User login
New and Noteworthy Information—January 2014
The Bacille Calmette-Guérin (BCG) vaccine may benefit patients with clinically isolated syndrome (CIS), according to research published online ahead of print December 4, 2013, in Neurology. A total of 82 participants with CIS were randomized to BCG or placebo and monitored monthly with brain MRI for six months. All patients subsequently received IM interferon β-1a for 12 months. In an open-label extension phase, patients received disease-modifying therapies (DMTs) recommended by their neurologists. During the initial six months, the number of cumulative lesions was significantly lower among vaccinated subjects. The number of total T1-hypointense lesions was lower in the BCG group at months 6, 12, and 18. After 60 months, the probability of clinically definite multiple sclerosis was lower in the BCG plus DMT arm, and more vaccinated people remained DMT-free.
Exercise programs may significantly improve the ability of people with dementia to perform activities of daily living, according to a study published online ahead of print December 4, 2013, in the Cochrane Library. Exercise also may improve cognition in these patients, but may not affect depression. Investigators reviewed randomized controlled trials in which older people diagnosed with dementia were allocated to exercise programs or to control groups, which received standard care or social contact. Sixteen trials with 937 participants met the inclusion criteria. The trials were highly heterogeneous in terms of subtype and severity of participants’ dementia, and type, duration, and frequency of exercise. The researchers found that informal caregivers’ burden may be reduced when the family member with dementia participates in an exercise program.
Thrombin activity may enable neurologists to detect multiple sclerosis (MS) before clinical signs of the disease are present, according to research published online ahead of print November 29, 2013, in Annals of Neurology. Using a novel molecular probe, investigators characterized the activity pattern of thrombin, the central protease of the coagulation cascade, in experimental autoimmune encephalomyelitis. Thrombin activity preceded the onset of neurologic signs; increased at disease peak; and correlated with fibrin deposition, microglial activation, demyelination, axonal damage, and clinical severity. Mice with a genetic deficit in prothrombin confirmed the specificity of the thrombin probe. Scientists may be able to use thrombin activity to develop sensitive probes for the preclinical detection and monitoring of neuroinflammation and MS progression, according to the investigators.
An athlete with concussion symptoms should not be allowed to return to play on the same day, according to the latest consensus statement on sports-related concussion, which was summarized in the December 2013 issue of Neurosurgery. The Concussion in Sport Group (CISG 4) based its recommendations on the advice of an expert panel that was sponsored by five international sports governing bodies. Between 80% and 90% of concussions resolve within seven to 10 days, but recovery may take longer in children and adolescents, according to the consensus statement. The updated statement emphasizes the distinction between concussion and mild traumatic brain injury. The CISG 4 suggests that patients with concussion have normal findings on brain neuroimaging studies (eg, CT scan), but those with traumatic brain injury have abnormal imaging findings.
Vitamin D may prevent multiple sclerosis (MS) by blocking T helper (TH) cells from migrating into the CNS, according to research published online ahead of print December 9, 2013, in Proceedings of the National Academy of Sciences. Investigators administered 1,25-dihydroxyvitamin D3 [1,25(OH)2D3], the bioactive form of vitamin D, to animals with experimental autoimmune encephalomyelitis, a mouse model of MS. Myelin-reactive TH cells were generated in the presence of 1,25(OH)2D3, secreted proinflammatory cytokines, and did not preferentially differentiate into suppressor T cells. The cells left the lymph node, entered the peripheral circulation, and migrated to the immunization sites. TH cells from 1,25(OH)2D3-treated mice were unable to enter the CNS parenchyma, however. Instead, the cells were maintained in the periphery. The mice developed experimental autoimmune encephalomyelitis when treatment ceased.
Among people with type 2 diabetes, dementia incidence may be highest among Native Americans and African Americans and lowest among Asians, according to a study published online ahead of print November 22, 2013, in Diabetes Care. Scientists identified 22,171 patients age 60 or older with diabetes and without preexisting dementia in the Kaiser Permanente Northern California Diabetes Registry. The investigators abstracted prevalent medical history and dementia incidence from medical records and calculated age-adjusted incidence densities. Dementia was diagnosed in 17.1% of patients. Age-adjusted dementia incidence densities were 34/1,000 person-years among Native Americans, 27/1,000 person-years among African Americans, and 19/1,000 person-years among Asians. Hazard ratios (relative to Asians) were 1.64 for Native Americans, 1.44 for African Americans, 1.30 for non-Hispanic whites, and 1.19 for Latinos.
Veterans with blast injuries have changes in brain tissue that may be apparent on imaging years later, according to data presented at the 99th Annual Meeting of the Radiological Society of North America. Researchers compared diffusion tensor imaging (DTI)-derived fractional anisotropy (FA) values in 10 veterans of Operations Iraqi Freedom and Enduring Freedom who had been diagnosed with mild traumatic brain injury with those of 10 healthy controls. The average time elapsed between the blast-induced injury and DTI scan among the patients was 51.3 months. FA values were significantly different between the two groups, and the researchers found significant correlations between FA values and attention, delayed memory, and psychomotor test scores. The results suggest that blast injury may have a long-term impact on the brain.
Among college athletes, head impact exposure may be related to white matter diffusion measures and cognition during the course of one playing season, even in the absence of diagnosed concussion, according to data published online ahead of print December 11, 2013, in Neurology. Researchers prospectively studied 79 noncontact sport athletes and 80 nonconcussed varsity football and ice hockey players who wore helmets that recorded the acceleration-time history of the head following impact. Mean diffusivity (MD) in the corpus callosum was significantly different between groups. Measures of head impact exposure correlated with white matter diffusivity measures in the corpus callosum, amygdala, cerebellar white matter, hippocampus, and thalamus. The magnitude of change in corpus callosum MD postseason was associated with poorer performance on a measure of verbal learning and memory.
Among veterans, traumatic brain injury (TBI) during the most recent deployment is the strongest predictor of postdeployment symptoms of post-traumatic stress disorder (PTSD), even when accounting for predeployment symptoms, prior TBI, and combat intensity, according to research published online ahead of print December 11, 2013, in JAMA Psychiatry. A total of 1,648 active-duty Marine and Navy servicemen underwent clinical interviews and completed self-assessments approximately one month before a seven-month deployment and three to six months after deployment. At the predeployment assessment, 56.8% of participants reported prior TBI. At postdeployment assessment, 19.8% reported sustaining TBI between predeployment and postdeployment assessments. Probability of PTSD was highest for participants with severe predeployment symptoms, high combat intensity, and deployment-related TBI. TBI doubled the PTSD rates for participants with less severe predeployment PTSD symptoms.
Fidgetin inhibition could promote tissue regeneration and repair the broken cell connections that occur in spinal cord injury and other conditions, according to research presented at the 2013 Annual Meeting of the American Society for Cell Biology. Fidgetin prunes unstable microtubule scaffolding in cells, as well as unneeded connections in the neuronal network as the latter grows. Researchers used a novel nanoparticle technology to block fidgetin in the injured nerves of adult rats. The nanoparticles were infused with small interfering RNA that bound the messenger RNA (mRNA) transcribed from the fidgetin gene. The mRNA for fidgetin was not translated, and the cell did not produce fidgetin. Blocking fidgetin restarted tissue growth in the animals. The technique could benefit patients with myocardial infarction or chronic cutaneous wounds.
Deep brain stimulation may improve driving ability for people with Parkinson’s disease, according to a study published online ahead of print December 18, 2013, in Neurology. Investigators studied 23 people who had deep brain stimulators, 21 people with Parkinson’s disease without stimulators, and 21 healthy individuals. Participants were tested with a driving simulator. Individuals with stimulators completed the test once with the stimulator on, once with it off, and once with the stimulator off after receiving levodopa. People with Parkinson’s disease without stimulators performed worse than controls in almost every category. People with stimulators did not perform significantly worse than the controls. Participants with stimulators had an average of 3.8 slight driving errors on the test, compared with 7.5 for the controls and 11.4 for people with Parkinson’s disease without stimulators.
Gadolinium-based contrast medium (Gd-CM) may be associated with abnormalities on brain MRI, according to research published online ahead of print December 17, 2013, in Radiology. Researchers compared unenhanced T1-weighted MR images of 19 patients who had undergone six or more contrast-enhanced brain scans with images of 16 people who had received six or fewer unenhanced scans. The hyperintensity of the dentate nucleus and globus pallidus correlated with the number of Gd-CM administrations. Hyperintensity in the dentate nucleus and globus pallidus on unenhanced MRI may be a consequence of the number of previous Gd-CM administrations, according to the researchers. Because gadolinium has a high signal intensity in the body, the data suggest that the toxic gadolinium component remains in the body in patients with normal renal function.
—Erik Greb
The Bacille Calmette-Guérin (BCG) vaccine may benefit patients with clinically isolated syndrome (CIS), according to research published online ahead of print December 4, 2013, in Neurology. A total of 82 participants with CIS were randomized to BCG or placebo and monitored monthly with brain MRI for six months. All patients subsequently received IM interferon β-1a for 12 months. In an open-label extension phase, patients received disease-modifying therapies (DMTs) recommended by their neurologists. During the initial six months, the number of cumulative lesions was significantly lower among vaccinated subjects. The number of total T1-hypointense lesions was lower in the BCG group at months 6, 12, and 18. After 60 months, the probability of clinically definite multiple sclerosis was lower in the BCG plus DMT arm, and more vaccinated people remained DMT-free.
Exercise programs may significantly improve the ability of people with dementia to perform activities of daily living, according to a study published online ahead of print December 4, 2013, in the Cochrane Library. Exercise also may improve cognition in these patients, but may not affect depression. Investigators reviewed randomized controlled trials in which older people diagnosed with dementia were allocated to exercise programs or to control groups, which received standard care or social contact. Sixteen trials with 937 participants met the inclusion criteria. The trials were highly heterogeneous in terms of subtype and severity of participants’ dementia, and type, duration, and frequency of exercise. The researchers found that informal caregivers’ burden may be reduced when the family member with dementia participates in an exercise program.
Thrombin activity may enable neurologists to detect multiple sclerosis (MS) before clinical signs of the disease are present, according to research published online ahead of print November 29, 2013, in Annals of Neurology. Using a novel molecular probe, investigators characterized the activity pattern of thrombin, the central protease of the coagulation cascade, in experimental autoimmune encephalomyelitis. Thrombin activity preceded the onset of neurologic signs; increased at disease peak; and correlated with fibrin deposition, microglial activation, demyelination, axonal damage, and clinical severity. Mice with a genetic deficit in prothrombin confirmed the specificity of the thrombin probe. Scientists may be able to use thrombin activity to develop sensitive probes for the preclinical detection and monitoring of neuroinflammation and MS progression, according to the investigators.
An athlete with concussion symptoms should not be allowed to return to play on the same day, according to the latest consensus statement on sports-related concussion, which was summarized in the December 2013 issue of Neurosurgery. The Concussion in Sport Group (CISG 4) based its recommendations on the advice of an expert panel that was sponsored by five international sports governing bodies. Between 80% and 90% of concussions resolve within seven to 10 days, but recovery may take longer in children and adolescents, according to the consensus statement. The updated statement emphasizes the distinction between concussion and mild traumatic brain injury. The CISG 4 suggests that patients with concussion have normal findings on brain neuroimaging studies (eg, CT scan), but those with traumatic brain injury have abnormal imaging findings.
Vitamin D may prevent multiple sclerosis (MS) by blocking T helper (TH) cells from migrating into the CNS, according to research published online ahead of print December 9, 2013, in Proceedings of the National Academy of Sciences. Investigators administered 1,25-dihydroxyvitamin D3 [1,25(OH)2D3], the bioactive form of vitamin D, to animals with experimental autoimmune encephalomyelitis, a mouse model of MS. Myelin-reactive TH cells were generated in the presence of 1,25(OH)2D3, secreted proinflammatory cytokines, and did not preferentially differentiate into suppressor T cells. The cells left the lymph node, entered the peripheral circulation, and migrated to the immunization sites. TH cells from 1,25(OH)2D3-treated mice were unable to enter the CNS parenchyma, however. Instead, the cells were maintained in the periphery. The mice developed experimental autoimmune encephalomyelitis when treatment ceased.
Among people with type 2 diabetes, dementia incidence may be highest among Native Americans and African Americans and lowest among Asians, according to a study published online ahead of print November 22, 2013, in Diabetes Care. Scientists identified 22,171 patients age 60 or older with diabetes and without preexisting dementia in the Kaiser Permanente Northern California Diabetes Registry. The investigators abstracted prevalent medical history and dementia incidence from medical records and calculated age-adjusted incidence densities. Dementia was diagnosed in 17.1% of patients. Age-adjusted dementia incidence densities were 34/1,000 person-years among Native Americans, 27/1,000 person-years among African Americans, and 19/1,000 person-years among Asians. Hazard ratios (relative to Asians) were 1.64 for Native Americans, 1.44 for African Americans, 1.30 for non-Hispanic whites, and 1.19 for Latinos.
Veterans with blast injuries have changes in brain tissue that may be apparent on imaging years later, according to data presented at the 99th Annual Meeting of the Radiological Society of North America. Researchers compared diffusion tensor imaging (DTI)-derived fractional anisotropy (FA) values in 10 veterans of Operations Iraqi Freedom and Enduring Freedom who had been diagnosed with mild traumatic brain injury with those of 10 healthy controls. The average time elapsed between the blast-induced injury and DTI scan among the patients was 51.3 months. FA values were significantly different between the two groups, and the researchers found significant correlations between FA values and attention, delayed memory, and psychomotor test scores. The results suggest that blast injury may have a long-term impact on the brain.
Among college athletes, head impact exposure may be related to white matter diffusion measures and cognition during the course of one playing season, even in the absence of diagnosed concussion, according to data published online ahead of print December 11, 2013, in Neurology. Researchers prospectively studied 79 noncontact sport athletes and 80 nonconcussed varsity football and ice hockey players who wore helmets that recorded the acceleration-time history of the head following impact. Mean diffusivity (MD) in the corpus callosum was significantly different between groups. Measures of head impact exposure correlated with white matter diffusivity measures in the corpus callosum, amygdala, cerebellar white matter, hippocampus, and thalamus. The magnitude of change in corpus callosum MD postseason was associated with poorer performance on a measure of verbal learning and memory.
Among veterans, traumatic brain injury (TBI) during the most recent deployment is the strongest predictor of postdeployment symptoms of post-traumatic stress disorder (PTSD), even when accounting for predeployment symptoms, prior TBI, and combat intensity, according to research published online ahead of print December 11, 2013, in JAMA Psychiatry. A total of 1,648 active-duty Marine and Navy servicemen underwent clinical interviews and completed self-assessments approximately one month before a seven-month deployment and three to six months after deployment. At the predeployment assessment, 56.8% of participants reported prior TBI. At postdeployment assessment, 19.8% reported sustaining TBI between predeployment and postdeployment assessments. Probability of PTSD was highest for participants with severe predeployment symptoms, high combat intensity, and deployment-related TBI. TBI doubled the PTSD rates for participants with less severe predeployment PTSD symptoms.
Fidgetin inhibition could promote tissue regeneration and repair the broken cell connections that occur in spinal cord injury and other conditions, according to research presented at the 2013 Annual Meeting of the American Society for Cell Biology. Fidgetin prunes unstable microtubule scaffolding in cells, as well as unneeded connections in the neuronal network as the latter grows. Researchers used a novel nanoparticle technology to block fidgetin in the injured nerves of adult rats. The nanoparticles were infused with small interfering RNA that bound the messenger RNA (mRNA) transcribed from the fidgetin gene. The mRNA for fidgetin was not translated, and the cell did not produce fidgetin. Blocking fidgetin restarted tissue growth in the animals. The technique could benefit patients with myocardial infarction or chronic cutaneous wounds.
Deep brain stimulation may improve driving ability for people with Parkinson’s disease, according to a study published online ahead of print December 18, 2013, in Neurology. Investigators studied 23 people who had deep brain stimulators, 21 people with Parkinson’s disease without stimulators, and 21 healthy individuals. Participants were tested with a driving simulator. Individuals with stimulators completed the test once with the stimulator on, once with it off, and once with the stimulator off after receiving levodopa. People with Parkinson’s disease without stimulators performed worse than controls in almost every category. People with stimulators did not perform significantly worse than the controls. Participants with stimulators had an average of 3.8 slight driving errors on the test, compared with 7.5 for the controls and 11.4 for people with Parkinson’s disease without stimulators.
Gadolinium-based contrast medium (Gd-CM) may be associated with abnormalities on brain MRI, according to research published online ahead of print December 17, 2013, in Radiology. Researchers compared unenhanced T1-weighted MR images of 19 patients who had undergone six or more contrast-enhanced brain scans with images of 16 people who had received six or fewer unenhanced scans. The hyperintensity of the dentate nucleus and globus pallidus correlated with the number of Gd-CM administrations. Hyperintensity in the dentate nucleus and globus pallidus on unenhanced MRI may be a consequence of the number of previous Gd-CM administrations, according to the researchers. Because gadolinium has a high signal intensity in the body, the data suggest that the toxic gadolinium component remains in the body in patients with normal renal function.
—Erik Greb
The Bacille Calmette-Guérin (BCG) vaccine may benefit patients with clinically isolated syndrome (CIS), according to research published online ahead of print December 4, 2013, in Neurology. A total of 82 participants with CIS were randomized to BCG or placebo and monitored monthly with brain MRI for six months. All patients subsequently received IM interferon β-1a for 12 months. In an open-label extension phase, patients received disease-modifying therapies (DMTs) recommended by their neurologists. During the initial six months, the number of cumulative lesions was significantly lower among vaccinated subjects. The number of total T1-hypointense lesions was lower in the BCG group at months 6, 12, and 18. After 60 months, the probability of clinically definite multiple sclerosis was lower in the BCG plus DMT arm, and more vaccinated people remained DMT-free.
Exercise programs may significantly improve the ability of people with dementia to perform activities of daily living, according to a study published online ahead of print December 4, 2013, in the Cochrane Library. Exercise also may improve cognition in these patients, but may not affect depression. Investigators reviewed randomized controlled trials in which older people diagnosed with dementia were allocated to exercise programs or to control groups, which received standard care or social contact. Sixteen trials with 937 participants met the inclusion criteria. The trials were highly heterogeneous in terms of subtype and severity of participants’ dementia, and type, duration, and frequency of exercise. The researchers found that informal caregivers’ burden may be reduced when the family member with dementia participates in an exercise program.
Thrombin activity may enable neurologists to detect multiple sclerosis (MS) before clinical signs of the disease are present, according to research published online ahead of print November 29, 2013, in Annals of Neurology. Using a novel molecular probe, investigators characterized the activity pattern of thrombin, the central protease of the coagulation cascade, in experimental autoimmune encephalomyelitis. Thrombin activity preceded the onset of neurologic signs; increased at disease peak; and correlated with fibrin deposition, microglial activation, demyelination, axonal damage, and clinical severity. Mice with a genetic deficit in prothrombin confirmed the specificity of the thrombin probe. Scientists may be able to use thrombin activity to develop sensitive probes for the preclinical detection and monitoring of neuroinflammation and MS progression, according to the investigators.
An athlete with concussion symptoms should not be allowed to return to play on the same day, according to the latest consensus statement on sports-related concussion, which was summarized in the December 2013 issue of Neurosurgery. The Concussion in Sport Group (CISG 4) based its recommendations on the advice of an expert panel that was sponsored by five international sports governing bodies. Between 80% and 90% of concussions resolve within seven to 10 days, but recovery may take longer in children and adolescents, according to the consensus statement. The updated statement emphasizes the distinction between concussion and mild traumatic brain injury. The CISG 4 suggests that patients with concussion have normal findings on brain neuroimaging studies (eg, CT scan), but those with traumatic brain injury have abnormal imaging findings.
Vitamin D may prevent multiple sclerosis (MS) by blocking T helper (TH) cells from migrating into the CNS, according to research published online ahead of print December 9, 2013, in Proceedings of the National Academy of Sciences. Investigators administered 1,25-dihydroxyvitamin D3 [1,25(OH)2D3], the bioactive form of vitamin D, to animals with experimental autoimmune encephalomyelitis, a mouse model of MS. Myelin-reactive TH cells were generated in the presence of 1,25(OH)2D3, secreted proinflammatory cytokines, and did not preferentially differentiate into suppressor T cells. The cells left the lymph node, entered the peripheral circulation, and migrated to the immunization sites. TH cells from 1,25(OH)2D3-treated mice were unable to enter the CNS parenchyma, however. Instead, the cells were maintained in the periphery. The mice developed experimental autoimmune encephalomyelitis when treatment ceased.
Among people with type 2 diabetes, dementia incidence may be highest among Native Americans and African Americans and lowest among Asians, according to a study published online ahead of print November 22, 2013, in Diabetes Care. Scientists identified 22,171 patients age 60 or older with diabetes and without preexisting dementia in the Kaiser Permanente Northern California Diabetes Registry. The investigators abstracted prevalent medical history and dementia incidence from medical records and calculated age-adjusted incidence densities. Dementia was diagnosed in 17.1% of patients. Age-adjusted dementia incidence densities were 34/1,000 person-years among Native Americans, 27/1,000 person-years among African Americans, and 19/1,000 person-years among Asians. Hazard ratios (relative to Asians) were 1.64 for Native Americans, 1.44 for African Americans, 1.30 for non-Hispanic whites, and 1.19 for Latinos.
Veterans with blast injuries have changes in brain tissue that may be apparent on imaging years later, according to data presented at the 99th Annual Meeting of the Radiological Society of North America. Researchers compared diffusion tensor imaging (DTI)-derived fractional anisotropy (FA) values in 10 veterans of Operations Iraqi Freedom and Enduring Freedom who had been diagnosed with mild traumatic brain injury with those of 10 healthy controls. The average time elapsed between the blast-induced injury and DTI scan among the patients was 51.3 months. FA values were significantly different between the two groups, and the researchers found significant correlations between FA values and attention, delayed memory, and psychomotor test scores. The results suggest that blast injury may have a long-term impact on the brain.
Among college athletes, head impact exposure may be related to white matter diffusion measures and cognition during the course of one playing season, even in the absence of diagnosed concussion, according to data published online ahead of print December 11, 2013, in Neurology. Researchers prospectively studied 79 noncontact sport athletes and 80 nonconcussed varsity football and ice hockey players who wore helmets that recorded the acceleration-time history of the head following impact. Mean diffusivity (MD) in the corpus callosum was significantly different between groups. Measures of head impact exposure correlated with white matter diffusivity measures in the corpus callosum, amygdala, cerebellar white matter, hippocampus, and thalamus. The magnitude of change in corpus callosum MD postseason was associated with poorer performance on a measure of verbal learning and memory.
Among veterans, traumatic brain injury (TBI) during the most recent deployment is the strongest predictor of postdeployment symptoms of post-traumatic stress disorder (PTSD), even when accounting for predeployment symptoms, prior TBI, and combat intensity, according to research published online ahead of print December 11, 2013, in JAMA Psychiatry. A total of 1,648 active-duty Marine and Navy servicemen underwent clinical interviews and completed self-assessments approximately one month before a seven-month deployment and three to six months after deployment. At the predeployment assessment, 56.8% of participants reported prior TBI. At postdeployment assessment, 19.8% reported sustaining TBI between predeployment and postdeployment assessments. Probability of PTSD was highest for participants with severe predeployment symptoms, high combat intensity, and deployment-related TBI. TBI doubled the PTSD rates for participants with less severe predeployment PTSD symptoms.
Fidgetin inhibition could promote tissue regeneration and repair the broken cell connections that occur in spinal cord injury and other conditions, according to research presented at the 2013 Annual Meeting of the American Society for Cell Biology. Fidgetin prunes unstable microtubule scaffolding in cells, as well as unneeded connections in the neuronal network as the latter grows. Researchers used a novel nanoparticle technology to block fidgetin in the injured nerves of adult rats. The nanoparticles were infused with small interfering RNA that bound the messenger RNA (mRNA) transcribed from the fidgetin gene. The mRNA for fidgetin was not translated, and the cell did not produce fidgetin. Blocking fidgetin restarted tissue growth in the animals. The technique could benefit patients with myocardial infarction or chronic cutaneous wounds.
Deep brain stimulation may improve driving ability for people with Parkinson’s disease, according to a study published online ahead of print December 18, 2013, in Neurology. Investigators studied 23 people who had deep brain stimulators, 21 people with Parkinson’s disease without stimulators, and 21 healthy individuals. Participants were tested with a driving simulator. Individuals with stimulators completed the test once with the stimulator on, once with it off, and once with the stimulator off after receiving levodopa. People with Parkinson’s disease without stimulators performed worse than controls in almost every category. People with stimulators did not perform significantly worse than the controls. Participants with stimulators had an average of 3.8 slight driving errors on the test, compared with 7.5 for the controls and 11.4 for people with Parkinson’s disease without stimulators.
Gadolinium-based contrast medium (Gd-CM) may be associated with abnormalities on brain MRI, according to research published online ahead of print December 17, 2013, in Radiology. Researchers compared unenhanced T1-weighted MR images of 19 patients who had undergone six or more contrast-enhanced brain scans with images of 16 people who had received six or fewer unenhanced scans. The hyperintensity of the dentate nucleus and globus pallidus correlated with the number of Gd-CM administrations. Hyperintensity in the dentate nucleus and globus pallidus on unenhanced MRI may be a consequence of the number of previous Gd-CM administrations, according to the researchers. Because gadolinium has a high signal intensity in the body, the data suggest that the toxic gadolinium component remains in the body in patients with normal renal function.
—Erik Greb
Ponatinib may be returning to market with new safety measures
The leukemia drug ponatinib is expected to return to market once the drug’s manufacturer has implemented measures to address the recently discovered safety risks.
The US Food and Drug Administration (FDA) is requiring that a number of safety measures be adopted, including changes to ponatinib’s label to narrow the drug’s indication and the addition of warnings about the increased risk of thrombosis and venous occlusion associated with ponatinib use.
In addition, dosing and administration recommendations must be revised, the patient medication guide must be updated, a risk evaluation and mitigation strategy (REMS) must be implemented, and postmarket investigations must be conducted to further characterize the drug’s safety and dosing.
Ponatinib was approved by the FDA in December 2012 to treat adults with chronic myeloid leukemia (CML) or Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) that is resistant to or intolerant of other tyrosine kinase inhibitors (TKIs).
But in October 2013, follow-up results of the phase 2 PACE trial suggested ponatinib can increase a patient’s risk of arterial and venous thrombotic events. So all trials of the drug were placed on partial clinical hold, with the exception of the phase 3 EPIC trial, which was discontinued.
Then, the FDA suspended sales and marketing of ponatinib, pending results of a safety evaluation. Now, the agency has decided ponatinib can return to the market if the new safety measures are implemented.
Safety measures in detail
The FDA is requiring that ponatinib use be restricted to:
- Adults with T315I-positive CML (chronic phase, accelerated phase, or blast phase)
- Adults with T315I-positive Ph+ ALL
- Adults with CML (chronic phase, accelerated phase, or blast phase) who cannot receive another TKI
- Adults with Ph+ ALL who cannot receive another TKI.
The Warnings and Precautions section of the drug’s label must be revised to include a description of the arterial and venous thrombosis and occlusions that have occurred in at least 27%—more than 1 in every 4—of patients treated with ponatinib.
The Dosage and Administration recommendations must be revised to state that the optimal dose of ponatinib has not been identified. The recommended starting dose remains 45 mg administered orally once daily, with or without food.
The patient Medication Guide must be revised to include additional safety information consistent with the safety information in the revised drug label.
The ponatinib REMS must inform prescribers about the approved indications for use and the serious risk of vascular occlusion and thromboembolism associated with the drug. The REMS must include the following:
- REMS letter to healthcare professionals who are known or likely to prescribe ponatinib
- REMS letter for professional societies to be distributed to their members
- REMS fact sheet for healthcare professionals
- Public statement to be published quarterly for 1 year in several professional journals
- Information to be prominently displayed at scientific meetings
- Ponatinib REMS website to provide access to all REMS materials for the duration of the REMS.
And postmarket investigations must further evaluate the dose selection, drug exposure, treatment response, and toxicity of ponatinib.
For more information, see the FDA’s safety communication. ![]()
The leukemia drug ponatinib is expected to return to market once the drug’s manufacturer has implemented measures to address the recently discovered safety risks.
The US Food and Drug Administration (FDA) is requiring that a number of safety measures be adopted, including changes to ponatinib’s label to narrow the drug’s indication and the addition of warnings about the increased risk of thrombosis and venous occlusion associated with ponatinib use.
In addition, dosing and administration recommendations must be revised, the patient medication guide must be updated, a risk evaluation and mitigation strategy (REMS) must be implemented, and postmarket investigations must be conducted to further characterize the drug’s safety and dosing.
Ponatinib was approved by the FDA in December 2012 to treat adults with chronic myeloid leukemia (CML) or Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) that is resistant to or intolerant of other tyrosine kinase inhibitors (TKIs).
But in October 2013, follow-up results of the phase 2 PACE trial suggested ponatinib can increase a patient’s risk of arterial and venous thrombotic events. So all trials of the drug were placed on partial clinical hold, with the exception of the phase 3 EPIC trial, which was discontinued.
Then, the FDA suspended sales and marketing of ponatinib, pending results of a safety evaluation. Now, the agency has decided ponatinib can return to the market if the new safety measures are implemented.
Safety measures in detail
The FDA is requiring that ponatinib use be restricted to:
- Adults with T315I-positive CML (chronic phase, accelerated phase, or blast phase)
- Adults with T315I-positive Ph+ ALL
- Adults with CML (chronic phase, accelerated phase, or blast phase) who cannot receive another TKI
- Adults with Ph+ ALL who cannot receive another TKI.
The Warnings and Precautions section of the drug’s label must be revised to include a description of the arterial and venous thrombosis and occlusions that have occurred in at least 27%—more than 1 in every 4—of patients treated with ponatinib.
The Dosage and Administration recommendations must be revised to state that the optimal dose of ponatinib has not been identified. The recommended starting dose remains 45 mg administered orally once daily, with or without food.
The patient Medication Guide must be revised to include additional safety information consistent with the safety information in the revised drug label.
The ponatinib REMS must inform prescribers about the approved indications for use and the serious risk of vascular occlusion and thromboembolism associated with the drug. The REMS must include the following:
- REMS letter to healthcare professionals who are known or likely to prescribe ponatinib
- REMS letter for professional societies to be distributed to their members
- REMS fact sheet for healthcare professionals
- Public statement to be published quarterly for 1 year in several professional journals
- Information to be prominently displayed at scientific meetings
- Ponatinib REMS website to provide access to all REMS materials for the duration of the REMS.
And postmarket investigations must further evaluate the dose selection, drug exposure, treatment response, and toxicity of ponatinib.
For more information, see the FDA’s safety communication. ![]()
The leukemia drug ponatinib is expected to return to market once the drug’s manufacturer has implemented measures to address the recently discovered safety risks.
The US Food and Drug Administration (FDA) is requiring that a number of safety measures be adopted, including changes to ponatinib’s label to narrow the drug’s indication and the addition of warnings about the increased risk of thrombosis and venous occlusion associated with ponatinib use.
In addition, dosing and administration recommendations must be revised, the patient medication guide must be updated, a risk evaluation and mitigation strategy (REMS) must be implemented, and postmarket investigations must be conducted to further characterize the drug’s safety and dosing.
Ponatinib was approved by the FDA in December 2012 to treat adults with chronic myeloid leukemia (CML) or Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL) that is resistant to or intolerant of other tyrosine kinase inhibitors (TKIs).
But in October 2013, follow-up results of the phase 2 PACE trial suggested ponatinib can increase a patient’s risk of arterial and venous thrombotic events. So all trials of the drug were placed on partial clinical hold, with the exception of the phase 3 EPIC trial, which was discontinued.
Then, the FDA suspended sales and marketing of ponatinib, pending results of a safety evaluation. Now, the agency has decided ponatinib can return to the market if the new safety measures are implemented.
Safety measures in detail
The FDA is requiring that ponatinib use be restricted to:
- Adults with T315I-positive CML (chronic phase, accelerated phase, or blast phase)
- Adults with T315I-positive Ph+ ALL
- Adults with CML (chronic phase, accelerated phase, or blast phase) who cannot receive another TKI
- Adults with Ph+ ALL who cannot receive another TKI.
The Warnings and Precautions section of the drug’s label must be revised to include a description of the arterial and venous thrombosis and occlusions that have occurred in at least 27%—more than 1 in every 4—of patients treated with ponatinib.
The Dosage and Administration recommendations must be revised to state that the optimal dose of ponatinib has not been identified. The recommended starting dose remains 45 mg administered orally once daily, with or without food.
The patient Medication Guide must be revised to include additional safety information consistent with the safety information in the revised drug label.
