User login
Utilization of Primary Care Physicians by Medical Residents: A Survey-Based Study
From the University of Michigan Medical School, Ann Arbor, MI.
Abstract
- Objective: Existing research has demonstrated overall low rates of residents establishing care with a primary care physician (PCP). We conducted a survey-based study to better understand chronic illness, PCP utilization, and prescription medication use patterns in resident physician populations.
- Methods: In 2017, we invited internal and family medicine trainees from a convenience sample of U.S. residency programs to participate in a survey. We compared the characteristics of residents who had established care with a PCP to those who had not.
- Results: The response rate was 45% (348/766 residents). The majority (n = 205, 59%) of respondents stated they had established care with a PCP primarily for routine preventative care (n = 159, 79%) and access in the event of an emergency (n = 132, 66%). However, 31% (n = 103) denied having had a wellness visit in over 3 years. Nearly a quarter of residents (n = 77, 23%) reported a chronic medical illness and 14% (n = 45) reported a preexisting mental health condition prior to residency. One-third (n = 111, 33%) reported taking a long-term prescription medication. Compared to residents who had not established care, those with a PCP (n = 205) more often reported a chronic condition (P < 0.001), seeing a subspecialist (P = 0.01), or taking long-term prescription medications (P < 0.001). One in 5 (n = 62,19%) respondents reported receiving prescriptions for an acute illness from an individual with whom they did not have a doctor-patient relationship.
- Conclusion: Medical residents have a substantial burden of chronic illness that may not be met through interactions with PCPs. Further understanding their medical needs and barriers to accessing care is necessary to ensure trainee well-being.
Keywords: Medical education-graduate, physician behavior, survey research, access to care.
Although internal medicine (IM) and family medicine (FM) residents must learn to provide high-quality primary care to their patients, little is known about whether they appropriately access such care themselves. Resident burnout and resilience has received attention [1,2], but there has been limited focus on understanding the burden of chronic medical and mental illness among residents. In particular, little is known about whether residents access primary care physicians (PCPs)—for either acute or chronic medical needs—and about resident self-medication practices.
Residency is often characterized by a life-changing geographic relocation. Even residents who do not relocate may still need to establish care with a new PCP due to health insurance or loss of access to a student clinic [3]. Establishing primary care with a new doctor typically requires scheduling a new patient visit, often with a wait time of several days to weeks [4,5]. Furthermore, lack of time, erratic schedules, and concerns about privacy and the stigma of being ill as a physician are barriers to establishing care [6-8]. Individuals who have not established primary care may experience delays in routine preventative health services, screening for chronic medical and mental health conditions, as well as access to care during acute illnesses [9,10]. Worse, they may engage in potentially unsafe practices, such as having colleagues write prescriptions for them, or even self-prescribing [8,11,12].
Existing research has demonstrated overall low rates of residents establishing care with a PCP [6–8,13]. However, these studies have either been limited to large academic centers or conducted outside the United States. Improving resident well-being may prove challenging without a clear understanding of current primary care utilization practices, the burden of chronic illness among residents, and patterns of prescription medication use and needs. Therefore, we conducted a survey-based study to understand primary care utilization and the burden of chronic illness among residents. We also assessed whether lack of primary care is associated with potentially risky behaviors, such as self-prescribing of medications.
Methods
Study Setting and Participants
The survey was distributed to current residents at IM and FM programs within the United States in 2017. Individual programs were recruited by directly contacting program directors or chief medical residents via email. Rather than contacting sites directly through standard templated emails, we identified programs both through personal contacts as well as the Electronic Residency Application Service list of accredited IM training programs. We elected to use this approach in order to increase response rates and to ensure that a sample representative of the trainee population was constructed. Programs were located in the Northeast, Midwest, South, and Pacific regions, and included small community-based programs and large academic centers.
Development of the Survey
The survey instrument was developed by the authors and reviewed by residents and PCPs at the University of Michigan to ensure relevance and comprehension of questions (The survey is available in the Appendix.). Once finalized, the survey was programmed into an online survey tool (Qualtrics, Provo, UT) and pilot-tested before being disseminated to the sampling frame. Data collected in the survey included: respondent’s utilization of a PCP, burden of chronic illness, long-term prescription medications, prescribing source, and demographic characteristics.
Each participating program distributed the survey to their residents through an email containing an anonymous hyperlink. The survey was available for completion for 4 weeks. We asked participating programs to send email reminders to encourage participation. Participants were given the option of receiving a $10 Amazon gift card after completion. All responses were recorded anonymously. The study received a “not regulated” status by the University of Michigan Institutional Review Board (HUM 00123888).
Statistical Analysis
Descriptive statistics were used to tabulate results. Respondents were encouraged, but not required, to answer all questions. Therefore, the response rate for each question was calculated using the total number of responses for that question as the denominator. Bivariable comparisons were made using Chi-squared or Fisher’s exact tests, as appropriate, for categorical data. A P value < 0.05, with 2-sided alpha, was considered statistically significant. All statistical analyses were conducted using Stata 13 SE (StataCorp, College Station, TX).
Results
Respondent Characteristics
Of the 29 programs contacted, 10 agreed to participate within the study timeframe. Of 766 potential respondents, 348 (45%) residents answered the survey (Table 1). The majority of respondents (n = 276, 82%) were from IM programs. Respondents were from all training years as follows: postgraduate year 1 residents (PGY-1, or interns; n = 130, 39%), PGY-2 residents (n = 98, 29%), PGY-3 residents (n = 93, 28%), and PGY-4 residents (n = 12, 4%). Most respondents were from the South (n = 130, 39%) and Midwest (n = 123, 37%) regions, and over half (n = 179, 54%) were female. Most respondents (n = 285, 86%) stated that they did not have children. The majority (n = 236, 71%) were completing residency in an area where they had not previously lived for more than 1 year.
Primary Care Utilization
Among the 348 respondents, 59% (n = 205) reported having established care with a PCP. An additional 6% (n = 21) had established care with an obstetrician/gynecologist for routine needs (Table 2). The 2 most common reasons for establishing care with a PCP were routine primary care needs, including contraception (n = 159, 79%), and access to a physician in the event of an acute medical need (n = 132, 66%).
Among respondents who had established care with a PCP, most (n = 188, 94%) had completed at least 1 appointment. However, among these 188 respondents, 68% (n = 127) stated that they had not made an acute visit in more than 12 months. When asked about wellness visits, almost one third of respondents (n = 103, 31%) stated that they had not been seen for a wellness visit in the past 3 years.
Burden of Chronic Illness
Most respondents (n = 223, 67%) stated that they did not have a chronic medical or mental health condition prior to residency (Table 3). However, 23% (n = 77) of respondents stated that they had been diagnosed with a chronic medical illness prior to residency, and 14% (n = 45) indicated they had been diagnosed with a mental health condition prior to residency. Almost one fifth of respondents (n = 60, 18%) reported seeing a subspecialist for a medical illness, and 33% (n = 111) reported taking a long-term prescription medication. With respect to major medical issues, the majority of residents (n = 239, 72%) denied experiencing events such as pregnancy, hospitalization, surgery, or an emergency department (ED) visit during training.
[polldaddy:10116940]
Inappropriate Prescriptions
While the majority of respondents denied writing a prescription for themselves for an acute or chronic medical condition, almost one fifth (n = 62, 19%) had received a prescription for an acute medical need from a provider outside of a clinical relationship (ie, from someone other than their PCP or specialty provider). Notably, 5% (n = 15) reported that this had occurred at least 2 or 3 times in the past 12 months (Table 4). Compared to respondents not taking long-term prescription medications, respondents who were already taking long-term prescription medications more frequently reported inappropriately receiving chronic prescriptions outside of an established clinical relationship (n = 14, 13% vs. n = 14, 6%; P = 0.05) and more often self-prescribed medications for acute needs (n = 12, 11% vs. n = 7, 3%; P = 0.005).
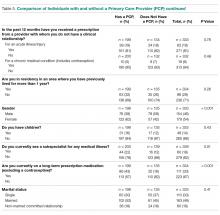
Comparison of Residents With and Without a PCP
Important differences were noted between residents who had a PCP versus those who did not (Table 5). For example, a higher percentage of residents with a PCP indicated they had been diagnosed with a chronic medical illness (n = 55, 28% vs. n = 22, 16%; P = 0.01) or a chronic mental health condition (n = 34, 17% vs. n = 11, 8%; P = 0.02) before residency. Additionally, a higher percentage of residents with a PCP (n = 70, 35% vs. n = 25, 18%; P = 0.001) reported experiencing medical events such as pregnancy, hospitalization, surgery, ED visit, or new diagnosis of a chronic medical illness during residency. Finally, a higher percentage of respondents with a PCP stated that they had visited a subspecialist for a medical illness (n = 44, 22% vs. n = 16,12%; P = 0.01) or were taking long-term prescription medications (n = 86, 43% vs. n = 25; 18%; P < 0.001). When comparing PGY-1 to PGY-2–PGY-4 residents, the former reported having established a medical relationship with a PCP significantly less frequently (n = 56, 43% vs. n = 142, 70%; P < 0.001).
Discussion
This survey-based study of medical residents across the United States suggests that a substantial proportion do not establish relationships with PCPs. Additionally, our data suggest that despite establishing care, few residents subsequently visited their PCP during training for wellness visits or routine care. Self-reported rates of chronic medical and mental health conditions were substantial in our sample. Furthermore, inappropriate self-prescription and the receipt of prescriptions outside of a medical relationship were also reported. These findings suggest that future studies that focus on the unique medical and mental health needs of physicians in training, as well as interventions to encourage care in this vulnerable period, are necessary.
We observed that most respondents that established primary care were female trainees. Although it is impossible to know with certainty, one hypothesis behind this discrepancy is that women routinely need to access preventative care for gynecologic needs such as pap smears, contraception, and potentially pregnancy and preconception counseling [14,15]. Similarly, residents with a chronic medical or mental health condition prior to residency established care with a local PCP at a significantly greater frequency than those without such diagnoses. While selection bias cannot be excluded, this finding suggests that illness is a driving factor in establishing care. There also appears to be an association between accessing the medical system (either for prescription medications or subspecialist care) and having established care with a PCP. Collectively, these data suggest that individuals without a compelling reason to access medical services might have barriers to accessing care in the event of medical needs or may not receive routine preventative care [9,10].
In general, we found that rates of reported inappropriate prescriptions were lower than those reported in prior studies where a comparable resident population was surveyed [8,12,16]. Inclusion of multiple institutions, differences in temporality, social desirability bias, and reporting bias might have influenced our findings in this regard. Surprisingly, we found that having a PCP did not influence likelihood of inappropriate prescription receipt, perhaps suggesting that this behavior reflects some degree of universal difficulty in accessing care. Alternatively, this finding might relate to a cultural tendency to self-prescribe among resident physicians. The fact that individuals on chronic medications more often both received and wrote inappropriate prescriptions suggests this problem might be more pronounced in individuals who take medications more often, as these residents have specific needs [12]. Future studies targeting these individuals thus appear warranted.
Our study has several limitations. First, our sample size was modest and the response rate of 45% was low. However, to our knowledge, this remains among the largest survey on this topic, and our response rate is comparable to similar trainee studies [8,11,13]. Second, we designed and created a novel survey for this study. While the questions were pilot-tested with users prior to dissemination, validation of the instrument was not performed. Third, since the study population was restricted to residents in fields that participate in primary care, our findings may not be generalizable to patterns of PCP use in other specialties [6].
These limitations aside, our study has important strengths. This is the first national study of its kind with specific questions addressing primary care access and utilization, prescription medication use and related practices, and the prevalence of medical conditions among trainees. Important differences in the rates of establishing primary care between male and female respondents, first- year and senior residents, and those with and without chronic disease suggest a need to target specific resident groups (males, interns, those without pre-existing conditions) for wellness-related interventions. Such interventions could include distribution of a list of local providers to first year residents, advanced protected time for doctor’s appointments, and safeguards to ensure health information is protected from potential supervisors. Future studies should also include residents from non-primary care oriented specialties such as surgery, emergency medicine, and anesthesiology to obtain results that are more generalizable to the resident population as a whole. Additionally, the rates of inappropriate prescriptions were not insignificant and warrant further evaluation of the driving forces behind these behaviors.
Conclusion
Medical residents have a substantial burden of chronic illness that may not be met through interactions with PCPs. More research into barriers that residents face while accessing care and an assessment of interventions to facilitate their access to care is important to promote trainee well-being. Without such direction and initiative, it may prove harder for physicians to heal themselves or those for whom they provide care.
Acknowledgments: We thank Suzanne Winter, the study coordinator, for her support with editing and formatting the manuscript, Latoya Kuhn for performing the statistical analysis and creating data tables, and Dr. Namita Sachdev and Dr. Renuka Tipirneni for providing feedback on the survey instrument. We also thank the involved programs for their participation.
Corresponding author: Vineet Chopra, NCRC 2800 Plymouth Rd., Bldg 16, 432, Ann Arbor, MI 48109, [email protected].
Financial disclosures: None.
Previous presentations: Results were presented at the Annual Michigan Medicine 2017 Internal Medicine Research Symposium.
1. Kassam A, Horton J, Shoimer I, Patten S. Predictors of well-being in resident physicians: a descriptive and psychometric study. J Grad Med Educ 2015;7:70–4.
2. Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med 2002;136:358–67.
3. Burstin HR, Swartz K, O’Neil AC, et al. The effect of change of health insurance on access to care. Inquiry 1998;35:389–97.
4. Rhodes KV, Basseyn S, Friedman AB, et al. Access to primary care appointments following 2014 insurance expansions. Ann Fam Med 2017;15:107–12.
5. Polsky D, Richards M, Basseyn S, et al. Appointment availability after increases in Medicaid payments for primary care. N Engl J Med 2015;372:537–45.
6. Gupta G, Schleinitz MD, Reinert SE, McGarry KA. Resident physician preventive health behaviors and perspectives on primary care. R I Med J (2013) 2013;96:43–7.
7. Rosen IM, Christine JD, Bellini LM, Asch DA. Health and health care among housestaff in four U.S. internal medicine residency programs. J Gen Intern Med 2000;15:116-21.
8. Campbell S, Delva D. Physician do not heal thyself. Survey of personal health practices among medical residents. Can Fam Physician 2003;49:1121–7.
9. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q 2005;83(3):457-502.
10. Weissman JS, Stern R, Fielding SL, et al. Delayed access to health care: risk factors, reasons, and consequences. Ann Intern Med 1991;114:325–31.
11. Guille C, Sen S. Prescription drug use and self-prescription among training physicians. Arch Intern Med 2012;172:371–2.
12. Roberts LW, Kim JP. Informal health care practices of residents: “curbside” consultation and self-diagnosis and treatment. Acad Psychiatry 2015;39:22-30.
13. Cohen JS, Patten S. Well-being in residency training: a survey examining resident physician satisfaction both within and outside of residency training and mental health in Alberta. BMC Med Educ 2005;5:21.
14. U.S. Preventive Services Task Force. Cervical cancer: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/cervical-cancer-screening. Published March 2012. Accessed August 21, 2018.
15. Health Resources and Services Administration. Women’s preventative services guidelines. https://www.hrsa.gov/womensguidelines2016/index.html. Updated October 2017. Accessed August 21, 2018.
16. Christie JD, Rosen IM, Bellini LM, et al. Prescription drug use and self-prescription among resident physicians. JAMA 1998;280(14):1253–5.
From the University of Michigan Medical School, Ann Arbor, MI.
Abstract
- Objective: Existing research has demonstrated overall low rates of residents establishing care with a primary care physician (PCP). We conducted a survey-based study to better understand chronic illness, PCP utilization, and prescription medication use patterns in resident physician populations.
- Methods: In 2017, we invited internal and family medicine trainees from a convenience sample of U.S. residency programs to participate in a survey. We compared the characteristics of residents who had established care with a PCP to those who had not.
- Results: The response rate was 45% (348/766 residents). The majority (n = 205, 59%) of respondents stated they had established care with a PCP primarily for routine preventative care (n = 159, 79%) and access in the event of an emergency (n = 132, 66%). However, 31% (n = 103) denied having had a wellness visit in over 3 years. Nearly a quarter of residents (n = 77, 23%) reported a chronic medical illness and 14% (n = 45) reported a preexisting mental health condition prior to residency. One-third (n = 111, 33%) reported taking a long-term prescription medication. Compared to residents who had not established care, those with a PCP (n = 205) more often reported a chronic condition (P < 0.001), seeing a subspecialist (P = 0.01), or taking long-term prescription medications (P < 0.001). One in 5 (n = 62,19%) respondents reported receiving prescriptions for an acute illness from an individual with whom they did not have a doctor-patient relationship.
- Conclusion: Medical residents have a substantial burden of chronic illness that may not be met through interactions with PCPs. Further understanding their medical needs and barriers to accessing care is necessary to ensure trainee well-being.
Keywords: Medical education-graduate, physician behavior, survey research, access to care.
Although internal medicine (IM) and family medicine (FM) residents must learn to provide high-quality primary care to their patients, little is known about whether they appropriately access such care themselves. Resident burnout and resilience has received attention [1,2], but there has been limited focus on understanding the burden of chronic medical and mental illness among residents. In particular, little is known about whether residents access primary care physicians (PCPs)—for either acute or chronic medical needs—and about resident self-medication practices.
Residency is often characterized by a life-changing geographic relocation. Even residents who do not relocate may still need to establish care with a new PCP due to health insurance or loss of access to a student clinic [3]. Establishing primary care with a new doctor typically requires scheduling a new patient visit, often with a wait time of several days to weeks [4,5]. Furthermore, lack of time, erratic schedules, and concerns about privacy and the stigma of being ill as a physician are barriers to establishing care [6-8]. Individuals who have not established primary care may experience delays in routine preventative health services, screening for chronic medical and mental health conditions, as well as access to care during acute illnesses [9,10]. Worse, they may engage in potentially unsafe practices, such as having colleagues write prescriptions for them, or even self-prescribing [8,11,12].
Existing research has demonstrated overall low rates of residents establishing care with a PCP [6–8,13]. However, these studies have either been limited to large academic centers or conducted outside the United States. Improving resident well-being may prove challenging without a clear understanding of current primary care utilization practices, the burden of chronic illness among residents, and patterns of prescription medication use and needs. Therefore, we conducted a survey-based study to understand primary care utilization and the burden of chronic illness among residents. We also assessed whether lack of primary care is associated with potentially risky behaviors, such as self-prescribing of medications.
Methods
Study Setting and Participants
The survey was distributed to current residents at IM and FM programs within the United States in 2017. Individual programs were recruited by directly contacting program directors or chief medical residents via email. Rather than contacting sites directly through standard templated emails, we identified programs both through personal contacts as well as the Electronic Residency Application Service list of accredited IM training programs. We elected to use this approach in order to increase response rates and to ensure that a sample representative of the trainee population was constructed. Programs were located in the Northeast, Midwest, South, and Pacific regions, and included small community-based programs and large academic centers.
Development of the Survey
The survey instrument was developed by the authors and reviewed by residents and PCPs at the University of Michigan to ensure relevance and comprehension of questions (The survey is available in the Appendix.). Once finalized, the survey was programmed into an online survey tool (Qualtrics, Provo, UT) and pilot-tested before being disseminated to the sampling frame. Data collected in the survey included: respondent’s utilization of a PCP, burden of chronic illness, long-term prescription medications, prescribing source, and demographic characteristics.
Each participating program distributed the survey to their residents through an email containing an anonymous hyperlink. The survey was available for completion for 4 weeks. We asked participating programs to send email reminders to encourage participation. Participants were given the option of receiving a $10 Amazon gift card after completion. All responses were recorded anonymously. The study received a “not regulated” status by the University of Michigan Institutional Review Board (HUM 00123888).
Statistical Analysis
Descriptive statistics were used to tabulate results. Respondents were encouraged, but not required, to answer all questions. Therefore, the response rate for each question was calculated using the total number of responses for that question as the denominator. Bivariable comparisons were made using Chi-squared or Fisher’s exact tests, as appropriate, for categorical data. A P value < 0.05, with 2-sided alpha, was considered statistically significant. All statistical analyses were conducted using Stata 13 SE (StataCorp, College Station, TX).
Results
Respondent Characteristics
Of the 29 programs contacted, 10 agreed to participate within the study timeframe. Of 766 potential respondents, 348 (45%) residents answered the survey (Table 1). The majority of respondents (n = 276, 82%) were from IM programs. Respondents were from all training years as follows: postgraduate year 1 residents (PGY-1, or interns; n = 130, 39%), PGY-2 residents (n = 98, 29%), PGY-3 residents (n = 93, 28%), and PGY-4 residents (n = 12, 4%). Most respondents were from the South (n = 130, 39%) and Midwest (n = 123, 37%) regions, and over half (n = 179, 54%) were female. Most respondents (n = 285, 86%) stated that they did not have children. The majority (n = 236, 71%) were completing residency in an area where they had not previously lived for more than 1 year.
