User login
Clindamycin Confers No Extra Benefit for Kids With SSSS
MINNEAPOLIS – A large single-site case review found that most pediatric patients with staphylococcal scalded skin syndrome (SSSS) had a classic presentation, often preceded by an upper respiratory tract infection.
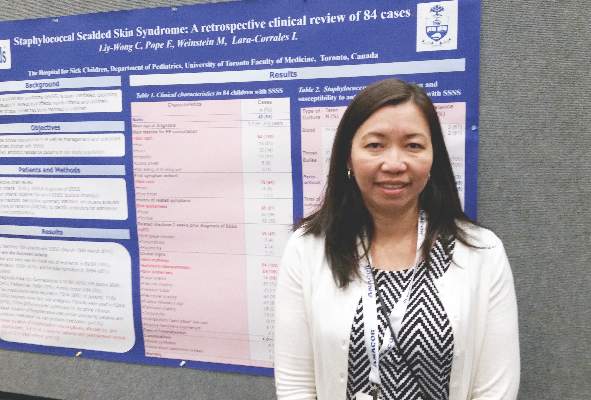
In the review, surgical debridement increased hospital length of stay, and the use of clindamycin gave none of the benefit that might be expected from an antitoxin-specific antibiotic, according to Carmen Liy-Wong, MD, a pediatric medicine fellow at the Hospital for Sick Children in Toronto.
All children in the 84-patient study had a skin rash, which was also the first symptom noticed for 94% of the patients (n = 79). All children also had the classic SSSS clinical signs of skin erythema and exfoliation or desquamation; most (88%, n = 74) had skin tenderness. In more than half of the children in the study, erythema, exfoliation, and bullae formation first presented on the head or neck.
Dr. Liy-Wong presented her findings at the annual meeting of the Society for Pediatric Dermatology. She and her collaborators used a retrospective chart review to develop the largest case series to date of SSSS in pediatric hospitalized children to describe both the clinical presentation of SSSS and antimicrobial use and susceptibilities. Study objectives, she said, included identifying the clinical characteristics of children with SSSS, as well as identifying management practices and associated outcomes for hospitalized children with SSSS.
Of the 84 patients who met inclusion criteria, 49 (58%) were male, and the mean age at SSSS diagnosis was 3.1 (plus or minus 2.4) years. Children, aged 0-18 years, were included if they had a clinical diagnosis of SSSS. Children with localized exfoliative staphylococcal infections, such as bullous impetigo, were excluded from the study.
In addition to erythema, exfoliation, and bullae formation, most children also had a history of skin tenderness (68%, n = 79); a little over a third had a history of fever or pruritus (38%, n = 32 for both). Thirty-five of the children (42%) had an upper respiratory tract infection in the 2 weeks preceding the SSSS diagnosis.
Facial edema, perioral or periocular crusting, and vesicles or bullae were seen in more than half of children. A few patients had conjunctivitis (11%, n = 9), mucous membrane involvement (5%, n = 4), or a sandpaper-like scarlatiniform rash (11%, n = 9).
No patients in the study died. Complications were rare: shock syndrome in one patient, and generalized bacteremia in three patients (4%).
Pain management was a mainstay of inpatient care for children with SSSS; 75 children (89%) required pain medication, and opioids were used in more than half. One in five children received morphine by continuous intravenous infusion.
Patients who underwent surgical debridement stayed a mean 5.8 (plus or minus 4.1) days, compared with a mean 3.6 (plus or minus 2.1) days for those children not receiving debridement (P = 0.03).
The study also aimed to identify antibiotic resistance patterns for SSSS in the single-site study population. Blood cultures were obtained from all but five patients and were positive in three patients. Bullae were cultured in 28 patients (33%), and periorificial lesions were cultured in 57 patients (68%). Throat cultures were obtained in 31 patients, but culture results were not reported.
“Periorificial cultures were more useful than other sites in identification of the causative organism,” Dr. Liy-Wong noted, since 74% (42 of 57) of periorificial cultures were positive. In all, 50 of 195 cultures (26%) were positive for Staphylococcus aureus. Almost all of the 50 isolates (98%, n = 49) were sensitive to oxacillin. Just under half of isolates were sensitive to clindamycin (48%, n = 24,) and erythromycin (46%, n = 23).
The use of clindamycin, an antibiotic known to be effective in inhibiting exotoxin production by staphylococcus species, was not associated with reduced hospital length of stay (P = .63 for comparison with nonantitoxin antibiotics). Dr. Liy-Wong and her collaborators noted that “no statistically significant difference in outcomes was found in patients treated with specific antitoxin medication (clindamycin),” a practice that requires further study.
SSSS was diagnosed by dermatologists in 35 of the 84 cases, followed by emergency department physicians in 29 cases (34%), pediatricians in 16 cases (19%), and family physicians in 4 cases (5%).
Dr. Liy-Wong and her colleagues reported no external sources of funding, and no conflicts of interest.
MINNEAPOLIS – A large single-site case review found that most pediatric patients with staphylococcal scalded skin syndrome (SSSS) had a classic presentation, often preceded by an upper respiratory tract infection.
In the review, surgical debridement increased hospital length of stay, and the use of clindamycin gave none of the benefit that might be expected from an antitoxin-specific antibiotic, according to Carmen Liy-Wong, MD, a pediatric medicine fellow at the Hospital for Sick Children in Toronto.
All children in the 84-patient study had a skin rash, which was also the first symptom noticed for 94% of the patients (n = 79). All children also had the classic SSSS clinical signs of skin erythema and exfoliation or desquamation; most (88%, n = 74) had skin tenderness. In more than half of the children in the study, erythema, exfoliation, and bullae formation first presented on the head or neck.
Dr. Liy-Wong presented her findings at the annual meeting of the Society for Pediatric Dermatology. She and her collaborators used a retrospective chart review to develop the largest case series to date of SSSS in pediatric hospitalized children to describe both the clinical presentation of SSSS and antimicrobial use and susceptibilities. Study objectives, she said, included identifying the clinical characteristics of children with SSSS, as well as identifying management practices and associated outcomes for hospitalized children with SSSS.
Of the 84 patients who met inclusion criteria, 49 (58%) were male, and the mean age at SSSS diagnosis was 3.1 (plus or minus 2.4) years. Children, aged 0-18 years, were included if they had a clinical diagnosis of SSSS. Children with localized exfoliative staphylococcal infections, such as bullous impetigo, were excluded from the study.
In addition to erythema, exfoliation, and bullae formation, most children also had a history of skin tenderness (68%, n = 79); a little over a third had a history of fever or pruritus (38%, n = 32 for both). Thirty-five of the children (42%) had an upper respiratory tract infection in the 2 weeks preceding the SSSS diagnosis.
Facial edema, perioral or periocular crusting, and vesicles or bullae were seen in more than half of children. A few patients had conjunctivitis (11%, n = 9), mucous membrane involvement (5%, n = 4), or a sandpaper-like scarlatiniform rash (11%, n = 9).
No patients in the study died. Complications were rare: shock syndrome in one patient, and generalized bacteremia in three patients (4%).
Pain management was a mainstay of inpatient care for children with SSSS; 75 children (89%) required pain medication, and opioids were used in more than half. One in five children received morphine by continuous intravenous infusion.
Patients who underwent surgical debridement stayed a mean 5.8 (plus or minus 4.1) days, compared with a mean 3.6 (plus or minus 2.1) days for those children not receiving debridement (P = 0.03).
The study also aimed to identify antibiotic resistance patterns for SSSS in the single-site study population. Blood cultures were obtained from all but five patients and were positive in three patients. Bullae were cultured in 28 patients (33%), and periorificial lesions were cultured in 57 patients (68%). Throat cultures were obtained in 31 patients, but culture results were not reported.
“Periorificial cultures were more useful than other sites in identification of the causative organism,” Dr. Liy-Wong noted, since 74% (42 of 57) of periorificial cultures were positive. In all, 50 of 195 cultures (26%) were positive for Staphylococcus aureus. Almost all of the 50 isolates (98%, n = 49) were sensitive to oxacillin. Just under half of isolates were sensitive to clindamycin (48%, n = 24,) and erythromycin (46%, n = 23).
The use of clindamycin, an antibiotic known to be effective in inhibiting exotoxin production by staphylococcus species, was not associated with reduced hospital length of stay (P = .63 for comparison with nonantitoxin antibiotics). Dr. Liy-Wong and her collaborators noted that “no statistically significant difference in outcomes was found in patients treated with specific antitoxin medication (clindamycin),” a practice that requires further study.
SSSS was diagnosed by dermatologists in 35 of the 84 cases, followed by emergency department physicians in 29 cases (34%), pediatricians in 16 cases (19%), and family physicians in 4 cases (5%).
Dr. Liy-Wong and her colleagues reported no external sources of funding, and no conflicts of interest.
MINNEAPOLIS – A large single-site case review found that most pediatric patients with staphylococcal scalded skin syndrome (SSSS) had a classic presentation, often preceded by an upper respiratory tract infection.
In the review, surgical debridement increased hospital length of stay, and the use of clindamycin gave none of the benefit that might be expected from an antitoxin-specific antibiotic, according to Carmen Liy-Wong, MD, a pediatric medicine fellow at the Hospital for Sick Children in Toronto.
All children in the 84-patient study had a skin rash, which was also the first symptom noticed for 94% of the patients (n = 79). All children also had the classic SSSS clinical signs of skin erythema and exfoliation or desquamation; most (88%, n = 74) had skin tenderness. In more than half of the children in the study, erythema, exfoliation, and bullae formation first presented on the head or neck.
Dr. Liy-Wong presented her findings at the annual meeting of the Society for Pediatric Dermatology. She and her collaborators used a retrospective chart review to develop the largest case series to date of SSSS in pediatric hospitalized children to describe both the clinical presentation of SSSS and antimicrobial use and susceptibilities. Study objectives, she said, included identifying the clinical characteristics of children with SSSS, as well as identifying management practices and associated outcomes for hospitalized children with SSSS.
Of the 84 patients who met inclusion criteria, 49 (58%) were male, and the mean age at SSSS diagnosis was 3.1 (plus or minus 2.4) years. Children, aged 0-18 years, were included if they had a clinical diagnosis of SSSS. Children with localized exfoliative staphylococcal infections, such as bullous impetigo, were excluded from the study.
In addition to erythema, exfoliation, and bullae formation, most children also had a history of skin tenderness (68%, n = 79); a little over a third had a history of fever or pruritus (38%, n = 32 for both). Thirty-five of the children (42%) had an upper respiratory tract infection in the 2 weeks preceding the SSSS diagnosis.
Facial edema, perioral or periocular crusting, and vesicles or bullae were seen in more than half of children. A few patients had conjunctivitis (11%, n = 9), mucous membrane involvement (5%, n = 4), or a sandpaper-like scarlatiniform rash (11%, n = 9).
No patients in the study died. Complications were rare: shock syndrome in one patient, and generalized bacteremia in three patients (4%).
Pain management was a mainstay of inpatient care for children with SSSS; 75 children (89%) required pain medication, and opioids were used in more than half. One in five children received morphine by continuous intravenous infusion.
Patients who underwent surgical debridement stayed a mean 5.8 (plus or minus 4.1) days, compared with a mean 3.6 (plus or minus 2.1) days for those children not receiving debridement (P = 0.03).
The study also aimed to identify antibiotic resistance patterns for SSSS in the single-site study population. Blood cultures were obtained from all but five patients and were positive in three patients. Bullae were cultured in 28 patients (33%), and periorificial lesions were cultured in 57 patients (68%). Throat cultures were obtained in 31 patients, but culture results were not reported.
“Periorificial cultures were more useful than other sites in identification of the causative organism,” Dr. Liy-Wong noted, since 74% (42 of 57) of periorificial cultures were positive. In all, 50 of 195 cultures (26%) were positive for Staphylococcus aureus. Almost all of the 50 isolates (98%, n = 49) were sensitive to oxacillin. Just under half of isolates were sensitive to clindamycin (48%, n = 24,) and erythromycin (46%, n = 23).
The use of clindamycin, an antibiotic known to be effective in inhibiting exotoxin production by staphylococcus species, was not associated with reduced hospital length of stay (P = .63 for comparison with nonantitoxin antibiotics). Dr. Liy-Wong and her collaborators noted that “no statistically significant difference in outcomes was found in patients treated with specific antitoxin medication (clindamycin),” a practice that requires further study.
SSSS was diagnosed by dermatologists in 35 of the 84 cases, followed by emergency department physicians in 29 cases (34%), pediatricians in 16 cases (19%), and family physicians in 4 cases (5%).
Dr. Liy-Wong and her colleagues reported no external sources of funding, and no conflicts of interest.
