User login
Following Patient Safety Practices
Healthcare delivery organizations are under increasing pressure to improve patient safety. The fundamental underpinning of efforts to improve safety has been the establishment of a no‐blame culture, one that focuses less on individual transgressions and more on system improvement.[1, 2] As evidence‐based practices to improve care have emerged, and the pressures to deliver tangible improvements in safety and quality have grown, providers, healthcare system leaders, and policymakers are struggling with how best to balance the need for accountability with this no‐blame paradigm.
In dealing with areas such as hand hygiene, where there is strong evidence for the value of the practice yet relatively poor adherence in many institutions, Wachter and Pronovost have argued that the scales need to tip more in the direction of accountability, including the imposition of penalties for clinicians who habitually fail to follow certain safety practices.[3] Although not obviating the critical importance of systems improvement, they argue that a failure to enforce such measures undermines trust in the system and invites external regulation. Chassin and colleagues made a similar point in arguing for the identification of certain accountability measures that could be used in public reporting and pay‐for‐performance programs.[4]
Few organizations have enacted robust systems to hold providers responsible for adhering to accountability measures.[4] Although many hospitals have policies to suspend clinical privileges for failing to sign discharge summaries or obtain a yearly purified protein derivative test, few have formal programs to identify and deal with clinicians whose behavior is persistently problematic.[3] Furthermore, existing modes of physician accountability, such as state licensing boards, only discipline physicians retroactively (and rarely) when healthcare organizations report poor performance. State boards typically do not consider prevention of injury, such as adherence to safety practices, to be part of their responsibility.[5] Similarly, credentialing boards (eg, the American Board of Internal Medicine) do not assess adherence to such practices in coming to their decisions.
It is estimated that strict adherence to infection control practices, such as hand hygiene, could prevent over 100,000 hospital deaths every year; adherence to other evidence‐based safety practices such as the use of a preoperative time‐out would likely prevent many more deaths and cases of medical injury.[3, 6] Although there are practical issues, such as how to audit individual clinician adherence in ways that are feasible and fair, that make enforcing individual provider accountability challenging, there seems little doubt that attitudes regarding the appropriateness of enacting penalties for safety transgressions will be key determinants of whether such measures are considered. Yet no study to date has assessed the opinions of different stakeholders (physicians, nurses, trainees, patients) regarding various strategies, including public reporting and penalties, to improve adherence to safety practices. We aimed to assess these attitudes across a variety of such stakeholders.
METHODS
Survey Development and Characteristics
To understand the perceptions of measures designed to improve patient safety, we designed a survey of patients, nurses, medical students, resident physicians, and attending physicians to be administered at hospitals associated with the University of California, San Francisco (UCSF). Institutional review board approval was obtained from the UCSF Committee on Human Research, and all respondents provided informed consent.
The survey was developed by the authors and pilot tested with 2 populations. First, the survey was administered to a group of 12 UCSF Division of Hospital Medicine research faculty; their feedback was used to revise the survey. Second, the survey was administered to a convenience sample of 2 UCSF medical students, and their feedback was used to further refine the survey.
The questionnaire presented 3 scenarios in which a healthcare provider committed a patient‐safety protocol lapse; participants were asked their opinions about the appropriate responses to each of the violations. The 3 scenarios were: (1) a healthcare provider not properly conducting hand hygiene before a patient encounter, (2) a healthcare provider not properly conducting a fall risk assessment on a hospitalized patient, and (3) a healthcare provider not properly conducting a preoperative timeout prior to surgery. For each scenario, a series of questions was asked about a variety of institutional responses toward a provider who did not adhere to each safety protocol. Potential responses included feedback (email feedback, verbal feedback, meeting with a supervisor, a quarterly performance review meeting, and a quarterly report card seen only by the provider), public reporting (posting the provider's infractions on a public website), and penalties (fines, suspension without pay, and firing).
We chose the 3 practices because they are backed by strong evidence, are relatively easy to perform, are inexpensive, are linked to important and common harms, and are generally supported within the patient‐safety community. Improved adherence to hand hygiene significantly reduces infection transmission in healthcare settings.[7, 8, 9, 10, 11] Performing fall risk assessments has been shown to reduce falls in hospitalized patients,[12] and using preoperative checklists, including a surgical time‐out, can reduce mortality and complication risks by approximately 40%.[13]
Respondents were asked how many cases of documented nonadherence would be necessary for the penalties to be appropriate (1 time, 25 times, 610 times, 1115 times, 16+ times, or would never be appropriate). Finally, respondents were asked to rate the potential harm to patients of each protocol lapse (nonelow, medium, or high).
Demographic information collected from the healthcare providers and medical students included age, gender, position, department, and years' experience in their current position. Demographic information collected from the patients included age, gender, insurance status, race, education level, household income level, and relationship status.
Survey Administration
Surveys were administered to convenience samples of 5 groups of individuals: attending physicians in the UCSF Department of Internal Medicine based at UCSF Medical Center and the San Francisco Veterans Affairs Medical Center, nurses at UCSF Medical Center, residents in the UCSF internal medicine residency program, medical students at UCSF, and inpatients in the internal medicine service at UCSF Medical Center's Moffitt‐Long Hospital. Attending physicians and nurses were surveyed at their respective departmental meetings. For resident physicians and medical students, surveys were distributed at the beginning of lectures and collected at the end.
Patients were eligible to participate if they spoke English and were noted to be alert and oriented to person, time, and place. A survey administrator located eligible patients in the internal medicine service via the electronic medical record system, determined if they were alert and oriented, and approached each patient in his or her room. If the patients verbally consented to consider participation, the surveys were given to them and retrieved after approximately 30 minutes.
Healthcare professionals were offered the opportunity to enter their e‐mail addresses at the end of the survey to become eligible for a drawing for a $100 gift card, but were informed that their e‐mail addresses would not be included in the analytic dataset. Inpatients were not offered any incentives to participate. All surveys were administered by a survey monitor in paper form between May 2011 and July 2012.
Data Analysis
Data analysis was conducted using the Statistical Analysis Software (SAS) package (SAS Institute Inc., Cary, NC) and Stata (StataCorp, College Station, TX). Descriptive analysis and frequency distributions were tallied for all responses. Responses to protocol lapses were grouped into 3 categories: feedback, public reporting, and penalty as described above. As all surveyed groups endorsed feedback as an appropriate response to all of the scenarios, we did not examine feedback, concentrating our analysis instead on public reporting and penalties.
Appropriateness ratings for each response to each protocol lapse were aggregated in 2 ways: ever appropriate (ie, the response would be appropriate after some number of documented lapses) versus never appropriate, and the threshold for the response. Whereas public reporting was only asked about as a single option, 3 separate responses were collapsed into the single response, penalties: fine, suspension, or firing. Individuals were classified as endorsing a penalty if they rated any 1 of these responses as ever appropriate. The threshold for penalty was the smallest number of occurrences at which 1 of the penalty responses was endorsed.
Differences among the 5 groups in the perceived harm of each protocol lapse were tested with 2 analyses. Group differences in ratings of whether public reporting and penalties were ever appropriate were tested with logistic regression analyses for each scenario separately, controlling for age, sex, and perceived harm of the protocol lapse. To determine if the 5 groups differed in their tendency to support public reporting or penalties regardless of the type of protocol lapse, we conducted logistic regression analyses across all 3 scenarios, accounting for multiple observations per individual through use of cluster‐correlated robust variance.[14] Differences among groups in the number of transgressions at which public reporting and penalties were supported were examined with log‐rank tests.
RESULTS
A total of 287 individuals were given surveys, and 183 completed them: 22 attending physicians, 33 resident physicians, 61 nurses, 47 medical students, and 20 patients (overall response rate 64%). Response rate for attending and resident physicians was 73%, for nurses 59%, and for medical students 54%. Among patients who were approached and agreed to accept a survey, 87% returned completed surveys (Table 1). The average age of attending physicians was 35.8 years (standard deviation [SD]: 5.3), residents was 28.3 years (SD: 1.7), nurses was 43.6 years (SD: 11.1), medical students was 26.6 years (SD: 2.9), and inpatients was 48.2 years (SD: 15.9). Thirty‐two percent of attending physicians were female, 67% of resident physicians were female, 88% of nurses were female, 66% of medical students were female, and 47% of inpatients were female.
| Attending Physician | Resident Physician | Nurse | Medical Student | Patient | |
|---|---|---|---|---|---|
| |||||
| No. | 22 | 33 | 61 | 47 | 20 |
| Response rate* | 73% | 73% | 59% | 54% | 87% |
| Age, y, meanSD | 365 | 282 | 4411 | 273 | 4816 |
| Sex, female, % (n) | 32% (7) | 67% (22) | 88% (53) | 66% (31) | 47% (9) |
Perceived Harm
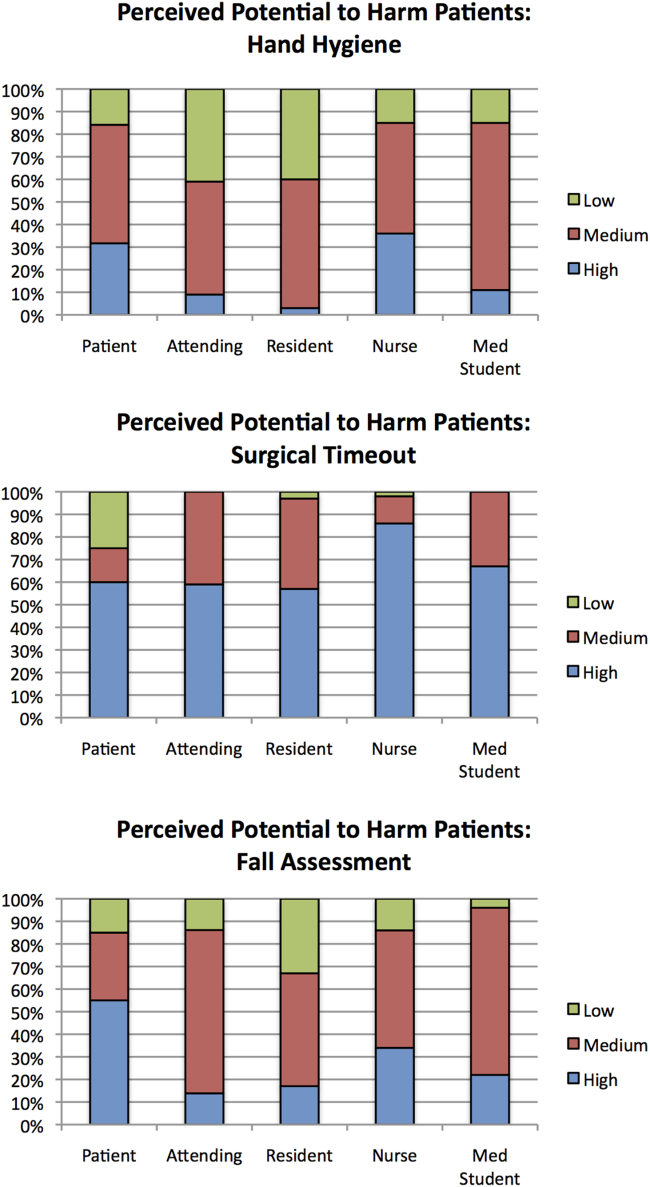
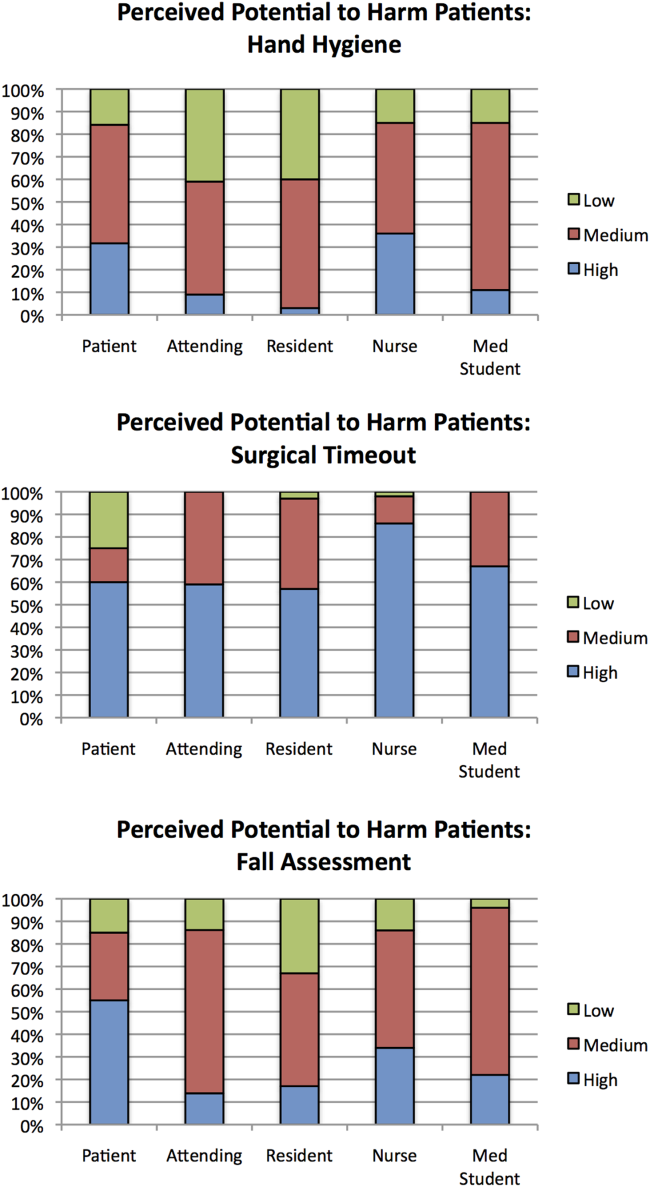
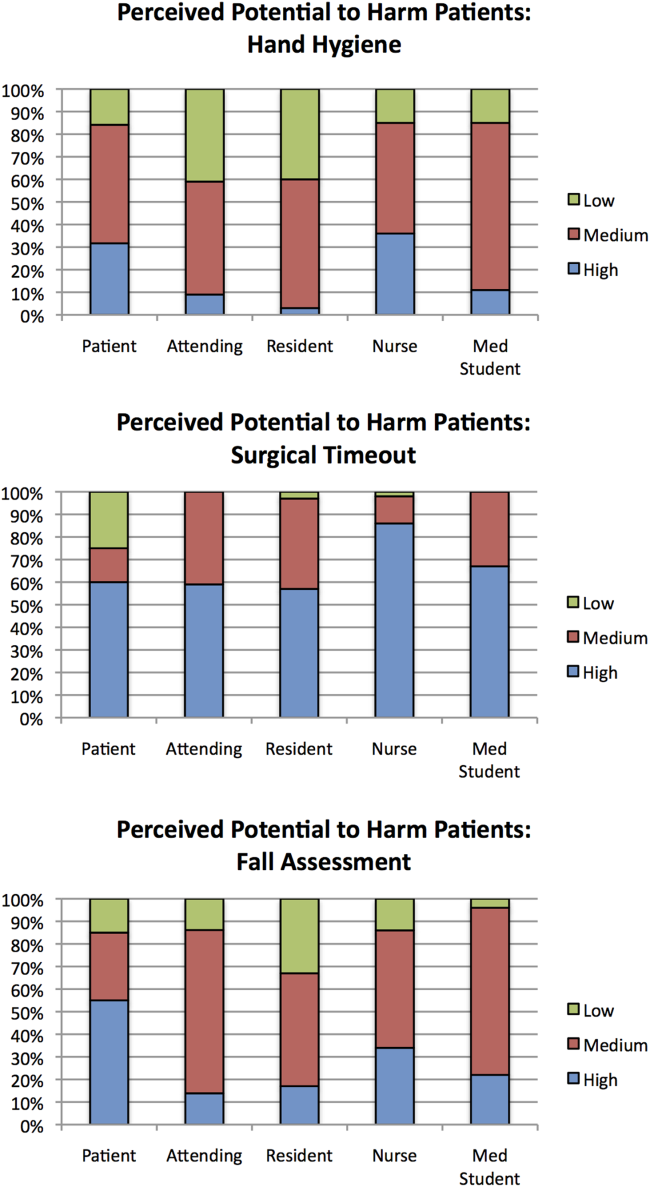
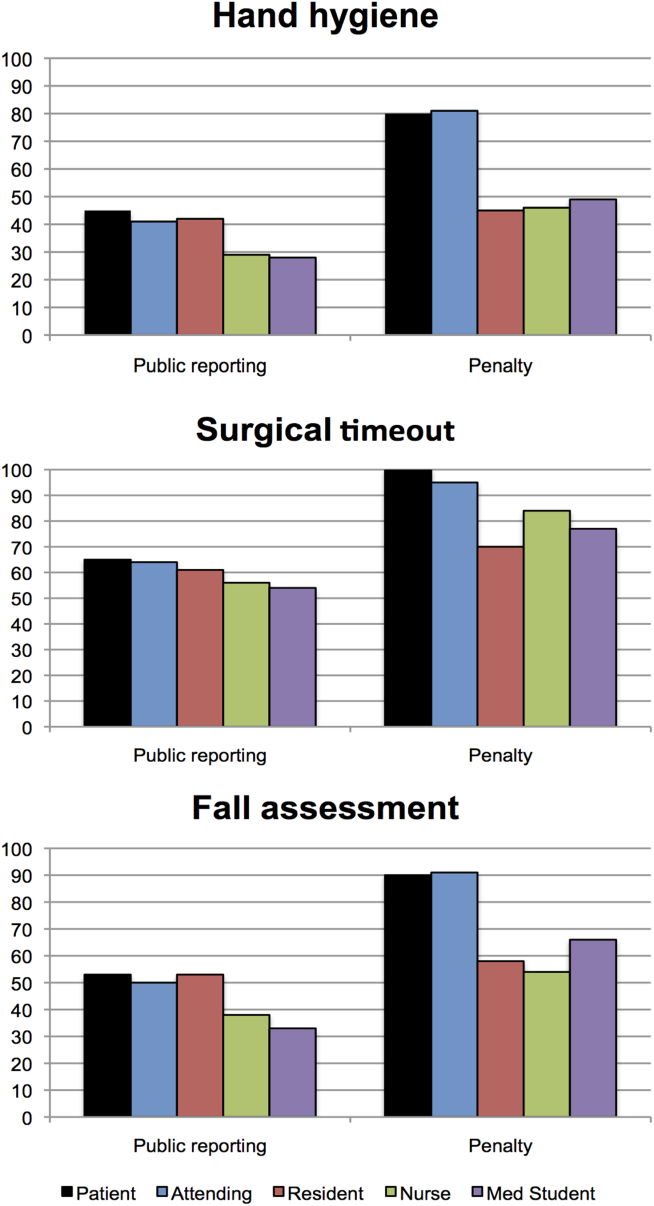
Out of the 3 scenarios presented in in the survey, participants believed that not conducting preoperative time‐outs in surgery presented the highest risk to patient safety, with 57% (residents) to 86% (nurses) rating the potential harm as high (Figure 1). Not conducting fall risk assessments was perceived as second most potentially harmful, and not properly practicing hand hygiene was perceived as least potentially harmful to patient safety. There were significant differences among groups in perceptions of potential harm for all 3 scenarios (P<0.001 for all).
