User login
MRD beats CR in prognostic value for MM, team confirms
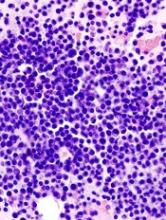
A team of researchers has confirmed that minimal residual disease (MRD) negativity is superior to complete response (CR) as a prognostic marker for progression-free survival (PFS) and overall survival (OS) in patients with multiple myeloma (MM).
MRD-positive patients who achieved CR had a similar survival to MRD-positive patients who achieved near CR (nCR) or partial response (PR). And this held true despite different induction regimens, disease stages, patient ages, cytogenetic groups, and whether the patients were transplant eligible or ineligible.
The team conducted the pooled analysis on behalf of the GEM (Grupo Español de Mieloma)/PETHEMA (Programa para el Estudio de la Terapéutica en Hemopatías Malignas) Cooperative Study Group.
They analyzed data from a large pool of 609 patients newly diagnosed with MM enrolled in 3 clinical trials—GEM 2000 (n=256), GEM2005MENOS65 (n=226), and GEM2010MAS65 (n=127). All patients had MRD assessments 9 months after study enrollment. The median follow-up was 71 months.
Juan-Jose Lahuerta, MD, PhD, of Hospital 12 de Octubre in Madrid, Spain, and colleagues reported the results in the Journal of Clinical Oncology.
Of the 609 patients, 286 (47%) achieved CR and had a significantly longer PFS (median, 49 months) than those who achieved nCR (median, 37 months), PR (median, 34 months) or less than PR (median, 11 months).
Patients who achieved CR also had a significantly longer OS (median, 128 months) than those who achieved PR (median, 75 months) or less than PR (median, 28 months), but not nCR (median, 77 months).
But patients who achieved CR and were still MRD-positive had a similar PFS (median, 27 months) to those patients who achieved nCR and PR and were MRD-positive (median 27 and 29 months, respectively). Median OS for MRD-positive patients in CR was a median 59 months, compared to 64 and 65 months, respectively, for MRD-positive patients in nCR and PR.
The team found that only MRD negativity significantly prolonged PFS and OS. Patients who were MRD-negative, even without achieving a CR, had a median PFS of 63 months (P<0.001) and the median OS not reached (P<0.001).
According to their paper, the investigators consider MRD negativity to be “one of the most relevant clinical end points and an aim of MM treatment of transplant-eligible and elderly patients who can tolerate intensive therapies.”
The team also investigated whether MRD negativity could be used as a meaningful clinical endpoint. They compared outcomes between patients who achieved CR according to MRD status before and after high-dose therapy and autologous stem cell transplant (ASCT).
Patients who were MRD-positive before transplant but MRD-negative afterwards had similar PFS and OS compared to patients who were MRD-negative before and after transplant. Patients who remained MRD-positive after transplant had inferior PFS and OS.
The team believes these results “support the adoption of MRD testing in routine practice to help discriminate between patients with clinically meaningful (MRD-negative) and misleading (MRD- positive) CRs.”
They noted, however, that a limitation of the study was the use of 2 different flow cytometries (8- and 4-color) with different sensitivities (10-5 and 10-4, respectively).
They also cautioned that these results should not be used to tailor treatments. Rather, new clinical trials that incorporate MRD assessments at additional time points need to be conducted.
A team of researchers has confirmed that minimal residual disease (MRD) negativity is superior to complete response (CR) as a prognostic marker for progression-free survival (PFS) and overall survival (OS) in patients with multiple myeloma (MM).
MRD-positive patients who achieved CR had a similar survival to MRD-positive patients who achieved near CR (nCR) or partial response (PR). And this held true despite different induction regimens, disease stages, patient ages, cytogenetic groups, and whether the patients were transplant eligible or ineligible.
The team conducted the pooled analysis on behalf of the GEM (Grupo Español de Mieloma)/PETHEMA (Programa para el Estudio de la Terapéutica en Hemopatías Malignas) Cooperative Study Group.
They analyzed data from a large pool of 609 patients newly diagnosed with MM enrolled in 3 clinical trials—GEM 2000 (n=256), GEM2005MENOS65 (n=226), and GEM2010MAS65 (n=127). All patients had MRD assessments 9 months after study enrollment. The median follow-up was 71 months.
Juan-Jose Lahuerta, MD, PhD, of Hospital 12 de Octubre in Madrid, Spain, and colleagues reported the results in the Journal of Clinical Oncology.
Of the 609 patients, 286 (47%) achieved CR and had a significantly longer PFS (median, 49 months) than those who achieved nCR (median, 37 months), PR (median, 34 months) or less than PR (median, 11 months).
Patients who achieved CR also had a significantly longer OS (median, 128 months) than those who achieved PR (median, 75 months) or less than PR (median, 28 months), but not nCR (median, 77 months).
But patients who achieved CR and were still MRD-positive had a similar PFS (median, 27 months) to those patients who achieved nCR and PR and were MRD-positive (median 27 and 29 months, respectively). Median OS for MRD-positive patients in CR was a median 59 months, compared to 64 and 65 months, respectively, for MRD-positive patients in nCR and PR.
The team found that only MRD negativity significantly prolonged PFS and OS. Patients who were MRD-negative, even without achieving a CR, had a median PFS of 63 months (P<0.001) and the median OS not reached (P<0.001).
According to their paper, the investigators consider MRD negativity to be “one of the most relevant clinical end points and an aim of MM treatment of transplant-eligible and elderly patients who can tolerate intensive therapies.”
The team also investigated whether MRD negativity could be used as a meaningful clinical endpoint. They compared outcomes between patients who achieved CR according to MRD status before and after high-dose therapy and autologous stem cell transplant (ASCT).
Patients who were MRD-positive before transplant but MRD-negative afterwards had similar PFS and OS compared to patients who were MRD-negative before and after transplant. Patients who remained MRD-positive after transplant had inferior PFS and OS.
The team believes these results “support the adoption of MRD testing in routine practice to help discriminate between patients with clinically meaningful (MRD-negative) and misleading (MRD- positive) CRs.”
They noted, however, that a limitation of the study was the use of 2 different flow cytometries (8- and 4-color) with different sensitivities (10-5 and 10-4, respectively).
They also cautioned that these results should not be used to tailor treatments. Rather, new clinical trials that incorporate MRD assessments at additional time points need to be conducted.
A team of researchers has confirmed that minimal residual disease (MRD) negativity is superior to complete response (CR) as a prognostic marker for progression-free survival (PFS) and overall survival (OS) in patients with multiple myeloma (MM).
MRD-positive patients who achieved CR had a similar survival to MRD-positive patients who achieved near CR (nCR) or partial response (PR). And this held true despite different induction regimens, disease stages, patient ages, cytogenetic groups, and whether the patients were transplant eligible or ineligible.
The team conducted the pooled analysis on behalf of the GEM (Grupo Español de Mieloma)/PETHEMA (Programa para el Estudio de la Terapéutica en Hemopatías Malignas) Cooperative Study Group.
They analyzed data from a large pool of 609 patients newly diagnosed with MM enrolled in 3 clinical trials—GEM 2000 (n=256), GEM2005MENOS65 (n=226), and GEM2010MAS65 (n=127). All patients had MRD assessments 9 months after study enrollment. The median follow-up was 71 months.
Juan-Jose Lahuerta, MD, PhD, of Hospital 12 de Octubre in Madrid, Spain, and colleagues reported the results in the Journal of Clinical Oncology.
Of the 609 patients, 286 (47%) achieved CR and had a significantly longer PFS (median, 49 months) than those who achieved nCR (median, 37 months), PR (median, 34 months) or less than PR (median, 11 months).
Patients who achieved CR also had a significantly longer OS (median, 128 months) than those who achieved PR (median, 75 months) or less than PR (median, 28 months), but not nCR (median, 77 months).
But patients who achieved CR and were still MRD-positive had a similar PFS (median, 27 months) to those patients who achieved nCR and PR and were MRD-positive (median 27 and 29 months, respectively). Median OS for MRD-positive patients in CR was a median 59 months, compared to 64 and 65 months, respectively, for MRD-positive patients in nCR and PR.
The team found that only MRD negativity significantly prolonged PFS and OS. Patients who were MRD-negative, even without achieving a CR, had a median PFS of 63 months (P<0.001) and the median OS not reached (P<0.001).
According to their paper, the investigators consider MRD negativity to be “one of the most relevant clinical end points and an aim of MM treatment of transplant-eligible and elderly patients who can tolerate intensive therapies.”
The team also investigated whether MRD negativity could be used as a meaningful clinical endpoint. They compared outcomes between patients who achieved CR according to MRD status before and after high-dose therapy and autologous stem cell transplant (ASCT).
Patients who were MRD-positive before transplant but MRD-negative afterwards had similar PFS and OS compared to patients who were MRD-negative before and after transplant. Patients who remained MRD-positive after transplant had inferior PFS and OS.
The team believes these results “support the adoption of MRD testing in routine practice to help discriminate between patients with clinically meaningful (MRD-negative) and misleading (MRD- positive) CRs.”
They noted, however, that a limitation of the study was the use of 2 different flow cytometries (8- and 4-color) with different sensitivities (10-5 and 10-4, respectively).
They also cautioned that these results should not be used to tailor treatments. Rather, new clinical trials that incorporate MRD assessments at additional time points need to be conducted.
Malaria drug could help identify bloodstains
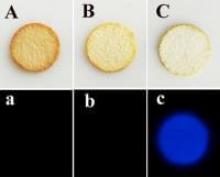
A new compound combining the antimalarial drug artemisinin and luminol could help crime scene technicians detect blood spots with fewer false identifications.
Luminol, which is often combined with hydrogen peroxide, reacts with the heme groups in blood, producing a bright blue glow, known as chemiluminescence.
However, luminol is subject to false positives due to interference from biomolecules and metal ions, and from the breakdown products of hydrogen peroxide.
Artemisinin is a natural peroxide that is more stable than hydrogen peroxide in the presence of common ions and more resistant to interference.
So investigators decided to combine artemisinin with luminol in an effort to minimize erroneous bloodstain identifications. They showed that the luminol-artemisinin combination is more selective than luminol-hydrogen peroxide.
They challenged the new combination with components of bleaches and disinfectants, which criminals often use to clean up a crime scene. The new compound could distinguish blood from coffee, tea, and brown sugar stains.
The investigators also successfully tested the new luminol-artemisinin compound using a smartphone to obtain results. This new method could provide highly accurate, cost-effective, on-scene analyses.
They believe the favorable sensitivity and selectivity of this method makes it promising in forensic pursuits.
Guobao Xu, PhD, of the Chinese Academy of Sciences in Beijing, People’s Republic of China, and colleagues reported these findings in the American Chemical Society’s journal, Analytical Chemistry.
The authors received funding from the National Natural Science Foundation of China, the National Key Research and Development Program of China, the Chinese Academy of Science President's International Fellowship Initiative Project, and the Chinese Academy of Sciences-the Academy of Sciences for the Developing World President's Fellowship Programme. ![]()
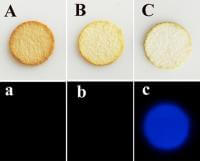
A new compound combining the antimalarial drug artemisinin and luminol could help crime scene technicians detect blood spots with fewer false identifications.
Luminol, which is often combined with hydrogen peroxide, reacts with the heme groups in blood, producing a bright blue glow, known as chemiluminescence.
However, luminol is subject to false positives due to interference from biomolecules and metal ions, and from the breakdown products of hydrogen peroxide.
Artemisinin is a natural peroxide that is more stable than hydrogen peroxide in the presence of common ions and more resistant to interference.
So investigators decided to combine artemisinin with luminol in an effort to minimize erroneous bloodstain identifications. They showed that the luminol-artemisinin combination is more selective than luminol-hydrogen peroxide.
They challenged the new combination with components of bleaches and disinfectants, which criminals often use to clean up a crime scene. The new compound could distinguish blood from coffee, tea, and brown sugar stains.
The investigators also successfully tested the new luminol-artemisinin compound using a smartphone to obtain results. This new method could provide highly accurate, cost-effective, on-scene analyses.
They believe the favorable sensitivity and selectivity of this method makes it promising in forensic pursuits.
Guobao Xu, PhD, of the Chinese Academy of Sciences in Beijing, People’s Republic of China, and colleagues reported these findings in the American Chemical Society’s journal, Analytical Chemistry.
The authors received funding from the National Natural Science Foundation of China, the National Key Research and Development Program of China, the Chinese Academy of Science President's International Fellowship Initiative Project, and the Chinese Academy of Sciences-the Academy of Sciences for the Developing World President's Fellowship Programme. ![]()
A new compound combining the antimalarial drug artemisinin and luminol could help crime scene technicians detect blood spots with fewer false identifications.
Luminol, which is often combined with hydrogen peroxide, reacts with the heme groups in blood, producing a bright blue glow, known as chemiluminescence.
However, luminol is subject to false positives due to interference from biomolecules and metal ions, and from the breakdown products of hydrogen peroxide.
Artemisinin is a natural peroxide that is more stable than hydrogen peroxide in the presence of common ions and more resistant to interference.
So investigators decided to combine artemisinin with luminol in an effort to minimize erroneous bloodstain identifications. They showed that the luminol-artemisinin combination is more selective than luminol-hydrogen peroxide.
They challenged the new combination with components of bleaches and disinfectants, which criminals often use to clean up a crime scene. The new compound could distinguish blood from coffee, tea, and brown sugar stains.
The investigators also successfully tested the new luminol-artemisinin compound using a smartphone to obtain results. This new method could provide highly accurate, cost-effective, on-scene analyses.
They believe the favorable sensitivity and selectivity of this method makes it promising in forensic pursuits.
Guobao Xu, PhD, of the Chinese Academy of Sciences in Beijing, People’s Republic of China, and colleagues reported these findings in the American Chemical Society’s journal, Analytical Chemistry.
