% in 2001 to 29% in 2009. There was no linear trend in adjusted cost per case, with $15,818 in 2001 and $15,987 in 2009 (in 2009 US dollars) (Table 1).
Ventilation Practices
Overall, 50.9% patients received ventilatory support (NIV or IMV or both) in 2001 and 49.7% in 2009 (P= 0.25). The use of NIV increased from 3.8% to 10.1% (P < 0.001), a 169% increase, whereas the utilization of IMV decreased from 48.5% in 2001 to 42.1% in 2009 (P for trend < 0.0001), a 13% decrease. Uses of both NIV and IMV during hospitalization were seen in 1.4% of cases in 2001 and 2.5% of cases in 2009.
2009 Data Analysis
In 2009 the 1,917,910 hospitalizations with ARF resulted in 381,155 (SD = 8965) deaths and a total inpatient cost of $54 billion. The most common etiologies in patients over 65 years old were pneumonia, CHF, COPD, ARDS, and sepsis. In patients younger than 45 years the most frequent diagnoses were pneumonia, ARDS, sepsis, asthma, drug ingestion, and trauma. Stratified analysis by gender and by age groups showed that mortality rates among men were higher than for women and were highest in patients older than 85 years (Table 3).
| Disease | Total | Age <45 Years | 4565 Years | 6584 Years | 85+ Years | Male | Female |
|---|---|---|---|---|---|---|---|
| |||||||
| Medical | |||||||
| Total, N (%) | 1,364,624 (71.2) | 144,715 (10.6) | 416,922 (30.6) | 615,009 (45.1) | 187,977 (13.8) | 647,894 (47.5) | 716,635 (52.5) |
| Pneumonia, %* | 46.1 | 41.7 | 42.8 | 46.9 | 54.3 | 48.8 | 43.7 |
| CHF, %* | 36.6 | 10.4 | 27.3 | 43.6 | 54.8 | 35.0 | 38.1 |
| ARDS, %* | 16.1 | 22.9 | 16.2 | 14.5 | 15.9 | 15.5 | 16.7 |
| Sepsis, %* | 21.2 | 18.1 | 21.3 | 21.3 | 23.1 | 22.8 | 19.8 |
| COPD, %* | 25.4 | 4.2 | 25.6 | 32.3 | 18.3 | 25.0 | 25.7 |
| AMI, %* | 9.0 | 2.6 | 7.1 | 10.5 | 13.3 | 9.3 | 8.8 |
| Asthma, %* | 9.2 | 18.1 | 11.6 | 6.7 | 5.4 | 6.2 | 12.0 |
| Stroke, %* | 4.8 | 2.3 | 4.1 | 5.5 | 6.0 | 5.0 | 4.7 |
| Trauma or burns, %* | 3.4 | 5.4 | 2.9 | 3.0 | 4.1 | 4.3 | 2.5 |
| Cardiorespiratory arrest, %* | 4.1 | 3.9 | 4.4 | 4.1 | 3.8 | 4.6 | 3.7 |
| Drug, %* | 3.7 | 16.6 | 5.1 | 0.8 | 0.3 | 3.8 | 3.6 |
| IMV, %* | 37.7 | 54.6 | 43.7 | 33.5 | 24.8 | 41.1 | 34.5 |
| NIV, %* | 11.9 | 7.1 | 11.5 | 13.0 | 12.7 | 11.4 | 12.3 |
| In‐hospital mortality (CI) | 22 (21.322.7) | 12.9 (11.913.9) | 18.5 (17.619.4) | 23.9 (23.024.9) | 31.8 (30.633.1) | 24.2 (23.325.1) | 20.9 (20.121.7) |
| Surgical | |||||||
| Total, N (%) | 552971 (28.8) | 64983 (11.8) | 190225 (34.4) | 254336 (46) | 43426 (7.9) | 295660 (53.5) | 257287 (46.5) |
| Pneumonia, %* | 34.9 | 33.0 | 34.0 | 35.0 | 40.5 | 37.1 | 32.2 |
| CHF, %* | 27.2 | 8.9 | 21.7 | 33.3 | 42.6 | 26.7 | 27.7 |
| ARDS, %* | 45.5 | 51.5 | 45.2 | 44.7 | 42.7 | 45.0 | 46.1 |
| Sepsis, %* | 25.1 | 22.8 | 25.4 | 25.2 | 26.1 | 25.4 | 24.7 |
| COPD, %* | 8.2 | 1.1 | 7.4 | 10.8 | 7.5 | 8.3 | 8.1 |
| AMI, %* | 16.9 | 4.9 | 17.0 | 19.8 | 17.9 | 19.1 | 14.4 |
| Asthma, %* | 6.1 | 7.6 | 7.2 | 5.4 | 3.6 | 4.1 | 8.5 |
| Stroke, %* | 8.9 | 6.6 | 9.2 | 9.4 | 7.2 | 8.9 | 8.8 |
| Trauma or burns, %* | 12.2 | 26.5 | 9.6 | 9.2 | 20.3 | 13.8 | 10.4 |
| Cardiorespiratory arrest, %* | 5.5 | 4.4 | 6.0 | 5.4 | 5.2 | 6.1 | 4.7 |
| Drug, %* | 0.5 | 1.3 | 0.7 | 0.2 | 0.2 | 0.4 | 0.6 |
| IMV, %* | 52.9 | 57.1 | 54.3 | 51.3 | 50.0 | 54.5 | 51.0 |
| NIV, %* | 5.8 | 3.5 | 5.5 | 6.4 | 6.4 | 5.6 | 6.0 |
| In‐hospital mortality, % (CI) | 18.6 (17.819.5) | 10.7 (9.312.0) | 15.5 (14.216.8) | 20.8 (19.821.9) | 29.4 (27.831.1) | 19.0 (18.219.8) | 18.3 (17.319.2) |
When we examined ventilation practices among medical patients we found that patients older than 85 years, when compared to patients younger than 45 years, were less likely to be treated with IMV (25% vs 55%) and more likely to be treated with NIV (12.7% vs 7%). At the same time, the average cost per case was lowest among patients 85 years and older, and hospital costs per case fell sharply after age 70 years. Costs were considerably higher for those who did not survive during hospitalization, particularly for patients younger than 45 years (Figure 2).
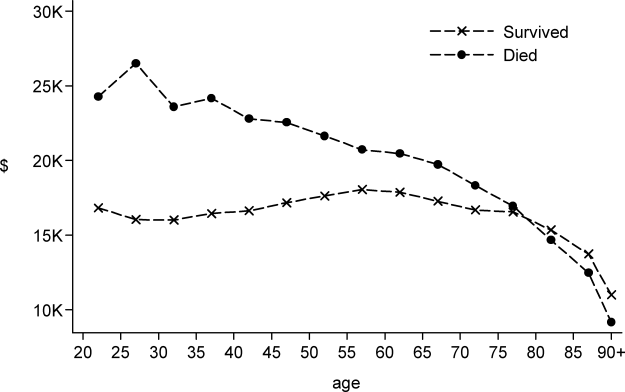
DISCUSSION
In this large population‐based study, we found that the number of hospitalizations associated with a diagnosis of ARF almost doubled over a 9‐year period. In 2009 there were nearly 2 million hospitalizations with ARF in the United States, resulting in approximately 380,000 deaths and inpatient costs of over $54 billion. The population‐adjusted ARF hospitalization rates increased in all age groups, and patients 85 years and older had the highest age‐specific hospitalization rate. Although overall rates of mechanical ventilation (NIV or IMV) remained stable over the 9‐year period, there was an important shift away from IMV (which decreased from 48% in 2001 to 42% in 2009) toward NIV (which increased from 4% in 2001 to 10% in 2009). Overall, there was a significant increase in the number of total deaths despite a decline in adjusted in‐hospital mortality rates. In‐hospital mortality rates decreased for all cases of ARF regardless of ventilation choice.
The findings of this study mirror results of others that have shown that although the incidence of critical care illnesses like sepsis[17, 20, 21, 26] and acute renal failure[27] has increased over the last decade, in‐hospital mortality rates have decreased.[20, 21, 28] Our results also compliment the results of a recent study that looked at hospitalizations for noncardiogenic ARF, which observed a 3.7‐fold increase in the number of cases and a steady decline in case fatality.[11]
Most prior studies addressing the incidence of ARF have included only patients receiving mechanical ventilation. In 1994, the estimated number of cases of ARF requiring IMV was 329,766,[9] which increased to 790,257 in 2005.[10] In our study we found that in 2009, the number of patients with ARF hospitalizations with IMV increased to 806,538. The increase in the overall number of cases with ARF was mainly driven by a surge in cases of sepsis and pneumonia. Our findings are consistent with national trends over time in noncardiogenic ARF[11] and in conditions that predispose patients to ARF such as sepsis[17, 20, 28] and acute renal failure.[27] As the number of claims for ARF doubled and the number of deaths increased, we found that adjusted hospital mortality improved from 27.6% in 2001 to 20.6% in 2009. This decline in hospital mortality was observed among all patients groups, regardless of ventilation choice. The decline in overall case fatality is consistent with prior findings in noncardiogenic ARF,[11] sepsis,[17, 28] and CHF.[29]
There are a number of potential explanations for the reduction in mortality observed over the study period, including improvements in hospital management of the underlying conditions leading to ARF, an increase in the proportion of patients being treated with NIV,[30] and advances in the care of critically ill patients such as the use of low‐tidal volume ventilation.[31, 32] Another contributor may be an increase in the proportion of discharges to nursing facilities, although this change in discharge disposition cannot fully explain our findings. For example, from 2007 to 2009, mortality decreased by 2 percentage points, and nursing home discharges increased by only 0.4 percentage points. Growth and aging of the US population only partially explain the increase we observed in the incidence of ARF, as age‐ and sex‐adjusted population rates increased by 56% from 2001 to 2009. In addition, the NIS captures data on hospital discharges and not individual patients; thus, a patient may have had multiple admissions. Over the last decade adoption of a more intensive practice style has been associated with improved in‐hospital mortality,[33, 34] and although these patients may be living longer they may have multiple readmissions.[35, 36]
We also observed that older patients were less likely to be treated with IMV, had a higher mortality rate, and less expensive care. These results are consistent with other studies and suggest that the intensity of treatment decreases with increasing age, and decisions to withhold or withdraw life‐supporting treatments are more frequent in the elderly.[26, 37] Prior research has shown that severity of illness is more important than age on patients' prognosis,[38, 39] and aggressive treatment strategies are not less cost‐effective when provided to older patients.[40]
Another important finding of this study is the marked increase in the use of NIV paired with a modest reduction in the use of IMV in the treatment of patients with ARF. This finding adds to evidence from other studies, which have similarly reported a dramatic increase in the use of NIV and a decrease in the use of IMV in patients with COPD as well as in ARF of other etiologies.[30, 41]
Our work has several limitations. First, we identified ARF based on ICD‐9‐CM codes and therefore cannot exclude disease misclassification. We did not find any studies in the literature addressing the accuracy and the completeness of ARF coding. However, we employed the same codes used to define ARF as has been used to define organ dysfunction in studies of severe sepsis,[17, 20] and the ICD‐9‐CM codes that we used to identify cases of ARDS have been used in prior studies.[11, 22, 23] Another limitation is that it is not clear to what extent the trends we observed may be due to changes over time in documentation and coding practices. Although this should be considered given the additional reimbursement associated with the diagnosis of ARF, our observation that rates of assisted ventilation have remained almost flat over the 9‐year period of the study suggest that would not wholly account for the rise in ARF. Second, because we did not have access to physiological data such as results of blood gas testing, we could not determine whether the threshold for applying the diagnosis of ARF or for delivering ventilatory support has changed over time. Third, for the purpose of this study we employed a broad definition of ARF, not limiting cases to those requiring mechanical ventilation, and this led to a more heterogeneous cohort including less severe cases of ARF. However, this is not dissimilar to the heterogeneity in disease severity observed among patients who receive a diagnosis of heart failure or acute renal failure. Fourth, survivors of ARF remain at high risk of death in the months after hospitalization,[42] but we assessed only in‐hospital mortality. It is possible that although in‐hospital mortality has improved, 30‐day mortality remained stable. Finally, as the NIS contains only discharge‐level data, we could not distinguish between patients admitted for ARF from those who developed ARF (potentially iatrogenic) after admission.
