User login
Teaching Physical Examination to Medical Students on Inpatient Medicine Teams: A Prospective, Mixed-Methods Descriptive Study
1Medical College of Wisconsin Affiliated Hospitals, Milwaukee, Wisconsin. At the time of this study, Dr. Bergl was with the Division of General Internal Medicine, Medical College of Wisconsin, Milwaukee, Wisconsin. 2Medical College of Wisconsin, Milwaukee, Wisconsin.Physical examination (PE) is a core clinical skill in undergraduate medical education.1 Although the optimal approach to teaching clinical skills is debated, robust preclinical curricula should generally be followed by iterative skill development during clinical rotations.2,3
The internal medicine rotation represents a critical time to enhance PE skills. Diagnostic decision making and PE are highly prioritized competencies for the internal medicine clerkship,4 and students will likely utilize many core examination skills1,2 during this time. Bedside teaching of PE during the internal medicine service also provides an opportunity for students to receive feedback based on direct observation,5 a sine qua non of competency-based assessment.
Unfortunately, current internal medicine training environments limit opportunities for workplace-based instruction in PE. Recent studies suggest diminishing time spent on bedside patient care and teaching, with computer-based “indirect patient care” dominating much of the clinical workday of internal medicine services.6-8 However, the literature does not delineate how often medical students are enhancing their PE skills during clinical rotations or describe how the educational environment may influence PE teaching.
We aimed to describe the content and context of PE instruction during the internal medicine clerkship workflow. Specifically, we sought to explore what strategies physician team members used to teach PE to students. We also sought to describe factors in the inpatient learning environment that might explain why physical examination (PE) instruction occurs infrequently.
METHODS
We conducted a prospective mixed-methods study using time motion analysis, checklists on clinical teaching, and daily open-ended observations written by a trained observer from June through August 2015 at a single academic medical center. Subjects were recruited from internal medicine teaching teams and were allowed to opt out. Teaching teams had 2 formats: (1) traditional team with an attending physician (hospitalist or general internist), a senior resident, 2 interns, a fourth-year medical student, and 2 third-year students or (2) hospitalist team in which a third-year student works directly with a hospitalist and advanced practitioner. The proposal was submitted to the Medical College of Wisconsin Institutional Review Board and deemed exempt from further review.
All observations were carried out by a single investigator (A.T.), who was a second-year medical student at the time. To train this observer and to pilot the data collection instruments, our lead investigator (P.B.) directly supervised our observer on 4 separate occasions, totaling over 12 hours of mentored co-observation. Immediately after each training session, both investigators (A.T. and P.B.) debriefed to compare notes, to review checklists on recorded observations, and to discuss areas of uncertainty. During the training period, formal metrics of agreement (eg, kappa coefficients) were not gathered, as data collection instruments were still being refined.
Observation periods were centered on third-year medical students and their interactions with patients and members of the teaching team. Observed activities included pre-rounding, teaching rounds with the attending physician, and new patient admissions during call days. Observations generally occurred between the hours of 7 AM and 6 PM, and we limited periods of observation to 3 consecutive hours to minimize observer fatigue. Observation periods were selected to maximize the number of subjects and teams observed, to adequately capture pre-rounding and new admissions activities, and to account for variations in rounding styles throughout the call cycle. Teams were excluded if a member of the study team was an attending physician on the clinical team or if any member of the patient care team had opted out of the study.
Data were collected on paper checklists that included idealized bedside teaching activities around PE. Teaching activities were identified through a review of relevant literature9,10 and were further informed by our senior investigator’s own experience with faculty development in this area11 and team members’ attendance at bedside teaching workshops. At the end of each day, our observer also wrote brief observations that summarized factors affecting bedside teaching of PE. Checklist data were transferred to an Excel file (Microsoft), and written observations were imported into NVivo 10 (QRS International, Melbourne, Australia) for coding and analysis.
Checklist data were analyzed using simple descriptive statistics. We compared time spent on various types of rounding using ANOVA, and we used a Student two-tailed t-test to compare the amount of time students spent examining patients on pre-rounds versus new admissions. To ascertain differences in the frequency of PE teaching activities by location, we used chi-squared tests. Statistical analysis was performed using embedded statistics functions in Microsoft Excel. A P value of <.05 was used as the cut-off for significance.
We analyzed the written observations using conventional qualitative content analysis. Two investigators (A.T. and P.B.) reviewed the written comments and used open coding to devise a preliminary inductive coding scheme. Codes were refined iteratively, and a schema of categories and nodes was outlined in a codebook that was periodically reviewed by the entire research team. The coding investigators met regularly to ensure consistency in coding, and a third team member remained available to reconcile significant disagreements in code definitions.
RESULTS
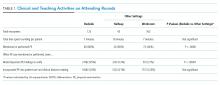
Eighty-one subjects participated in the study: 21 were attending physicians, 12 residents, 21 interns, 11 senior medical students, and 26 junior medical students. We observed 16 distinct inpatient teaching teams and 329 unique patient-related events (discussions and/or patient-clinician encounters), with most events being observed during attending rounds (269/329, or 82%). There were 123 encounters at the bedside, averaging 7 minutes; 43 encounters occurred in the hallway, averaging 8 minutes each; and 163 encounters occurred in a workroom and averaged 7 minutes per patient discussion. We also observed 28 student-patient encounters during pre-round activities and 30 student-patient encounters during new admissions.
Teaching and Direct Observation
During 28 pre-rounding encounters, students usually examined the patient (26 out of 28 instances, 93%) but were observed only 4 times doing so (out of 26 instances, or 15%). During 30 new patient admissions, students examined 27 patients (90%) and had their PE observed 6 times (out of 27 instances, or 22%). There were no significant differences in frequency of these activities (P > .05, chi-squared) between pre-rounds or new admissions.
Observations on Teaching Strategies
In the written observations, we categorized various methods being used to teach PE. Bedside teaching of PE most often involved teachers simply describing or discussing physical findings (42 mentions in observations) or verifying a student’s reported findings (15 mentions). Teachers were also observed to use bedside teaching to contextualize findings (13 mentions), such as relating the quality of bowel sounds to the patient’s constipation or to discuss expected pupillary light reflexes in a neurologically intact patient. Less commonly, attending physicians narrated steps in their PE technique (9 mentions). Students were infrequently encouraged to practice a specific PE skill again (7 mentions) or allowed to re-examine and reconsider their initial interpretations (5 mentions).
DISCUSSION
This observational study of clinical teaching on internal medicine teaching services demonstrates that PE teaching is most likely to occur during bedside rounding. However, even in bedside encounters, most PE instruction is limited to physician team members pointing out significant findings. Although physical findings were mentioned for the majority of patients seen on rounds, attending physicians infrequently verified students’ or residents’ findings, demonstrated technique, or incorporated PE into clinical decision making. We witnessed an alarming dearth of direct observation of students and almost no real-time feedback in performing and teaching PE. Thus, students rarely had opportunities to engage in higher-order learning activities related to PE on the internal medicine rotation.
We posit that the learning environment influenced PE instruction on the internal medicine rotation. To optimize inpatient teaching of PE, attending physicians need to consider the factors we identified in Table 2. Such teaching may be effective with a more limited number of participants and without distraction from technology. Time constraints are one of the major perceived barriers to bedside teaching of PE, and our data support this concern, as teams spent an average of only 7 minutes on each bedside encounter. However, many of the strategies observed to be used in real-time PE instruction, such as validating the learners’ findings or examining patients as a team, naturally fit into clinical routines and generally do not require extra thought or preparation.
One of the key strengths of our study is the use of direct observation of students and their teachers. This study is unique in its exclusive focus on PE and its description of factors affecting PE teaching activities on an internal medicine service. This observational, descriptive study also has obvious limitations. The study was conducted at a single institution during a limited time period. Moreover, the study period June through August, which was chosen based on our observer’s availability, includes the transition to a new academic year (July 1, 2015) when medical students and residents were becoming acclimated to their new roles. Additionally, the data were collected by a single researcher, and observer bias may affect the results of qualitative analysis of journal entries.
In conclusion, this study highlights the infrequency of applied PE skills in the daily clinical and educational workflow of internal medicine teaching teams. These findings may reflect a more widespread problem in clinical education, and replication of our findings at other teaching centers could galvanize faculty development around bedside PE teaching.
Disclosures
Dr. Bergl has nothing to disclose. Ms. Taylor reports grant support from the Cohen Endowment for Medical Student Research at the Medical College of Wisconsin during the conduct of the study. Mrs. Klumb, Ms. Quirk, Dr. Muntz, and Dr. Fletcher have nothing to disclose.
Funding
This work was funded in part by the Cohen Endowment for Medical Student Research at the Medical College of Wisconsin.
1. Corbett E, Berkow R, Bernstein L, et al on behalf of the AAMC Task Force on the Preclerkship Clinical Skills Education of Medical Students. Recommendations for clinical skills curricula for undergraduate medical education. Achieving excellence in basic clinical method through clinical skills education: The medical school clinical skills curriculum. Association of American Medical Colleges; 2008. https://www.aamc.org/download/130608/data/clinicalskills_oct09.qxd.pdf.pdf. Accessed July 12, 2017.
2. Gowda D, Blatt B, Fink MJ, Kosowicz LY, Baecker A, Silvestri RC. A core physical exam for medical students: Results of a national survey. Acad Med. 2014;89(3):436-442. PubMed
3. Uchida T, Farnan JM, Schwartz JE, Heiman HL. Teaching the physical examination: A longitudinal strategy for tomorrow’s physicians. Acad Med. 2014;89(3):373-375. PubMed
4. Fazio S, De Fer T, Goroll A . Core Medicine Clerkship Curriculum Guide: A resource for teachers and learners. Clerkship Directors in Internal Medicine and Society of General Internal Medicine; 2006. http://www.im.org/d/do/2285/. Accessed July 12, 2017.
5. Gonzalo J, Heist B, Duffy B, et al. Content and timing of feedback and reflection: A multi-center qualitative study of experienced bedside teachers. BMC Med Educ. 2014;(14):212. doi: 10.1186/1472-6920-14-212. PubMed
6. Stickrath C, Noble M, Prochazka A, et al. Attending rounds in the current era: What is and is not happening. JAMA Intern Med. 2013;173(12):1084-1089. PubMed
7. Block L, Habicht R, Wu AW, et al. In the wake of the 2003 and 2011 duty hours regulations, how do internal medicine interns spend their time? J Gen Intern Med. 2013;28(8):1042-1047. PubMed
8. Wenger N, Méan M, Castioni J, Marques-Vidal P, Waeber G, Garnier A. Allocation of internal medicine resident time in a Swiss Hospital: A time and motion study of day and evening shifts. Ann Intern Med. 2017;166(8):579-586. PubMed
9. Ramani S. Twelve tips for excellent physical examination teaching. Med Teach. 2008;30(9-10):851-856. PubMed
10. Gonzalo JD, Heist BS, Duffy BL, et al. The art of bedside rounds: A multi-center qualitative study of strategies used by experienced bedside teachers. J Gen Intern Med. 2013;28(3):412-420. PubMed
11. Janicik RW, Fletcher KE. Teaching at the bedside: A new model. Med Teach. 2003;25(2):127-130. PubMed
1Medical College of Wisconsin Affiliated Hospitals, Milwaukee, Wisconsin. At the time of this study, Dr. Bergl was with the Division of General Internal Medicine, Medical College of Wisconsin, Milwaukee, Wisconsin. 2Medical College of Wisconsin, Milwaukee, Wisconsin.Physical examination (PE) is a core clinical skill in undergraduate medical education.1 Although the optimal approach to teaching clinical skills is debated, robust preclinical curricula should generally be followed by iterative skill development during clinical rotations.2,3
The internal medicine rotation represents a critical time to enhance PE skills. Diagnostic decision making and PE are highly prioritized competencies for the internal medicine clerkship,4 and students will likely utilize many core examination skills1,2 during this time. Bedside teaching of PE during the internal medicine service also provides an opportunity for students to receive feedback based on direct observation,5 a sine qua non of competency-based assessment.
Unfortunately, current internal medicine training environments limit opportunities for workplace-based instruction in PE. Recent studies suggest diminishing time spent on bedside patient care and teaching, with computer-based “indirect patient care” dominating much of the clinical workday of internal medicine services.6-8 However, the literature does not delineate how often medical students are enhancing their PE skills during clinical rotations or describe how the educational environment may influence PE teaching.
We aimed to describe the content and context of PE instruction during the internal medicine clerkship workflow. Specifically, we sought to explore what strategies physician team members used to teach PE to students. We also sought to describe factors in the inpatient learning environment that might explain why physical examination (PE) instruction occurs infrequently.
METHODS
We conducted a prospective mixed-methods study using time motion analysis, checklists on clinical teaching, and daily open-ended observations written by a trained observer from June through August 2015 at a single academic medical center. Subjects were recruited from internal medicine teaching teams and were allowed to opt out. Teaching teams had 2 formats: (1) traditional team with an attending physician (hospitalist or general internist), a senior resident, 2 interns, a fourth-year medical student, and 2 third-year students or (2) hospitalist team in which a third-year student works directly with a hospitalist and advanced practitioner. The proposal was submitted to the Medical College of Wisconsin Institutional Review Board and deemed exempt from further review.
All observations were carried out by a single investigator (A.T.), who was a second-year medical student at the time. To train this observer and to pilot the data collection instruments, our lead investigator (P.B.) directly supervised our observer on 4 separate occasions, totaling over 12 hours of mentored co-observation. Immediately after each training session, both investigators (A.T. and P.B.) debriefed to compare notes, to review checklists on recorded observations, and to discuss areas of uncertainty. During the training period, formal metrics of agreement (eg, kappa coefficients) were not gathered, as data collection instruments were still being refined.
Observation periods were centered on third-year medical students and their interactions with patients and members of the teaching team. Observed activities included pre-rounding, teaching rounds with the attending physician, and new patient admissions during call days. Observations generally occurred between the hours of 7 AM and 6 PM, and we limited periods of observation to 3 consecutive hours to minimize observer fatigue. Observation periods were selected to maximize the number of subjects and teams observed, to adequately capture pre-rounding and new admissions activities, and to account for variations in rounding styles throughout the call cycle. Teams were excluded if a member of the study team was an attending physician on the clinical team or if any member of the patient care team had opted out of the study.
Data were collected on paper checklists that included idealized bedside teaching activities around PE. Teaching activities were identified through a review of relevant literature9,10 and were further informed by our senior investigator’s own experience with faculty development in this area11 and team members’ attendance at bedside teaching workshops. At the end of each day, our observer also wrote brief observations that summarized factors affecting bedside teaching of PE. Checklist data were transferred to an Excel file (Microsoft), and written observations were imported into NVivo 10 (QRS International, Melbourne, Australia) for coding and analysis.
Checklist data were analyzed using simple descriptive statistics. We compared time spent on various types of rounding using ANOVA, and we used a Student two-tailed t-test to compare the amount of time students spent examining patients on pre-rounds versus new admissions. To ascertain differences in the frequency of PE teaching activities by location, we used chi-squared tests. Statistical analysis was performed using embedded statistics functions in Microsoft Excel. A P value of <.05 was used as the cut-off for significance.
We analyzed the written observations using conventional qualitative content analysis. Two investigators (A.T. and P.B.) reviewed the written comments and used open coding to devise a preliminary inductive coding scheme. Codes were refined iteratively, and a schema of categories and nodes was outlined in a codebook that was periodically reviewed by the entire research team. The coding investigators met regularly to ensure consistency in coding, and a third team member remained available to reconcile significant disagreements in code definitions.
RESULTS
Eighty-one subjects participated in the study: 21 were attending physicians, 12 residents, 21 interns, 11 senior medical students, and 26 junior medical students. We observed 16 distinct inpatient teaching teams and 329 unique patient-related events (discussions and/or patient-clinician encounters), with most events being observed during attending rounds (269/329, or 82%). There were 123 encounters at the bedside, averaging 7 minutes; 43 encounters occurred in the hallway, averaging 8 minutes each; and 163 encounters occurred in a workroom and averaged 7 minutes per patient discussion. We also observed 28 student-patient encounters during pre-round activities and 30 student-patient encounters during new admissions.
Teaching and Direct Observation
During 28 pre-rounding encounters, students usually examined the patient (26 out of 28 instances, 93%) but were observed only 4 times doing so (out of 26 instances, or 15%). During 30 new patient admissions, students examined 27 patients (90%) and had their PE observed 6 times (out of 27 instances, or 22%). There were no significant differences in frequency of these activities (P > .05, chi-squared) between pre-rounds or new admissions.
Observations on Teaching Strategies
In the written observations, we categorized various methods being used to teach PE. Bedside teaching of PE most often involved teachers simply describing or discussing physical findings (42 mentions in observations) or verifying a student’s reported findings (15 mentions). Teachers were also observed to use bedside teaching to contextualize findings (13 mentions), such as relating the quality of bowel sounds to the patient’s constipation or to discuss expected pupillary light reflexes in a neurologically intact patient. Less commonly, attending physicians narrated steps in their PE technique (9 mentions). Students were infrequently encouraged to practice a specific PE skill again (7 mentions) or allowed to re-examine and reconsider their initial interpretations (5 mentions).
DISCUSSION
This observational study of clinical teaching on internal medicine teaching services demonstrates that PE teaching is most likely to occur during bedside rounding. However, even in bedside encounters, most PE instruction is limited to physician team members pointing out significant findings. Although physical findings were mentioned for the majority of patients seen on rounds, attending physicians infrequently verified students’ or residents’ findings, demonstrated technique, or incorporated PE into clinical decision making. We witnessed an alarming dearth of direct observation of students and almost no real-time feedback in performing and teaching PE. Thus, students rarely had opportunities to engage in higher-order learning activities related to PE on the internal medicine rotation.
We posit that the learning environment influenced PE instruction on the internal medicine rotation. To optimize inpatient teaching of PE, attending physicians need to consider the factors we identified in Table 2. Such teaching may be effective with a more limited number of participants and without distraction from technology. Time constraints are one of the major perceived barriers to bedside teaching of PE, and our data support this concern, as teams spent an average of only 7 minutes on each bedside encounter. However, many of the strategies observed to be used in real-time PE instruction, such as validating the learners’ findings or examining patients as a team, naturally fit into clinical routines and generally do not require extra thought or preparation.
One of the key strengths of our study is the use of direct observation of students and their teachers. This study is unique in its exclusive focus on PE and its description of factors affecting PE teaching activities on an internal medicine service. This observational, descriptive study also has obvious limitations. The study was conducted at a single institution during a limited time period. Moreover, the study period June through August, which was chosen based on our observer’s availability, includes the transition to a new academic year (July 1, 2015) when medical students and residents were becoming acclimated to their new roles. Additionally, the data were collected by a single researcher, and observer bias may affect the results of qualitative analysis of journal entries.
