User login
Team explains CD8 Treg dysfunction

Image by Kathryn T. Iacono
Research published in The Journal of Clinical Investigation provides new insights regarding CD8 regulatory T cells (Tregs).
Investigators found that, in young, healthy individuals, CD8 Tregs suppress the activation and expansion of CD4 T cells.
However, older individuals and patients with a rare form of vasculitis exhibit CD8 Treg dysfunction, which is tied to a drop in production of an enzyme called NADPH oxidase 2 (NOX2).
Cornelia Weyand, MD, of Stanford University Medical Center in California, and her colleagues conducted this research.
First, the team found that CD8 Tregs preferentially take up residence in lymph nodes, the spleen, and other regions where there are huge “armies” of CD4 T cells. This proximity puts the CD8 Tregs in a position to stamp out CD4 T-cell activation early on.
Further experiments demonstrated that CD8 Tregs manufacture copious amounts of NOX2, which they package into tiny membrane-bound packets and transfer to the surfaces of abutting CD4 T cells.
These NOX2-laden packets are then taken up by the CD4 T cells. Inside their new home, the enzymes produce large volumes of highly reactive signaling substances that dial down CD4 T cells’ activation and proliferation.
The investigators noted that contact between CD8 Tregs and CD4 T cells in the early stages of activation shuts down the CD4 T cells’ activity and reduces their proliferation by half or more, even several days after the CD8 Tregs have been removed. Transferring NOX2 alone onto activated CD4 T cells also produces this effect.
Next, the team analyzed blood samples from healthy individuals and observed that CD8 Tregs were only about half as common in blood from people age 60 and older as in blood from 20- to 30-year-olds.
Both CD8 Treg numbers and their ability to suppress CD4 T-cell proliferation declined with advancing age. Experiments traced this to a drop in NOX2 production by older donors’ CD8 Tregs.
The investigators also discovered CD8 Treg failure in giant-cell arteritis (GCA). The team compared blood from GCA patients to blood from age-matched healthy control subjects and from patients with 2 other autoimmune diseases—psoriatic arthritis and small-vessel vasculitis. This revealed a severe deficit among GCA patients in NOX2-producing CD8 Tregs.
“This tells us that the deficit in NOX2-producing CD8 Tregs is specific to GCA, not just driving or driven by inflammation,” Dr Weyand said. “That’s good news for our patients who have this disease, which has been an enigma. Now we know something about what’s causing it.”
The discovery of NOX2 on the surface of CD8 Tregs—but not on other T-cell types—makes them much easier to identify and count, Dr Weyand added.
She and her colleagues are taking advantage of the new-found biomarker to tally CD8 Tregs in patients with age-associated disorders now understood to be driven by chronic inflammation to see if CD8 Treg deficits underlie some of these conditions’ pathology and whether they may be amenable to potential NOX2-restoring treatments. ![]()

Image by Kathryn T. Iacono
Research published in The Journal of Clinical Investigation provides new insights regarding CD8 regulatory T cells (Tregs).
Investigators found that, in young, healthy individuals, CD8 Tregs suppress the activation and expansion of CD4 T cells.
However, older individuals and patients with a rare form of vasculitis exhibit CD8 Treg dysfunction, which is tied to a drop in production of an enzyme called NADPH oxidase 2 (NOX2).
Cornelia Weyand, MD, of Stanford University Medical Center in California, and her colleagues conducted this research.
First, the team found that CD8 Tregs preferentially take up residence in lymph nodes, the spleen, and other regions where there are huge “armies” of CD4 T cells. This proximity puts the CD8 Tregs in a position to stamp out CD4 T-cell activation early on.
Further experiments demonstrated that CD8 Tregs manufacture copious amounts of NOX2, which they package into tiny membrane-bound packets and transfer to the surfaces of abutting CD4 T cells.
These NOX2-laden packets are then taken up by the CD4 T cells. Inside their new home, the enzymes produce large volumes of highly reactive signaling substances that dial down CD4 T cells’ activation and proliferation.
The investigators noted that contact between CD8 Tregs and CD4 T cells in the early stages of activation shuts down the CD4 T cells’ activity and reduces their proliferation by half or more, even several days after the CD8 Tregs have been removed. Transferring NOX2 alone onto activated CD4 T cells also produces this effect.
Next, the team analyzed blood samples from healthy individuals and observed that CD8 Tregs were only about half as common in blood from people age 60 and older as in blood from 20- to 30-year-olds.
Both CD8 Treg numbers and their ability to suppress CD4 T-cell proliferation declined with advancing age. Experiments traced this to a drop in NOX2 production by older donors’ CD8 Tregs.
The investigators also discovered CD8 Treg failure in giant-cell arteritis (GCA). The team compared blood from GCA patients to blood from age-matched healthy control subjects and from patients with 2 other autoimmune diseases—psoriatic arthritis and small-vessel vasculitis. This revealed a severe deficit among GCA patients in NOX2-producing CD8 Tregs.
“This tells us that the deficit in NOX2-producing CD8 Tregs is specific to GCA, not just driving or driven by inflammation,” Dr Weyand said. “That’s good news for our patients who have this disease, which has been an enigma. Now we know something about what’s causing it.”
The discovery of NOX2 on the surface of CD8 Tregs—but not on other T-cell types—makes them much easier to identify and count, Dr Weyand added.
She and her colleagues are taking advantage of the new-found biomarker to tally CD8 Tregs in patients with age-associated disorders now understood to be driven by chronic inflammation to see if CD8 Treg deficits underlie some of these conditions’ pathology and whether they may be amenable to potential NOX2-restoring treatments. ![]()

Image by Kathryn T. Iacono
Research published in The Journal of Clinical Investigation provides new insights regarding CD8 regulatory T cells (Tregs).
Investigators found that, in young, healthy individuals, CD8 Tregs suppress the activation and expansion of CD4 T cells.
However, older individuals and patients with a rare form of vasculitis exhibit CD8 Treg dysfunction, which is tied to a drop in production of an enzyme called NADPH oxidase 2 (NOX2).
Cornelia Weyand, MD, of Stanford University Medical Center in California, and her colleagues conducted this research.
First, the team found that CD8 Tregs preferentially take up residence in lymph nodes, the spleen, and other regions where there are huge “armies” of CD4 T cells. This proximity puts the CD8 Tregs in a position to stamp out CD4 T-cell activation early on.
Further experiments demonstrated that CD8 Tregs manufacture copious amounts of NOX2, which they package into tiny membrane-bound packets and transfer to the surfaces of abutting CD4 T cells.
These NOX2-laden packets are then taken up by the CD4 T cells. Inside their new home, the enzymes produce large volumes of highly reactive signaling substances that dial down CD4 T cells’ activation and proliferation.
The investigators noted that contact between CD8 Tregs and CD4 T cells in the early stages of activation shuts down the CD4 T cells’ activity and reduces their proliferation by half or more, even several days after the CD8 Tregs have been removed. Transferring NOX2 alone onto activated CD4 T cells also produces this effect.
Next, the team analyzed blood samples from healthy individuals and observed that CD8 Tregs were only about half as common in blood from people age 60 and older as in blood from 20- to 30-year-olds.
Both CD8 Treg numbers and their ability to suppress CD4 T-cell proliferation declined with advancing age. Experiments traced this to a drop in NOX2 production by older donors’ CD8 Tregs.
The investigators also discovered CD8 Treg failure in giant-cell arteritis (GCA). The team compared blood from GCA patients to blood from age-matched healthy control subjects and from patients with 2 other autoimmune diseases—psoriatic arthritis and small-vessel vasculitis. This revealed a severe deficit among GCA patients in NOX2-producing CD8 Tregs.
“This tells us that the deficit in NOX2-producing CD8 Tregs is specific to GCA, not just driving or driven by inflammation,” Dr Weyand said. “That’s good news for our patients who have this disease, which has been an enigma. Now we know something about what’s causing it.”
The discovery of NOX2 on the surface of CD8 Tregs—but not on other T-cell types—makes them much easier to identify and count, Dr Weyand added.
She and her colleagues are taking advantage of the new-found biomarker to tally CD8 Tregs in patients with age-associated disorders now understood to be driven by chronic inflammation to see if CD8 Treg deficits underlie some of these conditions’ pathology and whether they may be amenable to potential NOX2-restoring treatments. ![]()
UnitedHealth Group leaving most ACA marketplaces
UnitedHealth Group will not sell policies next year in most of the health insurance marketplaces created by the Affordable Care Act, CEO Stephen Helmsley announced during an April 19 earnings call.
“Next year, we will remain in only a handful of states, and we will not carry financial exposure from exchanges into 2017,” Mr. Helmsley said, citing the company’s inability to offset the “shorter-term, higher-risk” population covered by the ACA exchange plans with large enough risk pools.
Mr. Helmsley did not say in which state marketplaces UnitedHealth Group (UHG) will continue to offer coverage.
Areas that could be hardest hit by the UHG withdrawal include Alabama, Arizona, Arkansas, Nebraska, North Carolina, and Tennessee, according to an analysis from the Kaiser Family Foundation.
For now, the decision by UHG is not likely to impact the average benchmark premium by more than a 1% increase, according to the analysis. That’s because the insurer was less likely than its competitors to offer lower-cost silver plans; when silver plans were offered, they were offered at or very near to the competitors’ prices. However, in states where the withdrawal of UHG means that two or fewer insurers are participating in the marketplace, benchmark premiums could rise substantially, according to the study.
The long-term effect of the UHG exit from most marketplaces is not clear, according to Kaiser’s analysts. “In areas with limited insurer participation, the remaining plans after a United exit may have more market power relative to providers, but in the absence of insurer competition, those savings may not be passed along to consumers,” they wrote.
ACA measures such as rate reviews and medical loss ratio provisions could mitigate adverse effects on consumers in these markets, giving regulators the power to force insurers to issue rebates if premiums outstrip the cost of care.
The insurer’s decision is simply evidence that typical market forces are in play, according to Jonathan Gold, a spokesperson for the Centers for Medicare & Medicaid Services.
“As with any new market, we expect changes and adjustments in the early years with issuers both entering and exiting states,” Mr. Gold said in an interview. The UHG decision was not unexpected, as company officials said they were contemplating the move last November.
“We have full confidence, based on data, that the marketplaces will continue to thrive for years ahead,” he said, noting that in 2016, 39 insurers exited the marketplace, while 40 entered.
On Twitter @whitneymcknight
UnitedHealth Group will not sell policies next year in most of the health insurance marketplaces created by the Affordable Care Act, CEO Stephen Helmsley announced during an April 19 earnings call.
“Next year, we will remain in only a handful of states, and we will not carry financial exposure from exchanges into 2017,” Mr. Helmsley said, citing the company’s inability to offset the “shorter-term, higher-risk” population covered by the ACA exchange plans with large enough risk pools.
Mr. Helmsley did not say in which state marketplaces UnitedHealth Group (UHG) will continue to offer coverage.
Areas that could be hardest hit by the UHG withdrawal include Alabama, Arizona, Arkansas, Nebraska, North Carolina, and Tennessee, according to an analysis from the Kaiser Family Foundation.
For now, the decision by UHG is not likely to impact the average benchmark premium by more than a 1% increase, according to the analysis. That’s because the insurer was less likely than its competitors to offer lower-cost silver plans; when silver plans were offered, they were offered at or very near to the competitors’ prices. However, in states where the withdrawal of UHG means that two or fewer insurers are participating in the marketplace, benchmark premiums could rise substantially, according to the study.
The long-term effect of the UHG exit from most marketplaces is not clear, according to Kaiser’s analysts. “In areas with limited insurer participation, the remaining plans after a United exit may have more market power relative to providers, but in the absence of insurer competition, those savings may not be passed along to consumers,” they wrote.
ACA measures such as rate reviews and medical loss ratio provisions could mitigate adverse effects on consumers in these markets, giving regulators the power to force insurers to issue rebates if premiums outstrip the cost of care.
The insurer’s decision is simply evidence that typical market forces are in play, according to Jonathan Gold, a spokesperson for the Centers for Medicare & Medicaid Services.
“As with any new market, we expect changes and adjustments in the early years with issuers both entering and exiting states,” Mr. Gold said in an interview. The UHG decision was not unexpected, as company officials said they were contemplating the move last November.
“We have full confidence, based on data, that the marketplaces will continue to thrive for years ahead,” he said, noting that in 2016, 39 insurers exited the marketplace, while 40 entered.
On Twitter @whitneymcknight
UnitedHealth Group will not sell policies next year in most of the health insurance marketplaces created by the Affordable Care Act, CEO Stephen Helmsley announced during an April 19 earnings call.
“Next year, we will remain in only a handful of states, and we will not carry financial exposure from exchanges into 2017,” Mr. Helmsley said, citing the company’s inability to offset the “shorter-term, higher-risk” population covered by the ACA exchange plans with large enough risk pools.
Mr. Helmsley did not say in which state marketplaces UnitedHealth Group (UHG) will continue to offer coverage.
Areas that could be hardest hit by the UHG withdrawal include Alabama, Arizona, Arkansas, Nebraska, North Carolina, and Tennessee, according to an analysis from the Kaiser Family Foundation.
For now, the decision by UHG is not likely to impact the average benchmark premium by more than a 1% increase, according to the analysis. That’s because the insurer was less likely than its competitors to offer lower-cost silver plans; when silver plans were offered, they were offered at or very near to the competitors’ prices. However, in states where the withdrawal of UHG means that two or fewer insurers are participating in the marketplace, benchmark premiums could rise substantially, according to the study.
The long-term effect of the UHG exit from most marketplaces is not clear, according to Kaiser’s analysts. “In areas with limited insurer participation, the remaining plans after a United exit may have more market power relative to providers, but in the absence of insurer competition, those savings may not be passed along to consumers,” they wrote.
ACA measures such as rate reviews and medical loss ratio provisions could mitigate adverse effects on consumers in these markets, giving regulators the power to force insurers to issue rebates if premiums outstrip the cost of care.
The insurer’s decision is simply evidence that typical market forces are in play, according to Jonathan Gold, a spokesperson for the Centers for Medicare & Medicaid Services.
“As with any new market, we expect changes and adjustments in the early years with issuers both entering and exiting states,” Mr. Gold said in an interview. The UHG decision was not unexpected, as company officials said they were contemplating the move last November.
“We have full confidence, based on data, that the marketplaces will continue to thrive for years ahead,” he said, noting that in 2016, 39 insurers exited the marketplace, while 40 entered.
On Twitter @whitneymcknight
AAN Updates Guidelines on Use of Botulinum Toxin for Four Disorders
VANCOUVER—The American Academy of Neurology (AAN) has updated its 2008 guidelines on the use of botulinum toxin for spasticity, cervical dystonia, blepharospasm, and migraine to reflect recent research. Unlike the 2008 guidelines, the current document describes the evidence for the four formulations of botulinum toxin individually. The guidelines were published online ahead of print April 18 in Neurology and presented at the 68th Annual Meeting of the AAN.
Botulinum toxin blocks the release of substances at nerve endings, generally resulting in reduced muscle contraction and decreased transmission of pain signals. The four preparations available in the United States are abobotulinumtoxinA, incobotulinumtoxinA, onabotulinumtoxinA, and rimabotulinumtoxinB.
To develop the guideline, David M. Simpson, MD, Professor of Neurology and Neuromuscular Diseases at the Icahn School of Medicine at Mount Sinai Hospital in New York, and colleagues reviewed all available scientific studies on these formulations in the four conditions specified. The authors concluded that botulinum toxin is generally safe and effective for treating spasticity in adults, cervical dystonia, blepharospasm, and chronic migraine.
The new guideline’s recommendation on chronic migraine is a major change from the earlier document, said Dr. Simpson. In 2008, not enough evidence was available to support any recommendation on the use of botulinum toxin for chronic migraine. Since that time, two pivotal Class I studies demonstrated the effectiveness of onabotulinumtoxinA in the treatment of chronic migraine. The magnitude of the drug’s efficacy was small, however. In the four weeks after the first treatments, onabotulinumtoxinA was associated with an approximately 15% reduction in headache days per month, compared with placebo. The difference was statistically significant, and the new guideline contains a Level A recommendation of onabotulinumtoxinA for chronic migraine.
On the other hand, the authors found Level A evidence indicating a lack of effectiveness of onabotulinumtoxinA in episodic migraine. “It’s an interesting question as to whether there’s a pathophysiologic difference between episodic migraine and chronic migraine,” but the evidence is unclear, said Dr. Simpson. Another possible explanation for botulinum toxin’s lack of efficacy in this indication is that studies of episodic migraine may reflect a floor effect, he added. “If you have so few headaches per month … how much does that need to reduce to see a significant difference from placebo? That is perhaps one obvious concern about getting a positive result of those studies.” In addition, the authors concluded that abobotulinumtoxinA, incobotulinumtoxinA, and onabotulinumtoxinA are effective in reducing excess muscle tone and should be offered to patients with upper limb spasticity. RimabotulinumtoxinB is probably effective for this indication and should be considered, according to the guideline. For lower limb spasticity, abobotulinumtoxinA and onabotulinumtoxinA are effective and should be offered.
