User login
Mediterranean diet cut Parkinson’s risk
‘Telereferrals’ improved mental health referral follow-through for children. How to take action to cut cardiovascular disease risk in rheumatoid patients. And the U.S. Preventive Services Task Force recommends counseling for perinatal depression prevention.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
‘Telereferrals’ improved mental health referral follow-through for children. How to take action to cut cardiovascular disease risk in rheumatoid patients. And the U.S. Preventive Services Task Force recommends counseling for perinatal depression prevention.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
‘Telereferrals’ improved mental health referral follow-through for children. How to take action to cut cardiovascular disease risk in rheumatoid patients. And the U.S. Preventive Services Task Force recommends counseling for perinatal depression prevention.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Umbilical cord milking tied to severe IVH in very premature neonates
Delayed cord clamping and cutting is safer
LAS VEGAS – Umbilical cord milking can cause severe intraventricular hemorrhage (IVH) in very premature neonates and should not be performed on these cerebrovascularly fragile premature babies.
Just six of these procedures would be needed to cause a case of severe IVH in neonates born at 23-27 weeks’ gestation, Michael W. Varner, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“Centers practicing umbilical cord milking should consider discontinuing this practice in infants 23-27 weeks’ gestation,” said Dr. Varner of the University of Utah, Salt Lake City.
The damage to the brains of very young preemies appears to be a direct result of the fluid overload caused by milking, he said. “From a mechanistic perspective, we can intuit that these findings are consistent with cord milking. This causes increasing venous return to the right atrium where it enters the foramen ovale and aorta. These very premature babies have more pulmonary vasoconstriction, which shunts more blood toward the brain. This results in fluctuations in flow in an immature brain with fragile germinal matrices and perhaps further compromised by chorioamnionitis inflammation, resulting in IVH.”
Premature Infants Receiving Milking or Delayed Cord Clamping (PREMOD2) was a noninferiority trial of umbilical cord milking compared to delayed cord clamping and cutting in preterm infants. Conducted at 11 sites in the United States and Europe, the study was halted prematurely when the data safety monitoring board determined that cord milking increased the risk of IVH in younger preemies and was no better than delayed cutting in the older preemies. The analysis presented at the meeting is the first public discussion of the data details.
The trial involved 474 premature neonates. They were randomized to placental transfusion via a 60-second delay in cord clamping and cutting or to umbilical cord milking, which involved grasping the cord and manually pushing the cord blood toward the infant four times before clamping. All participating sites received a video demonstrating the proper procedure. The cohort also was divided by gestational age: 23-27 weeks and 28-31 weeks.
The primary endpoint was a combination of severe IVH (grade 3 or higher) and neonatal death. Overall, the primary endpoint occurred in 29 of those randomized to cord milking (12%) and 20 randomized to delayed clamping (8%) – a significant difference.
This finding was largely driven by the treatment differences in the 23-27 week group, Dr. Varner said. Severe IVH occurred in 20 (22%) of those randomized to cord milking and five (6%) of those randomized to delayed clamping – a highly statistically significant difference with a P value of 0.0019.
In the 28-31 week group, there were no cases of severe IVH in the cord milking group, and three cases in the delayed clamping group; the difference was not statistically significant.
Overall, deaths were similar between the cord milking and cord clamping groups (17 and 15, respectively). Most of these deaths occurred in the younger group (14 in the cord milking group and 13 in the clamping group). There were five deaths in the older group: three in the cord milking group and two in the clamping group. None of these differences were statistically significant.
After seeing these data in a preplanned interim safety analysis, the Data Safety Monitoring Board stopped the study, saying that the intervention appeared dangerous for the younger babies, and no better than the delayed cutting and clamping for the older group, Dr. Varner said.
Since the trial was halted, investigators have been dissecting the data to identify any other intracranial hemorrhage risks particular to the infants. They found no significant differences in maternal characteristics at baseline, and – other than age and randomization– nothing significantly different between the infant groups. Severe persistent IVH occurred in almost 70% of the infants born at 23 weeks’ gestation but in only 7% in the delayed cord clamping group. The risks declined rapidly with increasing gestational age, although they were at all times greater than the risk of IVH in the cord clamping group.
“Looking at the data by gestational age, it’s clear that the majority of the severe IVH occurrences were in the 23 weekers, and also occurred in the first 7 days of life,” Dr. Varner said.
The cohort will be followed for at least another year, he added, as investigators track neurodevelopmental outcomes.
Investigators are particularly interested in differences in motor and language skills, as well as general cognitive development.
The study was sponsored by theEunice Kennedy Shriver National Institute of Child Health and Development. Neither Dr. Varner nor any of the coauthors had any financial declarations.
SOURCE: Katheria AC et al. The Pregnancy Meeting, late breaking abstract 1.
Delayed cord clamping and cutting is safer
Delayed cord clamping and cutting is safer
LAS VEGAS – Umbilical cord milking can cause severe intraventricular hemorrhage (IVH) in very premature neonates and should not be performed on these cerebrovascularly fragile premature babies.
Just six of these procedures would be needed to cause a case of severe IVH in neonates born at 23-27 weeks’ gestation, Michael W. Varner, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“Centers practicing umbilical cord milking should consider discontinuing this practice in infants 23-27 weeks’ gestation,” said Dr. Varner of the University of Utah, Salt Lake City.
The damage to the brains of very young preemies appears to be a direct result of the fluid overload caused by milking, he said. “From a mechanistic perspective, we can intuit that these findings are consistent with cord milking. This causes increasing venous return to the right atrium where it enters the foramen ovale and aorta. These very premature babies have more pulmonary vasoconstriction, which shunts more blood toward the brain. This results in fluctuations in flow in an immature brain with fragile germinal matrices and perhaps further compromised by chorioamnionitis inflammation, resulting in IVH.”
Premature Infants Receiving Milking or Delayed Cord Clamping (PREMOD2) was a noninferiority trial of umbilical cord milking compared to delayed cord clamping and cutting in preterm infants. Conducted at 11 sites in the United States and Europe, the study was halted prematurely when the data safety monitoring board determined that cord milking increased the risk of IVH in younger preemies and was no better than delayed cutting in the older preemies. The analysis presented at the meeting is the first public discussion of the data details.
The trial involved 474 premature neonates. They were randomized to placental transfusion via a 60-second delay in cord clamping and cutting or to umbilical cord milking, which involved grasping the cord and manually pushing the cord blood toward the infant four times before clamping. All participating sites received a video demonstrating the proper procedure. The cohort also was divided by gestational age: 23-27 weeks and 28-31 weeks.
The primary endpoint was a combination of severe IVH (grade 3 or higher) and neonatal death. Overall, the primary endpoint occurred in 29 of those randomized to cord milking (12%) and 20 randomized to delayed clamping (8%) – a significant difference.
This finding was largely driven by the treatment differences in the 23-27 week group, Dr. Varner said. Severe IVH occurred in 20 (22%) of those randomized to cord milking and five (6%) of those randomized to delayed clamping – a highly statistically significant difference with a P value of 0.0019.
In the 28-31 week group, there were no cases of severe IVH in the cord milking group, and three cases in the delayed clamping group; the difference was not statistically significant.
Overall, deaths were similar between the cord milking and cord clamping groups (17 and 15, respectively). Most of these deaths occurred in the younger group (14 in the cord milking group and 13 in the clamping group). There were five deaths in the older group: three in the cord milking group and two in the clamping group. None of these differences were statistically significant.
After seeing these data in a preplanned interim safety analysis, the Data Safety Monitoring Board stopped the study, saying that the intervention appeared dangerous for the younger babies, and no better than the delayed cutting and clamping for the older group, Dr. Varner said.
Since the trial was halted, investigators have been dissecting the data to identify any other intracranial hemorrhage risks particular to the infants. They found no significant differences in maternal characteristics at baseline, and – other than age and randomization– nothing significantly different between the infant groups. Severe persistent IVH occurred in almost 70% of the infants born at 23 weeks’ gestation but in only 7% in the delayed cord clamping group. The risks declined rapidly with increasing gestational age, although they were at all times greater than the risk of IVH in the cord clamping group.
“Looking at the data by gestational age, it’s clear that the majority of the severe IVH occurrences were in the 23 weekers, and also occurred in the first 7 days of life,” Dr. Varner said.
The cohort will be followed for at least another year, he added, as investigators track neurodevelopmental outcomes.
Investigators are particularly interested in differences in motor and language skills, as well as general cognitive development.
The study was sponsored by theEunice Kennedy Shriver National Institute of Child Health and Development. Neither Dr. Varner nor any of the coauthors had any financial declarations.
SOURCE: Katheria AC et al. The Pregnancy Meeting, late breaking abstract 1.
LAS VEGAS – Umbilical cord milking can cause severe intraventricular hemorrhage (IVH) in very premature neonates and should not be performed on these cerebrovascularly fragile premature babies.
Just six of these procedures would be needed to cause a case of severe IVH in neonates born at 23-27 weeks’ gestation, Michael W. Varner, MD, said at the meeting sponsored by the Society for Maternal-Fetal Medicine.
“Centers practicing umbilical cord milking should consider discontinuing this practice in infants 23-27 weeks’ gestation,” said Dr. Varner of the University of Utah, Salt Lake City.
The damage to the brains of very young preemies appears to be a direct result of the fluid overload caused by milking, he said. “From a mechanistic perspective, we can intuit that these findings are consistent with cord milking. This causes increasing venous return to the right atrium where it enters the foramen ovale and aorta. These very premature babies have more pulmonary vasoconstriction, which shunts more blood toward the brain. This results in fluctuations in flow in an immature brain with fragile germinal matrices and perhaps further compromised by chorioamnionitis inflammation, resulting in IVH.”
Premature Infants Receiving Milking or Delayed Cord Clamping (PREMOD2) was a noninferiority trial of umbilical cord milking compared to delayed cord clamping and cutting in preterm infants. Conducted at 11 sites in the United States and Europe, the study was halted prematurely when the data safety monitoring board determined that cord milking increased the risk of IVH in younger preemies and was no better than delayed cutting in the older preemies. The analysis presented at the meeting is the first public discussion of the data details.
The trial involved 474 premature neonates. They were randomized to placental transfusion via a 60-second delay in cord clamping and cutting or to umbilical cord milking, which involved grasping the cord and manually pushing the cord blood toward the infant four times before clamping. All participating sites received a video demonstrating the proper procedure. The cohort also was divided by gestational age: 23-27 weeks and 28-31 weeks.
The primary endpoint was a combination of severe IVH (grade 3 or higher) and neonatal death. Overall, the primary endpoint occurred in 29 of those randomized to cord milking (12%) and 20 randomized to delayed clamping (8%) – a significant difference.
This finding was largely driven by the treatment differences in the 23-27 week group, Dr. Varner said. Severe IVH occurred in 20 (22%) of those randomized to cord milking and five (6%) of those randomized to delayed clamping – a highly statistically significant difference with a P value of 0.0019.
In the 28-31 week group, there were no cases of severe IVH in the cord milking group, and three cases in the delayed clamping group; the difference was not statistically significant.
Overall, deaths were similar between the cord milking and cord clamping groups (17 and 15, respectively). Most of these deaths occurred in the younger group (14 in the cord milking group and 13 in the clamping group). There were five deaths in the older group: three in the cord milking group and two in the clamping group. None of these differences were statistically significant.
After seeing these data in a preplanned interim safety analysis, the Data Safety Monitoring Board stopped the study, saying that the intervention appeared dangerous for the younger babies, and no better than the delayed cutting and clamping for the older group, Dr. Varner said.
Since the trial was halted, investigators have been dissecting the data to identify any other intracranial hemorrhage risks particular to the infants. They found no significant differences in maternal characteristics at baseline, and – other than age and randomization– nothing significantly different between the infant groups. Severe persistent IVH occurred in almost 70% of the infants born at 23 weeks’ gestation but in only 7% in the delayed cord clamping group. The risks declined rapidly with increasing gestational age, although they were at all times greater than the risk of IVH in the cord clamping group.
“Looking at the data by gestational age, it’s clear that the majority of the severe IVH occurrences were in the 23 weekers, and also occurred in the first 7 days of life,” Dr. Varner said.
The cohort will be followed for at least another year, he added, as investigators track neurodevelopmental outcomes.
Investigators are particularly interested in differences in motor and language skills, as well as general cognitive development.
