User login
Highlights from AGA’s FDA engagement
AGA members and staff worked closely with representatives across the FDA on a number of key issues impacting gastroenterologists including duodenoscope reprocessing, fecal microbiota transplantation and new drug approvals for GI indications.
Center for Devices and Radiological Health (CDRH). The issue of duodenoscope reprocessing regained national attention when a safety communication issued by CDRH was covered by the New York Times.
The safety communication had noted that about one in 20 samples collected from reprocessed duodenoscopes tested positive for high-concern organisms such as E. coli and Pseudomonas aeruginosa.
AGA partnered with ACG, ASGE and SGNA to develop a letter to the editor and provided insights to AGA members in subsequent communications. CDRH issued another safety communication in August recommending a transition to disposable-component duodenoscopes and convened a public advisory committee meeting in November where AGA gave public testimony including several overarching principles for the evolution of clinical practice focusing on patient safety and outcomes. AGA has been at the forefront of this issue since risk of infection transmission during ERCP first came to light in 2015, and we will continue to work closely with FDA and industry to ensure solutions, like the recently approved disposable scopes and parts, meet the needs of our members.
Center for Biologics Evaluation and Research (CBER). Though it is not an approved therapy for Clostridioides difficile infection (CDI), FDA permits the use of fecal microbiota transplantation (FMT) for CDI unresponsive to standard antibiotic therapies under a temporary “enforcement policy” that has been in place since 2013. In response to concerns from the physician community that patient access to FMT may be discontinued once manufactured microbiota-based products come to market, AGA reengaged CBER in dialogue about the future of FMT through a meeting with CBER Director Peter Marks and eight senior CBER officials. In response to a June safety alert reporting a patient death from FMT using donor stool that was not screened for extended-spectrum beta-lactamase (ESBL)-producing E. coli, AGA requested clarification from CBER on new donor screening requirements announced for those who hold investigational new drug permits for FMT. Most recently, AGA was the only professional society to give public testimony at a November public hearing on the use of FMT to treat CDI. AGA will continue to engage CBER as the agency works to finalize its policy on FMT.
Center for Drug Evaluation and Research (CDER). AGA organized two joint scientific sessions at Digestive Disease Week® 2019 with representatives from CDER’s Division of Gastrointestinal and Inborn Errors Products: the inaugural FDA Town Hall and a session on controversies around measuring drug toxicity. The FDA Town Hall, which will continue at DDW 2020, featured four FDA speakers providing the data and rationale behind recent GI drug approvals. The session titled, “Controversies Around Measuring Drug Toxicity” gave FDA and gastroenterologists’ perspectives on 5-HT3 antagonists (e.g., alosetron) and 5-HT4 agonists (e.g., prucalopride), as well as proton pump inhibitors. These sessions aimed to promote an interchange of ideas among regulators, clinicians and pharmaceutical manufacturers to advance the development and use of new therapies for GI disorders.
AGA members and staff worked closely with representatives across the FDA on a number of key issues impacting gastroenterologists including duodenoscope reprocessing, fecal microbiota transplantation and new drug approvals for GI indications.
Center for Devices and Radiological Health (CDRH). The issue of duodenoscope reprocessing regained national attention when a safety communication issued by CDRH was covered by the New York Times.
The safety communication had noted that about one in 20 samples collected from reprocessed duodenoscopes tested positive for high-concern organisms such as E. coli and Pseudomonas aeruginosa.
AGA partnered with ACG, ASGE and SGNA to develop a letter to the editor and provided insights to AGA members in subsequent communications. CDRH issued another safety communication in August recommending a transition to disposable-component duodenoscopes and convened a public advisory committee meeting in November where AGA gave public testimony including several overarching principles for the evolution of clinical practice focusing on patient safety and outcomes. AGA has been at the forefront of this issue since risk of infection transmission during ERCP first came to light in 2015, and we will continue to work closely with FDA and industry to ensure solutions, like the recently approved disposable scopes and parts, meet the needs of our members.
Center for Biologics Evaluation and Research (CBER). Though it is not an approved therapy for Clostridioides difficile infection (CDI), FDA permits the use of fecal microbiota transplantation (FMT) for CDI unresponsive to standard antibiotic therapies under a temporary “enforcement policy” that has been in place since 2013. In response to concerns from the physician community that patient access to FMT may be discontinued once manufactured microbiota-based products come to market, AGA reengaged CBER in dialogue about the future of FMT through a meeting with CBER Director Peter Marks and eight senior CBER officials. In response to a June safety alert reporting a patient death from FMT using donor stool that was not screened for extended-spectrum beta-lactamase (ESBL)-producing E. coli, AGA requested clarification from CBER on new donor screening requirements announced for those who hold investigational new drug permits for FMT. Most recently, AGA was the only professional society to give public testimony at a November public hearing on the use of FMT to treat CDI. AGA will continue to engage CBER as the agency works to finalize its policy on FMT.