The ponatinib REMS must inform prescribers about the approved indications for use and the serious risk of vascular occlusion and thromboembolism associated with the drug. The REMS must include the following:
- REMS letter to healthcare professionals who are known or likely to prescribe ponatinib
- REMS letter for professional societies to be distributed to their members
- REMS fact sheet for healthcare professionals
- Public statement to be published quarterly for 1 year in several professional journals
- Information to be prominently displayed at scientific meetings
- Ponatinib REMS website to provide access to all REMS materials for the duration of the REMS.
And postmarket investigations must further evaluate the dose selection, drug exposure, treatment response, and toxicity of ponatinib.
For more information, see the FDA’s safety communication. ![]()
Emerging therapies for melanoma
Metastatic melanoma is a highly challenging cancer to treat. Like other solid tumors, it is a very heterogeneous disease both clinically and biologically. Consequently, the first decision point in its management is to assess the severity of an individual patient’s disease. This can be done based on the patient’s symptoms and how they have evolved over the preceding 1-2 months, performance status, the extent of disease as determined by physical examination, and staging workup, which should include either computed tomography scans of the body or a positron emission tomography/CT study as well as a brain magnetic resonance imaging scan. Patients with brain metastases as a subset (which is sizable – 20%-25% have brain metastases) require special attention because they may not respond to systemic therapies and will thus have to be managed with brain-targeted treatment options. Tumor testing for BRAF mutations is necessary in all patients with metastatic melanoma because the BRAF inhibitors (vemurafenib or dabrafenib) are a preferred choice of targeted therapy for this subset of patients, which constitutes about 50% of all melanoma patients. Immunotherapy plays an important role in nearly all patients with metastatic melanoma including those who have progressed after anti-BRAF therapy. Chemotherapy still has a significant (yet diminishing) role for patients who are no longer suitable for immunotherapy.
Metastatic melanoma is a highly challenging cancer to treat. Like other solid tumors, it is a very heterogeneous disease both clinically and biologically. Consequently, the first decision point in its management is to assess the severity of an individual patient’s disease. This can be done based on the patient’s symptoms and how they have evolved over the preceding 1-2 months, performance status, the extent of disease as determined by physical examination, and staging workup, which should include either computed tomography scans of the body or a positron emission tomography/CT study as well as a brain magnetic resonance imaging scan. Patients with brain metastases as a subset (which is sizable – 20%-25% have brain metastases) require special attention because they may not respond to systemic therapies and will thus have to be managed with brain-targeted treatment options. Tumor testing for BRAF mutations is necessary in all patients with metastatic melanoma because the BRAF inhibitors (vemurafenib or dabrafenib) are a preferred choice of targeted therapy for this subset of patients, which constitutes about 50% of all melanoma patients. Immunotherapy plays an important role in nearly all patients with metastatic melanoma including those who have progressed after anti-BRAF therapy. Chemotherapy still has a significant (yet diminishing) role for patients who are no longer suitable for immunotherapy.
Metastatic melanoma is a highly challenging cancer to treat. Like other solid tumors, it is a very heterogeneous disease both clinically and biologically. Consequently, the first decision point in its management is to assess the severity of an individual patient’s disease. This can be done based on the patient’s symptoms and how they have evolved over the preceding 1-2 months, performance status, the extent of disease as determined by physical examination, and staging workup, which should include either computed tomography scans of the body or a positron emission tomography/CT study as well as a brain magnetic resonance imaging scan. Patients with brain metastases as a subset (which is sizable – 20%-25% have brain metastases) require special attention because they may not respond to systemic therapies and will thus have to be managed with brain-targeted treatment options. Tumor testing for BRAF mutations is necessary in all patients with metastatic melanoma because the BRAF inhibitors (vemurafenib or dabrafenib) are a preferred choice of targeted therapy for this subset of patients, which constitutes about 50% of all melanoma patients. Immunotherapy plays an important role in nearly all patients with metastatic melanoma including those who have progressed after anti-BRAF therapy. Chemotherapy still has a significant (yet diminishing) role for patients who are no longer suitable for immunotherapy.
Nilotinib beats imatinib in newly diagnosed CML

Credit: CDC
NEW ORLEANS—New data indicate a trend for longer overall survival and event-free survival in newly diagnosed chronic myeloid leukemia (CML) patients on nilotinib versus imatinib.
Five-year data from the phase 3 ENESTnd study demonstrate higher rates of early and deeper molecular response in newly diagnosed CML patients taking nilotinib, as well as a reduced risk of progression compared to imatinib.
These results were presented at the 2013 ASH Annual Meeting as abstract 92.
“These new, updated data reaffirm the superiority of nilotinib over imatinib at achieving deeper molecular responses and provide even more evidence supporting nilotinib as an appropriate treatment of choice in newly diagnosed patients,” said Giuseppe Saglio, MD, of the University of Turin in Italy.
“Now, we are looking at how deeper molecular responses may help guide our approach towards how we treat CML in the future.”
The 5-year ENESTnd data showed that nilotinib can produce superior responses across various Philadelphia chromosome-positive CML patient populations, including newly diagnosed patients. Results showed higher rates of early and deeper sustained molecular response, known as MR4.5.
The difference in the rates of MR4.5 continued to be higher when nilotinib was given at 300 mg or 400 mg twice daily, when compared to imatinib (MR4.5: 6%-10% difference by 1 year, 21%-23% difference by 5 years).
“The most important endpoint is cumulative incidence of MR4.5,” Dr Saglio said. “At 5 years, this is achieved by 54% of those in nilotinib-300-mg group, 52% in the nilotinib-400-mg group, and 31% in the imatinib group. And the curves are still diverging.”
The data also indicate a trend for higher overall survival and event-free survival rates in patients treated with nilotinib.
Fifteen patients treated with imatinib had CML-related deaths, compared to 6 patients in the arm receiving nilotinib at 300 mg twice daily and 4 patients in the arm receiving nilotinib at 400 mg twice daily.
Few new adverse events and laboratory abnormalities were observed between year 4 and year 5. Rates of patients with adverse events leading to discontinuation were 11.1% in the 300-mg nilotinib group, 17.7% in the 400-mg nilotinib group, and 13.2% in the imatinib group.
Dr Saglio noted that select cardiac and vascular events are slightly more frequent on nilotinib versus imatinib. But there has been no increase in the annual incidence of these events over time.
Therefore, Dr Saglio concluded, “Nilotinib, a standard-of-care frontline therapy option for newly diagnosed, chronic-phase CML patients, affords superior efficacy compared with imatinib, including higher rates of early molecular response (which is associated with improved long-term outcomes), higher rates of deep molecular response, and a lower risk of disease progression. Nilotinib continues to show good tolerability with long-term follow-up.” ![]()

Credit: CDC
NEW ORLEANS—New data indicate a trend for longer overall survival and event-free survival in newly diagnosed chronic myeloid leukemia (CML) patients on nilotinib versus imatinib.
Five-year data from the phase 3 ENESTnd study demonstrate higher rates of early and deeper molecular response in newly diagnosed CML patients taking nilotinib, as well as a reduced risk of progression compared to imatinib.
These results were presented at the 2013 ASH Annual Meeting as abstract 92.
“These new, updated data reaffirm the superiority of nilotinib over imatinib at achieving deeper molecular responses and provide even more evidence supporting nilotinib as an appropriate treatment of choice in newly diagnosed patients,” said Giuseppe Saglio, MD, of the University of Turin in Italy.
“Now, we are looking at how deeper molecular responses may help guide our approach towards how we treat CML in the future.”
The 5-year ENESTnd data showed that nilotinib can produce superior responses across various Philadelphia chromosome-positive CML patient populations, including newly diagnosed patients. Results showed higher rates of early and deeper sustained molecular response, known as MR4.5.
The difference in the rates of MR4.5 continued to be higher when nilotinib was given at 300 mg or 400 mg twice daily, when compared to imatinib (MR4.5: 6%-10% difference by 1 year, 21%-23% difference by 5 years).
“The most important endpoint is cumulative incidence of MR4.5,” Dr Saglio said. “At 5 years, this is achieved by 54% of those in nilotinib-300-mg group, 52% in the nilotinib-400-mg group, and 31% in the imatinib group. And the curves are still diverging.”
The data also indicate a trend for higher overall survival and event-free survival rates in patients treated with nilotinib.
Fifteen patients treated with imatinib had CML-related deaths, compared to 6 patients in the arm receiving nilotinib at 300 mg twice daily and 4 patients in the arm receiving nilotinib at 400 mg twice daily.
Few new adverse events and laboratory abnormalities were observed between year 4 and year 5. Rates of patients with adverse events leading to discontinuation were 11.1% in the 300-mg nilotinib group, 17.7% in the 400-mg nilotinib group, and 13.2% in the imatinib group.
Dr Saglio noted that select cardiac and vascular events are slightly more frequent on nilotinib versus imatinib. But there has been no increase in the annual incidence of these events over time.
Therefore, Dr Saglio concluded, “Nilotinib, a standard-of-care frontline therapy option for newly diagnosed, chronic-phase CML patients, affords superior efficacy compared with imatinib, including higher rates of early molecular response (which is associated with improved long-term outcomes), higher rates of deep molecular response, and a lower risk of disease progression. Nilotinib continues to show good tolerability with long-term follow-up.” ![]()

Credit: CDC
NEW ORLEANS—New data indicate a trend for longer overall survival and event-free survival in newly diagnosed chronic myeloid leukemia (CML) patients on nilotinib versus imatinib.
Five-year data from the phase 3 ENESTnd study demonstrate higher rates of early and deeper molecular response in newly diagnosed CML patients taking nilotinib, as well as a reduced risk of progression compared to imatinib.
These results were presented at the 2013 ASH Annual Meeting as abstract 92.
“These new, updated data reaffirm the superiority of nilotinib over imatinib at achieving deeper molecular responses and provide even more evidence supporting nilotinib as an appropriate treatment of choice in newly diagnosed patients,” said Giuseppe Saglio, MD, of the University of Turin in Italy.
“Now, we are looking at how deeper molecular responses may help guide our approach towards how we treat CML in the future.”
The 5-year ENESTnd data showed that nilotinib can produce superior responses across various Philadelphia chromosome-positive CML patient populations, including newly diagnosed patients. Results showed higher rates of early and deeper sustained molecular response, known as MR4.5.
The difference in the rates of MR4.5 continued to be higher when nilotinib was given at 300 mg or 400 mg twice daily, when compared to imatinib (MR4.5: 6%-10% difference by 1 year, 21%-23% difference by 5 years).
“The most important endpoint is cumulative incidence of MR4.5,” Dr Saglio said. “At 5 years, this is achieved by 54% of those in nilotinib-300-mg group, 52% in the nilotinib-400-mg group, and 31% in the imatinib group. And the curves are still diverging.”
The data also indicate a trend for higher overall survival and event-free survival rates in patients treated with nilotinib.
Fifteen patients treated with imatinib had CML-related deaths, compared to 6 patients in the arm receiving nilotinib at 300 mg twice daily and 4 patients in the arm receiving nilotinib at 400 mg twice daily.
Few new adverse events and laboratory abnormalities were observed between year 4 and year 5. Rates of patients with adverse events leading to discontinuation were 11.1% in the 300-mg nilotinib group, 17.7% in the 400-mg nilotinib group, and 13.2% in the imatinib group.
Dr Saglio noted that select cardiac and vascular events are slightly more frequent on nilotinib versus imatinib. But there has been no increase in the annual incidence of these events over time.
Therefore, Dr Saglio concluded, “Nilotinib, a standard-of-care frontline therapy option for newly diagnosed, chronic-phase CML patients, affords superior efficacy compared with imatinib, including higher rates of early molecular response (which is associated with improved long-term outcomes), higher rates of deep molecular response, and a lower risk of disease progression. Nilotinib continues to show good tolerability with long-term follow-up.” ![]()
Pediatric Discharge Systematic Review
The process of discharging a pediatric patient from an acute care facility is currently fraught with difficulties. More than 20% of parents report problems in the transition of care from the hospital to the home and ambulatory care setting.[1] Clinical providers likewise note communication challenges around the time of discharge,[2, 3] especially when inpatient and outpatient providers are different, as with the hospitalist model.[4] Poor communication and problems in discharge transition and continuity of care often culminate in adverse events,[5, 6] including return to emergency department (ED) care and hospital readmission.[7]
Thirty‐day readmissions are common for certain pediatric conditions, such as oncologic diseases, transplantation, and sickle cell anemia and vary significantly across children's hospitals.[8] Discharge planning may decrease 30‐day readmissions in hospitalized adults[9]; however, it is not clear that the same is true in children. Both the preventability of pediatric readmissions[10] and the extent to which readmissions reflect suboptimal care[11] are subjects of debate. Despite these uncertainties, collaborative efforts intended to decrease pediatric readmissions[12] and improve discharge transitions[13, 14] are underway.
To inform these debates and efforts, we undertook a systematic review of the evidence of hospital‐initiated interventions to reduce repeat utilization of the ED and hospital. Acknowledging that existing evidence for condition‐specific discharge interventions in pediatrics might be limited, we sought to identify common elements of successful interventions across pediatric conditions.
METHODS
Search Strategy
With the assistance of a research librarian, we searched MEDLINE and CINAHL (Cumulative Index to Nursing and Allied Health Literature) from the inception of these databases through to March 28, 2012 (for search strategies, see the Supporting Information, Appendix, Part 1, in the online version of this article).
Study Selection
Two authors (K.A. and C.K.) independently reviewed abstracts identified by the initial search, as well as abstracts of references of included articles. Eligibility criteria for inclusion in full review included: (1) discharge‐oriented process or intervention initiated in the inpatient setting, (2) study outcomes related to subsequent utilization including hospital readmission or emergency department visit after hospitalization, (3) child‐ or adolescent‐focused or child‐specific results presented separately, and (4) written or available in English. If abstract review did not sufficiently clarify whether all eligibility criteria were met, the article was included in the full review. Two authors (K.A. and C.K.) independently reviewed articles meeting criteria for full review to determine eligibility. Disagreements regarding inclusion in the final analysis were discussed with all 4 authors. We excluded studies in countries with low or lower‐middle incomes,[15] as discharge interventions in these countries may not be broadly applicable.
Data Abstraction, Quality Assessment, and Data Synthesis
Two authors (K.A. and C.K.) independently abstracted data using a modified Cochrane Collaboration data collection form.[16] We independently scored the included studies using the Downs and Black checklist, which assesses the risk of bias and the quality of both randomized and nonrandomized studies.[17] This checklist yields a composite score of 0 to 28 points, excluding the item assessing power. As many studies either lacked power calculations or included power calculations based on outcomes not included in our review, we performed calculations to determine the sample size needed to detect a decrease in readmission or ED utilization by 20% from baseline or control rates. Due to the heterogeneous nature of included studies in terms of population, interventions, study design, and outcomes, meta‐analysis was not performed.
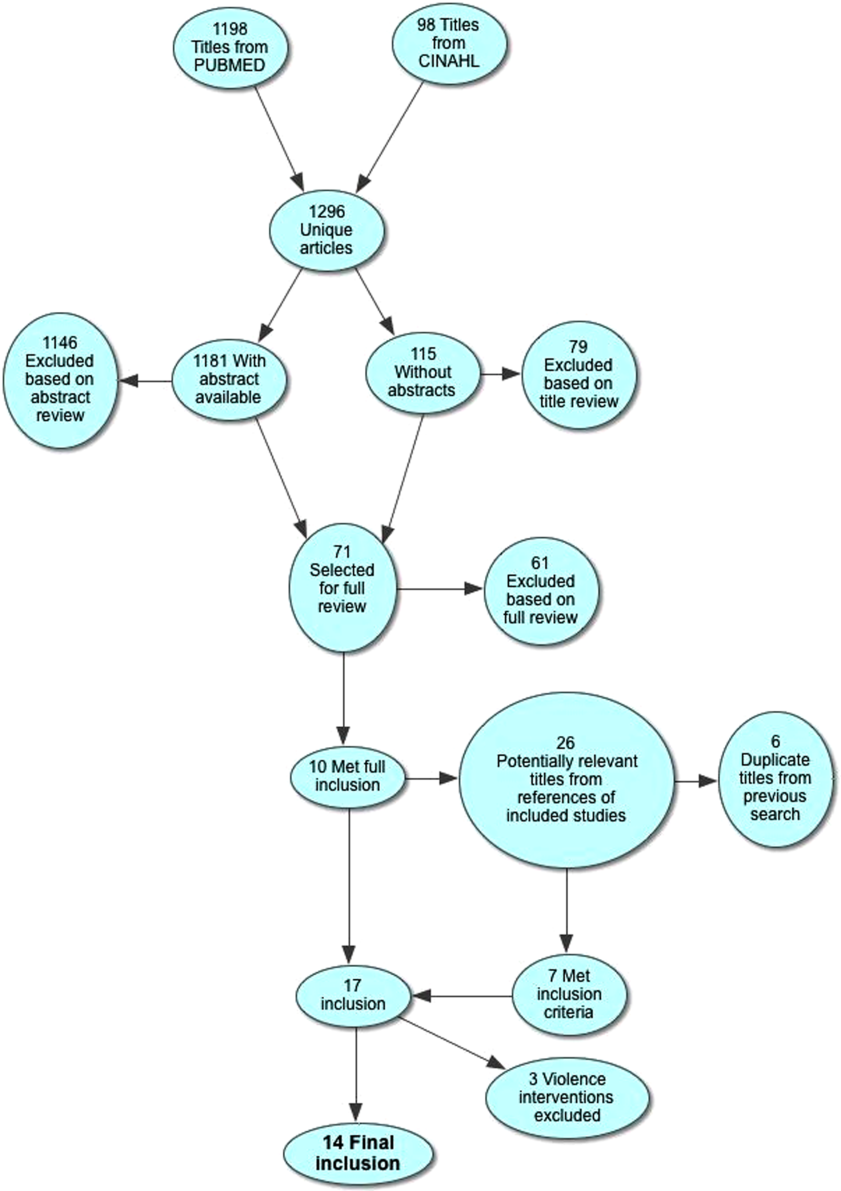
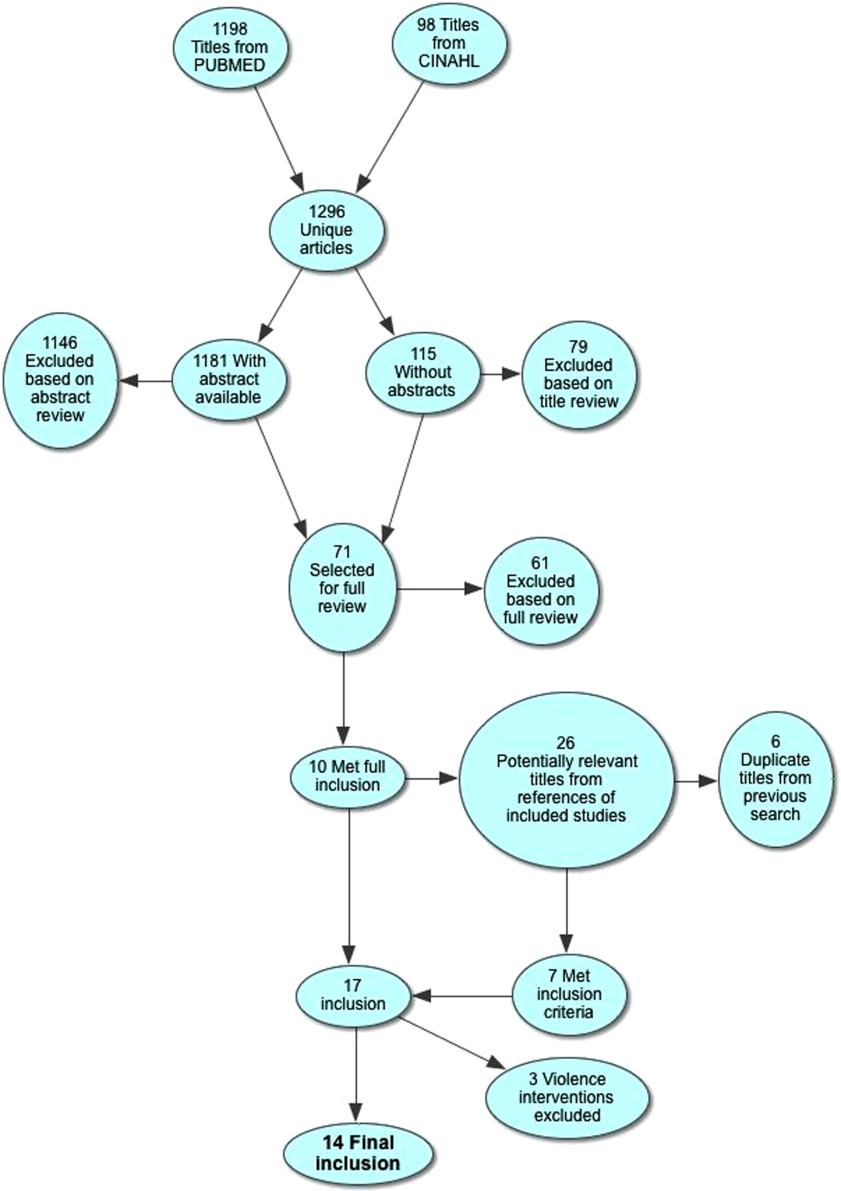
RESULTS
Electronic search yielded a total of 1296 unique citations. Review of abstracts identified 40 studies for full article review. We identified 10 articles that met all inclusion criteria. Subsequent review of references of included articles identified 20 additional articles for full review, 7 of which met all inclusion criteria. However, 3 articles[18, 19, 20] assessed the impact of violence interventions primarily on preventing reinjury and recidivism and thus were excluded (see Supporting Information, Appendix, Part 2, in the online version of this article for findings of the 3 articles). In total, we included 14 articles in our review[21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34] (Figure 1).
Patient Populations and Intervention Timing and Components
Studies varied regarding the specific medical conditions they evaluated. Eight of the papers reported discharge interventions for children with asthma, 5 papers focused on discharge from the neonatal intensive care unit (NICU), and a final study discussed a discharge intervention for children with cancer (Table 1). Although our primary goal was to synthesize discharge interventions across pediatric conditions, we provide a summary of discharge interventions by condition (see Supporting Information, Appendix, Part 3, in the online version of this article).
| Author, Year | Study Design | Age | Inclusion | Exclusion | Intervention | Control |
|---|---|---|---|---|---|---|
| ||||||
| Asthma | ||||||
| Davis, 2011[21] | Retrospective matched case control | 12 months18 years | Admitted for asthma at a single hospital in California. | 45 minutes of enhanced asthma education and phone call 3 weeks after discharge (n=698) | Patients were matched on age and past utilization who received standard education/care (n=698) | |
| Espinoza‐Palma, 2009[22] | RCT | 515 years | Admitted for asthma at a single hospital in Chile. | Chronic lung disease or neurologic alteration. | Self‐management education program with a postdischarge game to reinforce educational concepts (n=42) | Standard education (n=46) |
| Ng, 2006[23] | RCT | 215 years | Admitted for asthma in a pediatric ward at a single hospital in China. | Admitted to PICU or non‐Chinese speaking. | Evaluation by asthma nurse, animated asthma education booklet, 50‐minute discharge teaching session, follow‐up by phone at 1 week (n=55) | Evaluation by asthma nurse by physician referral, a written asthma education booklet, 30‐minute discharge teaching session (n=45) |
| Stevens, 2002[24] | RCT | 18 months5 years | In ED or admitted with primary diagnosis of asthma/wheezing at 2 hospitals in the United Kingdom. | Admitted when no researcher available. | Enhanced asthma education and follow‐up in a clinic 1 month after encounter (n=101) | Usual care (n=99) |
| Wesseldine, 1999[25] | RCT | 216 years | Admitted for asthma at a single hospital in the United Kingdom. | Admitted when no researcher available. | 20 minutes of enhanced asthma education including: guided self‐management plan, booklet, asthma hotline contact, and sometimes oral steroids (n=80) | Standard discharge that varied by provider (n=80) |
| Madge, 1997[26] | RCT | 214 years | Admitted for asthma at a single hospital in the United Kingdom. | Admitted on weekend. | 45 minutes of enhanced asthma education with written asthma plan, a nurse follow‐up visit 23 weeks postdischarge, telephone support, and a course of oral steroids (n=96) | Standard education (did not include written asthma plan) (n=105) |
| Taggart, 1991[27] | Pre‐post | 612 years | Admitted for asthma at single institution in Washington, DC with history of at least one ED visit in prior 6 months. | If resided outside of metro area. | Received written educational materials, adherence assistance, discussed emotions of asthma, video education provided, and tailored nursing interactions (n=40) | Enrolled patient's prior utilization |
| Mitchell, 1986[28] | RCT | >2 years | Admitted for asthma at single institution in New Zealand. | Having a previous life‐threatening attack. | 6 monthly postdischarge education sessions on lung anatomy/physiology, triggers and avoidance, asthma medication, advice on when and where to seek care (n=94 children of European descent, n=84 children of Polynesian descent) | Standard discharge (n=106 children of European descent; n=84 children of Polynesian descent) |
| Cancer | ||||||
| Caliskan Yilmaz, 2009[29] | Quasiexperimental | 18 years | New oncologic diagnoses in hospital in Turkey. | Children who died during follow‐up. | Frequent needs assessment, education, home visits, fever guidance, telephone consultation, and manual for home care; patients lived in Izmir (n=25) | Routine hospital services without formal education; patients lived outside of Izmir (n=24) |
| NICU | ||||||
| Broyles, 2000[30] | RCT | Neonate | Infants with birth weight 1500 g with mechanical vent use in 48 hours of life, born at single NICU in Texas. | Infant death, infant adopted or moved out of enrollment county. | Specialized follow‐up available 5 days a week for well or sick visits; access to medical advice via phone 24 hours a day, transportation to ED provided when needed; home visitation, parent education, and "foster grandmother" offered (n=446) | Specialized follow‐up available 2 mornings a week for well or sick visits; all other sick visits to be made through acute care clinic or ED (n=441) |
| Finello, 1998[31] | RCT | Neonate | Infants with birth weight between 750 and1750 g; discharged from 2 NICUs in California. | Infants with gross abnormalities. | Three separate intervention groups (n=20 in each): (1) home healthhome visits during the first 4 weeks after discharge, with physician consultation available at all times; (2) home visitinghealth and development support, parental support, support with referral services for 2 years after discharge; (3) home health and home visiting arms combined | Standard discharge (n=20). |
| Kotagal, 1995[32] | Pre‐post | Neonate | Infants discharged from a single NICU in Ohio. | Patients (n=257) discharged after restructuring of discharge practices including: removal of discharge weight criteria, engagement of family prior to discharge, evaluation of home environment prior to discharge, and arrangement of home health visits and follow‐up | Patients discharged before discharge restructuring (n=483) | |
| Casiro, 1993[33] | RCT | Neonate | Infants meeting discharge criteria from 1 of 2 NICUs in Canada. | Congenital anomalies, chronic neonatal illness, parent refusal, family complications, and death. | Early discharge based on prespecified criteria with 8 weeks of services including: assistance with infant care, sibling care and housekeeping; nurse availability via phone; follow‐up phone calls and home visitation tailored to family need (n=50) | Discharged at the discretion of their attending physicians; standard newborn public health referral for routine follow‐up (n=50) |
| Brooten, 1986[34] | RCT | Neonate | Infants born 1500 g at a single NICU in Pennsylvania. | Death, life‐threatening congenital anomalies, grade 4 IVH, surgical history, O2 requirement >10 weeks, family complications. | Early discharge based on prespecified criteria with weekly education prior to discharge, postdischarge follow‐up phone call, and home nurse visitation; consistent nurse availability via phone (n=39) | Standard discharge practices with a discharge weight minimum of 2.2 kg (n=40) |
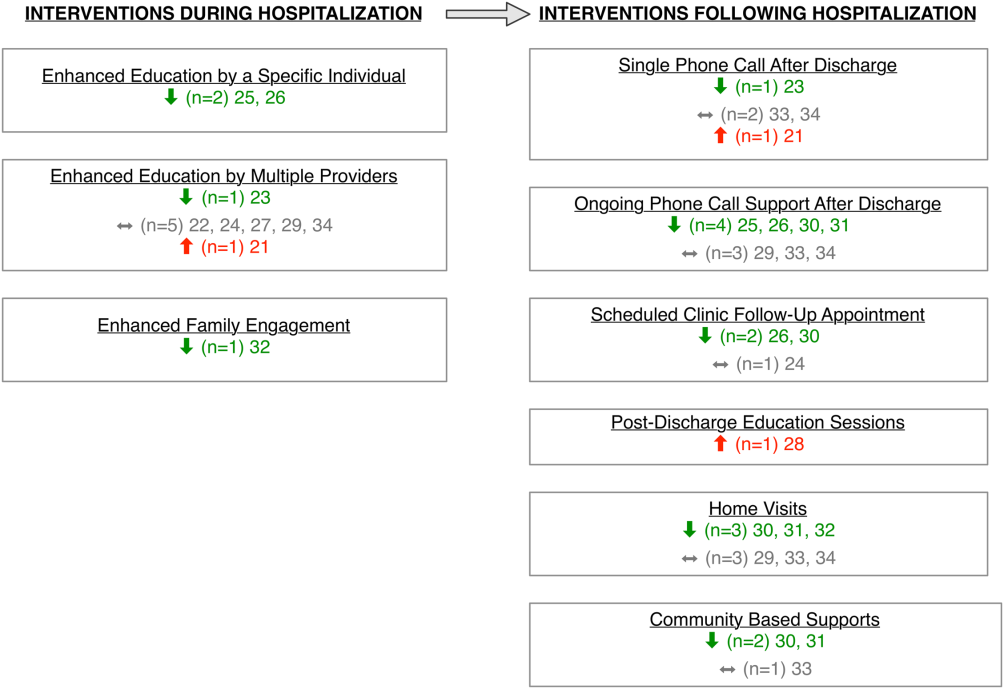
Studies varied regarding the timing and nature of the intervention components. Eight discharge interventions included a major inpatient component, in addition to outpatient support or follow‐up.[21, 23, 24, 25, 26, 29, 32, 34] Two studies included an inpatient education component only.[22, 27] The remainder were initiated during index hospitalization but focused primarily on home visitation, enhanced follow‐up, and support after discharge (Figure 2).[28, 30, 31, 33]
Outcome Assessment Methods
Readmission and subsequent ED utilization events were identified using multiple techniques. Some authors accessed claims records to capture all outcomes.[30, 33] Others relied on chart review.[21, 25, 26, 27, 28, 31, 32] One study supplemented hospital records with outpatient records.[24] Some investigators used parental reports.[22, 23, 31] Two studies did not describe methods for identifying postdischarge events.[29, 34]
Study Quality
The quality of the included studies varied (Table 2). Many of the studies had inadequate sample size to detect a difference in either readmission or ED visit subsequent to discharge. Eight studies found differences in either subsequent ED utilization, hospitalization, or both and were considered adequately powered for these specific outcomes.[21, 23, 25, 26, 28, 30, 31, 32] In contrast, among studies with readmission as an outcome, 6 were not adequately powered to detect a difference in this particular outcome.[24, 30, 31, 32, 33, 34] In these 6 studies, all except 1 study30 had 10% of the sample size required to detect differences in readmission. Further, 2 studies that examined ED utilization were underpowered to detect differences between intervention and control groups.[24, 26] We were unable to perform power calculations for 3 studies,[22, 27, 29] as the authors presented the number of events without clear denominators.