The study was sponsored by theEunice Kennedy Shriver National Institute of Child Health and Development. Neither Dr. Varner nor any of the coauthors had any financial declarations.
SOURCE: Katheria AC et al. The Pregnancy Meeting, late breaking abstract 1.
REPORTING FROM THE PREGNANCY MEETING
Researchers characterize new subtype of high-grade DLBCL
(DLBCL)
Patients with this subtype, dubbed “molecular high-grade” (MHG) DLBCL, were more likely to have germinal center B-cell-like (GCB) DLBCL, MYC rearrangements, and double-hit lymphoma.
When compared to other DLBCL patients, those with MHG DLBCL had inferior progression-free and overall survival.
Chulin Sha, PhD, of the University of Leeds (England), and colleagues reported these findings in the Journal of Clinical Oncology. The findings were published alongside a related editorial and a similar study from another group.
Dr. Sha and colleagues began their study by applying a previously developed gene expression classifier (Genome Med. 2015 Jul 1;7[1]:64) to 928 DLBCL patients enrolled in the REMoDL-B trial. REMoDL-B was designed to compare rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone (R-CHOP) to R-CHOP plus bortezomib (Hematol Oncol. 2017;35:130-1).
Dr. Sha and colleagues looked for somatic mutations in 400 REMoDL-B patient samples that were sequenced for a 70-gene panel.
The team also tested 360 samples for MYC, BCL2, and BCL6 chromosomal rearrangements using fluorescent in situ hybridization, and they tested 355 samples for MYC and BCL2 protein expression with immunohistochemistry.
Characteristics of MHG DLBCL
The researchers identified 83 REMoDL-B patients as having MHG DLBCL (9%). Most of the MHG patients had GCB DLBCL (90%), 48.6% had MYC rearrangements, and 36.1% had double-hit lymphoma.
Patients with MHG DLBCL had higher International Prognostic Index scores (P = .004), greater tumor bulk (P = .007), higher disease stage (P = .06), and higher lactate dehydrogenase levels (P less than .001) than patients with non-MHG DLBCL.
Although most MHG patients had GCB DLBCL, the researchers found key differences between patients with MHG DLBCL and non-MHG GCB DLBCL. MHG patients were significantly more likely than patients with non-MHG GCB DLBCL to have mutations in KMT2D, BCL2, MYC, and DDX3X. Additionally, some genes frequently mutated in GCB DLBCL — such as B2M, SGK1, and NFKBIA — were rare in MHG DLBCL.
Dr. Sha and colleagues also compared the MHG patients to 70 patients with Burkitt lymphoma (BL) who had been analyzed in a previous study (Genome Med. 2015 Jul 1;7[1]:64).
The researchers found that BL has more upregulated genes than GCB (2,483 genes) and MHG DLBCL (1,784 genes), and MHG DLBCL has more upregulated genes than GCB DLBCL (382 genes). The team observed a similar pattern with downregulated genes and said this suggests “MHG is an intermediate group but closer to GCB than to BL.”
The researchers also found, however, that “MHG and BL share high expression of signatures that contain cell-cycle genes, ribosome biogenesis, MYC overexpression, and TCF3 targets, which suggests a shared proliferative phenotype.”
The team determined that MHG has “a highly proliferative phenotype and shares features with centroblasts of the germinal center dark zone.”
Another discovery was that MHG patients in the REMoDL-B trial had worse progression-free survival (PFS) than their peers.
Among patients who received R-CHOP, the estimated 3-year PFS was:
- 37% for MHG patients
- 78% for patients with GCB DLBCL
- 64% for patients with activated B-cell like (ABC) DLBCL
- 65% for patients with unclassified DLBCL.
Among patients who received bortezomib plus R-CHOP, there was a trend toward improved PFS for patients with MHG DLBCL (58%; P = .08).
Validation cohort
Dr. Sha and colleagues validated their initial findings using RNA sequencing data from another group of DLBCL patients (Cell. 2017 Oct 5;171[2]:481-94.e15). This data set included 624 patients who received rituximab-based therapy.
Seventy-two patients in this group had MHG DLBCL (11.5%), and most MHG patients had GCB DLBCL (82%).
The researchers said the MHG group in this cohort “showed similar associations with clinical variables” and a “similar mutation spectrum” as the MHG group in the REMoDL-B cohort. Additionally, MHG patients in the validation cohort had inferior overall survival (P less than .001) compared to patients with non-MHG GCB DLBCL.
Dr. Sha and colleagues said the poor prognosis in MHG patients in both cohorts suggests a need for different treatment approaches in this group.
In the related editorial, Wing C. Chan, MD, of City of Hope Medical Center in Duarte, Calif., echoed that sentiment and said it will be important to include patients with high-risk DLBCL in clinical trials.
“Their tumors should be comprehensively characterize[d] for correlative analysis to determine the molecular lesions that underlie their biology and response to treatment,” Dr. Chan wrote.
Dr. Chan disclosed a patent for a diagnostic algorithm on GCB/ABC-type DLBCL and a patent on a diagnostic algorithm for peripheral T-cell lymphoma.
Dr. Sha and colleagues disclosed relationships with a range of pharmaceutical companies. The team’s research was supported by a grant from Bloodwise.
The REMoDL-B trial was endorsed by Cancer Research UK and was funded by Janssen-Cillag.
SOURCES: Sha C et al. J Clin Oncol. 2019 Jan 20;37(3):202-12. doi: 10.1200/JCO.18.01314; Chan WC. J Clin Oncol. 2019 Jan 20;37(3):175-7. doi: 10.1200/JCO.18.01910; Ennishi D et al. J Clin Oncol. 2019 Jan 20;37(3):190-201. doi: 10.1200/JCO.18.01583
(DLBCL)
Patients with this subtype, dubbed “molecular high-grade” (MHG) DLBCL, were more likely to have germinal center B-cell-like (GCB) DLBCL, MYC rearrangements, and double-hit lymphoma.
When compared to other DLBCL patients, those with MHG DLBCL had inferior progression-free and overall survival.
Chulin Sha, PhD, of the University of Leeds (England), and colleagues reported these findings in the Journal of Clinical Oncology. The findings were published alongside a related editorial and a similar study from another group.
Dr. Sha and colleagues began their study by applying a previously developed gene expression classifier (Genome Med. 2015 Jul 1;7[1]:64) to 928 DLBCL patients enrolled in the REMoDL-B trial. REMoDL-B was designed to compare rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone (R-CHOP) to R-CHOP plus bortezomib (Hematol Oncol. 2017;35:130-1).
Dr. Sha and colleagues looked for somatic mutations in 400 REMoDL-B patient samples that were sequenced for a 70-gene panel.
The team also tested 360 samples for MYC, BCL2, and BCL6 chromosomal rearrangements using fluorescent in situ hybridization, and they tested 355 samples for MYC and BCL2 protein expression with immunohistochemistry.
Characteristics of MHG DLBCL
The researchers identified 83 REMoDL-B patients as having MHG DLBCL (9%). Most of the MHG patients had GCB DLBCL (90%), 48.6% had MYC rearrangements, and 36.1% had double-hit lymphoma.
Patients with MHG DLBCL had higher International Prognostic Index scores (P = .004), greater tumor bulk (P = .007), higher disease stage (P = .06), and higher lactate dehydrogenase levels (P less than .001) than patients with non-MHG DLBCL.
Although most MHG patients had GCB DLBCL, the researchers found key differences between patients with MHG DLBCL and non-MHG GCB DLBCL. MHG patients were significantly more likely than patients with non-MHG GCB DLBCL to have mutations in KMT2D, BCL2, MYC, and DDX3X. Additionally, some genes frequently mutated in GCB DLBCL — such as B2M, SGK1, and NFKBIA — were rare in MHG DLBCL.
Dr. Sha and colleagues also compared the MHG patients to 70 patients with Burkitt lymphoma (BL) who had been analyzed in a previous study (Genome Med. 2015 Jul 1;7[1]:64).
The researchers found that BL has more upregulated genes than GCB (2,483 genes) and MHG DLBCL (1,784 genes), and MHG DLBCL has more upregulated genes than GCB DLBCL (382 genes). The team observed a similar pattern with downregulated genes and said this suggests “MHG is an intermediate group but closer to GCB than to BL.”
The researchers also found, however, that “MHG and BL share high expression of signatures that contain cell-cycle genes, ribosome biogenesis, MYC overexpression, and TCF3 targets, which suggests a shared proliferative phenotype.”
The team determined that MHG has “a highly proliferative phenotype and shares features with centroblasts of the germinal center dark zone.”
Another discovery was that MHG patients in the REMoDL-B trial had worse progression-free survival (PFS) than their peers.
Among patients who received R-CHOP, the estimated 3-year PFS was:
- 37% for MHG patients
- 78% for patients with GCB DLBCL
- 64% for patients with activated B-cell like (ABC) DLBCL
- 65% for patients with unclassified DLBCL.
Among patients who received bortezomib plus R-CHOP, there was a trend toward improved PFS for patients with MHG DLBCL (58%; P = .08).
Validation cohort
Dr. Sha and colleagues validated their initial findings using RNA sequencing data from another group of DLBCL patients (Cell. 2017 Oct 5;171[2]:481-94.e15). This data set included 624 patients who received rituximab-based therapy.
Seventy-two patients in this group had MHG DLBCL (11.5%), and most MHG patients had GCB DLBCL (82%).
The researchers said the MHG group in this cohort “showed similar associations with clinical variables” and a “similar mutation spectrum” as the MHG group in the REMoDL-B cohort. Additionally, MHG patients in the validation cohort had inferior overall survival (P less than .001) compared to patients with non-MHG GCB DLBCL.
Dr. Sha and colleagues said the poor prognosis in MHG patients in both cohorts suggests a need for different treatment approaches in this group.
In the related editorial, Wing C. Chan, MD, of City of Hope Medical Center in Duarte, Calif., echoed that sentiment and said it will be important to include patients with high-risk DLBCL in clinical trials.
“Their tumors should be comprehensively characterize[d] for correlative analysis to determine the molecular lesions that underlie their biology and response to treatment,” Dr. Chan wrote.
Dr. Chan disclosed a patent for a diagnostic algorithm on GCB/ABC-type DLBCL and a patent on a diagnostic algorithm for peripheral T-cell lymphoma.
Dr. Sha and colleagues disclosed relationships with a range of pharmaceutical companies. The team’s research was supported by a grant from Bloodwise.
The REMoDL-B trial was endorsed by Cancer Research UK and was funded by Janssen-Cillag.
SOURCES: Sha C et al. J Clin Oncol. 2019 Jan 20;37(3):202-12. doi: 10.1200/JCO.18.01314; Chan WC. J Clin Oncol. 2019 Jan 20;37(3):175-7. doi: 10.1200/JCO.18.01910; Ennishi D et al. J Clin Oncol. 2019 Jan 20;37(3):190-201. doi: 10.1200/JCO.18.01583
(DLBCL)
Patients with this subtype, dubbed “molecular high-grade” (MHG) DLBCL, were more likely to have germinal center B-cell-like (GCB) DLBCL, MYC rearrangements, and double-hit lymphoma.
When compared to other DLBCL patients, those with MHG DLBCL had inferior progression-free and overall survival.
Chulin Sha, PhD, of the University of Leeds (England), and colleagues reported these findings in the Journal of Clinical Oncology. The findings were published alongside a related editorial and a similar study from another group.
Dr. Sha and colleagues began their study by applying a previously developed gene expression classifier (Genome Med. 2015 Jul 1;7[1]:64) to 928 DLBCL patients enrolled in the REMoDL-B trial. REMoDL-B was designed to compare rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone (R-CHOP) to R-CHOP plus bortezomib (Hematol Oncol. 2017;35:130-1).
Dr. Sha and colleagues looked for somatic mutations in 400 REMoDL-B patient samples that were sequenced for a 70-gene panel.
The team also tested 360 samples for MYC, BCL2, and BCL6 chromosomal rearrangements using fluorescent in situ hybridization, and they tested 355 samples for MYC and BCL2 protein expression with immunohistochemistry.
Characteristics of MHG DLBCL
The researchers identified 83 REMoDL-B patients as having MHG DLBCL (9%). Most of the MHG patients had GCB DLBCL (90%), 48.6% had MYC rearrangements, and 36.1% had double-hit lymphoma.
