User login
Pigmentation Concerns: Assessment and Treatment [editorial]
Cosmetic Corner: Dermatologists Weigh in on Redness-Reducing Products
Leading dermatologists offered their recommendations on the top redness-reducing products. See what they’re recommending to their patients and why.
To improve patient care and outcomes, leading dermatologists offered their recommendations on the top redness-reducing products. Consideration must be given to:
· Brightening Serum
Scientific Skin
Recommended by Kenneth Beer, MD, West Palm Beach and Juniper, FL
· CeraVe Facial Moisturizing Lotion AM
Coria Laboratories, a division of Valeant Pharmaceuticals North America
“Sunscreen is a must. I recommend CeraVe.”—Gary Goldenberg, MD, New York, NY
· PÊCHE Redness Control
Neocutis Inc
“Patients have found [this product] to be soothing. Patients with rosacea have tolerated it well and found a decrease in redness.”—Mary P. Lupo, MD, New Orleans, LA
“ROSAPLEX [in this product] is an exclusive redness-balancing complex with dextran sulfate, zinc, caffeine, and glycerin, which helps to eliminate the appearance of blotchiness and blemishes, and improve overall skin tone. PÊCHE is a very versatile cream and can be used alone or in conjunction with prescription products for rosacea.”—Marta I. Rendon, MD, Boca Raton, FL
· Redness Solutions Daily Relief Cream
Clinique Laboratories, LLC
“This cream is safe for patients with rosacea to use as a general moisturizer and it has an underlying green base, which cuts the appearance of red.”—Anthony M. Rossi, MD, New York, NY
· Redness Solutions Soothing Cleanser
Clinique Laboratories, LLC
“[I recommend that patients] use the Redness Solutions Soothing Cleanser, then apply the Redness Solutions Daily Relief Cream.”—Gary Goldenberg, MD, New York, NY
· Replenix Products
Topix Pharmaceuticals, Inc
“The Replenix line really works well for redness associated with rosacea. It is high in antioxidants and is one of the few products that works.”—Kenneth Beer, MD, West Palm Beach and Juniper, FL
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cosmetic Dermatology® or Quadrant HealthCom Inc and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cosmetic Dermatology or Quadrant HealthCom Inc endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
Leading dermatologists offered their recommendations on the top redness-reducing products. See what they’re recommending to their patients and why.
To improve patient care and outcomes, leading dermatologists offered their recommendations on the top redness-reducing products. Consideration must be given to:
· Brightening Serum
Scientific Skin
Recommended by Kenneth Beer, MD, West Palm Beach and Juniper, FL
· CeraVe Facial Moisturizing Lotion AM
Coria Laboratories, a division of Valeant Pharmaceuticals North America
“Sunscreen is a must. I recommend CeraVe.”—Gary Goldenberg, MD, New York, NY
· PÊCHE Redness Control
Neocutis Inc
“Patients have found [this product] to be soothing. Patients with rosacea have tolerated it well and found a decrease in redness.”—Mary P. Lupo, MD, New Orleans, LA
“ROSAPLEX [in this product] is an exclusive redness-balancing complex with dextran sulfate, zinc, caffeine, and glycerin, which helps to eliminate the appearance of blotchiness and blemishes, and improve overall skin tone. PÊCHE is a very versatile cream and can be used alone or in conjunction with prescription products for rosacea.”—Marta I. Rendon, MD, Boca Raton, FL
· Redness Solutions Daily Relief Cream
Clinique Laboratories, LLC
“This cream is safe for patients with rosacea to use as a general moisturizer and it has an underlying green base, which cuts the appearance of red.”—Anthony M. Rossi, MD, New York, NY
· Redness Solutions Soothing Cleanser
Clinique Laboratories, LLC
“[I recommend that patients] use the Redness Solutions Soothing Cleanser, then apply the Redness Solutions Daily Relief Cream.”—Gary Goldenberg, MD, New York, NY
· Replenix Products
Topix Pharmaceuticals, Inc
“The Replenix line really works well for redness associated with rosacea. It is high in antioxidants and is one of the few products that works.”—Kenneth Beer, MD, West Palm Beach and Juniper, FL
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cosmetic Dermatology® or Quadrant HealthCom Inc and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cosmetic Dermatology or Quadrant HealthCom Inc endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
Leading dermatologists offered their recommendations on the top redness-reducing products. See what they’re recommending to their patients and why.
To improve patient care and outcomes, leading dermatologists offered their recommendations on the top redness-reducing products. Consideration must be given to:
· Brightening Serum
Scientific Skin
Recommended by Kenneth Beer, MD, West Palm Beach and Juniper, FL
· CeraVe Facial Moisturizing Lotion AM
Coria Laboratories, a division of Valeant Pharmaceuticals North America
“Sunscreen is a must. I recommend CeraVe.”—Gary Goldenberg, MD, New York, NY
· PÊCHE Redness Control
Neocutis Inc
“Patients have found [this product] to be soothing. Patients with rosacea have tolerated it well and found a decrease in redness.”—Mary P. Lupo, MD, New Orleans, LA
“ROSAPLEX [in this product] is an exclusive redness-balancing complex with dextran sulfate, zinc, caffeine, and glycerin, which helps to eliminate the appearance of blotchiness and blemishes, and improve overall skin tone. PÊCHE is a very versatile cream and can be used alone or in conjunction with prescription products for rosacea.”—Marta I. Rendon, MD, Boca Raton, FL
· Redness Solutions Daily Relief Cream
Clinique Laboratories, LLC
“This cream is safe for patients with rosacea to use as a general moisturizer and it has an underlying green base, which cuts the appearance of red.”—Anthony M. Rossi, MD, New York, NY
· Redness Solutions Soothing Cleanser
Clinique Laboratories, LLC
“[I recommend that patients] use the Redness Solutions Soothing Cleanser, then apply the Redness Solutions Daily Relief Cream.”—Gary Goldenberg, MD, New York, NY
· Replenix Products
Topix Pharmaceuticals, Inc
“The Replenix line really works well for redness associated with rosacea. It is high in antioxidants and is one of the few products that works.”—Kenneth Beer, MD, West Palm Beach and Juniper, FL
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cosmetic Dermatology® or Quadrant HealthCom Inc and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cosmetic Dermatology or Quadrant HealthCom Inc endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
Cosmetic Corner: Dermatologists Weigh in on Antiwrinkle Treatments
Leading dermatologists offered their recommendations on the top antiwrinkle treatments. See what they’re recommending to their patients and why.
To improve patient care and outcomes, leading dermatologists offered their recommendations on the top antiwrinkle treatments. Consideration must be given to:
· eCO2
Lutronic
“For antiwrinkle treatments, nothing beats a resurfacing procedure. At this time I believe that fractional CO2 laser resurfacing gives the best results with the least risk. You give up some efficacy compared to fully ablative CO2 laser resurfacing, but there is a markedly lower incidence of significant adverse events with the CO2 laser. We have been using the Lutronic eCO2 laser for the last few years and have been very happy with it.”—Mark G. Rubin, MD, Beverly Hills, CA
· Eucerin Q10 Anti-Wrinkle Sensitive Skin Creme
Beiersdorf Inc
Recommended by Deborah S. Sarnoff, MD, New York, NY
· Kinerase Pro+ Therapy Tretinoin Gel 0.05%
Valeant Pharmaceuticals North America LLC
“Kinerase tretinoin has superior tolerability to generic tretinoin. The vehicle is elegant, and our patients complain less about peeling and irritation.”—Amy J. Derick, MD, Barrington, IL
· Lifeline Skin Care
International Stem Cell Corporation
“Lifeline is a skin care line that is derived from pluripotent human stem cells, which have the ability to repair and renew damaged skin. Gene expression data reveal that collagen and elastin are upregulated after use of Lifeline, and I have definitely noticed an improvement in my skin quality and fine lines since I started using it regularly.”—Elizabeth K. Hale, MD, New York, NY
· Rapid Wrinkle Repair Night Moisturizer in conjunction with Olay Pro-X Wrinkle Smoothing Cream
Neutrogena Corporation and Procter & Gamble, respectively
Recommended by Marian Northington, MD, Birmingham, AL
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cosmetic Dermatology® or Quadrant HealthCom Inc and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cosmetic Dermatology or Quadrant HealthCom Inc endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
Leading dermatologists offered their recommendations on the top antiwrinkle treatments. See what they’re recommending to their patients and why.
To improve patient care and outcomes, leading dermatologists offered their recommendations on the top antiwrinkle treatments. Consideration must be given to:
· eCO2
Lutronic
“For antiwrinkle treatments, nothing beats a resurfacing procedure. At this time I believe that fractional CO2 laser resurfacing gives the best results with the least risk. You give up some efficacy compared to fully ablative CO2 laser resurfacing, but there is a markedly lower incidence of significant adverse events with the CO2 laser. We have been using the Lutronic eCO2 laser for the last few years and have been very happy with it.”—Mark G. Rubin, MD, Beverly Hills, CA
· Eucerin Q10 Anti-Wrinkle Sensitive Skin Creme
Beiersdorf Inc
Recommended by Deborah S. Sarnoff, MD, New York, NY
· Kinerase Pro+ Therapy Tretinoin Gel 0.05%
Valeant Pharmaceuticals North America LLC
“Kinerase tretinoin has superior tolerability to generic tretinoin. The vehicle is elegant, and our patients complain less about peeling and irritation.”—Amy J. Derick, MD, Barrington, IL
· Lifeline Skin Care
International Stem Cell Corporation
“Lifeline is a skin care line that is derived from pluripotent human stem cells, which have the ability to repair and renew damaged skin. Gene expression data reveal that collagen and elastin are upregulated after use of Lifeline, and I have definitely noticed an improvement in my skin quality and fine lines since I started using it regularly.”—Elizabeth K. Hale, MD, New York, NY
· Rapid Wrinkle Repair Night Moisturizer in conjunction with Olay Pro-X Wrinkle Smoothing Cream
Neutrogena Corporation and Procter & Gamble, respectively
Recommended by Marian Northington, MD, Birmingham, AL
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cosmetic Dermatology® or Quadrant HealthCom Inc and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cosmetic Dermatology or Quadrant HealthCom Inc endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
Leading dermatologists offered their recommendations on the top antiwrinkle treatments. See what they’re recommending to their patients and why.
