User login
Patients with Parkinson’s at elevated risk for suicidal thoughts, behavior
Adults with Parkinson’s disease are twice as likely to engage in suicidal behavior as the general population, results of a large meta-analysis show.
Given that up to half of patients with PD suffer from depression and anxiety, physicians should maintain a “high index of suspicion” for early recognition and management of suicidality, write the investigators, led by Eng-King Tan, MD, of Duke-NUS Medical School, Singapore.
“Management of both medical, such as sleep disorders, and psychosocial risk factors, such as feelings of loneliness, hopelessness, and depressed mood, could be useful in lowering suicide risk in patients with PD,” they add.
The study was published online in JAMA Neurology.
Suicide risk neglected in PD?
The analysis included 505,950 patients with PD across 28 cross-sectional, case-control, and cohort studies.
Across 14 studies, the prevalence of suicidal ideation in patients with PD was 22.2% (95% confidence interval, 14.6-32.3). In a sensitivity analysis excluding three outliers, the prevalence of suicidal ideation was higher at 24% (95% CI, 19.1-29.7).
Across 21 studies, the prevalence of suicidal behavior was “substantial” at 1.25% (95% CI, 0.64-2.41), the authors report. The prevalence of suicidal behavior was significantly higher in prospective studies (1.75%; 95% CI, 1.03-2.95) than retrospective studies (0.50%; 95% CI, 0.24 to 1.01).
Across 10 studies, the likelihood of suicidal behavior was about twofold higher among patients with PD than general population controls (odds ratio, 2.15; 95% CI, 1.22-3.78; P = .01). Across nine studies, the hazard ratio for suicidal behavior was 1.73 (95% CI, 1.40-2.14; P < .001).
There was no evidence of sex-related differences in suicidal behavior, although the analysis was limited by the paucity of data, the researchers note.
They note the quality of included studies was generally high, although eight of them did not explicitly identify and adjust for confounders.
Higher rate of mood, anxiety disorders
Paul Nestadt, MD, with Johns Hopkins Bloomberg School of Public Health, Baltimore, said this analysis reiterates what several reviews have found over the past few years, including his own.
“In general, rates of mood and anxiety disorders are much higher in PD than in other dementias, such as Alzheimer’s disease. This is reason enough to allocate resources to the mental health care of those diagnosed with PD and to pay special attention to at risk periods, such as early in the diagnosis, when suicide rates seem to be higher in dementias in general,” said Dr. Nestadt, who wasn’t involved in the study.
He noted that research has shown that suicides among people with PD are more likely to involve a firearm – likely because people with PD are more likely to be over age 65 and to be male – “both huge risk factors for firearm suicide.”
“Therefore, it is essential that caregivers be aware of the risks posed by firearms in the homes of people suffering from Parkinson’s or other dementias. It is the clinician’s responsibility to inform families of this risk, but it is all too often neglected,” Dr. Nestadt said.
Support for the study was provided in part by the National Medical Research Council. Dr. Tan reported honoraria from Eisai and Elsevier outside the submitted work. Dr. Nestadt reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Adults with Parkinson’s disease are twice as likely to engage in suicidal behavior as the general population, results of a large meta-analysis show.
Given that up to half of patients with PD suffer from depression and anxiety, physicians should maintain a “high index of suspicion” for early recognition and management of suicidality, write the investigators, led by Eng-King Tan, MD, of Duke-NUS Medical School, Singapore.
“Management of both medical, such as sleep disorders, and psychosocial risk factors, such as feelings of loneliness, hopelessness, and depressed mood, could be useful in lowering suicide risk in patients with PD,” they add.
The study was published online in JAMA Neurology.
Suicide risk neglected in PD?
The analysis included 505,950 patients with PD across 28 cross-sectional, case-control, and cohort studies.
Across 14 studies, the prevalence of suicidal ideation in patients with PD was 22.2% (95% confidence interval, 14.6-32.3). In a sensitivity analysis excluding three outliers, the prevalence of suicidal ideation was higher at 24% (95% CI, 19.1-29.7).
Across 21 studies, the prevalence of suicidal behavior was “substantial” at 1.25% (95% CI, 0.64-2.41), the authors report. The prevalence of suicidal behavior was significantly higher in prospective studies (1.75%; 95% CI, 1.03-2.95) than retrospective studies (0.50%; 95% CI, 0.24 to 1.01).
Across 10 studies, the likelihood of suicidal behavior was about twofold higher among patients with PD than general population controls (odds ratio, 2.15; 95% CI, 1.22-3.78; P = .01). Across nine studies, the hazard ratio for suicidal behavior was 1.73 (95% CI, 1.40-2.14; P < .001).
There was no evidence of sex-related differences in suicidal behavior, although the analysis was limited by the paucity of data, the researchers note.
They note the quality of included studies was generally high, although eight of them did not explicitly identify and adjust for confounders.
Higher rate of mood, anxiety disorders
Paul Nestadt, MD, with Johns Hopkins Bloomberg School of Public Health, Baltimore, said this analysis reiterates what several reviews have found over the past few years, including his own.
“In general, rates of mood and anxiety disorders are much higher in PD than in other dementias, such as Alzheimer’s disease. This is reason enough to allocate resources to the mental health care of those diagnosed with PD and to pay special attention to at risk periods, such as early in the diagnosis, when suicide rates seem to be higher in dementias in general,” said Dr. Nestadt, who wasn’t involved in the study.
He noted that research has shown that suicides among people with PD are more likely to involve a firearm – likely because people with PD are more likely to be over age 65 and to be male – “both huge risk factors for firearm suicide.”
“Therefore, it is essential that caregivers be aware of the risks posed by firearms in the homes of people suffering from Parkinson’s or other dementias. It is the clinician’s responsibility to inform families of this risk, but it is all too often neglected,” Dr. Nestadt said.
Support for the study was provided in part by the National Medical Research Council. Dr. Tan reported honoraria from Eisai and Elsevier outside the submitted work. Dr. Nestadt reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Adults with Parkinson’s disease are twice as likely to engage in suicidal behavior as the general population, results of a large meta-analysis show.
Given that up to half of patients with PD suffer from depression and anxiety, physicians should maintain a “high index of suspicion” for early recognition and management of suicidality, write the investigators, led by Eng-King Tan, MD, of Duke-NUS Medical School, Singapore.
“Management of both medical, such as sleep disorders, and psychosocial risk factors, such as feelings of loneliness, hopelessness, and depressed mood, could be useful in lowering suicide risk in patients with PD,” they add.
The study was published online in JAMA Neurology.
Suicide risk neglected in PD?
The analysis included 505,950 patients with PD across 28 cross-sectional, case-control, and cohort studies.
Across 14 studies, the prevalence of suicidal ideation in patients with PD was 22.2% (95% confidence interval, 14.6-32.3). In a sensitivity analysis excluding three outliers, the prevalence of suicidal ideation was higher at 24% (95% CI, 19.1-29.7).
Across 21 studies, the prevalence of suicidal behavior was “substantial” at 1.25% (95% CI, 0.64-2.41), the authors report. The prevalence of suicidal behavior was significantly higher in prospective studies (1.75%; 95% CI, 1.03-2.95) than retrospective studies (0.50%; 95% CI, 0.24 to 1.01).
Across 10 studies, the likelihood of suicidal behavior was about twofold higher among patients with PD than general population controls (odds ratio, 2.15; 95% CI, 1.22-3.78; P = .01). Across nine studies, the hazard ratio for suicidal behavior was 1.73 (95% CI, 1.40-2.14; P < .001).
There was no evidence of sex-related differences in suicidal behavior, although the analysis was limited by the paucity of data, the researchers note.
They note the quality of included studies was generally high, although eight of them did not explicitly identify and adjust for confounders.
Higher rate of mood, anxiety disorders
Paul Nestadt, MD, with Johns Hopkins Bloomberg School of Public Health, Baltimore, said this analysis reiterates what several reviews have found over the past few years, including his own.
“In general, rates of mood and anxiety disorders are much higher in PD than in other dementias, such as Alzheimer’s disease. This is reason enough to allocate resources to the mental health care of those diagnosed with PD and to pay special attention to at risk periods, such as early in the diagnosis, when suicide rates seem to be higher in dementias in general,” said Dr. Nestadt, who wasn’t involved in the study.
He noted that research has shown that suicides among people with PD are more likely to involve a firearm – likely because people with PD are more likely to be over age 65 and to be male – “both huge risk factors for firearm suicide.”
“Therefore, it is essential that caregivers be aware of the risks posed by firearms in the homes of people suffering from Parkinson’s or other dementias. It is the clinician’s responsibility to inform families of this risk, but it is all too often neglected,” Dr. Nestadt said.
Support for the study was provided in part by the National Medical Research Council. Dr. Tan reported honoraria from Eisai and Elsevier outside the submitted work. Dr. Nestadt reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Less severe strokes with LAA closure vs. DOAC in AFib?
TOPLINE:
Left atrial appendage closure was associated with about half as many disabling or fatal strokes and lower mortality after a stroke, compared with dual oral anticoagulant therapy in patients with atrial fibrillation (AFib), new observational research shows.
METHODOLOGY:
- The retrospective registry analysis included 447 adult patients with nonvalvular AFib, mean age 74 years, who were hospitalized with an ischemic stroke, 322 of whom were receiving direct oral anticoagulant (DOAC) therapy, mostly (84%) apixaban or rivaroxaban, and 125 were treated with left atrial appendage closure (LAAC), almost all (97%) with Watchman or Watchman-FLX devices.
- All patients received standard stroke care, monitoring, and treatment as well as physical therapy/rehabilitation.
- For the primary outcome, researchers used the modified Rankin Scale (mRS) to determine disabling (mRS score of 3-5) and fatal (mRS score of 6) strokes at discharge and at 3 months.
- The study adjusted for age, smoking, paroxysmal AFib, prior major bleeding, prior hemorrhagic stroke, medication adherence, and other risk factors.
TAKEAWAY:
- (38.3% vs. 70.3%; P < .001) and at 3 months (33.3% vs. 56.2%; P < .001), even though the LAAC group had more baseline comorbidity, for example, older age, more smokers, and more prior major bleeding.
- There was no significant difference in mortality between groups during hospitalization, but at 3 months, mortality was lower in the LAAC group (14.7% vs. 32.1%; P = .002).
- Multivariate linear regression analysis showed LAAC independently predicted more favorable mRS at discharge (2.8) and 3 months (1.4) (both P < .001) and was associated with less all-cause death at 3 months (odds ratio, 0.28; 95% confidence interval, 0.12-0.64; P = .002).
- Including those that excluded the 14.4% of LAAC patients who also received DOAC therapy, sensitivity analyses patients who got reduced dose DOACs and nonadherent patients yielded nearly identical outcomes to the full cohort analysis.
IN PRACTICE:
“Despite a higher baseline risk profile, patients treated with LAAC who developed IS had better outcomes than those receiving DOAC prophylaxis,” the authors conclude, adding that several ongoing prospective trials could, “shed light on the mechanism(s) responsible for differences in stroke severity.”
SOURCE:
The study was conducted by Mohit K. Turagam, MD, Icahn School of Medicine at Mount Sinai, New York, and colleagues. It was published online in JACC: Clinical Electrophysiology.
LIMITATIONS:
Despite sensitivity analyses and adjustment for risk factors, selection bias, missing data, and other confounding factors could have affected outcomes. The study didn’t evaluate recurrent IS or type and intensity of rehabilitation on outcomes. Lack of imaging data comparing stroke infarct size and volume limits understanding of exact mechanism driving higher stroke severity with DOACs. Because patients who died before reaching hospital weren’t captured in the registry, the actual mortality may be higher than reported.
DISCLOSURES:
Dr. Turagam has served as a consultant for Biosense Webster and Sanofi.
A version of this article first appeared on Medscape.com.
TOPLINE:
Left atrial appendage closure was associated with about half as many disabling or fatal strokes and lower mortality after a stroke, compared with dual oral anticoagulant therapy in patients with atrial fibrillation (AFib), new observational research shows.
METHODOLOGY:
- The retrospective registry analysis included 447 adult patients with nonvalvular AFib, mean age 74 years, who were hospitalized with an ischemic stroke, 322 of whom were receiving direct oral anticoagulant (DOAC) therapy, mostly (84%) apixaban or rivaroxaban, and 125 were treated with left atrial appendage closure (LAAC), almost all (97%) with Watchman or Watchman-FLX devices.
- All patients received standard stroke care, monitoring, and treatment as well as physical therapy/rehabilitation.
- For the primary outcome, researchers used the modified Rankin Scale (mRS) to determine disabling (mRS score of 3-5) and fatal (mRS score of 6) strokes at discharge and at 3 months.
- The study adjusted for age, smoking, paroxysmal AFib, prior major bleeding, prior hemorrhagic stroke, medication adherence, and other risk factors.
TAKEAWAY:
- (38.3% vs. 70.3%; P < .001) and at 3 months (33.3% vs. 56.2%; P < .001), even though the LAAC group had more baseline comorbidity, for example, older age, more smokers, and more prior major bleeding.
- There was no significant difference in mortality between groups during hospitalization, but at 3 months, mortality was lower in the LAAC group (14.7% vs. 32.1%; P = .002).
- Multivariate linear regression analysis showed LAAC independently predicted more favorable mRS at discharge (2.8) and 3 months (1.4) (both P < .001) and was associated with less all-cause death at 3 months (odds ratio, 0.28; 95% confidence interval, 0.12-0.64; P = .002).
