User login
HCV-infected patients in the ED should be tested for advanced liver fibrosis
More than one-third of hepatitis C virus-infected patients in the emergency department (ED) were found to have advanced liver fibrosis and higher mortality, according to the results of a retrospective study of 113 known patients with HCV at a single institution.
As part of an ongoing HCV linkage-to-care (LTC) program, HCV-infected ED patients were retrospectively identified. Components of FIB-4 (a noninvasive serum fibrosis index, which includes age, alanine aminotransferase, aspartate aminotransferase, and platelet count), were abstracted. Patients with an FIB-4 greater than 3.25 were classified with advanced fibrosis and characterized with regard to downstream outcomes at 1 year after enrollment.
The 1-year outcomes after the ED encounter for the 113 patients showed 38 with and 75 patients without advanced fibrosis. Among these, 72 (96%) and 34 (89.5%), respectively, agreed to be linked to HCV care. Ten patients of the total number of patients died within the 1-year follow-up. For those HCV-infected patients with advanced liver fibrosis compared to those without, all-cause mortality was more than fourfold higher, (18.4% [7 patients] vs. 4.0% [3 patients], P = .030), according to Yu-Hsiang Hsieh, PhD, associate professor of emergency medicine at Johns Hopkins University, Baltimore, and his colleagues (Am J Emerg Med. 2019;37[2]:286-90).
“Given the substantial burden of HCV-related illness in urban ED patients nationally, and the recognized fact that EDs are often the only point of contact with the health care system for many of these patients, we propose incorporating FIB-4 based rapid assessment into ED-based HCV screening and LTC programs in order to prioritize LTC for patients with advanced liver fibrosis, as well as routine ED clinical practice,” the researchers concluded.
They reported having no conflicts.
SOURCE: Yu-Hsiang Hsieh Y-H, Am J Emerg Med. 2019;37[2]:286-90.
More than one-third of hepatitis C virus-infected patients in the emergency department (ED) were found to have advanced liver fibrosis and higher mortality, according to the results of a retrospective study of 113 known patients with HCV at a single institution.
As part of an ongoing HCV linkage-to-care (LTC) program, HCV-infected ED patients were retrospectively identified. Components of FIB-4 (a noninvasive serum fibrosis index, which includes age, alanine aminotransferase, aspartate aminotransferase, and platelet count), were abstracted. Patients with an FIB-4 greater than 3.25 were classified with advanced fibrosis and characterized with regard to downstream outcomes at 1 year after enrollment.
The 1-year outcomes after the ED encounter for the 113 patients showed 38 with and 75 patients without advanced fibrosis. Among these, 72 (96%) and 34 (89.5%), respectively, agreed to be linked to HCV care. Ten patients of the total number of patients died within the 1-year follow-up. For those HCV-infected patients with advanced liver fibrosis compared to those without, all-cause mortality was more than fourfold higher, (18.4% [7 patients] vs. 4.0% [3 patients], P = .030), according to Yu-Hsiang Hsieh, PhD, associate professor of emergency medicine at Johns Hopkins University, Baltimore, and his colleagues (Am J Emerg Med. 2019;37[2]:286-90).
“Given the substantial burden of HCV-related illness in urban ED patients nationally, and the recognized fact that EDs are often the only point of contact with the health care system for many of these patients, we propose incorporating FIB-4 based rapid assessment into ED-based HCV screening and LTC programs in order to prioritize LTC for patients with advanced liver fibrosis, as well as routine ED clinical practice,” the researchers concluded.
They reported having no conflicts.
SOURCE: Yu-Hsiang Hsieh Y-H, Am J Emerg Med. 2019;37[2]:286-90.
More than one-third of hepatitis C virus-infected patients in the emergency department (ED) were found to have advanced liver fibrosis and higher mortality, according to the results of a retrospective study of 113 known patients with HCV at a single institution.
As part of an ongoing HCV linkage-to-care (LTC) program, HCV-infected ED patients were retrospectively identified. Components of FIB-4 (a noninvasive serum fibrosis index, which includes age, alanine aminotransferase, aspartate aminotransferase, and platelet count), were abstracted. Patients with an FIB-4 greater than 3.25 were classified with advanced fibrosis and characterized with regard to downstream outcomes at 1 year after enrollment.
The 1-year outcomes after the ED encounter for the 113 patients showed 38 with and 75 patients without advanced fibrosis. Among these, 72 (96%) and 34 (89.5%), respectively, agreed to be linked to HCV care. Ten patients of the total number of patients died within the 1-year follow-up. For those HCV-infected patients with advanced liver fibrosis compared to those without, all-cause mortality was more than fourfold higher, (18.4% [7 patients] vs. 4.0% [3 patients], P = .030), according to Yu-Hsiang Hsieh, PhD, associate professor of emergency medicine at Johns Hopkins University, Baltimore, and his colleagues (Am J Emerg Med. 2019;37[2]:286-90).
“Given the substantial burden of HCV-related illness in urban ED patients nationally, and the recognized fact that EDs are often the only point of contact with the health care system for many of these patients, we propose incorporating FIB-4 based rapid assessment into ED-based HCV screening and LTC programs in order to prioritize LTC for patients with advanced liver fibrosis, as well as routine ED clinical practice,” the researchers concluded.
They reported having no conflicts.
SOURCE: Yu-Hsiang Hsieh Y-H, Am J Emerg Med. 2019;37[2]:286-90.
FROM THE AMERICAN JOURNAL OF EMERGENCY MEDICINE
How to surf the rosacea treatment algorithm
WAIKOLOA, HAWAII – according to Linda Stein Gold, MD, director of dermatology research at Henry Ford Hospital in Detroit.

Papules and pustules need an oral or topical anti-inflammatory drug. Background erythema requires an alpha adrenergic agonist. Telangiectasia is best handled by a laser device, and if a patient has a phyma, “you’ve got to use a surgical approach,” she said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation. It sounds simple, but there are decisions to be made about what drugs and formulations to use, and when, and when to combine them.
In an interview, Dr. Stein Gold shared her approach to treatment, along with the latest on using ivermectin and brimonidine together, plus her thoughts on new medications under development and the role of the Demodex mite in rosacea.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – according to Linda Stein Gold, MD, director of dermatology research at Henry Ford Hospital in Detroit.

Papules and pustules need an oral or topical anti-inflammatory drug. Background erythema requires an alpha adrenergic agonist. Telangiectasia is best handled by a laser device, and if a patient has a phyma, “you’ve got to use a surgical approach,” she said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation. It sounds simple, but there are decisions to be made about what drugs and formulations to use, and when, and when to combine them.
In an interview, Dr. Stein Gold shared her approach to treatment, along with the latest on using ivermectin and brimonidine together, plus her thoughts on new medications under development and the role of the Demodex mite in rosacea.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – according to Linda Stein Gold, MD, director of dermatology research at Henry Ford Hospital in Detroit.

Papules and pustules need an oral or topical anti-inflammatory drug. Background erythema requires an alpha adrenergic agonist. Telangiectasia is best handled by a laser device, and if a patient has a phyma, “you’ve got to use a surgical approach,” she said at the Hawaii Dermatology Seminar provided by Global Academy for Medical Education/Skin Disease Education Foundation. It sounds simple, but there are decisions to be made about what drugs and formulations to use, and when, and when to combine them.
In an interview, Dr. Stein Gold shared her approach to treatment, along with the latest on using ivermectin and brimonidine together, plus her thoughts on new medications under development and the role of the Demodex mite in rosacea.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR
Noncardiac surgery has 7% covert stroke rate in elderly
HONOLULU – Covert strokes are relatively common in elderly patients who undergo noncardiac surgery, with a 7% incidence among a group of prospectively followed but generally unselected patients in a multicenter, international study.
By definition, these covert strokes were acutely asymptomatic, but showed evidence of clinical effects during the subsequent year. Twelve months after surgery, patients with acute, perioperative covert strokes found by systematic collection of postoperative MRI brain scans had a twofold increased rate of cognitive decline and a greater than twofold increased rate of delirium, compared with the patients who did not have evidence of a covert stroke, Marko Mrkobrada, MD, said at the International Stroke Conference sponsored by the American Heart Association.
The message from these findings is that, when elderly patients exhibit confusion or delirium after noncardiac surgery, their physicians should have a high index of suspicion that a covert stroke may have occurred, Dr. Mrkobrada said in a video interview. It’s possible that typical stroke symptoms do not appear in many of the covert stroke patients because they are masked in the immediate postoperative period, he added.
Right now, the only way to screen for a covert stroke is with a brain MR, a test that generally costs several hundred dollars, which is too expensive for routine screening. Dr. Mrkobrada said that his team hopes further study will identify a biomarker that can flag patients with a covert stroke at a lower cost. For example, colleagues of Dr. Mrkobrada have successfully used high-sensitivity troponin T, a biomarker of myocardial injury, to identify patients who have myocardial injury after noncardiac surgery (MINS; JAMA. 2017 April 25;371[16]:1642-51). Study results also established that treating MINS patients with dabigatran improved their long-term clinical outcomes (Lancet. 2018 June 9;391[10137]:2325-34).
Covert stroke after noncardiac surgery “is the same concept” as MINS, said Dr. Mrkobrada, a researcher at the London Health Sciences Centre in Canada. “We find strokes that do not get picked up after noncardiac surgery just like MIs that are not picked up,” he said. It’s also possible that certain interventions may improve outcomes in patients with covert strokes, just as they have helped MINS patients, he suggested. Potentially helpful interventions could include aspirin, a statin, and improved blood pressure control. A major goal for his research group is finding a biomarker that makes diagnosing covert stroke as easy as using high sensitivity troponin T to diagnose MINS.
The NeuroVISION (Detection and Neurological Impact of Cerebrovascular Events In Noncardiac Surgery Patients: A Cohort EvaluatioN) study enrolled and tested 1,114 people aged 65 years or older scheduled for elective noncardiac surgery anticipated to keep them hospitalized for at least 2 days at any of 12 participating centers in nine countries. Patients underwent cognitive function testing before surgery and had a brain MR scan 2-9 days after surgery, and they were excluded if they developed an overt stroke prior to the scan. Patients underwent a second round of cognitive testing a year after surgery. Patients averaged 73 years old.
The screening MR scans identified covert strokes in 78 of the study subjects (7%). The 1-year cognitive tests showed measurable drops in cognitive function in 42% of those who had experience covert strokes and in 29% of everyone else. Those rates translated to a doubled odds ratio for cognitive decline after covert stroke, compared with people without covert stroke after adjustment for baseline between-group differences, a highly statistically significant between-group difference for the study’s primary endpoint. Delirium occurred 2.2-fold more often in the covert stroke patients after adjustment, and overt strokes during 1-year follow-up were 4.1-fold more common patients who’d experienced a covert stroke, compared with everyone else, after adjustment, Dr. Mrkobrada reported. NeuroVISION is the first large-scale study to assess the incidence and associations of covert strokes after noncardiac surgery, he noted.