To improve patient care and outcomes, leading dermatologists offered their recommendations on the top antiwrinkle treatments. Consideration must be given to:
· eCO2
Lutronic
“For antiwrinkle treatments, nothing beats a resurfacing procedure. At this time I believe that fractional CO2 laser resurfacing gives the best results with the least risk. You give up some efficacy compared to fully ablative CO2 laser resurfacing, but there is a markedly lower incidence of significant adverse events with the CO2 laser. We have been using the Lutronic eCO2 laser for the last few years and have been very happy with it.”—Mark G. Rubin, MD, Beverly Hills, CA
· Eucerin Q10 Anti-Wrinkle Sensitive Skin Creme
Beiersdorf Inc
Recommended by Deborah S. Sarnoff, MD, New York, NY
· Kinerase Pro+ Therapy Tretinoin Gel 0.05%
Valeant Pharmaceuticals North America LLC
“Kinerase tretinoin has superior tolerability to generic tretinoin. The vehicle is elegant, and our patients complain less about peeling and irritation.”—Amy J. Derick, MD, Barrington, IL
· Lifeline Skin Care
International Stem Cell Corporation
“Lifeline is a skin care line that is derived from pluripotent human stem cells, which have the ability to repair and renew damaged skin. Gene expression data reveal that collagen and elastin are upregulated after use of Lifeline, and I have definitely noticed an improvement in my skin quality and fine lines since I started using it regularly.”—Elizabeth K. Hale, MD, New York, NY
· Rapid Wrinkle Repair Night Moisturizer in conjunction with Olay Pro-X Wrinkle Smoothing Cream
Neutrogena Corporation and Procter & Gamble, respectively
Recommended by Marian Northington, MD, Birmingham, AL
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cosmetic Dermatology® or Quadrant HealthCom Inc and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cosmetic Dermatology or Quadrant HealthCom Inc endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
Cosmetic Corner: Dermatologists Weigh in on Face Washes
Leading dermatologists offered their recommendations on the top face washes. See what they’re recommending to their patients and why.
To improve patient care and outcomes, leading dermatologists offered their recommendations on the top face washes. Consideration must be given to:
· Neutrogena Oil-Free Acne Wash Pink Grapefruit Facial Cleanser
Neutrogena Corporation
Recommended by Marian Northington, MD, Birmingham, AL
· pHaze 1 Facial Wash
PCA Skin
“It is an aloe-based cleanser with low level α-hydroxy acids in it. It is very well tolerated and leaves the skin with a squeaky clean feeling.”—Mark G. Rubin, MD, Beverly Hills, CA
· PURPOSE Gentle Cleansing Wash
Johnson & Johnson Consumer Companies Inc
Recommended by Marian Northington, MD, Birmingham, AL
· VIVITÉ Exfoliating Facial Cleanser
Allergan, Inc
“It is great for patients with oily or acne-prone skin. It is recommended to use several times per week, but I find that it can be used daily to decrease oil. It also helps with seborrheic dermatitis.”—Amy J. Derick, MD, Barrington, IL
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cosmetic Dermatology® or Quadrant HealthCom Inc and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cosmetic Dermatology or Quadrant HealthCom Inc endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
Leading dermatologists offered their recommendations on the top face washes. See what they’re recommending to their patients and why.
To improve patient care and outcomes, leading dermatologists offered their recommendations on the top face washes. Consideration must be given to:
· Neutrogena Oil-Free Acne Wash Pink Grapefruit Facial Cleanser
Neutrogena Corporation
Recommended by Marian Northington, MD, Birmingham, AL
· pHaze 1 Facial Wash
PCA Skin
“It is an aloe-based cleanser with low level α-hydroxy acids in it. It is very well tolerated and leaves the skin with a squeaky clean feeling.”—Mark G. Rubin, MD, Beverly Hills, CA
· PURPOSE Gentle Cleansing Wash
Johnson & Johnson Consumer Companies Inc
Recommended by Marian Northington, MD, Birmingham, AL
· VIVITÉ Exfoliating Facial Cleanser
Allergan, Inc
“It is great for patients with oily or acne-prone skin. It is recommended to use several times per week, but I find that it can be used daily to decrease oil. It also helps with seborrheic dermatitis.”—Amy J. Derick, MD, Barrington, IL
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cosmetic Dermatology® or Quadrant HealthCom Inc and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cosmetic Dermatology or Quadrant HealthCom Inc endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
Leading dermatologists offered their recommendations on the top face washes. See what they’re recommending to their patients and why.
To improve patient care and outcomes, leading dermatologists offered their recommendations on the top face washes. Consideration must be given to:
· Neutrogena Oil-Free Acne Wash Pink Grapefruit Facial Cleanser
Neutrogena Corporation
Recommended by Marian Northington, MD, Birmingham, AL
· pHaze 1 Facial Wash
PCA Skin
“It is an aloe-based cleanser with low level α-hydroxy acids in it. It is very well tolerated and leaves the skin with a squeaky clean feeling.”—Mark G. Rubin, MD, Beverly Hills, CA
· PURPOSE Gentle Cleansing Wash
Johnson & Johnson Consumer Companies Inc
Recommended by Marian Northington, MD, Birmingham, AL
· VIVITÉ Exfoliating Facial Cleanser
Allergan, Inc
“It is great for patients with oily or acne-prone skin. It is recommended to use several times per week, but I find that it can be used daily to decrease oil. It also helps with seborrheic dermatitis.”—Amy J. Derick, MD, Barrington, IL
Disclaimer: Opinions expressed herein do not necessarily reflect those of Cosmetic Dermatology® or Quadrant HealthCom Inc and shall not be used for product endorsement purposes. Any reference made to a specific commercial product does not indicate or imply that Cosmetic Dermatology or Quadrant HealthCom Inc endorses, recommends, or favors the product mentioned. No guarantee is given to the effects of recommended products.
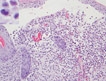
Heparin-Induced Bullous Hemorrhagic Dermatosis
Cutaneous Presentation of T-Cell Prolymphocytic Leukemia
Cutaneous Mastocytosis: A Case of Bullous Urticaria Pigmentosa
Langerhans Cell Histiocytosis
Postcoital vomiting after taking sildenafil?
When you think of sildenafil citrate for the treatment of erectile dysfunction (ED), what adverse effects come to mind? Chances are you think of some of the most common adverse reactions, such as headache (16%), flushing (10%), and dyspepsia (7%), with the latter more common (17%) at higher doses.1 Or perhaps you think of diarrhea (3%) or maybe even dizziness (2%). But chances are, you don’t think of vomiting, which is reported to occur in <2% of patients.1 In fact, an OVID search for the terms PDE5 inhibitors and vomiting revealed no reports of postcoital emesis. In the case we report here, however, postcoital vomiting secondary to sildenafil use did occur.
Our patient, a 43-year-old African-American man with a 23-year history of diabetes and hypertension, sought help for ED. His medications included insulin 70/30 and irbesartan/hydrochlorothiazide (Avalide) 150/12.5 mg daily, due to a history of ACE inhibitor-induced cough. He denied the use of tobacco and recreational drugs but admitted to consuming 6 to 10 beers on Friday nights. He followed no special diet or exercise regimen. A review of systems was negative except for the ED, presumed to be organic as the physical exam was unrevealing.
The patient was not using nitrates and had no known contraindications for sildenafil, and therapy was initiated at 50 mg as needed prior to sexual activity. On follow-up, he reported an acceptable erectile response but noted the onset of postcoital emesis. He denied associated nausea, but reported that on multiple occasions, emesis occurred soon after ejaculation, typically occurring about 90 minutes after ingestion of sildenafil.
The adverse effect profile of sildenafil may be divided into vasodilator effects and enzymatic inhibitor effects.2 It is postulated that an emetic response may be associated with PDE4 inhibitors secondary to release of mediators 5-HT, substance P, and noradrenaline analogous to presynaptic α2-adrenoreceptor inhibition.3
A study by Robichaud et al showed that administration of PDE4 inhibitors reduced the duration of anesthesia induced by a combination of xylazine and ketamine—a correlate of emesis in nonvomiting species (rodents).3 But it is not known if inhibition of PDE4 promotes emesis in humans or if a similar effect occurs with PDE5 inhibitors like sildenafil.3,4 Mild cross-reactivity of sildenafil with PDE6 (present in the retina) explains the visual disturbances associated with the drug (changes in color perception, blurry vision, and light sensitivity)5 and lends further credibility to possible cross-reactivity between PDE4 and PDE5.
Emesis in the absence of nausea or other gastrointestinal (GI) symptoms supports a drug-related effect, rather than a complication associated with type 2 diabetes or binge drinking. The patient denied symptoms of fullness, upper abdominal pain, or reduced hunger, all of which correlate better with delayed gastric emptying associated with diabetic gastroparesis than nausea or vomiting.5
The patient’s weekly consumption of beer meets the criteria for binge drinking defined by the National Institute of Alcohol Abuse and Alcoholism;6 however, emesis associated with ingestion of sildenafil occurred independent of alcohol ingestion, according to our patient.
