User login
Beware of natural fruit and nut ingredients in latex-allergic patients
It has been 40 years since the first reported case of IgE-mediated natural rubber latex allergy, which was soon followed by a global epidemic of allergic and anaphylactic reactions.1,2 Resolution came through insightful work in the 1990s that led to the removal of cornstarch powder and a switch to nonpowdered latex and synthetic examination gloves.2 Also discovered during this period was the cross-reactivity of many patients to latex and various fruits.
Research substantiates reports
Blanco et al. conducted a prospective study in their outpatient clinic in 25 patients diagnosed with latex allergy, published in 1994.They used a clinical questionnaire, skin-prick tests, skin test with a latex extract, and identification of total and specific IgE to help ascertain clinical characteristics and cross-reactivity. Of the 23 women and 2 men in the study (mean age 33, plus or minus 9 years), 9 (36%) experienced latex-induced reactions characterized by systemic anaphylaxis. In 13 patients (52%), 42 food allergies were identified, and 23 included systemic anaphylaxis. Avocado (9), chestnut (9), banana (7), kiwi (5), and papaya (3) were the most common foods to cause hypersensitivities. The researchers concluded that their small study supported the reality of a “latex-fruit syndrome.”3
Another study aimed to characterize the cross-reactivity of latex and foods and evaluate clinical significance. Beezhold et al. examined 47 patients allergic to latex and 46 nonallergic controls. The investigators found immunologic reactivity to foods to be prevalent (33 latex-allergic patients and seven controls), with 27% of food skin-prick tests positive in the latex-allergic group. In addition, clinical symptoms were linked to 27% of positive skin-prick tests. Among the 17 patients who displayed clinical allergies to at least one food, 14 showed local sensitivity reactions, with anaphylaxis noted in 11. Avocado (53%), potato (40%), banana (38%), tomato (28%), chestnut (28%), and kiwi (17%) were the foods most frequently cited for provoking a skin test reaction. The authors observed extensive cross-reactivity between latex sensitivity and particular foods, with potatoes and tomatoes reported for the first time.4
In 1997, Brehler et al. studied serum samples from 136 patients whose immediate hypersensitivity to latex proteins was clinically observable and documented. The samples were assessed for IgE antibodies against several fruits, with fruit-specific IgE antibodies recorded in 69.1%. Radioallergosorbent (RAST) -inhibition tests yielded the recognition of cross-reacting IgE antibodies in latex and multiple fruit allergens: avocado, banana, chestnut, fig, kiwi, mango, melon, papaya, passion fruit, peach, pineapple, and tomato. The investigators recorded 112 intolerance reactions and noted that 42.5% of their patients reported allergic symptoms after consuming these fruits. Fruit-specific IgE antibodies were detected in only 32.1% of these patients, suggesting to the researchers that serologic tests were suboptimal in forecasting food hypersensitivities in patients who are allergic to latex.5
Cross-reactivity with banana
Mäkinen-Kiljunen studied 47 patients to investigate banana allergy in patients with latex allergy in 1994, measuring latex-, banana-, and pollen-specific (birch, timothy, and mugwort) IgE. Thirty-one patients were also given skin-prick tests with banana and were queried about reactions after consuming bananas. Of the 47 sera samples, latex RAST results were positive in 31 and banana RAST results in 26. RAST results from latex and banana were correlated (25 of the 31 latex RAST-positive samples were also banana RAST-positive), but not with pollen. Sixteen of the 31 patients who ate banana reported symptoms, and 11 of the 31 patients given the banana skin-prick test showed positive results. The author confirmed the cross-reactivity of IgE antibodies for latex and banana, identifying for the first time a structurally similar antigen/allergen as at least one antigen from banana fused with an antigen from latex in crossed-line immunoelectrophoresis.6
In 1998, Mikkola et al. investigated whether proteins similar to hevein, a major natural rubber latex allergen, are present in banana and account for cross-reactivity between these botanicals. Immunoblotting revealed that 9 of 15 sera from latex-allergic patients with IgE to hevein also bound to 32- and 33-kd banana proteins. Studies using ELISA [enzyme-linked immunosorbent assay] showed that the common presentation of hypersensitivity to banana among patients allergic to latex could be attributed to cross-reacting IgE antibodies binding to epitopes in hevein and in the then-newly identified hevein-like endochitinase found in banana.7
Cross-reactivity with avocado
In response to reports of an association between allergy to natural rubber latex and avocado, Ahlroth et al. investigated cross-reactive proteins between natural rubber latex and avocado in 1995 by using skin-prick tests with fresh avocado on 11 patients and the sera of 18 patients with known latex allergy for IgE antibodies. Fourteen of the 18 sera were found to have IgE antibodies binding to 17 distinct avocado proteins, with multiple immunoblot experiments and skin-prick test results (positive in 7 of 11 patients) revealing marked immunologic cross-reactivity between latex and avocado.8
In 1998, Chen et al. set out to identify the cross-sensitizing allergen between latex and avocado, with hevein suspected. The researchers looked at sera samples from 118 health care workers allergic to latex and 78 patients with spina bifida who were allergic to latex. They noted a robust correlation between the prevalence of seropositive IgE antibodies to avocado in the presence of hevein-specific IgE antibodies in both groups. All members in the spina bifida group and 91 (73%) of the health care workers had positive IgE antibodies to hevein and high IgE values to avocado. Additional results supported the conclusion that sensitization to avocado in the majority of people allergic to latex is engendered by IgE-binding epitopes found in hevein.9
A year later, Diaz-Perales et al. considered the potential relevance of chitinases and complex glycans as factors in the then newly described latex/food syndrome, particularly in avocado, banana, and chestnuts. The investigators culled extracts from 20 various plant foods as well as latex. In immunoblot inhibition assays, the primary allergen and class I chitinase in avocado, Prs a 1, and the latex extract potently or completely blocked IgE binding by these constituents. Polyclonal antibodies to chitinases and sera from patients with latex/fruit allergy responded to reactive proteins of about 30-45 kd (putative class I chitinases) in chestnut, cherimoya, kiwi, mango, papaya, passion fruit, tomato, and wheat flour extracts. The glycans complex was deemed to be irrelevant in latex/fruit cross-reactivity, but the researchers found the putative class I chitinases to be notable players in the latex/fruit syndrome.10
According to Wagner and Breitender, anywhere from 30%-50% of people with known latex allergy also evince a related hypersensitivity or allergy to various plant-derived foods, with avocado, banana, chestnut, kiwi, peach, tomato, potato, and bell pepper among the foods most frequently linked to latex/fruit syndrome. They summarize that several plant defense proteins have been shown to be involved in the syndrome, with the most prominent, class I chitinases with an N-terminal hevein-like domain, having been found to cross-react with hevein (Hev b 6.02), a major IgE-binding allergen for individuals allergic to latex. A beta-1,3-glucanase, a key latex allergen, has also shown cross-reactivity with proteins of bell pepper, and another significant latex allergen, Hev b 7, a patatin-like protein, cross-reacts with its analogous protein in potato.11
Conclusion
It is unknown whether latex allergy precedes or follows food allergy.11 The latex/food syndrome itself merits attention as a significant source of hypersensitivity to natural cosmeceutical ingredients. Dermatologists should be aware of the lengthy list of cross-reacting plant-derived products, particularly when it comes to reviewing topical product ingredients with susceptible or allergic patients. Latex-allergic patients may react to these natural ingredients in food or when topically applied to the skin.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014), and a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC. Write to her at [email protected].
References
1. Nutter AF. Br J Dermatol 1979 Nov;101(5):597-8.
2. Kelly KJ et al. J Allergy Clin Immunol Pract. 2017 Sep-Oct;5(5):1212-16.
3. Blanco C et al. Ann Allergy. 1994 Oct;73(4):309-14.
4. Beezhold DH et al. Clin Exp Allergy. 1996 Apr;26(4):416-22.
5. Brehler R et al. Allergy. 1997 Apr;52(4):404-10.
6. Mäkinen-Kiljunen S. J Allergy Clin Immunol. 1994 Jun;93(6):990-6.
7. Mikkola JH et al. J Allergy Clin Immunol. 1998 Dec;102(6 Pt 1):1005-12.
8. Ahlroth M et al. J Allergy Clin Immunol. 1995 Aug;96(2):167-73.
9. Chen Z et al. J Allergy Clin Immunol. 1998 Sep;102(3):476-81.
10. Diaz-Perales A et al. J Allergy Clin Immunol. 1999 Sep;104(3 Pt 1):681-7.
11. Wagner S et al. Biochem Soc Trans. 2002 Nov;30(Pt 6):935-40.
It has been 40 years since the first reported case of IgE-mediated natural rubber latex allergy, which was soon followed by a global epidemic of allergic and anaphylactic reactions.1,2 Resolution came through insightful work in the 1990s that led to the removal of cornstarch powder and a switch to nonpowdered latex and synthetic examination gloves.2 Also discovered during this period was the cross-reactivity of many patients to latex and various fruits.
Research substantiates reports
Blanco et al. conducted a prospective study in their outpatient clinic in 25 patients diagnosed with latex allergy, published in 1994.They used a clinical questionnaire, skin-prick tests, skin test with a latex extract, and identification of total and specific IgE to help ascertain clinical characteristics and cross-reactivity. Of the 23 women and 2 men in the study (mean age 33, plus or minus 9 years), 9 (36%) experienced latex-induced reactions characterized by systemic anaphylaxis. In 13 patients (52%), 42 food allergies were identified, and 23 included systemic anaphylaxis. Avocado (9), chestnut (9), banana (7), kiwi (5), and papaya (3) were the most common foods to cause hypersensitivities. The researchers concluded that their small study supported the reality of a “latex-fruit syndrome.”3
Another study aimed to characterize the cross-reactivity of latex and foods and evaluate clinical significance. Beezhold et al. examined 47 patients allergic to latex and 46 nonallergic controls. The investigators found immunologic reactivity to foods to be prevalent (33 latex-allergic patients and seven controls), with 27% of food skin-prick tests positive in the latex-allergic group. In addition, clinical symptoms were linked to 27% of positive skin-prick tests. Among the 17 patients who displayed clinical allergies to at least one food, 14 showed local sensitivity reactions, with anaphylaxis noted in 11. Avocado (53%), potato (40%), banana (38%), tomato (28%), chestnut (28%), and kiwi (17%) were the foods most frequently cited for provoking a skin test reaction. The authors observed extensive cross-reactivity between latex sensitivity and particular foods, with potatoes and tomatoes reported for the first time.4
In 1997, Brehler et al. studied serum samples from 136 patients whose immediate hypersensitivity to latex proteins was clinically observable and documented. The samples were assessed for IgE antibodies against several fruits, with fruit-specific IgE antibodies recorded in 69.1%. Radioallergosorbent (RAST) -inhibition tests yielded the recognition of cross-reacting IgE antibodies in latex and multiple fruit allergens: avocado, banana, chestnut, fig, kiwi, mango, melon, papaya, passion fruit, peach, pineapple, and tomato. The investigators recorded 112 intolerance reactions and noted that 42.5% of their patients reported allergic symptoms after consuming these fruits. Fruit-specific IgE antibodies were detected in only 32.1% of these patients, suggesting to the researchers that serologic tests were suboptimal in forecasting food hypersensitivities in patients who are allergic to latex.5
Cross-reactivity with banana
Mäkinen-Kiljunen studied 47 patients to investigate banana allergy in patients with latex allergy in 1994, measuring latex-, banana-, and pollen-specific (birch, timothy, and mugwort) IgE. Thirty-one patients were also given skin-prick tests with banana and were queried about reactions after consuming bananas. Of the 47 sera samples, latex RAST results were positive in 31 and banana RAST results in 26. RAST results from latex and banana were correlated (25 of the 31 latex RAST-positive samples were also banana RAST-positive), but not with pollen. Sixteen of the 31 patients who ate banana reported symptoms, and 11 of the 31 patients given the banana skin-prick test showed positive results. The author confirmed the cross-reactivity of IgE antibodies for latex and banana, identifying for the first time a structurally similar antigen/allergen as at least one antigen from banana fused with an antigen from latex in crossed-line immunoelectrophoresis.6
In 1998, Mikkola et al. investigated whether proteins similar to hevein, a major natural rubber latex allergen, are present in banana and account for cross-reactivity between these botanicals. Immunoblotting revealed that 9 of 15 sera from latex-allergic patients with IgE to hevein also bound to 32- and 33-kd banana proteins. Studies using ELISA [enzyme-linked immunosorbent assay] showed that the common presentation of hypersensitivity to banana among patients allergic to latex could be attributed to cross-reacting IgE antibodies binding to epitopes in hevein and in the then-newly identified hevein-like endochitinase found in banana.7
Cross-reactivity with avocado
In response to reports of an association between allergy to natural rubber latex and avocado, Ahlroth et al. investigated cross-reactive proteins between natural rubber latex and avocado in 1995 by using skin-prick tests with fresh avocado on 11 patients and the sera of 18 patients with known latex allergy for IgE antibodies. Fourteen of the 18 sera were found to have IgE antibodies binding to 17 distinct avocado proteins, with multiple immunoblot experiments and skin-prick test results (positive in 7 of 11 patients) revealing marked immunologic cross-reactivity between latex and avocado.8
In 1998, Chen et al. set out to identify the cross-sensitizing allergen between latex and avocado, with hevein suspected. The researchers looked at sera samples from 118 health care workers allergic to latex and 78 patients with spina bifida who were allergic to latex. They noted a robust correlation between the prevalence of seropositive IgE antibodies to avocado in the presence of hevein-specific IgE antibodies in both groups. All members in the spina bifida group and 91 (73%) of the health care workers had positive IgE antibodies to hevein and high IgE values to avocado. Additional results supported the conclusion that sensitization to avocado in the majority of people allergic to latex is engendered by IgE-binding epitopes found in hevein.9
A year later, Diaz-Perales et al. considered the potential relevance of chitinases and complex glycans as factors in the then newly described latex/food syndrome, particularly in avocado, banana, and chestnuts. The investigators culled extracts from 20 various plant foods as well as latex. In immunoblot inhibition assays, the primary allergen and class I chitinase in avocado, Prs a 1, and the latex extract potently or completely blocked IgE binding by these constituents. Polyclonal antibodies to chitinases and sera from patients with latex/fruit allergy responded to reactive proteins of about 30-45 kd (putative class I chitinases) in chestnut, cherimoya, kiwi, mango, papaya, passion fruit, tomato, and wheat flour extracts. The glycans complex was deemed to be irrelevant in latex/fruit cross-reactivity, but the researchers found the putative class I chitinases to be notable players in the latex/fruit syndrome.10
According to Wagner and Breitender, anywhere from 30%-50% of people with known latex allergy also evince a related hypersensitivity or allergy to various plant-derived foods, with avocado, banana, chestnut, kiwi, peach, tomato, potato, and bell pepper among the foods most frequently linked to latex/fruit syndrome. They summarize that several plant defense proteins have been shown to be involved in the syndrome, with the most prominent, class I chitinases with an N-terminal hevein-like domain, having been found to cross-react with hevein (Hev b 6.02), a major IgE-binding allergen for individuals allergic to latex. A beta-1,3-glucanase, a key latex allergen, has also shown cross-reactivity with proteins of bell pepper, and another significant latex allergen, Hev b 7, a patatin-like protein, cross-reacts with its analogous protein in potato.11
Conclusion
It is unknown whether latex allergy precedes or follows food allergy.11 The latex/food syndrome itself merits attention as a significant source of hypersensitivity to natural cosmeceutical ingredients. Dermatologists should be aware of the lengthy list of cross-reacting plant-derived products, particularly when it comes to reviewing topical product ingredients with susceptible or allergic patients. Latex-allergic patients may react to these natural ingredients in food or when topically applied to the skin.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014), and a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC. Write to her at [email protected].