In conclusion, this study highlights the infrequency of applied PE skills in the daily clinical and educational workflow of internal medicine teaching teams. These findings may reflect a more widespread problem in clinical education, and replication of our findings at other teaching centers could galvanize faculty development around bedside PE teaching.
Disclosures
Dr. Bergl has nothing to disclose. Ms. Taylor reports grant support from the Cohen Endowment for Medical Student Research at the Medical College of Wisconsin during the conduct of the study. Mrs. Klumb, Ms. Quirk, Dr. Muntz, and Dr. Fletcher have nothing to disclose.
Funding
This work was funded in part by the Cohen Endowment for Medical Student Research at the Medical College of Wisconsin.
1Medical College of Wisconsin Affiliated Hospitals, Milwaukee, Wisconsin. At the time of this study, Dr. Bergl was with the Division of General Internal Medicine, Medical College of Wisconsin, Milwaukee, Wisconsin. 2Medical College of Wisconsin, Milwaukee, Wisconsin.Physical examination (PE) is a core clinical skill in undergraduate medical education.1 Although the optimal approach to teaching clinical skills is debated, robust preclinical curricula should generally be followed by iterative skill development during clinical rotations.2,3
The internal medicine rotation represents a critical time to enhance PE skills. Diagnostic decision making and PE are highly prioritized competencies for the internal medicine clerkship,4 and students will likely utilize many core examination skills1,2 during this time. Bedside teaching of PE during the internal medicine service also provides an opportunity for students to receive feedback based on direct observation,5 a sine qua non of competency-based assessment.
Unfortunately, current internal medicine training environments limit opportunities for workplace-based instruction in PE. Recent studies suggest diminishing time spent on bedside patient care and teaching, with computer-based “indirect patient care” dominating much of the clinical workday of internal medicine services.6-8 However, the literature does not delineate how often medical students are enhancing their PE skills during clinical rotations or describe how the educational environment may influence PE teaching.
We aimed to describe the content and context of PE instruction during the internal medicine clerkship workflow. Specifically, we sought to explore what strategies physician team members used to teach PE to students. We also sought to describe factors in the inpatient learning environment that might explain why physical examination (PE) instruction occurs infrequently.
METHODS
We conducted a prospective mixed-methods study using time motion analysis, checklists on clinical teaching, and daily open-ended observations written by a trained observer from June through August 2015 at a single academic medical center. Subjects were recruited from internal medicine teaching teams and were allowed to opt out. Teaching teams had 2 formats: (1) traditional team with an attending physician (hospitalist or general internist), a senior resident, 2 interns, a fourth-year medical student, and 2 third-year students or (2) hospitalist team in which a third-year student works directly with a hospitalist and advanced practitioner. The proposal was submitted to the Medical College of Wisconsin Institutional Review Board and deemed exempt from further review.
All observations were carried out by a single investigator (A.T.), who was a second-year medical student at the time. To train this observer and to pilot the data collection instruments, our lead investigator (P.B.) directly supervised our observer on 4 separate occasions, totaling over 12 hours of mentored co-observation. Immediately after each training session, both investigators (A.T. and P.B.) debriefed to compare notes, to review checklists on recorded observations, and to discuss areas of uncertainty. During the training period, formal metrics of agreement (eg, kappa coefficients) were not gathered, as data collection instruments were still being refined.
Observation periods were centered on third-year medical students and their interactions with patients and members of the teaching team. Observed activities included pre-rounding, teaching rounds with the attending physician, and new patient admissions during call days. Observations generally occurred between the hours of 7 AM and 6 PM, and we limited periods of observation to 3 consecutive hours to minimize observer fatigue. Observation periods were selected to maximize the number of subjects and teams observed, to adequately capture pre-rounding and new admissions activities, and to account for variations in rounding styles throughout the call cycle. Teams were excluded if a member of the study team was an attending physician on the clinical team or if any member of the patient care team had opted out of the study.
Data were collected on paper checklists that included idealized bedside teaching activities around PE. Teaching activities were identified through a review of relevant literature9,10 and were further informed by our senior investigator’s own experience with faculty development in this area11 and team members’ attendance at bedside teaching workshops. At the end of each day, our observer also wrote brief observations that summarized factors affecting bedside teaching of PE. Checklist data were transferred to an Excel file (Microsoft), and written observations were imported into NVivo 10 (QRS International, Melbourne, Australia) for coding and analysis.
Checklist data were analyzed using simple descriptive statistics. We compared time spent on various types of rounding using ANOVA, and we used a Student two-tailed t-test to compare the amount of time students spent examining patients on pre-rounds versus new admissions. To ascertain differences in the frequency of PE teaching activities by location, we used chi-squared tests. Statistical analysis was performed using embedded statistics functions in Microsoft Excel. A P value of <.05 was used as the cut-off for significance.
We analyzed the written observations using conventional qualitative content analysis. Two investigators (A.T. and P.B.) reviewed the written comments and used open coding to devise a preliminary inductive coding scheme. Codes were refined iteratively, and a schema of categories and nodes was outlined in a codebook that was periodically reviewed by the entire research team. The coding investigators met regularly to ensure consistency in coding, and a third team member remained available to reconcile significant disagreements in code definitions.
RESULTS
Eighty-one subjects participated in the study: 21 were attending physicians, 12 residents, 21 interns, 11 senior medical students, and 26 junior medical students. We observed 16 distinct inpatient teaching teams and 329 unique patient-related events (discussions and/or patient-clinician encounters), with most events being observed during attending rounds (269/329, or 82%). There were 123 encounters at the bedside, averaging 7 minutes; 43 encounters occurred in the hallway, averaging 8 minutes each; and 163 encounters occurred in a workroom and averaged 7 minutes per patient discussion. We also observed 28 student-patient encounters during pre-round activities and 30 student-patient encounters during new admissions.
Teaching and Direct Observation
During 28 pre-rounding encounters, students usually examined the patient (26 out of 28 instances, 93%) but were observed only 4 times doing so (out of 26 instances, or 15%). During 30 new patient admissions, students examined 27 patients (90%) and had their PE observed 6 times (out of 27 instances, or 22%). There were no significant differences in frequency of these activities (P > .05, chi-squared) between pre-rounds or new admissions.
Observations on Teaching Strategies
In the written observations, we categorized various methods being used to teach PE. Bedside teaching of PE most often involved teachers simply describing or discussing physical findings (42 mentions in observations) or verifying a student’s reported findings (15 mentions). Teachers were also observed to use bedside teaching to contextualize findings (13 mentions), such as relating the quality of bowel sounds to the patient’s constipation or to discuss expected pupillary light reflexes in a neurologically intact patient. Less commonly, attending physicians narrated steps in their PE technique (9 mentions). Students were infrequently encouraged to practice a specific PE skill again (7 mentions) or allowed to re-examine and reconsider their initial interpretations (5 mentions).
DISCUSSION
This observational study of clinical teaching on internal medicine teaching services demonstrates that PE teaching is most likely to occur during bedside rounding. However, even in bedside encounters, most PE instruction is limited to physician team members pointing out significant findings. Although physical findings were mentioned for the majority of patients seen on rounds, attending physicians infrequently verified students’ or residents’ findings, demonstrated technique, or incorporated PE into clinical decision making. We witnessed an alarming dearth of direct observation of students and almost no real-time feedback in performing and teaching PE. Thus, students rarely had opportunities to engage in higher-order learning activities related to PE on the internal medicine rotation.
We posit that the learning environment influenced PE instruction on the internal medicine rotation. To optimize inpatient teaching of PE, attending physicians need to consider the factors we identified in Table 2. Such teaching may be effective with a more limited number of participants and without distraction from technology. Time constraints are one of the major perceived barriers to bedside teaching of PE, and our data support this concern, as teams spent an average of only 7 minutes on each bedside encounter. However, many of the strategies observed to be used in real-time PE instruction, such as validating the learners’ findings or examining patients as a team, naturally fit into clinical routines and generally do not require extra thought or preparation.
One of the key strengths of our study is the use of direct observation of students and their teachers. This study is unique in its exclusive focus on PE and its description of factors affecting PE teaching activities on an internal medicine service. This observational, descriptive study also has obvious limitations. The study was conducted at a single institution during a limited time period. Moreover, the study period June through August, which was chosen based on our observer’s availability, includes the transition to a new academic year (July 1, 2015) when medical students and residents were becoming acclimated to their new roles. Additionally, the data were collected by a single researcher, and observer bias may affect the results of qualitative analysis of journal entries.
In conclusion, this study highlights the infrequency of applied PE skills in the daily clinical and educational workflow of internal medicine teaching teams. These findings may reflect a more widespread problem in clinical education, and replication of our findings at other teaching centers could galvanize faculty development around bedside PE teaching.
Disclosures
Dr. Bergl has nothing to disclose. Ms. Taylor reports grant support from the Cohen Endowment for Medical Student Research at the Medical College of Wisconsin during the conduct of the study. Mrs. Klumb, Ms. Quirk, Dr. Muntz, and Dr. Fletcher have nothing to disclose.
Funding
This work was funded in part by the Cohen Endowment for Medical Student Research at the Medical College of Wisconsin.
1. Corbett E, Berkow R, Bernstein L, et al on behalf of the AAMC Task Force on the Preclerkship Clinical Skills Education of Medical Students. Recommendations for clinical skills curricula for undergraduate medical education. Achieving excellence in basic clinical method through clinical skills education: The medical school clinical skills curriculum. Association of American Medical Colleges; 2008. https://www.aamc.org/download/130608/data/clinicalskills_oct09.qxd.pdf.pdf. Accessed July 12, 2017.
2. Gowda D, Blatt B, Fink MJ, Kosowicz LY, Baecker A, Silvestri RC. A core physical exam for medical students: Results of a national survey. Acad Med. 2014;89(3):436-442. PubMed
3. Uchida T, Farnan JM, Schwartz JE, Heiman HL. Teaching the physical examination: A longitudinal strategy for tomorrow’s physicians. Acad Med. 2014;89(3):373-375. PubMed
4. Fazio S, De Fer T, Goroll A . Core Medicine Clerkship Curriculum Guide: A resource for teachers and learners. Clerkship Directors in Internal Medicine and Society of General Internal Medicine; 2006. http://www.im.org/d/do/2285/. Accessed July 12, 2017.
5. Gonzalo J, Heist B, Duffy B, et al. Content and timing of feedback and reflection: A multi-center qualitative study of experienced bedside teachers. BMC Med Educ. 2014;(14):212. doi: 10.1186/1472-6920-14-212. PubMed
6. Stickrath C, Noble M, Prochazka A, et al. Attending rounds in the current era: What is and is not happening. JAMA Intern Med. 2013;173(12):1084-1089. PubMed
7. Block L, Habicht R, Wu AW, et al. In the wake of the 2003 and 2011 duty hours regulations, how do internal medicine interns spend their time? J Gen Intern Med. 2013;28(8):1042-1047. PubMed
8. Wenger N, Méan M, Castioni J, Marques-Vidal P, Waeber G, Garnier A. Allocation of internal medicine resident time in a Swiss Hospital: A time and motion study of day and evening shifts. Ann Intern Med. 2017;166(8):579-586. PubMed
9. Ramani S. Twelve tips for excellent physical examination teaching. Med Teach. 2008;30(9-10):851-856. PubMed
10. Gonzalo JD, Heist BS, Duffy BL, et al. The art of bedside rounds: A multi-center qualitative study of strategies used by experienced bedside teachers. J Gen Intern Med. 2013;28(3):412-420. PubMed
11. Janicik RW, Fletcher KE. Teaching at the bedside: A new model. Med Teach. 2003;25(2):127-130. PubMed
1. Corbett E, Berkow R, Bernstein L, et al on behalf of the AAMC Task Force on the Preclerkship Clinical Skills Education of Medical Students. Recommendations for clinical skills curricula for undergraduate medical education. Achieving excellence in basic clinical method through clinical skills education: The medical school clinical skills curriculum. Association of American Medical Colleges; 2008. https://www.aamc.org/download/130608/data/clinicalskills_oct09.qxd.pdf.pdf. Accessed July 12, 2017.
2. Gowda D, Blatt B, Fink MJ, Kosowicz LY, Baecker A, Silvestri RC. A core physical exam for medical students: Results of a national survey. Acad Med. 2014;89(3):436-442. PubMed
3. Uchida T, Farnan JM, Schwartz JE, Heiman HL. Teaching the physical examination: A longitudinal strategy for tomorrow’s physicians. Acad Med. 2014;89(3):373-375. PubMed
4. Fazio S, De Fer T, Goroll A . Core Medicine Clerkship Curriculum Guide: A resource for teachers and learners. Clerkship Directors in Internal Medicine and Society of General Internal Medicine; 2006. http://www.im.org/d/do/2285/. Accessed July 12, 2017.
5. Gonzalo J, Heist B, Duffy B, et al. Content and timing of feedback and reflection: A multi-center qualitative study of experienced bedside teachers. BMC Med Educ. 2014;(14):212. doi: 10.1186/1472-6920-14-212. PubMed
6. Stickrath C, Noble M, Prochazka A, et al. Attending rounds in the current era: What is and is not happening. JAMA Intern Med. 2013;173(12):1084-1089. PubMed
7. Block L, Habicht R, Wu AW, et al. In the wake of the 2003 and 2011 duty hours regulations, how do internal medicine interns spend their time? J Gen Intern Med. 2013;28(8):1042-1047. PubMed
8. Wenger N, Méan M, Castioni J, Marques-Vidal P, Waeber G, Garnier A. Allocation of internal medicine resident time in a Swiss Hospital: A time and motion study of day and evening shifts. Ann Intern Med. 2017;166(8):579-586. PubMed
9. Ramani S. Twelve tips for excellent physical examination teaching. Med Teach. 2008;30(9-10):851-856. PubMed
10. Gonzalo JD, Heist BS, Duffy BL, et al. The art of bedside rounds: A multi-center qualitative study of strategies used by experienced bedside teachers. J Gen Intern Med. 2013;28(3):412-420. PubMed
11. Janicik RW, Fletcher KE. Teaching at the bedside: A new model. Med Teach. 2003;25(2):127-130. PubMed
© 2018 Society of Hospital Medicine
Regular skin exams reduced advanced KCs in posttransplant patients
ORLANDO – Annual skin exams reduced the rate of advanced keratinocyte carcinoma (KC) after solid organ transplant by 34%, according to a review of 10,198 transplant patients in Ontario, Canada.
Transplant patients have a far higher risk of KC than the general public because of immunosuppression: A quarter of patients are affected within 5 years. Transplant guidelines have recommended annual skin exams.
Other studies have reported adherence rates of up to 50%, but the numbers were based largely on patient self-report. Instead, the Ontario study used billing codes and other administrative data to get an idea of how many patients actually followed through.
“I would be surprised if other jurisdictions have significantly better rates of adherence,” said lead investigator An-Wen Chan, MD, of the division of dermatology at the University of Toronto and director of a transplant dermatology clinic at the University Health Network.
Part of the problem is that there’s just not a lot of evidence that annual screenings improve KC outcomes, he noted.
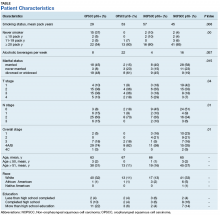
To help plug that evidence gap, Dr. Chan and his team reviewed transplant cases in Ontario going back to the mid-1990s; 62% of the patients had kidney transplants, 24% had liver transplants, and the rest had heart or lung transplants. The patients were all aged over 18 years; 60% were white, 15% Asian, 4% black, and the rest unknown. About two-thirds were men.
Adherence to annual dermatology checkups at least 75% of the time was associated with a marked reduction in the development of advanced KC, defined as lesions greater than 2 cm and requiring reconstruction and lymphadenectomy (adjusted hazard ratio, 0.66; 95% CI, 0.48-0.92).
Increasing age at transplant, white race, male sex, and past history of skin cancer were among the factors that were associated with increased risk. There was a trend toward increased risk with liver, lung, and heart transplants, as opposed to kidney transplants. Results were adjusted for demographic, transplant, and other variables.
In short, “adherence to annual dermatology assessments ... reduced KC-related morbidity and death. The highest risk patients were not necessarily the ones that saw their dermatologist annually,” Dr. Chan said.
Rates of adherence varied across transplant sites. It’s probably less of a problem at the University of Toronto, where Dr. Chan is embedded with the transplant team and where he can educate patients and providers on the importance of annual screening and help ensure that it’s done.
“We have a rigorous skin referral policy in place and really target transplant patients to be seen within a year. Having a dermatologist dedicated to transplant dermatology really helps,” he said. The next step is to define the optimal frequency of posttransplant skin cancer screening and to address barriers to screening.
There was no industry funding for the work, and Dr. Chan had no relevant disclosures.
SOURCE: Chan A et al. IID 2018, Abstract 522.
ORLANDO – Annual skin exams reduced the rate of advanced keratinocyte carcinoma (KC) after solid organ transplant by 34%, according to a review of 10,198 transplant patients in Ontario, Canada.
Transplant patients have a far higher risk of KC than the general public because of immunosuppression: A quarter of patients are affected within 5 years. Transplant guidelines have recommended annual skin exams.
Other studies have reported adherence rates of up to 50%, but the numbers were based largely on patient self-report. Instead, the Ontario study used billing codes and other administrative data to get an idea of how many patients actually followed through.
“I would be surprised if other jurisdictions have significantly better rates of adherence,” said lead investigator An-Wen Chan, MD, of the division of dermatology at the University of Toronto and director of a transplant dermatology clinic at the University Health Network.
Part of the problem is that there’s just not a lot of evidence that annual screenings improve KC outcomes, he noted.
To help plug that evidence gap, Dr. Chan and his team reviewed transplant cases in Ontario going back to the mid-1990s; 62% of the patients had kidney transplants, 24% had liver transplants, and the rest had heart or lung transplants. The patients were all aged over 18 years; 60% were white, 15% Asian, 4% black, and the rest unknown. About two-thirds were men.
Adherence to annual dermatology checkups at least 75% of the time was associated with a marked reduction in the development of advanced KC, defined as lesions greater than 2 cm and requiring reconstruction and lymphadenectomy (adjusted hazard ratio, 0.66; 95% CI, 0.48-0.92).
Increasing age at transplant, white race, male sex, and past history of skin cancer were among the factors that were associated with increased risk. There was a trend toward increased risk with liver, lung, and heart transplants, as opposed to kidney transplants. Results were adjusted for demographic, transplant, and other variables.
In short, “adherence to annual dermatology assessments ... reduced KC-related morbidity and death. The highest risk patients were not necessarily the ones that saw their dermatologist annually,” Dr. Chan said.
Rates of adherence varied across transplant sites. It’s probably less of a problem at the University of Toronto, where Dr. Chan is embedded with the transplant team and where he can educate patients and providers on the importance of annual screening and help ensure that it’s done.