| Author, Year | Study Design | D&B Score* | Adequately Powered (Yes/No)** | Timing of Outcome | Major Findings | Major Limitations |
|---|---|---|---|---|---|---|
| ||||||
| Asthma | ||||||
| Davis, 2011[21] | Retrospective matched case control | 14 | Readmission: N/A; ED: yes | 1 year | Patients with enhanced education had higher hazards of return to ED visit. | Intervention not randomized; only 29% of eligible children enrolled with unclear selection decisions due to lack of study personnel or caregiver presence in hospital; only 67% completed the intervention; 50% of patients were not local; follow‐up was not well described. |
| Espinoza‐Palma, 2009[22] | RCT | 19 | Readmission: b; ED:b | 1 year | No difference between the intervention and control in hospitalizations or ED visits. ED visits and hospitalizations decreased in year after compared to the year prior for both intervention and control. | Pre‐post analysis with similar effects in cases and controls, results may reflect regression to mean; follow‐up was not well described, and 12.5% who were lost to follow‐up were excluded from analysis; study was in Chile with different demographics than in the United States. |
| Ng, 2006[23] | RCT | 20 | Readmission: yes; ED: yes | 3 months | Patients in the intervention group were less likely to be readmitted or visit the ED. | Recruitment/refusal was not well described; number lost to follow‐up was not reported; study was in China with different demographics than the United States. |
| Stevens, 2002[24] | RCT | 20 | Readmission: no ED: no | 1 year | No differences between intervention and control for any outcomes. | 11% were lost to follow‐up; number of patients who refused was not reported; analysis did not adjust for site of recruitment (ED vs inpatient); 30% of children did not have a prior diagnosis of asthma; study was in England with different demographics than in the United States. |
| Wesseldine, 1999[25] | RCT | 20 | Readmission: yes; ED: yes | 6 months | Patients in intervention group less likely to be readmitted or visit ED. | Unclear if intervention group received oral steroids that might drive effect; number lost to follow‐up was not reported; high miss rate for recruitment; study was in England with different demographics than the United States. |
| Madge, 1997 [26] | RCT | 22 | Readmission: yes; ED: no | 214 months | Patients in intervention group were less likely to be readmitted compared to controls. No differences in repeat ED visits. | Unclear if education or oral steroids drove effect; number of patients who refused or were lost to follow‐not reported; time to outcome (214 months) varied for different patients, which may introduce bias given the seasonality of asthma; study was in Scotland with different demographics than the United States. |
| Taggart, 1991[27] | Pre‐post | 12 | Readmission:b; ED:b | 15 months | Overall there was no change in ED or hospitalization utilization from pre to post. When limited to children with severe asthma, there was a decrease in ED utilization after the intervention compared to prior ED use. | Use of historical utilization as a comparison does not account for potential effects of regression to mean or improvement with age; over one‐half of eligible patients were excluded due to lack of consent or inability to collect baseline data; inclusion criterion did not specify that prior utilization was necessarily for asthma exacerbation; number lost to follow‐up was not reported. |
| Mitchell, 1986[28] | RCT | 14 | Readmission: yesc; ED: N/A | 6 months and 618 months | Increase in percentage of readmission between 6 and 18 months for children of European descent. | Unclear exclusion criterion; full compliance with intervention only 52%; number of patients lost to follow‐up (outcome) was not reported; statistical analysis was not clearly described. |
| Cancer | ||||||
| Caliskan Yilmaz, 2009[29] | Quasiexperimental | 10 | Readmission:b; ED: N/A | Not specified | For the first readmission to the hospital, more of the readmissions were planned in the intervention group compared to the control group. Number of readmissions was not assessed. | Intervention was not randomized; children who died were excluded (4%); planned vs unplanned distinction not validated; unclear cointerventions regarding chemotherapy administration; recruitment and follow‐up was not well described; not all comparisons were described in methods. |
| NICU | ||||||
| Broyles, 2000[30] | RCT | 23 | Readmission: no; ED: yes | At 1 year adjusted age | Overall hospitalization rates were similar but there were fewer admissions to the ICU. Intervention group had fewer ED visits. Total costs were less in intervention group. | 10% refused to participate or consent was not sought, and 12% were excluded after randomization; different periods of follow‐up (outcomes observed at 1 year of life regardless of discharge timing); analysis did not adjust for site of recruitment (1 of 2 nurseries). |
| Finello, 1998[31] | RCT | 11 | Readmission: nod; ED: yes | At 6 months adjusted age and between 6 and 12 months adjusted age | No changes in hospitalization rates.d The home health+home visit arm had fewer ED visits between 6 and 12 months of life. Intervention was reported as saving money by decreasing initial length of stay. | Inclusion and exclusion criteria, recruitment/refusal, outcomes, and analysis plan were not clearly described; sample size was too small for effective randomization; different periods of follow‐up (outcomes observed at 1 year of life regardless of discharge timing); analysis did not adjust for site of recruitment; 15% of outcomes were missing. |
| Kotagal, 1995[32] | Pre‐post | 15 | Readmission: no; ED: yes | 14 days | Decreased number of ED visits in patients in intervention. No difference in readmission. Costs and length of stay were less in intervention. | Designed to decrease length of stay; pre‐post nature of study allows for possibility of other changes to practices other than the intervention. |
| Casiro, 1993[33] | RCT | 18 | Readmission: no; ED: N/A | 1 year of life | There were no differences in the readmissions or number of ambulatory care visits after discharge. Infants were discharged earlier in the intervention group, which resulted in cost savings. | Designed to decrease length of stay; 13% refused or were excluded due to family complications; and 8% were lost to follow‐up; different periods of follow‐up (outcomes observed at 1 year of life regardless of discharge timing); analysis did not adjust for site of recruitment (1 of 2 nurseries); 81% of infants were born to Caucasian women, which may limit generalizability. |
| Brooten, 1986[34] | RCT | 15 | Readmission: no; ED: N/A | 14 days and 18 months | No difference in readmission. Significantly lower charges during initial hospitalization for intervention group. | Designed to decrease length of stay; unclear when randomization occurred and exclusions unclear; 12.5% were excluded due to refusal or family issues; follow‐up not well described, and loss to follow‐up was unknown. |
Excluding the assessment of statistical power, Downs and Black scores ranged from 10 to 23 (maximum 28 possible points) indicating varying quality. As would be expected with discharge interventions, studies did not blind participants; 2 studies did, however, appropriately blind the outcome evaluators to intervention assignment.[22, 30] Even though 10 out of the 14 studies were randomized controlled trials, randomization may not have been completely effective due to sample size being too small for effective randomization,[31] large numbers of excluded subjects after randomization,[30] and unclear randomization process.[34] Several studies had varying follow‐up periods for patients within a given study. For example, 3 NICU studies assessed readmission at 1‐year corrected age,[30, 31, 33] creating the analytic difficulty that the amount of time a given patient was at risk for readmission was dependent on when the patient was discharged, yet this was not accounted for in the analyses. Only 2 studies demonstrated low rates of loss to follow‐up (10%).[30, 33] The remainder of the studies either had high incompletion/loss to follow‐up rates (>10%)[22, 24, 31] or did not report rates.[21, 23, 25, 26, 27, 28, 29, 32, 34] Finally, 3 studies recruited patients from multiple sites,[24, 31, 33] and none adjusted for potential differences in effect based on enrollment site.
Findings Across Patient Populations Regarding Readmission
Of the 4 studies that demonstrated change in overall readmission,[23, 25, 26, 28] all were asthma focused; 3 demonstrated a decrease in readmissions,[23, 25, 26] and 1 an increase in readmissions.[28] The 3 effective interventions included 1‐on‐1 inpatient education delivered by an asthma nurse, in addition to postdischarge follow‐up support, either by telephone or clinic visit. Two of these interventions provided rescue oral steroids to some patients on discharge.[25, 26] In contrast, a study from New Zealand evaluated a series of postdischarge visits using an existing public health nurse infrastructure and demonstrated an increase in readmission between 6 to 18 months after admission in European children.[28] An additional study focused on outpatient support after discharge from the NICU, and demonstrated a lower frequency of readmission to the intensive care unit without overall reduction of hospital readmission (Tables 1 and 2).[30]
Findings Across Patient Populations Regarding Subsequent ED Visits
Of all the discharge interventions, 6 demonstrated differences in return to the ED after discharge. Five studies described a decrease in ED visits after hospitalization,[23, 25, 30, 31, 32] and 1 showed an increase.[21] Three studies in the NICU population demonstrated decreased ED utilization through a combination of augmented family engagement during hospitalization and/or enhanced support after discharge. Two inpatient asthma education interventions with structured postdischarge follow‐up decreased return visitation to the ED.[23, 26] The intervention that worsened subsequent ED utilization (ie, increased ED visit hazard compared to matched controls) provided enhanced inpatient education to a nonrandom group of children hospitalized with asthma and provided a follow‐up phone call 3 weeks after discharge (Tables 1 and 2).[21]
DISCUSSION
In this review, we synthesized evidence regarding pediatric hospital discharge‐focused interventions intended to reduce subsequent utilization through decreased readmission and ED visits. Our review identified 14 studies clustered in 3 clinical areas: asthma, NICU care (chiefly prematurity), and cancer. Overall, 6 interventions demonstrated a reduction either in subsequent hospitalization or ED use. Four of the 6 positive interventions included both an enhanced inpatient education and engagement component as well as enhanced follow‐up after discharge. Importantly, all of the interventions were multifaceted; thus, we could not ascertain which specific aspects of the interventions mediated the change. Many of the included studies had significant methodological limitations.
Current Conceptual Framework
There are a number of existing discharge transitional care frameworks from prior studies[35, 36] and professional societies.[37] The Stepping Up to the Plate (SUTTP) alliance, a collaborative of 9 professional organizations, including the American Academy of Pediatrics, introduced 1 such framework in 2007. SUTTP sought to enhance care transitions by outlining principles of discharge transitional care including: (1) enhanced accountability, (2) creation of a central coordination hub charged with communicating expectations for care, (3) clear and direct communication of treatment plans and follow‐up, (4) timely feedback/feed‐forward of relevant information, and (5) involvement of family member at every stage.[38] In the context of the SUTTP framework, we present 3 hypotheses based on our findings to guide future work.
Hypothesis: Appointing a Dedicated Individual or Coordinating Hub Reduces Subsequent Utilization
Ostensibly, each discharge intervention included in this review sought to enhance accountability of providers or their health systems for discharge transitional care. Two of the asthma interventions appointed a particular provider to coordinate the discharge transition and demonstrated reductions in readmission.[25, 26] The successful NICU discharge interventions provided an integrated accountability structure across the health system, with a transition of accountability to an outpatient provider or central coordinating hub available to provide assistance and resources for an extended period following discharge.
By contrast, interventions with more than 1 individual intervener or without a centrally coordinated system for discharge transitional care tended not to demonstrate reduction in subsequent utilization.[21, 24, 27, 28] In fact, the 1 asthma intervention that utilized a previously existing public health nurse infrastructure demonstrated an increase in readmission.[28] Future efforts to enhance transitional care might investigate directly the impact of accountability structure on subsequent utilization by varying the number of effector individuals or the organization to which they report (eg, hospital system vs public health department).
Hypothesis: Individualized Task Learning and Feedback Enhances Effectiveness
Studies varied with respect to the extent they incorporated the principles of enhanced communication of the treatment and follow‐up plan and timely feedback/feed‐forward of relevant information. Successful efforts, however, seemed to embrace these strategies. Each of the 3 interventions that demonstrated readmission reduction[23, 25, 26] developed an individualized treatment plan during hospitalization, with either a specific follow‐up plan or resources for outpatient support. Two of these interventions assessed asthma inhaler technique prior to discharge, creating an inpatient audit and feedback loop allowing for assessment of competence prior to discharge. Audit and feedback has demonstrated promise modifying provider behavior[39] and is a plausible approach to enhancing patient and family self‐care.
Hypothesis: Timing of Intervention Enhances Effectiveness
Discrete sentinel events such as inpatient admission, may serve as a teachable moment[40, 41] or a tipping point[42] for some patients/families to initiate behavior change. Four of the 6 positive studies had a robust inpatient education component. By providing enhanced inpatient support, providers may be engaging the family at a timely opportunity to improve care. Both timing of the intervention (at admission vs discharge) and content (education‐ vs family‐engagement focused) are likely important to their effect and should be further explored with prospective study.
Persistent Literature Gaps
Follow‐up with a primary care provider after discharge is another intervention that might decrease postdischarge utilization. We did not identify any studies that specifically examined primary care follow‐up. However, 2 studies[43, 44] that did not meet our inclusion criteria (because they included adults and did not stratify by age group in the analysis) examined any outpatient follow‐up after discharge using state‐specific Medicaid claims. One study found that outpatient follow‐up after sickle cell hospitalization was associated with lower rates of readmission.[43] The other found no difference in readmission across multiple conditions.[44] One recent review of outpatient follow‐up from the ED for asthma found that even when increases in follow‐up were achieved, no reduction in the subsequent utilization was observed.[45]
Additional important questions remain underexplored. First, are condition‐specific interventions superior to those that span conditions? All of the interventions that demonstrated reductions in readmission were condition‐specific, yet no generic interventions met our inclusion criteria. Importantly, only 1 study[29] in our review examined discharge processes from 1 of the pediatric conditions with the most variation[8] in readmission. Further, no studies focused on children with complex medical conditions, who are known to be at increased risk of readmission,[46] indicating a sizable knowledge gap persists in understanding how to prevent readmissions in the most vulnerable pediatric populations.
Lastly, who are the most appropriate effector individuals for discharge‐focused transitional care interventions? Demographically matched effector individuals have shown promise in improving care using community health workers.[47, 48] The degree to which the identity of the intervener mediates subsequent ED and hospital utilization warrants further investigation.
Limitations of This Systematic Review
The studies included in this review assessed different outcomes at different intervals, precluding meta‐analysis. With greater consistency in the collection of data on the quality of discharge processes and their subsequent outcomes, future studies may offer further clarity as to which discharge‐oriented practices are more effective than others. Because we only identified literature in 3 pediatric conditions, generalizability beyond these conditions may be limited. The settings of the interventions also occurred in multiple countries; we excluded countries from low or low‐middle incomes to facilitate generalizability. As many of the discharge processes contained multiple interventions, it is not possible to ascertain which, if any, singular action may decrease posthospitalization utilization. Additionally, some of the included interventions are older, and it is plausible that discharge processes have evolved with the expansion of the hospitalist model.
Methods of data collection influence the quality of results in the included studies. Most of the studies included in this review used either medical record review or parental self‐report of utilization. Parental report may be sufficient for hospitalizations and ED utilization; however, it is subject to recall bias. Chart review likely underestimates the number of postdischarge events, depending on the individual institution's proportion of the market and the tendency of individuals to seek care at multiple institutions. Claims data may offer the most accurate assessments of ED and hospital utilization and cost, but can be more difficult to obtain and do not provide the same potential for granularity as parent report or medical records review.
Finally, subsequent ED visits, readmissions, and cost may not be the best measures of the quality of discharge transitional care. A number of tools have been developed to more specifically evaluate the quality of transitional care in adults,[49, 50] including a validated instrument that consists of only 3 items,[50] which primarily assesses the extent to which patients are prepared for self‐care upon discharge. For pediatric populations, validated tools assessing caregiver experience with discharge[51] and discharge readiness[52] are also available. These instruments may assist those interested in assessing process‐related outcomes that specifically assess discharge transitional care elements and may mediate subsequent ED visits or hospitalizations.
CONCLUSION
Successful discharge interventions to reduce pediatric readmission and ED have some common features, including an individual or team with specialized knowledge of the condition that assumed responsibility for the inpatient‐to‐outpatient transition and offered ongoing support to the family following discharge. All studies included in our review examined multiple discharge interventions; however, many did not have enough participants to detect differences in the outcomes of interest. Future studies might adapt common features of effective interventions, which are consistent with professional societies' recommendations.
Acknowledgements
The authors thank Marisa Conte for her help with developing the search algorithms for the review.
Disclosures: Drs. Auger and Kenyon received salary support from the Robert Wood Johnson Foundation Clinical Scholars program. Dr. Feudtner does not have any funding sources to disclose. Dr. Davis is funded in part by the Michigan Department of Community Health to serve as the Chief Medical Executive. The views expressed herein are not necessarily the views of the Department of Community Health. The authors have no conflicts of interest to report.
- , , , , . Are hospital characteristics associated with parental views of pediatric inpatient care quality? Pediatrics. 2003;111(2):308–314.
- , , , , , . Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841.
- , , , et al. Improving transitions of care at hospital discharge‐‐implications for pediatric hospitalists and primary care providers. J Healthc Qual. 2010;32(5):51–60.
- , . Hospitalists in children's hospitals: what we know now and what we need to know. J Pediatr. 2006;148(3):296–299.
- , , , , . The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–167.
- , , , et al. Adverse events among medical patients after discharge from hospital. CMAJ. 2004;170(3):345–349.
- , , , . Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003;18(8):646–651.
- , , , et al. Pediatric readmission prevalence and variability across hospitals. JAMA. 2013;309:372–380.
- , , , , , . Discharge planning from hospital to home. Cochrane Database Syst Rev. 2013;(1):CD000313.
- , , , , , . Preventability of early readmissions at a children's hospital. Pediatrics. 2012;131(1):e171–e181.
- , , , et al. State‐level child health system performance and the likelihood of readmission to children's hospitals. J Pediatr. 2010;157(1):98–102.e1.
- Ohio Children's Hospitals' solutions for patient safety. Available at: http://solutionsforpatientsafety.org/files/sps‐fact‐sheet.pdf. Accessed July 24, 2013.
- American Academy of Pediatrics. Value in inpatient pediatrics (VIP) network projects. Available at: http://www.aap.org/en‐us/professional‐resources/practice‐support/quality‐improvement/Quality‐Improvement‐Innovation‐Networks/Pages/Value‐in‐Inpatient‐Pediatrics‐Network‐Projects.aspx. Accessed July 24, 2013.
- Child Health Corporation of America. Resources for managing the patient discharge process. Available at: http://www.chca.com/news/index.html. Accessed October 31, 2013.
- The World Bank. World Development Indicators 2012. Available at: http://data.worldbank.org/sites/default/files/wdi‐2012‐ebook.pdf. Accessed July 5, 2013.
- The Cochrane Collaboration. Data collection form: Intervention review—RCTs and non‐RCTs. Available at: http://hiv.cochrane.org/sites/hiv.cochrane.org/files/uploads/Data%20extraction%20form_all%20studies.docx. Accessed July 24, 2013.
- , . The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non‐randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384.
- , , , et al. Brief violence interventions with community case management services are effective for high‐risk trauma patients. J Trauma. 2011;71(1):228–237.
- , , , , , . Benefits of a hospital‐based peer intervention program for violently injured youth. J Am Coll Surg. 2007;205(5):684–689.
- , , , , . Caught in the crossfire: the effects of a peer‐based intervention program for violently injured youth. J Adolesc Health. 2004;34(3):177–183.
- , , , , . A matched‐cohort evaluation of a bedside asthma intervention for patients hospitalized at a large urban children's hospital. J Urban Health. 2011;88(suppl 1):49–60.
- , , , et al. Effectiveness of asthma education with and without a self‐management plan in hospitalized children. J Asthma. 2009;46(9):906–910.
- , , , , And . Effect of a structured asthma education program on hospitalized asthmatic children: a randomized controlled study. Pediatr Int. 2006;48(2):158–162.
- , , , , , Parental education and guided self‐management of asthma and wheezing in the pre‐school child: a randomised controlled trial. Thorax. 2002;57(1):39–44.
- , , . Structured discharge procedure for children admitted to hospital with acute asthma: a randomised controlled trial of nursing practice. Arch Dis Child. 1999;80(2):110–114.
- , , . Impact of a nurse‐led home management training programme in children admitted to hospital with acute asthma: a randomised controlled study. Thorax. 1997;52(3):223–228.
- , , , et al. You Can Control Asthma: evaluation of an asthma education program for hospitalized inner‐city children. Patient Educ Couns. 1991;17(1):35–47.
- , , . Asthma education by community child health nurses. Arch Dis Child. 1986;61(12):1184–1189.
- , . Effectiveness of a discharge‐planning program and home visits for meeting the physical care needs of children with cancer. Support Care Cancer. 2009;18(2):243–253.
- , , , et al. Comprehensive follow‐up care and life‐threatening illnesses among high‐risk infants: a randomized controlled trial. JAMA. 2000;284(16):2070–2076.
- , , , . Very low birth weight infants and their families during the first year of life: comparisons of medical outcomes based on after care services. J Perinatol. 1998;18(5):365–371.
- , , , , . Description and evaluation of a program for the early discharge of infants from a neonatal intensive care unit. J Pediatr. 1995;127(2):285–290.
- , , , et al. Earlier discharge with community‐based intervention for low birth weight infants: a randomized trial. Pediatrics. 1993;92(1):128–134.
- , , , et al. A randomized clinical trial of early hospital discharge and home follow‐up of very‐low‐birth‐weight infants. N Engl J Med. 1986;315(15):934–939.
- , , . Care transitions from inpatient to outpatient settings: ongoing challenges and emerging best practices. Hosp Pract (1995). 2011;39(3):128–139.
- , , , , . Interventions to reduce 30‐day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–528.
- . Clinical report—physicians' roles in coordinating care of hospitalized children. Pediatrics. 2010;126(4):829–832.
- . White space or black hole: what can we do to improve care transitions? ABIM Foundation. Available at: http://www.abimfoundation.org/∼/media/Files/Publications/F06‐05‐2007_6.ashx. Accessed September 5, 2012.
- , , , et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;(6):CD000259.
- , , , , . A smoking cessation intervention for parents of children who are hospitalized for respiratory illness: the stop tobacco outreach program. Pediatrics. 2003;111(1):140–145.
- , . A randomized, controlled trial of smoking cessation counseling provided during child hospitalization for respiratory illness. Pediatr Pulmonol. 2008;43(6):561–566.
- , . Embracing chaos and complexity: a quantum change for public health. Am J Public Health. 2008;98(8):1382–1389.
- , , , , , . Outpatient follow‐up and rehospitalizations for sickle cell disease patients. Pediatr Blood Cancer. 2012;58(3):406–409.
- , , . Does having an outpatient visit after hospital discharge reduce the likelihood of readmission? Del Med J. 2003;75(8):291–298.
- , , . Follow‐up after acute asthma episodes. Proc Am Thorac Soc. 2009;6(4):386–393.
- , , , et al. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children's hospitals. JAMA. 2011;305(7):682–690.
- , , , et al. A randomized controlled evaluation of the effect of community health workers on hospitalization for asthma: the asthma coach. Arch Pediatr Adolesc Med. 2009;163(3):225–232.
- , , , . The Seattle‐King County Healthy Homes Project: a randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am J Public Health. 2005;95(4):652–659.
- , , , , , . Development and testing of a measure designed to assess the quality of care transitions. Int J Integr Care. 2002;2:e02.
- , , , . Assessing the quality of transitional care: further applications of the care transitions measure. Med Care. 2008;46(3):317–322.
- , , , et al. Hospital readmission and parent perceptions of their child's hospital discharge. Int J Qual Health Care. 2013;25(5):573–581.
- , . Psychometric properties of the Readiness for Hospital Discharge Scale. J Nurs Meas. 2006;14(3):163–180.
The process of discharging a pediatric patient from an acute care facility is currently fraught with difficulties. More than 20% of parents report problems in the transition of care from the hospital to the home and ambulatory care setting.[1] Clinical providers likewise note communication challenges around the time of discharge,[2, 3] especially when inpatient and outpatient providers are different, as with the hospitalist model.[4] Poor communication and problems in discharge transition and continuity of care often culminate in adverse events,[5, 6] including return to emergency department (ED) care and hospital readmission.[7]
Thirty‐day readmissions are common for certain pediatric conditions, such as oncologic diseases, transplantation, and sickle cell anemia and vary significantly across children's hospitals.[8] Discharge planning may decrease 30‐day readmissions in hospitalized adults[9]; however, it is not clear that the same is true in children. Both the preventability of pediatric readmissions[10] and the extent to which readmissions reflect suboptimal care[11] are subjects of debate. Despite these uncertainties, collaborative efforts intended to decrease pediatric readmissions[12] and improve discharge transitions[13, 14] are underway.
To inform these debates and efforts, we undertook a systematic review of the evidence of hospital‐initiated interventions to reduce repeat utilization of the ED and hospital. Acknowledging that existing evidence for condition‐specific discharge interventions in pediatrics might be limited, we sought to identify common elements of successful interventions across pediatric conditions.
METHODS
Search Strategy
With the assistance of a research librarian, we searched MEDLINE and CINAHL (Cumulative Index to Nursing and Allied Health Literature) from the inception of these databases through to March 28, 2012 (for search strategies, see the Supporting Information, Appendix, Part 1, in the online version of this article).
Study Selection
Two authors (K.A. and C.K.) independently reviewed abstracts identified by the initial search, as well as abstracts of references of included articles. Eligibility criteria for inclusion in full review included: (1) discharge‐oriented process or intervention initiated in the inpatient setting, (2) study outcomes related to subsequent utilization including hospital readmission or emergency department visit after hospitalization, (3) child‐ or adolescent‐focused or child‐specific results presented separately, and (4) written or available in English. If abstract review did not sufficiently clarify whether all eligibility criteria were met, the article was included in the full review. Two authors (K.A. and C.K.) independently reviewed articles meeting criteria for full review to determine eligibility. Disagreements regarding inclusion in the final analysis were discussed with all 4 authors. We excluded studies in countries with low or lower‐middle incomes,[15] as discharge interventions in these countries may not be broadly applicable.
Data Abstraction, Quality Assessment, and Data Synthesis
Two authors (K.A. and C.K.) independently abstracted data using a modified Cochrane Collaboration data collection form.[16] We independently scored the included studies using the Downs and Black checklist, which assesses the risk of bias and the quality of both randomized and nonrandomized studies.[17] This checklist yields a composite score of 0 to 28 points, excluding the item assessing power. As many studies either lacked power calculations or included power calculations based on outcomes not included in our review, we performed calculations to determine the sample size needed to detect a decrease in readmission or ED utilization by 20% from baseline or control rates. Due to the heterogeneous nature of included studies in terms of population, interventions, study design, and outcomes, meta‐analysis was not performed.
RESULTS
Electronic search yielded a total of 1296 unique citations. Review of abstracts identified 40 studies for full article review. We identified 10 articles that met all inclusion criteria. Subsequent review of references of included articles identified 20 additional articles for full review, 7 of which met all inclusion criteria. However, 3 articles[18, 19, 20] assessed the impact of violence interventions primarily on preventing reinjury and recidivism and thus were excluded (see Supporting Information, Appendix, Part 2, in the online version of this article for findings of the 3 articles). In total, we included 14 articles in our review[21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34] (Figure 1).
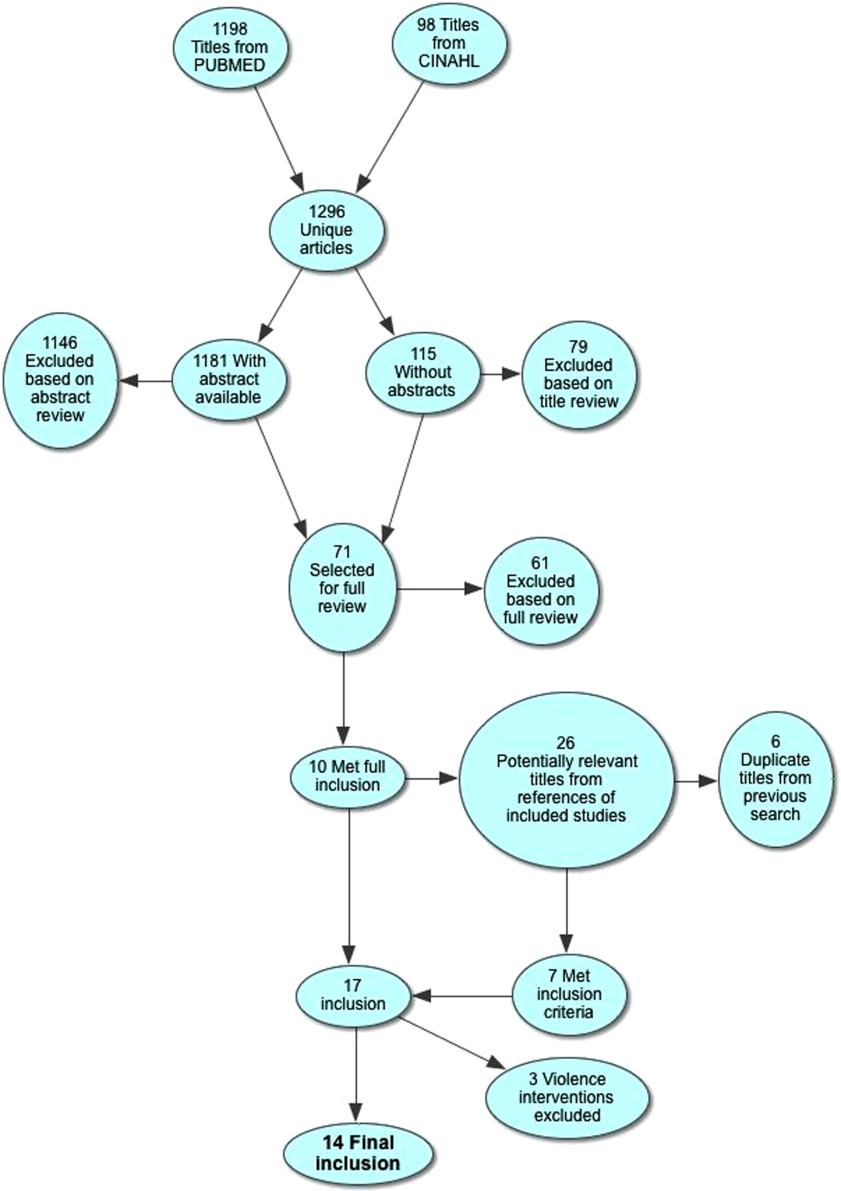
Patient Populations and Intervention Timing and Components
Studies varied regarding the specific medical conditions they evaluated. Eight of the papers reported discharge interventions for children with asthma, 5 papers focused on discharge from the neonatal intensive care unit (NICU), and a final study discussed a discharge intervention for children with cancer (Table 1). Although our primary goal was to synthesize discharge interventions across pediatric conditions, we provide a summary of discharge interventions by condition (see Supporting Information, Appendix, Part 3, in the online version of this article).