- Including those that excluded the 14.4% of LAAC patients who also received DOAC therapy, sensitivity analyses patients who got reduced dose DOACs and nonadherent patients yielded nearly identical outcomes to the full cohort analysis.
IN PRACTICE:
“Despite a higher baseline risk profile, patients treated with LAAC who developed IS had better outcomes than those receiving DOAC prophylaxis,” the authors conclude, adding that several ongoing prospective trials could, “shed light on the mechanism(s) responsible for differences in stroke severity.”
SOURCE:
The study was conducted by Mohit K. Turagam, MD, Icahn School of Medicine at Mount Sinai, New York, and colleagues. It was published online in JACC: Clinical Electrophysiology.
LIMITATIONS:
Despite sensitivity analyses and adjustment for risk factors, selection bias, missing data, and other confounding factors could have affected outcomes. The study didn’t evaluate recurrent IS or type and intensity of rehabilitation on outcomes. Lack of imaging data comparing stroke infarct size and volume limits understanding of exact mechanism driving higher stroke severity with DOACs. Because patients who died before reaching hospital weren’t captured in the registry, the actual mortality may be higher than reported.
DISCLOSURES:
Dr. Turagam has served as a consultant for Biosense Webster and Sanofi.
A version of this article first appeared on Medscape.com.
TOPLINE:
Left atrial appendage closure was associated with about half as many disabling or fatal strokes and lower mortality after a stroke, compared with dual oral anticoagulant therapy in patients with atrial fibrillation (AFib), new observational research shows.
METHODOLOGY:
- The retrospective registry analysis included 447 adult patients with nonvalvular AFib, mean age 74 years, who were hospitalized with an ischemic stroke, 322 of whom were receiving direct oral anticoagulant (DOAC) therapy, mostly (84%) apixaban or rivaroxaban, and 125 were treated with left atrial appendage closure (LAAC), almost all (97%) with Watchman or Watchman-FLX devices.
- All patients received standard stroke care, monitoring, and treatment as well as physical therapy/rehabilitation.
- For the primary outcome, researchers used the modified Rankin Scale (mRS) to determine disabling (mRS score of 3-5) and fatal (mRS score of 6) strokes at discharge and at 3 months.
- The study adjusted for age, smoking, paroxysmal AFib, prior major bleeding, prior hemorrhagic stroke, medication adherence, and other risk factors.
TAKEAWAY:
- (38.3% vs. 70.3%; P < .001) and at 3 months (33.3% vs. 56.2%; P < .001), even though the LAAC group had more baseline comorbidity, for example, older age, more smokers, and more prior major bleeding.
- There was no significant difference in mortality between groups during hospitalization, but at 3 months, mortality was lower in the LAAC group (14.7% vs. 32.1%; P = .002).
- Multivariate linear regression analysis showed LAAC independently predicted more favorable mRS at discharge (2.8) and 3 months (1.4) (both P < .001) and was associated with less all-cause death at 3 months (odds ratio, 0.28; 95% confidence interval, 0.12-0.64; P = .002).
- Including those that excluded the 14.4% of LAAC patients who also received DOAC therapy, sensitivity analyses patients who got reduced dose DOACs and nonadherent patients yielded nearly identical outcomes to the full cohort analysis.
IN PRACTICE:
“Despite a higher baseline risk profile, patients treated with LAAC who developed IS had better outcomes than those receiving DOAC prophylaxis,” the authors conclude, adding that several ongoing prospective trials could, “shed light on the mechanism(s) responsible for differences in stroke severity.”
SOURCE:
The study was conducted by Mohit K. Turagam, MD, Icahn School of Medicine at Mount Sinai, New York, and colleagues. It was published online in JACC: Clinical Electrophysiology.
LIMITATIONS:
Despite sensitivity analyses and adjustment for risk factors, selection bias, missing data, and other confounding factors could have affected outcomes. The study didn’t evaluate recurrent IS or type and intensity of rehabilitation on outcomes. Lack of imaging data comparing stroke infarct size and volume limits understanding of exact mechanism driving higher stroke severity with DOACs. Because patients who died before reaching hospital weren’t captured in the registry, the actual mortality may be higher than reported.
DISCLOSURES:
Dr. Turagam has served as a consultant for Biosense Webster and Sanofi.
A version of this article first appeared on Medscape.com.
Long-term organ preservation in rectal cancer is possible
TOPLINE:
with local tumor regrowth occurring mostly within the first 2 years.
METHODOLOGY:
- Many patients with locally advanced rectal cancer treated with total neoadjuvant therapy in the OPRA trial achieved a complete or near-complete tumor response and were initially offered a watch-and-wait strategy.
- However, nearly one-third of patients receiving watch-and-wait developed local tumor regrowth and ultimately required total mesorectal excision (TME).
- The study team reported updated organ preservation rates and oncologic outcomes in the OPRA trial of 324 patients with stage II/III rectal cancer randomized to induction chemotherapy followed by chemoradiation (n = 158) or chemoradiation followed by consolidation chemotherapy (n = 166).
- Among the 304 patients restaged a median of 7.8 weeks after finishing total neoadjuvant therapy, investigators recommended TME in 26% and watch-and-wait in 74% (n = 225).
TAKEAWAY:
- The researchers reported similar 5-year disease-free survival among patients in the induction chemotherapy group (71%) and the consolidation chemotherapy group (69%). The estimated 5-year overall survival rates were also similar in the two groups – 88% in the induction group vs. 85% in the consolidation group.
- Among the patients who received watch-and-wait, 36% (n = 81) experienced tumor regrowth; 94% occurred within 2 years and 99% occurred within 3 years.
- An estimated 39% of patients in the induction chemotherapy group and 54% in the consolidation chemotherapy group achieved organ preservation at 5 years, representing about half of patients overall.
- Among the patients who received watch-and-wait, salvage TME following tumor regrowth appeared to offer disease-free survival (64% of patients) similar to immediate TME after incomplete response to total neoadjuvant therapy (also 64%).
IN PRACTICE:
Total neoadjuvant therapy among patients with rectal cancer “resulted in long-term organ preservation in half of the patients,” the authors concluded. Although the order of therapy did not affect survival, consolidation chemotherapy “resulted in higher organ preservation at 5 years.”
“Our results support the recommendation that patients with rectal cancer offered [watch-and-wait] after neoadjuvant therapy should have very close surveillance during the first 3 years,” the authors added.
SOURCE:
The study, with first author Floris S. Verheij, BSc, Memorial Sloan Kettering Cancer Center, New York, was published online Oct. 26, 2023, in the Journal of Clinical Oncology.
LIMITATIONS:
The study, published as a clinical trials update, does not include a discussion of limitations.
DISCLOSURES:
Funding was provided by the National Cancer Institute. Several OPRA trialists disclosed relationships with a range of companies, including Sironax, Janssen Oncology, Toray Industries, Merck, and Intuitive Surgical.
A version of this article first appeared on Medscape.com.
TOPLINE:
with local tumor regrowth occurring mostly within the first 2 years.
METHODOLOGY:
- Many patients with locally advanced rectal cancer treated with total neoadjuvant therapy in the OPRA trial achieved a complete or near-complete tumor response and were initially offered a watch-and-wait strategy.
- However, nearly one-third of patients receiving watch-and-wait developed local tumor regrowth and ultimately required total mesorectal excision (TME).
- The study team reported updated organ preservation rates and oncologic outcomes in the OPRA trial of 324 patients with stage II/III rectal cancer randomized to induction chemotherapy followed by chemoradiation (n = 158) or chemoradiation followed by consolidation chemotherapy (n = 166).
- Among the 304 patients restaged a median of 7.8 weeks after finishing total neoadjuvant therapy, investigators recommended TME in 26% and watch-and-wait in 74% (n = 225).
TAKEAWAY:
- The researchers reported similar 5-year disease-free survival among patients in the induction chemotherapy group (71%) and the consolidation chemotherapy group (69%). The estimated 5-year overall survival rates were also similar in the two groups – 88% in the induction group vs. 85% in the consolidation group.
- Among the patients who received watch-and-wait, 36% (n = 81) experienced tumor regrowth; 94% occurred within 2 years and 99% occurred within 3 years.
- An estimated 39% of patients in the induction chemotherapy group and 54% in the consolidation chemotherapy group achieved organ preservation at 5 years, representing about half of patients overall.
- Among the patients who received watch-and-wait, salvage TME following tumor regrowth appeared to offer disease-free survival (64% of patients) similar to immediate TME after incomplete response to total neoadjuvant therapy (also 64%).
IN PRACTICE:
Total neoadjuvant therapy among patients with rectal cancer “resulted in long-term organ preservation in half of the patients,” the authors concluded. Although the order of therapy did not affect survival, consolidation chemotherapy “resulted in higher organ preservation at 5 years.”
“Our results support the recommendation that patients with rectal cancer offered [watch-and-wait] after neoadjuvant therapy should have very close surveillance during the first 3 years,” the authors added.
SOURCE:
The study, with first author Floris S. Verheij, BSc, Memorial Sloan Kettering Cancer Center, New York, was published online Oct. 26, 2023, in the Journal of Clinical Oncology.
LIMITATIONS:
The study, published as a clinical trials update, does not include a discussion of limitations.
DISCLOSURES:
Funding was provided by the National Cancer Institute. Several OPRA trialists disclosed relationships with a range of companies, including Sironax, Janssen Oncology, Toray Industries, Merck, and Intuitive Surgical.
A version of this article first appeared on Medscape.com.
TOPLINE:
with local tumor regrowth occurring mostly within the first 2 years.
METHODOLOGY:
- Many patients with locally advanced rectal cancer treated with total neoadjuvant therapy in the OPRA trial achieved a complete or near-complete tumor response and were initially offered a watch-and-wait strategy.
- However, nearly one-third of patients receiving watch-and-wait developed local tumor regrowth and ultimately required total mesorectal excision (TME).
- The study team reported updated organ preservation rates and oncologic outcomes in the OPRA trial of 324 patients with stage II/III rectal cancer randomized to induction chemotherapy followed by chemoradiation (n = 158) or chemoradiation followed by consolidation chemotherapy (n = 166).
- Among the 304 patients restaged a median of 7.8 weeks after finishing total neoadjuvant therapy, investigators recommended TME in 26% and watch-and-wait in 74% (n = 225).
TAKEAWAY:
- The researchers reported similar 5-year disease-free survival among patients in the induction chemotherapy group (71%) and the consolidation chemotherapy group (69%). The estimated 5-year overall survival rates were also similar in the two groups – 88% in the induction group vs. 85% in the consolidation group.
- Among the patients who received watch-and-wait, 36% (n = 81) experienced tumor regrowth; 94% occurred within 2 years and 99% occurred within 3 years.
- An estimated 39% of patients in the induction chemotherapy group and 54% in the consolidation chemotherapy group achieved organ preservation at 5 years, representing about half of patients overall.
- Among the patients who received watch-and-wait, salvage TME following tumor regrowth appeared to offer disease-free survival (64% of patients) similar to immediate TME after incomplete response to total neoadjuvant therapy (also 64%).
IN PRACTICE:
Total neoadjuvant therapy among patients with rectal cancer “resulted in long-term organ preservation in half of the patients,” the authors concluded. Although the order of therapy did not affect survival, consolidation chemotherapy “resulted in higher organ preservation at 5 years.”
“Our results support the recommendation that patients with rectal cancer offered [watch-and-wait] after neoadjuvant therapy should have very close surveillance during the first 3 years,” the authors added.
SOURCE:
The study, with first author Floris S. Verheij, BSc, Memorial Sloan Kettering Cancer Center, New York, was published online Oct. 26, 2023, in the Journal of Clinical Oncology.
LIMITATIONS:
The study, published as a clinical trials update, does not include a discussion of limitations.
DISCLOSURES:
Funding was provided by the National Cancer Institute. Several OPRA trialists disclosed relationships with a range of companies, including Sironax, Janssen Oncology, Toray Industries, Merck, and Intuitive Surgical.
A version of this article first appeared on Medscape.com.
New PCSK9 inhibitor allows 3-month treatment intervals
PHILADELPHIA – An investigational PCSK9 inhibitor that can be injected every 1-3 months as add-on therapy for patients with stubbornly high low-density lipoprotein (LDL) cholesterol has demonstrated cholesterol lowering for up to a year, in a clinical trial.
The results are from the phase 3 Recaticimab Add-On Therapy in Patients With Non-Familial Hypercholesterolemia and Mixed Hyperlipidemia (REMAIN-2) trial.
“It’s a new antibody that has a long half-life so each treatment can be prolonged,” investigator Xin Du, MD, professor of cardiology at Beijing Anzhen Hospital and the Capital Medical University, said in an interview. “Previous drugs like alirocumab and evolocumab have to be given every 2 weeks or every 4 weeks, and this new drug can be given even every 12 weeks, so it can get a very strong effect of LDL cholesterol lowering even when given every 3 months.”
Recaticimab has demonstrated a half-life of 18.6 to 27.4 days vs. 11 to 17 days for alirocumab and evolocumab, she said.
“Currently a high proportion of patients prescribed the PCSK9 inhibitors withdraw from therapy,” Dr. Du said. “After 36 months, only half of them are still on that therapy.”
Dr. Du presented the trial results at the annual scientific sessions of the American Heart Association.
