User login
Possible mechanism for fluoroquinolone-induced aortopathy uncovered
A new study finds that patients taking fluoroquinolone antibiotics may be at higher risk of aortopathy in part because of human aortic myofibroblast–mediated extracellular matrix (ECM) dysregulation.
“Emerging evidence supports pharmacologic-associated aortopathy in patients receiving fluoroquinolone [FQ] antibiotics,” said first author David G. Guzzardi, PhD, and his colleagues, citing previous research showing that, “compared with patients receiving amoxicillin antibiotics, those receiving FQ have a 66% higher risk of aneurysm or dissection within a 2-month period after commencing FQ use.”
Based upon such data, the Food and Drug Administration issued a December 2018 warning about the increased risk of ruptures or tears in the aorta with fluoroquinolone antibiotics in certain patients, updating their May 2017 warning regarding “disabling and potentially permanent side effects of the tendons, muscles, joints, nerves, and central nervous system that can occur together in the same patient,” upon exposure to this class of antibiotics. Earlier in 2018, the FDA had reinforced their safety information about serious and potentially fatal low blood sugar levels and mental health side effects with fluoroquinolone antibiotics.
Dr. Guzzardi and his colleagues at the University of Calgary (Alta.) performed a study to attempt to determine the possible cellular mechanisms for the observed aortopathy. In their study published in the Journal of Thoracic and Cardiovascular Surgery, Dr. Guzzardi and his colleagues isolated human aortic myofibroblasts from nine patients with aortopathy who were undergoing elective ascending aortic resection.
Following exposure of cells to FQ, the researchers assessed secreted matrix metalloproteinases relative to tissue inhibitors of matrix metalloproteinases (TIMPs). In addition, they examined ECM degradation by using a three-dimensional gelatin-fluorescein isothiocyanate fluorescence microgel assay. Aortic cellular collagen type I expression following FQ exposure was determined by immunoblotting and immunofluorescent staining. Dr. Guzzardi and his colleagues also looked at cell apoptosis, necrosis, and metabolic viability using two versions of vital staining.
They found that FQ exposure significantly decreased aortic cell TIMP-1 (P less than .004) and TIMP-2 (P less than .0004) protein expression, compared with controls, and the ratio of matrix metalloproteinase 9/TIMP-2 was increased (P less than .01). This suggests an increased capacity for ECM degradation after FQ exposure, according to the researchers.
In addition, FQ exposure attenuated collagen type I expression as assessed by immunoblotting (P less than .002) and immunofluorescence (P less than .02).
“FQ induces human aortic myofibroblast–mediated ECM dysregulation by decreasing TIMP expression and preventing compensatory collagen deposition. These data provide novel insights into the mechanisms that may underlie the clinical association of FQ exposure and increased risk of acute aortic events in the community. Our data suggest cautious use of FQ in selected patient populations with preexistent aortopathy and connective tissue disorders,” the researchers concluded.
In an accompanying editorial, while warning that these are preliminary observations based upon a small number of patients with aortopathy, Ari A. Mennander, MD, PhD, of Tampere (Finland) University, wrote that, “for the first time, the wild theory of fluoroquinolone-associated aortopathy has a molecular hint that is based on collagen degeneration and progression of aortic disease. ... This theory is in line with previous observations revealing antifibrotic activity and decreased collagen-1 protein expression with fluoroquinolones. The enigmatic puzzle of the progression of some aortic events may alarmingly be iatrogenic, and the clinician may wisely consider a prudent use of fluoroquinolones in patients with aortic dilatation.”
The authors and commentators reported that they had no commercial conflicts to disclose.
SOURCE: Guzzardi DG et al. J Thorac Cardiovasc Surg. 2019;157:109-19.
The issue of fluoroquinolones is certainly of concern. I wonder how many of my patients who have suffered a ruptured aneurysm were on one of these drugs? In the last few years, Cipro (ciprofloxacin) and Levaquin (levofloxacin) were commonly used by our family practice and internal medicine colleagues for almost all outpatient infections. It was so common that even my wife, who is not a physician, would request Cipro whenever she had a sneeze. We would also bring large bottles of Cipro every time we went traveling to some exotic destination, reassuring ourselves that the only “runs” we would have would be in the airport trying to catch a flight. A cousin of mine, prescribed Levaquin by a well-meaning physician while he was cruising the Nile River, ruptured his Achilles tendon.
Russell H. Samson, MD, FACS, DFSVS , is a clinical professor of surgery at Florida State University, Sarasota, a senior surgeon at Sarasota Vascular Specialists, and President of the Mote Vascular Foundation.
The issue of fluoroquinolones is certainly of concern. I wonder how many of my patients who have suffered a ruptured aneurysm were on one of these drugs? In the last few years, Cipro (ciprofloxacin) and Levaquin (levofloxacin) were commonly used by our family practice and internal medicine colleagues for almost all outpatient infections. It was so common that even my wife, who is not a physician, would request Cipro whenever she had a sneeze. We would also bring large bottles of Cipro every time we went traveling to some exotic destination, reassuring ourselves that the only “runs” we would have would be in the airport trying to catch a flight. A cousin of mine, prescribed Levaquin by a well-meaning physician while he was cruising the Nile River, ruptured his Achilles tendon.
Russell H. Samson, MD, FACS, DFSVS , is a clinical professor of surgery at Florida State University, Sarasota, a senior surgeon at Sarasota Vascular Specialists, and President of the Mote Vascular Foundation.
The issue of fluoroquinolones is certainly of concern. I wonder how many of my patients who have suffered a ruptured aneurysm were on one of these drugs? In the last few years, Cipro (ciprofloxacin) and Levaquin (levofloxacin) were commonly used by our family practice and internal medicine colleagues for almost all outpatient infections. It was so common that even my wife, who is not a physician, would request Cipro whenever she had a sneeze. We would also bring large bottles of Cipro every time we went traveling to some exotic destination, reassuring ourselves that the only “runs” we would have would be in the airport trying to catch a flight. A cousin of mine, prescribed Levaquin by a well-meaning physician while he was cruising the Nile River, ruptured his Achilles tendon.
Russell H. Samson, MD, FACS, DFSVS , is a clinical professor of surgery at Florida State University, Sarasota, a senior surgeon at Sarasota Vascular Specialists, and President of the Mote Vascular Foundation.
A new study finds that patients taking fluoroquinolone antibiotics may be at higher risk of aortopathy in part because of human aortic myofibroblast–mediated extracellular matrix (ECM) dysregulation.
“Emerging evidence supports pharmacologic-associated aortopathy in patients receiving fluoroquinolone [FQ] antibiotics,” said first author David G. Guzzardi, PhD, and his colleagues, citing previous research showing that, “compared with patients receiving amoxicillin antibiotics, those receiving FQ have a 66% higher risk of aneurysm or dissection within a 2-month period after commencing FQ use.”
Based upon such data, the Food and Drug Administration issued a December 2018 warning about the increased risk of ruptures or tears in the aorta with fluoroquinolone antibiotics in certain patients, updating their May 2017 warning regarding “disabling and potentially permanent side effects of the tendons, muscles, joints, nerves, and central nervous system that can occur together in the same patient,” upon exposure to this class of antibiotics. Earlier in 2018, the FDA had reinforced their safety information about serious and potentially fatal low blood sugar levels and mental health side effects with fluoroquinolone antibiotics.
Dr. Guzzardi and his colleagues at the University of Calgary (Alta.) performed a study to attempt to determine the possible cellular mechanisms for the observed aortopathy. In their study published in the Journal of Thoracic and Cardiovascular Surgery, Dr. Guzzardi and his colleagues isolated human aortic myofibroblasts from nine patients with aortopathy who were undergoing elective ascending aortic resection.
Following exposure of cells to FQ, the researchers assessed secreted matrix metalloproteinases relative to tissue inhibitors of matrix metalloproteinases (TIMPs). In addition, they examined ECM degradation by using a three-dimensional gelatin-fluorescein isothiocyanate fluorescence microgel assay. Aortic cellular collagen type I expression following FQ exposure was determined by immunoblotting and immunofluorescent staining. Dr. Guzzardi and his colleagues also looked at cell apoptosis, necrosis, and metabolic viability using two versions of vital staining.
They found that FQ exposure significantly decreased aortic cell TIMP-1 (P less than .004) and TIMP-2 (P less than .0004) protein expression, compared with controls, and the ratio of matrix metalloproteinase 9/TIMP-2 was increased (P less than .01). This suggests an increased capacity for ECM degradation after FQ exposure, according to the researchers.
In addition, FQ exposure attenuated collagen type I expression as assessed by immunoblotting (P less than .002) and immunofluorescence (P less than .02).
“FQ induces human aortic myofibroblast–mediated ECM dysregulation by decreasing TIMP expression and preventing compensatory collagen deposition. These data provide novel insights into the mechanisms that may underlie the clinical association of FQ exposure and increased risk of acute aortic events in the community. Our data suggest cautious use of FQ in selected patient populations with preexistent aortopathy and connective tissue disorders,” the researchers concluded.
In an accompanying editorial, while warning that these are preliminary observations based upon a small number of patients with aortopathy, Ari A. Mennander, MD, PhD, of Tampere (Finland) University, wrote that, “for the first time, the wild theory of fluoroquinolone-associated aortopathy has a molecular hint that is based on collagen degeneration and progression of aortic disease. ... This theory is in line with previous observations revealing antifibrotic activity and decreased collagen-1 protein expression with fluoroquinolones. The enigmatic puzzle of the progression of some aortic events may alarmingly be iatrogenic, and the clinician may wisely consider a prudent use of fluoroquinolones in patients with aortic dilatation.”
The authors and commentators reported that they had no commercial conflicts to disclose.
SOURCE: Guzzardi DG et al. J Thorac Cardiovasc Surg. 2019;157:109-19.
A new study finds that patients taking fluoroquinolone antibiotics may be at higher risk of aortopathy in part because of human aortic myofibroblast–mediated extracellular matrix (ECM) dysregulation.
“Emerging evidence supports pharmacologic-associated aortopathy in patients receiving fluoroquinolone [FQ] antibiotics,” said first author David G. Guzzardi, PhD, and his colleagues, citing previous research showing that, “compared with patients receiving amoxicillin antibiotics, those receiving FQ have a 66% higher risk of aneurysm or dissection within a 2-month period after commencing FQ use.”
Based upon such data, the Food and Drug Administration issued a December 2018 warning about the increased risk of ruptures or tears in the aorta with fluoroquinolone antibiotics in certain patients, updating their May 2017 warning regarding “disabling and potentially permanent side effects of the tendons, muscles, joints, nerves, and central nervous system that can occur together in the same patient,” upon exposure to this class of antibiotics. Earlier in 2018, the FDA had reinforced their safety information about serious and potentially fatal low blood sugar levels and mental health side effects with fluoroquinolone antibiotics.
Dr. Guzzardi and his colleagues at the University of Calgary (Alta.) performed a study to attempt to determine the possible cellular mechanisms for the observed aortopathy. In their study published in the Journal of Thoracic and Cardiovascular Surgery, Dr. Guzzardi and his colleagues isolated human aortic myofibroblasts from nine patients with aortopathy who were undergoing elective ascending aortic resection.
Following exposure of cells to FQ, the researchers assessed secreted matrix metalloproteinases relative to tissue inhibitors of matrix metalloproteinases (TIMPs). In addition, they examined ECM degradation by using a three-dimensional gelatin-fluorescein isothiocyanate fluorescence microgel assay. Aortic cellular collagen type I expression following FQ exposure was determined by immunoblotting and immunofluorescent staining. Dr. Guzzardi and his colleagues also looked at cell apoptosis, necrosis, and metabolic viability using two versions of vital staining.
They found that FQ exposure significantly decreased aortic cell TIMP-1 (P less than .004) and TIMP-2 (P less than .0004) protein expression, compared with controls, and the ratio of matrix metalloproteinase 9/TIMP-2 was increased (P less than .01). This suggests an increased capacity for ECM degradation after FQ exposure, according to the researchers.
In addition, FQ exposure attenuated collagen type I expression as assessed by immunoblotting (P less than .002) and immunofluorescence (P less than .02).
“FQ induces human aortic myofibroblast–mediated ECM dysregulation by decreasing TIMP expression and preventing compensatory collagen deposition. These data provide novel insights into the mechanisms that may underlie the clinical association of FQ exposure and increased risk of acute aortic events in the community. Our data suggest cautious use of FQ in selected patient populations with preexistent aortopathy and connective tissue disorders,” the researchers concluded.
In an accompanying editorial, while warning that these are preliminary observations based upon a small number of patients with aortopathy, Ari A. Mennander, MD, PhD, of Tampere (Finland) University, wrote that, “for the first time, the wild theory of fluoroquinolone-associated aortopathy has a molecular hint that is based on collagen degeneration and progression of aortic disease. ... This theory is in line with previous observations revealing antifibrotic activity and decreased collagen-1 protein expression with fluoroquinolones. The enigmatic puzzle of the progression of some aortic events may alarmingly be iatrogenic, and the clinician may wisely consider a prudent use of fluoroquinolones in patients with aortic dilatation.”
The authors and commentators reported that they had no commercial conflicts to disclose.
SOURCE: Guzzardi DG et al. J Thorac Cardiovasc Surg. 2019;157:109-19.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Growing Painful Nodule on the Lower Lip
The Diagnosis: Verrucous Carcinoma
An excisional biopsy revealed an endophytic and exophytic squamous proliferation with a papillomatous growth pattern, bulbous pushing border, and confluent parakeratosis (Figure). No fungal organisms were seen. Due to clinical and histological findings, a diagnosis of verrucous carcinoma (VC) was made.