AT THE SPD ANNUAL MEETING
Clindamycin confers no extra benefit for kids with SSSS
MINNEAPOLIS – A large single-site case review found that most pediatric patients with staphylococcal scalded skin syndrome (SSSS) had a classic presentation, often preceded by an upper respiratory tract infection.
In the review, surgical debridement increased hospital length of stay, and the use of clindamycin gave none of the benefit that might be expected from an antitoxin-specific antibiotic, according to Carmen Liy-Wong, MD, a pediatric medicine fellow at the Hospital for Sick Children in Toronto.
All children in the 84-patient study had a skin rash, which was also the first symptom noticed for 94% of the patients (n = 79). All children also had the classic SSSS clinical signs of skin erythema and exfoliation or desquamation; most (88%, n = 74) had skin tenderness. In more than half of the children in the study, erythema, exfoliation, and bullae formation first presented on the head or neck.
Dr. Liy-Wong presented her findings at the annual meeting of the Society for Pediatric Dermatology. She and her collaborators used a retrospective chart review to develop the largest case series to date of SSSS in pediatric hospitalized children to describe both the clinical presentation of SSSS and antimicrobial use and susceptibilities. Study objectives, she said, included identifying the clinical characteristics of children with SSSS, as well as identifying management practices and associated outcomes for hospitalized children with SSSS.
Of the 84 patients who met inclusion criteria, 49 (58%) were male, and the mean age at SSSS diagnosis was 3.1 (plus or minus 2.4) years. Children, aged 0-18 years, were included if they had a clinical diagnosis of SSSS. Children with localized exfoliative staphylococcal infections, such as bullous impetigo, were excluded from the study.
In addition to erythema, exfoliation, and bullae formation, most children also had a history of skin tenderness (68%, n = 79); a little over a third had a history of fever or pruritus (38%, n = 32 for both). Thirty-five of the children (42%) had an upper respiratory tract infection in the 2 weeks preceding the SSSS diagnosis.
Facial edema, perioral or periocular crusting, and vesicles or bullae were seen in more than half of children. A few patients had conjunctivitis (11%, n = 9), mucous membrane involvement (5%, n = 4), or a sandpaper-like scarlatiniform rash (11%, n = 9).
No patients in the study died. Complications were rare: shock syndrome in one patient, and generalized bacteremia in three patients (4%).
Pain management was a mainstay of inpatient care for children with SSSS; 75 children (89%) required pain medication, and opioids were used in more than half. One in five children received morphine by continuous intravenous infusion.
Patients who underwent surgical debridement stayed a mean 5.8 (plus or minus 4.1) days, compared with a mean 3.6 (plus or minus 2.1) days for those children not receiving debridement (P = 0.03).
The study also aimed to identify antibiotic resistance patterns for SSSS in the single-site study population. Blood cultures were obtained from all but five patients and were positive in three patients. Bullae were cultured in 28 patients (33%), and periorificial lesions were cultured in 57 patients (68%). Throat cultures were obtained in 31 patients, but culture results were not reported.
“Periorificial cultures were more useful than other sites in identification of the causative organism,” Dr. Liy-Wong noted, since 74% (42 of 57) of periorificial cultures were positive. In all, 50 of 195 cultures (26%) were positive for Staphylococcus aureus. Almost all of the 50 isolates (98%, n = 49) were sensitive to oxacillin. Just under half of isolates were sensitive to clindamycin (48%, n = 24,) and erythromycin (46%, n = 23).
The use of clindamycin, an antibiotic known to be effective in inhibiting exotoxin production by staphylococcus species, was not associated with reduced hospital length of stay (P = .63 for comparison with nonantitoxin antibiotics). Dr. Liy-Wong and her collaborators noted that “no statistically significant difference in outcomes was found in patients treated with specific antitoxin medication (clindamycin),” a practice that requires further study.
SSSS was diagnosed by dermatologists in 35 of the 84 cases, followed by emergency department physicians in 29 cases (34%), pediatricians in 16 cases (19%), and family physicians in 4 cases (5%).
Dr. Liy-Wong and her colleagues reported no external sources of funding, and no conflicts of interest.
On Twitter @karioakes
MINNEAPOLIS – A large single-site case review found that most pediatric patients with staphylococcal scalded skin syndrome (SSSS) had a classic presentation, often preceded by an upper respiratory tract infection.
In the review, surgical debridement increased hospital length of stay, and the use of clindamycin gave none of the benefit that might be expected from an antitoxin-specific antibiotic, according to Carmen Liy-Wong, MD, a pediatric medicine fellow at the Hospital for Sick Children in Toronto.
All children in the 84-patient study had a skin rash, which was also the first symptom noticed for 94% of the patients (n = 79). All children also had the classic SSSS clinical signs of skin erythema and exfoliation or desquamation; most (88%, n = 74) had skin tenderness. In more than half of the children in the study, erythema, exfoliation, and bullae formation first presented on the head or neck.
Dr. Liy-Wong presented her findings at the annual meeting of the Society for Pediatric Dermatology. She and her collaborators used a retrospective chart review to develop the largest case series to date of SSSS in pediatric hospitalized children to describe both the clinical presentation of SSSS and antimicrobial use and susceptibilities. Study objectives, she said, included identifying the clinical characteristics of children with SSSS, as well as identifying management practices and associated outcomes for hospitalized children with SSSS.
Of the 84 patients who met inclusion criteria, 49 (58%) were male, and the mean age at SSSS diagnosis was 3.1 (plus or minus 2.4) years. Children, aged 0-18 years, were included if they had a clinical diagnosis of SSSS. Children with localized exfoliative staphylococcal infections, such as bullous impetigo, were excluded from the study.
In addition to erythema, exfoliation, and bullae formation, most children also had a history of skin tenderness (68%, n = 79); a little over a third had a history of fever or pruritus (38%, n = 32 for both). Thirty-five of the children (42%) had an upper respiratory tract infection in the 2 weeks preceding the SSSS diagnosis.
Facial edema, perioral or periocular crusting, and vesicles or bullae were seen in more than half of children. A few patients had conjunctivitis (11%, n = 9), mucous membrane involvement (5%, n = 4), or a sandpaper-like scarlatiniform rash (11%, n = 9).
No patients in the study died. Complications were rare: shock syndrome in one patient, and generalized bacteremia in three patients (4%).
Pain management was a mainstay of inpatient care for children with SSSS; 75 children (89%) required pain medication, and opioids were used in more than half. One in five children received morphine by continuous intravenous infusion.
Patients who underwent surgical debridement stayed a mean 5.8 (plus or minus 4.1) days, compared with a mean 3.6 (plus or minus 2.1) days for those children not receiving debridement (P = 0.03).
The study also aimed to identify antibiotic resistance patterns for SSSS in the single-site study population. Blood cultures were obtained from all but five patients and were positive in three patients. Bullae were cultured in 28 patients (33%), and periorificial lesions were cultured in 57 patients (68%). Throat cultures were obtained in 31 patients, but culture results were not reported.
“Periorificial cultures were more useful than other sites in identification of the causative organism,” Dr. Liy-Wong noted, since 74% (42 of 57) of periorificial cultures were positive. In all, 50 of 195 cultures (26%) were positive for Staphylococcus aureus. Almost all of the 50 isolates (98%, n = 49) were sensitive to oxacillin. Just under half of isolates were sensitive to clindamycin (48%, n = 24,) and erythromycin (46%, n = 23).
The use of clindamycin, an antibiotic known to be effective in inhibiting exotoxin production by staphylococcus species, was not associated with reduced hospital length of stay (P = .63 for comparison with nonantitoxin antibiotics). Dr. Liy-Wong and her collaborators noted that “no statistically significant difference in outcomes was found in patients treated with specific antitoxin medication (clindamycin),” a practice that requires further study.
SSSS was diagnosed by dermatologists in 35 of the 84 cases, followed by emergency department physicians in 29 cases (34%), pediatricians in 16 cases (19%), and family physicians in 4 cases (5%).
Dr. Liy-Wong and her colleagues reported no external sources of funding, and no conflicts of interest.
On Twitter @karioakes
MINNEAPOLIS – A large single-site case review found that most pediatric patients with staphylococcal scalded skin syndrome (SSSS) had a classic presentation, often preceded by an upper respiratory tract infection.
In the review, surgical debridement increased hospital length of stay, and the use of clindamycin gave none of the benefit that might be expected from an antitoxin-specific antibiotic, according to Carmen Liy-Wong, MD, a pediatric medicine fellow at the Hospital for Sick Children in Toronto.
All children in the 84-patient study had a skin rash, which was also the first symptom noticed for 94% of the patients (n = 79). All children also had the classic SSSS clinical signs of skin erythema and exfoliation or desquamation; most (88%, n = 74) had skin tenderness. In more than half of the children in the study, erythema, exfoliation, and bullae formation first presented on the head or neck.
Dr. Liy-Wong presented her findings at the annual meeting of the Society for Pediatric Dermatology. She and her collaborators used a retrospective chart review to develop the largest case series to date of SSSS in pediatric hospitalized children to describe both the clinical presentation of SSSS and antimicrobial use and susceptibilities. Study objectives, she said, included identifying the clinical characteristics of children with SSSS, as well as identifying management practices and associated outcomes for hospitalized children with SSSS.
Of the 84 patients who met inclusion criteria, 49 (58%) were male, and the mean age at SSSS diagnosis was 3.1 (plus or minus 2.4) years. Children, aged 0-18 years, were included if they had a clinical diagnosis of SSSS. Children with localized exfoliative staphylococcal infections, such as bullous impetigo, were excluded from the study.
In addition to erythema, exfoliation, and bullae formation, most children also had a history of skin tenderness (68%, n = 79); a little over a third had a history of fever or pruritus (38%, n = 32 for both). Thirty-five of the children (42%) had an upper respiratory tract infection in the 2 weeks preceding the SSSS diagnosis.
Facial edema, perioral or periocular crusting, and vesicles or bullae were seen in more than half of children. A few patients had conjunctivitis (11%, n = 9), mucous membrane involvement (5%, n = 4), or a sandpaper-like scarlatiniform rash (11%, n = 9).
No patients in the study died. Complications were rare: shock syndrome in one patient, and generalized bacteremia in three patients (4%).
Pain management was a mainstay of inpatient care for children with SSSS; 75 children (89%) required pain medication, and opioids were used in more than half. One in five children received morphine by continuous intravenous infusion.
Patients who underwent surgical debridement stayed a mean 5.8 (plus or minus 4.1) days, compared with a mean 3.6 (plus or minus 2.1) days for those children not receiving debridement (P = 0.03).
The study also aimed to identify antibiotic resistance patterns for SSSS in the single-site study population. Blood cultures were obtained from all but five patients and were positive in three patients. Bullae were cultured in 28 patients (33%), and periorificial lesions were cultured in 57 patients (68%). Throat cultures were obtained in 31 patients, but culture results were not reported.
“Periorificial cultures were more useful than other sites in identification of the causative organism,” Dr. Liy-Wong noted, since 74% (42 of 57) of periorificial cultures were positive. In all, 50 of 195 cultures (26%) were positive for Staphylococcus aureus. Almost all of the 50 isolates (98%, n = 49) were sensitive to oxacillin. Just under half of isolates were sensitive to clindamycin (48%, n = 24,) and erythromycin (46%, n = 23).
The use of clindamycin, an antibiotic known to be effective in inhibiting exotoxin production by staphylococcus species, was not associated with reduced hospital length of stay (P = .63 for comparison with nonantitoxin antibiotics). Dr. Liy-Wong and her collaborators noted that “no statistically significant difference in outcomes was found in patients treated with specific antitoxin medication (clindamycin),” a practice that requires further study.
SSSS was diagnosed by dermatologists in 35 of the 84 cases, followed by emergency department physicians in 29 cases (34%), pediatricians in 16 cases (19%), and family physicians in 4 cases (5%).
Dr. Liy-Wong and her colleagues reported no external sources of funding, and no conflicts of interest.
On Twitter @karioakes
AT THE SPD ANNUAL MEETING
Key clinical point: Clindamycin did not benefit hospitalized children with staphylococcal scalded skin syndrome (SSSS).
Major finding: Clindamycin conferred no benefit in length of hospital stay compared with non-antitoxin antibiotics for SSSS (P = .63).
Data source: A retrospective chart review of 84 pediatric patients meeting SSSS criteria at a single children’s hospital.
Disclosures: Dr. Liy-Wong and her colleagues reported no external sources of funding, and no relevant disclosures.
Enhanced recovery protocol for colectomy patients reduced hospital stay
SAN DIEGO – Multihospital collaboration and implementation of enhanced recovery have the potential to improve outcomes, in particular, length of hospital stay, results from a pilot study showed.