Trial design and results
REMAIN-2 randomly assigned 692 patients to one of three recaticimab dosing arms vs. placebo: 150 mg/kg every 4 weeks; 300 mg/kg every 8 weeks; and 450 mg/kg every 12 weeks. The study was conducted from June 2021 to March 2023. The average age of the participants was 56 years and 64% were men. A high percentage of patients, 87% to 93.5%, completed the study across all groups. All participants had high LDL-C levels despite statin therapy: ≥ 70 mg/dL for those with cardiovascular disease and ≥ 100 mg/dL for those without.
Recaticimab enhanced LDL-C reduction by 53.4% to 62% vs. placebo at 24 weeks with a similar effect across all dosing regimens, Dr. Du said. That level of reduction was sustained out to 48 weeks, she said, at 48.4% to 64%.
At week 24, 86% to 94.5% of all patients across the three dosing arms achieved their LDL-C goal. The treatment had a positive impact on other lipid levels as well, Dr. Du said. Levels of non-HDL-C declined 55% to 47%. Apolipoprotein B (ApoB) levels fell 53% to 42% and lipoprotein (a), or Lp(a) readings declined 39.5% to 29%. The placebo arms had no change or small increases in non-HDL-C and ApoB levels and modest reductions in Lp(a).
The trial demonstrated acceptable safety and tolerability of recaticimab, Dr. Du said. At 48 weeks, the rates of injection site reactions were 3.9% in the treatment arms vs. 1.3% in the placebo arms. Common adverse events with a frequency ≥ 5% in patients receiving recaticimab were upper respiratory tract infection, hyperuricemia, urinary tract infection, increased blood creatine phosphokinase – a marker of damage to the heart – COVID-19 infection, and increased alanine transferase and aspartate transferase, both of which are markers of liver damage.
Larger, longer studies needed
Longer-term studies of recaticimab are still needed to determine its ability produce durable LDL-C reduction in a cost-effective manner, said discussant Stephen Nicholls, MD, director of Victorian Heart Institute and professor at Monash University in Australia. “It is important to note that these are still relatively short studies and the short treatment period cannot exclude the formation of neutralizing antibodies that have undermined development of other humanized antibodies,” he told attendees.
The every-12-week dosing, Dr. Nicholls said in an interview, “provides a dosing regimen that may be palatable to many patients.”
Besides the potential for the development of antibodies, Dr. Nicholls foresaw potential challenges with recaticimab. “The reality will lie in longer-term data,” he said. “If they can achieve durable lipid lowering without such neutralizing antibodies that would be very good.”
Dr. Nicholls added, “There’s a lot going on in the PCSK9 inhibitor space and the challenge for any new therapeutic, including this one, is where will it fit in given the space is getting crowded. So, data is important and clinical uptake will be equally important.”
Dr. Du disclosed relationships with Sanofi, AstraZeneca and Bayer. Dr. Nicholls disclosed relationships with AstraZeneca, Akcea, Amarin, Amgen, Anthera, Boehringer Ingelheim, Cerenis, CSL Behring, Eli Lilly, Esperion, Novartis, LipoScience, The Medicines Company, Merck, New Amsterdam Pharma, Omthera, Resverlogix, InfraReDx, Roche, Sanofi-Regeneron, Takeda, Vaxxinity, and Seqirus.
PHILADELPHIA – An investigational PCSK9 inhibitor that can be injected every 1-3 months as add-on therapy for patients with stubbornly high low-density lipoprotein (LDL) cholesterol has demonstrated cholesterol lowering for up to a year, in a clinical trial.
The results are from the phase 3 Recaticimab Add-On Therapy in Patients With Non-Familial Hypercholesterolemia and Mixed Hyperlipidemia (REMAIN-2) trial.
“It’s a new antibody that has a long half-life so each treatment can be prolonged,” investigator Xin Du, MD, professor of cardiology at Beijing Anzhen Hospital and the Capital Medical University, said in an interview. “Previous drugs like alirocumab and evolocumab have to be given every 2 weeks or every 4 weeks, and this new drug can be given even every 12 weeks, so it can get a very strong effect of LDL cholesterol lowering even when given every 3 months.”
Recaticimab has demonstrated a half-life of 18.6 to 27.4 days vs. 11 to 17 days for alirocumab and evolocumab, she said.
“Currently a high proportion of patients prescribed the PCSK9 inhibitors withdraw from therapy,” Dr. Du said. “After 36 months, only half of them are still on that therapy.”
Dr. Du presented the trial results at the annual scientific sessions of the American Heart Association.
Trial design and results
REMAIN-2 randomly assigned 692 patients to one of three recaticimab dosing arms vs. placebo: 150 mg/kg every 4 weeks; 300 mg/kg every 8 weeks; and 450 mg/kg every 12 weeks. The study was conducted from June 2021 to March 2023. The average age of the participants was 56 years and 64% were men. A high percentage of patients, 87% to 93.5%, completed the study across all groups. All participants had high LDL-C levels despite statin therapy: ≥ 70 mg/dL for those with cardiovascular disease and ≥ 100 mg/dL for those without.
Recaticimab enhanced LDL-C reduction by 53.4% to 62% vs. placebo at 24 weeks with a similar effect across all dosing regimens, Dr. Du said. That level of reduction was sustained out to 48 weeks, she said, at 48.4% to 64%.
At week 24, 86% to 94.5% of all patients across the three dosing arms achieved their LDL-C goal. The treatment had a positive impact on other lipid levels as well, Dr. Du said. Levels of non-HDL-C declined 55% to 47%. Apolipoprotein B (ApoB) levels fell 53% to 42% and lipoprotein (a), or Lp(a) readings declined 39.5% to 29%. The placebo arms had no change or small increases in non-HDL-C and ApoB levels and modest reductions in Lp(a).
The trial demonstrated acceptable safety and tolerability of recaticimab, Dr. Du said. At 48 weeks, the rates of injection site reactions were 3.9% in the treatment arms vs. 1.3% in the placebo arms. Common adverse events with a frequency ≥ 5% in patients receiving recaticimab were upper respiratory tract infection, hyperuricemia, urinary tract infection, increased blood creatine phosphokinase – a marker of damage to the heart – COVID-19 infection, and increased alanine transferase and aspartate transferase, both of which are markers of liver damage.
Larger, longer studies needed
Longer-term studies of recaticimab are still needed to determine its ability produce durable LDL-C reduction in a cost-effective manner, said discussant Stephen Nicholls, MD, director of Victorian Heart Institute and professor at Monash University in Australia. “It is important to note that these are still relatively short studies and the short treatment period cannot exclude the formation of neutralizing antibodies that have undermined development of other humanized antibodies,” he told attendees.
The every-12-week dosing, Dr. Nicholls said in an interview, “provides a dosing regimen that may be palatable to many patients.”
Besides the potential for the development of antibodies, Dr. Nicholls foresaw potential challenges with recaticimab. “The reality will lie in longer-term data,” he said. “If they can achieve durable lipid lowering without such neutralizing antibodies that would be very good.”
Dr. Nicholls added, “There’s a lot going on in the PCSK9 inhibitor space and the challenge for any new therapeutic, including this one, is where will it fit in given the space is getting crowded. So, data is important and clinical uptake will be equally important.”
Dr. Du disclosed relationships with Sanofi, AstraZeneca and Bayer. Dr. Nicholls disclosed relationships with AstraZeneca, Akcea, Amarin, Amgen, Anthera, Boehringer Ingelheim, Cerenis, CSL Behring, Eli Lilly, Esperion, Novartis, LipoScience, The Medicines Company, Merck, New Amsterdam Pharma, Omthera, Resverlogix, InfraReDx, Roche, Sanofi-Regeneron, Takeda, Vaxxinity, and Seqirus.
PHILADELPHIA – An investigational PCSK9 inhibitor that can be injected every 1-3 months as add-on therapy for patients with stubbornly high low-density lipoprotein (LDL) cholesterol has demonstrated cholesterol lowering for up to a year, in a clinical trial.
The results are from the phase 3 Recaticimab Add-On Therapy in Patients With Non-Familial Hypercholesterolemia and Mixed Hyperlipidemia (REMAIN-2) trial.
“It’s a new antibody that has a long half-life so each treatment can be prolonged,” investigator Xin Du, MD, professor of cardiology at Beijing Anzhen Hospital and the Capital Medical University, said in an interview. “Previous drugs like alirocumab and evolocumab have to be given every 2 weeks or every 4 weeks, and this new drug can be given even every 12 weeks, so it can get a very strong effect of LDL cholesterol lowering even when given every 3 months.”
Recaticimab has demonstrated a half-life of 18.6 to 27.4 days vs. 11 to 17 days for alirocumab and evolocumab, she said.
“Currently a high proportion of patients prescribed the PCSK9 inhibitors withdraw from therapy,” Dr. Du said. “After 36 months, only half of them are still on that therapy.”
Dr. Du presented the trial results at the annual scientific sessions of the American Heart Association.
Trial design and results
REMAIN-2 randomly assigned 692 patients to one of three recaticimab dosing arms vs. placebo: 150 mg/kg every 4 weeks; 300 mg/kg every 8 weeks; and 450 mg/kg every 12 weeks. The study was conducted from June 2021 to March 2023. The average age of the participants was 56 years and 64% were men. A high percentage of patients, 87% to 93.5%, completed the study across all groups. All participants had high LDL-C levels despite statin therapy: ≥ 70 mg/dL for those with cardiovascular disease and ≥ 100 mg/dL for those without.
Recaticimab enhanced LDL-C reduction by 53.4% to 62% vs. placebo at 24 weeks with a similar effect across all dosing regimens, Dr. Du said. That level of reduction was sustained out to 48 weeks, she said, at 48.4% to 64%.
At week 24, 86% to 94.5% of all patients across the three dosing arms achieved their LDL-C goal. The treatment had a positive impact on other lipid levels as well, Dr. Du said. Levels of non-HDL-C declined 55% to 47%. Apolipoprotein B (ApoB) levels fell 53% to 42% and lipoprotein (a), or Lp(a) readings declined 39.5% to 29%. The placebo arms had no change or small increases in non-HDL-C and ApoB levels and modest reductions in Lp(a).
The trial demonstrated acceptable safety and tolerability of recaticimab, Dr. Du said. At 48 weeks, the rates of injection site reactions were 3.9% in the treatment arms vs. 1.3% in the placebo arms. Common adverse events with a frequency ≥ 5% in patients receiving recaticimab were upper respiratory tract infection, hyperuricemia, urinary tract infection, increased blood creatine phosphokinase – a marker of damage to the heart – COVID-19 infection, and increased alanine transferase and aspartate transferase, both of which are markers of liver damage.
Larger, longer studies needed
Longer-term studies of recaticimab are still needed to determine its ability produce durable LDL-C reduction in a cost-effective manner, said discussant Stephen Nicholls, MD, director of Victorian Heart Institute and professor at Monash University in Australia. “It is important to note that these are still relatively short studies and the short treatment period cannot exclude the formation of neutralizing antibodies that have undermined development of other humanized antibodies,” he told attendees.
The every-12-week dosing, Dr. Nicholls said in an interview, “provides a dosing regimen that may be palatable to many patients.”
Besides the potential for the development of antibodies, Dr. Nicholls foresaw potential challenges with recaticimab. “The reality will lie in longer-term data,” he said. “If they can achieve durable lipid lowering without such neutralizing antibodies that would be very good.”
Dr. Nicholls added, “There’s a lot going on in the PCSK9 inhibitor space and the challenge for any new therapeutic, including this one, is where will it fit in given the space is getting crowded. So, data is important and clinical uptake will be equally important.”
Dr. Du disclosed relationships with Sanofi, AstraZeneca and Bayer. Dr. Nicholls disclosed relationships with AstraZeneca, Akcea, Amarin, Amgen, Anthera, Boehringer Ingelheim, Cerenis, CSL Behring, Eli Lilly, Esperion, Novartis, LipoScience, The Medicines Company, Merck, New Amsterdam Pharma, Omthera, Resverlogix, InfraReDx, Roche, Sanofi-Regeneron, Takeda, Vaxxinity, and Seqirus.
AT AHA 2023
Yoga linked to seizure, anxiety reduction in epilepsy
TOPLINE:
in people with epilepsy, a new study shows.
METHODOLOGY:
- Investigators included participants aged 18-60 years with epilepsy who scored ≥ 4 on the Kilifi Stigma Scale of Epilepsy. A score greater than the 66th percentile indicates the presence of strongly felt stigma.
- Patients (n = 160) had an average of one seizure per week, and most took at least two antiseizure medications.
- The intervention group (n = 80) participated in a yoga module with muscle-loosening exercises, slow and synchronized breathing, meditation, and positive affirmations. The control group (n = 80) participated in sham yoga sessions with no instructions on the breathing exercises or attention to the body movements and sensations during practice.
- Both groups participated in seven 1-hour supervised group yoga sessions over 3 months, were asked to practice the interventions at home five times per week, and received a psychoeducation module on epilepsy.
TAKEAWAY:
- Participants practicing the intervention module had significant reductions in self-perceived stigma, compared with those in the control group (P = .01).
- The proportion of participants in the intervention group who had a more than 50% seizure reduction (odds ratio, 4.11; P = .01) and complete seizure remission (OR, 7.4; P = .005) at the end of the 6-month follow-up was significantly higher than in the control group.
- Compared with those in the control group, there were also significant improvements in anxiety (P = .032) and quality of life (P < .001) in the intervention group.