Primary Care Utilization
Among the 348 respondents, 59% (n = 205) reported having established care with a PCP. An additional 6% (n = 21) had established care with an obstetrician/gynecologist for routine needs (Table 2). The 2 most common reasons for establishing care with a PCP were routine primary care needs, including contraception (n = 159, 79%), and access to a physician in the event of an acute medical need (n = 132, 66%).
Among respondents who had established care with a PCP, most (n = 188, 94%) had completed at least 1 appointment. However, among these 188 respondents, 68% (n = 127) stated that they had not made an acute visit in more than 12 months. When asked about wellness visits, almost one third of respondents (n = 103, 31%) stated that they had not been seen for a wellness visit in the past 3 years.
Burden of Chronic Illness
Most respondents (n = 223, 67%) stated that they did not have a chronic medical or mental health condition prior to residency (Table 3). However, 23% (n = 77) of respondents stated that they had been diagnosed with a chronic medical illness prior to residency, and 14% (n = 45) indicated they had been diagnosed with a mental health condition prior to residency. Almost one fifth of respondents (n = 60, 18%) reported seeing a subspecialist for a medical illness, and 33% (n = 111) reported taking a long-term prescription medication. With respect to major medical issues, the majority of residents (n = 239, 72%) denied experiencing events such as pregnancy, hospitalization, surgery, or an emergency department (ED) visit during training.
[polldaddy:10116940]
Inappropriate Prescriptions
While the majority of respondents denied writing a prescription for themselves for an acute or chronic medical condition, almost one fifth (n = 62, 19%) had received a prescription for an acute medical need from a provider outside of a clinical relationship (ie, from someone other than their PCP or specialty provider). Notably, 5% (n = 15) reported that this had occurred at least 2 or 3 times in the past 12 months (Table 4). Compared to respondents not taking long-term prescription medications, respondents who were already taking long-term prescription medications more frequently reported inappropriately receiving chronic prescriptions outside of an established clinical relationship (n = 14, 13% vs. n = 14, 6%; P = 0.05) and more often self-prescribed medications for acute needs (n = 12, 11% vs. n = 7, 3%; P = 0.005).
Comparison of Residents With and Without a PCP
Important differences were noted between residents who had a PCP versus those who did not (Table 5). For example, a higher percentage of residents with a PCP indicated they had been diagnosed with a chronic medical illness (n = 55, 28% vs. n = 22, 16%; P = 0.01) or a chronic mental health condition (n = 34, 17% vs. n = 11, 8%; P = 0.02) before residency. Additionally, a higher percentage of residents with a PCP (n = 70, 35% vs. n = 25, 18%; P = 0.001) reported experiencing medical events such as pregnancy, hospitalization, surgery, ED visit, or new diagnosis of a chronic medical illness during residency. Finally, a higher percentage of respondents with a PCP stated that they had visited a subspecialist for a medical illness (n = 44, 22% vs. n = 16,12%; P = 0.01) or were taking long-term prescription medications (n = 86, 43% vs. n = 25; 18%; P < 0.001). When comparing PGY-1 to PGY-2–PGY-4 residents, the former reported having established a medical relationship with a PCP significantly less frequently (n = 56, 43% vs. n = 142, 70%; P < 0.001).
Discussion
This survey-based study of medical residents across the United States suggests that a substantial proportion do not establish relationships with PCPs. Additionally, our data suggest that despite establishing care, few residents subsequently visited their PCP during training for wellness visits or routine care. Self-reported rates of chronic medical and mental health conditions were substantial in our sample. Furthermore, inappropriate self-prescription and the receipt of prescriptions outside of a medical relationship were also reported. These findings suggest that future studies that focus on the unique medical and mental health needs of physicians in training, as well as interventions to encourage care in this vulnerable period, are necessary.
We observed that most respondents that established primary care were female trainees. Although it is impossible to know with certainty, one hypothesis behind this discrepancy is that women routinely need to access preventative care for gynecologic needs such as pap smears, contraception, and potentially pregnancy and preconception counseling [14,15]. Similarly, residents with a chronic medical or mental health condition prior to residency established care with a local PCP at a significantly greater frequency than those without such diagnoses. While selection bias cannot be excluded, this finding suggests that illness is a driving factor in establishing care. There also appears to be an association between accessing the medical system (either for prescription medications or subspecialist care) and having established care with a PCP. Collectively, these data suggest that individuals without a compelling reason to access medical services might have barriers to accessing care in the event of medical needs or may not receive routine preventative care [9,10].
In general, we found that rates of reported inappropriate prescriptions were lower than those reported in prior studies where a comparable resident population was surveyed [8,12,16]. Inclusion of multiple institutions, differences in temporality, social desirability bias, and reporting bias might have influenced our findings in this regard. Surprisingly, we found that having a PCP did not influence likelihood of inappropriate prescription receipt, perhaps suggesting that this behavior reflects some degree of universal difficulty in accessing care. Alternatively, this finding might relate to a cultural tendency to self-prescribe among resident physicians. The fact that individuals on chronic medications more often both received and wrote inappropriate prescriptions suggests this problem might be more pronounced in individuals who take medications more often, as these residents have specific needs [12]. Future studies targeting these individuals thus appear warranted.
Our study has several limitations. First, our sample size was modest and the response rate of 45% was low. However, to our knowledge, this remains among the largest survey on this topic, and our response rate is comparable to similar trainee studies [8,11,13]. Second, we designed and created a novel survey for this study. While the questions were pilot-tested with users prior to dissemination, validation of the instrument was not performed. Third, since the study population was restricted to residents in fields that participate in primary care, our findings may not be generalizable to patterns of PCP use in other specialties [6].
These limitations aside, our study has important strengths. This is the first national study of its kind with specific questions addressing primary care access and utilization, prescription medication use and related practices, and the prevalence of medical conditions among trainees. Important differences in the rates of establishing primary care between male and female respondents, first- year and senior residents, and those with and without chronic disease suggest a need to target specific resident groups (males, interns, those without pre-existing conditions) for wellness-related interventions. Such interventions could include distribution of a list of local providers to first year residents, advanced protected time for doctor’s appointments, and safeguards to ensure health information is protected from potential supervisors. Future studies should also include residents from non-primary care oriented specialties such as surgery, emergency medicine, and anesthesiology to obtain results that are more generalizable to the resident population as a whole. Additionally, the rates of inappropriate prescriptions were not insignificant and warrant further evaluation of the driving forces behind these behaviors.
Conclusion
Medical residents have a substantial burden of chronic illness that may not be met through interactions with PCPs. More research into barriers that residents face while accessing care and an assessment of interventions to facilitate their access to care is important to promote trainee well-being. Without such direction and initiative, it may prove harder for physicians to heal themselves or those for whom they provide care.
Acknowledgments: We thank Suzanne Winter, the study coordinator, for her support with editing and formatting the manuscript, Latoya Kuhn for performing the statistical analysis and creating data tables, and Dr. Namita Sachdev and Dr. Renuka Tipirneni for providing feedback on the survey instrument. We also thank the involved programs for their participation.
Corresponding author: Vineet Chopra, NCRC 2800 Plymouth Rd., Bldg 16, 432, Ann Arbor, MI 48109, [email protected].
Financial disclosures: None.
Previous presentations: Results were presented at the Annual Michigan Medicine 2017 Internal Medicine Research Symposium.
From the University of Michigan Medical School, Ann Arbor, MI.
Abstract
- Objective: Existing research has demonstrated overall low rates of residents establishing care with a primary care physician (PCP). We conducted a survey-based study to better understand chronic illness, PCP utilization, and prescription medication use patterns in resident physician populations.
- Methods: In 2017, we invited internal and family medicine trainees from a convenience sample of U.S. residency programs to participate in a survey. We compared the characteristics of residents who had established care with a PCP to those who had not.
- Results: The response rate was 45% (348/766 residents). The majority (n = 205, 59%) of respondents stated they had established care with a PCP primarily for routine preventative care (n = 159, 79%) and access in the event of an emergency (n = 132, 66%). However, 31% (n = 103) denied having had a wellness visit in over 3 years. Nearly a quarter of residents (n = 77, 23%) reported a chronic medical illness and 14% (n = 45) reported a preexisting mental health condition prior to residency. One-third (n = 111, 33%) reported taking a long-term prescription medication. Compared to residents who had not established care, those with a PCP (n = 205) more often reported a chronic condition (P < 0.001), seeing a subspecialist (P = 0.01), or taking long-term prescription medications (P < 0.001). One in 5 (n = 62,19%) respondents reported receiving prescriptions for an acute illness from an individual with whom they did not have a doctor-patient relationship.
- Conclusion: Medical residents have a substantial burden of chronic illness that may not be met through interactions with PCPs. Further understanding their medical needs and barriers to accessing care is necessary to ensure trainee well-being.
Keywords: Medical education-graduate, physician behavior, survey research, access to care.
Although internal medicine (IM) and family medicine (FM) residents must learn to provide high-quality primary care to their patients, little is known about whether they appropriately access such care themselves. Resident burnout and resilience has received attention [1,2], but there has been limited focus on understanding the burden of chronic medical and mental illness among residents. In particular, little is known about whether residents access primary care physicians (PCPs)—for either acute or chronic medical needs—and about resident self-medication practices.
Residency is often characterized by a life-changing geographic relocation. Even residents who do not relocate may still need to establish care with a new PCP due to health insurance or loss of access to a student clinic [3]. Establishing primary care with a new doctor typically requires scheduling a new patient visit, often with a wait time of several days to weeks [4,5]. Furthermore, lack of time, erratic schedules, and concerns about privacy and the stigma of being ill as a physician are barriers to establishing care [6-8]. Individuals who have not established primary care may experience delays in routine preventative health services, screening for chronic medical and mental health conditions, as well as access to care during acute illnesses [9,10]. Worse, they may engage in potentially unsafe practices, such as having colleagues write prescriptions for them, or even self-prescribing [8,11,12].
Existing research has demonstrated overall low rates of residents establishing care with a PCP [6–8,13]. However, these studies have either been limited to large academic centers or conducted outside the United States. Improving resident well-being may prove challenging without a clear understanding of current primary care utilization practices, the burden of chronic illness among residents, and patterns of prescription medication use and needs. Therefore, we conducted a survey-based study to understand primary care utilization and the burden of chronic illness among residents. We also assessed whether lack of primary care is associated with potentially risky behaviors, such as self-prescribing of medications.
Methods
Study Setting and Participants
The survey was distributed to current residents at IM and FM programs within the United States in 2017. Individual programs were recruited by directly contacting program directors or chief medical residents via email. Rather than contacting sites directly through standard templated emails, we identified programs both through personal contacts as well as the Electronic Residency Application Service list of accredited IM training programs. We elected to use this approach in order to increase response rates and to ensure that a sample representative of the trainee population was constructed. Programs were located in the Northeast, Midwest, South, and Pacific regions, and included small community-based programs and large academic centers.
Development of the Survey
The survey instrument was developed by the authors and reviewed by residents and PCPs at the University of Michigan to ensure relevance and comprehension of questions (The survey is available in the Appendix.). Once finalized, the survey was programmed into an online survey tool (Qualtrics, Provo, UT) and pilot-tested before being disseminated to the sampling frame. Data collected in the survey included: respondent’s utilization of a PCP, burden of chronic illness, long-term prescription medications, prescribing source, and demographic characteristics.
Each participating program distributed the survey to their residents through an email containing an anonymous hyperlink. The survey was available for completion for 4 weeks. We asked participating programs to send email reminders to encourage participation. Participants were given the option of receiving a $10 Amazon gift card after completion. All responses were recorded anonymously. The study received a “not regulated” status by the University of Michigan Institutional Review Board (HUM 00123888).
Statistical Analysis
Descriptive statistics were used to tabulate results. Respondents were encouraged, but not required, to answer all questions. Therefore, the response rate for each question was calculated using the total number of responses for that question as the denominator. Bivariable comparisons were made using Chi-squared or Fisher’s exact tests, as appropriate, for categorical data. A P value < 0.05, with 2-sided alpha, was considered statistically significant. All statistical analyses were conducted using Stata 13 SE (StataCorp, College Station, TX).
Results
Respondent Characteristics
Of the 29 programs contacted, 10 agreed to participate within the study timeframe. Of 766 potential respondents, 348 (45%) residents answered the survey (Table 1). The majority of respondents (n = 276, 82%) were from IM programs. Respondents were from all training years as follows: postgraduate year 1 residents (PGY-1, or interns; n = 130, 39%), PGY-2 residents (n = 98, 29%), PGY-3 residents (n = 93, 28%), and PGY-4 residents (n = 12, 4%). Most respondents were from the South (n = 130, 39%) and Midwest (n = 123, 37%) regions, and over half (n = 179, 54%) were female. Most respondents (n = 285, 86%) stated that they did not have children. The majority (n = 236, 71%) were completing residency in an area where they had not previously lived for more than 1 year.
Primary Care Utilization
Among the 348 respondents, 59% (n = 205) reported having established care with a PCP. An additional 6% (n = 21) had established care with an obstetrician/gynecologist for routine needs (Table 2). The 2 most common reasons for establishing care with a PCP were routine primary care needs, including contraception (n = 159, 79%), and access to a physician in the event of an acute medical need (n = 132, 66%).
Among respondents who had established care with a PCP, most (n = 188, 94%) had completed at least 1 appointment. However, among these 188 respondents, 68% (n = 127) stated that they had not made an acute visit in more than 12 months. When asked about wellness visits, almost one third of respondents (n = 103, 31%) stated that they had not been seen for a wellness visit in the past 3 years.
Burden of Chronic Illness
Most respondents (n = 223, 67%) stated that they did not have a chronic medical or mental health condition prior to residency (Table 3). However, 23% (n = 77) of respondents stated that they had been diagnosed with a chronic medical illness prior to residency, and 14% (n = 45) indicated they had been diagnosed with a mental health condition prior to residency. Almost one fifth of respondents (n = 60, 18%) reported seeing a subspecialist for a medical illness, and 33% (n = 111) reported taking a long-term prescription medication. With respect to major medical issues, the majority of residents (n = 239, 72%) denied experiencing events such as pregnancy, hospitalization, surgery, or an emergency department (ED) visit during training.
[polldaddy:10116940]
Inappropriate Prescriptions
While the majority of respondents denied writing a prescription for themselves for an acute or chronic medical condition, almost one fifth (n = 62, 19%) had received a prescription for an acute medical need from a provider outside of a clinical relationship (ie, from someone other than their PCP or specialty provider). Notably, 5% (n = 15) reported that this had occurred at least 2 or 3 times in the past 12 months (Table 4). Compared to respondents not taking long-term prescription medications, respondents who were already taking long-term prescription medications more frequently reported inappropriately receiving chronic prescriptions outside of an established clinical relationship (n = 14, 13% vs. n = 14, 6%; P = 0.05) and more often self-prescribed medications for acute needs (n = 12, 11% vs. n = 7, 3%; P = 0.005).
Comparison of Residents With and Without a PCP
Important differences were noted between residents who had a PCP versus those who did not (Table 5). For example, a higher percentage of residents with a PCP indicated they had been diagnosed with a chronic medical illness (n = 55, 28% vs. n = 22, 16%; P = 0.01) or a chronic mental health condition (n = 34, 17% vs. n = 11, 8%; P = 0.02) before residency. Additionally, a higher percentage of residents with a PCP (n = 70, 35% vs. n = 25, 18%; P = 0.001) reported experiencing medical events such as pregnancy, hospitalization, surgery, ED visit, or new diagnosis of a chronic medical illness during residency. Finally, a higher percentage of respondents with a PCP stated that they had visited a subspecialist for a medical illness (n = 44, 22% vs. n = 16,12%; P = 0.01) or were taking long-term prescription medications (n = 86, 43% vs. n = 25; 18%; P < 0.001). When comparing PGY-1 to PGY-2–PGY-4 residents, the former reported having established a medical relationship with a PCP significantly less frequently (n = 56, 43% vs. n = 142, 70%; P < 0.001).
Discussion
This survey-based study of medical residents across the United States suggests that a substantial proportion do not establish relationships with PCPs. Additionally, our data suggest that despite establishing care, few residents subsequently visited their PCP during training for wellness visits or routine care. Self-reported rates of chronic medical and mental health conditions were substantial in our sample. Furthermore, inappropriate self-prescription and the receipt of prescriptions outside of a medical relationship were also reported. These findings suggest that future studies that focus on the unique medical and mental health needs of physicians in training, as well as interventions to encourage care in this vulnerable period, are necessary.
We observed that most respondents that established primary care were female trainees. Although it is impossible to know with certainty, one hypothesis behind this discrepancy is that women routinely need to access preventative care for gynecologic needs such as pap smears, contraception, and potentially pregnancy and preconception counseling [14,15]. Similarly, residents with a chronic medical or mental health condition prior to residency established care with a local PCP at a significantly greater frequency than those without such diagnoses. While selection bias cannot be excluded, this finding suggests that illness is a driving factor in establishing care. There also appears to be an association between accessing the medical system (either for prescription medications or subspecialist care) and having established care with a PCP. Collectively, these data suggest that individuals without a compelling reason to access medical services might have barriers to accessing care in the event of medical needs or may not receive routine preventative care [9,10].
In general, we found that rates of reported inappropriate prescriptions were lower than those reported in prior studies where a comparable resident population was surveyed [8,12,16]. Inclusion of multiple institutions, differences in temporality, social desirability bias, and reporting bias might have influenced our findings in this regard. Surprisingly, we found that having a PCP did not influence likelihood of inappropriate prescription receipt, perhaps suggesting that this behavior reflects some degree of universal difficulty in accessing care. Alternatively, this finding might relate to a cultural tendency to self-prescribe among resident physicians. The fact that individuals on chronic medications more often both received and wrote inappropriate prescriptions suggests this problem might be more pronounced in individuals who take medications more often, as these residents have specific needs [12]. Future studies targeting these individuals thus appear warranted.
Our study has several limitations. First, our sample size was modest and the response rate of 45% was low. However, to our knowledge, this remains among the largest survey on this topic, and our response rate is comparable to similar trainee studies [8,11,13]. Second, we designed and created a novel survey for this study. While the questions were pilot-tested with users prior to dissemination, validation of the instrument was not performed. Third, since the study population was restricted to residents in fields that participate in primary care, our findings may not be generalizable to patterns of PCP use in other specialties [6].
These limitations aside, our study has important strengths. This is the first national study of its kind with specific questions addressing primary care access and utilization, prescription medication use and related practices, and the prevalence of medical conditions among trainees. Important differences in the rates of establishing primary care between male and female respondents, first- year and senior residents, and those with and without chronic disease suggest a need to target specific resident groups (males, interns, those without pre-existing conditions) for wellness-related interventions. Such interventions could include distribution of a list of local providers to first year residents, advanced protected time for doctor’s appointments, and safeguards to ensure health information is protected from potential supervisors. Future studies should also include residents from non-primary care oriented specialties such as surgery, emergency medicine, and anesthesiology to obtain results that are more generalizable to the resident population as a whole. Additionally, the rates of inappropriate prescriptions were not insignificant and warrant further evaluation of the driving forces behind these behaviors.
Conclusion
Medical residents have a substantial burden of chronic illness that may not be met through interactions with PCPs. More research into barriers that residents face while accessing care and an assessment of interventions to facilitate their access to care is important to promote trainee well-being. Without such direction and initiative, it may prove harder for physicians to heal themselves or those for whom they provide care.
Acknowledgments: We thank Suzanne Winter, the study coordinator, for her support with editing and formatting the manuscript, Latoya Kuhn for performing the statistical analysis and creating data tables, and Dr. Namita Sachdev and Dr. Renuka Tipirneni for providing feedback on the survey instrument. We also thank the involved programs for their participation.
Corresponding author: Vineet Chopra, NCRC 2800 Plymouth Rd., Bldg 16, 432, Ann Arbor, MI 48109, [email protected].
Financial disclosures: None.
Previous presentations: Results were presented at the Annual Michigan Medicine 2017 Internal Medicine Research Symposium.
1. Kassam A, Horton J, Shoimer I, Patten S. Predictors of well-being in resident physicians: a descriptive and psychometric study. J Grad Med Educ 2015;7:70–4.
2. Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med 2002;136:358–67.
3. Burstin HR, Swartz K, O’Neil AC, et al. The effect of change of health insurance on access to care. Inquiry 1998;35:389–97.
4. Rhodes KV, Basseyn S, Friedman AB, et al. Access to primary care appointments following 2014 insurance expansions. Ann Fam Med 2017;15:107–12.
5. Polsky D, Richards M, Basseyn S, et al. Appointment availability after increases in Medicaid payments for primary care. N Engl J Med 2015;372:537–45.
6. Gupta G, Schleinitz MD, Reinert SE, McGarry KA. Resident physician preventive health behaviors and perspectives on primary care. R I Med J (2013) 2013;96:43–7.
7. Rosen IM, Christine JD, Bellini LM, Asch DA. Health and health care among housestaff in four U.S. internal medicine residency programs. J Gen Intern Med 2000;15:116-21.
8. Campbell S, Delva D. Physician do not heal thyself. Survey of personal health practices among medical residents. Can Fam Physician 2003;49:1121–7.
9. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q 2005;83(3):457-502.
