User login
Patients with severe mental illness can benefit from cognitive remediation training
Cognitive impairment seen in severely mentally ill people is well documented, and has been shown to affect as many as 98% of patients with schizophrenia.1 At this time, there are no FDA-approved medications for treating this cognitive impairment.2
Rusk State Hospital in Rusk, Texas, decided to put greater emphasis on improving cognitive impairment because of an increase in patients with a forensic commitment, either because of (1) not guilty by reason of insanity and (2) restoration of competency to stand trial, which typically require longer lengths of stay. Some of these patients experienced psychotic breaks while earning a college education, and one patient was a member of MENSA (an organization for people with a high IQ) before he became ill. Established programs were not adequate to address cognitive impairment.
How we developed and launched our program
Cognitive remediation is a new focus of psychiatry and is in its infancy; programs include cognitive remediation training (CRT) and cognitive enhancement therapy (CET) (Box3-9). CRT focuses more on practice and rote learning and CET is more inclusive, including aspects such as social skills training. These terms are interchangeable for programs designed to improve cognition. Because there is no standardized model, programs differ in content, length, use of computers vs manuals, social skills training, mentoring, and other modalities.
We could not find a program that could be adapted to our setting because of lack of funding and insufficient patient access to computers. Therefore, we developed our own program to address cognitive impairment in a population of individuals with severe mental illness in a state hospital setting.10 Our CRT program was designed for inpatient psychiatric patients, both on civil and forensic commitments.
The program includes >500 exercises and addresses several cognitive domains. Adding a facilitator or teacher in a group setting introduces an additional dimension to learning. Criteria to participate in the program included:
- behavior stable enough to participate
- ability to read and write English
- no traumatic brain injury that caused cognitive impairment
- the patient had to want to participate in the training program.
We tested each participant at the beginning and end of the 12-week training program, which consisted of 2 one-hour classes a week, with a target group size of 6 to 10 participants. As a rating tool, we used the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS), which has been shown to be an efficient approach to screening for cognitive impairment across several domains.11
We offered 2 levels of training: basic and advanced. Referral was based on the patient’s level of education and current cognitive function. Materials for the advanced group were at a high school or college level; the basic group used materials that were elementary school or mid-high school in scope. Assignment to the basic or advanced training was based on the recovery team’s or psychologist’s recommendation. The training was ongoing, meaning that a participant could begin at any time and continue until he (she) had completed the 12-week training program.
The weekly sessions in the CRT program were based on 12 categories (Table).10
1. Picture Puzzles: Part 1, Odd Man Out. Participants receive a series of 4 pictures and are asked to select the 1 that does not share a common link with the other 3 items. Targeted skills include pattern recognition, visual learning, reasoning, and creativity (looking for non-obvious answers). This plays a role in global cognition and everyday activities that are sight-related.
2. Word Problems. Participants receive math exercises with significant background information presented as text. Targeted skills include calculation, concentration, and reasoning. This helps with making change, figuring out the tip on a bill, balancing a checkbook, and assisting children with homework.
3. Picture Puzzles: Part 2, Matching.Participants view an illustration followed by a series of 4 other pictures, where ≥1 of which will have a close relationship to the example. The participant selects the item with the strongest link. Targeted skills include determining patterns, concentration, visual perception, and reasoning.
4. Verbal Challenge. Participants are provided a variety of word-based problems that involve word usage, definitions, games, and puzzles. Targeted skills include vocabulary, reading comprehension, reasoning, concentration, and global cognition.
5. Picture Puzzles: Part 3, Series Completion. Participants receive a sequence of 3 pictures followed by 4 possible solutions. The participant selects the item that completes the series or shares a common bond. Targeted skills include visual perception, picking up on patterns, creativity, reasoning, and concentration.
6. Mental Arithmetic: Part 1, Coin Counting. Participants are presented math problems related to money that can be solved by simple mental or quick paper calculation. Targeted skills include basic math, speed, concentration, and counting money. This helps with making change and balancing a checkbook.
7. Picture Puzzles: Part 4, Ratio. Participants receive presented analogy questions where the participant has to determine the ratio or proportional relation of the items. Targeted skills include memory, creativity, and decision-making.
8. Mental Arithmetic: Part 2, Potpourri. Participants receive a hodgepodge of math problems, including number sequences and word problems. Targeted skills include reasoning and computation.
9. Visual/spatial. Participants are presented exercises that require them to think in 3 dimensions and see “hidden” areas behind folds or on the other sides of figures. Targeted skills include spatial perception, reasoning, and decision-making.
10. Reasoning. Participants receive problems that involve taking in information, processing the data, analyzing the options based on previous experiences, and coming up with a decision that is factual and rational. Targeted skills include reasoning and decision-making.
11. Memory Exercise, Listening. Participants are provided a reading selection. After the reading, there is 20-minute waiting period during which the participant is engaged in other exercises before returning to answer questions about the reading. Targeted skills include listening, retention, and memory.
12. Speed Training. Participants receive exercises that provide practice in gathering and processing information and making decisions based on the given information. Targeted skills include decision-making, speed, and concentration.
Preliminary results, optimism about good outcomes
In the past 12 months, 28 participants have completed the CRT program: 11 in the basic training class and 17 in the advanced class. Of those, 7 in the basic program and 11 in the advanced program showed significant improvement as measured by the pre- and post-training RBANS; 64% of the participants improved. The average pre-test score in the basic group was 63 and post-test score was 72 (t10 = 3.148, P < .05). The average advanced pre-test score in the advanced class was 75 and post-test score was 80 (t16 = 2.476, P < .05) (Figure 1).
Because this program was developed as a treatment intervention for psychiatric inpatients, not a research study, we did not establish a control group.
In addition to the overall increase in cognitive functioning, individual successes have been noted. One participant who experienced a psychotic break while pursuing a college degree in literature scored 73 on his initial RBANS, indicating moderate impairment. After completing the 12-week program, his RBANS score increased to 95 (Figure 2). One year after completing the CRT program without additional cognitive training, the participant achieved an RBANS score of 104. Since then, the patient has been observed reading the classics in Latin and Greek, as he did before his psychotic break, and has been noted to be making more eye contact and engaging in conversations.
Success also has been noted for participants who did not see an increase in their RBANS scores. One participant historically had shown little interest in any programming or classes, but attended every CRT class, participated, and asked for additional worksheets to take back to the unit. Based on this feedback, each session now includes a worksheet that participants can take back with them.
Further findings of success
Cognitive impairment can be a significant disability in patients with severe mental illness. Longer lengths of stay present an opportunity to provide a CRT program over 12 weeks. However, some increase in cognitive functioning, as measured by the RBANS, was seen with participants who would not or could not complete all 24 classes. In addition to increased cognitive functioning, clinicians have noted improvements in patients’ participation in treatment and self-esteem.
The program engaged patients who previously were uninvolved in activities, and provided a sense of purpose and hope for them. One participant stated that he felt better about himself and had a more optimistic outlook for the future.
This program offers the possibility for participants to clear the mental fog caused by their illness or medication. The exercises stimulate cognitive activity when the goal is not to get the correct answer, but to think about and talk about possible solutions.
CRT, we have found, can greatly increase the quality of life of people with severe mental illness.
1. Keefe R, Easley C, Poe MP. Defining a cognitive function decrement in schizophrenia. Biol Psychiatry. 2005;57(6):688-691.
2. Nasrallah HA, Keefe RSE, Javitt DC. Cognitive deficits and poor functional outcomes in schizophrenia: clinical and neurobiological progress. Current Psychiatry. 2014;13(suppl 6):S1-S11.
3. Wykes T, Huddy V, Cellard C, et al. A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry. 2011;168(5):472-485.
4. Baharnoori M, Bartholomeusz C, Boucher A, et al. The 2nd Schizophrenia International Research Society Conference, 10-14 April 2010, Florence, Italy: summaries of oral sessions. Schizophr Res. 2010;124:e1-e62.
5. Antzoulatos EG, Miller EK. Increases in functional connectivity between prefrontal cortex and striatum during category learning. Neuron. 2014;83(1):216-225.
6. Hogarty G, Flesher S, Ulrich R, et al. Cognitive enhancement therapy for schizophrenia: effects of a 2-year randomized trial on cognition and behavior. Arch Gen Psychiatry. 2004;61(9):866-876.
7. Medalia A, Freilich B. The neuropsychological educational approach to cognitive remediation (NEAR) model: practice principles and outcome studies. Am J Psychiatr Rehabil. 2008;11(2):123-143.
8. Hurford IM, Kalkstein S, Hurford MO. Cognitive rehabilitation in schizophrenia. Psychiatric Times. http://www.psychiatrictimes.com/schizophrenia/cognitive-rehabilitation-schizophrenia. Published March 15, 2011. Accessed March 3, 2016.
9. Rogers P, Redoblado-Hodge A. A multi-site trial of cognitive remediation in schizophrenia: an Australian sample. Paper presented at: the 9th annual conference on Cognitive Remediation in Psychiatry; 2004; New York, NY.
10. Bates J. Making your brain hum: 12 weeks to a smarter you. Dallas, TX: Brown Books Publishing Group; 2016.
11. Hobart MP, Goldberg R, Bartko JJ, et al. Repeatable battery for the assessment of neuropsychological status as a screening test in schizophrenia, II: convergent/discriminant validity and diagnostic group comparisons. Am J Psychiatry. 1999;156(12):1951-1957.
Cognitive impairment seen in severely mentally ill people is well documented, and has been shown to affect as many as 98% of patients with schizophrenia.1 At this time, there are no FDA-approved medications for treating this cognitive impairment.2
Rusk State Hospital in Rusk, Texas, decided to put greater emphasis on improving cognitive impairment because of an increase in patients with a forensic commitment, either because of (1) not guilty by reason of insanity and (2) restoration of competency to stand trial, which typically require longer lengths of stay. Some of these patients experienced psychotic breaks while earning a college education, and one patient was a member of MENSA (an organization for people with a high IQ) before he became ill. Established programs were not adequate to address cognitive impairment.
How we developed and launched our program
Cognitive remediation is a new focus of psychiatry and is in its infancy; programs include cognitive remediation training (CRT) and cognitive enhancement therapy (CET) (Box3-9). CRT focuses more on practice and rote learning and CET is more inclusive, including aspects such as social skills training. These terms are interchangeable for programs designed to improve cognition. Because there is no standardized model, programs differ in content, length, use of computers vs manuals, social skills training, mentoring, and other modalities.
We could not find a program that could be adapted to our setting because of lack of funding and insufficient patient access to computers. Therefore, we developed our own program to address cognitive impairment in a population of individuals with severe mental illness in a state hospital setting.10 Our CRT program was designed for inpatient psychiatric patients, both on civil and forensic commitments.
The program includes >500 exercises and addresses several cognitive domains. Adding a facilitator or teacher in a group setting introduces an additional dimension to learning. Criteria to participate in the program included:
- behavior stable enough to participate
- ability to read and write English
- no traumatic brain injury that caused cognitive impairment
- the patient had to want to participate in the training program.
We tested each participant at the beginning and end of the 12-week training program, which consisted of 2 one-hour classes a week, with a target group size of 6 to 10 participants. As a rating tool, we used the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS), which has been shown to be an efficient approach to screening for cognitive impairment across several domains.11
We offered 2 levels of training: basic and advanced. Referral was based on the patient’s level of education and current cognitive function. Materials for the advanced group were at a high school or college level; the basic group used materials that were elementary school or mid-high school in scope. Assignment to the basic or advanced training was based on the recovery team’s or psychologist’s recommendation. The training was ongoing, meaning that a participant could begin at any time and continue until he (she) had completed the 12-week training program.
The weekly sessions in the CRT program were based on 12 categories (Table).10
1. Picture Puzzles: Part 1, Odd Man Out. Participants receive a series of 4 pictures and are asked to select the 1 that does not share a common link with the other 3 items. Targeted skills include pattern recognition, visual learning, reasoning, and creativity (looking for non-obvious answers). This plays a role in global cognition and everyday activities that are sight-related.
2. Word Problems. Participants receive math exercises with significant background information presented as text. Targeted skills include calculation, concentration, and reasoning. This helps with making change, figuring out the tip on a bill, balancing a checkbook, and assisting children with homework.
3. Picture Puzzles: Part 2, Matching.Participants view an illustration followed by a series of 4 other pictures, where ≥1 of which will have a close relationship to the example. The participant selects the item with the strongest link. Targeted skills include determining patterns, concentration, visual perception, and reasoning.
4. Verbal Challenge. Participants are provided a variety of word-based problems that involve word usage, definitions, games, and puzzles. Targeted skills include vocabulary, reading comprehension, reasoning, concentration, and global cognition.
5. Picture Puzzles: Part 3, Series Completion. Participants receive a sequence of 3 pictures followed by 4 possible solutions. The participant selects the item that completes the series or shares a common bond. Targeted skills include visual perception, picking up on patterns, creativity, reasoning, and concentration.
6. Mental Arithmetic: Part 1, Coin Counting. Participants are presented math problems related to money that can be solved by simple mental or quick paper calculation. Targeted skills include basic math, speed, concentration, and counting money. This helps with making change and balancing a checkbook.
7. Picture Puzzles: Part 4, Ratio. Participants receive presented analogy questions where the participant has to determine the ratio or proportional relation of the items. Targeted skills include memory, creativity, and decision-making.
8. Mental Arithmetic: Part 2, Potpourri. Participants receive a hodgepodge of math problems, including number sequences and word problems. Targeted skills include reasoning and computation.
9. Visual/spatial. Participants are presented exercises that require them to think in 3 dimensions and see “hidden” areas behind folds or on the other sides of figures. Targeted skills include spatial perception, reasoning, and decision-making.
10. Reasoning. Participants receive problems that involve taking in information, processing the data, analyzing the options based on previous experiences, and coming up with a decision that is factual and rational. Targeted skills include reasoning and decision-making.
11. Memory Exercise, Listening. Participants are provided a reading selection. After the reading, there is 20-minute waiting period during which the participant is engaged in other exercises before returning to answer questions about the reading. Targeted skills include listening, retention, and memory.
12. Speed Training. Participants receive exercises that provide practice in gathering and processing information and making decisions based on the given information. Targeted skills include decision-making, speed, and concentration.
Preliminary results, optimism about good outcomes
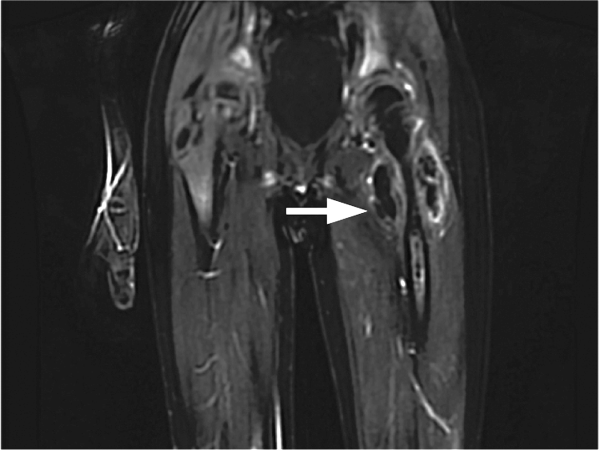
In the past 12 months, 28 participants have completed the CRT program: 11 in the basic training class and 17 in the advanced class. Of those, 7 in the basic program and 11 in the advanced program showed significant improvement as measured by the pre- and post-training RBANS; 64% of the participants improved. The average pre-test score in the basic group was 63 and post-test score was 72 (t10 = 3.148, P < .05). The average advanced pre-test score in the advanced class was 75 and post-test score was 80 (t16 = 2.476, P < .05) (Figure 1).
Because this program was developed as a treatment intervention for psychiatric inpatients, not a research study, we did not establish a control group.
In addition to the overall increase in cognitive functioning, individual successes have been noted. One participant who experienced a psychotic break while pursuing a college degree in literature scored 73 on his initial RBANS, indicating moderate impairment. After completing the 12-week program, his RBANS score increased to 95 (Figure 2). One year after completing the CRT program without additional cognitive training, the participant achieved an RBANS score of 104. Since then, the patient has been observed reading the classics in Latin and Greek, as he did before his psychotic break, and has been noted to be making more eye contact and engaging in conversations.
Success also has been noted for participants who did not see an increase in their RBANS scores. One participant historically had shown little interest in any programming or classes, but attended every CRT class, participated, and asked for additional worksheets to take back to the unit. Based on this feedback, each session now includes a worksheet that participants can take back with them.
Further findings of success
Cognitive impairment can be a significant disability in patients with severe mental illness. Longer lengths of stay present an opportunity to provide a CRT program over 12 weeks. However, some increase in cognitive functioning, as measured by the RBANS, was seen with participants who would not or could not complete all 24 classes. In addition to increased cognitive functioning, clinicians have noted improvements in patients’ participation in treatment and self-esteem.
The program engaged patients who previously were uninvolved in activities, and provided a sense of purpose and hope for them. One participant stated that he felt better about himself and had a more optimistic outlook for the future.
This program offers the possibility for participants to clear the mental fog caused by their illness or medication. The exercises stimulate cognitive activity when the goal is not to get the correct answer, but to think about and talk about possible solutions.
CRT, we have found, can greatly increase the quality of life of people with severe mental illness.
Cognitive impairment seen in severely mentally ill people is well documented, and has been shown to affect as many as 98% of patients with schizophrenia.1 At this time, there are no FDA-approved medications for treating this cognitive impairment.2
Rusk State Hospital in Rusk, Texas, decided to put greater emphasis on improving cognitive impairment because of an increase in patients with a forensic commitment, either because of (1) not guilty by reason of insanity and (2) restoration of competency to stand trial, which typically require longer lengths of stay. Some of these patients experienced psychotic breaks while earning a college education, and one patient was a member of MENSA (an organization for people with a high IQ) before he became ill. Established programs were not adequate to address cognitive impairment.
How we developed and launched our program
Cognitive remediation is a new focus of psychiatry and is in its infancy; programs include cognitive remediation training (CRT) and cognitive enhancement therapy (CET) (Box3-9). CRT focuses more on practice and rote learning and CET is more inclusive, including aspects such as social skills training. These terms are interchangeable for programs designed to improve cognition. Because there is no standardized model, programs differ in content, length, use of computers vs manuals, social skills training, mentoring, and other modalities.
We could not find a program that could be adapted to our setting because of lack of funding and insufficient patient access to computers. Therefore, we developed our own program to address cognitive impairment in a population of individuals with severe mental illness in a state hospital setting.10 Our CRT program was designed for inpatient psychiatric patients, both on civil and forensic commitments.
The program includes >500 exercises and addresses several cognitive domains. Adding a facilitator or teacher in a group setting introduces an additional dimension to learning. Criteria to participate in the program included:
- behavior stable enough to participate
- ability to read and write English
- no traumatic brain injury that caused cognitive impairment
- the patient had to want to participate in the training program.
We tested each participant at the beginning and end of the 12-week training program, which consisted of 2 one-hour classes a week, with a target group size of 6 to 10 participants. As a rating tool, we used the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS), which has been shown to be an efficient approach to screening for cognitive impairment across several domains.11
We offered 2 levels of training: basic and advanced. Referral was based on the patient’s level of education and current cognitive function. Materials for the advanced group were at a high school or college level; the basic group used materials that were elementary school or mid-high school in scope. Assignment to the basic or advanced training was based on the recovery team’s or psychologist’s recommendation. The training was ongoing, meaning that a participant could begin at any time and continue until he (she) had completed the 12-week training program.
The weekly sessions in the CRT program were based on 12 categories (Table).10
1. Picture Puzzles: Part 1, Odd Man Out. Participants receive a series of 4 pictures and are asked to select the 1 that does not share a common link with the other 3 items. Targeted skills include pattern recognition, visual learning, reasoning, and creativity (looking for non-obvious answers). This plays a role in global cognition and everyday activities that are sight-related.
2. Word Problems. Participants receive math exercises with significant background information presented as text. Targeted skills include calculation, concentration, and reasoning. This helps with making change, figuring out the tip on a bill, balancing a checkbook, and assisting children with homework.
3. Picture Puzzles: Part 2, Matching.Participants view an illustration followed by a series of 4 other pictures, where ≥1 of which will have a close relationship to the example. The participant selects the item with the strongest link. Targeted skills include determining patterns, concentration, visual perception, and reasoning.
4. Verbal Challenge. Participants are provided a variety of word-based problems that involve word usage, definitions, games, and puzzles. Targeted skills include vocabulary, reading comprehension, reasoning, concentration, and global cognition.
5. Picture Puzzles: Part 3, Series Completion. Participants receive a sequence of 3 pictures followed by 4 possible solutions. The participant selects the item that completes the series or shares a common bond. Targeted skills include visual perception, picking up on patterns, creativity, reasoning, and concentration.
6. Mental Arithmetic: Part 1, Coin Counting. Participants are presented math problems related to money that can be solved by simple mental or quick paper calculation. Targeted skills include basic math, speed, concentration, and counting money. This helps with making change and balancing a checkbook.
7. Picture Puzzles: Part 4, Ratio. Participants receive presented analogy questions where the participant has to determine the ratio or proportional relation of the items. Targeted skills include memory, creativity, and decision-making.
8. Mental Arithmetic: Part 2, Potpourri. Participants receive a hodgepodge of math problems, including number sequences and word problems. Targeted skills include reasoning and computation.
9. Visual/spatial. Participants are presented exercises that require them to think in 3 dimensions and see “hidden” areas behind folds or on the other sides of figures. Targeted skills include spatial perception, reasoning, and decision-making.
10. Reasoning. Participants receive problems that involve taking in information, processing the data, analyzing the options based on previous experiences, and coming up with a decision that is factual and rational. Targeted skills include reasoning and decision-making.
11. Memory Exercise, Listening. Participants are provided a reading selection. After the reading, there is 20-minute waiting period during which the participant is engaged in other exercises before returning to answer questions about the reading. Targeted skills include listening, retention, and memory.
12. Speed Training. Participants receive exercises that provide practice in gathering and processing information and making decisions based on the given information. Targeted skills include decision-making, speed, and concentration.
Preliminary results, optimism about good outcomes
In the past 12 months, 28 participants have completed the CRT program: 11 in the basic training class and 17 in the advanced class. Of those, 7 in the basic program and 11 in the advanced program showed significant improvement as measured by the pre- and post-training RBANS; 64% of the participants improved. The average pre-test score in the basic group was 63 and post-test score was 72 (t10 = 3.148, P < .05). The average advanced pre-test score in the advanced class was 75 and post-test score was 80 (t16 = 2.476, P < .05) (Figure 1).
Because this program was developed as a treatment intervention for psychiatric inpatients, not a research study, we did not establish a control group.
In addition to the overall increase in cognitive functioning, individual successes have been noted. One participant who experienced a psychotic break while pursuing a college degree in literature scored 73 on his initial RBANS, indicating moderate impairment. After completing the 12-week program, his RBANS score increased to 95 (Figure 2). One year after completing the CRT program without additional cognitive training, the participant achieved an RBANS score of 104. Since then, the patient has been observed reading the classics in Latin and Greek, as he did before his psychotic break, and has been noted to be making more eye contact and engaging in conversations.
Success also has been noted for participants who did not see an increase in their RBANS scores. One participant historically had shown little interest in any programming or classes, but attended every CRT class, participated, and asked for additional worksheets to take back to the unit. Based on this feedback, each session now includes a worksheet that participants can take back with them.