The patient was advised to try sildenafil both with and without food to determine if either scenario would ameliorate symptoms of vomiting, and to reduce the dosage to 25 mg. Since he now has another health care team, we do not know whether he tried again with sildenafil or another PDE5 inhibitor.
Another case in the literature struck us as remarkably similar. A case report published in 2002 described a 79-year-old man who experienced vestibular symptoms 2 hours after taking sildenafil for the first time, including horizontal nystagmus with rotator components and vomiting.2 The similar time frame as our patient’s complaints also indicates a drug-related phenomenon. The observation of vomiting appears to be unique in the literature and supports its inclusion in published reports that include the long list of sildenafil’s potential adverse effects.
Michelle Lamb, PharmD
Nancy Brahm, PharmD
Mark D. Fox, MD
Tulsa, Okla
1. Viagra (sildenafil citrate) tablets [package insert]. New York NY: Pfizer; 2010. Available at: http://media.pfizer.com/files/products/uspi_viagra.pdf. Accessed January 23, 2013.
2. Hamzavi J, Schmetterer L, Formanek M. Vestibular symptoms as a complication of sildenafil: a case report. Wein Klin Wochenschr. 2002;114:54-55.
3. Robichaud A, Stamatiou PB, Jin S-LC, et al. Deletion of phosphodiesterase 4D in mice shortens α2-adrenoreceptor-mediated anesthesia, a behavioral correlate of emesis. J Clin Invest. 2002;110:1045-1052.
4. Giembycz MA. 4D or not 4D - the emetogenic basis of PDE4 inhibitors uncovered? Trends Pharmacol Sci. 2002;23:548.-
5. Camilleri M, Bharucha AE, Farrugia G. Epidemiology mechanisms, and management of diabetic gastroparesis. Clin Gastroenterol Hepatol. 2011;9:5-12.
6. National Institute of Alcohol Abuse and Alcoholism. NIAAA council approves definition of binge drinking. NIAAA Newsletter. 2004;3:3.-
When you think of sildenafil citrate for the treatment of erectile dysfunction (ED), what adverse effects come to mind? Chances are you think of some of the most common adverse reactions, such as headache (16%), flushing (10%), and dyspepsia (7%), with the latter more common (17%) at higher doses.1 Or perhaps you think of diarrhea (3%) or maybe even dizziness (2%). But chances are, you don’t think of vomiting, which is reported to occur in <2% of patients.1 In fact, an OVID search for the terms PDE5 inhibitors and vomiting revealed no reports of postcoital emesis. In the case we report here, however, postcoital vomiting secondary to sildenafil use did occur.
Our patient, a 43-year-old African-American man with a 23-year history of diabetes and hypertension, sought help for ED. His medications included insulin 70/30 and irbesartan/hydrochlorothiazide (Avalide) 150/12.5 mg daily, due to a history of ACE inhibitor-induced cough. He denied the use of tobacco and recreational drugs but admitted to consuming 6 to 10 beers on Friday nights. He followed no special diet or exercise regimen. A review of systems was negative except for the ED, presumed to be organic as the physical exam was unrevealing.
The patient was not using nitrates and had no known contraindications for sildenafil, and therapy was initiated at 50 mg as needed prior to sexual activity. On follow-up, he reported an acceptable erectile response but noted the onset of postcoital emesis. He denied associated nausea, but reported that on multiple occasions, emesis occurred soon after ejaculation, typically occurring about 90 minutes after ingestion of sildenafil.
The adverse effect profile of sildenafil may be divided into vasodilator effects and enzymatic inhibitor effects.2 It is postulated that an emetic response may be associated with PDE4 inhibitors secondary to release of mediators 5-HT, substance P, and noradrenaline analogous to presynaptic α2-adrenoreceptor inhibition.3
A study by Robichaud et al showed that administration of PDE4 inhibitors reduced the duration of anesthesia induced by a combination of xylazine and ketamine—a correlate of emesis in nonvomiting species (rodents).3 But it is not known if inhibition of PDE4 promotes emesis in humans or if a similar effect occurs with PDE5 inhibitors like sildenafil.3,4 Mild cross-reactivity of sildenafil with PDE6 (present in the retina) explains the visual disturbances associated with the drug (changes in color perception, blurry vision, and light sensitivity)5 and lends further credibility to possible cross-reactivity between PDE4 and PDE5.
Emesis in the absence of nausea or other gastrointestinal (GI) symptoms supports a drug-related effect, rather than a complication associated with type 2 diabetes or binge drinking. The patient denied symptoms of fullness, upper abdominal pain, or reduced hunger, all of which correlate better with delayed gastric emptying associated with diabetic gastroparesis than nausea or vomiting.5
The patient’s weekly consumption of beer meets the criteria for binge drinking defined by the National Institute of Alcohol Abuse and Alcoholism;6 however, emesis associated with ingestion of sildenafil occurred independent of alcohol ingestion, according to our patient.
The patient was advised to try sildenafil both with and without food to determine if either scenario would ameliorate symptoms of vomiting, and to reduce the dosage to 25 mg. Since he now has another health care team, we do not know whether he tried again with sildenafil or another PDE5 inhibitor.
Another case in the literature struck us as remarkably similar. A case report published in 2002 described a 79-year-old man who experienced vestibular symptoms 2 hours after taking sildenafil for the first time, including horizontal nystagmus with rotator components and vomiting.2 The similar time frame as our patient’s complaints also indicates a drug-related phenomenon. The observation of vomiting appears to be unique in the literature and supports its inclusion in published reports that include the long list of sildenafil’s potential adverse effects.
Michelle Lamb, PharmD
Nancy Brahm, PharmD
Mark D. Fox, MD
Tulsa, Okla
When you think of sildenafil citrate for the treatment of erectile dysfunction (ED), what adverse effects come to mind? Chances are you think of some of the most common adverse reactions, such as headache (16%), flushing (10%), and dyspepsia (7%), with the latter more common (17%) at higher doses.1 Or perhaps you think of diarrhea (3%) or maybe even dizziness (2%). But chances are, you don’t think of vomiting, which is reported to occur in <2% of patients.1 In fact, an OVID search for the terms PDE5 inhibitors and vomiting revealed no reports of postcoital emesis. In the case we report here, however, postcoital vomiting secondary to sildenafil use did occur.
Our patient, a 43-year-old African-American man with a 23-year history of diabetes and hypertension, sought help for ED. His medications included insulin 70/30 and irbesartan/hydrochlorothiazide (Avalide) 150/12.5 mg daily, due to a history of ACE inhibitor-induced cough. He denied the use of tobacco and recreational drugs but admitted to consuming 6 to 10 beers on Friday nights. He followed no special diet or exercise regimen. A review of systems was negative except for the ED, presumed to be organic as the physical exam was unrevealing.
The patient was not using nitrates and had no known contraindications for sildenafil, and therapy was initiated at 50 mg as needed prior to sexual activity. On follow-up, he reported an acceptable erectile response but noted the onset of postcoital emesis. He denied associated nausea, but reported that on multiple occasions, emesis occurred soon after ejaculation, typically occurring about 90 minutes after ingestion of sildenafil.
The adverse effect profile of sildenafil may be divided into vasodilator effects and enzymatic inhibitor effects.2 It is postulated that an emetic response may be associated with PDE4 inhibitors secondary to release of mediators 5-HT, substance P, and noradrenaline analogous to presynaptic α2-adrenoreceptor inhibition.3
A study by Robichaud et al showed that administration of PDE4 inhibitors reduced the duration of anesthesia induced by a combination of xylazine and ketamine—a correlate of emesis in nonvomiting species (rodents).3 But it is not known if inhibition of PDE4 promotes emesis in humans or if a similar effect occurs with PDE5 inhibitors like sildenafil.3,4 Mild cross-reactivity of sildenafil with PDE6 (present in the retina) explains the visual disturbances associated with the drug (changes in color perception, blurry vision, and light sensitivity)5 and lends further credibility to possible cross-reactivity between PDE4 and PDE5.
Emesis in the absence of nausea or other gastrointestinal (GI) symptoms supports a drug-related effect, rather than a complication associated with type 2 diabetes or binge drinking. The patient denied symptoms of fullness, upper abdominal pain, or reduced hunger, all of which correlate better with delayed gastric emptying associated with diabetic gastroparesis than nausea or vomiting.5
The patient’s weekly consumption of beer meets the criteria for binge drinking defined by the National Institute of Alcohol Abuse and Alcoholism;6 however, emesis associated with ingestion of sildenafil occurred independent of alcohol ingestion, according to our patient.
The patient was advised to try sildenafil both with and without food to determine if either scenario would ameliorate symptoms of vomiting, and to reduce the dosage to 25 mg. Since he now has another health care team, we do not know whether he tried again with sildenafil or another PDE5 inhibitor.
Another case in the literature struck us as remarkably similar. A case report published in 2002 described a 79-year-old man who experienced vestibular symptoms 2 hours after taking sildenafil for the first time, including horizontal nystagmus with rotator components and vomiting.2 The similar time frame as our patient’s complaints also indicates a drug-related phenomenon. The observation of vomiting appears to be unique in the literature and supports its inclusion in published reports that include the long list of sildenafil’s potential adverse effects.
Michelle Lamb, PharmD
Nancy Brahm, PharmD
Mark D. Fox, MD
Tulsa, Okla
1. Viagra (sildenafil citrate) tablets [package insert]. New York NY: Pfizer; 2010. Available at: http://media.pfizer.com/files/products/uspi_viagra.pdf. Accessed January 23, 2013.