SOURCE: Mrkobrada M. ISC 2019, Late-Breaking Abstract LB18.
HONOLULU – Covert strokes are relatively common in elderly patients who undergo noncardiac surgery, with a 7% incidence among a group of prospectively followed but generally unselected patients in a multicenter, international study.
By definition, these covert strokes were acutely asymptomatic, but showed evidence of clinical effects during the subsequent year. Twelve months after surgery, patients with acute, perioperative covert strokes found by systematic collection of postoperative MRI brain scans had a twofold increased rate of cognitive decline and a greater than twofold increased rate of delirium, compared with the patients who did not have evidence of a covert stroke, Marko Mrkobrada, MD, said at the International Stroke Conference sponsored by the American Heart Association.
The message from these findings is that, when elderly patients exhibit confusion or delirium after noncardiac surgery, their physicians should have a high index of suspicion that a covert stroke may have occurred, Dr. Mrkobrada said in a video interview. It’s possible that typical stroke symptoms do not appear in many of the covert stroke patients because they are masked in the immediate postoperative period, he added.
Right now, the only way to screen for a covert stroke is with a brain MR, a test that generally costs several hundred dollars, which is too expensive for routine screening. Dr. Mrkobrada said that his team hopes further study will identify a biomarker that can flag patients with a covert stroke at a lower cost. For example, colleagues of Dr. Mrkobrada have successfully used high-sensitivity troponin T, a biomarker of myocardial injury, to identify patients who have myocardial injury after noncardiac surgery (MINS; JAMA. 2017 April 25;371[16]:1642-51). Study results also established that treating MINS patients with dabigatran improved their long-term clinical outcomes (Lancet. 2018 June 9;391[10137]:2325-34).
Covert stroke after noncardiac surgery “is the same concept” as MINS, said Dr. Mrkobrada, a researcher at the London Health Sciences Centre in Canada. “We find strokes that do not get picked up after noncardiac surgery just like MIs that are not picked up,” he said. It’s also possible that certain interventions may improve outcomes in patients with covert strokes, just as they have helped MINS patients, he suggested. Potentially helpful interventions could include aspirin, a statin, and improved blood pressure control. A major goal for his research group is finding a biomarker that makes diagnosing covert stroke as easy as using high sensitivity troponin T to diagnose MINS.
The NeuroVISION (Detection and Neurological Impact of Cerebrovascular Events In Noncardiac Surgery Patients: A Cohort EvaluatioN) study enrolled and tested 1,114 people aged 65 years or older scheduled for elective noncardiac surgery anticipated to keep them hospitalized for at least 2 days at any of 12 participating centers in nine countries. Patients underwent cognitive function testing before surgery and had a brain MR scan 2-9 days after surgery, and they were excluded if they developed an overt stroke prior to the scan. Patients underwent a second round of cognitive testing a year after surgery. Patients averaged 73 years old.
The screening MR scans identified covert strokes in 78 of the study subjects (7%). The 1-year cognitive tests showed measurable drops in cognitive function in 42% of those who had experience covert strokes and in 29% of everyone else. Those rates translated to a doubled odds ratio for cognitive decline after covert stroke, compared with people without covert stroke after adjustment for baseline between-group differences, a highly statistically significant between-group difference for the study’s primary endpoint. Delirium occurred 2.2-fold more often in the covert stroke patients after adjustment, and overt strokes during 1-year follow-up were 4.1-fold more common patients who’d experienced a covert stroke, compared with everyone else, after adjustment, Dr. Mrkobrada reported. NeuroVISION is the first large-scale study to assess the incidence and associations of covert strokes after noncardiac surgery, he noted.
SOURCE: Mrkobrada M. ISC 2019, Late-Breaking Abstract LB18.
HONOLULU – Covert strokes are relatively common in elderly patients who undergo noncardiac surgery, with a 7% incidence among a group of prospectively followed but generally unselected patients in a multicenter, international study.
By definition, these covert strokes were acutely asymptomatic, but showed evidence of clinical effects during the subsequent year. Twelve months after surgery, patients with acute, perioperative covert strokes found by systematic collection of postoperative MRI brain scans had a twofold increased rate of cognitive decline and a greater than twofold increased rate of delirium, compared with the patients who did not have evidence of a covert stroke, Marko Mrkobrada, MD, said at the International Stroke Conference sponsored by the American Heart Association.
The message from these findings is that, when elderly patients exhibit confusion or delirium after noncardiac surgery, their physicians should have a high index of suspicion that a covert stroke may have occurred, Dr. Mrkobrada said in a video interview. It’s possible that typical stroke symptoms do not appear in many of the covert stroke patients because they are masked in the immediate postoperative period, he added.
Right now, the only way to screen for a covert stroke is with a brain MR, a test that generally costs several hundred dollars, which is too expensive for routine screening. Dr. Mrkobrada said that his team hopes further study will identify a biomarker that can flag patients with a covert stroke at a lower cost. For example, colleagues of Dr. Mrkobrada have successfully used high-sensitivity troponin T, a biomarker of myocardial injury, to identify patients who have myocardial injury after noncardiac surgery (MINS; JAMA. 2017 April 25;371[16]:1642-51). Study results also established that treating MINS patients with dabigatran improved their long-term clinical outcomes (Lancet. 2018 June 9;391[10137]:2325-34).
Covert stroke after noncardiac surgery “is the same concept” as MINS, said Dr. Mrkobrada, a researcher at the London Health Sciences Centre in Canada. “We find strokes that do not get picked up after noncardiac surgery just like MIs that are not picked up,” he said. It’s also possible that certain interventions may improve outcomes in patients with covert strokes, just as they have helped MINS patients, he suggested. Potentially helpful interventions could include aspirin, a statin, and improved blood pressure control. A major goal for his research group is finding a biomarker that makes diagnosing covert stroke as easy as using high sensitivity troponin T to diagnose MINS.
The NeuroVISION (Detection and Neurological Impact of Cerebrovascular Events In Noncardiac Surgery Patients: A Cohort EvaluatioN) study enrolled and tested 1,114 people aged 65 years or older scheduled for elective noncardiac surgery anticipated to keep them hospitalized for at least 2 days at any of 12 participating centers in nine countries. Patients underwent cognitive function testing before surgery and had a brain MR scan 2-9 days after surgery, and they were excluded if they developed an overt stroke prior to the scan. Patients underwent a second round of cognitive testing a year after surgery. Patients averaged 73 years old.
The screening MR scans identified covert strokes in 78 of the study subjects (7%). The 1-year cognitive tests showed measurable drops in cognitive function in 42% of those who had experience covert strokes and in 29% of everyone else. Those rates translated to a doubled odds ratio for cognitive decline after covert stroke, compared with people without covert stroke after adjustment for baseline between-group differences, a highly statistically significant between-group difference for the study’s primary endpoint. Delirium occurred 2.2-fold more often in the covert stroke patients after adjustment, and overt strokes during 1-year follow-up were 4.1-fold more common patients who’d experienced a covert stroke, compared with everyone else, after adjustment, Dr. Mrkobrada reported. NeuroVISION is the first large-scale study to assess the incidence and associations of covert strokes after noncardiac surgery, he noted.
SOURCE: Mrkobrada M. ISC 2019, Late-Breaking Abstract LB18.
REPORTING FROM ISC 2019
Key clinical point:
Major finding: Elderly patients who underwent noncardiac surgery had a 7% incidence of covert stroke.
Study details: NeuroVISION, a prospective, multicenter, observational study with 1,114 patients.
Disclosures: NeuroVISION did not receive commercial funding. Dr. Mrkobrada had no disclosures.
Source: Mrkobrada M. ISC 2019, Late-Breaking Abstract LB18.
House committee passes AMA-endorsed firearm bill
WASHINGTON – A bill requiring universal background checks for firearm purchases passed the House Judiciary committee and is expected to pass the full House of Representatives when it comes up for consideration.
Rep. Mike Thompson (R-Calif.), chairman of the House Gun Violence Prevention Task Force, thanked the American Medical Association for its endorsement and support of the bill a day before its Feb. 13 committee passage during a speech at a national advocacy conference sponsored by the AMA.
“The new legislation, H.R. 8, which you have endorsed, would put in place universal background checks,” Rep. Thompson said. “This means anybody who buys a gun would have to go through a background check to make sure they are not a criminal, to make sure they are not dangerously mentally ill and a danger to themselves or others.”
The committee passed the Bipartisan Background Checks Act of 2019 by a 23-15 vote. It would require a background check on all firearms transfers, including private sales, with limited exemptions for firearms given as gifts between family members and those transferred for hunting, target shooting, and self-defense.
A second bill, the Enhanced Background Checks Act (H.R. 1112), passed 21-14 during the same session. That bill would close a loophole that currently allows a licensed dealer to transfer a firearm after 3 days if the background check system has not yet reported back.
Rep. Thompson credited the newest members of Congress with pushing these bills to the forefront.
“During the last midterm election, there was a sea change in attitude around gun violence prevention,” Rep. Thompson noted. “All 40 members of the Democratic-elected class who took a seat ran on gun violence prevention. So they came to Washington with more of a willingness to deal with this issue.”
H.R. 8 has 231 cosponsors – 226 Democrats and 5 Republicans – meaning it has more than enough support to pass in the full House, should all cosponsors remain on board.
Getting the bill passed in the Republican-controlled Senate will be a challenge and Rep. Thompson encouraged doctors to continue their advocacy on this legislation.
“You guys have been fabulous,” he said. “Without your help, we would not be where we are today. I can tell you that this bill will pass the House within the first 100 days and will go to the Senate. That is when you will have to start working again. ... Once it goes to the Senate, there is going to be a reluctance to take it up. We need to make sure that every U.S. senator hears from every doc and every doc’s family and every doc’s friend and every doc’s assistant and everybody else and their brother that this important so we can turn up the heat and make sure they take up the issue of background checks. It works. It saves lives.”
WASHINGTON – A bill requiring universal background checks for firearm purchases passed the House Judiciary committee and is expected to pass the full House of Representatives when it comes up for consideration.
Rep. Mike Thompson (R-Calif.), chairman of the House Gun Violence Prevention Task Force, thanked the American Medical Association for its endorsement and support of the bill a day before its Feb. 13 committee passage during a speech at a national advocacy conference sponsored by the AMA.
“The new legislation, H.R. 8, which you have endorsed, would put in place universal background checks,” Rep. Thompson said. “This means anybody who buys a gun would have to go through a background check to make sure they are not a criminal, to make sure they are not dangerously mentally ill and a danger to themselves or others.”
The committee passed the Bipartisan Background Checks Act of 2019 by a 23-15 vote. It would require a background check on all firearms transfers, including private sales, with limited exemptions for firearms given as gifts between family members and those transferred for hunting, target shooting, and self-defense.
