User login
May 2019 - Question 2
Q2. Correct Answer: B
Rationale:
The PRSS1 mutation has been shown to be the causative genetic factor in hereditary pancreatitis. Hereditary pancreatitis is an autosomal dominant gene mutation with 80% penetrance. Symptoms start in childhood with acute recurrent pancreatitis and progress to chronic pancreatitis, diabetes, and exocrine insufficiency. The incidence of pancreatic cancer is increased to 40% by age 70. BRCA1 mutations have been associated with familial pancreas cancer families. SPINK mutations have been associated with chronic tropical pancreatitis. Delta F508 is the most common mutation in cystic fibrosis that leads to pancreas insufficiency in childhood. The clinical scenario is classic for hereditary pancreatitis.
Reference
1. Shelton CA, Umapathy C, Stello K, Yadav D, Whitcomb DC. Hereditary pancreatitis in the United States: Survival and rates of pancreatic cancer. Am J Gastroenterol. 2018 Sep;113(9):1376-84.
Q2. Correct Answer: B
Rationale:
The PRSS1 mutation has been shown to be the causative genetic factor in hereditary pancreatitis. Hereditary pancreatitis is an autosomal dominant gene mutation with 80% penetrance. Symptoms start in childhood with acute recurrent pancreatitis and progress to chronic pancreatitis, diabetes, and exocrine insufficiency. The incidence of pancreatic cancer is increased to 40% by age 70. BRCA1 mutations have been associated with familial pancreas cancer families. SPINK mutations have been associated with chronic tropical pancreatitis. Delta F508 is the most common mutation in cystic fibrosis that leads to pancreas insufficiency in childhood. The clinical scenario is classic for hereditary pancreatitis.
Reference
1. Shelton CA, Umapathy C, Stello K, Yadav D, Whitcomb DC. Hereditary pancreatitis in the United States: Survival and rates of pancreatic cancer. Am J Gastroenterol. 2018 Sep;113(9):1376-84.
Q2. Correct Answer: B
Rationale:
The PRSS1 mutation has been shown to be the causative genetic factor in hereditary pancreatitis. Hereditary pancreatitis is an autosomal dominant gene mutation with 80% penetrance. Symptoms start in childhood with acute recurrent pancreatitis and progress to chronic pancreatitis, diabetes, and exocrine insufficiency. The incidence of pancreatic cancer is increased to 40% by age 70. BRCA1 mutations have been associated with familial pancreas cancer families. SPINK mutations have been associated with chronic tropical pancreatitis. Delta F508 is the most common mutation in cystic fibrosis that leads to pancreas insufficiency in childhood. The clinical scenario is classic for hereditary pancreatitis.
Reference
1. Shelton CA, Umapathy C, Stello K, Yadav D, Whitcomb DC. Hereditary pancreatitis in the United States: Survival and rates of pancreatic cancer. Am J Gastroenterol. 2018 Sep;113(9):1376-84.
Q2. A 25-year-old male presents to the emergency department with severe epigastric pain and mild elevations in lipase (3 x ULN) diagnostic of acute pancreatitis. The patient describes multiple episodes of pain and associated pancreas enzyme elevations since early childhood that generally respond to brief hospitalizations and conservative treatment including intravenous fluids and IV analgesics. CT imaging reveals parenchymal calcifications seen throughout the pancreas. Further history discloses two relatives with similar pain attacks.
May 2019 - Question 1
Q1. Correct Answer: A
Rationale:
This is an example of Yersinia infection. Transmission of yersiniosis is largely foodborne.
Risk factors associated with yersiniosis include consumption of undercooked or raw pork products and exposure to untreated water. Y. enterocolitica infection has also been associated with iron-overload states (such as hemochromatosis) and blood transfusions, because iron likely promotes virulence of this organism. The incubation period for yersiniosis is typically 4-6 days. Clinical manifestations of acute yersiniosis include diarrhea, abdominal pain, and fever; nausea and vomiting may also occur. Localization of abdominal pain to the right lower quadrant is also a diagnostic clue for yersiniosis. However, both Yersinia and Campylobacter can present with right lower quadrant pain that may be confused as appendicitis (pseudo appendicitis). Another diagnostic clue is pharyngitis, which may be an accompanying symptom. Yersinia causes diarrhea through penetration of the mucosa and proliferation in the submucosa. Pathogenic Y. enterocolitica pass through the stomach, adhere to gut epithelial cells, invade the gut wall, localize in lymphoid tissue within the gut wall and in regional mesenteric lymph nodes, and evade the host’s cell-mediated immune response. Vibrio cholerae and enterotoxigenic E. coli (ETEC) secrete enterotoxins that stimulate secretion and/or impair absorption.
Some bacteria produce toxins in contaminated food; when ingested, the toxins cause acute symptoms, usually nausea and vomiting. Examples of these are Staphylococcus aureus and Bacillus cereus. Enteropathogenic E. coli (EPEC) and enterohemorrhagic E. coli (EHEC) adhere to the intestinal mucosa, where they attach and cause effacement of the microvilli. Shigella, enteroinvasive E. coli, and Campylobacter jejuni penetrate the mucosa, spread, and cause mucosal damage with erosions and ulcers.
Reference
1. Cover TL, Aber RC. Yersinia enterocolitica. N Engl J Med. Jul 6 1989;321(1):16-24.
Q1. Correct Answer: A
Rationale:
This is an example of Yersinia infection. Transmission of yersiniosis is largely foodborne.
Risk factors associated with yersiniosis include consumption of undercooked or raw pork products and exposure to untreated water. Y. enterocolitica infection has also been associated with iron-overload states (such as hemochromatosis) and blood transfusions, because iron likely promotes virulence of this organism. The incubation period for yersiniosis is typically 4-6 days. Clinical manifestations of acute yersiniosis include diarrhea, abdominal pain, and fever; nausea and vomiting may also occur. Localization of abdominal pain to the right lower quadrant is also a diagnostic clue for yersiniosis. However, both Yersinia and Campylobacter can present with right lower quadrant pain that may be confused as appendicitis (pseudo appendicitis). Another diagnostic clue is pharyngitis, which may be an accompanying symptom. Yersinia causes diarrhea through penetration of the mucosa and proliferation in the submucosa. Pathogenic Y. enterocolitica pass through the stomach, adhere to gut epithelial cells, invade the gut wall, localize in lymphoid tissue within the gut wall and in regional mesenteric lymph nodes, and evade the host’s cell-mediated immune response. Vibrio cholerae and enterotoxigenic E. coli (ETEC) secrete enterotoxins that stimulate secretion and/or impair absorption.
Some bacteria produce toxins in contaminated food; when ingested, the toxins cause acute symptoms, usually nausea and vomiting. Examples of these are Staphylococcus aureus and Bacillus cereus. Enteropathogenic E. coli (EPEC) and enterohemorrhagic E. coli (EHEC) adhere to the intestinal mucosa, where they attach and cause effacement of the microvilli. Shigella, enteroinvasive E. coli, and Campylobacter jejuni penetrate the mucosa, spread, and cause mucosal damage with erosions and ulcers.
Reference
1. Cover TL, Aber RC. Yersinia enterocolitica. N Engl J Med. Jul 6 1989;321(1):16-24.
Q1. Correct Answer: A
Rationale:
This is an example of Yersinia infection. Transmission of yersiniosis is largely foodborne.
Risk factors associated with yersiniosis include consumption of undercooked or raw pork products and exposure to untreated water. Y. enterocolitica infection has also been associated with iron-overload states (such as hemochromatosis) and blood transfusions, because iron likely promotes virulence of this organism. The incubation period for yersiniosis is typically 4-6 days. Clinical manifestations of acute yersiniosis include diarrhea, abdominal pain, and fever; nausea and vomiting may also occur. Localization of abdominal pain to the right lower quadrant is also a diagnostic clue for yersiniosis. However, both Yersinia and Campylobacter can present with right lower quadrant pain that may be confused as appendicitis (pseudo appendicitis). Another diagnostic clue is pharyngitis, which may be an accompanying symptom. Yersinia causes diarrhea through penetration of the mucosa and proliferation in the submucosa. Pathogenic Y. enterocolitica pass through the stomach, adhere to gut epithelial cells, invade the gut wall, localize in lymphoid tissue within the gut wall and in regional mesenteric lymph nodes, and evade the host’s cell-mediated immune response. Vibrio cholerae and enterotoxigenic E. coli (ETEC) secrete enterotoxins that stimulate secretion and/or impair absorption.
Some bacteria produce toxins in contaminated food; when ingested, the toxins cause acute symptoms, usually nausea and vomiting. Examples of these are Staphylococcus aureus and Bacillus cereus. Enteropathogenic E. coli (EPEC) and enterohemorrhagic E. coli (EHEC) adhere to the intestinal mucosa, where they attach and cause effacement of the microvilli. Shigella, enteroinvasive E. coli, and Campylobacter jejuni penetrate the mucosa, spread, and cause mucosal damage with erosions and ulcers.
