User login
Gum Disease is Linked to Faster Cognitive Decline for Alzhemier's Patients
(Reuters Health) - For people with Alzheimer's disease, having gum disease is tied to faster cognitive decline, according to a new study.
"What we have shown is that regardless of the severity of dementia (within this mild to moderate impaired group) that patients with more severe gum disease are declining more rapidly," said senior author Clive Holmes of the University of Southampton in the UK.
In other studies, Holmes and his coauthors have found that conditions such as chest infections, urinary tract infections, rheumatoid arthritis and diabetes are associated with faster disease progression in Alzheimer's, he said.
"We hadn't previously looked at gum disease because MDs tendto leave this in the hands of dentists but it is an important common low grade chronic infection," Holmes told Reuters Health by email.
The researchers observed 60 people with mild to moderate Alzheimer's disease living at home for six months. The participants did not smoke, had not been treated for gum disease within the previous six months, and had at least 10 teeth.
At the start, each participant completed a cognitive assessment, gave a blood sample, was examined by a dental hygienist and their main caregiver was interviewed to provide a medical and dental history. The same tests and interviews were repeated six months later.
Of the 60 people in the study, 22 had moderate to severe gum disease at the beginning of the study. By six months later, one participant had died, three had withdrawn from the study and three were lost to follow-up.
Cognitive score declined more for those who had periodontitis to begin with than for those who did not, the researchers reported February 24 in PLoS One.
According to one theory, cognitive impairment leads to adverse oral health due to inattention to routine oral hygiene and care, said Dr. James M. Noble of the Taub Institute for Research on Alzheimer's Disease and the Aging Brain at Columbia University Medical Center in New York City, who was not part of the new study.
"The second, and the one I'm most intrigued by, is whether or not periodontal disease has an influence on cognitive outcomes of aging, either as an independent risk factor for (new-onset) cognitive impairment including Alzheimer's disease, or more rapid decline once (Alzheimer's disease) has been diagnosed, as was suggested by this study," Noble told Reuters Health by email.
Gum disease may cause chronic low-grade inflammation in the rest of the body, and inflammation is associated with changes in the brain, he said.
"It is known that gum disease is associated with increased markers of inflammation," Holmes said.
But the new study indicates a connection between gum disease and cognitive decline, not necessarily that one causes the other, he said. Further studies need to assess whether treatingthe gum disease would also slow cognitive decline.
"Periodontitis has been associated with heart disease and stroke among other conditions," Noble said. Based on this and other studies, "it seems to be good advice to brush and floss," Noble said.
(Reuters Health) - For people with Alzheimer's disease, having gum disease is tied to faster cognitive decline, according to a new study.
"What we have shown is that regardless of the severity of dementia (within this mild to moderate impaired group) that patients with more severe gum disease are declining more rapidly," said senior author Clive Holmes of the University of Southampton in the UK.
In other studies, Holmes and his coauthors have found that conditions such as chest infections, urinary tract infections, rheumatoid arthritis and diabetes are associated with faster disease progression in Alzheimer's, he said.
"We hadn't previously looked at gum disease because MDs tendto leave this in the hands of dentists but it is an important common low grade chronic infection," Holmes told Reuters Health by email.
The researchers observed 60 people with mild to moderate Alzheimer's disease living at home for six months. The participants did not smoke, had not been treated for gum disease within the previous six months, and had at least 10 teeth.
At the start, each participant completed a cognitive assessment, gave a blood sample, was examined by a dental hygienist and their main caregiver was interviewed to provide a medical and dental history. The same tests and interviews were repeated six months later.
Of the 60 people in the study, 22 had moderate to severe gum disease at the beginning of the study. By six months later, one participant had died, three had withdrawn from the study and three were lost to follow-up.
Cognitive score declined more for those who had periodontitis to begin with than for those who did not, the researchers reported February 24 in PLoS One.
According to one theory, cognitive impairment leads to adverse oral health due to inattention to routine oral hygiene and care, said Dr. James M. Noble of the Taub Institute for Research on Alzheimer's Disease and the Aging Brain at Columbia University Medical Center in New York City, who was not part of the new study.
"The second, and the one I'm most intrigued by, is whether or not periodontal disease has an influence on cognitive outcomes of aging, either as an independent risk factor for (new-onset) cognitive impairment including Alzheimer's disease, or more rapid decline once (Alzheimer's disease) has been diagnosed, as was suggested by this study," Noble told Reuters Health by email.
Gum disease may cause chronic low-grade inflammation in the rest of the body, and inflammation is associated with changes in the brain, he said.
"It is known that gum disease is associated with increased markers of inflammation," Holmes said.
But the new study indicates a connection between gum disease and cognitive decline, not necessarily that one causes the other, he said. Further studies need to assess whether treatingthe gum disease would also slow cognitive decline.
"Periodontitis has been associated with heart disease and stroke among other conditions," Noble said. Based on this and other studies, "it seems to be good advice to brush and floss," Noble said.
(Reuters Health) - For people with Alzheimer's disease, having gum disease is tied to faster cognitive decline, according to a new study.
"What we have shown is that regardless of the severity of dementia (within this mild to moderate impaired group) that patients with more severe gum disease are declining more rapidly," said senior author Clive Holmes of the University of Southampton in the UK.
In other studies, Holmes and his coauthors have found that conditions such as chest infections, urinary tract infections, rheumatoid arthritis and diabetes are associated with faster disease progression in Alzheimer's, he said.
"We hadn't previously looked at gum disease because MDs tendto leave this in the hands of dentists but it is an important common low grade chronic infection," Holmes told Reuters Health by email.
The researchers observed 60 people with mild to moderate Alzheimer's disease living at home for six months. The participants did not smoke, had not been treated for gum disease within the previous six months, and had at least 10 teeth.
At the start, each participant completed a cognitive assessment, gave a blood sample, was examined by a dental hygienist and their main caregiver was interviewed to provide a medical and dental history. The same tests and interviews were repeated six months later.
Of the 60 people in the study, 22 had moderate to severe gum disease at the beginning of the study. By six months later, one participant had died, three had withdrawn from the study and three were lost to follow-up.
Cognitive score declined more for those who had periodontitis to begin with than for those who did not, the researchers reported February 24 in PLoS One.
According to one theory, cognitive impairment leads to adverse oral health due to inattention to routine oral hygiene and care, said Dr. James M. Noble of the Taub Institute for Research on Alzheimer's Disease and the Aging Brain at Columbia University Medical Center in New York City, who was not part of the new study.
"The second, and the one I'm most intrigued by, is whether or not periodontal disease has an influence on cognitive outcomes of aging, either as an independent risk factor for (new-onset) cognitive impairment including Alzheimer's disease, or more rapid decline once (Alzheimer's disease) has been diagnosed, as was suggested by this study," Noble told Reuters Health by email.
Gum disease may cause chronic low-grade inflammation in the rest of the body, and inflammation is associated with changes in the brain, he said.
"It is known that gum disease is associated with increased markers of inflammation," Holmes said.
But the new study indicates a connection between gum disease and cognitive decline, not necessarily that one causes the other, he said. Further studies need to assess whether treatingthe gum disease would also slow cognitive decline.
"Periodontitis has been associated with heart disease and stroke among other conditions," Noble said. Based on this and other studies, "it seems to be good advice to brush and floss," Noble said.
Team traces evolution of malaria

Photo courtesy of
Sesh Sundararaman,
University of Pennsylvania
By studying malaria parasites found in chimpanzees, researchers believe they have gained new insights regarding a malaria parasite that infects humans.
The team used a selective amplification technique to sequence the genomes of 2 divergent Plasmodium species, P reichenowi and P gaboni, from chimpanzee blood.
This revealed clues about the evolution and pathogenicity of P falciparum, the deadliest malaria parasite that affects humans.
The researchers described this work in Nature Communications.
They noted that African apes harbor at least 6 Plasmodium species that have been classified into a separate subgenus, called Laverania. Three of these Laverania species, including P reichenowi and P gaboni, reside in chimps.
Three others—including P praefalciparum, which gave rise to P falciparum—reside in gorillas. The gorilla origin of P falciparum was discovered several years ago by this same group of investigators.
“We want to know why Plasmodium falciparum is so deadly,” said Beatrice Hahn, MD, of the University of Pennsylvania in Philadelphia.
“The answer must lie in the blueprint—the genome—of its chimpanzee and gorilla cousins. We also want to know how and when the gorilla precursor of Plasmodium falciparum jumped into humans and why this happened only once.”
In an attempt to answer these questions, Dr Hahn and her colleagues used their selective amplification method to sequence Laverania genomes.
They used small amounts of unprocessed blood collected during routine health screens of chimpanzees living in sanctuaries. With their technique, the team found they could generate “high-quality” Laverania genome sequences.
The researchers said the chimpanzee parasite genomes contain information about the evolutionary origins of the malaria parasites infecting humans. One of the first things to emerge from genome-wide analyses was that the parasites represent distinct, non-interbreeding species.
In addition, members of each chimpanzee parasite species display about 10 times more genetic diversity than human parasites.
“The chimpanzee parasites really highlight the lack of diversity in Plasmodium falciparum,” said Paul Sharp, PhD, of the University of Edinburgh in the UK.
“This is most likely because these parasites went through a severe bottleneck when first transmitted to humans, perhaps within the past 10,000 years.”
By comparing the different parasite genomes, the researchers found an expansion of a multi-gene family, which governs red blood cell remodeling and therefore helps the parasite to evade host immune cells and clearance by the spleen.
“The remodeling process is a key part of severe malaria pathology in human Plasmodium falciparum infections,” said Julian Rayner, PhD, of the Wellcome Trust Sanger Institute in Cambridge, UK.
“The expansion of this gene family from a single gene in all other Plasmodium parasites to up to 21 genes in Laverania suggests that remodeling evolved early in the radiation of this group of primate parasites and contributed not only to their unique biology but perhaps also to their successful expansion.”
“We also found a short region of the genome, including 2 essential invasion genes, where Plasmodium falciparum was much more different from its close relatives than we expected,” said Lindsey Plenderleith, PhD, of the University of Edinburgh.
Further analysis yielded the surprising finding that this fragment of DNA was horizontally transferred—from one species to another—into the gorilla ancestor of P falciparum.
“It is tempting to speculate that this unusual event somehow predisposed the precursor of Plasmodium falciparum to colonize humans,” Dr Hahn said. “However, this gene transfer clearly is not the entire story.”
Although the origin of P falciparum is considered well-established, nothing is known about the circumstances that led to its emergence.
“Coaxing entire parasite genome sequences out of small quantities of unprocessed ape blood will help us to better understand what happened and whether it can happen again,” said Sesh Sundararaman, an MD/PhD student at the University of Pennsylvania.
The team plans, as a next step, to use their select genome amplification technique to sequence additional ape parasite genomes to identify host-specific interactions and transmission requirements. They believe this would reveal vulnerabilities that might be exploited to combat malaria in humans. ![]()

Photo courtesy of
Sesh Sundararaman,
University of Pennsylvania
By studying malaria parasites found in chimpanzees, researchers believe they have gained new insights regarding a malaria parasite that infects humans.
