User login
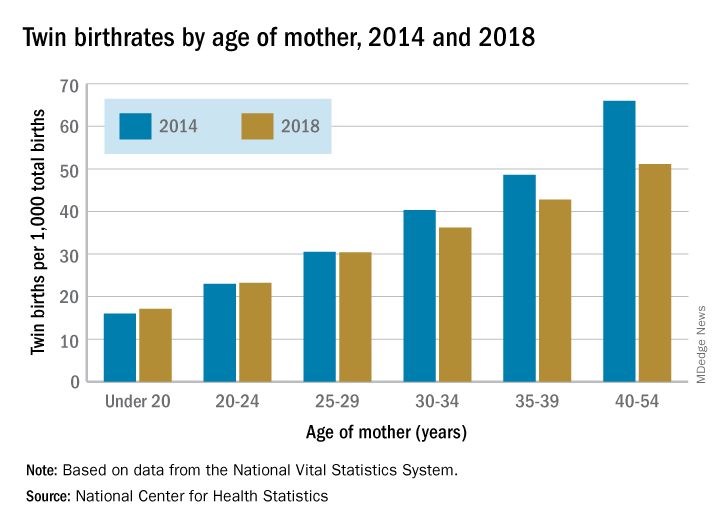
Twin births down among women 30 and older
according to the National Center for Health Statistics.
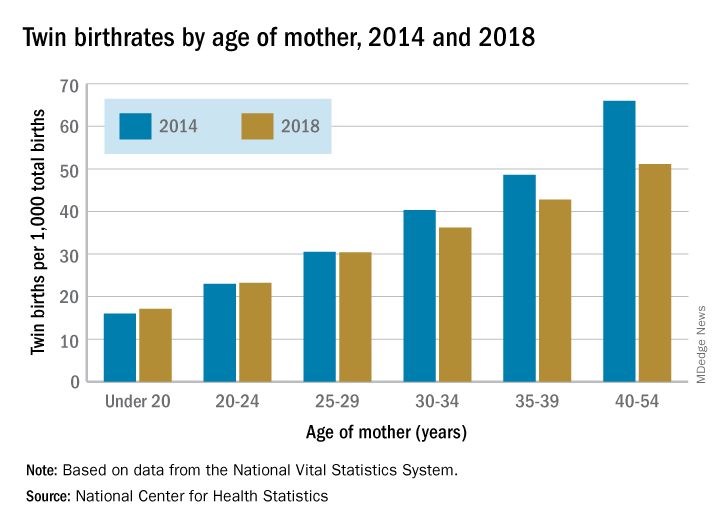
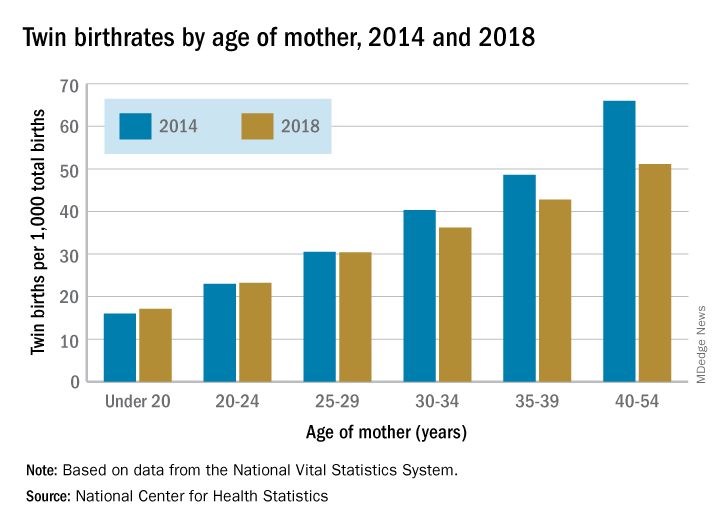
The twin birthrate, which had increased by 79% during 1980-2014, fell by 4% during 2014-2018, but that decline was “not universal across maternal age and race and Hispanic-origin groups,” the NCHS investigators said.
Twin birthrates fell by at least 10% for mothers aged 30 years and older from 2014 to 2018 but held steady for women in their twenties. Over that same period, the twin birthrate fell by a significant 7% among non-Hispanic white women (36.7 to 34.3 per 1,000 total births) but increased just slightly for non-Hispanic black women (40.0 to 40.5 per 1,000) and Hispanic women (24.1 to 24.4), the investigators reported.
For women 30 years and older, the drops in twin births got larger as age increased and were significant for each age group. The rate for women aged 30-34 years fell 10% as it went from 40.3 per 1,000 total births in 2014 to 36.2 per 1,000. The decrease was 12% (from 48.6 per 1,000 to 42.8) for women aged 35-39 and 23% (from 66.0 to 51.1) for those aged 40 years and older, they said based on data from the National Vital Statistics System.
The rates were basically unchanged for women in their 20s, from 23.0 to 23.2 in 20- to 24-year-olds and 30.5 to 30.4 in 25- to 29-year-olds – but there was a significant increase for the youngest group with rates among those younger than 20 years going from 16.0 to 17.1 per 1,000, the report showed.
according to the National Center for Health Statistics.
The twin birthrate, which had increased by 79% during 1980-2014, fell by 4% during 2014-2018, but that decline was “not universal across maternal age and race and Hispanic-origin groups,” the NCHS investigators said.
Twin birthrates fell by at least 10% for mothers aged 30 years and older from 2014 to 2018 but held steady for women in their twenties. Over that same period, the twin birthrate fell by a significant 7% among non-Hispanic white women (36.7 to 34.3 per 1,000 total births) but increased just slightly for non-Hispanic black women (40.0 to 40.5 per 1,000) and Hispanic women (24.1 to 24.4), the investigators reported.
For women 30 years and older, the drops in twin births got larger as age increased and were significant for each age group. The rate for women aged 30-34 years fell 10% as it went from 40.3 per 1,000 total births in 2014 to 36.2 per 1,000. The decrease was 12% (from 48.6 per 1,000 to 42.8) for women aged 35-39 and 23% (from 66.0 to 51.1) for those aged 40 years and older, they said based on data from the National Vital Statistics System.
The rates were basically unchanged for women in their 20s, from 23.0 to 23.2 in 20- to 24-year-olds and 30.5 to 30.4 in 25- to 29-year-olds – but there was a significant increase for the youngest group with rates among those younger than 20 years going from 16.0 to 17.1 per 1,000, the report showed.
according to the National Center for Health Statistics.
The twin birthrate, which had increased by 79% during 1980-2014, fell by 4% during 2014-2018, but that decline was “not universal across maternal age and race and Hispanic-origin groups,” the NCHS investigators said.
Twin birthrates fell by at least 10% for mothers aged 30 years and older from 2014 to 2018 but held steady for women in their twenties. Over that same period, the twin birthrate fell by a significant 7% among non-Hispanic white women (36.7 to 34.3 per 1,000 total births) but increased just slightly for non-Hispanic black women (40.0 to 40.5 per 1,000) and Hispanic women (24.1 to 24.4), the investigators reported.
For women 30 years and older, the drops in twin births got larger as age increased and were significant for each age group. The rate for women aged 30-34 years fell 10% as it went from 40.3 per 1,000 total births in 2014 to 36.2 per 1,000. The decrease was 12% (from 48.6 per 1,000 to 42.8) for women aged 35-39 and 23% (from 66.0 to 51.1) for those aged 40 years and older, they said based on data from the National Vital Statistics System.
The rates were basically unchanged for women in their 20s, from 23.0 to 23.2 in 20- to 24-year-olds and 30.5 to 30.4 in 25- to 29-year-olds – but there was a significant increase for the youngest group with rates among those younger than 20 years going from 16.0 to 17.1 per 1,000, the report showed.
Dismantling the opioid crisis
Dr. John Hickner’s editorial, “Doing our part to dismantle the opioid crisis” (J Fam Pract 2019;68:308) had important inaccuracies.
The Joint Commission, for which I serve as an executive vice president, did not “dub pain assessment the ‘fifth vital sign’. ” The concept of the fifth vital sign was developed by the American Pain Society in the 1990s.1 It gained national attention through a Veterans Health Administration initiative in 1999.2 And in 2001, the Joint Commission (then the Joint Commission on Accreditation of Healthcare Organizations or JCAHO) issued its Pain Standards.
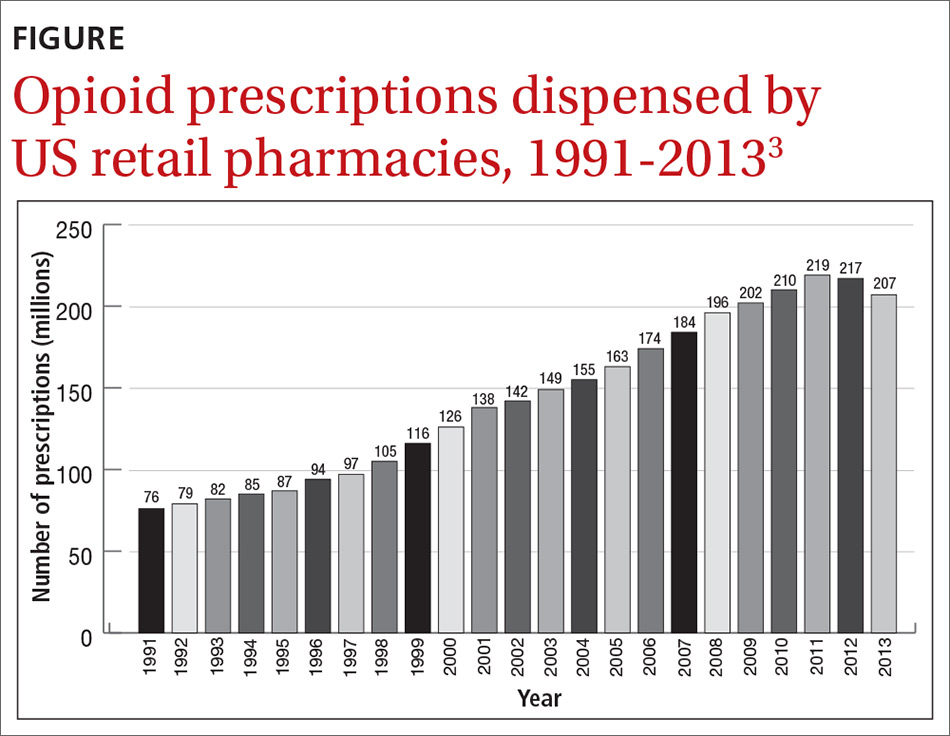
Dr. Hickner wrote that the push to assess for pain as the fifth vital sign was a central cause of the opioid epidemic; however, this is contrary to published data on the epidemic. Total opioid prescriptions had been steadily increasing in the United States for at least a decade before the Pain Standards went into effect in 2001 (FIGURE).3 Between 1991 and 1997, the number of prescriptions increased from 76 million to 97 million. The rate of increase from 1997 to 2011 appears to have been more rapid, which is likely due to the 1995 approval of the new sustained-release opioid OxyContin and the associated aggressive marketing campaigns to physicians.
Your readers should know that we, at the Joint Commission, are also “doing our part to dismantle the opioid crisis.” In 2016, we completely revised our Pain Standards, adding new criteria to help address the epidemic. Some adjustments include: requiring improved availability of nonpharmacologic therapy, encouraging engagement of patients in pain management plans, enhancing accessibility of Physician Drug Monitoring Program tools, and monitoring opioid prescribing.
David W. Baker, MD, FACP, executive vice president
The Joint Commission, Oakbrook Terrace, IL
1. American Pain Society. Principles of Analgesic Use in the Treatment of Acute Pain and Chronic Cancer Pain. 2nd ed. Skokie, Illinois: American Pain Society; 1989.
2. Department of Veteran’s Affairs. Pain: the fifth vital sign. www.va.gov/PAINMANAGEMENT/docs/Pain_As_the_5th_Vital_Sign_Toolkit.pdf. Published October 2000. Accessed September 30, 2019.
3 National Institute on Drug Abuse. America’s addiction to opioids: heroin and prescription drug abuse. https://archives.drugabuse.gov/testimonies/2014/americas-addiction-to-opioids-heroin-prescription-drug-abuse. Published May 14, 2014. Accessed September 30, 2019.
Dr. John Hickner’s editorial, “Doing our part to dismantle the opioid crisis” (J Fam Pract 2019;68:308) had important inaccuracies.
The Joint Commission, for which I serve as an executive vice president, did not “dub pain assessment the ‘fifth vital sign’. ” The concept of the fifth vital sign was developed by the American Pain Society in the 1990s.1 It gained national attention through a Veterans Health Administration initiative in 1999.2 And in 2001, the Joint Commission (then the Joint Commission on Accreditation of Healthcare Organizations or JCAHO) issued its Pain Standards.
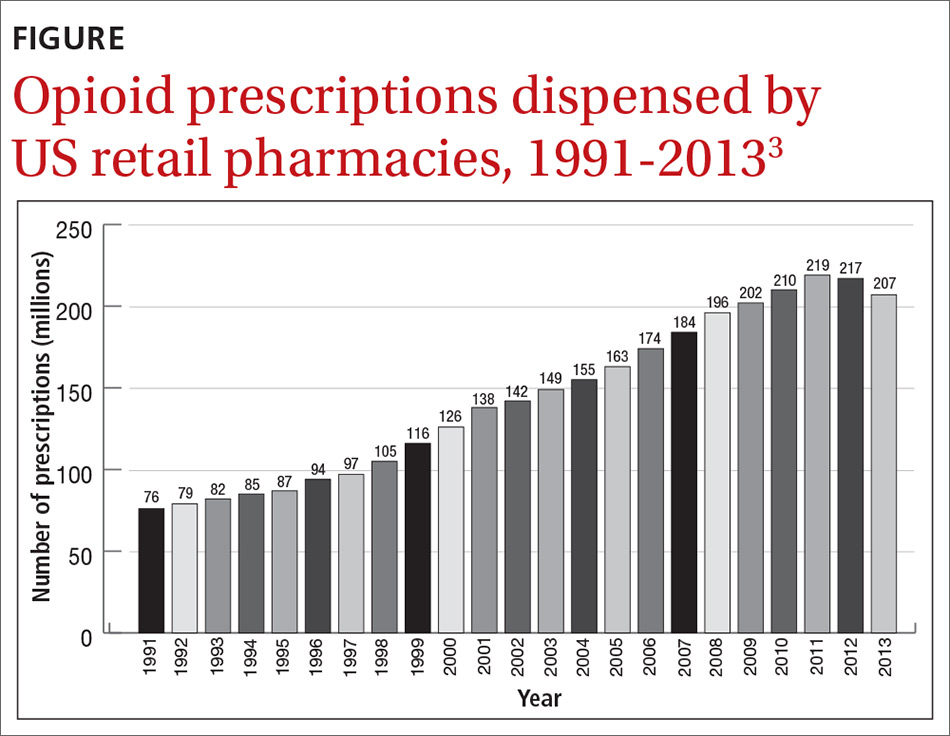
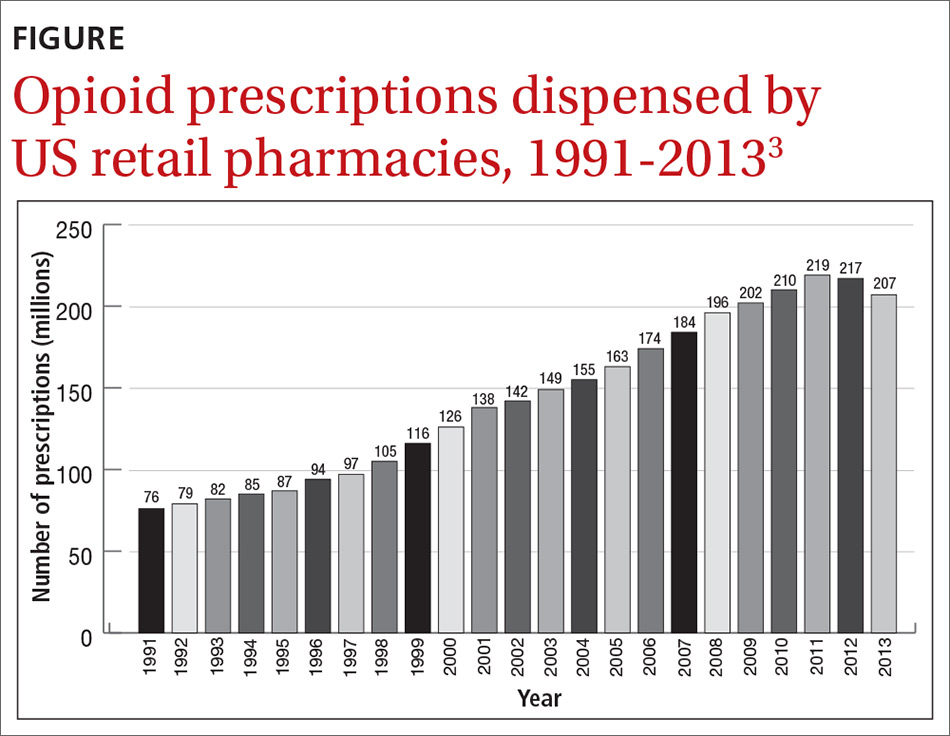
Dr. Hickner wrote that the push to assess for pain as the fifth vital sign was a central cause of the opioid epidemic; however, this is contrary to published data on the epidemic. Total opioid prescriptions had been steadily increasing in the United States for at least a decade before the Pain Standards went into effect in 2001 (FIGURE).3 Between 1991 and 1997, the number of prescriptions increased from 76 million to 97 million. The rate of increase from 1997 to 2011 appears to have been more rapid, which is likely due to the 1995 approval of the new sustained-release opioid OxyContin and the associated aggressive marketing campaigns to physicians.
Your readers should know that we, at the Joint Commission, are also “doing our part to dismantle the opioid crisis.” In 2016, we completely revised our Pain Standards, adding new criteria to help address the epidemic. Some adjustments include: requiring improved availability of nonpharmacologic therapy, encouraging engagement of patients in pain management plans, enhancing accessibility of Physician Drug Monitoring Program tools, and monitoring opioid prescribing.
David W. Baker, MD, FACP, executive vice president
The Joint Commission, Oakbrook Terrace, IL
Dr. John Hickner’s editorial, “Doing our part to dismantle the opioid crisis” (J Fam Pract 2019;68:308) had important inaccuracies.
The Joint Commission, for which I serve as an executive vice president, did not “dub pain assessment the ‘fifth vital sign’. ” The concept of the fifth vital sign was developed by the American Pain Society in the 1990s.1 It gained national attention through a Veterans Health Administration initiative in 1999.2 And in 2001, the Joint Commission (then the Joint Commission on Accreditation of Healthcare Organizations or JCAHO) issued its Pain Standards.
Dr. Hickner wrote that the push to assess for pain as the fifth vital sign was a central cause of the opioid epidemic; however, this is contrary to published data on the epidemic. Total opioid prescriptions had been steadily increasing in the United States for at least a decade before the Pain Standards went into effect in 2001 (FIGURE).3 Between 1991 and 1997, the number of prescriptions increased from 76 million to 97 million. The rate of increase from 1997 to 2011 appears to have been more rapid, which is likely due to the 1995 approval of the new sustained-release opioid OxyContin and the associated aggressive marketing campaigns to physicians.
Your readers should know that we, at the Joint Commission, are also “doing our part to dismantle the opioid crisis.” In 2016, we completely revised our Pain Standards, adding new criteria to help address the epidemic. Some adjustments include: requiring improved availability of nonpharmacologic therapy, encouraging engagement of patients in pain management plans, enhancing accessibility of Physician Drug Monitoring Program tools, and monitoring opioid prescribing.
David W. Baker, MD, FACP, executive vice president
The Joint Commission, Oakbrook Terrace, IL
1. American Pain Society. Principles of Analgesic Use in the Treatment of Acute Pain and Chronic Cancer Pain. 2nd ed. Skokie, Illinois: American Pain Society; 1989.
2. Department of Veteran’s Affairs. Pain: the fifth vital sign. www.va.gov/PAINMANAGEMENT/docs/Pain_As_the_5th_Vital_Sign_Toolkit.pdf. Published October 2000. Accessed September 30, 2019.
3 National Institute on Drug Abuse. America’s addiction to opioids: heroin and prescription drug abuse. https://archives.drugabuse.gov/testimonies/2014/americas-addiction-to-opioids-heroin-prescription-drug-abuse. Published May 14, 2014. Accessed September 30, 2019.
1. American Pain Society. Principles of Analgesic Use in the Treatment of Acute Pain and Chronic Cancer Pain. 2nd ed. Skokie, Illinois: American Pain Society; 1989.
2. Department of Veteran’s Affairs. Pain: the fifth vital sign. www.va.gov/PAINMANAGEMENT/docs/Pain_As_the_5th_Vital_Sign_Toolkit.pdf. Published October 2000. Accessed September 30, 2019.
3 National Institute on Drug Abuse. America’s addiction to opioids: heroin and prescription drug abuse. https://archives.drugabuse.gov/testimonies/2014/americas-addiction-to-opioids-heroin-prescription-drug-abuse. Published May 14, 2014. Accessed September 30, 2019.
Burned out? Change your practice
This month’s cover story addresses a phenomenon familiar to all of us: burnout. Mohanty and colleagues provide an excellent, concise summary of what burnout is, the probable causes of it, and possible solutions.
What has puzzled me about burnout is why there was no discussion of it 30 years ago when physicians worked easily as many hours but did not complain of being “burned out.” We just described ourselves as being tired. One could argue that the disconnect is due to a change in physicians’ expectations, but that theory does not hold up because burnout is common in both older and younger physicians.
I think that Dr. Wendy Dean, a psychiatrist at the Henry M. Jackson Foundation for the Advancement of Military Medicine, and her colleagues are correct in identifying a different culprit. They contend that the real issue is that we are “increasingly forced to consider the demands of other stakeholders—the electronic medical record (EMR), the insurers, the hospital, the health care system, even our own financial security—before the needs of our patients.”1 To redefine the problem of burnout, Dr. Dean uses a different term to label this phenomenon of exhaustion, demoralization, and depersonalization. She calls it “moral injury.”
“Moral injury . . . describes the challenge of simultaneously knowing what care patients need but being unable to provide it due to constraints that are beyond our control.”1
So what needs to change? No amount of yoga, mindfulness, meditation, or exercise will be sufficient, although these are great therapeutic activities. Office redesign, however, has already been shown to be highly effective in reducing physician burnout. For example, in an intensive practice redesign project in Colorado that included hiring more medical assistants, physician burnout declined from 56% to 25% in the first practice and from 40% to 0% in the second practice!2
One of the oldest examples of using team care to reduce physician burnout was implemented by Dr. Peter Anderson in 2003.3 Dr. Anderson was on the brink of throwing in the towel when he hired a second nurse and redistributed many tasks to the nurses. In a few years he had a thriving and satisfying practice for himself, his staff, and his patients.
These are only 2 examples of many successful redesign projects around the country. If you are getting burned out, change your practice, not yourself.
1. Dean W, Talbot S, Dean A. Reframing clinician distress: moral injury not burnout. Fed Pract. 2019;36:400-402.
2. Smith PC, Lyon C, English AF, et al. Practice transformation under the University of Colorado’s primary care redesign model. Ann Fam Med. 2019;17(suppl 1):S24-S32.
3. Anderson P, Halley MD. A new approach to making your doctor-nurse team more productive. Fam Pract Manag. 2008;15:35-40.
This month’s cover story addresses a phenomenon familiar to all of us: burnout. Mohanty and colleagues provide an excellent, concise summary of what burnout is, the probable causes of it, and possible solutions.
What has puzzled me about burnout is why there was no discussion of it 30 years ago when physicians worked easily as many hours but did not complain of being “burned out.” We just described ourselves as being tired. One could argue that the disconnect is due to a change in physicians’ expectations, but that theory does not hold up because burnout is common in both older and younger physicians.
I think that Dr. Wendy Dean, a psychiatrist at the Henry M. Jackson Foundation for the Advancement of Military Medicine, and her colleagues are correct in identifying a different culprit. They contend that the real issue is that we are “increasingly forced to consider the demands of other stakeholders—the electronic medical record (EMR), the insurers, the hospital, the health care system, even our own financial security—before the needs of our patients.”1 To redefine the problem of burnout, Dr. Dean uses a different term to label this phenomenon of exhaustion, demoralization, and depersonalization. She calls it “moral injury.”
“Moral injury . . . describes the challenge of simultaneously knowing what care patients need but being unable to provide it due to constraints that are beyond our control.”1
So what needs to change? No amount of yoga, mindfulness, meditation, or exercise will be sufficient, although these are great therapeutic activities. Office redesign, however, has already been shown to be highly effective in reducing physician burnout. For example, in an intensive practice redesign project in Colorado that included hiring more medical assistants, physician burnout declined from 56% to 25% in the first practice and from 40% to 0% in the second practice!2
One of the oldest examples of using team care to reduce physician burnout was implemented by Dr. Peter Anderson in 2003.3 Dr. Anderson was on the brink of throwing in the towel when he hired a second nurse and redistributed many tasks to the nurses. In a few years he had a thriving and satisfying practice for himself, his staff, and his patients.
These are only 2 examples of many successful redesign projects around the country. If you are getting burned out, change your practice, not yourself.
This month’s cover story addresses a phenomenon familiar to all of us: burnout. Mohanty and colleagues provide an excellent, concise summary of what burnout is, the probable causes of it, and possible solutions.
What has puzzled me about burnout is why there was no discussion of it 30 years ago when physicians worked easily as many hours but did not complain of being “burned out.” We just described ourselves as being tired. One could argue that the disconnect is due to a change in physicians’ expectations, but that theory does not hold up because burnout is common in both older and younger physicians.
I think that Dr. Wendy Dean, a psychiatrist at the Henry M. Jackson Foundation for the Advancement of Military Medicine, and her colleagues are correct in identifying a different culprit. They contend that the real issue is that we are “increasingly forced to consider the demands of other stakeholders—the electronic medical record (EMR), the insurers, the hospital, the health care system, even our own financial security—before the needs of our patients.”1 To redefine the problem of burnout, Dr. Dean uses a different term to label this phenomenon of exhaustion, demoralization, and depersonalization. She calls it “moral injury.”
“Moral injury . . . describes the challenge of simultaneously knowing what care patients need but being unable to provide it due to constraints that are beyond our control.”1
So what needs to change? No amount of yoga, mindfulness, meditation, or exercise will be sufficient, although these are great therapeutic activities. Office redesign, however, has already been shown to be highly effective in reducing physician burnout. For example, in an intensive practice redesign project in Colorado that included hiring more medical assistants, physician burnout declined from 56% to 25% in the first practice and from 40% to 0% in the second practice!2
One of the oldest examples of using team care to reduce physician burnout was implemented by Dr. Peter Anderson in 2003.3 Dr. Anderson was on the brink of throwing in the towel when he hired a second nurse and redistributed many tasks to the nurses. In a few years he had a thriving and satisfying practice for himself, his staff, and his patients.
These are only 2 examples of many successful redesign projects around the country. If you are getting burned out, change your practice, not yourself.
1. Dean W, Talbot S, Dean A. Reframing clinician distress: moral injury not burnout. Fed Pract. 2019;36:400-402.
2. Smith PC, Lyon C, English AF, et al. Practice transformation under the University of Colorado’s primary care redesign model. Ann Fam Med. 2019;17(suppl 1):S24-S32.
3. Anderson P, Halley MD. A new approach to making your doctor-nurse team more productive. Fam Pract Manag. 2008;15:35-40.
1. Dean W, Talbot S, Dean A. Reframing clinician distress: moral injury not burnout. Fed Pract. 2019;36:400-402.
2. Smith PC, Lyon C, English AF, et al. Practice transformation under the University of Colorado’s primary care redesign model. Ann Fam Med. 2019;17(suppl 1):S24-S32.
3. Anderson P, Halley MD. A new approach to making your doctor-nurse team more productive. Fam Pract Manag. 2008;15:35-40.
Time to conception after miscarriage: How long to wait?
EVIDENCE SUMMARY
To evaluate the longstanding belief that a short IPI after miscarriage is associated with adverse outcomes in subsequent pregnancies, a 2017 systematic review and meta-analysis of 16 studies (3 randomized controlled trials [RCTs] and 13 retrospective cohort studies) with a total of more than 1 million patients compared IPIs shorter and longer than 6 months (miscarriage was defined as any pregnancy loss before 24 weeks).1 The meta-analysis included 10 of the studies (2 RCTs and 8 cohort studies), with a total of 977,972 women and excluded 6 studies because of insufficient data. The outcomes investigated were recurrent miscarriage, preterm birth, stillbirth, pre-eclampsia, and low birthweight in the pregnancy following miscarriage.
Only 1 study reported the specific gestational age of the index miscarriage at 8.6 ± 2.8 weeks.2 All studies adjusted data for age, and some considered other confounders, such as race, smoking status, and body mass index (BMI).
Women included in the meta-analysis were from Asia, Europe, South America, and the United States and had a history of at least 1 miscarriage.1 A study of 257,908 subjects (Conde-Agudelo) also included women with a history of induced abortion from Latin American countries, where abortion is illegal, and made no distinction between spontaneous and induced abortions in those data sets.3 Women with a history of illegal abortion could be at greater risk of subsequent miscarriage than women who underwent a legally performed abortion.
IPI shorter than 6 months carries fewer risks
Excluding the Conde-Agudelo study, women with an IPI < 6 months, compared with > 6 months, had lower risks of subsequent miscarriage (7 studies, 46,313 women; risk ratio [RR] = 0.82; 95% confidence interval [CI], 0.78-0.86) and preterm delivery (7 studies, 60,772 women; RR = 0.79; 95% CI, 0.75-0.83); a higher rate of live births (4 studies, 44,586 women; RR = 1.06; 95% CI, 1.01-1.11); and no increase in stillbirths (4 studies, 44,586 women; RR = 0.88; 95% CI, 0.76-1.02), low birthweight (4 studies, 284,222 women; RR = 1.05; 95% CI, 0.48-2.29) or pre-eclampsia (5 studies, 284,899 women; RR = 0.95; 95% CI, 0.88-1.02) in the subsequent pregnancy.
Including the Conde-Agudelo study, the risk of preterm delivery was the same in women with an IPI < 6 months and > 6 months (8 studies, 318,880 women; RR = 0.93; 95% CI, 0.58-1.48).1 Four of the 10 studies evaluated the risk of miscarriage with an IPI < 3 months compared with > 3 months and found either no difference or a lower risk of subsequent miscarriage.2,4-6
IPI shorter than 3 months has lowest risk of all
A 2017 prospective cohort study examined the association between IPI length and risk of recurrent miscarriage in 514 women who had experienced recent miscarriage (defined as spontaneous pregnancy loss before 20 weeks of gestation).7 Average gestational age at the time of initial miscarriage wasn’t reported. Study participants were 30 years of age on average and predominantly white (76.8%); 12.3% were black.
The authors compared IPIs of < 3 months, 3 to 6 months, and > 18 months with IPIs of 6 to 18 months, which correlates with the IPIs recommended by the World Health Organization (WHO).8 They adjusted for maternal age, race, parity, BMI, and education. An IPI < 3 months was associated with the lowest risk of subsequent miscarriage (7.3% compared with 22.1%; adjusted hazard ratio = 0.33; 95% CI, 0.16-0.71). Women with IPIs of 3 to 6 months and > 18 months didn’t experience statistically significant differences in subsequent miscarriage rates compared with IPIs of 6 to 18 months.7
Continue to: But a short IPI after second-trimester loss increases risk of miscarriage
But a short IPI after second-trimester loss increases risk of miscarriage
By including all miscarriages, the meta-analysis effectively examined IPI after first-trimester loss because first-trimester loss occurs far more frequently than does second-trimester loss.1 A retrospective cohort study of Australian women, not included in the meta-analysis, assessed 4290 patients with a second-trimester pregnancy loss to specifically examine the association between IPI and risk of recurrent pregnancy loss.9
After a pregnancy loss at 14 to 19 weeks, women with an IPI < 3 months, compared with an IPI of 9 to 12 months, had an increased risk of recurrent pregnancy loss (21.9 vs 11.3%; P < .001). Women with an IPI > 9 to 12 months had rates of pregnancy loss similar to an IPI of 3 to 6 months (RR = 1.24; 95% CI, 0.89-1.7) and 6 to 9 months (RR = 1.02; 95% CI, 0.7-1.5). Women who experienced an initial loss at 20 to 23 weeks, for unclear reasons, showed no evidence that the IPI affected the risk of subsequent loss.
Short IPI may be linked to anxiety in first trimester of next pregnancy
A large cohort study of 20,308 pregnant Chinese women, including 1495 with a previous miscarriage, explored the mental health impact of IPI after miscarriage compared with no miscarriage.10 Investigators used the Self-Rating Anxiety Scale to evaluate anxiety and the Center for Epidemiologic Studies Depression Scale to evaluate depression.
Women with an IPI of < 7 months after miscarriage were more likely to experience anxiety symptoms in the subsequent pregnancy than were women with no previous miscarriage (adjusted odds ratio [AOR] = 2.76; 95% CI, 1.4-5.5), whereas women with a history of miscarriage and IPI > 6 months weren’t. Women with IPIs < 7 months and 7 to 12 months, compared with women who had no miscarriage, had an increased risk of depression (AOR = 2.5; 95% CI, 1.4-4.5, and AOR = 2.6; 95% CI, 1.3-5.2, respectively). Women with an IPI > 12 months had no increased risk of depression compared with women with no history of miscarriage.
The odds ratios were adjusted for age, education, BMI, income, and place of residence. The higher rates of depression and anxiety didn’t persist beyond the first trimester of the subsequent pregnancy.
Continue to: RECOMMENDATIONS
RECOMMENDATIONS
The American College of Obstetricians and Gynecologists’ Practice Bulletin on Early Pregnancy Loss states that no quality data exist to support delaying conception after early pregnancy loss (defined as loss of an intrauterine pregnancy in the first trimester) to prevent subsequent pregnancy loss or other pregnancy complications.11
WHO recommends a minimum IPI of at least 6 months after a spontaneous or elective abortion. This recommendation is based on a single multi-center cohort study in Latin America that included women with both spontaneous and induced abortions.8
Editor’s takeaway
High-quality evidence now shows that shorter IPIs after first-trimester miscarriages result in safe subsequent pregnancies. However, some concern remains about second-trimester miscarriages and maternal mental health following a shorter IPI, based on lower-quality evidence.