Reference
1. Cover TL, Aber RC. Yersinia enterocolitica. N Engl J Med. Jul 6 1989;321(1):16-24.
Q1. A 45-year-old man presents to the clinic with worsening right lower quadrant pain and diarrhea for the last 2 days. His past medical history is significant for hemochromatosis and he undergoes regular therapeutic phlebotomies. He admits to dining out in a newly-opened restaurant in his town 4 days ago. He describes having 5 nonbloody watery stools and also has been experiencing sore throat for the last 2 days. His physical examination is unremarkable except some mild abdominal tenderness at the right lower quadrant.
There was no rebound tenderness. Laboratory data shows mild leukocytosis.
HM19: Practice management tips for pediatric HMGs
Presenter
H. Barrett Fromme, MD, MHPE, FAAP
Session title
Sustainability Isn’t Just For The Forests: Practice management tips for long-term success in your Pediatric Hospital Medicine Group
Session summary
Dr. H. Barrett Fromme of the University of Chicago presented and facilitated a dialogue of sustainability. The audience was guided through a discussion of how efficiency and resources, workload and job demands, work-life integration and social support, and community at work can either lead to burnout or engagement within a Pediatric Hospital Medicine Group.
For each of the four topics, Dr. Fromme presented how individuals and leaders can leverage these areas to counteract burnout and promote engagement, ultimately leading to vitality within the practice group.
She closed her discussion stating that sustainability is a “process that maintains change in a balanced environment of resources, technology, and institutional change [that] are in harmony, and enhances current and future potential to meet human aspirations and needs.”
Key takeaways for HM
- Leaders can advocate with hospital leadership to optimize individual workload and job demands.
- Individuals and leaders can improve care process and clinical work flow to optimize efficiency and resources.
- Individuals and leaders can build high-functioning teams and cultivate communities of practice.
- Individuals and leaders can work together to develop goals to optimize work-life integration.
- Leaders can support values, autonomy, and growth to create an environment where individuals actively value and support their colleagues.
Dr. Kumar is a pediatric hospitalist at Cleveland Clinic Children’s and clinical assistant professor of pediatrics at Cleveland Clinic Lerner College of Medicine at Case Western Reserve University. She serves as the cochair of Pediatric Grand Rounds and is the research director for the Pediatric Hospital Medicine Fellowship at Cleveland Clinic Children’s.
Presenter
H. Barrett Fromme, MD, MHPE, FAAP
Session title
Sustainability Isn’t Just For The Forests: Practice management tips for long-term success in your Pediatric Hospital Medicine Group
Session summary
Dr. H. Barrett Fromme of the University of Chicago presented and facilitated a dialogue of sustainability. The audience was guided through a discussion of how efficiency and resources, workload and job demands, work-life integration and social support, and community at work can either lead to burnout or engagement within a Pediatric Hospital Medicine Group.
For each of the four topics, Dr. Fromme presented how individuals and leaders can leverage these areas to counteract burnout and promote engagement, ultimately leading to vitality within the practice group.
She closed her discussion stating that sustainability is a “process that maintains change in a balanced environment of resources, technology, and institutional change [that] are in harmony, and enhances current and future potential to meet human aspirations and needs.”
Key takeaways for HM
- Leaders can advocate with hospital leadership to optimize individual workload and job demands.
- Individuals and leaders can improve care process and clinical work flow to optimize efficiency and resources.
- Individuals and leaders can build high-functioning teams and cultivate communities of practice.
- Individuals and leaders can work together to develop goals to optimize work-life integration.
- Leaders can support values, autonomy, and growth to create an environment where individuals actively value and support their colleagues.
Dr. Kumar is a pediatric hospitalist at Cleveland Clinic Children’s and clinical assistant professor of pediatrics at Cleveland Clinic Lerner College of Medicine at Case Western Reserve University. She serves as the cochair of Pediatric Grand Rounds and is the research director for the Pediatric Hospital Medicine Fellowship at Cleveland Clinic Children’s.
Presenter
H. Barrett Fromme, MD, MHPE, FAAP
Session title
Sustainability Isn’t Just For The Forests: Practice management tips for long-term success in your Pediatric Hospital Medicine Group
Session summary
Dr. H. Barrett Fromme of the University of Chicago presented and facilitated a dialogue of sustainability. The audience was guided through a discussion of how efficiency and resources, workload and job demands, work-life integration and social support, and community at work can either lead to burnout or engagement within a Pediatric Hospital Medicine Group.
For each of the four topics, Dr. Fromme presented how individuals and leaders can leverage these areas to counteract burnout and promote engagement, ultimately leading to vitality within the practice group.
She closed her discussion stating that sustainability is a “process that maintains change in a balanced environment of resources, technology, and institutional change [that] are in harmony, and enhances current and future potential to meet human aspirations and needs.”
Key takeaways for HM
- Leaders can advocate with hospital leadership to optimize individual workload and job demands.
- Individuals and leaders can improve care process and clinical work flow to optimize efficiency and resources.
- Individuals and leaders can build high-functioning teams and cultivate communities of practice.
- Individuals and leaders can work together to develop goals to optimize work-life integration.
- Leaders can support values, autonomy, and growth to create an environment where individuals actively value and support their colleagues.
Dr. Kumar is a pediatric hospitalist at Cleveland Clinic Children’s and clinical assistant professor of pediatrics at Cleveland Clinic Lerner College of Medicine at Case Western Reserve University. She serves as the cochair of Pediatric Grand Rounds and is the research director for the Pediatric Hospital Medicine Fellowship at Cleveland Clinic Children’s.
Mavyret approved for children with any HCV genotype
The Food and Drug Administration has approved glecaprevir/pibrentasvir tablets (Mavyret) for treating any of six identified genotypes of hepatitis C virus in children ages 12-17 years.
The agency noted in its press announcement that, Dosing information now will be provided for patients aged 12 years and older or weighing at least 99 lbs, without cirrhosis or who have compensated cirrhosis. It is not recommended for patients with moderate cirrhosis, and it is contraindicated in patients with severe cirrhosis, as well as patients taking atazanavir and rifampin.
In clinical trials of 47 patients with genotype 1, 2, 3, or 4 HCV without cirrhosis or with only mild cirrhosis, results at 12 weeks after 8 or 16 weeks’ treatment suggested patients’ infections had been cured – 100% had no virus detected in their blood. Adverse reactions observed were consistent with those previously observed in adults during clinical trials.
The most common reactions were headache and fatigue. Hepatitis B virus reactivation has been reported in coinfected adults during or after treatment with direct-acting antivirals, and in those who were not receiving HBV antiviral treatment. Full prescribing information can be found on the FDA website, and more information about this approval can be found in the agency’s announcement.
The Food and Drug Administration has approved glecaprevir/pibrentasvir tablets (Mavyret) for treating any of six identified genotypes of hepatitis C virus in children ages 12-17 years.
The agency noted in its press announcement that, Dosing information now will be provided for patients aged 12 years and older or weighing at least 99 lbs, without cirrhosis or who have compensated cirrhosis. It is not recommended for patients with moderate cirrhosis, and it is contraindicated in patients with severe cirrhosis, as well as patients taking atazanavir and rifampin.
In clinical trials of 47 patients with genotype 1, 2, 3, or 4 HCV without cirrhosis or with only mild cirrhosis, results at 12 weeks after 8 or 16 weeks’ treatment suggested patients’ infections had been cured – 100% had no virus detected in their blood. Adverse reactions observed were consistent with those previously observed in adults during clinical trials.
The most common reactions were headache and fatigue. Hepatitis B virus reactivation has been reported in coinfected adults during or after treatment with direct-acting antivirals, and in those who were not receiving HBV antiviral treatment. Full prescribing information can be found on the FDA website, and more information about this approval can be found in the agency’s announcement.
The Food and Drug Administration has approved glecaprevir/pibrentasvir tablets (Mavyret) for treating any of six identified genotypes of hepatitis C virus in children ages 12-17 years.
The agency noted in its press announcement that, Dosing information now will be provided for patients aged 12 years and older or weighing at least 99 lbs, without cirrhosis or who have compensated cirrhosis. It is not recommended for patients with moderate cirrhosis, and it is contraindicated in patients with severe cirrhosis, as well as patients taking atazanavir and rifampin.
In clinical trials of 47 patients with genotype 1, 2, 3, or 4 HCV without cirrhosis or with only mild cirrhosis, results at 12 weeks after 8 or 16 weeks’ treatment suggested patients’ infections had been cured – 100% had no virus detected in their blood. Adverse reactions observed were consistent with those previously observed in adults during clinical trials.
The most common reactions were headache and fatigue. Hepatitis B virus reactivation has been reported in coinfected adults during or after treatment with direct-acting antivirals, and in those who were not receiving HBV antiviral treatment. Full prescribing information can be found on the FDA website, and more information about this approval can be found in the agency’s announcement.
SRA737 + anti–PD-L1 therapy and low-dose gemcitabine shows early promise for SCLC
ATLANTA – Combined treatment with a programmed death-ligand 1 (PD-L1) inhibitor, the oral CHK1 inhibitor SRA737, and low-dose gemcitabine for small cell lung cancer (SCLC) resulted in dramatic antitumor activity and established a strong antitumor microenvironment in a preclinical model.
The findings provide a “strong rationale” for combining these agents in patients with SCLC, Triparna Sen, PhD, reported in a late-breaking abstract presentation at the annual meeting of the American Association for Cancer Research.