The team used a selective amplification technique to sequence the genomes of 2 divergent Plasmodium species, P reichenowi and P gaboni, from chimpanzee blood.
This revealed clues about the evolution and pathogenicity of P falciparum, the deadliest malaria parasite that affects humans.
The researchers described this work in Nature Communications.
They noted that African apes harbor at least 6 Plasmodium species that have been classified into a separate subgenus, called Laverania. Three of these Laverania species, including P reichenowi and P gaboni, reside in chimps.
Three others—including P praefalciparum, which gave rise to P falciparum—reside in gorillas. The gorilla origin of P falciparum was discovered several years ago by this same group of investigators.
“We want to know why Plasmodium falciparum is so deadly,” said Beatrice Hahn, MD, of the University of Pennsylvania in Philadelphia.
“The answer must lie in the blueprint—the genome—of its chimpanzee and gorilla cousins. We also want to know how and when the gorilla precursor of Plasmodium falciparum jumped into humans and why this happened only once.”
In an attempt to answer these questions, Dr Hahn and her colleagues used their selective amplification method to sequence Laverania genomes.
They used small amounts of unprocessed blood collected during routine health screens of chimpanzees living in sanctuaries. With their technique, the team found they could generate “high-quality” Laverania genome sequences.
The researchers said the chimpanzee parasite genomes contain information about the evolutionary origins of the malaria parasites infecting humans. One of the first things to emerge from genome-wide analyses was that the parasites represent distinct, non-interbreeding species.
In addition, members of each chimpanzee parasite species display about 10 times more genetic diversity than human parasites.
“The chimpanzee parasites really highlight the lack of diversity in Plasmodium falciparum,” said Paul Sharp, PhD, of the University of Edinburgh in the UK.
“This is most likely because these parasites went through a severe bottleneck when first transmitted to humans, perhaps within the past 10,000 years.”
By comparing the different parasite genomes, the researchers found an expansion of a multi-gene family, which governs red blood cell remodeling and therefore helps the parasite to evade host immune cells and clearance by the spleen.
“The remodeling process is a key part of severe malaria pathology in human Plasmodium falciparum infections,” said Julian Rayner, PhD, of the Wellcome Trust Sanger Institute in Cambridge, UK.
“The expansion of this gene family from a single gene in all other Plasmodium parasites to up to 21 genes in Laverania suggests that remodeling evolved early in the radiation of this group of primate parasites and contributed not only to their unique biology but perhaps also to their successful expansion.”
“We also found a short region of the genome, including 2 essential invasion genes, where Plasmodium falciparum was much more different from its close relatives than we expected,” said Lindsey Plenderleith, PhD, of the University of Edinburgh.
Further analysis yielded the surprising finding that this fragment of DNA was horizontally transferred—from one species to another—into the gorilla ancestor of P falciparum.
“It is tempting to speculate that this unusual event somehow predisposed the precursor of Plasmodium falciparum to colonize humans,” Dr Hahn said. “However, this gene transfer clearly is not the entire story.”
Although the origin of P falciparum is considered well-established, nothing is known about the circumstances that led to its emergence.
“Coaxing entire parasite genome sequences out of small quantities of unprocessed ape blood will help us to better understand what happened and whether it can happen again,” said Sesh Sundararaman, an MD/PhD student at the University of Pennsylvania.
The team plans, as a next step, to use their select genome amplification technique to sequence additional ape parasite genomes to identify host-specific interactions and transmission requirements. They believe this would reveal vulnerabilities that might be exploited to combat malaria in humans. ![]()

Photo courtesy of
Sesh Sundararaman,
University of Pennsylvania
By studying malaria parasites found in chimpanzees, researchers believe they have gained new insights regarding a malaria parasite that infects humans.
The team used a selective amplification technique to sequence the genomes of 2 divergent Plasmodium species, P reichenowi and P gaboni, from chimpanzee blood.
This revealed clues about the evolution and pathogenicity of P falciparum, the deadliest malaria parasite that affects humans.
The researchers described this work in Nature Communications.
They noted that African apes harbor at least 6 Plasmodium species that have been classified into a separate subgenus, called Laverania. Three of these Laverania species, including P reichenowi and P gaboni, reside in chimps.
Three others—including P praefalciparum, which gave rise to P falciparum—reside in gorillas. The gorilla origin of P falciparum was discovered several years ago by this same group of investigators.
“We want to know why Plasmodium falciparum is so deadly,” said Beatrice Hahn, MD, of the University of Pennsylvania in Philadelphia.
“The answer must lie in the blueprint—the genome—of its chimpanzee and gorilla cousins. We also want to know how and when the gorilla precursor of Plasmodium falciparum jumped into humans and why this happened only once.”
In an attempt to answer these questions, Dr Hahn and her colleagues used their selective amplification method to sequence Laverania genomes.
They used small amounts of unprocessed blood collected during routine health screens of chimpanzees living in sanctuaries. With their technique, the team found they could generate “high-quality” Laverania genome sequences.
The researchers said the chimpanzee parasite genomes contain information about the evolutionary origins of the malaria parasites infecting humans. One of the first things to emerge from genome-wide analyses was that the parasites represent distinct, non-interbreeding species.
In addition, members of each chimpanzee parasite species display about 10 times more genetic diversity than human parasites.
“The chimpanzee parasites really highlight the lack of diversity in Plasmodium falciparum,” said Paul Sharp, PhD, of the University of Edinburgh in the UK.
“This is most likely because these parasites went through a severe bottleneck when first transmitted to humans, perhaps within the past 10,000 years.”
By comparing the different parasite genomes, the researchers found an expansion of a multi-gene family, which governs red blood cell remodeling and therefore helps the parasite to evade host immune cells and clearance by the spleen.
“The remodeling process is a key part of severe malaria pathology in human Plasmodium falciparum infections,” said Julian Rayner, PhD, of the Wellcome Trust Sanger Institute in Cambridge, UK.
“The expansion of this gene family from a single gene in all other Plasmodium parasites to up to 21 genes in Laverania suggests that remodeling evolved early in the radiation of this group of primate parasites and contributed not only to their unique biology but perhaps also to their successful expansion.”
“We also found a short region of the genome, including 2 essential invasion genes, where Plasmodium falciparum was much more different from its close relatives than we expected,” said Lindsey Plenderleith, PhD, of the University of Edinburgh.
Further analysis yielded the surprising finding that this fragment of DNA was horizontally transferred—from one species to another—into the gorilla ancestor of P falciparum.
“It is tempting to speculate that this unusual event somehow predisposed the precursor of Plasmodium falciparum to colonize humans,” Dr Hahn said. “However, this gene transfer clearly is not the entire story.”
Although the origin of P falciparum is considered well-established, nothing is known about the circumstances that led to its emergence.
“Coaxing entire parasite genome sequences out of small quantities of unprocessed ape blood will help us to better understand what happened and whether it can happen again,” said Sesh Sundararaman, an MD/PhD student at the University of Pennsylvania.
The team plans, as a next step, to use their select genome amplification technique to sequence additional ape parasite genomes to identify host-specific interactions and transmission requirements. They believe this would reveal vulnerabilities that might be exploited to combat malaria in humans. ![]()
EMA recommends orphan designation for EBV-CTLs

among uninfected cells (blue)
Image courtesy of Benjamin
Chaigne-Delalande
The European Medicines Agency (EMA) has recommended orphan designation for an allogeneic cytotoxic T-lymphocyte product that targets Epstein-Barr virus (EBV-CTLs) as a treatment for patients with EBV post-transplant lymphoproliferative disorder (EBV-PTLD).
The EMA’s opinion has been forwarded to the European Commission (EC), which makes the final decision.
The EC grants orphan designation to products intended to treat, prevent, or diagnose a life-threatening condition affecting up to 5 in 10,000 people in the European Union. The product must provide significant benefit to those affected by the condition.
Orphan designation from the EC provides companies with certain development incentives, including protocol assistance, a type of scientific advice specific for orphan drugs, and 10 years of market exclusivity once the drug is approved for use.
About EBV-CTLs
The EBV-CTL product utilizes a technology in which T cells are collected from the blood of third-party donors and then exposed to EBV antigens.
The activated T cells are then expanded, characterized, and stored for future use in a partially HLA-matched patient, providing an “off-the-shelf,” allogeneic, cellular therapeutic option for patients.
In the context of EBV-PTLD, the EBV-CTLs find the cancer cells expressing EBV and kill them.
Atara Biotherapeutics, Inc., the company developing the EBV-CTL product, is planning to launch a multi-center, early access clinical trial for EBV-CTLs in mid-2016, followed by 2 phase 3 trials in EBV-PTLD later in the year.
Results of a phase 1/2 study of EBV-CTLs were presented at the APHON 37th Annual Conference and Exhibit and at the 2015 ASCO Annual Meeting.
Atara’s EBV-CTL product already has orphan designation in the US for the treatment of patients with EBV-PTLD after hematopoietic stem cell transplant or solid organ transplant. The product has breakthrough designation for this indication as well. ![]()

among uninfected cells (blue)
Image courtesy of Benjamin
Chaigne-Delalande
The European Medicines Agency (EMA) has recommended orphan designation for an allogeneic cytotoxic T-lymphocyte product that targets Epstein-Barr virus (EBV-CTLs) as a treatment for patients with EBV post-transplant lymphoproliferative disorder (EBV-PTLD).
The EMA’s opinion has been forwarded to the European Commission (EC), which makes the final decision.
The EC grants orphan designation to products intended to treat, prevent, or diagnose a life-threatening condition affecting up to 5 in 10,000 people in the European Union. The product must provide significant benefit to those affected by the condition.
Orphan designation from the EC provides companies with certain development incentives, including protocol assistance, a type of scientific advice specific for orphan drugs, and 10 years of market exclusivity once the drug is approved for use.
About EBV-CTLs
The EBV-CTL product utilizes a technology in which T cells are collected from the blood of third-party donors and then exposed to EBV antigens.
The activated T cells are then expanded, characterized, and stored for future use in a partially HLA-matched patient, providing an “off-the-shelf,” allogeneic, cellular therapeutic option for patients.
In the context of EBV-PTLD, the EBV-CTLs find the cancer cells expressing EBV and kill them.
Atara Biotherapeutics, Inc., the company developing the EBV-CTL product, is planning to launch a multi-center, early access clinical trial for EBV-CTLs in mid-2016, followed by 2 phase 3 trials in EBV-PTLD later in the year.
Results of a phase 1/2 study of EBV-CTLs were presented at the APHON 37th Annual Conference and Exhibit and at the 2015 ASCO Annual Meeting.