“We have a rigorous skin referral policy in place and really target transplant patients to be seen within a year. Having a dermatologist dedicated to transplant dermatology really helps,” he said. The next step is to define the optimal frequency of posttransplant skin cancer screening and to address barriers to screening.
There was no industry funding for the work, and Dr. Chan had no relevant disclosures.
SOURCE: Chan A et al. IID 2018, Abstract 522.
ORLANDO – Annual skin exams reduced the rate of advanced keratinocyte carcinoma (KC) after solid organ transplant by 34%, according to a review of 10,198 transplant patients in Ontario, Canada.
Transplant patients have a far higher risk of KC than the general public because of immunosuppression: A quarter of patients are affected within 5 years. Transplant guidelines have recommended annual skin exams.
Other studies have reported adherence rates of up to 50%, but the numbers were based largely on patient self-report. Instead, the Ontario study used billing codes and other administrative data to get an idea of how many patients actually followed through.
“I would be surprised if other jurisdictions have significantly better rates of adherence,” said lead investigator An-Wen Chan, MD, of the division of dermatology at the University of Toronto and director of a transplant dermatology clinic at the University Health Network.
Part of the problem is that there’s just not a lot of evidence that annual screenings improve KC outcomes, he noted.
To help plug that evidence gap, Dr. Chan and his team reviewed transplant cases in Ontario going back to the mid-1990s; 62% of the patients had kidney transplants, 24% had liver transplants, and the rest had heart or lung transplants. The patients were all aged over 18 years; 60% were white, 15% Asian, 4% black, and the rest unknown. About two-thirds were men.
Adherence to annual dermatology checkups at least 75% of the time was associated with a marked reduction in the development of advanced KC, defined as lesions greater than 2 cm and requiring reconstruction and lymphadenectomy (adjusted hazard ratio, 0.66; 95% CI, 0.48-0.92).
Increasing age at transplant, white race, male sex, and past history of skin cancer were among the factors that were associated with increased risk. There was a trend toward increased risk with liver, lung, and heart transplants, as opposed to kidney transplants. Results were adjusted for demographic, transplant, and other variables.
In short, “adherence to annual dermatology assessments ... reduced KC-related morbidity and death. The highest risk patients were not necessarily the ones that saw their dermatologist annually,” Dr. Chan said.
Rates of adherence varied across transplant sites. It’s probably less of a problem at the University of Toronto, where Dr. Chan is embedded with the transplant team and where he can educate patients and providers on the importance of annual screening and help ensure that it’s done.
“We have a rigorous skin referral policy in place and really target transplant patients to be seen within a year. Having a dermatologist dedicated to transplant dermatology really helps,” he said. The next step is to define the optimal frequency of posttransplant skin cancer screening and to address barriers to screening.
There was no industry funding for the work, and Dr. Chan had no relevant disclosures.
SOURCE: Chan A et al. IID 2018, Abstract 522.
REPORTING FROM IID 2018
Key clinical point: Transplant patients need help to ensure they get annual dermatology checkups.
Major finding: Just 2.1% of the patients in the review had annual exams, and less than half saw a dermatologist even once during an average of 5-years follow-up.
Study details: A review of 10,198 solid organ transplant cases.
Disclosures: There was no industry funding, and the lead investigator had no disclosures.
Source: Chan A et al. IID 2018, Abstract 522
Epilepsy: Past, Present, and Future
Vijay M. Thadani,
Dr. Thadani is Professor of Neurology, Geisel School of Medicine at Dartmouth, Dartmouth-Hitchcock Medical Center in Lebanon, New Hampshire. He reports no conflict of interest.
As Neurology Reviews celebrates its 25th anniversary, we take this opportunity to look back and to look ahead in the area of epilepsy care and research. Epilepsy is a disease whose earliest descriptions date back to Egypt and Mesopotamia 3,000 years ago. A modern understanding of epilepsy as an electrical disorder of the brain dates back perhaps 150 years. The last 25 years have seen considerable progress in diagnosis and treatment, but in the Western world, the prevalence of epilepsy has held steady at around 1%, and a quarter of those patients have seizures that are not controlled, in spite of appropriate therapy.
While generalized and focal seizures remain the cornerstones of classification, the most recent theoretical advance is the network concept of epilepsy. By definition, a network must have nodes and connections. In generalized forms of epilepsy, these are recognized to be diffuse groupings of neurons and the fiber tracts that connect them. They are widely distributed and conducive to the rapid and bilateral spread of electrical abnormalities throughout the brain. In focal epilepsies, the abnormal electrical activity in the network is more constrained by traditional anatomic landmarks, but this does not preclude the possibility of secondary generalization. The elucidation of such networks by intracranial EEG and fMRI studies is a major triumph of the last 25 years.
All network activities, and therefore all forms of epilepsy, are ultimately based on the electrical behavior of individual neurons. At the cellular level, the last 25 years have seen enormous progress in the understanding of normal and abnormal electrical activity, and that progress is rooted in genetics. Genetic studies, correlated with electrophysiologic ones, have identified many mutations in ion channels that are responsible for various epilepsy syndromes. Examples of this are mutations in Na+ channels that lead to Dravet syndrome and mutations in GABA receptor subunits that are responsible for juvenile myoclonic epilepsy.
The mechanistic understanding of seizures and epilepsy has also been greatly enhanced in the last three decades by structural and developmental studies closely tied to genetics. Various forms of epilepsy are caused by aberrant neurogenesis and neuronal migration, leading to dysplastic cortex that has abnormal electrical activity and connectivity. The recent elucidation of the mTOR pathway, for example, has shown us how neuronal development and migration are controlled through several genetic steps, and mutations there can lead to tuberous sclerosis and related disorders that are accompanied by epilepsy.
Treatment
From the time that epilepsy was first recognized as a disease of the brain, treatment emphasized the control of seizures and not much else. A century after the introduction of bromide, there were, by 1967, perhaps half a dozen effective drugs available, including phenobarbital, phenytoin, and carbamazepine. Between 1967 and 1993, no new drugs for epilepsy were marketed in the USA, but the next 25 years saw a dramatic improvement. The years from 1993 to 2018 saw the introduction of perhaps 15 new drugs, most recently brivaracetam. However, in spite of this huge effort, at the expense of billions of dollars, each new drug makes less than 5% of previously refractory patients seizure-free.
Surgery
The idea of treating medically refractory epilepsy by surgical removal of the epileptic focus or network goes back more than a century, but advances in the last 25 years have been based on the revolution in imaging brought about by MRI. The easy and noninvasive identification of mesial temporal sclerosis and focal cortical dysplasias has enabled thousands of patients to become seizure-free. Complete control of seizures is obtained in only 50% to 75% of patients who undergo surgery, hardly better than a century ago, but advanced imaging and electrographic techniques have made surgery possible for many patients who previously would not have been candidates.
Looking Ahead
As they say, it is difficult to make predictions, especially about the future, but one can anticipate not only the identification of more gene mutations that cause epilepsy, but their correction with CRISPR/Cas9 and related technologies. Likewise, we can anticipate new antiepileptic drugs, but whether they will be broad-spectrum blockbusters like the cannabis derivatives are thought to be, or designer molecules tailored to specific types of seizures and epilepsy remains to be seen. In tuberous sclerosis, for example, drugs like tacrolimus that inhibit the mTOR pathway not only suppress abnormal cell proliferation, but also help with seizure control. Likewise, a small minority of epilepsies, now recognized to be autoimmune, will be treated with targeted immune suppression. A major goal is the discovery of drugs that will prevent the development of epilepsy or cure it in its early stages, as opposed to merely controlling the seizures.
Imaging of epileptic foci and networks of seizure spread will continue to improve with higher field strength MRI scans. EEG, MRI, and fMRI will probably coalesce, and PET scans will play a larger role. Combined images will guide epilepsy surgeons with regard to the boundaries of resections. The nature of EEG recording will also change. Until recently, owing to the properties of available amplifiers, we have looked at electrical oscillations between 1 Hz and 70 Hz. However, much higher frequencies are increasingly recognized as important in defining the epileptogenic zone and network. Epilepsy surgery that takes high-frequency oscillations into account will optimize the removal of epileptogenic lesions and the disruption of epileptic networks, while minimizing injury to normal brain functions.
Resective surgery may itself be rendered obsolete by cerebral stimulation, now in its infancy. Implanted devices such as Neuropace have shown promise in detecting seizures and delivering a counter-shock to abort them. Biologic stimulation is also on the horizon. In animal models, transplantation of GABA-producing cells has cured epilepsy, and optogenetic techniques may soon make it possible to activate particular classes of neurons that can turn off epileptic activity.
One can also anticipate a shift in treatment away from the exclusive emphasis on seizure control. We increasingly recognize that epilepsy is much more than seizures, and that patients with epilepsy may also have depression, impaired memory, and anxiety related to their illness. In the long run, the psychosocial problems of patients with epilepsy cannot be separated from social problems as a whole. Will, for example, the new, and doubtless expensive, treatments for epilepsy be made available to all who need them, or will we be obliged to work in a two-tier system? As health care providers, we can be cautiously optimistic regarding the medical aspects of epilepsy, but we will have to think in quite unanticipated ways to ensure equitable outcomes.
Vijay M. Thadani,
Dr. Thadani is Professor of Neurology, Geisel School of Medicine at Dartmouth, Dartmouth-Hitchcock Medical Center in Lebanon, New Hampshire. He reports no conflict of interest.
As Neurology Reviews celebrates its 25th anniversary, we take this opportunity to look back and to look ahead in the area of epilepsy care and research. Epilepsy is a disease whose earliest descriptions date back to Egypt and Mesopotamia 3,000 years ago. A modern understanding of epilepsy as an electrical disorder of the brain dates back perhaps 150 years. The last 25 years have seen considerable progress in diagnosis and treatment, but in the Western world, the prevalence of epilepsy has held steady at around 1%, and a quarter of those patients have seizures that are not controlled, in spite of appropriate therapy.
While generalized and focal seizures remain the cornerstones of classification, the most recent theoretical advance is the network concept of epilepsy. By definition, a network must have nodes and connections. In generalized forms of epilepsy, these are recognized to be diffuse groupings of neurons and the fiber tracts that connect them. They are widely distributed and conducive to the rapid and bilateral spread of electrical abnormalities throughout the brain. In focal epilepsies, the abnormal electrical activity in the network is more constrained by traditional anatomic landmarks, but this does not preclude the possibility of secondary generalization. The elucidation of such networks by intracranial EEG and fMRI studies is a major triumph of the last 25 years.
All network activities, and therefore all forms of epilepsy, are ultimately based on the electrical behavior of individual neurons. At the cellular level, the last 25 years have seen enormous progress in the understanding of normal and abnormal electrical activity, and that progress is rooted in genetics. Genetic studies, correlated with electrophysiologic ones, have identified many mutations in ion channels that are responsible for various epilepsy syndromes. Examples of this are mutations in Na+ channels that lead to Dravet syndrome and mutations in GABA receptor subunits that are responsible for juvenile myoclonic epilepsy.
The mechanistic understanding of seizures and epilepsy has also been greatly enhanced in the last three decades by structural and developmental studies closely tied to genetics. Various forms of epilepsy are caused by aberrant neurogenesis and neuronal migration, leading to dysplastic cortex that has abnormal electrical activity and connectivity. The recent elucidation of the mTOR pathway, for example, has shown us how neuronal development and migration are controlled through several genetic steps, and mutations there can lead to tuberous sclerosis and related disorders that are accompanied by epilepsy.
Treatment
From the time that epilepsy was first recognized as a disease of the brain, treatment emphasized the control of seizures and not much else. A century after the introduction of bromide, there were, by 1967, perhaps half a dozen effective drugs available, including phenobarbital, phenytoin, and carbamazepine. Between 1967 and 1993, no new drugs for epilepsy were marketed in the USA, but the next 25 years saw a dramatic improvement. The years from 1993 to 2018 saw the introduction of perhaps 15 new drugs, most recently brivaracetam. However, in spite of this huge effort, at the expense of billions of dollars, each new drug makes less than 5% of previously refractory patients seizure-free.
Surgery
The idea of treating medically refractory epilepsy by surgical removal of the epileptic focus or network goes back more than a century, but advances in the last 25 years have been based on the revolution in imaging brought about by MRI. The easy and noninvasive identification of mesial temporal sclerosis and focal cortical dysplasias has enabled thousands of patients to become seizure-free. Complete control of seizures is obtained in only 50% to 75% of patients who undergo surgery, hardly better than a century ago, but advanced imaging and electrographic techniques have made surgery possible for many patients who previously would not have been candidates.
Looking Ahead
As they say, it is difficult to make predictions, especially about the future, but one can anticipate not only the identification of more gene mutations that cause epilepsy, but their correction with CRISPR/Cas9 and related technologies. Likewise, we can anticipate new antiepileptic drugs, but whether they will be broad-spectrum blockbusters like the cannabis derivatives are thought to be, or designer molecules tailored to specific types of seizures and epilepsy remains to be seen. In tuberous sclerosis, for example, drugs like tacrolimus that inhibit the mTOR pathway not only suppress abnormal cell proliferation, but also help with seizure control. Likewise, a small minority of epilepsies, now recognized to be autoimmune, will be treated with targeted immune suppression. A major goal is the discovery of drugs that will prevent the development of epilepsy or cure it in its early stages, as opposed to merely controlling the seizures.
Imaging of epileptic foci and networks of seizure spread will continue to improve with higher field strength MRI scans. EEG, MRI, and fMRI will probably coalesce, and PET scans will play a larger role. Combined images will guide epilepsy surgeons with regard to the boundaries of resections. The nature of EEG recording will also change. Until recently, owing to the properties of available amplifiers, we have looked at electrical oscillations between 1 Hz and 70 Hz. However, much higher frequencies are increasingly recognized as important in defining the epileptogenic zone and network. Epilepsy surgery that takes high-frequency oscillations into account will optimize the removal of epileptogenic lesions and the disruption of epileptic networks, while minimizing injury to normal brain functions.
Resective surgery may itself be rendered obsolete by cerebral stimulation, now in its infancy. Implanted devices such as Neuropace have shown promise in detecting seizures and delivering a counter-shock to abort them. Biologic stimulation is also on the horizon. In animal models, transplantation of GABA-producing cells has cured epilepsy, and optogenetic techniques may soon make it possible to activate particular classes of neurons that can turn off epileptic activity.
One can also anticipate a shift in treatment away from the exclusive emphasis on seizure control. We increasingly recognize that epilepsy is much more than seizures, and that patients with epilepsy may also have depression, impaired memory, and anxiety related to their illness. In the long run, the psychosocial problems of patients with epilepsy cannot be separated from social problems as a whole. Will, for example, the new, and doubtless expensive, treatments for epilepsy be made available to all who need them, or will we be obliged to work in a two-tier system? As health care providers, we can be cautiously optimistic regarding the medical aspects of epilepsy, but we will have to think in quite unanticipated ways to ensure equitable outcomes.
Vijay M. Thadani,
Dr. Thadani is Professor of Neurology, Geisel School of Medicine at Dartmouth, Dartmouth-Hitchcock Medical Center in Lebanon, New Hampshire. He reports no conflict of interest.
As Neurology Reviews celebrates its 25th anniversary, we take this opportunity to look back and to look ahead in the area of epilepsy care and research. Epilepsy is a disease whose earliest descriptions date back to Egypt and Mesopotamia 3,000 years ago. A modern understanding of epilepsy as an electrical disorder of the brain dates back perhaps 150 years. The last 25 years have seen considerable progress in diagnosis and treatment, but in the Western world, the prevalence of epilepsy has held steady at around 1%, and a quarter of those patients have seizures that are not controlled, in spite of appropriate therapy.
While generalized and focal seizures remain the cornerstones of classification, the most recent theoretical advance is the network concept of epilepsy. By definition, a network must have nodes and connections. In generalized forms of epilepsy, these are recognized to be diffuse groupings of neurons and the fiber tracts that connect them. They are widely distributed and conducive to the rapid and bilateral spread of electrical abnormalities throughout the brain. In focal epilepsies, the abnormal electrical activity in the network is more constrained by traditional anatomic landmarks, but this does not preclude the possibility of secondary generalization. The elucidation of such networks by intracranial EEG and fMRI studies is a major triumph of the last 25 years.
All network activities, and therefore all forms of epilepsy, are ultimately based on the electrical behavior of individual neurons. At the cellular level, the last 25 years have seen enormous progress in the understanding of normal and abnormal electrical activity, and that progress is rooted in genetics. Genetic studies, correlated with electrophysiologic ones, have identified many mutations in ion channels that are responsible for various epilepsy syndromes. Examples of this are mutations in Na+ channels that lead to Dravet syndrome and mutations in GABA receptor subunits that are responsible for juvenile myoclonic epilepsy.
The mechanistic understanding of seizures and epilepsy has also been greatly enhanced in the last three decades by structural and developmental studies closely tied to genetics. Various forms of epilepsy are caused by aberrant neurogenesis and neuronal migration, leading to dysplastic cortex that has abnormal electrical activity and connectivity. The recent elucidation of the mTOR pathway, for example, has shown us how neuronal development and migration are controlled through several genetic steps, and mutations there can lead to tuberous sclerosis and related disorders that are accompanied by epilepsy.
Treatment
From the time that epilepsy was first recognized as a disease of the brain, treatment emphasized the control of seizures and not much else. A century after the introduction of bromide, there were, by 1967, perhaps half a dozen effective drugs available, including phenobarbital, phenytoin, and carbamazepine. Between 1967 and 1993, no new drugs for epilepsy were marketed in the USA, but the next 25 years saw a dramatic improvement. The years from 1993 to 2018 saw the introduction of perhaps 15 new drugs, most recently brivaracetam. However, in spite of this huge effort, at the expense of billions of dollars, each new drug makes less than 5% of previously refractory patients seizure-free.
Surgery
The idea of treating medically refractory epilepsy by surgical removal of the epileptic focus or network goes back more than a century, but advances in the last 25 years have been based on the revolution in imaging brought about by MRI. The easy and noninvasive identification of mesial temporal sclerosis and focal cortical dysplasias has enabled thousands of patients to become seizure-free. Complete control of seizures is obtained in only 50% to 75% of patients who undergo surgery, hardly better than a century ago, but advanced imaging and electrographic techniques have made surgery possible for many patients who previously would not have been candidates.
Looking Ahead
As they say, it is difficult to make predictions, especially about the future, but one can anticipate not only the identification of more gene mutations that cause epilepsy, but their correction with CRISPR/Cas9 and related technologies. Likewise, we can anticipate new antiepileptic drugs, but whether they will be broad-spectrum blockbusters like the cannabis derivatives are thought to be, or designer molecules tailored to specific types of seizures and epilepsy remains to be seen. In tuberous sclerosis, for example, drugs like tacrolimus that inhibit the mTOR pathway not only suppress abnormal cell proliferation, but also help with seizure control. Likewise, a small minority of epilepsies, now recognized to be autoimmune, will be treated with targeted immune suppression. A major goal is the discovery of drugs that will prevent the development of epilepsy or cure it in its early stages, as opposed to merely controlling the seizures.