References
1. Nutter AF. Br J Dermatol 1979 Nov;101(5):597-8.
2. Kelly KJ et al. J Allergy Clin Immunol Pract. 2017 Sep-Oct;5(5):1212-16.
3. Blanco C et al. Ann Allergy. 1994 Oct;73(4):309-14.
4. Beezhold DH et al. Clin Exp Allergy. 1996 Apr;26(4):416-22.
5. Brehler R et al. Allergy. 1997 Apr;52(4):404-10.
6. Mäkinen-Kiljunen S. J Allergy Clin Immunol. 1994 Jun;93(6):990-6.
7. Mikkola JH et al. J Allergy Clin Immunol. 1998 Dec;102(6 Pt 1):1005-12.
8. Ahlroth M et al. J Allergy Clin Immunol. 1995 Aug;96(2):167-73.
9. Chen Z et al. J Allergy Clin Immunol. 1998 Sep;102(3):476-81.
10. Diaz-Perales A et al. J Allergy Clin Immunol. 1999 Sep;104(3 Pt 1):681-7.
11. Wagner S et al. Biochem Soc Trans. 2002 Nov;30(Pt 6):935-40.
It has been 40 years since the first reported case of IgE-mediated natural rubber latex allergy, which was soon followed by a global epidemic of allergic and anaphylactic reactions.1,2 Resolution came through insightful work in the 1990s that led to the removal of cornstarch powder and a switch to nonpowdered latex and synthetic examination gloves.2 Also discovered during this period was the cross-reactivity of many patients to latex and various fruits.
Research substantiates reports
Blanco et al. conducted a prospective study in their outpatient clinic in 25 patients diagnosed with latex allergy, published in 1994.They used a clinical questionnaire, skin-prick tests, skin test with a latex extract, and identification of total and specific IgE to help ascertain clinical characteristics and cross-reactivity. Of the 23 women and 2 men in the study (mean age 33, plus or minus 9 years), 9 (36%) experienced latex-induced reactions characterized by systemic anaphylaxis. In 13 patients (52%), 42 food allergies were identified, and 23 included systemic anaphylaxis. Avocado (9), chestnut (9), banana (7), kiwi (5), and papaya (3) were the most common foods to cause hypersensitivities. The researchers concluded that their small study supported the reality of a “latex-fruit syndrome.”3
Another study aimed to characterize the cross-reactivity of latex and foods and evaluate clinical significance. Beezhold et al. examined 47 patients allergic to latex and 46 nonallergic controls. The investigators found immunologic reactivity to foods to be prevalent (33 latex-allergic patients and seven controls), with 27% of food skin-prick tests positive in the latex-allergic group. In addition, clinical symptoms were linked to 27% of positive skin-prick tests. Among the 17 patients who displayed clinical allergies to at least one food, 14 showed local sensitivity reactions, with anaphylaxis noted in 11. Avocado (53%), potato (40%), banana (38%), tomato (28%), chestnut (28%), and kiwi (17%) were the foods most frequently cited for provoking a skin test reaction. The authors observed extensive cross-reactivity between latex sensitivity and particular foods, with potatoes and tomatoes reported for the first time.4
In 1997, Brehler et al. studied serum samples from 136 patients whose immediate hypersensitivity to latex proteins was clinically observable and documented. The samples were assessed for IgE antibodies against several fruits, with fruit-specific IgE antibodies recorded in 69.1%. Radioallergosorbent (RAST) -inhibition tests yielded the recognition of cross-reacting IgE antibodies in latex and multiple fruit allergens: avocado, banana, chestnut, fig, kiwi, mango, melon, papaya, passion fruit, peach, pineapple, and tomato. The investigators recorded 112 intolerance reactions and noted that 42.5% of their patients reported allergic symptoms after consuming these fruits. Fruit-specific IgE antibodies were detected in only 32.1% of these patients, suggesting to the researchers that serologic tests were suboptimal in forecasting food hypersensitivities in patients who are allergic to latex.5
Cross-reactivity with banana
Mäkinen-Kiljunen studied 47 patients to investigate banana allergy in patients with latex allergy in 1994, measuring latex-, banana-, and pollen-specific (birch, timothy, and mugwort) IgE. Thirty-one patients were also given skin-prick tests with banana and were queried about reactions after consuming bananas. Of the 47 sera samples, latex RAST results were positive in 31 and banana RAST results in 26. RAST results from latex and banana were correlated (25 of the 31 latex RAST-positive samples were also banana RAST-positive), but not with pollen. Sixteen of the 31 patients who ate banana reported symptoms, and 11 of the 31 patients given the banana skin-prick test showed positive results. The author confirmed the cross-reactivity of IgE antibodies for latex and banana, identifying for the first time a structurally similar antigen/allergen as at least one antigen from banana fused with an antigen from latex in crossed-line immunoelectrophoresis.6
In 1998, Mikkola et al. investigated whether proteins similar to hevein, a major natural rubber latex allergen, are present in banana and account for cross-reactivity between these botanicals. Immunoblotting revealed that 9 of 15 sera from latex-allergic patients with IgE to hevein also bound to 32- and 33-kd banana proteins. Studies using ELISA [enzyme-linked immunosorbent assay] showed that the common presentation of hypersensitivity to banana among patients allergic to latex could be attributed to cross-reacting IgE antibodies binding to epitopes in hevein and in the then-newly identified hevein-like endochitinase found in banana.7
Cross-reactivity with avocado
In response to reports of an association between allergy to natural rubber latex and avocado, Ahlroth et al. investigated cross-reactive proteins between natural rubber latex and avocado in 1995 by using skin-prick tests with fresh avocado on 11 patients and the sera of 18 patients with known latex allergy for IgE antibodies. Fourteen of the 18 sera were found to have IgE antibodies binding to 17 distinct avocado proteins, with multiple immunoblot experiments and skin-prick test results (positive in 7 of 11 patients) revealing marked immunologic cross-reactivity between latex and avocado.8
In 1998, Chen et al. set out to identify the cross-sensitizing allergen between latex and avocado, with hevein suspected. The researchers looked at sera samples from 118 health care workers allergic to latex and 78 patients with spina bifida who were allergic to latex. They noted a robust correlation between the prevalence of seropositive IgE antibodies to avocado in the presence of hevein-specific IgE antibodies in both groups. All members in the spina bifida group and 91 (73%) of the health care workers had positive IgE antibodies to hevein and high IgE values to avocado. Additional results supported the conclusion that sensitization to avocado in the majority of people allergic to latex is engendered by IgE-binding epitopes found in hevein.9
A year later, Diaz-Perales et al. considered the potential relevance of chitinases and complex glycans as factors in the then newly described latex/food syndrome, particularly in avocado, banana, and chestnuts. The investigators culled extracts from 20 various plant foods as well as latex. In immunoblot inhibition assays, the primary allergen and class I chitinase in avocado, Prs a 1, and the latex extract potently or completely blocked IgE binding by these constituents. Polyclonal antibodies to chitinases and sera from patients with latex/fruit allergy responded to reactive proteins of about 30-45 kd (putative class I chitinases) in chestnut, cherimoya, kiwi, mango, papaya, passion fruit, tomato, and wheat flour extracts. The glycans complex was deemed to be irrelevant in latex/fruit cross-reactivity, but the researchers found the putative class I chitinases to be notable players in the latex/fruit syndrome.10
According to Wagner and Breitender, anywhere from 30%-50% of people with known latex allergy also evince a related hypersensitivity or allergy to various plant-derived foods, with avocado, banana, chestnut, kiwi, peach, tomato, potato, and bell pepper among the foods most frequently linked to latex/fruit syndrome. They summarize that several plant defense proteins have been shown to be involved in the syndrome, with the most prominent, class I chitinases with an N-terminal hevein-like domain, having been found to cross-react with hevein (Hev b 6.02), a major IgE-binding allergen for individuals allergic to latex. A beta-1,3-glucanase, a key latex allergen, has also shown cross-reactivity with proteins of bell pepper, and another significant latex allergen, Hev b 7, a patatin-like protein, cross-reacts with its analogous protein in potato.11
Conclusion
It is unknown whether latex allergy precedes or follows food allergy.11 The latex/food syndrome itself merits attention as a significant source of hypersensitivity to natural cosmeceutical ingredients. Dermatologists should be aware of the lengthy list of cross-reacting plant-derived products, particularly when it comes to reviewing topical product ingredients with susceptible or allergic patients. Latex-allergic patients may react to these natural ingredients in food or when topically applied to the skin.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur who practices in Miami. She founded the Cosmetic Dermatology Center at the University of Miami in 1997. Dr. Baumann wrote two textbooks: “Cosmetic Dermatology: Principles and Practice” (New York: McGraw-Hill, 2002), and “Cosmeceuticals and Cosmetic Ingredients” (New York: McGraw-Hill, 2014), and a New York Times Best Sellers book for consumers, “The Skin Type Solution” (New York: Bantam Dell, 2006). Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Evolus, Galderma, and Revance. She is the founder and CEO of Skin Type Solutions Franchise Systems LLC. Write to her at [email protected].