Appropriateness of Public Reporting and Penalties
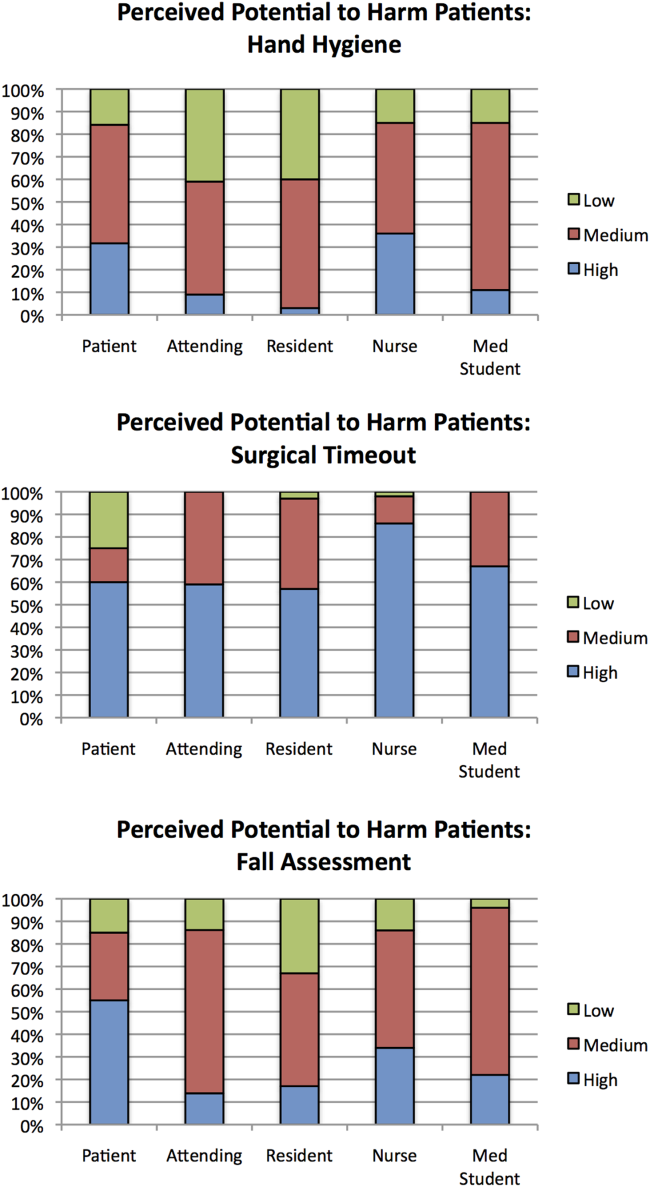
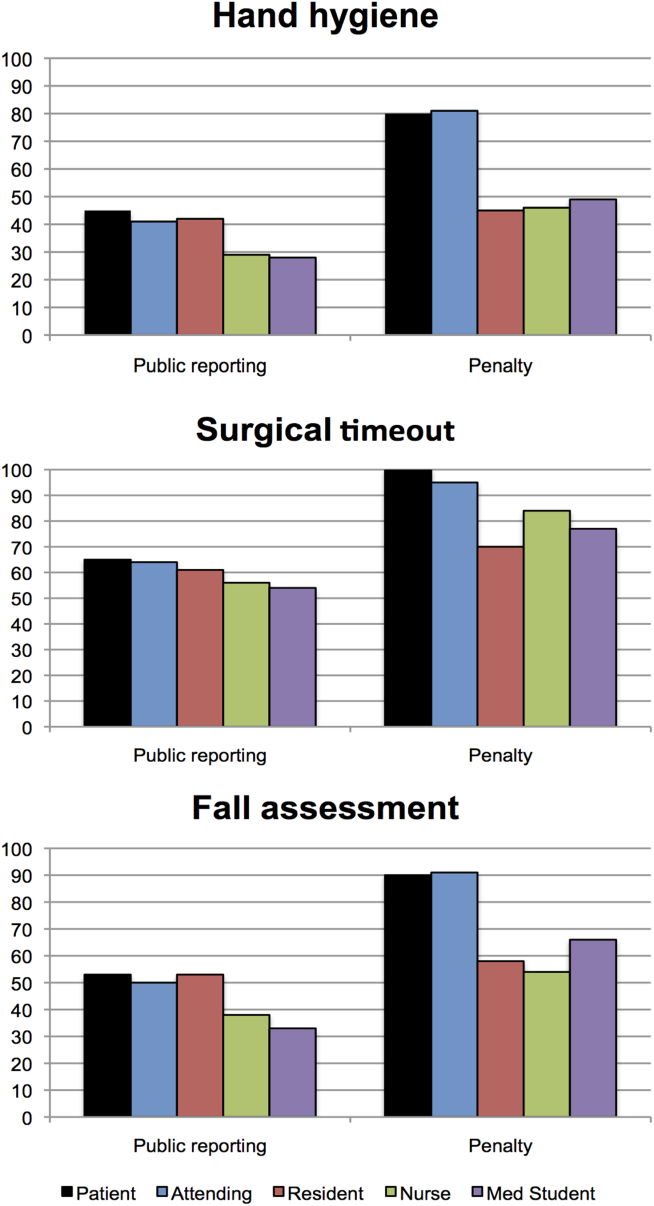
Public reporting was viewed as ever appropriate by 34% of all respondents for hand‐hygiene protocol lapses, 58% for surgical time‐out lapses, and 43% for fall risk assessment lapses. There were no significant differences among groups in endorsement of public reporting for individual scenarios (Figure 2). Penalties were endorsed more frequently than public reporting for all groups and all scenarios. The proportion of attending physicians and patients who rated penalties as ever appropriate were similar for each scenario. Residents, medical students, and nurses were less likely than patients and attending physicians to support penalties (P<0.05 for all differences).
The aggregated analysis revealed that nurses and medical students were significantly less likely than patients to endorse public reporting across scenarios. In terms of endorsement of penalties, we found no significant differences between attending physicians and patients, but residents (odds ratio [OR]: 0.09, 95% confidence interval [CI]: 0.03‐0.32), students (OR: 0.12, 95% CI: 0.04‐0.34), and nurses (OR: 0.17, 95% CI: 0.03‐0.41) had significantly lower odds of favoring penalties than did patients (Table 2).
| Odds Ratio (95% CI) | ||
|---|---|---|
| Public Reporting | Penalty | |
| ||
| Group, across all scenarios | ||
| Patients | Reference | Reference |
| Attending physicians | 0.58 (0.172.01) | 0.88 (0.203.84) |
| Resident physicians | 0.42 (0.121.52) | 0.09 (0.020.32) |
| Nurses | 0.32 (0.120.88) | 0.17 (0.030.41) |
| Medical students | 0.22 (0.060.80) | 0.12 (0.040.34) |
| Scenario, across all groups | ||
| Hand hygiene | Reference | Reference |
| Surgical time‐out | 2.82 (2.033.91) | 4.29 (2.976.20) |
| Fall assessment | 1.47 (1.091.98) | 1.74 (1.272.37) |
Across all surveyed groups, public reporting was more often supported for lapses of surgical timeout (OR: 2.82, 95% CI: 2.03‐3.91) and fall risk assessment protocols (OR: 1.47, 95% CI: 1.09‐1.98) than for the referent, hand‐hygiene lapses. Across all groups, penalties were more likely to be supported for surgical timeout (OR: 4.29, 95% CI: 2.97‐6.20) and fall risk assessment protocol lapses (OR: 1.74, 95% CI: 1.27‐2.37) than for hand‐hygiene lapses.
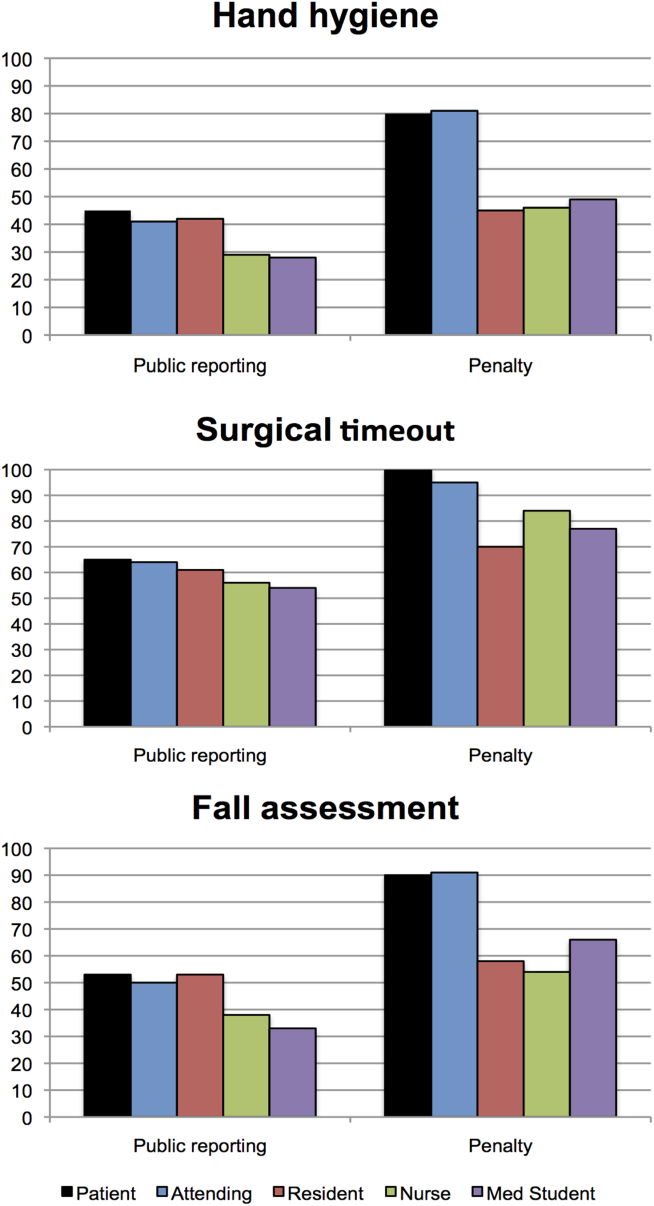
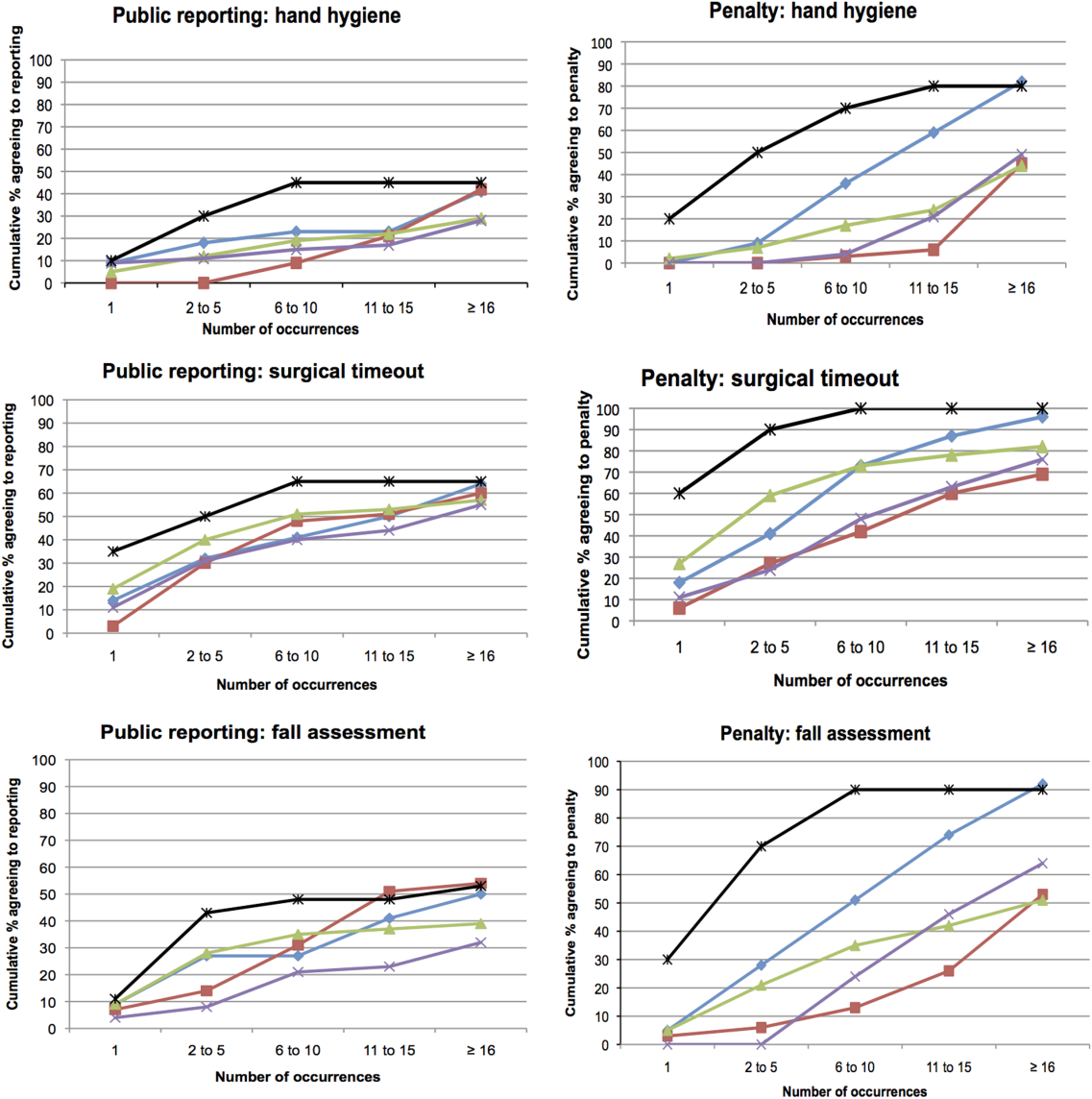
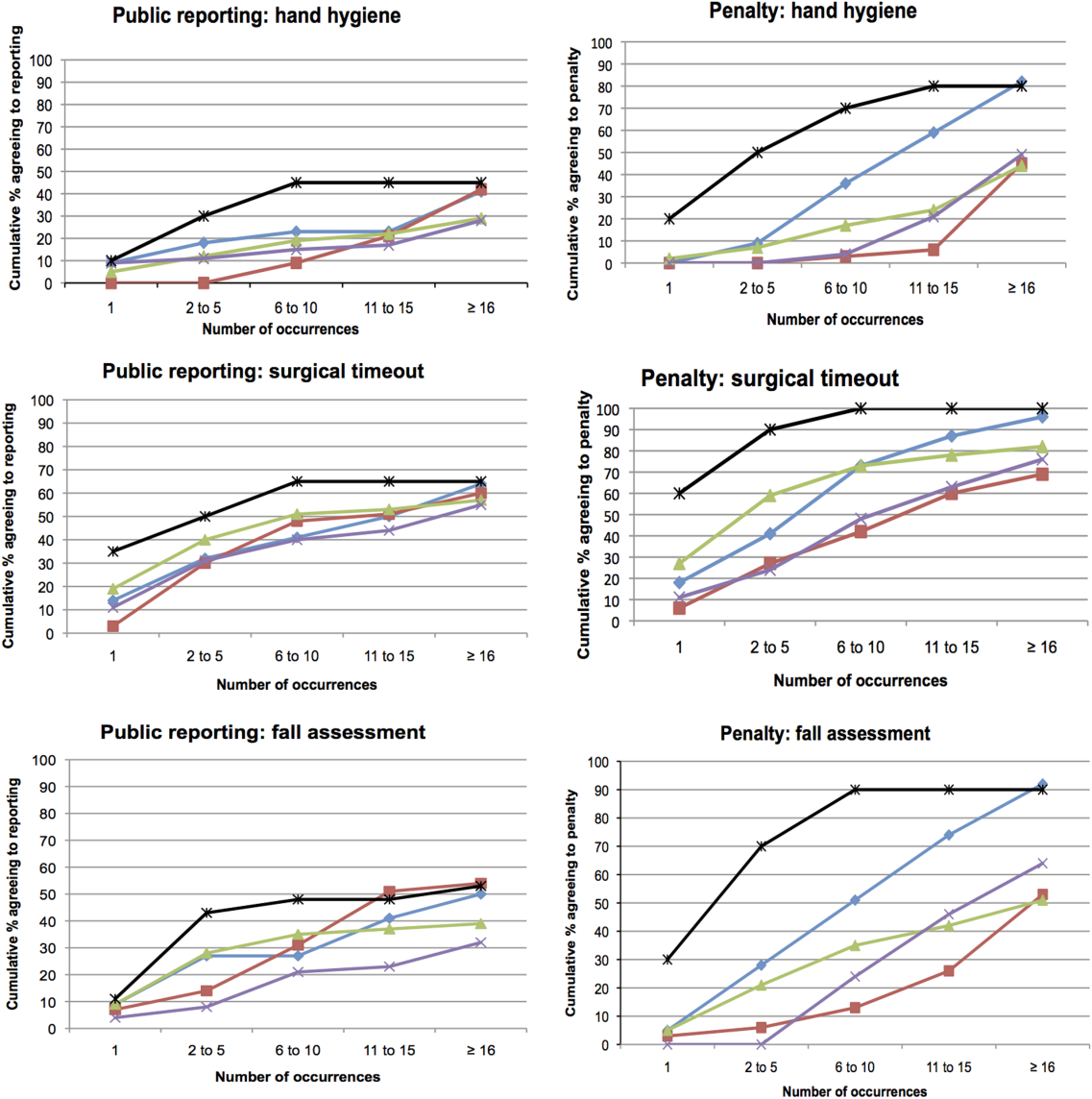
Thresholds for Public Reporting and Penalties
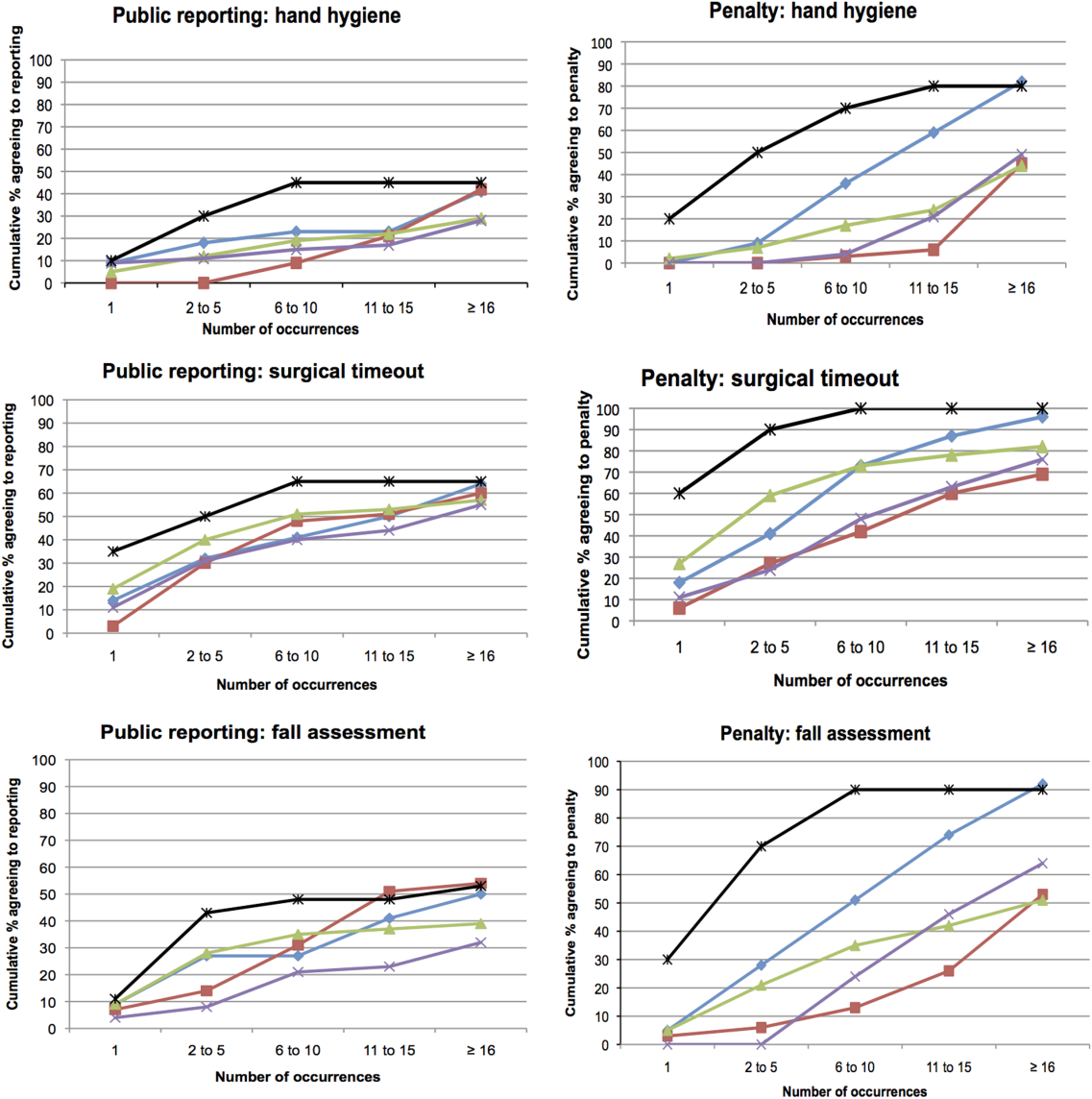
The log‐rank test showed no significant differences among the surveyed groups in the number of transgressions at which public reporting was deemed appropriate in any of the 3 scenarios (P=0.37, P=0.71, and P=0.32 for hand hygiene, surgical time‐out, and fall risk assessment, respectively) (Figure 3). However, patients endorsed penalties after significantly fewer occurrences than residents, medical students, and nurses for all 3 scenarios (P<0.001 for all differences), and at a significantly lower threshold than attending physicians for surgical timeout and fall risk assessment (P<0.001 and P=0.03, respectively).
DISCUSSION
This survey assessed attitudes of healthcare professionals, trainees, and inpatients toward public reporting and penalties when clinicians do not follow basic safety protocols. Respondents tended to favor more aggressive measures when they deemed the safety risk from protocol violations to be higher. Almost all participants favored providing feedback after safety protocol lapses. Healthcare professionals tended to favor punitive measures, such as fines, suspension, and firing, more than public reporting of transgressions. Patients had a lower threshold than both providers and trainees for public reporting and punitive measures. In aggregate, our study suggests that after a decade of emphasis on a no‐blame response to patient safety hazards, both healthcare providers and patients now believe clinicians should be held accountable for following basic safety protocols, though their thresholds and triggers vary.
A surprising finding was that providers were more likely to favor penalties (such as fines, suspension, or firing) than public reporting of safety transgressions. Multiple studies have suggested that public reporting of hospital quality data has improved adherence to care processes and may improve patient outcomes.[15, 16, 17] Although our data do not tell us why clinicians appear to be more worried about public reporting than penalties, they do help explain why transparency has been a relatively powerful strategy to motivate changes in practice, even when it is unaccompanied by significant shifts in consumer choices.[18] It would be natural to consider public reporting to be a softer strategy than fines, suspension, or firing; however, our results indicate that many clinicians do not see it that way. Alternatively, the results could also suggest that clinicians prefer measures that provide more immediate feedback than public reporting generally provides. These attitudes should be considered when enacting public reporting strategies.
Another interesting finding was that patients and attending physicians tended to track together regarding their attitudes toward penalties for safety lapses. Although patients had a lower threshold for favoring penalties than attendings, similar proportions of patients and attending physicians believed that penalties should be enacted for safety transgressions, and both groups were more penal than physician trainees and nurses. We speculate that attendings and patients may have the most skin in the game, patients as the ones directly harmed by a preventable adverse event, and attending physicians as the most responsible clinicians, at least in the eyes of the malpractice system, licensing boards, and credentials committees.
Even though our study illustrates relatively high levels of endorsement for aggressive measures to deal with clinicians who fail to follow evidence‐based safety practices, a shift in this direction has risks and benefits. The no‐blame paradigm in patient safety grew out of a need to encourage open discussion about medical mistakes.[2] Whereas shifting away from a purely no‐ blame approach may lead to greater adherence with safety practices, and one hopes fewer cases of preventable harm, it also risks stifling the open discussions about medical errors that characterize learning organizations.[13, 19] Because of this, a movement in this direction should be undertaken carefully, starting first with a small number of well‐established safety practices, and ensuring that robust education and system improvements precede and accompany the imposition of penalties for nonadherence.
Our study has limitations. The survey was developed using convenience samples of UCSF faculty and medical students, so broader inclusion of physicians, nurses, trainees, and patients may have yielded a different survey instrument. As a survey, we cannot be certain that any of the groups' responses in real life (eg, in a vote of the medical staff on a given policy) would mirror their survey response. Additionally, the responses to protocol lapses did not include all possible administrative responses, such as mandatory training/remediation or rewards for positive behaviors. The responses could have also been different if participants were presented with different patient safety scenarios. The study population was limited in several ways. Attending and resident physicians were drawn from an academic department of internal medicine; it is possible that other specialties would have different attitudes. Patients were relatively young (likely due to the inclusion criteria), as were attending physicians (due to oversampling of hospitalist physicians). The relatively small number of participants could also limit statistical power to detect differences among groups. Additionally, the study population was limited to patients and healthcare professionals in academic medical centers in San Francisco. It is possible that attitudes would be different in other regions and practice settings.
The no‐blame approach to patient safety has been crucial in refocusing the lens on systems failures and in encouraging the active engagement by clinicians, particularly physicians.[2, 3] On the other hand, there are legitimate concerns that a unidimensional no‐blame approach has permitted, perhaps even promoted, nonadherence to evidence‐based safety practices that could prevent many cases of harm. Although it may not be surprising that patients favor harsher consequences for providers who do not follow basic safety protocols, our study demonstrates relatively widespread support for such consequences even among clinicians and trainees. However, all groups appear to recognize the nuances underlying this set of issues, with varying levels of enthusiasm for punitive responses based on perceived risk and number of transgressions. Future studies are needed to investigate how best to implement public reporting and penalties in ways that can maximize the patient safety benefits.
Acknowledgements
The authors are grateful to the clinicians, trainees, and patients who participated in the survey.
- . Understanding Patient Safety. 2nd ed. New York, NY: McGraw Hill Medical; 2012.