A second bill, the Enhanced Background Checks Act (H.R. 1112), passed 21-14 during the same session. That bill would close a loophole that currently allows a licensed dealer to transfer a firearm after 3 days if the background check system has not yet reported back.
Rep. Thompson credited the newest members of Congress with pushing these bills to the forefront.
“During the last midterm election, there was a sea change in attitude around gun violence prevention,” Rep. Thompson noted. “All 40 members of the Democratic-elected class who took a seat ran on gun violence prevention. So they came to Washington with more of a willingness to deal with this issue.”
H.R. 8 has 231 cosponsors – 226 Democrats and 5 Republicans – meaning it has more than enough support to pass in the full House, should all cosponsors remain on board.
Getting the bill passed in the Republican-controlled Senate will be a challenge and Rep. Thompson encouraged doctors to continue their advocacy on this legislation.
“You guys have been fabulous,” he said. “Without your help, we would not be where we are today. I can tell you that this bill will pass the House within the first 100 days and will go to the Senate. That is when you will have to start working again. ... Once it goes to the Senate, there is going to be a reluctance to take it up. We need to make sure that every U.S. senator hears from every doc and every doc’s family and every doc’s friend and every doc’s assistant and everybody else and their brother that this important so we can turn up the heat and make sure they take up the issue of background checks. It works. It saves lives.”
WASHINGTON – A bill requiring universal background checks for firearm purchases passed the House Judiciary committee and is expected to pass the full House of Representatives when it comes up for consideration.
Rep. Mike Thompson (R-Calif.), chairman of the House Gun Violence Prevention Task Force, thanked the American Medical Association for its endorsement and support of the bill a day before its Feb. 13 committee passage during a speech at a national advocacy conference sponsored by the AMA.
“The new legislation, H.R. 8, which you have endorsed, would put in place universal background checks,” Rep. Thompson said. “This means anybody who buys a gun would have to go through a background check to make sure they are not a criminal, to make sure they are not dangerously mentally ill and a danger to themselves or others.”
The committee passed the Bipartisan Background Checks Act of 2019 by a 23-15 vote. It would require a background check on all firearms transfers, including private sales, with limited exemptions for firearms given as gifts between family members and those transferred for hunting, target shooting, and self-defense.
A second bill, the Enhanced Background Checks Act (H.R. 1112), passed 21-14 during the same session. That bill would close a loophole that currently allows a licensed dealer to transfer a firearm after 3 days if the background check system has not yet reported back.
Rep. Thompson credited the newest members of Congress with pushing these bills to the forefront.
“During the last midterm election, there was a sea change in attitude around gun violence prevention,” Rep. Thompson noted. “All 40 members of the Democratic-elected class who took a seat ran on gun violence prevention. So they came to Washington with more of a willingness to deal with this issue.”
H.R. 8 has 231 cosponsors – 226 Democrats and 5 Republicans – meaning it has more than enough support to pass in the full House, should all cosponsors remain on board.
Getting the bill passed in the Republican-controlled Senate will be a challenge and Rep. Thompson encouraged doctors to continue their advocacy on this legislation.
“You guys have been fabulous,” he said. “Without your help, we would not be where we are today. I can tell you that this bill will pass the House within the first 100 days and will go to the Senate. That is when you will have to start working again. ... Once it goes to the Senate, there is going to be a reluctance to take it up. We need to make sure that every U.S. senator hears from every doc and every doc’s family and every doc’s friend and every doc’s assistant and everybody else and their brother that this important so we can turn up the heat and make sure they take up the issue of background checks. It works. It saves lives.”
REPORTING FROM AMA NATIONAL ADVOCACY CONFERENCE
Don’t fear spironolactone, isotretinoin, OCs for acne
WAIKOLOA, HAWAII – There’s really , of the department of dermatology at the University of Alabama at Birmingham.
There have been concerns with all three in the past, but most of the worries have been recently laid to rest.
The news hasn’t reached everyone, though, so, by and large, they are “tools I think we are not using enough of,” Dr. Harper said in an interview. With isotretinoin, for instance, it really isn’t necessary to do blood work for lipids and liver function every month, a daunting prospect for patients; baseline testing with a repeat at 2 months is sufficient, as long as there’s no dose escalation and results are acceptable, with the exception of a monthly pregnancy test for women, she noted. Meanwhile, there’s no evidence of a link with inflammatory bowel disease, and wound healing isn’t as much of an issue as once thought.
It’s the same story with spironolactone. Hyperkalemia is a long-standing concern, but it turns out that “in healthy young women taking spironolactone for acne, we don’t need to be checking potassium.” As far as breast cancer goes, the potential risk with spironolactone hasn’t panned out in the literature, and there may not be “a link at all,” Dr. Harper said at the Hawaii Dermatology Seminar provided by the Global Academy for Medical Education/Skin Disease Education Foundation.
There are caveats, of course. Hormonal treatments shouldn’t be used in young women until they’ve established their menstrual cycle. OCs should not be used in smokers, or people who have hypertension or migraines, among other conditions. Also, elevated triglycerides remain a concern with isotretinoin. “The number I would want people to remember is 500 [mg/dL],” the threshold when triglycerides become a problem.
In the interview, Dr. Harper explained the new thinking on these three options, and shared her treatment tips, including what to do if patients’ triglycerides hit the 500 mg/dL mark.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – There’s really , of the department of dermatology at the University of Alabama at Birmingham.
There have been concerns with all three in the past, but most of the worries have been recently laid to rest.
The news hasn’t reached everyone, though, so, by and large, they are “tools I think we are not using enough of,” Dr. Harper said in an interview. With isotretinoin, for instance, it really isn’t necessary to do blood work for lipids and liver function every month, a daunting prospect for patients; baseline testing with a repeat at 2 months is sufficient, as long as there’s no dose escalation and results are acceptable, with the exception of a monthly pregnancy test for women, she noted. Meanwhile, there’s no evidence of a link with inflammatory bowel disease, and wound healing isn’t as much of an issue as once thought.
It’s the same story with spironolactone. Hyperkalemia is a long-standing concern, but it turns out that “in healthy young women taking spironolactone for acne, we don’t need to be checking potassium.” As far as breast cancer goes, the potential risk with spironolactone hasn’t panned out in the literature, and there may not be “a link at all,” Dr. Harper said at the Hawaii Dermatology Seminar provided by the Global Academy for Medical Education/Skin Disease Education Foundation.
There are caveats, of course. Hormonal treatments shouldn’t be used in young women until they’ve established their menstrual cycle. OCs should not be used in smokers, or people who have hypertension or migraines, among other conditions. Also, elevated triglycerides remain a concern with isotretinoin. “The number I would want people to remember is 500 [mg/dL],” the threshold when triglycerides become a problem.
In the interview, Dr. Harper explained the new thinking on these three options, and shared her treatment tips, including what to do if patients’ triglycerides hit the 500 mg/dL mark.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
WAIKOLOA, HAWAII – There’s really , of the department of dermatology at the University of Alabama at Birmingham.
There have been concerns with all three in the past, but most of the worries have been recently laid to rest.
The news hasn’t reached everyone, though, so, by and large, they are “tools I think we are not using enough of,” Dr. Harper said in an interview. With isotretinoin, for instance, it really isn’t necessary to do blood work for lipids and liver function every month, a daunting prospect for patients; baseline testing with a repeat at 2 months is sufficient, as long as there’s no dose escalation and results are acceptable, with the exception of a monthly pregnancy test for women, she noted. Meanwhile, there’s no evidence of a link with inflammatory bowel disease, and wound healing isn’t as much of an issue as once thought.
It’s the same story with spironolactone. Hyperkalemia is a long-standing concern, but it turns out that “in healthy young women taking spironolactone for acne, we don’t need to be checking potassium.” As far as breast cancer goes, the potential risk with spironolactone hasn’t panned out in the literature, and there may not be “a link at all,” Dr. Harper said at the Hawaii Dermatology Seminar provided by the Global Academy for Medical Education/Skin Disease Education Foundation.
There are caveats, of course. Hormonal treatments shouldn’t be used in young women until they’ve established their menstrual cycle. OCs should not be used in smokers, or people who have hypertension or migraines, among other conditions. Also, elevated triglycerides remain a concern with isotretinoin. “The number I would want people to remember is 500 [mg/dL],” the threshold when triglycerides become a problem.
In the interview, Dr. Harper explained the new thinking on these three options, and shared her treatment tips, including what to do if patients’ triglycerides hit the 500 mg/dL mark.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR
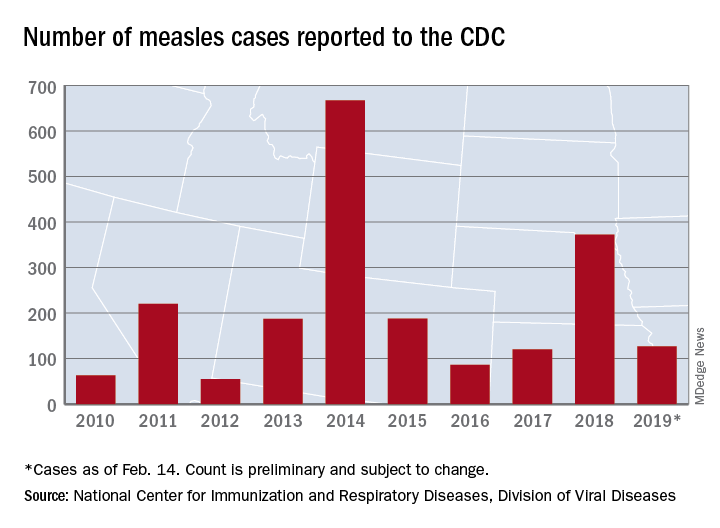
Measles: 26 new cases reported last week
according to the Centers for Disease Control and Prevention.
On Jan. 31, total measles cases stood at 79, which means that the number of individuals with measles has risen by 61% in just the last 2 weeks. Of the five outbreaks (defined as three or more cases) so far in 2019, three have occurred in New York (57 cases in three counties), one in Texas (8 cases in five counties), and one in Washington (62 cases in two counties), the CDC reported Feb. 18.
The majority of the Washington cases (61 of the 62) have occurred in Clark County, which is located just across the Columbia River from Portland, Ore. Oregon, in turn, has a higher percentage of kindergartners with nonmedical exemptions from vaccination (7.5%) than any other state, the CDC reported in October 2018. Washington’s rate of 3.9% was nearly double the national median of 2.0% for the 2017-2018 school year, while Texas (1.8%) and New York (1.0%) were below it, the CDC said.
In the Pacific Northwest, however, some parents may be changing their minds about vaccinations, according to the New York Times, which reported that “about triple the number of children have been vaccinated this year, compared with the same period in 2018,” in Oregon and southwest Washington.
Individual cases of measles have been reported to the CDC by seven other states: California, Colorado, Connecticut, Georgia, Illinois, Kentucky, and Oregon.
according to the Centers for Disease Control and Prevention.