References
1. Nutter AF. Br J Dermatol 1979 Nov;101(5):597-8.
2. Kelly KJ et al. J Allergy Clin Immunol Pract. 2017 Sep-Oct;5(5):1212-16.
3. Blanco C et al. Ann Allergy. 1994 Oct;73(4):309-14.
4. Beezhold DH et al. Clin Exp Allergy. 1996 Apr;26(4):416-22.
5. Brehler R et al. Allergy. 1997 Apr;52(4):404-10.
6. Mäkinen-Kiljunen S. J Allergy Clin Immunol. 1994 Jun;93(6):990-6.
7. Mikkola JH et al. J Allergy Clin Immunol. 1998 Dec;102(6 Pt 1):1005-12.
8. Ahlroth M et al. J Allergy Clin Immunol. 1995 Aug;96(2):167-73.
9. Chen Z et al. J Allergy Clin Immunol. 1998 Sep;102(3):476-81.
10. Diaz-Perales A et al. J Allergy Clin Immunol. 1999 Sep;104(3 Pt 1):681-7.
11. Wagner S et al. Biochem Soc Trans. 2002 Nov;30(Pt 6):935-40.
Progression in Huntington’s linked to CAG repeat number
The progression, not just age of onset, of Huntington’s disease can be predicted by a measurable genetic factor, researchers have learned.
Huntington’s, an inherited neurodegenerative disease that affects motor function and cognition, is caused by an expansion of the CAG trinucleotide sequence on the huntingtin gene. Scientists have previously linked younger age at onset to a higher number of CAG repeats on the gene, but the association between these and the rate of progression after onset was poorly understood.
In research published online August 12 in JAMA Neurology, investigators linked the rate of progression – which, like age at onset, is highly variable in Huntington’s – to CAG repeat length. CAG repeat length was strongly associated with distinct patterns of brain damage, as well as clinical measures of cognitive and motor decline.
For their research, Douglas R. Langbehn, MD, PhD, of the University of Iowa, Iowa City, and colleagues used data from two longitudinal observational studies in gene carriers for Huntington’s and nonrelated controls. The researchers looked at data from 443 participants (56% female; mean age, 44.4 years) who were followed for a mean of 4 years, with more than 2,000 study visits across the multisite cohort. Neuropsychiatric testing and brain imaging were conducted annually, using composite scoring systems of the investigators’ design. These composite scores sought to be more sensitive by combining results from several validated clinical and imaging tests.
Age and speed of decline in total functional capacity tracked with more CAG repeats, the researchers found. For example, in people with 40 CAG repeats, the estimated mean age of initial motor-cognitive score change was 42.46 years; for those with 45 repeats, 26.65 years, and for people with 50 CAG repeats, 18.49 years. Higher repeats were seen significantly associated with accelerated, nonlinear decline on both clinical and brain-volume measures, except gray matter volume, according to principal component analyses conducted on the data.
“We derived a single summary measure capturing the motor-cognitive phenotype and showed that the accelerating progression of the phenotype with aging is highly CAG repeat length dependent (i.e., those with higher CAG decline earlier and faster). Contrary to some previous assertions, this CAG dependence continues well past the onset of clinical illness,” Dr. Langbehn and colleagues wrote in their analysis. “By characterizing these CAG repeat length–dependent disease trajectories, we provide insights into disease progression that may guide future therapeutic approaches and identify the most appropriate intervention ages to prevent clinical decline.”
Dr. Langbehn and colleagues acknowledged as a limitation of their study its likely exclusion of the sickest subjects because of the cohorts’ design. The CHDI Foundation funded the study. Of the 16 coauthors, 13 reported receiving funding from CHDI and/or from pharmaceutical manufacturers.
SOURCE: Langbehn et al. JAMA Neurol. 2019 Aug 12. doi: 10.1001/jamaneurol.2019.2328
The progression, not just age of onset, of Huntington’s disease can be predicted by a measurable genetic factor, researchers have learned.
Huntington’s, an inherited neurodegenerative disease that affects motor function and cognition, is caused by an expansion of the CAG trinucleotide sequence on the huntingtin gene. Scientists have previously linked younger age at onset to a higher number of CAG repeats on the gene, but the association between these and the rate of progression after onset was poorly understood.
In research published online August 12 in JAMA Neurology, investigators linked the rate of progression – which, like age at onset, is highly variable in Huntington’s – to CAG repeat length. CAG repeat length was strongly associated with distinct patterns of brain damage, as well as clinical measures of cognitive and motor decline.
For their research, Douglas R. Langbehn, MD, PhD, of the University of Iowa, Iowa City, and colleagues used data from two longitudinal observational studies in gene carriers for Huntington’s and nonrelated controls. The researchers looked at data from 443 participants (56% female; mean age, 44.4 years) who were followed for a mean of 4 years, with more than 2,000 study visits across the multisite cohort. Neuropsychiatric testing and brain imaging were conducted annually, using composite scoring systems of the investigators’ design. These composite scores sought to be more sensitive by combining results from several validated clinical and imaging tests.
Age and speed of decline in total functional capacity tracked with more CAG repeats, the researchers found. For example, in people with 40 CAG repeats, the estimated mean age of initial motor-cognitive score change was 42.46 years; for those with 45 repeats, 26.65 years, and for people with 50 CAG repeats, 18.49 years. Higher repeats were seen significantly associated with accelerated, nonlinear decline on both clinical and brain-volume measures, except gray matter volume, according to principal component analyses conducted on the data.
“We derived a single summary measure capturing the motor-cognitive phenotype and showed that the accelerating progression of the phenotype with aging is highly CAG repeat length dependent (i.e., those with higher CAG decline earlier and faster). Contrary to some previous assertions, this CAG dependence continues well past the onset of clinical illness,” Dr. Langbehn and colleagues wrote in their analysis. “By characterizing these CAG repeat length–dependent disease trajectories, we provide insights into disease progression that may guide future therapeutic approaches and identify the most appropriate intervention ages to prevent clinical decline.”
Dr. Langbehn and colleagues acknowledged as a limitation of their study its likely exclusion of the sickest subjects because of the cohorts’ design. The CHDI Foundation funded the study. Of the 16 coauthors, 13 reported receiving funding from CHDI and/or from pharmaceutical manufacturers.
SOURCE: Langbehn et al. JAMA Neurol. 2019 Aug 12. doi: 10.1001/jamaneurol.2019.2328
The progression, not just age of onset, of Huntington’s disease can be predicted by a measurable genetic factor, researchers have learned.
Huntington’s, an inherited neurodegenerative disease that affects motor function and cognition, is caused by an expansion of the CAG trinucleotide sequence on the huntingtin gene. Scientists have previously linked younger age at onset to a higher number of CAG repeats on the gene, but the association between these and the rate of progression after onset was poorly understood.
In research published online August 12 in JAMA Neurology, investigators linked the rate of progression – which, like age at onset, is highly variable in Huntington’s – to CAG repeat length. CAG repeat length was strongly associated with distinct patterns of brain damage, as well as clinical measures of cognitive and motor decline.
For their research, Douglas R. Langbehn, MD, PhD, of the University of Iowa, Iowa City, and colleagues used data from two longitudinal observational studies in gene carriers for Huntington’s and nonrelated controls. The researchers looked at data from 443 participants (56% female; mean age, 44.4 years) who were followed for a mean of 4 years, with more than 2,000 study visits across the multisite cohort. Neuropsychiatric testing and brain imaging were conducted annually, using composite scoring systems of the investigators’ design. These composite scores sought to be more sensitive by combining results from several validated clinical and imaging tests.
Age and speed of decline in total functional capacity tracked with more CAG repeats, the researchers found. For example, in people with 40 CAG repeats, the estimated mean age of initial motor-cognitive score change was 42.46 years; for those with 45 repeats, 26.65 years, and for people with 50 CAG repeats, 18.49 years. Higher repeats were seen significantly associated with accelerated, nonlinear decline on both clinical and brain-volume measures, except gray matter volume, according to principal component analyses conducted on the data.
“We derived a single summary measure capturing the motor-cognitive phenotype and showed that the accelerating progression of the phenotype with aging is highly CAG repeat length dependent (i.e., those with higher CAG decline earlier and faster). Contrary to some previous assertions, this CAG dependence continues well past the onset of clinical illness,” Dr. Langbehn and colleagues wrote in their analysis. “By characterizing these CAG repeat length–dependent disease trajectories, we provide insights into disease progression that may guide future therapeutic approaches and identify the most appropriate intervention ages to prevent clinical decline.”
Dr. Langbehn and colleagues acknowledged as a limitation of their study its likely exclusion of the sickest subjects because of the cohorts’ design. The CHDI Foundation funded the study. Of the 16 coauthors, 13 reported receiving funding from CHDI and/or from pharmaceutical manufacturers.
SOURCE: Langbehn et al. JAMA Neurol. 2019 Aug 12. doi: 10.1001/jamaneurol.2019.2328
FROM JAMA NEUROLOGY
Key clinical point:
Major finding: CAG closely tracked the rate of cognitive and motor decline among patients with HD.
Study details: Brain imaging and neuropsychiatric testing data from 443 patients enrolled in cohort studies in people with HD-causing mutations
Disclosures: CHDI sponsored the study, and most coauthors disclosed financial relationships with the sponsor and/or pharmaceutical firms.
Source: Langbehn et al. JAMA Neurol. 2019 Aug 12. doi: 10.1001/jamaneurol.2019.2328.
FDA approves upadacitinib for rheumatoid arthritis
according to a release from its developer. The indication specifies that patients must have shown inadequate response or intolerance to methotrexate.
The approval is based on the SELECT program, which included 4,400 patients across five studies that tested the oral Janus kinase inhibitor in various settings, such as alone or with methotrexate. All primary and secondary endpoints were met in these trials. For example, among patients with inadequate response to methotrexate in one study, 68% of those treated with 15-mg upadacitinib monotherapy achieved 20% improvement in American College of Rheumatology response criteria (ACR20) at week 14 versus 41% of those who had continued on methotrexate. In another study of patients with in adequate response to methotrexate, 71% of those treated with upadacitinib/methotrexate combination therapy achieved ACR20 at week 12 versus 36% of those receiving placebo and methotrexate. Compared with other treatments, better rates of clinical remission and radiographic inhibition were seen with upadacitinib-based therapies, too.
Upadacitinib carries a boxed warning – the most serious warning the FDA issues – for risks of serious infection, malignancy, and thrombosis; these serious risks should be weighed against treatment benefits in any patients with increased risk for these problems or currently experiencing any of them. Concomitant use with other JAK inhibitors, biologic DMARDs, or with potent immunosuppressants is not recommended; its use also is not recommended for patients with severe hepatic impairment. The most common adverse reactions are upper respiratory tract infection, nausea, cough, and pyrexia. Live vaccines should be avoided with patients taking this drug, and patients who are breastfeeding should be advised against use of it.
More prescribing information can be found in the drug’s label, which can be found on the FDA’s website.
Upadacitinib is also being evaluated for treatment of other immune-mediated diseases.
according to a release from its developer. The indication specifies that patients must have shown inadequate response or intolerance to methotrexate.
The approval is based on the SELECT program, which included 4,400 patients across five studies that tested the oral Janus kinase inhibitor in various settings, such as alone or with methotrexate. All primary and secondary endpoints were met in these trials. For example, among patients with inadequate response to methotrexate in one study, 68% of those treated with 15-mg upadacitinib monotherapy achieved 20% improvement in American College of Rheumatology response criteria (ACR20) at week 14 versus 41% of those who had continued on methotrexate. In another study of patients with in adequate response to methotrexate, 71% of those treated with upadacitinib/methotrexate combination therapy achieved ACR20 at week 12 versus 36% of those receiving placebo and methotrexate. Compared with other treatments, better rates of clinical remission and radiographic inhibition were seen with upadacitinib-based therapies, too.
Upadacitinib carries a boxed warning – the most serious warning the FDA issues – for risks of serious infection, malignancy, and thrombosis; these serious risks should be weighed against treatment benefits in any patients with increased risk for these problems or currently experiencing any of them. Concomitant use with other JAK inhibitors, biologic DMARDs, or with potent immunosuppressants is not recommended; its use also is not recommended for patients with severe hepatic impairment. The most common adverse reactions are upper respiratory tract infection, nausea, cough, and pyrexia. Live vaccines should be avoided with patients taking this drug, and patients who are breastfeeding should be advised against use of it.
More prescribing information can be found in the drug’s label, which can be found on the FDA’s website.