Further findings of success
Cognitive impairment can be a significant disability in patients with severe mental illness. Longer lengths of stay present an opportunity to provide a CRT program over 12 weeks. However, some increase in cognitive functioning, as measured by the RBANS, was seen with participants who would not or could not complete all 24 classes. In addition to increased cognitive functioning, clinicians have noted improvements in patients’ participation in treatment and self-esteem.
The program engaged patients who previously were uninvolved in activities, and provided a sense of purpose and hope for them. One participant stated that he felt better about himself and had a more optimistic outlook for the future.
This program offers the possibility for participants to clear the mental fog caused by their illness or medication. The exercises stimulate cognitive activity when the goal is not to get the correct answer, but to think about and talk about possible solutions.
CRT, we have found, can greatly increase the quality of life of people with severe mental illness.
1. Keefe R, Easley C, Poe MP. Defining a cognitive function decrement in schizophrenia. Biol Psychiatry. 2005;57(6):688-691.
2. Nasrallah HA, Keefe RSE, Javitt DC. Cognitive deficits and poor functional outcomes in schizophrenia: clinical and neurobiological progress. Current Psychiatry. 2014;13(suppl 6):S1-S11.
3. Wykes T, Huddy V, Cellard C, et al. A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry. 2011;168(5):472-485.
4. Baharnoori M, Bartholomeusz C, Boucher A, et al. The 2nd Schizophrenia International Research Society Conference, 10-14 April 2010, Florence, Italy: summaries of oral sessions. Schizophr Res. 2010;124:e1-e62.
5. Antzoulatos EG, Miller EK. Increases in functional connectivity between prefrontal cortex and striatum during category learning. Neuron. 2014;83(1):216-225.
6. Hogarty G, Flesher S, Ulrich R, et al. Cognitive enhancement therapy for schizophrenia: effects of a 2-year randomized trial on cognition and behavior. Arch Gen Psychiatry. 2004;61(9):866-876.
7. Medalia A, Freilich B. The neuropsychological educational approach to cognitive remediation (NEAR) model: practice principles and outcome studies. Am J Psychiatr Rehabil. 2008;11(2):123-143.
8. Hurford IM, Kalkstein S, Hurford MO. Cognitive rehabilitation in schizophrenia. Psychiatric Times. http://www.psychiatrictimes.com/schizophrenia/cognitive-rehabilitation-schizophrenia. Published March 15, 2011. Accessed March 3, 2016.
9. Rogers P, Redoblado-Hodge A. A multi-site trial of cognitive remediation in schizophrenia: an Australian sample. Paper presented at: the 9th annual conference on Cognitive Remediation in Psychiatry; 2004; New York, NY.
10. Bates J. Making your brain hum: 12 weeks to a smarter you. Dallas, TX: Brown Books Publishing Group; 2016.
11. Hobart MP, Goldberg R, Bartko JJ, et al. Repeatable battery for the assessment of neuropsychological status as a screening test in schizophrenia, II: convergent/discriminant validity and diagnostic group comparisons. Am J Psychiatry. 1999;156(12):1951-1957.
1. Keefe R, Easley C, Poe MP. Defining a cognitive function decrement in schizophrenia. Biol Psychiatry. 2005;57(6):688-691.
2. Nasrallah HA, Keefe RSE, Javitt DC. Cognitive deficits and poor functional outcomes in schizophrenia: clinical and neurobiological progress. Current Psychiatry. 2014;13(suppl 6):S1-S11.
3. Wykes T, Huddy V, Cellard C, et al. A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry. 2011;168(5):472-485.
4. Baharnoori M, Bartholomeusz C, Boucher A, et al. The 2nd Schizophrenia International Research Society Conference, 10-14 April 2010, Florence, Italy: summaries of oral sessions. Schizophr Res. 2010;124:e1-e62.
5. Antzoulatos EG, Miller EK. Increases in functional connectivity between prefrontal cortex and striatum during category learning. Neuron. 2014;83(1):216-225.
6. Hogarty G, Flesher S, Ulrich R, et al. Cognitive enhancement therapy for schizophrenia: effects of a 2-year randomized trial on cognition and behavior. Arch Gen Psychiatry. 2004;61(9):866-876.
7. Medalia A, Freilich B. The neuropsychological educational approach to cognitive remediation (NEAR) model: practice principles and outcome studies. Am J Psychiatr Rehabil. 2008;11(2):123-143.
8. Hurford IM, Kalkstein S, Hurford MO. Cognitive rehabilitation in schizophrenia. Psychiatric Times. http://www.psychiatrictimes.com/schizophrenia/cognitive-rehabilitation-schizophrenia. Published March 15, 2011. Accessed March 3, 2016.
9. Rogers P, Redoblado-Hodge A. A multi-site trial of cognitive remediation in schizophrenia: an Australian sample. Paper presented at: the 9th annual conference on Cognitive Remediation in Psychiatry; 2004; New York, NY.
10. Bates J. Making your brain hum: 12 weeks to a smarter you. Dallas, TX: Brown Books Publishing Group; 2016.
11. Hobart MP, Goldberg R, Bartko JJ, et al. Repeatable battery for the assessment of neuropsychological status as a screening test in schizophrenia, II: convergent/discriminant validity and diagnostic group comparisons. Am J Psychiatry. 1999;156(12):1951-1957.
Genetic and related laboratory tests in psychiatry: What mental health practitioners need to know
What has been the history of the development of laboratory tests in the field of psychiatry?
During my almost-40-year academic medical career, I have been interested in the development and incorporation of laboratory tests into psychiatry.1 This interest initially focused on therapeutic drug monitoring (TDM) and the genetics of drug responsiveness, with an emphasis on drug metabolism. In addition to TDM—which I have long believed is vastly underutilized in psychiatry—there have been many failed attempts to develop diagnostic tests, including tests to distinguish between what were postulated to be serotonergic and noradrenergic forms of major depression in the 1970s2,3 and the dexamethasone suppression test for melancholia in the 1980s.4 Recently, a 51-analyte immunoassay test was marketed by Rules-Based Medicine, Inc. (RBM), as an aid in the diagnosis of schizophrenia, but the test was found to suffer a high false-positive rate and was withdrawn from the market.5 Given this track record, caution is warranted when examining claims for new tests.
What types of tests are being developed?
Most tests in development are pharmacogenomic (PG)-based or immunoassay (IA)-based.
PG tests examine single nucleotide polymorphisms (SNP) in genes that code for pharmacokinetic mechanisms, primarily cytochrome P450 (CYP) enzymes responsible for drug metabolism and P-glycoprotein, responsible for drug transportation. The next most common type of test examines pharmacodynamic mechanisms, such as SNPs of specific receptor genes, including serotonin (or 5-hydroxytryptophan [5-HT] transporter [SET or 5-HTT]) or the 5-HT2A receptor.
The fact that CYP enzymes lead the list is not surprising: These enzymes and their role in the metabolism of specific drugs have been extensively studied since the late 1980s. Considerable data has been accumulated regarding variants of CYP enzymes, which convey clinically meaningful differences among individuals in terms of their ability to metabolize drug via these pathways. Individuals are commonly divided into 4 phenotypic categories: ultra-rapid, extensive (or normal), intermediate, and poor metabolizers. Based on these phenotypes, clinical consequences can be quantitated in terms of changes in drug concentration, concentration-dependent beneficial or adverse effects, and associated/recommended changes in dosing.
Research into the role of pharmacodynamic variants, however, is still in infancy and more difficult to measure in terms of assessing endpoints, with related limitations in clinical utility.
IA assays generally measure a variety of proteins, particularly those reflecting inflammatory processes (eg, various cytokines, such as interleukin-6).6 As with pharmacodynamic measures, research into the role of inflammatory biomarkers is in early stages. The clinical utility of associated tests is, therefore, less certain; witness the recent study5 I noted that revealed a high false-positive rate for the RBM schizophrenia panel in healthy controls. Nevertheless, considerable research is being conducted in all of these areas so that new developments might lend themselves to greater clinical utility.
(Note that PG biomarkers are trait measures, whereas IA biomarkers are state measures, so that complementary use of both types of tests might prove useful in diagnosis and clinical management. Although such integrative use of these 2 different types of tests generally is not done today.)
What does it take to market these tests?
At a minimum, offering these tests for sale requires that the laboratory be certified by the Centers for Medicare & Medicaid Services, according to the Clinical Laboratory Improvement Amendments (CLIA) standards (www.fda.gov/medicaldevices/deviceregulationandguidance/ivdregulatoryassistance/ucm124105.htm). CLIA-certified laboratories are required to demonstrate the analytical validity of tests that they offer—ie, the accuracy and reliability of the test in measuring a parameter of interest—but not the clinical validity or utility of those tests. The fact that a test in fact measures what it claims to be measuring in and of itself does not mean it has clinical validity or utility (see the discussion below).
Must the FDA approve laboratory tests?
No, but that situation might be changing.
Currently, only tests used in a setting considered high risk—eg, a test intended to detect or diagnose a malignancy or guide its treatment—requires formal FDA approval. The approval of such a test requires submission to the FDA of clinical data supporting its clinical validity and utility, in addition to evidence of analytic validity.
Even in such cases, the degree and quality of the clinical data required are generally not as high as would be required for approval of a drug. That distinction is understandable, given the type and quantity of data necessary for drug approval and the many years and billions of dollars it takes to accumulate such data. For most laboratory tests, providing the same level of data required to have a drug approved would be neither necessary nor feasible given the business model underlying most laboratories providing laboratory tests.
What do ‘clinical validity’ and ‘clinical utility’ mean?
These are higher evidence thresholds than is needed for analytic validity, although the latter is a necessary first step on the path to achieving these higher thresholds.
Clinical validity is the ability of a test to detect:
- a clinically meaningful measure, such as clinical response
- an adverse effect
- a biologically meaningful measure (eg, a drug level or a change in the electrocardiographic pattern).
Above the threshold of clinical validity is clinical utility, which is proof that the test can reliably be used to guide clinical management and thus meaningfully improve outcomes, such as guiding drug or dosage selection.
Is the use of PG testing recommended? If so, in what instances?
Specific types of PG testing is recommended by the FDA recommended. The FDA has been incorporating PG information into the labels of specific medications for several years; the agency has a Web site (www.fda.gov/drugs/scienceresearch/researchareas/pharmacogenetics/ucm083378.htm) that continuously updates this information. The involved drugs are in all therapeutic classes—from oncology to psychiatry.
More than 30 psychotropic drugs have PG information in their label; some of those drugs’ labels contain specific recommendations, such as obtaining PG information before selecting or starting a drug in a specific patient. An example is carbamazepine, for which the recommendation is to obtain HLA testing before starting the drug in patients of Han Chinese ancestry, because members of this large ethnic group are at greater risk of serious dermatologic adverse effects, including Stevens-Johnson syndrome.
In other instances, the recommendation is to do the testing before increasing beyond a specific dose. Examples of psychiatric drugs whose labels contain such PG information include pimozide and iloperidone as well as citalopram. In the FDA-approved label, guidance is provided that these drugs can be started without testing if prescribed at a reduced recommended starting dosage range, rather than the full starting dosage range. The guidance on these drugs further recommends testing for genetic CYP2D6 poor metabolizer (PM) status before dosing above that initial recommended, limited, starting dosage range.
The rationale for this guidance is to reduce the risk that (1) patients in question will achieve an excessively high plasma drug level that can cause significant prolongation of intracardiac conduction (eg, QTc prolongation) and thus (2) develop the potentially fatal arrhythmia torsades de pointes. Guidance is based on thorough QTc studies that were performed on each drug,7,8 which makes them examples of instances in which the test has clinical validity and utility as well as analytical validity.
To find PG labeling in the package insert for these drugs, visit: www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm.
What about data for other tests that are marketed and promoted by developers?
Sometimes, there are—literally—no data on available tests beyond the analytical validity of the test; other times, the amount and quality of clinical data are quite variable, ranging from results of ≥1 small retrospective studies without controls to results of prospective, randomized, controlled studies. Even among the latter, the developer may conduct and analyze their studies without oversight by an independent agency, such as the FDA.
This situation (1) raises concern that study results are not independent of the developer’s business interests and, as one might expect, (2) leads to controversy about whether the data are compelling—or not.9-12
What is a critical difference between PG test results and results of most laboratory tests?
PG tests are, as noted, trait rather than state characteristics. That means that the results do not change except for a phenomenon known as phenocoversion, discussed below. (Of course, advances in gene therapy might make it possible someday to change a person’s genetic makeup and for mitochondrial genes that is already possible.)
For this reason, PG test results should not get buried in the medical record, as might happen with, say, a patient’s serum potassium level at a given point in time. Instead, PG test results need to be carried forward continuously. Results also should be given to the patient as part of his (her) personal health record and to all other health care providers that the patient is seeing or will see in the future. Each health care provider who obtains PG test results should consider sending them to all current clinicians providing care for the patient at the same time as they are.
Is your functional status at a given moment the same as your genetic status?
No. There is a phenomenon known as phenoconversion in which a person’s current functional status may be different from what would be expected based on their genetic status.
CYP2D6 functional status is susceptible to phenoconversion as follows: Administering fluoxetine and paroxetine, for example, at 20 or 40 mg/d converts 66% and 95%, respectively, of patients who are CYP2D6 extensive (ie, normal) metabolizers into phenocopies of people who, genetically, lack the ability to metabolize drugs via CYP2D6 (ie, genotypic CYP2D6 PM). Based on a recent study of 900 participants in routine clinical care who were taking an antidepressant, 4% of the general U.S. population are genetically CYP2D6 PM; an additional 24% are phenotypically CYP2D6 PM because of concomitant administration of a CYP2D6 substantial inhibitor, such as bupropion, fluoxetine, paroxetine, or terbenafine.13
That is the reason a provider needs to know what drugs a patient is taking concomitantly—to consider the possibility of phenoconversion and, when necessary, to dose accordingly.
What does the future hold?
Development of tests for use in psychiatric practice is likely to grow substantially, for at least 2 reasons:
- There is a huge unmet need for clinically meaningful tests to aid in the provision of optimal patient care and, therefore, a tremendous business opportunity
- Knowledge in the biological basis of psychiatric disorders is growing exponentially; with that knowledge comes the ability to develop new tests.
A recent example comes from a research group that devised a test that could predict suicidality.14 Time will tell whether this test or a derivative of it enters practice. Nevertheless, it is a harbinger of the likely dramatic changes in the landscape of clinical medicine particularly as it applies to psychiatry.
Given these developments, the syndromic diagnoses in DSM-5 will in the future likely be replaced by a new diagnostic schema that breaks down existing heterogenous syndromic diagnoses into pathophysiologically and etiologically meaningful entities using insights gained from genetic and biomarker data as well as functional brain imaging. Theoretically, those insights will lead to new modalities of treatment, including somatic treatments that target novel mechanisms of action, coupled to more effective psychosocial therapies—with both therapies guided by diagnostic tests to monitor response to specific treatment interventions.
During this transition from the past to the future, answers to the questions I’ve posed here about laboratory testing in psychiatry will, I hope, help the practitioner understand, evaluate, and incorporate these changes readily into practice.
1. Preskorn SH, Biggs JT. Use of tricyclic antidepressant blood levels. N Engl J Med. 1978;298(3):166.
2. Schildkraut JJ. Biogenic amines and affective disorders. Annu Rev Med. 1974;25(0):333-348.
3. Maas JW. Biogenic amines and depression. Biochemical and pharmacological separation of two types of depression. Arch Gen Psychiatry. 1975;32(11):1357-1361.
4. Carroll BJ, Feinberg M, Greden JF, et al. A specific laboratory test for the diagnosis of melancholia. Standardization, validation, and clinical utility. Arch Gen Psychiatry. 1981;38(1):15-22.
5. Wehler C, Preskorn S. High false-positive rate of a putative biomarker test to aid in the diagnosis of schizophrenia. J Clin Psychiatry. In press.
6. Savitz J, Preskorn S, Teague TK, et al. Minocycline and aspirin in the treatment of bipolar depression: a protocol for a proof-of-concept, randomised, double-blind, placebo-controlled, 2x2 clinical trial. BMJ Open. 2012;2(1):e000643. doi: 10.1136/bmjopen-2011-000643.
7. Rogers HL, Bhattaram A, Zineh I, et al. CYP2D6 genotype information to guide pimozide treatment in adult and pediatric patients: basis for the U.S. Food and Drug Administration’s new dosing recommendations. J Clin Psychiatry. 2012;73(9):1187-1190.
8. Potkin S, Preskorn S, Hochfeld M, et al. A thorough QTc study of 3 doses of iloperidone including metabolic inhibition via CYP2D6 and/or CYP3A4 inhibition and a comparison to quetiapine and ziprasidone. J Clin Psychopharmacol. 2013;33(1):3-10.
9. Howland RH. Pharmacogenetic testing in psychiatry: not (quite) ready for primetime. J Psychosoc Nurs Ment Health Serv. 2014;52(11):13-16.
10. Rosenblat JD, Lee Y, McIntyre RS. Does pharmacogenomics testing improve clinical outcomes for major depressive disorder? A systematic review of clinical trials and cost-effectiveness studies. J Clin Psychiatry. In press.
11. Nassan M, Nicholson WT, Elliott MA, et al. Pharmacokinetic pharmacogenetic prescribing guidelines for antidepressants: a template for psychiatric precision medicine. Mayo Clin Proc. In press.
12. Altar CA, Carhart JM, Allen JD, et al. Clinical validity: combinatorial pharmacogenomics predicts antidepressant responses and healthcare utilizations better than single gene phenotypes. Pharmacogenomics J. 2015;15(5):443-451.
13. Preskorn S, Kane C, Lobello K, et al. Cytochrome P450 2D6 phenoconversion is common in patients being treated for depression: implications for personalized medicine. J Clin Psychiatry. 2013;74(6):614-621.
14. Niculescu AB, Levey DF, Phalen PL, et al. Understanding and predicting suicidality using a combined genomic and clinical risk assessment approach. Mol Psychiatry. 2015;20(11):1266-1285.
What has been the history of the development of laboratory tests in the field of psychiatry?
During my almost-40-year academic medical career, I have been interested in the development and incorporation of laboratory tests into psychiatry.1 This interest initially focused on therapeutic drug monitoring (TDM) and the genetics of drug responsiveness, with an emphasis on drug metabolism. In addition to TDM—which I have long believed is vastly underutilized in psychiatry—there have been many failed attempts to develop diagnostic tests, including tests to distinguish between what were postulated to be serotonergic and noradrenergic forms of major depression in the 1970s2,3 and the dexamethasone suppression test for melancholia in the 1980s.4 Recently, a 51-analyte immunoassay test was marketed by Rules-Based Medicine, Inc. (RBM), as an aid in the diagnosis of schizophrenia, but the test was found to suffer a high false-positive rate and was withdrawn from the market.5 Given this track record, caution is warranted when examining claims for new tests.
What types of tests are being developed?
Most tests in development are pharmacogenomic (PG)-based or immunoassay (IA)-based.
PG tests examine single nucleotide polymorphisms (SNP) in genes that code for pharmacokinetic mechanisms, primarily cytochrome P450 (CYP) enzymes responsible for drug metabolism and P-glycoprotein, responsible for drug transportation. The next most common type of test examines pharmacodynamic mechanisms, such as SNPs of specific receptor genes, including serotonin (or 5-hydroxytryptophan [5-HT] transporter [SET or 5-HTT]) or the 5-HT2A receptor.
The fact that CYP enzymes lead the list is not surprising: These enzymes and their role in the metabolism of specific drugs have been extensively studied since the late 1980s. Considerable data has been accumulated regarding variants of CYP enzymes, which convey clinically meaningful differences among individuals in terms of their ability to metabolize drug via these pathways. Individuals are commonly divided into 4 phenotypic categories: ultra-rapid, extensive (or normal), intermediate, and poor metabolizers. Based on these phenotypes, clinical consequences can be quantitated in terms of changes in drug concentration, concentration-dependent beneficial or adverse effects, and associated/recommended changes in dosing.
Research into the role of pharmacodynamic variants, however, is still in infancy and more difficult to measure in terms of assessing endpoints, with related limitations in clinical utility.
IA assays generally measure a variety of proteins, particularly those reflecting inflammatory processes (eg, various cytokines, such as interleukin-6).6 As with pharmacodynamic measures, research into the role of inflammatory biomarkers is in early stages. The clinical utility of associated tests is, therefore, less certain; witness the recent study5 I noted that revealed a high false-positive rate for the RBM schizophrenia panel in healthy controls. Nevertheless, considerable research is being conducted in all of these areas so that new developments might lend themselves to greater clinical utility.
(Note that PG biomarkers are trait measures, whereas IA biomarkers are state measures, so that complementary use of both types of tests might prove useful in diagnosis and clinical management. Although such integrative use of these 2 different types of tests generally is not done today.)
What does it take to market these tests?
At a minimum, offering these tests for sale requires that the laboratory be certified by the Centers for Medicare & Medicaid Services, according to the Clinical Laboratory Improvement Amendments (CLIA) standards (www.fda.gov/medicaldevices/deviceregulationandguidance/ivdregulatoryassistance/ucm124105.htm). CLIA-certified laboratories are required to demonstrate the analytical validity of tests that they offer—ie, the accuracy and reliability of the test in measuring a parameter of interest—but not the clinical validity or utility of those tests. The fact that a test in fact measures what it claims to be measuring in and of itself does not mean it has clinical validity or utility (see the discussion below).
Must the FDA approve laboratory tests?
No, but that situation might be changing.
Currently, only tests used in a setting considered high risk—eg, a test intended to detect or diagnose a malignancy or guide its treatment—requires formal FDA approval. The approval of such a test requires submission to the FDA of clinical data supporting its clinical validity and utility, in addition to evidence of analytic validity.
Even in such cases, the degree and quality of the clinical data required are generally not as high as would be required for approval of a drug. That distinction is understandable, given the type and quantity of data necessary for drug approval and the many years and billions of dollars it takes to accumulate such data. For most laboratory tests, providing the same level of data required to have a drug approved would be neither necessary nor feasible given the business model underlying most laboratories providing laboratory tests.
What do ‘clinical validity’ and ‘clinical utility’ mean?
These are higher evidence thresholds than is needed for analytic validity, although the latter is a necessary first step on the path to achieving these higher thresholds.
Clinical validity is the ability of a test to detect:
- a clinically meaningful measure, such as clinical response
- an adverse effect
- a biologically meaningful measure (eg, a drug level or a change in the electrocardiographic pattern).
Above the threshold of clinical validity is clinical utility, which is proof that the test can reliably be used to guide clinical management and thus meaningfully improve outcomes, such as guiding drug or dosage selection.
Is the use of PG testing recommended? If so, in what instances?
Specific types of PG testing is recommended by the FDA recommended. The FDA has been incorporating PG information into the labels of specific medications for several years; the agency has a Web site (www.fda.gov/drugs/scienceresearch/researchareas/pharmacogenetics/ucm083378.htm) that continuously updates this information. The involved drugs are in all therapeutic classes—from oncology to psychiatry.
More than 30 psychotropic drugs have PG information in their label; some of those drugs’ labels contain specific recommendations, such as obtaining PG information before selecting or starting a drug in a specific patient. An example is carbamazepine, for which the recommendation is to obtain HLA testing before starting the drug in patients of Han Chinese ancestry, because members of this large ethnic group are at greater risk of serious dermatologic adverse effects, including Stevens-Johnson syndrome.
In other instances, the recommendation is to do the testing before increasing beyond a specific dose. Examples of psychiatric drugs whose labels contain such PG information include pimozide and iloperidone as well as citalopram. In the FDA-approved label, guidance is provided that these drugs can be started without testing if prescribed at a reduced recommended starting dosage range, rather than the full starting dosage range. The guidance on these drugs further recommends testing for genetic CYP2D6 poor metabolizer (PM) status before dosing above that initial recommended, limited, starting dosage range.