1. Kangatharan C, Labram S, Bhattacharya S. Interpregnancy interval following miscarriage and adverse pregnancy outcomes: systematic review and meta-analysis. Hum Reprod Update. 2017;23:221-231.
2. Wong LF, Schliep KC, Silver RM, et al. The effect of a very short interpregnancy interval and pregnancy outcomes following a previous pregnancy loss. Am J Obstet Gynecol. 2015;212:375.e1-375.e11.
3. Conde-Agudelo A, Belizan JM, Breman R, et al. Effect of the interpregnancy interval after an abortion on maternal and perinatal health in Latin America. Int J Gynaecol Obstet. 2005;89(suppl 1):S34-S40.
4. Bentolila Y, Ratzon R, Shoham-Vardi I, et al. Effect of interpregnancy interval on outcomes of pregnancy after recurrent pregnancy loss. J Matern Fetal Neonatal Med. 2013;26:1459-1464.
5. DaVanzo J, Hale L, Rahman M. How long after a miscarriage should women wait before becoming pregnant again? Multivariate analysis of cohort data from Matlab, Bangladesh. BMJ Open. 2012;2:e001591.
6. Wyss P, Biedermann K, Huch A. Relevance of the miscarriage-new pregnancy interval. J Perinat Med. 1994;22:235-241.
7. Sundermann AC, Hartmann KE, Jones SH, et al. Interpregnancy interval after pregnancy loss and risk of repeat miscarriage. Obstet Gynecol. 2017;130:1312-1318.
8. World Health Organization. Department of Reproductive Health and Research, Department of Making Pregnancy Safer. Report of a WHO Technical Consultation on Birth Spacing: Geneva, Switzerland 13-15 June 2005. Geneva: World Health Organization, 2007.
9. Roberts CL, Algert CS, Ford JB, et al. Association between interpregnancy interval and the risk of recurrent loss after a midtrimester loss. Hum Reprod. 2016;31:2834-2840.
10. Gong X, Hao J, Tao F, et al. Pregnancy loss and anxiety and depression during subsequent pregnancies: data from the C-ABC study. Eur J Obstet Gynecol Reprod Biol. 2013;166:30-36.
11. American College of Obstetricians and Gynecologists. Committee on Practice Bulletins-Gynecology. The American College of Obstetricians and Gynecologists Practice Bulletin no. 150. Early pregnancy loss. Obstet Gynecol. 2015;125:1258-1267.
EVIDENCE SUMMARY
To evaluate the longstanding belief that a short IPI after miscarriage is associated with adverse outcomes in subsequent pregnancies, a 2017 systematic review and meta-analysis of 16 studies (3 randomized controlled trials [RCTs] and 13 retrospective cohort studies) with a total of more than 1 million patients compared IPIs shorter and longer than 6 months (miscarriage was defined as any pregnancy loss before 24 weeks).1 The meta-analysis included 10 of the studies (2 RCTs and 8 cohort studies), with a total of 977,972 women and excluded 6 studies because of insufficient data. The outcomes investigated were recurrent miscarriage, preterm birth, stillbirth, pre-eclampsia, and low birthweight in the pregnancy following miscarriage.
Only 1 study reported the specific gestational age of the index miscarriage at 8.6 ± 2.8 weeks.2 All studies adjusted data for age, and some considered other confounders, such as race, smoking status, and body mass index (BMI).
Women included in the meta-analysis were from Asia, Europe, South America, and the United States and had a history of at least 1 miscarriage.1 A study of 257,908 subjects (Conde-Agudelo) also included women with a history of induced abortion from Latin American countries, where abortion is illegal, and made no distinction between spontaneous and induced abortions in those data sets.3 Women with a history of illegal abortion could be at greater risk of subsequent miscarriage than women who underwent a legally performed abortion.
IPI shorter than 6 months carries fewer risks
Excluding the Conde-Agudelo study, women with an IPI < 6 months, compared with > 6 months, had lower risks of subsequent miscarriage (7 studies, 46,313 women; risk ratio [RR] = 0.82; 95% confidence interval [CI], 0.78-0.86) and preterm delivery (7 studies, 60,772 women; RR = 0.79; 95% CI, 0.75-0.83); a higher rate of live births (4 studies, 44,586 women; RR = 1.06; 95% CI, 1.01-1.11); and no increase in stillbirths (4 studies, 44,586 women; RR = 0.88; 95% CI, 0.76-1.02), low birthweight (4 studies, 284,222 women; RR = 1.05; 95% CI, 0.48-2.29) or pre-eclampsia (5 studies, 284,899 women; RR = 0.95; 95% CI, 0.88-1.02) in the subsequent pregnancy.
Including the Conde-Agudelo study, the risk of preterm delivery was the same in women with an IPI < 6 months and > 6 months (8 studies, 318,880 women; RR = 0.93; 95% CI, 0.58-1.48).1 Four of the 10 studies evaluated the risk of miscarriage with an IPI < 3 months compared with > 3 months and found either no difference or a lower risk of subsequent miscarriage.2,4-6
IPI shorter than 3 months has lowest risk of all
A 2017 prospective cohort study examined the association between IPI length and risk of recurrent miscarriage in 514 women who had experienced recent miscarriage (defined as spontaneous pregnancy loss before 20 weeks of gestation).7 Average gestational age at the time of initial miscarriage wasn’t reported. Study participants were 30 years of age on average and predominantly white (76.8%); 12.3% were black.
The authors compared IPIs of < 3 months, 3 to 6 months, and > 18 months with IPIs of 6 to 18 months, which correlates with the IPIs recommended by the World Health Organization (WHO).8 They adjusted for maternal age, race, parity, BMI, and education. An IPI < 3 months was associated with the lowest risk of subsequent miscarriage (7.3% compared with 22.1%; adjusted hazard ratio = 0.33; 95% CI, 0.16-0.71). Women with IPIs of 3 to 6 months and > 18 months didn’t experience statistically significant differences in subsequent miscarriage rates compared with IPIs of 6 to 18 months.7
Continue to: But a short IPI after second-trimester loss increases risk of miscarriage
But a short IPI after second-trimester loss increases risk of miscarriage
By including all miscarriages, the meta-analysis effectively examined IPI after first-trimester loss because first-trimester loss occurs far more frequently than does second-trimester loss.1 A retrospective cohort study of Australian women, not included in the meta-analysis, assessed 4290 patients with a second-trimester pregnancy loss to specifically examine the association between IPI and risk of recurrent pregnancy loss.9
After a pregnancy loss at 14 to 19 weeks, women with an IPI < 3 months, compared with an IPI of 9 to 12 months, had an increased risk of recurrent pregnancy loss (21.9 vs 11.3%; P < .001). Women with an IPI > 9 to 12 months had rates of pregnancy loss similar to an IPI of 3 to 6 months (RR = 1.24; 95% CI, 0.89-1.7) and 6 to 9 months (RR = 1.02; 95% CI, 0.7-1.5). Women who experienced an initial loss at 20 to 23 weeks, for unclear reasons, showed no evidence that the IPI affected the risk of subsequent loss.
Short IPI may be linked to anxiety in first trimester of next pregnancy
A large cohort study of 20,308 pregnant Chinese women, including 1495 with a previous miscarriage, explored the mental health impact of IPI after miscarriage compared with no miscarriage.10 Investigators used the Self-Rating Anxiety Scale to evaluate anxiety and the Center for Epidemiologic Studies Depression Scale to evaluate depression.
Women with an IPI of < 7 months after miscarriage were more likely to experience anxiety symptoms in the subsequent pregnancy than were women with no previous miscarriage (adjusted odds ratio [AOR] = 2.76; 95% CI, 1.4-5.5), whereas women with a history of miscarriage and IPI > 6 months weren’t. Women with IPIs < 7 months and 7 to 12 months, compared with women who had no miscarriage, had an increased risk of depression (AOR = 2.5; 95% CI, 1.4-4.5, and AOR = 2.6; 95% CI, 1.3-5.2, respectively). Women with an IPI > 12 months had no increased risk of depression compared with women with no history of miscarriage.
The odds ratios were adjusted for age, education, BMI, income, and place of residence. The higher rates of depression and anxiety didn’t persist beyond the first trimester of the subsequent pregnancy.
Continue to: RECOMMENDATIONS
RECOMMENDATIONS
The American College of Obstetricians and Gynecologists’ Practice Bulletin on Early Pregnancy Loss states that no quality data exist to support delaying conception after early pregnancy loss (defined as loss of an intrauterine pregnancy in the first trimester) to prevent subsequent pregnancy loss or other pregnancy complications.11
WHO recommends a minimum IPI of at least 6 months after a spontaneous or elective abortion. This recommendation is based on a single multi-center cohort study in Latin America that included women with both spontaneous and induced abortions.8
Editor’s takeaway
High-quality evidence now shows that shorter IPIs after first-trimester miscarriages result in safe subsequent pregnancies. However, some concern remains about second-trimester miscarriages and maternal mental health following a shorter IPI, based on lower-quality evidence.
EVIDENCE SUMMARY
To evaluate the longstanding belief that a short IPI after miscarriage is associated with adverse outcomes in subsequent pregnancies, a 2017 systematic review and meta-analysis of 16 studies (3 randomized controlled trials [RCTs] and 13 retrospective cohort studies) with a total of more than 1 million patients compared IPIs shorter and longer than 6 months (miscarriage was defined as any pregnancy loss before 24 weeks).1 The meta-analysis included 10 of the studies (2 RCTs and 8 cohort studies), with a total of 977,972 women and excluded 6 studies because of insufficient data. The outcomes investigated were recurrent miscarriage, preterm birth, stillbirth, pre-eclampsia, and low birthweight in the pregnancy following miscarriage.
Only 1 study reported the specific gestational age of the index miscarriage at 8.6 ± 2.8 weeks.2 All studies adjusted data for age, and some considered other confounders, such as race, smoking status, and body mass index (BMI).
Women included in the meta-analysis were from Asia, Europe, South America, and the United States and had a history of at least 1 miscarriage.1 A study of 257,908 subjects (Conde-Agudelo) also included women with a history of induced abortion from Latin American countries, where abortion is illegal, and made no distinction between spontaneous and induced abortions in those data sets.3 Women with a history of illegal abortion could be at greater risk of subsequent miscarriage than women who underwent a legally performed abortion.
IPI shorter than 6 months carries fewer risks
Excluding the Conde-Agudelo study, women with an IPI < 6 months, compared with > 6 months, had lower risks of subsequent miscarriage (7 studies, 46,313 women; risk ratio [RR] = 0.82; 95% confidence interval [CI], 0.78-0.86) and preterm delivery (7 studies, 60,772 women; RR = 0.79; 95% CI, 0.75-0.83); a higher rate of live births (4 studies, 44,586 women; RR = 1.06; 95% CI, 1.01-1.11); and no increase in stillbirths (4 studies, 44,586 women; RR = 0.88; 95% CI, 0.76-1.02), low birthweight (4 studies, 284,222 women; RR = 1.05; 95% CI, 0.48-2.29) or pre-eclampsia (5 studies, 284,899 women; RR = 0.95; 95% CI, 0.88-1.02) in the subsequent pregnancy.
Including the Conde-Agudelo study, the risk of preterm delivery was the same in women with an IPI < 6 months and > 6 months (8 studies, 318,880 women; RR = 0.93; 95% CI, 0.58-1.48).1 Four of the 10 studies evaluated the risk of miscarriage with an IPI < 3 months compared with > 3 months and found either no difference or a lower risk of subsequent miscarriage.2,4-6
IPI shorter than 3 months has lowest risk of all
A 2017 prospective cohort study examined the association between IPI length and risk of recurrent miscarriage in 514 women who had experienced recent miscarriage (defined as spontaneous pregnancy loss before 20 weeks of gestation).7 Average gestational age at the time of initial miscarriage wasn’t reported. Study participants were 30 years of age on average and predominantly white (76.8%); 12.3% were black.
The authors compared IPIs of < 3 months, 3 to 6 months, and > 18 months with IPIs of 6 to 18 months, which correlates with the IPIs recommended by the World Health Organization (WHO).8 They adjusted for maternal age, race, parity, BMI, and education. An IPI < 3 months was associated with the lowest risk of subsequent miscarriage (7.3% compared with 22.1%; adjusted hazard ratio = 0.33; 95% CI, 0.16-0.71). Women with IPIs of 3 to 6 months and > 18 months didn’t experience statistically significant differences in subsequent miscarriage rates compared with IPIs of 6 to 18 months.7
Continue to: But a short IPI after second-trimester loss increases risk of miscarriage
But a short IPI after second-trimester loss increases risk of miscarriage
By including all miscarriages, the meta-analysis effectively examined IPI after first-trimester loss because first-trimester loss occurs far more frequently than does second-trimester loss.1 A retrospective cohort study of Australian women, not included in the meta-analysis, assessed 4290 patients with a second-trimester pregnancy loss to specifically examine the association between IPI and risk of recurrent pregnancy loss.9
After a pregnancy loss at 14 to 19 weeks, women with an IPI < 3 months, compared with an IPI of 9 to 12 months, had an increased risk of recurrent pregnancy loss (21.9 vs 11.3%; P < .001). Women with an IPI > 9 to 12 months had rates of pregnancy loss similar to an IPI of 3 to 6 months (RR = 1.24; 95% CI, 0.89-1.7) and 6 to 9 months (RR = 1.02; 95% CI, 0.7-1.5). Women who experienced an initial loss at 20 to 23 weeks, for unclear reasons, showed no evidence that the IPI affected the risk of subsequent loss.
Short IPI may be linked to anxiety in first trimester of next pregnancy
A large cohort study of 20,308 pregnant Chinese women, including 1495 with a previous miscarriage, explored the mental health impact of IPI after miscarriage compared with no miscarriage.10 Investigators used the Self-Rating Anxiety Scale to evaluate anxiety and the Center for Epidemiologic Studies Depression Scale to evaluate depression.
Women with an IPI of < 7 months after miscarriage were more likely to experience anxiety symptoms in the subsequent pregnancy than were women with no previous miscarriage (adjusted odds ratio [AOR] = 2.76; 95% CI, 1.4-5.5), whereas women with a history of miscarriage and IPI > 6 months weren’t. Women with IPIs < 7 months and 7 to 12 months, compared with women who had no miscarriage, had an increased risk of depression (AOR = 2.5; 95% CI, 1.4-4.5, and AOR = 2.6; 95% CI, 1.3-5.2, respectively). Women with an IPI > 12 months had no increased risk of depression compared with women with no history of miscarriage.
The odds ratios were adjusted for age, education, BMI, income, and place of residence. The higher rates of depression and anxiety didn’t persist beyond the first trimester of the subsequent pregnancy.
Continue to: RECOMMENDATIONS
RECOMMENDATIONS
The American College of Obstetricians and Gynecologists’ Practice Bulletin on Early Pregnancy Loss states that no quality data exist to support delaying conception after early pregnancy loss (defined as loss of an intrauterine pregnancy in the first trimester) to prevent subsequent pregnancy loss or other pregnancy complications.11
WHO recommends a minimum IPI of at least 6 months after a spontaneous or elective abortion. This recommendation is based on a single multi-center cohort study in Latin America that included women with both spontaneous and induced abortions.8
Editor’s takeaway
High-quality evidence now shows that shorter IPIs after first-trimester miscarriages result in safe subsequent pregnancies. However, some concern remains about second-trimester miscarriages and maternal mental health following a shorter IPI, based on lower-quality evidence.
1. Kangatharan C, Labram S, Bhattacharya S. Interpregnancy interval following miscarriage and adverse pregnancy outcomes: systematic review and meta-analysis. Hum Reprod Update. 2017;23:221-231.
2. Wong LF, Schliep KC, Silver RM, et al. The effect of a very short interpregnancy interval and pregnancy outcomes following a previous pregnancy loss. Am J Obstet Gynecol. 2015;212:375.e1-375.e11.
3. Conde-Agudelo A, Belizan JM, Breman R, et al. Effect of the interpregnancy interval after an abortion on maternal and perinatal health in Latin America. Int J Gynaecol Obstet. 2005;89(suppl 1):S34-S40.
4. Bentolila Y, Ratzon R, Shoham-Vardi I, et al. Effect of interpregnancy interval on outcomes of pregnancy after recurrent pregnancy loss. J Matern Fetal Neonatal Med. 2013;26:1459-1464.
5. DaVanzo J, Hale L, Rahman M. How long after a miscarriage should women wait before becoming pregnant again? Multivariate analysis of cohort data from Matlab, Bangladesh. BMJ Open. 2012;2:e001591.
6. Wyss P, Biedermann K, Huch A. Relevance of the miscarriage-new pregnancy interval. J Perinat Med. 1994;22:235-241.
7. Sundermann AC, Hartmann KE, Jones SH, et al. Interpregnancy interval after pregnancy loss and risk of repeat miscarriage. Obstet Gynecol. 2017;130:1312-1318.
8. World Health Organization. Department of Reproductive Health and Research, Department of Making Pregnancy Safer. Report of a WHO Technical Consultation on Birth Spacing: Geneva, Switzerland 13-15 June 2005. Geneva: World Health Organization, 2007.
9. Roberts CL, Algert CS, Ford JB, et al. Association between interpregnancy interval and the risk of recurrent loss after a midtrimester loss. Hum Reprod. 2016;31:2834-2840.
10. Gong X, Hao J, Tao F, et al. Pregnancy loss and anxiety and depression during subsequent pregnancies: data from the C-ABC study. Eur J Obstet Gynecol Reprod Biol. 2013;166:30-36.
11. American College of Obstetricians and Gynecologists. Committee on Practice Bulletins-Gynecology. The American College of Obstetricians and Gynecologists Practice Bulletin no. 150. Early pregnancy loss. Obstet Gynecol. 2015;125:1258-1267.
1. Kangatharan C, Labram S, Bhattacharya S. Interpregnancy interval following miscarriage and adverse pregnancy outcomes: systematic review and meta-analysis. Hum Reprod Update. 2017;23:221-231.
2. Wong LF, Schliep KC, Silver RM, et al. The effect of a very short interpregnancy interval and pregnancy outcomes following a previous pregnancy loss. Am J Obstet Gynecol. 2015;212:375.e1-375.e11.
3. Conde-Agudelo A, Belizan JM, Breman R, et al. Effect of the interpregnancy interval after an abortion on maternal and perinatal health in Latin America. Int J Gynaecol Obstet. 2005;89(suppl 1):S34-S40.
4. Bentolila Y, Ratzon R, Shoham-Vardi I, et al. Effect of interpregnancy interval on outcomes of pregnancy after recurrent pregnancy loss. J Matern Fetal Neonatal Med. 2013;26:1459-1464.
5. DaVanzo J, Hale L, Rahman M. How long after a miscarriage should women wait before becoming pregnant again? Multivariate analysis of cohort data from Matlab, Bangladesh. BMJ Open. 2012;2:e001591.
6. Wyss P, Biedermann K, Huch A. Relevance of the miscarriage-new pregnancy interval. J Perinat Med. 1994;22:235-241.
7. Sundermann AC, Hartmann KE, Jones SH, et al. Interpregnancy interval after pregnancy loss and risk of repeat miscarriage. Obstet Gynecol. 2017;130:1312-1318.
8. World Health Organization. Department of Reproductive Health and Research, Department of Making Pregnancy Safer. Report of a WHO Technical Consultation on Birth Spacing: Geneva, Switzerland 13-15 June 2005. Geneva: World Health Organization, 2007.
9. Roberts CL, Algert CS, Ford JB, et al. Association between interpregnancy interval and the risk of recurrent loss after a midtrimester loss. Hum Reprod. 2016;31:2834-2840.
10. Gong X, Hao J, Tao F, et al. Pregnancy loss and anxiety and depression during subsequent pregnancies: data from the C-ABC study. Eur J Obstet Gynecol Reprod Biol. 2013;166:30-36.
11. American College of Obstetricians and Gynecologists. Committee on Practice Bulletins-Gynecology. The American College of Obstetricians and Gynecologists Practice Bulletin no. 150. Early pregnancy loss. Obstet Gynecol. 2015;125:1258-1267.
EVIDENCE-BASED ANSWER:
An interpregnancy interval (IPI) of < 6 months following miscarriage is associated with an increased live birth rate in subsequent pregnancy, lower risks of preterm birth and subsequent miscarriage, and no difference in rates of stillbirth, pre-eclampsia, and low birth weight infants (strength of recommendation [SOR]: A, well-done meta-analysis). (IPI is defined as the time between the end of one pregnancy and the last menstrual period of a subsequent one.)
A very short IPI (< 3 months), when compared with an IPI of 6 to 18 months, is associated with the lowest rate of subsequent miscarriage (SOR: B, cohort study). However, for women who experience a pregnancy loss at 14 to 19 weeks’ gestation, an IPI < 3 months is associated with an increased risk of miscarriage or birth before 24 weeks’ gestation (SOR: B, cohort study).
Women with a short IPI following miscarriage may be at increased risk for anxiety and depression in the first trimester of the subsequent pregnancy (SOR: B, cohort study).
Persistent rash on the sole
A 52-year-old Chinese woman presented to a tertiary hospital in Singapore with a 3-month history of persistent and intermittently painful rashes over her right calf and foot (FIGURE). The patient had pancytopenia due to ongoing chemotherapy for metastatic nasopharyngeal carcinoma. She was systemically well and denied other dermatoses. Examination demonstrated scattered crops of tense hemorrhagic vesicles, each surrounded by a livid purpuric base, over the right plantar aspect of the foot, with areas of eschar over the right medial hallux. No allodynia, hyperaesthesia, or lymphadenopathy was noted.
A punch biopsy of an intact vesicle was performed.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis:
Herpes zoster
Histopathologic examination showed full-thickness epidermal necrosis with ballooning degeneration resulting in an intra-epidermal blister. Multinucleated keratinocytes with nuclear moulding were seen within the blister cavity. Grocott-Gomori methenamine-silver (GMS), acid-fast, and Gram stains were negative. Granular immunoglobulin (Ig) G, IgM, and C3 were seen intramurally. DNA analysis of vesicular fluid was positive for varicella zoster virus (VZV). A diagnosis of herpes zoster (HZ) of the right S1 dermatome with primary obliterative vasculitis was established.
Immunocompromised people—those who have impaired T-cell immunity (eg, recipients of organ or hematopoietic stem-cell transplants), take immunosuppressive therapy, or have lymphoma, leukemia, or human immunodeficiency virus (HIV) infection—have an increased risk for HZ. For example, in patients with acquired immunodeficiency syndrome (AIDS), HZ uniquely manifests as recurrent shingles. An estimated 20% to 30% of HIV-infected patients will have more than 1 episode of HZ, which may involve the same or different dermatomes.1,2 Furthermore, HZ in this population is more commonly associated with atypical presentations.3
What an atypical presentation may look like
In immunocompromised patients, HZ may present with atypical cutaneous manifestations or with atypical generalized symptoms.
Atypical cutaneous manifestations, as in disseminated zoster, manifest with multiple hyperkeratotic papules (3-20 mm in diameter) that follow no dermatomal pattern. These lesions may be chronic, persisting for months or years, and may be associated with acyclovir-resistant strains of VZV.2,3 Another dermatologic variant is ecthymatous VZV, which manifests with multiple large (10-30 mm) punched-out ulcerations with a central black eschar and a peripheral rim of vesicles.4 Viral folliculitis—in which infection is limited to the hair follicle, with no associated blisters—has also been reported in atypical HZ.5
Our patient presented with hemorrhagic vesicles mimicking vasculitic lesions, which had persisted over a 3-month period with intermittent localized pain. It has been proposed that in atypical presentations, the reactivated VZV spreads transaxonally from adjacent nerves to the outermost adventitial layer of the arterial wall, leading to a vasculitic appearance of the vesicles.6 Viral-induced vasculitis may also result either directly from infection of the blood vessels or secondary to vascular damage from an inflammatory immune complex–mediated reaction, cell-mediated hypersensitivity, or inflammation due to immune dysregulation.7,8
Continue to: Differential includes vesiculobullous conditions
Differential includes vesiculobullous conditions
There are several important items to consider in the differential.
Cutaneous vasculitis, in severe cases, may manifest with vesicles or bullae that resemble the lesions seen in HZ. However, its unilateral nature and distribution distinguish it.
Angioinvasive fungal infections in immunocompromised patients may manifest with scattered ulceronecrotic lesions to purpuric vesiculobullous dermatoses.9 However, no fungal organisms were seen on GMS staining of the biopsied tissue.
Atypical hand-foot-and-mouth disease tends to affect adults and is associated with Coxsackievirus A6 infection.10 It may manifest as generalized vesiculobullous exanthem resembling varicella. The chronic nature and restricted extent of the patient’s rash made this diagnosis unlikely.
Successful management depends on timely identification
Although most cases of HZ can be diagnosed clinically, atypical rashes may require a biopsy and direct immunofluorescence assay for VZV antigen or a polymerase-chain-reaction (PCR) assay for VZV DNA in cells from the base of blisters. Therefore, it is important to consider the diagnosis of HZ in immunocompromised patients presenting with an atypical rash to avoid misdiagnosis and costly testing.
Continue to: Our patient was treated...
Our patient was treated with oral acyclovir 800 mg 5 times/day for 10 days, with prompt resolution of her rash.
CORRESPONDENCE
Joel Hua-Liang Lim, MBBS, MRCP, MMed, 1 Mandalay Road, Singapore 308205; [email protected]
1. LeBoit PE, Limova M, Yen TS, et al. Chronic verrucous varicella-zoster virus infection in patients with the acquired immunodeficiency syndrome (AIDS): histologic and molecular biologic findings. Am J Dermatopathol. 1992;14:1-7.
2. Gnann JW Jr. Varicella-zoster virus: atypical presentations and unusual complications. J Infect Dis. 2002;186(suppl 1):S91-S98.
3. Weinberg JM, Mysliwiec A, Turiansky GW, et al. Viral folliculitis: atypical presentations of herpes simplex, herpes zoster, and molluscum contagiosum. Arch Dermatol. 1997;133:983-986.
4. Gilson IH, Barnett JH, Conant MA, et al. Disseminated ecthymatous herpes varicella zoster virus infection in patients with acquired immunodeficiency syndrome. J Am Acad Dermatol. 1989;20:637-642.
5. Løkke BJ, Weismann K, Mathiesen L, et al. Atypical varicella-zoster infection in AIDS. Acta Derm Venereol. 1993;73:123-125.
6. Uhoda I, Piérard-Franchimont C, Piérard GE. Varicella-zoster virus vasculitis: a case of recurrent varicella without epidermal involvement. Dermatology. 2000;200:173-175.
7. Teng GG, Chatham WW. Vasculitis related to viral and other microbial agents. Best Pract Res Clin Rheumatol. 2015;29:226-243.
8. Nagel MA, Gilden D. Developments in varicella zoster virus vasculopathy. Curr Neurol Neurosci Rep. 2016;16:12.
9. Pfaller MA, Diekema DJ. Epidemiology of invasive mycoses in North America. Crit Rev Microbiol. 2010;36:1-53.
10. Lott JP, Liu K, Landry M-L, et al. Atypical hand-foot-and-mouth disease associated with coxsackievirus A6 infection. J Am Acad Dermatol. 2013;69:736-741.
A 52-year-old Chinese woman presented to a tertiary hospital in Singapore with a 3-month history of persistent and intermittently painful rashes over her right calf and foot (FIGURE). The patient had pancytopenia due to ongoing chemotherapy for metastatic nasopharyngeal carcinoma. She was systemically well and denied other dermatoses. Examination demonstrated scattered crops of tense hemorrhagic vesicles, each surrounded by a livid purpuric base, over the right plantar aspect of the foot, with areas of eschar over the right medial hallux. No allodynia, hyperaesthesia, or lymphadenopathy was noted.
A punch biopsy of an intact vesicle was performed.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis:
Herpes zoster
Histopathologic examination showed full-thickness epidermal necrosis with ballooning degeneration resulting in an intra-epidermal blister. Multinucleated keratinocytes with nuclear moulding were seen within the blister cavity. Grocott-Gomori methenamine-silver (GMS), acid-fast, and Gram stains were negative. Granular immunoglobulin (Ig) G, IgM, and C3 were seen intramurally. DNA analysis of vesicular fluid was positive for varicella zoster virus (VZV). A diagnosis of herpes zoster (HZ) of the right S1 dermatome with primary obliterative vasculitis was established.
Immunocompromised people—those who have impaired T-cell immunity (eg, recipients of organ or hematopoietic stem-cell transplants), take immunosuppressive therapy, or have lymphoma, leukemia, or human immunodeficiency virus (HIV) infection—have an increased risk for HZ. For example, in patients with acquired immunodeficiency syndrome (AIDS), HZ uniquely manifests as recurrent shingles. An estimated 20% to 30% of HIV-infected patients will have more than 1 episode of HZ, which may involve the same or different dermatomes.1,2 Furthermore, HZ in this population is more commonly associated with atypical presentations.3
What an atypical presentation may look like
In immunocompromised patients, HZ may present with atypical cutaneous manifestations or with atypical generalized symptoms.
Atypical cutaneous manifestations, as in disseminated zoster, manifest with multiple hyperkeratotic papules (3-20 mm in diameter) that follow no dermatomal pattern. These lesions may be chronic, persisting for months or years, and may be associated with acyclovir-resistant strains of VZV.2,3 Another dermatologic variant is ecthymatous VZV, which manifests with multiple large (10-30 mm) punched-out ulcerations with a central black eschar and a peripheral rim of vesicles.4 Viral folliculitis—in which infection is limited to the hair follicle, with no associated blisters—has also been reported in atypical HZ.5
Our patient presented with hemorrhagic vesicles mimicking vasculitic lesions, which had persisted over a 3-month period with intermittent localized pain. It has been proposed that in atypical presentations, the reactivated VZV spreads transaxonally from adjacent nerves to the outermost adventitial layer of the arterial wall, leading to a vasculitic appearance of the vesicles.6 Viral-induced vasculitis may also result either directly from infection of the blood vessels or secondary to vascular damage from an inflammatory immune complex–mediated reaction, cell-mediated hypersensitivity, or inflammation due to immune dysregulation.7,8
Continue to: Differential includes vesiculobullous conditions
Differential includes vesiculobullous conditions
There are several important items to consider in the differential.
Cutaneous vasculitis, in severe cases, may manifest with vesicles or bullae that resemble the lesions seen in HZ. However, its unilateral nature and distribution distinguish it.
Angioinvasive fungal infections in immunocompromised patients may manifest with scattered ulceronecrotic lesions to purpuric vesiculobullous dermatoses.9 However, no fungal organisms were seen on GMS staining of the biopsied tissue.
Atypical hand-foot-and-mouth disease tends to affect adults and is associated with Coxsackievirus A6 infection.10 It may manifest as generalized vesiculobullous exanthem resembling varicella. The chronic nature and restricted extent of the patient’s rash made this diagnosis unlikely.
Successful management depends on timely identification
Although most cases of HZ can be diagnosed clinically, atypical rashes may require a biopsy and direct immunofluorescence assay for VZV antigen or a polymerase-chain-reaction (PCR) assay for VZV DNA in cells from the base of blisters. Therefore, it is important to consider the diagnosis of HZ in immunocompromised patients presenting with an atypical rash to avoid misdiagnosis and costly testing.
Continue to: Our patient was treated...
Our patient was treated with oral acyclovir 800 mg 5 times/day for 10 days, with prompt resolution of her rash.
CORRESPONDENCE
Joel Hua-Liang Lim, MBBS, MRCP, MMed, 1 Mandalay Road, Singapore 308205; [email protected]
A 52-year-old Chinese woman presented to a tertiary hospital in Singapore with a 3-month history of persistent and intermittently painful rashes over her right calf and foot (FIGURE). The patient had pancytopenia due to ongoing chemotherapy for metastatic nasopharyngeal carcinoma. She was systemically well and denied other dermatoses. Examination demonstrated scattered crops of tense hemorrhagic vesicles, each surrounded by a livid purpuric base, over the right plantar aspect of the foot, with areas of eschar over the right medial hallux. No allodynia, hyperaesthesia, or lymphadenopathy was noted.
A punch biopsy of an intact vesicle was performed.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis:
Herpes zoster
Histopathologic examination showed full-thickness epidermal necrosis with ballooning degeneration resulting in an intra-epidermal blister. Multinucleated keratinocytes with nuclear moulding were seen within the blister cavity. Grocott-Gomori methenamine-silver (GMS), acid-fast, and Gram stains were negative. Granular immunoglobulin (Ig) G, IgM, and C3 were seen intramurally. DNA analysis of vesicular fluid was positive for varicella zoster virus (VZV). A diagnosis of herpes zoster (HZ) of the right S1 dermatome with primary obliterative vasculitis was established.
Immunocompromised people—those who have impaired T-cell immunity (eg, recipients of organ or hematopoietic stem-cell transplants), take immunosuppressive therapy, or have lymphoma, leukemia, or human immunodeficiency virus (HIV) infection—have an increased risk for HZ. For example, in patients with acquired immunodeficiency syndrome (AIDS), HZ uniquely manifests as recurrent shingles. An estimated 20% to 30% of HIV-infected patients will have more than 1 episode of HZ, which may involve the same or different dermatomes.1,2 Furthermore, HZ in this population is more commonly associated with atypical presentations.3
What an atypical presentation may look like
In immunocompromised patients, HZ may present with atypical cutaneous manifestations or with atypical generalized symptoms.
Atypical cutaneous manifestations, as in disseminated zoster, manifest with multiple hyperkeratotic papules (3-20 mm in diameter) that follow no dermatomal pattern. These lesions may be chronic, persisting for months or years, and may be associated with acyclovir-resistant strains of VZV.2,3 Another dermatologic variant is ecthymatous VZV, which manifests with multiple large (10-30 mm) punched-out ulcerations with a central black eschar and a peripheral rim of vesicles.4 Viral folliculitis—in which infection is limited to the hair follicle, with no associated blisters—has also been reported in atypical HZ.5
Our patient presented with hemorrhagic vesicles mimicking vasculitic lesions, which had persisted over a 3-month period with intermittent localized pain. It has been proposed that in atypical presentations, the reactivated VZV spreads transaxonally from adjacent nerves to the outermost adventitial layer of the arterial wall, leading to a vasculitic appearance of the vesicles.6 Viral-induced vasculitis may also result either directly from infection of the blood vessels or secondary to vascular damage from an inflammatory immune complex–mediated reaction, cell-mediated hypersensitivity, or inflammation due to immune dysregulation.7,8
Continue to: Differential includes vesiculobullous conditions
Differential includes vesiculobullous conditions
There are several important items to consider in the differential.