“Given the importance of patient engagement, enhanced recovery has the potential to improve patient experience and provide high-value health care,” Julia R. Berian, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Dr. Berian, the James C. Thompson Geriatric Surgery Research Fellow at the University of Chicago Medical Center, presented findings from the Enhanced Recovery in NSQIP (ERIN) Pilot, a collaborative effort by 16 ACS-NSQIP hospitals to improve length of stay in patients who undergo colectomy, a procedure that has been shown to have an adverse event rate of 28.9% and an average length of stay of 9.8 days for those who experience an adverse event (J Am Coll Surg. 2008; 207[5]:698-704).
Implementation of the ERIN Pilot showed reductions in length of hospital stay and morbidity among colectomy patients. The average length of stay decreased by 1.2 days (from a mean of 6.6 among preimplementation cases to 5.4 days among post implementation cases; P less than .0001). Morbidity also decreased from 14% to 11% (P = .01), but the rate of readmission was 11% for both pre- and postimplementation cases. In the adjusted model, the enhanced recovery protocol decreased the risk of prolonged length of stay by 40% (odds ratio, 0.6; 95% confidence interval, 0.5-0.8).
For the ERIN Pilot, she and her associates participated in monthly conference calls for collaborative experience and expert guidance from project leaders Julie Thacker, MD, and Liane Feldman, MD. Enhanced recovery protocols were tailored to each individual hospital. Data were collected before and after implementation using 14 novel ERIN variables, including preoperative elements such as defining expectations and minimizing starvation, intraoperative variables such as optimizing fluid management and minimizing surgical trauma, and postoperative elements such as aggressive adherence to best practices including feeding, early ambulation, and minimizing the use of tethers such as urinary catheters.
The researchers evaluated procedure-targeted colectomy cases performed between July 2013 and June 2015, and excluded emergency cases or those with preoperative sepsis. They used bivariate analysis and multivariate logistic regression with forward selection, and the outcome of interest, prolonged hospital length of stay, was specified by the standard ACS NSQIP definition: greater than the 75th percentile of uncomplicated cases.
Dr. Berian reported results from 2,523 colectomies performed prior to implementation of the ERIN Pilot process and 823 colectomies performed after implementation of the process. The researchers observed no differences between the preimplementation and postimplementation cases in terms of sex, preoperative functional status, hypertension, renal failure, ascites, diabetes, disseminated cancer, or use of steroids for inflammatory bowel disease. However, compared with preimplementation colectomies, a significantly higher proportion of postimplementation cases were white (77% vs. 68%, respectively), had heart failure (2.8% vs. 1.2%), had chronic obstructive pulmonary disease (7.8% vs. 5.3%), were American Society of Anesthesiologists (ASA) class 1 and 2 ( 50.2% vs. 44.7%), were smokers (21.6% vs. 16.7%), had unintentional weight loss (7.7% vs. 5.7%), had used mechanical bowel prep (77% vs. 53%), and used more oral antibiotics (68% vs. 33%).
On the other hand, compared with preimplementation cases, there were significantly fewer bleeding disorders in the postimplementation colectomies (3.9% vs. 6.4%), as well as fewer cases with preoperative systemic inflammatory response syndrome (2.9% vs. 5.4%) and open surgery approaches (31.7% vs. 42.3%).
Dr. Berian disclosed that her fellowship position is funded by the John A. Hartford Foundation.
SAN DIEGO – Multihospital collaboration and implementation of enhanced recovery have the potential to improve outcomes, in particular, length of hospital stay, results from a pilot study showed.
“Given the importance of patient engagement, enhanced recovery has the potential to improve patient experience and provide high-value health care,” Julia R. Berian, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Dr. Berian, the James C. Thompson Geriatric Surgery Research Fellow at the University of Chicago Medical Center, presented findings from the Enhanced Recovery in NSQIP (ERIN) Pilot, a collaborative effort by 16 ACS-NSQIP hospitals to improve length of stay in patients who undergo colectomy, a procedure that has been shown to have an adverse event rate of 28.9% and an average length of stay of 9.8 days for those who experience an adverse event (J Am Coll Surg. 2008; 207[5]:698-704).
Implementation of the ERIN Pilot showed reductions in length of hospital stay and morbidity among colectomy patients. The average length of stay decreased by 1.2 days (from a mean of 6.6 among preimplementation cases to 5.4 days among post implementation cases; P less than .0001). Morbidity also decreased from 14% to 11% (P = .01), but the rate of readmission was 11% for both pre- and postimplementation cases. In the adjusted model, the enhanced recovery protocol decreased the risk of prolonged length of stay by 40% (odds ratio, 0.6; 95% confidence interval, 0.5-0.8).
For the ERIN Pilot, she and her associates participated in monthly conference calls for collaborative experience and expert guidance from project leaders Julie Thacker, MD, and Liane Feldman, MD. Enhanced recovery protocols were tailored to each individual hospital. Data were collected before and after implementation using 14 novel ERIN variables, including preoperative elements such as defining expectations and minimizing starvation, intraoperative variables such as optimizing fluid management and minimizing surgical trauma, and postoperative elements such as aggressive adherence to best practices including feeding, early ambulation, and minimizing the use of tethers such as urinary catheters.
The researchers evaluated procedure-targeted colectomy cases performed between July 2013 and June 2015, and excluded emergency cases or those with preoperative sepsis. They used bivariate analysis and multivariate logistic regression with forward selection, and the outcome of interest, prolonged hospital length of stay, was specified by the standard ACS NSQIP definition: greater than the 75th percentile of uncomplicated cases.
Dr. Berian reported results from 2,523 colectomies performed prior to implementation of the ERIN Pilot process and 823 colectomies performed after implementation of the process. The researchers observed no differences between the preimplementation and postimplementation cases in terms of sex, preoperative functional status, hypertension, renal failure, ascites, diabetes, disseminated cancer, or use of steroids for inflammatory bowel disease. However, compared with preimplementation colectomies, a significantly higher proportion of postimplementation cases were white (77% vs. 68%, respectively), had heart failure (2.8% vs. 1.2%), had chronic obstructive pulmonary disease (7.8% vs. 5.3%), were American Society of Anesthesiologists (ASA) class 1 and 2 ( 50.2% vs. 44.7%), were smokers (21.6% vs. 16.7%), had unintentional weight loss (7.7% vs. 5.7%), had used mechanical bowel prep (77% vs. 53%), and used more oral antibiotics (68% vs. 33%).
On the other hand, compared with preimplementation cases, there were significantly fewer bleeding disorders in the postimplementation colectomies (3.9% vs. 6.4%), as well as fewer cases with preoperative systemic inflammatory response syndrome (2.9% vs. 5.4%) and open surgery approaches (31.7% vs. 42.3%).
Dr. Berian disclosed that her fellowship position is funded by the John A. Hartford Foundation.
SAN DIEGO – Multihospital collaboration and implementation of enhanced recovery have the potential to improve outcomes, in particular, length of hospital stay, results from a pilot study showed.
“Given the importance of patient engagement, enhanced recovery has the potential to improve patient experience and provide high-value health care,” Julia R. Berian, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Dr. Berian, the James C. Thompson Geriatric Surgery Research Fellow at the University of Chicago Medical Center, presented findings from the Enhanced Recovery in NSQIP (ERIN) Pilot, a collaborative effort by 16 ACS-NSQIP hospitals to improve length of stay in patients who undergo colectomy, a procedure that has been shown to have an adverse event rate of 28.9% and an average length of stay of 9.8 days for those who experience an adverse event (J Am Coll Surg. 2008; 207[5]:698-704).
Implementation of the ERIN Pilot showed reductions in length of hospital stay and morbidity among colectomy patients. The average length of stay decreased by 1.2 days (from a mean of 6.6 among preimplementation cases to 5.4 days among post implementation cases; P less than .0001). Morbidity also decreased from 14% to 11% (P = .01), but the rate of readmission was 11% for both pre- and postimplementation cases. In the adjusted model, the enhanced recovery protocol decreased the risk of prolonged length of stay by 40% (odds ratio, 0.6; 95% confidence interval, 0.5-0.8).
For the ERIN Pilot, she and her associates participated in monthly conference calls for collaborative experience and expert guidance from project leaders Julie Thacker, MD, and Liane Feldman, MD. Enhanced recovery protocols were tailored to each individual hospital. Data were collected before and after implementation using 14 novel ERIN variables, including preoperative elements such as defining expectations and minimizing starvation, intraoperative variables such as optimizing fluid management and minimizing surgical trauma, and postoperative elements such as aggressive adherence to best practices including feeding, early ambulation, and minimizing the use of tethers such as urinary catheters.
The researchers evaluated procedure-targeted colectomy cases performed between July 2013 and June 2015, and excluded emergency cases or those with preoperative sepsis. They used bivariate analysis and multivariate logistic regression with forward selection, and the outcome of interest, prolonged hospital length of stay, was specified by the standard ACS NSQIP definition: greater than the 75th percentile of uncomplicated cases.
Dr. Berian reported results from 2,523 colectomies performed prior to implementation of the ERIN Pilot process and 823 colectomies performed after implementation of the process. The researchers observed no differences between the preimplementation and postimplementation cases in terms of sex, preoperative functional status, hypertension, renal failure, ascites, diabetes, disseminated cancer, or use of steroids for inflammatory bowel disease. However, compared with preimplementation colectomies, a significantly higher proportion of postimplementation cases were white (77% vs. 68%, respectively), had heart failure (2.8% vs. 1.2%), had chronic obstructive pulmonary disease (7.8% vs. 5.3%), were American Society of Anesthesiologists (ASA) class 1 and 2 ( 50.2% vs. 44.7%), were smokers (21.6% vs. 16.7%), had unintentional weight loss (7.7% vs. 5.7%), had used mechanical bowel prep (77% vs. 53%), and used more oral antibiotics (68% vs. 33%).
On the other hand, compared with preimplementation cases, there were significantly fewer bleeding disorders in the postimplementation colectomies (3.9% vs. 6.4%), as well as fewer cases with preoperative systemic inflammatory response syndrome (2.9% vs. 5.4%) and open surgery approaches (31.7% vs. 42.3%).
Dr. Berian disclosed that her fellowship position is funded by the John A. Hartford Foundation.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: A multihospital enhanced recovery process for colectomy patients decreased length of stay and morbidity.
Major finding: After implementation of an enhanced recovery protocol in colectomy patients, the average hospital length of stay decreased by 1.2 days (from a mean of 6.6 days among preimplementation cases to 5.4 days among post implementation cases; P less than .0001). Morbidity also decreased from 14% to 11% (P = .01).
Data source: An analysis of 2,523 colectomies performed prior to implementation of the Enhanced Recovery in NSQIP (ERIN) Pilot process and 823 colectomies performed after implementation of the process.
Disclosures: Dr. Berian disclosed that her fellowship position is funded by the John A. Hartford Foundation.
More states moving to require payment for abuse-deterrent opioids
LAKE BUENA VISTA, FLA. – The “Guidance for Industry” issued by the Food and Drug Administration last year has encouraged a systematic approach to the development and testing of opioid abuse-deterrent technologies that can be credited with spurring innovation, according to two pain specialists.
“Clinicians trying to understand these products are going to have to get used to hearing about likability studies and other types of evaluations that measure the efficacy of deterrence,” reported Jeffrey A. Gudin, MD, director of pain and palliative care, Englewood Hospital and Medical Center, New Jersey. He suggested that the outline provided by the FDA has been instrumental in defining standards with which different types of strategies can be compared.
At least eight opioids with abuse-deterrent properties already are on the market. Those include a product with a reservoir of the opioid-antagonist naloxone, which is designed for release in the event of tampering; pills constructed with complex polymers that produce a viscous gel when crushed or dissolved to prevent injection or snorting; and a tablet in which the opioid is accompanied with an aversion product. If the tablet is crushed, the aversion product mixes with the opioid, producing discomfort.
Four types of studies are recommended to evaluate abuse-deterrent strategies in the FDA manual for industry. Those include laboratory manipulation studies, pharmacokinetic studies, clinical abuse-deterrent studies, and postmarketing surveillance. The clinical abuse-deterrent studies are the ones that test likability. According to Dr. Gudin, those studies enroll drug-experienced recreational users who test whether pleasurable effects can be derived from the product despite the mechanism for deterrence.
Fulfilling the criteria for effect abuse deterrence “does not mean that the product is abuse proof,” cautioned Martin E. Hale, MD, an orthopedic surgeon and pain management specialist in private practice in Plantation, Fla. Rather, the goal is to provide a sufficient obstacle that the epidemic of opioid abuse and opioid-related deaths can be turned around. “Creating these types of deterrents may help,” Dr. Hale said.
Typically, addicts are seeking an immediate high, which is a very different goal from control of pain symptoms, according to Dr. Gudin. He reported that preventing the rapid onset of euphoria is one of the abuse-deterrent strategies being pursued. He cited one product in clinical development that requires 5 days before it crosses the blood-brain barrier. Such a product, he said, “would still work for the chronic pain patient, but it is not so good for the individuals who wants to get high.”
