User login
Surgeons can take steps to reduce excess opioids
NEW YORK – Surgeons prescribe approximately 10% of the 280 million schedule II prescriptions written every year. Because patients report taking on average 20%-30% of their opioid pills, a large amount of these drugs end up being diverted to nonpatients and contributing to the opioid epidemic in the United States, said Jonah J. Stulberg, MD.
”You can’t turn on the television, pick up the newspaper, do anything on social media without seeing a lot of headlines about the tragedies occurring because of opioid abuse,” said Dr. Stulberg, assistant professor of surgery at Northwestern University in Chicago.
The majority of opioid abusers are obtaining the drugs through diversion, he said. “So the prescriptions we’re writing and the excess pills we have available, they do make a difference. They’re making it down the pipeline.”
Some practical steps
There are practical actions surgeons can take to try to reduce the sheer volume of prescription opioids that end up in the hands of people for whom they are not intended, Dr. Stulberg said at the American College of Surgeons Quality and Safety Conference.
Sign up for a prescription monitoring program, he suggested. These programs are now available in 49 states (Missouri is the exception). “It’s really easy to create an account as a provider.” Just search online for your state’s prescription monitoring program and enter your contact information, he said. The state will then ask you for some basic information.
Take it one step further and integrate your prescription monitoring program into your electronic medical records, Dr. Stulberg said. “We’re starting to integrate it in all hospitals in Illinois. That means when the surgeon or the nurse providers look up the patient, they will know if the patient got two other prescriptions in the last 2 weeks.” He added, “You can ask if they need more pills before adding to the surplus.”
Another practical strategy is to give patients better access to opioid disposal. Find out where the nearest drug return receptacle or kiosk is located – a pharmacy, police station, or elsewhere – and inform your patients. “We put opioid retrieval boxes in our clinic. When patients are educated about this, they bring [excess pills] back.”
Minimizing opioid prescribing in surgery
“This is not a problem of one individual specialty,” Dr. Stulberg said. “We have a problem of culture, a problem of mindset. So we need to approach solving this problem, in my opinion, from that perspective.”
Start with setting patient expectations in the preoperative period. Explain what the surgery entails and the amount of pain they should expect. “Patients have to understand what we’re doing hurts but we can manage that pain. It can make a big difference in their satisfaction … and also in how much medication they end up taking.”
In addition, perform preoperative risk screening for opioid abuse. “There is very good evidence that patients with addictions to other drugs, alcohol, or who have previous drug use, are much more likely to continue using prescription pain medications after a surgical encounter – 6 months to 12 months later.”
In addition, a paradigm shift in thinking is needed. “When we’re talking about pain control in the clinic and minimizing opioids during a surgical episode, we should be focusing on function,” he said. Orthopedic surgery is a prime example, where physicians encourage patients to start mobility exercises the same day of surgery because evidence shows it helps restore function faster.
Surgeons should tell patients that “the goal of how we are treating your pain is getting you to your optimal function.” Then check on function recovery postoperatively, he added. “We don’t follow-up – that is not part of our standard postoperative pathway in any way.”
Consider prescribing fewer pills postoperatively
If surgeons have a prescription feedback mechanism in place, they might know how many opioid pills patients are actually taking. “If I gave 20 pills to the last 10 patients but they only took 8 on average – can I go lower?” Dr. Stulberg said.
Researchers conducted a study to determine opioid needs for 80% of the patients at their institution after certain types of surgery (Ann Surg. 2017;265:709-14).
The study determined the number of pills that 80% of patients found controlled their pain: after partial mastectomy, 5; after partial mastectomy with sentinel lymph node biopsy, 10; after laparoscopic cholecystectomy, 15; after laparoscopic inguinal hernia repair, 15; and after open inguinal hernia repair, 15. These numbers represent about 43% of the actual number prescribed overall, so many patients are getting more medications than they require.
Dr. Stulberg suggested that surgeons could use the data from this study to counter any pushback from others at their institution reluctant to prescribe fewer opioids for their patients.
Dr. Stulberg did not have any relevant disclosures.
NEW YORK – Surgeons prescribe approximately 10% of the 280 million schedule II prescriptions written every year. Because patients report taking on average 20%-30% of their opioid pills, a large amount of these drugs end up being diverted to nonpatients and contributing to the opioid epidemic in the United States, said Jonah J. Stulberg, MD.
”You can’t turn on the television, pick up the newspaper, do anything on social media without seeing a lot of headlines about the tragedies occurring because of opioid abuse,” said Dr. Stulberg, assistant professor of surgery at Northwestern University in Chicago.
The majority of opioid abusers are obtaining the drugs through diversion, he said. “So the prescriptions we’re writing and the excess pills we have available, they do make a difference. They’re making it down the pipeline.”
Some practical steps
There are practical actions surgeons can take to try to reduce the sheer volume of prescription opioids that end up in the hands of people for whom they are not intended, Dr. Stulberg said at the American College of Surgeons Quality and Safety Conference.
Sign up for a prescription monitoring program, he suggested. These programs are now available in 49 states (Missouri is the exception). “It’s really easy to create an account as a provider.” Just search online for your state’s prescription monitoring program and enter your contact information, he said. The state will then ask you for some basic information.
Take it one step further and integrate your prescription monitoring program into your electronic medical records, Dr. Stulberg said. “We’re starting to integrate it in all hospitals in Illinois. That means when the surgeon or the nurse providers look up the patient, they will know if the patient got two other prescriptions in the last 2 weeks.” He added, “You can ask if they need more pills before adding to the surplus.”
Another practical strategy is to give patients better access to opioid disposal. Find out where the nearest drug return receptacle or kiosk is located – a pharmacy, police station, or elsewhere – and inform your patients. “We put opioid retrieval boxes in our clinic. When patients are educated about this, they bring [excess pills] back.”
Minimizing opioid prescribing in surgery
“This is not a problem of one individual specialty,” Dr. Stulberg said. “We have a problem of culture, a problem of mindset. So we need to approach solving this problem, in my opinion, from that perspective.”
Start with setting patient expectations in the preoperative period. Explain what the surgery entails and the amount of pain they should expect. “Patients have to understand what we’re doing hurts but we can manage that pain. It can make a big difference in their satisfaction … and also in how much medication they end up taking.”
In addition, perform preoperative risk screening for opioid abuse. “There is very good evidence that patients with addictions to other drugs, alcohol, or who have previous drug use, are much more likely to continue using prescription pain medications after a surgical encounter – 6 months to 12 months later.”
In addition, a paradigm shift in thinking is needed. “When we’re talking about pain control in the clinic and minimizing opioids during a surgical episode, we should be focusing on function,” he said. Orthopedic surgery is a prime example, where physicians encourage patients to start mobility exercises the same day of surgery because evidence shows it helps restore function faster.
Surgeons should tell patients that “the goal of how we are treating your pain is getting you to your optimal function.” Then check on function recovery postoperatively, he added. “We don’t follow-up – that is not part of our standard postoperative pathway in any way.”
Consider prescribing fewer pills postoperatively
If surgeons have a prescription feedback mechanism in place, they might know how many opioid pills patients are actually taking. “If I gave 20 pills to the last 10 patients but they only took 8 on average – can I go lower?” Dr. Stulberg said.
Researchers conducted a study to determine opioid needs for 80% of the patients at their institution after certain types of surgery (Ann Surg. 2017;265:709-14).
The study determined the number of pills that 80% of patients found controlled their pain: after partial mastectomy, 5; after partial mastectomy with sentinel lymph node biopsy, 10; after laparoscopic cholecystectomy, 15; after laparoscopic inguinal hernia repair, 15; and after open inguinal hernia repair, 15. These numbers represent about 43% of the actual number prescribed overall, so many patients are getting more medications than they require.
Dr. Stulberg suggested that surgeons could use the data from this study to counter any pushback from others at their institution reluctant to prescribe fewer opioids for their patients.
Dr. Stulberg did not have any relevant disclosures.
NEW YORK – Surgeons prescribe approximately 10% of the 280 million schedule II prescriptions written every year. Because patients report taking on average 20%-30% of their opioid pills, a large amount of these drugs end up being diverted to nonpatients and contributing to the opioid epidemic in the United States, said Jonah J. Stulberg, MD.
”You can’t turn on the television, pick up the newspaper, do anything on social media without seeing a lot of headlines about the tragedies occurring because of opioid abuse,” said Dr. Stulberg, assistant professor of surgery at Northwestern University in Chicago.
The majority of opioid abusers are obtaining the drugs through diversion, he said. “So the prescriptions we’re writing and the excess pills we have available, they do make a difference. They’re making it down the pipeline.”
Some practical steps
There are practical actions surgeons can take to try to reduce the sheer volume of prescription opioids that end up in the hands of people for whom they are not intended, Dr. Stulberg said at the American College of Surgeons Quality and Safety Conference.
Sign up for a prescription monitoring program, he suggested. These programs are now available in 49 states (Missouri is the exception). “It’s really easy to create an account as a provider.” Just search online for your state’s prescription monitoring program and enter your contact information, he said. The state will then ask you for some basic information.
Take it one step further and integrate your prescription monitoring program into your electronic medical records, Dr. Stulberg said. “We’re starting to integrate it in all hospitals in Illinois. That means when the surgeon or the nurse providers look up the patient, they will know if the patient got two other prescriptions in the last 2 weeks.” He added, “You can ask if they need more pills before adding to the surplus.”
Another practical strategy is to give patients better access to opioid disposal. Find out where the nearest drug return receptacle or kiosk is located – a pharmacy, police station, or elsewhere – and inform your patients. “We put opioid retrieval boxes in our clinic. When patients are educated about this, they bring [excess pills] back.”
Minimizing opioid prescribing in surgery
“This is not a problem of one individual specialty,” Dr. Stulberg said. “We have a problem of culture, a problem of mindset. So we need to approach solving this problem, in my opinion, from that perspective.”
Start with setting patient expectations in the preoperative period. Explain what the surgery entails and the amount of pain they should expect. “Patients have to understand what we’re doing hurts but we can manage that pain. It can make a big difference in their satisfaction … and also in how much medication they end up taking.”
In addition, perform preoperative risk screening for opioid abuse. “There is very good evidence that patients with addictions to other drugs, alcohol, or who have previous drug use, are much more likely to continue using prescription pain medications after a surgical encounter – 6 months to 12 months later.”
In addition, a paradigm shift in thinking is needed. “When we’re talking about pain control in the clinic and minimizing opioids during a surgical episode, we should be focusing on function,” he said. Orthopedic surgery is a prime example, where physicians encourage patients to start mobility exercises the same day of surgery because evidence shows it helps restore function faster.
Surgeons should tell patients that “the goal of how we are treating your pain is getting you to your optimal function.” Then check on function recovery postoperatively, he added. “We don’t follow-up – that is not part of our standard postoperative pathway in any way.”
Consider prescribing fewer pills postoperatively
If surgeons have a prescription feedback mechanism in place, they might know how many opioid pills patients are actually taking. “If I gave 20 pills to the last 10 patients but they only took 8 on average – can I go lower?” Dr. Stulberg said.
Researchers conducted a study to determine opioid needs for 80% of the patients at their institution after certain types of surgery (Ann Surg. 2017;265:709-14).
The study determined the number of pills that 80% of patients found controlled their pain: after partial mastectomy, 5; after partial mastectomy with sentinel lymph node biopsy, 10; after laparoscopic cholecystectomy, 15; after laparoscopic inguinal hernia repair, 15; and after open inguinal hernia repair, 15. These numbers represent about 43% of the actual number prescribed overall, so many patients are getting more medications than they require.
Dr. Stulberg suggested that surgeons could use the data from this study to counter any pushback from others at their institution reluctant to prescribe fewer opioids for their patients.
Dr. Stulberg did not have any relevant disclosures.
EXPERT ANALYSIS AT THE ACS QUALITY & SAFETY CONFERENCE
Outcomes improved with ERAS pathway tailored to colorectal surgery
NEW YORK – A protocol that standardizes care before, during, and after colorectal surgery cut average hospital stays from almost 6 days to less than 3, reduced complications, and slashed costs an estimated $11,227 per procedure.
“We decided to take a look at our own data, and we saw that a couple of variables were higher than we wanted them to be,” said Deepa Bhat, MD, a second year surgery resident at Advocate Illinois Masonic Medical Center in Chicago. Length of stay was one. Colorectal surgery patients were staying in the hospital an average 5.65 days, for example.
Their surgical site infection rate also warranted attention, Dr. Bhat said during a poster session at the American College of Surgeons Quality and Safety Conference. The overall complication rate was 6.45%.
“So, we decided to implement this enhanced recovery pathway in the hope that it would, one, get patients out of the hospital faster and allow them to recover at home and, two, decrease the rate of complications, including surgical site infections.”
Prior to the protocol, individual surgeons chose when to initiate fluids, when to discharge a patient, and many other preoperative factors. “Now, care is standardized so that every patient experiences the same pre-, intra-, and postoperative protocol, which leads to better outcomes,” Dr. Bhat said.
The multidisciplinary Enhanced Recovery After Colorectal Surgery (ERACS) pathway also now emphasizes more patient education prior to surgery. “The patients go into surgery having a very clear idea of what they can expect, such as how their pain will be controlled, when they can start liquids, and what their expectations are for ambulation,” she said. “By making patients active participants in their own care, they tend to do better.”
The investigators studied 246 elective colorectal surgery patients at their large, urban, community teaching hospital. They compared outcomes in 2014, versus 2015, to gauge the effectiveness of the ERACS. “The change in length of stay was really rather remarkable,” Dr. Bhat said. In fact, the typical number of days in the hospital decreased by about half from 5.65 to 2.89 days, a statistically significant difference (P less than .0001).
Historically, “the whole reason we don’t send patients home sooner is we’re worried they’re going to bounce right back, and that’s an issue for the 30-day readmission rate,” Dr. Bhat said. However, the enhanced recovery protocol was designed to minimize that risk, and the study verified that it works. “We wanted to show that you can send patients home safely and also not worry that they would come back more often.”
Patient satisfaction seems higher too. Dr. Bhat added, “Who doesn’t feel better at home?”
“It is pretty remarkable that you can send somebody home in less than 3 days and they don’t come back to the hospital with complications, versus having them stay double that amount of time,” Dr. Bhat said. The direct variable cost was approximately $3,705 lower with the ERACS, and total hospitalization costs decreased by up to $11,227 per patient. For the institution overall, that outcome translated into savings of approximately $1 million for the year.
Dr. Bhat continues to see increasing gains from the protocol ERACS since the study period ended. “Our enhanced recovery pathway is getting better and better and more efficient.” The institution is now looking to expand enhanced recovery protocols to other types of surgery.
Dr. Deepa Bhat had no relevant financial disclosures.
NEW YORK – A protocol that standardizes care before, during, and after colorectal surgery cut average hospital stays from almost 6 days to less than 3, reduced complications, and slashed costs an estimated $11,227 per procedure.
“We decided to take a look at our own data, and we saw that a couple of variables were higher than we wanted them to be,” said Deepa Bhat, MD, a second year surgery resident at Advocate Illinois Masonic Medical Center in Chicago. Length of stay was one. Colorectal surgery patients were staying in the hospital an average 5.65 days, for example.
Their surgical site infection rate also warranted attention, Dr. Bhat said during a poster session at the American College of Surgeons Quality and Safety Conference. The overall complication rate was 6.45%.
“So, we decided to implement this enhanced recovery pathway in the hope that it would, one, get patients out of the hospital faster and allow them to recover at home and, two, decrease the rate of complications, including surgical site infections.”
Prior to the protocol, individual surgeons chose when to initiate fluids, when to discharge a patient, and many other preoperative factors. “Now, care is standardized so that every patient experiences the same pre-, intra-, and postoperative protocol, which leads to better outcomes,” Dr. Bhat said.
The multidisciplinary Enhanced Recovery After Colorectal Surgery (ERACS) pathway also now emphasizes more patient education prior to surgery. “The patients go into surgery having a very clear idea of what they can expect, such as how their pain will be controlled, when they can start liquids, and what their expectations are for ambulation,” she said. “By making patients active participants in their own care, they tend to do better.”
The investigators studied 246 elective colorectal surgery patients at their large, urban, community teaching hospital. They compared outcomes in 2014, versus 2015, to gauge the effectiveness of the ERACS. “The change in length of stay was really rather remarkable,” Dr. Bhat said. In fact, the typical number of days in the hospital decreased by about half from 5.65 to 2.89 days, a statistically significant difference (P less than .0001).
Historically, “the whole reason we don’t send patients home sooner is we’re worried they’re going to bounce right back, and that’s an issue for the 30-day readmission rate,” Dr. Bhat said. However, the enhanced recovery protocol was designed to minimize that risk, and the study verified that it works. “We wanted to show that you can send patients home safely and also not worry that they would come back more often.”
Patient satisfaction seems higher too. Dr. Bhat added, “Who doesn’t feel better at home?”
“It is pretty remarkable that you can send somebody home in less than 3 days and they don’t come back to the hospital with complications, versus having them stay double that amount of time,” Dr. Bhat said. The direct variable cost was approximately $3,705 lower with the ERACS, and total hospitalization costs decreased by up to $11,227 per patient. For the institution overall, that outcome translated into savings of approximately $1 million for the year.
Dr. Bhat continues to see increasing gains from the protocol ERACS since the study period ended. “Our enhanced recovery pathway is getting better and better and more efficient.” The institution is now looking to expand enhanced recovery protocols to other types of surgery.
Dr. Deepa Bhat had no relevant financial disclosures.
NEW YORK – A protocol that standardizes care before, during, and after colorectal surgery cut average hospital stays from almost 6 days to less than 3, reduced complications, and slashed costs an estimated $11,227 per procedure.
“We decided to take a look at our own data, and we saw that a couple of variables were higher than we wanted them to be,” said Deepa Bhat, MD, a second year surgery resident at Advocate Illinois Masonic Medical Center in Chicago. Length of stay was one. Colorectal surgery patients were staying in the hospital an average 5.65 days, for example.
Their surgical site infection rate also warranted attention, Dr. Bhat said during a poster session at the American College of Surgeons Quality and Safety Conference. The overall complication rate was 6.45%.
“So, we decided to implement this enhanced recovery pathway in the hope that it would, one, get patients out of the hospital faster and allow them to recover at home and, two, decrease the rate of complications, including surgical site infections.”
Prior to the protocol, individual surgeons chose when to initiate fluids, when to discharge a patient, and many other preoperative factors. “Now, care is standardized so that every patient experiences the same pre-, intra-, and postoperative protocol, which leads to better outcomes,” Dr. Bhat said.
The multidisciplinary Enhanced Recovery After Colorectal Surgery (ERACS) pathway also now emphasizes more patient education prior to surgery. “The patients go into surgery having a very clear idea of what they can expect, such as how their pain will be controlled, when they can start liquids, and what their expectations are for ambulation,” she said. “By making patients active participants in their own care, they tend to do better.”
The investigators studied 246 elective colorectal surgery patients at their large, urban, community teaching hospital. They compared outcomes in 2014, versus 2015, to gauge the effectiveness of the ERACS. “The change in length of stay was really rather remarkable,” Dr. Bhat said. In fact, the typical number of days in the hospital decreased by about half from 5.65 to 2.89 days, a statistically significant difference (P less than .0001).
Historically, “the whole reason we don’t send patients home sooner is we’re worried they’re going to bounce right back, and that’s an issue for the 30-day readmission rate,” Dr. Bhat said. However, the enhanced recovery protocol was designed to minimize that risk, and the study verified that it works. “We wanted to show that you can send patients home safely and also not worry that they would come back more often.”
Patient satisfaction seems higher too. Dr. Bhat added, “Who doesn’t feel better at home?”
“It is pretty remarkable that you can send somebody home in less than 3 days and they don’t come back to the hospital with complications, versus having them stay double that amount of time,” Dr. Bhat said. The direct variable cost was approximately $3,705 lower with the ERACS, and total hospitalization costs decreased by up to $11,227 per patient. For the institution overall, that outcome translated into savings of approximately $1 million for the year.
Dr. Bhat continues to see increasing gains from the protocol ERACS since the study period ended. “Our enhanced recovery pathway is getting better and better and more efficient.” The institution is now looking to expand enhanced recovery protocols to other types of surgery.
Dr. Deepa Bhat had no relevant financial disclosures.
AT THE ACS QUALITY AND SAFETY CONFERENCE
Key clinical point: An Enhanced Recovery After Colorectal Surgery (ERACS) protocol cut colorectal surgical site infections and reduced length of stay.
Major finding: The intervention decreased the hospital stays from an average of 6 days to 3 days and saved an estimated $11,227 per surgery.
Data source: A retrospective study of 246 patients undergoing elective colorectal surgery at a large, urban, community teaching hospital.
Disclosures: Dr. Deepa Bhat had no relevant financial disclosures.
From Obamacare to Trumpcare – implications for gastroenterologists
The June issue of CGH was the final column under my management. I have enjoyed the opportunity to provide you with information about practice management and health care reform. I also have enjoyed working with the Clinical Gastroenterology and Hepatology board of editors, and Erin Landis and Brook Simpson from AGA headquarters. Beginning in July 2017, this section will become the responsibility of Ziad Gellad, MD, MPH, AGAF, from Duke University. I have worked with Ziad for many years, and he serves on my board of editors for GI & Hepatology News. I have great confidence in his knowledge and ability.
During the last 5 years, we have published 58 columns beginning with an article where I made several broad predictions. I have tried to present important concepts and management tools related to private and academic clinical practice, health care reform, and health economics. This article was written in early January 2017 just before the inauguration of Donald Trump. As I wrote, we did not know the full extent or the pace of “Repeal and Replace,” as Obamacare becomes Trumpcare (www.healthaffairs.org/obamacare-to-trumpcare).
The extent of current Republican control of federal and state governments is unprecedented in modern political history. Per Newt Gingrich (The Economist, Jan. 7, 2017, p. 25), this will be the third attempt, after Ronald Reagan’s election in 1980 and Gingrich’s “Contract with America” in 1994, to break free from a “Big Government” mindset initiated by Franklin Roosevelt’s New Deal. In this article, I will speculate how a right-leaning shift in American health care policy might impact the business model of gastroenterology. No matter how government regulations or funds flow change, we (physicians) will ultimately be responsible for digestive care provided to our patients. In the words of Martin Luther King Jr. (as he paraphrased Theodore Parker), “The arc of the moral universe is long, but it bends toward justice.” What is remembered by fewer people, however, are words he then added during his speeches: “but only if we march.”
John I. Allen, MD, MBA, AGAF
Editor in Chief
The first column was published in July 2012.1 I wrote about five dominant themes that would alter our gastroenterology practices in the ensuing years. They were 1) an increasing requirement for us to demonstrate value, 2) the need to think about population management in addition to individual patient care, 3) consolidation that would occur at all levels of health care delivery, 4) increasing cost pressure, and 5) how medical decisions would be linked to reimbursement (now called value-based payment). I fully expected the Patient Protection and Affordable Care Act (ACA) would shape the health care landscape for the rest of our careers. After the article’s publication, I was invited to speak about health care reform at many academic centers and private practices. My last talk before the election was in Pasadena, Calif. (Oct. 28, 2016) where I confidently spoke about the implications of President Clinton’s cementing ACA into the fabric of U.S. medicine.
Donald Trump is now the 45th President of the United States. Republicans hold a 52-48 majority in the Senate and a 241-194 majority in the House. As of January 2017, one Supreme Court seat was available, and three more may open because of retirements (Justice Ginsburg is 83 years old, Justice Kennedy is 80, and Justice Breyer is 78). Republicans control all three branches of government in 25 states and dominate in 8 others. Conservative politicians control a large majority of county and city boards.
Until this year, Republicans have controlled all three branches of government only twice since 1945 (modern political history), and only once (George Bush in 2005) did the president have a Senate majority.2 With his win, Mr. Trump can lead a conservative revolution to reverse key initiatives begun when the Democratic Party held majority power. Repeal of the ACA, signed into legislation on March 23, 2010, is the Republican Party’s top priority.
Equally important, Congress can alter previously implemented federal regulations. Each year about 3,000 regulations are written by federal agencies that act with authority delegated by Congress (albeit Congress retains power to overturn them). Regulations are published in the Federal Register as preliminary rules during each year, and Final Rules are published after a public comment period and implemented shortly thereafter. Regulations carry the force of law and are codified in the Code of Federal Regulations. The Code of Federal Regulations is divided into 50 sections (Titles), with Title 42 (Public Health) and Title 45 (Public Welfare) most pertinent to us.
Other policies are created through executive orders, issued by the president (federal) or governors (states), without involvement of legislative or judicial branches (they were not mentioned in the Constitution, by the way). Executive orders issued by President Obama could, theoretically, be overturned by new executive orders.