Upadacitinib is also being evaluated for treatment of other immune-mediated diseases.
according to a release from its developer. The indication specifies that patients must have shown inadequate response or intolerance to methotrexate.
The approval is based on the SELECT program, which included 4,400 patients across five studies that tested the oral Janus kinase inhibitor in various settings, such as alone or with methotrexate. All primary and secondary endpoints were met in these trials. For example, among patients with inadequate response to methotrexate in one study, 68% of those treated with 15-mg upadacitinib monotherapy achieved 20% improvement in American College of Rheumatology response criteria (ACR20) at week 14 versus 41% of those who had continued on methotrexate. In another study of patients with in adequate response to methotrexate, 71% of those treated with upadacitinib/methotrexate combination therapy achieved ACR20 at week 12 versus 36% of those receiving placebo and methotrexate. Compared with other treatments, better rates of clinical remission and radiographic inhibition were seen with upadacitinib-based therapies, too.
Upadacitinib carries a boxed warning – the most serious warning the FDA issues – for risks of serious infection, malignancy, and thrombosis; these serious risks should be weighed against treatment benefits in any patients with increased risk for these problems or currently experiencing any of them. Concomitant use with other JAK inhibitors, biologic DMARDs, or with potent immunosuppressants is not recommended; its use also is not recommended for patients with severe hepatic impairment. The most common adverse reactions are upper respiratory tract infection, nausea, cough, and pyrexia. Live vaccines should be avoided with patients taking this drug, and patients who are breastfeeding should be advised against use of it.
More prescribing information can be found in the drug’s label, which can be found on the FDA’s website.
Upadacitinib is also being evaluated for treatment of other immune-mediated diseases.
Clicking override when the EHR system argues about an order
The EHR system at the hospital occasionally argues with me about my orders.
I may order a brain MRI, or CT angiography, or pretty much anything, and when I click to submit it a box pops up, telling me I shouldn’t be ordering that.
Sometimes it’s based on cost, saying that the MRI is more expensive than a CT, and according to some internal algorithm I should do that instead. Other times it says the test isn’t appropriate given the patient’s condition, age, zodiac sign, whatever. It might also say the test is redundant, because the patient just had a brain MRI during an admission last month.
I ignore them. There’s an override button to close the box and order the test, and that’s what I always click.
I have no objection to a reasonable review, but neither the computer nor its algorithms went through medical school, or residency, or read journals regularly, or have 20 years of experience in this field. I’d like to think (or hope) I know what I’m doing.
I don’t take this job lightly. When I order a test it’s because I’m trying to do the right thing for the patient. To find out what’s going on. To see what I can do to treat them. In short, to help as much as I can within the limitations of modern medical practice. Sometimes those things don’t always involve saving the insurance company money, or trying to get by with a previous study’s results.
Medicine is not a cookbook. While guidelines can be useful, every patient is different, and treatment plans have to be adjusted accordingly. It would be nice if this was the one-size-fits-all world the computer algorithms would like, but patient care is anything but.
I’d also rather “overcare” than “undercare.” To me, that’s just good practice. If I follow the computer’s advice and provide less care than needed and miss something, I’m pretty sure “because the computer told me not to” isn’t going to stand up as a defense in court.
I’m going to just keep on practicing medicine using, as one of my past attendings would say, “clinical correlation” and keeping what’s best for the patient in mind. Anything less may be fine for the computer, but not for me, and certainly not for those I’m trying to help.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The EHR system at the hospital occasionally argues with me about my orders.
I may order a brain MRI, or CT angiography, or pretty much anything, and when I click to submit it a box pops up, telling me I shouldn’t be ordering that.
Sometimes it’s based on cost, saying that the MRI is more expensive than a CT, and according to some internal algorithm I should do that instead. Other times it says the test isn’t appropriate given the patient’s condition, age, zodiac sign, whatever. It might also say the test is redundant, because the patient just had a brain MRI during an admission last month.
I ignore them. There’s an override button to close the box and order the test, and that’s what I always click.
I have no objection to a reasonable review, but neither the computer nor its algorithms went through medical school, or residency, or read journals regularly, or have 20 years of experience in this field. I’d like to think (or hope) I know what I’m doing.
I don’t take this job lightly. When I order a test it’s because I’m trying to do the right thing for the patient. To find out what’s going on. To see what I can do to treat them. In short, to help as much as I can within the limitations of modern medical practice. Sometimes those things don’t always involve saving the insurance company money, or trying to get by with a previous study’s results.
Medicine is not a cookbook. While guidelines can be useful, every patient is different, and treatment plans have to be adjusted accordingly. It would be nice if this was the one-size-fits-all world the computer algorithms would like, but patient care is anything but.
I’d also rather “overcare” than “undercare.” To me, that’s just good practice. If I follow the computer’s advice and provide less care than needed and miss something, I’m pretty sure “because the computer told me not to” isn’t going to stand up as a defense in court.
I’m going to just keep on practicing medicine using, as one of my past attendings would say, “clinical correlation” and keeping what’s best for the patient in mind. Anything less may be fine for the computer, but not for me, and certainly not for those I’m trying to help.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
The EHR system at the hospital occasionally argues with me about my orders.
I may order a brain MRI, or CT angiography, or pretty much anything, and when I click to submit it a box pops up, telling me I shouldn’t be ordering that.
Sometimes it’s based on cost, saying that the MRI is more expensive than a CT, and according to some internal algorithm I should do that instead. Other times it says the test isn’t appropriate given the patient’s condition, age, zodiac sign, whatever. It might also say the test is redundant, because the patient just had a brain MRI during an admission last month.
I ignore them. There’s an override button to close the box and order the test, and that’s what I always click.
I have no objection to a reasonable review, but neither the computer nor its algorithms went through medical school, or residency, or read journals regularly, or have 20 years of experience in this field. I’d like to think (or hope) I know what I’m doing.
I don’t take this job lightly. When I order a test it’s because I’m trying to do the right thing for the patient. To find out what’s going on. To see what I can do to treat them. In short, to help as much as I can within the limitations of modern medical practice. Sometimes those things don’t always involve saving the insurance company money, or trying to get by with a previous study’s results.
Medicine is not a cookbook. While guidelines can be useful, every patient is different, and treatment plans have to be adjusted accordingly. It would be nice if this was the one-size-fits-all world the computer algorithms would like, but patient care is anything but.
I’d also rather “overcare” than “undercare.” To me, that’s just good practice. If I follow the computer’s advice and provide less care than needed and miss something, I’m pretty sure “because the computer told me not to” isn’t going to stand up as a defense in court.
I’m going to just keep on practicing medicine using, as one of my past attendings would say, “clinical correlation” and keeping what’s best for the patient in mind. Anything less may be fine for the computer, but not for me, and certainly not for those I’m trying to help.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Pediatric, adolescent migraine treatment and prevention guidelines are updated
Two new guidelines on the treatment and prevention of migraines in children and adolescents have been released by the American Academy of Neurology and the American Headache Society.
This update to the previous guidelines released by the American Academy of Neurology in 2004 reflects the expansion in pharmacologic and nonpharmacologic approaches during the last 15 years, Andrew D. Hershey, MD, PhD, director of the division of neurology at Cincinnati Children’s Hospital and a fellow of the American Academy of Neurology, said in an interview.
“There has also been an increase in the number of randomized controlled studies, which have allowed for a more robust statement on acute and preventive treatments to be made,” said Dr. Hershey, who is also a senior author for both guidelines.
The two reports focused on separate issues: One guideline outlined the options for treatment of acute migraine, and the second guideline summarized the available studies on the effectiveness of preventive medications for migraine in children and adolescents.
The guidelines recommend a physical examination and history to establish a specific headache diagnosis and afford a treatment that provides fast and complete pain relief. Treatment should be initiated as soon as a patient realizes an attack is occurring. Patients with signs of secondary headache should be evaluated by a neurologist or a headache specialist.
Studies support the use of ibuprofen and acetaminophen for pain relief in cases of acute migraine, but only some triptans (such as almotriptan, rizatriptan, sumatriptan/naproxen, and zolmitriptan nasal spray) are approved for use in adolescents. Specifically, sumatriptan/naproxen was shown to be effective when compared with placebo in studies with adolescents, whose headache symptoms resolved within 2 hours.
It may be necessary to try more than one triptan, the guidelines noted, because patients respond differently to medications. A failure to respond to one triptan does not necessarily mean that treatment with another triptan will be unsuccessful.
The guidelines also focused on patient and family education to improve medication safety and adherence. Lifestyle modification, avoidance of migraine triggers, creating good sleep habits, and staying hydrated can help reduce migraines. While no medications improved associated symptoms of migraines such as nausea or vomiting, triptans did show a benefit in reducing phonophobia and photophobia.
Evidence for pharmacologic prevention of migraines in children and adolescents is limited, according to the guidelines. In the 15 studies included in a literature review, there was not sufficient evidence to show preventive treatments, such as divalproex, onabotulinumtoxinA, amitriptyline, nimodipine, and flunarizine, were more effective than placebo at reducing the frequency of headaches. There was some evidence to show propranolol in children and topiramate and cinnarizine in children and adolescents can reduce headache frequency. Children and adolescents who received cognitive-behavioral therapy together with amitriptyline were more likely to have reduced frequency of headaches than were those who received amitriptyline with patient education.
“The consensus conclusion was that a multidisciplinary approach that combines acute treatments, preventive treatments, and healthy habits is likely to have the best outcomes,” said Dr. Hershey.
Dr. Hershey acknowledged the many gaps between what is clinically observed and what the studies in the guidelines demonstrated.
“One of the biggest questions is how to minimize the expectation response in the controlled studies,” he said. “Additionally, we are moving toward a better recognition of the mechanism by which the various treatments work in a genetic-based disease that is polygenic in nature” with up to 38 different gene polymorphisms identified to date.
The guidelines also do not address newer treatments, such as calcitonin gene–related peptide (CGRP) antibodies, CGRP antagonists, serotonin antagonists, and devices because there are as yet no studies of their effectiveness in children and adolescents.
“They have been studied in adults, so will be prone to the expectation response; but given the large number of diverse therapies, one can hope that many of the gaps can be filled,” said Dr. Hershey.
The American Academy of Neurology provided funding for development of the guidelines and reimbursed authors who served as subcommittee members for travel expenses and in-person meetings. The authors reported personal and institutional relationships in the form of advisory board memberships, investigator appointments, speakers bureau positions, research support, grants, honorariums, consultancies, and publishing royalties for pharmaceutical companies and other organizations.
SOURCES: Oskoui M et al. Neurology. 2019 Aug 14. doi: 10.1212/WNL.0000000000008095. Oskoui M et al. Neurology. 2019 Aug 14. doi: 10.1212/WNL.0000000000008105.
Two new guidelines on the treatment and prevention of migraines in children and adolescents have been released by the American Academy of Neurology and the American Headache Society.
This update to the previous guidelines released by the American Academy of Neurology in 2004 reflects the expansion in pharmacologic and nonpharmacologic approaches during the last 15 years, Andrew D. Hershey, MD, PhD, director of the division of neurology at Cincinnati Children’s Hospital and a fellow of the American Academy of Neurology, said in an interview.
“There has also been an increase in the number of randomized controlled studies, which have allowed for a more robust statement on acute and preventive treatments to be made,” said Dr. Hershey, who is also a senior author for both guidelines.
The two reports focused on separate issues: One guideline outlined the options for treatment of acute migraine, and the second guideline summarized the available studies on the effectiveness of preventive medications for migraine in children and adolescents.
The guidelines recommend a physical examination and history to establish a specific headache diagnosis and afford a treatment that provides fast and complete pain relief. Treatment should be initiated as soon as a patient realizes an attack is occurring. Patients with signs of secondary headache should be evaluated by a neurologist or a headache specialist.
Studies support the use of ibuprofen and acetaminophen for pain relief in cases of acute migraine, but only some triptans (such as almotriptan, rizatriptan, sumatriptan/naproxen, and zolmitriptan nasal spray) are approved for use in adolescents. Specifically, sumatriptan/naproxen was shown to be effective when compared with placebo in studies with adolescents, whose headache symptoms resolved within 2 hours.
It may be necessary to try more than one triptan, the guidelines noted, because patients respond differently to medications. A failure to respond to one triptan does not necessarily mean that treatment with another triptan will be unsuccessful.
The guidelines also focused on patient and family education to improve medication safety and adherence. Lifestyle modification, avoidance of migraine triggers, creating good sleep habits, and staying hydrated can help reduce migraines. While no medications improved associated symptoms of migraines such as nausea or vomiting, triptans did show a benefit in reducing phonophobia and photophobia.