The rationale for this guidance is to reduce the risk that (1) patients in question will achieve an excessively high plasma drug level that can cause significant prolongation of intracardiac conduction (eg, QTc prolongation) and thus (2) develop the potentially fatal arrhythmia torsades de pointes. Guidance is based on thorough QTc studies that were performed on each drug,7,8 which makes them examples of instances in which the test has clinical validity and utility as well as analytical validity.
To find PG labeling in the package insert for these drugs, visit: www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm.
What about data for other tests that are marketed and promoted by developers?
Sometimes, there are—literally—no data on available tests beyond the analytical validity of the test; other times, the amount and quality of clinical data are quite variable, ranging from results of ≥1 small retrospective studies without controls to results of prospective, randomized, controlled studies. Even among the latter, the developer may conduct and analyze their studies without oversight by an independent agency, such as the FDA.
This situation (1) raises concern that study results are not independent of the developer’s business interests and, as one might expect, (2) leads to controversy about whether the data are compelling—or not.9-12
What is a critical difference between PG test results and results of most laboratory tests?
PG tests are, as noted, trait rather than state characteristics. That means that the results do not change except for a phenomenon known as phenocoversion, discussed below. (Of course, advances in gene therapy might make it possible someday to change a person’s genetic makeup and for mitochondrial genes that is already possible.)
For this reason, PG test results should not get buried in the medical record, as might happen with, say, a patient’s serum potassium level at a given point in time. Instead, PG test results need to be carried forward continuously. Results also should be given to the patient as part of his (her) personal health record and to all other health care providers that the patient is seeing or will see in the future. Each health care provider who obtains PG test results should consider sending them to all current clinicians providing care for the patient at the same time as they are.
Is your functional status at a given moment the same as your genetic status?
No. There is a phenomenon known as phenoconversion in which a person’s current functional status may be different from what would be expected based on their genetic status.
CYP2D6 functional status is susceptible to phenoconversion as follows: Administering fluoxetine and paroxetine, for example, at 20 or 40 mg/d converts 66% and 95%, respectively, of patients who are CYP2D6 extensive (ie, normal) metabolizers into phenocopies of people who, genetically, lack the ability to metabolize drugs via CYP2D6 (ie, genotypic CYP2D6 PM). Based on a recent study of 900 participants in routine clinical care who were taking an antidepressant, 4% of the general U.S. population are genetically CYP2D6 PM; an additional 24% are phenotypically CYP2D6 PM because of concomitant administration of a CYP2D6 substantial inhibitor, such as bupropion, fluoxetine, paroxetine, or terbenafine.13
That is the reason a provider needs to know what drugs a patient is taking concomitantly—to consider the possibility of phenoconversion and, when necessary, to dose accordingly.
What does the future hold?
Development of tests for use in psychiatric practice is likely to grow substantially, for at least 2 reasons:
- There is a huge unmet need for clinically meaningful tests to aid in the provision of optimal patient care and, therefore, a tremendous business opportunity
- Knowledge in the biological basis of psychiatric disorders is growing exponentially; with that knowledge comes the ability to develop new tests.
A recent example comes from a research group that devised a test that could predict suicidality.14 Time will tell whether this test or a derivative of it enters practice. Nevertheless, it is a harbinger of the likely dramatic changes in the landscape of clinical medicine particularly as it applies to psychiatry.
Given these developments, the syndromic diagnoses in DSM-5 will in the future likely be replaced by a new diagnostic schema that breaks down existing heterogenous syndromic diagnoses into pathophysiologically and etiologically meaningful entities using insights gained from genetic and biomarker data as well as functional brain imaging. Theoretically, those insights will lead to new modalities of treatment, including somatic treatments that target novel mechanisms of action, coupled to more effective psychosocial therapies—with both therapies guided by diagnostic tests to monitor response to specific treatment interventions.
During this transition from the past to the future, answers to the questions I’ve posed here about laboratory testing in psychiatry will, I hope, help the practitioner understand, evaluate, and incorporate these changes readily into practice.
What has been the history of the development of laboratory tests in the field of psychiatry?
During my almost-40-year academic medical career, I have been interested in the development and incorporation of laboratory tests into psychiatry.1 This interest initially focused on therapeutic drug monitoring (TDM) and the genetics of drug responsiveness, with an emphasis on drug metabolism. In addition to TDM—which I have long believed is vastly underutilized in psychiatry—there have been many failed attempts to develop diagnostic tests, including tests to distinguish between what were postulated to be serotonergic and noradrenergic forms of major depression in the 1970s2,3 and the dexamethasone suppression test for melancholia in the 1980s.4 Recently, a 51-analyte immunoassay test was marketed by Rules-Based Medicine, Inc. (RBM), as an aid in the diagnosis of schizophrenia, but the test was found to suffer a high false-positive rate and was withdrawn from the market.5 Given this track record, caution is warranted when examining claims for new tests.
What types of tests are being developed?
Most tests in development are pharmacogenomic (PG)-based or immunoassay (IA)-based.
PG tests examine single nucleotide polymorphisms (SNP) in genes that code for pharmacokinetic mechanisms, primarily cytochrome P450 (CYP) enzymes responsible for drug metabolism and P-glycoprotein, responsible for drug transportation. The next most common type of test examines pharmacodynamic mechanisms, such as SNPs of specific receptor genes, including serotonin (or 5-hydroxytryptophan [5-HT] transporter [SET or 5-HTT]) or the 5-HT2A receptor.
The fact that CYP enzymes lead the list is not surprising: These enzymes and their role in the metabolism of specific drugs have been extensively studied since the late 1980s. Considerable data has been accumulated regarding variants of CYP enzymes, which convey clinically meaningful differences among individuals in terms of their ability to metabolize drug via these pathways. Individuals are commonly divided into 4 phenotypic categories: ultra-rapid, extensive (or normal), intermediate, and poor metabolizers. Based on these phenotypes, clinical consequences can be quantitated in terms of changes in drug concentration, concentration-dependent beneficial or adverse effects, and associated/recommended changes in dosing.
Research into the role of pharmacodynamic variants, however, is still in infancy and more difficult to measure in terms of assessing endpoints, with related limitations in clinical utility.
IA assays generally measure a variety of proteins, particularly those reflecting inflammatory processes (eg, various cytokines, such as interleukin-6).6 As with pharmacodynamic measures, research into the role of inflammatory biomarkers is in early stages. The clinical utility of associated tests is, therefore, less certain; witness the recent study5 I noted that revealed a high false-positive rate for the RBM schizophrenia panel in healthy controls. Nevertheless, considerable research is being conducted in all of these areas so that new developments might lend themselves to greater clinical utility.
(Note that PG biomarkers are trait measures, whereas IA biomarkers are state measures, so that complementary use of both types of tests might prove useful in diagnosis and clinical management. Although such integrative use of these 2 different types of tests generally is not done today.)
What does it take to market these tests?
At a minimum, offering these tests for sale requires that the laboratory be certified by the Centers for Medicare & Medicaid Services, according to the Clinical Laboratory Improvement Amendments (CLIA) standards (www.fda.gov/medicaldevices/deviceregulationandguidance/ivdregulatoryassistance/ucm124105.htm). CLIA-certified laboratories are required to demonstrate the analytical validity of tests that they offer—ie, the accuracy and reliability of the test in measuring a parameter of interest—but not the clinical validity or utility of those tests. The fact that a test in fact measures what it claims to be measuring in and of itself does not mean it has clinical validity or utility (see the discussion below).
Must the FDA approve laboratory tests?
No, but that situation might be changing.
Currently, only tests used in a setting considered high risk—eg, a test intended to detect or diagnose a malignancy or guide its treatment—requires formal FDA approval. The approval of such a test requires submission to the FDA of clinical data supporting its clinical validity and utility, in addition to evidence of analytic validity.
Even in such cases, the degree and quality of the clinical data required are generally not as high as would be required for approval of a drug. That distinction is understandable, given the type and quantity of data necessary for drug approval and the many years and billions of dollars it takes to accumulate such data. For most laboratory tests, providing the same level of data required to have a drug approved would be neither necessary nor feasible given the business model underlying most laboratories providing laboratory tests.
What do ‘clinical validity’ and ‘clinical utility’ mean?
These are higher evidence thresholds than is needed for analytic validity, although the latter is a necessary first step on the path to achieving these higher thresholds.
Clinical validity is the ability of a test to detect:
- a clinically meaningful measure, such as clinical response
- an adverse effect
- a biologically meaningful measure (eg, a drug level or a change in the electrocardiographic pattern).
Above the threshold of clinical validity is clinical utility, which is proof that the test can reliably be used to guide clinical management and thus meaningfully improve outcomes, such as guiding drug or dosage selection.
Is the use of PG testing recommended? If so, in what instances?
Specific types of PG testing is recommended by the FDA recommended. The FDA has been incorporating PG information into the labels of specific medications for several years; the agency has a Web site (www.fda.gov/drugs/scienceresearch/researchareas/pharmacogenetics/ucm083378.htm) that continuously updates this information. The involved drugs are in all therapeutic classes—from oncology to psychiatry.
More than 30 psychotropic drugs have PG information in their label; some of those drugs’ labels contain specific recommendations, such as obtaining PG information before selecting or starting a drug in a specific patient. An example is carbamazepine, for which the recommendation is to obtain HLA testing before starting the drug in patients of Han Chinese ancestry, because members of this large ethnic group are at greater risk of serious dermatologic adverse effects, including Stevens-Johnson syndrome.
In other instances, the recommendation is to do the testing before increasing beyond a specific dose. Examples of psychiatric drugs whose labels contain such PG information include pimozide and iloperidone as well as citalopram. In the FDA-approved label, guidance is provided that these drugs can be started without testing if prescribed at a reduced recommended starting dosage range, rather than the full starting dosage range. The guidance on these drugs further recommends testing for genetic CYP2D6 poor metabolizer (PM) status before dosing above that initial recommended, limited, starting dosage range.
The rationale for this guidance is to reduce the risk that (1) patients in question will achieve an excessively high plasma drug level that can cause significant prolongation of intracardiac conduction (eg, QTc prolongation) and thus (2) develop the potentially fatal arrhythmia torsades de pointes. Guidance is based on thorough QTc studies that were performed on each drug,7,8 which makes them examples of instances in which the test has clinical validity and utility as well as analytical validity.
To find PG labeling in the package insert for these drugs, visit: www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm.
What about data for other tests that are marketed and promoted by developers?
Sometimes, there are—literally—no data on available tests beyond the analytical validity of the test; other times, the amount and quality of clinical data are quite variable, ranging from results of ≥1 small retrospective studies without controls to results of prospective, randomized, controlled studies. Even among the latter, the developer may conduct and analyze their studies without oversight by an independent agency, such as the FDA.
This situation (1) raises concern that study results are not independent of the developer’s business interests and, as one might expect, (2) leads to controversy about whether the data are compelling—or not.9-12
What is a critical difference between PG test results and results of most laboratory tests?
PG tests are, as noted, trait rather than state characteristics. That means that the results do not change except for a phenomenon known as phenocoversion, discussed below. (Of course, advances in gene therapy might make it possible someday to change a person’s genetic makeup and for mitochondrial genes that is already possible.)
For this reason, PG test results should not get buried in the medical record, as might happen with, say, a patient’s serum potassium level at a given point in time. Instead, PG test results need to be carried forward continuously. Results also should be given to the patient as part of his (her) personal health record and to all other health care providers that the patient is seeing or will see in the future. Each health care provider who obtains PG test results should consider sending them to all current clinicians providing care for the patient at the same time as they are.
Is your functional status at a given moment the same as your genetic status?
No. There is a phenomenon known as phenoconversion in which a person’s current functional status may be different from what would be expected based on their genetic status.
CYP2D6 functional status is susceptible to phenoconversion as follows: Administering fluoxetine and paroxetine, for example, at 20 or 40 mg/d converts 66% and 95%, respectively, of patients who are CYP2D6 extensive (ie, normal) metabolizers into phenocopies of people who, genetically, lack the ability to metabolize drugs via CYP2D6 (ie, genotypic CYP2D6 PM). Based on a recent study of 900 participants in routine clinical care who were taking an antidepressant, 4% of the general U.S. population are genetically CYP2D6 PM; an additional 24% are phenotypically CYP2D6 PM because of concomitant administration of a CYP2D6 substantial inhibitor, such as bupropion, fluoxetine, paroxetine, or terbenafine.13
That is the reason a provider needs to know what drugs a patient is taking concomitantly—to consider the possibility of phenoconversion and, when necessary, to dose accordingly.
What does the future hold?
Development of tests for use in psychiatric practice is likely to grow substantially, for at least 2 reasons:
- There is a huge unmet need for clinically meaningful tests to aid in the provision of optimal patient care and, therefore, a tremendous business opportunity
- Knowledge in the biological basis of psychiatric disorders is growing exponentially; with that knowledge comes the ability to develop new tests.
A recent example comes from a research group that devised a test that could predict suicidality.14 Time will tell whether this test or a derivative of it enters practice. Nevertheless, it is a harbinger of the likely dramatic changes in the landscape of clinical medicine particularly as it applies to psychiatry.
Given these developments, the syndromic diagnoses in DSM-5 will in the future likely be replaced by a new diagnostic schema that breaks down existing heterogenous syndromic diagnoses into pathophysiologically and etiologically meaningful entities using insights gained from genetic and biomarker data as well as functional brain imaging. Theoretically, those insights will lead to new modalities of treatment, including somatic treatments that target novel mechanisms of action, coupled to more effective psychosocial therapies—with both therapies guided by diagnostic tests to monitor response to specific treatment interventions.
During this transition from the past to the future, answers to the questions I’ve posed here about laboratory testing in psychiatry will, I hope, help the practitioner understand, evaluate, and incorporate these changes readily into practice.
1. Preskorn SH, Biggs JT. Use of tricyclic antidepressant blood levels. N Engl J Med. 1978;298(3):166.
2. Schildkraut JJ. Biogenic amines and affective disorders. Annu Rev Med. 1974;25(0):333-348.
3. Maas JW. Biogenic amines and depression. Biochemical and pharmacological separation of two types of depression. Arch Gen Psychiatry. 1975;32(11):1357-1361.
4. Carroll BJ, Feinberg M, Greden JF, et al. A specific laboratory test for the diagnosis of melancholia. Standardization, validation, and clinical utility. Arch Gen Psychiatry. 1981;38(1):15-22.
5. Wehler C, Preskorn S. High false-positive rate of a putative biomarker test to aid in the diagnosis of schizophrenia. J Clin Psychiatry. In press.
6. Savitz J, Preskorn S, Teague TK, et al. Minocycline and aspirin in the treatment of bipolar depression: a protocol for a proof-of-concept, randomised, double-blind, placebo-controlled, 2x2 clinical trial. BMJ Open. 2012;2(1):e000643. doi: 10.1136/bmjopen-2011-000643.
7. Rogers HL, Bhattaram A, Zineh I, et al. CYP2D6 genotype information to guide pimozide treatment in adult and pediatric patients: basis for the U.S. Food and Drug Administration’s new dosing recommendations. J Clin Psychiatry. 2012;73(9):1187-1190.
8. Potkin S, Preskorn S, Hochfeld M, et al. A thorough QTc study of 3 doses of iloperidone including metabolic inhibition via CYP2D6 and/or CYP3A4 inhibition and a comparison to quetiapine and ziprasidone. J Clin Psychopharmacol. 2013;33(1):3-10.
9. Howland RH. Pharmacogenetic testing in psychiatry: not (quite) ready for primetime. J Psychosoc Nurs Ment Health Serv. 2014;52(11):13-16.
10. Rosenblat JD, Lee Y, McIntyre RS. Does pharmacogenomics testing improve clinical outcomes for major depressive disorder? A systematic review of clinical trials and cost-effectiveness studies. J Clin Psychiatry. In press.
11. Nassan M, Nicholson WT, Elliott MA, et al. Pharmacokinetic pharmacogenetic prescribing guidelines for antidepressants: a template for psychiatric precision medicine. Mayo Clin Proc. In press.
12. Altar CA, Carhart JM, Allen JD, et al. Clinical validity: combinatorial pharmacogenomics predicts antidepressant responses and healthcare utilizations better than single gene phenotypes. Pharmacogenomics J. 2015;15(5):443-451.
13. Preskorn S, Kane C, Lobello K, et al. Cytochrome P450 2D6 phenoconversion is common in patients being treated for depression: implications for personalized medicine. J Clin Psychiatry. 2013;74(6):614-621.
14. Niculescu AB, Levey DF, Phalen PL, et al. Understanding and predicting suicidality using a combined genomic and clinical risk assessment approach. Mol Psychiatry. 2015;20(11):1266-1285.
1. Preskorn SH, Biggs JT. Use of tricyclic antidepressant blood levels. N Engl J Med. 1978;298(3):166.
2. Schildkraut JJ. Biogenic amines and affective disorders. Annu Rev Med. 1974;25(0):333-348.
3. Maas JW. Biogenic amines and depression. Biochemical and pharmacological separation of two types of depression. Arch Gen Psychiatry. 1975;32(11):1357-1361.
4. Carroll BJ, Feinberg M, Greden JF, et al. A specific laboratory test for the diagnosis of melancholia. Standardization, validation, and clinical utility. Arch Gen Psychiatry. 1981;38(1):15-22.
5. Wehler C, Preskorn S. High false-positive rate of a putative biomarker test to aid in the diagnosis of schizophrenia. J Clin Psychiatry. In press.
6. Savitz J, Preskorn S, Teague TK, et al. Minocycline and aspirin in the treatment of bipolar depression: a protocol for a proof-of-concept, randomised, double-blind, placebo-controlled, 2x2 clinical trial. BMJ Open. 2012;2(1):e000643. doi: 10.1136/bmjopen-2011-000643.
7. Rogers HL, Bhattaram A, Zineh I, et al. CYP2D6 genotype information to guide pimozide treatment in adult and pediatric patients: basis for the U.S. Food and Drug Administration’s new dosing recommendations. J Clin Psychiatry. 2012;73(9):1187-1190.
8. Potkin S, Preskorn S, Hochfeld M, et al. A thorough QTc study of 3 doses of iloperidone including metabolic inhibition via CYP2D6 and/or CYP3A4 inhibition and a comparison to quetiapine and ziprasidone. J Clin Psychopharmacol. 2013;33(1):3-10.
9. Howland RH. Pharmacogenetic testing in psychiatry: not (quite) ready for primetime. J Psychosoc Nurs Ment Health Serv. 2014;52(11):13-16.
10. Rosenblat JD, Lee Y, McIntyre RS. Does pharmacogenomics testing improve clinical outcomes for major depressive disorder? A systematic review of clinical trials and cost-effectiveness studies. J Clin Psychiatry. In press.
11. Nassan M, Nicholson WT, Elliott MA, et al. Pharmacokinetic pharmacogenetic prescribing guidelines for antidepressants: a template for psychiatric precision medicine. Mayo Clin Proc. In press.
12. Altar CA, Carhart JM, Allen JD, et al. Clinical validity: combinatorial pharmacogenomics predicts antidepressant responses and healthcare utilizations better than single gene phenotypes. Pharmacogenomics J. 2015;15(5):443-451.
13. Preskorn S, Kane C, Lobello K, et al. Cytochrome P450 2D6 phenoconversion is common in patients being treated for depression: implications for personalized medicine. J Clin Psychiatry. 2013;74(6):614-621.
14. Niculescu AB, Levey DF, Phalen PL, et al. Understanding and predicting suicidality using a combined genomic and clinical risk assessment approach. Mol Psychiatry. 2015;20(11):1266-1285.
No Mortality Benefit to Cardiac Catheterization in Patients with Stable Ischemic Heart Disease
Clinical question: Can cardiac catheterization prolong survival in patients with stable ischemic heart disease?
Background: Previous results from the COURAGE trial found no benefit of percutaneous intervention (PCI) as compared to medical therapy on a composite endpoint of death or nonfatal myocardial infarction or in total mortality at 4.6 years follow-up. The authors now report 15-year follow-up of the same patients.
Study design: Randomized, controlled trial.
Setting: The majority of the patients were from Veterans Affairs (VA) medical centers, although non-VA hospitals in the U.S. also were included.
Synopsis: Originally, 2,287 patients with stable ischemic heart disease and either an abnormal stress test or evidence of ischemia on ECG, as well at least 70% stenosis on angiography, were randomized to medical therapy or medical therapy plus PCI. Now, investigators have obtained extended follow-up information for 1,211 of the original patients (53%). They concluded that after 15 years of follow-up, there was no survival difference for the patients who initially received PCI in addition to medical management.
One limitation of the study was that it did not reflect important advances in both medical and interventional management of ischemic heart disease that have taken place since the study was conducted, which may affect patient mortality. It is also noteworthy that the investigators were unable to determine how many patients in the medical management group subsequently underwent revascularization after the study concluded and therefore may have crossed over between groups. Nevertheless, for now it appears that the major utility of PCI in stable ischemic heart disease is in symptomatic management.
Bottom Line: After 15 years of follow-up, there was still no mortality benefit to PCI as compared to optimal medical therapy for stable ischemic heart disease.
Citation: Sedlis SP, Hartigan PM, Teo KK, et al. Effect of PCI on long-term survival in patients with stable ischemic heart disease. N Engl J Med. 2015;373(20):1937-1946
Short Take
Cauti Infections Are Rarely Clinically Relevant and Associated with Low Complication Rate
A single-center retrospective study in the ICU setting shows that the definition of catheter-associated urinary tract infections (CAUTIs) is nonspecific and they’re mostly diagnosed when urine cultures are sent for workup of fever. Most of the time, there are alternative explanations for the fever.
Citation: Tedja R, Wentink J, O’Horo J, Thompson R, Sampathkumar P et al. Catheter-associated urinary tract infections in intensive care unit patients. Infect Control Hosp Epidemiol. 2015;36(11):1330-1334.
Clinical question: Can cardiac catheterization prolong survival in patients with stable ischemic heart disease?
Background: Previous results from the COURAGE trial found no benefit of percutaneous intervention (PCI) as compared to medical therapy on a composite endpoint of death or nonfatal myocardial infarction or in total mortality at 4.6 years follow-up. The authors now report 15-year follow-up of the same patients.
Study design: Randomized, controlled trial.
Setting: The majority of the patients were from Veterans Affairs (VA) medical centers, although non-VA hospitals in the U.S. also were included.
Synopsis: Originally, 2,287 patients with stable ischemic heart disease and either an abnormal stress test or evidence of ischemia on ECG, as well at least 70% stenosis on angiography, were randomized to medical therapy or medical therapy plus PCI. Now, investigators have obtained extended follow-up information for 1,211 of the original patients (53%). They concluded that after 15 years of follow-up, there was no survival difference for the patients who initially received PCI in addition to medical management.
One limitation of the study was that it did not reflect important advances in both medical and interventional management of ischemic heart disease that have taken place since the study was conducted, which may affect patient mortality. It is also noteworthy that the investigators were unable to determine how many patients in the medical management group subsequently underwent revascularization after the study concluded and therefore may have crossed over between groups. Nevertheless, for now it appears that the major utility of PCI in stable ischemic heart disease is in symptomatic management.
Bottom Line: After 15 years of follow-up, there was still no mortality benefit to PCI as compared to optimal medical therapy for stable ischemic heart disease.