Center for Drug Evaluation and Research (CDER). AGA organized two joint scientific sessions at Digestive Disease Week® 2019 with representatives from CDER’s Division of Gastrointestinal and Inborn Errors Products: the inaugural FDA Town Hall and a session on controversies around measuring drug toxicity. The FDA Town Hall, which will continue at DDW 2020, featured four FDA speakers providing the data and rationale behind recent GI drug approvals. The session titled, “Controversies Around Measuring Drug Toxicity” gave FDA and gastroenterologists’ perspectives on 5-HT3 antagonists (e.g., alosetron) and 5-HT4 agonists (e.g., prucalopride), as well as proton pump inhibitors. These sessions aimed to promote an interchange of ideas among regulators, clinicians and pharmaceutical manufacturers to advance the development and use of new therapies for GI disorders.
AGA members and staff worked closely with representatives across the FDA on a number of key issues impacting gastroenterologists including duodenoscope reprocessing, fecal microbiota transplantation and new drug approvals for GI indications.
Center for Devices and Radiological Health (CDRH). The issue of duodenoscope reprocessing regained national attention when a safety communication issued by CDRH was covered by the New York Times.
The safety communication had noted that about one in 20 samples collected from reprocessed duodenoscopes tested positive for high-concern organisms such as E. coli and Pseudomonas aeruginosa.
AGA partnered with ACG, ASGE and SGNA to develop a letter to the editor and provided insights to AGA members in subsequent communications. CDRH issued another safety communication in August recommending a transition to disposable-component duodenoscopes and convened a public advisory committee meeting in November where AGA gave public testimony including several overarching principles for the evolution of clinical practice focusing on patient safety and outcomes. AGA has been at the forefront of this issue since risk of infection transmission during ERCP first came to light in 2015, and we will continue to work closely with FDA and industry to ensure solutions, like the recently approved disposable scopes and parts, meet the needs of our members.
Center for Biologics Evaluation and Research (CBER). Though it is not an approved therapy for Clostridioides difficile infection (CDI), FDA permits the use of fecal microbiota transplantation (FMT) for CDI unresponsive to standard antibiotic therapies under a temporary “enforcement policy” that has been in place since 2013. In response to concerns from the physician community that patient access to FMT may be discontinued once manufactured microbiota-based products come to market, AGA reengaged CBER in dialogue about the future of FMT through a meeting with CBER Director Peter Marks and eight senior CBER officials. In response to a June safety alert reporting a patient death from FMT using donor stool that was not screened for extended-spectrum beta-lactamase (ESBL)-producing E. coli, AGA requested clarification from CBER on new donor screening requirements announced for those who hold investigational new drug permits for FMT. Most recently, AGA was the only professional society to give public testimony at a November public hearing on the use of FMT to treat CDI. AGA will continue to engage CBER as the agency works to finalize its policy on FMT.
Center for Drug Evaluation and Research (CDER). AGA organized two joint scientific sessions at Digestive Disease Week® 2019 with representatives from CDER’s Division of Gastrointestinal and Inborn Errors Products: the inaugural FDA Town Hall and a session on controversies around measuring drug toxicity. The FDA Town Hall, which will continue at DDW 2020, featured four FDA speakers providing the data and rationale behind recent GI drug approvals. The session titled, “Controversies Around Measuring Drug Toxicity” gave FDA and gastroenterologists’ perspectives on 5-HT3 antagonists (e.g., alosetron) and 5-HT4 agonists (e.g., prucalopride), as well as proton pump inhibitors. These sessions aimed to promote an interchange of ideas among regulators, clinicians and pharmaceutical manufacturers to advance the development and use of new therapies for GI disorders.
Many children who present to headache clinics have joint hypermobility
Key clinical point: About one-quarter of pediatric patients with headache have joint hypermobility.
Major finding: Among children with headache and joint hypermobility, 80% had severe headache disability.
Study details: A prospective, single-center study of 76 children with headache.
Disclosures: The study was not supported by funding, and the investigators had no disclosures.
Citation: Sahjwani D et al. CNS 2019, Abstract 101.
Key clinical point: About one-quarter of pediatric patients with headache have joint hypermobility.
Major finding: Among children with headache and joint hypermobility, 80% had severe headache disability.
Study details: A prospective, single-center study of 76 children with headache.
Disclosures: The study was not supported by funding, and the investigators had no disclosures.
Citation: Sahjwani D et al. CNS 2019, Abstract 101.
Key clinical point: About one-quarter of pediatric patients with headache have joint hypermobility.
Major finding: Among children with headache and joint hypermobility, 80% had severe headache disability.
Study details: A prospective, single-center study of 76 children with headache.
Disclosures: The study was not supported by funding, and the investigators had no disclosures.
Citation: Sahjwani D et al. CNS 2019, Abstract 101.
Researchers seek to characterize pediatric new daily persistent headache
Key clinical point: New daily persistent headache may be relatively common among children presenting to headache clinics.
