User login
Neoadjuvant degarelix more effective than triptorelin for ovarian suppression
Degarelix, the gonadotropin-releasing hormone (GnRH) antagonist approved for prostate cancer, was more effective than a GnRH agonist in achieving ovarian function suppression in women with breast cancer, results of a randomized trial show.
Ovarian function suppression was achieved more rapidly and maintained more effectively with degarelix, compared with triptorelin, in the premenopausal women who were receiving letrozole for neoadjuvant endocrine therapy, investigators said.
Adverse events including hot flashes and injection site reactions were reported more often with degarelix versus the GnRH agonist in this randomized, phase 2 trial of 51 subjects.
Additional research is needed to determine whether degarelix results in superior disease control versus the current standard of care, reported Silvia Dellapasqua, MD, of the European Institute of Oncology IRCCS in Milan, Italy, and coinvestigators.
“The study is hypothesis-generating, and supports later studies to assess whether maintenance of ovarian function suppression with degarelix translates into a better clinical outcome and is worth a trade-off of increased rate of some adverse events,” the researchers wrote. The report is in the Journal of Clinical Oncology.
Patients were randomly assigned to receive degarelix plus letrozole or triptorelin plus letrozole for six 28-day cycles. Degarelix was administered subcutaneously on day 1 of each cycle, while triptorelin was administered intramuscularly on day 1 of each cycle, and oral letrozole was to be taken daily. Surgery was performed a few weeks after the last injection.
All patients achieved optimal ovarian function suppression by the end of the first cycle. However, that endpoint was achieved significantly faster among patients in the degarelix arm, at a median of 3 days, versus a median of 14 days for the GnRH agonist, the investigators reported.
The optimal ovarian function suppression was seen three times faster with degarelix (hazard ratio, 3.05; 95% confidence interval, 1.65-5.65; P less than 001), they added.
One hundred percent of patients receiving degarelix and letrozole maintained optimal ovarian function suppression throughout the study, while about 15% of patients assigned to triptorelin had suboptimal suppression after that first cycle.
The group of patients receiving degarelix had a higher rate of node-negative disease at surgery, and a higher rate of breast-conserving surgery compared with the triptorelin group, the investigators said.
There were two grade 3 adverse events, hypertension and anemia, which both occurred in the triptorelin group, and no grade 4 adverse events. The most common adverse events reported were hot flashes, occurring in 80.0% and 69.2% of the degarelix and triptorelin groups, respectively; arthralgias in 32.0% and 53.8%; insomnia in 24.0% and 11.5%; injection site reactions in 24.0% and 0%; and nausea in 16.0% and 3.8%.
The study was supported by Ferring, and by the International Breast Cancer Study Group via Frontier Science and Technology Research Foundation, Swiss Group for Clinical Cancer Research, Cancer Research Switzerland, Oncosuisse, Swiss Cancer League, and the Foundation for Clinical Cancer Research of Eastern Switzerland. The authors reported disclosures related to Ferring, Novartis, Ipsen, DVAX, Roche, Genentech, Pfizer, Celgene, and Merck, among others.
SOURCE: Dellapasqua S et al. J Clin Oncol. 2018 Dec 27. doi: 10.1200/JCO.18.00296.
Degarelix, the gonadotropin-releasing hormone (GnRH) antagonist approved for prostate cancer, was more effective than a GnRH agonist in achieving ovarian function suppression in women with breast cancer, results of a randomized trial show.
Ovarian function suppression was achieved more rapidly and maintained more effectively with degarelix, compared with triptorelin, in the premenopausal women who were receiving letrozole for neoadjuvant endocrine therapy, investigators said.
Adverse events including hot flashes and injection site reactions were reported more often with degarelix versus the GnRH agonist in this randomized, phase 2 trial of 51 subjects.
Additional research is needed to determine whether degarelix results in superior disease control versus the current standard of care, reported Silvia Dellapasqua, MD, of the European Institute of Oncology IRCCS in Milan, Italy, and coinvestigators.
“The study is hypothesis-generating, and supports later studies to assess whether maintenance of ovarian function suppression with degarelix translates into a better clinical outcome and is worth a trade-off of increased rate of some adverse events,” the researchers wrote. The report is in the Journal of Clinical Oncology.
Patients were randomly assigned to receive degarelix plus letrozole or triptorelin plus letrozole for six 28-day cycles. Degarelix was administered subcutaneously on day 1 of each cycle, while triptorelin was administered intramuscularly on day 1 of each cycle, and oral letrozole was to be taken daily. Surgery was performed a few weeks after the last injection.
All patients achieved optimal ovarian function suppression by the end of the first cycle. However, that endpoint was achieved significantly faster among patients in the degarelix arm, at a median of 3 days, versus a median of 14 days for the GnRH agonist, the investigators reported.
The optimal ovarian function suppression was seen three times faster with degarelix (hazard ratio, 3.05; 95% confidence interval, 1.65-5.65; P less than 001), they added.
One hundred percent of patients receiving degarelix and letrozole maintained optimal ovarian function suppression throughout the study, while about 15% of patients assigned to triptorelin had suboptimal suppression after that first cycle.
The group of patients receiving degarelix had a higher rate of node-negative disease at surgery, and a higher rate of breast-conserving surgery compared with the triptorelin group, the investigators said.
There were two grade 3 adverse events, hypertension and anemia, which both occurred in the triptorelin group, and no grade 4 adverse events. The most common adverse events reported were hot flashes, occurring in 80.0% and 69.2% of the degarelix and triptorelin groups, respectively; arthralgias in 32.0% and 53.8%; insomnia in 24.0% and 11.5%; injection site reactions in 24.0% and 0%; and nausea in 16.0% and 3.8%.
The study was supported by Ferring, and by the International Breast Cancer Study Group via Frontier Science and Technology Research Foundation, Swiss Group for Clinical Cancer Research, Cancer Research Switzerland, Oncosuisse, Swiss Cancer League, and the Foundation for Clinical Cancer Research of Eastern Switzerland. The authors reported disclosures related to Ferring, Novartis, Ipsen, DVAX, Roche, Genentech, Pfizer, Celgene, and Merck, among others.
SOURCE: Dellapasqua S et al. J Clin Oncol. 2018 Dec 27. doi: 10.1200/JCO.18.00296.
Degarelix, the gonadotropin-releasing hormone (GnRH) antagonist approved for prostate cancer, was more effective than a GnRH agonist in achieving ovarian function suppression in women with breast cancer, results of a randomized trial show.
Ovarian function suppression was achieved more rapidly and maintained more effectively with degarelix, compared with triptorelin, in the premenopausal women who were receiving letrozole for neoadjuvant endocrine therapy, investigators said.
Adverse events including hot flashes and injection site reactions were reported more often with degarelix versus the GnRH agonist in this randomized, phase 2 trial of 51 subjects.
Additional research is needed to determine whether degarelix results in superior disease control versus the current standard of care, reported Silvia Dellapasqua, MD, of the European Institute of Oncology IRCCS in Milan, Italy, and coinvestigators.
“The study is hypothesis-generating, and supports later studies to assess whether maintenance of ovarian function suppression with degarelix translates into a better clinical outcome and is worth a trade-off of increased rate of some adverse events,” the researchers wrote. The report is in the Journal of Clinical Oncology.
Patients were randomly assigned to receive degarelix plus letrozole or triptorelin plus letrozole for six 28-day cycles. Degarelix was administered subcutaneously on day 1 of each cycle, while triptorelin was administered intramuscularly on day 1 of each cycle, and oral letrozole was to be taken daily. Surgery was performed a few weeks after the last injection.
All patients achieved optimal ovarian function suppression by the end of the first cycle. However, that endpoint was achieved significantly faster among patients in the degarelix arm, at a median of 3 days, versus a median of 14 days for the GnRH agonist, the investigators reported.
The optimal ovarian function suppression was seen three times faster with degarelix (hazard ratio, 3.05; 95% confidence interval, 1.65-5.65; P less than 001), they added.
One hundred percent of patients receiving degarelix and letrozole maintained optimal ovarian function suppression throughout the study, while about 15% of patients assigned to triptorelin had suboptimal suppression after that first cycle.
The group of patients receiving degarelix had a higher rate of node-negative disease at surgery, and a higher rate of breast-conserving surgery compared with the triptorelin group, the investigators said.
There were two grade 3 adverse events, hypertension and anemia, which both occurred in the triptorelin group, and no grade 4 adverse events. The most common adverse events reported were hot flashes, occurring in 80.0% and 69.2% of the degarelix and triptorelin groups, respectively; arthralgias in 32.0% and 53.8%; insomnia in 24.0% and 11.5%; injection site reactions in 24.0% and 0%; and nausea in 16.0% and 3.8%.
The study was supported by Ferring, and by the International Breast Cancer Study Group via Frontier Science and Technology Research Foundation, Swiss Group for Clinical Cancer Research, Cancer Research Switzerland, Oncosuisse, Swiss Cancer League, and the Foundation for Clinical Cancer Research of Eastern Switzerland. The authors reported disclosures related to Ferring, Novartis, Ipsen, DVAX, Roche, Genentech, Pfizer, Celgene, and Merck, among others.
SOURCE: Dellapasqua S et al. J Clin Oncol. 2018 Dec 27. doi: 10.1200/JCO.18.00296.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Degarelix, the gonadotropin-releasing hormone (GnRH) antagonist approved for prostate cancer, was more effective than the GnRH agonist triptorelin in achieving ovarian function suppression.
Major finding: Ovarian function suppression occurred three times faster with degarelix (hazard ratio, 3.05; 95% confidence interval, 1.65-5.65; P less than .001) and in contrast to the triptorelin group, none had suboptimal suppression on subsequent cycles.
Study details: A randomized phase 2 trial including 51 premenopausal women receiving letrozole for locally advanced, endocrine-responsive breast cancer.
Disclosures: The study was supported in part by Ferring. Authors reported disclosures related to Ferring, Novartis, Ipsen, DVAX, Roche, Genentech, Pfizer, Celgene, and Merck, among others.
Source: Dellapasqua S et al. J Clin Oncol. 2018 Dec 27. doi: 10.1200/JCO.18.00296.
Postprandial glucose responses to identical meals vary from person to person
LOS ANGELES – .
“The reason we got interested in nutrition in general is for its important role in health and disease, but also because, reading the literature on nutrition in general, it seemed that the science was relatively poor,” Eran Segal, PhD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “As a testament, you can see how frequently dietary recommendations for the public are changed. For example, 30 years ago, the cover of Time magazine said that eating cholesterol in the diet is very bad for you. Fifteen years later, Time magazine said that some cholesterol is actually good for you. There are other questions, like should you be eating dairy products? I think it shows that we have a poor understanding of what healthy nutrition is for human individuals. That’s why we wanted to start a study which would collect the right amount and the right kind of data to try to answer the question of what is a healthy diet for human individuals.”
In what is believed to be the first study of its kind, Dr. Segal, professor of computer science and applied mathematics at the Weizmann Institute of Science in Rehovot, Israel, and his associates recruited 1,000 individuals and asked them to wear a continuous glucose monitor (CGM) for 1 week (Cell 2015;163[5]:1079-94). For the study, known as The Personalized Nutrition Project, participants were asked to log everything they ate into a mobile app the researchers developed. “They would select a meal from a database of 10,000 foods,” Dr. Segal explained. “Each meal has full nutritional value so at the end of the study, we had about 50,000 meals that we had measurements of postprandial glucose response to, coupled with full nutritional values.” They also collected a comprehensive profile of individuals, which included body measurements, blood tests, medical background, food frequency questionnaires, and a measurement of the microbiome by both 16S rRNA sequencing and shotgun metagenomics.
For the first part of the study, researchers supplied a breakfast to all participants: either bread, bread with butter, glucose, or fructose, in each case 50 g of available carbohydrates. “The participants were asked to consume these the morning after the night fast,” Dr. Segal said. “This allowed us to compare how the same individual responds to eating the exact same food versus how different individuals respond to eating the same food.” The researchers found that, when the same person ate the same meal on 2 different days, the glucose response was highly reproducible. In contrast, different people had widely different postmeal glucose responses to identical meals. “Some individuals responded most highly to glucose; others responded most highly to bread,” Dr. Segal said. “There was about 10% of individuals who responded to bread and butter, compared to the other test foods. These results mean that any universal diet is going to have limited efficacy in its ability to balance blood glucose levels, because some foods will spike glucose levels in one person but not in another person. It also means that the concepts we’ve been using like the glycemic index are also going to have limited efficacy.”