Citation: Sedlis SP, Hartigan PM, Teo KK, et al. Effect of PCI on long-term survival in patients with stable ischemic heart disease. N Engl J Med. 2015;373(20):1937-1946
Short Take
Cauti Infections Are Rarely Clinically Relevant and Associated with Low Complication Rate
A single-center retrospective study in the ICU setting shows that the definition of catheter-associated urinary tract infections (CAUTIs) is nonspecific and they’re mostly diagnosed when urine cultures are sent for workup of fever. Most of the time, there are alternative explanations for the fever.
Citation: Tedja R, Wentink J, O’Horo J, Thompson R, Sampathkumar P et al. Catheter-associated urinary tract infections in intensive care unit patients. Infect Control Hosp Epidemiol. 2015;36(11):1330-1334.
Clinical question: Can cardiac catheterization prolong survival in patients with stable ischemic heart disease?
Background: Previous results from the COURAGE trial found no benefit of percutaneous intervention (PCI) as compared to medical therapy on a composite endpoint of death or nonfatal myocardial infarction or in total mortality at 4.6 years follow-up. The authors now report 15-year follow-up of the same patients.
Study design: Randomized, controlled trial.
Setting: The majority of the patients were from Veterans Affairs (VA) medical centers, although non-VA hospitals in the U.S. also were included.
Synopsis: Originally, 2,287 patients with stable ischemic heart disease and either an abnormal stress test or evidence of ischemia on ECG, as well at least 70% stenosis on angiography, were randomized to medical therapy or medical therapy plus PCI. Now, investigators have obtained extended follow-up information for 1,211 of the original patients (53%). They concluded that after 15 years of follow-up, there was no survival difference for the patients who initially received PCI in addition to medical management.
One limitation of the study was that it did not reflect important advances in both medical and interventional management of ischemic heart disease that have taken place since the study was conducted, which may affect patient mortality. It is also noteworthy that the investigators were unable to determine how many patients in the medical management group subsequently underwent revascularization after the study concluded and therefore may have crossed over between groups. Nevertheless, for now it appears that the major utility of PCI in stable ischemic heart disease is in symptomatic management.
Bottom Line: After 15 years of follow-up, there was still no mortality benefit to PCI as compared to optimal medical therapy for stable ischemic heart disease.
Citation: Sedlis SP, Hartigan PM, Teo KK, et al. Effect of PCI on long-term survival in patients with stable ischemic heart disease. N Engl J Med. 2015;373(20):1937-1946
Short Take
Cauti Infections Are Rarely Clinically Relevant and Associated with Low Complication Rate
A single-center retrospective study in the ICU setting shows that the definition of catheter-associated urinary tract infections (CAUTIs) is nonspecific and they’re mostly diagnosed when urine cultures are sent for workup of fever. Most of the time, there are alternative explanations for the fever.
Citation: Tedja R, Wentink J, O’Horo J, Thompson R, Sampathkumar P et al. Catheter-associated urinary tract infections in intensive care unit patients. Infect Control Hosp Epidemiol. 2015;36(11):1330-1334.
Increase in Broad-Spectrum Antibiotics Disproportionate to Rate of Resistant Organisms
Clinical question: Have healthcare-associated pneumonia (HCAP) guidelines improved treatment accuracy?
Background: Guidelines released in 2005 call for the use of broad-spectrum antibiotics for patients presenting with pneumonia who have had recent healthcare exposure. However, there is scant evidence to support the risk factors they identify, and the guidelines are likely to increase use of broad-spectrum antibiotics.
Study design: Observational, retrospective.
Setting: VA medical centers, 2006–2010.
Synopsis: In this study, VA medical center physicians evaluated 95,511 hospitalizations for pneumonia at 128 hospitals between 2006 and 2010, the years following the 2005 guidelines. Annual analyses were performed to assess antibiotics selection as well as evidence of resistant bacteria from blood and respiratory cultures. Researchers found that while the use of broad-spectrum antibiotics increased drastically during the study period (vancomycin from 16% to 31% and piperacillin-tazobactam from 16% to 27%, P<0.001 for both), the incidence of resistant organisms either decreased or remained stable.
Additionally, physicians were no better at matching broad-spectrum antibiotics to patients infected with resistant organisms at the end of the study period than they were at the start. They conclude that more research is urgently needed to identify patients at risk for resistant organisms in order to more appropriately prescribe broad-spectrum antibiotics.
This study did not evaluate patients’ clinical outcomes, so it is unclear whether they may have benefitted clinically from the implementation of the guidelines. For now, the optimal approach to empiric therapy for HCAP remains undefined.
Bottom line: Despite a marked increase in the use of broad-spectrum antibiotics for HCAP in the years following a change in treatment guidelines, doctors showed no improvement at matching these antibiotics to patients infected with resistant organisms.
Citation: Jones BE, Jones MM, Huttner B, et al. Trends in antibiotic use and nosocomial pathogens in hospitalized veterans with pneumonia at 128 medical centers, 2006-2010. Clin Infect Dis. 2015;61(9):1403-1410.
Clinical question: Have healthcare-associated pneumonia (HCAP) guidelines improved treatment accuracy?
Background: Guidelines released in 2005 call for the use of broad-spectrum antibiotics for patients presenting with pneumonia who have had recent healthcare exposure. However, there is scant evidence to support the risk factors they identify, and the guidelines are likely to increase use of broad-spectrum antibiotics.
Study design: Observational, retrospective.
Setting: VA medical centers, 2006–2010.
Synopsis: In this study, VA medical center physicians evaluated 95,511 hospitalizations for pneumonia at 128 hospitals between 2006 and 2010, the years following the 2005 guidelines. Annual analyses were performed to assess antibiotics selection as well as evidence of resistant bacteria from blood and respiratory cultures. Researchers found that while the use of broad-spectrum antibiotics increased drastically during the study period (vancomycin from 16% to 31% and piperacillin-tazobactam from 16% to 27%, P<0.001 for both), the incidence of resistant organisms either decreased or remained stable.
Additionally, physicians were no better at matching broad-spectrum antibiotics to patients infected with resistant organisms at the end of the study period than they were at the start. They conclude that more research is urgently needed to identify patients at risk for resistant organisms in order to more appropriately prescribe broad-spectrum antibiotics.
This study did not evaluate patients’ clinical outcomes, so it is unclear whether they may have benefitted clinically from the implementation of the guidelines. For now, the optimal approach to empiric therapy for HCAP remains undefined.
Bottom line: Despite a marked increase in the use of broad-spectrum antibiotics for HCAP in the years following a change in treatment guidelines, doctors showed no improvement at matching these antibiotics to patients infected with resistant organisms.
Citation: Jones BE, Jones MM, Huttner B, et al. Trends in antibiotic use and nosocomial pathogens in hospitalized veterans with pneumonia at 128 medical centers, 2006-2010. Clin Infect Dis. 2015;61(9):1403-1410.
Clinical question: Have healthcare-associated pneumonia (HCAP) guidelines improved treatment accuracy?
Background: Guidelines released in 2005 call for the use of broad-spectrum antibiotics for patients presenting with pneumonia who have had recent healthcare exposure. However, there is scant evidence to support the risk factors they identify, and the guidelines are likely to increase use of broad-spectrum antibiotics.
Study design: Observational, retrospective.
Setting: VA medical centers, 2006–2010.
Synopsis: In this study, VA medical center physicians evaluated 95,511 hospitalizations for pneumonia at 128 hospitals between 2006 and 2010, the years following the 2005 guidelines. Annual analyses were performed to assess antibiotics selection as well as evidence of resistant bacteria from blood and respiratory cultures. Researchers found that while the use of broad-spectrum antibiotics increased drastically during the study period (vancomycin from 16% to 31% and piperacillin-tazobactam from 16% to 27%, P<0.001 for both), the incidence of resistant organisms either decreased or remained stable.
Additionally, physicians were no better at matching broad-spectrum antibiotics to patients infected with resistant organisms at the end of the study period than they were at the start. They conclude that more research is urgently needed to identify patients at risk for resistant organisms in order to more appropriately prescribe broad-spectrum antibiotics.
This study did not evaluate patients’ clinical outcomes, so it is unclear whether they may have benefitted clinically from the implementation of the guidelines. For now, the optimal approach to empiric therapy for HCAP remains undefined.
Bottom line: Despite a marked increase in the use of broad-spectrum antibiotics for HCAP in the years following a change in treatment guidelines, doctors showed no improvement at matching these antibiotics to patients infected with resistant organisms.
Citation: Jones BE, Jones MM, Huttner B, et al. Trends in antibiotic use and nosocomial pathogens in hospitalized veterans with pneumonia at 128 medical centers, 2006-2010. Clin Infect Dis. 2015;61(9):1403-1410.
Considering Costs U.S. Hospitals choose Anticoagulant Rivaroxaban Over Warfarin
NEW YORK (Reuters Health) - U.S. hospitals save money when they use the novel oral anticoagulant rivaroxaban instead of warfarin to treat patients with venous thromboembolism (VTE), a new analysis finds.
"These days it's important to consider the cost of new drugs to the health system," Dr. Steven Deitelzweig from Ochsner Health System in New Orleans, Louisiana, noted in an interview with Reuters Health.
"This retrospective observational analysis had an ample number of patients, they had very good clinical outcomes with rivaroxaban, and we also demonstrated that those clinical outcomes could be achieved with a notable reduction in the all-important utilization side of healthcare," he said.
It's estimated that VTE affects more than 900,000 Americans each year, at a cost to the healthcare system between $13 and $27 billion.
Dr. Deitelzweig and his colleagues did an economic analysis of rivaroxaban versus low-molecular-weight heparin (LMWH)/warfarin for VTE in the hospital setting.
Using Truven MarketScan Hospital Drug Database, they identified more than 2,400 older adults hospitalized for primary VTE between 2012 and 2013. They created two groups of 1,223 patients each. Each group included 751 pulmonary embolism (PE) patients and 472 deep vein thrombosis (DVT) patients.
According to the analysis, total hospitalization costs - including room rate, laboratory tests, inpatient procedures, pharmacy costs and all other inpatient services - were significantly lower and length of stay was significantly shorter for patients treated with rivaroxaban rather than LMWH/warfarin.
Patients receiving rivaroxaban spent an average of 1.5 fewer days in the hospital than their peers on LMWH/warfarin (3.7 versus 5.2 days, p<0.001).
"This finding is consistent with the length of stay reduction found in the EINSTEIN VTE clinical trials," the researchers note in their poster presented March 7 at the Society of Hospital Medicine annual meeting in San Diego, California.
"Length of stay is one metric that we track quite closely and care about. Even one day less in a hospital is a significant cost savings and allows hospitals that are very busy to take care of the next patient, as appropriate," Dr. Deitelzweig told Reuters Health.
The rivaroxaban group had an adjusted average cost savings of $1,888 per admission compared with the LMWH/warfarin group ($8,387 versus $10,275; p<0.001), the study found.
Limitations of the study include the fact that patient medical history was limited to the patient's current admission. Outpatient treatment prior to admission, particularly whether they had received either rivaroxaban or LMWH/warfarin prior to admission was unknown. And despite propensity score matching and further statistical modeling, there remains the potential for unmeasured confounders, they note.
The study was funded by Janssen Scientific Affairs, LLC. Janssen Pharmaceuticals markets rivaroxaban under the trade name Xarelto. Four authors are employees of Janssen Research and Development, LLC.
NEW YORK (Reuters Health) - U.S. hospitals save money when they use the novel oral anticoagulant rivaroxaban instead of warfarin to treat patients with venous thromboembolism (VTE), a new analysis finds.
"These days it's important to consider the cost of new drugs to the health system," Dr. Steven Deitelzweig from Ochsner Health System in New Orleans, Louisiana, noted in an interview with Reuters Health.
"This retrospective observational analysis had an ample number of patients, they had very good clinical outcomes with rivaroxaban, and we also demonstrated that those clinical outcomes could be achieved with a notable reduction in the all-important utilization side of healthcare," he said.
It's estimated that VTE affects more than 900,000 Americans each year, at a cost to the healthcare system between $13 and $27 billion.
Dr. Deitelzweig and his colleagues did an economic analysis of rivaroxaban versus low-molecular-weight heparin (LMWH)/warfarin for VTE in the hospital setting.
Using Truven MarketScan Hospital Drug Database, they identified more than 2,400 older adults hospitalized for primary VTE between 2012 and 2013. They created two groups of 1,223 patients each. Each group included 751 pulmonary embolism (PE) patients and 472 deep vein thrombosis (DVT) patients.
According to the analysis, total hospitalization costs - including room rate, laboratory tests, inpatient procedures, pharmacy costs and all other inpatient services - were significantly lower and length of stay was significantly shorter for patients treated with rivaroxaban rather than LMWH/warfarin.
Patients receiving rivaroxaban spent an average of 1.5 fewer days in the hospital than their peers on LMWH/warfarin (3.7 versus 5.2 days, p<0.001).
"This finding is consistent with the length of stay reduction found in the EINSTEIN VTE clinical trials," the researchers note in their poster presented March 7 at the Society of Hospital Medicine annual meeting in San Diego, California.
"Length of stay is one metric that we track quite closely and care about. Even one day less in a hospital is a significant cost savings and allows hospitals that are very busy to take care of the next patient, as appropriate," Dr. Deitelzweig told Reuters Health.
The rivaroxaban group had an adjusted average cost savings of $1,888 per admission compared with the LMWH/warfarin group ($8,387 versus $10,275; p<0.001), the study found.
Limitations of the study include the fact that patient medical history was limited to the patient's current admission. Outpatient treatment prior to admission, particularly whether they had received either rivaroxaban or LMWH/warfarin prior to admission was unknown. And despite propensity score matching and further statistical modeling, there remains the potential for unmeasured confounders, they note.
The study was funded by Janssen Scientific Affairs, LLC. Janssen Pharmaceuticals markets rivaroxaban under the trade name Xarelto. Four authors are employees of Janssen Research and Development, LLC.
NEW YORK (Reuters Health) - U.S. hospitals save money when they use the novel oral anticoagulant rivaroxaban instead of warfarin to treat patients with venous thromboembolism (VTE), a new analysis finds.
"These days it's important to consider the cost of new drugs to the health system," Dr. Steven Deitelzweig from Ochsner Health System in New Orleans, Louisiana, noted in an interview with Reuters Health.
"This retrospective observational analysis had an ample number of patients, they had very good clinical outcomes with rivaroxaban, and we also demonstrated that those clinical outcomes could be achieved with a notable reduction in the all-important utilization side of healthcare," he said.
It's estimated that VTE affects more than 900,000 Americans each year, at a cost to the healthcare system between $13 and $27 billion.
Dr. Deitelzweig and his colleagues did an economic analysis of rivaroxaban versus low-molecular-weight heparin (LMWH)/warfarin for VTE in the hospital setting.
Using Truven MarketScan Hospital Drug Database, they identified more than 2,400 older adults hospitalized for primary VTE between 2012 and 2013. They created two groups of 1,223 patients each. Each group included 751 pulmonary embolism (PE) patients and 472 deep vein thrombosis (DVT) patients.
According to the analysis, total hospitalization costs - including room rate, laboratory tests, inpatient procedures, pharmacy costs and all other inpatient services - were significantly lower and length of stay was significantly shorter for patients treated with rivaroxaban rather than LMWH/warfarin.
Patients receiving rivaroxaban spent an average of 1.5 fewer days in the hospital than their peers on LMWH/warfarin (3.7 versus 5.2 days, p<0.001).
"This finding is consistent with the length of stay reduction found in the EINSTEIN VTE clinical trials," the researchers note in their poster presented March 7 at the Society of Hospital Medicine annual meeting in San Diego, California.
"Length of stay is one metric that we track quite closely and care about. Even one day less in a hospital is a significant cost savings and allows hospitals that are very busy to take care of the next patient, as appropriate," Dr. Deitelzweig told Reuters Health.
The rivaroxaban group had an adjusted average cost savings of $1,888 per admission compared with the LMWH/warfarin group ($8,387 versus $10,275; p<0.001), the study found.
Limitations of the study include the fact that patient medical history was limited to the patient's current admission. Outpatient treatment prior to admission, particularly whether they had received either rivaroxaban or LMWH/warfarin prior to admission was unknown. And despite propensity score matching and further statistical modeling, there remains the potential for unmeasured confounders, they note.
The study was funded by Janssen Scientific Affairs, LLC. Janssen Pharmaceuticals markets rivaroxaban under the trade name Xarelto. Four authors are employees of Janssen Research and Development, LLC.
Research helps explain how malaria evolved

Photo by Holly Lutz
A study published in Molecular Phylogenetics and Evolution has revealed a new hypothesis on the evolution of malaria.
Researchers tested malarial DNA found in birds, bats, and other small mammals from 5 East African countries and found evidence to suggest that malaria has its roots in bird hosts.
It then spread to bats and on to other mammals.
“We can’t begin to understand how malaria spread to humans until we understand its evolutionary history,” said Holly Lutz, a doctoral candidate at Cornell University in Ithaca, New York.
“In learning about its past, we may be better able to understand the effects it has on us.”
Lutz and her colleagues took blood samples from hundreds of East African birds, bats, and other small mammals and screened the blood for malaria parasites.
When they found malaria, the team took samples of the parasites’ DNA and sequenced it to identify mutations in the genetic code. From there, the researchers performed phylogenetic analyses to determine how different malaria species are related.
In analyzing the genetic codes of the parasites, the team was able to find places where the DNA differed from one species to the next. Then, the researchers used computing software to determine how the different species evolved and how they’re related to each other.
“[B]y looking at patterns of mutations in the DNA of the different malaria species, we’re able to see when it branched off from one host group into another,” Lutz explained. “It started out as a parasite in birds, and then it evolved to colonize bats, and from there, it’s evolved to affect other mammals.”
In addition to shedding light on the way malaria was able to evolve and spread, the study provides information about the manner in which animals and their parasites are connected.
“Each of these individual vertebrates is an ecosystem in and of itself,” Lutz said. “In learning more about how parasites live within their hosts, who is infecting who, and how these organisms coexist in these living, breathing ecosystems, we can learn more about how they are connected to and affected by the natural environments that we share with animals and plants.”
The researchers noted that this study doesn’t have direct implications for malaria treatment in humans. However, the team believes that having a better understanding of malaria’s evolutionary history could help scientists anticipate how it will change and evolve in the future. ![]()

Photo by Holly Lutz
A study published in Molecular Phylogenetics and Evolution has revealed a new hypothesis on the evolution of malaria.
Researchers tested malarial DNA found in birds, bats, and other small mammals from 5 East African countries and found evidence to suggest that malaria has its roots in bird hosts.
It then spread to bats and on to other mammals.
“We can’t begin to understand how malaria spread to humans until we understand its evolutionary history,” said Holly Lutz, a doctoral candidate at Cornell University in Ithaca, New York.
“In learning about its past, we may be better able to understand the effects it has on us.”
Lutz and her colleagues took blood samples from hundreds of East African birds, bats, and other small mammals and screened the blood for malaria parasites.
When they found malaria, the team took samples of the parasites’ DNA and sequenced it to identify mutations in the genetic code. From there, the researchers performed phylogenetic analyses to determine how different malaria species are related.
In analyzing the genetic codes of the parasites, the team was able to find places where the DNA differed from one species to the next. Then, the researchers used computing software to determine how the different species evolved and how they’re related to each other.
“[B]y looking at patterns of mutations in the DNA of the different malaria species, we’re able to see when it branched off from one host group into another,” Lutz explained. “It started out as a parasite in birds, and then it evolved to colonize bats, and from there, it’s evolved to affect other mammals.”
In addition to shedding light on the way malaria was able to evolve and spread, the study provides information about the manner in which animals and their parasites are connected.
“Each of these individual vertebrates is an ecosystem in and of itself,” Lutz said. “In learning more about how parasites live within their hosts, who is infecting who, and how these organisms coexist in these living, breathing ecosystems, we can learn more about how they are connected to and affected by the natural environments that we share with animals and plants.”
The researchers noted that this study doesn’t have direct implications for malaria treatment in humans. However, the team believes that having a better understanding of malaria’s evolutionary history could help scientists anticipate how it will change and evolve in the future. ![]()

Photo by Holly Lutz
A study published in Molecular Phylogenetics and Evolution has revealed a new hypothesis on the evolution of malaria.
Researchers tested malarial DNA found in birds, bats, and other small mammals from 5 East African countries and found evidence to suggest that malaria has its roots in bird hosts.
It then spread to bats and on to other mammals.
“We can’t begin to understand how malaria spread to humans until we understand its evolutionary history,” said Holly Lutz, a doctoral candidate at Cornell University in Ithaca, New York.
“In learning about its past, we may be better able to understand the effects it has on us.”
Lutz and her colleagues took blood samples from hundreds of East African birds, bats, and other small mammals and screened the blood for malaria parasites.
When they found malaria, the team took samples of the parasites’ DNA and sequenced it to identify mutations in the genetic code. From there, the researchers performed phylogenetic analyses to determine how different malaria species are related.
In analyzing the genetic codes of the parasites, the team was able to find places where the DNA differed from one species to the next. Then, the researchers used computing software to determine how the different species evolved and how they’re related to each other.
“[B]y looking at patterns of mutations in the DNA of the different malaria species, we’re able to see when it branched off from one host group into another,” Lutz explained. “It started out as a parasite in birds, and then it evolved to colonize bats, and from there, it’s evolved to affect other mammals.”
In addition to shedding light on the way malaria was able to evolve and spread, the study provides information about the manner in which animals and their parasites are connected.
“Each of these individual vertebrates is an ecosystem in and of itself,” Lutz said. “In learning more about how parasites live within their hosts, who is infecting who, and how these organisms coexist in these living, breathing ecosystems, we can learn more about how they are connected to and affected by the natural environments that we share with animals and plants.”
The researchers noted that this study doesn’t have direct implications for malaria treatment in humans. However, the team believes that having a better understanding of malaria’s evolutionary history could help scientists anticipate how it will change and evolve in the future. ![]()
Study: Dying at home doesn’t mean dying sooner

patient’s hand
Choosing to die at home does not hasten death for patients with terminal cancer, according to a study published in Cancer.
The research showed that cancer patients who died at home lived at least as long as patients who spent their last days in hospitals.
Investigators say these results suggest oncologists should not hesitate to refer patients for home-based palliative care simply because less medical treatment may be provided.
“The cancer patient and family tend to be concerned that the quality of medical treatment provided at home will be inferior to that given in a hospital and that survival might be shortened,” said study author Jun Hamano, MD, of the University of Tsukuba in Japan.
“However, our finding—that home death does not actually have a negative influence on the survival of cancer patients at all and, rather, may have a positive influence—could suggest that the patient and family can choose the place of death in terms of their preference and values.”
Dr Hamano and his colleagues conducted this research by prospectively studying 2069 patients—1582 receiving hospital-based palliative care and 487 receiving home-based palliative care.
In all, 1607 patients died in the hospital, and 462 died at home.
Among patients thought to have only days to live, the survival of those who died at home was significantly longer than the survival of those who died in a hospital. The estimated median survival times were 13 days and 9 days, respectively (P<0.006).
Similarly, survival was significantly longer in the home group than the hospital group among patients thought to have weeks to live. The estimated median survival times were 36 days and 29 days, respectively (P<0.007).
There was no significant difference between the home and hospital groups among patients thought to have months to live. The estimated median survival times were 59 days and 62 days, respectively (P=0.925).
Finally, analyses suggested the place of death had a significant influence on the survival time in both unadjusted and adjusted models. The hazard ratios were 0.86 (P<0.01) and 0.87 (P=0.01), respectively.