Major finding: Girls with new daily persistent headache report symptoms such as photophobia, phonophobia, and nausea significantly more frequently than boys do.
Study details: An observational study of 454 pediatric patients with new daily persistent headache.
Disclosures: The study was not supported by funding, and the investigators had no disclosures.
Citation: Pierce E et al. CNS 2019, Abstract 100.
Key clinical point: New daily persistent headache may be relatively common among children presenting to headache clinics.
Major finding: Girls with new daily persistent headache report symptoms such as photophobia, phonophobia, and nausea significantly more frequently than boys do.
Study details: An observational study of 454 pediatric patients with new daily persistent headache.
Disclosures: The study was not supported by funding, and the investigators had no disclosures.
Citation: Pierce E et al. CNS 2019, Abstract 100.
Key clinical point: New daily persistent headache may be relatively common among children presenting to headache clinics.
Major finding: Girls with new daily persistent headache report symptoms such as photophobia, phonophobia, and nausea significantly more frequently than boys do.
Study details: An observational study of 454 pediatric patients with new daily persistent headache.
Disclosures: The study was not supported by funding, and the investigators had no disclosures.
Citation: Pierce E et al. CNS 2019, Abstract 100.
Suicide rate higher than average for female clinicians
The suicide rate for women who provide health care is higher than that of all women of working age, while male health care practitioners are less likely to end their lives than working-age men as a whole, according to the Centers for Disease Control and Prevention.
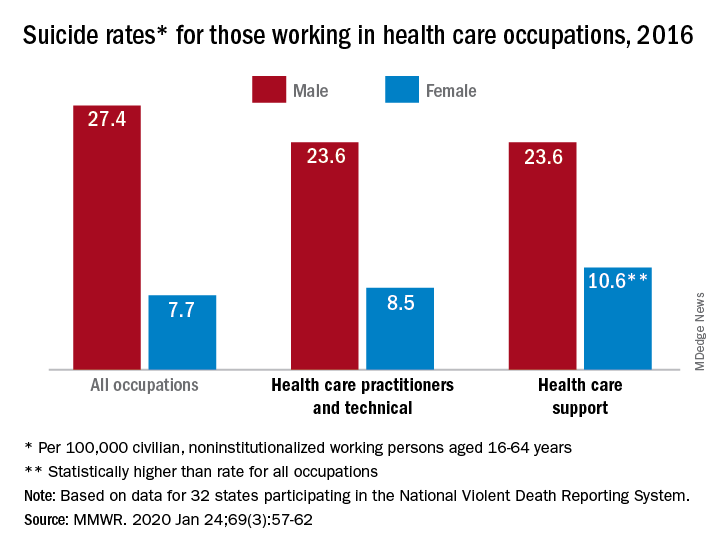
In 2016, the suicide rate for women classified as “healthcare practitioners and technical” – a category that includes physicians and surgeons, as well as chiropractors, physician assistants, and nurse practitioners – was 8.5 per 100,000 population, compared with 7.7 per 100,000 for all working women aged 16-64 years. That difference, however, was not statistically significant, Cora Peterson, PhD, and associates at the CDC said in the Morbidity and Mortality Weekly Report.
For females classified as “healthcare support” – medical assistants and transcriptionists, phlebotomists, and pharmacy aides – the suicide rate of 10.6 per 100,000 was significantly higher than that of all working women, the investigators noted.
The suicide rate for males in each of the two occupation categories was 23.6 per 100,000 population in 2016, lower than the rate of 27.4 per 100,000 for males of all occupations, they said, based on data from 32 states that participated in the 2016 National Violent Death Reporting System.
For males, the highest suicide rates in occupations meeting criteria for sample size were “construction and extraction” (49.4 per 100,000); “installation, maintenance, and repair” (36.9); and “arts, design, entertainment, sports, and media” (32.0). Among females, the highest rates were seen in “construction and extraction” (25.5 per 100,000), “protective service” (14.0), and “transportation and material moving” (12.5), with healthcare support next, Dr. Peterson and associates reported.
“Although relative comparisons of suicide rates in this manner are useful for prevention purposes, Therefore, all industry sectors and occupational groups can contribute to reducing suicide incidence,” they wrote.
SOURCE: Peterson C et al. MMWR. 2020 Jan 24;69(3):57-62.
The suicide rate for women who provide health care is higher than that of all women of working age, while male health care practitioners are less likely to end their lives than working-age men as a whole, according to the Centers for Disease Control and Prevention.