10. Weissman JS, Stern R, Fielding SL, et al. Delayed access to health care: risk factors, reasons, and consequences. Ann Intern Med 1991;114:325–31.
11. Guille C, Sen S. Prescription drug use and self-prescription among training physicians. Arch Intern Med 2012;172:371–2.
12. Roberts LW, Kim JP. Informal health care practices of residents: “curbside” consultation and self-diagnosis and treatment. Acad Psychiatry 2015;39:22-30.
13. Cohen JS, Patten S. Well-being in residency training: a survey examining resident physician satisfaction both within and outside of residency training and mental health in Alberta. BMC Med Educ 2005;5:21.
14. U.S. Preventive Services Task Force. Cervical cancer: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/cervical-cancer-screening. Published March 2012. Accessed August 21, 2018.
15. Health Resources and Services Administration. Women’s preventative services guidelines. https://www.hrsa.gov/womensguidelines2016/index.html. Updated October 2017. Accessed August 21, 2018.
16. Christie JD, Rosen IM, Bellini LM, et al. Prescription drug use and self-prescription among resident physicians. JAMA 1998;280(14):1253–5.
1. Kassam A, Horton J, Shoimer I, Patten S. Predictors of well-being in resident physicians: a descriptive and psychometric study. J Grad Med Educ 2015;7:70–4.
2. Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med 2002;136:358–67.
3. Burstin HR, Swartz K, O’Neil AC, et al. The effect of change of health insurance on access to care. Inquiry 1998;35:389–97.
4. Rhodes KV, Basseyn S, Friedman AB, et al. Access to primary care appointments following 2014 insurance expansions. Ann Fam Med 2017;15:107–12.
5. Polsky D, Richards M, Basseyn S, et al. Appointment availability after increases in Medicaid payments for primary care. N Engl J Med 2015;372:537–45.
6. Gupta G, Schleinitz MD, Reinert SE, McGarry KA. Resident physician preventive health behaviors and perspectives on primary care. R I Med J (2013) 2013;96:43–7.
7. Rosen IM, Christine JD, Bellini LM, Asch DA. Health and health care among housestaff in four U.S. internal medicine residency programs. J Gen Intern Med 2000;15:116-21.
8. Campbell S, Delva D. Physician do not heal thyself. Survey of personal health practices among medical residents. Can Fam Physician 2003;49:1121–7.
9. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q 2005;83(3):457-502.
10. Weissman JS, Stern R, Fielding SL, et al. Delayed access to health care: risk factors, reasons, and consequences. Ann Intern Med 1991;114:325–31.
11. Guille C, Sen S. Prescription drug use and self-prescription among training physicians. Arch Intern Med 2012;172:371–2.
12. Roberts LW, Kim JP. Informal health care practices of residents: “curbside” consultation and self-diagnosis and treatment. Acad Psychiatry 2015;39:22-30.
13. Cohen JS, Patten S. Well-being in residency training: a survey examining resident physician satisfaction both within and outside of residency training and mental health in Alberta. BMC Med Educ 2005;5:21.
14. U.S. Preventive Services Task Force. Cervical cancer: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/cervical-cancer-screening. Published March 2012. Accessed August 21, 2018.
15. Health Resources and Services Administration. Women’s preventative services guidelines. https://www.hrsa.gov/womensguidelines2016/index.html. Updated October 2017. Accessed August 21, 2018.
16. Christie JD, Rosen IM, Bellini LM, et al. Prescription drug use and self-prescription among resident physicians. JAMA 1998;280(14):1253–5.
Nocturnal Dexmedetomidine for Prevention of Delirium in the ICU
Study Overview
Objective. To determine if nocturnal dexmedetomidine prevents delirium and improves sleep in critically ill patients.
Design. Two-center, double-blind, placebo-controlled, randomized, trial.
Setting and participants. This study was conducted in the intensive care units (ICU) at 2 centers in North America between 2013 and 2016. Adults admitted to the ICU and receiving intermittent or continuous sedatives and expected to require at least 48 hours of ICU care were included in the study. Exclusion criteria were presence of delirium, severe dementia, acute neurologic injury, severe bradycardia, hepatic encephalopathy, end-stage liver disease, and expected death within 24 hours.
Intervention. Patients were randomized 1:1 to receive nocturnal dexmedetomidine (0.2–0.7 mcg/kg/hr) or dextrose 5% in water. Patients, clinicians, bedside nurses, and all study personnel were blinded to study drug assignment throughout the study. All sedatives were halved before the study drug was administered each evening. As-needed intravenous midazolam was used while titrating up the study drug. Study drug was administered nightly until either ICU discharge or an adverse event occurred. Decisions regarding use of other analgesic and sedative therapy, including opioids, oral benzodiazepines, acetaminophen, and nonsteroidal anti-inflammatory drugs, were left to the discretion of the clinician. Sleep-promoting agents such as melatonin or trazodone were not allowed.
Main outcome measures. The primary outcome was the proportion of patients who remained free of delirium during their critical illness. Secondary outcomes included ICU days spent without delirium; duration of delirium; sleep quality; proportion of patients who ever developed coma; proportion of nocturnal hours spent at each Richmond Agitation and Sedation Scale (RASS) score; maximal nocturnal pain levels; antipsychotic, corticosteroid, and oral analgesic use; days of mechanical ventilation; ICU and hospital stay duration; and ICU and hospital mortality.
Main results. 100 patients were randomized, with 50 patients in each group. 89% of patients were mechanically ventilated, and the Prediction of Delirium in ICU (PRE-DELIRIC) score [1] was 54 in the dexmedetomidine group and 51 in the placebo group. Continuous propofol and fentanyl infusion at randomization was used in 49% and 80%, respectively. Duration of median ICU stay was 10 days in the dexmedetomidine group and 9 days in the placebo group. More patients in the dexmedetomidine group (40 of 50 patients [80%]) than in the placebo group (27 of 50 patients [54%]) remained free of delirium (relative risk [RR], 0.44, 95% confidence interval {CI} 0.23 to 0.82; P = 0.006). The median (interquartile range [IQR]) duration of the first episode of delirium was similar between the dexmedetomidine (IQR 2.0 [0.6–2.7] days) and placebo (2.2 [0.7–3.2] days) groups (P = 0.73). The average Leeds Sleep Evaluation Questionnaire score also was similar (mean difference, 0.02, 95% CI 0.42 to 1.92) between the 2 groups. Incidence of hypotension or bradycardia did not differ significantly between the groups.
Conclusion. Nocturnal administration of low-dose dexmedetomidine in critically ill adults reduces the incidence of delirium during the ICU stay, and patient-reported sleep quality appears unchanged.
Commentary
Delirium is a sudden state of confusion and/or disturbance of consciousness and cognition that is believed to result from acute brain dysfunction, including neurochemical disequilibrium. It often occurs in association with a general medical condition, such as various types of shock, sepsis, surgery, anesthesia, or electrolyte imbalance. Studies have shown that delirium is associated with increased mortality in critically ill patients [2]. Most ICUs use a systematic assessment tool for early detection of delirium, such as the Confusion Assessment Method for the ICU (CAM-ICU), the Intensive Care Delirium Screening Checklist (ICDSC), or the DSM-IV TR score system. The CAM-ICU is the most frequently used tool to evaluate for the presence of delirium in critically ill patients; it is scored as positive if the patient manifests both an acute change in mental status and inattention, and has either a RASS greater than 0 or disorganized thinking [3].
The level of evidence regarding delirium prevention is low. Ear plugs, eye masks, educational staff, supportive reorientation, and music have been studied as nonpharmacologic methods for preventing delirium [4]. From a pharmacologic standpoint, the dopamine D2 antagonist haloperidol has been explored as a therapy for both treating and preventing delirium, since the condition is thought to be associated with anticholinergic and excessive dopaminergic mechanisms. A randomized controlled study in 142 patients who received haloperidol 2.5 mg intravenously every 8 hours found that the duration of delirium did not differ between the haloperidol and the placebo groups [5]. The most feared adverse effects of haloperidol, such as akathisia, muscle stiffness, arrhythmia, or QT prolongation, did not occur more frequently in the haloperidol group. Similar results have been reported by Al-Qadheeb et al [6]. Pharmacologic prophylaxis of delirium using atypical antipsychotics such as quetiapine has also been explored, but the level of evidence for this intervention remains very low. Current American College of Critical Care Medicine guidelines recommend nonpharmacologic management and do not firmly recommend any pharmacologic prevention for ICU delirium [7].
Dexmedetomidine is a selective alpha-2 adrenergic receptor agonist that acts at the locus ceruleus, providing sedation and analgesia. Studies assessing the choice of sedation in the ICU found that the use of dexmedetomidine or propofol, compared to benzodiazepines, is associated with a lower rate of delirium occurrence, especially in mechanically ventilated patients [8,9]. Dexmedetomidine offers several potential advantages over other sedative drugs: it has little effect on cognition, has minimal anticholinergic effect, and may restore a natural sleep pattern. While propofol causes hypotension, respiratory depression, and deeper sedation, dexmedetomidine is associated with lighter sedation, a minimal effect on respiratory drive, and a milder hemodynamic effect. In a randomized controlled trial involving post-surgery ICU patients, dexmedetomidine partially restored a normal sleep pattern (eg, increased percentage of stage 2 non-rapid eye movement sleep), prolonged total sleep time, improved sleep efficiency, and increased sleep quality [10]; by improving overall sleep quality, dexmedetomidine potentially may prevent delirium. Another study that randomly assigned 700 ICU patients who underwent noncardiac surgery to dexmedetomidine infusion (0.1 mcg/kg/hr from ICU admission on the day of surgery until the following morning) or placebo reported a significantly reduced incidence of delirium in the dexmedetomidine group [11]. On the other hand, a 2015 Cochrane meta-analysis that included 7 randomized controlled studies did not find a significant risk reduction of delirium with dexmedetomidine [12].
The current study by Skrobik et al was a randomized, placebo-controlled trial that examined the role of nocturnal dexmedetomidine in ICU delirium prevention in 100 ICU patients. Nocturnal administration of low-dose dexmedetomidine led to a statistically significant reduction in delirium incidence compared to placebo (RR of delirium, 0.44, 95% CI 0.23 to 0.82, which is similar to that suggested by previous studies). This study adds additional evidence regarding the use of dexmedetomidine for pharmacologic delirium prevention. It included many mechanically ventilated patients (89% of study population), strengthening the applicability of the result. Mechanical ventilation is a known risk factor for ICU delirium, and therefore this is an important population to study; previous trials largely included patients who were not mechanically ventilated. This study also supports the safety of dexmedetomidine infusion, especially in lower doses in critically ill patients, without significantly increasing the incidence of adverse events (mainly hypotension and bradycardia). The study protocol closely approximated real practice by allowing other analgesics, including opioids, and therefore suggests safety and real world applicability.
There are several confounding issues in this study. The study was blinded, and there was concern that the bedside nurses may have been able to identify the study drug based on the effects on heart rate. In addition, 50% of patients received antipsychotics. While baseline RASS score was significantly different between the 2 groups, patients in the dexmedetomidine group reached a deeper level of sedation during the study. Also, the protocol mandated halving the pre-existing sedative on the night of study drug initiation, which could have led to inadequate sedation in the placebo group. Placebo patients received propofol for a similar duration but at a higher dose compared to dexmedetomidine patients, and midazolam and fentanyl infusion was used in a similar pattern between the groups. The high exclusion rate (71%) limits the ability to generalize the results to all ICU patients.
Applications for Clinical Practice
ICU delirium is an important complication of critical illness and is potentially preventable. Benzodiazepines are associated with an increased risk of delirium, while there has been increasing interest in dexmedetomidine, a selective alpha-2 adrenergic receptor agonist, because of its potential for delirium prevention. Evidence to date does not strongly support routine use of pharmacologic prevention of delirium; however, dexmedetomidine may be an option for sedation, as opposed to benzodiazepines or propofol, in selected patients and may potentially prevent delirium.
—Minkyung Kwon, MD, Neal Patel, MD, and Vichaya Arunthari, MD, Pulmonary and Critical Care Medicine, Mayo Clinic Florida, Jacksonville, FL
1. van den Boogaard M, Pickkers P, Slooter AJ, et al. Development and validation of PRE-DELIRIC (PREdiction of DELIRium in ICu patients) delirium prediction model for intensive care patients: observational multicentre study. BMJ 2012;344:e420.
2. Slooter AJ, Van De Leur RR, Zaal IJ. Delirium in critically ill patients. Handb Clin Neurol 2017;141:449–66.
3. Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA 2001;286:2703–10.
4. Abraha I, Trotta F, Rimland JM, et al. Efficacy of non-pharmacological interventions to prevent and treat delirium in older patients: a systematic overview. The SENATOR project ONTOP Series. PLoS One 2015;10:e0123090.
5. Page VJ, Ely EW, Gates S, et al. Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (Hope-ICU): a randomised, double-blind, placebo-controlled trial. Lancet Respir Med 2013;1:515–23.
6. Al-Qadheeb NS, Skrobik Y, Schumaker G, et al. Preventing ICU subsyndromal delirium conversion to delirium with low-dose IV haloperidol: a double-blind, placebo-controlled pilot study. Crit Care Med 2016;44:583–91.
7. Barr J, Fraser GL, Puntillo K, et al; American College of Critical Care Medicine. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013;41:263–306.
8. Riker RR, Shehabi Y, Bokesch PM, et al. Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. JAMA 2009;301:489–99.
9. Pandharipande PP, Pun BT, Herr DL, et al. Effect of sedation with dexmedetomidine vs lorazepam on acute brain dysfunction in mechanically ventilated patients: the MENDS randomized controlled trial. JAMA 2007;298:2644–53.
10. Wu XH, Cui F, Zhang C, et al. Low-dose dexmedetomidine improves sleep quality pattern in elderly patients after noncardiac surgery in the intensive care unit: a pilot randomized controlled trial. Anesthesiology 2016;125:979–91.
11. Su X, Meng Z-T, Wu X-H, et al. Dexmedetomidine for prevention of delirium in elderly patients after non-cardiac surgery: a randomised, double-blind, placebo-controlled trial. Lancet 2016;388:1893–1902.
12. Chen K, Lu Z, Xin YC, et al. Alpha-2 agonists for long-term sedation during mechanical ventilation in critically ill patients. Cochrane Database Syst Rev 2015;1:CD010269.
Study Overview
Objective. To determine if nocturnal dexmedetomidine prevents delirium and improves sleep in critically ill patients.
Design. Two-center, double-blind, placebo-controlled, randomized, trial.
Setting and participants. This study was conducted in the intensive care units (ICU) at 2 centers in North America between 2013 and 2016. Adults admitted to the ICU and receiving intermittent or continuous sedatives and expected to require at least 48 hours of ICU care were included in the study. Exclusion criteria were presence of delirium, severe dementia, acute neurologic injury, severe bradycardia, hepatic encephalopathy, end-stage liver disease, and expected death within 24 hours.
Intervention. Patients were randomized 1:1 to receive nocturnal dexmedetomidine (0.2–0.7 mcg/kg/hr) or dextrose 5% in water. Patients, clinicians, bedside nurses, and all study personnel were blinded to study drug assignment throughout the study. All sedatives were halved before the study drug was administered each evening. As-needed intravenous midazolam was used while titrating up the study drug. Study drug was administered nightly until either ICU discharge or an adverse event occurred. Decisions regarding use of other analgesic and sedative therapy, including opioids, oral benzodiazepines, acetaminophen, and nonsteroidal anti-inflammatory drugs, were left to the discretion of the clinician. Sleep-promoting agents such as melatonin or trazodone were not allowed.
Main outcome measures. The primary outcome was the proportion of patients who remained free of delirium during their critical illness. Secondary outcomes included ICU days spent without delirium; duration of delirium; sleep quality; proportion of patients who ever developed coma; proportion of nocturnal hours spent at each Richmond Agitation and Sedation Scale (RASS) score; maximal nocturnal pain levels; antipsychotic, corticosteroid, and oral analgesic use; days of mechanical ventilation; ICU and hospital stay duration; and ICU and hospital mortality.
Main results. 100 patients were randomized, with 50 patients in each group. 89% of patients were mechanically ventilated, and the Prediction of Delirium in ICU (PRE-DELIRIC) score [1] was 54 in the dexmedetomidine group and 51 in the placebo group. Continuous propofol and fentanyl infusion at randomization was used in 49% and 80%, respectively. Duration of median ICU stay was 10 days in the dexmedetomidine group and 9 days in the placebo group. More patients in the dexmedetomidine group (40 of 50 patients [80%]) than in the placebo group (27 of 50 patients [54%]) remained free of delirium (relative risk [RR], 0.44, 95% confidence interval {CI} 0.23 to 0.82; P = 0.006). The median (interquartile range [IQR]) duration of the first episode of delirium was similar between the dexmedetomidine (IQR 2.0 [0.6–2.7] days) and placebo (2.2 [0.7–3.2] days) groups (P = 0.73). The average Leeds Sleep Evaluation Questionnaire score also was similar (mean difference, 0.02, 95% CI 0.42 to 1.92) between the 2 groups. Incidence of hypotension or bradycardia did not differ significantly between the groups.
Conclusion. Nocturnal administration of low-dose dexmedetomidine in critically ill adults reduces the incidence of delirium during the ICU stay, and patient-reported sleep quality appears unchanged.
Commentary
Delirium is a sudden state of confusion and/or disturbance of consciousness and cognition that is believed to result from acute brain dysfunction, including neurochemical disequilibrium. It often occurs in association with a general medical condition, such as various types of shock, sepsis, surgery, anesthesia, or electrolyte imbalance. Studies have shown that delirium is associated with increased mortality in critically ill patients [2]. Most ICUs use a systematic assessment tool for early detection of delirium, such as the Confusion Assessment Method for the ICU (CAM-ICU), the Intensive Care Delirium Screening Checklist (ICDSC), or the DSM-IV TR score system. The CAM-ICU is the most frequently used tool to evaluate for the presence of delirium in critically ill patients; it is scored as positive if the patient manifests both an acute change in mental status and inattention, and has either a RASS greater than 0 or disorganized thinking [3].
The level of evidence regarding delirium prevention is low. Ear plugs, eye masks, educational staff, supportive reorientation, and music have been studied as nonpharmacologic methods for preventing delirium [4]. From a pharmacologic standpoint, the dopamine D2 antagonist haloperidol has been explored as a therapy for both treating and preventing delirium, since the condition is thought to be associated with anticholinergic and excessive dopaminergic mechanisms. A randomized controlled study in 142 patients who received haloperidol 2.5 mg intravenously every 8 hours found that the duration of delirium did not differ between the haloperidol and the placebo groups [5]. The most feared adverse effects of haloperidol, such as akathisia, muscle stiffness, arrhythmia, or QT prolongation, did not occur more frequently in the haloperidol group. Similar results have been reported by Al-Qadheeb et al [6]. Pharmacologic prophylaxis of delirium using atypical antipsychotics such as quetiapine has also been explored, but the level of evidence for this intervention remains very low. Current American College of Critical Care Medicine guidelines recommend nonpharmacologic management and do not firmly recommend any pharmacologic prevention for ICU delirium [7].
Dexmedetomidine is a selective alpha-2 adrenergic receptor agonist that acts at the locus ceruleus, providing sedation and analgesia. Studies assessing the choice of sedation in the ICU found that the use of dexmedetomidine or propofol, compared to benzodiazepines, is associated with a lower rate of delirium occurrence, especially in mechanically ventilated patients [8,9]. Dexmedetomidine offers several potential advantages over other sedative drugs: it has little effect on cognition, has minimal anticholinergic effect, and may restore a natural sleep pattern. While propofol causes hypotension, respiratory depression, and deeper sedation, dexmedetomidine is associated with lighter sedation, a minimal effect on respiratory drive, and a milder hemodynamic effect. In a randomized controlled trial involving post-surgery ICU patients, dexmedetomidine partially restored a normal sleep pattern (eg, increased percentage of stage 2 non-rapid eye movement sleep), prolonged total sleep time, improved sleep efficiency, and increased sleep quality [10]; by improving overall sleep quality, dexmedetomidine potentially may prevent delirium. Another study that randomly assigned 700 ICU patients who underwent noncardiac surgery to dexmedetomidine infusion (0.1 mcg/kg/hr from ICU admission on the day of surgery until the following morning) or placebo reported a significantly reduced incidence of delirium in the dexmedetomidine group [11]. On the other hand, a 2015 Cochrane meta-analysis that included 7 randomized controlled studies did not find a significant risk reduction of delirium with dexmedetomidine [12].
The current study by Skrobik et al was a randomized, placebo-controlled trial that examined the role of nocturnal dexmedetomidine in ICU delirium prevention in 100 ICU patients. Nocturnal administration of low-dose dexmedetomidine led to a statistically significant reduction in delirium incidence compared to placebo (RR of delirium, 0.44, 95% CI 0.23 to 0.82, which is similar to that suggested by previous studies). This study adds additional evidence regarding the use of dexmedetomidine for pharmacologic delirium prevention. It included many mechanically ventilated patients (89% of study population), strengthening the applicability of the result. Mechanical ventilation is a known risk factor for ICU delirium, and therefore this is an important population to study; previous trials largely included patients who were not mechanically ventilated. This study also supports the safety of dexmedetomidine infusion, especially in lower doses in critically ill patients, without significantly increasing the incidence of adverse events (mainly hypotension and bradycardia). The study protocol closely approximated real practice by allowing other analgesics, including opioids, and therefore suggests safety and real world applicability.
