User login
When should nutritional support be implemented in a hospitalized patient?
Case
A 60-year-old male with a history of head & neck cancer, treated with radical neck dissection and radiation 5 years prior is admitted with community-acquired pneumonia and anasarca. Prior to admission, he was on a soft dysphagia diet and reports increased difficulty with solid foods and weight loss from 70 kg to 55 kg over 2.5 years. Should nutritional support be initiated?
Background
Malnutrition is associated with increased hospital mortality, decreased functional status and quality of life, infections, longer length of stay, higher hospital costs, and more frequent nonelective readmissions.1,2
Identifying patients who are malnourished or at risk for malnutrition
An international consensus committee recommended the following criteria for the diagnosis of undernutrition if two of six are present3:
- Insufficient energy intake.
- Weight loss.
- Loss of muscle mass.
- Loss of subcutaneous fat.
- Localized or generalized fluid accumulation that may sometimes mask weight loss.
- Diminished functional status as measured by handgrip strength.
The joint commission requires that all patients admitted to acute care hospitals be screened for risk of malnutrition within 24 hours. The American College of Gastroenterologists recommends using a validated score to assess nutritional risk, such as the Nutritional Risk Score (NRS) 2002 or the NUTRIC (Nutrition Risk in the Critically Ill) Score, which use a combination of nutritional status and diet-related factors – weight loss, body mass index, and food intake – and also severity of illness measurements.4
- Starvation-related malnutrition, such as anorexia nervosa, presents with a deficiency in calories and protein without inflammation, .
- Chronic disease–related malnutrition, such as that caused chronic obstructive pulmonary disease, cancer, and obesity, presents with mild to moderate inflammation.
- Acute disease or injury–related malnutrition, such as that caused by sepsis, burns, and trauma, presents with acute and severe inflammation.
Laboratory indicators such as albumin, prealbumin, and transferrin are not recommended for the determination of nutritional status. Instead, as negative acute-phase reactants, they can be used as surrogate markers of nutritional risk and degree of inflammation.4
Overview of the data
What are the indications for initiating nutritional support, and what is the optimal timing for initiation?
Patients who are malnourished or at significant risk for becoming malnourished should receive specialized nutrition support. Early enteral nutrition should be initiated within 24-48 hours of admission in critically ill patients with high nutritional risk who are unable to maintain volitional intake.6 In the absence of preexisting malnutrition, nutritional support should be provided for patients with inadequate oral intake for 7-14 days or for those in whom inadequate oral intake is expected over the same time period.7
How should nutritional support be administered?
Dietary modification and supplementation
In patients who can tolerate an oral diet, dietary modifications may be made in order to facilitate the provision of essential nutrients in a well-tolerated form. Modifications may include adjusting the consistency of foods, energy value of foods, types of nutrients consumed, and number and frequency of meals.8 Commercial meal replacement beverages are widely used to support a standard oral diet, but there is no data to support their routine use.7
Enteral nutrition
Enteral nutrition (EN) is the method of choice for administering nutrition support. Contraindications to enteral feeding include diffuse peritonitis, intestinal obstruction, and gastrointestinal ischemia.9 The potential advantages of EN over parenteral nutrition (PN) include decreased infection rate, decreased total complications, and shorter length of stay, but there has been no observed difference in mortality. EN is also suggested to have nonnutritional benefits related to providing luminal nutrients – these include maintaining gut integrity, beneficial immune responses, and favorable metabolic responses that help maintain euglycemia and enhance more physiologic fuel utilization.4
Enteral feeding can be administered through the following routes of access:
- Nasogastric tubes: A nasogastric or orogastric tube with radiologic confirmation of positioning is the first line of enteral access. Gastric feeding is preferred because it is well tolerated in the majority of patients, is more physiological, requires a lower level of expertise, and minimizes any delay in initiation of feeding.
- Postpyloric tubes: Postpyloric feeding tubes are indicated if gastric feeding is poorly tolerated or if the patient is at high risk for aspiration because jejunal feedings decrease the incidence of reflux, regurgitation, and aspiration.
- Percutaneous access: When long-term enteral access is required – that is, for greater than 4 weeks – a percutaneous enteral access device should be placed. Prolonged use of a nasoenteric tube may be associated with erosion of the nares and an increase in the incidence of aspiration pneumonia, sinusitis, and esophageal ulceration or stricture. Patients who have had a stroke are the most likely to benefit from percutaneous endoscopic gastrostomy placement, as 40% of patients can have continued dysphagia as long as 1 year after.4,10 Absolute contraindications for PEG placement include serious coagulation disorders (international normalized ratio greater than 1.5; fewer than 50,000 platelets/mcL), sepsis, abdominal wall infections, marked peritoneal carcinomatosis, peritonitis, severe gastroparesis, gastric outlet obstruction, or a history of total gastrectomy. Risks often outweigh benefits in patients who have cirrhosis with ascites, patients undergoing peritoneal dialysis, and patients who have portal hypertension with gastric varices, but PEG can be considered on a case-by-case basis.11
Parenteral nutrition
Parenteral nutrition is reserved for patients in whom enteral feeding is contraindicated or who fail to meet their nutritional needs with enteral feedings. If EN is not feasible, then parenteral nutrition should be initiated as soon as possible in patients who had high nutritional risk on admission. Otherwise, PN should not be initiated during the first week of hospitalization because there is evidence to suggest net harm when initiated early. Supplemental PN may be considered for patients already on EN who are unable to meet more than 60% of their energy and protein requirements by the enteral route alone, but again, this should only be considered after 7-10 days on EN. PN is generally stopped when the patients achieve more than 60% of their energy and protein goals from EN.4
How should patients be monitored while receiving nutritional support?
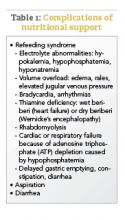
If a patient is severely malnourished and refeeding is initiated, serious complications can occur, which are summarized in Table 1; these complications can include severe electrolyte disorders, fluid shifts, and even death.12 Refeeding syndrome occurs in the first few days of initiating a diet in severely malnourished patients, and its severity is directly related to the severity of malnutrition prior to refeeding. The National Institute of Health and Clinical Excellence created criteria to identify patients at risk for refeeding syndrome; these criteria include having a BMI less than 18.5 kg/m2; unintentional weight loss of greater than 10% in the previous 3-6 months; little or no nutritional intake for more than 5 days; low levels of potassium, phosphorus, or magnesium before refeeding; and a history of alcohol misuse or taking certain drugs, such as insulin, chemotherapy, antacids, or diuretics.9
Aspiration is a risk with enteral feeding – the risk factors include being older than 70 years, altered mental status, supine position, and bolus rather than continuous infusion.4 Postpyloric feeding may reduce the risk of aspiration. Expert consensus suggests elevating the head of the bed by 30°-40° for all intubated patients receiving EN, as well as administering chlorhexidine mouthwash twice daily.6
Diarrhea is very common in patients receiving EN. After evaluating for other etiologies of diarrhea, tube feeding–associated diarrhea may be managed first by using a fiber-containing formulation. Fiber should be avoided in patients at risk for bowel ischemia or severe dysmotility. If diarrhea persists despite fiber, small peptide formulations, also known as elemental tube feeds, may be used.4,6
Gastric residual volume (GRV) is commonly monitored in patients receiving enteral nutrition. However, the American College of Gastroenterology does not recommend using GRVs to monitor EN feeding because it is a poor marker of clinically meaningful variables, such as gastric emptying, risk of aspiration, and risk of poor outcomes, and increases the risk of tube clogging and inadequate delivery of EN. If GRVs are being monitored, tube feedings should not be withheld because of high GRVs when there are no other signs of intolerance.4 Nausea may be managed by changing a patient from bolus to continuous feedings or by adding promotility agents such as metoclopramide or erythromycin.6
Special considerations in common conditions treated by hospitalists
The principles outlined above are general guidelines that are applicable to most patients requiring nutrition support. We have highlighted special considerations for common conditions in hospitalized patients who require nutritional support below.
Critical Illness
- Defer enteral nutrition until patient is fully resuscitated and hemodynamically stable.
- Severely malnourished or high nutritional-risk patients should be advanced toward goals as quickly as can be tolerated over 24-48 hours.
- Patients with acute respiratory distress syndrome or acute lung injury, or those expected to require mechanical ventilation for more than 72 hours, should receive trophic feeds or full nutrition by enteral route.6
Pancreatitis
- Oral feeding should be attempted as soon as abdominal pain is decreasing and inflammatory markers are improving.13
- A regular solid, low-fat diet should be initiated, rather than slowly advancing from a clear liquid diet.13
- In severe acute pancreatitis, initiation of enteral nutrition within 48 hours of presentation is associated with improved outcomes.13
- There is no difference in outcomes between gastric and postpyloric feeding.14
- Initiation of parenteral nutrition may be delayed for up to 5 days to allow for a trial of oral or enteral feeding.13
Surgical patients
- Consider postponing surgery to provide 7-10 days of preoperative nutrition supplementation in patients with risk of severe undernutrition.16
- Consider postoperative nutritional support if patients are at risk for severe undernutrition, are unable to eat for more than 7 days perioperatively, or are unable to maintain oral intake above 60% of recommended intake for more than 10 days.16
- Consider total parenteral nutrition in cases of impaired gastrointestinal function and absorption, high output enterocutaneous fistulae, obstructive lesions that do not allow enteral refeeding, or prolonged gastrointestinal failure.16
Prolonged Starvation
- Because of the high risk of refeeding syndrome, patients greater than 30% below ideal body weight should be hospitalized for close monitoring during refeeding.12
- Typical goal for weight gain is no greater than 2-3 pounds per week.10
- Total parenteral nutrition should be reserved for extreme cases, and if used, carbohydrate intake should not exceed 7 mg/kg/min.12
Stroke
- Enteral nutrition should be initiated within 24-48 hours of initial hospitalization if a patient is estimated to require feeding for more than 5 days and/or remain nil per os for 5-7 days.
- If a patient is intubated with increased intracranial pressure, this could delay gastric motility requiring a postpyloric tube placement.
- Initial placement of percutaneous endoscopic gastrostomy tubes can be considered if the hospitalized patient is expected to require nutritional support for greater than 30 days. Most patients will have improved dysphagia symptoms within 1 month of their acute stroke, although as many as 40% can have continued dysphagia up to 1 year.10
Back to the Case
The patient was admitted for a common general medical condition, but it is important to recognize that malnutrition was present on admission with weight loss and generalized fluid overload. Furthermore, he is at high nutritional risk because of his low body weight, poor oral intake, and dysphagia. Additionally, the acute inflammation from pneumonia places him in an increased catabolic state.
He was able to maintain some volitional oral intake, but after 7 days of close monitoring by a licensed dietician, it was determined that he was unable to meet his nutritional needs via the oral route. A percutaneous endoscopic gastrostomy tube was placed, and tube feeds were initiated, because his dysphagia – which was a significant factor contributing to his inability to meet his nutritional needs orally – was expected to persist for greater than 30 days.
Bottom Line
Nutrition support should be initiated in this patient with malnutrition on admission and high nutritional risk.
Dr. Abalos is an assistant professor at Georgetown University Medical Center in Washington. Dr. Corbett is an assistant professor at the University of Oklahoma Health Sciences Center in Oklahoma City.
References
1. Correia MI et al. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 2003 Jun;22(3):235-9.
2. Felder S et al. Association of nutritional risk and adverse medical outcomes across different medical inpatient populations. Nutrition. 2015 Nov-Dec;31(11-12):1385-93.
3. White JV et al. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: Characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Acad Nutr Diet. 2012 May;112(5):730-8.
4. McClave SA et al. ACG clinical guideline: Nutrition therapy in the adult hospitalized patient. Am J Gastroenterol. 2016 Mar;111(3):315-334.
5. Mueller C et al. A.S.P.E.N. clinical guidelines: Nutrition screening, assessment, and intervention in adults. JPEN J Parenter Enter Nutr. 2011 Jan;35(1):16-24.
6. McClave SA et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient. JPEN J Parenter Enter Nutr. 2016 Feb;40(2):159-211.
7. August D et al. Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. JPEN J Parenter Enter Nutr. 2002 Jan-Feb:26(1):SUPPL:1SA-138SA.
8. Kirkland LL et al. Nutrition in the hospitalized patient. J Hosp Med. 2013 Jan;8(1):52-8.
9. National Collaborating Centre for Acute Care, February 2006. Nutrition support in adults Oral nutrition support, enteral tube feeding and parenteral nutrition. National Collaborating Centre for Acute Care, London. Available from www.rcseng.ac.uk.
10. Corrigan ML et al. Nutrition in the stroke patient. Nutr Clin Pract. 2011 Jun;26(3):242-52.
11. Loser C et al. ESPEN guidelines on artificial enteral nutrition – Percutaneous endoscopic gastrostomy (PEG). Clin Nutr. 2005 Oct;24(5):848-61.
12. Mehler PS et al. Nutritional rehabilitation: Practical guidelines for refeeding the anorectic patient. J Nutr Metab. 2010. doi: 10.1155/2010/625782.
13. Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013 Jul-Aug;13(4 Suppl 2):e1-15.
14. Singh N et al. Evaluation of early enteral feeding through nasogastric and nasojejunal tube in severe acute pancreatitis: A noninferiority randomized controlled trial. Pancreas. 2012 Jan;41(1):153-9.
15. Braga M et al. ESPEN guidelines on parenteral nutrition: Surgery. Clin Nutr. 2009 Aug;28(4):378-86.
16. Weimann A et al. ESPEN Guidelines on enteral nutrition: Surgery including organ transplantation. Clin Nutr. 2006 Apr;25(2):224-44.
Additional reading
- Kirkland LL et al. Nutrition in the Hospitalized Patient. J Hosp Med. 2013 Jan;8(1):52-8.
- McClave SA et al. ACG Clinical Guideline: Nutrition Therapy in the Adult Hospitalized Patient. Am J Gastroenterol. 2016 Mar;111(3):315-334.
Quiz: Recognizing Malnutrition
Which of the following is not a criteria for the diagnosis of malnutrition?
A. Weight loss
B. Insufficient energy intake
C. Prealbumin
D. Diminished handgrip strength
Answer: C. Prealbumin. Laboratory indicators of nutrition, such as albumin, prealbumin, and transferrin, and markers of infection or inflammation are not recommended for the determination of nutritional status. Because negative acute-phase reactants, they instead can be used as surrogate markers of nutritional risk and degree of inflammation
Key Points
- At the time of admission to the hospital, malnutrition is present in 20-50% of patients. All hospitalized patients should be screened for nutritional risk and nutritional support should be considered if patients are not expected to be able to meet nutritional needs for more than 7 days.
- Patients with severe malnutrition on admission, severe critical illness, or severe acute pancreatitis should be provided nutritional support within 24-48 hours.
- Use the gut! Nutritional support should be provided via the most physiologic route possible. Total parenteral nutrition (TPN) should be reserved for patients in whom adequate nutrition cannot be provided enterally.
- Consider a percutaneous endoscopic gastrostomy (PEG) tube if the patient is expected to require tube feedings for more than 30 days.
- Patients with severe malnutrition who are given nutritional support are at high risk of developing refeeding syndrome, which manifests as electrolyte depletions and heart failure or volume overload.
Case
A 60-year-old male with a history of head & neck cancer, treated with radical neck dissection and radiation 5 years prior is admitted with community-acquired pneumonia and anasarca. Prior to admission, he was on a soft dysphagia diet and reports increased difficulty with solid foods and weight loss from 70 kg to 55 kg over 2.5 years. Should nutritional support be initiated?
Background
Malnutrition is associated with increased hospital mortality, decreased functional status and quality of life, infections, longer length of stay, higher hospital costs, and more frequent nonelective readmissions.1,2
Identifying patients who are malnourished or at risk for malnutrition
An international consensus committee recommended the following criteria for the diagnosis of undernutrition if two of six are present3:
- Insufficient energy intake.
- Weight loss.
- Loss of muscle mass.
- Loss of subcutaneous fat.
- Localized or generalized fluid accumulation that may sometimes mask weight loss.