The guideline also indicates that abobotulinumtoxinA and rimabotulinumtoxinB are effective for cervical dystonia and should be offered. OnabotulinumtoxinA and incobotulinumtoxinA are probably effective and should be considered for this indication.Researchers have conducted few well-designed studies on blepharospasm. OnabotulinumtoxinA and incobotulinumtoxinA are probably effective and should be considered for this indication, according to the guideline. AbobotulinumtoxinA is possibly effective and may be considered. The 2008 guidelines also discussed disorders such as essential tremor, hemifacial spasm, and disorders of the voice. No new evidence about botulinum toxin’s effect in these disorders was available at the time that the update was initiated, and they were not included.
—Erik Greb
Suggested Reading
Simpson DM, Hallett M, Ashman EJ, et al. Practice guideline update summary: Botulinum neurotoxin for the treatment of blepharospasm, cervical dystonia, adult spasticity, and headache: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2016 April 18 [Epub ahead of print].
VANCOUVER—The American Academy of Neurology (AAN) has updated its 2008 guidelines on the use of botulinum toxin for spasticity, cervical dystonia, blepharospasm, and migraine to reflect recent research. Unlike the 2008 guidelines, the current document describes the evidence for the four formulations of botulinum toxin individually. The guidelines were published online ahead of print April 18 in Neurology and presented at the 68th Annual Meeting of the AAN.
Botulinum toxin blocks the release of substances at nerve endings, generally resulting in reduced muscle contraction and decreased transmission of pain signals. The four preparations available in the United States are abobotulinumtoxinA, incobotulinumtoxinA, onabotulinumtoxinA, and rimabotulinumtoxinB.
To develop the guideline, David M. Simpson, MD, Professor of Neurology and Neuromuscular Diseases at the Icahn School of Medicine at Mount Sinai Hospital in New York, and colleagues reviewed all available scientific studies on these formulations in the four conditions specified. The authors concluded that botulinum toxin is generally safe and effective for treating spasticity in adults, cervical dystonia, blepharospasm, and chronic migraine.
The new guideline’s recommendation on chronic migraine is a major change from the earlier document, said Dr. Simpson. In 2008, not enough evidence was available to support any recommendation on the use of botulinum toxin for chronic migraine. Since that time, two pivotal Class I studies demonstrated the effectiveness of onabotulinumtoxinA in the treatment of chronic migraine. The magnitude of the drug’s efficacy was small, however. In the four weeks after the first treatments, onabotulinumtoxinA was associated with an approximately 15% reduction in headache days per month, compared with placebo. The difference was statistically significant, and the new guideline contains a Level A recommendation of onabotulinumtoxinA for chronic migraine.
On the other hand, the authors found Level A evidence indicating a lack of effectiveness of onabotulinumtoxinA in episodic migraine. “It’s an interesting question as to whether there’s a pathophysiologic difference between episodic migraine and chronic migraine,” but the evidence is unclear, said Dr. Simpson. Another possible explanation for botulinum toxin’s lack of efficacy in this indication is that studies of episodic migraine may reflect a floor effect, he added. “If you have so few headaches per month … how much does that need to reduce to see a significant difference from placebo? That is perhaps one obvious concern about getting a positive result of those studies.” In addition, the authors concluded that abobotulinumtoxinA, incobotulinumtoxinA, and onabotulinumtoxinA are effective in reducing excess muscle tone and should be offered to patients with upper limb spasticity. RimabotulinumtoxinB is probably effective for this indication and should be considered, according to the guideline. For lower limb spasticity, abobotulinumtoxinA and onabotulinumtoxinA are effective and should be offered.
The guideline also indicates that abobotulinumtoxinA and rimabotulinumtoxinB are effective for cervical dystonia and should be offered. OnabotulinumtoxinA and incobotulinumtoxinA are probably effective and should be considered for this indication.Researchers have conducted few well-designed studies on blepharospasm. OnabotulinumtoxinA and incobotulinumtoxinA are probably effective and should be considered for this indication, according to the guideline. AbobotulinumtoxinA is possibly effective and may be considered. The 2008 guidelines also discussed disorders such as essential tremor, hemifacial spasm, and disorders of the voice. No new evidence about botulinum toxin’s effect in these disorders was available at the time that the update was initiated, and they were not included.
—Erik Greb
VANCOUVER—The American Academy of Neurology (AAN) has updated its 2008 guidelines on the use of botulinum toxin for spasticity, cervical dystonia, blepharospasm, and migraine to reflect recent research. Unlike the 2008 guidelines, the current document describes the evidence for the four formulations of botulinum toxin individually. The guidelines were published online ahead of print April 18 in Neurology and presented at the 68th Annual Meeting of the AAN.
Botulinum toxin blocks the release of substances at nerve endings, generally resulting in reduced muscle contraction and decreased transmission of pain signals. The four preparations available in the United States are abobotulinumtoxinA, incobotulinumtoxinA, onabotulinumtoxinA, and rimabotulinumtoxinB.
To develop the guideline, David M. Simpson, MD, Professor of Neurology and Neuromuscular Diseases at the Icahn School of Medicine at Mount Sinai Hospital in New York, and colleagues reviewed all available scientific studies on these formulations in the four conditions specified. The authors concluded that botulinum toxin is generally safe and effective for treating spasticity in adults, cervical dystonia, blepharospasm, and chronic migraine.
The new guideline’s recommendation on chronic migraine is a major change from the earlier document, said Dr. Simpson. In 2008, not enough evidence was available to support any recommendation on the use of botulinum toxin for chronic migraine. Since that time, two pivotal Class I studies demonstrated the effectiveness of onabotulinumtoxinA in the treatment of chronic migraine. The magnitude of the drug’s efficacy was small, however. In the four weeks after the first treatments, onabotulinumtoxinA was associated with an approximately 15% reduction in headache days per month, compared with placebo. The difference was statistically significant, and the new guideline contains a Level A recommendation of onabotulinumtoxinA for chronic migraine.
On the other hand, the authors found Level A evidence indicating a lack of effectiveness of onabotulinumtoxinA in episodic migraine. “It’s an interesting question as to whether there’s a pathophysiologic difference between episodic migraine and chronic migraine,” but the evidence is unclear, said Dr. Simpson. Another possible explanation for botulinum toxin’s lack of efficacy in this indication is that studies of episodic migraine may reflect a floor effect, he added. “If you have so few headaches per month … how much does that need to reduce to see a significant difference from placebo? That is perhaps one obvious concern about getting a positive result of those studies.” In addition, the authors concluded that abobotulinumtoxinA, incobotulinumtoxinA, and onabotulinumtoxinA are effective in reducing excess muscle tone and should be offered to patients with upper limb spasticity. RimabotulinumtoxinB is probably effective for this indication and should be considered, according to the guideline. For lower limb spasticity, abobotulinumtoxinA and onabotulinumtoxinA are effective and should be offered.
The guideline also indicates that abobotulinumtoxinA and rimabotulinumtoxinB are effective for cervical dystonia and should be offered. OnabotulinumtoxinA and incobotulinumtoxinA are probably effective and should be considered for this indication.Researchers have conducted few well-designed studies on blepharospasm. OnabotulinumtoxinA and incobotulinumtoxinA are probably effective and should be considered for this indication, according to the guideline. AbobotulinumtoxinA is possibly effective and may be considered. The 2008 guidelines also discussed disorders such as essential tremor, hemifacial spasm, and disorders of the voice. No new evidence about botulinum toxin’s effect in these disorders was available at the time that the update was initiated, and they were not included.
—Erik Greb
Suggested Reading
Simpson DM, Hallett M, Ashman EJ, et al. Practice guideline update summary: Botulinum neurotoxin for the treatment of blepharospasm, cervical dystonia, adult spasticity, and headache: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2016 April 18 [Epub ahead of print].
Suggested Reading
Simpson DM, Hallett M, Ashman EJ, et al. Practice guideline update summary: Botulinum neurotoxin for the treatment of blepharospasm, cervical dystonia, adult spasticity, and headache: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology. 2016 April 18 [Epub ahead of print].
New data help guide the stopping of disease-modifying drugs in MS
VANCOUVER – Certain patient and disease characteristics may help guide decisions about starting and stopping therapy in progressive multiple sclerosis, according to a pair of longitudinal cohort studies reported at the annual meeting of the American Academy of Neurology.
In a cohort of patients transitioning from relapsing-remitting to progressive multiple sclerosis (MS), the age at onset of progression predicted the likelihood of subsequent relapses. The absolute lifetime risk ranged from 18% for patients younger than 35 years at the time to just 5% for those aged 55 years or older at the time.
And in a cohort of patients with secondary progressive MS, the annual rate of clinical relapse fell in the third year after immunomodulator discontinuation. Overall, 35% had a clinical relapse or radiologic disease activity. Patients had a lower risk of this outcome if they had greater disability at the time of discontinuation or if they had not had any radiologic disease activity in the antecedent years.
“These studies address a very important question, because not many people talk about stopping drugs,” commented session comoderator Helen Tremlett, Ph.D., of the division of neurology at the University of British Columbia, Vancouver, and the Canada Research Chair in Neuroepidemiology and Multiple Sclerosis. “I would like to see some of these findings validated in other cohorts. But I did like the questions they are asking.”
Age, risk of postprogression relapse
The first study focused on ongoing relapses in patients transitioning to progressive MS. “We have recently shown that these relapses indeed matter. People who continue to relapse after progressive MS onset develop a need for a cane 2 years earlier than those who don’t” continue to have relapses, explained senior author Dr. Orhun H. Kantarci of the department of neurology at the Mayo Clinic in Rochester, Minn. Therefore, continuation or initiation of disease-modifying drugs (DMDs) during this period of overlap may be beneficial.
He and his colleagues followed 946 patients with MS from a clinic- and population-based cohort, assessing the age at various disease landmarks.
Results showed the mean age at first relapse was 33 years, the mean age at the onset of progressive MS was 45 years, and the mean age at last relapse (whether it occurred before or after the onset of progressive disease) was 43 years.
The 95% overlap age range for age at first relapse and age at onset of progressive MS was 27-46 years, Dr. Kantarci reported. Therefore, DMDs would be expected to have a some impact during those years.
Further analyses showed that if the age of progressive MS onset was before 35 years, 35-44 years, 45-54 years, and 55 years or older, the absolute lifetime risk of relapse after progressive MS onset was 18%, 17%, 13%, and 5%, respectively. The corresponding last predicted relapse for these groups was before age 50, age 60, age 70, and age 70.
Taken together, the data suggest that in patients transitioning to progressive MS, initiation or continuation of a DMD is most likely to be beneficial if the patient is younger than 35, with some benefit, albeit less, up to the age of 54, according to Dr. Kantarci.
“But above 55, if a person has never been on a DMD, it is unlikely to be recommended, because I don’t expect it to do anything from the data we have,” he said. Furthermore, “DMD stopping can be offered to these patients. If a person is on a DMD and they are asking, ‘Can I stop it? I have been stable,’ and they are above age 55, it can be considered.”
The investigators are performing additional analyses of the data to assess the impact of DMDs on disease course, including the influence of initial and maintenance treatment choices, and factors that prompt physicians to switch treatments.
“What we haven’t done and will not be possible with this data ... the most interesting question is the impact of subclinical MRI disease, which is a different question,” Dr. Kantarci concluded. “And ultimately, we will have to have an actual stopping experiment and [assess] outcomes, which is an ongoing major planned effort.”
Outcomes after stopping immunomodulators
The second study assessed clinical and radiologic outcomes after discontinuation of immunomodulatory therapy in patients with secondary progressive MS.
“We have more and more patients [with secondary progressive disease] treated for several years, yet the natural history of the disease is less and less relapse, and progression of disability,” commented first author Dr. Julien Bonenfant, a neurologist at the Rennes University Hospital in France. Thus, the benefit of continuing treatment is unclear, especially given its cost and side effects.
He and his colleagues studied 106 consecutive patients with secondary progressive MS who had been on immunomodulators for at least 6 months, were taken off the immunomodulators, and were followed for a mean of 5 years.
Results showed that 16% of the patients had a clinical relapse after discontinuation, nearly all within the first 3 years. The annualized rate of clinical relapse actually fell from 0.13 in the 3 years before discontinuation to 0.07 in the 3 years afterward.
Overall, 35% of patients had either a clinical relapse and/or new contrast enhancement on MRI. Again, most of these events occurred within the first 3 years of discontinuation.
Patients had a lower risk of this outcome after treatment discontinuation if they had an Expanded Disability Status Scale (EDSS) score of 6 or greater at the time of discontinuation (hazard ratio, 0.4) and if they had not had any gadolinium enhancement on MRI in the 3 years before treatment discontinuation (HR, 0.4).
“Disease activity remained low after treatment withdrawal. We found no rebound of relapse rate in our population,” Dr. Bonenfant summarized. “There was no consequence on the slope of disability progression,” nor on the finding of enhancement on MRI alone.
Thirty patients were restarted on immunomodulators, about half of them solely because of MRI findings, he noted. This raises “the controversial question, is it relevant or not to resume treatment in these patients?”
“This study suggests that immunomodulatory treatment withdrawal seems reasonable for patients with advanced secondary progressive MS, especially with an EDSS of 6 or greater and no focal inflammatory disease [clinical or radiologic] at least in the past 3 years,” Dr. Bonenfant maintained. “It shows the importance of MRI monitoring to define the patients who are still in a focal immunoreactive state.”
“The results are far from being definitive, and further prospective studies are needed to provide evidence-based recommendations for clinical practice,” he concluded.
Dr. Kantarci disclosed that he has given scientific presentations at meetings supported by Novartis Pharmaceuticals and has presented as an invited speaker for Biogen but has received no personal compensation from either company. Dr. Bonenfant disclosed that he had no relevant conflicts of interest.
VANCOUVER – Certain patient and disease characteristics may help guide decisions about starting and stopping therapy in progressive multiple sclerosis, according to a pair of longitudinal cohort studies reported at the annual meeting of the American Academy of Neurology.
In a cohort of patients transitioning from relapsing-remitting to progressive multiple sclerosis (MS), the age at onset of progression predicted the likelihood of subsequent relapses. The absolute lifetime risk ranged from 18% for patients younger than 35 years at the time to just 5% for those aged 55 years or older at the time.
And in a cohort of patients with secondary progressive MS, the annual rate of clinical relapse fell in the third year after immunomodulator discontinuation. Overall, 35% had a clinical relapse or radiologic disease activity. Patients had a lower risk of this outcome if they had greater disability at the time of discontinuation or if they had not had any radiologic disease activity in the antecedent years.
“These studies address a very important question, because not many people talk about stopping drugs,” commented session comoderator Helen Tremlett, Ph.D., of the division of neurology at the University of British Columbia, Vancouver, and the Canada Research Chair in Neuroepidemiology and Multiple Sclerosis. “I would like to see some of these findings validated in other cohorts. But I did like the questions they are asking.”
Age, risk of postprogression relapse
The first study focused on ongoing relapses in patients transitioning to progressive MS. “We have recently shown that these relapses indeed matter. People who continue to relapse after progressive MS onset develop a need for a cane 2 years earlier than those who don’t” continue to have relapses, explained senior author Dr. Orhun H. Kantarci of the department of neurology at the Mayo Clinic in Rochester, Minn. Therefore, continuation or initiation of disease-modifying drugs (DMDs) during this period of overlap may be beneficial.
He and his colleagues followed 946 patients with MS from a clinic- and population-based cohort, assessing the age at various disease landmarks.
Results showed the mean age at first relapse was 33 years, the mean age at the onset of progressive MS was 45 years, and the mean age at last relapse (whether it occurred before or after the onset of progressive disease) was 43 years.
The 95% overlap age range for age at first relapse and age at onset of progressive MS was 27-46 years, Dr. Kantarci reported. Therefore, DMDs would be expected to have a some impact during those years.
Further analyses showed that if the age of progressive MS onset was before 35 years, 35-44 years, 45-54 years, and 55 years or older, the absolute lifetime risk of relapse after progressive MS onset was 18%, 17%, 13%, and 5%, respectively. The corresponding last predicted relapse for these groups was before age 50, age 60, age 70, and age 70.
Taken together, the data suggest that in patients transitioning to progressive MS, initiation or continuation of a DMD is most likely to be beneficial if the patient is younger than 35, with some benefit, albeit less, up to the age of 54, according to Dr. Kantarci.
“But above 55, if a person has never been on a DMD, it is unlikely to be recommended, because I don’t expect it to do anything from the data we have,” he said. Furthermore, “DMD stopping can be offered to these patients. If a person is on a DMD and they are asking, ‘Can I stop it? I have been stable,’ and they are above age 55, it can be considered.”
The investigators are performing additional analyses of the data to assess the impact of DMDs on disease course, including the influence of initial and maintenance treatment choices, and factors that prompt physicians to switch treatments.
“What we haven’t done and will not be possible with this data ... the most interesting question is the impact of subclinical MRI disease, which is a different question,” Dr. Kantarci concluded. “And ultimately, we will have to have an actual stopping experiment and [assess] outcomes, which is an ongoing major planned effort.”
Outcomes after stopping immunomodulators
The second study assessed clinical and radiologic outcomes after discontinuation of immunomodulatory therapy in patients with secondary progressive MS.
