User login
Feasibility—and safety—of reducing the traditional 14 prenatal visits to 8 or 10
CASE Low-risk maternity patient wants fewer prenatal visits
A recently pregnant patient asks her obstetrician if she can schedule fewer prenatal visits given that she is at low risk, wants to minimize missing work, and lives an hour away from the clinic office. Her physician tells her that she needs the standard 13 to 15 visits to have a healthy pregnancy.
Obstetric care in the United States largely remains a “one-size fits all” approach despite compelling data that fewer visits for low-risk women are medically acceptable and may be more cost-effective.
Prenatal care: One size does not fit all
With nearly 4 million births annually in the United States, prenatal care is one of the most widely used preventive health care strategies.1,2 The ideal method for providing prenatal care, however, remains controversial. At the inception of early 20th century prenatal care in the United States, preventive strategies focused in part on eclampsia-related maternal morbidity and mortality, which in turn informed the content and frequency of prenatal visits.2 Despite the dramatic changes in medical practice over the last 100 years, the basic timing and quantity of prenatal care has not changed substantively.
The lack of change is not because we have not explored other models of prenatal care and sought to introduce evidence-based change. Several studies have assessed the impact of reduced prenatal care visits for low-risk women.3-7 Systematic reviews evaluated 7 randomized trials, with more than 60,000 women enrolled, of prenatal care models with a reduced number of planned antenatal visits (4 to 9 visits vs the traditional 13 to 15 visits).3,8 There were no demonstrable differences in maternal or perinatal morbidity or mortality, particularly in higher resource settings.
Despite strong safety data and the potential cost-effectiveness of a reduced schedule of prenatal visits, US prenatal care practices generally continue to have a one-size-fits-all approach. Several organizations, however, have called for a change in practice.
Endorsing a reduced number of prenatal visits for low-risk women, the US Department of Health and Human Services Expert Panel on Prenatal Care issued a report in 1989 that stated “the specific content and timing of prenatal visits, contacts, and education should vary depending on the risk status of the pregnant woman and her fetus.”9 Consistent with that recommendation, the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (ACOG) jointly published guidelines that recommend a system of goal-oriented antenatal visits at specific gestational ages and that support a reduced schedule of prenatal visits, compared with traditional models, for low-risk, parous women.10 The World Health Organization also published recommendations for an 8 “contact” prenatal care system to reduce perinatal mortality and improve women’s prenatal experience.11
Is obstetric dogma the reason for lack of change?
Concerns about patient satisfaction may play a role in limiting the use of a reduced prenatal care visit model. In trials that evaluated a model of reduced prenatal care visits, women were less satisfied with a reduced visit schedule and the gap between provider contacts.3,8 Anecdotally, providers have expressed concerns about perceived liability. Most compelling, perhaps, is the idea that the traditional prenatal schedule has become obstetric dogma.
Continue to: Consciously or unconsciously, clinicians may feel...
Consciously or unconsciously, clinicians may feel uncomfortable diverging from a schedule of visits that is firmly entrenched in obstetric practice. Continuing the status quo is easier than restructuring prenatal care practice. Ultimately, a paradigm shift may be required to broadly adopt a model of fewer prenatal visits for low-risk pregnancies.12 With these issues propelling the historic patterns of prenatal care, it is easy to see why we have not yet changed despite convincing reasons to do so.
In this article, we detail the reduced-visit prenatal care models developed at 3 institutions and how they incorporate use of today’s technology.
Approach #1: University of Utah Virtual Prenatal Care Program
The University of Utah Virtual Prenatal Care Program was conceived as a “baby step” toward developing a model of fewer total prenatal visits. Virtual visits were intended to reduce the number of prenatal face-to-face visits while maintaining the same total number of visits. Since large clinical trials had established the safety of reduced visits, the primary objectives were to retain patient satisfaction and to facilitate provider adoption.
Would women be satisfied with remote prenatal care? A prospective randomized controlled trial was designed in which 200 women were assigned to receive either a combination of telemedicine and 5 scheduled in-clinic prenatal visits (remote care group) or traditional in-clinic prenatal care (usual care group). Low-risk multigravida pregnant women who were between 6 0/7 and 16 0/7 weeks’ gestation were enrolled. The primary outcome was patient satisfaction.
The face-to-face visits were goal oriented, with scheduled physical examination, laboratory tests, or ultrasonography, and were conducted by the patient’s established obstetric provider (physician or nurse midwife) to maintain continuity of care. The remote care group self-collected measurements for weight, blood pressure, and fetal heart rate by handheld Doppler device prior to each telemedicine visit and entered the information into the electronic medical record. The purpose of the self-collected data was patient engagement and satisfaction, as well as increased provider comfort with the change in prenatal care schedule, rather than medical necessity.
The primary outcome of overall patient satisfaction with prenatal care was ascertained by questionnaire after delivery. The sample size calculation of 200 patients was based on noninferiority testing, and analysis was by intent-to-treat. The details of the trial are pending publication.
As expected, the remote care group had significantly fewer in-clinic prenatal care visits compared with the usual care group (7.2 vs 11.3 visits); the total number of prenatal visits was not different between groups. Overall satisfaction with prenatal care was very high in both the remote care and the usual care group (100% vs 97%).
The virtual prenatal care model for low-risk pregnancies, consisting of a novel remote monitoring strategy and a reduced number of in-clinic visits, was not associated with lower patient satisfaction compared with traditional care.
New care strategy gives patients a choice. The success of this clinical trial has led to its programmatic adoption at the University of Utah, and low-risk women currently are offered a choice between participating in the Virtual Prenatal Care Program or receiving traditional prenatal care. The University of Utah is moving on from the one-size-fits-all approach to adopt new strategies that provide personalized evidence-based prenatal care at the lowest cost, while retaining high patient satisfaction. Formal cost-effectiveness analyses are underway.
Continue to: Approach #2: Mayo Clinic OB Nest...
Approach #2: Mayo Clinic OB Nest
In 2011, the Mayo Clinic Obstetric Division partnered with 2 other Mayo Clinic divisions, the Center for Innovation and the Center for the Science of Health Care Delivery, to redesign prenatal care for low-risk expectant mothers.Pregnant women and their obstetric health care teams (including obstetricians, certified nurse midwives, registered nurses, and clinical support staff) were convened to develop a novel model of prenatal care.4 The goal of this collaboration centered on:
- creating an evidence-driven prenatal care model for low-risk expectant women designed by relevant stakeholders
- focusing on meeting the on-demand needs of expectant mothers
- integrating innovative 21st century technology, and
- reducing the burden of prescheduled, low-value office visits.
Exploratory efforts to develop a novel care program. Based on feedback from the collaboration and guided by these goals, 141 expectant mothers participated in 19 different experiments, enabling the health care team to understand the impact of changing various components of prenatal care.
The experiments included integration of home monitoring (home fetal Doppler devices, drop-in fetal Doppler stations, home blood pressure monitoring devices), technology-enhanced communication with obstetric team members (video chats, tummy photos, virtual prenatal clinic appointments, proactive calls), and social media engagement (secure online prenatal care community).
Recommendations for the final components of OB Nest were based on feasibility and the potential impact on care. The recommendations included decreasing scheduled clinic appointments from 14 to 8, providing home monitoring devices to measure maternal blood pressure and fetal heart rate, establishing OB Nest virtual connected care visits with a registered nurse, and offering a secure online community of expectant mothers.
Trial assessed program’s efficacy, safety, satisfaction. A mixed-methods randomized controlled trial subsequently was conducted to evaluate the components of OB Nest.6 The trial included 300 pregnant women who were randomly assigned to standard prenatal care as recommended by ACOG or to OB Nest care.
OB Nest care consisted of 8 scheduled clinic appointments, 6 planned virtual (phone or online) connected care visits with a registered nurse dedicated to OB Nest, home monitoring of blood pressure (with a home digital sphygmomanometer) and fetal heart rate, and access to an online prenatal care community designated for OB Nest participants.
While publication of the trial results currently is pending, the OB Nest program appears to safely and effectively decrease the number of scheduled prenatal care visits for low-risk expectant mothers while improving the overall patient experience. OB Nest care now is offered as one of several options for low-risk expectant mothers at Mayo Clinic.
Additional avenues of study. Studies evaluating the impact of OB Nest in various nonacademic settings are now underway. Also under review is the potential cost savings of OB Nest as related to the productive lives of expectant mothers, while prenatal care safety is maintained.
The focus shift from a sick to a wellness perspective, stakeholder inclusion in the program design, and the integration of home monitoring tools are all major contributing factors to the success of OB Nest.
Continue to: Approach #3: Prisma Health utilizes mobile app technology...
Approach #3: Prisma Health utilizes mobile app technology
A third approach to reducing unnecessary visits for routine maternity care is to employ mobile app technology. Technology companies have developed app platforms for providers to use to educate and connect with patients; such apps reduce the number of routine obstetric office visits while maintaining patient satisfaction.
One group’s app experience. In a pilot study at a Prisma Health practice (South Carolina), 100 patients were placed on a reduced appointment schedule of 9 prenatal visits; the women self-monitored their weight gain and blood pressure using a remote monitoring system via an app called Babyscripts.7 Patient feedback was collected, with 45 of 100 patients responding.
Ninety-five percent of patients were satisfied with the mobile app, 94% reported positivity around pregnancy readiness, 90% were satisfied with their health care team, and 89% were happy with remote monitoring. Patients visited the app 3 times per week on average, and the top categories of interest were travel, exercise, genetics, and eating right.
One patient using the Babyscripts mobile health app and schedule optimization platform commented, “I am on my second pregnancy and wish this had been available for the first! The app is easy to use and I love seeing my weight on a graph. And I very much like the quality of the cuff” (personal data generated from Babyscripts).
In with the new
As clinicians strive to provide more patient-centered care, offering expectant families more than one way to receive their prenatal care is appropriate. Beyond the traditional 14-visit care model, we should offer use of novel options like mobile health apps, which improve the patient experience while decreasing the cost of care by reducing unnecessary visits.12 Note also that reducing visits for low-risk mothers opens space in the provider schedule for patients who need services more quickly.
Benefits for postpartum care. Traditionally, clinicians see the low-risk patient for a single follow-up appointment at 6 weeks postpartum. However, the World Health Organization recommends evaluating women at 3 days, 1 to 2 weeks, and 6 weeks postpartum.13 Further, the National Institute for Health and Care Excellence guidance recommends screening all women for resolution of postpartum blues at 10 to 14 days.14
ACOG also has made recommendations on optimizing postpartum care. In a committee opinion, ACOG recommends that all women have contact with their provider within the first 3 weeks postpartum.15 Recognizing that such an in-person visit may be difficult, ACOG has endorsed communication via text messaging, app-based support, and remote monitoring.15 An app such as Babyscripts would fill this need conveniently for both patient and provider.
In 2019, patients want choice. As maternity care providers, we should be open to considering novel, evidence-based options that may provide more cost-effective obstetric care.
- Martin JA, Hamilton BE, Osterman MJK, et al. Births: final data for 2017. Natl Vital Stat Rep. 2018;67:1-50.
- Alexander GR, Kotelchuck M. Assessing the role and effectiveness of prenatal care: history, challenges, and directions for future research. Public Health Rep. 2001;116:306-316.
- Dowswell T, Carroli G, Duley L, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev. 2015; (7):CD000934.
- de Mooij MJM, Hodny RL, O'Neil DA, et al. OB Nest: reimagining low-risk prenatal care. Mayo Clin Proc. 2018;93:458-466.
- Pflugeisen BM, McCarren C, Poore S, et al. Virtual visits: managing prenatal care with modern technology. MCN Am J Matern Child Nurs. 2016;41:24-30.
- Ridgeway JL, LeBlanc A, Branda M, et al. Implementation of a new prenatal care model to reduce office visits and increase connectivity and continuity of care: protocol for a mixed-methods study. BMC Pregnancy Childbirth. 2015;15:323.
- Marko KI, Krapf JM, Meltzer AC, et al. Testing the feasibility of remote patient monitoring in prenatal care using a mobile app and connected devices: a prospective observational trial. JMIR Res Protoc. 2016;5:e200.
- Carroli G, Villar J, Piaggio G, et al. WHO systematic review of randomised controlled trials of routine antenatal care. Lancet. 2001;357:1565-1570.
- Rosen MG, Merkatz IR, Hill JG. Caring for our future: a report by the expert panel on the content of prenatal care. Obstet Gynecol. 1991;77:782-787.
- American Academy of Pediatrics, American College of Obstetricians and Gynecologists. Guidelines for Perinatal Care. 8th edition. Elk Grove Village, IL: American Academy of Pediatrics, American College of Obstetricians and Gynecologists; 2017.
- World Health Organization. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience. Geneva, Switzerland: World Health Organization; 2016. https://apps.who.int/iris/bitstream/handle/10665/250796 /9789241549912-eng.pdf;jsessionid=C740C52F8AA1D7694CD9463152C193BA?sequence=1. Accessed June 19, 2019.
- Woo VG, Lundeen T, Matula S, et al. Achieving higher-value obstetrical care. Am J Obstet Gynecol. 2017;216:240e1-250e14.
- World Health Organization. WHO Recommendations on Postnatal Care of the Mother and Newborn. Geneva, Switzerland: WHO; 2014. https://apps.who.int/iris/bitstream/handle/10665/97603/9789241506649_eng.pdf?sequence=1. Accessed June 19, 2019.
- National Institute for Health and Care Excellence. Postnatal care up to 8 weeks after birth. Updated February 2015. https://www.nice.org.uk/guidance/cg37/chapter/1-Recommendations#maternal-health. Accessed June 19, 2019.
- American College of Obstetricians and Gynecologists. ACOG committee opinion no. 736. Optimizing postpartum care. Washington, DC: ACOG; 2018.
CASE Low-risk maternity patient wants fewer prenatal visits
A recently pregnant patient asks her obstetrician if she can schedule fewer prenatal visits given that she is at low risk, wants to minimize missing work, and lives an hour away from the clinic office. Her physician tells her that she needs the standard 13 to 15 visits to have a healthy pregnancy.
Obstetric care in the United States largely remains a “one-size fits all” approach despite compelling data that fewer visits for low-risk women are medically acceptable and may be more cost-effective.
Prenatal care: One size does not fit all
With nearly 4 million births annually in the United States, prenatal care is one of the most widely used preventive health care strategies.1,2 The ideal method for providing prenatal care, however, remains controversial. At the inception of early 20th century prenatal care in the United States, preventive strategies focused in part on eclampsia-related maternal morbidity and mortality, which in turn informed the content and frequency of prenatal visits.2 Despite the dramatic changes in medical practice over the last 100 years, the basic timing and quantity of prenatal care has not changed substantively.
The lack of change is not because we have not explored other models of prenatal care and sought to introduce evidence-based change. Several studies have assessed the impact of reduced prenatal care visits for low-risk women.3-7 Systematic reviews evaluated 7 randomized trials, with more than 60,000 women enrolled, of prenatal care models with a reduced number of planned antenatal visits (4 to 9 visits vs the traditional 13 to 15 visits).3,8 There were no demonstrable differences in maternal or perinatal morbidity or mortality, particularly in higher resource settings.
Despite strong safety data and the potential cost-effectiveness of a reduced schedule of prenatal visits, US prenatal care practices generally continue to have a one-size-fits-all approach. Several organizations, however, have called for a change in practice.
Endorsing a reduced number of prenatal visits for low-risk women, the US Department of Health and Human Services Expert Panel on Prenatal Care issued a report in 1989 that stated “the specific content and timing of prenatal visits, contacts, and education should vary depending on the risk status of the pregnant woman and her fetus.”9 Consistent with that recommendation, the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (ACOG) jointly published guidelines that recommend a system of goal-oriented antenatal visits at specific gestational ages and that support a reduced schedule of prenatal visits, compared with traditional models, for low-risk, parous women.10 The World Health Organization also published recommendations for an 8 “contact” prenatal care system to reduce perinatal mortality and improve women’s prenatal experience.11
Is obstetric dogma the reason for lack of change?
Concerns about patient satisfaction may play a role in limiting the use of a reduced prenatal care visit model. In trials that evaluated a model of reduced prenatal care visits, women were less satisfied with a reduced visit schedule and the gap between provider contacts.3,8 Anecdotally, providers have expressed concerns about perceived liability. Most compelling, perhaps, is the idea that the traditional prenatal schedule has become obstetric dogma.
Continue to: Consciously or unconsciously, clinicians may feel...
Consciously or unconsciously, clinicians may feel uncomfortable diverging from a schedule of visits that is firmly entrenched in obstetric practice. Continuing the status quo is easier than restructuring prenatal care practice. Ultimately, a paradigm shift may be required to broadly adopt a model of fewer prenatal visits for low-risk pregnancies.12 With these issues propelling the historic patterns of prenatal care, it is easy to see why we have not yet changed despite convincing reasons to do so.
In this article, we detail the reduced-visit prenatal care models developed at 3 institutions and how they incorporate use of today’s technology.
Approach #1: University of Utah Virtual Prenatal Care Program
The University of Utah Virtual Prenatal Care Program was conceived as a “baby step” toward developing a model of fewer total prenatal visits. Virtual visits were intended to reduce the number of prenatal face-to-face visits while maintaining the same total number of visits. Since large clinical trials had established the safety of reduced visits, the primary objectives were to retain patient satisfaction and to facilitate provider adoption.
Would women be satisfied with remote prenatal care? A prospective randomized controlled trial was designed in which 200 women were assigned to receive either a combination of telemedicine and 5 scheduled in-clinic prenatal visits (remote care group) or traditional in-clinic prenatal care (usual care group). Low-risk multigravida pregnant women who were between 6 0/7 and 16 0/7 weeks’ gestation were enrolled. The primary outcome was patient satisfaction.
The face-to-face visits were goal oriented, with scheduled physical examination, laboratory tests, or ultrasonography, and were conducted by the patient’s established obstetric provider (physician or nurse midwife) to maintain continuity of care. The remote care group self-collected measurements for weight, blood pressure, and fetal heart rate by handheld Doppler device prior to each telemedicine visit and entered the information into the electronic medical record. The purpose of the self-collected data was patient engagement and satisfaction, as well as increased provider comfort with the change in prenatal care schedule, rather than medical necessity.
The primary outcome of overall patient satisfaction with prenatal care was ascertained by questionnaire after delivery. The sample size calculation of 200 patients was based on noninferiority testing, and analysis was by intent-to-treat. The details of the trial are pending publication.
As expected, the remote care group had significantly fewer in-clinic prenatal care visits compared with the usual care group (7.2 vs 11.3 visits); the total number of prenatal visits was not different between groups. Overall satisfaction with prenatal care was very high in both the remote care and the usual care group (100% vs 97%).
The virtual prenatal care model for low-risk pregnancies, consisting of a novel remote monitoring strategy and a reduced number of in-clinic visits, was not associated with lower patient satisfaction compared with traditional care.
New care strategy gives patients a choice. The success of this clinical trial has led to its programmatic adoption at the University of Utah, and low-risk women currently are offered a choice between participating in the Virtual Prenatal Care Program or receiving traditional prenatal care. The University of Utah is moving on from the one-size-fits-all approach to adopt new strategies that provide personalized evidence-based prenatal care at the lowest cost, while retaining high patient satisfaction. Formal cost-effectiveness analyses are underway.
Continue to: Approach #2: Mayo Clinic OB Nest...
Approach #2: Mayo Clinic OB Nest
In 2011, the Mayo Clinic Obstetric Division partnered with 2 other Mayo Clinic divisions, the Center for Innovation and the Center for the Science of Health Care Delivery, to redesign prenatal care for low-risk expectant mothers.Pregnant women and their obstetric health care teams (including obstetricians, certified nurse midwives, registered nurses, and clinical support staff) were convened to develop a novel model of prenatal care.4 The goal of this collaboration centered on:
- creating an evidence-driven prenatal care model for low-risk expectant women designed by relevant stakeholders
- focusing on meeting the on-demand needs of expectant mothers
- integrating innovative 21st century technology, and
- reducing the burden of prescheduled, low-value office visits.
Exploratory efforts to develop a novel care program. Based on feedback from the collaboration and guided by these goals, 141 expectant mothers participated in 19 different experiments, enabling the health care team to understand the impact of changing various components of prenatal care.
The experiments included integration of home monitoring (home fetal Doppler devices, drop-in fetal Doppler stations, home blood pressure monitoring devices), technology-enhanced communication with obstetric team members (video chats, tummy photos, virtual prenatal clinic appointments, proactive calls), and social media engagement (secure online prenatal care community).
Recommendations for the final components of OB Nest were based on feasibility and the potential impact on care. The recommendations included decreasing scheduled clinic appointments from 14 to 8, providing home monitoring devices to measure maternal blood pressure and fetal heart rate, establishing OB Nest virtual connected care visits with a registered nurse, and offering a secure online community of expectant mothers.
Trial assessed program’s efficacy, safety, satisfaction. A mixed-methods randomized controlled trial subsequently was conducted to evaluate the components of OB Nest.6 The trial included 300 pregnant women who were randomly assigned to standard prenatal care as recommended by ACOG or to OB Nest care.
OB Nest care consisted of 8 scheduled clinic appointments, 6 planned virtual (phone or online) connected care visits with a registered nurse dedicated to OB Nest, home monitoring of blood pressure (with a home digital sphygmomanometer) and fetal heart rate, and access to an online prenatal care community designated for OB Nest participants.
While publication of the trial results currently is pending, the OB Nest program appears to safely and effectively decrease the number of scheduled prenatal care visits for low-risk expectant mothers while improving the overall patient experience. OB Nest care now is offered as one of several options for low-risk expectant mothers at Mayo Clinic.
Additional avenues of study. Studies evaluating the impact of OB Nest in various nonacademic settings are now underway. Also under review is the potential cost savings of OB Nest as related to the productive lives of expectant mothers, while prenatal care safety is maintained.
The focus shift from a sick to a wellness perspective, stakeholder inclusion in the program design, and the integration of home monitoring tools are all major contributing factors to the success of OB Nest.
Continue to: Approach #3: Prisma Health utilizes mobile app technology...
Approach #3: Prisma Health utilizes mobile app technology
A third approach to reducing unnecessary visits for routine maternity care is to employ mobile app technology. Technology companies have developed app platforms for providers to use to educate and connect with patients; such apps reduce the number of routine obstetric office visits while maintaining patient satisfaction.
One group’s app experience. In a pilot study at a Prisma Health practice (South Carolina), 100 patients were placed on a reduced appointment schedule of 9 prenatal visits; the women self-monitored their weight gain and blood pressure using a remote monitoring system via an app called Babyscripts.7 Patient feedback was collected, with 45 of 100 patients responding.
Ninety-five percent of patients were satisfied with the mobile app, 94% reported positivity around pregnancy readiness, 90% were satisfied with their health care team, and 89% were happy with remote monitoring. Patients visited the app 3 times per week on average, and the top categories of interest were travel, exercise, genetics, and eating right.
One patient using the Babyscripts mobile health app and schedule optimization platform commented, “I am on my second pregnancy and wish this had been available for the first! The app is easy to use and I love seeing my weight on a graph. And I very much like the quality of the cuff” (personal data generated from Babyscripts).
In with the new
As clinicians strive to provide more patient-centered care, offering expectant families more than one way to receive their prenatal care is appropriate. Beyond the traditional 14-visit care model, we should offer use of novel options like mobile health apps, which improve the patient experience while decreasing the cost of care by reducing unnecessary visits.12 Note also that reducing visits for low-risk mothers opens space in the provider schedule for patients who need services more quickly.
Benefits for postpartum care. Traditionally, clinicians see the low-risk patient for a single follow-up appointment at 6 weeks postpartum. However, the World Health Organization recommends evaluating women at 3 days, 1 to 2 weeks, and 6 weeks postpartum.13 Further, the National Institute for Health and Care Excellence guidance recommends screening all women for resolution of postpartum blues at 10 to 14 days.14
ACOG also has made recommendations on optimizing postpartum care. In a committee opinion, ACOG recommends that all women have contact with their provider within the first 3 weeks postpartum.15 Recognizing that such an in-person visit may be difficult, ACOG has endorsed communication via text messaging, app-based support, and remote monitoring.15 An app such as Babyscripts would fill this need conveniently for both patient and provider.
In 2019, patients want choice. As maternity care providers, we should be open to considering novel, evidence-based options that may provide more cost-effective obstetric care.
CASE Low-risk maternity patient wants fewer prenatal visits
A recently pregnant patient asks her obstetrician if she can schedule fewer prenatal visits given that she is at low risk, wants to minimize missing work, and lives an hour away from the clinic office. Her physician tells her that she needs the standard 13 to 15 visits to have a healthy pregnancy.
Obstetric care in the United States largely remains a “one-size fits all” approach despite compelling data that fewer visits for low-risk women are medically acceptable and may be more cost-effective.
Prenatal care: One size does not fit all
With nearly 4 million births annually in the United States, prenatal care is one of the most widely used preventive health care strategies.1,2 The ideal method for providing prenatal care, however, remains controversial. At the inception of early 20th century prenatal care in the United States, preventive strategies focused in part on eclampsia-related maternal morbidity and mortality, which in turn informed the content and frequency of prenatal visits.2 Despite the dramatic changes in medical practice over the last 100 years, the basic timing and quantity of prenatal care has not changed substantively.
The lack of change is not because we have not explored other models of prenatal care and sought to introduce evidence-based change. Several studies have assessed the impact of reduced prenatal care visits for low-risk women.3-7 Systematic reviews evaluated 7 randomized trials, with more than 60,000 women enrolled, of prenatal care models with a reduced number of planned antenatal visits (4 to 9 visits vs the traditional 13 to 15 visits).3,8 There were no demonstrable differences in maternal or perinatal morbidity or mortality, particularly in higher resource settings.
Despite strong safety data and the potential cost-effectiveness of a reduced schedule of prenatal visits, US prenatal care practices generally continue to have a one-size-fits-all approach. Several organizations, however, have called for a change in practice.
Endorsing a reduced number of prenatal visits for low-risk women, the US Department of Health and Human Services Expert Panel on Prenatal Care issued a report in 1989 that stated “the specific content and timing of prenatal visits, contacts, and education should vary depending on the risk status of the pregnant woman and her fetus.”9 Consistent with that recommendation, the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists (ACOG) jointly published guidelines that recommend a system of goal-oriented antenatal visits at specific gestational ages and that support a reduced schedule of prenatal visits, compared with traditional models, for low-risk, parous women.10 The World Health Organization also published recommendations for an 8 “contact” prenatal care system to reduce perinatal mortality and improve women’s prenatal experience.11
Is obstetric dogma the reason for lack of change?
Concerns about patient satisfaction may play a role in limiting the use of a reduced prenatal care visit model. In trials that evaluated a model of reduced prenatal care visits, women were less satisfied with a reduced visit schedule and the gap between provider contacts.3,8 Anecdotally, providers have expressed concerns about perceived liability. Most compelling, perhaps, is the idea that the traditional prenatal schedule has become obstetric dogma.
Continue to: Consciously or unconsciously, clinicians may feel...
Consciously or unconsciously, clinicians may feel uncomfortable diverging from a schedule of visits that is firmly entrenched in obstetric practice. Continuing the status quo is easier than restructuring prenatal care practice. Ultimately, a paradigm shift may be required to broadly adopt a model of fewer prenatal visits for low-risk pregnancies.12 With these issues propelling the historic patterns of prenatal care, it is easy to see why we have not yet changed despite convincing reasons to do so.
In this article, we detail the reduced-visit prenatal care models developed at 3 institutions and how they incorporate use of today’s technology.
Approach #1: University of Utah Virtual Prenatal Care Program
The University of Utah Virtual Prenatal Care Program was conceived as a “baby step” toward developing a model of fewer total prenatal visits. Virtual visits were intended to reduce the number of prenatal face-to-face visits while maintaining the same total number of visits. Since large clinical trials had established the safety of reduced visits, the primary objectives were to retain patient satisfaction and to facilitate provider adoption.
Would women be satisfied with remote prenatal care? A prospective randomized controlled trial was designed in which 200 women were assigned to receive either a combination of telemedicine and 5 scheduled in-clinic prenatal visits (remote care group) or traditional in-clinic prenatal care (usual care group). Low-risk multigravida pregnant women who were between 6 0/7 and 16 0/7 weeks’ gestation were enrolled. The primary outcome was patient satisfaction.
The face-to-face visits were goal oriented, with scheduled physical examination, laboratory tests, or ultrasonography, and were conducted by the patient’s established obstetric provider (physician or nurse midwife) to maintain continuity of care. The remote care group self-collected measurements for weight, blood pressure, and fetal heart rate by handheld Doppler device prior to each telemedicine visit and entered the information into the electronic medical record. The purpose of the self-collected data was patient engagement and satisfaction, as well as increased provider comfort with the change in prenatal care schedule, rather than medical necessity.
The primary outcome of overall patient satisfaction with prenatal care was ascertained by questionnaire after delivery. The sample size calculation of 200 patients was based on noninferiority testing, and analysis was by intent-to-treat. The details of the trial are pending publication.
As expected, the remote care group had significantly fewer in-clinic prenatal care visits compared with the usual care group (7.2 vs 11.3 visits); the total number of prenatal visits was not different between groups. Overall satisfaction with prenatal care was very high in both the remote care and the usual care group (100% vs 97%).
The virtual prenatal care model for low-risk pregnancies, consisting of a novel remote monitoring strategy and a reduced number of in-clinic visits, was not associated with lower patient satisfaction compared with traditional care.
New care strategy gives patients a choice. The success of this clinical trial has led to its programmatic adoption at the University of Utah, and low-risk women currently are offered a choice between participating in the Virtual Prenatal Care Program or receiving traditional prenatal care. The University of Utah is moving on from the one-size-fits-all approach to adopt new strategies that provide personalized evidence-based prenatal care at the lowest cost, while retaining high patient satisfaction. Formal cost-effectiveness analyses are underway.
Continue to: Approach #2: Mayo Clinic OB Nest...
Approach #2: Mayo Clinic OB Nest
In 2011, the Mayo Clinic Obstetric Division partnered with 2 other Mayo Clinic divisions, the Center for Innovation and the Center for the Science of Health Care Delivery, to redesign prenatal care for low-risk expectant mothers.Pregnant women and their obstetric health care teams (including obstetricians, certified nurse midwives, registered nurses, and clinical support staff) were convened to develop a novel model of prenatal care.4 The goal of this collaboration centered on:
- creating an evidence-driven prenatal care model for low-risk expectant women designed by relevant stakeholders
- focusing on meeting the on-demand needs of expectant mothers
- integrating innovative 21st century technology, and
- reducing the burden of prescheduled, low-value office visits.