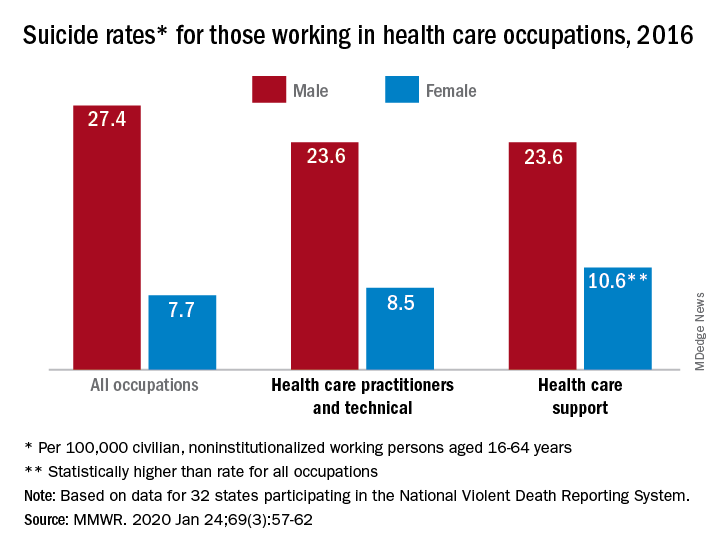
In 2016, the suicide rate for women classified as “healthcare practitioners and technical” – a category that includes physicians and surgeons, as well as chiropractors, physician assistants, and nurse practitioners – was 8.5 per 100,000 population, compared with 7.7 per 100,000 for all working women aged 16-64 years. That difference, however, was not statistically significant, Cora Peterson, PhD, and associates at the CDC said in the Morbidity and Mortality Weekly Report.
For females classified as “healthcare support” – medical assistants and transcriptionists, phlebotomists, and pharmacy aides – the suicide rate of 10.6 per 100,000 was significantly higher than that of all working women, the investigators noted.
The suicide rate for males in each of the two occupation categories was 23.6 per 100,000 population in 2016, lower than the rate of 27.4 per 100,000 for males of all occupations, they said, based on data from 32 states that participated in the 2016 National Violent Death Reporting System.
For males, the highest suicide rates in occupations meeting criteria for sample size were “construction and extraction” (49.4 per 100,000); “installation, maintenance, and repair” (36.9); and “arts, design, entertainment, sports, and media” (32.0). Among females, the highest rates were seen in “construction and extraction” (25.5 per 100,000), “protective service” (14.0), and “transportation and material moving” (12.5), with healthcare support next, Dr. Peterson and associates reported.
“Although relative comparisons of suicide rates in this manner are useful for prevention purposes, Therefore, all industry sectors and occupational groups can contribute to reducing suicide incidence,” they wrote.
SOURCE: Peterson C et al. MMWR. 2020 Jan 24;69(3):57-62.
The suicide rate for women who provide health care is higher than that of all women of working age, while male health care practitioners are less likely to end their lives than working-age men as a whole, according to the Centers for Disease Control and Prevention.
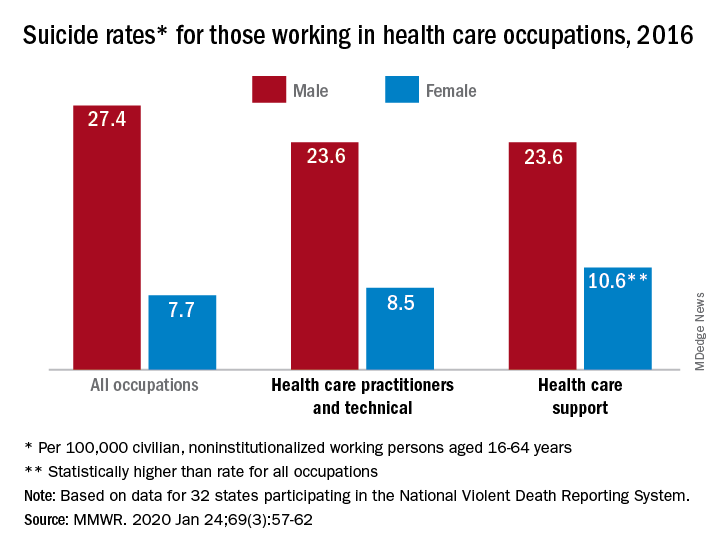
In 2016, the suicide rate for women classified as “healthcare practitioners and technical” – a category that includes physicians and surgeons, as well as chiropractors, physician assistants, and nurse practitioners – was 8.5 per 100,000 population, compared with 7.7 per 100,000 for all working women aged 16-64 years. That difference, however, was not statistically significant, Cora Peterson, PhD, and associates at the CDC said in the Morbidity and Mortality Weekly Report.
For females classified as “healthcare support” – medical assistants and transcriptionists, phlebotomists, and pharmacy aides – the suicide rate of 10.6 per 100,000 was significantly higher than that of all working women, the investigators noted.
The suicide rate for males in each of the two occupation categories was 23.6 per 100,000 population in 2016, lower than the rate of 27.4 per 100,000 for males of all occupations, they said, based on data from 32 states that participated in the 2016 National Violent Death Reporting System.