| Author, Year | Study Design | Age | Inclusion | Exclusion | Intervention | Control |
|---|---|---|---|---|---|---|
| ||||||
| Asthma | ||||||
| Davis, 2011[21] | Retrospective matched case control | 12 months18 years | Admitted for asthma at a single hospital in California. | 45 minutes of enhanced asthma education and phone call 3 weeks after discharge (n=698) | Patients were matched on age and past utilization who received standard education/care (n=698) | |
| Espinoza‐Palma, 2009[22] | RCT | 515 years | Admitted for asthma at a single hospital in Chile. | Chronic lung disease or neurologic alteration. | Self‐management education program with a postdischarge game to reinforce educational concepts (n=42) | Standard education (n=46) |
| Ng, 2006[23] | RCT | 215 years | Admitted for asthma in a pediatric ward at a single hospital in China. | Admitted to PICU or non‐Chinese speaking. | Evaluation by asthma nurse, animated asthma education booklet, 50‐minute discharge teaching session, follow‐up by phone at 1 week (n=55) | Evaluation by asthma nurse by physician referral, a written asthma education booklet, 30‐minute discharge teaching session (n=45) |
| Stevens, 2002[24] | RCT | 18 months5 years | In ED or admitted with primary diagnosis of asthma/wheezing at 2 hospitals in the United Kingdom. | Admitted when no researcher available. | Enhanced asthma education and follow‐up in a clinic 1 month after encounter (n=101) | Usual care (n=99) |
| Wesseldine, 1999[25] | RCT | 216 years | Admitted for asthma at a single hospital in the United Kingdom. | Admitted when no researcher available. | 20 minutes of enhanced asthma education including: guided self‐management plan, booklet, asthma hotline contact, and sometimes oral steroids (n=80) | Standard discharge that varied by provider (n=80) |
| Madge, 1997[26] | RCT | 214 years | Admitted for asthma at a single hospital in the United Kingdom. | Admitted on weekend. | 45 minutes of enhanced asthma education with written asthma plan, a nurse follow‐up visit 23 weeks postdischarge, telephone support, and a course of oral steroids (n=96) | Standard education (did not include written asthma plan) (n=105) |
| Taggart, 1991[27] | Pre‐post | 612 years | Admitted for asthma at single institution in Washington, DC with history of at least one ED visit in prior 6 months. | If resided outside of metro area. | Received written educational materials, adherence assistance, discussed emotions of asthma, video education provided, and tailored nursing interactions (n=40) | Enrolled patient's prior utilization |
| Mitchell, 1986[28] | RCT | >2 years | Admitted for asthma at single institution in New Zealand. | Having a previous life‐threatening attack. | 6 monthly postdischarge education sessions on lung anatomy/physiology, triggers and avoidance, asthma medication, advice on when and where to seek care (n=94 children of European descent, n=84 children of Polynesian descent) | Standard discharge (n=106 children of European descent; n=84 children of Polynesian descent) |
| Cancer | ||||||
| Caliskan Yilmaz, 2009[29] | Quasiexperimental | 18 years | New oncologic diagnoses in hospital in Turkey. | Children who died during follow‐up. | Frequent needs assessment, education, home visits, fever guidance, telephone consultation, and manual for home care; patients lived in Izmir (n=25) | Routine hospital services without formal education; patients lived outside of Izmir (n=24) |
| NICU | ||||||
| Broyles, 2000[30] | RCT | Neonate | Infants with birth weight 1500 g with mechanical vent use in 48 hours of life, born at single NICU in Texas. | Infant death, infant adopted or moved out of enrollment county. | Specialized follow‐up available 5 days a week for well or sick visits; access to medical advice via phone 24 hours a day, transportation to ED provided when needed; home visitation, parent education, and "foster grandmother" offered (n=446) | Specialized follow‐up available 2 mornings a week for well or sick visits; all other sick visits to be made through acute care clinic or ED (n=441) |
| Finello, 1998[31] | RCT | Neonate | Infants with birth weight between 750 and1750 g; discharged from 2 NICUs in California. | Infants with gross abnormalities. | Three separate intervention groups (n=20 in each): (1) home healthhome visits during the first 4 weeks after discharge, with physician consultation available at all times; (2) home visitinghealth and development support, parental support, support with referral services for 2 years after discharge; (3) home health and home visiting arms combined | Standard discharge (n=20). |
| Kotagal, 1995[32] | Pre‐post | Neonate | Infants discharged from a single NICU in Ohio. | Patients (n=257) discharged after restructuring of discharge practices including: removal of discharge weight criteria, engagement of family prior to discharge, evaluation of home environment prior to discharge, and arrangement of home health visits and follow‐up | Patients discharged before discharge restructuring (n=483) | |
| Casiro, 1993[33] | RCT | Neonate | Infants meeting discharge criteria from 1 of 2 NICUs in Canada. | Congenital anomalies, chronic neonatal illness, parent refusal, family complications, and death. | Early discharge based on prespecified criteria with 8 weeks of services including: assistance with infant care, sibling care and housekeeping; nurse availability via phone; follow‐up phone calls and home visitation tailored to family need (n=50) | Discharged at the discretion of their attending physicians; standard newborn public health referral for routine follow‐up (n=50) |
| Brooten, 1986[34] | RCT | Neonate | Infants born 1500 g at a single NICU in Pennsylvania. | Death, life‐threatening congenital anomalies, grade 4 IVH, surgical history, O2 requirement >10 weeks, family complications. | Early discharge based on prespecified criteria with weekly education prior to discharge, postdischarge follow‐up phone call, and home nurse visitation; consistent nurse availability via phone (n=39) | Standard discharge practices with a discharge weight minimum of 2.2 kg (n=40) |
Studies varied regarding the timing and nature of the intervention components. Eight discharge interventions included a major inpatient component, in addition to outpatient support or follow‐up.[21, 23, 24, 25, 26, 29, 32, 34] Two studies included an inpatient education component only.[22, 27] The remainder were initiated during index hospitalization but focused primarily on home visitation, enhanced follow‐up, and support after discharge (Figure 2).[28, 30, 31, 33]
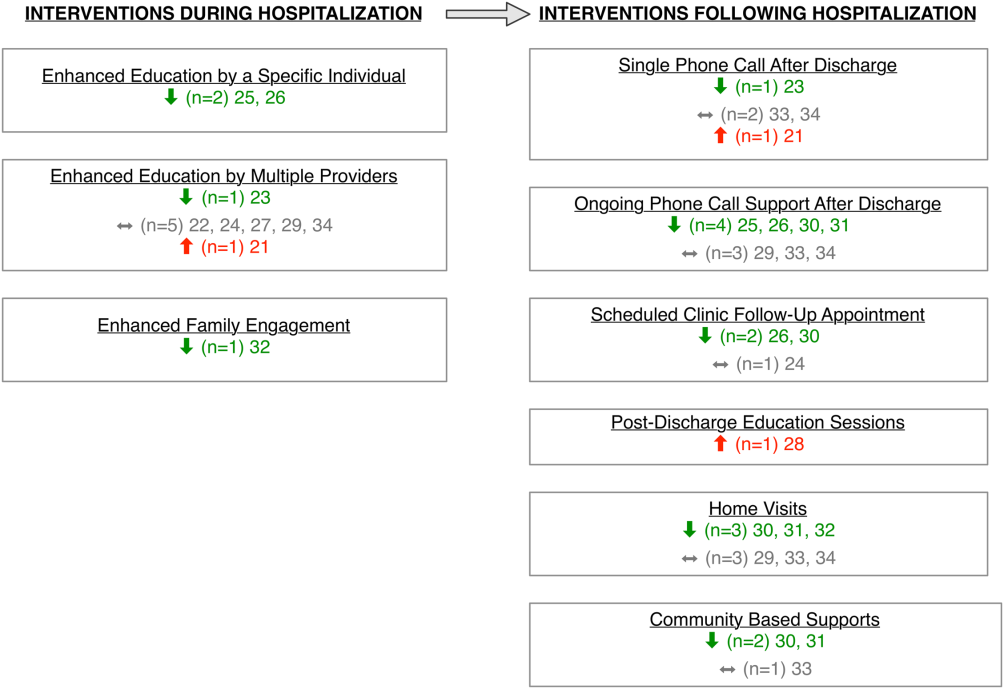
Outcome Assessment Methods
Readmission and subsequent ED utilization events were identified using multiple techniques. Some authors accessed claims records to capture all outcomes.[30, 33] Others relied on chart review.[21, 25, 26, 27, 28, 31, 32] One study supplemented hospital records with outpatient records.[24] Some investigators used parental reports.[22, 23, 31] Two studies did not describe methods for identifying postdischarge events.[29, 34]
Study Quality
The quality of the included studies varied (Table 2). Many of the studies had inadequate sample size to detect a difference in either readmission or ED visit subsequent to discharge. Eight studies found differences in either subsequent ED utilization, hospitalization, or both and were considered adequately powered for these specific outcomes.[21, 23, 25, 26, 28, 30, 31, 32] In contrast, among studies with readmission as an outcome, 6 were not adequately powered to detect a difference in this particular outcome.[24, 30, 31, 32, 33, 34] In these 6 studies, all except 1 study30 had 10% of the sample size required to detect differences in readmission. Further, 2 studies that examined ED utilization were underpowered to detect differences between intervention and control groups.[24, 26] We were unable to perform power calculations for 3 studies,[22, 27, 29] as the authors presented the number of events without clear denominators.
| Author, Year | Study Design | D&B Score* | Adequately Powered (Yes/No)** | Timing of Outcome | Major Findings | Major Limitations |
|---|---|---|---|---|---|---|
| ||||||
| Asthma | ||||||
| Davis, 2011[21] | Retrospective matched case control | 14 | Readmission: N/A; ED: yes | 1 year | Patients with enhanced education had higher hazards of return to ED visit. | Intervention not randomized; only 29% of eligible children enrolled with unclear selection decisions due to lack of study personnel or caregiver presence in hospital; only 67% completed the intervention; 50% of patients were not local; follow‐up was not well described. |
| Espinoza‐Palma, 2009[22] | RCT | 19 | Readmission: b; ED:b | 1 year | No difference between the intervention and control in hospitalizations or ED visits. ED visits and hospitalizations decreased in year after compared to the year prior for both intervention and control. | Pre‐post analysis with similar effects in cases and controls, results may reflect regression to mean; follow‐up was not well described, and 12.5% who were lost to follow‐up were excluded from analysis; study was in Chile with different demographics than in the United States. |
| Ng, 2006[23] | RCT | 20 | Readmission: yes; ED: yes | 3 months | Patients in the intervention group were less likely to be readmitted or visit the ED. | Recruitment/refusal was not well described; number lost to follow‐up was not reported; study was in China with different demographics than the United States. |
| Stevens, 2002[24] | RCT | 20 | Readmission: no ED: no | 1 year | No differences between intervention and control for any outcomes. | 11% were lost to follow‐up; number of patients who refused was not reported; analysis did not adjust for site of recruitment (ED vs inpatient); 30% of children did not have a prior diagnosis of asthma; study was in England with different demographics than in the United States. |
| Wesseldine, 1999[25] | RCT | 20 | Readmission: yes; ED: yes | 6 months | Patients in intervention group less likely to be readmitted or visit ED. | Unclear if intervention group received oral steroids that might drive effect; number lost to follow‐up was not reported; high miss rate for recruitment; study was in England with different demographics than the United States. |
| Madge, 1997 [26] | RCT | 22 | Readmission: yes; ED: no | 214 months | Patients in intervention group were less likely to be readmitted compared to controls. No differences in repeat ED visits. | Unclear if education or oral steroids drove effect; number of patients who refused or were lost to follow‐not reported; time to outcome (214 months) varied for different patients, which may introduce bias given the seasonality of asthma; study was in Scotland with different demographics than the United States. |
| Taggart, 1991[27] | Pre‐post | 12 | Readmission:b; ED:b | 15 months | Overall there was no change in ED or hospitalization utilization from pre to post. When limited to children with severe asthma, there was a decrease in ED utilization after the intervention compared to prior ED use. | Use of historical utilization as a comparison does not account for potential effects of regression to mean or improvement with age; over one‐half of eligible patients were excluded due to lack of consent or inability to collect baseline data; inclusion criterion did not specify that prior utilization was necessarily for asthma exacerbation; number lost to follow‐up was not reported. |
| Mitchell, 1986[28] | RCT | 14 | Readmission: yesc; ED: N/A | 6 months and 618 months | Increase in percentage of readmission between 6 and 18 months for children of European descent. | Unclear exclusion criterion; full compliance with intervention only 52%; number of patients lost to follow‐up (outcome) was not reported; statistical analysis was not clearly described. |
| Cancer | ||||||
| Caliskan Yilmaz, 2009[29] | Quasiexperimental | 10 | Readmission:b; ED: N/A | Not specified | For the first readmission to the hospital, more of the readmissions were planned in the intervention group compared to the control group. Number of readmissions was not assessed. | Intervention was not randomized; children who died were excluded (4%); planned vs unplanned distinction not validated; unclear cointerventions regarding chemotherapy administration; recruitment and follow‐up was not well described; not all comparisons were described in methods. |
| NICU | ||||||
| Broyles, 2000[30] | RCT | 23 | Readmission: no; ED: yes | At 1 year adjusted age | Overall hospitalization rates were similar but there were fewer admissions to the ICU. Intervention group had fewer ED visits. Total costs were less in intervention group. | 10% refused to participate or consent was not sought, and 12% were excluded after randomization; different periods of follow‐up (outcomes observed at 1 year of life regardless of discharge timing); analysis did not adjust for site of recruitment (1 of 2 nurseries). |
| Finello, 1998[31] | RCT | 11 | Readmission: nod; ED: yes | At 6 months adjusted age and between 6 and 12 months adjusted age | No changes in hospitalization rates.d The home health+home visit arm had fewer ED visits between 6 and 12 months of life. Intervention was reported as saving money by decreasing initial length of stay. | Inclusion and exclusion criteria, recruitment/refusal, outcomes, and analysis plan were not clearly described; sample size was too small for effective randomization; different periods of follow‐up (outcomes observed at 1 year of life regardless of discharge timing); analysis did not adjust for site of recruitment; 15% of outcomes were missing. |
| Kotagal, 1995[32] | Pre‐post | 15 | Readmission: no; ED: yes | 14 days | Decreased number of ED visits in patients in intervention. No difference in readmission. Costs and length of stay were less in intervention. | Designed to decrease length of stay; pre‐post nature of study allows for possibility of other changes to practices other than the intervention. |
| Casiro, 1993[33] | RCT | 18 | Readmission: no; ED: N/A | 1 year of life | There were no differences in the readmissions or number of ambulatory care visits after discharge. Infants were discharged earlier in the intervention group, which resulted in cost savings. | Designed to decrease length of stay; 13% refused or were excluded due to family complications; and 8% were lost to follow‐up; different periods of follow‐up (outcomes observed at 1 year of life regardless of discharge timing); analysis did not adjust for site of recruitment (1 of 2 nurseries); 81% of infants were born to Caucasian women, which may limit generalizability. |
| Brooten, 1986[34] | RCT | 15 | Readmission: no; ED: N/A | 14 days and 18 months | No difference in readmission. Significantly lower charges during initial hospitalization for intervention group. | Designed to decrease length of stay; unclear when randomization occurred and exclusions unclear; 12.5% were excluded due to refusal or family issues; follow‐up not well described, and loss to follow‐up was unknown. |
Excluding the assessment of statistical power, Downs and Black scores ranged from 10 to 23 (maximum 28 possible points) indicating varying quality. As would be expected with discharge interventions, studies did not blind participants; 2 studies did, however, appropriately blind the outcome evaluators to intervention assignment.[22, 30] Even though 10 out of the 14 studies were randomized controlled trials, randomization may not have been completely effective due to sample size being too small for effective randomization,[31] large numbers of excluded subjects after randomization,[30] and unclear randomization process.[34] Several studies had varying follow‐up periods for patients within a given study. For example, 3 NICU studies assessed readmission at 1‐year corrected age,[30, 31, 33] creating the analytic difficulty that the amount of time a given patient was at risk for readmission was dependent on when the patient was discharged, yet this was not accounted for in the analyses. Only 2 studies demonstrated low rates of loss to follow‐up (10%).[30, 33] The remainder of the studies either had high incompletion/loss to follow‐up rates (>10%)[22, 24, 31] or did not report rates.[21, 23, 25, 26, 27, 28, 29, 32, 34] Finally, 3 studies recruited patients from multiple sites,[24, 31, 33] and none adjusted for potential differences in effect based on enrollment site.
Findings Across Patient Populations Regarding Readmission
Of the 4 studies that demonstrated change in overall readmission,[23, 25, 26, 28] all were asthma focused; 3 demonstrated a decrease in readmissions,[23, 25, 26] and 1 an increase in readmissions.[28] The 3 effective interventions included 1‐on‐1 inpatient education delivered by an asthma nurse, in addition to postdischarge follow‐up support, either by telephone or clinic visit. Two of these interventions provided rescue oral steroids to some patients on discharge.[25, 26] In contrast, a study from New Zealand evaluated a series of postdischarge visits using an existing public health nurse infrastructure and demonstrated an increase in readmission between 6 to 18 months after admission in European children.[28] An additional study focused on outpatient support after discharge from the NICU, and demonstrated a lower frequency of readmission to the intensive care unit without overall reduction of hospital readmission (Tables 1 and 2).[30]
Findings Across Patient Populations Regarding Subsequent ED Visits
Of all the discharge interventions, 6 demonstrated differences in return to the ED after discharge. Five studies described a decrease in ED visits after hospitalization,[23, 25, 30, 31, 32] and 1 showed an increase.[21] Three studies in the NICU population demonstrated decreased ED utilization through a combination of augmented family engagement during hospitalization and/or enhanced support after discharge. Two inpatient asthma education interventions with structured postdischarge follow‐up decreased return visitation to the ED.[23, 26] The intervention that worsened subsequent ED utilization (ie, increased ED visit hazard compared to matched controls) provided enhanced inpatient education to a nonrandom group of children hospitalized with asthma and provided a follow‐up phone call 3 weeks after discharge (Tables 1 and 2).[21]
DISCUSSION
In this review, we synthesized evidence regarding pediatric hospital discharge‐focused interventions intended to reduce subsequent utilization through decreased readmission and ED visits. Our review identified 14 studies clustered in 3 clinical areas: asthma, NICU care (chiefly prematurity), and cancer. Overall, 6 interventions demonstrated a reduction either in subsequent hospitalization or ED use. Four of the 6 positive interventions included both an enhanced inpatient education and engagement component as well as enhanced follow‐up after discharge. Importantly, all of the interventions were multifaceted; thus, we could not ascertain which specific aspects of the interventions mediated the change. Many of the included studies had significant methodological limitations.
Current Conceptual Framework
There are a number of existing discharge transitional care frameworks from prior studies[35, 36] and professional societies.[37] The Stepping Up to the Plate (SUTTP) alliance, a collaborative of 9 professional organizations, including the American Academy of Pediatrics, introduced 1 such framework in 2007. SUTTP sought to enhance care transitions by outlining principles of discharge transitional care including: (1) enhanced accountability, (2) creation of a central coordination hub charged with communicating expectations for care, (3) clear and direct communication of treatment plans and follow‐up, (4) timely feedback/feed‐forward of relevant information, and (5) involvement of family member at every stage.[38] In the context of the SUTTP framework, we present 3 hypotheses based on our findings to guide future work.
Hypothesis: Appointing a Dedicated Individual or Coordinating Hub Reduces Subsequent Utilization
Ostensibly, each discharge intervention included in this review sought to enhance accountability of providers or their health systems for discharge transitional care. Two of the asthma interventions appointed a particular provider to coordinate the discharge transition and demonstrated reductions in readmission.[25, 26] The successful NICU discharge interventions provided an integrated accountability structure across the health system, with a transition of accountability to an outpatient provider or central coordinating hub available to provide assistance and resources for an extended period following discharge.
By contrast, interventions with more than 1 individual intervener or without a centrally coordinated system for discharge transitional care tended not to demonstrate reduction in subsequent utilization.[21, 24, 27, 28] In fact, the 1 asthma intervention that utilized a previously existing public health nurse infrastructure demonstrated an increase in readmission.[28] Future efforts to enhance transitional care might investigate directly the impact of accountability structure on subsequent utilization by varying the number of effector individuals or the organization to which they report (eg, hospital system vs public health department).
Hypothesis: Individualized Task Learning and Feedback Enhances Effectiveness
Studies varied with respect to the extent they incorporated the principles of enhanced communication of the treatment and follow‐up plan and timely feedback/feed‐forward of relevant information. Successful efforts, however, seemed to embrace these strategies. Each of the 3 interventions that demonstrated readmission reduction[23, 25, 26] developed an individualized treatment plan during hospitalization, with either a specific follow‐up plan or resources for outpatient support. Two of these interventions assessed asthma inhaler technique prior to discharge, creating an inpatient audit and feedback loop allowing for assessment of competence prior to discharge. Audit and feedback has demonstrated promise modifying provider behavior[39] and is a plausible approach to enhancing patient and family self‐care.
Hypothesis: Timing of Intervention Enhances Effectiveness
Discrete sentinel events such as inpatient admission, may serve as a teachable moment[40, 41] or a tipping point[42] for some patients/families to initiate behavior change. Four of the 6 positive studies had a robust inpatient education component. By providing enhanced inpatient support, providers may be engaging the family at a timely opportunity to improve care. Both timing of the intervention (at admission vs discharge) and content (education‐ vs family‐engagement focused) are likely important to their effect and should be further explored with prospective study.
Persistent Literature Gaps
Follow‐up with a primary care provider after discharge is another intervention that might decrease postdischarge utilization. We did not identify any studies that specifically examined primary care follow‐up. However, 2 studies[43, 44] that did not meet our inclusion criteria (because they included adults and did not stratify by age group in the analysis) examined any outpatient follow‐up after discharge using state‐specific Medicaid claims. One study found that outpatient follow‐up after sickle cell hospitalization was associated with lower rates of readmission.[43] The other found no difference in readmission across multiple conditions.[44] One recent review of outpatient follow‐up from the ED for asthma found that even when increases in follow‐up were achieved, no reduction in the subsequent utilization was observed.[45]
Additional important questions remain underexplored. First, are condition‐specific interventions superior to those that span conditions? All of the interventions that demonstrated reductions in readmission were condition‐specific, yet no generic interventions met our inclusion criteria. Importantly, only 1 study[29] in our review examined discharge processes from 1 of the pediatric conditions with the most variation[8] in readmission. Further, no studies focused on children with complex medical conditions, who are known to be at increased risk of readmission,[46] indicating a sizable knowledge gap persists in understanding how to prevent readmissions in the most vulnerable pediatric populations.
Lastly, who are the most appropriate effector individuals for discharge‐focused transitional care interventions? Demographically matched effector individuals have shown promise in improving care using community health workers.[47, 48] The degree to which the identity of the intervener mediates subsequent ED and hospital utilization warrants further investigation.
Limitations of This Systematic Review
The studies included in this review assessed different outcomes at different intervals, precluding meta‐analysis. With greater consistency in the collection of data on the quality of discharge processes and their subsequent outcomes, future studies may offer further clarity as to which discharge‐oriented practices are more effective than others. Because we only identified literature in 3 pediatric conditions, generalizability beyond these conditions may be limited. The settings of the interventions also occurred in multiple countries; we excluded countries from low or low‐middle incomes to facilitate generalizability. As many of the discharge processes contained multiple interventions, it is not possible to ascertain which, if any, singular action may decrease posthospitalization utilization. Additionally, some of the included interventions are older, and it is plausible that discharge processes have evolved with the expansion of the hospitalist model.
Methods of data collection influence the quality of results in the included studies. Most of the studies included in this review used either medical record review or parental self‐report of utilization. Parental report may be sufficient for hospitalizations and ED utilization; however, it is subject to recall bias. Chart review likely underestimates the number of postdischarge events, depending on the individual institution's proportion of the market and the tendency of individuals to seek care at multiple institutions. Claims data may offer the most accurate assessments of ED and hospital utilization and cost, but can be more difficult to obtain and do not provide the same potential for granularity as parent report or medical records review.
Finally, subsequent ED visits, readmissions, and cost may not be the best measures of the quality of discharge transitional care. A number of tools have been developed to more specifically evaluate the quality of transitional care in adults,[49, 50] including a validated instrument that consists of only 3 items,[50] which primarily assesses the extent to which patients are prepared for self‐care upon discharge. For pediatric populations, validated tools assessing caregiver experience with discharge[51] and discharge readiness[52] are also available. These instruments may assist those interested in assessing process‐related outcomes that specifically assess discharge transitional care elements and may mediate subsequent ED visits or hospitalizations.
CONCLUSION
Successful discharge interventions to reduce pediatric readmission and ED have some common features, including an individual or team with specialized knowledge of the condition that assumed responsibility for the inpatient‐to‐outpatient transition and offered ongoing support to the family following discharge. All studies included in our review examined multiple discharge interventions; however, many did not have enough participants to detect differences in the outcomes of interest. Future studies might adapt common features of effective interventions, which are consistent with professional societies' recommendations.
Acknowledgements
The authors thank Marisa Conte for her help with developing the search algorithms for the review.
Disclosures: Drs. Auger and Kenyon received salary support from the Robert Wood Johnson Foundation Clinical Scholars program. Dr. Feudtner does not have any funding sources to disclose. Dr. Davis is funded in part by the Michigan Department of Community Health to serve as the Chief Medical Executive. The views expressed herein are not necessarily the views of the Department of Community Health. The authors have no conflicts of interest to report.
The process of discharging a pediatric patient from an acute care facility is currently fraught with difficulties. More than 20% of parents report problems in the transition of care from the hospital to the home and ambulatory care setting.[1] Clinical providers likewise note communication challenges around the time of discharge,[2, 3] especially when inpatient and outpatient providers are different, as with the hospitalist model.[4] Poor communication and problems in discharge transition and continuity of care often culminate in adverse events,[5, 6] including return to emergency department (ED) care and hospital readmission.[7]
Thirty‐day readmissions are common for certain pediatric conditions, such as oncologic diseases, transplantation, and sickle cell anemia and vary significantly across children's hospitals.[8] Discharge planning may decrease 30‐day readmissions in hospitalized adults[9]; however, it is not clear that the same is true in children. Both the preventability of pediatric readmissions[10] and the extent to which readmissions reflect suboptimal care[11] are subjects of debate. Despite these uncertainties, collaborative efforts intended to decrease pediatric readmissions[12] and improve discharge transitions[13, 14] are underway.
To inform these debates and efforts, we undertook a systematic review of the evidence of hospital‐initiated interventions to reduce repeat utilization of the ED and hospital. Acknowledging that existing evidence for condition‐specific discharge interventions in pediatrics might be limited, we sought to identify common elements of successful interventions across pediatric conditions.
METHODS
Search Strategy
With the assistance of a research librarian, we searched MEDLINE and CINAHL (Cumulative Index to Nursing and Allied Health Literature) from the inception of these databases through to March 28, 2012 (for search strategies, see the Supporting Information, Appendix, Part 1, in the online version of this article).
Study Selection
Two authors (K.A. and C.K.) independently reviewed abstracts identified by the initial search, as well as abstracts of references of included articles. Eligibility criteria for inclusion in full review included: (1) discharge‐oriented process or intervention initiated in the inpatient setting, (2) study outcomes related to subsequent utilization including hospital readmission or emergency department visit after hospitalization, (3) child‐ or adolescent‐focused or child‐specific results presented separately, and (4) written or available in English. If abstract review did not sufficiently clarify whether all eligibility criteria were met, the article was included in the full review. Two authors (K.A. and C.K.) independently reviewed articles meeting criteria for full review to determine eligibility. Disagreements regarding inclusion in the final analysis were discussed with all 4 authors. We excluded studies in countries with low or lower‐middle incomes,[15] as discharge interventions in these countries may not be broadly applicable.
Data Abstraction, Quality Assessment, and Data Synthesis
Two authors (K.A. and C.K.) independently abstracted data using a modified Cochrane Collaboration data collection form.[16] We independently scored the included studies using the Downs and Black checklist, which assesses the risk of bias and the quality of both randomized and nonrandomized studies.[17] This checklist yields a composite score of 0 to 28 points, excluding the item assessing power. As many studies either lacked power calculations or included power calculations based on outcomes not included in our review, we performed calculations to determine the sample size needed to detect a decrease in readmission or ED utilization by 20% from baseline or control rates. Due to the heterogeneous nature of included studies in terms of population, interventions, study design, and outcomes, meta‐analysis was not performed.
RESULTS
Electronic search yielded a total of 1296 unique citations. Review of abstracts identified 40 studies for full article review. We identified 10 articles that met all inclusion criteria. Subsequent review of references of included articles identified 20 additional articles for full review, 7 of which met all inclusion criteria. However, 3 articles[18, 19, 20] assessed the impact of violence interventions primarily on preventing reinjury and recidivism and thus were excluded (see Supporting Information, Appendix, Part 2, in the online version of this article for findings of the 3 articles). In total, we included 14 articles in our review[21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34] (Figure 1).
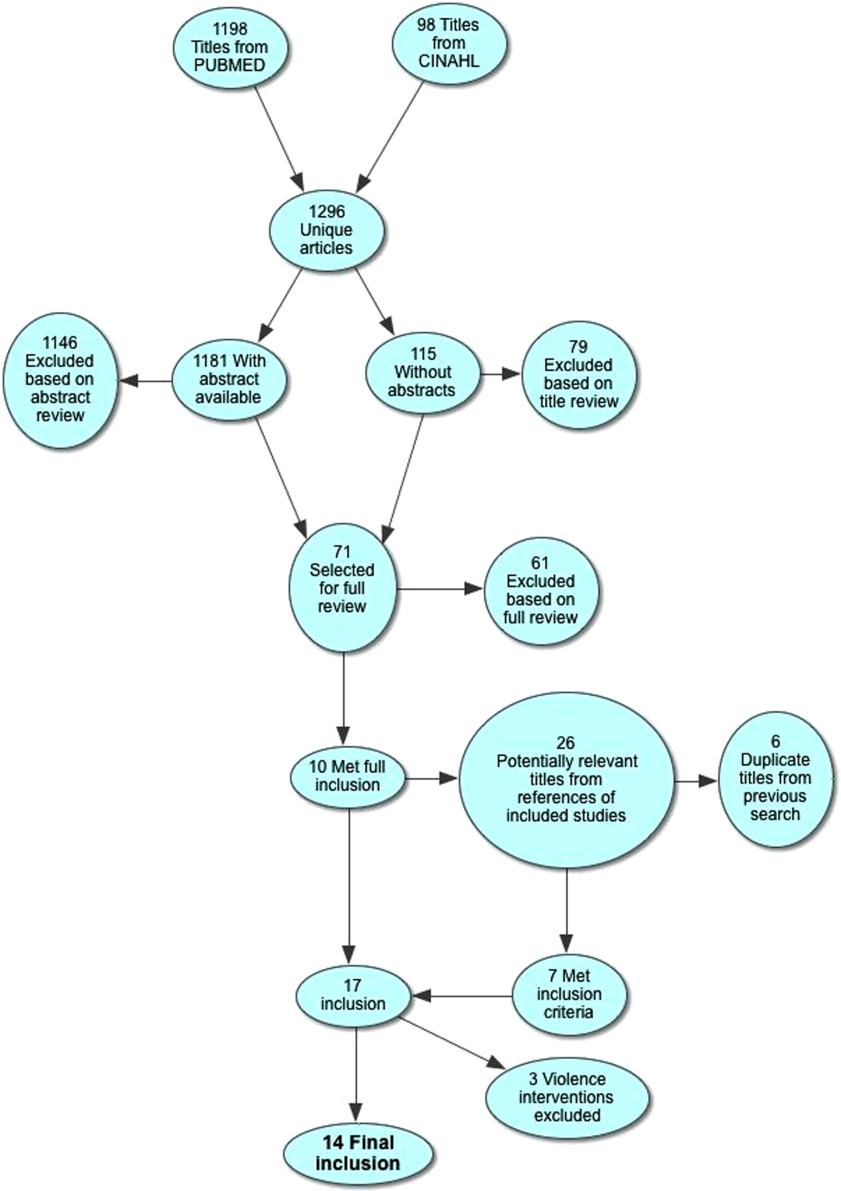
Patient Populations and Intervention Timing and Components
Studies varied regarding the specific medical conditions they evaluated. Eight of the papers reported discharge interventions for children with asthma, 5 papers focused on discharge from the neonatal intensive care unit (NICU), and a final study discussed a discharge intervention for children with cancer (Table 1). Although our primary goal was to synthesize discharge interventions across pediatric conditions, we provide a summary of discharge interventions by condition (see Supporting Information, Appendix, Part 3, in the online version of this article).