Not surprisingly, opioids with abuse deterrence cost more than those without, but the effort to remove this obstacle to encourage wider use is being addressed at the level of state legislatures, Dr. Gudin said. By his count, laws have been proposed in 30 states calling for third-party payers to make opioids with abuse deterrence available at the same cost as products without this technology. Four states have passed this legislation already, and an additional four have made passage contingent on studies demonstrating a change in risk of abuse.
In an informal poll at the meeting, a sizable majority of the attendees agreed that they would prefer to prescribe an opioid formulated with an abuse deterrent, particularly if third-party coverage was assured, but Dr. Gudin, like Dr. Hale, emphasized that no deterrent technology is foolproof.
For preventing inappropriate use of opioids, “abuse deterrence is just another tool in the toolkit,” Dr. Gudin said. He cautioned that all the other strategies aimed at keeping opioids out of the hands of abusers still should be employed. He predicted that most ER/LA opioids soon will have some form of abuse deterrence, and the same types of technologies are likely to offered in immediate-release opioids as well. Requiring third-party payers to provide reimbursement would accelerate the transition.
“Let’s face it, what is the downside if payers say they will work with you,” Dr. Gudin said.
Dr. Gudin reports a financial relationship with Teva, and Dr. Hale reports a financial relationship with Purdue.
The meeting was held by the American Pain Society and Global Academy for Medical Education. Global Academy and this news organization are owned by the same company.
LAKE BUENA VISTA, FLA. – The “Guidance for Industry” issued by the Food and Drug Administration last year has encouraged a systematic approach to the development and testing of opioid abuse-deterrent technologies that can be credited with spurring innovation, according to two pain specialists.
“Clinicians trying to understand these products are going to have to get used to hearing about likability studies and other types of evaluations that measure the efficacy of deterrence,” reported Jeffrey A. Gudin, MD, director of pain and palliative care, Englewood Hospital and Medical Center, New Jersey. He suggested that the outline provided by the FDA has been instrumental in defining standards with which different types of strategies can be compared.
At least eight opioids with abuse-deterrent properties already are on the market. Those include a product with a reservoir of the opioid-antagonist naloxone, which is designed for release in the event of tampering; pills constructed with complex polymers that produce a viscous gel when crushed or dissolved to prevent injection or snorting; and a tablet in which the opioid is accompanied with an aversion product. If the tablet is crushed, the aversion product mixes with the opioid, producing discomfort.
Four types of studies are recommended to evaluate abuse-deterrent strategies in the FDA manual for industry. Those include laboratory manipulation studies, pharmacokinetic studies, clinical abuse-deterrent studies, and postmarketing surveillance. The clinical abuse-deterrent studies are the ones that test likability. According to Dr. Gudin, those studies enroll drug-experienced recreational users who test whether pleasurable effects can be derived from the product despite the mechanism for deterrence.
Fulfilling the criteria for effect abuse deterrence “does not mean that the product is abuse proof,” cautioned Martin E. Hale, MD, an orthopedic surgeon and pain management specialist in private practice in Plantation, Fla. Rather, the goal is to provide a sufficient obstacle that the epidemic of opioid abuse and opioid-related deaths can be turned around. “Creating these types of deterrents may help,” Dr. Hale said.
Typically, addicts are seeking an immediate high, which is a very different goal from control of pain symptoms, according to Dr. Gudin. He reported that preventing the rapid onset of euphoria is one of the abuse-deterrent strategies being pursued. He cited one product in clinical development that requires 5 days before it crosses the blood-brain barrier. Such a product, he said, “would still work for the chronic pain patient, but it is not so good for the individuals who wants to get high.”
Not surprisingly, opioids with abuse deterrence cost more than those without, but the effort to remove this obstacle to encourage wider use is being addressed at the level of state legislatures, Dr. Gudin said. By his count, laws have been proposed in 30 states calling for third-party payers to make opioids with abuse deterrence available at the same cost as products without this technology. Four states have passed this legislation already, and an additional four have made passage contingent on studies demonstrating a change in risk of abuse.
In an informal poll at the meeting, a sizable majority of the attendees agreed that they would prefer to prescribe an opioid formulated with an abuse deterrent, particularly if third-party coverage was assured, but Dr. Gudin, like Dr. Hale, emphasized that no deterrent technology is foolproof.
For preventing inappropriate use of opioids, “abuse deterrence is just another tool in the toolkit,” Dr. Gudin said. He cautioned that all the other strategies aimed at keeping opioids out of the hands of abusers still should be employed. He predicted that most ER/LA opioids soon will have some form of abuse deterrence, and the same types of technologies are likely to offered in immediate-release opioids as well. Requiring third-party payers to provide reimbursement would accelerate the transition.
“Let’s face it, what is the downside if payers say they will work with you,” Dr. Gudin said.
Dr. Gudin reports a financial relationship with Teva, and Dr. Hale reports a financial relationship with Purdue.
The meeting was held by the American Pain Society and Global Academy for Medical Education. Global Academy and this news organization are owned by the same company.
LAKE BUENA VISTA, FLA. – The “Guidance for Industry” issued by the Food and Drug Administration last year has encouraged a systematic approach to the development and testing of opioid abuse-deterrent technologies that can be credited with spurring innovation, according to two pain specialists.
“Clinicians trying to understand these products are going to have to get used to hearing about likability studies and other types of evaluations that measure the efficacy of deterrence,” reported Jeffrey A. Gudin, MD, director of pain and palliative care, Englewood Hospital and Medical Center, New Jersey. He suggested that the outline provided by the FDA has been instrumental in defining standards with which different types of strategies can be compared.
At least eight opioids with abuse-deterrent properties already are on the market. Those include a product with a reservoir of the opioid-antagonist naloxone, which is designed for release in the event of tampering; pills constructed with complex polymers that produce a viscous gel when crushed or dissolved to prevent injection or snorting; and a tablet in which the opioid is accompanied with an aversion product. If the tablet is crushed, the aversion product mixes with the opioid, producing discomfort.
Four types of studies are recommended to evaluate abuse-deterrent strategies in the FDA manual for industry. Those include laboratory manipulation studies, pharmacokinetic studies, clinical abuse-deterrent studies, and postmarketing surveillance. The clinical abuse-deterrent studies are the ones that test likability. According to Dr. Gudin, those studies enroll drug-experienced recreational users who test whether pleasurable effects can be derived from the product despite the mechanism for deterrence.
Fulfilling the criteria for effect abuse deterrence “does not mean that the product is abuse proof,” cautioned Martin E. Hale, MD, an orthopedic surgeon and pain management specialist in private practice in Plantation, Fla. Rather, the goal is to provide a sufficient obstacle that the epidemic of opioid abuse and opioid-related deaths can be turned around. “Creating these types of deterrents may help,” Dr. Hale said.
Typically, addicts are seeking an immediate high, which is a very different goal from control of pain symptoms, according to Dr. Gudin. He reported that preventing the rapid onset of euphoria is one of the abuse-deterrent strategies being pursued. He cited one product in clinical development that requires 5 days before it crosses the blood-brain barrier. Such a product, he said, “would still work for the chronic pain patient, but it is not so good for the individuals who wants to get high.”
Not surprisingly, opioids with abuse deterrence cost more than those without, but the effort to remove this obstacle to encourage wider use is being addressed at the level of state legislatures, Dr. Gudin said. By his count, laws have been proposed in 30 states calling for third-party payers to make opioids with abuse deterrence available at the same cost as products without this technology. Four states have passed this legislation already, and an additional four have made passage contingent on studies demonstrating a change in risk of abuse.
In an informal poll at the meeting, a sizable majority of the attendees agreed that they would prefer to prescribe an opioid formulated with an abuse deterrent, particularly if third-party coverage was assured, but Dr. Gudin, like Dr. Hale, emphasized that no deterrent technology is foolproof.
For preventing inappropriate use of opioids, “abuse deterrence is just another tool in the toolkit,” Dr. Gudin said. He cautioned that all the other strategies aimed at keeping opioids out of the hands of abusers still should be employed. He predicted that most ER/LA opioids soon will have some form of abuse deterrence, and the same types of technologies are likely to offered in immediate-release opioids as well. Requiring third-party payers to provide reimbursement would accelerate the transition.
“Let’s face it, what is the downside if payers say they will work with you,” Dr. Gudin said.
Dr. Gudin reports a financial relationship with Teva, and Dr. Hale reports a financial relationship with Purdue.
The meeting was held by the American Pain Society and Global Academy for Medical Education. Global Academy and this news organization are owned by the same company.
EXPERT ANALYSIS FROM PAIN CARE FOR PRIMARY CARE
Graham Foundation Congratulates Latest 2016 Awardees
Every Heartbeat Valve Matters Fellowship
Sponsored by Edwards Lifesciences
CT surgeons treating patients from underserved populations spend time at an advanced heart valve disease training and educational institution to acquire skills that can be implemented in practice.
Chizoba Efobi, MD
University of Benin Teaching Hospital, Nigeria
Christian Kreutzer, MD
Hospital Nacional Alejandro Posadas, Argentina
Chartarooon Rimsukcharoenchai, MD
Chiang Mai University Hospital, Thailand
René Silva, MD
San Camilo - Holy Family Hospital, Brazil
Fellowship for Advanced Minimally Invasive Thoracic Surgery
Sponsored by Ethicon
Young thoracic or CT surgeons and their surgical teams visit clinical sites for one- and two-day training on VATS Lobectomy.
Mary Carolyn, MD
Saint Joseph’s Hospital
Alexander Kraev, MD
Billings Clinic
Roman Petrov, MD
Marietta Memorial Hospital
Nestor Villamizar Ortiz, MD
University of Miami
Graham Surgical Investigator Program
Supporting the clinical and translational research of young CT surgeons for up to two years.
Isaac George, MD
NewYork-Presbyterian Hospital Columbia University Medical Center
“Cardiac and Skeletal Muscle Metabolic Failure in Diabetic Heart Disease: Role of MSTN/AMPK Signaling”
Alexander Iribarne, MD
Dartmouth Medical School
“Geographic Variation in Screening and Frequency of Re-interventions after Thoracic Aortic Aneurysm Repair Among Medicare Recipients in the United States”
Ethicon Surgical Investigator Award
Ravi Ghanta, MD
University of Virginia
“Improving Stem Cell Engraftment by Optimization of the Mechanical Microenvironment in Ischemic Myocardium”
Intuitive Surgical Investigator Award
Michael Halkos, MD
Emory University
“Hybrid Coronary Revascularization Versus Coronary Artery Bypass Surgery For Patients With Multivessel Coronary Disease”
Oz Lemole Surgical Investigator Award
David Odell, MD
Northwestern University, Feinberg School of Medicine
“Development of a Novel Lung Cancer Quality Improvement Collaborative
North America Clinical Immersion in Advanced Minimally Invasive Thoracic Surgery
Sponsored by Medtronic
Young Chinese thoracic surgeons learn advanced minimally invasive thoracic surgery and comprehensive care screening and diagnosis at North American institutions.
Feng Jiang, MD
Jiangsu Cancer Hospital
Jiageng Li, MD
Cancer Institute and Hospital
Teng Mao, MD
Shanghai Chest Hospital
Hao Wang, MD
Zhongshan Hospital, Fudan University
Ruixiang Zhang, MD
Henan Cancer Hospital
Zhenrong Zhang, MD
China Japan Friendship Hospital
Feng Zhao, MD
Union Hospital, Hubei
Zuli Zhou, MD
Peking University People’s Hospital
Surgical Robotics Fellowship
Sponsored by Intuitive Surgical
North American general thoracic fellows and their attending surgeons spend two days receiving hands-on, advanced training in the Da Vinci robotics system.
Nicholas Baker, MD
University of Pittsburgh Medical Center
Adam Bograd, MD
Memorial Sloan Kettering Cancer Center
Edward Chan, MD
Houston Methodist Hospital
John Cleveland, MD
Keck School of Medicine University of Southern California
Mark Crye, MD
Allegheny Health Network-Allegheny General Hospital
Laura Donahoe, MD
University of Toronto
Crystal Erickson, MD
University of Michigan
Jinny Ha, MD
Johns Hopkins Hospital
Eric Jeng, MD
University of Florida
Peter Kneuertz, MD
New York-Presbyterian Hospital Weill Cornell Medical Center
Moshe Lapidot, MD
Brigham and Women’s Hospital
Antonio Lassaletta, MD
Harvard Medical School, Beth Israel Deaconess Medical Center
Jason Muesse, MD
Emory University
Christian Otero, MD
University of Miami/Jackson Memorial Medical Center
Janani Reisenauer, MD
Mayo Clinic
Smarika Shrestha, MD
Penn State Milton S. Hershey Medical Center
Nicholas Stephens, MD
The University of Texas Medical School at Houston
Huan Huan (Joanne) Sun, MD
NYU Langone Medical Center
John Waters, MD
The University of Texas Medical School at Houston
Brittany Zwischenberger, MD
Duke University
Thoracic Surgery Training Fellowship
Sponsored by Ethicon China
Chinese thoracic training fellows receive advanced training at North American institutions.