In summary, over the period of 2001 to 2009, there was a large increase in the number of patients given a diagnosis of ARF and a concomitant reduction in inpatient mortality. Although rates of mechanical ventilation remained relatively constant, there was a significant shift toward greater use of NIV at the expense of IMV.
Disclosures
Dr. Stefan is supported by KM1 CA156726 from the National Cancer Institute (NCI) and by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health (NIH), through grant UL1 RR025752. The work on this study was supported by a Charlton grant from Tufts University School of Medicine. Dr. Lindenauer and Dr. Pekow are supported by 1R18HL108810‐01 from the National Heart, Lung, and Blood Institute (NHLBI). The content of this publication is solely the responsibility of the authors and does not represent the official views of the NIH, NHLBI, or NCI.
All authors have read and approved the manuscript and none of them have any potential conflicts of interest to report.
Dr. Stefan had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Conception and design: Mihaela S. Stefan, Penelope S. Pekow, Michael B. Rothberg, Jay Steingrub, Peter K. Lindenauer; analysis and interpretation: Meng‐Shiou Shieh, Mihaela S. Stefan, Penelope S. Pekow, Michael B. Rothberg, Tara Lagu, Peter K. Lindenauer; drafting the manuscript for important intellectual content: Mihaela S. Stefan, Penelope S. Pekow, Michael B. Rothberg, Jay Steingrub, Tara Lagu, and Peter K. Lindenauer.
- , . Goldman's Cecil Medicine. 24th ed. Amsterdam, the Netherlands: Elsevier Inc.; 2012.
- , . Textbook of Respiratory Medicine. 5th ed. Philadelphia, PA: Saunders; 2010.
- , , . Epidemiology and outcome of acute respiratory failure in intensive care unit patients. Crit Care Med. 2003;31(4 suppl):S296–S299.
- , , , et al. Epidemiology of critical care syndromes, organ failures, and life‐support interventions in a suburban US community. Chest. 2011;140(6):1447–1455.
- , , , , . The changing epidemiology of mechanical ventilation: a population‐based study. J Intensive Care Med. 2006;21(3):173–182.
- , , , , . Mechanical ventilation in Ontario, 1992–2000: incidence, survival, and hospital bed utilization of noncardiac surgery adult patients. Crit Care Med. 2004;32(7):1504–1509.
- . Contributions to the epidemiology of acute respiratory failure. Crit Care. 2003;7(4):288–290.
- , , , et al. Incidence, severity, and mortality of acute respiratory failure in Berlin, Germany. Am J Respir Crit Care Med. 1995;151(4):1121–1125.
- . Acute respiratory failure in the United States: incidence and 31‐day survival. Chest. 2000;118(4):1100–1105.
- , , , , , . The epidemiology of mechanical ventilation use in the United States. Crit Care Med. 2010;38(10):1947–1953.
- , , , . Trends in the incidence of noncardiogenic acute respiratory failure: the role of race. Crit Care Med. 2012;40(5):1532–1538.
- , , , , . Secular trends in nosocomial infections and mortality associated with noninvasive ventilation in patients with exacerbation of COPD and pulmonary edema. JAMA. 2003;290(22):2985–2991.
- , , , et al. Association of noninvasive ventilation with nosocomial infections and survival in critically ill patients. JAMA. 2000;284(18):2361–2367.
- , , , , . Noninvasive versus conventional mechanical ventilation. An epidemiologic survey. Am J Respir Crit Care Med. 2001;163(4):874–880.
- , , , , , . Does noninvasive ventilation reduce the ICU nosocomial infection risk? A prospective clinical survey. Intensive Care Med. 1999;25(6):567–573.
- Heathcare Cost and Utilization Project (HCUP). Overview of the Nationwide Inpatient Sample. Available at: http://www.hcup‐us.ahrq.gov/nisoverview.jsp. Accessed December 6, 2011.
- , , , , , . Hospitalizations, costs, and outcomes of severe sepsis in the United States 2003 to 2007. Crit Care Med. 2011;40(3):754–761.
- , , , , . Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003–2009. JAMA. 2012;307(13):1405–1413.
- , , , , . Little evidence of correlation between growth in health care spending and reduced mortality. Health Aff (Millwood). 2010;29(8):1523–1531.
- , , , . The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–1554.
- , , , . Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003. Crit Care Med. 2007;35(5):1244–1250.
- , , . Risk factors for ARDS in the United States: analysis of the 1993 National Mortality Followback Study. Chest. 2001;119(4):1179–1184.
- , , , , , . Acute respiratory distress syndrome: estimated incidence and mortality rate in a 5 million‐person population base. Crit Care. 1998;2(1):29–34.
- , , . Validity of procedure codes in International Classification of Diseases, 9th Revision, Clinical Modification administrative data. Med Care. 2004;42(8):801–809.
- , , , . Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27.
- , . Epidemiology of sepsis: an update. Crit Care Med. 2001;29(7 suppl):S109–S116.
- , , , , , . Epidemiology and outcomes of acute renal failure in hospitalized patients: a national survey. Clin J Am Soc Nephrol. 2006;1(1):43–51.
- , , , . Facing the challenge: decreasing case fatality rates in severe sepsis despite increasing hospitalizations. Crit Care Med. 2005;33(11):2555–2562.
- , , , . National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries,1998–2008. JAMA. 2011;306(15):1669–1678.
- , , , et al. Outcomes of noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease in the United States, 1998–2008. Am J Respir Crit Care Med. 2011;185(2):152–159.
- , , , et al. A trial of goal‐oriented hemodynamic therapy in critically ill patients. SvO2 Collaborative Group. N Engl J Med. 1995;333(16):1025–1032.
- , . Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury. N Engl J Med. 2000;343(11):813; author reply 813–814.
- , , . Short‐ and long‐term survival of nonsurgical intensive care patients and its relation to diagnosis, severity of disease, age and comorbidities. Curr Aging Sci. 2009;2(3):240–248.
- , , , , , . The impact of COPD on management and outcomes of patients hospitalized with acute myocardial infarction—a ten‐year retrospective observational study. Chest. 2012;141(6):1441–1448.
- . The paradox of health. N Engl J Med. 1988;318(7):414–418.
- , , . Rehospitalizations among patients in the Medicare fee‐for‐service program. N Engl J Med. 2009;360(14):1418–1428.
- , , , et al. Outcomes and cost‐effectiveness of ventilator support and aggressive care for patients with acute respiratory failure due to pneumonia or acute respiratory distress syndrome. Am J Med. 2000;109(8):614–620.
- , , , et al. Older age, aggressiveness of care, and survival for seriously ill, hospitalized adults. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Ann Intern Med. 1999;131(10):721–728.
- , , , et al. Patient age and decisions to withhold life‐sustaining treatments from seriously ill, hospitalized adults. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. Ann Intern Med. 1999;130(2):116–125.
- , , , et al. Are aggressive treatment strategies less cost‐effective for older patients? The case of ventilator support and aggressive care for patients with acute respiratory failure. J Am Geriatr Soc. 2001;49(4):382–390.
- , . Utilization of non‐invasive ventilation in patients with acute respiratory failure from 2000–2009: a population‐based study. Am J Respir Crit Care Med. 2012;185:A6488.
- , , , et al. One‐year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;348(8):683–693.
- , . Goldman's Cecil Medicine. 24th ed. Amsterdam, the Netherlands: Elsevier Inc.; 2012.
- , . Textbook of Respiratory Medicine. 5th ed. Philadelphia, PA: Saunders; 2010.
- , , . Epidemiology and outcome of acute respiratory failure in intensive care unit patients. Crit Care Med. 2003;31(4 suppl):S296–S299.
- , , , et al. Epidemiology of critical care syndromes, organ failures, and life‐support interventions in a suburban US community. Chest. 2011;140(6):1447–1455.
- , , , , . The changing epidemiology of mechanical ventilation: a population‐based study. J Intensive Care Med. 2006;21(3):173–182.