Imaging of epileptic foci and networks of seizure spread will continue to improve with higher field strength MRI scans. EEG, MRI, and fMRI will probably coalesce, and PET scans will play a larger role. Combined images will guide epilepsy surgeons with regard to the boundaries of resections. The nature of EEG recording will also change. Until recently, owing to the properties of available amplifiers, we have looked at electrical oscillations between 1 Hz and 70 Hz. However, much higher frequencies are increasingly recognized as important in defining the epileptogenic zone and network. Epilepsy surgery that takes high-frequency oscillations into account will optimize the removal of epileptogenic lesions and the disruption of epileptic networks, while minimizing injury to normal brain functions.
Resective surgery may itself be rendered obsolete by cerebral stimulation, now in its infancy. Implanted devices such as Neuropace have shown promise in detecting seizures and delivering a counter-shock to abort them. Biologic stimulation is also on the horizon. In animal models, transplantation of GABA-producing cells has cured epilepsy, and optogenetic techniques may soon make it possible to activate particular classes of neurons that can turn off epileptic activity.
One can also anticipate a shift in treatment away from the exclusive emphasis on seizure control. We increasingly recognize that epilepsy is much more than seizures, and that patients with epilepsy may also have depression, impaired memory, and anxiety related to their illness. In the long run, the psychosocial problems of patients with epilepsy cannot be separated from social problems as a whole. Will, for example, the new, and doubtless expensive, treatments for epilepsy be made available to all who need them, or will we be obliged to work in a two-tier system? As health care providers, we can be cautiously optimistic regarding the medical aspects of epilepsy, but we will have to think in quite unanticipated ways to ensure equitable outcomes.
Staging System Classifies Nearly All Patients With Lewy Body Synucleinopathy
LOS ANGELES—The Unified Staging System for Lewy Body Disorders (USSLB) enables the categorization of almost all brains with Lewy body synucleinopathy, according to research described at the 70th Annual Meeting of the American Academy of Neurology. The USSLB’s stages correlate significantly with motor and nonmotor findings. “Wider use of the USSLB would help standardize research in synucleinopathies,” said Charles H. Adler, MD, PhD, Professor of Neurology at Mayo Clinic in Scottsdale, Arizona.
Investigators have developed several neuropathologic staging systems for Lewy body disorders, but many focus on specific diseases, such as Parkinson’s disease or dementia with Lewy bodies. They thus do not allow the classification of all patients with Lewy body disorders. In addition, the literature contains few data about how well these systems’ stages correlate with clinical and pathologic findings.
The Emergence of the USSLB
Dr. Adler and colleagues proposed the USSLB in research published in Acta Neuropathologica in 2009. Their goal was to enable the classification of patients with Lewy body disorders, regardless of their specific diagnoses. The USSLB includes four stages. Stage I denotes pathology limited to the olfactory bulb. Stage IIa denotes predominantly brainstem involvement. Stage IIb refers to pathology predominantly in the limbic system, rather than the brainstem. Stage III denotes pathology in the brainstem and limbic system. Stage IV represents neocortical pathology.
To examine the correlation between patients’ motor and nonmotor findings, including cognitive measures, and the extent of Lewy-type synucleinopathy, as categorized by the USSLB, Dr. Adler and others examined data from the Arizona Study of Aging and Neurodegenerative Disorders (AZSAND). That study includes participants in the Banner Sun Health Research Institute brain and body donation program. Participants undergo annual clinical exams that include movement testing, cognitive testing, sleep and autonomic questionnaires, and a smell test.
The investigators searched the AZSAND database for patients who presented from January 1997 through December 2015. They identified 641 autopsies. Clinical data and information on Lewy-type synucleinopathy were available for 280 of the cases. The population included cases with Lewy bodies and those with synuclein pathology within the neuropil and fibers. The population’s mean age at death was 83. Greater severity of synucleinopathy was associated with younger age at death.
Braak Staging Could Not Characterize Some Patients
The researchers classified 8.6% of cases as Stage I, 15.4% as Stage IIa, 13.6% as Stage IIb, 31.8% as Stage III, and 30.7% as Stage IV. Cognition was normal in 25.7% of the cases, 8.6% had mild cognitive impairment, and 65.7% had dementia.
Multiple measures of motor parkinsonism and cognitive impairment, as well as of hyposmia and probable REM sleep behavior disorder, correlated significantly with increasing USSLB stage. A few clinical features had no correlation with USSLB stage.
Dr. Adler and colleagues also applied the Braak staging criteria to the cases. To classify all cases, the investigators added an olfactory-bulb-only stage to the Braak criteria. Of the initial cohort, 70 cases could not be assigned a Braak stage. When the researchers removed cases with Alzheimer’s disease, 21% of cases could not be staged.
—Erik Greb
LOS ANGELES—The Unified Staging System for Lewy Body Disorders (USSLB) enables the categorization of almost all brains with Lewy body synucleinopathy, according to research described at the 70th Annual Meeting of the American Academy of Neurology. The USSLB’s stages correlate significantly with motor and nonmotor findings. “Wider use of the USSLB would help standardize research in synucleinopathies,” said Charles H. Adler, MD, PhD, Professor of Neurology at Mayo Clinic in Scottsdale, Arizona.
Investigators have developed several neuropathologic staging systems for Lewy body disorders, but many focus on specific diseases, such as Parkinson’s disease or dementia with Lewy bodies. They thus do not allow the classification of all patients with Lewy body disorders. In addition, the literature contains few data about how well these systems’ stages correlate with clinical and pathologic findings.
The Emergence of the USSLB
Dr. Adler and colleagues proposed the USSLB in research published in Acta Neuropathologica in 2009. Their goal was to enable the classification of patients with Lewy body disorders, regardless of their specific diagnoses. The USSLB includes four stages. Stage I denotes pathology limited to the olfactory bulb. Stage IIa denotes predominantly brainstem involvement. Stage IIb refers to pathology predominantly in the limbic system, rather than the brainstem. Stage III denotes pathology in the brainstem and limbic system. Stage IV represents neocortical pathology.
To examine the correlation between patients’ motor and nonmotor findings, including cognitive measures, and the extent of Lewy-type synucleinopathy, as categorized by the USSLB, Dr. Adler and others examined data from the Arizona Study of Aging and Neurodegenerative Disorders (AZSAND). That study includes participants in the Banner Sun Health Research Institute brain and body donation program. Participants undergo annual clinical exams that include movement testing, cognitive testing, sleep and autonomic questionnaires, and a smell test.
The investigators searched the AZSAND database for patients who presented from January 1997 through December 2015. They identified 641 autopsies. Clinical data and information on Lewy-type synucleinopathy were available for 280 of the cases. The population included cases with Lewy bodies and those with synuclein pathology within the neuropil and fibers. The population’s mean age at death was 83. Greater severity of synucleinopathy was associated with younger age at death.
Braak Staging Could Not Characterize Some Patients
The researchers classified 8.6% of cases as Stage I, 15.4% as Stage IIa, 13.6% as Stage IIb, 31.8% as Stage III, and 30.7% as Stage IV. Cognition was normal in 25.7% of the cases, 8.6% had mild cognitive impairment, and 65.7% had dementia.
Multiple measures of motor parkinsonism and cognitive impairment, as well as of hyposmia and probable REM sleep behavior disorder, correlated significantly with increasing USSLB stage. A few clinical features had no correlation with USSLB stage.
Dr. Adler and colleagues also applied the Braak staging criteria to the cases. To classify all cases, the investigators added an olfactory-bulb-only stage to the Braak criteria. Of the initial cohort, 70 cases could not be assigned a Braak stage. When the researchers removed cases with Alzheimer’s disease, 21% of cases could not be staged.
—Erik Greb
LOS ANGELES—The Unified Staging System for Lewy Body Disorders (USSLB) enables the categorization of almost all brains with Lewy body synucleinopathy, according to research described at the 70th Annual Meeting of the American Academy of Neurology. The USSLB’s stages correlate significantly with motor and nonmotor findings. “Wider use of the USSLB would help standardize research in synucleinopathies,” said Charles H. Adler, MD, PhD, Professor of Neurology at Mayo Clinic in Scottsdale, Arizona.
Investigators have developed several neuropathologic staging systems for Lewy body disorders, but many focus on specific diseases, such as Parkinson’s disease or dementia with Lewy bodies. They thus do not allow the classification of all patients with Lewy body disorders. In addition, the literature contains few data about how well these systems’ stages correlate with clinical and pathologic findings.
The Emergence of the USSLB
Dr. Adler and colleagues proposed the USSLB in research published in Acta Neuropathologica in 2009. Their goal was to enable the classification of patients with Lewy body disorders, regardless of their specific diagnoses. The USSLB includes four stages. Stage I denotes pathology limited to the olfactory bulb. Stage IIa denotes predominantly brainstem involvement. Stage IIb refers to pathology predominantly in the limbic system, rather than the brainstem. Stage III denotes pathology in the brainstem and limbic system. Stage IV represents neocortical pathology.
To examine the correlation between patients’ motor and nonmotor findings, including cognitive measures, and the extent of Lewy-type synucleinopathy, as categorized by the USSLB, Dr. Adler and others examined data from the Arizona Study of Aging and Neurodegenerative Disorders (AZSAND). That study includes participants in the Banner Sun Health Research Institute brain and body donation program. Participants undergo annual clinical exams that include movement testing, cognitive testing, sleep and autonomic questionnaires, and a smell test.
The investigators searched the AZSAND database for patients who presented from January 1997 through December 2015. They identified 641 autopsies. Clinical data and information on Lewy-type synucleinopathy were available for 280 of the cases. The population included cases with Lewy bodies and those with synuclein pathology within the neuropil and fibers. The population’s mean age at death was 83. Greater severity of synucleinopathy was associated with younger age at death.
Braak Staging Could Not Characterize Some Patients
The researchers classified 8.6% of cases as Stage I, 15.4% as Stage IIa, 13.6% as Stage IIb, 31.8% as Stage III, and 30.7% as Stage IV. Cognition was normal in 25.7% of the cases, 8.6% had mild cognitive impairment, and 65.7% had dementia.
Multiple measures of motor parkinsonism and cognitive impairment, as well as of hyposmia and probable REM sleep behavior disorder, correlated significantly with increasing USSLB stage. A few clinical features had no correlation with USSLB stage.
Dr. Adler and colleagues also applied the Braak staging criteria to the cases. To classify all cases, the investigators added an olfactory-bulb-only stage to the Braak criteria. Of the initial cohort, 70 cases could not be assigned a Braak stage. When the researchers removed cases with Alzheimer’s disease, 21% of cases could not be staged.
—Erik Greb
Ad hoc PCI dominates in elderly
ORLANDO – Ad hoc percutaneous coronary intervention is performed nearly six times more frequently than planned PCI in older patients undergoing elective PCI for stable coronary artery disease, according to a national study of Medicare claims data for 2009-2014.
The data showed no evident downside to ad hoc PCI in patients over age 65. Indeed, the ad hoc PCI strategy was associated with a significantly lower adjusted risk of in-hospital bleeding, compared with non–ad hoc PCI. The two approaches didn’t differ significantly in terms of in-hospital acute kidney injury or mortality, Kamil F. Faridi, MD, reported at the annual meeting of the American College of Cardiology.
In the past, concern had been voiced that ad hoc PCI – that is, PCI performed during the same session as diagnostic coronary angiography – doesn’t allow time for optimization of medical therapy prior to intervention, which might in theory result in worse outcomes. But such was not the case in a study of 169,434 patients age 65 years and up who underwent PCI for stable CAD with no evidence of acute coronary syndrome.
Moreover, ad hoc PCI offers several distinct advantages: a single vascular access, shorter net time in hospital, and lower cost, noted Dr. Faridi, of Beth Israel Deaconess Medical Center in Boston.
The proportion of elective PCIs that were performed on an ad hoc basis rose during the study years, from 77% in 2009 to 85% in 2014.
Patients who underwent ad hoc PCI were more likely to have angina symptoms before intervention. They were less likely to have peripheral vascular disease, heart failure, chronic kidney disease, complex lesion anatomy, or multivessel PCI than were patients who had planned PCI. Non–ad hoc PCI was more likely to occur at high-volume centers.
The in-hospital bleeding rate was 2.9% in the ad hoc PCI group, significantly lower than the 3.8% rate in the planned PCI patients. In an analysis adjusted for potential confounders, this translated to a 14% relative risk reduction. In-hospital acute kidney injury occurred in 8.0% of the ad hoc PCI group and 9.2% of the planned PCI group. The in-hospital mortality rate was 0.4% with ad hoc and 0.5% with planned PCI.
Dr. Faridi’s study was supported by the ACC National Cardiovascular Data Registry. He reported having no financial conflicts.
SOURCE: Faridi KF. ACC 2018, Abstract 1306-468/468
ORLANDO – Ad hoc percutaneous coronary intervention is performed nearly six times more frequently than planned PCI in older patients undergoing elective PCI for stable coronary artery disease, according to a national study of Medicare claims data for 2009-2014.
The data showed no evident downside to ad hoc PCI in patients over age 65. Indeed, the ad hoc PCI strategy was associated with a significantly lower adjusted risk of in-hospital bleeding, compared with non–ad hoc PCI. The two approaches didn’t differ significantly in terms of in-hospital acute kidney injury or mortality, Kamil F. Faridi, MD, reported at the annual meeting of the American College of Cardiology.
In the past, concern had been voiced that ad hoc PCI – that is, PCI performed during the same session as diagnostic coronary angiography – doesn’t allow time for optimization of medical therapy prior to intervention, which might in theory result in worse outcomes. But such was not the case in a study of 169,434 patients age 65 years and up who underwent PCI for stable CAD with no evidence of acute coronary syndrome.
Moreover, ad hoc PCI offers several distinct advantages: a single vascular access, shorter net time in hospital, and lower cost, noted Dr. Faridi, of Beth Israel Deaconess Medical Center in Boston.
The proportion of elective PCIs that were performed on an ad hoc basis rose during the study years, from 77% in 2009 to 85% in 2014.
Patients who underwent ad hoc PCI were more likely to have angina symptoms before intervention. They were less likely to have peripheral vascular disease, heart failure, chronic kidney disease, complex lesion anatomy, or multivessel PCI than were patients who had planned PCI. Non–ad hoc PCI was more likely to occur at high-volume centers.
The in-hospital bleeding rate was 2.9% in the ad hoc PCI group, significantly lower than the 3.8% rate in the planned PCI patients. In an analysis adjusted for potential confounders, this translated to a 14% relative risk reduction. In-hospital acute kidney injury occurred in 8.0% of the ad hoc PCI group and 9.2% of the planned PCI group. The in-hospital mortality rate was 0.4% with ad hoc and 0.5% with planned PCI.
Dr. Faridi’s study was supported by the ACC National Cardiovascular Data Registry. He reported having no financial conflicts.
SOURCE: Faridi KF. ACC 2018, Abstract 1306-468/468
ORLANDO – Ad hoc percutaneous coronary intervention is performed nearly six times more frequently than planned PCI in older patients undergoing elective PCI for stable coronary artery disease, according to a national study of Medicare claims data for 2009-2014.
The data showed no evident downside to ad hoc PCI in patients over age 65. Indeed, the ad hoc PCI strategy was associated with a significantly lower adjusted risk of in-hospital bleeding, compared with non–ad hoc PCI. The two approaches didn’t differ significantly in terms of in-hospital acute kidney injury or mortality, Kamil F. Faridi, MD, reported at the annual meeting of the American College of Cardiology.
In the past, concern had been voiced that ad hoc PCI – that is, PCI performed during the same session as diagnostic coronary angiography – doesn’t allow time for optimization of medical therapy prior to intervention, which might in theory result in worse outcomes. But such was not the case in a study of 169,434 patients age 65 years and up who underwent PCI for stable CAD with no evidence of acute coronary syndrome.
Moreover, ad hoc PCI offers several distinct advantages: a single vascular access, shorter net time in hospital, and lower cost, noted Dr. Faridi, of Beth Israel Deaconess Medical Center in Boston.
The proportion of elective PCIs that were performed on an ad hoc basis rose during the study years, from 77% in 2009 to 85% in 2014.
Patients who underwent ad hoc PCI were more likely to have angina symptoms before intervention. They were less likely to have peripheral vascular disease, heart failure, chronic kidney disease, complex lesion anatomy, or multivessel PCI than were patients who had planned PCI. Non–ad hoc PCI was more likely to occur at high-volume centers.
The in-hospital bleeding rate was 2.9% in the ad hoc PCI group, significantly lower than the 3.8% rate in the planned PCI patients. In an analysis adjusted for potential confounders, this translated to a 14% relative risk reduction. In-hospital acute kidney injury occurred in 8.0% of the ad hoc PCI group and 9.2% of the planned PCI group. The in-hospital mortality rate was 0.4% with ad hoc and 0.5% with planned PCI.
Dr. Faridi’s study was supported by the ACC National Cardiovascular Data Registry. He reported having no financial conflicts.
SOURCE: Faridi KF. ACC 2018, Abstract 1306-468/468
REPORTING FROM ACC 2018
Key clinical point: Ad hoc PCI in older patients has a lower bleeding risk than non–ad hoc PCI.
Major finding: Older patients undergoing ad hoc PCI for stable CAD were 14% less likely to experience significant in-hospital bleeding than were those undergoing planned PCI.
Study details: This was a retrospective study of nearly 170,000 patients age 65 years or older who underwent elective PCI for stable CAD.
Disclosures: The study was supported by the ACC National Cardiovascular Data Registry. The presenter reported having no financial conflicts.