There are several confounding issues in this study. The study was blinded, and there was concern that the bedside nurses may have been able to identify the study drug based on the effects on heart rate. In addition, 50% of patients received antipsychotics. While baseline RASS score was significantly different between the 2 groups, patients in the dexmedetomidine group reached a deeper level of sedation during the study. Also, the protocol mandated halving the pre-existing sedative on the night of study drug initiation, which could have led to inadequate sedation in the placebo group. Placebo patients received propofol for a similar duration but at a higher dose compared to dexmedetomidine patients, and midazolam and fentanyl infusion was used in a similar pattern between the groups. The high exclusion rate (71%) limits the ability to generalize the results to all ICU patients.
Applications for Clinical Practice
ICU delirium is an important complication of critical illness and is potentially preventable. Benzodiazepines are associated with an increased risk of delirium, while there has been increasing interest in dexmedetomidine, a selective alpha-2 adrenergic receptor agonist, because of its potential for delirium prevention. Evidence to date does not strongly support routine use of pharmacologic prevention of delirium; however, dexmedetomidine may be an option for sedation, as opposed to benzodiazepines or propofol, in selected patients and may potentially prevent delirium.
—Minkyung Kwon, MD, Neal Patel, MD, and Vichaya Arunthari, MD, Pulmonary and Critical Care Medicine, Mayo Clinic Florida, Jacksonville, FL
Study Overview
Objective. To determine if nocturnal dexmedetomidine prevents delirium and improves sleep in critically ill patients.
Design. Two-center, double-blind, placebo-controlled, randomized, trial.
Setting and participants. This study was conducted in the intensive care units (ICU) at 2 centers in North America between 2013 and 2016. Adults admitted to the ICU and receiving intermittent or continuous sedatives and expected to require at least 48 hours of ICU care were included in the study. Exclusion criteria were presence of delirium, severe dementia, acute neurologic injury, severe bradycardia, hepatic encephalopathy, end-stage liver disease, and expected death within 24 hours.
Intervention. Patients were randomized 1:1 to receive nocturnal dexmedetomidine (0.2–0.7 mcg/kg/hr) or dextrose 5% in water. Patients, clinicians, bedside nurses, and all study personnel were blinded to study drug assignment throughout the study. All sedatives were halved before the study drug was administered each evening. As-needed intravenous midazolam was used while titrating up the study drug. Study drug was administered nightly until either ICU discharge or an adverse event occurred. Decisions regarding use of other analgesic and sedative therapy, including opioids, oral benzodiazepines, acetaminophen, and nonsteroidal anti-inflammatory drugs, were left to the discretion of the clinician. Sleep-promoting agents such as melatonin or trazodone were not allowed.
Main outcome measures. The primary outcome was the proportion of patients who remained free of delirium during their critical illness. Secondary outcomes included ICU days spent without delirium; duration of delirium; sleep quality; proportion of patients who ever developed coma; proportion of nocturnal hours spent at each Richmond Agitation and Sedation Scale (RASS) score; maximal nocturnal pain levels; antipsychotic, corticosteroid, and oral analgesic use; days of mechanical ventilation; ICU and hospital stay duration; and ICU and hospital mortality.
Main results. 100 patients were randomized, with 50 patients in each group. 89% of patients were mechanically ventilated, and the Prediction of Delirium in ICU (PRE-DELIRIC) score [1] was 54 in the dexmedetomidine group and 51 in the placebo group. Continuous propofol and fentanyl infusion at randomization was used in 49% and 80%, respectively. Duration of median ICU stay was 10 days in the dexmedetomidine group and 9 days in the placebo group. More patients in the dexmedetomidine group (40 of 50 patients [80%]) than in the placebo group (27 of 50 patients [54%]) remained free of delirium (relative risk [RR], 0.44, 95% confidence interval {CI} 0.23 to 0.82; P = 0.006). The median (interquartile range [IQR]) duration of the first episode of delirium was similar between the dexmedetomidine (IQR 2.0 [0.6–2.7] days) and placebo (2.2 [0.7–3.2] days) groups (P = 0.73). The average Leeds Sleep Evaluation Questionnaire score also was similar (mean difference, 0.02, 95% CI 0.42 to 1.92) between the 2 groups. Incidence of hypotension or bradycardia did not differ significantly between the groups.
Conclusion. Nocturnal administration of low-dose dexmedetomidine in critically ill adults reduces the incidence of delirium during the ICU stay, and patient-reported sleep quality appears unchanged.
Commentary
Delirium is a sudden state of confusion and/or disturbance of consciousness and cognition that is believed to result from acute brain dysfunction, including neurochemical disequilibrium. It often occurs in association with a general medical condition, such as various types of shock, sepsis, surgery, anesthesia, or electrolyte imbalance. Studies have shown that delirium is associated with increased mortality in critically ill patients [2]. Most ICUs use a systematic assessment tool for early detection of delirium, such as the Confusion Assessment Method for the ICU (CAM-ICU), the Intensive Care Delirium Screening Checklist (ICDSC), or the DSM-IV TR score system. The CAM-ICU is the most frequently used tool to evaluate for the presence of delirium in critically ill patients; it is scored as positive if the patient manifests both an acute change in mental status and inattention, and has either a RASS greater than 0 or disorganized thinking [3].
The level of evidence regarding delirium prevention is low. Ear plugs, eye masks, educational staff, supportive reorientation, and music have been studied as nonpharmacologic methods for preventing delirium [4]. From a pharmacologic standpoint, the dopamine D2 antagonist haloperidol has been explored as a therapy for both treating and preventing delirium, since the condition is thought to be associated with anticholinergic and excessive dopaminergic mechanisms. A randomized controlled study in 142 patients who received haloperidol 2.5 mg intravenously every 8 hours found that the duration of delirium did not differ between the haloperidol and the placebo groups [5]. The most feared adverse effects of haloperidol, such as akathisia, muscle stiffness, arrhythmia, or QT prolongation, did not occur more frequently in the haloperidol group. Similar results have been reported by Al-Qadheeb et al [6]. Pharmacologic prophylaxis of delirium using atypical antipsychotics such as quetiapine has also been explored, but the level of evidence for this intervention remains very low. Current American College of Critical Care Medicine guidelines recommend nonpharmacologic management and do not firmly recommend any pharmacologic prevention for ICU delirium [7].
Dexmedetomidine is a selective alpha-2 adrenergic receptor agonist that acts at the locus ceruleus, providing sedation and analgesia. Studies assessing the choice of sedation in the ICU found that the use of dexmedetomidine or propofol, compared to benzodiazepines, is associated with a lower rate of delirium occurrence, especially in mechanically ventilated patients [8,9]. Dexmedetomidine offers several potential advantages over other sedative drugs: it has little effect on cognition, has minimal anticholinergic effect, and may restore a natural sleep pattern. While propofol causes hypotension, respiratory depression, and deeper sedation, dexmedetomidine is associated with lighter sedation, a minimal effect on respiratory drive, and a milder hemodynamic effect. In a randomized controlled trial involving post-surgery ICU patients, dexmedetomidine partially restored a normal sleep pattern (eg, increased percentage of stage 2 non-rapid eye movement sleep), prolonged total sleep time, improved sleep efficiency, and increased sleep quality [10]; by improving overall sleep quality, dexmedetomidine potentially may prevent delirium. Another study that randomly assigned 700 ICU patients who underwent noncardiac surgery to dexmedetomidine infusion (0.1 mcg/kg/hr from ICU admission on the day of surgery until the following morning) or placebo reported a significantly reduced incidence of delirium in the dexmedetomidine group [11]. On the other hand, a 2015 Cochrane meta-analysis that included 7 randomized controlled studies did not find a significant risk reduction of delirium with dexmedetomidine [12].
The current study by Skrobik et al was a randomized, placebo-controlled trial that examined the role of nocturnal dexmedetomidine in ICU delirium prevention in 100 ICU patients. Nocturnal administration of low-dose dexmedetomidine led to a statistically significant reduction in delirium incidence compared to placebo (RR of delirium, 0.44, 95% CI 0.23 to 0.82, which is similar to that suggested by previous studies). This study adds additional evidence regarding the use of dexmedetomidine for pharmacologic delirium prevention. It included many mechanically ventilated patients (89% of study population), strengthening the applicability of the result. Mechanical ventilation is a known risk factor for ICU delirium, and therefore this is an important population to study; previous trials largely included patients who were not mechanically ventilated. This study also supports the safety of dexmedetomidine infusion, especially in lower doses in critically ill patients, without significantly increasing the incidence of adverse events (mainly hypotension and bradycardia). The study protocol closely approximated real practice by allowing other analgesics, including opioids, and therefore suggests safety and real world applicability.
There are several confounding issues in this study. The study was blinded, and there was concern that the bedside nurses may have been able to identify the study drug based on the effects on heart rate. In addition, 50% of patients received antipsychotics. While baseline RASS score was significantly different between the 2 groups, patients in the dexmedetomidine group reached a deeper level of sedation during the study. Also, the protocol mandated halving the pre-existing sedative on the night of study drug initiation, which could have led to inadequate sedation in the placebo group. Placebo patients received propofol for a similar duration but at a higher dose compared to dexmedetomidine patients, and midazolam and fentanyl infusion was used in a similar pattern between the groups. The high exclusion rate (71%) limits the ability to generalize the results to all ICU patients.
Applications for Clinical Practice
ICU delirium is an important complication of critical illness and is potentially preventable. Benzodiazepines are associated with an increased risk of delirium, while there has been increasing interest in dexmedetomidine, a selective alpha-2 adrenergic receptor agonist, because of its potential for delirium prevention. Evidence to date does not strongly support routine use of pharmacologic prevention of delirium; however, dexmedetomidine may be an option for sedation, as opposed to benzodiazepines or propofol, in selected patients and may potentially prevent delirium.
—Minkyung Kwon, MD, Neal Patel, MD, and Vichaya Arunthari, MD, Pulmonary and Critical Care Medicine, Mayo Clinic Florida, Jacksonville, FL
1. van den Boogaard M, Pickkers P, Slooter AJ, et al. Development and validation of PRE-DELIRIC (PREdiction of DELIRium in ICu patients) delirium prediction model for intensive care patients: observational multicentre study. BMJ 2012;344:e420.
2. Slooter AJ, Van De Leur RR, Zaal IJ. Delirium in critically ill patients. Handb Clin Neurol 2017;141:449–66.
3. Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA 2001;286:2703–10.
4. Abraha I, Trotta F, Rimland JM, et al. Efficacy of non-pharmacological interventions to prevent and treat delirium in older patients: a systematic overview. The SENATOR project ONTOP Series. PLoS One 2015;10:e0123090.
5. Page VJ, Ely EW, Gates S, et al. Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (Hope-ICU): a randomised, double-blind, placebo-controlled trial. Lancet Respir Med 2013;1:515–23.
6. Al-Qadheeb NS, Skrobik Y, Schumaker G, et al. Preventing ICU subsyndromal delirium conversion to delirium with low-dose IV haloperidol: a double-blind, placebo-controlled pilot study. Crit Care Med 2016;44:583–91.
7. Barr J, Fraser GL, Puntillo K, et al; American College of Critical Care Medicine. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013;41:263–306.
8. Riker RR, Shehabi Y, Bokesch PM, et al. Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. JAMA 2009;301:489–99.
9. Pandharipande PP, Pun BT, Herr DL, et al. Effect of sedation with dexmedetomidine vs lorazepam on acute brain dysfunction in mechanically ventilated patients: the MENDS randomized controlled trial. JAMA 2007;298:2644–53.
10. Wu XH, Cui F, Zhang C, et al. Low-dose dexmedetomidine improves sleep quality pattern in elderly patients after noncardiac surgery in the intensive care unit: a pilot randomized controlled trial. Anesthesiology 2016;125:979–91.
11. Su X, Meng Z-T, Wu X-H, et al. Dexmedetomidine for prevention of delirium in elderly patients after non-cardiac surgery: a randomised, double-blind, placebo-controlled trial. Lancet 2016;388:1893–1902.
12. Chen K, Lu Z, Xin YC, et al. Alpha-2 agonists for long-term sedation during mechanical ventilation in critically ill patients. Cochrane Database Syst Rev 2015;1:CD010269.
1. van den Boogaard M, Pickkers P, Slooter AJ, et al. Development and validation of PRE-DELIRIC (PREdiction of DELIRium in ICu patients) delirium prediction model for intensive care patients: observational multicentre study. BMJ 2012;344:e420.
2. Slooter AJ, Van De Leur RR, Zaal IJ. Delirium in critically ill patients. Handb Clin Neurol 2017;141:449–66.
3. Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA 2001;286:2703–10.
4. Abraha I, Trotta F, Rimland JM, et al. Efficacy of non-pharmacological interventions to prevent and treat delirium in older patients: a systematic overview. The SENATOR project ONTOP Series. PLoS One 2015;10:e0123090.
5. Page VJ, Ely EW, Gates S, et al. Effect of intravenous haloperidol on the duration of delirium and coma in critically ill patients (Hope-ICU): a randomised, double-blind, placebo-controlled trial. Lancet Respir Med 2013;1:515–23.
6. Al-Qadheeb NS, Skrobik Y, Schumaker G, et al. Preventing ICU subsyndromal delirium conversion to delirium with low-dose IV haloperidol: a double-blind, placebo-controlled pilot study. Crit Care Med 2016;44:583–91.
7. Barr J, Fraser GL, Puntillo K, et al; American College of Critical Care Medicine. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 2013;41:263–306.
8. Riker RR, Shehabi Y, Bokesch PM, et al. Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. JAMA 2009;301:489–99.
9. Pandharipande PP, Pun BT, Herr DL, et al. Effect of sedation with dexmedetomidine vs lorazepam on acute brain dysfunction in mechanically ventilated patients: the MENDS randomized controlled trial. JAMA 2007;298:2644–53.
10. Wu XH, Cui F, Zhang C, et al. Low-dose dexmedetomidine improves sleep quality pattern in elderly patients after noncardiac surgery in the intensive care unit: a pilot randomized controlled trial. Anesthesiology 2016;125:979–91.
11. Su X, Meng Z-T, Wu X-H, et al. Dexmedetomidine for prevention of delirium in elderly patients after non-cardiac surgery: a randomised, double-blind, placebo-controlled trial. Lancet 2016;388:1893–1902.
12. Chen K, Lu Z, Xin YC, et al. Alpha-2 agonists for long-term sedation during mechanical ventilation in critically ill patients. Cochrane Database Syst Rev 2015;1:CD010269.
Dramatic response from pembrolizumab in patient with Lynch syndrome
A woman with two distinct primary tumors achieved complete regression of both after pembrolizumab therapy, investigators report.
This is the first documented instance of a checkpoint inhibitor leading to this kind of simultaneous regression, reported Benjamin Musher, MD, of Baylor College of Medicine, Houston, and his coauthors.
The patient was a 55-year-old woman with a family history of gastric, uterine, and colon cancer. After presenting with weight loss, fatigue, and abdominal pain, colonoscopy showed a 5-cm mucosal lesion. A subsequent PET-CT scan revealed a 12-cm hepatic mass with multiple other liver masses, and bulky lymph nodes nearby. Site biopsies showed two primary cancer types: colonic adenocarcinoma and intrahepatic cholangiocarcinoma.
“Additional staining ... for proteins that repair mismatched DNA showed an absence of MLH1 expression. Sequencing of the patient’s DNA revealed a deleterious mutation in MLH1, which confirmed that Lynch syndrome caused both types of cancer,” the authors wrote in Annals of Internal Medicine.
Lynch syndrome (also called hereditary nonpolyposis colorectal cancer), is an autosomal dominant condition that incurs a high risk of colorectal, pancreatic, bile duct, ovarian, gastric, and uterine cancer. Patients may present with more than one type of cancer simultaneously, as occurred in this case study.
Following diagnosis, the patient started pembrolizumab monotherapy (200 mg IV Q3W). After 16 months the tumors were undetectable by colonoscopy or PET-CT; 2 months later the patient was free of cancer symptoms.
“To our knowledge, our case report is the first to document complete regression of 2 simultaneous types of cancer after treatment with an immune checkpoint inhibitor,” the authors wrote.
But why the dramatic response?
“The types of cancer that develop because of a mismatch repair deficiency contain more mutations than most other kinds of cancer,” the authors explained. These highly mutated cells are recognized by the host immune system, but responses are limited, in part, by programmed cell death proteins. “These events make checkpoint inhibition an attractive and potentially effective treatment for mismatch repair deficient cancer.
“We believe that this case emphasizes the importance of eliciting a thorough family history in patients with cancer and considering the presence of multiple types of primary cancer in a patient with an extensive family history of cancer,” the authors concluded. “It also shows the value of identifying mismatch repair deficiency, [in which] immunotherapy can yield dramatic and durable benefit.”
Dr. Musher reported compensation from LOKON pharmaceuticals.
SOURCE: Musher et al. Ann Intern Med. 2018 Sep 24. doi: 10.7326/L18-0360.
A woman with two distinct primary tumors achieved complete regression of both after pembrolizumab therapy, investigators report.
This is the first documented instance of a checkpoint inhibitor leading to this kind of simultaneous regression, reported Benjamin Musher, MD, of Baylor College of Medicine, Houston, and his coauthors.
The patient was a 55-year-old woman with a family history of gastric, uterine, and colon cancer. After presenting with weight loss, fatigue, and abdominal pain, colonoscopy showed a 5-cm mucosal lesion. A subsequent PET-CT scan revealed a 12-cm hepatic mass with multiple other liver masses, and bulky lymph nodes nearby. Site biopsies showed two primary cancer types: colonic adenocarcinoma and intrahepatic cholangiocarcinoma.
“Additional staining ... for proteins that repair mismatched DNA showed an absence of MLH1 expression. Sequencing of the patient’s DNA revealed a deleterious mutation in MLH1, which confirmed that Lynch syndrome caused both types of cancer,” the authors wrote in Annals of Internal Medicine.
Lynch syndrome (also called hereditary nonpolyposis colorectal cancer), is an autosomal dominant condition that incurs a high risk of colorectal, pancreatic, bile duct, ovarian, gastric, and uterine cancer. Patients may present with more than one type of cancer simultaneously, as occurred in this case study.
Following diagnosis, the patient started pembrolizumab monotherapy (200 mg IV Q3W). After 16 months the tumors were undetectable by colonoscopy or PET-CT; 2 months later the patient was free of cancer symptoms.
“To our knowledge, our case report is the first to document complete regression of 2 simultaneous types of cancer after treatment with an immune checkpoint inhibitor,” the authors wrote.
But why the dramatic response?
“The types of cancer that develop because of a mismatch repair deficiency contain more mutations than most other kinds of cancer,” the authors explained. These highly mutated cells are recognized by the host immune system, but responses are limited, in part, by programmed cell death proteins. “These events make checkpoint inhibition an attractive and potentially effective treatment for mismatch repair deficient cancer.
“We believe that this case emphasizes the importance of eliciting a thorough family history in patients with cancer and considering the presence of multiple types of primary cancer in a patient with an extensive family history of cancer,” the authors concluded. “It also shows the value of identifying mismatch repair deficiency, [in which] immunotherapy can yield dramatic and durable benefit.”
Dr. Musher reported compensation from LOKON pharmaceuticals.
SOURCE: Musher et al. Ann Intern Med. 2018 Sep 24. doi: 10.7326/L18-0360.
A woman with two distinct primary tumors achieved complete regression of both after pembrolizumab therapy, investigators report.
This is the first documented instance of a checkpoint inhibitor leading to this kind of simultaneous regression, reported Benjamin Musher, MD, of Baylor College of Medicine, Houston, and his coauthors.
The patient was a 55-year-old woman with a family history of gastric, uterine, and colon cancer. After presenting with weight loss, fatigue, and abdominal pain, colonoscopy showed a 5-cm mucosal lesion. A subsequent PET-CT scan revealed a 12-cm hepatic mass with multiple other liver masses, and bulky lymph nodes nearby. Site biopsies showed two primary cancer types: colonic adenocarcinoma and intrahepatic cholangiocarcinoma.
“Additional staining ... for proteins that repair mismatched DNA showed an absence of MLH1 expression. Sequencing of the patient’s DNA revealed a deleterious mutation in MLH1, which confirmed that Lynch syndrome caused both types of cancer,” the authors wrote in Annals of Internal Medicine.
Lynch syndrome (also called hereditary nonpolyposis colorectal cancer), is an autosomal dominant condition that incurs a high risk of colorectal, pancreatic, bile duct, ovarian, gastric, and uterine cancer. Patients may present with more than one type of cancer simultaneously, as occurred in this case study.