- , , , , . Mechanical ventilation in Ontario, 1992–2000: incidence, survival, and hospital bed utilization of noncardiac surgery adult patients. Crit Care Med. 2004;32(7):1504–1509.
- . Contributions to the epidemiology of acute respiratory failure. Crit Care. 2003;7(4):288–290.
- , , , et al. Incidence, severity, and mortality of acute respiratory failure in Berlin, Germany. Am J Respir Crit Care Med. 1995;151(4):1121–1125.
- . Acute respiratory failure in the United States: incidence and 31‐day survival. Chest. 2000;118(4):1100–1105.
- , , , , , . The epidemiology of mechanical ventilation use in the United States. Crit Care Med. 2010;38(10):1947–1953.
- , , , . Trends in the incidence of noncardiogenic acute respiratory failure: the role of race. Crit Care Med. 2012;40(5):1532–1538.
- , , , , . Secular trends in nosocomial infections and mortality associated with noninvasive ventilation in patients with exacerbation of COPD and pulmonary edema. JAMA. 2003;290(22):2985–2991.
- , , , et al. Association of noninvasive ventilation with nosocomial infections and survival in critically ill patients. JAMA. 2000;284(18):2361–2367.
- , , , , . Noninvasive versus conventional mechanical ventilation. An epidemiologic survey. Am J Respir Crit Care Med. 2001;163(4):874–880.
- , , , , , . Does noninvasive ventilation reduce the ICU nosocomial infection risk? A prospective clinical survey. Intensive Care Med. 1999;25(6):567–573.
- Heathcare Cost and Utilization Project (HCUP). Overview of the Nationwide Inpatient Sample. Available at: http://www.hcup‐us.ahrq.gov/nisoverview.jsp. Accessed December 6, 2011.
- , , , , , . Hospitalizations, costs, and outcomes of severe sepsis in the United States 2003 to 2007. Crit Care Med. 2011;40(3):754–761.
- , , , , . Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003–2009. JAMA. 2012;307(13):1405–1413.
- , , , , . Little evidence of correlation between growth in health care spending and reduced mortality. Health Aff (Millwood). 2010;29(8):1523–1531.
- , , , . The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546–1554.
- , , , . Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003. Crit Care Med. 2007;35(5):1244–1250.
- , , . Risk factors for ARDS in the United States: analysis of the 1993 National Mortality Followback Study. Chest. 2001;119(4):1179–1184.
- , , , , , . Acute respiratory distress syndrome: estimated incidence and mortality rate in a 5 million‐person population base. Crit Care. 1998;2(1):29–34.
- , , . Validity of procedure codes in International Classification of Diseases, 9th Revision, Clinical Modification administrative data. Med Care. 2004;42(8):801–809.
- , , , . Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27.
- , . Epidemiology of sepsis: an update. Crit Care Med. 2001;29(7 suppl):S109–S116.
- , , , , , . Epidemiology and outcomes of acute renal failure in hospitalized patients: a national survey. Clin J Am Soc Nephrol. 2006;1(1):43–51.
- , , , . Facing the challenge: decreasing case fatality rates in severe sepsis despite increasing hospitalizations. Crit Care Med. 2005;33(11):2555–2562.
- , , , . National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries,1998–2008. JAMA. 2011;306(15):1669–1678.
- , , , et al. Outcomes of noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease in the United States, 1998–2008. Am J Respir Crit Care Med. 2011;185(2):152–159.
- , , , et al. A trial of goal‐oriented hemodynamic therapy in critically ill patients. SvO2 Collaborative Group. N Engl J Med. 1995;333(16):1025–1032.
- , . Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury. N Engl J Med. 2000;343(11):813; author reply 813–814.
- , , . Short‐ and long‐term survival of nonsurgical intensive care patients and its relation to diagnosis, severity of disease, age and comorbidities. Curr Aging Sci. 2009;2(3):240–248.
- , , , , , . The impact of COPD on management and outcomes of patients hospitalized with acute myocardial infarction—a ten‐year retrospective observational study. Chest. 2012;141(6):1441–1448.
- . The paradox of health. N Engl J Med. 1988;318(7):414–418.
- , , . Rehospitalizations among patients in the Medicare fee‐for‐service program. N Engl J Med. 2009;360(14):1418–1428.
- , , , et al. Outcomes and cost‐effectiveness of ventilator support and aggressive care for patients with acute respiratory failure due to pneumonia or acute respiratory distress syndrome. Am J Med. 2000;109(8):614–620.
- , , , et al. Older age, aggressiveness of care, and survival for seriously ill, hospitalized adults. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Ann Intern Med. 1999;131(10):721–728.
- , , , et al. Patient age and decisions to withhold life‐sustaining treatments from seriously ill, hospitalized adults. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. Ann Intern Med. 1999;130(2):116–125.
- , , , et al. Are aggressive treatment strategies less cost‐effective for older patients? The case of ventilator support and aggressive care for patients with acute respiratory failure. J Am Geriatr Soc. 2001;49(4):382–390.
- , . Utilization of non‐invasive ventilation in patients with acute respiratory failure from 2000–2009: a population‐based study. Am J Respir Crit Care Med. 2012;185:A6488.
- , , , et al. One‐year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;348(8):683–693.
Copyright © 2012 Society of Hospital Medicine
New Strategies to Combat an Old Foe
In the early part of the 20th century, pneumonia was a leading causes of death, particularly among older adults, for whom Osler termed it the Captain of the Men of Death.[1] Mortality rates from severe (bacteremic) pneumonia were typically 80% to 90%, and the introduction of antibacterial therapy in the 1940s reduced that mortality to 10% to 20%. However, as pointed out by Austrian and Gold in a landmark paper in the 1950s, mortality for patients dying within the first 4 to 5 days was not reduced in the postantibiotic era.[2] The survival rates for patients with severe community‐acquired pneumonia minimally improved over the ensuing 50 years, despite the introduction of numerous new antimicrobial drugs and other medical interventions.
One promising area for therapeutic intervention relates to the potential adverse effects of the host inflammatory response in the setting of pneumonia. A growing body of literature supports the conclusion that the window of optimal host response may be relatively narrow. Too little response and patients quickly succumb to overwhelming sepsis. Too much response and a patient's hyperactivated inflammatory system can set off a cascade of secondary events, triggering events such as acute lung injury or ischemic heart disease.[3] Studies have also established that the level of inflammation, as measured by biomarkers such as C‐reactive protein, tumor necrosis factor, and interleukins, can identify patients at increased risk of adverse outcomes.[4] Thus, it is logical to ask whether immune modulating therapies can improve outcomes for these patients.
In this issue of the Journal of Hospital Medicine, Shafiq and colleagues completed a systematic review and meta‐analysis of corticosteroid therapy for patients with pneumonia.[5] Updating prior reviews, they included 8 randomized controlled trials, all of which consisted of low‐dose, systemic, steroid therapy as the intervention and standard care as the control arm. The overall quality of the included studies was judged moderate, and the overall size of the pooled data was only 1119 patients. In their analysis, adjunctive steroid therapy did not reduce in‐hospital mortality, with 4 studies demonstrating effect sizes suggesting benefit, 3 studies demonstrating no benefit or harm, and 1 study favoring the nonsteroid arm. In these situations with grossly heterogeneous study results, it seems prudent to avoid overly interpreting pooled results, even if statistical tests for heterogeneity are nonsignificant. The investigators also reported a range of secondary outcomes, noting that hospital length of stay was significantly reduced in the pooled steroid treated arms.
The overall negative finding is clearly disappointing at a time when clinicians are looking for new treatments to improve outcomes for these patients. Pneumonia is a heterogeneous disorder, representing a wide range of microbial pathogens and underlying host risk factors. Current treatment guidelines for patients with community‐acquired pneumonia are largely empirical and do not focus on pathogen identification, host risk factor analysis, or biomarker distributions to select antimicrobial therapy.[6] In this regard, despite being 1 of the oldest conditions for which we have published guidelines for treatment, the treatment approach for pneumonia remains quite antiquated, ignoring recent advances in the incorporation of personalized treatment strategies for other illnesses. We may have reached the limits of one‐size‐fits‐all treatment strategies for hospitalized adults with community‐acquired pneumonia. To improve outcomes further, we need to understand the heterogeneity of the disorder and tailor therapies at an individual level. Rapid point‐of‐care tests for pathogens and host response offer the most promising approach toward this strategy.
It is notable that the majority of studies focus on in‐hospital mortality, even though the impact of steroid therapy may be observed over a longer period of follow‐up. Moreover, although mortality is clearly a relevant outcome, it is not the only patient‐centered outcome of importance. However, other outcomes that are typically assessed, such as length of hospitalization and cost, are not patient‐centered outcomes. These are process measures that reflect physician judgment as much as any patient response to treatment. We need to move the field forward by embracing patient outcomes beyond mortality to optimally evaluate new treatment strategies, particularly because the majority of patients will survive hospitalization for the illness. These outcomes would include time to resolution of major symptoms, such as cough and fatigue, and functional outcomes, including return to work and usual activities. Future comparative efficacy and effectiveness studies in pneumonia need to consider a much wider range of true patient outcomes.[7]
It is increasingly fashionable to adopt cross‐disease approaches toward optimizing patient care, particularly in the hospital. Important initiatives that aim to reduce hospital injuries and improve transitions of care are relatively agnostic to specific disease states. Much of the research agenda of hospital medicine avoids a disease‐specific focus, assuming such disease‐specific approaches are the domain of specialists. Yet, it is worth remembering that much of the progress for medical care can be traced to traditional considerations of disease pathophysiology and empirical studies of risk factors and treatments for specific disease. Hospitalists remain at the front line in dealing with most of the common illnesses that afflict patients. Battling those conditions 1 at a time should be an important component of the broader hospitalist research agenda. One hundred years after Osler charged the medical community to identify new strategies for treating an old enemy, we are still struggling to win the battle.
Disclosure
This work was supported in part by K24‐AI073957 (JPM) from the National Institute of Allergy and Infectious Diseases, National Institutes of Health. The author has no conflicts of interest to report.