Evidence for pharmacologic prevention of migraines in children and adolescents is limited, according to the guidelines. In the 15 studies included in a literature review, there was not sufficient evidence to show preventive treatments, such as divalproex, onabotulinumtoxinA, amitriptyline, nimodipine, and flunarizine, were more effective than placebo at reducing the frequency of headaches. There was some evidence to show propranolol in children and topiramate and cinnarizine in children and adolescents can reduce headache frequency. Children and adolescents who received cognitive-behavioral therapy together with amitriptyline were more likely to have reduced frequency of headaches than were those who received amitriptyline with patient education.
“The consensus conclusion was that a multidisciplinary approach that combines acute treatments, preventive treatments, and healthy habits is likely to have the best outcomes,” said Dr. Hershey.
Dr. Hershey acknowledged the many gaps between what is clinically observed and what the studies in the guidelines demonstrated.
“One of the biggest questions is how to minimize the expectation response in the controlled studies,” he said. “Additionally, we are moving toward a better recognition of the mechanism by which the various treatments work in a genetic-based disease that is polygenic in nature” with up to 38 different gene polymorphisms identified to date.
The guidelines also do not address newer treatments, such as calcitonin gene–related peptide (CGRP) antibodies, CGRP antagonists, serotonin antagonists, and devices because there are as yet no studies of their effectiveness in children and adolescents.
“They have been studied in adults, so will be prone to the expectation response; but given the large number of diverse therapies, one can hope that many of the gaps can be filled,” said Dr. Hershey.
The American Academy of Neurology provided funding for development of the guidelines and reimbursed authors who served as subcommittee members for travel expenses and in-person meetings. The authors reported personal and institutional relationships in the form of advisory board memberships, investigator appointments, speakers bureau positions, research support, grants, honorariums, consultancies, and publishing royalties for pharmaceutical companies and other organizations.
SOURCES: Oskoui M et al. Neurology. 2019 Aug 14. doi: 10.1212/WNL.0000000000008095. Oskoui M et al. Neurology. 2019 Aug 14. doi: 10.1212/WNL.0000000000008105.
Two new guidelines on the treatment and prevention of migraines in children and adolescents have been released by the American Academy of Neurology and the American Headache Society.
This update to the previous guidelines released by the American Academy of Neurology in 2004 reflects the expansion in pharmacologic and nonpharmacologic approaches during the last 15 years, Andrew D. Hershey, MD, PhD, director of the division of neurology at Cincinnati Children’s Hospital and a fellow of the American Academy of Neurology, said in an interview.
“There has also been an increase in the number of randomized controlled studies, which have allowed for a more robust statement on acute and preventive treatments to be made,” said Dr. Hershey, who is also a senior author for both guidelines.
The two reports focused on separate issues: One guideline outlined the options for treatment of acute migraine, and the second guideline summarized the available studies on the effectiveness of preventive medications for migraine in children and adolescents.
The guidelines recommend a physical examination and history to establish a specific headache diagnosis and afford a treatment that provides fast and complete pain relief. Treatment should be initiated as soon as a patient realizes an attack is occurring. Patients with signs of secondary headache should be evaluated by a neurologist or a headache specialist.
Studies support the use of ibuprofen and acetaminophen for pain relief in cases of acute migraine, but only some triptans (such as almotriptan, rizatriptan, sumatriptan/naproxen, and zolmitriptan nasal spray) are approved for use in adolescents. Specifically, sumatriptan/naproxen was shown to be effective when compared with placebo in studies with adolescents, whose headache symptoms resolved within 2 hours.
It may be necessary to try more than one triptan, the guidelines noted, because patients respond differently to medications. A failure to respond to one triptan does not necessarily mean that treatment with another triptan will be unsuccessful.
The guidelines also focused on patient and family education to improve medication safety and adherence. Lifestyle modification, avoidance of migraine triggers, creating good sleep habits, and staying hydrated can help reduce migraines. While no medications improved associated symptoms of migraines such as nausea or vomiting, triptans did show a benefit in reducing phonophobia and photophobia.
Evidence for pharmacologic prevention of migraines in children and adolescents is limited, according to the guidelines. In the 15 studies included in a literature review, there was not sufficient evidence to show preventive treatments, such as divalproex, onabotulinumtoxinA, amitriptyline, nimodipine, and flunarizine, were more effective than placebo at reducing the frequency of headaches. There was some evidence to show propranolol in children and topiramate and cinnarizine in children and adolescents can reduce headache frequency. Children and adolescents who received cognitive-behavioral therapy together with amitriptyline were more likely to have reduced frequency of headaches than were those who received amitriptyline with patient education.
“The consensus conclusion was that a multidisciplinary approach that combines acute treatments, preventive treatments, and healthy habits is likely to have the best outcomes,” said Dr. Hershey.
Dr. Hershey acknowledged the many gaps between what is clinically observed and what the studies in the guidelines demonstrated.
“One of the biggest questions is how to minimize the expectation response in the controlled studies,” he said. “Additionally, we are moving toward a better recognition of the mechanism by which the various treatments work in a genetic-based disease that is polygenic in nature” with up to 38 different gene polymorphisms identified to date.
The guidelines also do not address newer treatments, such as calcitonin gene–related peptide (CGRP) antibodies, CGRP antagonists, serotonin antagonists, and devices because there are as yet no studies of their effectiveness in children and adolescents.
“They have been studied in adults, so will be prone to the expectation response; but given the large number of diverse therapies, one can hope that many of the gaps can be filled,” said Dr. Hershey.
The American Academy of Neurology provided funding for development of the guidelines and reimbursed authors who served as subcommittee members for travel expenses and in-person meetings. The authors reported personal and institutional relationships in the form of advisory board memberships, investigator appointments, speakers bureau positions, research support, grants, honorariums, consultancies, and publishing royalties for pharmaceutical companies and other organizations.
SOURCES: Oskoui M et al. Neurology. 2019 Aug 14. doi: 10.1212/WNL.0000000000008095. Oskoui M et al. Neurology. 2019 Aug 14. doi: 10.1212/WNL.0000000000008105.
FROM NEUROLOGY
Ubrogepant shows acute migraine efficacy in triptan nonresponders
PHILADELPHIA – The oral, small molecule, calcitonin gene-related peptide receptor antagonist ubrogepant, currently under regulatory review for approval as a treatment for acute migraine headache, was as effective for migraine relief in patients with a history of triptan ineffectiveness as it was in patients for whom triptans had been effective, based on a post hoc analysis of data collected from 1,798 patients enrolled in two phase 3 trials.
In the roughly one-quarter of all patients who had a clinical history consistent with triptan ineffectiveness, one 50-mg dose of ubrogepant led to pain freedom 2 hours after treatment in 16% of patients, compared with a response rate of 8% in placebo-treated patients. Ubrogepant’s effectiveness rate that was about the same as seen in patients with a history of triptan effectiveness, who were about 37% of the study population, Susan Hutchinson, MD, said at the annual meeting of the American Headache Society.
Among those with a history of triptan effectiveness, 20% were pain free after 2 hours, compared with 11% of placebo-treated controls, said Dr. Hutchinson, a family physician and headache specialist who practices in Irvine, Calif. Both of these between-group differences were statistically significant. The remaining patients included in the analysis had no triptan history, and among these patients a single, 50-mg dose of ubrogepant produced pain freedom at 2 hours in 24% of patients, versus an 18% response in placebo-treated controls, a difference that fell short of statistical significance.
The analysis Dr. Hutchinson reported came from data collected in two pivotal trials of ubrogepant for treatment of an acute migraine headache, the ACHIEVE I and ACHIEVE II trials, which together randomized more than 2,600 migraine patients eligible for the study’s modified intention-to-treat analysis, and 1,798 patients from that analysis who received a 50-mg dose of ubrogepant or placebo. In March 2019, the company developing ubrogepant, Allergan, announced that the Food and Drug Administration had accepted the company’s application for marketing approval of ubrogepant as a treatment for acute migraine largely based on data from ACHIEVE I and ACHIEVE II.
The researchers defined a history of triptan ineffectiveness as a patient who never used a triptan because of a warning, precaution, or contraindication, a patient who recently used triptans but did not achieve pain freedom within 2 hours more than half the time taking the drugs, or a patient who no longer used triptans because of adverse effects or lack of efficacy. Patients who had used triptans in the past and had complete pain relief within 2 hours more than half the time were deemed triptan-effective patients.
The analysis also looked at two other endpoints in addition to complete pain freedom: complete relief of the most-bothersome symptom of the migraine headache (photophobia for most patients), which resolved in 39% and 36% of the triptan-effective and triptan-ineffective patients, respectively, compared with placebo response rates of 27% and 23%; both between-group differences were statistically significant. A third measure of efficacy was some degree of pain relief after 2 hours, which occurred in 62% of patients in whom triptans were effective and 55% in those in whom triptans were ineffective, which were again statistically significant higher rates than among patients who received placebo.
Safety findings from the two ubrogepant pivotal trials showed good drug tolerability, with no treatment-related serious adverse events, and a profile of modest numbers of treatment-related and total adverse events similar to what occurred among patients who received placebo.
ACHIEVE I and II were funded by Allergan, the company developing ubrogepant. Dr. Hutchinson has been an adviser to and a speaker on behalf of Allergan and several other companies.
SOURCE: Blumenfeld AM. Headache. 2019 June;59[S1]:1-208, Abstract IOR02.
PHILADELPHIA – The oral, small molecule, calcitonin gene-related peptide receptor antagonist ubrogepant, currently under regulatory review for approval as a treatment for acute migraine headache, was as effective for migraine relief in patients with a history of triptan ineffectiveness as it was in patients for whom triptans had been effective, based on a post hoc analysis of data collected from 1,798 patients enrolled in two phase 3 trials.
In the roughly one-quarter of all patients who had a clinical history consistent with triptan ineffectiveness, one 50-mg dose of ubrogepant led to pain freedom 2 hours after treatment in 16% of patients, compared with a response rate of 8% in placebo-treated patients. Ubrogepant’s effectiveness rate that was about the same as seen in patients with a history of triptan effectiveness, who were about 37% of the study population, Susan Hutchinson, MD, said at the annual meeting of the American Headache Society.
Among those with a history of triptan effectiveness, 20% were pain free after 2 hours, compared with 11% of placebo-treated controls, said Dr. Hutchinson, a family physician and headache specialist who practices in Irvine, Calif. Both of these between-group differences were statistically significant. The remaining patients included in the analysis had no triptan history, and among these patients a single, 50-mg dose of ubrogepant produced pain freedom at 2 hours in 24% of patients, versus an 18% response in placebo-treated controls, a difference that fell short of statistical significance.
The analysis Dr. Hutchinson reported came from data collected in two pivotal trials of ubrogepant for treatment of an acute migraine headache, the ACHIEVE I and ACHIEVE II trials, which together randomized more than 2,600 migraine patients eligible for the study’s modified intention-to-treat analysis, and 1,798 patients from that analysis who received a 50-mg dose of ubrogepant or placebo. In March 2019, the company developing ubrogepant, Allergan, announced that the Food and Drug Administration had accepted the company’s application for marketing approval of ubrogepant as a treatment for acute migraine largely based on data from ACHIEVE I and ACHIEVE II.
The researchers defined a history of triptan ineffectiveness as a patient who never used a triptan because of a warning, precaution, or contraindication, a patient who recently used triptans but did not achieve pain freedom within 2 hours more than half the time taking the drugs, or a patient who no longer used triptans because of adverse effects or lack of efficacy. Patients who had used triptans in the past and had complete pain relief within 2 hours more than half the time were deemed triptan-effective patients.
The analysis also looked at two other endpoints in addition to complete pain freedom: complete relief of the most-bothersome symptom of the migraine headache (photophobia for most patients), which resolved in 39% and 36% of the triptan-effective and triptan-ineffective patients, respectively, compared with placebo response rates of 27% and 23%; both between-group differences were statistically significant. A third measure of efficacy was some degree of pain relief after 2 hours, which occurred in 62% of patients in whom triptans were effective and 55% in those in whom triptans were ineffective, which were again statistically significant higher rates than among patients who received placebo.
Safety findings from the two ubrogepant pivotal trials showed good drug tolerability, with no treatment-related serious adverse events, and a profile of modest numbers of treatment-related and total adverse events similar to what occurred among patients who received placebo.