Based on these findings, Dr Hamano concluded that, “Patients, families, and clinicians should be reassured that good home hospice care does not shorten patient life and even may achieve longer survival.” ![]()

patient’s hand
Choosing to die at home does not hasten death for patients with terminal cancer, according to a study published in Cancer.
The research showed that cancer patients who died at home lived at least as long as patients who spent their last days in hospitals.
Investigators say these results suggest oncologists should not hesitate to refer patients for home-based palliative care simply because less medical treatment may be provided.
“The cancer patient and family tend to be concerned that the quality of medical treatment provided at home will be inferior to that given in a hospital and that survival might be shortened,” said study author Jun Hamano, MD, of the University of Tsukuba in Japan.
“However, our finding—that home death does not actually have a negative influence on the survival of cancer patients at all and, rather, may have a positive influence—could suggest that the patient and family can choose the place of death in terms of their preference and values.”
Dr Hamano and his colleagues conducted this research by prospectively studying 2069 patients—1582 receiving hospital-based palliative care and 487 receiving home-based palliative care.
In all, 1607 patients died in the hospital, and 462 died at home.
Among patients thought to have only days to live, the survival of those who died at home was significantly longer than the survival of those who died in a hospital. The estimated median survival times were 13 days and 9 days, respectively (P<0.006).
Similarly, survival was significantly longer in the home group than the hospital group among patients thought to have weeks to live. The estimated median survival times were 36 days and 29 days, respectively (P<0.007).
There was no significant difference between the home and hospital groups among patients thought to have months to live. The estimated median survival times were 59 days and 62 days, respectively (P=0.925).
Finally, analyses suggested the place of death had a significant influence on the survival time in both unadjusted and adjusted models. The hazard ratios were 0.86 (P<0.01) and 0.87 (P=0.01), respectively.
Based on these findings, Dr Hamano concluded that, “Patients, families, and clinicians should be reassured that good home hospice care does not shorten patient life and even may achieve longer survival.” ![]()

patient’s hand
Choosing to die at home does not hasten death for patients with terminal cancer, according to a study published in Cancer.
The research showed that cancer patients who died at home lived at least as long as patients who spent their last days in hospitals.
Investigators say these results suggest oncologists should not hesitate to refer patients for home-based palliative care simply because less medical treatment may be provided.
“The cancer patient and family tend to be concerned that the quality of medical treatment provided at home will be inferior to that given in a hospital and that survival might be shortened,” said study author Jun Hamano, MD, of the University of Tsukuba in Japan.
“However, our finding—that home death does not actually have a negative influence on the survival of cancer patients at all and, rather, may have a positive influence—could suggest that the patient and family can choose the place of death in terms of their preference and values.”
Dr Hamano and his colleagues conducted this research by prospectively studying 2069 patients—1582 receiving hospital-based palliative care and 487 receiving home-based palliative care.
In all, 1607 patients died in the hospital, and 462 died at home.
Among patients thought to have only days to live, the survival of those who died at home was significantly longer than the survival of those who died in a hospital. The estimated median survival times were 13 days and 9 days, respectively (P<0.006).
Similarly, survival was significantly longer in the home group than the hospital group among patients thought to have weeks to live. The estimated median survival times were 36 days and 29 days, respectively (P<0.007).
There was no significant difference between the home and hospital groups among patients thought to have months to live. The estimated median survival times were 59 days and 62 days, respectively (P=0.925).
Finally, analyses suggested the place of death had a significant influence on the survival time in both unadjusted and adjusted models. The hazard ratios were 0.86 (P<0.01) and 0.87 (P=0.01), respectively.
Based on these findings, Dr Hamano concluded that, “Patients, families, and clinicians should be reassured that good home hospice care does not shorten patient life and even may achieve longer survival.” ![]()
Another Spin
A previously healthy 11‐year‐old boy presented to the emergency department after referral from his pediatrician for 1 week of fevers. Seven days prior to admission he developed a fever to 40.8C, vomiting, and mild left knee pain. The vomiting resolved within 2 days. Five days prior to admission he developed a pruritic, pinpoint rash over his abdomen that resolved within 24 hours. He also developed red, cracked lips, redness of his tongue, redness surrounding his eyes, and slight swelling of his hands. Three days prior to admission his pediatrician noted a 1‐cm anterior cervical lymph node. His fevers occurred throughout each of the prior 7 days without a discernible pattern, and his mild knee pain persisted at the time of presentation.
This preteen has had high fevers for 1 week associated with arthralgia, pruritic rash, emesis, and oral mucosal erythema. His rash, lip and tongue erythema, and swollen hands are classic features of Kawasaki disease (KD), but he lacks the other characteristic physical examination findings. The diagnosis of KD requires fever for at least 5 days accompanied by 4 of the following 5 signs: polymorphous rash, oral mucous membrane changes, peripheral extremity changes such as swelling or skin desquamation, bilateral bulbar conjunctival injection, and cervical lymphadenopathy >1.5 cm in diameter. Children meeting fewer than 4 of these criteria may have an incomplete form of KD.
Because most patients with KD (80%) are under 5 years old, alternative diagnoses such as autoimmune illnesses or a hypersensitivity reaction should be considered. Travel, medication, and animal exposure histories may reveal clues to an infectious or drug‐induced etiology of his fever. Immunization status should be assessed, as measles is also associated with fever, rash, and mucosal changes. Arthralgia or arthritis may occur in KD, but these findings suggest the need to entertain other possibilities, including bone or joint infection, infective endocarditis, inflammatory bowel disease, juvenile idiopathic arthritis (JIA), or systemic lupus erythematosus (SLE).
The child's only past medical history was an episode of croup as an infant. There was no family history of autoimmune diseases. He was not taking any medications and had no known allergies. His immunizations were up to date, including measles, mumps, rubella, and varicella. He lived with his parents and his dog. He swam in fresh water during a trip to Maine 2 months earlier. Neither he nor his family recalled a tick bite. He had no exposure to raw meat or unpasteurized dairy products.
The travel to New England raises the possibility of Lyme disease, although a 2‐month interval between exposure and a high, prolonged fever would be very unusual. Knee arthralgia or arthritis is common in children with late‐stage Lyme disease, but can also be seen in early‐disseminated disease. The prior description of the rash is not suggestive of erythema chronicum migrans, which is seen in early‐stage Lyme disease.
C‐reactive protein (CRP) was 189 mg/L (normal 6.3 mg/L). An echocardiogram was normal. Intravenous immunoglobulin (IVIG) was administered for presumed KD, with immediate improvement of the periorbital erythema, tongue redness, and hand swelling. He was discharged the next day on aspirin with cardiology clinic follow‐up.
Improvement after IVIG supports the diagnosis of KD. It is typical to discharge KD patients from the hospital when they have been afebrile for 24 hours or when the CRP level has declined by approximately 50%.
Over the next 48 hours he felt unwell with high‐grade fevers, continued left knee pain, and new left hip pain. He was readmitted to the hospital. His temperature was 39.4C, respiratory rate was 22 breaths per minute, heart rate was 122 beats per minute, blood pressure was 103/50 mm Hg, and oxygen saturation was 100% while breathing ambient air. He appeared mildly uncomfortable. His conjunctivae were normal. His lips were dry, red, and cracked, and his tongue was red with prominent papillae. His neck was supple without lymphadenopathy. His lungs were clear to auscultation. His heart exam was without murmurs. His abdomen was soft, and the liver and spleen were not enlarged. He had no swelling or erythema of his joints; however, he experienced pain with range of motion of his left knee, and tenderness and restricted range of motion of his left hip. His neurologic exam was normal. There were no rashes.
He has persistent fever, tachycardia, and tachypnea, now without features of KD except oral mucosal changes including prominent tongue papillae consistent with a strawberry tongue. Continued or recurrent fever may suggest persistent KD with ongoing inflammation or the need to search for an alternative diagnoses. An echocardiogram should be repeated, as the coronary artery abnormalities in KD can evolve rapidly, particularly when inflammation persists. Additional findings may include decreased left ventricular function, mitral regurgitation, or pericardial effusion. A second dose of IVIG is necessary to control fever and inflammation in about 15% of patients with KD, although in this case IVIG should be withheld pending further evaluation.
Arthralgia occurs commonly in KD, whereas frank arthritis is less typical. Polyarticular or oligoarticular arthritis involving small or large joints (especially knee or ankle) affects 5% to 10% of patients. The severity of findings in his left hip warrants consideration of septic arthritis with pain referred to the knee; pelvic or femoral osteomyelitis; psoas abscess; or pyomyositis. Following basic lab tests, imaging of the left hip region is indicated.
Laboratory evaluation revealed: white blood cell (WBC) count 10,000/L (absolute neutrophil count 8,460/L, absolute lymphocyte count 530/L), hemoglobin 10.6 g/dL, platelet count 208,000/L, serum sodium 130 mmol/L, serum potassium 3.3 mmol/L, serum urea nitrogen 11 mg/dL, serum creatinine 0.54 mg/dL, aspartate transaminase (AST) 26 U/L, alanine transaminase (ALT) 31 U/L, albumin 1.7 g/dL, erythrocyte sedimentation rate (ESR) > 100 mm/h, and CRP 263 mg/L. No blast cells were seen on peripheral blood smear.
Hypoalbuminemia and markedly elevated inflammatory markers indicate an inflammatory condition that has been active for more than a week. Assessing ESR after IVIG therapy is not useful because exogenous globulins increase the ESR; however, CRP is useful to monitor inflammation and remains elevated here.
Incomplete KD is still possible. Hyponatremia, hypoalbuminemia, and anemia are all features of persistent KD, and have been utilized in several clinical scoring systems in Japan to identify KD patients at increased risk for developing coronary complications. A neoplastic process cannot be excluded, but does not appear likely based on the acuity of his presentation and peripheral blood smear review.
Upon readmission he received a second dose of 2 g/kg IVIG. He remained on aspirin and continued to have fevers. A repeat echocardiogram was normal. He had worsening pain in his left knee and hip with difficulty straightening his left leg. Physical examination was notable for tenderness to palpation over his left hip joint, refusal to bear weight, and resistance to passive range of motion. On hospital day 2, an ultrasound of his left hip and knee revealed a complex left hip effusion and small left knee effusion.
KD becomes less likely in the presence of persistent fevers after IVIG and a repeatedly normal echocardiogram. Worsening left leg symptoms including impaired hip extension with a complex hip effusion suggests an infectious process in or adjacent to the left hip, such as septic arthritis, myositis, or osteomyelitis of the pelvis or proximal femur. A complex hip effusion is less likely to be present with arthritis related to JIA or SLE. The patient needs an emergent hip aspiration and possibly magnetic resonance imaging (MRI) to evaluate adjacent structures.
Arthrotomy and open drainage of his left hip revealed purulent fluid with a WBC count of 49,000/L with 89% neutrophils and 2% lymphocytes. Gram stain was negative. A left knee aspirate demonstrated straw‐colored synovial fluid (which was not sent for cell counts). Bacterial, fungal, and acid‐fast bacilli cultures were requested from hip and knee aspirates. Intravenous ceftriaxone and vancomycin were administered.
The most likely organism in pediatric pyogenic arthritis is Staphylococcus aureus, but there is a long list of other potential pathogens, including Streptococcus pyogenes (group A streptococcus) and Streptococcus pneumoniae. Most pediatric patients with acute pyogenic arthritis have synovial fluid WBC counts in excess of 75,000 to 100,000/L. The protracted course and the initial lack of hip symptoms raise the possibility of a primary osteomyelitis of the femur (particularly the intracapsular portion of the femoral neck or head) or of the acetabulum, with subsequent extension into the hip joint. Pyogenic myositis involving muscle groups adjacent to the hip would be unlikely to spread into the hip space, but can lead to synovial irritation, characterized by sterile joint fluid and WBC counts that fall short of the usual numbers seen in septic arthritis. The blood supply to the femoral head can become compromised with prolonged inflammation and increased intracapsular pressure, resulting in aseptic necrosis.
All cultures from his hip and knee aspirations were sterile. He continued to have daily fevers and persistent tachycardia while receiving intravenous ceftriaxone and vancomycin. Additional testing was notable for: antinuclear antibody (ANA) 1:80, anti‐streptolysin O (ASO) titer 344 IU (normal 150 IU), AST and ALT within normal limits, ferritin 568 ng/mL (normal 322 ng/mL), and lactate dehydrogenase (LDH) 212 units/L (normal 257 units/L). Abdominal ultrasound revealed borderline hepatosplenomegaly. An ophthalmologic examination was normal.
On postoperative day 4 he developed left upper thigh swelling. An MRI showed rim‐enhancing juxta‐articular complex fluid collections surrounding the left femur with decreased marrow enhancement of the left proximal femur (Figure 1).
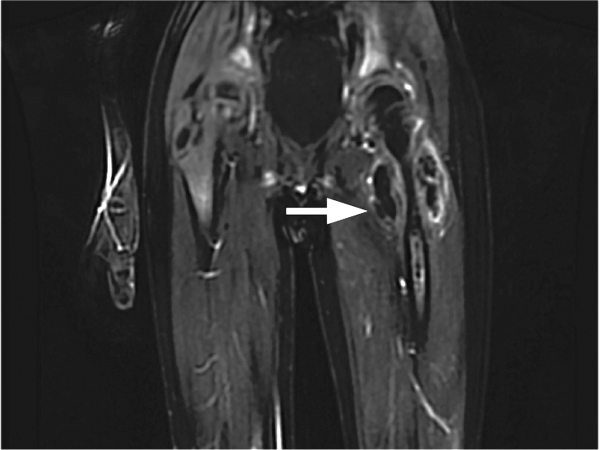
The limited rheumatologic evaluation is unrevealing; the ANA result is nondiagnostic and the ASO titer is normal for age. Laboratories generally report adult normal values for streptococcal antibodies regardless of the patient's age; children from ages 7 to 12 years are at their life peak frequency of group A streptococcal pharyngitis and typically have higher normal values of streptococcal antibodies, including ASO (up to about 480640 IU). The moderately elevated ferritin level is most likely an acute phase reactant and not high enough to suggest macrophage activation syndrome, which is unlikely with the normal AST, ALT, and LDH levels, the absence of significant splenomegaly, and the lack of cytopenias. Continued fever with progressive left upper thigh swelling point to osteomyelitis of the proximal femur, which may have initially ruptured into the hip and then infiltrated the femoral cortex and spread infection into the adjacent soft tissues. Surgical debridement is indicated.
The relative prevalence of methicillin‐sensitive S aureus (MSSA) and methicillin‐resistant S aureus vary widely with geography. MSSA strains are more likely to be highly toxigenic. The elaboration of 1 or more extracellular toxins could account for the patient's initial symptoms.
The patient was brought back to the operating room for drainage of the juxta‐articular fluid collections and a biopsy of his femur. The fluid collections were grossly purulent. His intraoperative cultures were positive for MSSA. The bone biopsy revealed necrotic tissue, acute inflammation, and bacterial colonies, consistent with acute osteomyelitis. Further testing of his S aureus isolate was positive for staphylococcal enterotoxin B. He completed a 4‐week course of oral clindamycin with subsequent normalization of his hip exam and inflammatory markers. At a follow‐up visit the patient was feeling better, but had developed skin peeling on the lateral aspects of his feet consistent with late sequelae of toxin‐mediated disease (Figure 2). Three months after discharge the patient had returned to his baseline activity level and remained asymptomatic.
COMMENTARY
The patient presented with a constellation of symptoms that was initially mistaken for incomplete KD until focal progression of his symptoms exposed an underlying femoral osteomyelitis with periarticular abscess formation. Bacterial cultures and subsequent toxin assay revealed an enterotoxin B‐producing strain of S aureus.
Certain staphylococcal strains secrete superantigens that may lead to the development of a systemic toxin‐mediated syndrome. Toxins elaborated by S aureus include toxic shock syndrome toxin‐1 (TSST‐1) and enterotoxins, which have been implicated in menstrual and nonmenstrual toxic shock syndromes.[1, 2] Enterotoxin B is a staphylococcal superantigen found in most strains of the USA400 clonal group, and has been frequently associated with skin and soft tissue infections.[3] Enterotoxin B production has been reported in nearly half of S aureus isolates from skin, soft tissue, and bone infections.[4]
Staphylococcal and streptococcal toxin‐mediated diseases can mimic vasculitis, systemic juvenile idiopathic arthritis, viral infections, and Stevens‐Johnson syndrome. Glossitis in toxin‐mediated syndromes manifests with a swollen, red tongue with overlying enlarged papillae, giving the appearance of a strawberry. Although pediatric providers often equate strawberry tongue, conjunctival injection, rash, and erythematous lips with KD, these findings are also seen in toxin‐mediated diseases, such as scarlet fever or staphylococcal toxic shock syndrome. Enterotoxin B mediated staphylococcal disease masquerading as KD has been reported in 2 cases: a 7‐month‐old boy with multifocal S aureus osteomyelitis and a 5‐year‐old boy with S aureus bacteremia. Both staphylococcal isolates produced enterotoxin B but were negative for other staphylococcus‐related toxins including TSST‐1.[5]
The Institute of Medicine (IOM) recently released its report Improving Diagnosis in Health Care, highlighting the under‐recognized quality and safety issue of diagnostic error.[6] The report uses the following broad and patient‐centered definition of diagnostic error: the failure to (a) establish an accurate and timely explanation of the patient's health problem(s) or (b) communicate that explanation to the patient. The IOM's conceptual model of diagnosis emphasizes the iterative nature of the diagnostic process, including the importance of generating a working diagnosis, gathering and incorporating new information in the reassessment of that diagnosis, and integrating treatment response into the formulation of the final diagnosis (Figure 3).

Even though the patient initially had several features consistent with KD, the increasing number of atypical features could have prompted the clinical team to reconsider their working diagnosis. The patient's age was atypical for KD, he had progressive knee and hip arthritis, and his fevers persisted after IVIG. An expanded differential should have included toxic shock syndrome; the resolution of conjunctival and mucosal injection and edema after IVIG may have been the result of antibodies in the IVIG preparation with neutralizing activity against superantigens. This antitoxin activity has established a role for IVIG in the management of staphylococcal toxic shock syndrome.[7] Ultimately, his imaging and surgical drainage revealed a focal staphylococcal toxin‐producing infectious source from which his fevers, rash, and mucosal and extremity changes emanated. This case reminds us that the more atypical a working diagnosis iseither in its presentation or treatment responsethe more readily clinicians should take it for another spin around the diagnostic wheel in search of a more suitable alternative.
KEY LEARNING POINTS
- Staphylococcal toxin‐mediated disease may mimic KD, with common features including strawberry tongue, oral and conjunctival injection, and skin desquamation.
- Improvement after treatment with IVIG is characteristic but not diagnostic of KD, and may be seen in toxin‐mediated disease.
- KD may present with arthralgia or arthritis, but severe joint abnormalities warrant consideration of infectious and other autoimmune conditions.
- The more atypical a working diagnosis iseither in its presentation or treatment responsethe more readily clinicians should gather, interpret, and integrate new information in search of a more suitable alternative.
Disclosure: Nothing to report.
- . Staphylococcal enterotoxin B and toxic shock syndrome toxin‐1 are significantly associated with non‐menstrual TSS. Lancet. 1986;1:1149–1150.
- , , , , . Toxic shock syndrome caused by a strain of staphylococcus aureus that produces enterotoxin C but not toxic shock syndrome toxin‐1. Am J Dis Child. 1989;143 (7):848–849.
- , , , , , . Staphylococcus aureus isolates encode variant staphylococcal enterotoxin B proteins that are diverse in superantigenicity and lethality. PLoS One. 2012;7(7):e41157.
- , , , et al. Variability of antibiotic susceptibility and toxin production of Staphylococcal aureus stains isolated from skin, soft tissue, and bone related infections. BMC Microbiol. 2013;13:188.
- , , , , . Kawasaki syndrome‐like illness associated with infection caused by enterotoxin B‐secreting Staphylococcus aureus. Clin Microbiol Rev. 2013;26:422–447.
- National Academies of Sciences, Engineering, and Medicine. Improving Diagnosis in Health Care. Washington, DC: The National Academies Press; 2015.
- , , , et al. Intravenous immunoglobulin G therapy in streptococcal toxic shock syndrome: a European randomized, double‐blind, placebo‐controlled trial. Clin Infect Dis. 2003;37(3):333–340.
A previously healthy 11‐year‐old boy presented to the emergency department after referral from his pediatrician for 1 week of fevers. Seven days prior to admission he developed a fever to 40.8C, vomiting, and mild left knee pain. The vomiting resolved within 2 days. Five days prior to admission he developed a pruritic, pinpoint rash over his abdomen that resolved within 24 hours. He also developed red, cracked lips, redness of his tongue, redness surrounding his eyes, and slight swelling of his hands. Three days prior to admission his pediatrician noted a 1‐cm anterior cervical lymph node. His fevers occurred throughout each of the prior 7 days without a discernible pattern, and his mild knee pain persisted at the time of presentation.
This preteen has had high fevers for 1 week associated with arthralgia, pruritic rash, emesis, and oral mucosal erythema. His rash, lip and tongue erythema, and swollen hands are classic features of Kawasaki disease (KD), but he lacks the other characteristic physical examination findings. The diagnosis of KD requires fever for at least 5 days accompanied by 4 of the following 5 signs: polymorphous rash, oral mucous membrane changes, peripheral extremity changes such as swelling or skin desquamation, bilateral bulbar conjunctival injection, and cervical lymphadenopathy >1.5 cm in diameter. Children meeting fewer than 4 of these criteria may have an incomplete form of KD.
Because most patients with KD (80%) are under 5 years old, alternative diagnoses such as autoimmune illnesses or a hypersensitivity reaction should be considered. Travel, medication, and animal exposure histories may reveal clues to an infectious or drug‐induced etiology of his fever. Immunization status should be assessed, as measles is also associated with fever, rash, and mucosal changes. Arthralgia or arthritis may occur in KD, but these findings suggest the need to entertain other possibilities, including bone or joint infection, infective endocarditis, inflammatory bowel disease, juvenile idiopathic arthritis (JIA), or systemic lupus erythematosus (SLE).
The child's only past medical history was an episode of croup as an infant. There was no family history of autoimmune diseases. He was not taking any medications and had no known allergies. His immunizations were up to date, including measles, mumps, rubella, and varicella. He lived with his parents and his dog. He swam in fresh water during a trip to Maine 2 months earlier. Neither he nor his family recalled a tick bite. He had no exposure to raw meat or unpasteurized dairy products.
The travel to New England raises the possibility of Lyme disease, although a 2‐month interval between exposure and a high, prolonged fever would be very unusual. Knee arthralgia or arthritis is common in children with late‐stage Lyme disease, but can also be seen in early‐disseminated disease. The prior description of the rash is not suggestive of erythema chronicum migrans, which is seen in early‐stage Lyme disease.
C‐reactive protein (CRP) was 189 mg/L (normal 6.3 mg/L). An echocardiogram was normal. Intravenous immunoglobulin (IVIG) was administered for presumed KD, with immediate improvement of the periorbital erythema, tongue redness, and hand swelling. He was discharged the next day on aspirin with cardiology clinic follow‐up.
Improvement after IVIG supports the diagnosis of KD. It is typical to discharge KD patients from the hospital when they have been afebrile for 24 hours or when the CRP level has declined by approximately 50%.