- . The Principles and Practices of Medicine. 7th ed. New York, London: D. Appleton and Co.; 1909.
- , . Pneumococcal bacteremia with special reference to bacteremic pneumococcal pneumonia. Ann Intern Med. 1964;60:759–776.
- , , , et al. Acute bacterial pneumonia is associated with the occurrence of acute coronary syndromes. Medicine (Baltimore). 2009;88(3):154–159.
- , , , et al. Understanding the inflammatory cytokine response in pneumonia and sepsis: results of the Genetic and Inflammatory Markers of Sepsis (GenIMS) Study. Arch Intern Med. 2007;167(15):1655–1663.
- , , , , . Adjuvant steroid therapy in community‐acquired pneumonia: a systematic review and meta‐analysis. J Hosp Med. 2013.
- , , , et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community‐acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27–S72.
- . Reassessing the design, conduct, and analysis of clinical trials of therapy for community‐acquired pneumonia. Clin Infect Dis. 2008;46(8):1152–1156.
In the early part of the 20th century, pneumonia was a leading causes of death, particularly among older adults, for whom Osler termed it the Captain of the Men of Death.[1] Mortality rates from severe (bacteremic) pneumonia were typically 80% to 90%, and the introduction of antibacterial therapy in the 1940s reduced that mortality to 10% to 20%. However, as pointed out by Austrian and Gold in a landmark paper in the 1950s, mortality for patients dying within the first 4 to 5 days was not reduced in the postantibiotic era.[2] The survival rates for patients with severe community‐acquired pneumonia minimally improved over the ensuing 50 years, despite the introduction of numerous new antimicrobial drugs and other medical interventions.
One promising area for therapeutic intervention relates to the potential adverse effects of the host inflammatory response in the setting of pneumonia. A growing body of literature supports the conclusion that the window of optimal host response may be relatively narrow. Too little response and patients quickly succumb to overwhelming sepsis. Too much response and a patient's hyperactivated inflammatory system can set off a cascade of secondary events, triggering events such as acute lung injury or ischemic heart disease.[3] Studies have also established that the level of inflammation, as measured by biomarkers such as C‐reactive protein, tumor necrosis factor, and interleukins, can identify patients at increased risk of adverse outcomes.[4] Thus, it is logical to ask whether immune modulating therapies can improve outcomes for these patients.
In this issue of the Journal of Hospital Medicine, Shafiq and colleagues completed a systematic review and meta‐analysis of corticosteroid therapy for patients with pneumonia.[5] Updating prior reviews, they included 8 randomized controlled trials, all of which consisted of low‐dose, systemic, steroid therapy as the intervention and standard care as the control arm. The overall quality of the included studies was judged moderate, and the overall size of the pooled data was only 1119 patients. In their analysis, adjunctive steroid therapy did not reduce in‐hospital mortality, with 4 studies demonstrating effect sizes suggesting benefit, 3 studies demonstrating no benefit or harm, and 1 study favoring the nonsteroid arm. In these situations with grossly heterogeneous study results, it seems prudent to avoid overly interpreting pooled results, even if statistical tests for heterogeneity are nonsignificant. The investigators also reported a range of secondary outcomes, noting that hospital length of stay was significantly reduced in the pooled steroid treated arms.
The overall negative finding is clearly disappointing at a time when clinicians are looking for new treatments to improve outcomes for these patients. Pneumonia is a heterogeneous disorder, representing a wide range of microbial pathogens and underlying host risk factors. Current treatment guidelines for patients with community‐acquired pneumonia are largely empirical and do not focus on pathogen identification, host risk factor analysis, or biomarker distributions to select antimicrobial therapy.[6] In this regard, despite being 1 of the oldest conditions for which we have published guidelines for treatment, the treatment approach for pneumonia remains quite antiquated, ignoring recent advances in the incorporation of personalized treatment strategies for other illnesses. We may have reached the limits of one‐size‐fits‐all treatment strategies for hospitalized adults with community‐acquired pneumonia. To improve outcomes further, we need to understand the heterogeneity of the disorder and tailor therapies at an individual level. Rapid point‐of‐care tests for pathogens and host response offer the most promising approach toward this strategy.
It is notable that the majority of studies focus on in‐hospital mortality, even though the impact of steroid therapy may be observed over a longer period of follow‐up. Moreover, although mortality is clearly a relevant outcome, it is not the only patient‐centered outcome of importance. However, other outcomes that are typically assessed, such as length of hospitalization and cost, are not patient‐centered outcomes. These are process measures that reflect physician judgment as much as any patient response to treatment. We need to move the field forward by embracing patient outcomes beyond mortality to optimally evaluate new treatment strategies, particularly because the majority of patients will survive hospitalization for the illness. These outcomes would include time to resolution of major symptoms, such as cough and fatigue, and functional outcomes, including return to work and usual activities. Future comparative efficacy and effectiveness studies in pneumonia need to consider a much wider range of true patient outcomes.[7]
It is increasingly fashionable to adopt cross‐disease approaches toward optimizing patient care, particularly in the hospital. Important initiatives that aim to reduce hospital injuries and improve transitions of care are relatively agnostic to specific disease states. Much of the research agenda of hospital medicine avoids a disease‐specific focus, assuming such disease‐specific approaches are the domain of specialists. Yet, it is worth remembering that much of the progress for medical care can be traced to traditional considerations of disease pathophysiology and empirical studies of risk factors and treatments for specific disease. Hospitalists remain at the front line in dealing with most of the common illnesses that afflict patients. Battling those conditions 1 at a time should be an important component of the broader hospitalist research agenda. One hundred years after Osler charged the medical community to identify new strategies for treating an old enemy, we are still struggling to win the battle.
Disclosure
This work was supported in part by K24‐AI073957 (JPM) from the National Institute of Allergy and Infectious Diseases, National Institutes of Health. The author has no conflicts of interest to report.
In the early part of the 20th century, pneumonia was a leading causes of death, particularly among older adults, for whom Osler termed it the Captain of the Men of Death.[1] Mortality rates from severe (bacteremic) pneumonia were typically 80% to 90%, and the introduction of antibacterial therapy in the 1940s reduced that mortality to 10% to 20%. However, as pointed out by Austrian and Gold in a landmark paper in the 1950s, mortality for patients dying within the first 4 to 5 days was not reduced in the postantibiotic era.[2] The survival rates for patients with severe community‐acquired pneumonia minimally improved over the ensuing 50 years, despite the introduction of numerous new antimicrobial drugs and other medical interventions.
One promising area for therapeutic intervention relates to the potential adverse effects of the host inflammatory response in the setting of pneumonia. A growing body of literature supports the conclusion that the window of optimal host response may be relatively narrow. Too little response and patients quickly succumb to overwhelming sepsis. Too much response and a patient's hyperactivated inflammatory system can set off a cascade of secondary events, triggering events such as acute lung injury or ischemic heart disease.[3] Studies have also established that the level of inflammation, as measured by biomarkers such as C‐reactive protein, tumor necrosis factor, and interleukins, can identify patients at increased risk of adverse outcomes.[4] Thus, it is logical to ask whether immune modulating therapies can improve outcomes for these patients.
In this issue of the Journal of Hospital Medicine, Shafiq and colleagues completed a systematic review and meta‐analysis of corticosteroid therapy for patients with pneumonia.[5] Updating prior reviews, they included 8 randomized controlled trials, all of which consisted of low‐dose, systemic, steroid therapy as the intervention and standard care as the control arm. The overall quality of the included studies was judged moderate, and the overall size of the pooled data was only 1119 patients. In their analysis, adjunctive steroid therapy did not reduce in‐hospital mortality, with 4 studies demonstrating effect sizes suggesting benefit, 3 studies demonstrating no benefit or harm, and 1 study favoring the nonsteroid arm. In these situations with grossly heterogeneous study results, it seems prudent to avoid overly interpreting pooled results, even if statistical tests for heterogeneity are nonsignificant. The investigators also reported a range of secondary outcomes, noting that hospital length of stay was significantly reduced in the pooled steroid treated arms.
The overall negative finding is clearly disappointing at a time when clinicians are looking for new treatments to improve outcomes for these patients. Pneumonia is a heterogeneous disorder, representing a wide range of microbial pathogens and underlying host risk factors. Current treatment guidelines for patients with community‐acquired pneumonia are largely empirical and do not focus on pathogen identification, host risk factor analysis, or biomarker distributions to select antimicrobial therapy.[6] In this regard, despite being 1 of the oldest conditions for which we have published guidelines for treatment, the treatment approach for pneumonia remains quite antiquated, ignoring recent advances in the incorporation of personalized treatment strategies for other illnesses. We may have reached the limits of one‐size‐fits‐all treatment strategies for hospitalized adults with community‐acquired pneumonia. To improve outcomes further, we need to understand the heterogeneity of the disorder and tailor therapies at an individual level. Rapid point‐of‐care tests for pathogens and host response offer the most promising approach toward this strategy.
It is notable that the majority of studies focus on in‐hospital mortality, even though the impact of steroid therapy may be observed over a longer period of follow‐up. Moreover, although mortality is clearly a relevant outcome, it is not the only patient‐centered outcome of importance. However, other outcomes that are typically assessed, such as length of hospitalization and cost, are not patient‐centered outcomes. These are process measures that reflect physician judgment as much as any patient response to treatment. We need to move the field forward by embracing patient outcomes beyond mortality to optimally evaluate new treatment strategies, particularly because the majority of patients will survive hospitalization for the illness. These outcomes would include time to resolution of major symptoms, such as cough and fatigue, and functional outcomes, including return to work and usual activities. Future comparative efficacy and effectiveness studies in pneumonia need to consider a much wider range of true patient outcomes.[7]
It is increasingly fashionable to adopt cross‐disease approaches toward optimizing patient care, particularly in the hospital. Important initiatives that aim to reduce hospital injuries and improve transitions of care are relatively agnostic to specific disease states. Much of the research agenda of hospital medicine avoids a disease‐specific focus, assuming such disease‐specific approaches are the domain of specialists. Yet, it is worth remembering that much of the progress for medical care can be traced to traditional considerations of disease pathophysiology and empirical studies of risk factors and treatments for specific disease. Hospitalists remain at the front line in dealing with most of the common illnesses that afflict patients. Battling those conditions 1 at a time should be an important component of the broader hospitalist research agenda. One hundred years after Osler charged the medical community to identify new strategies for treating an old enemy, we are still struggling to win the battle.