Source: Faridi KF. ACC 2018, Abstract 1306-468/468
Positivity Rates in Oropharyngeal and Nonoropharyngeal Head and Neck Cancer in the VA
Head and neck cancer (HNC) continues to be a major health issue with an estimated 51,540 cases in the US in 2018, making it the eighth most common cancer among men with an estimated 4% of all new cancer diagnoses.1 Over the past decade, human papillomavirus (HPV) has emerged as a major prognostic factor for survival in squamous cell carcinomas of the oropharynx. Patients who are HPV-positive (HPV+) have a much higher survival rate than patients who have HPV-negative (HPV-) cancers of the oropharynx. The 8th edition of the American Joint Committee on Cancer (AJCC) staging manual has 2 distinct stagings for HPV+ and HPV- oropharyngeal tumors using p16-positivity (p16+) as a surrogate marker.2
Squamous cell carcinomas of the oropharynx that are HPV+ have about half the risk of death of HPV- tumors, are highly responsive to treatment, and are more often seen in younger and healthier patients with little to no tobacco use.2,3 As such, there also is a movement to de-escalate HPV+ oropharyngeal cancers with multiple trials by either replacing cytotoxic chemotherapy with a targeted agent (cisplatin vs cetuximab in RTOG 1016) or reducing the radiation dose (ECOG 1308, NRG HN002, Quarterback, and OPTIMA trials).3
The focus of many epidemiologic studies has been in the HNC general population. A recent epidemiologic analysis of the HNC general population found a p16 positivity rate of 60% in oropharyngeal squamous cell carcinomas (OPSCC) and 10% in nonoropharyngeal squamous cell carcinomas (NOPSCC).4 There has been a lack of studies focusing on the US Department of Veterans Administration (VA) population. The VA HNC population consists mostly of older white male smokers; whereas the rise of OPSCC in the general population consists primarily of males aged < 60 years often with little or no tobacco use.5 Furthermore, the importance of p16 positivity in NOPSCC also may be prognostic.6 Population data on this subset in the VA are lacking as well.This study’s purpose is to analyze the p16 positivity rate in both the OPSCC and NOPSCC in the VA population. Elucidation of epidemiologic factors that are associated with these groups may bring to light important differences between the VA and general HNC populations.
Methods
A review of the Kansas City VA Medical Center database for patients with HNC was performed from 2011 to 2017. The review consisted of 183 patient records (second primaries were scored separately), and 123 were deemed eligible for the study. Epidemiologic data were collected, including site, OPSCC vs NOPSCC, age, race, education level, tobacco use, alcohol use, TNM stage, and marital status (Table).
Results
The NOPSCC p16+ group had the greatest mean pack-year use (57). The lowest was in the OPSCC p16+ group (29). The OPSCC p16+ group had 37% never smokers compared with ≤ 10% for the other groups. Both the OPSCC and NOPSCC p16- groups had much more alcohol use per week than that of the p16+ groups. The differences in marital status included a lower rate of never married individuals in the p16+ group and a higher rate of marriage in the NOPSCC p16- group. The T stage distribution within the OPSCC groups was similar, but NOPSCC groups saw more T1 lesions in the NOPSCC p16- group (42% p16- vs 18% p16+). Conversely, more T4 lesions were found in the NOPSCC p16+ patients (7% p16- vs 29% p16+).
Discussion
The overall HPV positivity rate in the general population of patients with HNC has been reported as between 57% and 72% for OPSCC and between 1.3% and 7% for NOPSCC.6 One study, however, examined the p16 positivity rate in NOPSCC patients enrolled in major trials (RTOG 0129, 0234, and 0522 studies) and found that up to 19.3% of NOPSCC patients had p16 positivity.6 Even with the near 20% rate in those aforementioned trials that are above the reported norm, the current study found that nearly 30% of its VA population had p16+ NOPSCC. It has been shown that regardless of site, HPV-driven head and neck tumors share a similar gene expression and DNA methylation profiles (nonkeratinizing, basaloid histopathologic features, and lack of TP53 or CDKN2A alterations).5 p16+ NOPSCC has a different immune microenvironment with less lymphocyte infiltration, and there is some debate in the literature about the effects on tumor outcomes for NOPSCC cancer.5
In the aforementioned RTOG trials, p16- NOPSCC had worse outcomes compared with those of p16+ NOPSCC.6 This result is in contrast to the Danish Head and Neck Cancer Group (DAHANCA) and the combined Johns Hopkins University (JHU) and University of California, San Francisco (UCSF) data that found no difference between p16+ NOPSCC or p16- NOPSCC.7,8 In regards to race, this study did not find any differences. Another UCSF and JHU study showed lower p16+ rates in African American patients with OPSCC, but no distinction between race in the NOPSCC group. This result is consistent with the data in the current study as the distribution of race was no different among the 4 groups; however, this study's cohort was 90% white, 10% African American, and only < 1% Native American.4 This study's cohort population also was consistent with HPV-positive tumors presenting with earlier T, but higher N staging.9
Smoking is known to decrease survival in HPV-positive HNC, with the RTOG 0129 study separating head and neck tumors into low, medium, and high risk, based on HPV status, smoking, and stage.10 Although the average smoking pack-years in the current study’s OPC p16+ group was high at 29 pack-years, there was still a significant number of nonsmokers in that same group (37%). The University of Michigan conducted a study that had a similar profile of patients with an average age of 56.5 and 32.4% never smokers in their p16+ OPSCC cohort; thus, the VA p16+ OPSCC group in this study may be similar to the general population's p16+ OPSCC group.11 Nonmonogamous relationships also have been shown to be a risk factor for HPV positivity, and there was a difference in marital status (assuming it was a surrogate for monogamy) between the 4 groups; however, in contrast, the p16+ group in the current study had a high number of married patients, 45% in OPC p16+ group, and may not have been a good surrogate for monogamy in this VA population.
Limitations
Limitations of this study include all the caveats that come with a retrospective study, such as confounding variables, unbalanced groups, and selection bias. A detailed sexual history was not included, although it is well known that sexual activity is linked with oral HPV positivity.12 Human papillomavirus positivity based on p16 immunohistochemical analysis also was used as a surrogate marker for HPV instead of DNA in situ hybridization. The data also may be skewed due to the study patient’s being predominantly white and male: Both groups have a higher predilection for HPV-driven HNCs.13
Conclusion
The proportion of p16+ VA OPSCC cases was similar to that of the general population at 75% with 37% never smokers, but the percentage in NOPSCC was higher at 29% with only 10% never smokers. The p16+ NOPSCC also presented with more T4 lesions and a higher overall stage compared with p16- NOPSCC. Further studies are needed to compare these subgroups in the VA and in the general HNC populations.
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7-30.
2. Lydiatt WM, Patel SG, O’Sullivan B, et al. Head and neck cancers major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67(2):122-137.
3. Mirghani H, Blanchard P. Treatment de-escalation for HPV-driven oropharyngeal cancer: where do we stand? Clin Transl Radiat Oncol. 2017;8:4-11.
4. D’Souza G, Westra WH, Wang SJ, et al. Differences in the prevalence of human papillomavirus (HPV) in head and neck squamous cell cancers by sex, race, anatomic tumor site, and HPV detection method. JAMA Oncol. 2017;3(2):169-177.
5. Chakravarthy A, Henderson S, Thirdborough SM, et al. Human papillomavirus drives tumor development throughout the head and neck: improved prognosis is associated with an immune response largely restricted to the oropharynx. J Clin Oncol. 2016;34(34):4132-4141.
6. Chung CH, Zhang Q, Kong CS, et al. p16 protein expression and human papillomavirus status as prognostic biomarkers of nonoropharyngeal head and neck squamous cell carcinoma. J Clin Oncol. 2014;32(35):3930-3938.
7. Lassen P, Primdahl H, Johansen J, et al; Danish Head and Neck Cancer Group (DAHANCA). Impact of HPV-associated p16-expression on radiotherapy outcome in advanced oropharynx and non-oropharynx cancer. Radiother Oncol. 2014;113(3):310-316.
8. Fakhry C, Westra WH, Wang SJ, et al. The prognostic role of sex, race, and human papillomavirus in oropharyngeal and nonoropharyngeal head and neck squamous cell cancer. Cancer. 2017;123(9):1566-1575.
9. Elrefaey S, Massaro MA, Chiocca S, Chiesa F, Ansarin M. HPV in oropharyngeal cancer: the basics to know in clinical practice. Acta Otorhinolaryngol Ital. 2014;34(5):299-309.
10. Ang KK, Harris J, Wheeler R, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363(1):24-35.
11. Maxwell, JH, Kumar B, Feng FY, et al. Tobacco use in HPV-positive advanced oropharynx cancer patients related to increased risk of distant metastases and tumor recurrence. Clin Cancer Res. 2010;16(4):1226-1235.
12. Gillison ML, Broutian T, Pickard RK, et al. Prevalence of oral HPV infection in the United States, 2009-2010. JAMA. 2012;307(7):693-703.
13. Benson E, Li R, Eisele D, Fakhry C. The clinical impact of HPV tumor status upon head and neck squamous cell carcinomas. Oral Oncol. 2014;50(6):565-574.
Head and neck cancer (HNC) continues to be a major health issue with an estimated 51,540 cases in the US in 2018, making it the eighth most common cancer among men with an estimated 4% of all new cancer diagnoses.1 Over the past decade, human papillomavirus (HPV) has emerged as a major prognostic factor for survival in squamous cell carcinomas of the oropharynx. Patients who are HPV-positive (HPV+) have a much higher survival rate than patients who have HPV-negative (HPV-) cancers of the oropharynx. The 8th edition of the American Joint Committee on Cancer (AJCC) staging manual has 2 distinct stagings for HPV+ and HPV- oropharyngeal tumors using p16-positivity (p16+) as a surrogate marker.2
Squamous cell carcinomas of the oropharynx that are HPV+ have about half the risk of death of HPV- tumors, are highly responsive to treatment, and are more often seen in younger and healthier patients with little to no tobacco use.2,3 As such, there also is a movement to de-escalate HPV+ oropharyngeal cancers with multiple trials by either replacing cytotoxic chemotherapy with a targeted agent (cisplatin vs cetuximab in RTOG 1016) or reducing the radiation dose (ECOG 1308, NRG HN002, Quarterback, and OPTIMA trials).3
The focus of many epidemiologic studies has been in the HNC general population. A recent epidemiologic analysis of the HNC general population found a p16 positivity rate of 60% in oropharyngeal squamous cell carcinomas (OPSCC) and 10% in nonoropharyngeal squamous cell carcinomas (NOPSCC).4 There has been a lack of studies focusing on the US Department of Veterans Administration (VA) population. The VA HNC population consists mostly of older white male smokers; whereas the rise of OPSCC in the general population consists primarily of males aged < 60 years often with little or no tobacco use.5 Furthermore, the importance of p16 positivity in NOPSCC also may be prognostic.6 Population data on this subset in the VA are lacking as well.This study’s purpose is to analyze the p16 positivity rate in both the OPSCC and NOPSCC in the VA population. Elucidation of epidemiologic factors that are associated with these groups may bring to light important differences between the VA and general HNC populations.
Methods
A review of the Kansas City VA Medical Center database for patients with HNC was performed from 2011 to 2017. The review consisted of 183 patient records (second primaries were scored separately), and 123 were deemed eligible for the study. Epidemiologic data were collected, including site, OPSCC vs NOPSCC, age, race, education level, tobacco use, alcohol use, TNM stage, and marital status (Table).
Results
The NOPSCC p16+ group had the greatest mean pack-year use (57). The lowest was in the OPSCC p16+ group (29). The OPSCC p16+ group had 37% never smokers compared with ≤ 10% for the other groups. Both the OPSCC and NOPSCC p16- groups had much more alcohol use per week than that of the p16+ groups. The differences in marital status included a lower rate of never married individuals in the p16+ group and a higher rate of marriage in the NOPSCC p16- group. The T stage distribution within the OPSCC groups was similar, but NOPSCC groups saw more T1 lesions in the NOPSCC p16- group (42% p16- vs 18% p16+). Conversely, more T4 lesions were found in the NOPSCC p16+ patients (7% p16- vs 29% p16+).
Discussion
The overall HPV positivity rate in the general population of patients with HNC has been reported as between 57% and 72% for OPSCC and between 1.3% and 7% for NOPSCC.6 One study, however, examined the p16 positivity rate in NOPSCC patients enrolled in major trials (RTOG 0129, 0234, and 0522 studies) and found that up to 19.3% of NOPSCC patients had p16 positivity.6 Even with the near 20% rate in those aforementioned trials that are above the reported norm, the current study found that nearly 30% of its VA population had p16+ NOPSCC. It has been shown that regardless of site, HPV-driven head and neck tumors share a similar gene expression and DNA methylation profiles (nonkeratinizing, basaloid histopathologic features, and lack of TP53 or CDKN2A alterations).5 p16+ NOPSCC has a different immune microenvironment with less lymphocyte infiltration, and there is some debate in the literature about the effects on tumor outcomes for NOPSCC cancer.5
In the aforementioned RTOG trials, p16- NOPSCC had worse outcomes compared with those of p16+ NOPSCC.6 This result is in contrast to the Danish Head and Neck Cancer Group (DAHANCA) and the combined Johns Hopkins University (JHU) and University of California, San Francisco (UCSF) data that found no difference between p16+ NOPSCC or p16- NOPSCC.7,8 In regards to race, this study did not find any differences. Another UCSF and JHU study showed lower p16+ rates in African American patients with OPSCC, but no distinction between race in the NOPSCC group. This result is consistent with the data in the current study as the distribution of race was no different among the 4 groups; however, this study's cohort was 90% white, 10% African American, and only < 1% Native American.4 This study's cohort population also was consistent with HPV-positive tumors presenting with earlier T, but higher N staging.9
Smoking is known to decrease survival in HPV-positive HNC, with the RTOG 0129 study separating head and neck tumors into low, medium, and high risk, based on HPV status, smoking, and stage.10 Although the average smoking pack-years in the current study’s OPC p16+ group was high at 29 pack-years, there was still a significant number of nonsmokers in that same group (37%). The University of Michigan conducted a study that had a similar profile of patients with an average age of 56.5 and 32.4% never smokers in their p16+ OPSCC cohort; thus, the VA p16+ OPSCC group in this study may be similar to the general population's p16+ OPSCC group.11 Nonmonogamous relationships also have been shown to be a risk factor for HPV positivity, and there was a difference in marital status (assuming it was a surrogate for monogamy) between the 4 groups; however, in contrast, the p16+ group in the current study had a high number of married patients, 45% in OPC p16+ group, and may not have been a good surrogate for monogamy in this VA population.
Limitations
Limitations of this study include all the caveats that come with a retrospective study, such as confounding variables, unbalanced groups, and selection bias. A detailed sexual history was not included, although it is well known that sexual activity is linked with oral HPV positivity.12 Human papillomavirus positivity based on p16 immunohistochemical analysis also was used as a surrogate marker for HPV instead of DNA in situ hybridization. The data also may be skewed due to the study patient’s being predominantly white and male: Both groups have a higher predilection for HPV-driven HNCs.13
Conclusion
The proportion of p16+ VA OPSCC cases was similar to that of the general population at 75% with 37% never smokers, but the percentage in NOPSCC was higher at 29% with only 10% never smokers. The p16+ NOPSCC also presented with more T4 lesions and a higher overall stage compared with p16- NOPSCC. Further studies are needed to compare these subgroups in the VA and in the general HNC populations.
Head and neck cancer (HNC) continues to be a major health issue with an estimated 51,540 cases in the US in 2018, making it the eighth most common cancer among men with an estimated 4% of all new cancer diagnoses.1 Over the past decade, human papillomavirus (HPV) has emerged as a major prognostic factor for survival in squamous cell carcinomas of the oropharynx. Patients who are HPV-positive (HPV+) have a much higher survival rate than patients who have HPV-negative (HPV-) cancers of the oropharynx. The 8th edition of the American Joint Committee on Cancer (AJCC) staging manual has 2 distinct stagings for HPV+ and HPV- oropharyngeal tumors using p16-positivity (p16+) as a surrogate marker.2
Squamous cell carcinomas of the oropharynx that are HPV+ have about half the risk of death of HPV- tumors, are highly responsive to treatment, and are more often seen in younger and healthier patients with little to no tobacco use.2,3 As such, there also is a movement to de-escalate HPV+ oropharyngeal cancers with multiple trials by either replacing cytotoxic chemotherapy with a targeted agent (cisplatin vs cetuximab in RTOG 1016) or reducing the radiation dose (ECOG 1308, NRG HN002, Quarterback, and OPTIMA trials).3
The focus of many epidemiologic studies has been in the HNC general population. A recent epidemiologic analysis of the HNC general population found a p16 positivity rate of 60% in oropharyngeal squamous cell carcinomas (OPSCC) and 10% in nonoropharyngeal squamous cell carcinomas (NOPSCC).4 There has been a lack of studies focusing on the US Department of Veterans Administration (VA) population. The VA HNC population consists mostly of older white male smokers; whereas the rise of OPSCC in the general population consists primarily of males aged < 60 years often with little or no tobacco use.5 Furthermore, the importance of p16 positivity in NOPSCC also may be prognostic.6 Population data on this subset in the VA are lacking as well.This study’s purpose is to analyze the p16 positivity rate in both the OPSCC and NOPSCC in the VA population. Elucidation of epidemiologic factors that are associated with these groups may bring to light important differences between the VA and general HNC populations.
Methods
A review of the Kansas City VA Medical Center database for patients with HNC was performed from 2011 to 2017. The review consisted of 183 patient records (second primaries were scored separately), and 123 were deemed eligible for the study. Epidemiologic data were collected, including site, OPSCC vs NOPSCC, age, race, education level, tobacco use, alcohol use, TNM stage, and marital status (Table).
Results
The NOPSCC p16+ group had the greatest mean pack-year use (57). The lowest was in the OPSCC p16+ group (29). The OPSCC p16+ group had 37% never smokers compared with ≤ 10% for the other groups. Both the OPSCC and NOPSCC p16- groups had much more alcohol use per week than that of the p16+ groups. The differences in marital status included a lower rate of never married individuals in the p16+ group and a higher rate of marriage in the NOPSCC p16- group. The T stage distribution within the OPSCC groups was similar, but NOPSCC groups saw more T1 lesions in the NOPSCC p16- group (42% p16- vs 18% p16+). Conversely, more T4 lesions were found in the NOPSCC p16+ patients (7% p16- vs 29% p16+).
Discussion
The overall HPV positivity rate in the general population of patients with HNC has been reported as between 57% and 72% for OPSCC and between 1.3% and 7% for NOPSCC.6 One study, however, examined the p16 positivity rate in NOPSCC patients enrolled in major trials (RTOG 0129, 0234, and 0522 studies) and found that up to 19.3% of NOPSCC patients had p16 positivity.6 Even with the near 20% rate in those aforementioned trials that are above the reported norm, the current study found that nearly 30% of its VA population had p16+ NOPSCC. It has been shown that regardless of site, HPV-driven head and neck tumors share a similar gene expression and DNA methylation profiles (nonkeratinizing, basaloid histopathologic features, and lack of TP53 or CDKN2A alterations).5 p16+ NOPSCC has a different immune microenvironment with less lymphocyte infiltration, and there is some debate in the literature about the effects on tumor outcomes for NOPSCC cancer.5
In the aforementioned RTOG trials, p16- NOPSCC had worse outcomes compared with those of p16+ NOPSCC.6 This result is in contrast to the Danish Head and Neck Cancer Group (DAHANCA) and the combined Johns Hopkins University (JHU) and University of California, San Francisco (UCSF) data that found no difference between p16+ NOPSCC or p16- NOPSCC.7,8 In regards to race, this study did not find any differences. Another UCSF and JHU study showed lower p16+ rates in African American patients with OPSCC, but no distinction between race in the NOPSCC group. This result is consistent with the data in the current study as the distribution of race was no different among the 4 groups; however, this study's cohort was 90% white, 10% African American, and only < 1% Native American.4 This study's cohort population also was consistent with HPV-positive tumors presenting with earlier T, but higher N staging.9
Smoking is known to decrease survival in HPV-positive HNC, with the RTOG 0129 study separating head and neck tumors into low, medium, and high risk, based on HPV status, smoking, and stage.10 Although the average smoking pack-years in the current study’s OPC p16+ group was high at 29 pack-years, there was still a significant number of nonsmokers in that same group (37%). The University of Michigan conducted a study that had a similar profile of patients with an average age of 56.5 and 32.4% never smokers in their p16+ OPSCC cohort; thus, the VA p16+ OPSCC group in this study may be similar to the general population's p16+ OPSCC group.11 Nonmonogamous relationships also have been shown to be a risk factor for HPV positivity, and there was a difference in marital status (assuming it was a surrogate for monogamy) between the 4 groups; however, in contrast, the p16+ group in the current study had a high number of married patients, 45% in OPC p16+ group, and may not have been a good surrogate for monogamy in this VA population.