Cutaneous vasculitis, in severe cases, may manifest with vesicles or bullae that resemble the lesions seen in HZ. However, its unilateral nature and distribution distinguish it.
Angioinvasive fungal infections in immunocompromised patients may manifest with scattered ulceronecrotic lesions to purpuric vesiculobullous dermatoses.9 However, no fungal organisms were seen on GMS staining of the biopsied tissue.
Atypical hand-foot-and-mouth disease tends to affect adults and is associated with Coxsackievirus A6 infection.10 It may manifest as generalized vesiculobullous exanthem resembling varicella. The chronic nature and restricted extent of the patient’s rash made this diagnosis unlikely.
Successful management depends on timely identification
Although most cases of HZ can be diagnosed clinically, atypical rashes may require a biopsy and direct immunofluorescence assay for VZV antigen or a polymerase-chain-reaction (PCR) assay for VZV DNA in cells from the base of blisters. Therefore, it is important to consider the diagnosis of HZ in immunocompromised patients presenting with an atypical rash to avoid misdiagnosis and costly testing.
Continue to: Our patient was treated...
Our patient was treated with oral acyclovir 800 mg 5 times/day for 10 days, with prompt resolution of her rash.
CORRESPONDENCE
Joel Hua-Liang Lim, MBBS, MRCP, MMed, 1 Mandalay Road, Singapore 308205; [email protected]
1. LeBoit PE, Limova M, Yen TS, et al. Chronic verrucous varicella-zoster virus infection in patients with the acquired immunodeficiency syndrome (AIDS): histologic and molecular biologic findings. Am J Dermatopathol. 1992;14:1-7.
2. Gnann JW Jr. Varicella-zoster virus: atypical presentations and unusual complications. J Infect Dis. 2002;186(suppl 1):S91-S98.
3. Weinberg JM, Mysliwiec A, Turiansky GW, et al. Viral folliculitis: atypical presentations of herpes simplex, herpes zoster, and molluscum contagiosum. Arch Dermatol. 1997;133:983-986.
4. Gilson IH, Barnett JH, Conant MA, et al. Disseminated ecthymatous herpes varicella zoster virus infection in patients with acquired immunodeficiency syndrome. J Am Acad Dermatol. 1989;20:637-642.
5. Løkke BJ, Weismann K, Mathiesen L, et al. Atypical varicella-zoster infection in AIDS. Acta Derm Venereol. 1993;73:123-125.
6. Uhoda I, Piérard-Franchimont C, Piérard GE. Varicella-zoster virus vasculitis: a case of recurrent varicella without epidermal involvement. Dermatology. 2000;200:173-175.
7. Teng GG, Chatham WW. Vasculitis related to viral and other microbial agents. Best Pract Res Clin Rheumatol. 2015;29:226-243.
8. Nagel MA, Gilden D. Developments in varicella zoster virus vasculopathy. Curr Neurol Neurosci Rep. 2016;16:12.
9. Pfaller MA, Diekema DJ. Epidemiology of invasive mycoses in North America. Crit Rev Microbiol. 2010;36:1-53.
10. Lott JP, Liu K, Landry M-L, et al. Atypical hand-foot-and-mouth disease associated with coxsackievirus A6 infection. J Am Acad Dermatol. 2013;69:736-741.
1. LeBoit PE, Limova M, Yen TS, et al. Chronic verrucous varicella-zoster virus infection in patients with the acquired immunodeficiency syndrome (AIDS): histologic and molecular biologic findings. Am J Dermatopathol. 1992;14:1-7.
2. Gnann JW Jr. Varicella-zoster virus: atypical presentations and unusual complications. J Infect Dis. 2002;186(suppl 1):S91-S98.
3. Weinberg JM, Mysliwiec A, Turiansky GW, et al. Viral folliculitis: atypical presentations of herpes simplex, herpes zoster, and molluscum contagiosum. Arch Dermatol. 1997;133:983-986.
4. Gilson IH, Barnett JH, Conant MA, et al. Disseminated ecthymatous herpes varicella zoster virus infection in patients with acquired immunodeficiency syndrome. J Am Acad Dermatol. 1989;20:637-642.
5. Løkke BJ, Weismann K, Mathiesen L, et al. Atypical varicella-zoster infection in AIDS. Acta Derm Venereol. 1993;73:123-125.
6. Uhoda I, Piérard-Franchimont C, Piérard GE. Varicella-zoster virus vasculitis: a case of recurrent varicella without epidermal involvement. Dermatology. 2000;200:173-175.
7. Teng GG, Chatham WW. Vasculitis related to viral and other microbial agents. Best Pract Res Clin Rheumatol. 2015;29:226-243.
8. Nagel MA, Gilden D. Developments in varicella zoster virus vasculopathy. Curr Neurol Neurosci Rep. 2016;16:12.
9. Pfaller MA, Diekema DJ. Epidemiology of invasive mycoses in North America. Crit Rev Microbiol. 2010;36:1-53.
10. Lott JP, Liu K, Landry M-L, et al. Atypical hand-foot-and-mouth disease associated with coxsackievirus A6 infection. J Am Acad Dermatol. 2013;69:736-741.
Presentation is key to diagnosing salivary gland disorders
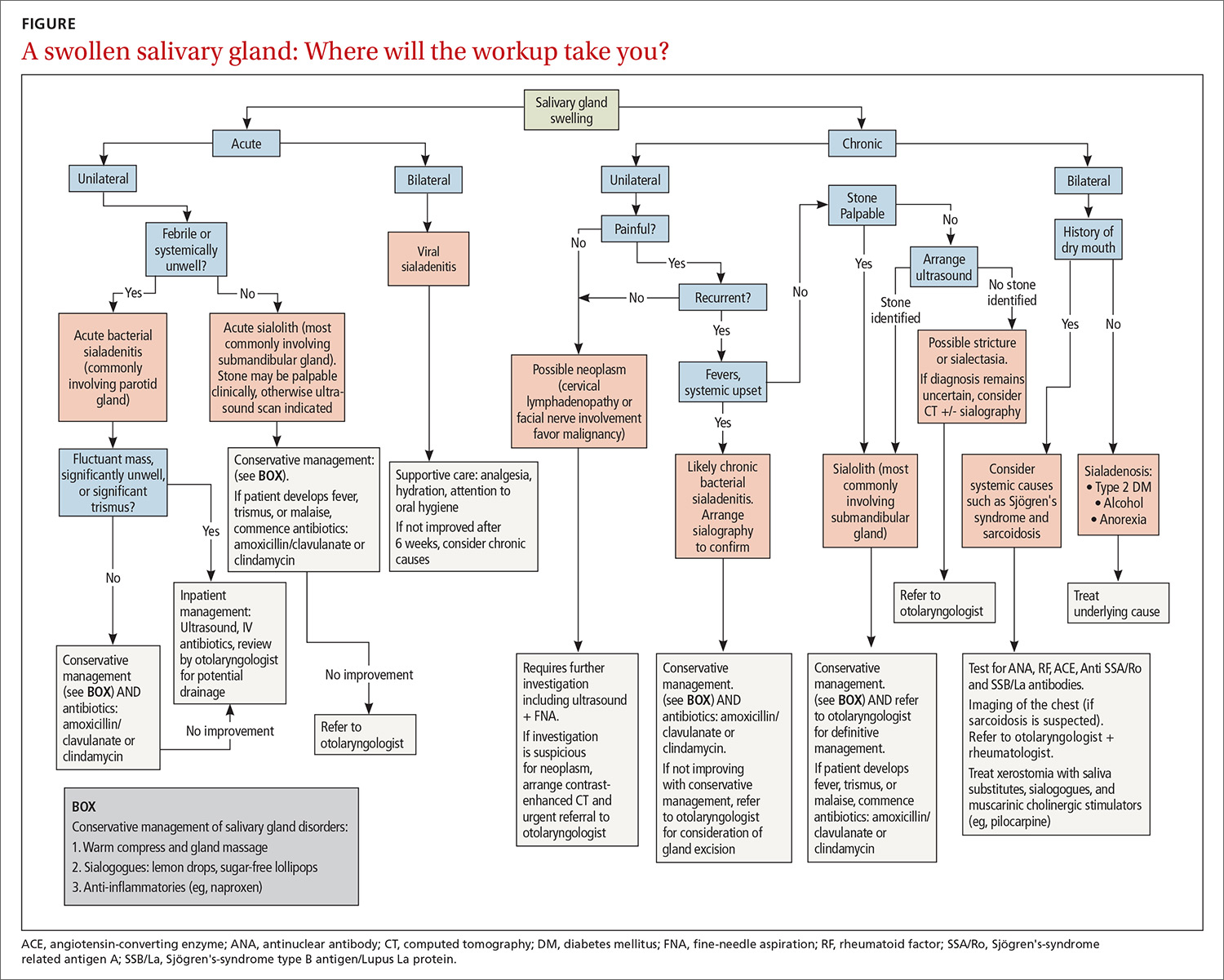
Making a diagnosis of a salivary gland disorder can be difficult. Common presentations, such as a painful or swollen gland, can be caused by numerous disorders of strikingly variable severity and consequences, including inflammatory, infectious, and neoplastic conditions, for which treatment can differ significantly, and referral for specialty care is sometimes necessary.
Yet it is the patient’s presentation that can aid you in making the diagnosis that will guide management. Consider that acute symptoms often result from infection, for example, and chronic or recurrent symptoms are caused more often by obstructive or nonobstructive inflammatory conditions and neoplasms. Diagnosis of an apparent neoplasm, prompted by clinical findings, is made using imaging and fine-needle aspiration (FNA) biopsy. Acute infection usually resolves with antibiotics and supportive management; calculi that cause persistent symptoms warrant referral for consideration of stone or gland removal; and malignant neoplasms usually require excision as well as neck dissection and chemotherapy or radiotherapy, or both—calling for multidisciplinary care.
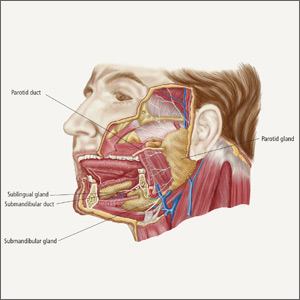
In this article, we clarify what can be an imprecise and perplexing path from the presentation to diagnosis to treatment of disorders of the salivary glands. To begin, see “Geography of the salivary glands,” for an overview of the location, structure, and corresponding ducts of the component salivary glands (parotid, submandibular, sublingual, and minor glands).
SIDEBAR
Geography of the salivary glands
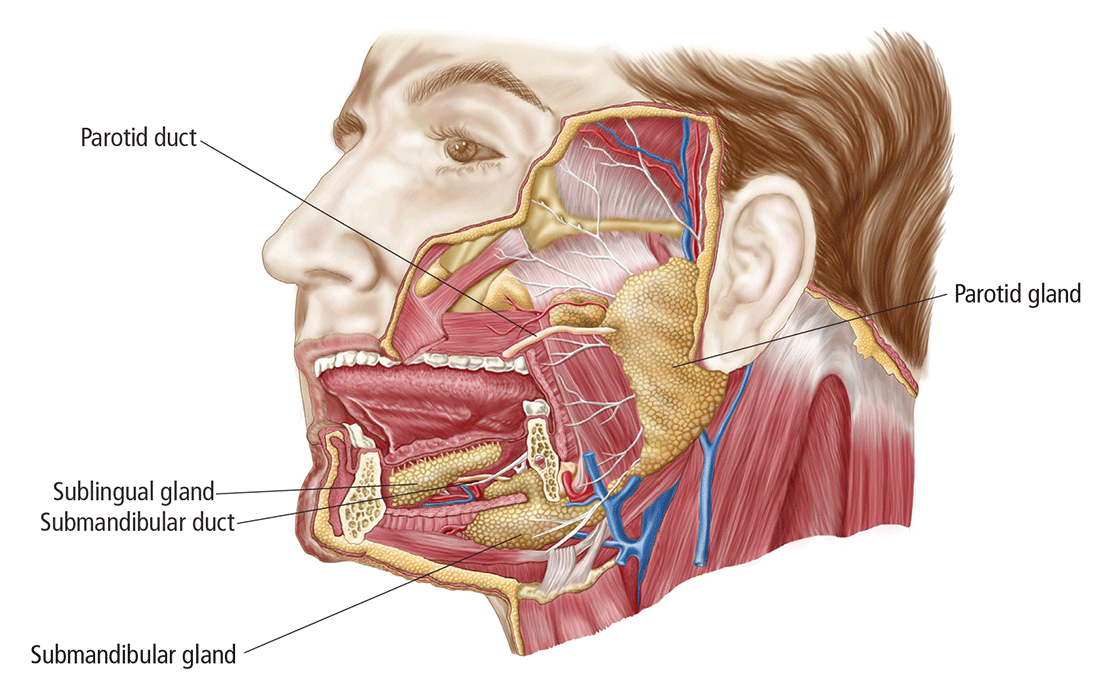
The salivary glands comprise the major paired parotid, submandibular, and sublingual glands, as well as minor salivary glands that line the oropharyngeal mucosa. Secretion of saliva is modulated by both autonomic and humoral factors.
The parotid gland sits between the mastoid process, the ramus of the mandible, and the styloid process, extend- ing from the external auditory meatus superiorly to below the angle of the mandible and into the neck inferiorly. The gland is surrounded by a tough capsule. Embedded within the gland is the facial nerve, which divides into its 5 branches within the substance of the gland. The parotid (Stensen’s) duct passes anteriorly before turning medially to pierce the buccinator muscle, opening onto the mucous membrane of the cheek opposite the second upper molar.
The submandibular gland comprises (1) a large superficial part that fills the space between the mandible and the floor of the mouth and (2) a small deep part that wraps around the posterior border of the mylohyoid muscle. The submandibular (Wharton’s) duct runs anteriorly to open onto the floor of the mouth, alongside the frenulum.
The sublingual gland, the smallest of the major salivary glands, lies anteriorly in the floor of the mouth, with many small ducts opening either into the submandibular duct or directly into the mouth.
Basic secretory units of salivary glands are clusters of cells, each called an acinus. These cells secrete a fluid that contains water, electrolytes, mucous, and enzymes, all of which flow out of the acini into collecting ducts. The saliva produced by the parotid is mainly serous; by the submandibular gland, mixed; and by the sublingual and minor salivary glands, mucoid.
Presentation helps establish the differential Dx
Ask: Are the glands swollen?
Painless salivary gland swelling has a variety of causes, including neoplasm, sialadenosis, and the eating disorders bulimia and anorexia nervosa. There is significant overlap of presentations among those causes (FIGURE). Pain accompanying swelling is uncommon but not unheard of.
Neoplasms. Tumors of the salivary gland are relatively uncommon, constituting approximately 2% of head and neck neoplasms; most (80%) occur in the parotid gland, and most of those are benign.1 Although benign and malignant salivary gland neoplasms do not usually present with pain, pain can be associated with a neoplasm secondary to suppuration, hemorrhage into a mass, or infiltration of a malignancy into adjacent tissue.
Benign tumors. The majority of benign tumors are pleomorphic adenomas of the parotid, accounting for approximately 60% of salivary gland neoplasms.1,2 Tumors localized to the submandibular gland are often (in 50% of cases) malignant, however.3
Benign tumors are typically slow-growing and, generally, painless. On examination, they are well-circumscribed, mobile, and nontender. Patients presenting late with a large tumor might, however, experience pain secondary to stretching of the parotid capsule or compression of local structures.
Continue to: Ultrasonograhpy (US) is an excellent...
Ultrasonography (US) is an excellent initial imaging choice for investigating a possible salivary gland tumor; US is combined with FNA, which is safe and highly reliable for differentiating neoplastic and non-neoplastic disorders.4 (Avoid open biopsy of a neoplasm because of the risk of tumor spillage.) In patients with suspected neoplasm, contrast-enhanced computed tomography (CT) or magnetic resonance imaging (MRI) should also be performed, because both modalities allow delineation of the tumor mass and demonstration of any infiltration of surrounding structures.
Treatment of benign neoplasms involves complete excision because, with some tumors, particularly pleomorphic adenomas, there is risk of malignant transformation over time. Superficial parotidectomy is the most common procedure, because most benign tumors occur in the superficial lobe of the parotid gland. Delicate dissection of the facial nerve is integral to the operation, although temporary facial nerve palsy will still occur in 5% to 10% of patients undergoing superficial parotidectomy for a benign tumor, with permanent injury occurring in fewer than 1%.5
Malignancy. Features of a tumor that raise concern of malignancy include6:
- rapid growth
- pain
- tethering to underlying structures or overlying skin
- firm mass
- associated cervical lymphadenopathy
- facial-nerve palsy.
The workup of a malignant tumor is the same as it is for a benign neoplasm: US-guided FNA, essential for diagnosis, and contrast-enhanced CT or MRI to delineate the tumor.
Malignant salivary gland neoplasms usually require excision as well as neck dissection and chemotherapy or radiotherapy, or both, necessitating a multidisciplinary approach. Also, there is potential for squamous-cell carcinoma and melanoma of the head to metastasize to salivary gland lymph nodes; it is important, therefore, to examine for, and elicit any history of, cutaneous malignancy of the scalp or face.
Continue to: Sialadenosis...
Sialadenosis presents with asymptomatic bilateral hypertrophy of the salivary glands—more commonly the parotids and rarely the submandibular glands. Swelling is persistent, symmetrical, painless, and of normal tone on palpation.
Causes of sialadenosis include alcoholism and, less commonly, diabetes mellitus and malnutrition; some cases are idiopathic. An autonomic neuropathy, causing excessive salivary acinar protein synthesis or failure of adequate secretion, or both, is common to alcoholism, diabetes, and malnutrition.7 Subsequent engorgement of acinar cells leads to clinical parotid hypertrophy.
Diagnosis is based on history and examination, as well as on the findings of US or CT, which will reveal bilateral gland enlargement and increased density. The glands appear dense because adipose cells are displaced by acinar cell hypertrophy; however, end-stage changes can result in the opposite appearance: a lucent enlargement caused by fatty infiltration.2 FNA is unnecessary, unless there is suspicion of neoplasm, as there would be in patients with asymmetrical parotid enlargement, pain, lymph node enlargement, or facial-nerve involvement. In patients with sialadenosis, in contrast, acinar cell hypertrophy alone will be present.
Treatment of sialadenosis is best aimed at rectifying the underlying medical condition, which might, over time, lead to some reduction in the size of the gland. There is no specific effective therapy for elimination of glandular swelling.
Bulimia and anorexia nervosa. Bulimia nervosa, the induction of vomiting after binge eating, can be associated with bilateral or occasionally unilateral parotid swelling. Anorexia, a form of self-starvation, can occur in association with bulimia, with patients also presenting with parotid swelling. Associated parotid swelling is similar to what is seen in sialadenosis: painless, persistent, and of nonpathologic consistency.
The pathophysiology of bulimia- and anorexia-associated parotid-gland swelling is identical to what is seen in sialadenosis: dysregulation of acinar cell sympathetic nerve supply that leads to enlargement of individual parenchymal cells.8 Contrast-enhanced CT can reveal increased vascularity associated with active bulimia. FNA and CT, however, are required only in patients in whom the diagnosis is not clear and when neoplasm is suspected.
Continue to: Treatment includes...
Treatment includes correcting electrolyte abnormalities and, more importantly, addressing underlying emotional issues to stop purging episodes. Psychiatric input and social support are invaluable. Parotid gland swelling generally improves with cessation of vomiting episodes.
Ask: Is the patient in pain?
Causes of salivary gland pain include sialolithiasis, sialadenitis, and recurrent parotitis of childhood. Pain occurs secondary to stretching of the fibrous capsule in which the parotid or submandibular gland is surrounded, compression of pain fibers by an expanding mass, or infiltration of nerves by neoplasia.
Sialolithiasis. Sialolithiasis, or salivary stones, are primarily calcium carbonate concentrations within the salivary ductal system. More than 80% occur in the submandibular gland or duct9 as a result of production of mixed mucoid and serous saliva and a tortuous duct path.
Patients usually present with a history of intermittent swelling and pain of the involved gland associated with eating. Increased production of saliva during meals, which then passes through a partially obstructed salivary duct, leads to salivary retention and glandular swelling. Thus, a recurring pattern can develop, with varying periods of remission,7 eventually leading to an acute suppurative process or sialadenitis (described below). Chronic salivary disease can also be caused by stricture of a duct or, rarely, external compression by a tumor mass.
Examination often reveals an enlarged and often tender gland; conversely, chronic disease can lead to gland atrophy. Usually, only minimal saliva is able to be expressed from an obstructed duct. For a submandibular duct stone, bimanual palpation might reveal its position if it is located distally in the floor of the mouth; a proximal stone might not be palpable.
Continue to: Although US is operator-dependent...
Although US is operator-dependent, it is the imaging modality of choice for identifying sialolithiasis10 because it can identify gland architecture, duct dilation, and both radiolucent and radiopaque stones. For patients in whom US findings are normal despite a convincing clinical presentation of sialolithiasis, CT should be performed because small stones can be missed on US.11
Supportive measures for sialolithiasis are listed in the TABLE. Reserve antibiotics for patients who have signs or symptoms of infection, including pyrexia, trismus, and malaise. A beta-lactam antibiotic, such as amoxicillin–clavulanate, 875 mg orally bid, or a cephalosporin, such as cephalexin, 500 mg orally qid, are appropriate first-line options. Clindamycin, 300 mg orally tid, or metronidazole, 500 mg orally tid, are acceptable alternatives. When signs or symptoms are persistent or recurrent, refer the patient for a surgical opinion.
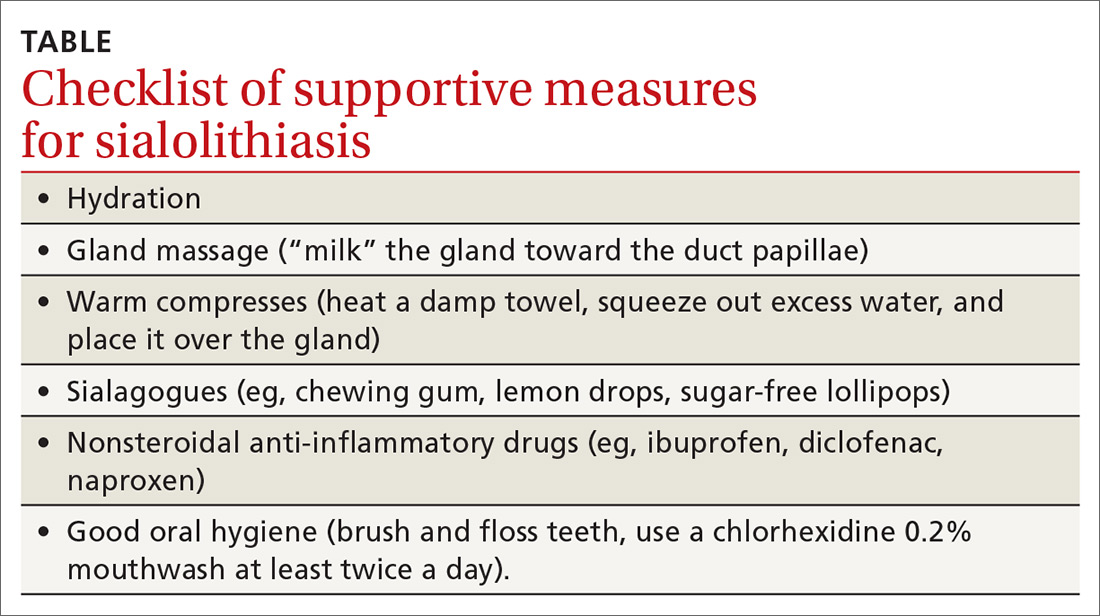
Stones located in the floor of the mouth are usually excised through an intraoral approach. In the past, gland excision was advocated when a sialolith was found more proximally within the gland parenchyma. More recently, however, sialendoscopy, involving insertion of a small, semirigid endoscope into the salivary duct, has been shown safe and effective for removing a stone; successful removal, in as many as 80% of cases, increases to 90% when performed using a minimally invasive surgical technique.12 Although sialendoscopy is effective, the technique cannot always treat the underlying abnormality of the salivary gland; gland excision is therefore warranted in some cases.
Last, extracorporeal shock wave therapy is aimed at fragmenting salivary stones before retrieval. Results are variable, however, and treatment should be guided by an otolaryngologist.13,14
Sialadenitis (bacterial and viral infection). Acute suppurative sialadenitis occurs secondary to retrograde ductal bacterial infection. The parotid gland is most frequently involved,15 although submandibular sialadenitis is not uncommon. Patients usually present with sudden-onset unilateral, painful swelling.
Continue to: Pathophysiology involves...
Pathophysiology involves dehydration or decreased oral intake leading to salivary stasis and subsequent bacterial migration into the gland. Medically debilitated and postoperative patients are therefore at greater risk; so are patients with diabetes mellitus, poor oral hygiene, Sjögren’s syndrome, hypothyroidism, or renal failure.16 Certain medications, including anticholinergics, can also predispose to hyposalivation.17
(As discussed, sialolithiasis and stricture of salivary ducts can also cause acute bacterial infection; in such cases, however, the typical presentation is one of chronic or recurrent infection.)
Examination might reveal an exquisitely tender, indurated, and inflamed gland; pus can often be expressed from the respective intraoral orifice. Any expressed pus should be sent for culture to guide antibiotic therapy.
Treatment should focus on hydration, oral hygiene, and antibiotics, while reversing or minimizing any underlying contributing medical condition. Warm compresses applied to the involved gland, massage, and sialagogues, such as lemon drops or sugar-free lollipops, can stimulate salivary flow and prevent stasis.
More than 80% of infections are caused by Staphylococcus aureus17; anaerobic and mixed infections have also been recognized.A beta-lactam penicillin, such as amoxicillin-clavulanate, is the antibiotic of choice. A patient who is systemically unwell should be treated as an inpatient with nafcillin and metronidazole. Methicillin-resistant S aureus must also be considered in patients with comorbid disease, such as diabetes mellitus or intravenous drug use, or in patients residing in an area of substantial incidence of methicillin-resistant S aureus. In those cases, substitute vancomycin or linezolid for nafcillin.18
Continue to: Less commonly...
Less commonly, abscess can form, with the patient presenting as systemically unwell with a fluctuant mass. If the diagnosis is unclear or the patient does not improve, abscess can be confirmed by US. Expedient surgical review and inpatient admission can then be arranged.
Unlike bacterial sialadenitis, causes of viral sialadenitis are often bilateral. Mumps (a paramyxovirus) is the most common viral cause, affecting primarily children < 15 years.19 The parotid glands are most often involved, with inflammation and edema causing significant pain because of increasing intraparotid pressure as expansion of the gland is limited by its tense fibrous capsule. Complications of mumps include orchitis, meningitis, pancreatitis, and oophoritis.
Mumps is highly contagious; it is spread through contact with airborne saliva droplets, with viral entry through the nose or mouth, followed by proliferation in the salivary glands or on surface epithelium of the respiratory tract.7 Diagnosis is confirmed by viral serology. A positive test of serum immunoglobulin M confirms the diagnosis, but this test should not be performed until 3 days after onset of symptoms because a false-negative result is otherwise possible.20 Immunoglobulin G serologic testing can further aid diagnosis; the titer is measured approximately 4 days after onset of symptoms and again 2 to 3 weeks later. A 4-fold rise in titer confirms mumps.
Other viral infections that can cause sialadenitis include Epstein-Barr virus, cytomegalovirus, human immunodeficiency virus, coxsackievirus, and influenza. Treatment is supportive: analgesia, hydration, oral hygiene, and rest. Inflammation might take weeks to resolve, but expect complete resolution. For a patient who has significant trismus, poor oral intake, or a potentially threatened airway, inpatient care should be provided.
Recurrent parotitis of childhood is an inflammatory condition that usually affects one, but at times both, parotid glands. It is characterized by episodes of painful swelling. Incidence peaks at 3 to 6 years of age.7 Episodes can be frequent, occurring 1 to 5 times a year and lasting 3 to 7 days—sometimes longer—and usually resolving without treatment.
Continue to: The precise etiology...
The precise etiology of recurrent parotitis of childhood is unclear; possibly, saliva aggregates to form obstructive mucous plugs, thus causing stasis and swelling of the gland. As pressure builds, spontaneous plug extrusion occurs and symptoms resolve, provided infection is not a factor. US demonstrates multiple round, hypoechoic areas consistent with duct dilation, and surrounding infiltration by lymphocytes.1
Supportive care—adequate hydration, gland massage, warm compresses, and sialogogues—are mainstays of treatment. Fever and malaise warrant treatment with oral antibiotics. Sialadenoscopy, which can be considered in children with frequent episodes, can decrease the frequency and severity of episodes.21 The condition usually resolves spontaneously at puberty.
Ask: Does the patient have dry mouth?
In-depth review of xerostomia is beyond the scope of this article. Causes include Sjögren's syndrome, immunoglobulin G4-related sialadenitis, sarcoidosis, radiation therapy, diabetes, chronic infection, and medications—in particular those with anticholinergic effects.
Treatment of xerostomia includes saliva substitutes, sialagogues, and, for oral candidiasis, antifungals. Muscarinic cholinergic stimulators, such as pilocarpine, 5 mg qid have been used with some success22; patients should be advised of potential adverse effects with these agents, including sweating, urinary frequency, flushing, and chills.
CORRESPONDENCE
Shankar Haran, MBBS, ENT Department, Townsville Hospital, 100 Angus Smith Dr, Douglas, Queensland, Australia 4814; [email protected].
1. de Oliveira FA, Duarte EC, Taveira CT, et al. Salivary gland tumor: a review of 599 cases in a Brazilian population. Head Neck Pathol. 2009;3:271-275.
2. Spiro RH. Salivary neoplasms: overview of a 35-year experience with 2,807 patients. Head Neck Surg. 1986;8:177-184.
3. Bova R. A guide to salivary gland disorders. Medicine Today. 2006;7:44-48.
4. Zhang S, Bao R, Bagby J, et al. Fine needle aspiration of salivary glands: 5-year experience from a single academic center. Acta Cytol. 2009;53:375-382.
5. Bova R, Saylor A, Coman WB. Parotidectomy: review of treatment and outcomes. ANZ J Surg. 2004;74:563-568.
6. Sood S, McGurk M, Vaz F. Management of salivary gland tumours: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol. 2016;130:S142-S149.
7. Mandel L. Salivary gland disorders. Med Clin North Am. 2014;98:1407-1449.
8. Mandel L, Abai S. Diagnosing bulimia nervosa with parotid gland swelling. J Am Dent Assoc. 2004;135:613–616.
9. Lustmann J, Regev E, Melamed Y. Sialolithiasis. A survey on 245 patients and a review of literature. Int J Oral Maxillofac Surg. 1990;19:135–138.
10. Vogl TJ, Al-Nawas B, Beutner D, et al. Updated S2K AWMF guideline for the diagnosis and follow-up of obstructive sialadenitis—relevance for radiologic imaging. Rofo. 2014;186:843-846.
11. Schwarz D, Kabbasch C, Scheer M, et al. Comparative analysis of sialendoscopy, sonography, and CBCT in the detection of sialolithiasis. Laryngoscope. 2015;125:1098–1101.
12. Atienza G, López-Cedrún JL. Management of obstructive salivary disorders by sialendoscopy: a systematic review. Br J Oral Maxillofac Surg. 2015;53:507-519.
13. Escudier MP, Brown JE, Putcha V, et al. Factors influencing the outcome of extracorporeal shock wave lithotripsy in the management of salivary calculi. Laryngoscope. 2010;120:1545-1549.
14. Koch M, Schapher M, Mantsopoulos K, et al. Multimodal treatment in difficult sialolithiasis: Role of extracorporeal shock-wave lithotripsy and intraductal pneumatic lithotripsy. Laryngoscope. 2018;128:E332-E338.
15. McQuone SJ. Acute viral and bacterial infections of the salivary glands. Otolaryngol Clin North Am. 1999;32:793-811.
16. O’Neil C, Sidhu S. Salivary gland disorders. Australian Doctor. 2011;28:19-25.
17. Mandel L. Differentiating acute suppurative parotitis from acute exacerbation of a chronic parotitis: case reports. J Oral Maxillofac Surg. 2008;66:1964-1968.
18. Chow AW. Suppurative parotitis in adults. UpToDate.com. www.uptodate.com/contents/suppurative-parotitis-in-adults. Accessed September 25, 2019.
19. Katz SL, Gershon AA, Hotez PJ. Infectious Diseases of Children. New York, NY: Mosby Year Book; 1998:280-289.
20. Krause CH, Molyneaux PJ, Ho-Yen DO, et al. Comparison of mumps-IgM ELISAs in acute infection. J Clin Virol. 2007;38:153-156.
21. Quenin S, Plouin-Gaudon I, Marchal F, et al. Juvenile recurrent parotitis: sialendoscopic approach. Arch Otolaryngol Head Neck Surg. 2008;134:715-719.
22. Papas AS, Sherrer YS, Charney M, et al. Successful treatment of dry mouth and dry eye symptoms in Sjögren’s syndrome patients with oral pilocarpine: a randomized, placebo-controlled, dose-adjustment study. J Clin Rheumatol. 2004;10:169-177.
Making a diagnosis of a salivary gland disorder can be difficult. Common presentations, such as a painful or swollen gland, can be caused by numerous disorders of strikingly variable severity and consequences, including inflammatory, infectious, and neoplastic conditions, for which treatment can differ significantly, and referral for specialty care is sometimes necessary.
Yet it is the patient’s presentation that can aid you in making the diagnosis that will guide management. Consider that acute symptoms often result from infection, for example, and chronic or recurrent symptoms are caused more often by obstructive or nonobstructive inflammatory conditions and neoplasms. Diagnosis of an apparent neoplasm, prompted by clinical findings, is made using imaging and fine-needle aspiration (FNA) biopsy. Acute infection usually resolves with antibiotics and supportive management; calculi that cause persistent symptoms warrant referral for consideration of stone or gland removal; and malignant neoplasms usually require excision as well as neck dissection and chemotherapy or radiotherapy, or both—calling for multidisciplinary care.
In this article, we clarify what can be an imprecise and perplexing path from the presentation to diagnosis to treatment of disorders of the salivary glands. To begin, see “Geography of the salivary glands,” for an overview of the location, structure, and corresponding ducts of the component salivary glands (parotid, submandibular, sublingual, and minor glands).