- The intervention group also experienced significant improvement in mindfulness (P < .001) and cognitive impairment, compared with the control group (P < .004).
IN PRACTICE:
“This stigma can affect a person’s life in many ways, including treatment, emergency department visits, and poor mental health,” study investigator Majari Tripathi, MD, of All India Institute of Medical Sciences, New Delhi, said in a press release. “Our study showed that doing yoga can alleviate the burden of epilepsy and improve the overall quality of life by reducing this perceived stigma.”
SOURCE:
Dr. Tripathi and Kirandeep Kaur, MD, also of All India Institute of Medical Sciences, conducted the study with their colleagues. It was published online in Neurology.
LIMITATIONS:
There was no passive control or treatment as usual group, which would indicate the effect size of the intervention. In addition, there was no monitoring of seizure frequency before the study began, which may have biased the change of seizure frequency as an outcome.
DISCLOSURES:
The study investigators reported no study funding or reported disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
in people with epilepsy, a new study shows.
METHODOLOGY:
- Investigators included participants aged 18-60 years with epilepsy who scored ≥ 4 on the Kilifi Stigma Scale of Epilepsy. A score greater than the 66th percentile indicates the presence of strongly felt stigma.
- Patients (n = 160) had an average of one seizure per week, and most took at least two antiseizure medications.
- The intervention group (n = 80) participated in a yoga module with muscle-loosening exercises, slow and synchronized breathing, meditation, and positive affirmations. The control group (n = 80) participated in sham yoga sessions with no instructions on the breathing exercises or attention to the body movements and sensations during practice.
- Both groups participated in seven 1-hour supervised group yoga sessions over 3 months, were asked to practice the interventions at home five times per week, and received a psychoeducation module on epilepsy.
TAKEAWAY:
- Participants practicing the intervention module had significant reductions in self-perceived stigma, compared with those in the control group (P = .01).
- The proportion of participants in the intervention group who had a more than 50% seizure reduction (odds ratio, 4.11; P = .01) and complete seizure remission (OR, 7.4; P = .005) at the end of the 6-month follow-up was significantly higher than in the control group.
- Compared with those in the control group, there were also significant improvements in anxiety (P = .032) and quality of life (P < .001) in the intervention group.
- The intervention group also experienced significant improvement in mindfulness (P < .001) and cognitive impairment, compared with the control group (P < .004).
IN PRACTICE:
“This stigma can affect a person’s life in many ways, including treatment, emergency department visits, and poor mental health,” study investigator Majari Tripathi, MD, of All India Institute of Medical Sciences, New Delhi, said in a press release. “Our study showed that doing yoga can alleviate the burden of epilepsy and improve the overall quality of life by reducing this perceived stigma.”
SOURCE:
Dr. Tripathi and Kirandeep Kaur, MD, also of All India Institute of Medical Sciences, conducted the study with their colleagues. It was published online in Neurology.
LIMITATIONS:
There was no passive control or treatment as usual group, which would indicate the effect size of the intervention. In addition, there was no monitoring of seizure frequency before the study began, which may have biased the change of seizure frequency as an outcome.
DISCLOSURES:
The study investigators reported no study funding or reported disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
in people with epilepsy, a new study shows.
METHODOLOGY:
- Investigators included participants aged 18-60 years with epilepsy who scored ≥ 4 on the Kilifi Stigma Scale of Epilepsy. A score greater than the 66th percentile indicates the presence of strongly felt stigma.
- Patients (n = 160) had an average of one seizure per week, and most took at least two antiseizure medications.
- The intervention group (n = 80) participated in a yoga module with muscle-loosening exercises, slow and synchronized breathing, meditation, and positive affirmations. The control group (n = 80) participated in sham yoga sessions with no instructions on the breathing exercises or attention to the body movements and sensations during practice.
- Both groups participated in seven 1-hour supervised group yoga sessions over 3 months, were asked to practice the interventions at home five times per week, and received a psychoeducation module on epilepsy.
TAKEAWAY:
- Participants practicing the intervention module had significant reductions in self-perceived stigma, compared with those in the control group (P = .01).
- The proportion of participants in the intervention group who had a more than 50% seizure reduction (odds ratio, 4.11; P = .01) and complete seizure remission (OR, 7.4; P = .005) at the end of the 6-month follow-up was significantly higher than in the control group.
- Compared with those in the control group, there were also significant improvements in anxiety (P = .032) and quality of life (P < .001) in the intervention group.
- The intervention group also experienced significant improvement in mindfulness (P < .001) and cognitive impairment, compared with the control group (P < .004).
IN PRACTICE:
“This stigma can affect a person’s life in many ways, including treatment, emergency department visits, and poor mental health,” study investigator Majari Tripathi, MD, of All India Institute of Medical Sciences, New Delhi, said in a press release. “Our study showed that doing yoga can alleviate the burden of epilepsy and improve the overall quality of life by reducing this perceived stigma.”
SOURCE:
Dr. Tripathi and Kirandeep Kaur, MD, also of All India Institute of Medical Sciences, conducted the study with their colleagues. It was published online in Neurology.
LIMITATIONS:
There was no passive control or treatment as usual group, which would indicate the effect size of the intervention. In addition, there was no monitoring of seizure frequency before the study began, which may have biased the change of seizure frequency as an outcome.
DISCLOSURES:
The study investigators reported no study funding or reported disclosures.
A version of this article appeared on Medscape.com.
Bariatric surgery still best option for some with obesity
Bariatric surgery continues to play a major role in obesity management despite the emergence of potent new weight-loss medications, according to two experts who spoke at an Endocrine Society science writers briefing.
“Bariatric surgery is safe, effective, and unfortunately underutilized for treating obesity and its complications,” said Jaime Almandoz, MD, medical director of the Weight Wellness Program at the University of Texas Southwestern Medical Center, Dallas.
Added Dr. Almandoz, who is triple board-certified in internal medicine, endocrinology, and obesity medicine, “Sometimes this gets presented in a linear fashion. ‘We’ll try lifestyle first, and if that doesn’t work, we’ll try medications, and if that doesn’t work, we’ll try surgery.’ But sometimes we might need to go straight to surgery instead of going through medications first, because it may be the most effective and evidence-based treatment for the person in the office in front of you.”
Moreover, he pointed out that currently, Medicare and many private insurers don’t cover antiobesity medications but do cover bariatric surgery.
Indeed, Srividya Kidambi, MD, professor and chief of endocrinology and molecular medicine at the Medical College of Wisconsin/Froedtert Hospital, Milwaukee, said there are certain types of patients for whom she might consider bariatric surgery first. One would be a person with a body mass index (BMI) greater than 40 kg/m2 or with a BMI greater than 35 kg/m2 and severe comorbidities.
Another, she said, would be young, relatively healthy people with obesity who have no comorbid conditions. “We know that if we stop the medication, the weight comes back. So, if I see a 20- to 25-year-old, am I really to commit them to lifelong therapy, or is bariatric surgery a better option in these cases? These drugs have not been around that long ... so I tend to recommend bariatric surgery in some patients.”
During the recent briefing, Dr. Almandoz summarized the evidence base for the benefits of bariatric surgery beyond weight loss, which include remission of type 2 diabetes and fatty liver disease, reduction of the risks of cardiovascular disease and cancer, and increased life expectancy.
“Everyone seems to be talking about GLP-1s for facilitating weight loss and treating obesity. ... What I want to do is provide a counterpoint to accessible therapies that are covered by more insurance plans and that may, in fact, have a better evidence base for treating obesity and its related complications,” he said in his introduction.
Bariatric surgery has been used for decades, and many centers of excellence perform it, with greatly reduced complication rates seen today than in the past. “It’s comparable to having a gallbladder surgery in terms of perioperative risk,” he noted.
Medicare and private insurers generally cover bariatric surgery for people with BMI greater than 40 kg/m2 or 35-39 kg/m2 and at least one weight-related comorbidity, including type 2 diabetes, obstructive sleep apnea, hypertension, atherosclerotic disease, hyperlipidemia, and fatty liver disease.
Data suggest that weight reduction of about 3% can lead to meaningful reductions in blood glucose and triglyceride levels, but weight loss of 15% or greater is associated with reductions in cardiovascular events and type 2 diabetes remission. Lifestyle modification typically produces about 5% weight loss, compared with 20%-35% with bariatric surgery with sleeve gastrectomy or gastric bypass.
Older weight loss medications produced weight loss of 5%-10%; only the newer medications, semaglutide 2.4 mg and tirzepatide, come close to that. Weight loss with semaglutide is about 15%, while tirzepatide can produce weight loss of up to 22%. But, there are still issues with affordability, access, and lack of coverage, Dr. Almandoz noted.
One recent randomized trial of more than 400 individuals showed that bariatric surgery was more effective than lifestyle and medical therapies for treating metabolic-associated steatohepatitis without worsening of fibrosis.
Another showed that the surgery was associated with fewer major adverse liver outcomes among people who already had MASH. That same study showed a 70% reduction in cardiovascular events with bariatric surgery.
For patients with type 2 diabetes, numerous trials have demonstrated long-term remission and reduced A1c at 5 years and 10 years post surgery, along with reductions in microvascular and macrovascular complications.
Other data suggest that a shorter history of type 2 diabetes is among the factors predicting remission with bariatric surgery. “Oftentimes, both patients and providers will wait until the diabetes is quite advanced before they even have the conversation about weight loss or even bariatric surgery. This suggests that if we intervene earlier in the course of disease, when it is less severe and less advanced, we have a higher rate of causing remission in the diabetes,” Dr. Almandoz said.
The American Diabetes Association’s Standards of Care incorporate bariatric surgery as either “recommended” or “may be considered” to treat type 2 diabetes, depending on BMI level, for those who don’t achieve durable weight loss with nonsurgical methods, he noted.
A retrospective cohort study showed significant reductions in cardiovascular outcomes with bariatric surgery among people with baseline cardiovascular disease. “This is not just about bariatric surgery to cause weight loss. This is about the multitude of effects that happen when we treat obesity as a disease with highly effective therapies such as surgery,” he said.
Even cancer risk and cancer-related mortality were significantly reduced with bariatric surgery, another study found.
And in the long-term Swedish Obese Subjects Study, among people with obesity, bariatric surgery was associated with a 3-year increase in life expectancy, compared with not undergoing surgery.
However, Dr. Almandoz also pointed out that some patients may benefit from both weight-loss medication and bariatric surgery. “Once someone has undergone pharmacotherapy, there may still be a role for bariatric procedures in helping to optimize body weight and control body weight long term. And likewise for those who have undergone bariatric surgery, there’s also a role for pharmacotherapy in terms of treating insufficient weight loss or weight recurrence after bariatric surgery. ... So I think there’s clearly a role for integration of therapies.”
Dr. Almandoz serves as consultant/advisory board member for Novo Nordisk, Boehringer Ingelheim, and Eli Lilly. Dr. Kidambi is director of TOPS Center for Metabolic Research and is medical editor of TOPS Magazine, for which her institution receives an honorarium.
A version of this article first appeared on Medscape.com.
Bariatric surgery continues to play a major role in obesity management despite the emergence of potent new weight-loss medications, according to two experts who spoke at an Endocrine Society science writers briefing.
“Bariatric surgery is safe, effective, and unfortunately underutilized for treating obesity and its complications,” said Jaime Almandoz, MD, medical director of the Weight Wellness Program at the University of Texas Southwestern Medical Center, Dallas.
Added Dr. Almandoz, who is triple board-certified in internal medicine, endocrinology, and obesity medicine, “Sometimes this gets presented in a linear fashion. ‘We’ll try lifestyle first, and if that doesn’t work, we’ll try medications, and if that doesn’t work, we’ll try surgery.’ But sometimes we might need to go straight to surgery instead of going through medications first, because it may be the most effective and evidence-based treatment for the person in the office in front of you.”
Moreover, he pointed out that currently, Medicare and many private insurers don’t cover antiobesity medications but do cover bariatric surgery.
Indeed, Srividya Kidambi, MD, professor and chief of endocrinology and molecular medicine at the Medical College of Wisconsin/Froedtert Hospital, Milwaukee, said there are certain types of patients for whom she might consider bariatric surgery first. One would be a person with a body mass index (BMI) greater than 40 kg/m2 or with a BMI greater than 35 kg/m2 and severe comorbidities.
Another, she said, would be young, relatively healthy people with obesity who have no comorbid conditions. “We know that if we stop the medication, the weight comes back. So, if I see a 20- to 25-year-old, am I really to commit them to lifelong therapy, or is bariatric surgery a better option in these cases? These drugs have not been around that long ... so I tend to recommend bariatric surgery in some patients.”
During the recent briefing, Dr. Almandoz summarized the evidence base for the benefits of bariatric surgery beyond weight loss, which include remission of type 2 diabetes and fatty liver disease, reduction of the risks of cardiovascular disease and cancer, and increased life expectancy.
“Everyone seems to be talking about GLP-1s for facilitating weight loss and treating obesity. ... What I want to do is provide a counterpoint to accessible therapies that are covered by more insurance plans and that may, in fact, have a better evidence base for treating obesity and its related complications,” he said in his introduction.
Bariatric surgery has been used for decades, and many centers of excellence perform it, with greatly reduced complication rates seen today than in the past. “It’s comparable to having a gallbladder surgery in terms of perioperative risk,” he noted.