Repeal and replace
Destruction of the ACA is a top priority of President Trump and Republican leaders of both houses of Congress. The ACA was a Democratic bill (passed with no Republican support), although it had many similarities to previous Republican legislative ideas dating from 1993.3
Although outright repeal could be blocked by a Democratic filibuster, the law could be drastically modified through budget reconciliation whose passage takes only a simple Senate majority. Thus, a simple budget-related bill could serve as a vehicle to defund many parts of ACA, including money for Medicaid expansion, insurance risk corridors, money to offset out-of-pocket expenses and individual premium subsidies, for example.4,5
There would be substantial problems if ACA were repealed even with a 2- or 3-year delay, a scenario proposed to provide time for a replacement bill. On Jan. 4, 2017, the House Republican Study Committee introduced the American Health Care Reform Act (AHCRA) as a replacement proposal, with the stipulation that ACA would be repealed as of Jan. 1, 2018. This initial bill hinted at Republican intent and was detailed in a Health Affairs blog.6 Importantly, there were distinct similarities between this and prior Republican proposals put forward by Representative Tom Price (nominated to head the Department of Health & Human Services under President Trump) and Speaker of the House Paul Ryan.7,8
Consistently, Republicans have advocated for expansion of health savings accounts, altering the tax code to allow individuals to deduct health insurance premiums, establishment of association risk pools, imposition of malpractice limits, protections for people with preexisting conditions, and further restrictions on abortion coverage. The AHCRA changes financial subsidies for purchasing insurance from a tax credit (which can be paid to people even if they do not pay taxes) to a tax deduction (only applicable to people who pay taxes). Analysis of a similar proposal made by President Trump during the campaign found that this plan would increase the number of uninsured people by more than 15 million.
If ACA is repealed, effects would be broader than just factors related to insurance coverage.9 ACA provides for preventive care (including colonoscopy) without copays, education of additional medical personnel, closing the donut hole for Medicare Part D (medications), approval of generic biologics, and Medicaid expansions, among other initiatives. If ACA were defunded without restoring pre-ACA support for Disproportion Share Hospital charity care, research, and graduate medical education, then safety-net hospitals and many academic medical centers (AMCs) could face enormous funding cuts.10 Defunding Medicaid expansion would adversely affect states in many ways, as pointed out by Ayanian et al.11 Medicaid expansion had broad economic impact in states that accepted federal money to expand. In Michigan for example, 30,900 jobs were added to the state in 2016 because of Medicaid expansion, with two-thirds outside of the health care industry. President Obama defined his view about the effects of ACA repeal in the New England Journal of Medicine.12
Lessons learned
Economic principles and unique characteristics of United States health care help explain why solutions to its high cost and uneven coverage are so difficult to achieve. These include higher prices for goods in the United States compared with other countries, variation in price (unrelated to quality), restraints on government price negotiations, inefficiencies due to variation in size of delivery systems, and “moral hazard” related to rich insurance coverage, which are some of the factors that doom any simple solutions. These are reviewed by Victor Fuchs13 in an excellent article in Annals of Internal Medicine. Payment methods for health care services also distort resource use and efficiencies. Understanding the eight basic payment methodologies in health care and current predictions about future health care spending will be important in shaping reimbursement policies.14,15
Disruptions in health care are unpopular and, as Uve Reinardt stated: “Our health care financing system will always remain a horrendous mess and a fountain for such dismay among the providers of health care as well as among patients.”4 Lessons to inform the next iteration of health care policy, learned from the 2009-2010 experience, might be as follows:
1. If a bill is to be passed, the president must personally lead in explaining the bill to the public in simple terms.
2. Even the threat of repeal may disrupt the current market and force insurance companies to exit quickly.
3. Coverage must be affordable to individuals, state budgets, and health care providers. Because expansion states saw positive impacts to state budgets8 and mental health and substance abuse services became part of Medicaid benefits, how will a replacement bill maintain coverage and compensate for new state moneys used now for other imperatives such as education and infrastructure?
4. Health care is like a massive cargo ship, not a sports car, so a bill to replace the ACA may take a long time (and might never be passed).
5. Health care is intensely personal, so it will always be politically charged.
Ultimately, physicians will need to make strategic guesses and rapid adjustments to sustain financial viability and provide high-value care. Strategies differ depending on your practice situation. Keep in mind the five principles listed in the opening paragraph of this article. It is likely that the most important principle to factor into your practice strategy is continuing reduction in reimbursements. No matter what model is adopted to reform the ACA, the financial pot (Medicare, Medicaid, commercial insurance, bundled payments, fee-for-service payments) will be reduced, and the number of uninsured patients will increase. How would you change your practice if Medicare was your best payer (“manage to Medicare”)?
Independent practices
Physicians in small- to medium-size independent practices continue to struggle with reducing reimbursements, reporting burdens, increasing overhead expenses, crushing regulatory requirements, and provider burnout. Trumpcare will favor small practices more than Obamacare from a policy (not necessarily a financial) perspective. Regulations on small business and reporting burdens may ease, but the move toward value-based reimbursement as outlined in the MACRA (passed with overwhelming bipartisan support) will not end.16 Practices in small communities continue to thrive because they give excellent care with limited competition and low overhead. Some practices in suburban and urban centers struggle because payers tend to favor (with enhanced managed care rates) larger practices and health systems. Large, horizontally integrated, efficient gastroenterology practices will continue to thrive because they can develop a “must-have” position with payers. Building remote patient monitoring, teleconsulting, and capabilities around value demonstration will be strategically advantageous.
Options for independent physicians include 1) maintaining status quo, 2) retiring, or 3) exiting the independent business model through a practice sale. Traditionally, physicians who wanted to sell their practices turned to hospitals or health systems. Recently, a physician-run model funded by venture capital has emerged where reduced overhead (through centralization of services) is combined with enhanced power during payer negotiations (because of scale). This model has allowed practices to merge into a physician organization and remain free from health system employment.17
Large health systems
Physicians employed by large health systems, whether they are nonprofit, for-profit, or AMCs, will see their future tied directly to health system success. If bundled payment, alternative payment, and capitation models of health care financing continue to grow in popularity, then success will be determined by a health system’s market share and its ability to form true clinical integration. In a capitated environment, expansion of market share (especially of relatively healthy patients) will help support margins. However, financial success will come from a system’s ability to manage high-cost patients, those 5% of patients who consume 50% of health care resources.18
Hospitals with a financially challenged patient base (safety-net hospitals) will have enormous financial pressures going forward. Repeal of ACA without restoration of pre-ACA funding will affect directly the financial health of systems including AMCs. AMCs and other health systems will be forced to reduce fixed overhead, enhance productivity of faculty, and restrict nonfunded activities (teaching for example). Although most AMCs are now in an active acquisition mode, this strategy is naturally limited by the number of remaining acquisition targets. Traditional high managed care rates enjoyed by AMCs will shrink, as will federal research funding (which typically comes with high indirect financial support). Health systems and GI societies will need to dedicate much more attention to state policy makers as Trumpcare progresses.
Finally, all providers will need to manage the business implications of retail health. As people assume higher deductibles and copays and health savings accounts grow, patients will change their patterns of purchasing services. Reputation counts for less when people are facing large price differences, so attention to patient-centric amenities, price, patient engagement, and patient satisfaction will become even more important.
Conclusion
The United States has undergone a massive and rapid political transformation. The mandate felt by conservative politicians, perhaps not supported by numbers, will carry a conservative platform forward. In areas where progressive Democrats emphasized federal power and socialized regulation (religion, education, civil rights, income security, and health policy), conservatives will transfer decision power as much as possible to states, local communities, and individuals. Maintaining the concept of “health as a right” will test the conscience of all of us.
References
1. Allen, J.I. The road ahead. Clin Gastroenterol Hepatol. 2012;10:692-6.
2. Gill KE. Visual guide: the balance of power between Congress and the Presidency (1901-2016). Wired Pen. November 2016. Available from http://wiredpen.com/resources/political-commentary-and-analysis/a-visual-guide-balance-of-power-congress-presidency/. Accessed Dec. 30, 2016.
3. Mertens M. Chart: comparing health reform bills – Democrats and Republicans 2009, Republics 1993. Kaiser Health News. Feb. 24, 2010. Available from http://khn.org/022310-bill-comparison/. Accessed Jan. 8, 2017.
4. Hotchkiss M. Q&A: what a Trump presidency means for the Affordable Care Act. Nov. 16, 2016 News at Princeton. Princeton University. Available from https://www.princeton.edu/main/news/archive/S47/93/09C11/index.xml?section=topstories. Accessed Dec. 30, 2016.
5. Jost T. Taking stock of health reform: where we’ve been, where we’re going. Health Affairs Blog. Available from http://healthaffairs.org/blog/2016/12/06/taking-stock-of-health-reform-where-weve-been-where-were-going/. Accessed Dec. 30, 2016.
6. Jost T. The Republican Study Committee’s ACA replacement proposal (updated). Health Affairs Blog. Available from http://healthaffairs.org/blog/2017/01/05/the-republican-study-committees-aca-replacement-proposal/. Accessed Jan. 10, 2017.
7. Price T. Empowering patients first. Available from http://tomprice.house.gov/sites/tomprice.house.gov/files/HR%202300%20Empowering%20Patients%20First%20Act%202015.pdf. Accessed Dec. 30, 2016.
8. Ryan P. A better way. Available from https://abetterway.speaker.gov/_assets/pdf/ABetterWay-HealthCare-PolicyPaper.pdf. Accessed Dec. 30, 2016.
9. Oberlander, J. The end of Obamacare. N Engl J Med. 2017;376:1-3.
10. Goodnough A. Hospitals in safety net brace for health care law’s repeal. New York Times. Dec. 28, 2016. Available from http://www.nytimes.com/2016/12/28/health/hospitals-medicaid-obamacare-trump.html?smprod=nytcore-iphone&smid=nytcore-iphone-share&_r=0. Accessed Jan. 10, 2017.
11. Ayanian, J.Z., Ehrlich, G.M., Grimes, D.R., et al. Economic effects of Medicaid expansion in Michigan. N Engl J Med. 2017;376:407-10.
12. Obama, B.H. Repealing the ACA without a replacement: the risks to American health care. N Engl J Med. 2017;376:297-9.
13. Fuchs, V.R. Major concepts of health economics. Ann Intern Med. 2015;162:380-3.
14. Quinn, K. The 8 basic payment methods in health care. Ann Intern Med. 2015;163:300-6.
15. Schoenman JA. A detailed look at US health care spending: a presentation from the National Institute for Health Care Management (NIHCM). Oct. 25, 2012. Available from http://www.nihcm.org/images/stories/Health_care_spending_slides_-_MILI_-_Schoenman.pdf. Accessed Dec. 30, 2016.
16. Allen, J.I., Allen, C.C., Brill, J.V. Gastroenterology 2020: no time for WIMPs. Gastroenterology. 2016;150:295-9.
17. Sciacca R. Weekly Byte: GI roundtable and navigating uncharted waters in health care. The PMD Blog. Available from https://www.pmd.com/blog/post/weekly-byte-gi-roundtable-and-navigating-uncharted-waters-in-health-care. Accessed Jan. 10, 2017.
18. Powers, B.W., Chaguturu, S.K. ACOs and high-cost patients. N Engl J Med. 2016;374:203-5.
Dr. Allen is professor of medicine, University of Michigan School of Medicine, Institute for Health Care Policy and Innovations, and associate medical director of Network Strategy and Business Development – Michigan Medicine, Ann Arbor. He discloses no conflicts.
The June issue of CGH was the final column under my management. I have enjoyed the opportunity to provide you with information about practice management and health care reform. I also have enjoyed working with the Clinical Gastroenterology and Hepatology board of editors, and Erin Landis and Brook Simpson from AGA headquarters. Beginning in July 2017, this section will become the responsibility of Ziad Gellad, MD, MPH, AGAF, from Duke University. I have worked with Ziad for many years, and he serves on my board of editors for GI & Hepatology News. I have great confidence in his knowledge and ability.
During the last 5 years, we have published 58 columns beginning with an article where I made several broad predictions. I have tried to present important concepts and management tools related to private and academic clinical practice, health care reform, and health economics. This article was written in early January 2017 just before the inauguration of Donald Trump. As I wrote, we did not know the full extent or the pace of “Repeal and Replace,” as Obamacare becomes Trumpcare (www.healthaffairs.org/obamacare-to-trumpcare).
The extent of current Republican control of federal and state governments is unprecedented in modern political history. Per Newt Gingrich (The Economist, Jan. 7, 2017, p. 25), this will be the third attempt, after Ronald Reagan’s election in 1980 and Gingrich’s “Contract with America” in 1994, to break free from a “Big Government” mindset initiated by Franklin Roosevelt’s New Deal. In this article, I will speculate how a right-leaning shift in American health care policy might impact the business model of gastroenterology. No matter how government regulations or funds flow change, we (physicians) will ultimately be responsible for digestive care provided to our patients. In the words of Martin Luther King Jr. (as he paraphrased Theodore Parker), “The arc of the moral universe is long, but it bends toward justice.” What is remembered by fewer people, however, are words he then added during his speeches: “but only if we march.”
John I. Allen, MD, MBA, AGAF
Editor in Chief
The first column was published in July 2012.1 I wrote about five dominant themes that would alter our gastroenterology practices in the ensuing years. They were 1) an increasing requirement for us to demonstrate value, 2) the need to think about population management in addition to individual patient care, 3) consolidation that would occur at all levels of health care delivery, 4) increasing cost pressure, and 5) how medical decisions would be linked to reimbursement (now called value-based payment). I fully expected the Patient Protection and Affordable Care Act (ACA) would shape the health care landscape for the rest of our careers. After the article’s publication, I was invited to speak about health care reform at many academic centers and private practices. My last talk before the election was in Pasadena, Calif. (Oct. 28, 2016) where I confidently spoke about the implications of President Clinton’s cementing ACA into the fabric of U.S. medicine.
Donald Trump is now the 45th President of the United States. Republicans hold a 52-48 majority in the Senate and a 241-194 majority in the House. As of January 2017, one Supreme Court seat was available, and three more may open because of retirements (Justice Ginsburg is 83 years old, Justice Kennedy is 80, and Justice Breyer is 78). Republicans control all three branches of government in 25 states and dominate in 8 others. Conservative politicians control a large majority of county and city boards.
Until this year, Republicans have controlled all three branches of government only twice since 1945 (modern political history), and only once (George Bush in 2005) did the president have a Senate majority.2 With his win, Mr. Trump can lead a conservative revolution to reverse key initiatives begun when the Democratic Party held majority power. Repeal of the ACA, signed into legislation on March 23, 2010, is the Republican Party’s top priority.
Equally important, Congress can alter previously implemented federal regulations. Each year about 3,000 regulations are written by federal agencies that act with authority delegated by Congress (albeit Congress retains power to overturn them). Regulations are published in the Federal Register as preliminary rules during each year, and Final Rules are published after a public comment period and implemented shortly thereafter. Regulations carry the force of law and are codified in the Code of Federal Regulations. The Code of Federal Regulations is divided into 50 sections (Titles), with Title 42 (Public Health) and Title 45 (Public Welfare) most pertinent to us.
Other policies are created through executive orders, issued by the president (federal) or governors (states), without involvement of legislative or judicial branches (they were not mentioned in the Constitution, by the way). Executive orders issued by President Obama could, theoretically, be overturned by new executive orders.
Repeal and replace
Destruction of the ACA is a top priority of President Trump and Republican leaders of both houses of Congress. The ACA was a Democratic bill (passed with no Republican support), although it had many similarities to previous Republican legislative ideas dating from 1993.3
Although outright repeal could be blocked by a Democratic filibuster, the law could be drastically modified through budget reconciliation whose passage takes only a simple Senate majority. Thus, a simple budget-related bill could serve as a vehicle to defund many parts of ACA, including money for Medicaid expansion, insurance risk corridors, money to offset out-of-pocket expenses and individual premium subsidies, for example.4,5
There would be substantial problems if ACA were repealed even with a 2- or 3-year delay, a scenario proposed to provide time for a replacement bill. On Jan. 4, 2017, the House Republican Study Committee introduced the American Health Care Reform Act (AHCRA) as a replacement proposal, with the stipulation that ACA would be repealed as of Jan. 1, 2018. This initial bill hinted at Republican intent and was detailed in a Health Affairs blog.6 Importantly, there were distinct similarities between this and prior Republican proposals put forward by Representative Tom Price (nominated to head the Department of Health & Human Services under President Trump) and Speaker of the House Paul Ryan.7,8
Consistently, Republicans have advocated for expansion of health savings accounts, altering the tax code to allow individuals to deduct health insurance premiums, establishment of association risk pools, imposition of malpractice limits, protections for people with preexisting conditions, and further restrictions on abortion coverage. The AHCRA changes financial subsidies for purchasing insurance from a tax credit (which can be paid to people even if they do not pay taxes) to a tax deduction (only applicable to people who pay taxes). Analysis of a similar proposal made by President Trump during the campaign found that this plan would increase the number of uninsured people by more than 15 million.
If ACA is repealed, effects would be broader than just factors related to insurance coverage.9 ACA provides for preventive care (including colonoscopy) without copays, education of additional medical personnel, closing the donut hole for Medicare Part D (medications), approval of generic biologics, and Medicaid expansions, among other initiatives. If ACA were defunded without restoring pre-ACA support for Disproportion Share Hospital charity care, research, and graduate medical education, then safety-net hospitals and many academic medical centers (AMCs) could face enormous funding cuts.10 Defunding Medicaid expansion would adversely affect states in many ways, as pointed out by Ayanian et al.11 Medicaid expansion had broad economic impact in states that accepted federal money to expand. In Michigan for example, 30,900 jobs were added to the state in 2016 because of Medicaid expansion, with two-thirds outside of the health care industry. President Obama defined his view about the effects of ACA repeal in the New England Journal of Medicine.12
Lessons learned
Economic principles and unique characteristics of United States health care help explain why solutions to its high cost and uneven coverage are so difficult to achieve. These include higher prices for goods in the United States compared with other countries, variation in price (unrelated to quality), restraints on government price negotiations, inefficiencies due to variation in size of delivery systems, and “moral hazard” related to rich insurance coverage, which are some of the factors that doom any simple solutions. These are reviewed by Victor Fuchs13 in an excellent article in Annals of Internal Medicine. Payment methods for health care services also distort resource use and efficiencies. Understanding the eight basic payment methodologies in health care and current predictions about future health care spending will be important in shaping reimbursement policies.14,15
Disruptions in health care are unpopular and, as Uve Reinardt stated: “Our health care financing system will always remain a horrendous mess and a fountain for such dismay among the providers of health care as well as among patients.”4 Lessons to inform the next iteration of health care policy, learned from the 2009-2010 experience, might be as follows:
1. If a bill is to be passed, the president must personally lead in explaining the bill to the public in simple terms.
2. Even the threat of repeal may disrupt the current market and force insurance companies to exit quickly.
3. Coverage must be affordable to individuals, state budgets, and health care providers. Because expansion states saw positive impacts to state budgets8 and mental health and substance abuse services became part of Medicaid benefits, how will a replacement bill maintain coverage and compensate for new state moneys used now for other imperatives such as education and infrastructure?
4. Health care is like a massive cargo ship, not a sports car, so a bill to replace the ACA may take a long time (and might never be passed).
5. Health care is intensely personal, so it will always be politically charged.
Ultimately, physicians will need to make strategic guesses and rapid adjustments to sustain financial viability and provide high-value care. Strategies differ depending on your practice situation. Keep in mind the five principles listed in the opening paragraph of this article. It is likely that the most important principle to factor into your practice strategy is continuing reduction in reimbursements. No matter what model is adopted to reform the ACA, the financial pot (Medicare, Medicaid, commercial insurance, bundled payments, fee-for-service payments) will be reduced, and the number of uninsured patients will increase. How would you change your practice if Medicare was your best payer (“manage to Medicare”)?
Independent practices
Physicians in small- to medium-size independent practices continue to struggle with reducing reimbursements, reporting burdens, increasing overhead expenses, crushing regulatory requirements, and provider burnout. Trumpcare will favor small practices more than Obamacare from a policy (not necessarily a financial) perspective. Regulations on small business and reporting burdens may ease, but the move toward value-based reimbursement as outlined in the MACRA (passed with overwhelming bipartisan support) will not end.16 Practices in small communities continue to thrive because they give excellent care with limited competition and low overhead. Some practices in suburban and urban centers struggle because payers tend to favor (with enhanced managed care rates) larger practices and health systems. Large, horizontally integrated, efficient gastroenterology practices will continue to thrive because they can develop a “must-have” position with payers. Building remote patient monitoring, teleconsulting, and capabilities around value demonstration will be strategically advantageous.
Options for independent physicians include 1) maintaining status quo, 2) retiring, or 3) exiting the independent business model through a practice sale. Traditionally, physicians who wanted to sell their practices turned to hospitals or health systems. Recently, a physician-run model funded by venture capital has emerged where reduced overhead (through centralization of services) is combined with enhanced power during payer negotiations (because of scale). This model has allowed practices to merge into a physician organization and remain free from health system employment.17
Large health systems
Physicians employed by large health systems, whether they are nonprofit, for-profit, or AMCs, will see their future tied directly to health system success. If bundled payment, alternative payment, and capitation models of health care financing continue to grow in popularity, then success will be determined by a health system’s market share and its ability to form true clinical integration. In a capitated environment, expansion of market share (especially of relatively healthy patients) will help support margins. However, financial success will come from a system’s ability to manage high-cost patients, those 5% of patients who consume 50% of health care resources.18
Hospitals with a financially challenged patient base (safety-net hospitals) will have enormous financial pressures going forward. Repeal of ACA without restoration of pre-ACA funding will affect directly the financial health of systems including AMCs. AMCs and other health systems will be forced to reduce fixed overhead, enhance productivity of faculty, and restrict nonfunded activities (teaching for example). Although most AMCs are now in an active acquisition mode, this strategy is naturally limited by the number of remaining acquisition targets. Traditional high managed care rates enjoyed by AMCs will shrink, as will federal research funding (which typically comes with high indirect financial support). Health systems and GI societies will need to dedicate much more attention to state policy makers as Trumpcare progresses.
Finally, all providers will need to manage the business implications of retail health. As people assume higher deductibles and copays and health savings accounts grow, patients will change their patterns of purchasing services. Reputation counts for less when people are facing large price differences, so attention to patient-centric amenities, price, patient engagement, and patient satisfaction will become even more important.
Conclusion
The United States has undergone a massive and rapid political transformation. The mandate felt by conservative politicians, perhaps not supported by numbers, will carry a conservative platform forward. In areas where progressive Democrats emphasized federal power and socialized regulation (religion, education, civil rights, income security, and health policy), conservatives will transfer decision power as much as possible to states, local communities, and individuals. Maintaining the concept of “health as a right” will test the conscience of all of us.
References
1. Allen, J.I. The road ahead. Clin Gastroenterol Hepatol. 2012;10:692-6.
2. Gill KE. Visual guide: the balance of power between Congress and the Presidency (1901-2016). Wired Pen. November 2016. Available from http://wiredpen.com/resources/political-commentary-and-analysis/a-visual-guide-balance-of-power-congress-presidency/. Accessed Dec. 30, 2016.
3. Mertens M. Chart: comparing health reform bills – Democrats and Republicans 2009, Republics 1993. Kaiser Health News. Feb. 24, 2010. Available from http://khn.org/022310-bill-comparison/. Accessed Jan. 8, 2017.
4. Hotchkiss M. Q&A: what a Trump presidency means for the Affordable Care Act. Nov. 16, 2016 News at Princeton. Princeton University. Available from https://www.princeton.edu/main/news/archive/S47/93/09C11/index.xml?section=topstories. Accessed Dec. 30, 2016.
5. Jost T. Taking stock of health reform: where we’ve been, where we’re going. Health Affairs Blog. Available from http://healthaffairs.org/blog/2016/12/06/taking-stock-of-health-reform-where-weve-been-where-were-going/. Accessed Dec. 30, 2016.
6. Jost T. The Republican Study Committee’s ACA replacement proposal (updated). Health Affairs Blog. Available from http://healthaffairs.org/blog/2017/01/05/the-republican-study-committees-aca-replacement-proposal/. Accessed Jan. 10, 2017.
7. Price T. Empowering patients first. Available from http://tomprice.house.gov/sites/tomprice.house.gov/files/HR%202300%20Empowering%20Patients%20First%20Act%202015.pdf. Accessed Dec. 30, 2016.
8. Ryan P. A better way. Available from https://abetterway.speaker.gov/_assets/pdf/ABetterWay-HealthCare-PolicyPaper.pdf. Accessed Dec. 30, 2016.