Disclosure
This work was supported in part by K24‐AI073957 (JPM) from the National Institute of Allergy and Infectious Diseases, National Institutes of Health. The author has no conflicts of interest to report.
- . The Principles and Practices of Medicine. 7th ed. New York, London: D. Appleton and Co.; 1909.
- , . Pneumococcal bacteremia with special reference to bacteremic pneumococcal pneumonia. Ann Intern Med. 1964;60:759–776.
- , , , et al. Acute bacterial pneumonia is associated with the occurrence of acute coronary syndromes. Medicine (Baltimore). 2009;88(3):154–159.
- , , , et al. Understanding the inflammatory cytokine response in pneumonia and sepsis: results of the Genetic and Inflammatory Markers of Sepsis (GenIMS) Study. Arch Intern Med. 2007;167(15):1655–1663.
- , , , , . Adjuvant steroid therapy in community‐acquired pneumonia: a systematic review and meta‐analysis. J Hosp Med. 2013.
- , , , et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community‐acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27–S72.
- . Reassessing the design, conduct, and analysis of clinical trials of therapy for community‐acquired pneumonia. Clin Infect Dis. 2008;46(8):1152–1156.
- . The Principles and Practices of Medicine. 7th ed. New York, London: D. Appleton and Co.; 1909.
- , . Pneumococcal bacteremia with special reference to bacteremic pneumococcal pneumonia. Ann Intern Med. 1964;60:759–776.
- , , , et al. Acute bacterial pneumonia is associated with the occurrence of acute coronary syndromes. Medicine (Baltimore). 2009;88(3):154–159.
- , , , et al. Understanding the inflammatory cytokine response in pneumonia and sepsis: results of the Genetic and Inflammatory Markers of Sepsis (GenIMS) Study. Arch Intern Med. 2007;167(15):1655–1663.
- , , , , . Adjuvant steroid therapy in community‐acquired pneumonia: a systematic review and meta‐analysis. J Hosp Med. 2013.
- , , , et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community‐acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27–S72.
- . Reassessing the design, conduct, and analysis of clinical trials of therapy for community‐acquired pneumonia. Clin Infect Dis. 2008;46(8):1152–1156.
Resting better with more zolpidem info
"Seriously? ... Okay. Get a stat x-ray of the pelvis and hips and tell the family I’ll be up within 5 minutes."
You hang up the phone incredulous! After 4 weeks in the critical care unit, 2 weeks in a step-down unit, and an additional 8 days on the general medical ward, your patient was finally on the launching pad.
You had spent 90 minutes the night before meticulously reviewing every nursing note, physical therapy recommendation, and a myriad of consultants notes to make sure your discharge summary thoroughly reflected her very complicated hospital course. Last night, she was alert and chatting up a storm. At times, she did not even know if she would ever make it out of the hospital (and neither did you), and here it was, the long-awaited day of discharge, and she wakes up groggy and takes a bad fall on her way to the bathroom.
The list of possible explanations for her new-onset grogginess race through your mind. The likelihood of a stroke is remote. Her vital signs and morning labs are all normal. She was weaned off pain meds weeks ago, and her only complaint for the past few days had been insomnia, for which you ordered zolpidem PRN. Surely that could not be the culprit ... or could it?
Recent evidence shows that sleep aids containing the popular drug zolpidem may be linked to decreased alertness the morning after use, particularly the long-acting formulations. In some patients, blood levels of the drug may remain high enough to put patients at risk when performing tasks that require mental alertness. Evidence of this association was so compelling, the Food and Drug Administration recently announced that it is requiring manufacturers of Ambien, Ambien CR, Zolpimist, and Edluar, sleep aids that contain zolpidem, to lower recommended doses. Women are at particular risk, since they eliminate the drug more slowly than do men. Accordingly, the new FDA-recommended dose for women was cut in half – 5 mg for immediate-release products and 6.25 mg for extended-release products.
Of course, zolpidem is not alone in its propensity to cause grogginess. Virtually any sleep aid can do so because, well, that is what it they are designed to do – make patients sleepy.
This recent drug-safety information was so interesting because we often have a false sense of security when prescribing this drug, and we prescribe it very often. It is our "safer" alternative to valium-type medications. We are now encouraged to order a safer dose of this frequently prescribed drug.
I ordered a lower dose myself right after reading the latest FDA report.
The bottom line is that we need to be aware what this study showed so we can alter our prescribing habits and order the lower dose. All medications have the potential to have side effects in a minority of patients, but it is very important for us to know and react when new recommendations come out that have the potential to be so far reaching.
Dr. Hester is a hospitalist with Baltimore-Washington Medical Center, Glen Burnie, Md., who has a passion for empowering patients to partner in their health care.
"Seriously? ... Okay. Get a stat x-ray of the pelvis and hips and tell the family I’ll be up within 5 minutes."
You hang up the phone incredulous! After 4 weeks in the critical care unit, 2 weeks in a step-down unit, and an additional 8 days on the general medical ward, your patient was finally on the launching pad.
You had spent 90 minutes the night before meticulously reviewing every nursing note, physical therapy recommendation, and a myriad of consultants notes to make sure your discharge summary thoroughly reflected her very complicated hospital course. Last night, she was alert and chatting up a storm. At times, she did not even know if she would ever make it out of the hospital (and neither did you), and here it was, the long-awaited day of discharge, and she wakes up groggy and takes a bad fall on her way to the bathroom.
The list of possible explanations for her new-onset grogginess race through your mind. The likelihood of a stroke is remote. Her vital signs and morning labs are all normal. She was weaned off pain meds weeks ago, and her only complaint for the past few days had been insomnia, for which you ordered zolpidem PRN. Surely that could not be the culprit ... or could it?
Recent evidence shows that sleep aids containing the popular drug zolpidem may be linked to decreased alertness the morning after use, particularly the long-acting formulations. In some patients, blood levels of the drug may remain high enough to put patients at risk when performing tasks that require mental alertness. Evidence of this association was so compelling, the Food and Drug Administration recently announced that it is requiring manufacturers of Ambien, Ambien CR, Zolpimist, and Edluar, sleep aids that contain zolpidem, to lower recommended doses. Women are at particular risk, since they eliminate the drug more slowly than do men. Accordingly, the new FDA-recommended dose for women was cut in half – 5 mg for immediate-release products and 6.25 mg for extended-release products.
Of course, zolpidem is not alone in its propensity to cause grogginess. Virtually any sleep aid can do so because, well, that is what it they are designed to do – make patients sleepy.
This recent drug-safety information was so interesting because we often have a false sense of security when prescribing this drug, and we prescribe it very often. It is our "safer" alternative to valium-type medications. We are now encouraged to order a safer dose of this frequently prescribed drug.
I ordered a lower dose myself right after reading the latest FDA report.
The bottom line is that we need to be aware what this study showed so we can alter our prescribing habits and order the lower dose. All medications have the potential to have side effects in a minority of patients, but it is very important for us to know and react when new recommendations come out that have the potential to be so far reaching.
Dr. Hester is a hospitalist with Baltimore-Washington Medical Center, Glen Burnie, Md., who has a passion for empowering patients to partner in their health care.
"Seriously? ... Okay. Get a stat x-ray of the pelvis and hips and tell the family I’ll be up within 5 minutes."
You hang up the phone incredulous! After 4 weeks in the critical care unit, 2 weeks in a step-down unit, and an additional 8 days on the general medical ward, your patient was finally on the launching pad.
You had spent 90 minutes the night before meticulously reviewing every nursing note, physical therapy recommendation, and a myriad of consultants notes to make sure your discharge summary thoroughly reflected her very complicated hospital course. Last night, she was alert and chatting up a storm. At times, she did not even know if she would ever make it out of the hospital (and neither did you), and here it was, the long-awaited day of discharge, and she wakes up groggy and takes a bad fall on her way to the bathroom.
The list of possible explanations for her new-onset grogginess race through your mind. The likelihood of a stroke is remote. Her vital signs and morning labs are all normal. She was weaned off pain meds weeks ago, and her only complaint for the past few days had been insomnia, for which you ordered zolpidem PRN. Surely that could not be the culprit ... or could it?
Recent evidence shows that sleep aids containing the popular drug zolpidem may be linked to decreased alertness the morning after use, particularly the long-acting formulations. In some patients, blood levels of the drug may remain high enough to put patients at risk when performing tasks that require mental alertness. Evidence of this association was so compelling, the Food and Drug Administration recently announced that it is requiring manufacturers of Ambien, Ambien CR, Zolpimist, and Edluar, sleep aids that contain zolpidem, to lower recommended doses. Women are at particular risk, since they eliminate the drug more slowly than do men. Accordingly, the new FDA-recommended dose for women was cut in half – 5 mg for immediate-release products and 6.25 mg for extended-release products.
Of course, zolpidem is not alone in its propensity to cause grogginess. Virtually any sleep aid can do so because, well, that is what it they are designed to do – make patients sleepy.
This recent drug-safety information was so interesting because we often have a false sense of security when prescribing this drug, and we prescribe it very often. It is our "safer" alternative to valium-type medications. We are now encouraged to order a safer dose of this frequently prescribed drug.
I ordered a lower dose myself right after reading the latest FDA report.
The bottom line is that we need to be aware what this study showed so we can alter our prescribing habits and order the lower dose. All medications have the potential to have side effects in a minority of patients, but it is very important for us to know and react when new recommendations come out that have the potential to be so far reaching.
Dr. Hester is a hospitalist with Baltimore-Washington Medical Center, Glen Burnie, Md., who has a passion for empowering patients to partner in their health care.
The Patient-Doctor Relationship Gap
Physicians who rank poorly in their communication skills with patients were associated with reduced rates of medication adherence in a new report.