Mingsong Wang, MD
Shanghai Xinhua Hospital
Song Xu, MD
Tianjin Medical University General Hospital
Wanpu Yan, MD
Beijing Cancer Hospital
Yong Zhang, MD
First Affiliated Hospital of Xi’an Jiaotong University
Every Heartbeat Valve Matters Fellowship
Sponsored by Edwards Lifesciences
CT surgeons treating patients from underserved populations spend time at an advanced heart valve disease training and educational institution to acquire skills that can be implemented in practice.
Chizoba Efobi, MD
University of Benin Teaching Hospital, Nigeria
Christian Kreutzer, MD
Hospital Nacional Alejandro Posadas, Argentina
Chartarooon Rimsukcharoenchai, MD
Chiang Mai University Hospital, Thailand
René Silva, MD
San Camilo - Holy Family Hospital, Brazil
Fellowship for Advanced Minimally Invasive Thoracic Surgery
Sponsored by Ethicon
Young thoracic or CT surgeons and their surgical teams visit clinical sites for one- and two-day training on VATS Lobectomy.
Mary Carolyn, MD
Saint Joseph’s Hospital
Alexander Kraev, MD
Billings Clinic
Roman Petrov, MD
Marietta Memorial Hospital
Nestor Villamizar Ortiz, MD
University of Miami
Graham Surgical Investigator Program
Supporting the clinical and translational research of young CT surgeons for up to two years.
Isaac George, MD
NewYork-Presbyterian Hospital Columbia University Medical Center
“Cardiac and Skeletal Muscle Metabolic Failure in Diabetic Heart Disease: Role of MSTN/AMPK Signaling”
Alexander Iribarne, MD
Dartmouth Medical School
“Geographic Variation in Screening and Frequency of Re-interventions after Thoracic Aortic Aneurysm Repair Among Medicare Recipients in the United States”
Ethicon Surgical Investigator Award
Ravi Ghanta, MD
University of Virginia
“Improving Stem Cell Engraftment by Optimization of the Mechanical Microenvironment in Ischemic Myocardium”
Intuitive Surgical Investigator Award
Michael Halkos, MD
Emory University
“Hybrid Coronary Revascularization Versus Coronary Artery Bypass Surgery For Patients With Multivessel Coronary Disease”
Oz Lemole Surgical Investigator Award
David Odell, MD
Northwestern University, Feinberg School of Medicine
“Development of a Novel Lung Cancer Quality Improvement Collaborative
North America Clinical Immersion in Advanced Minimally Invasive Thoracic Surgery
Sponsored by Medtronic
Young Chinese thoracic surgeons learn advanced minimally invasive thoracic surgery and comprehensive care screening and diagnosis at North American institutions.
Feng Jiang, MD
Jiangsu Cancer Hospital
Jiageng Li, MD
Cancer Institute and Hospital
Teng Mao, MD
Shanghai Chest Hospital
Hao Wang, MD
Zhongshan Hospital, Fudan University
Ruixiang Zhang, MD
Henan Cancer Hospital
Zhenrong Zhang, MD
China Japan Friendship Hospital
Feng Zhao, MD
Union Hospital, Hubei
Zuli Zhou, MD
Peking University People’s Hospital
Surgical Robotics Fellowship
Sponsored by Intuitive Surgical
North American general thoracic fellows and their attending surgeons spend two days receiving hands-on, advanced training in the Da Vinci robotics system.
Nicholas Baker, MD
University of Pittsburgh Medical Center
Adam Bograd, MD
Memorial Sloan Kettering Cancer Center
Edward Chan, MD
Houston Methodist Hospital
John Cleveland, MD
Keck School of Medicine University of Southern California
Mark Crye, MD
Allegheny Health Network-Allegheny General Hospital
Laura Donahoe, MD
University of Toronto
Crystal Erickson, MD
University of Michigan
Jinny Ha, MD
Johns Hopkins Hospital
Eric Jeng, MD
University of Florida
Peter Kneuertz, MD
New York-Presbyterian Hospital Weill Cornell Medical Center
Moshe Lapidot, MD
Brigham and Women’s Hospital
Antonio Lassaletta, MD
Harvard Medical School, Beth Israel Deaconess Medical Center
Jason Muesse, MD
Emory University
Christian Otero, MD
University of Miami/Jackson Memorial Medical Center
Janani Reisenauer, MD
Mayo Clinic
Smarika Shrestha, MD
Penn State Milton S. Hershey Medical Center
Nicholas Stephens, MD
The University of Texas Medical School at Houston
Huan Huan (Joanne) Sun, MD
NYU Langone Medical Center
John Waters, MD
The University of Texas Medical School at Houston
Brittany Zwischenberger, MD
Duke University
Thoracic Surgery Training Fellowship
Sponsored by Ethicon China
Chinese thoracic training fellows receive advanced training at North American institutions.
Mingsong Wang, MD
Shanghai Xinhua Hospital
Song Xu, MD
Tianjin Medical University General Hospital
Wanpu Yan, MD
Beijing Cancer Hospital
Yong Zhang, MD
First Affiliated Hospital of Xi’an Jiaotong University
Every Heartbeat Valve Matters Fellowship
Sponsored by Edwards Lifesciences
CT surgeons treating patients from underserved populations spend time at an advanced heart valve disease training and educational institution to acquire skills that can be implemented in practice.
Chizoba Efobi, MD
University of Benin Teaching Hospital, Nigeria
Christian Kreutzer, MD
Hospital Nacional Alejandro Posadas, Argentina
Chartarooon Rimsukcharoenchai, MD
Chiang Mai University Hospital, Thailand
René Silva, MD
San Camilo - Holy Family Hospital, Brazil
Fellowship for Advanced Minimally Invasive Thoracic Surgery
Sponsored by Ethicon
Young thoracic or CT surgeons and their surgical teams visit clinical sites for one- and two-day training on VATS Lobectomy.
Mary Carolyn, MD
Saint Joseph’s Hospital
Alexander Kraev, MD
Billings Clinic
Roman Petrov, MD
Marietta Memorial Hospital
Nestor Villamizar Ortiz, MD
University of Miami
Graham Surgical Investigator Program
Supporting the clinical and translational research of young CT surgeons for up to two years.
Isaac George, MD
NewYork-Presbyterian Hospital Columbia University Medical Center
“Cardiac and Skeletal Muscle Metabolic Failure in Diabetic Heart Disease: Role of MSTN/AMPK Signaling”
Alexander Iribarne, MD
Dartmouth Medical School
“Geographic Variation in Screening and Frequency of Re-interventions after Thoracic Aortic Aneurysm Repair Among Medicare Recipients in the United States”
Ethicon Surgical Investigator Award
Ravi Ghanta, MD
University of Virginia
“Improving Stem Cell Engraftment by Optimization of the Mechanical Microenvironment in Ischemic Myocardium”
Intuitive Surgical Investigator Award
Michael Halkos, MD
Emory University
“Hybrid Coronary Revascularization Versus Coronary Artery Bypass Surgery For Patients With Multivessel Coronary Disease”
Oz Lemole Surgical Investigator Award
David Odell, MD
Northwestern University, Feinberg School of Medicine
“Development of a Novel Lung Cancer Quality Improvement Collaborative
North America Clinical Immersion in Advanced Minimally Invasive Thoracic Surgery
Sponsored by Medtronic
Young Chinese thoracic surgeons learn advanced minimally invasive thoracic surgery and comprehensive care screening and diagnosis at North American institutions.
Feng Jiang, MD
Jiangsu Cancer Hospital
Jiageng Li, MD
Cancer Institute and Hospital
Teng Mao, MD
Shanghai Chest Hospital
Hao Wang, MD
Zhongshan Hospital, Fudan University
Ruixiang Zhang, MD
Henan Cancer Hospital
Zhenrong Zhang, MD
China Japan Friendship Hospital
Feng Zhao, MD
Union Hospital, Hubei
Zuli Zhou, MD
Peking University People’s Hospital
Surgical Robotics Fellowship
Sponsored by Intuitive Surgical
North American general thoracic fellows and their attending surgeons spend two days receiving hands-on, advanced training in the Da Vinci robotics system.
Nicholas Baker, MD
University of Pittsburgh Medical Center
Adam Bograd, MD
Memorial Sloan Kettering Cancer Center
Edward Chan, MD
Houston Methodist Hospital
John Cleveland, MD
Keck School of Medicine University of Southern California
Mark Crye, MD
Allegheny Health Network-Allegheny General Hospital
Laura Donahoe, MD
University of Toronto
Crystal Erickson, MD
University of Michigan
Jinny Ha, MD
Johns Hopkins Hospital
Eric Jeng, MD
University of Florida
Peter Kneuertz, MD
New York-Presbyterian Hospital Weill Cornell Medical Center
Moshe Lapidot, MD
Brigham and Women’s Hospital
Antonio Lassaletta, MD
Harvard Medical School, Beth Israel Deaconess Medical Center
Jason Muesse, MD
Emory University
Christian Otero, MD
University of Miami/Jackson Memorial Medical Center
Janani Reisenauer, MD
Mayo Clinic
Smarika Shrestha, MD
Penn State Milton S. Hershey Medical Center
Nicholas Stephens, MD
The University of Texas Medical School at Houston
Huan Huan (Joanne) Sun, MD
NYU Langone Medical Center
John Waters, MD
The University of Texas Medical School at Houston
Brittany Zwischenberger, MD
Duke University
Thoracic Surgery Training Fellowship
Sponsored by Ethicon China
Chinese thoracic training fellows receive advanced training at North American institutions.
Mingsong Wang, MD
Shanghai Xinhua Hospital
Song Xu, MD
Tianjin Medical University General Hospital
Wanpu Yan, MD
Beijing Cancer Hospital
Yong Zhang, MD
First Affiliated Hospital of Xi’an Jiaotong University
SB-generated CAR T cells show promise

Image by NIAID
Researchers have reported “favorable” long-term results from a pair of phase 1 trials in which they used the non-viral Sleeping Beauty (SB) transposon/transposase system to create CD19-specific chimeric antigen receptor (CAR) T cells.
These CAR T cells appeared to be safe, and results suggested they can provide additional control of leukemia and lymphoma when given after autologous or allogeneic hematopoietic stem cell transplant (HSCT).
In addition, the researchers said use of the SB transposon/transposase platform could reduce the costs and complexity associated with recombinant viral vector-based immunotherapy.
The team described their results with the SB system in The Journal of Clinical Investigation. Results from these trials were previously reported at the inaugural CRI-CIMT-EATI-AACR International Cancer Immunotherapy Conference.
The trials were sponsored by MD Anderson Cancer Center in collaboration with the National Cancer Institute, National Center for Research Resources, Intrexon Corporation, and Ziopharm Oncology.
The trials included 26 patients with multiply relapsed B-lineage acute lymphoblastic leukemia (ALL, n=17) or B-cell non-Hodgkin lymphoma (NHL, n=9).
The patients received SB-modified T cells after autologous (n=7) or allogeneic (n=19) HSCT.
The researchers said SB-mediated gene transfer and stimulation resulted in large ex vivo expansion of T cells while retaining CAR expression and without integration hotspots.
Autologous and allogeneic T cells survived after infusion an average of 201 days and 51 days, respectively.
Safety
The researchers said there were no unexpected acute infusion or delayed toxicities. Mild elevations in cytokines were observed but not cytokine storm.
Three allogeneic HSCT recipients developed graft-vs-host disease (GVHD). One patient developed grade 1 acute skin GVHD that resolved with topical steroids, and 1 developed chronic skin GVHD that responded to systemic steroids.
The third patient, who had a history of drug-induced liver toxicity, developed recurrent liver toxicity with a component of liver GVHD 1 month after T-cell infusion. This patient died of liver failure.
There were 5 other deaths, all of them due to disease relapse.
Efficacy: Autologous HSCT
Seven patients with advanced NHL were treated with autologous HSCT, followed by the administration of patient-derived CAR T cells.
Six of the 7 patients were in complete remission (CR) at a median follow-up of 25.5 months (range, 6.4 to 32.7 months).
The 30-month progression-free survival (PFS) rate was 83%, and the overall survival (OS) rate was 100%.
Efficacy: Allogeneic HSCT
Nineteen patients (ALL n=17, NHL n=2) received donor-derived CAR T cells after allogeneic HSCT. The patients had advanced disease at the time of HSCT, and CAR T cells were administered without additional lymphodepletion.