9. Oberlander, J. The end of Obamacare. N Engl J Med. 2017;376:1-3.
10. Goodnough A. Hospitals in safety net brace for health care law’s repeal. New York Times. Dec. 28, 2016. Available from http://www.nytimes.com/2016/12/28/health/hospitals-medicaid-obamacare-trump.html?smprod=nytcore-iphone&smid=nytcore-iphone-share&_r=0. Accessed Jan. 10, 2017.
11. Ayanian, J.Z., Ehrlich, G.M., Grimes, D.R., et al. Economic effects of Medicaid expansion in Michigan. N Engl J Med. 2017;376:407-10.
12. Obama, B.H. Repealing the ACA without a replacement: the risks to American health care. N Engl J Med. 2017;376:297-9.
13. Fuchs, V.R. Major concepts of health economics. Ann Intern Med. 2015;162:380-3.
14. Quinn, K. The 8 basic payment methods in health care. Ann Intern Med. 2015;163:300-6.
15. Schoenman JA. A detailed look at US health care spending: a presentation from the National Institute for Health Care Management (NIHCM). Oct. 25, 2012. Available from http://www.nihcm.org/images/stories/Health_care_spending_slides_-_MILI_-_Schoenman.pdf. Accessed Dec. 30, 2016.
16. Allen, J.I., Allen, C.C., Brill, J.V. Gastroenterology 2020: no time for WIMPs. Gastroenterology. 2016;150:295-9.
17. Sciacca R. Weekly Byte: GI roundtable and navigating uncharted waters in health care. The PMD Blog. Available from https://www.pmd.com/blog/post/weekly-byte-gi-roundtable-and-navigating-uncharted-waters-in-health-care. Accessed Jan. 10, 2017.
18. Powers, B.W., Chaguturu, S.K. ACOs and high-cost patients. N Engl J Med. 2016;374:203-5.
Dr. Allen is professor of medicine, University of Michigan School of Medicine, Institute for Health Care Policy and Innovations, and associate medical director of Network Strategy and Business Development – Michigan Medicine, Ann Arbor. He discloses no conflicts.
The June issue of CGH was the final column under my management. I have enjoyed the opportunity to provide you with information about practice management and health care reform. I also have enjoyed working with the Clinical Gastroenterology and Hepatology board of editors, and Erin Landis and Brook Simpson from AGA headquarters. Beginning in July 2017, this section will become the responsibility of Ziad Gellad, MD, MPH, AGAF, from Duke University. I have worked with Ziad for many years, and he serves on my board of editors for GI & Hepatology News. I have great confidence in his knowledge and ability.
During the last 5 years, we have published 58 columns beginning with an article where I made several broad predictions. I have tried to present important concepts and management tools related to private and academic clinical practice, health care reform, and health economics. This article was written in early January 2017 just before the inauguration of Donald Trump. As I wrote, we did not know the full extent or the pace of “Repeal and Replace,” as Obamacare becomes Trumpcare (www.healthaffairs.org/obamacare-to-trumpcare).
The extent of current Republican control of federal and state governments is unprecedented in modern political history. Per Newt Gingrich (The Economist, Jan. 7, 2017, p. 25), this will be the third attempt, after Ronald Reagan’s election in 1980 and Gingrich’s “Contract with America” in 1994, to break free from a “Big Government” mindset initiated by Franklin Roosevelt’s New Deal. In this article, I will speculate how a right-leaning shift in American health care policy might impact the business model of gastroenterology. No matter how government regulations or funds flow change, we (physicians) will ultimately be responsible for digestive care provided to our patients. In the words of Martin Luther King Jr. (as he paraphrased Theodore Parker), “The arc of the moral universe is long, but it bends toward justice.” What is remembered by fewer people, however, are words he then added during his speeches: “but only if we march.”
John I. Allen, MD, MBA, AGAF
Editor in Chief
The first column was published in July 2012.1 I wrote about five dominant themes that would alter our gastroenterology practices in the ensuing years. They were 1) an increasing requirement for us to demonstrate value, 2) the need to think about population management in addition to individual patient care, 3) consolidation that would occur at all levels of health care delivery, 4) increasing cost pressure, and 5) how medical decisions would be linked to reimbursement (now called value-based payment). I fully expected the Patient Protection and Affordable Care Act (ACA) would shape the health care landscape for the rest of our careers. After the article’s publication, I was invited to speak about health care reform at many academic centers and private practices. My last talk before the election was in Pasadena, Calif. (Oct. 28, 2016) where I confidently spoke about the implications of President Clinton’s cementing ACA into the fabric of U.S. medicine.
Donald Trump is now the 45th President of the United States. Republicans hold a 52-48 majority in the Senate and a 241-194 majority in the House. As of January 2017, one Supreme Court seat was available, and three more may open because of retirements (Justice Ginsburg is 83 years old, Justice Kennedy is 80, and Justice Breyer is 78). Republicans control all three branches of government in 25 states and dominate in 8 others. Conservative politicians control a large majority of county and city boards.
Until this year, Republicans have controlled all three branches of government only twice since 1945 (modern political history), and only once (George Bush in 2005) did the president have a Senate majority.2 With his win, Mr. Trump can lead a conservative revolution to reverse key initiatives begun when the Democratic Party held majority power. Repeal of the ACA, signed into legislation on March 23, 2010, is the Republican Party’s top priority.
Equally important, Congress can alter previously implemented federal regulations. Each year about 3,000 regulations are written by federal agencies that act with authority delegated by Congress (albeit Congress retains power to overturn them). Regulations are published in the Federal Register as preliminary rules during each year, and Final Rules are published after a public comment period and implemented shortly thereafter. Regulations carry the force of law and are codified in the Code of Federal Regulations. The Code of Federal Regulations is divided into 50 sections (Titles), with Title 42 (Public Health) and Title 45 (Public Welfare) most pertinent to us.
Other policies are created through executive orders, issued by the president (federal) or governors (states), without involvement of legislative or judicial branches (they were not mentioned in the Constitution, by the way). Executive orders issued by President Obama could, theoretically, be overturned by new executive orders.
Repeal and replace
Destruction of the ACA is a top priority of President Trump and Republican leaders of both houses of Congress. The ACA was a Democratic bill (passed with no Republican support), although it had many similarities to previous Republican legislative ideas dating from 1993.3
Although outright repeal could be blocked by a Democratic filibuster, the law could be drastically modified through budget reconciliation whose passage takes only a simple Senate majority. Thus, a simple budget-related bill could serve as a vehicle to defund many parts of ACA, including money for Medicaid expansion, insurance risk corridors, money to offset out-of-pocket expenses and individual premium subsidies, for example.4,5
There would be substantial problems if ACA were repealed even with a 2- or 3-year delay, a scenario proposed to provide time for a replacement bill. On Jan. 4, 2017, the House Republican Study Committee introduced the American Health Care Reform Act (AHCRA) as a replacement proposal, with the stipulation that ACA would be repealed as of Jan. 1, 2018. This initial bill hinted at Republican intent and was detailed in a Health Affairs blog.6 Importantly, there were distinct similarities between this and prior Republican proposals put forward by Representative Tom Price (nominated to head the Department of Health & Human Services under President Trump) and Speaker of the House Paul Ryan.7,8
Consistently, Republicans have advocated for expansion of health savings accounts, altering the tax code to allow individuals to deduct health insurance premiums, establishment of association risk pools, imposition of malpractice limits, protections for people with preexisting conditions, and further restrictions on abortion coverage. The AHCRA changes financial subsidies for purchasing insurance from a tax credit (which can be paid to people even if they do not pay taxes) to a tax deduction (only applicable to people who pay taxes). Analysis of a similar proposal made by President Trump during the campaign found that this plan would increase the number of uninsured people by more than 15 million.
If ACA is repealed, effects would be broader than just factors related to insurance coverage.9 ACA provides for preventive care (including colonoscopy) without copays, education of additional medical personnel, closing the donut hole for Medicare Part D (medications), approval of generic biologics, and Medicaid expansions, among other initiatives. If ACA were defunded without restoring pre-ACA support for Disproportion Share Hospital charity care, research, and graduate medical education, then safety-net hospitals and many academic medical centers (AMCs) could face enormous funding cuts.10 Defunding Medicaid expansion would adversely affect states in many ways, as pointed out by Ayanian et al.11 Medicaid expansion had broad economic impact in states that accepted federal money to expand. In Michigan for example, 30,900 jobs were added to the state in 2016 because of Medicaid expansion, with two-thirds outside of the health care industry. President Obama defined his view about the effects of ACA repeal in the New England Journal of Medicine.12
Lessons learned
Economic principles and unique characteristics of United States health care help explain why solutions to its high cost and uneven coverage are so difficult to achieve. These include higher prices for goods in the United States compared with other countries, variation in price (unrelated to quality), restraints on government price negotiations, inefficiencies due to variation in size of delivery systems, and “moral hazard” related to rich insurance coverage, which are some of the factors that doom any simple solutions. These are reviewed by Victor Fuchs13 in an excellent article in Annals of Internal Medicine. Payment methods for health care services also distort resource use and efficiencies. Understanding the eight basic payment methodologies in health care and current predictions about future health care spending will be important in shaping reimbursement policies.14,15
Disruptions in health care are unpopular and, as Uve Reinardt stated: “Our health care financing system will always remain a horrendous mess and a fountain for such dismay among the providers of health care as well as among patients.”4 Lessons to inform the next iteration of health care policy, learned from the 2009-2010 experience, might be as follows:
1. If a bill is to be passed, the president must personally lead in explaining the bill to the public in simple terms.
2. Even the threat of repeal may disrupt the current market and force insurance companies to exit quickly.
3. Coverage must be affordable to individuals, state budgets, and health care providers. Because expansion states saw positive impacts to state budgets8 and mental health and substance abuse services became part of Medicaid benefits, how will a replacement bill maintain coverage and compensate for new state moneys used now for other imperatives such as education and infrastructure?
4. Health care is like a massive cargo ship, not a sports car, so a bill to replace the ACA may take a long time (and might never be passed).
5. Health care is intensely personal, so it will always be politically charged.
Ultimately, physicians will need to make strategic guesses and rapid adjustments to sustain financial viability and provide high-value care. Strategies differ depending on your practice situation. Keep in mind the five principles listed in the opening paragraph of this article. It is likely that the most important principle to factor into your practice strategy is continuing reduction in reimbursements. No matter what model is adopted to reform the ACA, the financial pot (Medicare, Medicaid, commercial insurance, bundled payments, fee-for-service payments) will be reduced, and the number of uninsured patients will increase. How would you change your practice if Medicare was your best payer (“manage to Medicare”)?
Independent practices
Physicians in small- to medium-size independent practices continue to struggle with reducing reimbursements, reporting burdens, increasing overhead expenses, crushing regulatory requirements, and provider burnout. Trumpcare will favor small practices more than Obamacare from a policy (not necessarily a financial) perspective. Regulations on small business and reporting burdens may ease, but the move toward value-based reimbursement as outlined in the MACRA (passed with overwhelming bipartisan support) will not end.16 Practices in small communities continue to thrive because they give excellent care with limited competition and low overhead. Some practices in suburban and urban centers struggle because payers tend to favor (with enhanced managed care rates) larger practices and health systems. Large, horizontally integrated, efficient gastroenterology practices will continue to thrive because they can develop a “must-have” position with payers. Building remote patient monitoring, teleconsulting, and capabilities around value demonstration will be strategically advantageous.
Options for independent physicians include 1) maintaining status quo, 2) retiring, or 3) exiting the independent business model through a practice sale. Traditionally, physicians who wanted to sell their practices turned to hospitals or health systems. Recently, a physician-run model funded by venture capital has emerged where reduced overhead (through centralization of services) is combined with enhanced power during payer negotiations (because of scale). This model has allowed practices to merge into a physician organization and remain free from health system employment.17
Large health systems
Physicians employed by large health systems, whether they are nonprofit, for-profit, or AMCs, will see their future tied directly to health system success. If bundled payment, alternative payment, and capitation models of health care financing continue to grow in popularity, then success will be determined by a health system’s market share and its ability to form true clinical integration. In a capitated environment, expansion of market share (especially of relatively healthy patients) will help support margins. However, financial success will come from a system’s ability to manage high-cost patients, those 5% of patients who consume 50% of health care resources.18
Hospitals with a financially challenged patient base (safety-net hospitals) will have enormous financial pressures going forward. Repeal of ACA without restoration of pre-ACA funding will affect directly the financial health of systems including AMCs. AMCs and other health systems will be forced to reduce fixed overhead, enhance productivity of faculty, and restrict nonfunded activities (teaching for example). Although most AMCs are now in an active acquisition mode, this strategy is naturally limited by the number of remaining acquisition targets. Traditional high managed care rates enjoyed by AMCs will shrink, as will federal research funding (which typically comes with high indirect financial support). Health systems and GI societies will need to dedicate much more attention to state policy makers as Trumpcare progresses.
Finally, all providers will need to manage the business implications of retail health. As people assume higher deductibles and copays and health savings accounts grow, patients will change their patterns of purchasing services. Reputation counts for less when people are facing large price differences, so attention to patient-centric amenities, price, patient engagement, and patient satisfaction will become even more important.
Conclusion
The United States has undergone a massive and rapid political transformation. The mandate felt by conservative politicians, perhaps not supported by numbers, will carry a conservative platform forward. In areas where progressive Democrats emphasized federal power and socialized regulation (religion, education, civil rights, income security, and health policy), conservatives will transfer decision power as much as possible to states, local communities, and individuals. Maintaining the concept of “health as a right” will test the conscience of all of us.
References
1. Allen, J.I. The road ahead. Clin Gastroenterol Hepatol. 2012;10:692-6.
2. Gill KE. Visual guide: the balance of power between Congress and the Presidency (1901-2016). Wired Pen. November 2016. Available from http://wiredpen.com/resources/political-commentary-and-analysis/a-visual-guide-balance-of-power-congress-presidency/. Accessed Dec. 30, 2016.
3. Mertens M. Chart: comparing health reform bills – Democrats and Republicans 2009, Republics 1993. Kaiser Health News. Feb. 24, 2010. Available from http://khn.org/022310-bill-comparison/. Accessed Jan. 8, 2017.
4. Hotchkiss M. Q&A: what a Trump presidency means for the Affordable Care Act. Nov. 16, 2016 News at Princeton. Princeton University. Available from https://www.princeton.edu/main/news/archive/S47/93/09C11/index.xml?section=topstories. Accessed Dec. 30, 2016.
5. Jost T. Taking stock of health reform: where we’ve been, where we’re going. Health Affairs Blog. Available from http://healthaffairs.org/blog/2016/12/06/taking-stock-of-health-reform-where-weve-been-where-were-going/. Accessed Dec. 30, 2016.
6. Jost T. The Republican Study Committee’s ACA replacement proposal (updated). Health Affairs Blog. Available from http://healthaffairs.org/blog/2017/01/05/the-republican-study-committees-aca-replacement-proposal/. Accessed Jan. 10, 2017.
7. Price T. Empowering patients first. Available from http://tomprice.house.gov/sites/tomprice.house.gov/files/HR%202300%20Empowering%20Patients%20First%20Act%202015.pdf. Accessed Dec. 30, 2016.
8. Ryan P. A better way. Available from https://abetterway.speaker.gov/_assets/pdf/ABetterWay-HealthCare-PolicyPaper.pdf. Accessed Dec. 30, 2016.
9. Oberlander, J. The end of Obamacare. N Engl J Med. 2017;376:1-3.
10. Goodnough A. Hospitals in safety net brace for health care law’s repeal. New York Times. Dec. 28, 2016. Available from http://www.nytimes.com/2016/12/28/health/hospitals-medicaid-obamacare-trump.html?smprod=nytcore-iphone&smid=nytcore-iphone-share&_r=0. Accessed Jan. 10, 2017.
11. Ayanian, J.Z., Ehrlich, G.M., Grimes, D.R., et al. Economic effects of Medicaid expansion in Michigan. N Engl J Med. 2017;376:407-10.
12. Obama, B.H. Repealing the ACA without a replacement: the risks to American health care. N Engl J Med. 2017;376:297-9.
13. Fuchs, V.R. Major concepts of health economics. Ann Intern Med. 2015;162:380-3.
14. Quinn, K. The 8 basic payment methods in health care. Ann Intern Med. 2015;163:300-6.
15. Schoenman JA. A detailed look at US health care spending: a presentation from the National Institute for Health Care Management (NIHCM). Oct. 25, 2012. Available from http://www.nihcm.org/images/stories/Health_care_spending_slides_-_MILI_-_Schoenman.pdf. Accessed Dec. 30, 2016.
16. Allen, J.I., Allen, C.C., Brill, J.V. Gastroenterology 2020: no time for WIMPs. Gastroenterology. 2016;150:295-9.
17. Sciacca R. Weekly Byte: GI roundtable and navigating uncharted waters in health care. The PMD Blog. Available from https://www.pmd.com/blog/post/weekly-byte-gi-roundtable-and-navigating-uncharted-waters-in-health-care. Accessed Jan. 10, 2017.
18. Powers, B.W., Chaguturu, S.K. ACOs and high-cost patients. N Engl J Med. 2016;374:203-5.
Dr. Allen is professor of medicine, University of Michigan School of Medicine, Institute for Health Care Policy and Innovations, and associate medical director of Network Strategy and Business Development – Michigan Medicine, Ann Arbor. He discloses no conflicts.
New cryoballoon treatment eradicated esophageal squamous cell neoplasias
For the first time, endoscopists have used focal cryoballoon ablation to eradicate early esophageal squamous cell neoplasias, including high-grade lesions in treatment-experienced patients.
A single session of treatment with the novel, portable nitrous oxide system (C2 Therapeutics, Redwood City, Calif.) produced complete pathologic and endoscopic responses at 3 months in 8 of 10 patients, reported Marcia Irene Canto, MD, of Johns Hopkins University in Baltimore, with her associates. Two to five sessions produced complete responses in the other two patients, and all patients were disease-free at their last visit (median follow-up, 10.7 months; interquartile range, 4-14 months). The study was published online July 15 in Gastrointestinal Endoscopy (2017. doi: 10.1016/j.gie.2017.07.013).
Standard treatments for esophageal squamous cell neoplasia have drawbacks. Submucosal dissection can cause bleeding, perforation, and stenosis, and radiofrequency ablation (RFA) is associated with stricture. To test an alternative, the researchers used a portable, hand-held, battery-powered cryoballoon ablation system that successfully eradicated Barrett’s esophagus lesions in two prior studies. The machine contains liquid nitrous oxide, which turns to gas when released into a balloon catheter in the endoscope. The gas inflates the balloon, enabling the endoscopist to see through it to the neoplastic mucosa, which is pretreated with Lugol chromoendoscopy. The endoscopist then cryoablates the target lesion across the balloon wall. Unlike cryospray, the entire dose of cryogen hits the lesion, the investigators noted. Also, the gas is automatically evacuated without the need for suctioning or decompression, and the treatment process does not require heavy gas tanks or repeated freeze-thaw cycles.
In this study, all 10 patients achieved complete endoscopic and pathologic responses at 3 months. Seven patients were followed for 1 year, and none showed biopsy evidence of neoplastic progression. In contrast, a prospective trial of circumferential radiofrequency ablation without endoscopic mucosal resection or endoscopic submucosal dissection reported a 12-month rate of complete response of 84%, the researchers noted (Endoscopy. 2015;47:398-408). There were no serious treatment-related adverse events. Pain was usually self-limited, although one patient required 2 days of narcotics. Two patients developed symptomatic strictures 6-8 weeks after treatment that resolved with balloon dilation. Both of these patients had undergone extensive multifocal ablation. “Circumferential treatment of ESCN [esophageal squamous cell neoplasia] remains problematic for all endoscopic ablative therapies, with a high stricture rate of 20% in our small pilot study of cryoablation and 20%-23% with RFA,” the investigators wrote. “The risk for postablation stricture appears to be related to a long length of ESCN. Optimizing the cryogen dose, technique, and decrease in Lugol’s solution concentration might alter the incidence of postablation strictures for ablative treatments.”
Study participants were 55-90 years old, and six were female. Four were treatment naive, and six had progressed despite endoscopic mucosal resection, RFA, spray cryotherapy, argon plasma coagulation, or multiple therapies. Seven patients had high-grade lesions, two had low-grade lesions, and one had early esophageal squamous cell carcinoma. Most lesions were distally located, but two were in the middle esophagus and one was proximal. The largest lesion measured 4 cm and the maximum length of all lesions in a single patient was 10 cm. Patients did not have visible esophageal masses or evidence of advanced or metastatic disease.
“Comparative effectiveness trials might eventually determine the role of cryoablation in the treatment of early ESCN,” the researchers concluded. An open-label, nonrandomized clinical trial of the balloon cryotherapy device is underway in China (NCT02605759). The article did not list funding sources or disclosures.
For the first time, endoscopists have used focal cryoballoon ablation to eradicate early esophageal squamous cell neoplasias, including high-grade lesions in treatment-experienced patients.
A single session of treatment with the novel, portable nitrous oxide system (C2 Therapeutics, Redwood City, Calif.) produced complete pathologic and endoscopic responses at 3 months in 8 of 10 patients, reported Marcia Irene Canto, MD, of Johns Hopkins University in Baltimore, with her associates. Two to five sessions produced complete responses in the other two patients, and all patients were disease-free at their last visit (median follow-up, 10.7 months; interquartile range, 4-14 months). The study was published online July 15 in Gastrointestinal Endoscopy (2017. doi: 10.1016/j.gie.2017.07.013).
Standard treatments for esophageal squamous cell neoplasia have drawbacks. Submucosal dissection can cause bleeding, perforation, and stenosis, and radiofrequency ablation (RFA) is associated with stricture. To test an alternative, the researchers used a portable, hand-held, battery-powered cryoballoon ablation system that successfully eradicated Barrett’s esophagus lesions in two prior studies. The machine contains liquid nitrous oxide, which turns to gas when released into a balloon catheter in the endoscope. The gas inflates the balloon, enabling the endoscopist to see through it to the neoplastic mucosa, which is pretreated with Lugol chromoendoscopy. The endoscopist then cryoablates the target lesion across the balloon wall. Unlike cryospray, the entire dose of cryogen hits the lesion, the investigators noted. Also, the gas is automatically evacuated without the need for suctioning or decompression, and the treatment process does not require heavy gas tanks or repeated freeze-thaw cycles.
In this study, all 10 patients achieved complete endoscopic and pathologic responses at 3 months. Seven patients were followed for 1 year, and none showed biopsy evidence of neoplastic progression. In contrast, a prospective trial of circumferential radiofrequency ablation without endoscopic mucosal resection or endoscopic submucosal dissection reported a 12-month rate of complete response of 84%, the researchers noted (Endoscopy. 2015;47:398-408). There were no serious treatment-related adverse events. Pain was usually self-limited, although one patient required 2 days of narcotics. Two patients developed symptomatic strictures 6-8 weeks after treatment that resolved with balloon dilation. Both of these patients had undergone extensive multifocal ablation. “Circumferential treatment of ESCN [esophageal squamous cell neoplasia] remains problematic for all endoscopic ablative therapies, with a high stricture rate of 20% in our small pilot study of cryoablation and 20%-23% with RFA,” the investigators wrote. “The risk for postablation stricture appears to be related to a long length of ESCN. Optimizing the cryogen dose, technique, and decrease in Lugol’s solution concentration might alter the incidence of postablation strictures for ablative treatments.”
Study participants were 55-90 years old, and six were female. Four were treatment naive, and six had progressed despite endoscopic mucosal resection, RFA, spray cryotherapy, argon plasma coagulation, or multiple therapies. Seven patients had high-grade lesions, two had low-grade lesions, and one had early esophageal squamous cell carcinoma. Most lesions were distally located, but two were in the middle esophagus and one was proximal. The largest lesion measured 4 cm and the maximum length of all lesions in a single patient was 10 cm. Patients did not have visible esophageal masses or evidence of advanced or metastatic disease.
“Comparative effectiveness trials might eventually determine the role of cryoablation in the treatment of early ESCN,” the researchers concluded. An open-label, nonrandomized clinical trial of the balloon cryotherapy device is underway in China (NCT02605759). The article did not list funding sources or disclosures.
For the first time, endoscopists have used focal cryoballoon ablation to eradicate early esophageal squamous cell neoplasias, including high-grade lesions in treatment-experienced patients.
A single session of treatment with the novel, portable nitrous oxide system (C2 Therapeutics, Redwood City, Calif.) produced complete pathologic and endoscopic responses at 3 months in 8 of 10 patients, reported Marcia Irene Canto, MD, of Johns Hopkins University in Baltimore, with her associates. Two to five sessions produced complete responses in the other two patients, and all patients were disease-free at their last visit (median follow-up, 10.7 months; interquartile range, 4-14 months). The study was published online July 15 in Gastrointestinal Endoscopy (2017. doi: 10.1016/j.gie.2017.07.013).