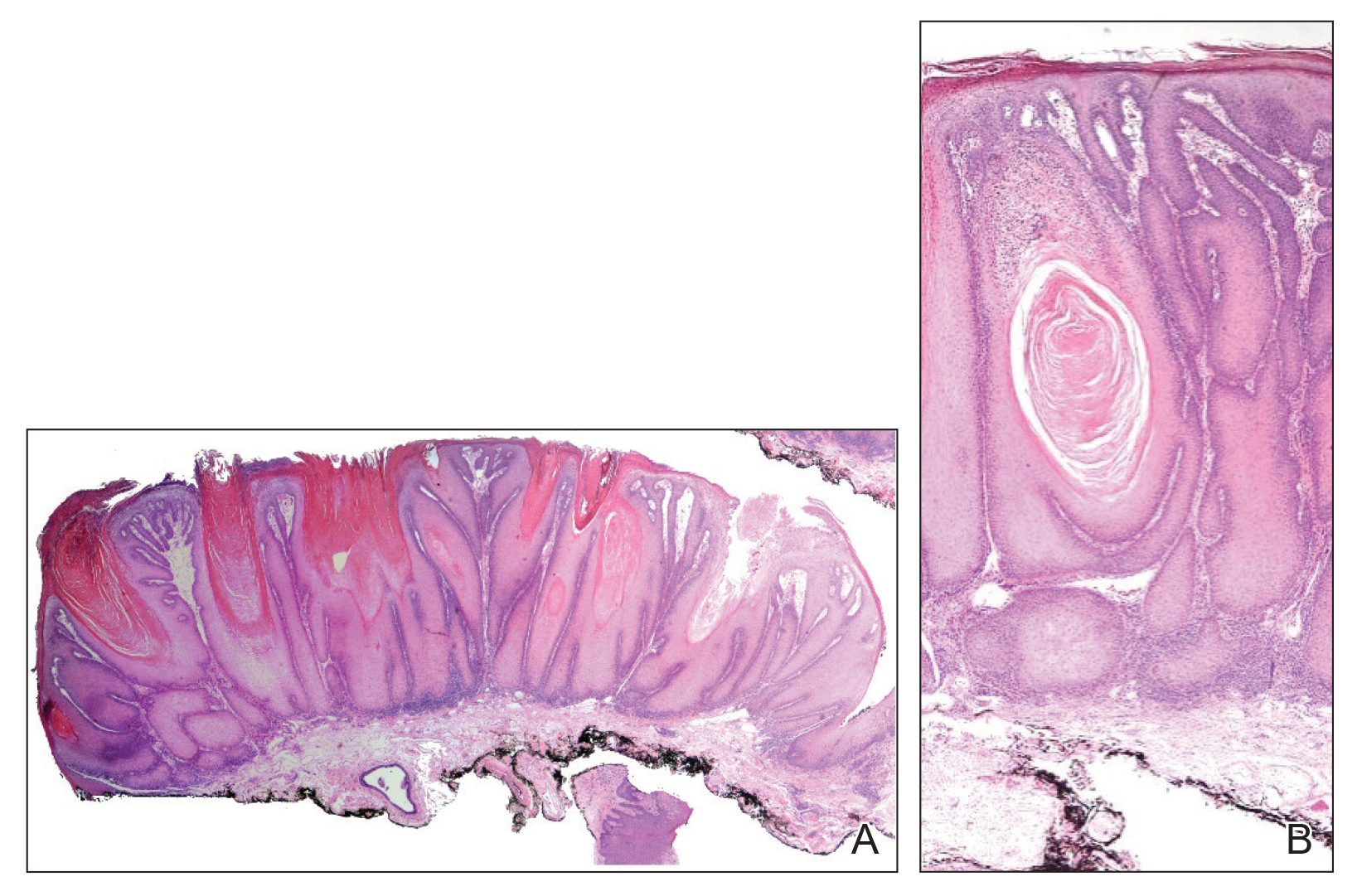
Verrucous carcinoma is a rare variant of squamous cell carcinoma (SCC) with specific clinical and histological features.1 These tumors have a slow and localized growth pattern but can be locally aggressive. Metastasis of VC is rare, giving VC an overall good prognosis, with a 5-year survival rate greater than 75%.2 Verrucous carcinoma typically occurs in 1 of 3 locations: the oropharynx, genitals, or soles of the feet. Depending on the site of involvement, various names have been used in the literature to describe this entity, including Ackerman tumor (solitary oral mucosal lesion), Buschke-Lowenstein tumor (genital involvement), florid oral papillomatosis (multiple oral lesions), and carcinoma cuniculatum (sole of the foot).3 The most common sites for VC in the oral cavity are the buccal mucosa and gingiva.4
Verrucous carcinoma occurs more often among men in the sixth decade of life.3 The etiology of oral VC remains unclear; however, use of chewing tobacco, chemical carcinogens, chronic irritation, human papillomavirus (HPV), and poor oral hygiene have been reported as predisposing risk factors.4,5 The role of HPV in the pathogenesis of VC remains controversial, but both low-risk types HPV-6 and HPV-11 and high-risk types HPV-16 and HPV-18 have been found in association with VC.5,6
Clinically, oral VC lesions most often present as pink-white erythematous papules or plaques with exophytic cauliflowerlike surface alterations. Although the tumors are slow growing with little risk for metastasis, they may be locally invasive with deep involvement of the surrounding
structures.1 Histopathologically, VC displays proliferation of the epithelium with downward growth into the connective tissue but usually without a pattern of true invasion. The epithelium is well differentiated and displays little pleomorphism or mitoses.5,7 Obtaining a generous biopsy specimen is essential to view the diagnostic architecture of VC and rule out other entities, such as viral verruca, blastomycosis, SCC, and verruciform xanthoma. Squamous cell carcinoma characteristically has a more infiltrative border as opposed to the bulbous border of VC. In addition, the distribution of p53 and Ki-67 staining differs between SCC and VC. Squamous cell carcinoma shows positive p53 and Ki-67 staining for the full thickness of the epidermis, while VC has positive staining only in the lower third of the epidermis.5
Surgical resection is considered the first-line treatment of VC through excision or Mohs micrographic surgery. Radiation therapy is controversial due to the risk for anaplastic transformation. When surgery is not ideal due to the tumor size or location or the patient’s preference, other treatment modalities with reported success include intralesional interferon alfa; cryosurgery; topical imiquimod; and topical or systemic cytostatic agents such as bleomycin, 5-fluorouracil, cisplatin, or methotrexate.1,2
- Pattee SF, Bordeaux J, Mahalingam M, et al. Verrucous carcinoma of the scalp. J Am Acad Dermatol. 2006;56:506-508.
- Nikkels AF, Thirion L, Quatresooz P, et al. Photodynamic therapy for cutaneous verrucous carcinoma. J Am Acad Dermatol. 2007;57:516-519.
- Ho J, Diven DG, Butler PJ, et al. An ulcerating verrucous plaque on the foot. Arch Dermatol. 2000;136:547-552.
- Sonalika WG, Anand T. Oral verrucous carcinoma: a retrospective analysis for clinicopathologic features. J Cancer Res Ther. 2016;12:142-145.
- Dubina M, Goldenberg G. Viral-associated nonmelanoma skin cancers: a review. Am J Dermatopathol. 2009;31:561-573.
- Geusau A, Heinz-Peer G, Volc-Platzer B, et al. Regression of deeply infiltrating giant condyloma (Buschke-Lowenstein tumor) following long-term intralesional interferon alpha therapy. Arch Dermatol. 2000;136:707-710.
- Ansai S, Kimura T, Hayashi M. Fatal genital verrucous carcinoma. Am J Dermatopathol. 2007;29:68-71.
The Diagnosis: Verrucous Carcinoma
An excisional biopsy revealed an endophytic and exophytic squamous proliferation with a papillomatous growth pattern, bulbous pushing border, and confluent parakeratosis (Figure). No fungal organisms were seen. Due to clinical and histological findings, a diagnosis of verrucous carcinoma (VC) was made.
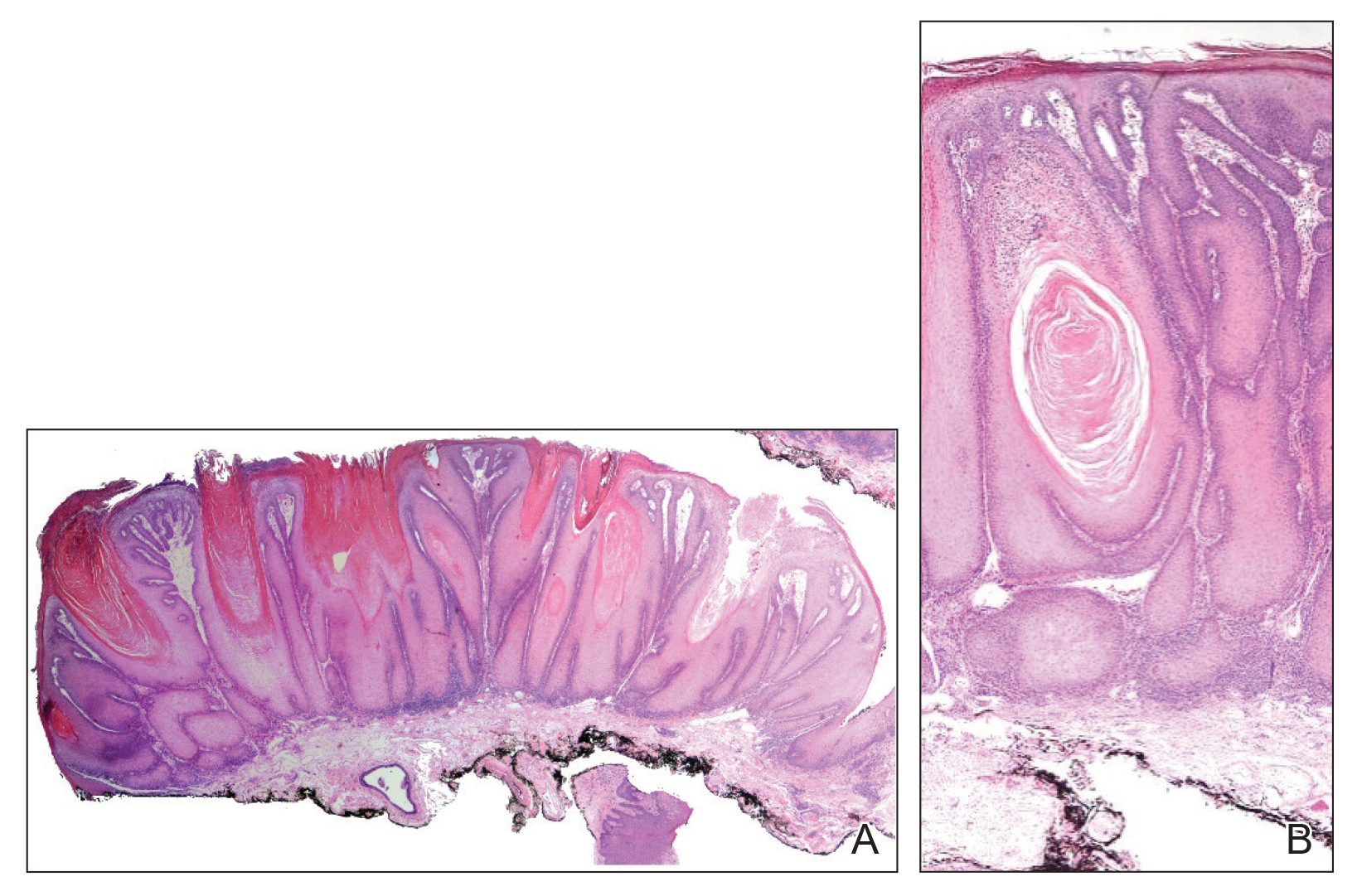
Verrucous carcinoma is a rare variant of squamous cell carcinoma (SCC) with specific clinical and histological features.1 These tumors have a slow and localized growth pattern but can be locally aggressive. Metastasis of VC is rare, giving VC an overall good prognosis, with a 5-year survival rate greater than 75%.2 Verrucous carcinoma typically occurs in 1 of 3 locations: the oropharynx, genitals, or soles of the feet. Depending on the site of involvement, various names have been used in the literature to describe this entity, including Ackerman tumor (solitary oral mucosal lesion), Buschke-Lowenstein tumor (genital involvement), florid oral papillomatosis (multiple oral lesions), and carcinoma cuniculatum (sole of the foot).3 The most common sites for VC in the oral cavity are the buccal mucosa and gingiva.4
Verrucous carcinoma occurs more often among men in the sixth decade of life.3 The etiology of oral VC remains unclear; however, use of chewing tobacco, chemical carcinogens, chronic irritation, human papillomavirus (HPV), and poor oral hygiene have been reported as predisposing risk factors.4,5 The role of HPV in the pathogenesis of VC remains controversial, but both low-risk types HPV-6 and HPV-11 and high-risk types HPV-16 and HPV-18 have been found in association with VC.5,6
Clinically, oral VC lesions most often present as pink-white erythematous papules or plaques with exophytic cauliflowerlike surface alterations. Although the tumors are slow growing with little risk for metastasis, they may be locally invasive with deep involvement of the surrounding
structures.1 Histopathologically, VC displays proliferation of the epithelium with downward growth into the connective tissue but usually without a pattern of true invasion. The epithelium is well differentiated and displays little pleomorphism or mitoses.5,7 Obtaining a generous biopsy specimen is essential to view the diagnostic architecture of VC and rule out other entities, such as viral verruca, blastomycosis, SCC, and verruciform xanthoma. Squamous cell carcinoma characteristically has a more infiltrative border as opposed to the bulbous border of VC. In addition, the distribution of p53 and Ki-67 staining differs between SCC and VC. Squamous cell carcinoma shows positive p53 and Ki-67 staining for the full thickness of the epidermis, while VC has positive staining only in the lower third of the epidermis.5
Surgical resection is considered the first-line treatment of VC through excision or Mohs micrographic surgery. Radiation therapy is controversial due to the risk for anaplastic transformation. When surgery is not ideal due to the tumor size or location or the patient’s preference, other treatment modalities with reported success include intralesional interferon alfa; cryosurgery; topical imiquimod; and topical or systemic cytostatic agents such as bleomycin, 5-fluorouracil, cisplatin, or methotrexate.1,2
The Diagnosis: Verrucous Carcinoma
An excisional biopsy revealed an endophytic and exophytic squamous proliferation with a papillomatous growth pattern, bulbous pushing border, and confluent parakeratosis (Figure). No fungal organisms were seen. Due to clinical and histological findings, a diagnosis of verrucous carcinoma (VC) was made.