Exploratory efforts to develop a novel care program. Based on feedback from the collaboration and guided by these goals, 141 expectant mothers participated in 19 different experiments, enabling the health care team to understand the impact of changing various components of prenatal care.
The experiments included integration of home monitoring (home fetal Doppler devices, drop-in fetal Doppler stations, home blood pressure monitoring devices), technology-enhanced communication with obstetric team members (video chats, tummy photos, virtual prenatal clinic appointments, proactive calls), and social media engagement (secure online prenatal care community).
Recommendations for the final components of OB Nest were based on feasibility and the potential impact on care. The recommendations included decreasing scheduled clinic appointments from 14 to 8, providing home monitoring devices to measure maternal blood pressure and fetal heart rate, establishing OB Nest virtual connected care visits with a registered nurse, and offering a secure online community of expectant mothers.
Trial assessed program’s efficacy, safety, satisfaction. A mixed-methods randomized controlled trial subsequently was conducted to evaluate the components of OB Nest.6 The trial included 300 pregnant women who were randomly assigned to standard prenatal care as recommended by ACOG or to OB Nest care.
OB Nest care consisted of 8 scheduled clinic appointments, 6 planned virtual (phone or online) connected care visits with a registered nurse dedicated to OB Nest, home monitoring of blood pressure (with a home digital sphygmomanometer) and fetal heart rate, and access to an online prenatal care community designated for OB Nest participants.
While publication of the trial results currently is pending, the OB Nest program appears to safely and effectively decrease the number of scheduled prenatal care visits for low-risk expectant mothers while improving the overall patient experience. OB Nest care now is offered as one of several options for low-risk expectant mothers at Mayo Clinic.
Additional avenues of study. Studies evaluating the impact of OB Nest in various nonacademic settings are now underway. Also under review is the potential cost savings of OB Nest as related to the productive lives of expectant mothers, while prenatal care safety is maintained.
The focus shift from a sick to a wellness perspective, stakeholder inclusion in the program design, and the integration of home monitoring tools are all major contributing factors to the success of OB Nest.
Continue to: Approach #3: Prisma Health utilizes mobile app technology...
Approach #3: Prisma Health utilizes mobile app technology
A third approach to reducing unnecessary visits for routine maternity care is to employ mobile app technology. Technology companies have developed app platforms for providers to use to educate and connect with patients; such apps reduce the number of routine obstetric office visits while maintaining patient satisfaction.
One group’s app experience. In a pilot study at a Prisma Health practice (South Carolina), 100 patients were placed on a reduced appointment schedule of 9 prenatal visits; the women self-monitored their weight gain and blood pressure using a remote monitoring system via an app called Babyscripts.7 Patient feedback was collected, with 45 of 100 patients responding.
Ninety-five percent of patients were satisfied with the mobile app, 94% reported positivity around pregnancy readiness, 90% were satisfied with their health care team, and 89% were happy with remote monitoring. Patients visited the app 3 times per week on average, and the top categories of interest were travel, exercise, genetics, and eating right.
One patient using the Babyscripts mobile health app and schedule optimization platform commented, “I am on my second pregnancy and wish this had been available for the first! The app is easy to use and I love seeing my weight on a graph. And I very much like the quality of the cuff” (personal data generated from Babyscripts).
In with the new
As clinicians strive to provide more patient-centered care, offering expectant families more than one way to receive their prenatal care is appropriate. Beyond the traditional 14-visit care model, we should offer use of novel options like mobile health apps, which improve the patient experience while decreasing the cost of care by reducing unnecessary visits.12 Note also that reducing visits for low-risk mothers opens space in the provider schedule for patients who need services more quickly.
Benefits for postpartum care. Traditionally, clinicians see the low-risk patient for a single follow-up appointment at 6 weeks postpartum. However, the World Health Organization recommends evaluating women at 3 days, 1 to 2 weeks, and 6 weeks postpartum.13 Further, the National Institute for Health and Care Excellence guidance recommends screening all women for resolution of postpartum blues at 10 to 14 days.14
ACOG also has made recommendations on optimizing postpartum care. In a committee opinion, ACOG recommends that all women have contact with their provider within the first 3 weeks postpartum.15 Recognizing that such an in-person visit may be difficult, ACOG has endorsed communication via text messaging, app-based support, and remote monitoring.15 An app such as Babyscripts would fill this need conveniently for both patient and provider.
In 2019, patients want choice. As maternity care providers, we should be open to considering novel, evidence-based options that may provide more cost-effective obstetric care.
- Martin JA, Hamilton BE, Osterman MJK, et al. Births: final data for 2017. Natl Vital Stat Rep. 2018;67:1-50.
- Alexander GR, Kotelchuck M. Assessing the role and effectiveness of prenatal care: history, challenges, and directions for future research. Public Health Rep. 2001;116:306-316.
- Dowswell T, Carroli G, Duley L, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev. 2015; (7):CD000934.
- de Mooij MJM, Hodny RL, O'Neil DA, et al. OB Nest: reimagining low-risk prenatal care. Mayo Clin Proc. 2018;93:458-466.
- Pflugeisen BM, McCarren C, Poore S, et al. Virtual visits: managing prenatal care with modern technology. MCN Am J Matern Child Nurs. 2016;41:24-30.
- Ridgeway JL, LeBlanc A, Branda M, et al. Implementation of a new prenatal care model to reduce office visits and increase connectivity and continuity of care: protocol for a mixed-methods study. BMC Pregnancy Childbirth. 2015;15:323.
- Marko KI, Krapf JM, Meltzer AC, et al. Testing the feasibility of remote patient monitoring in prenatal care using a mobile app and connected devices: a prospective observational trial. JMIR Res Protoc. 2016;5:e200.
- Carroli G, Villar J, Piaggio G, et al. WHO systematic review of randomised controlled trials of routine antenatal care. Lancet. 2001;357:1565-1570.
- Rosen MG, Merkatz IR, Hill JG. Caring for our future: a report by the expert panel on the content of prenatal care. Obstet Gynecol. 1991;77:782-787.
- American Academy of Pediatrics, American College of Obstetricians and Gynecologists. Guidelines for Perinatal Care. 8th edition. Elk Grove Village, IL: American Academy of Pediatrics, American College of Obstetricians and Gynecologists; 2017.
- World Health Organization. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience. Geneva, Switzerland: World Health Organization; 2016. https://apps.who.int/iris/bitstream/handle/10665/250796 /9789241549912-eng.pdf;jsessionid=C740C52F8AA1D7694CD9463152C193BA?sequence=1. Accessed June 19, 2019.
- Woo VG, Lundeen T, Matula S, et al. Achieving higher-value obstetrical care. Am J Obstet Gynecol. 2017;216:240e1-250e14.
- World Health Organization. WHO Recommendations on Postnatal Care of the Mother and Newborn. Geneva, Switzerland: WHO; 2014. https://apps.who.int/iris/bitstream/handle/10665/97603/9789241506649_eng.pdf?sequence=1. Accessed June 19, 2019.
- National Institute for Health and Care Excellence. Postnatal care up to 8 weeks after birth. Updated February 2015. https://www.nice.org.uk/guidance/cg37/chapter/1-Recommendations#maternal-health. Accessed June 19, 2019.
- American College of Obstetricians and Gynecologists. ACOG committee opinion no. 736. Optimizing postpartum care. Washington, DC: ACOG; 2018.
- Martin JA, Hamilton BE, Osterman MJK, et al. Births: final data for 2017. Natl Vital Stat Rep. 2018;67:1-50.
- Alexander GR, Kotelchuck M. Assessing the role and effectiveness of prenatal care: history, challenges, and directions for future research. Public Health Rep. 2001;116:306-316.
- Dowswell T, Carroli G, Duley L, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev. 2015; (7):CD000934.
- de Mooij MJM, Hodny RL, O'Neil DA, et al. OB Nest: reimagining low-risk prenatal care. Mayo Clin Proc. 2018;93:458-466.
- Pflugeisen BM, McCarren C, Poore S, et al. Virtual visits: managing prenatal care with modern technology. MCN Am J Matern Child Nurs. 2016;41:24-30.
- Ridgeway JL, LeBlanc A, Branda M, et al. Implementation of a new prenatal care model to reduce office visits and increase connectivity and continuity of care: protocol for a mixed-methods study. BMC Pregnancy Childbirth. 2015;15:323.
- Marko KI, Krapf JM, Meltzer AC, et al. Testing the feasibility of remote patient monitoring in prenatal care using a mobile app and connected devices: a prospective observational trial. JMIR Res Protoc. 2016;5:e200.
- Carroli G, Villar J, Piaggio G, et al. WHO systematic review of randomised controlled trials of routine antenatal care. Lancet. 2001;357:1565-1570.
- Rosen MG, Merkatz IR, Hill JG. Caring for our future: a report by the expert panel on the content of prenatal care. Obstet Gynecol. 1991;77:782-787.
- American Academy of Pediatrics, American College of Obstetricians and Gynecologists. Guidelines for Perinatal Care. 8th edition. Elk Grove Village, IL: American Academy of Pediatrics, American College of Obstetricians and Gynecologists; 2017.
- World Health Organization. WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience. Geneva, Switzerland: World Health Organization; 2016. https://apps.who.int/iris/bitstream/handle/10665/250796 /9789241549912-eng.pdf;jsessionid=C740C52F8AA1D7694CD9463152C193BA?sequence=1. Accessed June 19, 2019.
- Woo VG, Lundeen T, Matula S, et al. Achieving higher-value obstetrical care. Am J Obstet Gynecol. 2017;216:240e1-250e14.
- World Health Organization. WHO Recommendations on Postnatal Care of the Mother and Newborn. Geneva, Switzerland: WHO; 2014. https://apps.who.int/iris/bitstream/handle/10665/97603/9789241506649_eng.pdf?sequence=1. Accessed June 19, 2019.
- National Institute for Health and Care Excellence. Postnatal care up to 8 weeks after birth. Updated February 2015. https://www.nice.org.uk/guidance/cg37/chapter/1-Recommendations#maternal-health. Accessed June 19, 2019.
- American College of Obstetricians and Gynecologists. ACOG committee opinion no. 736. Optimizing postpartum care. Washington, DC: ACOG; 2018.
Comment & Controversy
WHAT IS YOUR APPROACH TO THE PERSISTENT OCCIPUT POSTERIOR MALPOSITION?
ROBERT L. BARBIERI, MD
(EDITORIAL; MARCH 2019)
A classic approach for managing fetal malposition
For those of us who trained and practiced obstetrics in the days of the 6% primary cesarean delivery (CD) rate, we never considered the management of the persistent occiput
- The cervix must be fully dilated.
- Dense regional anesthesia must be achieved.
- The vertex must have reached +1 station.
- The position must be clearly established, and this does not require anything other than the ability to palpate an ear, as it can be pointed only in one direction. If you feel ultrasonography is needed, be my guest.
- Use an obstetric lubricant to reduce resistance and minimize lacerations.
- While a trial of manual rotation is reasonable, it commonly will not succeed and requires that an operator’s hand be inserted rather than a slender and less traumatic device (forceps).
- Next, palpate the sagittal suture to determine whether the position is straight OP versus left OP or right OP. This should not be difficult unless the poor woman has gone through 2 or 3 hours of unproductive pushing, thereby creating caput.
- After proper forceps application is confirmed, gently apply upward pressure. This will make rotation easier.
- Dr. Irving’s recommendations notwithstanding, the forceps handles are not carried in a wide sweep. One should use Kielland’s forceps, which do not have a pelvic curve and were invented for this precise indication. The forceps are simply rotated.
- Try to avoid delivery as an OP, as this pulls a much larger diameter deflexed head through the pelvis and usually results in significant lacerations.
- Episiotomy is not always required if rotation has succeeded.
- Once descent to the outlet has been achieved, it is probably best to switch to a forceps with a pelvic curve to achieve easier extension.
- This should complete the delivery, but as a general rule, if more than minimal resistance is met in any of the above steps, abandon the procedure and move to CD.
- This process should result in at least a 70% success rate.
As is most likely understood by the current generation of obstetricians who appear to be satisfied with a 30% to 40% primary CD rate, the above reflects the views of a long-retired ObGyn (whose CD rate never exceeded 10%) and may be inappropriate for those who are not adequately trained in or comfortable with vaginal obstetrics.
David M. Priver, MD
San Diego, California
Continue to: HOW DO YOU FEEL ABOUT EXPECTANTLY MANAGING A WELL-DATED PREGNANCY PAST 41 WEEKS’ GESTATION?
HOW DO YOU FEEL ABOUT EXPECTANTLY MANAGING A WELL-DATED PREGNANCY PAST 41 WEEKS’ GESTATION?
ROBERT L. BARBIERI, MD
(EDITORIAL; FEBRUARY 2019)
Membrane stripping can be problematic
The recent discussion on stripping membranes to facilitate the initiation of labor and delivery was intriguing. This practice was reviewed extensively during my training in the 1960s and abandoned when the results were disappointing or contradictory. Although the practice has been revitalized recently, I am concerned that potential risks and the absence of a recommended protocol of safeguards may allow new problems to develop.
In a metropolitan community where I provide consultative services, the only patients I see for evaluation of pregnancies beyond 40 to 41 weeks come from providers who are non-physicians. Apparently, they are concerned that they may have to turn their patients over to physician providers for interventions that they are not capable of doing. My advice to them is simply that nothing good happens after 40 to 41 weeks.
Well-grown babies may continue to grow if they are healthy, and they may incur greater risks of dystotic labor and delivery resulting in injury or the need for physician-administered surgical assistance. If, on the other hand, growth markedly diminishes or ceases, fetal harm or neonatal complications may occur through asphyxia, meconium aspiration, or trauma. In either event, physician-based assistance is strongly encouraged, as long as due diligence in determining gestational age has been done.
Promoting membrane stripping without having a protocol for ascertainment of risk factors is worrisome to me. In my opinion, large population studies that fail to demonstrate increased risks of infection may fail to demonstrate that membrane stripping may induce a degree of perinatal infection comparable to that of prolonged labor with multiple internal examinations with or without ultimate cesarean birth. Prior to considering membrane stripping as a strategy, one should recognize certain important considerations, namely:
- Patients most in need of active intervention may have the least favorable cervical findings, and as a result they are potentially at risk for the greatest discomfort.
- The frequency of group B streptococcal colonization of the vagina at term should be recognized, and a culture should be obtained immediately prior to intervention. When a culture is a positive, membrane stripping should be avoided, or at least a sober consideration of its use and appropriate antibiotic coverage should occur.
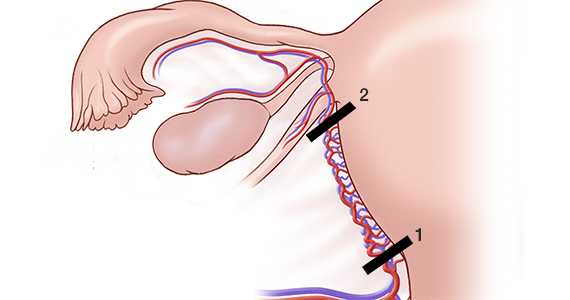
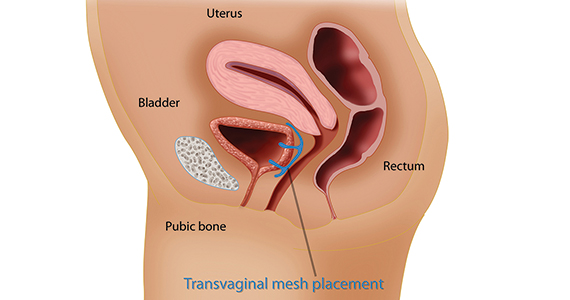
- Consider performing transvaginal ultrasonography prior to membrane stripping to exclude the possibility of a placental edge close enough to be encountered and compromised, with resultant hemorrhage in an outpatient venue ill equipped to provide adequate emergency support.
- The comparative effectiveness of other direct cervical conditioning therapies, including use of a Foley catheter or regional prostaglandin medication, has been well explored and found effective. Also, if one takes seriously the need for any intervention, admission to the hospital for overnight cervical conditioning allows for surveillance and avoids the patient experience of being sent home cramping, bleeding, brooding infection, and questioning her trust in the provider.
Continue to: I am concerned that the promotion...
I am concerned that the promotion of this potentially rather brutish practice by highly reputable advisors can result in its growing utilization by providers some of whom may be least qualified to apply proper judgment and sensitivity to its selection. In the most primitive of circumstances, it may have utility. Personally, however, I feel that medically based strategies initiated and monitored by professionals capable of dealing with any untoward departures from the expected results must be considered in the best traditions of what we do. The appeal of simplicity must not encourage the adoption of interventions that lack the proper application of thought and plan and whose only appeal is that of simplicity.
Richard P. Perkins, MD
Fort Myers, Florida; Stockton, California
Dr. Barbieri responds
I thank Dr. Priver for his excellent description of how to use forceps to resolve a persistent occiput posterior position. I also thank Dr. Perkins for his valuable comments and agree with him that in the United States among the options available for outpatient cervical ripening, misoprostol or a balloon are more commonly used than membrane stripping. Membrane stripping is an outpatient cervical ripening technique that is commonly used in the United Kingdom.
WHAT IS YOUR APPROACH TO THE PERSISTENT OCCIPUT POSTERIOR MALPOSITION?
ROBERT L. BARBIERI, MD
(EDITORIAL; MARCH 2019)
A classic approach for managing fetal malposition
For those of us who trained and practiced obstetrics in the days of the 6% primary cesarean delivery (CD) rate, we never considered the management of the persistent occiput
- The cervix must be fully dilated.
- Dense regional anesthesia must be achieved.
- The vertex must have reached +1 station.
- The position must be clearly established, and this does not require anything other than the ability to palpate an ear, as it can be pointed only in one direction. If you feel ultrasonography is needed, be my guest.
- Use an obstetric lubricant to reduce resistance and minimize lacerations.
- While a trial of manual rotation is reasonable, it commonly will not succeed and requires that an operator’s hand be inserted rather than a slender and less traumatic device (forceps).
- Next, palpate the sagittal suture to determine whether the position is straight OP versus left OP or right OP. This should not be difficult unless the poor woman has gone through 2 or 3 hours of unproductive pushing, thereby creating caput.
- After proper forceps application is confirmed, gently apply upward pressure. This will make rotation easier.
- Dr. Irving’s recommendations notwithstanding, the forceps handles are not carried in a wide sweep. One should use Kielland’s forceps, which do not have a pelvic curve and were invented for this precise indication. The forceps are simply rotated.
- Try to avoid delivery as an OP, as this pulls a much larger diameter deflexed head through the pelvis and usually results in significant lacerations.
- Episiotomy is not always required if rotation has succeeded.
- Once descent to the outlet has been achieved, it is probably best to switch to a forceps with a pelvic curve to achieve easier extension.
- This should complete the delivery, but as a general rule, if more than minimal resistance is met in any of the above steps, abandon the procedure and move to CD.
- This process should result in at least a 70% success rate.
As is most likely understood by the current generation of obstetricians who appear to be satisfied with a 30% to 40% primary CD rate, the above reflects the views of a long-retired ObGyn (whose CD rate never exceeded 10%) and may be inappropriate for those who are not adequately trained in or comfortable with vaginal obstetrics.
David M. Priver, MD
San Diego, California
Continue to: HOW DO YOU FEEL ABOUT EXPECTANTLY MANAGING A WELL-DATED PREGNANCY PAST 41 WEEKS’ GESTATION?
HOW DO YOU FEEL ABOUT EXPECTANTLY MANAGING A WELL-DATED PREGNANCY PAST 41 WEEKS’ GESTATION?
ROBERT L. BARBIERI, MD
(EDITORIAL; FEBRUARY 2019)
Membrane stripping can be problematic
The recent discussion on stripping membranes to facilitate the initiation of labor and delivery was intriguing. This practice was reviewed extensively during my training in the 1960s and abandoned when the results were disappointing or contradictory. Although the practice has been revitalized recently, I am concerned that potential risks and the absence of a recommended protocol of safeguards may allow new problems to develop.
In a metropolitan community where I provide consultative services, the only patients I see for evaluation of pregnancies beyond 40 to 41 weeks come from providers who are non-physicians. Apparently, they are concerned that they may have to turn their patients over to physician providers for interventions that they are not capable of doing. My advice to them is simply that nothing good happens after 40 to 41 weeks.
Well-grown babies may continue to grow if they are healthy, and they may incur greater risks of dystotic labor and delivery resulting in injury or the need for physician-administered surgical assistance. If, on the other hand, growth markedly diminishes or ceases, fetal harm or neonatal complications may occur through asphyxia, meconium aspiration, or trauma. In either event, physician-based assistance is strongly encouraged, as long as due diligence in determining gestational age has been done.
Promoting membrane stripping without having a protocol for ascertainment of risk factors is worrisome to me. In my opinion, large population studies that fail to demonstrate increased risks of infection may fail to demonstrate that membrane stripping may induce a degree of perinatal infection comparable to that of prolonged labor with multiple internal examinations with or without ultimate cesarean birth. Prior to considering membrane stripping as a strategy, one should recognize certain important considerations, namely:
- Patients most in need of active intervention may have the least favorable cervical findings, and as a result they are potentially at risk for the greatest discomfort.
- The frequency of group B streptococcal colonization of the vagina at term should be recognized, and a culture should be obtained immediately prior to intervention. When a culture is a positive, membrane stripping should be avoided, or at least a sober consideration of its use and appropriate antibiotic coverage should occur.
- Consider performing transvaginal ultrasonography prior to membrane stripping to exclude the possibility of a placental edge close enough to be encountered and compromised, with resultant hemorrhage in an outpatient venue ill equipped to provide adequate emergency support.
- The comparative effectiveness of other direct cervical conditioning therapies, including use of a Foley catheter or regional prostaglandin medication, has been well explored and found effective. Also, if one takes seriously the need for any intervention, admission to the hospital for overnight cervical conditioning allows for surveillance and avoids the patient experience of being sent home cramping, bleeding, brooding infection, and questioning her trust in the provider.
Continue to: I am concerned that the promotion...
I am concerned that the promotion of this potentially rather brutish practice by highly reputable advisors can result in its growing utilization by providers some of whom may be least qualified to apply proper judgment and sensitivity to its selection. In the most primitive of circumstances, it may have utility. Personally, however, I feel that medically based strategies initiated and monitored by professionals capable of dealing with any untoward departures from the expected results must be considered in the best traditions of what we do. The appeal of simplicity must not encourage the adoption of interventions that lack the proper application of thought and plan and whose only appeal is that of simplicity.
Richard P. Perkins, MD
Fort Myers, Florida; Stockton, California
Dr. Barbieri responds
I thank Dr. Priver for his excellent description of how to use forceps to resolve a persistent occiput posterior position. I also thank Dr. Perkins for his valuable comments and agree with him that in the United States among the options available for outpatient cervical ripening, misoprostol or a balloon are more commonly used than membrane stripping. Membrane stripping is an outpatient cervical ripening technique that is commonly used in the United Kingdom.
WHAT IS YOUR APPROACH TO THE PERSISTENT OCCIPUT POSTERIOR MALPOSITION?
ROBERT L. BARBIERI, MD
(EDITORIAL; MARCH 2019)
A classic approach for managing fetal malposition
For those of us who trained and practiced obstetrics in the days of the 6% primary cesarean delivery (CD) rate, we never considered the management of the persistent occiput
- The cervix must be fully dilated.
- Dense regional anesthesia must be achieved.
- The vertex must have reached +1 station.
- The position must be clearly established, and this does not require anything other than the ability to palpate an ear, as it can be pointed only in one direction. If you feel ultrasonography is needed, be my guest.
- Use an obstetric lubricant to reduce resistance and minimize lacerations.
- While a trial of manual rotation is reasonable, it commonly will not succeed and requires that an operator’s hand be inserted rather than a slender and less traumatic device (forceps).
- Next, palpate the sagittal suture to determine whether the position is straight OP versus left OP or right OP. This should not be difficult unless the poor woman has gone through 2 or 3 hours of unproductive pushing, thereby creating caput.
- After proper forceps application is confirmed, gently apply upward pressure. This will make rotation easier.
- Dr. Irving’s recommendations notwithstanding, the forceps handles are not carried in a wide sweep. One should use Kielland’s forceps, which do not have a pelvic curve and were invented for this precise indication. The forceps are simply rotated.
- Try to avoid delivery as an OP, as this pulls a much larger diameter deflexed head through the pelvis and usually results in significant lacerations.
- Episiotomy is not always required if rotation has succeeded.
- Once descent to the outlet has been achieved, it is probably best to switch to a forceps with a pelvic curve to achieve easier extension.
- This should complete the delivery, but as a general rule, if more than minimal resistance is met in any of the above steps, abandon the procedure and move to CD.
- This process should result in at least a 70% success rate.
As is most likely understood by the current generation of obstetricians who appear to be satisfied with a 30% to 40% primary CD rate, the above reflects the views of a long-retired ObGyn (whose CD rate never exceeded 10%) and may be inappropriate for those who are not adequately trained in or comfortable with vaginal obstetrics.
David M. Priver, MD
San Diego, California
Continue to: HOW DO YOU FEEL ABOUT EXPECTANTLY MANAGING A WELL-DATED PREGNANCY PAST 41 WEEKS’ GESTATION?
HOW DO YOU FEEL ABOUT EXPECTANTLY MANAGING A WELL-DATED PREGNANCY PAST 41 WEEKS’ GESTATION?
ROBERT L. BARBIERI, MD
(EDITORIAL; FEBRUARY 2019)
Membrane stripping can be problematic
The recent discussion on stripping membranes to facilitate the initiation of labor and delivery was intriguing. This practice was reviewed extensively during my training in the 1960s and abandoned when the results were disappointing or contradictory. Although the practice has been revitalized recently, I am concerned that potential risks and the absence of a recommended protocol of safeguards may allow new problems to develop.
In a metropolitan community where I provide consultative services, the only patients I see for evaluation of pregnancies beyond 40 to 41 weeks come from providers who are non-physicians. Apparently, they are concerned that they may have to turn their patients over to physician providers for interventions that they are not capable of doing. My advice to them is simply that nothing good happens after 40 to 41 weeks.
Well-grown babies may continue to grow if they are healthy, and they may incur greater risks of dystotic labor and delivery resulting in injury or the need for physician-administered surgical assistance. If, on the other hand, growth markedly diminishes or ceases, fetal harm or neonatal complications may occur through asphyxia, meconium aspiration, or trauma. In either event, physician-based assistance is strongly encouraged, as long as due diligence in determining gestational age has been done.
Promoting membrane stripping without having a protocol for ascertainment of risk factors is worrisome to me. In my opinion, large population studies that fail to demonstrate increased risks of infection may fail to demonstrate that membrane stripping may induce a degree of perinatal infection comparable to that of prolonged labor with multiple internal examinations with or without ultimate cesarean birth. Prior to considering membrane stripping as a strategy, one should recognize certain important considerations, namely:
- Patients most in need of active intervention may have the least favorable cervical findings, and as a result they are potentially at risk for the greatest discomfort.
- The frequency of group B streptococcal colonization of the vagina at term should be recognized, and a culture should be obtained immediately prior to intervention. When a culture is a positive, membrane stripping should be avoided, or at least a sober consideration of its use and appropriate antibiotic coverage should occur.
- Consider performing transvaginal ultrasonography prior to membrane stripping to exclude the possibility of a placental edge close enough to be encountered and compromised, with resultant hemorrhage in an outpatient venue ill equipped to provide adequate emergency support.
- The comparative effectiveness of other direct cervical conditioning therapies, including use of a Foley catheter or regional prostaglandin medication, has been well explored and found effective. Also, if one takes seriously the need for any intervention, admission to the hospital for overnight cervical conditioning allows for surveillance and avoids the patient experience of being sent home cramping, bleeding, brooding infection, and questioning her trust in the provider.
Continue to: I am concerned that the promotion...
I am concerned that the promotion of this potentially rather brutish practice by highly reputable advisors can result in its growing utilization by providers some of whom may be least qualified to apply proper judgment and sensitivity to its selection. In the most primitive of circumstances, it may have utility. Personally, however, I feel that medically based strategies initiated and monitored by professionals capable of dealing with any untoward departures from the expected results must be considered in the best traditions of what we do. The appeal of simplicity must not encourage the adoption of interventions that lack the proper application of thought and plan and whose only appeal is that of simplicity.
Richard P. Perkins, MD
Fort Myers, Florida; Stockton, California
Dr. Barbieri responds
I thank Dr. Priver for his excellent description of how to use forceps to resolve a persistent occiput posterior position. I also thank Dr. Perkins for his valuable comments and agree with him that in the United States among the options available for outpatient cervical ripening, misoprostol or a balloon are more commonly used than membrane stripping. Membrane stripping is an outpatient cervical ripening technique that is commonly used in the United Kingdom.
Flying acid zombies, poster face-lifts, and feces of champions
The flying dead
Just when you thought cicada infestations couldn’t get worse – the cicadas are now zombies on an acid trip.
West Virginia University researchers recently discovered that a fungus called Massopora, which has compounds similar to those found in psychedelic mushrooms, can infect cicadas and cause seriously weird behavior.
How weird, you ask? Well, male cicadas try to mate with everything they encounter, even though the fungus has eaten away their limbs … and their genitals. Talk about a bad trip.
It gets worse. These zombie-like cicadas are flying around and exposing their healthy brethren to the fungus. So, now we have to worry about potentially billions of these buggers becoming rotting, flying, hypersexual machines.
Makes a person really want to stay inside for the whole summer, perhaps in a fortified bunker. Just in case.
Also, for the curious: One of the study’s authors concedes that if a person were “motivated enough,” they might be able to get high off the cicada fungus. Not interested in finding out exactly how many cicadas you’d have to crunch on before you start tasting colors?
Poster do-over
It’s time to get ready for a revolution – and just in time for 4th of July. No, we’re not redeclaring independence from Britain. It’s something much, much more radical, at least to the scientific community.
Get ready for … the redesign of the science poster.
Mike Morrison, a doctoral student in psychology, has proposed a new way to present information at meetings that breathes new life into the tired poster design. While fascinating insights could be held on a poster, the reality of meetings and conferences is that people often skim over the posters they see, barely registering the information.
Morrison is taking advantage of the ever-present smartphone to ramp up the classic science poster to a new level. He proposes a format where the key research finding is smack in the middle, in big, readable language. Accompanying this is a QR code you can scan, which would take you to a page with the full details of the study.
Morrison tweeted out his idea, and it spread quickly through the scientific community, gaining traction from younger scientists and students who love the idea.