Atara’s EBV-CTL product already has orphan designation in the US for the treatment of patients with EBV-PTLD after hematopoietic stem cell transplant or solid organ transplant. The product has breakthrough designation for this indication as well. ![]()

among uninfected cells (blue)
Image courtesy of Benjamin
Chaigne-Delalande
The European Medicines Agency (EMA) has recommended orphan designation for an allogeneic cytotoxic T-lymphocyte product that targets Epstein-Barr virus (EBV-CTLs) as a treatment for patients with EBV post-transplant lymphoproliferative disorder (EBV-PTLD).
The EMA’s opinion has been forwarded to the European Commission (EC), which makes the final decision.
The EC grants orphan designation to products intended to treat, prevent, or diagnose a life-threatening condition affecting up to 5 in 10,000 people in the European Union. The product must provide significant benefit to those affected by the condition.
Orphan designation from the EC provides companies with certain development incentives, including protocol assistance, a type of scientific advice specific for orphan drugs, and 10 years of market exclusivity once the drug is approved for use.
About EBV-CTLs
The EBV-CTL product utilizes a technology in which T cells are collected from the blood of third-party donors and then exposed to EBV antigens.
The activated T cells are then expanded, characterized, and stored for future use in a partially HLA-matched patient, providing an “off-the-shelf,” allogeneic, cellular therapeutic option for patients.
In the context of EBV-PTLD, the EBV-CTLs find the cancer cells expressing EBV and kill them.
Atara Biotherapeutics, Inc., the company developing the EBV-CTL product, is planning to launch a multi-center, early access clinical trial for EBV-CTLs in mid-2016, followed by 2 phase 3 trials in EBV-PTLD later in the year.
Results of a phase 1/2 study of EBV-CTLs were presented at the APHON 37th Annual Conference and Exhibit and at the 2015 ASCO Annual Meeting.
Atara’s EBV-CTL product already has orphan designation in the US for the treatment of patients with EBV-PTLD after hematopoietic stem cell transplant or solid organ transplant. The product has breakthrough designation for this indication as well. ![]()
Drug shows early promise for rel/ref NHL

Blinatumomab, a CD19/CD3 bispecific T-cell engager antibody construct, can produce durable responses in patients with relapsed/refractory B-cell non-Hodgkin lymphoma (NHL), according to a phase 1 study.
Among patients who received the maximum-tolerated dose (MTD) of blinatumomab, the overall response rate (ORR) was nearly 70%, and the median duration of response was more than 400 days.
However, there was a high rate of neurologic events, particularly among patients who received higher doses of the drug.
Ralph Bargou, MD, of Wuerzburg University Hospital in Germany, and his colleagues conducted this study and reported the results in the Journal of Clinical Oncology.
The study was supported by Amgen (and Micromet before its acquisition by Amgen), the companies developing blinatumomab.
The study enrolled 76 patients with relapsed/refractory NHL. Most patients (n=52) had indolent NHL. Subtypes included follicular lymphoma (FL, n=28), mantle cell lymphoma (MCL, n=24), diffuse large B-cell lymphoma (DLBCL, n=14), and “other” (n=10).
The “other” category included lymphoplasmacytic lymphoma (n=2), small lymphoplasmacytic lymphoma (n=1), immunocytoma (n=1), Waldenstrom’s macroglobulinemia (n=1), marginal zone NHL (n=1), marginal zone B-cell lymphoma (n=1), marginal zone lymphoma (n=1), chronic lymphocytic leukemia (n=1), and small lymphoplasmacytic lymphoma/chronic lymphocytic leukemia (n=1).
The patients’ median age was 65 (range, 20-80), and the median number of prior treatment regimens was 3 (range, 1-10).
Dosing, toxicity, and discontinuation
This phase 1, dose-escalation study had a 3 + 3 design. Blinatumomab was given over 4 or 8 weeks at 7 different dose levels, ranging from 0.5 μg/m2/day to 90 μg/m2/day.
The researchers found that neurologic events were dose-limiting, and 60 μg/m2/day was the MTD.
Five patients experienced dose-limiting toxicities, including a grade 2 mental disorder (15 μg/m2/day), a case of grade 4 metabolic acidosis due to grand mal seizure (30 μg/m2/day), 2 cases of grade 3 encephalopathy (90 μg/m2/day), and 1 case of grade 3 seizure and aphasia (90 μg/m2/day).
Forty-two patients received treatment in the formal dose-escalation phase. Thirty-four additional patients were recruited to evaluate the antilymphoma activity of blinatumomab and test strategies for mitigating neurologic events at the MTD.
The researchers found that stepwise dosing (5 μg/m2/day to 60 μg/m2/day) plus pentosan polysulfate SP54 (n=3) prompted no treatment discontinuations.
However, single-step (n=5) dosing led to 2 discontinuations, and double-step (n=24) dosing led to 7 discontinuations. All were due to neurologic events.
The most clinically relevant adverse events were neurologic in nature. The overall incidence of these events, regardless of causality, was 71%. The incidence of grade 3 neurologic events was 22%.
Twenty percent of patients experienced serious neurologic events, including encephalopathy (8%), aphasia (4%), and headache (3%). There were no grade 4 or 5 neurologic events.
Response
Among patients treated at the MTD (60 μg/m2/day), the ORR was 69% (24/35). The ORR was 50% at 90 μg/m2/day (2/4), 20% at 15 μg/m2/day (3/15), and 17% at 30 μg/m2/day (1/6).
Complete responses (CRs) occurred in 1 patient at the 15 μg/m2/day dose, 1 at the 30 μg/m2/day dose, 1 at the 90 μg/m2/day dose, and 8 at the 60 μg/m2/day dose. Unconfirmed CRs (CRus) occurred in 5 patients at the 60 μg/m2/day dose.
Among patients who received the MTD, the ORR was 80% in FL patients, 71% in MCL patients, 55% in DLBCL patients, and 50% in the “other” category. There were 6 CR/CRus among FL patients, 3 CR/CRus among MCL patients, and 4 CR/CRus among DLBCL patients.
The median duration of response for patients who received the MTD was 404 days (95% CI, 207 to 1129). The median duration of CR/CRu was 508 days (95% CI, 213 to not estimable). And the median duration of partial response was 185 days (95% CI, 28 to 754).
Nine patients were still in remission at the time of the analysis, and 12 patients had remissions lasting more than 1 year.
“Blinatumomab continues to demonstrate a long duration of response in heavily pretreated non-Hodgkin lymphoma patients,” Dr Bargou said. “Results of the expanded phase 1 experience suggest that blinatumomab has the potential to alter the clinical course of disease in patients with a variety of NHL subtypes.” ![]()

Blinatumomab, a CD19/CD3 bispecific T-cell engager antibody construct, can produce durable responses in patients with relapsed/refractory B-cell non-Hodgkin lymphoma (NHL), according to a phase 1 study.
Among patients who received the maximum-tolerated dose (MTD) of blinatumomab, the overall response rate (ORR) was nearly 70%, and the median duration of response was more than 400 days.
However, there was a high rate of neurologic events, particularly among patients who received higher doses of the drug.
Ralph Bargou, MD, of Wuerzburg University Hospital in Germany, and his colleagues conducted this study and reported the results in the Journal of Clinical Oncology.
The study was supported by Amgen (and Micromet before its acquisition by Amgen), the companies developing blinatumomab.
The study enrolled 76 patients with relapsed/refractory NHL. Most patients (n=52) had indolent NHL. Subtypes included follicular lymphoma (FL, n=28), mantle cell lymphoma (MCL, n=24), diffuse large B-cell lymphoma (DLBCL, n=14), and “other” (n=10).
The “other” category included lymphoplasmacytic lymphoma (n=2), small lymphoplasmacytic lymphoma (n=1), immunocytoma (n=1), Waldenstrom’s macroglobulinemia (n=1), marginal zone NHL (n=1), marginal zone B-cell lymphoma (n=1), marginal zone lymphoma (n=1), chronic lymphocytic leukemia (n=1), and small lymphoplasmacytic lymphoma/chronic lymphocytic leukemia (n=1).
The patients’ median age was 65 (range, 20-80), and the median number of prior treatment regimens was 3 (range, 1-10).
Dosing, toxicity, and discontinuation
This phase 1, dose-escalation study had a 3 + 3 design. Blinatumomab was given over 4 or 8 weeks at 7 different dose levels, ranging from 0.5 μg/m2/day to 90 μg/m2/day.
The researchers found that neurologic events were dose-limiting, and 60 μg/m2/day was the MTD.
Five patients experienced dose-limiting toxicities, including a grade 2 mental disorder (15 μg/m2/day), a case of grade 4 metabolic acidosis due to grand mal seizure (30 μg/m2/day), 2 cases of grade 3 encephalopathy (90 μg/m2/day), and 1 case of grade 3 seizure and aphasia (90 μg/m2/day).
Forty-two patients received treatment in the formal dose-escalation phase. Thirty-four additional patients were recruited to evaluate the antilymphoma activity of blinatumomab and test strategies for mitigating neurologic events at the MTD.
The researchers found that stepwise dosing (5 μg/m2/day to 60 μg/m2/day) plus pentosan polysulfate SP54 (n=3) prompted no treatment discontinuations.
However, single-step (n=5) dosing led to 2 discontinuations, and double-step (n=24) dosing led to 7 discontinuations. All were due to neurologic events.
The most clinically relevant adverse events were neurologic in nature. The overall incidence of these events, regardless of causality, was 71%. The incidence of grade 3 neurologic events was 22%.
Twenty percent of patients experienced serious neurologic events, including encephalopathy (8%), aphasia (4%), and headache (3%). There were no grade 4 or 5 neurologic events.
Response
Among patients treated at the MTD (60 μg/m2/day), the ORR was 69% (24/35). The ORR was 50% at 90 μg/m2/day (2/4), 20% at 15 μg/m2/day (3/15), and 17% at 30 μg/m2/day (1/6).
Complete responses (CRs) occurred in 1 patient at the 15 μg/m2/day dose, 1 at the 30 μg/m2/day dose, 1 at the 90 μg/m2/day dose, and 8 at the 60 μg/m2/day dose. Unconfirmed CRs (CRus) occurred in 5 patients at the 60 μg/m2/day dose.
Among patients who received the MTD, the ORR was 80% in FL patients, 71% in MCL patients, 55% in DLBCL patients, and 50% in the “other” category. There were 6 CR/CRus among FL patients, 3 CR/CRus among MCL patients, and 4 CR/CRus among DLBCL patients.
The median duration of response for patients who received the MTD was 404 days (95% CI, 207 to 1129). The median duration of CR/CRu was 508 days (95% CI, 213 to not estimable). And the median duration of partial response was 185 days (95% CI, 28 to 754).
Nine patients were still in remission at the time of the analysis, and 12 patients had remissions lasting more than 1 year.