On Jan. 31, total measles cases stood at 79, which means that the number of individuals with measles has risen by 61% in just the last 2 weeks. Of the five outbreaks (defined as three or more cases) so far in 2019, three have occurred in New York (57 cases in three counties), one in Texas (8 cases in five counties), and one in Washington (62 cases in two counties), the CDC reported Feb. 18.
The majority of the Washington cases (61 of the 62) have occurred in Clark County, which is located just across the Columbia River from Portland, Ore. Oregon, in turn, has a higher percentage of kindergartners with nonmedical exemptions from vaccination (7.5%) than any other state, the CDC reported in October 2018. Washington’s rate of 3.9% was nearly double the national median of 2.0% for the 2017-2018 school year, while Texas (1.8%) and New York (1.0%) were below it, the CDC said.
In the Pacific Northwest, however, some parents may be changing their minds about vaccinations, according to the New York Times, which reported that “about triple the number of children have been vaccinated this year, compared with the same period in 2018,” in Oregon and southwest Washington.
Individual cases of measles have been reported to the CDC by seven other states: California, Colorado, Connecticut, Georgia, Illinois, Kentucky, and Oregon.
according to the Centers for Disease Control and Prevention.
On Jan. 31, total measles cases stood at 79, which means that the number of individuals with measles has risen by 61% in just the last 2 weeks. Of the five outbreaks (defined as three or more cases) so far in 2019, three have occurred in New York (57 cases in three counties), one in Texas (8 cases in five counties), and one in Washington (62 cases in two counties), the CDC reported Feb. 18.
The majority of the Washington cases (61 of the 62) have occurred in Clark County, which is located just across the Columbia River from Portland, Ore. Oregon, in turn, has a higher percentage of kindergartners with nonmedical exemptions from vaccination (7.5%) than any other state, the CDC reported in October 2018. Washington’s rate of 3.9% was nearly double the national median of 2.0% for the 2017-2018 school year, while Texas (1.8%) and New York (1.0%) were below it, the CDC said.
In the Pacific Northwest, however, some parents may be changing their minds about vaccinations, according to the New York Times, which reported that “about triple the number of children have been vaccinated this year, compared with the same period in 2018,” in Oregon and southwest Washington.
Individual cases of measles have been reported to the CDC by seven other states: California, Colorado, Connecticut, Georgia, Illinois, Kentucky, and Oregon.
List of medications linked to drug-induced lupus expands
leaving the overall number now standing at 118.
Among the 118 suspected drugs found in VigiBase, the WHO’s global deduplicated individual case safety reports (ICSR) database, 42 had not been previously reported in association with drug-induced lupus (DIL) and 76 had been previously reported in association with DIL in Medline. DIL was reported as a serious adverse event in 55.4% of cases, according to French researchers led by Laurent Arnaud, MD, PhD, of the department of rheumatology at Hôpitaux Universitaires de Strasbourg and Centre National de Références des Maladies Systémiques Rares, Strasbourg, France.
Dr. Arnaud and his colleagues conducted a case-noncase analysis for each drug associated with DIL in order to compare the proportion of specific adverse drug reactions (ADRs) reported for a single drug with the proportion of the same ADR for all other treatments in VigiBase, which receives reports from more than 130 country members of the WHO Programme for International Drug Monitoring and contains over 16 million deduplicated ICSRs recorded by pharmacovigilance centers since 1967. They searched for cases classified as systemic lupus erythematosus (SLE) and identified 12,166 ICSRs of DIL; from these they found 118 suspected drugs with significant pharmacovigilance signal from 8,163 ICSRs that mostly originated from the Americas (65%) and Europe (23%).
In line with what the study authors expected, the drugs associated with the highest number of DIL cases were the antitumor necrosis factor agents infliximab, adalimumab, and etanercept, and the drugs associated with the highest disproportional reporting of DIL were procainamide and hydralazine.
“This is an important finding because these are the two drugs associated with the highest risk of DIL in the literature, therefore confirming the reliability of our approach using a large pharmacovigilance database,” the researchers wrote in Annals of the Rheumatic Diseases.
Overall, DIL was considered definite for 9 drugs (procainamide, hydralazine, minocycline, quinidine, isoniazid, terbinafine, methyldopa, dihydralazine, and chlorpromazine), probable for 19 drugs, and possible for 45 drugs.
The median age of DIL onset was 49 years, which the authors noted was about 2 decades older than that of spontaneous SLE.
They also observed a marked predominance in females (female to male sex ratio, 4.3), a finding that contrasted with previous studies reporting a female to male sex ratio closer to 1:1.
Dr. Arnaud and his colleagues stated that their finding of a median delay between the reported start of suspected treatment and DIL occurrence of 172 days (interquartile range, 35-610 days) suggested that DIL mostly appears after a few months and usually within the first 2 years of treatment with the suspected drug.
“The analysis of the median reporting years for each suspected drug shows a clear evolution of suspected drugs during the past decades. This further underlines that the constantly changing spectrum of DIL should be monitored continuously, and further validates the interest of our approach using the WHO international pharmacovigilance database, the biggest database of this kind with over 16 million deduplicated ICSRs,” they wrote.
The researchers added that distinguishing DIL from SLE is important because its prognosis is usually good when the drug is withdrawn, but the spectrum of DIL is constantly evolving, with drugs once described as strongly linked to DIL now prescribed less frequently.
“The first case of DIL was reported in 1945 with sulfadiazine, while hydralazine DIL was first reported in 1953. Since then, pharmacopoeia has strongly evolved, and one could hypothesize that so has the spectrum of drugs that can induce DIL,” they wrote.
“The detailed list of suspected drugs may prove useful to physicians when confronted with potential DIL cases. Altogether, these findings may help in improving the identification of this constantly evolving disease,” they concluded.
The current study was limited by the lack of a uniform set of criteria for the diagnosis of DIL and by the level of reported details available in VigiBase.
The authors had no outside funding for the study and reported having no conflicts of interest.
SOURCE: Arnaud L et al. Ann Rheum Dis. 2019 Feb 4. doi: 10.1136/annrheumdis-2018-214598.
This new and updated list of possible lupus-inducing drugs includes a growing range of treatment categories, chemical structures, and pharmacologic actions. Yet it is still unclear what the common denominator is that links them.
Drug-induced lupus (DIL) is a peculiar adverse drug reaction that appears to be unrelated to any known property of the inducing agent, although cytokine modulating biologics are a possible exception. Nevertheless, the in vivo metabolism of dissimilar drugs to products with a common, reactive property may go some way to explaining how compounds with different pharmacologic and chemical structures could induce similar adverse reactions.
The findings by Arnaud et al. need better documentation than just positive pharmacovigilance signals. For example, a drug with a relatively high signal does not necessarily translate to a high propensity for causing lupus-like symptoms. It may be a reflection of high drug usage or an awareness of the report contributors for detecting new-onset systemic lupus erythematosus.
Regardless, this research serves to help and inform the medical community to increase the vigilance of previously unreported DIL and perhaps motivate the publication of novel, convincing case reports.
Robert L. Rubin, PhD, is with the University of New Mexico, Albuquerque. His comments are adapted from an editorial accompanying the report by Arnaud et al. (Ann Rheum Dis. 2019 Feb 13. doi: annrheumdis-2018-214785). He reported having no relevant disclosures.
This new and updated list of possible lupus-inducing drugs includes a growing range of treatment categories, chemical structures, and pharmacologic actions. Yet it is still unclear what the common denominator is that links them.
Drug-induced lupus (DIL) is a peculiar adverse drug reaction that appears to be unrelated to any known property of the inducing agent, although cytokine modulating biologics are a possible exception. Nevertheless, the in vivo metabolism of dissimilar drugs to products with a common, reactive property may go some way to explaining how compounds with different pharmacologic and chemical structures could induce similar adverse reactions.
The findings by Arnaud et al. need better documentation than just positive pharmacovigilance signals. For example, a drug with a relatively high signal does not necessarily translate to a high propensity for causing lupus-like symptoms. It may be a reflection of high drug usage or an awareness of the report contributors for detecting new-onset systemic lupus erythematosus.
Regardless, this research serves to help and inform the medical community to increase the vigilance of previously unreported DIL and perhaps motivate the publication of novel, convincing case reports.
Robert L. Rubin, PhD, is with the University of New Mexico, Albuquerque. His comments are adapted from an editorial accompanying the report by Arnaud et al. (Ann Rheum Dis. 2019 Feb 13. doi: annrheumdis-2018-214785). He reported having no relevant disclosures.
This new and updated list of possible lupus-inducing drugs includes a growing range of treatment categories, chemical structures, and pharmacologic actions. Yet it is still unclear what the common denominator is that links them.
Drug-induced lupus (DIL) is a peculiar adverse drug reaction that appears to be unrelated to any known property of the inducing agent, although cytokine modulating biologics are a possible exception. Nevertheless, the in vivo metabolism of dissimilar drugs to products with a common, reactive property may go some way to explaining how compounds with different pharmacologic and chemical structures could induce similar adverse reactions.
The findings by Arnaud et al. need better documentation than just positive pharmacovigilance signals. For example, a drug with a relatively high signal does not necessarily translate to a high propensity for causing lupus-like symptoms. It may be a reflection of high drug usage or an awareness of the report contributors for detecting new-onset systemic lupus erythematosus.
Regardless, this research serves to help and inform the medical community to increase the vigilance of previously unreported DIL and perhaps motivate the publication of novel, convincing case reports.
Robert L. Rubin, PhD, is with the University of New Mexico, Albuquerque. His comments are adapted from an editorial accompanying the report by Arnaud et al. (Ann Rheum Dis. 2019 Feb 13. doi: annrheumdis-2018-214785). He reported having no relevant disclosures.
leaving the overall number now standing at 118.
Among the 118 suspected drugs found in VigiBase, the WHO’s global deduplicated individual case safety reports (ICSR) database, 42 had not been previously reported in association with drug-induced lupus (DIL) and 76 had been previously reported in association with DIL in Medline. DIL was reported as a serious adverse event in 55.4% of cases, according to French researchers led by Laurent Arnaud, MD, PhD, of the department of rheumatology at Hôpitaux Universitaires de Strasbourg and Centre National de Références des Maladies Systémiques Rares, Strasbourg, France.
Dr. Arnaud and his colleagues conducted a case-noncase analysis for each drug associated with DIL in order to compare the proportion of specific adverse drug reactions (ADRs) reported for a single drug with the proportion of the same ADR for all other treatments in VigiBase, which receives reports from more than 130 country members of the WHO Programme for International Drug Monitoring and contains over 16 million deduplicated ICSRs recorded by pharmacovigilance centers since 1967. They searched for cases classified as systemic lupus erythematosus (SLE) and identified 12,166 ICSRs of DIL; from these they found 118 suspected drugs with significant pharmacovigilance signal from 8,163 ICSRs that mostly originated from the Americas (65%) and Europe (23%).