2. Hamzavi J, Schmetterer L, Formanek M. Vestibular symptoms as a complication of sildenafil: a case report. Wein Klin Wochenschr. 2002;114:54-55.
3. Robichaud A, Stamatiou PB, Jin S-LC, et al. Deletion of phosphodiesterase 4D in mice shortens α2-adrenoreceptor-mediated anesthesia, a behavioral correlate of emesis. J Clin Invest. 2002;110:1045-1052.
4. Giembycz MA. 4D or not 4D - the emetogenic basis of PDE4 inhibitors uncovered? Trends Pharmacol Sci. 2002;23:548.-
5. Camilleri M, Bharucha AE, Farrugia G. Epidemiology mechanisms, and management of diabetic gastroparesis. Clin Gastroenterol Hepatol. 2011;9:5-12.
6. National Institute of Alcohol Abuse and Alcoholism. NIAAA council approves definition of binge drinking. NIAAA Newsletter. 2004;3:3.-
1. Viagra (sildenafil citrate) tablets [package insert]. New York NY: Pfizer; 2010. Available at: http://media.pfizer.com/files/products/uspi_viagra.pdf. Accessed January 23, 2013.
2. Hamzavi J, Schmetterer L, Formanek M. Vestibular symptoms as a complication of sildenafil: a case report. Wein Klin Wochenschr. 2002;114:54-55.
3. Robichaud A, Stamatiou PB, Jin S-LC, et al. Deletion of phosphodiesterase 4D in mice shortens α2-adrenoreceptor-mediated anesthesia, a behavioral correlate of emesis. J Clin Invest. 2002;110:1045-1052.
4. Giembycz MA. 4D or not 4D - the emetogenic basis of PDE4 inhibitors uncovered? Trends Pharmacol Sci. 2002;23:548.-
5. Camilleri M, Bharucha AE, Farrugia G. Epidemiology mechanisms, and management of diabetic gastroparesis. Clin Gastroenterol Hepatol. 2011;9:5-12.
6. National Institute of Alcohol Abuse and Alcoholism. NIAAA council approves definition of binge drinking. NIAAA Newsletter. 2004;3:3.-
Bipolar disorder or something else?
CASE: Unclear diagnosis
Police find Ms. S, age 31, extremely intoxicated and drinking alcohol in her car in a city park parking lot. In the emergency room, she becomes increasingly somnolent and clinicians intubate her trachea to protect her airway. Lab testing shows she has elevated acetaminophen and lithium serum levels, and she is transferred to our hospital for further management after being started on N-acetylcysteine to treat acetaminophen toxicity. Her “ex-fiancé,” the father of her 2 children, saw her earlier the day of the episode and says she was distraught, intoxicated, and had several empty pill bottles in her purse.
In our hospital, Ms. S’ lithium level increases from 2.3 mEq/L to a peak of 5.32 mEq/L, and she undergoes hemodialysis. On hospital day 2, her serum lithium level is trending downward. After Ms. S is able to breathe spontaneously, her trachea is extubated and her hemodialysis line is removed. A psychiatric consultation is obtained, but she is unable to provide a coherent history and the treating clinicians believe she has delirium caused by multiple factors.
On hospital day 3, Ms. S’ delirium clears enough for her to engage in an interview, and she is transferred to our inpatient psychiatry ward for further monitoring and stabilization.
She reports that she was diagnosed with bipolar disorder (BD) at age 12, when she faced multiple psychosocial stressors, including physical abuse by her mother’s boyfriend. She took several psychotropics—although she cannot remember which ones—until age 14, when she stopped all medications until the year before her current hospitalization. Although throughout adolescence and adulthood Ms. S experienced chronic irritability, anxiety, impulsive behavior, poor self-esteem, abusive relationships, self-cutting, and depressed mood, she maintains that she felt worse when she was taking psychotropics and doubts the BD diagnosis. She attributes her longstanding mood issues to low self-worth, a “codependent nature,” and a tendency to gravitate toward abusive relationships. Although she admits to experimenting with several illicit drugs during adolescence, she denies more recent substance use and states she drinks alcohol only once every few months.
The authors’ observations
BD is underdiagnosed in several patient populations, such as individuals previously diagnosed with MDD.1-3 Misdiagnosis can have severe implications, including delay in receiving treatment with effective medications (eg, mood stabilizers) or use of agents that can induce mania or rapid-cycling, such as antidepressants. Perhaps in response to this concern, in recent years clinicians increasingly have diagnosed BD in adolescents and adults. An analysis of a national database of physician practices found a 40-fold increase in office visits for BD among youth and a near doubling among adults from 1994 to 2003.4
Although underdiagnosis of BD remains important, some researchers have suggested that overdiagnosis may be more prevalent and equally harmful. In a study of 180 patients being treated for depression in a family care clinic, there was a 21.6% initial underdiagnosis rate among those eventually found to have BD.1 However, among 43 patients with a prior BD diagnosis, the diagnosis was not confirmed in 33%.1 In a study of 700 psychiatric outpatients in Rhode Island, only 43% of 145 patients who reported a prior BD diagnosis had that diagnosis confirmed.5 Three times as many patients were overdiagnosed with BD as underdiagnosed.
Are there characteristics common to individuals incorrectly diagnosed with BD? In a study that compared patients who had been mistakenly diagnosed with BD with those who had not been diagnosed with BD, the overdiagnosis group was significantly more likely to be diagnosed with a personality disorder, in particular borderline or antisocial personality disorder.6 Only lifetime and current BPD, current posttraumatic stress disorder (PTSD), and lifetime impulse control disorders were independently associated with BD overdiagnosis. The odds ratio for overdiagnosis of BD in patients found to have BPD was 3.7.
EVALUATION: Rethink the diagnosis
In the last few months, Ms. S had complained to her primary care provider (PCP) of worsening anxiety and depressed mood. She was the victim of ongoing physical and emotional abuse by her ex-fiancé and was concerned that she may lose custody of her 2 sons. Approximately 8 months before admission, Ms. S’ PCP prescribed lithium, 450 mg, 3 times a day, for “mood stabilization” and depression because she’d already been diagnosed with BD. This was the first mood stabilizer she’d taken since she was 14. She also was taking unknown doses of hydrocodone/acetaminophen, cyclobenzaprine, and tramadol for pain and temazepam for insomnia. Ms. S continued to suffer from labile and depressed mood, and fought with her ex-fiancé and legal authorities to maintain custody of her 2 children until she was found in the park.
Throughout her hospitalization she denies that she attempted suicide that day, and maintains that this incident was caused by unintentional mismanagement of her medications. Although she continues to have a sense of low self-worth, she denies feeling depressed; in contrast, she says she feels like she has a “new lease on life.” During several interviews she cannot provide a history of any prolonged (ie, several days) episodes of elevated mood, increased goal-directed behavior, decreased need for sleep, tangential thought, pressured speech, or other symptoms that suggest hypomania or mania. She does not endorse prolonged periods of neurovegetative symptoms that would indicate a major depressive episode.
We feel that Ms. S’ symptoms of affective dysregulation, impulsivity, and interpersonal dysfunction are consistent with BPD, and we determine that she meets 6 of the 9 DSM-IV-TR diagnostic features of BPD (≥5 are required for a BPD diagnosis) (Table 1).7 Ms. S describes efforts to avoid abandonment, unstable and intense interpersonal relationships, marked and persistent unstable self-image, recurrent suicidal and self-mutilating behavior, affective instability, and chronic feelings of emptiness. She is discharged to follow up with a psychotherapist and family practitioner. She is not continued on any psychotropic medications.
The authors’ observations
Although it can be difficult to accurately diagnose psychiatric illness during a brief inpatient hospitalization, several clinicians who cared for Ms. S felt that her presentation was more consistent with BPD than BD. Her case is an example of the potential harm of incorrectly diagnosing personality-disordered patients with BD. Ms. S is impulsive and used lithium—a medication that is the standard of care for BD—in an overdose, which lead to a costly and dangerous hospitalization marked by a difficult tracheal intubation and hemodialysis.
Table 1
DSM-IV-TR diagnostic criteria for borderline personality disorder
| A pervasive pattern of instability of interpersonal relationships, self-image, and affects, and marked impulsivity, as indicated by ≥5 of the following: |
|
| Source: Reference 7 |
Distinguishing BD and BPD
There is considerable overlap in symptoms of BD and BPD. Although the episodic nature of BD is well differentiated from the more chronic course of BPD, many hypomania and mania symptoms are similar to those of BPD (Table 2).7 For example, patients with BD or BPD may exhibit impulsive behavior and labile moods. Substance use, risky and self-destructive behaviors, and inflammatory interpersonal relationships can occur in both disorders. Some researchers have suggested that pathophysiologically, BPD may fall on a spectrum of bipolar illness, and have proposed a clinical entity they call bipolar type IV or ultra-rapid cycling BD.2,8,9 There may be more co-occurrence of BD with BPD than would be expected by chance10; 1 review of BPD studies found the rate of comorbid BD ranged from 5.6% to 19%.11 However, because of differences in several factors—including phenomenology, family prevalence, longitudinal course, and medication response—some researchers have concluded that evidence does not support categorizing BPD as part of a bipolar spectrum.10-14 Nonetheless, BPD and other personality disorders often co-occur with axis I disorders, including MDD, BD, or PTSD.