We’re in the age of remakes now – in which classics are reinvented for a new audience. It’s time the science poster got a face-lift, too.
Running a marathon, one Veillonella at a time
What’s the difference between an elite athlete and a person who’s out of juice after running for 30 seconds?
Well, many things, we’re sure. A proper diet, rigorous training, not spending 12 hours a day sitting behind a computer screen. But just to add insult to injury, according to a study published in Nature Medicine, athletes even poop better than us normal people.
That may require a bit of explanation. A group of researchers from Harvard University, Boston, analyzed stool samples from elite marathon runners before and just after they participated in the 2015 Boston Marathon. They found that, following the race, the athletes had significantly higher amounts of Veillonella in their microbiota. This bacteria breaks down lactic acid, which is made during intense exercise and causes muscle fatigue and stress.
Naturally, the next step was to take that bacteria, feed it to mice, then get them running on a treadmill.
While not every mouse fed Veillonella saw increased performance, on average, mice that received the bacteria saw a 13% improvement over their non–Veillonella enhanced friends.
The researchers noted that this sort of probiotic treatment could be useful to patients with metabolic diseases, such as diabetes. Plus, there’s the obvious benefit to athletes. We look forward to hearing advertisements swearing by Veillonella-infused Wheaties, the true breakfast of champions.
Put a little boredom in your life
Is your job an endless, soul-sucking vortex of dreariness? Do you stare at the wall for hours at a time while you’re at work, wishing you had something better to do? Do you look forward to leaving early to go to the dentist? [Editor query: What does this have to do with health care? LOTME: You’ll see. We’re building dramatic tension.]
Did you answer yes to any of these questions? Way to go! You’ve taken the first step on the road to creativity. [Still waiting. We’re almost there.]
A recent study examined the effects of boredom by assigning people to either a really boring task – sorting a bowl of red and green beans by color for 30 minutes using only one hand – or a nonboring art project using paper, glue, and, of course, beans. [What’s with the beans? It’s not our fault they used beans.]
The next task was the same for both groups: Come up with some reasons for being late for work and think of ideas for a new product by a hypothetical company. The answers were graded on their uniqueness, and the bean-sorting group had more creative ideas than did the art-project group.
The point is, ladies and gentlemen, that boredom is good. Boredom is right. Boredom works. [A Gordon Gekko reference? Couldn’t you find something from this century? No.]
By now you’re probably wondering: “But how can I get one of those really boring jobs? After all, I’m a doctor. I heal the sick and care for the needy. My work is way too interesting to inspire true creativity.” Have you ever considered writing a medical humor column?
[Note to readers: We’ve pulled the staff away from their building blocks and crayons and given them a timeout. Hopefully things will be a little better by next week.]
The flying dead
Just when you thought cicada infestations couldn’t get worse – the cicadas are now zombies on an acid trip.
West Virginia University researchers recently discovered that a fungus called Massopora, which has compounds similar to those found in psychedelic mushrooms, can infect cicadas and cause seriously weird behavior.
How weird, you ask? Well, male cicadas try to mate with everything they encounter, even though the fungus has eaten away their limbs … and their genitals. Talk about a bad trip.
It gets worse. These zombie-like cicadas are flying around and exposing their healthy brethren to the fungus. So, now we have to worry about potentially billions of these buggers becoming rotting, flying, hypersexual machines.
Makes a person really want to stay inside for the whole summer, perhaps in a fortified bunker. Just in case.
Also, for the curious: One of the study’s authors concedes that if a person were “motivated enough,” they might be able to get high off the cicada fungus. Not interested in finding out exactly how many cicadas you’d have to crunch on before you start tasting colors?
Poster do-over
It’s time to get ready for a revolution – and just in time for 4th of July. No, we’re not redeclaring independence from Britain. It’s something much, much more radical, at least to the scientific community.
Get ready for … the redesign of the science poster.
Mike Morrison, a doctoral student in psychology, has proposed a new way to present information at meetings that breathes new life into the tired poster design. While fascinating insights could be held on a poster, the reality of meetings and conferences is that people often skim over the posters they see, barely registering the information.
Morrison is taking advantage of the ever-present smartphone to ramp up the classic science poster to a new level. He proposes a format where the key research finding is smack in the middle, in big, readable language. Accompanying this is a QR code you can scan, which would take you to a page with the full details of the study.
Morrison tweeted out his idea, and it spread quickly through the scientific community, gaining traction from younger scientists and students who love the idea.
We’re in the age of remakes now – in which classics are reinvented for a new audience. It’s time the science poster got a face-lift, too.
Running a marathon, one Veillonella at a time
What’s the difference between an elite athlete and a person who’s out of juice after running for 30 seconds?
Well, many things, we’re sure. A proper diet, rigorous training, not spending 12 hours a day sitting behind a computer screen. But just to add insult to injury, according to a study published in Nature Medicine, athletes even poop better than us normal people.
That may require a bit of explanation. A group of researchers from Harvard University, Boston, analyzed stool samples from elite marathon runners before and just after they participated in the 2015 Boston Marathon. They found that, following the race, the athletes had significantly higher amounts of Veillonella in their microbiota. This bacteria breaks down lactic acid, which is made during intense exercise and causes muscle fatigue and stress.
Naturally, the next step was to take that bacteria, feed it to mice, then get them running on a treadmill.
While not every mouse fed Veillonella saw increased performance, on average, mice that received the bacteria saw a 13% improvement over their non–Veillonella enhanced friends.
The researchers noted that this sort of probiotic treatment could be useful to patients with metabolic diseases, such as diabetes. Plus, there’s the obvious benefit to athletes. We look forward to hearing advertisements swearing by Veillonella-infused Wheaties, the true breakfast of champions.
Put a little boredom in your life
Is your job an endless, soul-sucking vortex of dreariness? Do you stare at the wall for hours at a time while you’re at work, wishing you had something better to do? Do you look forward to leaving early to go to the dentist? [Editor query: What does this have to do with health care? LOTME: You’ll see. We’re building dramatic tension.]
Did you answer yes to any of these questions? Way to go! You’ve taken the first step on the road to creativity. [Still waiting. We’re almost there.]
A recent study examined the effects of boredom by assigning people to either a really boring task – sorting a bowl of red and green beans by color for 30 minutes using only one hand – or a nonboring art project using paper, glue, and, of course, beans. [What’s with the beans? It’s not our fault they used beans.]
The next task was the same for both groups: Come up with some reasons for being late for work and think of ideas for a new product by a hypothetical company. The answers were graded on their uniqueness, and the bean-sorting group had more creative ideas than did the art-project group.
The point is, ladies and gentlemen, that boredom is good. Boredom is right. Boredom works. [A Gordon Gekko reference? Couldn’t you find something from this century? No.]
By now you’re probably wondering: “But how can I get one of those really boring jobs? After all, I’m a doctor. I heal the sick and care for the needy. My work is way too interesting to inspire true creativity.” Have you ever considered writing a medical humor column?
[Note to readers: We’ve pulled the staff away from their building blocks and crayons and given them a timeout. Hopefully things will be a little better by next week.]
The flying dead
Just when you thought cicada infestations couldn’t get worse – the cicadas are now zombies on an acid trip.
West Virginia University researchers recently discovered that a fungus called Massopora, which has compounds similar to those found in psychedelic mushrooms, can infect cicadas and cause seriously weird behavior.
How weird, you ask? Well, male cicadas try to mate with everything they encounter, even though the fungus has eaten away their limbs … and their genitals. Talk about a bad trip.
It gets worse. These zombie-like cicadas are flying around and exposing their healthy brethren to the fungus. So, now we have to worry about potentially billions of these buggers becoming rotting, flying, hypersexual machines.
Makes a person really want to stay inside for the whole summer, perhaps in a fortified bunker. Just in case.
Also, for the curious: One of the study’s authors concedes that if a person were “motivated enough,” they might be able to get high off the cicada fungus. Not interested in finding out exactly how many cicadas you’d have to crunch on before you start tasting colors?
Poster do-over
It’s time to get ready for a revolution – and just in time for 4th of July. No, we’re not redeclaring independence from Britain. It’s something much, much more radical, at least to the scientific community.
Get ready for … the redesign of the science poster.
Mike Morrison, a doctoral student in psychology, has proposed a new way to present information at meetings that breathes new life into the tired poster design. While fascinating insights could be held on a poster, the reality of meetings and conferences is that people often skim over the posters they see, barely registering the information.
Morrison is taking advantage of the ever-present smartphone to ramp up the classic science poster to a new level. He proposes a format where the key research finding is smack in the middle, in big, readable language. Accompanying this is a QR code you can scan, which would take you to a page with the full details of the study.
Morrison tweeted out his idea, and it spread quickly through the scientific community, gaining traction from younger scientists and students who love the idea.
We’re in the age of remakes now – in which classics are reinvented for a new audience. It’s time the science poster got a face-lift, too.
Running a marathon, one Veillonella at a time
What’s the difference between an elite athlete and a person who’s out of juice after running for 30 seconds?
Well, many things, we’re sure. A proper diet, rigorous training, not spending 12 hours a day sitting behind a computer screen. But just to add insult to injury, according to a study published in Nature Medicine, athletes even poop better than us normal people.
That may require a bit of explanation. A group of researchers from Harvard University, Boston, analyzed stool samples from elite marathon runners before and just after they participated in the 2015 Boston Marathon. They found that, following the race, the athletes had significantly higher amounts of Veillonella in their microbiota. This bacteria breaks down lactic acid, which is made during intense exercise and causes muscle fatigue and stress.
Naturally, the next step was to take that bacteria, feed it to mice, then get them running on a treadmill.
While not every mouse fed Veillonella saw increased performance, on average, mice that received the bacteria saw a 13% improvement over their non–Veillonella enhanced friends.
The researchers noted that this sort of probiotic treatment could be useful to patients with metabolic diseases, such as diabetes. Plus, there’s the obvious benefit to athletes. We look forward to hearing advertisements swearing by Veillonella-infused Wheaties, the true breakfast of champions.
Put a little boredom in your life
Is your job an endless, soul-sucking vortex of dreariness? Do you stare at the wall for hours at a time while you’re at work, wishing you had something better to do? Do you look forward to leaving early to go to the dentist? [Editor query: What does this have to do with health care? LOTME: You’ll see. We’re building dramatic tension.]
Did you answer yes to any of these questions? Way to go! You’ve taken the first step on the road to creativity. [Still waiting. We’re almost there.]
A recent study examined the effects of boredom by assigning people to either a really boring task – sorting a bowl of red and green beans by color for 30 minutes using only one hand – or a nonboring art project using paper, glue, and, of course, beans. [What’s with the beans? It’s not our fault they used beans.]
The next task was the same for both groups: Come up with some reasons for being late for work and think of ideas for a new product by a hypothetical company. The answers were graded on their uniqueness, and the bean-sorting group had more creative ideas than did the art-project group.
The point is, ladies and gentlemen, that boredom is good. Boredom is right. Boredom works. [A Gordon Gekko reference? Couldn’t you find something from this century? No.]
By now you’re probably wondering: “But how can I get one of those really boring jobs? After all, I’m a doctor. I heal the sick and care for the needy. My work is way too interesting to inspire true creativity.” Have you ever considered writing a medical humor column?
[Note to readers: We’ve pulled the staff away from their building blocks and crayons and given them a timeout. Hopefully things will be a little better by next week.]
RNase drug shows promise for Sjögren’s fatigue
MADRID – RSLV-132, a novel drug that eliminates circulating nucleic acids, improved the symptoms of mental fatigue in patients with primary Sjögren’s syndrome (pSS) in a phase 2, double-blind, randomized, placebo-controlled “proof-of-concept” study.

The mental component of fatigue on the Profile of Fatigue (PRO-F) scale improved by 1.53 points among the patients given RSLV-132, while there was a worsening of 0.06 points in the placebo group (P = .046). Scores range from 0 to 7 on the PRO-F.
There were also improvements in some patient-reported outcomes, namely the EULAR pSS Patient Reported Index (ESSPRI) and the Functional Assessment of Chronic Illness Therapy (FACIT)-Fatigue (FACIT-F), and improvement of neuropsychological measures of cognitive function, but none were statistically significant. All of these outcomes, including fatigue, were secondary outcomes of the study.
“Fatigue is a major issue for patients with Sjögren’s syndrome,” Wan-Fai Ng, MBChB, PhD, said in an interview at the European Congress of Rheumatology. Indeed, fatigue can be disabling in the majority of individuals, he added.
Currently, the best way to manage fatigue is to first ask about it, said Dr. Ng, who is professor of rheumatology at the Institute of Cellular Medicine at Newcastle University, Newcastle-upon-Tyne, England. He then checks for any underlying problem that could be better managed – sleep problems or anemia, for example – and optimizes treatment for any underlying disease. “I think many people would at least feel satisfied that people take the symptoms seriously.”
Dr. Ng and his coauthors investigated the effects of RSLV-132, a first-in-class human RNase fused to the human Fc domain of human immunoglobulin (Ig) G1, in the RESOLVE 132-04 study. This novel drug been designed to increase serum RNase activity to digest RNA-associated immune complexes, Dr. Ng and associates observed in their abstract. As a consequence of this, they say, activation of toll-like receptors and the production of interferon (IFN) is affected, as is B-cell proliferation and the production of autoantibodies – all mechanisms that are “key to pSS pathogenesis.”
The IFN pathway has been implicated in fatigue, Dr. Ng observed when he presented the RESOLVE 132-04 study’s findings, which involved 30 patients with pSS who had been treated for 3 months. Inclusion criteria were pSS as defined by the American-European Consensus Group 2002 criteria, anti-Ro antibody positivity, and increased expression of three IFN-regulated genes: HERC5, EPSTI1, and CMPK2. Exclusion criteria were the use of hydroxychloroquine, prednisolone at daily doses above 10 mg, and the use of biologic disease-modifying antirheumatic drugs.
Patients were randomized in a 3:1 ratio to receive either 10 mg/kg of RSLV-132 (n = 20) or placebo (n = 8) at weeks 0, 1, 2, and then every fortnight until week 12. Dr. Ng noted that although 30 patients were randomized, two patients had dropped out in the placebo group before they could be “treated.”
The primary endpoint was the change in the blood cell gene expression or serum protein levels indicative of reduced inflammation. The results indicated reductions in noncoding RNA molecules in patients who received RSLV-132 versus placebo, “consistent with the mode of action of the molecule.” In addition, “the majority of inflammatory markers were reduced,” Dr. Ng said.
Another finding showed a nonsignificant trend for improvement of 0.8 units in the physical component in the RSLV-132 group, compared against 0.06 units with placebo (P = .142).
Patients who received RSLV-132 reduced the time needed to complete the Digital Symbol Substitution Test by 16.4 s, compared with an increase of 2.8 s for placebo (P = .024).
Similar trends were observed for ESSPRI and FACIT-F scores.
These are very early data and clearly a bigger study would be needed before any conclusions could be drawn, Dr. Ng said in an interview. What these data suggest is that “maybe there is some way that we could manage fatigue, and we just need to go and explore that.”
RSLV-132 has also been studied in patients with systemic lupus erythematosus (Lupus. 2017;26:825-34).
The trial was sponsored by Resolve Therapeutics. Dr. Ng was an investigator in the trial and disclosed other research collaborations with electroCore, GlaxoSmithKline, and AbbVie. He also disclosed acting as a consultant for Novartis, GlaxoSmithKline, AbbVie, MedImmune, Pfizer, and Bristol-Myers Squibb.
Source: Fisher B et al. Ann Rheum Dis. 2019 Jun;78(suppl 2):177, Abstract OP0202. doi: 10.1136/annrheumdis-2019-eular.3098.
MADRID – RSLV-132, a novel drug that eliminates circulating nucleic acids, improved the symptoms of mental fatigue in patients with primary Sjögren’s syndrome (pSS) in a phase 2, double-blind, randomized, placebo-controlled “proof-of-concept” study.

The mental component of fatigue on the Profile of Fatigue (PRO-F) scale improved by 1.53 points among the patients given RSLV-132, while there was a worsening of 0.06 points in the placebo group (P = .046). Scores range from 0 to 7 on the PRO-F.
There were also improvements in some patient-reported outcomes, namely the EULAR pSS Patient Reported Index (ESSPRI) and the Functional Assessment of Chronic Illness Therapy (FACIT)-Fatigue (FACIT-F), and improvement of neuropsychological measures of cognitive function, but none were statistically significant. All of these outcomes, including fatigue, were secondary outcomes of the study.
“Fatigue is a major issue for patients with Sjögren’s syndrome,” Wan-Fai Ng, MBChB, PhD, said in an interview at the European Congress of Rheumatology. Indeed, fatigue can be disabling in the majority of individuals, he added.
Currently, the best way to manage fatigue is to first ask about it, said Dr. Ng, who is professor of rheumatology at the Institute of Cellular Medicine at Newcastle University, Newcastle-upon-Tyne, England. He then checks for any underlying problem that could be better managed – sleep problems or anemia, for example – and optimizes treatment for any underlying disease. “I think many people would at least feel satisfied that people take the symptoms seriously.”
Dr. Ng and his coauthors investigated the effects of RSLV-132, a first-in-class human RNase fused to the human Fc domain of human immunoglobulin (Ig) G1, in the RESOLVE 132-04 study. This novel drug been designed to increase serum RNase activity to digest RNA-associated immune complexes, Dr. Ng and associates observed in their abstract. As a consequence of this, they say, activation of toll-like receptors and the production of interferon (IFN) is affected, as is B-cell proliferation and the production of autoantibodies – all mechanisms that are “key to pSS pathogenesis.”
The IFN pathway has been implicated in fatigue, Dr. Ng observed when he presented the RESOLVE 132-04 study’s findings, which involved 30 patients with pSS who had been treated for 3 months. Inclusion criteria were pSS as defined by the American-European Consensus Group 2002 criteria, anti-Ro antibody positivity, and increased expression of three IFN-regulated genes: HERC5, EPSTI1, and CMPK2. Exclusion criteria were the use of hydroxychloroquine, prednisolone at daily doses above 10 mg, and the use of biologic disease-modifying antirheumatic drugs.
Patients were randomized in a 3:1 ratio to receive either 10 mg/kg of RSLV-132 (n = 20) or placebo (n = 8) at weeks 0, 1, 2, and then every fortnight until week 12. Dr. Ng noted that although 30 patients were randomized, two patients had dropped out in the placebo group before they could be “treated.”
The primary endpoint was the change in the blood cell gene expression or serum protein levels indicative of reduced inflammation. The results indicated reductions in noncoding RNA molecules in patients who received RSLV-132 versus placebo, “consistent with the mode of action of the molecule.” In addition, “the majority of inflammatory markers were reduced,” Dr. Ng said.
Another finding showed a nonsignificant trend for improvement of 0.8 units in the physical component in the RSLV-132 group, compared against 0.06 units with placebo (P = .142).
Patients who received RSLV-132 reduced the time needed to complete the Digital Symbol Substitution Test by 16.4 s, compared with an increase of 2.8 s for placebo (P = .024).
Similar trends were observed for ESSPRI and FACIT-F scores.
These are very early data and clearly a bigger study would be needed before any conclusions could be drawn, Dr. Ng said in an interview. What these data suggest is that “maybe there is some way that we could manage fatigue, and we just need to go and explore that.”
RSLV-132 has also been studied in patients with systemic lupus erythematosus (Lupus. 2017;26:825-34).
The trial was sponsored by Resolve Therapeutics. Dr. Ng was an investigator in the trial and disclosed other research collaborations with electroCore, GlaxoSmithKline, and AbbVie. He also disclosed acting as a consultant for Novartis, GlaxoSmithKline, AbbVie, MedImmune, Pfizer, and Bristol-Myers Squibb.
Source: Fisher B et al. Ann Rheum Dis. 2019 Jun;78(suppl 2):177, Abstract OP0202. doi: 10.1136/annrheumdis-2019-eular.3098.
MADRID – RSLV-132, a novel drug that eliminates circulating nucleic acids, improved the symptoms of mental fatigue in patients with primary Sjögren’s syndrome (pSS) in a phase 2, double-blind, randomized, placebo-controlled “proof-of-concept” study.

The mental component of fatigue on the Profile of Fatigue (PRO-F) scale improved by 1.53 points among the patients given RSLV-132, while there was a worsening of 0.06 points in the placebo group (P = .046). Scores range from 0 to 7 on the PRO-F.
There were also improvements in some patient-reported outcomes, namely the EULAR pSS Patient Reported Index (ESSPRI) and the Functional Assessment of Chronic Illness Therapy (FACIT)-Fatigue (FACIT-F), and improvement of neuropsychological measures of cognitive function, but none were statistically significant. All of these outcomes, including fatigue, were secondary outcomes of the study.
“Fatigue is a major issue for patients with Sjögren’s syndrome,” Wan-Fai Ng, MBChB, PhD, said in an interview at the European Congress of Rheumatology. Indeed, fatigue can be disabling in the majority of individuals, he added.
Currently, the best way to manage fatigue is to first ask about it, said Dr. Ng, who is professor of rheumatology at the Institute of Cellular Medicine at Newcastle University, Newcastle-upon-Tyne, England. He then checks for any underlying problem that could be better managed – sleep problems or anemia, for example – and optimizes treatment for any underlying disease. “I think many people would at least feel satisfied that people take the symptoms seriously.”
Dr. Ng and his coauthors investigated the effects of RSLV-132, a first-in-class human RNase fused to the human Fc domain of human immunoglobulin (Ig) G1, in the RESOLVE 132-04 study. This novel drug been designed to increase serum RNase activity to digest RNA-associated immune complexes, Dr. Ng and associates observed in their abstract. As a consequence of this, they say, activation of toll-like receptors and the production of interferon (IFN) is affected, as is B-cell proliferation and the production of autoantibodies – all mechanisms that are “key to pSS pathogenesis.”
The IFN pathway has been implicated in fatigue, Dr. Ng observed when he presented the RESOLVE 132-04 study’s findings, which involved 30 patients with pSS who had been treated for 3 months. Inclusion criteria were pSS as defined by the American-European Consensus Group 2002 criteria, anti-Ro antibody positivity, and increased expression of three IFN-regulated genes: HERC5, EPSTI1, and CMPK2. Exclusion criteria were the use of hydroxychloroquine, prednisolone at daily doses above 10 mg, and the use of biologic disease-modifying antirheumatic drugs.
Patients were randomized in a 3:1 ratio to receive either 10 mg/kg of RSLV-132 (n = 20) or placebo (n = 8) at weeks 0, 1, 2, and then every fortnight until week 12. Dr. Ng noted that although 30 patients were randomized, two patients had dropped out in the placebo group before they could be “treated.”
The primary endpoint was the change in the blood cell gene expression or serum protein levels indicative of reduced inflammation. The results indicated reductions in noncoding RNA molecules in patients who received RSLV-132 versus placebo, “consistent with the mode of action of the molecule.” In addition, “the majority of inflammatory markers were reduced,” Dr. Ng said.
Another finding showed a nonsignificant trend for improvement of 0.8 units in the physical component in the RSLV-132 group, compared against 0.06 units with placebo (P = .142).
Patients who received RSLV-132 reduced the time needed to complete the Digital Symbol Substitution Test by 16.4 s, compared with an increase of 2.8 s for placebo (P = .024).
Similar trends were observed for ESSPRI and FACIT-F scores.
These are very early data and clearly a bigger study would be needed before any conclusions could be drawn, Dr. Ng said in an interview. What these data suggest is that “maybe there is some way that we could manage fatigue, and we just need to go and explore that.”
RSLV-132 has also been studied in patients with systemic lupus erythematosus (Lupus. 2017;26:825-34).
The trial was sponsored by Resolve Therapeutics. Dr. Ng was an investigator in the trial and disclosed other research collaborations with electroCore, GlaxoSmithKline, and AbbVie. He also disclosed acting as a consultant for Novartis, GlaxoSmithKline, AbbVie, MedImmune, Pfizer, and Bristol-Myers Squibb.
Source: Fisher B et al. Ann Rheum Dis. 2019 Jun;78(suppl 2):177, Abstract OP0202. doi: 10.1136/annrheumdis-2019-eular.3098.
REPORTING FROM EULAR 2019 CONGRESS
Cancer deaths cost over $94 billion in lost earnings in 2015
Cancer led to 492,000 deaths for Americans aged 16-84 years in 2015, and those deaths cost $94.4 billion in lost earnings that year, according to a study published in JAMA Oncology.
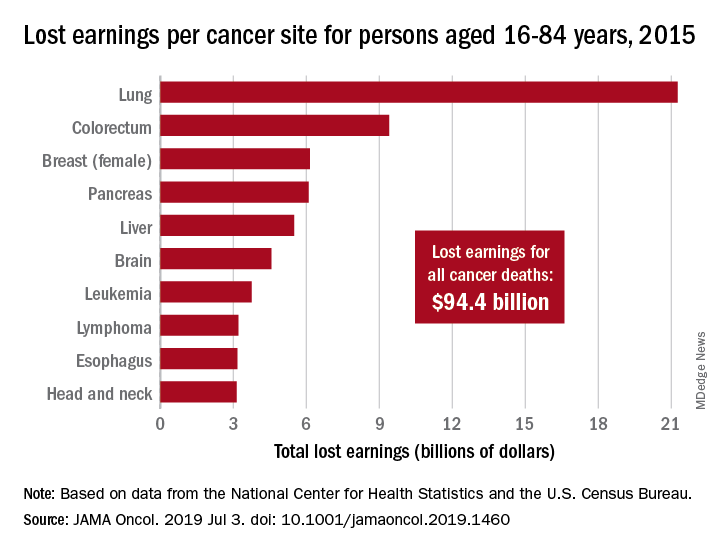
Cancer also took more than 8.7 million years of life from those individuals, with lung cancer being the most costly in terms of both lost earnings and years of life lost, said Farhad Islami, MD, PhD, and associates at the American Cancer Society, Atlanta.
“Person-years of life lost and lost earnings were high for many cancers associated with modifiable risk factors and effective screening and treatment, suggesting that a substantial proportion of the mortality burden is potentially avoidable,” they wrote, adding that “implementation of comprehensive cancer prevention interventions and equitable access to high-quality care across all states could reduce the burden of cancer and associated geographic and other differences in the country.”
In 2015, lung cancer took more than 2.2 million years of life and $21.3 billion in earnings from Americans aged 16-84 years. Colorectal cancer was next with 766,000 years of life lost and $9.4 billion in lost earnings, followed by female breast cancer with losses of 746,000 years of life and 6.2 billion in earnings, Dr. Islami and associated reported.
For all cancers, the cost in lost earnings per death was almost $192,000, with the highest costs coming from cancers of the brain and nervous system ($315,000) and cervix ($311,000). On that basis, lung cancer cost was lower than average at $159,000 per death, they noted.
At the state level, lost-earnings rates were lowest in Utah ($19.6 million per 100,000 persons) and highest in Kentucky ($35.3 million per 100,000). “If all states had Utah’s lost earnings rate in 2015, lost earnings in the U.S. would have been reduced by 29.3%, or $27.7 billion, and life years lost nationwide in 2015 would be reduced by 2.4 million,” Dr. Islami and his associates said in a written statement.
Data for the study were obtained from the National Center for Health Statistics (mortality) and the U.S. Census Bureau (earnings). The study was supported by the Intramural Research Department of the American Cancer Society, and all of the investigators are employees of the society.
SOURCE: Islami F et al. JAMA Oncol. 2019 Jul 3. doi: 10.1001/jamaoncol.2019.1460.
Cancer led to 492,000 deaths for Americans aged 16-84 years in 2015, and those deaths cost $94.4 billion in lost earnings that year, according to a study published in JAMA Oncology.
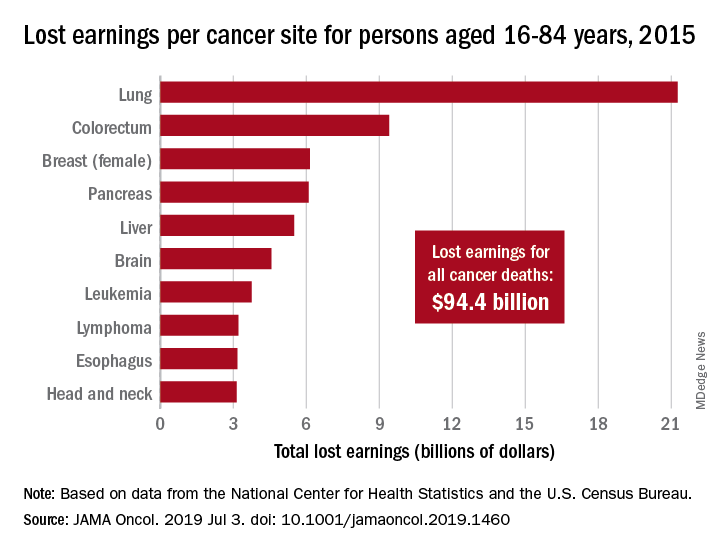
Cancer also took more than 8.7 million years of life from those individuals, with lung cancer being the most costly in terms of both lost earnings and years of life lost, said Farhad Islami, MD, PhD, and associates at the American Cancer Society, Atlanta.
“Person-years of life lost and lost earnings were high for many cancers associated with modifiable risk factors and effective screening and treatment, suggesting that a substantial proportion of the mortality burden is potentially avoidable,” they wrote, adding that “implementation of comprehensive cancer prevention interventions and equitable access to high-quality care across all states could reduce the burden of cancer and associated geographic and other differences in the country.”
In 2015, lung cancer took more than 2.2 million years of life and $21.3 billion in earnings from Americans aged 16-84 years. Colorectal cancer was next with 766,000 years of life lost and $9.4 billion in lost earnings, followed by female breast cancer with losses of 746,000 years of life and 6.2 billion in earnings, Dr. Islami and associated reported.
For all cancers, the cost in lost earnings per death was almost $192,000, with the highest costs coming from cancers of the brain and nervous system ($315,000) and cervix ($311,000). On that basis, lung cancer cost was lower than average at $159,000 per death, they noted.
At the state level, lost-earnings rates were lowest in Utah ($19.6 million per 100,000 persons) and highest in Kentucky ($35.3 million per 100,000). “If all states had Utah’s lost earnings rate in 2015, lost earnings in the U.S. would have been reduced by 29.3%, or $27.7 billion, and life years lost nationwide in 2015 would be reduced by 2.4 million,” Dr. Islami and his associates said in a written statement.
Data for the study were obtained from the National Center for Health Statistics (mortality) and the U.S. Census Bureau (earnings). The study was supported by the Intramural Research Department of the American Cancer Society, and all of the investigators are employees of the society.
SOURCE: Islami F et al. JAMA Oncol. 2019 Jul 3. doi: 10.1001/jamaoncol.2019.1460.