- . Error in medicine. JAMA. 1994;272(23):1851–1857.
- , . Balancing "no blame" with accountability in patient safety. N Engl J Med. 2009;361(14):1401–1406.
- , , , . Accountability measures—using measurement to promote quality improvement. N Engl J Med. 2010;363(7):683–688.
- , . Problem doctors: is there a system‐level solution? Ann Intern Med. 2006;144(2):107–115.
- , , , et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360(5):491–499.
- , , , , . Effectiveness of a comprehensive hand hygiene program for reduction of infection rates in a long‐term care facility. Am J Infect Control. 2013;41(1):39–44.
- , . Impact of a hospital‐wide hand hygiene promotion strategy on healthcare‐associated infections. Antimicrob Resist Infect Control. 2012;1(1):13.
- , , , et al. Determinants of hand hygiene noncompliance in intensive care units. Am J Infect Control. 2013;41(2):131–135.
- , , , , , . Impact of a hospital‐wide hand hygiene initiative on healthcare‐associated infections: results of an interrupted time series. BMJ Qual Saf. 2012;21(12):1019–1026.
- , , , . Effectiveness of multifaceted hand hygiene interventions in long‐term care facilities in Hong Kong: a cluster‐randomized controlled trial. Infect Control Hosp Epidemiol. 2012;33(8):761–767.
- , , , , . Development, implementation, and evaluation of a comprehensive fall risk program. J Spec Pediatr Nurs 2011;16(2):130–139.
- , , , . A systematic review of the effectiveness, compliance, and critical factors for implementation of safety checklists in surgery. Ann Surg. 2012;256(6):925–933.
- . A note on robust variance estimation for cluster‐correlated data. Biometrics. 2000;56(2):645–646.
- , , , et al. Public reporting and pay for performance in hospital quality improvement. N Engl J Med. 2007;356(5):486–496.
- , , , , . Improving the outcomes of coronary artery bypass surgery in New York State. JAMA. 1994;271(10):761–766.
- , , . Declines in hospital mortality associated with a regional initiative to measure hospital performance. Am J Med Qual. 1997;12(2):103–112.
- , , , . The public release of performance data: what do we expect to gain? A review of the evidence. JAMA. 2000;283(14):1866–1874.
- . Continuing education meets the learning organization: the challenge of a systems approach to patient safety. J Contin Educ Health Prof. 2000;20(4):197–207.
Healthcare delivery organizations are under increasing pressure to improve patient safety. The fundamental underpinning of efforts to improve safety has been the establishment of a no‐blame culture, one that focuses less on individual transgressions and more on system improvement.[1, 2] As evidence‐based practices to improve care have emerged, and the pressures to deliver tangible improvements in safety and quality have grown, providers, healthcare system leaders, and policymakers are struggling with how best to balance the need for accountability with this no‐blame paradigm.
In dealing with areas such as hand hygiene, where there is strong evidence for the value of the practice yet relatively poor adherence in many institutions, Wachter and Pronovost have argued that the scales need to tip more in the direction of accountability, including the imposition of penalties for clinicians who habitually fail to follow certain safety practices.[3] Although not obviating the critical importance of systems improvement, they argue that a failure to enforce such measures undermines trust in the system and invites external regulation. Chassin and colleagues made a similar point in arguing for the identification of certain accountability measures that could be used in public reporting and pay‐for‐performance programs.[4]
Few organizations have enacted robust systems to hold providers responsible for adhering to accountability measures.[4] Although many hospitals have policies to suspend clinical privileges for failing to sign discharge summaries or obtain a yearly purified protein derivative test, few have formal programs to identify and deal with clinicians whose behavior is persistently problematic.[3] Furthermore, existing modes of physician accountability, such as state licensing boards, only discipline physicians retroactively (and rarely) when healthcare organizations report poor performance. State boards typically do not consider prevention of injury, such as adherence to safety practices, to be part of their responsibility.[5] Similarly, credentialing boards (eg, the American Board of Internal Medicine) do not assess adherence to such practices in coming to their decisions.
It is estimated that strict adherence to infection control practices, such as hand hygiene, could prevent over 100,000 hospital deaths every year; adherence to other evidence‐based safety practices such as the use of a preoperative time‐out would likely prevent many more deaths and cases of medical injury.[3, 6] Although there are practical issues, such as how to audit individual clinician adherence in ways that are feasible and fair, that make enforcing individual provider accountability challenging, there seems little doubt that attitudes regarding the appropriateness of enacting penalties for safety transgressions will be key determinants of whether such measures are considered. Yet no study to date has assessed the opinions of different stakeholders (physicians, nurses, trainees, patients) regarding various strategies, including public reporting and penalties, to improve adherence to safety practices. We aimed to assess these attitudes across a variety of such stakeholders.
METHODS
Survey Development and Characteristics
To understand the perceptions of measures designed to improve patient safety, we designed a survey of patients, nurses, medical students, resident physicians, and attending physicians to be administered at hospitals associated with the University of California, San Francisco (UCSF). Institutional review board approval was obtained from the UCSF Committee on Human Research, and all respondents provided informed consent.
The survey was developed by the authors and pilot tested with 2 populations. First, the survey was administered to a group of 12 UCSF Division of Hospital Medicine research faculty; their feedback was used to revise the survey. Second, the survey was administered to a convenience sample of 2 UCSF medical students, and their feedback was used to further refine the survey.
The questionnaire presented 3 scenarios in which a healthcare provider committed a patient‐safety protocol lapse; participants were asked their opinions about the appropriate responses to each of the violations. The 3 scenarios were: (1) a healthcare provider not properly conducting hand hygiene before a patient encounter, (2) a healthcare provider not properly conducting a fall risk assessment on a hospitalized patient, and (3) a healthcare provider not properly conducting a preoperative timeout prior to surgery. For each scenario, a series of questions was asked about a variety of institutional responses toward a provider who did not adhere to each safety protocol. Potential responses included feedback (email feedback, verbal feedback, meeting with a supervisor, a quarterly performance review meeting, and a quarterly report card seen only by the provider), public reporting (posting the provider's infractions on a public website), and penalties (fines, suspension without pay, and firing).
We chose the 3 practices because they are backed by strong evidence, are relatively easy to perform, are inexpensive, are linked to important and common harms, and are generally supported within the patient‐safety community. Improved adherence to hand hygiene significantly reduces infection transmission in healthcare settings.[7, 8, 9, 10, 11] Performing fall risk assessments has been shown to reduce falls in hospitalized patients,[12] and using preoperative checklists, including a surgical time‐out, can reduce mortality and complication risks by approximately 40%.[13]
Respondents were asked how many cases of documented nonadherence would be necessary for the penalties to be appropriate (1 time, 25 times, 610 times, 1115 times, 16+ times, or would never be appropriate). Finally, respondents were asked to rate the potential harm to patients of each protocol lapse (nonelow, medium, or high).
Demographic information collected from the healthcare providers and medical students included age, gender, position, department, and years' experience in their current position. Demographic information collected from the patients included age, gender, insurance status, race, education level, household income level, and relationship status.
Survey Administration
Surveys were administered to convenience samples of 5 groups of individuals: attending physicians in the UCSF Department of Internal Medicine based at UCSF Medical Center and the San Francisco Veterans Affairs Medical Center, nurses at UCSF Medical Center, residents in the UCSF internal medicine residency program, medical students at UCSF, and inpatients in the internal medicine service at UCSF Medical Center's Moffitt‐Long Hospital. Attending physicians and nurses were surveyed at their respective departmental meetings. For resident physicians and medical students, surveys were distributed at the beginning of lectures and collected at the end.