Some research has suggested that the increasing availability and marketing campaigns of medications to treat BD may promote diagnosis of the disorder.15 Zimmerman15 hypothesizes that physicians may be more likely to diagnose a condition that responds to medication (ie, BD) than one that is less responsive (ie, BPD). Financial compensation for treating axis I disorders is significantly better than for treating personality disorders.16 The inpatient setting confers barriers to accurately diagnosing personality disorders, including limits on the amount of time that clinicians can spend with patients or ability to communicate with sources of collateral information. A patient’s observed personality and behaviors while hospitalized may not accurately reflect his or her personality and behaviors in that patient’s “natural” environment.
Several diagnostic strategies can help distinguish BPD from BD. For BD to be the primary diagnosis, a patient must have had a hypomanic or manic episode. Sustained episodes of elation or extreme irritability without evident stressors suggest BD rather than BPD.10 According to Gunderson et al,10 “repeated angry outbursts, suicide attempts, or acts of deliberate self harm that are reactive to interpersonal stress and reflect extreme rejection sensitivity are axiomatic of borderline personality disorder.” In a review of clinical practice, Gunderson17 found that hypersensitivity to rejection and fearful preoccupation with expected abandonment are the most distinctive characteristics of BPD patients. He suggested that clinicians can establish the diagnosis by asking patients directly if they believe the criteria for BPD characterize them, which also can help a patient to accept the diagnosis.
Finally, during a short hospitalization, it can be helpful to obtain collateral information from the patient’s friends and family or further characterize the time course of symptoms and diagnostic features in the patient’s natural environment. Clinicians who are reluctant to diagnose BPD in an inpatient setting could suggest the presence of borderline traits or discuss the possibility of the BPD diagnosis in documentation (eg, in the assessment or formulation). Doing so would avoid a premature BPD diagnosis and allow outpatient providers to confirm or rule out personality disorder diagnoses over time. It is important to screen patients with BPD for co-occurring axis I disorders, including BD, MDD, PTSD, and substance abuse.
A false-positive BD diagnosis in patients with BPD has serious treatment implications. Antipsychotics, antidepressants, and anticonvulsants have been used to target BPD symptoms such as affective dysregulation, impulsivity, and cognitive/perceptual abnormalities, but no medications are FDA-approved for treating BPD. American Psychiatric Association guidelines recommend symptom-based pharmacologic strategies for BPD,18 although some researchers believe that these recommendations are out-of-date and not evidence-based.17,19 Some evidence suggests pharmacotherapy can have modest short-term benefits on specific BPD symptoms, but no data suggest that medication can reduce the severity of BPD or lead to remission.19-23 Just 1 randomized controlled trial (N = 17) has examined lithium for BPD and found no effect on mood.11,24
Misdiagnosis of BD in the context of BPD may create unrealistic expectations regarding the potential efficacy of medications for relieving symptoms. Patients may be diverted from potentially helpful psychotherapeutic treatments—such as DBT or mentalization therapy—which evidence suggests can effectively reduce symptoms, the need for additional treatments, and self-harm or suicidal behaviors.10,17,19 Evidence from long-term longitudinal studies suggests that psychosocial or psychotherapeutic treatment may protect against suicide in BPD patients.25
Table 2
DSM-IV-TR diagnostic criteria for a manic episode
|
The DSM-IV-TR diagnostic criteria for a hypomanic episode are similar to criteria for a manic episode, except:
|
| Source: Reference 7 |
Related Resources
- National Education Alliance Borderline Personality Disorder. www.borderlinepersonalitydisorder.com.
- Hoffman PD, Steiner-Grossman P. Borderline personality disorder: meeting the challenges to successful treatment. Philadelphia, PA: Haworth Press; 2008.
Drug Brand Names
- Cyclobenzaprine • Flexeril
- Hydrocodone/acetaminophen • Lorcet, Vicodin, others
- Lithium • Eskalith, Lithobid
- Temazepam • Restoril
- Tramadol • Ultram
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Hirschfeld RM, Cass AR, Holt DC, et al. Screening for bipolar disorder in patients treated for depression in a family medicine clinic. J Am Board Fam Pract. 2005;18(4):233-239.
2. Ghaemi SN, Ko JY, Goodwin FK. “Cade’s disease” and beyond: Misdiagnosis antidepressant use, and a proposed definition for bipolar spectrum disorder. Can J Psychiatry. 2002;47(2):125-134.
3. Bowden CL. Strategies to reduce misdiagnosis of bipolar depression. Psychiatr Serv. 2001;52(1):51-55.
4. Moreno C, Laje G, Blanco C, et al. National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Arch Gen Psychiatry. 2007;64(9):1032-1039.
5. Zimmerman M, Ruggero CJ, Chelminski I, et al. Is bipolar disorder overdiagnosed? J Clin Psychiatry. 2008;69(6):935-940.
6. Zimmerman M, Ruggero CJ, Chelminski I, et al. Psychiatric diagnoses in patients previously overdiagnosed with bipolar disorder. J Clin Psychiatry. 2010;71(1):26-31.
7. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
8. Akiskal HS. The bipolar spectrum-the shaping of a new paradigm in psychiatry. Curr Psychiatry Rep. 2002;4(1):1-3.
9. Akiskal HS, Pinto O. The evolving bipolar spectrum. Prototypes I II, III, and IV. Psychiatr Clin North Am. 1999;22(3):517-534, vii.
10. Gunderson JG, Weinberg I, Daversa MT, et al. Descriptive and longitudinal observations on the relationship of borderline personality disorder and bipolar disorder. Am J Psychiatry. 2006;163(7):1173-1178.
11. Paris J, Gunderson J, Weinberg I. The interface between borderline personality disorder and bipolar spectrum disorders. Compr Psychiatry. 2007;48(2):145-154.
12. Paris J. Why psychiatrists are reluctant to diagnose: borderline personality disorder. Psychiatry (Edgmont). 2007;4(1):35-39.
13. Paris J. Borderline or bipolar? Distinguishing borderline personality disorder from bipolar spectrum disorders. Harv Rev Psychiatry. 2004;12(3):140-145.
14. Ruggero CJ, Zimmerman M, Chelminski I, et al. Borderline personality disorder and the misdiagnosis of bipolar disorder. J Psychiatr Res. 2010;44(6):405-408.
15. Zimmerman M. Problems diagnosing bipolar disorder in clinical practice. Expert Rev Neurother. 2010;10(7):1019-1021.
16. Stone MH. Relationship of borderline personality disorder and bipolar disorder. Am J Psychiatry. 2006;163(7):1126-1128.
17. Gunderson JG. Clinical practice. Borderline personality disorder. N Engl J Med. 2011;364(21):2037-2042.
18. American Psychiatric Association. Practice guideline for the treatment of patients with borderline personality disorder. Washington D.C.: American Psychiatric Association; 2001.
19. Paris J. The treatment of borderline personality disorder: implications of research on diagnosis etiology, and outcome. Annu Rev Clin Psychol. 2009;5:277-290.
20. Stoffers J, Völlm BA, Rücker G, et al. Pharmacological interventions for borderline personality disorder. Cochrane Database Syst Rev. 2010;(6):CD005653.-
21. Ripoll LH, Triebwasser J, Siever LJ. Evidence-based pharmacotherapy for personality disorders. Int J Neuropsychopharmacol. 2011;14(9):1257-1288.
22. Mercer D, Douglass AB, Links PS. Meta-analyses of mood stabilizers antidepressants and antipsychotics in the treatment of borderline personality disorder: effectiveness for depression and anger symptoms. J Pers Disord. 2009;23(2):156-174.
23. Lieb K, Völlm B, Rücker G, et al. Pharmacotherapy for borderline personality disorder: Cochrane systematic review of randomised trials. Br J Psychiatry. 2010;196(1):4-12.
24. Links PS, Steiner M, Boiago I, et al. Lithium therapy for borderline patients: preliminary findings. J Pers Disord. 1990;4(2):173-181.
25. Goodman M, Roiff T, Oakes AH, et al. Suicidal risk and management in borderline personality disorder. Curr Psychiatry Rep. 2012;14(1):79-85.
CASE: Unclear diagnosis
Police find Ms. S, age 31, extremely intoxicated and drinking alcohol in her car in a city park parking lot. In the emergency room, she becomes increasingly somnolent and clinicians intubate her trachea to protect her airway. Lab testing shows she has elevated acetaminophen and lithium serum levels, and she is transferred to our hospital for further management after being started on N-acetylcysteine to treat acetaminophen toxicity. Her “ex-fiancé,” the father of her 2 children, saw her earlier the day of the episode and says she was distraught, intoxicated, and had several empty pill bottles in her purse.
In our hospital, Ms. S’ lithium level increases from 2.3 mEq/L to a peak of 5.32 mEq/L, and she undergoes hemodialysis. On hospital day 2, her serum lithium level is trending downward. After Ms. S is able to breathe spontaneously, her trachea is extubated and her hemodialysis line is removed. A psychiatric consultation is obtained, but she is unable to provide a coherent history and the treating clinicians believe she has delirium caused by multiple factors.
On hospital day 3, Ms. S’ delirium clears enough for her to engage in an interview, and she is transferred to our inpatient psychiatry ward for further monitoring and stabilization.
She reports that she was diagnosed with bipolar disorder (BD) at age 12, when she faced multiple psychosocial stressors, including physical abuse by her mother’s boyfriend. She took several psychotropics—although she cannot remember which ones—until age 14, when she stopped all medications until the year before her current hospitalization. Although throughout adolescence and adulthood Ms. S experienced chronic irritability, anxiety, impulsive behavior, poor self-esteem, abusive relationships, self-cutting, and depressed mood, she maintains that she felt worse when she was taking psychotropics and doubts the BD diagnosis. She attributes her longstanding mood issues to low self-worth, a “codependent nature,” and a tendency to gravitate toward abusive relationships. Although she admits to experimenting with several illicit drugs during adolescence, she denies more recent substance use and states she drinks alcohol only once every few months.