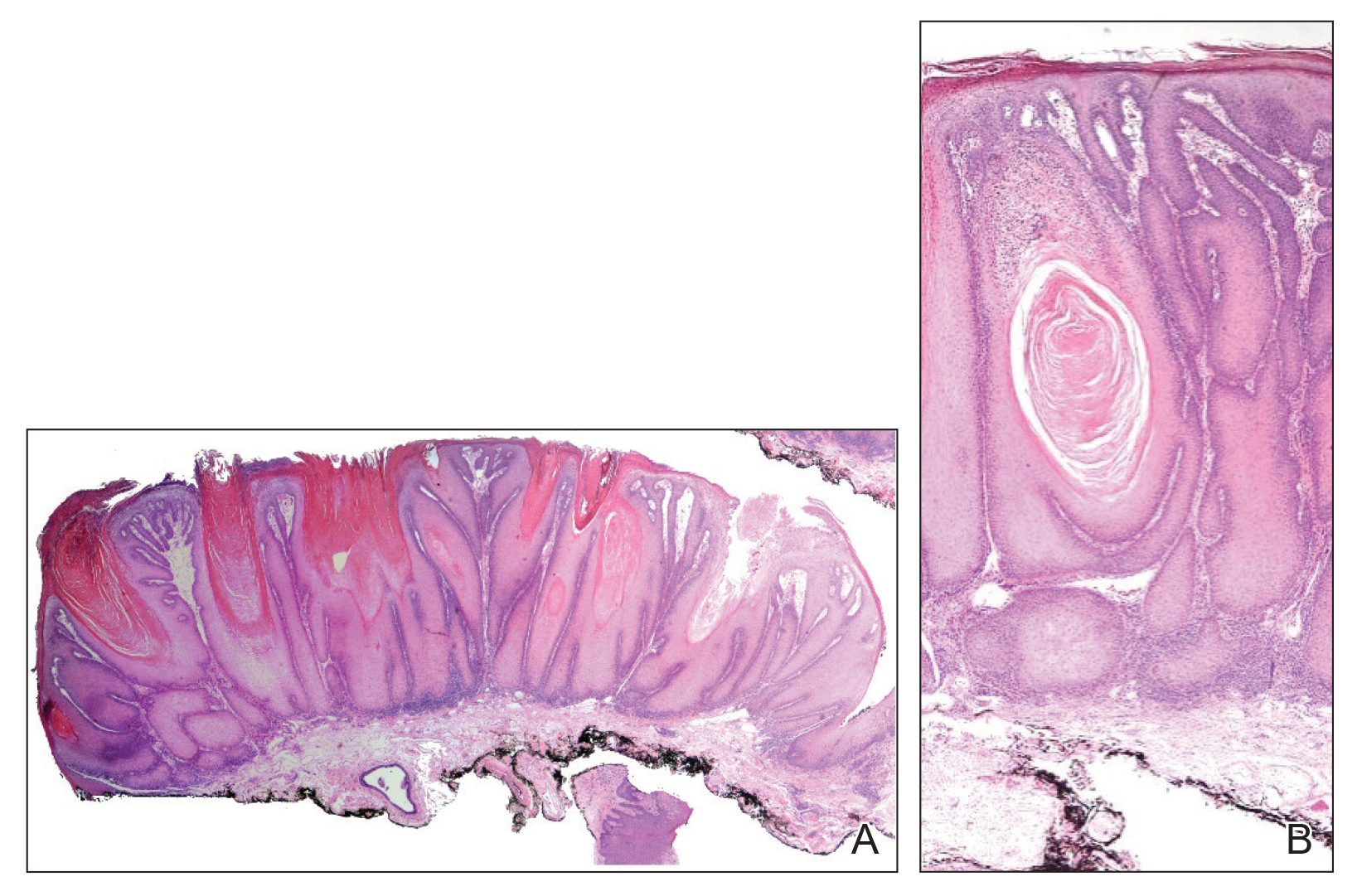
Verrucous carcinoma is a rare variant of squamous cell carcinoma (SCC) with specific clinical and histological features.1 These tumors have a slow and localized growth pattern but can be locally aggressive. Metastasis of VC is rare, giving VC an overall good prognosis, with a 5-year survival rate greater than 75%.2 Verrucous carcinoma typically occurs in 1 of 3 locations: the oropharynx, genitals, or soles of the feet. Depending on the site of involvement, various names have been used in the literature to describe this entity, including Ackerman tumor (solitary oral mucosal lesion), Buschke-Lowenstein tumor (genital involvement), florid oral papillomatosis (multiple oral lesions), and carcinoma cuniculatum (sole of the foot).3 The most common sites for VC in the oral cavity are the buccal mucosa and gingiva.4
Verrucous carcinoma occurs more often among men in the sixth decade of life.3 The etiology of oral VC remains unclear; however, use of chewing tobacco, chemical carcinogens, chronic irritation, human papillomavirus (HPV), and poor oral hygiene have been reported as predisposing risk factors.4,5 The role of HPV in the pathogenesis of VC remains controversial, but both low-risk types HPV-6 and HPV-11 and high-risk types HPV-16 and HPV-18 have been found in association with VC.5,6
Clinically, oral VC lesions most often present as pink-white erythematous papules or plaques with exophytic cauliflowerlike surface alterations. Although the tumors are slow growing with little risk for metastasis, they may be locally invasive with deep involvement of the surrounding
structures.1 Histopathologically, VC displays proliferation of the epithelium with downward growth into the connective tissue but usually without a pattern of true invasion. The epithelium is well differentiated and displays little pleomorphism or mitoses.5,7 Obtaining a generous biopsy specimen is essential to view the diagnostic architecture of VC and rule out other entities, such as viral verruca, blastomycosis, SCC, and verruciform xanthoma. Squamous cell carcinoma characteristically has a more infiltrative border as opposed to the bulbous border of VC. In addition, the distribution of p53 and Ki-67 staining differs between SCC and VC. Squamous cell carcinoma shows positive p53 and Ki-67 staining for the full thickness of the epidermis, while VC has positive staining only in the lower third of the epidermis.5
Surgical resection is considered the first-line treatment of VC through excision or Mohs micrographic surgery. Radiation therapy is controversial due to the risk for anaplastic transformation. When surgery is not ideal due to the tumor size or location or the patient’s preference, other treatment modalities with reported success include intralesional interferon alfa; cryosurgery; topical imiquimod; and topical or systemic cytostatic agents such as bleomycin, 5-fluorouracil, cisplatin, or methotrexate.1,2
- Pattee SF, Bordeaux J, Mahalingam M, et al. Verrucous carcinoma of the scalp. J Am Acad Dermatol. 2006;56:506-508.
- Nikkels AF, Thirion L, Quatresooz P, et al. Photodynamic therapy for cutaneous verrucous carcinoma. J Am Acad Dermatol. 2007;57:516-519.
- Ho J, Diven DG, Butler PJ, et al. An ulcerating verrucous plaque on the foot. Arch Dermatol. 2000;136:547-552.
- Sonalika WG, Anand T. Oral verrucous carcinoma: a retrospective analysis for clinicopathologic features. J Cancer Res Ther. 2016;12:142-145.
- Dubina M, Goldenberg G. Viral-associated nonmelanoma skin cancers: a review. Am J Dermatopathol. 2009;31:561-573.
- Geusau A, Heinz-Peer G, Volc-Platzer B, et al. Regression of deeply infiltrating giant condyloma (Buschke-Lowenstein tumor) following long-term intralesional interferon alpha therapy. Arch Dermatol. 2000;136:707-710.
- Ansai S, Kimura T, Hayashi M. Fatal genital verrucous carcinoma. Am J Dermatopathol. 2007;29:68-71.
- Pattee SF, Bordeaux J, Mahalingam M, et al. Verrucous carcinoma of the scalp. J Am Acad Dermatol. 2006;56:506-508.
- Nikkels AF, Thirion L, Quatresooz P, et al. Photodynamic therapy for cutaneous verrucous carcinoma. J Am Acad Dermatol. 2007;57:516-519.
- Ho J, Diven DG, Butler PJ, et al. An ulcerating verrucous plaque on the foot. Arch Dermatol. 2000;136:547-552.
- Sonalika WG, Anand T. Oral verrucous carcinoma: a retrospective analysis for clinicopathologic features. J Cancer Res Ther. 2016;12:142-145.
- Dubina M, Goldenberg G. Viral-associated nonmelanoma skin cancers: a review. Am J Dermatopathol. 2009;31:561-573.
- Geusau A, Heinz-Peer G, Volc-Platzer B, et al. Regression of deeply infiltrating giant condyloma (Buschke-Lowenstein tumor) following long-term intralesional interferon alpha therapy. Arch Dermatol. 2000;136:707-710.
- Ansai S, Kimura T, Hayashi M. Fatal genital verrucous carcinoma. Am J Dermatopathol. 2007;29:68-71.

Enterovirus in at-risk children associated with later celiac disease
“We found a significant association between exposure to enterovirus and subsequent risk of celiac disease,” wrote lead author Christian R. Kahrs of the University of Oslo and his coauthors, adding that “adenovirus was not associated with celiac disease.” The study was published in the BMJ.
From 2001 to 2007, 46,939 newborns in Norway were screened for the HLA-DQ2/DQ8 genotype, which is associated with an increased risk of celiac disease. The genotype was identified in 912 children, and blood and stool sample collection began at 3 months. Children who were still contributing blood samples by 2014-2016 were invited to be screened for celiac disease.
Of the 220 children screened, 25 were diagnosed with celiac disease. Enterovirus was detected in 370 (17%) of the 2,135 stool samples and was more frequent in children who developed celiac disease antibodies than in matched controls (adjusted odds ratio, 1.49; 95% confidence interval, 1.07-2.06; P = .02). There was a significant association between later development of celiac disease and the commonly identified enterovirus A (aOR, 1.62; 95% CI, 1.04-2.53; P = .03) and enterovirus B (aOR, 2.27; 95% CI, 1.33-3.88; P = .003). No adenovirus types were associated with development of celiac disease.
The authors acknowledged their study’s limitations, including the possibility that children might be diagnosed with celiac disease later than the study’s roughly 10-year follow-up and the limited number of children with the disease despite a large number of analyzed samples. They noted that, “given the limited number of cases, we call for corroboration in similar studies and preferably interventional studies to reach conclusions about causality.”
The study was funded by the Research Council of Norway, the Project for the Conceptual Development of Research Organization, and the Norwegian Coeliac Society. Two authors reported grant support from trusts and foundations in Norway and Switzerland; no conflicts of interest were reported.
SOURCE: Kahrs CR et al. BMJ. 2019 Feb 13. doi: 10.1136/bmj.l231.
“We found a significant association between exposure to enterovirus and subsequent risk of celiac disease,” wrote lead author Christian R. Kahrs of the University of Oslo and his coauthors, adding that “adenovirus was not associated with celiac disease.” The study was published in the BMJ.
From 2001 to 2007, 46,939 newborns in Norway were screened for the HLA-DQ2/DQ8 genotype, which is associated with an increased risk of celiac disease. The genotype was identified in 912 children, and blood and stool sample collection began at 3 months. Children who were still contributing blood samples by 2014-2016 were invited to be screened for celiac disease.
Of the 220 children screened, 25 were diagnosed with celiac disease. Enterovirus was detected in 370 (17%) of the 2,135 stool samples and was more frequent in children who developed celiac disease antibodies than in matched controls (adjusted odds ratio, 1.49; 95% confidence interval, 1.07-2.06; P = .02). There was a significant association between later development of celiac disease and the commonly identified enterovirus A (aOR, 1.62; 95% CI, 1.04-2.53; P = .03) and enterovirus B (aOR, 2.27; 95% CI, 1.33-3.88; P = .003). No adenovirus types were associated with development of celiac disease.
The authors acknowledged their study’s limitations, including the possibility that children might be diagnosed with celiac disease later than the study’s roughly 10-year follow-up and the limited number of children with the disease despite a large number of analyzed samples. They noted that, “given the limited number of cases, we call for corroboration in similar studies and preferably interventional studies to reach conclusions about causality.”
The study was funded by the Research Council of Norway, the Project for the Conceptual Development of Research Organization, and the Norwegian Coeliac Society. Two authors reported grant support from trusts and foundations in Norway and Switzerland; no conflicts of interest were reported.
SOURCE: Kahrs CR et al. BMJ. 2019 Feb 13. doi: 10.1136/bmj.l231.
“We found a significant association between exposure to enterovirus and subsequent risk of celiac disease,” wrote lead author Christian R. Kahrs of the University of Oslo and his coauthors, adding that “adenovirus was not associated with celiac disease.” The study was published in the BMJ.
From 2001 to 2007, 46,939 newborns in Norway were screened for the HLA-DQ2/DQ8 genotype, which is associated with an increased risk of celiac disease. The genotype was identified in 912 children, and blood and stool sample collection began at 3 months. Children who were still contributing blood samples by 2014-2016 were invited to be screened for celiac disease.
Of the 220 children screened, 25 were diagnosed with celiac disease. Enterovirus was detected in 370 (17%) of the 2,135 stool samples and was more frequent in children who developed celiac disease antibodies than in matched controls (adjusted odds ratio, 1.49; 95% confidence interval, 1.07-2.06; P = .02). There was a significant association between later development of celiac disease and the commonly identified enterovirus A (aOR, 1.62; 95% CI, 1.04-2.53; P = .03) and enterovirus B (aOR, 2.27; 95% CI, 1.33-3.88; P = .003). No adenovirus types were associated with development of celiac disease.
The authors acknowledged their study’s limitations, including the possibility that children might be diagnosed with celiac disease later than the study’s roughly 10-year follow-up and the limited number of children with the disease despite a large number of analyzed samples. They noted that, “given the limited number of cases, we call for corroboration in similar studies and preferably interventional studies to reach conclusions about causality.”