Eleven of 19 patients were still in CR at a median follow-up of 7.5 months (range, 2.7 to 17.9 months). The 1-year PFS rate was 53%, and the OS rate was 63%.
The researchers also looked at the subset of allogeneic HSCT recipients who received haplo-identical CAR T cells. These 8 patients had a 1-year PFS rate of 75% and an OS rate of 100%.
“By following these patients over an extended duration, as we do in these studies, we can better understand the added benefit of CAR-T over HSCT alone,” said Francois Lebel, MD, of Ziopharm Oncology.
“Although the primary objective of these trials was not to establish efficacy, the recipients’ outcomes are encouraging, with apparent doubling of survivals compared to historical controls. We are encouraged by these clinical data and look forward to results from our phase 1 study infusing our next-generation CD19-specific CAR T cells in patients with advanced lymphoid malignancies.” ![]()

Image by NIAID
Researchers have reported “favorable” long-term results from a pair of phase 1 trials in which they used the non-viral Sleeping Beauty (SB) transposon/transposase system to create CD19-specific chimeric antigen receptor (CAR) T cells.
These CAR T cells appeared to be safe, and results suggested they can provide additional control of leukemia and lymphoma when given after autologous or allogeneic hematopoietic stem cell transplant (HSCT).
In addition, the researchers said use of the SB transposon/transposase platform could reduce the costs and complexity associated with recombinant viral vector-based immunotherapy.
The team described their results with the SB system in The Journal of Clinical Investigation. Results from these trials were previously reported at the inaugural CRI-CIMT-EATI-AACR International Cancer Immunotherapy Conference.
The trials were sponsored by MD Anderson Cancer Center in collaboration with the National Cancer Institute, National Center for Research Resources, Intrexon Corporation, and Ziopharm Oncology.
The trials included 26 patients with multiply relapsed B-lineage acute lymphoblastic leukemia (ALL, n=17) or B-cell non-Hodgkin lymphoma (NHL, n=9).
The patients received SB-modified T cells after autologous (n=7) or allogeneic (n=19) HSCT.
The researchers said SB-mediated gene transfer and stimulation resulted in large ex vivo expansion of T cells while retaining CAR expression and without integration hotspots.
Autologous and allogeneic T cells survived after infusion an average of 201 days and 51 days, respectively.
Safety
The researchers said there were no unexpected acute infusion or delayed toxicities. Mild elevations in cytokines were observed but not cytokine storm.
Three allogeneic HSCT recipients developed graft-vs-host disease (GVHD). One patient developed grade 1 acute skin GVHD that resolved with topical steroids, and 1 developed chronic skin GVHD that responded to systemic steroids.
The third patient, who had a history of drug-induced liver toxicity, developed recurrent liver toxicity with a component of liver GVHD 1 month after T-cell infusion. This patient died of liver failure.
There were 5 other deaths, all of them due to disease relapse.
Efficacy: Autologous HSCT
Seven patients with advanced NHL were treated with autologous HSCT, followed by the administration of patient-derived CAR T cells.
Six of the 7 patients were in complete remission (CR) at a median follow-up of 25.5 months (range, 6.4 to 32.7 months).
The 30-month progression-free survival (PFS) rate was 83%, and the overall survival (OS) rate was 100%.
Efficacy: Allogeneic HSCT
Nineteen patients (ALL n=17, NHL n=2) received donor-derived CAR T cells after allogeneic HSCT. The patients had advanced disease at the time of HSCT, and CAR T cells were administered without additional lymphodepletion.
Eleven of 19 patients were still in CR at a median follow-up of 7.5 months (range, 2.7 to 17.9 months). The 1-year PFS rate was 53%, and the OS rate was 63%.
The researchers also looked at the subset of allogeneic HSCT recipients who received haplo-identical CAR T cells. These 8 patients had a 1-year PFS rate of 75% and an OS rate of 100%.
“By following these patients over an extended duration, as we do in these studies, we can better understand the added benefit of CAR-T over HSCT alone,” said Francois Lebel, MD, of Ziopharm Oncology.
“Although the primary objective of these trials was not to establish efficacy, the recipients’ outcomes are encouraging, with apparent doubling of survivals compared to historical controls. We are encouraged by these clinical data and look forward to results from our phase 1 study infusing our next-generation CD19-specific CAR T cells in patients with advanced lymphoid malignancies.” ![]()

Image by NIAID
Researchers have reported “favorable” long-term results from a pair of phase 1 trials in which they used the non-viral Sleeping Beauty (SB) transposon/transposase system to create CD19-specific chimeric antigen receptor (CAR) T cells.
These CAR T cells appeared to be safe, and results suggested they can provide additional control of leukemia and lymphoma when given after autologous or allogeneic hematopoietic stem cell transplant (HSCT).
In addition, the researchers said use of the SB transposon/transposase platform could reduce the costs and complexity associated with recombinant viral vector-based immunotherapy.
The team described their results with the SB system in The Journal of Clinical Investigation. Results from these trials were previously reported at the inaugural CRI-CIMT-EATI-AACR International Cancer Immunotherapy Conference.
The trials were sponsored by MD Anderson Cancer Center in collaboration with the National Cancer Institute, National Center for Research Resources, Intrexon Corporation, and Ziopharm Oncology.
The trials included 26 patients with multiply relapsed B-lineage acute lymphoblastic leukemia (ALL, n=17) or B-cell non-Hodgkin lymphoma (NHL, n=9).
The patients received SB-modified T cells after autologous (n=7) or allogeneic (n=19) HSCT.
The researchers said SB-mediated gene transfer and stimulation resulted in large ex vivo expansion of T cells while retaining CAR expression and without integration hotspots.
Autologous and allogeneic T cells survived after infusion an average of 201 days and 51 days, respectively.
Safety
The researchers said there were no unexpected acute infusion or delayed toxicities. Mild elevations in cytokines were observed but not cytokine storm.
Three allogeneic HSCT recipients developed graft-vs-host disease (GVHD). One patient developed grade 1 acute skin GVHD that resolved with topical steroids, and 1 developed chronic skin GVHD that responded to systemic steroids.
The third patient, who had a history of drug-induced liver toxicity, developed recurrent liver toxicity with a component of liver GVHD 1 month after T-cell infusion. This patient died of liver failure.
There were 5 other deaths, all of them due to disease relapse.
Efficacy: Autologous HSCT
Seven patients with advanced NHL were treated with autologous HSCT, followed by the administration of patient-derived CAR T cells.
Six of the 7 patients were in complete remission (CR) at a median follow-up of 25.5 months (range, 6.4 to 32.7 months).
The 30-month progression-free survival (PFS) rate was 83%, and the overall survival (OS) rate was 100%.
Efficacy: Allogeneic HSCT
Nineteen patients (ALL n=17, NHL n=2) received donor-derived CAR T cells after allogeneic HSCT. The patients had advanced disease at the time of HSCT, and CAR T cells were administered without additional lymphodepletion.
Eleven of 19 patients were still in CR at a median follow-up of 7.5 months (range, 2.7 to 17.9 months). The 1-year PFS rate was 53%, and the OS rate was 63%.
The researchers also looked at the subset of allogeneic HSCT recipients who received haplo-identical CAR T cells. These 8 patients had a 1-year PFS rate of 75% and an OS rate of 100%.
“By following these patients over an extended duration, as we do in these studies, we can better understand the added benefit of CAR-T over HSCT alone,” said Francois Lebel, MD, of Ziopharm Oncology.
“Although the primary objective of these trials was not to establish efficacy, the recipients’ outcomes are encouraging, with apparent doubling of survivals compared to historical controls. We are encouraged by these clinical data and look forward to results from our phase 1 study infusing our next-generation CD19-specific CAR T cells in patients with advanced lymphoid malignancies.” ![]()
Pediatric Hospitalist Michael Beck, MD, FAAP, Measures Success By Others’ Success
Young boys sometimes see a firefighter or a police officer in the line of duty and decide that’s what they want to be when they get older. Michael Beck, MD, FAAP, saw his pediatrician that way.
“He was a very humanistic provider and found joy in serving children and their families,” Dr. Beck says. “I saw how a pediatrician could influence others and make the world a better place and still have fun serving a vulnerable patient population.”
His career in pediatric hospital medicine, though?
“It was largely pure luck,” Dr. Beck admits. “When I was seeking my first job, I was offered a position that was 50/50 internal medicine and pediatrics but purely a hospitalist position.”
Dr. Beck has risen through academic hospitalist ranks the past 15 years and now serves as the division chief of pediatric hospital medicine at Penn State Children’s Hospital at Milton S. Hershey (Pa.) Medical Center. He is one of eight new members of Team Hospitalist, The Hospitalist’s volunteer editorial advisory board.
Question: What was medical school and residency like for you? Was there a single moment you knew “I can do this”?
Answer: I always have been filled with self-doubt, which is a perpetual motivator for me. I guess I believed I could do hospital-based work when I started knowing the majority of what was going on with patients after hearing residents discuss cases and I knew what the labs, studies, and exam findings were going to be before I saw the patient.
Q: What do you like most about working as a hospitalist?
A: The acuity and pathology of cases. I get to see cases that some people only read about. It is very intellectual challenging, and I get to work with and learn from specialists every day.
Q: What do you dislike most?
A: Some of the cases are devastating to families. It is always important to remind yourself—and the team—that some of the diagnoses we help make affect families and the patient in very profound ways.
Q: Did you have a mentor during your training or early career? If so, who was the mentor, and what were the most important lessons you learned from him/her?
A: Dr. Barbara Ostrov. I learned what it really means to be a servant-leader. I witnessed her work ethic and saw that a leader of others should lead by example and be willing to work twice what is expected of others. She is always nonjudgmental and professional, yet forthright, when dealing with contentious situations. She trumpets the work of others, not her own, and sees others’ successes as her success. In the end, I believed she worked for me, not the other way around.
Q: Have you tried to mentor others? Why or why not?
A: Yes. As a division chief, I want others to succeed. The best quote I have read was by Richard Branson [CEO of Virgin]: “Train people so that they can leave, but treat them so they want to stay.”
Q: What’s the biggest change you’ve seen in HM in your career?
A: It has moved from a clinical service to a robust area of research and strong researchers.
Q: What’s the biggest change you would like to see in HM?
A: If hospital medicine is positioning itself to be a specialty with fellowship training, with access to knowledge different from PCPs, then I believe we should function like other specialty services with a different skill set. We should own our discharge process and follow-up plans. We should follow up with patients in a discharge clinic setting to review clinical course, health literacy issues, labs, and studies and even order follow-up studies based on incoming results.
Q: For group leaders, why is it important for you to continue seeing patients?
A: As a clinician leader, my charge is to foster teamwork and create a shared vision for improvement and change. This is not possible to do from an office space or conference room separate from where the work gets done.
Q: As a hospitalist, seeing most of your patients for the very first time, what aspect of patient care is most challenging?
A: Establishing trust and rapport in five to 10 minutes. Caring for a hospitalized patient, when they are surrounded by loved ones, is stressful and anxiety-provoking. Delivering information in a way that is honest and empathetic and timely without the benefit of having a personal historic connection with a patient is always challenging.
Q: What aspect of patient care is most rewarding?
A: Making a diagnosis in a patient that has eluded diagnosis for weeks or months.
Q: What aspect of teaching in the 21st century is most difficult? And what is most enjoyable?
A: Today’s learners have different expectations from mine [in terms] of what they want to get from a career in medicine. While I don’t always agree with them, it is the reality and puts me in a position to discuss and understand the rationale of a changing mindset. As a physician leader, it is important to understand this because it helps me create an environment that fosters successful recruitment and retention.
Q: You mention wanting to tackle the issue of physician burnout? Why is that something important to you?
A: I personally lived through it and felt the effects it had on the relationships I had with family, friends, medical students, residents, and patients. I know what it felt like to be angry, cynical, and distanced from those I cared about and from those whom I was charged with caring for. I never forgot how isolated [you] can feel in an academic center even when surrounded by hundreds. I vowed that if I ever found my way to a leadership position, I would begin by creating an environment that emphasized morale, honesty, integrity, and professionalism. If I succeeded in this, the other organizational missions of education, patient care, quality, and value would follow.
Since 2012, our division has monitored burnout, work-life balance, and, more recently, physician engagement. Although we take care of the sickest children in the region, our group supports each other, recognizing and respectful of the fact that we each have different comfort levels, skill sets, but we also have fun. Patients, nurses, social workers, care coordinators, and clerks see this. Like I teach the residents, you never get a second chance to make a first impression, but you also never get a second chance to make a last one, so make all interactions count. TH
Richard Quinn is a freelance writer in New Jersey.