Standard treatments for esophageal squamous cell neoplasia have drawbacks. Submucosal dissection can cause bleeding, perforation, and stenosis, and radiofrequency ablation (RFA) is associated with stricture. To test an alternative, the researchers used a portable, hand-held, battery-powered cryoballoon ablation system that successfully eradicated Barrett’s esophagus lesions in two prior studies. The machine contains liquid nitrous oxide, which turns to gas when released into a balloon catheter in the endoscope. The gas inflates the balloon, enabling the endoscopist to see through it to the neoplastic mucosa, which is pretreated with Lugol chromoendoscopy. The endoscopist then cryoablates the target lesion across the balloon wall. Unlike cryospray, the entire dose of cryogen hits the lesion, the investigators noted. Also, the gas is automatically evacuated without the need for suctioning or decompression, and the treatment process does not require heavy gas tanks or repeated freeze-thaw cycles.
In this study, all 10 patients achieved complete endoscopic and pathologic responses at 3 months. Seven patients were followed for 1 year, and none showed biopsy evidence of neoplastic progression. In contrast, a prospective trial of circumferential radiofrequency ablation without endoscopic mucosal resection or endoscopic submucosal dissection reported a 12-month rate of complete response of 84%, the researchers noted (Endoscopy. 2015;47:398-408). There were no serious treatment-related adverse events. Pain was usually self-limited, although one patient required 2 days of narcotics. Two patients developed symptomatic strictures 6-8 weeks after treatment that resolved with balloon dilation. Both of these patients had undergone extensive multifocal ablation. “Circumferential treatment of ESCN [esophageal squamous cell neoplasia] remains problematic for all endoscopic ablative therapies, with a high stricture rate of 20% in our small pilot study of cryoablation and 20%-23% with RFA,” the investigators wrote. “The risk for postablation stricture appears to be related to a long length of ESCN. Optimizing the cryogen dose, technique, and decrease in Lugol’s solution concentration might alter the incidence of postablation strictures for ablative treatments.”
Study participants were 55-90 years old, and six were female. Four were treatment naive, and six had progressed despite endoscopic mucosal resection, RFA, spray cryotherapy, argon plasma coagulation, or multiple therapies. Seven patients had high-grade lesions, two had low-grade lesions, and one had early esophageal squamous cell carcinoma. Most lesions were distally located, but two were in the middle esophagus and one was proximal. The largest lesion measured 4 cm and the maximum length of all lesions in a single patient was 10 cm. Patients did not have visible esophageal masses or evidence of advanced or metastatic disease.
“Comparative effectiveness trials might eventually determine the role of cryoablation in the treatment of early ESCN,” the researchers concluded. An open-label, nonrandomized clinical trial of the balloon cryotherapy device is underway in China (NCT02605759). The article did not list funding sources or disclosures.
FROM GIE
Key clinical point: In a first-in-kind study, endoscopists used focal cryoballoon ablation to eradicate early esophageal squamous cell neoplasias.
Major finding: All 10 patients had a complete response at 3 months. All remained disease free at last follow-up (median, 10.7 months).
Data source: A multicenter study of 10 patients with early high-grade or low-grade esophageal squamous cell neoplasias or early squamous cell carcinomas.
Disclosures: The article did not list funding sources or disclosures.
Same-day antiretroviral treatment increased viral suppression in HIV patients
Patients who received antiretroviral treatment (ART) on the day they underwent HIV testing were more likely to continue treatment and have a lower mortality rate, a study conducted in Port-au-Prince, Haiti, showed.
According to the World Health Organization, ART treatment is essential in stopping the spread of HIV; however, one-quarter to one-third of patients do not continue the treatment process after starting ART, the investigators reported.
Starting ART treatment the same day as HIV testing showed the potential to reduce this problem. “Our findings suggest that ART initiation as soon as possible after HIV testing may be beneficial for clinically stable patients,” wrote Serena Koenig, MD, of the department of infectious diseases at Brigham and Women’s Hospital, Boston, and her coinvestigators. “In resource-poor settings with fragile delivery systems, such as Haiti, the provision of immediate support by care providers at the time of HIV diagnosis can have both structural and individual impact.”
In a randomized, controlled study of 703 patients, 277 of 347 same-day ART patients (80%) retained care, and 10 (3%) died, compared with 256 of 356 patients (72%) in the standard care group, 20 (6%) of whom died (PLoS Med. 2017 Jul 25. doi: 10.1371/journal.pmed.1002357).
Retention of care was defined as attending one clinic visit between 12 months and 15 months after testing, the investigators reported.
The median age of participating patients was 37 years; the median CD4 count was 247 cells/mm3 in the standard care group and 249 cells/mm3 in the same-day group.
At the end of the study, the adjusted mortality risk among patients in the same-day ART group was less than half that of the standard care group (risk ratio, 0.43; P = .033).
Care retention might be related to a more positive mindset among those who start ART immediately after diagnosis, the investigators said.
“Making treatment initiation logistically easier for patients, we believe that same-day counseling and ART initiation increase the sense of hope, optimism, and overall connectedness to the health care system for patients, which have been shown to be important for retention,” Dr. Koenig and her colleagues wrote.
The findings update the 2016 World Health Organization standard guidelines for ART treatment, which report that there is not enough information to recommend same-day treatment. The study was limited by the single-center patient population. Patients also had lower than usual CD4 counts, which may have exaggerated successful results.
The National Institute of Allergy and Infectious Diseases funded the study. The investigators reported they had no relevant financial disclosures.
[email protected]On Twitter @eaztweets
Patients who received antiretroviral treatment (ART) on the day they underwent HIV testing were more likely to continue treatment and have a lower mortality rate, a study conducted in Port-au-Prince, Haiti, showed.
According to the World Health Organization, ART treatment is essential in stopping the spread of HIV; however, one-quarter to one-third of patients do not continue the treatment process after starting ART, the investigators reported.
Starting ART treatment the same day as HIV testing showed the potential to reduce this problem. “Our findings suggest that ART initiation as soon as possible after HIV testing may be beneficial for clinically stable patients,” wrote Serena Koenig, MD, of the department of infectious diseases at Brigham and Women’s Hospital, Boston, and her coinvestigators. “In resource-poor settings with fragile delivery systems, such as Haiti, the provision of immediate support by care providers at the time of HIV diagnosis can have both structural and individual impact.”
In a randomized, controlled study of 703 patients, 277 of 347 same-day ART patients (80%) retained care, and 10 (3%) died, compared with 256 of 356 patients (72%) in the standard care group, 20 (6%) of whom died (PLoS Med. 2017 Jul 25. doi: 10.1371/journal.pmed.1002357).
Retention of care was defined as attending one clinic visit between 12 months and 15 months after testing, the investigators reported.
The median age of participating patients was 37 years; the median CD4 count was 247 cells/mm3 in the standard care group and 249 cells/mm3 in the same-day group.
At the end of the study, the adjusted mortality risk among patients in the same-day ART group was less than half that of the standard care group (risk ratio, 0.43; P = .033).
Care retention might be related to a more positive mindset among those who start ART immediately after diagnosis, the investigators said.
“Making treatment initiation logistically easier for patients, we believe that same-day counseling and ART initiation increase the sense of hope, optimism, and overall connectedness to the health care system for patients, which have been shown to be important for retention,” Dr. Koenig and her colleagues wrote.
The findings update the 2016 World Health Organization standard guidelines for ART treatment, which report that there is not enough information to recommend same-day treatment. The study was limited by the single-center patient population. Patients also had lower than usual CD4 counts, which may have exaggerated successful results.
The National Institute of Allergy and Infectious Diseases funded the study. The investigators reported they had no relevant financial disclosures.
[email protected]On Twitter @eaztweets
Patients who received antiretroviral treatment (ART) on the day they underwent HIV testing were more likely to continue treatment and have a lower mortality rate, a study conducted in Port-au-Prince, Haiti, showed.
According to the World Health Organization, ART treatment is essential in stopping the spread of HIV; however, one-quarter to one-third of patients do not continue the treatment process after starting ART, the investigators reported.
Starting ART treatment the same day as HIV testing showed the potential to reduce this problem. “Our findings suggest that ART initiation as soon as possible after HIV testing may be beneficial for clinically stable patients,” wrote Serena Koenig, MD, of the department of infectious diseases at Brigham and Women’s Hospital, Boston, and her coinvestigators. “In resource-poor settings with fragile delivery systems, such as Haiti, the provision of immediate support by care providers at the time of HIV diagnosis can have both structural and individual impact.”
In a randomized, controlled study of 703 patients, 277 of 347 same-day ART patients (80%) retained care, and 10 (3%) died, compared with 256 of 356 patients (72%) in the standard care group, 20 (6%) of whom died (PLoS Med. 2017 Jul 25. doi: 10.1371/journal.pmed.1002357).
Retention of care was defined as attending one clinic visit between 12 months and 15 months after testing, the investigators reported.
The median age of participating patients was 37 years; the median CD4 count was 247 cells/mm3 in the standard care group and 249 cells/mm3 in the same-day group.
At the end of the study, the adjusted mortality risk among patients in the same-day ART group was less than half that of the standard care group (risk ratio, 0.43; P = .033).
Care retention might be related to a more positive mindset among those who start ART immediately after diagnosis, the investigators said.
“Making treatment initiation logistically easier for patients, we believe that same-day counseling and ART initiation increase the sense of hope, optimism, and overall connectedness to the health care system for patients, which have been shown to be important for retention,” Dr. Koenig and her colleagues wrote.
The findings update the 2016 World Health Organization standard guidelines for ART treatment, which report that there is not enough information to recommend same-day treatment. The study was limited by the single-center patient population. Patients also had lower than usual CD4 counts, which may have exaggerated successful results.
The National Institute of Allergy and Infectious Diseases funded the study. The investigators reported they had no relevant financial disclosures.
[email protected]On Twitter @eaztweets
FROM PLOS MEDICINE
Key clinical point:
Major finding: Of 347 same-day ART patients, 277 (80%) retained care, and 10 (3%) died, compared with 256 (72%) and 20 (6%) in the standard treatment group.
Data source: An unblinded, randomized controlled study of 703 HIV patients from the Haitian Study Group for the Study of Kaposi’s Sarcoma and Opportunistic Infections between August 2013 and October 2015.
Disclosures: The National Institute of Allergy and Infectious Diseases sponsored the study. The investigators reported they had no relevant financial disclosures.
Evaluating the Clinical and Demographic Features of Extrafacial Granuloma Faciale
Granuloma faciale (GF) is a chronic benign leukocytoclastic vasculitis that can be difficult to treat. It is characterized by single or multiple, soft, well-circumscribed papules, plaques, or nodules ranging in color from red, violet, or yellow to brown that may darken with sun exposure.1 Lesions usually are smooth with follicular orifices that are accentuated, thus producing a peau d’orange appearance. Lesions generally are slow to develop and asymptomatic, though some patients report pruritus or burning.2,3 Diagnosis of GF is based on the presence of distinct histologic features. The epidermis usually is spared, with a prominent grenz zone of normal collagen separating the epidermis from a dense infiltrate of neutrophils, lymphocytes, and eosinophils. This mixed inflammatory infiltrate is seen mainly in the superficial dermis but occasionally spreads to the lower dermis and subcutaneous tissues.4
As the name implies, GF usually is confined to the face but occasionally involves extrafacial sites.5-15 The clinical characteristics of these rare extrafacial lesions are not well understood. The purpose of this study was to identify the clinical and demographic features of extrafacial GF in patients treated at Mayo Clinic (Rochester, Minnesota) during a 54-year period.
Methods
This study was approved by the Mayo institutional review board. We searched the Mayo Clinic Rochester dermatology database for all patients with a diagnosis of GF from 1959 through 2013. All histopathology slides were reviewed by a board-certified dermatologist (A.G.B.) and dermatopathologist (A.G.B.) before inclusion in this study. Histologic criteria for diagnosis of GF included the presence of a mixed inflammatory infiltrate of neutrophils, eosinophils, lymphocytes, and histiocytes in the superficial or deep dermis; a prominent grenz zone separating the uninvolved epidermis; and the presence of vascular damage, as seen by fibrin deposition in dermal blood vessels.
Medical records were reviewed for patient demographics and for history pertinent to the diagnosis of GF, including sites involved, appearance, histopathology reports, symptoms, treatments, and outcomes.
Literature Search Strategy
A computerized Ovid MEDLINE database search was undertaken to identify English-language articles concerning GF in humans using the search terms granuloma faciale with extrafacial or disseminated. To ensure that no articles were overlooked, we conducted another search for English-language articles in the Embase database (1946-2013) using the terms granuloma faciale and extrafacial or disseminated.
Statistical Analysis
Descriptive clinical and histopathologic data were summarized using means, medians, and ranges or proportions as appropriate; statistical analysis was performed using SAS software (JMP package).
Results
Ninety-six patients with a diagnosis of GF were identified, and 12 (13%) had a diagnosis of extrafacial GF. Of them, 2 patients had a diagnosis of extrafacial GF supported only by histopathology slides without accompanying clinical records and therefore were excluded from the study. Thus, 10 cases of extrafacial GF were identified from our search and were included in the study group. Clinical data for these patients are summarized in Table 1. The mean age was 58.7 years (range, 26–87 years). Six (60%) patients were male, and all patients were white. Seven patients (70%) had facial GF in addition to extrafacial GF. Six patients reported no symptoms (60%), and 4 (40%) reported pruritus, discomfort, or both associated with their GF lesions.

Extrafacial GF was diagnosed in the following anatomic locations: scalp (n=3 [30%]), posterior auricular area (n=3 [30%]), mid upper back (n=1 [10%]), right shoulder (n=1 [10%]), both ears (n=1 [10%]), right elbow (n=1 [10%]), and left infra-auricular area (n=1 [10%]). Only 1 (10%) patient had multiple extrafacial sites identified.
The lesions were characterized clinically as violet, red, and yellow to brown smooth papules, plaques, and nodules (Figure 1). Biopsies from these lesions showed a subepidermal and adnexal grenz zone; a polymorphous perivascular and periadnexal dermal infiltrate composed of neutrophils, eosinophils, lymphocytes, histiocytes, and plasma cells; and a mild subtle leukocytoclastic vasculitis with subtle mild vascular necrosis (Figure 2).

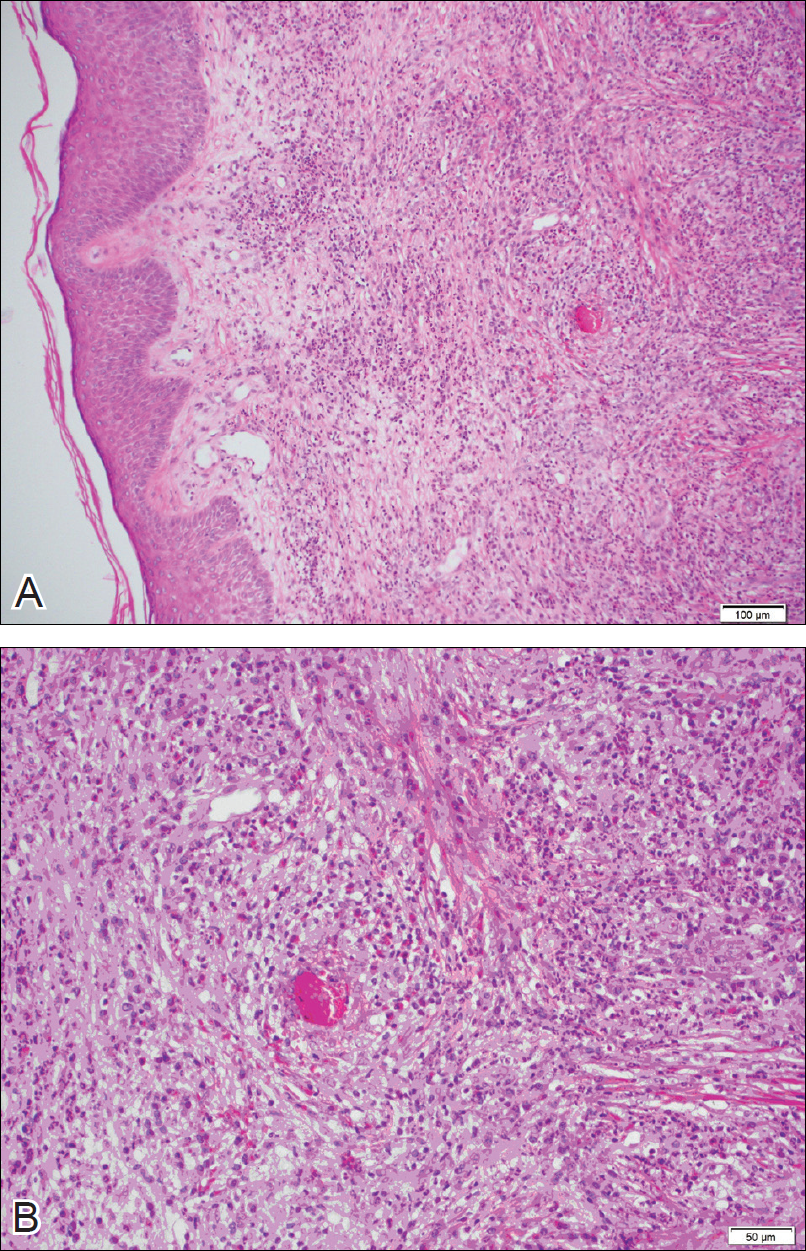
For the 9 patients who elected to undergo GF treatment, the average number of treatments attempted was 2.8 (range, 1–5). The most common method of treatment was a combination of intralesional and topical corticosteroids (n=5 [50%]). Other methods included surgery (n=3 [30%]), dapsone (n=2 [20%]), radiation therapy (n=2 [20%]), cryosurgery (n=1 [10%]), nitrogen mustard (n=1 [10%]), liquid nitrogen (n=1 [10%]), and tar shampoo and fluocinolone acetonide solution 0.01% (n=1 [10%]).
Treatment outcomes were available for 8 of 9 treated patients. Three patients (patients 7, 8, and 10) had long-term successful resolution of their lesions. Patient 7 had an extrafacial lesion that was successfully treated with intralesional and topical corticosteroids, but the facial lesions recurred. The extrafacial GF lesion in patient 8 was found adjacent to a squamous cell carcinoma and was removed with a wide surgical excision that included both lesions. Patient 10 was successfully treated with a combination of liquid nitrogen and topical corticosteroid. Patients 2 and 4 were well controlled while on dapsone; however, once the treatment was discontinued, primarily due to adverse effects, the lesions returned.
Literature Search
Our search of the English-language literature identified 20 patients with extrafacial GF (Table 2). Fifteen (75%) patients were male, which was similar to our study (6/10 [60%]). Our patient population was slightly older with a mean age of 58.7 years compared to a median age of 54 years among those identified in the literature. Additionally, 3 (30%) patients in our study had no facial lesions, as seen in classic GF, which is comparable to 8 (40%) patients identified in the literature.
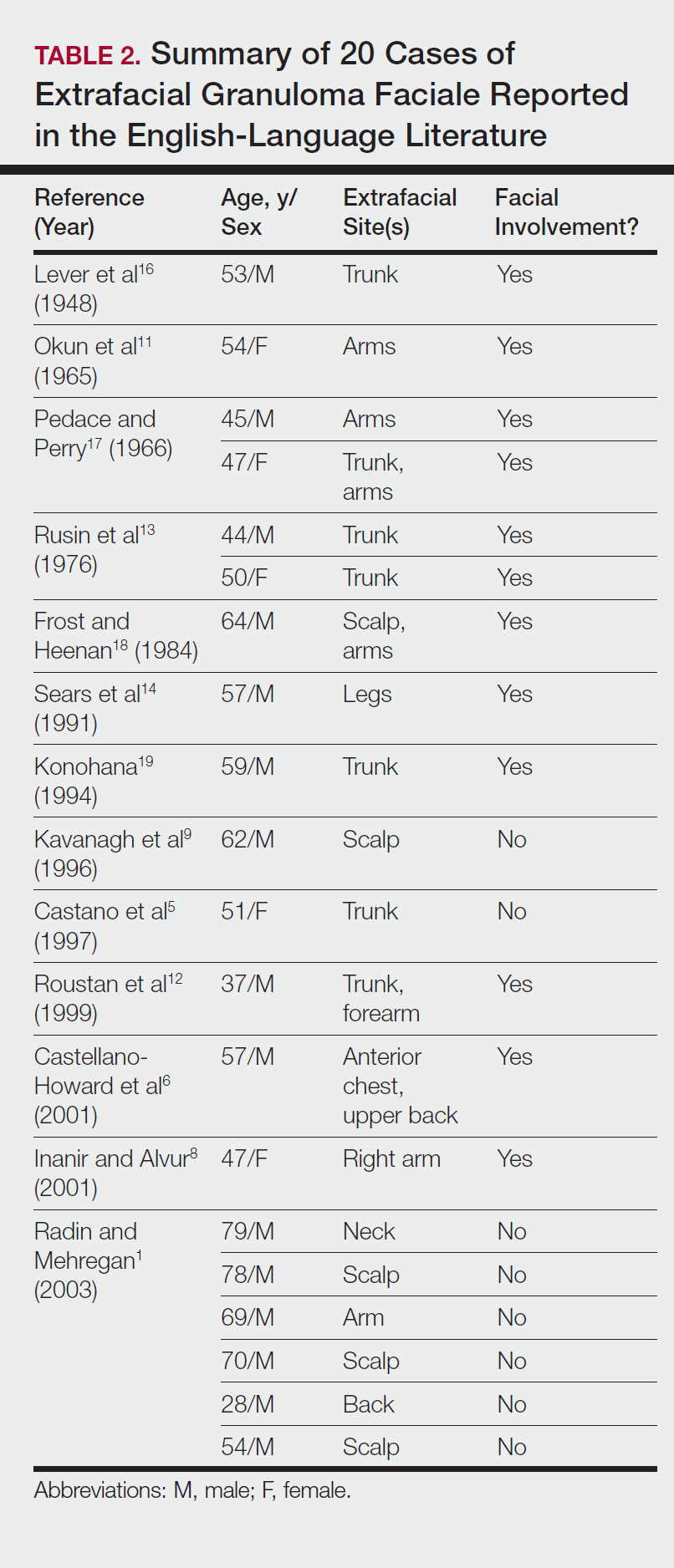
Comment
Extrafacial GF primarily affects white individuals and is more prevalent in men, as demonstrated in our study. Extrafacial GF was most often found in association with facial lesions, with only 3 patients having exclusively extrafacial sites.
Data from the current study indicate that diverse modalities were used to treat extrafacial GF with variable outcomes (chronic recurrence to complete resolution). The most common first-line treatment, intralesional corticosteroid injection, was used in 5 (50%) patients but resulted in only 1 (10%) successful resolution. Other methods frequently used in our study and prior studies were surgical excision, cryotherapy, electrosurgery, and dermabrasion.1,20 These treatments do not appear to be uniformly definitive, and the ablative methods may result in scarring.1 Different laser treatments are emerging for the management of GF lesions. Prior reports of treating facial GF with argon and CO2 lasers have indicated minimized residual scarring and pigmentation.21-23 The use of pulsed dye lasers has resulted in complete clearance of facial GF lesions, without recurrence on long-term follow-up.20,24-26
The latest investigations of immunomodulatory drugs indicate these agents are promising for the management of facial GF. Eetam et al27 reported the successful use of topical tacrolimus to treat facial GF. The relatively low cost and ease of use make these topical medications a competitive alternative to currently available surgical and laser methods. The appearance of all of these novel therapeutic modalities creates the necessity for a randomized trial to establish their efficacy on extrafacial GF lesions.
The wide array of treatments reflects the recalcitrant nature of extrafacial GF lesions. Further insight into the etiology of these lesions is needed to understand their tendency to recur. The important contribution of our study is the observed
Conclusion
The findings from this study and the cases reviewed in the literature provide a unique contribution to the understanding of the clinical and demographic characteristics of extrafacial GF. The rarity of this condition is the single most important constraint of our study, reflected in the emblematic limitations of a retrospective analysis in a select group of patients. The results of analysis of data from our patients were similar to the findings reported in the English-language medical literature. Serious consideration should be given to the development of a national registry for patients with GF. A database containing the clinicopathologic features, treatments, and outcomes for patients with both facial and extrafacial manifestations of GF may be invaluable in evaluating various treatment options and increasing understanding of the etiology and epidemiology of the disease.
- Radin DA, Mehregan DR. Granuloma faciale: distribution of the lesions and review of the literature. Cutis. 2003;72:213-219.