Over the next 48 hours he felt unwell with high‐grade fevers, continued left knee pain, and new left hip pain. He was readmitted to the hospital. His temperature was 39.4C, respiratory rate was 22 breaths per minute, heart rate was 122 beats per minute, blood pressure was 103/50 mm Hg, and oxygen saturation was 100% while breathing ambient air. He appeared mildly uncomfortable. His conjunctivae were normal. His lips were dry, red, and cracked, and his tongue was red with prominent papillae. His neck was supple without lymphadenopathy. His lungs were clear to auscultation. His heart exam was without murmurs. His abdomen was soft, and the liver and spleen were not enlarged. He had no swelling or erythema of his joints; however, he experienced pain with range of motion of his left knee, and tenderness and restricted range of motion of his left hip. His neurologic exam was normal. There were no rashes.
He has persistent fever, tachycardia, and tachypnea, now without features of KD except oral mucosal changes including prominent tongue papillae consistent with a strawberry tongue. Continued or recurrent fever may suggest persistent KD with ongoing inflammation or the need to search for an alternative diagnoses. An echocardiogram should be repeated, as the coronary artery abnormalities in KD can evolve rapidly, particularly when inflammation persists. Additional findings may include decreased left ventricular function, mitral regurgitation, or pericardial effusion. A second dose of IVIG is necessary to control fever and inflammation in about 15% of patients with KD, although in this case IVIG should be withheld pending further evaluation.
Arthralgia occurs commonly in KD, whereas frank arthritis is less typical. Polyarticular or oligoarticular arthritis involving small or large joints (especially knee or ankle) affects 5% to 10% of patients. The severity of findings in his left hip warrants consideration of septic arthritis with pain referred to the knee; pelvic or femoral osteomyelitis; psoas abscess; or pyomyositis. Following basic lab tests, imaging of the left hip region is indicated.
Laboratory evaluation revealed: white blood cell (WBC) count 10,000/L (absolute neutrophil count 8,460/L, absolute lymphocyte count 530/L), hemoglobin 10.6 g/dL, platelet count 208,000/L, serum sodium 130 mmol/L, serum potassium 3.3 mmol/L, serum urea nitrogen 11 mg/dL, serum creatinine 0.54 mg/dL, aspartate transaminase (AST) 26 U/L, alanine transaminase (ALT) 31 U/L, albumin 1.7 g/dL, erythrocyte sedimentation rate (ESR) > 100 mm/h, and CRP 263 mg/L. No blast cells were seen on peripheral blood smear.
Hypoalbuminemia and markedly elevated inflammatory markers indicate an inflammatory condition that has been active for more than a week. Assessing ESR after IVIG therapy is not useful because exogenous globulins increase the ESR; however, CRP is useful to monitor inflammation and remains elevated here.
Incomplete KD is still possible. Hyponatremia, hypoalbuminemia, and anemia are all features of persistent KD, and have been utilized in several clinical scoring systems in Japan to identify KD patients at increased risk for developing coronary complications. A neoplastic process cannot be excluded, but does not appear likely based on the acuity of his presentation and peripheral blood smear review.
Upon readmission he received a second dose of 2 g/kg IVIG. He remained on aspirin and continued to have fevers. A repeat echocardiogram was normal. He had worsening pain in his left knee and hip with difficulty straightening his left leg. Physical examination was notable for tenderness to palpation over his left hip joint, refusal to bear weight, and resistance to passive range of motion. On hospital day 2, an ultrasound of his left hip and knee revealed a complex left hip effusion and small left knee effusion.
KD becomes less likely in the presence of persistent fevers after IVIG and a repeatedly normal echocardiogram. Worsening left leg symptoms including impaired hip extension with a complex hip effusion suggests an infectious process in or adjacent to the left hip, such as septic arthritis, myositis, or osteomyelitis of the pelvis or proximal femur. A complex hip effusion is less likely to be present with arthritis related to JIA or SLE. The patient needs an emergent hip aspiration and possibly magnetic resonance imaging (MRI) to evaluate adjacent structures.
Arthrotomy and open drainage of his left hip revealed purulent fluid with a WBC count of 49,000/L with 89% neutrophils and 2% lymphocytes. Gram stain was negative. A left knee aspirate demonstrated straw‐colored synovial fluid (which was not sent for cell counts). Bacterial, fungal, and acid‐fast bacilli cultures were requested from hip and knee aspirates. Intravenous ceftriaxone and vancomycin were administered.
The most likely organism in pediatric pyogenic arthritis is Staphylococcus aureus, but there is a long list of other potential pathogens, including Streptococcus pyogenes (group A streptococcus) and Streptococcus pneumoniae. Most pediatric patients with acute pyogenic arthritis have synovial fluid WBC counts in excess of 75,000 to 100,000/L. The protracted course and the initial lack of hip symptoms raise the possibility of a primary osteomyelitis of the femur (particularly the intracapsular portion of the femoral neck or head) or of the acetabulum, with subsequent extension into the hip joint. Pyogenic myositis involving muscle groups adjacent to the hip would be unlikely to spread into the hip space, but can lead to synovial irritation, characterized by sterile joint fluid and WBC counts that fall short of the usual numbers seen in septic arthritis. The blood supply to the femoral head can become compromised with prolonged inflammation and increased intracapsular pressure, resulting in aseptic necrosis.
All cultures from his hip and knee aspirations were sterile. He continued to have daily fevers and persistent tachycardia while receiving intravenous ceftriaxone and vancomycin. Additional testing was notable for: antinuclear antibody (ANA) 1:80, anti‐streptolysin O (ASO) titer 344 IU (normal 150 IU), AST and ALT within normal limits, ferritin 568 ng/mL (normal 322 ng/mL), and lactate dehydrogenase (LDH) 212 units/L (normal 257 units/L). Abdominal ultrasound revealed borderline hepatosplenomegaly. An ophthalmologic examination was normal.
On postoperative day 4 he developed left upper thigh swelling. An MRI showed rim‐enhancing juxta‐articular complex fluid collections surrounding the left femur with decreased marrow enhancement of the left proximal femur (Figure 1).
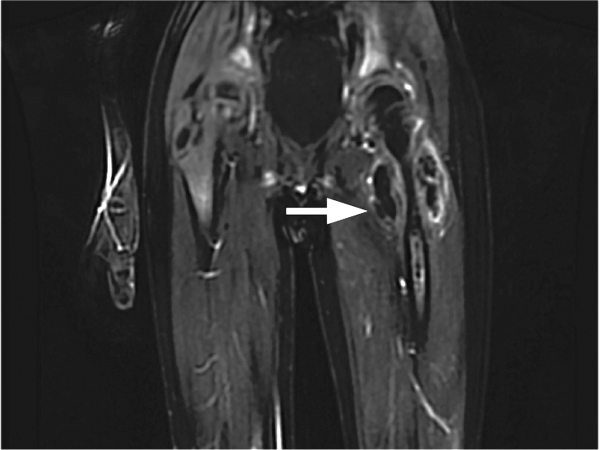
The limited rheumatologic evaluation is unrevealing; the ANA result is nondiagnostic and the ASO titer is normal for age. Laboratories generally report adult normal values for streptococcal antibodies regardless of the patient's age; children from ages 7 to 12 years are at their life peak frequency of group A streptococcal pharyngitis and typically have higher normal values of streptococcal antibodies, including ASO (up to about 480640 IU). The moderately elevated ferritin level is most likely an acute phase reactant and not high enough to suggest macrophage activation syndrome, which is unlikely with the normal AST, ALT, and LDH levels, the absence of significant splenomegaly, and the lack of cytopenias. Continued fever with progressive left upper thigh swelling point to osteomyelitis of the proximal femur, which may have initially ruptured into the hip and then infiltrated the femoral cortex and spread infection into the adjacent soft tissues. Surgical debridement is indicated.
The relative prevalence of methicillin‐sensitive S aureus (MSSA) and methicillin‐resistant S aureus vary widely with geography. MSSA strains are more likely to be highly toxigenic. The elaboration of 1 or more extracellular toxins could account for the patient's initial symptoms.
The patient was brought back to the operating room for drainage of the juxta‐articular fluid collections and a biopsy of his femur. The fluid collections were grossly purulent. His intraoperative cultures were positive for MSSA. The bone biopsy revealed necrotic tissue, acute inflammation, and bacterial colonies, consistent with acute osteomyelitis. Further testing of his S aureus isolate was positive for staphylococcal enterotoxin B. He completed a 4‐week course of oral clindamycin with subsequent normalization of his hip exam and inflammatory markers. At a follow‐up visit the patient was feeling better, but had developed skin peeling on the lateral aspects of his feet consistent with late sequelae of toxin‐mediated disease (Figure 2). Three months after discharge the patient had returned to his baseline activity level and remained asymptomatic.
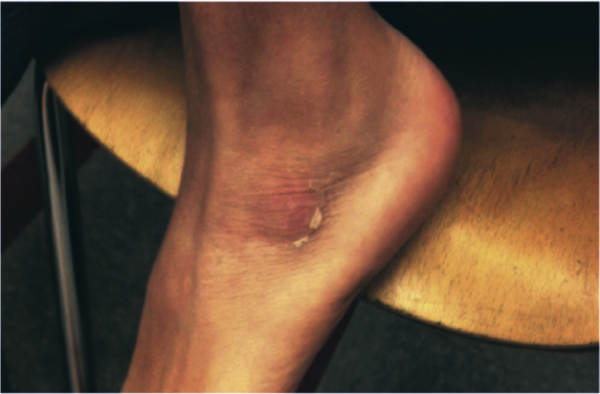
COMMENTARY
The patient presented with a constellation of symptoms that was initially mistaken for incomplete KD until focal progression of his symptoms exposed an underlying femoral osteomyelitis with periarticular abscess formation. Bacterial cultures and subsequent toxin assay revealed an enterotoxin B‐producing strain of S aureus.
Certain staphylococcal strains secrete superantigens that may lead to the development of a systemic toxin‐mediated syndrome. Toxins elaborated by S aureus include toxic shock syndrome toxin‐1 (TSST‐1) and enterotoxins, which have been implicated in menstrual and nonmenstrual toxic shock syndromes.[1, 2] Enterotoxin B is a staphylococcal superantigen found in most strains of the USA400 clonal group, and has been frequently associated with skin and soft tissue infections.[3] Enterotoxin B production has been reported in nearly half of S aureus isolates from skin, soft tissue, and bone infections.[4]
Staphylococcal and streptococcal toxin‐mediated diseases can mimic vasculitis, systemic juvenile idiopathic arthritis, viral infections, and Stevens‐Johnson syndrome. Glossitis in toxin‐mediated syndromes manifests with a swollen, red tongue with overlying enlarged papillae, giving the appearance of a strawberry. Although pediatric providers often equate strawberry tongue, conjunctival injection, rash, and erythematous lips with KD, these findings are also seen in toxin‐mediated diseases, such as scarlet fever or staphylococcal toxic shock syndrome. Enterotoxin B mediated staphylococcal disease masquerading as KD has been reported in 2 cases: a 7‐month‐old boy with multifocal S aureus osteomyelitis and a 5‐year‐old boy with S aureus bacteremia. Both staphylococcal isolates produced enterotoxin B but were negative for other staphylococcus‐related toxins including TSST‐1.[5]
The Institute of Medicine (IOM) recently released its report Improving Diagnosis in Health Care, highlighting the under‐recognized quality and safety issue of diagnostic error.[6] The report uses the following broad and patient‐centered definition of diagnostic error: the failure to (a) establish an accurate and timely explanation of the patient's health problem(s) or (b) communicate that explanation to the patient. The IOM's conceptual model of diagnosis emphasizes the iterative nature of the diagnostic process, including the importance of generating a working diagnosis, gathering and incorporating new information in the reassessment of that diagnosis, and integrating treatment response into the formulation of the final diagnosis (Figure 3).

Even though the patient initially had several features consistent with KD, the increasing number of atypical features could have prompted the clinical team to reconsider their working diagnosis. The patient's age was atypical for KD, he had progressive knee and hip arthritis, and his fevers persisted after IVIG. An expanded differential should have included toxic shock syndrome; the resolution of conjunctival and mucosal injection and edema after IVIG may have been the result of antibodies in the IVIG preparation with neutralizing activity against superantigens. This antitoxin activity has established a role for IVIG in the management of staphylococcal toxic shock syndrome.[7] Ultimately, his imaging and surgical drainage revealed a focal staphylococcal toxin‐producing infectious source from which his fevers, rash, and mucosal and extremity changes emanated. This case reminds us that the more atypical a working diagnosis iseither in its presentation or treatment responsethe more readily clinicians should take it for another spin around the diagnostic wheel in search of a more suitable alternative.
KEY LEARNING POINTS
- Staphylococcal toxin‐mediated disease may mimic KD, with common features including strawberry tongue, oral and conjunctival injection, and skin desquamation.
- Improvement after treatment with IVIG is characteristic but not diagnostic of KD, and may be seen in toxin‐mediated disease.
- KD may present with arthralgia or arthritis, but severe joint abnormalities warrant consideration of infectious and other autoimmune conditions.
- The more atypical a working diagnosis iseither in its presentation or treatment responsethe more readily clinicians should gather, interpret, and integrate new information in search of a more suitable alternative.
Disclosure: Nothing to report.
A previously healthy 11‐year‐old boy presented to the emergency department after referral from his pediatrician for 1 week of fevers. Seven days prior to admission he developed a fever to 40.8C, vomiting, and mild left knee pain. The vomiting resolved within 2 days. Five days prior to admission he developed a pruritic, pinpoint rash over his abdomen that resolved within 24 hours. He also developed red, cracked lips, redness of his tongue, redness surrounding his eyes, and slight swelling of his hands. Three days prior to admission his pediatrician noted a 1‐cm anterior cervical lymph node. His fevers occurred throughout each of the prior 7 days without a discernible pattern, and his mild knee pain persisted at the time of presentation.
This preteen has had high fevers for 1 week associated with arthralgia, pruritic rash, emesis, and oral mucosal erythema. His rash, lip and tongue erythema, and swollen hands are classic features of Kawasaki disease (KD), but he lacks the other characteristic physical examination findings. The diagnosis of KD requires fever for at least 5 days accompanied by 4 of the following 5 signs: polymorphous rash, oral mucous membrane changes, peripheral extremity changes such as swelling or skin desquamation, bilateral bulbar conjunctival injection, and cervical lymphadenopathy >1.5 cm in diameter. Children meeting fewer than 4 of these criteria may have an incomplete form of KD.
Because most patients with KD (80%) are under 5 years old, alternative diagnoses such as autoimmune illnesses or a hypersensitivity reaction should be considered. Travel, medication, and animal exposure histories may reveal clues to an infectious or drug‐induced etiology of his fever. Immunization status should be assessed, as measles is also associated with fever, rash, and mucosal changes. Arthralgia or arthritis may occur in KD, but these findings suggest the need to entertain other possibilities, including bone or joint infection, infective endocarditis, inflammatory bowel disease, juvenile idiopathic arthritis (JIA), or systemic lupus erythematosus (SLE).
The child's only past medical history was an episode of croup as an infant. There was no family history of autoimmune diseases. He was not taking any medications and had no known allergies. His immunizations were up to date, including measles, mumps, rubella, and varicella. He lived with his parents and his dog. He swam in fresh water during a trip to Maine 2 months earlier. Neither he nor his family recalled a tick bite. He had no exposure to raw meat or unpasteurized dairy products.
The travel to New England raises the possibility of Lyme disease, although a 2‐month interval between exposure and a high, prolonged fever would be very unusual. Knee arthralgia or arthritis is common in children with late‐stage Lyme disease, but can also be seen in early‐disseminated disease. The prior description of the rash is not suggestive of erythema chronicum migrans, which is seen in early‐stage Lyme disease.
C‐reactive protein (CRP) was 189 mg/L (normal 6.3 mg/L). An echocardiogram was normal. Intravenous immunoglobulin (IVIG) was administered for presumed KD, with immediate improvement of the periorbital erythema, tongue redness, and hand swelling. He was discharged the next day on aspirin with cardiology clinic follow‐up.
Improvement after IVIG supports the diagnosis of KD. It is typical to discharge KD patients from the hospital when they have been afebrile for 24 hours or when the CRP level has declined by approximately 50%.
Over the next 48 hours he felt unwell with high‐grade fevers, continued left knee pain, and new left hip pain. He was readmitted to the hospital. His temperature was 39.4C, respiratory rate was 22 breaths per minute, heart rate was 122 beats per minute, blood pressure was 103/50 mm Hg, and oxygen saturation was 100% while breathing ambient air. He appeared mildly uncomfortable. His conjunctivae were normal. His lips were dry, red, and cracked, and his tongue was red with prominent papillae. His neck was supple without lymphadenopathy. His lungs were clear to auscultation. His heart exam was without murmurs. His abdomen was soft, and the liver and spleen were not enlarged. He had no swelling or erythema of his joints; however, he experienced pain with range of motion of his left knee, and tenderness and restricted range of motion of his left hip. His neurologic exam was normal. There were no rashes.
He has persistent fever, tachycardia, and tachypnea, now without features of KD except oral mucosal changes including prominent tongue papillae consistent with a strawberry tongue. Continued or recurrent fever may suggest persistent KD with ongoing inflammation or the need to search for an alternative diagnoses. An echocardiogram should be repeated, as the coronary artery abnormalities in KD can evolve rapidly, particularly when inflammation persists. Additional findings may include decreased left ventricular function, mitral regurgitation, or pericardial effusion. A second dose of IVIG is necessary to control fever and inflammation in about 15% of patients with KD, although in this case IVIG should be withheld pending further evaluation.
Arthralgia occurs commonly in KD, whereas frank arthritis is less typical. Polyarticular or oligoarticular arthritis involving small or large joints (especially knee or ankle) affects 5% to 10% of patients. The severity of findings in his left hip warrants consideration of septic arthritis with pain referred to the knee; pelvic or femoral osteomyelitis; psoas abscess; or pyomyositis. Following basic lab tests, imaging of the left hip region is indicated.
Laboratory evaluation revealed: white blood cell (WBC) count 10,000/L (absolute neutrophil count 8,460/L, absolute lymphocyte count 530/L), hemoglobin 10.6 g/dL, platelet count 208,000/L, serum sodium 130 mmol/L, serum potassium 3.3 mmol/L, serum urea nitrogen 11 mg/dL, serum creatinine 0.54 mg/dL, aspartate transaminase (AST) 26 U/L, alanine transaminase (ALT) 31 U/L, albumin 1.7 g/dL, erythrocyte sedimentation rate (ESR) > 100 mm/h, and CRP 263 mg/L. No blast cells were seen on peripheral blood smear.
Hypoalbuminemia and markedly elevated inflammatory markers indicate an inflammatory condition that has been active for more than a week. Assessing ESR after IVIG therapy is not useful because exogenous globulins increase the ESR; however, CRP is useful to monitor inflammation and remains elevated here.
Incomplete KD is still possible. Hyponatremia, hypoalbuminemia, and anemia are all features of persistent KD, and have been utilized in several clinical scoring systems in Japan to identify KD patients at increased risk for developing coronary complications. A neoplastic process cannot be excluded, but does not appear likely based on the acuity of his presentation and peripheral blood smear review.
Upon readmission he received a second dose of 2 g/kg IVIG. He remained on aspirin and continued to have fevers. A repeat echocardiogram was normal. He had worsening pain in his left knee and hip with difficulty straightening his left leg. Physical examination was notable for tenderness to palpation over his left hip joint, refusal to bear weight, and resistance to passive range of motion. On hospital day 2, an ultrasound of his left hip and knee revealed a complex left hip effusion and small left knee effusion.
KD becomes less likely in the presence of persistent fevers after IVIG and a repeatedly normal echocardiogram. Worsening left leg symptoms including impaired hip extension with a complex hip effusion suggests an infectious process in or adjacent to the left hip, such as septic arthritis, myositis, or osteomyelitis of the pelvis or proximal femur. A complex hip effusion is less likely to be present with arthritis related to JIA or SLE. The patient needs an emergent hip aspiration and possibly magnetic resonance imaging (MRI) to evaluate adjacent structures.
Arthrotomy and open drainage of his left hip revealed purulent fluid with a WBC count of 49,000/L with 89% neutrophils and 2% lymphocytes. Gram stain was negative. A left knee aspirate demonstrated straw‐colored synovial fluid (which was not sent for cell counts). Bacterial, fungal, and acid‐fast bacilli cultures were requested from hip and knee aspirates. Intravenous ceftriaxone and vancomycin were administered.
The most likely organism in pediatric pyogenic arthritis is Staphylococcus aureus, but there is a long list of other potential pathogens, including Streptococcus pyogenes (group A streptococcus) and Streptococcus pneumoniae. Most pediatric patients with acute pyogenic arthritis have synovial fluid WBC counts in excess of 75,000 to 100,000/L. The protracted course and the initial lack of hip symptoms raise the possibility of a primary osteomyelitis of the femur (particularly the intracapsular portion of the femoral neck or head) or of the acetabulum, with subsequent extension into the hip joint. Pyogenic myositis involving muscle groups adjacent to the hip would be unlikely to spread into the hip space, but can lead to synovial irritation, characterized by sterile joint fluid and WBC counts that fall short of the usual numbers seen in septic arthritis. The blood supply to the femoral head can become compromised with prolonged inflammation and increased intracapsular pressure, resulting in aseptic necrosis.
All cultures from his hip and knee aspirations were sterile. He continued to have daily fevers and persistent tachycardia while receiving intravenous ceftriaxone and vancomycin. Additional testing was notable for: antinuclear antibody (ANA) 1:80, anti‐streptolysin O (ASO) titer 344 IU (normal 150 IU), AST and ALT within normal limits, ferritin 568 ng/mL (normal 322 ng/mL), and lactate dehydrogenase (LDH) 212 units/L (normal 257 units/L). Abdominal ultrasound revealed borderline hepatosplenomegaly. An ophthalmologic examination was normal.
On postoperative day 4 he developed left upper thigh swelling. An MRI showed rim‐enhancing juxta‐articular complex fluid collections surrounding the left femur with decreased marrow enhancement of the left proximal femur (Figure 1).
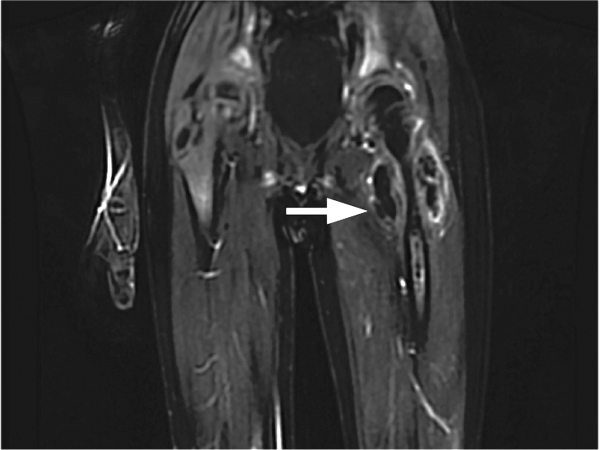
The limited rheumatologic evaluation is unrevealing; the ANA result is nondiagnostic and the ASO titer is normal for age. Laboratories generally report adult normal values for streptococcal antibodies regardless of the patient's age; children from ages 7 to 12 years are at their life peak frequency of group A streptococcal pharyngitis and typically have higher normal values of streptococcal antibodies, including ASO (up to about 480640 IU). The moderately elevated ferritin level is most likely an acute phase reactant and not high enough to suggest macrophage activation syndrome, which is unlikely with the normal AST, ALT, and LDH levels, the absence of significant splenomegaly, and the lack of cytopenias. Continued fever with progressive left upper thigh swelling point to osteomyelitis of the proximal femur, which may have initially ruptured into the hip and then infiltrated the femoral cortex and spread infection into the adjacent soft tissues. Surgical debridement is indicated.