SIDEBAR
Geography of the salivary glands
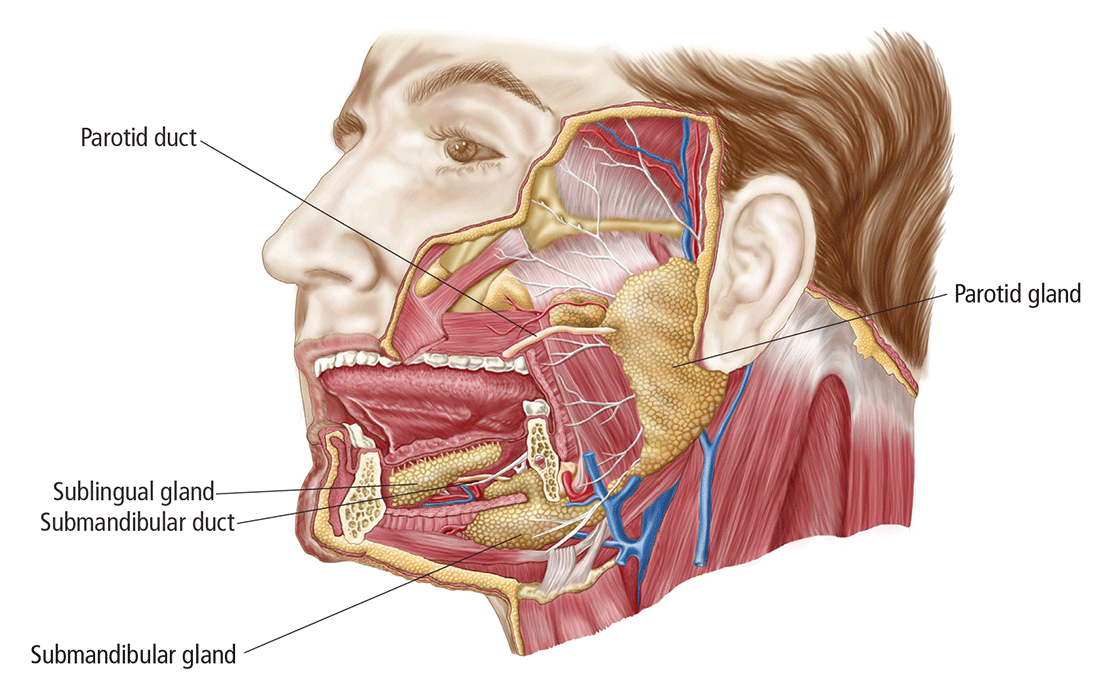
The salivary glands comprise the major paired parotid, submandibular, and sublingual glands, as well as minor salivary glands that line the oropharyngeal mucosa. Secretion of saliva is modulated by both autonomic and humoral factors.
The parotid gland sits between the mastoid process, the ramus of the mandible, and the styloid process, extend- ing from the external auditory meatus superiorly to below the angle of the mandible and into the neck inferiorly. The gland is surrounded by a tough capsule. Embedded within the gland is the facial nerve, which divides into its 5 branches within the substance of the gland. The parotid (Stensen’s) duct passes anteriorly before turning medially to pierce the buccinator muscle, opening onto the mucous membrane of the cheek opposite the second upper molar.
The submandibular gland comprises (1) a large superficial part that fills the space between the mandible and the floor of the mouth and (2) a small deep part that wraps around the posterior border of the mylohyoid muscle. The submandibular (Wharton’s) duct runs anteriorly to open onto the floor of the mouth, alongside the frenulum.
The sublingual gland, the smallest of the major salivary glands, lies anteriorly in the floor of the mouth, with many small ducts opening either into the submandibular duct or directly into the mouth.
Basic secretory units of salivary glands are clusters of cells, each called an acinus. These cells secrete a fluid that contains water, electrolytes, mucous, and enzymes, all of which flow out of the acini into collecting ducts. The saliva produced by the parotid is mainly serous; by the submandibular gland, mixed; and by the sublingual and minor salivary glands, mucoid.
Presentation helps establish the differential Dx
Ask: Are the glands swollen?
Painless salivary gland swelling has a variety of causes, including neoplasm, sialadenosis, and the eating disorders bulimia and anorexia nervosa. There is significant overlap of presentations among those causes (FIGURE). Pain accompanying swelling is uncommon but not unheard of.
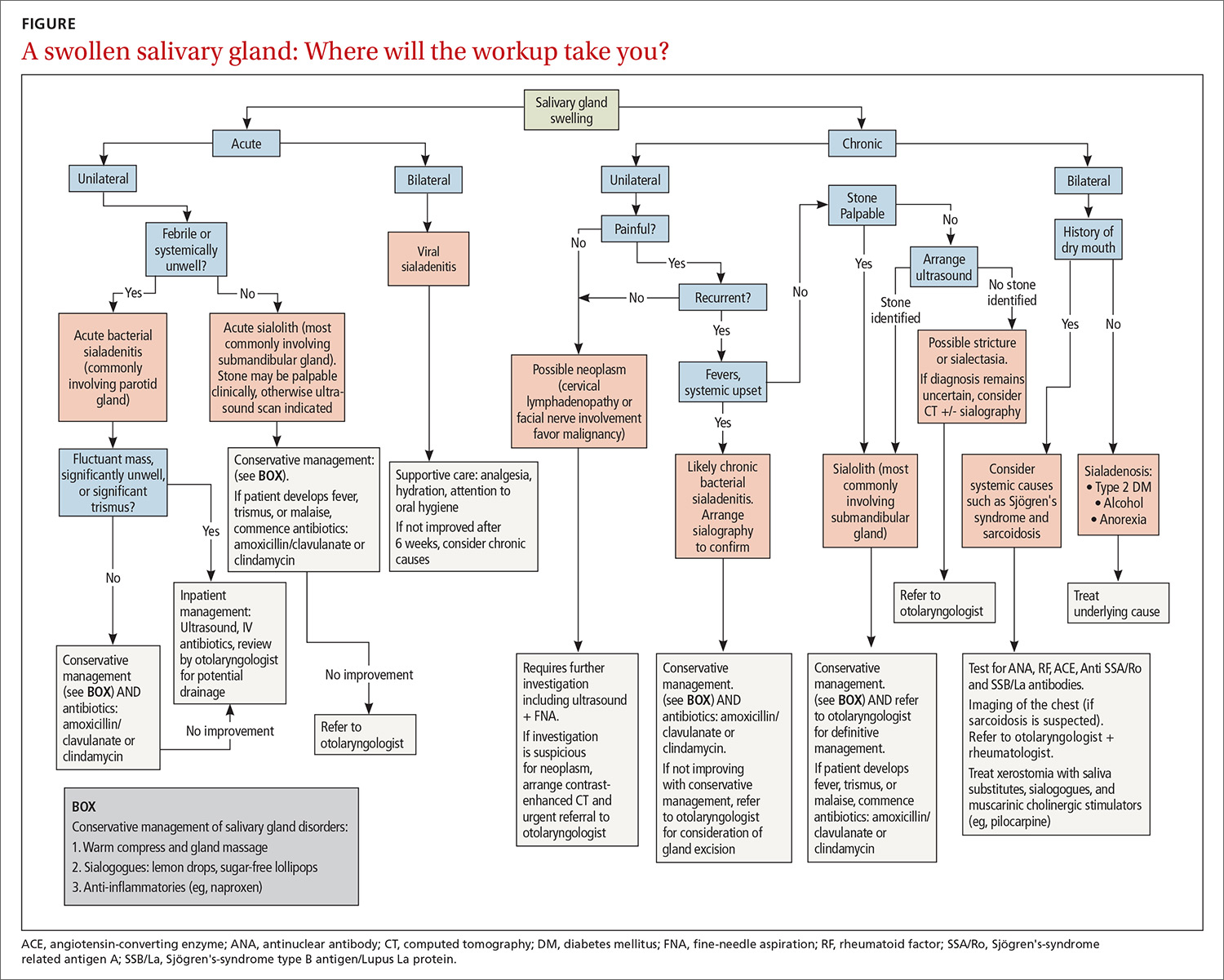
Neoplasms. Tumors of the salivary gland are relatively uncommon, constituting approximately 2% of head and neck neoplasms; most (80%) occur in the parotid gland, and most of those are benign.1 Although benign and malignant salivary gland neoplasms do not usually present with pain, pain can be associated with a neoplasm secondary to suppuration, hemorrhage into a mass, or infiltration of a malignancy into adjacent tissue.
Benign tumors. The majority of benign tumors are pleomorphic adenomas of the parotid, accounting for approximately 60% of salivary gland neoplasms.1,2 Tumors localized to the submandibular gland are often (in 50% of cases) malignant, however.3
Benign tumors are typically slow-growing and, generally, painless. On examination, they are well-circumscribed, mobile, and nontender. Patients presenting late with a large tumor might, however, experience pain secondary to stretching of the parotid capsule or compression of local structures.
Continue to: Ultrasonograhpy (US) is an excellent...
Ultrasonography (US) is an excellent initial imaging choice for investigating a possible salivary gland tumor; US is combined with FNA, which is safe and highly reliable for differentiating neoplastic and non-neoplastic disorders.4 (Avoid open biopsy of a neoplasm because of the risk of tumor spillage.) In patients with suspected neoplasm, contrast-enhanced computed tomography (CT) or magnetic resonance imaging (MRI) should also be performed, because both modalities allow delineation of the tumor mass and demonstration of any infiltration of surrounding structures.
Treatment of benign neoplasms involves complete excision because, with some tumors, particularly pleomorphic adenomas, there is risk of malignant transformation over time. Superficial parotidectomy is the most common procedure, because most benign tumors occur in the superficial lobe of the parotid gland. Delicate dissection of the facial nerve is integral to the operation, although temporary facial nerve palsy will still occur in 5% to 10% of patients undergoing superficial parotidectomy for a benign tumor, with permanent injury occurring in fewer than 1%.5
Malignancy. Features of a tumor that raise concern of malignancy include6:
- rapid growth
- pain
- tethering to underlying structures or overlying skin
- firm mass
- associated cervical lymphadenopathy
- facial-nerve palsy.
The workup of a malignant tumor is the same as it is for a benign neoplasm: US-guided FNA, essential for diagnosis, and contrast-enhanced CT or MRI to delineate the tumor.
Malignant salivary gland neoplasms usually require excision as well as neck dissection and chemotherapy or radiotherapy, or both, necessitating a multidisciplinary approach. Also, there is potential for squamous-cell carcinoma and melanoma of the head to metastasize to salivary gland lymph nodes; it is important, therefore, to examine for, and elicit any history of, cutaneous malignancy of the scalp or face.
Continue to: Sialadenosis...
Sialadenosis presents with asymptomatic bilateral hypertrophy of the salivary glands—more commonly the parotids and rarely the submandibular glands. Swelling is persistent, symmetrical, painless, and of normal tone on palpation.
Causes of sialadenosis include alcoholism and, less commonly, diabetes mellitus and malnutrition; some cases are idiopathic. An autonomic neuropathy, causing excessive salivary acinar protein synthesis or failure of adequate secretion, or both, is common to alcoholism, diabetes, and malnutrition.7 Subsequent engorgement of acinar cells leads to clinical parotid hypertrophy.
Diagnosis is based on history and examination, as well as on the findings of US or CT, which will reveal bilateral gland enlargement and increased density. The glands appear dense because adipose cells are displaced by acinar cell hypertrophy; however, end-stage changes can result in the opposite appearance: a lucent enlargement caused by fatty infiltration.2 FNA is unnecessary, unless there is suspicion of neoplasm, as there would be in patients with asymmetrical parotid enlargement, pain, lymph node enlargement, or facial-nerve involvement. In patients with sialadenosis, in contrast, acinar cell hypertrophy alone will be present.
Treatment of sialadenosis is best aimed at rectifying the underlying medical condition, which might, over time, lead to some reduction in the size of the gland. There is no specific effective therapy for elimination of glandular swelling.
Bulimia and anorexia nervosa. Bulimia nervosa, the induction of vomiting after binge eating, can be associated with bilateral or occasionally unilateral parotid swelling. Anorexia, a form of self-starvation, can occur in association with bulimia, with patients also presenting with parotid swelling. Associated parotid swelling is similar to what is seen in sialadenosis: painless, persistent, and of nonpathologic consistency.
The pathophysiology of bulimia- and anorexia-associated parotid-gland swelling is identical to what is seen in sialadenosis: dysregulation of acinar cell sympathetic nerve supply that leads to enlargement of individual parenchymal cells.8 Contrast-enhanced CT can reveal increased vascularity associated with active bulimia. FNA and CT, however, are required only in patients in whom the diagnosis is not clear and when neoplasm is suspected.
Continue to: Treatment includes...
Treatment includes correcting electrolyte abnormalities and, more importantly, addressing underlying emotional issues to stop purging episodes. Psychiatric input and social support are invaluable. Parotid gland swelling generally improves with cessation of vomiting episodes.
Ask: Is the patient in pain?
Causes of salivary gland pain include sialolithiasis, sialadenitis, and recurrent parotitis of childhood. Pain occurs secondary to stretching of the fibrous capsule in which the parotid or submandibular gland is surrounded, compression of pain fibers by an expanding mass, or infiltration of nerves by neoplasia.
Sialolithiasis. Sialolithiasis, or salivary stones, are primarily calcium carbonate concentrations within the salivary ductal system. More than 80% occur in the submandibular gland or duct9 as a result of production of mixed mucoid and serous saliva and a tortuous duct path.
Patients usually present with a history of intermittent swelling and pain of the involved gland associated with eating. Increased production of saliva during meals, which then passes through a partially obstructed salivary duct, leads to salivary retention and glandular swelling. Thus, a recurring pattern can develop, with varying periods of remission,7 eventually leading to an acute suppurative process or sialadenitis (described below). Chronic salivary disease can also be caused by stricture of a duct or, rarely, external compression by a tumor mass.
Examination often reveals an enlarged and often tender gland; conversely, chronic disease can lead to gland atrophy. Usually, only minimal saliva is able to be expressed from an obstructed duct. For a submandibular duct stone, bimanual palpation might reveal its position if it is located distally in the floor of the mouth; a proximal stone might not be palpable.
Continue to: Although US is operator-dependent...
Although US is operator-dependent, it is the imaging modality of choice for identifying sialolithiasis10 because it can identify gland architecture, duct dilation, and both radiolucent and radiopaque stones. For patients in whom US findings are normal despite a convincing clinical presentation of sialolithiasis, CT should be performed because small stones can be missed on US.11
Supportive measures for sialolithiasis are listed in the TABLE. Reserve antibiotics for patients who have signs or symptoms of infection, including pyrexia, trismus, and malaise. A beta-lactam antibiotic, such as amoxicillin–clavulanate, 875 mg orally bid, or a cephalosporin, such as cephalexin, 500 mg orally qid, are appropriate first-line options. Clindamycin, 300 mg orally tid, or metronidazole, 500 mg orally tid, are acceptable alternatives. When signs or symptoms are persistent or recurrent, refer the patient for a surgical opinion.
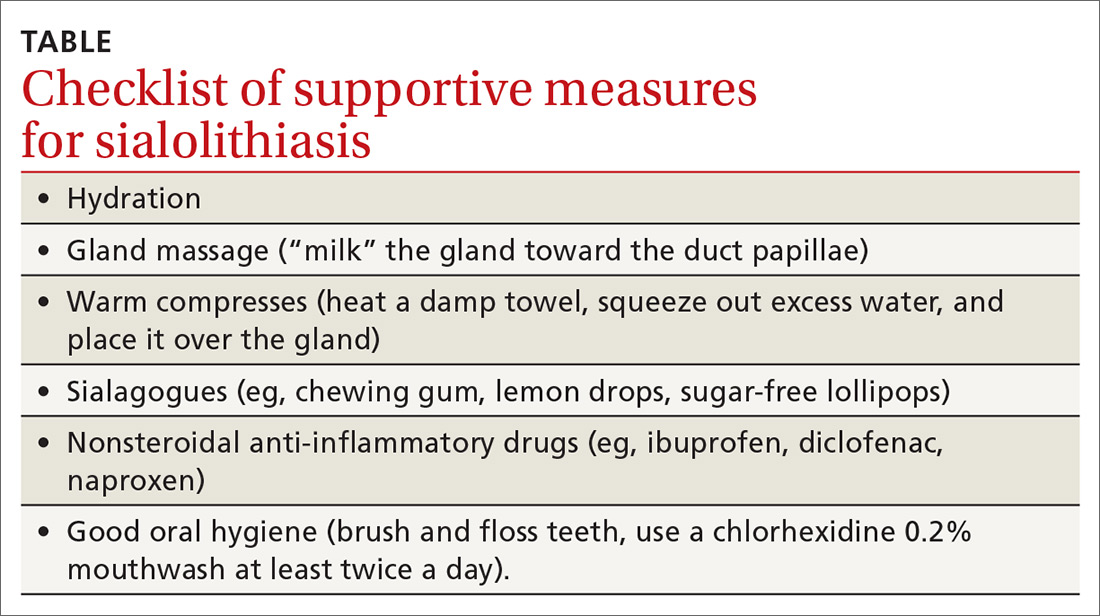
Stones located in the floor of the mouth are usually excised through an intraoral approach. In the past, gland excision was advocated when a sialolith was found more proximally within the gland parenchyma. More recently, however, sialendoscopy, involving insertion of a small, semirigid endoscope into the salivary duct, has been shown safe and effective for removing a stone; successful removal, in as many as 80% of cases, increases to 90% when performed using a minimally invasive surgical technique.12 Although sialendoscopy is effective, the technique cannot always treat the underlying abnormality of the salivary gland; gland excision is therefore warranted in some cases.
Last, extracorporeal shock wave therapy is aimed at fragmenting salivary stones before retrieval. Results are variable, however, and treatment should be guided by an otolaryngologist.13,14
Sialadenitis (bacterial and viral infection). Acute suppurative sialadenitis occurs secondary to retrograde ductal bacterial infection. The parotid gland is most frequently involved,15 although submandibular sialadenitis is not uncommon. Patients usually present with sudden-onset unilateral, painful swelling.
Continue to: Pathophysiology involves...
Pathophysiology involves dehydration or decreased oral intake leading to salivary stasis and subsequent bacterial migration into the gland. Medically debilitated and postoperative patients are therefore at greater risk; so are patients with diabetes mellitus, poor oral hygiene, Sjögren’s syndrome, hypothyroidism, or renal failure.16 Certain medications, including anticholinergics, can also predispose to hyposalivation.17
(As discussed, sialolithiasis and stricture of salivary ducts can also cause acute bacterial infection; in such cases, however, the typical presentation is one of chronic or recurrent infection.)
Examination might reveal an exquisitely tender, indurated, and inflamed gland; pus can often be expressed from the respective intraoral orifice. Any expressed pus should be sent for culture to guide antibiotic therapy.
Treatment should focus on hydration, oral hygiene, and antibiotics, while reversing or minimizing any underlying contributing medical condition. Warm compresses applied to the involved gland, massage, and sialagogues, such as lemon drops or sugar-free lollipops, can stimulate salivary flow and prevent stasis.
More than 80% of infections are caused by Staphylococcus aureus17; anaerobic and mixed infections have also been recognized.A beta-lactam penicillin, such as amoxicillin-clavulanate, is the antibiotic of choice. A patient who is systemically unwell should be treated as an inpatient with nafcillin and metronidazole. Methicillin-resistant S aureus must also be considered in patients with comorbid disease, such as diabetes mellitus or intravenous drug use, or in patients residing in an area of substantial incidence of methicillin-resistant S aureus. In those cases, substitute vancomycin or linezolid for nafcillin.18
Continue to: Less commonly...
Less commonly, abscess can form, with the patient presenting as systemically unwell with a fluctuant mass. If the diagnosis is unclear or the patient does not improve, abscess can be confirmed by US. Expedient surgical review and inpatient admission can then be arranged.
Unlike bacterial sialadenitis, causes of viral sialadenitis are often bilateral. Mumps (a paramyxovirus) is the most common viral cause, affecting primarily children < 15 years.19 The parotid glands are most often involved, with inflammation and edema causing significant pain because of increasing intraparotid pressure as expansion of the gland is limited by its tense fibrous capsule. Complications of mumps include orchitis, meningitis, pancreatitis, and oophoritis.
Mumps is highly contagious; it is spread through contact with airborne saliva droplets, with viral entry through the nose or mouth, followed by proliferation in the salivary glands or on surface epithelium of the respiratory tract.7 Diagnosis is confirmed by viral serology. A positive test of serum immunoglobulin M confirms the diagnosis, but this test should not be performed until 3 days after onset of symptoms because a false-negative result is otherwise possible.20 Immunoglobulin G serologic testing can further aid diagnosis; the titer is measured approximately 4 days after onset of symptoms and again 2 to 3 weeks later. A 4-fold rise in titer confirms mumps.
Other viral infections that can cause sialadenitis include Epstein-Barr virus, cytomegalovirus, human immunodeficiency virus, coxsackievirus, and influenza. Treatment is supportive: analgesia, hydration, oral hygiene, and rest. Inflammation might take weeks to resolve, but expect complete resolution. For a patient who has significant trismus, poor oral intake, or a potentially threatened airway, inpatient care should be provided.
Recurrent parotitis of childhood is an inflammatory condition that usually affects one, but at times both, parotid glands. It is characterized by episodes of painful swelling. Incidence peaks at 3 to 6 years of age.7 Episodes can be frequent, occurring 1 to 5 times a year and lasting 3 to 7 days—sometimes longer—and usually resolving without treatment.
Continue to: The precise etiology...
The precise etiology of recurrent parotitis of childhood is unclear; possibly, saliva aggregates to form obstructive mucous plugs, thus causing stasis and swelling of the gland. As pressure builds, spontaneous plug extrusion occurs and symptoms resolve, provided infection is not a factor. US demonstrates multiple round, hypoechoic areas consistent with duct dilation, and surrounding infiltration by lymphocytes.1
Supportive care—adequate hydration, gland massage, warm compresses, and sialogogues—are mainstays of treatment. Fever and malaise warrant treatment with oral antibiotics. Sialadenoscopy, which can be considered in children with frequent episodes, can decrease the frequency and severity of episodes.21 The condition usually resolves spontaneously at puberty.
Ask: Does the patient have dry mouth?
In-depth review of xerostomia is beyond the scope of this article. Causes include Sjögren's syndrome, immunoglobulin G4-related sialadenitis, sarcoidosis, radiation therapy, diabetes, chronic infection, and medications—in particular those with anticholinergic effects.
Treatment of xerostomia includes saliva substitutes, sialagogues, and, for oral candidiasis, antifungals. Muscarinic cholinergic stimulators, such as pilocarpine, 5 mg qid have been used with some success22; patients should be advised of potential adverse effects with these agents, including sweating, urinary frequency, flushing, and chills.
CORRESPONDENCE
Shankar Haran, MBBS, ENT Department, Townsville Hospital, 100 Angus Smith Dr, Douglas, Queensland, Australia 4814; [email protected].
Making a diagnosis of a salivary gland disorder can be difficult. Common presentations, such as a painful or swollen gland, can be caused by numerous disorders of strikingly variable severity and consequences, including inflammatory, infectious, and neoplastic conditions, for which treatment can differ significantly, and referral for specialty care is sometimes necessary.
Yet it is the patient’s presentation that can aid you in making the diagnosis that will guide management. Consider that acute symptoms often result from infection, for example, and chronic or recurrent symptoms are caused more often by obstructive or nonobstructive inflammatory conditions and neoplasms. Diagnosis of an apparent neoplasm, prompted by clinical findings, is made using imaging and fine-needle aspiration (FNA) biopsy. Acute infection usually resolves with antibiotics and supportive management; calculi that cause persistent symptoms warrant referral for consideration of stone or gland removal; and malignant neoplasms usually require excision as well as neck dissection and chemotherapy or radiotherapy, or both—calling for multidisciplinary care.
In this article, we clarify what can be an imprecise and perplexing path from the presentation to diagnosis to treatment of disorders of the salivary glands. To begin, see “Geography of the salivary glands,” for an overview of the location, structure, and corresponding ducts of the component salivary glands (parotid, submandibular, sublingual, and minor glands).
SIDEBAR
Geography of the salivary glands
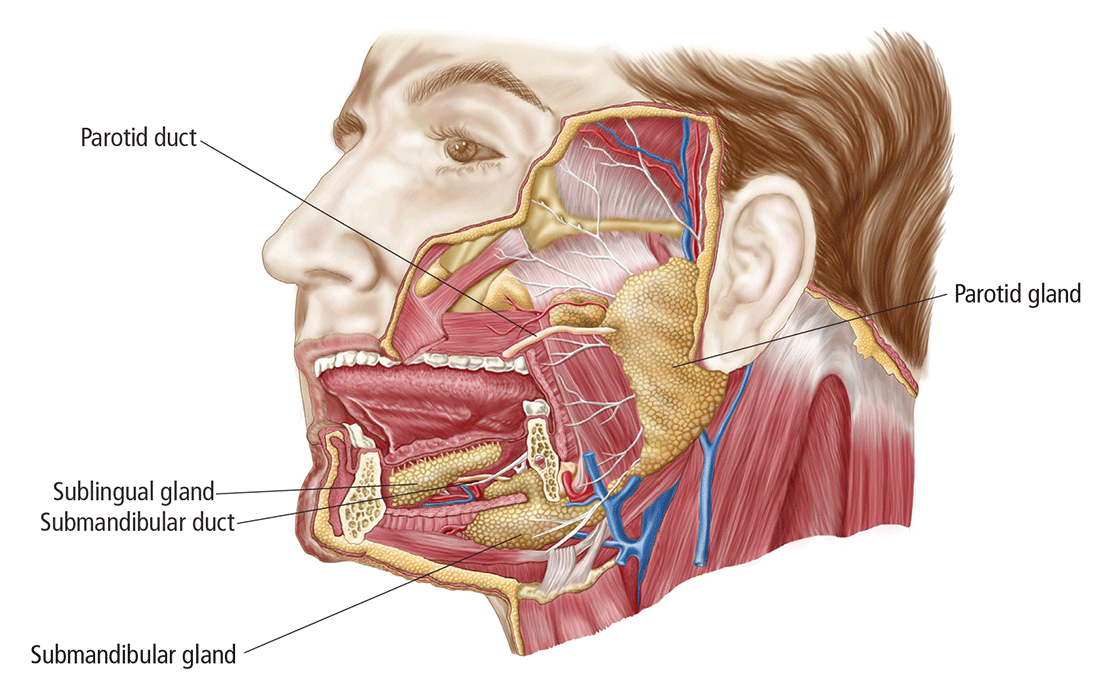
The salivary glands comprise the major paired parotid, submandibular, and sublingual glands, as well as minor salivary glands that line the oropharyngeal mucosa. Secretion of saliva is modulated by both autonomic and humoral factors.
The parotid gland sits between the mastoid process, the ramus of the mandible, and the styloid process, extend- ing from the external auditory meatus superiorly to below the angle of the mandible and into the neck inferiorly. The gland is surrounded by a tough capsule. Embedded within the gland is the facial nerve, which divides into its 5 branches within the substance of the gland. The parotid (Stensen’s) duct passes anteriorly before turning medially to pierce the buccinator muscle, opening onto the mucous membrane of the cheek opposite the second upper molar.
The submandibular gland comprises (1) a large superficial part that fills the space between the mandible and the floor of the mouth and (2) a small deep part that wraps around the posterior border of the mylohyoid muscle. The submandibular (Wharton’s) duct runs anteriorly to open onto the floor of the mouth, alongside the frenulum.
The sublingual gland, the smallest of the major salivary glands, lies anteriorly in the floor of the mouth, with many small ducts opening either into the submandibular duct or directly into the mouth.
Basic secretory units of salivary glands are clusters of cells, each called an acinus. These cells secrete a fluid that contains water, electrolytes, mucous, and enzymes, all of which flow out of the acini into collecting ducts. The saliva produced by the parotid is mainly serous; by the submandibular gland, mixed; and by the sublingual and minor salivary glands, mucoid.
Presentation helps establish the differential Dx
Ask: Are the glands swollen?
Painless salivary gland swelling has a variety of causes, including neoplasm, sialadenosis, and the eating disorders bulimia and anorexia nervosa. There is significant overlap of presentations among those causes (FIGURE). Pain accompanying swelling is uncommon but not unheard of.
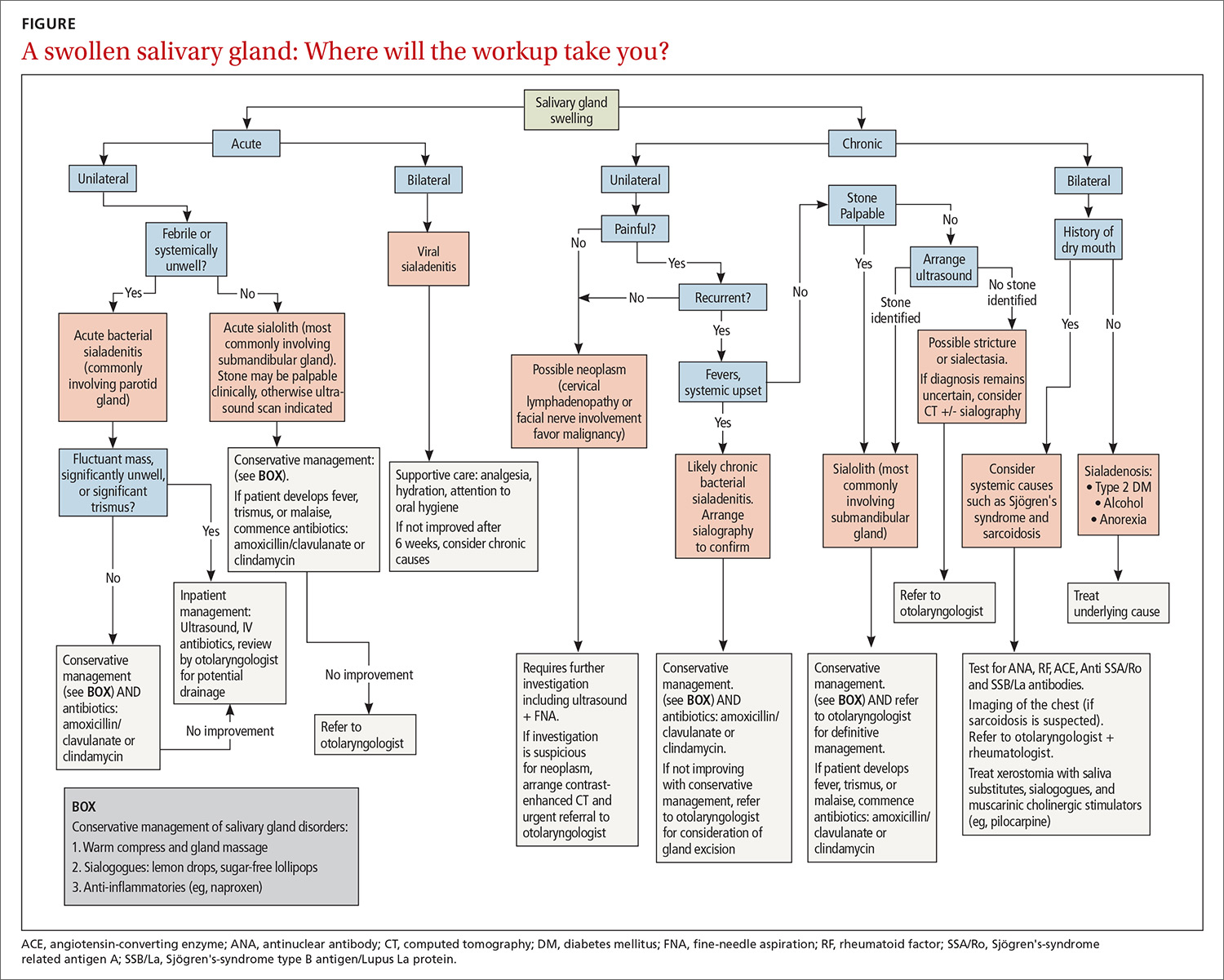
Neoplasms. Tumors of the salivary gland are relatively uncommon, constituting approximately 2% of head and neck neoplasms; most (80%) occur in the parotid gland, and most of those are benign.1 Although benign and malignant salivary gland neoplasms do not usually present with pain, pain can be associated with a neoplasm secondary to suppuration, hemorrhage into a mass, or infiltration of a malignancy into adjacent tissue.
Benign tumors. The majority of benign tumors are pleomorphic adenomas of the parotid, accounting for approximately 60% of salivary gland neoplasms.1,2 Tumors localized to the submandibular gland are often (in 50% of cases) malignant, however.3
Benign tumors are typically slow-growing and, generally, painless. On examination, they are well-circumscribed, mobile, and nontender. Patients presenting late with a large tumor might, however, experience pain secondary to stretching of the parotid capsule or compression of local structures.
Continue to: Ultrasonograhpy (US) is an excellent...
Ultrasonography (US) is an excellent initial imaging choice for investigating a possible salivary gland tumor; US is combined with FNA, which is safe and highly reliable for differentiating neoplastic and non-neoplastic disorders.4 (Avoid open biopsy of a neoplasm because of the risk of tumor spillage.) In patients with suspected neoplasm, contrast-enhanced computed tomography (CT) or magnetic resonance imaging (MRI) should also be performed, because both modalities allow delineation of the tumor mass and demonstration of any infiltration of surrounding structures.
Treatment of benign neoplasms involves complete excision because, with some tumors, particularly pleomorphic adenomas, there is risk of malignant transformation over time. Superficial parotidectomy is the most common procedure, because most benign tumors occur in the superficial lobe of the parotid gland. Delicate dissection of the facial nerve is integral to the operation, although temporary facial nerve palsy will still occur in 5% to 10% of patients undergoing superficial parotidectomy for a benign tumor, with permanent injury occurring in fewer than 1%.5
Malignancy. Features of a tumor that raise concern of malignancy include6:
- rapid growth
- pain
- tethering to underlying structures or overlying skin
- firm mass
- associated cervical lymphadenopathy
- facial-nerve palsy.
The workup of a malignant tumor is the same as it is for a benign neoplasm: US-guided FNA, essential for diagnosis, and contrast-enhanced CT or MRI to delineate the tumor.
Malignant salivary gland neoplasms usually require excision as well as neck dissection and chemotherapy or radiotherapy, or both, necessitating a multidisciplinary approach. Also, there is potential for squamous-cell carcinoma and melanoma of the head to metastasize to salivary gland lymph nodes; it is important, therefore, to examine for, and elicit any history of, cutaneous malignancy of the scalp or face.