“Blinatumomab continues to demonstrate a long duration of response in heavily pretreated non-Hodgkin lymphoma patients,” Dr Bargou said. “Results of the expanded phase 1 experience suggest that blinatumomab has the potential to alter the clinical course of disease in patients with a variety of NHL subtypes.” ![]()

Blinatumomab, a CD19/CD3 bispecific T-cell engager antibody construct, can produce durable responses in patients with relapsed/refractory B-cell non-Hodgkin lymphoma (NHL), according to a phase 1 study.
Among patients who received the maximum-tolerated dose (MTD) of blinatumomab, the overall response rate (ORR) was nearly 70%, and the median duration of response was more than 400 days.
However, there was a high rate of neurologic events, particularly among patients who received higher doses of the drug.
Ralph Bargou, MD, of Wuerzburg University Hospital in Germany, and his colleagues conducted this study and reported the results in the Journal of Clinical Oncology.
The study was supported by Amgen (and Micromet before its acquisition by Amgen), the companies developing blinatumomab.
The study enrolled 76 patients with relapsed/refractory NHL. Most patients (n=52) had indolent NHL. Subtypes included follicular lymphoma (FL, n=28), mantle cell lymphoma (MCL, n=24), diffuse large B-cell lymphoma (DLBCL, n=14), and “other” (n=10).
The “other” category included lymphoplasmacytic lymphoma (n=2), small lymphoplasmacytic lymphoma (n=1), immunocytoma (n=1), Waldenstrom’s macroglobulinemia (n=1), marginal zone NHL (n=1), marginal zone B-cell lymphoma (n=1), marginal zone lymphoma (n=1), chronic lymphocytic leukemia (n=1), and small lymphoplasmacytic lymphoma/chronic lymphocytic leukemia (n=1).
The patients’ median age was 65 (range, 20-80), and the median number of prior treatment regimens was 3 (range, 1-10).
Dosing, toxicity, and discontinuation
This phase 1, dose-escalation study had a 3 + 3 design. Blinatumomab was given over 4 or 8 weeks at 7 different dose levels, ranging from 0.5 μg/m2/day to 90 μg/m2/day.
The researchers found that neurologic events were dose-limiting, and 60 μg/m2/day was the MTD.
Five patients experienced dose-limiting toxicities, including a grade 2 mental disorder (15 μg/m2/day), a case of grade 4 metabolic acidosis due to grand mal seizure (30 μg/m2/day), 2 cases of grade 3 encephalopathy (90 μg/m2/day), and 1 case of grade 3 seizure and aphasia (90 μg/m2/day).
Forty-two patients received treatment in the formal dose-escalation phase. Thirty-four additional patients were recruited to evaluate the antilymphoma activity of blinatumomab and test strategies for mitigating neurologic events at the MTD.
The researchers found that stepwise dosing (5 μg/m2/day to 60 μg/m2/day) plus pentosan polysulfate SP54 (n=3) prompted no treatment discontinuations.
However, single-step (n=5) dosing led to 2 discontinuations, and double-step (n=24) dosing led to 7 discontinuations. All were due to neurologic events.
The most clinically relevant adverse events were neurologic in nature. The overall incidence of these events, regardless of causality, was 71%. The incidence of grade 3 neurologic events was 22%.
Twenty percent of patients experienced serious neurologic events, including encephalopathy (8%), aphasia (4%), and headache (3%). There were no grade 4 or 5 neurologic events.
Response
Among patients treated at the MTD (60 μg/m2/day), the ORR was 69% (24/35). The ORR was 50% at 90 μg/m2/day (2/4), 20% at 15 μg/m2/day (3/15), and 17% at 30 μg/m2/day (1/6).
Complete responses (CRs) occurred in 1 patient at the 15 μg/m2/day dose, 1 at the 30 μg/m2/day dose, 1 at the 90 μg/m2/day dose, and 8 at the 60 μg/m2/day dose. Unconfirmed CRs (CRus) occurred in 5 patients at the 60 μg/m2/day dose.
Among patients who received the MTD, the ORR was 80% in FL patients, 71% in MCL patients, 55% in DLBCL patients, and 50% in the “other” category. There were 6 CR/CRus among FL patients, 3 CR/CRus among MCL patients, and 4 CR/CRus among DLBCL patients.
The median duration of response for patients who received the MTD was 404 days (95% CI, 207 to 1129). The median duration of CR/CRu was 508 days (95% CI, 213 to not estimable). And the median duration of partial response was 185 days (95% CI, 28 to 754).
Nine patients were still in remission at the time of the analysis, and 12 patients had remissions lasting more than 1 year.
“Blinatumomab continues to demonstrate a long duration of response in heavily pretreated non-Hodgkin lymphoma patients,” Dr Bargou said. “Results of the expanded phase 1 experience suggest that blinatumomab has the potential to alter the clinical course of disease in patients with a variety of NHL subtypes.” ![]()
A Double Dose of Trouble
ANSWER
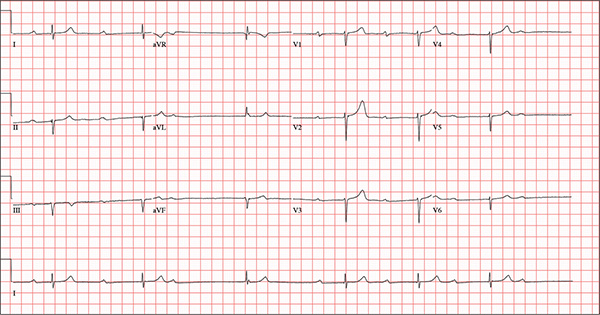
This ECG demonstrates marked sinus bradycardia with a second-degree atrioventricular (AV) block (Mobitz I). Other findings include left-axis deviation, an old inferior MI, and poor R-wave progression.
Second-degree Mobitz I block is present in a 3:1 pattern of progressive prolongation of the PR interval until the third beat, where there is block in the AV node preventing conduction of the P wave to the ventricles. This is typically caused by progressive fatigue within the AV node until block occurs, then the cycle repeats.
Left-axis deviation is evidenced by a QRS axis of –78°. An old inferior MI is signified by the significant Q waves in leads II, III, and aVF. Finally, poor R-wave progression is demonstrated by small R waves in all of the precordial leads.
This ECG represented a significant change from one obtained three months earlier, during a routine outpatient visit. Careful review of the records at the Alzheimer facility revealed that the patient had received twice his usual dose of propranolol on three consecutive days. His rhythm returned to a baseline sinus rhythm (at 68 beats/min) after his ß-blocker was withheld for two days, and no further intervention was needed.
ANSWER
This ECG demonstrates marked sinus bradycardia with a second-degree atrioventricular (AV) block (Mobitz I). Other findings include left-axis deviation, an old inferior MI, and poor R-wave progression.
Second-degree Mobitz I block is present in a 3:1 pattern of progressive prolongation of the PR interval until the third beat, where there is block in the AV node preventing conduction of the P wave to the ventricles. This is typically caused by progressive fatigue within the AV node until block occurs, then the cycle repeats.
Left-axis deviation is evidenced by a QRS axis of –78°. An old inferior MI is signified by the significant Q waves in leads II, III, and aVF. Finally, poor R-wave progression is demonstrated by small R waves in all of the precordial leads.
This ECG represented a significant change from one obtained three months earlier, during a routine outpatient visit. Careful review of the records at the Alzheimer facility revealed that the patient had received twice his usual dose of propranolol on three consecutive days. His rhythm returned to a baseline sinus rhythm (at 68 beats/min) after his ß-blocker was withheld for two days, and no further intervention was needed.
ANSWER
This ECG demonstrates marked sinus bradycardia with a second-degree atrioventricular (AV) block (Mobitz I). Other findings include left-axis deviation, an old inferior MI, and poor R-wave progression.
Second-degree Mobitz I block is present in a 3:1 pattern of progressive prolongation of the PR interval until the third beat, where there is block in the AV node preventing conduction of the P wave to the ventricles. This is typically caused by progressive fatigue within the AV node until block occurs, then the cycle repeats.
Left-axis deviation is evidenced by a QRS axis of –78°. An old inferior MI is signified by the significant Q waves in leads II, III, and aVF. Finally, poor R-wave progression is demonstrated by small R waves in all of the precordial leads.
This ECG represented a significant change from one obtained three months earlier, during a routine outpatient visit. Careful review of the records at the Alzheimer facility revealed that the patient had received twice his usual dose of propranolol on three consecutive days. His rhythm returned to a baseline sinus rhythm (at 68 beats/min) after his ß-blocker was withheld for two days, and no further intervention was needed.
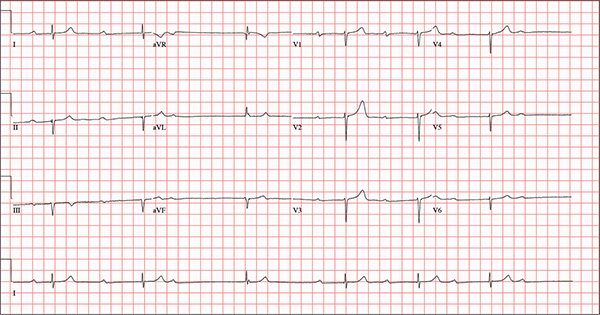
An 82-year-old man is referred from a nearby Alzheimer care facility following an episode of postural hypotension. While trying to get out of bed, he experienced near-syncope, which was observed by a nurse caring for another patient in the same room. The patient was helped back into bed, and the resident care provider was summoned. A careful examination ruled out any injury sustained when the patient’s knees buckled and he fell to the ground. However, he was found to have profound bradycardia with a pulse of 30 beats/min. Emergency medical services were called, and the patient was transported to your facility for further evaluation. You find the patient to be pleasant but mildly confused. He is in no distress. A review of the limited available records shows that he has had Alzheimer disease for four years; it has been relatively stable, with no recent changes in cognition. His history includes an inferior myocardial infarction (MI) at age 68 and hypertension. The latter has been treated with diuretics and ß-blockers, although the doses have not been changed since his MI. Other remarkable items in the history include hypothyroidism, type 2 diabetes, cholecystectomy, and appendectomy. He has significant osteoarthritis in both knees but does not require a cane or other device to ambulate. The patient is a retired iron worker from the local foundry. He is a widower with two adult children who live remotely and do not visit. He was a heavy drinker in his younger years and smoked one to two packs of cigarettes per day until his MI. He has abstained from alcohol and tobacco since his wife’s death six years ago. His medication list includes a daily aspirin, furosemide, potassium chloride, propranolol, and levothyroxine. He is said to be allergic to penicillin, but there is no record of him ever receiving it. The review of systems is difficult to obtain due to the patient’s confusion. He has not had any recent infectious illnesses, according to the accompanying nurse from the Alzheimer facility. Physical exam reveals a disheveled but otherwise pleasant man. He can remember only one out of three words when asked to recite immediately after hearing them. Vital signs include a blood pressure of 86/48 mm Hg; pulse, 40 beats/min; respiratory rate, 14 breaths/min-1; and temperature, 98.4°F. His weight is 163 lb and his height, 66 in. The patient wears corrective lenses and hearing aids, but the batteries in the latter are dead. Regardless, he can hear you if you speak loudly. Pertinent physical findings include scattered crackles in both lung bases, a regularly irregular slow heart rate, a grade III/VI systolic murmur that radiates to the neck, and well-healed surgical scars on the abdomen consistent with the surgeries described in the history. There appear to be no gross focal neurologic findings. An ECG reveals a ventricular rate of 38 beats/min; PR interval, not measured; QRS duration, 78 ms; QT/QTc interval, 434/345 ms; P axis, 25°; R axis, –78°; and T axis, 13°. What is your interpretation of this ECG?