| Author, Year | Study Design | Age | Inclusion | Exclusion | Intervention | Control |
|---|---|---|---|---|---|---|
| ||||||
| Asthma | ||||||
| Davis, 2011[21] | Retrospective matched case control | 12 months18 years | Admitted for asthma at a single hospital in California. | 45 minutes of enhanced asthma education and phone call 3 weeks after discharge (n=698) | Patients were matched on age and past utilization who received standard education/care (n=698) | |
| Espinoza‐Palma, 2009[22] | RCT | 515 years | Admitted for asthma at a single hospital in Chile. | Chronic lung disease or neurologic alteration. | Self‐management education program with a postdischarge game to reinforce educational concepts (n=42) | Standard education (n=46) |
| Ng, 2006[23] | RCT | 215 years | Admitted for asthma in a pediatric ward at a single hospital in China. | Admitted to PICU or non‐Chinese speaking. | Evaluation by asthma nurse, animated asthma education booklet, 50‐minute discharge teaching session, follow‐up by phone at 1 week (n=55) | Evaluation by asthma nurse by physician referral, a written asthma education booklet, 30‐minute discharge teaching session (n=45) |
| Stevens, 2002[24] | RCT | 18 months5 years | In ED or admitted with primary diagnosis of asthma/wheezing at 2 hospitals in the United Kingdom. | Admitted when no researcher available. | Enhanced asthma education and follow‐up in a clinic 1 month after encounter (n=101) | Usual care (n=99) |
| Wesseldine, 1999[25] | RCT | 216 years | Admitted for asthma at a single hospital in the United Kingdom. | Admitted when no researcher available. | 20 minutes of enhanced asthma education including: guided self‐management plan, booklet, asthma hotline contact, and sometimes oral steroids (n=80) | Standard discharge that varied by provider (n=80) |
| Madge, 1997[26] | RCT | 214 years | Admitted for asthma at a single hospital in the United Kingdom. | Admitted on weekend. | 45 minutes of enhanced asthma education with written asthma plan, a nurse follow‐up visit 23 weeks postdischarge, telephone support, and a course of oral steroids (n=96) | Standard education (did not include written asthma plan) (n=105) |
| Taggart, 1991[27] | Pre‐post | 612 years | Admitted for asthma at single institution in Washington, DC with history of at least one ED visit in prior 6 months. | If resided outside of metro area. | Received written educational materials, adherence assistance, discussed emotions of asthma, video education provided, and tailored nursing interactions (n=40) | Enrolled patient's prior utilization |
| Mitchell, 1986[28] | RCT | >2 years | Admitted for asthma at single institution in New Zealand. | Having a previous life‐threatening attack. | 6 monthly postdischarge education sessions on lung anatomy/physiology, triggers and avoidance, asthma medication, advice on when and where to seek care (n=94 children of European descent, n=84 children of Polynesian descent) | Standard discharge (n=106 children of European descent; n=84 children of Polynesian descent) |
| Cancer | ||||||
| Caliskan Yilmaz, 2009[29] | Quasiexperimental | 18 years | New oncologic diagnoses in hospital in Turkey. | Children who died during follow‐up. | Frequent needs assessment, education, home visits, fever guidance, telephone consultation, and manual for home care; patients lived in Izmir (n=25) | Routine hospital services without formal education; patients lived outside of Izmir (n=24) |
| NICU | ||||||
| Broyles, 2000[30] | RCT | Neonate | Infants with birth weight 1500 g with mechanical vent use in 48 hours of life, born at single NICU in Texas. | Infant death, infant adopted or moved out of enrollment county. | Specialized follow‐up available 5 days a week for well or sick visits; access to medical advice via phone 24 hours a day, transportation to ED provided when needed; home visitation, parent education, and "foster grandmother" offered (n=446) | Specialized follow‐up available 2 mornings a week for well or sick visits; all other sick visits to be made through acute care clinic or ED (n=441) |
| Finello, 1998[31] | RCT | Neonate | Infants with birth weight between 750 and1750 g; discharged from 2 NICUs in California. | Infants with gross abnormalities. | Three separate intervention groups (n=20 in each): (1) home healthhome visits during the first 4 weeks after discharge, with physician consultation available at all times; (2) home visitinghealth and development support, parental support, support with referral services for 2 years after discharge; (3) home health and home visiting arms combined | Standard discharge (n=20). |
| Kotagal, 1995[32] | Pre‐post | Neonate | Infants discharged from a single NICU in Ohio. | Patients (n=257) discharged after restructuring of discharge practices including: removal of discharge weight criteria, engagement of family prior to discharge, evaluation of home environment prior to discharge, and arrangement of home health visits and follow‐up | Patients discharged before discharge restructuring (n=483) | |
| Casiro, 1993[33] | RCT | Neonate | Infants meeting discharge criteria from 1 of 2 NICUs in Canada. | Congenital anomalies, chronic neonatal illness, parent refusal, family complications, and death. | Early discharge based on prespecified criteria with 8 weeks of services including: assistance with infant care, sibling care and housekeeping; nurse availability via phone; follow‐up phone calls and home visitation tailored to family need (n=50) | Discharged at the discretion of their attending physicians; standard newborn public health referral for routine follow‐up (n=50) |
| Brooten, 1986[34] | RCT | Neonate | Infants born 1500 g at a single NICU in Pennsylvania. | Death, life‐threatening congenital anomalies, grade 4 IVH, surgical history, O2 requirement >10 weeks, family complications. | Early discharge based on prespecified criteria with weekly education prior to discharge, postdischarge follow‐up phone call, and home nurse visitation; consistent nurse availability via phone (n=39) | Standard discharge practices with a discharge weight minimum of 2.2 kg (n=40) |
Studies varied regarding the timing and nature of the intervention components. Eight discharge interventions included a major inpatient component, in addition to outpatient support or follow‐up.[21, 23, 24, 25, 26, 29, 32, 34] Two studies included an inpatient education component only.[22, 27] The remainder were initiated during index hospitalization but focused primarily on home visitation, enhanced follow‐up, and support after discharge (Figure 2).[28, 30, 31, 33]
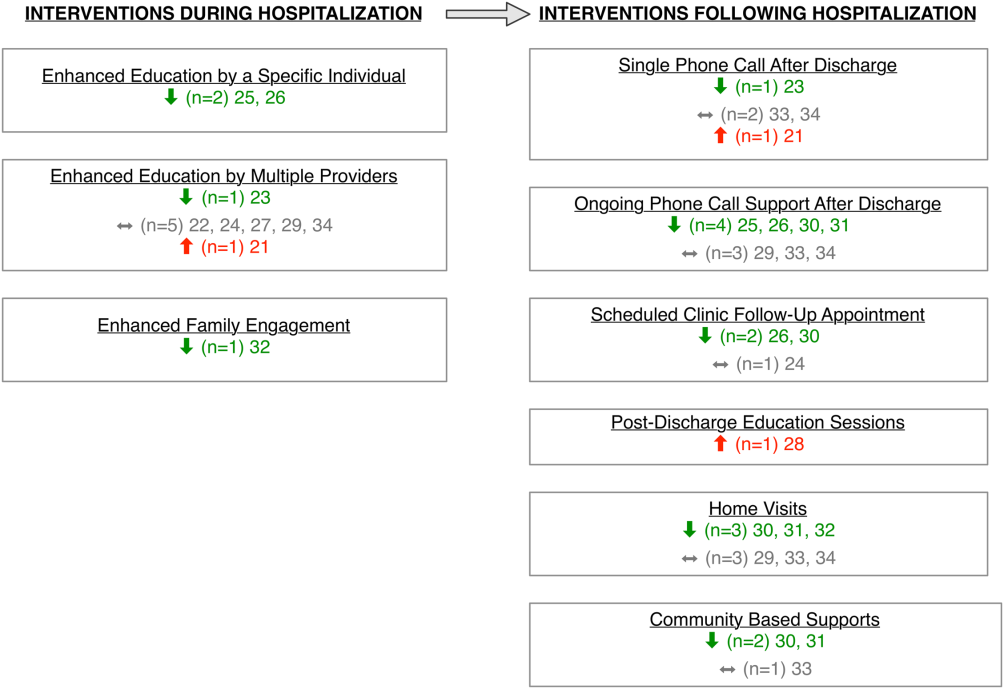
Outcome Assessment Methods
Readmission and subsequent ED utilization events were identified using multiple techniques. Some authors accessed claims records to capture all outcomes.[30, 33] Others relied on chart review.[21, 25, 26, 27, 28, 31, 32] One study supplemented hospital records with outpatient records.[24] Some investigators used parental reports.[22, 23, 31] Two studies did not describe methods for identifying postdischarge events.[29, 34]
Study Quality
The quality of the included studies varied (Table 2). Many of the studies had inadequate sample size to detect a difference in either readmission or ED visit subsequent to discharge. Eight studies found differences in either subsequent ED utilization, hospitalization, or both and were considered adequately powered for these specific outcomes.[21, 23, 25, 26, 28, 30, 31, 32] In contrast, among studies with readmission as an outcome, 6 were not adequately powered to detect a difference in this particular outcome.[24, 30, 31, 32, 33, 34] In these 6 studies, all except 1 study30 had 10% of the sample size required to detect differences in readmission. Further, 2 studies that examined ED utilization were underpowered to detect differences between intervention and control groups.[24, 26] We were unable to perform power calculations for 3 studies,[22, 27, 29] as the authors presented the number of events without clear denominators.
| Author, Year | Study Design | D&B Score* | Adequately Powered (Yes/No)** | Timing of Outcome | Major Findings | Major Limitations |
|---|---|---|---|---|---|---|
| ||||||
| Asthma | ||||||
| Davis, 2011[21] | Retrospective matched case control | 14 | Readmission: N/A; ED: yes | 1 year | Patients with enhanced education had higher hazards of return to ED visit. | Intervention not randomized; only 29% of eligible children enrolled with unclear selection decisions due to lack of study personnel or caregiver presence in hospital; only 67% completed the intervention; 50% of patients were not local; follow‐up was not well described. |
| Espinoza‐Palma, 2009[22] | RCT | 19 | Readmission: b; ED:b | 1 year | No difference between the intervention and control in hospitalizations or ED visits. ED visits and hospitalizations decreased in year after compared to the year prior for both intervention and control. | Pre‐post analysis with similar effects in cases and controls, results may reflect regression to mean; follow‐up was not well described, and 12.5% who were lost to follow‐up were excluded from analysis; study was in Chile with different demographics than in the United States. |
| Ng, 2006[23] | RCT | 20 | Readmission: yes; ED: yes | 3 months | Patients in the intervention group were less likely to be readmitted or visit the ED. | Recruitment/refusal was not well described; number lost to follow‐up was not reported; study was in China with different demographics than the United States. |
| Stevens, 2002[24] | RCT | 20 | Readmission: no ED: no | 1 year | No differences between intervention and control for any outcomes. | 11% were lost to follow‐up; number of patients who refused was not reported; analysis did not adjust for site of recruitment (ED vs inpatient); 30% of children did not have a prior diagnosis of asthma; study was in England with different demographics than in the United States. |
| Wesseldine, 1999[25] | RCT | 20 | Readmission: yes; ED: yes | 6 months | Patients in intervention group less likely to be readmitted or visit ED. | Unclear if intervention group received oral steroids that might drive effect; number lost to follow‐up was not reported; high miss rate for recruitment; study was in England with different demographics than the United States. |
| Madge, 1997 [26] | RCT | 22 | Readmission: yes; ED: no | 214 months | Patients in intervention group were less likely to be readmitted compared to controls. No differences in repeat ED visits. | Unclear if education or oral steroids drove effect; number of patients who refused or were lost to follow‐not reported; time to outcome (214 months) varied for different patients, which may introduce bias given the seasonality of asthma; study was in Scotland with different demographics than the United States. |
| Taggart, 1991[27] | Pre‐post | 12 | Readmission:b; ED:b | 15 months | Overall there was no change in ED or hospitalization utilization from pre to post. When limited to children with severe asthma, there was a decrease in ED utilization after the intervention compared to prior ED use. | Use of historical utilization as a comparison does not account for potential effects of regression to mean or improvement with age; over one‐half of eligible patients were excluded due to lack of consent or inability to collect baseline data; inclusion criterion did not specify that prior utilization was necessarily for asthma exacerbation; number lost to follow‐up was not reported. |
| Mitchell, 1986[28] | RCT | 14 | Readmission: yesc; ED: N/A | 6 months and 618 months | Increase in percentage of readmission between 6 and 18 months for children of European descent. | Unclear exclusion criterion; full compliance with intervention only 52%; number of patients lost to follow‐up (outcome) was not reported; statistical analysis was not clearly described. |
| Cancer | ||||||
| Caliskan Yilmaz, 2009[29] | Quasiexperimental | 10 | Readmission:b; ED: N/A | Not specified | For the first readmission to the hospital, more of the readmissions were planned in the intervention group compared to the control group. Number of readmissions was not assessed. | Intervention was not randomized; children who died were excluded (4%); planned vs unplanned distinction not validated; unclear cointerventions regarding chemotherapy administration; recruitment and follow‐up was not well described; not all comparisons were described in methods. |
| NICU | ||||||
| Broyles, 2000[30] | RCT | 23 | Readmission: no; ED: yes | At 1 year adjusted age | Overall hospitalization rates were similar but there were fewer admissions to the ICU. Intervention group had fewer ED visits. Total costs were less in intervention group. | 10% refused to participate or consent was not sought, and 12% were excluded after randomization; different periods of follow‐up (outcomes observed at 1 year of life regardless of discharge timing); analysis did not adjust for site of recruitment (1 of 2 nurseries). |
| Finello, 1998[31] | RCT | 11 | Readmission: nod; ED: yes | At 6 months adjusted age and between 6 and 12 months adjusted age | No changes in hospitalization rates.d The home health+home visit arm had fewer ED visits between 6 and 12 months of life. Intervention was reported as saving money by decreasing initial length of stay. | Inclusion and exclusion criteria, recruitment/refusal, outcomes, and analysis plan were not clearly described; sample size was too small for effective randomization; different periods of follow‐up (outcomes observed at 1 year of life regardless of discharge timing); analysis did not adjust for site of recruitment; 15% of outcomes were missing. |
| Kotagal, 1995[32] | Pre‐post | 15 | Readmission: no; ED: yes | 14 days | Decreased number of ED visits in patients in intervention. No difference in readmission. Costs and length of stay were less in intervention. | Designed to decrease length of stay; pre‐post nature of study allows for possibility of other changes to practices other than the intervention. |
| Casiro, 1993[33] | RCT | 18 | Readmission: no; ED: N/A | 1 year of life | There were no differences in the readmissions or number of ambulatory care visits after discharge. Infants were discharged earlier in the intervention group, which resulted in cost savings. | Designed to decrease length of stay; 13% refused or were excluded due to family complications; and 8% were lost to follow‐up; different periods of follow‐up (outcomes observed at 1 year of life regardless of discharge timing); analysis did not adjust for site of recruitment (1 of 2 nurseries); 81% of infants were born to Caucasian women, which may limit generalizability. |
| Brooten, 1986[34] | RCT | 15 | Readmission: no; ED: N/A | 14 days and 18 months | No difference in readmission. Significantly lower charges during initial hospitalization for intervention group. | Designed to decrease length of stay; unclear when randomization occurred and exclusions unclear; 12.5% were excluded due to refusal or family issues; follow‐up not well described, and loss to follow‐up was unknown. |
Excluding the assessment of statistical power, Downs and Black scores ranged from 10 to 23 (maximum 28 possible points) indicating varying quality. As would be expected with discharge interventions, studies did not blind participants; 2 studies did, however, appropriately blind the outcome evaluators to intervention assignment.[22, 30] Even though 10 out of the 14 studies were randomized controlled trials, randomization may not have been completely effective due to sample size being too small for effective randomization,[31] large numbers of excluded subjects after randomization,[30] and unclear randomization process.[34] Several studies had varying follow‐up periods for patients within a given study. For example, 3 NICU studies assessed readmission at 1‐year corrected age,[30, 31, 33] creating the analytic difficulty that the amount of time a given patient was at risk for readmission was dependent on when the patient was discharged, yet this was not accounted for in the analyses. Only 2 studies demonstrated low rates of loss to follow‐up (10%).[30, 33] The remainder of the studies either had high incompletion/loss to follow‐up rates (>10%)[22, 24, 31] or did not report rates.[21, 23, 25, 26, 27, 28, 29, 32, 34] Finally, 3 studies recruited patients from multiple sites,[24, 31, 33] and none adjusted for potential differences in effect based on enrollment site.
Findings Across Patient Populations Regarding Readmission
Of the 4 studies that demonstrated change in overall readmission,[23, 25, 26, 28] all were asthma focused; 3 demonstrated a decrease in readmissions,[23, 25, 26] and 1 an increase in readmissions.[28] The 3 effective interventions included 1‐on‐1 inpatient education delivered by an asthma nurse, in addition to postdischarge follow‐up support, either by telephone or clinic visit. Two of these interventions provided rescue oral steroids to some patients on discharge.[25, 26] In contrast, a study from New Zealand evaluated a series of postdischarge visits using an existing public health nurse infrastructure and demonstrated an increase in readmission between 6 to 18 months after admission in European children.[28] An additional study focused on outpatient support after discharge from the NICU, and demonstrated a lower frequency of readmission to the intensive care unit without overall reduction of hospital readmission (Tables 1 and 2).[30]
Findings Across Patient Populations Regarding Subsequent ED Visits
Of all the discharge interventions, 6 demonstrated differences in return to the ED after discharge. Five studies described a decrease in ED visits after hospitalization,[23, 25, 30, 31, 32] and 1 showed an increase.[21] Three studies in the NICU population demonstrated decreased ED utilization through a combination of augmented family engagement during hospitalization and/or enhanced support after discharge. Two inpatient asthma education interventions with structured postdischarge follow‐up decreased return visitation to the ED.[23, 26] The intervention that worsened subsequent ED utilization (ie, increased ED visit hazard compared to matched controls) provided enhanced inpatient education to a nonrandom group of children hospitalized with asthma and provided a follow‐up phone call 3 weeks after discharge (Tables 1 and 2).[21]
DISCUSSION
In this review, we synthesized evidence regarding pediatric hospital discharge‐focused interventions intended to reduce subsequent utilization through decreased readmission and ED visits. Our review identified 14 studies clustered in 3 clinical areas: asthma, NICU care (chiefly prematurity), and cancer. Overall, 6 interventions demonstrated a reduction either in subsequent hospitalization or ED use. Four of the 6 positive interventions included both an enhanced inpatient education and engagement component as well as enhanced follow‐up after discharge. Importantly, all of the interventions were multifaceted; thus, we could not ascertain which specific aspects of the interventions mediated the change. Many of the included studies had significant methodological limitations.
Current Conceptual Framework
There are a number of existing discharge transitional care frameworks from prior studies[35, 36] and professional societies.[37] The Stepping Up to the Plate (SUTTP) alliance, a collaborative of 9 professional organizations, including the American Academy of Pediatrics, introduced 1 such framework in 2007. SUTTP sought to enhance care transitions by outlining principles of discharge transitional care including: (1) enhanced accountability, (2) creation of a central coordination hub charged with communicating expectations for care, (3) clear and direct communication of treatment plans and follow‐up, (4) timely feedback/feed‐forward of relevant information, and (5) involvement of family member at every stage.[38] In the context of the SUTTP framework, we present 3 hypotheses based on our findings to guide future work.
Hypothesis: Appointing a Dedicated Individual or Coordinating Hub Reduces Subsequent Utilization
Ostensibly, each discharge intervention included in this review sought to enhance accountability of providers or their health systems for discharge transitional care. Two of the asthma interventions appointed a particular provider to coordinate the discharge transition and demonstrated reductions in readmission.[25, 26] The successful NICU discharge interventions provided an integrated accountability structure across the health system, with a transition of accountability to an outpatient provider or central coordinating hub available to provide assistance and resources for an extended period following discharge.
By contrast, interventions with more than 1 individual intervener or without a centrally coordinated system for discharge transitional care tended not to demonstrate reduction in subsequent utilization.[21, 24, 27, 28] In fact, the 1 asthma intervention that utilized a previously existing public health nurse infrastructure demonstrated an increase in readmission.[28] Future efforts to enhance transitional care might investigate directly the impact of accountability structure on subsequent utilization by varying the number of effector individuals or the organization to which they report (eg, hospital system vs public health department).
Hypothesis: Individualized Task Learning and Feedback Enhances Effectiveness
Studies varied with respect to the extent they incorporated the principles of enhanced communication of the treatment and follow‐up plan and timely feedback/feed‐forward of relevant information. Successful efforts, however, seemed to embrace these strategies. Each of the 3 interventions that demonstrated readmission reduction[23, 25, 26] developed an individualized treatment plan during hospitalization, with either a specific follow‐up plan or resources for outpatient support. Two of these interventions assessed asthma inhaler technique prior to discharge, creating an inpatient audit and feedback loop allowing for assessment of competence prior to discharge. Audit and feedback has demonstrated promise modifying provider behavior[39] and is a plausible approach to enhancing patient and family self‐care.
Hypothesis: Timing of Intervention Enhances Effectiveness
Discrete sentinel events such as inpatient admission, may serve as a teachable moment[40, 41] or a tipping point[42] for some patients/families to initiate behavior change. Four of the 6 positive studies had a robust inpatient education component. By providing enhanced inpatient support, providers may be engaging the family at a timely opportunity to improve care. Both timing of the intervention (at admission vs discharge) and content (education‐ vs family‐engagement focused) are likely important to their effect and should be further explored with prospective study.
Persistent Literature Gaps
Follow‐up with a primary care provider after discharge is another intervention that might decrease postdischarge utilization. We did not identify any studies that specifically examined primary care follow‐up. However, 2 studies[43, 44] that did not meet our inclusion criteria (because they included adults and did not stratify by age group in the analysis) examined any outpatient follow‐up after discharge using state‐specific Medicaid claims. One study found that outpatient follow‐up after sickle cell hospitalization was associated with lower rates of readmission.[43] The other found no difference in readmission across multiple conditions.[44] One recent review of outpatient follow‐up from the ED for asthma found that even when increases in follow‐up were achieved, no reduction in the subsequent utilization was observed.[45]
Additional important questions remain underexplored. First, are condition‐specific interventions superior to those that span conditions? All of the interventions that demonstrated reductions in readmission were condition‐specific, yet no generic interventions met our inclusion criteria. Importantly, only 1 study[29] in our review examined discharge processes from 1 of the pediatric conditions with the most variation[8] in readmission. Further, no studies focused on children with complex medical conditions, who are known to be at increased risk of readmission,[46] indicating a sizable knowledge gap persists in understanding how to prevent readmissions in the most vulnerable pediatric populations.
Lastly, who are the most appropriate effector individuals for discharge‐focused transitional care interventions? Demographically matched effector individuals have shown promise in improving care using community health workers.[47, 48] The degree to which the identity of the intervener mediates subsequent ED and hospital utilization warrants further investigation.
Limitations of This Systematic Review
The studies included in this review assessed different outcomes at different intervals, precluding meta‐analysis. With greater consistency in the collection of data on the quality of discharge processes and their subsequent outcomes, future studies may offer further clarity as to which discharge‐oriented practices are more effective than others. Because we only identified literature in 3 pediatric conditions, generalizability beyond these conditions may be limited. The settings of the interventions also occurred in multiple countries; we excluded countries from low or low‐middle incomes to facilitate generalizability. As many of the discharge processes contained multiple interventions, it is not possible to ascertain which, if any, singular action may decrease posthospitalization utilization. Additionally, some of the included interventions are older, and it is plausible that discharge processes have evolved with the expansion of the hospitalist model.
Methods of data collection influence the quality of results in the included studies. Most of the studies included in this review used either medical record review or parental self‐report of utilization. Parental report may be sufficient for hospitalizations and ED utilization; however, it is subject to recall bias. Chart review likely underestimates the number of postdischarge events, depending on the individual institution's proportion of the market and the tendency of individuals to seek care at multiple institutions. Claims data may offer the most accurate assessments of ED and hospital utilization and cost, but can be more difficult to obtain and do not provide the same potential for granularity as parent report or medical records review.
Finally, subsequent ED visits, readmissions, and cost may not be the best measures of the quality of discharge transitional care. A number of tools have been developed to more specifically evaluate the quality of transitional care in adults,[49, 50] including a validated instrument that consists of only 3 items,[50] which primarily assesses the extent to which patients are prepared for self‐care upon discharge. For pediatric populations, validated tools assessing caregiver experience with discharge[51] and discharge readiness[52] are also available. These instruments may assist those interested in assessing process‐related outcomes that specifically assess discharge transitional care elements and may mediate subsequent ED visits or hospitalizations.
CONCLUSION
Successful discharge interventions to reduce pediatric readmission and ED have some common features, including an individual or team with specialized knowledge of the condition that assumed responsibility for the inpatient‐to‐outpatient transition and offered ongoing support to the family following discharge. All studies included in our review examined multiple discharge interventions; however, many did not have enough participants to detect differences in the outcomes of interest. Future studies might adapt common features of effective interventions, which are consistent with professional societies' recommendations.
Acknowledgements
The authors thank Marisa Conte for her help with developing the search algorithms for the review.
Disclosures: Drs. Auger and Kenyon received salary support from the Robert Wood Johnson Foundation Clinical Scholars program. Dr. Feudtner does not have any funding sources to disclose. Dr. Davis is funded in part by the Michigan Department of Community Health to serve as the Chief Medical Executive. The views expressed herein are not necessarily the views of the Department of Community Health. The authors have no conflicts of interest to report.
- , , , , . Are hospital characteristics associated with parental views of pediatric inpatient care quality? Pediatrics. 2003;111(2):308–314.
- , , , , , . Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841.
- , , , et al. Improving transitions of care at hospital discharge‐‐implications for pediatric hospitalists and primary care providers. J Healthc Qual. 2010;32(5):51–60.
- , . Hospitalists in children's hospitals: what we know now and what we need to know. J Pediatr. 2006;148(3):296–299.
- , , , , . The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–167.
- , , , et al. Adverse events among medical patients after discharge from hospital. CMAJ. 2004;170(3):345–349.
- , , , . Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003;18(8):646–651.
- , , , et al. Pediatric readmission prevalence and variability across hospitals. JAMA. 2013;309:372–380.
- , , , , , . Discharge planning from hospital to home. Cochrane Database Syst Rev. 2013;(1):CD000313.
- , , , , , . Preventability of early readmissions at a children's hospital. Pediatrics. 2012;131(1):e171–e181.
- , , , et al. State‐level child health system performance and the likelihood of readmission to children's hospitals. J Pediatr. 2010;157(1):98–102.e1.
- Ohio Children's Hospitals' solutions for patient safety. Available at: http://solutionsforpatientsafety.org/files/sps‐fact‐sheet.pdf. Accessed July 24, 2013.
- American Academy of Pediatrics. Value in inpatient pediatrics (VIP) network projects. Available at: http://www.aap.org/en‐us/professional‐resources/practice‐support/quality‐improvement/Quality‐Improvement‐Innovation‐Networks/Pages/Value‐in‐Inpatient‐Pediatrics‐Network‐Projects.aspx. Accessed July 24, 2013.
- Child Health Corporation of America. Resources for managing the patient discharge process. Available at: http://www.chca.com/news/index.html. Accessed October 31, 2013.
- The World Bank. World Development Indicators 2012. Available at: http://data.worldbank.org/sites/default/files/wdi‐2012‐ebook.pdf. Accessed July 5, 2013.
- The Cochrane Collaboration. Data collection form: Intervention review—RCTs and non‐RCTs. Available at: http://hiv.cochrane.org/sites/hiv.cochrane.org/files/uploads/Data%20extraction%20form_all%20studies.docx. Accessed July 24, 2013.
- , . The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non‐randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384.
- , , , et al. Brief violence interventions with community case management services are effective for high‐risk trauma patients. J Trauma. 2011;71(1):228–237.
- , , , , , . Benefits of a hospital‐based peer intervention program for violently injured youth. J Am Coll Surg. 2007;205(5):684–689.
- , , , , . Caught in the crossfire: the effects of a peer‐based intervention program for violently injured youth. J Adolesc Health. 2004;34(3):177–183.
- , , , , . A matched‐cohort evaluation of a bedside asthma intervention for patients hospitalized at a large urban children's hospital. J Urban Health. 2011;88(suppl 1):49–60.
- , , , et al. Effectiveness of asthma education with and without a self‐management plan in hospitalized children. J Asthma. 2009;46(9):906–910.
- , , , , And . Effect of a structured asthma education program on hospitalized asthmatic children: a randomized controlled study. Pediatr Int. 2006;48(2):158–162.
- , , , , , Parental education and guided self‐management of asthma and wheezing in the pre‐school child: a randomised controlled trial. Thorax. 2002;57(1):39–44.
- , , . Structured discharge procedure for children admitted to hospital with acute asthma: a randomised controlled trial of nursing practice. Arch Dis Child. 1999;80(2):110–114.
- , , . Impact of a nurse‐led home management training programme in children admitted to hospital with acute asthma: a randomised controlled study. Thorax. 1997;52(3):223–228.
- , , , et al. You Can Control Asthma: evaluation of an asthma education program for hospitalized inner‐city children. Patient Educ Couns. 1991;17(1):35–47.
- , , . Asthma education by community child health nurses. Arch Dis Child. 1986;61(12):1184–1189.
- , . Effectiveness of a discharge‐planning program and home visits for meeting the physical care needs of children with cancer. Support Care Cancer. 2009;18(2):243–253.
- , , , et al. Comprehensive follow‐up care and life‐threatening illnesses among high‐risk infants: a randomized controlled trial. JAMA. 2000;284(16):2070–2076.
- , , , . Very low birth weight infants and their families during the first year of life: comparisons of medical outcomes based on after care services. J Perinatol. 1998;18(5):365–371.
- , , , , . Description and evaluation of a program for the early discharge of infants from a neonatal intensive care unit. J Pediatr. 1995;127(2):285–290.
- , , , et al. Earlier discharge with community‐based intervention for low birth weight infants: a randomized trial. Pediatrics. 1993;92(1):128–134.
- , , , et al. A randomized clinical trial of early hospital discharge and home follow‐up of very‐low‐birth‐weight infants. N Engl J Med. 1986;315(15):934–939.
- , , . Care transitions from inpatient to outpatient settings: ongoing challenges and emerging best practices. Hosp Pract (1995). 2011;39(3):128–139.
- , , , , . Interventions to reduce 30‐day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–528.
- . Clinical report—physicians' roles in coordinating care of hospitalized children. Pediatrics. 2010;126(4):829–832.
- . White space or black hole: what can we do to improve care transitions? ABIM Foundation. Available at: http://www.abimfoundation.org/∼/media/Files/Publications/F06‐05‐2007_6.ashx. Accessed September 5, 2012.
- , , , et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;(6):CD000259.
- , , , , . A smoking cessation intervention for parents of children who are hospitalized for respiratory illness: the stop tobacco outreach program. Pediatrics. 2003;111(1):140–145.
- , . A randomized, controlled trial of smoking cessation counseling provided during child hospitalization for respiratory illness. Pediatr Pulmonol. 2008;43(6):561–566.
- , . Embracing chaos and complexity: a quantum change for public health. Am J Public Health. 2008;98(8):1382–1389.
- , , , , , . Outpatient follow‐up and rehospitalizations for sickle cell disease patients. Pediatr Blood Cancer. 2012;58(3):406–409.
- , , . Does having an outpatient visit after hospital discharge reduce the likelihood of readmission? Del Med J. 2003;75(8):291–298.
- , , . Follow‐up after acute asthma episodes. Proc Am Thorac Soc. 2009;6(4):386–393.
- , , , et al. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children's hospitals. JAMA. 2011;305(7):682–690.
- , , , et al. A randomized controlled evaluation of the effect of community health workers on hospitalization for asthma: the asthma coach. Arch Pediatr Adolesc Med. 2009;163(3):225–232.
- , , , . The Seattle‐King County Healthy Homes Project: a randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am J Public Health. 2005;95(4):652–659.
- , , , , , . Development and testing of a measure designed to assess the quality of care transitions. Int J Integr Care. 2002;2:e02.
- , , , . Assessing the quality of transitional care: further applications of the care transitions measure. Med Care. 2008;46(3):317–322.
- , , , et al. Hospital readmission and parent perceptions of their child's hospital discharge. Int J Qual Health Care. 2013;25(5):573–581.
- , . Psychometric properties of the Readiness for Hospital Discharge Scale. J Nurs Meas. 2006;14(3):163–180.
- , , , , . Are hospital characteristics associated with parental views of pediatric inpatient care quality? Pediatrics. 2003;111(2):308–314.
- , , , , , . Deficits in communication and information transfer between hospital‐based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297(8):831–841.
- , , , et al. Improving transitions of care at hospital discharge‐‐implications for pediatric hospitalists and primary care providers. J Healthc Qual. 2010;32(5):51–60.
- , . Hospitalists in children's hospitals: what we know now and what we need to know. J Pediatr. 2006;148(3):296–299.
- , , , , . The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–167.
- , , , et al. Adverse events among medical patients after discharge from hospital. CMAJ. 2004;170(3):345–349.
- , , , . Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med. 2003;18(8):646–651.
- , , , et al. Pediatric readmission prevalence and variability across hospitals. JAMA. 2013;309:372–380.
- , , , , , . Discharge planning from hospital to home. Cochrane Database Syst Rev. 2013;(1):CD000313.
- , , , , , . Preventability of early readmissions at a children's hospital. Pediatrics. 2012;131(1):e171–e181.
- , , , et al. State‐level child health system performance and the likelihood of readmission to children's hospitals. J Pediatr. 2010;157(1):98–102.e1.
- Ohio Children's Hospitals' solutions for patient safety. Available at: http://solutionsforpatientsafety.org/files/sps‐fact‐sheet.pdf. Accessed July 24, 2013.
- American Academy of Pediatrics. Value in inpatient pediatrics (VIP) network projects. Available at: http://www.aap.org/en‐us/professional‐resources/practice‐support/quality‐improvement/Quality‐Improvement‐Innovation‐Networks/Pages/Value‐in‐Inpatient‐Pediatrics‐Network‐Projects.aspx. Accessed July 24, 2013.
- Child Health Corporation of America. Resources for managing the patient discharge process. Available at: http://www.chca.com/news/index.html. Accessed October 31, 2013.
- The World Bank. World Development Indicators 2012. Available at: http://data.worldbank.org/sites/default/files/wdi‐2012‐ebook.pdf. Accessed July 5, 2013.
- The Cochrane Collaboration. Data collection form: Intervention review—RCTs and non‐RCTs. Available at: http://hiv.cochrane.org/sites/hiv.cochrane.org/files/uploads/Data%20extraction%20form_all%20studies.docx. Accessed July 24, 2013.
- , . The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non‐randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384.
- , , , et al. Brief violence interventions with community case management services are effective for high‐risk trauma patients. J Trauma. 2011;71(1):228–237.
- , , , , , . Benefits of a hospital‐based peer intervention program for violently injured youth. J Am Coll Surg. 2007;205(5):684–689.
- , , , , . Caught in the crossfire: the effects of a peer‐based intervention program for violently injured youth. J Adolesc Health. 2004;34(3):177–183.
- , , , , . A matched‐cohort evaluation of a bedside asthma intervention for patients hospitalized at a large urban children's hospital. J Urban Health. 2011;88(suppl 1):49–60.
- , , , et al. Effectiveness of asthma education with and without a self‐management plan in hospitalized children. J Asthma. 2009;46(9):906–910.
- , , , , And . Effect of a structured asthma education program on hospitalized asthmatic children: a randomized controlled study. Pediatr Int. 2006;48(2):158–162.
- , , , , , Parental education and guided self‐management of asthma and wheezing in the pre‐school child: a randomised controlled trial. Thorax. 2002;57(1):39–44.
- , , . Structured discharge procedure for children admitted to hospital with acute asthma: a randomised controlled trial of nursing practice. Arch Dis Child. 1999;80(2):110–114.
- , , . Impact of a nurse‐led home management training programme in children admitted to hospital with acute asthma: a randomised controlled study. Thorax. 1997;52(3):223–228.
- , , , et al. You Can Control Asthma: evaluation of an asthma education program for hospitalized inner‐city children. Patient Educ Couns. 1991;17(1):35–47.