- Diminished functional status as measured by handgrip strength.
The joint commission requires that all patients admitted to acute care hospitals be screened for risk of malnutrition within 24 hours. The American College of Gastroenterologists recommends using a validated score to assess nutritional risk, such as the Nutritional Risk Score (NRS) 2002 or the NUTRIC (Nutrition Risk in the Critically Ill) Score, which use a combination of nutritional status and diet-related factors – weight loss, body mass index, and food intake – and also severity of illness measurements.4
- Starvation-related malnutrition, such as anorexia nervosa, presents with a deficiency in calories and protein without inflammation, .
- Chronic disease–related malnutrition, such as that caused chronic obstructive pulmonary disease, cancer, and obesity, presents with mild to moderate inflammation.
- Acute disease or injury–related malnutrition, such as that caused by sepsis, burns, and trauma, presents with acute and severe inflammation.
Laboratory indicators such as albumin, prealbumin, and transferrin are not recommended for the determination of nutritional status. Instead, as negative acute-phase reactants, they can be used as surrogate markers of nutritional risk and degree of inflammation.4
Overview of the data
What are the indications for initiating nutritional support, and what is the optimal timing for initiation?
Patients who are malnourished or at significant risk for becoming malnourished should receive specialized nutrition support. Early enteral nutrition should be initiated within 24-48 hours of admission in critically ill patients with high nutritional risk who are unable to maintain volitional intake.6 In the absence of preexisting malnutrition, nutritional support should be provided for patients with inadequate oral intake for 7-14 days or for those in whom inadequate oral intake is expected over the same time period.7
How should nutritional support be administered?
Dietary modification and supplementation
In patients who can tolerate an oral diet, dietary modifications may be made in order to facilitate the provision of essential nutrients in a well-tolerated form. Modifications may include adjusting the consistency of foods, energy value of foods, types of nutrients consumed, and number and frequency of meals.8 Commercial meal replacement beverages are widely used to support a standard oral diet, but there is no data to support their routine use.7
Enteral nutrition
Enteral nutrition (EN) is the method of choice for administering nutrition support. Contraindications to enteral feeding include diffuse peritonitis, intestinal obstruction, and gastrointestinal ischemia.9 The potential advantages of EN over parenteral nutrition (PN) include decreased infection rate, decreased total complications, and shorter length of stay, but there has been no observed difference in mortality. EN is also suggested to have nonnutritional benefits related to providing luminal nutrients – these include maintaining gut integrity, beneficial immune responses, and favorable metabolic responses that help maintain euglycemia and enhance more physiologic fuel utilization.4
Enteral feeding can be administered through the following routes of access:
- Nasogastric tubes: A nasogastric or orogastric tube with radiologic confirmation of positioning is the first line of enteral access. Gastric feeding is preferred because it is well tolerated in the majority of patients, is more physiological, requires a lower level of expertise, and minimizes any delay in initiation of feeding.
- Postpyloric tubes: Postpyloric feeding tubes are indicated if gastric feeding is poorly tolerated or if the patient is at high risk for aspiration because jejunal feedings decrease the incidence of reflux, regurgitation, and aspiration.
- Percutaneous access: When long-term enteral access is required – that is, for greater than 4 weeks – a percutaneous enteral access device should be placed. Prolonged use of a nasoenteric tube may be associated with erosion of the nares and an increase in the incidence of aspiration pneumonia, sinusitis, and esophageal ulceration or stricture. Patients who have had a stroke are the most likely to benefit from percutaneous endoscopic gastrostomy placement, as 40% of patients can have continued dysphagia as long as 1 year after.4,10 Absolute contraindications for PEG placement include serious coagulation disorders (international normalized ratio greater than 1.5; fewer than 50,000 platelets/mcL), sepsis, abdominal wall infections, marked peritoneal carcinomatosis, peritonitis, severe gastroparesis, gastric outlet obstruction, or a history of total gastrectomy. Risks often outweigh benefits in patients who have cirrhosis with ascites, patients undergoing peritoneal dialysis, and patients who have portal hypertension with gastric varices, but PEG can be considered on a case-by-case basis.11
Parenteral nutrition
Parenteral nutrition is reserved for patients in whom enteral feeding is contraindicated or who fail to meet their nutritional needs with enteral feedings. If EN is not feasible, then parenteral nutrition should be initiated as soon as possible in patients who had high nutritional risk on admission. Otherwise, PN should not be initiated during the first week of hospitalization because there is evidence to suggest net harm when initiated early. Supplemental PN may be considered for patients already on EN who are unable to meet more than 60% of their energy and protein requirements by the enteral route alone, but again, this should only be considered after 7-10 days on EN. PN is generally stopped when the patients achieve more than 60% of their energy and protein goals from EN.4
How should patients be monitored while receiving nutritional support?
If a patient is severely malnourished and refeeding is initiated, serious complications can occur, which are summarized in Table 1; these complications can include severe electrolyte disorders, fluid shifts, and even death.12 Refeeding syndrome occurs in the first few days of initiating a diet in severely malnourished patients, and its severity is directly related to the severity of malnutrition prior to refeeding. The National Institute of Health and Clinical Excellence created criteria to identify patients at risk for refeeding syndrome; these criteria include having a BMI less than 18.5 kg/m2; unintentional weight loss of greater than 10% in the previous 3-6 months; little or no nutritional intake for more than 5 days; low levels of potassium, phosphorus, or magnesium before refeeding; and a history of alcohol misuse or taking certain drugs, such as insulin, chemotherapy, antacids, or diuretics.9
Aspiration is a risk with enteral feeding – the risk factors include being older than 70 years, altered mental status, supine position, and bolus rather than continuous infusion.4 Postpyloric feeding may reduce the risk of aspiration. Expert consensus suggests elevating the head of the bed by 30°-40° for all intubated patients receiving EN, as well as administering chlorhexidine mouthwash twice daily.6
Diarrhea is very common in patients receiving EN. After evaluating for other etiologies of diarrhea, tube feeding–associated diarrhea may be managed first by using a fiber-containing formulation. Fiber should be avoided in patients at risk for bowel ischemia or severe dysmotility. If diarrhea persists despite fiber, small peptide formulations, also known as elemental tube feeds, may be used.4,6
Gastric residual volume (GRV) is commonly monitored in patients receiving enteral nutrition. However, the American College of Gastroenterology does not recommend using GRVs to monitor EN feeding because it is a poor marker of clinically meaningful variables, such as gastric emptying, risk of aspiration, and risk of poor outcomes, and increases the risk of tube clogging and inadequate delivery of EN. If GRVs are being monitored, tube feedings should not be withheld because of high GRVs when there are no other signs of intolerance.4 Nausea may be managed by changing a patient from bolus to continuous feedings or by adding promotility agents such as metoclopramide or erythromycin.6
Special considerations in common conditions treated by hospitalists
The principles outlined above are general guidelines that are applicable to most patients requiring nutrition support. We have highlighted special considerations for common conditions in hospitalized patients who require nutritional support below.
Critical Illness
- Defer enteral nutrition until patient is fully resuscitated and hemodynamically stable.
- Severely malnourished or high nutritional-risk patients should be advanced toward goals as quickly as can be tolerated over 24-48 hours.
- Patients with acute respiratory distress syndrome or acute lung injury, or those expected to require mechanical ventilation for more than 72 hours, should receive trophic feeds or full nutrition by enteral route.6
Pancreatitis
- Oral feeding should be attempted as soon as abdominal pain is decreasing and inflammatory markers are improving.13
- A regular solid, low-fat diet should be initiated, rather than slowly advancing from a clear liquid diet.13
- In severe acute pancreatitis, initiation of enteral nutrition within 48 hours of presentation is associated with improved outcomes.13
- There is no difference in outcomes between gastric and postpyloric feeding.14
- Initiation of parenteral nutrition may be delayed for up to 5 days to allow for a trial of oral or enteral feeding.13
Surgical patients
- Consider postponing surgery to provide 7-10 days of preoperative nutrition supplementation in patients with risk of severe undernutrition.16
- Consider postoperative nutritional support if patients are at risk for severe undernutrition, are unable to eat for more than 7 days perioperatively, or are unable to maintain oral intake above 60% of recommended intake for more than 10 days.16
- Consider total parenteral nutrition in cases of impaired gastrointestinal function and absorption, high output enterocutaneous fistulae, obstructive lesions that do not allow enteral refeeding, or prolonged gastrointestinal failure.16
Prolonged Starvation
- Because of the high risk of refeeding syndrome, patients greater than 30% below ideal body weight should be hospitalized for close monitoring during refeeding.12
- Typical goal for weight gain is no greater than 2-3 pounds per week.10
- Total parenteral nutrition should be reserved for extreme cases, and if used, carbohydrate intake should not exceed 7 mg/kg/min.12
Stroke
- Enteral nutrition should be initiated within 24-48 hours of initial hospitalization if a patient is estimated to require feeding for more than 5 days and/or remain nil per os for 5-7 days.
- If a patient is intubated with increased intracranial pressure, this could delay gastric motility requiring a postpyloric tube placement.
- Initial placement of percutaneous endoscopic gastrostomy tubes can be considered if the hospitalized patient is expected to require nutritional support for greater than 30 days. Most patients will have improved dysphagia symptoms within 1 month of their acute stroke, although as many as 40% can have continued dysphagia up to 1 year.10
Back to the Case
The patient was admitted for a common general medical condition, but it is important to recognize that malnutrition was present on admission with weight loss and generalized fluid overload. Furthermore, he is at high nutritional risk because of his low body weight, poor oral intake, and dysphagia. Additionally, the acute inflammation from pneumonia places him in an increased catabolic state.
He was able to maintain some volitional oral intake, but after 7 days of close monitoring by a licensed dietician, it was determined that he was unable to meet his nutritional needs via the oral route. A percutaneous endoscopic gastrostomy tube was placed, and tube feeds were initiated, because his dysphagia – which was a significant factor contributing to his inability to meet his nutritional needs orally – was expected to persist for greater than 30 days.
Bottom Line
Nutrition support should be initiated in this patient with malnutrition on admission and high nutritional risk.
Dr. Abalos is an assistant professor at Georgetown University Medical Center in Washington. Dr. Corbett is an assistant professor at the University of Oklahoma Health Sciences Center in Oklahoma City.
References
1. Correia MI et al. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 2003 Jun;22(3):235-9.
2. Felder S et al. Association of nutritional risk and adverse medical outcomes across different medical inpatient populations. Nutrition. 2015 Nov-Dec;31(11-12):1385-93.
3. White JV et al. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: Characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Acad Nutr Diet. 2012 May;112(5):730-8.
4. McClave SA et al. ACG clinical guideline: Nutrition therapy in the adult hospitalized patient. Am J Gastroenterol. 2016 Mar;111(3):315-334.
5. Mueller C et al. A.S.P.E.N. clinical guidelines: Nutrition screening, assessment, and intervention in adults. JPEN J Parenter Enter Nutr. 2011 Jan;35(1):16-24.
6. McClave SA et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient. JPEN J Parenter Enter Nutr. 2016 Feb;40(2):159-211.
7. August D et al. Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. JPEN J Parenter Enter Nutr. 2002 Jan-Feb:26(1):SUPPL:1SA-138SA.
8. Kirkland LL et al. Nutrition in the hospitalized patient. J Hosp Med. 2013 Jan;8(1):52-8.
9. National Collaborating Centre for Acute Care, February 2006. Nutrition support in adults Oral nutrition support, enteral tube feeding and parenteral nutrition. National Collaborating Centre for Acute Care, London. Available from www.rcseng.ac.uk.
10. Corrigan ML et al. Nutrition in the stroke patient. Nutr Clin Pract. 2011 Jun;26(3):242-52.
11. Loser C et al. ESPEN guidelines on artificial enteral nutrition – Percutaneous endoscopic gastrostomy (PEG). Clin Nutr. 2005 Oct;24(5):848-61.
12. Mehler PS et al. Nutritional rehabilitation: Practical guidelines for refeeding the anorectic patient. J Nutr Metab. 2010. doi: 10.1155/2010/625782.
13. Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013 Jul-Aug;13(4 Suppl 2):e1-15.
14. Singh N et al. Evaluation of early enteral feeding through nasogastric and nasojejunal tube in severe acute pancreatitis: A noninferiority randomized controlled trial. Pancreas. 2012 Jan;41(1):153-9.
15. Braga M et al. ESPEN guidelines on parenteral nutrition: Surgery. Clin Nutr. 2009 Aug;28(4):378-86.
16. Weimann A et al. ESPEN Guidelines on enteral nutrition: Surgery including organ transplantation. Clin Nutr. 2006 Apr;25(2):224-44.
Additional reading
- Kirkland LL et al. Nutrition in the Hospitalized Patient. J Hosp Med. 2013 Jan;8(1):52-8.
- McClave SA et al. ACG Clinical Guideline: Nutrition Therapy in the Adult Hospitalized Patient. Am J Gastroenterol. 2016 Mar;111(3):315-334.
Quiz: Recognizing Malnutrition
Which of the following is not a criteria for the diagnosis of malnutrition?
A. Weight loss
B. Insufficient energy intake
C. Prealbumin
D. Diminished handgrip strength
Answer: C. Prealbumin. Laboratory indicators of nutrition, such as albumin, prealbumin, and transferrin, and markers of infection or inflammation are not recommended for the determination of nutritional status. Because negative acute-phase reactants, they instead can be used as surrogate markers of nutritional risk and degree of inflammation
Key Points
- At the time of admission to the hospital, malnutrition is present in 20-50% of patients. All hospitalized patients should be screened for nutritional risk and nutritional support should be considered if patients are not expected to be able to meet nutritional needs for more than 7 days.
- Patients with severe malnutrition on admission, severe critical illness, or severe acute pancreatitis should be provided nutritional support within 24-48 hours.
- Use the gut! Nutritional support should be provided via the most physiologic route possible. Total parenteral nutrition (TPN) should be reserved for patients in whom adequate nutrition cannot be provided enterally.
- Consider a percutaneous endoscopic gastrostomy (PEG) tube if the patient is expected to require tube feedings for more than 30 days.
- Patients with severe malnutrition who are given nutritional support are at high risk of developing refeeding syndrome, which manifests as electrolyte depletions and heart failure or volume overload.
Case
A 60-year-old male with a history of head & neck cancer, treated with radical neck dissection and radiation 5 years prior is admitted with community-acquired pneumonia and anasarca. Prior to admission, he was on a soft dysphagia diet and reports increased difficulty with solid foods and weight loss from 70 kg to 55 kg over 2.5 years. Should nutritional support be initiated?
Background
Malnutrition is associated with increased hospital mortality, decreased functional status and quality of life, infections, longer length of stay, higher hospital costs, and more frequent nonelective readmissions.1,2
Identifying patients who are malnourished or at risk for malnutrition
An international consensus committee recommended the following criteria for the diagnosis of undernutrition if two of six are present3:
- Insufficient energy intake.
- Weight loss.
- Loss of muscle mass.
- Loss of subcutaneous fat.
- Localized or generalized fluid accumulation that may sometimes mask weight loss.
- Diminished functional status as measured by handgrip strength.
The joint commission requires that all patients admitted to acute care hospitals be screened for risk of malnutrition within 24 hours. The American College of Gastroenterologists recommends using a validated score to assess nutritional risk, such as the Nutritional Risk Score (NRS) 2002 or the NUTRIC (Nutrition Risk in the Critically Ill) Score, which use a combination of nutritional status and diet-related factors – weight loss, body mass index, and food intake – and also severity of illness measurements.4
- Starvation-related malnutrition, such as anorexia nervosa, presents with a deficiency in calories and protein without inflammation, .
- Chronic disease–related malnutrition, such as that caused chronic obstructive pulmonary disease, cancer, and obesity, presents with mild to moderate inflammation.
- Acute disease or injury–related malnutrition, such as that caused by sepsis, burns, and trauma, presents with acute and severe inflammation.