Patients with MHG DLBCL had higher International Prognostic Index scores (P = .004), greater tumor bulk (P = .007), higher disease stage (P = .06), and higher lactate dehydrogenase levels (P less than .001) than patients with non-MHG DLBCL.
Although most MHG patients had GCB DLBCL, the researchers found key differences between patients with MHG DLBCL and non-MHG GCB DLBCL. MHG patients were significantly more likely than patients with non-MHG GCB DLBCL to have mutations in KMT2D, BCL2, MYC, and DDX3X. Additionally, some genes frequently mutated in GCB DLBCL — such as B2M, SGK1, and NFKBIA — were rare in MHG DLBCL.
Dr. Sha and colleagues also compared the MHG patients to 70 patients with Burkitt lymphoma (BL) who had been analyzed in a previous study (Genome Med. 2015 Jul 1;7[1]:64).
The researchers found that BL has more upregulated genes than GCB (2,483 genes) and MHG DLBCL (1,784 genes), and MHG DLBCL has more upregulated genes than GCB DLBCL (382 genes). The team observed a similar pattern with downregulated genes and said this suggests “MHG is an intermediate group but closer to GCB than to BL.”
The researchers also found, however, that “MHG and BL share high expression of signatures that contain cell-cycle genes, ribosome biogenesis, MYC overexpression, and TCF3 targets, which suggests a shared proliferative phenotype.”
The team determined that MHG has “a highly proliferative phenotype and shares features with centroblasts of the germinal center dark zone.”
Another discovery was that MHG patients in the REMoDL-B trial had worse progression-free survival (PFS) than their peers.
Among patients who received R-CHOP, the estimated 3-year PFS was:
- 37% for MHG patients
- 78% for patients with GCB DLBCL
- 64% for patients with activated B-cell like (ABC) DLBCL
- 65% for patients with unclassified DLBCL.
Among patients who received bortezomib plus R-CHOP, there was a trend toward improved PFS for patients with MHG DLBCL (58%; P = .08).
Validation cohort
Dr. Sha and colleagues validated their initial findings using RNA sequencing data from another group of DLBCL patients (Cell. 2017 Oct 5;171[2]:481-94.e15). This data set included 624 patients who received rituximab-based therapy.
Seventy-two patients in this group had MHG DLBCL (11.5%), and most MHG patients had GCB DLBCL (82%).
The researchers said the MHG group in this cohort “showed similar associations with clinical variables” and a “similar mutation spectrum” as the MHG group in the REMoDL-B cohort. Additionally, MHG patients in the validation cohort had inferior overall survival (P less than .001) compared to patients with non-MHG GCB DLBCL.
Dr. Sha and colleagues said the poor prognosis in MHG patients in both cohorts suggests a need for different treatment approaches in this group.
In the related editorial, Wing C. Chan, MD, of City of Hope Medical Center in Duarte, Calif., echoed that sentiment and said it will be important to include patients with high-risk DLBCL in clinical trials.
“Their tumors should be comprehensively characterize[d] for correlative analysis to determine the molecular lesions that underlie their biology and response to treatment,” Dr. Chan wrote.
Dr. Chan disclosed a patent for a diagnostic algorithm on GCB/ABC-type DLBCL and a patent on a diagnostic algorithm for peripheral T-cell lymphoma.
Dr. Sha and colleagues disclosed relationships with a range of pharmaceutical companies. The team’s research was supported by a grant from Bloodwise.
The REMoDL-B trial was endorsed by Cancer Research UK and was funded by Janssen-Cillag.
SOURCES: Sha C et al. J Clin Oncol. 2019 Jan 20;37(3):202-12. doi: 10.1200/JCO.18.01314; Chan WC. J Clin Oncol. 2019 Jan 20;37(3):175-7. doi: 10.1200/JCO.18.01910; Ennishi D et al. J Clin Oncol. 2019 Jan 20;37(3):190-201. doi: 10.1200/JCO.18.01583
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Culture change needed to improve gender inequalities in medicine
LONDON –
“Gender equality is everyone’s business,” Sarah Hawkes, MBBS, PhD, a professor of global public health at University College London (England), said at the event.
“We’re not talking about women taking over the shop, but women being given an equal opportunity to run the shop. It doesn’t matter where we place ourselves on the gender spectrum as far as advancing equality in science is concerned. What matters is that we all, irrespective of gender, call ourselves feminists.”
For years, women have been “underrepresented in positions of power and leadership, undervalued, and experience discrimination and gender-based violence in scientific and health disciplines across the world,” according to an editorial in the British-based journal (Lancet. 2019;393:493). Such inequalities are compounded and hard to separate from other inequalities, including ethnicity, disability, class, geography, and sexuality.
Despite efforts to readdress the predominantly male culture of medicine, the problem of gender inequality remains “stubbornly persistent,” the editorial said.
“We have spent years being told that the problem lies with us as individuals and that we just need to be better, stronger, more vocal, as women,” Dr. Hawkes observed. “But what really needs to happen is for change to happen in places that hold power.” She further argued: “We don’t need any more individual change; we need organizational and institutional norm change.”
Gender inequality has a long history, and not just in medicine, said British journalist Caroline Criado-Perez OBE, who gave a keynote speech. Ms. Criado-Perez, who is a well-respected feminist campaigner, noted that the world was largely “modeled to fit men.” From architecture to transport, and even crash-test dummies, everything was largely modeled on, or to accommodate, the male rather than the female body.
“I don’t need to tell you that women are 50% more likely to be misdiagnosed following a heart attack” than men. There is no more urgent need to challenge gender inequality than in medicine, Women are dying because of the gender data gap in medicine,” she asserted. “In medical research, in medical education, in medical practice, it needs to be closed as a matter of urgency.”
Original data published in the Advancing Women in Science, Medicine and Global Health special edition of The Lancet found that only 31% of biomedical research papers published in 2016 reported outcomes for both men and women (Lancet. 2019;393:550-9). Reporting of sex differences was somewhat better in clinical or public health-related research papers, at 67% and 69%, respectively. Sex-differences were more likely to be reported if a woman was one of the key authors, Cassidy R. Sugimoto, PhD, associate professor of informatics at Indiana University in Bloomington, and associates, observed in their paper.
That said, women often have to fight to be included as an author on a paper, even when they have done the majority of the work, the event participants highlighted. Women were still less likely than men to be named as the first or last author on a paper, as well as be less likely to receive research funding to enable them to do the work in the first place (Lancet. 2018;393:531-40).
“Was it really you?” was a question sometimes asked of a woman named as a lead or first author, noted Sonia Gandhi, MD, PhD, group leader of the Neurodegeneration Biology Laboratory at the Francis Crick Institute in Cambridge (England). Women network differently to men, Dr. Gandhi observed, and not necessarily in networks that forward careers. Women were also often questioned about their productivity, and regardless of any training on unconscious bias, women were still at a disadvantage if they took a career break to have children.
Women’s credentials and capabilities were often felt to be less respected by male colleagues, and there was talk of being met with microaggressions in the workplace, as in one example given by Nana Odom, MSc, a clinical engineer at the Royal United Hospital Bath (England). She was told “you’re not an engineer, because I have not got a set of screwdrivers and sit at a computer and program.” Such comments can deeply affect a person, Dr. Odom said. “Sometimes I feel that if I don’t go into the workshop and open up a bit of kit that I am not an engineer, but it’s so unconscious, it carries on with you.” These types of stories need to be told so then they can be properly addressed when they do happen, she said.
Female representation is so important, said F. Gigi Osler, MD, head of otolaryngology-head and neck surgery at St. Boniface Hospital in Winnipeg. Dr. Osler is the 2018-2019 president of the Canadian Medical Association, the eighth woman to hold this prestigious position in the organization’s 151 years of operation. She also happens to be the first female surgeon and the first woman of color in the role. “When I stepped into the presidency last August, I thought very long and very hard about how I was going to use my voice and this platform,” Dr. Osler said. “It became very clear to me after I started how important representation was. I can’t tell you how many women, young women, and women of color...have come up to me to say, ‘I’m so excited to have you in this position. I’ve never seen someone who looks like me in that type of leadership position,’ ” she observed.
“As leaders, I think we can advocate for structures and processes,” Dr. Osler added, “I think we set the culture.” Leaders have the responsibility for creating and nurturing and fostering a professional, respectful, and inclusive environment, she said.
“We need more strong leaders, we need more diversity in leadership.” Dr. Osler was keen to point out that greater diversity does not mean only women, but other groups as well. “Look around the room. Who is not here? How can I make it easier for them to get here?”
Another strong female role model at the event was Dame Sally Davies, the Chief Medical Officer for England, a hematologist by training. Not only is she the first female in that role, she will also become the first female Master of Trinity College Cambridge starting in October 2019, a role dominated by men for more than 500 years.
All people, women and men, need to be given fair opportunity, Dame Sally said. Addressing structural issues can help, she said. “We need role models, mentors, and champions,” she said, noting that there were differences between the three. “Mentors give you advice, they get to know you, and they help you think through your issue. Champions may not have time for that, but they know you are good,” and they are putting you forward for opportunities.
“If the system isn’t right, or we are treated badly, we need to call it out,” Dame Sally said. “I do think that we often let things pass that we shouldn’t.” A classic situation is where a woman may suggest something at a meeting and it is ignored, but when a man says the same thing it is taken on board. That kind of behavior needs to stop and be addressed when it happens, by everyone at the table, she said.
Dr. Hawkes observed in her summing up of the day: “Throughout the history of health, change comes about not just through action at the top, but also from action from the bottom up.” She added: “The question is how do we make that change happen?” That’s where the next phase of research needs to take place, she suggested, “we need to actually see, in a very evidence-informed way, what actually works to make and sustain change.”
No financial disclosures were reported by any of the speakers quoted.
SOURCE: Lancet. 2019;393:493–610, e6-e28
LONDON –
“Gender equality is everyone’s business,” Sarah Hawkes, MBBS, PhD, a professor of global public health at University College London (England), said at the event.
“We’re not talking about women taking over the shop, but women being given an equal opportunity to run the shop. It doesn’t matter where we place ourselves on the gender spectrum as far as advancing equality in science is concerned. What matters is that we all, irrespective of gender, call ourselves feminists.”
For years, women have been “underrepresented in positions of power and leadership, undervalued, and experience discrimination and gender-based violence in scientific and health disciplines across the world,” according to an editorial in the British-based journal (Lancet. 2019;393:493). Such inequalities are compounded and hard to separate from other inequalities, including ethnicity, disability, class, geography, and sexuality.
Despite efforts to readdress the predominantly male culture of medicine, the problem of gender inequality remains “stubbornly persistent,” the editorial said.
“We have spent years being told that the problem lies with us as individuals and that we just need to be better, stronger, more vocal, as women,” Dr. Hawkes observed. “But what really needs to happen is for change to happen in places that hold power.” She further argued: “We don’t need any more individual change; we need organizational and institutional norm change.”
Gender inequality has a long history, and not just in medicine, said British journalist Caroline Criado-Perez OBE, who gave a keynote speech. Ms. Criado-Perez, who is a well-respected feminist campaigner, noted that the world was largely “modeled to fit men.” From architecture to transport, and even crash-test dummies, everything was largely modeled on, or to accommodate, the male rather than the female body.
“I don’t need to tell you that women are 50% more likely to be misdiagnosed following a heart attack” than men. There is no more urgent need to challenge gender inequality than in medicine, Women are dying because of the gender data gap in medicine,” she asserted. “In medical research, in medical education, in medical practice, it needs to be closed as a matter of urgency.”
Original data published in the Advancing Women in Science, Medicine and Global Health special edition of The Lancet found that only 31% of biomedical research papers published in 2016 reported outcomes for both men and women (Lancet. 2019;393:550-9). Reporting of sex differences was somewhat better in clinical or public health-related research papers, at 67% and 69%, respectively. Sex-differences were more likely to be reported if a woman was one of the key authors, Cassidy R. Sugimoto, PhD, associate professor of informatics at Indiana University in Bloomington, and associates, observed in their paper.
That said, women often have to fight to be included as an author on a paper, even when they have done the majority of the work, the event participants highlighted. Women were still less likely than men to be named as the first or last author on a paper, as well as be less likely to receive research funding to enable them to do the work in the first place (Lancet. 2018;393:531-40).