Young boys sometimes see a firefighter or a police officer in the line of duty and decide that’s what they want to be when they get older. Michael Beck, MD, FAAP, saw his pediatrician that way.
“He was a very humanistic provider and found joy in serving children and their families,” Dr. Beck says. “I saw how a pediatrician could influence others and make the world a better place and still have fun serving a vulnerable patient population.”
His career in pediatric hospital medicine, though?
“It was largely pure luck,” Dr. Beck admits. “When I was seeking my first job, I was offered a position that was 50/50 internal medicine and pediatrics but purely a hospitalist position.”
Dr. Beck has risen through academic hospitalist ranks the past 15 years and now serves as the division chief of pediatric hospital medicine at Penn State Children’s Hospital at Milton S. Hershey (Pa.) Medical Center. He is one of eight new members of Team Hospitalist, The Hospitalist’s volunteer editorial advisory board.
Question: What was medical school and residency like for you? Was there a single moment you knew “I can do this”?
Answer: I always have been filled with self-doubt, which is a perpetual motivator for me. I guess I believed I could do hospital-based work when I started knowing the majority of what was going on with patients after hearing residents discuss cases and I knew what the labs, studies, and exam findings were going to be before I saw the patient.
Q: What do you like most about working as a hospitalist?
A: The acuity and pathology of cases. I get to see cases that some people only read about. It is very intellectual challenging, and I get to work with and learn from specialists every day.
Q: What do you dislike most?
A: Some of the cases are devastating to families. It is always important to remind yourself—and the team—that some of the diagnoses we help make affect families and the patient in very profound ways.
Q: Did you have a mentor during your training or early career? If so, who was the mentor, and what were the most important lessons you learned from him/her?
A: Dr. Barbara Ostrov. I learned what it really means to be a servant-leader. I witnessed her work ethic and saw that a leader of others should lead by example and be willing to work twice what is expected of others. She is always nonjudgmental and professional, yet forthright, when dealing with contentious situations. She trumpets the work of others, not her own, and sees others’ successes as her success. In the end, I believed she worked for me, not the other way around.
Q: Have you tried to mentor others? Why or why not?
A: Yes. As a division chief, I want others to succeed. The best quote I have read was by Richard Branson [CEO of Virgin]: “Train people so that they can leave, but treat them so they want to stay.”
Q: What’s the biggest change you’ve seen in HM in your career?
A: It has moved from a clinical service to a robust area of research and strong researchers.
Q: What’s the biggest change you would like to see in HM?
A: If hospital medicine is positioning itself to be a specialty with fellowship training, with access to knowledge different from PCPs, then I believe we should function like other specialty services with a different skill set. We should own our discharge process and follow-up plans. We should follow up with patients in a discharge clinic setting to review clinical course, health literacy issues, labs, and studies and even order follow-up studies based on incoming results.
Q: For group leaders, why is it important for you to continue seeing patients?
A: As a clinician leader, my charge is to foster teamwork and create a shared vision for improvement and change. This is not possible to do from an office space or conference room separate from where the work gets done.
Q: As a hospitalist, seeing most of your patients for the very first time, what aspect of patient care is most challenging?
A: Establishing trust and rapport in five to 10 minutes. Caring for a hospitalized patient, when they are surrounded by loved ones, is stressful and anxiety-provoking. Delivering information in a way that is honest and empathetic and timely without the benefit of having a personal historic connection with a patient is always challenging.
Q: What aspect of patient care is most rewarding?
A: Making a diagnosis in a patient that has eluded diagnosis for weeks or months.
Q: What aspect of teaching in the 21st century is most difficult? And what is most enjoyable?
A: Today’s learners have different expectations from mine [in terms] of what they want to get from a career in medicine. While I don’t always agree with them, it is the reality and puts me in a position to discuss and understand the rationale of a changing mindset. As a physician leader, it is important to understand this because it helps me create an environment that fosters successful recruitment and retention.
Q: You mention wanting to tackle the issue of physician burnout? Why is that something important to you?
A: I personally lived through it and felt the effects it had on the relationships I had with family, friends, medical students, residents, and patients. I know what it felt like to be angry, cynical, and distanced from those I cared about and from those whom I was charged with caring for. I never forgot how isolated [you] can feel in an academic center even when surrounded by hundreds. I vowed that if I ever found my way to a leadership position, I would begin by creating an environment that emphasized morale, honesty, integrity, and professionalism. If I succeeded in this, the other organizational missions of education, patient care, quality, and value would follow.
Since 2012, our division has monitored burnout, work-life balance, and, more recently, physician engagement. Although we take care of the sickest children in the region, our group supports each other, recognizing and respectful of the fact that we each have different comfort levels, skill sets, but we also have fun. Patients, nurses, social workers, care coordinators, and clerks see this. Like I teach the residents, you never get a second chance to make a first impression, but you also never get a second chance to make a last one, so make all interactions count. TH
Richard Quinn is a freelance writer in New Jersey.
Young boys sometimes see a firefighter or a police officer in the line of duty and decide that’s what they want to be when they get older. Michael Beck, MD, FAAP, saw his pediatrician that way.
“He was a very humanistic provider and found joy in serving children and their families,” Dr. Beck says. “I saw how a pediatrician could influence others and make the world a better place and still have fun serving a vulnerable patient population.”
His career in pediatric hospital medicine, though?
“It was largely pure luck,” Dr. Beck admits. “When I was seeking my first job, I was offered a position that was 50/50 internal medicine and pediatrics but purely a hospitalist position.”
Dr. Beck has risen through academic hospitalist ranks the past 15 years and now serves as the division chief of pediatric hospital medicine at Penn State Children’s Hospital at Milton S. Hershey (Pa.) Medical Center. He is one of eight new members of Team Hospitalist, The Hospitalist’s volunteer editorial advisory board.
Question: What was medical school and residency like for you? Was there a single moment you knew “I can do this”?
Answer: I always have been filled with self-doubt, which is a perpetual motivator for me. I guess I believed I could do hospital-based work when I started knowing the majority of what was going on with patients after hearing residents discuss cases and I knew what the labs, studies, and exam findings were going to be before I saw the patient.
Q: What do you like most about working as a hospitalist?
A: The acuity and pathology of cases. I get to see cases that some people only read about. It is very intellectual challenging, and I get to work with and learn from specialists every day.
Q: What do you dislike most?
A: Some of the cases are devastating to families. It is always important to remind yourself—and the team—that some of the diagnoses we help make affect families and the patient in very profound ways.
Q: Did you have a mentor during your training or early career? If so, who was the mentor, and what were the most important lessons you learned from him/her?
A: Dr. Barbara Ostrov. I learned what it really means to be a servant-leader. I witnessed her work ethic and saw that a leader of others should lead by example and be willing to work twice what is expected of others. She is always nonjudgmental and professional, yet forthright, when dealing with contentious situations. She trumpets the work of others, not her own, and sees others’ successes as her success. In the end, I believed she worked for me, not the other way around.
Q: Have you tried to mentor others? Why or why not?
A: Yes. As a division chief, I want others to succeed. The best quote I have read was by Richard Branson [CEO of Virgin]: “Train people so that they can leave, but treat them so they want to stay.”
Q: What’s the biggest change you’ve seen in HM in your career?
A: It has moved from a clinical service to a robust area of research and strong researchers.
Q: What’s the biggest change you would like to see in HM?
A: If hospital medicine is positioning itself to be a specialty with fellowship training, with access to knowledge different from PCPs, then I believe we should function like other specialty services with a different skill set. We should own our discharge process and follow-up plans. We should follow up with patients in a discharge clinic setting to review clinical course, health literacy issues, labs, and studies and even order follow-up studies based on incoming results.
Q: For group leaders, why is it important for you to continue seeing patients?
A: As a clinician leader, my charge is to foster teamwork and create a shared vision for improvement and change. This is not possible to do from an office space or conference room separate from where the work gets done.
Q: As a hospitalist, seeing most of your patients for the very first time, what aspect of patient care is most challenging?
A: Establishing trust and rapport in five to 10 minutes. Caring for a hospitalized patient, when they are surrounded by loved ones, is stressful and anxiety-provoking. Delivering information in a way that is honest and empathetic and timely without the benefit of having a personal historic connection with a patient is always challenging.
Q: What aspect of patient care is most rewarding?
A: Making a diagnosis in a patient that has eluded diagnosis for weeks or months.
Q: What aspect of teaching in the 21st century is most difficult? And what is most enjoyable?
A: Today’s learners have different expectations from mine [in terms] of what they want to get from a career in medicine. While I don’t always agree with them, it is the reality and puts me in a position to discuss and understand the rationale of a changing mindset. As a physician leader, it is important to understand this because it helps me create an environment that fosters successful recruitment and retention.
Q: You mention wanting to tackle the issue of physician burnout? Why is that something important to you?
A: I personally lived through it and felt the effects it had on the relationships I had with family, friends, medical students, residents, and patients. I know what it felt like to be angry, cynical, and distanced from those I cared about and from those whom I was charged with caring for. I never forgot how isolated [you] can feel in an academic center even when surrounded by hundreds. I vowed that if I ever found my way to a leadership position, I would begin by creating an environment that emphasized morale, honesty, integrity, and professionalism. If I succeeded in this, the other organizational missions of education, patient care, quality, and value would follow.
Since 2012, our division has monitored burnout, work-life balance, and, more recently, physician engagement. Although we take care of the sickest children in the region, our group supports each other, recognizing and respectful of the fact that we each have different comfort levels, skill sets, but we also have fun. Patients, nurses, social workers, care coordinators, and clerks see this. Like I teach the residents, you never get a second chance to make a first impression, but you also never get a second chance to make a last one, so make all interactions count. TH
Richard Quinn is a freelance writer in New Jersey.
Plant sugars influence malaria transmission

feeding on Barleria lupilina.
Photo from Domonbabele
F. d. S. Hien et al.
A study published in PLOS Pathogens suggests the plant-based part of Anopheles mosquitoes’ diet affects malaria transmission by influencing the interaction between the mosquitoes and Plasmodium parasites.
Recent studies have shown that Anopheles female mosquitoes, which can transmit the malaria parasite P falciparum, locate and display preferences for natural sources of plant sugar.
These studies also suggested that environmental sugars influence the lifespan and blood-feeding rate of mosquitoes and, therefore, their malaria transmission potential.
Whether the type of plant sugar could also affect the malaria host-pathogen interactions was unclear.
To find out, Thierry Lefevre, PhD, of the Institut de Recherche en Sciences de la Santé in Bobo Dioulasso, Burkina Faso, and his colleagues examined the impact of plant diversity on mosquito susceptibility to malaria parasites.
The team studied the natural interactions between the P falciparum parasite, the Anopheles coluzzii mosquito (a major vector of P falciparum in Africa), and several natural plant-derived sugar sources growing in the vicinity of human dwellings in Burkina Faso.
The latter included 2 ornamental flowering plants (Barleria lupilina and Thevetia neriifolia) as well as mangoes and the grape-like fruit from the Lannea microcarpa tree.
The researchers raised groups of Anopheles mosquitos in cages and provided each of them with a different plant sugar source or with a 5% glucose solution.
Sugar-fed mosquitoes were then starved for 24 hours before being offered a parasite-containing blood meal. The blood was drawn from healthy Plasmodium-infected local human volunteers and diluted to a consistent concentration of parasites.
Blood-fed female mosquitoes were housed in a biosafety room and continued to be fed their assigned plant sugar source.
Seven or 14 days after the blood-meal, roughly 30 mosquitoes from each group were examined under the microscope for traits that influence malaria transmission.
The researchers found that different sugar sources had different effects on all traits examined, including the infection and survival rates of the mosquitoes and the survival rate of the parasites 7 days after the blood meal.
The plant sugar source also influenced the proportion of mosquitoes harboring sporozoites and the timing of sporozoite release.
To predict the relative contribution of the different plants to overall malaria transmission, the researchers used the various experimental results in an epidemiological model.
This suggested that plant sugar source can be a significant driver of malaria transmission dynamics.
Compared to the baseline scenario with the 5% glucose solution, both L microcarpa and B lupilina increased malaria transmission by an estimated 30% and 40%, respectively, mainly because of increased infection rates among mosquitoes exposed to parasites through their blood-meal.
In contrast, T neriifolia, with its negative effect on infection rate and decreased longevity, was predicted to decrease malaria transmission by 30% compared with sugar water.
The researchers said these findings suggest that planting anti-Plasmodium plant sugar sources could be a promising alternative strategy for controlling malaria. ![]()

feeding on Barleria lupilina.
Photo from Domonbabele
F. d. S. Hien et al.
A study published in PLOS Pathogens suggests the plant-based part of Anopheles mosquitoes’ diet affects malaria transmission by influencing the interaction between the mosquitoes and Plasmodium parasites.