Continue to: Sialadenosis...
Sialadenosis presents with asymptomatic bilateral hypertrophy of the salivary glands—more commonly the parotids and rarely the submandibular glands. Swelling is persistent, symmetrical, painless, and of normal tone on palpation.
Causes of sialadenosis include alcoholism and, less commonly, diabetes mellitus and malnutrition; some cases are idiopathic. An autonomic neuropathy, causing excessive salivary acinar protein synthesis or failure of adequate secretion, or both, is common to alcoholism, diabetes, and malnutrition.7 Subsequent engorgement of acinar cells leads to clinical parotid hypertrophy.
Diagnosis is based on history and examination, as well as on the findings of US or CT, which will reveal bilateral gland enlargement and increased density. The glands appear dense because adipose cells are displaced by acinar cell hypertrophy; however, end-stage changes can result in the opposite appearance: a lucent enlargement caused by fatty infiltration.2 FNA is unnecessary, unless there is suspicion of neoplasm, as there would be in patients with asymmetrical parotid enlargement, pain, lymph node enlargement, or facial-nerve involvement. In patients with sialadenosis, in contrast, acinar cell hypertrophy alone will be present.
Treatment of sialadenosis is best aimed at rectifying the underlying medical condition, which might, over time, lead to some reduction in the size of the gland. There is no specific effective therapy for elimination of glandular swelling.
Bulimia and anorexia nervosa. Bulimia nervosa, the induction of vomiting after binge eating, can be associated with bilateral or occasionally unilateral parotid swelling. Anorexia, a form of self-starvation, can occur in association with bulimia, with patients also presenting with parotid swelling. Associated parotid swelling is similar to what is seen in sialadenosis: painless, persistent, and of nonpathologic consistency.
The pathophysiology of bulimia- and anorexia-associated parotid-gland swelling is identical to what is seen in sialadenosis: dysregulation of acinar cell sympathetic nerve supply that leads to enlargement of individual parenchymal cells.8 Contrast-enhanced CT can reveal increased vascularity associated with active bulimia. FNA and CT, however, are required only in patients in whom the diagnosis is not clear and when neoplasm is suspected.
Continue to: Treatment includes...
Treatment includes correcting electrolyte abnormalities and, more importantly, addressing underlying emotional issues to stop purging episodes. Psychiatric input and social support are invaluable. Parotid gland swelling generally improves with cessation of vomiting episodes.
Ask: Is the patient in pain?
Causes of salivary gland pain include sialolithiasis, sialadenitis, and recurrent parotitis of childhood. Pain occurs secondary to stretching of the fibrous capsule in which the parotid or submandibular gland is surrounded, compression of pain fibers by an expanding mass, or infiltration of nerves by neoplasia.
Sialolithiasis. Sialolithiasis, or salivary stones, are primarily calcium carbonate concentrations within the salivary ductal system. More than 80% occur in the submandibular gland or duct9 as a result of production of mixed mucoid and serous saliva and a tortuous duct path.
Patients usually present with a history of intermittent swelling and pain of the involved gland associated with eating. Increased production of saliva during meals, which then passes through a partially obstructed salivary duct, leads to salivary retention and glandular swelling. Thus, a recurring pattern can develop, with varying periods of remission,7 eventually leading to an acute suppurative process or sialadenitis (described below). Chronic salivary disease can also be caused by stricture of a duct or, rarely, external compression by a tumor mass.
Examination often reveals an enlarged and often tender gland; conversely, chronic disease can lead to gland atrophy. Usually, only minimal saliva is able to be expressed from an obstructed duct. For a submandibular duct stone, bimanual palpation might reveal its position if it is located distally in the floor of the mouth; a proximal stone might not be palpable.
Continue to: Although US is operator-dependent...
Although US is operator-dependent, it is the imaging modality of choice for identifying sialolithiasis10 because it can identify gland architecture, duct dilation, and both radiolucent and radiopaque stones. For patients in whom US findings are normal despite a convincing clinical presentation of sialolithiasis, CT should be performed because small stones can be missed on US.11
Supportive measures for sialolithiasis are listed in the TABLE. Reserve antibiotics for patients who have signs or symptoms of infection, including pyrexia, trismus, and malaise. A beta-lactam antibiotic, such as amoxicillin–clavulanate, 875 mg orally bid, or a cephalosporin, such as cephalexin, 500 mg orally qid, are appropriate first-line options. Clindamycin, 300 mg orally tid, or metronidazole, 500 mg orally tid, are acceptable alternatives. When signs or symptoms are persistent or recurrent, refer the patient for a surgical opinion.
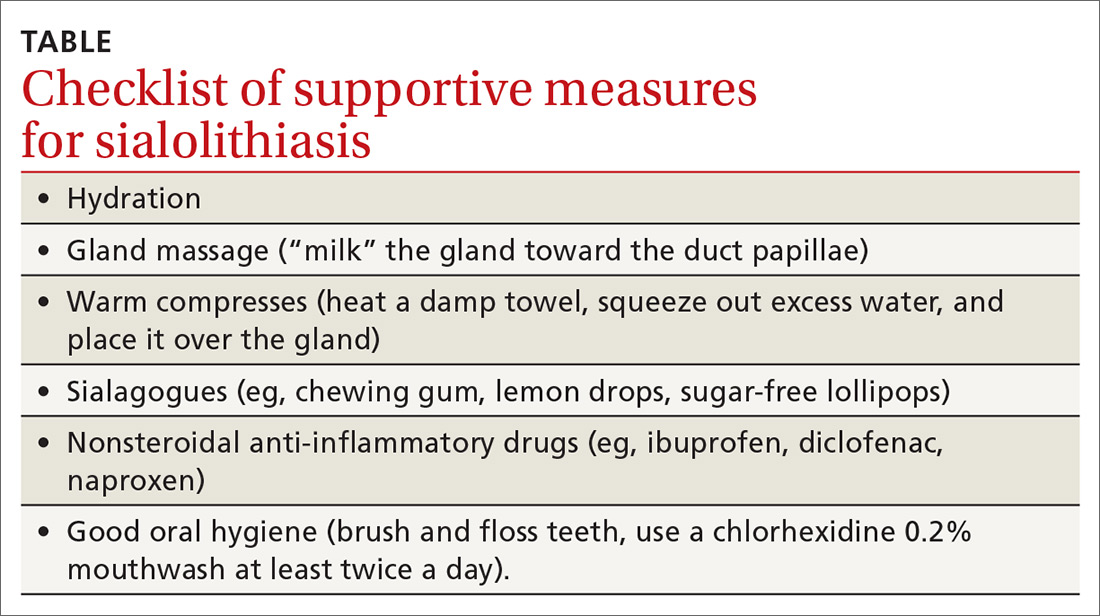
Stones located in the floor of the mouth are usually excised through an intraoral approach. In the past, gland excision was advocated when a sialolith was found more proximally within the gland parenchyma. More recently, however, sialendoscopy, involving insertion of a small, semirigid endoscope into the salivary duct, has been shown safe and effective for removing a stone; successful removal, in as many as 80% of cases, increases to 90% when performed using a minimally invasive surgical technique.12 Although sialendoscopy is effective, the technique cannot always treat the underlying abnormality of the salivary gland; gland excision is therefore warranted in some cases.
Last, extracorporeal shock wave therapy is aimed at fragmenting salivary stones before retrieval. Results are variable, however, and treatment should be guided by an otolaryngologist.13,14
Sialadenitis (bacterial and viral infection). Acute suppurative sialadenitis occurs secondary to retrograde ductal bacterial infection. The parotid gland is most frequently involved,15 although submandibular sialadenitis is not uncommon. Patients usually present with sudden-onset unilateral, painful swelling.
Continue to: Pathophysiology involves...
Pathophysiology involves dehydration or decreased oral intake leading to salivary stasis and subsequent bacterial migration into the gland. Medically debilitated and postoperative patients are therefore at greater risk; so are patients with diabetes mellitus, poor oral hygiene, Sjögren’s syndrome, hypothyroidism, or renal failure.16 Certain medications, including anticholinergics, can also predispose to hyposalivation.17
(As discussed, sialolithiasis and stricture of salivary ducts can also cause acute bacterial infection; in such cases, however, the typical presentation is one of chronic or recurrent infection.)
Examination might reveal an exquisitely tender, indurated, and inflamed gland; pus can often be expressed from the respective intraoral orifice. Any expressed pus should be sent for culture to guide antibiotic therapy.
Treatment should focus on hydration, oral hygiene, and antibiotics, while reversing or minimizing any underlying contributing medical condition. Warm compresses applied to the involved gland, massage, and sialagogues, such as lemon drops or sugar-free lollipops, can stimulate salivary flow and prevent stasis.
More than 80% of infections are caused by Staphylococcus aureus17; anaerobic and mixed infections have also been recognized.A beta-lactam penicillin, such as amoxicillin-clavulanate, is the antibiotic of choice. A patient who is systemically unwell should be treated as an inpatient with nafcillin and metronidazole. Methicillin-resistant S aureus must also be considered in patients with comorbid disease, such as diabetes mellitus or intravenous drug use, or in patients residing in an area of substantial incidence of methicillin-resistant S aureus. In those cases, substitute vancomycin or linezolid for nafcillin.18
Continue to: Less commonly...
Less commonly, abscess can form, with the patient presenting as systemically unwell with a fluctuant mass. If the diagnosis is unclear or the patient does not improve, abscess can be confirmed by US. Expedient surgical review and inpatient admission can then be arranged.
Unlike bacterial sialadenitis, causes of viral sialadenitis are often bilateral. Mumps (a paramyxovirus) is the most common viral cause, affecting primarily children < 15 years.19 The parotid glands are most often involved, with inflammation and edema causing significant pain because of increasing intraparotid pressure as expansion of the gland is limited by its tense fibrous capsule. Complications of mumps include orchitis, meningitis, pancreatitis, and oophoritis.
Mumps is highly contagious; it is spread through contact with airborne saliva droplets, with viral entry through the nose or mouth, followed by proliferation in the salivary glands or on surface epithelium of the respiratory tract.7 Diagnosis is confirmed by viral serology. A positive test of serum immunoglobulin M confirms the diagnosis, but this test should not be performed until 3 days after onset of symptoms because a false-negative result is otherwise possible.20 Immunoglobulin G serologic testing can further aid diagnosis; the titer is measured approximately 4 days after onset of symptoms and again 2 to 3 weeks later. A 4-fold rise in titer confirms mumps.
Other viral infections that can cause sialadenitis include Epstein-Barr virus, cytomegalovirus, human immunodeficiency virus, coxsackievirus, and influenza. Treatment is supportive: analgesia, hydration, oral hygiene, and rest. Inflammation might take weeks to resolve, but expect complete resolution. For a patient who has significant trismus, poor oral intake, or a potentially threatened airway, inpatient care should be provided.
Recurrent parotitis of childhood is an inflammatory condition that usually affects one, but at times both, parotid glands. It is characterized by episodes of painful swelling. Incidence peaks at 3 to 6 years of age.7 Episodes can be frequent, occurring 1 to 5 times a year and lasting 3 to 7 days—sometimes longer—and usually resolving without treatment.
Continue to: The precise etiology...
The precise etiology of recurrent parotitis of childhood is unclear; possibly, saliva aggregates to form obstructive mucous plugs, thus causing stasis and swelling of the gland. As pressure builds, spontaneous plug extrusion occurs and symptoms resolve, provided infection is not a factor. US demonstrates multiple round, hypoechoic areas consistent with duct dilation, and surrounding infiltration by lymphocytes.1
Supportive care—adequate hydration, gland massage, warm compresses, and sialogogues—are mainstays of treatment. Fever and malaise warrant treatment with oral antibiotics. Sialadenoscopy, which can be considered in children with frequent episodes, can decrease the frequency and severity of episodes.21 The condition usually resolves spontaneously at puberty.
Ask: Does the patient have dry mouth?
In-depth review of xerostomia is beyond the scope of this article. Causes include Sjögren's syndrome, immunoglobulin G4-related sialadenitis, sarcoidosis, radiation therapy, diabetes, chronic infection, and medications—in particular those with anticholinergic effects.
Treatment of xerostomia includes saliva substitutes, sialagogues, and, for oral candidiasis, antifungals. Muscarinic cholinergic stimulators, such as pilocarpine, 5 mg qid have been used with some success22; patients should be advised of potential adverse effects with these agents, including sweating, urinary frequency, flushing, and chills.
CORRESPONDENCE
Shankar Haran, MBBS, ENT Department, Townsville Hospital, 100 Angus Smith Dr, Douglas, Queensland, Australia 4814; [email protected].
1. de Oliveira FA, Duarte EC, Taveira CT, et al. Salivary gland tumor: a review of 599 cases in a Brazilian population. Head Neck Pathol. 2009;3:271-275.
2. Spiro RH. Salivary neoplasms: overview of a 35-year experience with 2,807 patients. Head Neck Surg. 1986;8:177-184.
3. Bova R. A guide to salivary gland disorders. Medicine Today. 2006;7:44-48.
4. Zhang S, Bao R, Bagby J, et al. Fine needle aspiration of salivary glands: 5-year experience from a single academic center. Acta Cytol. 2009;53:375-382.
5. Bova R, Saylor A, Coman WB. Parotidectomy: review of treatment and outcomes. ANZ J Surg. 2004;74:563-568.
6. Sood S, McGurk M, Vaz F. Management of salivary gland tumours: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol. 2016;130:S142-S149.
7. Mandel L. Salivary gland disorders. Med Clin North Am. 2014;98:1407-1449.
8. Mandel L, Abai S. Diagnosing bulimia nervosa with parotid gland swelling. J Am Dent Assoc. 2004;135:613–616.
9. Lustmann J, Regev E, Melamed Y. Sialolithiasis. A survey on 245 patients and a review of literature. Int J Oral Maxillofac Surg. 1990;19:135–138.
10. Vogl TJ, Al-Nawas B, Beutner D, et al. Updated S2K AWMF guideline for the diagnosis and follow-up of obstructive sialadenitis—relevance for radiologic imaging. Rofo. 2014;186:843-846.
11. Schwarz D, Kabbasch C, Scheer M, et al. Comparative analysis of sialendoscopy, sonography, and CBCT in the detection of sialolithiasis. Laryngoscope. 2015;125:1098–1101.
12. Atienza G, López-Cedrún JL. Management of obstructive salivary disorders by sialendoscopy: a systematic review. Br J Oral Maxillofac Surg. 2015;53:507-519.
13. Escudier MP, Brown JE, Putcha V, et al. Factors influencing the outcome of extracorporeal shock wave lithotripsy in the management of salivary calculi. Laryngoscope. 2010;120:1545-1549.
14. Koch M, Schapher M, Mantsopoulos K, et al. Multimodal treatment in difficult sialolithiasis: Role of extracorporeal shock-wave lithotripsy and intraductal pneumatic lithotripsy. Laryngoscope. 2018;128:E332-E338.
15. McQuone SJ. Acute viral and bacterial infections of the salivary glands. Otolaryngol Clin North Am. 1999;32:793-811.
16. O’Neil C, Sidhu S. Salivary gland disorders. Australian Doctor. 2011;28:19-25.
17. Mandel L. Differentiating acute suppurative parotitis from acute exacerbation of a chronic parotitis: case reports. J Oral Maxillofac Surg. 2008;66:1964-1968.
18. Chow AW. Suppurative parotitis in adults. UpToDate.com. www.uptodate.com/contents/suppurative-parotitis-in-adults. Accessed September 25, 2019.
19. Katz SL, Gershon AA, Hotez PJ. Infectious Diseases of Children. New York, NY: Mosby Year Book; 1998:280-289.
20. Krause CH, Molyneaux PJ, Ho-Yen DO, et al. Comparison of mumps-IgM ELISAs in acute infection. J Clin Virol. 2007;38:153-156.
21. Quenin S, Plouin-Gaudon I, Marchal F, et al. Juvenile recurrent parotitis: sialendoscopic approach. Arch Otolaryngol Head Neck Surg. 2008;134:715-719.
22. Papas AS, Sherrer YS, Charney M, et al. Successful treatment of dry mouth and dry eye symptoms in Sjögren’s syndrome patients with oral pilocarpine: a randomized, placebo-controlled, dose-adjustment study. J Clin Rheumatol. 2004;10:169-177.
1. de Oliveira FA, Duarte EC, Taveira CT, et al. Salivary gland tumor: a review of 599 cases in a Brazilian population. Head Neck Pathol. 2009;3:271-275.
2. Spiro RH. Salivary neoplasms: overview of a 35-year experience with 2,807 patients. Head Neck Surg. 1986;8:177-184.
3. Bova R. A guide to salivary gland disorders. Medicine Today. 2006;7:44-48.
4. Zhang S, Bao R, Bagby J, et al. Fine needle aspiration of salivary glands: 5-year experience from a single academic center. Acta Cytol. 2009;53:375-382.
5. Bova R, Saylor A, Coman WB. Parotidectomy: review of treatment and outcomes. ANZ J Surg. 2004;74:563-568.
6. Sood S, McGurk M, Vaz F. Management of salivary gland tumours: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol. 2016;130:S142-S149.
7. Mandel L. Salivary gland disorders. Med Clin North Am. 2014;98:1407-1449.
8. Mandel L, Abai S. Diagnosing bulimia nervosa with parotid gland swelling. J Am Dent Assoc. 2004;135:613–616.
9. Lustmann J, Regev E, Melamed Y. Sialolithiasis. A survey on 245 patients and a review of literature. Int J Oral Maxillofac Surg. 1990;19:135–138.
10. Vogl TJ, Al-Nawas B, Beutner D, et al. Updated S2K AWMF guideline for the diagnosis and follow-up of obstructive sialadenitis—relevance for radiologic imaging. Rofo. 2014;186:843-846.
11. Schwarz D, Kabbasch C, Scheer M, et al. Comparative analysis of sialendoscopy, sonography, and CBCT in the detection of sialolithiasis. Laryngoscope. 2015;125:1098–1101.
12. Atienza G, López-Cedrún JL. Management of obstructive salivary disorders by sialendoscopy: a systematic review. Br J Oral Maxillofac Surg. 2015;53:507-519.
13. Escudier MP, Brown JE, Putcha V, et al. Factors influencing the outcome of extracorporeal shock wave lithotripsy in the management of salivary calculi. Laryngoscope. 2010;120:1545-1549.
14. Koch M, Schapher M, Mantsopoulos K, et al. Multimodal treatment in difficult sialolithiasis: Role of extracorporeal shock-wave lithotripsy and intraductal pneumatic lithotripsy. Laryngoscope. 2018;128:E332-E338.
15. McQuone SJ. Acute viral and bacterial infections of the salivary glands. Otolaryngol Clin North Am. 1999;32:793-811.
16. O’Neil C, Sidhu S. Salivary gland disorders. Australian Doctor. 2011;28:19-25.
17. Mandel L. Differentiating acute suppurative parotitis from acute exacerbation of a chronic parotitis: case reports. J Oral Maxillofac Surg. 2008;66:1964-1968.
18. Chow AW. Suppurative parotitis in adults. UpToDate.com. www.uptodate.com/contents/suppurative-parotitis-in-adults. Accessed September 25, 2019.
19. Katz SL, Gershon AA, Hotez PJ. Infectious Diseases of Children. New York, NY: Mosby Year Book; 1998:280-289.
20. Krause CH, Molyneaux PJ, Ho-Yen DO, et al. Comparison of mumps-IgM ELISAs in acute infection. J Clin Virol. 2007;38:153-156.
21. Quenin S, Plouin-Gaudon I, Marchal F, et al. Juvenile recurrent parotitis: sialendoscopic approach. Arch Otolaryngol Head Neck Surg. 2008;134:715-719.
22. Papas AS, Sherrer YS, Charney M, et al. Successful treatment of dry mouth and dry eye symptoms in Sjögren’s syndrome patients with oral pilocarpine: a randomized, placebo-controlled, dose-adjustment study. J Clin Rheumatol. 2004;10:169-177.
PRACTICE RECOMMENDATIONS
› Use ultrasonography for initial imaging of a salivary gland. A
› Refer patients with the following findings for further specialty evaluation: abscess, inflammation unresponsive to medical care, recurrent or chronic symptoms, suspected neoplasm (for excision), and suspected sialolithiasis. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Painful ulcers on gingiva, tongue, and buccal mucosa
A 29-year-old man with no prior history of mouth sores abruptly developed many 1- to 1.5-mm blisters on the gingiva (FIGURE 1A),tongue (FIGURE 1B), and buccal mucosa (FIGURE 1C), which evolved into small erosions accompanied by a low-grade fever 5 days prior to presentation. The patient had no history of any dermatologic conditions or systemic illnesses and was taking no medication.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Acute primary herpetic gingivostomatitis
Herpes simplex virus (HSV) is the causative agent for acute primary herpetic gingivostomatitis.1 HSV-1 is primarily responsible for oral mucosal infections, while HSV-2 is implicated in most genital and cutaneous lower body lesions.1 Herpetic gingivostomatitis often presents as a sudden vesiculoulcerative eruption anywhere in the mouth, including the perioral skin, vermillion border, gingiva, tongue, or buccal mucosa.2 Associated symptoms include malaise, headache, fever, and cervical lymphadenopathy; however, most occurrences are subclinical or asymptomatic.2
A diagnosis that’s more common in children. Primary HSV occurs in people who have not previously been exposed to the virus. While it is an infection that classically presents in childhood, it is not limited to this group. Manifestations often are more severe in adults.1
Following an incubation period of a few days to 3 weeks, the primary infection typically lasts 10 to 14 days.1,2 Recurrence is highly variable and generally less severe than primary infection, with grouped vesicles often recurring in the same spot with each recurrence on the vermillion border of the lip. Triggers for reactivation include immunosuppression, pregnancy, fever, UV radiation, or trauma.1,2
Differential includes other conditions with mucosal lesions
Acute herpetic gingivostomatitis must be distinguished from other disease processes that cause ulcerative mucosal lesions.
Aphthous stomatitis (canker sores) is the most common ulcerative disease of the oral mucosa.3 It presents as painful, punched-out, shallow ulcers with a yellowish gray pseudomembranous center and surrounding erythema.3 No definitive etiology has been established; however, aphthae often occur after trauma.
Continue to: Herpangina...
Herpangina is caused by coxsackie A virus and primarily is seen in infants and children younger than 5.4 The papulovesicular lesions primarily affect the posterior oral cavity, including the soft palate, anterior tonsillar pillars, and uvula.4
Allergic contact dermatitis is precipitated by contact with an allergen and presents with pain or pruritus. Lesions are erythematous with vesicles, erosions, ulcers, or hyperkeratosis that gradually resolve after withdrawal of the causative allergen.5
Pemphigus vulgaris. Oral ulcerations of the buccal mucosa and gingiva are the first manifestation of pemphigus vulgaris in the majority of patients, with skin blisters occurring months to years later over areas exposed to frictional stress.6 Skin sloughs may be seen in response to frictional stress (Nikolsky sign).6
The new Dx gold standard is PCR
Acute herpetic gingivostomatitis usually is diagnosed by history and hallmark clinical signs and symptoms.1 In this case, our patient presented with a sudden eruption of painful blisters on multiple areas of the oral mucosa associated with fever. The diagnosis can be confirmed by viral culture, serology with anti-HSV IgM and IgG, Tzanck preparation, immunofluorescence, and polymerase chain reaction (PCR).1 Viral culture has been the gold standard for mucosal HSV diagnosis; however, PCR is emerging as the new gold standard because of its unrivaled sensitivity, specificity, and rapid turnaround time.7,8 Specimens for PCR are submitted using a swab of infected cells placed in the same viral transport medium used for HSV cultures.
Our patient’s culture was positive for HSV-1.
Continue to: Prompt use of antivirals is key
Prompt use of antivirals is key
Treatment of acute HSV gingivostomatitis involves symptomatic management with topical anesthetics, oral analgesics, and normal saline rinses.1 Acyclovir is an established therapy; however, it has poor bioavailability and gastrointestinal absorption.1 Valacyclovir has improved bioavailability and is well tolerated.1 For primary herpes gingivostomatitis, we favor 1 g twice daily for 7 days.1 Our patient responded well to this valacyclovir regimen and healed completely in 1 week.
CORRESPONDENCE
Robert T. Brodell, MD, 2500 N State St, Jackson, MS 39216; [email protected]
1. Ajar AH, Chauvin PJ. Acute herpetic gingivostomatitis in adults: a review of 13 cases, including diagnosis and management. J Can Dent Assoc. 2002;68:247-251.
2. George AK, Anil S. Acute herpetic gingivostomatitis associated with herpes simplex virus 2: report of a case. J Int Oral Health. 2014;6:99-102.
3. Akintoye SO, Greenburg MS. Recurrent aphthous stomatitis. Dent Clin N Am. 2014;58:281-297.
4. Scott LA, Stone MS. Viral exanthems. Dermatol Online J. 2003;9:4.
5. Feller L, Wood NH, Khammissa RA, et al. Review: allergic contact stomatitis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017;123:559-565.
6. Bascones-Martinez A, Munoz-Corcuera M, Bascones-Ilundain C, et al. Oral manifestations of pemphigus vulgaris: clinical presentation, differential diagnosis and management. J Clin Exp Dermatol Res. 2010;1:112.
7. LeGoff J, Péré H, Bélec L. Diagnosis of genital herpes simplex virus infection in the clinical laboratory. Virol J. 2014;11:83.
8. Centers for Disease Control and Prevention. Genital HSV infections. www.cdc.gov/std/tg2015/herpes.htm. Updated June 4, 2015. Accessed September 26, 2019.
A 29-year-old man with no prior history of mouth sores abruptly developed many 1- to 1.5-mm blisters on the gingiva (FIGURE 1A),tongue (FIGURE 1B), and buccal mucosa (FIGURE 1C), which evolved into small erosions accompanied by a low-grade fever 5 days prior to presentation. The patient had no history of any dermatologic conditions or systemic illnesses and was taking no medication.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Acute primary herpetic gingivostomatitis
Herpes simplex virus (HSV) is the causative agent for acute primary herpetic gingivostomatitis.1 HSV-1 is primarily responsible for oral mucosal infections, while HSV-2 is implicated in most genital and cutaneous lower body lesions.1 Herpetic gingivostomatitis often presents as a sudden vesiculoulcerative eruption anywhere in the mouth, including the perioral skin, vermillion border, gingiva, tongue, or buccal mucosa.2 Associated symptoms include malaise, headache, fever, and cervical lymphadenopathy; however, most occurrences are subclinical or asymptomatic.2
A diagnosis that’s more common in children. Primary HSV occurs in people who have not previously been exposed to the virus. While it is an infection that classically presents in childhood, it is not limited to this group. Manifestations often are more severe in adults.1
Following an incubation period of a few days to 3 weeks, the primary infection typically lasts 10 to 14 days.1,2 Recurrence is highly variable and generally less severe than primary infection, with grouped vesicles often recurring in the same spot with each recurrence on the vermillion border of the lip. Triggers for reactivation include immunosuppression, pregnancy, fever, UV radiation, or trauma.1,2
Differential includes other conditions with mucosal lesions
Acute herpetic gingivostomatitis must be distinguished from other disease processes that cause ulcerative mucosal lesions.
Aphthous stomatitis (canker sores) is the most common ulcerative disease of the oral mucosa.3 It presents as painful, punched-out, shallow ulcers with a yellowish gray pseudomembranous center and surrounding erythema.3 No definitive etiology has been established; however, aphthae often occur after trauma.
Continue to: Herpangina...
Herpangina is caused by coxsackie A virus and primarily is seen in infants and children younger than 5.4 The papulovesicular lesions primarily affect the posterior oral cavity, including the soft palate, anterior tonsillar pillars, and uvula.4
Allergic contact dermatitis is precipitated by contact with an allergen and presents with pain or pruritus. Lesions are erythematous with vesicles, erosions, ulcers, or hyperkeratosis that gradually resolve after withdrawal of the causative allergen.5
Pemphigus vulgaris. Oral ulcerations of the buccal mucosa and gingiva are the first manifestation of pemphigus vulgaris in the majority of patients, with skin blisters occurring months to years later over areas exposed to frictional stress.6 Skin sloughs may be seen in response to frictional stress (Nikolsky sign).6
The new Dx gold standard is PCR
Acute herpetic gingivostomatitis usually is diagnosed by history and hallmark clinical signs and symptoms.1 In this case, our patient presented with a sudden eruption of painful blisters on multiple areas of the oral mucosa associated with fever. The diagnosis can be confirmed by viral culture, serology with anti-HSV IgM and IgG, Tzanck preparation, immunofluorescence, and polymerase chain reaction (PCR).1 Viral culture has been the gold standard for mucosal HSV diagnosis; however, PCR is emerging as the new gold standard because of its unrivaled sensitivity, specificity, and rapid turnaround time.7,8 Specimens for PCR are submitted using a swab of infected cells placed in the same viral transport medium used for HSV cultures.
Our patient’s culture was positive for HSV-1.
Continue to: Prompt use of antivirals is key
Prompt use of antivirals is key
Treatment of acute HSV gingivostomatitis involves symptomatic management with topical anesthetics, oral analgesics, and normal saline rinses.1 Acyclovir is an established therapy; however, it has poor bioavailability and gastrointestinal absorption.1 Valacyclovir has improved bioavailability and is well tolerated.1 For primary herpes gingivostomatitis, we favor 1 g twice daily for 7 days.1 Our patient responded well to this valacyclovir regimen and healed completely in 1 week.
CORRESPONDENCE
Robert T. Brodell, MD, 2500 N State St, Jackson, MS 39216; [email protected]
A 29-year-old man with no prior history of mouth sores abruptly developed many 1- to 1.5-mm blisters on the gingiva (FIGURE 1A),tongue (FIGURE 1B), and buccal mucosa (FIGURE 1C), which evolved into small erosions accompanied by a low-grade fever 5 days prior to presentation. The patient had no history of any dermatologic conditions or systemic illnesses and was taking no medication.

WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Acute primary herpetic gingivostomatitis
Herpes simplex virus (HSV) is the causative agent for acute primary herpetic gingivostomatitis.1 HSV-1 is primarily responsible for oral mucosal infections, while HSV-2 is implicated in most genital and cutaneous lower body lesions.1 Herpetic gingivostomatitis often presents as a sudden vesiculoulcerative eruption anywhere in the mouth, including the perioral skin, vermillion border, gingiva, tongue, or buccal mucosa.2 Associated symptoms include malaise, headache, fever, and cervical lymphadenopathy; however, most occurrences are subclinical or asymptomatic.2
A diagnosis that’s more common in children. Primary HSV occurs in people who have not previously been exposed to the virus. While it is an infection that classically presents in childhood, it is not limited to this group. Manifestations often are more severe in adults.1
Following an incubation period of a few days to 3 weeks, the primary infection typically lasts 10 to 14 days.1,2 Recurrence is highly variable and generally less severe than primary infection, with grouped vesicles often recurring in the same spot with each recurrence on the vermillion border of the lip. Triggers for reactivation include immunosuppression, pregnancy, fever, UV radiation, or trauma.1,2
Differential includes other conditions with mucosal lesions
Acute herpetic gingivostomatitis must be distinguished from other disease processes that cause ulcerative mucosal lesions.
Aphthous stomatitis (canker sores) is the most common ulcerative disease of the oral mucosa.3 It presents as painful, punched-out, shallow ulcers with a yellowish gray pseudomembranous center and surrounding erythema.3 No definitive etiology has been established; however, aphthae often occur after trauma.
Continue to: Herpangina...
Herpangina is caused by coxsackie A virus and primarily is seen in infants and children younger than 5.4 The papulovesicular lesions primarily affect the posterior oral cavity, including the soft palate, anterior tonsillar pillars, and uvula.4
Allergic contact dermatitis is precipitated by contact with an allergen and presents with pain or pruritus. Lesions are erythematous with vesicles, erosions, ulcers, or hyperkeratosis that gradually resolve after withdrawal of the causative allergen.5
Pemphigus vulgaris. Oral ulcerations of the buccal mucosa and gingiva are the first manifestation of pemphigus vulgaris in the majority of patients, with skin blisters occurring months to years later over areas exposed to frictional stress.6 Skin sloughs may be seen in response to frictional stress (Nikolsky sign).6
The new Dx gold standard is PCR
Acute herpetic gingivostomatitis usually is diagnosed by history and hallmark clinical signs and symptoms.1 In this case, our patient presented with a sudden eruption of painful blisters on multiple areas of the oral mucosa associated with fever. The diagnosis can be confirmed by viral culture, serology with anti-HSV IgM and IgG, Tzanck preparation, immunofluorescence, and polymerase chain reaction (PCR).1 Viral culture has been the gold standard for mucosal HSV diagnosis; however, PCR is emerging as the new gold standard because of its unrivaled sensitivity, specificity, and rapid turnaround time.7,8 Specimens for PCR are submitted using a swab of infected cells placed in the same viral transport medium used for HSV cultures.
Our patient’s culture was positive for HSV-1.
Continue to: Prompt use of antivirals is key
Prompt use of antivirals is key
Treatment of acute HSV gingivostomatitis involves symptomatic management with topical anesthetics, oral analgesics, and normal saline rinses.1 Acyclovir is an established therapy; however, it has poor bioavailability and gastrointestinal absorption.1 Valacyclovir has improved bioavailability and is well tolerated.1 For primary herpes gingivostomatitis, we favor 1 g twice daily for 7 days.1 Our patient responded well to this valacyclovir regimen and healed completely in 1 week.
CORRESPONDENCE
Robert T. Brodell, MD, 2500 N State St, Jackson, MS 39216; [email protected]
1. Ajar AH, Chauvin PJ. Acute herpetic gingivostomatitis in adults: a review of 13 cases, including diagnosis and management. J Can Dent Assoc. 2002;68:247-251.
2. George AK, Anil S. Acute herpetic gingivostomatitis associated with herpes simplex virus 2: report of a case. J Int Oral Health. 2014;6:99-102.
3. Akintoye SO, Greenburg MS. Recurrent aphthous stomatitis. Dent Clin N Am. 2014;58:281-297.
4. Scott LA, Stone MS. Viral exanthems. Dermatol Online J. 2003;9:4.
5. Feller L, Wood NH, Khammissa RA, et al. Review: allergic contact stomatitis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017;123:559-565.