The authors’ observations
BD is underdiagnosed in several patient populations, such as individuals previously diagnosed with MDD.1-3 Misdiagnosis can have severe implications, including delay in receiving treatment with effective medications (eg, mood stabilizers) or use of agents that can induce mania or rapid-cycling, such as antidepressants. Perhaps in response to this concern, in recent years clinicians increasingly have diagnosed BD in adolescents and adults. An analysis of a national database of physician practices found a 40-fold increase in office visits for BD among youth and a near doubling among adults from 1994 to 2003.4
Although underdiagnosis of BD remains important, some researchers have suggested that overdiagnosis may be more prevalent and equally harmful. In a study of 180 patients being treated for depression in a family care clinic, there was a 21.6% initial underdiagnosis rate among those eventually found to have BD.1 However, among 43 patients with a prior BD diagnosis, the diagnosis was not confirmed in 33%.1 In a study of 700 psychiatric outpatients in Rhode Island, only 43% of 145 patients who reported a prior BD diagnosis had that diagnosis confirmed.5 Three times as many patients were overdiagnosed with BD as underdiagnosed.
Are there characteristics common to individuals incorrectly diagnosed with BD? In a study that compared patients who had been mistakenly diagnosed with BD with those who had not been diagnosed with BD, the overdiagnosis group was significantly more likely to be diagnosed with a personality disorder, in particular borderline or antisocial personality disorder.6 Only lifetime and current BPD, current posttraumatic stress disorder (PTSD), and lifetime impulse control disorders were independently associated with BD overdiagnosis. The odds ratio for overdiagnosis of BD in patients found to have BPD was 3.7.
EVALUATION: Rethink the diagnosis
In the last few months, Ms. S had complained to her primary care provider (PCP) of worsening anxiety and depressed mood. She was the victim of ongoing physical and emotional abuse by her ex-fiancé and was concerned that she may lose custody of her 2 sons. Approximately 8 months before admission, Ms. S’ PCP prescribed lithium, 450 mg, 3 times a day, for “mood stabilization” and depression because she’d already been diagnosed with BD. This was the first mood stabilizer she’d taken since she was 14. She also was taking unknown doses of hydrocodone/acetaminophen, cyclobenzaprine, and tramadol for pain and temazepam for insomnia. Ms. S continued to suffer from labile and depressed mood, and fought with her ex-fiancé and legal authorities to maintain custody of her 2 children until she was found in the park.
Throughout her hospitalization she denies that she attempted suicide that day, and maintains that this incident was caused by unintentional mismanagement of her medications. Although she continues to have a sense of low self-worth, she denies feeling depressed; in contrast, she says she feels like she has a “new lease on life.” During several interviews she cannot provide a history of any prolonged (ie, several days) episodes of elevated mood, increased goal-directed behavior, decreased need for sleep, tangential thought, pressured speech, or other symptoms that suggest hypomania or mania. She does not endorse prolonged periods of neurovegetative symptoms that would indicate a major depressive episode.
We feel that Ms. S’ symptoms of affective dysregulation, impulsivity, and interpersonal dysfunction are consistent with BPD, and we determine that she meets 6 of the 9 DSM-IV-TR diagnostic features of BPD (≥5 are required for a BPD diagnosis) (Table 1).7 Ms. S describes efforts to avoid abandonment, unstable and intense interpersonal relationships, marked and persistent unstable self-image, recurrent suicidal and self-mutilating behavior, affective instability, and chronic feelings of emptiness. She is discharged to follow up with a psychotherapist and family practitioner. She is not continued on any psychotropic medications.
The authors’ observations
Although it can be difficult to accurately diagnose psychiatric illness during a brief inpatient hospitalization, several clinicians who cared for Ms. S felt that her presentation was more consistent with BPD than BD. Her case is an example of the potential harm of incorrectly diagnosing personality-disordered patients with BD. Ms. S is impulsive and used lithium—a medication that is the standard of care for BD—in an overdose, which lead to a costly and dangerous hospitalization marked by a difficult tracheal intubation and hemodialysis.
Table 1
DSM-IV-TR diagnostic criteria for borderline personality disorder
| A pervasive pattern of instability of interpersonal relationships, self-image, and affects, and marked impulsivity, as indicated by ≥5 of the following: |
|
| Source: Reference 7 |
Distinguishing BD and BPD
There is considerable overlap in symptoms of BD and BPD. Although the episodic nature of BD is well differentiated from the more chronic course of BPD, many hypomania and mania symptoms are similar to those of BPD (Table 2).7 For example, patients with BD or BPD may exhibit impulsive behavior and labile moods. Substance use, risky and self-destructive behaviors, and inflammatory interpersonal relationships can occur in both disorders. Some researchers have suggested that pathophysiologically, BPD may fall on a spectrum of bipolar illness, and have proposed a clinical entity they call bipolar type IV or ultra-rapid cycling BD.2,8,9 There may be more co-occurrence of BD with BPD than would be expected by chance10; 1 review of BPD studies found the rate of comorbid BD ranged from 5.6% to 19%.11 However, because of differences in several factors—including phenomenology, family prevalence, longitudinal course, and medication response—some researchers have concluded that evidence does not support categorizing BPD as part of a bipolar spectrum.10-14 Nonetheless, BPD and other personality disorders often co-occur with axis I disorders, including MDD, BD, or PTSD.
Some research has suggested that the increasing availability and marketing campaigns of medications to treat BD may promote diagnosis of the disorder.15 Zimmerman15 hypothesizes that physicians may be more likely to diagnose a condition that responds to medication (ie, BD) than one that is less responsive (ie, BPD). Financial compensation for treating axis I disorders is significantly better than for treating personality disorders.16 The inpatient setting confers barriers to accurately diagnosing personality disorders, including limits on the amount of time that clinicians can spend with patients or ability to communicate with sources of collateral information. A patient’s observed personality and behaviors while hospitalized may not accurately reflect his or her personality and behaviors in that patient’s “natural” environment.
Several diagnostic strategies can help distinguish BPD from BD. For BD to be the primary diagnosis, a patient must have had a hypomanic or manic episode. Sustained episodes of elation or extreme irritability without evident stressors suggest BD rather than BPD.10 According to Gunderson et al,10 “repeated angry outbursts, suicide attempts, or acts of deliberate self harm that are reactive to interpersonal stress and reflect extreme rejection sensitivity are axiomatic of borderline personality disorder.” In a review of clinical practice, Gunderson17 found that hypersensitivity to rejection and fearful preoccupation with expected abandonment are the most distinctive characteristics of BPD patients. He suggested that clinicians can establish the diagnosis by asking patients directly if they believe the criteria for BPD characterize them, which also can help a patient to accept the diagnosis.
Finally, during a short hospitalization, it can be helpful to obtain collateral information from the patient’s friends and family or further characterize the time course of symptoms and diagnostic features in the patient’s natural environment. Clinicians who are reluctant to diagnose BPD in an inpatient setting could suggest the presence of borderline traits or discuss the possibility of the BPD diagnosis in documentation (eg, in the assessment or formulation). Doing so would avoid a premature BPD diagnosis and allow outpatient providers to confirm or rule out personality disorder diagnoses over time. It is important to screen patients with BPD for co-occurring axis I disorders, including BD, MDD, PTSD, and substance abuse.
A false-positive BD diagnosis in patients with BPD has serious treatment implications. Antipsychotics, antidepressants, and anticonvulsants have been used to target BPD symptoms such as affective dysregulation, impulsivity, and cognitive/perceptual abnormalities, but no medications are FDA-approved for treating BPD. American Psychiatric Association guidelines recommend symptom-based pharmacologic strategies for BPD,18 although some researchers believe that these recommendations are out-of-date and not evidence-based.17,19 Some evidence suggests pharmacotherapy can have modest short-term benefits on specific BPD symptoms, but no data suggest that medication can reduce the severity of BPD or lead to remission.19-23 Just 1 randomized controlled trial (N = 17) has examined lithium for BPD and found no effect on mood.11,24
Misdiagnosis of BD in the context of BPD may create unrealistic expectations regarding the potential efficacy of medications for relieving symptoms. Patients may be diverted from potentially helpful psychotherapeutic treatments—such as DBT or mentalization therapy—which evidence suggests can effectively reduce symptoms, the need for additional treatments, and self-harm or suicidal behaviors.10,17,19 Evidence from long-term longitudinal studies suggests that psychosocial or psychotherapeutic treatment may protect against suicide in BPD patients.25
Table 2
DSM-IV-TR diagnostic criteria for a manic episode
|
The DSM-IV-TR diagnostic criteria for a hypomanic episode are similar to criteria for a manic episode, except:
|
| Source: Reference 7 |
Related Resources
- National Education Alliance Borderline Personality Disorder. www.borderlinepersonalitydisorder.com.
- Hoffman PD, Steiner-Grossman P. Borderline personality disorder: meeting the challenges to successful treatment. Philadelphia, PA: Haworth Press; 2008.
Drug Brand Names
- Cyclobenzaprine • Flexeril
- Hydrocodone/acetaminophen • Lorcet, Vicodin, others
- Lithium • Eskalith, Lithobid
- Temazepam • Restoril
- Tramadol • Ultram
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Unclear diagnosis
Police find Ms. S, age 31, extremely intoxicated and drinking alcohol in her car in a city park parking lot. In the emergency room, she becomes increasingly somnolent and clinicians intubate her trachea to protect her airway. Lab testing shows she has elevated acetaminophen and lithium serum levels, and she is transferred to our hospital for further management after being started on N-acetylcysteine to treat acetaminophen toxicity. Her “ex-fiancé,” the father of her 2 children, saw her earlier the day of the episode and says she was distraught, intoxicated, and had several empty pill bottles in her purse.
