User login
COVID-19: What now?
“There are decades where nothing happens,” wrote Vladimir Lenin, “and there are weeks where decades happen.” Barely a dozen weeks ago, no one knew that the SARS-CoV-2 virus existed. Now, it has spread to almost every country on Earth, infecting over 1.8 million people whom we know about, and many more whom we do not. In so doing, it has crashed economies and health care systems, filled hospitals, emptied public spaces, and separated people from their workplaces and their friends on a scale that few of us have ever witnessed.
It has also triggered an avalanche of questions as to why our initial response was so thoroughly lethargic, rudderless, and uncoordinated; while there is plenty of blame to go around, that is for another time. The glaring question for many – including physicians trying to keep our private practices viable – is: What now?
The answer depends, of course, on how the pandemic plays out. No one yet knows exactly what will happen, but much depends on two properties of the virus, both of which are currently unknown. First: seasonality. Coronaviruses tend to thrive in winter and wane in the summer. That may also be true for SARS-CoV-2, but seasonal variations might not sufficiently slow the virus when it has so many immunologically naive hosts to infect. As I write this in mid-April, we wait anxiously to see what – if anything – summer temperatures do to its transmission in the Northern Hemisphere.
The second wild card is duration of immunity. Determining that will involve developing accurate serologic tests and administering them widely. Immune citizens, once identified, can return to work, care for the vulnerable, and anchor the economy during future outbreaks.
Even if we do get a summer hiatus, seasonal viruses typically return as winter approaches. We could conceivably still be mopping up from this outbreak when the virus – if it is seasonal – comes roaring back in October or November. Will we be ready? Or will it catch us with our pants amidships yet again?
I can envision two possibilities: Assuming we luck into a seasonal reprieve in the next few weeks, infection rates should drop, which could allow our private practices to return toward some semblance of normal – if health workers and patients alike can be convinced that our offices and clinics are safe. This might be accomplished as part of our overall preparation for a potential winter recurrence, by checking every patient’s temperature at the waiting room door. Similarly, all students should get a daily temperature check at school, as should all commuters, airline passengers, and individuals at any sizable gathering. Every fever should trigger a COVID-19 test, and every positive test should launch aggressive contact tracing and quarantines. Meanwhile, treatments and vaccines should get fast-tracked.
That’s what should happen. If it doesn’t, and COVID-19 recurs next winter, worse than before, it is anybody’s guess whether most private medical practices will be able to weather a second onslaught. Further government funding is not assured. We won’t have a vaccine by November. Chloroquine, hydroxychloroquine, and azithromycin might turn out to be helpful, but we can’t count on them.
Even if we do get lucky with seasonality, the question remains of how long it will take to restore public confidence and reboot the economy. Economies generally do not function like light switches that can be turned off for a while then simply turned back on, but act more like campfires. If you pour a bucket of water on one, it takes some time to get it cranked up again. After the “Great Recession” of 2008, it took nearly 10 years.
So now, with great reluctance, I must trot out a hoary old cliché: Hope for the best, but plan for the worst. Everyone’s situation will be different, of course, but I can make a few general suggestions. Perform a difficult mental exercise: What will you do if SARS-CoV-2 outlasts emergency funds from the Paycheck Protection and Economic Injury Disaster programs? Do the math – how long can you keep your practice afloat without floating further loans or dipping into personal savings? If you don’t know how many patients you need to see per day to break even, figure it out – now. On what day will you run out of money? When will you start putting your future at risk?
None of us thought we would ever have to face questions like these, of course – and how ironic is it that a medical emergency has forced them upon us? I sincerely hope that none of us will need to actually confront this Hobson’s choice in the coming months, but far better to address the hypothetical now than the reality later. As always, consult with your own attorney, accountant, and other business advisors before making any life-altering decisions.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected]. He has no disclosures.
“There are decades where nothing happens,” wrote Vladimir Lenin, “and there are weeks where decades happen.” Barely a dozen weeks ago, no one knew that the SARS-CoV-2 virus existed. Now, it has spread to almost every country on Earth, infecting over 1.8 million people whom we know about, and many more whom we do not. In so doing, it has crashed economies and health care systems, filled hospitals, emptied public spaces, and separated people from their workplaces and their friends on a scale that few of us have ever witnessed.
It has also triggered an avalanche of questions as to why our initial response was so thoroughly lethargic, rudderless, and uncoordinated; while there is plenty of blame to go around, that is for another time. The glaring question for many – including physicians trying to keep our private practices viable – is: What now?