A cross-sectional study of nearly 9,4000 patients in the Diabetes Study of Northern California (DISTANCE) found roughly 30% of patients who gave their physicians poor ratings when it came to involving them in decisions, understanding their problems with medications, and eliciting their trust were less likely to refill their cardiometabolic medications than those whose doctors were deemed to be good communicators, researchers found. For each 10-point decrease in the Consumer Assessment of Healthcare Providers and Systems Survey (CAHPS), the prevalence of poor medication adherence increased by 0.9% (P +0.1), the researchers added.
“One of the tricks is that medication adherence is an inherently physician-centric concept,” says lead author Neda Ratanawongsa, MD, MPH, assistant professor in the department of medicine at the University of California at San Francisco (UCSF). “We’re asking you to take medicine that we think will be best for you. That’s been the way that physicians operate for years, often appropriately so. But part of this is figuring out how to encourage the patients to disclose their decision that ‘Yes, I do want to take that medicine’ or ‘No, here’s why I don’t want to take that medicine.’”
Dr. Ratanawongsa adds that hospitalists and other physicians have to develop a sense of trust with patients to build relationships. Future studies could then track patient satisfaction and adherence over time to see if a corollary exists. Also, she says, hospitalists shouldn’t be discouraged that most of their relationships aren’t long-term ones like those found in other specialties.
“I wouldn’t underestimate the impact a hospitalist could have, whether one-time interaction or not, to change an existing therapy program,” Dr. Ratanawongsa says. “It’s important for hospitalists to understand the power of their words.”
Visit our website for more information about medication reconciliation.
Physicians who rank poorly in their communication skills with patients were associated with reduced rates of medication adherence in a new report.
A cross-sectional study of nearly 9,4000 patients in the Diabetes Study of Northern California (DISTANCE) found roughly 30% of patients who gave their physicians poor ratings when it came to involving them in decisions, understanding their problems with medications, and eliciting their trust were less likely to refill their cardiometabolic medications than those whose doctors were deemed to be good communicators, researchers found. For each 10-point decrease in the Consumer Assessment of Healthcare Providers and Systems Survey (CAHPS), the prevalence of poor medication adherence increased by 0.9% (P +0.1), the researchers added.
“One of the tricks is that medication adherence is an inherently physician-centric concept,” says lead author Neda Ratanawongsa, MD, MPH, assistant professor in the department of medicine at the University of California at San Francisco (UCSF). “We’re asking you to take medicine that we think will be best for you. That’s been the way that physicians operate for years, often appropriately so. But part of this is figuring out how to encourage the patients to disclose their decision that ‘Yes, I do want to take that medicine’ or ‘No, here’s why I don’t want to take that medicine.’”
Dr. Ratanawongsa adds that hospitalists and other physicians have to develop a sense of trust with patients to build relationships. Future studies could then track patient satisfaction and adherence over time to see if a corollary exists. Also, she says, hospitalists shouldn’t be discouraged that most of their relationships aren’t long-term ones like those found in other specialties.
“I wouldn’t underestimate the impact a hospitalist could have, whether one-time interaction or not, to change an existing therapy program,” Dr. Ratanawongsa says. “It’s important for hospitalists to understand the power of their words.”
Visit our website for more information about medication reconciliation.
Physicians who rank poorly in their communication skills with patients were associated with reduced rates of medication adherence in a new report.
A cross-sectional study of nearly 9,4000 patients in the Diabetes Study of Northern California (DISTANCE) found roughly 30% of patients who gave their physicians poor ratings when it came to involving them in decisions, understanding their problems with medications, and eliciting their trust were less likely to refill their cardiometabolic medications than those whose doctors were deemed to be good communicators, researchers found. For each 10-point decrease in the Consumer Assessment of Healthcare Providers and Systems Survey (CAHPS), the prevalence of poor medication adherence increased by 0.9% (P +0.1), the researchers added.
“One of the tricks is that medication adherence is an inherently physician-centric concept,” says lead author Neda Ratanawongsa, MD, MPH, assistant professor in the department of medicine at the University of California at San Francisco (UCSF). “We’re asking you to take medicine that we think will be best for you. That’s been the way that physicians operate for years, often appropriately so. But part of this is figuring out how to encourage the patients to disclose their decision that ‘Yes, I do want to take that medicine’ or ‘No, here’s why I don’t want to take that medicine.’”
Dr. Ratanawongsa adds that hospitalists and other physicians have to develop a sense of trust with patients to build relationships. Future studies could then track patient satisfaction and adherence over time to see if a corollary exists. Also, she says, hospitalists shouldn’t be discouraged that most of their relationships aren’t long-term ones like those found in other specialties.
“I wouldn’t underestimate the impact a hospitalist could have, whether one-time interaction or not, to change an existing therapy program,” Dr. Ratanawongsa says. “It’s important for hospitalists to understand the power of their words.”
Visit our website for more information about medication reconciliation.
Pharmacist-Hospitalist Collaboration Can Improve Care, Save Money
A healthy collaboration between hospitalists and pharmacists can generate cost savings and promote positive outcomes, such as preventing adverse drug events and improving care transitions, says Jonathan Edwards, PharmD, BCPS, a clinical pharmacy specialist at Huntsville Hospital in Alabama.
At the 2012 national conference of the American College of Clinical Pharmacy in Hollywood, Fla., Edwards presented a poster that detailed the effectiveness of such interdisciplinary collaboration at Huntsville Hospital, where pharmacists and physicians developed six order sets, a collaborative practice, and a patient interaction program from November 2011 to February 2012. During the study period, researchers documented a total cost savings of $9,825 resulting from 156 patient interventions.
Edwards’ collaborative study at Huntsville started with two physicians who had launched a service teaching hospitalists what pharmacists do, and how they could help in their efforts.
“We got together and developed an order set for treating acute alcohol withdrawal. That went well, so we did five more order sets,” Edwards says. “Then we thought: What if pharmacists got more involved by meeting directly with patients in the hospital to optimize their medication management and help them reach their goals for treatment? We now evaluate patients on the hospitalist service in three units.”
For Edwards, key factors that make the hospitalist-pharmacist relationship work include communicating the pharmacist’s availability to help with the hospitalist’s patients, identifying the physician’s openness to help, and clarifying how the physician prefers to be contacted.
Last October, the American Society of Health-System Pharmacists (ASHP) and the American Pharmacists Association (APhA) recognized eight care-transitions programs for best practices that improved patient outcomes and reduced hospital readmissions as part of the Medication Management in Care Transitions (MMCT) Project.
“The MMCT project highlights the valuable role pharmacists can play in addressing medication-related problems that can lead to hospital readmissions,” APhA chief executive officer Thomas E. Menighan, BSPharm, MBA, ScD (Hon), FAPhA, said in a news release. “By putting together these best practices, our goal is to provide a model for better coordination of care and better connectivity between pharmacists and healthcare providers in different practice settings that leads to improved patient health.”
Visit our website for more information about maximizing patient care through pharmacist-hospitalist collaboration.
A healthy collaboration between hospitalists and pharmacists can generate cost savings and promote positive outcomes, such as preventing adverse drug events and improving care transitions, says Jonathan Edwards, PharmD, BCPS, a clinical pharmacy specialist at Huntsville Hospital in Alabama.
At the 2012 national conference of the American College of Clinical Pharmacy in Hollywood, Fla., Edwards presented a poster that detailed the effectiveness of such interdisciplinary collaboration at Huntsville Hospital, where pharmacists and physicians developed six order sets, a collaborative practice, and a patient interaction program from November 2011 to February 2012. During the study period, researchers documented a total cost savings of $9,825 resulting from 156 patient interventions.
Edwards’ collaborative study at Huntsville started with two physicians who had launched a service teaching hospitalists what pharmacists do, and how they could help in their efforts.
“We got together and developed an order set for treating acute alcohol withdrawal. That went well, so we did five more order sets,” Edwards says. “Then we thought: What if pharmacists got more involved by meeting directly with patients in the hospital to optimize their medication management and help them reach their goals for treatment? We now evaluate patients on the hospitalist service in three units.”
For Edwards, key factors that make the hospitalist-pharmacist relationship work include communicating the pharmacist’s availability to help with the hospitalist’s patients, identifying the physician’s openness to help, and clarifying how the physician prefers to be contacted.
Last October, the American Society of Health-System Pharmacists (ASHP) and the American Pharmacists Association (APhA) recognized eight care-transitions programs for best practices that improved patient outcomes and reduced hospital readmissions as part of the Medication Management in Care Transitions (MMCT) Project.
“The MMCT project highlights the valuable role pharmacists can play in addressing medication-related problems that can lead to hospital readmissions,” APhA chief executive officer Thomas E. Menighan, BSPharm, MBA, ScD (Hon), FAPhA, said in a news release. “By putting together these best practices, our goal is to provide a model for better coordination of care and better connectivity between pharmacists and healthcare providers in different practice settings that leads to improved patient health.”
Visit our website for more information about maximizing patient care through pharmacist-hospitalist collaboration.
A healthy collaboration between hospitalists and pharmacists can generate cost savings and promote positive outcomes, such as preventing adverse drug events and improving care transitions, says Jonathan Edwards, PharmD, BCPS, a clinical pharmacy specialist at Huntsville Hospital in Alabama.
At the 2012 national conference of the American College of Clinical Pharmacy in Hollywood, Fla., Edwards presented a poster that detailed the effectiveness of such interdisciplinary collaboration at Huntsville Hospital, where pharmacists and physicians developed six order sets, a collaborative practice, and a patient interaction program from November 2011 to February 2012. During the study period, researchers documented a total cost savings of $9,825 resulting from 156 patient interventions.
Edwards’ collaborative study at Huntsville started with two physicians who had launched a service teaching hospitalists what pharmacists do, and how they could help in their efforts.
“We got together and developed an order set for treating acute alcohol withdrawal. That went well, so we did five more order sets,” Edwards says. “Then we thought: What if pharmacists got more involved by meeting directly with patients in the hospital to optimize their medication management and help them reach their goals for treatment? We now evaluate patients on the hospitalist service in three units.”
For Edwards, key factors that make the hospitalist-pharmacist relationship work include communicating the pharmacist’s availability to help with the hospitalist’s patients, identifying the physician’s openness to help, and clarifying how the physician prefers to be contacted.