Dr. Sen and her colleagues assessed this triple regimen based on encouraging prior findings, including their own recent finding that DNA damage response (DDR) inhibition “actually increases antitumor immunity in this cancer type” by activating the STING/TBK1/RF3 innate immune pathway and increasing levels of chemokines-CXCL10 and CCL5 that induced activation of cytotoxic T lymphocytes.
“Based on this background and studies published in other cancer types, we hypothesized that ... SRA737... a very highly selective potent checkpoint inhibitor ... will upregulate the innate immune signaling, resulting in improved antitumor immune response in combination with anti–PD-L1,” she said, noting that bladder and colorectal cancer models were also studied.
The results varied by cancer type, but encouraging results in SCLC led to in vivo study, said Dr. Sen, who was a postdoctoral fellow, instructor, and member of the Byers Laboratory at MD Anderson Cancer Center, Houston, at the time the research was conducted.
She and her colleagues injected immunocompetent mice with Trp53, Rb1, and p130 triple-knockout SCLC cell lines that are “very highly representative of what we see in patients,” and resulting tumors were treated with SRA737 alone or in combination with an anti–PD-L1 agent.
PD-L1 alone did not work, and SRA737 with 5- out of 7-day dosing was associated with a significant delay in tumor growth.
“However, the combination does much better than either of the single agents alone. ... we never had tumor growth beyond baseline and there was regression as early as 12 days,” she said, noting that the combination activates the STING pathway.
Similar findings were seen for bladder and colorectal cancer models, she noted.
The next question is how chemotherapy plus immune checkpoint blockade – the currently approved first-line therapy in SCLC – can be improved, and how chemotherapy modulates the immune microenvironment in SCLC, she said.
To explore this, she and her colleagues treated the mice with subtherapeutic doses of SRA737 on 2 out of 7 days with low-dose gemcitabine, followed by anti–PD-L1 therapy, or with single-agent therapy and various double-agent combinations.
Again, none of the agents worked on their own.
“Even with the double combinations you see very, very modest benefit,” she said. “With the triple combination we wipe out the tumors; as early as 14 days we have 8 out of 10 complete responses, and we have followed the tumors up to 2 months and they stay gone.”
“In a nutshell, this works,” she added.
Additional analyses showed that the CD3+ T cells increase with the gemcitabine/SRA737 combination, and even more so with the triple-combination therapy.
“So we not only increase the CD3+ total T cells, we do increase CD8+ cytotoxic T cells,” she said. “Interestingly, we also decrease exhausted T-cell populations, and also [regulatory T] cells.”
Additionally, the M1 macrophage population was significantly higher with the triple regimen, there was a trend toward a decrease in the antimacrophage population, and there was a higher population of dendritic cells and myeloid-derived suppressor cells.
“What I believe is we are still scratching the surface, and we need to go deeper into the tumor microenvironment and see how these combinations really work,” she said, concluding that SRA737 is cytotoxic and induces micro-nuclei formation in a subset of SCLC and other cancer models in vitro, that in combination with anti–PD-L1 it activates innate immune signaling and causes tumor regression in SCLC, and that with low-dose gemcitabine it results in durable tumor regression in combination with SRA737 and anti–PD-L1.
“What is the most interesting is that this triple combination enhances antitumor immunity by increasing cytotoxic T-cell infiltration, decreasing T-cell exhaustion, and a favorable modulation of antigen presenting cells,” she said. “Why do we care? The anti–PD-L1 drug ... atezolizumab ... is right now FDA approved as a first-line treatment in combination with chemotherapy, and we already have DDR inhibitors in the clinic, we have PARP inhibitors in the clinic, we have checkpoint inhibitors in the clinic, SRA737 is in the clinic.
“So our preclinical data provides a strong rationale for combining low-dose gemcitabine with checkpoint inhibition and with anti–PD-L1 to enhance the clinical efficacy of these drugs,” she concluded.
Dr. Sen reported having no disclosures.
SOURCE: Sen T et al. AACR 2019, Abstract LB-148.
ATLANTA – Combined treatment with a programmed death-ligand 1 (PD-L1) inhibitor, the oral CHK1 inhibitor SRA737, and low-dose gemcitabine for small cell lung cancer (SCLC) resulted in dramatic antitumor activity and established a strong antitumor microenvironment in a preclinical model.
The findings provide a “strong rationale” for combining these agents in patients with SCLC, Triparna Sen, PhD, reported in a late-breaking abstract presentation at the annual meeting of the American Association for Cancer Research.
Dr. Sen and her colleagues assessed this triple regimen based on encouraging prior findings, including their own recent finding that DNA damage response (DDR) inhibition “actually increases antitumor immunity in this cancer type” by activating the STING/TBK1/RF3 innate immune pathway and increasing levels of chemokines-CXCL10 and CCL5 that induced activation of cytotoxic T lymphocytes.
“Based on this background and studies published in other cancer types, we hypothesized that ... SRA737... a very highly selective potent checkpoint inhibitor ... will upregulate the innate immune signaling, resulting in improved antitumor immune response in combination with anti–PD-L1,” she said, noting that bladder and colorectal cancer models were also studied.
The results varied by cancer type, but encouraging results in SCLC led to in vivo study, said Dr. Sen, who was a postdoctoral fellow, instructor, and member of the Byers Laboratory at MD Anderson Cancer Center, Houston, at the time the research was conducted.
She and her colleagues injected immunocompetent mice with Trp53, Rb1, and p130 triple-knockout SCLC cell lines that are “very highly representative of what we see in patients,” and resulting tumors were treated with SRA737 alone or in combination with an anti–PD-L1 agent.
PD-L1 alone did not work, and SRA737 with 5- out of 7-day dosing was associated with a significant delay in tumor growth.
“However, the combination does much better than either of the single agents alone. ... we never had tumor growth beyond baseline and there was regression as early as 12 days,” she said, noting that the combination activates the STING pathway.
Similar findings were seen for bladder and colorectal cancer models, she noted.
The next question is how chemotherapy plus immune checkpoint blockade – the currently approved first-line therapy in SCLC – can be improved, and how chemotherapy modulates the immune microenvironment in SCLC, she said.
To explore this, she and her colleagues treated the mice with subtherapeutic doses of SRA737 on 2 out of 7 days with low-dose gemcitabine, followed by anti–PD-L1 therapy, or with single-agent therapy and various double-agent combinations.
Again, none of the agents worked on their own.
“Even with the double combinations you see very, very modest benefit,” she said. “With the triple combination we wipe out the tumors; as early as 14 days we have 8 out of 10 complete responses, and we have followed the tumors up to 2 months and they stay gone.”
“In a nutshell, this works,” she added.
Additional analyses showed that the CD3+ T cells increase with the gemcitabine/SRA737 combination, and even more so with the triple-combination therapy.
“So we not only increase the CD3+ total T cells, we do increase CD8+ cytotoxic T cells,” she said. “Interestingly, we also decrease exhausted T-cell populations, and also [regulatory T] cells.”
Additionally, the M1 macrophage population was significantly higher with the triple regimen, there was a trend toward a decrease in the antimacrophage population, and there was a higher population of dendritic cells and myeloid-derived suppressor cells.
“What I believe is we are still scratching the surface, and we need to go deeper into the tumor microenvironment and see how these combinations really work,” she said, concluding that SRA737 is cytotoxic and induces micro-nuclei formation in a subset of SCLC and other cancer models in vitro, that in combination with anti–PD-L1 it activates innate immune signaling and causes tumor regression in SCLC, and that with low-dose gemcitabine it results in durable tumor regression in combination with SRA737 and anti–PD-L1.
“What is the most interesting is that this triple combination enhances antitumor immunity by increasing cytotoxic T-cell infiltration, decreasing T-cell exhaustion, and a favorable modulation of antigen presenting cells,” she said. “Why do we care? The anti–PD-L1 drug ... atezolizumab ... is right now FDA approved as a first-line treatment in combination with chemotherapy, and we already have DDR inhibitors in the clinic, we have PARP inhibitors in the clinic, we have checkpoint inhibitors in the clinic, SRA737 is in the clinic.
“So our preclinical data provides a strong rationale for combining low-dose gemcitabine with checkpoint inhibition and with anti–PD-L1 to enhance the clinical efficacy of these drugs,” she concluded.
Dr. Sen reported having no disclosures.
SOURCE: Sen T et al. AACR 2019, Abstract LB-148.
ATLANTA – Combined treatment with a programmed death-ligand 1 (PD-L1) inhibitor, the oral CHK1 inhibitor SRA737, and low-dose gemcitabine for small cell lung cancer (SCLC) resulted in dramatic antitumor activity and established a strong antitumor microenvironment in a preclinical model.
The findings provide a “strong rationale” for combining these agents in patients with SCLC, Triparna Sen, PhD, reported in a late-breaking abstract presentation at the annual meeting of the American Association for Cancer Research.
Dr. Sen and her colleagues assessed this triple regimen based on encouraging prior findings, including their own recent finding that DNA damage response (DDR) inhibition “actually increases antitumor immunity in this cancer type” by activating the STING/TBK1/RF3 innate immune pathway and increasing levels of chemokines-CXCL10 and CCL5 that induced activation of cytotoxic T lymphocytes.