In line with what the study authors expected, the drugs associated with the highest number of DIL cases were the antitumor necrosis factor agents infliximab, adalimumab, and etanercept, and the drugs associated with the highest disproportional reporting of DIL were procainamide and hydralazine.
“This is an important finding because these are the two drugs associated with the highest risk of DIL in the literature, therefore confirming the reliability of our approach using a large pharmacovigilance database,” the researchers wrote in Annals of the Rheumatic Diseases.
Overall, DIL was considered definite for 9 drugs (procainamide, hydralazine, minocycline, quinidine, isoniazid, terbinafine, methyldopa, dihydralazine, and chlorpromazine), probable for 19 drugs, and possible for 45 drugs.
The median age of DIL onset was 49 years, which the authors noted was about 2 decades older than that of spontaneous SLE.
They also observed a marked predominance in females (female to male sex ratio, 4.3), a finding that contrasted with previous studies reporting a female to male sex ratio closer to 1:1.
Dr. Arnaud and his colleagues stated that their finding of a median delay between the reported start of suspected treatment and DIL occurrence of 172 days (interquartile range, 35-610 days) suggested that DIL mostly appears after a few months and usually within the first 2 years of treatment with the suspected drug.
“The analysis of the median reporting years for each suspected drug shows a clear evolution of suspected drugs during the past decades. This further underlines that the constantly changing spectrum of DIL should be monitored continuously, and further validates the interest of our approach using the WHO international pharmacovigilance database, the biggest database of this kind with over 16 million deduplicated ICSRs,” they wrote.
The researchers added that distinguishing DIL from SLE is important because its prognosis is usually good when the drug is withdrawn, but the spectrum of DIL is constantly evolving, with drugs once described as strongly linked to DIL now prescribed less frequently.
“The first case of DIL was reported in 1945 with sulfadiazine, while hydralazine DIL was first reported in 1953. Since then, pharmacopoeia has strongly evolved, and one could hypothesize that so has the spectrum of drugs that can induce DIL,” they wrote.
“The detailed list of suspected drugs may prove useful to physicians when confronted with potential DIL cases. Altogether, these findings may help in improving the identification of this constantly evolving disease,” they concluded.
The current study was limited by the lack of a uniform set of criteria for the diagnosis of DIL and by the level of reported details available in VigiBase.
The authors had no outside funding for the study and reported having no conflicts of interest.
SOURCE: Arnaud L et al. Ann Rheum Dis. 2019 Feb 4. doi: 10.1136/annrheumdis-2018-214598.
leaving the overall number now standing at 118.
Among the 118 suspected drugs found in VigiBase, the WHO’s global deduplicated individual case safety reports (ICSR) database, 42 had not been previously reported in association with drug-induced lupus (DIL) and 76 had been previously reported in association with DIL in Medline. DIL was reported as a serious adverse event in 55.4% of cases, according to French researchers led by Laurent Arnaud, MD, PhD, of the department of rheumatology at Hôpitaux Universitaires de Strasbourg and Centre National de Références des Maladies Systémiques Rares, Strasbourg, France.
Dr. Arnaud and his colleagues conducted a case-noncase analysis for each drug associated with DIL in order to compare the proportion of specific adverse drug reactions (ADRs) reported for a single drug with the proportion of the same ADR for all other treatments in VigiBase, which receives reports from more than 130 country members of the WHO Programme for International Drug Monitoring and contains over 16 million deduplicated ICSRs recorded by pharmacovigilance centers since 1967. They searched for cases classified as systemic lupus erythematosus (SLE) and identified 12,166 ICSRs of DIL; from these they found 118 suspected drugs with significant pharmacovigilance signal from 8,163 ICSRs that mostly originated from the Americas (65%) and Europe (23%).
In line with what the study authors expected, the drugs associated with the highest number of DIL cases were the antitumor necrosis factor agents infliximab, adalimumab, and etanercept, and the drugs associated with the highest disproportional reporting of DIL were procainamide and hydralazine.
“This is an important finding because these are the two drugs associated with the highest risk of DIL in the literature, therefore confirming the reliability of our approach using a large pharmacovigilance database,” the researchers wrote in Annals of the Rheumatic Diseases.
Overall, DIL was considered definite for 9 drugs (procainamide, hydralazine, minocycline, quinidine, isoniazid, terbinafine, methyldopa, dihydralazine, and chlorpromazine), probable for 19 drugs, and possible for 45 drugs.
The median age of DIL onset was 49 years, which the authors noted was about 2 decades older than that of spontaneous SLE.
They also observed a marked predominance in females (female to male sex ratio, 4.3), a finding that contrasted with previous studies reporting a female to male sex ratio closer to 1:1.
Dr. Arnaud and his colleagues stated that their finding of a median delay between the reported start of suspected treatment and DIL occurrence of 172 days (interquartile range, 35-610 days) suggested that DIL mostly appears after a few months and usually within the first 2 years of treatment with the suspected drug.
“The analysis of the median reporting years for each suspected drug shows a clear evolution of suspected drugs during the past decades. This further underlines that the constantly changing spectrum of DIL should be monitored continuously, and further validates the interest of our approach using the WHO international pharmacovigilance database, the biggest database of this kind with over 16 million deduplicated ICSRs,” they wrote.
The researchers added that distinguishing DIL from SLE is important because its prognosis is usually good when the drug is withdrawn, but the spectrum of DIL is constantly evolving, with drugs once described as strongly linked to DIL now prescribed less frequently.
“The first case of DIL was reported in 1945 with sulfadiazine, while hydralazine DIL was first reported in 1953. Since then, pharmacopoeia has strongly evolved, and one could hypothesize that so has the spectrum of drugs that can induce DIL,” they wrote.
“The detailed list of suspected drugs may prove useful to physicians when confronted with potential DIL cases. Altogether, these findings may help in improving the identification of this constantly evolving disease,” they concluded.
The current study was limited by the lack of a uniform set of criteria for the diagnosis of DIL and by the level of reported details available in VigiBase.
The authors had no outside funding for the study and reported having no conflicts of interest.
SOURCE: Arnaud L et al. Ann Rheum Dis. 2019 Feb 4. doi: 10.1136/annrheumdis-2018-214598.
FROM ANNALS OF THE RHEUMATIC DISEASES
Meta-analysis: Combo therapies best for neuroendocrine tumors
Multiple treatment options, which have shown to be safe and effective for patients with neuroendocrine tumors (NET), are presently available, according to a systematic review and meta-analysis of 30 randomized clinical trials.
“We aimed to identify all [randomized clinical trials] comparing therapeutic interventions in [neuroendocrine tumors],” Reto M. Kaderli, MD, of the University of Bern in Switzerland, and his colleagues wrote in JAMA Oncology.
The researchers searched major databases for studies that compared treatment options for patients with neuroendocrine tumors. After applying the search criteria, the team found 38 studies that included a total of 30 randomized trials.
Various outcome measures were used, including progression-free survival, overall survival, disease control, quality of life, and adverse events. The majority of studies compared an intervention to a comparator of unclear efficacy or placebo. In addition, Dr. Kaderli and his colleagues completed a network meta-analysis to analyze the efficacy of each treatment option.
“The results suggest a superiority of combination therapies, especially of those including somatostatin analogues. In pNETs [pancreatic NETs], somatostatin analogues plus interferon, everolimus, or everolimus plus bevacizumab were highly efficacious. The certainty of evidence for these therapies was variable and was the highest for somatostatin analogues plus everolimus,” Dr. Kaderli and his associates wrote.
Furthermore, the results “suggest a range of monotherapies that are superior to placebo, including everolimus, interferon, and sunitinib in pNETs, and somatostatin analogues in pNETs and GI [gastrointestinal]-NETs,” they said.
The researchers acknowledged that a key limitation of the study was the inability to acquire unpublished data. Consequently, Dr. Kaderli and his colleagues reported there may be a risk of publication bias.
The study was supported by funding from the Insula Stiftung zur Förderung der viszeralchirurgischen Forschung. The authors reported no conflicts of interest.
SOURCE: Kaderli RM et al. JAMA Oncol. 2019 Feb 14. doi: 10.1001/jamaoncol.2018.6720.
One question that remains from the study by Reto M. Kaderli, MD, and his colleagues is the comparative advantages and disadvantages of the various therapies used to treat patients with neuroendocrine tumors.
Recently, several novel therapies have been approved for the treatment of pancreatic and gastrointestinal neuroendocrine tumors, which include agents used for both tumor and symptom control. The majority of studies that evaluated these agents compared them with a comparator of unclear efficacy or placebo. As a result, it is challenging to compare and contrast these competing therapies with respect to efficacy and safety.
Other challenges also exist, such as the biological and clinical diversity seen with neuroendocrine tumors. The current body of literature contains studies that examined different tumor types, including pancreatic, midgut, or gastroenteropancreatic neuroendocrine tumors, which caused significant variation in outcomes. Similar difficulties were seen with the response criteria across these studies.
These results support the active recruitment of patients into randomized comparison studies, which compare these therapies directly. While these types of studies will require larger sample sizes versus placebo-controlled trials, they are necessary to better understand which agents are best in different subtypes of neuroendocrine tumors.
Jonathan R. Strosberg, MD, and Taymeyah Al-Toubah, MPH, are affiliated with the department of gastrointestinal oncology at H. Lee Moffitt Cancer Center and Research Institute in Tampa. Mauro Cives, MD, is affiliated with the department of biomedical sciences and human oncology at the University of Bari in Italy. Dr. Strosberg reported having financial affiliations with Ipsen, Lexicon, and Novartis. These comments are adapted from their accompanying editorial (JAMA Oncol. 2019 Feb 14. doi: 10.1001/jamaoncol.2018.6694 .
One question that remains from the study by Reto M. Kaderli, MD, and his colleagues is the comparative advantages and disadvantages of the various therapies used to treat patients with neuroendocrine tumors.
Recently, several novel therapies have been approved for the treatment of pancreatic and gastrointestinal neuroendocrine tumors, which include agents used for both tumor and symptom control. The majority of studies that evaluated these agents compared them with a comparator of unclear efficacy or placebo. As a result, it is challenging to compare and contrast these competing therapies with respect to efficacy and safety.
Other challenges also exist, such as the biological and clinical diversity seen with neuroendocrine tumors. The current body of literature contains studies that examined different tumor types, including pancreatic, midgut, or gastroenteropancreatic neuroendocrine tumors, which caused significant variation in outcomes. Similar difficulties were seen with the response criteria across these studies.
These results support the active recruitment of patients into randomized comparison studies, which compare these therapies directly. While these types of studies will require larger sample sizes versus placebo-controlled trials, they are necessary to better understand which agents are best in different subtypes of neuroendocrine tumors.