Medicare and private insurers generally cover bariatric surgery for people with BMI greater than 40 kg/m2 or 35-39 kg/m2 and at least one weight-related comorbidity, including type 2 diabetes, obstructive sleep apnea, hypertension, atherosclerotic disease, hyperlipidemia, and fatty liver disease.
Data suggest that weight reduction of about 3% can lead to meaningful reductions in blood glucose and triglyceride levels, but weight loss of 15% or greater is associated with reductions in cardiovascular events and type 2 diabetes remission. Lifestyle modification typically produces about 5% weight loss, compared with 20%-35% with bariatric surgery with sleeve gastrectomy or gastric bypass.
Older weight loss medications produced weight loss of 5%-10%; only the newer medications, semaglutide 2.4 mg and tirzepatide, come close to that. Weight loss with semaglutide is about 15%, while tirzepatide can produce weight loss of up to 22%. But, there are still issues with affordability, access, and lack of coverage, Dr. Almandoz noted.
One recent randomized trial of more than 400 individuals showed that bariatric surgery was more effective than lifestyle and medical therapies for treating metabolic-associated steatohepatitis without worsening of fibrosis.
Another showed that the surgery was associated with fewer major adverse liver outcomes among people who already had MASH. That same study showed a 70% reduction in cardiovascular events with bariatric surgery.
For patients with type 2 diabetes, numerous trials have demonstrated long-term remission and reduced A1c at 5 years and 10 years post surgery, along with reductions in microvascular and macrovascular complications.
Other data suggest that a shorter history of type 2 diabetes is among the factors predicting remission with bariatric surgery. “Oftentimes, both patients and providers will wait until the diabetes is quite advanced before they even have the conversation about weight loss or even bariatric surgery. This suggests that if we intervene earlier in the course of disease, when it is less severe and less advanced, we have a higher rate of causing remission in the diabetes,” Dr. Almandoz said.
The American Diabetes Association’s Standards of Care incorporate bariatric surgery as either “recommended” or “may be considered” to treat type 2 diabetes, depending on BMI level, for those who don’t achieve durable weight loss with nonsurgical methods, he noted.
A retrospective cohort study showed significant reductions in cardiovascular outcomes with bariatric surgery among people with baseline cardiovascular disease. “This is not just about bariatric surgery to cause weight loss. This is about the multitude of effects that happen when we treat obesity as a disease with highly effective therapies such as surgery,” he said.
Even cancer risk and cancer-related mortality were significantly reduced with bariatric surgery, another study found.
And in the long-term Swedish Obese Subjects Study, among people with obesity, bariatric surgery was associated with a 3-year increase in life expectancy, compared with not undergoing surgery.
However, Dr. Almandoz also pointed out that some patients may benefit from both weight-loss medication and bariatric surgery. “Once someone has undergone pharmacotherapy, there may still be a role for bariatric procedures in helping to optimize body weight and control body weight long term. And likewise for those who have undergone bariatric surgery, there’s also a role for pharmacotherapy in terms of treating insufficient weight loss or weight recurrence after bariatric surgery. ... So I think there’s clearly a role for integration of therapies.”
Dr. Almandoz serves as consultant/advisory board member for Novo Nordisk, Boehringer Ingelheim, and Eli Lilly. Dr. Kidambi is director of TOPS Center for Metabolic Research and is medical editor of TOPS Magazine, for which her institution receives an honorarium.
A version of this article first appeared on Medscape.com.
Bariatric surgery continues to play a major role in obesity management despite the emergence of potent new weight-loss medications, according to two experts who spoke at an Endocrine Society science writers briefing.
“Bariatric surgery is safe, effective, and unfortunately underutilized for treating obesity and its complications,” said Jaime Almandoz, MD, medical director of the Weight Wellness Program at the University of Texas Southwestern Medical Center, Dallas.
Added Dr. Almandoz, who is triple board-certified in internal medicine, endocrinology, and obesity medicine, “Sometimes this gets presented in a linear fashion. ‘We’ll try lifestyle first, and if that doesn’t work, we’ll try medications, and if that doesn’t work, we’ll try surgery.’ But sometimes we might need to go straight to surgery instead of going through medications first, because it may be the most effective and evidence-based treatment for the person in the office in front of you.”
Moreover, he pointed out that currently, Medicare and many private insurers don’t cover antiobesity medications but do cover bariatric surgery.
Indeed, Srividya Kidambi, MD, professor and chief of endocrinology and molecular medicine at the Medical College of Wisconsin/Froedtert Hospital, Milwaukee, said there are certain types of patients for whom she might consider bariatric surgery first. One would be a person with a body mass index (BMI) greater than 40 kg/m2 or with a BMI greater than 35 kg/m2 and severe comorbidities.
Another, she said, would be young, relatively healthy people with obesity who have no comorbid conditions. “We know that if we stop the medication, the weight comes back. So, if I see a 20- to 25-year-old, am I really to commit them to lifelong therapy, or is bariatric surgery a better option in these cases? These drugs have not been around that long ... so I tend to recommend bariatric surgery in some patients.”
During the recent briefing, Dr. Almandoz summarized the evidence base for the benefits of bariatric surgery beyond weight loss, which include remission of type 2 diabetes and fatty liver disease, reduction of the risks of cardiovascular disease and cancer, and increased life expectancy.
“Everyone seems to be talking about GLP-1s for facilitating weight loss and treating obesity. ... What I want to do is provide a counterpoint to accessible therapies that are covered by more insurance plans and that may, in fact, have a better evidence base for treating obesity and its related complications,” he said in his introduction.
Bariatric surgery has been used for decades, and many centers of excellence perform it, with greatly reduced complication rates seen today than in the past. “It’s comparable to having a gallbladder surgery in terms of perioperative risk,” he noted.
Medicare and private insurers generally cover bariatric surgery for people with BMI greater than 40 kg/m2 or 35-39 kg/m2 and at least one weight-related comorbidity, including type 2 diabetes, obstructive sleep apnea, hypertension, atherosclerotic disease, hyperlipidemia, and fatty liver disease.
Data suggest that weight reduction of about 3% can lead to meaningful reductions in blood glucose and triglyceride levels, but weight loss of 15% or greater is associated with reductions in cardiovascular events and type 2 diabetes remission. Lifestyle modification typically produces about 5% weight loss, compared with 20%-35% with bariatric surgery with sleeve gastrectomy or gastric bypass.
Older weight loss medications produced weight loss of 5%-10%; only the newer medications, semaglutide 2.4 mg and tirzepatide, come close to that. Weight loss with semaglutide is about 15%, while tirzepatide can produce weight loss of up to 22%. But, there are still issues with affordability, access, and lack of coverage, Dr. Almandoz noted.
One recent randomized trial of more than 400 individuals showed that bariatric surgery was more effective than lifestyle and medical therapies for treating metabolic-associated steatohepatitis without worsening of fibrosis.
Another showed that the surgery was associated with fewer major adverse liver outcomes among people who already had MASH. That same study showed a 70% reduction in cardiovascular events with bariatric surgery.
For patients with type 2 diabetes, numerous trials have demonstrated long-term remission and reduced A1c at 5 years and 10 years post surgery, along with reductions in microvascular and macrovascular complications.
Other data suggest that a shorter history of type 2 diabetes is among the factors predicting remission with bariatric surgery. “Oftentimes, both patients and providers will wait until the diabetes is quite advanced before they even have the conversation about weight loss or even bariatric surgery. This suggests that if we intervene earlier in the course of disease, when it is less severe and less advanced, we have a higher rate of causing remission in the diabetes,” Dr. Almandoz said.
The American Diabetes Association’s Standards of Care incorporate bariatric surgery as either “recommended” or “may be considered” to treat type 2 diabetes, depending on BMI level, for those who don’t achieve durable weight loss with nonsurgical methods, he noted.
A retrospective cohort study showed significant reductions in cardiovascular outcomes with bariatric surgery among people with baseline cardiovascular disease. “This is not just about bariatric surgery to cause weight loss. This is about the multitude of effects that happen when we treat obesity as a disease with highly effective therapies such as surgery,” he said.
Even cancer risk and cancer-related mortality were significantly reduced with bariatric surgery, another study found.
And in the long-term Swedish Obese Subjects Study, among people with obesity, bariatric surgery was associated with a 3-year increase in life expectancy, compared with not undergoing surgery.
However, Dr. Almandoz also pointed out that some patients may benefit from both weight-loss medication and bariatric surgery. “Once someone has undergone pharmacotherapy, there may still be a role for bariatric procedures in helping to optimize body weight and control body weight long term. And likewise for those who have undergone bariatric surgery, there’s also a role for pharmacotherapy in terms of treating insufficient weight loss or weight recurrence after bariatric surgery. ... So I think there’s clearly a role for integration of therapies.”
Dr. Almandoz serves as consultant/advisory board member for Novo Nordisk, Boehringer Ingelheim, and Eli Lilly. Dr. Kidambi is director of TOPS Center for Metabolic Research and is medical editor of TOPS Magazine, for which her institution receives an honorarium.
A version of this article first appeared on Medscape.com.
Low-dose aspirin provokes no flares in patients with IBD during pregnancy
, shows new research presented in October at the American College of Gastroenterology (ACG) Annual Scientific Meeting.
Low-dose aspirin is recommended for pregnant women who are at risk of hypertensive disorders, such as eclampsia, preeclampsia, and gestational diabetes, said Uma Mahadevan, MD, AGAF, a gastroenterologist and director of the University of California, San Francisco Colitis and Crohn’s Disease Center, who presented the research at the meeting. Regular nonsteroidal anti-inflammatory drug use has been associated with increased disease activity in patients with inflammatory bowel disease (IBD), but the impact of low-dose aspirin on IBD during pregnancy has not been well studied, she said.
The study, which was conducted between January 2013 and December 2022 at a single clinic, included 325 women (mean age 34 years) with IBD who had at least one pregnancy. Of these, 53% had ulcerative colitis and 47% had Crohn’s disease. The primary outcome was IBD flare during pregnancy or within 6 months postpartum. Flares were defined as an IBD-related hospitalization and/or surgery, new initiation of IBD therapy, elevated level of fecal calprotectin greater than 150 micrograms per milligram, or new active endoscopic disease.
A total of 95 patients (29%) used low-dose aspirin during pregnancy; 59 took 81 mg and 36 took 162 mg. The cumulative flare rate was similar between patients who took low-dose aspirin and those who did not (24% vs. 26%, P = .83). However, patients who took low-dose aspirin were significantly more likely than were those who did not to experience preterm birth, younger gestational age at delivery, and cesarean delivery (22.1% vs. 6.1%, 38 weeks vs. 39 weeks, 51% vs. 27%, respectively, P < .01 for all).
Overall rates of hypertensive disorders of pregnancy were similar between the low-dose aspirin and non–low-dose aspirin groups (22% vs. 19%, respectively, P = .59), but individuals on low-dose aspirin were more likely to experience preeclampsia than were those not on low-dose aspirin (11.6% vs 4.3%, P = .03).
The study findings support the benefits of aspirin for pregnant women at increased risk for these conditions. “Pregnant patients with IBD should be offered low-dose aspirin without concern for increased risk of flares,” Dr. Mahadevan said.
“This is a very practical study with high relevance in our everyday management of IBD patients,” Shannon Chang, MD, a specialist in IBD with NYU Langone Health, said in an interview. “Having this study helps us understand the risk of increased IBD activity in the setting of aspirin use during pregnancy.”
Dr. Chang was not surprised by the findings. “Since the [ACOG] guidelines changed several years ago, there have been more and more patients with IBD who have taken aspirin during their pregnancies and the results of this study seem to match what we see in clinical practice,” she said. “This study will help us counsel our patients on the safety of aspirin use during pregnancy, and the findings will also be useful for discussions with our obstetrics colleagues who may seek guidance on the safety of aspirin [use] in our pregnant IBD patients.”
The study received no outside funding. Dr. Mahadevan disclosed relationships with AbbVie, Boehringer Ingelheim, Bristol Myers Squibb, Celltrion, Eli Lilly, Gilead, Janssen, Pfizer, Prometheus Biosciences, Protagonist Therapeutics, Rani Therapeutics, Roivant, and Takeda. Dr. Chang disclosed serving as a consultant for Pfizer, AbbVie, and BMS.
, shows new research presented in October at the American College of Gastroenterology (ACG) Annual Scientific Meeting.
Low-dose aspirin is recommended for pregnant women who are at risk of hypertensive disorders, such as eclampsia, preeclampsia, and gestational diabetes, said Uma Mahadevan, MD, AGAF, a gastroenterologist and director of the University of California, San Francisco Colitis and Crohn’s Disease Center, who presented the research at the meeting. Regular nonsteroidal anti-inflammatory drug use has been associated with increased disease activity in patients with inflammatory bowel disease (IBD), but the impact of low-dose aspirin on IBD during pregnancy has not been well studied, she said.
The study, which was conducted between January 2013 and December 2022 at a single clinic, included 325 women (mean age 34 years) with IBD who had at least one pregnancy. Of these, 53% had ulcerative colitis and 47% had Crohn’s disease. The primary outcome was IBD flare during pregnancy or within 6 months postpartum. Flares were defined as an IBD-related hospitalization and/or surgery, new initiation of IBD therapy, elevated level of fecal calprotectin greater than 150 micrograms per milligram, or new active endoscopic disease.