Patients were eligible to participate if they spoke English and were noted to be alert and oriented to person, time, and place. A survey administrator located eligible patients in the internal medicine service via the electronic medical record system, determined if they were alert and oriented, and approached each patient in his or her room. If the patients verbally consented to consider participation, the surveys were given to them and retrieved after approximately 30 minutes.
Healthcare professionals were offered the opportunity to enter their e‐mail addresses at the end of the survey to become eligible for a drawing for a $100 gift card, but were informed that their e‐mail addresses would not be included in the analytic dataset. Inpatients were not offered any incentives to participate. All surveys were administered by a survey monitor in paper form between May 2011 and July 2012.
Data Analysis
Data analysis was conducted using the Statistical Analysis Software (SAS) package (SAS Institute Inc., Cary, NC) and Stata (StataCorp, College Station, TX). Descriptive analysis and frequency distributions were tallied for all responses. Responses to protocol lapses were grouped into 3 categories: feedback, public reporting, and penalty as described above. As all surveyed groups endorsed feedback as an appropriate response to all of the scenarios, we did not examine feedback, concentrating our analysis instead on public reporting and penalties.
Appropriateness ratings for each response to each protocol lapse were aggregated in 2 ways: ever appropriate (ie, the response would be appropriate after some number of documented lapses) versus never appropriate, and the threshold for the response. Whereas public reporting was only asked about as a single option, 3 separate responses were collapsed into the single response, penalties: fine, suspension, or firing. Individuals were classified as endorsing a penalty if they rated any 1 of these responses as ever appropriate. The threshold for penalty was the smallest number of occurrences at which 1 of the penalty responses was endorsed.
Differences among the 5 groups in the perceived harm of each protocol lapse were tested with 2 analyses. Group differences in ratings of whether public reporting and penalties were ever appropriate were tested with logistic regression analyses for each scenario separately, controlling for age, sex, and perceived harm of the protocol lapse. To determine if the 5 groups differed in their tendency to support public reporting or penalties regardless of the type of protocol lapse, we conducted logistic regression analyses across all 3 scenarios, accounting for multiple observations per individual through use of cluster‐correlated robust variance.[14] Differences among groups in the number of transgressions at which public reporting and penalties were supported were examined with log‐rank tests.
RESULTS
A total of 287 individuals were given surveys, and 183 completed them: 22 attending physicians, 33 resident physicians, 61 nurses, 47 medical students, and 20 patients (overall response rate 64%). Response rate for attending and resident physicians was 73%, for nurses 59%, and for medical students 54%. Among patients who were approached and agreed to accept a survey, 87% returned completed surveys (Table 1). The average age of attending physicians was 35.8 years (standard deviation [SD]: 5.3), residents was 28.3 years (SD: 1.7), nurses was 43.6 years (SD: 11.1), medical students was 26.6 years (SD: 2.9), and inpatients was 48.2 years (SD: 15.9). Thirty‐two percent of attending physicians were female, 67% of resident physicians were female, 88% of nurses were female, 66% of medical students were female, and 47% of inpatients were female.
| Attending Physician | Resident Physician | Nurse | Medical Student | Patient | |
|---|---|---|---|---|---|
| |||||
| No. | 22 | 33 | 61 | 47 | 20 |
| Response rate* | 73% | 73% | 59% | 54% | 87% |
| Age, y, meanSD | 365 | 282 | 4411 | 273 | 4816 |
| Sex, female, % (n) | 32% (7) | 67% (22) | 88% (53) | 66% (31) | 47% (9) |
Perceived Harm
Out of the 3 scenarios presented in in the survey, participants believed that not conducting preoperative time‐outs in surgery presented the highest risk to patient safety, with 57% (residents) to 86% (nurses) rating the potential harm as high (Figure 1). Not conducting fall risk assessments was perceived as second most potentially harmful, and not properly practicing hand hygiene was perceived as least potentially harmful to patient safety. There were significant differences among groups in perceptions of potential harm for all 3 scenarios (P<0.001 for all).
Appropriateness of Public Reporting and Penalties
Public reporting was viewed as ever appropriate by 34% of all respondents for hand‐hygiene protocol lapses, 58% for surgical time‐out lapses, and 43% for fall risk assessment lapses. There were no significant differences among groups in endorsement of public reporting for individual scenarios (Figure 2). Penalties were endorsed more frequently than public reporting for all groups and all scenarios. The proportion of attending physicians and patients who rated penalties as ever appropriate were similar for each scenario. Residents, medical students, and nurses were less likely than patients and attending physicians to support penalties (P<0.05 for all differences).
The aggregated analysis revealed that nurses and medical students were significantly less likely than patients to endorse public reporting across scenarios. In terms of endorsement of penalties, we found no significant differences between attending physicians and patients, but residents (odds ratio [OR]: 0.09, 95% confidence interval [CI]: 0.03‐0.32), students (OR: 0.12, 95% CI: 0.04‐0.34), and nurses (OR: 0.17, 95% CI: 0.03‐0.41) had significantly lower odds of favoring penalties than did patients (Table 2).
| Odds Ratio (95% CI) | ||
|---|---|---|
| Public Reporting | Penalty | |
| ||
| Group, across all scenarios | ||
| Patients | Reference | Reference |
| Attending physicians | 0.58 (0.172.01) | 0.88 (0.203.84) |
| Resident physicians | 0.42 (0.121.52) | 0.09 (0.020.32) |
| Nurses | 0.32 (0.120.88) | 0.17 (0.030.41) |
| Medical students | 0.22 (0.060.80) | 0.12 (0.040.34) |
| Scenario, across all groups | ||
| Hand hygiene | Reference | Reference |
| Surgical time‐out | 2.82 (2.033.91) | 4.29 (2.976.20) |
| Fall assessment | 1.47 (1.091.98) | 1.74 (1.272.37) |
Across all surveyed groups, public reporting was more often supported for lapses of surgical timeout (OR: 2.82, 95% CI: 2.03‐3.91) and fall risk assessment protocols (OR: 1.47, 95% CI: 1.09‐1.98) than for the referent, hand‐hygiene lapses. Across all groups, penalties were more likely to be supported for surgical timeout (OR: 4.29, 95% CI: 2.97‐6.20) and fall risk assessment protocol lapses (OR: 1.74, 95% CI: 1.27‐2.37) than for hand‐hygiene lapses.
Thresholds for Public Reporting and Penalties
The log‐rank test showed no significant differences among the surveyed groups in the number of transgressions at which public reporting was deemed appropriate in any of the 3 scenarios (P=0.37, P=0.71, and P=0.32 for hand hygiene, surgical time‐out, and fall risk assessment, respectively) (Figure 3). However, patients endorsed penalties after significantly fewer occurrences than residents, medical students, and nurses for all 3 scenarios (P<0.001 for all differences), and at a significantly lower threshold than attending physicians for surgical timeout and fall risk assessment (P<0.001 and P=0.03, respectively).
DISCUSSION
This survey assessed attitudes of healthcare professionals, trainees, and inpatients toward public reporting and penalties when clinicians do not follow basic safety protocols. Respondents tended to favor more aggressive measures when they deemed the safety risk from protocol violations to be higher. Almost all participants favored providing feedback after safety protocol lapses. Healthcare professionals tended to favor punitive measures, such as fines, suspension, and firing, more than public reporting of transgressions. Patients had a lower threshold than both providers and trainees for public reporting and punitive measures. In aggregate, our study suggests that after a decade of emphasis on a no‐blame response to patient safety hazards, both healthcare providers and patients now believe clinicians should be held accountable for following basic safety protocols, though their thresholds and triggers vary.
A surprising finding was that providers were more likely to favor penalties (such as fines, suspension, or firing) than public reporting of safety transgressions. Multiple studies have suggested that public reporting of hospital quality data has improved adherence to care processes and may improve patient outcomes.[15, 16, 17] Although our data do not tell us why clinicians appear to be more worried about public reporting than penalties, they do help explain why transparency has been a relatively powerful strategy to motivate changes in practice, even when it is unaccompanied by significant shifts in consumer choices.[18] It would be natural to consider public reporting to be a softer strategy than fines, suspension, or firing; however, our results indicate that many clinicians do not see it that way. Alternatively, the results could also suggest that clinicians prefer measures that provide more immediate feedback than public reporting generally provides. These attitudes should be considered when enacting public reporting strategies.
Another interesting finding was that patients and attending physicians tended to track together regarding their attitudes toward penalties for safety lapses. Although patients had a lower threshold for favoring penalties than attendings, similar proportions of patients and attending physicians believed that penalties should be enacted for safety transgressions, and both groups were more penal than physician trainees and nurses. We speculate that attendings and patients may have the most skin in the game, patients as the ones directly harmed by a preventable adverse event, and attending physicians as the most responsible clinicians, at least in the eyes of the malpractice system, licensing boards, and credentials committees.
Even though our study illustrates relatively high levels of endorsement for aggressive measures to deal with clinicians who fail to follow evidence‐based safety practices, a shift in this direction has risks and benefits. The no‐blame paradigm in patient safety grew out of a need to encourage open discussion about medical mistakes.[2] Whereas shifting away from a purely no‐ blame approach may lead to greater adherence with safety practices, and one hopes fewer cases of preventable harm, it also risks stifling the open discussions about medical errors that characterize learning organizations.[13, 19] Because of this, a movement in this direction should be undertaken carefully, starting first with a small number of well‐established safety practices, and ensuring that robust education and system improvements precede and accompany the imposition of penalties for nonadherence.
Our study has limitations. The survey was developed using convenience samples of UCSF faculty and medical students, so broader inclusion of physicians, nurses, trainees, and patients may have yielded a different survey instrument. As a survey, we cannot be certain that any of the groups' responses in real life (eg, in a vote of the medical staff on a given policy) would mirror their survey response. Additionally, the responses to protocol lapses did not include all possible administrative responses, such as mandatory training/remediation or rewards for positive behaviors. The responses could have also been different if participants were presented with different patient safety scenarios. The study population was limited in several ways. Attending and resident physicians were drawn from an academic department of internal medicine; it is possible that other specialties would have different attitudes. Patients were relatively young (likely due to the inclusion criteria), as were attending physicians (due to oversampling of hospitalist physicians). The relatively small number of participants could also limit statistical power to detect differences among groups. Additionally, the study population was limited to patients and healthcare professionals in academic medical centers in San Francisco. It is possible that attitudes would be different in other regions and practice settings.
The no‐blame approach to patient safety has been crucial in refocusing the lens on systems failures and in encouraging the active engagement by clinicians, particularly physicians.[2, 3] On the other hand, there are legitimate concerns that a unidimensional no‐blame approach has permitted, perhaps even promoted, nonadherence to evidence‐based safety practices that could prevent many cases of harm. Although it may not be surprising that patients favor harsher consequences for providers who do not follow basic safety protocols, our study demonstrates relatively widespread support for such consequences even among clinicians and trainees. However, all groups appear to recognize the nuances underlying this set of issues, with varying levels of enthusiasm for punitive responses based on perceived risk and number of transgressions. Future studies are needed to investigate how best to implement public reporting and penalties in ways that can maximize the patient safety benefits.
Acknowledgements
The authors are grateful to the clinicians, trainees, and patients who participated in the survey.
Healthcare delivery organizations are under increasing pressure to improve patient safety. The fundamental underpinning of efforts to improve safety has been the establishment of a no‐blame culture, one that focuses less on individual transgressions and more on system improvement.[1, 2] As evidence‐based practices to improve care have emerged, and the pressures to deliver tangible improvements in safety and quality have grown, providers, healthcare system leaders, and policymakers are struggling with how best to balance the need for accountability with this no‐blame paradigm.
In dealing with areas such as hand hygiene, where there is strong evidence for the value of the practice yet relatively poor adherence in many institutions, Wachter and Pronovost have argued that the scales need to tip more in the direction of accountability, including the imposition of penalties for clinicians who habitually fail to follow certain safety practices.[3] Although not obviating the critical importance of systems improvement, they argue that a failure to enforce such measures undermines trust in the system and invites external regulation. Chassin and colleagues made a similar point in arguing for the identification of certain accountability measures that could be used in public reporting and pay‐for‐performance programs.[4]
Few organizations have enacted robust systems to hold providers responsible for adhering to accountability measures.[4] Although many hospitals have policies to suspend clinical privileges for failing to sign discharge summaries or obtain a yearly purified protein derivative test, few have formal programs to identify and deal with clinicians whose behavior is persistently problematic.[3] Furthermore, existing modes of physician accountability, such as state licensing boards, only discipline physicians retroactively (and rarely) when healthcare organizations report poor performance. State boards typically do not consider prevention of injury, such as adherence to safety practices, to be part of their responsibility.[5] Similarly, credentialing boards (eg, the American Board of Internal Medicine) do not assess adherence to such practices in coming to their decisions.
It is estimated that strict adherence to infection control practices, such as hand hygiene, could prevent over 100,000 hospital deaths every year; adherence to other evidence‐based safety practices such as the use of a preoperative time‐out would likely prevent many more deaths and cases of medical injury.[3, 6] Although there are practical issues, such as how to audit individual clinician adherence in ways that are feasible and fair, that make enforcing individual provider accountability challenging, there seems little doubt that attitudes regarding the appropriateness of enacting penalties for safety transgressions will be key determinants of whether such measures are considered. Yet no study to date has assessed the opinions of different stakeholders (physicians, nurses, trainees, patients) regarding various strategies, including public reporting and penalties, to improve adherence to safety practices. We aimed to assess these attitudes across a variety of such stakeholders.
METHODS
Survey Development and Characteristics
To understand the perceptions of measures designed to improve patient safety, we designed a survey of patients, nurses, medical students, resident physicians, and attending physicians to be administered at hospitals associated with the University of California, San Francisco (UCSF). Institutional review board approval was obtained from the UCSF Committee on Human Research, and all respondents provided informed consent.
The survey was developed by the authors and pilot tested with 2 populations. First, the survey was administered to a group of 12 UCSF Division of Hospital Medicine research faculty; their feedback was used to revise the survey. Second, the survey was administered to a convenience sample of 2 UCSF medical students, and their feedback was used to further refine the survey.
The questionnaire presented 3 scenarios in which a healthcare provider committed a patient‐safety protocol lapse; participants were asked their opinions about the appropriate responses to each of the violations. The 3 scenarios were: (1) a healthcare provider not properly conducting hand hygiene before a patient encounter, (2) a healthcare provider not properly conducting a fall risk assessment on a hospitalized patient, and (3) a healthcare provider not properly conducting a preoperative timeout prior to surgery. For each scenario, a series of questions was asked about a variety of institutional responses toward a provider who did not adhere to each safety protocol. Potential responses included feedback (email feedback, verbal feedback, meeting with a supervisor, a quarterly performance review meeting, and a quarterly report card seen only by the provider), public reporting (posting the provider's infractions on a public website), and penalties (fines, suspension without pay, and firing).
We chose the 3 practices because they are backed by strong evidence, are relatively easy to perform, are inexpensive, are linked to important and common harms, and are generally supported within the patient‐safety community. Improved adherence to hand hygiene significantly reduces infection transmission in healthcare settings.[7, 8, 9, 10, 11] Performing fall risk assessments has been shown to reduce falls in hospitalized patients,[12] and using preoperative checklists, including a surgical time‐out, can reduce mortality and complication risks by approximately 40%.[13]
Respondents were asked how many cases of documented nonadherence would be necessary for the penalties to be appropriate (1 time, 25 times, 610 times, 1115 times, 16+ times, or would never be appropriate). Finally, respondents were asked to rate the potential harm to patients of each protocol lapse (nonelow, medium, or high).
Demographic information collected from the healthcare providers and medical students included age, gender, position, department, and years' experience in their current position. Demographic information collected from the patients included age, gender, insurance status, race, education level, household income level, and relationship status.
Survey Administration
Surveys were administered to convenience samples of 5 groups of individuals: attending physicians in the UCSF Department of Internal Medicine based at UCSF Medical Center and the San Francisco Veterans Affairs Medical Center, nurses at UCSF Medical Center, residents in the UCSF internal medicine residency program, medical students at UCSF, and inpatients in the internal medicine service at UCSF Medical Center's Moffitt‐Long Hospital. Attending physicians and nurses were surveyed at their respective departmental meetings. For resident physicians and medical students, surveys were distributed at the beginning of lectures and collected at the end.
Patients were eligible to participate if they spoke English and were noted to be alert and oriented to person, time, and place. A survey administrator located eligible patients in the internal medicine service via the electronic medical record system, determined if they were alert and oriented, and approached each patient in his or her room. If the patients verbally consented to consider participation, the surveys were given to them and retrieved after approximately 30 minutes.
Healthcare professionals were offered the opportunity to enter their e‐mail addresses at the end of the survey to become eligible for a drawing for a $100 gift card, but were informed that their e‐mail addresses would not be included in the analytic dataset. Inpatients were not offered any incentives to participate. All surveys were administered by a survey monitor in paper form between May 2011 and July 2012.
Data Analysis
Data analysis was conducted using the Statistical Analysis Software (SAS) package (SAS Institute Inc., Cary, NC) and Stata (StataCorp, College Station, TX). Descriptive analysis and frequency distributions were tallied for all responses. Responses to protocol lapses were grouped into 3 categories: feedback, public reporting, and penalty as described above. As all surveyed groups endorsed feedback as an appropriate response to all of the scenarios, we did not examine feedback, concentrating our analysis instead on public reporting and penalties.
Appropriateness ratings for each response to each protocol lapse were aggregated in 2 ways: ever appropriate (ie, the response would be appropriate after some number of documented lapses) versus never appropriate, and the threshold for the response. Whereas public reporting was only asked about as a single option, 3 separate responses were collapsed into the single response, penalties: fine, suspension, or firing. Individuals were classified as endorsing a penalty if they rated any 1 of these responses as ever appropriate. The threshold for penalty was the smallest number of occurrences at which 1 of the penalty responses was endorsed.