Last October, the American Society of Health-System Pharmacists (ASHP) and the American Pharmacists Association (APhA) recognized eight care-transitions programs for best practices that improved patient outcomes and reduced hospital readmissions as part of the Medication Management in Care Transitions (MMCT) Project.
“The MMCT project highlights the valuable role pharmacists can play in addressing medication-related problems that can lead to hospital readmissions,” APhA chief executive officer Thomas E. Menighan, BSPharm, MBA, ScD (Hon), FAPhA, said in a news release. “By putting together these best practices, our goal is to provide a model for better coordination of care and better connectivity between pharmacists and healthcare providers in different practice settings that leads to improved patient health.”
Visit our website for more information about maximizing patient care through pharmacist-hospitalist collaboration.
Trial bolsters fecal infusion efficacy against C. difficile
The infusion of donor feces into the duodenum of patients with recurrent, often intractable Clostridium difficile infection led to a much higher rate of cure than did either vancomycin therapy or bowel lavage in a small, randomized, open-label clinical trial.
The trial was closed early to new enrollment after only 43 of its planned 120 patients had undergone randomization because an interim analysis by the trial’s data safety and monitoring board found that almost all patients in the two control groups had a recurrence, compared with ultimate resolution of diarrhea in 15 of 16 patients treated with fecal infusion.
There were no infectious complications from the fecal infusions, and the only adverse event was transient diarrhea immediately following the procedure, which resolved in all patients within 3 hours, according to Dr. Els van Nood of the University of Amsterdam Academic Medical Center and her associates. They reported their findings online Jan. 16 in the New England Journal of Medicine.
"We found that the infusion of donor feces is a potential therapeutic strategy against recurrent C. difficile infection. In our study, infusion of a relatively large amount of feces through a nasoduodenal tube had an acceptable adverse-event profile and was logistically manageable," they noted.
Currently there is no effective therapy for recurrent C. difficile infection of the gastrointestinal tract. Extended and repeated courses of vancomycin usually are prescribed, but the antibiotic’s efficacy is estimated to be only 60% for the first recurrence and declines substantially with each subsequent recurrence.
The reason for the waning of antibiotic effectiveness is not known for certain. Experts have proposed that C. difficile spores may persist in the gut and get reactivated over time; that antibody responses to Clostridium toxins diminish over time; or that persistent disturbance of the native intestinal microbiota causes reduced diversity, which in turn reduces natural resistance to C. difficile.
It was hoped that infusion of feces from healthy donors would address the last mechanism, restoring the normal microbiota and boosting host defenses against C. difficile. Several preliminary studies have produced promising results, but "experience with this procedure is limited by a lack of randomized trials supporting its efficacy and the unappealing nature of the treatment," Dr. van Nood and her colleagues said.
All the study subjects had persistent C. difficile infection, as evidenced by severe diarrhea with positive stool tests for the organism, after multiple courses of vancomycin and/or metronidazole.
Both patients and physicians are reluctant to choose donor-feces infusion until other measures have failed repeatedly. "It seems reasonable to initiate treatment with donor-feces infusion after the second or third relapse," the investigators wrote.
A total of 41 patients completed the study protocol. The trial compared the infusion of donor feces after pretreatment with a brief (4-day) course of vancomycin and bowel lavage (16 patients), a standard vancomycin regimen (12 patients), and a standard vancomycin regimen plus bowel lavage (13 patients). Bowel lavage was included because it has been used in previous studies of this new treatment and is thought to "reduce the pathogenic bowel content, facilitating colonization of healthy donor microbiota."
Most of the study subjects were elderly, with mean ages of 73 years, 66 years, and 69 years, respectively, in the three study arms.
Feces donors included 15 healthy volunteers aged 60 years and older who were screened for numerous potentially transmissible diseases. Fecal samples were collected just before the infusion was scheduled, and they were screened for parasites, C. difficile, and enteropathogenic bacteria. The samples were diluted with 500 mL of sterile saline, and the mixture was strained and poured into a sterile bottle.
A mean of 141 g of feces was infused through a nasoduodenal tube, and patients were monitored for 2 hours. Analysis of patients’ phylogenetic microarray profiles before and after treatment demonstrated "a major shift in the patients’ microbiota" from abnormal to normal diversity of organisms, Dr. van Nood and her associates said (N. Engl. J. Med. 2013 Jan. 16 [doi: 10.1056/NEJMoa1205037]).
The primary endpoint was cure without relapse within 10 weeks of treatment. Thirteen patients in the infusion group (81%) reached this endpoint after a single infusion. The remaining 3 patients had a second treatment, and 2 of them were cured, for an overall cure rate of 94% (15 of 16 patients).
In comparison, the cure rate with vancomycin alone was 31% (4 of 13 patients), and with vancomycin plus bowel lavage it was 23% (3 of 13).
At an interim follow-up of 5 weeks following initial treatment, C. difficile infection recurred in 1 patient (6%) in the infusion group, compared with 8 (62%) in the vancomycin-only group and 7 (54%) in the vancomycin-plus-lavage group.
Eighteen patients from the two control groups who relapsed after antibiotic treatment switched to off-protocol infusions of donor feces. Fifteen of them (83%) were cured: 11 after a single fecal infusion and 4 after two infusions.
All but one of the patients who received fecal infusions experienced immediate diarrhea, sometimes with cramping (31%) and belching (19%). These symptoms resolved in all of them within 3 hours. The only other adverse event that may have been related to the treatment was constipation, which developed in three patients.
Although the exact mechanism of action of this "unconventional" therapy is not yet known, Dr. van Nood and her colleagues speculated that donor-feces infusion probably restores the normal intestinal microbiota, enhancing the host defense against C. difficile.
Future research must determine the optimal protocol for donor-feces infusion, including the amount of feces required. Alternative routes of infusion, such as via enema or colonoscopy, also should be explored, they added.
This study was supported by the Netherlands Organization for Health Research and Development and the Netherlands Organization for Scientific Research. Four of the study’s 13 authors reported ties to Astellas. Two of those four also reported ties to Microbex.
This trial addresses one of the main impediments to the routine use of fecal microbiota transplantation (FMT) since it was first performed in 1958: a lack of efficacy data from randomized controlled trials. The results support an earlier systematic review of uncontrolled case series in which the overall response rates of FMT were 80% through the stomach or small intestine and 92% through colonoscopy or enema.

|
|
Despite the resurgence of FMT in recent years as a result of the past decade’s increase in the incidence and severity of C. difficile–associated diarrhea, it has not become mainstream, and only the most recalcitrant cases are likely to undergo it, "usually out of desperation after multiple treatment approaches have failed."
The trial’s findings "will provide added stimulus to the ongoing efforts to address the other main impediments to the routine and widespread use of FMT": unappealing aesthetics and the logistical challenge of harvesting and processing donor material.
Ciarán P. Kelly, M.D., is a professor of medicine in the division of gastroenterology at Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston. He reported having financial ties to many companies developing therapies for treating C. difficile infection. These comments are taken from his editorial accompanying Dr. van Nood’s report (N. Engl. J. Med. 2013 Jan. 16 [doi: 10.1056/NEJMe1214816]).
This trial addresses one of the main impediments to the routine use of fecal microbiota transplantation (FMT) since it was first performed in 1958: a lack of efficacy data from randomized controlled trials. The results support an earlier systematic review of uncontrolled case series in which the overall response rates of FMT were 80% through the stomach or small intestine and 92% through colonoscopy or enema.

|
|
Despite the resurgence of FMT in recent years as a result of the past decade’s increase in the incidence and severity of C. difficile–associated diarrhea, it has not become mainstream, and only the most recalcitrant cases are likely to undergo it, "usually out of desperation after multiple treatment approaches have failed."
The trial’s findings "will provide added stimulus to the ongoing efforts to address the other main impediments to the routine and widespread use of FMT": unappealing aesthetics and the logistical challenge of harvesting and processing donor material.
Ciarán P. Kelly, M.D., is a professor of medicine in the division of gastroenterology at Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston. He reported having financial ties to many companies developing therapies for treating C. difficile infection. These comments are taken from his editorial accompanying Dr. van Nood’s report (N. Engl. J. Med. 2013 Jan. 16 [doi: 10.1056/NEJMe1214816]).
This trial addresses one of the main impediments to the routine use of fecal microbiota transplantation (FMT) since it was first performed in 1958: a lack of efficacy data from randomized controlled trials. The results support an earlier systematic review of uncontrolled case series in which the overall response rates of FMT were 80% through the stomach or small intestine and 92% through colonoscopy or enema.

|
|
Despite the resurgence of FMT in recent years as a result of the past decade’s increase in the incidence and severity of C. difficile–associated diarrhea, it has not become mainstream, and only the most recalcitrant cases are likely to undergo it, "usually out of desperation after multiple treatment approaches have failed."
The trial’s findings "will provide added stimulus to the ongoing efforts to address the other main impediments to the routine and widespread use of FMT": unappealing aesthetics and the logistical challenge of harvesting and processing donor material.
Ciarán P. Kelly, M.D., is a professor of medicine in the division of gastroenterology at Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston. He reported having financial ties to many companies developing therapies for treating C. difficile infection. These comments are taken from his editorial accompanying Dr. van Nood’s report (N. Engl. J. Med. 2013 Jan. 16 [doi: 10.1056/NEJMe1214816]).
The infusion of donor feces into the duodenum of patients with recurrent, often intractable Clostridium difficile infection led to a much higher rate of cure than did either vancomycin therapy or bowel lavage in a small, randomized, open-label clinical trial.
The trial was closed early to new enrollment after only 43 of its planned 120 patients had undergone randomization because an interim analysis by the trial’s data safety and monitoring board found that almost all patients in the two control groups had a recurrence, compared with ultimate resolution of diarrhea in 15 of 16 patients treated with fecal infusion.
There were no infectious complications from the fecal infusions, and the only adverse event was transient diarrhea immediately following the procedure, which resolved in all patients within 3 hours, according to Dr. Els van Nood of the University of Amsterdam Academic Medical Center and her associates. They reported their findings online Jan. 16 in the New England Journal of Medicine.