For males, the highest suicide rates in occupations meeting criteria for sample size were “construction and extraction” (49.4 per 100,000); “installation, maintenance, and repair” (36.9); and “arts, design, entertainment, sports, and media” (32.0). Among females, the highest rates were seen in “construction and extraction” (25.5 per 100,000), “protective service” (14.0), and “transportation and material moving” (12.5), with healthcare support next, Dr. Peterson and associates reported.
“Although relative comparisons of suicide rates in this manner are useful for prevention purposes, Therefore, all industry sectors and occupational groups can contribute to reducing suicide incidence,” they wrote.
SOURCE: Peterson C et al. MMWR. 2020 Jan 24;69(3):57-62.
FROM MMWR
Ubrogepant May Relieve Migraine Pain at 2 Hours
Key clinical point: Ubrogepant, an oral calcitonin gene–related peptide (CGRP)–receptor antagonist, may relieve patients’ migraine pain and their most bothersome associated symptom, such as photophobia, phonophobia, or nausea, at 2 hours after acute treatment.
Major finding: At 2 hours, pain freedom was reported by 101 of 464 participants in the ubrogepant 50-mg group (21.8%), 90 of 435 in the ubrogepant 25-mg group (20.7%), and 65 of 456 in the placebo group (14.3%).
Study details: ACHIEVE II was a randomized, double-blind, placebo-controlled, single-attack clinical trial that included more than 1,300 adults with migraine.
Disclosures: The trial was sponsored by Allergan, the company developing the drug. Several authors are Allergan employees. Dr. Lipton is a consultant, advisory board member, or has received honoraria from Allergan and other companies.
Citation: Lipton RB et al. JAMA. 2019;322(19):1887-98. doi: 10.1001/jama.2019.16711.
Key clinical point: Ubrogepant, an oral calcitonin gene–related peptide (CGRP)–receptor antagonist, may relieve patients’ migraine pain and their most bothersome associated symptom, such as photophobia, phonophobia, or nausea, at 2 hours after acute treatment.
Major finding: At 2 hours, pain freedom was reported by 101 of 464 participants in the ubrogepant 50-mg group (21.8%), 90 of 435 in the ubrogepant 25-mg group (20.7%), and 65 of 456 in the placebo group (14.3%).
Study details: ACHIEVE II was a randomized, double-blind, placebo-controlled, single-attack clinical trial that included more than 1,300 adults with migraine.
Disclosures: The trial was sponsored by Allergan, the company developing the drug. Several authors are Allergan employees. Dr. Lipton is a consultant, advisory board member, or has received honoraria from Allergan and other companies.
Citation: Lipton RB et al. JAMA. 2019;322(19):1887-98. doi: 10.1001/jama.2019.16711.
Key clinical point: Ubrogepant, an oral calcitonin gene–related peptide (CGRP)–receptor antagonist, may relieve patients’ migraine pain and their most bothersome associated symptom, such as photophobia, phonophobia, or nausea, at 2 hours after acute treatment.
Major finding: At 2 hours, pain freedom was reported by 101 of 464 participants in the ubrogepant 50-mg group (21.8%), 90 of 435 in the ubrogepant 25-mg group (20.7%), and 65 of 456 in the placebo group (14.3%).
Study details: ACHIEVE II was a randomized, double-blind, placebo-controlled, single-attack clinical trial that included more than 1,300 adults with migraine.
Disclosures: The trial was sponsored by Allergan, the company developing the drug. Several authors are Allergan employees. Dr. Lipton is a consultant, advisory board member, or has received honoraria from Allergan and other companies.
Citation: Lipton RB et al. JAMA. 2019;322(19):1887-98. doi: 10.1001/jama.2019.16711.
Headache may be a significant outcome of pediatric hemispherectomy
Key clinical point: Headache is a significant concern after pediatric hemispherectomy.
Major finding: Of 22 children who underwent hemispherectomy, 19 (86.4%) had headaches after the surgery.
Study details: A retrospective chart review and follow-up questionnaires that were administered to 22 children with hemispherectomy.
Citation: Pandit I et al. CNS 2019. Abstract 99.
Key clinical point: Headache is a significant concern after pediatric hemispherectomy.
Major finding: Of 22 children who underwent hemispherectomy, 19 (86.4%) had headaches after the surgery.
Study details: A retrospective chart review and follow-up questionnaires that were administered to 22 children with hemispherectomy.
Citation: Pandit I et al. CNS 2019. Abstract 99.
Key clinical point: Headache is a significant concern after pediatric hemispherectomy.
Major finding: Of 22 children who underwent hemispherectomy, 19 (86.4%) had headaches after the surgery.
Study details: A retrospective chart review and follow-up questionnaires that were administered to 22 children with hemispherectomy.
Citation: Pandit I et al. CNS 2019. Abstract 99.
New nomogram better predicts bladder cancer risk
A new and simple nomogram for predicting the risk of bladder cancer in patients with microscopic hematuria could optimize the diagnostic work up process, according to a recent study.
The tool may help improve patient understanding about their risk of bladder cancer, as well as alleviate unnecessary diagnostic evaluations for some patients.