Jonathan R. Strosberg, MD, and Taymeyah Al-Toubah, MPH, are affiliated with the department of gastrointestinal oncology at H. Lee Moffitt Cancer Center and Research Institute in Tampa. Mauro Cives, MD, is affiliated with the department of biomedical sciences and human oncology at the University of Bari in Italy. Dr. Strosberg reported having financial affiliations with Ipsen, Lexicon, and Novartis. These comments are adapted from their accompanying editorial (JAMA Oncol. 2019 Feb 14. doi: 10.1001/jamaoncol.2018.6694 .
One question that remains from the study by Reto M. Kaderli, MD, and his colleagues is the comparative advantages and disadvantages of the various therapies used to treat patients with neuroendocrine tumors.
Recently, several novel therapies have been approved for the treatment of pancreatic and gastrointestinal neuroendocrine tumors, which include agents used for both tumor and symptom control. The majority of studies that evaluated these agents compared them with a comparator of unclear efficacy or placebo. As a result, it is challenging to compare and contrast these competing therapies with respect to efficacy and safety.
Other challenges also exist, such as the biological and clinical diversity seen with neuroendocrine tumors. The current body of literature contains studies that examined different tumor types, including pancreatic, midgut, or gastroenteropancreatic neuroendocrine tumors, which caused significant variation in outcomes. Similar difficulties were seen with the response criteria across these studies.
These results support the active recruitment of patients into randomized comparison studies, which compare these therapies directly. While these types of studies will require larger sample sizes versus placebo-controlled trials, they are necessary to better understand which agents are best in different subtypes of neuroendocrine tumors.
Jonathan R. Strosberg, MD, and Taymeyah Al-Toubah, MPH, are affiliated with the department of gastrointestinal oncology at H. Lee Moffitt Cancer Center and Research Institute in Tampa. Mauro Cives, MD, is affiliated with the department of biomedical sciences and human oncology at the University of Bari in Italy. Dr. Strosberg reported having financial affiliations with Ipsen, Lexicon, and Novartis. These comments are adapted from their accompanying editorial (JAMA Oncol. 2019 Feb 14. doi: 10.1001/jamaoncol.2018.6694 .
Multiple treatment options, which have shown to be safe and effective for patients with neuroendocrine tumors (NET), are presently available, according to a systematic review and meta-analysis of 30 randomized clinical trials.
“We aimed to identify all [randomized clinical trials] comparing therapeutic interventions in [neuroendocrine tumors],” Reto M. Kaderli, MD, of the University of Bern in Switzerland, and his colleagues wrote in JAMA Oncology.
The researchers searched major databases for studies that compared treatment options for patients with neuroendocrine tumors. After applying the search criteria, the team found 38 studies that included a total of 30 randomized trials.
Various outcome measures were used, including progression-free survival, overall survival, disease control, quality of life, and adverse events. The majority of studies compared an intervention to a comparator of unclear efficacy or placebo. In addition, Dr. Kaderli and his colleagues completed a network meta-analysis to analyze the efficacy of each treatment option.
“The results suggest a superiority of combination therapies, especially of those including somatostatin analogues. In pNETs [pancreatic NETs], somatostatin analogues plus interferon, everolimus, or everolimus plus bevacizumab were highly efficacious. The certainty of evidence for these therapies was variable and was the highest for somatostatin analogues plus everolimus,” Dr. Kaderli and his associates wrote.
Furthermore, the results “suggest a range of monotherapies that are superior to placebo, including everolimus, interferon, and sunitinib in pNETs, and somatostatin analogues in pNETs and GI [gastrointestinal]-NETs,” they said.
The researchers acknowledged that a key limitation of the study was the inability to acquire unpublished data. Consequently, Dr. Kaderli and his colleagues reported there may be a risk of publication bias.
The study was supported by funding from the Insula Stiftung zur Förderung der viszeralchirurgischen Forschung. The authors reported no conflicts of interest.
SOURCE: Kaderli RM et al. JAMA Oncol. 2019 Feb 14. doi: 10.1001/jamaoncol.2018.6720.
Multiple treatment options, which have shown to be safe and effective for patients with neuroendocrine tumors (NET), are presently available, according to a systematic review and meta-analysis of 30 randomized clinical trials.
“We aimed to identify all [randomized clinical trials] comparing therapeutic interventions in [neuroendocrine tumors],” Reto M. Kaderli, MD, of the University of Bern in Switzerland, and his colleagues wrote in JAMA Oncology.
The researchers searched major databases for studies that compared treatment options for patients with neuroendocrine tumors. After applying the search criteria, the team found 38 studies that included a total of 30 randomized trials.
Various outcome measures were used, including progression-free survival, overall survival, disease control, quality of life, and adverse events. The majority of studies compared an intervention to a comparator of unclear efficacy or placebo. In addition, Dr. Kaderli and his colleagues completed a network meta-analysis to analyze the efficacy of each treatment option.
“The results suggest a superiority of combination therapies, especially of those including somatostatin analogues. In pNETs [pancreatic NETs], somatostatin analogues plus interferon, everolimus, or everolimus plus bevacizumab were highly efficacious. The certainty of evidence for these therapies was variable and was the highest for somatostatin analogues plus everolimus,” Dr. Kaderli and his associates wrote.
Furthermore, the results “suggest a range of monotherapies that are superior to placebo, including everolimus, interferon, and sunitinib in pNETs, and somatostatin analogues in pNETs and GI [gastrointestinal]-NETs,” they said.
The researchers acknowledged that a key limitation of the study was the inability to acquire unpublished data. Consequently, Dr. Kaderli and his colleagues reported there may be a risk of publication bias.
The study was supported by funding from the Insula Stiftung zur Förderung der viszeralchirurgischen Forschung. The authors reported no conflicts of interest.
SOURCE: Kaderli RM et al. JAMA Oncol. 2019 Feb 14. doi: 10.1001/jamaoncol.2018.6720.
FROM JAMA ONCOLOGY
Shaping the future of hospital medicine
Dr. Therese Franco leads SHM’s Pacific Northwest chapter
Therese Franco, MD, SFHM, a hospitalist at the Virginia Mason Medical Center in Seattle, is the current president of SHM’s Pacific Northwest chapter.
The Hospitalist recently sat down with her to learn about her background and discuss some of the initiatives that the Pacific Northwest chapter has been working on.
Can you tell us about your education and training on the way to becoming a hospitalist?
My undergraduate degree is in engineering from Michigan State University. I then went to the University of Michigan in Ann Arbor and did one degree at the School of Public Health in environmental and industrial health, and another degree in the College of Engineering in industrial and operations engineering. In my work with the safety department at an automotive company, I found I was spending a lot of time looking at data, and not talking to people. I got into a conversation with one of the occupational medicine physicians there, and he said, “You ought to try this.” I spoke with a good friend, who was a medical student, and she agreed.
So then I went to medical school thinking that I would practice occupational medicine. I went to medical school at Wayne State University in Detroit and did a couple of rotations in occupational medicine. I wasn’t sure that was the right fit, so I then went off to residency in internal medicine at the University of Connecticut and really enjoyed my wards experience. I liked the pace, I liked the variety, and just really liked all of hospital medicine. So that’s what I decided to do.
What are your areas of research interest?
This year I’m doing a research fellowship through the Center for Healthcare Improvement Science, at Virginia Mason. Through SHM’s mentored implementation program, I have done a lot of work on diabetes and glycemic control but never really published much of it. I think it is so important to share what you learn, so I’m working on publishing some of our results from the diabetes work.
Another area of interest is advanced-practice providers in hospital medicine, which I think is very important, given all the issues that health care is facing. I think that medicine has gotten more complex and that we’re going to have to look at working in a collaborative, inter-professional, multidisciplinary way. I think that advanced practice can really improve the care of hospitalized patients, if we practice appropriate skill-task alignment, develop a culture of mutual respect, and find the best ways to deploy our advanced-practice providers and our physicians.
That can be challenging. Some people, I think, are worried about losing their jobs, and some people feel like they want to “own” all of the patient, because it’s such a part of the culture of medicine. So it’s a really complicated issue, and I think that doctors are going to have to get used to delegating tasks that they used to perform.
So a collaborative practice requires both a professional and a cultural shift?
I think so. I was our inaugural program director for an advanced-practice fellowship in hospital medicine, and in that role, I attended conferences and learning events for program development. I think that many institutions are facing some of the same challenges. For the most part, I’m optimistic about things. I think we’re on the right track, and help is on the way – we just have to figure out how to use it.
Has your institution made any changes along these lines?
We’re primarily using the fellowship as a tool to recruit and retain some of the brightest and best. We’ve got three fellows that matriculated from our program and are currently working in the section of hospital medicine. Everyone’s been really flexible and open to the idea that the job description is emerging. I think my colleagues are very appreciative of our advanced-practice providers. We’ve got two nurse practitioners and one physician assistant who is also a PhD-trained pharmacist. They’ve been great additions to our team.
What are some of the other issues that the Pacific Northwest chapter members are concerned about?
One of our most successful meetings was around telemedicine. There’s a lot of interest in that, and it’s very financially and technically complex. Some hospitals in the area are really doing novel things. One of the most interesting things is an addiction medicine teleconsult.
That’s out of Swedish Medical Center, Seattle. Of course there’s telestroke, which I think is picking up in popularity. We had speakers from Virginia Mason who presented on telestroke. Some institutions are even doing admissions this way. The University of Washington is doing some good antimicrobial stewardship work. They present cases and they teleconference and have an infectious disease consultant. It’s not a program directed at revenue generation, but is focused instead on sharing and spreading expertise.
Our chapter also hosted a presentation on burnout that was pretty well attended. And then, unfortunately, we did lose a hospitalist to suicide over the summer. That was the inspiration for offering the screening of the movie, “Do No Harm: Exposing the Hippocratic Hoax.”
What was the program that you put together around the screening?
We had the filmmaker come for the screening, and we organized a panel discussion with a wellness officer from a local clinic and a psychiatrist who used to be on the board of the Physician Health Program. John Nelson, MD, MHM, one of SHM’s cofounders and a local hospitalist here, also participated as a panelist.
Overall, the event was well received. There were some things that I didn’t really expect. I’m not sure that the film resonated with too many people in the room. It is very much directed at the educational process – med students and residents – and at times the dialogue is a little inflammatory.
I learned a few important things from the film. I did not realize that the tragedy of physician suicide is not unique to the United States – it’s an international issue. And we sometimes use the term “pimping” to talk about questioning interns or residents on rounds. Apparently, that stands for “put in my place,” which is very condescending and unacceptable. I will not use the term again.
I think future conversations need to come from thoughtful, rational, respectful leaders who are willing to work with regulatory agencies, hospitals, and administrators. If we want to move forward, physicians, administrators, and the public need to come together in the best interest of the patient and of public health. And I don’t know who leads that conversation.
Will your chapter have another event around that subject?
We will do what our membership wants and needs. We meet quarterly, and once a year we hold a people’s choice meeting and I solicit topics. If members want to keep the conversation moving, I’m going to do what I can to support them.
What are some other issues that stand out as important to your chapter?