Laboratory indicators such as albumin, prealbumin, and transferrin are not recommended for the determination of nutritional status. Instead, as negative acute-phase reactants, they can be used as surrogate markers of nutritional risk and degree of inflammation.4
Overview of the data
What are the indications for initiating nutritional support, and what is the optimal timing for initiation?
Patients who are malnourished or at significant risk for becoming malnourished should receive specialized nutrition support. Early enteral nutrition should be initiated within 24-48 hours of admission in critically ill patients with high nutritional risk who are unable to maintain volitional intake.6 In the absence of preexisting malnutrition, nutritional support should be provided for patients with inadequate oral intake for 7-14 days or for those in whom inadequate oral intake is expected over the same time period.7
How should nutritional support be administered?
Dietary modification and supplementation
In patients who can tolerate an oral diet, dietary modifications may be made in order to facilitate the provision of essential nutrients in a well-tolerated form. Modifications may include adjusting the consistency of foods, energy value of foods, types of nutrients consumed, and number and frequency of meals.8 Commercial meal replacement beverages are widely used to support a standard oral diet, but there is no data to support their routine use.7
Enteral nutrition
Enteral nutrition (EN) is the method of choice for administering nutrition support. Contraindications to enteral feeding include diffuse peritonitis, intestinal obstruction, and gastrointestinal ischemia.9 The potential advantages of EN over parenteral nutrition (PN) include decreased infection rate, decreased total complications, and shorter length of stay, but there has been no observed difference in mortality. EN is also suggested to have nonnutritional benefits related to providing luminal nutrients – these include maintaining gut integrity, beneficial immune responses, and favorable metabolic responses that help maintain euglycemia and enhance more physiologic fuel utilization.4
Enteral feeding can be administered through the following routes of access:
- Nasogastric tubes: A nasogastric or orogastric tube with radiologic confirmation of positioning is the first line of enteral access. Gastric feeding is preferred because it is well tolerated in the majority of patients, is more physiological, requires a lower level of expertise, and minimizes any delay in initiation of feeding.
- Postpyloric tubes: Postpyloric feeding tubes are indicated if gastric feeding is poorly tolerated or if the patient is at high risk for aspiration because jejunal feedings decrease the incidence of reflux, regurgitation, and aspiration.
- Percutaneous access: When long-term enteral access is required – that is, for greater than 4 weeks – a percutaneous enteral access device should be placed. Prolonged use of a nasoenteric tube may be associated with erosion of the nares and an increase in the incidence of aspiration pneumonia, sinusitis, and esophageal ulceration or stricture. Patients who have had a stroke are the most likely to benefit from percutaneous endoscopic gastrostomy placement, as 40% of patients can have continued dysphagia as long as 1 year after.4,10 Absolute contraindications for PEG placement include serious coagulation disorders (international normalized ratio greater than 1.5; fewer than 50,000 platelets/mcL), sepsis, abdominal wall infections, marked peritoneal carcinomatosis, peritonitis, severe gastroparesis, gastric outlet obstruction, or a history of total gastrectomy. Risks often outweigh benefits in patients who have cirrhosis with ascites, patients undergoing peritoneal dialysis, and patients who have portal hypertension with gastric varices, but PEG can be considered on a case-by-case basis.11
Parenteral nutrition
Parenteral nutrition is reserved for patients in whom enteral feeding is contraindicated or who fail to meet their nutritional needs with enteral feedings. If EN is not feasible, then parenteral nutrition should be initiated as soon as possible in patients who had high nutritional risk on admission. Otherwise, PN should not be initiated during the first week of hospitalization because there is evidence to suggest net harm when initiated early. Supplemental PN may be considered for patients already on EN who are unable to meet more than 60% of their energy and protein requirements by the enteral route alone, but again, this should only be considered after 7-10 days on EN. PN is generally stopped when the patients achieve more than 60% of their energy and protein goals from EN.4
How should patients be monitored while receiving nutritional support?
If a patient is severely malnourished and refeeding is initiated, serious complications can occur, which are summarized in Table 1; these complications can include severe electrolyte disorders, fluid shifts, and even death.12 Refeeding syndrome occurs in the first few days of initiating a diet in severely malnourished patients, and its severity is directly related to the severity of malnutrition prior to refeeding. The National Institute of Health and Clinical Excellence created criteria to identify patients at risk for refeeding syndrome; these criteria include having a BMI less than 18.5 kg/m2; unintentional weight loss of greater than 10% in the previous 3-6 months; little or no nutritional intake for more than 5 days; low levels of potassium, phosphorus, or magnesium before refeeding; and a history of alcohol misuse or taking certain drugs, such as insulin, chemotherapy, antacids, or diuretics.9
Aspiration is a risk with enteral feeding – the risk factors include being older than 70 years, altered mental status, supine position, and bolus rather than continuous infusion.4 Postpyloric feeding may reduce the risk of aspiration. Expert consensus suggests elevating the head of the bed by 30°-40° for all intubated patients receiving EN, as well as administering chlorhexidine mouthwash twice daily.6
Diarrhea is very common in patients receiving EN. After evaluating for other etiologies of diarrhea, tube feeding–associated diarrhea may be managed first by using a fiber-containing formulation. Fiber should be avoided in patients at risk for bowel ischemia or severe dysmotility. If diarrhea persists despite fiber, small peptide formulations, also known as elemental tube feeds, may be used.4,6
Gastric residual volume (GRV) is commonly monitored in patients receiving enteral nutrition. However, the American College of Gastroenterology does not recommend using GRVs to monitor EN feeding because it is a poor marker of clinically meaningful variables, such as gastric emptying, risk of aspiration, and risk of poor outcomes, and increases the risk of tube clogging and inadequate delivery of EN. If GRVs are being monitored, tube feedings should not be withheld because of high GRVs when there are no other signs of intolerance.4 Nausea may be managed by changing a patient from bolus to continuous feedings or by adding promotility agents such as metoclopramide or erythromycin.6
Special considerations in common conditions treated by hospitalists
The principles outlined above are general guidelines that are applicable to most patients requiring nutrition support. We have highlighted special considerations for common conditions in hospitalized patients who require nutritional support below.
Critical Illness
- Defer enteral nutrition until patient is fully resuscitated and hemodynamically stable.
- Severely malnourished or high nutritional-risk patients should be advanced toward goals as quickly as can be tolerated over 24-48 hours.
- Patients with acute respiratory distress syndrome or acute lung injury, or those expected to require mechanical ventilation for more than 72 hours, should receive trophic feeds or full nutrition by enteral route.6
Pancreatitis
- Oral feeding should be attempted as soon as abdominal pain is decreasing and inflammatory markers are improving.13
- A regular solid, low-fat diet should be initiated, rather than slowly advancing from a clear liquid diet.13
- In severe acute pancreatitis, initiation of enteral nutrition within 48 hours of presentation is associated with improved outcomes.13
- There is no difference in outcomes between gastric and postpyloric feeding.14
- Initiation of parenteral nutrition may be delayed for up to 5 days to allow for a trial of oral or enteral feeding.13
Surgical patients
- Consider postponing surgery to provide 7-10 days of preoperative nutrition supplementation in patients with risk of severe undernutrition.16
- Consider postoperative nutritional support if patients are at risk for severe undernutrition, are unable to eat for more than 7 days perioperatively, or are unable to maintain oral intake above 60% of recommended intake for more than 10 days.16
- Consider total parenteral nutrition in cases of impaired gastrointestinal function and absorption, high output enterocutaneous fistulae, obstructive lesions that do not allow enteral refeeding, or prolonged gastrointestinal failure.16
Prolonged Starvation
- Because of the high risk of refeeding syndrome, patients greater than 30% below ideal body weight should be hospitalized for close monitoring during refeeding.12
- Typical goal for weight gain is no greater than 2-3 pounds per week.10
- Total parenteral nutrition should be reserved for extreme cases, and if used, carbohydrate intake should not exceed 7 mg/kg/min.12
Stroke
- Enteral nutrition should be initiated within 24-48 hours of initial hospitalization if a patient is estimated to require feeding for more than 5 days and/or remain nil per os for 5-7 days.
- If a patient is intubated with increased intracranial pressure, this could delay gastric motility requiring a postpyloric tube placement.
- Initial placement of percutaneous endoscopic gastrostomy tubes can be considered if the hospitalized patient is expected to require nutritional support for greater than 30 days. Most patients will have improved dysphagia symptoms within 1 month of their acute stroke, although as many as 40% can have continued dysphagia up to 1 year.10
Back to the Case
The patient was admitted for a common general medical condition, but it is important to recognize that malnutrition was present on admission with weight loss and generalized fluid overload. Furthermore, he is at high nutritional risk because of his low body weight, poor oral intake, and dysphagia. Additionally, the acute inflammation from pneumonia places him in an increased catabolic state.
He was able to maintain some volitional oral intake, but after 7 days of close monitoring by a licensed dietician, it was determined that he was unable to meet his nutritional needs via the oral route. A percutaneous endoscopic gastrostomy tube was placed, and tube feeds were initiated, because his dysphagia – which was a significant factor contributing to his inability to meet his nutritional needs orally – was expected to persist for greater than 30 days.
Bottom Line
Nutrition support should be initiated in this patient with malnutrition on admission and high nutritional risk.
Dr. Abalos is an assistant professor at Georgetown University Medical Center in Washington. Dr. Corbett is an assistant professor at the University of Oklahoma Health Sciences Center in Oklahoma City.
References
1. Correia MI et al. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 2003 Jun;22(3):235-9.
2. Felder S et al. Association of nutritional risk and adverse medical outcomes across different medical inpatient populations. Nutrition. 2015 Nov-Dec;31(11-12):1385-93.
3. White JV et al. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: Characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). J Acad Nutr Diet. 2012 May;112(5):730-8.
4. McClave SA et al. ACG clinical guideline: Nutrition therapy in the adult hospitalized patient. Am J Gastroenterol. 2016 Mar;111(3):315-334.
5. Mueller C et al. A.S.P.E.N. clinical guidelines: Nutrition screening, assessment, and intervention in adults. JPEN J Parenter Enter Nutr. 2011 Jan;35(1):16-24.
6. McClave SA et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient. JPEN J Parenter Enter Nutr. 2016 Feb;40(2):159-211.
7. August D et al. Guidelines for the use of parenteral and enteral nutrition in adult and pediatric patients. JPEN J Parenter Enter Nutr. 2002 Jan-Feb:26(1):SUPPL:1SA-138SA.
8. Kirkland LL et al. Nutrition in the hospitalized patient. J Hosp Med. 2013 Jan;8(1):52-8.
9. National Collaborating Centre for Acute Care, February 2006. Nutrition support in adults Oral nutrition support, enteral tube feeding and parenteral nutrition. National Collaborating Centre for Acute Care, London. Available from www.rcseng.ac.uk.
10. Corrigan ML et al. Nutrition in the stroke patient. Nutr Clin Pract. 2011 Jun;26(3):242-52.
11. Loser C et al. ESPEN guidelines on artificial enteral nutrition – Percutaneous endoscopic gastrostomy (PEG). Clin Nutr. 2005 Oct;24(5):848-61.
12. Mehler PS et al. Nutritional rehabilitation: Practical guidelines for refeeding the anorectic patient. J Nutr Metab. 2010. doi: 10.1155/2010/625782.
13. Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013 Jul-Aug;13(4 Suppl 2):e1-15.
14. Singh N et al. Evaluation of early enteral feeding through nasogastric and nasojejunal tube in severe acute pancreatitis: A noninferiority randomized controlled trial. Pancreas. 2012 Jan;41(1):153-9.
15. Braga M et al. ESPEN guidelines on parenteral nutrition: Surgery. Clin Nutr. 2009 Aug;28(4):378-86.
16. Weimann A et al. ESPEN Guidelines on enteral nutrition: Surgery including organ transplantation. Clin Nutr. 2006 Apr;25(2):224-44.
Additional reading
- Kirkland LL et al. Nutrition in the Hospitalized Patient. J Hosp Med. 2013 Jan;8(1):52-8.
- McClave SA et al. ACG Clinical Guideline: Nutrition Therapy in the Adult Hospitalized Patient. Am J Gastroenterol. 2016 Mar;111(3):315-334.
Quiz: Recognizing Malnutrition
Which of the following is not a criteria for the diagnosis of malnutrition?
A. Weight loss
B. Insufficient energy intake
C. Prealbumin
D. Diminished handgrip strength
Answer: C. Prealbumin. Laboratory indicators of nutrition, such as albumin, prealbumin, and transferrin, and markers of infection or inflammation are not recommended for the determination of nutritional status. Because negative acute-phase reactants, they instead can be used as surrogate markers of nutritional risk and degree of inflammation
Key Points
- At the time of admission to the hospital, malnutrition is present in 20-50% of patients. All hospitalized patients should be screened for nutritional risk and nutritional support should be considered if patients are not expected to be able to meet nutritional needs for more than 7 days.
- Patients with severe malnutrition on admission, severe critical illness, or severe acute pancreatitis should be provided nutritional support within 24-48 hours.
- Use the gut! Nutritional support should be provided via the most physiologic route possible. Total parenteral nutrition (TPN) should be reserved for patients in whom adequate nutrition cannot be provided enterally.
- Consider a percutaneous endoscopic gastrostomy (PEG) tube if the patient is expected to require tube feedings for more than 30 days.
- Patients with severe malnutrition who are given nutritional support are at high risk of developing refeeding syndrome, which manifests as electrolyte depletions and heart failure or volume overload.
Myasthenia Gravis: Challenges and Burdens of Disease
Click Here to Read Supplement.
In a new supplement to Neurology Reviews, expert Richard J. Nowak, MD, MS, discusses the burden of myasthenia gravis and challenges in treating the disease.
Topics in this supplement include:
- Pathophysiology of Myasthenia Gravis
- Treatment Resistant Myasthenia Gravis
- Burden and Cost
Click Here to Read Supplement.
US/UNB-gMG/18/0033
Click Here to Read Supplement.
In a new supplement to Neurology Reviews, expert Richard J. Nowak, MD, MS, discusses the burden of myasthenia gravis and challenges in treating the disease.
Topics in this supplement include:
- Pathophysiology of Myasthenia Gravis
- Treatment Resistant Myasthenia Gravis
- Burden and Cost
Click Here to Read Supplement.
US/UNB-gMG/18/0033
Click Here to Read Supplement.
In a new supplement to Neurology Reviews, expert Richard J. Nowak, MD, MS, discusses the burden of myasthenia gravis and challenges in treating the disease.
Topics in this supplement include:
- Pathophysiology of Myasthenia Gravis
- Treatment Resistant Myasthenia Gravis
- Burden and Cost
Click Here to Read Supplement.
US/UNB-gMG/18/0033
Chlamydia infections associated with more than a doubling of ovarian cancer risk
Pelvic inflammatory disease caused by chlamydia appears to significantly increase the risk of ovarian cancer, according to research to be presented at the annual meeting of the American Association for Cancer Research.
The finding, replicated in two large databases, suggests that promptly treating the infection might reduce the lifetime risk of developing ovarian cancer, Britton Trabert, PhD, said during a press briefing held in advance of the meeting.
The study portends both promise and challenge, according to Elaine R. Mardis, PhD, who comoderated the session.
“Ovarian cancer is typically diagnosed at a late stage and therefore has a poor prognosis,” said Dr. Mardis of The Nationwide Hospital, Columbus, Ohio. “Chlamydia will be an important point of study here, both because of the frequency of this infection, and because it is quite difficult to detect, due to its asymptomatic nature. But the most important take-home point is that we might be able to go a long way in terms of preventing ovarian cancer by routinely screening for infective agents.”
Pelvic inflammatory disease is known to be associated with ovarian cancer, and chlamydia is a leading cause of the disease, noted Dr. Trabert. “But chlamydia infections can be asymptomatic and persist for months or even years, so ascertainment of past chlamydia infections is challenging.”
To investigate the potential link between these infections and ovarian cancer, Dr. Trabert and her colleagues examined associations between antibodies to several infectious agents, including chlamydia, in two large ovarian cancer databases: a population-based case/control study in Poland and a case-control study nested into the U.S. Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial.