The relative prevalence of methicillin‐sensitive S aureus (MSSA) and methicillin‐resistant S aureus vary widely with geography. MSSA strains are more likely to be highly toxigenic. The elaboration of 1 or more extracellular toxins could account for the patient's initial symptoms.
The patient was brought back to the operating room for drainage of the juxta‐articular fluid collections and a biopsy of his femur. The fluid collections were grossly purulent. His intraoperative cultures were positive for MSSA. The bone biopsy revealed necrotic tissue, acute inflammation, and bacterial colonies, consistent with acute osteomyelitis. Further testing of his S aureus isolate was positive for staphylococcal enterotoxin B. He completed a 4‐week course of oral clindamycin with subsequent normalization of his hip exam and inflammatory markers. At a follow‐up visit the patient was feeling better, but had developed skin peeling on the lateral aspects of his feet consistent with late sequelae of toxin‐mediated disease (Figure 2). Three months after discharge the patient had returned to his baseline activity level and remained asymptomatic.
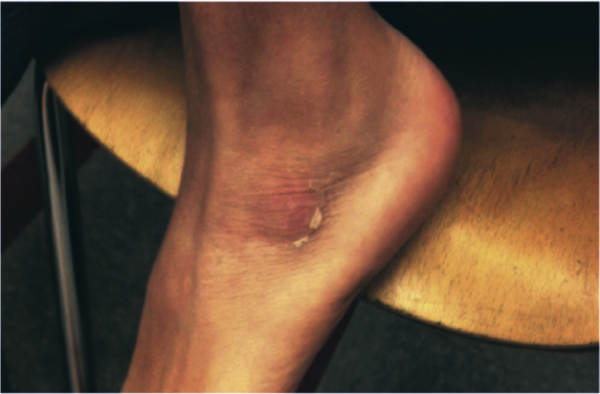
COMMENTARY
The patient presented with a constellation of symptoms that was initially mistaken for incomplete KD until focal progression of his symptoms exposed an underlying femoral osteomyelitis with periarticular abscess formation. Bacterial cultures and subsequent toxin assay revealed an enterotoxin B‐producing strain of S aureus.
Certain staphylococcal strains secrete superantigens that may lead to the development of a systemic toxin‐mediated syndrome. Toxins elaborated by S aureus include toxic shock syndrome toxin‐1 (TSST‐1) and enterotoxins, which have been implicated in menstrual and nonmenstrual toxic shock syndromes.[1, 2] Enterotoxin B is a staphylococcal superantigen found in most strains of the USA400 clonal group, and has been frequently associated with skin and soft tissue infections.[3] Enterotoxin B production has been reported in nearly half of S aureus isolates from skin, soft tissue, and bone infections.[4]
Staphylococcal and streptococcal toxin‐mediated diseases can mimic vasculitis, systemic juvenile idiopathic arthritis, viral infections, and Stevens‐Johnson syndrome. Glossitis in toxin‐mediated syndromes manifests with a swollen, red tongue with overlying enlarged papillae, giving the appearance of a strawberry. Although pediatric providers often equate strawberry tongue, conjunctival injection, rash, and erythematous lips with KD, these findings are also seen in toxin‐mediated diseases, such as scarlet fever or staphylococcal toxic shock syndrome. Enterotoxin B mediated staphylococcal disease masquerading as KD has been reported in 2 cases: a 7‐month‐old boy with multifocal S aureus osteomyelitis and a 5‐year‐old boy with S aureus bacteremia. Both staphylococcal isolates produced enterotoxin B but were negative for other staphylococcus‐related toxins including TSST‐1.[5]
The Institute of Medicine (IOM) recently released its report Improving Diagnosis in Health Care, highlighting the under‐recognized quality and safety issue of diagnostic error.[6] The report uses the following broad and patient‐centered definition of diagnostic error: the failure to (a) establish an accurate and timely explanation of the patient's health problem(s) or (b) communicate that explanation to the patient. The IOM's conceptual model of diagnosis emphasizes the iterative nature of the diagnostic process, including the importance of generating a working diagnosis, gathering and incorporating new information in the reassessment of that diagnosis, and integrating treatment response into the formulation of the final diagnosis (Figure 3).

Even though the patient initially had several features consistent with KD, the increasing number of atypical features could have prompted the clinical team to reconsider their working diagnosis. The patient's age was atypical for KD, he had progressive knee and hip arthritis, and his fevers persisted after IVIG. An expanded differential should have included toxic shock syndrome; the resolution of conjunctival and mucosal injection and edema after IVIG may have been the result of antibodies in the IVIG preparation with neutralizing activity against superantigens. This antitoxin activity has established a role for IVIG in the management of staphylococcal toxic shock syndrome.[7] Ultimately, his imaging and surgical drainage revealed a focal staphylococcal toxin‐producing infectious source from which his fevers, rash, and mucosal and extremity changes emanated. This case reminds us that the more atypical a working diagnosis iseither in its presentation or treatment responsethe more readily clinicians should take it for another spin around the diagnostic wheel in search of a more suitable alternative.
KEY LEARNING POINTS
- Staphylococcal toxin‐mediated disease may mimic KD, with common features including strawberry tongue, oral and conjunctival injection, and skin desquamation.
- Improvement after treatment with IVIG is characteristic but not diagnostic of KD, and may be seen in toxin‐mediated disease.
- KD may present with arthralgia or arthritis, but severe joint abnormalities warrant consideration of infectious and other autoimmune conditions.
- The more atypical a working diagnosis iseither in its presentation or treatment responsethe more readily clinicians should gather, interpret, and integrate new information in search of a more suitable alternative.
Disclosure: Nothing to report.
- . Staphylococcal enterotoxin B and toxic shock syndrome toxin‐1 are significantly associated with non‐menstrual TSS. Lancet. 1986;1:1149–1150.
- , , , , . Toxic shock syndrome caused by a strain of staphylococcus aureus that produces enterotoxin C but not toxic shock syndrome toxin‐1. Am J Dis Child. 1989;143 (7):848–849.
- , , , , , . Staphylococcus aureus isolates encode variant staphylococcal enterotoxin B proteins that are diverse in superantigenicity and lethality. PLoS One. 2012;7(7):e41157.
- , , , et al. Variability of antibiotic susceptibility and toxin production of Staphylococcal aureus stains isolated from skin, soft tissue, and bone related infections. BMC Microbiol. 2013;13:188.
- , , , , . Kawasaki syndrome‐like illness associated with infection caused by enterotoxin B‐secreting Staphylococcus aureus. Clin Microbiol Rev. 2013;26:422–447.
- National Academies of Sciences, Engineering, and Medicine. Improving Diagnosis in Health Care. Washington, DC: The National Academies Press; 2015.
- , , , et al. Intravenous immunoglobulin G therapy in streptococcal toxic shock syndrome: a European randomized, double‐blind, placebo‐controlled trial. Clin Infect Dis. 2003;37(3):333–340.
- . Staphylococcal enterotoxin B and toxic shock syndrome toxin‐1 are significantly associated with non‐menstrual TSS. Lancet. 1986;1:1149–1150.
- , , , , . Toxic shock syndrome caused by a strain of staphylococcus aureus that produces enterotoxin C but not toxic shock syndrome toxin‐1. Am J Dis Child. 1989;143 (7):848–849.
- , , , , , . Staphylococcus aureus isolates encode variant staphylococcal enterotoxin B proteins that are diverse in superantigenicity and lethality. PLoS One. 2012;7(7):e41157.
- , , , et al. Variability of antibiotic susceptibility and toxin production of Staphylococcal aureus stains isolated from skin, soft tissue, and bone related infections. BMC Microbiol. 2013;13:188.
- , , , , . Kawasaki syndrome‐like illness associated with infection caused by enterotoxin B‐secreting Staphylococcus aureus. Clin Microbiol Rev. 2013;26:422–447.
- National Academies of Sciences, Engineering, and Medicine. Improving Diagnosis in Health Care. Washington, DC: The National Academies Press; 2015.
- , , , et al. Intravenous immunoglobulin G therapy in streptococcal toxic shock syndrome: a European randomized, double‐blind, placebo‐controlled trial. Clin Infect Dis. 2003;37(3):333–340.
10 Reasons to Attend the Quality and Safety Educators Academy
Teaching quality improvement and patient safety is no longer an elective—it’s a necessity. The Quality and Safety Educators Academy (QSEA, sites.hospitalmedicine.org/qsea) provides medical educators with the knowledge and tools to integrate quality improvement and safety concepts into their curricula. This year, QSEA will be held May 23–25 at Tempe Mission Palms Hotel and Conference Center in Arizona.
Here are the top 10 reasons you can’t afford to miss it—and will be glad you went!
- Unparalleled Education: Develop and refine your knowledge in the field of quality and patient safety.
- Curriculum Development: Return to your institution with a collection of new curriculum ideas from QSEA faculty and peers.
- Professional Development: Spend focused time developing and reflecting on your career goals as a physician educator in quality and safety.
- Networking: Build a network of quality and safety educators with both faculty mentors and colleagues with similar career interests.
- Institutional Support: Learn strategies to engage your institutional and program leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education (ACGME) Next Accreditation System/Clinical Learning Environment Review (CLER) expectations and improve patient care.
- Hands-On Activities: Dive in to an interactive learning environment with a 10-to-1 student-to-faculty ratio, including facilitated large group sessions, small group activities, and mentor groups.
- Variety of Content: Each day features a variety of topics, such as the principles of quality improvement and patient safety, mentoring trainees in quality improvement project work, high-value care curriculum, curriculum development and assessment in medical education, and many others.
- Distinguished Faculty: All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Valuable Resources: Leave with a tool kit of educational resources for quality and safety education.
- Desert Beauty: Enjoy sunny Tempe, Arizona, or travel to nearby Phoenix or Scottsdale!
It’s no surprise that QSEA sold out each of the past four years, so don’t delay—it’s almost here! Register online or via phone at 800-843-3360. Questions? Email [email protected].
Teaching quality improvement and patient safety is no longer an elective—it’s a necessity. The Quality and Safety Educators Academy (QSEA, sites.hospitalmedicine.org/qsea) provides medical educators with the knowledge and tools to integrate quality improvement and safety concepts into their curricula. This year, QSEA will be held May 23–25 at Tempe Mission Palms Hotel and Conference Center in Arizona.
Here are the top 10 reasons you can’t afford to miss it—and will be glad you went!
- Unparalleled Education: Develop and refine your knowledge in the field of quality and patient safety.
- Curriculum Development: Return to your institution with a collection of new curriculum ideas from QSEA faculty and peers.
- Professional Development: Spend focused time developing and reflecting on your career goals as a physician educator in quality and safety.
- Networking: Build a network of quality and safety educators with both faculty mentors and colleagues with similar career interests.
- Institutional Support: Learn strategies to engage your institutional and program leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education (ACGME) Next Accreditation System/Clinical Learning Environment Review (CLER) expectations and improve patient care.
- Hands-On Activities: Dive in to an interactive learning environment with a 10-to-1 student-to-faculty ratio, including facilitated large group sessions, small group activities, and mentor groups.
- Variety of Content: Each day features a variety of topics, such as the principles of quality improvement and patient safety, mentoring trainees in quality improvement project work, high-value care curriculum, curriculum development and assessment in medical education, and many others.
- Distinguished Faculty: All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Valuable Resources: Leave with a tool kit of educational resources for quality and safety education.
- Desert Beauty: Enjoy sunny Tempe, Arizona, or travel to nearby Phoenix or Scottsdale!
It’s no surprise that QSEA sold out each of the past four years, so don’t delay—it’s almost here! Register online or via phone at 800-843-3360. Questions? Email [email protected].
Teaching quality improvement and patient safety is no longer an elective—it’s a necessity. The Quality and Safety Educators Academy (QSEA, sites.hospitalmedicine.org/qsea) provides medical educators with the knowledge and tools to integrate quality improvement and safety concepts into their curricula. This year, QSEA will be held May 23–25 at Tempe Mission Palms Hotel and Conference Center in Arizona.
Here are the top 10 reasons you can’t afford to miss it—and will be glad you went!
- Unparalleled Education: Develop and refine your knowledge in the field of quality and patient safety.
- Curriculum Development: Return to your institution with a collection of new curriculum ideas from QSEA faculty and peers.
- Professional Development: Spend focused time developing and reflecting on your career goals as a physician educator in quality and safety.
- Networking: Build a network of quality and safety educators with both faculty mentors and colleagues with similar career interests.
- Institutional Support: Learn strategies to engage your institutional and program leaders to support and implement a quality and patient safety curriculum to meet the Accreditation Council for Graduate Medical Education (ACGME) Next Accreditation System/Clinical Learning Environment Review (CLER) expectations and improve patient care.
- Hands-On Activities: Dive in to an interactive learning environment with a 10-to-1 student-to-faculty ratio, including facilitated large group sessions, small group activities, and mentor groups.
- Variety of Content: Each day features a variety of topics, such as the principles of quality improvement and patient safety, mentoring trainees in quality improvement project work, high-value care curriculum, curriculum development and assessment in medical education, and many others.
- Distinguished Faculty: All sessions are led by experienced physicians known for their ability to practice and teach quality improvement and patient safety, mentor junior faculty, and guide educators in curriculum development.
- Valuable Resources: Leave with a tool kit of educational resources for quality and safety education.
- Desert Beauty: Enjoy sunny Tempe, Arizona, or travel to nearby Phoenix or Scottsdale!
It’s no surprise that QSEA sold out each of the past four years, so don’t delay—it’s almost here! Register online or via phone at 800-843-3360. Questions? Email [email protected].
2016 Fellows in Hospital Medicine
MHM
Tina Budnitz, MPH, MHM
Greg Maynard, MD, MHM
Eric Howell, MD, MHM
FHM
Nicole Adler, MD, FHM
Tochukwu Agbata, MD, FHM
Alka Aggarwal, MD, FHM
Gaurav Ahuja, MD, MBBS, FHM
Sameena Akhtar, MD, FHM
Karan Singh S. Alag, MD, MBBS, FHM
Venkata N. Allada, MD, FACP, FHM
Margaret M. Ameyaw, MBChB, FHM
Robert L. Anderson, MD, FHM
Jorge Arboleda, DO, FHM
Michael Aref, MD, PhD, FACP, FHM
Elizabeth M. Arias, MD, FACP, FHM
Amarpreet S. Bains, MD, FHM
Ebrahim Barkoudah, MD, MPH, FACP, FHM
Wanes Barsemian, MD, FHM
Jeffrey T. Bates, MD, FACP, FHM
John F. Bell, MD, MPH, FHM
Kjell Benson, MD, FHM
Azmina Bhaiji, MD, FHM
Sai-Sridhar Boddupalli, MD, FHM
Ani Bodoutchian, MD, MBA, FAAFP, FHM
Tanya M. Boldenow, MD, FHM
Dennis T. Bolger Jr., MD, FHM
Greg D. Bowling, MD, FHM
David A. Bozaan, MD, FHM
Marcia Carbo, MD, FAAP, FHM
Donna Cardoza, MD, FHM
Frank R. Carson Jr., MD, FHM
Kelly Caverzagie, MD, FACP, FHM
Elizabeth A. Cerceo, MD, FACP, FHM
Jeffrey M. Ceresnak, MD, FHM
Romil Chadha, MD, MPH, FACP, FHM
Charles Charman, MD, FHM
Bushra I. Chaudhry, MD, FHM
Justin J. Chow, MD, FHM
Douglas E. Cohen, MD, FHM
John M. Colombo Jr., MD, FHM
Steven Connelly, MD, FACP, FHM
David Corman, MD, FHM
Christopher C. Costa, MD, FHM
William C. Crowe Jr., DNP, ACNP, FNP, MSN, RN, FHM
Ria Dancel, MD, FAAP, FHM
Zubaer Dawlah, MD, FHM
Chandrasekhar R. Dinasarapu, MD, MBBS, MPH, FHM
Vijay Saradhi Dontu, MD, FHM
Oleg Dulkin, MD, FHM
Kevin C. Eaton, PA-C, FHM
Eric Edwards, MD, FHM
Mary E. Fedor, MD, FHM
John W. Fowler Jr., MD, FACP, FHM
Maria G. Frank, MD, FACP, FHM
Yelena Galumyan, MD, FHM
Christopher D. Gamble, MD, FACP, FHM
David J. Goldstein, MD, FHM
Kalpana Gorthi, MD, FHM
Manjula V. Gunawardane, MD, FHM
Craig G. Gunderson, MD, FHM
Theodore J. Haland, MD, FHM
Aaron C. Hamilton, MD, MBA, FHM
Anil Hanuman, DO, FHM
Catriona M. Harrop, MD, FHM
Hossan Hassan, FAAFP, FHM
Eileen Hennrikus, MD, FHM
Arif Hussain, MD, FHM
Javid Iqbal, MD, FHM
Shadi Jarjous, MD, FHM
Jeremy Jaskunas, MD, FHM
John David Johnston, MD, FHM
Gurmeet Kaur Kalra, MD, FHM
Stephen K. Keiser, FHM
Sirajabid Khatib, MD, FHM
Joanna Kipnes, MD, FHM
Mukesh Kumar, MBBS, MD, FACP, FHM
Rumman A. Langah, MD, FACP, FHM
Rebecca Lauderdale, MD, FHM
Lajide R. Lawoyin, MD, FACP, FHM
Lien Le, MD, FHM
Alex Leung, FHM
William I. Levin, MD, FHM
David Lichtman, PA, FHM
Doris Wei-Hwa Lin, MD, FHM
Caroline E. Lyon, MD, MPH, FHM
John D. Machado, DO, FHM
Yvonne Maduka, MD, FHM
Lawrence L. Magras, MD, MBA, FHM
Anamaria Massier, MD, FHM
Daniel McFarlane, MD, FHM
Tresa A. McNeal, MD, FHM
Johnny Mei, MD, MHA, FACP, FHM
Rovie Mesola, MD, FHM