Limitations
Limitations of this study include all the caveats that come with a retrospective study, such as confounding variables, unbalanced groups, and selection bias. A detailed sexual history was not included, although it is well known that sexual activity is linked with oral HPV positivity.12 Human papillomavirus positivity based on p16 immunohistochemical analysis also was used as a surrogate marker for HPV instead of DNA in situ hybridization. The data also may be skewed due to the study patient’s being predominantly white and male: Both groups have a higher predilection for HPV-driven HNCs.13
Conclusion
The proportion of p16+ VA OPSCC cases was similar to that of the general population at 75% with 37% never smokers, but the percentage in NOPSCC was higher at 29% with only 10% never smokers. The p16+ NOPSCC also presented with more T4 lesions and a higher overall stage compared with p16- NOPSCC. Further studies are needed to compare these subgroups in the VA and in the general HNC populations.
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7-30.
2. Lydiatt WM, Patel SG, O’Sullivan B, et al. Head and neck cancers major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67(2):122-137.
3. Mirghani H, Blanchard P. Treatment de-escalation for HPV-driven oropharyngeal cancer: where do we stand? Clin Transl Radiat Oncol. 2017;8:4-11.
4. D’Souza G, Westra WH, Wang SJ, et al. Differences in the prevalence of human papillomavirus (HPV) in head and neck squamous cell cancers by sex, race, anatomic tumor site, and HPV detection method. JAMA Oncol. 2017;3(2):169-177.
5. Chakravarthy A, Henderson S, Thirdborough SM, et al. Human papillomavirus drives tumor development throughout the head and neck: improved prognosis is associated with an immune response largely restricted to the oropharynx. J Clin Oncol. 2016;34(34):4132-4141.
6. Chung CH, Zhang Q, Kong CS, et al. p16 protein expression and human papillomavirus status as prognostic biomarkers of nonoropharyngeal head and neck squamous cell carcinoma. J Clin Oncol. 2014;32(35):3930-3938.
7. Lassen P, Primdahl H, Johansen J, et al; Danish Head and Neck Cancer Group (DAHANCA). Impact of HPV-associated p16-expression on radiotherapy outcome in advanced oropharynx and non-oropharynx cancer. Radiother Oncol. 2014;113(3):310-316.
8. Fakhry C, Westra WH, Wang SJ, et al. The prognostic role of sex, race, and human papillomavirus in oropharyngeal and nonoropharyngeal head and neck squamous cell cancer. Cancer. 2017;123(9):1566-1575.
9. Elrefaey S, Massaro MA, Chiocca S, Chiesa F, Ansarin M. HPV in oropharyngeal cancer: the basics to know in clinical practice. Acta Otorhinolaryngol Ital. 2014;34(5):299-309.
10. Ang KK, Harris J, Wheeler R, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363(1):24-35.
11. Maxwell, JH, Kumar B, Feng FY, et al. Tobacco use in HPV-positive advanced oropharynx cancer patients related to increased risk of distant metastases and tumor recurrence. Clin Cancer Res. 2010;16(4):1226-1235.
12. Gillison ML, Broutian T, Pickard RK, et al. Prevalence of oral HPV infection in the United States, 2009-2010. JAMA. 2012;307(7):693-703.
13. Benson E, Li R, Eisele D, Fakhry C. The clinical impact of HPV tumor status upon head and neck squamous cell carcinomas. Oral Oncol. 2014;50(6):565-574.
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7-30.
2. Lydiatt WM, Patel SG, O’Sullivan B, et al. Head and neck cancers major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67(2):122-137.
3. Mirghani H, Blanchard P. Treatment de-escalation for HPV-driven oropharyngeal cancer: where do we stand? Clin Transl Radiat Oncol. 2017;8:4-11.
4. D’Souza G, Westra WH, Wang SJ, et al. Differences in the prevalence of human papillomavirus (HPV) in head and neck squamous cell cancers by sex, race, anatomic tumor site, and HPV detection method. JAMA Oncol. 2017;3(2):169-177.
5. Chakravarthy A, Henderson S, Thirdborough SM, et al. Human papillomavirus drives tumor development throughout the head and neck: improved prognosis is associated with an immune response largely restricted to the oropharynx. J Clin Oncol. 2016;34(34):4132-4141.
6. Chung CH, Zhang Q, Kong CS, et al. p16 protein expression and human papillomavirus status as prognostic biomarkers of nonoropharyngeal head and neck squamous cell carcinoma. J Clin Oncol. 2014;32(35):3930-3938.
7. Lassen P, Primdahl H, Johansen J, et al; Danish Head and Neck Cancer Group (DAHANCA). Impact of HPV-associated p16-expression on radiotherapy outcome in advanced oropharynx and non-oropharynx cancer. Radiother Oncol. 2014;113(3):310-316.
8. Fakhry C, Westra WH, Wang SJ, et al. The prognostic role of sex, race, and human papillomavirus in oropharyngeal and nonoropharyngeal head and neck squamous cell cancer. Cancer. 2017;123(9):1566-1575.
9. Elrefaey S, Massaro MA, Chiocca S, Chiesa F, Ansarin M. HPV in oropharyngeal cancer: the basics to know in clinical practice. Acta Otorhinolaryngol Ital. 2014;34(5):299-309.
10. Ang KK, Harris J, Wheeler R, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363(1):24-35.
11. Maxwell, JH, Kumar B, Feng FY, et al. Tobacco use in HPV-positive advanced oropharynx cancer patients related to increased risk of distant metastases and tumor recurrence. Clin Cancer Res. 2010;16(4):1226-1235.
12. Gillison ML, Broutian T, Pickard RK, et al. Prevalence of oral HPV infection in the United States, 2009-2010. JAMA. 2012;307(7):693-703.
13. Benson E, Li R, Eisele D, Fakhry C. The clinical impact of HPV tumor status upon head and neck squamous cell carcinomas. Oral Oncol. 2014;50(6):565-574.
Renal denervation for hypertension rebounds
PARIS – Endovascular device–delivered renal denervation has been dramatically resuscitated as a promisingly safe and effective nonpharmacologic treatment for hypertension on the basis of two rigorous positive, prospective, sham-controlled, randomized trials presented at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
“These two trials are proof of concept. They were not intended to show superiority of denervation over drug therapy. They provide the proof of principle that when we interfere with the renal sympathetic nervous system we are able to lower blood pressure,” according to Felix Mahfoud, MD, an interventional cardiologist at Saarland University Hospital in Homburg, Germany, who was a coinvestigator in both trials.
As a longtime investigator in the field, he was selected by the EuroPCR 2018 organizers to present an official statement to attendees in conjunction with presentation of the two late-breaking clinical trials. The essence of the official commentary was that, despite what physicians have heard based on earlier major setbacks, renal denervation (RDN) therapy for hypertension is alive and well; it’s an active area of investigation; and it holds promise for addressing the vast unmet need for better control of hypertension.
“It’s an interesting field. EuroPCR is committed to further support of the field. Stay tuned; there’s more to come. It’s been a bumpy road up until now, but I think we’re back on track with renal denervation,” Dr. Mahfoud said.
A few years ago RDN was widely dismissed as a failed treatment strategy on the basis of the negative results of the phase 3 SYMPLICITY HTN-3 trial conducted in patients with multidrug-resistant hypertension (N Engl J Med. 2014 Apr 10;370[15]:1393-401). Since then, two European consensus conferences on device-based hypertension therapies were held in 2015 and 2017. Those meetings analyzed key mistakes in earlier research and identified three key confounders that need to be standardized in order for high-quality research to move forward: The use of antihypertensive medications, or lack thereof, must be fixed and consistent; patients with severe treatment-resistant hypertension for whom basically nothing works are not the population to study initially; and key trial design and procedural details for the various endovascular therapies in development must be agreed upon.
The two sham-controlled trials presented at EuroPCR 2018 utilized different ablative energy sources: The RADIANCE-HTN SOLO study employed an ultrasound catheter, while the SPYRAL HTN-ON MED trial used a radiofrequency device. Both devices remain investigational. Each aims to ablate both the afferent and efferent renal sympathetic nerves located in the adventitia that run to and from the brain.
RADIANCE-HTN SOLO
Laura Mauri, MD, professor of medicine at Harvard Medical School, Boston, reported on 146 patients with mild to moderate hypertension at 39 U.S. and European centers, all of whom were deemed anatomically suitable for device therapy on the basis of the results of renal angiography. After a 4-week antihypertensive medication washout period, by which point their average blood pressure had climbed to 150/93 mm Hg, they were randomized in single-blind fashion to endovascular ultrasound RDN using ReCor Medical’s Paradise system or to renal angiography as a sham procedure.
The primary endpoint was the change in daytime ambulatory systolic blood pressure at 2 months’ follow-up post procedure in an intent-to-treat analysis. The RDN group had an 8.5–mm Hg reduction from baseline, compared with a 2.2–mm Hg reduction in sham-treated controls.
In a per protocol analysis excluding the five patients in the RDN group and 13 controls who required antihypertensive medication during the 2-month follow-up period, the average reduction in daytime ambulatory SBP was 8.5 mm Hg in the RDN group and 0.1 mm Hg in controls.
Similar statistically significant and clinically important placebo-controlled reductions in blood pressure were seen in all other endpoints, including 24-hour ambulatory, office, and home blood pressure.
“To put this in context, the magnitude of effect observed both on ambulatory blood pressure as well as office blood pressure is comparable with differences in blood pressure associated with reduction in cardiovascular events in population-based studies and meta-analyses of antihypertensive medication randomized trials,” Dr. Mauri observed.
At 2 months, 20% of the RDN group had a blood pressure below 135/85 mm Hg in the absence of antihypertensive medication, compared with 3% of controls.
No major adverse events such as renal failure, major vascular complications, embolism with end organ damage, or hypertensive crisis occurred during 2 months of follow-up. Follow-up will continue out to 3 years to evaluate the durability of therapeutic benefit.
The Paradise ultrasound system achieves circumferential ablation at a controllable depth of 1-6 mm in order to interrupt renal nerve traffic. Two or three ablations, each lasting 7 seconds, are delivered to each of the main renal arteries. The arterial wall is protected by water circulating through the balloon. The results were published simultaneously with Dr. Mauri’s presentation (Lancet 2018 May 23; doi: 10.1016/S0140-6736[18]31082-1).
SPYRAL HTN-ON MED
David E. Kandzari, MD, reported on the first 80 patients to complete 6 months of prospective follow-up in this ongoing international, single-blind, randomized trial of more than 400 patients with inadequately controlled hypertension on one to three commonly prescribed antihypertensive medications. Participants are being randomized to RDN via circumferential radiofrequency ablation using Medtronic’s Symplicity Spyral catheter or a sham control procedure. Although in this trial patients remain on their antihypertensive medications, an earlier randomized trial established proof of principle for efficacy in the absence of antihypertensive drugs.
In the real RDN group, 24-hour ambulatory blood pressure fell from baseline to 6 months of follow-up to a statistically significant and clinically meaningful degree: by 9.0 mm Hg systolic, compared with 1.6 mm Hg in controls, and by 6.0 mm Hg diastolic versus 1.9 mm Hg with the sham procedure. Similarly, office blood pressure fell by 9.4/5.2 mm Hg with RDN, compared with 2.6/1.7 mm Hg in controls.
Notably, 24-hour ambulatory systolic blood pressure was significantly lower in the RDN group around the clock.
“This may have important considerations with regard to pharmacotherapies with pharmacokinetic peaks and troughs in the early morning hours and late evening, or perhaps for groups with hypertension who are at especially high risk for cardiovascular events, such as those with nocturnal or early morning hypertension,” observed Dr. Kandzari, director of interventional cardiology and chief scientific officer at the Piedmont Heart Institute in Atlanta.
“This raises the concept of an ‘always on’ effect for renal denervation therapy that may be in distinction to pharmacotherapy and independent of adherence issues,” he added.
And speaking of adherence, a key feature of SPYRAL HTN-ON MED was that the trial incorporated periodic drug adherence monitoring using both urine and blood testing. The results, Dr. Kandzari said, were eye opening: At any given time, roughly 40% of patients in both study arms were nonadherent to their antihypertensive medications. Moreover, nonadherence was dynamic: It was not predictable for any single patient at any time point.
This 40% nonadherence rate was surprisingly high given that participants in SPYRAL HTN-ON MED were volunteers eager to participate in a non–drug treatment study and were informed up front that they would be undergoing adherence testing.
As in RADIANCE-HTN SOLO, no safety issues arose during follow-up in SPYRAL HTN-ON MED. The results were published simultaneously with Dr. Kandzari’s presentation (Lancet 2018 May 23; doi: 10.1016/S0140-6736[18]30951-6).
One difference between the two technologies is that, unlike the ReCor Paradise ultrasound catheter, which ablates in the main renal arteries, the Medtronic radiofrequency device is placed in the side branches.
Asked whether he sees RDN, provided it is established as safe and effective, being used primarily in hypertensive patients who are on or off medication, Dr. Kandzari replied that his personal view is it will have a role in both. Some patients would prefer not to take drugs. For others with uncontrolled hypertension despite multidrug therapy, RDN could serve as adjunctive therapy that reduces their need for medication.
Unanswered questions
Additional studies of both technologies are ongoing, and pivotal large phase 3 trials are being planned, with results expected in the next year or 2. Asked if regulatory agencies are going to require large, long-term trials with hard cardiovascular endpoints as a condition for approval, Dr. Mauri said a strong case can be made for bypassing this step.
“Blood pressure is remarkable,” she replied. “It’s one of the strongest surrogate endpoints that we have in the medical literature. It’s supported by multiple randomized trials of antihypertensive therapies, which have shown that reductions in blood pressure are associated with reductions in mortality from cardiovascular events. That’s really the gold standard for a surrogate endpoint. So I think it’s convincing. That being said, I would be very interested to also see hard endpoints in the long term, but that will take time.”
And time is a luxury in light of the escalating global hypertension pandemic. Dr. Mahfoud noted that it’s estimated that in 2015, 950 million people around the world had a systolic blood pressure in excess of 140 mm Hg. By 2025, that figure is expected to climb to 2.5 billion people. The Centers for Disease Control and Prevention estimates that more than 360,000 deaths per year in the United States have hypertension as the primary or a contributing cause. Blood pressure control rates remain unacceptably low, in the 50% range. Nonadherence is high. So there is a pressing unmet need for new forms of treatment.
Dr. Mahfoud cited three major remaining research priorities for RDN therapy. There is a need for some form of intraprocedural feedback to inform the interventionalist while still in the catheterization lab that the denervation is successfully completed. A reliable predictor of response is desirable so that likely nonresponders to RDN aren’t needlessly exposed to the procedure. And of course, the sustainability of benefit for RDN requires longer-term study.
Dr. Kandzari reported receiving institutional research support and consulting fees from Medtronic and several other medical device companies. Dr. Mauri reported receiving institutional research support from ReCor and other device companies and serving as a consultant to ReCor and Medtronic; in addition, she has accepted a position as a vice president at Medtronic to begin in September.
PARIS – Endovascular device–delivered renal denervation has been dramatically resuscitated as a promisingly safe and effective nonpharmacologic treatment for hypertension on the basis of two rigorous positive, prospective, sham-controlled, randomized trials presented at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
“These two trials are proof of concept. They were not intended to show superiority of denervation over drug therapy. They provide the proof of principle that when we interfere with the renal sympathetic nervous system we are able to lower blood pressure,” according to Felix Mahfoud, MD, an interventional cardiologist at Saarland University Hospital in Homburg, Germany, who was a coinvestigator in both trials.
As a longtime investigator in the field, he was selected by the EuroPCR 2018 organizers to present an official statement to attendees in conjunction with presentation of the two late-breaking clinical trials. The essence of the official commentary was that, despite what physicians have heard based on earlier major setbacks, renal denervation (RDN) therapy for hypertension is alive and well; it’s an active area of investigation; and it holds promise for addressing the vast unmet need for better control of hypertension.
“It’s an interesting field. EuroPCR is committed to further support of the field. Stay tuned; there’s more to come. It’s been a bumpy road up until now, but I think we’re back on track with renal denervation,” Dr. Mahfoud said.
A few years ago RDN was widely dismissed as a failed treatment strategy on the basis of the negative results of the phase 3 SYMPLICITY HTN-3 trial conducted in patients with multidrug-resistant hypertension (N Engl J Med. 2014 Apr 10;370[15]:1393-401). Since then, two European consensus conferences on device-based hypertension therapies were held in 2015 and 2017. Those meetings analyzed key mistakes in earlier research and identified three key confounders that need to be standardized in order for high-quality research to move forward: The use of antihypertensive medications, or lack thereof, must be fixed and consistent; patients with severe treatment-resistant hypertension for whom basically nothing works are not the population to study initially; and key trial design and procedural details for the various endovascular therapies in development must be agreed upon.
The two sham-controlled trials presented at EuroPCR 2018 utilized different ablative energy sources: The RADIANCE-HTN SOLO study employed an ultrasound catheter, while the SPYRAL HTN-ON MED trial used a radiofrequency device. Both devices remain investigational. Each aims to ablate both the afferent and efferent renal sympathetic nerves located in the adventitia that run to and from the brain.
RADIANCE-HTN SOLO
Laura Mauri, MD, professor of medicine at Harvard Medical School, Boston, reported on 146 patients with mild to moderate hypertension at 39 U.S. and European centers, all of whom were deemed anatomically suitable for device therapy on the basis of the results of renal angiography. After a 4-week antihypertensive medication washout period, by which point their average blood pressure had climbed to 150/93 mm Hg, they were randomized in single-blind fashion to endovascular ultrasound RDN using ReCor Medical’s Paradise system or to renal angiography as a sham procedure.