One key topic is the financial side of hospitalist practice, and dealing with issues that seem to create inefficiencies – regulatory issues, documentation issues, things that are important because we want to tell the story of what we’re doing. We certainly want to be reimbursed for the value-added work that we’re doing, but a lot of value-added work creates inefficiencies of practice, and I hear a lot of dissatisfaction around documentation, coding, billing, and other issues related to reimbursement. While people are concerned about these problems, nobody wants to talk about them. They just want somebody to fix it. So I’m not sure what to do with that, because I think if I had a meeting about coding and billing, I would have three attendees.
But our annual poster meeting is always well attended. We always do it at the end of the year, to kick off the holiday season. It’s a nice opportunity to connect socially with colleagues because you mix and you mingle and look at the posters. We had some really great posters, and our top three prize winners were medical students, which is inspirational. They make you feel good about the future.
Our chapter is trying to diversify geographically and clinically. We were fortunate to receive a development funds grant to use technology to do streaming meetings. Our hope is that we can host streaming meetings and eventually transition hosting to rotate around the state. Once there’s large enough attendance, the different delegates can develop their own leadership teams and, eventually, their own chapter. We’re hoping to grow the organization that way.
What else is on the horizon for hospitalists in the Pacific Northwest?
I’d like to see more frequent meetings and a greater variety of meetings. I think there’s interest in adding some kind of service element to the chapter. Maybe we can do a blood pressure screening at a sporting event.
I think we’ll also be focusing on students and residents and trying to create support for them. We held a student event around financial planning, and that was very well attended. I think we would like to do something around mentorship. Of course it’s hard to find mentors, because everybody is so busy.
Our chapter really needs to leverage our technology if we want to have the reach that I’m talking about. I’m looking forward to piloting the streaming meeting concept, and I hope to do some live polling of our meeting attendees to get them engaged. I hope we continue to grow and keep the dialogue going about what matters in hospital medicine, and do our part to shape the future in the way we want it.
Dr. Therese Franco leads SHM’s Pacific Northwest chapter
Dr. Therese Franco leads SHM’s Pacific Northwest chapter
Therese Franco, MD, SFHM, a hospitalist at the Virginia Mason Medical Center in Seattle, is the current president of SHM’s Pacific Northwest chapter.
The Hospitalist recently sat down with her to learn about her background and discuss some of the initiatives that the Pacific Northwest chapter has been working on.
Can you tell us about your education and training on the way to becoming a hospitalist?
My undergraduate degree is in engineering from Michigan State University. I then went to the University of Michigan in Ann Arbor and did one degree at the School of Public Health in environmental and industrial health, and another degree in the College of Engineering in industrial and operations engineering. In my work with the safety department at an automotive company, I found I was spending a lot of time looking at data, and not talking to people. I got into a conversation with one of the occupational medicine physicians there, and he said, “You ought to try this.” I spoke with a good friend, who was a medical student, and she agreed.
So then I went to medical school thinking that I would practice occupational medicine. I went to medical school at Wayne State University in Detroit and did a couple of rotations in occupational medicine. I wasn’t sure that was the right fit, so I then went off to residency in internal medicine at the University of Connecticut and really enjoyed my wards experience. I liked the pace, I liked the variety, and just really liked all of hospital medicine. So that’s what I decided to do.
What are your areas of research interest?
This year I’m doing a research fellowship through the Center for Healthcare Improvement Science, at Virginia Mason. Through SHM’s mentored implementation program, I have done a lot of work on diabetes and glycemic control but never really published much of it. I think it is so important to share what you learn, so I’m working on publishing some of our results from the diabetes work.
Another area of interest is advanced-practice providers in hospital medicine, which I think is very important, given all the issues that health care is facing. I think that medicine has gotten more complex and that we’re going to have to look at working in a collaborative, inter-professional, multidisciplinary way. I think that advanced practice can really improve the care of hospitalized patients, if we practice appropriate skill-task alignment, develop a culture of mutual respect, and find the best ways to deploy our advanced-practice providers and our physicians.
That can be challenging. Some people, I think, are worried about losing their jobs, and some people feel like they want to “own” all of the patient, because it’s such a part of the culture of medicine. So it’s a really complicated issue, and I think that doctors are going to have to get used to delegating tasks that they used to perform.
So a collaborative practice requires both a professional and a cultural shift?
I think so. I was our inaugural program director for an advanced-practice fellowship in hospital medicine, and in that role, I attended conferences and learning events for program development. I think that many institutions are facing some of the same challenges. For the most part, I’m optimistic about things. I think we’re on the right track, and help is on the way – we just have to figure out how to use it.
Has your institution made any changes along these lines?
We’re primarily using the fellowship as a tool to recruit and retain some of the brightest and best. We’ve got three fellows that matriculated from our program and are currently working in the section of hospital medicine. Everyone’s been really flexible and open to the idea that the job description is emerging. I think my colleagues are very appreciative of our advanced-practice providers. We’ve got two nurse practitioners and one physician assistant who is also a PhD-trained pharmacist. They’ve been great additions to our team.
What are some of the other issues that the Pacific Northwest chapter members are concerned about?
One of our most successful meetings was around telemedicine. There’s a lot of interest in that, and it’s very financially and technically complex. Some hospitals in the area are really doing novel things. One of the most interesting things is an addiction medicine teleconsult.
That’s out of Swedish Medical Center, Seattle. Of course there’s telestroke, which I think is picking up in popularity. We had speakers from Virginia Mason who presented on telestroke. Some institutions are even doing admissions this way. The University of Washington is doing some good antimicrobial stewardship work. They present cases and they teleconference and have an infectious disease consultant. It’s not a program directed at revenue generation, but is focused instead on sharing and spreading expertise.
Our chapter also hosted a presentation on burnout that was pretty well attended. And then, unfortunately, we did lose a hospitalist to suicide over the summer. That was the inspiration for offering the screening of the movie, “Do No Harm: Exposing the Hippocratic Hoax.”
What was the program that you put together around the screening?
We had the filmmaker come for the screening, and we organized a panel discussion with a wellness officer from a local clinic and a psychiatrist who used to be on the board of the Physician Health Program. John Nelson, MD, MHM, one of SHM’s cofounders and a local hospitalist here, also participated as a panelist.
Overall, the event was well received. There were some things that I didn’t really expect. I’m not sure that the film resonated with too many people in the room. It is very much directed at the educational process – med students and residents – and at times the dialogue is a little inflammatory.
I learned a few important things from the film. I did not realize that the tragedy of physician suicide is not unique to the United States – it’s an international issue. And we sometimes use the term “pimping” to talk about questioning interns or residents on rounds. Apparently, that stands for “put in my place,” which is very condescending and unacceptable. I will not use the term again.
I think future conversations need to come from thoughtful, rational, respectful leaders who are willing to work with regulatory agencies, hospitals, and administrators. If we want to move forward, physicians, administrators, and the public need to come together in the best interest of the patient and of public health. And I don’t know who leads that conversation.
Will your chapter have another event around that subject?
We will do what our membership wants and needs. We meet quarterly, and once a year we hold a people’s choice meeting and I solicit topics. If members want to keep the conversation moving, I’m going to do what I can to support them.
What are some other issues that stand out as important to your chapter?
One key topic is the financial side of hospitalist practice, and dealing with issues that seem to create inefficiencies – regulatory issues, documentation issues, things that are important because we want to tell the story of what we’re doing. We certainly want to be reimbursed for the value-added work that we’re doing, but a lot of value-added work creates inefficiencies of practice, and I hear a lot of dissatisfaction around documentation, coding, billing, and other issues related to reimbursement. While people are concerned about these problems, nobody wants to talk about them. They just want somebody to fix it. So I’m not sure what to do with that, because I think if I had a meeting about coding and billing, I would have three attendees.
But our annual poster meeting is always well attended. We always do it at the end of the year, to kick off the holiday season. It’s a nice opportunity to connect socially with colleagues because you mix and you mingle and look at the posters. We had some really great posters, and our top three prize winners were medical students, which is inspirational. They make you feel good about the future.
Our chapter is trying to diversify geographically and clinically. We were fortunate to receive a development funds grant to use technology to do streaming meetings. Our hope is that we can host streaming meetings and eventually transition hosting to rotate around the state. Once there’s large enough attendance, the different delegates can develop their own leadership teams and, eventually, their own chapter. We’re hoping to grow the organization that way.
What else is on the horizon for hospitalists in the Pacific Northwest?
I’d like to see more frequent meetings and a greater variety of meetings. I think there’s interest in adding some kind of service element to the chapter. Maybe we can do a blood pressure screening at a sporting event.
I think we’ll also be focusing on students and residents and trying to create support for them. We held a student event around financial planning, and that was very well attended. I think we would like to do something around mentorship. Of course it’s hard to find mentors, because everybody is so busy.
Our chapter really needs to leverage our technology if we want to have the reach that I’m talking about. I’m looking forward to piloting the streaming meeting concept, and I hope to do some live polling of our meeting attendees to get them engaged. I hope we continue to grow and keep the dialogue going about what matters in hospital medicine, and do our part to shape the future in the way we want it.
Therese Franco, MD, SFHM, a hospitalist at the Virginia Mason Medical Center in Seattle, is the current president of SHM’s Pacific Northwest chapter.
The Hospitalist recently sat down with her to learn about her background and discuss some of the initiatives that the Pacific Northwest chapter has been working on.
Can you tell us about your education and training on the way to becoming a hospitalist?
My undergraduate degree is in engineering from Michigan State University. I then went to the University of Michigan in Ann Arbor and did one degree at the School of Public Health in environmental and industrial health, and another degree in the College of Engineering in industrial and operations engineering. In my work with the safety department at an automotive company, I found I was spending a lot of time looking at data, and not talking to people. I got into a conversation with one of the occupational medicine physicians there, and he said, “You ought to try this.” I spoke with a good friend, who was a medical student, and she agreed.
So then I went to medical school thinking that I would practice occupational medicine. I went to medical school at Wayne State University in Detroit and did a couple of rotations in occupational medicine. I wasn’t sure that was the right fit, so I then went off to residency in internal medicine at the University of Connecticut and really enjoyed my wards experience. I liked the pace, I liked the variety, and just really liked all of hospital medicine. So that’s what I decided to do.
What are your areas of research interest?
This year I’m doing a research fellowship through the Center for Healthcare Improvement Science, at Virginia Mason. Through SHM’s mentored implementation program, I have done a lot of work on diabetes and glycemic control but never really published much of it. I think it is so important to share what you learn, so I’m working on publishing some of our results from the diabetes work.
Another area of interest is advanced-practice providers in hospital medicine, which I think is very important, given all the issues that health care is facing. I think that medicine has gotten more complex and that we’re going to have to look at working in a collaborative, inter-professional, multidisciplinary way. I think that advanced practice can really improve the care of hospitalized patients, if we practice appropriate skill-task alignment, develop a culture of mutual respect, and find the best ways to deploy our advanced-practice providers and our physicians.