The authors received funding from the National Natural Science Foundation of China, the National Key Research and Development Program of China, the Chinese Academy of Science President's International Fellowship Initiative Project, and the Chinese Academy of Sciences-the Academy of Sciences for the Developing World President's Fellowship Programme. ![]()
Common Variable Immunodeficiency: A Clinical Overview
IN THIS ARTICLE
- Diagnosis
- Treatment/management
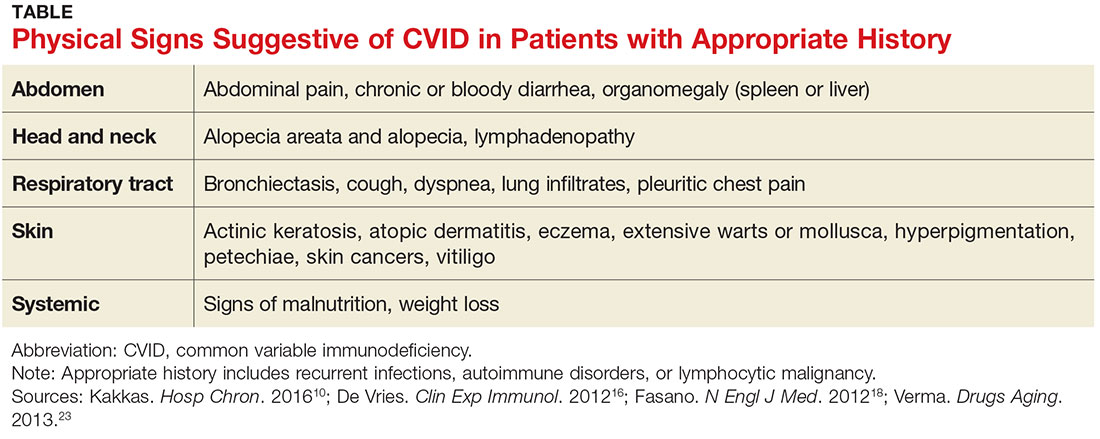
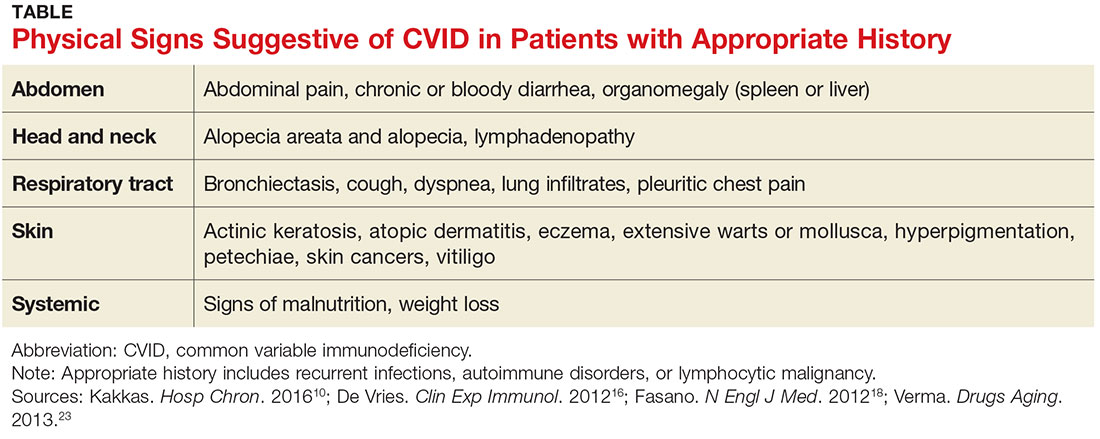
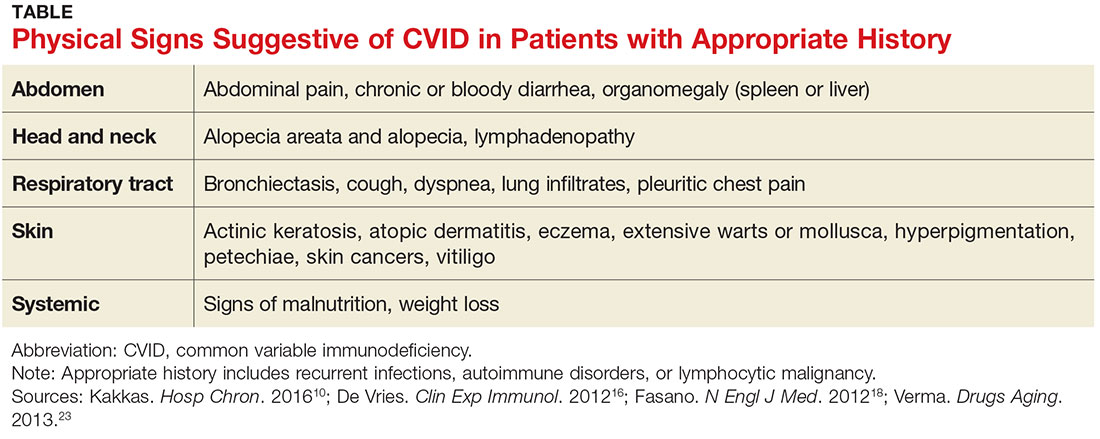
- Physcial signs suggestive of CVID in patients with appropriate history
- Case outcome
A 60-year-old woman with a recent history of air and cruise ship travel presented with symptoms consistent with acute sinusitis. She had a 34–pack-year history of cigarette smoking but had quit at age 50. Her medical history was significant for hypothyroidism, hypertension, coronary artery disease, mild asthma, and COPD. Past surgical history included coronary artery bypass, abdominal hysterectomy, and cholecystectomy. Her medications included inhaled bronchodilators, thyroxin, hydrochlorothiazide, nitrates, ß-blockers, and calcium channel blockers.
Over the next five years, she presented with frequent episodes of respiratory illness for which she received multiple courses of antibiotics, inhaled bronchodilators, and oral as well as inhaled corticosteroids. She consequently became increasingly sensitized to multiple antibiotic classes and was frequently hospitalized for the treatment of her respiratory illnesses.
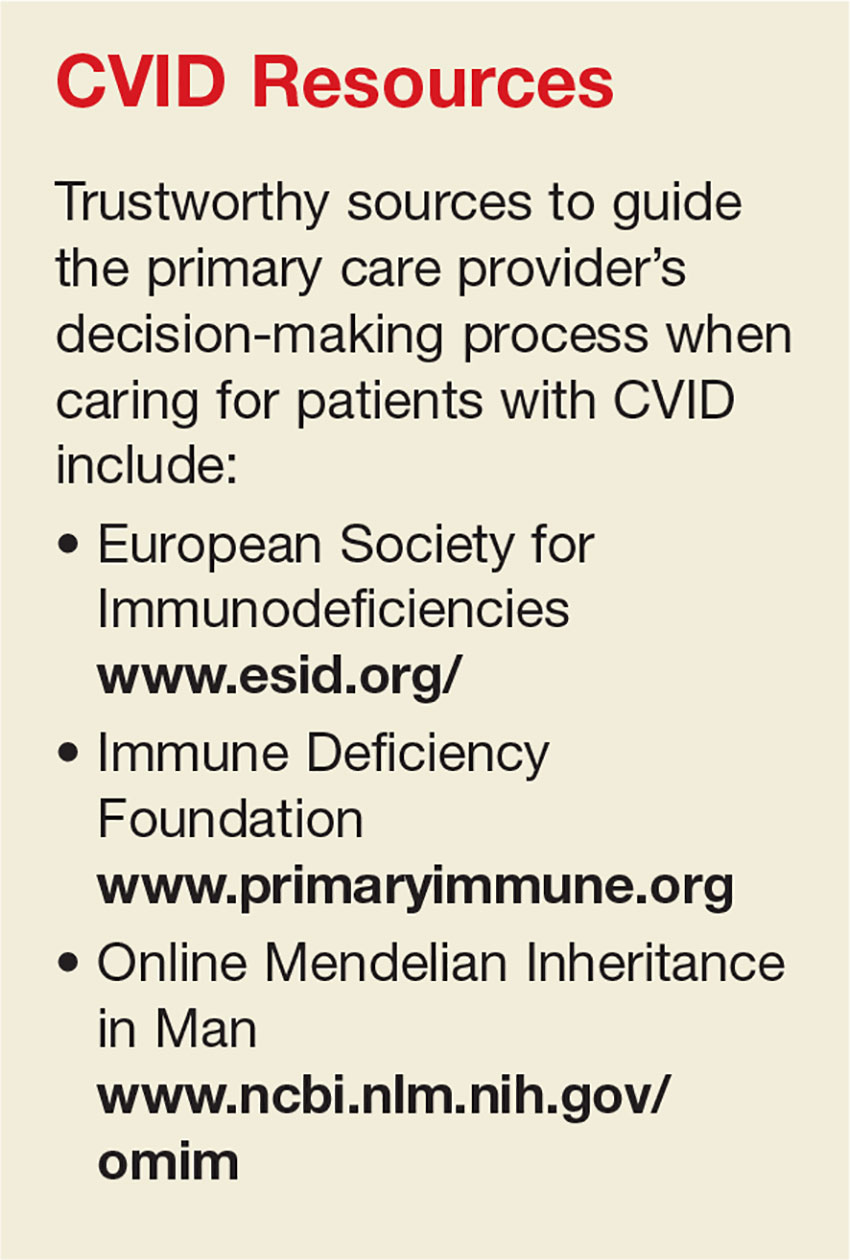
Common variable immunodeficiency disorders (collectively known as CVID) are the most common clinically significant immunodeficiency diseases among adults.1 Manifesting clinically as frequent, unusually severe or recalcitrant bacterial infections of the ear, sinus, respiratory tree, and/or gastrointestinal tract, CVID is genetically induced.2 Additionally, these disorders can predispose individuals to autoimmune conditions and to cancers involving B lymphocytes.3 Often thought to be a disease of younger people, CVID can occur across the age span.4
The immune dysfunction that characterizes CVID is believed to result from underlying genetic defects that affect the differentiation of B cells, leading to faulty immunoglobulin (Ig) synthesis. Recent advances that allow the detection of multiple novel susceptibility loci for CVID have dramatically increased our understanding of the pathophysiology and pathogenesis of this disorder.5 These advances are being used to refine the diagnostic parameters of CVID and in the future may help clinicians tailor treatment protocols to specific genetic defects.5,6
Although considered rare, CVID is often unrecognized; the incidence is likely much higher than the current estimates of 1:10,000 to 1:50,000.7 About 13% to 23% of individuals with chronic sinusitis are thought to be affected by CVID.8 While it is most commonly diagnosed during the second and third decades of life, it can be diagnosed at any time during the lifespan.4 A high burden of disease is associated with this disorder, as hospitalizations and costly, aggressive treatment regimens are needed to manage the resultant bacterial infections and sequelae.2
Increased awareness of CVID among primary care providers is needed to assure prompt diagnosis and to avoid unnecessary complications associated with delayed treatment. The diagnostic workup is complex, and referral to immunology for specific diagnosis and treatment is strongly advised. Recognition is the first step, and primary care providers must include primary immunodeficiency disorders, including CVID, in their differential to avert a missed diagnosis and to ensure optimal treatment.9
CLINICAL MANIFESTATIONS/PATIENT HISTORY
Frequent and severe infections are a hallmark of CVID. The most common types of infections seen in CVID are sinusitis, conjunctivitis, otitis media, bronchitis, pneumonia, and gastroenteritis.10 These primary bacterial infections can disseminate, causing septicemia and/or central nervous system infection.11 The usual infectious pathogens are encapsulated bacteria such as Streptococcus pneumoniae and Haemophilus influenzae, but atypical infections due to organisms such as Pneumocystis carinii and Mycoplasma pneumoniae also occur in some patients.12,13
Although the majority of CVID cases occur sporadically, family history is helpful in securing the correct diagnosis.15 Known immunodeficiency, unusual susceptibility to infections, autoimmune diseases, hematologic malignancy, or death caused by infection in other family members should increase the provider’s index of suspicion for CVID.16
Many genetic defects have been implicated in CVID, yet the wide phenotypic expression found even in persons with similar genetic profiles implies that CVID has a complex genetic transmission pattern.15 Known or suspected consanguinity in parents or grandparents increases the risk for CVID.6
Although these family history elements occur infrequently, they increase the likelihood of severe opportunistic infection, which can cause organ damage or even death.1,17 Being alert for these elements of family history can help to avoid delays in diagnosis and treatment and eventual organ damage.2
DIFFERENTIAL DIAGNOSIS
When considering the differential diagnosis for the primary features of CVID, other etiologies that should be considered include allergies, environmental exposures, uncontrolled gastroesophageal reflux disease, structural abnormalities of the upper respiratory tract, and celiac disease.5,10,18,19 Far less common but still worthy of consideration are other genetic conditions, such as primary ciliary dyskinesia, cystic fibrosis, thymic dysfunction or carcinoma, and protein-losing enteropathies.20,21
A number of conditions can cause immunosuppression. Transient reductions in serum Ig levels can occur in the presence of serious infections.22 Long-term, high-dose use of some medications, such as corticosteroids, or use of anticonvulsants may reduce antibody availability. Chronic illnesses, malignancy, and malnutrition can also play a role in immunosuppression.19 CVID shares features with a large number of primary immune diseases, and these as well as other causes of hypogammaglobulinemia must be excluded before the diagnosis of CVID can be made.1
DIAGNOSIS
While infectious disease is a common reason patients seek medical care, few patients presenting with one will have CVID. Nevertheless, immunologic evaluations should be performed and appropriate referral to an immunology specialist is strongly recommended when more than one severe infection arises in a year’s time; when a pattern of severe or unusual infections presents over a period of time; when bronchiectasis is present; or when infections do not resolve with conventional treatment.16 In addition, the physical findings noted in the Table, when combined with a history of recurrent infections, autoimmune disorders, or lymphocytic malignancy, should prompt evaluation for CVID.10,16,18,23
The diagnosis of CVID requires testing for low serum levels of total IgG, IgG subclasses, IgA, and IgM. In CVID, IgG and IgA levels will be reduced, and occasionally IgM levels will also be diminished.24 Unless an active infection is present, there will be no change in the patient’s routine blood tests, such as the complete blood count and total complement levels.
The diagnosis is also based on demonstration of a deficient antibody response to protein (tetanus) and polysaccharide (pneumonia) vaccine antigens.21 A minimal reaction to these vaccines should prompt referral to an immunology specialist for additional testing and a plan of care.25 However, whenever the index of suspicion for CVID is high, prompt referral to immunology should not be delayed to perform further testing.16
TREATMENT/MANAGEMENT
IgG replacement therapy, which treats the underlying pathophysiology of CVID by supplementing one of the deficient antibodies, is the standard treatment for CVID. IgG is considered a blood product since it is made from human plasma. Patients may experience untoward reactions to IgG replacement therapy, similar to transfusion reactions; such reactions commonly include back pain, low-grade fever, muscle and joint discomfort, and fatigue. These unpleasant effects can be minimized with the prophylactic use of antihistamines, antipyretics, or even glucocorticoids.26
Although IgG replacement therapy has high upfront costs, it increases patients’ well-being considerably by preventing multiple or recurrent infections and the resultant hospitalizations for antibiotic therapy.27 Home infusion of IgG can minimize costs as well as increase patient autonomy.28 With home infusions, IgG is administered via a multisite subcutaneous route using a slow-infusion mechanical pump. Subcutaneous infusions generally take four to six hours, depending on the number of sites used. Some patients can infuse while they sleep, which increases patient satisfaction with the treatment.27
Infections in persons with CVID can be severe and may lead to organ-system compromise, requiring aggressive therapy aimed at supporting the function of the affected organ systems. For example, patients with CVID can develop unrelenting vomiting and diarrhea, which may require inpatient admission for rehydration and stabilization until the infection can be treated adequately.32
Treatment options remain limited for the subset of CVID patients who develop severe complications, such as interstitial lung disease or neoplasms. These complications are associated with a significant increase in patient mortality, and allogeneic hematopoietic stem cell transplantation may be indicated for patients who develop them. This potentially curative treatment is being explored in ongoing research trials.33
PATIENT EDUCATION
Scrupulous hand hygiene, careful avoidance of infectious exposures, watchful food handling and preparation, and lifestyle choices that support good general health are key elements of self-care for patients who have CVID. Preventive measures serve this population well by helping to reduce some of the complications of this serious disease.