“Was it really you?” was a question sometimes asked of a woman named as a lead or first author, noted Sonia Gandhi, MD, PhD, group leader of the Neurodegeneration Biology Laboratory at the Francis Crick Institute in Cambridge (England). Women network differently to men, Dr. Gandhi observed, and not necessarily in networks that forward careers. Women were also often questioned about their productivity, and regardless of any training on unconscious bias, women were still at a disadvantage if they took a career break to have children.
Women’s credentials and capabilities were often felt to be less respected by male colleagues, and there was talk of being met with microaggressions in the workplace, as in one example given by Nana Odom, MSc, a clinical engineer at the Royal United Hospital Bath (England). She was told “you’re not an engineer, because I have not got a set of screwdrivers and sit at a computer and program.” Such comments can deeply affect a person, Dr. Odom said. “Sometimes I feel that if I don’t go into the workshop and open up a bit of kit that I am not an engineer, but it’s so unconscious, it carries on with you.” These types of stories need to be told so then they can be properly addressed when they do happen, she said.
Female representation is so important, said F. Gigi Osler, MD, head of otolaryngology-head and neck surgery at St. Boniface Hospital in Winnipeg. Dr. Osler is the 2018-2019 president of the Canadian Medical Association, the eighth woman to hold this prestigious position in the organization’s 151 years of operation. She also happens to be the first female surgeon and the first woman of color in the role. “When I stepped into the presidency last August, I thought very long and very hard about how I was going to use my voice and this platform,” Dr. Osler said. “It became very clear to me after I started how important representation was. I can’t tell you how many women, young women, and women of color...have come up to me to say, ‘I’m so excited to have you in this position. I’ve never seen someone who looks like me in that type of leadership position,’ ” she observed.
“As leaders, I think we can advocate for structures and processes,” Dr. Osler added, “I think we set the culture.” Leaders have the responsibility for creating and nurturing and fostering a professional, respectful, and inclusive environment, she said.
“We need more strong leaders, we need more diversity in leadership.” Dr. Osler was keen to point out that greater diversity does not mean only women, but other groups as well. “Look around the room. Who is not here? How can I make it easier for them to get here?”
Another strong female role model at the event was Dame Sally Davies, the Chief Medical Officer for England, a hematologist by training. Not only is she the first female in that role, she will also become the first female Master of Trinity College Cambridge starting in October 2019, a role dominated by men for more than 500 years.
All people, women and men, need to be given fair opportunity, Dame Sally said. Addressing structural issues can help, she said. “We need role models, mentors, and champions,” she said, noting that there were differences between the three. “Mentors give you advice, they get to know you, and they help you think through your issue. Champions may not have time for that, but they know you are good,” and they are putting you forward for opportunities.
“If the system isn’t right, or we are treated badly, we need to call it out,” Dame Sally said. “I do think that we often let things pass that we shouldn’t.” A classic situation is where a woman may suggest something at a meeting and it is ignored, but when a man says the same thing it is taken on board. That kind of behavior needs to stop and be addressed when it happens, by everyone at the table, she said.
Dr. Hawkes observed in her summing up of the day: “Throughout the history of health, change comes about not just through action at the top, but also from action from the bottom up.” She added: “The question is how do we make that change happen?” That’s where the next phase of research needs to take place, she suggested, “we need to actually see, in a very evidence-informed way, what actually works to make and sustain change.”
No financial disclosures were reported by any of the speakers quoted.
SOURCE: Lancet. 2019;393:493–610, e6-e28
LONDON –
“Gender equality is everyone’s business,” Sarah Hawkes, MBBS, PhD, a professor of global public health at University College London (England), said at the event.
“We’re not talking about women taking over the shop, but women being given an equal opportunity to run the shop. It doesn’t matter where we place ourselves on the gender spectrum as far as advancing equality in science is concerned. What matters is that we all, irrespective of gender, call ourselves feminists.”
For years, women have been “underrepresented in positions of power and leadership, undervalued, and experience discrimination and gender-based violence in scientific and health disciplines across the world,” according to an editorial in the British-based journal (Lancet. 2019;393:493). Such inequalities are compounded and hard to separate from other inequalities, including ethnicity, disability, class, geography, and sexuality.
Despite efforts to readdress the predominantly male culture of medicine, the problem of gender inequality remains “stubbornly persistent,” the editorial said.
“We have spent years being told that the problem lies with us as individuals and that we just need to be better, stronger, more vocal, as women,” Dr. Hawkes observed. “But what really needs to happen is for change to happen in places that hold power.” She further argued: “We don’t need any more individual change; we need organizational and institutional norm change.”
Gender inequality has a long history, and not just in medicine, said British journalist Caroline Criado-Perez OBE, who gave a keynote speech. Ms. Criado-Perez, who is a well-respected feminist campaigner, noted that the world was largely “modeled to fit men.” From architecture to transport, and even crash-test dummies, everything was largely modeled on, or to accommodate, the male rather than the female body.
“I don’t need to tell you that women are 50% more likely to be misdiagnosed following a heart attack” than men. There is no more urgent need to challenge gender inequality than in medicine, Women are dying because of the gender data gap in medicine,” she asserted. “In medical research, in medical education, in medical practice, it needs to be closed as a matter of urgency.”
Original data published in the Advancing Women in Science, Medicine and Global Health special edition of The Lancet found that only 31% of biomedical research papers published in 2016 reported outcomes for both men and women (Lancet. 2019;393:550-9). Reporting of sex differences was somewhat better in clinical or public health-related research papers, at 67% and 69%, respectively. Sex-differences were more likely to be reported if a woman was one of the key authors, Cassidy R. Sugimoto, PhD, associate professor of informatics at Indiana University in Bloomington, and associates, observed in their paper.
That said, women often have to fight to be included as an author on a paper, even when they have done the majority of the work, the event participants highlighted. Women were still less likely than men to be named as the first or last author on a paper, as well as be less likely to receive research funding to enable them to do the work in the first place (Lancet. 2018;393:531-40).
“Was it really you?” was a question sometimes asked of a woman named as a lead or first author, noted Sonia Gandhi, MD, PhD, group leader of the Neurodegeneration Biology Laboratory at the Francis Crick Institute in Cambridge (England). Women network differently to men, Dr. Gandhi observed, and not necessarily in networks that forward careers. Women were also often questioned about their productivity, and regardless of any training on unconscious bias, women were still at a disadvantage if they took a career break to have children.
Women’s credentials and capabilities were often felt to be less respected by male colleagues, and there was talk of being met with microaggressions in the workplace, as in one example given by Nana Odom, MSc, a clinical engineer at the Royal United Hospital Bath (England). She was told “you’re not an engineer, because I have not got a set of screwdrivers and sit at a computer and program.” Such comments can deeply affect a person, Dr. Odom said. “Sometimes I feel that if I don’t go into the workshop and open up a bit of kit that I am not an engineer, but it’s so unconscious, it carries on with you.” These types of stories need to be told so then they can be properly addressed when they do happen, she said.
Female representation is so important, said F. Gigi Osler, MD, head of otolaryngology-head and neck surgery at St. Boniface Hospital in Winnipeg. Dr. Osler is the 2018-2019 president of the Canadian Medical Association, the eighth woman to hold this prestigious position in the organization’s 151 years of operation. She also happens to be the first female surgeon and the first woman of color in the role. “When I stepped into the presidency last August, I thought very long and very hard about how I was going to use my voice and this platform,” Dr. Osler said. “It became very clear to me after I started how important representation was. I can’t tell you how many women, young women, and women of color...have come up to me to say, ‘I’m so excited to have you in this position. I’ve never seen someone who looks like me in that type of leadership position,’ ” she observed.
“As leaders, I think we can advocate for structures and processes,” Dr. Osler added, “I think we set the culture.” Leaders have the responsibility for creating and nurturing and fostering a professional, respectful, and inclusive environment, she said.
“We need more strong leaders, we need more diversity in leadership.” Dr. Osler was keen to point out that greater diversity does not mean only women, but other groups as well. “Look around the room. Who is not here? How can I make it easier for them to get here?”
Another strong female role model at the event was Dame Sally Davies, the Chief Medical Officer for England, a hematologist by training. Not only is she the first female in that role, she will also become the first female Master of Trinity College Cambridge starting in October 2019, a role dominated by men for more than 500 years.
All people, women and men, need to be given fair opportunity, Dame Sally said. Addressing structural issues can help, she said. “We need role models, mentors, and champions,” she said, noting that there were differences between the three. “Mentors give you advice, they get to know you, and they help you think through your issue. Champions may not have time for that, but they know you are good,” and they are putting you forward for opportunities.
“If the system isn’t right, or we are treated badly, we need to call it out,” Dame Sally said. “I do think that we often let things pass that we shouldn’t.” A classic situation is where a woman may suggest something at a meeting and it is ignored, but when a man says the same thing it is taken on board. That kind of behavior needs to stop and be addressed when it happens, by everyone at the table, she said.
Dr. Hawkes observed in her summing up of the day: “Throughout the history of health, change comes about not just through action at the top, but also from action from the bottom up.” She added: “The question is how do we make that change happen?” That’s where the next phase of research needs to take place, she suggested, “we need to actually see, in a very evidence-informed way, what actually works to make and sustain change.”
No financial disclosures were reported by any of the speakers quoted.
SOURCE: Lancet. 2019;393:493–610, e6-e28
FROM A LAUNCH EVENT HELD BY THE LANCET
Ehlers-Danlos syndrome: Increased IUGR risk reported
LAS VEGAS – Women with Ehlers-Danlos syndrome who became pregnant were more likely to experience antepartum hemorrhage, placenta previa, cervical incompetence, and preterm birth, according to a retrospective cohort study of national birth data. Long hospital stays also were more likely among these women.
Infants born to women with Ehlers-Danlos syndrome (EDS) were significantly more likely to have intrauterine growth retardation (IUGR) as well, an unexpected and as-yet unexplained finding, said the study’s first author, Laura Nicholls-Dempsey, MD, speaking at a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Complications were infrequent overall, with a very low rate of intrauterine demise and no maternal mortality seen in the 910 women with EDS who were studied, said Dr. Nicholls-Dempsey, an ob.gyn. resident at McGill University, Montreal.
In counseling women with EDS, Dr. Nicholls-Dempsey said that she would advise them that “these are the types of things we’re going to watch out for, and we’ll see how the pregnancy goes. But we have to be careful about these: preterm birth, antepartum bleeding, placenta previa. We’ll watch the growth of the baby; we just have to be more careful about these specific things.”
Compared with women without EDS, those with the inherited connective tissue disorder had adjusted odds ratios (AORs) of 3.2 for cervical incompetence (95% confidence interval, 2.0-5.1) and 2.2 for placenta previa (95% CI, 1.3-3.9; P less than .01 for both). Absolute rates for these complications were 0.8% and 0.7% for women without EDS and 2.1% and 1.4% for women with EDS, respectively.
Women with EDS also had AORs of 1.8 for antepartum hemorrhage (2.8% versus 1.6%; 95% CI, 1.2-2.7; P less than .01). Cesarean delivery was more likely in women with EDS, with an AOR of 1.6 (37.4% versus 26.9%; 95% CI, 2.0-5.1); conversely, instrumental vaginal delivery was less likely in women with EDS (AOR = 0.5; 95% CI, 0.4-0.7; P less than .01 for both), meaning that spontaneous vaginal delivery was less likely in the EDS cohort.
The higher frequency of Cesarean deliveries may be attributable to anticipatory management by physicians seeking to avoid such complications as antepartum hemorrhage, as well as to the increased rate of placenta previa seen among the EDS cohort, Dr. Nicholls-Dempsey said.
After statistical adjustment, women in the EDS cohort were more than three times as likely to have hospital stays of both more than 7 days and 14 days (5.7% versus 2.1%, AOR = 3.1 for 7 days; 2.3% versus 0.7%, AOR = 3.8 for 14 days; P less than .01 for both).
Rates of some other maternal complications, such as pre-eclampsia, eclampsia, and gestational hypertension, were not elevated in the EDS cohort. Rates of premature rupture of membranes, chorioamnionitis, uterine rupture, postpartum hemorrhage, perineal laceration, and venous thromboembolism were also similar between groups.
However, not only was the AOR for preterm birth 1.5 for infants of women with EDS, but IUGR was more common in these neonates as well (AOR = 1.7, P less than .01 for both). The latter finding was unexpected, and Dr. Nicholls-Dempsey and her colleagues currently don’t have a mechanistic explanation for the higher IUGR rate.