"We found that the infusion of donor feces is a potential therapeutic strategy against recurrent C. difficile infection. In our study, infusion of a relatively large amount of feces through a nasoduodenal tube had an acceptable adverse-event profile and was logistically manageable," they noted.
Currently there is no effective therapy for recurrent C. difficile infection of the gastrointestinal tract. Extended and repeated courses of vancomycin usually are prescribed, but the antibiotic’s efficacy is estimated to be only 60% for the first recurrence and declines substantially with each subsequent recurrence.
The reason for the waning of antibiotic effectiveness is not known for certain. Experts have proposed that C. difficile spores may persist in the gut and get reactivated over time; that antibody responses to Clostridium toxins diminish over time; or that persistent disturbance of the native intestinal microbiota causes reduced diversity, which in turn reduces natural resistance to C. difficile.
It was hoped that infusion of feces from healthy donors would address the last mechanism, restoring the normal microbiota and boosting host defenses against C. difficile. Several preliminary studies have produced promising results, but "experience with this procedure is limited by a lack of randomized trials supporting its efficacy and the unappealing nature of the treatment," Dr. van Nood and her colleagues said.
All the study subjects had persistent C. difficile infection, as evidenced by severe diarrhea with positive stool tests for the organism, after multiple courses of vancomycin and/or metronidazole.
Both patients and physicians are reluctant to choose donor-feces infusion until other measures have failed repeatedly. "It seems reasonable to initiate treatment with donor-feces infusion after the second or third relapse," the investigators wrote.
A total of 41 patients completed the study protocol. The trial compared the infusion of donor feces after pretreatment with a brief (4-day) course of vancomycin and bowel lavage (16 patients), a standard vancomycin regimen (12 patients), and a standard vancomycin regimen plus bowel lavage (13 patients). Bowel lavage was included because it has been used in previous studies of this new treatment and is thought to "reduce the pathogenic bowel content, facilitating colonization of healthy donor microbiota."
Most of the study subjects were elderly, with mean ages of 73 years, 66 years, and 69 years, respectively, in the three study arms.
Feces donors included 15 healthy volunteers aged 60 years and older who were screened for numerous potentially transmissible diseases. Fecal samples were collected just before the infusion was scheduled, and they were screened for parasites, C. difficile, and enteropathogenic bacteria. The samples were diluted with 500 mL of sterile saline, and the mixture was strained and poured into a sterile bottle.
A mean of 141 g of feces was infused through a nasoduodenal tube, and patients were monitored for 2 hours. Analysis of patients’ phylogenetic microarray profiles before and after treatment demonstrated "a major shift in the patients’ microbiota" from abnormal to normal diversity of organisms, Dr. van Nood and her associates said (N. Engl. J. Med. 2013 Jan. 16 [doi: 10.1056/NEJMoa1205037]).
The primary endpoint was cure without relapse within 10 weeks of treatment. Thirteen patients in the infusion group (81%) reached this endpoint after a single infusion. The remaining 3 patients had a second treatment, and 2 of them were cured, for an overall cure rate of 94% (15 of 16 patients).
In comparison, the cure rate with vancomycin alone was 31% (4 of 13 patients), and with vancomycin plus bowel lavage it was 23% (3 of 13).
At an interim follow-up of 5 weeks following initial treatment, C. difficile infection recurred in 1 patient (6%) in the infusion group, compared with 8 (62%) in the vancomycin-only group and 7 (54%) in the vancomycin-plus-lavage group.
Eighteen patients from the two control groups who relapsed after antibiotic treatment switched to off-protocol infusions of donor feces. Fifteen of them (83%) were cured: 11 after a single fecal infusion and 4 after two infusions.
All but one of the patients who received fecal infusions experienced immediate diarrhea, sometimes with cramping (31%) and belching (19%). These symptoms resolved in all of them within 3 hours. The only other adverse event that may have been related to the treatment was constipation, which developed in three patients.
Although the exact mechanism of action of this "unconventional" therapy is not yet known, Dr. van Nood and her colleagues speculated that donor-feces infusion probably restores the normal intestinal microbiota, enhancing the host defense against C. difficile.
Future research must determine the optimal protocol for donor-feces infusion, including the amount of feces required. Alternative routes of infusion, such as via enema or colonoscopy, also should be explored, they added.
This study was supported by the Netherlands Organization for Health Research and Development and the Netherlands Organization for Scientific Research. Four of the study’s 13 authors reported ties to Astellas. Two of those four also reported ties to Microbex.
The infusion of donor feces into the duodenum of patients with recurrent, often intractable Clostridium difficile infection led to a much higher rate of cure than did either vancomycin therapy or bowel lavage in a small, randomized, open-label clinical trial.
The trial was closed early to new enrollment after only 43 of its planned 120 patients had undergone randomization because an interim analysis by the trial’s data safety and monitoring board found that almost all patients in the two control groups had a recurrence, compared with ultimate resolution of diarrhea in 15 of 16 patients treated with fecal infusion.
There were no infectious complications from the fecal infusions, and the only adverse event was transient diarrhea immediately following the procedure, which resolved in all patients within 3 hours, according to Dr. Els van Nood of the University of Amsterdam Academic Medical Center and her associates. They reported their findings online Jan. 16 in the New England Journal of Medicine.
"We found that the infusion of donor feces is a potential therapeutic strategy against recurrent C. difficile infection. In our study, infusion of a relatively large amount of feces through a nasoduodenal tube had an acceptable adverse-event profile and was logistically manageable," they noted.
Currently there is no effective therapy for recurrent C. difficile infection of the gastrointestinal tract. Extended and repeated courses of vancomycin usually are prescribed, but the antibiotic’s efficacy is estimated to be only 60% for the first recurrence and declines substantially with each subsequent recurrence.
The reason for the waning of antibiotic effectiveness is not known for certain. Experts have proposed that C. difficile spores may persist in the gut and get reactivated over time; that antibody responses to Clostridium toxins diminish over time; or that persistent disturbance of the native intestinal microbiota causes reduced diversity, which in turn reduces natural resistance to C. difficile.
It was hoped that infusion of feces from healthy donors would address the last mechanism, restoring the normal microbiota and boosting host defenses against C. difficile. Several preliminary studies have produced promising results, but "experience with this procedure is limited by a lack of randomized trials supporting its efficacy and the unappealing nature of the treatment," Dr. van Nood and her colleagues said.
All the study subjects had persistent C. difficile infection, as evidenced by severe diarrhea with positive stool tests for the organism, after multiple courses of vancomycin and/or metronidazole.
Both patients and physicians are reluctant to choose donor-feces infusion until other measures have failed repeatedly. "It seems reasonable to initiate treatment with donor-feces infusion after the second or third relapse," the investigators wrote.
A total of 41 patients completed the study protocol. The trial compared the infusion of donor feces after pretreatment with a brief (4-day) course of vancomycin and bowel lavage (16 patients), a standard vancomycin regimen (12 patients), and a standard vancomycin regimen plus bowel lavage (13 patients). Bowel lavage was included because it has been used in previous studies of this new treatment and is thought to "reduce the pathogenic bowel content, facilitating colonization of healthy donor microbiota."
Most of the study subjects were elderly, with mean ages of 73 years, 66 years, and 69 years, respectively, in the three study arms.
Feces donors included 15 healthy volunteers aged 60 years and older who were screened for numerous potentially transmissible diseases. Fecal samples were collected just before the infusion was scheduled, and they were screened for parasites, C. difficile, and enteropathogenic bacteria. The samples were diluted with 500 mL of sterile saline, and the mixture was strained and poured into a sterile bottle.
A mean of 141 g of feces was infused through a nasoduodenal tube, and patients were monitored for 2 hours. Analysis of patients’ phylogenetic microarray profiles before and after treatment demonstrated "a major shift in the patients’ microbiota" from abnormal to normal diversity of organisms, Dr. van Nood and her associates said (N. Engl. J. Med. 2013 Jan. 16 [doi: 10.1056/NEJMoa1205037]).
The primary endpoint was cure without relapse within 10 weeks of treatment. Thirteen patients in the infusion group (81%) reached this endpoint after a single infusion. The remaining 3 patients had a second treatment, and 2 of them were cured, for an overall cure rate of 94% (15 of 16 patients).
In comparison, the cure rate with vancomycin alone was 31% (4 of 13 patients), and with vancomycin plus bowel lavage it was 23% (3 of 13).
At an interim follow-up of 5 weeks following initial treatment, C. difficile infection recurred in 1 patient (6%) in the infusion group, compared with 8 (62%) in the vancomycin-only group and 7 (54%) in the vancomycin-plus-lavage group.
Eighteen patients from the two control groups who relapsed after antibiotic treatment switched to off-protocol infusions of donor feces. Fifteen of them (83%) were cured: 11 after a single fecal infusion and 4 after two infusions.
All but one of the patients who received fecal infusions experienced immediate diarrhea, sometimes with cramping (31%) and belching (19%). These symptoms resolved in all of them within 3 hours. The only other adverse event that may have been related to the treatment was constipation, which developed in three patients.
Although the exact mechanism of action of this "unconventional" therapy is not yet known, Dr. van Nood and her colleagues speculated that donor-feces infusion probably restores the normal intestinal microbiota, enhancing the host defense against C. difficile.
Future research must determine the optimal protocol for donor-feces infusion, including the amount of feces required. Alternative routes of infusion, such as via enema or colonoscopy, also should be explored, they added.
This study was supported by the Netherlands Organization for Health Research and Development and the Netherlands Organization for Scientific Research. Four of the study’s 13 authors reported ties to Astellas. Two of those four also reported ties to Microbex.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Major Finding: The overall cure rate of C. difficile infection was 94% with donor-feces infusion, 31% with vancomycin alone, and 23% with vancomycin plus bowel lavage.
Data Source: An open-label, randomized controlled trial comparing three treatment regimens in 41 patients with recurrent C. difficile infection of the GI tract.
Disclosures: This study was supported by the Netherlands Organization for Health Research and Development and the Netherlands Organization for Scientific Research. Four of the study’s 13 authors reported ties to Astellas. Two of those four also reported ties to Microbex.