6. Bascones-Martinez A, Munoz-Corcuera M, Bascones-Ilundain C, et al. Oral manifestations of pemphigus vulgaris: clinical presentation, differential diagnosis and management. J Clin Exp Dermatol Res. 2010;1:112.
7. LeGoff J, Péré H, Bélec L. Diagnosis of genital herpes simplex virus infection in the clinical laboratory. Virol J. 2014;11:83.
8. Centers for Disease Control and Prevention. Genital HSV infections. www.cdc.gov/std/tg2015/herpes.htm. Updated June 4, 2015. Accessed September 26, 2019.
1. Ajar AH, Chauvin PJ. Acute herpetic gingivostomatitis in adults: a review of 13 cases, including diagnosis and management. J Can Dent Assoc. 2002;68:247-251.
2. George AK, Anil S. Acute herpetic gingivostomatitis associated with herpes simplex virus 2: report of a case. J Int Oral Health. 2014;6:99-102.
3. Akintoye SO, Greenburg MS. Recurrent aphthous stomatitis. Dent Clin N Am. 2014;58:281-297.
4. Scott LA, Stone MS. Viral exanthems. Dermatol Online J. 2003;9:4.
5. Feller L, Wood NH, Khammissa RA, et al. Review: allergic contact stomatitis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017;123:559-565.
6. Bascones-Martinez A, Munoz-Corcuera M, Bascones-Ilundain C, et al. Oral manifestations of pemphigus vulgaris: clinical presentation, differential diagnosis and management. J Clin Exp Dermatol Res. 2010;1:112.
7. LeGoff J, Péré H, Bélec L. Diagnosis of genital herpes simplex virus infection in the clinical laboratory. Virol J. 2014;11:83.
8. Centers for Disease Control and Prevention. Genital HSV infections. www.cdc.gov/std/tg2015/herpes.htm. Updated June 4, 2015. Accessed September 26, 2019.
20-year-old male college basketball prospect • wrist pain after falling on wrist • normal ROM • pain with active/passive wrist extension • Dx?
THE CASE
A 20-year-old man presented to our family medicine clinic with right wrist pain 4 days after falling on his wrist and hand while playing basketball. He denied any other previous injury or trauma. The pain was unchanged since the injury occurred.
Examination demonstrated mild edema over the palmar and ulnar aspect of the patient’s right wrist with no apparent ecchymosis. He had normal range of motion of his right wrist and hand. However, he experienced pain with active and passive wrist extension and ulnar deviation. There was significant tenderness in the palmar and ulnar aspects of his right wrist just distal to the ulnar styloid process.
THE DIAGNOSIS
Standard plain x-rays of the right wrist revealed an isolated fracture of the body of the triquetrum (FIGURE 1). Since the patient refused to have a cast placed, his wrist was immobilized with a wrist brace. By Day 16 post injury, the pain and edema had improved significantly. After talking with the patient about the potential risks and benefits of continuing to play basketball—and despite our recommendation that he not play—he decided to continue playing since he was a college basketball prospect.
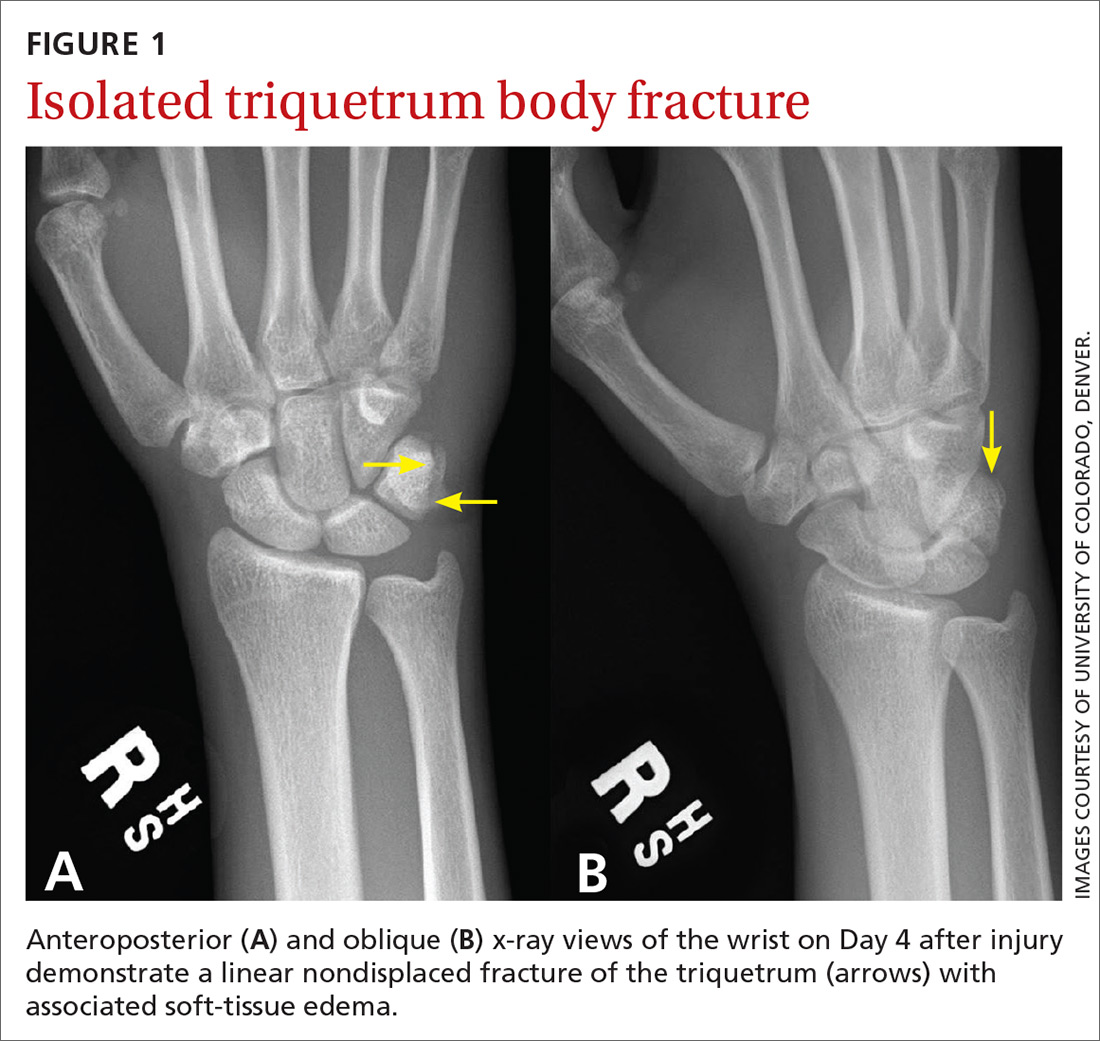
At 4 weeks post injury, x-rays demonstrated mild interval healing (FIGURE 2). At the 8-week visit, the patient had only very mild pain and tenderness, and x-ray images showed improvement (FIGURE 3). Within a few months, his symptoms resolved completely. No further imaging was performed.
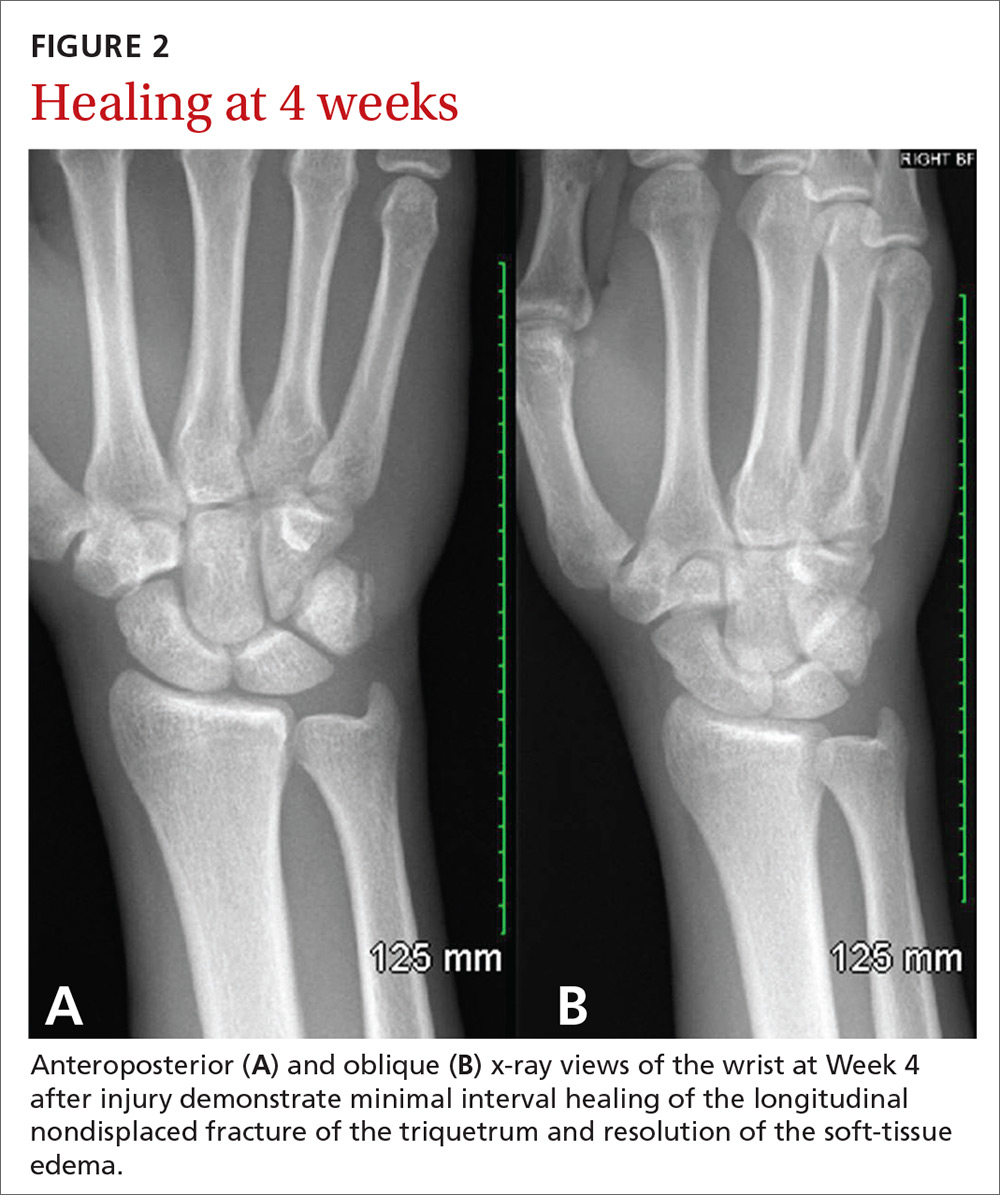
DISCUSSION
In general, carpal fractures are uncommon.1 The triquetrum is the second most commonly injured carpal bone, involved in up to 18% of all carpal fractures.2,3 Triquetrum fractures most commonly occur as isolated injuries and are typically classified in 2 general categories: avulsion fractures (dorsal cortex or volar cortex) and fractures of the triquetrum body.4-8 Isolated avulsion fractures of the triquetral dorsal cortex are relatively common, occurring in about 95% of triquetrum injuries.4-9 Isolated fractures of the triquetrum body are less common, occurring in about 4% of triquetrum injuries, and can go unnoticed on conventional x-rays.4-9

Basketball presents a unique risk for hand or wrist fracture due to its high-impact nature, hard playing surfaces, and frequent use of the hands for dribbling, shooting, rebounding, and passing the ball.
In a retrospective study of sports-related fractures conducted at the Royal Infirmary of Edinburgh, basketball had the highest incidence of carpal injuries compared with other sports, including football, rugby, skiing, snowboarding, and ice-skating.4 Similarly, a retrospective study conducted at the University of California, Los Angeles, found that of all Division 1 collegiate athletes at the school, basketball players had the highest incidence of primary fractures, and the most common fracture location was the hand.10
Continue to: An injury that's easy to miss
An injury that’s easy to miss
Because the incidence of hand and wrist injuries is high among basketball players, it is imperative that triquetrum body fractures are not missed or misdiagnosed as more common hand and wrist injuries, such as triquetral dorsal avulsion fractures.
Our patient, who had an isolated triquetrum body fracture, presented with focal tenderness on the palmar and ulnar aspects of his wrist and pain with ulnar deviation. Since triquetral body fractures often have a clinical presentation quite similar to that of triquetral dorsal avulsion fractures, patients presenting with symptoms of wrist tenderness and pain should be treated with a high degree of clinical suspicion.
With our patient, anteroposterior and lateral x-rays were sufficient to demonstrate an isolated triquetrum body fracture; however, triquetral fractures can be missed in up to 20% of x-rays.4 Both magnetic resonance imaging and computerized tomography are useful in diagnosing occult triquetrum fractures and should be used to confirm clinical suspicion when traditional x-rays are inconclusive.11,12
Management varies
Management of isolated triquetrum body fractures varies depending on the fracture pattern and the status of bone consolidation. Triquetral body fractures typically heal well; it’s very rare that there is a nonunion. As our patient’s fracture was nondisplaced and stable, brace immobilization for 4 weeks was sufficient to facilitate healing and restore long-term hand and wrist functionality. This course of treatment is consistent with other cases of nondisplaced triquetrum body fractures reported in the literature.13
Long-term outcomes. The literature is sparse regarding the long-term functional outcome of nonsurgical treatment for nondisplaced triquetrum body fractures. Multiple carpal fractures, displaced triquetrum body fractures, and persistent pain for multiple months after nonsurgical management all indicate the need for referral to orthopedic surgery. In instances of fracture displacement or nonunion, management tends to be surgical, with open reduction and internal fixation (ORIF) used in multiple cases of nonunion for isolated triquetrum body fractures.3,14 Any diagnostic imaging that reveals displacement, malunion, or nonunion of the fracture is an indication for referral to an orthopedic surgeon.
Continue to: Return to play
Return to play. There is no evidence-based return-to-play recommendation for patients with a triquetrum fracture. However, our patient continued to play basketball through the early stages of injury management because he was a collegiate prospect. While medical, social, and economic factors should be considered when discussing treatment options with athletes, injuries should be managed so that there is no long-term loss of function or risk of injury exacerbation. When discussing early return from injury with athletes who have outside pressure to return to play, it’s important to make them aware of the associated long- and short-term risks.15
THE TAKEAWAY
Management of an isolated triquetrum body fracture is typically straightforward; however, if the fracture is displaced, refer the patient to an orthopedic surgeon as ORIF may be required. For this reason, it’s important to be able to promptly identify isolated triquetrum body fractures and to avoid confusing them with triquetrum dorsal avulsion fractures.
Depending on the sport played and the severity of the injury, athletes with conservatively managed nondisplaced triquetral body fractures may be candidates for early return to play. Nonetheless, athletes should understand both the short- and the long-term risks of playing with an injury, and they should never be advised to continue playing with an injury if it jeopardizes their well-being or the long-term functionality of the affected body part.
CORRESPONDENCE
Morteza Khodaee, MD, MPH, University of Colorado School of Medicine, AFW Clinic, 3055 Roslyn Street, Denver, CO 80238; [email protected]
1. Suh N, Ek ET, Wolfe SW. Carpal fractures. J Hand Surg Am. 2014;39:785-791.
2. Hey HW, Chong AK, Murphy D. Prevalence of carpal fracture in Singapore. J Hand Surg Am. 2011;36:278-283.
3. Al Rashid M, Rasoli S, Khan WS. Non-union of isolated displaced triquetral body fracture—a case report. Ortop Traumatol Rehabil. 2012;14:71-74.
4. Becce F, Theumann N, Bollmann C, et al. Dorsal fractures of the triquetrum: MRI findings with an emphasis on dorsal carpal ligament injuries. AJR Am J Roentgenol. 2013;200:608-617.
5. Court-Brown CM, Wood AM, Aitken S. The epidemiology of acute sports-related fractures in adults. Injury. 2008;39:1365-1372.
6. Urch EY, Lee SK. Carpal fractures other than scaphoid. Clin Sports Med. 2015;34:51-67.
7. deWeber K. Triquetrum fractures. UpToDate. 2016. www.uptodate.com/contents/triquetrum-fractures. Accessed September 3, 2019.
8. Höcker K, Menschik A. Chip fractures of the triquetrum. Mechanism, classification and results. J Hand Surg Br. 1994;19:584-588.
9. Jarraya M, Hayashi D, Roemer FW, et al. Radiographically occult and subtle fractures: a pictorial review. Radiol Res Pract. 2013;2013:370169.
10. Hame SL, LaFemina JM, McAllister DR, et al. Fractures in the collegiate athlete. Am J Sports Med. 2004;32:446-451.
11. Hindman BW, Kulik WJ, Lee G, et al. Occult fractures of the carpals and metacarpals: demonstration by CT. AJR Am J Roentgenol. 1989;153:529-532.
12. Pierre-Jerome C, Moncayo V, Albastaki U, et al. Multiple occult wrist bone injuries and joint effusions: prevalence and distribution on MRI. Emerg Radiol. 2010;17:179-184.
13. Yildirim C, Akmaz I, Keklikçi K, et al. An unusual combined fracture pattern of the triquetrum. J Hand Surg Eur Vol. 2008;33:385-386.
14. Rasoli S, Ricks M, Packer G. Isolated displaced non-union of a triquetral body fracture: a case report. J Med Case Rep. 2012;6:54.
15. Strickland JW. Considerations for the treatment of the injured athlete. Clin Sports Med. 1998;17:397-400.
THE CASE
A 20-year-old man presented to our family medicine clinic with right wrist pain 4 days after falling on his wrist and hand while playing basketball. He denied any other previous injury or trauma. The pain was unchanged since the injury occurred.
Examination demonstrated mild edema over the palmar and ulnar aspect of the patient’s right wrist with no apparent ecchymosis. He had normal range of motion of his right wrist and hand. However, he experienced pain with active and passive wrist extension and ulnar deviation. There was significant tenderness in the palmar and ulnar aspects of his right wrist just distal to the ulnar styloid process.
THE DIAGNOSIS
Standard plain x-rays of the right wrist revealed an isolated fracture of the body of the triquetrum (FIGURE 1). Since the patient refused to have a cast placed, his wrist was immobilized with a wrist brace. By Day 16 post injury, the pain and edema had improved significantly. After talking with the patient about the potential risks and benefits of continuing to play basketball—and despite our recommendation that he not play—he decided to continue playing since he was a college basketball prospect.
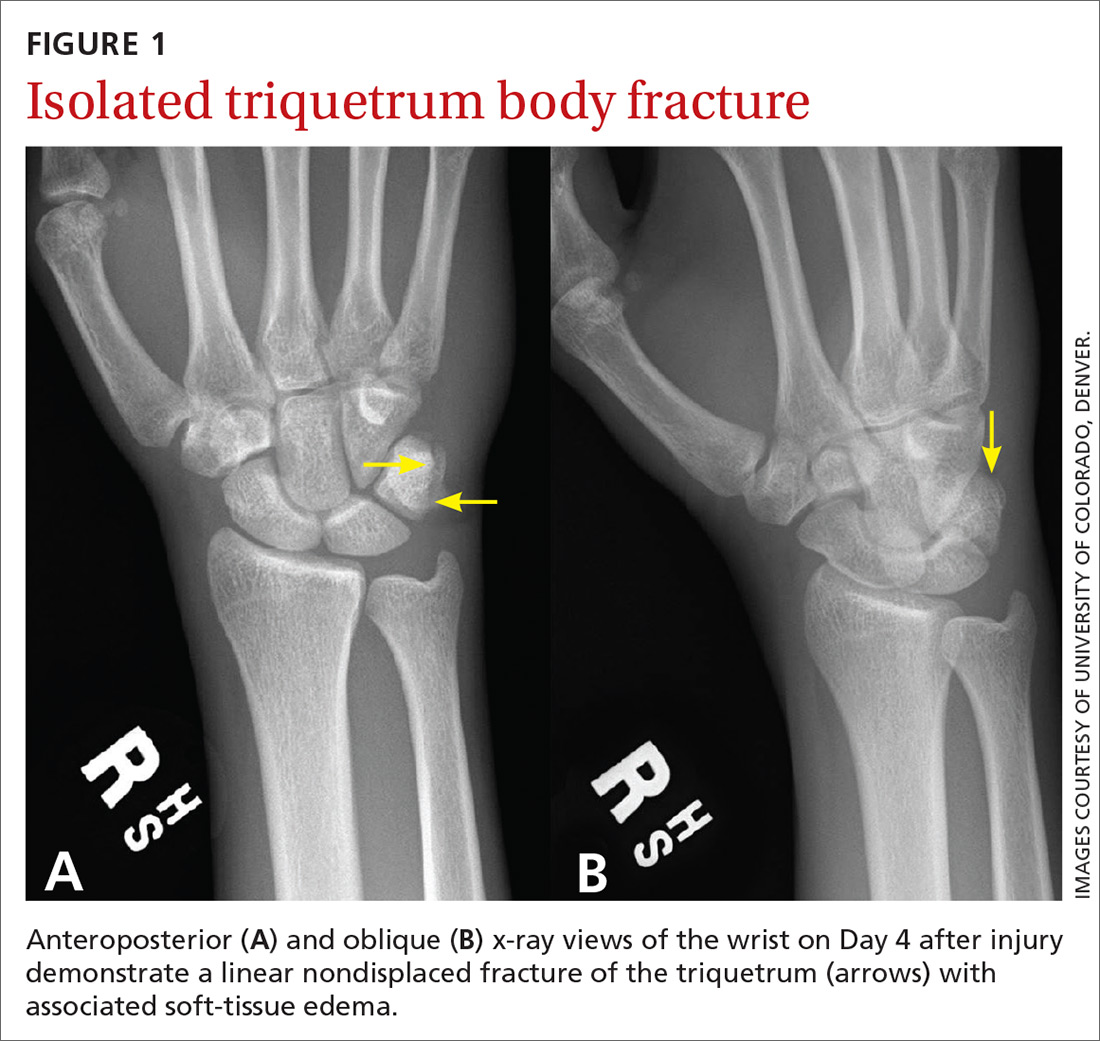
At 4 weeks post injury, x-rays demonstrated mild interval healing (FIGURE 2). At the 8-week visit, the patient had only very mild pain and tenderness, and x-ray images showed improvement (FIGURE 3). Within a few months, his symptoms resolved completely. No further imaging was performed.
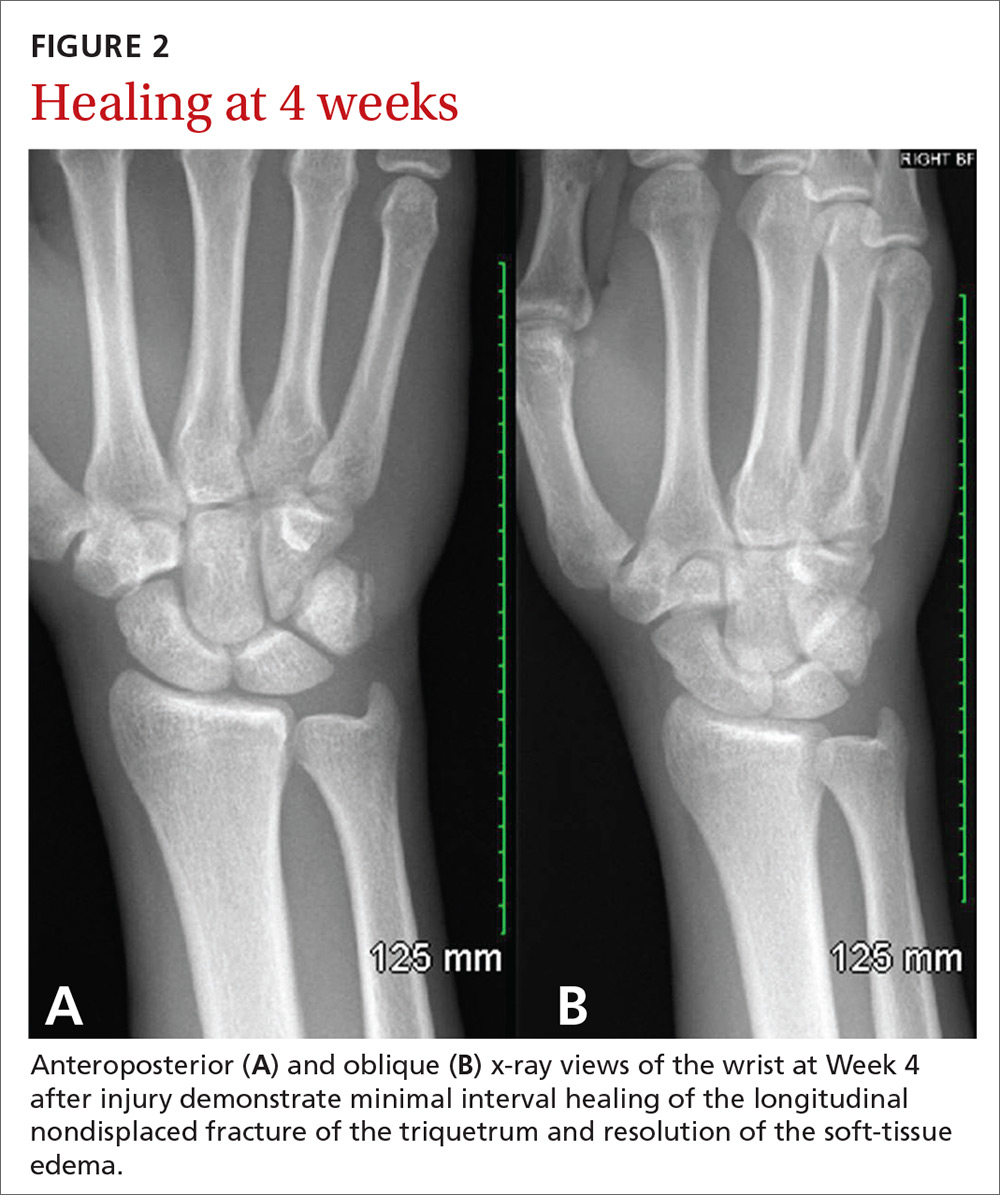
DISCUSSION
In general, carpal fractures are uncommon.1 The triquetrum is the second most commonly injured carpal bone, involved in up to 18% of all carpal fractures.2,3 Triquetrum fractures most commonly occur as isolated injuries and are typically classified in 2 general categories: avulsion fractures (dorsal cortex or volar cortex) and fractures of the triquetrum body.4-8 Isolated avulsion fractures of the triquetral dorsal cortex are relatively common, occurring in about 95% of triquetrum injuries.4-9 Isolated fractures of the triquetrum body are less common, occurring in about 4% of triquetrum injuries, and can go unnoticed on conventional x-rays.4-9

Basketball presents a unique risk for hand or wrist fracture due to its high-impact nature, hard playing surfaces, and frequent use of the hands for dribbling, shooting, rebounding, and passing the ball.
In a retrospective study of sports-related fractures conducted at the Royal Infirmary of Edinburgh, basketball had the highest incidence of carpal injuries compared with other sports, including football, rugby, skiing, snowboarding, and ice-skating.4 Similarly, a retrospective study conducted at the University of California, Los Angeles, found that of all Division 1 collegiate athletes at the school, basketball players had the highest incidence of primary fractures, and the most common fracture location was the hand.10
Continue to: An injury that's easy to miss
An injury that’s easy to miss
Because the incidence of hand and wrist injuries is high among basketball players, it is imperative that triquetrum body fractures are not missed or misdiagnosed as more common hand and wrist injuries, such as triquetral dorsal avulsion fractures.
Our patient, who had an isolated triquetrum body fracture, presented with focal tenderness on the palmar and ulnar aspects of his wrist and pain with ulnar deviation. Since triquetral body fractures often have a clinical presentation quite similar to that of triquetral dorsal avulsion fractures, patients presenting with symptoms of wrist tenderness and pain should be treated with a high degree of clinical suspicion.
With our patient, anteroposterior and lateral x-rays were sufficient to demonstrate an isolated triquetrum body fracture; however, triquetral fractures can be missed in up to 20% of x-rays.4 Both magnetic resonance imaging and computerized tomography are useful in diagnosing occult triquetrum fractures and should be used to confirm clinical suspicion when traditional x-rays are inconclusive.11,12
Management varies
Management of isolated triquetrum body fractures varies depending on the fracture pattern and the status of bone consolidation. Triquetral body fractures typically heal well; it’s very rare that there is a nonunion. As our patient’s fracture was nondisplaced and stable, brace immobilization for 4 weeks was sufficient to facilitate healing and restore long-term hand and wrist functionality. This course of treatment is consistent with other cases of nondisplaced triquetrum body fractures reported in the literature.13
Long-term outcomes. The literature is sparse regarding the long-term functional outcome of nonsurgical treatment for nondisplaced triquetrum body fractures. Multiple carpal fractures, displaced triquetrum body fractures, and persistent pain for multiple months after nonsurgical management all indicate the need for referral to orthopedic surgery. In instances of fracture displacement or nonunion, management tends to be surgical, with open reduction and internal fixation (ORIF) used in multiple cases of nonunion for isolated triquetrum body fractures.3,14 Any diagnostic imaging that reveals displacement, malunion, or nonunion of the fracture is an indication for referral to an orthopedic surgeon.
Continue to: Return to play
Return to play. There is no evidence-based return-to-play recommendation for patients with a triquetrum fracture. However, our patient continued to play basketball through the early stages of injury management because he was a collegiate prospect. While medical, social, and economic factors should be considered when discussing treatment options with athletes, injuries should be managed so that there is no long-term loss of function or risk of injury exacerbation. When discussing early return from injury with athletes who have outside pressure to return to play, it’s important to make them aware of the associated long- and short-term risks.15
THE TAKEAWAY
Management of an isolated triquetrum body fracture is typically straightforward; however, if the fracture is displaced, refer the patient to an orthopedic surgeon as ORIF may be required. For this reason, it’s important to be able to promptly identify isolated triquetrum body fractures and to avoid confusing them with triquetrum dorsal avulsion fractures.
Depending on the sport played and the severity of the injury, athletes with conservatively managed nondisplaced triquetral body fractures may be candidates for early return to play. Nonetheless, athletes should understand both the short- and the long-term risks of playing with an injury, and they should never be advised to continue playing with an injury if it jeopardizes their well-being or the long-term functionality of the affected body part.
CORRESPONDENCE
Morteza Khodaee, MD, MPH, University of Colorado School of Medicine, AFW Clinic, 3055 Roslyn Street, Denver, CO 80238; [email protected]
THE CASE
A 20-year-old man presented to our family medicine clinic with right wrist pain 4 days after falling on his wrist and hand while playing basketball. He denied any other previous injury or trauma. The pain was unchanged since the injury occurred.
Examination demonstrated mild edema over the palmar and ulnar aspect of the patient’s right wrist with no apparent ecchymosis. He had normal range of motion of his right wrist and hand. However, he experienced pain with active and passive wrist extension and ulnar deviation. There was significant tenderness in the palmar and ulnar aspects of his right wrist just distal to the ulnar styloid process.
THE DIAGNOSIS
Standard plain x-rays of the right wrist revealed an isolated fracture of the body of the triquetrum (FIGURE 1). Since the patient refused to have a cast placed, his wrist was immobilized with a wrist brace. By Day 16 post injury, the pain and edema had improved significantly. After talking with the patient about the potential risks and benefits of continuing to play basketball—and despite our recommendation that he not play—he decided to continue playing since he was a college basketball prospect.
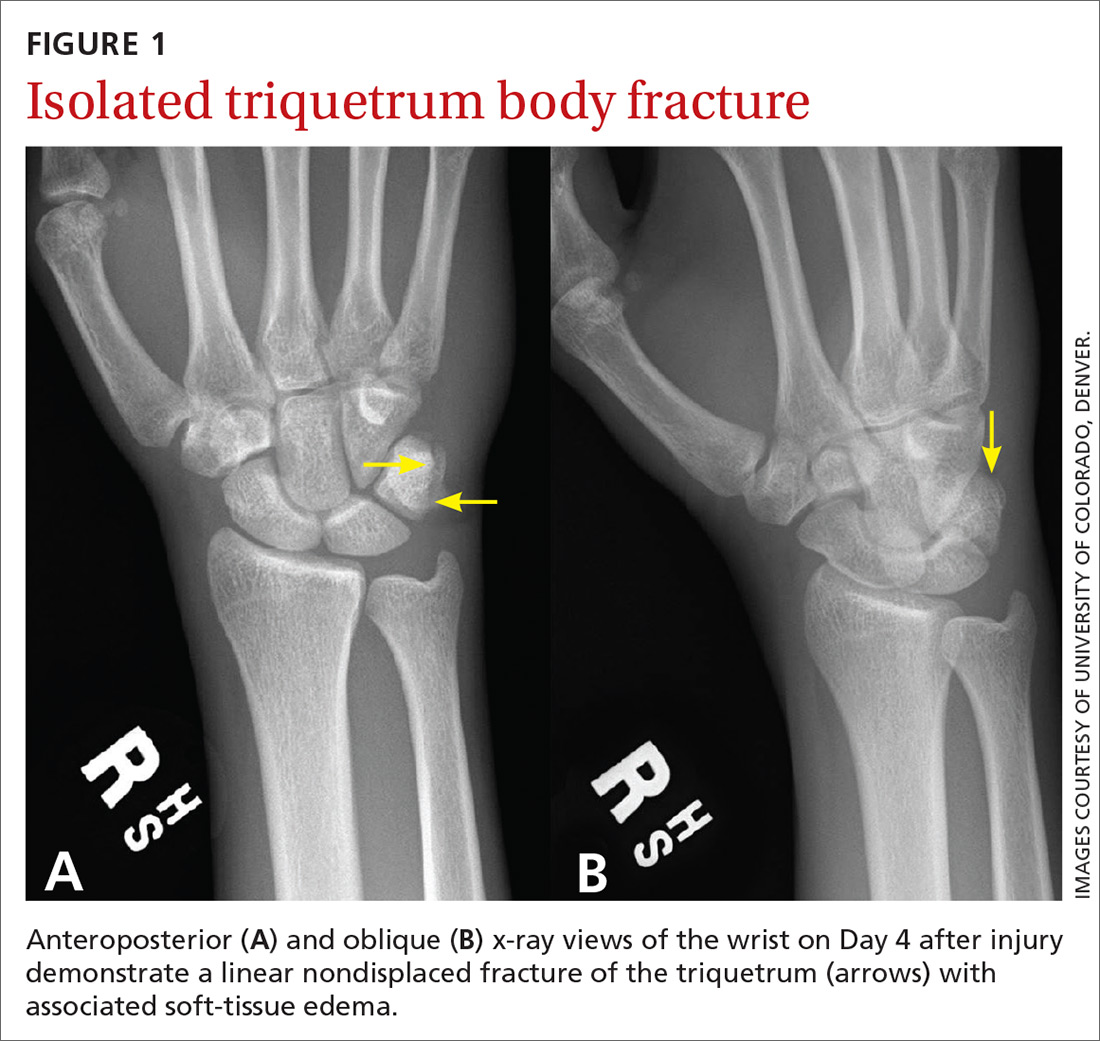
At 4 weeks post injury, x-rays demonstrated mild interval healing (FIGURE 2). At the 8-week visit, the patient had only very mild pain and tenderness, and x-ray images showed improvement (FIGURE 3). Within a few months, his symptoms resolved completely. No further imaging was performed.