Patients with CVID should understand keys aspects regarding its diagnosis, treatment, and prognosis. Specifically, they should know that people who have CVID are born missing some of the body’s immune defenses, which increases their risk for infection, especially of the sinuses, lungs, and gut. Sometimes it takes years to make this diagnosis, because it is a rare cause of common symptoms.
The patient was referred to immunology, and a diagnosis of CVID was made. She was successfully treated with subcutaneous IgG replacement therapy. She died due to overwhelming sepsis after an episode of pneumonia at age 84.
CONCLUSION
The secret to prompt detection of CVID is adding it to the differential diagnosis of recurrent infections. Timely recognition and appropriate referral prevent serious complications, since successful treatment options are available.
Special thanks to Doug Bartelt, DNP, APNP, NP-C.
1. Bonilla FA, Barlan I, Chapel H, et al. International Consensus Document (ICON): Common Variable Immunodeficiency Disorders. J Allergy Clin Immunol Pract. 2016;4(1):38-59.
2. Jolles S. The variable in common variable immunodeficiency: a disease of complex phenotypes. J Allergy Clin Immunol Pract. 2013;1(6):545-556.
3. Barsotti NS, Almeida RR, Costa PR, et al. IL-10-Producing regulatory B cells are decreased in patients with common variable immunodeficiency. PLoS One. 2016;11(3): e0151761.
4. Rosenberg E, Dent PB, Denburg JA. Primary immune deficiencies in the adult: a previously underrecognized common condition. J Allergy Clin Immunol Pract. 2016;4(6):1101-1107.
5. Orange JS, Glessner JT, Resnick E,Genome-wide association identifies diverse causes of common variable immunodeficiency. J Allergy Clin Immunol. 2011;127(6):1360-1367.e6.
6. Stray-Pedersen A, Sorte HS, Samarakoon P, et al. Primary immunodeficiency diseases: genomic approaches delineate heterogeneous Mendelian disorders. J Allergy Clin Immunol. 2017;139(1):232-245.
7. Salzer U, Warnatz K, Peter HH. Common variable immunodeficiency—an update. Arthritis Res Ther. 2012;14(5):223.
8. Schwitzguébel AJ, Jandus P, Lacroix JS, et al. Immunoglobulin deficiency in patients with chronic rhinosinusitis: systematic review of the literature and meta-analysis. J Allergy Clin Immunol. 2015;136(6):1523-1531.
9. Chapel H. Common variable immunodeficiency disorders (CVID)—diagnoses of exclusion, especially combined immune defects. J Allergy Clin Immunol Pract. 2016;4(6):1158-1159.
10. Kakkas I. Clinical heterogeneity of common variable immunodeficiency. Hosp Chron. 2016;11(1):10-14.
11. Bonilla FA, Khan DA, Ballas ZK, et al. Practice parameter for the diagnosis and management of primary immunodeficiency. J Allergy Clin Immunol. 2015;136(5):1186-1205.
12. Schussler E, Beasley MB, Maglione PJ. Lung disease in primary antibody deficiencies. J Allergy Clin Immunol Pract. 2016;4(6):1039-1052.
13. Harville TO. Could better categorization of pulmonary disease in common variable immunodeficiency ultimately allow for better treatment outcomes? Ann Allergy Asthma Immunol. 2014;113(4):336-337.
14. Oliveira JB, Fleisher TA. Laboratory evaluation of primary immunodeficiencies. J Allergy Clin Immunol. 2010;125(2):S297-S305.
15. Bogaert DJ, Dullaers M, Lambrecht BN, et al. Genes associated with common variable immunodeficiency: one diagnosis to rule them all? J Med Genet. 2016;53(9):575-590.
16. De Vries E; European Society for Immunodeficiencies (ESID) members. Patient-centered screening for primary immunodeficiency, a multi-stage diagnostic protocol designed for non-immunologists: 2011 update. Clin Exp Immunol. 2012; 167(1):108-119.
17. Bertinchamp R, Gérard L, Boutboul D, et al. Exclusion of patients with a severe T-cell defect improves the definition of common variable immunodeficiency. J Allergy Clin Immunol Pract. 2016;4(6):1147-1157.
18. Fasano A, Catassi C. Celiac disease. N Engl J Med. 2012;367(25):2419-2426.
19. Park MA, Li JT, Hagan JB, et al. Common variable immunodeficiency: a new look at an old disease. Lancet. 2008;372(9637):489-502.
20. Cunningham-Rundles C, Maglione PJ. Common variable immunodeficiency. J Allergy Clin Immunol. 2012;129(5):1425-1426.
21. Bonilla FA, Barlan I, Chapel H, et al. International consensus document (ICON): Common variable immunodeficiency disorders. J Allergy Clin Immunol Pract. 2016;4(1):38-59.
22. Chinen J, Notarangelo LD, Shearer WT. Advances in basic and clinical immunology in 2014. J Allergy Clin Immunol Pract. 2015;135(5):1132-1141.
23. Verma N, Thaventhiran A, Gathmann B, et al. Therapeutic management of primary immunodeficiency in older patients. Drugs Aging. 2013;30(7):503-512.
24. Jolles S. The variable in common variable immunodeficiency: a disease of complex phenotypes. J Allergy Clin Immunol Pract. 2013;1(6):545-556.
25. McCullagh BN, Comellas AP, Ballas ZK, et al. Antibody deficiency in patients with frequent exacerbations of chronic obstructive pulmonary disease (COPD). PLoS One. 2017;12(2):e0172437.
26. Wasserman RL. The nuts and bolts of immunoglobulin treatment for antibody deficiency. J Allergy Clin Immunol Pract. 2016;4(6):1076-1081.
27. Lingman-Framme J, Fasth A. Subcutaneous immunoglobulin for primary and secondary immunodeficiencies: an evidence-based review. Drugs. 2013;73(12):1307-1319.
28. Ducruet T, Levasseur M, Des Roches A, et al. Pharmacoeconomic advantages of subcutaneous versus intravenous immunoglobulin treatment in a Canadian pediatric center. J Allergy Clin Immunol Pract. 2013;131(2):585-587.
29. Driessen G, van der Burg M. Primary antibody deficiencies [educational paper]. Eur J Pediatr. 2011;170(6):693-702.
30. Kuruvilla M, de la Morena MT. Antibiotic prophylaxis in primary immune deficiency disorders. J Allergy Clin Immunol Pract. 2013;1(6):573-582.
31. Norlin AC, Hansen S, Wahren-Borgström E, et al. Vitamin D3 supplementation and antibiotic consumption—results from a prospective, observational study at an immune-deficiency unit in Sweden. PLoS One. 2016;11(9):e0163451.
32. Lougaris V, Ravelli A, Villanacci V, et al. Gastrointestinal pathologic abnormalities in pediatric- and adult-onset common variable immunodeficiency. Dig Dis Sci. 2015;60(8):2384-2389.
33. Wehr C, Gennery AR, Lindemans C, et al. Multicenter experience in hematopoietic stem cell transplantation for serious complications of common variable immunodeficiency. J Allergy Clin Immunol. 2015;135(4):988-997.
34. Shearer WT, Fleisher TA, Buckley RH, et al; Medical Advisory Committee of the Immune Deficiency Foundation. Recommendations for live viral and bacterial vaccines in immunodeficient patients and their close contacts. J Allergy Clin Immunol. 2014;133(4):961-966.
IN THIS ARTICLE
- Diagnosis
- Treatment/management
- Physcial signs suggestive of CVID in patients with appropriate history
- Case outcome
A 60-year-old woman with a recent history of air and cruise ship travel presented with symptoms consistent with acute sinusitis. She had a 34–pack-year history of cigarette smoking but had quit at age 50. Her medical history was significant for hypothyroidism, hypertension, coronary artery disease, mild asthma, and COPD. Past surgical history included coronary artery bypass, abdominal hysterectomy, and cholecystectomy. Her medications included inhaled bronchodilators, thyroxin, hydrochlorothiazide, nitrates, ß-blockers, and calcium channel blockers.
Over the next five years, she presented with frequent episodes of respiratory illness for which she received multiple courses of antibiotics, inhaled bronchodilators, and oral as well as inhaled corticosteroids. She consequently became increasingly sensitized to multiple antibiotic classes and was frequently hospitalized for the treatment of her respiratory illnesses.
Common variable immunodeficiency disorders (collectively known as CVID) are the most common clinically significant immunodeficiency diseases among adults.1 Manifesting clinically as frequent, unusually severe or recalcitrant bacterial infections of the ear, sinus, respiratory tree, and/or gastrointestinal tract, CVID is genetically induced.2 Additionally, these disorders can predispose individuals to autoimmune conditions and to cancers involving B lymphocytes.3 Often thought to be a disease of younger people, CVID can occur across the age span.4
The immune dysfunction that characterizes CVID is believed to result from underlying genetic defects that affect the differentiation of B cells, leading to faulty immunoglobulin (Ig) synthesis. Recent advances that allow the detection of multiple novel susceptibility loci for CVID have dramatically increased our understanding of the pathophysiology and pathogenesis of this disorder.5 These advances are being used to refine the diagnostic parameters of CVID and in the future may help clinicians tailor treatment protocols to specific genetic defects.5,6
Although considered rare, CVID is often unrecognized; the incidence is likely much higher than the current estimates of 1:10,000 to 1:50,000.7 About 13% to 23% of individuals with chronic sinusitis are thought to be affected by CVID.8 While it is most commonly diagnosed during the second and third decades of life, it can be diagnosed at any time during the lifespan.4 A high burden of disease is associated with this disorder, as hospitalizations and costly, aggressive treatment regimens are needed to manage the resultant bacterial infections and sequelae.2
Increased awareness of CVID among primary care providers is needed to assure prompt diagnosis and to avoid unnecessary complications associated with delayed treatment. The diagnostic workup is complex, and referral to immunology for specific diagnosis and treatment is strongly advised. Recognition is the first step, and primary care providers must include primary immunodeficiency disorders, including CVID, in their differential to avert a missed diagnosis and to ensure optimal treatment.9
CLINICAL MANIFESTATIONS/PATIENT HISTORY
Frequent and severe infections are a hallmark of CVID. The most common types of infections seen in CVID are sinusitis, conjunctivitis, otitis media, bronchitis, pneumonia, and gastroenteritis.10 These primary bacterial infections can disseminate, causing septicemia and/or central nervous system infection.11 The usual infectious pathogens are encapsulated bacteria such as Streptococcus pneumoniae and Haemophilus influenzae, but atypical infections due to organisms such as Pneumocystis carinii and Mycoplasma pneumoniae also occur in some patients.12,13
Although the majority of CVID cases occur sporadically, family history is helpful in securing the correct diagnosis.15 Known immunodeficiency, unusual susceptibility to infections, autoimmune diseases, hematologic malignancy, or death caused by infection in other family members should increase the provider’s index of suspicion for CVID.16
Many genetic defects have been implicated in CVID, yet the wide phenotypic expression found even in persons with similar genetic profiles implies that CVID has a complex genetic transmission pattern.15 Known or suspected consanguinity in parents or grandparents increases the risk for CVID.6
Although these family history elements occur infrequently, they increase the likelihood of severe opportunistic infection, which can cause organ damage or even death.1,17 Being alert for these elements of family history can help to avoid delays in diagnosis and treatment and eventual organ damage.2
DIFFERENTIAL DIAGNOSIS
When considering the differential diagnosis for the primary features of CVID, other etiologies that should be considered include allergies, environmental exposures, uncontrolled gastroesophageal reflux disease, structural abnormalities of the upper respiratory tract, and celiac disease.5,10,18,19 Far less common but still worthy of consideration are other genetic conditions, such as primary ciliary dyskinesia, cystic fibrosis, thymic dysfunction or carcinoma, and protein-losing enteropathies.20,21
A number of conditions can cause immunosuppression. Transient reductions in serum Ig levels can occur in the presence of serious infections.22 Long-term, high-dose use of some medications, such as corticosteroids, or use of anticonvulsants may reduce antibody availability. Chronic illnesses, malignancy, and malnutrition can also play a role in immunosuppression.19 CVID shares features with a large number of primary immune diseases, and these as well as other causes of hypogammaglobulinemia must be excluded before the diagnosis of CVID can be made.1
DIAGNOSIS
While infectious disease is a common reason patients seek medical care, few patients presenting with one will have CVID. Nevertheless, immunologic evaluations should be performed and appropriate referral to an immunology specialist is strongly recommended when more than one severe infection arises in a year’s time; when a pattern of severe or unusual infections presents over a period of time; when bronchiectasis is present; or when infections do not resolve with conventional treatment.16 In addition, the physical findings noted in the Table, when combined with a history of recurrent infections, autoimmune disorders, or lymphocytic malignancy, should prompt evaluation for CVID.10,16,18,23
The diagnosis of CVID requires testing for low serum levels of total IgG, IgG subclasses, IgA, and IgM. In CVID, IgG and IgA levels will be reduced, and occasionally IgM levels will also be diminished.24 Unless an active infection is present, there will be no change in the patient’s routine blood tests, such as the complete blood count and total complement levels.
The diagnosis is also based on demonstration of a deficient antibody response to protein (tetanus) and polysaccharide (pneumonia) vaccine antigens.21 A minimal reaction to these vaccines should prompt referral to an immunology specialist for additional testing and a plan of care.25 However, whenever the index of suspicion for CVID is high, prompt referral to immunology should not be delayed to perform further testing.16
TREATMENT/MANAGEMENT
IgG replacement therapy, which treats the underlying pathophysiology of CVID by supplementing one of the deficient antibodies, is the standard treatment for CVID. IgG is considered a blood product since it is made from human plasma. Patients may experience untoward reactions to IgG replacement therapy, similar to transfusion reactions; such reactions commonly include back pain, low-grade fever, muscle and joint discomfort, and fatigue. These unpleasant effects can be minimized with the prophylactic use of antihistamines, antipyretics, or even glucocorticoids.26
Although IgG replacement therapy has high upfront costs, it increases patients’ well-being considerably by preventing multiple or recurrent infections and the resultant hospitalizations for antibiotic therapy.27 Home infusion of IgG can minimize costs as well as increase patient autonomy.28 With home infusions, IgG is administered via a multisite subcutaneous route using a slow-infusion mechanical pump. Subcutaneous infusions generally take four to six hours, depending on the number of sites used. Some patients can infuse while they sleep, which increases patient satisfaction with the treatment.27
Infections in persons with CVID can be severe and may lead to organ-system compromise, requiring aggressive therapy aimed at supporting the function of the affected organ systems. For example, patients with CVID can develop unrelenting vomiting and diarrhea, which may require inpatient admission for rehydration and stabilization until the infection can be treated adequately.32
Treatment options remain limited for the subset of CVID patients who develop severe complications, such as interstitial lung disease or neoplasms. These complications are associated with a significant increase in patient mortality, and allogeneic hematopoietic stem cell transplantation may be indicated for patients who develop them. This potentially curative treatment is being explored in ongoing research trials.33
PATIENT EDUCATION
Scrupulous hand hygiene, careful avoidance of infectious exposures, watchful food handling and preparation, and lifestyle choices that support good general health are key elements of self-care for patients who have CVID. Preventive measures serve this population well by helping to reduce some of the complications of this serious disease.