The researchers screened for antibodies to chlamydia, Mycoplasma genitalium, Epstein-Barre virus, human papillomavirus, herpes simplex virus-1 and -2, polyomavirus, hepatitis B and C, and cytomegalovirus. The chlamydia antibody selected was plasmid-encoded Pgp3 protein, considered the gold standard measurement for prior or existing chlamydia infections.
The patient cohorts comprised 278 cases vs. 556 controls from the Polish study, and 160 cases vs. 159 controls from the PLCO study. Serum samples were collected at the time of ovarian cancer diagnosis in the Polish cohort, and before diagnosis in the PLCO cohort.
Dr. Trabert presented odds ratios for a Pgp3 antibody titer cut point indicative of past chlamydia infection, and a “more stringent” higher cut point indicative of current or chronic infection. She and her colleagues found statistically significant associations for each cut point in both studies.
In the Polish cohort, the lower Pgp3 cut point was associated with a 63% increased risk of ovarian cancer (odds ratio, 1.63). The higher cut point was associated with a doubling of risk (OR, 2.0).
In the PLCO cohort, the lower cut point was associated with a 43% increased risk (OR, 1.43). The higher cut point more than doubled the risk of ovarian cancer (OR, 2.25).
Neither cohort showed any significant association of ovarian cancer with any of the other antibodies, Dr. Trabert said.
The NCI Intramural Research Program supported the study. Dr. Trabert and her colleagues declared no conflicts of interest.
SOURCE: Trabert et al. Abstract 4942.
Pelvic inflammatory disease caused by chlamydia appears to significantly increase the risk of ovarian cancer, according to research to be presented at the annual meeting of the American Association for Cancer Research.
The finding, replicated in two large databases, suggests that promptly treating the infection might reduce the lifetime risk of developing ovarian cancer, Britton Trabert, PhD, said during a press briefing held in advance of the meeting.
The study portends both promise and challenge, according to Elaine R. Mardis, PhD, who comoderated the session.
“Ovarian cancer is typically diagnosed at a late stage and therefore has a poor prognosis,” said Dr. Mardis of The Nationwide Hospital, Columbus, Ohio. “Chlamydia will be an important point of study here, both because of the frequency of this infection, and because it is quite difficult to detect, due to its asymptomatic nature. But the most important take-home point is that we might be able to go a long way in terms of preventing ovarian cancer by routinely screening for infective agents.”
Pelvic inflammatory disease is known to be associated with ovarian cancer, and chlamydia is a leading cause of the disease, noted Dr. Trabert. “But chlamydia infections can be asymptomatic and persist for months or even years, so ascertainment of past chlamydia infections is challenging.”
To investigate the potential link between these infections and ovarian cancer, Dr. Trabert and her colleagues examined associations between antibodies to several infectious agents, including chlamydia, in two large ovarian cancer databases: a population-based case/control study in Poland and a case-control study nested into the U.S. Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial.
The researchers screened for antibodies to chlamydia, Mycoplasma genitalium, Epstein-Barre virus, human papillomavirus, herpes simplex virus-1 and -2, polyomavirus, hepatitis B and C, and cytomegalovirus. The chlamydia antibody selected was plasmid-encoded Pgp3 protein, considered the gold standard measurement for prior or existing chlamydia infections.
The patient cohorts comprised 278 cases vs. 556 controls from the Polish study, and 160 cases vs. 159 controls from the PLCO study. Serum samples were collected at the time of ovarian cancer diagnosis in the Polish cohort, and before diagnosis in the PLCO cohort.
Dr. Trabert presented odds ratios for a Pgp3 antibody titer cut point indicative of past chlamydia infection, and a “more stringent” higher cut point indicative of current or chronic infection. She and her colleagues found statistically significant associations for each cut point in both studies.
In the Polish cohort, the lower Pgp3 cut point was associated with a 63% increased risk of ovarian cancer (odds ratio, 1.63). The higher cut point was associated with a doubling of risk (OR, 2.0).
In the PLCO cohort, the lower cut point was associated with a 43% increased risk (OR, 1.43). The higher cut point more than doubled the risk of ovarian cancer (OR, 2.25).
Neither cohort showed any significant association of ovarian cancer with any of the other antibodies, Dr. Trabert said.
The NCI Intramural Research Program supported the study. Dr. Trabert and her colleagues declared no conflicts of interest.
SOURCE: Trabert et al. Abstract 4942.
Pelvic inflammatory disease caused by chlamydia appears to significantly increase the risk of ovarian cancer, according to research to be presented at the annual meeting of the American Association for Cancer Research.
The finding, replicated in two large databases, suggests that promptly treating the infection might reduce the lifetime risk of developing ovarian cancer, Britton Trabert, PhD, said during a press briefing held in advance of the meeting.
The study portends both promise and challenge, according to Elaine R. Mardis, PhD, who comoderated the session.
“Ovarian cancer is typically diagnosed at a late stage and therefore has a poor prognosis,” said Dr. Mardis of The Nationwide Hospital, Columbus, Ohio. “Chlamydia will be an important point of study here, both because of the frequency of this infection, and because it is quite difficult to detect, due to its asymptomatic nature. But the most important take-home point is that we might be able to go a long way in terms of preventing ovarian cancer by routinely screening for infective agents.”
Pelvic inflammatory disease is known to be associated with ovarian cancer, and chlamydia is a leading cause of the disease, noted Dr. Trabert. “But chlamydia infections can be asymptomatic and persist for months or even years, so ascertainment of past chlamydia infections is challenging.”
To investigate the potential link between these infections and ovarian cancer, Dr. Trabert and her colleagues examined associations between antibodies to several infectious agents, including chlamydia, in two large ovarian cancer databases: a population-based case/control study in Poland and a case-control study nested into the U.S. Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial.
The researchers screened for antibodies to chlamydia, Mycoplasma genitalium, Epstein-Barre virus, human papillomavirus, herpes simplex virus-1 and -2, polyomavirus, hepatitis B and C, and cytomegalovirus. The chlamydia antibody selected was plasmid-encoded Pgp3 protein, considered the gold standard measurement for prior or existing chlamydia infections.
The patient cohorts comprised 278 cases vs. 556 controls from the Polish study, and 160 cases vs. 159 controls from the PLCO study. Serum samples were collected at the time of ovarian cancer diagnosis in the Polish cohort, and before diagnosis in the PLCO cohort.
Dr. Trabert presented odds ratios for a Pgp3 antibody titer cut point indicative of past chlamydia infection, and a “more stringent” higher cut point indicative of current or chronic infection. She and her colleagues found statistically significant associations for each cut point in both studies.
In the Polish cohort, the lower Pgp3 cut point was associated with a 63% increased risk of ovarian cancer (odds ratio, 1.63). The higher cut point was associated with a doubling of risk (OR, 2.0).
In the PLCO cohort, the lower cut point was associated with a 43% increased risk (OR, 1.43). The higher cut point more than doubled the risk of ovarian cancer (OR, 2.25).
Neither cohort showed any significant association of ovarian cancer with any of the other antibodies, Dr. Trabert said.
The NCI Intramural Research Program supported the study. Dr. Trabert and her colleagues declared no conflicts of interest.
SOURCE: Trabert et al. Abstract 4942.
FROM THE AACR ANNUAL MEETING
Key clinical point: Chlamydia infections appear to increase the risk of ovarian cancer.
Major finding: The presence of an antibody to chlamydia increased the chance of ovarian cancer by up to 2.25-fold (OR 2.25).
Study details: The cohorts comprised 278 cases vs. 556 controls from a Polish study, and 160 cases vs. 159 controls from a U.S. study.
Disclosures: The NCI Intramural Research Program supported the study. The researchers declared no conflicts of interest.
Source: Trabet et al. Abstract 4942.
I am not your burnout expert
Look, I am not a burnout expert. And neither are you (presumably). None of us know much, but that won’t stop the regulations from coming. Program directors are already being asked to provide “wellness plans.” Through the SVS, experts have been enlisted to help, but it is now clear that what works for others won’t necessarily work for vascular surgeons. The next step is up to us. We are the only ones with detailed knowledge of our lives. I believe we are moving closer to answers but still face a few significant hurdles. Don’t worry, there are solutions. Hear me out …
Previously, I shared three studies with you, which found that vascular surgeons had the highest rates of suicidal ideation and career dissatisfaction among surgeons while spending more hours in the hospital than any other specialty. So what has been done to address these horrific numbers? Very little. We need answers now, but most of the data are over 10 years old. Much has changed in our specialty. The endovascular revolution created an entirely new working paradigm. A busy vascular surgeon used to perform 300 cases annually; now this number approaches 1,000. More procedures means more clerical work. Lead aprons and radiation exposure have added new ergonomic and medical concerns. Reimbursement dynamics now favor shorter, more frequent patient interactions over longer, more complex cases. We are benchmarked against old work standards while CPT bundling continuously lowers current RVU designations. EMR was supposed to make our lives better; it has done the opposite. Patient-centered health care has become a mantra, but the measures taken often backfire. Practicing medicine where the desired outcome is a high score on patient satisfaction surveys will likely lead to unnecessary tests, poor cost allocation, and low physician fulfillment. Quality of care is now measured scrupulously while the quality of our lives remains undocumented.
In the absence of organized reform, burnout appears to be increasing. A recent Mayo Clinic–AMA study found the current prevalence to be 54% among physicians. All of this has not happened overnight. I believe practicing vascular surgeons are resilient by default. The majority of us trained prior to the enforcement of duty hour restrictions. Out of high school, I enrolled in a 6-year BA/MD program (skipping 2 years of college seemed like a great idea in high school, less so when I got there). Half of my class never finished. In my intern year, six of the eight categorical residents dropped out. My odds of reaching PGY 2 were 12.5%. Fuzzy math aside, all of your stories are similar. We have proved our resilience over and over again. What is happening here is different.
Burnout is described as emotional exhaustion, low self-esteem, and depersonalization/cynicism. It develops slowly, progressively as stressors increase. A common thread seems to be the feeling that you alone are not enough. Examine your daily life. What are your most common stressors? For me, they relate to time management, clinical documentation, and whatever fresh hell my kids’ teachers have cooked up for “school projects.”
*****Scene*****
Wife: Can you help Luke (kindergarten) finish his diorama? It needs to be a scale depiction of his 3 favorite scenes from Wagner’s Ring cycle.
Me: Sure, I just need to complete the wind tunnel testing on Jack’s (3rd grade) carbon-neutral peanut-free alternative fuel source rocket booster.
Off stage – 7th Grade Son: The genetically modified spiders got loose again!
*****End Scene*****
We want to do a good job, but more hurdles are placed in our way. A recent AMA/Dartmouth Hitchcock study found that 50% of physicians’ time is spent performing data entry and other administrative work. Only 27% of time was spent on patient care. Every hour of face-to-face patient time requires 2 hours of EMR/clerical work. We are trapped in a bureaucratic prison. For years, every quality initiative was solved with a new form. To enter a simple note today, we must first “establish our relationship” with the patient, then ably click through a minefield of “warning boxes” signifying impending DVT prophylaxis catastrophes and antibiotic crimes and misdemeanors, next we scroll through a pre-populated postapocalyptic hellscape of minute- by-minute vital sign entries and lab values dating back to inception. Then, and only then, finally, ON PAGE 11, we can meagerly type: Patient at wound care, will come back on evening rounds.
Another important component of the burnout syndrome is dehumanization. Recently I spoke with Donald Zimmerman, PhD, author of the textbook “Person-Focused Health Care Management.” His thoughts on health care were dramatically altered after spending 43 days in an ICU following abdominal aortic aneurysm repair. He describes the experience as “my worst nightmare that then got worse and then never ended.” While we can learn from his experience, how many of us were trained to face this horror? Dehumanization is a natural protective response, especially when we have so little time for patient interactions. Compassion fatigue sets in when we don’t have the time and resources to care for our patients.While poor outcomes have been cited as a result of burnout, this appears to be an end-stage result. The Minimizing Error, Maximizing Outcome (MEMO) study funded by the AHRQ found that physicians often served as a buffer between their patients and poor medical environments. The organizational flaws that led to burnout also independently resulted in substandard patient care. The burnout physicians experienced was a symptom of the defective health care system and not causative of the poor care. Doctors were literally sacrificing their well-being to care for their patients.
Not surprisingly, attitudes regarding burnout vary significantly between health care executives and physicians. A New England Journal of Medicine survey of their Insights Council found that 96% of respondents agreed that burnout is a moderate or serious problem, although physicians were significantly more likely than executives to rate the problem as “serious.” Opinions on solutions varied as well, with executives more likely to support redesign of EMR, while physicians favored reduction of documentation and clerical work. Obviously the physicians’ solution would be more costly to the corporation as the executives deflected the problem back to the EMR designers. Neither group favored the use of resilience/wellness programs as a primary solution.
Of all the remedies proposed, I find resilience training to be especially egregious. Studies consistently show a 40%-50% prevalence of burnout among physicians. How can this be an individual problem? Why train doctors to endure a broken system? This type of problem solving is why burnout continues to flourish. Doctors are not suffering from a disease but rather exhibiting a symptom.
To arrive at possible solutions, let’s look at the elite athlete analogy. What are you trained to do? What are your exceptional skills? For me it is clearly EMR documentation (just checking to see if any of my residents have read this far). How many of us would describe ourselves as expert at billing? Paperwork? Medication reconciliation? Discharge summaries? Should LeBron James hawk 16-ounce Miller Lites in the nosebleeds during halftime? This may sound like I am expressing a cocky attitude that these tasks are beneath us, but we now have concrete evidence that forcing physicians to perform these duties hurts patient care and literally kills us. Full stop. Physician burnout can lead to suicide in the absence of clinical depression.
While hopelessness is part and parcel of the burnout syndrome, there are now potential solutions within our grasp. Clearly a reduction in clerical duties will be a key component of any realistic plan. Our time must be proportioned. Few of us are asking to work less. Reducing patient interactions while increasing the average time of these encounters has been shown to reduce burnout without decreasing work hours. We want to do a good job. It is time to remove these barriers.
Our next steps have already been taken, and for me it represents the best example of the potential of Vascular Specialist and the SVS. Under the leadership of SVS President Clem Darling, MD, and Executive Director Ken Slaw, PhD, a task force was created to address this issue. Ably chaired by Dawn Coleman, MD, and including Sam Money, MD, from the SVS Executive Council and Past SVS President Julie Freischlag, MD, the task force has collaborated with actual burnout experts Tait Shanafelt, MD, and Susan Hallbeck, PhD, to create a survey designed to identify the causes, prevalence, and potential solutions to the burnout problem in vascular surgery.
The first survey has been completed and will be issued to all SVS members this month to coincide with the SCVS annual symposium. The second, which will focus more on physical issues, will be released during the VAM in June.
Look, no one hates surveys more than I do. We simply have to get this information. Each survey is designed to only take 10 minutes. Things are going to change one way or another. Let’s lead, not wait to follow. With your help this will be the last time I write this ignorantly on this crisis. Vascular surgeons are few in number but this gives us the potential to deliver the most comprehensive self-assessment any specialty has ever performed. Lend your voice to the coming change.
Finally, there are now innovations in use which have proved beneficial in mitigating burnout. A Stanford University School of Medicine program allows physicians to “bank” time spent on committees, teaching, or other administrative duties and exchange these credits for home delivery meals, cleaning services, or even work tasks such as grant applications and paper writing. While the physicians could certainly afford to pay for these assistances, the success of the program demonstrates it is the time saved in arranging the services that the doctors truly valued. Our happiness seems to excel when we spend our time performing the tasks for which we are best suited.
It is time to change. When a system reaches this point, something breaks. Let’s stop being the thing that breaks. Fill out the survey. Get involved. There is time to act before we all burn out on burnout.
Dr. Sheahan is the Claude C. Craighead Jr. Professor and Chair, Division of Vascular and Endovascular Surgery, Louisiana State University Health Sciences Center, New Orleans.