Cancer led to 492,000 deaths for Americans aged 16-84 years in 2015, and those deaths cost $94.4 billion in lost earnings that year, according to a study published in JAMA Oncology.
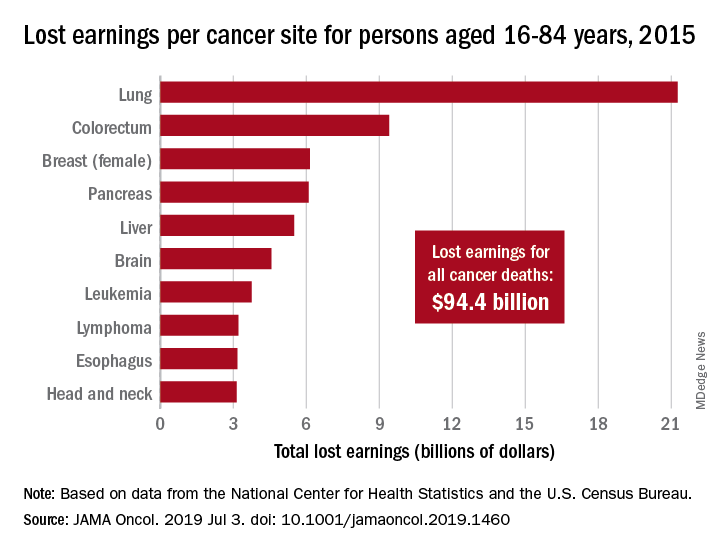
Cancer also took more than 8.7 million years of life from those individuals, with lung cancer being the most costly in terms of both lost earnings and years of life lost, said Farhad Islami, MD, PhD, and associates at the American Cancer Society, Atlanta.
“Person-years of life lost and lost earnings were high for many cancers associated with modifiable risk factors and effective screening and treatment, suggesting that a substantial proportion of the mortality burden is potentially avoidable,” they wrote, adding that “implementation of comprehensive cancer prevention interventions and equitable access to high-quality care across all states could reduce the burden of cancer and associated geographic and other differences in the country.”
In 2015, lung cancer took more than 2.2 million years of life and $21.3 billion in earnings from Americans aged 16-84 years. Colorectal cancer was next with 766,000 years of life lost and $9.4 billion in lost earnings, followed by female breast cancer with losses of 746,000 years of life and 6.2 billion in earnings, Dr. Islami and associated reported.
For all cancers, the cost in lost earnings per death was almost $192,000, with the highest costs coming from cancers of the brain and nervous system ($315,000) and cervix ($311,000). On that basis, lung cancer cost was lower than average at $159,000 per death, they noted.
At the state level, lost-earnings rates were lowest in Utah ($19.6 million per 100,000 persons) and highest in Kentucky ($35.3 million per 100,000). “If all states had Utah’s lost earnings rate in 2015, lost earnings in the U.S. would have been reduced by 29.3%, or $27.7 billion, and life years lost nationwide in 2015 would be reduced by 2.4 million,” Dr. Islami and his associates said in a written statement.
Data for the study were obtained from the National Center for Health Statistics (mortality) and the U.S. Census Bureau (earnings). The study was supported by the Intramural Research Department of the American Cancer Society, and all of the investigators are employees of the society.
SOURCE: Islami F et al. JAMA Oncol. 2019 Jul 3. doi: 10.1001/jamaoncol.2019.1460.
FROM JAMA ONCOLOGY
Is the vaginal or buccal route more effective when administering prostaglandins for cervical ripening at term?
Haas DM, Daggy J, Flannery KM, et al. A comparison of vaginal versus buccal misoprostol for cervical ripening in women for labor induction at term (the IMPROVE trial): a triple masked randomized controlled trial. Am J Obstet Gynecol. 2019. doi:10.1016/j.ajog.2019.04.037.
EXPERT COMMENTARY
Cervical ripening is routine practice in women undergoing induction of labor who have an unfavorable cervical examination.1 This is because generating contractions against a long thick cervix is more likely to lead to failed induction and cesarean delivery. Cervical ripening can be achieved using mechanical or pharmacologic methods.
Misoprostol (a prostaglandin E1 [PGE1] analog) is approved by the US Food and Drug Administration for the treatment of peptic ulcer disease, but it also is widely used off-label for cervical ripening, partly due to its low cost. Misoprostol’s optimal dosing regimen and route of administration are not known. The IMPROVE trial was designed to address this knowledge gap, specifically to compare the efficacy and safety of VM versus BM in women undergoing labor induction at term.
Details of the study
The IMPROVE trial was a prospective, randomized, noninferiority, triple-masked, placebo-controlled trial of 300 women with a singleton vertex fetus requiring cervical ripening for induction of labor at term.2 Enrolled women were randomly assigned to VM or BM (same dosing regimen) and to a matching placebo administered via the opposite route.
Primary outcomes included time-to-vaginal-delivery from first dose, which was reduced in VM vs BM (20.1 vs 28.1 hours; P = .006), and urgent cesarean delivery for nonreassuring fetal testing, which was similarly reduced in VM (3.3% vs 9.5%; P = .33). These differences persisted after controlling for covariates. There was also a greater difference seen in multiparous versus nulliparous women.
Secondary outcomes also favored VM over BM, including more vaginal deliverieswithin 24 hours, fewer doses to achieve active labor, and a lower maximum dose of oxytocin.
Overall cesarean delivery rates were similar in the 2 groups (VM, 15.8%; BM, 22.3%; P = .15). There were no significant differences in other delivery characteristics or in maternal or fetal adverse events.
While a number of studies have evaluated the risk of cesarean delivery (CD) with the use of cervical ripening agents by different routes of administration, Handal-Orefice and colleagues studied this outcome specifically in a predominantly overweight population at a tertiary care center.1
The retrospective study included 276 women, of whom 91% had a body mass index (BMI) of 25 kg/m2 or more and 61% had a BMI of 30 kg/m2 or more at the time of delivery.
For cervical ripening, 138 women received vaginal misoprostol (25 µg) and 138 received oral misoprostol (50 µg). The frequency of CD (the primary study outcome) was significantly higher with oral compared with vaginal misoprostol use (32% vs 21%; P = .04). When the analysis was adjusted for age, BMI, parity, indication for induction, and Foley catheter use, the risk of CD remained significantly higher for the oral misoprostol group (adjusted odds ratio [aOR], 2.01; 95% confidence interval [CI], 1.07-3.76).
Other key findings:
- frequency of CD among nulliparous women: 41% in the oral misoprostol group, 28% in the vaginal misoprostol group (aOR, 2.79; 95% CI, 1.26-6.19)
- time to vaginal delivery: 41 hours for the oral misoprostol group, 31 hours for the vaginal misoprostol group (P = .01)
- uterine tachysystole: 11% in the oral misoprostol group, 20% in the vaginal misoprostol group (P = .04).
The authors noted that the strengths of the study, including the racial and ethnic diversity of the population (72% of women were of either black or Hispanic race or ethnicity), the commonly used doses of misoprostol, and the performance of inductions outside a research protocol, add to the generalizability of the results.
Reference
1. Handal-Orefice R, Friedman AM, Chouinard SM, et al. Oral or vaginal misoprostol for labor induction and cesarean delivery risk. Obstet Gynecol. 2019. doi:10.1097/AOG.0000000000003274.
Continue to: Study strengths and limitations...
Study strengths and limitations
The IMPROVE trial had a triple-blinded study design with an intention-to-treat paradigm and good follow-up. There was also standardization of PGE1 administration criteria, which was consistent with the American College of Obstetricians and Gynecologists standards of care. Results were similar to those of prior studies regarding rates of tachysystole, urgent cesarean delivery, and vaginal delivery.
The study has good generalizability as it included both elective and medically indicated inductions; however, patients with ruptured membranes were excluded. Although there was no difference in the overall cesarean delivery rates, the study was underpowered to look at this outcome. The authors included a patient satisfaction survey, but this is hard to interpret since study participants all received tablets orally and vaginally. The study did not address efficacy of VM versus BM administration at different doses or time intervals.
Labor induction has doubled over the past 2 decades, with almost 25% of parturients currently undergoing induction in the United States.3 This number is likely to increase given recent data suggesting that routine induction at 39 weeks may significantly decrease cesarean delivery rates.4 It is critical, therefore, that we identify the optimal technique for cervical ripening, including the ideal dosing regimen and route of administration. Results of the IMPROVE trial suggest that vaginal administration of misoprostol (25 μg initial dose, 50 μg subsequent doses) may be superior to the buccal route, with more rapid vaginal delivery, more vaginal deliveries within 24 hours, and fewer urgent cesareans for nonreassuring fetal testing (although the overall cesarean delivery rate was not significantly different).
ERROL R. NORWITZ, MD, PHD, MBA; JULIE M. STONE, MD
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 107. Induction of labor. Obstet Gynecol. 2009;114(2 pt 1):386-397.
- Haas DM, Daggy J, Flannery KM, et al. A comparison of vaginal versus buccal misoprostol for cervical ripening in women for labor induction at term (the IMPROVE trial): a triple masked randomized controlled trial. Am J Obstet Gynecol. 2019. doi:10.1016/j.ajog.2019.04.037.
- Martin JA, Hamilton BE, Osterman M, et al. Births: final data for 2016. Nat Vital Stat Rep. 2018;67:1-55.
- Grobman WA, Rice MM, Reddy UM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
Haas DM, Daggy J, Flannery KM, et al. A comparison of vaginal versus buccal misoprostol for cervical ripening in women for labor induction at term (the IMPROVE trial): a triple masked randomized controlled trial. Am J Obstet Gynecol. 2019. doi:10.1016/j.ajog.2019.04.037.
EXPERT COMMENTARY
Cervical ripening is routine practice in women undergoing induction of labor who have an unfavorable cervical examination.1 This is because generating contractions against a long thick cervix is more likely to lead to failed induction and cesarean delivery. Cervical ripening can be achieved using mechanical or pharmacologic methods.
Misoprostol (a prostaglandin E1 [PGE1] analog) is approved by the US Food and Drug Administration for the treatment of peptic ulcer disease, but it also is widely used off-label for cervical ripening, partly due to its low cost. Misoprostol’s optimal dosing regimen and route of administration are not known. The IMPROVE trial was designed to address this knowledge gap, specifically to compare the efficacy and safety of VM versus BM in women undergoing labor induction at term.
Details of the study
The IMPROVE trial was a prospective, randomized, noninferiority, triple-masked, placebo-controlled trial of 300 women with a singleton vertex fetus requiring cervical ripening for induction of labor at term.2 Enrolled women were randomly assigned to VM or BM (same dosing regimen) and to a matching placebo administered via the opposite route.
Primary outcomes included time-to-vaginal-delivery from first dose, which was reduced in VM vs BM (20.1 vs 28.1 hours; P = .006), and urgent cesarean delivery for nonreassuring fetal testing, which was similarly reduced in VM (3.3% vs 9.5%; P = .33). These differences persisted after controlling for covariates. There was also a greater difference seen in multiparous versus nulliparous women.
Secondary outcomes also favored VM over BM, including more vaginal deliverieswithin 24 hours, fewer doses to achieve active labor, and a lower maximum dose of oxytocin.
Overall cesarean delivery rates were similar in the 2 groups (VM, 15.8%; BM, 22.3%; P = .15). There were no significant differences in other delivery characteristics or in maternal or fetal adverse events.
While a number of studies have evaluated the risk of cesarean delivery (CD) with the use of cervical ripening agents by different routes of administration, Handal-Orefice and colleagues studied this outcome specifically in a predominantly overweight population at a tertiary care center.1
The retrospective study included 276 women, of whom 91% had a body mass index (BMI) of 25 kg/m2 or more and 61% had a BMI of 30 kg/m2 or more at the time of delivery.
For cervical ripening, 138 women received vaginal misoprostol (25 µg) and 138 received oral misoprostol (50 µg). The frequency of CD (the primary study outcome) was significantly higher with oral compared with vaginal misoprostol use (32% vs 21%; P = .04). When the analysis was adjusted for age, BMI, parity, indication for induction, and Foley catheter use, the risk of CD remained significantly higher for the oral misoprostol group (adjusted odds ratio [aOR], 2.01; 95% confidence interval [CI], 1.07-3.76).
Other key findings:
- frequency of CD among nulliparous women: 41% in the oral misoprostol group, 28% in the vaginal misoprostol group (aOR, 2.79; 95% CI, 1.26-6.19)
- time to vaginal delivery: 41 hours for the oral misoprostol group, 31 hours for the vaginal misoprostol group (P = .01)
- uterine tachysystole: 11% in the oral misoprostol group, 20% in the vaginal misoprostol group (P = .04).
The authors noted that the strengths of the study, including the racial and ethnic diversity of the population (72% of women were of either black or Hispanic race or ethnicity), the commonly used doses of misoprostol, and the performance of inductions outside a research protocol, add to the generalizability of the results.
Reference
1. Handal-Orefice R, Friedman AM, Chouinard SM, et al. Oral or vaginal misoprostol for labor induction and cesarean delivery risk. Obstet Gynecol. 2019. doi:10.1097/AOG.0000000000003274.
Continue to: Study strengths and limitations...
Study strengths and limitations
The IMPROVE trial had a triple-blinded study design with an intention-to-treat paradigm and good follow-up. There was also standardization of PGE1 administration criteria, which was consistent with the American College of Obstetricians and Gynecologists standards of care. Results were similar to those of prior studies regarding rates of tachysystole, urgent cesarean delivery, and vaginal delivery.
The study has good generalizability as it included both elective and medically indicated inductions; however, patients with ruptured membranes were excluded. Although there was no difference in the overall cesarean delivery rates, the study was underpowered to look at this outcome. The authors included a patient satisfaction survey, but this is hard to interpret since study participants all received tablets orally and vaginally. The study did not address efficacy of VM versus BM administration at different doses or time intervals.
Labor induction has doubled over the past 2 decades, with almost 25% of parturients currently undergoing induction in the United States.3 This number is likely to increase given recent data suggesting that routine induction at 39 weeks may significantly decrease cesarean delivery rates.4 It is critical, therefore, that we identify the optimal technique for cervical ripening, including the ideal dosing regimen and route of administration. Results of the IMPROVE trial suggest that vaginal administration of misoprostol (25 μg initial dose, 50 μg subsequent doses) may be superior to the buccal route, with more rapid vaginal delivery, more vaginal deliveries within 24 hours, and fewer urgent cesareans for nonreassuring fetal testing (although the overall cesarean delivery rate was not significantly different).
ERROL R. NORWITZ, MD, PHD, MBA; JULIE M. STONE, MD
Haas DM, Daggy J, Flannery KM, et al. A comparison of vaginal versus buccal misoprostol for cervical ripening in women for labor induction at term (the IMPROVE trial): a triple masked randomized controlled trial. Am J Obstet Gynecol. 2019. doi:10.1016/j.ajog.2019.04.037.
EXPERT COMMENTARY
Cervical ripening is routine practice in women undergoing induction of labor who have an unfavorable cervical examination.1 This is because generating contractions against a long thick cervix is more likely to lead to failed induction and cesarean delivery. Cervical ripening can be achieved using mechanical or pharmacologic methods.
Misoprostol (a prostaglandin E1 [PGE1] analog) is approved by the US Food and Drug Administration for the treatment of peptic ulcer disease, but it also is widely used off-label for cervical ripening, partly due to its low cost. Misoprostol’s optimal dosing regimen and route of administration are not known. The IMPROVE trial was designed to address this knowledge gap, specifically to compare the efficacy and safety of VM versus BM in women undergoing labor induction at term.
Details of the study
The IMPROVE trial was a prospective, randomized, noninferiority, triple-masked, placebo-controlled trial of 300 women with a singleton vertex fetus requiring cervical ripening for induction of labor at term.2 Enrolled women were randomly assigned to VM or BM (same dosing regimen) and to a matching placebo administered via the opposite route.
Primary outcomes included time-to-vaginal-delivery from first dose, which was reduced in VM vs BM (20.1 vs 28.1 hours; P = .006), and urgent cesarean delivery for nonreassuring fetal testing, which was similarly reduced in VM (3.3% vs 9.5%; P = .33). These differences persisted after controlling for covariates. There was also a greater difference seen in multiparous versus nulliparous women.
Secondary outcomes also favored VM over BM, including more vaginal deliverieswithin 24 hours, fewer doses to achieve active labor, and a lower maximum dose of oxytocin.
Overall cesarean delivery rates were similar in the 2 groups (VM, 15.8%; BM, 22.3%; P = .15). There were no significant differences in other delivery characteristics or in maternal or fetal adverse events.
While a number of studies have evaluated the risk of cesarean delivery (CD) with the use of cervical ripening agents by different routes of administration, Handal-Orefice and colleagues studied this outcome specifically in a predominantly overweight population at a tertiary care center.1
The retrospective study included 276 women, of whom 91% had a body mass index (BMI) of 25 kg/m2 or more and 61% had a BMI of 30 kg/m2 or more at the time of delivery.
For cervical ripening, 138 women received vaginal misoprostol (25 µg) and 138 received oral misoprostol (50 µg). The frequency of CD (the primary study outcome) was significantly higher with oral compared with vaginal misoprostol use (32% vs 21%; P = .04). When the analysis was adjusted for age, BMI, parity, indication for induction, and Foley catheter use, the risk of CD remained significantly higher for the oral misoprostol group (adjusted odds ratio [aOR], 2.01; 95% confidence interval [CI], 1.07-3.76).
Other key findings:
- frequency of CD among nulliparous women: 41% in the oral misoprostol group, 28% in the vaginal misoprostol group (aOR, 2.79; 95% CI, 1.26-6.19)
- time to vaginal delivery: 41 hours for the oral misoprostol group, 31 hours for the vaginal misoprostol group (P = .01)
- uterine tachysystole: 11% in the oral misoprostol group, 20% in the vaginal misoprostol group (P = .04).
The authors noted that the strengths of the study, including the racial and ethnic diversity of the population (72% of women were of either black or Hispanic race or ethnicity), the commonly used doses of misoprostol, and the performance of inductions outside a research protocol, add to the generalizability of the results.
Reference
1. Handal-Orefice R, Friedman AM, Chouinard SM, et al. Oral or vaginal misoprostol for labor induction and cesarean delivery risk. Obstet Gynecol. 2019. doi:10.1097/AOG.0000000000003274.
Continue to: Study strengths and limitations...
Study strengths and limitations
The IMPROVE trial had a triple-blinded study design with an intention-to-treat paradigm and good follow-up. There was also standardization of PGE1 administration criteria, which was consistent with the American College of Obstetricians and Gynecologists standards of care. Results were similar to those of prior studies regarding rates of tachysystole, urgent cesarean delivery, and vaginal delivery.
The study has good generalizability as it included both elective and medically indicated inductions; however, patients with ruptured membranes were excluded. Although there was no difference in the overall cesarean delivery rates, the study was underpowered to look at this outcome. The authors included a patient satisfaction survey, but this is hard to interpret since study participants all received tablets orally and vaginally. The study did not address efficacy of VM versus BM administration at different doses or time intervals.
Labor induction has doubled over the past 2 decades, with almost 25% of parturients currently undergoing induction in the United States.3 This number is likely to increase given recent data suggesting that routine induction at 39 weeks may significantly decrease cesarean delivery rates.4 It is critical, therefore, that we identify the optimal technique for cervical ripening, including the ideal dosing regimen and route of administration. Results of the IMPROVE trial suggest that vaginal administration of misoprostol (25 μg initial dose, 50 μg subsequent doses) may be superior to the buccal route, with more rapid vaginal delivery, more vaginal deliveries within 24 hours, and fewer urgent cesareans for nonreassuring fetal testing (although the overall cesarean delivery rate was not significantly different).
ERROL R. NORWITZ, MD, PHD, MBA; JULIE M. STONE, MD
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 107. Induction of labor. Obstet Gynecol. 2009;114(2 pt 1):386-397.
- Haas DM, Daggy J, Flannery KM, et al. A comparison of vaginal versus buccal misoprostol for cervical ripening in women for labor induction at term (the IMPROVE trial): a triple masked randomized controlled trial. Am J Obstet Gynecol. 2019. doi:10.1016/j.ajog.2019.04.037.
- Martin JA, Hamilton BE, Osterman M, et al. Births: final data for 2016. Nat Vital Stat Rep. 2018;67:1-55.
- Grobman WA, Rice MM, Reddy UM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
- American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 107. Induction of labor. Obstet Gynecol. 2009;114(2 pt 1):386-397.
- Haas DM, Daggy J, Flannery KM, et al. A comparison of vaginal versus buccal misoprostol for cervical ripening in women for labor induction at term (the IMPROVE trial): a triple masked randomized controlled trial. Am J Obstet Gynecol. 2019. doi:10.1016/j.ajog.2019.04.037.
- Martin JA, Hamilton BE, Osterman M, et al. Births: final data for 2016. Nat Vital Stat Rep. 2018;67:1-55.
- Grobman WA, Rice MM, Reddy UM, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379:513-523.
Adjustment for characteristics not used by Medicare reduces hospital variations in readmission rates
Clinical question: Can differences in hospital readmission rates be explained by patient characteristics not accounted for by Medicare?
Background: In its Pay for Performance program, Medicare ties payments to readmission rates but adjusts these rates only for limited patient characteristics. Hospitals serving higher-risk patients have received greater penalties. These programs may have the unintended consequence of penalizing hospitals that provide care to higher-risk patients.
Study design: Observational study.
Setting: Medicare admissions claims from 2013 through 2014 in 2,215 hospitals.
Synopsis: Using Medicare claims for admission and linked U.S. census data, the study assessed several clinical and social characteristics not currently used for risk adjustment. A sample of 1,169,014 index admissions among 1,003,664 unique beneficiaries was analyzed. The study compared rates with and without these additional adjustments.
Additional adjustments reduced overall variation in hospital readmission by 9.6%, changed rates upward or downward by 0.4%-0.7% for the 10% of hospitals most affected by the readjustments, and they would be expected to reduce penalties by 52%, 46%, and 41% for hospitals with the largest 1%, 5%, and 10% of penalty reductions, respectively.
Bottom line: Hospitals serving higher-risk patients may be penalized because of the patients they serve rather that the quality of care they provide.
Citation: Roberts ET et al. Assessment of the effect of adjustment for patient characteristics on hospital readmission rates: Implications for Pay for Performance. JAMA Intern Med. 2018;178(11)1498-1507.
Dr. Asuen is an assistant professor of medicine in the division of hospital medicine at Mount Sinai Hospital, New York.
Clinical question: Can differences in hospital readmission rates be explained by patient characteristics not accounted for by Medicare?
Background: In its Pay for Performance program, Medicare ties payments to readmission rates but adjusts these rates only for limited patient characteristics. Hospitals serving higher-risk patients have received greater penalties. These programs may have the unintended consequence of penalizing hospitals that provide care to higher-risk patients.
Study design: Observational study.
Setting: Medicare admissions claims from 2013 through 2014 in 2,215 hospitals.
Synopsis: Using Medicare claims for admission and linked U.S. census data, the study assessed several clinical and social characteristics not currently used for risk adjustment. A sample of 1,169,014 index admissions among 1,003,664 unique beneficiaries was analyzed. The study compared rates with and without these additional adjustments.
Additional adjustments reduced overall variation in hospital readmission by 9.6%, changed rates upward or downward by 0.4%-0.7% for the 10% of hospitals most affected by the readjustments, and they would be expected to reduce penalties by 52%, 46%, and 41% for hospitals with the largest 1%, 5%, and 10% of penalty reductions, respectively.
Bottom line: Hospitals serving higher-risk patients may be penalized because of the patients they serve rather that the quality of care they provide.
Citation: Roberts ET et al. Assessment of the effect of adjustment for patient characteristics on hospital readmission rates: Implications for Pay for Performance. JAMA Intern Med. 2018;178(11)1498-1507.
Dr. Asuen is an assistant professor of medicine in the division of hospital medicine at Mount Sinai Hospital, New York.
Clinical question: Can differences in hospital readmission rates be explained by patient characteristics not accounted for by Medicare?
Background: In its Pay for Performance program, Medicare ties payments to readmission rates but adjusts these rates only for limited patient characteristics. Hospitals serving higher-risk patients have received greater penalties. These programs may have the unintended consequence of penalizing hospitals that provide care to higher-risk patients.
Study design: Observational study.
Setting: Medicare admissions claims from 2013 through 2014 in 2,215 hospitals.
Synopsis: Using Medicare claims for admission and linked U.S. census data, the study assessed several clinical and social characteristics not currently used for risk adjustment. A sample of 1,169,014 index admissions among 1,003,664 unique beneficiaries was analyzed. The study compared rates with and without these additional adjustments.
Additional adjustments reduced overall variation in hospital readmission by 9.6%, changed rates upward or downward by 0.4%-0.7% for the 10% of hospitals most affected by the readjustments, and they would be expected to reduce penalties by 52%, 46%, and 41% for hospitals with the largest 1%, 5%, and 10% of penalty reductions, respectively.
Bottom line: Hospitals serving higher-risk patients may be penalized because of the patients they serve rather that the quality of care they provide.
Citation: Roberts ET et al. Assessment of the effect of adjustment for patient characteristics on hospital readmission rates: Implications for Pay for Performance. JAMA Intern Med. 2018;178(11)1498-1507.
Dr. Asuen is an assistant professor of medicine in the division of hospital medicine at Mount Sinai Hospital, New York.
Uterus-sparing interventions to treat postpartum hemorrhage during cesarean delivery surgery
Postpartum blood loss greater than 1,000 mL occurs in approximately 7% of cesarean delivery (CD) procedures with the administration of oxytocin alone or oxytocin plus misoprostol.1 Rapid identification and control of hemorrhage is essential to avoid escalating coagulopathy and maternal instability. In cases of excess blood loss, clinicians request assistance from colleagues, endeavor to identify the cause of the bleeding, utilize additional uterotonics (methylergonovine, carboprost, misoprostol), perform uterine massage, warm the uterus, repair lacerations and replace blood products. If blood loss continues after these initial measures, obstetricians may consider uterine artery embolization (UAE) or hysterectomy. While UAE is a highly effective measure to control postpartum hemorrhage, it is not available at all obstetric hospitals. Even when available, there may be a significant time delay from the decision to consult an interventional radiologist to completion of the embolization procedure.
To avoid the permanent sterilization of a hysterectomy, or to obtain time for UAE or correction of coagulopathy, additional uterus-sparing surgical interventions should be considered. These include: 1) progressive uterine devascularization, 2) uterine compression sutures, and 3) intrauterine balloon tamponade. One caveat is that there is very little high-quality evidence from randomized trials to compare the efficacy or outcome of these uterine-sparing surgical interventions. Most of our evidence is based on limited case series and expert recommendations.
Uterine devascularization
Many techniques have been described for performing progressive uterine devascularization. Most experts recommend first performing an O’Leary suture, ligating both ascending uterine arteries and accompanying veins at a point approximately 2 cm closer to the cervix than the uterine incision (FIGURE 1). An absorbable suture is passed through the myometrium, being sure to remain medial to the ascending uterine vessels. Clear visualization of the vessels posteriorly is essential, usually necessitating exteriorization of the uterus. The needle is then driven through an avascular space in the broad ligament close to the uterine vessels, and the suture is tied down. Ureteral injury can be avoided by extending the bladder flap laterally to the level of the round ligament and mobilizing the vesicouterine peritoneum inferiorly, with the suture placed directly on endopelvic fascia. If necessary, the utero-ovarian ligament can be ligated in a second step, just below the uterine-tubal junction. The progressive devascularization intervention can be limited to the first or second steps if bleeding is well controlled.
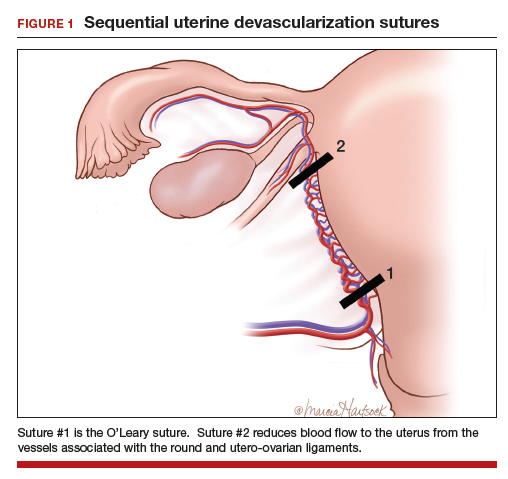
In our experience, bilateral O’Leary sutures are highly effective at controlling ongoing uterine bleeding, particularly from the lower uterine segment. In the event that they are not successful, placement does not preclude later use of UAE.
Uterine compression sutures
Compression sutures are most often used in the setting of refractory uterine atony. They also may be helpful for controlling focal atony or bleeding from a placental implantation site. More than a dozen different types of uterine compression sutures have been reported in the literature; the B-Lynch, Hyman, and Pereira sutures are most commonly performed.2
Continue to: The B-Lynch suture3 is performed with...
The B-Lynch suture3 is performed with a long, rapidly absorbable suture on a large needle (FIGURE 2). We use a 60-inch #1 or #2 chromic suture on a TP-1 needle in the following steps:
- Take bites on either side of the right edge of the hysterotomy incision (A and B). Place these bites approximately 3 cm from the edge of the hysterotomy incision.
- Loop the suture around the fundus and reenter the uterus through the posterior uterine wall at point C, which is directly posterior to point B.
- Exit the posterior wall of the uterus through point D.
- Loop the suture over the uterine fundus.
- Anchor the suture in the lower uterine segment by taking bites on either side of the left edge of the uterine hysterotomy incision (points E and F).
- Pull the two ends of the suture tight while an assistant squeezes the uterus to aid compression.
- Place a surgical knot to secure the suture.
- Close the hysterotomy incision.
The B-Lynch suture was described with an open hysterotomy incision,3 which avoids closing off the lower uterine segment. We have successfully performed a modific tion on a closed uterus, taking care to not drive the lower uterine sutures through both the anterior and posterior walls.