- , , . Asthma education by community child health nurses. Arch Dis Child. 1986;61(12):1184–1189.
- , . Effectiveness of a discharge‐planning program and home visits for meeting the physical care needs of children with cancer. Support Care Cancer. 2009;18(2):243–253.
- , , , et al. Comprehensive follow‐up care and life‐threatening illnesses among high‐risk infants: a randomized controlled trial. JAMA. 2000;284(16):2070–2076.
- , , , . Very low birth weight infants and their families during the first year of life: comparisons of medical outcomes based on after care services. J Perinatol. 1998;18(5):365–371.
- , , , , . Description and evaluation of a program for the early discharge of infants from a neonatal intensive care unit. J Pediatr. 1995;127(2):285–290.
- , , , et al. Earlier discharge with community‐based intervention for low birth weight infants: a randomized trial. Pediatrics. 1993;92(1):128–134.
- , , , et al. A randomized clinical trial of early hospital discharge and home follow‐up of very‐low‐birth‐weight infants. N Engl J Med. 1986;315(15):934–939.
- , , . Care transitions from inpatient to outpatient settings: ongoing challenges and emerging best practices. Hosp Pract (1995). 2011;39(3):128–139.
- , , , , . Interventions to reduce 30‐day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–528.
- . Clinical report—physicians' roles in coordinating care of hospitalized children. Pediatrics. 2010;126(4):829–832.
- . White space or black hole: what can we do to improve care transitions? ABIM Foundation. Available at: http://www.abimfoundation.org/∼/media/Files/Publications/F06‐05‐2007_6.ashx. Accessed September 5, 2012.
- , , , et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;(6):CD000259.
- , , , , . A smoking cessation intervention for parents of children who are hospitalized for respiratory illness: the stop tobacco outreach program. Pediatrics. 2003;111(1):140–145.
- , . A randomized, controlled trial of smoking cessation counseling provided during child hospitalization for respiratory illness. Pediatr Pulmonol. 2008;43(6):561–566.
- , . Embracing chaos and complexity: a quantum change for public health. Am J Public Health. 2008;98(8):1382–1389.
- , , , , , . Outpatient follow‐up and rehospitalizations for sickle cell disease patients. Pediatr Blood Cancer. 2012;58(3):406–409.
- , , . Does having an outpatient visit after hospital discharge reduce the likelihood of readmission? Del Med J. 2003;75(8):291–298.
- , , . Follow‐up after acute asthma episodes. Proc Am Thorac Soc. 2009;6(4):386–393.
- , , , et al. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children's hospitals. JAMA. 2011;305(7):682–690.
- , , , et al. A randomized controlled evaluation of the effect of community health workers on hospitalization for asthma: the asthma coach. Arch Pediatr Adolesc Med. 2009;163(3):225–232.
- , , , . The Seattle‐King County Healthy Homes Project: a randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am J Public Health. 2005;95(4):652–659.
- , , , , , . Development and testing of a measure designed to assess the quality of care transitions. Int J Integr Care. 2002;2:e02.
- , , , . Assessing the quality of transitional care: further applications of the care transitions measure. Med Care. 2008;46(3):317–322.
- , , , et al. Hospital readmission and parent perceptions of their child's hospital discharge. Int J Qual Health Care. 2013;25(5):573–581.
- , . Psychometric properties of the Readiness for Hospital Discharge Scale. J Nurs Meas. 2006;14(3):163–180.
Fewer Catheter-Related Complications with Central Access in ICU Patients
Clinical question
What type of venous access -- central or peripheral -- is better for patients in the intensive care unit who have no absolute indication for central access?
Bottom line
As compared with central venous catheters (CVCs), the initial use of peripheral venous catheters (PVCs) in patients in the intensive care unit (ICU) leads to more complications, primarily related to the difficulty in inserting of these catheters. Furthermore, the majority of patients in the PVC group may eventually require a CVC because of an increase in the rate of venotoxic drug infusions or because they have difficulty maintaining the PVC. (LOE = 1b-)
Reference
Ricard J, Salomon L, Boyer A, et al. Central or peripheral catheters for initial venous access of ICU patients. Crit Care Med 2013;41(9):2108-2115.
Study design
Randomized controlled trial (nonblinded)
Funding source
Government
Allocation
Concealed
Setting
Inpatient (ICU only)
Synopsis
Using concealed allocation, these investigators randomized ICU patients requiring venous access to receive either a CVC or PVC. Only patients without any absolute indications for CVCs were included. CVCs could be inserted into jugular, subclavian, or femoral sites at the discretion of the clinician. PVCs were 18-gauge or 20-gauge short catheters. Patients with a predefined increase in the rate of venotoxic drug infusions or those with difficulty maintaining a PVC were able to cross-over to the CVC group. More than half the patients in the PVC group ultimately received a CVC. Baseline characteristics were comparable between the 2 groups, with a mean age of 64 years, similar predicted mortality scores, and the majority of patients requiring mechanical ventilation. The primary outcome was the number of catheter-related complications defined as major mechanical, maintenance-related, infectious, or thrombotic complications. The determination of what constituted a major or minor complication was made a priori by the investigators. They also used a validated classification system of adverse events that rated the complications from grade 1 (minimal symptoms) to grade 5 (death). For example, one major mechanical CVC complication was the need to change insertion site, whereas a major mechanical PVC complication was needing more than 5 attempts to place a PVC. Overall, the PVC group had a greater number of major complications (133 vs 87; P = .02), the majority of which were PVC insertion difficulties (n = 56), erythema at insertion site (n = 20), and subcutaneous diffusion (n = 19). None were life threatening. When the complications were categorized using the grading classification, there were again more complications per patient in the PVC group (1.54 vs 0.89; P = .0001), mainly due to a larger number of grade 1 and grade 2 complications. Finally, more time was spent by doctors and nurses in managing catheters in the PVC group.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question
What type of venous access -- central or peripheral -- is better for patients in the intensive care unit who have no absolute indication for central access?
Bottom line
As compared with central venous catheters (CVCs), the initial use of peripheral venous catheters (PVCs) in patients in the intensive care unit (ICU) leads to more complications, primarily related to the difficulty in inserting of these catheters. Furthermore, the majority of patients in the PVC group may eventually require a CVC because of an increase in the rate of venotoxic drug infusions or because they have difficulty maintaining the PVC. (LOE = 1b-)
Reference
Ricard J, Salomon L, Boyer A, et al. Central or peripheral catheters for initial venous access of ICU patients. Crit Care Med 2013;41(9):2108-2115.
Study design
Randomized controlled trial (nonblinded)
Funding source
Government
Allocation
Concealed
Setting
Inpatient (ICU only)
Synopsis
Using concealed allocation, these investigators randomized ICU patients requiring venous access to receive either a CVC or PVC. Only patients without any absolute indications for CVCs were included. CVCs could be inserted into jugular, subclavian, or femoral sites at the discretion of the clinician. PVCs were 18-gauge or 20-gauge short catheters. Patients with a predefined increase in the rate of venotoxic drug infusions or those with difficulty maintaining a PVC were able to cross-over to the CVC group. More than half the patients in the PVC group ultimately received a CVC. Baseline characteristics were comparable between the 2 groups, with a mean age of 64 years, similar predicted mortality scores, and the majority of patients requiring mechanical ventilation. The primary outcome was the number of catheter-related complications defined as major mechanical, maintenance-related, infectious, or thrombotic complications. The determination of what constituted a major or minor complication was made a priori by the investigators. They also used a validated classification system of adverse events that rated the complications from grade 1 (minimal symptoms) to grade 5 (death). For example, one major mechanical CVC complication was the need to change insertion site, whereas a major mechanical PVC complication was needing more than 5 attempts to place a PVC. Overall, the PVC group had a greater number of major complications (133 vs 87; P = .02), the majority of which were PVC insertion difficulties (n = 56), erythema at insertion site (n = 20), and subcutaneous diffusion (n = 19). None were life threatening. When the complications were categorized using the grading classification, there were again more complications per patient in the PVC group (1.54 vs 0.89; P = .0001), mainly due to a larger number of grade 1 and grade 2 complications. Finally, more time was spent by doctors and nurses in managing catheters in the PVC group.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question
What type of venous access -- central or peripheral -- is better for patients in the intensive care unit who have no absolute indication for central access?
Bottom line
As compared with central venous catheters (CVCs), the initial use of peripheral venous catheters (PVCs) in patients in the intensive care unit (ICU) leads to more complications, primarily related to the difficulty in inserting of these catheters. Furthermore, the majority of patients in the PVC group may eventually require a CVC because of an increase in the rate of venotoxic drug infusions or because they have difficulty maintaining the PVC. (LOE = 1b-)
Reference
Ricard J, Salomon L, Boyer A, et al. Central or peripheral catheters for initial venous access of ICU patients. Crit Care Med 2013;41(9):2108-2115.
Study design
Randomized controlled trial (nonblinded)
Funding source
Government
Allocation
Concealed
Setting
Inpatient (ICU only)
Synopsis
Using concealed allocation, these investigators randomized ICU patients requiring venous access to receive either a CVC or PVC. Only patients without any absolute indications for CVCs were included. CVCs could be inserted into jugular, subclavian, or femoral sites at the discretion of the clinician. PVCs were 18-gauge or 20-gauge short catheters. Patients with a predefined increase in the rate of venotoxic drug infusions or those with difficulty maintaining a PVC were able to cross-over to the CVC group. More than half the patients in the PVC group ultimately received a CVC. Baseline characteristics were comparable between the 2 groups, with a mean age of 64 years, similar predicted mortality scores, and the majority of patients requiring mechanical ventilation. The primary outcome was the number of catheter-related complications defined as major mechanical, maintenance-related, infectious, or thrombotic complications. The determination of what constituted a major or minor complication was made a priori by the investigators. They also used a validated classification system of adverse events that rated the complications from grade 1 (minimal symptoms) to grade 5 (death). For example, one major mechanical CVC complication was the need to change insertion site, whereas a major mechanical PVC complication was needing more than 5 attempts to place a PVC. Overall, the PVC group had a greater number of major complications (133 vs 87; P = .02), the majority of which were PVC insertion difficulties (n = 56), erythema at insertion site (n = 20), and subcutaneous diffusion (n = 19). None were life threatening. When the complications were categorized using the grading classification, there were again more complications per patient in the PVC group (1.54 vs 0.89; P = .0001), mainly due to a larger number of grade 1 and grade 2 complications. Finally, more time was spent by doctors and nurses in managing catheters in the PVC group.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Colchicine Effective for First Episode of Acute Pericarditis
Clinical question
Does the addition of colchicine improve outcomes in the treatment of an initial episode of acute pericarditis?
Bottom line
When used in addition to conventional anti-inflammatory therapy, colchicine decreases the rate of incessant or recurrent pericarditis. You would need to treat 4 patients with colchicine to prevent one such episode. (LOE = 1b)
Reference
Imazio M, Brucato A, Cemin R, et al, for the ICAP Investigators. A randomized trial of colchicine for acute pericarditis. N Engl J Med 2013;369(16):1522-1528.
Study design
Randomized controlled trial (double-blinded)
Funding source
Government
Concealed
Setting
Inpatient (any location) with outpatient follow-up
Synopsis
Colchicine has been previously shown effective in the prevention of recurrent pericarditis (Daily POEM 12-16-2011). In this study, patients with a first episode of acute pericarditis were randomized to receive either colchicine (0.5 mg - 1 mg daily for 3 months; n = 120) or matching placebo (n = 120). All patients also received conventional treatment for acute pericarditis, either aspirin 800 mg or ibuprofen 600 mg every 8 hours for 7 to 10 days, followed by a taper, or (for those with contraindications to aspirin or ibuprofen) glucorticoid therapy for 2 weeks, followed by a taper. Baseline characteristics in the 2 groups were similar: mean age was 52 years, 60% were male, and the most common cause of pericarditis was idiopathic. The majority of patients received aspirin rather than ibuprofen or glucocorticoids as concomitant therapy. Adherence to the study drug was higher than 95% and did not differ between the 2 groups. Patients were followed up for a mean of 22 months and none were lost to follow-up. Analysis was by intention to treat. The primary outcome of incessant or recurrent pericarditis was decreased in the colchicine group as compared with the placebo group (16.7% vs 37.5%; relative risk = 0.56; 95% CI, 0.30-0.72; P < .001). In addition, the colchicine group had significantly better outcomes with regard to the number of patients with persistent symptoms at 72 hours (19% vs 40%), rate of remission within 1 week (85% vs 58%), time to first recurrence (25 weeks vs 18 weeks), and rate of percarditis-related hospitalizations (5% vs 14%). There was no difference in either overall side effects or gastrointestinal side effects between the 2 groups.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question
Does the addition of colchicine improve outcomes in the treatment of an initial episode of acute pericarditis?
Bottom line
When used in addition to conventional anti-inflammatory therapy, colchicine decreases the rate of incessant or recurrent pericarditis. You would need to treat 4 patients with colchicine to prevent one such episode. (LOE = 1b)
Reference
Imazio M, Brucato A, Cemin R, et al, for the ICAP Investigators. A randomized trial of colchicine for acute pericarditis. N Engl J Med 2013;369(16):1522-1528.
Study design
Randomized controlled trial (double-blinded)
Funding source
Government
Concealed
Setting
Inpatient (any location) with outpatient follow-up
Synopsis
Colchicine has been previously shown effective in the prevention of recurrent pericarditis (Daily POEM 12-16-2011). In this study, patients with a first episode of acute pericarditis were randomized to receive either colchicine (0.5 mg - 1 mg daily for 3 months; n = 120) or matching placebo (n = 120). All patients also received conventional treatment for acute pericarditis, either aspirin 800 mg or ibuprofen 600 mg every 8 hours for 7 to 10 days, followed by a taper, or (for those with contraindications to aspirin or ibuprofen) glucorticoid therapy for 2 weeks, followed by a taper. Baseline characteristics in the 2 groups were similar: mean age was 52 years, 60% were male, and the most common cause of pericarditis was idiopathic. The majority of patients received aspirin rather than ibuprofen or glucocorticoids as concomitant therapy. Adherence to the study drug was higher than 95% and did not differ between the 2 groups. Patients were followed up for a mean of 22 months and none were lost to follow-up. Analysis was by intention to treat. The primary outcome of incessant or recurrent pericarditis was decreased in the colchicine group as compared with the placebo group (16.7% vs 37.5%; relative risk = 0.56; 95% CI, 0.30-0.72; P < .001). In addition, the colchicine group had significantly better outcomes with regard to the number of patients with persistent symptoms at 72 hours (19% vs 40%), rate of remission within 1 week (85% vs 58%), time to first recurrence (25 weeks vs 18 weeks), and rate of percarditis-related hospitalizations (5% vs 14%). There was no difference in either overall side effects or gastrointestinal side effects between the 2 groups.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
Clinical question
Does the addition of colchicine improve outcomes in the treatment of an initial episode of acute pericarditis?
Bottom line
When used in addition to conventional anti-inflammatory therapy, colchicine decreases the rate of incessant or recurrent pericarditis. You would need to treat 4 patients with colchicine to prevent one such episode. (LOE = 1b)
Reference
Imazio M, Brucato A, Cemin R, et al, for the ICAP Investigators. A randomized trial of colchicine for acute pericarditis. N Engl J Med 2013;369(16):1522-1528.
Study design
Randomized controlled trial (double-blinded)
Funding source
Government
Concealed
Setting
Inpatient (any location) with outpatient follow-up
Synopsis
Colchicine has been previously shown effective in the prevention of recurrent pericarditis (Daily POEM 12-16-2011). In this study, patients with a first episode of acute pericarditis were randomized to receive either colchicine (0.5 mg - 1 mg daily for 3 months; n = 120) or matching placebo (n = 120). All patients also received conventional treatment for acute pericarditis, either aspirin 800 mg or ibuprofen 600 mg every 8 hours for 7 to 10 days, followed by a taper, or (for those with contraindications to aspirin or ibuprofen) glucorticoid therapy for 2 weeks, followed by a taper. Baseline characteristics in the 2 groups were similar: mean age was 52 years, 60% were male, and the most common cause of pericarditis was idiopathic. The majority of patients received aspirin rather than ibuprofen or glucocorticoids as concomitant therapy. Adherence to the study drug was higher than 95% and did not differ between the 2 groups. Patients were followed up for a mean of 22 months and none were lost to follow-up. Analysis was by intention to treat. The primary outcome of incessant or recurrent pericarditis was decreased in the colchicine group as compared with the placebo group (16.7% vs 37.5%; relative risk = 0.56; 95% CI, 0.30-0.72; P < .001). In addition, the colchicine group had significantly better outcomes with regard to the number of patients with persistent symptoms at 72 hours (19% vs 40%), rate of remission within 1 week (85% vs 58%), time to first recurrence (25 weeks vs 18 weeks), and rate of percarditis-related hospitalizations (5% vs 14%). There was no difference in either overall side effects or gastrointestinal side effects between the 2 groups.
Dr. Kulkarni is an assistant professor of hospital medicine at Northwestern University in Chicago.
The danger of measles
First the good news: According to a study commissioned by the Centers for Disease Control and Prevention and published in JAMA Pediatrics on Dec. 5, measles was officially eliminated in the United States in 2000, and that elimination persisted until 2011. This shows that the vaccine, first approved in 1963, has been effective at "eliminating" the disease, defined as the absence of endemic disease transmission.
This is no small feat. Measles is highly contagious, and prior to 1963, resulted in about 500 deaths per year in the United States, and tens of thousands of hospitalizations. Because it’s so highly contagious, vaccinating a large chunk of susceptible patients was the only way to effectively combat the disease. The "elimination" of the disease marks the success of vaccination strategies. Globally, there are now 500,000 fewer deaths per year from measles than there were a decade ago. If we continue with vaccination programs as we do, there is a chance we can eradicate the disease (JAMA Pediatrics 2013 [doi:10.1001/jamapediatrics.2013.4342]).
Now the bad news: This year, according to a statement that the CDC put out on Dec. 5, there have been 175 cases of measles. This is three times the annual median number of about 60. These cases have been concentrated in communities that are against vaccination, usually brought in from other places where antivaccination sentiments are also high, like Europe, or where vaccination strategies are lagging, like the developing world.
In a well-publicized outbreak in Texas in August, 21 unvaccinated people belonging to the Eagle Mountain International Church contracted the disease when an unvaccinated man travelled to Indonesia and came back ill. The pastor, Terri Copeland Pearsons, daughter of a televangelist Kenneth Copeland, clarifies that she is not against vaccinations but she has reservations about them. "The concerns we have had are primarily with very young children who have family history of autism and with bundling too many immunizations at one time."
Ms. Pearsons further says: "the facts are the facts, but then we know the truth. That always overcomes facts." When did fact become the enemy? How does faith trump science? Why do people treat science with such skepticism, and yet take anecdotes as gospel truth? How is it that despite the best efforts of infectious disease and pediatric societies to dispel such mistaken notions, these ideas survive?
In studies exploring the psychology of vaccine refusal, the factors that parents take into consideration include, but are not limited to, the perceptions of vulnerability of the children, severity of the disease, and safety of the vaccine.
People have forgotten just how severe measles can be. In addition, the unfounded belief that the vaccine can cause autism has just taken on a life of its own, given credibility by celebrities.
I understand that for some people anecdotes often tell a more powerful story than data does. So here’s one anecdote from the personal anecdote library of a doctor from a developing country.
I knew Albert through mutual friends. He played bass in a rock band, belonged to a fraternity in medical school, was involved in intramural basketball, and was in a loving relationship. By the time we graduated from medical school, he was the proud father of a baby girl.
But then things seemed to fall out of place. He failed the medical boards. He uncharacteristically sank into a deep depression that was so severe that he required inpatient treatment, and even then the treatments were not working. Still the assumption was that he had depression from his life’s circumstances.
And then he had a seizure.
That was when the diagnosis of subacute sclerosing panencephalitis, or SSPE, was made. It explained the personality change, intellectual difficulty, and seizures. He had contracted measles 10 years earlier, and this is a known complication of measles, one that hospitals in the Philippines are unfortunately all too familiar with. He died within a few weeks of diagnosis.
Society has forgotten how severe measles can be. We have an effective vaccine and effective global vaccination programs. We therefore have a chance to eradicate this disease altogether, like we did with smallpox and like we’re trying to do with polio. One parent’s strongly held but erroneous beliefs can cause trouble for large segments of the population. Ignoring the antivaccination rhetoric won’t make it go away.
Dr. Chan practices rheumatology in Pawtucket, R.I.
First the good news: According to a study commissioned by the Centers for Disease Control and Prevention and published in JAMA Pediatrics on Dec. 5, measles was officially eliminated in the United States in 2000, and that elimination persisted until 2011. This shows that the vaccine, first approved in 1963, has been effective at "eliminating" the disease, defined as the absence of endemic disease transmission.
This is no small feat. Measles is highly contagious, and prior to 1963, resulted in about 500 deaths per year in the United States, and tens of thousands of hospitalizations. Because it’s so highly contagious, vaccinating a large chunk of susceptible patients was the only way to effectively combat the disease. The "elimination" of the disease marks the success of vaccination strategies. Globally, there are now 500,000 fewer deaths per year from measles than there were a decade ago. If we continue with vaccination programs as we do, there is a chance we can eradicate the disease (JAMA Pediatrics 2013 [doi:10.1001/jamapediatrics.2013.4342]).
Now the bad news: This year, according to a statement that the CDC put out on Dec. 5, there have been 175 cases of measles. This is three times the annual median number of about 60. These cases have been concentrated in communities that are against vaccination, usually brought in from other places where antivaccination sentiments are also high, like Europe, or where vaccination strategies are lagging, like the developing world.
In a well-publicized outbreak in Texas in August, 21 unvaccinated people belonging to the Eagle Mountain International Church contracted the disease when an unvaccinated man travelled to Indonesia and came back ill. The pastor, Terri Copeland Pearsons, daughter of a televangelist Kenneth Copeland, clarifies that she is not against vaccinations but she has reservations about them. "The concerns we have had are primarily with very young children who have family history of autism and with bundling too many immunizations at one time."
Ms. Pearsons further says: "the facts are the facts, but then we know the truth. That always overcomes facts." When did fact become the enemy? How does faith trump science? Why do people treat science with such skepticism, and yet take anecdotes as gospel truth? How is it that despite the best efforts of infectious disease and pediatric societies to dispel such mistaken notions, these ideas survive?
In studies exploring the psychology of vaccine refusal, the factors that parents take into consideration include, but are not limited to, the perceptions of vulnerability of the children, severity of the disease, and safety of the vaccine.
People have forgotten just how severe measles can be. In addition, the unfounded belief that the vaccine can cause autism has just taken on a life of its own, given credibility by celebrities.
I understand that for some people anecdotes often tell a more powerful story than data does. So here’s one anecdote from the personal anecdote library of a doctor from a developing country.
I knew Albert through mutual friends. He played bass in a rock band, belonged to a fraternity in medical school, was involved in intramural basketball, and was in a loving relationship. By the time we graduated from medical school, he was the proud father of a baby girl.
But then things seemed to fall out of place. He failed the medical boards. He uncharacteristically sank into a deep depression that was so severe that he required inpatient treatment, and even then the treatments were not working. Still the assumption was that he had depression from his life’s circumstances.
And then he had a seizure.
That was when the diagnosis of subacute sclerosing panencephalitis, or SSPE, was made. It explained the personality change, intellectual difficulty, and seizures. He had contracted measles 10 years earlier, and this is a known complication of measles, one that hospitals in the Philippines are unfortunately all too familiar with. He died within a few weeks of diagnosis.
Society has forgotten how severe measles can be. We have an effective vaccine and effective global vaccination programs. We therefore have a chance to eradicate this disease altogether, like we did with smallpox and like we’re trying to do with polio. One parent’s strongly held but erroneous beliefs can cause trouble for large segments of the population. Ignoring the antivaccination rhetoric won’t make it go away.
Dr. Chan practices rheumatology in Pawtucket, R.I.
First the good news: According to a study commissioned by the Centers for Disease Control and Prevention and published in JAMA Pediatrics on Dec. 5, measles was officially eliminated in the United States in 2000, and that elimination persisted until 2011. This shows that the vaccine, first approved in 1963, has been effective at "eliminating" the disease, defined as the absence of endemic disease transmission.
This is no small feat. Measles is highly contagious, and prior to 1963, resulted in about 500 deaths per year in the United States, and tens of thousands of hospitalizations. Because it’s so highly contagious, vaccinating a large chunk of susceptible patients was the only way to effectively combat the disease. The "elimination" of the disease marks the success of vaccination strategies. Globally, there are now 500,000 fewer deaths per year from measles than there were a decade ago. If we continue with vaccination programs as we do, there is a chance we can eradicate the disease (JAMA Pediatrics 2013 [doi:10.1001/jamapediatrics.2013.4342]).
Now the bad news: This year, according to a statement that the CDC put out on Dec. 5, there have been 175 cases of measles. This is three times the annual median number of about 60. These cases have been concentrated in communities that are against vaccination, usually brought in from other places where antivaccination sentiments are also high, like Europe, or where vaccination strategies are lagging, like the developing world.
In a well-publicized outbreak in Texas in August, 21 unvaccinated people belonging to the Eagle Mountain International Church contracted the disease when an unvaccinated man travelled to Indonesia and came back ill. The pastor, Terri Copeland Pearsons, daughter of a televangelist Kenneth Copeland, clarifies that she is not against vaccinations but she has reservations about them. "The concerns we have had are primarily with very young children who have family history of autism and with bundling too many immunizations at one time."
Ms. Pearsons further says: "the facts are the facts, but then we know the truth. That always overcomes facts." When did fact become the enemy? How does faith trump science? Why do people treat science with such skepticism, and yet take anecdotes as gospel truth? How is it that despite the best efforts of infectious disease and pediatric societies to dispel such mistaken notions, these ideas survive?
In studies exploring the psychology of vaccine refusal, the factors that parents take into consideration include, but are not limited to, the perceptions of vulnerability of the children, severity of the disease, and safety of the vaccine.
People have forgotten just how severe measles can be. In addition, the unfounded belief that the vaccine can cause autism has just taken on a life of its own, given credibility by celebrities.
I understand that for some people anecdotes often tell a more powerful story than data does. So here’s one anecdote from the personal anecdote library of a doctor from a developing country.
I knew Albert through mutual friends. He played bass in a rock band, belonged to a fraternity in medical school, was involved in intramural basketball, and was in a loving relationship. By the time we graduated from medical school, he was the proud father of a baby girl.
But then things seemed to fall out of place. He failed the medical boards. He uncharacteristically sank into a deep depression that was so severe that he required inpatient treatment, and even then the treatments were not working. Still the assumption was that he had depression from his life’s circumstances.
And then he had a seizure.
That was when the diagnosis of subacute sclerosing panencephalitis, or SSPE, was made. It explained the personality change, intellectual difficulty, and seizures. He had contracted measles 10 years earlier, and this is a known complication of measles, one that hospitals in the Philippines are unfortunately all too familiar with. He died within a few weeks of diagnosis.
Society has forgotten how severe measles can be. We have an effective vaccine and effective global vaccination programs. We therefore have a chance to eradicate this disease altogether, like we did with smallpox and like we’re trying to do with polio. One parent’s strongly held but erroneous beliefs can cause trouble for large segments of the population. Ignoring the antivaccination rhetoric won’t make it go away.
Dr. Chan practices rheumatology in Pawtucket, R.I.
Psychiatric medications and lactation: Informing clinical decisions
Over the last 2 decades, abundant data on the reproductive safety of medications used to treat psychiatric disorders have become available, filling in many gaps with respect to our knowledge about the safety of commonly used psychiatric medications during pregnancy. But the availability of such safety data with respect to the use of these agents during breastfeeding is less complete.
Because of fears of potential adverse effects on infants associated with psychotropic drug use during lactation, many women with a psychiatric disorder who are treated with a range of psychiatric medications are advised not to breastfeed; or if they choose to breastfeed, they are counseled to avoid taking the essential medication that has made them well. This has been a somewhat intuitive, cautious approach. However, in my 25 years of clinical experience taking care of pregnant and postpartum women with a range of psychiatric disorders, one sad scenario I have frequently witnessed is the woman who decides to defer pharmacologic treatment for severe postpartum psychiatric illness after being counseled to defer treatment given a wish to breastfeed. Those women often have been psychiatrically ill for months while breastfeeding after having decided to defer their own treatment because they do not want to expose the baby to even scant amounts of medication secreted into breast milk associated with use of a needed medicine during lactation.
In a recently published clinical report from the American Academy of Pediatrics committee on drugs, authors suggest that advice not to breastfeed or to uniformly avoid medications while nursing because of possible adverse effects in the infant is often not evidence based and may not be necessary in many cases. The committee states that most drugs do not pose a risk to the mother or infant who is nursing, and that "the benefits of breastfeeding outweigh the risks of exposure to most therapeutic agents via human breast milk" (Pediatrics 2013;132:e796-e809).
The report points out that for certain drugs, a careful risk-benefit analysis is needed, especially for drugs that are concentrated in human milk, those with unproven benefits, and those with long half-lives. Importantly, the report notes say that decisions about the use of medications during lactation have to be made on a case-by-case basis. A concrete example would be exercising appropriate vigilance about the use of these medicines in premature infants with immature metabolism.
The report, published on-line in Pediatrics in August 2013, includes a section on antidepressants, anxiolytics, and antipsychotics. As a resource for clinicians, the report highlights LactMed, part of the National Library of Medicine’s toxicology data network (TOXNET), which provides real-time updated scientific information on the excretion of drugs into breast milk.
The report makes the important distinction regarding the range of clinical decisions that get made in the context of different clinical situations. For example, at our center, patients frequently present with questions about whether to use psychiatric medications while breastfeeding when these women have already been taking the medication during pregnancy for treatment of underlying psychiatric disorder. Others make queries about introduction of pharmacologic therapy in the early postpartum period in the context, for example, of new-onset postpartum depression. Specifically, a woman with a history of psychiatric disorder who is treated with antidepressant during pregnancy may continue that medication across the postpartum period to attenuate risk for postpartum depression, particularly if she has a history of recurrent disease, or depressive relapse when medication has been discontinued. That is clinical scenario differs from that of a woman who develops new onset of depression during the postpartum period.
One part of the AAP report addresses use of certain psychiatric medications in the context of available information from the literature regarding extent of excretion of these medications into breast milk. This section states that many antianxiety drugs, antidepressants, and mood stabilizers are excreted in low concentrations into human milk, with the estimated infant doses under 2% of the weight-adjusted maternal dose. However, the authors also cite small series or case reports where infant plasma levels of some drugs were reported to exceed 10% of maternal plasma concentrations. They list 13 such drugs, which include selective serotonin reuptake inhibitors (SSRIs), antipsychotics, anxiolytics, and mood stabilizers. It is important to keep in mind that the number of these cases is small and represent a very small proportion of cases, when the total denominator of reports in the literature of psychotropic drug use during lactation is considered. For example, olanzapine, a second generation antipsychotic is highlighted as an agent of concern based on one case report (J. Psychopharmacol. 2010;24:121-3).
The take-home message for the clinician is that all psychotropics are excreted into breast milk, even if quantification of the agents in breast milk or infant plasma reveals relatively scant concentration (J. Clin. Psychiatry 2003;64:73-80). If mom takes the medicine coincident with lactation, baby is exposed. At our center, we are usually reluctant to discontinue a medication such as an atypical antipsychotic to treat bipolar disorder in the postpartum period even if the mom chooses to breastfeed considering the extent to which women with bipolar disorder are at a high risk for relapse during the puerperium.
Ironically, we probably have more information regarding the excretion of antidepressants and drugs such as lamotrigine, used as a mood stabilizer, into breast milk than most medicines women take during the postpartum period, with data over the past 15 years suggesting that these medications, like other medications, are excreted into breast milk and are present in infant plasma in extremely sparse concentrations. It is noteworthy that cases of frank newborn toxicity directly associated with mothers who breastfeed on psychiatric medications are extremely few and far between, and are anecdotal at best. For some context, the literature on the effects of SSRI use during pregnancy is vast and prevalence of use of these medications during pregnancy and the postpartum period is substantial; that being said, reports of adverse effects reported in the babies of women who breastfeed while taking an SSRI are scant and thus at least somewhat reassuring.
And yet, consistently, I have witnessed that psychiatric medications are highlighted in the literature as particular agents of concern when it comes to lactation, compared with other medicines, for which only sparse data are available. Whether this reflects a bias about the necessity of treating psychiatric disorders during the postpartum period is unknown. Certainly, the long-term implications for the infant of exposure to low concentrations of psychiatric and nonpsychiatric medications in the context of breastfeeding exposure have yet to be clarified.