Next, the researchers aimed to determine what factors influence the variability in people’s responses to the same food. “We found many different correlations between the various blood markers and physical measurements that we obtained, but what was most novel was the variability in postmeal glucose response across people associated with microbiota composition and function,” Dr. Segal said. From this, he and his colleagues developed a machine-learning algorithm that integrates blood parameters, dietary habits, anthropometrics, physical activity, and gut microbiota. Using this algorithm, the prediction accuracy of personalized glucose responses achieved an r value of 0.68, which explains about 50% of the variability. For the final component of the study, the researchers randomized 26 participants to one of five dietary arms and followed for 1 week by continuous glucose monitoring. They were able to demonstrate that personally tailored diets lower the postprandial glucose response.
As a follow-up to this work, Dr. Segal and his associates enrolled 200 people with an hemoglobin A1c between 5.7% and 6.5% into the Personalized Nutrition Project for Prediabetes (PNP3) study, which investigates whether personalized diet intervention will improve postprandial blood glucose levels and other metabolic health factors in individuals with prediabetes, compared with the standard Mediterranean-style low-fat diet (NCT03222791). Participants were randomized to 6 months of standard of care following Dietary Guidelines for Americans 2015-2020, Eighth Edition, or to an algorithm diet. Primary outcomes are reduction in average glucose levels and evaluation of the total daily time of plasma glucose levels were below 140 mg/dL. Participants wore the continuous glucose monitor for the entire 6 months of intervention. “I don’t think this was ever done before,” he said. “We’re also looking at secondary metabolic endpoints and exploratory endpoints such as changes in the microbiome. We’re asking people to log everything they eat for the entire 6 months of intervention. It gives us a lot of power in terms assessing compliance. It’s an immense amount of data.”
Evaluation of the data are not yet complete, but interim results are promising. For example, he discussed results from one study participant on the algorithm diet. “Across 1 month, this person was able to entirely reduce the peaks in glucose levels and dramatic reductions in the time above 140 mg/dL in the 6-month treatment period,” said Dr. Segal, who is one of the study’s principal investigators. He disclosed that he is a paid consultant to DayTwo.
LOS ANGELES – .
“The reason we got interested in nutrition in general is for its important role in health and disease, but also because, reading the literature on nutrition in general, it seemed that the science was relatively poor,” Eran Segal, PhD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “As a testament, you can see how frequently dietary recommendations for the public are changed. For example, 30 years ago, the cover of Time magazine said that eating cholesterol in the diet is very bad for you. Fifteen years later, Time magazine said that some cholesterol is actually good for you. There are other questions, like should you be eating dairy products? I think it shows that we have a poor understanding of what healthy nutrition is for human individuals. That’s why we wanted to start a study which would collect the right amount and the right kind of data to try to answer the question of what is a healthy diet for human individuals.”
In what is believed to be the first study of its kind, Dr. Segal, professor of computer science and applied mathematics at the Weizmann Institute of Science in Rehovot, Israel, and his associates recruited 1,000 individuals and asked them to wear a continuous glucose monitor (CGM) for 1 week (Cell 2015;163[5]:1079-94). For the study, known as The Personalized Nutrition Project, participants were asked to log everything they ate into a mobile app the researchers developed. “They would select a meal from a database of 10,000 foods,” Dr. Segal explained. “Each meal has full nutritional value so at the end of the study, we had about 50,000 meals that we had measurements of postprandial glucose response to, coupled with full nutritional values.” They also collected a comprehensive profile of individuals, which included body measurements, blood tests, medical background, food frequency questionnaires, and a measurement of the microbiome by both 16S rRNA sequencing and shotgun metagenomics.
For the first part of the study, researchers supplied a breakfast to all participants: either bread, bread with butter, glucose, or fructose, in each case 50 g of available carbohydrates. “The participants were asked to consume these the morning after the night fast,” Dr. Segal said. “This allowed us to compare how the same individual responds to eating the exact same food versus how different individuals respond to eating the same food.” The researchers found that, when the same person ate the same meal on 2 different days, the glucose response was highly reproducible. In contrast, different people had widely different postmeal glucose responses to identical meals. “Some individuals responded most highly to glucose; others responded most highly to bread,” Dr. Segal said. “There was about 10% of individuals who responded to bread and butter, compared to the other test foods. These results mean that any universal diet is going to have limited efficacy in its ability to balance blood glucose levels, because some foods will spike glucose levels in one person but not in another person. It also means that the concepts we’ve been using like the glycemic index are also going to have limited efficacy.”
Next, the researchers aimed to determine what factors influence the variability in people’s responses to the same food. “We found many different correlations between the various blood markers and physical measurements that we obtained, but what was most novel was the variability in postmeal glucose response across people associated with microbiota composition and function,” Dr. Segal said. From this, he and his colleagues developed a machine-learning algorithm that integrates blood parameters, dietary habits, anthropometrics, physical activity, and gut microbiota. Using this algorithm, the prediction accuracy of personalized glucose responses achieved an r value of 0.68, which explains about 50% of the variability. For the final component of the study, the researchers randomized 26 participants to one of five dietary arms and followed for 1 week by continuous glucose monitoring. They were able to demonstrate that personally tailored diets lower the postprandial glucose response.
As a follow-up to this work, Dr. Segal and his associates enrolled 200 people with an hemoglobin A1c between 5.7% and 6.5% into the Personalized Nutrition Project for Prediabetes (PNP3) study, which investigates whether personalized diet intervention will improve postprandial blood glucose levels and other metabolic health factors in individuals with prediabetes, compared with the standard Mediterranean-style low-fat diet (NCT03222791). Participants were randomized to 6 months of standard of care following Dietary Guidelines for Americans 2015-2020, Eighth Edition, or to an algorithm diet. Primary outcomes are reduction in average glucose levels and evaluation of the total daily time of plasma glucose levels were below 140 mg/dL. Participants wore the continuous glucose monitor for the entire 6 months of intervention. “I don’t think this was ever done before,” he said. “We’re also looking at secondary metabolic endpoints and exploratory endpoints such as changes in the microbiome. We’re asking people to log everything they eat for the entire 6 months of intervention. It gives us a lot of power in terms assessing compliance. It’s an immense amount of data.”
Evaluation of the data are not yet complete, but interim results are promising. For example, he discussed results from one study participant on the algorithm diet. “Across 1 month, this person was able to entirely reduce the peaks in glucose levels and dramatic reductions in the time above 140 mg/dL in the 6-month treatment period,” said Dr. Segal, who is one of the study’s principal investigators. He disclosed that he is a paid consultant to DayTwo.
LOS ANGELES – .
“The reason we got interested in nutrition in general is for its important role in health and disease, but also because, reading the literature on nutrition in general, it seemed that the science was relatively poor,” Eran Segal, PhD, said at the World Congress on Insulin Resistance, Diabetes & Cardiovascular Disease. “As a testament, you can see how frequently dietary recommendations for the public are changed. For example, 30 years ago, the cover of Time magazine said that eating cholesterol in the diet is very bad for you. Fifteen years later, Time magazine said that some cholesterol is actually good for you. There are other questions, like should you be eating dairy products? I think it shows that we have a poor understanding of what healthy nutrition is for human individuals. That’s why we wanted to start a study which would collect the right amount and the right kind of data to try to answer the question of what is a healthy diet for human individuals.”
In what is believed to be the first study of its kind, Dr. Segal, professor of computer science and applied mathematics at the Weizmann Institute of Science in Rehovot, Israel, and his associates recruited 1,000 individuals and asked them to wear a continuous glucose monitor (CGM) for 1 week (Cell 2015;163[5]:1079-94). For the study, known as The Personalized Nutrition Project, participants were asked to log everything they ate into a mobile app the researchers developed. “They would select a meal from a database of 10,000 foods,” Dr. Segal explained. “Each meal has full nutritional value so at the end of the study, we had about 50,000 meals that we had measurements of postprandial glucose response to, coupled with full nutritional values.” They also collected a comprehensive profile of individuals, which included body measurements, blood tests, medical background, food frequency questionnaires, and a measurement of the microbiome by both 16S rRNA sequencing and shotgun metagenomics.
For the first part of the study, researchers supplied a breakfast to all participants: either bread, bread with butter, glucose, or fructose, in each case 50 g of available carbohydrates. “The participants were asked to consume these the morning after the night fast,” Dr. Segal said. “This allowed us to compare how the same individual responds to eating the exact same food versus how different individuals respond to eating the same food.” The researchers found that, when the same person ate the same meal on 2 different days, the glucose response was highly reproducible. In contrast, different people had widely different postmeal glucose responses to identical meals. “Some individuals responded most highly to glucose; others responded most highly to bread,” Dr. Segal said. “There was about 10% of individuals who responded to bread and butter, compared to the other test foods. These results mean that any universal diet is going to have limited efficacy in its ability to balance blood glucose levels, because some foods will spike glucose levels in one person but not in another person. It also means that the concepts we’ve been using like the glycemic index are also going to have limited efficacy.”
Next, the researchers aimed to determine what factors influence the variability in people’s responses to the same food. “We found many different correlations between the various blood markers and physical measurements that we obtained, but what was most novel was the variability in postmeal glucose response across people associated with microbiota composition and function,” Dr. Segal said. From this, he and his colleagues developed a machine-learning algorithm that integrates blood parameters, dietary habits, anthropometrics, physical activity, and gut microbiota. Using this algorithm, the prediction accuracy of personalized glucose responses achieved an r value of 0.68, which explains about 50% of the variability. For the final component of the study, the researchers randomized 26 participants to one of five dietary arms and followed for 1 week by continuous glucose monitoring. They were able to demonstrate that personally tailored diets lower the postprandial glucose response.
As a follow-up to this work, Dr. Segal and his associates enrolled 200 people with an hemoglobin A1c between 5.7% and 6.5% into the Personalized Nutrition Project for Prediabetes (PNP3) study, which investigates whether personalized diet intervention will improve postprandial blood glucose levels and other metabolic health factors in individuals with prediabetes, compared with the standard Mediterranean-style low-fat diet (NCT03222791). Participants were randomized to 6 months of standard of care following Dietary Guidelines for Americans 2015-2020, Eighth Edition, or to an algorithm diet. Primary outcomes are reduction in average glucose levels and evaluation of the total daily time of plasma glucose levels were below 140 mg/dL. Participants wore the continuous glucose monitor for the entire 6 months of intervention. “I don’t think this was ever done before,” he said. “We’re also looking at secondary metabolic endpoints and exploratory endpoints such as changes in the microbiome. We’re asking people to log everything they eat for the entire 6 months of intervention. It gives us a lot of power in terms assessing compliance. It’s an immense amount of data.”
Evaluation of the data are not yet complete, but interim results are promising. For example, he discussed results from one study participant on the algorithm diet. “Across 1 month, this person was able to entirely reduce the peaks in glucose levels and dramatic reductions in the time above 140 mg/dL in the 6-month treatment period,” said Dr. Segal, who is one of the study’s principal investigators. He disclosed that he is a paid consultant to DayTwo.
EXPERT ANALYSIS FROM WCIRDC 2018
Gout’s Golden Globe, resistance is fecal, eucalyptus eulogy
Eucalyptus eulogy
(“Taps” quietly plays in the background ... ) In some sad news, Quincy the diabetic koala has passed on to that great eucalyptus tree in the sky. The furry type 1 diabetic lived in San Diego, where he was recently fitted with a cutting-edge continuous glucose monitor (CGM). This allowed Quincy more time for his favorite activities (chewing and sleeping) and less time spent with pesky skin pricks.
Quincy died of pneumonia, and it is unclear whether his death was diabetes related. All we know is that he will be missed greatly. He was beloved by those with diabetes everywhere, animal or otherwise. Quincy’s successful CGM procedure also gives endocrinologists hope that the technology could eventually be used for similarly fragile humans, like babies. R.I.P., Quincy; we loved you. In lieu of flowers, donations may be made to his favorite charity, the Drop Bear Awareness Association.