A total of 95 patients (29%) used low-dose aspirin during pregnancy; 59 took 81 mg and 36 took 162 mg. The cumulative flare rate was similar between patients who took low-dose aspirin and those who did not (24% vs. 26%, P = .83). However, patients who took low-dose aspirin were significantly more likely than were those who did not to experience preterm birth, younger gestational age at delivery, and cesarean delivery (22.1% vs. 6.1%, 38 weeks vs. 39 weeks, 51% vs. 27%, respectively, P < .01 for all).
Overall rates of hypertensive disorders of pregnancy were similar between the low-dose aspirin and non–low-dose aspirin groups (22% vs. 19%, respectively, P = .59), but individuals on low-dose aspirin were more likely to experience preeclampsia than were those not on low-dose aspirin (11.6% vs 4.3%, P = .03).
The study findings support the benefits of aspirin for pregnant women at increased risk for these conditions. “Pregnant patients with IBD should be offered low-dose aspirin without concern for increased risk of flares,” Dr. Mahadevan said.
“This is a very practical study with high relevance in our everyday management of IBD patients,” Shannon Chang, MD, a specialist in IBD with NYU Langone Health, said in an interview. “Having this study helps us understand the risk of increased IBD activity in the setting of aspirin use during pregnancy.”
Dr. Chang was not surprised by the findings. “Since the [ACOG] guidelines changed several years ago, there have been more and more patients with IBD who have taken aspirin during their pregnancies and the results of this study seem to match what we see in clinical practice,” she said. “This study will help us counsel our patients on the safety of aspirin use during pregnancy, and the findings will also be useful for discussions with our obstetrics colleagues who may seek guidance on the safety of aspirin [use] in our pregnant IBD patients.”
The study received no outside funding. Dr. Mahadevan disclosed relationships with AbbVie, Boehringer Ingelheim, Bristol Myers Squibb, Celltrion, Eli Lilly, Gilead, Janssen, Pfizer, Prometheus Biosciences, Protagonist Therapeutics, Rani Therapeutics, Roivant, and Takeda. Dr. Chang disclosed serving as a consultant for Pfizer, AbbVie, and BMS.
, shows new research presented in October at the American College of Gastroenterology (ACG) Annual Scientific Meeting.
Low-dose aspirin is recommended for pregnant women who are at risk of hypertensive disorders, such as eclampsia, preeclampsia, and gestational diabetes, said Uma Mahadevan, MD, AGAF, a gastroenterologist and director of the University of California, San Francisco Colitis and Crohn’s Disease Center, who presented the research at the meeting. Regular nonsteroidal anti-inflammatory drug use has been associated with increased disease activity in patients with inflammatory bowel disease (IBD), but the impact of low-dose aspirin on IBD during pregnancy has not been well studied, she said.
The study, which was conducted between January 2013 and December 2022 at a single clinic, included 325 women (mean age 34 years) with IBD who had at least one pregnancy. Of these, 53% had ulcerative colitis and 47% had Crohn’s disease. The primary outcome was IBD flare during pregnancy or within 6 months postpartum. Flares were defined as an IBD-related hospitalization and/or surgery, new initiation of IBD therapy, elevated level of fecal calprotectin greater than 150 micrograms per milligram, or new active endoscopic disease.
A total of 95 patients (29%) used low-dose aspirin during pregnancy; 59 took 81 mg and 36 took 162 mg. The cumulative flare rate was similar between patients who took low-dose aspirin and those who did not (24% vs. 26%, P = .83). However, patients who took low-dose aspirin were significantly more likely than were those who did not to experience preterm birth, younger gestational age at delivery, and cesarean delivery (22.1% vs. 6.1%, 38 weeks vs. 39 weeks, 51% vs. 27%, respectively, P < .01 for all).
Overall rates of hypertensive disorders of pregnancy were similar between the low-dose aspirin and non–low-dose aspirin groups (22% vs. 19%, respectively, P = .59), but individuals on low-dose aspirin were more likely to experience preeclampsia than were those not on low-dose aspirin (11.6% vs 4.3%, P = .03).
The study findings support the benefits of aspirin for pregnant women at increased risk for these conditions. “Pregnant patients with IBD should be offered low-dose aspirin without concern for increased risk of flares,” Dr. Mahadevan said.
“This is a very practical study with high relevance in our everyday management of IBD patients,” Shannon Chang, MD, a specialist in IBD with NYU Langone Health, said in an interview. “Having this study helps us understand the risk of increased IBD activity in the setting of aspirin use during pregnancy.”
Dr. Chang was not surprised by the findings. “Since the [ACOG] guidelines changed several years ago, there have been more and more patients with IBD who have taken aspirin during their pregnancies and the results of this study seem to match what we see in clinical practice,” she said. “This study will help us counsel our patients on the safety of aspirin use during pregnancy, and the findings will also be useful for discussions with our obstetrics colleagues who may seek guidance on the safety of aspirin [use] in our pregnant IBD patients.”
The study received no outside funding. Dr. Mahadevan disclosed relationships with AbbVie, Boehringer Ingelheim, Bristol Myers Squibb, Celltrion, Eli Lilly, Gilead, Janssen, Pfizer, Prometheus Biosciences, Protagonist Therapeutics, Rani Therapeutics, Roivant, and Takeda. Dr. Chang disclosed serving as a consultant for Pfizer, AbbVie, and BMS.
FROM ACG 2023
Quitting medical school
A few weeks ago I shared by concerns about the dwindling numbers of primary care physicians. The early exodus of practicing providers and an obvious disinterest by future physicians in what they see as the unpalatable work/life balance of frontline hands-on medicine are among the causes.
A recent study published in the journal Pediatrics highlights personal finance as a contributor to the drain on the primary care workforce. The investigators found “high self-reported educational debt ($200,000 to < $300,000) was positively associated with training in a positive lifetime earnings potential subspecialty.” In other words, why would a physician who was burdened with student loans enter a subspecialty that would limit his or her ability to pay it off? I suspect that money has always been a factor in career selection, but the ballooning cost of college and medical school has certainly not nudged graduates toward the low lifetime earnings potential of primary care pediatrics.
Another recently released survey adds the perspective of current medical school students to the murky future of the primary health care workforce. The Clinician of the Future 2023: Education Edition, published by Elsevier Health, reports on insights of more than 2,000 nursing and medical school student from around the world. The headline shocker was that while across the board a not surprising 12% of medical students were considering quitting their studies, in the United States this number was 25%.
Overall, more than 60% of the students worried about their future income, how workforce shortages would effect them and whether they would join the ranks of those clinicians suffering from burnout. While the students surveyed acknowledged that artificial intelligence could have some negative repercussions, 62% were excited about its use in their education. Similarly, they anticipated the positive contribution of digital technology while acknowledging its potential downsides.
Given the current mental health climate in this country, I was not surprised that almost a quarter of medical students in this country are considering quitting school. I would like to see a larger sample surveyed and repeated over time. But, the discrepancy between the United States and the rest of the world is troubling.
The number that really jumped out at me was that 54% of medical students (nurses, 62%) viewed “ their current studies as a stepping-stone toward a broader career in health care.” As an example, the authors quoted one medical student who plans to “look for other possibilities where I don’t directly treat patients.”
Whether this disinterest in direct patient care is an attitude that preceded their entry into medical school or a change reflecting a major reversal induced by the realty of face-to-face patient encounters in school was not addressed in the survey. I think the general population would be surprised and maybe disappointed to learn that half the students in medical school weren’t planning on seeing patients.
I went off to medical school with a rather naive Norman Rockwellian view of a physician. I was a little surprised that a few of my classmates seemed to be gravitating toward administrative and research careers, but by far most of us were heading toward opportunities that would place us face to face with patients. Some would become specialists but primary care still had an appeal for many of us.
In my last letter about primary care training, I suggested that traditional medical school was probably a poor investment for the person who shares a bit of my old-school image of the primary care physician. In addition to cost and the time invested, the curriculum would likely be overly broad and deep and not terribly applicable to the patient mix he or she would eventually be seeing. This global survey may suggest that medical students have already discovered, or are just now discovering, this mismatch between medical school and the realities of primary care.
Our challenge is to first deal with deterrent of student debt and then to develop a new, affordable and efficient pathway to primary care that attracts those people who are looking for a face to face style of medicine on the front line. The patients know we need specialists and administrators but they also want a bit more of Norman Rockwell.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
A few weeks ago I shared by concerns about the dwindling numbers of primary care physicians. The early exodus of practicing providers and an obvious disinterest by future physicians in what they see as the unpalatable work/life balance of frontline hands-on medicine are among the causes.
A recent study published in the journal Pediatrics highlights personal finance as a contributor to the drain on the primary care workforce. The investigators found “high self-reported educational debt ($200,000 to < $300,000) was positively associated with training in a positive lifetime earnings potential subspecialty.” In other words, why would a physician who was burdened with student loans enter a subspecialty that would limit his or her ability to pay it off? I suspect that money has always been a factor in career selection, but the ballooning cost of college and medical school has certainly not nudged graduates toward the low lifetime earnings potential of primary care pediatrics.
Another recently released survey adds the perspective of current medical school students to the murky future of the primary health care workforce. The Clinician of the Future 2023: Education Edition, published by Elsevier Health, reports on insights of more than 2,000 nursing and medical school student from around the world. The headline shocker was that while across the board a not surprising 12% of medical students were considering quitting their studies, in the United States this number was 25%.
Overall, more than 60% of the students worried about their future income, how workforce shortages would effect them and whether they would join the ranks of those clinicians suffering from burnout. While the students surveyed acknowledged that artificial intelligence could have some negative repercussions, 62% were excited about its use in their education. Similarly, they anticipated the positive contribution of digital technology while acknowledging its potential downsides.
Given the current mental health climate in this country, I was not surprised that almost a quarter of medical students in this country are considering quitting school. I would like to see a larger sample surveyed and repeated over time. But, the discrepancy between the United States and the rest of the world is troubling.
The number that really jumped out at me was that 54% of medical students (nurses, 62%) viewed “ their current studies as a stepping-stone toward a broader career in health care.” As an example, the authors quoted one medical student who plans to “look for other possibilities where I don’t directly treat patients.”
Whether this disinterest in direct patient care is an attitude that preceded their entry into medical school or a change reflecting a major reversal induced by the realty of face-to-face patient encounters in school was not addressed in the survey. I think the general population would be surprised and maybe disappointed to learn that half the students in medical school weren’t planning on seeing patients.
I went off to medical school with a rather naive Norman Rockwellian view of a physician. I was a little surprised that a few of my classmates seemed to be gravitating toward administrative and research careers, but by far most of us were heading toward opportunities that would place us face to face with patients. Some would become specialists but primary care still had an appeal for many of us.
In my last letter about primary care training, I suggested that traditional medical school was probably a poor investment for the person who shares a bit of my old-school image of the primary care physician. In addition to cost and the time invested, the curriculum would likely be overly broad and deep and not terribly applicable to the patient mix he or she would eventually be seeing. This global survey may suggest that medical students have already discovered, or are just now discovering, this mismatch between medical school and the realities of primary care.
Our challenge is to first deal with deterrent of student debt and then to develop a new, affordable and efficient pathway to primary care that attracts those people who are looking for a face to face style of medicine on the front line. The patients know we need specialists and administrators but they also want a bit more of Norman Rockwell.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
A few weeks ago I shared by concerns about the dwindling numbers of primary care physicians. The early exodus of practicing providers and an obvious disinterest by future physicians in what they see as the unpalatable work/life balance of frontline hands-on medicine are among the causes.
A recent study published in the journal Pediatrics highlights personal finance as a contributor to the drain on the primary care workforce. The investigators found “high self-reported educational debt ($200,000 to < $300,000) was positively associated with training in a positive lifetime earnings potential subspecialty.” In other words, why would a physician who was burdened with student loans enter a subspecialty that would limit his or her ability to pay it off? I suspect that money has always been a factor in career selection, but the ballooning cost of college and medical school has certainly not nudged graduates toward the low lifetime earnings potential of primary care pediatrics.
Another recently released survey adds the perspective of current medical school students to the murky future of the primary health care workforce. The Clinician of the Future 2023: Education Edition, published by Elsevier Health, reports on insights of more than 2,000 nursing and medical school student from around the world. The headline shocker was that while across the board a not surprising 12% of medical students were considering quitting their studies, in the United States this number was 25%.
Overall, more than 60% of the students worried about their future income, how workforce shortages would effect them and whether they would join the ranks of those clinicians suffering from burnout. While the students surveyed acknowledged that artificial intelligence could have some negative repercussions, 62% were excited about its use in their education. Similarly, they anticipated the positive contribution of digital technology while acknowledging its potential downsides.
Given the current mental health climate in this country, I was not surprised that almost a quarter of medical students in this country are considering quitting school. I would like to see a larger sample surveyed and repeated over time. But, the discrepancy between the United States and the rest of the world is troubling.
The number that really jumped out at me was that 54% of medical students (nurses, 62%) viewed “ their current studies as a stepping-stone toward a broader career in health care.” As an example, the authors quoted one medical student who plans to “look for other possibilities where I don’t directly treat patients.”
Whether this disinterest in direct patient care is an attitude that preceded their entry into medical school or a change reflecting a major reversal induced by the realty of face-to-face patient encounters in school was not addressed in the survey. I think the general population would be surprised and maybe disappointed to learn that half the students in medical school weren’t planning on seeing patients.
I went off to medical school with a rather naive Norman Rockwellian view of a physician. I was a little surprised that a few of my classmates seemed to be gravitating toward administrative and research careers, but by far most of us were heading toward opportunities that would place us face to face with patients. Some would become specialists but primary care still had an appeal for many of us.