The primary endpoint was the change in daytime ambulatory systolic blood pressure at 2 months’ follow-up post procedure in an intent-to-treat analysis. The RDN group had an 8.5–mm Hg reduction from baseline, compared with a 2.2–mm Hg reduction in sham-treated controls.
In a per protocol analysis excluding the five patients in the RDN group and 13 controls who required antihypertensive medication during the 2-month follow-up period, the average reduction in daytime ambulatory SBP was 8.5 mm Hg in the RDN group and 0.1 mm Hg in controls.
Similar statistically significant and clinically important placebo-controlled reductions in blood pressure were seen in all other endpoints, including 24-hour ambulatory, office, and home blood pressure.
“To put this in context, the magnitude of effect observed both on ambulatory blood pressure as well as office blood pressure is comparable with differences in blood pressure associated with reduction in cardiovascular events in population-based studies and meta-analyses of antihypertensive medication randomized trials,” Dr. Mauri observed.
At 2 months, 20% of the RDN group had a blood pressure below 135/85 mm Hg in the absence of antihypertensive medication, compared with 3% of controls.
No major adverse events such as renal failure, major vascular complications, embolism with end organ damage, or hypertensive crisis occurred during 2 months of follow-up. Follow-up will continue out to 3 years to evaluate the durability of therapeutic benefit.
The Paradise ultrasound system achieves circumferential ablation at a controllable depth of 1-6 mm in order to interrupt renal nerve traffic. Two or three ablations, each lasting 7 seconds, are delivered to each of the main renal arteries. The arterial wall is protected by water circulating through the balloon. The results were published simultaneously with Dr. Mauri’s presentation (Lancet 2018 May 23; doi: 10.1016/S0140-6736[18]31082-1).
SPYRAL HTN-ON MED
David E. Kandzari, MD, reported on the first 80 patients to complete 6 months of prospective follow-up in this ongoing international, single-blind, randomized trial of more than 400 patients with inadequately controlled hypertension on one to three commonly prescribed antihypertensive medications. Participants are being randomized to RDN via circumferential radiofrequency ablation using Medtronic’s Symplicity Spyral catheter or a sham control procedure. Although in this trial patients remain on their antihypertensive medications, an earlier randomized trial established proof of principle for efficacy in the absence of antihypertensive drugs.
In the real RDN group, 24-hour ambulatory blood pressure fell from baseline to 6 months of follow-up to a statistically significant and clinically meaningful degree: by 9.0 mm Hg systolic, compared with 1.6 mm Hg in controls, and by 6.0 mm Hg diastolic versus 1.9 mm Hg with the sham procedure. Similarly, office blood pressure fell by 9.4/5.2 mm Hg with RDN, compared with 2.6/1.7 mm Hg in controls.
Notably, 24-hour ambulatory systolic blood pressure was significantly lower in the RDN group around the clock.
“This may have important considerations with regard to pharmacotherapies with pharmacokinetic peaks and troughs in the early morning hours and late evening, or perhaps for groups with hypertension who are at especially high risk for cardiovascular events, such as those with nocturnal or early morning hypertension,” observed Dr. Kandzari, director of interventional cardiology and chief scientific officer at the Piedmont Heart Institute in Atlanta.
“This raises the concept of an ‘always on’ effect for renal denervation therapy that may be in distinction to pharmacotherapy and independent of adherence issues,” he added.
And speaking of adherence, a key feature of SPYRAL HTN-ON MED was that the trial incorporated periodic drug adherence monitoring using both urine and blood testing. The results, Dr. Kandzari said, were eye opening: At any given time, roughly 40% of patients in both study arms were nonadherent to their antihypertensive medications. Moreover, nonadherence was dynamic: It was not predictable for any single patient at any time point.
This 40% nonadherence rate was surprisingly high given that participants in SPYRAL HTN-ON MED were volunteers eager to participate in a non–drug treatment study and were informed up front that they would be undergoing adherence testing.
As in RADIANCE-HTN SOLO, no safety issues arose during follow-up in SPYRAL HTN-ON MED. The results were published simultaneously with Dr. Kandzari’s presentation (Lancet 2018 May 23; doi: 10.1016/S0140-6736[18]30951-6).
One difference between the two technologies is that, unlike the ReCor Paradise ultrasound catheter, which ablates in the main renal arteries, the Medtronic radiofrequency device is placed in the side branches.
Asked whether he sees RDN, provided it is established as safe and effective, being used primarily in hypertensive patients who are on or off medication, Dr. Kandzari replied that his personal view is it will have a role in both. Some patients would prefer not to take drugs. For others with uncontrolled hypertension despite multidrug therapy, RDN could serve as adjunctive therapy that reduces their need for medication.
Unanswered questions
Additional studies of both technologies are ongoing, and pivotal large phase 3 trials are being planned, with results expected in the next year or 2. Asked if regulatory agencies are going to require large, long-term trials with hard cardiovascular endpoints as a condition for approval, Dr. Mauri said a strong case can be made for bypassing this step.
“Blood pressure is remarkable,” she replied. “It’s one of the strongest surrogate endpoints that we have in the medical literature. It’s supported by multiple randomized trials of antihypertensive therapies, which have shown that reductions in blood pressure are associated with reductions in mortality from cardiovascular events. That’s really the gold standard for a surrogate endpoint. So I think it’s convincing. That being said, I would be very interested to also see hard endpoints in the long term, but that will take time.”
And time is a luxury in light of the escalating global hypertension pandemic. Dr. Mahfoud noted that it’s estimated that in 2015, 950 million people around the world had a systolic blood pressure in excess of 140 mm Hg. By 2025, that figure is expected to climb to 2.5 billion people. The Centers for Disease Control and Prevention estimates that more than 360,000 deaths per year in the United States have hypertension as the primary or a contributing cause. Blood pressure control rates remain unacceptably low, in the 50% range. Nonadherence is high. So there is a pressing unmet need for new forms of treatment.
Dr. Mahfoud cited three major remaining research priorities for RDN therapy. There is a need for some form of intraprocedural feedback to inform the interventionalist while still in the catheterization lab that the denervation is successfully completed. A reliable predictor of response is desirable so that likely nonresponders to RDN aren’t needlessly exposed to the procedure. And of course, the sustainability of benefit for RDN requires longer-term study.
Dr. Kandzari reported receiving institutional research support and consulting fees from Medtronic and several other medical device companies. Dr. Mauri reported receiving institutional research support from ReCor and other device companies and serving as a consultant to ReCor and Medtronic; in addition, she has accepted a position as a vice president at Medtronic to begin in September.
PARIS – Endovascular device–delivered renal denervation has been dramatically resuscitated as a promisingly safe and effective nonpharmacologic treatment for hypertension on the basis of two rigorous positive, prospective, sham-controlled, randomized trials presented at the annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
“These two trials are proof of concept. They were not intended to show superiority of denervation over drug therapy. They provide the proof of principle that when we interfere with the renal sympathetic nervous system we are able to lower blood pressure,” according to Felix Mahfoud, MD, an interventional cardiologist at Saarland University Hospital in Homburg, Germany, who was a coinvestigator in both trials.
As a longtime investigator in the field, he was selected by the EuroPCR 2018 organizers to present an official statement to attendees in conjunction with presentation of the two late-breaking clinical trials. The essence of the official commentary was that, despite what physicians have heard based on earlier major setbacks, renal denervation (RDN) therapy for hypertension is alive and well; it’s an active area of investigation; and it holds promise for addressing the vast unmet need for better control of hypertension.
“It’s an interesting field. EuroPCR is committed to further support of the field. Stay tuned; there’s more to come. It’s been a bumpy road up until now, but I think we’re back on track with renal denervation,” Dr. Mahfoud said.
A few years ago RDN was widely dismissed as a failed treatment strategy on the basis of the negative results of the phase 3 SYMPLICITY HTN-3 trial conducted in patients with multidrug-resistant hypertension (N Engl J Med. 2014 Apr 10;370[15]:1393-401). Since then, two European consensus conferences on device-based hypertension therapies were held in 2015 and 2017. Those meetings analyzed key mistakes in earlier research and identified three key confounders that need to be standardized in order for high-quality research to move forward: The use of antihypertensive medications, or lack thereof, must be fixed and consistent; patients with severe treatment-resistant hypertension for whom basically nothing works are not the population to study initially; and key trial design and procedural details for the various endovascular therapies in development must be agreed upon.
The two sham-controlled trials presented at EuroPCR 2018 utilized different ablative energy sources: The RADIANCE-HTN SOLO study employed an ultrasound catheter, while the SPYRAL HTN-ON MED trial used a radiofrequency device. Both devices remain investigational. Each aims to ablate both the afferent and efferent renal sympathetic nerves located in the adventitia that run to and from the brain.
RADIANCE-HTN SOLO
Laura Mauri, MD, professor of medicine at Harvard Medical School, Boston, reported on 146 patients with mild to moderate hypertension at 39 U.S. and European centers, all of whom were deemed anatomically suitable for device therapy on the basis of the results of renal angiography. After a 4-week antihypertensive medication washout period, by which point their average blood pressure had climbed to 150/93 mm Hg, they were randomized in single-blind fashion to endovascular ultrasound RDN using ReCor Medical’s Paradise system or to renal angiography as a sham procedure.
The primary endpoint was the change in daytime ambulatory systolic blood pressure at 2 months’ follow-up post procedure in an intent-to-treat analysis. The RDN group had an 8.5–mm Hg reduction from baseline, compared with a 2.2–mm Hg reduction in sham-treated controls.
In a per protocol analysis excluding the five patients in the RDN group and 13 controls who required antihypertensive medication during the 2-month follow-up period, the average reduction in daytime ambulatory SBP was 8.5 mm Hg in the RDN group and 0.1 mm Hg in controls.
Similar statistically significant and clinically important placebo-controlled reductions in blood pressure were seen in all other endpoints, including 24-hour ambulatory, office, and home blood pressure.
“To put this in context, the magnitude of effect observed both on ambulatory blood pressure as well as office blood pressure is comparable with differences in blood pressure associated with reduction in cardiovascular events in population-based studies and meta-analyses of antihypertensive medication randomized trials,” Dr. Mauri observed.
At 2 months, 20% of the RDN group had a blood pressure below 135/85 mm Hg in the absence of antihypertensive medication, compared with 3% of controls.
No major adverse events such as renal failure, major vascular complications, embolism with end organ damage, or hypertensive crisis occurred during 2 months of follow-up. Follow-up will continue out to 3 years to evaluate the durability of therapeutic benefit.
The Paradise ultrasound system achieves circumferential ablation at a controllable depth of 1-6 mm in order to interrupt renal nerve traffic. Two or three ablations, each lasting 7 seconds, are delivered to each of the main renal arteries. The arterial wall is protected by water circulating through the balloon. The results were published simultaneously with Dr. Mauri’s presentation (Lancet 2018 May 23; doi: 10.1016/S0140-6736[18]31082-1).
SPYRAL HTN-ON MED
David E. Kandzari, MD, reported on the first 80 patients to complete 6 months of prospective follow-up in this ongoing international, single-blind, randomized trial of more than 400 patients with inadequately controlled hypertension on one to three commonly prescribed antihypertensive medications. Participants are being randomized to RDN via circumferential radiofrequency ablation using Medtronic’s Symplicity Spyral catheter or a sham control procedure. Although in this trial patients remain on their antihypertensive medications, an earlier randomized trial established proof of principle for efficacy in the absence of antihypertensive drugs.
In the real RDN group, 24-hour ambulatory blood pressure fell from baseline to 6 months of follow-up to a statistically significant and clinically meaningful degree: by 9.0 mm Hg systolic, compared with 1.6 mm Hg in controls, and by 6.0 mm Hg diastolic versus 1.9 mm Hg with the sham procedure. Similarly, office blood pressure fell by 9.4/5.2 mm Hg with RDN, compared with 2.6/1.7 mm Hg in controls.
Notably, 24-hour ambulatory systolic blood pressure was significantly lower in the RDN group around the clock.
“This may have important considerations with regard to pharmacotherapies with pharmacokinetic peaks and troughs in the early morning hours and late evening, or perhaps for groups with hypertension who are at especially high risk for cardiovascular events, such as those with nocturnal or early morning hypertension,” observed Dr. Kandzari, director of interventional cardiology and chief scientific officer at the Piedmont Heart Institute in Atlanta.
“This raises the concept of an ‘always on’ effect for renal denervation therapy that may be in distinction to pharmacotherapy and independent of adherence issues,” he added.
And speaking of adherence, a key feature of SPYRAL HTN-ON MED was that the trial incorporated periodic drug adherence monitoring using both urine and blood testing. The results, Dr. Kandzari said, were eye opening: At any given time, roughly 40% of patients in both study arms were nonadherent to their antihypertensive medications. Moreover, nonadherence was dynamic: It was not predictable for any single patient at any time point.
This 40% nonadherence rate was surprisingly high given that participants in SPYRAL HTN-ON MED were volunteers eager to participate in a non–drug treatment study and were informed up front that they would be undergoing adherence testing.
As in RADIANCE-HTN SOLO, no safety issues arose during follow-up in SPYRAL HTN-ON MED. The results were published simultaneously with Dr. Kandzari’s presentation (Lancet 2018 May 23; doi: 10.1016/S0140-6736[18]30951-6).
One difference between the two technologies is that, unlike the ReCor Paradise ultrasound catheter, which ablates in the main renal arteries, the Medtronic radiofrequency device is placed in the side branches.
Asked whether he sees RDN, provided it is established as safe and effective, being used primarily in hypertensive patients who are on or off medication, Dr. Kandzari replied that his personal view is it will have a role in both. Some patients would prefer not to take drugs. For others with uncontrolled hypertension despite multidrug therapy, RDN could serve as adjunctive therapy that reduces their need for medication.
Unanswered questions
Additional studies of both technologies are ongoing, and pivotal large phase 3 trials are being planned, with results expected in the next year or 2. Asked if regulatory agencies are going to require large, long-term trials with hard cardiovascular endpoints as a condition for approval, Dr. Mauri said a strong case can be made for bypassing this step.
“Blood pressure is remarkable,” she replied. “It’s one of the strongest surrogate endpoints that we have in the medical literature. It’s supported by multiple randomized trials of antihypertensive therapies, which have shown that reductions in blood pressure are associated with reductions in mortality from cardiovascular events. That’s really the gold standard for a surrogate endpoint. So I think it’s convincing. That being said, I would be very interested to also see hard endpoints in the long term, but that will take time.”
And time is a luxury in light of the escalating global hypertension pandemic. Dr. Mahfoud noted that it’s estimated that in 2015, 950 million people around the world had a systolic blood pressure in excess of 140 mm Hg. By 2025, that figure is expected to climb to 2.5 billion people. The Centers for Disease Control and Prevention estimates that more than 360,000 deaths per year in the United States have hypertension as the primary or a contributing cause. Blood pressure control rates remain unacceptably low, in the 50% range. Nonadherence is high. So there is a pressing unmet need for new forms of treatment.
Dr. Mahfoud cited three major remaining research priorities for RDN therapy. There is a need for some form of intraprocedural feedback to inform the interventionalist while still in the catheterization lab that the denervation is successfully completed. A reliable predictor of response is desirable so that likely nonresponders to RDN aren’t needlessly exposed to the procedure. And of course, the sustainability of benefit for RDN requires longer-term study.
Dr. Kandzari reported receiving institutional research support and consulting fees from Medtronic and several other medical device companies. Dr. Mauri reported receiving institutional research support from ReCor and other device companies and serving as a consultant to ReCor and Medtronic; in addition, she has accepted a position as a vice president at Medtronic to begin in September.
REPORTING FROM EUROPCR 2018
High testosterone in postmenopausal women may add CVD risk
In postmenopausal women, a higher level of testosterone in comparison to estrogen may increase the cardiovascular disease risk later in life, results of a recent analysis suggest.
A higher ratio of testosterone to estradiol was associated with the development of cardiovascular disease, coronary heart disease, and heart failure in postmenopausal women, according to results from an analysis based on 2,834 postmenopausal women in MESA (Multi-Ethnic Study of Atherosclerosis).
In addition, total testosterone levels were associated with increased cardiovascular disease and coronary heart disease, while estradiol is associated with a reduced risk of coronary heart disease and heart failure with reduced ejection fraction, investigators reported in the Journal of the American College of Cardiology.
Without any interventional studies as guidance, it’s not clear what the “best strategy” would be to modify sex hormone levels and reduce cardiovascular disease risk, wrote investigator Di Zhao, PhD, of the department of epidemiology at Johns Hopkins University Bloomberg School of Public Health, Baltimore, and her study coauthors.
“Nonetheless, a more androgenic sex hormone profile may identify a woman at higher risk for cardiovascular disease who may benefit from other risk-reducing strategies,” Dr. Zhao and her colleagues wrote in their report.
The postmenopausal women included in this analysis all had baseline measurements of testosterone, estradiol, dehydroepiandrosterone, and sex hormone–binding globulin levels between 2000 and 2002, according to the report.
After more than 12 years of follow-up, investigators found that a higher total testosterone to estradiol ratio was independently associated with an increased risk of incident cardiovascular disease (hazard ratio, 1.19; 95% confidence interval, 1.02-1.40), coronary heart disease (HR, 1.45; 95% CI, 1.19-1.78), and heart failure (HR, 1.31; 95% CI, 1.01-1.70).
Investigators also reported a statistically significant association between total testosterone levels and risk of cardiovascular disease and coronary heart disease but not risk of heart failure.
In a subgroup analysis of postmenopausal women with heart failure, investigators found a significant positive association with the testosterone to estradiol ratio (HR, 1.65; 95% CI, 1.07-2.54) and inverse associations for estradiol (HR, 0.60; 95% CI, 0.39-0.93) and for dehydroepiandrosterone (HR, 0.59; 95% CI, 0.44-0.78).
On their own, estradiol levels had no association with cardiovascular disease events overall, but they were associated with lower coronary heart disease risk, according to investigators. Estradiol also was associated with a lower heart failure risk, though the trend did not reach statistical significance.
The study was partially funded by the American Heart Association’s Go Red for Women Research Network. Study authors reported disclosures related to Cordex Systems, Siemens Diagnostics, and other entities.
SOURCE: Zhao D et al. J Am Coll Cardiol. 2018 Jun 5; 71:2555-66.
This study offers new insights into the relationships between endogenous hormones and how they influence cardiovascular event risk, according to Virginia M. Miller, PhD, and Rekha Mankad, MD.
Previous observational studies have established that decreases in endogenous estrogen led to increases in cardiovascular event risk and incidence, Dr. Miller and Dr. Mankad said in an editorial referencing the study.
What’s less clear is the role of testosterone in cardiovascular risk and event incidence, both by itself and in relation to other endogenous hormones.
“Few studies have gone beyond singular associations of hormone levels with cardiovascular events,” the editorial authors wrote in the Journal of the American College of Cardiology.