What’s Latin for ‘poop’?
The study of the human microbiota has become incredibly important in recent years, but there’s no getting away from the fact that it entails experimenting on poop. Remarkably, no one’s come up with a proper technical name for this unsavory activity. However, thanks to a collaboration between a gastroenterologist and a classics professor at the University of North Carolina, that deficiency is no more. You’ve met the in vivo and in vitro study. Now, please welcome the “in vimo” study!
Why in vimo? The term fecal or “in feco” might seem obvious. But the Latin root word never referred to poop, and if there’s one thing scientists can’t have, it’s improper Latin usage. The Romans, it turns out, had lots of words for poop. The root word of laetamen referred to fertility, richness, and happiness – a tempting prospect – but was mostly used to refer to farm animal dung. Merda mostly referred to smell or stench, and stercus shared the same root word as scatology, which refers to obscene literature. Fimus, which specifically refers to manure, was thus the most precise, and it was used by literary giants such as Livy, Virgil, and Tacitus. A clear winner, and the in vimo study flushed the rest of the competition away.
And just in case you think these researchers are no fun, the name they chose for the active enzymes collected from their in vimo samples? Poopernatants. Yes, even doctors enjoy a good poop joke.
The new Breakfast Club
Researchers at the University of Illinois and the University of Texas have collaborated to study something that most of us fear greatly: high school cliques. The researchers, who may or may not have peaked in high school, took a look at high school peer crowds and influences that form those tight-knit bonds that last all of 4 years.
The study found that most of the classic cliques – the jocks, the popular crowd, the brains, the stoners, the loners – are still alive and well in today’s American school system. However, at least one new group has emerged in the last decade: the “anime/manga fans.” Researchers noted that although schools have become much more diverse, racial and ethnic stereotypes are alive and well. Thank God we only have to do high school once.
Resistance is fecal
And now, just in case you were wondering how long it would take to put our newfound knowledge of “in vimo” to use, here comes a study that has “in vimo” written all over it (metaphorically speaking, of course).
Researchers in Sweden and Finland decided to take a look at antibiotic resistance genes in sewage, because “antibiotics consumed by humans and animals are released into the environment in urine and fecal material contained in treated wastewaters and sludge applied to land.” Then they compared the abundance of the mobile antibiotic resistance genes with the abundance of a human fecal pollution marker.
That marker – a virus that infects bacteria in human feces but is rare in other animals – was “highly correlated to the abundance of antibiotic resistance genes in environmental samples,” they said in a separate written statement, which “indicates that fecal pollution can largely explain the increase in resistant bacteria often found in human-impacted environments.” The name of that marker, the virus found in feces, happens to be “crAssphage.” And yes, the A really is capitalized. Really. We are not making this up.
Gout wins a Golden Globe
Gout has a new poster girl: Great Britain’s Queen Anne. She’s been dead for more than 4 centuries, but a Hollywood version of this stout monarch is turning a famously royal affliction into the disease of the moment.
The credit goes to actress Olivia Colman, who just won a Golden Globe award for her brilliant performance in the earthy comedy “The Favourite.” Ms. Colman transforms the pain-wracked Queen Anne into a needy, manipulative, and loopy monarch who still manages to draw our sympathy.
Besides flummoxing American spell-checkers with its title, The Favourite glories in stretching the truth about the queen’s private life. But she really does seem to have had the “disease of kings,” which has long been linked to the rich, fatty diets enjoyed by blue bloods.
Now, there’s talk that high-protein, meat-friendly keto and paleo diets are boosting rates among the young. This theory got an airing last week in a New York Magazine article titled “Why Gout Is Making a Comeback.”
The truth may be more complicated. Over the last few years, researchers have cast doubt on the keto-leads-to-gout theory and suggested that fructose in sugar may be the real culprit. According to this hypothesis, gout afflicted British royals as they developed a communal sweet tooth during the early days of the sugar trade. Gout then spread to the general population as sugar became more accessible.
The gout debate will continue. As for Olivia Colman, she will soon grace smaller screens with her performance as Queen Elizabeth II in Netflix’s series “The Crown.”
QE II isn’t known for having suffered from any major diseases. But at her next checkup, we do think she should have that stiff upper lip looked at.

Eucalyptus eulogy
(“Taps” quietly plays in the background ... ) In some sad news, Quincy the diabetic koala has passed on to that great eucalyptus tree in the sky. The furry type 1 diabetic lived in San Diego, where he was recently fitted with a cutting-edge continuous glucose monitor (CGM). This allowed Quincy more time for his favorite activities (chewing and sleeping) and less time spent with pesky skin pricks.
Quincy died of pneumonia, and it is unclear whether his death was diabetes related. All we know is that he will be missed greatly. He was beloved by those with diabetes everywhere, animal or otherwise. Quincy’s successful CGM procedure also gives endocrinologists hope that the technology could eventually be used for similarly fragile humans, like babies. R.I.P., Quincy; we loved you. In lieu of flowers, donations may be made to his favorite charity, the Drop Bear Awareness Association.
What’s Latin for ‘poop’?
The study of the human microbiota has become incredibly important in recent years, but there’s no getting away from the fact that it entails experimenting on poop. Remarkably, no one’s come up with a proper technical name for this unsavory activity. However, thanks to a collaboration between a gastroenterologist and a classics professor at the University of North Carolina, that deficiency is no more. You’ve met the in vivo and in vitro study. Now, please welcome the “in vimo” study!
Why in vimo? The term fecal or “in feco” might seem obvious. But the Latin root word never referred to poop, and if there’s one thing scientists can’t have, it’s improper Latin usage. The Romans, it turns out, had lots of words for poop. The root word of laetamen referred to fertility, richness, and happiness – a tempting prospect – but was mostly used to refer to farm animal dung. Merda mostly referred to smell or stench, and stercus shared the same root word as scatology, which refers to obscene literature. Fimus, which specifically refers to manure, was thus the most precise, and it was used by literary giants such as Livy, Virgil, and Tacitus. A clear winner, and the in vimo study flushed the rest of the competition away.
And just in case you think these researchers are no fun, the name they chose for the active enzymes collected from their in vimo samples? Poopernatants. Yes, even doctors enjoy a good poop joke.
The new Breakfast Club
Researchers at the University of Illinois and the University of Texas have collaborated to study something that most of us fear greatly: high school cliques. The researchers, who may or may not have peaked in high school, took a look at high school peer crowds and influences that form those tight-knit bonds that last all of 4 years.
The study found that most of the classic cliques – the jocks, the popular crowd, the brains, the stoners, the loners – are still alive and well in today’s American school system. However, at least one new group has emerged in the last decade: the “anime/manga fans.” Researchers noted that although schools have become much more diverse, racial and ethnic stereotypes are alive and well. Thank God we only have to do high school once.
Resistance is fecal
And now, just in case you were wondering how long it would take to put our newfound knowledge of “in vimo” to use, here comes a study that has “in vimo” written all over it (metaphorically speaking, of course).
Researchers in Sweden and Finland decided to take a look at antibiotic resistance genes in sewage, because “antibiotics consumed by humans and animals are released into the environment in urine and fecal material contained in treated wastewaters and sludge applied to land.” Then they compared the abundance of the mobile antibiotic resistance genes with the abundance of a human fecal pollution marker.
That marker – a virus that infects bacteria in human feces but is rare in other animals – was “highly correlated to the abundance of antibiotic resistance genes in environmental samples,” they said in a separate written statement, which “indicates that fecal pollution can largely explain the increase in resistant bacteria often found in human-impacted environments.” The name of that marker, the virus found in feces, happens to be “crAssphage.” And yes, the A really is capitalized. Really. We are not making this up.
Gout wins a Golden Globe
Gout has a new poster girl: Great Britain’s Queen Anne. She’s been dead for more than 4 centuries, but a Hollywood version of this stout monarch is turning a famously royal affliction into the disease of the moment.
The credit goes to actress Olivia Colman, who just won a Golden Globe award for her brilliant performance in the earthy comedy “The Favourite.” Ms. Colman transforms the pain-wracked Queen Anne into a needy, manipulative, and loopy monarch who still manages to draw our sympathy.
Besides flummoxing American spell-checkers with its title, The Favourite glories in stretching the truth about the queen’s private life. But she really does seem to have had the “disease of kings,” which has long been linked to the rich, fatty diets enjoyed by blue bloods.
Now, there’s talk that high-protein, meat-friendly keto and paleo diets are boosting rates among the young. This theory got an airing last week in a New York Magazine article titled “Why Gout Is Making a Comeback.”
The truth may be more complicated. Over the last few years, researchers have cast doubt on the keto-leads-to-gout theory and suggested that fructose in sugar may be the real culprit. According to this hypothesis, gout afflicted British royals as they developed a communal sweet tooth during the early days of the sugar trade. Gout then spread to the general population as sugar became more accessible.
The gout debate will continue. As for Olivia Colman, she will soon grace smaller screens with her performance as Queen Elizabeth II in Netflix’s series “The Crown.”
QE II isn’t known for having suffered from any major diseases. But at her next checkup, we do think she should have that stiff upper lip looked at.

Eucalyptus eulogy
(“Taps” quietly plays in the background ... ) In some sad news, Quincy the diabetic koala has passed on to that great eucalyptus tree in the sky. The furry type 1 diabetic lived in San Diego, where he was recently fitted with a cutting-edge continuous glucose monitor (CGM). This allowed Quincy more time for his favorite activities (chewing and sleeping) and less time spent with pesky skin pricks.
Quincy died of pneumonia, and it is unclear whether his death was diabetes related. All we know is that he will be missed greatly. He was beloved by those with diabetes everywhere, animal or otherwise. Quincy’s successful CGM procedure also gives endocrinologists hope that the technology could eventually be used for similarly fragile humans, like babies. R.I.P., Quincy; we loved you. In lieu of flowers, donations may be made to his favorite charity, the Drop Bear Awareness Association.
What’s Latin for ‘poop’?
The study of the human microbiota has become incredibly important in recent years, but there’s no getting away from the fact that it entails experimenting on poop. Remarkably, no one’s come up with a proper technical name for this unsavory activity. However, thanks to a collaboration between a gastroenterologist and a classics professor at the University of North Carolina, that deficiency is no more. You’ve met the in vivo and in vitro study. Now, please welcome the “in vimo” study!
Why in vimo? The term fecal or “in feco” might seem obvious. But the Latin root word never referred to poop, and if there’s one thing scientists can’t have, it’s improper Latin usage. The Romans, it turns out, had lots of words for poop. The root word of laetamen referred to fertility, richness, and happiness – a tempting prospect – but was mostly used to refer to farm animal dung. Merda mostly referred to smell or stench, and stercus shared the same root word as scatology, which refers to obscene literature. Fimus, which specifically refers to manure, was thus the most precise, and it was used by literary giants such as Livy, Virgil, and Tacitus. A clear winner, and the in vimo study flushed the rest of the competition away.
And just in case you think these researchers are no fun, the name they chose for the active enzymes collected from their in vimo samples? Poopernatants. Yes, even doctors enjoy a good poop joke.
The new Breakfast Club
Researchers at the University of Illinois and the University of Texas have collaborated to study something that most of us fear greatly: high school cliques. The researchers, who may or may not have peaked in high school, took a look at high school peer crowds and influences that form those tight-knit bonds that last all of 4 years.
The study found that most of the classic cliques – the jocks, the popular crowd, the brains, the stoners, the loners – are still alive and well in today’s American school system. However, at least one new group has emerged in the last decade: the “anime/manga fans.” Researchers noted that although schools have become much more diverse, racial and ethnic stereotypes are alive and well. Thank God we only have to do high school once.
Resistance is fecal
And now, just in case you were wondering how long it would take to put our newfound knowledge of “in vimo” to use, here comes a study that has “in vimo” written all over it (metaphorically speaking, of course).
Researchers in Sweden and Finland decided to take a look at antibiotic resistance genes in sewage, because “antibiotics consumed by humans and animals are released into the environment in urine and fecal material contained in treated wastewaters and sludge applied to land.” Then they compared the abundance of the mobile antibiotic resistance genes with the abundance of a human fecal pollution marker.