“We have more and more patients [with secondary progressive disease] treated for several years, yet the natural history of the disease is less and less relapse, and progression of disability,” commented first author Dr. Julien Bonenfant, a neurologist at the Rennes University Hospital in France. Thus, the benefit of continuing treatment is unclear, especially given its cost and side effects.
He and his colleagues studied 106 consecutive patients with secondary progressive MS who had been on immunomodulators for at least 6 months, were taken off the immunomodulators, and were followed for a mean of 5 years.
Results showed that 16% of the patients had a clinical relapse after discontinuation, nearly all within the first 3 years. The annualized rate of clinical relapse actually fell from 0.13 in the 3 years before discontinuation to 0.07 in the 3 years afterward.
Overall, 35% of patients had either a clinical relapse and/or new contrast enhancement on MRI. Again, most of these events occurred within the first 3 years of discontinuation.
Patients had a lower risk of this outcome after treatment discontinuation if they had an Expanded Disability Status Scale (EDSS) score of 6 or greater at the time of discontinuation (hazard ratio, 0.4) and if they had not had any gadolinium enhancement on MRI in the 3 years before treatment discontinuation (HR, 0.4).
“Disease activity remained low after treatment withdrawal. We found no rebound of relapse rate in our population,” Dr. Bonenfant summarized. “There was no consequence on the slope of disability progression,” nor on the finding of enhancement on MRI alone.
Thirty patients were restarted on immunomodulators, about half of them solely because of MRI findings, he noted. This raises “the controversial question, is it relevant or not to resume treatment in these patients?”
“This study suggests that immunomodulatory treatment withdrawal seems reasonable for patients with advanced secondary progressive MS, especially with an EDSS of 6 or greater and no focal inflammatory disease [clinical or radiologic] at least in the past 3 years,” Dr. Bonenfant maintained. “It shows the importance of MRI monitoring to define the patients who are still in a focal immunoreactive state.”
“The results are far from being definitive, and further prospective studies are needed to provide evidence-based recommendations for clinical practice,” he concluded.
Dr. Kantarci disclosed that he has given scientific presentations at meetings supported by Novartis Pharmaceuticals and has presented as an invited speaker for Biogen but has received no personal compensation from either company. Dr. Bonenfant disclosed that he had no relevant conflicts of interest.
VANCOUVER – Certain patient and disease characteristics may help guide decisions about starting and stopping therapy in progressive multiple sclerosis, according to a pair of longitudinal cohort studies reported at the annual meeting of the American Academy of Neurology.
In a cohort of patients transitioning from relapsing-remitting to progressive multiple sclerosis (MS), the age at onset of progression predicted the likelihood of subsequent relapses. The absolute lifetime risk ranged from 18% for patients younger than 35 years at the time to just 5% for those aged 55 years or older at the time.
And in a cohort of patients with secondary progressive MS, the annual rate of clinical relapse fell in the third year after immunomodulator discontinuation. Overall, 35% had a clinical relapse or radiologic disease activity. Patients had a lower risk of this outcome if they had greater disability at the time of discontinuation or if they had not had any radiologic disease activity in the antecedent years.
“These studies address a very important question, because not many people talk about stopping drugs,” commented session comoderator Helen Tremlett, Ph.D., of the division of neurology at the University of British Columbia, Vancouver, and the Canada Research Chair in Neuroepidemiology and Multiple Sclerosis. “I would like to see some of these findings validated in other cohorts. But I did like the questions they are asking.”
Age, risk of postprogression relapse
The first study focused on ongoing relapses in patients transitioning to progressive MS. “We have recently shown that these relapses indeed matter. People who continue to relapse after progressive MS onset develop a need for a cane 2 years earlier than those who don’t” continue to have relapses, explained senior author Dr. Orhun H. Kantarci of the department of neurology at the Mayo Clinic in Rochester, Minn. Therefore, continuation or initiation of disease-modifying drugs (DMDs) during this period of overlap may be beneficial.
He and his colleagues followed 946 patients with MS from a clinic- and population-based cohort, assessing the age at various disease landmarks.
Results showed the mean age at first relapse was 33 years, the mean age at the onset of progressive MS was 45 years, and the mean age at last relapse (whether it occurred before or after the onset of progressive disease) was 43 years.
The 95% overlap age range for age at first relapse and age at onset of progressive MS was 27-46 years, Dr. Kantarci reported. Therefore, DMDs would be expected to have a some impact during those years.
Further analyses showed that if the age of progressive MS onset was before 35 years, 35-44 years, 45-54 years, and 55 years or older, the absolute lifetime risk of relapse after progressive MS onset was 18%, 17%, 13%, and 5%, respectively. The corresponding last predicted relapse for these groups was before age 50, age 60, age 70, and age 70.
Taken together, the data suggest that in patients transitioning to progressive MS, initiation or continuation of a DMD is most likely to be beneficial if the patient is younger than 35, with some benefit, albeit less, up to the age of 54, according to Dr. Kantarci.
“But above 55, if a person has never been on a DMD, it is unlikely to be recommended, because I don’t expect it to do anything from the data we have,” he said. Furthermore, “DMD stopping can be offered to these patients. If a person is on a DMD and they are asking, ‘Can I stop it? I have been stable,’ and they are above age 55, it can be considered.”
The investigators are performing additional analyses of the data to assess the impact of DMDs on disease course, including the influence of initial and maintenance treatment choices, and factors that prompt physicians to switch treatments.
“What we haven’t done and will not be possible with this data ... the most interesting question is the impact of subclinical MRI disease, which is a different question,” Dr. Kantarci concluded. “And ultimately, we will have to have an actual stopping experiment and [assess] outcomes, which is an ongoing major planned effort.”
Outcomes after stopping immunomodulators
The second study assessed clinical and radiologic outcomes after discontinuation of immunomodulatory therapy in patients with secondary progressive MS.
“We have more and more patients [with secondary progressive disease] treated for several years, yet the natural history of the disease is less and less relapse, and progression of disability,” commented first author Dr. Julien Bonenfant, a neurologist at the Rennes University Hospital in France. Thus, the benefit of continuing treatment is unclear, especially given its cost and side effects.
He and his colleagues studied 106 consecutive patients with secondary progressive MS who had been on immunomodulators for at least 6 months, were taken off the immunomodulators, and were followed for a mean of 5 years.
Results showed that 16% of the patients had a clinical relapse after discontinuation, nearly all within the first 3 years. The annualized rate of clinical relapse actually fell from 0.13 in the 3 years before discontinuation to 0.07 in the 3 years afterward.
Overall, 35% of patients had either a clinical relapse and/or new contrast enhancement on MRI. Again, most of these events occurred within the first 3 years of discontinuation.
Patients had a lower risk of this outcome after treatment discontinuation if they had an Expanded Disability Status Scale (EDSS) score of 6 or greater at the time of discontinuation (hazard ratio, 0.4) and if they had not had any gadolinium enhancement on MRI in the 3 years before treatment discontinuation (HR, 0.4).
“Disease activity remained low after treatment withdrawal. We found no rebound of relapse rate in our population,” Dr. Bonenfant summarized. “There was no consequence on the slope of disability progression,” nor on the finding of enhancement on MRI alone.
Thirty patients were restarted on immunomodulators, about half of them solely because of MRI findings, he noted. This raises “the controversial question, is it relevant or not to resume treatment in these patients?”
“This study suggests that immunomodulatory treatment withdrawal seems reasonable for patients with advanced secondary progressive MS, especially with an EDSS of 6 or greater and no focal inflammatory disease [clinical or radiologic] at least in the past 3 years,” Dr. Bonenfant maintained. “It shows the importance of MRI monitoring to define the patients who are still in a focal immunoreactive state.”
“The results are far from being definitive, and further prospective studies are needed to provide evidence-based recommendations for clinical practice,” he concluded.
Dr. Kantarci disclosed that he has given scientific presentations at meetings supported by Novartis Pharmaceuticals and has presented as an invited speaker for Biogen but has received no personal compensation from either company. Dr. Bonenfant disclosed that he had no relevant conflicts of interest.
AT THE AAN 2016 ANNUAL MEETING
Key clinical point: Patient and disease characteristics may help guide decisions about starting and stopping therapy in progressive MS.
Major finding: The absolute risk of symptomatic relapse after the onset of progressive disease fell with the age at this onset, from 18% for patients younger than 35 at that time to 5% in patients 55 and older. In patients with secondary progressive disease, the annualized clinical relapse rate was 0.13 in the 3 years before and 0.07 in the 3 years after immunomodulator discontinuation.
Data source: A pair of longitudinal cohort studies in 964 patients transitioning to progressive MS and 106 patients with secondary progressive MS.
Disclosures: Dr. Kantarci disclosed that he has given scientific presentations at meetings supported by Novartis Pharmaceuticals and has presented as an invited speaker for Biogen, but has received no personal compensation from either company. Dr. Bonenfant disclosed that he had no relevant conflicts of interest.
Get to Know NO: Deconstructing the Data on Nitric Oxide–Releasing Technologies for Acne
In addition to the standard fare at the 74th Annual Meeting of the American Academy of Dermatology (AAD) in Washington, DC (March 4–8, 2016), this year there were several lectures addressing the use of nitric oxide (NO) for the treatment of acne. Therefore, I would like to review how NO gets delivered and the therapeutic implications as well as provide some context and understanding of the varying NO delivery systems being investigated.
Let’s start with some basics: Why should we even consider NO, a diatomic lipophilic gaseous molecule, for acne? It may be a surprise, but you already use NO for this purpose.
- NO is produced on the surface of the skin by action of commensal bacteria and plays a physiologic role in inhibition of infection by pathogenic organisms including bacteria, fungi, and viruses, and a microbicidal role against Propionibacterium acnes.
- NO minimizes inflammation by inhibiting neutrophil chemotaxis; production of lipases by P acnes (minimizes production of immunogenic free fatty acids); production of multiple cytokines such as tumor necrosis factor α, IL-8, and IL-6; antigen-presenting cell recognition of P acnes; and multiple elements of the NLRP3 (NOD-like receptor family, pyrin domain containing 3) inflammasome, the specific inflammasome reported to be impressively activated when monocytes, and even sebocytes, are exposed to P acnes, thereby inhibiting the conversion of pro–IL-1β to IL-1β.
However, NO’s direct biological action is not enough to explain these effects. It is S-nitrosylation, the covalent modification of a protein cysteine thiol by a NO group to generate an S-nitrosothiol such as nitrosoglutathione, that explains NO’s potent modulation of gene expression and enzymatic functions.
Nitric oxide was first featured in the late-breaking research session presented by Lawrence F. Eichenfield, MD, at the AAD (Efficacy and Safety of SB204 Gel in the Treatment of Acne Vulgaris)(F053). Results were presented from a phase 2b, multicenter, randomized, double-blind study comparing the efficacy, safety, and tolerability of SB204 NO-releasing gel 4% to vehicle in participants with acne vulgaris. The investigators concluded that SB204 once daily was safe and effective for the treatment of acne vulgaris, though they did not present data on the technology itself.
The NO-releasing technology being used in SB204 is an NO donor that falls under a class of NO donors called the diazeniumdiolates, or NONOates, which have been used experimentally for more than 50 years. These compounds consist of a diolate group (N[O-]N=O) bound to a nucleophile adduct (a primary or secondary amine or polyamine) by means of a nitrogen atom. Thus, you have NO bound to a donor that under appropriate environmental conditions will release its NO following first-order kinetics. It simply releases NO, rather then generate or create it.
Two issues are to be raised in relation to Dr. Eichenfield’s presentation:
- The anti-inflammatory mechanism data cited in the study by Qin et al and discussed was not generated using the NONOate SB204.
Here is the most important point to be made: Not all NO-releasing platforms are created equal. The technology used to demonstrate the anti-inflammatory impact of NO, specifically inhibition of IL-1β through the NLRP3 inflammasome, was a different platform than SB204, and one I developed at the Albert Einstein College of Medicine (Bronx, New York) and is currently under development. This NO generator, as opposed to donor, has been shown to uniquely facilitate the formation of NO from nitrite salt through a stable and potent NO intermediate N2O3 (designated NO-np).
N2O3 can effectively facilitate trans-nitrosylation under both aerobic and anaerobic conditions, a feat my research group has found that NONOates cannot accomplish. It is both NO and its effect when placed on cellular thiols that together generate its biological impact. Therefore, it cannot be assumed that efficacy data produced from the use of NO-np would result from using any NONOate.
- A highlight of this presentation was safety. First, a reality check: When do we ever use a topical agent for only 12 weeks, as in the study discussed by Dr. Eichenfield? In fact, given the mechanism by which NO exerts its anti-inflammatory activity, the efficacy will be short-lived and require continued use.
Accumulation of amines and their metabolites released from NONOates have been shown to induce cytotoxicity in a study by Saavedra et al (J Med Chem. 1997;40:1947-1954). In the study by Blecher et al (Nanomedicine. 2012;8:1364-1371), topical application of DETA (diethylenetriamine) NONOate, another type of NONOate, actually delayed wound closure in NOD-SCID (nonobese diabetic severe combined immunodeficiency) mice as compared to untreated controls in a study by Blecher et al. Systemic infusion at concentrations required to reduce blood pressure resulted in methemoglobinemia and diminished oxygen-carrying capacity in a study by Cabrales et al (Free Radic Biol Med. 2010;49:530-538). The NONOate utilized in SB204 is encapsulated in a hydrogel particle to prevent permeation of said metabolites and donor compounds through the skin; however, a 12-week safety evaluation is certainly not long enough to determine whether local or systemic absorption has occurred. Of note, the NO-np has undergone extensive safety testing from cell culture of embryonic zebra fish to Syrian hamsters and even pigs showing no significant toxicity at any of the effective concentrations in animal studies.
Data published on the NO-np’s preclinical efficacy for the treatment of acne, infected excisions, and burn wounds were presented in 2 of my lectures at the AAD (Nanotechnology and Immunomodulators [F085] and Antimicrobial Dressings: Silver and Beyond [S056])(Chouake et al [J Drugs Dermatol. 2012;11:1471-1477]; Friedman et al [Virulence. 2011;2:217-221]; Han et al [PLoS One. 2009;4:e7804]; Marcherla et al [Front Microbiol. 2012;3:193]; Martinez et al [J Invest Dermatol. 2009;129:2463-2469]; Qin et al [J Invest Dermatol. 2015;135:2723-2731]; Blecher et al [Nanomedicine. 2012;8:1364-1371]). These data can be found within the suggested reading below.
What’s the issue?
Know the awesome biological power of NO. Know the differences between delivery systems, including donors and generators. Know the differences in therapeutic relevance, including efficacy and safety.
Do you know NO?
We want to know your views! Tell us what you think.
Suggested Readings
Multidrug-Resistant Bacterial and Fungal Skin and Soft Tissue Infections
- Ahmadi M, Lee H, Sanchez D, et al. Sustained nitric oxide releasing nanoparticles induce cell death in Candida albicans yeast and hyphal cells preventing biofilm formation in vitro and in a rodent central venous catheter model. Antimicrob Agents Chemother. 2016;60:2185-2194.
- Chouake J, Schairer D, Kutner A, et al. Nitrosoglutathione generating nitric oxide nanoparticles as an improved strategy for combating Pseudomonas aeruginosa–infected wounds. J Drugs Dermatol. 2012;11:1471-1477.
- Friedman A, Blecher K, Sanchez D, et al. Susceptibility of gram positive and negative bacteria to novel nitric oxide-releasing nanoparticle technology. Virulence. 2011;2:217-221.
- Friedman A, Blecher K, Schairer D, et al. Improved antimicrobial efficacy with nitric oxide releasing nanoparticle generated S-nitrosoglutathione. Nitric Oxide. 2011;25:381-386.
- Han G, Martinez LM, Mihu MR, et al. Nitric oxide releasing nanoparticles are therapeutic for Staphylococcus aureus abscesses in murine model of infection. PLoS One. 2009;4:e7804.
- Landriscina A, Rosen J, Blecher-Paz K, et al. Nitric oxide-releasing nanoparticles as a treatment for cutaneous dermatophyte infections. Sci Lett. 2015,4:193.
- Marcherla C, Sanchez DA, Ahmadi M, et al. Nitric oxide releasing nanoparticles for the treatment of Candida albicans burn infections [published online June 8, 2012]. Front Microbiol. 2012;3:193.
- Martinez L, Han G, Chacko M, et al. Antimicrobial and healing efficacy of sustained release nitric oxide nanoparticles against Staphylococcus aureus skin infections. J Invest Dermatol. 2009;129:2463-2469.
- Mihu MR, Sandkovsky U, Han G, et al. The use of nitric oxide releasing nanoparticles as a treatment against Acinetobacter baumannii in wound infections. Virulence. 2010;1:62-67.
- Mordorski B, Pelgrift R, Adler B, et al. S-nitrosocaptopril nanoparticles as nitric oxide-liberating and transnitrosylating anti-infective technology. Nanomedicine. 2015;11:283-291.
- Qin M, Landriscina A, Rosen JM, et al. Nitric oxide-releasing nanoparticles prevent Propionibacterium acnes-induced inflammation by both clearing the organism and inhibiting microbial stimulation of the innate immune response. J Invest Dermatol. 2015;135:2723-2731.