Following diagnosis, the patient started pembrolizumab monotherapy (200 mg IV Q3W). After 16 months the tumors were undetectable by colonoscopy or PET-CT; 2 months later the patient was free of cancer symptoms.
“To our knowledge, our case report is the first to document complete regression of 2 simultaneous types of cancer after treatment with an immune checkpoint inhibitor,” the authors wrote.
But why the dramatic response?
“The types of cancer that develop because of a mismatch repair deficiency contain more mutations than most other kinds of cancer,” the authors explained. These highly mutated cells are recognized by the host immune system, but responses are limited, in part, by programmed cell death proteins. “These events make checkpoint inhibition an attractive and potentially effective treatment for mismatch repair deficient cancer.
“We believe that this case emphasizes the importance of eliciting a thorough family history in patients with cancer and considering the presence of multiple types of primary cancer in a patient with an extensive family history of cancer,” the authors concluded. “It also shows the value of identifying mismatch repair deficiency, [in which] immunotherapy can yield dramatic and durable benefit.”
Dr. Musher reported compensation from LOKON pharmaceuticals.
SOURCE: Musher et al. Ann Intern Med. 2018 Sep 24. doi: 10.7326/L18-0360.
FROM ANNALS OF INTERNAL MEDICINE
Key clinical point: Pembrolizumab may provide complete tumor regression in patients with mismatch repair deficiency (Lynch syndrome) who have more than one type of cancer.
Major finding: A woman with primary colonic adenocarcinoma and primary intrahepatic cholangiocarcinoma achieved complete regression of both tumor types after pembrolizumab therapy.
Study details: A case study of a 55-year-old woman with Lynch syndrome who had a family history of gastric, uterine, and colon cancer.
Disclosures: Dr. Musher reported receiving compensation from Lokon.
Source: Musher et al. Ann Intern Med. 2018 Sep 24. doi: 10.7326/L18-0360.
Laser tattoo removal plume ‘probably safer’ than laser hair removal plume
SAN DIEGO – results from a novel study demonstrated.
“The laser plume is known to contain possible hazards,” Yakir Levin, MD, PhD, said at the annual Masters of Aesthetics Symposium. “Intact human papillomavirus DNA has been demonstrated in the CO2 laser plume of common wart treatments,” he noted, and transmission of bovine papillomavirus has been shown in a bovine model of CO2 laser treatment (Arch Dermatol 2002;138[10]:1303-7). “In addition, aerosolized human cells have been demonstrated in laser tattoo removal.”
In a more recent study, Gary S. Chuang, MD, and his colleagues demonstrated hazards in the laser hair removal plume (JAMA Dermatol 2016;152[12]:1320-6). “These include ultrafine particles that become lodged in pulmonary alveoli and cause long-term respiratory problems, as well as volatile organic compounds, which can be carcinogens and environmental toxins,” said Dr. Levin of the Massachusetts General Hospital department of dermatology and the Wellman Center for Photomedicine, both in Boston. “They showed that this can be improved but not cured by proper use of a smoke evacuator; they also emphasized the importance of wearing a mask.”
Dr. Levin and his colleagues chose to study laser tattoo removal plume because more than 40 million Americans have tattoos, especially younger adults. In addition, 17% regret having their tattoo and 11% are undergoing or have undergone tattoo removal procedures. In what is believed to be the first study of its kind, the researchers performed a study in ex vivo pig skin and in humans undergoing routine laser tattoo removal. They measured the concentration of nanoparticles as well as the presence of heavy metals, volatile organic compounds, and airborne bacteria.
For the swine study, the excised pig skin was tattooed with several differently colored inks. Dr. Levin and his colleagues found that the concentration of airborne nanoparticles measured during laser tattoo removal was elevated and varied with different inks and different lasers used. Fine metals were measured in mcg/m3 air and were below safe occupational exposure limits. The same effect was seen for volatile organic compounds.
Next, the researchers analyzed the laser plume in humans undergoing removal of blue, black, and multicolored tattoos. “Here, the results were a little bit different,” Dr. Levin said. “Airborne particle concentrations were higher in the dermatologist’s breathing zone and near the tattoo removal site than in the remainder of the room or outside of the room. However, concentrations were 30 times lower for human skin than for pig skin. That’s because the pig study was somewhat artificial in that the tattoos were done when the pig was dead.”
Metals were detected in the plume in the human study, but they were all below occupational exposure limits. The same effect was seen for volatile organic compounds.
Dr. Levin said that airborne nanoparticle concentrations for laser tattoo removal of ex vivo tattooed swine skin were comparable to those reported for hair removal, while airborne nanoparticle concentrations for laser removal of in vivo human skin were much lower than those reported for laser hair removal. “So it’s probably true that the potential health hazards from laser tattoo removal are lower than for laser hair removal, but we did not study viral particles or the presence of viable human cells in the plume,” he said.
Current methods to limit laser plume exposure include suction of the plume with a smoke evacuator, use of a barrier device placed over the skin, and wearing a face mask constructed to filter nanoparticles, such as an N95 mask.
Other safety issues to consider
Dr. Levin discussed additional safety considerations in performing laser treatments.
“We want to protect the epidermis from injury during the laser exposure, which is currently done with spray cooling, air cooling, and/or contact cooling,” he said. “We want to limit the pain experienced by patients throughout the laser treatment before and after the brief laser exposure. This is often accomplished with the use of ice packs or air cooling. We also want to avoid double pulsing and skip areas. This can sometimes but not always be achieved by paying close attention to clinical endpoints.”
He and his associates are currently developing a device to accomplish all of those safety goals with a multilayer approach. “One of the layers would be a hydrogel, which serves to protect the epidermis and to provide pain relief throughout the laser treatment,” he said. “Above that layer is an indicator layer that is not aqueous, and on top of that is a fine layer of particles. The idea is, if you’re looking at this from above, when you fire the laser, you would see a change of color or some other indicator to show you exactly where you fired the laser. Finally, the multilayer patch also serves to obstruct the laser plume.”
Dr. Levin acknowledged research support from the American Society for Dermatologic Surgery’s Fredric S. Brandt, MD, Innovations in Aesthetics Fellowship Fund and assistance from the Health Hazard Evaluation Program of National Institute for Occupational Safety and Health.
SAN DIEGO – results from a novel study demonstrated.
“The laser plume is known to contain possible hazards,” Yakir Levin, MD, PhD, said at the annual Masters of Aesthetics Symposium. “Intact human papillomavirus DNA has been demonstrated in the CO2 laser plume of common wart treatments,” he noted, and transmission of bovine papillomavirus has been shown in a bovine model of CO2 laser treatment (Arch Dermatol 2002;138[10]:1303-7). “In addition, aerosolized human cells have been demonstrated in laser tattoo removal.”
In a more recent study, Gary S. Chuang, MD, and his colleagues demonstrated hazards in the laser hair removal plume (JAMA Dermatol 2016;152[12]:1320-6). “These include ultrafine particles that become lodged in pulmonary alveoli and cause long-term respiratory problems, as well as volatile organic compounds, which can be carcinogens and environmental toxins,” said Dr. Levin of the Massachusetts General Hospital department of dermatology and the Wellman Center for Photomedicine, both in Boston. “They showed that this can be improved but not cured by proper use of a smoke evacuator; they also emphasized the importance of wearing a mask.”
Dr. Levin and his colleagues chose to study laser tattoo removal plume because more than 40 million Americans have tattoos, especially younger adults. In addition, 17% regret having their tattoo and 11% are undergoing or have undergone tattoo removal procedures. In what is believed to be the first study of its kind, the researchers performed a study in ex vivo pig skin and in humans undergoing routine laser tattoo removal. They measured the concentration of nanoparticles as well as the presence of heavy metals, volatile organic compounds, and airborne bacteria.
For the swine study, the excised pig skin was tattooed with several differently colored inks. Dr. Levin and his colleagues found that the concentration of airborne nanoparticles measured during laser tattoo removal was elevated and varied with different inks and different lasers used. Fine metals were measured in mcg/m3 air and were below safe occupational exposure limits. The same effect was seen for volatile organic compounds.
Next, the researchers analyzed the laser plume in humans undergoing removal of blue, black, and multicolored tattoos. “Here, the results were a little bit different,” Dr. Levin said. “Airborne particle concentrations were higher in the dermatologist’s breathing zone and near the tattoo removal site than in the remainder of the room or outside of the room. However, concentrations were 30 times lower for human skin than for pig skin. That’s because the pig study was somewhat artificial in that the tattoos were done when the pig was dead.”
Metals were detected in the plume in the human study, but they were all below occupational exposure limits. The same effect was seen for volatile organic compounds.
Dr. Levin said that airborne nanoparticle concentrations for laser tattoo removal of ex vivo tattooed swine skin were comparable to those reported for hair removal, while airborne nanoparticle concentrations for laser removal of in vivo human skin were much lower than those reported for laser hair removal. “So it’s probably true that the potential health hazards from laser tattoo removal are lower than for laser hair removal, but we did not study viral particles or the presence of viable human cells in the plume,” he said.
Current methods to limit laser plume exposure include suction of the plume with a smoke evacuator, use of a barrier device placed over the skin, and wearing a face mask constructed to filter nanoparticles, such as an N95 mask.
Other safety issues to consider
Dr. Levin discussed additional safety considerations in performing laser treatments.
“We want to protect the epidermis from injury during the laser exposure, which is currently done with spray cooling, air cooling, and/or contact cooling,” he said. “We want to limit the pain experienced by patients throughout the laser treatment before and after the brief laser exposure. This is often accomplished with the use of ice packs or air cooling. We also want to avoid double pulsing and skip areas. This can sometimes but not always be achieved by paying close attention to clinical endpoints.”
He and his associates are currently developing a device to accomplish all of those safety goals with a multilayer approach. “One of the layers would be a hydrogel, which serves to protect the epidermis and to provide pain relief throughout the laser treatment,” he said. “Above that layer is an indicator layer that is not aqueous, and on top of that is a fine layer of particles. The idea is, if you’re looking at this from above, when you fire the laser, you would see a change of color or some other indicator to show you exactly where you fired the laser. Finally, the multilayer patch also serves to obstruct the laser plume.”
Dr. Levin acknowledged research support from the American Society for Dermatologic Surgery’s Fredric S. Brandt, MD, Innovations in Aesthetics Fellowship Fund and assistance from the Health Hazard Evaluation Program of National Institute for Occupational Safety and Health.
SAN DIEGO – results from a novel study demonstrated.
“The laser plume is known to contain possible hazards,” Yakir Levin, MD, PhD, said at the annual Masters of Aesthetics Symposium. “Intact human papillomavirus DNA has been demonstrated in the CO2 laser plume of common wart treatments,” he noted, and transmission of bovine papillomavirus has been shown in a bovine model of CO2 laser treatment (Arch Dermatol 2002;138[10]:1303-7). “In addition, aerosolized human cells have been demonstrated in laser tattoo removal.”
In a more recent study, Gary S. Chuang, MD, and his colleagues demonstrated hazards in the laser hair removal plume (JAMA Dermatol 2016;152[12]:1320-6). “These include ultrafine particles that become lodged in pulmonary alveoli and cause long-term respiratory problems, as well as volatile organic compounds, which can be carcinogens and environmental toxins,” said Dr. Levin of the Massachusetts General Hospital department of dermatology and the Wellman Center for Photomedicine, both in Boston. “They showed that this can be improved but not cured by proper use of a smoke evacuator; they also emphasized the importance of wearing a mask.”
Dr. Levin and his colleagues chose to study laser tattoo removal plume because more than 40 million Americans have tattoos, especially younger adults. In addition, 17% regret having their tattoo and 11% are undergoing or have undergone tattoo removal procedures. In what is believed to be the first study of its kind, the researchers performed a study in ex vivo pig skin and in humans undergoing routine laser tattoo removal. They measured the concentration of nanoparticles as well as the presence of heavy metals, volatile organic compounds, and airborne bacteria.
For the swine study, the excised pig skin was tattooed with several differently colored inks. Dr. Levin and his colleagues found that the concentration of airborne nanoparticles measured during laser tattoo removal was elevated and varied with different inks and different lasers used. Fine metals were measured in mcg/m3 air and were below safe occupational exposure limits. The same effect was seen for volatile organic compounds.
Next, the researchers analyzed the laser plume in humans undergoing removal of blue, black, and multicolored tattoos. “Here, the results were a little bit different,” Dr. Levin said. “Airborne particle concentrations were higher in the dermatologist’s breathing zone and near the tattoo removal site than in the remainder of the room or outside of the room. However, concentrations were 30 times lower for human skin than for pig skin. That’s because the pig study was somewhat artificial in that the tattoos were done when the pig was dead.”
Metals were detected in the plume in the human study, but they were all below occupational exposure limits. The same effect was seen for volatile organic compounds.
Dr. Levin said that airborne nanoparticle concentrations for laser tattoo removal of ex vivo tattooed swine skin were comparable to those reported for hair removal, while airborne nanoparticle concentrations for laser removal of in vivo human skin were much lower than those reported for laser hair removal. “So it’s probably true that the potential health hazards from laser tattoo removal are lower than for laser hair removal, but we did not study viral particles or the presence of viable human cells in the plume,” he said.
Current methods to limit laser plume exposure include suction of the plume with a smoke evacuator, use of a barrier device placed over the skin, and wearing a face mask constructed to filter nanoparticles, such as an N95 mask.
Other safety issues to consider
Dr. Levin discussed additional safety considerations in performing laser treatments.
“We want to protect the epidermis from injury during the laser exposure, which is currently done with spray cooling, air cooling, and/or contact cooling,” he said. “We want to limit the pain experienced by patients throughout the laser treatment before and after the brief laser exposure. This is often accomplished with the use of ice packs or air cooling. We also want to avoid double pulsing and skip areas. This can sometimes but not always be achieved by paying close attention to clinical endpoints.”
He and his associates are currently developing a device to accomplish all of those safety goals with a multilayer approach. “One of the layers would be a hydrogel, which serves to protect the epidermis and to provide pain relief throughout the laser treatment,” he said. “Above that layer is an indicator layer that is not aqueous, and on top of that is a fine layer of particles. The idea is, if you’re looking at this from above, when you fire the laser, you would see a change of color or some other indicator to show you exactly where you fired the laser. Finally, the multilayer patch also serves to obstruct the laser plume.”
Dr. Levin acknowledged research support from the American Society for Dermatologic Surgery’s Fredric S. Brandt, MD, Innovations in Aesthetics Fellowship Fund and assistance from the Health Hazard Evaluation Program of National Institute for Occupational Safety and Health.
REPORTING FROM MOAS 2018
Trump administration proposes weakening rules governing organ transplant centers
This article was produced in collaboration with the Houston Chronicle.
The Trump administration on Sept. 17 proposed eliminating a decade-old regulation that puts hospitals at risk of losing their Medicare funding if too many of their patients die or suffer organ failure after receiving transplants.
The rule the government is proposing to scrap is the same one that led the Centers for Medicare & Medicaid Services to cut off funding in August for heart transplants at Baylor St. Luke’s Medical Center in Houston after an investigation by ProPublica and the Houston Chronicle revealed an outsized number of patient deaths and complications in recent years.
The proposal was unveiled Sept. 17 as part of the White House’s push to “cut the red tape” and do away with “burdensome regulation” that officials said put paperwork ahead of patients. In a speech announcing the proposed changes, CMS Administrator Seema Verma said the agency’s existing policies have “put lives in danger.”
“We are proposing to remove those inefficiencies to reduce the amount of time patients have to wait, so that they can begin healing,” Ms. Verma said.
The proposal, now subject to public comment and revision before it is finalized, surprised many transplant physicians who have long called for relaxed federal oversight. They’ve argued that the rules requiring that hospitals meet certain survival thresholds for transplants discourage them from taking on risky patients or accepting less-than-perfect organs, lengthening the time patients spend on the waiting list.
The regulation was put in place in 2007 after a series of scandals at transplant programs revealed lax federal oversight. Several transplant programs had compiled abysmal patient survival statistics for years while continuing to receive Medicare funding.
Even though it has the authority to do so, Medicare rarely terminates programs for poor outcomes. It is far more common for the government to force underperforming programs into systems-improvement agreements, in which hospitals agree to make certain changes and be subject to stepped-up oversight.
Medicare bypassed that process and cut off funding for heart transplants at St. Luke’s in August after the hospital’s 1-year patient survival rate fell below national norms from 2014 to mid-2016. A few St. Luke’s cardiologists grew so concerned that they started sending some of their patients to other hospitals for transplants.
St. Luke’s has appealed its Medicare termination, saying, “we do not believe CMS’ recent decisions reflect our ongoing progress and accomplishments to improve the quality of our care.” A spokeswoman said officials are still reviewing the Medicare proposal and declined to comment.
In a statement to reporters Sept. 21, CMS said it would continue to monitoring transplant programs and is strengthening its process for inspecting transplant programs to ensure they provide safe, quality care.
“CMS will continue to collect the data on each transplant program’s performance with regards to patient and graft survival,” the agency said in the statement. “These data, rather than being a stand-alone measure, will be used as a component of the survey process to further inform and direct the survey.”
If the proposed regulatory change had been in place previously, it’s not clear whether St. Luke’s would have faced punitive action from Medicare.
“I am probably in the minority in the transplant community, but I think, based on what is proposed, this is a bad idea,” said Laura J. Aguiar, an Arizona-based transplant consultant who has spent years helping programs improve their outcomes to stave off Medicare penalties. “I have been around long enough to remember that there were very valid reasons why CMS, in the George W. Bush administration, took the steps they took in implementing all of this.”
Since the rules were put in place 11 years ago, the percentage of patients who survive at least 1 year after receiving heart, kidney, lung, and other organ transplants has increased nationally. But some experts say those gains have come at a cost.
Jesse D. Schold, PhD, a researcher in quantitative health sciences at the Cleveland Clinic, has spent years chronicling what he calls the “unintended consequences” of holding transplant programs accountable for poor outcomes. Even though CMS relies on data that has been adjusted to ensure that programs aren’t punished for treating sicker patients or accepting riskier donor organs, Dr. Schold said the rules have created a perception that programs need to turn away some ailing patients and reject less-than-ideal organs in order to meet outcome targets.
As a result, Dr. Schold said, some potentially viable donor organs are discarded while thousands of patients die on waiting lists each year. Dr. Schold said he was surprised to learn a study he coauthored was among the research cited by CMS as justification for the policy change, which he said would be a “significant net positive” for patients.
“I don’t want anything to in any way imply that I’m a fan of the current administration,” Dr. Schold said, referencing the Trump administration’s aggressive and often controversial efforts to slash regulations. “However, in this case, I think it is something that is beneficial.”
Joel Adler, MD, a liver surgeon at the University of Wisconsin–Madison, whose research also was cited by CMS, said a major weakness of the current regulation is that it focuses only on the survival of patients fortunate enough to have received a transplant. Medicare, he said, does not take into account the percentage of patients who die awaiting a transplant. That can discourage programs from accepting organs for patients who might be less likely to survive afterward.
Despite identifying problems with the current rules, Dr. Adler and his coauthor did not propose eliminating Medicare’s standards, but they instead suggested ways to improve outcome measures and create incentives for programs to perform more, not fewer, transplants.
“Should we get rid of (the regulation) entirely?” Dr. Adler asked. “I don’t know. I suspect we’ll swing back to somewhere in the middle, because there has to be some mechanism of capturing things when they are really, really bad. That has to exist.”
Medicare isn’t the only organization that oversees transplant centers. The United Network for Organ Sharing, a federal contractor that operates the national waiting list for organs, can put programs on probation or even revoke their good standing for continued poor results, though it rarely takes such actions. Similarly, another federal contractor, the Scientific Registry of Transplant Recipients, analyzes transplant outcomes and publicly reports which centers have mortality rates that are higher than expected based on the characteristics of their patients.
Even if the proposal is approved, it would not mean CMS would stop regulating transplant programs. Last year, for example, CMS cut off funding to the Medical University Hospital in Charleston, South Carolina, after the program failed to perform the minimum number of heart transplants required by CMS to maintain certification. That provision, also added during the reforms of 2007, would not be affected by the changes proposed Sept. 17.
The Charleston hospital, South Carolina’s only heart transplant program, made necessary changes and regained Medicare certification this year.
Alexander Aussi, a San Antonio–based consultant who specializes in helping transplant programs satisfy regulatory requirements, said he understands the desire to reduce the number of rules and regulations that transplant centers must follow. But he said he fears that the CMS proposal would return the transplant field to an earlier era when “some programs were cowboyish about their outcomes.”
“I cannot tell you in good conscience that if you remove those guidelines and metrics … that you’re going to have better outcomes,” Mr. Aussi said. “On the contrary, I believe you’re going to have a lot of transplant programs reversing course.”
Ms. Aguiar, the Arizona-based consultant, shares those concerns. Even without strict CMS oversight, she said, many transplant programs will continue providing high-quality care; but some won’t.
“There will be others that will take the removal of these requirements as a blessing to go back to the bad old days,” she said, “and it is patients who will end up paying the price for it.”