“Based on this background and studies published in other cancer types, we hypothesized that ... SRA737... a very highly selective potent checkpoint inhibitor ... will upregulate the innate immune signaling, resulting in improved antitumor immune response in combination with anti–PD-L1,” she said, noting that bladder and colorectal cancer models were also studied.
The results varied by cancer type, but encouraging results in SCLC led to in vivo study, said Dr. Sen, who was a postdoctoral fellow, instructor, and member of the Byers Laboratory at MD Anderson Cancer Center, Houston, at the time the research was conducted.
She and her colleagues injected immunocompetent mice with Trp53, Rb1, and p130 triple-knockout SCLC cell lines that are “very highly representative of what we see in patients,” and resulting tumors were treated with SRA737 alone or in combination with an anti–PD-L1 agent.
PD-L1 alone did not work, and SRA737 with 5- out of 7-day dosing was associated with a significant delay in tumor growth.
“However, the combination does much better than either of the single agents alone. ... we never had tumor growth beyond baseline and there was regression as early as 12 days,” she said, noting that the combination activates the STING pathway.
Similar findings were seen for bladder and colorectal cancer models, she noted.
The next question is how chemotherapy plus immune checkpoint blockade – the currently approved first-line therapy in SCLC – can be improved, and how chemotherapy modulates the immune microenvironment in SCLC, she said.
To explore this, she and her colleagues treated the mice with subtherapeutic doses of SRA737 on 2 out of 7 days with low-dose gemcitabine, followed by anti–PD-L1 therapy, or with single-agent therapy and various double-agent combinations.
Again, none of the agents worked on their own.
“Even with the double combinations you see very, very modest benefit,” she said. “With the triple combination we wipe out the tumors; as early as 14 days we have 8 out of 10 complete responses, and we have followed the tumors up to 2 months and they stay gone.”
“In a nutshell, this works,” she added.
Additional analyses showed that the CD3+ T cells increase with the gemcitabine/SRA737 combination, and even more so with the triple-combination therapy.
“So we not only increase the CD3+ total T cells, we do increase CD8+ cytotoxic T cells,” she said. “Interestingly, we also decrease exhausted T-cell populations, and also [regulatory T] cells.”
Additionally, the M1 macrophage population was significantly higher with the triple regimen, there was a trend toward a decrease in the antimacrophage population, and there was a higher population of dendritic cells and myeloid-derived suppressor cells.
“What I believe is we are still scratching the surface, and we need to go deeper into the tumor microenvironment and see how these combinations really work,” she said, concluding that SRA737 is cytotoxic and induces micro-nuclei formation in a subset of SCLC and other cancer models in vitro, that in combination with anti–PD-L1 it activates innate immune signaling and causes tumor regression in SCLC, and that with low-dose gemcitabine it results in durable tumor regression in combination with SRA737 and anti–PD-L1.
“What is the most interesting is that this triple combination enhances antitumor immunity by increasing cytotoxic T-cell infiltration, decreasing T-cell exhaustion, and a favorable modulation of antigen presenting cells,” she said. “Why do we care? The anti–PD-L1 drug ... atezolizumab ... is right now FDA approved as a first-line treatment in combination with chemotherapy, and we already have DDR inhibitors in the clinic, we have PARP inhibitors in the clinic, we have checkpoint inhibitors in the clinic, SRA737 is in the clinic.
“So our preclinical data provides a strong rationale for combining low-dose gemcitabine with checkpoint inhibition and with anti–PD-L1 to enhance the clinical efficacy of these drugs,” she concluded.
Dr. Sen reported having no disclosures.
SOURCE: Sen T et al. AACR 2019, Abstract LB-148.
REPORTING FROM AACR 2019
Early childhood infections tied to psychosis risk
ORLANDO – Infections before the age of 4 are linked to the risk of nonaffective psychosis (NAP) in adulthood, according to a study presented at the annual congress of the Schizophrenia International Research Society. Researchers also found that a lower IQ seems to make the psychosis risk more likely.
It’s well-established in the literature that infections are tied to schizophrenia and that a premorbid IQ deficit is linked as well. Researchers looked to a huge data pool from the Swedish population to try to better define these risks.
“We know that there is an association between infection and schizophrenia,” said Golam Khandaker, MRCPsych, PhD, head of the inflammation and psychiatry research group at the University of Cambridge (England). “We know that there is premorbid IQ deficit in schizophrenia. So, we wanted to know, is there a sensitive period during childhood when exposure to infection is more harmful?”
Researchers analyzed data for 647,000 people in the Swedish population who were born between 1973 and 1997, and conscripted for military service through 2010. Exposure to infection was considered to be any hospitalization with any serious infection between birth and age 13. IQ measurements were taken during military conscription at the age of 18. And researchers looked for risk of nonaffective psychosis from the age of 18 on.
There was a significant increase in risk of nonaffective psychosis in adulthood among those who’d had an infection, with a hazard ratio of 1.16 (95% confidence interval, 1.08-1.24). But when researchers broke down this risk into smaller age spans, they found that only infection between birth and 1 year old (HR, 1.19; 95% CI, 1.06-1.33) and between age 2 and 4 (HR, 1.11; 95% CI, 1.02-1.22) was linked with a significantly elevated risk of NAP. Researchers also saw a link between infection and IQ.
Researchers assessed whether familial factors could be confounding this link. They looked at rates of NAP among those with an early infection and no early infection in the general population and found that it was no different statistically than among full siblings with an early infection, compared with those with no early infection. In other words, the infection-psychosis risk was the same – whether someone was a close family member or not.
Dr. Khandaker said the findings more definitively establish a link between infection and psychosis risk and suggest that the early years are when children are at their most vulnerable.
“The association between adult nonaffective psychosis with premorbid IQ and childhood infection are not explained by shared familial confounding,” he said. “So these associations could be causal.”
When they looked at the role of IQ and the link between infection and psychosis risk, researchers found an interaction: With every 1-point decrease in IQ score, there was a corresponding increased risk of NAP among those with childhood infections (odds ratio, 1.006; P = .02).
“Childhood infections,” Dr. Khandaker said, “increase psychosis risk partly by interfering with neurodevelopment, and partly by exaggerating the effects of cognitive vulnerability to psychosis.”
Dr. Khandaker disclosed no relevant financial relationships.
ORLANDO – Infections before the age of 4 are linked to the risk of nonaffective psychosis (NAP) in adulthood, according to a study presented at the annual congress of the Schizophrenia International Research Society. Researchers also found that a lower IQ seems to make the psychosis risk more likely.
It’s well-established in the literature that infections are tied to schizophrenia and that a premorbid IQ deficit is linked as well. Researchers looked to a huge data pool from the Swedish population to try to better define these risks.
“We know that there is an association between infection and schizophrenia,” said Golam Khandaker, MRCPsych, PhD, head of the inflammation and psychiatry research group at the University of Cambridge (England). “We know that there is premorbid IQ deficit in schizophrenia. So, we wanted to know, is there a sensitive period during childhood when exposure to infection is more harmful?”
Researchers analyzed data for 647,000 people in the Swedish population who were born between 1973 and 1997, and conscripted for military service through 2010. Exposure to infection was considered to be any hospitalization with any serious infection between birth and age 13. IQ measurements were taken during military conscription at the age of 18. And researchers looked for risk of nonaffective psychosis from the age of 18 on.
There was a significant increase in risk of nonaffective psychosis in adulthood among those who’d had an infection, with a hazard ratio of 1.16 (95% confidence interval, 1.08-1.24). But when researchers broke down this risk into smaller age spans, they found that only infection between birth and 1 year old (HR, 1.19; 95% CI, 1.06-1.33) and between age 2 and 4 (HR, 1.11; 95% CI, 1.02-1.22) was linked with a significantly elevated risk of NAP. Researchers also saw a link between infection and IQ.
Researchers assessed whether familial factors could be confounding this link. They looked at rates of NAP among those with an early infection and no early infection in the general population and found that it was no different statistically than among full siblings with an early infection, compared with those with no early infection. In other words, the infection-psychosis risk was the same – whether someone was a close family member or not.
Dr. Khandaker said the findings more definitively establish a link between infection and psychosis risk and suggest that the early years are when children are at their most vulnerable.
“The association between adult nonaffective psychosis with premorbid IQ and childhood infection are not explained by shared familial confounding,” he said. “So these associations could be causal.”
When they looked at the role of IQ and the link between infection and psychosis risk, researchers found an interaction: With every 1-point decrease in IQ score, there was a corresponding increased risk of NAP among those with childhood infections (odds ratio, 1.006; P = .02).
“Childhood infections,” Dr. Khandaker said, “increase psychosis risk partly by interfering with neurodevelopment, and partly by exaggerating the effects of cognitive vulnerability to psychosis.”
Dr. Khandaker disclosed no relevant financial relationships.
ORLANDO – Infections before the age of 4 are linked to the risk of nonaffective psychosis (NAP) in adulthood, according to a study presented at the annual congress of the Schizophrenia International Research Society. Researchers also found that a lower IQ seems to make the psychosis risk more likely.
It’s well-established in the literature that infections are tied to schizophrenia and that a premorbid IQ deficit is linked as well. Researchers looked to a huge data pool from the Swedish population to try to better define these risks.