- Schairer D, Martinez L, Blecher K, et al. Nitric oxide nanoparticles: pre-clinical utility as a therapeutic for intramuscular abscesses. Virulence. 2012;3:1-6.
Wound Healing
- Blecher K, Martinez LR, Tuckman-Vernon C, et al. Nitric oxide-releasing nanoparticles accelerate wound healing in NOD-SCID mice. Nanomedicine. 2012;8:1364-1371.
- Han G, Nguyen LN, Macherla C, et al. Nitric oxide-releasing nanoparticles accelerate wound healing by promoting fibroblast migration and collagen deposition. Am J Pathol. 2012;180:1465-1473.
Erectile Dysfunction
- Han G, Tar M, Kuppam DS, et al. Nanoparticles as a novel delivery vehicle for therapeutics targeting erectile dysfunction [published online September 18, 2009. J Sex Med. 2010;7(1 pt 1):224-333.
- Tar M, CabralesP, Navati M, et al. Topically applied NO-releasing nanoparticles can increase intracorporal pressure and elicit spontaneous erections in a rat model of radical prostatectomy. J Sex Med. 2014;11:2903-2914.
Cardiovascular Disease
- Cabrales P, Han G, Nacharaju P, et al. Reversal of hemoglobin-induced vasoconstriction with sustained release of nitric oxide [published online November 5, 2010]. Am J Physiol Heart Circ Physiol. 2011;300:H49-H56.
- Cabrales P, Han G, Roche C, et al. Sustained release nitric oxide from long-lived circulation nanoparticles. Free Radic Biol Med. 2010;49:530-538.
- Nacharaju P, Friedman AJ, Friedman JM, et al. Exogenous nitric oxide prevents collapse during hemorrhagic shock. Resuscitation. 2011;82:607-613.
Safety of NO Donors
- Friedman A, Friedman JM. Novel biomaterials for the sustained release of nitric oxide: past, present, and future. Expert Opin Drug Deliv. 2009;6:1113-1122.
- Liang H, Nacharaju P, Friedman A, et al. Nitric oxide generating/releasing materials. Future Sci OA. 2015;1. doi:10.4155/fso.15.54.
- Saavedra JE, Billiar TR, Williams DL, et al. Targeting nitric oxide (NO) delivery in vivo. design of a liver-selective NO donor prodrug that blocks tumor necrosis factor-alpha-induced apoptosis and toxicity in the liver. J Med Chem. 1997;40:1947-1954.
In addition to the standard fare at the 74th Annual Meeting of the American Academy of Dermatology (AAD) in Washington, DC (March 4–8, 2016), this year there were several lectures addressing the use of nitric oxide (NO) for the treatment of acne. Therefore, I would like to review how NO gets delivered and the therapeutic implications as well as provide some context and understanding of the varying NO delivery systems being investigated.
Let’s start with some basics: Why should we even consider NO, a diatomic lipophilic gaseous molecule, for acne? It may be a surprise, but you already use NO for this purpose.
- NO is produced on the surface of the skin by action of commensal bacteria and plays a physiologic role in inhibition of infection by pathogenic organisms including bacteria, fungi, and viruses, and a microbicidal role against Propionibacterium acnes.
- NO minimizes inflammation by inhibiting neutrophil chemotaxis; production of lipases by P acnes (minimizes production of immunogenic free fatty acids); production of multiple cytokines such as tumor necrosis factor α, IL-8, and IL-6; antigen-presenting cell recognition of P acnes; and multiple elements of the NLRP3 (NOD-like receptor family, pyrin domain containing 3) inflammasome, the specific inflammasome reported to be impressively activated when monocytes, and even sebocytes, are exposed to P acnes, thereby inhibiting the conversion of pro–IL-1β to IL-1β.
However, NO’s direct biological action is not enough to explain these effects. It is S-nitrosylation, the covalent modification of a protein cysteine thiol by a NO group to generate an S-nitrosothiol such as nitrosoglutathione, that explains NO’s potent modulation of gene expression and enzymatic functions.
Nitric oxide was first featured in the late-breaking research session presented by Lawrence F. Eichenfield, MD, at the AAD (Efficacy and Safety of SB204 Gel in the Treatment of Acne Vulgaris)(F053). Results were presented from a phase 2b, multicenter, randomized, double-blind study comparing the efficacy, safety, and tolerability of SB204 NO-releasing gel 4% to vehicle in participants with acne vulgaris. The investigators concluded that SB204 once daily was safe and effective for the treatment of acne vulgaris, though they did not present data on the technology itself.
The NO-releasing technology being used in SB204 is an NO donor that falls under a class of NO donors called the diazeniumdiolates, or NONOates, which have been used experimentally for more than 50 years. These compounds consist of a diolate group (N[O-]N=O) bound to a nucleophile adduct (a primary or secondary amine or polyamine) by means of a nitrogen atom. Thus, you have NO bound to a donor that under appropriate environmental conditions will release its NO following first-order kinetics. It simply releases NO, rather then generate or create it.
Two issues are to be raised in relation to Dr. Eichenfield’s presentation:
- The anti-inflammatory mechanism data cited in the study by Qin et al and discussed was not generated using the NONOate SB204.
Here is the most important point to be made: Not all NO-releasing platforms are created equal. The technology used to demonstrate the anti-inflammatory impact of NO, specifically inhibition of IL-1β through the NLRP3 inflammasome, was a different platform than SB204, and one I developed at the Albert Einstein College of Medicine (Bronx, New York) and is currently under development. This NO generator, as opposed to donor, has been shown to uniquely facilitate the formation of NO from nitrite salt through a stable and potent NO intermediate N2O3 (designated NO-np).
N2O3 can effectively facilitate trans-nitrosylation under both aerobic and anaerobic conditions, a feat my research group has found that NONOates cannot accomplish. It is both NO and its effect when placed on cellular thiols that together generate its biological impact. Therefore, it cannot be assumed that efficacy data produced from the use of NO-np would result from using any NONOate.
- A highlight of this presentation was safety. First, a reality check: When do we ever use a topical agent for only 12 weeks, as in the study discussed by Dr. Eichenfield? In fact, given the mechanism by which NO exerts its anti-inflammatory activity, the efficacy will be short-lived and require continued use.
Accumulation of amines and their metabolites released from NONOates have been shown to induce cytotoxicity in a study by Saavedra et al (J Med Chem. 1997;40:1947-1954). In the study by Blecher et al (Nanomedicine. 2012;8:1364-1371), topical application of DETA (diethylenetriamine) NONOate, another type of NONOate, actually delayed wound closure in NOD-SCID (nonobese diabetic severe combined immunodeficiency) mice as compared to untreated controls in a study by Blecher et al. Systemic infusion at concentrations required to reduce blood pressure resulted in methemoglobinemia and diminished oxygen-carrying capacity in a study by Cabrales et al (Free Radic Biol Med. 2010;49:530-538). The NONOate utilized in SB204 is encapsulated in a hydrogel particle to prevent permeation of said metabolites and donor compounds through the skin; however, a 12-week safety evaluation is certainly not long enough to determine whether local or systemic absorption has occurred. Of note, the NO-np has undergone extensive safety testing from cell culture of embryonic zebra fish to Syrian hamsters and even pigs showing no significant toxicity at any of the effective concentrations in animal studies.
Data published on the NO-np’s preclinical efficacy for the treatment of acne, infected excisions, and burn wounds were presented in 2 of my lectures at the AAD (Nanotechnology and Immunomodulators [F085] and Antimicrobial Dressings: Silver and Beyond [S056])(Chouake et al [J Drugs Dermatol. 2012;11:1471-1477]; Friedman et al [Virulence. 2011;2:217-221]; Han et al [PLoS One. 2009;4:e7804]; Marcherla et al [Front Microbiol. 2012;3:193]; Martinez et al [J Invest Dermatol. 2009;129:2463-2469]; Qin et al [J Invest Dermatol. 2015;135:2723-2731]; Blecher et al [Nanomedicine. 2012;8:1364-1371]). These data can be found within the suggested reading below.
What’s the issue?
Know the awesome biological power of NO. Know the differences between delivery systems, including donors and generators. Know the differences in therapeutic relevance, including efficacy and safety.
Do you know NO?
We want to know your views! Tell us what you think.
Suggested Readings
Multidrug-Resistant Bacterial and Fungal Skin and Soft Tissue Infections
- Ahmadi M, Lee H, Sanchez D, et al. Sustained nitric oxide releasing nanoparticles induce cell death in Candida albicans yeast and hyphal cells preventing biofilm formation in vitro and in a rodent central venous catheter model. Antimicrob Agents Chemother. 2016;60:2185-2194.
- Chouake J, Schairer D, Kutner A, et al. Nitrosoglutathione generating nitric oxide nanoparticles as an improved strategy for combating Pseudomonas aeruginosa–infected wounds. J Drugs Dermatol. 2012;11:1471-1477.
- Friedman A, Blecher K, Sanchez D, et al. Susceptibility of gram positive and negative bacteria to novel nitric oxide-releasing nanoparticle technology. Virulence. 2011;2:217-221.
- Friedman A, Blecher K, Schairer D, et al. Improved antimicrobial efficacy with nitric oxide releasing nanoparticle generated S-nitrosoglutathione. Nitric Oxide. 2011;25:381-386.
- Han G, Martinez LM, Mihu MR, et al. Nitric oxide releasing nanoparticles are therapeutic for Staphylococcus aureus abscesses in murine model of infection. PLoS One. 2009;4:e7804.
- Landriscina A, Rosen J, Blecher-Paz K, et al. Nitric oxide-releasing nanoparticles as a treatment for cutaneous dermatophyte infections. Sci Lett. 2015,4:193.
- Marcherla C, Sanchez DA, Ahmadi M, et al. Nitric oxide releasing nanoparticles for the treatment of Candida albicans burn infections [published online June 8, 2012]. Front Microbiol. 2012;3:193.
- Martinez L, Han G, Chacko M, et al. Antimicrobial and healing efficacy of sustained release nitric oxide nanoparticles against Staphylococcus aureus skin infections. J Invest Dermatol. 2009;129:2463-2469.
- Mihu MR, Sandkovsky U, Han G, et al. The use of nitric oxide releasing nanoparticles as a treatment against Acinetobacter baumannii in wound infections. Virulence. 2010;1:62-67.
- Mordorski B, Pelgrift R, Adler B, et al. S-nitrosocaptopril nanoparticles as nitric oxide-liberating and transnitrosylating anti-infective technology. Nanomedicine. 2015;11:283-291.
- Qin M, Landriscina A, Rosen JM, et al. Nitric oxide-releasing nanoparticles prevent Propionibacterium acnes-induced inflammation by both clearing the organism and inhibiting microbial stimulation of the innate immune response. J Invest Dermatol. 2015;135:2723-2731.
- Schairer D, Martinez L, Blecher K, et al. Nitric oxide nanoparticles: pre-clinical utility as a therapeutic for intramuscular abscesses. Virulence. 2012;3:1-6.
Wound Healing
- Blecher K, Martinez LR, Tuckman-Vernon C, et al. Nitric oxide-releasing nanoparticles accelerate wound healing in NOD-SCID mice. Nanomedicine. 2012;8:1364-1371.
- Han G, Nguyen LN, Macherla C, et al. Nitric oxide-releasing nanoparticles accelerate wound healing by promoting fibroblast migration and collagen deposition. Am J Pathol. 2012;180:1465-1473.
Erectile Dysfunction
- Han G, Tar M, Kuppam DS, et al. Nanoparticles as a novel delivery vehicle for therapeutics targeting erectile dysfunction [published online September 18, 2009. J Sex Med. 2010;7(1 pt 1):224-333.
- Tar M, CabralesP, Navati M, et al. Topically applied NO-releasing nanoparticles can increase intracorporal pressure and elicit spontaneous erections in a rat model of radical prostatectomy. J Sex Med. 2014;11:2903-2914.
Cardiovascular Disease
- Cabrales P, Han G, Nacharaju P, et al. Reversal of hemoglobin-induced vasoconstriction with sustained release of nitric oxide [published online November 5, 2010]. Am J Physiol Heart Circ Physiol. 2011;300:H49-H56.
- Cabrales P, Han G, Roche C, et al. Sustained release nitric oxide from long-lived circulation nanoparticles. Free Radic Biol Med. 2010;49:530-538.
- Nacharaju P, Friedman AJ, Friedman JM, et al. Exogenous nitric oxide prevents collapse during hemorrhagic shock. Resuscitation. 2011;82:607-613.
Safety of NO Donors
- Friedman A, Friedman JM. Novel biomaterials for the sustained release of nitric oxide: past, present, and future. Expert Opin Drug Deliv. 2009;6:1113-1122.
- Liang H, Nacharaju P, Friedman A, et al. Nitric oxide generating/releasing materials. Future Sci OA. 2015;1. doi:10.4155/fso.15.54.
- Saavedra JE, Billiar TR, Williams DL, et al. Targeting nitric oxide (NO) delivery in vivo. design of a liver-selective NO donor prodrug that blocks tumor necrosis factor-alpha-induced apoptosis and toxicity in the liver. J Med Chem. 1997;40:1947-1954.
In addition to the standard fare at the 74th Annual Meeting of the American Academy of Dermatology (AAD) in Washington, DC (March 4–8, 2016), this year there were several lectures addressing the use of nitric oxide (NO) for the treatment of acne. Therefore, I would like to review how NO gets delivered and the therapeutic implications as well as provide some context and understanding of the varying NO delivery systems being investigated.
Let’s start with some basics: Why should we even consider NO, a diatomic lipophilic gaseous molecule, for acne? It may be a surprise, but you already use NO for this purpose.
- NO is produced on the surface of the skin by action of commensal bacteria and plays a physiologic role in inhibition of infection by pathogenic organisms including bacteria, fungi, and viruses, and a microbicidal role against Propionibacterium acnes.
- NO minimizes inflammation by inhibiting neutrophil chemotaxis; production of lipases by P acnes (minimizes production of immunogenic free fatty acids); production of multiple cytokines such as tumor necrosis factor α, IL-8, and IL-6; antigen-presenting cell recognition of P acnes; and multiple elements of the NLRP3 (NOD-like receptor family, pyrin domain containing 3) inflammasome, the specific inflammasome reported to be impressively activated when monocytes, and even sebocytes, are exposed to P acnes, thereby inhibiting the conversion of pro–IL-1β to IL-1β.
However, NO’s direct biological action is not enough to explain these effects. It is S-nitrosylation, the covalent modification of a protein cysteine thiol by a NO group to generate an S-nitrosothiol such as nitrosoglutathione, that explains NO’s potent modulation of gene expression and enzymatic functions.
Nitric oxide was first featured in the late-breaking research session presented by Lawrence F. Eichenfield, MD, at the AAD (Efficacy and Safety of SB204 Gel in the Treatment of Acne Vulgaris)(F053). Results were presented from a phase 2b, multicenter, randomized, double-blind study comparing the efficacy, safety, and tolerability of SB204 NO-releasing gel 4% to vehicle in participants with acne vulgaris. The investigators concluded that SB204 once daily was safe and effective for the treatment of acne vulgaris, though they did not present data on the technology itself.
The NO-releasing technology being used in SB204 is an NO donor that falls under a class of NO donors called the diazeniumdiolates, or NONOates, which have been used experimentally for more than 50 years. These compounds consist of a diolate group (N[O-]N=O) bound to a nucleophile adduct (a primary or secondary amine or polyamine) by means of a nitrogen atom. Thus, you have NO bound to a donor that under appropriate environmental conditions will release its NO following first-order kinetics. It simply releases NO, rather then generate or create it.
Two issues are to be raised in relation to Dr. Eichenfield’s presentation:
- The anti-inflammatory mechanism data cited in the study by Qin et al and discussed was not generated using the NONOate SB204.
Here is the most important point to be made: Not all NO-releasing platforms are created equal. The technology used to demonstrate the anti-inflammatory impact of NO, specifically inhibition of IL-1β through the NLRP3 inflammasome, was a different platform than SB204, and one I developed at the Albert Einstein College of Medicine (Bronx, New York) and is currently under development. This NO generator, as opposed to donor, has been shown to uniquely facilitate the formation of NO from nitrite salt through a stable and potent NO intermediate N2O3 (designated NO-np).
N2O3 can effectively facilitate trans-nitrosylation under both aerobic and anaerobic conditions, a feat my research group has found that NONOates cannot accomplish. It is both NO and its effect when placed on cellular thiols that together generate its biological impact. Therefore, it cannot be assumed that efficacy data produced from the use of NO-np would result from using any NONOate.
- A highlight of this presentation was safety. First, a reality check: When do we ever use a topical agent for only 12 weeks, as in the study discussed by Dr. Eichenfield? In fact, given the mechanism by which NO exerts its anti-inflammatory activity, the efficacy will be short-lived and require continued use.