The study was funded by the Research Council of Norway, the Project for the Conceptual Development of Research Organization, and the Norwegian Coeliac Society. Two authors reported grant support from trusts and foundations in Norway and Switzerland; no conflicts of interest were reported.
SOURCE: Kahrs CR et al. BMJ. 2019 Feb 13. doi: 10.1136/bmj.l231.
FROM THE BMJ
Delays of 1-2+ years in IBD diagnosis are common, patients say
LAS VEGAS – Delays in diagnosis of inflammatory bowel disease (IBD) appear to be very common and often extensive, a new survey of U.S. patients suggests. Nearly two-thirds said their diagnosis was delayed past symptom onset for more than a year, and almost half reported a delay of more than 2 years.
On average, patients who experienced diagnosis delays said they’d seen an average of 3.5 physicians. “Most patients reported that they received an uncertain or wrong diagnosis by their primary care physician or gastroenterologist,” said study coauthor Ryan C. Ungaro, MD, of Icahn School of Medicine at Mount Sinai, New York, in an interview prior to the presentation of the study findings at the Crohn’s & Colitis Congress - a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
“Working at a tertiary care IBD center, we noticed that many patients tell us it took them a long time to get diagnosed with Crohn’s disease [CD] or ulcerative colitis [UC],” said Dr. Ungaro. “There are some studies on delay in diagnosis in Europe but none in the U.S. We hypothesized that diagnostic delay is a major issue for IBD patients in the U.S.”
The study authors offered a survey to 2,341 patients with IBD; 1,121 responded to the questions. Of those, 68% reported their diagnosis was delayed, with 64% reporting a delay of over 1 year and 48% reporting a delay over 2 years.
Compared with those with UC, patients with CD were more likely to report more than 1-year delays (70% vs. 48%; P less than .0001) and more than 2-year delays (52% vs. 37%; P = .0008).
Patients who reported delays said they saw an average of 3.5 physicians before getting an IBD diagnosis. The patients most commonly blamed their incorrect diagnosis on primary care providers (58%) and gastroenterologists (28%).
“Most likely, CD may be misdiagnosed because the common presenting symptoms – abdominal pain, diarrhea – are also seen in other common gastrointestinal conditions such as irritable bowel syndrome,” Dr. Ungaro said. “In contrast, most patients with UC present with rectal bleeding which is a ‘red flag’ symptom that is more likely to get worked up.”
In some cases, patients blamed themselves, reporting “that they personally did not feel their symptoms warranted work-up or were too embarrassed by their symptoms to tell anyone,” Dr. Ungaro said. “The other theme that was noted was access – delay or difficulty seeing a gastroenterologist.”
Going forward, “diagnostic delay may be improved through patient education regarding awareness of alarm symptoms for IBD,” said gastroenterologist and study lead author Zane Gallinger, MD, FRCPC, of the University of Toronto at Mount Sinai Hospital, in an interview. According to him, these symptoms include diarrhea, abdominal pain, weight loss, family history of CD, perianal abscess, and fistula and fever.
At the primary care level, Dr. Gallinger said that noninvasive tests such as fecal calprotectin can help identify patients with inflammatory conditions and that “more rapid access to gastroenterologists for earlier diagnosis of IBD can improve patient outcomes.”
The Crohn’s and Colitis Foundation funded the study. Dr. Gallinger reported relationships with Takeda and AbbVie.
SOURCE: Gallinger Z et al. Crohn’s & Colitis Congress, Abstract P030.
LAS VEGAS – Delays in diagnosis of inflammatory bowel disease (IBD) appear to be very common and often extensive, a new survey of U.S. patients suggests. Nearly two-thirds said their diagnosis was delayed past symptom onset for more than a year, and almost half reported a delay of more than 2 years.
On average, patients who experienced diagnosis delays said they’d seen an average of 3.5 physicians. “Most patients reported that they received an uncertain or wrong diagnosis by their primary care physician or gastroenterologist,” said study coauthor Ryan C. Ungaro, MD, of Icahn School of Medicine at Mount Sinai, New York, in an interview prior to the presentation of the study findings at the Crohn’s & Colitis Congress - a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
“Working at a tertiary care IBD center, we noticed that many patients tell us it took them a long time to get diagnosed with Crohn’s disease [CD] or ulcerative colitis [UC],” said Dr. Ungaro. “There are some studies on delay in diagnosis in Europe but none in the U.S. We hypothesized that diagnostic delay is a major issue for IBD patients in the U.S.”
The study authors offered a survey to 2,341 patients with IBD; 1,121 responded to the questions. Of those, 68% reported their diagnosis was delayed, with 64% reporting a delay of over 1 year and 48% reporting a delay over 2 years.
Compared with those with UC, patients with CD were more likely to report more than 1-year delays (70% vs. 48%; P less than .0001) and more than 2-year delays (52% vs. 37%; P = .0008).
Patients who reported delays said they saw an average of 3.5 physicians before getting an IBD diagnosis. The patients most commonly blamed their incorrect diagnosis on primary care providers (58%) and gastroenterologists (28%).
“Most likely, CD may be misdiagnosed because the common presenting symptoms – abdominal pain, diarrhea – are also seen in other common gastrointestinal conditions such as irritable bowel syndrome,” Dr. Ungaro said. “In contrast, most patients with UC present with rectal bleeding which is a ‘red flag’ symptom that is more likely to get worked up.”
In some cases, patients blamed themselves, reporting “that they personally did not feel their symptoms warranted work-up or were too embarrassed by their symptoms to tell anyone,” Dr. Ungaro said. “The other theme that was noted was access – delay or difficulty seeing a gastroenterologist.”
Going forward, “diagnostic delay may be improved through patient education regarding awareness of alarm symptoms for IBD,” said gastroenterologist and study lead author Zane Gallinger, MD, FRCPC, of the University of Toronto at Mount Sinai Hospital, in an interview. According to him, these symptoms include diarrhea, abdominal pain, weight loss, family history of CD, perianal abscess, and fistula and fever.
At the primary care level, Dr. Gallinger said that noninvasive tests such as fecal calprotectin can help identify patients with inflammatory conditions and that “more rapid access to gastroenterologists for earlier diagnosis of IBD can improve patient outcomes.”
The Crohn’s and Colitis Foundation funded the study. Dr. Gallinger reported relationships with Takeda and AbbVie.
SOURCE: Gallinger Z et al. Crohn’s & Colitis Congress, Abstract P030.
LAS VEGAS – Delays in diagnosis of inflammatory bowel disease (IBD) appear to be very common and often extensive, a new survey of U.S. patients suggests. Nearly two-thirds said their diagnosis was delayed past symptom onset for more than a year, and almost half reported a delay of more than 2 years.
On average, patients who experienced diagnosis delays said they’d seen an average of 3.5 physicians. “Most patients reported that they received an uncertain or wrong diagnosis by their primary care physician or gastroenterologist,” said study coauthor Ryan C. Ungaro, MD, of Icahn School of Medicine at Mount Sinai, New York, in an interview prior to the presentation of the study findings at the Crohn’s & Colitis Congress - a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association.
“Working at a tertiary care IBD center, we noticed that many patients tell us it took them a long time to get diagnosed with Crohn’s disease [CD] or ulcerative colitis [UC],” said Dr. Ungaro. “There are some studies on delay in diagnosis in Europe but none in the U.S. We hypothesized that diagnostic delay is a major issue for IBD patients in the U.S.”
The study authors offered a survey to 2,341 patients with IBD; 1,121 responded to the questions. Of those, 68% reported their diagnosis was delayed, with 64% reporting a delay of over 1 year and 48% reporting a delay over 2 years.
Compared with those with UC, patients with CD were more likely to report more than 1-year delays (70% vs. 48%; P less than .0001) and more than 2-year delays (52% vs. 37%; P = .0008).
Patients who reported delays said they saw an average of 3.5 physicians before getting an IBD diagnosis. The patients most commonly blamed their incorrect diagnosis on primary care providers (58%) and gastroenterologists (28%).
“Most likely, CD may be misdiagnosed because the common presenting symptoms – abdominal pain, diarrhea – are also seen in other common gastrointestinal conditions such as irritable bowel syndrome,” Dr. Ungaro said. “In contrast, most patients with UC present with rectal bleeding which is a ‘red flag’ symptom that is more likely to get worked up.”
In some cases, patients blamed themselves, reporting “that they personally did not feel their symptoms warranted work-up or were too embarrassed by their symptoms to tell anyone,” Dr. Ungaro said. “The other theme that was noted was access – delay or difficulty seeing a gastroenterologist.”
Going forward, “diagnostic delay may be improved through patient education regarding awareness of alarm symptoms for IBD,” said gastroenterologist and study lead author Zane Gallinger, MD, FRCPC, of the University of Toronto at Mount Sinai Hospital, in an interview. According to him, these symptoms include diarrhea, abdominal pain, weight loss, family history of CD, perianal abscess, and fistula and fever.
At the primary care level, Dr. Gallinger said that noninvasive tests such as fecal calprotectin can help identify patients with inflammatory conditions and that “more rapid access to gastroenterologists for earlier diagnosis of IBD can improve patient outcomes.”
The Crohn’s and Colitis Foundation funded the study. Dr. Gallinger reported relationships with Takeda and AbbVie.
SOURCE: Gallinger Z et al. Crohn’s & Colitis Congress, Abstract P030.
REPORTING FROM THE CROHN’S & COLITIS CONGRESS
One postdelivery antibiotic dose nearly halves infection in operative delivery
LAS VEGAS – A randomized controlled trial comparing a single postdelivery intravenous dose of antibiotic after operative delivery found that antibiotics nearly halved the risk for maternal infection.
For women who received a single dose of amoxicillin-clavulanic acid, the risk ratio was 0.58 for suspected or confirmed infection, compared with those who received an intravenous dose of saline solution (95% confidence interval, 0.49-0.69, P less than .001). Culture-confirmed systemic infections were similarly reduced by a risk ratio (RR) of 0.44 (95% CI, 0.22-0.89; P =.018).
Superficial and deep incisional infections were also significantly less likely in the women who had received antibiotics (RRs 0.53 and 0.46, respectively; P less than .001 for both). Although sepsis occurred in numerically fewer women who received antibiotics, the numbers were, overall, small and not statistically significant.
By 6 weeks after delivery, patients receiving antibiotics were less likely to have outpatient or home visits for perineal problems or concerns as well (P less than .001).
“This trial shows clear benefit of a single dose of prophylactic antibiotic after operative vaginal birth, and this should be introduced into routine practice,” said Marian Knight, MBChB, DPhil.
Dr. Knight presented findings of the randomized trial, dubbed ANODE, at a late-breaking abstract session of the meeting, which was sponsored by the Society for Maternal-Fetal Medicine. Dr. Knight, professor of maternal and child population health at the University of Oxford (England), explained that ANODE aimed to determine whether a single dose of prophylactic amoxicillin-clavulanic acid was clinically effective in preventing confirmed or suspected maternal infection after operative vaginal birth.
The study tips the scales in favor of the anti-infective properties of the single antibiotic dose after operative delivery, and comes at a time when unacceptable levels of maternal morbidity and mortality coexist with pressing worries about antibiotic resistance, Dr. Knight said.
The multicenter randomized, blinded, placebo-controlled trial was conducted at 27 sites in the United Kingdom between March 2016 and June 2018.
Women at the study sites who underwent operative delivery, whether by forceps or vacuum extraction, received either a single dose of intravenous amoxicillin-clavulanic acid (1 gm/200 mg), or a placebo dose of saline solution. Antibiotics were given in the window of 0 to 6 hours post-delivery.
The primary outcome measure was confirmed or suspected maternal infection within 6 weeks of delivery. Women were positive for infection if they were prescribed antibiotics for perineal wound infections, if they experienced endometrial or uterine infections, if they had urinary tract infections with “systemic features, or if they had other systemic infections. Other criteria for infection were culture-confirmed systemic infection, or endometritis by criteria established by the Centers for Disease Control and Prevention.
Dr. Knight and her colleagues used an intention-to-treat analysis that looked at the primary outcome as a risk ratio, with a 95% CI. Secondary outcomes, also presented as risk ratios, were considered with a 99% CI.
A total of 3,427 women were randomized. In all, 1,715 women in the active arm and 1,705 in the placebo arm were included in the outcomes analyses. Women were interviewed by telephone, they completed questionnaires, and they received a questionnaire by mail or completed one online. Slightly more than 1,500 women in each arm completed the phone interview, and nearly 1,300 in each arm completed the initial questionnaire.
The mean age was 30 years, and most of the participants (84%-87%) were white. Most were of normal weight, with a median body mass index at the initial prenatal visit of 25 kg/m2.
Though women with multiple pregnancies were included in the study, just 11 in the active arm and 9 in the placebo arm delivered twins. There were no triplets. Most women (76%-78%) were primiparous, and just 7%-8% of women had prior cesarean delivery.
The mode of operative delivery for most of the participants (63%-67%) was forceps, with all but 10 of the remaining women receiving vacuum extraction (the remaining 10 had spontaneous vaginal deliveries).
The reasons for instrumental delivery were approximately evenly divided between failure of labor to progress and fetal compromise.
Nearly 90% of the women – more than 1,500 in each study arm – received episiotomies, a figure that Dr. Knight said she found surprising. She noted that mediolateral incisions are the standard of care in the United Kingdom. Still, 29%-33% of the women experienced a tear, with most being second-degree tears. Third- and fourth-degree tears occurred in two women overall. Almost all of the women (99%) had their wounds sutured.
Three serious adverse events were reported. One woman in the placebo arm required intensive care unit admission for severe sepsis, and another placebo participant required a transfusion after postpartum hemorrhage. One patient who received antibiotic had immediate diffuse itching and a swollen throat. However, antibiotic side effects were reported in only 2 of the 1,715 active arm participants, Dr. Knight said.