That marker – a virus that infects bacteria in human feces but is rare in other animals – was “highly correlated to the abundance of antibiotic resistance genes in environmental samples,” they said in a separate written statement, which “indicates that fecal pollution can largely explain the increase in resistant bacteria often found in human-impacted environments.” The name of that marker, the virus found in feces, happens to be “crAssphage.” And yes, the A really is capitalized. Really. We are not making this up.
Gout wins a Golden Globe
Gout has a new poster girl: Great Britain’s Queen Anne. She’s been dead for more than 4 centuries, but a Hollywood version of this stout monarch is turning a famously royal affliction into the disease of the moment.
The credit goes to actress Olivia Colman, who just won a Golden Globe award for her brilliant performance in the earthy comedy “The Favourite.” Ms. Colman transforms the pain-wracked Queen Anne into a needy, manipulative, and loopy monarch who still manages to draw our sympathy.
Besides flummoxing American spell-checkers with its title, The Favourite glories in stretching the truth about the queen’s private life. But she really does seem to have had the “disease of kings,” which has long been linked to the rich, fatty diets enjoyed by blue bloods.
Now, there’s talk that high-protein, meat-friendly keto and paleo diets are boosting rates among the young. This theory got an airing last week in a New York Magazine article titled “Why Gout Is Making a Comeback.”
The truth may be more complicated. Over the last few years, researchers have cast doubt on the keto-leads-to-gout theory and suggested that fructose in sugar may be the real culprit. According to this hypothesis, gout afflicted British royals as they developed a communal sweet tooth during the early days of the sugar trade. Gout then spread to the general population as sugar became more accessible.
The gout debate will continue. As for Olivia Colman, she will soon grace smaller screens with her performance as Queen Elizabeth II in Netflix’s series “The Crown.”
QE II isn’t known for having suffered from any major diseases. But at her next checkup, we do think she should have that stiff upper lip looked at.

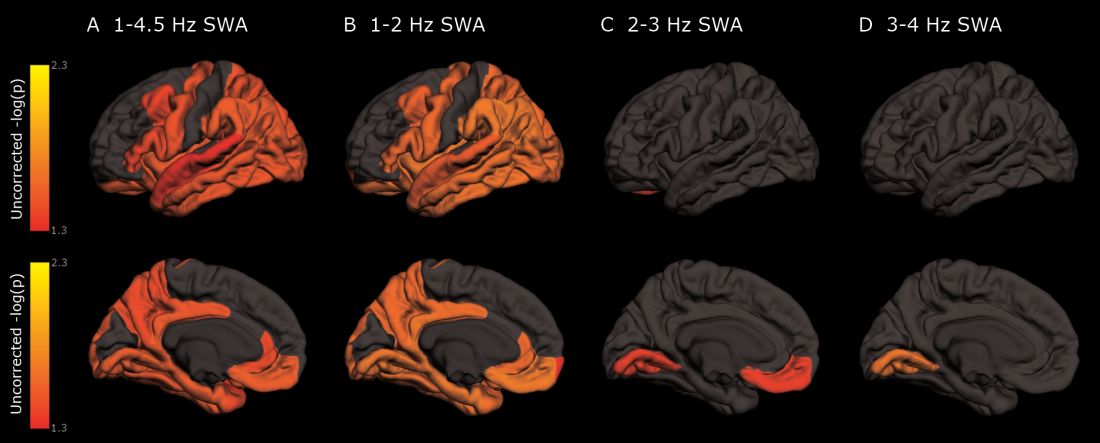
As deep sleep decreases, Alzheimer’s pathology – particularly tau – increases
The protein was evident in areas associated with memory consolidation, typically affected in Alzheimer’s disease: the entorhinal, parahippocampal, inferior parietal, insula, isthmus cingulate, lingual, supramarginal, and orbitofrontal regions.
Because the findings were observed in a population of cognitively normal and minimally impaired subjects, they suggest a role for sleep studies in assessing the risk for cognitive decline and Alzheimer’s disease, and in monitoring patients with the disease, reported Brendan P. Lucey, MD, and his colleagues. The report is in Science and Translational Medicine (Sci Transl Med. 2019 Jan 9;11:eaau6550).
“With the rising incidence of Alzheimer’s disease in an aging population, our findings have potential application in both clinical trials and patient screening for Alzheimer’s disease to noninvasively monitor for progression of Alzheimer’s disease pathology,” wrote Dr. Lucey, director of the Sleep Medicine Center and assistant professor of neurology at Washington University in St. Louis. “For instance, periodically measuring non-REM slow wave activity, in conjunction with other biomarkers, may have utility for monitoring Alzheimer’s disease risk or response to an Alzheimer’s disease treatment.”
Dr. Lucey and his colleagues examined sleep architecture and tau and amyloid deposition in 119 subjects enrolled in longitudinal aging studies. For 6 nights, subjects slept with a single-channel EEG monitor on. They also underwent cognitive testing and genotyping for Alzheimer’s disease risk factors.
Subjects were a mean of 74 years old. Almost 80% had normal cognition as measured by the Clinical Dementia Rating Scale (CDR); the remainder had very mild cognitive impairment (CDR 0.5)
Among those with positive biomarker findings, sleep architecture was altered in several ways: lower REM latency, lower wake after sleep onset, prolonged sleep-onset latency, and longer self-reported total sleep time. The differences were evident in those with normal cognition, but even more pronounced in those with mild cognitive impairment. Despite the longer sleep times, however, sleep efficiency was decreased.
Decreased non-REM slow wave activity was associated with increased tau deposition. The protein was largely concentrated in areas of typical Alzheimer’s disease pathology (entorhinal, parahippocampal, orbital frontal, precuneus, inferior parietal, and inferior temporal regions). There were no significant associations between non-REM slow wave activity and amyloid deposits.
Other sleep parameters, however, were associated with amyloid, including REM latency and sleep latency, “suggesting that as amyloid-beta deposition increased, the time to fall asleep and enter REM sleep decreased,” the investigators said.
Those with tau pathology also slept longer, reporting more daytime naps. “This suggests that participants with greater tau pathology experienced daytime sleepiness despite increased total sleep time.”
“These results, coupled with the non-REM slow wave activity findings, suggest that the quality of sleep decreases with increasing tau despite increased sleep time.” Questions about napping should probably be included in dementia screening discussions, they said.
The study was largely funded by the National Institutes of Health. Dr. Lucey had no financial conflicts.
SOURCE: Lucey BP et al. Sci Transl Med 2019 Jan 9;11:eaau6550.
The protein was evident in areas associated with memory consolidation, typically affected in Alzheimer’s disease: the entorhinal, parahippocampal, inferior parietal, insula, isthmus cingulate, lingual, supramarginal, and orbitofrontal regions.
Because the findings were observed in a population of cognitively normal and minimally impaired subjects, they suggest a role for sleep studies in assessing the risk for cognitive decline and Alzheimer’s disease, and in monitoring patients with the disease, reported Brendan P. Lucey, MD, and his colleagues. The report is in Science and Translational Medicine (Sci Transl Med. 2019 Jan 9;11:eaau6550).
“With the rising incidence of Alzheimer’s disease in an aging population, our findings have potential application in both clinical trials and patient screening for Alzheimer’s disease to noninvasively monitor for progression of Alzheimer’s disease pathology,” wrote Dr. Lucey, director of the Sleep Medicine Center and assistant professor of neurology at Washington University in St. Louis. “For instance, periodically measuring non-REM slow wave activity, in conjunction with other biomarkers, may have utility for monitoring Alzheimer’s disease risk or response to an Alzheimer’s disease treatment.”
Dr. Lucey and his colleagues examined sleep architecture and tau and amyloid deposition in 119 subjects enrolled in longitudinal aging studies. For 6 nights, subjects slept with a single-channel EEG monitor on. They also underwent cognitive testing and genotyping for Alzheimer’s disease risk factors.
Subjects were a mean of 74 years old. Almost 80% had normal cognition as measured by the Clinical Dementia Rating Scale (CDR); the remainder had very mild cognitive impairment (CDR 0.5)
Among those with positive biomarker findings, sleep architecture was altered in several ways: lower REM latency, lower wake after sleep onset, prolonged sleep-onset latency, and longer self-reported total sleep time. The differences were evident in those with normal cognition, but even more pronounced in those with mild cognitive impairment. Despite the longer sleep times, however, sleep efficiency was decreased.
Decreased non-REM slow wave activity was associated with increased tau deposition. The protein was largely concentrated in areas of typical Alzheimer’s disease pathology (entorhinal, parahippocampal, orbital frontal, precuneus, inferior parietal, and inferior temporal regions). There were no significant associations between non-REM slow wave activity and amyloid deposits.
Other sleep parameters, however, were associated with amyloid, including REM latency and sleep latency, “suggesting that as amyloid-beta deposition increased, the time to fall asleep and enter REM sleep decreased,” the investigators said.
Those with tau pathology also slept longer, reporting more daytime naps. “This suggests that participants with greater tau pathology experienced daytime sleepiness despite increased total sleep time.”
“These results, coupled with the non-REM slow wave activity findings, suggest that the quality of sleep decreases with increasing tau despite increased sleep time.” Questions about napping should probably be included in dementia screening discussions, they said.
The study was largely funded by the National Institutes of Health. Dr. Lucey had no financial conflicts.
SOURCE: Lucey BP et al. Sci Transl Med 2019 Jan 9;11:eaau6550.
The protein was evident in areas associated with memory consolidation, typically affected in Alzheimer’s disease: the entorhinal, parahippocampal, inferior parietal, insula, isthmus cingulate, lingual, supramarginal, and orbitofrontal regions.
Because the findings were observed in a population of cognitively normal and minimally impaired subjects, they suggest a role for sleep studies in assessing the risk for cognitive decline and Alzheimer’s disease, and in monitoring patients with the disease, reported Brendan P. Lucey, MD, and his colleagues. The report is in Science and Translational Medicine (Sci Transl Med. 2019 Jan 9;11:eaau6550).
“With the rising incidence of Alzheimer’s disease in an aging population, our findings have potential application in both clinical trials and patient screening for Alzheimer’s disease to noninvasively monitor for progression of Alzheimer’s disease pathology,” wrote Dr. Lucey, director of the Sleep Medicine Center and assistant professor of neurology at Washington University in St. Louis. “For instance, periodically measuring non-REM slow wave activity, in conjunction with other biomarkers, may have utility for monitoring Alzheimer’s disease risk or response to an Alzheimer’s disease treatment.”
Dr. Lucey and his colleagues examined sleep architecture and tau and amyloid deposition in 119 subjects enrolled in longitudinal aging studies. For 6 nights, subjects slept with a single-channel EEG monitor on. They also underwent cognitive testing and genotyping for Alzheimer’s disease risk factors.
Subjects were a mean of 74 years old. Almost 80% had normal cognition as measured by the Clinical Dementia Rating Scale (CDR); the remainder had very mild cognitive impairment (CDR 0.5)
Among those with positive biomarker findings, sleep architecture was altered in several ways: lower REM latency, lower wake after sleep onset, prolonged sleep-onset latency, and longer self-reported total sleep time. The differences were evident in those with normal cognition, but even more pronounced in those with mild cognitive impairment. Despite the longer sleep times, however, sleep efficiency was decreased.
Decreased non-REM slow wave activity was associated with increased tau deposition. The protein was largely concentrated in areas of typical Alzheimer’s disease pathology (entorhinal, parahippocampal, orbital frontal, precuneus, inferior parietal, and inferior temporal regions). There were no significant associations between non-REM slow wave activity and amyloid deposits.
Other sleep parameters, however, were associated with amyloid, including REM latency and sleep latency, “suggesting that as amyloid-beta deposition increased, the time to fall asleep and enter REM sleep decreased,” the investigators said.
Those with tau pathology also slept longer, reporting more daytime naps. “This suggests that participants with greater tau pathology experienced daytime sleepiness despite increased total sleep time.”
“These results, coupled with the non-REM slow wave activity findings, suggest that the quality of sleep decreases with increasing tau despite increased sleep time.” Questions about napping should probably be included in dementia screening discussions, they said.
The study was largely funded by the National Institutes of Health. Dr. Lucey had no financial conflicts.
SOURCE: Lucey BP et al. Sci Transl Med 2019 Jan 9;11:eaau6550.
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point: Cognitively normal subjects with tau deposition experience altered sleep patterns.