Accumulation of amines and their metabolites released from NONOates have been shown to induce cytotoxicity in a study by Saavedra et al (J Med Chem. 1997;40:1947-1954). In the study by Blecher et al (Nanomedicine. 2012;8:1364-1371), topical application of DETA (diethylenetriamine) NONOate, another type of NONOate, actually delayed wound closure in NOD-SCID (nonobese diabetic severe combined immunodeficiency) mice as compared to untreated controls in a study by Blecher et al. Systemic infusion at concentrations required to reduce blood pressure resulted in methemoglobinemia and diminished oxygen-carrying capacity in a study by Cabrales et al (Free Radic Biol Med. 2010;49:530-538). The NONOate utilized in SB204 is encapsulated in a hydrogel particle to prevent permeation of said metabolites and donor compounds through the skin; however, a 12-week safety evaluation is certainly not long enough to determine whether local or systemic absorption has occurred. Of note, the NO-np has undergone extensive safety testing from cell culture of embryonic zebra fish to Syrian hamsters and even pigs showing no significant toxicity at any of the effective concentrations in animal studies.
Data published on the NO-np’s preclinical efficacy for the treatment of acne, infected excisions, and burn wounds were presented in 2 of my lectures at the AAD (Nanotechnology and Immunomodulators [F085] and Antimicrobial Dressings: Silver and Beyond [S056])(Chouake et al [J Drugs Dermatol. 2012;11:1471-1477]; Friedman et al [Virulence. 2011;2:217-221]; Han et al [PLoS One. 2009;4:e7804]; Marcherla et al [Front Microbiol. 2012;3:193]; Martinez et al [J Invest Dermatol. 2009;129:2463-2469]; Qin et al [J Invest Dermatol. 2015;135:2723-2731]; Blecher et al [Nanomedicine. 2012;8:1364-1371]). These data can be found within the suggested reading below.
What’s the issue?
Know the awesome biological power of NO. Know the differences between delivery systems, including donors and generators. Know the differences in therapeutic relevance, including efficacy and safety.
Do you know NO?
We want to know your views! Tell us what you think.
Suggested Readings
Multidrug-Resistant Bacterial and Fungal Skin and Soft Tissue Infections
- Ahmadi M, Lee H, Sanchez D, et al. Sustained nitric oxide releasing nanoparticles induce cell death in Candida albicans yeast and hyphal cells preventing biofilm formation in vitro and in a rodent central venous catheter model. Antimicrob Agents Chemother. 2016;60:2185-2194.
- Chouake J, Schairer D, Kutner A, et al. Nitrosoglutathione generating nitric oxide nanoparticles as an improved strategy for combating Pseudomonas aeruginosa–infected wounds. J Drugs Dermatol. 2012;11:1471-1477.
- Friedman A, Blecher K, Sanchez D, et al. Susceptibility of gram positive and negative bacteria to novel nitric oxide-releasing nanoparticle technology. Virulence. 2011;2:217-221.
- Friedman A, Blecher K, Schairer D, et al. Improved antimicrobial efficacy with nitric oxide releasing nanoparticle generated S-nitrosoglutathione. Nitric Oxide. 2011;25:381-386.
- Han G, Martinez LM, Mihu MR, et al. Nitric oxide releasing nanoparticles are therapeutic for Staphylococcus aureus abscesses in murine model of infection. PLoS One. 2009;4:e7804.
- Landriscina A, Rosen J, Blecher-Paz K, et al. Nitric oxide-releasing nanoparticles as a treatment for cutaneous dermatophyte infections. Sci Lett. 2015,4:193.
- Marcherla C, Sanchez DA, Ahmadi M, et al. Nitric oxide releasing nanoparticles for the treatment of Candida albicans burn infections [published online June 8, 2012]. Front Microbiol. 2012;3:193.
- Martinez L, Han G, Chacko M, et al. Antimicrobial and healing efficacy of sustained release nitric oxide nanoparticles against Staphylococcus aureus skin infections. J Invest Dermatol. 2009;129:2463-2469.
- Mihu MR, Sandkovsky U, Han G, et al. The use of nitric oxide releasing nanoparticles as a treatment against Acinetobacter baumannii in wound infections. Virulence. 2010;1:62-67.
- Mordorski B, Pelgrift R, Adler B, et al. S-nitrosocaptopril nanoparticles as nitric oxide-liberating and transnitrosylating anti-infective technology. Nanomedicine. 2015;11:283-291.
- Qin M, Landriscina A, Rosen JM, et al. Nitric oxide-releasing nanoparticles prevent Propionibacterium acnes-induced inflammation by both clearing the organism and inhibiting microbial stimulation of the innate immune response. J Invest Dermatol. 2015;135:2723-2731.
- Schairer D, Martinez L, Blecher K, et al. Nitric oxide nanoparticles: pre-clinical utility as a therapeutic for intramuscular abscesses. Virulence. 2012;3:1-6.
Wound Healing
- Blecher K, Martinez LR, Tuckman-Vernon C, et al. Nitric oxide-releasing nanoparticles accelerate wound healing in NOD-SCID mice. Nanomedicine. 2012;8:1364-1371.
- Han G, Nguyen LN, Macherla C, et al. Nitric oxide-releasing nanoparticles accelerate wound healing by promoting fibroblast migration and collagen deposition. Am J Pathol. 2012;180:1465-1473.
Erectile Dysfunction
- Han G, Tar M, Kuppam DS, et al. Nanoparticles as a novel delivery vehicle for therapeutics targeting erectile dysfunction [published online September 18, 2009. J Sex Med. 2010;7(1 pt 1):224-333.
- Tar M, CabralesP, Navati M, et al. Topically applied NO-releasing nanoparticles can increase intracorporal pressure and elicit spontaneous erections in a rat model of radical prostatectomy. J Sex Med. 2014;11:2903-2914.
Cardiovascular Disease
- Cabrales P, Han G, Nacharaju P, et al. Reversal of hemoglobin-induced vasoconstriction with sustained release of nitric oxide [published online November 5, 2010]. Am J Physiol Heart Circ Physiol. 2011;300:H49-H56.
- Cabrales P, Han G, Roche C, et al. Sustained release nitric oxide from long-lived circulation nanoparticles. Free Radic Biol Med. 2010;49:530-538.
- Nacharaju P, Friedman AJ, Friedman JM, et al. Exogenous nitric oxide prevents collapse during hemorrhagic shock. Resuscitation. 2011;82:607-613.
Safety of NO Donors
- Friedman A, Friedman JM. Novel biomaterials for the sustained release of nitric oxide: past, present, and future. Expert Opin Drug Deliv. 2009;6:1113-1122.
- Liang H, Nacharaju P, Friedman A, et al. Nitric oxide generating/releasing materials. Future Sci OA. 2015;1. doi:10.4155/fso.15.54.
- Saavedra JE, Billiar TR, Williams DL, et al. Targeting nitric oxide (NO) delivery in vivo. design of a liver-selective NO donor prodrug that blocks tumor necrosis factor-alpha-induced apoptosis and toxicity in the liver. J Med Chem. 1997;40:1947-1954.
Targeting gene rearrangements shows promise in early study
Entrectinib, an investigational drug that targets several abnormal fusion proteins, showed antitumor activity and was safe in patients with several different types of advanced solid tumors. The patients had never before been exposed to drugs targeting these same genetic alterations.
“Responses can be very rapid and durable … which include colorectal, primary brain tumor, astrocytoma, fibrosarcoma, lung, and mammary analog secretory carcinoma,” Dr. Alexander Drilon of Memorial Sloan Kettering Cancer Center in New York said in a news conference at the annual meeting of the American Association for Cancer Research. “Dramatic intracranial activity … has been demonstrated both in primary brain tumor and also in metastatic.”
NTRK1/2/3, ROS1, and ALK gene–rearranged cancers produce fusion proteins that are ligand independent for their activity and thus constitutively active, driving tumor growth. Entrectinib is a pan-TRK, ROS1, ALK tyrosine kinase inhibitor that targets the abnormal fusion protein products of the genes, is highly potent at low concentrations, and has been designed to cross the blood-brain barrier (BBB). The targeted proteins are present across multiple cancers and are especially prevalent (greater than 80%) among some rare adult and pediatric cancers.
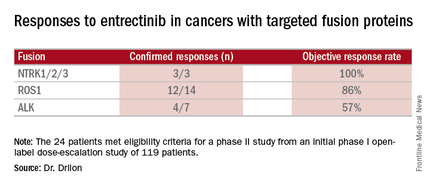
Combined data on 119 patients in two phase I trials established 600 mg orally once daily as the recommended dose to go into phase II trials. Among the 24 patients meeting eligibility criteria for a phase II trial (presence of the targeted gene fusions in their tumors, no prior treatment against these targets, and treatment at or above 600 mg daily), the confirmed response rate was 79% (19/24). Most were partial responses in terms of tumor shrinkage, but two patients had complete responses. Response rates appeared to vary according to the specific fusion protein defect.
All three cases of CNS disease with NTRK-rearranged cancers had intracranial responses, demonstrating that the drug crosses the BBB and is active. In one case, a 46-year-old man with brain metastases heavily pretreated for non–small cell lung cancer with an NTRK1 rearrangement experienced a dramatic response.
“The patient at that point was actually on hospice and was doing extremely poorly on supplemental oxygen,” Dr. Drilon said. “Within a few weeks, the patient had a dramatic clinical response to therapy … At day 26 there was almost a 50% reduction in tumor burden.” At day 317 scans showed he had a complete intracranial response to entrectinib, but he still has visceral disease on therapy past 1 year.
Responses often occurred within the first month of therapy, and many persisted for several months without disease progression, with one patient being followed for more than 2 years with clinical benefit. Nineteen of 24 patients have been on the therapy for more than 6 months, and the therapy appears to be safe and well tolerated.
Commenting on this study and others targeting specific genetic alterations leading to cancer, Dr. Louis Weiner, director of the Georgetown Lombardi Comprehensive Cancer Center in Washington, said, “You’re seeing a series of clinical trials described that aren’t necessarily targeting people with a particular cancer but rather people who have cancers characterized by particular molecular abnormalities.” Not all cancers will have identified molecular abnormalities driving them. “However, I think where you have these drivers, the proper thing to do is not to worry about whether [a drug] works in a given disease but rather whether it works for people with that particular abnormality,” he said.
For the future, the investigators plan a phase II trial called STARTRK-2. It is a multicenter, open-label, global basket study to include any solid tumors with the targeted rearrangements.
Dr. Drilon disclosed ties with Ignyta, which funded the study, and has received research funding from Foundation Medicine. Dr. Weiner disclosed ties with several pharmaceutical companies.
Entrectinib, an investigational drug that targets several abnormal fusion proteins, showed antitumor activity and was safe in patients with several different types of advanced solid tumors. The patients had never before been exposed to drugs targeting these same genetic alterations.
“Responses can be very rapid and durable … which include colorectal, primary brain tumor, astrocytoma, fibrosarcoma, lung, and mammary analog secretory carcinoma,” Dr. Alexander Drilon of Memorial Sloan Kettering Cancer Center in New York said in a news conference at the annual meeting of the American Association for Cancer Research. “Dramatic intracranial activity … has been demonstrated both in primary brain tumor and also in metastatic.”
NTRK1/2/3, ROS1, and ALK gene–rearranged cancers produce fusion proteins that are ligand independent for their activity and thus constitutively active, driving tumor growth. Entrectinib is a pan-TRK, ROS1, ALK tyrosine kinase inhibitor that targets the abnormal fusion protein products of the genes, is highly potent at low concentrations, and has been designed to cross the blood-brain barrier (BBB). The targeted proteins are present across multiple cancers and are especially prevalent (greater than 80%) among some rare adult and pediatric cancers.
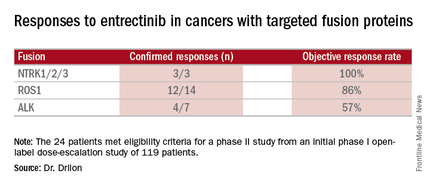
Combined data on 119 patients in two phase I trials established 600 mg orally once daily as the recommended dose to go into phase II trials. Among the 24 patients meeting eligibility criteria for a phase II trial (presence of the targeted gene fusions in their tumors, no prior treatment against these targets, and treatment at or above 600 mg daily), the confirmed response rate was 79% (19/24). Most were partial responses in terms of tumor shrinkage, but two patients had complete responses. Response rates appeared to vary according to the specific fusion protein defect.
All three cases of CNS disease with NTRK-rearranged cancers had intracranial responses, demonstrating that the drug crosses the BBB and is active. In one case, a 46-year-old man with brain metastases heavily pretreated for non–small cell lung cancer with an NTRK1 rearrangement experienced a dramatic response.
“The patient at that point was actually on hospice and was doing extremely poorly on supplemental oxygen,” Dr. Drilon said. “Within a few weeks, the patient had a dramatic clinical response to therapy … At day 26 there was almost a 50% reduction in tumor burden.” At day 317 scans showed he had a complete intracranial response to entrectinib, but he still has visceral disease on therapy past 1 year.
Responses often occurred within the first month of therapy, and many persisted for several months without disease progression, with one patient being followed for more than 2 years with clinical benefit. Nineteen of 24 patients have been on the therapy for more than 6 months, and the therapy appears to be safe and well tolerated.
Commenting on this study and others targeting specific genetic alterations leading to cancer, Dr. Louis Weiner, director of the Georgetown Lombardi Comprehensive Cancer Center in Washington, said, “You’re seeing a series of clinical trials described that aren’t necessarily targeting people with a particular cancer but rather people who have cancers characterized by particular molecular abnormalities.” Not all cancers will have identified molecular abnormalities driving them. “However, I think where you have these drivers, the proper thing to do is not to worry about whether [a drug] works in a given disease but rather whether it works for people with that particular abnormality,” he said.
For the future, the investigators plan a phase II trial called STARTRK-2. It is a multicenter, open-label, global basket study to include any solid tumors with the targeted rearrangements.
Dr. Drilon disclosed ties with Ignyta, which funded the study, and has received research funding from Foundation Medicine. Dr. Weiner disclosed ties with several pharmaceutical companies.
Entrectinib, an investigational drug that targets several abnormal fusion proteins, showed antitumor activity and was safe in patients with several different types of advanced solid tumors. The patients had never before been exposed to drugs targeting these same genetic alterations.
“Responses can be very rapid and durable … which include colorectal, primary brain tumor, astrocytoma, fibrosarcoma, lung, and mammary analog secretory carcinoma,” Dr. Alexander Drilon of Memorial Sloan Kettering Cancer Center in New York said in a news conference at the annual meeting of the American Association for Cancer Research. “Dramatic intracranial activity … has been demonstrated both in primary brain tumor and also in metastatic.”
NTRK1/2/3, ROS1, and ALK gene–rearranged cancers produce fusion proteins that are ligand independent for their activity and thus constitutively active, driving tumor growth. Entrectinib is a pan-TRK, ROS1, ALK tyrosine kinase inhibitor that targets the abnormal fusion protein products of the genes, is highly potent at low concentrations, and has been designed to cross the blood-brain barrier (BBB). The targeted proteins are present across multiple cancers and are especially prevalent (greater than 80%) among some rare adult and pediatric cancers.
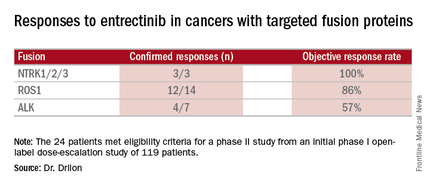
Combined data on 119 patients in two phase I trials established 600 mg orally once daily as the recommended dose to go into phase II trials. Among the 24 patients meeting eligibility criteria for a phase II trial (presence of the targeted gene fusions in their tumors, no prior treatment against these targets, and treatment at or above 600 mg daily), the confirmed response rate was 79% (19/24). Most were partial responses in terms of tumor shrinkage, but two patients had complete responses. Response rates appeared to vary according to the specific fusion protein defect.
All three cases of CNS disease with NTRK-rearranged cancers had intracranial responses, demonstrating that the drug crosses the BBB and is active. In one case, a 46-year-old man with brain metastases heavily pretreated for non–small cell lung cancer with an NTRK1 rearrangement experienced a dramatic response.
“The patient at that point was actually on hospice and was doing extremely poorly on supplemental oxygen,” Dr. Drilon said. “Within a few weeks, the patient had a dramatic clinical response to therapy … At day 26 there was almost a 50% reduction in tumor burden.” At day 317 scans showed he had a complete intracranial response to entrectinib, but he still has visceral disease on therapy past 1 year.
Responses often occurred within the first month of therapy, and many persisted for several months without disease progression, with one patient being followed for more than 2 years with clinical benefit. Nineteen of 24 patients have been on the therapy for more than 6 months, and the therapy appears to be safe and well tolerated.
Commenting on this study and others targeting specific genetic alterations leading to cancer, Dr. Louis Weiner, director of the Georgetown Lombardi Comprehensive Cancer Center in Washington, said, “You’re seeing a series of clinical trials described that aren’t necessarily targeting people with a particular cancer but rather people who have cancers characterized by particular molecular abnormalities.” Not all cancers will have identified molecular abnormalities driving them. “However, I think where you have these drivers, the proper thing to do is not to worry about whether [a drug] works in a given disease but rather whether it works for people with that particular abnormality,” he said.
For the future, the investigators plan a phase II trial called STARTRK-2. It is a multicenter, open-label, global basket study to include any solid tumors with the targeted rearrangements.
Dr. Drilon disclosed ties with Ignyta, which funded the study, and has received research funding from Foundation Medicine. Dr. Weiner disclosed ties with several pharmaceutical companies.