When Trauma Changes the Picture
Answer
The radiograph has several findings. First, there are multiple fractures along the left lateral ribs. Second, there is a small left apical pneumothorax. Most significant, though, is an elevated left hemidiaphragm. There appears to be stomach or possibly bowel protruding into it.
Although a large hiatal hernia could yield similar findings, in the setting of trauma, one must be concerned about a traumatic diaphragmatic hernia. Subsequent CT of the chest, abdomen, and pelvis confirmed a defect within the diaphragm, with a significant portion of the stomach herniating into the left chest.
Surgical consultation was obtained. The patient was admitted and ultimately underwent surgical intervention to repair the problem.
Answer
The radiograph has several findings. First, there are multiple fractures along the left lateral ribs. Second, there is a small left apical pneumothorax. Most significant, though, is an elevated left hemidiaphragm. There appears to be stomach or possibly bowel protruding into it.
Although a large hiatal hernia could yield similar findings, in the setting of trauma, one must be concerned about a traumatic diaphragmatic hernia. Subsequent CT of the chest, abdomen, and pelvis confirmed a defect within the diaphragm, with a significant portion of the stomach herniating into the left chest.
Surgical consultation was obtained. The patient was admitted and ultimately underwent surgical intervention to repair the problem.
Answer
The radiograph has several findings. First, there are multiple fractures along the left lateral ribs. Second, there is a small left apical pneumothorax. Most significant, though, is an elevated left hemidiaphragm. There appears to be stomach or possibly bowel protruding into it.
Although a large hiatal hernia could yield similar findings, in the setting of trauma, one must be concerned about a traumatic diaphragmatic hernia. Subsequent CT of the chest, abdomen, and pelvis confirmed a defect within the diaphragm, with a significant portion of the stomach herniating into the left chest.
Surgical consultation was obtained. The patient was admitted and ultimately underwent surgical intervention to repair the problem.

A 75-year-old man is brought to your emergency center following a fall from his attic. He slipped and fell approximately 10 feet, landing on his left side. He did not hit his head and denies any loss of consciousness. His primary complaint is left-side chest wall pain. Medical history is significant for hypertension, diabetes, reflux, and atrial fibrillation. On primary survey, you note an elderly male who is somewhat uncomfortable but in no obvious distress. His vital signs are stable; O2 saturation is 98% on room air. The patient exhibits moderate tenderness along the anterior lateral aspect of his chest, as well as mild generalized tenderness in his abdomen. Good inspiratory effort is limited secondary to his pain. While you enter orders into the computer, a portable chest radiograph is obtained. What is your impression?
Brain imaging suggests link between stress and cardiovascular events
Stress seems to be a strong driver of cardiovascular events, including heart attack, stroke, and even death.
For the first time, brain imaging has confirmed a link that has long been suspected: Activation of one of the brain’s prime emotional centers, the amygdala, directly correlates with the risk of cardiovascular events.
“This study illustrates a clear relationship between the activity of the amygdala and heart disease,” Dr. Ahmed A. Tawakol said at a press teleconference leading up to the annual meeting of the American College of Cardiology.
“Stress is known to be associated with an increase in the risk of cardiovascular events, and the risk is on par with that exerted by smoking, hypertension, and diabetes, but we don’t address it,” said Dr. Tawakol, codirector of the Cardiac MRI PET CT Program at Massachusetts General Hospital, Boston.
The findings also highlight a possible pathway for this relationship, suggesting that stress-related noradrenalin stimulates extramedullary hematopoiesis, a key driver of inflammation. This can contribute to atherosclerotic inflammation, which increases the likelihood of a heart attack or stroke, said Dr. Tawakol.
His study comprised 293 subjects who had undergone a PET or CT scan for cancer evaluation, but were determined to be cancer free. All scans contained brain and bone imaging data. Dr. Tawakol assessed amygdala and bone marrow activation, and evaluated inflammatory response in arteries.
These findings were then correlated with any cardiovascular events occurring in the next 5 years; the median follow-up was 3.8 years. Events were significantly more common among those with high levels of amygdala activation, occurring in 35% of this group, but in just 5% of those with low activation.
After adjusting for risk factors in the Framingham model, Dr. Tawakol found that high amygdala activation conferred a 14-fold increase in the risk of a cardiovascular event. These were likely to be precipitous as well, he said: The higher the level of activation, the more likely the event was to happen within the first year of follow-up.
He had no financial disclosures.
Stress seems to be a strong driver of cardiovascular events, including heart attack, stroke, and even death.
For the first time, brain imaging has confirmed a link that has long been suspected: Activation of one of the brain’s prime emotional centers, the amygdala, directly correlates with the risk of cardiovascular events.
“This study illustrates a clear relationship between the activity of the amygdala and heart disease,” Dr. Ahmed A. Tawakol said at a press teleconference leading up to the annual meeting of the American College of Cardiology.
“Stress is known to be associated with an increase in the risk of cardiovascular events, and the risk is on par with that exerted by smoking, hypertension, and diabetes, but we don’t address it,” said Dr. Tawakol, codirector of the Cardiac MRI PET CT Program at Massachusetts General Hospital, Boston.
The findings also highlight a possible pathway for this relationship, suggesting that stress-related noradrenalin stimulates extramedullary hematopoiesis, a key driver of inflammation. This can contribute to atherosclerotic inflammation, which increases the likelihood of a heart attack or stroke, said Dr. Tawakol.
His study comprised 293 subjects who had undergone a PET or CT scan for cancer evaluation, but were determined to be cancer free. All scans contained brain and bone imaging data. Dr. Tawakol assessed amygdala and bone marrow activation, and evaluated inflammatory response in arteries.
These findings were then correlated with any cardiovascular events occurring in the next 5 years; the median follow-up was 3.8 years. Events were significantly more common among those with high levels of amygdala activation, occurring in 35% of this group, but in just 5% of those with low activation.
After adjusting for risk factors in the Framingham model, Dr. Tawakol found that high amygdala activation conferred a 14-fold increase in the risk of a cardiovascular event. These were likely to be precipitous as well, he said: The higher the level of activation, the more likely the event was to happen within the first year of follow-up.
He had no financial disclosures.
Stress seems to be a strong driver of cardiovascular events, including heart attack, stroke, and even death.
For the first time, brain imaging has confirmed a link that has long been suspected: Activation of one of the brain’s prime emotional centers, the amygdala, directly correlates with the risk of cardiovascular events.
“This study illustrates a clear relationship between the activity of the amygdala and heart disease,” Dr. Ahmed A. Tawakol said at a press teleconference leading up to the annual meeting of the American College of Cardiology.
“Stress is known to be associated with an increase in the risk of cardiovascular events, and the risk is on par with that exerted by smoking, hypertension, and diabetes, but we don’t address it,” said Dr. Tawakol, codirector of the Cardiac MRI PET CT Program at Massachusetts General Hospital, Boston.
The findings also highlight a possible pathway for this relationship, suggesting that stress-related noradrenalin stimulates extramedullary hematopoiesis, a key driver of inflammation. This can contribute to atherosclerotic inflammation, which increases the likelihood of a heart attack or stroke, said Dr. Tawakol.
His study comprised 293 subjects who had undergone a PET or CT scan for cancer evaluation, but were determined to be cancer free. All scans contained brain and bone imaging data. Dr. Tawakol assessed amygdala and bone marrow activation, and evaluated inflammatory response in arteries.
These findings were then correlated with any cardiovascular events occurring in the next 5 years; the median follow-up was 3.8 years. Events were significantly more common among those with high levels of amygdala activation, occurring in 35% of this group, but in just 5% of those with low activation.
After adjusting for risk factors in the Framingham model, Dr. Tawakol found that high amygdala activation conferred a 14-fold increase in the risk of a cardiovascular event. These were likely to be precipitous as well, he said: The higher the level of activation, the more likely the event was to happen within the first year of follow-up.
He had no financial disclosures.
FROM ACC 16
Key clinical point: Activation of the amygdala, the brain’s fear response center, was directly correlated with the occurrence of cardiovascular events.
Major finding: High amygdala activation conferred a 14-fold increase in the risk of a heart attack, stroke, or cardiac death.
Data source: An imaging study in 293 patients.
Disclosures: Dr. Tawakol had no financial disclosures.
Heart attack patients getting younger, fatter, and less healthy
Despite advances in the prevention and early detection of cardiovascular disease, heart attack patients are getting younger, fatter, and less health conscious.
A look at 10 years’ worth of patient data reveals these and other “alarming trends,” according to Dr. Samir R. Kapadia of the Cleveland Clinic.
“What we found was so very contradictory to what we expected,” he said at a press briefing held in advance of the annual meeting of the American College of Cardiology. “Amazingly, we saw that patients presenting with myocardial infarction were getting younger, and their body mass index was going up. There was more smoking, more hypertension, and more diabetes. And all of this despite our better understanding of cardiovascular risk factors.”
The findings seem to point to a serious gap between gathering scientific knowledge and putting that knowledge into practice.
“We have to extend our efforts and put a lot more into educating patients,” Dr. Kapadia said. “Maybe it’s not enough to just tell people to eat right and exercise – maybe we should also be providing them with a structured program. But this is not just the job of the cardiologist. Primary care physicians have to also have this insight, communicate it to the patients, and get them the resources they need to help prevent heart attacks.”
His retrospective study comprised 3,912 consecutive patients who were treated for ST-segment elevation MI (STEMI) from 1995 to 2014. Data were collected on age, gender, diabetes, hypertension, smoking, lipid levels, chronic renal impairment, and obesity. The group was divided into four epochs: 1995-1999, 2000-2004, 2005-2009, and 2010-2014. The researchers examined these factors both in the entire cohort and in a subset of 1,325 who had a diagnosis of coronary artery disease at the time of their MI.
Patients became significantly younger over the entire study period. In epoch 1, the mean age of the entire cohort was 63.6 years. By epoch 3, this had declined to 60.3 years – a significant drop. The change was also evident in the CAD subset; among these patients, mean age declined from 64.1 years in epoch 1 to 61.8 years in epoch 4.
Tobacco use increased significantly in both groups as well. In the overall cohort, the rate was 27.7% in epoch 1 and 45.4% in epoch 4. In the CAD subset, it rose from 24.6% to 42.7%.
Hypertension in the entire cohort increased from 56.7% to 77.3%. In the CAD subset, it increased from 60.9% to 89%.