Dr. Nicholls-Dempsey explained that she and her colleagues used data from the United States’ Health Care Cost and Utilization Project’s Nationwide Inpatient Sample (HCUP-NIS) to compare outcomes of women with EDS with the national sample as a whole.
Between 1999 and 2013, 13,881,592 births occurred in the HCUP-NIS cohort, with 910 deliveries to women who had EDS. These women were identified by ICD-9 codes, she said.
Comparing women with EDS to the non-EDS cohort, women with EDS were more likely to be Caucasian, have a higher income, and to be smokers; the cohorts were otherwise similar.
Ehlers-Danlos syndrome is a heterogeneous disorder involving abnormalities of collagen synthesis, with 13 known subtypes not captured in the HCUP-NIS data, Dr. Nicholls-Dempsey acknowledged. She characterized this as both a limitation but also a potential strength of the study.
“I really like this study because ... we know there’s 13 types of EDS that are genetically different ... They have their overlapping symptoms, but each one is different,” she said. “In an ideal world, we would have each subtype, and we would run this type of analysis on each subtype, to really be able to say to a patient, ‘You have this mutation, and this complication is going to be a big problem for you.’” The numbers of each subtype are so small that this is infeasible, she noted.
Still, the national sample acquired over many years offers real-world outcomes that clinicians can use in shared decision-making with EDS patients who are contemplating pregnancy or are already pregnant. Also, knowing which complications are more likely in patients with EDS can help plan optimal management of labor and delivery, Dr. Nicholls-Dempsey said.
Over the study’s 14-year span, the overall arc of EDS pregnancy outcomes is well captured regardless of mutation type. “It’s very applicable to the general population” of individuals with EDS, she noted. “Because it’s not type-specific, it’s really a good overview of what you can expect in EDS patients, regardless of the type.”
Dr. Nicholls-Dempsey reported no conflicts of interest and no outside sources of funding.
SOURCE: Nicholls-Dempsey L et al. Am J Obstet Gynecol. 2019 Jan;220(1):S381-382. Abstract 574
LAS VEGAS – Women with Ehlers-Danlos syndrome who became pregnant were more likely to experience antepartum hemorrhage, placenta previa, cervical incompetence, and preterm birth, according to a retrospective cohort study of national birth data. Long hospital stays also were more likely among these women.
Infants born to women with Ehlers-Danlos syndrome (EDS) were significantly more likely to have intrauterine growth retardation (IUGR) as well, an unexpected and as-yet unexplained finding, said the study’s first author, Laura Nicholls-Dempsey, MD, speaking at a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Complications were infrequent overall, with a very low rate of intrauterine demise and no maternal mortality seen in the 910 women with EDS who were studied, said Dr. Nicholls-Dempsey, an ob.gyn. resident at McGill University, Montreal.
In counseling women with EDS, Dr. Nicholls-Dempsey said that she would advise them that “these are the types of things we’re going to watch out for, and we’ll see how the pregnancy goes. But we have to be careful about these: preterm birth, antepartum bleeding, placenta previa. We’ll watch the growth of the baby; we just have to be more careful about these specific things.”
Compared with women without EDS, those with the inherited connective tissue disorder had adjusted odds ratios (AORs) of 3.2 for cervical incompetence (95% confidence interval, 2.0-5.1) and 2.2 for placenta previa (95% CI, 1.3-3.9; P less than .01 for both). Absolute rates for these complications were 0.8% and 0.7% for women without EDS and 2.1% and 1.4% for women with EDS, respectively.
Women with EDS also had AORs of 1.8 for antepartum hemorrhage (2.8% versus 1.6%; 95% CI, 1.2-2.7; P less than .01). Cesarean delivery was more likely in women with EDS, with an AOR of 1.6 (37.4% versus 26.9%; 95% CI, 2.0-5.1); conversely, instrumental vaginal delivery was less likely in women with EDS (AOR = 0.5; 95% CI, 0.4-0.7; P less than .01 for both), meaning that spontaneous vaginal delivery was less likely in the EDS cohort.
The higher frequency of Cesarean deliveries may be attributable to anticipatory management by physicians seeking to avoid such complications as antepartum hemorrhage, as well as to the increased rate of placenta previa seen among the EDS cohort, Dr. Nicholls-Dempsey said.
After statistical adjustment, women in the EDS cohort were more than three times as likely to have hospital stays of both more than 7 days and 14 days (5.7% versus 2.1%, AOR = 3.1 for 7 days; 2.3% versus 0.7%, AOR = 3.8 for 14 days; P less than .01 for both).
Rates of some other maternal complications, such as pre-eclampsia, eclampsia, and gestational hypertension, were not elevated in the EDS cohort. Rates of premature rupture of membranes, chorioamnionitis, uterine rupture, postpartum hemorrhage, perineal laceration, and venous thromboembolism were also similar between groups.
However, not only was the AOR for preterm birth 1.5 for infants of women with EDS, but IUGR was more common in these neonates as well (AOR = 1.7, P less than .01 for both). The latter finding was unexpected, and Dr. Nicholls-Dempsey and her colleagues currently don’t have a mechanistic explanation for the higher IUGR rate.
Dr. Nicholls-Dempsey explained that she and her colleagues used data from the United States’ Health Care Cost and Utilization Project’s Nationwide Inpatient Sample (HCUP-NIS) to compare outcomes of women with EDS with the national sample as a whole.
Between 1999 and 2013, 13,881,592 births occurred in the HCUP-NIS cohort, with 910 deliveries to women who had EDS. These women were identified by ICD-9 codes, she said.
Comparing women with EDS to the non-EDS cohort, women with EDS were more likely to be Caucasian, have a higher income, and to be smokers; the cohorts were otherwise similar.
Ehlers-Danlos syndrome is a heterogeneous disorder involving abnormalities of collagen synthesis, with 13 known subtypes not captured in the HCUP-NIS data, Dr. Nicholls-Dempsey acknowledged. She characterized this as both a limitation but also a potential strength of the study.
“I really like this study because ... we know there’s 13 types of EDS that are genetically different ... They have their overlapping symptoms, but each one is different,” she said. “In an ideal world, we would have each subtype, and we would run this type of analysis on each subtype, to really be able to say to a patient, ‘You have this mutation, and this complication is going to be a big problem for you.’” The numbers of each subtype are so small that this is infeasible, she noted.
Still, the national sample acquired over many years offers real-world outcomes that clinicians can use in shared decision-making with EDS patients who are contemplating pregnancy or are already pregnant. Also, knowing which complications are more likely in patients with EDS can help plan optimal management of labor and delivery, Dr. Nicholls-Dempsey said.
Over the study’s 14-year span, the overall arc of EDS pregnancy outcomes is well captured regardless of mutation type. “It’s very applicable to the general population” of individuals with EDS, she noted. “Because it’s not type-specific, it’s really a good overview of what you can expect in EDS patients, regardless of the type.”
Dr. Nicholls-Dempsey reported no conflicts of interest and no outside sources of funding.
SOURCE: Nicholls-Dempsey L et al. Am J Obstet Gynecol. 2019 Jan;220(1):S381-382. Abstract 574
LAS VEGAS – Women with Ehlers-Danlos syndrome who became pregnant were more likely to experience antepartum hemorrhage, placenta previa, cervical incompetence, and preterm birth, according to a retrospective cohort study of national birth data. Long hospital stays also were more likely among these women.
Infants born to women with Ehlers-Danlos syndrome (EDS) were significantly more likely to have intrauterine growth retardation (IUGR) as well, an unexpected and as-yet unexplained finding, said the study’s first author, Laura Nicholls-Dempsey, MD, speaking at a poster session at the meeting sponsored by the Society for Maternal-Fetal Medicine.
Complications were infrequent overall, with a very low rate of intrauterine demise and no maternal mortality seen in the 910 women with EDS who were studied, said Dr. Nicholls-Dempsey, an ob.gyn. resident at McGill University, Montreal.
In counseling women with EDS, Dr. Nicholls-Dempsey said that she would advise them that “these are the types of things we’re going to watch out for, and we’ll see how the pregnancy goes. But we have to be careful about these: preterm birth, antepartum bleeding, placenta previa. We’ll watch the growth of the baby; we just have to be more careful about these specific things.”
Compared with women without EDS, those with the inherited connective tissue disorder had adjusted odds ratios (AORs) of 3.2 for cervical incompetence (95% confidence interval, 2.0-5.1) and 2.2 for placenta previa (95% CI, 1.3-3.9; P less than .01 for both). Absolute rates for these complications were 0.8% and 0.7% for women without EDS and 2.1% and 1.4% for women with EDS, respectively.
Women with EDS also had AORs of 1.8 for antepartum hemorrhage (2.8% versus 1.6%; 95% CI, 1.2-2.7; P less than .01). Cesarean delivery was more likely in women with EDS, with an AOR of 1.6 (37.4% versus 26.9%; 95% CI, 2.0-5.1); conversely, instrumental vaginal delivery was less likely in women with EDS (AOR = 0.5; 95% CI, 0.4-0.7; P less than .01 for both), meaning that spontaneous vaginal delivery was less likely in the EDS cohort.
The higher frequency of Cesarean deliveries may be attributable to anticipatory management by physicians seeking to avoid such complications as antepartum hemorrhage, as well as to the increased rate of placenta previa seen among the EDS cohort, Dr. Nicholls-Dempsey said.
After statistical adjustment, women in the EDS cohort were more than three times as likely to have hospital stays of both more than 7 days and 14 days (5.7% versus 2.1%, AOR = 3.1 for 7 days; 2.3% versus 0.7%, AOR = 3.8 for 14 days; P less than .01 for both).
Rates of some other maternal complications, such as pre-eclampsia, eclampsia, and gestational hypertension, were not elevated in the EDS cohort. Rates of premature rupture of membranes, chorioamnionitis, uterine rupture, postpartum hemorrhage, perineal laceration, and venous thromboembolism were also similar between groups.
However, not only was the AOR for preterm birth 1.5 for infants of women with EDS, but IUGR was more common in these neonates as well (AOR = 1.7, P less than .01 for both). The latter finding was unexpected, and Dr. Nicholls-Dempsey and her colleagues currently don’t have a mechanistic explanation for the higher IUGR rate.
Dr. Nicholls-Dempsey explained that she and her colleagues used data from the United States’ Health Care Cost and Utilization Project’s Nationwide Inpatient Sample (HCUP-NIS) to compare outcomes of women with EDS with the national sample as a whole.
Between 1999 and 2013, 13,881,592 births occurred in the HCUP-NIS cohort, with 910 deliveries to women who had EDS. These women were identified by ICD-9 codes, she said.
Comparing women with EDS to the non-EDS cohort, women with EDS were more likely to be Caucasian, have a higher income, and to be smokers; the cohorts were otherwise similar.
Ehlers-Danlos syndrome is a heterogeneous disorder involving abnormalities of collagen synthesis, with 13 known subtypes not captured in the HCUP-NIS data, Dr. Nicholls-Dempsey acknowledged. She characterized this as both a limitation but also a potential strength of the study.
“I really like this study because ... we know there’s 13 types of EDS that are genetically different ... They have their overlapping symptoms, but each one is different,” she said. “In an ideal world, we would have each subtype, and we would run this type of analysis on each subtype, to really be able to say to a patient, ‘You have this mutation, and this complication is going to be a big problem for you.’” The numbers of each subtype are so small that this is infeasible, she noted.
Still, the national sample acquired over many years offers real-world outcomes that clinicians can use in shared decision-making with EDS patients who are contemplating pregnancy or are already pregnant. Also, knowing which complications are more likely in patients with EDS can help plan optimal management of labor and delivery, Dr. Nicholls-Dempsey said.
Over the study’s 14-year span, the overall arc of EDS pregnancy outcomes is well captured regardless of mutation type. “It’s very applicable to the general population” of individuals with EDS, she noted. “Because it’s not type-specific, it’s really a good overview of what you can expect in EDS patients, regardless of the type.”
Dr. Nicholls-Dempsey reported no conflicts of interest and no outside sources of funding.
SOURCE: Nicholls-Dempsey L et al. Am J Obstet Gynecol. 2019 Jan;220(1):S381-382. Abstract 574
REPORTING FROM THE PREGNANCY MEETING
CAR T-cell therapies difficult to compare
One chimeric antigen receptor (CAR) T-cell therapy may appear better than another, but confounding factors make it difficult to compare these therapies effectively, according to a review published in the Journal of Clinical Oncology.