“The goal of this study was to identify objective clinical factors associated with a bladder cancer diagnosis and to use these factors to create a nomogram that accurately predicts risk of bladder cancer,” wrote Richard S. Matulewicz, MD, MS, of Northwestern University, Chicago, and colleagues in Urologic Oncology.
Researchers identified 4,178 patients with a new diagnosis of microscopic hematuria from 2007 to 2015. Data was collected from an enterprise data repository of the Northwestern Medicine healthcare system. Study participants who underwent a full microhematuria evaluation were randomized to either a training or validation subgroup. In the training cohort, logistic regression analysis was used to detect factors linked to the diagnosis of bladder cancer. In the model, receiver operating curves were built to predict a diagnosis of bladder cancer among participants. In addition, calibration plots were computed for both subgroups to evaluate the discriminative ability of the model. After analysis, the researchers found significant differences in urinalysis results and demographics among patients with and without a diagnosis of bladder cancer. Patients with bladder cancer had a higher amount of microhematuria (RBC/hpf) on urinalysis (P less than .0001), were more likely previous or current smokers (P = .001), were more often male (68.2% vs. 49.7%; P = .0002), and were older (69.1 vs. 58.2 years; P less than .0001).
With respect to the predictive ability of the model, the area under the curve (AUC) in the training and validation set was 0.79 (95% confidence interval, 0.75-0.83) and 0.74 (95% CI, 0.67-0.80), respectively.
In addition, calibration plots demonstrated that the tool was able to predict the risk of bladder cancer diagnosis for patients with a probability of 0.3 or below.
“These results indicate that the model works best for a range of probabilities of (0-0.30), which is the vast majority of patients clinically and in our data,” the researchers explained.
The team acknowledged that characterizing risk beyond these levels should be done with caution given poor calibration beyond this threshold.
“External validation [of the model] and continued evolution of risk stratification models are needed,” they concluded.
The study was funded by the National Institutes of Health and the American Association of Medical Colleges. The authors reported having no conflicts of interest.
SOURCE: Matulewicz RS et al. Urol Oncol. 2020 Jan 14. doi: 10.1016/j.urolonc.2019.12.010.
A new and simple nomogram for predicting the risk of bladder cancer in patients with microscopic hematuria could optimize the diagnostic work up process, according to a recent study.
The tool may help improve patient understanding about their risk of bladder cancer, as well as alleviate unnecessary diagnostic evaluations for some patients.
“The goal of this study was to identify objective clinical factors associated with a bladder cancer diagnosis and to use these factors to create a nomogram that accurately predicts risk of bladder cancer,” wrote Richard S. Matulewicz, MD, MS, of Northwestern University, Chicago, and colleagues in Urologic Oncology.
Researchers identified 4,178 patients with a new diagnosis of microscopic hematuria from 2007 to 2015. Data was collected from an enterprise data repository of the Northwestern Medicine healthcare system. Study participants who underwent a full microhematuria evaluation were randomized to either a training or validation subgroup. In the training cohort, logistic regression analysis was used to detect factors linked to the diagnosis of bladder cancer. In the model, receiver operating curves were built to predict a diagnosis of bladder cancer among participants. In addition, calibration plots were computed for both subgroups to evaluate the discriminative ability of the model. After analysis, the researchers found significant differences in urinalysis results and demographics among patients with and without a diagnosis of bladder cancer. Patients with bladder cancer had a higher amount of microhematuria (RBC/hpf) on urinalysis (P less than .0001), were more likely previous or current smokers (P = .001), were more often male (68.2% vs. 49.7%; P = .0002), and were older (69.1 vs. 58.2 years; P less than .0001).
With respect to the predictive ability of the model, the area under the curve (AUC) in the training and validation set was 0.79 (95% confidence interval, 0.75-0.83) and 0.74 (95% CI, 0.67-0.80), respectively.
In addition, calibration plots demonstrated that the tool was able to predict the risk of bladder cancer diagnosis for patients with a probability of 0.3 or below.
“These results indicate that the model works best for a range of probabilities of (0-0.30), which is the vast majority of patients clinically and in our data,” the researchers explained.
The team acknowledged that characterizing risk beyond these levels should be done with caution given poor calibration beyond this threshold.
“External validation [of the model] and continued evolution of risk stratification models are needed,” they concluded.
The study was funded by the National Institutes of Health and the American Association of Medical Colleges. The authors reported having no conflicts of interest.
SOURCE: Matulewicz RS et al. Urol Oncol. 2020 Jan 14. doi: 10.1016/j.urolonc.2019.12.010.
A new and simple nomogram for predicting the risk of bladder cancer in patients with microscopic hematuria could optimize the diagnostic work up process, according to a recent study.
The tool may help improve patient understanding about their risk of bladder cancer, as well as alleviate unnecessary diagnostic evaluations for some patients.