Obesity increased in both cohorts in overlapping trends, from about 30% in epoch 1 to 40% in epoch 4.
Diabetes increased as well. In the entire cohort, it rose from 24.6% to 30.6%. In the CAD subset, it rose from 25.4% to 41.5%.
Dr. Kapadia noted that the proportion of patients with at least three major risk factors rose from 65% to 85%, and that the incidence of chronic obstructive pulmonary disease increased from 5% to 12%, although he didn’t break this trend down by group.
He had no financial disclosures.
Despite advances in the prevention and early detection of cardiovascular disease, heart attack patients are getting younger, fatter, and less health conscious.
A look at 10 years’ worth of patient data reveals these and other “alarming trends,” according to Dr. Samir R. Kapadia of the Cleveland Clinic.
“What we found was so very contradictory to what we expected,” he said at a press briefing held in advance of the annual meeting of the American College of Cardiology. “Amazingly, we saw that patients presenting with myocardial infarction were getting younger, and their body mass index was going up. There was more smoking, more hypertension, and more diabetes. And all of this despite our better understanding of cardiovascular risk factors.”
The findings seem to point to a serious gap between gathering scientific knowledge and putting that knowledge into practice.
“We have to extend our efforts and put a lot more into educating patients,” Dr. Kapadia said. “Maybe it’s not enough to just tell people to eat right and exercise – maybe we should also be providing them with a structured program. But this is not just the job of the cardiologist. Primary care physicians have to also have this insight, communicate it to the patients, and get them the resources they need to help prevent heart attacks.”
His retrospective study comprised 3,912 consecutive patients who were treated for ST-segment elevation MI (STEMI) from 1995 to 2014. Data were collected on age, gender, diabetes, hypertension, smoking, lipid levels, chronic renal impairment, and obesity. The group was divided into four epochs: 1995-1999, 2000-2004, 2005-2009, and 2010-2014. The researchers examined these factors both in the entire cohort and in a subset of 1,325 who had a diagnosis of coronary artery disease at the time of their MI.
Patients became significantly younger over the entire study period. In epoch 1, the mean age of the entire cohort was 63.6 years. By epoch 3, this had declined to 60.3 years – a significant drop. The change was also evident in the CAD subset; among these patients, mean age declined from 64.1 years in epoch 1 to 61.8 years in epoch 4.
Tobacco use increased significantly in both groups as well. In the overall cohort, the rate was 27.7% in epoch 1 and 45.4% in epoch 4. In the CAD subset, it rose from 24.6% to 42.7%.
Hypertension in the entire cohort increased from 56.7% to 77.3%. In the CAD subset, it increased from 60.9% to 89%.
Obesity increased in both cohorts in overlapping trends, from about 30% in epoch 1 to 40% in epoch 4.
Diabetes increased as well. In the entire cohort, it rose from 24.6% to 30.6%. In the CAD subset, it rose from 25.4% to 41.5%.
Dr. Kapadia noted that the proportion of patients with at least three major risk factors rose from 65% to 85%, and that the incidence of chronic obstructive pulmonary disease increased from 5% to 12%, although he didn’t break this trend down by group.
He had no financial disclosures.
Despite advances in the prevention and early detection of cardiovascular disease, heart attack patients are getting younger, fatter, and less health conscious.
A look at 10 years’ worth of patient data reveals these and other “alarming trends,” according to Dr. Samir R. Kapadia of the Cleveland Clinic.
“What we found was so very contradictory to what we expected,” he said at a press briefing held in advance of the annual meeting of the American College of Cardiology. “Amazingly, we saw that patients presenting with myocardial infarction were getting younger, and their body mass index was going up. There was more smoking, more hypertension, and more diabetes. And all of this despite our better understanding of cardiovascular risk factors.”
The findings seem to point to a serious gap between gathering scientific knowledge and putting that knowledge into practice.
“We have to extend our efforts and put a lot more into educating patients,” Dr. Kapadia said. “Maybe it’s not enough to just tell people to eat right and exercise – maybe we should also be providing them with a structured program. But this is not just the job of the cardiologist. Primary care physicians have to also have this insight, communicate it to the patients, and get them the resources they need to help prevent heart attacks.”
His retrospective study comprised 3,912 consecutive patients who were treated for ST-segment elevation MI (STEMI) from 1995 to 2014. Data were collected on age, gender, diabetes, hypertension, smoking, lipid levels, chronic renal impairment, and obesity. The group was divided into four epochs: 1995-1999, 2000-2004, 2005-2009, and 2010-2014. The researchers examined these factors both in the entire cohort and in a subset of 1,325 who had a diagnosis of coronary artery disease at the time of their MI.
Patients became significantly younger over the entire study period. In epoch 1, the mean age of the entire cohort was 63.6 years. By epoch 3, this had declined to 60.3 years – a significant drop. The change was also evident in the CAD subset; among these patients, mean age declined from 64.1 years in epoch 1 to 61.8 years in epoch 4.
Tobacco use increased significantly in both groups as well. In the overall cohort, the rate was 27.7% in epoch 1 and 45.4% in epoch 4. In the CAD subset, it rose from 24.6% to 42.7%.
Hypertension in the entire cohort increased from 56.7% to 77.3%. In the CAD subset, it increased from 60.9% to 89%.
Obesity increased in both cohorts in overlapping trends, from about 30% in epoch 1 to 40% in epoch 4.
Diabetes increased as well. In the entire cohort, it rose from 24.6% to 30.6%. In the CAD subset, it rose from 25.4% to 41.5%.
Dr. Kapadia noted that the proportion of patients with at least three major risk factors rose from 65% to 85%, and that the incidence of chronic obstructive pulmonary disease increased from 5% to 12%, although he didn’t break this trend down by group.
He had no financial disclosures.
FROM ACC 16
Key clinical point: Despite advances in understanding heart disease prevention, patients with heart attack are younger and less healthy than they were 10 years ago.
Major finding: Patients are an average of 3 years younger than in 1994, and more are obese and use tobacco.
Data source: A retrospective study of 3,912 patients with acute ST-segment elevation MI.
Disclosures: Dr. Samir Kapadia had no financial disclosures.
Chaplains play important part of integrated palliative care
WASHINGTON – Hospital chaplains are key partners in meeting the needs of palliative care patients and, as such, have much to offer psychiatry, according to an expert.
“I think we should work with chaplains,” Dr. Laura B. Dunn, professor of psychiatry and behavioral sciences at Stanford (Calif.) University, said in an interview at the annual meeting of the American Association for Geriatric Psychiatry. “It’s very helpful to know what they do, and for them to know what we do in terms of diagnosing and using a biopsychosocial model.”
Dr. Dunn said the relegation of chaplaincy and spiritual care in medicine has been unfortunate. After all, the level of a patient’s spiritual health is an inherent aspect of quality of life in palliative care, particularly for those over age 60 who often want help reconciling with loved ones, data collected by Dr. Dunn show. Viewing those patients in terms of their core needs rather than seeking a psychiatric diagnosis can make them more satisfied with their overall palliative care experience, she said.
How is spiritual health measured? There are few models and even fewer empirical studies, but Dr. Dunn said in addition learning how to deliver pastoral care, professional chaplains are trained to assess, intervene, and observe outcomes in spiritual health.
To begin with, spirituality is defined not in terms of “religiosity” but more as following an ethical path, similar to the idea of the Golden Rule or the ethic of reciprocity: Love your neighbor as yourself, in other words. The spiritual maturity to follow such a path requires the ability to love oneself that is balanced with a connection to others, and God, “if your belief includes God,” said Dr. Dunn, who pointed out that chaplaincy programs for atheists also exist.
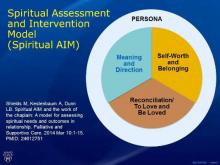
By observing a person’s behavior and conversing with him or her, paying close attention to the person’s attributions of blame, if any, and expressions of chief concerns, a chaplain will assess where on the continuum that person is in three key components of spiritual health: the need for meaning and direction, a sense of self-worth and belonging, and an ability to love and be loved. This latter component often is facilitated through seeking reconciliation when relationships are broken.
In the face of crisis, such as with terminal illness, one of those needs typically supersedes the others. This is what is known as the person’s “core spiritual need,” said Dr. Dunn, who also serves director of the university’s Geriatric Psychiatry Fellowship Training Program, and has extensive research and clinical experience evaluating and managing older adults with mood, anxiety, and cognitive disorders. As part of her research, she and her colleagues have developed a schematic called the Spiritual AIM (Spiritual Assessment and Intervention Model), which depicts those three concerns in relation to one another (Palliat Support Care. 2015 Feb;13:75-89).
Chaplains also are trained to rely on their own feelings about people, similar to the way in which psychiatrists use countertransference. “It is not intrapersonal; it is interpersonal,” Dr. Dunn said. “Healing happens in relationship, and the focus is on that relationship.”
Chaplains undergo standardized clinical pastoral training programs predicated on a combination of theological reflection and psychological theory, plus critique from professional peers and students.
“Their model is very similar to what we [geriatric psychiatrists] do when we assess a patient,” Dr. Dunn said. “We might be more structured trying to ferret out a diagnosis, but we’re assessing all the time.”
Depending on which aspect of spiritual health is most lacking, the chaplain will choose the role of either a “guide” to help with balancing the need for meaning and direction, a “valuer” to help restore feelings of worth and belonging, or a “truth-teller” who will explore with the patient ways he or she might have contributed to broken relationships, and actions the patient might take in order to heal them. This is all done within the context of an interdisciplinary team, Dr. Dunn said.
She and a team of researchers, including a chaplain, conducted a study of 31 advanced-stage adult cancer patients in an outpatient palliative care service, that measured self-reported changes in their spiritual, psychological, and physical symptoms both before and after Spiritual AIM sessions with a chaplain.
The need for balancing one of the three key components of spiritual health was determined by the chaplain to be fairly equal across the cohort, although just more than half of patients younger than 60 years of age struggled more with self-worth and belonging (P = .030). Those over 60 years were equally concerned with either reconciliation or meaning and direction (P less than .05). Two-thirds of the cohort were women, although a relationship between gender and spiritual assessment needs was not determined. Two-thirds also identified themselves as Christian, just over one-third were Jewish, and the rest identified as either Buddhist or nondenominational.
Using a variety of validated palliative care scales, such as the Edmonton Symptom Assessment Syndrome (ESAS) for physical complaints, the Center for Epidemiologic Studies Short Depression Scale, the Mini Mental Adjustment to Cancer scale (Mini-MAC), and the positive and negative RCOPE questionnaire for religious coping, among other scales, Dr. Dunn and her associates found that the change in baseline of overall spiritual health after intervention from the chaplain improved slightly in most measures. Mean baseline scores for the ESAS went from 25 to 24.4 post-intervention. The difference between baseline depression scores fell from 4.2 to 4.1.