FROM THE AACR ANNUAL MEETING
Key clinical point: Entrectinib showed antitumor activity including intracranial responses.
Major finding: Patients with the targeted abnormalities had a 79% response rate.
Data source: Twenty-four patients meeting eligibility criteria for a phase II study from an initial phase I open-label dose-escalation study of 119 patients.
Disclosures: Dr. Drilon disclosed ties with Ignyta, which funded the study, and has received research funding from Foundation Medicine. Dr. Weiner disclosed ties with several pharmaceutical companies.
Smooth hair – an acne-causing epidemic
Do you ask your acne patients about which hair products they use? This common question has recently brought our attention to popular hair products that are causing an acne epidemic. Have we forgotten about “Pomade acne”? Well, it’s making a comeback. Originally described in ethnic women, new frizz-fighting hair products have resurged and so has pomade acne in all skin types and in both men and women.
Smoothing serums, heat styling sprays, leave-in products popularly known as “It’s-a-10,” “Biosilk,” “anti-frizz serums,” “heat-protectants,” “thermal setting sprays,” and “shine sprays,” contain silicone-derived ingredients and oils to control frizz, add shine, and detangle the hair. They work by smoothing the hair cuticle, and for women with difficult-to-manage hair, they have become an essential part of the daily beauty regimen.
Men are not in the clear either. Hair waxes and pomades used to style men’s hair contain greasy wax-based ingredients that also clog pores, trap bacteria, and cause inflammatory breakouts.
As a general rule in skin and body care, most products work well for what they are made to do, but when misused, they can cause mishaps. You wouldn’t moisturize your face with your hair serum would you? It seems obvious that this could cause some skin issues; however, most people will not think to correlate their acne breakouts with their hair products until we mention it. These products rub off on the face or on the pillow at night. In addition, the less we wash our hair, the more we are going to bed and getting the daytime products all over our pillowcases. Our faces are rolling around in oily, waxy, hair products all night.
Makeup is known to cause acne, and some of the makeups that are well known culprits contain the same ingredients as in hair products. Foundations, primers, and popular “BB” creams often contain cyclopentasiloxane and dimethicone. They serve a similar purpose: smoothing the skin and smoothing the hair. Both should be avoided in acne-prone patients.
Common culprits in hair products include PVP/DMAPA acrylates, cyclopentasiloxane, panthenol, dimethicone, silicone, Quaternium-70, oils, and petrolatum.
The only way to eliminate acne caused by hair products is to completely eliminate the hair product from the daily routine. However, if your patients can’t live without their hair products, here are some tips to share with them to reduce breakouts:
• Choose a hairstyle that keeps the hair away from the face, or wear hair up to avoid prolonged contact with the face, particularly while sleeping.
• Change pillowcase often (every day if possible), especially for side sleepers. Regardless of the fabric, pillowcases trap oil, dirt, and bacteria.
• Shower at night and sleep with clean hair and clean skin.
• Style hair before applying makeup. Wash hands thoroughly to remove all hair products before touching the skin.
• Cover the face prior to applying any hair sprays.
• Cover the hair at bedtime; however, tight head coverings can stimulate sweat and cause scalp breakouts.
As a general rule, any patient with difficult-to-control acne, recalcitrant acne, or acne in areas on the cheeks or hairline should eliminate these hair products in their daily routine or avoid skin contact with these products.
References
1. J Clin Aesthet Dermatol. 2010 Apr;3(4):24-38.
2. Arch Dermatol. 1972;106 (6):843-50.
3. J Am Acad Dermatol. 2003; 48:S127-33.
4. Arch Dermatol. 1970;101(5):580-584.
5. “Cosmetics in Dermatology,” Second Edition, by Zoe Diana Draelos (New York: Churchill Livingstone, 1995).
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub.
Do you ask your acne patients about which hair products they use? This common question has recently brought our attention to popular hair products that are causing an acne epidemic. Have we forgotten about “Pomade acne”? Well, it’s making a comeback. Originally described in ethnic women, new frizz-fighting hair products have resurged and so has pomade acne in all skin types and in both men and women.
Smoothing serums, heat styling sprays, leave-in products popularly known as “It’s-a-10,” “Biosilk,” “anti-frizz serums,” “heat-protectants,” “thermal setting sprays,” and “shine sprays,” contain silicone-derived ingredients and oils to control frizz, add shine, and detangle the hair. They work by smoothing the hair cuticle, and for women with difficult-to-manage hair, they have become an essential part of the daily beauty regimen.
Men are not in the clear either. Hair waxes and pomades used to style men’s hair contain greasy wax-based ingredients that also clog pores, trap bacteria, and cause inflammatory breakouts.
As a general rule in skin and body care, most products work well for what they are made to do, but when misused, they can cause mishaps. You wouldn’t moisturize your face with your hair serum would you? It seems obvious that this could cause some skin issues; however, most people will not think to correlate their acne breakouts with their hair products until we mention it. These products rub off on the face or on the pillow at night. In addition, the less we wash our hair, the more we are going to bed and getting the daytime products all over our pillowcases. Our faces are rolling around in oily, waxy, hair products all night.
Makeup is known to cause acne, and some of the makeups that are well known culprits contain the same ingredients as in hair products. Foundations, primers, and popular “BB” creams often contain cyclopentasiloxane and dimethicone. They serve a similar purpose: smoothing the skin and smoothing the hair. Both should be avoided in acne-prone patients.
Common culprits in hair products include PVP/DMAPA acrylates, cyclopentasiloxane, panthenol, dimethicone, silicone, Quaternium-70, oils, and petrolatum.
The only way to eliminate acne caused by hair products is to completely eliminate the hair product from the daily routine. However, if your patients can’t live without their hair products, here are some tips to share with them to reduce breakouts:
• Choose a hairstyle that keeps the hair away from the face, or wear hair up to avoid prolonged contact with the face, particularly while sleeping.
• Change pillowcase often (every day if possible), especially for side sleepers. Regardless of the fabric, pillowcases trap oil, dirt, and bacteria.
• Shower at night and sleep with clean hair and clean skin.
• Style hair before applying makeup. Wash hands thoroughly to remove all hair products before touching the skin.
• Cover the face prior to applying any hair sprays.
• Cover the hair at bedtime; however, tight head coverings can stimulate sweat and cause scalp breakouts.
As a general rule, any patient with difficult-to-control acne, recalcitrant acne, or acne in areas on the cheeks or hairline should eliminate these hair products in their daily routine or avoid skin contact with these products.
References
1. J Clin Aesthet Dermatol. 2010 Apr;3(4):24-38.
2. Arch Dermatol. 1972;106 (6):843-50.
3. J Am Acad Dermatol. 2003; 48:S127-33.
4. Arch Dermatol. 1970;101(5):580-584.
5. “Cosmetics in Dermatology,” Second Edition, by Zoe Diana Draelos (New York: Churchill Livingstone, 1995).
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub.
Do you ask your acne patients about which hair products they use? This common question has recently brought our attention to popular hair products that are causing an acne epidemic. Have we forgotten about “Pomade acne”? Well, it’s making a comeback. Originally described in ethnic women, new frizz-fighting hair products have resurged and so has pomade acne in all skin types and in both men and women.
Smoothing serums, heat styling sprays, leave-in products popularly known as “It’s-a-10,” “Biosilk,” “anti-frizz serums,” “heat-protectants,” “thermal setting sprays,” and “shine sprays,” contain silicone-derived ingredients and oils to control frizz, add shine, and detangle the hair. They work by smoothing the hair cuticle, and for women with difficult-to-manage hair, they have become an essential part of the daily beauty regimen.
Men are not in the clear either. Hair waxes and pomades used to style men’s hair contain greasy wax-based ingredients that also clog pores, trap bacteria, and cause inflammatory breakouts.
As a general rule in skin and body care, most products work well for what they are made to do, but when misused, they can cause mishaps. You wouldn’t moisturize your face with your hair serum would you? It seems obvious that this could cause some skin issues; however, most people will not think to correlate their acne breakouts with their hair products until we mention it. These products rub off on the face or on the pillow at night. In addition, the less we wash our hair, the more we are going to bed and getting the daytime products all over our pillowcases. Our faces are rolling around in oily, waxy, hair products all night.
Makeup is known to cause acne, and some of the makeups that are well known culprits contain the same ingredients as in hair products. Foundations, primers, and popular “BB” creams often contain cyclopentasiloxane and dimethicone. They serve a similar purpose: smoothing the skin and smoothing the hair. Both should be avoided in acne-prone patients.
Common culprits in hair products include PVP/DMAPA acrylates, cyclopentasiloxane, panthenol, dimethicone, silicone, Quaternium-70, oils, and petrolatum.
The only way to eliminate acne caused by hair products is to completely eliminate the hair product from the daily routine. However, if your patients can’t live without their hair products, here are some tips to share with them to reduce breakouts:
• Choose a hairstyle that keeps the hair away from the face, or wear hair up to avoid prolonged contact with the face, particularly while sleeping.
• Change pillowcase often (every day if possible), especially for side sleepers. Regardless of the fabric, pillowcases trap oil, dirt, and bacteria.
• Shower at night and sleep with clean hair and clean skin.
• Style hair before applying makeup. Wash hands thoroughly to remove all hair products before touching the skin.
• Cover the face prior to applying any hair sprays.
• Cover the hair at bedtime; however, tight head coverings can stimulate sweat and cause scalp breakouts.
As a general rule, any patient with difficult-to-control acne, recalcitrant acne, or acne in areas on the cheeks or hairline should eliminate these hair products in their daily routine or avoid skin contact with these products.
References
1. J Clin Aesthet Dermatol. 2010 Apr;3(4):24-38.
2. Arch Dermatol. 1972;106 (6):843-50.
3. J Am Acad Dermatol. 2003; 48:S127-33.
4. Arch Dermatol. 1970;101(5):580-584.
5. “Cosmetics in Dermatology,” Second Edition, by Zoe Diana Draelos (New York: Churchill Livingstone, 1995).
Dr. Wesley and Dr. Talakoub are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub.
Myth of the Month: Retired myths from yesteryear
I appreciate the opportunity to share medical myths each month, hopefully to highlight topics where new knowledge and data may help change ways we approach common problems in medicine. I have been researching medical myths since the early 1990s, and some have actually evolved in such a way that they are no longer myths – that is, accepted practice now is very different than it was decades ago, and has incorporated updated research.
Some myths are timeless. The vitamin B12 myth I shared in this column last year continues to this day, despite evidence that has been present since the 1960s.
I will share with you two of my all-time favorite myths that have now been retired, where current practice now does not perpetuate these myths.
When I was in medical school, I was taught that the best way to treat a corneal abrasion was to patch the affected eye.1 Pretty much everyone who was seen in an emergency department for a corneal abrasion before the 1990s left the ED with an eye patch. This standard approach was not based on any evidence of benefit of healing or decreased pain.
Dr. Harold Jackson reported in a study of patients with corneal abrasions published in 1960 that there was no difference in healing between eyes that were patched and eyes that were left unpatched.2 The largest published study on eye patches for corneal abrasions involved 201 patients who were evaluated for corneal abrasions.3 The patients who did not receive an eye patch had less pain and quicker healing of the corneal abrasions. Other studies all showed no benefit to eye patches.4,5
A Cochrane Review published in 2006 concluded: “Treating simple corneal abrasions with a patch does not improve healing rates on the first day post-injury and does not reduce pain. In addition, use of patches results in a loss of binocular vision. Therefore, it is recommended that patches should not be used for simple corneal abrasions.”6
A more recent study by Dr. Moreno Menghini and colleagues showed no differences in healing of traumatic corneal abrasions between groups who received an eye patch, a contact lens, or no eye covering.7
Another longstanding myth that is less commonly seen now is the avoidance of use of narcotics for the treatment of acute, severe abdominal pain.
The long-term teaching was that by treating abdominal pain with narcotics, you could mask the important physical exam findings in patients presenting with an acute abdomen. The source of this myth wasn’t hard to uncover. The following are quotes from Cope’s Early Diagnosis of the Acute Abdomen 15th and 16th editions (these were the editions available back when I was a medical student in the early 1980s).
From the 15th edition: “If morphine be given, it is possible for a patient to die happy in the belief that he is on the road to recovery, and in some cases the medical attendant may for a time be induced to share the elusive hope.”8
An even stronger position was taken in the next edition of Cope’s text: “The patient cried out for relief, the relatives are insistent that something should be done, and the humane disciple of Aesculapius may think it is his first duty to diminish or banish the too obvious agony by administering a narcotic. Such a policy is a mistake. Though it may appear cruel, it is really kind to withhold morphine until a reasonable diagnosis has been made.”9
No controlled trials ever questioned this long-held belief until a study done by Dr. Alex Attard and colleagues published in 1992.10 In this study, 100 patients were evaluated by an admitting officer and given an intramuscular injection of either a narcotic or saline. Surgeons who subsequently followed the patients felt equally confident in diagnosis and management in both groups. The decision to operate or observe was incorrect in two patients in the narcotic group and nine in the saline group.
Dr. H. A. Amoli and colleagues studied whether administering morphine changed exam findings in patients with acute appendiciits.11 In a randomized, double-blind study design, half the patients received morphine and half received saline. Patients were examined by surgeons not involved in their care before and after drug administration, and their pain intensity and signs were recorded at each visit. The administration of morphine did not alter clinical signs or physician management plans.
In a study by Dr. Steven Pace and colleagues of patients presenting with acute abdominal pain, intravenous morphine or placebo was administered in 71 patients early in their presentation to the ED.12 There were no differences in accuracy of diagnosis between groups. Three diagnostic or management errors were made in each group.
I think the standard of care now for corneal abrasion treatment does not include eye patching. I also believe that the old teaching of no pain medication until the surgeon has examined the patient has also been replaced with appropriate pain management occurring early in the care plan for patients presenting with acute abdominal pain.
In the case of corneal abrasions, overwhelming data showing no benefit won out. I believe that the change in the management of acute abdominal pain was a combination of data along with advances in diagnostic imaging.
References
1. Wilkins. Emergency Medicine. 1989 Williams and Wilkins, Baltimore, Md.
2. Br Med J. 1960 Sep 3;2(5200):713.
3. Ophthalmology. 1995 Dec;102(12):1936-42.
4. Lancet. 1991 Mar 16;337(8742):643.
6. Cochrane Database Syst Rev. 2006 Apr 19;(2):CD004764.
7. Ophthalmic Res. 2013;50(1):13-8.
8. Cope’s Early Diagnosis of the Acute Abdomen, 15th Edition, Oxford University Press, 1979.
9. Cope’s Early Diagnosis of the Acute Abdomen, 16th Edition, Oxford University Press, 1983.
10. BMJ. 1992 Sep 5;305(6853):554-6.
11. Emerg Med J. 2008 Sep;25(9):586-9.
12. Acad Emerg Med. 1996 Dec;3(12):1086-92.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
I appreciate the opportunity to share medical myths each month, hopefully to highlight topics where new knowledge and data may help change ways we approach common problems in medicine. I have been researching medical myths since the early 1990s, and some have actually evolved in such a way that they are no longer myths – that is, accepted practice now is very different than it was decades ago, and has incorporated updated research.
Some myths are timeless. The vitamin B12 myth I shared in this column last year continues to this day, despite evidence that has been present since the 1960s.
I will share with you two of my all-time favorite myths that have now been retired, where current practice now does not perpetuate these myths.
When I was in medical school, I was taught that the best way to treat a corneal abrasion was to patch the affected eye.1 Pretty much everyone who was seen in an emergency department for a corneal abrasion before the 1990s left the ED with an eye patch. This standard approach was not based on any evidence of benefit of healing or decreased pain.
Dr. Harold Jackson reported in a study of patients with corneal abrasions published in 1960 that there was no difference in healing between eyes that were patched and eyes that were left unpatched.2 The largest published study on eye patches for corneal abrasions involved 201 patients who were evaluated for corneal abrasions.3 The patients who did not receive an eye patch had less pain and quicker healing of the corneal abrasions. Other studies all showed no benefit to eye patches.4,5
A Cochrane Review published in 2006 concluded: “Treating simple corneal abrasions with a patch does not improve healing rates on the first day post-injury and does not reduce pain. In addition, use of patches results in a loss of binocular vision. Therefore, it is recommended that patches should not be used for simple corneal abrasions.”6
A more recent study by Dr. Moreno Menghini and colleagues showed no differences in healing of traumatic corneal abrasions between groups who received an eye patch, a contact lens, or no eye covering.7
Another longstanding myth that is less commonly seen now is the avoidance of use of narcotics for the treatment of acute, severe abdominal pain.
The long-term teaching was that by treating abdominal pain with narcotics, you could mask the important physical exam findings in patients presenting with an acute abdomen. The source of this myth wasn’t hard to uncover. The following are quotes from Cope’s Early Diagnosis of the Acute Abdomen 15th and 16th editions (these were the editions available back when I was a medical student in the early 1980s).