That can be challenging. Some people, I think, are worried about losing their jobs, and some people feel like they want to “own” all of the patient, because it’s such a part of the culture of medicine. So it’s a really complicated issue, and I think that doctors are going to have to get used to delegating tasks that they used to perform.
So a collaborative practice requires both a professional and a cultural shift?
I think so. I was our inaugural program director for an advanced-practice fellowship in hospital medicine, and in that role, I attended conferences and learning events for program development. I think that many institutions are facing some of the same challenges. For the most part, I’m optimistic about things. I think we’re on the right track, and help is on the way – we just have to figure out how to use it.
Has your institution made any changes along these lines?
We’re primarily using the fellowship as a tool to recruit and retain some of the brightest and best. We’ve got three fellows that matriculated from our program and are currently working in the section of hospital medicine. Everyone’s been really flexible and open to the idea that the job description is emerging. I think my colleagues are very appreciative of our advanced-practice providers. We’ve got two nurse practitioners and one physician assistant who is also a PhD-trained pharmacist. They’ve been great additions to our team.
What are some of the other issues that the Pacific Northwest chapter members are concerned about?
One of our most successful meetings was around telemedicine. There’s a lot of interest in that, and it’s very financially and technically complex. Some hospitals in the area are really doing novel things. One of the most interesting things is an addiction medicine teleconsult.
That’s out of Swedish Medical Center, Seattle. Of course there’s telestroke, which I think is picking up in popularity. We had speakers from Virginia Mason who presented on telestroke. Some institutions are even doing admissions this way. The University of Washington is doing some good antimicrobial stewardship work. They present cases and they teleconference and have an infectious disease consultant. It’s not a program directed at revenue generation, but is focused instead on sharing and spreading expertise.
Our chapter also hosted a presentation on burnout that was pretty well attended. And then, unfortunately, we did lose a hospitalist to suicide over the summer. That was the inspiration for offering the screening of the movie, “Do No Harm: Exposing the Hippocratic Hoax.”
What was the program that you put together around the screening?
We had the filmmaker come for the screening, and we organized a panel discussion with a wellness officer from a local clinic and a psychiatrist who used to be on the board of the Physician Health Program. John Nelson, MD, MHM, one of SHM’s cofounders and a local hospitalist here, also participated as a panelist.
Overall, the event was well received. There were some things that I didn’t really expect. I’m not sure that the film resonated with too many people in the room. It is very much directed at the educational process – med students and residents – and at times the dialogue is a little inflammatory.
I learned a few important things from the film. I did not realize that the tragedy of physician suicide is not unique to the United States – it’s an international issue. And we sometimes use the term “pimping” to talk about questioning interns or residents on rounds. Apparently, that stands for “put in my place,” which is very condescending and unacceptable. I will not use the term again.
I think future conversations need to come from thoughtful, rational, respectful leaders who are willing to work with regulatory agencies, hospitals, and administrators. If we want to move forward, physicians, administrators, and the public need to come together in the best interest of the patient and of public health. And I don’t know who leads that conversation.
Will your chapter have another event around that subject?
We will do what our membership wants and needs. We meet quarterly, and once a year we hold a people’s choice meeting and I solicit topics. If members want to keep the conversation moving, I’m going to do what I can to support them.
What are some other issues that stand out as important to your chapter?
One key topic is the financial side of hospitalist practice, and dealing with issues that seem to create inefficiencies – regulatory issues, documentation issues, things that are important because we want to tell the story of what we’re doing. We certainly want to be reimbursed for the value-added work that we’re doing, but a lot of value-added work creates inefficiencies of practice, and I hear a lot of dissatisfaction around documentation, coding, billing, and other issues related to reimbursement. While people are concerned about these problems, nobody wants to talk about them. They just want somebody to fix it. So I’m not sure what to do with that, because I think if I had a meeting about coding and billing, I would have three attendees.
But our annual poster meeting is always well attended. We always do it at the end of the year, to kick off the holiday season. It’s a nice opportunity to connect socially with colleagues because you mix and you mingle and look at the posters. We had some really great posters, and our top three prize winners were medical students, which is inspirational. They make you feel good about the future.
Our chapter is trying to diversify geographically and clinically. We were fortunate to receive a development funds grant to use technology to do streaming meetings. Our hope is that we can host streaming meetings and eventually transition hosting to rotate around the state. Once there’s large enough attendance, the different delegates can develop their own leadership teams and, eventually, their own chapter. We’re hoping to grow the organization that way.
What else is on the horizon for hospitalists in the Pacific Northwest?
I’d like to see more frequent meetings and a greater variety of meetings. I think there’s interest in adding some kind of service element to the chapter. Maybe we can do a blood pressure screening at a sporting event.
I think we’ll also be focusing on students and residents and trying to create support for them. We held a student event around financial planning, and that was very well attended. I think we would like to do something around mentorship. Of course it’s hard to find mentors, because everybody is so busy.
Our chapter really needs to leverage our technology if we want to have the reach that I’m talking about. I’m looking forward to piloting the streaming meeting concept, and I hope to do some live polling of our meeting attendees to get them engaged. I hope we continue to grow and keep the dialogue going about what matters in hospital medicine, and do our part to shape the future in the way we want it.
Outcomes similar for skin graft, synthetic mesh in incisional hernia repair
Giant incisional , according to findings published in Hernia.
In a prospective, randomized study of 52 patients (24 who received FTSG and 28 who received synthetic mesh), two recurrences were found at 1-year follow up in each group. Results for pain, patient satisfaction, and aesthetic outcome did not differ significantly between the groups, reported Viktor Holmdahl of the department of surgery and perioperative sciences at Umeå (Sweden) University and his coauthors.
Patients were aged 18 years or older, with symptomatic giant (greater than 10 cm) ventral incisional hernia. All patients had computerized tomography (CT) imaging of the abdominal wall, and were assessed for abdominal wall muscle strength via the Biodex Multi-Joint System-4.
The synthetic mesh used was a polypropylene mesh overlapping the repaired hernia defect by at least 5 cm. The FTSG was always placed in an onlay position, and was taken from excess skin adjacent to the midline incision made for the hernia repair. Postoperative care was identical for both groups, Dr. Holmdahl and his colleagues reported.
At 1 year, all patients received a follow-up Biodex assessment and were evaluated for recurrence. Aesthetic outcomes such as scar appearance and wound healing were assessed. Patients self-reported pain levels using a visual analogue scale.
Two patients in both the FTSG group (8.3%) and the synthetic mesh group (7.1%) had recurrence (P = 1.000). Differences between groups for the other measures were not significant, including for well-healed scars (91.3% for FTSG vs. 96.4% for synthetic mesh) and excess skin (60.9% vs. 57.1%). Biodex results also did not differ significantly between the groups.
The similarities in results between the two techniques “indicate that FTSG possibly has a future role in hernia repair, but more research is needed,” the authors concluded.
The study was supported by the Swedish Research Council and by a regional agreement between Umeå University and Västerbotten County Council. The investigators declared no conflicts of interest.
SOURCE: Holmdahl V et al. Hernia 2019 Feb 8. doi: 10.1007/s10029-019-01900-4.
Giant incisional , according to findings published in Hernia.
In a prospective, randomized study of 52 patients (24 who received FTSG and 28 who received synthetic mesh), two recurrences were found at 1-year follow up in each group. Results for pain, patient satisfaction, and aesthetic outcome did not differ significantly between the groups, reported Viktor Holmdahl of the department of surgery and perioperative sciences at Umeå (Sweden) University and his coauthors.
Patients were aged 18 years or older, with symptomatic giant (greater than 10 cm) ventral incisional hernia. All patients had computerized tomography (CT) imaging of the abdominal wall, and were assessed for abdominal wall muscle strength via the Biodex Multi-Joint System-4.
The synthetic mesh used was a polypropylene mesh overlapping the repaired hernia defect by at least 5 cm. The FTSG was always placed in an onlay position, and was taken from excess skin adjacent to the midline incision made for the hernia repair. Postoperative care was identical for both groups, Dr. Holmdahl and his colleagues reported.
At 1 year, all patients received a follow-up Biodex assessment and were evaluated for recurrence. Aesthetic outcomes such as scar appearance and wound healing were assessed. Patients self-reported pain levels using a visual analogue scale.
Two patients in both the FTSG group (8.3%) and the synthetic mesh group (7.1%) had recurrence (P = 1.000). Differences between groups for the other measures were not significant, including for well-healed scars (91.3% for FTSG vs. 96.4% for synthetic mesh) and excess skin (60.9% vs. 57.1%). Biodex results also did not differ significantly between the groups.
The similarities in results between the two techniques “indicate that FTSG possibly has a future role in hernia repair, but more research is needed,” the authors concluded.
The study was supported by the Swedish Research Council and by a regional agreement between Umeå University and Västerbotten County Council. The investigators declared no conflicts of interest.
SOURCE: Holmdahl V et al. Hernia 2019 Feb 8. doi: 10.1007/s10029-019-01900-4.
Giant incisional , according to findings published in Hernia.
In a prospective, randomized study of 52 patients (24 who received FTSG and 28 who received synthetic mesh), two recurrences were found at 1-year follow up in each group. Results for pain, patient satisfaction, and aesthetic outcome did not differ significantly between the groups, reported Viktor Holmdahl of the department of surgery and perioperative sciences at Umeå (Sweden) University and his coauthors.
Patients were aged 18 years or older, with symptomatic giant (greater than 10 cm) ventral incisional hernia. All patients had computerized tomography (CT) imaging of the abdominal wall, and were assessed for abdominal wall muscle strength via the Biodex Multi-Joint System-4.
The synthetic mesh used was a polypropylene mesh overlapping the repaired hernia defect by at least 5 cm. The FTSG was always placed in an onlay position, and was taken from excess skin adjacent to the midline incision made for the hernia repair. Postoperative care was identical for both groups, Dr. Holmdahl and his colleagues reported.
At 1 year, all patients received a follow-up Biodex assessment and were evaluated for recurrence. Aesthetic outcomes such as scar appearance and wound healing were assessed. Patients self-reported pain levels using a visual analogue scale.
Two patients in both the FTSG group (8.3%) and the synthetic mesh group (7.1%) had recurrence (P = 1.000). Differences between groups for the other measures were not significant, including for well-healed scars (91.3% for FTSG vs. 96.4% for synthetic mesh) and excess skin (60.9% vs. 57.1%). Biodex results also did not differ significantly between the groups.
The similarities in results between the two techniques “indicate that FTSG possibly has a future role in hernia repair, but more research is needed,” the authors concluded.
The study was supported by the Swedish Research Council and by a regional agreement between Umeå University and Västerbotten County Council. The investigators declared no conflicts of interest.
SOURCE: Holmdahl V et al. Hernia 2019 Feb 8. doi: 10.1007/s10029-019-01900-4.
FROM HERNIA