Mini-MAC scores improved, particularly in “fighting spirit” and levels of fatalism (P = .084 and P = .036, respectively). In addition, maladaptive coping skills also improved (P = .018).The findings have helped Dr. Dunn in her work as a geriatric psychiatrist, especially when treating cancer patients, or in settings where there is not as much time for a full clinical assessment. “I think of patients in terms of their core needs and what I can do right now to help patients meet those needs.” Dr. Dunn cited, as an example, patients who feel like they don’t belong and are lonely. “If they’re in an assisted living home, can I get them to enter [the communal space]? That’s very different than thinking of them in terms only of depression.”
On Twitter @whitneymcknight
One reason chaplains are such a key part of the palliative care team is that they are seen by patients from a different perspective, Dr. Gurprit S. Lamba said. “Chaplains lend their ears, act as friends, and provide company to these patients,” Dr. Lamba said in an interview. “Discussing spiritual/religious matters helps these individuals cope better. Chaplains can provide more meaningful services with knowledge about different cultures, doctrines, and traditions, so that they can tailor their meetings accordingly.
“Studies have shown that psychiatrists are less religious and show less religious affiliation than their patients and than the population in general. As Dr. Dunn mentioned, chaplaincy programs for atheists also exist. Psychiatrists, with chaplains, can work with any individual to improve and optimize treatment. The critical part lies in assessment of patients’ religious views and spirituality along with their families’ opinions before offering meeting with chaplains.”
Dr. Lamba is a geriatric psychiatrist affiliated with BayRidge Hospital in Lynn, Mass.
One reason chaplains are such a key part of the palliative care team is that they are seen by patients from a different perspective, Dr. Gurprit S. Lamba said. “Chaplains lend their ears, act as friends, and provide company to these patients,” Dr. Lamba said in an interview. “Discussing spiritual/religious matters helps these individuals cope better. Chaplains can provide more meaningful services with knowledge about different cultures, doctrines, and traditions, so that they can tailor their meetings accordingly.
“Studies have shown that psychiatrists are less religious and show less religious affiliation than their patients and than the population in general. As Dr. Dunn mentioned, chaplaincy programs for atheists also exist. Psychiatrists, with chaplains, can work with any individual to improve and optimize treatment. The critical part lies in assessment of patients’ religious views and spirituality along with their families’ opinions before offering meeting with chaplains.”
Dr. Lamba is a geriatric psychiatrist affiliated with BayRidge Hospital in Lynn, Mass.
One reason chaplains are such a key part of the palliative care team is that they are seen by patients from a different perspective, Dr. Gurprit S. Lamba said. “Chaplains lend their ears, act as friends, and provide company to these patients,” Dr. Lamba said in an interview. “Discussing spiritual/religious matters helps these individuals cope better. Chaplains can provide more meaningful services with knowledge about different cultures, doctrines, and traditions, so that they can tailor their meetings accordingly.
“Studies have shown that psychiatrists are less religious and show less religious affiliation than their patients and than the population in general. As Dr. Dunn mentioned, chaplaincy programs for atheists also exist. Psychiatrists, with chaplains, can work with any individual to improve and optimize treatment. The critical part lies in assessment of patients’ religious views and spirituality along with their families’ opinions before offering meeting with chaplains.”
Dr. Lamba is a geriatric psychiatrist affiliated with BayRidge Hospital in Lynn, Mass.
WASHINGTON – Hospital chaplains are key partners in meeting the needs of palliative care patients and, as such, have much to offer psychiatry, according to an expert.
“I think we should work with chaplains,” Dr. Laura B. Dunn, professor of psychiatry and behavioral sciences at Stanford (Calif.) University, said in an interview at the annual meeting of the American Association for Geriatric Psychiatry. “It’s very helpful to know what they do, and for them to know what we do in terms of diagnosing and using a biopsychosocial model.”
Dr. Dunn said the relegation of chaplaincy and spiritual care in medicine has been unfortunate. After all, the level of a patient’s spiritual health is an inherent aspect of quality of life in palliative care, particularly for those over age 60 who often want help reconciling with loved ones, data collected by Dr. Dunn show. Viewing those patients in terms of their core needs rather than seeking a psychiatric diagnosis can make them more satisfied with their overall palliative care experience, she said.
How is spiritual health measured? There are few models and even fewer empirical studies, but Dr. Dunn said in addition learning how to deliver pastoral care, professional chaplains are trained to assess, intervene, and observe outcomes in spiritual health.
To begin with, spirituality is defined not in terms of “religiosity” but more as following an ethical path, similar to the idea of the Golden Rule or the ethic of reciprocity: Love your neighbor as yourself, in other words. The spiritual maturity to follow such a path requires the ability to love oneself that is balanced with a connection to others, and God, “if your belief includes God,” said Dr. Dunn, who pointed out that chaplaincy programs for atheists also exist.
By observing a person’s behavior and conversing with him or her, paying close attention to the person’s attributions of blame, if any, and expressions of chief concerns, a chaplain will assess where on the continuum that person is in three key components of spiritual health: the need for meaning and direction, a sense of self-worth and belonging, and an ability to love and be loved. This latter component often is facilitated through seeking reconciliation when relationships are broken.
In the face of crisis, such as with terminal illness, one of those needs typically supersedes the others. This is what is known as the person’s “core spiritual need,” said Dr. Dunn, who also serves director of the university’s Geriatric Psychiatry Fellowship Training Program, and has extensive research and clinical experience evaluating and managing older adults with mood, anxiety, and cognitive disorders. As part of her research, she and her colleagues have developed a schematic called the Spiritual AIM (Spiritual Assessment and Intervention Model), which depicts those three concerns in relation to one another (Palliat Support Care. 2015 Feb;13:75-89).
Chaplains also are trained to rely on their own feelings about people, similar to the way in which psychiatrists use countertransference. “It is not intrapersonal; it is interpersonal,” Dr. Dunn said. “Healing happens in relationship, and the focus is on that relationship.”
Chaplains undergo standardized clinical pastoral training programs predicated on a combination of theological reflection and psychological theory, plus critique from professional peers and students.
“Their model is very similar to what we [geriatric psychiatrists] do when we assess a patient,” Dr. Dunn said. “We might be more structured trying to ferret out a diagnosis, but we’re assessing all the time.”
Depending on which aspect of spiritual health is most lacking, the chaplain will choose the role of either a “guide” to help with balancing the need for meaning and direction, a “valuer” to help restore feelings of worth and belonging, or a “truth-teller” who will explore with the patient ways he or she might have contributed to broken relationships, and actions the patient might take in order to heal them. This is all done within the context of an interdisciplinary team, Dr. Dunn said.
She and a team of researchers, including a chaplain, conducted a study of 31 advanced-stage adult cancer patients in an outpatient palliative care service, that measured self-reported changes in their spiritual, psychological, and physical symptoms both before and after Spiritual AIM sessions with a chaplain.
The need for balancing one of the three key components of spiritual health was determined by the chaplain to be fairly equal across the cohort, although just more than half of patients younger than 60 years of age struggled more with self-worth and belonging (P = .030). Those over 60 years were equally concerned with either reconciliation or meaning and direction (P less than .05). Two-thirds of the cohort were women, although a relationship between gender and spiritual assessment needs was not determined. Two-thirds also identified themselves as Christian, just over one-third were Jewish, and the rest identified as either Buddhist or nondenominational.
Using a variety of validated palliative care scales, such as the Edmonton Symptom Assessment Syndrome (ESAS) for physical complaints, the Center for Epidemiologic Studies Short Depression Scale, the Mini Mental Adjustment to Cancer scale (Mini-MAC), and the positive and negative RCOPE questionnaire for religious coping, among other scales, Dr. Dunn and her associates found that the change in baseline of overall spiritual health after intervention from the chaplain improved slightly in most measures. Mean baseline scores for the ESAS went from 25 to 24.4 post-intervention. The difference between baseline depression scores fell from 4.2 to 4.1.
Mini-MAC scores improved, particularly in “fighting spirit” and levels of fatalism (P = .084 and P = .036, respectively). In addition, maladaptive coping skills also improved (P = .018).The findings have helped Dr. Dunn in her work as a geriatric psychiatrist, especially when treating cancer patients, or in settings where there is not as much time for a full clinical assessment. “I think of patients in terms of their core needs and what I can do right now to help patients meet those needs.” Dr. Dunn cited, as an example, patients who feel like they don’t belong and are lonely. “If they’re in an assisted living home, can I get them to enter [the communal space]? That’s very different than thinking of them in terms only of depression.”
On Twitter @whitneymcknight
WASHINGTON – Hospital chaplains are key partners in meeting the needs of palliative care patients and, as such, have much to offer psychiatry, according to an expert.
“I think we should work with chaplains,” Dr. Laura B. Dunn, professor of psychiatry and behavioral sciences at Stanford (Calif.) University, said in an interview at the annual meeting of the American Association for Geriatric Psychiatry. “It’s very helpful to know what they do, and for them to know what we do in terms of diagnosing and using a biopsychosocial model.”
Dr. Dunn said the relegation of chaplaincy and spiritual care in medicine has been unfortunate. After all, the level of a patient’s spiritual health is an inherent aspect of quality of life in palliative care, particularly for those over age 60 who often want help reconciling with loved ones, data collected by Dr. Dunn show. Viewing those patients in terms of their core needs rather than seeking a psychiatric diagnosis can make them more satisfied with their overall palliative care experience, she said.
How is spiritual health measured? There are few models and even fewer empirical studies, but Dr. Dunn said in addition learning how to deliver pastoral care, professional chaplains are trained to assess, intervene, and observe outcomes in spiritual health.
To begin with, spirituality is defined not in terms of “religiosity” but more as following an ethical path, similar to the idea of the Golden Rule or the ethic of reciprocity: Love your neighbor as yourself, in other words. The spiritual maturity to follow such a path requires the ability to love oneself that is balanced with a connection to others, and God, “if your belief includes God,” said Dr. Dunn, who pointed out that chaplaincy programs for atheists also exist.
By observing a person’s behavior and conversing with him or her, paying close attention to the person’s attributions of blame, if any, and expressions of chief concerns, a chaplain will assess where on the continuum that person is in three key components of spiritual health: the need for meaning and direction, a sense of self-worth and belonging, and an ability to love and be loved. This latter component often is facilitated through seeking reconciliation when relationships are broken.
In the face of crisis, such as with terminal illness, one of those needs typically supersedes the others. This is what is known as the person’s “core spiritual need,” said Dr. Dunn, who also serves director of the university’s Geriatric Psychiatry Fellowship Training Program, and has extensive research and clinical experience evaluating and managing older adults with mood, anxiety, and cognitive disorders. As part of her research, she and her colleagues have developed a schematic called the Spiritual AIM (Spiritual Assessment and Intervention Model), which depicts those three concerns in relation to one another (Palliat Support Care. 2015 Feb;13:75-89).
Chaplains also are trained to rely on their own feelings about people, similar to the way in which psychiatrists use countertransference. “It is not intrapersonal; it is interpersonal,” Dr. Dunn said. “Healing happens in relationship, and the focus is on that relationship.”