Henry J. Michtalik, MD, MHS, MPH, FHM
Prateek Mishra, MD, FHM
Adrian M. Mogos, MD, FHM
Wajahath A. Mohsini, MD, FACP, FHM
Ashwin Narasimhan, MD, FACP, FHM
Sivakumar Natanasabapathy, MRCP, FHM
Monica C. Necula, MD, FHM
Naomi Nomizu, MD, FHM
Shervin Nourparvar, MD, FHM
Allan L. Ong, MD, FHM
Pia Ong, MD, FHM
Chike Onyejekwe, MD, FHM
Binu T. Pappachen, MD, FHM
Akash Parashar MD, MBBS, FHM
Hiren B. Parikh, MD, MBA, FHM
Jung Hyun Park, MD, FHM
Shailesh Mansukh Patel, DO, FHM
Frank A. Perry, MD, FHM
Jeffrey W. Petry, MD, MMM, FHM
John R. Pierce Jr., MD, MPH, FHM
Jeffrey Poulos, MD, FHM
Richard N. Pulido, MD, FHM
Charu Puri, MD, FHM
Carolyn Quan, MD, FHM
Saraswathi V. Racherla, MD, FHM
Aisha Rahim, MD, FHM
Edwin Q. Ravano, MD, FHM
Behzad Razavi, MD, FACP, FHM
Erin N. Reis, MD, FHM
Maria Anaizza Aurora Reyna, MD, FHM
Mark Safalow, MD, FHM
Javaid Saleem, MD, MBBS, FHM
Mandeep S. Saluja, MD, FHM
Edward R. Sampt, MD, FHM
Jorge Santibanez, MD, FHM
Anne E. Sayers, MD, FHM
Brian Schroeder, FACHE, MHA, FHM
Scott E. Sears, MD, FACP, FHM
Meghan M. Sebasky, MD, FHM
Patricia L. Seymour, MD, FHM
Neel B. Shah, MB, BCh, FACP, FACMG, FHM
Poonam Sharma, MD, FHM
Umesh Sharma, MD, MS, FACP, FHM
Ashwin B. Shivakumar, MD, MSPH, FHM
Mohammed Fazil Siddiqi, MD, FHM
Sonya Sidhu-Izzo, MD, FHM
Alana E. Sigmund, MD, FHM
Shantnu Singh, MBBS, FHM
Amith Skandhan, MD, FHM
Christopher G. Skinner, MD, FACP, FHM
Dustin T. Smith, MD, FHM
Todd I. Smith, MD, FHM
Jeffrey D. Solomon, MD, FHM
Alberto Enrique Soyano, MD, FHM
Rodney R. Story, MD, FHM
John R. Sullivan, MD, FHM
Joseph G. Surber, DO, FHM
Heather R. Swanson, MD, FHM
Preetham Talari, MD, FHM
Sofia Teferi, MD, FAAP, FHM
Rafael A. Teran, MD, FHM
Abey K. Thomas, MD, FACP, FHM
Anca R. Udrea, MD, FHM
Shawn N. Usery, MD, FHM
Moncy Varughese, MD, FACP, FHM
Leigh Vaughan, MD, FHM
Manivannan Veerasamy, MD, FACP, FHM
Ruvan Chandika Wickramasinghe, MD, FHM
Michael Williams, DO, FHM
Sandra C. Wilson, MD, FACP, MA, FHM
Kareem Z. Yahya, MD, FHM
Deyun Yang, MD, PhD, FACP, FHM
Hector L. Yordan, MD, FHM
Elham A. Yousef, MD, MSc, FHM
Anthony M. Zepeda, MD, FHM
SFHM
Ashfaq Ahmad, MD, MBA, SFHM
Aziz Ansari, DO, SFHM
Anna M. Arroyo Plasencia, MD, SFHM
Andy Arwari, MD, FACP, SFHM
Jonathan G. Bae, MD, SFHM
Ankush K. Bansal, MD, FACP, SFHM
Jitendra Barmecha, MD, MPH, SFHM
Bishara A. Bates, BS, MHA, SFHM
Valerie F. Briones-Pryor, MD, FACP, SFHM
Michael E. Burton, MD, SFHM
Tracy E. Cardin, ACNP-BC, SFHM
Chris Cockerham, MD, SFHM
Timothy J. Crone, MD, SFHM
Debasish Dasgupta, MBBS, MHA, FACP, FACHE, SFHM, CPE, CPHQ
Kapil J. Dave, MD, SFHM
Shaker M. Eid, MD, MBA, SFHM
Howard R. Epstein, MD, SFHM
Christopher M. Frost, MD, SFHM
Timothy M. Gawronski, PA-C, SFHM
Amy S. Giarrusso, MD, SFHM
Jeffrey A. Gindi, MD, SFHM
Jason A. Green, MD, SFHM
Paul William Helgerson, MD, SFHM
Maliha Iqbal, MD, SFHM
James J. Jeffries II, MD, FACP, SFHM
Ian H. Jenkins, MD, SFHM
Scott Kaatz, DO, MSc, FACP, SFHM
Khurram Kamran, MD, SFHM
Anand Kartha, MD, MS, SFHM
Attila Kasza, MD, SFHM
Amy M. Keech, MD, SFHM
William A. Landis, MD, SFHM
Jimmie E. Lewis Jr., MD, MHA, SFHM
James W. Leyhane, MD, SFHM
Michael Lin, MD, SFHM
Julianna Lindsey, MD, SFHM
Madaiah Lokeshwari, MD, SFHM
Laszlo I. Madaras, MD, MPH, SFHM
Murthy V. Madduri, MD, SFHM
Arun V. Mohan, MD, SFHM
David R. Munoz, MD, SFHM
Mark A. Murray, MD, SFHM
Vasantha Natarajan, MD, SFHM
G. Xon Ng, MD, SFHM
Andy Odden, MD, SFHM
Tiffani M. Panek, MA, CLHM, SFHM
Shannon Connor Phillips, MD, MPH, SFHM
Preethi Prakash, MD, FACP, SFHM
Alberto Puig, MD, PhD, SFHM
Rebecca P. Ramirez, MD, SFHM
Allen B. Repp, MD, FACP, MS, SFHM
Scott C. Rissmiller, MD, SFHM
Frank Romero Jr., MD, SFHM
Marcus Lindley Scarbrough, MD, FACP, SFHM
Anneliese M. Schleyer, MD, SFHM
Eric R. Schumacher, DO, SFHM
Noppon Pooh Setji, MD, SFHM
Mohammad R. Shaheed, MD, SFHM
Jeffrey Scott Shapiro, MD, SFHM
Ann Sheehy, MD, MS, SFHM
R. Lucas Shelly, DO, SFHM
Andres F. Soto, MD, SFHM
John R. Stephens, MD, SFHM
Camille N. Upchurch, MD, SFHM
Fernando S. Waldemar, MD, SFHM
Michael D. Wang, MD, SFHM
Charlotta Weaver, MD, SFHM
Andrew White, MD, SFHM
Anthony Williams, MD, MBA, SFHM
MHM
Tina Budnitz, MPH, MHM
Greg Maynard, MD, MHM
Eric Howell, MD, MHM
FHM
Nicole Adler, MD, FHM
Tochukwu Agbata, MD, FHM
Alka Aggarwal, MD, FHM
Gaurav Ahuja, MD, MBBS, FHM
Sameena Akhtar, MD, FHM
Karan Singh S. Alag, MD, MBBS, FHM
Venkata N. Allada, MD, FACP, FHM
Margaret M. Ameyaw, MBChB, FHM
Robert L. Anderson, MD, FHM
Jorge Arboleda, DO, FHM
Michael Aref, MD, PhD, FACP, FHM
Elizabeth M. Arias, MD, FACP, FHM
Amarpreet S. Bains, MD, FHM
Ebrahim Barkoudah, MD, MPH, FACP, FHM
Wanes Barsemian, MD, FHM
Jeffrey T. Bates, MD, FACP, FHM
John F. Bell, MD, MPH, FHM
Kjell Benson, MD, FHM
Azmina Bhaiji, MD, FHM
Sai-Sridhar Boddupalli, MD, FHM
Ani Bodoutchian, MD, MBA, FAAFP, FHM
Tanya M. Boldenow, MD, FHM
Dennis T. Bolger Jr., MD, FHM
Greg D. Bowling, MD, FHM
David A. Bozaan, MD, FHM
Marcia Carbo, MD, FAAP, FHM
Donna Cardoza, MD, FHM
Frank R. Carson Jr., MD, FHM
Kelly Caverzagie, MD, FACP, FHM
Elizabeth A. Cerceo, MD, FACP, FHM
Jeffrey M. Ceresnak, MD, FHM
Romil Chadha, MD, MPH, FACP, FHM
Charles Charman, MD, FHM
Bushra I. Chaudhry, MD, FHM
Justin J. Chow, MD, FHM
Douglas E. Cohen, MD, FHM
John M. Colombo Jr., MD, FHM
Steven Connelly, MD, FACP, FHM
David Corman, MD, FHM
Christopher C. Costa, MD, FHM
William C. Crowe Jr., DNP, ACNP, FNP, MSN, RN, FHM
Ria Dancel, MD, FAAP, FHM
Zubaer Dawlah, MD, FHM
Chandrasekhar R. Dinasarapu, MD, MBBS, MPH, FHM
Vijay Saradhi Dontu, MD, FHM
Oleg Dulkin, MD, FHM
Kevin C. Eaton, PA-C, FHM
Eric Edwards, MD, FHM
Mary E. Fedor, MD, FHM
John W. Fowler Jr., MD, FACP, FHM
Maria G. Frank, MD, FACP, FHM
Yelena Galumyan, MD, FHM
Christopher D. Gamble, MD, FACP, FHM
David J. Goldstein, MD, FHM
Kalpana Gorthi, MD, FHM
Manjula V. Gunawardane, MD, FHM
Craig G. Gunderson, MD, FHM
Theodore J. Haland, MD, FHM
Aaron C. Hamilton, MD, MBA, FHM
Anil Hanuman, DO, FHM
Catriona M. Harrop, MD, FHM
Hossan Hassan, FAAFP, FHM
Eileen Hennrikus, MD, FHM
Arif Hussain, MD, FHM
Javid Iqbal, MD, FHM
Shadi Jarjous, MD, FHM
Jeremy Jaskunas, MD, FHM
John David Johnston, MD, FHM
Gurmeet Kaur Kalra, MD, FHM
Stephen K. Keiser, FHM
Sirajabid Khatib, MD, FHM
Joanna Kipnes, MD, FHM
Mukesh Kumar, MBBS, MD, FACP, FHM
Rumman A. Langah, MD, FACP, FHM
Rebecca Lauderdale, MD, FHM
Lajide R. Lawoyin, MD, FACP, FHM
Lien Le, MD, FHM
Alex Leung, FHM
William I. Levin, MD, FHM
David Lichtman, PA, FHM
Doris Wei-Hwa Lin, MD, FHM
Caroline E. Lyon, MD, MPH, FHM
John D. Machado, DO, FHM
Yvonne Maduka, MD, FHM
Lawrence L. Magras, MD, MBA, FHM
Anamaria Massier, MD, FHM
Daniel McFarlane, MD, FHM
Tresa A. McNeal, MD, FHM
Johnny Mei, MD, MHA, FACP, FHM
Rovie Mesola, MD, FHM
Henry J. Michtalik, MD, MHS, MPH, FHM
Prateek Mishra, MD, FHM
Adrian M. Mogos, MD, FHM
Wajahath A. Mohsini, MD, FACP, FHM
Ashwin Narasimhan, MD, FACP, FHM
Sivakumar Natanasabapathy, MRCP, FHM
Monica C. Necula, MD, FHM
Naomi Nomizu, MD, FHM
Shervin Nourparvar, MD, FHM
Allan L. Ong, MD, FHM
Pia Ong, MD, FHM
Chike Onyejekwe, MD, FHM
Binu T. Pappachen, MD, FHM
Akash Parashar MD, MBBS, FHM
Hiren B. Parikh, MD, MBA, FHM
Jung Hyun Park, MD, FHM
Shailesh Mansukh Patel, DO, FHM
Frank A. Perry, MD, FHM
Jeffrey W. Petry, MD, MMM, FHM
John R. Pierce Jr., MD, MPH, FHM
Jeffrey Poulos, MD, FHM
Richard N. Pulido, MD, FHM
Charu Puri, MD, FHM
Carolyn Quan, MD, FHM
Saraswathi V. Racherla, MD, FHM
Aisha Rahim, MD, FHM
Edwin Q. Ravano, MD, FHM
Behzad Razavi, MD, FACP, FHM
Erin N. Reis, MD, FHM
Maria Anaizza Aurora Reyna, MD, FHM
Mark Safalow, MD, FHM
Javaid Saleem, MD, MBBS, FHM
Mandeep S. Saluja, MD, FHM
Edward R. Sampt, MD, FHM
Jorge Santibanez, MD, FHM
Anne E. Sayers, MD, FHM
Brian Schroeder, FACHE, MHA, FHM
Scott E. Sears, MD, FACP, FHM
Meghan M. Sebasky, MD, FHM
Patricia L. Seymour, MD, FHM
Neel B. Shah, MB, BCh, FACP, FACMG, FHM
Poonam Sharma, MD, FHM
Umesh Sharma, MD, MS, FACP, FHM
Ashwin B. Shivakumar, MD, MSPH, FHM
Mohammed Fazil Siddiqi, MD, FHM
Sonya Sidhu-Izzo, MD, FHM
Alana E. Sigmund, MD, FHM
Shantnu Singh, MBBS, FHM
Amith Skandhan, MD, FHM
Christopher G. Skinner, MD, FACP, FHM
Dustin T. Smith, MD, FHM
Todd I. Smith, MD, FHM
Jeffrey D. Solomon, MD, FHM
Alberto Enrique Soyano, MD, FHM
Rodney R. Story, MD, FHM
John R. Sullivan, MD, FHM
Joseph G. Surber, DO, FHM
Heather R. Swanson, MD, FHM
Preetham Talari, MD, FHM
Sofia Teferi, MD, FAAP, FHM
Rafael A. Teran, MD, FHM
Abey K. Thomas, MD, FACP, FHM
Anca R. Udrea, MD, FHM
Shawn N. Usery, MD, FHM
Moncy Varughese, MD, FACP, FHM
Leigh Vaughan, MD, FHM
Manivannan Veerasamy, MD, FACP, FHM
Ruvan Chandika Wickramasinghe, MD, FHM
Michael Williams, DO, FHM
Sandra C. Wilson, MD, FACP, MA, FHM
Kareem Z. Yahya, MD, FHM
Deyun Yang, MD, PhD, FACP, FHM
Hector L. Yordan, MD, FHM
Elham A. Yousef, MD, MSc, FHM
Anthony M. Zepeda, MD, FHM
SFHM
Ashfaq Ahmad, MD, MBA, SFHM
Aziz Ansari, DO, SFHM
Anna M. Arroyo Plasencia, MD, SFHM
Andy Arwari, MD, FACP, SFHM
Jonathan G. Bae, MD, SFHM
Ankush K. Bansal, MD, FACP, SFHM
Jitendra Barmecha, MD, MPH, SFHM
Bishara A. Bates, BS, MHA, SFHM
Valerie F. Briones-Pryor, MD, FACP, SFHM
Michael E. Burton, MD, SFHM
Tracy E. Cardin, ACNP-BC, SFHM
Chris Cockerham, MD, SFHM
Timothy J. Crone, MD, SFHM
Debasish Dasgupta, MBBS, MHA, FACP, FACHE, SFHM, CPE, CPHQ
Kapil J. Dave, MD, SFHM
Shaker M. Eid, MD, MBA, SFHM
Howard R. Epstein, MD, SFHM
Christopher M. Frost, MD, SFHM
Timothy M. Gawronski, PA-C, SFHM
Amy S. Giarrusso, MD, SFHM
Jeffrey A. Gindi, MD, SFHM
Jason A. Green, MD, SFHM
Paul William Helgerson, MD, SFHM
Maliha Iqbal, MD, SFHM
James J. Jeffries II, MD, FACP, SFHM
Ian H. Jenkins, MD, SFHM
Scott Kaatz, DO, MSc, FACP, SFHM
Khurram Kamran, MD, SFHM
Anand Kartha, MD, MS, SFHM
Attila Kasza, MD, SFHM
Amy M. Keech, MD, SFHM
William A. Landis, MD, SFHM
Jimmie E. Lewis Jr., MD, MHA, SFHM
James W. Leyhane, MD, SFHM
Michael Lin, MD, SFHM
Julianna Lindsey, MD, SFHM
Madaiah Lokeshwari, MD, SFHM
Laszlo I. Madaras, MD, MPH, SFHM
Murthy V. Madduri, MD, SFHM
Arun V. Mohan, MD, SFHM
David R. Munoz, MD, SFHM
Mark A. Murray, MD, SFHM
Vasantha Natarajan, MD, SFHM
G. Xon Ng, MD, SFHM
Andy Odden, MD, SFHM
Tiffani M. Panek, MA, CLHM, SFHM
Shannon Connor Phillips, MD, MPH, SFHM
Preethi Prakash, MD, FACP, SFHM
Alberto Puig, MD, PhD, SFHM
Rebecca P. Ramirez, MD, SFHM
Allen B. Repp, MD, FACP, MS, SFHM
Scott C. Rissmiller, MD, SFHM
Frank Romero Jr., MD, SFHM
Marcus Lindley Scarbrough, MD, FACP, SFHM
Anneliese M. Schleyer, MD, SFHM
Eric R. Schumacher, DO, SFHM
Noppon Pooh Setji, MD, SFHM
Mohammad R. Shaheed, MD, SFHM
Jeffrey Scott Shapiro, MD, SFHM
Ann Sheehy, MD, MS, SFHM
R. Lucas Shelly, DO, SFHM
Andres F. Soto, MD, SFHM
John R. Stephens, MD, SFHM
Camille N. Upchurch, MD, SFHM
Fernando S. Waldemar, MD, SFHM
Michael D. Wang, MD, SFHM
Charlotta Weaver, MD, SFHM
Andrew White, MD, SFHM
Anthony Williams, MD, MBA, SFHM
MHM
Tina Budnitz, MPH, MHM
Greg Maynard, MD, MHM
Eric Howell, MD, MHM
FHM
Nicole Adler, MD, FHM
Tochukwu Agbata, MD, FHM
Alka Aggarwal, MD, FHM
Gaurav Ahuja, MD, MBBS, FHM
Sameena Akhtar, MD, FHM
Karan Singh S. Alag, MD, MBBS, FHM
Venkata N. Allada, MD, FACP, FHM
Margaret M. Ameyaw, MBChB, FHM
Robert L. Anderson, MD, FHM
Jorge Arboleda, DO, FHM
Michael Aref, MD, PhD, FACP, FHM
Elizabeth M. Arias, MD, FACP, FHM
Amarpreet S. Bains, MD, FHM
Ebrahim Barkoudah, MD, MPH, FACP, FHM
Wanes Barsemian, MD, FHM
Jeffrey T. Bates, MD, FACP, FHM
John F. Bell, MD, MPH, FHM
Kjell Benson, MD, FHM
Azmina Bhaiji, MD, FHM
Sai-Sridhar Boddupalli, MD, FHM
Ani Bodoutchian, MD, MBA, FAAFP, FHM
Tanya M. Boldenow, MD, FHM
Dennis T. Bolger Jr., MD, FHM
Greg D. Bowling, MD, FHM
David A. Bozaan, MD, FHM
Marcia Carbo, MD, FAAP, FHM
Donna Cardoza, MD, FHM
Frank R. Carson Jr., MD, FHM
Kelly Caverzagie, MD, FACP, FHM
Elizabeth A. Cerceo, MD, FACP, FHM
Jeffrey M. Ceresnak, MD, FHM
Romil Chadha, MD, MPH, FACP, FHM
Charles Charman, MD, FHM
Bushra I. Chaudhry, MD, FHM
Justin J. Chow, MD, FHM
Douglas E. Cohen, MD, FHM
John M. Colombo Jr., MD, FHM
Steven Connelly, MD, FACP, FHM
David Corman, MD, FHM
Christopher C. Costa, MD, FHM
William C. Crowe Jr., DNP, ACNP, FNP, MSN, RN, FHM
Ria Dancel, MD, FAAP, FHM
Zubaer Dawlah, MD, FHM
Chandrasekhar R. Dinasarapu, MD, MBBS, MPH, FHM
Vijay Saradhi Dontu, MD, FHM
Oleg Dulkin, MD, FHM
Kevin C. Eaton, PA-C, FHM
Eric Edwards, MD, FHM
Mary E. Fedor, MD, FHM
John W. Fowler Jr., MD, FACP, FHM
Maria G. Frank, MD, FACP, FHM
Yelena Galumyan, MD, FHM
Christopher D. Gamble, MD, FACP, FHM
David J. Goldstein, MD, FHM
Kalpana Gorthi, MD, FHM
Manjula V. Gunawardane, MD, FHM
Craig G. Gunderson, MD, FHM
Theodore J. Haland, MD, FHM
Aaron C. Hamilton, MD, MBA, FHM
Anil Hanuman, DO, FHM
Catriona M. Harrop, MD, FHM
Hossan Hassan, FAAFP, FHM
Eileen Hennrikus, MD, FHM
Arif Hussain, MD, FHM
Javid Iqbal, MD, FHM
Shadi Jarjous, MD, FHM
Jeremy Jaskunas, MD, FHM
John David Johnston, MD, FHM
Gurmeet Kaur Kalra, MD, FHM
Stephen K. Keiser, FHM
Sirajabid Khatib, MD, FHM
Joanna Kipnes, MD, FHM
Mukesh Kumar, MBBS, MD, FACP, FHM
Rumman A. Langah, MD, FACP, FHM
Rebecca Lauderdale, MD, FHM
Lajide R. Lawoyin, MD, FACP, FHM
Lien Le, MD, FHM
Alex Leung, FHM
William I. Levin, MD, FHM
David Lichtman, PA, FHM
Doris Wei-Hwa Lin, MD, FHM
Caroline E. Lyon, MD, MPH, FHM
John D. Machado, DO, FHM
Yvonne Maduka, MD, FHM
Lawrence L. Magras, MD, MBA, FHM
Anamaria Massier, MD, FHM
Daniel McFarlane, MD, FHM
Tresa A. McNeal, MD, FHM
Johnny Mei, MD, MHA, FACP, FHM
Rovie Mesola, MD, FHM
Henry J. Michtalik, MD, MHS, MPH, FHM
Prateek Mishra, MD, FHM
Adrian M. Mogos, MD, FHM
Wajahath A. Mohsini, MD, FACP, FHM
Ashwin Narasimhan, MD, FACP, FHM
Sivakumar Natanasabapathy, MRCP, FHM
Monica C. Necula, MD, FHM
Naomi Nomizu, MD, FHM
Shervin Nourparvar, MD, FHM
Allan L. Ong, MD, FHM
Pia Ong, MD, FHM
Chike Onyejekwe, MD, FHM
Binu T. Pappachen, MD, FHM
Akash Parashar MD, MBBS, FHM
Hiren B. Parikh, MD, MBA, FHM
Jung Hyun Park, MD, FHM
Shailesh Mansukh Patel, DO, FHM
Frank A. Perry, MD, FHM
Jeffrey W. Petry, MD, MMM, FHM
John R. Pierce Jr., MD, MPH, FHM
Jeffrey Poulos, MD, FHM
Richard N. Pulido, MD, FHM
Charu Puri, MD, FHM
Carolyn Quan, MD, FHM
Saraswathi V. Racherla, MD, FHM
Aisha Rahim, MD, FHM
Edwin Q. Ravano, MD, FHM
Behzad Razavi, MD, FACP, FHM
Erin N. Reis, MD, FHM
Maria Anaizza Aurora Reyna, MD, FHM
Mark Safalow, MD, FHM
Javaid Saleem, MD, MBBS, FHM
Mandeep S. Saluja, MD, FHM
Edward R. Sampt, MD, FHM
Jorge Santibanez, MD, FHM
Anne E. Sayers, MD, FHM
Brian Schroeder, FACHE, MHA, FHM
Scott E. Sears, MD, FACP, FHM
Meghan M. Sebasky, MD, FHM
Patricia L. Seymour, MD, FHM
Neel B. Shah, MB, BCh, FACP, FACMG, FHM
Poonam Sharma, MD, FHM
Umesh Sharma, MD, MS, FACP, FHM
Ashwin B. Shivakumar, MD, MSPH, FHM
Mohammed Fazil Siddiqi, MD, FHM
Sonya Sidhu-Izzo, MD, FHM
Alana E. Sigmund, MD, FHM
Shantnu Singh, MBBS, FHM
Amith Skandhan, MD, FHM
Christopher G. Skinner, MD, FACP, FHM
Dustin T. Smith, MD, FHM
Todd I. Smith, MD, FHM
Jeffrey D. Solomon, MD, FHM
Alberto Enrique Soyano, MD, FHM
Rodney R. Story, MD, FHM
John R. Sullivan, MD, FHM
Joseph G. Surber, DO, FHM
Heather R. Swanson, MD, FHM
Preetham Talari, MD, FHM
Sofia Teferi, MD, FAAP, FHM
Rafael A. Teran, MD, FHM
Abey K. Thomas, MD, FACP, FHM
Anca R. Udrea, MD, FHM
Shawn N. Usery, MD, FHM
Moncy Varughese, MD, FACP, FHM
Leigh Vaughan, MD, FHM
Manivannan Veerasamy, MD, FACP, FHM
Ruvan Chandika Wickramasinghe, MD, FHM
Michael Williams, DO, FHM
Sandra C. Wilson, MD, FACP, MA, FHM
Kareem Z. Yahya, MD, FHM
Deyun Yang, MD, PhD, FACP, FHM
Hector L. Yordan, MD, FHM
Elham A. Yousef, MD, MSc, FHM
Anthony M. Zepeda, MD, FHM
SFHM
Ashfaq Ahmad, MD, MBA, SFHM
Aziz Ansari, DO, SFHM
Anna M. Arroyo Plasencia, MD, SFHM
Andy Arwari, MD, FACP, SFHM
Jonathan G. Bae, MD, SFHM
Ankush K. Bansal, MD, FACP, SFHM
Jitendra Barmecha, MD, MPH, SFHM
Bishara A. Bates, BS, MHA, SFHM
Valerie F. Briones-Pryor, MD, FACP, SFHM
Michael E. Burton, MD, SFHM
Tracy E. Cardin, ACNP-BC, SFHM
Chris Cockerham, MD, SFHM
Timothy J. Crone, MD, SFHM
Debasish Dasgupta, MBBS, MHA, FACP, FACHE, SFHM, CPE, CPHQ
Kapil J. Dave, MD, SFHM
Shaker M. Eid, MD, MBA, SFHM
Howard R. Epstein, MD, SFHM
Christopher M. Frost, MD, SFHM
Timothy M. Gawronski, PA-C, SFHM
Amy S. Giarrusso, MD, SFHM
Jeffrey A. Gindi, MD, SFHM
Jason A. Green, MD, SFHM
Paul William Helgerson, MD, SFHM
Maliha Iqbal, MD, SFHM
James J. Jeffries II, MD, FACP, SFHM
Ian H. Jenkins, MD, SFHM
Scott Kaatz, DO, MSc, FACP, SFHM
Khurram Kamran, MD, SFHM
Anand Kartha, MD, MS, SFHM
Attila Kasza, MD, SFHM
Amy M. Keech, MD, SFHM
William A. Landis, MD, SFHM
Jimmie E. Lewis Jr., MD, MHA, SFHM
James W. Leyhane, MD, SFHM
Michael Lin, MD, SFHM
Julianna Lindsey, MD, SFHM
Madaiah Lokeshwari, MD, SFHM
Laszlo I. Madaras, MD, MPH, SFHM
Murthy V. Madduri, MD, SFHM
Arun V. Mohan, MD, SFHM
David R. Munoz, MD, SFHM
Mark A. Murray, MD, SFHM
Vasantha Natarajan, MD, SFHM
G. Xon Ng, MD, SFHM
Andy Odden, MD, SFHM
Tiffani M. Panek, MA, CLHM, SFHM
Shannon Connor Phillips, MD, MPH, SFHM
Preethi Prakash, MD, FACP, SFHM
Alberto Puig, MD, PhD, SFHM
Rebecca P. Ramirez, MD, SFHM
Allen B. Repp, MD, FACP, MS, SFHM
Scott C. Rissmiller, MD, SFHM
Frank Romero Jr., MD, SFHM
Marcus Lindley Scarbrough, MD, FACP, SFHM
Anneliese M. Schleyer, MD, SFHM
Eric R. Schumacher, DO, SFHM
Noppon Pooh Setji, MD, SFHM
Mohammad R. Shaheed, MD, SFHM
Jeffrey Scott Shapiro, MD, SFHM
Ann Sheehy, MD, MS, SFHM
R. Lucas Shelly, DO, SFHM
Andres F. Soto, MD, SFHM
John R. Stephens, MD, SFHM
Camille N. Upchurch, MD, SFHM
Fernando S. Waldemar, MD, SFHM
Michael D. Wang, MD, SFHM
Charlotta Weaver, MD, SFHM
Andrew White, MD, SFHM
Anthony Williams, MD, MBA, SFHM