“We know that there is an association between infection and schizophrenia,” said Golam Khandaker, MRCPsych, PhD, head of the inflammation and psychiatry research group at the University of Cambridge (England). “We know that there is premorbid IQ deficit in schizophrenia. So, we wanted to know, is there a sensitive period during childhood when exposure to infection is more harmful?”
Researchers analyzed data for 647,000 people in the Swedish population who were born between 1973 and 1997, and conscripted for military service through 2010. Exposure to infection was considered to be any hospitalization with any serious infection between birth and age 13. IQ measurements were taken during military conscription at the age of 18. And researchers looked for risk of nonaffective psychosis from the age of 18 on.
There was a significant increase in risk of nonaffective psychosis in adulthood among those who’d had an infection, with a hazard ratio of 1.16 (95% confidence interval, 1.08-1.24). But when researchers broke down this risk into smaller age spans, they found that only infection between birth and 1 year old (HR, 1.19; 95% CI, 1.06-1.33) and between age 2 and 4 (HR, 1.11; 95% CI, 1.02-1.22) was linked with a significantly elevated risk of NAP. Researchers also saw a link between infection and IQ.
Researchers assessed whether familial factors could be confounding this link. They looked at rates of NAP among those with an early infection and no early infection in the general population and found that it was no different statistically than among full siblings with an early infection, compared with those with no early infection. In other words, the infection-psychosis risk was the same – whether someone was a close family member or not.
Dr. Khandaker said the findings more definitively establish a link between infection and psychosis risk and suggest that the early years are when children are at their most vulnerable.
“The association between adult nonaffective psychosis with premorbid IQ and childhood infection are not explained by shared familial confounding,” he said. “So these associations could be causal.”
When they looked at the role of IQ and the link between infection and psychosis risk, researchers found an interaction: With every 1-point decrease in IQ score, there was a corresponding increased risk of NAP among those with childhood infections (odds ratio, 1.006; P = .02).
“Childhood infections,” Dr. Khandaker said, “increase psychosis risk partly by interfering with neurodevelopment, and partly by exaggerating the effects of cognitive vulnerability to psychosis.”
Dr. Khandaker disclosed no relevant financial relationships.
REPORTING FROM SIRS 2019
AD biomarker not tied to increased interest in physician-assisted death
Being diagnosed with an elevated amyloid-beta biomarker that indicates greater risk of Alzheimer’s disease did not lead to increased consideration of physician-assisted death (PAD), according to an analysis of patients interviewed during clinical trials on cognitive decline.
“Our findings suggest that learning one’s amyloid imaging result does not change baseline attitudes regarding the acceptability of PAD,” wrote Emily A. Largent, PhD, of the department of medical ethics and health policy at the University of Pennsylvania, Philadelphia, and coauthors. The study was published as a research letter in JAMA Neurology.
Participants were recruited from two ongoing clinical trials, one of which included patients with elevated amyloid-beta (n = 50), whereas the other did not (n = 30). All participants completed an interview 4-12 weeks after receiving their biomarker results; 47 and 30 participants, respectively, also completed a follow-up interview at 12 months.
When asked whether they had considered PAD, nearly two-thirds of interviewees with the Alzheimer’s disease biomarker stated that they neither had nor would. Roughly one in five from that group said they would pursue PAD if they began to suffer from cognitive impairment or became a burden on others. Interviewees who did not have elevated amyloid beta, when asked whether a reversed result would have led to PAD or suicide, showed interest in roughly similar proportion to their at-risk counterparts.
The coauthors acknowledged the limitations of their study, including not asking about other end-of-life preferences or perceived quality of life for people with dementia. They also noted that, although their sample mirrors the populations of the two studies they drew from, “its homogeneity limits generalizability.” As such, they stressed that
The study was supported by grants from the Alzheimer’s Association and the National Institute on Aging. One author reported receiving grants from those two organizations during the study; another reported receiving grants from Lilly and Novartis. No other conflicts of interest were reported.
SOURCE: Largent EA et al. JAMA Neurol. 2019 Apr 29. doi: 10.1001/jamaneurol.2019.0797.
The fascinating thing about this study is that the idea for it arose when some of the individuals spontaneously mentioned assisted suicide during their initial interview, Annette L. Hanson, MD, said in an interview.
“Would these subjects have thought of suicide in the absence of the Brittany Maynard publicity campaign? I doubt it.”
Dr. Hanson, a forensic psychiatrist, is assistant professor of psychiatry at the University of Maryland and at Johns Hopkins University, both in Baltimore.
The fascinating thing about this study is that the idea for it arose when some of the individuals spontaneously mentioned assisted suicide during their initial interview, Annette L. Hanson, MD, said in an interview.
“Would these subjects have thought of suicide in the absence of the Brittany Maynard publicity campaign? I doubt it.”
Dr. Hanson, a forensic psychiatrist, is assistant professor of psychiatry at the University of Maryland and at Johns Hopkins University, both in Baltimore.
The fascinating thing about this study is that the idea for it arose when some of the individuals spontaneously mentioned assisted suicide during their initial interview, Annette L. Hanson, MD, said in an interview.
“Would these subjects have thought of suicide in the absence of the Brittany Maynard publicity campaign? I doubt it.”
Dr. Hanson, a forensic psychiatrist, is assistant professor of psychiatry at the University of Maryland and at Johns Hopkins University, both in Baltimore.
Being diagnosed with an elevated amyloid-beta biomarker that indicates greater risk of Alzheimer’s disease did not lead to increased consideration of physician-assisted death (PAD), according to an analysis of patients interviewed during clinical trials on cognitive decline.
“Our findings suggest that learning one’s amyloid imaging result does not change baseline attitudes regarding the acceptability of PAD,” wrote Emily A. Largent, PhD, of the department of medical ethics and health policy at the University of Pennsylvania, Philadelphia, and coauthors. The study was published as a research letter in JAMA Neurology.
Participants were recruited from two ongoing clinical trials, one of which included patients with elevated amyloid-beta (n = 50), whereas the other did not (n = 30). All participants completed an interview 4-12 weeks after receiving their biomarker results; 47 and 30 participants, respectively, also completed a follow-up interview at 12 months.
When asked whether they had considered PAD, nearly two-thirds of interviewees with the Alzheimer’s disease biomarker stated that they neither had nor would. Roughly one in five from that group said they would pursue PAD if they began to suffer from cognitive impairment or became a burden on others. Interviewees who did not have elevated amyloid beta, when asked whether a reversed result would have led to PAD or suicide, showed interest in roughly similar proportion to their at-risk counterparts.
The coauthors acknowledged the limitations of their study, including not asking about other end-of-life preferences or perceived quality of life for people with dementia. They also noted that, although their sample mirrors the populations of the two studies they drew from, “its homogeneity limits generalizability.” As such, they stressed that
The study was supported by grants from the Alzheimer’s Association and the National Institute on Aging. One author reported receiving grants from those two organizations during the study; another reported receiving grants from Lilly and Novartis. No other conflicts of interest were reported.
SOURCE: Largent EA et al. JAMA Neurol. 2019 Apr 29. doi: 10.1001/jamaneurol.2019.0797.
Being diagnosed with an elevated amyloid-beta biomarker that indicates greater risk of Alzheimer’s disease did not lead to increased consideration of physician-assisted death (PAD), according to an analysis of patients interviewed during clinical trials on cognitive decline.
“Our findings suggest that learning one’s amyloid imaging result does not change baseline attitudes regarding the acceptability of PAD,” wrote Emily A. Largent, PhD, of the department of medical ethics and health policy at the University of Pennsylvania, Philadelphia, and coauthors. The study was published as a research letter in JAMA Neurology.
Participants were recruited from two ongoing clinical trials, one of which included patients with elevated amyloid-beta (n = 50), whereas the other did not (n = 30). All participants completed an interview 4-12 weeks after receiving their biomarker results; 47 and 30 participants, respectively, also completed a follow-up interview at 12 months.
When asked whether they had considered PAD, nearly two-thirds of interviewees with the Alzheimer’s disease biomarker stated that they neither had nor would. Roughly one in five from that group said they would pursue PAD if they began to suffer from cognitive impairment or became a burden on others. Interviewees who did not have elevated amyloid beta, when asked whether a reversed result would have led to PAD or suicide, showed interest in roughly similar proportion to their at-risk counterparts.
The coauthors acknowledged the limitations of their study, including not asking about other end-of-life preferences or perceived quality of life for people with dementia. They also noted that, although their sample mirrors the populations of the two studies they drew from, “its homogeneity limits generalizability.” As such, they stressed that
The study was supported by grants from the Alzheimer’s Association and the National Institute on Aging. One author reported receiving grants from those two organizations during the study; another reported receiving grants from Lilly and Novartis. No other conflicts of interest were reported.
SOURCE: Largent EA et al. JAMA Neurol. 2019 Apr 29. doi: 10.1001/jamaneurol.2019.0797.
FROM JAMA NEUROLOGY
Weight loss improves psoriatic arthritis
MAUI, HAWAII – Serious weight loss brings big improvement in psoriatic arthritis in obese patients, at least short term, according to a Swedish, single-arm, prospective, proof-of-concept study.
A dose-response effect was evident: the greater the lost poundage, the bigger the improvement across multiple dimensions of psoriatic arthritis.