Chaplains undergo standardized clinical pastoral training programs predicated on a combination of theological reflection and psychological theory, plus critique from professional peers and students.
“Their model is very similar to what we [geriatric psychiatrists] do when we assess a patient,” Dr. Dunn said. “We might be more structured trying to ferret out a diagnosis, but we’re assessing all the time.”
Depending on which aspect of spiritual health is most lacking, the chaplain will choose the role of either a “guide” to help with balancing the need for meaning and direction, a “valuer” to help restore feelings of worth and belonging, or a “truth-teller” who will explore with the patient ways he or she might have contributed to broken relationships, and actions the patient might take in order to heal them. This is all done within the context of an interdisciplinary team, Dr. Dunn said.
She and a team of researchers, including a chaplain, conducted a study of 31 advanced-stage adult cancer patients in an outpatient palliative care service, that measured self-reported changes in their spiritual, psychological, and physical symptoms both before and after Spiritual AIM sessions with a chaplain.
The need for balancing one of the three key components of spiritual health was determined by the chaplain to be fairly equal across the cohort, although just more than half of patients younger than 60 years of age struggled more with self-worth and belonging (P = .030). Those over 60 years were equally concerned with either reconciliation or meaning and direction (P less than .05). Two-thirds of the cohort were women, although a relationship between gender and spiritual assessment needs was not determined. Two-thirds also identified themselves as Christian, just over one-third were Jewish, and the rest identified as either Buddhist or nondenominational.
Using a variety of validated palliative care scales, such as the Edmonton Symptom Assessment Syndrome (ESAS) for physical complaints, the Center for Epidemiologic Studies Short Depression Scale, the Mini Mental Adjustment to Cancer scale (Mini-MAC), and the positive and negative RCOPE questionnaire for religious coping, among other scales, Dr. Dunn and her associates found that the change in baseline of overall spiritual health after intervention from the chaplain improved slightly in most measures. Mean baseline scores for the ESAS went from 25 to 24.4 post-intervention. The difference between baseline depression scores fell from 4.2 to 4.1.
Mini-MAC scores improved, particularly in “fighting spirit” and levels of fatalism (P = .084 and P = .036, respectively). In addition, maladaptive coping skills also improved (P = .018).The findings have helped Dr. Dunn in her work as a geriatric psychiatrist, especially when treating cancer patients, or in settings where there is not as much time for a full clinical assessment. “I think of patients in terms of their core needs and what I can do right now to help patients meet those needs.” Dr. Dunn cited, as an example, patients who feel like they don’t belong and are lonely. “If they’re in an assisted living home, can I get them to enter [the communal space]? That’s very different than thinking of them in terms only of depression.”
On Twitter @whitneymcknight
EXPERT ANALYSIS FROM AAGP 2016
Randomized corporate clinical trials
The randomized clinical trial (RCT) has been the bulwark of the development of effective and safe medical and surgical therapy. Developed over the last half-century, they have proved the benefit and safety of new drugs and procedures and provided guidance to physicians in choosing therapeutic choices for their patients. They have replaced intuitive care that had largely directed medical care for centuries with a degree of science in making therapeutic decisions.
Although less than perfect, the RCT has been the reason for the remarkable success that we have achieved in decreasing the mortality of heart disease. This success has been driven largely by scientific altruism modified to some degree by the financial benefits of both the medical profession and the pharmaceutical industry.
As corporate hospital and third-party payers expand their role in the pattern of health care, there is the potential to make changes in how care is rendered beyond the choice of medical or surgical therapy. The expansion of care regionally and nationally provides tempting targets to modify the quality and efficacy on a large scale. It also provides potential cost-saving targets and generates corporate profits. Decisions at the corporate or administrative area in the past have been initiated on the basis of competitive costs and on intuitive decision making. The size of the market, however, provides an opportunity to test a variety of administrative plans that can lead to cost saving. These initiatives, well-meaning in their genesis, may result in patient participation in “studies” in which the patient may have a limited knowledge and benefit and uncertain risks.
RCTs demand informed consent by patients and unbiased temporal oversight by safety boards when searching for answers to questions based on contemporary knowledge. At present, there is no specific role for the patient’s voluntary and informed participation should a corporate representative initiate a “study” to answer a corporate question. Before we embark on “research” in patient care, it is imperative that we consider the principles established by RCTs. I propose two scenarios that may provide illustrative insight:
1. A nurse administrator wishes to explore the question of the cost savings achieved on a general medical ward by changing the current nurse staffing of eight professional nurses to a staffing with two professional nurses and six nursing assistants. The administrator will use personnel costs as the endpoint of the study and consider a variety of secondary issues such as the duration of time to respond to a call, sacral erythema, and wrong-dose administration, or other quality measurements.
2. The administrator of the catheterization laboratory decides to compare two catheters in the laboratory driven again by the costs of the catheters. The primary endpoint of the study will be cost savings. Secondary measurements will be time in the catheterization laboratory and postprocedure bleeding.
In both cases, the patient may or not have been informed about the research project in which they have been enrolled. In addition, there is no temporal assessment of the occurrence of adverse events that could occur during the progress of the “study” to ensure its safety. Many of the safeguards that have been developed around the RCT need to be incorporated into the design of these investigations.
This, of course, is all hypothetical, but on the other hand, it is not beyond the realm of possibility; as we move from “local care” to a system driven by anonymous personnel, it is important to obtain the consent of the patient and to establish procedures to ensure their safety.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
The randomized clinical trial (RCT) has been the bulwark of the development of effective and safe medical and surgical therapy. Developed over the last half-century, they have proved the benefit and safety of new drugs and procedures and provided guidance to physicians in choosing therapeutic choices for their patients. They have replaced intuitive care that had largely directed medical care for centuries with a degree of science in making therapeutic decisions.
Although less than perfect, the RCT has been the reason for the remarkable success that we have achieved in decreasing the mortality of heart disease. This success has been driven largely by scientific altruism modified to some degree by the financial benefits of both the medical profession and the pharmaceutical industry.
As corporate hospital and third-party payers expand their role in the pattern of health care, there is the potential to make changes in how care is rendered beyond the choice of medical or surgical therapy. The expansion of care regionally and nationally provides tempting targets to modify the quality and efficacy on a large scale. It also provides potential cost-saving targets and generates corporate profits. Decisions at the corporate or administrative area in the past have been initiated on the basis of competitive costs and on intuitive decision making. The size of the market, however, provides an opportunity to test a variety of administrative plans that can lead to cost saving. These initiatives, well-meaning in their genesis, may result in patient participation in “studies” in which the patient may have a limited knowledge and benefit and uncertain risks.
RCTs demand informed consent by patients and unbiased temporal oversight by safety boards when searching for answers to questions based on contemporary knowledge. At present, there is no specific role for the patient’s voluntary and informed participation should a corporate representative initiate a “study” to answer a corporate question. Before we embark on “research” in patient care, it is imperative that we consider the principles established by RCTs. I propose two scenarios that may provide illustrative insight:
1. A nurse administrator wishes to explore the question of the cost savings achieved on a general medical ward by changing the current nurse staffing of eight professional nurses to a staffing with two professional nurses and six nursing assistants. The administrator will use personnel costs as the endpoint of the study and consider a variety of secondary issues such as the duration of time to respond to a call, sacral erythema, and wrong-dose administration, or other quality measurements.
2. The administrator of the catheterization laboratory decides to compare two catheters in the laboratory driven again by the costs of the catheters. The primary endpoint of the study will be cost savings. Secondary measurements will be time in the catheterization laboratory and postprocedure bleeding.
In both cases, the patient may or not have been informed about the research project in which they have been enrolled. In addition, there is no temporal assessment of the occurrence of adverse events that could occur during the progress of the “study” to ensure its safety. Many of the safeguards that have been developed around the RCT need to be incorporated into the design of these investigations.
This, of course, is all hypothetical, but on the other hand, it is not beyond the realm of possibility; as we move from “local care” to a system driven by anonymous personnel, it is important to obtain the consent of the patient and to establish procedures to ensure their safety.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.
The randomized clinical trial (RCT) has been the bulwark of the development of effective and safe medical and surgical therapy. Developed over the last half-century, they have proved the benefit and safety of new drugs and procedures and provided guidance to physicians in choosing therapeutic choices for their patients. They have replaced intuitive care that had largely directed medical care for centuries with a degree of science in making therapeutic decisions.
Although less than perfect, the RCT has been the reason for the remarkable success that we have achieved in decreasing the mortality of heart disease. This success has been driven largely by scientific altruism modified to some degree by the financial benefits of both the medical profession and the pharmaceutical industry.
As corporate hospital and third-party payers expand their role in the pattern of health care, there is the potential to make changes in how care is rendered beyond the choice of medical or surgical therapy. The expansion of care regionally and nationally provides tempting targets to modify the quality and efficacy on a large scale. It also provides potential cost-saving targets and generates corporate profits. Decisions at the corporate or administrative area in the past have been initiated on the basis of competitive costs and on intuitive decision making. The size of the market, however, provides an opportunity to test a variety of administrative plans that can lead to cost saving. These initiatives, well-meaning in their genesis, may result in patient participation in “studies” in which the patient may have a limited knowledge and benefit and uncertain risks.
RCTs demand informed consent by patients and unbiased temporal oversight by safety boards when searching for answers to questions based on contemporary knowledge. At present, there is no specific role for the patient’s voluntary and informed participation should a corporate representative initiate a “study” to answer a corporate question. Before we embark on “research” in patient care, it is imperative that we consider the principles established by RCTs. I propose two scenarios that may provide illustrative insight:
1. A nurse administrator wishes to explore the question of the cost savings achieved on a general medical ward by changing the current nurse staffing of eight professional nurses to a staffing with two professional nurses and six nursing assistants. The administrator will use personnel costs as the endpoint of the study and consider a variety of secondary issues such as the duration of time to respond to a call, sacral erythema, and wrong-dose administration, or other quality measurements.
2. The administrator of the catheterization laboratory decides to compare two catheters in the laboratory driven again by the costs of the catheters. The primary endpoint of the study will be cost savings. Secondary measurements will be time in the catheterization laboratory and postprocedure bleeding.
In both cases, the patient may or not have been informed about the research project in which they have been enrolled. In addition, there is no temporal assessment of the occurrence of adverse events that could occur during the progress of the “study” to ensure its safety. Many of the safeguards that have been developed around the RCT need to be incorporated into the design of these investigations.
This, of course, is all hypothetical, but on the other hand, it is not beyond the realm of possibility; as we move from “local care” to a system driven by anonymous personnel, it is important to obtain the consent of the patient and to establish procedures to ensure their safety.
Dr. Goldstein, medical editor of Cardiology News, is professor of medicine at Wayne State University and division head emeritus of cardiovascular medicine at Henry Ford Hospital, both in Detroit. He is on data safety monitoring committees for the National Institutes of Health and several pharmaceutical companies.