Major finding: Decreased time in non-REM deep sleep was associated with increased tau pathology in Alzheimer’s-affected brain regions and in cerebrospinal fluid.
Study details: The prospective longitudinal study comprised 119 subjects.
Disclosures: The authors reported no relevant financial disclosures.
Source: Lucey BP et al. Sci Transl Med. 2019 Jan 9;11:eaau6550.
January 2019 Highlights
Autologous Hematopoietic Stem Cells May Treat Aggressive MS Effectively
The therapy may halt disease activity and promote sustained functional improvement.
BERLIN—Autologous hematopoietic stem cell transplantation (HSCT) could prevent disease activity and promote functional recovery in patients with aggressive multiple sclerosis (MS), according to a retrospective case series presented at ECTRIMS 2018.
A review article suggested that the likelihood of achieving no evidence of disease activity (NEDA) after two years of treatment ranges between 10% and 60%
Like other highly effective therapies, HSCT has been considered to entail significant safety risks. When the European Society for Blood and Marrow Transplantation (EBMT) reviewed their data, however, they identified one death related to HSCT between 2012 and 2016. The estimated risk of death from HSCT is thus approximately 0.2%. “Mortality associated with transplantation has decreased so much that it is almost into the range of other standard disease-modifying therapies,” said Joyutpal Das, MBBS, a neuroscientist at Royal Hallamshire Hospital in Sheffield, United Kingdom.
EBMT recommended that neurologists consider HSCT for patients with highly active radiologic and clinical disease who have failed to respond to standard disease-modifying therapy. The treatment can be considered as first-line therapy for patients with exceptionally active disease who have become disabled, they added.
A Retrospective Case Series
To examine the efficacy of HSCT in this patient population, Dr. Das and colleagues conducted a retrospective case series of 20 patients with MS from five centers in various countries. The patients’ treating physicians decided that HSCT should be their first-line therapy. Dr. Das and colleagues used NEDA-3 (which includes relapses, disability progression, and MRI activity) as their primary outcome. Each patient underwent brain MRI during the first six months of treatment and at six- to 12-month intervals thereafter.
The case series included equal numbers of men and women. All patients had frequent relapses, incomplete recovery, and multiple gadolinium enhancing lesions on serial MRI scans. The lesions often affected the brainstem, cerebellum, and spine. Patients’ median age of diagnosis and median age of treatment were 28. The time between the first onset of symptoms and treatment was nine months, and that between diagnosis and treatment was five months. Patients’ median pretreatment Expanded Disability Status Scale (EDSS) score was 6.5. Median follow-up duration was 2.5 years.
EDSS Score Improved
Three patients had new lesions during the first six months of treatment, but no patients had new lesions on subsequent MRI scans. “It has been suggested … that if you want to use NEDA to measure efficacy, the patient should have rebaseline imaging after the initiation of treatment,” said Dr. Das. “If we use our six-month scan as rebaseline imaging, then we have no further disease activity on MRI scan.”
After treatment initiation, the median EDSS score decreased from 6.5 to 2. Patients’ median improvement on EDSS score was 2.5 points, which was statistically significant. Seven patients had an EDSS score improvement of 3 points or greater. EDSS score improved for all but one patient. The results suggest that HSCT induced rapid and sustained remission, said Dr. Das.
The investigators observed typical transplant-related toxicity in the population, and no patient died. One woman conceived and gave birth to a healthy baby, and one man fathered a healthy baby.
—Erik Greb
Suggested Reading
Sormani MP, Muraro PA, Saccardi R, Mancardi G. NEDA status in highly active MS can be more easily obtained with autologous hematopoietic stem cell transplantation than other drugs. Mult Scler. 2017;23(2):201-204.
The therapy may halt disease activity and promote sustained functional improvement.
The therapy may halt disease activity and promote sustained functional improvement.
BERLIN—Autologous hematopoietic stem cell transplantation (HSCT) could prevent disease activity and promote functional recovery in patients with aggressive multiple sclerosis (MS), according to a retrospective case series presented at ECTRIMS 2018.
A review article suggested that the likelihood of achieving no evidence of disease activity (NEDA) after two years of treatment ranges between 10% and 60%
Like other highly effective therapies, HSCT has been considered to entail significant safety risks. When the European Society for Blood and Marrow Transplantation (EBMT) reviewed their data, however, they identified one death related to HSCT between 2012 and 2016. The estimated risk of death from HSCT is thus approximately 0.2%. “Mortality associated with transplantation has decreased so much that it is almost into the range of other standard disease-modifying therapies,” said Joyutpal Das, MBBS, a neuroscientist at Royal Hallamshire Hospital in Sheffield, United Kingdom.
EBMT recommended that neurologists consider HSCT for patients with highly active radiologic and clinical disease who have failed to respond to standard disease-modifying therapy. The treatment can be considered as first-line therapy for patients with exceptionally active disease who have become disabled, they added.
A Retrospective Case Series
To examine the efficacy of HSCT in this patient population, Dr. Das and colleagues conducted a retrospective case series of 20 patients with MS from five centers in various countries. The patients’ treating physicians decided that HSCT should be their first-line therapy. Dr. Das and colleagues used NEDA-3 (which includes relapses, disability progression, and MRI activity) as their primary outcome. Each patient underwent brain MRI during the first six months of treatment and at six- to 12-month intervals thereafter.
The case series included equal numbers of men and women. All patients had frequent relapses, incomplete recovery, and multiple gadolinium enhancing lesions on serial MRI scans. The lesions often affected the brainstem, cerebellum, and spine. Patients’ median age of diagnosis and median age of treatment were 28. The time between the first onset of symptoms and treatment was nine months, and that between diagnosis and treatment was five months. Patients’ median pretreatment Expanded Disability Status Scale (EDSS) score was 6.5. Median follow-up duration was 2.5 years.
EDSS Score Improved
Three patients had new lesions during the first six months of treatment, but no patients had new lesions on subsequent MRI scans. “It has been suggested … that if you want to use NEDA to measure efficacy, the patient should have rebaseline imaging after the initiation of treatment,” said Dr. Das. “If we use our six-month scan as rebaseline imaging, then we have no further disease activity on MRI scan.”
After treatment initiation, the median EDSS score decreased from 6.5 to 2. Patients’ median improvement on EDSS score was 2.5 points, which was statistically significant. Seven patients had an EDSS score improvement of 3 points or greater. EDSS score improved for all but one patient. The results suggest that HSCT induced rapid and sustained remission, said Dr. Das.
The investigators observed typical transplant-related toxicity in the population, and no patient died. One woman conceived and gave birth to a healthy baby, and one man fathered a healthy baby.
—Erik Greb
Suggested Reading
Sormani MP, Muraro PA, Saccardi R, Mancardi G. NEDA status in highly active MS can be more easily obtained with autologous hematopoietic stem cell transplantation than other drugs. Mult Scler. 2017;23(2):201-204.
BERLIN—Autologous hematopoietic stem cell transplantation (HSCT) could prevent disease activity and promote functional recovery in patients with aggressive multiple sclerosis (MS), according to a retrospective case series presented at ECTRIMS 2018.
A review article suggested that the likelihood of achieving no evidence of disease activity (NEDA) after two years of treatment ranges between 10% and 60%
Like other highly effective therapies, HSCT has been considered to entail significant safety risks. When the European Society for Blood and Marrow Transplantation (EBMT) reviewed their data, however, they identified one death related to HSCT between 2012 and 2016. The estimated risk of death from HSCT is thus approximately 0.2%. “Mortality associated with transplantation has decreased so much that it is almost into the range of other standard disease-modifying therapies,” said Joyutpal Das, MBBS, a neuroscientist at Royal Hallamshire Hospital in Sheffield, United Kingdom.
EBMT recommended that neurologists consider HSCT for patients with highly active radiologic and clinical disease who have failed to respond to standard disease-modifying therapy. The treatment can be considered as first-line therapy for patients with exceptionally active disease who have become disabled, they added.
A Retrospective Case Series
To examine the efficacy of HSCT in this patient population, Dr. Das and colleagues conducted a retrospective case series of 20 patients with MS from five centers in various countries. The patients’ treating physicians decided that HSCT should be their first-line therapy. Dr. Das and colleagues used NEDA-3 (which includes relapses, disability progression, and MRI activity) as their primary outcome. Each patient underwent brain MRI during the first six months of treatment and at six- to 12-month intervals thereafter.
The case series included equal numbers of men and women. All patients had frequent relapses, incomplete recovery, and multiple gadolinium enhancing lesions on serial MRI scans. The lesions often affected the brainstem, cerebellum, and spine. Patients’ median age of diagnosis and median age of treatment were 28. The time between the first onset of symptoms and treatment was nine months, and that between diagnosis and treatment was five months. Patients’ median pretreatment Expanded Disability Status Scale (EDSS) score was 6.5. Median follow-up duration was 2.5 years.
EDSS Score Improved
Three patients had new lesions during the first six months of treatment, but no patients had new lesions on subsequent MRI scans. “It has been suggested … that if you want to use NEDA to measure efficacy, the patient should have rebaseline imaging after the initiation of treatment,” said Dr. Das. “If we use our six-month scan as rebaseline imaging, then we have no further disease activity on MRI scan.”
After treatment initiation, the median EDSS score decreased from 6.5 to 2. Patients’ median improvement on EDSS score was 2.5 points, which was statistically significant. Seven patients had an EDSS score improvement of 3 points or greater. EDSS score improved for all but one patient. The results suggest that HSCT induced rapid and sustained remission, said Dr. Das.
The investigators observed typical transplant-related toxicity in the population, and no patient died. One woman conceived and gave birth to a healthy baby, and one man fathered a healthy baby.
—Erik Greb
Suggested Reading
Sormani MP, Muraro PA, Saccardi R, Mancardi G. NEDA status in highly active MS can be more easily obtained with autologous hematopoietic stem cell transplantation than other drugs. Mult Scler. 2017;23(2):201-204.
Interferon Beta May Not Affect Pregnancy Outcomes in MS
The rates of live births and congenital anomalies are similar between exposed and nonexposed patients.
BERLIN—European registry data do not support the hypothesis that exposure to interferon beta before conception or during pregnancy adversely affects pregnancy outcome or infant outcome, according to an analysis presented at ECTRIMS 2018.
In women, diagnosis of multiple sclerosis (MS) and treatment initiation often occur during childbearing years, but neurologists have not reached consensus about treatment before or during pregnancy. The European Interferon Beta Pregnancy Registry was created to gather evidence about the effect of this treatment on maternal and fetal outcomes. A separate population-based cohort study examined health care registry data from Finland and Sweden (ie, Nordic registries) for the same purpose.
An Analysis of Prospective Data
Kerstin Hellwig, MD, Senior Consultant Neurologist and researcher at St. Joseph and St. Elizabeth Hospital and Ruhr University in Bochum, Germany, and colleagues examined these databases to evaluate the prevalence of pregnancy and infant outcomes in women with MS who had been exposed to interferon beta. The investigators analyzed 948 pregnancy reports with recorded pregnancy outcomes from the European Interferon Beta Pregnancy Registry. They also examined 875 pregnancy events in the Nordic registries among patients exposed to interferon beta and other treatments and 1,831 events among untreated patients.
Treatment Did Not Affect Birth Weight
Approximately 82% of pregnancies in the European registry had an outcome of live birth without congenital anomalies. The prevalence of spontaneous abortions and live births with congenital anomalies were similar to those reported in the general population.
About 98% of pregnancies in the exposed cohort of the Nordic registries had an outcome of live birth without congenital anomalies. This result is similar to the corresponding 97% rate in the nonexposed cohort. The prevalence of spontaneous abortions and congenital anomalies also were similar between the exposed and nonexposed cohorts of the Nordic registries.
Birth weights ranged from 580 g to 5,160 g in the Nordic registries. The proportion of babies with low or very low birth weight was 5.0% in the interferon-exposed cohort, 4.7% among babies exposed to interferon and other treatments, and 5.8% among nonexposed babies. Mean birth weight was 3,421.2 g in the interferon-exposed cohort, 3,434.3 g in the cohort exposed to interferon and other treatments, and 3,389.3 g in the nonexposed cohort. These weights were consistent with results from the prospective German pregnancy registry, according to the authors. Birth weights were not recorded systematically in the European registry.