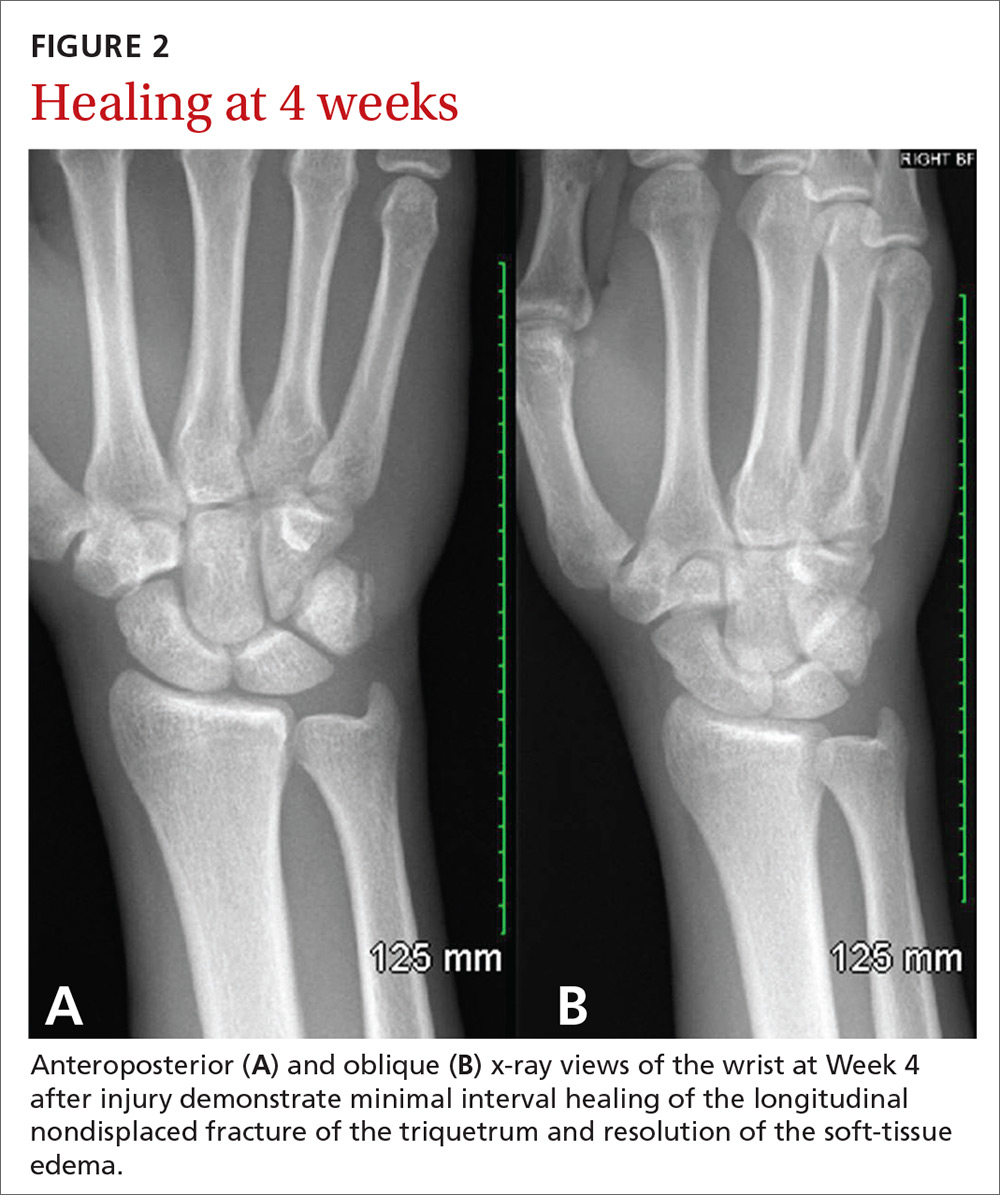
DISCUSSION
In general, carpal fractures are uncommon.1 The triquetrum is the second most commonly injured carpal bone, involved in up to 18% of all carpal fractures.2,3 Triquetrum fractures most commonly occur as isolated injuries and are typically classified in 2 general categories: avulsion fractures (dorsal cortex or volar cortex) and fractures of the triquetrum body.4-8 Isolated avulsion fractures of the triquetral dorsal cortex are relatively common, occurring in about 95% of triquetrum injuries.4-9 Isolated fractures of the triquetrum body are less common, occurring in about 4% of triquetrum injuries, and can go unnoticed on conventional x-rays.4-9

Basketball presents a unique risk for hand or wrist fracture due to its high-impact nature, hard playing surfaces, and frequent use of the hands for dribbling, shooting, rebounding, and passing the ball.
In a retrospective study of sports-related fractures conducted at the Royal Infirmary of Edinburgh, basketball had the highest incidence of carpal injuries compared with other sports, including football, rugby, skiing, snowboarding, and ice-skating.4 Similarly, a retrospective study conducted at the University of California, Los Angeles, found that of all Division 1 collegiate athletes at the school, basketball players had the highest incidence of primary fractures, and the most common fracture location was the hand.10
Continue to: An injury that's easy to miss
An injury that’s easy to miss
Because the incidence of hand and wrist injuries is high among basketball players, it is imperative that triquetrum body fractures are not missed or misdiagnosed as more common hand and wrist injuries, such as triquetral dorsal avulsion fractures.
Our patient, who had an isolated triquetrum body fracture, presented with focal tenderness on the palmar and ulnar aspects of his wrist and pain with ulnar deviation. Since triquetral body fractures often have a clinical presentation quite similar to that of triquetral dorsal avulsion fractures, patients presenting with symptoms of wrist tenderness and pain should be treated with a high degree of clinical suspicion.
With our patient, anteroposterior and lateral x-rays were sufficient to demonstrate an isolated triquetrum body fracture; however, triquetral fractures can be missed in up to 20% of x-rays.4 Both magnetic resonance imaging and computerized tomography are useful in diagnosing occult triquetrum fractures and should be used to confirm clinical suspicion when traditional x-rays are inconclusive.11,12
Management varies
Management of isolated triquetrum body fractures varies depending on the fracture pattern and the status of bone consolidation. Triquetral body fractures typically heal well; it’s very rare that there is a nonunion. As our patient’s fracture was nondisplaced and stable, brace immobilization for 4 weeks was sufficient to facilitate healing and restore long-term hand and wrist functionality. This course of treatment is consistent with other cases of nondisplaced triquetrum body fractures reported in the literature.13
Long-term outcomes. The literature is sparse regarding the long-term functional outcome of nonsurgical treatment for nondisplaced triquetrum body fractures. Multiple carpal fractures, displaced triquetrum body fractures, and persistent pain for multiple months after nonsurgical management all indicate the need for referral to orthopedic surgery. In instances of fracture displacement or nonunion, management tends to be surgical, with open reduction and internal fixation (ORIF) used in multiple cases of nonunion for isolated triquetrum body fractures.3,14 Any diagnostic imaging that reveals displacement, malunion, or nonunion of the fracture is an indication for referral to an orthopedic surgeon.
Continue to: Return to play
Return to play. There is no evidence-based return-to-play recommendation for patients with a triquetrum fracture. However, our patient continued to play basketball through the early stages of injury management because he was a collegiate prospect. While medical, social, and economic factors should be considered when discussing treatment options with athletes, injuries should be managed so that there is no long-term loss of function or risk of injury exacerbation. When discussing early return from injury with athletes who have outside pressure to return to play, it’s important to make them aware of the associated long- and short-term risks.15
THE TAKEAWAY
Management of an isolated triquetrum body fracture is typically straightforward; however, if the fracture is displaced, refer the patient to an orthopedic surgeon as ORIF may be required. For this reason, it’s important to be able to promptly identify isolated triquetrum body fractures and to avoid confusing them with triquetrum dorsal avulsion fractures.
Depending on the sport played and the severity of the injury, athletes with conservatively managed nondisplaced triquetral body fractures may be candidates for early return to play. Nonetheless, athletes should understand both the short- and the long-term risks of playing with an injury, and they should never be advised to continue playing with an injury if it jeopardizes their well-being or the long-term functionality of the affected body part.
CORRESPONDENCE
Morteza Khodaee, MD, MPH, University of Colorado School of Medicine, AFW Clinic, 3055 Roslyn Street, Denver, CO 80238; [email protected]
1. Suh N, Ek ET, Wolfe SW. Carpal fractures. J Hand Surg Am. 2014;39:785-791.
2. Hey HW, Chong AK, Murphy D. Prevalence of carpal fracture in Singapore. J Hand Surg Am. 2011;36:278-283.
3. Al Rashid M, Rasoli S, Khan WS. Non-union of isolated displaced triquetral body fracture—a case report. Ortop Traumatol Rehabil. 2012;14:71-74.
4. Becce F, Theumann N, Bollmann C, et al. Dorsal fractures of the triquetrum: MRI findings with an emphasis on dorsal carpal ligament injuries. AJR Am J Roentgenol. 2013;200:608-617.
5. Court-Brown CM, Wood AM, Aitken S. The epidemiology of acute sports-related fractures in adults. Injury. 2008;39:1365-1372.
6. Urch EY, Lee SK. Carpal fractures other than scaphoid. Clin Sports Med. 2015;34:51-67.
7. deWeber K. Triquetrum fractures. UpToDate. 2016. www.uptodate.com/contents/triquetrum-fractures. Accessed September 3, 2019.
8. Höcker K, Menschik A. Chip fractures of the triquetrum. Mechanism, classification and results. J Hand Surg Br. 1994;19:584-588.
9. Jarraya M, Hayashi D, Roemer FW, et al. Radiographically occult and subtle fractures: a pictorial review. Radiol Res Pract. 2013;2013:370169.
10. Hame SL, LaFemina JM, McAllister DR, et al. Fractures in the collegiate athlete. Am J Sports Med. 2004;32:446-451.
11. Hindman BW, Kulik WJ, Lee G, et al. Occult fractures of the carpals and metacarpals: demonstration by CT. AJR Am J Roentgenol. 1989;153:529-532.
12. Pierre-Jerome C, Moncayo V, Albastaki U, et al. Multiple occult wrist bone injuries and joint effusions: prevalence and distribution on MRI. Emerg Radiol. 2010;17:179-184.
13. Yildirim C, Akmaz I, Keklikçi K, et al. An unusual combined fracture pattern of the triquetrum. J Hand Surg Eur Vol. 2008;33:385-386.
14. Rasoli S, Ricks M, Packer G. Isolated displaced non-union of a triquetral body fracture: a case report. J Med Case Rep. 2012;6:54.
15. Strickland JW. Considerations for the treatment of the injured athlete. Clin Sports Med. 1998;17:397-400.
1. Suh N, Ek ET, Wolfe SW. Carpal fractures. J Hand Surg Am. 2014;39:785-791.
2. Hey HW, Chong AK, Murphy D. Prevalence of carpal fracture in Singapore. J Hand Surg Am. 2011;36:278-283.
3. Al Rashid M, Rasoli S, Khan WS. Non-union of isolated displaced triquetral body fracture—a case report. Ortop Traumatol Rehabil. 2012;14:71-74.
4. Becce F, Theumann N, Bollmann C, et al. Dorsal fractures of the triquetrum: MRI findings with an emphasis on dorsal carpal ligament injuries. AJR Am J Roentgenol. 2013;200:608-617.
5. Court-Brown CM, Wood AM, Aitken S. The epidemiology of acute sports-related fractures in adults. Injury. 2008;39:1365-1372.
6. Urch EY, Lee SK. Carpal fractures other than scaphoid. Clin Sports Med. 2015;34:51-67.
7. deWeber K. Triquetrum fractures. UpToDate. 2016. www.uptodate.com/contents/triquetrum-fractures. Accessed September 3, 2019.
8. Höcker K, Menschik A. Chip fractures of the triquetrum. Mechanism, classification and results. J Hand Surg Br. 1994;19:584-588.
9. Jarraya M, Hayashi D, Roemer FW, et al. Radiographically occult and subtle fractures: a pictorial review. Radiol Res Pract. 2013;2013:370169.
10. Hame SL, LaFemina JM, McAllister DR, et al. Fractures in the collegiate athlete. Am J Sports Med. 2004;32:446-451.
11. Hindman BW, Kulik WJ, Lee G, et al. Occult fractures of the carpals and metacarpals: demonstration by CT. AJR Am J Roentgenol. 1989;153:529-532.
12. Pierre-Jerome C, Moncayo V, Albastaki U, et al. Multiple occult wrist bone injuries and joint effusions: prevalence and distribution on MRI. Emerg Radiol. 2010;17:179-184.
13. Yildirim C, Akmaz I, Keklikçi K, et al. An unusual combined fracture pattern of the triquetrum. J Hand Surg Eur Vol. 2008;33:385-386.
14. Rasoli S, Ricks M, Packer G. Isolated displaced non-union of a triquetral body fracture: a case report. J Med Case Rep. 2012;6:54.
15. Strickland JW. Considerations for the treatment of the injured athlete. Clin Sports Med. 1998;17:397-400.
Can sleep apnea be accurately diagnosed at home?
ILLUSTRATIVE CASE
A 50-year-old overweight male with a history of hypertension presents to your office for a yearly physical. On review of symptoms, he notes feeling constantly tired, despite reported good sleep hygiene practices. He scores 11 on the Epworth Sleepiness Scale, and his wife complains about his snoring. You have a high suspicion of obstructive sleep apnea. What is your next step?
Obstructive sleep apnea (OSA) is quite common, affecting at least 2% to 4% of the general adult population.2 The gold standard for OSA diagnosis has been laboratory polysomnography (PSG) to measure the apnea-hypopnea index (AHI), which is the average number of apneas and hypopneas per hour of sleep, and the respiratory event index (REI), which is the average number of apneas, hypopneas, and respiratory effort-related arousals per hour of sleep. A minimum of 5 on the AHI or REI, along with clinical symptoms, is required for diagnosis.
Many adults go undiagnosed and untreated, however, due to barriers to diagnosis including the inconvenience of laboratory PSG.3 Sleep laboratories often have a significant wait time for evaluation, and sleeping in an unfamiliar place can be inconvenient or intolerable for some patients, making diagnosis difficult despite high clinical suspicion. Untreated sleep apnea is associated with an increased risk of hypertension, coronary artery disease, congestive heart failure, stroke, atrial fibrillation, and type 2 diabetes.4
Home sleep studies are an alternative for patients with a high risk of OSA without comorbid sleep conditions, heart failure, or chronic obstructive pulmonary disease (COPD). This study investigated the long-term effectiveness of diagnosis by home respiratory polygraphy (HRP) vs laboratory PSG in patients with an intermediate to high clinical suspicion for OSA.
STUDY SUMMARY
Home Dx is noninferior to lab Dx in all aspects studied
This multicenter, noninferiority randomized controlled trial and cost analysis study conducted in Spain randomized 430 adults referred to pulmonology for suspected OSA to receive either in-lab PSG or HRP. Patients received treatment with continuous positive airway pressure (CPAP) if their REI was ≥ 5 for HRP or their AHI was ≥ 5 for PSG with significant clinical symptoms, which is consistent with the Spanish Sleep Network guidelines.5 All patients in both arms received sleep hygiene instruction, nutrition education, and single-session auto-CPAP titration, and were evaluated at 1 and 3 months to assess for compliance. At 6 months, all patients were evaluated with PSG.
HRP was found to be non-inferior to PSG based on Epworth Sleepiness Scale (ESS) scores evaluated at baseline and at 6-month follow-up (HRP mean = -4.2 points; 95% confidence interval [CI], -4.8 to -3.6 and PSG mean -4.9; 95% CI, -5.4 to -4.3; P = .14). Both groups had similar secondary outcomes. Quality-of-life as measured by the 30-point Functional Outcomes of Sleep Questionnaire improved by an average of 6.7 (standard deviation [SD] = 16.7) in the HRP group vs 6.5 (SD = 18.1) in the PSG group (P = .92). Systolic and diastolic blood pressure improved significantly in both groups without any statistically significant difference between the groups. HRP was also found to be more cost-effective than PSG with a savings equivalent to more than half the cost of PSG, or about $450 per study (depending on the exchange rate).
WHAT’S NEW
HRP offers advantages for low-risk patients
In the majority of patients, OSA can be diagnosed at home with outcomes similar to those for lab diagnosis, decreased cost, and decreased time from suspected diagnosis to treatment. HRP is acceptable for patients with a high probability of OSA without significant comorbidities if monitoring includes at least airflow, respiratory effort, and blood oxygenation.6
Continue to: CAVEATS
CAVEATS
Recommendations are somewhat ambiguous
This study, as well as current guidelines, recommend home sleep studies for patients with a high clinical suspicion or high pre-test probability of OSA and who lack comorbid conditions that could affect sleep. The comorbid conditions are well identified: COPD, heart failure hypoventilation syndromes, insomnia, hypersomnia, parasomnia, periodic limb movement disorder, narcolepsy, and chronic opioid use.6 However, what constitutes “a high clinical suspicion” or “high pre-test probability” was not well defined in this study.
Several clinical screening tools are available and include the ESS, Berlin Questionnaire, and STOP-BANG Scoring System (Snoring, Tiredness, Observed apnea, Pressure [systemic hypertension], Body mass index > 35, Age > 50 years, Neck circumference > 16 inches, male Gender). An ESS score ≥ 10 warrants further evaluation, but is not very sensitive. Two or more positive categories on the Berlin Questionnaire indicates a high risk of OSA with a sensitivity of 76%, 77%, and 77% for mild, moderate, and severe OSA, respectively.7 A score of ≥ 3 on the STOP-BANG Scoring System has been validated and has a sensitivity of 83.6%, 92.9%, and 100% for an AHI > 5, > 15, and > 30, respectively.8
Home sleep studies should not be used to screen the general population.
CHALLENGES TO IMPLEMENTATION
Recommendations may present a challenge but insurance should not
The American Academy of Sleep Medicine recommends that portable monitoring must record airflow, respiratory effort, and blood oxygenation, and the device must be able to display the raw data to be interpreted by a board-certified sleep medicine physician according to current published standards.6 Implementation would require appropriate selection of a home monitoring device, consultation with a sleep medicine specialist, and significant patient education to ensure interpretable results.
Insurance should not be a barrier to implementation as the Centers for Medicare and Medicaid Services accept home sleep apnea testing results for CPAP prescriptions.9 However, variability currently exists regarding the extent to which private insurers provide coverage for home sleep apnea testing.
ACKNOWLEDGMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Corral J, Sánchez-Quiroga MÁ, Carmona-Bernal C, et al. Conventional polysomnography is not necessary for the management of most patients with suspected obstructive sleep apnea. Noninferiority, randomized controlled trial. Am J Respir Crit Care Med. 2017;196:1181-1190.
2. Epstein LJ, Kristo D, Strollo PJ, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5:263-276.
3. Colten H, Abboud F, Block G, et al. Sleep disorders and sleep deprivation: an unmet public health problem. 2006. Washington, DC: National Academy of Sciences.
4. Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5:136-143.
5. Lloberes P, Durán-Cantolla J, Martinez-Garcia MA, et al. Diagnosis and treatment of sleep apnea-hypopnea syndrome. Spanish Society of Pulmonology and Thoracic Surgery. Arch Bronconeumol. 2011;47:143-156.
6. Rosen IM, Kirsch DB, Chervin RD; American Academy of Sleep Medicine Board of Directors. Clinical use of a home sleep apnea test: an American Academy of Sleep Medicine position statement. J Clin Sleep Med. 2017;13:1205-1207.
7. Chiu HY, Chen PY, Chuang, LP, et al. Diagnostic accuracy of the Berlin questionnaire, STOP-BANG, STOP and Epworth Sleepiness scale in detecting obstructive sleep apnea: a bivariate meta-analysis. Sleep Med Rev. 2017;36:57-70.
8. Chung, F, Yegneswaran B, Lio P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108:812-821.
9. Centers for Medicare and Medicaid Services. Decision Memo for Continuous Positive Airway Pressure (CPAP) Therapy for Obstructive Sleep Apnea (OSA) (CAG-00093R2). March 13, 2008. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=204. Accessed September 6, 2019.
ILLUSTRATIVE CASE
A 50-year-old overweight male with a history of hypertension presents to your office for a yearly physical. On review of symptoms, he notes feeling constantly tired, despite reported good sleep hygiene practices. He scores 11 on the Epworth Sleepiness Scale, and his wife complains about his snoring. You have a high suspicion of obstructive sleep apnea. What is your next step?
Obstructive sleep apnea (OSA) is quite common, affecting at least 2% to 4% of the general adult population.2 The gold standard for OSA diagnosis has been laboratory polysomnography (PSG) to measure the apnea-hypopnea index (AHI), which is the average number of apneas and hypopneas per hour of sleep, and the respiratory event index (REI), which is the average number of apneas, hypopneas, and respiratory effort-related arousals per hour of sleep. A minimum of 5 on the AHI or REI, along with clinical symptoms, is required for diagnosis.
Many adults go undiagnosed and untreated, however, due to barriers to diagnosis including the inconvenience of laboratory PSG.3 Sleep laboratories often have a significant wait time for evaluation, and sleeping in an unfamiliar place can be inconvenient or intolerable for some patients, making diagnosis difficult despite high clinical suspicion. Untreated sleep apnea is associated with an increased risk of hypertension, coronary artery disease, congestive heart failure, stroke, atrial fibrillation, and type 2 diabetes.4
Home sleep studies are an alternative for patients with a high risk of OSA without comorbid sleep conditions, heart failure, or chronic obstructive pulmonary disease (COPD). This study investigated the long-term effectiveness of diagnosis by home respiratory polygraphy (HRP) vs laboratory PSG in patients with an intermediate to high clinical suspicion for OSA.
STUDY SUMMARY
Home Dx is noninferior to lab Dx in all aspects studied
This multicenter, noninferiority randomized controlled trial and cost analysis study conducted in Spain randomized 430 adults referred to pulmonology for suspected OSA to receive either in-lab PSG or HRP. Patients received treatment with continuous positive airway pressure (CPAP) if their REI was ≥ 5 for HRP or their AHI was ≥ 5 for PSG with significant clinical symptoms, which is consistent with the Spanish Sleep Network guidelines.5 All patients in both arms received sleep hygiene instruction, nutrition education, and single-session auto-CPAP titration, and were evaluated at 1 and 3 months to assess for compliance. At 6 months, all patients were evaluated with PSG.
HRP was found to be non-inferior to PSG based on Epworth Sleepiness Scale (ESS) scores evaluated at baseline and at 6-month follow-up (HRP mean = -4.2 points; 95% confidence interval [CI], -4.8 to -3.6 and PSG mean -4.9; 95% CI, -5.4 to -4.3; P = .14). Both groups had similar secondary outcomes. Quality-of-life as measured by the 30-point Functional Outcomes of Sleep Questionnaire improved by an average of 6.7 (standard deviation [SD] = 16.7) in the HRP group vs 6.5 (SD = 18.1) in the PSG group (P = .92). Systolic and diastolic blood pressure improved significantly in both groups without any statistically significant difference between the groups. HRP was also found to be more cost-effective than PSG with a savings equivalent to more than half the cost of PSG, or about $450 per study (depending on the exchange rate).
WHAT’S NEW
HRP offers advantages for low-risk patients
In the majority of patients, OSA can be diagnosed at home with outcomes similar to those for lab diagnosis, decreased cost, and decreased time from suspected diagnosis to treatment. HRP is acceptable for patients with a high probability of OSA without significant comorbidities if monitoring includes at least airflow, respiratory effort, and blood oxygenation.6
Continue to: CAVEATS
CAVEATS
Recommendations are somewhat ambiguous
This study, as well as current guidelines, recommend home sleep studies for patients with a high clinical suspicion or high pre-test probability of OSA and who lack comorbid conditions that could affect sleep. The comorbid conditions are well identified: COPD, heart failure hypoventilation syndromes, insomnia, hypersomnia, parasomnia, periodic limb movement disorder, narcolepsy, and chronic opioid use.6 However, what constitutes “a high clinical suspicion” or “high pre-test probability” was not well defined in this study.
Several clinical screening tools are available and include the ESS, Berlin Questionnaire, and STOP-BANG Scoring System (Snoring, Tiredness, Observed apnea, Pressure [systemic hypertension], Body mass index > 35, Age > 50 years, Neck circumference > 16 inches, male Gender). An ESS score ≥ 10 warrants further evaluation, but is not very sensitive. Two or more positive categories on the Berlin Questionnaire indicates a high risk of OSA with a sensitivity of 76%, 77%, and 77% for mild, moderate, and severe OSA, respectively.7 A score of ≥ 3 on the STOP-BANG Scoring System has been validated and has a sensitivity of 83.6%, 92.9%, and 100% for an AHI > 5, > 15, and > 30, respectively.8
Home sleep studies should not be used to screen the general population.
CHALLENGES TO IMPLEMENTATION
Recommendations may present a challenge but insurance should not
The American Academy of Sleep Medicine recommends that portable monitoring must record airflow, respiratory effort, and blood oxygenation, and the device must be able to display the raw data to be interpreted by a board-certified sleep medicine physician according to current published standards.6 Implementation would require appropriate selection of a home monitoring device, consultation with a sleep medicine specialist, and significant patient education to ensure interpretable results.
Insurance should not be a barrier to implementation as the Centers for Medicare and Medicaid Services accept home sleep apnea testing results for CPAP prescriptions.9 However, variability currently exists regarding the extent to which private insurers provide coverage for home sleep apnea testing.
ACKNOWLEDGMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
ILLUSTRATIVE CASE
A 50-year-old overweight male with a history of hypertension presents to your office for a yearly physical. On review of symptoms, he notes feeling constantly tired, despite reported good sleep hygiene practices. He scores 11 on the Epworth Sleepiness Scale, and his wife complains about his snoring. You have a high suspicion of obstructive sleep apnea. What is your next step?
Obstructive sleep apnea (OSA) is quite common, affecting at least 2% to 4% of the general adult population.2 The gold standard for OSA diagnosis has been laboratory polysomnography (PSG) to measure the apnea-hypopnea index (AHI), which is the average number of apneas and hypopneas per hour of sleep, and the respiratory event index (REI), which is the average number of apneas, hypopneas, and respiratory effort-related arousals per hour of sleep. A minimum of 5 on the AHI or REI, along with clinical symptoms, is required for diagnosis.
Many adults go undiagnosed and untreated, however, due to barriers to diagnosis including the inconvenience of laboratory PSG.3 Sleep laboratories often have a significant wait time for evaluation, and sleeping in an unfamiliar place can be inconvenient or intolerable for some patients, making diagnosis difficult despite high clinical suspicion. Untreated sleep apnea is associated with an increased risk of hypertension, coronary artery disease, congestive heart failure, stroke, atrial fibrillation, and type 2 diabetes.4
Home sleep studies are an alternative for patients with a high risk of OSA without comorbid sleep conditions, heart failure, or chronic obstructive pulmonary disease (COPD). This study investigated the long-term effectiveness of diagnosis by home respiratory polygraphy (HRP) vs laboratory PSG in patients with an intermediate to high clinical suspicion for OSA.
STUDY SUMMARY
Home Dx is noninferior to lab Dx in all aspects studied
This multicenter, noninferiority randomized controlled trial and cost analysis study conducted in Spain randomized 430 adults referred to pulmonology for suspected OSA to receive either in-lab PSG or HRP. Patients received treatment with continuous positive airway pressure (CPAP) if their REI was ≥ 5 for HRP or their AHI was ≥ 5 for PSG with significant clinical symptoms, which is consistent with the Spanish Sleep Network guidelines.5 All patients in both arms received sleep hygiene instruction, nutrition education, and single-session auto-CPAP titration, and were evaluated at 1 and 3 months to assess for compliance. At 6 months, all patients were evaluated with PSG.
HRP was found to be non-inferior to PSG based on Epworth Sleepiness Scale (ESS) scores evaluated at baseline and at 6-month follow-up (HRP mean = -4.2 points; 95% confidence interval [CI], -4.8 to -3.6 and PSG mean -4.9; 95% CI, -5.4 to -4.3; P = .14). Both groups had similar secondary outcomes. Quality-of-life as measured by the 30-point Functional Outcomes of Sleep Questionnaire improved by an average of 6.7 (standard deviation [SD] = 16.7) in the HRP group vs 6.5 (SD = 18.1) in the PSG group (P = .92). Systolic and diastolic blood pressure improved significantly in both groups without any statistically significant difference between the groups. HRP was also found to be more cost-effective than PSG with a savings equivalent to more than half the cost of PSG, or about $450 per study (depending on the exchange rate).
WHAT’S NEW
HRP offers advantages for low-risk patients
In the majority of patients, OSA can be diagnosed at home with outcomes similar to those for lab diagnosis, decreased cost, and decreased time from suspected diagnosis to treatment. HRP is acceptable for patients with a high probability of OSA without significant comorbidities if monitoring includes at least airflow, respiratory effort, and blood oxygenation.6
Continue to: CAVEATS
CAVEATS
Recommendations are somewhat ambiguous
This study, as well as current guidelines, recommend home sleep studies for patients with a high clinical suspicion or high pre-test probability of OSA and who lack comorbid conditions that could affect sleep. The comorbid conditions are well identified: COPD, heart failure hypoventilation syndromes, insomnia, hypersomnia, parasomnia, periodic limb movement disorder, narcolepsy, and chronic opioid use.6 However, what constitutes “a high clinical suspicion” or “high pre-test probability” was not well defined in this study.
Several clinical screening tools are available and include the ESS, Berlin Questionnaire, and STOP-BANG Scoring System (Snoring, Tiredness, Observed apnea, Pressure [systemic hypertension], Body mass index > 35, Age > 50 years, Neck circumference > 16 inches, male Gender). An ESS score ≥ 10 warrants further evaluation, but is not very sensitive. Two or more positive categories on the Berlin Questionnaire indicates a high risk of OSA with a sensitivity of 76%, 77%, and 77% for mild, moderate, and severe OSA, respectively.7 A score of ≥ 3 on the STOP-BANG Scoring System has been validated and has a sensitivity of 83.6%, 92.9%, and 100% for an AHI > 5, > 15, and > 30, respectively.8
Home sleep studies should not be used to screen the general population.
CHALLENGES TO IMPLEMENTATION
Recommendations may present a challenge but insurance should not
The American Academy of Sleep Medicine recommends that portable monitoring must record airflow, respiratory effort, and blood oxygenation, and the device must be able to display the raw data to be interpreted by a board-certified sleep medicine physician according to current published standards.6 Implementation would require appropriate selection of a home monitoring device, consultation with a sleep medicine specialist, and significant patient education to ensure interpretable results.
Insurance should not be a barrier to implementation as the Centers for Medicare and Medicaid Services accept home sleep apnea testing results for CPAP prescriptions.9 However, variability currently exists regarding the extent to which private insurers provide coverage for home sleep apnea testing.
ACKNOWLEDGMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
1. Corral J, Sánchez-Quiroga MÁ, Carmona-Bernal C, et al. Conventional polysomnography is not necessary for the management of most patients with suspected obstructive sleep apnea. Noninferiority, randomized controlled trial. Am J Respir Crit Care Med. 2017;196:1181-1190.
2. Epstein LJ, Kristo D, Strollo PJ, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5:263-276.
3. Colten H, Abboud F, Block G, et al. Sleep disorders and sleep deprivation: an unmet public health problem. 2006. Washington, DC: National Academy of Sciences.
4. Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5:136-143.
5. Lloberes P, Durán-Cantolla J, Martinez-Garcia MA, et al. Diagnosis and treatment of sleep apnea-hypopnea syndrome. Spanish Society of Pulmonology and Thoracic Surgery. Arch Bronconeumol. 2011;47:143-156.
6. Rosen IM, Kirsch DB, Chervin RD; American Academy of Sleep Medicine Board of Directors. Clinical use of a home sleep apnea test: an American Academy of Sleep Medicine position statement. J Clin Sleep Med. 2017;13:1205-1207.
7. Chiu HY, Chen PY, Chuang, LP, et al. Diagnostic accuracy of the Berlin questionnaire, STOP-BANG, STOP and Epworth Sleepiness scale in detecting obstructive sleep apnea: a bivariate meta-analysis. Sleep Med Rev. 2017;36:57-70.
8. Chung, F, Yegneswaran B, Lio P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108:812-821.
9. Centers for Medicare and Medicaid Services. Decision Memo for Continuous Positive Airway Pressure (CPAP) Therapy for Obstructive Sleep Apnea (OSA) (CAG-00093R2). March 13, 2008. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=204. Accessed September 6, 2019.
1. Corral J, Sánchez-Quiroga MÁ, Carmona-Bernal C, et al. Conventional polysomnography is not necessary for the management of most patients with suspected obstructive sleep apnea. Noninferiority, randomized controlled trial. Am J Respir Crit Care Med. 2017;196:1181-1190.
2. Epstein LJ, Kristo D, Strollo PJ, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5:263-276.
3. Colten H, Abboud F, Block G, et al. Sleep disorders and sleep deprivation: an unmet public health problem. 2006. Washington, DC: National Academy of Sciences.
4. Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5:136-143.
5. Lloberes P, Durán-Cantolla J, Martinez-Garcia MA, et al. Diagnosis and treatment of sleep apnea-hypopnea syndrome. Spanish Society of Pulmonology and Thoracic Surgery. Arch Bronconeumol. 2011;47:143-156.
6. Rosen IM, Kirsch DB, Chervin RD; American Academy of Sleep Medicine Board of Directors. Clinical use of a home sleep apnea test: an American Academy of Sleep Medicine position statement. J Clin Sleep Med. 2017;13:1205-1207.