From the 15th edition: “If morphine be given, it is possible for a patient to die happy in the belief that he is on the road to recovery, and in some cases the medical attendant may for a time be induced to share the elusive hope.”8
An even stronger position was taken in the next edition of Cope’s text: “The patient cried out for relief, the relatives are insistent that something should be done, and the humane disciple of Aesculapius may think it is his first duty to diminish or banish the too obvious agony by administering a narcotic. Such a policy is a mistake. Though it may appear cruel, it is really kind to withhold morphine until a reasonable diagnosis has been made.”9
No controlled trials ever questioned this long-held belief until a study done by Dr. Alex Attard and colleagues published in 1992.10 In this study, 100 patients were evaluated by an admitting officer and given an intramuscular injection of either a narcotic or saline. Surgeons who subsequently followed the patients felt equally confident in diagnosis and management in both groups. The decision to operate or observe was incorrect in two patients in the narcotic group and nine in the saline group.
Dr. H. A. Amoli and colleagues studied whether administering morphine changed exam findings in patients with acute appendiciits.11 In a randomized, double-blind study design, half the patients received morphine and half received saline. Patients were examined by surgeons not involved in their care before and after drug administration, and their pain intensity and signs were recorded at each visit. The administration of morphine did not alter clinical signs or physician management plans.
In a study by Dr. Steven Pace and colleagues of patients presenting with acute abdominal pain, intravenous morphine or placebo was administered in 71 patients early in their presentation to the ED.12 There were no differences in accuracy of diagnosis between groups. Three diagnostic or management errors were made in each group.
I think the standard of care now for corneal abrasion treatment does not include eye patching. I also believe that the old teaching of no pain medication until the surgeon has examined the patient has also been replaced with appropriate pain management occurring early in the care plan for patients presenting with acute abdominal pain.
In the case of corneal abrasions, overwhelming data showing no benefit won out. I believe that the change in the management of acute abdominal pain was a combination of data along with advances in diagnostic imaging.
References
1. Wilkins. Emergency Medicine. 1989 Williams and Wilkins, Baltimore, Md.
2. Br Med J. 1960 Sep 3;2(5200):713.
3. Ophthalmology. 1995 Dec;102(12):1936-42.
4. Lancet. 1991 Mar 16;337(8742):643.
6. Cochrane Database Syst Rev. 2006 Apr 19;(2):CD004764.
7. Ophthalmic Res. 2013;50(1):13-8.
8. Cope’s Early Diagnosis of the Acute Abdomen, 15th Edition, Oxford University Press, 1979.
9. Cope’s Early Diagnosis of the Acute Abdomen, 16th Edition, Oxford University Press, 1983.
10. BMJ. 1992 Sep 5;305(6853):554-6.
11. Emerg Med J. 2008 Sep;25(9):586-9.
12. Acad Emerg Med. 1996 Dec;3(12):1086-92.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
I appreciate the opportunity to share medical myths each month, hopefully to highlight topics where new knowledge and data may help change ways we approach common problems in medicine. I have been researching medical myths since the early 1990s, and some have actually evolved in such a way that they are no longer myths – that is, accepted practice now is very different than it was decades ago, and has incorporated updated research.
Some myths are timeless. The vitamin B12 myth I shared in this column last year continues to this day, despite evidence that has been present since the 1960s.
I will share with you two of my all-time favorite myths that have now been retired, where current practice now does not perpetuate these myths.
When I was in medical school, I was taught that the best way to treat a corneal abrasion was to patch the affected eye.1 Pretty much everyone who was seen in an emergency department for a corneal abrasion before the 1990s left the ED with an eye patch. This standard approach was not based on any evidence of benefit of healing or decreased pain.
Dr. Harold Jackson reported in a study of patients with corneal abrasions published in 1960 that there was no difference in healing between eyes that were patched and eyes that were left unpatched.2 The largest published study on eye patches for corneal abrasions involved 201 patients who were evaluated for corneal abrasions.3 The patients who did not receive an eye patch had less pain and quicker healing of the corneal abrasions. Other studies all showed no benefit to eye patches.4,5
A Cochrane Review published in 2006 concluded: “Treating simple corneal abrasions with a patch does not improve healing rates on the first day post-injury and does not reduce pain. In addition, use of patches results in a loss of binocular vision. Therefore, it is recommended that patches should not be used for simple corneal abrasions.”6
A more recent study by Dr. Moreno Menghini and colleagues showed no differences in healing of traumatic corneal abrasions between groups who received an eye patch, a contact lens, or no eye covering.7
Another longstanding myth that is less commonly seen now is the avoidance of use of narcotics for the treatment of acute, severe abdominal pain.
The long-term teaching was that by treating abdominal pain with narcotics, you could mask the important physical exam findings in patients presenting with an acute abdomen. The source of this myth wasn’t hard to uncover. The following are quotes from Cope’s Early Diagnosis of the Acute Abdomen 15th and 16th editions (these were the editions available back when I was a medical student in the early 1980s).
From the 15th edition: “If morphine be given, it is possible for a patient to die happy in the belief that he is on the road to recovery, and in some cases the medical attendant may for a time be induced to share the elusive hope.”8
An even stronger position was taken in the next edition of Cope’s text: “The patient cried out for relief, the relatives are insistent that something should be done, and the humane disciple of Aesculapius may think it is his first duty to diminish or banish the too obvious agony by administering a narcotic. Such a policy is a mistake. Though it may appear cruel, it is really kind to withhold morphine until a reasonable diagnosis has been made.”9
No controlled trials ever questioned this long-held belief until a study done by Dr. Alex Attard and colleagues published in 1992.10 In this study, 100 patients were evaluated by an admitting officer and given an intramuscular injection of either a narcotic or saline. Surgeons who subsequently followed the patients felt equally confident in diagnosis and management in both groups. The decision to operate or observe was incorrect in two patients in the narcotic group and nine in the saline group.
Dr. H. A. Amoli and colleagues studied whether administering morphine changed exam findings in patients with acute appendiciits.11 In a randomized, double-blind study design, half the patients received morphine and half received saline. Patients were examined by surgeons not involved in their care before and after drug administration, and their pain intensity and signs were recorded at each visit. The administration of morphine did not alter clinical signs or physician management plans.
In a study by Dr. Steven Pace and colleagues of patients presenting with acute abdominal pain, intravenous morphine or placebo was administered in 71 patients early in their presentation to the ED.12 There were no differences in accuracy of diagnosis between groups. Three diagnostic or management errors were made in each group.
I think the standard of care now for corneal abrasion treatment does not include eye patching. I also believe that the old teaching of no pain medication until the surgeon has examined the patient has also been replaced with appropriate pain management occurring early in the care plan for patients presenting with acute abdominal pain.
In the case of corneal abrasions, overwhelming data showing no benefit won out. I believe that the change in the management of acute abdominal pain was a combination of data along with advances in diagnostic imaging.
References
1. Wilkins. Emergency Medicine. 1989 Williams and Wilkins, Baltimore, Md.
2. Br Med J. 1960 Sep 3;2(5200):713.
3. Ophthalmology. 1995 Dec;102(12):1936-42.
4. Lancet. 1991 Mar 16;337(8742):643.
6. Cochrane Database Syst Rev. 2006 Apr 19;(2):CD004764.
7. Ophthalmic Res. 2013;50(1):13-8.
8. Cope’s Early Diagnosis of the Acute Abdomen, 15th Edition, Oxford University Press, 1979.
9. Cope’s Early Diagnosis of the Acute Abdomen, 16th Edition, Oxford University Press, 1983.
10. BMJ. 1992 Sep 5;305(6853):554-6.
11. Emerg Med J. 2008 Sep;25(9):586-9.
12. Acad Emerg Med. 1996 Dec;3(12):1086-92.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
Women with epilepsy conceive at normal rate
VANCOUVER – Women with epilepsy have fertility rates comparable with healthy women in the general population, according to results from the first prospective observational cohort study to make the comparison.
During the year-long Women With Epilepsy: Pregnancy Outcomes and Deliveries (WEPOD) study, 70% of women with epilepsy and 67% of healthy control women became pregnant, and there was no significant difference in the mean time to pregnancy between those with and without epilepsy (6 months vs. 9 months, respectively), Dr. Page Pennell reported at the annual meeting of the American Academy of Neurology.
Live births occurred in 82% of pregnancies of women with epilepsy and 80% of controls, while miscarriages occurred in 13% and 20%, respectively. Both of those rates are very similar to the general population. Another 5% of pregnancies in women with epilepsy were ectopic, terminated due to chromosomal abnormality, or lost to follow-up.
“These findings should reassure women with epilepsy and clinicians when counseling women with epilepsy who are planning pregnancy,” said Dr. Pennell, director of research for the division of epilepsy in the department of neurology at Brigham and Women’s Hospital in Boston. She is a primary investigator of the study along with Dr. Jacqueline French, professor of neurology at NYU Langone Medical Center and Dr. Cynthia Harden, system director of epilepsy services at Mount Sinai Beth Israel, both in New York.
“I think overall the findings are more in the light of myth busting. ... We don’t necessarily see a lot of problems with fertility, yet the literature suggests that the birth rates are much lower,” Dr. Harden said in an interview.
“It’s really the first solid evidence, and it’s nice because in a sea of bad news for women when it comes to family planning and achieving pregnancy and pregnancy outcomes, I think this was very positive to say that their ability to achieve pregnancy was no different than what was reported by a control population without epilepsy,” Dr. Katherine Noe, an epilepsy specialist at the Mayo Clinic in Scottsdale, Ariz., said when asked to comment on the study.
“There was certainly reason to be concerned,” said Dr. Noe, who was not involved in the study. “We have a lot of data saying that babies exposed to antiepileptic drugs are more likely to have malformations, and so you could have a baby that already early in pregnancy has severe malformations that would be more likely to end in spontaneous abortion.”
Dr. Noe said that pregnancy registry data indicate that women with epilepsy may be more likely to have a pregnancy that ends in a miscarriage. Investigators for several studies published in 2015 reported that women with epilepsy face greater risk for morbidity and adverse outcomes at the time of delivery and during pregnancy than women without epilepsy (JAMA Neurol. 2015;72[9]:981-8 and Lancet. 2016;386[10006]:1845–52). Women with epilepsy also have been thought to be more prone to infertility for various reasons, including menstrual irregularities, polycystic ovarian syndrome related to antiepileptic medications, and early menopause, she said.
Three previous studies had reported that women with epilepsy had birth rates as low as only one-quarter to one-third that of women without epilepsy. There have been many reasons reported for why that might be the case, including lower marriage rates, sexual dysfunction, lower libido (in both men and women with epilepsy), and increased number of anovulatory cycles, or greater choice to not become pregnant, Dr. Pennell said.
The WEPOD study enrolled 89 women with epilepsy and 109 healthy controls who were seeking to become pregnant and had stopped using contraception within 6 months of enrollment or were about to stop using it. The investigators excluded women with infertility, polycystic ovarian syndrome, endometriosis, endocrine disorder, and heavy smoking, or who were not in an exclusive heterosexual relationship with a significant other or spouse.
Participants received iPod touch devices with an app with which they tracked menses and intercourse, as well as antiepileptic drug use and seizures in women with epilepsy. “This was a particularly novel part of the study,” Dr. Harden said. It allowed the investigators to track adherence very well. Participants logged about 87% of their days in the app, and the investigators could see when the entries were made.
Women in both groups had a mean age of about 31 years and mean body mass index of about 25 kg/m2. Overall, 52%-58% had undergone a prior pregnancy. Women with epilepsy, compared with controls, were less often Asian (17% vs. 6%) or African American (16% vs. 1%). The education level of participants was “fairly similar” between the groups, and slightly more women with epilepsy were unemployed (21% vs. 10%). Women with epilepsy also were more often married than were controls (89% vs. 75%).
During the study, 36% of women with epilepsy were still having seizures. At enrollment, most of the women’s seizure types were generalized (30%) or focal only (63%). Dr. Pennell noted that the antiseizure medications that the women were taking were typical for women of reproductive age: lamotrigine monotherapy (44%), levetiracetam monotherapy (28%), monotherapy with a strong enzyme-inducing drug (12%), other polytherapy (10%), polytherapy with a strong enzyme-inducing drug (6%), other monotherapy (3%), or no antiseizure medication (2%). A few women either added or stopped drugs during the study. A total of 18 women with epilepsy and 15 healthy controls dropped out.
As expected, age affected the likelihood of becoming pregnant, as well as number of prior pregnancies. Body mass index did not affect the likelihood of becoming pregnant, while white race and being married increased the likelihood.
In future analyses, the investigators are planning on checking whether ovulatory rates, frequency of intercourse, and time of intercourse had any impact on pregnancy, and in women with epilepsy, they will check the effect of the type of antiseizure medication and seizure-related factors.
“I think our findings will stand with future analyses.” Dr. Harden said. “The most interesting future findings may come from within the epilepsy group,” she said, noting that older antiepileptic medications have been previously associated with difficulty conceiving.
The WEPOD study was funded by the Milken Family Foundation, the Epilepsy Therapy Project, and the Epilepsy Foundation.
VANCOUVER – Women with epilepsy have fertility rates comparable with healthy women in the general population, according to results from the first prospective observational cohort study to make the comparison.
During the year-long Women With Epilepsy: Pregnancy Outcomes and Deliveries (WEPOD) study, 70% of women with epilepsy and 67% of healthy control women became pregnant, and there was no significant difference in the mean time to pregnancy between those with and without epilepsy (6 months vs. 9 months, respectively), Dr. Page Pennell reported at the annual meeting of the American Academy of Neurology.
Live births occurred in 82% of pregnancies of women with epilepsy and 80% of controls, while miscarriages occurred in 13% and 20%, respectively. Both of those rates are very similar to the general population. Another 5% of pregnancies in women with epilepsy were ectopic, terminated due to chromosomal abnormality, or lost to follow-up.
“These findings should reassure women with epilepsy and clinicians when counseling women with epilepsy who are planning pregnancy,” said Dr. Pennell, director of research for the division of epilepsy in the department of neurology at Brigham and Women’s Hospital in Boston. She is a primary investigator of the study along with Dr. Jacqueline French, professor of neurology at NYU Langone Medical Center and Dr. Cynthia Harden, system director of epilepsy services at Mount Sinai Beth Israel, both in New York.
“I think overall the findings are more in the light of myth busting. ... We don’t necessarily see a lot of problems with fertility, yet the literature suggests that the birth rates are much lower,” Dr. Harden said in an interview.
“It’s really the first solid evidence, and it’s nice because in a sea of bad news for women when it comes to family planning and achieving pregnancy and pregnancy outcomes, I think this was very positive to say that their ability to achieve pregnancy was no different than what was reported by a control population without epilepsy,” Dr. Katherine Noe, an epilepsy specialist at the Mayo Clinic in Scottsdale, Ariz., said when asked to comment on the study.
“There was certainly reason to be concerned,” said Dr. Noe, who was not involved in the study. “We have a lot of data saying that babies exposed to antiepileptic drugs are more likely to have malformations, and so you could have a baby that already early in pregnancy has severe malformations that would be more likely to end in spontaneous abortion.”
Dr. Noe said that pregnancy registry data indicate that women with epilepsy may be more likely to have a pregnancy that ends in a miscarriage. Investigators for several studies published in 2015 reported that women with epilepsy face greater risk for morbidity and adverse outcomes at the time of delivery and during pregnancy than women without epilepsy (JAMA Neurol. 2015;72[9]:981-8 and Lancet. 2016;386[10006]:1845–52). Women with epilepsy also have been thought to be more prone to infertility for various reasons, including menstrual irregularities, polycystic ovarian syndrome related to antiepileptic medications, and early menopause, she said.
Three previous studies had reported that women with epilepsy had birth rates as low as only one-quarter to one-third that of women without epilepsy. There have been many reasons reported for why that might be the case, including lower marriage rates, sexual dysfunction, lower libido (in both men and women with epilepsy), and increased number of anovulatory cycles, or greater choice to not become pregnant, Dr. Pennell said.
The WEPOD study enrolled 89 women with epilepsy and 109 healthy controls who were seeking to become pregnant and had stopped using contraception within 6 months of enrollment or were about to stop using it. The investigators excluded women with infertility, polycystic ovarian syndrome, endometriosis, endocrine disorder, and heavy smoking, or who were not in an exclusive heterosexual relationship with a significant other or spouse.
Participants received iPod touch devices with an app with which they tracked menses and intercourse, as well as antiepileptic drug use and seizures in women with epilepsy. “This was a particularly novel part of the study,” Dr. Harden said. It allowed the investigators to track adherence very well. Participants logged about 87% of their days in the app, and the investigators could see when the entries were made.
Women in both groups had a mean age of about 31 years and mean body mass index of about 25 kg/m2. Overall, 52%-58% had undergone a prior pregnancy. Women with epilepsy, compared with controls, were less often Asian (17% vs. 6%) or African American (16% vs. 1%). The education level of participants was “fairly similar” between the groups, and slightly more women with epilepsy were unemployed (21% vs. 10%). Women with epilepsy also were more often married than were controls (89% vs. 75%).
During the study, 36% of women with epilepsy were still having seizures. At enrollment, most of the women’s seizure types were generalized (30%) or focal only (63%). Dr. Pennell noted that the antiseizure medications that the women were taking were typical for women of reproductive age: lamotrigine monotherapy (44%), levetiracetam monotherapy (28%), monotherapy with a strong enzyme-inducing drug (12%), other polytherapy (10%), polytherapy with a strong enzyme-inducing drug (6%), other monotherapy (3%), or no antiseizure medication (2%). A few women either added or stopped drugs during the study. A total of 18 women with epilepsy and 15 healthy controls dropped out.