Patients with CVID should understand keys aspects regarding its diagnosis, treatment, and prognosis. Specifically, they should know that people who have CVID are born missing some of the body’s immune defenses, which increases their risk for infection, especially of the sinuses, lungs, and gut. Sometimes it takes years to make this diagnosis, because it is a rare cause of common symptoms.
The patient was referred to immunology, and a diagnosis of CVID was made. She was successfully treated with subcutaneous IgG replacement therapy. She died due to overwhelming sepsis after an episode of pneumonia at age 84.
CONCLUSION
The secret to prompt detection of CVID is adding it to the differential diagnosis of recurrent infections. Timely recognition and appropriate referral prevent serious complications, since successful treatment options are available.
Special thanks to Doug Bartelt, DNP, APNP, NP-C.
IN THIS ARTICLE
- Diagnosis
- Treatment/management
- Physcial signs suggestive of CVID in patients with appropriate history
- Case outcome
A 60-year-old woman with a recent history of air and cruise ship travel presented with symptoms consistent with acute sinusitis. She had a 34–pack-year history of cigarette smoking but had quit at age 50. Her medical history was significant for hypothyroidism, hypertension, coronary artery disease, mild asthma, and COPD. Past surgical history included coronary artery bypass, abdominal hysterectomy, and cholecystectomy. Her medications included inhaled bronchodilators, thyroxin, hydrochlorothiazide, nitrates, ß-blockers, and calcium channel blockers.
Over the next five years, she presented with frequent episodes of respiratory illness for which she received multiple courses of antibiotics, inhaled bronchodilators, and oral as well as inhaled corticosteroids. She consequently became increasingly sensitized to multiple antibiotic classes and was frequently hospitalized for the treatment of her respiratory illnesses.
Common variable immunodeficiency disorders (collectively known as CVID) are the most common clinically significant immunodeficiency diseases among adults.1 Manifesting clinically as frequent, unusually severe or recalcitrant bacterial infections of the ear, sinus, respiratory tree, and/or gastrointestinal tract, CVID is genetically induced.2 Additionally, these disorders can predispose individuals to autoimmune conditions and to cancers involving B lymphocytes.3 Often thought to be a disease of younger people, CVID can occur across the age span.4
The immune dysfunction that characterizes CVID is believed to result from underlying genetic defects that affect the differentiation of B cells, leading to faulty immunoglobulin (Ig) synthesis. Recent advances that allow the detection of multiple novel susceptibility loci for CVID have dramatically increased our understanding of the pathophysiology and pathogenesis of this disorder.5 These advances are being used to refine the diagnostic parameters of CVID and in the future may help clinicians tailor treatment protocols to specific genetic defects.5,6
Although considered rare, CVID is often unrecognized; the incidence is likely much higher than the current estimates of 1:10,000 to 1:50,000.7 About 13% to 23% of individuals with chronic sinusitis are thought to be affected by CVID.8 While it is most commonly diagnosed during the second and third decades of life, it can be diagnosed at any time during the lifespan.4 A high burden of disease is associated with this disorder, as hospitalizations and costly, aggressive treatment regimens are needed to manage the resultant bacterial infections and sequelae.2
Increased awareness of CVID among primary care providers is needed to assure prompt diagnosis and to avoid unnecessary complications associated with delayed treatment. The diagnostic workup is complex, and referral to immunology for specific diagnosis and treatment is strongly advised. Recognition is the first step, and primary care providers must include primary immunodeficiency disorders, including CVID, in their differential to avert a missed diagnosis and to ensure optimal treatment.9
CLINICAL MANIFESTATIONS/PATIENT HISTORY
Frequent and severe infections are a hallmark of CVID. The most common types of infections seen in CVID are sinusitis, conjunctivitis, otitis media, bronchitis, pneumonia, and gastroenteritis.10 These primary bacterial infections can disseminate, causing septicemia and/or central nervous system infection.11 The usual infectious pathogens are encapsulated bacteria such as Streptococcus pneumoniae and Haemophilus influenzae, but atypical infections due to organisms such as Pneumocystis carinii and Mycoplasma pneumoniae also occur in some patients.12,13
Although the majority of CVID cases occur sporadically, family history is helpful in securing the correct diagnosis.15 Known immunodeficiency, unusual susceptibility to infections, autoimmune diseases, hematologic malignancy, or death caused by infection in other family members should increase the provider’s index of suspicion for CVID.16
Many genetic defects have been implicated in CVID, yet the wide phenotypic expression found even in persons with similar genetic profiles implies that CVID has a complex genetic transmission pattern.15 Known or suspected consanguinity in parents or grandparents increases the risk for CVID.6
Although these family history elements occur infrequently, they increase the likelihood of severe opportunistic infection, which can cause organ damage or even death.1,17 Being alert for these elements of family history can help to avoid delays in diagnosis and treatment and eventual organ damage.2
DIFFERENTIAL DIAGNOSIS
When considering the differential diagnosis for the primary features of CVID, other etiologies that should be considered include allergies, environmental exposures, uncontrolled gastroesophageal reflux disease, structural abnormalities of the upper respiratory tract, and celiac disease.5,10,18,19 Far less common but still worthy of consideration are other genetic conditions, such as primary ciliary dyskinesia, cystic fibrosis, thymic dysfunction or carcinoma, and protein-losing enteropathies.20,21
A number of conditions can cause immunosuppression. Transient reductions in serum Ig levels can occur in the presence of serious infections.22 Long-term, high-dose use of some medications, such as corticosteroids, or use of anticonvulsants may reduce antibody availability. Chronic illnesses, malignancy, and malnutrition can also play a role in immunosuppression.19 CVID shares features with a large number of primary immune diseases, and these as well as other causes of hypogammaglobulinemia must be excluded before the diagnosis of CVID can be made.1
DIAGNOSIS
While infectious disease is a common reason patients seek medical care, few patients presenting with one will have CVID. Nevertheless, immunologic evaluations should be performed and appropriate referral to an immunology specialist is strongly recommended when more than one severe infection arises in a year’s time; when a pattern of severe or unusual infections presents over a period of time; when bronchiectasis is present; or when infections do not resolve with conventional treatment.16 In addition, the physical findings noted in the Table, when combined with a history of recurrent infections, autoimmune disorders, or lymphocytic malignancy, should prompt evaluation for CVID.10,16,18,23
The diagnosis of CVID requires testing for low serum levels of total IgG, IgG subclasses, IgA, and IgM. In CVID, IgG and IgA levels will be reduced, and occasionally IgM levels will also be diminished.24 Unless an active infection is present, there will be no change in the patient’s routine blood tests, such as the complete blood count and total complement levels.
The diagnosis is also based on demonstration of a deficient antibody response to protein (tetanus) and polysaccharide (pneumonia) vaccine antigens.21 A minimal reaction to these vaccines should prompt referral to an immunology specialist for additional testing and a plan of care.25 However, whenever the index of suspicion for CVID is high, prompt referral to immunology should not be delayed to perform further testing.16
TREATMENT/MANAGEMENT
IgG replacement therapy, which treats the underlying pathophysiology of CVID by supplementing one of the deficient antibodies, is the standard treatment for CVID. IgG is considered a blood product since it is made from human plasma. Patients may experience untoward reactions to IgG replacement therapy, similar to transfusion reactions; such reactions commonly include back pain, low-grade fever, muscle and joint discomfort, and fatigue. These unpleasant effects can be minimized with the prophylactic use of antihistamines, antipyretics, or even glucocorticoids.26
Although IgG replacement therapy has high upfront costs, it increases patients’ well-being considerably by preventing multiple or recurrent infections and the resultant hospitalizations for antibiotic therapy.27 Home infusion of IgG can minimize costs as well as increase patient autonomy.28 With home infusions, IgG is administered via a multisite subcutaneous route using a slow-infusion mechanical pump. Subcutaneous infusions generally take four to six hours, depending on the number of sites used. Some patients can infuse while they sleep, which increases patient satisfaction with the treatment.27
Infections in persons with CVID can be severe and may lead to organ-system compromise, requiring aggressive therapy aimed at supporting the function of the affected organ systems. For example, patients with CVID can develop unrelenting vomiting and diarrhea, which may require inpatient admission for rehydration and stabilization until the infection can be treated adequately.32
Treatment options remain limited for the subset of CVID patients who develop severe complications, such as interstitial lung disease or neoplasms. These complications are associated with a significant increase in patient mortality, and allogeneic hematopoietic stem cell transplantation may be indicated for patients who develop them. This potentially curative treatment is being explored in ongoing research trials.33
PATIENT EDUCATION
Scrupulous hand hygiene, careful avoidance of infectious exposures, watchful food handling and preparation, and lifestyle choices that support good general health are key elements of self-care for patients who have CVID. Preventive measures serve this population well by helping to reduce some of the complications of this serious disease.
Patients with CVID should understand keys aspects regarding its diagnosis, treatment, and prognosis. Specifically, they should know that people who have CVID are born missing some of the body’s immune defenses, which increases their risk for infection, especially of the sinuses, lungs, and gut. Sometimes it takes years to make this diagnosis, because it is a rare cause of common symptoms.
The patient was referred to immunology, and a diagnosis of CVID was made. She was successfully treated with subcutaneous IgG replacement therapy. She died due to overwhelming sepsis after an episode of pneumonia at age 84.
CONCLUSION
The secret to prompt detection of CVID is adding it to the differential diagnosis of recurrent infections. Timely recognition and appropriate referral prevent serious complications, since successful treatment options are available.
Special thanks to Doug Bartelt, DNP, APNP, NP-C.
1. Bonilla FA, Barlan I, Chapel H, et al. International Consensus Document (ICON): Common Variable Immunodeficiency Disorders. J Allergy Clin Immunol Pract. 2016;4(1):38-59.
2. Jolles S. The variable in common variable immunodeficiency: a disease of complex phenotypes. J Allergy Clin Immunol Pract. 2013;1(6):545-556.
3. Barsotti NS, Almeida RR, Costa PR, et al. IL-10-Producing regulatory B cells are decreased in patients with common variable immunodeficiency. PLoS One. 2016;11(3): e0151761.
4. Rosenberg E, Dent PB, Denburg JA. Primary immune deficiencies in the adult: a previously underrecognized common condition. J Allergy Clin Immunol Pract. 2016;4(6):1101-1107.
5. Orange JS, Glessner JT, Resnick E,Genome-wide association identifies diverse causes of common variable immunodeficiency. J Allergy Clin Immunol. 2011;127(6):1360-1367.e6.
6. Stray-Pedersen A, Sorte HS, Samarakoon P, et al. Primary immunodeficiency diseases: genomic approaches delineate heterogeneous Mendelian disorders. J Allergy Clin Immunol. 2017;139(1):232-245.
7. Salzer U, Warnatz K, Peter HH. Common variable immunodeficiency—an update. Arthritis Res Ther. 2012;14(5):223.
8. Schwitzguébel AJ, Jandus P, Lacroix JS, et al. Immunoglobulin deficiency in patients with chronic rhinosinusitis: systematic review of the literature and meta-analysis. J Allergy Clin Immunol. 2015;136(6):1523-1531.
9. Chapel H. Common variable immunodeficiency disorders (CVID)—diagnoses of exclusion, especially combined immune defects. J Allergy Clin Immunol Pract. 2016;4(6):1158-1159.
10. Kakkas I. Clinical heterogeneity of common variable immunodeficiency. Hosp Chron. 2016;11(1):10-14.
11. Bonilla FA, Khan DA, Ballas ZK, et al. Practice parameter for the diagnosis and management of primary immunodeficiency. J Allergy Clin Immunol. 2015;136(5):1186-1205.
12. Schussler E, Beasley MB, Maglione PJ. Lung disease in primary antibody deficiencies. J Allergy Clin Immunol Pract. 2016;4(6):1039-1052.
13. Harville TO. Could better categorization of pulmonary disease in common variable immunodeficiency ultimately allow for better treatment outcomes? Ann Allergy Asthma Immunol. 2014;113(4):336-337.
14. Oliveira JB, Fleisher TA. Laboratory evaluation of primary immunodeficiencies. J Allergy Clin Immunol. 2010;125(2):S297-S305.
15. Bogaert DJ, Dullaers M, Lambrecht BN, et al. Genes associated with common variable immunodeficiency: one diagnosis to rule them all? J Med Genet. 2016;53(9):575-590.
16. De Vries E; European Society for Immunodeficiencies (ESID) members. Patient-centered screening for primary immunodeficiency, a multi-stage diagnostic protocol designed for non-immunologists: 2011 update. Clin Exp Immunol. 2012; 167(1):108-119.
17. Bertinchamp R, Gérard L, Boutboul D, et al. Exclusion of patients with a severe T-cell defect improves the definition of common variable immunodeficiency. J Allergy Clin Immunol Pract. 2016;4(6):1147-1157.
18. Fasano A, Catassi C. Celiac disease. N Engl J Med. 2012;367(25):2419-2426.
19. Park MA, Li JT, Hagan JB, et al. Common variable immunodeficiency: a new look at an old disease. Lancet. 2008;372(9637):489-502.
20. Cunningham-Rundles C, Maglione PJ. Common variable immunodeficiency. J Allergy Clin Immunol. 2012;129(5):1425-1426.
21. Bonilla FA, Barlan I, Chapel H, et al. International consensus document (ICON): Common variable immunodeficiency disorders. J Allergy Clin Immunol Pract. 2016;4(1):38-59.
22. Chinen J, Notarangelo LD, Shearer WT. Advances in basic and clinical immunology in 2014. J Allergy Clin Immunol Pract. 2015;135(5):1132-1141.
23. Verma N, Thaventhiran A, Gathmann B, et al. Therapeutic management of primary immunodeficiency in older patients. Drugs Aging. 2013;30(7):503-512.
24. Jolles S. The variable in common variable immunodeficiency: a disease of complex phenotypes. J Allergy Clin Immunol Pract. 2013;1(6):545-556.
25. McCullagh BN, Comellas AP, Ballas ZK, et al. Antibody deficiency in patients with frequent exacerbations of chronic obstructive pulmonary disease (COPD). PLoS One. 2017;12(2):e0172437.
26. Wasserman RL. The nuts and bolts of immunoglobulin treatment for antibody deficiency. J Allergy Clin Immunol Pract. 2016;4(6):1076-1081.