Whether a woman treated with a psychiatric medication during the post partum should breastfeed is a prime example of a clinical scenario in which there is no perfect decision, and we need to make the best decision possible, taking into account the available data, and the mother’s psychiatric disorder and her wishes. Some women may be extremely committed to breastfeeding and may choose to breastfeed, acknowledging some of the unknowns regarding these medications during lactation, while other women consider some of the ambiguity associated with the long-term effects of exposure while lactating and may choose not to breastfeed.
It is noteworthy that the AAP committee on drugs concluded the benefits of breastfeeding outweigh the risk of exposure to most therapeutic agents via human milk. And those at our center would certainly suggest that this is the case for psychiatric medications, particularly those used to sustain postpartum maternal psychiatric well-being, which is so critical. As is the case with any clinical decision, and certainly with respect to the use of psychiatric medications during pregnancy and lactation, the decision to treat is contingent on a careful risk-benefit analysis, where the risks of exposure to a medicine is weighed against the risk of untreated psychiatric illness. Even with the well-documented benefits of breastfeeding, nothing should trump the treatment of postpartum psychiatric illness, even if the cost is deferring breastfeeding. Treatment cannot be deferred because of the impact of untreated maternal psychiatric illness on maternal morbidity and on the development of children.
Dr. Cohen is the director of the Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information about reproductive mental health at www.womensmentalhealth.org. To comment, e-mail him at [email protected]. Dr. Cohen has been a consultant to manufacturers of antidepressants and antipsychotic medications.
Over the last 2 decades, abundant data on the reproductive safety of medications used to treat psychiatric disorders have become available, filling in many gaps with respect to our knowledge about the safety of commonly used psychiatric medications during pregnancy. But the availability of such safety data with respect to the use of these agents during breastfeeding is less complete.
Because of fears of potential adverse effects on infants associated with psychotropic drug use during lactation, many women with a psychiatric disorder who are treated with a range of psychiatric medications are advised not to breastfeed; or if they choose to breastfeed, they are counseled to avoid taking the essential medication that has made them well. This has been a somewhat intuitive, cautious approach. However, in my 25 years of clinical experience taking care of pregnant and postpartum women with a range of psychiatric disorders, one sad scenario I have frequently witnessed is the woman who decides to defer pharmacologic treatment for severe postpartum psychiatric illness after being counseled to defer treatment given a wish to breastfeed. Those women often have been psychiatrically ill for months while breastfeeding after having decided to defer their own treatment because they do not want to expose the baby to even scant amounts of medication secreted into breast milk associated with use of a needed medicine during lactation.
In a recently published clinical report from the American Academy of Pediatrics committee on drugs, authors suggest that advice not to breastfeed or to uniformly avoid medications while nursing because of possible adverse effects in the infant is often not evidence based and may not be necessary in many cases. The committee states that most drugs do not pose a risk to the mother or infant who is nursing, and that "the benefits of breastfeeding outweigh the risks of exposure to most therapeutic agents via human breast milk" (Pediatrics 2013;132:e796-e809).
The report points out that for certain drugs, a careful risk-benefit analysis is needed, especially for drugs that are concentrated in human milk, those with unproven benefits, and those with long half-lives. Importantly, the report notes say that decisions about the use of medications during lactation have to be made on a case-by-case basis. A concrete example would be exercising appropriate vigilance about the use of these medicines in premature infants with immature metabolism.
The report, published on-line in Pediatrics in August 2013, includes a section on antidepressants, anxiolytics, and antipsychotics. As a resource for clinicians, the report highlights LactMed, part of the National Library of Medicine’s toxicology data network (TOXNET), which provides real-time updated scientific information on the excretion of drugs into breast milk.
The report makes the important distinction regarding the range of clinical decisions that get made in the context of different clinical situations. For example, at our center, patients frequently present with questions about whether to use psychiatric medications while breastfeeding when these women have already been taking the medication during pregnancy for treatment of underlying psychiatric disorder. Others make queries about introduction of pharmacologic therapy in the early postpartum period in the context, for example, of new-onset postpartum depression. Specifically, a woman with a history of psychiatric disorder who is treated with antidepressant during pregnancy may continue that medication across the postpartum period to attenuate risk for postpartum depression, particularly if she has a history of recurrent disease, or depressive relapse when medication has been discontinued. That is clinical scenario differs from that of a woman who develops new onset of depression during the postpartum period.
One part of the AAP report addresses use of certain psychiatric medications in the context of available information from the literature regarding extent of excretion of these medications into breast milk. This section states that many antianxiety drugs, antidepressants, and mood stabilizers are excreted in low concentrations into human milk, with the estimated infant doses under 2% of the weight-adjusted maternal dose. However, the authors also cite small series or case reports where infant plasma levels of some drugs were reported to exceed 10% of maternal plasma concentrations. They list 13 such drugs, which include selective serotonin reuptake inhibitors (SSRIs), antipsychotics, anxiolytics, and mood stabilizers. It is important to keep in mind that the number of these cases is small and represent a very small proportion of cases, when the total denominator of reports in the literature of psychotropic drug use during lactation is considered. For example, olanzapine, a second generation antipsychotic is highlighted as an agent of concern based on one case report (J. Psychopharmacol. 2010;24:121-3).
The take-home message for the clinician is that all psychotropics are excreted into breast milk, even if quantification of the agents in breast milk or infant plasma reveals relatively scant concentration (J. Clin. Psychiatry 2003;64:73-80). If mom takes the medicine coincident with lactation, baby is exposed. At our center, we are usually reluctant to discontinue a medication such as an atypical antipsychotic to treat bipolar disorder in the postpartum period even if the mom chooses to breastfeed considering the extent to which women with bipolar disorder are at a high risk for relapse during the puerperium.
Ironically, we probably have more information regarding the excretion of antidepressants and drugs such as lamotrigine, used as a mood stabilizer, into breast milk than most medicines women take during the postpartum period, with data over the past 15 years suggesting that these medications, like other medications, are excreted into breast milk and are present in infant plasma in extremely sparse concentrations. It is noteworthy that cases of frank newborn toxicity directly associated with mothers who breastfeed on psychiatric medications are extremely few and far between, and are anecdotal at best. For some context, the literature on the effects of SSRI use during pregnancy is vast and prevalence of use of these medications during pregnancy and the postpartum period is substantial; that being said, reports of adverse effects reported in the babies of women who breastfeed while taking an SSRI are scant and thus at least somewhat reassuring.
And yet, consistently, I have witnessed that psychiatric medications are highlighted in the literature as particular agents of concern when it comes to lactation, compared with other medicines, for which only sparse data are available. Whether this reflects a bias about the necessity of treating psychiatric disorders during the postpartum period is unknown. Certainly, the long-term implications for the infant of exposure to low concentrations of psychiatric and nonpsychiatric medications in the context of breastfeeding exposure have yet to be clarified.
Whether a woman treated with a psychiatric medication during the post partum should breastfeed is a prime example of a clinical scenario in which there is no perfect decision, and we need to make the best decision possible, taking into account the available data, and the mother’s psychiatric disorder and her wishes. Some women may be extremely committed to breastfeeding and may choose to breastfeed, acknowledging some of the unknowns regarding these medications during lactation, while other women consider some of the ambiguity associated with the long-term effects of exposure while lactating and may choose not to breastfeed.
It is noteworthy that the AAP committee on drugs concluded the benefits of breastfeeding outweigh the risk of exposure to most therapeutic agents via human milk. And those at our center would certainly suggest that this is the case for psychiatric medications, particularly those used to sustain postpartum maternal psychiatric well-being, which is so critical. As is the case with any clinical decision, and certainly with respect to the use of psychiatric medications during pregnancy and lactation, the decision to treat is contingent on a careful risk-benefit analysis, where the risks of exposure to a medicine is weighed against the risk of untreated psychiatric illness. Even with the well-documented benefits of breastfeeding, nothing should trump the treatment of postpartum psychiatric illness, even if the cost is deferring breastfeeding. Treatment cannot be deferred because of the impact of untreated maternal psychiatric illness on maternal morbidity and on the development of children.
Dr. Cohen is the director of the Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information about reproductive mental health at www.womensmentalhealth.org. To comment, e-mail him at [email protected]. Dr. Cohen has been a consultant to manufacturers of antidepressants and antipsychotic medications.
Over the last 2 decades, abundant data on the reproductive safety of medications used to treat psychiatric disorders have become available, filling in many gaps with respect to our knowledge about the safety of commonly used psychiatric medications during pregnancy. But the availability of such safety data with respect to the use of these agents during breastfeeding is less complete.
Because of fears of potential adverse effects on infants associated with psychotropic drug use during lactation, many women with a psychiatric disorder who are treated with a range of psychiatric medications are advised not to breastfeed; or if they choose to breastfeed, they are counseled to avoid taking the essential medication that has made them well. This has been a somewhat intuitive, cautious approach. However, in my 25 years of clinical experience taking care of pregnant and postpartum women with a range of psychiatric disorders, one sad scenario I have frequently witnessed is the woman who decides to defer pharmacologic treatment for severe postpartum psychiatric illness after being counseled to defer treatment given a wish to breastfeed. Those women often have been psychiatrically ill for months while breastfeeding after having decided to defer their own treatment because they do not want to expose the baby to even scant amounts of medication secreted into breast milk associated with use of a needed medicine during lactation.
In a recently published clinical report from the American Academy of Pediatrics committee on drugs, authors suggest that advice not to breastfeed or to uniformly avoid medications while nursing because of possible adverse effects in the infant is often not evidence based and may not be necessary in many cases. The committee states that most drugs do not pose a risk to the mother or infant who is nursing, and that "the benefits of breastfeeding outweigh the risks of exposure to most therapeutic agents via human breast milk" (Pediatrics 2013;132:e796-e809).
The report points out that for certain drugs, a careful risk-benefit analysis is needed, especially for drugs that are concentrated in human milk, those with unproven benefits, and those with long half-lives. Importantly, the report notes say that decisions about the use of medications during lactation have to be made on a case-by-case basis. A concrete example would be exercising appropriate vigilance about the use of these medicines in premature infants with immature metabolism.
The report, published on-line in Pediatrics in August 2013, includes a section on antidepressants, anxiolytics, and antipsychotics. As a resource for clinicians, the report highlights LactMed, part of the National Library of Medicine’s toxicology data network (TOXNET), which provides real-time updated scientific information on the excretion of drugs into breast milk.
The report makes the important distinction regarding the range of clinical decisions that get made in the context of different clinical situations. For example, at our center, patients frequently present with questions about whether to use psychiatric medications while breastfeeding when these women have already been taking the medication during pregnancy for treatment of underlying psychiatric disorder. Others make queries about introduction of pharmacologic therapy in the early postpartum period in the context, for example, of new-onset postpartum depression. Specifically, a woman with a history of psychiatric disorder who is treated with antidepressant during pregnancy may continue that medication across the postpartum period to attenuate risk for postpartum depression, particularly if she has a history of recurrent disease, or depressive relapse when medication has been discontinued. That is clinical scenario differs from that of a woman who develops new onset of depression during the postpartum period.
One part of the AAP report addresses use of certain psychiatric medications in the context of available information from the literature regarding extent of excretion of these medications into breast milk. This section states that many antianxiety drugs, antidepressants, and mood stabilizers are excreted in low concentrations into human milk, with the estimated infant doses under 2% of the weight-adjusted maternal dose. However, the authors also cite small series or case reports where infant plasma levels of some drugs were reported to exceed 10% of maternal plasma concentrations. They list 13 such drugs, which include selective serotonin reuptake inhibitors (SSRIs), antipsychotics, anxiolytics, and mood stabilizers. It is important to keep in mind that the number of these cases is small and represent a very small proportion of cases, when the total denominator of reports in the literature of psychotropic drug use during lactation is considered. For example, olanzapine, a second generation antipsychotic is highlighted as an agent of concern based on one case report (J. Psychopharmacol. 2010;24:121-3).
The take-home message for the clinician is that all psychotropics are excreted into breast milk, even if quantification of the agents in breast milk or infant plasma reveals relatively scant concentration (J. Clin. Psychiatry 2003;64:73-80). If mom takes the medicine coincident with lactation, baby is exposed. At our center, we are usually reluctant to discontinue a medication such as an atypical antipsychotic to treat bipolar disorder in the postpartum period even if the mom chooses to breastfeed considering the extent to which women with bipolar disorder are at a high risk for relapse during the puerperium.
Ironically, we probably have more information regarding the excretion of antidepressants and drugs such as lamotrigine, used as a mood stabilizer, into breast milk than most medicines women take during the postpartum period, with data over the past 15 years suggesting that these medications, like other medications, are excreted into breast milk and are present in infant plasma in extremely sparse concentrations. It is noteworthy that cases of frank newborn toxicity directly associated with mothers who breastfeed on psychiatric medications are extremely few and far between, and are anecdotal at best. For some context, the literature on the effects of SSRI use during pregnancy is vast and prevalence of use of these medications during pregnancy and the postpartum period is substantial; that being said, reports of adverse effects reported in the babies of women who breastfeed while taking an SSRI are scant and thus at least somewhat reassuring.
And yet, consistently, I have witnessed that psychiatric medications are highlighted in the literature as particular agents of concern when it comes to lactation, compared with other medicines, for which only sparse data are available. Whether this reflects a bias about the necessity of treating psychiatric disorders during the postpartum period is unknown. Certainly, the long-term implications for the infant of exposure to low concentrations of psychiatric and nonpsychiatric medications in the context of breastfeeding exposure have yet to be clarified.
Whether a woman treated with a psychiatric medication during the post partum should breastfeed is a prime example of a clinical scenario in which there is no perfect decision, and we need to make the best decision possible, taking into account the available data, and the mother’s psychiatric disorder and her wishes. Some women may be extremely committed to breastfeeding and may choose to breastfeed, acknowledging some of the unknowns regarding these medications during lactation, while other women consider some of the ambiguity associated with the long-term effects of exposure while lactating and may choose not to breastfeed.
It is noteworthy that the AAP committee on drugs concluded the benefits of breastfeeding outweigh the risk of exposure to most therapeutic agents via human milk. And those at our center would certainly suggest that this is the case for psychiatric medications, particularly those used to sustain postpartum maternal psychiatric well-being, which is so critical. As is the case with any clinical decision, and certainly with respect to the use of psychiatric medications during pregnancy and lactation, the decision to treat is contingent on a careful risk-benefit analysis, where the risks of exposure to a medicine is weighed against the risk of untreated psychiatric illness. Even with the well-documented benefits of breastfeeding, nothing should trump the treatment of postpartum psychiatric illness, even if the cost is deferring breastfeeding. Treatment cannot be deferred because of the impact of untreated maternal psychiatric illness on maternal morbidity and on the development of children.
Dr. Cohen is the director of the Center for Women’s Mental Health at Massachusetts General Hospital in Boston, which provides information about reproductive mental health at www.womensmentalhealth.org. To comment, e-mail him at [email protected]. Dr. Cohen has been a consultant to manufacturers of antidepressants and antipsychotic medications.
Measuring the MEWS and the Rothman Index
Bedside calculation of early warning system (EWS) scores is standard practice in many hospitals to predict clinical deterioration. These systems were designed for periodic hand‐scoring, typically using a half‐dozen variables dominated by vital signs. Most derive from the Modified Early Warning Score (MEWS).[1, 2] Despite years of modification, EWSs have had only modest impact on outcomes.[3, 4] Major improvement is possible only by adding more information than is contained in vital signs. Thus, the next generation of EWSs must analyze electronic medical records (EMRs). Analysis would be performed by computer, displayed automatically, and updated whenever new data are entered into the EMR. Such systems could deliver timely, accurate, longitudinally trended acuity information that could aid in earlier detection of declining patient condition as well as improving sensitivity and specificity of EWS alarms.
Advancing this endeavor along with others,[5, 6] we previously published a patient acuity metric, the Rothman Index (RI), which automatically updates when asynchronous vital signs, laboratory test results, Braden Scale,[7] cardiac rhythm, and nursing assessments are entered into the EMR.[8] Our goal was to enable clinicians to visualize changes in acuity by simple line graphs personalized to each patient at any point in time across the trajectory of care. In our model validation studies,[8] we made no attempt to identify generalizable thresholds, though others[9] have defined decision cut points for RI in a nonemergent context. To examine decision support feasibility in an emergent context, and to compare RI with a general EWS standard, we compare the accuracy of the RI with the MEWS in predicting hospital death within 24 hours.
METHODS
Site Description and Ethics
The institutional review board of Abington Memorial Hospital (Abington, PA) approved collection of retrospective data obtained from their 665‐bed, regional referral center and teaching hospital. Handling of patient information complied with the Health Insurance Portability and Accountability Act of 1996 regulations.
Patient Inclusion
The analysis included all patients, aged 18 years or older, admitted from July 2009 through June 2010, when there were sufficient data in the EMR to compute the RI. Obstetric and psychiatric patients were excluded because nursing documentation is insufficient in this dataset.
Data Collection/Data Sources
Clinical variables were extracted from the EMR (AllScripts Sunrise Clinical Manager, Chicago, IL) by SQL query and placed into a database. RI[8] and MEWS[1] were computed according to published methods. Table 1 shows definitions of standards for each nursing assessment,[8] and Table 2 identifies all clinical variables employed for each system. Briefly, RI utilizes 26 variables related to clinical care and routinely available in the EMR. These include vital signs, laboratory results, cardiac rhythms, and nursing assessments. Excess risk associated with any value of a variable is defined as percent absolute increase in 1‐year mortality relative to minimum 1‐year mortality identified for that variable. Excess risk is summed on a linear scale to reflect cumulative risk for individual patients at any given time. RI was computed at every new observation during a patient visit, when input values were available. Laboratory results are included when measured, but after 24 hours their weighting is reduced by 50%, and after 48 hours they are excluded. Data input intervals were a function of institutional patient care protocols and physician orders. All observations during a patient's stay were included in the analysis, per the method of Prytherch et al.[4] Because data did not contain the simplified alert/voice/pain/unresponsive (A/V/P/U) score, computation of MEWS used appropriate mapping of the Glasgow Coma Scale.[10] A corresponding MEWS was calculated for each RI. The relationship between RI and MEWS is inverse. RI ranges from 91 to 100, with lower scores indicating increasing acuity. MEWS ranges from 0 to 14, with higher scores indicating increasing acuity.
| |
| Cardiac | Pulse regular, rate 60100 bpm, skin warm and dry. Blood pressure 140/90 and no symptoms of hypotension. |
| Food/nutrition | No difficulty with chewing, swallowing, or manual dexterity. Patient consuming >50% of daily diet ordered as observed or stated. |
| Gastrointestinal | Abdomen soft and nontender. Bowel sounds present. No nausea or vomiting. Continent. Bowel pattern normal as observed or stated. |
| Genitourinary | Voids without difficulty. Continent. Urine clear, yellow to amber as observed or stated. Urinary catheter patent if present. |
| Musculoskeletal | Independently able to move all extremities and perform functional activities as observed or stated (includes assistive devices). |
| Neurological | Alert and oriented to person, place, time, situation. Speech is coherent. |
| Peripheral‐vascular | Extremities are normal or pink and warm. Peripheral pulses palpable. Capillary refill 3 seconds. No edema, numbness or tingling. |
| Psychosocial | Behavior appropriate to situation. Expressed concerns and fears being addressed. Adequate support system. |
| Respiratory | Respiration 1224/minute at rest, quiet and regular. Bilateral breath sounds clear. Nail beds and mucous membranes pink. Sputum clear, if present. |
| Safety/fall risk | Safety/fall risk factors not present. Not a risk to self or others. |
| Skin/tissue | Skin clean, dry, and intact with no reddened areas. Patient is alert, cooperative and able to reposition self independently. Braden Scale >15. |
| Input Variable | A: Alive in 24 Hours, Mean (SD) | B: Dead Within 24 Hours, Mean (SD) | P Value |
|---|---|---|---|
| |||
| Diastolic blood pressure, mm Hg | 66.8 (13.5) | 56.6 (16.8) | 0.0001 |
| Systolic blood pressure, mm Hga | 127.3 (23.8) | 105.2 (29.4) | 0.0001 |
| Temperature, Fa | 98.2 (1.1) | 98.2 (2.0) | 0.1165 |
| Respiration, breaths per minutea | 20.1 (4.7) | 23.6 (9.1) | 0.0001 |
| Heart rate, bpma | 81.1 (16.5) | 96.9 (22.2) | 0.0001 |
| Pulse oximetry, % O2 saturation | 96.3 (3.3) | 93.8 (10.1) | 0.0001 |
| Creatinine, mg/dL | 1.2 (1.2) | 1.8 (1.5) | 0.0001 |
| Blood urea nitrogen, mg/dL | 23.9 (17.9) | 42.1 (26.4) | 0.0001 |
| Serum chloride, mmol/L | 104.3 (5.4) | 106.9 (9.7) | 0.0001 |
| Serum potassium, mmol/L | 4.2 (0.5) | 4.4 (0.8) | 0.0001 |
| Serum sodium, mmol/L | 139.0 (4.1) | 140.7 (8.5) | 0.0001 |
| Hemoglobin, gm/dL | 11.2 (2.1) | 10.6 (2.1) | 0.0001 |
| White blood cell count, 103 cell/L | 9.9 (6.3) | 15.0 (10.9) | 0.0001 |
| Braden Scale, total points | 17.7 (3.4) | 12.2 (3.1) | 0.0001 |
| NURSING ASSESSMENTS | A: Alive in 24 Hours and Failed Standard | B: Dead Within 24 Hours and Failed Standard | P Value |
| Neurological | 38.7% | 91.4% | 0.0001 |
| Genitourinary | 46.6% | 90.0% | 0.0001 |
| Respiratory | 55.6% | 89.0% | 0.0001 |
| Peripheral vascular | 54.1% | 86.9% | 0.0001 |
| Food | 28.3% | 80.6% | 0.0001 |
| Skin | 56.3% | 75.0% | 0.0001 |
| Gastrointestinal | 49.3% | 75.0% | 0.0001 |
| Musculoskeletal | 50.3% | 72.4% | 0.0001 |
| Cardiac | 30.4% | 59.8% | 0.0001 |
| Psychosocial | 24.6% | 40.9% | 0.0001 |
| Safety | 25.5% | 29.0% | 0.0001 |
| A/V/P/U scorea | 96.3/2.1/1.4/0.2% | 88.6/21.6/4.6/5.3% | 0.0001 |
| Sinus rhythm (absent)b | 34.9% | 53.3% | 0.0001 |
Outcome Ascertainment
In‐hospital death was determined by merging the date and time of discharge with clinical inputs from the hospital's EMR. Data points were judged to be within 24 hours of death if the timestamp of the data point collection was within 24 hours of the discharge time with expired as the discharge disposition.
Statistical Methods
Demographics and input variables from the 2 groups of observations, those who were within 24 hours of death and those who were not, were compared using a t test with a Cochran and Cox[11] approximation of the probability level of the approximate t statistic for unequal variances. Mean, standard deviation, and P values are reported. Discrimination of RI and MEWS to predict 24‐hour mortality was estimated using area under the receiver operating characteristic (ROC) curve (AUC), and null hypothesis was tested using 2. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive and negative likelihood ratios (LR+, LR) were computed. Analyses were performed with SAS 9.3 (procedures ttest, freq, logistic, nlmixed; SAS Institute, Cary, NC). Typically MEWS=4 triggers a protocol to increase level of assessment and/or care, often a transfer to the intensive care unit (ICU). We denoted the point on ROC curve where MEWS=4 and identified an RI point of similar LR and sensitivity to compare false alarm rate. Then we identified an RI point of similar LR+ for comparison of LR and sensitivity.
RESULTS
A total of 1,794,910 observations during 32,472 patient visits were included; 617 patients died (1.9%). Physiological characteristics for all input variables used by RI or MEWS are shown in Table 2, comparing observations taken within 24 hours of death to all other observations.
RI versus MEWS demonstrated superior discrimination of 24‐hour mortality (AUC was 0.93 [95% confidence interval {CI}: 0.92‐0.93] vs 0.82 [95% CI: 0.82‐0.83]; difference, 0.11 [95% CI: 0.10‐0.11]; P0.0001). ROC curves for RI and MEWS are shown in Figure 1; the MEWS is subsumed by RI across the entire range. Further, paired comparisons at points of clinical importance are presented in Table 3 for LR+, LR, sensitivity, specificity, PPV, and NPV. In the first pair of columns, MEWS=4 (typical trigger point for alarms) is matched to RI using sensitivity or LR; the corresponding point is RI=16, which generates twice the LR+ and reduces false alarms by 53%. In the second pair of columns, MEWS=4 is matched to RI using PPV or LR+; the corresponding point is RI=30, which captures 54% more of those patients who will die within 24 hours.
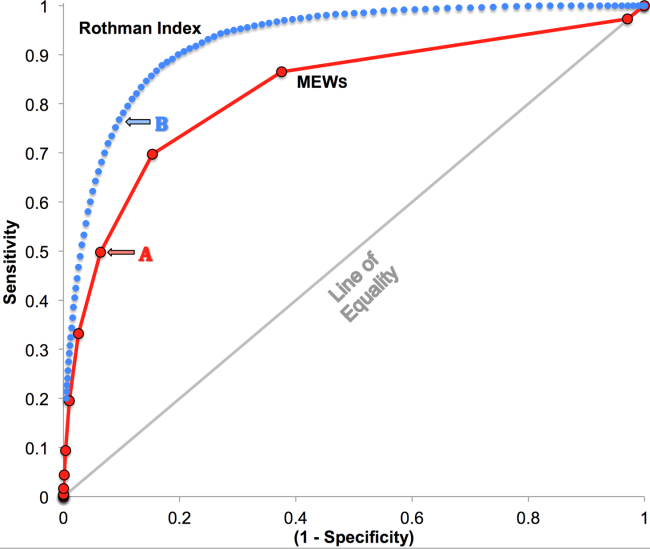
| Cut Points | MEWS=4 | RI=16a | MEWS=4 | RI=30b |
|---|---|---|---|---|
| ||||
| Likelihood ratio, positive | 7.8 | 16.9 | 7.8c | 7.9c |
| Likelihood ratio, negative | 0.54c | 0.53c | 0.54 | 0.26 |
| Sensitivity | 49.8% | 48.9% | 49.8% | 76.8% |
| Specificity | 93.6% | 97.1% | 93.6% | 90.4% |
| Positive predictive value | 5.2% | 10.6% | 5.2% | 5.3% |
| Negative predictive value | 99.6% | 99.6% | 99.6% | 99.8% |
DISCUSSION
We have shown that a general acuity metric (RI) computed using data routinely entered into an EMR outperforms MEWS in identifying hospitalized patients likely to die within 24 hours. At similar sensitivity, RI yields an LR+ more than 2‐fold greater, at a value often considered conclusive. MEWS is derived using 4 vital signs and a neurologic assessment. Such a focus on vital signs may limit responsiveness to changes in acuity, especially during early clinical deterioration. Indeed, threshold breach tools may inadvertently induce a false sense of an individual patient's condition and safety.[12] The present findings suggest the performance of RI over MEWS may be due to inclusion of nursing assessments, laboratory test results, and heart rhythm. Relative contributions of each category are: vital signs (35%), nursing assessments (34%), and laboratory test results (31%). We found in previous work that failed nursing assessments strongly correlate with mortality,[13] as illustrated in Table 2 by sharp differences between patients dying within 24 hours and those who did not.
Sensitivity to detect early deterioration, especially when not evidenced by compromised vital signs, is crucial for acuity vigilance and preemptive interventions. Others[14] have demonstrated that our approach to longitudinal modeling of the acuity continuum is well positioned to investigate clinical pathophysiology preceding adverse events and to identify actionable trends in patients at high risk of complications and sepsis after colorectal operations. Future research may reveal both clinical and administrative advantages to having this real‐time acuity measure available for all patients during the entire hospital visit, with efficacy in applications beyond use as a trigger for EWS alarms.
Study limitations include retrospective design, single‐center cohort, no exclusion of expected hospital deaths, and EMR requirement. For MEWS, the Glasgow Coma Scale was mapped to A/V/P/U, which does not appear to affect results, as our c‐statistic is identical to the literature.[4] Any hospital with an EMR collects the data necessary for computation of RI values. The RI algorithms are available in software compatible with systems from numerous EMR manufacturers (eg, Epic, Cerner, McKesson, Siemens, AllScripts, Phillips).
The advent of the EMR in hospitals marries well with an EWS that leverages from additional data more information than is contained in vital signs, permitting complex numeric computations of acuity scores, a process simply not possible with paper systems. Further, the automatic recalculation of the score reduces the burden on clinicians, and broadens potential use over a wide range, from minute‐by‐minute recalculations when attached to sensors in the ICU, to comparative metrics of hospital performance, to nonclinical financial resource applications. This new information technology is guiding methods to achieve a significant performance increment over current EWS and may assist earlier detection of deterioration, providing a chance to avoid medical crises.[15]
Acknowledgements
The authors express their appreciation to Abington Memorial Hospital. Particular thanks are extended to Steven I. Rothman, MSEM, for extensive discussions and technical support. The authors thank Alan Solinger, PhD, for his assistance in reviewing the manuscript.
Disclosures: One author (RAS) declares no conflict of interest. Two authors (GDF, MJR) are employees and shareholders in PeraHealth, Inc. of Charlotte, North Carolina, a health information technology company that offers products utilizing the Rothman Index. All of the original research defining the Rothman Index was performed prior to the formation of the company and is now published in peer‐reviewed journals. The index is freely available to all qualified researchers and is currently installed at several major medical research centers and hospital systems. This present work is under the auspices and partly funded by an independent foundation, F.A.R. Institute of Sarasota, Florida. Early research defining the Rothman Index was funded by grants from Sarasota Memorial Healthcare Foundation and the Goldsmith Fund of Greenfield Foundation. Continuing research has been funded by the F.A.R. Institute.
- , , , . Validation of a modified Early Warning Score in medical admissions. QJM Mon J Assoc Physicians. 2001;94:521–526.
- , , . Monitoring vital signs using early warning scoring systems: a review of the literature. J Nurs Manag. 2011;19:311–330.
- , , , et al. A clinical deterioration prediction tool for internal medicine patients. Am J Med Qual. 2013;28:135–142.
- , , , . ViEWS—towards a national early warning score for detecting adult inpatient deterioration. Resuscitation. 2010;81:932–937.
- , , , , , . Early detection of impending physiologic deterioration among patients who are not in intensive care: development of predictive models using data from an automated electronic medical record. J Hosp Med. 2012;7:388–395.
- , , , et al. Predicting out of intensive care unit cardiopulmonary arrest or death using electronic medical record data. BMC Med Inform Decis Mak. 2013;13:28.
- , , , The Braden Scale for predicting pressure sore risk. Nurs Res. 1987;36:205–210.
- , , . Development and validation of a continuous measure of patient condition using the electronic medical record. J Biomed Inform. 2013;46:837–848.
- , , , , . Identifying patients at increased risk for unplanned readmission. Med Care. 2013;51:761–766.
- , , . Comparison of consciousness level assessment in the poisoned patient using the alert/verbal/painful/unresponsive scale and the Glasgow Coma Scale. Ann Emerg Med. 2004;44:108–113.
- , . Experimental Design. New York, NY: John Wiley 1950.
- , . Patterns of unexpected in‐hospital deaths: a root cause analysis. Patient Saf Surg. 2011;5:3.
- , , , . Clinical implications and validity of nursing assessments: a longitudinal measure of patient condition from analysis of the Electronic Medical Record. BMJ Open. 2012;2(4):pii: e000646.
- , , , . Automated analysis of electronic medical record data reflects the pathophysiology of operative complications. Surgery. 2013;154:918–926.
- , , Not getting better means getting worse—trends in Early Warning Scores suggest that there might only be a short time span to rescue those threatening to fall off a “physiological” cliff? Resuscitation. 2013;84:409–410.
Bedside calculation of early warning system (EWS) scores is standard practice in many hospitals to predict clinical deterioration. These systems were designed for periodic hand‐scoring, typically using a half‐dozen variables dominated by vital signs. Most derive from the Modified Early Warning Score (MEWS).[1, 2] Despite years of modification, EWSs have had only modest impact on outcomes.[3, 4] Major improvement is possible only by adding more information than is contained in vital signs. Thus, the next generation of EWSs must analyze electronic medical records (EMRs). Analysis would be performed by computer, displayed automatically, and updated whenever new data are entered into the EMR. Such systems could deliver timely, accurate, longitudinally trended acuity information that could aid in earlier detection of declining patient condition as well as improving sensitivity and specificity of EWS alarms.
Advancing this endeavor along with others,[5, 6] we previously published a patient acuity metric, the Rothman Index (RI), which automatically updates when asynchronous vital signs, laboratory test results, Braden Scale,[7] cardiac rhythm, and nursing assessments are entered into the EMR.[8] Our goal was to enable clinicians to visualize changes in acuity by simple line graphs personalized to each patient at any point in time across the trajectory of care. In our model validation studies,[8] we made no attempt to identify generalizable thresholds, though others[9] have defined decision cut points for RI in a nonemergent context. To examine decision support feasibility in an emergent context, and to compare RI with a general EWS standard, we compare the accuracy of the RI with the MEWS in predicting hospital death within 24 hours.