As expected, age affected the likelihood of becoming pregnant, as well as number of prior pregnancies. Body mass index did not affect the likelihood of becoming pregnant, while white race and being married increased the likelihood.
In future analyses, the investigators are planning on checking whether ovulatory rates, frequency of intercourse, and time of intercourse had any impact on pregnancy, and in women with epilepsy, they will check the effect of the type of antiseizure medication and seizure-related factors.
“I think our findings will stand with future analyses.” Dr. Harden said. “The most interesting future findings may come from within the epilepsy group,” she said, noting that older antiepileptic medications have been previously associated with difficulty conceiving.
The WEPOD study was funded by the Milken Family Foundation, the Epilepsy Therapy Project, and the Epilepsy Foundation.
VANCOUVER – Women with epilepsy have fertility rates comparable with healthy women in the general population, according to results from the first prospective observational cohort study to make the comparison.
During the year-long Women With Epilepsy: Pregnancy Outcomes and Deliveries (WEPOD) study, 70% of women with epilepsy and 67% of healthy control women became pregnant, and there was no significant difference in the mean time to pregnancy between those with and without epilepsy (6 months vs. 9 months, respectively), Dr. Page Pennell reported at the annual meeting of the American Academy of Neurology.
Live births occurred in 82% of pregnancies of women with epilepsy and 80% of controls, while miscarriages occurred in 13% and 20%, respectively. Both of those rates are very similar to the general population. Another 5% of pregnancies in women with epilepsy were ectopic, terminated due to chromosomal abnormality, or lost to follow-up.
“These findings should reassure women with epilepsy and clinicians when counseling women with epilepsy who are planning pregnancy,” said Dr. Pennell, director of research for the division of epilepsy in the department of neurology at Brigham and Women’s Hospital in Boston. She is a primary investigator of the study along with Dr. Jacqueline French, professor of neurology at NYU Langone Medical Center and Dr. Cynthia Harden, system director of epilepsy services at Mount Sinai Beth Israel, both in New York.
“I think overall the findings are more in the light of myth busting. ... We don’t necessarily see a lot of problems with fertility, yet the literature suggests that the birth rates are much lower,” Dr. Harden said in an interview.
“It’s really the first solid evidence, and it’s nice because in a sea of bad news for women when it comes to family planning and achieving pregnancy and pregnancy outcomes, I think this was very positive to say that their ability to achieve pregnancy was no different than what was reported by a control population without epilepsy,” Dr. Katherine Noe, an epilepsy specialist at the Mayo Clinic in Scottsdale, Ariz., said when asked to comment on the study.
“There was certainly reason to be concerned,” said Dr. Noe, who was not involved in the study. “We have a lot of data saying that babies exposed to antiepileptic drugs are more likely to have malformations, and so you could have a baby that already early in pregnancy has severe malformations that would be more likely to end in spontaneous abortion.”
Dr. Noe said that pregnancy registry data indicate that women with epilepsy may be more likely to have a pregnancy that ends in a miscarriage. Investigators for several studies published in 2015 reported that women with epilepsy face greater risk for morbidity and adverse outcomes at the time of delivery and during pregnancy than women without epilepsy (JAMA Neurol. 2015;72[9]:981-8 and Lancet. 2016;386[10006]:1845–52). Women with epilepsy also have been thought to be more prone to infertility for various reasons, including menstrual irregularities, polycystic ovarian syndrome related to antiepileptic medications, and early menopause, she said.
Three previous studies had reported that women with epilepsy had birth rates as low as only one-quarter to one-third that of women without epilepsy. There have been many reasons reported for why that might be the case, including lower marriage rates, sexual dysfunction, lower libido (in both men and women with epilepsy), and increased number of anovulatory cycles, or greater choice to not become pregnant, Dr. Pennell said.
The WEPOD study enrolled 89 women with epilepsy and 109 healthy controls who were seeking to become pregnant and had stopped using contraception within 6 months of enrollment or were about to stop using it. The investigators excluded women with infertility, polycystic ovarian syndrome, endometriosis, endocrine disorder, and heavy smoking, or who were not in an exclusive heterosexual relationship with a significant other or spouse.
Participants received iPod touch devices with an app with which they tracked menses and intercourse, as well as antiepileptic drug use and seizures in women with epilepsy. “This was a particularly novel part of the study,” Dr. Harden said. It allowed the investigators to track adherence very well. Participants logged about 87% of their days in the app, and the investigators could see when the entries were made.
Women in both groups had a mean age of about 31 years and mean body mass index of about 25 kg/m2. Overall, 52%-58% had undergone a prior pregnancy. Women with epilepsy, compared with controls, were less often Asian (17% vs. 6%) or African American (16% vs. 1%). The education level of participants was “fairly similar” between the groups, and slightly more women with epilepsy were unemployed (21% vs. 10%). Women with epilepsy also were more often married than were controls (89% vs. 75%).
During the study, 36% of women with epilepsy were still having seizures. At enrollment, most of the women’s seizure types were generalized (30%) or focal only (63%). Dr. Pennell noted that the antiseizure medications that the women were taking were typical for women of reproductive age: lamotrigine monotherapy (44%), levetiracetam monotherapy (28%), monotherapy with a strong enzyme-inducing drug (12%), other polytherapy (10%), polytherapy with a strong enzyme-inducing drug (6%), other monotherapy (3%), or no antiseizure medication (2%). A few women either added or stopped drugs during the study. A total of 18 women with epilepsy and 15 healthy controls dropped out.
As expected, age affected the likelihood of becoming pregnant, as well as number of prior pregnancies. Body mass index did not affect the likelihood of becoming pregnant, while white race and being married increased the likelihood.
In future analyses, the investigators are planning on checking whether ovulatory rates, frequency of intercourse, and time of intercourse had any impact on pregnancy, and in women with epilepsy, they will check the effect of the type of antiseizure medication and seizure-related factors.
“I think our findings will stand with future analyses.” Dr. Harden said. “The most interesting future findings may come from within the epilepsy group,” she said, noting that older antiepileptic medications have been previously associated with difficulty conceiving.
The WEPOD study was funded by the Milken Family Foundation, the Epilepsy Therapy Project, and the Epilepsy Foundation.
AT THE AAN 2016 ANNUAL MEETING
Key clinical point: Women with epilepsy do not have lower ability to conceive.
Major finding: 70% of women with epilepsy and 67% of healthy control women became pregnant.
Data source: A prospective case-control study of 89 women with epilepsy and 109 healthy controls.
Disclosures: The WEPOD study was funded by the Milken Family Foundation, the Epilepsy Therapy Project, and the Epilepsy Foundation.
STAMPEDE: Metabolic surgery bests medical therapy long term
CHICAGO – The superiority of metabolic surgery over intensive medical therapy for achieving glycemic control in patients with type 2 diabetes was largely maintained at the final 5-year follow-up evaluation in the randomized, controlled STAMPEDE trial.
The 150 subjects, who had “fairly severe diabetes” with an average disease duration of 8 years, were randomized to receive intensive medical therapy alone, or intensive medical therapy with Roux-en-Y gastric bypass surgery or sleeve gastrectomy surgery. The primary endpoint of hemoglobin A1c less than 6% was achieved in 5%, 29%, and 23% of patients in the groups, respectively. The difference was statistically significant in favor of both types of surgery, Dr. Philip Raymond Schauer reported at the annual meeting of the American College of Cardiology.
Furthermore, patients in the surgery groups fared better than those in the intensive medical therapy group on several other measures, including disease remission (defied as HbA1c less than 6% without diabetes medication), HbA1c less than 7% (the American Diabetes Association target for therapy), change in fasting plasma glucose from baseline, and changes in high- and low-density lipoprotein cholesterol levels, said Dr. Schauer, director of the Cleveland Clinic Bariatric and Metabolic Institute.
Patients in the surgery groups also experienced a significantly greater reduction in the use of antihypertensive medications and lipid-lowering agents, he added.
The “very dramatic drop” in HbA1c seen early on in the surgical patients was, for the most part, sustained out to 5 years, he said.
The results for both surgeries were significantly better than those for intensive medical therapy, but the results with gastric bypass were more effective at 5 years than were those for sleeve gastrectomy, he added, noting that the surgery patients had better quality of life, compared with the intensive medical therapy patients.
As for adverse events in the surgery groups, no perioperative deaths occurred, and while there were some surgical complications, none resulted in long-term disability, Dr. Schauer said.
Anemia was more common in the surgery patients, but was fairly mild. The most common complication was weight gain in 20% of patients, and the overall reoperation rate was 7%.
Of note, patients in the study had body mass index ranging from 27 to 43 kg/m2, and those with BMI less than 35 had similar benefits as those with more severe obesity. This is important, as many insurance companies won’t cover metabolic surgery for patients with BMI less than 35, he explained.
These findings represent the longest follow-up to date comparing the efficacy of the two most common metabolic surgery procedures with medical treatment of type 2 diabetes for maintaining glycemic control or reducing end-organ complications. Three-year outcomes of STAMPEDE (Surgical Treatment and Medications Potentially Eradicate Diabetes Efficiently) were reported in 2014 (N Engl J Med. 2014;370:2002-13).
The participants ranged in age from 20 to 60 years. The average HbA1c was about 9%, the average BMI was 36, and most were on at least three antidiabetic medications at baseline. Half were on insulin.
The findings are important, because of the roughly 25 million Americans with type 2 diabetes, only about half have good glycemic control on their current medical treatment strategies, Dr. Schauer said.
Though limited by the single-center study design, the STAMPEDE findings show that metabolic surgery is more effective long term than intensive medical therapy in patients with uncontrolled type 2 diabetes and should be considered a treatment option in this population, he concluded, adding that multicenter studies would be helpful for determining the generalizability of the findings.
Dr. Schauer reported receiving consulting fees/honoraria from Ethicon Endosurgery and The Medicines Company, and having ownership interest in Surgical Excellence.
CHICAGO – The superiority of metabolic surgery over intensive medical therapy for achieving glycemic control in patients with type 2 diabetes was largely maintained at the final 5-year follow-up evaluation in the randomized, controlled STAMPEDE trial.
The 150 subjects, who had “fairly severe diabetes” with an average disease duration of 8 years, were randomized to receive intensive medical therapy alone, or intensive medical therapy with Roux-en-Y gastric bypass surgery or sleeve gastrectomy surgery. The primary endpoint of hemoglobin A1c less than 6% was achieved in 5%, 29%, and 23% of patients in the groups, respectively. The difference was statistically significant in favor of both types of surgery, Dr. Philip Raymond Schauer reported at the annual meeting of the American College of Cardiology.
Furthermore, patients in the surgery groups fared better than those in the intensive medical therapy group on several other measures, including disease remission (defied as HbA1c less than 6% without diabetes medication), HbA1c less than 7% (the American Diabetes Association target for therapy), change in fasting plasma glucose from baseline, and changes in high- and low-density lipoprotein cholesterol levels, said Dr. Schauer, director of the Cleveland Clinic Bariatric and Metabolic Institute.
Patients in the surgery groups also experienced a significantly greater reduction in the use of antihypertensive medications and lipid-lowering agents, he added.
The “very dramatic drop” in HbA1c seen early on in the surgical patients was, for the most part, sustained out to 5 years, he said.
The results for both surgeries were significantly better than those for intensive medical therapy, but the results with gastric bypass were more effective at 5 years than were those for sleeve gastrectomy, he added, noting that the surgery patients had better quality of life, compared with the intensive medical therapy patients.
As for adverse events in the surgery groups, no perioperative deaths occurred, and while there were some surgical complications, none resulted in long-term disability, Dr. Schauer said.
Anemia was more common in the surgery patients, but was fairly mild. The most common complication was weight gain in 20% of patients, and the overall reoperation rate was 7%.
Of note, patients in the study had body mass index ranging from 27 to 43 kg/m2, and those with BMI less than 35 had similar benefits as those with more severe obesity. This is important, as many insurance companies won’t cover metabolic surgery for patients with BMI less than 35, he explained.
These findings represent the longest follow-up to date comparing the efficacy of the two most common metabolic surgery procedures with medical treatment of type 2 diabetes for maintaining glycemic control or reducing end-organ complications. Three-year outcomes of STAMPEDE (Surgical Treatment and Medications Potentially Eradicate Diabetes Efficiently) were reported in 2014 (N Engl J Med. 2014;370:2002-13).
The participants ranged in age from 20 to 60 years. The average HbA1c was about 9%, the average BMI was 36, and most were on at least three antidiabetic medications at baseline. Half were on insulin.
The findings are important, because of the roughly 25 million Americans with type 2 diabetes, only about half have good glycemic control on their current medical treatment strategies, Dr. Schauer said.
Though limited by the single-center study design, the STAMPEDE findings show that metabolic surgery is more effective long term than intensive medical therapy in patients with uncontrolled type 2 diabetes and should be considered a treatment option in this population, he concluded, adding that multicenter studies would be helpful for determining the generalizability of the findings.
Dr. Schauer reported receiving consulting fees/honoraria from Ethicon Endosurgery and The Medicines Company, and having ownership interest in Surgical Excellence.
CHICAGO – The superiority of metabolic surgery over intensive medical therapy for achieving glycemic control in patients with type 2 diabetes was largely maintained at the final 5-year follow-up evaluation in the randomized, controlled STAMPEDE trial.
The 150 subjects, who had “fairly severe diabetes” with an average disease duration of 8 years, were randomized to receive intensive medical therapy alone, or intensive medical therapy with Roux-en-Y gastric bypass surgery or sleeve gastrectomy surgery. The primary endpoint of hemoglobin A1c less than 6% was achieved in 5%, 29%, and 23% of patients in the groups, respectively. The difference was statistically significant in favor of both types of surgery, Dr. Philip Raymond Schauer reported at the annual meeting of the American College of Cardiology.
Furthermore, patients in the surgery groups fared better than those in the intensive medical therapy group on several other measures, including disease remission (defied as HbA1c less than 6% without diabetes medication), HbA1c less than 7% (the American Diabetes Association target for therapy), change in fasting plasma glucose from baseline, and changes in high- and low-density lipoprotein cholesterol levels, said Dr. Schauer, director of the Cleveland Clinic Bariatric and Metabolic Institute.
Patients in the surgery groups also experienced a significantly greater reduction in the use of antihypertensive medications and lipid-lowering agents, he added.
The “very dramatic drop” in HbA1c seen early on in the surgical patients was, for the most part, sustained out to 5 years, he said.
The results for both surgeries were significantly better than those for intensive medical therapy, but the results with gastric bypass were more effective at 5 years than were those for sleeve gastrectomy, he added, noting that the surgery patients had better quality of life, compared with the intensive medical therapy patients.
As for adverse events in the surgery groups, no perioperative deaths occurred, and while there were some surgical complications, none resulted in long-term disability, Dr. Schauer said.
Anemia was more common in the surgery patients, but was fairly mild. The most common complication was weight gain in 20% of patients, and the overall reoperation rate was 7%.
Of note, patients in the study had body mass index ranging from 27 to 43 kg/m2, and those with BMI less than 35 had similar benefits as those with more severe obesity. This is important, as many insurance companies won’t cover metabolic surgery for patients with BMI less than 35, he explained.
These findings represent the longest follow-up to date comparing the efficacy of the two most common metabolic surgery procedures with medical treatment of type 2 diabetes for maintaining glycemic control or reducing end-organ complications. Three-year outcomes of STAMPEDE (Surgical Treatment and Medications Potentially Eradicate Diabetes Efficiently) were reported in 2014 (N Engl J Med. 2014;370:2002-13).
The participants ranged in age from 20 to 60 years. The average HbA1c was about 9%, the average BMI was 36, and most were on at least three antidiabetic medications at baseline. Half were on insulin.
The findings are important, because of the roughly 25 million Americans with type 2 diabetes, only about half have good glycemic control on their current medical treatment strategies, Dr. Schauer said.
Though limited by the single-center study design, the STAMPEDE findings show that metabolic surgery is more effective long term than intensive medical therapy in patients with uncontrolled type 2 diabetes and should be considered a treatment option in this population, he concluded, adding that multicenter studies would be helpful for determining the generalizability of the findings.
Dr. Schauer reported receiving consulting fees/honoraria from Ethicon Endosurgery and The Medicines Company, and having ownership interest in Surgical Excellence.
AT ACC 16
Key clinical point: The superiority of metabolic surgery over intensive medical therapy for achieving glycemic control among patients with type 2 diabetes in the randomized, controlled STAMPEDE persisted at the final 5-year follow-up evaluation.
Major finding: The primary endpoint of HbA1c less than 6% was achieved in 5%, 29%, and 23% of patients in the medication and medication plus Roux-en-Y or sleeve gastrectomy groups, respectively.
Data source: The randomized, controlled STAMPEDE trial in 150 subjects.
Disclosures: Dr. Schauer reported receiving consulting fees/honoraria from Ethicon Endosurgery and The Medicines Company, and having ownership interest in Surgical Excellence.