In our hospital, Ms. S’ lithium level increases from 2.3 mEq/L to a peak of 5.32 mEq/L, and she undergoes hemodialysis. On hospital day 2, her serum lithium level is trending downward. After Ms. S is able to breathe spontaneously, her trachea is extubated and her hemodialysis line is removed. A psychiatric consultation is obtained, but she is unable to provide a coherent history and the treating clinicians believe she has delirium caused by multiple factors.
On hospital day 3, Ms. S’ delirium clears enough for her to engage in an interview, and she is transferred to our inpatient psychiatry ward for further monitoring and stabilization.
She reports that she was diagnosed with bipolar disorder (BD) at age 12, when she faced multiple psychosocial stressors, including physical abuse by her mother’s boyfriend. She took several psychotropics—although she cannot remember which ones—until age 14, when she stopped all medications until the year before her current hospitalization. Although throughout adolescence and adulthood Ms. S experienced chronic irritability, anxiety, impulsive behavior, poor self-esteem, abusive relationships, self-cutting, and depressed mood, she maintains that she felt worse when she was taking psychotropics and doubts the BD diagnosis. She attributes her longstanding mood issues to low self-worth, a “codependent nature,” and a tendency to gravitate toward abusive relationships. Although she admits to experimenting with several illicit drugs during adolescence, she denies more recent substance use and states she drinks alcohol only once every few months.
The authors’ observations
BD is underdiagnosed in several patient populations, such as individuals previously diagnosed with MDD.1-3 Misdiagnosis can have severe implications, including delay in receiving treatment with effective medications (eg, mood stabilizers) or use of agents that can induce mania or rapid-cycling, such as antidepressants. Perhaps in response to this concern, in recent years clinicians increasingly have diagnosed BD in adolescents and adults. An analysis of a national database of physician practices found a 40-fold increase in office visits for BD among youth and a near doubling among adults from 1994 to 2003.4
Although underdiagnosis of BD remains important, some researchers have suggested that overdiagnosis may be more prevalent and equally harmful. In a study of 180 patients being treated for depression in a family care clinic, there was a 21.6% initial underdiagnosis rate among those eventually found to have BD.1 However, among 43 patients with a prior BD diagnosis, the diagnosis was not confirmed in 33%.1 In a study of 700 psychiatric outpatients in Rhode Island, only 43% of 145 patients who reported a prior BD diagnosis had that diagnosis confirmed.5 Three times as many patients were overdiagnosed with BD as underdiagnosed.
Are there characteristics common to individuals incorrectly diagnosed with BD? In a study that compared patients who had been mistakenly diagnosed with BD with those who had not been diagnosed with BD, the overdiagnosis group was significantly more likely to be diagnosed with a personality disorder, in particular borderline or antisocial personality disorder.6 Only lifetime and current BPD, current posttraumatic stress disorder (PTSD), and lifetime impulse control disorders were independently associated with BD overdiagnosis. The odds ratio for overdiagnosis of BD in patients found to have BPD was 3.7.
EVALUATION: Rethink the diagnosis
In the last few months, Ms. S had complained to her primary care provider (PCP) of worsening anxiety and depressed mood. She was the victim of ongoing physical and emotional abuse by her ex-fiancé and was concerned that she may lose custody of her 2 sons. Approximately 8 months before admission, Ms. S’ PCP prescribed lithium, 450 mg, 3 times a day, for “mood stabilization” and depression because she’d already been diagnosed with BD. This was the first mood stabilizer she’d taken since she was 14. She also was taking unknown doses of hydrocodone/acetaminophen, cyclobenzaprine, and tramadol for pain and temazepam for insomnia. Ms. S continued to suffer from labile and depressed mood, and fought with her ex-fiancé and legal authorities to maintain custody of her 2 children until she was found in the park.
Throughout her hospitalization she denies that she attempted suicide that day, and maintains that this incident was caused by unintentional mismanagement of her medications. Although she continues to have a sense of low self-worth, she denies feeling depressed; in contrast, she says she feels like she has a “new lease on life.” During several interviews she cannot provide a history of any prolonged (ie, several days) episodes of elevated mood, increased goal-directed behavior, decreased need for sleep, tangential thought, pressured speech, or other symptoms that suggest hypomania or mania. She does not endorse prolonged periods of neurovegetative symptoms that would indicate a major depressive episode.
We feel that Ms. S’ symptoms of affective dysregulation, impulsivity, and interpersonal dysfunction are consistent with BPD, and we determine that she meets 6 of the 9 DSM-IV-TR diagnostic features of BPD (≥5 are required for a BPD diagnosis) (Table 1).7 Ms. S describes efforts to avoid abandonment, unstable and intense interpersonal relationships, marked and persistent unstable self-image, recurrent suicidal and self-mutilating behavior, affective instability, and chronic feelings of emptiness. She is discharged to follow up with a psychotherapist and family practitioner. She is not continued on any psychotropic medications.
The authors’ observations
Although it can be difficult to accurately diagnose psychiatric illness during a brief inpatient hospitalization, several clinicians who cared for Ms. S felt that her presentation was more consistent with BPD than BD. Her case is an example of the potential harm of incorrectly diagnosing personality-disordered patients with BD. Ms. S is impulsive and used lithium—a medication that is the standard of care for BD—in an overdose, which lead to a costly and dangerous hospitalization marked by a difficult tracheal intubation and hemodialysis.
Table 1
DSM-IV-TR diagnostic criteria for borderline personality disorder
| A pervasive pattern of instability of interpersonal relationships, self-image, and affects, and marked impulsivity, as indicated by ≥5 of the following: |
|
| Source: Reference 7 |
Distinguishing BD and BPD
There is considerable overlap in symptoms of BD and BPD. Although the episodic nature of BD is well differentiated from the more chronic course of BPD, many hypomania and mania symptoms are similar to those of BPD (Table 2).7 For example, patients with BD or BPD may exhibit impulsive behavior and labile moods. Substance use, risky and self-destructive behaviors, and inflammatory interpersonal relationships can occur in both disorders. Some researchers have suggested that pathophysiologically, BPD may fall on a spectrum of bipolar illness, and have proposed a clinical entity they call bipolar type IV or ultra-rapid cycling BD.2,8,9 There may be more co-occurrence of BD with BPD than would be expected by chance10; 1 review of BPD studies found the rate of comorbid BD ranged from 5.6% to 19%.11 However, because of differences in several factors—including phenomenology, family prevalence, longitudinal course, and medication response—some researchers have concluded that evidence does not support categorizing BPD as part of a bipolar spectrum.10-14 Nonetheless, BPD and other personality disorders often co-occur with axis I disorders, including MDD, BD, or PTSD.
Some research has suggested that the increasing availability and marketing campaigns of medications to treat BD may promote diagnosis of the disorder.15 Zimmerman15 hypothesizes that physicians may be more likely to diagnose a condition that responds to medication (ie, BD) than one that is less responsive (ie, BPD). Financial compensation for treating axis I disorders is significantly better than for treating personality disorders.16 The inpatient setting confers barriers to accurately diagnosing personality disorders, including limits on the amount of time that clinicians can spend with patients or ability to communicate with sources of collateral information. A patient’s observed personality and behaviors while hospitalized may not accurately reflect his or her personality and behaviors in that patient’s “natural” environment.
Several diagnostic strategies can help distinguish BPD from BD. For BD to be the primary diagnosis, a patient must have had a hypomanic or manic episode. Sustained episodes of elation or extreme irritability without evident stressors suggest BD rather than BPD.10 According to Gunderson et al,10 “repeated angry outbursts, suicide attempts, or acts of deliberate self harm that are reactive to interpersonal stress and reflect extreme rejection sensitivity are axiomatic of borderline personality disorder.” In a review of clinical practice, Gunderson17 found that hypersensitivity to rejection and fearful preoccupation with expected abandonment are the most distinctive characteristics of BPD patients. He suggested that clinicians can establish the diagnosis by asking patients directly if they believe the criteria for BPD characterize them, which also can help a patient to accept the diagnosis.
Finally, during a short hospitalization, it can be helpful to obtain collateral information from the patient’s friends and family or further characterize the time course of symptoms and diagnostic features in the patient’s natural environment. Clinicians who are reluctant to diagnose BPD in an inpatient setting could suggest the presence of borderline traits or discuss the possibility of the BPD diagnosis in documentation (eg, in the assessment or formulation). Doing so would avoid a premature BPD diagnosis and allow outpatient providers to confirm or rule out personality disorder diagnoses over time. It is important to screen patients with BPD for co-occurring axis I disorders, including BD, MDD, PTSD, and substance abuse.
A false-positive BD diagnosis in patients with BPD has serious treatment implications. Antipsychotics, antidepressants, and anticonvulsants have been used to target BPD symptoms such as affective dysregulation, impulsivity, and cognitive/perceptual abnormalities, but no medications are FDA-approved for treating BPD. American Psychiatric Association guidelines recommend symptom-based pharmacologic strategies for BPD,18 although some researchers believe that these recommendations are out-of-date and not evidence-based.17,19 Some evidence suggests pharmacotherapy can have modest short-term benefits on specific BPD symptoms, but no data suggest that medication can reduce the severity of BPD or lead to remission.19-23 Just 1 randomized controlled trial (N = 17) has examined lithium for BPD and found no effect on mood.11,24
Misdiagnosis of BD in the context of BPD may create unrealistic expectations regarding the potential efficacy of medications for relieving symptoms. Patients may be diverted from potentially helpful psychotherapeutic treatments—such as DBT or mentalization therapy—which evidence suggests can effectively reduce symptoms, the need for additional treatments, and self-harm or suicidal behaviors.10,17,19 Evidence from long-term longitudinal studies suggests that psychosocial or psychotherapeutic treatment may protect against suicide in BPD patients.25
Table 2
DSM-IV-TR diagnostic criteria for a manic episode
|
The DSM-IV-TR diagnostic criteria for a hypomanic episode are similar to criteria for a manic episode, except:
|
| Source: Reference 7 |
Related Resources
- National Education Alliance Borderline Personality Disorder. www.borderlinepersonalitydisorder.com.