Mike Hixenbaugh is an investigative reporter at the Houston Chronicle. Email him at [email protected] and follow him on Twitter at @Mike_Hixenbaugh. Charles Ornstein is a senior editor at ProPublica, overseeing the Local Reporting Network. Follow him on Twitter at @charlesornstein.
This article was produced in collaboration with the Houston Chronicle.
The Trump administration on Sept. 17 proposed eliminating a decade-old regulation that puts hospitals at risk of losing their Medicare funding if too many of their patients die or suffer organ failure after receiving transplants.
The rule the government is proposing to scrap is the same one that led the Centers for Medicare & Medicaid Services to cut off funding in August for heart transplants at Baylor St. Luke’s Medical Center in Houston after an investigation by ProPublica and the Houston Chronicle revealed an outsized number of patient deaths and complications in recent years.
The proposal was unveiled Sept. 17 as part of the White House’s push to “cut the red tape” and do away with “burdensome regulation” that officials said put paperwork ahead of patients. In a speech announcing the proposed changes, CMS Administrator Seema Verma said the agency’s existing policies have “put lives in danger.”
“We are proposing to remove those inefficiencies to reduce the amount of time patients have to wait, so that they can begin healing,” Ms. Verma said.
The proposal, now subject to public comment and revision before it is finalized, surprised many transplant physicians who have long called for relaxed federal oversight. They’ve argued that the rules requiring that hospitals meet certain survival thresholds for transplants discourage them from taking on risky patients or accepting less-than-perfect organs, lengthening the time patients spend on the waiting list.
The regulation was put in place in 2007 after a series of scandals at transplant programs revealed lax federal oversight. Several transplant programs had compiled abysmal patient survival statistics for years while continuing to receive Medicare funding.
Even though it has the authority to do so, Medicare rarely terminates programs for poor outcomes. It is far more common for the government to force underperforming programs into systems-improvement agreements, in which hospitals agree to make certain changes and be subject to stepped-up oversight.
Medicare bypassed that process and cut off funding for heart transplants at St. Luke’s in August after the hospital’s 1-year patient survival rate fell below national norms from 2014 to mid-2016. A few St. Luke’s cardiologists grew so concerned that they started sending some of their patients to other hospitals for transplants.
St. Luke’s has appealed its Medicare termination, saying, “we do not believe CMS’ recent decisions reflect our ongoing progress and accomplishments to improve the quality of our care.” A spokeswoman said officials are still reviewing the Medicare proposal and declined to comment.
In a statement to reporters Sept. 21, CMS said it would continue to monitoring transplant programs and is strengthening its process for inspecting transplant programs to ensure they provide safe, quality care.
“CMS will continue to collect the data on each transplant program’s performance with regards to patient and graft survival,” the agency said in the statement. “These data, rather than being a stand-alone measure, will be used as a component of the survey process to further inform and direct the survey.”
If the proposed regulatory change had been in place previously, it’s not clear whether St. Luke’s would have faced punitive action from Medicare.
“I am probably in the minority in the transplant community, but I think, based on what is proposed, this is a bad idea,” said Laura J. Aguiar, an Arizona-based transplant consultant who has spent years helping programs improve their outcomes to stave off Medicare penalties. “I have been around long enough to remember that there were very valid reasons why CMS, in the George W. Bush administration, took the steps they took in implementing all of this.”
Since the rules were put in place 11 years ago, the percentage of patients who survive at least 1 year after receiving heart, kidney, lung, and other organ transplants has increased nationally. But some experts say those gains have come at a cost.
Jesse D. Schold, PhD, a researcher in quantitative health sciences at the Cleveland Clinic, has spent years chronicling what he calls the “unintended consequences” of holding transplant programs accountable for poor outcomes. Even though CMS relies on data that has been adjusted to ensure that programs aren’t punished for treating sicker patients or accepting riskier donor organs, Dr. Schold said the rules have created a perception that programs need to turn away some ailing patients and reject less-than-ideal organs in order to meet outcome targets.
As a result, Dr. Schold said, some potentially viable donor organs are discarded while thousands of patients die on waiting lists each year. Dr. Schold said he was surprised to learn a study he coauthored was among the research cited by CMS as justification for the policy change, which he said would be a “significant net positive” for patients.
“I don’t want anything to in any way imply that I’m a fan of the current administration,” Dr. Schold said, referencing the Trump administration’s aggressive and often controversial efforts to slash regulations. “However, in this case, I think it is something that is beneficial.”
Joel Adler, MD, a liver surgeon at the University of Wisconsin–Madison, whose research also was cited by CMS, said a major weakness of the current regulation is that it focuses only on the survival of patients fortunate enough to have received a transplant. Medicare, he said, does not take into account the percentage of patients who die awaiting a transplant. That can discourage programs from accepting organs for patients who might be less likely to survive afterward.
Despite identifying problems with the current rules, Dr. Adler and his coauthor did not propose eliminating Medicare’s standards, but they instead suggested ways to improve outcome measures and create incentives for programs to perform more, not fewer, transplants.
“Should we get rid of (the regulation) entirely?” Dr. Adler asked. “I don’t know. I suspect we’ll swing back to somewhere in the middle, because there has to be some mechanism of capturing things when they are really, really bad. That has to exist.”
Medicare isn’t the only organization that oversees transplant centers. The United Network for Organ Sharing, a federal contractor that operates the national waiting list for organs, can put programs on probation or even revoke their good standing for continued poor results, though it rarely takes such actions. Similarly, another federal contractor, the Scientific Registry of Transplant Recipients, analyzes transplant outcomes and publicly reports which centers have mortality rates that are higher than expected based on the characteristics of their patients.
Even if the proposal is approved, it would not mean CMS would stop regulating transplant programs. Last year, for example, CMS cut off funding to the Medical University Hospital in Charleston, South Carolina, after the program failed to perform the minimum number of heart transplants required by CMS to maintain certification. That provision, also added during the reforms of 2007, would not be affected by the changes proposed Sept. 17.
The Charleston hospital, South Carolina’s only heart transplant program, made necessary changes and regained Medicare certification this year.
Alexander Aussi, a San Antonio–based consultant who specializes in helping transplant programs satisfy regulatory requirements, said he understands the desire to reduce the number of rules and regulations that transplant centers must follow. But he said he fears that the CMS proposal would return the transplant field to an earlier era when “some programs were cowboyish about their outcomes.”
“I cannot tell you in good conscience that if you remove those guidelines and metrics … that you’re going to have better outcomes,” Mr. Aussi said. “On the contrary, I believe you’re going to have a lot of transplant programs reversing course.”
Ms. Aguiar, the Arizona-based consultant, shares those concerns. Even without strict CMS oversight, she said, many transplant programs will continue providing high-quality care; but some won’t.
“There will be others that will take the removal of these requirements as a blessing to go back to the bad old days,” she said, “and it is patients who will end up paying the price for it.”
Mike Hixenbaugh is an investigative reporter at the Houston Chronicle. Email him at [email protected] and follow him on Twitter at @Mike_Hixenbaugh. Charles Ornstein is a senior editor at ProPublica, overseeing the Local Reporting Network. Follow him on Twitter at @charlesornstein.
This article was produced in collaboration with the Houston Chronicle.
The Trump administration on Sept. 17 proposed eliminating a decade-old regulation that puts hospitals at risk of losing their Medicare funding if too many of their patients die or suffer organ failure after receiving transplants.
The rule the government is proposing to scrap is the same one that led the Centers for Medicare & Medicaid Services to cut off funding in August for heart transplants at Baylor St. Luke’s Medical Center in Houston after an investigation by ProPublica and the Houston Chronicle revealed an outsized number of patient deaths and complications in recent years.
The proposal was unveiled Sept. 17 as part of the White House’s push to “cut the red tape” and do away with “burdensome regulation” that officials said put paperwork ahead of patients. In a speech announcing the proposed changes, CMS Administrator Seema Verma said the agency’s existing policies have “put lives in danger.”
“We are proposing to remove those inefficiencies to reduce the amount of time patients have to wait, so that they can begin healing,” Ms. Verma said.
The proposal, now subject to public comment and revision before it is finalized, surprised many transplant physicians who have long called for relaxed federal oversight. They’ve argued that the rules requiring that hospitals meet certain survival thresholds for transplants discourage them from taking on risky patients or accepting less-than-perfect organs, lengthening the time patients spend on the waiting list.
The regulation was put in place in 2007 after a series of scandals at transplant programs revealed lax federal oversight. Several transplant programs had compiled abysmal patient survival statistics for years while continuing to receive Medicare funding.
Even though it has the authority to do so, Medicare rarely terminates programs for poor outcomes. It is far more common for the government to force underperforming programs into systems-improvement agreements, in which hospitals agree to make certain changes and be subject to stepped-up oversight.
Medicare bypassed that process and cut off funding for heart transplants at St. Luke’s in August after the hospital’s 1-year patient survival rate fell below national norms from 2014 to mid-2016. A few St. Luke’s cardiologists grew so concerned that they started sending some of their patients to other hospitals for transplants.
St. Luke’s has appealed its Medicare termination, saying, “we do not believe CMS’ recent decisions reflect our ongoing progress and accomplishments to improve the quality of our care.” A spokeswoman said officials are still reviewing the Medicare proposal and declined to comment.
In a statement to reporters Sept. 21, CMS said it would continue to monitoring transplant programs and is strengthening its process for inspecting transplant programs to ensure they provide safe, quality care.
“CMS will continue to collect the data on each transplant program’s performance with regards to patient and graft survival,” the agency said in the statement. “These data, rather than being a stand-alone measure, will be used as a component of the survey process to further inform and direct the survey.”
If the proposed regulatory change had been in place previously, it’s not clear whether St. Luke’s would have faced punitive action from Medicare.
“I am probably in the minority in the transplant community, but I think, based on what is proposed, this is a bad idea,” said Laura J. Aguiar, an Arizona-based transplant consultant who has spent years helping programs improve their outcomes to stave off Medicare penalties. “I have been around long enough to remember that there were very valid reasons why CMS, in the George W. Bush administration, took the steps they took in implementing all of this.”
Since the rules were put in place 11 years ago, the percentage of patients who survive at least 1 year after receiving heart, kidney, lung, and other organ transplants has increased nationally. But some experts say those gains have come at a cost.
Jesse D. Schold, PhD, a researcher in quantitative health sciences at the Cleveland Clinic, has spent years chronicling what he calls the “unintended consequences” of holding transplant programs accountable for poor outcomes. Even though CMS relies on data that has been adjusted to ensure that programs aren’t punished for treating sicker patients or accepting riskier donor organs, Dr. Schold said the rules have created a perception that programs need to turn away some ailing patients and reject less-than-ideal organs in order to meet outcome targets.
As a result, Dr. Schold said, some potentially viable donor organs are discarded while thousands of patients die on waiting lists each year. Dr. Schold said he was surprised to learn a study he coauthored was among the research cited by CMS as justification for the policy change, which he said would be a “significant net positive” for patients.
“I don’t want anything to in any way imply that I’m a fan of the current administration,” Dr. Schold said, referencing the Trump administration’s aggressive and often controversial efforts to slash regulations. “However, in this case, I think it is something that is beneficial.”
Joel Adler, MD, a liver surgeon at the University of Wisconsin–Madison, whose research also was cited by CMS, said a major weakness of the current regulation is that it focuses only on the survival of patients fortunate enough to have received a transplant. Medicare, he said, does not take into account the percentage of patients who die awaiting a transplant. That can discourage programs from accepting organs for patients who might be less likely to survive afterward.
Despite identifying problems with the current rules, Dr. Adler and his coauthor did not propose eliminating Medicare’s standards, but they instead suggested ways to improve outcome measures and create incentives for programs to perform more, not fewer, transplants.
“Should we get rid of (the regulation) entirely?” Dr. Adler asked. “I don’t know. I suspect we’ll swing back to somewhere in the middle, because there has to be some mechanism of capturing things when they are really, really bad. That has to exist.”
Medicare isn’t the only organization that oversees transplant centers. The United Network for Organ Sharing, a federal contractor that operates the national waiting list for organs, can put programs on probation or even revoke their good standing for continued poor results, though it rarely takes such actions. Similarly, another federal contractor, the Scientific Registry of Transplant Recipients, analyzes transplant outcomes and publicly reports which centers have mortality rates that are higher than expected based on the characteristics of their patients.
Even if the proposal is approved, it would not mean CMS would stop regulating transplant programs. Last year, for example, CMS cut off funding to the Medical University Hospital in Charleston, South Carolina, after the program failed to perform the minimum number of heart transplants required by CMS to maintain certification. That provision, also added during the reforms of 2007, would not be affected by the changes proposed Sept. 17.
The Charleston hospital, South Carolina’s only heart transplant program, made necessary changes and regained Medicare certification this year.
Alexander Aussi, a San Antonio–based consultant who specializes in helping transplant programs satisfy regulatory requirements, said he understands the desire to reduce the number of rules and regulations that transplant centers must follow. But he said he fears that the CMS proposal would return the transplant field to an earlier era when “some programs were cowboyish about their outcomes.”
“I cannot tell you in good conscience that if you remove those guidelines and metrics … that you’re going to have better outcomes,” Mr. Aussi said. “On the contrary, I believe you’re going to have a lot of transplant programs reversing course.”
Ms. Aguiar, the Arizona-based consultant, shares those concerns. Even without strict CMS oversight, she said, many transplant programs will continue providing high-quality care; but some won’t.
“There will be others that will take the removal of these requirements as a blessing to go back to the bad old days,” she said, “and it is patients who will end up paying the price for it.”
Mike Hixenbaugh is an investigative reporter at the Houston Chronicle. Email him at [email protected] and follow him on Twitter at @Mike_Hixenbaugh. Charles Ornstein is a senior editor at ProPublica, overseeing the Local Reporting Network. Follow him on Twitter at @charlesornstein.
Prosthesis-patient mismatch post TAVR ups death risk 19%
SAN DIEGO – Severe prosthesis-patient mismatch (PPM) after transcatheter aortic valve replacement (TAVR) increases risk of adverse outcomes and may be preventable in some cases with careful preprocedural planning, suggests a registry-based retrospective cohort study of 62,125 patients treated in the contemporary era.
The study – the largest to date of this patient population – determined that about one in every eight patients undergoing TAVR ultimately had a severe mismatch between the hemodynamics of the valve prosthesis and the requirements for cardiac output. Compared with counterparts that have moderate or no PPM, these patients with severe PPM had a 12% higher adjusted risk of heart failure rehospitalization and a 19% higher adjusted risk of death, according to results reported at the Transcatheter Cardiovascular Therapeutics annual meeting and simultaneously published online (J Am Coll Cardiol. 2018 Sep 23. doi: 10.1016/j.jacc.2018.09.001).
Notably, some of the predictors of severe PPM, such as use of smaller-diameter valves and performance of a valve-in-valve procedure, were potentially modifiable.
“Our findings suggest that efforts should be made to identify this problem and limit the risk for PPM after TAVR,” concluded lead investigator Howard C. Herrmann, MD, a professor at the University of Pennsylvania and director of the cardiac catheterization laboratories, Hospital of the University of Pennsylvania, both in Philadelphia. “Awareness is really the first step in trying to fix it.”
“We spend a lot of time in the heart-team meetings looking at the CT scans for annular dimensions and the vascular access, but we don’t really talk too much about severe PPM or the risk of that,” he elaborated. “This [study] allows us to start to predict it, based on patient factors and what prosthesis we might be choosing for a patient, and it allows us to have that conversation and think about alternatives.
“There are alternatives to try to avoid PPM, everything from which prosthesis we choose to the size of the prosthesis, to whether we fracture a patient’s valve if we are doing a valve-in-valve procedure. In the future, in some situations, we might even choose a low-risk or low-intermediate-risk patient for surgery with an enlargement operation in order to get a larger effective orifice area. So there are choices that we can make, and we should start thinking about that in the heart-team approach.”
Findings in context
The new study reinforces the message “that hemodynamics matter,” he said. “To the extent that we can get larger valves in and get better results from those valves, it will reduce the frequency of PPM. That’s something as operators we don’t spend as much time focusing on, and this will refocus our attention in trying to prevent PPM by being more diligent in terms of prosthesis choice and some operator characteristics, to try to reduce the gradients and improve the effective orifice areas as much as we can.”
Panelist Jeffrey J. Popma, MD, an interventional cardiologist at Beth Israel Deaconess Medical Center, Boston, noted that he and his colleagues have observed similar trends in their smaller studies but had difficulty teasing out contributors. “It really goes back to the preprocedural planning about what valve you can get in, and larger orifice area is certainly better,” he concurred. “So I do think that this is a phenomenal addition.”
Study details
For the study, Dr. Herrmann and his colleagues analyzed 2014-2107 data from the STS/ACC Transcatheter Valve Therapy Registry, a national surveillance and quality improvement system. They identified enrollees aged 65 years or older at the time of their TAVR procedure who had fee-for-service Medicare and linked them to Centers for Medicare & Medicaid Services claims data to assess outcomes.
Overall, 12.1% of patients had severe PPM, defined as an effective valve orifice area indexed to body surface area of less than 0.65 cm2/m2 on discharge echocardiography, and another 24.6% had moderate PPM, Dr. Herrmann reported at the meeting, sponsored by the Cardiovascular Research Foundation.
The strongest multivariate predictors of severe PPM were small prosthetic valve size (up to 23 mm in diameter) (odds ratio, 2.77), a valve-in-valve procedure (OR, 2.78), larger body surface area (OR, 1.71 per 0.2-U increase), and female sex (OR, 1.46). Odds also increased with decreasing age and were elevated for patients of nonwhite/Hispanic race and those having a lower ejection fraction, atrial fibrillation or flutter, or severe mitral or tricuspid regurgitation.
It was not possible to assess specific valves as predictors of mismatch because the registry prohibits comparisons across manufacturers, according to Dr. Herrmann.
One-year mortality, the study’s primary endpoint, was 17.2% in patients with severe PPM, compared with 15.8% in patients with moderate or no PPM (adjusted hazard ratio, 1.19; P less than .001). Findings were similar across subgroups.
The 1-year rate of heart failure rehospitalization was 14.7% in patients with severe PPM, compared with 12.2% in patients with moderate or no PPM (AHR, 1.12; P = .017).
“I would point out that these [outcome] curves are divergent at 1 year,” Dr. Herrmann noted. “So if we look at low-intermediate-risk and low-risk patients and younger patients, who may be more active and who see the effects of PPM more commonly and who are going to be living more than 1 year, we are going to have to consider this going forward in a more important way.”
Severe PPM did not significantly influence the rate of stroke (which stood at about 4% in each group) or worsen quality of life score at 1 year.
Dr. Herrmann disclosed receiving institutional grant/research support from Abbott Vascular, Bayer, Boston Scientific, Corvia Medical, Edwards Lifesciences, Medtronic, and St. Jude Medical, as well as consulting fees/honoraria from Edwards, Medtronic, and Siemens Healthineers.
SAN DIEGO – Severe prosthesis-patient mismatch (PPM) after transcatheter aortic valve replacement (TAVR) increases risk of adverse outcomes and may be preventable in some cases with careful preprocedural planning, suggests a registry-based retrospective cohort study of 62,125 patients treated in the contemporary era.
The study – the largest to date of this patient population – determined that about one in every eight patients undergoing TAVR ultimately had a severe mismatch between the hemodynamics of the valve prosthesis and the requirements for cardiac output. Compared with counterparts that have moderate or no PPM, these patients with severe PPM had a 12% higher adjusted risk of heart failure rehospitalization and a 19% higher adjusted risk of death, according to results reported at the Transcatheter Cardiovascular Therapeutics annual meeting and simultaneously published online (J Am Coll Cardiol. 2018 Sep 23. doi: 10.1016/j.jacc.2018.09.001).
Notably, some of the predictors of severe PPM, such as use of smaller-diameter valves and performance of a valve-in-valve procedure, were potentially modifiable.
“Our findings suggest that efforts should be made to identify this problem and limit the risk for PPM after TAVR,” concluded lead investigator Howard C. Herrmann, MD, a professor at the University of Pennsylvania and director of the cardiac catheterization laboratories, Hospital of the University of Pennsylvania, both in Philadelphia. “Awareness is really the first step in trying to fix it.”
“We spend a lot of time in the heart-team meetings looking at the CT scans for annular dimensions and the vascular access, but we don’t really talk too much about severe PPM or the risk of that,” he elaborated. “This [study] allows us to start to predict it, based on patient factors and what prosthesis we might be choosing for a patient, and it allows us to have that conversation and think about alternatives.
“There are alternatives to try to avoid PPM, everything from which prosthesis we choose to the size of the prosthesis, to whether we fracture a patient’s valve if we are doing a valve-in-valve procedure. In the future, in some situations, we might even choose a low-risk or low-intermediate-risk patient for surgery with an enlargement operation in order to get a larger effective orifice area. So there are choices that we can make, and we should start thinking about that in the heart-team approach.”
Findings in context
The new study reinforces the message “that hemodynamics matter,” he said. “To the extent that we can get larger valves in and get better results from those valves, it will reduce the frequency of PPM. That’s something as operators we don’t spend as much time focusing on, and this will refocus our attention in trying to prevent PPM by being more diligent in terms of prosthesis choice and some operator characteristics, to try to reduce the gradients and improve the effective orifice areas as much as we can.”