- Dowlati B, Firooz A, Dowlati Y. Granuloma faciale: successful treatment of nine cases with a combination of cryotherapy and intralesional corticosteroid injection. Int J Dermatol. 1997;36:548-551.
- Guill MA, Aton JK. Facial granuloma responsive to dapsone therapy. Arch Dermatol. 1982;118:332-335.
- Ryan TJ. Cutaneous vasculitis. In: Champion RH, Burton JL, Burns DA, et al, eds. Rook/Wilkins/Ebling Textbook of Dermatology. 7th ed. Malden, MA: Blackwell Science; 2004.
- Castano E, Segurado A, Iglesias L, et al. Granuloma faciale entirely in an extrafacial location. Br J Dermatol. 1997;136:978-979.
- Castellano-Howard L, Fairbee SI, Hogan DJ, et al. Extrafacial granuloma faciale: report of a case and response to treatment. Cutis. 2001;67:413-415.
- Cecchi R, Paoli S, Giomi A. Granuloma faciale with extrafacial lesions. Eur J Dermatol. 2002;12:438.
- Inanir I, Alvur Y. Granuloma faciale with extrafacial lesions. Br J Dermatol. 2001;14:360-362.
- Kavanagh GM, McLaren KM, Hunter JA. Extensive extrafacial granuloma faciale of the scalp. Br J Dermatol. 1996;134:595-596.
- Marcoval J, Moreno A, Peyr J. Granuloma faciale: a clinicopathological study of 11 cases. J Am Acad Dermatol. 2004;51:269-273.
- Okun MR, Bauman L, Minor D. Granuloma faciale with lesions on the face and hand. Arch Dermatol. 1965;92:78-80.
- Roustan G, Sanchez Yus E, Salas C, et al. Granuloma faciale with extrafacial lesions. Dermatology. 1999;198:79-82.
- Rusin LJ, Dubin HV, Taylor WB. Disseminated granuloma faciale. Arch Dermatol. 1976;112:1575-1577.
- Sears JK, Gitter DG, Stone MS. Extrafacial granuloma faciale. Arch Dermatol. 1991;127:742-743.
- Zargari O. Disseminated granuloma faciale. Int J Dermatol. 2004;43:210-212.
- Lever WF, Lane CG, Downing JG, et al. Eosinophilic granuloma of the skin: report of three cases. Arch Derm Syphilol. 1948;58:430-438.
- Pedace FJ, Perry HO. Granuloma faciale: a clinical and histopathologic review. Arch Dermatol. 1966;94:387-395.
- Frost FA, Heenan PJ. Facial granuloma. Australas J Dermatol. 1984;25:121-124.
Konohana A. Extrafacial granuloma faciale. J Dermatol. 1994;21:680-682.- Ludwig E, Allam JP, Bieber T, et al. New treatment modalities for granuloma faciale. Br J Dermatol. 2003;149:634-637.
- Apfelberg DB, Druker D, Maser MR, et al. Granuloma faciale: treatment with the argon laser. Arch Dermatol. 1983;119:573-576.
- Apfelberg DB, Maser MR, Lash H, et al. Expanded role of the argon laser in plastic surgery. J Dermatol Surg Oncol. 1983;9:145-151.
- Wheeland RG, Ashley JR, Smith DA, et al. Carbon dioxide laser treatment of granuloma faciale. J Dermatol Surg Oncol. 1984;10:730-733.
- Cheung ST, Lanigan SW. Granuloma faciale treated with the pulsed-dye laser: a case series. Clin Exp Dermatol. 2005;30:373-375.
- Chatrath V, Rohrer TE. Granuloma faciale successfully treated with long-pulsed tunable dye laser. Dermatol Surg. 2002;28:527-529.
- Elston DM. Treatment of granuloma faciale with the pulsed dye laser. Cutis. 2000;65:97-98.
- Eetam I, Ertekin B, Unal I, et al. Granuloma faciale: is it a new indication for pimecrolimus? a case report. J Dermatolog Treat. 2006;17:238-240.
- Johnson WC, Higdon RS, Helwig EB. Granuloma faciale. AMA Arch Derm. 1959;79:42-52.
Granuloma faciale (GF) is a chronic benign leukocytoclastic vasculitis that can be difficult to treat. It is characterized by single or multiple, soft, well-circumscribed papules, plaques, or nodules ranging in color from red, violet, or yellow to brown that may darken with sun exposure.1 Lesions usually are smooth with follicular orifices that are accentuated, thus producing a peau d’orange appearance. Lesions generally are slow to develop and asymptomatic, though some patients report pruritus or burning.2,3 Diagnosis of GF is based on the presence of distinct histologic features. The epidermis usually is spared, with a prominent grenz zone of normal collagen separating the epidermis from a dense infiltrate of neutrophils, lymphocytes, and eosinophils. This mixed inflammatory infiltrate is seen mainly in the superficial dermis but occasionally spreads to the lower dermis and subcutaneous tissues.4
As the name implies, GF usually is confined to the face but occasionally involves extrafacial sites.5-15 The clinical characteristics of these rare extrafacial lesions are not well understood. The purpose of this study was to identify the clinical and demographic features of extrafacial GF in patients treated at Mayo Clinic (Rochester, Minnesota) during a 54-year period.
Methods
This study was approved by the Mayo institutional review board. We searched the Mayo Clinic Rochester dermatology database for all patients with a diagnosis of GF from 1959 through 2013. All histopathology slides were reviewed by a board-certified dermatologist (A.G.B.) and dermatopathologist (A.G.B.) before inclusion in this study. Histologic criteria for diagnosis of GF included the presence of a mixed inflammatory infiltrate of neutrophils, eosinophils, lymphocytes, and histiocytes in the superficial or deep dermis; a prominent grenz zone separating the uninvolved epidermis; and the presence of vascular damage, as seen by fibrin deposition in dermal blood vessels.
Medical records were reviewed for patient demographics and for history pertinent to the diagnosis of GF, including sites involved, appearance, histopathology reports, symptoms, treatments, and outcomes.
Literature Search Strategy
A computerized Ovid MEDLINE database search was undertaken to identify English-language articles concerning GF in humans using the search terms granuloma faciale with extrafacial or disseminated. To ensure that no articles were overlooked, we conducted another search for English-language articles in the Embase database (1946-2013) using the terms granuloma faciale and extrafacial or disseminated.
Statistical Analysis
Descriptive clinical and histopathologic data were summarized using means, medians, and ranges or proportions as appropriate; statistical analysis was performed using SAS software (JMP package).
Results
Ninety-six patients with a diagnosis of GF were identified, and 12 (13%) had a diagnosis of extrafacial GF. Of them, 2 patients had a diagnosis of extrafacial GF supported only by histopathology slides without accompanying clinical records and therefore were excluded from the study. Thus, 10 cases of extrafacial GF were identified from our search and were included in the study group. Clinical data for these patients are summarized in Table 1. The mean age was 58.7 years (range, 26–87 years). Six (60%) patients were male, and all patients were white. Seven patients (70%) had facial GF in addition to extrafacial GF. Six patients reported no symptoms (60%), and 4 (40%) reported pruritus, discomfort, or both associated with their GF lesions.

Extrafacial GF was diagnosed in the following anatomic locations: scalp (n=3 [30%]), posterior auricular area (n=3 [30%]), mid upper back (n=1 [10%]), right shoulder (n=1 [10%]), both ears (n=1 [10%]), right elbow (n=1 [10%]), and left infra-auricular area (n=1 [10%]). Only 1 (10%) patient had multiple extrafacial sites identified.
The lesions were characterized clinically as violet, red, and yellow to brown smooth papules, plaques, and nodules (Figure 1). Biopsies from these lesions showed a subepidermal and adnexal grenz zone; a polymorphous perivascular and periadnexal dermal infiltrate composed of neutrophils, eosinophils, lymphocytes, histiocytes, and plasma cells; and a mild subtle leukocytoclastic vasculitis with subtle mild vascular necrosis (Figure 2).

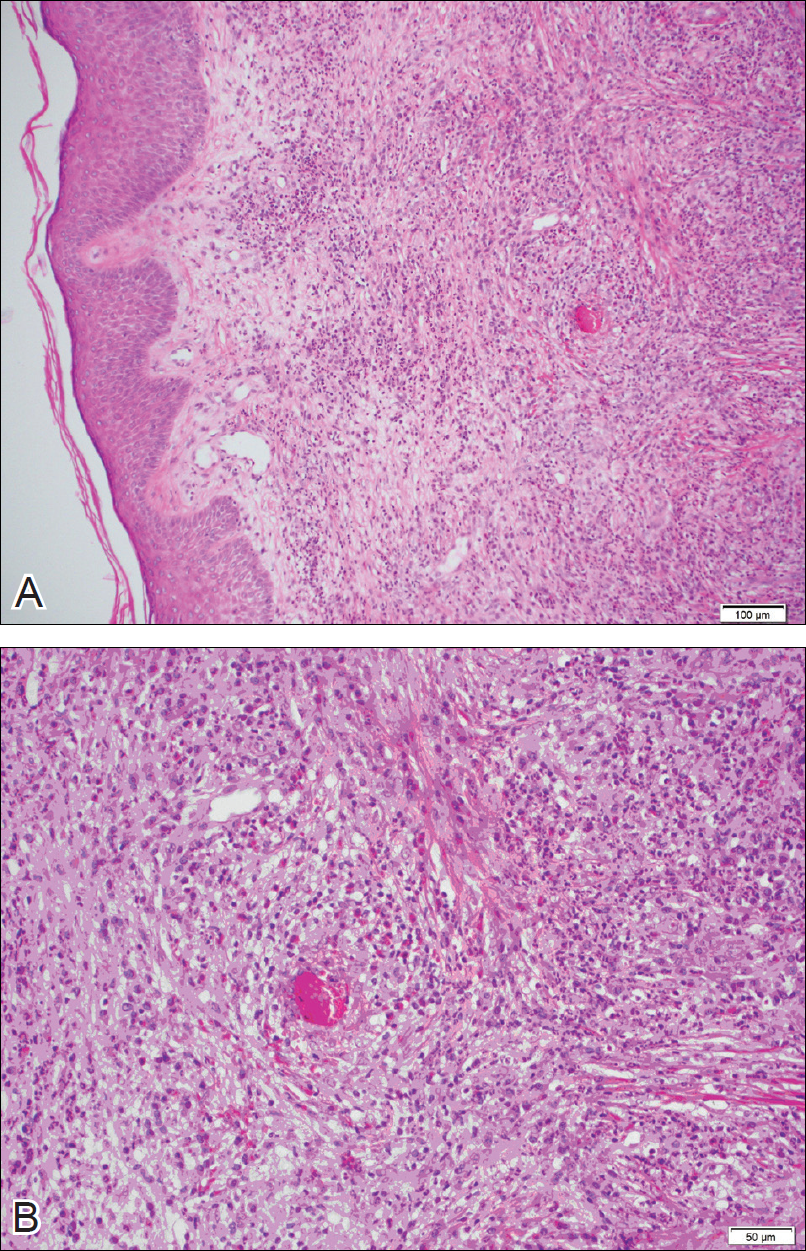
For the 9 patients who elected to undergo GF treatment, the average number of treatments attempted was 2.8 (range, 1–5). The most common method of treatment was a combination of intralesional and topical corticosteroids (n=5 [50%]). Other methods included surgery (n=3 [30%]), dapsone (n=2 [20%]), radiation therapy (n=2 [20%]), cryosurgery (n=1 [10%]), nitrogen mustard (n=1 [10%]), liquid nitrogen (n=1 [10%]), and tar shampoo and fluocinolone acetonide solution 0.01% (n=1 [10%]).
Treatment outcomes were available for 8 of 9 treated patients. Three patients (patients 7, 8, and 10) had long-term successful resolution of their lesions. Patient 7 had an extrafacial lesion that was successfully treated with intralesional and topical corticosteroids, but the facial lesions recurred. The extrafacial GF lesion in patient 8 was found adjacent to a squamous cell carcinoma and was removed with a wide surgical excision that included both lesions. Patient 10 was successfully treated with a combination of liquid nitrogen and topical corticosteroid. Patients 2 and 4 were well controlled while on dapsone; however, once the treatment was discontinued, primarily due to adverse effects, the lesions returned.
Literature Search
Our search of the English-language literature identified 20 patients with extrafacial GF (Table 2). Fifteen (75%) patients were male, which was similar to our study (6/10 [60%]). Our patient population was slightly older with a mean age of 58.7 years compared to a median age of 54 years among those identified in the literature. Additionally, 3 (30%) patients in our study had no facial lesions, as seen in classic GF, which is comparable to 8 (40%) patients identified in the literature.
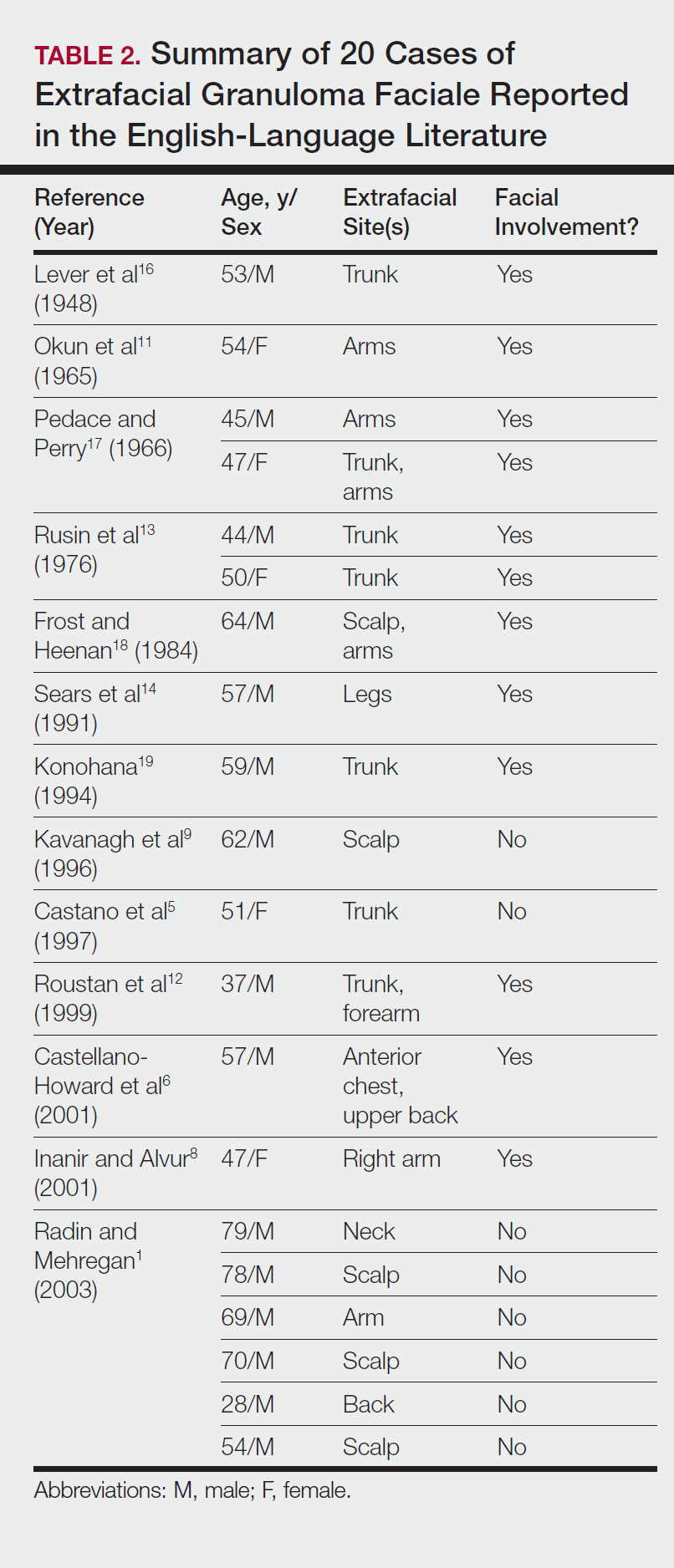
Comment
Extrafacial GF primarily affects white individuals and is more prevalent in men, as demonstrated in our study. Extrafacial GF was most often found in association with facial lesions, with only 3 patients having exclusively extrafacial sites.
Data from the current study indicate that diverse modalities were used to treat extrafacial GF with variable outcomes (chronic recurrence to complete resolution). The most common first-line treatment, intralesional corticosteroid injection, was used in 5 (50%) patients but resulted in only 1 (10%) successful resolution. Other methods frequently used in our study and prior studies were surgical excision, cryotherapy, electrosurgery, and dermabrasion.1,20 These treatments do not appear to be uniformly definitive, and the ablative methods may result in scarring.1 Different laser treatments are emerging for the management of GF lesions. Prior reports of treating facial GF with argon and CO2 lasers have indicated minimized residual scarring and pigmentation.21-23 The use of pulsed dye lasers has resulted in complete clearance of facial GF lesions, without recurrence on long-term follow-up.20,24-26
The latest investigations of immunomodulatory drugs indicate these agents are promising for the management of facial GF. Eetam et al27 reported the successful use of topical tacrolimus to treat facial GF. The relatively low cost and ease of use make these topical medications a competitive alternative to currently available surgical and laser methods. The appearance of all of these novel therapeutic modalities creates the necessity for a randomized trial to establish their efficacy on extrafacial GF lesions.
The wide array of treatments reflects the recalcitrant nature of extrafacial GF lesions. Further insight into the etiology of these lesions is needed to understand their tendency to recur. The important contribution of our study is the observed
Conclusion
The findings from this study and the cases reviewed in the literature provide a unique contribution to the understanding of the clinical and demographic characteristics of extrafacial GF. The rarity of this condition is the single most important constraint of our study, reflected in the emblematic limitations of a retrospective analysis in a select group of patients. The results of analysis of data from our patients were similar to the findings reported in the English-language medical literature. Serious consideration should be given to the development of a national registry for patients with GF. A database containing the clinicopathologic features, treatments, and outcomes for patients with both facial and extrafacial manifestations of GF may be invaluable in evaluating various treatment options and increasing understanding of the etiology and epidemiology of the disease.
Granuloma faciale (GF) is a chronic benign leukocytoclastic vasculitis that can be difficult to treat. It is characterized by single or multiple, soft, well-circumscribed papules, plaques, or nodules ranging in color from red, violet, or yellow to brown that may darken with sun exposure.1 Lesions usually are smooth with follicular orifices that are accentuated, thus producing a peau d’orange appearance. Lesions generally are slow to develop and asymptomatic, though some patients report pruritus or burning.2,3 Diagnosis of GF is based on the presence of distinct histologic features. The epidermis usually is spared, with a prominent grenz zone of normal collagen separating the epidermis from a dense infiltrate of neutrophils, lymphocytes, and eosinophils. This mixed inflammatory infiltrate is seen mainly in the superficial dermis but occasionally spreads to the lower dermis and subcutaneous tissues.4
As the name implies, GF usually is confined to the face but occasionally involves extrafacial sites.5-15 The clinical characteristics of these rare extrafacial lesions are not well understood. The purpose of this study was to identify the clinical and demographic features of extrafacial GF in patients treated at Mayo Clinic (Rochester, Minnesota) during a 54-year period.
Methods
This study was approved by the Mayo institutional review board. We searched the Mayo Clinic Rochester dermatology database for all patients with a diagnosis of GF from 1959 through 2013. All histopathology slides were reviewed by a board-certified dermatologist (A.G.B.) and dermatopathologist (A.G.B.) before inclusion in this study. Histologic criteria for diagnosis of GF included the presence of a mixed inflammatory infiltrate of neutrophils, eosinophils, lymphocytes, and histiocytes in the superficial or deep dermis; a prominent grenz zone separating the uninvolved epidermis; and the presence of vascular damage, as seen by fibrin deposition in dermal blood vessels.
Medical records were reviewed for patient demographics and for history pertinent to the diagnosis of GF, including sites involved, appearance, histopathology reports, symptoms, treatments, and outcomes.
Literature Search Strategy
A computerized Ovid MEDLINE database search was undertaken to identify English-language articles concerning GF in humans using the search terms granuloma faciale with extrafacial or disseminated. To ensure that no articles were overlooked, we conducted another search for English-language articles in the Embase database (1946-2013) using the terms granuloma faciale and extrafacial or disseminated.
Statistical Analysis
Descriptive clinical and histopathologic data were summarized using means, medians, and ranges or proportions as appropriate; statistical analysis was performed using SAS software (JMP package).
Results
Ninety-six patients with a diagnosis of GF were identified, and 12 (13%) had a diagnosis of extrafacial GF. Of them, 2 patients had a diagnosis of extrafacial GF supported only by histopathology slides without accompanying clinical records and therefore were excluded from the study. Thus, 10 cases of extrafacial GF were identified from our search and were included in the study group. Clinical data for these patients are summarized in Table 1. The mean age was 58.7 years (range, 26–87 years). Six (60%) patients were male, and all patients were white. Seven patients (70%) had facial GF in addition to extrafacial GF. Six patients reported no symptoms (60%), and 4 (40%) reported pruritus, discomfort, or both associated with their GF lesions.

Extrafacial GF was diagnosed in the following anatomic locations: scalp (n=3 [30%]), posterior auricular area (n=3 [30%]), mid upper back (n=1 [10%]), right shoulder (n=1 [10%]), both ears (n=1 [10%]), right elbow (n=1 [10%]), and left infra-auricular area (n=1 [10%]). Only 1 (10%) patient had multiple extrafacial sites identified.
The lesions were characterized clinically as violet, red, and yellow to brown smooth papules, plaques, and nodules (Figure 1). Biopsies from these lesions showed a subepidermal and adnexal grenz zone; a polymorphous perivascular and periadnexal dermal infiltrate composed of neutrophils, eosinophils, lymphocytes, histiocytes, and plasma cells; and a mild subtle leukocytoclastic vasculitis with subtle mild vascular necrosis (Figure 2).

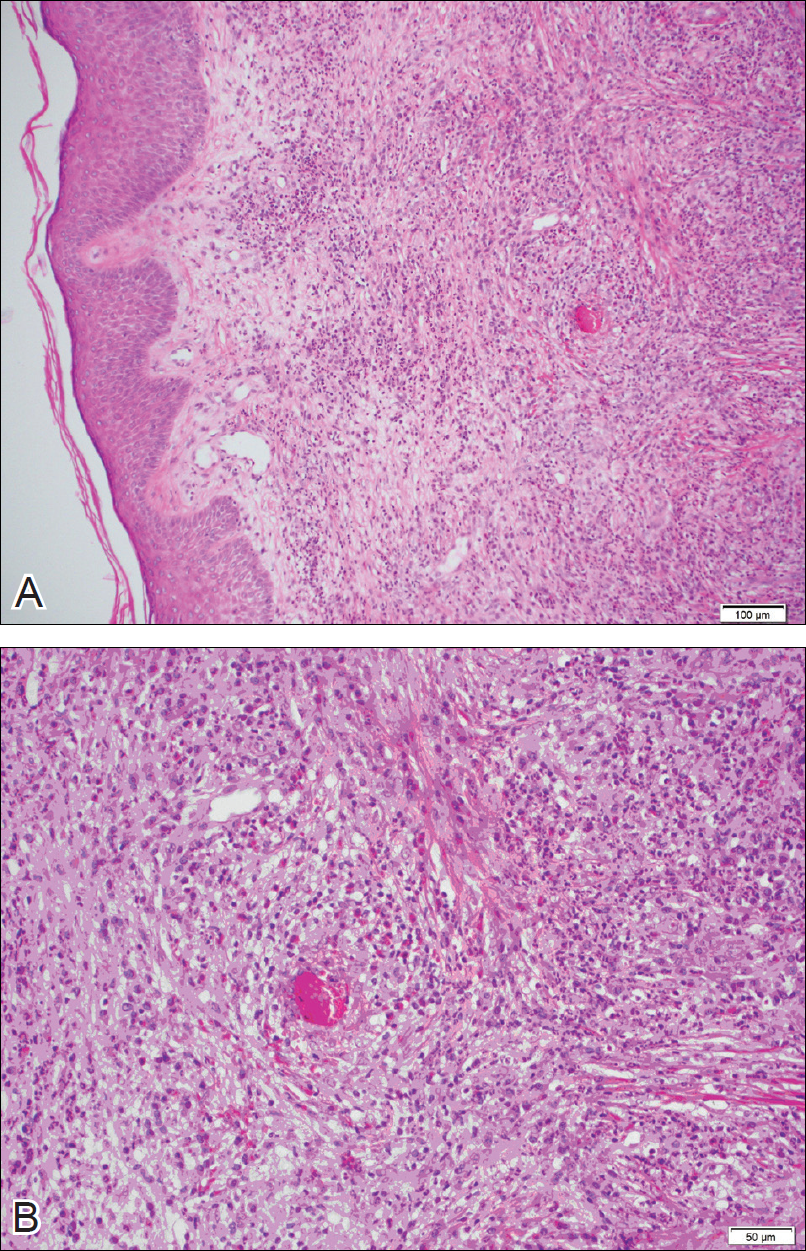
For the 9 patients who elected to undergo GF treatment, the average number of treatments attempted was 2.8 (range, 1–5). The most common method of treatment was a combination of intralesional and topical corticosteroids (n=5 [50%]). Other methods included surgery (n=3 [30%]), dapsone (n=2 [20%]), radiation therapy (n=2 [20%]), cryosurgery (n=1 [10%]), nitrogen mustard (n=1 [10%]), liquid nitrogen (n=1 [10%]), and tar shampoo and fluocinolone acetonide solution 0.01% (n=1 [10%]).