Differences among the 5 groups in the perceived harm of each protocol lapse were tested with 2 analyses. Group differences in ratings of whether public reporting and penalties were ever appropriate were tested with logistic regression analyses for each scenario separately, controlling for age, sex, and perceived harm of the protocol lapse. To determine if the 5 groups differed in their tendency to support public reporting or penalties regardless of the type of protocol lapse, we conducted logistic regression analyses across all 3 scenarios, accounting for multiple observations per individual through use of cluster‐correlated robust variance.[14] Differences among groups in the number of transgressions at which public reporting and penalties were supported were examined with log‐rank tests.
RESULTS
A total of 287 individuals were given surveys, and 183 completed them: 22 attending physicians, 33 resident physicians, 61 nurses, 47 medical students, and 20 patients (overall response rate 64%). Response rate for attending and resident physicians was 73%, for nurses 59%, and for medical students 54%. Among patients who were approached and agreed to accept a survey, 87% returned completed surveys (Table 1). The average age of attending physicians was 35.8 years (standard deviation [SD]: 5.3), residents was 28.3 years (SD: 1.7), nurses was 43.6 years (SD: 11.1), medical students was 26.6 years (SD: 2.9), and inpatients was 48.2 years (SD: 15.9). Thirty‐two percent of attending physicians were female, 67% of resident physicians were female, 88% of nurses were female, 66% of medical students were female, and 47% of inpatients were female.
| Attending Physician | Resident Physician | Nurse | Medical Student | Patient | |
|---|---|---|---|---|---|
| |||||
| No. | 22 | 33 | 61 | 47 | 20 |
| Response rate* | 73% | 73% | 59% | 54% | 87% |
| Age, y, meanSD | 365 | 282 | 4411 | 273 | 4816 |
| Sex, female, % (n) | 32% (7) | 67% (22) | 88% (53) | 66% (31) | 47% (9) |
Perceived Harm
Out of the 3 scenarios presented in in the survey, participants believed that not conducting preoperative time‐outs in surgery presented the highest risk to patient safety, with 57% (residents) to 86% (nurses) rating the potential harm as high (Figure 1). Not conducting fall risk assessments was perceived as second most potentially harmful, and not properly practicing hand hygiene was perceived as least potentially harmful to patient safety. There were significant differences among groups in perceptions of potential harm for all 3 scenarios (P<0.001 for all).
Appropriateness of Public Reporting and Penalties
Public reporting was viewed as ever appropriate by 34% of all respondents for hand‐hygiene protocol lapses, 58% for surgical time‐out lapses, and 43% for fall risk assessment lapses. There were no significant differences among groups in endorsement of public reporting for individual scenarios (Figure 2). Penalties were endorsed more frequently than public reporting for all groups and all scenarios. The proportion of attending physicians and patients who rated penalties as ever appropriate were similar for each scenario. Residents, medical students, and nurses were less likely than patients and attending physicians to support penalties (P<0.05 for all differences).
The aggregated analysis revealed that nurses and medical students were significantly less likely than patients to endorse public reporting across scenarios. In terms of endorsement of penalties, we found no significant differences between attending physicians and patients, but residents (odds ratio [OR]: 0.09, 95% confidence interval [CI]: 0.03‐0.32), students (OR: 0.12, 95% CI: 0.04‐0.34), and nurses (OR: 0.17, 95% CI: 0.03‐0.41) had significantly lower odds of favoring penalties than did patients (Table 2).
| Odds Ratio (95% CI) | ||
|---|---|---|
| Public Reporting | Penalty | |
| ||
| Group, across all scenarios | ||
| Patients | Reference | Reference |
| Attending physicians | 0.58 (0.172.01) | 0.88 (0.203.84) |
| Resident physicians | 0.42 (0.121.52) | 0.09 (0.020.32) |
| Nurses | 0.32 (0.120.88) | 0.17 (0.030.41) |
| Medical students | 0.22 (0.060.80) | 0.12 (0.040.34) |
| Scenario, across all groups | ||
| Hand hygiene | Reference | Reference |
| Surgical time‐out | 2.82 (2.033.91) | 4.29 (2.976.20) |
| Fall assessment | 1.47 (1.091.98) | 1.74 (1.272.37) |
Across all surveyed groups, public reporting was more often supported for lapses of surgical timeout (OR: 2.82, 95% CI: 2.03‐3.91) and fall risk assessment protocols (OR: 1.47, 95% CI: 1.09‐1.98) than for the referent, hand‐hygiene lapses. Across all groups, penalties were more likely to be supported for surgical timeout (OR: 4.29, 95% CI: 2.97‐6.20) and fall risk assessment protocol lapses (OR: 1.74, 95% CI: 1.27‐2.37) than for hand‐hygiene lapses.
Thresholds for Public Reporting and Penalties
The log‐rank test showed no significant differences among the surveyed groups in the number of transgressions at which public reporting was deemed appropriate in any of the 3 scenarios (P=0.37, P=0.71, and P=0.32 for hand hygiene, surgical time‐out, and fall risk assessment, respectively) (Figure 3). However, patients endorsed penalties after significantly fewer occurrences than residents, medical students, and nurses for all 3 scenarios (P<0.001 for all differences), and at a significantly lower threshold than attending physicians for surgical timeout and fall risk assessment (P<0.001 and P=0.03, respectively).
DISCUSSION
This survey assessed attitudes of healthcare professionals, trainees, and inpatients toward public reporting and penalties when clinicians do not follow basic safety protocols. Respondents tended to favor more aggressive measures when they deemed the safety risk from protocol violations to be higher. Almost all participants favored providing feedback after safety protocol lapses. Healthcare professionals tended to favor punitive measures, such as fines, suspension, and firing, more than public reporting of transgressions. Patients had a lower threshold than both providers and trainees for public reporting and punitive measures. In aggregate, our study suggests that after a decade of emphasis on a no‐blame response to patient safety hazards, both healthcare providers and patients now believe clinicians should be held accountable for following basic safety protocols, though their thresholds and triggers vary.
A surprising finding was that providers were more likely to favor penalties (such as fines, suspension, or firing) than public reporting of safety transgressions. Multiple studies have suggested that public reporting of hospital quality data has improved adherence to care processes and may improve patient outcomes.[15, 16, 17] Although our data do not tell us why clinicians appear to be more worried about public reporting than penalties, they do help explain why transparency has been a relatively powerful strategy to motivate changes in practice, even when it is unaccompanied by significant shifts in consumer choices.[18] It would be natural to consider public reporting to be a softer strategy than fines, suspension, or firing; however, our results indicate that many clinicians do not see it that way. Alternatively, the results could also suggest that clinicians prefer measures that provide more immediate feedback than public reporting generally provides. These attitudes should be considered when enacting public reporting strategies.
Another interesting finding was that patients and attending physicians tended to track together regarding their attitudes toward penalties for safety lapses. Although patients had a lower threshold for favoring penalties than attendings, similar proportions of patients and attending physicians believed that penalties should be enacted for safety transgressions, and both groups were more penal than physician trainees and nurses. We speculate that attendings and patients may have the most skin in the game, patients as the ones directly harmed by a preventable adverse event, and attending physicians as the most responsible clinicians, at least in the eyes of the malpractice system, licensing boards, and credentials committees.
Even though our study illustrates relatively high levels of endorsement for aggressive measures to deal with clinicians who fail to follow evidence‐based safety practices, a shift in this direction has risks and benefits. The no‐blame paradigm in patient safety grew out of a need to encourage open discussion about medical mistakes.[2] Whereas shifting away from a purely no‐ blame approach may lead to greater adherence with safety practices, and one hopes fewer cases of preventable harm, it also risks stifling the open discussions about medical errors that characterize learning organizations.[13, 19] Because of this, a movement in this direction should be undertaken carefully, starting first with a small number of well‐established safety practices, and ensuring that robust education and system improvements precede and accompany the imposition of penalties for nonadherence.
Our study has limitations. The survey was developed using convenience samples of UCSF faculty and medical students, so broader inclusion of physicians, nurses, trainees, and patients may have yielded a different survey instrument. As a survey, we cannot be certain that any of the groups' responses in real life (eg, in a vote of the medical staff on a given policy) would mirror their survey response. Additionally, the responses to protocol lapses did not include all possible administrative responses, such as mandatory training/remediation or rewards for positive behaviors. The responses could have also been different if participants were presented with different patient safety scenarios. The study population was limited in several ways. Attending and resident physicians were drawn from an academic department of internal medicine; it is possible that other specialties would have different attitudes. Patients were relatively young (likely due to the inclusion criteria), as were attending physicians (due to oversampling of hospitalist physicians). The relatively small number of participants could also limit statistical power to detect differences among groups. Additionally, the study population was limited to patients and healthcare professionals in academic medical centers in San Francisco. It is possible that attitudes would be different in other regions and practice settings.
The no‐blame approach to patient safety has been crucial in refocusing the lens on systems failures and in encouraging the active engagement by clinicians, particularly physicians.[2, 3] On the other hand, there are legitimate concerns that a unidimensional no‐blame approach has permitted, perhaps even promoted, nonadherence to evidence‐based safety practices that could prevent many cases of harm. Although it may not be surprising that patients favor harsher consequences for providers who do not follow basic safety protocols, our study demonstrates relatively widespread support for such consequences even among clinicians and trainees. However, all groups appear to recognize the nuances underlying this set of issues, with varying levels of enthusiasm for punitive responses based on perceived risk and number of transgressions. Future studies are needed to investigate how best to implement public reporting and penalties in ways that can maximize the patient safety benefits.
Acknowledgements
The authors are grateful to the clinicians, trainees, and patients who participated in the survey.
- . Understanding Patient Safety. 2nd ed. New York, NY: McGraw Hill Medical; 2012.
- . Error in medicine. JAMA. 1994;272(23):1851–1857.
- , . Balancing "no blame" with accountability in patient safety. N Engl J Med. 2009;361(14):1401–1406.
- , , , . Accountability measures—using measurement to promote quality improvement. N Engl J Med. 2010;363(7):683–688.
- , . Problem doctors: is there a system‐level solution? Ann Intern Med. 2006;144(2):107–115.
- , , , et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360(5):491–499.
- , , , , . Effectiveness of a comprehensive hand hygiene program for reduction of infection rates in a long‐term care facility. Am J Infect Control. 2013;41(1):39–44.
- , . Impact of a hospital‐wide hand hygiene promotion strategy on healthcare‐associated infections. Antimicrob Resist Infect Control. 2012;1(1):13.
- , , , et al. Determinants of hand hygiene noncompliance in intensive care units. Am J Infect Control. 2013;41(2):131–135.
- , , , , , . Impact of a hospital‐wide hand hygiene initiative on healthcare‐associated infections: results of an interrupted time series. BMJ Qual Saf. 2012;21(12):1019–1026.
- , , , . Effectiveness of multifaceted hand hygiene interventions in long‐term care facilities in Hong Kong: a cluster‐randomized controlled trial. Infect Control Hosp Epidemiol. 2012;33(8):761–767.
- , , , , . Development, implementation, and evaluation of a comprehensive fall risk program. J Spec Pediatr Nurs 2011;16(2):130–139.
- , , , . A systematic review of the effectiveness, compliance, and critical factors for implementation of safety checklists in surgery. Ann Surg. 2012;256(6):925–933.
- . A note on robust variance estimation for cluster‐correlated data. Biometrics. 2000;56(2):645–646.
- , , , et al. Public reporting and pay for performance in hospital quality improvement. N Engl J Med. 2007;356(5):486–496.
- , , , , . Improving the outcomes of coronary artery bypass surgery in New York State. JAMA. 1994;271(10):761–766.
- , , . Declines in hospital mortality associated with a regional initiative to measure hospital performance. Am J Med Qual. 1997;12(2):103–112.
- , , , . The public release of performance data: what do we expect to gain? A review of the evidence. JAMA. 2000;283(14):1866–1874.
- . Continuing education meets the learning organization: the challenge of a systems approach to patient safety. J Contin Educ Health Prof. 2000;20(4):197–207.
- . Understanding Patient Safety. 2nd ed. New York, NY: McGraw Hill Medical; 2012.
- . Error in medicine. JAMA. 1994;272(23):1851–1857.
- , . Balancing "no blame" with accountability in patient safety. N Engl J Med. 2009;361(14):1401–1406.
- , , , . Accountability measures—using measurement to promote quality improvement. N Engl J Med. 2010;363(7):683–688.
- , . Problem doctors: is there a system‐level solution? Ann Intern Med. 2006;144(2):107–115.
- , , , et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med. 2009;360(5):491–499.
- , , , , . Effectiveness of a comprehensive hand hygiene program for reduction of infection rates in a long‐term care facility. Am J Infect Control. 2013;41(1):39–44.
- , . Impact of a hospital‐wide hand hygiene promotion strategy on healthcare‐associated infections. Antimicrob Resist Infect Control. 2012;1(1):13.
- , , , et al. Determinants of hand hygiene noncompliance in intensive care units. Am J Infect Control. 2013;41(2):131–135.
- , , , , , . Impact of a hospital‐wide hand hygiene initiative on healthcare‐associated infections: results of an interrupted time series. BMJ Qual Saf. 2012;21(12):1019–1026.
- , , , . Effectiveness of multifaceted hand hygiene interventions in long‐term care facilities in Hong Kong: a cluster‐randomized controlled trial. Infect Control Hosp Epidemiol. 2012;33(8):761–767.
- , , , , . Development, implementation, and evaluation of a comprehensive fall risk program. J Spec Pediatr Nurs 2011;16(2):130–139.
- , , , . A systematic review of the effectiveness, compliance, and critical factors for implementation of safety checklists in surgery. Ann Surg. 2012;256(6):925–933.
- . A note on robust variance estimation for cluster‐correlated data. Biometrics. 2000;56(2):645–646.
- , , , et al. Public reporting and pay for performance in hospital quality improvement. N Engl J Med. 2007;356(5):486–496.
- , , , , . Improving the outcomes of coronary artery bypass surgery in New York State. JAMA. 1994;271(10):761–766.
- , , . Declines in hospital mortality associated with a regional initiative to measure hospital performance. Am J Med Qual. 1997;12(2):103–112.
- , , , . The public release of performance data: what do we expect to gain? A review of the evidence. JAMA. 2000;283(14):1866–1874.
- . Continuing education meets the learning organization: the challenge of a systems approach to patient safety. J Contin Educ Health Prof. 2000;20(4):197–207.
© 2013 Society of Hospital Medicine
In reference to “Discharge against medical advice: How often do we intervene?”
In their study of against medical advice (AMA) discharges, Edwards et al.[1] express surprise that prescriptions were given and follow‐up arranged at a much lower rate than the frequency of warning of impending AMA discharge. The authors assume that when doctors know a patient wants to leave AMA, they will and should, as a matter of course, write prescriptions and arrange follow‐up. Not considered is the possibility that doctors may decide for selected patients that the better response is not to prescribe and not to arrange follow‐up. Prescribing medications to a patient who has already shown disinterest in heeding doctors' advice may be considered dangerous. Similarly, making an appointment for a patient who has already demonstrated a lack of adherence, thereby depriving another patient of that appointment, may be considered an imprudent use of resources. The authors do not provide data on how many AMA discharges may have been averted by this approach. Attempts to minimize the negative impact of capable patients' decisions neglect that some patients do not categorically prioritize health, and that true autonomy entails not just decision making but bearing responsibility for those decisions' consequences. Medical risk reduction is not the only value at play in these complex situations.
- , , . Discharge against medical advice: how often do we intervene? J Hosp Med. 2013;8(10):574–577.
In their study of against medical advice (AMA) discharges, Edwards et al.[1] express surprise that prescriptions were given and follow‐up arranged at a much lower rate than the frequency of warning of impending AMA discharge. The authors assume that when doctors know a patient wants to leave AMA, they will and should, as a matter of course, write prescriptions and arrange follow‐up. Not considered is the possibility that doctors may decide for selected patients that the better response is not to prescribe and not to arrange follow‐up. Prescribing medications to a patient who has already shown disinterest in heeding doctors' advice may be considered dangerous. Similarly, making an appointment for a patient who has already demonstrated a lack of adherence, thereby depriving another patient of that appointment, may be considered an imprudent use of resources. The authors do not provide data on how many AMA discharges may have been averted by this approach. Attempts to minimize the negative impact of capable patients' decisions neglect that some patients do not categorically prioritize health, and that true autonomy entails not just decision making but bearing responsibility for those decisions' consequences. Medical risk reduction is not the only value at play in these complex situations.
In their study of against medical advice (AMA) discharges, Edwards et al.[1] express surprise that prescriptions were given and follow‐up arranged at a much lower rate than the frequency of warning of impending AMA discharge. The authors assume that when doctors know a patient wants to leave AMA, they will and should, as a matter of course, write prescriptions and arrange follow‐up. Not considered is the possibility that doctors may decide for selected patients that the better response is not to prescribe and not to arrange follow‐up. Prescribing medications to a patient who has already shown disinterest in heeding doctors' advice may be considered dangerous. Similarly, making an appointment for a patient who has already demonstrated a lack of adherence, thereby depriving another patient of that appointment, may be considered an imprudent use of resources. The authors do not provide data on how many AMA discharges may have been averted by this approach. Attempts to minimize the negative impact of capable patients' decisions neglect that some patients do not categorically prioritize health, and that true autonomy entails not just decision making but bearing responsibility for those decisions' consequences. Medical risk reduction is not the only value at play in these complex situations.
- , , . Discharge against medical advice: how often do we intervene? J Hosp Med. 2013;8(10):574–577.
- , , . Discharge against medical advice: how often do we intervene? J Hosp Med. 2013;8(10):574–577.
Letters to the Editor
We believe medications can safely be prescribed to most patients who leave against medical advice (AMA), and that follow‐up should be offered to most if not all such patients. Why should we do this? Consider a wheezing asthma patient who leaves AMA. She or he is probably more likely to return to the emergency department (somewhere) or be readmitted (somewhere) and cost more money (to the system) than if given an inhaler and steroid taper.