The competing concerns of maternal safety and antibiotic stewardship are weighed against a global backdrop of high maternal infection rates, Dr. Knight said. Sepsis causes 11% of global maternal deaths, a rate that drops to about 5% in higher-income nations. However, she pointed out, that figure rises to about 13% in the United States.
“For every woman that dies from pregnancy-related infection, a further 70 have severe infection and survive,” she said.
Known risk factors for infection include operative vaginal delivery and cesarean deliveries. For cesareans performed after the onset of labor, the adjusted odds ratio reaches 6.7 for severe infection, Dr. Knight said (PLoS Med. 2014;11:e1001672). A systematic review estimated that the rate for any infection following cesarean delivery approaches one in four women, she said (Cochrane Database Syst Rev. 2014 Oct 28;[10]:CD007482).
The same systematic review found that prophylactic antibiotics reduced incidence of wound infection, endometritis, and serious maternal wound infection after cesarean delivery (RR 0.40, 0.38, and 0.31, respectively).
For operative vaginal deliveries, however, a Cochrane review found one study of 393 women. Although no women given antibiotics developed endometritis compared with seven cases of endometritis in the no-antibiotics group for a RR of .07, the 95% confidence interval in the Cochrane analysis included zero, so the findings weren’t statistically significant. Hospital length of stay didn’t differ between the two groups (Cochrane Database Syst Rev. 2014 Oct 13;[10]:CD004455).
Citing this review, the United Kingdom’s Royal College of Gynecologists had concluded that evidence was insufficient to support routine antibiotic prophylaxis in operative deliveries. The American College of Obstetricians and Gynecologists make no mention of antibiotic prophylaxis or postdelivery infection in its guidelines for operative delivery, Dr. Knight said.
Since confirmed or suspected infection was still seen in 11% of women who received antibiotics, further analysis “is needed to investigate whether early administration, prenatal administration, or repeated administration is more likely to be effective,” she said. Women in the ANODE trial received their dose at a median of 3 hours after delivery.
“Until these analyses are completed, there is no indication for administration of more than a single dose of prophylactic antibiotic, or for predelivery administration,” she said.
Dr. Knight reported that ANODE was funded by the U.K.’s National Institute for Health Research. She reported that she had no conflicts of interest.
SOURCE: Knight M et al. Am J Obstet Gynecol. 2019 Jan;220;1:S685. Abstract LB 3.
LAS VEGAS – A randomized controlled trial comparing a single postdelivery intravenous dose of antibiotic after operative delivery found that antibiotics nearly halved the risk for maternal infection.
For women who received a single dose of amoxicillin-clavulanic acid, the risk ratio was 0.58 for suspected or confirmed infection, compared with those who received an intravenous dose of saline solution (95% confidence interval, 0.49-0.69, P less than .001). Culture-confirmed systemic infections were similarly reduced by a risk ratio (RR) of 0.44 (95% CI, 0.22-0.89; P =.018).
Superficial and deep incisional infections were also significantly less likely in the women who had received antibiotics (RRs 0.53 and 0.46, respectively; P less than .001 for both). Although sepsis occurred in numerically fewer women who received antibiotics, the numbers were, overall, small and not statistically significant.
By 6 weeks after delivery, patients receiving antibiotics were less likely to have outpatient or home visits for perineal problems or concerns as well (P less than .001).
“This trial shows clear benefit of a single dose of prophylactic antibiotic after operative vaginal birth, and this should be introduced into routine practice,” said Marian Knight, MBChB, DPhil.
Dr. Knight presented findings of the randomized trial, dubbed ANODE, at a late-breaking abstract session of the meeting, which was sponsored by the Society for Maternal-Fetal Medicine. Dr. Knight, professor of maternal and child population health at the University of Oxford (England), explained that ANODE aimed to determine whether a single dose of prophylactic amoxicillin-clavulanic acid was clinically effective in preventing confirmed or suspected maternal infection after operative vaginal birth.
The study tips the scales in favor of the anti-infective properties of the single antibiotic dose after operative delivery, and comes at a time when unacceptable levels of maternal morbidity and mortality coexist with pressing worries about antibiotic resistance, Dr. Knight said.
The multicenter randomized, blinded, placebo-controlled trial was conducted at 27 sites in the United Kingdom between March 2016 and June 2018.
Women at the study sites who underwent operative delivery, whether by forceps or vacuum extraction, received either a single dose of intravenous amoxicillin-clavulanic acid (1 gm/200 mg), or a placebo dose of saline solution. Antibiotics were given in the window of 0 to 6 hours post-delivery.
The primary outcome measure was confirmed or suspected maternal infection within 6 weeks of delivery. Women were positive for infection if they were prescribed antibiotics for perineal wound infections, if they experienced endometrial or uterine infections, if they had urinary tract infections with “systemic features, or if they had other systemic infections. Other criteria for infection were culture-confirmed systemic infection, or endometritis by criteria established by the Centers for Disease Control and Prevention.
Dr. Knight and her colleagues used an intention-to-treat analysis that looked at the primary outcome as a risk ratio, with a 95% CI. Secondary outcomes, also presented as risk ratios, were considered with a 99% CI.
A total of 3,427 women were randomized. In all, 1,715 women in the active arm and 1,705 in the placebo arm were included in the outcomes analyses. Women were interviewed by telephone, they completed questionnaires, and they received a questionnaire by mail or completed one online. Slightly more than 1,500 women in each arm completed the phone interview, and nearly 1,300 in each arm completed the initial questionnaire.
The mean age was 30 years, and most of the participants (84%-87%) were white. Most were of normal weight, with a median body mass index at the initial prenatal visit of 25 kg/m2.
Though women with multiple pregnancies were included in the study, just 11 in the active arm and 9 in the placebo arm delivered twins. There were no triplets. Most women (76%-78%) were primiparous, and just 7%-8% of women had prior cesarean delivery.
The mode of operative delivery for most of the participants (63%-67%) was forceps, with all but 10 of the remaining women receiving vacuum extraction (the remaining 10 had spontaneous vaginal deliveries).
The reasons for instrumental delivery were approximately evenly divided between failure of labor to progress and fetal compromise.
Nearly 90% of the women – more than 1,500 in each study arm – received episiotomies, a figure that Dr. Knight said she found surprising. She noted that mediolateral incisions are the standard of care in the United Kingdom. Still, 29%-33% of the women experienced a tear, with most being second-degree tears. Third- and fourth-degree tears occurred in two women overall. Almost all of the women (99%) had their wounds sutured.
Three serious adverse events were reported. One woman in the placebo arm required intensive care unit admission for severe sepsis, and another placebo participant required a transfusion after postpartum hemorrhage. One patient who received antibiotic had immediate diffuse itching and a swollen throat. However, antibiotic side effects were reported in only 2 of the 1,715 active arm participants, Dr. Knight said.
The competing concerns of maternal safety and antibiotic stewardship are weighed against a global backdrop of high maternal infection rates, Dr. Knight said. Sepsis causes 11% of global maternal deaths, a rate that drops to about 5% in higher-income nations. However, she pointed out, that figure rises to about 13% in the United States.
“For every woman that dies from pregnancy-related infection, a further 70 have severe infection and survive,” she said.
Known risk factors for infection include operative vaginal delivery and cesarean deliveries. For cesareans performed after the onset of labor, the adjusted odds ratio reaches 6.7 for severe infection, Dr. Knight said (PLoS Med. 2014;11:e1001672). A systematic review estimated that the rate for any infection following cesarean delivery approaches one in four women, she said (Cochrane Database Syst Rev. 2014 Oct 28;[10]:CD007482).
The same systematic review found that prophylactic antibiotics reduced incidence of wound infection, endometritis, and serious maternal wound infection after cesarean delivery (RR 0.40, 0.38, and 0.31, respectively).
For operative vaginal deliveries, however, a Cochrane review found one study of 393 women. Although no women given antibiotics developed endometritis compared with seven cases of endometritis in the no-antibiotics group for a RR of .07, the 95% confidence interval in the Cochrane analysis included zero, so the findings weren’t statistically significant. Hospital length of stay didn’t differ between the two groups (Cochrane Database Syst Rev. 2014 Oct 13;[10]:CD004455).
Citing this review, the United Kingdom’s Royal College of Gynecologists had concluded that evidence was insufficient to support routine antibiotic prophylaxis in operative deliveries. The American College of Obstetricians and Gynecologists make no mention of antibiotic prophylaxis or postdelivery infection in its guidelines for operative delivery, Dr. Knight said.
Since confirmed or suspected infection was still seen in 11% of women who received antibiotics, further analysis “is needed to investigate whether early administration, prenatal administration, or repeated administration is more likely to be effective,” she said. Women in the ANODE trial received their dose at a median of 3 hours after delivery.
“Until these analyses are completed, there is no indication for administration of more than a single dose of prophylactic antibiotic, or for predelivery administration,” she said.
Dr. Knight reported that ANODE was funded by the U.K.’s National Institute for Health Research. She reported that she had no conflicts of interest.
SOURCE: Knight M et al. Am J Obstet Gynecol. 2019 Jan;220;1:S685. Abstract LB 3.
LAS VEGAS – A randomized controlled trial comparing a single postdelivery intravenous dose of antibiotic after operative delivery found that antibiotics nearly halved the risk for maternal infection.
For women who received a single dose of amoxicillin-clavulanic acid, the risk ratio was 0.58 for suspected or confirmed infection, compared with those who received an intravenous dose of saline solution (95% confidence interval, 0.49-0.69, P less than .001). Culture-confirmed systemic infections were similarly reduced by a risk ratio (RR) of 0.44 (95% CI, 0.22-0.89; P =.018).
Superficial and deep incisional infections were also significantly less likely in the women who had received antibiotics (RRs 0.53 and 0.46, respectively; P less than .001 for both). Although sepsis occurred in numerically fewer women who received antibiotics, the numbers were, overall, small and not statistically significant.
By 6 weeks after delivery, patients receiving antibiotics were less likely to have outpatient or home visits for perineal problems or concerns as well (P less than .001).
“This trial shows clear benefit of a single dose of prophylactic antibiotic after operative vaginal birth, and this should be introduced into routine practice,” said Marian Knight, MBChB, DPhil.
Dr. Knight presented findings of the randomized trial, dubbed ANODE, at a late-breaking abstract session of the meeting, which was sponsored by the Society for Maternal-Fetal Medicine. Dr. Knight, professor of maternal and child population health at the University of Oxford (England), explained that ANODE aimed to determine whether a single dose of prophylactic amoxicillin-clavulanic acid was clinically effective in preventing confirmed or suspected maternal infection after operative vaginal birth.
The study tips the scales in favor of the anti-infective properties of the single antibiotic dose after operative delivery, and comes at a time when unacceptable levels of maternal morbidity and mortality coexist with pressing worries about antibiotic resistance, Dr. Knight said.
The multicenter randomized, blinded, placebo-controlled trial was conducted at 27 sites in the United Kingdom between March 2016 and June 2018.
Women at the study sites who underwent operative delivery, whether by forceps or vacuum extraction, received either a single dose of intravenous amoxicillin-clavulanic acid (1 gm/200 mg), or a placebo dose of saline solution. Antibiotics were given in the window of 0 to 6 hours post-delivery.
The primary outcome measure was confirmed or suspected maternal infection within 6 weeks of delivery. Women were positive for infection if they were prescribed antibiotics for perineal wound infections, if they experienced endometrial or uterine infections, if they had urinary tract infections with “systemic features, or if they had other systemic infections. Other criteria for infection were culture-confirmed systemic infection, or endometritis by criteria established by the Centers for Disease Control and Prevention.
Dr. Knight and her colleagues used an intention-to-treat analysis that looked at the primary outcome as a risk ratio, with a 95% CI. Secondary outcomes, also presented as risk ratios, were considered with a 99% CI.
A total of 3,427 women were randomized. In all, 1,715 women in the active arm and 1,705 in the placebo arm were included in the outcomes analyses. Women were interviewed by telephone, they completed questionnaires, and they received a questionnaire by mail or completed one online. Slightly more than 1,500 women in each arm completed the phone interview, and nearly 1,300 in each arm completed the initial questionnaire.
The mean age was 30 years, and most of the participants (84%-87%) were white. Most were of normal weight, with a median body mass index at the initial prenatal visit of 25 kg/m2.
Though women with multiple pregnancies were included in the study, just 11 in the active arm and 9 in the placebo arm delivered twins. There were no triplets. Most women (76%-78%) were primiparous, and just 7%-8% of women had prior cesarean delivery.
The mode of operative delivery for most of the participants (63%-67%) was forceps, with all but 10 of the remaining women receiving vacuum extraction (the remaining 10 had spontaneous vaginal deliveries).
The reasons for instrumental delivery were approximately evenly divided between failure of labor to progress and fetal compromise.
Nearly 90% of the women – more than 1,500 in each study arm – received episiotomies, a figure that Dr. Knight said she found surprising. She noted that mediolateral incisions are the standard of care in the United Kingdom. Still, 29%-33% of the women experienced a tear, with most being second-degree tears. Third- and fourth-degree tears occurred in two women overall. Almost all of the women (99%) had their wounds sutured.
Three serious adverse events were reported. One woman in the placebo arm required intensive care unit admission for severe sepsis, and another placebo participant required a transfusion after postpartum hemorrhage. One patient who received antibiotic had immediate diffuse itching and a swollen throat. However, antibiotic side effects were reported in only 2 of the 1,715 active arm participants, Dr. Knight said.
The competing concerns of maternal safety and antibiotic stewardship are weighed against a global backdrop of high maternal infection rates, Dr. Knight said. Sepsis causes 11% of global maternal deaths, a rate that drops to about 5% in higher-income nations. However, she pointed out, that figure rises to about 13% in the United States.
“For every woman that dies from pregnancy-related infection, a further 70 have severe infection and survive,” she said.
Known risk factors for infection include operative vaginal delivery and cesarean deliveries. For cesareans performed after the onset of labor, the adjusted odds ratio reaches 6.7 for severe infection, Dr. Knight said (PLoS Med. 2014;11:e1001672). A systematic review estimated that the rate for any infection following cesarean delivery approaches one in four women, she said (Cochrane Database Syst Rev. 2014 Oct 28;[10]:CD007482).