Look, I am not a burnout expert. And neither are you (presumably). None of us know much, but that won’t stop the regulations from coming. Program directors are already being asked to provide “wellness plans.” Through the SVS, experts have been enlisted to help, but it is now clear that what works for others won’t necessarily work for vascular surgeons. The next step is up to us. We are the only ones with detailed knowledge of our lives. I believe we are moving closer to answers but still face a few significant hurdles. Don’t worry, there are solutions. Hear me out …
Previously, I shared three studies with you, which found that vascular surgeons had the highest rates of suicidal ideation and career dissatisfaction among surgeons while spending more hours in the hospital than any other specialty. So what has been done to address these horrific numbers? Very little. We need answers now, but most of the data are over 10 years old. Much has changed in our specialty. The endovascular revolution created an entirely new working paradigm. A busy vascular surgeon used to perform 300 cases annually; now this number approaches 1,000. More procedures means more clerical work. Lead aprons and radiation exposure have added new ergonomic and medical concerns. Reimbursement dynamics now favor shorter, more frequent patient interactions over longer, more complex cases. We are benchmarked against old work standards while CPT bundling continuously lowers current RVU designations. EMR was supposed to make our lives better; it has done the opposite. Patient-centered health care has become a mantra, but the measures taken often backfire. Practicing medicine where the desired outcome is a high score on patient satisfaction surveys will likely lead to unnecessary tests, poor cost allocation, and low physician fulfillment. Quality of care is now measured scrupulously while the quality of our lives remains undocumented.
In the absence of organized reform, burnout appears to be increasing. A recent Mayo Clinic–AMA study found the current prevalence to be 54% among physicians. All of this has not happened overnight. I believe practicing vascular surgeons are resilient by default. The majority of us trained prior to the enforcement of duty hour restrictions. Out of high school, I enrolled in a 6-year BA/MD program (skipping 2 years of college seemed like a great idea in high school, less so when I got there). Half of my class never finished. In my intern year, six of the eight categorical residents dropped out. My odds of reaching PGY 2 were 12.5%. Fuzzy math aside, all of your stories are similar. We have proved our resilience over and over again. What is happening here is different.
Burnout is described as emotional exhaustion, low self-esteem, and depersonalization/cynicism. It develops slowly, progressively as stressors increase. A common thread seems to be the feeling that you alone are not enough. Examine your daily life. What are your most common stressors? For me, they relate to time management, clinical documentation, and whatever fresh hell my kids’ teachers have cooked up for “school projects.”
*****Scene*****
Wife: Can you help Luke (kindergarten) finish his diorama? It needs to be a scale depiction of his 3 favorite scenes from Wagner’s Ring cycle.
Me: Sure, I just need to complete the wind tunnel testing on Jack’s (3rd grade) carbon-neutral peanut-free alternative fuel source rocket booster.
Off stage – 7th Grade Son: The genetically modified spiders got loose again!
*****End Scene*****
We want to do a good job, but more hurdles are placed in our way. A recent AMA/Dartmouth Hitchcock study found that 50% of physicians’ time is spent performing data entry and other administrative work. Only 27% of time was spent on patient care. Every hour of face-to-face patient time requires 2 hours of EMR/clerical work. We are trapped in a bureaucratic prison. For years, every quality initiative was solved with a new form. To enter a simple note today, we must first “establish our relationship” with the patient, then ably click through a minefield of “warning boxes” signifying impending DVT prophylaxis catastrophes and antibiotic crimes and misdemeanors, next we scroll through a pre-populated postapocalyptic hellscape of minute- by-minute vital sign entries and lab values dating back to inception. Then, and only then, finally, ON PAGE 11, we can meagerly type: Patient at wound care, will come back on evening rounds.
Another important component of the burnout syndrome is dehumanization. Recently I spoke with Donald Zimmerman, PhD, author of the textbook “Person-Focused Health Care Management.” His thoughts on health care were dramatically altered after spending 43 days in an ICU following abdominal aortic aneurysm repair. He describes the experience as “my worst nightmare that then got worse and then never ended.” While we can learn from his experience, how many of us were trained to face this horror? Dehumanization is a natural protective response, especially when we have so little time for patient interactions. Compassion fatigue sets in when we don’t have the time and resources to care for our patients.While poor outcomes have been cited as a result of burnout, this appears to be an end-stage result. The Minimizing Error, Maximizing Outcome (MEMO) study funded by the AHRQ found that physicians often served as a buffer between their patients and poor medical environments. The organizational flaws that led to burnout also independently resulted in substandard patient care. The burnout physicians experienced was a symptom of the defective health care system and not causative of the poor care. Doctors were literally sacrificing their well-being to care for their patients.
Not surprisingly, attitudes regarding burnout vary significantly between health care executives and physicians. A New England Journal of Medicine survey of their Insights Council found that 96% of respondents agreed that burnout is a moderate or serious problem, although physicians were significantly more likely than executives to rate the problem as “serious.” Opinions on solutions varied as well, with executives more likely to support redesign of EMR, while physicians favored reduction of documentation and clerical work. Obviously the physicians’ solution would be more costly to the corporation as the executives deflected the problem back to the EMR designers. Neither group favored the use of resilience/wellness programs as a primary solution.
Of all the remedies proposed, I find resilience training to be especially egregious. Studies consistently show a 40%-50% prevalence of burnout among physicians. How can this be an individual problem? Why train doctors to endure a broken system? This type of problem solving is why burnout continues to flourish. Doctors are not suffering from a disease but rather exhibiting a symptom.
To arrive at possible solutions, let’s look at the elite athlete analogy. What are you trained to do? What are your exceptional skills? For me it is clearly EMR documentation (just checking to see if any of my residents have read this far). How many of us would describe ourselves as expert at billing? Paperwork? Medication reconciliation? Discharge summaries? Should LeBron James hawk 16-ounce Miller Lites in the nosebleeds during halftime? This may sound like I am expressing a cocky attitude that these tasks are beneath us, but we now have concrete evidence that forcing physicians to perform these duties hurts patient care and literally kills us. Full stop. Physician burnout can lead to suicide in the absence of clinical depression.
While hopelessness is part and parcel of the burnout syndrome, there are now potential solutions within our grasp. Clearly a reduction in clerical duties will be a key component of any realistic plan. Our time must be proportioned. Few of us are asking to work less. Reducing patient interactions while increasing the average time of these encounters has been shown to reduce burnout without decreasing work hours. We want to do a good job. It is time to remove these barriers.
Our next steps have already been taken, and for me it represents the best example of the potential of Vascular Specialist and the SVS. Under the leadership of SVS President Clem Darling, MD, and Executive Director Ken Slaw, PhD, a task force was created to address this issue. Ably chaired by Dawn Coleman, MD, and including Sam Money, MD, from the SVS Executive Council and Past SVS President Julie Freischlag, MD, the task force has collaborated with actual burnout experts Tait Shanafelt, MD, and Susan Hallbeck, PhD, to create a survey designed to identify the causes, prevalence, and potential solutions to the burnout problem in vascular surgery.
The first survey has been completed and will be issued to all SVS members this month to coincide with the SCVS annual symposium. The second, which will focus more on physical issues, will be released during the VAM in June.
Look, no one hates surveys more than I do. We simply have to get this information. Each survey is designed to only take 10 minutes. Things are going to change one way or another. Let’s lead, not wait to follow. With your help this will be the last time I write this ignorantly on this crisis. Vascular surgeons are few in number but this gives us the potential to deliver the most comprehensive self-assessment any specialty has ever performed. Lend your voice to the coming change.
Finally, there are now innovations in use which have proved beneficial in mitigating burnout. A Stanford University School of Medicine program allows physicians to “bank” time spent on committees, teaching, or other administrative duties and exchange these credits for home delivery meals, cleaning services, or even work tasks such as grant applications and paper writing. While the physicians could certainly afford to pay for these assistances, the success of the program demonstrates it is the time saved in arranging the services that the doctors truly valued. Our happiness seems to excel when we spend our time performing the tasks for which we are best suited.
It is time to change. When a system reaches this point, something breaks. Let’s stop being the thing that breaks. Fill out the survey. Get involved. There is time to act before we all burn out on burnout.
Dr. Sheahan is the Claude C. Craighead Jr. Professor and Chair, Division of Vascular and Endovascular Surgery, Louisiana State University Health Sciences Center, New Orleans.
Look, I am not a burnout expert. And neither are you (presumably). None of us know much, but that won’t stop the regulations from coming. Program directors are already being asked to provide “wellness plans.” Through the SVS, experts have been enlisted to help, but it is now clear that what works for others won’t necessarily work for vascular surgeons. The next step is up to us. We are the only ones with detailed knowledge of our lives. I believe we are moving closer to answers but still face a few significant hurdles. Don’t worry, there are solutions. Hear me out …
Previously, I shared three studies with you, which found that vascular surgeons had the highest rates of suicidal ideation and career dissatisfaction among surgeons while spending more hours in the hospital than any other specialty. So what has been done to address these horrific numbers? Very little. We need answers now, but most of the data are over 10 years old. Much has changed in our specialty. The endovascular revolution created an entirely new working paradigm. A busy vascular surgeon used to perform 300 cases annually; now this number approaches 1,000. More procedures means more clerical work. Lead aprons and radiation exposure have added new ergonomic and medical concerns. Reimbursement dynamics now favor shorter, more frequent patient interactions over longer, more complex cases. We are benchmarked against old work standards while CPT bundling continuously lowers current RVU designations. EMR was supposed to make our lives better; it has done the opposite. Patient-centered health care has become a mantra, but the measures taken often backfire. Practicing medicine where the desired outcome is a high score on patient satisfaction surveys will likely lead to unnecessary tests, poor cost allocation, and low physician fulfillment. Quality of care is now measured scrupulously while the quality of our lives remains undocumented.
In the absence of organized reform, burnout appears to be increasing. A recent Mayo Clinic–AMA study found the current prevalence to be 54% among physicians. All of this has not happened overnight. I believe practicing vascular surgeons are resilient by default. The majority of us trained prior to the enforcement of duty hour restrictions. Out of high school, I enrolled in a 6-year BA/MD program (skipping 2 years of college seemed like a great idea in high school, less so when I got there). Half of my class never finished. In my intern year, six of the eight categorical residents dropped out. My odds of reaching PGY 2 were 12.5%. Fuzzy math aside, all of your stories are similar. We have proved our resilience over and over again. What is happening here is different.
Burnout is described as emotional exhaustion, low self-esteem, and depersonalization/cynicism. It develops slowly, progressively as stressors increase. A common thread seems to be the feeling that you alone are not enough. Examine your daily life. What are your most common stressors? For me, they relate to time management, clinical documentation, and whatever fresh hell my kids’ teachers have cooked up for “school projects.”
*****Scene*****
Wife: Can you help Luke (kindergarten) finish his diorama? It needs to be a scale depiction of his 3 favorite scenes from Wagner’s Ring cycle.
Me: Sure, I just need to complete the wind tunnel testing on Jack’s (3rd grade) carbon-neutral peanut-free alternative fuel source rocket booster.
Off stage – 7th Grade Son: The genetically modified spiders got loose again!
*****End Scene*****
We want to do a good job, but more hurdles are placed in our way. A recent AMA/Dartmouth Hitchcock study found that 50% of physicians’ time is spent performing data entry and other administrative work. Only 27% of time was spent on patient care. Every hour of face-to-face patient time requires 2 hours of EMR/clerical work. We are trapped in a bureaucratic prison. For years, every quality initiative was solved with a new form. To enter a simple note today, we must first “establish our relationship” with the patient, then ably click through a minefield of “warning boxes” signifying impending DVT prophylaxis catastrophes and antibiotic crimes and misdemeanors, next we scroll through a pre-populated postapocalyptic hellscape of minute- by-minute vital sign entries and lab values dating back to inception. Then, and only then, finally, ON PAGE 11, we can meagerly type: Patient at wound care, will come back on evening rounds.
Another important component of the burnout syndrome is dehumanization. Recently I spoke with Donald Zimmerman, PhD, author of the textbook “Person-Focused Health Care Management.” His thoughts on health care were dramatically altered after spending 43 days in an ICU following abdominal aortic aneurysm repair. He describes the experience as “my worst nightmare that then got worse and then never ended.” While we can learn from his experience, how many of us were trained to face this horror? Dehumanization is a natural protective response, especially when we have so little time for patient interactions. Compassion fatigue sets in when we don’t have the time and resources to care for our patients.While poor outcomes have been cited as a result of burnout, this appears to be an end-stage result. The Minimizing Error, Maximizing Outcome (MEMO) study funded by the AHRQ found that physicians often served as a buffer between their patients and poor medical environments. The organizational flaws that led to burnout also independently resulted in substandard patient care. The burnout physicians experienced was a symptom of the defective health care system and not causative of the poor care. Doctors were literally sacrificing their well-being to care for their patients.
Not surprisingly, attitudes regarding burnout vary significantly between health care executives and physicians. A New England Journal of Medicine survey of their Insights Council found that 96% of respondents agreed that burnout is a moderate or serious problem, although physicians were significantly more likely than executives to rate the problem as “serious.” Opinions on solutions varied as well, with executives more likely to support redesign of EMR, while physicians favored reduction of documentation and clerical work. Obviously the physicians’ solution would be more costly to the corporation as the executives deflected the problem back to the EMR designers. Neither group favored the use of resilience/wellness programs as a primary solution.
Of all the remedies proposed, I find resilience training to be especially egregious. Studies consistently show a 40%-50% prevalence of burnout among physicians. How can this be an individual problem? Why train doctors to endure a broken system? This type of problem solving is why burnout continues to flourish. Doctors are not suffering from a disease but rather exhibiting a symptom.
To arrive at possible solutions, let’s look at the elite athlete analogy. What are you trained to do? What are your exceptional skills? For me it is clearly EMR documentation (just checking to see if any of my residents have read this far). How many of us would describe ourselves as expert at billing? Paperwork? Medication reconciliation? Discharge summaries? Should LeBron James hawk 16-ounce Miller Lites in the nosebleeds during halftime? This may sound like I am expressing a cocky attitude that these tasks are beneath us, but we now have concrete evidence that forcing physicians to perform these duties hurts patient care and literally kills us. Full stop. Physician burnout can lead to suicide in the absence of clinical depression.
While hopelessness is part and parcel of the burnout syndrome, there are now potential solutions within our grasp. Clearly a reduction in clerical duties will be a key component of any realistic plan. Our time must be proportioned. Few of us are asking to work less. Reducing patient interactions while increasing the average time of these encounters has been shown to reduce burnout without decreasing work hours. We want to do a good job. It is time to remove these barriers.
Our next steps have already been taken, and for me it represents the best example of the potential of Vascular Specialist and the SVS. Under the leadership of SVS President Clem Darling, MD, and Executive Director Ken Slaw, PhD, a task force was created to address this issue. Ably chaired by Dawn Coleman, MD, and including Sam Money, MD, from the SVS Executive Council and Past SVS President Julie Freischlag, MD, the task force has collaborated with actual burnout experts Tait Shanafelt, MD, and Susan Hallbeck, PhD, to create a survey designed to identify the causes, prevalence, and potential solutions to the burnout problem in vascular surgery.
The first survey has been completed and will be issued to all SVS members this month to coincide with the SCVS annual symposium. The second, which will focus more on physical issues, will be released during the VAM in June.
Look, no one hates surveys more than I do. We simply have to get this information. Each survey is designed to only take 10 minutes. Things are going to change one way or another. Let’s lead, not wait to follow. With your help this will be the last time I write this ignorantly on this crisis. Vascular surgeons are few in number but this gives us the potential to deliver the most comprehensive self-assessment any specialty has ever performed. Lend your voice to the coming change.
Finally, there are now innovations in use which have proved beneficial in mitigating burnout. A Stanford University School of Medicine program allows physicians to “bank” time spent on committees, teaching, or other administrative duties and exchange these credits for home delivery meals, cleaning services, or even work tasks such as grant applications and paper writing. While the physicians could certainly afford to pay for these assistances, the success of the program demonstrates it is the time saved in arranging the services that the doctors truly valued. Our happiness seems to excel when we spend our time performing the tasks for which we are best suited.