Dr. Querques et al. suggest that doctors should potentially not prescribe and should not offer follow‐up to certain patients who want to leave AMA, particularly those who show disinterest in heeding the doctor's advice and have already demonstrated a lack of adherence. How should doctors make those judgments? Patients leave AMA for a variety of reasons: for example to avoid cost, because they feel better, or poor communication. Certainly, not all patients who want to leave AMA are categorically nonadherent. Conversely, up to 50% of all continuity patients are not fully adherent to the lifestyle changes and medications their physicians prescribe,[1] yet they would rarely if ever threaten AMA. Is withholding treatments that are likely to be effective and have minimal risk worth the potential benefit of increasing a patient's priority on their own healthcare? As emphasized by Berger (2008),[2] interventions with low risk and high potential for efficacy (assistance with establishing a follow‐up) should be pursued, and those with potential risks (starting new long‐term medications) should be avoided. At minimum, considering these options is an ethical requirement in the care of patients. We maintain that this reasoning should be explained and documented, which often is not being done in healthcare today.
How many AMAs are avoided by truly collaborative relationships with patients (nonevents), and how many are fueled by a more paternalistic relationship? For example, if a patient truly has a sick family member or child to take care of or has financial problems or no insurance, then it seems reasonable, perhaps even responsible, to leave the hospital even if maximal benefits of care have not been reached. In a collaborative relationship, providers may then tailor treatment to the patient's circumstances, even if this means the patient is not getting the best possible care.
- , . Medication adherence: WHO cares? Mayo Clin Proc. 2011;86(4):304–314.
- . Discharge against medical advice: ethical considerations and professional obligations. J Hosp Med. 2008;3(5):403–408.
We believe medications can safely be prescribed to most patients who leave against medical advice (AMA), and that follow‐up should be offered to most if not all such patients. Why should we do this? Consider a wheezing asthma patient who leaves AMA. She or he is probably more likely to return to the emergency department (somewhere) or be readmitted (somewhere) and cost more money (to the system) than if given an inhaler and steroid taper.
Dr. Querques et al. suggest that doctors should potentially not prescribe and should not offer follow‐up to certain patients who want to leave AMA, particularly those who show disinterest in heeding the doctor's advice and have already demonstrated a lack of adherence. How should doctors make those judgments? Patients leave AMA for a variety of reasons: for example to avoid cost, because they feel better, or poor communication. Certainly, not all patients who want to leave AMA are categorically nonadherent. Conversely, up to 50% of all continuity patients are not fully adherent to the lifestyle changes and medications their physicians prescribe,[1] yet they would rarely if ever threaten AMA. Is withholding treatments that are likely to be effective and have minimal risk worth the potential benefit of increasing a patient's priority on their own healthcare? As emphasized by Berger (2008),[2] interventions with low risk and high potential for efficacy (assistance with establishing a follow‐up) should be pursued, and those with potential risks (starting new long‐term medications) should be avoided. At minimum, considering these options is an ethical requirement in the care of patients. We maintain that this reasoning should be explained and documented, which often is not being done in healthcare today.
How many AMAs are avoided by truly collaborative relationships with patients (nonevents), and how many are fueled by a more paternalistic relationship? For example, if a patient truly has a sick family member or child to take care of or has financial problems or no insurance, then it seems reasonable, perhaps even responsible, to leave the hospital even if maximal benefits of care have not been reached. In a collaborative relationship, providers may then tailor treatment to the patient's circumstances, even if this means the patient is not getting the best possible care.
We believe medications can safely be prescribed to most patients who leave against medical advice (AMA), and that follow‐up should be offered to most if not all such patients. Why should we do this? Consider a wheezing asthma patient who leaves AMA. She or he is probably more likely to return to the emergency department (somewhere) or be readmitted (somewhere) and cost more money (to the system) than if given an inhaler and steroid taper.
Dr. Querques et al. suggest that doctors should potentially not prescribe and should not offer follow‐up to certain patients who want to leave AMA, particularly those who show disinterest in heeding the doctor's advice and have already demonstrated a lack of adherence. How should doctors make those judgments? Patients leave AMA for a variety of reasons: for example to avoid cost, because they feel better, or poor communication. Certainly, not all patients who want to leave AMA are categorically nonadherent. Conversely, up to 50% of all continuity patients are not fully adherent to the lifestyle changes and medications their physicians prescribe,[1] yet they would rarely if ever threaten AMA. Is withholding treatments that are likely to be effective and have minimal risk worth the potential benefit of increasing a patient's priority on their own healthcare? As emphasized by Berger (2008),[2] interventions with low risk and high potential for efficacy (assistance with establishing a follow‐up) should be pursued, and those with potential risks (starting new long‐term medications) should be avoided. At minimum, considering these options is an ethical requirement in the care of patients. We maintain that this reasoning should be explained and documented, which often is not being done in healthcare today.
How many AMAs are avoided by truly collaborative relationships with patients (nonevents), and how many are fueled by a more paternalistic relationship? For example, if a patient truly has a sick family member or child to take care of or has financial problems or no insurance, then it seems reasonable, perhaps even responsible, to leave the hospital even if maximal benefits of care have not been reached. In a collaborative relationship, providers may then tailor treatment to the patient's circumstances, even if this means the patient is not getting the best possible care.
- , . Medication adherence: WHO cares? Mayo Clin Proc. 2011;86(4):304–314.
- . Discharge against medical advice: ethical considerations and professional obligations. J Hosp Med. 2008;3(5):403–408.
- , . Medication adherence: WHO cares? Mayo Clin Proc. 2011;86(4):304–314.
- . Discharge against medical advice: ethical considerations and professional obligations. J Hosp Med. 2008;3(5):403–408.
Why social media are here to stay
A new year holds so much potential. It’s often when we’re at our most ambitious and optimistic. A time when we’re more likely to try something new – learn a language, take up CrossFit, or, even, dive into the social media ocean.
In this column over the last year, I have written about many different social media platforms including Facebook, YouTube, and Pinterest. Many physicians have e-mailed me asking, "Do I really need to be doing social media? Is it more than just a fad?" My answer was and still is, Yes!
The medical landscape is continually evolving, and social media continue to disrupt the traditional roles of doctor and patient. We now have "e-patients," "digital doctors," and doctor-rating sites; hospitals have Facebook pages, and surgeons are tweeting live surgery. Never has the field of medicine been so transparent.
Although I don’t have a crystal ball, I can assure you that social media are here to stay for a long time. So, if you’ve only dipped your toe in the social media waters so far, keep reading; you might find some inspiration to take the plunge in 2014:
• 90% of adults aged 18-24 said they would trust medical information shared by others in their social media networks. Social media communications are simply word of mouth enhanced by technology. Instead of telling their immediate family about you at the dinner table, your patients now have the ability to tell hundreds or thousands of people about you on social media. Create compelling content, make it shareable, and you’ll help build positive word of mouth.
• Social media users are more likely to trust health-related content written by physicians than by any other group. There is a tremendous amount of health care information online, much of it inaccurate. That means content produced by you (for example, through Facebook updates, YouTube videos, and blog posts) is likely to be shared more frequently and to help build your brand as a trusted physician.
• 47% of patients share their medical information online with doctors, and 43% do so with hospitals.
• 77% of patients used search engines prior to booking their medical appointment. If you’re not online, patients won’t find you.
• 41% of patients said social media would affect their choice of a specific doctor, hospital, or medical facility. Online word of mouth has an impact on you and your practice.
• 58% of health care marketers use blogs vs. 74% of all marketers. Maintaining a blog helps you build brand loyalty and gives you a competitive edge against physicians who aren’t online.
• YouTube traffic to hospital websites has increased 119% year to year. Because they’re visual, videos tend to be more memorable for social media users. Whether videos are used to share poignant patient stories, educate patients about specific diseases and treatments, or show how a clinical procedure is performed, they allow you to connect more intimately with patients and prospective patients, and put a human face on your practice.
• Parents are more likely to seek medical information online. Data show that 22% of parents use Facebook vs. 14% of nonparents, and 20% of parents use YouTube vs. 12% of nonparents. Parents want online information they can trust; that means information created by you.
• 51% of patients said they would feel more valued if their health care provider communicated with them digitally. This means exploring other modes of communication such as e-mail, newsletters, blog posts, and Facebook updates.
• 60% of physicians surveyed said social media improve the quality of care delivered to their patients. From physician online communities to Google hangouts, physicians are learning from one another, and often from patients, making them better clinicians.
Sources include DC Interactive Group, Demi and Cooper Advertising, Media Bistro, PWC Health Research Institute, and TeleVox.
Dr. Benabio is a practicing dermatologist and physician director of health care transformation at Kaiser Permanente in San Diego. Connect with him on Twitter @Dermdoc or drop him a line at [email protected].
A new year holds so much potential. It’s often when we’re at our most ambitious and optimistic. A time when we’re more likely to try something new – learn a language, take up CrossFit, or, even, dive into the social media ocean.
In this column over the last year, I have written about many different social media platforms including Facebook, YouTube, and Pinterest. Many physicians have e-mailed me asking, "Do I really need to be doing social media? Is it more than just a fad?" My answer was and still is, Yes!
The medical landscape is continually evolving, and social media continue to disrupt the traditional roles of doctor and patient. We now have "e-patients," "digital doctors," and doctor-rating sites; hospitals have Facebook pages, and surgeons are tweeting live surgery. Never has the field of medicine been so transparent.
Although I don’t have a crystal ball, I can assure you that social media are here to stay for a long time. So, if you’ve only dipped your toe in the social media waters so far, keep reading; you might find some inspiration to take the plunge in 2014:
• 90% of adults aged 18-24 said they would trust medical information shared by others in their social media networks. Social media communications are simply word of mouth enhanced by technology. Instead of telling their immediate family about you at the dinner table, your patients now have the ability to tell hundreds or thousands of people about you on social media. Create compelling content, make it shareable, and you’ll help build positive word of mouth.
• Social media users are more likely to trust health-related content written by physicians than by any other group. There is a tremendous amount of health care information online, much of it inaccurate. That means content produced by you (for example, through Facebook updates, YouTube videos, and blog posts) is likely to be shared more frequently and to help build your brand as a trusted physician.
• 47% of patients share their medical information online with doctors, and 43% do so with hospitals.
• 77% of patients used search engines prior to booking their medical appointment. If you’re not online, patients won’t find you.
• 41% of patients said social media would affect their choice of a specific doctor, hospital, or medical facility. Online word of mouth has an impact on you and your practice.
• 58% of health care marketers use blogs vs. 74% of all marketers. Maintaining a blog helps you build brand loyalty and gives you a competitive edge against physicians who aren’t online.
• YouTube traffic to hospital websites has increased 119% year to year. Because they’re visual, videos tend to be more memorable for social media users. Whether videos are used to share poignant patient stories, educate patients about specific diseases and treatments, or show how a clinical procedure is performed, they allow you to connect more intimately with patients and prospective patients, and put a human face on your practice.
• Parents are more likely to seek medical information online. Data show that 22% of parents use Facebook vs. 14% of nonparents, and 20% of parents use YouTube vs. 12% of nonparents. Parents want online information they can trust; that means information created by you.
• 51% of patients said they would feel more valued if their health care provider communicated with them digitally. This means exploring other modes of communication such as e-mail, newsletters, blog posts, and Facebook updates.
• 60% of physicians surveyed said social media improve the quality of care delivered to their patients. From physician online communities to Google hangouts, physicians are learning from one another, and often from patients, making them better clinicians.
Sources include DC Interactive Group, Demi and Cooper Advertising, Media Bistro, PWC Health Research Institute, and TeleVox.
Dr. Benabio is a practicing dermatologist and physician director of health care transformation at Kaiser Permanente in San Diego. Connect with him on Twitter @Dermdoc or drop him a line at [email protected].
A new year holds so much potential. It’s often when we’re at our most ambitious and optimistic. A time when we’re more likely to try something new – learn a language, take up CrossFit, or, even, dive into the social media ocean.
In this column over the last year, I have written about many different social media platforms including Facebook, YouTube, and Pinterest. Many physicians have e-mailed me asking, "Do I really need to be doing social media? Is it more than just a fad?" My answer was and still is, Yes!
The medical landscape is continually evolving, and social media continue to disrupt the traditional roles of doctor and patient. We now have "e-patients," "digital doctors," and doctor-rating sites; hospitals have Facebook pages, and surgeons are tweeting live surgery. Never has the field of medicine been so transparent.
Although I don’t have a crystal ball, I can assure you that social media are here to stay for a long time. So, if you’ve only dipped your toe in the social media waters so far, keep reading; you might find some inspiration to take the plunge in 2014:
• 90% of adults aged 18-24 said they would trust medical information shared by others in their social media networks. Social media communications are simply word of mouth enhanced by technology. Instead of telling their immediate family about you at the dinner table, your patients now have the ability to tell hundreds or thousands of people about you on social media. Create compelling content, make it shareable, and you’ll help build positive word of mouth.
• Social media users are more likely to trust health-related content written by physicians than by any other group. There is a tremendous amount of health care information online, much of it inaccurate. That means content produced by you (for example, through Facebook updates, YouTube videos, and blog posts) is likely to be shared more frequently and to help build your brand as a trusted physician.
• 47% of patients share their medical information online with doctors, and 43% do so with hospitals.
• 77% of patients used search engines prior to booking their medical appointment. If you’re not online, patients won’t find you.
• 41% of patients said social media would affect their choice of a specific doctor, hospital, or medical facility. Online word of mouth has an impact on you and your practice.
• 58% of health care marketers use blogs vs. 74% of all marketers. Maintaining a blog helps you build brand loyalty and gives you a competitive edge against physicians who aren’t online.
• YouTube traffic to hospital websites has increased 119% year to year. Because they’re visual, videos tend to be more memorable for social media users. Whether videos are used to share poignant patient stories, educate patients about specific diseases and treatments, or show how a clinical procedure is performed, they allow you to connect more intimately with patients and prospective patients, and put a human face on your practice.
• Parents are more likely to seek medical information online. Data show that 22% of parents use Facebook vs. 14% of nonparents, and 20% of parents use YouTube vs. 12% of nonparents. Parents want online information they can trust; that means information created by you.
• 51% of patients said they would feel more valued if their health care provider communicated with them digitally. This means exploring other modes of communication such as e-mail, newsletters, blog posts, and Facebook updates.
• 60% of physicians surveyed said social media improve the quality of care delivered to their patients. From physician online communities to Google hangouts, physicians are learning from one another, and often from patients, making them better clinicians.
Sources include DC Interactive Group, Demi and Cooper Advertising, Media Bistro, PWC Health Research Institute, and TeleVox.
Dr. Benabio is a practicing dermatologist and physician director of health care transformation at Kaiser Permanente in San Diego. Connect with him on Twitter @Dermdoc or drop him a line at [email protected].
Promises, promises
For many, the making and breaking of New Year’s resolutions have become a humorless cliché. Still, the beginning of a new year is as good a time as any for reflection and inspiration; and if you restrict your fix-it list to a few realistic promises that can actually be kept, resolution time does not have to remain an exercise in futility.
I can’t presume to know what needs improving in your practice, but I do know the issues I get the most questions about. Perhaps the following Top Ten list will inspire you to create a realistic list of your own.
1. Do a HIPAA risk assessment. The new HIPAA rules are now in effect, as I discussed a few months ago. Is your office up to speed? Review every procedure that involves confidential information; make sure there are no violations. Penalties for carelessness are much stiffer now.
2. Encrypt your mobile devices. This is a subset of item 1. The biggest HIPAA vulnerability in many practices is laptops and tablets that carry confidential patient information; losing one could be a disaster. Encryption software is cheap and readily available, and a lost or stolen mobile device will probably not be treated as a HIPAA breach if it is properly encrypted.
3. Reduce your accounts receivable by keeping a credit card number on file for each patient, and charging patient-owed balances as they come in. A series of my past columns in the archives at edermatologynews.com explains exactly how to do it. Every hotel in the world does this, and you should too.
4. Review your coding habits. For example, are you billing for 99213 each and every time your evaluation and treatment meet the criteria for that code? If not, you’re leaving money on the table; and that will become a more and more significant issue if reimbursements tighten up in the next few years – as they almost surely will.
5. Clear your "horizontal file cabinet." That’s the mess on your desk, all the paperwork you never seem to get to (probably because you’re tweeting or answering e-mail). Set aside an hour or two and get it all done. You’ll find some interesting stuff in there. Then, for every piece of paper that arrives on your desk from now on, follow the DDD Rule: Do it, Delegate it, or Destroy it. Don’t start a new mess.
6. Keep a closer eye on your office finances. Most physicians delegate the bookkeeping, and that’s fine. But ignoring the financial side creates an atmosphere that facilitates embezzlement. Set aside a few hours each month to review the books personally. And make sure your employees know you’re doing it.
7. Make sure your long-range financial planning is on track. This is another task physicians tend to "set and forget," but the Great Recession was an eye-opener for many of us. Once a year, sit down with your accountant and planner and make sure your investments are well diversified and all other aspects of your finances – budgets, credit ratings, insurance coverage, tax situations, college savings, estate plans, and retirement accounts – are in the best shape possible. Now would be a good time.
8. Back up your data. Now is also an excellent time to verify that the information on your office and personal computers is being backed up – locally and online – on a regular schedule. Don’t wait until something crashes.
9. Take more vacations. Remember Eastern’s First Law: Your last words will not be, "I wish I had spent more time in the office." This is the year to start spending more time enjoying your life, your friends and family, and the world. As John Lennon said, "Life is what happens to you while you’re busy making other plans."