ACHIEVE I and II were funded by Allergan, the company developing ubrogepant. Dr. Hutchinson has been an adviser to and a speaker on behalf of Allergan and several other companies.
SOURCE: Blumenfeld AM. Headache. 2019 June;59[S1]:1-208, Abstract IOR02.
PHILADELPHIA – The oral, small molecule, calcitonin gene-related peptide receptor antagonist ubrogepant, currently under regulatory review for approval as a treatment for acute migraine headache, was as effective for migraine relief in patients with a history of triptan ineffectiveness as it was in patients for whom triptans had been effective, based on a post hoc analysis of data collected from 1,798 patients enrolled in two phase 3 trials.
In the roughly one-quarter of all patients who had a clinical history consistent with triptan ineffectiveness, one 50-mg dose of ubrogepant led to pain freedom 2 hours after treatment in 16% of patients, compared with a response rate of 8% in placebo-treated patients. Ubrogepant’s effectiveness rate that was about the same as seen in patients with a history of triptan effectiveness, who were about 37% of the study population, Susan Hutchinson, MD, said at the annual meeting of the American Headache Society.
Among those with a history of triptan effectiveness, 20% were pain free after 2 hours, compared with 11% of placebo-treated controls, said Dr. Hutchinson, a family physician and headache specialist who practices in Irvine, Calif. Both of these between-group differences were statistically significant. The remaining patients included in the analysis had no triptan history, and among these patients a single, 50-mg dose of ubrogepant produced pain freedom at 2 hours in 24% of patients, versus an 18% response in placebo-treated controls, a difference that fell short of statistical significance.
The analysis Dr. Hutchinson reported came from data collected in two pivotal trials of ubrogepant for treatment of an acute migraine headache, the ACHIEVE I and ACHIEVE II trials, which together randomized more than 2,600 migraine patients eligible for the study’s modified intention-to-treat analysis, and 1,798 patients from that analysis who received a 50-mg dose of ubrogepant or placebo. In March 2019, the company developing ubrogepant, Allergan, announced that the Food and Drug Administration had accepted the company’s application for marketing approval of ubrogepant as a treatment for acute migraine largely based on data from ACHIEVE I and ACHIEVE II.
The researchers defined a history of triptan ineffectiveness as a patient who never used a triptan because of a warning, precaution, or contraindication, a patient who recently used triptans but did not achieve pain freedom within 2 hours more than half the time taking the drugs, or a patient who no longer used triptans because of adverse effects or lack of efficacy. Patients who had used triptans in the past and had complete pain relief within 2 hours more than half the time were deemed triptan-effective patients.
The analysis also looked at two other endpoints in addition to complete pain freedom: complete relief of the most-bothersome symptom of the migraine headache (photophobia for most patients), which resolved in 39% and 36% of the triptan-effective and triptan-ineffective patients, respectively, compared with placebo response rates of 27% and 23%; both between-group differences were statistically significant. A third measure of efficacy was some degree of pain relief after 2 hours, which occurred in 62% of patients in whom triptans were effective and 55% in those in whom triptans were ineffective, which were again statistically significant higher rates than among patients who received placebo.
Safety findings from the two ubrogepant pivotal trials showed good drug tolerability, with no treatment-related serious adverse events, and a profile of modest numbers of treatment-related and total adverse events similar to what occurred among patients who received placebo.
ACHIEVE I and II were funded by Allergan, the company developing ubrogepant. Dr. Hutchinson has been an adviser to and a speaker on behalf of Allergan and several other companies.
SOURCE: Blumenfeld AM. Headache. 2019 June;59[S1]:1-208, Abstract IOR02.
REPORTING FROM AHS 2019
TAVR valves now FDA approved for low-risk patients
The Food and Drug Administration has expanded the indication for the Sapien 3, Sapien 3 Ultra, CoreValve Evolut R, and CoreValve Evolut PRO transcatheter heart valves to include patients with severe aortic valve stenosis at low risk for death or major complications associated with open-heart surgery.
The announcement was based on results of a pair of clinical trials involving patients with severe aortic valve stenosis. In the first, 1,000 patients were randomly sorted to receive either transcatheter aortic valve replacement (TAVR) with the Edwards Lifescience’s Sapien 3 device or open-heart surgery. In the second, 1,468 patients received either Medtronic’s CoreValve Evolut R or CoreValve Evolut PRO or open heart surgery. In both studies, after an average follow-up time of 15-17 months, outcomes such as all-cause mortality and stroke were similar in patients who underwent open heart surgery and who received the transcatheter heart valve.
Serious adverse events associated with transcatheter heart valves include death, stroke, acute kidney injury, heart attack, bleeding, and the need for a permanent pacemaker. Patients who cannot tolerate blood-thinning medication or have an infection in the heart are contraindicated; in addition, the CoreValve devices should not be used in patients sensitive to titanium or nickel. Because the longevity of transcatheter heart valves, compared with open-heart surgery, has not been established, younger patients should discuss options with their health care provider.
“This new approval significantly expands the number of patients that can be treated with this less invasive procedure for aortic valve replacement and follows a thorough review of data demonstrating these devices are safe and effective for this larger population,” Bram Zuckerman, MD, director of the Office of Cardiovascular Devices in the FDA’s Center for Devices and Radiological Health, said in the press release.
Find the full press release on the FDA website.
The Food and Drug Administration has expanded the indication for the Sapien 3, Sapien 3 Ultra, CoreValve Evolut R, and CoreValve Evolut PRO transcatheter heart valves to include patients with severe aortic valve stenosis at low risk for death or major complications associated with open-heart surgery.
The announcement was based on results of a pair of clinical trials involving patients with severe aortic valve stenosis. In the first, 1,000 patients were randomly sorted to receive either transcatheter aortic valve replacement (TAVR) with the Edwards Lifescience’s Sapien 3 device or open-heart surgery. In the second, 1,468 patients received either Medtronic’s CoreValve Evolut R or CoreValve Evolut PRO or open heart surgery. In both studies, after an average follow-up time of 15-17 months, outcomes such as all-cause mortality and stroke were similar in patients who underwent open heart surgery and who received the transcatheter heart valve.
Serious adverse events associated with transcatheter heart valves include death, stroke, acute kidney injury, heart attack, bleeding, and the need for a permanent pacemaker. Patients who cannot tolerate blood-thinning medication or have an infection in the heart are contraindicated; in addition, the CoreValve devices should not be used in patients sensitive to titanium or nickel. Because the longevity of transcatheter heart valves, compared with open-heart surgery, has not been established, younger patients should discuss options with their health care provider.
“This new approval significantly expands the number of patients that can be treated with this less invasive procedure for aortic valve replacement and follows a thorough review of data demonstrating these devices are safe and effective for this larger population,” Bram Zuckerman, MD, director of the Office of Cardiovascular Devices in the FDA’s Center for Devices and Radiological Health, said in the press release.
Find the full press release on the FDA website.
The Food and Drug Administration has expanded the indication for the Sapien 3, Sapien 3 Ultra, CoreValve Evolut R, and CoreValve Evolut PRO transcatheter heart valves to include patients with severe aortic valve stenosis at low risk for death or major complications associated with open-heart surgery.
The announcement was based on results of a pair of clinical trials involving patients with severe aortic valve stenosis. In the first, 1,000 patients were randomly sorted to receive either transcatheter aortic valve replacement (TAVR) with the Edwards Lifescience’s Sapien 3 device or open-heart surgery. In the second, 1,468 patients received either Medtronic’s CoreValve Evolut R or CoreValve Evolut PRO or open heart surgery. In both studies, after an average follow-up time of 15-17 months, outcomes such as all-cause mortality and stroke were similar in patients who underwent open heart surgery and who received the transcatheter heart valve.
Serious adverse events associated with transcatheter heart valves include death, stroke, acute kidney injury, heart attack, bleeding, and the need for a permanent pacemaker. Patients who cannot tolerate blood-thinning medication or have an infection in the heart are contraindicated; in addition, the CoreValve devices should not be used in patients sensitive to titanium or nickel. Because the longevity of transcatheter heart valves, compared with open-heart surgery, has not been established, younger patients should discuss options with their health care provider.
“This new approval significantly expands the number of patients that can be treated with this less invasive procedure for aortic valve replacement and follows a thorough review of data demonstrating these devices are safe and effective for this larger population,” Bram Zuckerman, MD, director of the Office of Cardiovascular Devices in the FDA’s Center for Devices and Radiological Health, said in the press release.
Find the full press release on the FDA website.
Prescription drug use varies between U.S. and Canada
The United States and Canada deliver health care in different ways, and patterns of prescription drug use also vary between the two countries, according to the National Center for Health Statistics.
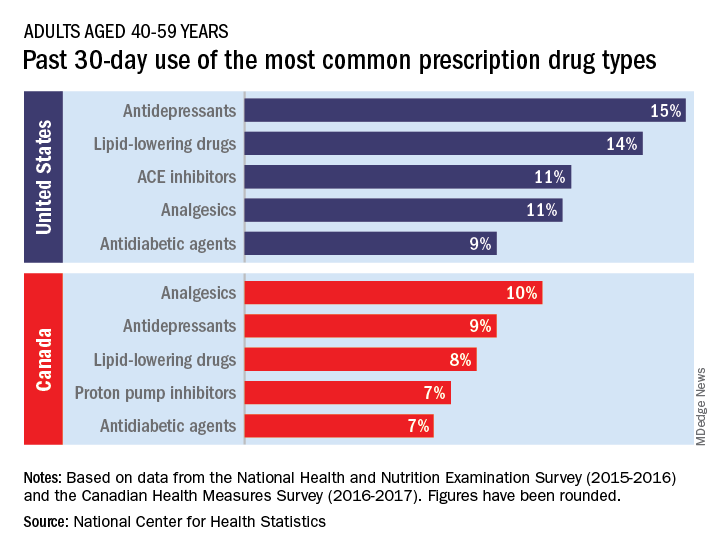
The populations of the two countries, however, have similar age distributions – adults aged 40-79 years made up 44% of the population in the United States and 48% in Canada in 2016 – so “monitoring the use of prescription drugs provides insights into the health and health care of U.S. and Canadian adults,” the NCHS investigators wrote.
Data from the 2015-2016 National Health and Nutritional Examination Survey show that 15% of Americans aged 40-59 years had used antidepressants in the past 30 days, putting them ahead of lipid-lowering drugs (14%) and ACE inhibitors (11%), the NCHS said in a recent Data Brief.
Analgesics were the leading drug type in Canada, with 10% of adults aged 40-59 years reporting use in the past month, although that’s still lower than in the United States (11%), where they were fourth in popularity. The American top two were second and third among Canadians, while proton pump inhibitors were fourth in Canada but did not crack the top five in the United States, the NCHS reported based on 2016-2017 data from the Canadian Health Measures Survey.
Older adults (60-79 years) in the two countries managed to share some common ground: Lipid-lowering drugs were the most commonly used prescription medication both north and south of the border, although past 30-day use was considerably higher in the United States (45% vs. 34%), the NCHS investigators said.
There were differences to be found, however, in the older age group. Analgesics were the second most commonly used drug type in Canada but did not even reach the top five in the United States, while beta-blockers were third among Americans but missed the Canadian top five, they noted.
(60% vs. 53%) and to have used at least five such drugs (15% vs. 10%). The differences among adults aged 60-79 were not significant, although American use was higher for at least one drug (84% vs. 83%) and for at least five (35% vs. 31%), according to the report.
The United States and Canada deliver health care in different ways, and patterns of prescription drug use also vary between the two countries, according to the National Center for Health Statistics.
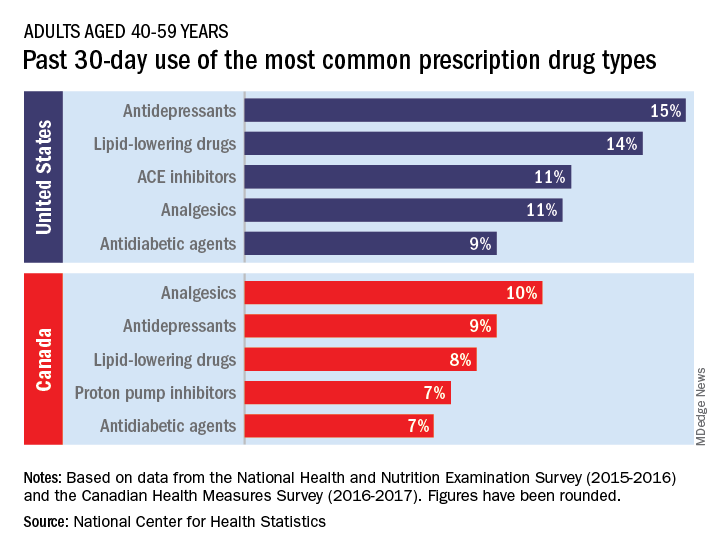
The populations of the two countries, however, have similar age distributions – adults aged 40-79 years made up 44% of the population in the United States and 48% in Canada in 2016 – so “monitoring the use of prescription drugs provides insights into the health and health care of U.S. and Canadian adults,” the NCHS investigators wrote.