In my last letter about primary care training, I suggested that traditional medical school was probably a poor investment for the person who shares a bit of my old-school image of the primary care physician. In addition to cost and the time invested, the curriculum would likely be overly broad and deep and not terribly applicable to the patient mix he or she would eventually be seeing. This global survey may suggest that medical students have already discovered, or are just now discovering, this mismatch between medical school and the realities of primary care.
Our challenge is to first deal with deterrent of student debt and then to develop a new, affordable and efficient pathway to primary care that attracts those people who are looking for a face to face style of medicine on the front line. The patients know we need specialists and administrators but they also want a bit more of Norman Rockwell.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
U.S. kids are taking melatonin for sleep, despite evidence gap
according to a recent study.
These findings should prompt clinicians to discuss with parents the various factors that could be driving sleep disturbances, and potential safety issues associated with melatonin usage, lead author Lauren E. Hartstein, PhD, a postdoctoral fellow in the Sleep and Development Lab at the University of Colorado, Boulder, and colleagues reported.
Writing in JAMA Pediatrics, the investigators noted that melatonin products are notorious for mislabeling, with active ingredient quantities as much as three times higher than the labeled amount. This issue is particularly concerning, they added, as calls to poison control for melatonin ingestion jumped more than fivefold from 2012 to 2021, with most cases involving children younger than 5 years. Meanwhile, scant evidence is available to characterize intentional usage in the same population.
“Current data are lacking on the prevalence of melatonin use and the frequency, dosing, and timing of melatonin administration in U.S. youth,” Dr. Hartstein and colleagues wrote.
To address this knowledge gap, the investigators conducted an online survey of parents with children and adolescents aged 1.0-13.9 years. The survey asked parents to report any melatonin usage in their children in the past 30 days.
Parents reporting melatonin usage were asked about frequency, dose, timing of administration before bedtime, and duration of use.
Findings were reported within three age groups: preschool (1-4 years), school aged (5-9 years), and preteen (10-13 years).
The survey revealed that almost one in five children in the older age groups were using melatonin, with a rate of 18.5% in the school-aged group and 19.4% in the preteen group. In comparison, 5.6% of preschool children had received melatonin for sleep in the past 30 days.
A significant uptick in usage
These findings point to a significant uptick in usage, according to Dr. Hartstein and colleagues, who cited a 2017-2018 study that found just 1.3% of U.S. children had taken melatonin in the past 30 days.
In the present study, melatonin was typically administered 30 minutes before bedtime, most often as a gummy (64.3%) or chewable tablet (27.0%).
Frequency of administration was similar between age groups and trended toward a bimodal pattern, with melatonin often given either 1 day per week or 7 days per week.
Median dose increased significantly with age, from 0.5 mg in the preschool group to 1.0 mg in the school-aged group and 2.0 mg in the preteen group. Median duration also showed a significant upward trend, with 12-month, 18-month, and 21-month durations, respectively, for ascending age groups.
The investigators concluded that melatonin usage among U.S. adolescents and children is “exceedingly common,” despite a lack of evidence to support long-term safety or guide optimal dosing.
Is melatonin use masking other sleep issues?
“Widespread melatonin use across developmental stages may suggest a high prevalence of sleep disruption, which deserves accurate diagnosis and effective treatment,” Dr. Hartstein and colleagues wrote. “Dissemination of information regarding safety concerns, such as overdose and supplement mislabeling, is necessary. Clinicians should discuss with parents the factors associated with sleep difficulties and effective behavioral strategies.”
Large-scale, long-term studies are needed, they added, to generate relevant safety and efficacy data, and to characterize the factors driving melatonin administration by parents.
“Studies like these add to our knowledge base and give us insight into what patients or parents may be doing that can impact overall health,” said Alfonso J. Padilla, MD, assistant clinical professor of sleep medicine at the University of California, Los Angeles, in a written comment. “Often, in normal encounters with our patients we may not be able to gather this information easily. It may help open conversations about sleep issues that are not being addressed.”
Dr. Padilla suggested that parents may believe that melatonin is safe because it is not regulated by the Food and Drug Administration, when in fact they could be negatively impacting their children’s sleep. He noted that short-term risks include altered circadian rhythm and vivid dreams or nightmares, while long-term safety remains unclear.
“As a sleep physician, I use melatonin for specific indications only,” Dr. Padilla said. “I may use it in small children that are having difficulty falling asleep, especially in children with autism or special needs. I also use it for help in adjustment in circadian rhythm, especially in adolescents.”
He recommends melatonin, he added, if he has a complete case history, and melatonin is suitable for that patient.
Typically, it’s not.
“Most often a medication is not the answer for the sleep concern that parents are having about their child,” he said.
The investigators disclosed grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the Colorado Clinical and Translational Science Award Program of the National Center for Advancing Translational Sciences of the National Institutes of Health. They reported no conflicts of interest.
according to a recent study.
These findings should prompt clinicians to discuss with parents the various factors that could be driving sleep disturbances, and potential safety issues associated with melatonin usage, lead author Lauren E. Hartstein, PhD, a postdoctoral fellow in the Sleep and Development Lab at the University of Colorado, Boulder, and colleagues reported.
Writing in JAMA Pediatrics, the investigators noted that melatonin products are notorious for mislabeling, with active ingredient quantities as much as three times higher than the labeled amount. This issue is particularly concerning, they added, as calls to poison control for melatonin ingestion jumped more than fivefold from 2012 to 2021, with most cases involving children younger than 5 years. Meanwhile, scant evidence is available to characterize intentional usage in the same population.
“Current data are lacking on the prevalence of melatonin use and the frequency, dosing, and timing of melatonin administration in U.S. youth,” Dr. Hartstein and colleagues wrote.
To address this knowledge gap, the investigators conducted an online survey of parents with children and adolescents aged 1.0-13.9 years. The survey asked parents to report any melatonin usage in their children in the past 30 days.
Parents reporting melatonin usage were asked about frequency, dose, timing of administration before bedtime, and duration of use.
Findings were reported within three age groups: preschool (1-4 years), school aged (5-9 years), and preteen (10-13 years).
The survey revealed that almost one in five children in the older age groups were using melatonin, with a rate of 18.5% in the school-aged group and 19.4% in the preteen group. In comparison, 5.6% of preschool children had received melatonin for sleep in the past 30 days.
A significant uptick in usage
These findings point to a significant uptick in usage, according to Dr. Hartstein and colleagues, who cited a 2017-2018 study that found just 1.3% of U.S. children had taken melatonin in the past 30 days.
In the present study, melatonin was typically administered 30 minutes before bedtime, most often as a gummy (64.3%) or chewable tablet (27.0%).
Frequency of administration was similar between age groups and trended toward a bimodal pattern, with melatonin often given either 1 day per week or 7 days per week.
Median dose increased significantly with age, from 0.5 mg in the preschool group to 1.0 mg in the school-aged group and 2.0 mg in the preteen group. Median duration also showed a significant upward trend, with 12-month, 18-month, and 21-month durations, respectively, for ascending age groups.
The investigators concluded that melatonin usage among U.S. adolescents and children is “exceedingly common,” despite a lack of evidence to support long-term safety or guide optimal dosing.
Is melatonin use masking other sleep issues?
“Widespread melatonin use across developmental stages may suggest a high prevalence of sleep disruption, which deserves accurate diagnosis and effective treatment,” Dr. Hartstein and colleagues wrote. “Dissemination of information regarding safety concerns, such as overdose and supplement mislabeling, is necessary. Clinicians should discuss with parents the factors associated with sleep difficulties and effective behavioral strategies.”
Large-scale, long-term studies are needed, they added, to generate relevant safety and efficacy data, and to characterize the factors driving melatonin administration by parents.
“Studies like these add to our knowledge base and give us insight into what patients or parents may be doing that can impact overall health,” said Alfonso J. Padilla, MD, assistant clinical professor of sleep medicine at the University of California, Los Angeles, in a written comment. “Often, in normal encounters with our patients we may not be able to gather this information easily. It may help open conversations about sleep issues that are not being addressed.”
Dr. Padilla suggested that parents may believe that melatonin is safe because it is not regulated by the Food and Drug Administration, when in fact they could be negatively impacting their children’s sleep. He noted that short-term risks include altered circadian rhythm and vivid dreams or nightmares, while long-term safety remains unclear.
“As a sleep physician, I use melatonin for specific indications only,” Dr. Padilla said. “I may use it in small children that are having difficulty falling asleep, especially in children with autism or special needs. I also use it for help in adjustment in circadian rhythm, especially in adolescents.”
He recommends melatonin, he added, if he has a complete case history, and melatonin is suitable for that patient.
Typically, it’s not.
“Most often a medication is not the answer for the sleep concern that parents are having about their child,” he said.
The investigators disclosed grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the Colorado Clinical and Translational Science Award Program of the National Center for Advancing Translational Sciences of the National Institutes of Health. They reported no conflicts of interest.
according to a recent study.
These findings should prompt clinicians to discuss with parents the various factors that could be driving sleep disturbances, and potential safety issues associated with melatonin usage, lead author Lauren E. Hartstein, PhD, a postdoctoral fellow in the Sleep and Development Lab at the University of Colorado, Boulder, and colleagues reported.
Writing in JAMA Pediatrics, the investigators noted that melatonin products are notorious for mislabeling, with active ingredient quantities as much as three times higher than the labeled amount. This issue is particularly concerning, they added, as calls to poison control for melatonin ingestion jumped more than fivefold from 2012 to 2021, with most cases involving children younger than 5 years. Meanwhile, scant evidence is available to characterize intentional usage in the same population.
“Current data are lacking on the prevalence of melatonin use and the frequency, dosing, and timing of melatonin administration in U.S. youth,” Dr. Hartstein and colleagues wrote.
To address this knowledge gap, the investigators conducted an online survey of parents with children and adolescents aged 1.0-13.9 years. The survey asked parents to report any melatonin usage in their children in the past 30 days.
Parents reporting melatonin usage were asked about frequency, dose, timing of administration before bedtime, and duration of use.
Findings were reported within three age groups: preschool (1-4 years), school aged (5-9 years), and preteen (10-13 years).
The survey revealed that almost one in five children in the older age groups were using melatonin, with a rate of 18.5% in the school-aged group and 19.4% in the preteen group. In comparison, 5.6% of preschool children had received melatonin for sleep in the past 30 days.
A significant uptick in usage
These findings point to a significant uptick in usage, according to Dr. Hartstein and colleagues, who cited a 2017-2018 study that found just 1.3% of U.S. children had taken melatonin in the past 30 days.
In the present study, melatonin was typically administered 30 minutes before bedtime, most often as a gummy (64.3%) or chewable tablet (27.0%).
Frequency of administration was similar between age groups and trended toward a bimodal pattern, with melatonin often given either 1 day per week or 7 days per week.
Median dose increased significantly with age, from 0.5 mg in the preschool group to 1.0 mg in the school-aged group and 2.0 mg in the preteen group. Median duration also showed a significant upward trend, with 12-month, 18-month, and 21-month durations, respectively, for ascending age groups.
The investigators concluded that melatonin usage among U.S. adolescents and children is “exceedingly common,” despite a lack of evidence to support long-term safety or guide optimal dosing.
Is melatonin use masking other sleep issues?
“Widespread melatonin use across developmental stages may suggest a high prevalence of sleep disruption, which deserves accurate diagnosis and effective treatment,” Dr. Hartstein and colleagues wrote. “Dissemination of information regarding safety concerns, such as overdose and supplement mislabeling, is necessary. Clinicians should discuss with parents the factors associated with sleep difficulties and effective behavioral strategies.”
Large-scale, long-term studies are needed, they added, to generate relevant safety and efficacy data, and to characterize the factors driving melatonin administration by parents.
“Studies like these add to our knowledge base and give us insight into what patients or parents may be doing that can impact overall health,” said Alfonso J. Padilla, MD, assistant clinical professor of sleep medicine at the University of California, Los Angeles, in a written comment. “Often, in normal encounters with our patients we may not be able to gather this information easily. It may help open conversations about sleep issues that are not being addressed.”
Dr. Padilla suggested that parents may believe that melatonin is safe because it is not regulated by the Food and Drug Administration, when in fact they could be negatively impacting their children’s sleep. He noted that short-term risks include altered circadian rhythm and vivid dreams or nightmares, while long-term safety remains unclear.
“As a sleep physician, I use melatonin for specific indications only,” Dr. Padilla said. “I may use it in small children that are having difficulty falling asleep, especially in children with autism or special needs. I also use it for help in adjustment in circadian rhythm, especially in adolescents.”
He recommends melatonin, he added, if he has a complete case history, and melatonin is suitable for that patient.
Typically, it’s not.
“Most often a medication is not the answer for the sleep concern that parents are having about their child,” he said.
The investigators disclosed grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the Colorado Clinical and Translational Science Award Program of the National Center for Advancing Translational Sciences of the National Institutes of Health. They reported no conflicts of interest.
FROM JAMA PEDIATRICS
Is air filtration the best public health intervention against respiratory viruses?
This transcript has been edited for clarity.