“The European Interferon Beta Pregnancy Registry showed no evidence that interferon beta exposure before conception or during pregnancy adversely affected pregnancy or infant outcomes,” said Dr. Hellwig and colleagues. “This is consistent with data collected from the Nordic registers.”
This study was supported by Merck in
—Erik Greb
Suggested Reading
Alroughani R, Altintas A, Al Jumah M, et al. Pregnancy and the use of disease-modifying therapies in patients with multiple sclerosis: benefits versus risks. Mult Scler Int. 2016;2016:1034912.
Friend S, Richman S, Bloomgren G, et al. Evaluation of pregnancy outcomes from the Tysabri (natalizumab) pregnancy exposure registry: a global, observational, follow-up study. BMC Neurol. 2016;16(1):150.
The rates of live births and congenital anomalies are similar between exposed and nonexposed patients.
The rates of live births and congenital anomalies are similar between exposed and nonexposed patients.
BERLIN—European registry data do not support the hypothesis that exposure to interferon beta before conception or during pregnancy adversely affects pregnancy outcome or infant outcome, according to an analysis presented at ECTRIMS 2018.
In women, diagnosis of multiple sclerosis (MS) and treatment initiation often occur during childbearing years, but neurologists have not reached consensus about treatment before or during pregnancy. The European Interferon Beta Pregnancy Registry was created to gather evidence about the effect of this treatment on maternal and fetal outcomes. A separate population-based cohort study examined health care registry data from Finland and Sweden (ie, Nordic registries) for the same purpose.
An Analysis of Prospective Data
Kerstin Hellwig, MD, Senior Consultant Neurologist and researcher at St. Joseph and St. Elizabeth Hospital and Ruhr University in Bochum, Germany, and colleagues examined these databases to evaluate the prevalence of pregnancy and infant outcomes in women with MS who had been exposed to interferon beta. The investigators analyzed 948 pregnancy reports with recorded pregnancy outcomes from the European Interferon Beta Pregnancy Registry. They also examined 875 pregnancy events in the Nordic registries among patients exposed to interferon beta and other treatments and 1,831 events among untreated patients.
Treatment Did Not Affect Birth Weight
Approximately 82% of pregnancies in the European registry had an outcome of live birth without congenital anomalies. The prevalence of spontaneous abortions and live births with congenital anomalies were similar to those reported in the general population.
About 98% of pregnancies in the exposed cohort of the Nordic registries had an outcome of live birth without congenital anomalies. This result is similar to the corresponding 97% rate in the nonexposed cohort. The prevalence of spontaneous abortions and congenital anomalies also were similar between the exposed and nonexposed cohorts of the Nordic registries.
Birth weights ranged from 580 g to 5,160 g in the Nordic registries. The proportion of babies with low or very low birth weight was 5.0% in the interferon-exposed cohort, 4.7% among babies exposed to interferon and other treatments, and 5.8% among nonexposed babies. Mean birth weight was 3,421.2 g in the interferon-exposed cohort, 3,434.3 g in the cohort exposed to interferon and other treatments, and 3,389.3 g in the nonexposed cohort. These weights were consistent with results from the prospective German pregnancy registry, according to the authors. Birth weights were not recorded systematically in the European registry.
“The European Interferon Beta Pregnancy Registry showed no evidence that interferon beta exposure before conception or during pregnancy adversely affected pregnancy or infant outcomes,” said Dr. Hellwig and colleagues. “This is consistent with data collected from the Nordic registers.”
This study was supported by Merck in
—Erik Greb
Suggested Reading
Alroughani R, Altintas A, Al Jumah M, et al. Pregnancy and the use of disease-modifying therapies in patients with multiple sclerosis: benefits versus risks. Mult Scler Int. 2016;2016:1034912.
Friend S, Richman S, Bloomgren G, et al. Evaluation of pregnancy outcomes from the Tysabri (natalizumab) pregnancy exposure registry: a global, observational, follow-up study. BMC Neurol. 2016;16(1):150.
BERLIN—European registry data do not support the hypothesis that exposure to interferon beta before conception or during pregnancy adversely affects pregnancy outcome or infant outcome, according to an analysis presented at ECTRIMS 2018.
In women, diagnosis of multiple sclerosis (MS) and treatment initiation often occur during childbearing years, but neurologists have not reached consensus about treatment before or during pregnancy. The European Interferon Beta Pregnancy Registry was created to gather evidence about the effect of this treatment on maternal and fetal outcomes. A separate population-based cohort study examined health care registry data from Finland and Sweden (ie, Nordic registries) for the same purpose.
An Analysis of Prospective Data
Kerstin Hellwig, MD, Senior Consultant Neurologist and researcher at St. Joseph and St. Elizabeth Hospital and Ruhr University in Bochum, Germany, and colleagues examined these databases to evaluate the prevalence of pregnancy and infant outcomes in women with MS who had been exposed to interferon beta. The investigators analyzed 948 pregnancy reports with recorded pregnancy outcomes from the European Interferon Beta Pregnancy Registry. They also examined 875 pregnancy events in the Nordic registries among patients exposed to interferon beta and other treatments and 1,831 events among untreated patients.
Treatment Did Not Affect Birth Weight
Approximately 82% of pregnancies in the European registry had an outcome of live birth without congenital anomalies. The prevalence of spontaneous abortions and live births with congenital anomalies were similar to those reported in the general population.
About 98% of pregnancies in the exposed cohort of the Nordic registries had an outcome of live birth without congenital anomalies. This result is similar to the corresponding 97% rate in the nonexposed cohort. The prevalence of spontaneous abortions and congenital anomalies also were similar between the exposed and nonexposed cohorts of the Nordic registries.
Birth weights ranged from 580 g to 5,160 g in the Nordic registries. The proportion of babies with low or very low birth weight was 5.0% in the interferon-exposed cohort, 4.7% among babies exposed to interferon and other treatments, and 5.8% among nonexposed babies. Mean birth weight was 3,421.2 g in the interferon-exposed cohort, 3,434.3 g in the cohort exposed to interferon and other treatments, and 3,389.3 g in the nonexposed cohort. These weights were consistent with results from the prospective German pregnancy registry, according to the authors. Birth weights were not recorded systematically in the European registry.
“The European Interferon Beta Pregnancy Registry showed no evidence that interferon beta exposure before conception or during pregnancy adversely affected pregnancy or infant outcomes,” said Dr. Hellwig and colleagues. “This is consistent with data collected from the Nordic registers.”
This study was supported by Merck in
—Erik Greb
Suggested Reading
Alroughani R, Altintas A, Al Jumah M, et al. Pregnancy and the use of disease-modifying therapies in patients with multiple sclerosis: benefits versus risks. Mult Scler Int. 2016;2016:1034912.
Friend S, Richman S, Bloomgren G, et al. Evaluation of pregnancy outcomes from the Tysabri (natalizumab) pregnancy exposure registry: a global, observational, follow-up study. BMC Neurol. 2016;16(1):150.
Alcohol use, psychological distress associated with possible RBD
(RBD), according to a population-based cohort study published in Neurology. In addition, the results also replicate previous findings of an association between possible RBD and smoking, low education, and male sex.
The risk factors for RBD have been studied comparatively little. “While much is still unknown about RBD, it can be caused by medications or it may be an early sign of another neurologic condition like Parkinson’s disease, dementia with Lewy bodies, or multiple system atrophy,” according to Ronald B. Postuma, MD, an associate professor at McGill University, Montreal. “Identifying lifestyle and personal risk factors linked to this sleep disorder may lead to finding ways to reduce the chances of developing it.”
To assess sociodemographic, socioeconomic, and clinical correlates of possible RBD, Dr. Postuma and his colleagues examined baseline data collected between 2012 and 2015 in the Canadian Longitudinal Study on Aging (CLSA), which included 30,097 participants. To screen for possible RBD, the CLSA researchers asked patients, “Have you ever been told, or suspected yourself, that you seem to ‘act out your dreams’ while asleep [e.g., punching, flailing your arms in the air, making running movements, etc.]?” Participants answered additional questions to rule out RBD mimics. Patients with symptom onset before age 20 years, positive apnea screen, or a diagnosis of dementia, Alzheimer’s disease, parkinsonism, or Parkinson’s disease were excluded from analysis.
In all, 3,271 participants screened positive for possible RBD. After the investigators excluded participants with potential mimics, 958 patients (about 3.2% of the total population) remained in the analysis. Approximately 59% of patients with possible RBD were male, compared with 42% of controls. Patients with possible RBD were more likely to be married, in a common-law relationship, or widowed.
Participants with possible RBD had slightly less education (estimated mean, 13.2 years vs. 13.6 years) and lower income, compared with controls. Participants with possible RBD retired at a slightly younger age (57.5 years vs. 58.6 years) and were more likely to have retired because of health concerns (28.9% vs. 22.0%), compared with controls.
In addition, patients with possible RBD were more likely to drink more and to be moderate to heavy drinkers than controls; they were also more likely to be current or past smokers. Antidepressant use was more frequent and psychological distress was greater among participants with possible RBD.
When the investigators performed a multivariable logistic regression analysis, the associations between possible RBD and male sex and relationship status remained. Lower educational level, but not income level, also remained associated with possible RBD. Furthermore, retirement age and having reported retirement because of health concerns remained significantly associated with possible RBD, as did the amount of alcohol consumed weekly and moderate to heavy drinking. Sensitivity analyses did not change the results significantly.
One of the study’s limitations is its reliance on self-report to identify participants with possible RBD, the authors wrote. The prevalence of possible RBD in the study was 3.2%, but research using polysomnography has found a prevalence of about 1%. Thus, the majority of cases in this study may have other disorders such as restless legs syndrome or periodic limb movements. Furthermore, many participants who enact their dreams (such as unmarried people) are likely unaware of it. Finally, the researchers did not measure several variables of interest, such as consumption of caffeinated products.
“The main advantages of our current study are the large sample size; the systematic population-based sampling; the capacity to adjust for diverse potential confounding variables, including mental illness; and the ability to screen out RBD mimics,” the authors concluded.
SOURCE: Postuma RB et al. Neurology. 2018 Dec 26. doi: 10.1212/WNL.0000000000006849.
(RBD), according to a population-based cohort study published in Neurology. In addition, the results also replicate previous findings of an association between possible RBD and smoking, low education, and male sex.
The risk factors for RBD have been studied comparatively little. “While much is still unknown about RBD, it can be caused by medications or it may be an early sign of another neurologic condition like Parkinson’s disease, dementia with Lewy bodies, or multiple system atrophy,” according to Ronald B. Postuma, MD, an associate professor at McGill University, Montreal. “Identifying lifestyle and personal risk factors linked to this sleep disorder may lead to finding ways to reduce the chances of developing it.”
To assess sociodemographic, socioeconomic, and clinical correlates of possible RBD, Dr. Postuma and his colleagues examined baseline data collected between 2012 and 2015 in the Canadian Longitudinal Study on Aging (CLSA), which included 30,097 participants. To screen for possible RBD, the CLSA researchers asked patients, “Have you ever been told, or suspected yourself, that you seem to ‘act out your dreams’ while asleep [e.g., punching, flailing your arms in the air, making running movements, etc.]?” Participants answered additional questions to rule out RBD mimics. Patients with symptom onset before age 20 years, positive apnea screen, or a diagnosis of dementia, Alzheimer’s disease, parkinsonism, or Parkinson’s disease were excluded from analysis.
In all, 3,271 participants screened positive for possible RBD. After the investigators excluded participants with potential mimics, 958 patients (about 3.2% of the total population) remained in the analysis. Approximately 59% of patients with possible RBD were male, compared with 42% of controls. Patients with possible RBD were more likely to be married, in a common-law relationship, or widowed.
Participants with possible RBD had slightly less education (estimated mean, 13.2 years vs. 13.6 years) and lower income, compared with controls. Participants with possible RBD retired at a slightly younger age (57.5 years vs. 58.6 years) and were more likely to have retired because of health concerns (28.9% vs. 22.0%), compared with controls.
In addition, patients with possible RBD were more likely to drink more and to be moderate to heavy drinkers than controls; they were also more likely to be current or past smokers. Antidepressant use was more frequent and psychological distress was greater among participants with possible RBD.