10. Look at yourself. A private practice lives or dies on the personalities of its physicians, and your staff copies your personality and style. Take a hard, honest look at yourself. Identify your negative personality traits and work to eliminate them. If you have any difficulty finding the things that need changing ... ask your spouse. He or she will be happy to outline them for you in great detail.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is a clinical associate professor of dermatology at Seton Hall University School of Graduate Medical Education in South Orange, N.J. Dr. Eastern is a two-time past president of the Dermatological Society of New Jersey, and currently serves on its executive board. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
For many, the making and breaking of New Year’s resolutions have become a humorless cliché. Still, the beginning of a new year is as good a time as any for reflection and inspiration; and if you restrict your fix-it list to a few realistic promises that can actually be kept, resolution time does not have to remain an exercise in futility.
I can’t presume to know what needs improving in your practice, but I do know the issues I get the most questions about. Perhaps the following Top Ten list will inspire you to create a realistic list of your own.
1. Do a HIPAA risk assessment. The new HIPAA rules are now in effect, as I discussed a few months ago. Is your office up to speed? Review every procedure that involves confidential information; make sure there are no violations. Penalties for carelessness are much stiffer now.
2. Encrypt your mobile devices. This is a subset of item 1. The biggest HIPAA vulnerability in many practices is laptops and tablets that carry confidential patient information; losing one could be a disaster. Encryption software is cheap and readily available, and a lost or stolen mobile device will probably not be treated as a HIPAA breach if it is properly encrypted.
3. Reduce your accounts receivable by keeping a credit card number on file for each patient, and charging patient-owed balances as they come in. A series of my past columns in the archives at edermatologynews.com explains exactly how to do it. Every hotel in the world does this, and you should too.
4. Review your coding habits. For example, are you billing for 99213 each and every time your evaluation and treatment meet the criteria for that code? If not, you’re leaving money on the table; and that will become a more and more significant issue if reimbursements tighten up in the next few years – as they almost surely will.
5. Clear your "horizontal file cabinet." That’s the mess on your desk, all the paperwork you never seem to get to (probably because you’re tweeting or answering e-mail). Set aside an hour or two and get it all done. You’ll find some interesting stuff in there. Then, for every piece of paper that arrives on your desk from now on, follow the DDD Rule: Do it, Delegate it, or Destroy it. Don’t start a new mess.
6. Keep a closer eye on your office finances. Most physicians delegate the bookkeeping, and that’s fine. But ignoring the financial side creates an atmosphere that facilitates embezzlement. Set aside a few hours each month to review the books personally. And make sure your employees know you’re doing it.
7. Make sure your long-range financial planning is on track. This is another task physicians tend to "set and forget," but the Great Recession was an eye-opener for many of us. Once a year, sit down with your accountant and planner and make sure your investments are well diversified and all other aspects of your finances – budgets, credit ratings, insurance coverage, tax situations, college savings, estate plans, and retirement accounts – are in the best shape possible. Now would be a good time.
8. Back up your data. Now is also an excellent time to verify that the information on your office and personal computers is being backed up – locally and online – on a regular schedule. Don’t wait until something crashes.
9. Take more vacations. Remember Eastern’s First Law: Your last words will not be, "I wish I had spent more time in the office." This is the year to start spending more time enjoying your life, your friends and family, and the world. As John Lennon said, "Life is what happens to you while you’re busy making other plans."
10. Look at yourself. A private practice lives or dies on the personalities of its physicians, and your staff copies your personality and style. Take a hard, honest look at yourself. Identify your negative personality traits and work to eliminate them. If you have any difficulty finding the things that need changing ... ask your spouse. He or she will be happy to outline them for you in great detail.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is a clinical associate professor of dermatology at Seton Hall University School of Graduate Medical Education in South Orange, N.J. Dr. Eastern is a two-time past president of the Dermatological Society of New Jersey, and currently serves on its executive board. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
For many, the making and breaking of New Year’s resolutions have become a humorless cliché. Still, the beginning of a new year is as good a time as any for reflection and inspiration; and if you restrict your fix-it list to a few realistic promises that can actually be kept, resolution time does not have to remain an exercise in futility.
I can’t presume to know what needs improving in your practice, but I do know the issues I get the most questions about. Perhaps the following Top Ten list will inspire you to create a realistic list of your own.
1. Do a HIPAA risk assessment. The new HIPAA rules are now in effect, as I discussed a few months ago. Is your office up to speed? Review every procedure that involves confidential information; make sure there are no violations. Penalties for carelessness are much stiffer now.
2. Encrypt your mobile devices. This is a subset of item 1. The biggest HIPAA vulnerability in many practices is laptops and tablets that carry confidential patient information; losing one could be a disaster. Encryption software is cheap and readily available, and a lost or stolen mobile device will probably not be treated as a HIPAA breach if it is properly encrypted.
3. Reduce your accounts receivable by keeping a credit card number on file for each patient, and charging patient-owed balances as they come in. A series of my past columns in the archives at edermatologynews.com explains exactly how to do it. Every hotel in the world does this, and you should too.
4. Review your coding habits. For example, are you billing for 99213 each and every time your evaluation and treatment meet the criteria for that code? If not, you’re leaving money on the table; and that will become a more and more significant issue if reimbursements tighten up in the next few years – as they almost surely will.
5. Clear your "horizontal file cabinet." That’s the mess on your desk, all the paperwork you never seem to get to (probably because you’re tweeting or answering e-mail). Set aside an hour or two and get it all done. You’ll find some interesting stuff in there. Then, for every piece of paper that arrives on your desk from now on, follow the DDD Rule: Do it, Delegate it, or Destroy it. Don’t start a new mess.
6. Keep a closer eye on your office finances. Most physicians delegate the bookkeeping, and that’s fine. But ignoring the financial side creates an atmosphere that facilitates embezzlement. Set aside a few hours each month to review the books personally. And make sure your employees know you’re doing it.
7. Make sure your long-range financial planning is on track. This is another task physicians tend to "set and forget," but the Great Recession was an eye-opener for many of us. Once a year, sit down with your accountant and planner and make sure your investments are well diversified and all other aspects of your finances – budgets, credit ratings, insurance coverage, tax situations, college savings, estate plans, and retirement accounts – are in the best shape possible. Now would be a good time.
8. Back up your data. Now is also an excellent time to verify that the information on your office and personal computers is being backed up – locally and online – on a regular schedule. Don’t wait until something crashes.
9. Take more vacations. Remember Eastern’s First Law: Your last words will not be, "I wish I had spent more time in the office." This is the year to start spending more time enjoying your life, your friends and family, and the world. As John Lennon said, "Life is what happens to you while you’re busy making other plans."
10. Look at yourself. A private practice lives or dies on the personalities of its physicians, and your staff copies your personality and style. Take a hard, honest look at yourself. Identify your negative personality traits and work to eliminate them. If you have any difficulty finding the things that need changing ... ask your spouse. He or she will be happy to outline them for you in great detail.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is a clinical associate professor of dermatology at Seton Hall University School of Graduate Medical Education in South Orange, N.J. Dr. Eastern is a two-time past president of the Dermatological Society of New Jersey, and currently serves on its executive board. He holds teaching positions at several hospitals and has delivered more than 500 academic speaking presentations. He is the author of numerous articles and textbook chapters, and is a long-time monthly columnist for Skin & Allergy News.
Vitamin D deficiency in ethnic populations
Many clinicians are unaware that ethnic populations in North America do not achieve optimal serum 25-hydroxyvitamin D (abbreviated 25[OH]D) because of the increased pigmentation in their skin, which reduces vitamin D production. Vitamin D insufficiency is more prevalent among individuals with darker skin, compared with those with lighter skin at any time of year, even during the winter months. Contributing to the deficiency, the dietary intake of vitamin D intake among African Americans in particular is often below the recommended intakes in every age group after puberty. However, data have shown vitamin D protects against Sjögren’s syndrome, psoriasis, type 1 and type 2 diabetes, multiple sclerosis, and rheumatoid arthritis.
Vitamin D also may protect against cardiovascular disease through its anti-inflammatory effects and may reduce the risk for colorectal cancer, breast cancer, and prostate cancer by promoting cell differentiation and down-regulating hyperproliferative cell growth. Most of these conditions have been shown to be as prevalent, if not more prevalent, among blacks than whites.
While vitamin D can be obtained from sun exposure, this is not always a viable option. UV exposure is linked to skin cancer, which leads clinicians to encourage sun avoidance, but they may disregard the need for vitamin D. In addition, darker pigmentation of the skin reduces vitamin D synthesis in the skin.
How can you help your skin of color patients get enough vitamin D, especially in the winter? Nutritional sources of vitamin D include salmon, sardines, and cows’ milk; however, many individuals do not achieve optimal vitamin D status from food intake alone.
Since UV exposure and diet are not sufficient sources of vitamin D, supplementation has become crucial to our patients, particularly those with darker skin. Dietary reference intakes for vitamin D have been under considerable scrutiny, and many experts now believe that intakes of 25 mcg/d (1,000 IU) or more may be needed for most people to achieve optimal blood levels of 25(OH)D. The two forms of vitamin D used in dietary supplements are ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3). Cholecalciferol, the D3 form of the vitamin, is the form of choice when supplementing with vitamin D. Types of D3 supplements include gel caps, liquid, powders, and tablets. Vitamin D is often measured in International Units (IU) or mcg. One mcg of cholecalciferol is equal to 40 IU of vitamin D.
The debate continues over the most effective forms of vitamin D acquisition; however, many health professionals agree that vitamin D supplementation, particularly in winter months, should be an integral part of our armamentarium of therapeutics for ethnic patients, and especially those who suffer from psoriasis and other autoimmune and inflammatory skin conditions.
Dr. Talakoub is in private practice in McLean, Va.
Do you have questions about treating patients with dark skin? If so, send them to [email protected].
Many clinicians are unaware that ethnic populations in North America do not achieve optimal serum 25-hydroxyvitamin D (abbreviated 25[OH]D) because of the increased pigmentation in their skin, which reduces vitamin D production. Vitamin D insufficiency is more prevalent among individuals with darker skin, compared with those with lighter skin at any time of year, even during the winter months. Contributing to the deficiency, the dietary intake of vitamin D intake among African Americans in particular is often below the recommended intakes in every age group after puberty. However, data have shown vitamin D protects against Sjögren’s syndrome, psoriasis, type 1 and type 2 diabetes, multiple sclerosis, and rheumatoid arthritis.
Vitamin D also may protect against cardiovascular disease through its anti-inflammatory effects and may reduce the risk for colorectal cancer, breast cancer, and prostate cancer by promoting cell differentiation and down-regulating hyperproliferative cell growth. Most of these conditions have been shown to be as prevalent, if not more prevalent, among blacks than whites.
While vitamin D can be obtained from sun exposure, this is not always a viable option. UV exposure is linked to skin cancer, which leads clinicians to encourage sun avoidance, but they may disregard the need for vitamin D. In addition, darker pigmentation of the skin reduces vitamin D synthesis in the skin.
How can you help your skin of color patients get enough vitamin D, especially in the winter? Nutritional sources of vitamin D include salmon, sardines, and cows’ milk; however, many individuals do not achieve optimal vitamin D status from food intake alone.
Since UV exposure and diet are not sufficient sources of vitamin D, supplementation has become crucial to our patients, particularly those with darker skin. Dietary reference intakes for vitamin D have been under considerable scrutiny, and many experts now believe that intakes of 25 mcg/d (1,000 IU) or more may be needed for most people to achieve optimal blood levels of 25(OH)D. The two forms of vitamin D used in dietary supplements are ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3). Cholecalciferol, the D3 form of the vitamin, is the form of choice when supplementing with vitamin D. Types of D3 supplements include gel caps, liquid, powders, and tablets. Vitamin D is often measured in International Units (IU) or mcg. One mcg of cholecalciferol is equal to 40 IU of vitamin D.
The debate continues over the most effective forms of vitamin D acquisition; however, many health professionals agree that vitamin D supplementation, particularly in winter months, should be an integral part of our armamentarium of therapeutics for ethnic patients, and especially those who suffer from psoriasis and other autoimmune and inflammatory skin conditions.
Dr. Talakoub is in private practice in McLean, Va.
Do you have questions about treating patients with dark skin? If so, send them to [email protected].
Many clinicians are unaware that ethnic populations in North America do not achieve optimal serum 25-hydroxyvitamin D (abbreviated 25[OH]D) because of the increased pigmentation in their skin, which reduces vitamin D production. Vitamin D insufficiency is more prevalent among individuals with darker skin, compared with those with lighter skin at any time of year, even during the winter months. Contributing to the deficiency, the dietary intake of vitamin D intake among African Americans in particular is often below the recommended intakes in every age group after puberty. However, data have shown vitamin D protects against Sjögren’s syndrome, psoriasis, type 1 and type 2 diabetes, multiple sclerosis, and rheumatoid arthritis.
Vitamin D also may protect against cardiovascular disease through its anti-inflammatory effects and may reduce the risk for colorectal cancer, breast cancer, and prostate cancer by promoting cell differentiation and down-regulating hyperproliferative cell growth. Most of these conditions have been shown to be as prevalent, if not more prevalent, among blacks than whites.
While vitamin D can be obtained from sun exposure, this is not always a viable option. UV exposure is linked to skin cancer, which leads clinicians to encourage sun avoidance, but they may disregard the need for vitamin D. In addition, darker pigmentation of the skin reduces vitamin D synthesis in the skin.
How can you help your skin of color patients get enough vitamin D, especially in the winter? Nutritional sources of vitamin D include salmon, sardines, and cows’ milk; however, many individuals do not achieve optimal vitamin D status from food intake alone.
Since UV exposure and diet are not sufficient sources of vitamin D, supplementation has become crucial to our patients, particularly those with darker skin. Dietary reference intakes for vitamin D have been under considerable scrutiny, and many experts now believe that intakes of 25 mcg/d (1,000 IU) or more may be needed for most people to achieve optimal blood levels of 25(OH)D. The two forms of vitamin D used in dietary supplements are ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3). Cholecalciferol, the D3 form of the vitamin, is the form of choice when supplementing with vitamin D. Types of D3 supplements include gel caps, liquid, powders, and tablets. Vitamin D is often measured in International Units (IU) or mcg. One mcg of cholecalciferol is equal to 40 IU of vitamin D.
The debate continues over the most effective forms of vitamin D acquisition; however, many health professionals agree that vitamin D supplementation, particularly in winter months, should be an integral part of our armamentarium of therapeutics for ethnic patients, and especially those who suffer from psoriasis and other autoimmune and inflammatory skin conditions.
Dr. Talakoub is in private practice in McLean, Va.
Do you have questions about treating patients with dark skin? If so, send them to [email protected].
Cost and response criteria are the new challenges
Although the concept of using immunotherapy to target an immune response against tumors is not new, this treatment modality is only now beginning to realize its full potential. Here, we take a look at the role of immunotherapy in cancer and some of the most exciting areas of clinical development.
*Click on the link to the left for a PDF of the full article.
Although the concept of using immunotherapy to target an immune response against tumors is not new, this treatment modality is only now beginning to realize its full potential. Here, we take a look at the role of immunotherapy in cancer and some of the most exciting areas of clinical development.
*Click on the link to the left for a PDF of the full article.
Although the concept of using immunotherapy to target an immune response against tumors is not new, this treatment modality is only now beginning to realize its full potential. Here, we take a look at the role of immunotherapy in cancer and some of the most exciting areas of clinical development.
*Click on the link to the left for a PDF of the full article.
Key issues in the management of gastrointestinal immune-related adverse events associated with ipilimumab administration
Ipilimumab is an anticytotoxic T lymphocyte antigen-4 (CTLA-4) monoclonal antibody that attenuates negative signaling from CTLA-4 and potentiates T-cell activation and proliferation. Two phase 3 randomized trials in advanced melanoma demonstrated a significant improvement in overall survival, the first of which led to regulatory approval in the United States and Europe for treatment of unresectable or metastatic melanoma. Ipilimumab administration is associated with immune-related adverse events (irAEs). Gastrointestinal (GI) irAEs are among the most common and although they are typically mild to moderate in severity, if they are left unrecognized or untreated, they can become life-threatening. These toxicities can be managed effectively in almost all patients by using established guidelines that stress vigilance and the use of corticosteroids and other immunosuppressive agents when necessary. The goal of this review is to educate physicians on the recognition and challenges associated with management of GI irAEs.
*Click on the link to the left for a PDF of the full article.
Ipilimumab is an anticytotoxic T lymphocyte antigen-4 (CTLA-4) monoclonal antibody that attenuates negative signaling from CTLA-4 and potentiates T-cell activation and proliferation. Two phase 3 randomized trials in advanced melanoma demonstrated a significant improvement in overall survival, the first of which led to regulatory approval in the United States and Europe for treatment of unresectable or metastatic melanoma. Ipilimumab administration is associated with immune-related adverse events (irAEs). Gastrointestinal (GI) irAEs are among the most common and although they are typically mild to moderate in severity, if they are left unrecognized or untreated, they can become life-threatening. These toxicities can be managed effectively in almost all patients by using established guidelines that stress vigilance and the use of corticosteroids and other immunosuppressive agents when necessary. The goal of this review is to educate physicians on the recognition and challenges associated with management of GI irAEs.
*Click on the link to the left for a PDF of the full article.
Ipilimumab is an anticytotoxic T lymphocyte antigen-4 (CTLA-4) monoclonal antibody that attenuates negative signaling from CTLA-4 and potentiates T-cell activation and proliferation. Two phase 3 randomized trials in advanced melanoma demonstrated a significant improvement in overall survival, the first of which led to regulatory approval in the United States and Europe for treatment of unresectable or metastatic melanoma. Ipilimumab administration is associated with immune-related adverse events (irAEs). Gastrointestinal (GI) irAEs are among the most common and although they are typically mild to moderate in severity, if they are left unrecognized or untreated, they can become life-threatening. These toxicities can be managed effectively in almost all patients by using established guidelines that stress vigilance and the use of corticosteroids and other immunosuppressive agents when necessary. The goal of this review is to educate physicians on the recognition and challenges associated with management of GI irAEs.