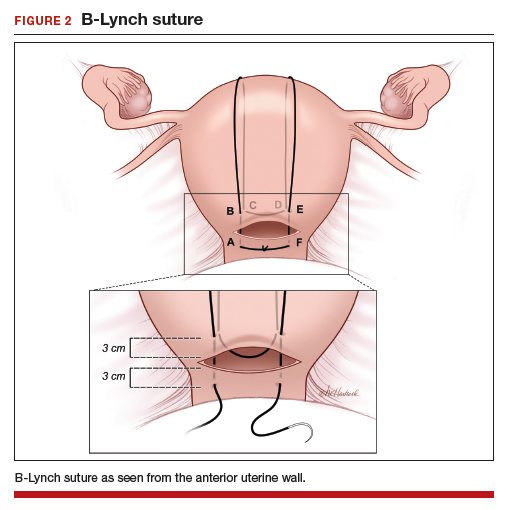
The Hayman suture4 was proposed with two important modifications: The suture is placed through-and-through the lower uterine segment with a closed hysterotomy, and the suture can be fixed to the uterine fundus to avoid slippage. This vertical compression suture (FIGURE 3) is performed by placing two to four vertical #2 chromic sutures directly through the anterior to posterior uterine wall, tying the suture on the fundus using a 3-throw technique to minimize slippage of the first knot. In the original description, Hayman also described injecting carboprost into the uterine fundus to stimulate uterine contraction and regularly inspecting the vagina to evaluate the extent of continued bleeding.4
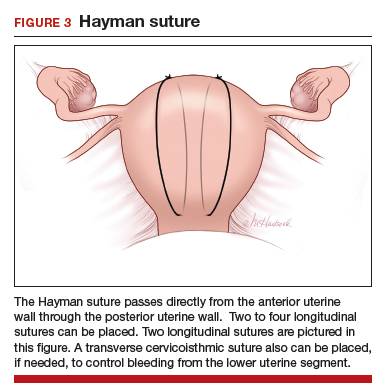
The Pereira sutures,5 also described on a closed uterus, combine vertical and horizontal sutures placed as a series of bites into the submucosal myometrium using #1 polyglactin 910 (Vicryl) sutures (FIGURE 4). The sutures do not enter the uterine cavity. Two to three transverse sutures are initially placed followed by two vertical sutures. When placing the transverse sutures, it is important to cross the broad ligament in an avascular area and avoid trauma to blood vessels, ureters, gonadal vessels and fallopian tubes. The vertical sutures begin and end at the level of the transverse suture closest to the cervix.
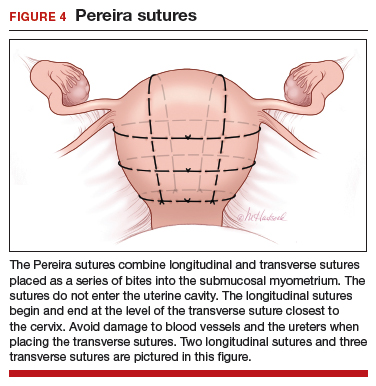
Intrauterine balloon tamponade
Many types of balloon tamponade devices have been developed, ranging from the humble condom tied to a Foley urinary catheter to the sophisticated Bakri6,7 and Belfort-Dildy8 balloon tamponade devices. Intrauterine balloon tamponade is highly effective in controlling excess bleeding following vaginal delivery and less effective when used following a CD. In one study of 226 women with postpartum hemorrhage treated with a Bakri balloon the success rate was 89% and 66% following vaginal delivery and CD, respectively.9
Continue to: When using balloon tamponade during a CD...
When using balloon tamponade during a CD, some experts recommend partially closing the transverse hysterotomy incision by placing sutures to close edges of the hysterotomy, followed by insertion of the balloon into the uterus and the stem through the cervix into the vagina. Attachment of the stem to a collection bag should help to quickly assess the rate of blood loss. The balloon is inflated after the hysterotomy is closed. Following inflation of an intrauterine balloon, blood loss should decrease almost immediately.10 If excessive blood loss continues for more than 10 minutes, additional uterus-sparing interventions or hysterectomy may be required. Following successful balloon tamponade, the balloon may be deflated 12 to 24 hours postpartum when maternal stabilization and normal coagulation have been achieved. If bleeding resumes, the balloon may be reinflated and UAE should be considered.
Combined interventions: Uterine devascularization plus uterine compression sutures
There are no high-quality randomized trials comparing the devascularization plus compression sutures versus a single intervention alone, and case series and case reports on this topic are lacking. If uterine devascularization alone does not sufficiently control bleeding, adding a uterine compression stitch might resolve the hemorrhage. Both procedures require only suture material, which is immediately available in all operating rooms. Hence, this combination of interventions can be executed quickly.
Uterine sandwich: Intrauterine balloon tamponade plus uterine compression sutures
CD for placenta previa is associated with an increased risk of postpartum hemorrhage, with bleeding from the lower uterine segment greatly contributing to total blood loss. While O’Leary sutures can stem the flow of bleeding in this area, the use of both an intrauterine balloon tamponade plus uterine compression sutures—a so-called uterine sandwich—may result in maximal reduction in blood loss.11,12
In one randomized trial, 106 women undergoing CD for a placenta previa were randomly assigned to uterine devascularization alone or double transverse compression suture at the lower uterine segment plus intrauterine Foley catheter balloon. Compared with women receiving devascularization alone, the combination of compression suture plus intrauterine balloon significantly reduced blood loss (1,350 mL vs 750 mL, respectively; P = .0001).13
Underutilization of uterine-sparing interventions
In a nationwide study of 50 consecutive Danish peripartum hysterectomy cases, an audit committee concluded that 24% of the hysterectomies could have been avoided, and an additional 30% of hysterectomies might have been avoided, if uterine-sparing surgical interventions had been utilized.14 In a recent survey of senior ObGyn residents in France, greater than 70% of respondents reported that they had not mastered uterine-sparing techniques of uterine devascularization and compression sutures, nor peripartum hysterectomy.15 Together, these studies suggest that uterine-sparing interventions are underutilized and that with more training and practice clinicians would become facile with these interventions.
The cornerstones of uterine-sparing surgical interventions are simplicity, safety, and efficacy. If a combination of pharmacologic and multiple uterine-sparing surgical interventions do not control the bleeding, the patient may need an emergency hysterectomy or, if stable, a UAE. While devascularization and compression sutures are described during CD, it is reasonable to use them after vaginal delivery if the next reasonable step would be a laparotomy. When you next face the clinical challenge of a postpartum hemorrhage, rapid recognition of excess blood loss, early identification of the cause, swift pharmacologic treatment, and timely escalation of surgical interventions will help you reduce the risk of hysterectomy and severe maternal morbidity.
- Gallos ID, Papadopoulou A, Man R, et al. Uterotonic agents for preventing postpartum haemorrhage: a network meta-analysis. Cochrane Database of Syst Rev. 2018;12:CD011689.
- Li GT, Li XF, Wu BP, et al. Three cornerstones of uterine compression sutures: simplicity, safety, and efficacy. Arch Gynecol Obstet. 2015;292:949-952.
- B-Lynch C, Coker A, Lawal AH, et al. The B-Lynch surgical technique for the control of massive postpartum hemorrhage: an alternative to hysterectomy? Five cases reported. Br J Obstet Gynaecol. 1997;104:372-375.
- Hayman RG, Arulkumaran S, Steer PJ. Uterine compression sutures: surgical management of postpartum hemorrhage. Obstet Gynecol. 2002;99:502-506.
- Pereira A, Nunes F, Pedroso S, et al. Compressive sutures to treat postpartum bleeding secondary to uterine atony. Obstet Gynecol. 2005;106:569-572.
- Bakri YN. Uterine tamponade-drain for hemorrhage secondary to placenta previa-accreta. Int J Gynaecol Obstet. 1992;37:302-303.
- Bakri YN, Amri A, Abdul Jabbar F. Tamponade-balloon for obstetrical bleeding. Int J Gynaecol Obstet. 2001;74:139-142.
- Dildy GA, Belfort MA, Adair CD, et al; ebb Surveillance Study Team. Initial experience with a dual-balloon catheter for the management of postpartum hemorrhage. Am J Obstet Gynecol. 2014;210:136.e1-e6.
- Revert M, Cottenet J, Raynal P, et al. Intrauterine balloon tamponade for management of severe postpartum hemorrhage in a perinatal network: a prospective cohort study. BJOG. 2017;124:1255-1262.
- Condous GS, Arulkumaran S, Symonds I, et al. The “tamponade test” in the management of massive postpartum hemorrhage. Obstet Gynecol. 2003;101:767-772.
- Nelson WL, O’Brien JM. The uterine sandwich for persistent uterine atony: combining the B-Lynch compression suture and an intrauterine Bakri balloon. Am J Obstet Gynecol. 2007;196:e9-e10.
- Matsubara S, Kuwata T, Baba Y, et al. A novel “uterine sandwich” for haemorrhage at cesarean section for placenta praevia. Aust N Z J Obstet Gynaecol. 2014;54:283-286.
- Sallam HF, Shady NW. A sandwich technique (N&H variation technique) to reduce blood loss during cesarean delivery for complete placenta previa: a randomized controlled trial. J Matern Fetal Neonatal Med. 2018:1-8.
- Colmorn LB, Krebs L, Langhoff-Roos J; NOSS study group. Potentially avoidable peripartum hysterectomies in Denmark: a population based clinical audit. PLoS One. 2016;11:e0161302.
- Bouet PE, Madar H, Froeliger A, et al. Surgical treatment of postpartum haemorrhage: national survey of French residents in obstetrics and gynecology. BMC Pregnancy Childbirth. 2019;19:91.
Postpartum blood loss greater than 1,000 mL occurs in approximately 7% of cesarean delivery (CD) procedures with the administration of oxytocin alone or oxytocin plus misoprostol.1 Rapid identification and control of hemorrhage is essential to avoid escalating coagulopathy and maternal instability. In cases of excess blood loss, clinicians request assistance from colleagues, endeavor to identify the cause of the bleeding, utilize additional uterotonics (methylergonovine, carboprost, misoprostol), perform uterine massage, warm the uterus, repair lacerations and replace blood products. If blood loss continues after these initial measures, obstetricians may consider uterine artery embolization (UAE) or hysterectomy. While UAE is a highly effective measure to control postpartum hemorrhage, it is not available at all obstetric hospitals. Even when available, there may be a significant time delay from the decision to consult an interventional radiologist to completion of the embolization procedure.
To avoid the permanent sterilization of a hysterectomy, or to obtain time for UAE or correction of coagulopathy, additional uterus-sparing surgical interventions should be considered. These include: 1) progressive uterine devascularization, 2) uterine compression sutures, and 3) intrauterine balloon tamponade. One caveat is that there is very little high-quality evidence from randomized trials to compare the efficacy or outcome of these uterine-sparing surgical interventions. Most of our evidence is based on limited case series and expert recommendations.
Uterine devascularization
Many techniques have been described for performing progressive uterine devascularization. Most experts recommend first performing an O’Leary suture, ligating both ascending uterine arteries and accompanying veins at a point approximately 2 cm closer to the cervix than the uterine incision (FIGURE 1). An absorbable suture is passed through the myometrium, being sure to remain medial to the ascending uterine vessels. Clear visualization of the vessels posteriorly is essential, usually necessitating exteriorization of the uterus. The needle is then driven through an avascular space in the broad ligament close to the uterine vessels, and the suture is tied down. Ureteral injury can be avoided by extending the bladder flap laterally to the level of the round ligament and mobilizing the vesicouterine peritoneum inferiorly, with the suture placed directly on endopelvic fascia. If necessary, the utero-ovarian ligament can be ligated in a second step, just below the uterine-tubal junction. The progressive devascularization intervention can be limited to the first or second steps if bleeding is well controlled.
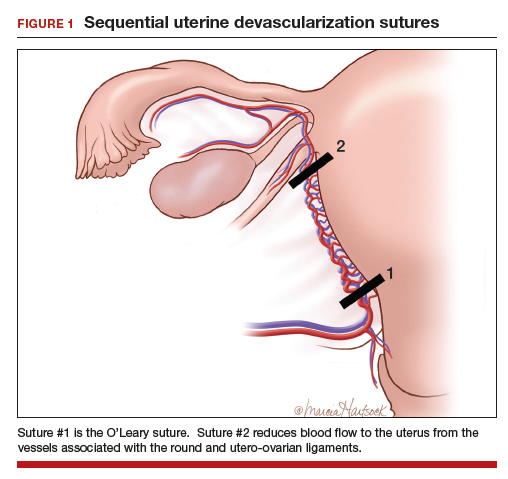
In our experience, bilateral O’Leary sutures are highly effective at controlling ongoing uterine bleeding, particularly from the lower uterine segment. In the event that they are not successful, placement does not preclude later use of UAE.
Uterine compression sutures
Compression sutures are most often used in the setting of refractory uterine atony. They also may be helpful for controlling focal atony or bleeding from a placental implantation site. More than a dozen different types of uterine compression sutures have been reported in the literature; the B-Lynch, Hyman, and Pereira sutures are most commonly performed.2
Continue to: The B-Lynch suture3 is performed with...
The B-Lynch suture3 is performed with a long, rapidly absorbable suture on a large needle (FIGURE 2). We use a 60-inch #1 or #2 chromic suture on a TP-1 needle in the following steps:
- Take bites on either side of the right edge of the hysterotomy incision (A and B). Place these bites approximately 3 cm from the edge of the hysterotomy incision.
- Loop the suture around the fundus and reenter the uterus through the posterior uterine wall at point C, which is directly posterior to point B.
- Exit the posterior wall of the uterus through point D.
- Loop the suture over the uterine fundus.
- Anchor the suture in the lower uterine segment by taking bites on either side of the left edge of the uterine hysterotomy incision (points E and F).
- Pull the two ends of the suture tight while an assistant squeezes the uterus to aid compression.
- Place a surgical knot to secure the suture.
- Close the hysterotomy incision.
The B-Lynch suture was described with an open hysterotomy incision,3 which avoids closing off the lower uterine segment. We have successfully performed a modific tion on a closed uterus, taking care to not drive the lower uterine sutures through both the anterior and posterior walls.
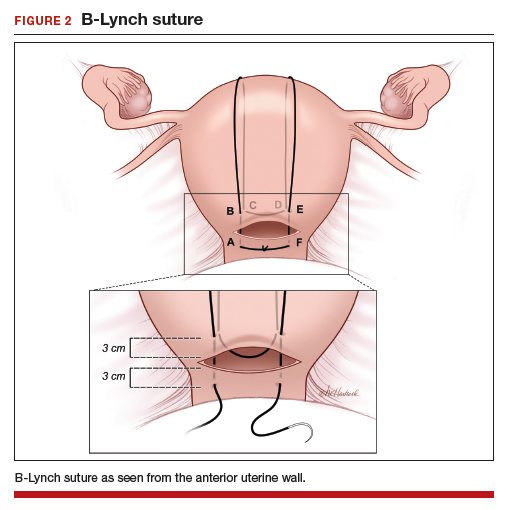
The Hayman suture4 was proposed with two important modifications: The suture is placed through-and-through the lower uterine segment with a closed hysterotomy, and the suture can be fixed to the uterine fundus to avoid slippage. This vertical compression suture (FIGURE 3) is performed by placing two to four vertical #2 chromic sutures directly through the anterior to posterior uterine wall, tying the suture on the fundus using a 3-throw technique to minimize slippage of the first knot. In the original description, Hayman also described injecting carboprost into the uterine fundus to stimulate uterine contraction and regularly inspecting the vagina to evaluate the extent of continued bleeding.4
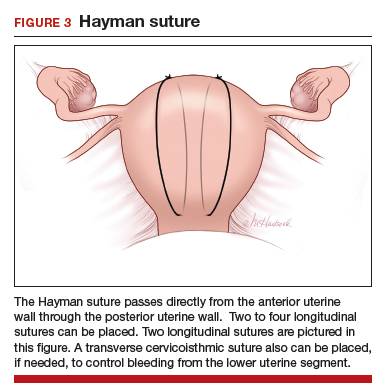
The Pereira sutures,5 also described on a closed uterus, combine vertical and horizontal sutures placed as a series of bites into the submucosal myometrium using #1 polyglactin 910 (Vicryl) sutures (FIGURE 4). The sutures do not enter the uterine cavity. Two to three transverse sutures are initially placed followed by two vertical sutures. When placing the transverse sutures, it is important to cross the broad ligament in an avascular area and avoid trauma to blood vessels, ureters, gonadal vessels and fallopian tubes. The vertical sutures begin and end at the level of the transverse suture closest to the cervix.
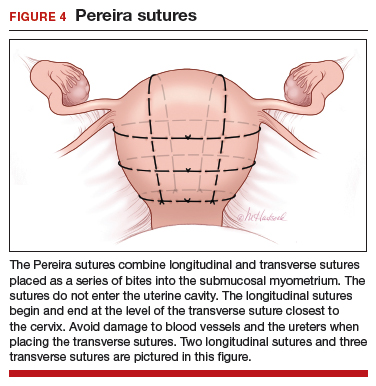
Intrauterine balloon tamponade
Many types of balloon tamponade devices have been developed, ranging from the humble condom tied to a Foley urinary catheter to the sophisticated Bakri6,7 and Belfort-Dildy8 balloon tamponade devices. Intrauterine balloon tamponade is highly effective in controlling excess bleeding following vaginal delivery and less effective when used following a CD. In one study of 226 women with postpartum hemorrhage treated with a Bakri balloon the success rate was 89% and 66% following vaginal delivery and CD, respectively.9
Continue to: When using balloon tamponade during a CD...
When using balloon tamponade during a CD, some experts recommend partially closing the transverse hysterotomy incision by placing sutures to close edges of the hysterotomy, followed by insertion of the balloon into the uterus and the stem through the cervix into the vagina. Attachment of the stem to a collection bag should help to quickly assess the rate of blood loss. The balloon is inflated after the hysterotomy is closed. Following inflation of an intrauterine balloon, blood loss should decrease almost immediately.10 If excessive blood loss continues for more than 10 minutes, additional uterus-sparing interventions or hysterectomy may be required. Following successful balloon tamponade, the balloon may be deflated 12 to 24 hours postpartum when maternal stabilization and normal coagulation have been achieved. If bleeding resumes, the balloon may be reinflated and UAE should be considered.
Combined interventions: Uterine devascularization plus uterine compression sutures
There are no high-quality randomized trials comparing the devascularization plus compression sutures versus a single intervention alone, and case series and case reports on this topic are lacking. If uterine devascularization alone does not sufficiently control bleeding, adding a uterine compression stitch might resolve the hemorrhage. Both procedures require only suture material, which is immediately available in all operating rooms. Hence, this combination of interventions can be executed quickly.
Uterine sandwich: Intrauterine balloon tamponade plus uterine compression sutures
CD for placenta previa is associated with an increased risk of postpartum hemorrhage, with bleeding from the lower uterine segment greatly contributing to total blood loss. While O’Leary sutures can stem the flow of bleeding in this area, the use of both an intrauterine balloon tamponade plus uterine compression sutures—a so-called uterine sandwich—may result in maximal reduction in blood loss.11,12
In one randomized trial, 106 women undergoing CD for a placenta previa were randomly assigned to uterine devascularization alone or double transverse compression suture at the lower uterine segment plus intrauterine Foley catheter balloon. Compared with women receiving devascularization alone, the combination of compression suture plus intrauterine balloon significantly reduced blood loss (1,350 mL vs 750 mL, respectively; P = .0001).13
Underutilization of uterine-sparing interventions
In a nationwide study of 50 consecutive Danish peripartum hysterectomy cases, an audit committee concluded that 24% of the hysterectomies could have been avoided, and an additional 30% of hysterectomies might have been avoided, if uterine-sparing surgical interventions had been utilized.14 In a recent survey of senior ObGyn residents in France, greater than 70% of respondents reported that they had not mastered uterine-sparing techniques of uterine devascularization and compression sutures, nor peripartum hysterectomy.15 Together, these studies suggest that uterine-sparing interventions are underutilized and that with more training and practice clinicians would become facile with these interventions.
The cornerstones of uterine-sparing surgical interventions are simplicity, safety, and efficacy. If a combination of pharmacologic and multiple uterine-sparing surgical interventions do not control the bleeding, the patient may need an emergency hysterectomy or, if stable, a UAE. While devascularization and compression sutures are described during CD, it is reasonable to use them after vaginal delivery if the next reasonable step would be a laparotomy. When you next face the clinical challenge of a postpartum hemorrhage, rapid recognition of excess blood loss, early identification of the cause, swift pharmacologic treatment, and timely escalation of surgical interventions will help you reduce the risk of hysterectomy and severe maternal morbidity.
Postpartum blood loss greater than 1,000 mL occurs in approximately 7% of cesarean delivery (CD) procedures with the administration of oxytocin alone or oxytocin plus misoprostol.1 Rapid identification and control of hemorrhage is essential to avoid escalating coagulopathy and maternal instability. In cases of excess blood loss, clinicians request assistance from colleagues, endeavor to identify the cause of the bleeding, utilize additional uterotonics (methylergonovine, carboprost, misoprostol), perform uterine massage, warm the uterus, repair lacerations and replace blood products. If blood loss continues after these initial measures, obstetricians may consider uterine artery embolization (UAE) or hysterectomy. While UAE is a highly effective measure to control postpartum hemorrhage, it is not available at all obstetric hospitals. Even when available, there may be a significant time delay from the decision to consult an interventional radiologist to completion of the embolization procedure.
To avoid the permanent sterilization of a hysterectomy, or to obtain time for UAE or correction of coagulopathy, additional uterus-sparing surgical interventions should be considered. These include: 1) progressive uterine devascularization, 2) uterine compression sutures, and 3) intrauterine balloon tamponade. One caveat is that there is very little high-quality evidence from randomized trials to compare the efficacy or outcome of these uterine-sparing surgical interventions. Most of our evidence is based on limited case series and expert recommendations.
Uterine devascularization
Many techniques have been described for performing progressive uterine devascularization. Most experts recommend first performing an O’Leary suture, ligating both ascending uterine arteries and accompanying veins at a point approximately 2 cm closer to the cervix than the uterine incision (FIGURE 1). An absorbable suture is passed through the myometrium, being sure to remain medial to the ascending uterine vessels. Clear visualization of the vessels posteriorly is essential, usually necessitating exteriorization of the uterus. The needle is then driven through an avascular space in the broad ligament close to the uterine vessels, and the suture is tied down. Ureteral injury can be avoided by extending the bladder flap laterally to the level of the round ligament and mobilizing the vesicouterine peritoneum inferiorly, with the suture placed directly on endopelvic fascia. If necessary, the utero-ovarian ligament can be ligated in a second step, just below the uterine-tubal junction. The progressive devascularization intervention can be limited to the first or second steps if bleeding is well controlled.
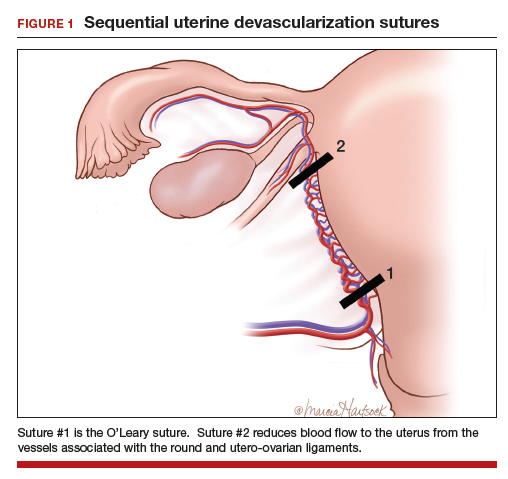
In our experience, bilateral O’Leary sutures are highly effective at controlling ongoing uterine bleeding, particularly from the lower uterine segment. In the event that they are not successful, placement does not preclude later use of UAE.
Uterine compression sutures
Compression sutures are most often used in the setting of refractory uterine atony. They also may be helpful for controlling focal atony or bleeding from a placental implantation site. More than a dozen different types of uterine compression sutures have been reported in the literature; the B-Lynch, Hyman, and Pereira sutures are most commonly performed.2
Continue to: The B-Lynch suture3 is performed with...
The B-Lynch suture3 is performed with a long, rapidly absorbable suture on a large needle (FIGURE 2). We use a 60-inch #1 or #2 chromic suture on a TP-1 needle in the following steps:
- Take bites on either side of the right edge of the hysterotomy incision (A and B). Place these bites approximately 3 cm from the edge of the hysterotomy incision.
- Loop the suture around the fundus and reenter the uterus through the posterior uterine wall at point C, which is directly posterior to point B.
- Exit the posterior wall of the uterus through point D.
- Loop the suture over the uterine fundus.
- Anchor the suture in the lower uterine segment by taking bites on either side of the left edge of the uterine hysterotomy incision (points E and F).
- Pull the two ends of the suture tight while an assistant squeezes the uterus to aid compression.
- Place a surgical knot to secure the suture.
- Close the hysterotomy incision.
The B-Lynch suture was described with an open hysterotomy incision,3 which avoids closing off the lower uterine segment. We have successfully performed a modific tion on a closed uterus, taking care to not drive the lower uterine sutures through both the anterior and posterior walls.
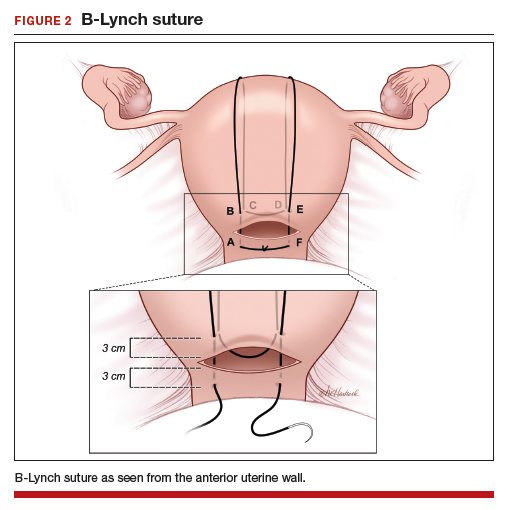
The Hayman suture4 was proposed with two important modifications: The suture is placed through-and-through the lower uterine segment with a closed hysterotomy, and the suture can be fixed to the uterine fundus to avoid slippage. This vertical compression suture (FIGURE 3) is performed by placing two to four vertical #2 chromic sutures directly through the anterior to posterior uterine wall, tying the suture on the fundus using a 3-throw technique to minimize slippage of the first knot. In the original description, Hayman also described injecting carboprost into the uterine fundus to stimulate uterine contraction and regularly inspecting the vagina to evaluate the extent of continued bleeding.4
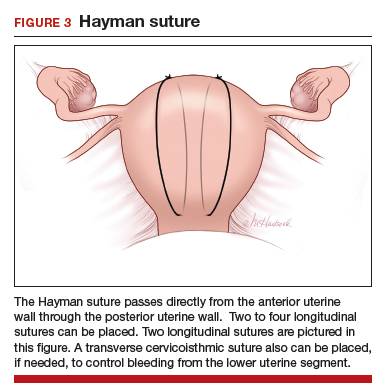
The Pereira sutures,5 also described on a closed uterus, combine vertical and horizontal sutures placed as a series of bites into the submucosal myometrium using #1 polyglactin 910 (Vicryl) sutures (FIGURE 4). The sutures do not enter the uterine cavity. Two to three transverse sutures are initially placed followed by two vertical sutures. When placing the transverse sutures, it is important to cross the broad ligament in an avascular area and avoid trauma to blood vessels, ureters, gonadal vessels and fallopian tubes. The vertical sutures begin and end at the level of the transverse suture closest to the cervix.
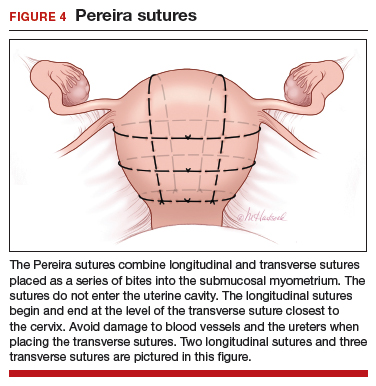
Intrauterine balloon tamponade
Many types of balloon tamponade devices have been developed, ranging from the humble condom tied to a Foley urinary catheter to the sophisticated Bakri6,7 and Belfort-Dildy8 balloon tamponade devices. Intrauterine balloon tamponade is highly effective in controlling excess bleeding following vaginal delivery and less effective when used following a CD. In one study of 226 women with postpartum hemorrhage treated with a Bakri balloon the success rate was 89% and 66% following vaginal delivery and CD, respectively.9
Continue to: When using balloon tamponade during a CD...
When using balloon tamponade during a CD, some experts recommend partially closing the transverse hysterotomy incision by placing sutures to close edges of the hysterotomy, followed by insertion of the balloon into the uterus and the stem through the cervix into the vagina. Attachment of the stem to a collection bag should help to quickly assess the rate of blood loss. The balloon is inflated after the hysterotomy is closed. Following inflation of an intrauterine balloon, blood loss should decrease almost immediately.10 If excessive blood loss continues for more than 10 minutes, additional uterus-sparing interventions or hysterectomy may be required. Following successful balloon tamponade, the balloon may be deflated 12 to 24 hours postpartum when maternal stabilization and normal coagulation have been achieved. If bleeding resumes, the balloon may be reinflated and UAE should be considered.
Combined interventions: Uterine devascularization plus uterine compression sutures
There are no high-quality randomized trials comparing the devascularization plus compression sutures versus a single intervention alone, and case series and case reports on this topic are lacking. If uterine devascularization alone does not sufficiently control bleeding, adding a uterine compression stitch might resolve the hemorrhage. Both procedures require only suture material, which is immediately available in all operating rooms. Hence, this combination of interventions can be executed quickly.
Uterine sandwich: Intrauterine balloon tamponade plus uterine compression sutures
CD for placenta previa is associated with an increased risk of postpartum hemorrhage, with bleeding from the lower uterine segment greatly contributing to total blood loss. While O’Leary sutures can stem the flow of bleeding in this area, the use of both an intrauterine balloon tamponade plus uterine compression sutures—a so-called uterine sandwich—may result in maximal reduction in blood loss.11,12
In one randomized trial, 106 women undergoing CD for a placenta previa were randomly assigned to uterine devascularization alone or double transverse compression suture at the lower uterine segment plus intrauterine Foley catheter balloon. Compared with women receiving devascularization alone, the combination of compression suture plus intrauterine balloon significantly reduced blood loss (1,350 mL vs 750 mL, respectively; P = .0001).13
Underutilization of uterine-sparing interventions
In a nationwide study of 50 consecutive Danish peripartum hysterectomy cases, an audit committee concluded that 24% of the hysterectomies could have been avoided, and an additional 30% of hysterectomies might have been avoided, if uterine-sparing surgical interventions had been utilized.14 In a recent survey of senior ObGyn residents in France, greater than 70% of respondents reported that they had not mastered uterine-sparing techniques of uterine devascularization and compression sutures, nor peripartum hysterectomy.15 Together, these studies suggest that uterine-sparing interventions are underutilized and that with more training and practice clinicians would become facile with these interventions.