“The goal of this study was to identify objective clinical factors associated with a bladder cancer diagnosis and to use these factors to create a nomogram that accurately predicts risk of bladder cancer,” wrote Richard S. Matulewicz, MD, MS, of Northwestern University, Chicago, and colleagues in Urologic Oncology.
Researchers identified 4,178 patients with a new diagnosis of microscopic hematuria from 2007 to 2015. Data was collected from an enterprise data repository of the Northwestern Medicine healthcare system. Study participants who underwent a full microhematuria evaluation were randomized to either a training or validation subgroup. In the training cohort, logistic regression analysis was used to detect factors linked to the diagnosis of bladder cancer. In the model, receiver operating curves were built to predict a diagnosis of bladder cancer among participants. In addition, calibration plots were computed for both subgroups to evaluate the discriminative ability of the model. After analysis, the researchers found significant differences in urinalysis results and demographics among patients with and without a diagnosis of bladder cancer. Patients with bladder cancer had a higher amount of microhematuria (RBC/hpf) on urinalysis (P less than .0001), were more likely previous or current smokers (P = .001), were more often male (68.2% vs. 49.7%; P = .0002), and were older (69.1 vs. 58.2 years; P less than .0001).
With respect to the predictive ability of the model, the area under the curve (AUC) in the training and validation set was 0.79 (95% confidence interval, 0.75-0.83) and 0.74 (95% CI, 0.67-0.80), respectively.
In addition, calibration plots demonstrated that the tool was able to predict the risk of bladder cancer diagnosis for patients with a probability of 0.3 or below.
“These results indicate that the model works best for a range of probabilities of (0-0.30), which is the vast majority of patients clinically and in our data,” the researchers explained.
The team acknowledged that characterizing risk beyond these levels should be done with caution given poor calibration beyond this threshold.
“External validation [of the model] and continued evolution of risk stratification models are needed,” they concluded.
The study was funded by the National Institutes of Health and the American Association of Medical Colleges. The authors reported having no conflicts of interest.
SOURCE: Matulewicz RS et al. Urol Oncol. 2020 Jan 14. doi: 10.1016/j.urolonc.2019.12.010.
FROM UROLOGIC ONCOLOGY
Late-Onset MS is Often More Severe Than Earlier-Onset MS
Adolescent Lung Inflammation May Trigger Later MS
Key clinical point: Inflammatory pulmonary events occurring at age 11-15 years may be a risk factor for subsequent multiple sclerosis.
Major finding: Swedes who experienced pneumonia at age 11-15 years had an adjusted 2.8-fold increased risk of MS later in life.
Study details: This Swedish national registry cohort study included 6,109 MS patients and 49,479 controls matched for age, gender, and locale.
Disclosures: The presenter reported receiving research funding from F. Hoffmann–La Roche, Novartis, and AstraZeneca and serving on an advisory board for IQVIA.
Citation: Montgomery S. ECTRIMS 2019, Abstract 270.
Key clinical point: Inflammatory pulmonary events occurring at age 11-15 years may be a risk factor for subsequent multiple sclerosis.
Major finding: Swedes who experienced pneumonia at age 11-15 years had an adjusted 2.8-fold increased risk of MS later in life.
Study details: This Swedish national registry cohort study included 6,109 MS patients and 49,479 controls matched for age, gender, and locale.
Disclosures: The presenter reported receiving research funding from F. Hoffmann–La Roche, Novartis, and AstraZeneca and serving on an advisory board for IQVIA.
Citation: Montgomery S. ECTRIMS 2019, Abstract 270.
Key clinical point: Inflammatory pulmonary events occurring at age 11-15 years may be a risk factor for subsequent multiple sclerosis.
Major finding: Swedes who experienced pneumonia at age 11-15 years had an adjusted 2.8-fold increased risk of MS later in life.
Study details: This Swedish national registry cohort study included 6,109 MS patients and 49,479 controls matched for age, gender, and locale.
Disclosures: The presenter reported receiving research funding from F. Hoffmann–La Roche, Novartis, and AstraZeneca and serving on an advisory board for IQVIA.
Citation: Montgomery S. ECTRIMS 2019, Abstract 270.
Creating best practices for APPs
A holistic approach to integration
Hospital medicine groups (HMGs) nationally are confronted with a host of challenging issues: increased patient volume/complexities, resident duty-hour restrictions, and a rise in provider burnout. Many are turning to advanced practice providers (APPs) to help lighten these burdens.
But no practical guidelines exist around how to successfully incorporate APPs in a way that meets the needs of the patients, the providers, the HMG, and the health system, according to Kasey Bowden, MSN, FNP, AG-ACNP, lead author of a HM19 abstract on that subject.
“Much of the recent literature around APP utilization involves descriptive anecdotes on how individual HMGs have utilized APPs, and what metrics this helped them to achieve,” she said. “While these stories are often compelling, they provide no tangible value to HMGs looking to incorporate APPs into practice, as they do not address unique elements that limit successful APP integration, including diverse educational backgrounds of APPs and exceedingly high turnover rates (12.6% nationally).”