When the investigators performed a multivariable logistic regression analysis, the associations between possible RBD and male sex and relationship status remained. Lower educational level, but not income level, also remained associated with possible RBD. Furthermore, retirement age and having reported retirement because of health concerns remained significantly associated with possible RBD, as did the amount of alcohol consumed weekly and moderate to heavy drinking. Sensitivity analyses did not change the results significantly.
One of the study’s limitations is its reliance on self-report to identify participants with possible RBD, the authors wrote. The prevalence of possible RBD in the study was 3.2%, but research using polysomnography has found a prevalence of about 1%. Thus, the majority of cases in this study may have other disorders such as restless legs syndrome or periodic limb movements. Furthermore, many participants who enact their dreams (such as unmarried people) are likely unaware of it. Finally, the researchers did not measure several variables of interest, such as consumption of caffeinated products.
“The main advantages of our current study are the large sample size; the systematic population-based sampling; the capacity to adjust for diverse potential confounding variables, including mental illness; and the ability to screen out RBD mimics,” the authors concluded.
SOURCE: Postuma RB et al. Neurology. 2018 Dec 26. doi: 10.1212/WNL.0000000000006849.
(RBD), according to a population-based cohort study published in Neurology. In addition, the results also replicate previous findings of an association between possible RBD and smoking, low education, and male sex.
The risk factors for RBD have been studied comparatively little. “While much is still unknown about RBD, it can be caused by medications or it may be an early sign of another neurologic condition like Parkinson’s disease, dementia with Lewy bodies, or multiple system atrophy,” according to Ronald B. Postuma, MD, an associate professor at McGill University, Montreal. “Identifying lifestyle and personal risk factors linked to this sleep disorder may lead to finding ways to reduce the chances of developing it.”
To assess sociodemographic, socioeconomic, and clinical correlates of possible RBD, Dr. Postuma and his colleagues examined baseline data collected between 2012 and 2015 in the Canadian Longitudinal Study on Aging (CLSA), which included 30,097 participants. To screen for possible RBD, the CLSA researchers asked patients, “Have you ever been told, or suspected yourself, that you seem to ‘act out your dreams’ while asleep [e.g., punching, flailing your arms in the air, making running movements, etc.]?” Participants answered additional questions to rule out RBD mimics. Patients with symptom onset before age 20 years, positive apnea screen, or a diagnosis of dementia, Alzheimer’s disease, parkinsonism, or Parkinson’s disease were excluded from analysis.
In all, 3,271 participants screened positive for possible RBD. After the investigators excluded participants with potential mimics, 958 patients (about 3.2% of the total population) remained in the analysis. Approximately 59% of patients with possible RBD were male, compared with 42% of controls. Patients with possible RBD were more likely to be married, in a common-law relationship, or widowed.
Participants with possible RBD had slightly less education (estimated mean, 13.2 years vs. 13.6 years) and lower income, compared with controls. Participants with possible RBD retired at a slightly younger age (57.5 years vs. 58.6 years) and were more likely to have retired because of health concerns (28.9% vs. 22.0%), compared with controls.
In addition, patients with possible RBD were more likely to drink more and to be moderate to heavy drinkers than controls; they were also more likely to be current or past smokers. Antidepressant use was more frequent and psychological distress was greater among participants with possible RBD.
When the investigators performed a multivariable logistic regression analysis, the associations between possible RBD and male sex and relationship status remained. Lower educational level, but not income level, also remained associated with possible RBD. Furthermore, retirement age and having reported retirement because of health concerns remained significantly associated with possible RBD, as did the amount of alcohol consumed weekly and moderate to heavy drinking. Sensitivity analyses did not change the results significantly.
One of the study’s limitations is its reliance on self-report to identify participants with possible RBD, the authors wrote. The prevalence of possible RBD in the study was 3.2%, but research using polysomnography has found a prevalence of about 1%. Thus, the majority of cases in this study may have other disorders such as restless legs syndrome or periodic limb movements. Furthermore, many participants who enact their dreams (such as unmarried people) are likely unaware of it. Finally, the researchers did not measure several variables of interest, such as consumption of caffeinated products.
“The main advantages of our current study are the large sample size; the systematic population-based sampling; the capacity to adjust for diverse potential confounding variables, including mental illness; and the ability to screen out RBD mimics,” the authors concluded.
SOURCE: Postuma RB et al. Neurology. 2018 Dec 26. doi: 10.1212/WNL.0000000000006849.
FROM NEUROLOGY
Key clinical point: Alcohol use and psychological distress are associated with possible REM sleep behavior disorder.
Major finding: A self-report questionnaire yielded a 3.2% prevalence of possible REM sleep behavior disorder.
Study details: A prospective, population-based cohort study of 30,097 participants.
Disclosures: The Canadian government provided funding for the research.
Source: Postuma RB et al. Neurology. 2018 Dec 26. doi: 10.1212/WNL.0000000000006849.
ACOG updates guidance on chronic hypertension in pregnancy, gestational hypertension
Ob.gyns. will need to focus more on individualized care as they use the two new practice bulletins, one on chronic hypertension in pregnancy and one on gestational hypertension and preeclampsia, released by the American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins–Obstetrics.
The bulletins will replace the 2013 ACOG hypertension in pregnancy task force report and are published in the January issue of Obstetrics & Gynecology.
“The task force was a tour de force in creating a comprehensive view of hypertensive diseases of pregnancy, including research,” Christian M. Pettker, MD, who helped develop both practice bulletins, stated in a press release. “The updated guidance provides clearer recommendations for the management of gestational hypertension with severe-range blood pressure, an emphasis on and instructions for timely treatment of acutely elevated blood pressures, and more defined recommendations for the management of pain in postoperative patients with hypertension.”
“Ob.gyns. will need to focus more on individualized care and may find it’s best to err on the side of caution because the appropriate treatment of hypertensive diseases in pregnancy may be the most important focus of our attempts to improve maternal mortality and morbidity in the United States,” he said.*
Gestational hypertension or preeclampsia
For women with gestational hypertension or preeclampsia at 37 weeks of gestation or later without severe features, the guidelines recommend delivery rather than expectant management.
Those patients with severe features of gestational hypertension or preeclampsia or eclampsia should receive magnesium sulfate to prevent or treat seizures.
Patients should receive low-dose aspirin (81 mg/day) for preeclampsia prophylaxis between 12 weeks and 28 weeks of gestation if they have high-risk factors of preeclampsia such as multifetal gestation, a previous pregnancy with preeclampsia, renal disease, autoimmune disease, type 1 or type 2 diabetes mellitus, chronic hypertension, or a previous pregnancy with preeclampsia; or more than one moderate risk factor such as a family history of preeclampsia, maternal age greater than 35 years, first pregnancy, body mass index greater than 30, personal history factors, or sociodemographic characteristics.
NSAIDs should continue to be used in preference to opioid analgesics.
The guidance also discusses mode of delivery, antihypertensive drugs and thresholds for treatment, management of acute complications for preeclampsia with HELLP (hemolysis, elevated liver enzymes, low platelet count) syndrome, the optimal treatment for eclampsia, and postpartum hypertension and headache.
Chronic hypertension
Pregnant women with chronic hypertension also should receive low-dose aspirin between 12 weeks and 28 weeks of gestation. Antihypertensive therapy should be initiated for women with persistent chronic hypertension at systolic pressure of 160 mm Hg or higher and/or diastolic pressure of 110 mm Hg or higher. Consider treating patients at lower blood pressure (BP) thresholds depending on comorbidities or underlying impaired renal function.
ACOG has recommended treating pregnant patients as chronically hypertensive according to recently changed criteria from the American College of Cardiology and the American Heart Association, which call for classifying blood pressure into the following categories:
- Normal. Systolic BP less than 120 mm Hg; diastolic BP less than 80 mm Hg.
- Elevated. Systolic BP greater than or equal to 120-129 mm Hg; diastolic BP greater than 80 mm Hg.
- Stage 1 hypertension. Systolic BP, 130-139 mm Hg; diastolic BP, 80-89 mm Hg.
- Stage 2 hypertension. Systolic BP greater than or equal to 140 mm Hg; diastolic BP greater than or equal to 90 mm Hg.
“The new blood pressure ranges for nonpregnant women have a lower threshold for hypertension diagnosis compared to ACOG’s criteria,” Dr. Pettker said. “This will likely cause a general increase in patients classified as chronic hypertensive and will require shared decision making by the ob.gyn. and the patient regarding appropriate management in pregnancy.”
The guideline also discusses chronic hypertension with superimposed preeclampsia; tests for baseline evaluation of chronic hypertension in pregnancy; common oral antihypertensive agents to use in pregnancy and those to use for urgent blood pressure control in pregnancy; control of acute-onset severe-range hypertension; and postpartum considerations in patients with chronic hypertension.
SOURCE: Gestational hypertension and preeclampsia. ACOG Practice Bulletin No. 202. Obstet Gynecol. 2019;133:e1-25; Chronic hypertension in pregnancy. ACOG Practice Bulletin No. 203. Obstet Gynecol. 2019;133:e26-50.
This article was updated 1/11/19 and 11/19/19.
Ob.gyns. will need to focus more on individualized care as they use the two new practice bulletins, one on chronic hypertension in pregnancy and one on gestational hypertension and preeclampsia, released by the American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins–Obstetrics.
The bulletins will replace the 2013 ACOG hypertension in pregnancy task force report and are published in the January issue of Obstetrics & Gynecology.
“The task force was a tour de force in creating a comprehensive view of hypertensive diseases of pregnancy, including research,” Christian M. Pettker, MD, who helped develop both practice bulletins, stated in a press release. “The updated guidance provides clearer recommendations for the management of gestational hypertension with severe-range blood pressure, an emphasis on and instructions for timely treatment of acutely elevated blood pressures, and more defined recommendations for the management of pain in postoperative patients with hypertension.”
“Ob.gyns. will need to focus more on individualized care and may find it’s best to err on the side of caution because the appropriate treatment of hypertensive diseases in pregnancy may be the most important focus of our attempts to improve maternal mortality and morbidity in the United States,” he said.*
Gestational hypertension or preeclampsia
For women with gestational hypertension or preeclampsia at 37 weeks of gestation or later without severe features, the guidelines recommend delivery rather than expectant management.
Those patients with severe features of gestational hypertension or preeclampsia or eclampsia should receive magnesium sulfate to prevent or treat seizures.
Patients should receive low-dose aspirin (81 mg/day) for preeclampsia prophylaxis between 12 weeks and 28 weeks of gestation if they have high-risk factors of preeclampsia such as multifetal gestation, a previous pregnancy with preeclampsia, renal disease, autoimmune disease, type 1 or type 2 diabetes mellitus, chronic hypertension, or a previous pregnancy with preeclampsia; or more than one moderate risk factor such as a family history of preeclampsia, maternal age greater than 35 years, first pregnancy, body mass index greater than 30, personal history factors, or sociodemographic characteristics.
NSAIDs should continue to be used in preference to opioid analgesics.
The guidance also discusses mode of delivery, antihypertensive drugs and thresholds for treatment, management of acute complications for preeclampsia with HELLP (hemolysis, elevated liver enzymes, low platelet count) syndrome, the optimal treatment for eclampsia, and postpartum hypertension and headache.
Chronic hypertension
Pregnant women with chronic hypertension also should receive low-dose aspirin between 12 weeks and 28 weeks of gestation. Antihypertensive therapy should be initiated for women with persistent chronic hypertension at systolic pressure of 160 mm Hg or higher and/or diastolic pressure of 110 mm Hg or higher. Consider treating patients at lower blood pressure (BP) thresholds depending on comorbidities or underlying impaired renal function.
ACOG has recommended treating pregnant patients as chronically hypertensive according to recently changed criteria from the American College of Cardiology and the American Heart Association, which call for classifying blood pressure into the following categories:
- Normal. Systolic BP less than 120 mm Hg; diastolic BP less than 80 mm Hg.
- Elevated. Systolic BP greater than or equal to 120-129 mm Hg; diastolic BP greater than 80 mm Hg.
- Stage 1 hypertension. Systolic BP, 130-139 mm Hg; diastolic BP, 80-89 mm Hg.