7. Chiu HY, Chen PY, Chuang, LP, et al. Diagnostic accuracy of the Berlin questionnaire, STOP-BANG, STOP and Epworth Sleepiness scale in detecting obstructive sleep apnea: a bivariate meta-analysis. Sleep Med Rev. 2017;36:57-70.
8. Chung, F, Yegneswaran B, Lio P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108:812-821.
9. Centers for Medicare and Medicaid Services. Decision Memo for Continuous Positive Airway Pressure (CPAP) Therapy for Obstructive Sleep Apnea (OSA) (CAG-00093R2). March 13, 2008. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=204. Accessed September 6, 2019.
PRACTICE CHANGER
Consider ordering home respiratory polygraphy vs laboratory sleep studies for patients suspected of having obstructive sleep apnea.1
Corral J, Sánchez-Quiroga MÁ, Carmona-Bernal C, et al. Conventional polysomnography is not necessary for the management of most patients with suspected obstructive sleep apnea. Noninferiority, randomized controlled trial. Am J Respir Crit Care Med. 2017;196:1181-1190.
STRENGTH OF RECOMMENDATION
B: Based on a multicenter, noninferiority randomized controlled trial and cost analysis study.
Influenza update
2018-2019 season retrospective
Last year’s influenza season was longer than usual. Infections, as measured by the percentage of outpatient visits due to influenza-like illness, increased in early November 2018, peaked in early February to mid-March of 2019, and remained above baseline levels through mid-May.1,2 Ninety six percent of influenza-positive samples were influenza A,1 and 57% of those were H1N1.2 In the second half of the season, H3N2 became the predominant circulating virus and there was a genetic shift in this strain that caused a decrease in the effectiveness of influenza vaccines (FIGURE).1 The influenza-confirmed hospitalization rate was 65.3/100,000, with the highest rate (221.7/100,000) occurring among those 65 years of age and older.2 Of those hospitalized with influenza, 93% of adults and 55% of children had an underlying medical condition and 29% of women of childbearing age were pregnant.2
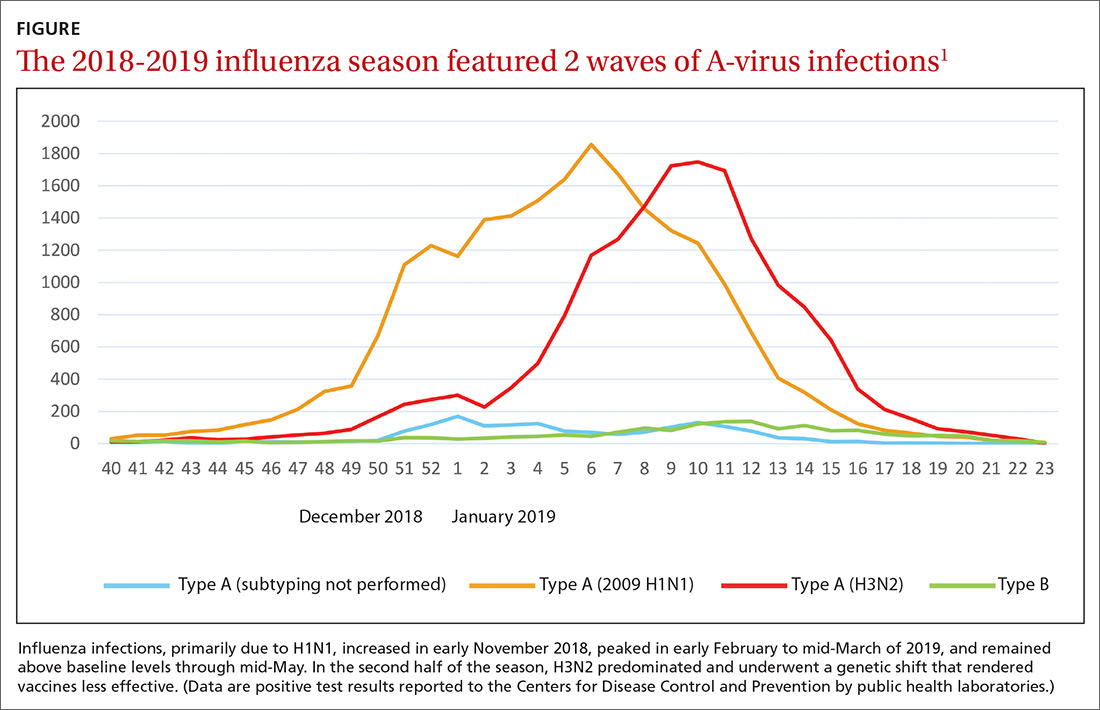
Morbidity and mortality from influenza during the 2018-2019 influenza season were moderate compared with previous years. Pneumonia and influenza mortality reached close to 8% of all deaths during the peak of the season (considered a modest peak), but stayed above the epidemic threshold for 10 weeks.2 There were 119 pediatric deaths.1 Overall, in the United States, there were an estimated 37 to 43 million influenza-related illnesses, 17 to 20 million flu-related medical visits, 531,000 to 647,000 flu-related hospitalizations, and 36,400 to 61,200 deaths.1
Influenza viral resistance to oseltamivir remained very low throughout the season for both A and B viruses.2
Vaccine effectiveness was subpar
The effectiveness of influenza vaccine last season was disappointing. When assessed using laboratory-confirmed medically attended influenza, the vaccine was 29% effective; when assessed by age group, the confidence intervals included 0 in ages 9 to 17 years and 50 years and older.3 In the age group 6 months to 8 years, the vaccine was 49% effective.3 The vaccine was not effective against the predominant H3N2 strain circulating. It was 25% effective in preventing hospitalization, with a lack of benefit seen in individuals ages 18 to 49 years and those 65 and older.3
Vaccination was associated with increased rates of hospitalizations from infections cause by H3N2. It is not known if this finding was due to chance, unstable results from small numbers, an unknown bias, or some biological cause not yet understood. This is a topic of ongoing research.
Effectiveness in preventing pediatric hospitalizations was estimated at 31%, again with no effectiveness against H3N2.3 The estimate of vaccine effectiveness in the United States was similar to that in Canada.2
While these results are much lower than desired, influenza vaccine did prevent an estimated 40,000 to 90,000 hospitalizations and decreased influenza-like illnesses by 44%.3
Continue to: A look at vaccine safety
A look at vaccine safety
Numerous studies of influenza vaccine safety were presented at the June 2019 meeting of the Advisory Committee on Immunization Practices (ACIP).4 These studies included assessments using the Vaccine Adverse Events Reporting System; the Vaccine Safety Datalink (VSD), which conducts ongoing rapid analysis of adverse events throughout the influenza season; and Food and Drug Administration (FDA)-sponsored studies of Medicare patients. These vaccine safety monitoring systems have been described in a prior Practice Alert.5
Possible vaccine reactions studied included Guillain-Barre Syndrome (GBS), anaphylaxis, encephalitis, Bell’s palsy, febrile seizures, and pregnancy-related adverse events such as miscarriage and congenital anomalies. While preliminary safety signals were detected for anaphylaxis, Bell’s palsy, febrile seizures, and GBS, a more in-depth investigation found no association of any adverse events with vaccination except for febrile seizures, with an attributable risk of 4.24/100,000 doses in children ages 6 to 23 months and 1.8/100,000 in those ages 24 to 59 months.4 The incidence of febrile seizures was similar to that of previous seasons and primarily occurred when the vaccine was administered in conjunction with another vaccine. A preliminary FDA analysis found a small elevated risk of GBS with high-dose trivalent inactivated vaccine, with an attributable risk of 0.98 per million doses, but this was not confirmed by the VSD analysis.4
What you need to know about the upcoming season
ACIP recommendations on influenza vaccines for 2019 to 2020 are essentially unchanged from last year.6 All individuals ages 6 months and older, who do not have a contraindication, should receive a flu vaccine in the fall of 2019. The composition of this season’s vaccine contains new H1N1 and H3N2 variants to more closely match the circulating strains. ACIP has updated or clarified 4 logistical issues in this year’s recommendations:
- Four inactivated-influenza vaccines are now available for children ages 6 to 35 months. Dose volumes are not the same for all 4 (TABLE).7
- Vaccination is now encouraged for September or later for those requiring only 1 dose of vaccine. Earlier administration can result in waning immunity by the end of the flu season, especially in older adults.7
- Children ages 6 months to 8 years may require 2 doses if they haven’t received any previous influenza vaccine, and the second dose should be given even if the child turns 9 between doses 1 and 2.7
- One adjuvanted influenza vaccine containing MF59—the trivalent inactivated influenza vaccine, Fluad—is approved for those ages 65 years and older. One note of caution is that licensed vaccines for other conditions also contain new nonaluminum adjuvants and there are few data on the safety and effectiveness of simultaneous or sequential administration of Fluad with the 2 novel nonaluminum adjuvant-containing vaccines. These vaccines are the recombinant zoster subunit vaccine (Shingrix), which contains the liposome-based adjuvant ASO1, and the recombinant hepatitis B surface antigen vaccine (Heplisav-B), which contains cytosine phosphoguanine oligodeoxynucleotide. Given the lack of data and the availability of other influenza vaccine options, ACIP advises that selecting a nonadjuvanted influenza vaccine may be the best option when an older adult needs both an influenza vaccine and either Shingrix or Heplisav-B. However, do not delay giving any vaccine if a specific alternate product is unavailable.7
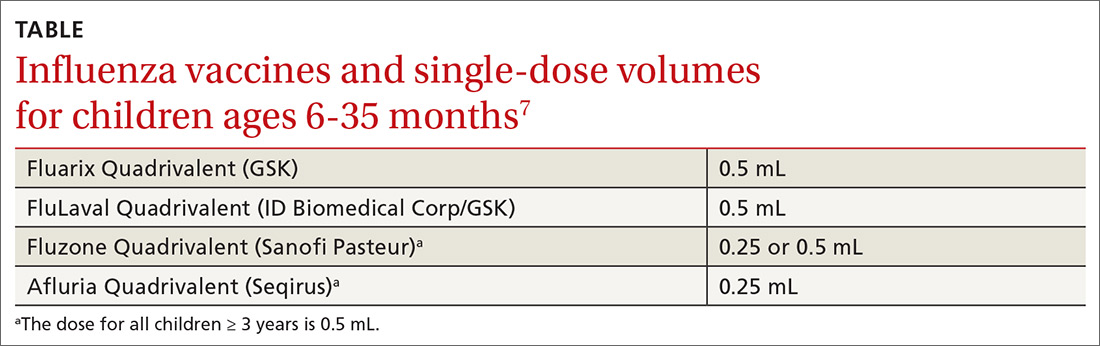
All recommendations concerning the use of influenza vaccine for the 2019-2020 influenza season and a listing of all available influenza vaccine products can be found on the ACIP Web site (cdc.gov/vaccines/acip/index.html) or in the Morbidity and Mortality Weekly Report.8
1. Brammer L. Influenza Surveillance Update. Presented to the ACIP June 27, 2019. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2019-06/flu-2-Brammer-508.pdf. Accessed August 21, 2019.
2. Hammond A, Hundal K, Laurenson-Shafer H, et al. Review of the 2018–2019 influenza season in the northern hemisphere. WHO Wkly Epidemiol Record. 2019;94:345-364.
3. Flannery B, Chung J, Ferdinands J, et al. Preliminary estimates of the 2018-2019 seasonal influenza vaccine effectiveness against medically attended influenza from three U.S. networks. Presented to ACIP June 27, 2019. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2019-06/flu-3-flannery-508.pdf. Accessed August 21, 2019.
4. Shimabukuro T. End-of-season update: 2018-2019 influenza vaccine safety monitoring. Presented to the ACIP meeting June 27, 2019. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2019-06/flu-4-Shimabukuro-508.pdf. Accessed August 21, 2019.
5. Campos-Outcalt D. Facts to help you keep pace with the vaccine conversation. J Fam Pract. 2019;68:341-346.
6. Campos-Outcalt D. CDC recommendations for the 2018-2019 influenza season. J Fam Pract. 2018;67:550-553.
7. Grohskopf L. Influenza work group considerations and proposed 2019-2020 season recommendations. Presented to the ACIP June 27, 2019. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2019-06/flu-5-grohskopf-508.pdf. Accessed August 21, 2019.
8. Grohskopf LA, Alyanak E, Broder KR, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices —United States, 2019-20 influenza season. MMWR Recomm Rep. 2019;68:1-21.
2018-2019 season retrospective
Last year’s influenza season was longer than usual. Infections, as measured by the percentage of outpatient visits due to influenza-like illness, increased in early November 2018, peaked in early February to mid-March of 2019, and remained above baseline levels through mid-May.1,2 Ninety six percent of influenza-positive samples were influenza A,1 and 57% of those were H1N1.2 In the second half of the season, H3N2 became the predominant circulating virus and there was a genetic shift in this strain that caused a decrease in the effectiveness of influenza vaccines (FIGURE).1 The influenza-confirmed hospitalization rate was 65.3/100,000, with the highest rate (221.7/100,000) occurring among those 65 years of age and older.2 Of those hospitalized with influenza, 93% of adults and 55% of children had an underlying medical condition and 29% of women of childbearing age were pregnant.2
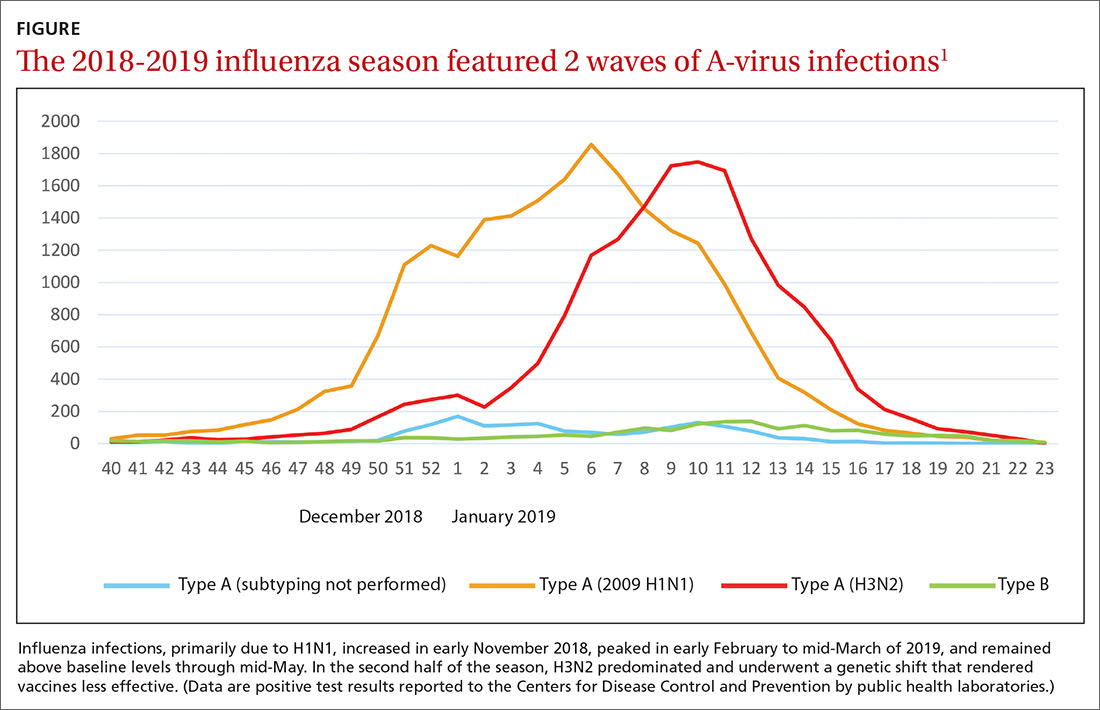
Morbidity and mortality from influenza during the 2018-2019 influenza season were moderate compared with previous years. Pneumonia and influenza mortality reached close to 8% of all deaths during the peak of the season (considered a modest peak), but stayed above the epidemic threshold for 10 weeks.2 There were 119 pediatric deaths.1 Overall, in the United States, there were an estimated 37 to 43 million influenza-related illnesses, 17 to 20 million flu-related medical visits, 531,000 to 647,000 flu-related hospitalizations, and 36,400 to 61,200 deaths.1
Influenza viral resistance to oseltamivir remained very low throughout the season for both A and B viruses.2
Vaccine effectiveness was subpar
The effectiveness of influenza vaccine last season was disappointing. When assessed using laboratory-confirmed medically attended influenza, the vaccine was 29% effective; when assessed by age group, the confidence intervals included 0 in ages 9 to 17 years and 50 years and older.3 In the age group 6 months to 8 years, the vaccine was 49% effective.3 The vaccine was not effective against the predominant H3N2 strain circulating. It was 25% effective in preventing hospitalization, with a lack of benefit seen in individuals ages 18 to 49 years and those 65 and older.3
Vaccination was associated with increased rates of hospitalizations from infections cause by H3N2. It is not known if this finding was due to chance, unstable results from small numbers, an unknown bias, or some biological cause not yet understood. This is a topic of ongoing research.
Effectiveness in preventing pediatric hospitalizations was estimated at 31%, again with no effectiveness against H3N2.3 The estimate of vaccine effectiveness in the United States was similar to that in Canada.2
While these results are much lower than desired, influenza vaccine did prevent an estimated 40,000 to 90,000 hospitalizations and decreased influenza-like illnesses by 44%.3
Continue to: A look at vaccine safety
A look at vaccine safety
Numerous studies of influenza vaccine safety were presented at the June 2019 meeting of the Advisory Committee on Immunization Practices (ACIP).4 These studies included assessments using the Vaccine Adverse Events Reporting System; the Vaccine Safety Datalink (VSD), which conducts ongoing rapid analysis of adverse events throughout the influenza season; and Food and Drug Administration (FDA)-sponsored studies of Medicare patients. These vaccine safety monitoring systems have been described in a prior Practice Alert.5
Possible vaccine reactions studied included Guillain-Barre Syndrome (GBS), anaphylaxis, encephalitis, Bell’s palsy, febrile seizures, and pregnancy-related adverse events such as miscarriage and congenital anomalies. While preliminary safety signals were detected for anaphylaxis, Bell’s palsy, febrile seizures, and GBS, a more in-depth investigation found no association of any adverse events with vaccination except for febrile seizures, with an attributable risk of 4.24/100,000 doses in children ages 6 to 23 months and 1.8/100,000 in those ages 24 to 59 months.4 The incidence of febrile seizures was similar to that of previous seasons and primarily occurred when the vaccine was administered in conjunction with another vaccine. A preliminary FDA analysis found a small elevated risk of GBS with high-dose trivalent inactivated vaccine, with an attributable risk of 0.98 per million doses, but this was not confirmed by the VSD analysis.4
What you need to know about the upcoming season
ACIP recommendations on influenza vaccines for 2019 to 2020 are essentially unchanged from last year.6 All individuals ages 6 months and older, who do not have a contraindication, should receive a flu vaccine in the fall of 2019. The composition of this season’s vaccine contains new H1N1 and H3N2 variants to more closely match the circulating strains. ACIP has updated or clarified 4 logistical issues in this year’s recommendations:
- Four inactivated-influenza vaccines are now available for children ages 6 to 35 months. Dose volumes are not the same for all 4 (TABLE).7
- Vaccination is now encouraged for September or later for those requiring only 1 dose of vaccine. Earlier administration can result in waning immunity by the end of the flu season, especially in older adults.7
- Children ages 6 months to 8 years may require 2 doses if they haven’t received any previous influenza vaccine, and the second dose should be given even if the child turns 9 between doses 1 and 2.7
- One adjuvanted influenza vaccine containing MF59—the trivalent inactivated influenza vaccine, Fluad—is approved for those ages 65 years and older. One note of caution is that licensed vaccines for other conditions also contain new nonaluminum adjuvants and there are few data on the safety and effectiveness of simultaneous or sequential administration of Fluad with the 2 novel nonaluminum adjuvant-containing vaccines. These vaccines are the recombinant zoster subunit vaccine (Shingrix), which contains the liposome-based adjuvant ASO1, and the recombinant hepatitis B surface antigen vaccine (Heplisav-B), which contains cytosine phosphoguanine oligodeoxynucleotide. Given the lack of data and the availability of other influenza vaccine options, ACIP advises that selecting a nonadjuvanted influenza vaccine may be the best option when an older adult needs both an influenza vaccine and either Shingrix or Heplisav-B. However, do not delay giving any vaccine if a specific alternate product is unavailable.7
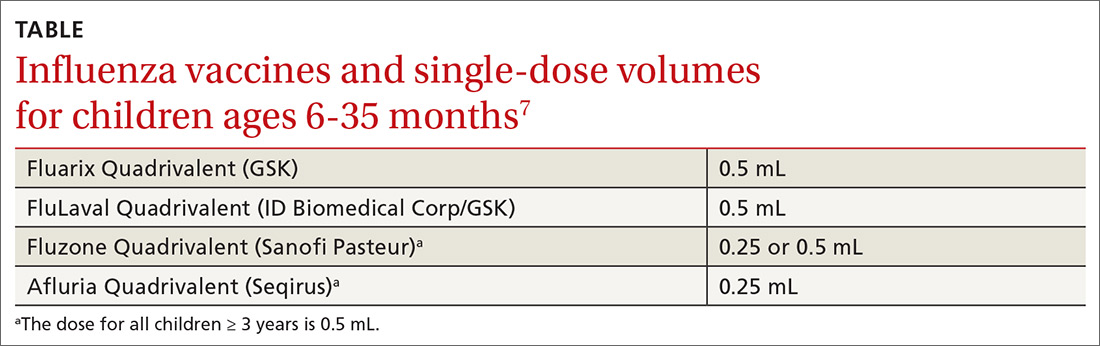
All recommendations concerning the use of influenza vaccine for the 2019-2020 influenza season and a listing of all available influenza vaccine products can be found on the ACIP Web site (cdc.gov/vaccines/acip/index.html) or in the Morbidity and Mortality Weekly Report.8
2018-2019 season retrospective
Last year’s influenza season was longer than usual. Infections, as measured by the percentage of outpatient visits due to influenza-like illness, increased in early November 2018, peaked in early February to mid-March of 2019, and remained above baseline levels through mid-May.1,2 Ninety six percent of influenza-positive samples were influenza A,1 and 57% of those were H1N1.2 In the second half of the season, H3N2 became the predominant circulating virus and there was a genetic shift in this strain that caused a decrease in the effectiveness of influenza vaccines (FIGURE).1 The influenza-confirmed hospitalization rate was 65.3/100,000, with the highest rate (221.7/100,000) occurring among those 65 years of age and older.2 Of those hospitalized with influenza, 93% of adults and 55% of children had an underlying medical condition and 29% of women of childbearing age were pregnant.2
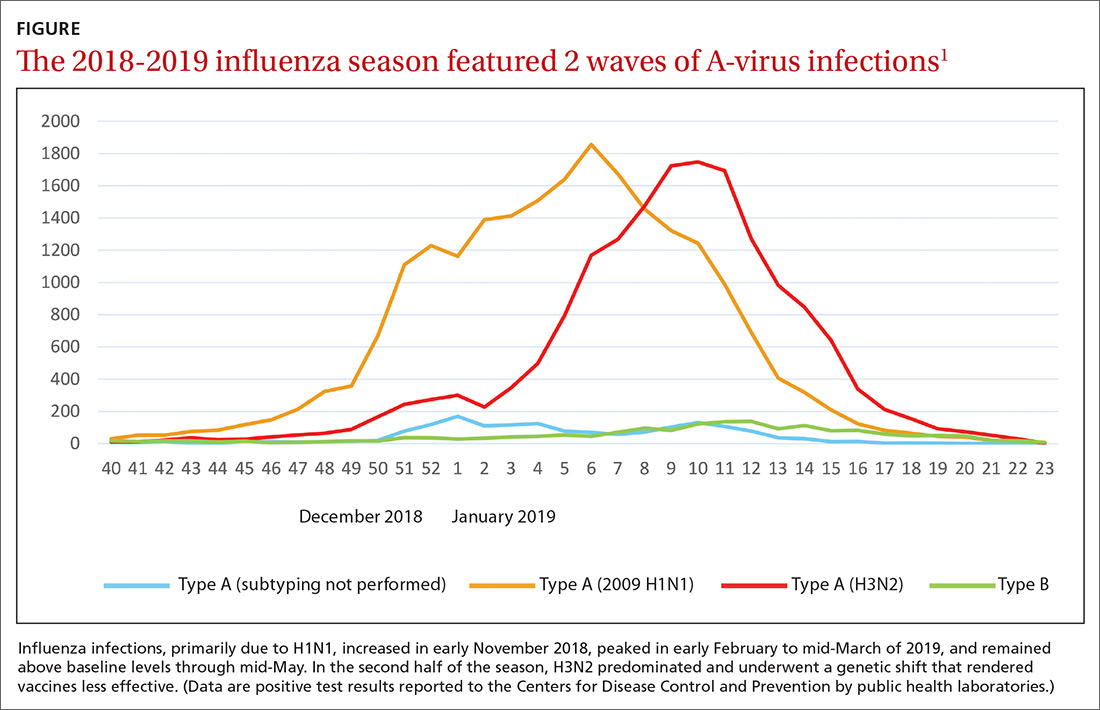
Morbidity and mortality from influenza during the 2018-2019 influenza season were moderate compared with previous years. Pneumonia and influenza mortality reached close to 8% of all deaths during the peak of the season (considered a modest peak), but stayed above the epidemic threshold for 10 weeks.2 There were 119 pediatric deaths.1 Overall, in the United States, there were an estimated 37 to 43 million influenza-related illnesses, 17 to 20 million flu-related medical visits, 531,000 to 647,000 flu-related hospitalizations, and 36,400 to 61,200 deaths.1
Influenza viral resistance to oseltamivir remained very low throughout the season for both A and B viruses.2
Vaccine effectiveness was subpar
The effectiveness of influenza vaccine last season was disappointing. When assessed using laboratory-confirmed medically attended influenza, the vaccine was 29% effective; when assessed by age group, the confidence intervals included 0 in ages 9 to 17 years and 50 years and older.3 In the age group 6 months to 8 years, the vaccine was 49% effective.3 The vaccine was not effective against the predominant H3N2 strain circulating. It was 25% effective in preventing hospitalization, with a lack of benefit seen in individuals ages 18 to 49 years and those 65 and older.3
Vaccination was associated with increased rates of hospitalizations from infections cause by H3N2. It is not known if this finding was due to chance, unstable results from small numbers, an unknown bias, or some biological cause not yet understood. This is a topic of ongoing research.
Effectiveness in preventing pediatric hospitalizations was estimated at 31%, again with no effectiveness against H3N2.3 The estimate of vaccine effectiveness in the United States was similar to that in Canada.2
While these results are much lower than desired, influenza vaccine did prevent an estimated 40,000 to 90,000 hospitalizations and decreased influenza-like illnesses by 44%.3
Continue to: A look at vaccine safety
A look at vaccine safety
Numerous studies of influenza vaccine safety were presented at the June 2019 meeting of the Advisory Committee on Immunization Practices (ACIP).4 These studies included assessments using the Vaccine Adverse Events Reporting System; the Vaccine Safety Datalink (VSD), which conducts ongoing rapid analysis of adverse events throughout the influenza season; and Food and Drug Administration (FDA)-sponsored studies of Medicare patients. These vaccine safety monitoring systems have been described in a prior Practice Alert.5
Possible vaccine reactions studied included Guillain-Barre Syndrome (GBS), anaphylaxis, encephalitis, Bell’s palsy, febrile seizures, and pregnancy-related adverse events such as miscarriage and congenital anomalies. While preliminary safety signals were detected for anaphylaxis, Bell’s palsy, febrile seizures, and GBS, a more in-depth investigation found no association of any adverse events with vaccination except for febrile seizures, with an attributable risk of 4.24/100,000 doses in children ages 6 to 23 months and 1.8/100,000 in those ages 24 to 59 months.4 The incidence of febrile seizures was similar to that of previous seasons and primarily occurred when the vaccine was administered in conjunction with another vaccine. A preliminary FDA analysis found a small elevated risk of GBS with high-dose trivalent inactivated vaccine, with an attributable risk of 0.98 per million doses, but this was not confirmed by the VSD analysis.4
What you need to know about the upcoming season
ACIP recommendations on influenza vaccines for 2019 to 2020 are essentially unchanged from last year.6 All individuals ages 6 months and older, who do not have a contraindication, should receive a flu vaccine in the fall of 2019. The composition of this season’s vaccine contains new H1N1 and H3N2 variants to more closely match the circulating strains. ACIP has updated or clarified 4 logistical issues in this year’s recommendations:
- Four inactivated-influenza vaccines are now available for children ages 6 to 35 months. Dose volumes are not the same for all 4 (TABLE).7
- Vaccination is now encouraged for September or later for those requiring only 1 dose of vaccine. Earlier administration can result in waning immunity by the end of the flu season, especially in older adults.7
- Children ages 6 months to 8 years may require 2 doses if they haven’t received any previous influenza vaccine, and the second dose should be given even if the child turns 9 between doses 1 and 2.7
- One adjuvanted influenza vaccine containing MF59—the trivalent inactivated influenza vaccine, Fluad—is approved for those ages 65 years and older. One note of caution is that licensed vaccines for other conditions also contain new nonaluminum adjuvants and there are few data on the safety and effectiveness of simultaneous or sequential administration of Fluad with the 2 novel nonaluminum adjuvant-containing vaccines. These vaccines are the recombinant zoster subunit vaccine (Shingrix), which contains the liposome-based adjuvant ASO1, and the recombinant hepatitis B surface antigen vaccine (Heplisav-B), which contains cytosine phosphoguanine oligodeoxynucleotide. Given the lack of data and the availability of other influenza vaccine options, ACIP advises that selecting a nonadjuvanted influenza vaccine may be the best option when an older adult needs both an influenza vaccine and either Shingrix or Heplisav-B. However, do not delay giving any vaccine if a specific alternate product is unavailable.7
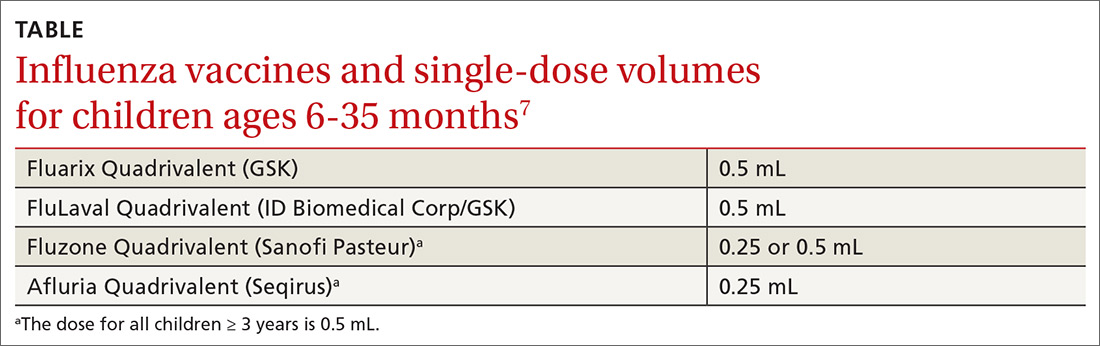
All recommendations concerning the use of influenza vaccine for the 2019-2020 influenza season and a listing of all available influenza vaccine products can be found on the ACIP Web site (cdc.gov/vaccines/acip/index.html) or in the Morbidity and Mortality Weekly Report.8
1. Brammer L. Influenza Surveillance Update. Presented to the ACIP June 27, 2019. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2019-06/flu-2-Brammer-508.pdf. Accessed August 21, 2019.
2. Hammond A, Hundal K, Laurenson-Shafer H, et al. Review of the 2018–2019 influenza season in the northern hemisphere. WHO Wkly Epidemiol Record. 2019;94:345-364.
3. Flannery B, Chung J, Ferdinands J, et al. Preliminary estimates of the 2018-2019 seasonal influenza vaccine effectiveness against medically attended influenza from three U.S. networks. Presented to ACIP June 27, 2019. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2019-06/flu-3-flannery-508.pdf. Accessed August 21, 2019.
4. Shimabukuro T. End-of-season update: 2018-2019 influenza vaccine safety monitoring. Presented to the ACIP meeting June 27, 2019. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2019-06/flu-4-Shimabukuro-508.pdf. Accessed August 21, 2019.
5. Campos-Outcalt D. Facts to help you keep pace with the vaccine conversation. J Fam Pract. 2019;68:341-346.
6. Campos-Outcalt D. CDC recommendations for the 2018-2019 influenza season. J Fam Pract. 2018;67:550-553.
7. Grohskopf L. Influenza work group considerations and proposed 2019-2020 season recommendations. Presented to the ACIP June 27, 2019. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2019-06/flu-5-grohskopf-508.pdf. Accessed August 21, 2019.
8. Grohskopf LA, Alyanak E, Broder KR, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices —United States, 2019-20 influenza season. MMWR Recomm Rep. 2019;68:1-21.
1. Brammer L. Influenza Surveillance Update. Presented to the ACIP June 27, 2019. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2019-06/flu-2-Brammer-508.pdf. Accessed August 21, 2019.
2. Hammond A, Hundal K, Laurenson-Shafer H, et al. Review of the 2018–2019 influenza season in the northern hemisphere. WHO Wkly Epidemiol Record. 2019;94:345-364.
3. Flannery B, Chung J, Ferdinands J, et al. Preliminary estimates of the 2018-2019 seasonal influenza vaccine effectiveness against medically attended influenza from three U.S. networks. Presented to ACIP June 27, 2019. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2019-06/flu-3-flannery-508.pdf. Accessed August 21, 2019.
4. Shimabukuro T. End-of-season update: 2018-2019 influenza vaccine safety monitoring. Presented to the ACIP meeting June 27, 2019. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2019-06/flu-4-Shimabukuro-508.pdf. Accessed August 21, 2019.
5. Campos-Outcalt D. Facts to help you keep pace with the vaccine conversation. J Fam Pract. 2019;68:341-346.
6. Campos-Outcalt D. CDC recommendations for the 2018-2019 influenza season. J Fam Pract. 2018;67:550-553.
7. Grohskopf L. Influenza work group considerations and proposed 2019-2020 season recommendations. Presented to the ACIP June 27, 2019. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2019-06/flu-5-grohskopf-508.pdf. Accessed August 21, 2019.
8. Grohskopf LA, Alyanak E, Broder KR, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices —United States, 2019-20 influenza season. MMWR Recomm Rep. 2019;68:1-21.