Treatment outcomes were available for 8 of 9 treated patients. Three patients (patients 7, 8, and 10) had long-term successful resolution of their lesions. Patient 7 had an extrafacial lesion that was successfully treated with intralesional and topical corticosteroids, but the facial lesions recurred. The extrafacial GF lesion in patient 8 was found adjacent to a squamous cell carcinoma and was removed with a wide surgical excision that included both lesions. Patient 10 was successfully treated with a combination of liquid nitrogen and topical corticosteroid. Patients 2 and 4 were well controlled while on dapsone; however, once the treatment was discontinued, primarily due to adverse effects, the lesions returned.
Literature Search
Our search of the English-language literature identified 20 patients with extrafacial GF (Table 2). Fifteen (75%) patients were male, which was similar to our study (6/10 [60%]). Our patient population was slightly older with a mean age of 58.7 years compared to a median age of 54 years among those identified in the literature. Additionally, 3 (30%) patients in our study had no facial lesions, as seen in classic GF, which is comparable to 8 (40%) patients identified in the literature.
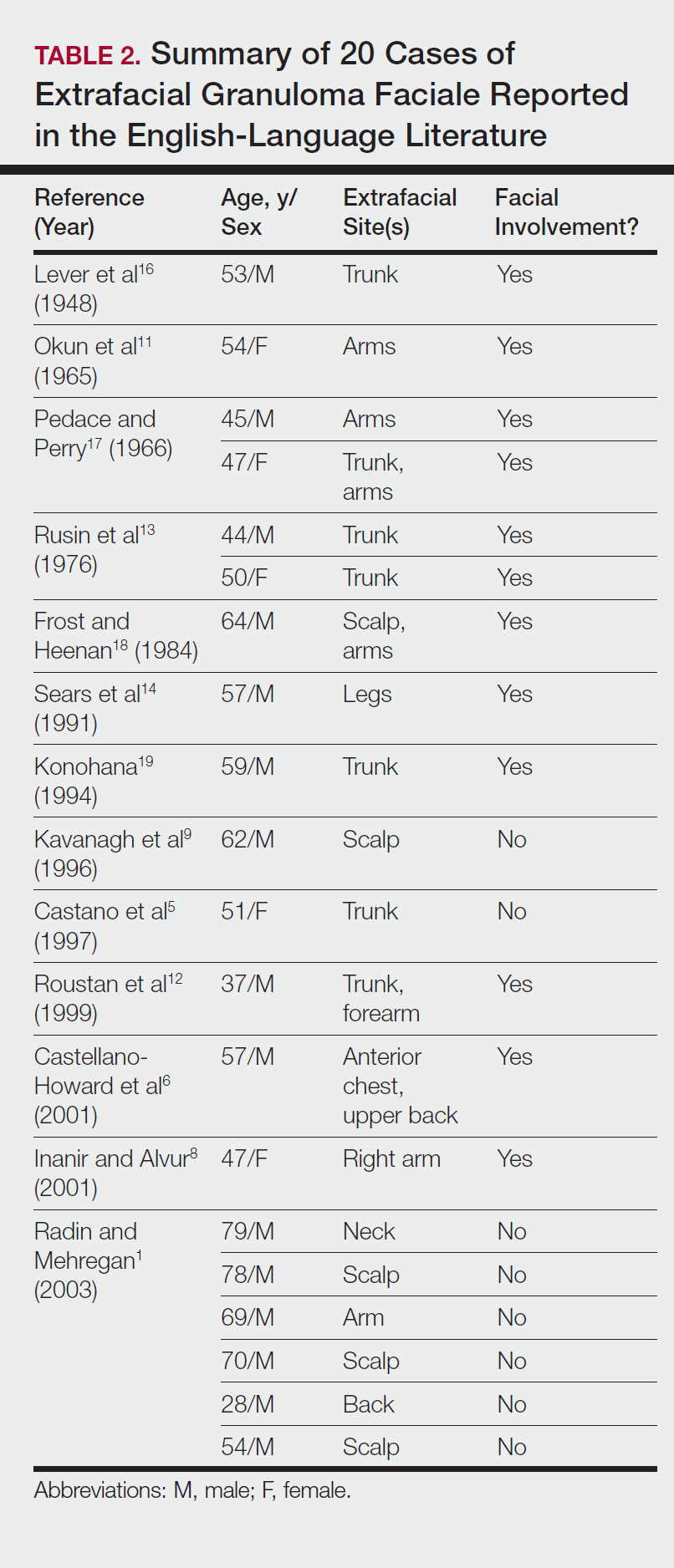
Comment
Extrafacial GF primarily affects white individuals and is more prevalent in men, as demonstrated in our study. Extrafacial GF was most often found in association with facial lesions, with only 3 patients having exclusively extrafacial sites.
Data from the current study indicate that diverse modalities were used to treat extrafacial GF with variable outcomes (chronic recurrence to complete resolution). The most common first-line treatment, intralesional corticosteroid injection, was used in 5 (50%) patients but resulted in only 1 (10%) successful resolution. Other methods frequently used in our study and prior studies were surgical excision, cryotherapy, electrosurgery, and dermabrasion.1,20 These treatments do not appear to be uniformly definitive, and the ablative methods may result in scarring.1 Different laser treatments are emerging for the management of GF lesions. Prior reports of treating facial GF with argon and CO2 lasers have indicated minimized residual scarring and pigmentation.21-23 The use of pulsed dye lasers has resulted in complete clearance of facial GF lesions, without recurrence on long-term follow-up.20,24-26
The latest investigations of immunomodulatory drugs indicate these agents are promising for the management of facial GF. Eetam et al27 reported the successful use of topical tacrolimus to treat facial GF. The relatively low cost and ease of use make these topical medications a competitive alternative to currently available surgical and laser methods. The appearance of all of these novel therapeutic modalities creates the necessity for a randomized trial to establish their efficacy on extrafacial GF lesions.
The wide array of treatments reflects the recalcitrant nature of extrafacial GF lesions. Further insight into the etiology of these lesions is needed to understand their tendency to recur. The important contribution of our study is the observed
Conclusion
The findings from this study and the cases reviewed in the literature provide a unique contribution to the understanding of the clinical and demographic characteristics of extrafacial GF. The rarity of this condition is the single most important constraint of our study, reflected in the emblematic limitations of a retrospective analysis in a select group of patients. The results of analysis of data from our patients were similar to the findings reported in the English-language medical literature. Serious consideration should be given to the development of a national registry for patients with GF. A database containing the clinicopathologic features, treatments, and outcomes for patients with both facial and extrafacial manifestations of GF may be invaluable in evaluating various treatment options and increasing understanding of the etiology and epidemiology of the disease.
- Radin DA, Mehregan DR. Granuloma faciale: distribution of the lesions and review of the literature. Cutis. 2003;72:213-219.
- Dowlati B, Firooz A, Dowlati Y. Granuloma faciale: successful treatment of nine cases with a combination of cryotherapy and intralesional corticosteroid injection. Int J Dermatol. 1997;36:548-551.
- Guill MA, Aton JK. Facial granuloma responsive to dapsone therapy. Arch Dermatol. 1982;118:332-335.
- Ryan TJ. Cutaneous vasculitis. In: Champion RH, Burton JL, Burns DA, et al, eds. Rook/Wilkins/Ebling Textbook of Dermatology. 7th ed. Malden, MA: Blackwell Science; 2004.
- Castano E, Segurado A, Iglesias L, et al. Granuloma faciale entirely in an extrafacial location. Br J Dermatol. 1997;136:978-979.
- Castellano-Howard L, Fairbee SI, Hogan DJ, et al. Extrafacial granuloma faciale: report of a case and response to treatment. Cutis. 2001;67:413-415.
- Cecchi R, Paoli S, Giomi A. Granuloma faciale with extrafacial lesions. Eur J Dermatol. 2002;12:438.
- Inanir I, Alvur Y. Granuloma faciale with extrafacial lesions. Br J Dermatol. 2001;14:360-362.
- Kavanagh GM, McLaren KM, Hunter JA. Extensive extrafacial granuloma faciale of the scalp. Br J Dermatol. 1996;134:595-596.
- Marcoval J, Moreno A, Peyr J. Granuloma faciale: a clinicopathological study of 11 cases. J Am Acad Dermatol. 2004;51:269-273.
- Okun MR, Bauman L, Minor D. Granuloma faciale with lesions on the face and hand. Arch Dermatol. 1965;92:78-80.
- Roustan G, Sanchez Yus E, Salas C, et al. Granuloma faciale with extrafacial lesions. Dermatology. 1999;198:79-82.
- Rusin LJ, Dubin HV, Taylor WB. Disseminated granuloma faciale. Arch Dermatol. 1976;112:1575-1577.
- Sears JK, Gitter DG, Stone MS. Extrafacial granuloma faciale. Arch Dermatol. 1991;127:742-743.
- Zargari O. Disseminated granuloma faciale. Int J Dermatol. 2004;43:210-212.
- Lever WF, Lane CG, Downing JG, et al. Eosinophilic granuloma of the skin: report of three cases. Arch Derm Syphilol. 1948;58:430-438.
- Pedace FJ, Perry HO. Granuloma faciale: a clinical and histopathologic review. Arch Dermatol. 1966;94:387-395.
- Frost FA, Heenan PJ. Facial granuloma. Australas J Dermatol. 1984;25:121-124.
Konohana A. Extrafacial granuloma faciale. J Dermatol. 1994;21:680-682.- Ludwig E, Allam JP, Bieber T, et al. New treatment modalities for granuloma faciale. Br J Dermatol. 2003;149:634-637.
- Apfelberg DB, Druker D, Maser MR, et al. Granuloma faciale: treatment with the argon laser. Arch Dermatol. 1983;119:573-576.
- Apfelberg DB, Maser MR, Lash H, et al. Expanded role of the argon laser in plastic surgery. J Dermatol Surg Oncol. 1983;9:145-151.
- Wheeland RG, Ashley JR, Smith DA, et al. Carbon dioxide laser treatment of granuloma faciale. J Dermatol Surg Oncol. 1984;10:730-733.
- Cheung ST, Lanigan SW. Granuloma faciale treated with the pulsed-dye laser: a case series. Clin Exp Dermatol. 2005;30:373-375.
- Chatrath V, Rohrer TE. Granuloma faciale successfully treated with long-pulsed tunable dye laser. Dermatol Surg. 2002;28:527-529.
- Elston DM. Treatment of granuloma faciale with the pulsed dye laser. Cutis. 2000;65:97-98.
- Eetam I, Ertekin B, Unal I, et al. Granuloma faciale: is it a new indication for pimecrolimus? a case report. J Dermatolog Treat. 2006;17:238-240.
- Johnson WC, Higdon RS, Helwig EB. Granuloma faciale. AMA Arch Derm. 1959;79:42-52.
- Radin DA, Mehregan DR. Granuloma faciale: distribution of the lesions and review of the literature. Cutis. 2003;72:213-219.
- Dowlati B, Firooz A, Dowlati Y. Granuloma faciale: successful treatment of nine cases with a combination of cryotherapy and intralesional corticosteroid injection. Int J Dermatol. 1997;36:548-551.
- Guill MA, Aton JK. Facial granuloma responsive to dapsone therapy. Arch Dermatol. 1982;118:332-335.
- Ryan TJ. Cutaneous vasculitis. In: Champion RH, Burton JL, Burns DA, et al, eds. Rook/Wilkins/Ebling Textbook of Dermatology. 7th ed. Malden, MA: Blackwell Science; 2004.
- Castano E, Segurado A, Iglesias L, et al. Granuloma faciale entirely in an extrafacial location. Br J Dermatol. 1997;136:978-979.
- Castellano-Howard L, Fairbee SI, Hogan DJ, et al. Extrafacial granuloma faciale: report of a case and response to treatment. Cutis. 2001;67:413-415.
- Cecchi R, Paoli S, Giomi A. Granuloma faciale with extrafacial lesions. Eur J Dermatol. 2002;12:438.
- Inanir I, Alvur Y. Granuloma faciale with extrafacial lesions. Br J Dermatol. 2001;14:360-362.
- Kavanagh GM, McLaren KM, Hunter JA. Extensive extrafacial granuloma faciale of the scalp. Br J Dermatol. 1996;134:595-596.
- Marcoval J, Moreno A, Peyr J. Granuloma faciale: a clinicopathological study of 11 cases. J Am Acad Dermatol. 2004;51:269-273.
- Okun MR, Bauman L, Minor D. Granuloma faciale with lesions on the face and hand. Arch Dermatol. 1965;92:78-80.
- Roustan G, Sanchez Yus E, Salas C, et al. Granuloma faciale with extrafacial lesions. Dermatology. 1999;198:79-82.
- Rusin LJ, Dubin HV, Taylor WB. Disseminated granuloma faciale. Arch Dermatol. 1976;112:1575-1577.
- Sears JK, Gitter DG, Stone MS. Extrafacial granuloma faciale. Arch Dermatol. 1991;127:742-743.
- Zargari O. Disseminated granuloma faciale. Int J Dermatol. 2004;43:210-212.
- Lever WF, Lane CG, Downing JG, et al. Eosinophilic granuloma of the skin: report of three cases. Arch Derm Syphilol. 1948;58:430-438.
- Pedace FJ, Perry HO. Granuloma faciale: a clinical and histopathologic review. Arch Dermatol. 1966;94:387-395.
- Frost FA, Heenan PJ. Facial granuloma. Australas J Dermatol. 1984;25:121-124.
Konohana A. Extrafacial granuloma faciale. J Dermatol. 1994;21:680-682.- Ludwig E, Allam JP, Bieber T, et al. New treatment modalities for granuloma faciale. Br J Dermatol. 2003;149:634-637.
- Apfelberg DB, Druker D, Maser MR, et al. Granuloma faciale: treatment with the argon laser. Arch Dermatol. 1983;119:573-576.
- Apfelberg DB, Maser MR, Lash H, et al. Expanded role of the argon laser in plastic surgery. J Dermatol Surg Oncol. 1983;9:145-151.
- Wheeland RG, Ashley JR, Smith DA, et al. Carbon dioxide laser treatment of granuloma faciale. J Dermatol Surg Oncol. 1984;10:730-733.
- Cheung ST, Lanigan SW. Granuloma faciale treated with the pulsed-dye laser: a case series. Clin Exp Dermatol. 2005;30:373-375.
- Chatrath V, Rohrer TE. Granuloma faciale successfully treated with long-pulsed tunable dye laser. Dermatol Surg. 2002;28:527-529.
- Elston DM. Treatment of granuloma faciale with the pulsed dye laser. Cutis. 2000;65:97-98.
- Eetam I, Ertekin B, Unal I, et al. Granuloma faciale: is it a new indication for pimecrolimus? a case report. J Dermatolog Treat. 2006;17:238-240.
- Johnson WC, Higdon RS, Helwig EB. Granuloma faciale. AMA Arch Derm. 1959;79:42-52.
Practice Points
- Extrafacial lesions are rare in granuloma faciale (GF).
- Extrafacial GF should be included in the differential diagnosis of well-demarcated plaques and nodules found on the trunk or extremities.
- Diagnosis of extrafacial GF is based on the presence of distinct histologic features identical to GF.
- Granuloma faciale is a chronic benign leukocytoclastic vasculitis that can be difficult to treat.
VIDEO: Further CTE correlation found in deceased American football players
Evidence of a correlation between chronic traumatic encephalopathy (CTE) and playing American football was strengthened in the largest retrospective study cohort to date.
The progressive neurodegenerative disease associated with recurrent head trauma has been linked to football over the past decade. However, this new study took steps to solidify the connection by studying 202 deceased brains, more than double the size of a previous 2013 report.
First author Jesse Mez, MD, of Boston University, and his colleagues examined the brains donated to a brain bank jointly run by the VA Boston Healthcare System, Boston University, and the Concussion Legacy Foundation. They correlated their findings with interviews and questionnaires filled out in 2014 by those close to the donors (JAMA. 2017 Jul 25. doi: 10.1001/jama.2017.8334).
The donors were male, and a majority (79%) were white. The average age at death was 67 years. In the mild cases, there was an average of 13 years of play; in severe cases, the average was 15.8 years.
The researchers found evidence of CTE in 177 (88%) of the 202 brains of football players, with cases found in 3 (21%) who played only in high school, 48 (91%) who played in college, 9 (64%) semiprofessional players, 7 (88%) Canadian Football League players, and 110 (99%) NFL players, according to investigators.
“Nearly all of the former NFL players in this study had CTE pathology, and this pathology was frequently severe,” noted Dr. Mez and his coinvestigators. ”These findings suggest that CTE may be related to prior participation in football and that a high level of play may be related to substantial disease burden.”
Severity of CTE positively correlated with longer playing history and more competitive levels of play. According to the investigators, severe cases of CTE were found in none of the high school players, 27 college players (56%), 5 semiprofessional players (56%), 6 Canadian professional players (86%), and 95 NFL players (86%).
All participants with CTE commonly displayed certain symptoms regardless of severity level.
Impulsiveness occurred in 23 mild cases (89%) and 65 severe cases (80%). Depression was seen in 18 mild cases (67%) and 46 severe cases (56%). A total of 13 players (50%) with mild symptoms showed apathy, compared with 43 with severe symptoms (52%). Anxiety was reported for 14 mild cases (52%) and 41 severe cases (50%). Cognitive symptoms such as problems with memory and attention were also common at both levels of severity, with 19 cases (73%) and 18 cases (69%), respectively, among donors with mild CTE, and 76 (92%) and 67 (81%) among donors with severe CTE.
Those interviewed who were close to the donors also reported other behavior or mood symptoms that the investigators inferred to be related to CTE.
“Many of these participants had a substance use disorder, demonstrated suicidality, or had a family history of psychiatric illness,” the investigators wrote. “Behavior or mood symptoms may be the initial presentation for a subset of individuals with CTE, or alternatively, CTE [phosphorylated tau] pathology may lower the threshold for psychiatric manifestations in susceptible individuals.”
The investigators asserted that the correlation of CTE diagnosis and severity may be more nuanced than just how many times a player is hit.
“Several other football-related factors may influence CTE risk and disease severity, including but not limited to age at first exposure to football, duration of play, player position, cumulative hits, and linear and rotational acceleration of hits,” Dr. Mez and his associates wrote. “Recent work in living former football players has shown that age at first exposure may be related to impaired cognitive performance and altered corpus callosum white matter and that cumulative hits may be related to impairment on self-report and objective measures of cognition, mood, and behavior, although it is unclear if any of these outcomes are related to CTE pathology.”
This study was limited by the potential bias of donors who participated in the program. Researchers acknowledge that public awareness of the issue of CTE and head trauma may have influenced players with symptoms to donate their brains, thereby increasing the CTE frequency in the sample.
In addition, the brain bank where the sample was taken is not representative of the entire population of American football players, as most donors played at the college, semi-professional, and professional level, as opposed to only high school or youth leagues.
The senior author of the study, Ann C. McKee, MD, discussed the study further in a related video interview.
The National Institute of Neurological Disorders and Stroke, the National Institute of Aging, the U.S. Department of Defense, the U.S. Department of Veterans Affairs, the National Operating Committee on Standards for Athletic Equipment, the Alzheimer’s Association, the Concussion Legacy Foundation, the Andlinger Family Foundation, the WWE, and the NFL supported the study. Five authors reported receiving support from relevant sources, including the NFL.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @eaztweets
Traumatic brain injuries (TBIs) are a serious health concern that currently affect 10 million people per year worldwide.
While a majority of TBIs are caused by car crashes, contact sports are estimated to cause between 1.6-3.8 million concussions in the United States every year, making the root of this study – to learn more about CTE among those in contact sports – imperative.
This study used the largest CTE cohort to date, but it is important to read the results, which are concerning, within the context of the study.
Results from the informants who filled out the questionnaires – most commonly friends or family of the deceased – showed cognitive symptoms in 88% of donors and behavioral symptoms in 95%, compared with 5% and 20% prevalence, respectively, among a questionnaire-based study filled out by retired National Football League players. This may mean that rates of symptomatic CTE may be lower outside of a selected cohort of former players.
While early-stage CTE was found in some high school players, most individuals do not play football beyond a high school level, and the link between high school football and future neurological decline was not well established in this study.
This study is a good example of the progress that has been made in TBI research, but there are still many fundamental questions that need to be answered. The next step will be improving disease models and expanding the studies of at-risk populations.
It is of the utmost importance that these improvements are made immediately; increasing our knowledge and public awareness of TBIs is paramount.
Gil Rabinovici, MD, is associate professor of neurology at the University of California–San Francisco, and an associate editor for JAMA Neurology. He receives research support from Avid Radiopharmaceuticals, Eli Lilly, GE Healthcare, and Piramal. He has received consulting or speaking honoraria from Eisai, Genentech, Lundbeck, Merck, Putnam, and Roche. These comments were taken from an editorial (JAMA 2017 Jul 25. doi: 10.1001/jama.2017.9353 ).
Traumatic brain injuries (TBIs) are a serious health concern that currently affect 10 million people per year worldwide.
While a majority of TBIs are caused by car crashes, contact sports are estimated to cause between 1.6-3.8 million concussions in the United States every year, making the root of this study – to learn more about CTE among those in contact sports – imperative.
This study used the largest CTE cohort to date, but it is important to read the results, which are concerning, within the context of the study.
Results from the informants who filled out the questionnaires – most commonly friends or family of the deceased – showed cognitive symptoms in 88% of donors and behavioral symptoms in 95%, compared with 5% and 20% prevalence, respectively, among a questionnaire-based study filled out by retired National Football League players. This may mean that rates of symptomatic CTE may be lower outside of a selected cohort of former players.
While early-stage CTE was found in some high school players, most individuals do not play football beyond a high school level, and the link between high school football and future neurological decline was not well established in this study.
This study is a good example of the progress that has been made in TBI research, but there are still many fundamental questions that need to be answered. The next step will be improving disease models and expanding the studies of at-risk populations.
It is of the utmost importance that these improvements are made immediately; increasing our knowledge and public awareness of TBIs is paramount.
Gil Rabinovici, MD, is associate professor of neurology at the University of California–San Francisco, and an associate editor for JAMA Neurology. He receives research support from Avid Radiopharmaceuticals, Eli Lilly, GE Healthcare, and Piramal. He has received consulting or speaking honoraria from Eisai, Genentech, Lundbeck, Merck, Putnam, and Roche. These comments were taken from an editorial (JAMA 2017 Jul 25. doi: 10.1001/jama.2017.9353 ).
Traumatic brain injuries (TBIs) are a serious health concern that currently affect 10 million people per year worldwide.
While a majority of TBIs are caused by car crashes, contact sports are estimated to cause between 1.6-3.8 million concussions in the United States every year, making the root of this study – to learn more about CTE among those in contact sports – imperative.
This study used the largest CTE cohort to date, but it is important to read the results, which are concerning, within the context of the study.
Results from the informants who filled out the questionnaires – most commonly friends or family of the deceased – showed cognitive symptoms in 88% of donors and behavioral symptoms in 95%, compared with 5% and 20% prevalence, respectively, among a questionnaire-based study filled out by retired National Football League players. This may mean that rates of symptomatic CTE may be lower outside of a selected cohort of former players.
While early-stage CTE was found in some high school players, most individuals do not play football beyond a high school level, and the link between high school football and future neurological decline was not well established in this study.
This study is a good example of the progress that has been made in TBI research, but there are still many fundamental questions that need to be answered. The next step will be improving disease models and expanding the studies of at-risk populations.
It is of the utmost importance that these improvements are made immediately; increasing our knowledge and public awareness of TBIs is paramount.