The same systematic review found that prophylactic antibiotics reduced incidence of wound infection, endometritis, and serious maternal wound infection after cesarean delivery (RR 0.40, 0.38, and 0.31, respectively).
For operative vaginal deliveries, however, a Cochrane review found one study of 393 women. Although no women given antibiotics developed endometritis compared with seven cases of endometritis in the no-antibiotics group for a RR of .07, the 95% confidence interval in the Cochrane analysis included zero, so the findings weren’t statistically significant. Hospital length of stay didn’t differ between the two groups (Cochrane Database Syst Rev. 2014 Oct 13;[10]:CD004455).
Citing this review, the United Kingdom’s Royal College of Gynecologists had concluded that evidence was insufficient to support routine antibiotic prophylaxis in operative deliveries. The American College of Obstetricians and Gynecologists make no mention of antibiotic prophylaxis or postdelivery infection in its guidelines for operative delivery, Dr. Knight said.
Since confirmed or suspected infection was still seen in 11% of women who received antibiotics, further analysis “is needed to investigate whether early administration, prenatal administration, or repeated administration is more likely to be effective,” she said. Women in the ANODE trial received their dose at a median of 3 hours after delivery.
“Until these analyses are completed, there is no indication for administration of more than a single dose of prophylactic antibiotic, or for predelivery administration,” she said.
Dr. Knight reported that ANODE was funded by the U.K.’s National Institute for Health Research. She reported that she had no conflicts of interest.
SOURCE: Knight M et al. Am J Obstet Gynecol. 2019 Jan;220;1:S685. Abstract LB 3.
REPORTING FROM THE PREGNANCY MEETING
Severe skin reaction to AEDs
Also today, adherence to statins is lower among younger patients, women, and minorities, the flu season rages on, and how medication-assisted treatment impacts pregnant women with opioid use disorder.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, adherence to statins is lower among younger patients, women, and minorities, the flu season rages on, and how medication-assisted treatment impacts pregnant women with opioid use disorder.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, adherence to statins is lower among younger patients, women, and minorities, the flu season rages on, and how medication-assisted treatment impacts pregnant women with opioid use disorder.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Bag-mask ventilation during intubation reduces severe hypoxemia
, according to data presented at the Critical Care Congress, sponsored by the Society of Critical Care Medicine.

A multicenter study, published simultaneously in the Feb. 18 issue of the New England Journal of Medicine, randomized 401 critically-ill patients in the ICU who were undergoing tracheal intubation to receive either ventilation with a bag-mask device during induction for intubation or no ventilation.
The median lowest oxygen saturation between induction and 2 minutes after intubation was 96% in the bag-mask ventilated patients and 93% in the no-ventilation group, representing a 4.7% difference after adjusting for prespecified covariates (P = .01).
In a post-hoc analysis that adjusted for other factors such as the provision of preoxygenation, the preoxygenation device, pneumonia, and gastrointestinal bleeding, there was a 5.2% difference between the two groups in median lowest oxygen saturation, favoring the bag-mask group.
Bag-mask ventilation was also associated with almost a halving in the incidence of severe hypoxemia – defined as an oxygen saturation below 80% – compared with no-ventilation (10.9% vs. 22.8%; relative risk = 0.48). There was also a lower incidence of patients with an oxygen saturation below 90% and below 70% in the bag-mask ventilation group, compared with the no-ventilation group.
Overall, the median decrease in oxygen saturation from induction to the lowest point was 1% in the bag-mask group, and 5% in the no-ventilation group.
The study saw no effects of factors such as body-mass index, operator experience, or Acute Physiology and Chronic Health Evaluation (APACHE II) score. The patients had a median age of 60 years, about half had sepsis or septic shock, and close to 60% had hypoxemic respiratory failure as an indication for tracheal intubation.
Jonathan D. Casey, MD, of Vanderbilt University, Nashville, Tenn., and his coauthors wrote that their results suggested for every nine critically ill patients undergoing tracheal intubation, bag-mask ventilation would prevent severe hypoxemia in one patient.
“These findings are important because oxygen saturation is an established endpoint in airway management trials and is a contributing factor to periprocedural cardiac arrest and death,” they wrote.
They noted that there are conflicting guidelines on the use of bag-mask ventilation during tracheal intubation, with some recommending its use for all patients – even those who are not hypoxemic – and others advising their use only for patients with hypoxemia. This study excluded patients who were identified as hypoxemic or in whom bag-mask ventilation was contraindicated.
Despite concerns about bag-mask ventilation increasing the risk the aspiration, the study showed no significant difference between the two groups in the incidence of operator-reported aspiration or the presence of a new opacity on chest radiograph in the 48 hours after intubation.
The authors acknowledged that, given the low incidence of operator-reported aspiration during tracheal intubation, a much larger study would be needed to show whether bag-mask ventilation did increase the risk of aspiration.
“However, our trial provides some reassurance, since the incidence of operator-reported aspiration was numerically lower in the bag-mask ventilation group than in the no-ventilation group,” they wrote.
There were also no significant differences between the two groups in oxygen saturation, fraction of inspired oxygen or positive end-expiratory pressure in the 24 hours after intubation. Bag-mask ventilation was also associated with similar rates of in-hospital mortality, number of ventilator-free days, and days out of the ICU as no-ventilation.
The authors noted that their trial focused on critically-ill patients in the ICU, so the results may not be generalizable to patients in the emergency department or in a prehospital setting.
The study and some authors were supported by the National Institutes of Health. Two authors declared personal fees from the pharmaceutical industry unrelated to the study, and no other conflicts of interest were declared.
SOURCE: Casey J et al. N Engl J Med. 2019 Feb 18. doi: 10.1056/NEJMoa1812405
Debate around the question of whether to use bag-mask ventilation in critically-ill patients has been limited by the lack of high-quality evidence on the risk of aspiration or on the benefits of this approach. This study found no evidence of an increase in the incidence of aspiration, despite using multiple measures to detect it, which provide some reassurance that manual ventilation during tracheal intubation is not likely to cause significant harm.
One significant limitation of this trial, however, is that it did not standardize the preoxygenation strategy across the two groups, so significantly more patients in the bag-mask group received bag-mask ventilation before induction. Median oxygen saturation before induction was the same in the two groups, but this does not rule out the possibility of differences in the arterial pressure of oxygen.
This study may not settle the question of whether to use bag-mask ventilation during tracheal intubation, but it provides strong suggestion that the practice is not harmful.
Patricia A. Kritek, MD, and Andrew M. Luks, MD, are with the division of pulmonary, critical care, and sleep medicine at the University of Washington in Seattle. These comments are adapted from their editorial accompanying the paper by Casey et al. (N Engl J Med. 2019 Feb 18. doi: 10.1056/NEJMe1900708). Dr. Luks declared personal fees from private industry outside the submitted work. Dr. Kritek reported having nothing to disclose.
Debate around the question of whether to use bag-mask ventilation in critically-ill patients has been limited by the lack of high-quality evidence on the risk of aspiration or on the benefits of this approach. This study found no evidence of an increase in the incidence of aspiration, despite using multiple measures to detect it, which provide some reassurance that manual ventilation during tracheal intubation is not likely to cause significant harm.
One significant limitation of this trial, however, is that it did not standardize the preoxygenation strategy across the two groups, so significantly more patients in the bag-mask group received bag-mask ventilation before induction. Median oxygen saturation before induction was the same in the two groups, but this does not rule out the possibility of differences in the arterial pressure of oxygen.
This study may not settle the question of whether to use bag-mask ventilation during tracheal intubation, but it provides strong suggestion that the practice is not harmful.
Patricia A. Kritek, MD, and Andrew M. Luks, MD, are with the division of pulmonary, critical care, and sleep medicine at the University of Washington in Seattle. These comments are adapted from their editorial accompanying the paper by Casey et al. (N Engl J Med. 2019 Feb 18. doi: 10.1056/NEJMe1900708). Dr. Luks declared personal fees from private industry outside the submitted work. Dr. Kritek reported having nothing to disclose.
Debate around the question of whether to use bag-mask ventilation in critically-ill patients has been limited by the lack of high-quality evidence on the risk of aspiration or on the benefits of this approach. This study found no evidence of an increase in the incidence of aspiration, despite using multiple measures to detect it, which provide some reassurance that manual ventilation during tracheal intubation is not likely to cause significant harm.
One significant limitation of this trial, however, is that it did not standardize the preoxygenation strategy across the two groups, so significantly more patients in the bag-mask group received bag-mask ventilation before induction. Median oxygen saturation before induction was the same in the two groups, but this does not rule out the possibility of differences in the arterial pressure of oxygen.
This study may not settle the question of whether to use bag-mask ventilation during tracheal intubation, but it provides strong suggestion that the practice is not harmful.
Patricia A. Kritek, MD, and Andrew M. Luks, MD, are with the division of pulmonary, critical care, and sleep medicine at the University of Washington in Seattle. These comments are adapted from their editorial accompanying the paper by Casey et al. (N Engl J Med. 2019 Feb 18. doi: 10.1056/NEJMe1900708). Dr. Luks declared personal fees from private industry outside the submitted work. Dr. Kritek reported having nothing to disclose.
, according to data presented at the Critical Care Congress, sponsored by the Society of Critical Care Medicine.

A multicenter study, published simultaneously in the Feb. 18 issue of the New England Journal of Medicine, randomized 401 critically-ill patients in the ICU who were undergoing tracheal intubation to receive either ventilation with a bag-mask device during induction for intubation or no ventilation.
The median lowest oxygen saturation between induction and 2 minutes after intubation was 96% in the bag-mask ventilated patients and 93% in the no-ventilation group, representing a 4.7% difference after adjusting for prespecified covariates (P = .01).
In a post-hoc analysis that adjusted for other factors such as the provision of preoxygenation, the preoxygenation device, pneumonia, and gastrointestinal bleeding, there was a 5.2% difference between the two groups in median lowest oxygen saturation, favoring the bag-mask group.
Bag-mask ventilation was also associated with almost a halving in the incidence of severe hypoxemia – defined as an oxygen saturation below 80% – compared with no-ventilation (10.9% vs. 22.8%; relative risk = 0.48). There was also a lower incidence of patients with an oxygen saturation below 90% and below 70% in the bag-mask ventilation group, compared with the no-ventilation group.
Overall, the median decrease in oxygen saturation from induction to the lowest point was 1% in the bag-mask group, and 5% in the no-ventilation group.
The study saw no effects of factors such as body-mass index, operator experience, or Acute Physiology and Chronic Health Evaluation (APACHE II) score. The patients had a median age of 60 years, about half had sepsis or septic shock, and close to 60% had hypoxemic respiratory failure as an indication for tracheal intubation.
Jonathan D. Casey, MD, of Vanderbilt University, Nashville, Tenn., and his coauthors wrote that their results suggested for every nine critically ill patients undergoing tracheal intubation, bag-mask ventilation would prevent severe hypoxemia in one patient.
“These findings are important because oxygen saturation is an established endpoint in airway management trials and is a contributing factor to periprocedural cardiac arrest and death,” they wrote.
They noted that there are conflicting guidelines on the use of bag-mask ventilation during tracheal intubation, with some recommending its use for all patients – even those who are not hypoxemic – and others advising their use only for patients with hypoxemia. This study excluded patients who were identified as hypoxemic or in whom bag-mask ventilation was contraindicated.
Despite concerns about bag-mask ventilation increasing the risk the aspiration, the study showed no significant difference between the two groups in the incidence of operator-reported aspiration or the presence of a new opacity on chest radiograph in the 48 hours after intubation.
The authors acknowledged that, given the low incidence of operator-reported aspiration during tracheal intubation, a much larger study would be needed to show whether bag-mask ventilation did increase the risk of aspiration.
“However, our trial provides some reassurance, since the incidence of operator-reported aspiration was numerically lower in the bag-mask ventilation group than in the no-ventilation group,” they wrote.
There were also no significant differences between the two groups in oxygen saturation, fraction of inspired oxygen or positive end-expiratory pressure in the 24 hours after intubation. Bag-mask ventilation was also associated with similar rates of in-hospital mortality, number of ventilator-free days, and days out of the ICU as no-ventilation.
The authors noted that their trial focused on critically-ill patients in the ICU, so the results may not be generalizable to patients in the emergency department or in a prehospital setting.
The study and some authors were supported by the National Institutes of Health. Two authors declared personal fees from the pharmaceutical industry unrelated to the study, and no other conflicts of interest were declared.
SOURCE: Casey J et al. N Engl J Med. 2019 Feb 18. doi: 10.1056/NEJMoa1812405
, according to data presented at the Critical Care Congress, sponsored by the Society of Critical Care Medicine.

A multicenter study, published simultaneously in the Feb. 18 issue of the New England Journal of Medicine, randomized 401 critically-ill patients in the ICU who were undergoing tracheal intubation to receive either ventilation with a bag-mask device during induction for intubation or no ventilation.
The median lowest oxygen saturation between induction and 2 minutes after intubation was 96% in the bag-mask ventilated patients and 93% in the no-ventilation group, representing a 4.7% difference after adjusting for prespecified covariates (P = .01).
In a post-hoc analysis that adjusted for other factors such as the provision of preoxygenation, the preoxygenation device, pneumonia, and gastrointestinal bleeding, there was a 5.2% difference between the two groups in median lowest oxygen saturation, favoring the bag-mask group.
Bag-mask ventilation was also associated with almost a halving in the incidence of severe hypoxemia – defined as an oxygen saturation below 80% – compared with no-ventilation (10.9% vs. 22.8%; relative risk = 0.48). There was also a lower incidence of patients with an oxygen saturation below 90% and below 70% in the bag-mask ventilation group, compared with the no-ventilation group.
Overall, the median decrease in oxygen saturation from induction to the lowest point was 1% in the bag-mask group, and 5% in the no-ventilation group.