Panelist Jeffrey J. Popma, MD, an interventional cardiologist at Beth Israel Deaconess Medical Center, Boston, noted that he and his colleagues have observed similar trends in their smaller studies but had difficulty teasing out contributors. “It really goes back to the preprocedural planning about what valve you can get in, and larger orifice area is certainly better,” he concurred. “So I do think that this is a phenomenal addition.”
Study details
For the study, Dr. Herrmann and his colleagues analyzed 2014-2107 data from the STS/ACC Transcatheter Valve Therapy Registry, a national surveillance and quality improvement system. They identified enrollees aged 65 years or older at the time of their TAVR procedure who had fee-for-service Medicare and linked them to Centers for Medicare & Medicaid Services claims data to assess outcomes.
Overall, 12.1% of patients had severe PPM, defined as an effective valve orifice area indexed to body surface area of less than 0.65 cm2/m2 on discharge echocardiography, and another 24.6% had moderate PPM, Dr. Herrmann reported at the meeting, sponsored by the Cardiovascular Research Foundation.
The strongest multivariate predictors of severe PPM were small prosthetic valve size (up to 23 mm in diameter) (odds ratio, 2.77), a valve-in-valve procedure (OR, 2.78), larger body surface area (OR, 1.71 per 0.2-U increase), and female sex (OR, 1.46). Odds also increased with decreasing age and were elevated for patients of nonwhite/Hispanic race and those having a lower ejection fraction, atrial fibrillation or flutter, or severe mitral or tricuspid regurgitation.
It was not possible to assess specific valves as predictors of mismatch because the registry prohibits comparisons across manufacturers, according to Dr. Herrmann.
One-year mortality, the study’s primary endpoint, was 17.2% in patients with severe PPM, compared with 15.8% in patients with moderate or no PPM (adjusted hazard ratio, 1.19; P less than .001). Findings were similar across subgroups.
The 1-year rate of heart failure rehospitalization was 14.7% in patients with severe PPM, compared with 12.2% in patients with moderate or no PPM (AHR, 1.12; P = .017).
“I would point out that these [outcome] curves are divergent at 1 year,” Dr. Herrmann noted. “So if we look at low-intermediate-risk and low-risk patients and younger patients, who may be more active and who see the effects of PPM more commonly and who are going to be living more than 1 year, we are going to have to consider this going forward in a more important way.”
Severe PPM did not significantly influence the rate of stroke (which stood at about 4% in each group) or worsen quality of life score at 1 year.
Dr. Herrmann disclosed receiving institutional grant/research support from Abbott Vascular, Bayer, Boston Scientific, Corvia Medical, Edwards Lifesciences, Medtronic, and St. Jude Medical, as well as consulting fees/honoraria from Edwards, Medtronic, and Siemens Healthineers.
SAN DIEGO – Severe prosthesis-patient mismatch (PPM) after transcatheter aortic valve replacement (TAVR) increases risk of adverse outcomes and may be preventable in some cases with careful preprocedural planning, suggests a registry-based retrospective cohort study of 62,125 patients treated in the contemporary era.
The study – the largest to date of this patient population – determined that about one in every eight patients undergoing TAVR ultimately had a severe mismatch between the hemodynamics of the valve prosthesis and the requirements for cardiac output. Compared with counterparts that have moderate or no PPM, these patients with severe PPM had a 12% higher adjusted risk of heart failure rehospitalization and a 19% higher adjusted risk of death, according to results reported at the Transcatheter Cardiovascular Therapeutics annual meeting and simultaneously published online (J Am Coll Cardiol. 2018 Sep 23. doi: 10.1016/j.jacc.2018.09.001).
Notably, some of the predictors of severe PPM, such as use of smaller-diameter valves and performance of a valve-in-valve procedure, were potentially modifiable.
“Our findings suggest that efforts should be made to identify this problem and limit the risk for PPM after TAVR,” concluded lead investigator Howard C. Herrmann, MD, a professor at the University of Pennsylvania and director of the cardiac catheterization laboratories, Hospital of the University of Pennsylvania, both in Philadelphia. “Awareness is really the first step in trying to fix it.”
“We spend a lot of time in the heart-team meetings looking at the CT scans for annular dimensions and the vascular access, but we don’t really talk too much about severe PPM or the risk of that,” he elaborated. “This [study] allows us to start to predict it, based on patient factors and what prosthesis we might be choosing for a patient, and it allows us to have that conversation and think about alternatives.
“There are alternatives to try to avoid PPM, everything from which prosthesis we choose to the size of the prosthesis, to whether we fracture a patient’s valve if we are doing a valve-in-valve procedure. In the future, in some situations, we might even choose a low-risk or low-intermediate-risk patient for surgery with an enlargement operation in order to get a larger effective orifice area. So there are choices that we can make, and we should start thinking about that in the heart-team approach.”
Findings in context
The new study reinforces the message “that hemodynamics matter,” he said. “To the extent that we can get larger valves in and get better results from those valves, it will reduce the frequency of PPM. That’s something as operators we don’t spend as much time focusing on, and this will refocus our attention in trying to prevent PPM by being more diligent in terms of prosthesis choice and some operator characteristics, to try to reduce the gradients and improve the effective orifice areas as much as we can.”
Panelist Jeffrey J. Popma, MD, an interventional cardiologist at Beth Israel Deaconess Medical Center, Boston, noted that he and his colleagues have observed similar trends in their smaller studies but had difficulty teasing out contributors. “It really goes back to the preprocedural planning about what valve you can get in, and larger orifice area is certainly better,” he concurred. “So I do think that this is a phenomenal addition.”
Study details
For the study, Dr. Herrmann and his colleagues analyzed 2014-2107 data from the STS/ACC Transcatheter Valve Therapy Registry, a national surveillance and quality improvement system. They identified enrollees aged 65 years or older at the time of their TAVR procedure who had fee-for-service Medicare and linked them to Centers for Medicare & Medicaid Services claims data to assess outcomes.
Overall, 12.1% of patients had severe PPM, defined as an effective valve orifice area indexed to body surface area of less than 0.65 cm2/m2 on discharge echocardiography, and another 24.6% had moderate PPM, Dr. Herrmann reported at the meeting, sponsored by the Cardiovascular Research Foundation.
The strongest multivariate predictors of severe PPM were small prosthetic valve size (up to 23 mm in diameter) (odds ratio, 2.77), a valve-in-valve procedure (OR, 2.78), larger body surface area (OR, 1.71 per 0.2-U increase), and female sex (OR, 1.46). Odds also increased with decreasing age and were elevated for patients of nonwhite/Hispanic race and those having a lower ejection fraction, atrial fibrillation or flutter, or severe mitral or tricuspid regurgitation.
It was not possible to assess specific valves as predictors of mismatch because the registry prohibits comparisons across manufacturers, according to Dr. Herrmann.
One-year mortality, the study’s primary endpoint, was 17.2% in patients with severe PPM, compared with 15.8% in patients with moderate or no PPM (adjusted hazard ratio, 1.19; P less than .001). Findings were similar across subgroups.
The 1-year rate of heart failure rehospitalization was 14.7% in patients with severe PPM, compared with 12.2% in patients with moderate or no PPM (AHR, 1.12; P = .017).
“I would point out that these [outcome] curves are divergent at 1 year,” Dr. Herrmann noted. “So if we look at low-intermediate-risk and low-risk patients and younger patients, who may be more active and who see the effects of PPM more commonly and who are going to be living more than 1 year, we are going to have to consider this going forward in a more important way.”
Severe PPM did not significantly influence the rate of stroke (which stood at about 4% in each group) or worsen quality of life score at 1 year.
Dr. Herrmann disclosed receiving institutional grant/research support from Abbott Vascular, Bayer, Boston Scientific, Corvia Medical, Edwards Lifesciences, Medtronic, and St. Jude Medical, as well as consulting fees/honoraria from Edwards, Medtronic, and Siemens Healthineers.
REPORTING FROM TCT 2018
Key clinical point:
Major finding: Patients with severe PPM after TAVR had elevated risks of heart failure rehospitalization (adjusted hazard ratio, 1.12) and death (AHR, 1.19).
Study details: A retrospective cohort study of 62,125 patients aged 65 years or older who underwent TAVR and were captured in the national STS/ACC Transcatheter Valve Therapy Registry.
Disclosures: Dr. Herrmann disclosed receiving institutional grant/research support from Abbott Vascular, Bayer, Boston Scientific, Corvia Medical, Edwards Lifesciences, Medtronic, and St. Jude Medical, as well as consulting fees/honoraria from Edwards, Medtronic, and Siemens Healthineers.
Novel device improves mitral regurgitation 30% in REDUCE-FMR
SAN DIEGO – In patients with heart failure and functional mitral regurgitation, implantation of an investigational device led to reduced MR and improved left ventricular remodeling at 1 year, compared with patients who received sham treatment in the REDUCE-FMR trial.
The device showed promise in this trial, despite a small sample size, and its nature makes it possible to follow up with other procedures if the disease progresses. “The advantage of this technique is that all other options are still open,” Horst Sievert, MD, director of the CardioVascular Center in Frankfurt, said during a press conference at the Transcatheter Cardiovascular Therapeutics annual meeting.
The Carillon Mitral Counter System includes two anchors, one in the great cardiac vein and one in the coronary sinus, connected by a shaping ribbon. The tension of the ribbon bolsters the mitral annulus, which in turn reduces mitral regurgitation.
REDUCE-FMR recruited 120 patients from centers in eight countries and randomized 87 to the Carillon device (73 implanted) and 33 to a sham procedure. Sham patients were sedated and received a coronary sinus angiogram. Patients were included if they had dilated ischemic or nonischemic cardiomyopathy and moderate to severe functional MR, among other requirements. Exclusion criteria included existing coronary artery stents in the implant target zone, severe mitral annular calcification, and significant organic mitral valve pathology.
The primary endpoint was the mean reduction of regurgitant volume at 1 year. The treated patients had a 22% reduction of 7.1 mL, while the sham group on average had an 8% increase of 3.3 mL (P = .03). In the as-treated subpopulation, which comprised 45 patients in the treatment group and 13 controls, the values were –7.5 mL and +3.3 mL (P = .02). A per-protocol analysis, which excluded patients who did not meet protocol criteria, led to an amplification of the effect when the study design was adhered to (–12.5 mL vs. +1.3 mL), though this result did not achieve statistical significance owing to the small sample size.
For the safety endpoints, the researchers examined the frequency of major adverse events (MAE), including death, myocardial infarction, cardiac perforation, device embolism, and surgery or percutaneous coronary intervention related to the device at 1 year. In the treatment group, 16.1% experienced a MAE, compared with 18.2% of control patients, a statistically nonsignificant difference.
A secondary efficacy endpoint of change in left ventricular end-diastolic volume showed improvements in the treatment group at 6 months (–12.4 mL) and 12 months (–8.6 mL), compared with increases in the sham group at 6 months (+5.4 mL) and 12 months (+6.5 mL). A similar trend occurred in left ventricular end-systolic volume (–7.8 mL and –4.8 mL; +3.4 mL and +6.1 mL, respectively).
The study was conducted in a patient population similar to that of the COAPT trial, which examined implantation of Abbott’s MitraClip. That study, presented here at TCT 2018 and simultaneously published in the New England Journal of Medicine, also examined patients with heart failure and secondary MR.
However, in REDUCE-FMR, many of the patients had milder heart failure than the researchers had expected: 44.8% in the treatment group had NYHA class II, as did 48.5% in the sham group. That surprise may help identify an appropriate patient population. “I think this device may have a nice spot in between medical therapy and MitraClip implantation, because we have, by chance, a patient population with mild heart insufficiency and mild MR,” said Dr. Sievert.
The two devices also showed different physiologic effects, Michael Mack, MD, said at a press conference. “One subtle difference is that, in this trial, the difference is due to both positive left ventricular remodeling in the treatment arm and continued progression in the sham control. In COAPT, the difference in improvement that we saw was totally due to prevention of progression of disease. We just stabilized the disease to where it was at. So that’s an intriguing difference here, that you actually were able to demonstrate positive left ventricular remodeling,” noted Dr. Mack, medical director for cardiovascular surgery at Baylor Scott & White Medical Center, Plano, Tex. He was a coinvestigator in the COAPT trial.
REDUCE-FMR was funded by Cardiac Dimensions. Dr. Sievert has received consulting fees, travel expenses, and study honoraria from Cardiac Dimensions, and 35 other companies. Dr. Mack has received grant support or had a research contract with Abbott Vascular, Medtronic, and Edwards Lifesciences.
SAN DIEGO – In patients with heart failure and functional mitral regurgitation, implantation of an investigational device led to reduced MR and improved left ventricular remodeling at 1 year, compared with patients who received sham treatment in the REDUCE-FMR trial.
The device showed promise in this trial, despite a small sample size, and its nature makes it possible to follow up with other procedures if the disease progresses. “The advantage of this technique is that all other options are still open,” Horst Sievert, MD, director of the CardioVascular Center in Frankfurt, said during a press conference at the Transcatheter Cardiovascular Therapeutics annual meeting.
The Carillon Mitral Counter System includes two anchors, one in the great cardiac vein and one in the coronary sinus, connected by a shaping ribbon. The tension of the ribbon bolsters the mitral annulus, which in turn reduces mitral regurgitation.
REDUCE-FMR recruited 120 patients from centers in eight countries and randomized 87 to the Carillon device (73 implanted) and 33 to a sham procedure. Sham patients were sedated and received a coronary sinus angiogram. Patients were included if they had dilated ischemic or nonischemic cardiomyopathy and moderate to severe functional MR, among other requirements. Exclusion criteria included existing coronary artery stents in the implant target zone, severe mitral annular calcification, and significant organic mitral valve pathology.
The primary endpoint was the mean reduction of regurgitant volume at 1 year. The treated patients had a 22% reduction of 7.1 mL, while the sham group on average had an 8% increase of 3.3 mL (P = .03). In the as-treated subpopulation, which comprised 45 patients in the treatment group and 13 controls, the values were –7.5 mL and +3.3 mL (P = .02). A per-protocol analysis, which excluded patients who did not meet protocol criteria, led to an amplification of the effect when the study design was adhered to (–12.5 mL vs. +1.3 mL), though this result did not achieve statistical significance owing to the small sample size.
For the safety endpoints, the researchers examined the frequency of major adverse events (MAE), including death, myocardial infarction, cardiac perforation, device embolism, and surgery or percutaneous coronary intervention related to the device at 1 year. In the treatment group, 16.1% experienced a MAE, compared with 18.2% of control patients, a statistically nonsignificant difference.
A secondary efficacy endpoint of change in left ventricular end-diastolic volume showed improvements in the treatment group at 6 months (–12.4 mL) and 12 months (–8.6 mL), compared with increases in the sham group at 6 months (+5.4 mL) and 12 months (+6.5 mL). A similar trend occurred in left ventricular end-systolic volume (–7.8 mL and –4.8 mL; +3.4 mL and +6.1 mL, respectively).
The study was conducted in a patient population similar to that of the COAPT trial, which examined implantation of Abbott’s MitraClip. That study, presented here at TCT 2018 and simultaneously published in the New England Journal of Medicine, also examined patients with heart failure and secondary MR.
However, in REDUCE-FMR, many of the patients had milder heart failure than the researchers had expected: 44.8% in the treatment group had NYHA class II, as did 48.5% in the sham group. That surprise may help identify an appropriate patient population. “I think this device may have a nice spot in between medical therapy and MitraClip implantation, because we have, by chance, a patient population with mild heart insufficiency and mild MR,” said Dr. Sievert.
The two devices also showed different physiologic effects, Michael Mack, MD, said at a press conference. “One subtle difference is that, in this trial, the difference is due to both positive left ventricular remodeling in the treatment arm and continued progression in the sham control. In COAPT, the difference in improvement that we saw was totally due to prevention of progression of disease. We just stabilized the disease to where it was at. So that’s an intriguing difference here, that you actually were able to demonstrate positive left ventricular remodeling,” noted Dr. Mack, medical director for cardiovascular surgery at Baylor Scott & White Medical Center, Plano, Tex. He was a coinvestigator in the COAPT trial.
REDUCE-FMR was funded by Cardiac Dimensions. Dr. Sievert has received consulting fees, travel expenses, and study honoraria from Cardiac Dimensions, and 35 other companies. Dr. Mack has received grant support or had a research contract with Abbott Vascular, Medtronic, and Edwards Lifesciences.
SAN DIEGO – In patients with heart failure and functional mitral regurgitation, implantation of an investigational device led to reduced MR and improved left ventricular remodeling at 1 year, compared with patients who received sham treatment in the REDUCE-FMR trial.
The device showed promise in this trial, despite a small sample size, and its nature makes it possible to follow up with other procedures if the disease progresses. “The advantage of this technique is that all other options are still open,” Horst Sievert, MD, director of the CardioVascular Center in Frankfurt, said during a press conference at the Transcatheter Cardiovascular Therapeutics annual meeting.
The Carillon Mitral Counter System includes two anchors, one in the great cardiac vein and one in the coronary sinus, connected by a shaping ribbon. The tension of the ribbon bolsters the mitral annulus, which in turn reduces mitral regurgitation.
REDUCE-FMR recruited 120 patients from centers in eight countries and randomized 87 to the Carillon device (73 implanted) and 33 to a sham procedure. Sham patients were sedated and received a coronary sinus angiogram. Patients were included if they had dilated ischemic or nonischemic cardiomyopathy and moderate to severe functional MR, among other requirements. Exclusion criteria included existing coronary artery stents in the implant target zone, severe mitral annular calcification, and significant organic mitral valve pathology.
The primary endpoint was the mean reduction of regurgitant volume at 1 year. The treated patients had a 22% reduction of 7.1 mL, while the sham group on average had an 8% increase of 3.3 mL (P = .03). In the as-treated subpopulation, which comprised 45 patients in the treatment group and 13 controls, the values were –7.5 mL and +3.3 mL (P = .02). A per-protocol analysis, which excluded patients who did not meet protocol criteria, led to an amplification of the effect when the study design was adhered to (–12.5 mL vs. +1.3 mL), though this result did not achieve statistical significance owing to the small sample size.
For the safety endpoints, the researchers examined the frequency of major adverse events (MAE), including death, myocardial infarction, cardiac perforation, device embolism, and surgery or percutaneous coronary intervention related to the device at 1 year. In the treatment group, 16.1% experienced a MAE, compared with 18.2% of control patients, a statistically nonsignificant difference.
A secondary efficacy endpoint of change in left ventricular end-diastolic volume showed improvements in the treatment group at 6 months (–12.4 mL) and 12 months (–8.6 mL), compared with increases in the sham group at 6 months (+5.4 mL) and 12 months (+6.5 mL). A similar trend occurred in left ventricular end-systolic volume (–7.8 mL and –4.8 mL; +3.4 mL and +6.1 mL, respectively).
The study was conducted in a patient population similar to that of the COAPT trial, which examined implantation of Abbott’s MitraClip. That study, presented here at TCT 2018 and simultaneously published in the New England Journal of Medicine, also examined patients with heart failure and secondary MR.
However, in REDUCE-FMR, many of the patients had milder heart failure than the researchers had expected: 44.8% in the treatment group had NYHA class II, as did 48.5% in the sham group. That surprise may help identify an appropriate patient population. “I think this device may have a nice spot in between medical therapy and MitraClip implantation, because we have, by chance, a patient population with mild heart insufficiency and mild MR,” said Dr. Sievert.
The two devices also showed different physiologic effects, Michael Mack, MD, said at a press conference. “One subtle difference is that, in this trial, the difference is due to both positive left ventricular remodeling in the treatment arm and continued progression in the sham control. In COAPT, the difference in improvement that we saw was totally due to prevention of progression of disease. We just stabilized the disease to where it was at. So that’s an intriguing difference here, that you actually were able to demonstrate positive left ventricular remodeling,” noted Dr. Mack, medical director for cardiovascular surgery at Baylor Scott & White Medical Center, Plano, Tex. He was a coinvestigator in the COAPT trial.
REDUCE-FMR was funded by Cardiac Dimensions. Dr. Sievert has received consulting fees, travel expenses, and study honoraria from Cardiac Dimensions, and 35 other companies. Dr. Mack has received grant support or had a research contract with Abbott Vascular, Medtronic, and Edwards Lifesciences.
REPORTING FROM TCT 2018
Key clinical point: The device led to improvement in mitral regurgitation as well as ventricular remodeling.
Major finding:
Study details: REDUCE-FMR, a randomized, sham controlled trial of 120 patients from 8 countries.
Disclosures: REDUCE-FMR was funded by Cardiac Dimensions. Dr. Sievert has received consulting fees, travel expenses, and study honoraria from Cardiac Dimensions, and 35 other companies. Dr. Mack has received grant support or had a research contract with Abbott Vascular, Medtronic, and Edwards Lifesciences.
CGP guides cancer patient management, facilitates trial enrollment
TORONTO – according to findings from a retrospective study of 46 patients who were followed for 3 years after CGP.