Data from the 2015-2016 National Health and Nutritional Examination Survey show that 15% of Americans aged 40-59 years had used antidepressants in the past 30 days, putting them ahead of lipid-lowering drugs (14%) and ACE inhibitors (11%), the NCHS said in a recent Data Brief.
Analgesics were the leading drug type in Canada, with 10% of adults aged 40-59 years reporting use in the past month, although that’s still lower than in the United States (11%), where they were fourth in popularity. The American top two were second and third among Canadians, while proton pump inhibitors were fourth in Canada but did not crack the top five in the United States, the NCHS reported based on 2016-2017 data from the Canadian Health Measures Survey.
Older adults (60-79 years) in the two countries managed to share some common ground: Lipid-lowering drugs were the most commonly used prescription medication both north and south of the border, although past 30-day use was considerably higher in the United States (45% vs. 34%), the NCHS investigators said.
There were differences to be found, however, in the older age group. Analgesics were the second most commonly used drug type in Canada but did not even reach the top five in the United States, while beta-blockers were third among Americans but missed the Canadian top five, they noted.
(60% vs. 53%) and to have used at least five such drugs (15% vs. 10%). The differences among adults aged 60-79 were not significant, although American use was higher for at least one drug (84% vs. 83%) and for at least five (35% vs. 31%), according to the report.
The United States and Canada deliver health care in different ways, and patterns of prescription drug use also vary between the two countries, according to the National Center for Health Statistics.
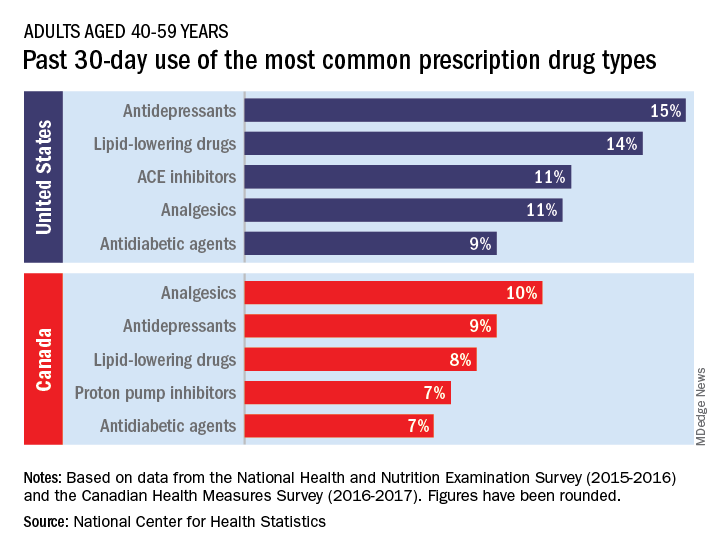
The populations of the two countries, however, have similar age distributions – adults aged 40-79 years made up 44% of the population in the United States and 48% in Canada in 2016 – so “monitoring the use of prescription drugs provides insights into the health and health care of U.S. and Canadian adults,” the NCHS investigators wrote.
Data from the 2015-2016 National Health and Nutritional Examination Survey show that 15% of Americans aged 40-59 years had used antidepressants in the past 30 days, putting them ahead of lipid-lowering drugs (14%) and ACE inhibitors (11%), the NCHS said in a recent Data Brief.
Analgesics were the leading drug type in Canada, with 10% of adults aged 40-59 years reporting use in the past month, although that’s still lower than in the United States (11%), where they were fourth in popularity. The American top two were second and third among Canadians, while proton pump inhibitors were fourth in Canada but did not crack the top five in the United States, the NCHS reported based on 2016-2017 data from the Canadian Health Measures Survey.
Older adults (60-79 years) in the two countries managed to share some common ground: Lipid-lowering drugs were the most commonly used prescription medication both north and south of the border, although past 30-day use was considerably higher in the United States (45% vs. 34%), the NCHS investigators said.
There were differences to be found, however, in the older age group. Analgesics were the second most commonly used drug type in Canada but did not even reach the top five in the United States, while beta-blockers were third among Americans but missed the Canadian top five, they noted.
(60% vs. 53%) and to have used at least five such drugs (15% vs. 10%). The differences among adults aged 60-79 were not significant, although American use was higher for at least one drug (84% vs. 83%) and for at least five (35% vs. 31%), according to the report.
Is your office ready for a case of measles?
It’s a typically busy Friday and the doctor is running 20 minutes behind schedule. He enters the next exam room and the sight of the patient makes him forget the apology he had prepared.
The 10 month old looks miserable. Red eyes. Snot dripping from his nose. A red rash that extends from his face and involves most of the chest, arms, and upper thighs.
“When did this start?” he asks the mother as he searches for a surgical mask in the cabinet next to the exam table.
“Two days after we returned from our vacation in France,” the worried young woman replies. “Do you think it could be measles?”
Between Jan. 1 and Aug. 8, 2019, 1,182 cases of measles had been confirmed in the United States. That’s more than three times the number of cases reported in all of 2018, and the highest number of cases reported in a single year in more than a quarter century. While 75% of the cases this year have been linked to outbreaks in New York, individuals from 30 states have been affected.
Given the widespread nature of the outbreak, With measles in particular, time is limited to deliver effective postexposure prophylaxis and prevent the spread of measles in the community, making it difficult to develop a plan on the fly.
Schedule strategically. You don’t want a patient with measles hanging out in your waiting room. According to the American Academy of Pediatrics, measures to prevent the transmission of contagious infectious agents in ambulatory facilities begin at the time the visit is scheduled. When there is measles transmission in the community, consider using a standardized script when scheduling patients that includes questions about fever, rash, other symptoms typical for measles, and possible exposures. Some offices will have procedures in place that can be adapted to care for patients with suspected measles. When a patient presents for suspected chicken pox, do you advise them to come at the end of the day to minimize exposures? Enter through a side door? Perform a car visit?
Triage promptly. Mask patients with fever and rash, move to a private room, and close the door.
Once measles is suspected, only health care personnel who are immune to measles should enter the exam room. According to the Centers for Disease Control and Prevention, presumptive evidence of measles immunity in health care providers is written documentation of vaccination with two doses of live measles or MMR vaccine administered at least 28 days apart, laboratory evidence of immunity (that is, positive measles IgG), laboratory confirmation of disease, or birth before 1957.
Even though health care providers born before 1957 are presumed to have had the disease at some point and have traditionally been considered immune, the CDC suggests that health care facilities consider giving these individuals two doses of MMR vaccine unless they have prior laboratory confirmation of disease immunity. Do you know who in your office is immune or would you need to scramble if you had an exposure?
When measles is suspected, health care personnel should wear an N-95 if they have been fit tested and the appropriate mask is available. Practically, most ambulatory offices do not stock N-95 masks and the next best choice is a regular surgical mask.
Order the recommended tests to confirm the diagnosis, but do not wait for the results to confirm the diagnosis. The CDC recommends testing serum for IgM antibodies and sending a throat or nasopharyngeal swab to look for the virus by polymerase chain reaction testing. Measles virus also is shed in the urine so collecting a urine specimen for testing may increase the chances of finding the virus. Depending on where you practice, the tests may take 3 days or more to result. Contact your local health department as soon as you consider a measles diagnosis.
Discharge patients home or transferred to a higher level of care if this is necessary as quickly as possible. Fortunately, most patients with measles do not require hospitalization. Do not send patients to the hospital simply for the purpose of laboratory testing if this can be accomplished quickly in your office or for evaluation by other providers. This just creates the potential for more exposures. If a patient does require higher-level care, provider-to-provider communication about the suspected diagnosis and the need for airborne isolation should take place.
Keep the door closed. Once a patient with suspected measles is discharged from a regular exam room, the door should remain closed, and it should not be used for at least 1 hour. Remember that infectious virus can remain in the air for 1-2 hours after a patient leaves an area. The same is true for the waiting room.
Develop the exposure list. In general, patients and family members who were in the waiting room at the same time as the index patient and up to 1-2 hours after the index patient left are considered exposed. Measles is highly contagious and 9 out of 10 susceptible people who are exposed will develop disease. How many infants aged less than 1 year might be in your waiting room at any given time? How many immunocompromised patients or family members? Public health authorities can help determine who needs prophylaxis.
Don’t get anxious and start testing everyone for measles, especially patients who lack typical signs and symptoms or exposures. Ordering a test in a patient who has a low likelihood of measles is more likely to result in a false-positive test than a true-positive test. False-positive measles IgM tests can be seen with some viral infections, including parvovirus and Epstein-Barr. Some rheumatologic disorders also can contribute to false-positive tests.
Review your office procedure for vaccine counseling. The 10 month old with measles in the opening vignette should have been given an MMR vaccine before travel. The vaccine is recommended for infants aged 6-11 months who are traveling outside the United States, but it doesn’t count toward the vaccine series. Reimmunize young travelers at 12-15 months and again at 4-6 years. The CDC has developed a toolkit that contains resources for taking to parents about vaccines. It is available at https://www.cdc.gov/measles/toolkit/healthcare-providers.html.
It’s a typically busy Friday and the doctor is running 20 minutes behind schedule. He enters the next exam room and the sight of the patient makes him forget the apology he had prepared.
The 10 month old looks miserable. Red eyes. Snot dripping from his nose. A red rash that extends from his face and involves most of the chest, arms, and upper thighs.
“When did this start?” he asks the mother as he searches for a surgical mask in the cabinet next to the exam table.
“Two days after we returned from our vacation in France,” the worried young woman replies. “Do you think it could be measles?”
Between Jan. 1 and Aug. 8, 2019, 1,182 cases of measles had been confirmed in the United States. That’s more than three times the number of cases reported in all of 2018, and the highest number of cases reported in a single year in more than a quarter century. While 75% of the cases this year have been linked to outbreaks in New York, individuals from 30 states have been affected.
Given the widespread nature of the outbreak, With measles in particular, time is limited to deliver effective postexposure prophylaxis and prevent the spread of measles in the community, making it difficult to develop a plan on the fly.
Schedule strategically. You don’t want a patient with measles hanging out in your waiting room. According to the American Academy of Pediatrics, measures to prevent the transmission of contagious infectious agents in ambulatory facilities begin at the time the visit is scheduled. When there is measles transmission in the community, consider using a standardized script when scheduling patients that includes questions about fever, rash, other symptoms typical for measles, and possible exposures. Some offices will have procedures in place that can be adapted to care for patients with suspected measles. When a patient presents for suspected chicken pox, do you advise them to come at the end of the day to minimize exposures? Enter through a side door? Perform a car visit?
Triage promptly. Mask patients with fever and rash, move to a private room, and close the door.
Once measles is suspected, only health care personnel who are immune to measles should enter the exam room. According to the Centers for Disease Control and Prevention, presumptive evidence of measles immunity in health care providers is written documentation of vaccination with two doses of live measles or MMR vaccine administered at least 28 days apart, laboratory evidence of immunity (that is, positive measles IgG), laboratory confirmation of disease, or birth before 1957.
Even though health care providers born before 1957 are presumed to have had the disease at some point and have traditionally been considered immune, the CDC suggests that health care facilities consider giving these individuals two doses of MMR vaccine unless they have prior laboratory confirmation of disease immunity. Do you know who in your office is immune or would you need to scramble if you had an exposure?
When measles is suspected, health care personnel should wear an N-95 if they have been fit tested and the appropriate mask is available. Practically, most ambulatory offices do not stock N-95 masks and the next best choice is a regular surgical mask.
Order the recommended tests to confirm the diagnosis, but do not wait for the results to confirm the diagnosis. The CDC recommends testing serum for IgM antibodies and sending a throat or nasopharyngeal swab to look for the virus by polymerase chain reaction testing. Measles virus also is shed in the urine so collecting a urine specimen for testing may increase the chances of finding the virus. Depending on where you practice, the tests may take 3 days or more to result. Contact your local health department as soon as you consider a measles diagnosis.