27. Lingman-Framme J, Fasth A. Subcutaneous immunoglobulin for primary and secondary immunodeficiencies: an evidence-based review. Drugs. 2013;73(12):1307-1319.
28. Ducruet T, Levasseur M, Des Roches A, et al. Pharmacoeconomic advantages of subcutaneous versus intravenous immunoglobulin treatment in a Canadian pediatric center. J Allergy Clin Immunol Pract. 2013;131(2):585-587.
29. Driessen G, van der Burg M. Primary antibody deficiencies [educational paper]. Eur J Pediatr. 2011;170(6):693-702.
30. Kuruvilla M, de la Morena MT. Antibiotic prophylaxis in primary immune deficiency disorders. J Allergy Clin Immunol Pract. 2013;1(6):573-582.
31. Norlin AC, Hansen S, Wahren-Borgström E, et al. Vitamin D3 supplementation and antibiotic consumption—results from a prospective, observational study at an immune-deficiency unit in Sweden. PLoS One. 2016;11(9):e0163451.
32. Lougaris V, Ravelli A, Villanacci V, et al. Gastrointestinal pathologic abnormalities in pediatric- and adult-onset common variable immunodeficiency. Dig Dis Sci. 2015;60(8):2384-2389.
33. Wehr C, Gennery AR, Lindemans C, et al. Multicenter experience in hematopoietic stem cell transplantation for serious complications of common variable immunodeficiency. J Allergy Clin Immunol. 2015;135(4):988-997.
34. Shearer WT, Fleisher TA, Buckley RH, et al; Medical Advisory Committee of the Immune Deficiency Foundation. Recommendations for live viral and bacterial vaccines in immunodeficient patients and their close contacts. J Allergy Clin Immunol. 2014;133(4):961-966.
1. Bonilla FA, Barlan I, Chapel H, et al. International Consensus Document (ICON): Common Variable Immunodeficiency Disorders. J Allergy Clin Immunol Pract. 2016;4(1):38-59.
2. Jolles S. The variable in common variable immunodeficiency: a disease of complex phenotypes. J Allergy Clin Immunol Pract. 2013;1(6):545-556.
3. Barsotti NS, Almeida RR, Costa PR, et al. IL-10-Producing regulatory B cells are decreased in patients with common variable immunodeficiency. PLoS One. 2016;11(3): e0151761.
4. Rosenberg E, Dent PB, Denburg JA. Primary immune deficiencies in the adult: a previously underrecognized common condition. J Allergy Clin Immunol Pract. 2016;4(6):1101-1107.
5. Orange JS, Glessner JT, Resnick E,Genome-wide association identifies diverse causes of common variable immunodeficiency. J Allergy Clin Immunol. 2011;127(6):1360-1367.e6.
6. Stray-Pedersen A, Sorte HS, Samarakoon P, et al. Primary immunodeficiency diseases: genomic approaches delineate heterogeneous Mendelian disorders. J Allergy Clin Immunol. 2017;139(1):232-245.
7. Salzer U, Warnatz K, Peter HH. Common variable immunodeficiency—an update. Arthritis Res Ther. 2012;14(5):223.
8. Schwitzguébel AJ, Jandus P, Lacroix JS, et al. Immunoglobulin deficiency in patients with chronic rhinosinusitis: systematic review of the literature and meta-analysis. J Allergy Clin Immunol. 2015;136(6):1523-1531.
9. Chapel H. Common variable immunodeficiency disorders (CVID)—diagnoses of exclusion, especially combined immune defects. J Allergy Clin Immunol Pract. 2016;4(6):1158-1159.
10. Kakkas I. Clinical heterogeneity of common variable immunodeficiency. Hosp Chron. 2016;11(1):10-14.
11. Bonilla FA, Khan DA, Ballas ZK, et al. Practice parameter for the diagnosis and management of primary immunodeficiency. J Allergy Clin Immunol. 2015;136(5):1186-1205.
12. Schussler E, Beasley MB, Maglione PJ. Lung disease in primary antibody deficiencies. J Allergy Clin Immunol Pract. 2016;4(6):1039-1052.
13. Harville TO. Could better categorization of pulmonary disease in common variable immunodeficiency ultimately allow for better treatment outcomes? Ann Allergy Asthma Immunol. 2014;113(4):336-337.
14. Oliveira JB, Fleisher TA. Laboratory evaluation of primary immunodeficiencies. J Allergy Clin Immunol. 2010;125(2):S297-S305.
15. Bogaert DJ, Dullaers M, Lambrecht BN, et al. Genes associated with common variable immunodeficiency: one diagnosis to rule them all? J Med Genet. 2016;53(9):575-590.
16. De Vries E; European Society for Immunodeficiencies (ESID) members. Patient-centered screening for primary immunodeficiency, a multi-stage diagnostic protocol designed for non-immunologists: 2011 update. Clin Exp Immunol. 2012; 167(1):108-119.
17. Bertinchamp R, Gérard L, Boutboul D, et al. Exclusion of patients with a severe T-cell defect improves the definition of common variable immunodeficiency. J Allergy Clin Immunol Pract. 2016;4(6):1147-1157.
18. Fasano A, Catassi C. Celiac disease. N Engl J Med. 2012;367(25):2419-2426.
19. Park MA, Li JT, Hagan JB, et al. Common variable immunodeficiency: a new look at an old disease. Lancet. 2008;372(9637):489-502.
20. Cunningham-Rundles C, Maglione PJ. Common variable immunodeficiency. J Allergy Clin Immunol. 2012;129(5):1425-1426.
21. Bonilla FA, Barlan I, Chapel H, et al. International consensus document (ICON): Common variable immunodeficiency disorders. J Allergy Clin Immunol Pract. 2016;4(1):38-59.
22. Chinen J, Notarangelo LD, Shearer WT. Advances in basic and clinical immunology in 2014. J Allergy Clin Immunol Pract. 2015;135(5):1132-1141.
23. Verma N, Thaventhiran A, Gathmann B, et al. Therapeutic management of primary immunodeficiency in older patients. Drugs Aging. 2013;30(7):503-512.
24. Jolles S. The variable in common variable immunodeficiency: a disease of complex phenotypes. J Allergy Clin Immunol Pract. 2013;1(6):545-556.
25. McCullagh BN, Comellas AP, Ballas ZK, et al. Antibody deficiency in patients with frequent exacerbations of chronic obstructive pulmonary disease (COPD). PLoS One. 2017;12(2):e0172437.
26. Wasserman RL. The nuts and bolts of immunoglobulin treatment for antibody deficiency. J Allergy Clin Immunol Pract. 2016;4(6):1076-1081.
27. Lingman-Framme J, Fasth A. Subcutaneous immunoglobulin for primary and secondary immunodeficiencies: an evidence-based review. Drugs. 2013;73(12):1307-1319.
28. Ducruet T, Levasseur M, Des Roches A, et al. Pharmacoeconomic advantages of subcutaneous versus intravenous immunoglobulin treatment in a Canadian pediatric center. J Allergy Clin Immunol Pract. 2013;131(2):585-587.
29. Driessen G, van der Burg M. Primary antibody deficiencies [educational paper]. Eur J Pediatr. 2011;170(6):693-702.
30. Kuruvilla M, de la Morena MT. Antibiotic prophylaxis in primary immune deficiency disorders. J Allergy Clin Immunol Pract. 2013;1(6):573-582.
31. Norlin AC, Hansen S, Wahren-Borgström E, et al. Vitamin D3 supplementation and antibiotic consumption—results from a prospective, observational study at an immune-deficiency unit in Sweden. PLoS One. 2016;11(9):e0163451.
32. Lougaris V, Ravelli A, Villanacci V, et al. Gastrointestinal pathologic abnormalities in pediatric- and adult-onset common variable immunodeficiency. Dig Dis Sci. 2015;60(8):2384-2389.
33. Wehr C, Gennery AR, Lindemans C, et al. Multicenter experience in hematopoietic stem cell transplantation for serious complications of common variable immunodeficiency. J Allergy Clin Immunol. 2015;135(4):988-997.
34. Shearer WT, Fleisher TA, Buckley RH, et al; Medical Advisory Committee of the Immune Deficiency Foundation. Recommendations for live viral and bacterial vaccines in immunodeficient patients and their close contacts. J Allergy Clin Immunol. 2014;133(4):961-966.
HHS proposal may limit birth control access
The Trump administration has drafted a plan that would allow more employers to opt out of offering no-cost contraception coverage to women based on religious or moral grounds, according to a leaked copy of the interim rule.
The proposed rule, first obtained by the media outlet Vox, would greatly expand the religious exemption under the Affordable Care Act for employers otherwise subject to the ACA’s contraception mandate. If approved, the rule would allow additional entities and employers that object to the mandate for religious or moral reasons to be exempt from providing coverage. The exception would apply to plans sponsored by objecting employers, whether or not they operate as a nonprofit, according to the leaked rule.
The American Congress of Obstetricians and Gynecologists denounced the rule, saying the proposal would wipe away women’s access to care and put women in all insurance plans at risk of losing coverage they have today.
“Contraception is an integral part of preventive care and a medical necessity for women during approximately 30 years of their lives. Access to contraception allows women to achieve, lead, and reach their full potentials, becoming key drivers of our Nation’s economic success,” Haywood L. Brown, MD, ACOG president, said in a statement. “Since the Affordable Care Act increased access to contraceptives, our nation has achieved a 30-year low in its unintended pregnancy rate, including among teens. Any move to decrease access to these vital services would have damaging effects on public health. Women, families, and our nation all benefit from seamless, affordable access to contraception.”
The White House has declined to comment about the leaked proposal. However, in early May, HHS Secretary Tom Price, MD, said he welcomed the chance to reexamine the ACA’s contraception mandate.
Since the ACA’s contraceptive mandate took effect, it has been the subject of multiple court challenges across the country. The mandate requires nearly all employers to provide coverage of birth control to employees, except for group health plans of “religious employers,” which are deemed exempt. Those religious employers are for the most part churches and other houses of worship.
The Obama administration later created a workaround for another group – nonprofit religious employers – to opt out of the mandate, but critics argued the process itself was a violation of their religious freedom. The issue led to the case of Zubik v. Burwell, a legal challenge over the mandate exemption that went before the U.S. Supreme Court in March 2016.
But the issue remained unresolved. In May 2016, the Supreme Court vacated the lower court rulings related to Zubik v. Burwell and remanded the case back to the four appeals courts that had originally ruled on the issue.
[email protected]
On Twitter @legal_med
The Trump administration has drafted a plan that would allow more employers to opt out of offering no-cost contraception coverage to women based on religious or moral grounds, according to a leaked copy of the interim rule.
The proposed rule, first obtained by the media outlet Vox, would greatly expand the religious exemption under the Affordable Care Act for employers otherwise subject to the ACA’s contraception mandate. If approved, the rule would allow additional entities and employers that object to the mandate for religious or moral reasons to be exempt from providing coverage. The exception would apply to plans sponsored by objecting employers, whether or not they operate as a nonprofit, according to the leaked rule.
The American Congress of Obstetricians and Gynecologists denounced the rule, saying the proposal would wipe away women’s access to care and put women in all insurance plans at risk of losing coverage they have today.
“Contraception is an integral part of preventive care and a medical necessity for women during approximately 30 years of their lives. Access to contraception allows women to achieve, lead, and reach their full potentials, becoming key drivers of our Nation’s economic success,” Haywood L. Brown, MD, ACOG president, said in a statement. “Since the Affordable Care Act increased access to contraceptives, our nation has achieved a 30-year low in its unintended pregnancy rate, including among teens. Any move to decrease access to these vital services would have damaging effects on public health. Women, families, and our nation all benefit from seamless, affordable access to contraception.”
The White House has declined to comment about the leaked proposal. However, in early May, HHS Secretary Tom Price, MD, said he welcomed the chance to reexamine the ACA’s contraception mandate.
Since the ACA’s contraceptive mandate took effect, it has been the subject of multiple court challenges across the country. The mandate requires nearly all employers to provide coverage of birth control to employees, except for group health plans of “religious employers,” which are deemed exempt. Those religious employers are for the most part churches and other houses of worship.
The Obama administration later created a workaround for another group – nonprofit religious employers – to opt out of the mandate, but critics argued the process itself was a violation of their religious freedom. The issue led to the case of Zubik v. Burwell, a legal challenge over the mandate exemption that went before the U.S. Supreme Court in March 2016.
But the issue remained unresolved. In May 2016, the Supreme Court vacated the lower court rulings related to Zubik v. Burwell and remanded the case back to the four appeals courts that had originally ruled on the issue.
[email protected]
On Twitter @legal_med
The Trump administration has drafted a plan that would allow more employers to opt out of offering no-cost contraception coverage to women based on religious or moral grounds, according to a leaked copy of the interim rule.
The proposed rule, first obtained by the media outlet Vox, would greatly expand the religious exemption under the Affordable Care Act for employers otherwise subject to the ACA’s contraception mandate. If approved, the rule would allow additional entities and employers that object to the mandate for religious or moral reasons to be exempt from providing coverage. The exception would apply to plans sponsored by objecting employers, whether or not they operate as a nonprofit, according to the leaked rule.
The American Congress of Obstetricians and Gynecologists denounced the rule, saying the proposal would wipe away women’s access to care and put women in all insurance plans at risk of losing coverage they have today.
“Contraception is an integral part of preventive care and a medical necessity for women during approximately 30 years of their lives. Access to contraception allows women to achieve, lead, and reach their full potentials, becoming key drivers of our Nation’s economic success,” Haywood L. Brown, MD, ACOG president, said in a statement. “Since the Affordable Care Act increased access to contraceptives, our nation has achieved a 30-year low in its unintended pregnancy rate, including among teens. Any move to decrease access to these vital services would have damaging effects on public health. Women, families, and our nation all benefit from seamless, affordable access to contraception.”
The White House has declined to comment about the leaked proposal. However, in early May, HHS Secretary Tom Price, MD, said he welcomed the chance to reexamine the ACA’s contraception mandate.
Since the ACA’s contraceptive mandate took effect, it has been the subject of multiple court challenges across the country. The mandate requires nearly all employers to provide coverage of birth control to employees, except for group health plans of “religious employers,” which are deemed exempt. Those religious employers are for the most part churches and other houses of worship.
The Obama administration later created a workaround for another group – nonprofit religious employers – to opt out of the mandate, but critics argued the process itself was a violation of their religious freedom. The issue led to the case of Zubik v. Burwell, a legal challenge over the mandate exemption that went before the U.S. Supreme Court in March 2016.
But the issue remained unresolved. In May 2016, the Supreme Court vacated the lower court rulings related to Zubik v. Burwell and remanded the case back to the four appeals courts that had originally ruled on the issue.