The study saw no effects of factors such as body-mass index, operator experience, or Acute Physiology and Chronic Health Evaluation (APACHE II) score. The patients had a median age of 60 years, about half had sepsis or septic shock, and close to 60% had hypoxemic respiratory failure as an indication for tracheal intubation.
Jonathan D. Casey, MD, of Vanderbilt University, Nashville, Tenn., and his coauthors wrote that their results suggested for every nine critically ill patients undergoing tracheal intubation, bag-mask ventilation would prevent severe hypoxemia in one patient.
“These findings are important because oxygen saturation is an established endpoint in airway management trials and is a contributing factor to periprocedural cardiac arrest and death,” they wrote.
They noted that there are conflicting guidelines on the use of bag-mask ventilation during tracheal intubation, with some recommending its use for all patients – even those who are not hypoxemic – and others advising their use only for patients with hypoxemia. This study excluded patients who were identified as hypoxemic or in whom bag-mask ventilation was contraindicated.
Despite concerns about bag-mask ventilation increasing the risk the aspiration, the study showed no significant difference between the two groups in the incidence of operator-reported aspiration or the presence of a new opacity on chest radiograph in the 48 hours after intubation.
The authors acknowledged that, given the low incidence of operator-reported aspiration during tracheal intubation, a much larger study would be needed to show whether bag-mask ventilation did increase the risk of aspiration.
“However, our trial provides some reassurance, since the incidence of operator-reported aspiration was numerically lower in the bag-mask ventilation group than in the no-ventilation group,” they wrote.
There were also no significant differences between the two groups in oxygen saturation, fraction of inspired oxygen or positive end-expiratory pressure in the 24 hours after intubation. Bag-mask ventilation was also associated with similar rates of in-hospital mortality, number of ventilator-free days, and days out of the ICU as no-ventilation.
The authors noted that their trial focused on critically-ill patients in the ICU, so the results may not be generalizable to patients in the emergency department or in a prehospital setting.
The study and some authors were supported by the National Institutes of Health. Two authors declared personal fees from the pharmaceutical industry unrelated to the study, and no other conflicts of interest were declared.
SOURCE: Casey J et al. N Engl J Med. 2019 Feb 18. doi: 10.1056/NEJMoa1812405
FROM CCC48
Key clinical point: Bag-mask ventilation during tracheal intubation reduces the risk of severe hypoxemia.
Major finding: For every nine patients who receive bag-mask ventilation during tracheal intubation, one case of severe hypoxemia is avoided.
Study details: Randomized, controlled trial in 401 critically-ill patients undergoing tracheal intubation.
Disclosures: The study and some authors were supported by the National Institutes of Health. Two authors declared personal fees from the pharmaceutical industry unrelated to the study.
Source: Casey J et al. N Engl J Med. 2019 Feb 18. doi: 10.1056/NEJMoa1812405
Lower prices drive OTC insulin sales at Walmart
than the OTC insulin sold elsewhere, according to a national survey of pharmacy employees.
The survey was undertaken by Jennifer N. Goldstein, MD, of Christiana Care Health System in Newark, Del., and her colleagues and published online Feb. 18 in JAMA Internal Medicine.
As Walmart does not make its sales data public, Dr. Goldstein and her colleagues conducted a national telephone-based survey of Walmart and chain pharmacies in the 49 states where OTC insulin is available. They administered a five-item questionnaire that sought to determine the frequency of OTC insulin sales.
Of the 561 pharmacies that completed the questionnaire, 500 (89.1%) responded that they did sell OTC insulin; this included 284 of 292 Walmart pharmacies. Among those Walmart pharmacies, 247 (87%) said sales of OTC insulin occurred daily; 31 (10.9%) sold it weekly; and 3 (1.1%) sold it monthly.
The chains (CVS, Walgreens, Rite Aid) reported far less frequent sales of OTC insulin; 100 out of 216 (46.3%) pharmacies said they made sales only “a few times a year,” and none reported daily sales.
A majority of respondents (54.9%) also answered yes when asked if they believed patients purchased OTC insulin because they could not afford the copayment on prescription insulin; 70.1% of those positive responses came from Walmart pharmacies.
The coauthors acknowledged that their survey represents the impressions of pharmacy employees as opposed to actual sales data. The numbers, however, do “support an estimate of daily sales of more than 18,000 vials of over-the-counter insulin at Walmart pharmacies.” As for next steps, they noted that “further studies should explore clinical and safety outcomes related to the use of over-the-counter insulin.”
One author was supported by a grant from the National Institutes of Health. No conflicts of interest were reported.
SOURCE: Goldstein JN et al. JAMA Intern Med. 2019 Feb 18. doi: 10.1001/jamainternmed.2018.7279
than the OTC insulin sold elsewhere, according to a national survey of pharmacy employees.
The survey was undertaken by Jennifer N. Goldstein, MD, of Christiana Care Health System in Newark, Del., and her colleagues and published online Feb. 18 in JAMA Internal Medicine.
As Walmart does not make its sales data public, Dr. Goldstein and her colleagues conducted a national telephone-based survey of Walmart and chain pharmacies in the 49 states where OTC insulin is available. They administered a five-item questionnaire that sought to determine the frequency of OTC insulin sales.
Of the 561 pharmacies that completed the questionnaire, 500 (89.1%) responded that they did sell OTC insulin; this included 284 of 292 Walmart pharmacies. Among those Walmart pharmacies, 247 (87%) said sales of OTC insulin occurred daily; 31 (10.9%) sold it weekly; and 3 (1.1%) sold it monthly.
The chains (CVS, Walgreens, Rite Aid) reported far less frequent sales of OTC insulin; 100 out of 216 (46.3%) pharmacies said they made sales only “a few times a year,” and none reported daily sales.
A majority of respondents (54.9%) also answered yes when asked if they believed patients purchased OTC insulin because they could not afford the copayment on prescription insulin; 70.1% of those positive responses came from Walmart pharmacies.
The coauthors acknowledged that their survey represents the impressions of pharmacy employees as opposed to actual sales data. The numbers, however, do “support an estimate of daily sales of more than 18,000 vials of over-the-counter insulin at Walmart pharmacies.” As for next steps, they noted that “further studies should explore clinical and safety outcomes related to the use of over-the-counter insulin.”
One author was supported by a grant from the National Institutes of Health. No conflicts of interest were reported.
SOURCE: Goldstein JN et al. JAMA Intern Med. 2019 Feb 18. doi: 10.1001/jamainternmed.2018.7279
than the OTC insulin sold elsewhere, according to a national survey of pharmacy employees.
The survey was undertaken by Jennifer N. Goldstein, MD, of Christiana Care Health System in Newark, Del., and her colleagues and published online Feb. 18 in JAMA Internal Medicine.
As Walmart does not make its sales data public, Dr. Goldstein and her colleagues conducted a national telephone-based survey of Walmart and chain pharmacies in the 49 states where OTC insulin is available. They administered a five-item questionnaire that sought to determine the frequency of OTC insulin sales.
Of the 561 pharmacies that completed the questionnaire, 500 (89.1%) responded that they did sell OTC insulin; this included 284 of 292 Walmart pharmacies. Among those Walmart pharmacies, 247 (87%) said sales of OTC insulin occurred daily; 31 (10.9%) sold it weekly; and 3 (1.1%) sold it monthly.
The chains (CVS, Walgreens, Rite Aid) reported far less frequent sales of OTC insulin; 100 out of 216 (46.3%) pharmacies said they made sales only “a few times a year,” and none reported daily sales.
A majority of respondents (54.9%) also answered yes when asked if they believed patients purchased OTC insulin because they could not afford the copayment on prescription insulin; 70.1% of those positive responses came from Walmart pharmacies.
The coauthors acknowledged that their survey represents the impressions of pharmacy employees as opposed to actual sales data. The numbers, however, do “support an estimate of daily sales of more than 18,000 vials of over-the-counter insulin at Walmart pharmacies.” As for next steps, they noted that “further studies should explore clinical and safety outcomes related to the use of over-the-counter insulin.”
One author was supported by a grant from the National Institutes of Health. No conflicts of interest were reported.
SOURCE: Goldstein JN et al. JAMA Intern Med. 2019 Feb 18. doi: 10.1001/jamainternmed.2018.7279
FROM JAMA INTERNAL MEDICINE
Key clinical point: Patients who purchase over-the-counter insulin typically do so at Walmart, likely because they charge much less than chain pharmacies.
Major finding: 87% of Walmart pharmacies report daily sales of over-the-counter insulin, compared with 0% of chain pharmacies.
Study details: A national telephone-based survey of Walmart and chain pharmacies in the 49 states where over-the-counter insulin is sold.
Disclosures: One author was supported by a grant from the National Institutes of Health. No conflicts of interest were reported.
Source: Goldstein JN et al. JAMA Intern Med. 2019 Feb 18. doi: 10.1001/jamainternmed.2018.7279
Early intensive treatment of MS may benefit patients
First-line treatment of multiple sclerosis with a high-efficacy therapy may produce better long-term outcomes than does an escalation treatment approach, data from a real-world cohort study suggest.
In a population-based cohort of patients with multiple sclerosis (MS) in southeast Wales, those who initiated treatment with a high-efficacy therapy had a smaller average increase in Expanded Disability Status Scale (EDSS) score after 5 years, compared with patients who started on moderate-efficacy therapy, researchers reported Feb. 18 in JAMA Neurology. These outcomes occurred “despite clinical surveillance and targeted escalation” in the group of patients who started on moderate-efficacy drugs, said first author Katharine Harding, PhD, of Cardiff University and the University Hospital of Wales in Cardiff and the Royal Gwent Hospital, Newport, Wales, and her colleagues. “These findings suggest that real-world escalation approaches may be inadequate to prevent unfavorable long-term outcomes and support the need for a prospective clinical trial to compare disease-modifying therapy algorithms.”
The investigators analyzed data collected between January 1998 and December 2016 from 592 patients with MS. Of the 592 patients, 104 initiated treatment with alemtuzumab (Lemtrada) or natalizumab (Tysabri), which the researchers classified as high-efficacy therapies (i.e., early intensive treatment), and 488 initiated treatment with interferons, glatiramer acetate (Copaxone), dimethyl fumarate (Tecfidera), fingolimod (Gilenya), or teriflunomide (Aubagio), which were considered moderate-efficacy therapies (i.e., escalation approach).
At baseline, patients who received early intensive treatment had higher average EDSS scores, compared with patients treated with an escalation approach (4.2 vs. 3.5). After 5 years, the average increase in EDSS score was lower among patients who received early intensive treatment, compared with patients treated with an escalation approach (0.3 vs. 1.2). The researchers adjusted for patients’ sex, age at treatment, year of starting treatment, and escalation to high-efficacy treatment in the escalation treatment approach group.
Median time to sustained accumulation of disability was 6.0 years for the early intensive therapy group and 3.1 years for the escalation therapy group, but the risk of sustained accumulation of disability did not differ between the groups after adjustment for covariates.
“Although patients were selected to receive early intensive treatment on the basis of poor prognostic factors, including more active disease, it was this patient group that had better long-term outcomes,” Dr. Harding and her colleagues wrote.
There were no treatment-related deaths in the study. Among patients who received alemtuzumab, 87% developed infusion-related adverse events, and 47% developed autoimmunity. Among patients receiving natalizumab, there were no serious adverse events and no cases of progressive multifocal leukoencephalopathy. In patients receiving moderate-efficacy disease-modifying therapies, there were seven serious adverse events (1.4%).
Dr. Harding disclosed grants from Novartis UK outside the present study. Coauthors reported honoraria, support to attend educational meetings, and travel expenses, as well as grants and salary outside the present study, from various pharmaceutical companies, including Biogen, Teva, Roche, MedDay Pharma, Merck, Genzyme, and Novartis.
SOURCE: Harding K et al. JAMA Neurol. 2019 Feb 18. doi: 10.1001/jamaneurol.2018.4905
First-line treatment of multiple sclerosis with a high-efficacy therapy may produce better long-term outcomes than does an escalation treatment approach, data from a real-world cohort study suggest.
In a population-based cohort of patients with multiple sclerosis (MS) in southeast Wales, those who initiated treatment with a high-efficacy therapy had a smaller average increase in Expanded Disability Status Scale (EDSS) score after 5 years, compared with patients who started on moderate-efficacy therapy, researchers reported Feb. 18 in JAMA Neurology. These outcomes occurred “despite clinical surveillance and targeted escalation” in the group of patients who started on moderate-efficacy drugs, said first author Katharine Harding, PhD, of Cardiff University and the University Hospital of Wales in Cardiff and the Royal Gwent Hospital, Newport, Wales, and her colleagues. “These findings suggest that real-world escalation approaches may be inadequate to prevent unfavorable long-term outcomes and support the need for a prospective clinical trial to compare disease-modifying therapy algorithms.”
The investigators analyzed data collected between January 1998 and December 2016 from 592 patients with MS. Of the 592 patients, 104 initiated treatment with alemtuzumab (Lemtrada) or natalizumab (Tysabri), which the researchers classified as high-efficacy therapies (i.e., early intensive treatment), and 488 initiated treatment with interferons, glatiramer acetate (Copaxone), dimethyl fumarate (Tecfidera), fingolimod (Gilenya), or teriflunomide (Aubagio), which were considered moderate-efficacy therapies (i.e., escalation approach).
At baseline, patients who received early intensive treatment had higher average EDSS scores, compared with patients treated with an escalation approach (4.2 vs. 3.5). After 5 years, the average increase in EDSS score was lower among patients who received early intensive treatment, compared with patients treated with an escalation approach (0.3 vs. 1.2). The researchers adjusted for patients’ sex, age at treatment, year of starting treatment, and escalation to high-efficacy treatment in the escalation treatment approach group.
Median time to sustained accumulation of disability was 6.0 years for the early intensive therapy group and 3.1 years for the escalation therapy group, but the risk of sustained accumulation of disability did not differ between the groups after adjustment for covariates.