A total of 263 genomic alterations were identified in the patients, leading to a change of therapy in 26% of cases and referral to a clinical trial in 13%, Kimberly Rohan, APN, reported at the World Conference on Lung Cancer.
The 13% referral rate was surprising, “because that’s way above the national average for enrollment in a clinical trial,” Ms. Rohan, of the Edward Cancer Center in Naperville, Ill., said during a press briefing at the meeting, sponsored by the International Association for the Study of Lung Cancer.
“Among those diagnosed with lung cancer, 6% were referred to clinical trials and 34% had a change of therapy,” she said, noting that all but one of the patients had non–small cell lung cancer, and the other had small cell lung cancer and many alterations.
Of note, three patients enrolled in hospice care based on the findings; sometimes, palliative care is the most appropriate option, and this information helps patients and their families make those decisions, Ms. Rohan said.
Patients were tested between 2014 and 2017, and the review looked at the number of genomic alterations identified in each, what treatments were associated with potential clinical trial benefits, what therapies were associated with lack of response, and the effects of the CGP findings on decision making.
An important next step is to work with payors to get them to pay for CGP testing, she said. “These tests are expensive so a lot of [insurance companies] don’t want to pay for them, but this data will help support the fact that [these tests] do allow better treatments for patients and allow patients to make better decisions for themselves in regard to treatment.”
Ms. Rohan is a speaker or advisory board member for Merck, Genentech, and AstraZeneca.
TORONTO – according to findings from a retrospective study of 46 patients who were followed for 3 years after CGP.
A total of 263 genomic alterations were identified in the patients, leading to a change of therapy in 26% of cases and referral to a clinical trial in 13%, Kimberly Rohan, APN, reported at the World Conference on Lung Cancer.
The 13% referral rate was surprising, “because that’s way above the national average for enrollment in a clinical trial,” Ms. Rohan, of the Edward Cancer Center in Naperville, Ill., said during a press briefing at the meeting, sponsored by the International Association for the Study of Lung Cancer.
“Among those diagnosed with lung cancer, 6% were referred to clinical trials and 34% had a change of therapy,” she said, noting that all but one of the patients had non–small cell lung cancer, and the other had small cell lung cancer and many alterations.
Of note, three patients enrolled in hospice care based on the findings; sometimes, palliative care is the most appropriate option, and this information helps patients and their families make those decisions, Ms. Rohan said.
Patients were tested between 2014 and 2017, and the review looked at the number of genomic alterations identified in each, what treatments were associated with potential clinical trial benefits, what therapies were associated with lack of response, and the effects of the CGP findings on decision making.
An important next step is to work with payors to get them to pay for CGP testing, she said. “These tests are expensive so a lot of [insurance companies] don’t want to pay for them, but this data will help support the fact that [these tests] do allow better treatments for patients and allow patients to make better decisions for themselves in regard to treatment.”
Ms. Rohan is a speaker or advisory board member for Merck, Genentech, and AstraZeneca.
TORONTO – according to findings from a retrospective study of 46 patients who were followed for 3 years after CGP.
A total of 263 genomic alterations were identified in the patients, leading to a change of therapy in 26% of cases and referral to a clinical trial in 13%, Kimberly Rohan, APN, reported at the World Conference on Lung Cancer.
The 13% referral rate was surprising, “because that’s way above the national average for enrollment in a clinical trial,” Ms. Rohan, of the Edward Cancer Center in Naperville, Ill., said during a press briefing at the meeting, sponsored by the International Association for the Study of Lung Cancer.
“Among those diagnosed with lung cancer, 6% were referred to clinical trials and 34% had a change of therapy,” she said, noting that all but one of the patients had non–small cell lung cancer, and the other had small cell lung cancer and many alterations.
Of note, three patients enrolled in hospice care based on the findings; sometimes, palliative care is the most appropriate option, and this information helps patients and their families make those decisions, Ms. Rohan said.
Patients were tested between 2014 and 2017, and the review looked at the number of genomic alterations identified in each, what treatments were associated with potential clinical trial benefits, what therapies were associated with lack of response, and the effects of the CGP findings on decision making.
An important next step is to work with payors to get them to pay for CGP testing, she said. “These tests are expensive so a lot of [insurance companies] don’t want to pay for them, but this data will help support the fact that [these tests] do allow better treatments for patients and allow patients to make better decisions for themselves in regard to treatment.”
Ms. Rohan is a speaker or advisory board member for Merck, Genentech, and AstraZeneca.
REPORTING FROM WCLC 2018
Key clinical point: Comprehensive genetic profiling (GCP) is useful for guiding the care of cancer patients.
Major finding: CGP led to a change of therapy in 26% of cases and referral to a clinical trial in 13% of cases.
Study details: A retrospective study of CGP for 46 cancer patients.
Disclosures: Ms. Rohan is a speaker or advisory board member for Merck, Genentech, and AstraZeneca.
Eltrombopag irons out kinks in hematopoiesis
The hematopoietic action of the thrombopoietin receptor (TPO-R) agonist eltrombopag (Promacta) occurs at the stem cell level through its effects on iron chelation that in turn leads to hematopoietic stem cell (HSC) stimulation and self-renewal, investigators report.
Studying the effects of eltrombopag treatment in mouse models and in bone marrow cells isolated from patients, Britta Will, PhD, from the Albert Einstein College of Medicine, New York, and her colleagues found that eltrombopag’s stimulatory effects on stem cell self-renewal were independent of the thrombopoietin receptor.
“The iron chelation–dependent mechanism of [eltrombopag] is very likely to confer clinical relevance in the context of enhancing TPO-R–dependent HSC stimulation and reinforcing stem cell identity through wide-ranging iron-dependent metabolic reprogramming, which increases healthy stem cells without causing their exhaustion in bone marrow failure syndromes, as well as aid in preserving functional HSCs under cellular stress (such as transplantation, cytotoxic treatment, or irradiation),” they wrote in Science Translational Medicine.
To gain insight into the effects of eltrombopag on the earliest stages of hematopoiesis, the investigators conducted a series of experiments, starting with an assessment of the effects of the agent on the functional hallmarks of primary human stem cells.
Using assays for differentiation, self-renewal, and cell proliferation in human bone marrow cell lines, they found that eltrombopag acts directly on multilineage hematopoiesis by fostering commitment to differentiation at the multipotent progenitor (MPP) cell level and by enhancing self-renewal of hematopoietic stem cells.
Next, they investigated whether eltrombopag promoted hematopoiesis by activating the TPO-R, or through a different mechanism, and found that its action was independent of the thrombopoietin receptor. Specifically, they found that eltrombopag “elicits gene expression alterations in HSCs consistent with a molecular response to reduced intracellular iron content, consisting of decreased glycolysis and enhanced lipid and protein catabolic pathway activation.”
To show that the effect was independent of TPO-R, they then turned to mouse models (eltrombopag is known to activate TPO-R signaling in primate cells, including in humans, but cannot do so in mice, they explained). They showed that in mice, eltrombopag is capable of stimulating HSCs even in the absence of action on the TPO-R.
They also demonstrated that HSCs from both humans and mice have evidence of changes in metabolism and in gene expression that were consistent with reduction of labile iron pools that stem cells rely on for maintenance. When they preloaded cells with iron, the stimulatory effects of eltrombopag were negated, further supporting the iron-chelating effects of the drug on HSC stimulation.
Finally, they looked at HSC function in bone marrow mononuclear cells from patients with immune thrombocytopenia who were being treated with eltrombopag and found a threefold greater increase in the number of functional HSCs, compared with samples from patients treated with the TPO-R agonist romiplostim (Nplate), which does not have iron-chelating properties.
“Together, our data demonstrate a TPO-R–independent stem cell stimulatory function of EP and suggest that free intracellular iron pools may serve as a rheostat for HSC maintenance,” the investigators wrote.
The study was supported by the New York State Department of Health. Dr. Will and two coauthors reported research support from GlaxoSmithKline and Novartis, and serving as consultants for Novartis. Two of the co-authors are employees of Novartis.
SOURCE: Kao YR et al. Sci Transl Med. 2018 Sep 12;10(458). doi: 10.1126/scitranslmed.aas9563.
The hematopoietic action of the thrombopoietin receptor (TPO-R) agonist eltrombopag (Promacta) occurs at the stem cell level through its effects on iron chelation that in turn leads to hematopoietic stem cell (HSC) stimulation and self-renewal, investigators report.
Studying the effects of eltrombopag treatment in mouse models and in bone marrow cells isolated from patients, Britta Will, PhD, from the Albert Einstein College of Medicine, New York, and her colleagues found that eltrombopag’s stimulatory effects on stem cell self-renewal were independent of the thrombopoietin receptor.
“The iron chelation–dependent mechanism of [eltrombopag] is very likely to confer clinical relevance in the context of enhancing TPO-R–dependent HSC stimulation and reinforcing stem cell identity through wide-ranging iron-dependent metabolic reprogramming, which increases healthy stem cells without causing their exhaustion in bone marrow failure syndromes, as well as aid in preserving functional HSCs under cellular stress (such as transplantation, cytotoxic treatment, or irradiation),” they wrote in Science Translational Medicine.
To gain insight into the effects of eltrombopag on the earliest stages of hematopoiesis, the investigators conducted a series of experiments, starting with an assessment of the effects of the agent on the functional hallmarks of primary human stem cells.
Using assays for differentiation, self-renewal, and cell proliferation in human bone marrow cell lines, they found that eltrombopag acts directly on multilineage hematopoiesis by fostering commitment to differentiation at the multipotent progenitor (MPP) cell level and by enhancing self-renewal of hematopoietic stem cells.
Next, they investigated whether eltrombopag promoted hematopoiesis by activating the TPO-R, or through a different mechanism, and found that its action was independent of the thrombopoietin receptor. Specifically, they found that eltrombopag “elicits gene expression alterations in HSCs consistent with a molecular response to reduced intracellular iron content, consisting of decreased glycolysis and enhanced lipid and protein catabolic pathway activation.”
To show that the effect was independent of TPO-R, they then turned to mouse models (eltrombopag is known to activate TPO-R signaling in primate cells, including in humans, but cannot do so in mice, they explained). They showed that in mice, eltrombopag is capable of stimulating HSCs even in the absence of action on the TPO-R.
They also demonstrated that HSCs from both humans and mice have evidence of changes in metabolism and in gene expression that were consistent with reduction of labile iron pools that stem cells rely on for maintenance. When they preloaded cells with iron, the stimulatory effects of eltrombopag were negated, further supporting the iron-chelating effects of the drug on HSC stimulation.
Finally, they looked at HSC function in bone marrow mononuclear cells from patients with immune thrombocytopenia who were being treated with eltrombopag and found a threefold greater increase in the number of functional HSCs, compared with samples from patients treated with the TPO-R agonist romiplostim (Nplate), which does not have iron-chelating properties.
“Together, our data demonstrate a TPO-R–independent stem cell stimulatory function of EP and suggest that free intracellular iron pools may serve as a rheostat for HSC maintenance,” the investigators wrote.
The study was supported by the New York State Department of Health. Dr. Will and two coauthors reported research support from GlaxoSmithKline and Novartis, and serving as consultants for Novartis. Two of the co-authors are employees of Novartis.
SOURCE: Kao YR et al. Sci Transl Med. 2018 Sep 12;10(458). doi: 10.1126/scitranslmed.aas9563.
The hematopoietic action of the thrombopoietin receptor (TPO-R) agonist eltrombopag (Promacta) occurs at the stem cell level through its effects on iron chelation that in turn leads to hematopoietic stem cell (HSC) stimulation and self-renewal, investigators report.
Studying the effects of eltrombopag treatment in mouse models and in bone marrow cells isolated from patients, Britta Will, PhD, from the Albert Einstein College of Medicine, New York, and her colleagues found that eltrombopag’s stimulatory effects on stem cell self-renewal were independent of the thrombopoietin receptor.
“The iron chelation–dependent mechanism of [eltrombopag] is very likely to confer clinical relevance in the context of enhancing TPO-R–dependent HSC stimulation and reinforcing stem cell identity through wide-ranging iron-dependent metabolic reprogramming, which increases healthy stem cells without causing their exhaustion in bone marrow failure syndromes, as well as aid in preserving functional HSCs under cellular stress (such as transplantation, cytotoxic treatment, or irradiation),” they wrote in Science Translational Medicine.
To gain insight into the effects of eltrombopag on the earliest stages of hematopoiesis, the investigators conducted a series of experiments, starting with an assessment of the effects of the agent on the functional hallmarks of primary human stem cells.
Using assays for differentiation, self-renewal, and cell proliferation in human bone marrow cell lines, they found that eltrombopag acts directly on multilineage hematopoiesis by fostering commitment to differentiation at the multipotent progenitor (MPP) cell level and by enhancing self-renewal of hematopoietic stem cells.
Next, they investigated whether eltrombopag promoted hematopoiesis by activating the TPO-R, or through a different mechanism, and found that its action was independent of the thrombopoietin receptor. Specifically, they found that eltrombopag “elicits gene expression alterations in HSCs consistent with a molecular response to reduced intracellular iron content, consisting of decreased glycolysis and enhanced lipid and protein catabolic pathway activation.”
To show that the effect was independent of TPO-R, they then turned to mouse models (eltrombopag is known to activate TPO-R signaling in primate cells, including in humans, but cannot do so in mice, they explained). They showed that in mice, eltrombopag is capable of stimulating HSCs even in the absence of action on the TPO-R.
They also demonstrated that HSCs from both humans and mice have evidence of changes in metabolism and in gene expression that were consistent with reduction of labile iron pools that stem cells rely on for maintenance. When they preloaded cells with iron, the stimulatory effects of eltrombopag were negated, further supporting the iron-chelating effects of the drug on HSC stimulation.
Finally, they looked at HSC function in bone marrow mononuclear cells from patients with immune thrombocytopenia who were being treated with eltrombopag and found a threefold greater increase in the number of functional HSCs, compared with samples from patients treated with the TPO-R agonist romiplostim (Nplate), which does not have iron-chelating properties.
“Together, our data demonstrate a TPO-R–independent stem cell stimulatory function of EP and suggest that free intracellular iron pools may serve as a rheostat for HSC maintenance,” the investigators wrote.
The study was supported by the New York State Department of Health. Dr. Will and two coauthors reported research support from GlaxoSmithKline and Novartis, and serving as consultants for Novartis. Two of the co-authors are employees of Novartis.
SOURCE: Kao YR et al. Sci Transl Med. 2018 Sep 12;10(458). doi: 10.1126/scitranslmed.aas9563.
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point:
Major finding: Eltrombopag stimulates hematopoiesis through iron-chelating effects at the stem cell level, independent of its effect on the thrombopoietin receptor.
Study details: Basic science experiments in mouse models, human bone marrow cells lines, and samples from patients with immune thrombocytopenia.
Disclosures: The study was supported by the New York State Department of Health. Dr. Will and two coauthors reported research support from GlaxoSmithKline and Novartis and serving as consultants for Novartis. Two of the coauthors are employees of Novartis.
Source: Kao Y-R et al. Sci Transl Med. 2018 Sep 12;10(458). doi: 10.1126/scitranslmed.aas9563.
NICE looks likely to reject use of Kymriah for DLBCL
The National Institute for Health and Care Excellence (NICE) has issued draft guidance recommending against tisagenlecleucel (Kymriah) as a treatment for adults with diffuse large B-cell lymphoma (DLBCL).

Tisagenlecleucel is a chimeric antigen receptor (CAR) T-cell therapy that was recently approved by the European Commission to treat adults with relapsed or refractory DLBCL who have received two or more lines of systemic therapy.
Tisagenlecleucel is also European Commission–approved to treat patients up to age 25 years who have B-cell acute lymphoblastic leukemia (ALL) that is refractory, in relapse posttransplant, or in second or later relapse.
In September 2018, the National Health Service (NHS) in England announced tisagenlecleucel will be made available for these ALL patients through the Cancer Drugs Fund.
However, in who have received two or more lines of systemic therapy. NICE noted that there is no standard treatment for this patient group, and that salvage chemotherapy is the most common treatment option.
Although the latest results from the JULIET trial suggest tisagenlecleucel can produce responses in patients with relapsed/refractory DLBCL, there are no data comparing tisagenlecleucel with salvage chemotherapy. Additionally, tisagenlecleucel cannot be considered a life-extending treatment at the end of life, according to NICE criteria.
All cost-effectiveness estimates for tisagenlecleucel are above the range NICE normally considers acceptable, and tisagenlecleucel does not meet criteria for inclusion in the Cancer Drugs Fund.
The list price for tisagenlecleucel is 282,000 pounds. However, Novartis, the company developing tisagenlecleucel, has a confidential commercial arrangement with the NHS that lowers the price of tisagenlecleucel for the ALL indication. This arrangement would apply if tisagenlecleucel were recommended for the DLBCL indication.
In August, NICE issued a similar draft guidance document recommending against use of another CAR T-cell therapy, axicabtagene ciloleucel (Yescarta). Axicabtagene ciloleucel is approved in Europe for the treatment of patients with relapsed/refractory DLBCL or primary mediastinal B-cell lymphoma who have received two or more lines of systemic therapy.
The National Institute for Health and Care Excellence (NICE) has issued draft guidance recommending against tisagenlecleucel (Kymriah) as a treatment for adults with diffuse large B-cell lymphoma (DLBCL).

Tisagenlecleucel is a chimeric antigen receptor (CAR) T-cell therapy that was recently approved by the European Commission to treat adults with relapsed or refractory DLBCL who have received two or more lines of systemic therapy.
Tisagenlecleucel is also European Commission–approved to treat patients up to age 25 years who have B-cell acute lymphoblastic leukemia (ALL) that is refractory, in relapse posttransplant, or in second or later relapse.
In September 2018, the National Health Service (NHS) in England announced tisagenlecleucel will be made available for these ALL patients through the Cancer Drugs Fund.
However, in who have received two or more lines of systemic therapy. NICE noted that there is no standard treatment for this patient group, and that salvage chemotherapy is the most common treatment option.
Although the latest results from the JULIET trial suggest tisagenlecleucel can produce responses in patients with relapsed/refractory DLBCL, there are no data comparing tisagenlecleucel with salvage chemotherapy. Additionally, tisagenlecleucel cannot be considered a life-extending treatment at the end of life, according to NICE criteria.
All cost-effectiveness estimates for tisagenlecleucel are above the range NICE normally considers acceptable, and tisagenlecleucel does not meet criteria for inclusion in the Cancer Drugs Fund.
The list price for tisagenlecleucel is 282,000 pounds. However, Novartis, the company developing tisagenlecleucel, has a confidential commercial arrangement with the NHS that lowers the price of tisagenlecleucel for the ALL indication. This arrangement would apply if tisagenlecleucel were recommended for the DLBCL indication.
In August, NICE issued a similar draft guidance document recommending against use of another CAR T-cell therapy, axicabtagene ciloleucel (Yescarta). Axicabtagene ciloleucel is approved in Europe for the treatment of patients with relapsed/refractory DLBCL or primary mediastinal B-cell lymphoma who have received two or more lines of systemic therapy.
The National Institute for Health and Care Excellence (NICE) has issued draft guidance recommending against tisagenlecleucel (Kymriah) as a treatment for adults with diffuse large B-cell lymphoma (DLBCL).

Tisagenlecleucel is a chimeric antigen receptor (CAR) T-cell therapy that was recently approved by the European Commission to treat adults with relapsed or refractory DLBCL who have received two or more lines of systemic therapy.
Tisagenlecleucel is also European Commission–approved to treat patients up to age 25 years who have B-cell acute lymphoblastic leukemia (ALL) that is refractory, in relapse posttransplant, or in second or later relapse.
In September 2018, the National Health Service (NHS) in England announced tisagenlecleucel will be made available for these ALL patients through the Cancer Drugs Fund.
However, in who have received two or more lines of systemic therapy. NICE noted that there is no standard treatment for this patient group, and that salvage chemotherapy is the most common treatment option.
Although the latest results from the JULIET trial suggest tisagenlecleucel can produce responses in patients with relapsed/refractory DLBCL, there are no data comparing tisagenlecleucel with salvage chemotherapy. Additionally, tisagenlecleucel cannot be considered a life-extending treatment at the end of life, according to NICE criteria.
All cost-effectiveness estimates for tisagenlecleucel are above the range NICE normally considers acceptable, and tisagenlecleucel does not meet criteria for inclusion in the Cancer Drugs Fund.
The list price for tisagenlecleucel is 282,000 pounds. However, Novartis, the company developing tisagenlecleucel, has a confidential commercial arrangement with the NHS that lowers the price of tisagenlecleucel for the ALL indication. This arrangement would apply if tisagenlecleucel were recommended for the DLBCL indication.
In August, NICE issued a similar draft guidance document recommending against use of another CAR T-cell therapy, axicabtagene ciloleucel (Yescarta). Axicabtagene ciloleucel is approved in Europe for the treatment of patients with relapsed/refractory DLBCL or primary mediastinal B-cell lymphoma who have received two or more lines of systemic therapy.