The short-term efficacy was eye-catching, especially in view of the well-recognized increased prevalence of obesity in psoriatic arthritis patients. But the jury is still out as to the long-term impact of this nonpharmacologic therapy, Eric M. Ruderman, MD, said at the 2019 Rheumatology Winter Clinical Symposium.
He has spoken with the Swedish investigators and was happy to learn they’re continuing to follow study participants long term.
“That’s going to be the key, right? Because if you do this for 12 weeks, like every other fad crash diet, and then you let the weight go right back on again, you haven’t really accomplished anything. I think the key will be what happens at a year,” according to Dr. Ruderman, professor of medicine and associate chief for clinical affairs in the division of rheumatology at Northwestern University, Chicago.
The study included 46 obese psoriatic arthritis patients who signed on for a structured, medically supervised very-low-energy diet lasting 12-16 weeks, depending upon their baseline obesity level. The commercially available liquid diet (Cambridge Weight Plan Limited) is a type of therapy widely prescribed by Swedish physicians, clocking in at a mere 640 kcal/day.
“I don’t know about you, but I ate that at breakfast this morning,” quipped symposium director Arthur Kavanaugh, MD, professor of medicine at the University of California, San Diego.
Following completion of the strict very-low-energy diet, patients were gradually reintroduced to a less-draconian, solid-food, energy-restricted diet, to be followed through the 12-month mark. The full 12-month protocol was supervised by staff in the obesity unit at Sahlgrenska University Hospital in Gothenburg, Sweden. The 12-month results will be presented at the annual European Congress of Rheumatology in Madrid.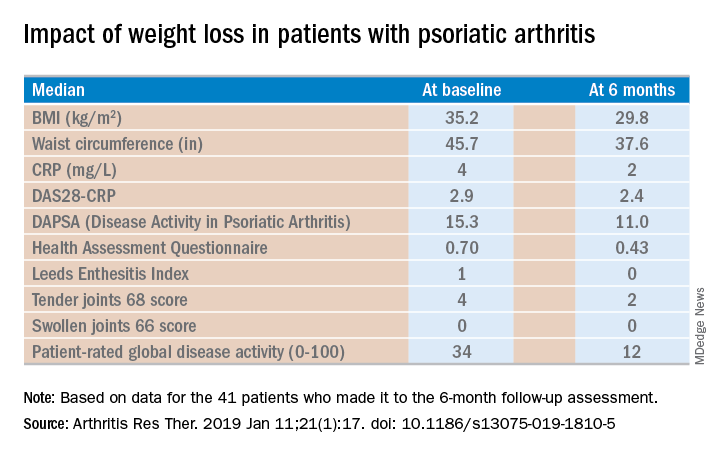
Of the 46 starters, 41 made it to the 6-month follow-up assessment. At that point they’d lost a median of 18.2 kg, or 18.6% of their baseline body weight. Their body mass index had dropped from an average of 35.2 to 29.8 kg/m2. And their psoriatic arthritis had improved significantly. For example, their median Disease Activity Score using 28 joint counts based upon C-reactive protein (DAS28-CRP) decreased from 2.9 at baseline to 2.4 at 6 months, with ACR 20, -50, and -70 responses of 51.2%, 34.1%, and 7.3% while disease-directed medications were held constant (Arthritis Res Ther. 2019 Jan 11;21[1]:17. doi: 10.1186/s13075-019-1810-5).
The investigators reported the very-low-energy diet phase was generally well tolerated. A total of 34 of the 41 patients deemed it “easier or much easier” than expected, prompting Dr. Ruderman to comment: “Because they thought it was going to be awful.”
Dr. Ruderman and Dr. Kavanaugh reported serving as consultants to numerous pharmaceutical companies.
MAUI, HAWAII – Serious weight loss brings big improvement in psoriatic arthritis in obese patients, at least short term, according to a Swedish, single-arm, prospective, proof-of-concept study.
A dose-response effect was evident: the greater the lost poundage, the bigger the improvement across multiple dimensions of psoriatic arthritis.
The short-term efficacy was eye-catching, especially in view of the well-recognized increased prevalence of obesity in psoriatic arthritis patients. But the jury is still out as to the long-term impact of this nonpharmacologic therapy, Eric M. Ruderman, MD, said at the 2019 Rheumatology Winter Clinical Symposium.
He has spoken with the Swedish investigators and was happy to learn they’re continuing to follow study participants long term.
“That’s going to be the key, right? Because if you do this for 12 weeks, like every other fad crash diet, and then you let the weight go right back on again, you haven’t really accomplished anything. I think the key will be what happens at a year,” according to Dr. Ruderman, professor of medicine and associate chief for clinical affairs in the division of rheumatology at Northwestern University, Chicago.
The study included 46 obese psoriatic arthritis patients who signed on for a structured, medically supervised very-low-energy diet lasting 12-16 weeks, depending upon their baseline obesity level. The commercially available liquid diet (Cambridge Weight Plan Limited) is a type of therapy widely prescribed by Swedish physicians, clocking in at a mere 640 kcal/day.
“I don’t know about you, but I ate that at breakfast this morning,” quipped symposium director Arthur Kavanaugh, MD, professor of medicine at the University of California, San Diego.
Following completion of the strict very-low-energy diet, patients were gradually reintroduced to a less-draconian, solid-food, energy-restricted diet, to be followed through the 12-month mark. The full 12-month protocol was supervised by staff in the obesity unit at Sahlgrenska University Hospital in Gothenburg, Sweden. The 12-month results will be presented at the annual European Congress of Rheumatology in Madrid.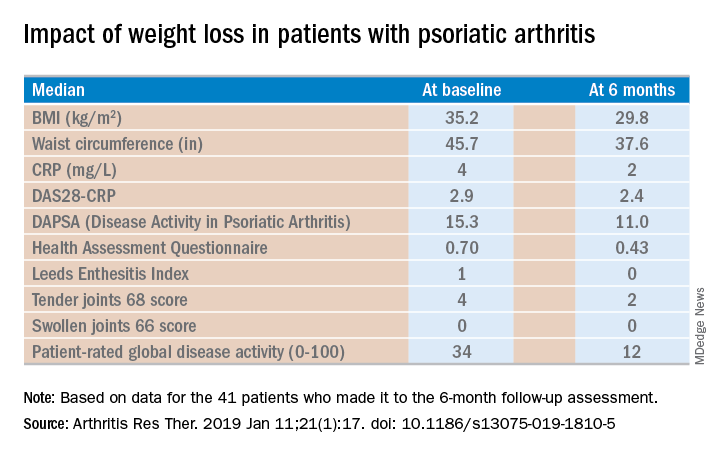
Of the 46 starters, 41 made it to the 6-month follow-up assessment. At that point they’d lost a median of 18.2 kg, or 18.6% of their baseline body weight. Their body mass index had dropped from an average of 35.2 to 29.8 kg/m2. And their psoriatic arthritis had improved significantly. For example, their median Disease Activity Score using 28 joint counts based upon C-reactive protein (DAS28-CRP) decreased from 2.9 at baseline to 2.4 at 6 months, with ACR 20, -50, and -70 responses of 51.2%, 34.1%, and 7.3% while disease-directed medications were held constant (Arthritis Res Ther. 2019 Jan 11;21[1]:17. doi: 10.1186/s13075-019-1810-5).
The investigators reported the very-low-energy diet phase was generally well tolerated. A total of 34 of the 41 patients deemed it “easier or much easier” than expected, prompting Dr. Ruderman to comment: “Because they thought it was going to be awful.”
Dr. Ruderman and Dr. Kavanaugh reported serving as consultants to numerous pharmaceutical companies.
MAUI, HAWAII – Serious weight loss brings big improvement in psoriatic arthritis in obese patients, at least short term, according to a Swedish, single-arm, prospective, proof-of-concept study.
A dose-response effect was evident: the greater the lost poundage, the bigger the improvement across multiple dimensions of psoriatic arthritis.
The short-term efficacy was eye-catching, especially in view of the well-recognized increased prevalence of obesity in psoriatic arthritis patients. But the jury is still out as to the long-term impact of this nonpharmacologic therapy, Eric M. Ruderman, MD, said at the 2019 Rheumatology Winter Clinical Symposium.
He has spoken with the Swedish investigators and was happy to learn they’re continuing to follow study participants long term.
“That’s going to be the key, right? Because if you do this for 12 weeks, like every other fad crash diet, and then you let the weight go right back on again, you haven’t really accomplished anything. I think the key will be what happens at a year,” according to Dr. Ruderman, professor of medicine and associate chief for clinical affairs in the division of rheumatology at Northwestern University, Chicago.
The study included 46 obese psoriatic arthritis patients who signed on for a structured, medically supervised very-low-energy diet lasting 12-16 weeks, depending upon their baseline obesity level. The commercially available liquid diet (Cambridge Weight Plan Limited) is a type of therapy widely prescribed by Swedish physicians, clocking in at a mere 640 kcal/day.
“I don’t know about you, but I ate that at breakfast this morning,” quipped symposium director Arthur Kavanaugh, MD, professor of medicine at the University of California, San Diego.