Caron A. Jacobson, MD, of the Dana-Farber Cancer Institute in Boston, reviewed results from three trials of CAR T-cell therapies in patients with B-cell non-Hodgkin lymphoma (B-NHL).
She noted that cross-trial comparisons are always limited, but such comparisons of CAR T-cell therapies are hindered by several confounding factors.
Dr. Jacobson said differences in manufacturing procedures and turnaround time, differences in patient eligibility and management, and the complexity of CAR T-cell therapies make it difficult to compare results from three CAR-T trials in B-NHL:
• The ZUMA-1 trial (NCT02348216) of axicabtagene ciloleucel (axi-cel, Yescarta)
• The JULIET trial (NCT02445248) of tisagenlecleucel (t-cel, Kymriah)
• The TRANSCEND-NHL-001 trial (NCT02631044) of lisocabtagene maraleucel (liso-cel, JCAR017).
Looking at response rates alone, axi-cel appears the most promising. The overall response rate (ORR) was 82% with axi-cel, 75% with liso-cel, and 52% with t-cel.
When considering cytokine release syndrome (CRS), liso-cel appears the safest. The rate of CRS was 93% with axi-cel (13% grade 3 or higher), 58% with t-cel (22% grade 3 or higher), and 39% with liso-cel (1% grade 3 or higher).
However, as Dr. Jacobson pointed out, it’s impossible to know if these differences in efficacy and toxicity are “statistically meaningful.”
Dr. Jacobson also noted that bridging therapy may have affected these results, as it might reduce tumor burden and increase toxicity, but bridging therapy was not used uniformly across these trials.
Most patients received bridging therapy before t-cel, none received it before axi-cel, and the use of bridging therapy was not reported in the trial of liso-cel.
“It is not possible to know whether patients treated on the ZUMA-1 trial, who were more likely to receive their CAR T cells, were healthier and more fit than patients on other studies or, because they were not allowed to receive bridging therapy, were actually sicker with a higher tumor burden and were therefore at risk for greater toxicity,” Dr. Jacobson wrote.
The fact that ZUMA-1 patients were more likely to receive CAR T cells brings up another issue—the difference between the reported results and the intent-to-treat (ITT) results in these trials. Since most patients on ZUMA-1 received the study treatment, there isn't much difference between the reported results and ITT results. However, about a third of patients who underwent apheresis on the JULIET trial did not ultimately receive CAR T cells, which means a bigger difference between the reported results and ITT results.
In ZUMA-1, 111 patients underwent leukapheresis, and 101 received treatment with axi-cel and were evaluable for efficacy. So the ORR was 75% (83/111) in the ITT population, compared to 82% in the population evaluable for efficacy.
In JULIET, 165 patients underwent leukapheresis, 111 received t-cel, and 93 were evaluable. The ORR was 30% (48/161) in the ITT population, compared to 52% in the evaluable population.
In TRANSCEND-NHL-001, 134 patients underwent leukapheresis, 114 patients received liso-cel, and 102 were evaluable. The ORR was 63% (77/122) in the ITT population, compared to 75% in the evaluable population.
Dr. Jacobson said these differences can be explained, in part, by differences in manufacturing. The time to manufacture cells was longer on the JULIET trial than on ZUMA-1, which may have been due to differences in transfection and manufacturing procedures as well as manufacturing ability.
In addition, differences in patient eligibility may have played a role, as healthier patients might be able to tolerate a longer manufacturing period than sicker patients.
Unfortunately, these differences cannot be accounted for without a randomized trial, but Dr. Jacobson said a randomized trial of these therapies is unlikely to occur.
“[S]o perhaps the best answers will come from institutions that have experience with all three products,” she wrote. “And in these cases, physicians and institutions will have to decide to what extent they would sacrifice efficacy for improved safety or sacrifice safety for improved reliability and consistency of treatment delivery.”
Dr. Jacobson disclosed relationships with Kite Pharma/Gilead Sciences, Bayer AG, Pfizer, Precision BioSciences, Novartis, Celgene, and Cowen.
SOURCE: Jacobson CA. J Clin Oncol. 2019 Feb 1;37(4):328-35. doi: 10.1200/JCO.18.01457
One chimeric antigen receptor (CAR) T-cell therapy may appear better than another, but confounding factors make it difficult to compare these therapies effectively, according to a review published in the Journal of Clinical Oncology.
Caron A. Jacobson, MD, of the Dana-Farber Cancer Institute in Boston, reviewed results from three trials of CAR T-cell therapies in patients with B-cell non-Hodgkin lymphoma (B-NHL).
She noted that cross-trial comparisons are always limited, but such comparisons of CAR T-cell therapies are hindered by several confounding factors.
Dr. Jacobson said differences in manufacturing procedures and turnaround time, differences in patient eligibility and management, and the complexity of CAR T-cell therapies make it difficult to compare results from three CAR-T trials in B-NHL:
• The ZUMA-1 trial (NCT02348216) of axicabtagene ciloleucel (axi-cel, Yescarta)
• The JULIET trial (NCT02445248) of tisagenlecleucel (t-cel, Kymriah)
• The TRANSCEND-NHL-001 trial (NCT02631044) of lisocabtagene maraleucel (liso-cel, JCAR017).
Looking at response rates alone, axi-cel appears the most promising. The overall response rate (ORR) was 82% with axi-cel, 75% with liso-cel, and 52% with t-cel.
When considering cytokine release syndrome (CRS), liso-cel appears the safest. The rate of CRS was 93% with axi-cel (13% grade 3 or higher), 58% with t-cel (22% grade 3 or higher), and 39% with liso-cel (1% grade 3 or higher).
However, as Dr. Jacobson pointed out, it’s impossible to know if these differences in efficacy and toxicity are “statistically meaningful.”
Dr. Jacobson also noted that bridging therapy may have affected these results, as it might reduce tumor burden and increase toxicity, but bridging therapy was not used uniformly across these trials.
Most patients received bridging therapy before t-cel, none received it before axi-cel, and the use of bridging therapy was not reported in the trial of liso-cel.
“It is not possible to know whether patients treated on the ZUMA-1 trial, who were more likely to receive their CAR T cells, were healthier and more fit than patients on other studies or, because they were not allowed to receive bridging therapy, were actually sicker with a higher tumor burden and were therefore at risk for greater toxicity,” Dr. Jacobson wrote.
The fact that ZUMA-1 patients were more likely to receive CAR T cells brings up another issue—the difference between the reported results and the intent-to-treat (ITT) results in these trials. Since most patients on ZUMA-1 received the study treatment, there isn't much difference between the reported results and ITT results. However, about a third of patients who underwent apheresis on the JULIET trial did not ultimately receive CAR T cells, which means a bigger difference between the reported results and ITT results.
In ZUMA-1, 111 patients underwent leukapheresis, and 101 received treatment with axi-cel and were evaluable for efficacy. So the ORR was 75% (83/111) in the ITT population, compared to 82% in the population evaluable for efficacy.
In JULIET, 165 patients underwent leukapheresis, 111 received t-cel, and 93 were evaluable. The ORR was 30% (48/161) in the ITT population, compared to 52% in the evaluable population.
In TRANSCEND-NHL-001, 134 patients underwent leukapheresis, 114 patients received liso-cel, and 102 were evaluable. The ORR was 63% (77/122) in the ITT population, compared to 75% in the evaluable population.
Dr. Jacobson said these differences can be explained, in part, by differences in manufacturing. The time to manufacture cells was longer on the JULIET trial than on ZUMA-1, which may have been due to differences in transfection and manufacturing procedures as well as manufacturing ability.
In addition, differences in patient eligibility may have played a role, as healthier patients might be able to tolerate a longer manufacturing period than sicker patients.
Unfortunately, these differences cannot be accounted for without a randomized trial, but Dr. Jacobson said a randomized trial of these therapies is unlikely to occur.
“[S]o perhaps the best answers will come from institutions that have experience with all three products,” she wrote. “And in these cases, physicians and institutions will have to decide to what extent they would sacrifice efficacy for improved safety or sacrifice safety for improved reliability and consistency of treatment delivery.”
Dr. Jacobson disclosed relationships with Kite Pharma/Gilead Sciences, Bayer AG, Pfizer, Precision BioSciences, Novartis, Celgene, and Cowen.
SOURCE: Jacobson CA. J Clin Oncol. 2019 Feb 1;37(4):328-35. doi: 10.1200/JCO.18.01457
One chimeric antigen receptor (CAR) T-cell therapy may appear better than another, but confounding factors make it difficult to compare these therapies effectively, according to a review published in the Journal of Clinical Oncology.
Caron A. Jacobson, MD, of the Dana-Farber Cancer Institute in Boston, reviewed results from three trials of CAR T-cell therapies in patients with B-cell non-Hodgkin lymphoma (B-NHL).
She noted that cross-trial comparisons are always limited, but such comparisons of CAR T-cell therapies are hindered by several confounding factors.
Dr. Jacobson said differences in manufacturing procedures and turnaround time, differences in patient eligibility and management, and the complexity of CAR T-cell therapies make it difficult to compare results from three CAR-T trials in B-NHL:
• The ZUMA-1 trial (NCT02348216) of axicabtagene ciloleucel (axi-cel, Yescarta)
• The JULIET trial (NCT02445248) of tisagenlecleucel (t-cel, Kymriah)
• The TRANSCEND-NHL-001 trial (NCT02631044) of lisocabtagene maraleucel (liso-cel, JCAR017).
Looking at response rates alone, axi-cel appears the most promising. The overall response rate (ORR) was 82% with axi-cel, 75% with liso-cel, and 52% with t-cel.
When considering cytokine release syndrome (CRS), liso-cel appears the safest. The rate of CRS was 93% with axi-cel (13% grade 3 or higher), 58% with t-cel (22% grade 3 or higher), and 39% with liso-cel (1% grade 3 or higher).
However, as Dr. Jacobson pointed out, it’s impossible to know if these differences in efficacy and toxicity are “statistically meaningful.”
Dr. Jacobson also noted that bridging therapy may have affected these results, as it might reduce tumor burden and increase toxicity, but bridging therapy was not used uniformly across these trials.
Most patients received bridging therapy before t-cel, none received it before axi-cel, and the use of bridging therapy was not reported in the trial of liso-cel.
“It is not possible to know whether patients treated on the ZUMA-1 trial, who were more likely to receive their CAR T cells, were healthier and more fit than patients on other studies or, because they were not allowed to receive bridging therapy, were actually sicker with a higher tumor burden and were therefore at risk for greater toxicity,” Dr. Jacobson wrote.
The fact that ZUMA-1 patients were more likely to receive CAR T cells brings up another issue—the difference between the reported results and the intent-to-treat (ITT) results in these trials. Since most patients on ZUMA-1 received the study treatment, there isn't much difference between the reported results and ITT results. However, about a third of patients who underwent apheresis on the JULIET trial did not ultimately receive CAR T cells, which means a bigger difference between the reported results and ITT results.
In ZUMA-1, 111 patients underwent leukapheresis, and 101 received treatment with axi-cel and were evaluable for efficacy. So the ORR was 75% (83/111) in the ITT population, compared to 82% in the population evaluable for efficacy.
In JULIET, 165 patients underwent leukapheresis, 111 received t-cel, and 93 were evaluable. The ORR was 30% (48/161) in the ITT population, compared to 52% in the evaluable population.
In TRANSCEND-NHL-001, 134 patients underwent leukapheresis, 114 patients received liso-cel, and 102 were evaluable. The ORR was 63% (77/122) in the ITT population, compared to 75% in the evaluable population.
Dr. Jacobson said these differences can be explained, in part, by differences in manufacturing. The time to manufacture cells was longer on the JULIET trial than on ZUMA-1, which may have been due to differences in transfection and manufacturing procedures as well as manufacturing ability.
In addition, differences in patient eligibility may have played a role, as healthier patients might be able to tolerate a longer manufacturing period than sicker patients.
Unfortunately, these differences cannot be accounted for without a randomized trial, but Dr. Jacobson said a randomized trial of these therapies is unlikely to occur.
“[S]o perhaps the best answers will come from institutions that have experience with all three products,” she wrote. “And in these cases, physicians and institutions will have to decide to what extent they would sacrifice efficacy for improved safety or sacrifice safety for improved reliability and consistency of treatment delivery.”
Dr. Jacobson disclosed relationships with Kite Pharma/Gilead Sciences, Bayer AG, Pfizer, Precision BioSciences, Novartis, Celgene, and Cowen.