It is time to change. When a system reaches this point, something breaks. Let’s stop being the thing that breaks. Fill out the survey. Get involved. There is time to act before we all burn out on burnout.
Dr. Sheahan is the Claude C. Craighead Jr. Professor and Chair, Division of Vascular and Endovascular Surgery, Louisiana State University Health Sciences Center, New Orleans.
Closure of High-Risk PFOs Reduces Risk of Recurrent Stroke
Closure of a patent foramen ovale (PFO) with an atrial septal aneurysm, hypermobility, or size of 2 mm or greater reduces the risk of stroke recurrence in patients with cryptogenic stroke, according to research published online ahead of print March 12 in the Journal of the American College of Cardiology.
“Considering the high prevalence of PFO in the general population and cryptogenic stroke patients, the key to appropriate use of this medical device is determining how to select optimal candidates for the procedure,” said Jae-Kwan Song, MD, PhD, a Professor in the Department of Medicine at Asan Medical Center, University of Ulsan College of Medicine, in Seoul, South Korea. “With our study and other recent trials, the criteria for selecting patients for the procedure are becoming clearer; in particular, the results suggest that closure is beneficial for those with high-risk PFO.”
A Multisite Superiority Trial
Previous research has not offered a definitive answer to the question of whether physicians can determine the potential benefit of PFO closure according to the PFO’s morphologic characteristics. In an earlier study, Dr. Song and colleagues found that high-risk PFO, as defined by transesophageal echocardiography (TEE), helped to predict stroke recurrence. The investigators then initiated the DEFENSE-PFO trial to evaluate whether restricting treatment to patients with cryptogenic stroke and PFO morphology associated with a higher rate of recurrent stroke would enhance the benefits of PFO closure.
Dr. Song and colleagues conducted DEFENSE-PFO, an open-label superiority trial, at two sites in South Korea from June 2011 through October 2017. Eligible patients had an ischemic stroke within the previous six months with no identifiable cause other than a high-risk PFO with left-to-right shunting. The researchers performed a standardized evaluation to rule out other identifiable mechanisms of stroke. The exclusion criteria were at least 50% stenosis of a major vessel, occlusion of a major vessel, and stroke resulting from small-vessel occlusive disease. Dr. Song and colleagues performed Holter monitoring or prolonged monitoring of cardiac rhythm to rule out paroxysmal atrial fibrillation.
A high-risk PFO was defined as one with an atrial septal aneurysm (ie, protrusion of the dilated segment of the septum at least 15 mm beyond the level surface of the atrial septum), hypermobility (ie, phasic septal excursion of 10 mm or more into either atrium), or size (ie, maximum separation of the septum primum from the secundum during the Valsalva maneuver) of 2 mm or greater on TEE.
Patients were randomized in equal groups to transcatheter PFO closure with the Amplatzer PFO Occluder plus medical therapy or medical therapy alone. All participants received antiplatelet therapy or anticoagulation chosen by the local investigator. During follow-up visits at one, three, six, 12, and 24 months, investigators recorded clinical data.
The primary end point was a composite of stroke, vascular death, or Thrombolysis in Myocardial Infarction (TIMI)-defined major bleeding during two years of follow-up. The secondary end point was asymptomatic ischemic stroke on follow-up MRI.
No End-Point Events After PFO Closure
Dr. Song and colleagues identified 450 patients with cryptogenic stoke and PFO, of whom 175 had high-risk PFO. They randomized 60 patients to each study arm. Participants’ mean age was 51.8. The groups were well balanced in terms of age, sex, medical history, qualifying event, modified Rankin scale score at discharge, and the anatomic characteristics of the PFO and atrial septum.
Seven patients randomized to PFO closure declined the treatment. Dual antiplatelet therapy was the most common medication in both groups at 30 days after randomization. This trend continued for as long as 12 months in the medication-only group, but single antiplatelet therapy became the most common strategy after six months in the PFO-closure group. About 17% of patients in the PFO-closure group stopped medication after the intervention. The median duration of follow-up was 2.8 years.
In the intention-to-treat analysis, no patient in the PFO-closure group had a primary end point event, compared with six patients in the medication-only group. Events recorded in the latter group included five ischemic strokes, one cerebral hemorrhage, two TIMI-defined major bleeding events, and one transient ischemic attack. The Kaplan-Meier two-year cumulative estimate of the probability of stroke was 10.5% in the medication-only group. The number of patients needed to treat with PFO closure to avoid one stroke at two years thus was 10.
Implications for Selection Criteria
The DEFENSE-PFO study differs from two previous trials that found benefits of PFO closure, but did not consider the anatomic features of the atrial septum or PFO. “The only trial with stringent entry criteria similar to ours is the CLOSE trial, which required that patients have a large interatrial right-to-left shunt (more than 30 microbubbles in the left atrium within three cardiac cycles after opacification of the right atrium) or an atrial septal aneurysm (a septum primum excursion greater than 10 mm),” said Dr. Song and colleagues. “Both the CLOSE trial and our trial showed no occurrence of stroke in patients who underwent PFO closure, suggesting that the beneficial effect of percutaneous device closure of PFO can be maximized by adding the morphologic characteristics of PFO, as evaluated by TEE, to the selection criteria for the procedure.”
Because the DEFENSE-PFO study was terminated early for patient safety, it was underpowered to provide a hazard ratio for its primary end point. In addition, selection bias may have affected the study, since it was conducted at a small number of centers.
—Erik Greb
Suggested Reading
Lee PH, Song J-K, Kim JS, et al. Cryptogenic stroke and high-risk patent foramen ovale: The DEFENSE-PFO trial. J Am Coll Cardiol. 2018 Mar 12 [Epub ahead of print].
Mas JL, Derumeaux G, Guillon B, et al. Patent foramen ovale closure or anticoagulation vs. antiplatelets after stroke. N Engl J Med. 2017;377(11):1011-1021.
Closure of a patent foramen ovale (PFO) with an atrial septal aneurysm, hypermobility, or size of 2 mm or greater reduces the risk of stroke recurrence in patients with cryptogenic stroke, according to research published online ahead of print March 12 in the Journal of the American College of Cardiology.
“Considering the high prevalence of PFO in the general population and cryptogenic stroke patients, the key to appropriate use of this medical device is determining how to select optimal candidates for the procedure,” said Jae-Kwan Song, MD, PhD, a Professor in the Department of Medicine at Asan Medical Center, University of Ulsan College of Medicine, in Seoul, South Korea. “With our study and other recent trials, the criteria for selecting patients for the procedure are becoming clearer; in particular, the results suggest that closure is beneficial for those with high-risk PFO.”
A Multisite Superiority Trial
Previous research has not offered a definitive answer to the question of whether physicians can determine the potential benefit of PFO closure according to the PFO’s morphologic characteristics. In an earlier study, Dr. Song and colleagues found that high-risk PFO, as defined by transesophageal echocardiography (TEE), helped to predict stroke recurrence. The investigators then initiated the DEFENSE-PFO trial to evaluate whether restricting treatment to patients with cryptogenic stroke and PFO morphology associated with a higher rate of recurrent stroke would enhance the benefits of PFO closure.
Dr. Song and colleagues conducted DEFENSE-PFO, an open-label superiority trial, at two sites in South Korea from June 2011 through October 2017. Eligible patients had an ischemic stroke within the previous six months with no identifiable cause other than a high-risk PFO with left-to-right shunting. The researchers performed a standardized evaluation to rule out other identifiable mechanisms of stroke. The exclusion criteria were at least 50% stenosis of a major vessel, occlusion of a major vessel, and stroke resulting from small-vessel occlusive disease. Dr. Song and colleagues performed Holter monitoring or prolonged monitoring of cardiac rhythm to rule out paroxysmal atrial fibrillation.
A high-risk PFO was defined as one with an atrial septal aneurysm (ie, protrusion of the dilated segment of the septum at least 15 mm beyond the level surface of the atrial septum), hypermobility (ie, phasic septal excursion of 10 mm or more into either atrium), or size (ie, maximum separation of the septum primum from the secundum during the Valsalva maneuver) of 2 mm or greater on TEE.
Patients were randomized in equal groups to transcatheter PFO closure with the Amplatzer PFO Occluder plus medical therapy or medical therapy alone. All participants received antiplatelet therapy or anticoagulation chosen by the local investigator. During follow-up visits at one, three, six, 12, and 24 months, investigators recorded clinical data.
The primary end point was a composite of stroke, vascular death, or Thrombolysis in Myocardial Infarction (TIMI)-defined major bleeding during two years of follow-up. The secondary end point was asymptomatic ischemic stroke on follow-up MRI.
No End-Point Events After PFO Closure
Dr. Song and colleagues identified 450 patients with cryptogenic stoke and PFO, of whom 175 had high-risk PFO. They randomized 60 patients to each study arm. Participants’ mean age was 51.8. The groups were well balanced in terms of age, sex, medical history, qualifying event, modified Rankin scale score at discharge, and the anatomic characteristics of the PFO and atrial septum.
Seven patients randomized to PFO closure declined the treatment. Dual antiplatelet therapy was the most common medication in both groups at 30 days after randomization. This trend continued for as long as 12 months in the medication-only group, but single antiplatelet therapy became the most common strategy after six months in the PFO-closure group. About 17% of patients in the PFO-closure group stopped medication after the intervention. The median duration of follow-up was 2.8 years.
In the intention-to-treat analysis, no patient in the PFO-closure group had a primary end point event, compared with six patients in the medication-only group. Events recorded in the latter group included five ischemic strokes, one cerebral hemorrhage, two TIMI-defined major bleeding events, and one transient ischemic attack. The Kaplan-Meier two-year cumulative estimate of the probability of stroke was 10.5% in the medication-only group. The number of patients needed to treat with PFO closure to avoid one stroke at two years thus was 10.
Implications for Selection Criteria
The DEFENSE-PFO study differs from two previous trials that found benefits of PFO closure, but did not consider the anatomic features of the atrial septum or PFO. “The only trial with stringent entry criteria similar to ours is the CLOSE trial, which required that patients have a large interatrial right-to-left shunt (more than 30 microbubbles in the left atrium within three cardiac cycles after opacification of the right atrium) or an atrial septal aneurysm (a septum primum excursion greater than 10 mm),” said Dr. Song and colleagues. “Both the CLOSE trial and our trial showed no occurrence of stroke in patients who underwent PFO closure, suggesting that the beneficial effect of percutaneous device closure of PFO can be maximized by adding the morphologic characteristics of PFO, as evaluated by TEE, to the selection criteria for the procedure.”
Because the DEFENSE-PFO study was terminated early for patient safety, it was underpowered to provide a hazard ratio for its primary end point. In addition, selection bias may have affected the study, since it was conducted at a small number of centers.
—Erik Greb
Suggested Reading
Lee PH, Song J-K, Kim JS, et al. Cryptogenic stroke and high-risk patent foramen ovale: The DEFENSE-PFO trial. J Am Coll Cardiol. 2018 Mar 12 [Epub ahead of print].
Mas JL, Derumeaux G, Guillon B, et al. Patent foramen ovale closure or anticoagulation vs. antiplatelets after stroke. N Engl J Med. 2017;377(11):1011-1021.
Closure of a patent foramen ovale (PFO) with an atrial septal aneurysm, hypermobility, or size of 2 mm or greater reduces the risk of stroke recurrence in patients with cryptogenic stroke, according to research published online ahead of print March 12 in the Journal of the American College of Cardiology.
“Considering the high prevalence of PFO in the general population and cryptogenic stroke patients, the key to appropriate use of this medical device is determining how to select optimal candidates for the procedure,” said Jae-Kwan Song, MD, PhD, a Professor in the Department of Medicine at Asan Medical Center, University of Ulsan College of Medicine, in Seoul, South Korea. “With our study and other recent trials, the criteria for selecting patients for the procedure are becoming clearer; in particular, the results suggest that closure is beneficial for those with high-risk PFO.”
A Multisite Superiority Trial
Previous research has not offered a definitive answer to the question of whether physicians can determine the potential benefit of PFO closure according to the PFO’s morphologic characteristics. In an earlier study, Dr. Song and colleagues found that high-risk PFO, as defined by transesophageal echocardiography (TEE), helped to predict stroke recurrence. The investigators then initiated the DEFENSE-PFO trial to evaluate whether restricting treatment to patients with cryptogenic stroke and PFO morphology associated with a higher rate of recurrent stroke would enhance the benefits of PFO closure.
Dr. Song and colleagues conducted DEFENSE-PFO, an open-label superiority trial, at two sites in South Korea from June 2011 through October 2017. Eligible patients had an ischemic stroke within the previous six months with no identifiable cause other than a high-risk PFO with left-to-right shunting. The researchers performed a standardized evaluation to rule out other identifiable mechanisms of stroke. The exclusion criteria were at least 50% stenosis of a major vessel, occlusion of a major vessel, and stroke resulting from small-vessel occlusive disease. Dr. Song and colleagues performed Holter monitoring or prolonged monitoring of cardiac rhythm to rule out paroxysmal atrial fibrillation.
A high-risk PFO was defined as one with an atrial septal aneurysm (ie, protrusion of the dilated segment of the septum at least 15 mm beyond the level surface of the atrial septum), hypermobility (ie, phasic septal excursion of 10 mm or more into either atrium), or size (ie, maximum separation of the septum primum from the secundum during the Valsalva maneuver) of 2 mm or greater on TEE.
Patients were randomized in equal groups to transcatheter PFO closure with the Amplatzer PFO Occluder plus medical therapy or medical therapy alone. All participants received antiplatelet therapy or anticoagulation chosen by the local investigator. During follow-up visits at one, three, six, 12, and 24 months, investigators recorded clinical data.
The primary end point was a composite of stroke, vascular death, or Thrombolysis in Myocardial Infarction (TIMI)-defined major bleeding during two years of follow-up. The secondary end point was asymptomatic ischemic stroke on follow-up MRI.
No End-Point Events After PFO Closure
Dr. Song and colleagues identified 450 patients with cryptogenic stoke and PFO, of whom 175 had high-risk PFO. They randomized 60 patients to each study arm. Participants’ mean age was 51.8. The groups were well balanced in terms of age, sex, medical history, qualifying event, modified Rankin scale score at discharge, and the anatomic characteristics of the PFO and atrial septum.
Seven patients randomized to PFO closure declined the treatment. Dual antiplatelet therapy was the most common medication in both groups at 30 days after randomization. This trend continued for as long as 12 months in the medication-only group, but single antiplatelet therapy became the most common strategy after six months in the PFO-closure group. About 17% of patients in the PFO-closure group stopped medication after the intervention. The median duration of follow-up was 2.8 years.
In the intention-to-treat analysis, no patient in the PFO-closure group had a primary end point event, compared with six patients in the medication-only group. Events recorded in the latter group included five ischemic strokes, one cerebral hemorrhage, two TIMI-defined major bleeding events, and one transient ischemic attack. The Kaplan-Meier two-year cumulative estimate of the probability of stroke was 10.5% in the medication-only group. The number of patients needed to treat with PFO closure to avoid one stroke at two years thus was 10.
Implications for Selection Criteria
The DEFENSE-PFO study differs from two previous trials that found benefits of PFO closure, but did not consider the anatomic features of the atrial septum or PFO. “The only trial with stringent entry criteria similar to ours is the CLOSE trial, which required that patients have a large interatrial right-to-left shunt (more than 30 microbubbles in the left atrium within three cardiac cycles after opacification of the right atrium) or an atrial septal aneurysm (a septum primum excursion greater than 10 mm),” said Dr. Song and colleagues. “Both the CLOSE trial and our trial showed no occurrence of stroke in patients who underwent PFO closure, suggesting that the beneficial effect of percutaneous device closure of PFO can be maximized by adding the morphologic characteristics of PFO, as evaluated by TEE, to the selection criteria for the procedure.”
Because the DEFENSE-PFO study was terminated early for patient safety, it was underpowered to provide a hazard ratio for its primary end point. In addition, selection bias may have affected the study, since it was conducted at a small number of centers.