Following completion of the strict very-low-energy diet, patients were gradually reintroduced to a less-draconian, solid-food, energy-restricted diet, to be followed through the 12-month mark. The full 12-month protocol was supervised by staff in the obesity unit at Sahlgrenska University Hospital in Gothenburg, Sweden. The 12-month results will be presented at the annual European Congress of Rheumatology in Madrid.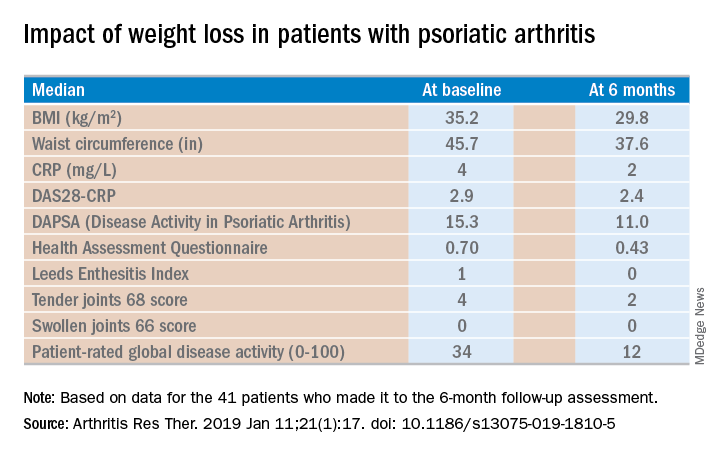
Of the 46 starters, 41 made it to the 6-month follow-up assessment. At that point they’d lost a median of 18.2 kg, or 18.6% of their baseline body weight. Their body mass index had dropped from an average of 35.2 to 29.8 kg/m2. And their psoriatic arthritis had improved significantly. For example, their median Disease Activity Score using 28 joint counts based upon C-reactive protein (DAS28-CRP) decreased from 2.9 at baseline to 2.4 at 6 months, with ACR 20, -50, and -70 responses of 51.2%, 34.1%, and 7.3% while disease-directed medications were held constant (Arthritis Res Ther. 2019 Jan 11;21[1]:17. doi: 10.1186/s13075-019-1810-5).
The investigators reported the very-low-energy diet phase was generally well tolerated. A total of 34 of the 41 patients deemed it “easier or much easier” than expected, prompting Dr. Ruderman to comment: “Because they thought it was going to be awful.”
Dr. Ruderman and Dr. Kavanaugh reported serving as consultants to numerous pharmaceutical companies.
REPORTING FROM RWCS 2019
Patient education material often fails to meet readability standards
Most of the online patient education materials provided by eight nationally recognized ob.gyn. societies are written at levels above the readability guidelines set by the American Medical Association, National Institutes of Health, and Department of Health & Human Services, according to Fatimah Z. Fahimuddin, MD, of the University of California, San Francisco, Fresno, and her associates.
According to the AMA, NIH, and HHS, all patient education material should be written at or below a sixth-grade reading level.
In a study published in Obstetrics & Gynecology, the investigators analyzed the readability of 410 online patient education documents from the American Association of Gynecologic Laparoscopists, the American College of Obstetricians and Gynecologists, the American Society for Reproductive Medicine, the American Urogynecologic Society, the Association of Reproductive Health Professionals, the Society of Gynecologic Oncology, the Society for Maternal-Fetal Medicine, and Voices for Pelvic Floor Disorders.
The mean Flesch-Kincaid Grade Level score was 8.9 for the 69 obstetrics-related documents analyzed; for the 341 gynecology-related documents, the mean score was 8.7. The American Urogynecologic Society had the most readable documents, with a mean grade level score of 6.4; the American Association of Gynecologic Laparoscopists had the least readable, with a mean grade level score of 12.7. For the other three readability scales utilized in the analysis, mean scores generally ranged in the 8th-12th grade reading levels.
“It is not surprising that writing patient education materials at an appropriate reading level is difficult. With readability scales utilizing syllable count, common words such as ‘menstruation,’ ‘uterus,’ and ‘contractions’ will lead to higher readability scores. Thus, higher reading levels in both specialties is seen and expected,” the investigators wrote. Measures such as the addition of glossaries to define words and visuals to illustrate complex procedures would be helpful for reading comprehension and have been used by other medical societies.
The study authors reported no conflicts of interest.
SOURCE: Fahimuddin FZ et al. Obstet Gynecol. 2019;133:888-94.
Most of the online patient education materials provided by eight nationally recognized ob.gyn. societies are written at levels above the readability guidelines set by the American Medical Association, National Institutes of Health, and Department of Health & Human Services, according to Fatimah Z. Fahimuddin, MD, of the University of California, San Francisco, Fresno, and her associates.
According to the AMA, NIH, and HHS, all patient education material should be written at or below a sixth-grade reading level.
In a study published in Obstetrics & Gynecology, the investigators analyzed the readability of 410 online patient education documents from the American Association of Gynecologic Laparoscopists, the American College of Obstetricians and Gynecologists, the American Society for Reproductive Medicine, the American Urogynecologic Society, the Association of Reproductive Health Professionals, the Society of Gynecologic Oncology, the Society for Maternal-Fetal Medicine, and Voices for Pelvic Floor Disorders.
The mean Flesch-Kincaid Grade Level score was 8.9 for the 69 obstetrics-related documents analyzed; for the 341 gynecology-related documents, the mean score was 8.7. The American Urogynecologic Society had the most readable documents, with a mean grade level score of 6.4; the American Association of Gynecologic Laparoscopists had the least readable, with a mean grade level score of 12.7. For the other three readability scales utilized in the analysis, mean scores generally ranged in the 8th-12th grade reading levels.
“It is not surprising that writing patient education materials at an appropriate reading level is difficult. With readability scales utilizing syllable count, common words such as ‘menstruation,’ ‘uterus,’ and ‘contractions’ will lead to higher readability scores. Thus, higher reading levels in both specialties is seen and expected,” the investigators wrote. Measures such as the addition of glossaries to define words and visuals to illustrate complex procedures would be helpful for reading comprehension and have been used by other medical societies.
The study authors reported no conflicts of interest.
SOURCE: Fahimuddin FZ et al. Obstet Gynecol. 2019;133:888-94.
Most of the online patient education materials provided by eight nationally recognized ob.gyn. societies are written at levels above the readability guidelines set by the American Medical Association, National Institutes of Health, and Department of Health & Human Services, according to Fatimah Z. Fahimuddin, MD, of the University of California, San Francisco, Fresno, and her associates.
According to the AMA, NIH, and HHS, all patient education material should be written at or below a sixth-grade reading level.
In a study published in Obstetrics & Gynecology, the investigators analyzed the readability of 410 online patient education documents from the American Association of Gynecologic Laparoscopists, the American College of Obstetricians and Gynecologists, the American Society for Reproductive Medicine, the American Urogynecologic Society, the Association of Reproductive Health Professionals, the Society of Gynecologic Oncology, the Society for Maternal-Fetal Medicine, and Voices for Pelvic Floor Disorders.
The mean Flesch-Kincaid Grade Level score was 8.9 for the 69 obstetrics-related documents analyzed; for the 341 gynecology-related documents, the mean score was 8.7. The American Urogynecologic Society had the most readable documents, with a mean grade level score of 6.4; the American Association of Gynecologic Laparoscopists had the least readable, with a mean grade level score of 12.7. For the other three readability scales utilized in the analysis, mean scores generally ranged in the 8th-12th grade reading levels.
“It is not surprising that writing patient education materials at an appropriate reading level is difficult. With readability scales utilizing syllable count, common words such as ‘menstruation,’ ‘uterus,’ and ‘contractions’ will lead to higher readability scores. Thus, higher reading levels in both specialties is seen and expected,” the investigators wrote. Measures such as the addition of glossaries to define words and visuals to illustrate complex procedures would be helpful for reading comprehension and have been used by other medical societies.
The study authors reported no conflicts of interest.
SOURCE: Fahimuddin FZ et al. Obstet Gynecol. 2019;133:888-94.
FROM OBSTETRICS & GYNECOLOGY
Laparoscopic magnetic sphincter augmentation may accrue savings over time
BALTIMORE – because the former procedure is associated with lower medical therapy costs after the procedure.
The finding comes from to a prospective observational study from the Allegheny Health Network in Pittsburgh, reported by Shahin Ayazi, MD, at the annual meeting of the American Society of Gastrointestinal Endoscopic Surgeons.
“Magnetic sphincter augmentation (MSA) results in comparable symptom control, proton-pump inhibitor (PPI) elimination rate, and GERD health-related quality of life and Reflux Symptom Index measures compared to values reported for laparoscopic Nissen fundoplication (LNF) in the literature,” said Dr. Ayazi of the University of Rochester (N.Y.). “Unlike reported values for LNF, the majority of patients after MSA were discharged on the same day of surgery.”
Dr. Ayazi reported on 180 patients who had MSA and 1,131 who had LNF over a 2-year period beginning in September 2015 at Allegheny Health, a network of eight hospitals and related facilities in western Pennsylvania and western New York State. The study analyzed Highmark claims data to calculate costs for 12 months before and after surgery in four categories: total procedure payer cost, payer costs of PPI, disease-related costs, and all medical costs.
Dr. Ayazi noted that many payers have been reluctant to cover the costs of MSA because the device costs around $5,000 on average. “There’s also a paucity of data in the literature in regard to the cost analysis of MSA in the management of reflux disease,” he said, adding that this is the first study that uses payer data to analyze the cost of antireflux surgery.