Ms. Bowden and coauthors created a conceptual framework, which recognizes that, without taking a holistic approach, many HMGs will fail to successfully integrate APPs. “Our hope is that by utilizing this framework to define APP-physician best practices, we will be able to create a useful tool for all HMGs that will promote successful APP-physician collaborative practice models.”
She thinks that hospitalists could also use this framework to examine their current practice models and to see where there may be opportunity for improvement. For example, a group may look at their own APP turnover rate. “If turnover rate is high in the first year, it may suggest inadequate onboarding/training, if it is high after 3 years, this may suggest minimal opportunities for professional growth and advancement,” Ms. Bowden said. “I would love to see a consensus group form within SHM of physician and APP leaders to utilize this framework to establish ‘APP-Physician best practices,’ and create a guideline available to all HMGs so that they can successfully incorporate APPs into their practice,” she said.
Reference
1. Bowden K et al. Creation of APP-physician best practices: A necessary tool for the growing APP workforce. Hospital Medicine 2019, Abstract 436.
A holistic approach to integration
A holistic approach to integration
Hospital medicine groups (HMGs) nationally are confronted with a host of challenging issues: increased patient volume/complexities, resident duty-hour restrictions, and a rise in provider burnout. Many are turning to advanced practice providers (APPs) to help lighten these burdens.
But no practical guidelines exist around how to successfully incorporate APPs in a way that meets the needs of the patients, the providers, the HMG, and the health system, according to Kasey Bowden, MSN, FNP, AG-ACNP, lead author of a HM19 abstract on that subject.
“Much of the recent literature around APP utilization involves descriptive anecdotes on how individual HMGs have utilized APPs, and what metrics this helped them to achieve,” she said. “While these stories are often compelling, they provide no tangible value to HMGs looking to incorporate APPs into practice, as they do not address unique elements that limit successful APP integration, including diverse educational backgrounds of APPs and exceedingly high turnover rates (12.6% nationally).”
Ms. Bowden and coauthors created a conceptual framework, which recognizes that, without taking a holistic approach, many HMGs will fail to successfully integrate APPs. “Our hope is that by utilizing this framework to define APP-physician best practices, we will be able to create a useful tool for all HMGs that will promote successful APP-physician collaborative practice models.”
She thinks that hospitalists could also use this framework to examine their current practice models and to see where there may be opportunity for improvement. For example, a group may look at their own APP turnover rate. “If turnover rate is high in the first year, it may suggest inadequate onboarding/training, if it is high after 3 years, this may suggest minimal opportunities for professional growth and advancement,” Ms. Bowden said. “I would love to see a consensus group form within SHM of physician and APP leaders to utilize this framework to establish ‘APP-Physician best practices,’ and create a guideline available to all HMGs so that they can successfully incorporate APPs into their practice,” she said.
Reference
1. Bowden K et al. Creation of APP-physician best practices: A necessary tool for the growing APP workforce. Hospital Medicine 2019, Abstract 436.
Hospital medicine groups (HMGs) nationally are confronted with a host of challenging issues: increased patient volume/complexities, resident duty-hour restrictions, and a rise in provider burnout. Many are turning to advanced practice providers (APPs) to help lighten these burdens.
But no practical guidelines exist around how to successfully incorporate APPs in a way that meets the needs of the patients, the providers, the HMG, and the health system, according to Kasey Bowden, MSN, FNP, AG-ACNP, lead author of a HM19 abstract on that subject.
“Much of the recent literature around APP utilization involves descriptive anecdotes on how individual HMGs have utilized APPs, and what metrics this helped them to achieve,” she said. “While these stories are often compelling, they provide no tangible value to HMGs looking to incorporate APPs into practice, as they do not address unique elements that limit successful APP integration, including diverse educational backgrounds of APPs and exceedingly high turnover rates (12.6% nationally).”
Ms. Bowden and coauthors created a conceptual framework, which recognizes that, without taking a holistic approach, many HMGs will fail to successfully integrate APPs. “Our hope is that by utilizing this framework to define APP-physician best practices, we will be able to create a useful tool for all HMGs that will promote successful APP-physician collaborative practice models.”
She thinks that hospitalists could also use this framework to examine their current practice models and to see where there may be opportunity for improvement. For example, a group may look at their own APP turnover rate. “If turnover rate is high in the first year, it may suggest inadequate onboarding/training, if it is high after 3 years, this may suggest minimal opportunities for professional growth and advancement,” Ms. Bowden said. “I would love to see a consensus group form within SHM of physician and APP leaders to utilize this framework to establish ‘APP-Physician best practices,’ and create a guideline available to all HMGs so that they can successfully incorporate APPs into their practice,” she said.
Reference
1. Bowden K et al. Creation of APP-physician best practices: A necessary tool for the growing APP workforce. Hospital Medicine 2019, Abstract 436.