Gil Rabinovici, MD, is associate professor of neurology at the University of California–San Francisco, and an associate editor for JAMA Neurology. He receives research support from Avid Radiopharmaceuticals, Eli Lilly, GE Healthcare, and Piramal. He has received consulting or speaking honoraria from Eisai, Genentech, Lundbeck, Merck, Putnam, and Roche. These comments were taken from an editorial (JAMA 2017 Jul 25. doi: 10.1001/jama.2017.9353 ).
Evidence of a correlation between chronic traumatic encephalopathy (CTE) and playing American football was strengthened in the largest retrospective study cohort to date.
The progressive neurodegenerative disease associated with recurrent head trauma has been linked to football over the past decade. However, this new study took steps to solidify the connection by studying 202 deceased brains, more than double the size of a previous 2013 report.
First author Jesse Mez, MD, of Boston University, and his colleagues examined the brains donated to a brain bank jointly run by the VA Boston Healthcare System, Boston University, and the Concussion Legacy Foundation. They correlated their findings with interviews and questionnaires filled out in 2014 by those close to the donors (JAMA. 2017 Jul 25. doi: 10.1001/jama.2017.8334).
The donors were male, and a majority (79%) were white. The average age at death was 67 years. In the mild cases, there was an average of 13 years of play; in severe cases, the average was 15.8 years.
The researchers found evidence of CTE in 177 (88%) of the 202 brains of football players, with cases found in 3 (21%) who played only in high school, 48 (91%) who played in college, 9 (64%) semiprofessional players, 7 (88%) Canadian Football League players, and 110 (99%) NFL players, according to investigators.
“Nearly all of the former NFL players in this study had CTE pathology, and this pathology was frequently severe,” noted Dr. Mez and his coinvestigators. ”These findings suggest that CTE may be related to prior participation in football and that a high level of play may be related to substantial disease burden.”
Severity of CTE positively correlated with longer playing history and more competitive levels of play. According to the investigators, severe cases of CTE were found in none of the high school players, 27 college players (56%), 5 semiprofessional players (56%), 6 Canadian professional players (86%), and 95 NFL players (86%).
All participants with CTE commonly displayed certain symptoms regardless of severity level.
Impulsiveness occurred in 23 mild cases (89%) and 65 severe cases (80%). Depression was seen in 18 mild cases (67%) and 46 severe cases (56%). A total of 13 players (50%) with mild symptoms showed apathy, compared with 43 with severe symptoms (52%). Anxiety was reported for 14 mild cases (52%) and 41 severe cases (50%). Cognitive symptoms such as problems with memory and attention were also common at both levels of severity, with 19 cases (73%) and 18 cases (69%), respectively, among donors with mild CTE, and 76 (92%) and 67 (81%) among donors with severe CTE.
Those interviewed who were close to the donors also reported other behavior or mood symptoms that the investigators inferred to be related to CTE.
“Many of these participants had a substance use disorder, demonstrated suicidality, or had a family history of psychiatric illness,” the investigators wrote. “Behavior or mood symptoms may be the initial presentation for a subset of individuals with CTE, or alternatively, CTE [phosphorylated tau] pathology may lower the threshold for psychiatric manifestations in susceptible individuals.”
The investigators asserted that the correlation of CTE diagnosis and severity may be more nuanced than just how many times a player is hit.
“Several other football-related factors may influence CTE risk and disease severity, including but not limited to age at first exposure to football, duration of play, player position, cumulative hits, and linear and rotational acceleration of hits,” Dr. Mez and his associates wrote. “Recent work in living former football players has shown that age at first exposure may be related to impaired cognitive performance and altered corpus callosum white matter and that cumulative hits may be related to impairment on self-report and objective measures of cognition, mood, and behavior, although it is unclear if any of these outcomes are related to CTE pathology.”
This study was limited by the potential bias of donors who participated in the program. Researchers acknowledge that public awareness of the issue of CTE and head trauma may have influenced players with symptoms to donate their brains, thereby increasing the CTE frequency in the sample.
In addition, the brain bank where the sample was taken is not representative of the entire population of American football players, as most donors played at the college, semi-professional, and professional level, as opposed to only high school or youth leagues.
The senior author of the study, Ann C. McKee, MD, discussed the study further in a related video interview.
The National Institute of Neurological Disorders and Stroke, the National Institute of Aging, the U.S. Department of Defense, the U.S. Department of Veterans Affairs, the National Operating Committee on Standards for Athletic Equipment, the Alzheimer’s Association, the Concussion Legacy Foundation, the Andlinger Family Foundation, the WWE, and the NFL supported the study. Five authors reported receiving support from relevant sources, including the NFL.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @eaztweets
Evidence of a correlation between chronic traumatic encephalopathy (CTE) and playing American football was strengthened in the largest retrospective study cohort to date.
The progressive neurodegenerative disease associated with recurrent head trauma has been linked to football over the past decade. However, this new study took steps to solidify the connection by studying 202 deceased brains, more than double the size of a previous 2013 report.
First author Jesse Mez, MD, of Boston University, and his colleagues examined the brains donated to a brain bank jointly run by the VA Boston Healthcare System, Boston University, and the Concussion Legacy Foundation. They correlated their findings with interviews and questionnaires filled out in 2014 by those close to the donors (JAMA. 2017 Jul 25. doi: 10.1001/jama.2017.8334).
The donors were male, and a majority (79%) were white. The average age at death was 67 years. In the mild cases, there was an average of 13 years of play; in severe cases, the average was 15.8 years.
The researchers found evidence of CTE in 177 (88%) of the 202 brains of football players, with cases found in 3 (21%) who played only in high school, 48 (91%) who played in college, 9 (64%) semiprofessional players, 7 (88%) Canadian Football League players, and 110 (99%) NFL players, according to investigators.
“Nearly all of the former NFL players in this study had CTE pathology, and this pathology was frequently severe,” noted Dr. Mez and his coinvestigators. ”These findings suggest that CTE may be related to prior participation in football and that a high level of play may be related to substantial disease burden.”
Severity of CTE positively correlated with longer playing history and more competitive levels of play. According to the investigators, severe cases of CTE were found in none of the high school players, 27 college players (56%), 5 semiprofessional players (56%), 6 Canadian professional players (86%), and 95 NFL players (86%).
All participants with CTE commonly displayed certain symptoms regardless of severity level.
Impulsiveness occurred in 23 mild cases (89%) and 65 severe cases (80%). Depression was seen in 18 mild cases (67%) and 46 severe cases (56%). A total of 13 players (50%) with mild symptoms showed apathy, compared with 43 with severe symptoms (52%). Anxiety was reported for 14 mild cases (52%) and 41 severe cases (50%). Cognitive symptoms such as problems with memory and attention were also common at both levels of severity, with 19 cases (73%) and 18 cases (69%), respectively, among donors with mild CTE, and 76 (92%) and 67 (81%) among donors with severe CTE.
Those interviewed who were close to the donors also reported other behavior or mood symptoms that the investigators inferred to be related to CTE.
“Many of these participants had a substance use disorder, demonstrated suicidality, or had a family history of psychiatric illness,” the investigators wrote. “Behavior or mood symptoms may be the initial presentation for a subset of individuals with CTE, or alternatively, CTE [phosphorylated tau] pathology may lower the threshold for psychiatric manifestations in susceptible individuals.”
The investigators asserted that the correlation of CTE diagnosis and severity may be more nuanced than just how many times a player is hit.
“Several other football-related factors may influence CTE risk and disease severity, including but not limited to age at first exposure to football, duration of play, player position, cumulative hits, and linear and rotational acceleration of hits,” Dr. Mez and his associates wrote. “Recent work in living former football players has shown that age at first exposure may be related to impaired cognitive performance and altered corpus callosum white matter and that cumulative hits may be related to impairment on self-report and objective measures of cognition, mood, and behavior, although it is unclear if any of these outcomes are related to CTE pathology.”
This study was limited by the potential bias of donors who participated in the program. Researchers acknowledge that public awareness of the issue of CTE and head trauma may have influenced players with symptoms to donate their brains, thereby increasing the CTE frequency in the sample.
In addition, the brain bank where the sample was taken is not representative of the entire population of American football players, as most donors played at the college, semi-professional, and professional level, as opposed to only high school or youth leagues.
The senior author of the study, Ann C. McKee, MD, discussed the study further in a related video interview.
The National Institute of Neurological Disorders and Stroke, the National Institute of Aging, the U.S. Department of Defense, the U.S. Department of Veterans Affairs, the National Operating Committee on Standards for Athletic Equipment, the Alzheimer’s Association, the Concussion Legacy Foundation, the Andlinger Family Foundation, the WWE, and the NFL supported the study. Five authors reported receiving support from relevant sources, including the NFL.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
[email protected]
On Twitter @eaztweets
FROM JAMA
Key clinical point:
Major finding: Of 202 deceased football players who played at levels ranging from high school to the NFL and who donated their brains, 177 (88%) were diagnosed with CTE.
Data source: A blinded, retrospective study of 202 donated brains, as well as questionnaires and interviews with informants close to the deceased.
Disclosures: The National Institute of Neurological Disorders and Stroke, the National Institute of Aging, U.S. Department of Defense, U.S. Department of Veterans Affairs, the National Operating Committee on Standards for Athletic Equipment, the Alzheimer’s Association, the Concussion Legacy Foundation, the Andlinger Family Foundation, the WWE, and the NFL supported the study. Five authors reported receiving support from relevant sources, including the NFL.
Mobile messages support safe sleep practices
Mobile health interventions targeting mothers of healthy newborns significantly improved safe sleep practices, compared with controls, in a randomized trial of 1,600 mothers published online July 25 in JAMA.
Despite the success of the Back to Sleep campaign in reducing rates of sudden infant death syndrome, approximately 3,500 infant deaths due to SIDS, accidental suffocation, or strangulation in bed occurred in 2014, wrote Rachel Y. Moon, MD, of the University of Virginia, Charlottesville, and her colleagues (JAMA. 2017;318:351-9).
A total of 1,263 mothers completed the study, and mothers who received the mobile messages about safe sleep were significantly more likely than those who received the control messages to engage in safe sleep practices, including placing babies on their backs (89% vs. 80%), sharing a room without cosleeping (83% vs. 70%), avoiding the use of soft bedding (79% vs. 68%), and use of pacifiers (69% vs. 60%). The initial nursing quality intervention alone had no significant impact on any of the safe sleep practices, the researchers noted.
The results were limited by several factors, including the 21% lost to follow up and lack of data on adverse events and clinical outcomes, the researchers said. However, the results suggest that mobile messages could be cost effective and easily implemented by hospitals.
“Furthermore, because the rates of opening and viewing messages in this study were consistently higher than 50%, and almost all adults now have cell phones or email access, it is likely that this type of intervention would be feasible and well received by parents,” Dr. Moon and her associates added. “Whether widespread implementation is feasible or if it reduces sudden and unexpected infant death rates remains to be studied.”
“The messages and videos were timed to address challenges and questions that arise at specific time points; therefore, providing this additional information to parents at critical times may have been important in assuaging concerns about adherence to recommended practices. Furthermore, receiving frequent videos and email or text messages may have served as a virtual support system for mothers, reinforcing safe parental practices,” Dr. Moon and her associates noted.
The researchers had no financial conflicts to disclose. The study was supported in part by the National Institute of Child Health and Human Development and by the CJ Foundation for SIDS.
In this study by Dr. Moon and her associates, new mothers who received both the nursing educational intervention and mobile intervention for safe sleep reported the highest percentages for adhering to safe sleep practices, and moms who received the safe sleep mobile intervention alone had the second-highest percentages.
However, the study was underpowered and too short termed to determine whether this intervention actually will reduce the occurrence of SIDS.
Limitations of this study include that the mothers who did not respond at follow-up were more likely to be younger, black, single, and less educated – all risk factors for SIDS. The study also was restricted to healthy term infants, and preterm babies are another high-risk SIDS group.
Nonetheless, the fact that this study chose to use multifaceted approaches was promising, combining “health messaging, education of health care professionals, and interventions aimed at reducing barriers to safe sleep practices for infant caregivers.” Whatever interventions are tried, they “need to be adapted for implementation among the highest-risk groups such as non-Hispanic black, American Indian, and Alaskan Native mothers and families because these are the populations with the highest rates of SIDS and sleep-related infant death.”
Carrie K. Shapiro-Mendoza, PhD, MPH is affiliated with the division of reproductive health at the Centers for Disease Control and Prevention in Atlanta, Georgia. She commented in an editorial accompanying the report by Moon et al. (JAMA. 2017;318:336-8). Dr. Shapiro-Mendoza had no financial conflicts to disclose.
In this study by Dr. Moon and her associates, new mothers who received both the nursing educational intervention and mobile intervention for safe sleep reported the highest percentages for adhering to safe sleep practices, and moms who received the safe sleep mobile intervention alone had the second-highest percentages.
However, the study was underpowered and too short termed to determine whether this intervention actually will reduce the occurrence of SIDS.
Limitations of this study include that the mothers who did not respond at follow-up were more likely to be younger, black, single, and less educated – all risk factors for SIDS. The study also was restricted to healthy term infants, and preterm babies are another high-risk SIDS group.
Nonetheless, the fact that this study chose to use multifaceted approaches was promising, combining “health messaging, education of health care professionals, and interventions aimed at reducing barriers to safe sleep practices for infant caregivers.” Whatever interventions are tried, they “need to be adapted for implementation among the highest-risk groups such as non-Hispanic black, American Indian, and Alaskan Native mothers and families because these are the populations with the highest rates of SIDS and sleep-related infant death.”
Carrie K. Shapiro-Mendoza, PhD, MPH is affiliated with the division of reproductive health at the Centers for Disease Control and Prevention in Atlanta, Georgia. She commented in an editorial accompanying the report by Moon et al. (JAMA. 2017;318:336-8). Dr. Shapiro-Mendoza had no financial conflicts to disclose.
In this study by Dr. Moon and her associates, new mothers who received both the nursing educational intervention and mobile intervention for safe sleep reported the highest percentages for adhering to safe sleep practices, and moms who received the safe sleep mobile intervention alone had the second-highest percentages.
However, the study was underpowered and too short termed to determine whether this intervention actually will reduce the occurrence of SIDS.
Limitations of this study include that the mothers who did not respond at follow-up were more likely to be younger, black, single, and less educated – all risk factors for SIDS. The study also was restricted to healthy term infants, and preterm babies are another high-risk SIDS group.
Nonetheless, the fact that this study chose to use multifaceted approaches was promising, combining “health messaging, education of health care professionals, and interventions aimed at reducing barriers to safe sleep practices for infant caregivers.” Whatever interventions are tried, they “need to be adapted for implementation among the highest-risk groups such as non-Hispanic black, American Indian, and Alaskan Native mothers and families because these are the populations with the highest rates of SIDS and sleep-related infant death.”
Carrie K. Shapiro-Mendoza, PhD, MPH is affiliated with the division of reproductive health at the Centers for Disease Control and Prevention in Atlanta, Georgia. She commented in an editorial accompanying the report by Moon et al. (JAMA. 2017;318:336-8). Dr. Shapiro-Mendoza had no financial conflicts to disclose.
Mobile health interventions targeting mothers of healthy newborns significantly improved safe sleep practices, compared with controls, in a randomized trial of 1,600 mothers published online July 25 in JAMA.
Despite the success of the Back to Sleep campaign in reducing rates of sudden infant death syndrome, approximately 3,500 infant deaths due to SIDS, accidental suffocation, or strangulation in bed occurred in 2014, wrote Rachel Y. Moon, MD, of the University of Virginia, Charlottesville, and her colleagues (JAMA. 2017;318:351-9).
A total of 1,263 mothers completed the study, and mothers who received the mobile messages about safe sleep were significantly more likely than those who received the control messages to engage in safe sleep practices, including placing babies on their backs (89% vs. 80%), sharing a room without cosleeping (83% vs. 70%), avoiding the use of soft bedding (79% vs. 68%), and use of pacifiers (69% vs. 60%). The initial nursing quality intervention alone had no significant impact on any of the safe sleep practices, the researchers noted.
The results were limited by several factors, including the 21% lost to follow up and lack of data on adverse events and clinical outcomes, the researchers said. However, the results suggest that mobile messages could be cost effective and easily implemented by hospitals.
“Furthermore, because the rates of opening and viewing messages in this study were consistently higher than 50%, and almost all adults now have cell phones or email access, it is likely that this type of intervention would be feasible and well received by parents,” Dr. Moon and her associates added. “Whether widespread implementation is feasible or if it reduces sudden and unexpected infant death rates remains to be studied.”
“The messages and videos were timed to address challenges and questions that arise at specific time points; therefore, providing this additional information to parents at critical times may have been important in assuaging concerns about adherence to recommended practices. Furthermore, receiving frequent videos and email or text messages may have served as a virtual support system for mothers, reinforcing safe parental practices,” Dr. Moon and her associates noted.
The researchers had no financial conflicts to disclose. The study was supported in part by the National Institute of Child Health and Human Development and by the CJ Foundation for SIDS.
Mobile health interventions targeting mothers of healthy newborns significantly improved safe sleep practices, compared with controls, in a randomized trial of 1,600 mothers published online July 25 in JAMA.
Despite the success of the Back to Sleep campaign in reducing rates of sudden infant death syndrome, approximately 3,500 infant deaths due to SIDS, accidental suffocation, or strangulation in bed occurred in 2014, wrote Rachel Y. Moon, MD, of the University of Virginia, Charlottesville, and her colleagues (JAMA. 2017;318:351-9).
A total of 1,263 mothers completed the study, and mothers who received the mobile messages about safe sleep were significantly more likely than those who received the control messages to engage in safe sleep practices, including placing babies on their backs (89% vs. 80%), sharing a room without cosleeping (83% vs. 70%), avoiding the use of soft bedding (79% vs. 68%), and use of pacifiers (69% vs. 60%). The initial nursing quality intervention alone had no significant impact on any of the safe sleep practices, the researchers noted.
The results were limited by several factors, including the 21% lost to follow up and lack of data on adverse events and clinical outcomes, the researchers said. However, the results suggest that mobile messages could be cost effective and easily implemented by hospitals.
“Furthermore, because the rates of opening and viewing messages in this study were consistently higher than 50%, and almost all adults now have cell phones or email access, it is likely that this type of intervention would be feasible and well received by parents,” Dr. Moon and her associates added. “Whether widespread implementation is feasible or if it reduces sudden and unexpected infant death rates remains to be studied.”
“The messages and videos were timed to address challenges and questions that arise at specific time points; therefore, providing this additional information to parents at critical times may have been important in assuaging concerns about adherence to recommended practices. Furthermore, receiving frequent videos and email or text messages may have served as a virtual support system for mothers, reinforcing safe parental practices,” Dr. Moon and her associates noted.
The researchers had no financial conflicts to disclose. The study was supported in part by the National Institute of Child Health and Human Development and by the CJ Foundation for SIDS.
FROM JAMA
Key clinical point: Email and text messages effectively communicated safe infant sleep practices to mothers.
Major finding: Overall,
Data source: The data come from a randomized trial of 1,600 mothers with healthy newborns.
Disclosures: The researchers had no financial conflicts to disclose. The study was supported in part by the National Institute of Child Health and Human Development and by the CJ Foundation for SIDS.
Little treatments show big promise for youth psychiatric problems
SAN FRANCISCO – Very brief, outside-the-box therapeutic interventions are racking up respectable efficacy scores in randomized, controlled trials addressing a variety of common psychiatric problems in youths, Jessica L. Schleider observed at the annual conference of the Anxiety and Depression Association of America.
The impetus for developing very brief interventions – or VBIs, as they are known in psychotherapy research parlance – is mounting recognition that conventional treatment approaches have by and large failed children and adolescents who have mental health problems, explained Ms. Schleider, a doctoral candidate in clinical psychology at Harvard University in Cambridge, Mass.
According to data from the Centers for Disease Control and Prevention and the Child Mind Institute, only 20% of American children and adolescents who have significant mental health problems access mental health services. And among those who do, only a minority complete their planned course of treatment.
Reimbursable treatment plans for youth mental health problems typically entail about 16 sessions. Yet national insurance reimbursement data indicate those youths who do access treatment attend on average fewer than four sessions.
“Given that the current model just doesn’t seem to be meeting the needs of kids and families across the country, novel approaches are going to be necessary to really reduce the burden of youth mental illness on a broad scale,” Ms. Schleider asserted.
She characterized VBIs as an example of what is often referred to in TED Talks as “disruptive innovation.” VBIs are intended to extend the reach of youth mental health services by offering interventions that are brief, affordable, accessible, and scalable. It’s a concept that has captured the imagination of officials at the National Institute of Mental Health, which is funding her VBI work and that of others under the institute’s experimental therapeutics initiative.
Ms. Schleider coauthored a recent meta-analysis of 50 randomized, controlled trials of single-session interventions (SSIs) for mental health problems in a collective 10,508 youths. The investigators found that the treatment effect size varied by the target problem. The largest effect size documented – 1.05, which is a strong benefit – was for SSIs targeting eating disorders. The weakest was for the 18 randomized trials addressing substance abuse, with an effect size of a mere 0.08 (J Am Acad Child Adolesc Psychiatry. 2017 Feb;56[2]:107-15).
“The mean effect size across all categories is 0.32, which is decent. It’s in the small-to-medium range,” she noted. “But if you zoom in on the most common types of youth mental health problems – anxiety, conduct, and depression – we see that the overall effect of those single-session programs compares surprisingly well to the full-length treatments that we have, further supporting a possible value as an element of our mental health system.”
For SSIs addressing anxiety, for example, the mean posttreatment effect size was 0.56, compared with 0.61 for conventional multisession programs. For conduct problems, SSIs produced a mean effect size of 0.54, versus 0.46 for full-length treatment programs. And while the effect size of SSIs for depression was small, at 0.18, the same might be said for the 0.28 mean effect size for standard depression therapy programs.
Mean SSI treatment effect sizes were larger for children than for adolescents, at 0.42, compared with 0.19.
Ms. Schleider also presented highlights of a published randomized, double-blind trial of a self-administered computer-guided SSI she and her coauthor have developed. That SSI is designed to briefly teach troubled adolescents a growth personality mindset: that is, the belief that personal traits such as shyness, sadness, and intelligence are malleable through effort and hard work, rather than static and unchangeable.
“Kids with fixed mindsets tend to fare worse than those with growth mindsets,” she said. “They give up prematurely in response to social and academic stress, and they engage in a lot more negative self talk.
The intervention borrows from the achievement motivation theory developed by Carol S. Dweck, Ph.D., professor of psychology at Stanford (Calif.) University and author of the book, “Mindset: the New Psychology of Success.”
The trial randomized 96 subjects aged 12-15 years to a half hour spent on a computer with the growth mindset intervention or a shared feelings control. These were teens with elevated levels of internalizing problems. Eighty-four percent of them met criteria for anxiety by the SCARED CHILD (Screen for Child Anxiety Related Disorders – Child Version) or for depression via the CDI (Children’s Depression Inventory). Subjects were followed up immediately post treatment and again at 3, 6, and 9 months, with 74% of the original group participating in the final follow-up.
The guided growth mindset group showed significant reductions from baseline in CDI and SCARED scores at every follow-up point, while the control group remained unchanged.
“What I see as the bottom line are the 9-month follow-up effects: All effect sizes for youth- and parent-reported outcomes of anxiety and depression are in the small-to-medium range,” Ms. Schleider said. “But this is quite promising, I think, for a 30-minute intervention that kids can complete on their own.”
Also, the mindset intervention strengthened postintervention measures of the adolescents’ perceived control. On a postintervention, laboratory-based, standardized social stress test, the mindset intervention group achieved physiologic recovery more than three times faster than did the controls, as assessed via electrodermal activity.
Ms. Schleider called the study results “promising and exciting.” She is now working with therapists at McLean Hospital, Belmont, Mass., to see whether administering the growth mindset intervention at the start of youth intensive cognitive-behavioral therapy for anxiety results in improved treatment outcomes.
“By teaching kids that change is possible, it might improve their engagement in CBT or reduce their dropout rates,” she noted.
Ms. Schleider is also pilot studying a parent-directed growth mindset intervention to learn whether it improves parents’ attitude toward psychotherapy and seeking services for a troubled child.
Her randomized trial was supported by the National Institute of Mental Health, the American Psychological Association, and the Harvard Center on the Developing Child. She reported having no financial conflicts.
SAN FRANCISCO – Very brief, outside-the-box therapeutic interventions are racking up respectable efficacy scores in randomized, controlled trials addressing a variety of common psychiatric problems in youths, Jessica L. Schleider observed at the annual conference of the Anxiety and Depression Association of America.
The impetus for developing very brief interventions – or VBIs, as they are known in psychotherapy research parlance – is mounting recognition that conventional treatment approaches have by and large failed children and adolescents who have mental health problems, explained Ms. Schleider, a doctoral candidate in clinical psychology at Harvard University in Cambridge, Mass.