- Hoffman PD, Steiner-Grossman P. Borderline personality disorder: meeting the challenges to successful treatment. Philadelphia, PA: Haworth Press; 2008.
Drug Brand Names
- Cyclobenzaprine • Flexeril
- Hydrocodone/acetaminophen • Lorcet, Vicodin, others
- Lithium • Eskalith, Lithobid
- Temazepam • Restoril
- Tramadol • Ultram
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Hirschfeld RM, Cass AR, Holt DC, et al. Screening for bipolar disorder in patients treated for depression in a family medicine clinic. J Am Board Fam Pract. 2005;18(4):233-239.
2. Ghaemi SN, Ko JY, Goodwin FK. “Cade’s disease” and beyond: Misdiagnosis antidepressant use, and a proposed definition for bipolar spectrum disorder. Can J Psychiatry. 2002;47(2):125-134.
3. Bowden CL. Strategies to reduce misdiagnosis of bipolar depression. Psychiatr Serv. 2001;52(1):51-55.
4. Moreno C, Laje G, Blanco C, et al. National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Arch Gen Psychiatry. 2007;64(9):1032-1039.
5. Zimmerman M, Ruggero CJ, Chelminski I, et al. Is bipolar disorder overdiagnosed? J Clin Psychiatry. 2008;69(6):935-940.
6. Zimmerman M, Ruggero CJ, Chelminski I, et al. Psychiatric diagnoses in patients previously overdiagnosed with bipolar disorder. J Clin Psychiatry. 2010;71(1):26-31.
7. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
8. Akiskal HS. The bipolar spectrum-the shaping of a new paradigm in psychiatry. Curr Psychiatry Rep. 2002;4(1):1-3.
9. Akiskal HS, Pinto O. The evolving bipolar spectrum. Prototypes I II, III, and IV. Psychiatr Clin North Am. 1999;22(3):517-534, vii.
10. Gunderson JG, Weinberg I, Daversa MT, et al. Descriptive and longitudinal observations on the relationship of borderline personality disorder and bipolar disorder. Am J Psychiatry. 2006;163(7):1173-1178.
11. Paris J, Gunderson J, Weinberg I. The interface between borderline personality disorder and bipolar spectrum disorders. Compr Psychiatry. 2007;48(2):145-154.
12. Paris J. Why psychiatrists are reluctant to diagnose: borderline personality disorder. Psychiatry (Edgmont). 2007;4(1):35-39.
13. Paris J. Borderline or bipolar? Distinguishing borderline personality disorder from bipolar spectrum disorders. Harv Rev Psychiatry. 2004;12(3):140-145.
14. Ruggero CJ, Zimmerman M, Chelminski I, et al. Borderline personality disorder and the misdiagnosis of bipolar disorder. J Psychiatr Res. 2010;44(6):405-408.
15. Zimmerman M. Problems diagnosing bipolar disorder in clinical practice. Expert Rev Neurother. 2010;10(7):1019-1021.
16. Stone MH. Relationship of borderline personality disorder and bipolar disorder. Am J Psychiatry. 2006;163(7):1126-1128.
17. Gunderson JG. Clinical practice. Borderline personality disorder. N Engl J Med. 2011;364(21):2037-2042.
18. American Psychiatric Association. Practice guideline for the treatment of patients with borderline personality disorder. Washington D.C.: American Psychiatric Association; 2001.
19. Paris J. The treatment of borderline personality disorder: implications of research on diagnosis etiology, and outcome. Annu Rev Clin Psychol. 2009;5:277-290.
20. Stoffers J, Völlm BA, Rücker G, et al. Pharmacological interventions for borderline personality disorder. Cochrane Database Syst Rev. 2010;(6):CD005653.-
21. Ripoll LH, Triebwasser J, Siever LJ. Evidence-based pharmacotherapy for personality disorders. Int J Neuropsychopharmacol. 2011;14(9):1257-1288.
22. Mercer D, Douglass AB, Links PS. Meta-analyses of mood stabilizers antidepressants and antipsychotics in the treatment of borderline personality disorder: effectiveness for depression and anger symptoms. J Pers Disord. 2009;23(2):156-174.
23. Lieb K, Völlm B, Rücker G, et al. Pharmacotherapy for borderline personality disorder: Cochrane systematic review of randomised trials. Br J Psychiatry. 2010;196(1):4-12.
24. Links PS, Steiner M, Boiago I, et al. Lithium therapy for borderline patients: preliminary findings. J Pers Disord. 1990;4(2):173-181.
25. Goodman M, Roiff T, Oakes AH, et al. Suicidal risk and management in borderline personality disorder. Curr Psychiatry Rep. 2012;14(1):79-85.
1. Hirschfeld RM, Cass AR, Holt DC, et al. Screening for bipolar disorder in patients treated for depression in a family medicine clinic. J Am Board Fam Pract. 2005;18(4):233-239.
2. Ghaemi SN, Ko JY, Goodwin FK. “Cade’s disease” and beyond: Misdiagnosis antidepressant use, and a proposed definition for bipolar spectrum disorder. Can J Psychiatry. 2002;47(2):125-134.
3. Bowden CL. Strategies to reduce misdiagnosis of bipolar depression. Psychiatr Serv. 2001;52(1):51-55.
4. Moreno C, Laje G, Blanco C, et al. National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Arch Gen Psychiatry. 2007;64(9):1032-1039.
5. Zimmerman M, Ruggero CJ, Chelminski I, et al. Is bipolar disorder overdiagnosed? J Clin Psychiatry. 2008;69(6):935-940.
6. Zimmerman M, Ruggero CJ, Chelminski I, et al. Psychiatric diagnoses in patients previously overdiagnosed with bipolar disorder. J Clin Psychiatry. 2010;71(1):26-31.
7. Diagnostic and statistical manual of mental disorders, 4th ed, text rev. Washington DC: American Psychiatric Association; 2000.
8. Akiskal HS. The bipolar spectrum-the shaping of a new paradigm in psychiatry. Curr Psychiatry Rep. 2002;4(1):1-3.
9. Akiskal HS, Pinto O. The evolving bipolar spectrum. Prototypes I II, III, and IV. Psychiatr Clin North Am. 1999;22(3):517-534, vii.
10. Gunderson JG, Weinberg I, Daversa MT, et al. Descriptive and longitudinal observations on the relationship of borderline personality disorder and bipolar disorder. Am J Psychiatry. 2006;163(7):1173-1178.
11. Paris J, Gunderson J, Weinberg I. The interface between borderline personality disorder and bipolar spectrum disorders. Compr Psychiatry. 2007;48(2):145-154.
12. Paris J. Why psychiatrists are reluctant to diagnose: borderline personality disorder. Psychiatry (Edgmont). 2007;4(1):35-39.
13. Paris J. Borderline or bipolar? Distinguishing borderline personality disorder from bipolar spectrum disorders. Harv Rev Psychiatry. 2004;12(3):140-145.
14. Ruggero CJ, Zimmerman M, Chelminski I, et al. Borderline personality disorder and the misdiagnosis of bipolar disorder. J Psychiatr Res. 2010;44(6):405-408.
15. Zimmerman M. Problems diagnosing bipolar disorder in clinical practice. Expert Rev Neurother. 2010;10(7):1019-1021.
16. Stone MH. Relationship of borderline personality disorder and bipolar disorder. Am J Psychiatry. 2006;163(7):1126-1128.
17. Gunderson JG. Clinical practice. Borderline personality disorder. N Engl J Med. 2011;364(21):2037-2042.
18. American Psychiatric Association. Practice guideline for the treatment of patients with borderline personality disorder. Washington D.C.: American Psychiatric Association; 2001.
19. Paris J. The treatment of borderline personality disorder: implications of research on diagnosis etiology, and outcome. Annu Rev Clin Psychol. 2009;5:277-290.
20. Stoffers J, Völlm BA, Rücker G, et al. Pharmacological interventions for borderline personality disorder. Cochrane Database Syst Rev. 2010;(6):CD005653.-
21. Ripoll LH, Triebwasser J, Siever LJ. Evidence-based pharmacotherapy for personality disorders. Int J Neuropsychopharmacol. 2011;14(9):1257-1288.
22. Mercer D, Douglass AB, Links PS. Meta-analyses of mood stabilizers antidepressants and antipsychotics in the treatment of borderline personality disorder: effectiveness for depression and anger symptoms. J Pers Disord. 2009;23(2):156-174.
23. Lieb K, Völlm B, Rücker G, et al. Pharmacotherapy for borderline personality disorder: Cochrane systematic review of randomised trials. Br J Psychiatry. 2010;196(1):4-12.
24. Links PS, Steiner M, Boiago I, et al. Lithium therapy for borderline patients: preliminary findings. J Pers Disord. 1990;4(2):173-181.
25. Goodman M, Roiff T, Oakes AH, et al. Suicidal risk and management in borderline personality disorder. Curr Psychiatry Rep. 2012;14(1):79-85.