The study by Zhao and her colleagues is unique in part because their analysis considers the ratio of testosterone to estradiol. In particular, they found that a higher testosterone to estradiol level was associated with a higher incidence of cardiovascular events overall and of coronary heart disease.
What was unexpected, according to Dr. Miller and Dr. Mankad, was a U-shaped association with incident heart failure. In subgroup analysis, investigators found a positive association between testosterone to estradiol ratio and heart failure with reduced ejection fraction but not with heart failure with preserved ejection fraction.
“By addressing a set of defined incident events, this study provides new information needed to develop mechanistic hypotheses of causal relationships of hormones with specific aspects of cardiac function,” the editorial authors wrote.
Dr. Miller and Dr. Mankad are both with the women’s health research center and department of cardiovascular disease at the Women’s Heart Clinic at the Mayo Clinic, Rochester, Minn. These comments are derived from their editorial in the Journal of the American College of Cardiology. Dr. Mankad had no disclosures, while Dr. Miller reported support from a National Institutes of Health grant.
This study offers new insights into the relationships between endogenous hormones and how they influence cardiovascular event risk, according to Virginia M. Miller, PhD, and Rekha Mankad, MD.
Previous observational studies have established that decreases in endogenous estrogen led to increases in cardiovascular event risk and incidence, Dr. Miller and Dr. Mankad said in an editorial referencing the study.
What’s less clear is the role of testosterone in cardiovascular risk and event incidence, both by itself and in relation to other endogenous hormones.
“Few studies have gone beyond singular associations of hormone levels with cardiovascular events,” the editorial authors wrote in the Journal of the American College of Cardiology.
The study by Zhao and her colleagues is unique in part because their analysis considers the ratio of testosterone to estradiol. In particular, they found that a higher testosterone to estradiol level was associated with a higher incidence of cardiovascular events overall and of coronary heart disease.
What was unexpected, according to Dr. Miller and Dr. Mankad, was a U-shaped association with incident heart failure. In subgroup analysis, investigators found a positive association between testosterone to estradiol ratio and heart failure with reduced ejection fraction but not with heart failure with preserved ejection fraction.
“By addressing a set of defined incident events, this study provides new information needed to develop mechanistic hypotheses of causal relationships of hormones with specific aspects of cardiac function,” the editorial authors wrote.
Dr. Miller and Dr. Mankad are both with the women’s health research center and department of cardiovascular disease at the Women’s Heart Clinic at the Mayo Clinic, Rochester, Minn. These comments are derived from their editorial in the Journal of the American College of Cardiology. Dr. Mankad had no disclosures, while Dr. Miller reported support from a National Institutes of Health grant.
This study offers new insights into the relationships between endogenous hormones and how they influence cardiovascular event risk, according to Virginia M. Miller, PhD, and Rekha Mankad, MD.
Previous observational studies have established that decreases in endogenous estrogen led to increases in cardiovascular event risk and incidence, Dr. Miller and Dr. Mankad said in an editorial referencing the study.
What’s less clear is the role of testosterone in cardiovascular risk and event incidence, both by itself and in relation to other endogenous hormones.
“Few studies have gone beyond singular associations of hormone levels with cardiovascular events,” the editorial authors wrote in the Journal of the American College of Cardiology.
The study by Zhao and her colleagues is unique in part because their analysis considers the ratio of testosterone to estradiol. In particular, they found that a higher testosterone to estradiol level was associated with a higher incidence of cardiovascular events overall and of coronary heart disease.
What was unexpected, according to Dr. Miller and Dr. Mankad, was a U-shaped association with incident heart failure. In subgroup analysis, investigators found a positive association between testosterone to estradiol ratio and heart failure with reduced ejection fraction but not with heart failure with preserved ejection fraction.
“By addressing a set of defined incident events, this study provides new information needed to develop mechanistic hypotheses of causal relationships of hormones with specific aspects of cardiac function,” the editorial authors wrote.
Dr. Miller and Dr. Mankad are both with the women’s health research center and department of cardiovascular disease at the Women’s Heart Clinic at the Mayo Clinic, Rochester, Minn. These comments are derived from their editorial in the Journal of the American College of Cardiology. Dr. Mankad had no disclosures, while Dr. Miller reported support from a National Institutes of Health grant.
In postmenopausal women, a higher level of testosterone in comparison to estrogen may increase the cardiovascular disease risk later in life, results of a recent analysis suggest.
A higher ratio of testosterone to estradiol was associated with the development of cardiovascular disease, coronary heart disease, and heart failure in postmenopausal women, according to results from an analysis based on 2,834 postmenopausal women in MESA (Multi-Ethnic Study of Atherosclerosis).
In addition, total testosterone levels were associated with increased cardiovascular disease and coronary heart disease, while estradiol is associated with a reduced risk of coronary heart disease and heart failure with reduced ejection fraction, investigators reported in the Journal of the American College of Cardiology.
Without any interventional studies as guidance, it’s not clear what the “best strategy” would be to modify sex hormone levels and reduce cardiovascular disease risk, wrote investigator Di Zhao, PhD, of the department of epidemiology at Johns Hopkins University Bloomberg School of Public Health, Baltimore, and her study coauthors.
“Nonetheless, a more androgenic sex hormone profile may identify a woman at higher risk for cardiovascular disease who may benefit from other risk-reducing strategies,” Dr. Zhao and her colleagues wrote in their report.
The postmenopausal women included in this analysis all had baseline measurements of testosterone, estradiol, dehydroepiandrosterone, and sex hormone–binding globulin levels between 2000 and 2002, according to the report.
After more than 12 years of follow-up, investigators found that a higher total testosterone to estradiol ratio was independently associated with an increased risk of incident cardiovascular disease (hazard ratio, 1.19; 95% confidence interval, 1.02-1.40), coronary heart disease (HR, 1.45; 95% CI, 1.19-1.78), and heart failure (HR, 1.31; 95% CI, 1.01-1.70).
Investigators also reported a statistically significant association between total testosterone levels and risk of cardiovascular disease and coronary heart disease but not risk of heart failure.
In a subgroup analysis of postmenopausal women with heart failure, investigators found a significant positive association with the testosterone to estradiol ratio (HR, 1.65; 95% CI, 1.07-2.54) and inverse associations for estradiol (HR, 0.60; 95% CI, 0.39-0.93) and for dehydroepiandrosterone (HR, 0.59; 95% CI, 0.44-0.78).
On their own, estradiol levels had no association with cardiovascular disease events overall, but they were associated with lower coronary heart disease risk, according to investigators. Estradiol also was associated with a lower heart failure risk, though the trend did not reach statistical significance.
The study was partially funded by the American Heart Association’s Go Red for Women Research Network. Study authors reported disclosures related to Cordex Systems, Siemens Diagnostics, and other entities.
SOURCE: Zhao D et al. J Am Coll Cardiol. 2018 Jun 5; 71:2555-66.
In postmenopausal women, a higher level of testosterone in comparison to estrogen may increase the cardiovascular disease risk later in life, results of a recent analysis suggest.
A higher ratio of testosterone to estradiol was associated with the development of cardiovascular disease, coronary heart disease, and heart failure in postmenopausal women, according to results from an analysis based on 2,834 postmenopausal women in MESA (Multi-Ethnic Study of Atherosclerosis).
In addition, total testosterone levels were associated with increased cardiovascular disease and coronary heart disease, while estradiol is associated with a reduced risk of coronary heart disease and heart failure with reduced ejection fraction, investigators reported in the Journal of the American College of Cardiology.
Without any interventional studies as guidance, it’s not clear what the “best strategy” would be to modify sex hormone levels and reduce cardiovascular disease risk, wrote investigator Di Zhao, PhD, of the department of epidemiology at Johns Hopkins University Bloomberg School of Public Health, Baltimore, and her study coauthors.
“Nonetheless, a more androgenic sex hormone profile may identify a woman at higher risk for cardiovascular disease who may benefit from other risk-reducing strategies,” Dr. Zhao and her colleagues wrote in their report.
The postmenopausal women included in this analysis all had baseline measurements of testosterone, estradiol, dehydroepiandrosterone, and sex hormone–binding globulin levels between 2000 and 2002, according to the report.
After more than 12 years of follow-up, investigators found that a higher total testosterone to estradiol ratio was independently associated with an increased risk of incident cardiovascular disease (hazard ratio, 1.19; 95% confidence interval, 1.02-1.40), coronary heart disease (HR, 1.45; 95% CI, 1.19-1.78), and heart failure (HR, 1.31; 95% CI, 1.01-1.70).
Investigators also reported a statistically significant association between total testosterone levels and risk of cardiovascular disease and coronary heart disease but not risk of heart failure.
In a subgroup analysis of postmenopausal women with heart failure, investigators found a significant positive association with the testosterone to estradiol ratio (HR, 1.65; 95% CI, 1.07-2.54) and inverse associations for estradiol (HR, 0.60; 95% CI, 0.39-0.93) and for dehydroepiandrosterone (HR, 0.59; 95% CI, 0.44-0.78).
On their own, estradiol levels had no association with cardiovascular disease events overall, but they were associated with lower coronary heart disease risk, according to investigators. Estradiol also was associated with a lower heart failure risk, though the trend did not reach statistical significance.
The study was partially funded by the American Heart Association’s Go Red for Women Research Network. Study authors reported disclosures related to Cordex Systems, Siemens Diagnostics, and other entities.
SOURCE: Zhao D et al. J Am Coll Cardiol. 2018 Jun 5; 71:2555-66.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point: Levels of testosterone and estradiol after menopause correlated with increased cardiovascular risks later in life.
Major finding: A higher total testosterone to estradiol ratio was independently associated with increased risk of incident cardiovascular disease (hazard ratio, 1.19; 95% confidence interval, 1.02-1.40).
Study details: Analysis including 2,834 postmenopausal women in the MESA (Multi-Ethnic Study of Atherosclerosis) study.
Disclosures: Partial funding came from the American Heart Association’s Go Red for Women Research Network. Study authors reported disclosures related to Cordex Systems, Siemens Diagnostics, and other entities.
Source: Zhao D et al. J Am Coll Cardiol. 2018 Jun 5; 71:2555-66.
Which Factors Predict Successful Epilepsy Reoperations?
LOS ANGELES—Among patients with intractable focal epilepsy who have failed one or more epilepsy surgeries, reoperation may provide long-term seizure control, according to research presented at the 70th Annual Meeting of the American Academy of Neurology. Patients with prior epilepsy surgery are less likely to achieve seizure freedom, however, compared with patients undergoing initial epilepsy surgery, the researchers said.
“It is possible to achieve long-term seizure control in patients with failed prior epilepsy surgery,” said Ruta Yardi, MD, a researcher at the Cleveland Clinic, and colleagues. “A lesional MRI, specific prior postoperative pathology, and fewer prior resections seem to predict better outcomes.” These results may be helpful in identifying candidates for reoperation, the investigators said.
Epilepsy surgery is the most effective treatment option for patients with medically refractory focal epilepsy, but initial surgeries may not be successful, Dr. Yardi and colleagues said. A small percentage of patients who do not benefit from a first surgery may be evaluated for another resection. Data for how outcomes vary with successive surgeries are limited, however, the researchers said.
To assess longitudinal seizure outcomes following reoperations in patients with intractable focal epilepsy and identify prognostic factors that influence these outcomes, Dr. Yardi and colleagues retrospectively studied 898 patients (448 female; about a third pediatric) who underwent epilepsy surgery at the Cleveland Clinic between 1995 and 2016. The investigators analyzed baseline characteristics, known predictors of seizure outcome, surgical data, pathology, and postoperative seizure recurrence. The primary outcome was complete seizure freedom (ie, Engel Class IA) at last follow-up.
The researchers analyzed the data using Kaplan–Meier survival curves and univariate and multivariate hazard modeling. The analysis included 788 patients without prior surgery, 92 patients with one prior surgery, and 18 patients with two or more prior surgeries. Two years after the most recent epilepsy surgery, 58% of patients with no prior surgery were seizure-free, compared with 49% of patients who had one prior surgery and 39% of patients who had two or more prior surgeries. Patients with more than one surgery were more likely to have an Engel outcome score of greater than Class I.
Variables that correlated with better seizu
—Jake Remaly
LOS ANGELES—Among patients with intractable focal epilepsy who have failed one or more epilepsy surgeries, reoperation may provide long-term seizure control, according to research presented at the 70th Annual Meeting of the American Academy of Neurology. Patients with prior epilepsy surgery are less likely to achieve seizure freedom, however, compared with patients undergoing initial epilepsy surgery, the researchers said.
“It is possible to achieve long-term seizure control in patients with failed prior epilepsy surgery,” said Ruta Yardi, MD, a researcher at the Cleveland Clinic, and colleagues. “A lesional MRI, specific prior postoperative pathology, and fewer prior resections seem to predict better outcomes.” These results may be helpful in identifying candidates for reoperation, the investigators said.
Epilepsy surgery is the most effective treatment option for patients with medically refractory focal epilepsy, but initial surgeries may not be successful, Dr. Yardi and colleagues said. A small percentage of patients who do not benefit from a first surgery may be evaluated for another resection. Data for how outcomes vary with successive surgeries are limited, however, the researchers said.
To assess longitudinal seizure outcomes following reoperations in patients with intractable focal epilepsy and identify prognostic factors that influence these outcomes, Dr. Yardi and colleagues retrospectively studied 898 patients (448 female; about a third pediatric) who underwent epilepsy surgery at the Cleveland Clinic between 1995 and 2016. The investigators analyzed baseline characteristics, known predictors of seizure outcome, surgical data, pathology, and postoperative seizure recurrence. The primary outcome was complete seizure freedom (ie, Engel Class IA) at last follow-up.
The researchers analyzed the data using Kaplan–Meier survival curves and univariate and multivariate hazard modeling. The analysis included 788 patients without prior surgery, 92 patients with one prior surgery, and 18 patients with two or more prior surgeries. Two years after the most recent epilepsy surgery, 58% of patients with no prior surgery were seizure-free, compared with 49% of patients who had one prior surgery and 39% of patients who had two or more prior surgeries. Patients with more than one surgery were more likely to have an Engel outcome score of greater than Class I.
Variables that correlated with better seizu
—Jake Remaly
LOS ANGELES—Among patients with intractable focal epilepsy who have failed one or more epilepsy surgeries, reoperation may provide long-term seizure control, according to research presented at the 70th Annual Meeting of the American Academy of Neurology. Patients with prior epilepsy surgery are less likely to achieve seizure freedom, however, compared with patients undergoing initial epilepsy surgery, the researchers said.
“It is possible to achieve long-term seizure control in patients with failed prior epilepsy surgery,” said Ruta Yardi, MD, a researcher at the Cleveland Clinic, and colleagues. “A lesional MRI, specific prior postoperative pathology, and fewer prior resections seem to predict better outcomes.” These results may be helpful in identifying candidates for reoperation, the investigators said.
Epilepsy surgery is the most effective treatment option for patients with medically refractory focal epilepsy, but initial surgeries may not be successful, Dr. Yardi and colleagues said. A small percentage of patients who do not benefit from a first surgery may be evaluated for another resection. Data for how outcomes vary with successive surgeries are limited, however, the researchers said.
To assess longitudinal seizure outcomes following reoperations in patients with intractable focal epilepsy and identify prognostic factors that influence these outcomes, Dr. Yardi and colleagues retrospectively studied 898 patients (448 female; about a third pediatric) who underwent epilepsy surgery at the Cleveland Clinic between 1995 and 2016. The investigators analyzed baseline characteristics, known predictors of seizure outcome, surgical data, pathology, and postoperative seizure recurrence. The primary outcome was complete seizure freedom (ie, Engel Class IA) at last follow-up.
The researchers analyzed the data using Kaplan–Meier survival curves and univariate and multivariate hazard modeling. The analysis included 788 patients without prior surgery, 92 patients with one prior surgery, and 18 patients with two or more prior surgeries. Two years after the most recent epilepsy surgery, 58% of patients with no prior surgery were seizure-free, compared with 49% of patients who had one prior surgery and 39% of patients who had two or more prior surgeries. Patients with more than one surgery were more likely to have an Engel outcome score of greater than Class I.
Variables that correlated with better seizu
—Jake Remaly
Effects of psoriatic arthritis not just physical
conducted by the Harris Poll on behalf of Pfizer.
Over 90% of respondents said that their psoriatic arthritis had negatively impacted their emotional and mental well-being and 75% reported negative effects on their relationships with friends and family, Pfizer reported. Among the 301 adults aged 18 years and older who responded to the survey, 58% had stopped participating in sports or recreational activities and 51% had stopped participating in social activities.
The effects on patients’ professional lives also were considerable: Almost 74% said that it had a negative effect on their career path, 41% had experienced decreased productivity, and 13% had quit or been let go from a job, Pfizer said.
Some of the survey results suggested a disconnect between patients and their physicians. Of the 89% of patients who were very or somewhat satisfied with their prescription medication, 90% said that they would like to make changes to their treatment regimen and 89% described their illness as moderate to severe, Pfizer reported.
The survey was conducted online from Nov. 2 to Dec. 1, 2017.
conducted by the Harris Poll on behalf of Pfizer.
Over 90% of respondents said that their psoriatic arthritis had negatively impacted their emotional and mental well-being and 75% reported negative effects on their relationships with friends and family, Pfizer reported. Among the 301 adults aged 18 years and older who responded to the survey, 58% had stopped participating in sports or recreational activities and 51% had stopped participating in social activities.
The effects on patients’ professional lives also were considerable: Almost 74% said that it had a negative effect on their career path, 41% had experienced decreased productivity, and 13% had quit or been let go from a job, Pfizer said.
Some of the survey results suggested a disconnect between patients and their physicians. Of the 89% of patients who were very or somewhat satisfied with their prescription medication, 90% said that they would like to make changes to their treatment regimen and 89% described their illness as moderate to severe, Pfizer reported.
The survey was conducted online from Nov. 2 to Dec. 1, 2017.
conducted by the Harris Poll on behalf of Pfizer.
Over 90% of respondents said that their psoriatic arthritis had negatively impacted their emotional and mental well-being and 75% reported negative effects on their relationships with friends and family, Pfizer reported. Among the 301 adults aged 18 years and older who responded to the survey, 58% had stopped participating in sports or recreational activities and 51% had stopped participating in social activities.
The effects on patients’ professional lives also were considerable: Almost 74% said that it had a negative effect on their career path, 41% had experienced decreased productivity, and 13% had quit or been let go from a job, Pfizer said.
Some of the survey results suggested a disconnect between patients and their physicians. Of the 89% of patients who were very or somewhat satisfied with their prescription medication, 90% said that they would like to make changes to their treatment regimen and 89% described their illness as moderate to severe, Pfizer reported.
The survey was conducted online from Nov. 2 to Dec. 1, 2017.