SOURCE: Jacobson CA. J Clin Oncol. 2019 Feb 1;37(4):328-35. doi: 10.1200/JCO.18.01457
FROM JOURNAL OF CLINICAL ONCOLOGY
ICYMI: Andexanet alfa reduces anti–factor Xa activity from apixaban, rivaroxaban
Patients with acute major bleeding associated with factor Xa inhibitor usage who received andexanet alfa experienced a significant decrease in anti–factor Xa activity, with more than three-quarters of patients experiencing good or excellent hemostatic efficiency after 12 hours. That finding emerged from the multicenter, prospective, open-label, single-group ANNEXA-4 trial published in the New England Journal of Medicine (2019 Feb 11. doi: 10.1056/NEJMoa1814051).
We reported this story at the annual meeting of the American College of Cardiology before it was published in the journal. Find our coverage at the link below.
Patients with acute major bleeding associated with factor Xa inhibitor usage who received andexanet alfa experienced a significant decrease in anti–factor Xa activity, with more than three-quarters of patients experiencing good or excellent hemostatic efficiency after 12 hours. That finding emerged from the multicenter, prospective, open-label, single-group ANNEXA-4 trial published in the New England Journal of Medicine (2019 Feb 11. doi: 10.1056/NEJMoa1814051).
We reported this story at the annual meeting of the American College of Cardiology before it was published in the journal. Find our coverage at the link below.
Patients with acute major bleeding associated with factor Xa inhibitor usage who received andexanet alfa experienced a significant decrease in anti–factor Xa activity, with more than three-quarters of patients experiencing good or excellent hemostatic efficiency after 12 hours. That finding emerged from the multicenter, prospective, open-label, single-group ANNEXA-4 trial published in the New England Journal of Medicine (2019 Feb 11. doi: 10.1056/NEJMoa1814051).
We reported this story at the annual meeting of the American College of Cardiology before it was published in the journal. Find our coverage at the link below.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
FDA approves first interoperable insulin infusion pump
, for insulin delivery in children and adults with diabetes.
The pump delivers insulin under the skin at a variable or fixed rate. It can function on its own, or it can be digitally connected to automatically communicate with and receive drug-dosing commands from other diabetes management devices, such as automated insulin-dosing systems, the agency announced.
The approval was based on a review of performance data demonstrating that the device can deliver insulin accurately and reliably and at the rates and volumes programmed by the user. The agency also assessed the pump’s ability to connect reliably with other devices, as well as its cybersecurity and fail-safe modes.
Risks associated with the device were similar to those of other infusion pumps and include infection, bleeding, pain, or skin irritations. Blockages and air bubbles can occur in the tubing, which will affect drug delivery. Risks associated with incorrect drug delivery include hypo- and hyperglycemia as well as diabetic ketoacidosis.
“The marketing authorization of the [pump] has the potential to aid patients who seek more individualized diabetes therapy systems and opens the door for developers of future connected diabetes devices to get other safe and effective products to patients more efficiently,” FDA Commissioner Scott Gottlieb, MD, said in the announcement.
, for insulin delivery in children and adults with diabetes.
The pump delivers insulin under the skin at a variable or fixed rate. It can function on its own, or it can be digitally connected to automatically communicate with and receive drug-dosing commands from other diabetes management devices, such as automated insulin-dosing systems, the agency announced.
The approval was based on a review of performance data demonstrating that the device can deliver insulin accurately and reliably and at the rates and volumes programmed by the user. The agency also assessed the pump’s ability to connect reliably with other devices, as well as its cybersecurity and fail-safe modes.
Risks associated with the device were similar to those of other infusion pumps and include infection, bleeding, pain, or skin irritations. Blockages and air bubbles can occur in the tubing, which will affect drug delivery. Risks associated with incorrect drug delivery include hypo- and hyperglycemia as well as diabetic ketoacidosis.
“The marketing authorization of the [pump] has the potential to aid patients who seek more individualized diabetes therapy systems and opens the door for developers of future connected diabetes devices to get other safe and effective products to patients more efficiently,” FDA Commissioner Scott Gottlieb, MD, said in the announcement.
, for insulin delivery in children and adults with diabetes.
The pump delivers insulin under the skin at a variable or fixed rate. It can function on its own, or it can be digitally connected to automatically communicate with and receive drug-dosing commands from other diabetes management devices, such as automated insulin-dosing systems, the agency announced.
The approval was based on a review of performance data demonstrating that the device can deliver insulin accurately and reliably and at the rates and volumes programmed by the user. The agency also assessed the pump’s ability to connect reliably with other devices, as well as its cybersecurity and fail-safe modes.
Risks associated with the device were similar to those of other infusion pumps and include infection, bleeding, pain, or skin irritations. Blockages and air bubbles can occur in the tubing, which will affect drug delivery. Risks associated with incorrect drug delivery include hypo- and hyperglycemia as well as diabetic ketoacidosis.
“The marketing authorization of the [pump] has the potential to aid patients who seek more individualized diabetes therapy systems and opens the door for developers of future connected diabetes devices to get other safe and effective products to patients more efficiently,” FDA Commissioner Scott Gottlieb, MD, said in the announcement.
Flu season showing its staying power
Like an unwelcome guest, the 2018-2019 flu season seems to be settling in for a lengthy stay as three more states have reached the highest level of influenza-like illness (ILI) activity, according to the Centers for Disease Control and Prevention.
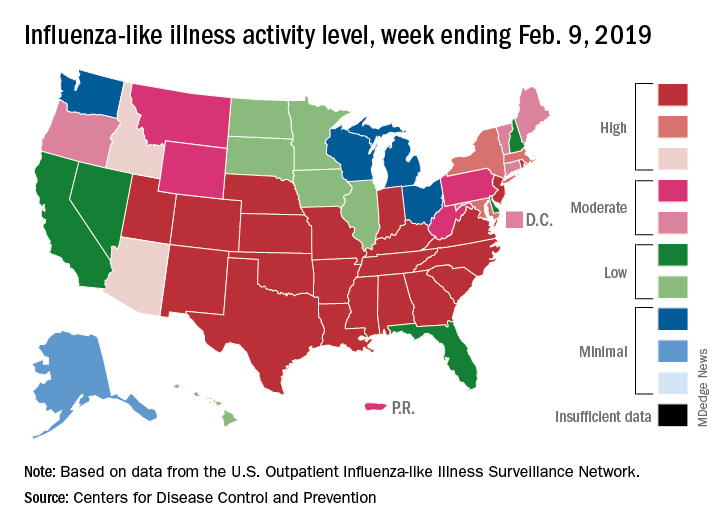
There are now 21 states at level 10 on the CDC’s 1-10 scale, with the South showing up almost solidly red on the flu activity map for the week ending Feb. 9. Another five states are at levels 8 and 9, bringing the total in the high range to 26 for the week, compared with 24 the previous week, the CDC’s influenza division reported Feb. 15.
National activity, reflected in the proportion of outpatient visits involving ILI, took a step up from 4.3% the week before to 4.8% for the week ending Feb. 9. The national baseline rate is 2.2% for ILI, which the CDC defines “as fever (temperature of 100°F [37.8°C] or greater) and cough and/or sore throat.”
Two flu-related pediatric deaths occurred during the week ending Feb. 9, and another four were reported from earlier weeks, which brings the total for the 2018-2019 season to 34, the CDC said. At the same point in last year’s flu season, there had been 84 flu-related deaths in children.
In a separate report, the CDC said that, based on data collected from Nov. 23, 2018 to Feb. 2, 2019, “the influenza vaccine has been 47% effective in preventing medically attended acute respiratory virus infection across all age groups and specifically was 46% effective in preventing medical visits associated with influenza A(H1N1)pdm09.” The effectiveness of the vaccine was 61% for children aged 6 months to 17 years, the CDC said (MMWR. 2019 Feb 15;68[6];135-9).
Flu vaccination during the 2017-2018 season prevented 7.1 million illnesses, 3.7 million medical visits, 109,000 hospitalizations, and 8,000 flu-related deaths, the CDC said, adding that “vaccination has been found to reduce deaths, intensive care unit admissions and length of stay, and overall duration of hospitalization among hospitalized influenza patients.”
Forecasts for the rest of the 2018-2019 season “predict that elevated influenza activity in parts of the United States will continue for several more weeks,” the CDC said.
Like an unwelcome guest, the 2018-2019 flu season seems to be settling in for a lengthy stay as three more states have reached the highest level of influenza-like illness (ILI) activity, according to the Centers for Disease Control and Prevention.
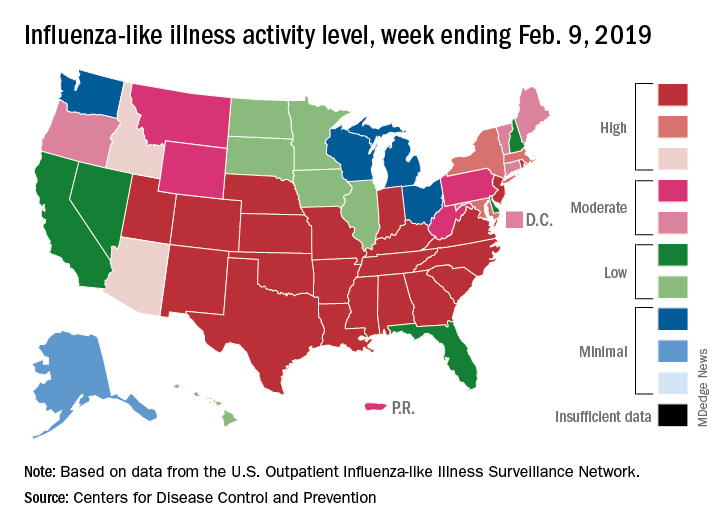
There are now 21 states at level 10 on the CDC’s 1-10 scale, with the South showing up almost solidly red on the flu activity map for the week ending Feb. 9. Another five states are at levels 8 and 9, bringing the total in the high range to 26 for the week, compared with 24 the previous week, the CDC’s influenza division reported Feb. 15.
National activity, reflected in the proportion of outpatient visits involving ILI, took a step up from 4.3% the week before to 4.8% for the week ending Feb. 9. The national baseline rate is 2.2% for ILI, which the CDC defines “as fever (temperature of 100°F [37.8°C] or greater) and cough and/or sore throat.”
Two flu-related pediatric deaths occurred during the week ending Feb. 9, and another four were reported from earlier weeks, which brings the total for the 2018-2019 season to 34, the CDC said. At the same point in last year’s flu season, there had been 84 flu-related deaths in children.
In a separate report, the CDC said that, based on data collected from Nov. 23, 2018 to Feb. 2, 2019, “the influenza vaccine has been 47% effective in preventing medically attended acute respiratory virus infection across all age groups and specifically was 46% effective in preventing medical visits associated with influenza A(H1N1)pdm09.” The effectiveness of the vaccine was 61% for children aged 6 months to 17 years, the CDC said (MMWR. 2019 Feb 15;68[6];135-9).
Flu vaccination during the 2017-2018 season prevented 7.1 million illnesses, 3.7 million medical visits, 109,000 hospitalizations, and 8,000 flu-related deaths, the CDC said, adding that “vaccination has been found to reduce deaths, intensive care unit admissions and length of stay, and overall duration of hospitalization among hospitalized influenza patients.”
Forecasts for the rest of the 2018-2019 season “predict that elevated influenza activity in parts of the United States will continue for several more weeks,” the CDC said.
Like an unwelcome guest, the 2018-2019 flu season seems to be settling in for a lengthy stay as three more states have reached the highest level of influenza-like illness (ILI) activity, according to the Centers for Disease Control and Prevention.