Recent studies have shown that Anopheles female mosquitoes, which can transmit the malaria parasite P falciparum, locate and display preferences for natural sources of plant sugar.
These studies also suggested that environmental sugars influence the lifespan and blood-feeding rate of mosquitoes and, therefore, their malaria transmission potential.
Whether the type of plant sugar could also affect the malaria host-pathogen interactions was unclear.
To find out, Thierry Lefevre, PhD, of the Institut de Recherche en Sciences de la Santé in Bobo Dioulasso, Burkina Faso, and his colleagues examined the impact of plant diversity on mosquito susceptibility to malaria parasites.
The team studied the natural interactions between the P falciparum parasite, the Anopheles coluzzii mosquito (a major vector of P falciparum in Africa), and several natural plant-derived sugar sources growing in the vicinity of human dwellings in Burkina Faso.
The latter included 2 ornamental flowering plants (Barleria lupilina and Thevetia neriifolia) as well as mangoes and the grape-like fruit from the Lannea microcarpa tree.
The researchers raised groups of Anopheles mosquitos in cages and provided each of them with a different plant sugar source or with a 5% glucose solution.
Sugar-fed mosquitoes were then starved for 24 hours before being offered a parasite-containing blood meal. The blood was drawn from healthy Plasmodium-infected local human volunteers and diluted to a consistent concentration of parasites.
Blood-fed female mosquitoes were housed in a biosafety room and continued to be fed their assigned plant sugar source.
Seven or 14 days after the blood-meal, roughly 30 mosquitoes from each group were examined under the microscope for traits that influence malaria transmission.
The researchers found that different sugar sources had different effects on all traits examined, including the infection and survival rates of the mosquitoes and the survival rate of the parasites 7 days after the blood meal.
The plant sugar source also influenced the proportion of mosquitoes harboring sporozoites and the timing of sporozoite release.
To predict the relative contribution of the different plants to overall malaria transmission, the researchers used the various experimental results in an epidemiological model.
This suggested that plant sugar source can be a significant driver of malaria transmission dynamics.
Compared to the baseline scenario with the 5% glucose solution, both L microcarpa and B lupilina increased malaria transmission by an estimated 30% and 40%, respectively, mainly because of increased infection rates among mosquitoes exposed to parasites through their blood-meal.
In contrast, T neriifolia, with its negative effect on infection rate and decreased longevity, was predicted to decrease malaria transmission by 30% compared with sugar water.
The researchers said these findings suggest that planting anti-Plasmodium plant sugar sources could be a promising alternative strategy for controlling malaria. ![]()

feeding on Barleria lupilina.
Photo from Domonbabele
F. d. S. Hien et al.
A study published in PLOS Pathogens suggests the plant-based part of Anopheles mosquitoes’ diet affects malaria transmission by influencing the interaction between the mosquitoes and Plasmodium parasites.
Recent studies have shown that Anopheles female mosquitoes, which can transmit the malaria parasite P falciparum, locate and display preferences for natural sources of plant sugar.
These studies also suggested that environmental sugars influence the lifespan and blood-feeding rate of mosquitoes and, therefore, their malaria transmission potential.
Whether the type of plant sugar could also affect the malaria host-pathogen interactions was unclear.
To find out, Thierry Lefevre, PhD, of the Institut de Recherche en Sciences de la Santé in Bobo Dioulasso, Burkina Faso, and his colleagues examined the impact of plant diversity on mosquito susceptibility to malaria parasites.
The team studied the natural interactions between the P falciparum parasite, the Anopheles coluzzii mosquito (a major vector of P falciparum in Africa), and several natural plant-derived sugar sources growing in the vicinity of human dwellings in Burkina Faso.
The latter included 2 ornamental flowering plants (Barleria lupilina and Thevetia neriifolia) as well as mangoes and the grape-like fruit from the Lannea microcarpa tree.
The researchers raised groups of Anopheles mosquitos in cages and provided each of them with a different plant sugar source or with a 5% glucose solution.
Sugar-fed mosquitoes were then starved for 24 hours before being offered a parasite-containing blood meal. The blood was drawn from healthy Plasmodium-infected local human volunteers and diluted to a consistent concentration of parasites.
Blood-fed female mosquitoes were housed in a biosafety room and continued to be fed their assigned plant sugar source.
Seven or 14 days after the blood-meal, roughly 30 mosquitoes from each group were examined under the microscope for traits that influence malaria transmission.
The researchers found that different sugar sources had different effects on all traits examined, including the infection and survival rates of the mosquitoes and the survival rate of the parasites 7 days after the blood meal.
The plant sugar source also influenced the proportion of mosquitoes harboring sporozoites and the timing of sporozoite release.
To predict the relative contribution of the different plants to overall malaria transmission, the researchers used the various experimental results in an epidemiological model.
This suggested that plant sugar source can be a significant driver of malaria transmission dynamics.
Compared to the baseline scenario with the 5% glucose solution, both L microcarpa and B lupilina increased malaria transmission by an estimated 30% and 40%, respectively, mainly because of increased infection rates among mosquitoes exposed to parasites through their blood-meal.
In contrast, T neriifolia, with its negative effect on infection rate and decreased longevity, was predicted to decrease malaria transmission by 30% compared with sugar water.
The researchers said these findings suggest that planting anti-Plasmodium plant sugar sources could be a promising alternative strategy for controlling malaria. ![]()
Drug interferes with testing for blood transfusion

Photo by Daniel Gay
Research has shown that daratumumab, a monoclonal antibody approved to treat multiple myeloma, interferes with routine compatibility testing for blood transfusion.
And this interference can cause delays in providing patients with compatible blood.
Investigators have discovered ways to eliminate or circumvent the interference, but implementing these methods in hospital blood banks may be challenging.
Michael F. Murphy, MD, of John Radcliffe Hospital in Oxford, UK, and his colleagues discussed this issue in a letter to NEJM.
In a phase 1/2 trial of daratumumab, investigators at different study sites observed that the drug consistently interfered with routine blood compatibility testing. This meant that daratumumab-treated patients sometimes experienced delays in receiving blood transfusions.
Investigation revealed that daratumumab in patient plasma directly binds to CD38 on reagent red blood cells used in the blood bank, which causes false-positive antibody screens.
Unfortunately, standard serological methods to eliminate panreactive antibodies did not affect daratumumab’s interference.
However, an investigator-initiated study revealed a dithiothreitol-based method that can eliminate the interference.1
Another method, involving an anti-daratumumab idiotype, also appears effective, though not readily available.2 And a third method is to issue phenotypically or genotypically matched red cell units.3,4
However, establishing these approaches as routine methods in hospital blood banks will be a major challenge, according to Dr Murphy and his colleagues.
The team also said this issue with daratumumab suggests there is a pressing need to investigate whether new drugs interfere with routine blood bank testing.
Investigations should be performed early during drug development. And if interference with compatibility tests is found, it should be brought to the attention of clinicians and blood banks with advice about how to overcome the interference. ![]()

Photo by Daniel Gay
Research has shown that daratumumab, a monoclonal antibody approved to treat multiple myeloma, interferes with routine compatibility testing for blood transfusion.
And this interference can cause delays in providing patients with compatible blood.
Investigators have discovered ways to eliminate or circumvent the interference, but implementing these methods in hospital blood banks may be challenging.
Michael F. Murphy, MD, of John Radcliffe Hospital in Oxford, UK, and his colleagues discussed this issue in a letter to NEJM.
In a phase 1/2 trial of daratumumab, investigators at different study sites observed that the drug consistently interfered with routine blood compatibility testing. This meant that daratumumab-treated patients sometimes experienced delays in receiving blood transfusions.
Investigation revealed that daratumumab in patient plasma directly binds to CD38 on reagent red blood cells used in the blood bank, which causes false-positive antibody screens.
Unfortunately, standard serological methods to eliminate panreactive antibodies did not affect daratumumab’s interference.
However, an investigator-initiated study revealed a dithiothreitol-based method that can eliminate the interference.1
Another method, involving an anti-daratumumab idiotype, also appears effective, though not readily available.2 And a third method is to issue phenotypically or genotypically matched red cell units.3,4
However, establishing these approaches as routine methods in hospital blood banks will be a major challenge, according to Dr Murphy and his colleagues.
The team also said this issue with daratumumab suggests there is a pressing need to investigate whether new drugs interfere with routine blood bank testing.
Investigations should be performed early during drug development. And if interference with compatibility tests is found, it should be brought to the attention of clinicians and blood banks with advice about how to overcome the interference. ![]()

Photo by Daniel Gay
Research has shown that daratumumab, a monoclonal antibody approved to treat multiple myeloma, interferes with routine compatibility testing for blood transfusion.
And this interference can cause delays in providing patients with compatible blood.
Investigators have discovered ways to eliminate or circumvent the interference, but implementing these methods in hospital blood banks may be challenging.
Michael F. Murphy, MD, of John Radcliffe Hospital in Oxford, UK, and his colleagues discussed this issue in a letter to NEJM.
In a phase 1/2 trial of daratumumab, investigators at different study sites observed that the drug consistently interfered with routine blood compatibility testing. This meant that daratumumab-treated patients sometimes experienced delays in receiving blood transfusions.
Investigation revealed that daratumumab in patient plasma directly binds to CD38 on reagent red blood cells used in the blood bank, which causes false-positive antibody screens.
Unfortunately, standard serological methods to eliminate panreactive antibodies did not affect daratumumab’s interference.
However, an investigator-initiated study revealed a dithiothreitol-based method that can eliminate the interference.1
Another method, involving an anti-daratumumab idiotype, also appears effective, though not readily available.2 And a third method is to issue phenotypically or genotypically matched red cell units.3,4
However, establishing these approaches as routine methods in hospital blood banks will be a major challenge, according to Dr Murphy and his colleagues.
The team also said this issue with daratumumab suggests there is a pressing need to investigate whether new drugs interfere with routine blood bank testing.
Investigations should be performed early during drug development. And if interference with compatibility tests is found, it should be brought to the attention of clinicians and blood banks with advice about how to overcome the interference. ![]()
Team creates database of autophagy-related proteins

Image by Sarah Pfau
Scientists have identified previously undiscovered proteins related to autophagy and created a database containing them.
The team believes this database will enable the scientific community to find ways to activate autophagy inside human cells.
And it could aid the development of drugs to treat age-related conditions such as cancer.
The team described the creation of the database in the journal Autophagy.
The database is available here: https://ilir.warwick.ac.uk/.
“Our novel database resource will open a lot of new avenues in basic and translational science,” said Ioannis Nezis, PhD, of the University of Warwick in Coventry, UK.
“Identifying novel selective autophagy-related proteins will help for the development of novel pharmaceutical drug targets for a large variety of diseases like cancer, neurodegeneration, and other aging-related diseases, infections, diabetes, obesity, and Crohn’s disease.”
“Importantly, understanding the molecular mechanisms of selective autophagy will help researchers to find interventions to activate the autophagic pathway to prevent aging and promote healthy well-being during the life course.” ![]()

Image by Sarah Pfau
Scientists have identified previously undiscovered proteins related to autophagy and created a database containing them.
The team believes this database will enable the scientific community to find ways to activate autophagy inside human cells.
And it could aid the development of drugs to treat age-related conditions such as cancer.
The team described the creation of the database in the journal Autophagy.
The database is available here: https://ilir.warwick.ac.uk/.
“Our novel database resource will open a lot of new avenues in basic and translational science,” said Ioannis Nezis, PhD, of the University of Warwick in Coventry, UK.
“Identifying novel selective autophagy-related proteins will help for the development of novel pharmaceutical drug targets for a large variety of diseases like cancer, neurodegeneration, and other aging-related diseases, infections, diabetes, obesity, and Crohn’s disease.”
“Importantly, understanding the molecular mechanisms of selective autophagy will help researchers to find interventions to activate the autophagic pathway to prevent aging and promote healthy well-being during the life course.” ![]()

Image by Sarah Pfau
Scientists have identified previously undiscovered proteins related to autophagy and created a database containing them.
The team believes this database will enable the scientific community to find ways to activate autophagy inside human cells.
And it could aid the development of drugs to treat age-related conditions such as cancer.
The team described the creation of the database in the journal Autophagy.
The database is available here: https://ilir.warwick.ac.uk/.
“Our novel database resource will open a lot of new avenues in basic and translational science,” said Ioannis Nezis, PhD, of the University of Warwick in Coventry, UK.
“Identifying novel selective autophagy-related proteins will help for the development of novel pharmaceutical drug targets for a large variety of diseases like cancer, neurodegeneration, and other aging-related diseases, infections, diabetes, obesity, and Crohn’s disease.”
“Importantly, understanding the molecular mechanisms of selective autophagy will help researchers to find interventions to activate the autophagic pathway to prevent aging and promote healthy well-being during the life course.” ![]()