*Click on the link to the left for a PDF of the full article.
Multimodality therapy for uterine serous carcinoma and the association with overall and relapse-free survival
Objective To identify prognostic factors for overall survival (OS) and relapse-free survival (RFS) for patients with uterine serous carcinoma.
Methods From January 1, 2000 to January 1, 2010, 44 patients with uterine serous carcinoma were analyzed to determine prognostic and predictive factors for OS and RFS using the Kaplan-Meier product-limit method and log-rank tests.
Results Median follow-up was 4.1 years, median OS was 4.2 years, 2-year OS was 83% and decreased to 48% at 5 years. Two-year RFS was 82% and decreased to 75% at 5 years. Age, stage, tumor size, tumor not arising from a polyp, parametrial involvement, lymphovascular invasion, and no adjuvant treatment were prognostic factors associated with shorter OS. Higher stage and parametrial involvement were prognostic factors associated with shorter RFS. Combined adjuvant chemotherapy and radiation therapy was significantly associated with longer OS rates.
Conclusions Adjuvant chemotherapy and radiation therapy as well as tumors arising from a polyp are associated with increased overall survival in patients with uterine serous carcinoma. Early-stage disease is associated with increased relapse-free and overall survival. Adjuvant chemotherapy with a platinum and paclitaxol-based regimen and radiation therapy should be attempted in patients with uterine serous carcinoma.
*To read the full article, click on the PDF icon at the top of this introduction.
Objective To identify prognostic factors for overall survival (OS) and relapse-free survival (RFS) for patients with uterine serous carcinoma.
Methods From January 1, 2000 to January 1, 2010, 44 patients with uterine serous carcinoma were analyzed to determine prognostic and predictive factors for OS and RFS using the Kaplan-Meier product-limit method and log-rank tests.
Results Median follow-up was 4.1 years, median OS was 4.2 years, 2-year OS was 83% and decreased to 48% at 5 years. Two-year RFS was 82% and decreased to 75% at 5 years. Age, stage, tumor size, tumor not arising from a polyp, parametrial involvement, lymphovascular invasion, and no adjuvant treatment were prognostic factors associated with shorter OS. Higher stage and parametrial involvement were prognostic factors associated with shorter RFS. Combined adjuvant chemotherapy and radiation therapy was significantly associated with longer OS rates.
Conclusions Adjuvant chemotherapy and radiation therapy as well as tumors arising from a polyp are associated with increased overall survival in patients with uterine serous carcinoma. Early-stage disease is associated with increased relapse-free and overall survival. Adjuvant chemotherapy with a platinum and paclitaxol-based regimen and radiation therapy should be attempted in patients with uterine serous carcinoma.
*To read the full article, click on the PDF icon at the top of this introduction.
Objective To identify prognostic factors for overall survival (OS) and relapse-free survival (RFS) for patients with uterine serous carcinoma.
Methods From January 1, 2000 to January 1, 2010, 44 patients with uterine serous carcinoma were analyzed to determine prognostic and predictive factors for OS and RFS using the Kaplan-Meier product-limit method and log-rank tests.
Results Median follow-up was 4.1 years, median OS was 4.2 years, 2-year OS was 83% and decreased to 48% at 5 years. Two-year RFS was 82% and decreased to 75% at 5 years. Age, stage, tumor size, tumor not arising from a polyp, parametrial involvement, lymphovascular invasion, and no adjuvant treatment were prognostic factors associated with shorter OS. Higher stage and parametrial involvement were prognostic factors associated with shorter RFS. Combined adjuvant chemotherapy and radiation therapy was significantly associated with longer OS rates.
Conclusions Adjuvant chemotherapy and radiation therapy as well as tumors arising from a polyp are associated with increased overall survival in patients with uterine serous carcinoma. Early-stage disease is associated with increased relapse-free and overall survival. Adjuvant chemotherapy with a platinum and paclitaxol-based regimen and radiation therapy should be attempted in patients with uterine serous carcinoma.
*To read the full article, click on the PDF icon at the top of this introduction.
Enzastaurin no better than placebo in DLBCL
Convention Center, site of the
2013 ASH Annual Meeting
NEW ORLEANS—In a phase 3 study, patients with diffuse large B-cell lymphoma (DLBCL) who received post-induction therapy with enzastaurin saw no improvements in survival over patients who received placebo.
All patients were in their first remission after treatment with R-CHOP, but they were thought to have a high risk of relapse.
The patients who received 3 years of treatment with enzastaurin had similar rates of event-free survival (EFS), disease-free survival (DFS), and overall survival (OS) as patients who received placebo.
Michael Crump, MD, of Princess Margaret Cancer Centre in Toronto, Canada, reported these results at the 2013 ASH Annual Meeting as abstract 371.
Dr Crump noted that enzastaurin is a potent and selective inhibitor of PKCβ, the major isoform expressed in normal and malignant B cells. The kinase is required for signaling through the B-cell receptor, is necessary for activation of NF-κB, and is involved in VEGF-mediated angiogenesis.
“It was a little more than 10 years ago that Margaret Shipp and her colleagues demonstrated that overexpression of PKCβ mRNA and protein was associated with relapsed and fatal diffuse large B-cell lymphoma,” Dr Crump said.
“Since that time, other investigators have also shown that overexpression of either protein or mRNA is associated with a worse outcome in patients receiving CHOP chemotherapy as well as R-CHOP. So [PKCβ] seems to be a rational therapeutic target.”
With this in mind, Dr Crump and his colleagues conducted the phase 3 PRELUDE trial, comparing enzastaurin to placebo in DLBCL patients.
Patient population
The researchers enrolled 866 patients who had a complete response, unconfirmed complete response, or negative FDG-PET scan following treatment with R-CHOP14 or R-CHOP21.
The team randomized 758 of the patients to receive placebo or oral enzastaurin at 500 mg once daily, with a 1125 mg loading dose on day 1. A total of 263 patients in the enzastaurin arm and 129 patients in the placebo arm completed 3 years of treatment.
The rates of discontinuation were similar between the arms—46.7% (n=230) in the enzastaurin arm and 48.2% (n=120) in the placebo arm. In both groups, the most common reason for discontinuation was disease progression (n=103 and 60, respectively). Adverse events were the second most common reason (n=72 and 28, respectively).
Baseline characteristics were similar between the 2 groups. The median age was 64, most patients were Caucasian, most had an ECOG performance status of 0, most had stage IV disease, and more than half of the patients in each arm were PET-negative (although about 40% of patients in each arm did not have a PET scan).
Survival outcomes
The 2-year OS rate was 87% in the enzastaurin arm and 89% in the placebo arm. The 4-year OS rates were 81% and 82%, respectively. And the hazard ratio was 1.04 (P=0.807).
The 2-year EFS rate was 78% in the enzastaurin arm and 73% in the placebo arm. The 4-year EFS rates were 69% and 70%, respectively. And the hazard ratio was 0.90 (P=0.460).
The 2-year DFS rate was 79% in the enzastaurin arm and 75% in the placebo arm. The 4-year DFS rates were 70% and 71%, respectively. And the hazard ratio was 0.92 (P=0.541).
The researchers also assessed DFS according to cell of origin. And they found no difference between patients who had germinal center B-cell (GCB) DLBCL and patients who did not.
Overall, the hazard ratio for GCB vs non-GCB DLBCL was 0.92 (P=0.74). In the enzastaurin arm, the hazard ratio was 0.77 (P=0.40). And in the placebo arm, the hazard ratio was 1.31 (P=0.54).
“One would anticipate a drug that interferes with B-cell receptor signaling might have benefitted patients with tumors that are not of germinal center origin,” Dr Crump said. “Altogether, however . . ., there was actually no difference in GCB vs non-GCB, in terms of outcome.”
“Perhaps [the patients] being in a complete response is one of the reasons why we don’t actually see a difference in outcomes,” he added. “These are all patients who’ve had very good responses to their primary treatment.”
Adverse events
Dr Crump said there were a number of adverse events that could be related to enzastaurin treatment.
Chromaturia occurred in 18.5% of patients in the enzastaurin arm and 0.4% of patients in the placebo arm (P<0.001). Prolonged QT interval was an issue in 10.8% and 3.6%, respectively; diarrhea occurred in 10.3% and 2.8%, respectively; and discolored feces arose in 7.7% and 0%, respectively (P<0.001 for all).
Other adverse events (occurring in 5% of patients or greater) included neutropenia, rash, fatigue, and nausea. But the rates of these events were similar between the treatment arms.
Dr Crump noted that these results are consistent with the established safety profile of enzastaurin when it’s used as a single agent in lymphoma and other cancers. ![]()
Convention Center, site of the
2013 ASH Annual Meeting
NEW ORLEANS—In a phase 3 study, patients with diffuse large B-cell lymphoma (DLBCL) who received post-induction therapy with enzastaurin saw no improvements in survival over patients who received placebo.
All patients were in their first remission after treatment with R-CHOP, but they were thought to have a high risk of relapse.
The patients who received 3 years of treatment with enzastaurin had similar rates of event-free survival (EFS), disease-free survival (DFS), and overall survival (OS) as patients who received placebo.
Michael Crump, MD, of Princess Margaret Cancer Centre in Toronto, Canada, reported these results at the 2013 ASH Annual Meeting as abstract 371.
Dr Crump noted that enzastaurin is a potent and selective inhibitor of PKCβ, the major isoform expressed in normal and malignant B cells. The kinase is required for signaling through the B-cell receptor, is necessary for activation of NF-κB, and is involved in VEGF-mediated angiogenesis.
“It was a little more than 10 years ago that Margaret Shipp and her colleagues demonstrated that overexpression of PKCβ mRNA and protein was associated with relapsed and fatal diffuse large B-cell lymphoma,” Dr Crump said.
“Since that time, other investigators have also shown that overexpression of either protein or mRNA is associated with a worse outcome in patients receiving CHOP chemotherapy as well as R-CHOP. So [PKCβ] seems to be a rational therapeutic target.”
With this in mind, Dr Crump and his colleagues conducted the phase 3 PRELUDE trial, comparing enzastaurin to placebo in DLBCL patients.
Patient population
The researchers enrolled 866 patients who had a complete response, unconfirmed complete response, or negative FDG-PET scan following treatment with R-CHOP14 or R-CHOP21.
The team randomized 758 of the patients to receive placebo or oral enzastaurin at 500 mg once daily, with a 1125 mg loading dose on day 1. A total of 263 patients in the enzastaurin arm and 129 patients in the placebo arm completed 3 years of treatment.
The rates of discontinuation were similar between the arms—46.7% (n=230) in the enzastaurin arm and 48.2% (n=120) in the placebo arm. In both groups, the most common reason for discontinuation was disease progression (n=103 and 60, respectively). Adverse events were the second most common reason (n=72 and 28, respectively).
Baseline characteristics were similar between the 2 groups. The median age was 64, most patients were Caucasian, most had an ECOG performance status of 0, most had stage IV disease, and more than half of the patients in each arm were PET-negative (although about 40% of patients in each arm did not have a PET scan).
Survival outcomes
The 2-year OS rate was 87% in the enzastaurin arm and 89% in the placebo arm. The 4-year OS rates were 81% and 82%, respectively. And the hazard ratio was 1.04 (P=0.807).
The 2-year EFS rate was 78% in the enzastaurin arm and 73% in the placebo arm. The 4-year EFS rates were 69% and 70%, respectively. And the hazard ratio was 0.90 (P=0.460).
The 2-year DFS rate was 79% in the enzastaurin arm and 75% in the placebo arm. The 4-year DFS rates were 70% and 71%, respectively. And the hazard ratio was 0.92 (P=0.541).
The researchers also assessed DFS according to cell of origin. And they found no difference between patients who had germinal center B-cell (GCB) DLBCL and patients who did not.
Overall, the hazard ratio for GCB vs non-GCB DLBCL was 0.92 (P=0.74). In the enzastaurin arm, the hazard ratio was 0.77 (P=0.40). And in the placebo arm, the hazard ratio was 1.31 (P=0.54).
“One would anticipate a drug that interferes with B-cell receptor signaling might have benefitted patients with tumors that are not of germinal center origin,” Dr Crump said. “Altogether, however . . ., there was actually no difference in GCB vs non-GCB, in terms of outcome.”
“Perhaps [the patients] being in a complete response is one of the reasons why we don’t actually see a difference in outcomes,” he added. “These are all patients who’ve had very good responses to their primary treatment.”
Adverse events
Dr Crump said there were a number of adverse events that could be related to enzastaurin treatment.
Chromaturia occurred in 18.5% of patients in the enzastaurin arm and 0.4% of patients in the placebo arm (P<0.001). Prolonged QT interval was an issue in 10.8% and 3.6%, respectively; diarrhea occurred in 10.3% and 2.8%, respectively; and discolored feces arose in 7.7% and 0%, respectively (P<0.001 for all).
Other adverse events (occurring in 5% of patients or greater) included neutropenia, rash, fatigue, and nausea. But the rates of these events were similar between the treatment arms.
Dr Crump noted that these results are consistent with the established safety profile of enzastaurin when it’s used as a single agent in lymphoma and other cancers. ![]()
Convention Center, site of the
2013 ASH Annual Meeting
NEW ORLEANS—In a phase 3 study, patients with diffuse large B-cell lymphoma (DLBCL) who received post-induction therapy with enzastaurin saw no improvements in survival over patients who received placebo.
All patients were in their first remission after treatment with R-CHOP, but they were thought to have a high risk of relapse.
The patients who received 3 years of treatment with enzastaurin had similar rates of event-free survival (EFS), disease-free survival (DFS), and overall survival (OS) as patients who received placebo.
Michael Crump, MD, of Princess Margaret Cancer Centre in Toronto, Canada, reported these results at the 2013 ASH Annual Meeting as abstract 371.
Dr Crump noted that enzastaurin is a potent and selective inhibitor of PKCβ, the major isoform expressed in normal and malignant B cells. The kinase is required for signaling through the B-cell receptor, is necessary for activation of NF-κB, and is involved in VEGF-mediated angiogenesis.
“It was a little more than 10 years ago that Margaret Shipp and her colleagues demonstrated that overexpression of PKCβ mRNA and protein was associated with relapsed and fatal diffuse large B-cell lymphoma,” Dr Crump said.
“Since that time, other investigators have also shown that overexpression of either protein or mRNA is associated with a worse outcome in patients receiving CHOP chemotherapy as well as R-CHOP. So [PKCβ] seems to be a rational therapeutic target.”
With this in mind, Dr Crump and his colleagues conducted the phase 3 PRELUDE trial, comparing enzastaurin to placebo in DLBCL patients.
Patient population
The researchers enrolled 866 patients who had a complete response, unconfirmed complete response, or negative FDG-PET scan following treatment with R-CHOP14 or R-CHOP21.
The team randomized 758 of the patients to receive placebo or oral enzastaurin at 500 mg once daily, with a 1125 mg loading dose on day 1. A total of 263 patients in the enzastaurin arm and 129 patients in the placebo arm completed 3 years of treatment.
The rates of discontinuation were similar between the arms—46.7% (n=230) in the enzastaurin arm and 48.2% (n=120) in the placebo arm. In both groups, the most common reason for discontinuation was disease progression (n=103 and 60, respectively). Adverse events were the second most common reason (n=72 and 28, respectively).
Baseline characteristics were similar between the 2 groups. The median age was 64, most patients were Caucasian, most had an ECOG performance status of 0, most had stage IV disease, and more than half of the patients in each arm were PET-negative (although about 40% of patients in each arm did not have a PET scan).
Survival outcomes
The 2-year OS rate was 87% in the enzastaurin arm and 89% in the placebo arm. The 4-year OS rates were 81% and 82%, respectively. And the hazard ratio was 1.04 (P=0.807).
The 2-year EFS rate was 78% in the enzastaurin arm and 73% in the placebo arm. The 4-year EFS rates were 69% and 70%, respectively. And the hazard ratio was 0.90 (P=0.460).
The 2-year DFS rate was 79% in the enzastaurin arm and 75% in the placebo arm. The 4-year DFS rates were 70% and 71%, respectively. And the hazard ratio was 0.92 (P=0.541).
The researchers also assessed DFS according to cell of origin. And they found no difference between patients who had germinal center B-cell (GCB) DLBCL and patients who did not.
Overall, the hazard ratio for GCB vs non-GCB DLBCL was 0.92 (P=0.74). In the enzastaurin arm, the hazard ratio was 0.77 (P=0.40). And in the placebo arm, the hazard ratio was 1.31 (P=0.54).
“One would anticipate a drug that interferes with B-cell receptor signaling might have benefitted patients with tumors that are not of germinal center origin,” Dr Crump said. “Altogether, however . . ., there was actually no difference in GCB vs non-GCB, in terms of outcome.”
“Perhaps [the patients] being in a complete response is one of the reasons why we don’t actually see a difference in outcomes,” he added. “These are all patients who’ve had very good responses to their primary treatment.”
Adverse events
Dr Crump said there were a number of adverse events that could be related to enzastaurin treatment.
Chromaturia occurred in 18.5% of patients in the enzastaurin arm and 0.4% of patients in the placebo arm (P<0.001). Prolonged QT interval was an issue in 10.8% and 3.6%, respectively; diarrhea occurred in 10.3% and 2.8%, respectively; and discolored feces arose in 7.7% and 0%, respectively (P<0.001 for all).
Other adverse events (occurring in 5% of patients or greater) included neutropenia, rash, fatigue, and nausea. But the rates of these events were similar between the treatment arms.
Dr Crump noted that these results are consistent with the established safety profile of enzastaurin when it’s used as a single agent in lymphoma and other cancers. ![]()