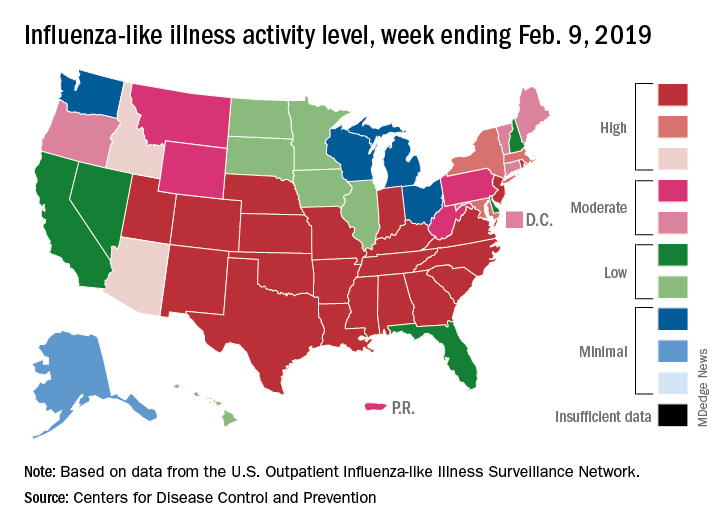
There are now 21 states at level 10 on the CDC’s 1-10 scale, with the South showing up almost solidly red on the flu activity map for the week ending Feb. 9. Another five states are at levels 8 and 9, bringing the total in the high range to 26 for the week, compared with 24 the previous week, the CDC’s influenza division reported Feb. 15.
National activity, reflected in the proportion of outpatient visits involving ILI, took a step up from 4.3% the week before to 4.8% for the week ending Feb. 9. The national baseline rate is 2.2% for ILI, which the CDC defines “as fever (temperature of 100°F [37.8°C] or greater) and cough and/or sore throat.”
Two flu-related pediatric deaths occurred during the week ending Feb. 9, and another four were reported from earlier weeks, which brings the total for the 2018-2019 season to 34, the CDC said. At the same point in last year’s flu season, there had been 84 flu-related deaths in children.
In a separate report, the CDC said that, based on data collected from Nov. 23, 2018 to Feb. 2, 2019, “the influenza vaccine has been 47% effective in preventing medically attended acute respiratory virus infection across all age groups and specifically was 46% effective in preventing medical visits associated with influenza A(H1N1)pdm09.” The effectiveness of the vaccine was 61% for children aged 6 months to 17 years, the CDC said (MMWR. 2019 Feb 15;68[6];135-9).
Flu vaccination during the 2017-2018 season prevented 7.1 million illnesses, 3.7 million medical visits, 109,000 hospitalizations, and 8,000 flu-related deaths, the CDC said, adding that “vaccination has been found to reduce deaths, intensive care unit admissions and length of stay, and overall duration of hospitalization among hospitalized influenza patients.”
Forecasts for the rest of the 2018-2019 season “predict that elevated influenza activity in parts of the United States will continue for several more weeks,” the CDC said.
CMS proposes coverage of CAR T-cell therapy in trials
The Centers for Medicare & Medicaid Services has proposed to cover chimeric antigen receptor (CAR) T-cell therapy for cancer patients participating in clinical trials that study the treatment’s effectiveness, according to a Feb. 15 announcement.
The proposed national coverage determination would require CMS to cover CAR T-cell therapies nationwide when the treatment is offered in CMS-approved registries or clinical studies in which patients are monitored for 2 or more years following treatment.
Results from the studies would help CMS identify which patients benefit most from CAR T-cell therapies and inform future coverage decisions, CMS Administrator Seema Verma said.
“CAR T-cell therapy was the first FDA-approved gene therapy, marking the beginning of an entirely new approach to treating serious and even life-threatening diseases,” Ms. Verma said in a statement. “Today’s proposed coverage decision would improve access to this therapy while deepening CMS’s understanding of how patients in Medicare respond to it, so the agency can ensure that it is paying for CAR T-cell therapy for cases in which the benefits outweigh the risks.”
As part of the proposal, CMS would cover autologous treatment with T cells expressing at least one chimeric antigen receptor (CAR) through coverage with evidence development when prescribed by a treating oncologist and performed in a hospital, according to a summary of the proposal.
The patient and hospital must meet specific criteria to be eligible for coverage, including that patients have relapsed or refractory cancer and do not have a comorbidity that would otherwise preclude patient benefit.
Hospitals, meanwhile, must have a cellular therapy program consisting of an integrated medical team that includes a clinical program director, a quality manager, and at least one physician experienced in cellular therapy, among other requirements.
CMS also would require that treatment is an FDA-approved biologic, providing targeted therapy for a known antigen expressed in the patient’s cancer according to an FDA indication. Repeat treatment would be covered only when a new primary cancer diagnosis is made by the treating oncologist and certain patient conditions are met.
Both inpatient and outpatient settings for the CAR T-cell therapy treatment are acceptable under the proposal. In either case, the patient and the hospital must be participating in a prospective, national, audited registry that consecutively enrolls patients, accepts all manufactured products, follows the patient for at least 2 years, and addresses a set of approved evidence-development questions. Additionally, all registries must be reviewed and approved by CMS.
The proposed national coverage determination was the result of an Aug. 22, 2018 meeting of the Medicare Evidence Development & Coverage Advisory Committee. The committee provides CMS with an external assessment of the appropriateness of therapies under review.
Public comments about the CAR T-cell therapy proposal will be accepted online here until March 15. A final decision on the proposal is expected by May 2019.
The agency’s proposal follows an Aug. 17 final rule by CMS that sets a new payment scheme for inpatient administration of two CAR T-cell therapies. The rule categorizes CAR T-cell therapies under the umbrella of the renamed Medicare Severity–Diagnosis Related Groups 016 – Autologous Bone Marrow Transplant with CC/MCC or T-cell Immunotherapy – and assigns ICD-10 PCS procedure codes XW033C3 and XW043C3 to the use of axicabtagene ciloleucel (Yescarta) and tisagenlecleucel (Kymriah) in the inpatient setting for fiscal year 2019, which began in October 2018. CMS also approved a temporary New Technology Add-On Payment for use of the therapies with a maximum threshold of $186,500.
In April 2018, CMS announced payment rates for outpatient administration of the two drugs, settling on $395,380 for axicabtagene ciloleucel and $500,839 for tisagenlecleucel. The two medications have list prices of $373,000 and $475,000, respectively.
The Centers for Medicare & Medicaid Services has proposed to cover chimeric antigen receptor (CAR) T-cell therapy for cancer patients participating in clinical trials that study the treatment’s effectiveness, according to a Feb. 15 announcement.
The proposed national coverage determination would require CMS to cover CAR T-cell therapies nationwide when the treatment is offered in CMS-approved registries or clinical studies in which patients are monitored for 2 or more years following treatment.
Results from the studies would help CMS identify which patients benefit most from CAR T-cell therapies and inform future coverage decisions, CMS Administrator Seema Verma said.
“CAR T-cell therapy was the first FDA-approved gene therapy, marking the beginning of an entirely new approach to treating serious and even life-threatening diseases,” Ms. Verma said in a statement. “Today’s proposed coverage decision would improve access to this therapy while deepening CMS’s understanding of how patients in Medicare respond to it, so the agency can ensure that it is paying for CAR T-cell therapy for cases in which the benefits outweigh the risks.”
As part of the proposal, CMS would cover autologous treatment with T cells expressing at least one chimeric antigen receptor (CAR) through coverage with evidence development when prescribed by a treating oncologist and performed in a hospital, according to a summary of the proposal.
The patient and hospital must meet specific criteria to be eligible for coverage, including that patients have relapsed or refractory cancer and do not have a comorbidity that would otherwise preclude patient benefit.
Hospitals, meanwhile, must have a cellular therapy program consisting of an integrated medical team that includes a clinical program director, a quality manager, and at least one physician experienced in cellular therapy, among other requirements.
CMS also would require that treatment is an FDA-approved biologic, providing targeted therapy for a known antigen expressed in the patient’s cancer according to an FDA indication. Repeat treatment would be covered only when a new primary cancer diagnosis is made by the treating oncologist and certain patient conditions are met.
Both inpatient and outpatient settings for the CAR T-cell therapy treatment are acceptable under the proposal. In either case, the patient and the hospital must be participating in a prospective, national, audited registry that consecutively enrolls patients, accepts all manufactured products, follows the patient for at least 2 years, and addresses a set of approved evidence-development questions. Additionally, all registries must be reviewed and approved by CMS.
The proposed national coverage determination was the result of an Aug. 22, 2018 meeting of the Medicare Evidence Development & Coverage Advisory Committee. The committee provides CMS with an external assessment of the appropriateness of therapies under review.
Public comments about the CAR T-cell therapy proposal will be accepted online here until March 15. A final decision on the proposal is expected by May 2019.
The agency’s proposal follows an Aug. 17 final rule by CMS that sets a new payment scheme for inpatient administration of two CAR T-cell therapies. The rule categorizes CAR T-cell therapies under the umbrella of the renamed Medicare Severity–Diagnosis Related Groups 016 – Autologous Bone Marrow Transplant with CC/MCC or T-cell Immunotherapy – and assigns ICD-10 PCS procedure codes XW033C3 and XW043C3 to the use of axicabtagene ciloleucel (Yescarta) and tisagenlecleucel (Kymriah) in the inpatient setting for fiscal year 2019, which began in October 2018. CMS also approved a temporary New Technology Add-On Payment for use of the therapies with a maximum threshold of $186,500.
In April 2018, CMS announced payment rates for outpatient administration of the two drugs, settling on $395,380 for axicabtagene ciloleucel and $500,839 for tisagenlecleucel. The two medications have list prices of $373,000 and $475,000, respectively.
The Centers for Medicare & Medicaid Services has proposed to cover chimeric antigen receptor (CAR) T-cell therapy for cancer patients participating in clinical trials that study the treatment’s effectiveness, according to a Feb. 15 announcement.
The proposed national coverage determination would require CMS to cover CAR T-cell therapies nationwide when the treatment is offered in CMS-approved registries or clinical studies in which patients are monitored for 2 or more years following treatment.
Results from the studies would help CMS identify which patients benefit most from CAR T-cell therapies and inform future coverage decisions, CMS Administrator Seema Verma said.
“CAR T-cell therapy was the first FDA-approved gene therapy, marking the beginning of an entirely new approach to treating serious and even life-threatening diseases,” Ms. Verma said in a statement. “Today’s proposed coverage decision would improve access to this therapy while deepening CMS’s understanding of how patients in Medicare respond to it, so the agency can ensure that it is paying for CAR T-cell therapy for cases in which the benefits outweigh the risks.”
As part of the proposal, CMS would cover autologous treatment with T cells expressing at least one chimeric antigen receptor (CAR) through coverage with evidence development when prescribed by a treating oncologist and performed in a hospital, according to a summary of the proposal.
The patient and hospital must meet specific criteria to be eligible for coverage, including that patients have relapsed or refractory cancer and do not have a comorbidity that would otherwise preclude patient benefit.
Hospitals, meanwhile, must have a cellular therapy program consisting of an integrated medical team that includes a clinical program director, a quality manager, and at least one physician experienced in cellular therapy, among other requirements.
CMS also would require that treatment is an FDA-approved biologic, providing targeted therapy for a known antigen expressed in the patient’s cancer according to an FDA indication. Repeat treatment would be covered only when a new primary cancer diagnosis is made by the treating oncologist and certain patient conditions are met.
Both inpatient and outpatient settings for the CAR T-cell therapy treatment are acceptable under the proposal. In either case, the patient and the hospital must be participating in a prospective, national, audited registry that consecutively enrolls patients, accepts all manufactured products, follows the patient for at least 2 years, and addresses a set of approved evidence-development questions. Additionally, all registries must be reviewed and approved by CMS.
The proposed national coverage determination was the result of an Aug. 22, 2018 meeting of the Medicare Evidence Development & Coverage Advisory Committee. The committee provides CMS with an external assessment of the appropriateness of therapies under review.
Public comments about the CAR T-cell therapy proposal will be accepted online here until March 15. A final decision on the proposal is expected by May 2019.
The agency’s proposal follows an Aug. 17 final rule by CMS that sets a new payment scheme for inpatient administration of two CAR T-cell therapies. The rule categorizes CAR T-cell therapies under the umbrella of the renamed Medicare Severity–Diagnosis Related Groups 016 – Autologous Bone Marrow Transplant with CC/MCC or T-cell Immunotherapy – and assigns ICD-10 PCS procedure codes XW033C3 and XW043C3 to the use of axicabtagene ciloleucel (Yescarta) and tisagenlecleucel (Kymriah) in the inpatient setting for fiscal year 2019, which began in October 2018. CMS also approved a temporary New Technology Add-On Payment for use of the therapies with a maximum threshold of $186,500.
In April 2018, CMS announced payment rates for outpatient administration of the two drugs, settling on $395,380 for axicabtagene ciloleucel and $500,839 for tisagenlecleucel. The two medications have list prices of $373,000 and $475,000, respectively.