METHODS
Site Description and Ethics
The institutional review board of Abington Memorial Hospital (Abington, PA) approved collection of retrospective data obtained from their 665‐bed, regional referral center and teaching hospital. Handling of patient information complied with the Health Insurance Portability and Accountability Act of 1996 regulations.
Patient Inclusion
The analysis included all patients, aged 18 years or older, admitted from July 2009 through June 2010, when there were sufficient data in the EMR to compute the RI. Obstetric and psychiatric patients were excluded because nursing documentation is insufficient in this dataset.
Data Collection/Data Sources
Clinical variables were extracted from the EMR (AllScripts Sunrise Clinical Manager, Chicago, IL) by SQL query and placed into a database. RI[8] and MEWS[1] were computed according to published methods. Table 1 shows definitions of standards for each nursing assessment,[8] and Table 2 identifies all clinical variables employed for each system. Briefly, RI utilizes 26 variables related to clinical care and routinely available in the EMR. These include vital signs, laboratory results, cardiac rhythms, and nursing assessments. Excess risk associated with any value of a variable is defined as percent absolute increase in 1‐year mortality relative to minimum 1‐year mortality identified for that variable. Excess risk is summed on a linear scale to reflect cumulative risk for individual patients at any given time. RI was computed at every new observation during a patient visit, when input values were available. Laboratory results are included when measured, but after 24 hours their weighting is reduced by 50%, and after 48 hours they are excluded. Data input intervals were a function of institutional patient care protocols and physician orders. All observations during a patient's stay were included in the analysis, per the method of Prytherch et al.[4] Because data did not contain the simplified alert/voice/pain/unresponsive (A/V/P/U) score, computation of MEWS used appropriate mapping of the Glasgow Coma Scale.[10] A corresponding MEWS was calculated for each RI. The relationship between RI and MEWS is inverse. RI ranges from 91 to 100, with lower scores indicating increasing acuity. MEWS ranges from 0 to 14, with higher scores indicating increasing acuity.
| |
| Cardiac | Pulse regular, rate 60100 bpm, skin warm and dry. Blood pressure 140/90 and no symptoms of hypotension. |
| Food/nutrition | No difficulty with chewing, swallowing, or manual dexterity. Patient consuming >50% of daily diet ordered as observed or stated. |
| Gastrointestinal | Abdomen soft and nontender. Bowel sounds present. No nausea or vomiting. Continent. Bowel pattern normal as observed or stated. |
| Genitourinary | Voids without difficulty. Continent. Urine clear, yellow to amber as observed or stated. Urinary catheter patent if present. |
| Musculoskeletal | Independently able to move all extremities and perform functional activities as observed or stated (includes assistive devices). |
| Neurological | Alert and oriented to person, place, time, situation. Speech is coherent. |
| Peripheral‐vascular | Extremities are normal or pink and warm. Peripheral pulses palpable. Capillary refill 3 seconds. No edema, numbness or tingling. |
| Psychosocial | Behavior appropriate to situation. Expressed concerns and fears being addressed. Adequate support system. |
| Respiratory | Respiration 1224/minute at rest, quiet and regular. Bilateral breath sounds clear. Nail beds and mucous membranes pink. Sputum clear, if present. |
| Safety/fall risk | Safety/fall risk factors not present. Not a risk to self or others. |
| Skin/tissue | Skin clean, dry, and intact with no reddened areas. Patient is alert, cooperative and able to reposition self independently. Braden Scale >15. |
| Input Variable | A: Alive in 24 Hours, Mean (SD) | B: Dead Within 24 Hours, Mean (SD) | P Value |
|---|---|---|---|
| |||
| Diastolic blood pressure, mm Hg | 66.8 (13.5) | 56.6 (16.8) | 0.0001 |
| Systolic blood pressure, mm Hga | 127.3 (23.8) | 105.2 (29.4) | 0.0001 |
| Temperature, Fa | 98.2 (1.1) | 98.2 (2.0) | 0.1165 |
| Respiration, breaths per minutea | 20.1 (4.7) | 23.6 (9.1) | 0.0001 |
| Heart rate, bpma | 81.1 (16.5) | 96.9 (22.2) | 0.0001 |
| Pulse oximetry, % O2 saturation | 96.3 (3.3) | 93.8 (10.1) | 0.0001 |
| Creatinine, mg/dL | 1.2 (1.2) | 1.8 (1.5) | 0.0001 |
| Blood urea nitrogen, mg/dL | 23.9 (17.9) | 42.1 (26.4) | 0.0001 |
| Serum chloride, mmol/L | 104.3 (5.4) | 106.9 (9.7) | 0.0001 |
| Serum potassium, mmol/L | 4.2 (0.5) | 4.4 (0.8) | 0.0001 |
| Serum sodium, mmol/L | 139.0 (4.1) | 140.7 (8.5) | 0.0001 |
| Hemoglobin, gm/dL | 11.2 (2.1) | 10.6 (2.1) | 0.0001 |
| White blood cell count, 103 cell/L | 9.9 (6.3) | 15.0 (10.9) | 0.0001 |
| Braden Scale, total points | 17.7 (3.4) | 12.2 (3.1) | 0.0001 |
| NURSING ASSESSMENTS | A: Alive in 24 Hours and Failed Standard | B: Dead Within 24 Hours and Failed Standard | P Value |
| Neurological | 38.7% | 91.4% | 0.0001 |
| Genitourinary | 46.6% | 90.0% | 0.0001 |
| Respiratory | 55.6% | 89.0% | 0.0001 |
| Peripheral vascular | 54.1% | 86.9% | 0.0001 |
| Food | 28.3% | 80.6% | 0.0001 |
| Skin | 56.3% | 75.0% | 0.0001 |
| Gastrointestinal | 49.3% | 75.0% | 0.0001 |
| Musculoskeletal | 50.3% | 72.4% | 0.0001 |
| Cardiac | 30.4% | 59.8% | 0.0001 |
| Psychosocial | 24.6% | 40.9% | 0.0001 |
| Safety | 25.5% | 29.0% | 0.0001 |
| A/V/P/U scorea | 96.3/2.1/1.4/0.2% | 88.6/21.6/4.6/5.3% | 0.0001 |
| Sinus rhythm (absent)b | 34.9% | 53.3% | 0.0001 |
Outcome Ascertainment
In‐hospital death was determined by merging the date and time of discharge with clinical inputs from the hospital's EMR. Data points were judged to be within 24 hours of death if the timestamp of the data point collection was within 24 hours of the discharge time with expired as the discharge disposition.
Statistical Methods
Demographics and input variables from the 2 groups of observations, those who were within 24 hours of death and those who were not, were compared using a t test with a Cochran and Cox[11] approximation of the probability level of the approximate t statistic for unequal variances. Mean, standard deviation, and P values are reported. Discrimination of RI and MEWS to predict 24‐hour mortality was estimated using area under the receiver operating characteristic (ROC) curve (AUC), and null hypothesis was tested using 2. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive and negative likelihood ratios (LR+, LR) were computed. Analyses were performed with SAS 9.3 (procedures ttest, freq, logistic, nlmixed; SAS Institute, Cary, NC). Typically MEWS=4 triggers a protocol to increase level of assessment and/or care, often a transfer to the intensive care unit (ICU). We denoted the point on ROC curve where MEWS=4 and identified an RI point of similar LR and sensitivity to compare false alarm rate. Then we identified an RI point of similar LR+ for comparison of LR and sensitivity.
RESULTS
A total of 1,794,910 observations during 32,472 patient visits were included; 617 patients died (1.9%). Physiological characteristics for all input variables used by RI or MEWS are shown in Table 2, comparing observations taken within 24 hours of death to all other observations.
RI versus MEWS demonstrated superior discrimination of 24‐hour mortality (AUC was 0.93 [95% confidence interval {CI}: 0.92‐0.93] vs 0.82 [95% CI: 0.82‐0.83]; difference, 0.11 [95% CI: 0.10‐0.11]; P0.0001). ROC curves for RI and MEWS are shown in Figure 1; the MEWS is subsumed by RI across the entire range. Further, paired comparisons at points of clinical importance are presented in Table 3 for LR+, LR, sensitivity, specificity, PPV, and NPV. In the first pair of columns, MEWS=4 (typical trigger point for alarms) is matched to RI using sensitivity or LR; the corresponding point is RI=16, which generates twice the LR+ and reduces false alarms by 53%. In the second pair of columns, MEWS=4 is matched to RI using PPV or LR+; the corresponding point is RI=30, which captures 54% more of those patients who will die within 24 hours.
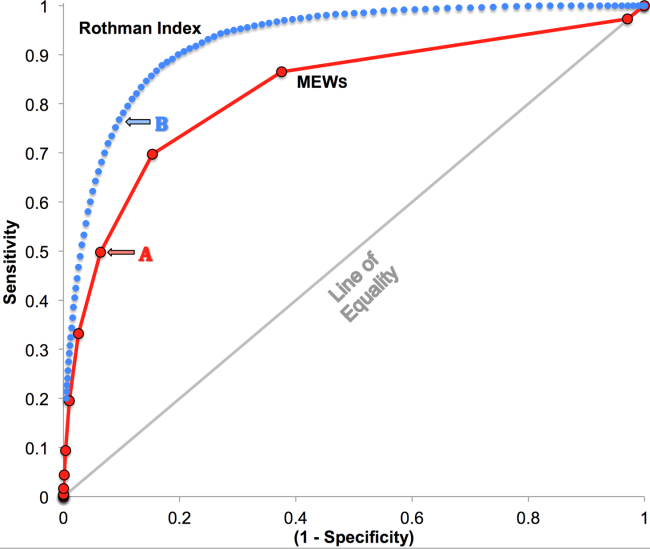
| Cut Points | MEWS=4 | RI=16a | MEWS=4 | RI=30b |
|---|---|---|---|---|
| ||||
| Likelihood ratio, positive | 7.8 | 16.9 | 7.8c | 7.9c |
| Likelihood ratio, negative | 0.54c | 0.53c | 0.54 | 0.26 |
| Sensitivity | 49.8% | 48.9% | 49.8% | 76.8% |
| Specificity | 93.6% | 97.1% | 93.6% | 90.4% |
| Positive predictive value | 5.2% | 10.6% | 5.2% | 5.3% |
| Negative predictive value | 99.6% | 99.6% | 99.6% | 99.8% |
DISCUSSION
We have shown that a general acuity metric (RI) computed using data routinely entered into an EMR outperforms MEWS in identifying hospitalized patients likely to die within 24 hours. At similar sensitivity, RI yields an LR+ more than 2‐fold greater, at a value often considered conclusive. MEWS is derived using 4 vital signs and a neurologic assessment. Such a focus on vital signs may limit responsiveness to changes in acuity, especially during early clinical deterioration. Indeed, threshold breach tools may inadvertently induce a false sense of an individual patient's condition and safety.[12] The present findings suggest the performance of RI over MEWS may be due to inclusion of nursing assessments, laboratory test results, and heart rhythm. Relative contributions of each category are: vital signs (35%), nursing assessments (34%), and laboratory test results (31%). We found in previous work that failed nursing assessments strongly correlate with mortality,[13] as illustrated in Table 2 by sharp differences between patients dying within 24 hours and those who did not.
Sensitivity to detect early deterioration, especially when not evidenced by compromised vital signs, is crucial for acuity vigilance and preemptive interventions. Others[14] have demonstrated that our approach to longitudinal modeling of the acuity continuum is well positioned to investigate clinical pathophysiology preceding adverse events and to identify actionable trends in patients at high risk of complications and sepsis after colorectal operations. Future research may reveal both clinical and administrative advantages to having this real‐time acuity measure available for all patients during the entire hospital visit, with efficacy in applications beyond use as a trigger for EWS alarms.
Study limitations include retrospective design, single‐center cohort, no exclusion of expected hospital deaths, and EMR requirement. For MEWS, the Glasgow Coma Scale was mapped to A/V/P/U, which does not appear to affect results, as our c‐statistic is identical to the literature.[4] Any hospital with an EMR collects the data necessary for computation of RI values. The RI algorithms are available in software compatible with systems from numerous EMR manufacturers (eg, Epic, Cerner, McKesson, Siemens, AllScripts, Phillips).
The advent of the EMR in hospitals marries well with an EWS that leverages from additional data more information than is contained in vital signs, permitting complex numeric computations of acuity scores, a process simply not possible with paper systems. Further, the automatic recalculation of the score reduces the burden on clinicians, and broadens potential use over a wide range, from minute‐by‐minute recalculations when attached to sensors in the ICU, to comparative metrics of hospital performance, to nonclinical financial resource applications. This new information technology is guiding methods to achieve a significant performance increment over current EWS and may assist earlier detection of deterioration, providing a chance to avoid medical crises.[15]
Acknowledgements
The authors express their appreciation to Abington Memorial Hospital. Particular thanks are extended to Steven I. Rothman, MSEM, for extensive discussions and technical support. The authors thank Alan Solinger, PhD, for his assistance in reviewing the manuscript.
Disclosures: One author (RAS) declares no conflict of interest. Two authors (GDF, MJR) are employees and shareholders in PeraHealth, Inc. of Charlotte, North Carolina, a health information technology company that offers products utilizing the Rothman Index. All of the original research defining the Rothman Index was performed prior to the formation of the company and is now published in peer‐reviewed journals. The index is freely available to all qualified researchers and is currently installed at several major medical research centers and hospital systems. This present work is under the auspices and partly funded by an independent foundation, F.A.R. Institute of Sarasota, Florida. Early research defining the Rothman Index was funded by grants from Sarasota Memorial Healthcare Foundation and the Goldsmith Fund of Greenfield Foundation. Continuing research has been funded by the F.A.R. Institute.
Bedside calculation of early warning system (EWS) scores is standard practice in many hospitals to predict clinical deterioration. These systems were designed for periodic hand‐scoring, typically using a half‐dozen variables dominated by vital signs. Most derive from the Modified Early Warning Score (MEWS).[1, 2] Despite years of modification, EWSs have had only modest impact on outcomes.[3, 4] Major improvement is possible only by adding more information than is contained in vital signs. Thus, the next generation of EWSs must analyze electronic medical records (EMRs). Analysis would be performed by computer, displayed automatically, and updated whenever new data are entered into the EMR. Such systems could deliver timely, accurate, longitudinally trended acuity information that could aid in earlier detection of declining patient condition as well as improving sensitivity and specificity of EWS alarms.
Advancing this endeavor along with others,[5, 6] we previously published a patient acuity metric, the Rothman Index (RI), which automatically updates when asynchronous vital signs, laboratory test results, Braden Scale,[7] cardiac rhythm, and nursing assessments are entered into the EMR.[8] Our goal was to enable clinicians to visualize changes in acuity by simple line graphs personalized to each patient at any point in time across the trajectory of care. In our model validation studies,[8] we made no attempt to identify generalizable thresholds, though others[9] have defined decision cut points for RI in a nonemergent context. To examine decision support feasibility in an emergent context, and to compare RI with a general EWS standard, we compare the accuracy of the RI with the MEWS in predicting hospital death within 24 hours.
METHODS
Site Description and Ethics
The institutional review board of Abington Memorial Hospital (Abington, PA) approved collection of retrospective data obtained from their 665‐bed, regional referral center and teaching hospital. Handling of patient information complied with the Health Insurance Portability and Accountability Act of 1996 regulations.
Patient Inclusion
The analysis included all patients, aged 18 years or older, admitted from July 2009 through June 2010, when there were sufficient data in the EMR to compute the RI. Obstetric and psychiatric patients were excluded because nursing documentation is insufficient in this dataset.
Data Collection/Data Sources
Clinical variables were extracted from the EMR (AllScripts Sunrise Clinical Manager, Chicago, IL) by SQL query and placed into a database. RI[8] and MEWS[1] were computed according to published methods. Table 1 shows definitions of standards for each nursing assessment,[8] and Table 2 identifies all clinical variables employed for each system. Briefly, RI utilizes 26 variables related to clinical care and routinely available in the EMR. These include vital signs, laboratory results, cardiac rhythms, and nursing assessments. Excess risk associated with any value of a variable is defined as percent absolute increase in 1‐year mortality relative to minimum 1‐year mortality identified for that variable. Excess risk is summed on a linear scale to reflect cumulative risk for individual patients at any given time. RI was computed at every new observation during a patient visit, when input values were available. Laboratory results are included when measured, but after 24 hours their weighting is reduced by 50%, and after 48 hours they are excluded. Data input intervals were a function of institutional patient care protocols and physician orders. All observations during a patient's stay were included in the analysis, per the method of Prytherch et al.[4] Because data did not contain the simplified alert/voice/pain/unresponsive (A/V/P/U) score, computation of MEWS used appropriate mapping of the Glasgow Coma Scale.[10] A corresponding MEWS was calculated for each RI. The relationship between RI and MEWS is inverse. RI ranges from 91 to 100, with lower scores indicating increasing acuity. MEWS ranges from 0 to 14, with higher scores indicating increasing acuity.
| |
| Cardiac | Pulse regular, rate 60100 bpm, skin warm and dry. Blood pressure 140/90 and no symptoms of hypotension. |
| Food/nutrition | No difficulty with chewing, swallowing, or manual dexterity. Patient consuming >50% of daily diet ordered as observed or stated. |
| Gastrointestinal | Abdomen soft and nontender. Bowel sounds present. No nausea or vomiting. Continent. Bowel pattern normal as observed or stated. |
| Genitourinary | Voids without difficulty. Continent. Urine clear, yellow to amber as observed or stated. Urinary catheter patent if present. |
| Musculoskeletal | Independently able to move all extremities and perform functional activities as observed or stated (includes assistive devices). |
| Neurological | Alert and oriented to person, place, time, situation. Speech is coherent. |
| Peripheral‐vascular | Extremities are normal or pink and warm. Peripheral pulses palpable. Capillary refill 3 seconds. No edema, numbness or tingling. |
| Psychosocial | Behavior appropriate to situation. Expressed concerns and fears being addressed. Adequate support system. |
| Respiratory | Respiration 1224/minute at rest, quiet and regular. Bilateral breath sounds clear. Nail beds and mucous membranes pink. Sputum clear, if present. |
| Safety/fall risk | Safety/fall risk factors not present. Not a risk to self or others. |
| Skin/tissue | Skin clean, dry, and intact with no reddened areas. Patient is alert, cooperative and able to reposition self independently. Braden Scale >15. |
| Input Variable | A: Alive in 24 Hours, Mean (SD) | B: Dead Within 24 Hours, Mean (SD) | P Value |
|---|---|---|---|
| |||
| Diastolic blood pressure, mm Hg | 66.8 (13.5) | 56.6 (16.8) | 0.0001 |
| Systolic blood pressure, mm Hga | 127.3 (23.8) | 105.2 (29.4) | 0.0001 |
| Temperature, Fa | 98.2 (1.1) | 98.2 (2.0) | 0.1165 |
| Respiration, breaths per minutea | 20.1 (4.7) | 23.6 (9.1) | 0.0001 |
| Heart rate, bpma | 81.1 (16.5) | 96.9 (22.2) | 0.0001 |
| Pulse oximetry, % O2 saturation | 96.3 (3.3) | 93.8 (10.1) | 0.0001 |
| Creatinine, mg/dL | 1.2 (1.2) | 1.8 (1.5) | 0.0001 |
| Blood urea nitrogen, mg/dL | 23.9 (17.9) | 42.1 (26.4) | 0.0001 |
| Serum chloride, mmol/L | 104.3 (5.4) | 106.9 (9.7) | 0.0001 |
| Serum potassium, mmol/L | 4.2 (0.5) | 4.4 (0.8) | 0.0001 |
| Serum sodium, mmol/L | 139.0 (4.1) | 140.7 (8.5) | 0.0001 |
| Hemoglobin, gm/dL | 11.2 (2.1) | 10.6 (2.1) | 0.0001 |
| White blood cell count, 103 cell/L | 9.9 (6.3) | 15.0 (10.9) | 0.0001 |
| Braden Scale, total points | 17.7 (3.4) | 12.2 (3.1) | 0.0001 |
| NURSING ASSESSMENTS | A: Alive in 24 Hours and Failed Standard | B: Dead Within 24 Hours and Failed Standard | P Value |
| Neurological | 38.7% | 91.4% | 0.0001 |
| Genitourinary | 46.6% | 90.0% | 0.0001 |
| Respiratory | 55.6% | 89.0% | 0.0001 |
| Peripheral vascular | 54.1% | 86.9% | 0.0001 |
| Food | 28.3% | 80.6% | 0.0001 |
| Skin | 56.3% | 75.0% | 0.0001 |
| Gastrointestinal | 49.3% | 75.0% | 0.0001 |
| Musculoskeletal | 50.3% | 72.4% | 0.0001 |
| Cardiac | 30.4% | 59.8% | 0.0001 |
| Psychosocial | 24.6% | 40.9% | 0.0001 |
| Safety | 25.5% | 29.0% | 0.0001 |
| A/V/P/U scorea | 96.3/2.1/1.4/0.2% | 88.6/21.6/4.6/5.3% | 0.0001 |
| Sinus rhythm (absent)b | 34.9% | 53.3% | 0.0001 |
Outcome Ascertainment
In‐hospital death was determined by merging the date and time of discharge with clinical inputs from the hospital's EMR. Data points were judged to be within 24 hours of death if the timestamp of the data point collection was within 24 hours of the discharge time with expired as the discharge disposition.
Statistical Methods
Demographics and input variables from the 2 groups of observations, those who were within 24 hours of death and those who were not, were compared using a t test with a Cochran and Cox[11] approximation of the probability level of the approximate t statistic for unequal variances. Mean, standard deviation, and P values are reported. Discrimination of RI and MEWS to predict 24‐hour mortality was estimated using area under the receiver operating characteristic (ROC) curve (AUC), and null hypothesis was tested using 2. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive and negative likelihood ratios (LR+, LR) were computed. Analyses were performed with SAS 9.3 (procedures ttest, freq, logistic, nlmixed; SAS Institute, Cary, NC). Typically MEWS=4 triggers a protocol to increase level of assessment and/or care, often a transfer to the intensive care unit (ICU). We denoted the point on ROC curve where MEWS=4 and identified an RI point of similar LR and sensitivity to compare false alarm rate. Then we identified an RI point of similar LR+ for comparison of LR and sensitivity.
RESULTS
A total of 1,794,910 observations during 32,472 patient visits were included; 617 patients died (1.9%). Physiological characteristics for all input variables used by RI or MEWS are shown in Table 2, comparing observations taken within 24 hours of death to all other observations.
RI versus MEWS demonstrated superior discrimination of 24‐hour mortality (AUC was 0.93 [95% confidence interval {CI}: 0.92‐0.93] vs 0.82 [95% CI: 0.82‐0.83]; difference, 0.11 [95% CI: 0.10‐0.11]; P0.0001). ROC curves for RI and MEWS are shown in Figure 1; the MEWS is subsumed by RI across the entire range. Further, paired comparisons at points of clinical importance are presented in Table 3 for LR+, LR, sensitivity, specificity, PPV, and NPV. In the first pair of columns, MEWS=4 (typical trigger point for alarms) is matched to RI using sensitivity or LR; the corresponding point is RI=16, which generates twice the LR+ and reduces false alarms by 53%. In the second pair of columns, MEWS=4 is matched to RI using PPV or LR+; the corresponding point is RI=30, which captures 54% more of those patients who will die within 24 hours.
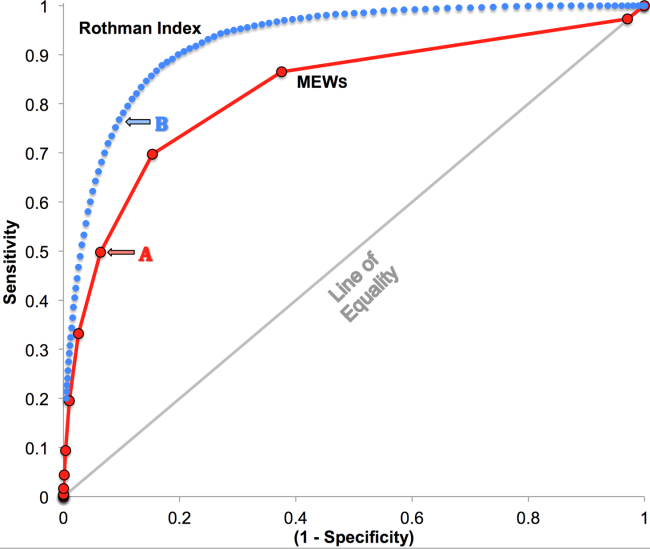
| Cut Points | MEWS=4 | RI=16a | MEWS=4 | RI=30b |
|---|---|---|---|---|
| ||||
| Likelihood ratio, positive | 7.8 | 16.9 | 7.8c | 7.9c |
| Likelihood ratio, negative | 0.54c | 0.53c | 0.54 | 0.26 |
| Sensitivity | 49.8% | 48.9% | 49.8% | 76.8% |
| Specificity | 93.6% | 97.1% | 93.6% | 90.4% |
| Positive predictive value | 5.2% | 10.6% | 5.2% | 5.3% |
| Negative predictive value | 99.6% | 99.6% | 99.6% | 99.8% |
DISCUSSION
We have shown that a general acuity metric (RI) computed using data routinely entered into an EMR outperforms MEWS in identifying hospitalized patients likely to die within 24 hours. At similar sensitivity, RI yields an LR+ more than 2‐fold greater, at a value often considered conclusive. MEWS is derived using 4 vital signs and a neurologic assessment. Such a focus on vital signs may limit responsiveness to changes in acuity, especially during early clinical deterioration. Indeed, threshold breach tools may inadvertently induce a false sense of an individual patient's condition and safety.[12] The present findings suggest the performance of RI over MEWS may be due to inclusion of nursing assessments, laboratory test results, and heart rhythm. Relative contributions of each category are: vital signs (35%), nursing assessments (34%), and laboratory test results (31%). We found in previous work that failed nursing assessments strongly correlate with mortality,[13] as illustrated in Table 2 by sharp differences between patients dying within 24 hours and those who did not.
Sensitivity to detect early deterioration, especially when not evidenced by compromised vital signs, is crucial for acuity vigilance and preemptive interventions. Others[14] have demonstrated that our approach to longitudinal modeling of the acuity continuum is well positioned to investigate clinical pathophysiology preceding adverse events and to identify actionable trends in patients at high risk of complications and sepsis after colorectal operations. Future research may reveal both clinical and administrative advantages to having this real‐time acuity measure available for all patients during the entire hospital visit, with efficacy in applications beyond use as a trigger for EWS alarms.
Study limitations include retrospective design, single‐center cohort, no exclusion of expected hospital deaths, and EMR requirement. For MEWS, the Glasgow Coma Scale was mapped to A/V/P/U, which does not appear to affect results, as our c‐statistic is identical to the literature.[4] Any hospital with an EMR collects the data necessary for computation of RI values. The RI algorithms are available in software compatible with systems from numerous EMR manufacturers (eg, Epic, Cerner, McKesson, Siemens, AllScripts, Phillips).
The advent of the EMR in hospitals marries well with an EWS that leverages from additional data more information than is contained in vital signs, permitting complex numeric computations of acuity scores, a process simply not possible with paper systems. Further, the automatic recalculation of the score reduces the burden on clinicians, and broadens potential use over a wide range, from minute‐by‐minute recalculations when attached to sensors in the ICU, to comparative metrics of hospital performance, to nonclinical financial resource applications. This new information technology is guiding methods to achieve a significant performance increment over current EWS and may assist earlier detection of deterioration, providing a chance to avoid medical crises.[15]
Acknowledgements
The authors express their appreciation to Abington Memorial Hospital. Particular thanks are extended to Steven I. Rothman, MSEM, for extensive discussions and technical support. The authors thank Alan Solinger, PhD, for his assistance in reviewing the manuscript.
Disclosures: One author (RAS) declares no conflict of interest. Two authors (GDF, MJR) are employees and shareholders in PeraHealth, Inc. of Charlotte, North Carolina, a health information technology company that offers products utilizing the Rothman Index. All of the original research defining the Rothman Index was performed prior to the formation of the company and is now published in peer‐reviewed journals. The index is freely available to all qualified researchers and is currently installed at several major medical research centers and hospital systems. This present work is under the auspices and partly funded by an independent foundation, F.A.R. Institute of Sarasota, Florida. Early research defining the Rothman Index was funded by grants from Sarasota Memorial Healthcare Foundation and the Goldsmith Fund of Greenfield Foundation. Continuing research has been funded by the F.A.R. Institute.
- , , , . Validation of a modified Early Warning Score in medical admissions. QJM Mon J Assoc Physicians. 2001;94:521–526.
- , , . Monitoring vital signs using early warning scoring systems: a review of the literature. J Nurs Manag. 2011;19:311–330.
- , , , et al. A clinical deterioration prediction tool for internal medicine patients. Am J Med Qual. 2013;28:135–142.
- , , , . ViEWS—towards a national early warning score for detecting adult inpatient deterioration. Resuscitation. 2010;81:932–937.
- , , , , , . Early detection of impending physiologic deterioration among patients who are not in intensive care: development of predictive models using data from an automated electronic medical record. J Hosp Med. 2012;7:388–395.
- , , , et al. Predicting out of intensive care unit cardiopulmonary arrest or death using electronic medical record data. BMC Med Inform Decis Mak. 2013;13:28.
- , , , The Braden Scale for predicting pressure sore risk. Nurs Res. 1987;36:205–210.
- , , . Development and validation of a continuous measure of patient condition using the electronic medical record. J Biomed Inform. 2013;46:837–848.
- , , , , . Identifying patients at increased risk for unplanned readmission. Med Care. 2013;51:761–766.
- , , . Comparison of consciousness level assessment in the poisoned patient using the alert/verbal/painful/unresponsive scale and the Glasgow Coma Scale. Ann Emerg Med. 2004;44:108–113.
- , . Experimental Design. New York, NY: John Wiley 1950.
- , . Patterns of unexpected in‐hospital deaths: a root cause analysis. Patient Saf Surg. 2011;5:3.
- , , , . Clinical implications and validity of nursing assessments: a longitudinal measure of patient condition from analysis of the Electronic Medical Record. BMJ Open. 2012;2(4):pii: e000646.
- , , , . Automated analysis of electronic medical record data reflects the pathophysiology of operative complications. Surgery. 2013;154:918–926.
- , , Not getting better means getting worse—trends in Early Warning Scores suggest that there might only be a short time span to rescue those threatening to fall off a “physiological” cliff? Resuscitation. 2013;84:409–410.
- , , , . Validation of a modified Early Warning Score in medical admissions. QJM Mon J Assoc Physicians. 2001;94:521–526.
- , , . Monitoring vital signs using early warning scoring systems: a review of the literature. J Nurs Manag. 2011;19:311–330.
- , , , et al. A clinical deterioration prediction tool for internal medicine patients. Am J Med Qual. 2013;28:135–142.
- , , , . ViEWS—towards a national early warning score for detecting adult inpatient deterioration. Resuscitation. 2010;81:932–937.
- , , , , , . Early detection of impending physiologic deterioration among patients who are not in intensive care: development of predictive models using data from an automated electronic medical record. J Hosp Med. 2012;7:388–395.
- , , , et al. Predicting out of intensive care unit cardiopulmonary arrest or death using electronic medical record data. BMC Med Inform Decis Mak. 2013;13:28.
- , , , The Braden Scale for predicting pressure sore risk. Nurs Res. 1987;36:205–210.
- , , . Development and validation of a continuous measure of patient condition using the electronic medical record. J Biomed Inform. 2013;46:837–848.
- , , , , . Identifying patients at increased risk for unplanned readmission. Med Care. 2013;51:761–766.
- , , . Comparison of consciousness level assessment in the poisoned patient using the alert/verbal/painful/unresponsive scale and the Glasgow Coma Scale. Ann Emerg Med. 2004;44:108–113.
- , . Experimental Design. New York, NY: John Wiley 1950.
- , . Patterns of unexpected in‐hospital deaths: a root cause analysis. Patient Saf Surg. 2011;5:3.
- , , , . Clinical implications and validity of nursing assessments: a longitudinal measure of patient condition from analysis of the Electronic Medical Record. BMJ Open. 2012;2(4):pii: e000646.
- , , , . Automated analysis of electronic medical record data reflects the pathophysiology of operative complications. Surgery. 2013;154:918–926.
- , , Not getting better means getting worse—trends in Early Warning Scores suggest that there might only be a short time span to rescue those threatening to fall off a “physiological” cliff? Resuscitation. 2013;84:409–410.