The cornerstones of uterine-sparing surgical interventions are simplicity, safety, and efficacy. If a combination of pharmacologic and multiple uterine-sparing surgical interventions do not control the bleeding, the patient may need an emergency hysterectomy or, if stable, a UAE. While devascularization and compression sutures are described during CD, it is reasonable to use them after vaginal delivery if the next reasonable step would be a laparotomy. When you next face the clinical challenge of a postpartum hemorrhage, rapid recognition of excess blood loss, early identification of the cause, swift pharmacologic treatment, and timely escalation of surgical interventions will help you reduce the risk of hysterectomy and severe maternal morbidity.
- Gallos ID, Papadopoulou A, Man R, et al. Uterotonic agents for preventing postpartum haemorrhage: a network meta-analysis. Cochrane Database of Syst Rev. 2018;12:CD011689.
- Li GT, Li XF, Wu BP, et al. Three cornerstones of uterine compression sutures: simplicity, safety, and efficacy. Arch Gynecol Obstet. 2015;292:949-952.
- B-Lynch C, Coker A, Lawal AH, et al. The B-Lynch surgical technique for the control of massive postpartum hemorrhage: an alternative to hysterectomy? Five cases reported. Br J Obstet Gynaecol. 1997;104:372-375.
- Hayman RG, Arulkumaran S, Steer PJ. Uterine compression sutures: surgical management of postpartum hemorrhage. Obstet Gynecol. 2002;99:502-506.
- Pereira A, Nunes F, Pedroso S, et al. Compressive sutures to treat postpartum bleeding secondary to uterine atony. Obstet Gynecol. 2005;106:569-572.
- Bakri YN. Uterine tamponade-drain for hemorrhage secondary to placenta previa-accreta. Int J Gynaecol Obstet. 1992;37:302-303.
- Bakri YN, Amri A, Abdul Jabbar F. Tamponade-balloon for obstetrical bleeding. Int J Gynaecol Obstet. 2001;74:139-142.
- Dildy GA, Belfort MA, Adair CD, et al; ebb Surveillance Study Team. Initial experience with a dual-balloon catheter for the management of postpartum hemorrhage. Am J Obstet Gynecol. 2014;210:136.e1-e6.
- Revert M, Cottenet J, Raynal P, et al. Intrauterine balloon tamponade for management of severe postpartum hemorrhage in a perinatal network: a prospective cohort study. BJOG. 2017;124:1255-1262.
- Condous GS, Arulkumaran S, Symonds I, et al. The “tamponade test” in the management of massive postpartum hemorrhage. Obstet Gynecol. 2003;101:767-772.
- Nelson WL, O’Brien JM. The uterine sandwich for persistent uterine atony: combining the B-Lynch compression suture and an intrauterine Bakri balloon. Am J Obstet Gynecol. 2007;196:e9-e10.
- Matsubara S, Kuwata T, Baba Y, et al. A novel “uterine sandwich” for haemorrhage at cesarean section for placenta praevia. Aust N Z J Obstet Gynaecol. 2014;54:283-286.
- Sallam HF, Shady NW. A sandwich technique (N&H variation technique) to reduce blood loss during cesarean delivery for complete placenta previa: a randomized controlled trial. J Matern Fetal Neonatal Med. 2018:1-8.
- Colmorn LB, Krebs L, Langhoff-Roos J; NOSS study group. Potentially avoidable peripartum hysterectomies in Denmark: a population based clinical audit. PLoS One. 2016;11:e0161302.
- Bouet PE, Madar H, Froeliger A, et al. Surgical treatment of postpartum haemorrhage: national survey of French residents in obstetrics and gynecology. BMC Pregnancy Childbirth. 2019;19:91.
- Gallos ID, Papadopoulou A, Man R, et al. Uterotonic agents for preventing postpartum haemorrhage: a network meta-analysis. Cochrane Database of Syst Rev. 2018;12:CD011689.
- Li GT, Li XF, Wu BP, et al. Three cornerstones of uterine compression sutures: simplicity, safety, and efficacy. Arch Gynecol Obstet. 2015;292:949-952.
- B-Lynch C, Coker A, Lawal AH, et al. The B-Lynch surgical technique for the control of massive postpartum hemorrhage: an alternative to hysterectomy? Five cases reported. Br J Obstet Gynaecol. 1997;104:372-375.
- Hayman RG, Arulkumaran S, Steer PJ. Uterine compression sutures: surgical management of postpartum hemorrhage. Obstet Gynecol. 2002;99:502-506.
- Pereira A, Nunes F, Pedroso S, et al. Compressive sutures to treat postpartum bleeding secondary to uterine atony. Obstet Gynecol. 2005;106:569-572.
- Bakri YN. Uterine tamponade-drain for hemorrhage secondary to placenta previa-accreta. Int J Gynaecol Obstet. 1992;37:302-303.
- Bakri YN, Amri A, Abdul Jabbar F. Tamponade-balloon for obstetrical bleeding. Int J Gynaecol Obstet. 2001;74:139-142.
- Dildy GA, Belfort MA, Adair CD, et al; ebb Surveillance Study Team. Initial experience with a dual-balloon catheter for the management of postpartum hemorrhage. Am J Obstet Gynecol. 2014;210:136.e1-e6.
- Revert M, Cottenet J, Raynal P, et al. Intrauterine balloon tamponade for management of severe postpartum hemorrhage in a perinatal network: a prospective cohort study. BJOG. 2017;124:1255-1262.
- Condous GS, Arulkumaran S, Symonds I, et al. The “tamponade test” in the management of massive postpartum hemorrhage. Obstet Gynecol. 2003;101:767-772.
- Nelson WL, O’Brien JM. The uterine sandwich for persistent uterine atony: combining the B-Lynch compression suture and an intrauterine Bakri balloon. Am J Obstet Gynecol. 2007;196:e9-e10.
- Matsubara S, Kuwata T, Baba Y, et al. A novel “uterine sandwich” for haemorrhage at cesarean section for placenta praevia. Aust N Z J Obstet Gynaecol. 2014;54:283-286.
- Sallam HF, Shady NW. A sandwich technique (N&H variation technique) to reduce blood loss during cesarean delivery for complete placenta previa: a randomized controlled trial. J Matern Fetal Neonatal Med. 2018:1-8.
- Colmorn LB, Krebs L, Langhoff-Roos J; NOSS study group. Potentially avoidable peripartum hysterectomies in Denmark: a population based clinical audit. PLoS One. 2016;11:e0161302.
- Bouet PE, Madar H, Froeliger A, et al. Surgical treatment of postpartum haemorrhage: national survey of French residents in obstetrics and gynecology. BMC Pregnancy Childbirth. 2019;19:91.
Genomic study reveals five subtypes of colorectal cancer
Colorectal cancer can be divided into five DNA methylation subtypes that predict molecular and clinical behavior and may offer future therapeutic targets, according to investigators.
In 216 unselected colorectal cancers, five subtypes of the CpG island methylator phenotype (CIMP) showed “striking” associations with sex, age, and tumor location, reported lead author Lochlan Fennell, MD, of the QIMR Berghofer Medical Research Institute in Queensland, Australia, and colleagues. CIMP level increased with age in a stepwise fashion, they noted.
Further associations with CIMP subtype and BRAF mutation status support the investigators’ recent report that sessile serrated adenomas are rare in young patients and pose little risk of malignancy. With additional research, these findings could “inform the development of patient-centric surveillance for young and older patients who present with sessile serrated adenomas,” the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology.
“CIMP can be detected using a standardized marker panel to stratify tumors as CIMP-high, CIMP-low, or CIMP-negative.” In the present study, the investigators expanded these three existing subtypes into five subtypes, allowing for better prediction of clinical and molecular characteristics associated with disease progression.
Initial genomic testing showed that 13.4% of cases carried a BRAF V600E mutation, 34.7% were mutated at KRAS codon 12 or 13, and almost half of the patients (42.2%) had a TP53 mutation. Sorted into the three previously described subtypes, CIMP negative was most common (68.5%), followed by CIMP low (20.4%), and CIMP high (11.1%). About two-thirds (66%) of BRAF mutant cancers were CIMP high, compared with just 3% of BRAF wild-type cases (P less than .0001). KRAS mutated cases were more often CIMP-low than KRAS wild-type cancers (34.6% vs. 12.8%; P less than .001).
With use of Illumina HumanMethylation450 Bead Chip arrays and recursively partitioned mixed model clustering, five methylation clusters were identified; specifically, these were CIMP-H1 and CIMP-H2 (high methylation levels), CIMP-L1 and CIMP-L2 (intermediate methylation levels), and CIMP-negative (low methylation level). As described above, methylation level demonstrated a direct relationship with age, ranging from CIMP-negative (61.9 years) to CIMP-H1 (75.2 years). The investigators also reported unique characteristics of each new subtype. For instance, the CIMP-H1 cluster had many features in common with cases of serrated neoplasia, such as BRAF mutation positivity (73.9%; P less than .0001).
“BRAF mutations are a hallmark of the serrated neoplasia pathway, and indicate that these cancers probably arose in serrated precursor lesions,” the investigators wrote. “We previously showed that the colonoscopic incidence of sessile serrated adenomas does not differ between patients aged in their 30s and patients who are much older, whereas BRAF mutant cancers were restricted to older individuals, suggesting these BRAF mutant polyps may have limited malignant potential in young patients.”
In contrast with the CIMP-H1 cases, CIMP-H2 cancers were more often KRAS mutant (54.5% vs. 17.4%). Other findings revealed associations with subtype and location; for example, CIMP-L1 cases were located equally in the distal and proximal colon, whereas CIMP-L2 cases more often localized to the distal colon and rectum. Of note for CIMP-negative cancers, most (62.3%) occurred in the distal colon, and none had a BRAF mutation.
The five methylation subtypes also showed associations with consensus molecular subtypes (CMS) to varying degrees. The two strongest correlations were found in CIMP-H1 cancers and CIMP-H2 cancers, which were most frequently classified as CMS1 (69.6%) and CMS3 (54.5%), respectively.
Using CIBERSORT, the investigators detected a variety of associations between the five subtypes and stromal immune cell composition. For example, CIMP-H1 cases were enriched for macrophages, compared with the other subtypes, except CIMP-L2. Mast cells showed a stepwise relationship with subtype; they contributed the most to the immune microenvironment of CIMP-negative cancers and the least to cases classified as CIMP-H1. A converse trend was found with natural killer cells.
Of note, in CIMP-H1 and CIMP-H2 cancers, oncogenes were significantly more likely than tumor-suppressor genes to undergo gene body methylation, which is positively correlated with gene expression, and oncogenes in these subtypes had significantly greater gene body methylation than normal colonic mucosa.
“The five subtypes identified in this study are highly correlated with key clinical and molecular features, including patient age, tumor location, microsatellite instability, and oncogenic mitogen-activated protein kinase mutations,” they wrote. “We show that cancers with high DNA methylation show an increased preponderance for mutating genes involved in epigenetic regulation, and namely those that are implicated in the chromatin remodeling process.”
Concluding, the investigators explained the role of their research in future therapy development. “Our analyses have identified potentially druggable vulnerabilities in cancers of different methylation subtypes,” they wrote. “Inhibitors targeting synthetic lethalities, such as SWI/SNF component inhibitors for those with ARID mutations, should be evaluated because these agents may be clinically beneficial to certain patient subsets.”
The study was funded by the National Health and Medical Research Council, the US National Institutes of Health, Pathology Queensland, and others. The investigators disclosed no conflicts of interest.
SOURCE: Fennell L et al. CMGH. 2019 Apr 4. doi: 10.1016/j.jcmgh.2019.04.002.
Genomic, epigenomic, and transcriptomic information has revealed molecular subclasses of CRC, which has refined our understanding of the molecular and cellular biology of CRC and improved our treatment of patients with CRC. Several reliable and clinically useful molecular subtypes of colorectal cancer have been identified, including microsatellite unstable (MSI), chromosomal unstable (CIN), CpG island methylator phenotype (CIMP), and CMS 1-4 subtypes. Despite these substantial advances, it is also clear that we still only partially grasp the molecular and cellular biology driving CRC.
The studies by Fennell et al. provide new insights into the CIMP subtype of CRC that address this knowledge gap. Using a large CRC cohort and more detailed molecular information than available in prior studies, they have identified previously unrecognized CRC CIMP subtypes that have unique methylomes and mutation patterns. These 5 CIMP subclasses vary with regard to location in the colon, frequency of mutations in KRAS, BRAF, and MSI, as well as alterations in epigenetic regulatory genes. The observations related to differences in frequencies of MSI, and mutations in KRAS and BRAF help demystify the heterogeneity in clinical and cellular behavior that has been seen in the broader class of CIMP cancers. Perhaps most importantly, their studies identify plausible driver molecular alterations unique to the CIMP subclasses, such as subclass specific mutations in epigenetic regulatory genes and activated oncogenes. These are promising novel targets for chemoprevention strategies and therapies. Fennell and colleagues have now set the stage for functional studies of these molecular alterations to determine their true role in the cellular and clinical behavior of CRC.
William M. Grady, MD, is the Rodger C. Haggitt Professor of Medicine, department of medicine, division of gastroenterology, University of Washington School of Medicine, and clinical research division, Fred Hutchinson Cancer Research Center, Seattle. He is an advisory board member for Freenome and SEngine; has consulted for DiaCarta, Boehringer Ingelheim, and Guardant Health; and has conducted industry-sponsored research for Jannsenn and Cambridge Epigenetic.
Genomic, epigenomic, and transcriptomic information has revealed molecular subclasses of CRC, which has refined our understanding of the molecular and cellular biology of CRC and improved our treatment of patients with CRC. Several reliable and clinically useful molecular subtypes of colorectal cancer have been identified, including microsatellite unstable (MSI), chromosomal unstable (CIN), CpG island methylator phenotype (CIMP), and CMS 1-4 subtypes. Despite these substantial advances, it is also clear that we still only partially grasp the molecular and cellular biology driving CRC.
The studies by Fennell et al. provide new insights into the CIMP subtype of CRC that address this knowledge gap. Using a large CRC cohort and more detailed molecular information than available in prior studies, they have identified previously unrecognized CRC CIMP subtypes that have unique methylomes and mutation patterns. These 5 CIMP subclasses vary with regard to location in the colon, frequency of mutations in KRAS, BRAF, and MSI, as well as alterations in epigenetic regulatory genes. The observations related to differences in frequencies of MSI, and mutations in KRAS and BRAF help demystify the heterogeneity in clinical and cellular behavior that has been seen in the broader class of CIMP cancers. Perhaps most importantly, their studies identify plausible driver molecular alterations unique to the CIMP subclasses, such as subclass specific mutations in epigenetic regulatory genes and activated oncogenes. These are promising novel targets for chemoprevention strategies and therapies. Fennell and colleagues have now set the stage for functional studies of these molecular alterations to determine their true role in the cellular and clinical behavior of CRC.
William M. Grady, MD, is the Rodger C. Haggitt Professor of Medicine, department of medicine, division of gastroenterology, University of Washington School of Medicine, and clinical research division, Fred Hutchinson Cancer Research Center, Seattle. He is an advisory board member for Freenome and SEngine; has consulted for DiaCarta, Boehringer Ingelheim, and Guardant Health; and has conducted industry-sponsored research for Jannsenn and Cambridge Epigenetic.
Genomic, epigenomic, and transcriptomic information has revealed molecular subclasses of CRC, which has refined our understanding of the molecular and cellular biology of CRC and improved our treatment of patients with CRC. Several reliable and clinically useful molecular subtypes of colorectal cancer have been identified, including microsatellite unstable (MSI), chromosomal unstable (CIN), CpG island methylator phenotype (CIMP), and CMS 1-4 subtypes. Despite these substantial advances, it is also clear that we still only partially grasp the molecular and cellular biology driving CRC.
The studies by Fennell et al. provide new insights into the CIMP subtype of CRC that address this knowledge gap. Using a large CRC cohort and more detailed molecular information than available in prior studies, they have identified previously unrecognized CRC CIMP subtypes that have unique methylomes and mutation patterns. These 5 CIMP subclasses vary with regard to location in the colon, frequency of mutations in KRAS, BRAF, and MSI, as well as alterations in epigenetic regulatory genes. The observations related to differences in frequencies of MSI, and mutations in KRAS and BRAF help demystify the heterogeneity in clinical and cellular behavior that has been seen in the broader class of CIMP cancers. Perhaps most importantly, their studies identify plausible driver molecular alterations unique to the CIMP subclasses, such as subclass specific mutations in epigenetic regulatory genes and activated oncogenes. These are promising novel targets for chemoprevention strategies and therapies. Fennell and colleagues have now set the stage for functional studies of these molecular alterations to determine their true role in the cellular and clinical behavior of CRC.
William M. Grady, MD, is the Rodger C. Haggitt Professor of Medicine, department of medicine, division of gastroenterology, University of Washington School of Medicine, and clinical research division, Fred Hutchinson Cancer Research Center, Seattle. He is an advisory board member for Freenome and SEngine; has consulted for DiaCarta, Boehringer Ingelheim, and Guardant Health; and has conducted industry-sponsored research for Jannsenn and Cambridge Epigenetic.
Colorectal cancer can be divided into five DNA methylation subtypes that predict molecular and clinical behavior and may offer future therapeutic targets, according to investigators.
In 216 unselected colorectal cancers, five subtypes of the CpG island methylator phenotype (CIMP) showed “striking” associations with sex, age, and tumor location, reported lead author Lochlan Fennell, MD, of the QIMR Berghofer Medical Research Institute in Queensland, Australia, and colleagues. CIMP level increased with age in a stepwise fashion, they noted.
Further associations with CIMP subtype and BRAF mutation status support the investigators’ recent report that sessile serrated adenomas are rare in young patients and pose little risk of malignancy. With additional research, these findings could “inform the development of patient-centric surveillance for young and older patients who present with sessile serrated adenomas,” the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology.
“CIMP can be detected using a standardized marker panel to stratify tumors as CIMP-high, CIMP-low, or CIMP-negative.” In the present study, the investigators expanded these three existing subtypes into five subtypes, allowing for better prediction of clinical and molecular characteristics associated with disease progression.
Initial genomic testing showed that 13.4% of cases carried a BRAF V600E mutation, 34.7% were mutated at KRAS codon 12 or 13, and almost half of the patients (42.2%) had a TP53 mutation. Sorted into the three previously described subtypes, CIMP negative was most common (68.5%), followed by CIMP low (20.4%), and CIMP high (11.1%). About two-thirds (66%) of BRAF mutant cancers were CIMP high, compared with just 3% of BRAF wild-type cases (P less than .0001). KRAS mutated cases were more often CIMP-low than KRAS wild-type cancers (34.6% vs. 12.8%; P less than .001).
With use of Illumina HumanMethylation450 Bead Chip arrays and recursively partitioned mixed model clustering, five methylation clusters were identified; specifically, these were CIMP-H1 and CIMP-H2 (high methylation levels), CIMP-L1 and CIMP-L2 (intermediate methylation levels), and CIMP-negative (low methylation level). As described above, methylation level demonstrated a direct relationship with age, ranging from CIMP-negative (61.9 years) to CIMP-H1 (75.2 years). The investigators also reported unique characteristics of each new subtype. For instance, the CIMP-H1 cluster had many features in common with cases of serrated neoplasia, such as BRAF mutation positivity (73.9%; P less than .0001).
“BRAF mutations are a hallmark of the serrated neoplasia pathway, and indicate that these cancers probably arose in serrated precursor lesions,” the investigators wrote. “We previously showed that the colonoscopic incidence of sessile serrated adenomas does not differ between patients aged in their 30s and patients who are much older, whereas BRAF mutant cancers were restricted to older individuals, suggesting these BRAF mutant polyps may have limited malignant potential in young patients.”
In contrast with the CIMP-H1 cases, CIMP-H2 cancers were more often KRAS mutant (54.5% vs. 17.4%). Other findings revealed associations with subtype and location; for example, CIMP-L1 cases were located equally in the distal and proximal colon, whereas CIMP-L2 cases more often localized to the distal colon and rectum. Of note for CIMP-negative cancers, most (62.3%) occurred in the distal colon, and none had a BRAF mutation.
The five methylation subtypes also showed associations with consensus molecular subtypes (CMS) to varying degrees. The two strongest correlations were found in CIMP-H1 cancers and CIMP-H2 cancers, which were most frequently classified as CMS1 (69.6%) and CMS3 (54.5%), respectively.
Using CIBERSORT, the investigators detected a variety of associations between the five subtypes and stromal immune cell composition. For example, CIMP-H1 cases were enriched for macrophages, compared with the other subtypes, except CIMP-L2. Mast cells showed a stepwise relationship with subtype; they contributed the most to the immune microenvironment of CIMP-negative cancers and the least to cases classified as CIMP-H1. A converse trend was found with natural killer cells.
Of note, in CIMP-H1 and CIMP-H2 cancers, oncogenes were significantly more likely than tumor-suppressor genes to undergo gene body methylation, which is positively correlated with gene expression, and oncogenes in these subtypes had significantly greater gene body methylation than normal colonic mucosa.
“The five subtypes identified in this study are highly correlated with key clinical and molecular features, including patient age, tumor location, microsatellite instability, and oncogenic mitogen-activated protein kinase mutations,” they wrote. “We show that cancers with high DNA methylation show an increased preponderance for mutating genes involved in epigenetic regulation, and namely those that are implicated in the chromatin remodeling process.”
Concluding, the investigators explained the role of their research in future therapy development. “Our analyses have identified potentially druggable vulnerabilities in cancers of different methylation subtypes,” they wrote. “Inhibitors targeting synthetic lethalities, such as SWI/SNF component inhibitors for those with ARID mutations, should be evaluated because these agents may be clinically beneficial to certain patient subsets.”
The study was funded by the National Health and Medical Research Council, the US National Institutes of Health, Pathology Queensland, and others. The investigators disclosed no conflicts of interest.
SOURCE: Fennell L et al. CMGH. 2019 Apr 4. doi: 10.1016/j.jcmgh.2019.04.002.
Colorectal cancer can be divided into five DNA methylation subtypes that predict molecular and clinical behavior and may offer future therapeutic targets, according to investigators.
In 216 unselected colorectal cancers, five subtypes of the CpG island methylator phenotype (CIMP) showed “striking” associations with sex, age, and tumor location, reported lead author Lochlan Fennell, MD, of the QIMR Berghofer Medical Research Institute in Queensland, Australia, and colleagues. CIMP level increased with age in a stepwise fashion, they noted.
Further associations with CIMP subtype and BRAF mutation status support the investigators’ recent report that sessile serrated adenomas are rare in young patients and pose little risk of malignancy. With additional research, these findings could “inform the development of patient-centric surveillance for young and older patients who present with sessile serrated adenomas,” the investigators wrote in Cellular and Molecular Gastroenterology and Hepatology.
“CIMP can be detected using a standardized marker panel to stratify tumors as CIMP-high, CIMP-low, or CIMP-negative.” In the present study, the investigators expanded these three existing subtypes into five subtypes, allowing for better prediction of clinical and molecular characteristics associated with disease progression.
Initial genomic testing showed that 13.4% of cases carried a BRAF V600E mutation, 34.7% were mutated at KRAS codon 12 or 13, and almost half of the patients (42.2%) had a TP53 mutation. Sorted into the three previously described subtypes, CIMP negative was most common (68.5%), followed by CIMP low (20.4%), and CIMP high (11.1%). About two-thirds (66%) of BRAF mutant cancers were CIMP high, compared with just 3% of BRAF wild-type cases (P less than .0001). KRAS mutated cases were more often CIMP-low than KRAS wild-type cancers (34.6% vs. 12.8%; P less than .001).
With use of Illumina HumanMethylation450 Bead Chip arrays and recursively partitioned mixed model clustering, five methylation clusters were identified; specifically, these were CIMP-H1 and CIMP-H2 (high methylation levels), CIMP-L1 and CIMP-L2 (intermediate methylation levels), and CIMP-negative (low methylation level). As described above, methylation level demonstrated a direct relationship with age, ranging from CIMP-negative (61.9 years) to CIMP-H1 (75.2 years). The investigators also reported unique characteristics of each new subtype. For instance, the CIMP-H1 cluster had many features in common with cases of serrated neoplasia, such as BRAF mutation positivity (73.9%; P less than .0001).
“BRAF mutations are a hallmark of the serrated neoplasia pathway, and indicate that these cancers probably arose in serrated precursor lesions,” the investigators wrote. “We previously showed that the colonoscopic incidence of sessile serrated adenomas does not differ between patients aged in their 30s and patients who are much older, whereas BRAF mutant cancers were restricted to older individuals, suggesting these BRAF mutant polyps may have limited malignant potential in young patients.”
In contrast with the CIMP-H1 cases, CIMP-H2 cancers were more often KRAS mutant (54.5% vs. 17.4%). Other findings revealed associations with subtype and location; for example, CIMP-L1 cases were located equally in the distal and proximal colon, whereas CIMP-L2 cases more often localized to the distal colon and rectum. Of note for CIMP-negative cancers, most (62.3%) occurred in the distal colon, and none had a BRAF mutation.
The five methylation subtypes also showed associations with consensus molecular subtypes (CMS) to varying degrees. The two strongest correlations were found in CIMP-H1 cancers and CIMP-H2 cancers, which were most frequently classified as CMS1 (69.6%) and CMS3 (54.5%), respectively.
Using CIBERSORT, the investigators detected a variety of associations between the five subtypes and stromal immune cell composition. For example, CIMP-H1 cases were enriched for macrophages, compared with the other subtypes, except CIMP-L2. Mast cells showed a stepwise relationship with subtype; they contributed the most to the immune microenvironment of CIMP-negative cancers and the least to cases classified as CIMP-H1. A converse trend was found with natural killer cells.
Of note, in CIMP-H1 and CIMP-H2 cancers, oncogenes were significantly more likely than tumor-suppressor genes to undergo gene body methylation, which is positively correlated with gene expression, and oncogenes in these subtypes had significantly greater gene body methylation than normal colonic mucosa.
“The five subtypes identified in this study are highly correlated with key clinical and molecular features, including patient age, tumor location, microsatellite instability, and oncogenic mitogen-activated protein kinase mutations,” they wrote. “We show that cancers with high DNA methylation show an increased preponderance for mutating genes involved in epigenetic regulation, and namely those that are implicated in the chromatin remodeling process.”
Concluding, the investigators explained the role of their research in future therapy development. “Our analyses have identified potentially druggable vulnerabilities in cancers of different methylation subtypes,” they wrote. “Inhibitors targeting synthetic lethalities, such as SWI/SNF component inhibitors for those with ARID mutations, should be evaluated because these agents may be clinically beneficial to certain patient subsets.”
The study was funded by the National Health and Medical Research Council, the US National Institutes of Health, Pathology Queensland, and others. The investigators disclosed no conflicts of interest.
SOURCE: Fennell L et al. CMGH. 2019 Apr 4. doi: 10.1016/j.jcmgh.2019.04.002.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
The mesh mess, enmeshed in controversy
CASE Complications with mesh placement for SUI
A 47-year-old woman (G4 P3013) presents 5 months posthysterectomy with evidence of urinary tract infection (UTI). Escherichia coli is isolated, and she responds to antibiotic therapy.
Her surgical history includes a mini-sling procedure using a needleless device and mesh placement in order to correct progressive worsening of loss of urine when coughing and sneezing. She also reported slight pelvic pain, dysuria, and urgency upon urination at that time. After subsequent development of pelvic organ prolapse (POP), she underwent the vaginal hysterectomy.
Following her UTI treatment, a host of problems occur for the patient, including pelvic pain and dyspareunia. Her male partner reports “feeling something during sex,” especially at the anterior vaginal wall. A plain radiograph of the abdomen identifies a 2 cm x 2 cm stone over the vaginal mesh. In consultation with female pelvic medicine and reconstructive surgery subspecialists, lithotripsy is performed, with the stone fragmented. The patient remains symptomatic, however.
The mesh is noted to be eroding through the vaginal wall. An attempt is made to excise the mesh, initially via transuretheral resection, then through a laparoscopic approach. Due to the mesh being embedded in the tissue, however, an open approach is undertaken. Extensive excision of the mesh and stone fragments is performed. Postoperatively, the patient reports “dry vagina,” with no other genitourinary complaints.
The patient sues. She sues the mesh manufacturer. She also seeks to sue the gynecologist who placed the sling and vaginal mesh (as she says she was not informed of “all the risks” of vaginal mesh placement. She is part of a class action lawsuit, along with thousands of other women.
WHAT’S THE VERDICT?
The device manufacturer settled out of court with the class action suit. (The gynecologist was never formally a defendant because the patient/plaintiff was advised to “drop the physician from the suit.”) The attorneys representing the class action received 40% of the award plus presented costs for the representation. The class as a whole received a little more than 50% of the negotiated award. The patient in this case received $60,000.
Medical background
Stress urinary incontinence (SUI) is a prevalent condition; it affects 35% of women.1 Overall, 80% of women aged 80 or younger will undergo some form of surgery for POP during their lifetime.2 The pathophysiology of SUI includes urethral hypermobility and intrinsic sphincter deficiency.3
Surgical correction for urinary incontinence: A timeline
Use of the gracilis muscle flap to surgically correct urinary incontinence was introduced in 1907. This technique has been replaced by today’s more common Burch procedure, which was first described in 1961. Surgical mesh use dates back to the 1950s, when it was primarily used for abdominal hernia repair. Tension-free tape was introduced in 1995.4-6
Continue to: In the late 1990s the US Food and Drug Administration...
In the late 1990s the US Food and Drug Administration (FDA) permitted use of the first transvaginal meshes, which were designed to treat SUI—the midurethral sling. These mesh slings were so successful that similar meshes were developed to treat POP.7 Almost immediately there were problems with the new POP devices, and 3 years later Boston Scientific recalled its device.8 Nonetheless, the FDA cleared more than 150 devices using surgical mesh for urogynecologic indications (FIGURE).9
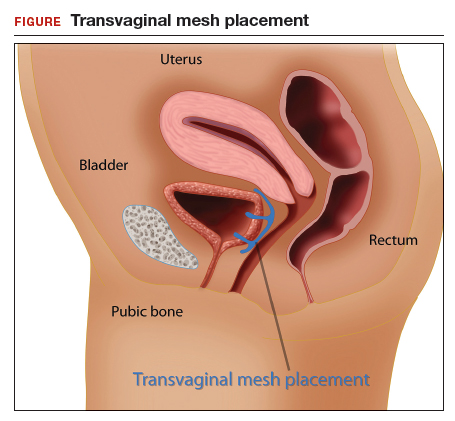
Mesh complications
Managing complications from intravesical mesh is a clinically challenging problem. Bladder perforation, stone formation, and penetration through the vagina can occur. Bladder-related complications can manifest as recurrent UTIs and obstructive urinary symptoms, especially in association with stone formation. From the gynecologic perspective, the more common complications with mesh utilization are pelvic pain, groin pain, dyspareunia, contracture and scarring of mesh, and narrowing of the vaginal canal.10 Mesh erosion problems will occur in an estimated 10% to 25% of transvaginal mesh POP implants.11
In 2008, a comparison of transvaginal mesh to native tissue repair (suture-based) or other (biologic) grafts was published.12 The bottom line: there is insufficient evidence to suggest that transvaginal mesh significantly improves outcomes for both posterior and apical defects.