[email protected]
On Twitter @legal_med
Biomarker panel promising for early endometriosis diagnosis
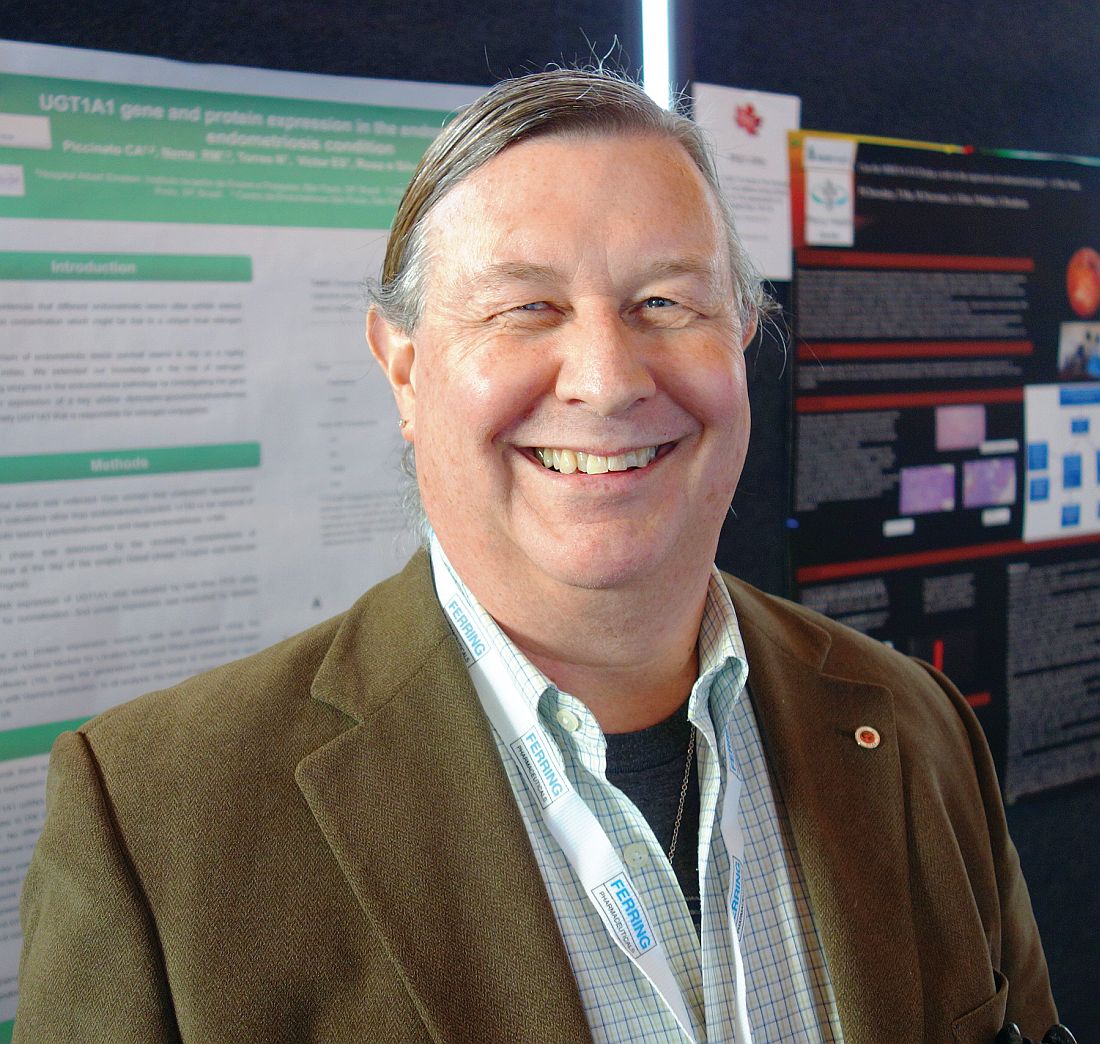
VANCOUVER – Investigators at McMaster University in Hamilton, Ontario, are zeroing in on a biomarker blood test panel to diagnose endometriosis without surgery.
At the World Congress on Endometriosis, they described a decision tree incorporating blood levels of brain-derived neurotrophic factor (BDNF), glycodelin, and zinc-alpha2-glycoprotein (ZAG), quantified by enzyme-linked immunosorbent assay. ZAG levels above 91.58 ng/mL – the first cut in the decision tree, glycodelin above 39.19 ng/mL – the second cut, and BDNF above 953.9 pg/mL identified endometriosis with a sensitivity of 89.2% and a specificity of 70.0%. The combination outperformed any biomarker on its own.
BDNF is a protein involved in neurogenesis, angiogenesis, and apoptosis resistance, all hallmark pathogenic features of endometriosis. Glycodelin and ZAG are associated with secretory endometrium.
The findings come from a comparison of blood levels in 65 women undergoing endometriosis surgery with the blood levels in 14 women undergoing surgery for benign gynecological problems, and in 16 healthy controls with no history of pelvic pain.
The need is great for a noninvasive test to diagnose endometriosis. Currently, diagnosis is made during surgery and can be delayed for several years. Like investigators at other institutions, the research team at McMaster is hoping to develop an easy, accurate way to catch and treat the disease early before complications set in.
Early diagnosis has “resisted our best efforts for years, but we are slowly moving closer to the end zone,” said senior investigator Warren Foster, PhD, a professor of obstetrics and gynecology at McMaster.
Other teams have reported favorable results for microRNAs, circulating endometrial stem cells, biomarker combinations, and other approaches. “It seems to me that there is a lot of progress being made. One of the big issues that we still have to solve is reproducibility, but there’s so much coming forward,” Dr. Foster said. “It’s an exciting time to be looking for novel diagnostic markers for endometriosis.”
The McMaster team next plans to test its panel prospectively in women with suspected early stage disease.
The work was funded by the Canadian Institutes of Health Research. Dr. Foster is in talks with industry to license the algorithm.
VANCOUVER – Investigators at McMaster University in Hamilton, Ontario, are zeroing in on a biomarker blood test panel to diagnose endometriosis without surgery.
At the World Congress on Endometriosis, they described a decision tree incorporating blood levels of brain-derived neurotrophic factor (BDNF), glycodelin, and zinc-alpha2-glycoprotein (ZAG), quantified by enzyme-linked immunosorbent assay. ZAG levels above 91.58 ng/mL – the first cut in the decision tree, glycodelin above 39.19 ng/mL – the second cut, and BDNF above 953.9 pg/mL identified endometriosis with a sensitivity of 89.2% and a specificity of 70.0%. The combination outperformed any biomarker on its own.
BDNF is a protein involved in neurogenesis, angiogenesis, and apoptosis resistance, all hallmark pathogenic features of endometriosis. Glycodelin and ZAG are associated with secretory endometrium.
The findings come from a comparison of blood levels in 65 women undergoing endometriosis surgery with the blood levels in 14 women undergoing surgery for benign gynecological problems, and in 16 healthy controls with no history of pelvic pain.
The need is great for a noninvasive test to diagnose endometriosis. Currently, diagnosis is made during surgery and can be delayed for several years. Like investigators at other institutions, the research team at McMaster is hoping to develop an easy, accurate way to catch and treat the disease early before complications set in.
Early diagnosis has “resisted our best efforts for years, but we are slowly moving closer to the end zone,” said senior investigator Warren Foster, PhD, a professor of obstetrics and gynecology at McMaster.
Other teams have reported favorable results for microRNAs, circulating endometrial stem cells, biomarker combinations, and other approaches. “It seems to me that there is a lot of progress being made. One of the big issues that we still have to solve is reproducibility, but there’s so much coming forward,” Dr. Foster said. “It’s an exciting time to be looking for novel diagnostic markers for endometriosis.”
The McMaster team next plans to test its panel prospectively in women with suspected early stage disease.
The work was funded by the Canadian Institutes of Health Research. Dr. Foster is in talks with industry to license the algorithm.
VANCOUVER – Investigators at McMaster University in Hamilton, Ontario, are zeroing in on a biomarker blood test panel to diagnose endometriosis without surgery.
At the World Congress on Endometriosis, they described a decision tree incorporating blood levels of brain-derived neurotrophic factor (BDNF), glycodelin, and zinc-alpha2-glycoprotein (ZAG), quantified by enzyme-linked immunosorbent assay. ZAG levels above 91.58 ng/mL – the first cut in the decision tree, glycodelin above 39.19 ng/mL – the second cut, and BDNF above 953.9 pg/mL identified endometriosis with a sensitivity of 89.2% and a specificity of 70.0%. The combination outperformed any biomarker on its own.
BDNF is a protein involved in neurogenesis, angiogenesis, and apoptosis resistance, all hallmark pathogenic features of endometriosis. Glycodelin and ZAG are associated with secretory endometrium.
The findings come from a comparison of blood levels in 65 women undergoing endometriosis surgery with the blood levels in 14 women undergoing surgery for benign gynecological problems, and in 16 healthy controls with no history of pelvic pain.
The need is great for a noninvasive test to diagnose endometriosis. Currently, diagnosis is made during surgery and can be delayed for several years. Like investigators at other institutions, the research team at McMaster is hoping to develop an easy, accurate way to catch and treat the disease early before complications set in.
Early diagnosis has “resisted our best efforts for years, but we are slowly moving closer to the end zone,” said senior investigator Warren Foster, PhD, a professor of obstetrics and gynecology at McMaster.
Other teams have reported favorable results for microRNAs, circulating endometrial stem cells, biomarker combinations, and other approaches. “It seems to me that there is a lot of progress being made. One of the big issues that we still have to solve is reproducibility, but there’s so much coming forward,” Dr. Foster said. “It’s an exciting time to be looking for novel diagnostic markers for endometriosis.”
The McMaster team next plans to test its panel prospectively in women with suspected early stage disease.
The work was funded by the Canadian Institutes of Health Research. Dr. Foster is in talks with industry to license the algorithm.
AT WCE 2017
Key clinical point:
Major finding: Zinc-alpha2-glycoprotein levels above 91.58 ng/mL, glycodelin above 39.19 ng/mL, and brain-derived neurotrophic factor above 953.30 pg/mL identified endometriosis with a sensitivity of 89.2% and a specificity of 70.0%.
Data source: A case-control review of 95 women.
Disclosures: The work was funded by the Canadian Institutes of Health Research. The investigators are in talks with industry to license the algorithm.
Medical treatments for uterine fibroids show promise in efficacy and safety studies
Up to 80% of women who are of reproductive age have uterine fibroids that cause heavy and prolonged bleeding.1 Additional concerns include infertility and pain, says James Simon, MD, Clinical Professor at George Washington University in Washington, DC. Black women are more likely than white women to undergo hysterectomy for uterine fibroids. They also are more likely to experience severe or very severe symptoms from fibroids and report that these symptoms interfere with physical activities, relationships, and work.2
Current medical treatments include on- and off-label use of oral contraceptives, gonadotropin-releasing hormone (GnRH) receptor agonists, and progestins. Data on investigational oral GnRH antagonists and oral selective progesterone-receptor modulators (SPRMs) were presented at the 2017 Annual Clinical and Scientific Meeting of the American College of Obstetricians and Gynecologists.
Details of VENUS I
In the phase 3, randomized, controlled VENUS I trial, investigators assessed the efficacy and safety of ulipristal acetate (UPA), an SPRM, by race and body mass index (BMI) in premenopausal women (aged 18 to 50) with symptomatic uterine fibroids.1
Simon and colleagues randomly assigned participants to UPA 5 mg, UPA 10 mg, or placebo once daily for 12 weeks, followed by a 12-week treatment-free follow-up period. UPA, at 5 and 10 mg, was significantly more efficacious than placebo in rate of and time to amenorrhea (P<.0001). The superiority was observed regardless of race and BMI. In addition, women taking UPA versus placebo reported significantly less impact on activities due to uterine fibroids. The study authors concluded that “UPA treatment provides effective control of bleeding and improvement in physical and social activities for women with symptomatic uterine fibroids, regardless of race and BMI.”1
Establishing the ideal treatment period for UPA to avoid progesterone-associated endometrial changes (in this study it was 12 weeks of once-daily therapy) is a current goal, said Simon.
Details of elagolix phase 2b study
Simon also presented data on another investigational drug, elagolix, an orally administered GnRH antagonist, which has an inhibiting effect on luteinizing hormone and follicle-stimulating hormone secretion. This in turn reduces production of estradiol and progesterone. Elagolix also is being studied for the treatment of endometriosis.3
In the uterine fibroids study, a 24-week, multicenter, double-blind, randomized controlled, parallel group trial, 567 premenopausal women aged 18 to 51 with heavy menstrual bleeding of >80 mL of blood loss were assigned to placebo or elagolix 300 mg twice per day or 600 mg once per day alone or in combination with add-back therapy (with estradiol/norethindrone acetate) to prevent bone loss and menopausal symptoms.4
Compared with placebo, women treated with elagolix with or without add-back therapy had significant reductions from baseline in mean menstrual blood loss. Women treated with elagolix also had significant increases in hemoglobin concentration from baseline to month 6 compared with placebo.4
Adverse effects were similar to menopause symptoms: bone loss, hot flashes, night sweats, headaches, and disturbed sleep, said Simon. With the add-back treatments, adverse effects were mitigated in a dose-dependent fashion, he pointed out, and were most likely tolerable compared with the heavy bleeding experienced by women at the start of the study.
- Simon JA, Catherino W, Blakesley RE, Chan A, Sriukiene V, Al-Hendy A. Ulipristal acetate treatment of uterine fibroids in black and obese women. VENUS I subgroup analyses. Paper presented at: 2017 Annual Clinical and Scientific Meeting of The American College of Obstetricians and Gynecologists; May 6, 2017; San Diego, CA.
- Stewart EA, Nicholson WK, Bradley L, Borah BJ. The burden of uterine fibroids for African-American women: results of a national survey. J Womens Health (Larchmnt). 2013;22(10):807–816.
- Taylor HS, Guidice LC, Lessey BA, et al. Treatment of endometriosis-associated pain with elagolix, an oral GnRH antagonist. NEJM. doi:10.1056/NEJMoa1700089.
- Stewart EA, Owens C, Duan WR, Gao J, Chwalisz K, Simon JA. Elagolix alone and with add-back decreases heavy menstrual bleeding in women with uterine fibroids. Paper presented at: 2017 Annual Clinical and Scientific Meeting of The American College of Obstetricians and Gynecologists; May 6, 2017; San Diego, CA.
Up to 80% of women who are of reproductive age have uterine fibroids that cause heavy and prolonged bleeding.1 Additional concerns include infertility and pain, says James Simon, MD, Clinical Professor at George Washington University in Washington, DC. Black women are more likely than white women to undergo hysterectomy for uterine fibroids. They also are more likely to experience severe or very severe symptoms from fibroids and report that these symptoms interfere with physical activities, relationships, and work.2
Current medical treatments include on- and off-label use of oral contraceptives, gonadotropin-releasing hormone (GnRH) receptor agonists, and progestins. Data on investigational oral GnRH antagonists and oral selective progesterone-receptor modulators (SPRMs) were presented at the 2017 Annual Clinical and Scientific Meeting of the American College of Obstetricians and Gynecologists.