In this study, MSA costs slightly more up front than LNF ($13,522 vs. $13,388, respectively; P = .02). Per-member/per-month (PMPM) costs in the 12 months before their procedures were higher in the MSA group ($305 vs. $233). After surgery, these costs were significantly lower at $104 for MSA patients versus $126 for LNF patients, Dr. Ayazi said.
In the MSA group, 89% of patients were discharged on the same day as surgery, 90.7% said they were satisfied with the outcome, and 91.8% discontinued PPI therapy, Dr. Ayazi said.
He noted the claims data did not provide access to clinical data, Highmark did not provide information on the etiology of the costs differences, and the follow-up for cost analysis is relatively short-term.
During the discussion, Michel Gagner, MD, of Westmount, Quebec, warned against reading too much into the study because of its short duration and gave the example of experience with the laparoscopic adjustable gastric band. “The 10 years after, when you look at the reoperation, the removal, the conversions, some of the disasters in this area – all this needs to be added to the cost, and then when you looked at this, it was no longer cost effective. So I’m wondering if the same story could happen in the next 10 years. You may find that your conclusions are totally reversed.”
Peter Crookes, MD, of the University of Southern California, Los Angeles, challenged the study’s comparison of procedure cost, noting that the trend is toward same-day discharge after LNF, whereas study patients were hospitalized after LNF. Dr. Ayazi noted that the data presented reported procedure cost, not the hospital stay costs, because Highmark did not provide that data.
Lead researcher Blair Jobe, MD, director of the Esophageal and Lung Institute at Allegheny Health Network, added, “The higher initial cost of a LINX (Ethicon) procedure compared to a Nissen fundoplication is perceived as a drawback by insurers, which can make getting insurance approvals challenging. This study suggests that perception may be short sighted in that insurance plans can provide better care for their GERD patients at a similar cost to laparoscopic Nissen fundoplication when you factor in the greater reductions in medical costs after the procedure.”
Dr. Ayazi has no relevant financial relationships to disclose. Dr. Jobe reported he is a consultant for Ethicon.
SOURCE: Ayazi S et al. SAGES 2019, Session SS04.
BALTIMORE – because the former procedure is associated with lower medical therapy costs after the procedure.
The finding comes from to a prospective observational study from the Allegheny Health Network in Pittsburgh, reported by Shahin Ayazi, MD, at the annual meeting of the American Society of Gastrointestinal Endoscopic Surgeons.
“Magnetic sphincter augmentation (MSA) results in comparable symptom control, proton-pump inhibitor (PPI) elimination rate, and GERD health-related quality of life and Reflux Symptom Index measures compared to values reported for laparoscopic Nissen fundoplication (LNF) in the literature,” said Dr. Ayazi of the University of Rochester (N.Y.). “Unlike reported values for LNF, the majority of patients after MSA were discharged on the same day of surgery.”
Dr. Ayazi reported on 180 patients who had MSA and 1,131 who had LNF over a 2-year period beginning in September 2015 at Allegheny Health, a network of eight hospitals and related facilities in western Pennsylvania and western New York State. The study analyzed Highmark claims data to calculate costs for 12 months before and after surgery in four categories: total procedure payer cost, payer costs of PPI, disease-related costs, and all medical costs.
Dr. Ayazi noted that many payers have been reluctant to cover the costs of MSA because the device costs around $5,000 on average. “There’s also a paucity of data in the literature in regard to the cost analysis of MSA in the management of reflux disease,” he said, adding that this is the first study that uses payer data to analyze the cost of antireflux surgery.
In this study, MSA costs slightly more up front than LNF ($13,522 vs. $13,388, respectively; P = .02). Per-member/per-month (PMPM) costs in the 12 months before their procedures were higher in the MSA group ($305 vs. $233). After surgery, these costs were significantly lower at $104 for MSA patients versus $126 for LNF patients, Dr. Ayazi said.
In the MSA group, 89% of patients were discharged on the same day as surgery, 90.7% said they were satisfied with the outcome, and 91.8% discontinued PPI therapy, Dr. Ayazi said.
He noted the claims data did not provide access to clinical data, Highmark did not provide information on the etiology of the costs differences, and the follow-up for cost analysis is relatively short-term.
During the discussion, Michel Gagner, MD, of Westmount, Quebec, warned against reading too much into the study because of its short duration and gave the example of experience with the laparoscopic adjustable gastric band. “The 10 years after, when you look at the reoperation, the removal, the conversions, some of the disasters in this area – all this needs to be added to the cost, and then when you looked at this, it was no longer cost effective. So I’m wondering if the same story could happen in the next 10 years. You may find that your conclusions are totally reversed.”
Peter Crookes, MD, of the University of Southern California, Los Angeles, challenged the study’s comparison of procedure cost, noting that the trend is toward same-day discharge after LNF, whereas study patients were hospitalized after LNF. Dr. Ayazi noted that the data presented reported procedure cost, not the hospital stay costs, because Highmark did not provide that data.
Lead researcher Blair Jobe, MD, director of the Esophageal and Lung Institute at Allegheny Health Network, added, “The higher initial cost of a LINX (Ethicon) procedure compared to a Nissen fundoplication is perceived as a drawback by insurers, which can make getting insurance approvals challenging. This study suggests that perception may be short sighted in that insurance plans can provide better care for their GERD patients at a similar cost to laparoscopic Nissen fundoplication when you factor in the greater reductions in medical costs after the procedure.”
Dr. Ayazi has no relevant financial relationships to disclose. Dr. Jobe reported he is a consultant for Ethicon.
SOURCE: Ayazi S et al. SAGES 2019, Session SS04.
BALTIMORE – because the former procedure is associated with lower medical therapy costs after the procedure.
The finding comes from to a prospective observational study from the Allegheny Health Network in Pittsburgh, reported by Shahin Ayazi, MD, at the annual meeting of the American Society of Gastrointestinal Endoscopic Surgeons.
“Magnetic sphincter augmentation (MSA) results in comparable symptom control, proton-pump inhibitor (PPI) elimination rate, and GERD health-related quality of life and Reflux Symptom Index measures compared to values reported for laparoscopic Nissen fundoplication (LNF) in the literature,” said Dr. Ayazi of the University of Rochester (N.Y.). “Unlike reported values for LNF, the majority of patients after MSA were discharged on the same day of surgery.”
Dr. Ayazi reported on 180 patients who had MSA and 1,131 who had LNF over a 2-year period beginning in September 2015 at Allegheny Health, a network of eight hospitals and related facilities in western Pennsylvania and western New York State. The study analyzed Highmark claims data to calculate costs for 12 months before and after surgery in four categories: total procedure payer cost, payer costs of PPI, disease-related costs, and all medical costs.
Dr. Ayazi noted that many payers have been reluctant to cover the costs of MSA because the device costs around $5,000 on average. “There’s also a paucity of data in the literature in regard to the cost analysis of MSA in the management of reflux disease,” he said, adding that this is the first study that uses payer data to analyze the cost of antireflux surgery.
In this study, MSA costs slightly more up front than LNF ($13,522 vs. $13,388, respectively; P = .02). Per-member/per-month (PMPM) costs in the 12 months before their procedures were higher in the MSA group ($305 vs. $233). After surgery, these costs were significantly lower at $104 for MSA patients versus $126 for LNF patients, Dr. Ayazi said.
In the MSA group, 89% of patients were discharged on the same day as surgery, 90.7% said they were satisfied with the outcome, and 91.8% discontinued PPI therapy, Dr. Ayazi said.
He noted the claims data did not provide access to clinical data, Highmark did not provide information on the etiology of the costs differences, and the follow-up for cost analysis is relatively short-term.
During the discussion, Michel Gagner, MD, of Westmount, Quebec, warned against reading too much into the study because of its short duration and gave the example of experience with the laparoscopic adjustable gastric band. “The 10 years after, when you look at the reoperation, the removal, the conversions, some of the disasters in this area – all this needs to be added to the cost, and then when you looked at this, it was no longer cost effective. So I’m wondering if the same story could happen in the next 10 years. You may find that your conclusions are totally reversed.”
Peter Crookes, MD, of the University of Southern California, Los Angeles, challenged the study’s comparison of procedure cost, noting that the trend is toward same-day discharge after LNF, whereas study patients were hospitalized after LNF. Dr. Ayazi noted that the data presented reported procedure cost, not the hospital stay costs, because Highmark did not provide that data.
Lead researcher Blair Jobe, MD, director of the Esophageal and Lung Institute at Allegheny Health Network, added, “The higher initial cost of a LINX (Ethicon) procedure compared to a Nissen fundoplication is perceived as a drawback by insurers, which can make getting insurance approvals challenging. This study suggests that perception may be short sighted in that insurance plans can provide better care for their GERD patients at a similar cost to laparoscopic Nissen fundoplication when you factor in the greater reductions in medical costs after the procedure.”
Dr. Ayazi has no relevant financial relationships to disclose. Dr. Jobe reported he is a consultant for Ethicon.
SOURCE: Ayazi S et al. SAGES 2019, Session SS04.
REPORTING FROM SAGES 2019