—Erik Greb
Suggested Reading
Lee PH, Song J-K, Kim JS, et al. Cryptogenic stroke and high-risk patent foramen ovale: The DEFENSE-PFO trial. J Am Coll Cardiol. 2018 Mar 12 [Epub ahead of print].
Mas JL, Derumeaux G, Guillon B, et al. Patent foramen ovale closure or anticoagulation vs. antiplatelets after stroke. N Engl J Med. 2017;377(11):1011-1021.
Analytics, board support are quality improvement keys
Jeffrey Glasheen, MD, had not considered focusing on quality improvement (QI) while studying at the University of Wisconsin, Madison. It was not until a medical error led to the death of a family member that his eyes were opened to the potential consequences of a system not invested in care quality.
“I couldn’t square with it because I had spent the last two to three years of my life working with some of the most dedicated, passionate, hard working people who all were trying to improve lives, and the fact that what I was seeing could result in a family member dying just didn’t make sense,” said Dr. Glasheen. “At the time I thought ‘This must be one of those unfortunate things that happens once in a lifetime,’ and I put it on the back burner.”
As more research on medical errors emerged, however, Dr. Glasheen realized his family’s experience was not as unique as he had thought.
It was after reading the now famous Institute of Medicine report, “To err is human,” which found that medical errors were responsible for 44,000-98,000 deaths a year, that Dr. Glasheen resolved to pursue a career in quality improvement.
Because it was early in his medical career, he began on a small level, teaching his residents about the importance of patient safety and giving lessons on core competencies involved in quality care and higher liability. But he quickly expanded his efforts.
“I started with what I had control over,” Dr. Glasheen explained. “From there, I moved to teaching more medical students, which lead to teaching in front of classrooms, which opened the door to the idea of starting a hospitalist training program.”
In 2003, Dr. Glasheen pitched the program to the University of Colorado at Denver, Aurora, where he completed his residency; this pitch led to the development of a hospitalist training program that focused on improving safety outcomes.
He served as the director of the University of Colorado Hospital Medicine Group from 2003 to 2015, during which time he was approached by the dean to assist in creating and leading the hospitalist training program for internal medicine residents.
The first of its kind, the rigorous University of Colorado program was designed to give residents tools useful beyond the clinical setting to become successful health system leaders.
In 2013, Dr. Glasheen and his colleagues founded the Institute for Healthcare Quality, Safety & Efficiency, which is guided by the mission to improve the quality of care provided on the local level. He has since become the chief quality officer for UCHealth and the University of Colorado Hospital Authority and an associate dean for clinical affairs in quality and safety education, as well as continuing to be a professor of medicine.
For those hoping to pursue quality improvement, Dr. Glasheen stressed the importance of a strong basis in data analytics.
“One of the most common things I see with data is people start to chase what’s called common cause variation, which means they’ll look at a run chart over the course of 12 months and react to every up and down when those are essentially random,” Dr. Glasheen said. “Being able to understand when something is particularly significant and when your interventions are actually making an impact is a skill set I think people who are new to quality improvement don’t often have.”
Having support from board members is also critical to success, although starting without such support should not deter future QI leaders.
“There needs to be a vision from the leadership that this work is important, and not just through words but through deeds, because no board in the country will say that quality is not important,” Dr. Glasheen said. “I would say start with small projects you can control, that tie back not only to patient lives but financial performance as well. If you can tell a board you saved the lives of 40 patients who would have died during the year and saved $1-$2 million in the process, the question will shift from whether the board should invest in QI resources to how much should be invested.”
Looking ahead, Dr. Glasheen highlighted the growing importance of hospital-acquired infections, such as surgical-site infections, catheter-associated urinary tract infections, and ventilator-associated pneumonia, as areas that need to be focused on in the QI sphere.
Jeffrey Glasheen, MD, had not considered focusing on quality improvement (QI) while studying at the University of Wisconsin, Madison. It was not until a medical error led to the death of a family member that his eyes were opened to the potential consequences of a system not invested in care quality.
“I couldn’t square with it because I had spent the last two to three years of my life working with some of the most dedicated, passionate, hard working people who all were trying to improve lives, and the fact that what I was seeing could result in a family member dying just didn’t make sense,” said Dr. Glasheen. “At the time I thought ‘This must be one of those unfortunate things that happens once in a lifetime,’ and I put it on the back burner.”
As more research on medical errors emerged, however, Dr. Glasheen realized his family’s experience was not as unique as he had thought.
It was after reading the now famous Institute of Medicine report, “To err is human,” which found that medical errors were responsible for 44,000-98,000 deaths a year, that Dr. Glasheen resolved to pursue a career in quality improvement.
Because it was early in his medical career, he began on a small level, teaching his residents about the importance of patient safety and giving lessons on core competencies involved in quality care and higher liability. But he quickly expanded his efforts.
“I started with what I had control over,” Dr. Glasheen explained. “From there, I moved to teaching more medical students, which lead to teaching in front of classrooms, which opened the door to the idea of starting a hospitalist training program.”
In 2003, Dr. Glasheen pitched the program to the University of Colorado at Denver, Aurora, where he completed his residency; this pitch led to the development of a hospitalist training program that focused on improving safety outcomes.
He served as the director of the University of Colorado Hospital Medicine Group from 2003 to 2015, during which time he was approached by the dean to assist in creating and leading the hospitalist training program for internal medicine residents.
The first of its kind, the rigorous University of Colorado program was designed to give residents tools useful beyond the clinical setting to become successful health system leaders.
In 2013, Dr. Glasheen and his colleagues founded the Institute for Healthcare Quality, Safety & Efficiency, which is guided by the mission to improve the quality of care provided on the local level. He has since become the chief quality officer for UCHealth and the University of Colorado Hospital Authority and an associate dean for clinical affairs in quality and safety education, as well as continuing to be a professor of medicine.
For those hoping to pursue quality improvement, Dr. Glasheen stressed the importance of a strong basis in data analytics.
“One of the most common things I see with data is people start to chase what’s called common cause variation, which means they’ll look at a run chart over the course of 12 months and react to every up and down when those are essentially random,” Dr. Glasheen said. “Being able to understand when something is particularly significant and when your interventions are actually making an impact is a skill set I think people who are new to quality improvement don’t often have.”
Having support from board members is also critical to success, although starting without such support should not deter future QI leaders.
“There needs to be a vision from the leadership that this work is important, and not just through words but through deeds, because no board in the country will say that quality is not important,” Dr. Glasheen said. “I would say start with small projects you can control, that tie back not only to patient lives but financial performance as well. If you can tell a board you saved the lives of 40 patients who would have died during the year and saved $1-$2 million in the process, the question will shift from whether the board should invest in QI resources to how much should be invested.”
Looking ahead, Dr. Glasheen highlighted the growing importance of hospital-acquired infections, such as surgical-site infections, catheter-associated urinary tract infections, and ventilator-associated pneumonia, as areas that need to be focused on in the QI sphere.
Jeffrey Glasheen, MD, had not considered focusing on quality improvement (QI) while studying at the University of Wisconsin, Madison. It was not until a medical error led to the death of a family member that his eyes were opened to the potential consequences of a system not invested in care quality.
“I couldn’t square with it because I had spent the last two to three years of my life working with some of the most dedicated, passionate, hard working people who all were trying to improve lives, and the fact that what I was seeing could result in a family member dying just didn’t make sense,” said Dr. Glasheen. “At the time I thought ‘This must be one of those unfortunate things that happens once in a lifetime,’ and I put it on the back burner.”
As more research on medical errors emerged, however, Dr. Glasheen realized his family’s experience was not as unique as he had thought.
It was after reading the now famous Institute of Medicine report, “To err is human,” which found that medical errors were responsible for 44,000-98,000 deaths a year, that Dr. Glasheen resolved to pursue a career in quality improvement.
Because it was early in his medical career, he began on a small level, teaching his residents about the importance of patient safety and giving lessons on core competencies involved in quality care and higher liability. But he quickly expanded his efforts.
“I started with what I had control over,” Dr. Glasheen explained. “From there, I moved to teaching more medical students, which lead to teaching in front of classrooms, which opened the door to the idea of starting a hospitalist training program.”
In 2003, Dr. Glasheen pitched the program to the University of Colorado at Denver, Aurora, where he completed his residency; this pitch led to the development of a hospitalist training program that focused on improving safety outcomes.
He served as the director of the University of Colorado Hospital Medicine Group from 2003 to 2015, during which time he was approached by the dean to assist in creating and leading the hospitalist training program for internal medicine residents.
The first of its kind, the rigorous University of Colorado program was designed to give residents tools useful beyond the clinical setting to become successful health system leaders.
In 2013, Dr. Glasheen and his colleagues founded the Institute for Healthcare Quality, Safety & Efficiency, which is guided by the mission to improve the quality of care provided on the local level. He has since become the chief quality officer for UCHealth and the University of Colorado Hospital Authority and an associate dean for clinical affairs in quality and safety education, as well as continuing to be a professor of medicine.
For those hoping to pursue quality improvement, Dr. Glasheen stressed the importance of a strong basis in data analytics.
“One of the most common things I see with data is people start to chase what’s called common cause variation, which means they’ll look at a run chart over the course of 12 months and react to every up and down when those are essentially random,” Dr. Glasheen said. “Being able to understand when something is particularly significant and when your interventions are actually making an impact is a skill set I think people who are new to quality improvement don’t often have.”
Having support from board members is also critical to success, although starting without such support should not deter future QI leaders.
“There needs to be a vision from the leadership that this work is important, and not just through words but through deeds, because no board in the country will say that quality is not important,” Dr. Glasheen said. “I would say start with small projects you can control, that tie back not only to patient lives but financial performance as well. If you can tell a board you saved the lives of 40 patients who would have died during the year and saved $1-$2 million in the process, the question will shift from whether the board should invest in QI resources to how much should be invested.”
Looking ahead, Dr. Glasheen highlighted the growing importance of hospital-acquired infections, such as surgical-site infections, catheter-associated urinary tract infections, and ventilator-associated pneumonia, as areas that need to be focused on in the QI sphere.
Make The Diagnosis - April 2018
Once an individual has been exposed to varicella-zoster virus, either from primary infection (chickenpox) or vaccination, the virus remains dormant in dorsal root ganglion cells. It may become reactivated at a later time, which results in herpes zoster. Typically, immunosuppression (hematologic malignancy and HIV infection) and age are factors that play a role in reactivation, although young people may develop shingles as well. Older age increases the incidence of herpes zoster.
More than 90% of patients will experience a prodrome of pain, burning, or tingling in the dermatome prior to the development of cutaneous lesions. Occasionally, there will be no symptoms prior. Papules and plaques begin to form, which quickly develop into vesicles and blisters. After a few days, lesions become crusted. Bullae or necrosis may occur in more severe cases. Typically, the condition resolves in 2-3 weeks, but can take 6 weeks or longer in elderly patients. In zoster sine herpete, patients have pain but no skin lesions.
In typical herpes zoster, lesions can be scattered outside the dermatome as well. When more than 20 lesions are scattered outside the area of primary or adjacent dermatomes, this is defined as disseminated herpes zoster. This occurs more commonly in debilitated or immune-compromised individuals. The outlying vesicles are often singular, not grouped, and resemble the “dew drop on a rose petal” look of varicella-zoster lesions. Dissemination necessitates systemic antiviral therapy, preferably intravenous followed by oral treatment once stable. Central nervous system and pulmonary involvement can occur.
Complications of zoster can occur. Postherpetic neuralgia and pain is more common in patients over the age of 50 and may become chronic. Ramsay Hunt syndrome may result in facial paralysis and hearing loss when there is involvement of the facial or auditory nerve. Occasionally, inflammatory lesions can occur within the affected area after the infection has resolved. Secondary bacterial infection, scarring, and motor paralysis can occur.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at edermatologynews.com. To submit a case for possible publication, send an email to [email protected]. This case and photo were submitted by Dr. Bilu Martin.
Once an individual has been exposed to varicella-zoster virus, either from primary infection (chickenpox) or vaccination, the virus remains dormant in dorsal root ganglion cells. It may become reactivated at a later time, which results in herpes zoster. Typically, immunosuppression (hematologic malignancy and HIV infection) and age are factors that play a role in reactivation, although young people may develop shingles as well. Older age increases the incidence of herpes zoster.
More than 90% of patients will experience a prodrome of pain, burning, or tingling in the dermatome prior to the development of cutaneous lesions. Occasionally, there will be no symptoms prior. Papules and plaques begin to form, which quickly develop into vesicles and blisters. After a few days, lesions become crusted. Bullae or necrosis may occur in more severe cases. Typically, the condition resolves in 2-3 weeks, but can take 6 weeks or longer in elderly patients. In zoster sine herpete, patients have pain but no skin lesions.
In typical herpes zoster, lesions can be scattered outside the dermatome as well. When more than 20 lesions are scattered outside the area of primary or adjacent dermatomes, this is defined as disseminated herpes zoster. This occurs more commonly in debilitated or immune-compromised individuals. The outlying vesicles are often singular, not grouped, and resemble the “dew drop on a rose petal” look of varicella-zoster lesions. Dissemination necessitates systemic antiviral therapy, preferably intravenous followed by oral treatment once stable. Central nervous system and pulmonary involvement can occur.
Complications of zoster can occur. Postherpetic neuralgia and pain is more common in patients over the age of 50 and may become chronic. Ramsay Hunt syndrome may result in facial paralysis and hearing loss when there is involvement of the facial or auditory nerve. Occasionally, inflammatory lesions can occur within the affected area after the infection has resolved. Secondary bacterial infection, scarring, and motor paralysis can occur.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at edermatologynews.com. To submit a case for possible publication, send an email to [email protected]. This case and photo were submitted by Dr. Bilu Martin.
Once an individual has been exposed to varicella-zoster virus, either from primary infection (chickenpox) or vaccination, the virus remains dormant in dorsal root ganglion cells. It may become reactivated at a later time, which results in herpes zoster. Typically, immunosuppression (hematologic malignancy and HIV infection) and age are factors that play a role in reactivation, although young people may develop shingles as well. Older age increases the incidence of herpes zoster.
More than 90% of patients will experience a prodrome of pain, burning, or tingling in the dermatome prior to the development of cutaneous lesions. Occasionally, there will be no symptoms prior. Papules and plaques begin to form, which quickly develop into vesicles and blisters. After a few days, lesions become crusted. Bullae or necrosis may occur in more severe cases. Typically, the condition resolves in 2-3 weeks, but can take 6 weeks or longer in elderly patients. In zoster sine herpete, patients have pain but no skin lesions.
In typical herpes zoster, lesions can be scattered outside the dermatome as well. When more than 20 lesions are scattered outside the area of primary or adjacent dermatomes, this is defined as disseminated herpes zoster. This occurs more commonly in debilitated or immune-compromised individuals. The outlying vesicles are often singular, not grouped, and resemble the “dew drop on a rose petal” look of varicella-zoster lesions. Dissemination necessitates systemic antiviral therapy, preferably intravenous followed by oral treatment once stable. Central nervous system and pulmonary involvement can occur.
Complications of zoster can occur. Postherpetic neuralgia and pain is more common in patients over the age of 50 and may become chronic. Ramsay Hunt syndrome may result in facial paralysis and hearing loss when there is involvement of the facial or auditory nerve. Occasionally, inflammatory lesions can occur within the affected area after the infection has resolved. Secondary bacterial infection, scarring, and motor paralysis can occur.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at edermatologynews.com. To submit a case for possible publication, send an email to [email protected]. This case and photo were submitted by Dr. Bilu Martin.
A healthy 70-year-old white male presented with an 8-day history of fatigue and a tingling, erythematous plaque with crusting on the left flank. Four days after the flank lesions appeared, he developed vesicles with an erythematous base on the right abdomen and back. There were more than 20 vesicles present on the abdomen and back, but there were no lesions on other parts of the body.
Tanning addiction associated with multiple behavioral comorbidities
said Kimberly A. Miller, PhD, of the University of Southern California, Los Angeles, and her associates.