“Although patients were selected to receive early intensive treatment on the basis of poor prognostic factors, including more active disease, it was this patient group that had better long-term outcomes,” Dr. Harding and her colleagues wrote.
There were no treatment-related deaths in the study. Among patients who received alemtuzumab, 87% developed infusion-related adverse events, and 47% developed autoimmunity. Among patients receiving natalizumab, there were no serious adverse events and no cases of progressive multifocal leukoencephalopathy. In patients receiving moderate-efficacy disease-modifying therapies, there were seven serious adverse events (1.4%).
Dr. Harding disclosed grants from Novartis UK outside the present study. Coauthors reported honoraria, support to attend educational meetings, and travel expenses, as well as grants and salary outside the present study, from various pharmaceutical companies, including Biogen, Teva, Roche, MedDay Pharma, Merck, Genzyme, and Novartis.
SOURCE: Harding K et al. JAMA Neurol. 2019 Feb 18. doi: 10.1001/jamaneurol.2018.4905
First-line treatment of multiple sclerosis with a high-efficacy therapy may produce better long-term outcomes than does an escalation treatment approach, data from a real-world cohort study suggest.
In a population-based cohort of patients with multiple sclerosis (MS) in southeast Wales, those who initiated treatment with a high-efficacy therapy had a smaller average increase in Expanded Disability Status Scale (EDSS) score after 5 years, compared with patients who started on moderate-efficacy therapy, researchers reported Feb. 18 in JAMA Neurology. These outcomes occurred “despite clinical surveillance and targeted escalation” in the group of patients who started on moderate-efficacy drugs, said first author Katharine Harding, PhD, of Cardiff University and the University Hospital of Wales in Cardiff and the Royal Gwent Hospital, Newport, Wales, and her colleagues. “These findings suggest that real-world escalation approaches may be inadequate to prevent unfavorable long-term outcomes and support the need for a prospective clinical trial to compare disease-modifying therapy algorithms.”
The investigators analyzed data collected between January 1998 and December 2016 from 592 patients with MS. Of the 592 patients, 104 initiated treatment with alemtuzumab (Lemtrada) or natalizumab (Tysabri), which the researchers classified as high-efficacy therapies (i.e., early intensive treatment), and 488 initiated treatment with interferons, glatiramer acetate (Copaxone), dimethyl fumarate (Tecfidera), fingolimod (Gilenya), or teriflunomide (Aubagio), which were considered moderate-efficacy therapies (i.e., escalation approach).
At baseline, patients who received early intensive treatment had higher average EDSS scores, compared with patients treated with an escalation approach (4.2 vs. 3.5). After 5 years, the average increase in EDSS score was lower among patients who received early intensive treatment, compared with patients treated with an escalation approach (0.3 vs. 1.2). The researchers adjusted for patients’ sex, age at treatment, year of starting treatment, and escalation to high-efficacy treatment in the escalation treatment approach group.
Median time to sustained accumulation of disability was 6.0 years for the early intensive therapy group and 3.1 years for the escalation therapy group, but the risk of sustained accumulation of disability did not differ between the groups after adjustment for covariates.
“Although patients were selected to receive early intensive treatment on the basis of poor prognostic factors, including more active disease, it was this patient group that had better long-term outcomes,” Dr. Harding and her colleagues wrote.
There were no treatment-related deaths in the study. Among patients who received alemtuzumab, 87% developed infusion-related adverse events, and 47% developed autoimmunity. Among patients receiving natalizumab, there were no serious adverse events and no cases of progressive multifocal leukoencephalopathy. In patients receiving moderate-efficacy disease-modifying therapies, there were seven serious adverse events (1.4%).
Dr. Harding disclosed grants from Novartis UK outside the present study. Coauthors reported honoraria, support to attend educational meetings, and travel expenses, as well as grants and salary outside the present study, from various pharmaceutical companies, including Biogen, Teva, Roche, MedDay Pharma, Merck, Genzyme, and Novartis.
SOURCE: Harding K et al. JAMA Neurol. 2019 Feb 18. doi: 10.1001/jamaneurol.2018.4905
FROM JAMA NEUROLOGY
Key clinical point:
Major finding: After 5 years, the average increase in Expanded Disability Status Scale score was lower among patients who received early intensive treatment, compared with patients treated with an escalation approach (0.3 vs. 1.2).
Study details: A population-based cohort study of 592 patients with MS in southeast Wales.
Disclosures: Dr. Harding disclosed grants from Novartis UK outside the present study. Coauthors reported honoraria, support to attend educational meetings, and travel expenses, as well as grants and salary outside the present study, from various pharmaceutical companies, including Biogen, Teva, Roche, MedDay Pharma, Merck, Genzyme, and Novartis.
Source: Harding K et al. JAMA Neurol. 2019 Feb 18. doi: 10.1001/jamaneurol.2018.4905.
Hormone therapy in transgender individuals may up risk of CV events
when compared with the general population, according to a study that analyzed medical records of more than 6,000 patients.
“In light of our results, we urge both physicians and transgender individuals to be aware of this increased cardiovascular risk,” first author Nienke M. Nota, MD, said in a press release for the study, which was published online Feb. 18 in Circulation. “It may be helpful to reduce risk factors by stopping smoking, exercising, eating a healthy diet, and losing weight, if needed, before starting therapy, and clinicians should continue to evaluate patients on an ongoing basis thereafter.”Dr. Nota and her colleagues at the Amsterdam University Medical Center analyzed the risk of cardiovascular events by comparing the medical records of 6,793 individuals, including only patients who received hormone therapy at their center or affiliate. They did not include those who had discontinued hormone therapy for an extended period or had alternated female and male sex hormones.
They defined transmen as indiviuals assigned female sex at birth but who had male gender identity, and transwomen as those assigned male sex at birth but with female gender identity.*
Researchers analyzed 2,517 transwomen (median age 30 years) and 1,358 transmen (median age 23 years) who received hormone therapy (defined as estrogen with and without androgen-suppressors for transwomen and testosterone for transmen) at the center gender’s clinic between 1972 and 2015. These records were compared with those of cisgender women and men (individuals whose gender identity matches their assigned birth gender).
The mean follow-up duration was 9.07 years for transwomen and 8.10 years for transmen. The researchers compared observed cases of stroke, myocardial infarction (MI), and venous thromboembolism (VTE) with expected cases using cisgender reference women and men. There were 29 stroke events, 30 MIs, and 73 VTE events for transwomen and 6 stroke, 11 MIs, and 2 VTE events for transmen.
There was a greater risk of stroke for transwomen, compared with cisgender women (standardized incidence ratio [SIR] = 2.42) and cisgender men (1.80), and a significantly greater risk of VTE, compared with cisgender women (5.52) and cisgender men (4.55).
The rate of MI was also significantly higher in transwomen, compared with cisgender women (2.64) and in transmen compared with cisgender women (3.69).
In a subgroup analysis, the researchers found ethinylestradiol use prior to 2001 did not significantly change the incident rate of cardiovascular events, but noted there was a lower rate of VTE when transwomen who began hormone therapy prior to 2001 were excluded from the analysis.
The researchers noted that hormone therapy may increase the risk of cardiovascular events in transgender individuals, in part, due to hormone therapy’s effect on cardiovascular risk factors such as lipid levels. Although a previous study analyzed the risk of cardiovascular events in transwomen and transmen, the researchers said that study could not conclude there was an increased risk of cardiovascular events for transmen.
The researchers said the results may be limited by study design, and their analysis of medical records could not account for potential confounders such as psychosocial stressors and smoking, as well as the decreasing risk of cardiovascular events over the period of the study, and assessing cardiovascular events differently than reference studies used.
The study had no specific funding, and the authors reported no relevant conflicts of interest.
SOURCE: Nota NM et al. Circulation. 2019 Feb 18. doi: 10.1161/CIRCULATIONAHA.118.038584
*Correction 2/25/2019: An earlier version of this story incorrectly defined transwomen and transmen. The definitions are now accurate.
when compared with the general population, according to a study that analyzed medical records of more than 6,000 patients.
“In light of our results, we urge both physicians and transgender individuals to be aware of this increased cardiovascular risk,” first author Nienke M. Nota, MD, said in a press release for the study, which was published online Feb. 18 in Circulation. “It may be helpful to reduce risk factors by stopping smoking, exercising, eating a healthy diet, and losing weight, if needed, before starting therapy, and clinicians should continue to evaluate patients on an ongoing basis thereafter.”Dr. Nota and her colleagues at the Amsterdam University Medical Center analyzed the risk of cardiovascular events by comparing the medical records of 6,793 individuals, including only patients who received hormone therapy at their center or affiliate. They did not include those who had discontinued hormone therapy for an extended period or had alternated female and male sex hormones.
They defined transmen as indiviuals assigned female sex at birth but who had male gender identity, and transwomen as those assigned male sex at birth but with female gender identity.*
Researchers analyzed 2,517 transwomen (median age 30 years) and 1,358 transmen (median age 23 years) who received hormone therapy (defined as estrogen with and without androgen-suppressors for transwomen and testosterone for transmen) at the center gender’s clinic between 1972 and 2015. These records were compared with those of cisgender women and men (individuals whose gender identity matches their assigned birth gender).
The mean follow-up duration was 9.07 years for transwomen and 8.10 years for transmen. The researchers compared observed cases of stroke, myocardial infarction (MI), and venous thromboembolism (VTE) with expected cases using cisgender reference women and men. There were 29 stroke events, 30 MIs, and 73 VTE events for transwomen and 6 stroke, 11 MIs, and 2 VTE events for transmen.
There was a greater risk of stroke for transwomen, compared with cisgender women (standardized incidence ratio [SIR] = 2.42) and cisgender men (1.80), and a significantly greater risk of VTE, compared with cisgender women (5.52) and cisgender men (4.55).
The rate of MI was also significantly higher in transwomen, compared with cisgender women (2.64) and in transmen compared with cisgender women (3.69).
In a subgroup analysis, the researchers found ethinylestradiol use prior to 2001 did not significantly change the incident rate of cardiovascular events, but noted there was a lower rate of VTE when transwomen who began hormone therapy prior to 2001 were excluded from the analysis.
The researchers noted that hormone therapy may increase the risk of cardiovascular events in transgender individuals, in part, due to hormone therapy’s effect on cardiovascular risk factors such as lipid levels. Although a previous study analyzed the risk of cardiovascular events in transwomen and transmen, the researchers said that study could not conclude there was an increased risk of cardiovascular events for transmen.
The researchers said the results may be limited by study design, and their analysis of medical records could not account for potential confounders such as psychosocial stressors and smoking, as well as the decreasing risk of cardiovascular events over the period of the study, and assessing cardiovascular events differently than reference studies used.
The study had no specific funding, and the authors reported no relevant conflicts of interest.
SOURCE: Nota NM et al. Circulation. 2019 Feb 18. doi: 10.1161/CIRCULATIONAHA.118.038584
*Correction 2/25/2019: An earlier version of this story incorrectly defined transwomen and transmen. The definitions are now accurate.
when compared with the general population, according to a study that analyzed medical records of more than 6,000 patients.
“In light of our results, we urge both physicians and transgender individuals to be aware of this increased cardiovascular risk,” first author Nienke M. Nota, MD, said in a press release for the study, which was published online Feb. 18 in Circulation. “It may be helpful to reduce risk factors by stopping smoking, exercising, eating a healthy diet, and losing weight, if needed, before starting therapy, and clinicians should continue to evaluate patients on an ongoing basis thereafter.”Dr. Nota and her colleagues at the Amsterdam University Medical Center analyzed the risk of cardiovascular events by comparing the medical records of 6,793 individuals, including only patients who received hormone therapy at their center or affiliate. They did not include those who had discontinued hormone therapy for an extended period or had alternated female and male sex hormones.
They defined transmen as indiviuals assigned female sex at birth but who had male gender identity, and transwomen as those assigned male sex at birth but with female gender identity.*
Researchers analyzed 2,517 transwomen (median age 30 years) and 1,358 transmen (median age 23 years) who received hormone therapy (defined as estrogen with and without androgen-suppressors for transwomen and testosterone for transmen) at the center gender’s clinic between 1972 and 2015. These records were compared with those of cisgender women and men (individuals whose gender identity matches their assigned birth gender).
The mean follow-up duration was 9.07 years for transwomen and 8.10 years for transmen. The researchers compared observed cases of stroke, myocardial infarction (MI), and venous thromboembolism (VTE) with expected cases using cisgender reference women and men. There were 29 stroke events, 30 MIs, and 73 VTE events for transwomen and 6 stroke, 11 MIs, and 2 VTE events for transmen.
There was a greater risk of stroke for transwomen, compared with cisgender women (standardized incidence ratio [SIR] = 2.42) and cisgender men (1.80), and a significantly greater risk of VTE, compared with cisgender women (5.52) and cisgender men (4.55).
The rate of MI was also significantly higher in transwomen, compared with cisgender women (2.64) and in transmen compared with cisgender women (3.69).
In a subgroup analysis, the researchers found ethinylestradiol use prior to 2001 did not significantly change the incident rate of cardiovascular events, but noted there was a lower rate of VTE when transwomen who began hormone therapy prior to 2001 were excluded from the analysis.
The researchers noted that hormone therapy may increase the risk of cardiovascular events in transgender individuals, in part, due to hormone therapy’s effect on cardiovascular risk factors such as lipid levels. Although a previous study analyzed the risk of cardiovascular events in transwomen and transmen, the researchers said that study could not conclude there was an increased risk of cardiovascular events for transmen.
The researchers said the results may be limited by study design, and their analysis of medical records could not account for potential confounders such as psychosocial stressors and smoking, as well as the decreasing risk of cardiovascular events over the period of the study, and assessing cardiovascular events differently than reference studies used.
The study had no specific funding, and the authors reported no relevant conflicts of interest.
SOURCE: Nota NM et al. Circulation. 2019 Feb 18. doi: 10.1161/CIRCULATIONAHA.118.038584
*Correction 2/25/2019: An earlier version of this story incorrectly defined transwomen and transmen. The definitions are now accurate.
FROM CIRCULATION