Legal background
Mesh used for surgical purposes is a medical device, which legally is a product—a special product to be sure, but a product nonetheless. Products are subject to product liability rules. Mesh is also subject to an FDA regulatory system. We will briefly discuss products liability and the regulation of devices, both of which have played important roles in mesh-related injuries.
Products liability
As a general matter, defective products subject their manufacturer and seller to liability. There are several legal theories regarding product liability: negligence (in which the defect was caused through carelessness), breach of warranty or guarantee (in addition to express warranties, there are a number of implied warranties for products, including that it is fit for its intended purpose), and strict liability (there was a defect in the product, but it may not have been because of negligence). The product may be defective in the way it was designed, manufactured, or packaged, or it may be defective because adequate instructions and warning were not given to consumers.
Of course, not every product involved in an injury is defective—most automobile accidents, for example, are not the result of any defect in the automobile. In medicine, almost no product (device or pharmaceutical) is entirely safe. In some ways they are unavoidably unsafe and bound to cause some injuries. But when injuries are caused by a defect in the product (design or manufacturing defect or failure to warn), then there may be products liability. Most products liability cases arise under state law.
FDA’s device regulations
Both drugs and medical devices are subject to FDA review and ordinarily require some form of FDA clearance before they may be marketed. In the case of devices, the FDA has 3 classes, with an increase in risk to the user from Class I to III. Various levels of FDA review are required before marketing of the device is permitted, again with the intensity of review increasing from I to III as follows:
- Class I devices pose the least risk, have the least regulation, and are subject to general controls (ie, manufacturing and marketing practices).
- Class II devices pose slightly higher risks and are subject to special controls in addition to the criteria for Class I.
- Class III devices pose the most risk to patients and require premarket approval (scientific review and studies are required to ensure efficacy and safety).13
Continue to: There are a number of limits on manufacturer liability for defective devices...
There are a number of limits on manufacturer liability for defective devices. For Class III devices, the thorough FDA review of the safety of a device may limit the ability of an injured patient to sue based on the state product liability laws.14 For the most part, this “preemption” of state law has not played a major role in mesh litigation because they were initially classified as Class II devices which did not require or include a detailed FDA review.15
The duty to warn of the dangers and risk of medical devices means that manufacturers (or sellers) of devices are obligated to inform health care providers and other medical personnel of the risks. Unlike other manufacturers, device manufacturers do not have to directly warn consumers—because physicians deal directly with patients and prescribe the devices. Therefore, the health care providers, rather than the manufacturers, are obligated to inform the patient.16 This is known as the learned intermediary rule. Manufacturers may still be liable for failure to warn if they do not convey to health care providers proper warnings.
Manufacturers and sellers are not the only entities that may be subject to liability caused by medical devices. Hospitals or other entities that stock and care for devices are responsible for maintaining the safety and functionality of devices in their care.
Health care providers also may be responsible for injuries from medical devices. Generally, that liability is based on negligence. Negligence may relate to selecting an improper device, installing or using it incorrectly, or failing to give the patient adequate information (or informed consent) about the device and alternatives to it.17
A look at the mesh mess
There are a lot of distressing problems and professional disappointments in dissecting the “mesh mess,” including a failure of the FDA to regulate effectively, the extended sale and promotion of intrinsic sphincter deficiency mesh products, the improper use of mesh by physicians even after the risks were known, and, in some instances, the taking advantage of injured patients by attorneys and businesses.18 A lot of finger pointing also has occurred.19 We will recount some of the lowlights of this unfortunate tale.
Continue to: The FDA, in the 1990s, classified the first POP and SUI mesh...
The FDA, in the 1990s, classified the first POP and SUI mesh as Class II after deciding these products were “substantially equivalent” to older surgical meshes. This, of course, proved not to be the case.20 The FDA started receiving thousands of reports of adverse events and, in 2008, warned physicians to be vigilant for adverse events from the mesh. The FDA’s notification recommendations regarding mesh included the following13:
- Obtain specialized training for each mesh implantation technique, and be cognizant of risks.
- Be vigilant for potential adverse events from mesh, including erosion and infection.
- Be observant for complications associated with tools of transvaginal placement (ie, bowel, bladder, and vessel perforation).
- Inform patients that implantation of mesh is permanent and complications may require additional surgery for correction.
- Be aware that complications may affect quality of life—eg, pain with intercourse, scarring, and vaginal wall narrowing (POP repair).
- Provide patients with written copy of patient labeling from the surgical mesh manufacturer.
In 2011, the FDA issued a formal warning to providers that transvaginal mesh posed meaningful risks beyond nonmesh surgery. The FDA’s bulletin draws attention to how the mesh is placed more so than the material per se.19,21 Mesh was a Class II device for sacrocolpopexy or midurethral sling and, similarly, the transvaginal kit was also a Class II device. Overall, use of mesh midurethral slings has been well received as treatment for SUI. The FDA also accepted it for POP, however, but with increasingly strong warnings. The FDA’s 2011 communication stated, “This update is to inform you that serious complications associated with surgical mesh for transvaginal repair of POP are not rare….Furthermore, it is not clear that transvaginal POP repair with mesh is more effective than traditional non-mesh repair in all patients with POP and it may expose patients to greater risk.”7,13
In 2014 the FDA proposed reclassifying mesh to a Class III device, which would require that manufacturers obtain approval, based on safety and effectiveness, before selling mesh. Not until 2016 did the FDA actually reclassify the mess as Class III. Of course, during this time, mesh manufacturers were well aware of the substantial problems the products were causing.13
After serious problems with mesh became well known, and especially after FDA warnings, the use of mesh other than as indicated by the FDA was increasingly risky from a legal (as well as a health) standpoint. As long as mesh was still on the market, of course, it was available for use. But use of mesh for POP procedures without good indications in a way that was contrary to the FDA warnings might well be negligent.
Changes to informed consent
The FDA warnings also should have changed the informed consent for the use of mesh.22 Informed consent commonly consists of the following:
- informing the patient of the proposed procedure
- describing risks (and benefits) of the proposed process
- explaining reasonable alternatives
- noting the risks of taking no action.
Information that is material to a decision should be disclosed. If mesh were going to be used, after the problems of mesh were known and identified by the FDA (other than midurethral slings as treatment of SUI), the risks should have been clearly identified for patients, with alternatives outlined. The American College of Obstetricians and Gynecologists Committee on Ethics has 8 fundamental concepts with regard to informed consent that are worth keeping in mind23:
- Obtaining informed consent for medical treatment and research is an ethical requirement.
- The process expresses respect for the patient as a person.
- It protects patients against unwanted treatment and allows patients’ active involvement in medical planning and care.
- Communication is of paramount importance.
- Informed consent is a process and not a signature on a form.
- A commitment to informed consent and to provision of medical benefit to the patient are linked to provision of care.
- If obtaining informed consent is impossible, a designated surrogate should be identified representing the patient’s best interests.
- Knowledge on the part of the provider regarding state and federal requirements is necessary.
Continue to: Lawsuits line up...
Lawsuits line up
The widespread use of a product with a significant percentage of injuries and eventually with warnings about injuries from use sounds like the formula for a lot of lawsuits. This certainly has happened. A large number of suits—both class actions and individual actions—were filed as a result of mesh injuries.24 These suits were overwhelmingly against the manufacturer, although some included physicians.7 Device makers are more attractive defendants for several reasons. First, they have very deep pockets. In addition, jurors are generally much less sympathetic to large companies than to doctors. Large class actions meant that there were many different patients among the plaintiffs, and medical malpractice claims in most states have a number of trial difficulties not present in other product liability cases. Common defendants have included Johnson & Johnson, Boston Scientific, and Medtronic.
Some of the cases resulted in very large damage awards against manufacturers based on various kinds of product(s) liability. Many other cases were settled or tried with relatively small damages. There were, in addition, a number of instances in which the manufacturers were not liable. Of the 32 plaintiffs who have gone to trial thus far, 24 have obtained verdicts totaling $345 million ($14 million average). The cases that have settled have been for much less—perhaps $60,000 on average. A number of cases remain unresolved. To date, the estimate is that 100,000 women have received almost $8 billion from 7 device manufacturers to resolve claims.25
Some state attorneys general have gotten into the process as well. Attorneys general from California, Kentucky, Mississippi, and Washington have filed lawsuits against Johnson & Johnson, claiming that they deceived doctors and patients about the risks of their pelvic mesh. The states claim that marketing and instructional literature should have contained more information about the risks. Some physicians in these states have expressed concern that these lawsuit risks may do more harm than good because the suits conflate mesh used to treat incontinence with the more risky mesh for POP.26
The “ugly” of class action lawsuits
We have discussed both the sad (the injuries to patients) and the bad (the slow regulatory response and continuing injuries). (The ethics of the marketing by the manufacturers might also be raised as the bad.27) Next, let’s look briefly at the ugly.
Some of the patients affected by mesh injuries have been victimized a second time by medical “lenders” and some of their attorneys. Press reports describe patients with modest awards paying 40% in attorney fees (on the high side for personal injury settlements) plus extravagant costs—leaving modest amounts of actual recovery.25
Worse still, a process of “medical lending” has arisen in mesh cases.28 Medical lenders may contact mesh victims offering to pay up front for surgery to remove mesh, and then place a lien against the settlement for repayment at a much higher rate. They might pay the surgeon $2,500 for the surgery, but place a lien on the settlement amount for $60,000.29,30 In addition, there are allegations that lawyers may recruit the doctors to overstate the injuries or do unnecessary removal surgery because that will likely up the award.31 A quick Google search indicates dozens of offers of cash now for your mesh lawsuit (transvaginal and hernia repair).
The patient in our hypothetical case at the beginning had a fairly typical experience. She was a member of a class filing and received a modest settlement. The attorneys representing the class were allowed by the court to charge substantial attorneys’ fees and costs. The patient had the good sense to avoid medical lenders, although other members of the class did use medical lenders and are now filing complaints about the way they were treated by these lenders.
- Maintain surgical skills and be open to new technology. Medical practice requires constant updating and use of new and improved technology as it comes along. By definition, new technology often requires new skills and understanding. A significant portion of surgeons using mesh indicated that they had not read the instructions for use, or had done so only once.1 CME programs that include surgical education remain of particular value.
- Whether new technology or old, it is essential to keep up to date on all FDA bulletins pertinent to devices and pharmaceuticals that you use and prescribe. For example, in 2016 and 2018 the FDA warned that the use of a very old class of drugs (fluoroquinolones) should be limited. It advised "that the serious side effects associated with fluoroquinolones generally outweigh the benefits for patients with acute sinusitis, acute bronchitis, and uncomplicated urinary tract infections who have other treatment options. For patients with these conditions, fluoroquinolones should be reserved for those who do not have alternative treatment options."2 Continued, unnecessary prescriptions for fluoroquinolones would put a physician at some legal risk whether or not the physician had paid any attention to the warning.
- Informed consent is a very important legal and medical process. Take it seriously, and make sure the patient has the information necessary to make informed decisions about treatment. Document the process and the information provided. In some cases consider directing patients to appropriate literature or websites of the manufacturers.
- As to the use of mesh, if not following FDA advice, it is important to document the reason for this and to document the informed consent especially carefully.
- Follow patients after mesh placement for a minimum of 1 year and emphasize to patients they should convey signs and symptoms of complications from initial placement.3 High-risk patients should be of particular concern and be monitored very closely.
References
- Kirkpatrick G, Faber KD, Fromer DL. Transvaginal mesh placement and the instructions for use: a survey of North American urologists. J Urol. https://doi.org/10.1016/j.urpr.2018.05.004.
- FDA Drug Safety Communication: FDA advises restricting fluoroquinolone antibiotic use for certain uncomplicated infections; warns about disabling side effects that can occur together. July 26, 2016. https://www.fda.gov/Drugs/DrugSafety/ucm500143.htm. Accessed June 19, 2019.
- Karlovsky ME. How to avoid and deal with pelvic mesh litigation. Curr Urol Rep. 2016;17:55.
- Maral I, Ozkardeş H, Peşkircioğlu L, et al. Prevalence of stress urinary incontinence in both sexes at or after age 15 years: a cross-sectional study. J Urol. 2001;165:408-412.
- Olsen AL, Smith VJ, Bergstrom JO, et al. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89:501-506.
- Chang J, Lee D. Midurethral slings in the mesh litigation era. Transl Androl Urol. 2017;6(suppl 2): S68-S75.
- Mattingly R, ed. TeLinde's Operative Gynecology, 5th edition. Lippincott, William, and Wilkins: Philadelphia, PA; 1997.
- Burch J. Urethrovaginal fixation to Cooper's ligament for correction of stress incontinence, cystocele, and prolapse. Am J Obstet Gynecol. 1961;81:281-290.
- Ulmsten U, Falconer C, Johnson P, et al. A multicenter study of tension-free vaginal tape (TVT) for surgical treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1998;9:210-213.
- Kuhlmann-Capek MJ, Kilic GS, Shah AB, et al. Enmeshed in controversy: use of vaginal mesh in the current medicolegal environment. Female Pelvic Med Reconstr Surg. 2015;21:241-243.
- Powell SF. Changing our minds: reforming the FDA medical device reclassification process. Food Drug Law J. 2018;73:177-209.
- US Food and Drug Administration. Surgical Mesh for Treatment of Women with Pelvic Organ Prolapse and Stress Urinary Incontinence. September 2011. https://www.thesenatorsfirm.com/documents/OBS.pdf. Accessed June 19, 2019.
- Maher C, Feiner B, Baessler K, et al. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;(4):CD004014.
- Ganj FA, Ibeanu OA, Bedestani A, Nolan TE, Chesson RR. Complications of transvaginal monofilament polypropylene mesh in pelvic organ prolapse repair. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:919-925.
- Sung VW, Rogers RG, Schaffer JI, et al. Graft use in transvaginal pelvic organ prolapse repair: a systematic review. Obstet Gynecol. 2008;112:1131-1142.
- FDA public health notification: serious complications associated with transvaginal placement of surgical mesh in repair of pelvic organ prolapse and stress urinary incontinence. October 20, 2008. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/PublicHealthNotifications/ucm061976.htm. Accessed February 14, 2019.
- Riegel v. Medtronic, 552 U.S. 312 (2008).
- Whitney DW. Guide to preemption of state-law claims against Class III PMA medical devices. Food Drug Law J. 2010;65:113-139.
- Alam P, Iglesia CB. Informed consent for reconstructive pelvic surgery. Obstet Gynecol Clin North Am. 2016;43:131-139.
- Nosti PA, Iglesia CB. Medicolegal issues surrounding devices and mesh for surgical treatment of prolapse and incontinence. Clin Obstet Gynecol. 2013;56:221-228.
- Shepherd CG. Transvaginal mesh litigation: a new opportunity to resolve mass medical device failure claims. Tennessee Law Rev. 2012;80:3:477-94.
- Karlovsky ME. How to avoid and deal with pelvic mesh litigation. Curr Urol Rep. 2016;17:55.
- Cohn JA, Timbrook Brown E, Kowalik CG, et al. The mesh controversy. F1000Research website. https://f1000research.com/articles/5-2423/v1. Accessed June 17, 2019.
- Obstetrics and Gynecology Devices Panel Meeting, February 12, 2019. US Food and Drug Administration website. https://www.fda.gov/media/122867/download. Accessed June 19, 2019.
- Mucowski SJ, Jurnalov C, Phelps JY. Use of vaginal mesh in the face of recent FDA warnings and litigation. Am J Obstet Gynecol. 2010;203:103.e1-e4.
- American College of Obstetricians and Gynecologists Committee on Ethics. ACOG Committee Opinion No. 439: informed consent. Obstet Gynecol. 2009;114(2 pt 1):401-408.
- Souders CP, Eilber KS, McClelland L, et al. The truth behind transvaginal mesh litigation: devices, timelines, and provider characteristics. Female Pelvic Med Reconstr Surg. 2018;24:21-25.
- Goldstein M. As pelvic mesh settlements near $8 billion, women question lawyers' fees. New York Times. February 1, 2019. https://www.nytimes.com/2019/02/01/business/pelvic-mesh-settlements-lawyers.html. Accessed June 19, 2019.
- Johnson G. Surgeons fear pelvic mesh lawsuits will spook patients. Associated Press News. January 10, 2019. https://www.apnews.com/25777c3c33e3489283b1dc2ebdde6b55. Accessed June 19, 2019.
- Clarke RN. Medical device marketing and the ethics of vaginal mesh kit marketing. In The Innovation and Evolution of Medical Devices. New York, NY: Springer; 2019:103-123.
- Top 5 drug and medical device developments of 2018. Law 360. January 1, 2019. Accessed through LexisNexis.
- Frankel A, Dye J. The Lien Machine. New breed of investor profits by financing surgeries for desperate women patients. Reuters. August 18, 2015. https://www.reuters.com/investigates/special-report/usa-litigation-mesh/. Accessed June 19, 2019.
- Sullivan T. New report looks at intersection of "medical lending" and pelvic mesh lawsuits. Policy & Medicine. May 5, 2018. https://www.policymed.com/2015/08/medical-lending-and-pelvic-mesh-litigation.html. Accessed June 19, 2019.
- Goldstein M, Sliver-Greensberg J. How profiteers lure women into often-unneeded surgery. New York Times. April 14, 2018. https://www.nytimes.com/2018/04/14/business/vaginal-mesh-surgery-lawsuits-financing.html. Accessed June 19, 2019.
CASE Complications with mesh placement for SUI
A 47-year-old woman (G4 P3013) presents 5 months posthysterectomy with evidence of urinary tract infection (UTI). Escherichia coli is isolated, and she responds to antibiotic therapy.
Her surgical history includes a mini-sling procedure using a needleless device and mesh placement in order to correct progressive worsening of loss of urine when coughing and sneezing. She also reported slight pelvic pain, dysuria, and urgency upon urination at that time. After subsequent development of pelvic organ prolapse (POP), she underwent the vaginal hysterectomy.
Following her UTI treatment, a host of problems occur for the patient, including pelvic pain and dyspareunia. Her male partner reports “feeling something during sex,” especially at the anterior vaginal wall. A plain radiograph of the abdomen identifies a 2 cm x 2 cm stone over the vaginal mesh. In consultation with female pelvic medicine and reconstructive surgery subspecialists, lithotripsy is performed, with the stone fragmented. The patient remains symptomatic, however.
The mesh is noted to be eroding through the vaginal wall. An attempt is made to excise the mesh, initially via transuretheral resection, then through a laparoscopic approach. Due to the mesh being embedded in the tissue, however, an open approach is undertaken. Extensive excision of the mesh and stone fragments is performed. Postoperatively, the patient reports “dry vagina,” with no other genitourinary complaints.
The patient sues. She sues the mesh manufacturer. She also seeks to sue the gynecologist who placed the sling and vaginal mesh (as she says she was not informed of “all the risks” of vaginal mesh placement. She is part of a class action lawsuit, along with thousands of other women.
WHAT’S THE VERDICT?
The device manufacturer settled out of court with the class action suit. (The gynecologist was never formally a defendant because the patient/plaintiff was advised to “drop the physician from the suit.”) The attorneys representing the class action received 40% of the award plus presented costs for the representation. The class as a whole received a little more than 50% of the negotiated award. The patient in this case received $60,000.
Medical background
Stress urinary incontinence (SUI) is a prevalent condition; it affects 35% of women.1 Overall, 80% of women aged 80 or younger will undergo some form of surgery for POP during their lifetime.2 The pathophysiology of SUI includes urethral hypermobility and intrinsic sphincter deficiency.3
Surgical correction for urinary incontinence: A timeline
Use of the gracilis muscle flap to surgically correct urinary incontinence was introduced in 1907. This technique has been replaced by today’s more common Burch procedure, which was first described in 1961. Surgical mesh use dates back to the 1950s, when it was primarily used for abdominal hernia repair. Tension-free tape was introduced in 1995.4-6
Continue to: In the late 1990s the US Food and Drug Administration...
In the late 1990s the US Food and Drug Administration (FDA) permitted use of the first transvaginal meshes, which were designed to treat SUI—the midurethral sling. These mesh slings were so successful that similar meshes were developed to treat POP.7 Almost immediately there were problems with the new POP devices, and 3 years later Boston Scientific recalled its device.8 Nonetheless, the FDA cleared more than 150 devices using surgical mesh for urogynecologic indications (FIGURE).9
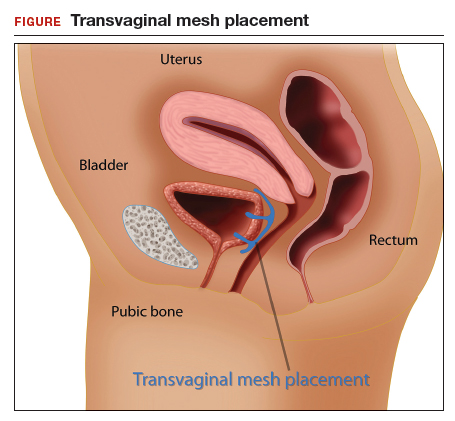
Mesh complications
Managing complications from intravesical mesh is a clinically challenging problem. Bladder perforation, stone formation, and penetration through the vagina can occur. Bladder-related complications can manifest as recurrent UTIs and obstructive urinary symptoms, especially in association with stone formation. From the gynecologic perspective, the more common complications with mesh utilization are pelvic pain, groin pain, dyspareunia, contracture and scarring of mesh, and narrowing of the vaginal canal.10 Mesh erosion problems will occur in an estimated 10% to 25% of transvaginal mesh POP implants.11
In 2008, a comparison of transvaginal mesh to native tissue repair (suture-based) or other (biologic) grafts was published.12 The bottom line: there is insufficient evidence to suggest that transvaginal mesh significantly improves outcomes for both posterior and apical defects.
Legal background
Mesh used for surgical purposes is a medical device, which legally is a product—a special product to be sure, but a product nonetheless. Products are subject to product liability rules. Mesh is also subject to an FDA regulatory system. We will briefly discuss products liability and the regulation of devices, both of which have played important roles in mesh-related injuries.
Products liability
As a general matter, defective products subject their manufacturer and seller to liability. There are several legal theories regarding product liability: negligence (in which the defect was caused through carelessness), breach of warranty or guarantee (in addition to express warranties, there are a number of implied warranties for products, including that it is fit for its intended purpose), and strict liability (there was a defect in the product, but it may not have been because of negligence). The product may be defective in the way it was designed, manufactured, or packaged, or it may be defective because adequate instructions and warning were not given to consumers.
Of course, not every product involved in an injury is defective—most automobile accidents, for example, are not the result of any defect in the automobile. In medicine, almost no product (device or pharmaceutical) is entirely safe. In some ways they are unavoidably unsafe and bound to cause some injuries. But when injuries are caused by a defect in the product (design or manufacturing defect or failure to warn), then there may be products liability. Most products liability cases arise under state law.
FDA’s device regulations
Both drugs and medical devices are subject to FDA review and ordinarily require some form of FDA clearance before they may be marketed. In the case of devices, the FDA has 3 classes, with an increase in risk to the user from Class I to III. Various levels of FDA review are required before marketing of the device is permitted, again with the intensity of review increasing from I to III as follows:
- Class I devices pose the least risk, have the least regulation, and are subject to general controls (ie, manufacturing and marketing practices).
- Class II devices pose slightly higher risks and are subject to special controls in addition to the criteria for Class I.
- Class III devices pose the most risk to patients and require premarket approval (scientific review and studies are required to ensure efficacy and safety).13
Continue to: There are a number of limits on manufacturer liability for defective devices...
There are a number of limits on manufacturer liability for defective devices. For Class III devices, the thorough FDA review of the safety of a device may limit the ability of an injured patient to sue based on the state product liability laws.14 For the most part, this “preemption” of state law has not played a major role in mesh litigation because they were initially classified as Class II devices which did not require or include a detailed FDA review.15
The duty to warn of the dangers and risk of medical devices means that manufacturers (or sellers) of devices are obligated to inform health care providers and other medical personnel of the risks. Unlike other manufacturers, device manufacturers do not have to directly warn consumers—because physicians deal directly with patients and prescribe the devices. Therefore, the health care providers, rather than the manufacturers, are obligated to inform the patient.16 This is known as the learned intermediary rule. Manufacturers may still be liable for failure to warn if they do not convey to health care providers proper warnings.
Manufacturers and sellers are not the only entities that may be subject to liability caused by medical devices. Hospitals or other entities that stock and care for devices are responsible for maintaining the safety and functionality of devices in their care.
Health care providers also may be responsible for injuries from medical devices. Generally, that liability is based on negligence. Negligence may relate to selecting an improper device, installing or using it incorrectly, or failing to give the patient adequate information (or informed consent) about the device and alternatives to it.17
A look at the mesh mess
There are a lot of distressing problems and professional disappointments in dissecting the “mesh mess,” including a failure of the FDA to regulate effectively, the extended sale and promotion of intrinsic sphincter deficiency mesh products, the improper use of mesh by physicians even after the risks were known, and, in some instances, the taking advantage of injured patients by attorneys and businesses.18 A lot of finger pointing also has occurred.19 We will recount some of the lowlights of this unfortunate tale.
Continue to: The FDA, in the 1990s, classified the first POP and SUI mesh...
The FDA, in the 1990s, classified the first POP and SUI mesh as Class II after deciding these products were “substantially equivalent” to older surgical meshes. This, of course, proved not to be the case.20 The FDA started receiving thousands of reports of adverse events and, in 2008, warned physicians to be vigilant for adverse events from the mesh. The FDA’s notification recommendations regarding mesh included the following13:
- Obtain specialized training for each mesh implantation technique, and be cognizant of risks.
- Be vigilant for potential adverse events from mesh, including erosion and infection.
- Be observant for complications associated with tools of transvaginal placement (ie, bowel, bladder, and vessel perforation).
- Inform patients that implantation of mesh is permanent and complications may require additional surgery for correction.
- Be aware that complications may affect quality of life—eg, pain with intercourse, scarring, and vaginal wall narrowing (POP repair).
- Provide patients with written copy of patient labeling from the surgical mesh manufacturer.
In 2011, the FDA issued a formal warning to providers that transvaginal mesh posed meaningful risks beyond nonmesh surgery. The FDA’s bulletin draws attention to how the mesh is placed more so than the material per se.19,21 Mesh was a Class II device for sacrocolpopexy or midurethral sling and, similarly, the transvaginal kit was also a Class II device. Overall, use of mesh midurethral slings has been well received as treatment for SUI. The FDA also accepted it for POP, however, but with increasingly strong warnings. The FDA’s 2011 communication stated, “This update is to inform you that serious complications associated with surgical mesh for transvaginal repair of POP are not rare….Furthermore, it is not clear that transvaginal POP repair with mesh is more effective than traditional non-mesh repair in all patients with POP and it may expose patients to greater risk.”7,13
In 2014 the FDA proposed reclassifying mesh to a Class III device, which would require that manufacturers obtain approval, based on safety and effectiveness, before selling mesh. Not until 2016 did the FDA actually reclassify the mess as Class III. Of course, during this time, mesh manufacturers were well aware of the substantial problems the products were causing.13
After serious problems with mesh became well known, and especially after FDA warnings, the use of mesh other than as indicated by the FDA was increasingly risky from a legal (as well as a health) standpoint. As long as mesh was still on the market, of course, it was available for use. But use of mesh for POP procedures without good indications in a way that was contrary to the FDA warnings might well be negligent.
Changes to informed consent
The FDA warnings also should have changed the informed consent for the use of mesh.22 Informed consent commonly consists of the following:
- informing the patient of the proposed procedure
- describing risks (and benefits) of the proposed process
- explaining reasonable alternatives
- noting the risks of taking no action.
Information that is material to a decision should be disclosed. If mesh were going to be used, after the problems of mesh were known and identified by the FDA (other than midurethral slings as treatment of SUI), the risks should have been clearly identified for patients, with alternatives outlined. The American College of Obstetricians and Gynecologists Committee on Ethics has 8 fundamental concepts with regard to informed consent that are worth keeping in mind23:
- Obtaining informed consent for medical treatment and research is an ethical requirement.
- The process expresses respect for the patient as a person.
- It protects patients against unwanted treatment and allows patients’ active involvement in medical planning and care.
- Communication is of paramount importance.
- Informed consent is a process and not a signature on a form.
- A commitment to informed consent and to provision of medical benefit to the patient are linked to provision of care.
- If obtaining informed consent is impossible, a designated surrogate should be identified representing the patient’s best interests.
- Knowledge on the part of the provider regarding state and federal requirements is necessary.
Continue to: Lawsuits line up...
Lawsuits line up
The widespread use of a product with a significant percentage of injuries and eventually with warnings about injuries from use sounds like the formula for a lot of lawsuits. This certainly has happened. A large number of suits—both class actions and individual actions—were filed as a result of mesh injuries.24 These suits were overwhelmingly against the manufacturer, although some included physicians.7 Device makers are more attractive defendants for several reasons. First, they have very deep pockets. In addition, jurors are generally much less sympathetic to large companies than to doctors. Large class actions meant that there were many different patients among the plaintiffs, and medical malpractice claims in most states have a number of trial difficulties not present in other product liability cases. Common defendants have included Johnson & Johnson, Boston Scientific, and Medtronic.
Some of the cases resulted in very large damage awards against manufacturers based on various kinds of product(s) liability. Many other cases were settled or tried with relatively small damages. There were, in addition, a number of instances in which the manufacturers were not liable. Of the 32 plaintiffs who have gone to trial thus far, 24 have obtained verdicts totaling $345 million ($14 million average). The cases that have settled have been for much less—perhaps $60,000 on average. A number of cases remain unresolved. To date, the estimate is that 100,000 women have received almost $8 billion from 7 device manufacturers to resolve claims.25
Some state attorneys general have gotten into the process as well. Attorneys general from California, Kentucky, Mississippi, and Washington have filed lawsuits against Johnson & Johnson, claiming that they deceived doctors and patients about the risks of their pelvic mesh. The states claim that marketing and instructional literature should have contained more information about the risks. Some physicians in these states have expressed concern that these lawsuit risks may do more harm than good because the suits conflate mesh used to treat incontinence with the more risky mesh for POP.26
The “ugly” of class action lawsuits
We have discussed both the sad (the injuries to patients) and the bad (the slow regulatory response and continuing injuries). (The ethics of the marketing by the manufacturers might also be raised as the bad.27) Next, let’s look briefly at the ugly.