When it comes to the public health fight against respiratory viruses – COVID, flu, RSV, and so on – it has always struck me as strange how staunchly basically any intervention is opposed. Masking was, of course, the prototypical entrenched warfare of opposing ideologies, with advocates pointing to studies suggesting the efficacy of masking to prevent transmission and advocating for broad masking recommendations, and detractors citing studies that suggested masks were ineffective and characterizing masking policies as fascist overreach. I’ll admit that I was always perplexed by this a bit, as that particular intervention seemed so benign – a bit annoying, I guess, but not crazy.
I have come to appreciate what I call status quo bias, which is the tendency to reject any policy, advice, or intervention that would force you, as an individual, to change your usual behavior. We just don’t like to do that. It has made me think that the most successful public health interventions might be the ones that take the individual out of the loop. And air quality control seems an ideal fit here. Here is a potential intervention where you, the individual, have to do precisely nothing. The status quo is preserved. We just, you know, have cleaner indoor air.
But even the suggestion of air treatment systems as a bulwark against respiratory virus transmission has been met with not just skepticism but cynicism, and perhaps even defeatism. It seems that there are those out there who think there really is nothing we can do. Sickness is interpreted in a Calvinistic framework: You become ill because it is your pre-destiny. But maybe air treatment could actually work. It seems like it might, if a new paper from PLOS One is to be believed.
What we’re talking about is a study titled “Bipolar Ionization Rapidly Inactivates Real-World, Airborne Concentrations of Infective Respiratory Viruses” – a highly controlled, laboratory-based analysis of a bipolar ionization system which seems to rapidly reduce viral counts in the air.
The proposed mechanism of action is pretty simple. The ionization system – which, don’t worry, has been shown not to produce ozone – spits out positively and negatively charged particles, which float around the test chamber, designed to look like a pretty standard room that you might find in an office or a school.
Virus is then injected into the chamber through an aerosolization machine, to achieve concentrations on the order of what you might get standing within 6 feet or so of someone actively infected with COVID while they are breathing and talking.
The idea is that those ions stick to the virus particles, similar to how a balloon sticks to the wall after you rub it on your hair, and that tends to cause them to clump together and settle on surfaces more rapidly, and thus get farther away from their ports of entry to the human system: nose, mouth, and eyes. But the ions may also interfere with viruses’ ability to bind to cellular receptors, even in the air.
To quantify viral infectivity, the researchers used a biological system. Basically, you take air samples and expose a petri dish of cells to them and see how many cells die. Fewer cells dying, less infective. Under control conditions, you can see that virus infectivity does decrease over time. Time zero here is the end of a SARS-CoV-2 aerosolization.
This may simply reflect the fact that virus particles settle out of the air. But As you can see, within about an hour, you have almost no infective virus detectable. That’s fairly impressive.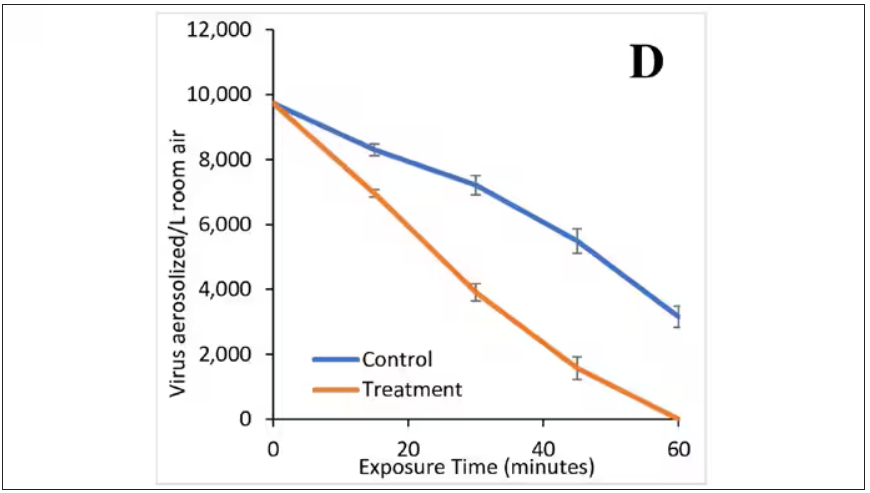
Now, I’m not saying that this is a panacea, but it is certainly worth considering the use of technologies like these if we are going to revamp the infrastructure of our offices and schools. And, of course, it would be nice to see this tested in a rigorous clinical trial with actual infected people, not cells, as the outcome. But I continue to be encouraged by interventions like this which, to be honest, ask very little of us as individuals. Maybe it’s time we accept the things, or people, that we cannot change.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
When it comes to the public health fight against respiratory viruses – COVID, flu, RSV, and so on – it has always struck me as strange how staunchly basically any intervention is opposed. Masking was, of course, the prototypical entrenched warfare of opposing ideologies, with advocates pointing to studies suggesting the efficacy of masking to prevent transmission and advocating for broad masking recommendations, and detractors citing studies that suggested masks were ineffective and characterizing masking policies as fascist overreach. I’ll admit that I was always perplexed by this a bit, as that particular intervention seemed so benign – a bit annoying, I guess, but not crazy.
I have come to appreciate what I call status quo bias, which is the tendency to reject any policy, advice, or intervention that would force you, as an individual, to change your usual behavior. We just don’t like to do that. It has made me think that the most successful public health interventions might be the ones that take the individual out of the loop. And air quality control seems an ideal fit here. Here is a potential intervention where you, the individual, have to do precisely nothing. The status quo is preserved. We just, you know, have cleaner indoor air.
But even the suggestion of air treatment systems as a bulwark against respiratory virus transmission has been met with not just skepticism but cynicism, and perhaps even defeatism. It seems that there are those out there who think there really is nothing we can do. Sickness is interpreted in a Calvinistic framework: You become ill because it is your pre-destiny. But maybe air treatment could actually work. It seems like it might, if a new paper from PLOS One is to be believed.
What we’re talking about is a study titled “Bipolar Ionization Rapidly Inactivates Real-World, Airborne Concentrations of Infective Respiratory Viruses” – a highly controlled, laboratory-based analysis of a bipolar ionization system which seems to rapidly reduce viral counts in the air.
The proposed mechanism of action is pretty simple. The ionization system – which, don’t worry, has been shown not to produce ozone – spits out positively and negatively charged particles, which float around the test chamber, designed to look like a pretty standard room that you might find in an office or a school.
Virus is then injected into the chamber through an aerosolization machine, to achieve concentrations on the order of what you might get standing within 6 feet or so of someone actively infected with COVID while they are breathing and talking.
The idea is that those ions stick to the virus particles, similar to how a balloon sticks to the wall after you rub it on your hair, and that tends to cause them to clump together and settle on surfaces more rapidly, and thus get farther away from their ports of entry to the human system: nose, mouth, and eyes. But the ions may also interfere with viruses’ ability to bind to cellular receptors, even in the air.
To quantify viral infectivity, the researchers used a biological system. Basically, you take air samples and expose a petri dish of cells to them and see how many cells die. Fewer cells dying, less infective. Under control conditions, you can see that virus infectivity does decrease over time. Time zero here is the end of a SARS-CoV-2 aerosolization.
This may simply reflect the fact that virus particles settle out of the air. But As you can see, within about an hour, you have almost no infective virus detectable. That’s fairly impressive.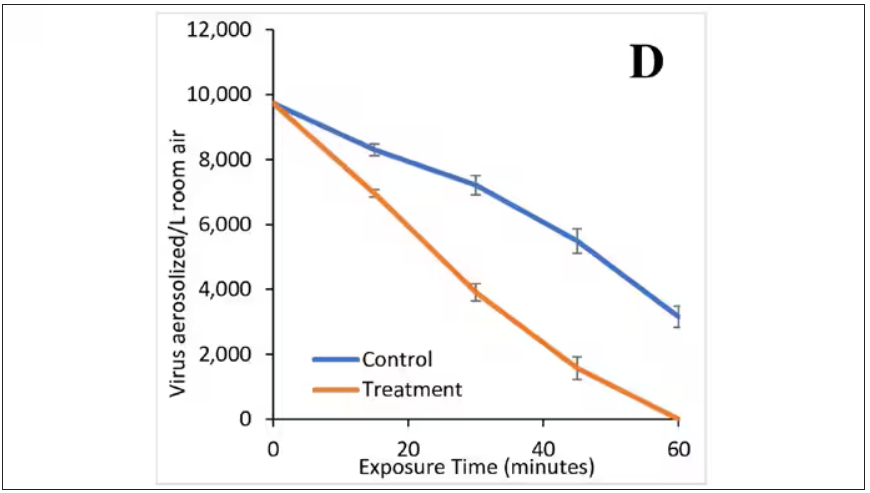
Now, I’m not saying that this is a panacea, but it is certainly worth considering the use of technologies like these if we are going to revamp the infrastructure of our offices and schools. And, of course, it would be nice to see this tested in a rigorous clinical trial with actual infected people, not cells, as the outcome. But I continue to be encouraged by interventions like this which, to be honest, ask very little of us as individuals. Maybe it’s time we accept the things, or people, that we cannot change.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
When it comes to the public health fight against respiratory viruses – COVID, flu, RSV, and so on – it has always struck me as strange how staunchly basically any intervention is opposed. Masking was, of course, the prototypical entrenched warfare of opposing ideologies, with advocates pointing to studies suggesting the efficacy of masking to prevent transmission and advocating for broad masking recommendations, and detractors citing studies that suggested masks were ineffective and characterizing masking policies as fascist overreach. I’ll admit that I was always perplexed by this a bit, as that particular intervention seemed so benign – a bit annoying, I guess, but not crazy.
I have come to appreciate what I call status quo bias, which is the tendency to reject any policy, advice, or intervention that would force you, as an individual, to change your usual behavior. We just don’t like to do that. It has made me think that the most successful public health interventions might be the ones that take the individual out of the loop. And air quality control seems an ideal fit here. Here is a potential intervention where you, the individual, have to do precisely nothing. The status quo is preserved. We just, you know, have cleaner indoor air.
But even the suggestion of air treatment systems as a bulwark against respiratory virus transmission has been met with not just skepticism but cynicism, and perhaps even defeatism. It seems that there are those out there who think there really is nothing we can do. Sickness is interpreted in a Calvinistic framework: You become ill because it is your pre-destiny. But maybe air treatment could actually work. It seems like it might, if a new paper from PLOS One is to be believed.
What we’re talking about is a study titled “Bipolar Ionization Rapidly Inactivates Real-World, Airborne Concentrations of Infective Respiratory Viruses” – a highly controlled, laboratory-based analysis of a bipolar ionization system which seems to rapidly reduce viral counts in the air.
The proposed mechanism of action is pretty simple. The ionization system – which, don’t worry, has been shown not to produce ozone – spits out positively and negatively charged particles, which float around the test chamber, designed to look like a pretty standard room that you might find in an office or a school.
Virus is then injected into the chamber through an aerosolization machine, to achieve concentrations on the order of what you might get standing within 6 feet or so of someone actively infected with COVID while they are breathing and talking.
The idea is that those ions stick to the virus particles, similar to how a balloon sticks to the wall after you rub it on your hair, and that tends to cause them to clump together and settle on surfaces more rapidly, and thus get farther away from their ports of entry to the human system: nose, mouth, and eyes. But the ions may also interfere with viruses’ ability to bind to cellular receptors, even in the air.
To quantify viral infectivity, the researchers used a biological system. Basically, you take air samples and expose a petri dish of cells to them and see how many cells die. Fewer cells dying, less infective. Under control conditions, you can see that virus infectivity does decrease over time. Time zero here is the end of a SARS-CoV-2 aerosolization.
This may simply reflect the fact that virus particles settle out of the air. But As you can see, within about an hour, you have almost no infective virus detectable. That’s fairly impressive.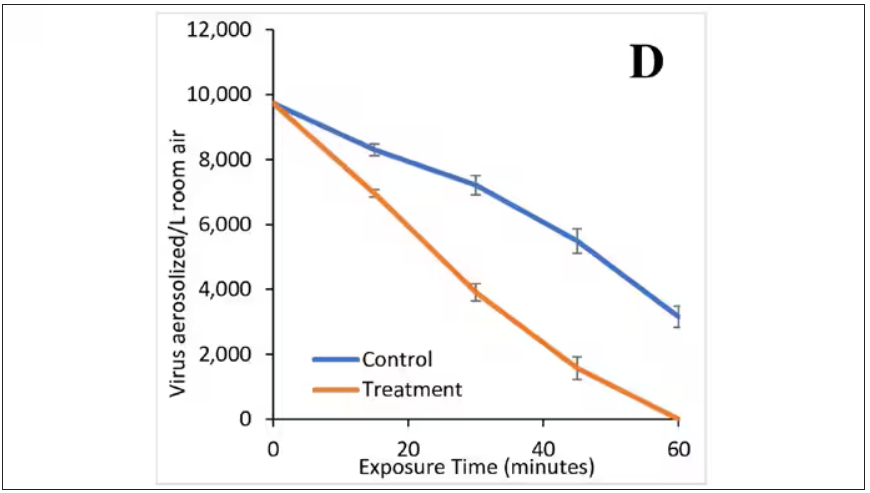
Now, I’m not saying that this is a panacea, but it is certainly worth considering the use of technologies like these if we are going to revamp the infrastructure of our offices and schools. And, of course, it would be nice to see this tested in a rigorous clinical trial with actual infected people, not cells, as the outcome. But I continue to be encouraged by interventions like this which, to be honest, ask very little of us as individuals. Maybe it’s time we accept the things, or people, that we cannot change.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.