Details of VENUS I
In the phase 3, randomized, controlled VENUS I trial, investigators assessed the efficacy and safety of ulipristal acetate (UPA), an SPRM, by race and body mass index (BMI) in premenopausal women (aged 18 to 50) with symptomatic uterine fibroids.1
Simon and colleagues randomly assigned participants to UPA 5 mg, UPA 10 mg, or placebo once daily for 12 weeks, followed by a 12-week treatment-free follow-up period. UPA, at 5 and 10 mg, was significantly more efficacious than placebo in rate of and time to amenorrhea (P<.0001). The superiority was observed regardless of race and BMI. In addition, women taking UPA versus placebo reported significantly less impact on activities due to uterine fibroids. The study authors concluded that “UPA treatment provides effective control of bleeding and improvement in physical and social activities for women with symptomatic uterine fibroids, regardless of race and BMI.”1
Establishing the ideal treatment period for UPA to avoid progesterone-associated endometrial changes (in this study it was 12 weeks of once-daily therapy) is a current goal, said Simon.
Details of elagolix phase 2b study
Simon also presented data on another investigational drug, elagolix, an orally administered GnRH antagonist, which has an inhibiting effect on luteinizing hormone and follicle-stimulating hormone secretion. This in turn reduces production of estradiol and progesterone. Elagolix also is being studied for the treatment of endometriosis.3
In the uterine fibroids study, a 24-week, multicenter, double-blind, randomized controlled, parallel group trial, 567 premenopausal women aged 18 to 51 with heavy menstrual bleeding of >80 mL of blood loss were assigned to placebo or elagolix 300 mg twice per day or 600 mg once per day alone or in combination with add-back therapy (with estradiol/norethindrone acetate) to prevent bone loss and menopausal symptoms.4
Compared with placebo, women treated with elagolix with or without add-back therapy had significant reductions from baseline in mean menstrual blood loss. Women treated with elagolix also had significant increases in hemoglobin concentration from baseline to month 6 compared with placebo.4
Adverse effects were similar to menopause symptoms: bone loss, hot flashes, night sweats, headaches, and disturbed sleep, said Simon. With the add-back treatments, adverse effects were mitigated in a dose-dependent fashion, he pointed out, and were most likely tolerable compared with the heavy bleeding experienced by women at the start of the study.
Up to 80% of women who are of reproductive age have uterine fibroids that cause heavy and prolonged bleeding.1 Additional concerns include infertility and pain, says James Simon, MD, Clinical Professor at George Washington University in Washington, DC. Black women are more likely than white women to undergo hysterectomy for uterine fibroids. They also are more likely to experience severe or very severe symptoms from fibroids and report that these symptoms interfere with physical activities, relationships, and work.2
Current medical treatments include on- and off-label use of oral contraceptives, gonadotropin-releasing hormone (GnRH) receptor agonists, and progestins. Data on investigational oral GnRH antagonists and oral selective progesterone-receptor modulators (SPRMs) were presented at the 2017 Annual Clinical and Scientific Meeting of the American College of Obstetricians and Gynecologists.
Details of VENUS I
In the phase 3, randomized, controlled VENUS I trial, investigators assessed the efficacy and safety of ulipristal acetate (UPA), an SPRM, by race and body mass index (BMI) in premenopausal women (aged 18 to 50) with symptomatic uterine fibroids.1
Simon and colleagues randomly assigned participants to UPA 5 mg, UPA 10 mg, or placebo once daily for 12 weeks, followed by a 12-week treatment-free follow-up period. UPA, at 5 and 10 mg, was significantly more efficacious than placebo in rate of and time to amenorrhea (P<.0001). The superiority was observed regardless of race and BMI. In addition, women taking UPA versus placebo reported significantly less impact on activities due to uterine fibroids. The study authors concluded that “UPA treatment provides effective control of bleeding and improvement in physical and social activities for women with symptomatic uterine fibroids, regardless of race and BMI.”1
Establishing the ideal treatment period for UPA to avoid progesterone-associated endometrial changes (in this study it was 12 weeks of once-daily therapy) is a current goal, said Simon.
Details of elagolix phase 2b study
Simon also presented data on another investigational drug, elagolix, an orally administered GnRH antagonist, which has an inhibiting effect on luteinizing hormone and follicle-stimulating hormone secretion. This in turn reduces production of estradiol and progesterone. Elagolix also is being studied for the treatment of endometriosis.3
In the uterine fibroids study, a 24-week, multicenter, double-blind, randomized controlled, parallel group trial, 567 premenopausal women aged 18 to 51 with heavy menstrual bleeding of >80 mL of blood loss were assigned to placebo or elagolix 300 mg twice per day or 600 mg once per day alone or in combination with add-back therapy (with estradiol/norethindrone acetate) to prevent bone loss and menopausal symptoms.4
Compared with placebo, women treated with elagolix with or without add-back therapy had significant reductions from baseline in mean menstrual blood loss. Women treated with elagolix also had significant increases in hemoglobin concentration from baseline to month 6 compared with placebo.4
Adverse effects were similar to menopause symptoms: bone loss, hot flashes, night sweats, headaches, and disturbed sleep, said Simon. With the add-back treatments, adverse effects were mitigated in a dose-dependent fashion, he pointed out, and were most likely tolerable compared with the heavy bleeding experienced by women at the start of the study.
- Simon JA, Catherino W, Blakesley RE, Chan A, Sriukiene V, Al-Hendy A. Ulipristal acetate treatment of uterine fibroids in black and obese women. VENUS I subgroup analyses. Paper presented at: 2017 Annual Clinical and Scientific Meeting of The American College of Obstetricians and Gynecologists; May 6, 2017; San Diego, CA.
- Stewart EA, Nicholson WK, Bradley L, Borah BJ. The burden of uterine fibroids for African-American women: results of a national survey. J Womens Health (Larchmnt). 2013;22(10):807–816.
- Taylor HS, Guidice LC, Lessey BA, et al. Treatment of endometriosis-associated pain with elagolix, an oral GnRH antagonist. NEJM. doi:10.1056/NEJMoa1700089.
- Stewart EA, Owens C, Duan WR, Gao J, Chwalisz K, Simon JA. Elagolix alone and with add-back decreases heavy menstrual bleeding in women with uterine fibroids. Paper presented at: 2017 Annual Clinical and Scientific Meeting of The American College of Obstetricians and Gynecologists; May 6, 2017; San Diego, CA.
- Simon JA, Catherino W, Blakesley RE, Chan A, Sriukiene V, Al-Hendy A. Ulipristal acetate treatment of uterine fibroids in black and obese women. VENUS I subgroup analyses. Paper presented at: 2017 Annual Clinical and Scientific Meeting of The American College of Obstetricians and Gynecologists; May 6, 2017; San Diego, CA.
- Stewart EA, Nicholson WK, Bradley L, Borah BJ. The burden of uterine fibroids for African-American women: results of a national survey. J Womens Health (Larchmnt). 2013;22(10):807–816.
- Taylor HS, Guidice LC, Lessey BA, et al. Treatment of endometriosis-associated pain with elagolix, an oral GnRH antagonist. NEJM. doi:10.1056/NEJMoa1700089.
- Stewart EA, Owens C, Duan WR, Gao J, Chwalisz K, Simon JA. Elagolix alone and with add-back decreases heavy menstrual bleeding in women with uterine fibroids. Paper presented at: 2017 Annual Clinical and Scientific Meeting of The American College of Obstetricians and Gynecologists; May 6, 2017; San Diego, CA.
Minimally invasive cosmetic procedures more popular than ever
The total number of minimally invasive cosmetic procedures topped 15 million for the first time in 2016, with onabotulinumtoxinA injections leading the way, according to the American Society of Plastic Surgeons.
An estimated 15.4 million minimally invasive cosmetic procedures were performed last year, with onabotulinumtoxinA making up over 45% – approximately 7.1 million anatomic sites injected – of that total, ASPS data show.
Next in popularity was injection of soft tissue fillers, with just over 2.6 million procedures – almost 17% of the procedures performed in 2016 – followed by chemical peels with almost 1.4 million procedures, laser hair removal with 1.1 million procedures, and microdermabrasion at 775,000, the ASPS reported.
The total number of minimally invasive procedures was up 3% from the 14.96 million performed in 2015, while onabotulinumtoxinA was up 4%, soft tissue fillers were up 2%, chemical peels were up 4%, laser hair removal was down 1%, and microdermabrasion was down 3%. Larger changes were seen among some less common procedures: injection lipolysis was up 18% (55,660 procedures in 2016), fat injection was up 13% (79,208 procedures in 2016), and acellular dermal matrix procedures were down 18% (7,809 in 2016), according to the ASPS Tracking Operations and Outcomes for Plastic Surgeons database and an annual survey of board-certified dermatologists, otolaryngologists, and plastic surgeons (final sample = 703).
The total number of minimally invasive cosmetic procedures topped 15 million for the first time in 2016, with onabotulinumtoxinA injections leading the way, according to the American Society of Plastic Surgeons.
An estimated 15.4 million minimally invasive cosmetic procedures were performed last year, with onabotulinumtoxinA making up over 45% – approximately 7.1 million anatomic sites injected – of that total, ASPS data show.
Next in popularity was injection of soft tissue fillers, with just over 2.6 million procedures – almost 17% of the procedures performed in 2016 – followed by chemical peels with almost 1.4 million procedures, laser hair removal with 1.1 million procedures, and microdermabrasion at 775,000, the ASPS reported.
The total number of minimally invasive procedures was up 3% from the 14.96 million performed in 2015, while onabotulinumtoxinA was up 4%, soft tissue fillers were up 2%, chemical peels were up 4%, laser hair removal was down 1%, and microdermabrasion was down 3%. Larger changes were seen among some less common procedures: injection lipolysis was up 18% (55,660 procedures in 2016), fat injection was up 13% (79,208 procedures in 2016), and acellular dermal matrix procedures were down 18% (7,809 in 2016), according to the ASPS Tracking Operations and Outcomes for Plastic Surgeons database and an annual survey of board-certified dermatologists, otolaryngologists, and plastic surgeons (final sample = 703).
The total number of minimally invasive cosmetic procedures topped 15 million for the first time in 2016, with onabotulinumtoxinA injections leading the way, according to the American Society of Plastic Surgeons.
An estimated 15.4 million minimally invasive cosmetic procedures were performed last year, with onabotulinumtoxinA making up over 45% – approximately 7.1 million anatomic sites injected – of that total, ASPS data show.
Next in popularity was injection of soft tissue fillers, with just over 2.6 million procedures – almost 17% of the procedures performed in 2016 – followed by chemical peels with almost 1.4 million procedures, laser hair removal with 1.1 million procedures, and microdermabrasion at 775,000, the ASPS reported.
The total number of minimally invasive procedures was up 3% from the 14.96 million performed in 2015, while onabotulinumtoxinA was up 4%, soft tissue fillers were up 2%, chemical peels were up 4%, laser hair removal was down 1%, and microdermabrasion was down 3%. Larger changes were seen among some less common procedures: injection lipolysis was up 18% (55,660 procedures in 2016), fat injection was up 13% (79,208 procedures in 2016), and acellular dermal matrix procedures were down 18% (7,809 in 2016), according to the ASPS Tracking Operations and Outcomes for Plastic Surgeons database and an annual survey of board-certified dermatologists, otolaryngologists, and plastic surgeons (final sample = 703).
State e-cigarette laws linked to reduced youth use
Several state regulations governing the sales or use of e-cigarettes and related products were associated with lower proportions of youth trying or regularly using vaping products, a new study found.
Restricting sales of electronic vapor products to minors, however, was not linked to a lower risk of vaping among teens.
Dr. Keim and her associates investigated possible associations between various state laws related to vaping products, all passed before 2015, and youth use of the products. They relied on 2015 data from 35 state-specific surveys of youth regarding use of vaping products and from the Youth Risk Behavior Survey from the Centers for Disease Control and Prevention, a nationally representative, biannual survey of students in grades 9-12. The Tobacco Control Laws Database of the American Nonsmokers’ Rights Foundation provided information on state laws related to electronic vapor products.
Among the 200,513 teens whose responses were included in the study, 44% had ever used any kind of electronic vapor product. Rates were similar between girls and boys for ever having tried one or currently using one, Dr. Keim reported at the Pediatric Academic Societies annual meeting.
The researchers looked at associations with each of the following types of laws:
• Statewide prohibition of vaping products on school property or in workplaces, which includes Arizona, New Hampshire, Vermont, and Virginia for schools and North Dakota for workplaces.
• Prohibition of sales to minors under age 18 years, present in 24 states.
• Prohibition or restriction of sales of e-cigarette products from vending machines, present in 17 states.
• Prohibition or restriction of self-service displays of vaping products, present in 11 states.
• Prohibition or restriction of sampling of electronic vapor products, present in Arizona, Delaware, Kentucky, Maryland, New Hampshire, North Carolina, Oklahoma, and South Carolina.
For most of the regulations, teens had a reduced likelihood of trying or currently using vaping products after adjusting for age, ethnicity, grade level, race, region, and sex. Risk of ever trying a vaping product was 12% lower in states that prohibited their use on school grounds or in workplaces, 6% lower in states that barred sales to those under age 18, and 7% lower in states that restricted or prohibited self-service vaping displays.
The risk of youth currently using electronic vapor products was 5% lower in states with the school grounds and workplace restrictions, and 13% lower in states that restricted self-service displays. Laws restricting minor sales were unrelated to the risk of current vaping among youth. Restricting vending machine sales of vaping products had no association with the risk of a teen ever trying vaping, but it was linked to a 7% lower risk of current use of the products among teens. All these associations were statistically significant based on confidence interval values.
Interestingly, a statistically significant risk increase in vaping use occurred for teens in states that restricted or outlawed sampling of vaping products. The risk was 8% higher for ever trying a product and 20% higher for current use. But those findings also could indicate the possibility of reverse causation.
“It’s possible that states that were particularly concerned about sampling had the worst problems – were the ones more likely to institute a ban on that practice, and that would generate the counterintuitive finding,” Dr. Keim said in an interview. “With the data currently available, we can’t look at teen use both before and after the restrictions, just afterwards, but with more data for 2017, it would provide a clearer picture of all of the associations we examined.”
Aside from these laws, other interventions have the potential to reduce vaping among teens as well.
“Restrictions on use in various types of public places and on school grounds may be additional helpful approaches, similar to what has been done with cigarettes,” Dr. Keim said. Although their analysis included laws that prohibited use on school grounds, only four states have one of these laws.
Several state regulations governing the sales or use of e-cigarettes and related products were associated with lower proportions of youth trying or regularly using vaping products, a new study found.
Restricting sales of electronic vapor products to minors, however, was not linked to a lower risk of vaping among teens.
Dr. Keim and her associates investigated possible associations between various state laws related to vaping products, all passed before 2015, and youth use of the products. They relied on 2015 data from 35 state-specific surveys of youth regarding use of vaping products and from the Youth Risk Behavior Survey from the Centers for Disease Control and Prevention, a nationally representative, biannual survey of students in grades 9-12. The Tobacco Control Laws Database of the American Nonsmokers’ Rights Foundation provided information on state laws related to electronic vapor products.