Discharge patients home or transferred to a higher level of care if this is necessary as quickly as possible. Fortunately, most patients with measles do not require hospitalization. Do not send patients to the hospital simply for the purpose of laboratory testing if this can be accomplished quickly in your office or for evaluation by other providers. This just creates the potential for more exposures. If a patient does require higher-level care, provider-to-provider communication about the suspected diagnosis and the need for airborne isolation should take place.
Keep the door closed. Once a patient with suspected measles is discharged from a regular exam room, the door should remain closed, and it should not be used for at least 1 hour. Remember that infectious virus can remain in the air for 1-2 hours after a patient leaves an area. The same is true for the waiting room.
Develop the exposure list. In general, patients and family members who were in the waiting room at the same time as the index patient and up to 1-2 hours after the index patient left are considered exposed. Measles is highly contagious and 9 out of 10 susceptible people who are exposed will develop disease. How many infants aged less than 1 year might be in your waiting room at any given time? How many immunocompromised patients or family members? Public health authorities can help determine who needs prophylaxis.
Don’t get anxious and start testing everyone for measles, especially patients who lack typical signs and symptoms or exposures. Ordering a test in a patient who has a low likelihood of measles is more likely to result in a false-positive test than a true-positive test. False-positive measles IgM tests can be seen with some viral infections, including parvovirus and Epstein-Barr. Some rheumatologic disorders also can contribute to false-positive tests.
Review your office procedure for vaccine counseling. The 10 month old with measles in the opening vignette should have been given an MMR vaccine before travel. The vaccine is recommended for infants aged 6-11 months who are traveling outside the United States, but it doesn’t count toward the vaccine series. Reimmunize young travelers at 12-15 months and again at 4-6 years. The CDC has developed a toolkit that contains resources for taking to parents about vaccines. It is available at https://www.cdc.gov/measles/toolkit/healthcare-providers.html.
It’s a typically busy Friday and the doctor is running 20 minutes behind schedule. He enters the next exam room and the sight of the patient makes him forget the apology he had prepared.
The 10 month old looks miserable. Red eyes. Snot dripping from his nose. A red rash that extends from his face and involves most of the chest, arms, and upper thighs.
“When did this start?” he asks the mother as he searches for a surgical mask in the cabinet next to the exam table.
“Two days after we returned from our vacation in France,” the worried young woman replies. “Do you think it could be measles?”
Between Jan. 1 and Aug. 8, 2019, 1,182 cases of measles had been confirmed in the United States. That’s more than three times the number of cases reported in all of 2018, and the highest number of cases reported in a single year in more than a quarter century. While 75% of the cases this year have been linked to outbreaks in New York, individuals from 30 states have been affected.
Given the widespread nature of the outbreak, With measles in particular, time is limited to deliver effective postexposure prophylaxis and prevent the spread of measles in the community, making it difficult to develop a plan on the fly.
Schedule strategically. You don’t want a patient with measles hanging out in your waiting room. According to the American Academy of Pediatrics, measures to prevent the transmission of contagious infectious agents in ambulatory facilities begin at the time the visit is scheduled. When there is measles transmission in the community, consider using a standardized script when scheduling patients that includes questions about fever, rash, other symptoms typical for measles, and possible exposures. Some offices will have procedures in place that can be adapted to care for patients with suspected measles. When a patient presents for suspected chicken pox, do you advise them to come at the end of the day to minimize exposures? Enter through a side door? Perform a car visit?
Triage promptly. Mask patients with fever and rash, move to a private room, and close the door.
Once measles is suspected, only health care personnel who are immune to measles should enter the exam room. According to the Centers for Disease Control and Prevention, presumptive evidence of measles immunity in health care providers is written documentation of vaccination with two doses of live measles or MMR vaccine administered at least 28 days apart, laboratory evidence of immunity (that is, positive measles IgG), laboratory confirmation of disease, or birth before 1957.
Even though health care providers born before 1957 are presumed to have had the disease at some point and have traditionally been considered immune, the CDC suggests that health care facilities consider giving these individuals two doses of MMR vaccine unless they have prior laboratory confirmation of disease immunity. Do you know who in your office is immune or would you need to scramble if you had an exposure?
When measles is suspected, health care personnel should wear an N-95 if they have been fit tested and the appropriate mask is available. Practically, most ambulatory offices do not stock N-95 masks and the next best choice is a regular surgical mask.
Order the recommended tests to confirm the diagnosis, but do not wait for the results to confirm the diagnosis. The CDC recommends testing serum for IgM antibodies and sending a throat or nasopharyngeal swab to look for the virus by polymerase chain reaction testing. Measles virus also is shed in the urine so collecting a urine specimen for testing may increase the chances of finding the virus. Depending on where you practice, the tests may take 3 days or more to result. Contact your local health department as soon as you consider a measles diagnosis.
Discharge patients home or transferred to a higher level of care if this is necessary as quickly as possible. Fortunately, most patients with measles do not require hospitalization. Do not send patients to the hospital simply for the purpose of laboratory testing if this can be accomplished quickly in your office or for evaluation by other providers. This just creates the potential for more exposures. If a patient does require higher-level care, provider-to-provider communication about the suspected diagnosis and the need for airborne isolation should take place.
Keep the door closed. Once a patient with suspected measles is discharged from a regular exam room, the door should remain closed, and it should not be used for at least 1 hour. Remember that infectious virus can remain in the air for 1-2 hours after a patient leaves an area. The same is true for the waiting room.
Develop the exposure list. In general, patients and family members who were in the waiting room at the same time as the index patient and up to 1-2 hours after the index patient left are considered exposed. Measles is highly contagious and 9 out of 10 susceptible people who are exposed will develop disease. How many infants aged less than 1 year might be in your waiting room at any given time? How many immunocompromised patients or family members? Public health authorities can help determine who needs prophylaxis.
Don’t get anxious and start testing everyone for measles, especially patients who lack typical signs and symptoms or exposures. Ordering a test in a patient who has a low likelihood of measles is more likely to result in a false-positive test than a true-positive test. False-positive measles IgM tests can be seen with some viral infections, including parvovirus and Epstein-Barr. Some rheumatologic disorders also can contribute to false-positive tests.
Review your office procedure for vaccine counseling. The 10 month old with measles in the opening vignette should have been given an MMR vaccine before travel. The vaccine is recommended for infants aged 6-11 months who are traveling outside the United States, but it doesn’t count toward the vaccine series. Reimmunize young travelers at 12-15 months and again at 4-6 years. The CDC has developed a toolkit that contains resources for taking to parents about vaccines. It is available at https://www.cdc.gov/measles/toolkit/healthcare-providers.html.
Nebraska issues SUNucate-based guidance for schools
Nebraska’s Department of Education recommended in a guidance that children be allowed to possess and use sunscreen products in school and at school-sponsored events, according to an Aug. 2 release from the American Society for Dermatologic Surgery.
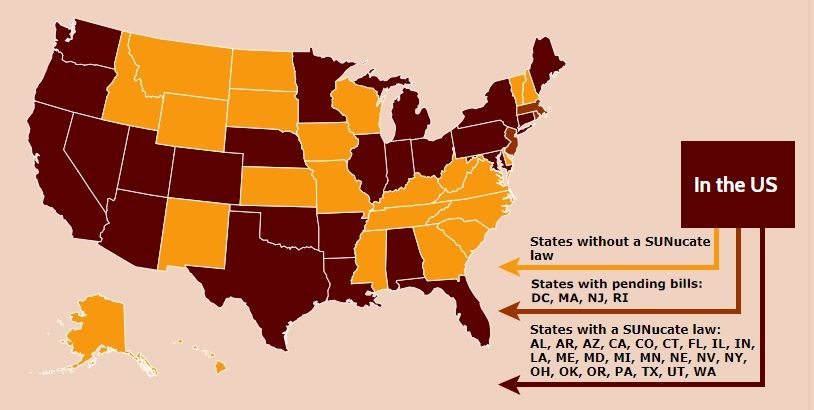
The department’s guidance is based on model legislation developed by the SUNucate Coalition, which was created by the American Society for Dermatologic Surgery Association and “works to address barriers to sunscreen use in school and camps and promote sun-safe behavior.” The coalition was created in 2016 because of reports that some U.S. schools had banned sunscreen products as part of broader medication bans because of these products’ classification as an over-the-counter medication.
Twenty-three other states have moved to lift such bans; these states were joined by Arkansas, Connecticut, Illinois, Maine, Minnesota, Nevada, and now Nebraska in 2019 alone. The District of Columbia, Massachusetts, New Jersey, and Rhode Island are expected to follow suit.
Nebraska’s Department of Education recommended in a guidance that children be allowed to possess and use sunscreen products in school and at school-sponsored events, according to an Aug. 2 release from the American Society for Dermatologic Surgery.
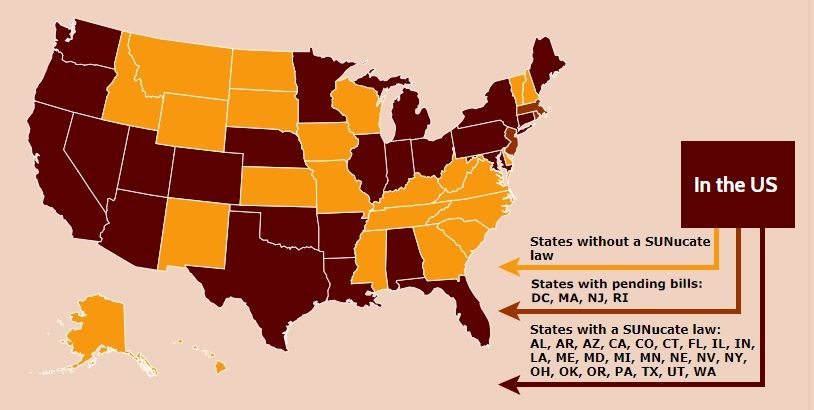
The department’s guidance is based on model legislation developed by the SUNucate Coalition, which was created by the American Society for Dermatologic Surgery Association and “works to address barriers to sunscreen use in school and camps and promote sun-safe behavior.” The coalition was created in 2016 because of reports that some U.S. schools had banned sunscreen products as part of broader medication bans because of these products’ classification as an over-the-counter medication.
Twenty-three other states have moved to lift such bans; these states were joined by Arkansas, Connecticut, Illinois, Maine, Minnesota, Nevada, and now Nebraska in 2019 alone. The District of Columbia, Massachusetts, New Jersey, and Rhode Island are expected to follow suit.
Nebraska’s Department of Education recommended in a guidance that children be allowed to possess and use sunscreen products in school and at school-sponsored events, according to an Aug. 2 release from the American Society for Dermatologic Surgery.
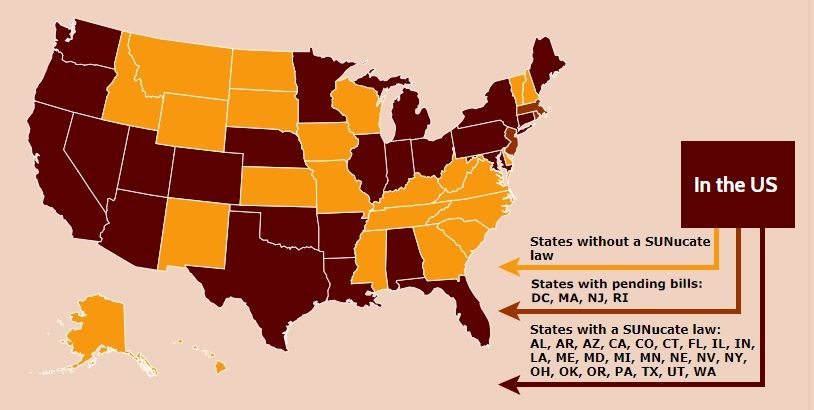
The department’s guidance is based on model legislation developed by the SUNucate Coalition, which was created by the American Society for Dermatologic Surgery Association and “works to address barriers to sunscreen use in school and camps and promote sun-safe behavior.” The coalition was created in 2016 because of reports that some U.S. schools had banned sunscreen products as part of broader medication bans because of these products’ classification as an over-the-counter medication.
Twenty-three other states have moved to lift such bans; these states were joined by Arkansas, Connecticut, Illinois, Maine, Minnesota, Nevada, and now Nebraska in 2019 alone. The District of Columbia, Massachusetts, New Jersey, and Rhode Island are expected to follow suit.