According to data from the Centers for Disease Control and Prevention and the Child Mind Institute, only 20% of American children and adolescents who have significant mental health problems access mental health services. And among those who do, only a minority complete their planned course of treatment.
Reimbursable treatment plans for youth mental health problems typically entail about 16 sessions. Yet national insurance reimbursement data indicate those youths who do access treatment attend on average fewer than four sessions.
“Given that the current model just doesn’t seem to be meeting the needs of kids and families across the country, novel approaches are going to be necessary to really reduce the burden of youth mental illness on a broad scale,” Ms. Schleider asserted.
She characterized VBIs as an example of what is often referred to in TED Talks as “disruptive innovation.” VBIs are intended to extend the reach of youth mental health services by offering interventions that are brief, affordable, accessible, and scalable. It’s a concept that has captured the imagination of officials at the National Institute of Mental Health, which is funding her VBI work and that of others under the institute’s experimental therapeutics initiative.
Ms. Schleider coauthored a recent meta-analysis of 50 randomized, controlled trials of single-session interventions (SSIs) for mental health problems in a collective 10,508 youths. The investigators found that the treatment effect size varied by the target problem. The largest effect size documented – 1.05, which is a strong benefit – was for SSIs targeting eating disorders. The weakest was for the 18 randomized trials addressing substance abuse, with an effect size of a mere 0.08 (J Am Acad Child Adolesc Psychiatry. 2017 Feb;56[2]:107-15).
“The mean effect size across all categories is 0.32, which is decent. It’s in the small-to-medium range,” she noted. “But if you zoom in on the most common types of youth mental health problems – anxiety, conduct, and depression – we see that the overall effect of those single-session programs compares surprisingly well to the full-length treatments that we have, further supporting a possible value as an element of our mental health system.”
For SSIs addressing anxiety, for example, the mean posttreatment effect size was 0.56, compared with 0.61 for conventional multisession programs. For conduct problems, SSIs produced a mean effect size of 0.54, versus 0.46 for full-length treatment programs. And while the effect size of SSIs for depression was small, at 0.18, the same might be said for the 0.28 mean effect size for standard depression therapy programs.
Mean SSI treatment effect sizes were larger for children than for adolescents, at 0.42, compared with 0.19.
Ms. Schleider also presented highlights of a published randomized, double-blind trial of a self-administered computer-guided SSI she and her coauthor have developed. That SSI is designed to briefly teach troubled adolescents a growth personality mindset: that is, the belief that personal traits such as shyness, sadness, and intelligence are malleable through effort and hard work, rather than static and unchangeable.
“Kids with fixed mindsets tend to fare worse than those with growth mindsets,” she said. “They give up prematurely in response to social and academic stress, and they engage in a lot more negative self talk.
The intervention borrows from the achievement motivation theory developed by Carol S. Dweck, Ph.D., professor of psychology at Stanford (Calif.) University and author of the book, “Mindset: the New Psychology of Success.”
The trial randomized 96 subjects aged 12-15 years to a half hour spent on a computer with the growth mindset intervention or a shared feelings control. These were teens with elevated levels of internalizing problems. Eighty-four percent of them met criteria for anxiety by the SCARED CHILD (Screen for Child Anxiety Related Disorders – Child Version) or for depression via the CDI (Children’s Depression Inventory). Subjects were followed up immediately post treatment and again at 3, 6, and 9 months, with 74% of the original group participating in the final follow-up.
The guided growth mindset group showed significant reductions from baseline in CDI and SCARED scores at every follow-up point, while the control group remained unchanged.
“What I see as the bottom line are the 9-month follow-up effects: All effect sizes for youth- and parent-reported outcomes of anxiety and depression are in the small-to-medium range,” Ms. Schleider said. “But this is quite promising, I think, for a 30-minute intervention that kids can complete on their own.”
Also, the mindset intervention strengthened postintervention measures of the adolescents’ perceived control. On a postintervention, laboratory-based, standardized social stress test, the mindset intervention group achieved physiologic recovery more than three times faster than did the controls, as assessed via electrodermal activity.
Ms. Schleider called the study results “promising and exciting.” She is now working with therapists at McLean Hospital, Belmont, Mass., to see whether administering the growth mindset intervention at the start of youth intensive cognitive-behavioral therapy for anxiety results in improved treatment outcomes.
“By teaching kids that change is possible, it might improve their engagement in CBT or reduce their dropout rates,” she noted.
Ms. Schleider is also pilot studying a parent-directed growth mindset intervention to learn whether it improves parents’ attitude toward psychotherapy and seeking services for a troubled child.
Her randomized trial was supported by the National Institute of Mental Health, the American Psychological Association, and the Harvard Center on the Developing Child. She reported having no financial conflicts.
SAN FRANCISCO – Very brief, outside-the-box therapeutic interventions are racking up respectable efficacy scores in randomized, controlled trials addressing a variety of common psychiatric problems in youths, Jessica L. Schleider observed at the annual conference of the Anxiety and Depression Association of America.
The impetus for developing very brief interventions – or VBIs, as they are known in psychotherapy research parlance – is mounting recognition that conventional treatment approaches have by and large failed children and adolescents who have mental health problems, explained Ms. Schleider, a doctoral candidate in clinical psychology at Harvard University in Cambridge, Mass.
According to data from the Centers for Disease Control and Prevention and the Child Mind Institute, only 20% of American children and adolescents who have significant mental health problems access mental health services. And among those who do, only a minority complete their planned course of treatment.
Reimbursable treatment plans for youth mental health problems typically entail about 16 sessions. Yet national insurance reimbursement data indicate those youths who do access treatment attend on average fewer than four sessions.
“Given that the current model just doesn’t seem to be meeting the needs of kids and families across the country, novel approaches are going to be necessary to really reduce the burden of youth mental illness on a broad scale,” Ms. Schleider asserted.
She characterized VBIs as an example of what is often referred to in TED Talks as “disruptive innovation.” VBIs are intended to extend the reach of youth mental health services by offering interventions that are brief, affordable, accessible, and scalable. It’s a concept that has captured the imagination of officials at the National Institute of Mental Health, which is funding her VBI work and that of others under the institute’s experimental therapeutics initiative.
Ms. Schleider coauthored a recent meta-analysis of 50 randomized, controlled trials of single-session interventions (SSIs) for mental health problems in a collective 10,508 youths. The investigators found that the treatment effect size varied by the target problem. The largest effect size documented – 1.05, which is a strong benefit – was for SSIs targeting eating disorders. The weakest was for the 18 randomized trials addressing substance abuse, with an effect size of a mere 0.08 (J Am Acad Child Adolesc Psychiatry. 2017 Feb;56[2]:107-15).
“The mean effect size across all categories is 0.32, which is decent. It’s in the small-to-medium range,” she noted. “But if you zoom in on the most common types of youth mental health problems – anxiety, conduct, and depression – we see that the overall effect of those single-session programs compares surprisingly well to the full-length treatments that we have, further supporting a possible value as an element of our mental health system.”
For SSIs addressing anxiety, for example, the mean posttreatment effect size was 0.56, compared with 0.61 for conventional multisession programs. For conduct problems, SSIs produced a mean effect size of 0.54, versus 0.46 for full-length treatment programs. And while the effect size of SSIs for depression was small, at 0.18, the same might be said for the 0.28 mean effect size for standard depression therapy programs.
Mean SSI treatment effect sizes were larger for children than for adolescents, at 0.42, compared with 0.19.
Ms. Schleider also presented highlights of a published randomized, double-blind trial of a self-administered computer-guided SSI she and her coauthor have developed. That SSI is designed to briefly teach troubled adolescents a growth personality mindset: that is, the belief that personal traits such as shyness, sadness, and intelligence are malleable through effort and hard work, rather than static and unchangeable.
“Kids with fixed mindsets tend to fare worse than those with growth mindsets,” she said. “They give up prematurely in response to social and academic stress, and they engage in a lot more negative self talk.
The intervention borrows from the achievement motivation theory developed by Carol S. Dweck, Ph.D., professor of psychology at Stanford (Calif.) University and author of the book, “Mindset: the New Psychology of Success.”
The trial randomized 96 subjects aged 12-15 years to a half hour spent on a computer with the growth mindset intervention or a shared feelings control. These were teens with elevated levels of internalizing problems. Eighty-four percent of them met criteria for anxiety by the SCARED CHILD (Screen for Child Anxiety Related Disorders – Child Version) or for depression via the CDI (Children’s Depression Inventory). Subjects were followed up immediately post treatment and again at 3, 6, and 9 months, with 74% of the original group participating in the final follow-up.
The guided growth mindset group showed significant reductions from baseline in CDI and SCARED scores at every follow-up point, while the control group remained unchanged.
“What I see as the bottom line are the 9-month follow-up effects: All effect sizes for youth- and parent-reported outcomes of anxiety and depression are in the small-to-medium range,” Ms. Schleider said. “But this is quite promising, I think, for a 30-minute intervention that kids can complete on their own.”
Also, the mindset intervention strengthened postintervention measures of the adolescents’ perceived control. On a postintervention, laboratory-based, standardized social stress test, the mindset intervention group achieved physiologic recovery more than three times faster than did the controls, as assessed via electrodermal activity.
Ms. Schleider called the study results “promising and exciting.” She is now working with therapists at McLean Hospital, Belmont, Mass., to see whether administering the growth mindset intervention at the start of youth intensive cognitive-behavioral therapy for anxiety results in improved treatment outcomes.
“By teaching kids that change is possible, it might improve their engagement in CBT or reduce their dropout rates,” she noted.
Ms. Schleider is also pilot studying a parent-directed growth mindset intervention to learn whether it improves parents’ attitude toward psychotherapy and seeking services for a troubled child.
Her randomized trial was supported by the National Institute of Mental Health, the American Psychological Association, and the Harvard Center on the Developing Child. She reported having no financial conflicts.
EXPERT ANALYSIS FROM THE ANXIETY AND DEPRESSION CONFERENCE 2017
Many aspects to caring for epidermolysis bullosa patients
CHICAGO – Ask patients with recessive dystrophic epidermolysis bullosa (EB) to name their most bothersome symptom, and they’re likely to say itch, followed closely by pain, according to Jemima Mellerio, MD.
“We don’t really understand a lot about the mechanism of itch in patients with this disease, which is one of the reasons why we don’t have good treatments,” Prof. Mellerio said at the World Congress of Pediatric Dermatology.
A key resource for patients with EB and clinicians who care for them is Debra International, a network of national groups working on behalf of people with EB, which is undertaking a longterm initiative to develop clinical practice guidelines for the disorder. “This has been going on for about five years and is gathering momentum,” Prof. Mellerio said. “In the EB literature, there is very little that is good quality, evidence-based medicine.” Links to existing guidelines can be accessed DEBRA website.
She shared clinical tips for managing various aspects of EB, including pain, which was the subject of a recent 23-page clinical practice guideline (BMC Med. 2014;12:178). “It’s important to take a proper history: What kind of pain is it and when do they get it?” she commented. “Is there anything that is triggering it?” Basic treatment principles are to start with simple options like acetaminophen/NSAIDs and add in weak opiates as appropriate. Go a bit stronger if necessary, titrating to get the desired effect. “If you have specialist pain services, that can be extremely useful in some of the more complex cases,” she said.
Many EB patients are plagued by neuropathic pain that burns and stings. “For these cases, you might try tricyclic antidepressants or anticonvulsants like gabapentin and pregabalin,” she noted. Anxiolytics such as midazolam can be used to reduce anxiety during procedures, bathing, and dressings. A wide range of pain formulations exist to meet patient needs or preferences, including oral tablets or suspensions, lozenges, intranasal preparations, transdermal patches and intramuscular and intravenous injections.
Topical measures for isolated, painful wounds include ibuprofen-impregnated dressings such as Biatain Ibu and topical morphine gel. “You can get this made up by using morphine sulfate and mixing it in a hydrogel,” Prof. Mellerio said. “You apply that when you have a limited number of painful wounds, so you don’t get the systemic effects from having morphine but you get the local beneficial effects.” [This approach was described in Arch Dis Child. 2004;89:679-81.] Adding salt to a bath can also ameliorate pain for patients. She recommends adding 90g of salt to 10L bath water for a 0.9% solution, which translates into about 800g salt for a half-full tub of water.
Basic skin care is another challenge for EB patients. For those with extremely fragile skin, Prof. Mellerio recommends applying a primary layer of a soft silicone or lipidocolloid dressing under a secondary dressing layer. “There’s a whole range of soft silicone foam dressings or polymeric membrane, which is a nice soft dressing that can go over a primary dressing or directly on the skin if fragility is not a problem,” she said. “Really, it comes down to patient and carer choice as to what to use. It depends on many factors including site, exudate, pain, and dressing size. The frequency of wound changes will also vary. So, if you’ve got an infected, more heavily exuding wound, the dressing changes will be more frequent.”
Critical colonization and infection are significant problems for EB patients and are ideally managed with topical antimicrobials such as hydrogen peroxide cream, enzymatic antimicrobials, polyhexamethylene biguanide, and medical grade honey. “Topical antibiotics such as mupirocin can also be used, but there are problems with resistance if you’re using it long-term and potential for sensitization,” Prof. Mellerio said. “Other options include antimicrobial dressings such as polymeric membrane, polyhexamethylene biguanide, and silver. With silver dressings, there is the potential to absorb silver, so, if you’re a child and you have a lot of wounds on your skin, you can absorb silver at significant levels, which could be a problem.”
If patients don’t respond to topical measures, consider using oral antibiotics for 10-14 days, she said. Swab first for sensitivity and to look for Streptococcal carriage “because you can get a lot of problems like renal damage,” and use IV antibiotics only for severe infections, she said. “Best Practice Guidelines for Skin and Wound Care in Epidermolysis Bullosa,” supported by an award from the Urgo Foundation and produced by Wounds International/Wounds UK, are available.
Prof. Mellerio noted that EB can also adversely affect oral health and lead to the formation of painful blisters, scarring, microstomia, and ankyloglossia, which “can contribute to difficulties eating and speaking and make it hard to keep the teeth clean.” Analgesics can be helpful, as can an NSAID mouthwash or spray or mucoprotectants like Episil that coat the surface of lesions. “Alcohol-free chlorhexidine washes and fluoride mouth washes can help, as can high fluoride toothpaste and trying to limit the consumption of sugary foods and snacks,” she said. “You can adapt things like toothbrushes with a grip, which means that it’s a bit easier for somebody with EB to be able to keep their teeth clean.”
Keeping bones strong is also a concern, since osteopenia and osteoporosis are common in EB. “We’ve seen vertebral crush fractures in children as young as five years old,” Prof. Mellerio said. “Optimize calcium and vitamin D and mobility, which is important in helping people accrue their bone mineral density throughout life. Sometimes we have to use bisphosphonate therapies, but there isn’t a great deal in the literature to support what the best way of doing this is.”
Prof. Mellerio reported having no financial disclosures.
CHICAGO – Ask patients with recessive dystrophic epidermolysis bullosa (EB) to name their most bothersome symptom, and they’re likely to say itch, followed closely by pain, according to Jemima Mellerio, MD.
“We don’t really understand a lot about the mechanism of itch in patients with this disease, which is one of the reasons why we don’t have good treatments,” Prof. Mellerio said at the World Congress of Pediatric Dermatology.
A key resource for patients with EB and clinicians who care for them is Debra International, a network of national groups working on behalf of people with EB, which is undertaking a longterm initiative to develop clinical practice guidelines for the disorder. “This has been going on for about five years and is gathering momentum,” Prof. Mellerio said. “In the EB literature, there is very little that is good quality, evidence-based medicine.” Links to existing guidelines can be accessed DEBRA website.
She shared clinical tips for managing various aspects of EB, including pain, which was the subject of a recent 23-page clinical practice guideline (BMC Med. 2014;12:178). “It’s important to take a proper history: What kind of pain is it and when do they get it?” she commented. “Is there anything that is triggering it?” Basic treatment principles are to start with simple options like acetaminophen/NSAIDs and add in weak opiates as appropriate. Go a bit stronger if necessary, titrating to get the desired effect. “If you have specialist pain services, that can be extremely useful in some of the more complex cases,” she said.
Many EB patients are plagued by neuropathic pain that burns and stings. “For these cases, you might try tricyclic antidepressants or anticonvulsants like gabapentin and pregabalin,” she noted. Anxiolytics such as midazolam can be used to reduce anxiety during procedures, bathing, and dressings. A wide range of pain formulations exist to meet patient needs or preferences, including oral tablets or suspensions, lozenges, intranasal preparations, transdermal patches and intramuscular and intravenous injections.
Topical measures for isolated, painful wounds include ibuprofen-impregnated dressings such as Biatain Ibu and topical morphine gel. “You can get this made up by using morphine sulfate and mixing it in a hydrogel,” Prof. Mellerio said. “You apply that when you have a limited number of painful wounds, so you don’t get the systemic effects from having morphine but you get the local beneficial effects.” [This approach was described in Arch Dis Child. 2004;89:679-81.] Adding salt to a bath can also ameliorate pain for patients. She recommends adding 90g of salt to 10L bath water for a 0.9% solution, which translates into about 800g salt for a half-full tub of water.
Basic skin care is another challenge for EB patients. For those with extremely fragile skin, Prof. Mellerio recommends applying a primary layer of a soft silicone or lipidocolloid dressing under a secondary dressing layer. “There’s a whole range of soft silicone foam dressings or polymeric membrane, which is a nice soft dressing that can go over a primary dressing or directly on the skin if fragility is not a problem,” she said. “Really, it comes down to patient and carer choice as to what to use. It depends on many factors including site, exudate, pain, and dressing size. The frequency of wound changes will also vary. So, if you’ve got an infected, more heavily exuding wound, the dressing changes will be more frequent.”
Critical colonization and infection are significant problems for EB patients and are ideally managed with topical antimicrobials such as hydrogen peroxide cream, enzymatic antimicrobials, polyhexamethylene biguanide, and medical grade honey. “Topical antibiotics such as mupirocin can also be used, but there are problems with resistance if you’re using it long-term and potential for sensitization,” Prof. Mellerio said. “Other options include antimicrobial dressings such as polymeric membrane, polyhexamethylene biguanide, and silver. With silver dressings, there is the potential to absorb silver, so, if you’re a child and you have a lot of wounds on your skin, you can absorb silver at significant levels, which could be a problem.”
If patients don’t respond to topical measures, consider using oral antibiotics for 10-14 days, she said. Swab first for sensitivity and to look for Streptococcal carriage “because you can get a lot of problems like renal damage,” and use IV antibiotics only for severe infections, she said. “Best Practice Guidelines for Skin and Wound Care in Epidermolysis Bullosa,” supported by an award from the Urgo Foundation and produced by Wounds International/Wounds UK, are available.
Prof. Mellerio noted that EB can also adversely affect oral health and lead to the formation of painful blisters, scarring, microstomia, and ankyloglossia, which “can contribute to difficulties eating and speaking and make it hard to keep the teeth clean.” Analgesics can be helpful, as can an NSAID mouthwash or spray or mucoprotectants like Episil that coat the surface of lesions. “Alcohol-free chlorhexidine washes and fluoride mouth washes can help, as can high fluoride toothpaste and trying to limit the consumption of sugary foods and snacks,” she said. “You can adapt things like toothbrushes with a grip, which means that it’s a bit easier for somebody with EB to be able to keep their teeth clean.”
Keeping bones strong is also a concern, since osteopenia and osteoporosis are common in EB. “We’ve seen vertebral crush fractures in children as young as five years old,” Prof. Mellerio said. “Optimize calcium and vitamin D and mobility, which is important in helping people accrue their bone mineral density throughout life. Sometimes we have to use bisphosphonate therapies, but there isn’t a great deal in the literature to support what the best way of doing this is.”
Prof. Mellerio reported having no financial disclosures.
CHICAGO – Ask patients with recessive dystrophic epidermolysis bullosa (EB) to name their most bothersome symptom, and they’re likely to say itch, followed closely by pain, according to Jemima Mellerio, MD.
“We don’t really understand a lot about the mechanism of itch in patients with this disease, which is one of the reasons why we don’t have good treatments,” Prof. Mellerio said at the World Congress of Pediatric Dermatology.
A key resource for patients with EB and clinicians who care for them is Debra International, a network of national groups working on behalf of people with EB, which is undertaking a longterm initiative to develop clinical practice guidelines for the disorder. “This has been going on for about five years and is gathering momentum,” Prof. Mellerio said. “In the EB literature, there is very little that is good quality, evidence-based medicine.” Links to existing guidelines can be accessed DEBRA website.
She shared clinical tips for managing various aspects of EB, including pain, which was the subject of a recent 23-page clinical practice guideline (BMC Med. 2014;12:178). “It’s important to take a proper history: What kind of pain is it and when do they get it?” she commented. “Is there anything that is triggering it?” Basic treatment principles are to start with simple options like acetaminophen/NSAIDs and add in weak opiates as appropriate. Go a bit stronger if necessary, titrating to get the desired effect. “If you have specialist pain services, that can be extremely useful in some of the more complex cases,” she said.
Many EB patients are plagued by neuropathic pain that burns and stings. “For these cases, you might try tricyclic antidepressants or anticonvulsants like gabapentin and pregabalin,” she noted. Anxiolytics such as midazolam can be used to reduce anxiety during procedures, bathing, and dressings. A wide range of pain formulations exist to meet patient needs or preferences, including oral tablets or suspensions, lozenges, intranasal preparations, transdermal patches and intramuscular and intravenous injections.
Topical measures for isolated, painful wounds include ibuprofen-impregnated dressings such as Biatain Ibu and topical morphine gel. “You can get this made up by using morphine sulfate and mixing it in a hydrogel,” Prof. Mellerio said. “You apply that when you have a limited number of painful wounds, so you don’t get the systemic effects from having morphine but you get the local beneficial effects.” [This approach was described in Arch Dis Child. 2004;89:679-81.] Adding salt to a bath can also ameliorate pain for patients. She recommends adding 90g of salt to 10L bath water for a 0.9% solution, which translates into about 800g salt for a half-full tub of water.
Basic skin care is another challenge for EB patients. For those with extremely fragile skin, Prof. Mellerio recommends applying a primary layer of a soft silicone or lipidocolloid dressing under a secondary dressing layer. “There’s a whole range of soft silicone foam dressings or polymeric membrane, which is a nice soft dressing that can go over a primary dressing or directly on the skin if fragility is not a problem,” she said. “Really, it comes down to patient and carer choice as to what to use. It depends on many factors including site, exudate, pain, and dressing size. The frequency of wound changes will also vary. So, if you’ve got an infected, more heavily exuding wound, the dressing changes will be more frequent.”
Critical colonization and infection are significant problems for EB patients and are ideally managed with topical antimicrobials such as hydrogen peroxide cream, enzymatic antimicrobials, polyhexamethylene biguanide, and medical grade honey. “Topical antibiotics such as mupirocin can also be used, but there are problems with resistance if you’re using it long-term and potential for sensitization,” Prof. Mellerio said. “Other options include antimicrobial dressings such as polymeric membrane, polyhexamethylene biguanide, and silver. With silver dressings, there is the potential to absorb silver, so, if you’re a child and you have a lot of wounds on your skin, you can absorb silver at significant levels, which could be a problem.”
If patients don’t respond to topical measures, consider using oral antibiotics for 10-14 days, she said. Swab first for sensitivity and to look for Streptococcal carriage “because you can get a lot of problems like renal damage,” and use IV antibiotics only for severe infections, she said. “Best Practice Guidelines for Skin and Wound Care in Epidermolysis Bullosa,” supported by an award from the Urgo Foundation and produced by Wounds International/Wounds UK, are available.
Prof. Mellerio noted that EB can also adversely affect oral health and lead to the formation of painful blisters, scarring, microstomia, and ankyloglossia, which “can contribute to difficulties eating and speaking and make it hard to keep the teeth clean.” Analgesics can be helpful, as can an NSAID mouthwash or spray or mucoprotectants like Episil that coat the surface of lesions. “Alcohol-free chlorhexidine washes and fluoride mouth washes can help, as can high fluoride toothpaste and trying to limit the consumption of sugary foods and snacks,” she said. “You can adapt things like toothbrushes with a grip, which means that it’s a bit easier for somebody with EB to be able to keep their teeth clean.”
Keeping bones strong is also a concern, since osteopenia and osteoporosis are common in EB. “We’ve seen vertebral crush fractures in children as young as five years old,” Prof. Mellerio said. “Optimize calcium and vitamin D and mobility, which is important in helping people accrue their bone mineral density throughout life. Sometimes we have to use bisphosphonate therapies, but there isn’t a great deal in the literature to support what the best way of doing this is.”
Prof. Mellerio reported having no financial disclosures.
AT WCPD 2017