Among the 200,513 teens whose responses were included in the study, 44% had ever used any kind of electronic vapor product. Rates were similar between girls and boys for ever having tried one or currently using one, Dr. Keim reported at the Pediatric Academic Societies annual meeting.
The researchers looked at associations with each of the following types of laws:
• Statewide prohibition of vaping products on school property or in workplaces, which includes Arizona, New Hampshire, Vermont, and Virginia for schools and North Dakota for workplaces.
• Prohibition of sales to minors under age 18 years, present in 24 states.
• Prohibition or restriction of sales of e-cigarette products from vending machines, present in 17 states.
• Prohibition or restriction of self-service displays of vaping products, present in 11 states.
• Prohibition or restriction of sampling of electronic vapor products, present in Arizona, Delaware, Kentucky, Maryland, New Hampshire, North Carolina, Oklahoma, and South Carolina.
For most of the regulations, teens had a reduced likelihood of trying or currently using vaping products after adjusting for age, ethnicity, grade level, race, region, and sex. Risk of ever trying a vaping product was 12% lower in states that prohibited their use on school grounds or in workplaces, 6% lower in states that barred sales to those under age 18, and 7% lower in states that restricted or prohibited self-service vaping displays.
The risk of youth currently using electronic vapor products was 5% lower in states with the school grounds and workplace restrictions, and 13% lower in states that restricted self-service displays. Laws restricting minor sales were unrelated to the risk of current vaping among youth. Restricting vending machine sales of vaping products had no association with the risk of a teen ever trying vaping, but it was linked to a 7% lower risk of current use of the products among teens. All these associations were statistically significant based on confidence interval values.
Interestingly, a statistically significant risk increase in vaping use occurred for teens in states that restricted or outlawed sampling of vaping products. The risk was 8% higher for ever trying a product and 20% higher for current use. But those findings also could indicate the possibility of reverse causation.
“It’s possible that states that were particularly concerned about sampling had the worst problems – were the ones more likely to institute a ban on that practice, and that would generate the counterintuitive finding,” Dr. Keim said in an interview. “With the data currently available, we can’t look at teen use both before and after the restrictions, just afterwards, but with more data for 2017, it would provide a clearer picture of all of the associations we examined.”
Aside from these laws, other interventions have the potential to reduce vaping among teens as well.
“Restrictions on use in various types of public places and on school grounds may be additional helpful approaches, similar to what has been done with cigarettes,” Dr. Keim said. Although their analysis included laws that prohibited use on school grounds, only four states have one of these laws.
Several state regulations governing the sales or use of e-cigarettes and related products were associated with lower proportions of youth trying or regularly using vaping products, a new study found.
Restricting sales of electronic vapor products to minors, however, was not linked to a lower risk of vaping among teens.
Dr. Keim and her associates investigated possible associations between various state laws related to vaping products, all passed before 2015, and youth use of the products. They relied on 2015 data from 35 state-specific surveys of youth regarding use of vaping products and from the Youth Risk Behavior Survey from the Centers for Disease Control and Prevention, a nationally representative, biannual survey of students in grades 9-12. The Tobacco Control Laws Database of the American Nonsmokers’ Rights Foundation provided information on state laws related to electronic vapor products.
Among the 200,513 teens whose responses were included in the study, 44% had ever used any kind of electronic vapor product. Rates were similar between girls and boys for ever having tried one or currently using one, Dr. Keim reported at the Pediatric Academic Societies annual meeting.
The researchers looked at associations with each of the following types of laws:
• Statewide prohibition of vaping products on school property or in workplaces, which includes Arizona, New Hampshire, Vermont, and Virginia for schools and North Dakota for workplaces.
• Prohibition of sales to minors under age 18 years, present in 24 states.
• Prohibition or restriction of sales of e-cigarette products from vending machines, present in 17 states.
• Prohibition or restriction of self-service displays of vaping products, present in 11 states.
• Prohibition or restriction of sampling of electronic vapor products, present in Arizona, Delaware, Kentucky, Maryland, New Hampshire, North Carolina, Oklahoma, and South Carolina.
For most of the regulations, teens had a reduced likelihood of trying or currently using vaping products after adjusting for age, ethnicity, grade level, race, region, and sex. Risk of ever trying a vaping product was 12% lower in states that prohibited their use on school grounds or in workplaces, 6% lower in states that barred sales to those under age 18, and 7% lower in states that restricted or prohibited self-service vaping displays.
The risk of youth currently using electronic vapor products was 5% lower in states with the school grounds and workplace restrictions, and 13% lower in states that restricted self-service displays. Laws restricting minor sales were unrelated to the risk of current vaping among youth. Restricting vending machine sales of vaping products had no association with the risk of a teen ever trying vaping, but it was linked to a 7% lower risk of current use of the products among teens. All these associations were statistically significant based on confidence interval values.
Interestingly, a statistically significant risk increase in vaping use occurred for teens in states that restricted or outlawed sampling of vaping products. The risk was 8% higher for ever trying a product and 20% higher for current use. But those findings also could indicate the possibility of reverse causation.
“It’s possible that states that were particularly concerned about sampling had the worst problems – were the ones more likely to institute a ban on that practice, and that would generate the counterintuitive finding,” Dr. Keim said in an interview. “With the data currently available, we can’t look at teen use both before and after the restrictions, just afterwards, but with more data for 2017, it would provide a clearer picture of all of the associations we examined.”
Aside from these laws, other interventions have the potential to reduce vaping among teens as well.
“Restrictions on use in various types of public places and on school grounds may be additional helpful approaches, similar to what has been done with cigarettes,” Dr. Keim said. Although their analysis included laws that prohibited use on school grounds, only four states have one of these laws.
FROM PAS 2017
Key clinical point: The two state laws associated with lower risks of teens trying or currently using e-cigarette products were prohibiting their use at school or work and prohibiting or restricting self-service displays.
Major finding: , depending on the law.
Data source: The findings are based on an analysis of 200,513 high school students’ use of electronic vapor products and their states’ laws regarding vaping use, marketing, or sales.
Disclosures: The research did not use any external funding, and Dr. Keim had no relevant financial disclosures.
Limitations with molecular techniques in detecting onychomycosis
Real-time PCR techniques for identifying the pathogens responsible for onychomycosis can offer some advantages over conventional diagnostic approaches but also have their limitations, say the authors of a study published in Mycoses.
Anissa Z. Hafirassou of Frères-Mentouri, Constantine University, Algeria, and colleagues analyzed nail samples from 70 patients with clinical signs of onychomycosis and 15 healthy controls using four different real-time PCR assays – a panfungal, a pandermatophyte, an assay for Candida and one for Aspergillus – and conventional methods.
Most samples were of Trichophyton species and were found in patients with proven onychomycosis. In contrast, the sequencing results from the healthy samples were all negative.
The pandermatophyte analysis found dermatophyte DNA in 60% of cases – most of were proven cases of onychomycosis – representing a sensitivity of 90% compared to positive culture. This analysis showed 90% sensitivity compared to cultures, but there was no correlation between culture results and pandermatophyte RT-PCR in nine cases.
This technique also detected Trichophyton cases in 15 patients who had negative culture results, but found amplification products in three of the control subjects, two of which were Penicillium chrysogenum. However two culture-positive samples showed up as negative with both the panfungal and pandermatophyte methods.
“Due to the low sensitivity of the panfungal assay and the lack of correlation between cultures and PCR results, the possibility of the presence of environmental and colonizing species together with pathological species in nail samples, was studied,” the authors wrote.
Twenty-five fingernail samples that were negative on the panfungal analysis were also tested for Candida and Aspergillus. Candida species were detected in 76% of these samples, and Aspergillus in 60%, while 64% contained mixed populations. Ten samples contained more than one species of Candida and one had two species of Aspergillus.
“Conventional diagnostic methods have several limitations such as time-cost, low sensitivity and the need of skilled personnel,” the authors wrote, noting that the molecular methods also had limitations to their usefulness.
The panfungal method showed low sensitivity, which may have been due to the mix of fungal populations that was found even in healthy controls, the researchers added.
“The pandermatophyte assay was sensitive and specific but only detected dermatophyte species and did not allow differentiation among them,” they wrote.
The role of nondermatophyte species isolated from onychomycosis should be considered carefully, as these are also found in healthy nails, the researchers noted.
The study and one author were supported by the Spanish Fondo de Investigaciones Sanitarias of the Instituto de Salud Carlos III. No conflicts of interest were declared.
Real-time PCR techniques for identifying the pathogens responsible for onychomycosis can offer some advantages over conventional diagnostic approaches but also have their limitations, say the authors of a study published in Mycoses.
Anissa Z. Hafirassou of Frères-Mentouri, Constantine University, Algeria, and colleagues analyzed nail samples from 70 patients with clinical signs of onychomycosis and 15 healthy controls using four different real-time PCR assays – a panfungal, a pandermatophyte, an assay for Candida and one for Aspergillus – and conventional methods.
Most samples were of Trichophyton species and were found in patients with proven onychomycosis. In contrast, the sequencing results from the healthy samples were all negative.
The pandermatophyte analysis found dermatophyte DNA in 60% of cases – most of were proven cases of onychomycosis – representing a sensitivity of 90% compared to positive culture. This analysis showed 90% sensitivity compared to cultures, but there was no correlation between culture results and pandermatophyte RT-PCR in nine cases.
This technique also detected Trichophyton cases in 15 patients who had negative culture results, but found amplification products in three of the control subjects, two of which were Penicillium chrysogenum. However two culture-positive samples showed up as negative with both the panfungal and pandermatophyte methods.
“Due to the low sensitivity of the panfungal assay and the lack of correlation between cultures and PCR results, the possibility of the presence of environmental and colonizing species together with pathological species in nail samples, was studied,” the authors wrote.
Twenty-five fingernail samples that were negative on the panfungal analysis were also tested for Candida and Aspergillus. Candida species were detected in 76% of these samples, and Aspergillus in 60%, while 64% contained mixed populations. Ten samples contained more than one species of Candida and one had two species of Aspergillus.
“Conventional diagnostic methods have several limitations such as time-cost, low sensitivity and the need of skilled personnel,” the authors wrote, noting that the molecular methods also had limitations to their usefulness.
The panfungal method showed low sensitivity, which may have been due to the mix of fungal populations that was found even in healthy controls, the researchers added.
“The pandermatophyte assay was sensitive and specific but only detected dermatophyte species and did not allow differentiation among them,” they wrote.
The role of nondermatophyte species isolated from onychomycosis should be considered carefully, as these are also found in healthy nails, the researchers noted.
The study and one author were supported by the Spanish Fondo de Investigaciones Sanitarias of the Instituto de Salud Carlos III. No conflicts of interest were declared.
Real-time PCR techniques for identifying the pathogens responsible for onychomycosis can offer some advantages over conventional diagnostic approaches but also have their limitations, say the authors of a study published in Mycoses.
Anissa Z. Hafirassou of Frères-Mentouri, Constantine University, Algeria, and colleagues analyzed nail samples from 70 patients with clinical signs of onychomycosis and 15 healthy controls using four different real-time PCR assays – a panfungal, a pandermatophyte, an assay for Candida and one for Aspergillus – and conventional methods.
Most samples were of Trichophyton species and were found in patients with proven onychomycosis. In contrast, the sequencing results from the healthy samples were all negative.
The pandermatophyte analysis found dermatophyte DNA in 60% of cases – most of were proven cases of onychomycosis – representing a sensitivity of 90% compared to positive culture. This analysis showed 90% sensitivity compared to cultures, but there was no correlation between culture results and pandermatophyte RT-PCR in nine cases.
This technique also detected Trichophyton cases in 15 patients who had negative culture results, but found amplification products in three of the control subjects, two of which were Penicillium chrysogenum. However two culture-positive samples showed up as negative with both the panfungal and pandermatophyte methods.
“Due to the low sensitivity of the panfungal assay and the lack of correlation between cultures and PCR results, the possibility of the presence of environmental and colonizing species together with pathological species in nail samples, was studied,” the authors wrote.
Twenty-five fingernail samples that were negative on the panfungal analysis were also tested for Candida and Aspergillus. Candida species were detected in 76% of these samples, and Aspergillus in 60%, while 64% contained mixed populations. Ten samples contained more than one species of Candida and one had two species of Aspergillus.
“Conventional diagnostic methods have several limitations such as time-cost, low sensitivity and the need of skilled personnel,” the authors wrote, noting that the molecular methods also had limitations to their usefulness.
The panfungal method showed low sensitivity, which may have been due to the mix of fungal populations that was found even in healthy controls, the researchers added.
“The pandermatophyte assay was sensitive and specific but only detected dermatophyte species and did not allow differentiation among them,” they wrote.
The role of nondermatophyte species isolated from onychomycosis should be considered carefully, as these are also found in healthy nails, the researchers noted.
The study and one author were supported by the Spanish Fondo de Investigaciones Sanitarias of the Instituto de Salud Carlos III. No conflicts of interest were declared.
FROM MYCOSES
Key clinical point: Real-time PCR techniques for identifying the pathogens in onychomycosis have some advantages over culture but also have their limitations.
Major finding: Panfungal real-time PCR had a sensitivity of 47% and pandermatophyte RT-PCR had a sensitivity of 90% compared to positive culture.
Data source: Analysis of toenail samples from 70 patients with onychomycosis and 15 healthy controls.
Disclosures: The study and one author were supported by the Spanish Fondo de Investigaciones Sanitarias of the Instituto de Salud Carlos III. No conflicts of interest were declared.
Check Out the SVS Expanded Member Benefits Portfolio
The Society for Vascular Surgery has its very own member affinity program, offering members access to best-in-class products and services coupled with special member discounts.
The portfolio includes a number of insurance, financial and private-practice related products that will assist members in their day-to-day lives. The result: a selection of financial and practice solutions to protect and benefit your families, incomes, practices, offices and staff – even your own slice of cyberspace.
For more information, visit vsweb.org/AffinityProgram, call 855-533-1776 or email [email protected].
The Society for Vascular Surgery has its very own member affinity program, offering members access to best-in-class products and services coupled with special member discounts.
The portfolio includes a number of insurance, financial and private-practice related products that will assist members in their day-to-day lives. The result: a selection of financial and practice solutions to protect and benefit your families, incomes, practices, offices and staff – even your own slice of cyberspace.
For more information, visit vsweb.org/AffinityProgram, call 855-533-1776 or email [email protected].
The Society for Vascular Surgery has its very own member affinity program, offering members access to best-in-class products and services coupled with special member discounts.
The portfolio includes a number of insurance, financial and private-practice related products that will assist members in their day-to-day lives. The result: a selection of financial and practice solutions to protect and benefit your families, incomes, practices, offices and staff – even your own slice of cyberspace.
For more information, visit vsweb.org/AffinityProgram, call 855-533-1776 or email [email protected].