Some of the patients affected by mesh injuries have been victimized a second time by medical “lenders” and some of their attorneys. Press reports describe patients with modest awards paying 40% in attorney fees (on the high side for personal injury settlements) plus extravagant costs—leaving modest amounts of actual recovery.25
Worse still, a process of “medical lending” has arisen in mesh cases.28 Medical lenders may contact mesh victims offering to pay up front for surgery to remove mesh, and then place a lien against the settlement for repayment at a much higher rate. They might pay the surgeon $2,500 for the surgery, but place a lien on the settlement amount for $60,000.29,30 In addition, there are allegations that lawyers may recruit the doctors to overstate the injuries or do unnecessary removal surgery because that will likely up the award.31 A quick Google search indicates dozens of offers of cash now for your mesh lawsuit (transvaginal and hernia repair).
The patient in our hypothetical case at the beginning had a fairly typical experience. She was a member of a class filing and received a modest settlement. The attorneys representing the class were allowed by the court to charge substantial attorneys’ fees and costs. The patient had the good sense to avoid medical lenders, although other members of the class did use medical lenders and are now filing complaints about the way they were treated by these lenders.
- Maintain surgical skills and be open to new technology. Medical practice requires constant updating and use of new and improved technology as it comes along. By definition, new technology often requires new skills and understanding. A significant portion of surgeons using mesh indicated that they had not read the instructions for use, or had done so only once.1 CME programs that include surgical education remain of particular value.
- Whether new technology or old, it is essential to keep up to date on all FDA bulletins pertinent to devices and pharmaceuticals that you use and prescribe. For example, in 2016 and 2018 the FDA warned that the use of a very old class of drugs (fluoroquinolones) should be limited. It advised "that the serious side effects associated with fluoroquinolones generally outweigh the benefits for patients with acute sinusitis, acute bronchitis, and uncomplicated urinary tract infections who have other treatment options. For patients with these conditions, fluoroquinolones should be reserved for those who do not have alternative treatment options."2 Continued, unnecessary prescriptions for fluoroquinolones would put a physician at some legal risk whether or not the physician had paid any attention to the warning.
- Informed consent is a very important legal and medical process. Take it seriously, and make sure the patient has the information necessary to make informed decisions about treatment. Document the process and the information provided. In some cases consider directing patients to appropriate literature or websites of the manufacturers.
- As to the use of mesh, if not following FDA advice, it is important to document the reason for this and to document the informed consent especially carefully.
- Follow patients after mesh placement for a minimum of 1 year and emphasize to patients they should convey signs and symptoms of complications from initial placement.3 High-risk patients should be of particular concern and be monitored very closely.
References
- Kirkpatrick G, Faber KD, Fromer DL. Transvaginal mesh placement and the instructions for use: a survey of North American urologists. J Urol. https://doi.org/10.1016/j.urpr.2018.05.004.
- FDA Drug Safety Communication: FDA advises restricting fluoroquinolone antibiotic use for certain uncomplicated infections; warns about disabling side effects that can occur together. July 26, 2016. https://www.fda.gov/Drugs/DrugSafety/ucm500143.htm. Accessed June 19, 2019.
- Karlovsky ME. How to avoid and deal with pelvic mesh litigation. Curr Urol Rep. 2016;17:55.
CASE Complications with mesh placement for SUI
A 47-year-old woman (G4 P3013) presents 5 months posthysterectomy with evidence of urinary tract infection (UTI). Escherichia coli is isolated, and she responds to antibiotic therapy.
Her surgical history includes a mini-sling procedure using a needleless device and mesh placement in order to correct progressive worsening of loss of urine when coughing and sneezing. She also reported slight pelvic pain, dysuria, and urgency upon urination at that time. After subsequent development of pelvic organ prolapse (POP), she underwent the vaginal hysterectomy.
Following her UTI treatment, a host of problems occur for the patient, including pelvic pain and dyspareunia. Her male partner reports “feeling something during sex,” especially at the anterior vaginal wall. A plain radiograph of the abdomen identifies a 2 cm x 2 cm stone over the vaginal mesh. In consultation with female pelvic medicine and reconstructive surgery subspecialists, lithotripsy is performed, with the stone fragmented. The patient remains symptomatic, however.
The mesh is noted to be eroding through the vaginal wall. An attempt is made to excise the mesh, initially via transuretheral resection, then through a laparoscopic approach. Due to the mesh being embedded in the tissue, however, an open approach is undertaken. Extensive excision of the mesh and stone fragments is performed. Postoperatively, the patient reports “dry vagina,” with no other genitourinary complaints.
The patient sues. She sues the mesh manufacturer. She also seeks to sue the gynecologist who placed the sling and vaginal mesh (as she says she was not informed of “all the risks” of vaginal mesh placement. She is part of a class action lawsuit, along with thousands of other women.
WHAT’S THE VERDICT?
The device manufacturer settled out of court with the class action suit. (The gynecologist was never formally a defendant because the patient/plaintiff was advised to “drop the physician from the suit.”) The attorneys representing the class action received 40% of the award plus presented costs for the representation. The class as a whole received a little more than 50% of the negotiated award. The patient in this case received $60,000.
Medical background
Stress urinary incontinence (SUI) is a prevalent condition; it affects 35% of women.1 Overall, 80% of women aged 80 or younger will undergo some form of surgery for POP during their lifetime.2 The pathophysiology of SUI includes urethral hypermobility and intrinsic sphincter deficiency.3
Surgical correction for urinary incontinence: A timeline
Use of the gracilis muscle flap to surgically correct urinary incontinence was introduced in 1907. This technique has been replaced by today’s more common Burch procedure, which was first described in 1961. Surgical mesh use dates back to the 1950s, when it was primarily used for abdominal hernia repair. Tension-free tape was introduced in 1995.4-6
Continue to: In the late 1990s the US Food and Drug Administration...
In the late 1990s the US Food and Drug Administration (FDA) permitted use of the first transvaginal meshes, which were designed to treat SUI—the midurethral sling. These mesh slings were so successful that similar meshes were developed to treat POP.7 Almost immediately there were problems with the new POP devices, and 3 years later Boston Scientific recalled its device.8 Nonetheless, the FDA cleared more than 150 devices using surgical mesh for urogynecologic indications (FIGURE).9
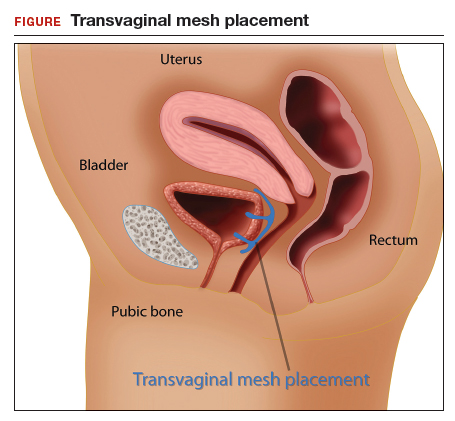
Mesh complications
Managing complications from intravesical mesh is a clinically challenging problem. Bladder perforation, stone formation, and penetration through the vagina can occur. Bladder-related complications can manifest as recurrent UTIs and obstructive urinary symptoms, especially in association with stone formation. From the gynecologic perspective, the more common complications with mesh utilization are pelvic pain, groin pain, dyspareunia, contracture and scarring of mesh, and narrowing of the vaginal canal.10 Mesh erosion problems will occur in an estimated 10% to 25% of transvaginal mesh POP implants.11
In 2008, a comparison of transvaginal mesh to native tissue repair (suture-based) or other (biologic) grafts was published.12 The bottom line: there is insufficient evidence to suggest that transvaginal mesh significantly improves outcomes for both posterior and apical defects.
Legal background
Mesh used for surgical purposes is a medical device, which legally is a product—a special product to be sure, but a product nonetheless. Products are subject to product liability rules. Mesh is also subject to an FDA regulatory system. We will briefly discuss products liability and the regulation of devices, both of which have played important roles in mesh-related injuries.
Products liability
As a general matter, defective products subject their manufacturer and seller to liability. There are several legal theories regarding product liability: negligence (in which the defect was caused through carelessness), breach of warranty or guarantee (in addition to express warranties, there are a number of implied warranties for products, including that it is fit for its intended purpose), and strict liability (there was a defect in the product, but it may not have been because of negligence). The product may be defective in the way it was designed, manufactured, or packaged, or it may be defective because adequate instructions and warning were not given to consumers.
Of course, not every product involved in an injury is defective—most automobile accidents, for example, are not the result of any defect in the automobile. In medicine, almost no product (device or pharmaceutical) is entirely safe. In some ways they are unavoidably unsafe and bound to cause some injuries. But when injuries are caused by a defect in the product (design or manufacturing defect or failure to warn), then there may be products liability. Most products liability cases arise under state law.
FDA’s device regulations
Both drugs and medical devices are subject to FDA review and ordinarily require some form of FDA clearance before they may be marketed. In the case of devices, the FDA has 3 classes, with an increase in risk to the user from Class I to III. Various levels of FDA review are required before marketing of the device is permitted, again with the intensity of review increasing from I to III as follows:
- Class I devices pose the least risk, have the least regulation, and are subject to general controls (ie, manufacturing and marketing practices).
- Class II devices pose slightly higher risks and are subject to special controls in addition to the criteria for Class I.
- Class III devices pose the most risk to patients and require premarket approval (scientific review and studies are required to ensure efficacy and safety).13
Continue to: There are a number of limits on manufacturer liability for defective devices...
There are a number of limits on manufacturer liability for defective devices. For Class III devices, the thorough FDA review of the safety of a device may limit the ability of an injured patient to sue based on the state product liability laws.14 For the most part, this “preemption” of state law has not played a major role in mesh litigation because they were initially classified as Class II devices which did not require or include a detailed FDA review.15
The duty to warn of the dangers and risk of medical devices means that manufacturers (or sellers) of devices are obligated to inform health care providers and other medical personnel of the risks. Unlike other manufacturers, device manufacturers do not have to directly warn consumers—because physicians deal directly with patients and prescribe the devices. Therefore, the health care providers, rather than the manufacturers, are obligated to inform the patient.16 This is known as the learned intermediary rule. Manufacturers may still be liable for failure to warn if they do not convey to health care providers proper warnings.
Manufacturers and sellers are not the only entities that may be subject to liability caused by medical devices. Hospitals or other entities that stock and care for devices are responsible for maintaining the safety and functionality of devices in their care.
Health care providers also may be responsible for injuries from medical devices. Generally, that liability is based on negligence. Negligence may relate to selecting an improper device, installing or using it incorrectly, or failing to give the patient adequate information (or informed consent) about the device and alternatives to it.17
A look at the mesh mess
There are a lot of distressing problems and professional disappointments in dissecting the “mesh mess,” including a failure of the FDA to regulate effectively, the extended sale and promotion of intrinsic sphincter deficiency mesh products, the improper use of mesh by physicians even after the risks were known, and, in some instances, the taking advantage of injured patients by attorneys and businesses.18 A lot of finger pointing also has occurred.19 We will recount some of the lowlights of this unfortunate tale.
Continue to: The FDA, in the 1990s, classified the first POP and SUI mesh...
The FDA, in the 1990s, classified the first POP and SUI mesh as Class II after deciding these products were “substantially equivalent” to older surgical meshes. This, of course, proved not to be the case.20 The FDA started receiving thousands of reports of adverse events and, in 2008, warned physicians to be vigilant for adverse events from the mesh. The FDA’s notification recommendations regarding mesh included the following13:
- Obtain specialized training for each mesh implantation technique, and be cognizant of risks.
- Be vigilant for potential adverse events from mesh, including erosion and infection.
- Be observant for complications associated with tools of transvaginal placement (ie, bowel, bladder, and vessel perforation).
- Inform patients that implantation of mesh is permanent and complications may require additional surgery for correction.
- Be aware that complications may affect quality of life—eg, pain with intercourse, scarring, and vaginal wall narrowing (POP repair).
- Provide patients with written copy of patient labeling from the surgical mesh manufacturer.
In 2011, the FDA issued a formal warning to providers that transvaginal mesh posed meaningful risks beyond nonmesh surgery. The FDA’s bulletin draws attention to how the mesh is placed more so than the material per se.19,21 Mesh was a Class II device for sacrocolpopexy or midurethral sling and, similarly, the transvaginal kit was also a Class II device. Overall, use of mesh midurethral slings has been well received as treatment for SUI. The FDA also accepted it for POP, however, but with increasingly strong warnings. The FDA’s 2011 communication stated, “This update is to inform you that serious complications associated with surgical mesh for transvaginal repair of POP are not rare….Furthermore, it is not clear that transvaginal POP repair with mesh is more effective than traditional non-mesh repair in all patients with POP and it may expose patients to greater risk.”7,13
In 2014 the FDA proposed reclassifying mesh to a Class III device, which would require that manufacturers obtain approval, based on safety and effectiveness, before selling mesh. Not until 2016 did the FDA actually reclassify the mess as Class III. Of course, during this time, mesh manufacturers were well aware of the substantial problems the products were causing.13
After serious problems with mesh became well known, and especially after FDA warnings, the use of mesh other than as indicated by the FDA was increasingly risky from a legal (as well as a health) standpoint. As long as mesh was still on the market, of course, it was available for use. But use of mesh for POP procedures without good indications in a way that was contrary to the FDA warnings might well be negligent.
Changes to informed consent
The FDA warnings also should have changed the informed consent for the use of mesh.22 Informed consent commonly consists of the following:
- informing the patient of the proposed procedure
- describing risks (and benefits) of the proposed process
- explaining reasonable alternatives
- noting the risks of taking no action.
Information that is material to a decision should be disclosed. If mesh were going to be used, after the problems of mesh were known and identified by the FDA (other than midurethral slings as treatment of SUI), the risks should have been clearly identified for patients, with alternatives outlined. The American College of Obstetricians and Gynecologists Committee on Ethics has 8 fundamental concepts with regard to informed consent that are worth keeping in mind23:
- Obtaining informed consent for medical treatment and research is an ethical requirement.
- The process expresses respect for the patient as a person.
- It protects patients against unwanted treatment and allows patients’ active involvement in medical planning and care.
- Communication is of paramount importance.
- Informed consent is a process and not a signature on a form.
- A commitment to informed consent and to provision of medical benefit to the patient are linked to provision of care.
- If obtaining informed consent is impossible, a designated surrogate should be identified representing the patient’s best interests.
- Knowledge on the part of the provider regarding state and federal requirements is necessary.
Continue to: Lawsuits line up...
Lawsuits line up
The widespread use of a product with a significant percentage of injuries and eventually with warnings about injuries from use sounds like the formula for a lot of lawsuits. This certainly has happened. A large number of suits—both class actions and individual actions—were filed as a result of mesh injuries.24 These suits were overwhelmingly against the manufacturer, although some included physicians.7 Device makers are more attractive defendants for several reasons. First, they have very deep pockets. In addition, jurors are generally much less sympathetic to large companies than to doctors. Large class actions meant that there were many different patients among the plaintiffs, and medical malpractice claims in most states have a number of trial difficulties not present in other product liability cases. Common defendants have included Johnson & Johnson, Boston Scientific, and Medtronic.
Some of the cases resulted in very large damage awards against manufacturers based on various kinds of product(s) liability. Many other cases were settled or tried with relatively small damages. There were, in addition, a number of instances in which the manufacturers were not liable. Of the 32 plaintiffs who have gone to trial thus far, 24 have obtained verdicts totaling $345 million ($14 million average). The cases that have settled have been for much less—perhaps $60,000 on average. A number of cases remain unresolved. To date, the estimate is that 100,000 women have received almost $8 billion from 7 device manufacturers to resolve claims.25
Some state attorneys general have gotten into the process as well. Attorneys general from California, Kentucky, Mississippi, and Washington have filed lawsuits against Johnson & Johnson, claiming that they deceived doctors and patients about the risks of their pelvic mesh. The states claim that marketing and instructional literature should have contained more information about the risks. Some physicians in these states have expressed concern that these lawsuit risks may do more harm than good because the suits conflate mesh used to treat incontinence with the more risky mesh for POP.26
The “ugly” of class action lawsuits
We have discussed both the sad (the injuries to patients) and the bad (the slow regulatory response and continuing injuries). (The ethics of the marketing by the manufacturers might also be raised as the bad.27) Next, let’s look briefly at the ugly.
Some of the patients affected by mesh injuries have been victimized a second time by medical “lenders” and some of their attorneys. Press reports describe patients with modest awards paying 40% in attorney fees (on the high side for personal injury settlements) plus extravagant costs—leaving modest amounts of actual recovery.25
Worse still, a process of “medical lending” has arisen in mesh cases.28 Medical lenders may contact mesh victims offering to pay up front for surgery to remove mesh, and then place a lien against the settlement for repayment at a much higher rate. They might pay the surgeon $2,500 for the surgery, but place a lien on the settlement amount for $60,000.29,30 In addition, there are allegations that lawyers may recruit the doctors to overstate the injuries or do unnecessary removal surgery because that will likely up the award.31 A quick Google search indicates dozens of offers of cash now for your mesh lawsuit (transvaginal and hernia repair).
The patient in our hypothetical case at the beginning had a fairly typical experience. She was a member of a class filing and received a modest settlement. The attorneys representing the class were allowed by the court to charge substantial attorneys’ fees and costs. The patient had the good sense to avoid medical lenders, although other members of the class did use medical lenders and are now filing complaints about the way they were treated by these lenders.
- Maintain surgical skills and be open to new technology. Medical practice requires constant updating and use of new and improved technology as it comes along. By definition, new technology often requires new skills and understanding. A significant portion of surgeons using mesh indicated that they had not read the instructions for use, or had done so only once.1 CME programs that include surgical education remain of particular value.
- Whether new technology or old, it is essential to keep up to date on all FDA bulletins pertinent to devices and pharmaceuticals that you use and prescribe. For example, in 2016 and 2018 the FDA warned that the use of a very old class of drugs (fluoroquinolones) should be limited. It advised "that the serious side effects associated with fluoroquinolones generally outweigh the benefits for patients with acute sinusitis, acute bronchitis, and uncomplicated urinary tract infections who have other treatment options. For patients with these conditions, fluoroquinolones should be reserved for those who do not have alternative treatment options."2 Continued, unnecessary prescriptions for fluoroquinolones would put a physician at some legal risk whether or not the physician had paid any attention to the warning.
- Informed consent is a very important legal and medical process. Take it seriously, and make sure the patient has the information necessary to make informed decisions about treatment. Document the process and the information provided. In some cases consider directing patients to appropriate literature or websites of the manufacturers.
- As to the use of mesh, if not following FDA advice, it is important to document the reason for this and to document the informed consent especially carefully.
- Follow patients after mesh placement for a minimum of 1 year and emphasize to patients they should convey signs and symptoms of complications from initial placement.3 High-risk patients should be of particular concern and be monitored very closely.
References
- Kirkpatrick G, Faber KD, Fromer DL. Transvaginal mesh placement and the instructions for use: a survey of North American urologists. J Urol. https://doi.org/10.1016/j.urpr.2018.05.004.
- FDA Drug Safety Communication: FDA advises restricting fluoroquinolone antibiotic use for certain uncomplicated infections; warns about disabling side effects that can occur together. July 26, 2016. https://www.fda.gov/Drugs/DrugSafety/ucm500143.htm. Accessed June 19, 2019.
- Karlovsky ME. How to avoid and deal with pelvic mesh litigation. Curr Urol Rep. 2016;17:55.
- Maral I, Ozkardeş H, Peşkircioğlu L, et al. Prevalence of stress urinary incontinence in both sexes at or after age 15 years: a cross-sectional study. J Urol. 2001;165:408-412.
- Olsen AL, Smith VJ, Bergstrom JO, et al. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89:501-506.
- Chang J, Lee D. Midurethral slings in the mesh litigation era. Transl Androl Urol. 2017;6(suppl 2): S68-S75.
- Mattingly R, ed. TeLinde's Operative Gynecology, 5th edition. Lippincott, William, and Wilkins: Philadelphia, PA; 1997.
- Burch J. Urethrovaginal fixation to Cooper's ligament for correction of stress incontinence, cystocele, and prolapse. Am J Obstet Gynecol. 1961;81:281-290.
- Ulmsten U, Falconer C, Johnson P, et al. A multicenter study of tension-free vaginal tape (TVT) for surgical treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1998;9:210-213.
- Kuhlmann-Capek MJ, Kilic GS, Shah AB, et al. Enmeshed in controversy: use of vaginal mesh in the current medicolegal environment. Female Pelvic Med Reconstr Surg. 2015;21:241-243.
- Powell SF. Changing our minds: reforming the FDA medical device reclassification process. Food Drug Law J. 2018;73:177-209.
- US Food and Drug Administration. Surgical Mesh for Treatment of Women with Pelvic Organ Prolapse and Stress Urinary Incontinence. September 2011. https://www.thesenatorsfirm.com/documents/OBS.pdf. Accessed June 19, 2019.
- Maher C, Feiner B, Baessler K, et al. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;(4):CD004014.
- Ganj FA, Ibeanu OA, Bedestani A, Nolan TE, Chesson RR. Complications of transvaginal monofilament polypropylene mesh in pelvic organ prolapse repair. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:919-925.
- Sung VW, Rogers RG, Schaffer JI, et al. Graft use in transvaginal pelvic organ prolapse repair: a systematic review. Obstet Gynecol. 2008;112:1131-1142.
- FDA public health notification: serious complications associated with transvaginal placement of surgical mesh in repair of pelvic organ prolapse and stress urinary incontinence. October 20, 2008. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/PublicHealthNotifications/ucm061976.htm. Accessed February 14, 2019.
- Riegel v. Medtronic, 552 U.S. 312 (2008).
- Whitney DW. Guide to preemption of state-law claims against Class III PMA medical devices. Food Drug Law J. 2010;65:113-139.
- Alam P, Iglesia CB. Informed consent for reconstructive pelvic surgery. Obstet Gynecol Clin North Am. 2016;43:131-139.
- Nosti PA, Iglesia CB. Medicolegal issues surrounding devices and mesh for surgical treatment of prolapse and incontinence. Clin Obstet Gynecol. 2013;56:221-228.
- Shepherd CG. Transvaginal mesh litigation: a new opportunity to resolve mass medical device failure claims. Tennessee Law Rev. 2012;80:3:477-94.
- Karlovsky ME. How to avoid and deal with pelvic mesh litigation. Curr Urol Rep. 2016;17:55.
- Cohn JA, Timbrook Brown E, Kowalik CG, et al. The mesh controversy. F1000Research website. https://f1000research.com/articles/5-2423/v1. Accessed June 17, 2019.
- Obstetrics and Gynecology Devices Panel Meeting, February 12, 2019. US Food and Drug Administration website. https://www.fda.gov/media/122867/download. Accessed June 19, 2019.
- Mucowski SJ, Jurnalov C, Phelps JY. Use of vaginal mesh in the face of recent FDA warnings and litigation. Am J Obstet Gynecol. 2010;203:103.e1-e4.
- American College of Obstetricians and Gynecologists Committee on Ethics. ACOG Committee Opinion No. 439: informed consent. Obstet Gynecol. 2009;114(2 pt 1):401-408.
- Souders CP, Eilber KS, McClelland L, et al. The truth behind transvaginal mesh litigation: devices, timelines, and provider characteristics. Female Pelvic Med Reconstr Surg. 2018;24:21-25.
- Goldstein M. As pelvic mesh settlements near $8 billion, women question lawyers' fees. New York Times. February 1, 2019. https://www.nytimes.com/2019/02/01/business/pelvic-mesh-settlements-lawyers.html. Accessed June 19, 2019.
- Johnson G. Surgeons fear pelvic mesh lawsuits will spook patients. Associated Press News. January 10, 2019. https://www.apnews.com/25777c3c33e3489283b1dc2ebdde6b55. Accessed June 19, 2019.
- Clarke RN. Medical device marketing and the ethics of vaginal mesh kit marketing. In The Innovation and Evolution of Medical Devices. New York, NY: Springer; 2019:103-123.
- Top 5 drug and medical device developments of 2018. Law 360. January 1, 2019. Accessed through LexisNexis.
- Frankel A, Dye J. The Lien Machine. New breed of investor profits by financing surgeries for desperate women patients. Reuters. August 18, 2015. https://www.reuters.com/investigates/special-report/usa-litigation-mesh/. Accessed June 19, 2019.
- Sullivan T. New report looks at intersection of "medical lending" and pelvic mesh lawsuits. Policy & Medicine. May 5, 2018. https://www.policymed.com/2015/08/medical-lending-and-pelvic-mesh-litigation.html. Accessed June 19, 2019.
- Goldstein M, Sliver-Greensberg J. How profiteers lure women into often-unneeded surgery. New York Times. April 14, 2018. https://www.nytimes.com/2018/04/14/business/vaginal-mesh-surgery-lawsuits-financing.html. Accessed June 19, 2019.
- Maral I, Ozkardeş H, Peşkircioğlu L, et al. Prevalence of stress urinary incontinence in both sexes at or after age 15 years: a cross-sectional study. J Urol. 2001;165:408-412.
- Olsen AL, Smith VJ, Bergstrom JO, et al. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89:501-506.
- Chang J, Lee D. Midurethral slings in the mesh litigation era. Transl Androl Urol. 2017;6(suppl 2): S68-S75.
- Mattingly R, ed. TeLinde's Operative Gynecology, 5th edition. Lippincott, William, and Wilkins: Philadelphia, PA; 1997.
- Burch J. Urethrovaginal fixation to Cooper's ligament for correction of stress incontinence, cystocele, and prolapse. Am J Obstet Gynecol. 1961;81:281-290.
- Ulmsten U, Falconer C, Johnson P, et al. A multicenter study of tension-free vaginal tape (TVT) for surgical treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1998;9:210-213.
- Kuhlmann-Capek MJ, Kilic GS, Shah AB, et al. Enmeshed in controversy: use of vaginal mesh in the current medicolegal environment. Female Pelvic Med Reconstr Surg. 2015;21:241-243.
- Powell SF. Changing our minds: reforming the FDA medical device reclassification process. Food Drug Law J. 2018;73:177-209.
- US Food and Drug Administration. Surgical Mesh for Treatment of Women with Pelvic Organ Prolapse and Stress Urinary Incontinence. September 2011. https://www.thesenatorsfirm.com/documents/OBS.pdf. Accessed June 19, 2019.
- Maher C, Feiner B, Baessler K, et al. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;(4):CD004014.
- Ganj FA, Ibeanu OA, Bedestani A, Nolan TE, Chesson RR. Complications of transvaginal monofilament polypropylene mesh in pelvic organ prolapse repair. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:919-925.
- Sung VW, Rogers RG, Schaffer JI, et al. Graft use in transvaginal pelvic organ prolapse repair: a systematic review. Obstet Gynecol. 2008;112:1131-1142.
- FDA public health notification: serious complications associated with transvaginal placement of surgical mesh in repair of pelvic organ prolapse and stress urinary incontinence. October 20, 2008. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/PublicHealthNotifications/ucm061976.htm. Accessed February 14, 2019.
- Riegel v. Medtronic, 552 U.S. 312 (2008).
- Whitney DW. Guide to preemption of state-law claims against Class III PMA medical devices. Food Drug Law J. 2010;65:113-139.
- Alam P, Iglesia CB. Informed consent for reconstructive pelvic surgery. Obstet Gynecol Clin North Am. 2016;43:131-139.
- Nosti PA, Iglesia CB. Medicolegal issues surrounding devices and mesh for surgical treatment of prolapse and incontinence. Clin Obstet Gynecol. 2013;56:221-228.
- Shepherd CG. Transvaginal mesh litigation: a new opportunity to resolve mass medical device failure claims. Tennessee Law Rev. 2012;80:3:477-94.
- Karlovsky ME. How to avoid and deal with pelvic mesh litigation. Curr Urol Rep. 2016;17:55.
- Cohn JA, Timbrook Brown E, Kowalik CG, et al. The mesh controversy. F1000Research website. https://f1000research.com/articles/5-2423/v1. Accessed June 17, 2019.
- Obstetrics and Gynecology Devices Panel Meeting, February 12, 2019. US Food and Drug Administration website. https://www.fda.gov/media/122867/download. Accessed June 19, 2019.
- Mucowski SJ, Jurnalov C, Phelps JY. Use of vaginal mesh in the face of recent FDA warnings and litigation. Am J Obstet Gynecol. 2010;203:103.e1-e4.
- American College of Obstetricians and Gynecologists Committee on Ethics. ACOG Committee Opinion No. 439: informed consent. Obstet Gynecol. 2009;114(2 pt 1):401-408.
- Souders CP, Eilber KS, McClelland L, et al. The truth behind transvaginal mesh litigation: devices, timelines, and provider characteristics. Female Pelvic Med Reconstr Surg. 2018;24:21-25.
- Goldstein M. As pelvic mesh settlements near $8 billion, women question lawyers' fees. New York Times. February 1, 2019. https://www.nytimes.com/2019/02/01/business/pelvic-mesh-settlements-lawyers.html. Accessed June 19, 2019.
- Johnson G. Surgeons fear pelvic mesh lawsuits will spook patients. Associated Press News. January 10, 2019. https://www.apnews.com/25777c3c33e3489283b1dc2ebdde6b55. Accessed June 19, 2019.
- Clarke RN. Medical device marketing and the ethics of vaginal mesh kit marketing. In The Innovation and Evolution of Medical Devices. New York, NY: Springer; 2019:103-123.
- Top 5 drug and medical device developments of 2018. Law 360. January 1, 2019. Accessed through LexisNexis.
- Frankel A, Dye J. The Lien Machine. New breed of investor profits by financing surgeries for desperate women patients. Reuters. August 18, 2015. https://www.reuters.com/investigates/special-report/usa-litigation-mesh/. Accessed June 19, 2019.
- Sullivan T. New report looks at intersection of "medical lending" and pelvic mesh lawsuits. Policy & Medicine. May 5, 2018. https://www.policymed.com/2015/08/medical-lending-and-pelvic-mesh-litigation.html. Accessed June 19, 2019.
- Goldstein M, Sliver-Greensberg J. How profiteers lure women into often-unneeded surgery. New York Times. April 14, 2018. https://www.nytimes.com/2018/04/14/business/vaginal-mesh-surgery-lawsuits-financing.html. Accessed June 19, 2019.