- Stage 2 hypertension. Systolic BP greater than or equal to 140 mm Hg; diastolic BP greater than or equal to 90 mm Hg.
“The new blood pressure ranges for nonpregnant women have a lower threshold for hypertension diagnosis compared to ACOG’s criteria,” Dr. Pettker said. “This will likely cause a general increase in patients classified as chronic hypertensive and will require shared decision making by the ob.gyn. and the patient regarding appropriate management in pregnancy.”
The guideline also discusses chronic hypertension with superimposed preeclampsia; tests for baseline evaluation of chronic hypertension in pregnancy; common oral antihypertensive agents to use in pregnancy and those to use for urgent blood pressure control in pregnancy; control of acute-onset severe-range hypertension; and postpartum considerations in patients with chronic hypertension.
SOURCE: Gestational hypertension and preeclampsia. ACOG Practice Bulletin No. 202. Obstet Gynecol. 2019;133:e1-25; Chronic hypertension in pregnancy. ACOG Practice Bulletin No. 203. Obstet Gynecol. 2019;133:e26-50.
This article was updated 1/11/19 and 11/19/19.
Ob.gyns. will need to focus more on individualized care as they use the two new practice bulletins, one on chronic hypertension in pregnancy and one on gestational hypertension and preeclampsia, released by the American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins–Obstetrics.
The bulletins will replace the 2013 ACOG hypertension in pregnancy task force report and are published in the January issue of Obstetrics & Gynecology.
“The task force was a tour de force in creating a comprehensive view of hypertensive diseases of pregnancy, including research,” Christian M. Pettker, MD, who helped develop both practice bulletins, stated in a press release. “The updated guidance provides clearer recommendations for the management of gestational hypertension with severe-range blood pressure, an emphasis on and instructions for timely treatment of acutely elevated blood pressures, and more defined recommendations for the management of pain in postoperative patients with hypertension.”
“Ob.gyns. will need to focus more on individualized care and may find it’s best to err on the side of caution because the appropriate treatment of hypertensive diseases in pregnancy may be the most important focus of our attempts to improve maternal mortality and morbidity in the United States,” he said.*
Gestational hypertension or preeclampsia
For women with gestational hypertension or preeclampsia at 37 weeks of gestation or later without severe features, the guidelines recommend delivery rather than expectant management.
Those patients with severe features of gestational hypertension or preeclampsia or eclampsia should receive magnesium sulfate to prevent or treat seizures.
Patients should receive low-dose aspirin (81 mg/day) for preeclampsia prophylaxis between 12 weeks and 28 weeks of gestation if they have high-risk factors of preeclampsia such as multifetal gestation, a previous pregnancy with preeclampsia, renal disease, autoimmune disease, type 1 or type 2 diabetes mellitus, chronic hypertension, or a previous pregnancy with preeclampsia; or more than one moderate risk factor such as a family history of preeclampsia, maternal age greater than 35 years, first pregnancy, body mass index greater than 30, personal history factors, or sociodemographic characteristics.
NSAIDs should continue to be used in preference to opioid analgesics.
The guidance also discusses mode of delivery, antihypertensive drugs and thresholds for treatment, management of acute complications for preeclampsia with HELLP (hemolysis, elevated liver enzymes, low platelet count) syndrome, the optimal treatment for eclampsia, and postpartum hypertension and headache.
Chronic hypertension
Pregnant women with chronic hypertension also should receive low-dose aspirin between 12 weeks and 28 weeks of gestation. Antihypertensive therapy should be initiated for women with persistent chronic hypertension at systolic pressure of 160 mm Hg or higher and/or diastolic pressure of 110 mm Hg or higher. Consider treating patients at lower blood pressure (BP) thresholds depending on comorbidities or underlying impaired renal function.
ACOG has recommended treating pregnant patients as chronically hypertensive according to recently changed criteria from the American College of Cardiology and the American Heart Association, which call for classifying blood pressure into the following categories:
- Normal. Systolic BP less than 120 mm Hg; diastolic BP less than 80 mm Hg.
- Elevated. Systolic BP greater than or equal to 120-129 mm Hg; diastolic BP greater than 80 mm Hg.
- Stage 1 hypertension. Systolic BP, 130-139 mm Hg; diastolic BP, 80-89 mm Hg.
- Stage 2 hypertension. Systolic BP greater than or equal to 140 mm Hg; diastolic BP greater than or equal to 90 mm Hg.
“The new blood pressure ranges for nonpregnant women have a lower threshold for hypertension diagnosis compared to ACOG’s criteria,” Dr. Pettker said. “This will likely cause a general increase in patients classified as chronic hypertensive and will require shared decision making by the ob.gyn. and the patient regarding appropriate management in pregnancy.”
The guideline also discusses chronic hypertension with superimposed preeclampsia; tests for baseline evaluation of chronic hypertension in pregnancy; common oral antihypertensive agents to use in pregnancy and those to use for urgent blood pressure control in pregnancy; control of acute-onset severe-range hypertension; and postpartum considerations in patients with chronic hypertension.
SOURCE: Gestational hypertension and preeclampsia. ACOG Practice Bulletin No. 202. Obstet Gynecol. 2019;133:e1-25; Chronic hypertension in pregnancy. ACOG Practice Bulletin No. 203. Obstet Gynecol. 2019;133:e26-50.
This article was updated 1/11/19 and 11/19/19.
FROM OBSTETRICS & GYNECOLOGY
Heberden’s nodes linked to knee OA progression
according to a review of 575 participants in a substudy of the Osteoarthritis Initiative cohort.
After assessing Heberden’s nodes (HNs) – bony enlargements of the last finger joint – and knee MRI findings at baseline and 24 months, the investigators found that HNs were associated with periarticular bone area expansion in the knee. The investigators reported their findings in Arthritis & Rheumatology.
Comparing the 395 subjects with HNs with the 180 without, there was more periarticular bone area expansion among HN patients at 2 years in the knee joint (adjusted odds ratio, 1.39; 95% confidence interval, 1.06-1.83), especially in the medial femur (aOR, 1.49; 95% CI, 1.05-2.13), lateral femur (aOR, 2.51; 95% CI, 1.58-3.97), femoral notch (aOR, 1.37; 95% CI, 1.02-1.84), and lateral trochlea (aOR, 1.44; 95% CI, 1.08-1.9). The comparisons were adjusted for age, sex, body mass index, and bone remodeling agent use.
“The presence of Heberden’s nodes in a physical examination is associated with a distinct pattern of worsening of osteoarthritis-related structural damage in the knee joint,” lead investigator Arya Haj-Mirzaian, MD, a radiologist and postdoctoral fellow at Johns Hopkins University, Baltimore, said in a press release.
However, HNs were also associated with less worsening of knee osteophytes, especially at the femoral end of the knee joint (aOR, 0.54; 95% CI, 0.31-0.95); the finding seemed to contradict the overall picture of worsening knee osteoarthritis with HNs.
“Although osteophytes are thought to be a late secondary sequel or compensatory repair mechanism in OA and indicator of advanced knee OA, less worsening in osteophytes’ score ... may propose that less ossification is involved in the pathophysiology of knee OA in the presence of HNs,” the investigators wrote. It’s a subject for future research.
Patients with HNs were older, more often female, and had a lower frequency for other knee OA risk factors, such as excessive body mass index and knee injury. Patients with gout were excluded.
There was no external funding, and the investigators reported no disclosures.
SOURCE: Haj-Mirzaian A et al. Arthritis Rheumatol. 2019 Jan 9. doi: 10.1002/art.40811.
according to a review of 575 participants in a substudy of the Osteoarthritis Initiative cohort.
After assessing Heberden’s nodes (HNs) – bony enlargements of the last finger joint – and knee MRI findings at baseline and 24 months, the investigators found that HNs were associated with periarticular bone area expansion in the knee. The investigators reported their findings in Arthritis & Rheumatology.
Comparing the 395 subjects with HNs with the 180 without, there was more periarticular bone area expansion among HN patients at 2 years in the knee joint (adjusted odds ratio, 1.39; 95% confidence interval, 1.06-1.83), especially in the medial femur (aOR, 1.49; 95% CI, 1.05-2.13), lateral femur (aOR, 2.51; 95% CI, 1.58-3.97), femoral notch (aOR, 1.37; 95% CI, 1.02-1.84), and lateral trochlea (aOR, 1.44; 95% CI, 1.08-1.9). The comparisons were adjusted for age, sex, body mass index, and bone remodeling agent use.
“The presence of Heberden’s nodes in a physical examination is associated with a distinct pattern of worsening of osteoarthritis-related structural damage in the knee joint,” lead investigator Arya Haj-Mirzaian, MD, a radiologist and postdoctoral fellow at Johns Hopkins University, Baltimore, said in a press release.
However, HNs were also associated with less worsening of knee osteophytes, especially at the femoral end of the knee joint (aOR, 0.54; 95% CI, 0.31-0.95); the finding seemed to contradict the overall picture of worsening knee osteoarthritis with HNs.
“Although osteophytes are thought to be a late secondary sequel or compensatory repair mechanism in OA and indicator of advanced knee OA, less worsening in osteophytes’ score ... may propose that less ossification is involved in the pathophysiology of knee OA in the presence of HNs,” the investigators wrote. It’s a subject for future research.
Patients with HNs were older, more often female, and had a lower frequency for other knee OA risk factors, such as excessive body mass index and knee injury. Patients with gout were excluded.
There was no external funding, and the investigators reported no disclosures.
SOURCE: Haj-Mirzaian A et al. Arthritis Rheumatol. 2019 Jan 9. doi: 10.1002/art.40811.
according to a review of 575 participants in a substudy of the Osteoarthritis Initiative cohort.
After assessing Heberden’s nodes (HNs) – bony enlargements of the last finger joint – and knee MRI findings at baseline and 24 months, the investigators found that HNs were associated with periarticular bone area expansion in the knee. The investigators reported their findings in Arthritis & Rheumatology.
Comparing the 395 subjects with HNs with the 180 without, there was more periarticular bone area expansion among HN patients at 2 years in the knee joint (adjusted odds ratio, 1.39; 95% confidence interval, 1.06-1.83), especially in the medial femur (aOR, 1.49; 95% CI, 1.05-2.13), lateral femur (aOR, 2.51; 95% CI, 1.58-3.97), femoral notch (aOR, 1.37; 95% CI, 1.02-1.84), and lateral trochlea (aOR, 1.44; 95% CI, 1.08-1.9). The comparisons were adjusted for age, sex, body mass index, and bone remodeling agent use.
“The presence of Heberden’s nodes in a physical examination is associated with a distinct pattern of worsening of osteoarthritis-related structural damage in the knee joint,” lead investigator Arya Haj-Mirzaian, MD, a radiologist and postdoctoral fellow at Johns Hopkins University, Baltimore, said in a press release.
However, HNs were also associated with less worsening of knee osteophytes, especially at the femoral end of the knee joint (aOR, 0.54; 95% CI, 0.31-0.95); the finding seemed to contradict the overall picture of worsening knee osteoarthritis with HNs.
“Although osteophytes are thought to be a late secondary sequel or compensatory repair mechanism in OA and indicator of advanced knee OA, less worsening in osteophytes’ score ... may propose that less ossification is involved in the pathophysiology of knee OA in the presence of HNs,” the investigators wrote. It’s a subject for future research.
Patients with HNs were older, more often female, and had a lower frequency for other knee OA risk factors, such as excessive body mass index and knee injury. Patients with gout were excluded.
There was no external funding, and the investigators reported no disclosures.
SOURCE: Haj-Mirzaian A et al. Arthritis Rheumatol. 2019 Jan 9. doi: 10.1002/art.40811.
FROM ARTHRITIS & RHEUMATOLOGY
Key clinical point: Heberden’s nodes may be an indicator of knee OA progression.
Major finding: There was more periarticular bone area expansion among patients with Heberden’s nodes at 2 years in the knee joint (adjusted odds ratio, 1.39; 95% confidence interval, 1.06-1.83).
Study details: A substudy of 575 participants in the Osteoarthritis Initiative cohort
Disclosures: There was no external funding, and the investigators reported no disclosures.
Source: Haj-Mirzaian A et al. Arthritis Rheumatol. 2019 Jan 9. doi: 10.1002/art.40811.