Of a multiethnic sample of 2,637 high school students aged 16-17 years from Los Angeles, 7% met the modified CAGE criteria for tanning addiction, a compulsive drive to use indoor tanning beds frequently. The rate was similar in Hispanic teens and non-Hispanic white adolescents (7.6% versus 7.9%, respectively). Asian and Asian American teens had the lowest prevalence of tanning addiction (4.3%), while Native Hawaiian/Pacific Islanders had the highest (10.5%). Slightly more females than males met the criteria (9% vs. 5%), Dr. Miller and her associates reported in the Journal of Investigative Dermatology.
Past 30-day tobacco and marijuana use was significantly associated with tanning addiction, and teens with problem drinking were 3.4 times as likely to meet tanning addiction criteria as were those without problem drinking. Adolescents with panic disorder symptoms were two times more likely to meet tanning addiction criteria than were those without symptoms, and those with obsessive-compulsive disorder symptoms were three times more likely, Dr. Miller and associates said.
“ for each additional psychological symptom, this figure was 30%,” the researchers said.
Dr. Miller and her associates cited several limitations. One was the cross-sectional design of the study. Another was the study’s focus on adolescents from Los Angeles, which limits the generalizability of the findings.
The authors declared no conflicts of interest.
SOURCE: Miller KA et al. J Investig Dermatol. 2018. doi: 10.1016/j.jid.2018.02.018.
said Kimberly A. Miller, PhD, of the University of Southern California, Los Angeles, and her associates.
Of a multiethnic sample of 2,637 high school students aged 16-17 years from Los Angeles, 7% met the modified CAGE criteria for tanning addiction, a compulsive drive to use indoor tanning beds frequently. The rate was similar in Hispanic teens and non-Hispanic white adolescents (7.6% versus 7.9%, respectively). Asian and Asian American teens had the lowest prevalence of tanning addiction (4.3%), while Native Hawaiian/Pacific Islanders had the highest (10.5%). Slightly more females than males met the criteria (9% vs. 5%), Dr. Miller and her associates reported in the Journal of Investigative Dermatology.
Past 30-day tobacco and marijuana use was significantly associated with tanning addiction, and teens with problem drinking were 3.4 times as likely to meet tanning addiction criteria as were those without problem drinking. Adolescents with panic disorder symptoms were two times more likely to meet tanning addiction criteria than were those without symptoms, and those with obsessive-compulsive disorder symptoms were three times more likely, Dr. Miller and associates said.
“ for each additional psychological symptom, this figure was 30%,” the researchers said.
Dr. Miller and her associates cited several limitations. One was the cross-sectional design of the study. Another was the study’s focus on adolescents from Los Angeles, which limits the generalizability of the findings.
The authors declared no conflicts of interest.
SOURCE: Miller KA et al. J Investig Dermatol. 2018. doi: 10.1016/j.jid.2018.02.018.
said Kimberly A. Miller, PhD, of the University of Southern California, Los Angeles, and her associates.
Of a multiethnic sample of 2,637 high school students aged 16-17 years from Los Angeles, 7% met the modified CAGE criteria for tanning addiction, a compulsive drive to use indoor tanning beds frequently. The rate was similar in Hispanic teens and non-Hispanic white adolescents (7.6% versus 7.9%, respectively). Asian and Asian American teens had the lowest prevalence of tanning addiction (4.3%), while Native Hawaiian/Pacific Islanders had the highest (10.5%). Slightly more females than males met the criteria (9% vs. 5%), Dr. Miller and her associates reported in the Journal of Investigative Dermatology.
Past 30-day tobacco and marijuana use was significantly associated with tanning addiction, and teens with problem drinking were 3.4 times as likely to meet tanning addiction criteria as were those without problem drinking. Adolescents with panic disorder symptoms were two times more likely to meet tanning addiction criteria than were those without symptoms, and those with obsessive-compulsive disorder symptoms were three times more likely, Dr. Miller and associates said.
“ for each additional psychological symptom, this figure was 30%,” the researchers said.
Dr. Miller and her associates cited several limitations. One was the cross-sectional design of the study. Another was the study’s focus on adolescents from Los Angeles, which limits the generalizability of the findings.
The authors declared no conflicts of interest.
SOURCE: Miller KA et al. J Investig Dermatol. 2018. doi: 10.1016/j.jid.2018.02.018.
FROM THE JOURNAL OF INVESTIGATIVE DERMATOLOGY
MDedge Daily News: Alcohol dependence ages your brain
Artificial intelligence comes to glucose monitoring. There’s a promising combo treatment for allergic rhinitis. And evidence mounts for the importance of thrombectomy in stroke.
Listen to the MDedge Daily News podcast for all the details on today’s top news.
Artificial intelligence comes to glucose monitoring. There’s a promising combo treatment for allergic rhinitis. And evidence mounts for the importance of thrombectomy in stroke.
Listen to the MDedge Daily News podcast for all the details on today’s top news.
Artificial intelligence comes to glucose monitoring. There’s a promising combo treatment for allergic rhinitis. And evidence mounts for the importance of thrombectomy in stroke.
Listen to the MDedge Daily News podcast for all the details on today’s top news.
AML patients may fare better at NCI centers
New research suggests patients with acute myeloid leukemia (AML) may have a lower risk of early mortality if they receive treatment at a National Cancer Institute (NCI) cancer center.
In a study of AML patients in California, the risk of 60-day mortality was 53% lower among patients treated at NCI cancer centers than among those treated at other centers.
These findings were reported in Cancer.
“We found the early mortality, deaths less than 60 days after diagnosis, was significantly lower at the NCI-designated cancer centers compared to non-NCI-designated cancer centers in California,” said study author Brian Jonas, MD, PhD, of the University of California at Davis School of Medicine in Sacramento, California.
To conduct this study, Dr Jonas and his colleagues analyzed data from the California Cancer Registry and the California Office of Statewide Health Planning and Development Patient Discharge Database.
The California Cancer Registry provides sociodemographic and clinical data for all California cancer patients. The California Office of Statewide Health Planning and Development Patient Discharge Database has data on diagnoses and procedures for all hospital patients in California, excluding 14 Veterans Affairs and military hospitals.
Patients
The study included data on AML patients 18 and older who received inpatient chemotherapy between 1999 and 2014. There were 7007 patients, 1762 (25%) of whom were treated at NCI-designated cancer centers.
The median number of new AML patients per year was 13.5 (range, 0-43) at the NCI centers and 2 (range, 1-17) at non-NCI centers that admitted at least 1 patient with AML. More than half of the non-NCI centers had a median of 0 new AML patients per year.
NCI patients were more likely to be younger (≤65) than non-NCI patients (P<0.0001), to live in neighborhoods with higher socioeconomic status (P<0.0001), have fewer comorbidities (P<0.0001), and have public health insurance (P<0.0001).
Results
There were several types of complications that differed significantly between center types.
Patients treated at NCI centers were significantly more likely to have leukapheresis (5.5% vs 2.7%; P<0.001) and renal failure (22.8% vs 19.9%; P=0.010).
But they were significantly less likely to have respiratory failure (11.6% vs 14.3%; P=0.003) and cardiac arrest (1.1% vs 2.0%; P=0.014).
Sixty-day survival was significantly higher among NCI patients (88.0% vs 76.3%; P<0.001).
In an inverse-probability-weighted analysis adjusted for sociodemographic factors and comorbidities, treatment at an NCI center was associated with significantly lower early mortality, with an odds ratio (OR) of 0.46 (P<0.001).
This analysis also revealed a significant association between increased early mortality and major bleeding (OR=1.79, P<0.001), renal failure (OR=2.33, P<0.001), respiratory failure (OR=6.46, P<0.001), and cardiac arrest (OR=13.33, P<0.001).
For the most part, the impact of complications on early mortality did not differ significantly by treatment center.
The exception was respiratory failure. Patients with respiratory failure had a significantly greater risk of early mortality if they were treated at a non-NCI center (OR=9.48) than at an NCI center (OR=4.20).
Potential explanations
The researchers believe the variations in early mortality they observed point to inconsistent supportive care. However, more work must be done to fully understand the differences in care driving these issues.
“This is clearly provocative data that makes you want to understand exactly why,” Dr Jonas said. “We’re going to have to dive into that question in a more significant way.”
In the absence of data that could identify the exact causes, the researchers noted that other studies have shown higher patient volumes may contribute to better care.
“I see 60 or more AML cases per year,” Dr Jonas said. “High volume/low volume must play a role.”
The researchers believe other potential contributing factors could be access to clinical trials, better nursing ratios, and more sophisticated intensive care units.
The team hopes this research will spawn more intensive efforts to identify the causes that underlie variations in early mortality between hospital sites.
“This is a provocative and hopeful paper in terms of improving outcomes,” Dr Jonas said. “It sends a positive message that there are things we could probably do that could help everyone.”
New research suggests patients with acute myeloid leukemia (AML) may have a lower risk of early mortality if they receive treatment at a National Cancer Institute (NCI) cancer center.
In a study of AML patients in California, the risk of 60-day mortality was 53% lower among patients treated at NCI cancer centers than among those treated at other centers.
These findings were reported in Cancer.
“We found the early mortality, deaths less than 60 days after diagnosis, was significantly lower at the NCI-designated cancer centers compared to non-NCI-designated cancer centers in California,” said study author Brian Jonas, MD, PhD, of the University of California at Davis School of Medicine in Sacramento, California.
To conduct this study, Dr Jonas and his colleagues analyzed data from the California Cancer Registry and the California Office of Statewide Health Planning and Development Patient Discharge Database.
The California Cancer Registry provides sociodemographic and clinical data for all California cancer patients. The California Office of Statewide Health Planning and Development Patient Discharge Database has data on diagnoses and procedures for all hospital patients in California, excluding 14 Veterans Affairs and military hospitals.
Patients
The study included data on AML patients 18 and older who received inpatient chemotherapy between 1999 and 2014. There were 7007 patients, 1762 (25%) of whom were treated at NCI-designated cancer centers.
The median number of new AML patients per year was 13.5 (range, 0-43) at the NCI centers and 2 (range, 1-17) at non-NCI centers that admitted at least 1 patient with AML. More than half of the non-NCI centers had a median of 0 new AML patients per year.
NCI patients were more likely to be younger (≤65) than non-NCI patients (P<0.0001), to live in neighborhoods with higher socioeconomic status (P<0.0001), have fewer comorbidities (P<0.0001), and have public health insurance (P<0.0001).
Results
There were several types of complications that differed significantly between center types.
Patients treated at NCI centers were significantly more likely to have leukapheresis (5.5% vs 2.7%; P<0.001) and renal failure (22.8% vs 19.9%; P=0.010).
But they were significantly less likely to have respiratory failure (11.6% vs 14.3%; P=0.003) and cardiac arrest (1.1% vs 2.0%; P=0.014).
Sixty-day survival was significantly higher among NCI patients (88.0% vs 76.3%; P<0.001).
In an inverse-probability-weighted analysis adjusted for sociodemographic factors and comorbidities, treatment at an NCI center was associated with significantly lower early mortality, with an odds ratio (OR) of 0.46 (P<0.001).
This analysis also revealed a significant association between increased early mortality and major bleeding (OR=1.79, P<0.001), renal failure (OR=2.33, P<0.001), respiratory failure (OR=6.46, P<0.001), and cardiac arrest (OR=13.33, P<0.001).
For the most part, the impact of complications on early mortality did not differ significantly by treatment center.
The exception was respiratory failure. Patients with respiratory failure had a significantly greater risk of early mortality if they were treated at a non-NCI center (OR=9.48) than at an NCI center (OR=4.20).
Potential explanations
The researchers believe the variations in early mortality they observed point to inconsistent supportive care. However, more work must be done to fully understand the differences in care driving these issues.
“This is clearly provocative data that makes you want to understand exactly why,” Dr Jonas said. “We’re going to have to dive into that question in a more significant way.”
In the absence of data that could identify the exact causes, the researchers noted that other studies have shown higher patient volumes may contribute to better care.
“I see 60 or more AML cases per year,” Dr Jonas said. “High volume/low volume must play a role.”
The researchers believe other potential contributing factors could be access to clinical trials, better nursing ratios, and more sophisticated intensive care units.
The team hopes this research will spawn more intensive efforts to identify the causes that underlie variations in early mortality between hospital sites.
“This is a provocative and hopeful paper in terms of improving outcomes,” Dr Jonas said. “It sends a positive message that there are things we could probably do that could help everyone.”
New research suggests patients with acute myeloid leukemia (AML) may have a lower risk of early mortality if they receive treatment at a National Cancer Institute (NCI) cancer center.
In a study of AML patients in California, the risk of 60-day mortality was 53% lower among patients treated at NCI cancer centers than among those treated at other centers.
These findings were reported in Cancer.
“We found the early mortality, deaths less than 60 days after diagnosis, was significantly lower at the NCI-designated cancer centers compared to non-NCI-designated cancer centers in California,” said study author Brian Jonas, MD, PhD, of the University of California at Davis School of Medicine in Sacramento, California.
To conduct this study, Dr Jonas and his colleagues analyzed data from the California Cancer Registry and the California Office of Statewide Health Planning and Development Patient Discharge Database.
The California Cancer Registry provides sociodemographic and clinical data for all California cancer patients. The California Office of Statewide Health Planning and Development Patient Discharge Database has data on diagnoses and procedures for all hospital patients in California, excluding 14 Veterans Affairs and military hospitals.
Patients
The study included data on AML patients 18 and older who received inpatient chemotherapy between 1999 and 2014. There were 7007 patients, 1762 (25%) of whom were treated at NCI-designated cancer centers.
The median number of new AML patients per year was 13.5 (range, 0-43) at the NCI centers and 2 (range, 1-17) at non-NCI centers that admitted at least 1 patient with AML. More than half of the non-NCI centers had a median of 0 new AML patients per year.
NCI patients were more likely to be younger (≤65) than non-NCI patients (P<0.0001), to live in neighborhoods with higher socioeconomic status (P<0.0001), have fewer comorbidities (P<0.0001), and have public health insurance (P<0.0001).
Results
There were several types of complications that differed significantly between center types.
Patients treated at NCI centers were significantly more likely to have leukapheresis (5.5% vs 2.7%; P<0.001) and renal failure (22.8% vs 19.9%; P=0.010).
But they were significantly less likely to have respiratory failure (11.6% vs 14.3%; P=0.003) and cardiac arrest (1.1% vs 2.0%; P=0.014).
Sixty-day survival was significantly higher among NCI patients (88.0% vs 76.3%; P<0.001).
In an inverse-probability-weighted analysis adjusted for sociodemographic factors and comorbidities, treatment at an NCI center was associated with significantly lower early mortality, with an odds ratio (OR) of 0.46 (P<0.001).
This analysis also revealed a significant association between increased early mortality and major bleeding (OR=1.79, P<0.001), renal failure (OR=2.33, P<0.001), respiratory failure (OR=6.46, P<0.001), and cardiac arrest (OR=13.33, P<0.001).
For the most part, the impact of complications on early mortality did not differ significantly by treatment center.
The exception was respiratory failure. Patients with respiratory failure had a significantly greater risk of early mortality if they were treated at a non-NCI center (OR=9.48) than at an NCI center (OR=4.20).
Potential explanations
The researchers believe the variations in early mortality they observed point to inconsistent supportive care. However, more work must be done to fully understand the differences in care driving these issues.
“This is clearly provocative data that makes you want to understand exactly why,” Dr Jonas said. “We’re going to have to dive into that question in a more significant way.”
In the absence of data that could identify the exact causes, the researchers noted that other studies have shown higher patient volumes may contribute to better care.
“I see 60 or more AML cases per year,” Dr Jonas said. “High volume/low volume must play a role.”
The researchers believe other potential contributing factors could be access to clinical trials, better nursing ratios, and more sophisticated intensive care units.
The team hopes this research will spawn more intensive efforts to identify the causes that underlie variations in early mortality between hospital sites.
“This is a provocative and hopeful paper in terms of improving outcomes,” Dr Jonas said. “It sends a positive message that there are things we could probably do that could help everyone.”