The answer depends, of course, on how the pandemic plays out. No one yet knows exactly what will happen, but much depends on two properties of the virus, both of which are currently unknown. First: seasonality. Coronaviruses tend to thrive in winter and wane in the summer. That may also be true for SARS-CoV-2, but seasonal variations might not sufficiently slow the virus when it has so many immunologically naive hosts to infect. As I write this in mid-April, we wait anxiously to see what – if anything – summer temperatures do to its transmission in the Northern Hemisphere.
The second wild card is duration of immunity. Determining that will involve developing accurate serologic tests and administering them widely. Immune citizens, once identified, can return to work, care for the vulnerable, and anchor the economy during future outbreaks.
Even if we do get a summer hiatus, seasonal viruses typically return as winter approaches. We could conceivably still be mopping up from this outbreak when the virus – if it is seasonal – comes roaring back in October or November. Will we be ready? Or will it catch us with our pants amidships yet again?
I can envision two possibilities: Assuming we luck into a seasonal reprieve in the next few weeks, infection rates should drop, which could allow our private practices to return toward some semblance of normal – if health workers and patients alike can be convinced that our offices and clinics are safe. This might be accomplished as part of our overall preparation for a potential winter recurrence, by checking every patient’s temperature at the waiting room door. Similarly, all students should get a daily temperature check at school, as should all commuters, airline passengers, and individuals at any sizable gathering. Every fever should trigger a COVID-19 test, and every positive test should launch aggressive contact tracing and quarantines. Meanwhile, treatments and vaccines should get fast-tracked.
That’s what should happen. If it doesn’t, and COVID-19 recurs next winter, worse than before, it is anybody’s guess whether most private medical practices will be able to weather a second onslaught. Further government funding is not assured. We won’t have a vaccine by November. Chloroquine, hydroxychloroquine, and azithromycin might turn out to be helpful, but we can’t count on them.
Even if we do get lucky with seasonality, the question remains of how long it will take to restore public confidence and reboot the economy. Economies generally do not function like light switches that can be turned off for a while then simply turned back on, but act more like campfires. If you pour a bucket of water on one, it takes some time to get it cranked up again. After the “Great Recession” of 2008, it took nearly 10 years.
So now, with great reluctance, I must trot out a hoary old cliché: Hope for the best, but plan for the worst. Everyone’s situation will be different, of course, but I can make a few general suggestions. Perform a difficult mental exercise: What will you do if SARS-CoV-2 outlasts emergency funds from the Paycheck Protection and Economic Injury Disaster programs? Do the math – how long can you keep your practice afloat without floating further loans or dipping into personal savings? If you don’t know how many patients you need to see per day to break even, figure it out – now. On what day will you run out of money? When will you start putting your future at risk?
None of us thought we would ever have to face questions like these, of course – and how ironic is it that a medical emergency has forced them upon us? I sincerely hope that none of us will need to actually confront this Hobson’s choice in the coming months, but far better to address the hypothetical now than the reality later. As always, consult with your own attorney, accountant, and other business advisors before making any life-altering decisions.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected]. He has no disclosures.
“There are decades where nothing happens,” wrote Vladimir Lenin, “and there are weeks where decades happen.” Barely a dozen weeks ago, no one knew that the SARS-CoV-2 virus existed. Now, it has spread to almost every country on Earth, infecting over 1.8 million people whom we know about, and many more whom we do not. In so doing, it has crashed economies and health care systems, filled hospitals, emptied public spaces, and separated people from their workplaces and their friends on a scale that few of us have ever witnessed.
It has also triggered an avalanche of questions as to why our initial response was so thoroughly lethargic, rudderless, and uncoordinated; while there is plenty of blame to go around, that is for another time. The glaring question for many – including physicians trying to keep our private practices viable – is: What now?
The answer depends, of course, on how the pandemic plays out. No one yet knows exactly what will happen, but much depends on two properties of the virus, both of which are currently unknown. First: seasonality. Coronaviruses tend to thrive in winter and wane in the summer. That may also be true for SARS-CoV-2, but seasonal variations might not sufficiently slow the virus when it has so many immunologically naive hosts to infect. As I write this in mid-April, we wait anxiously to see what – if anything – summer temperatures do to its transmission in the Northern Hemisphere.
The second wild card is duration of immunity. Determining that will involve developing accurate serologic tests and administering them widely. Immune citizens, once identified, can return to work, care for the vulnerable, and anchor the economy during future outbreaks.
Even if we do get a summer hiatus, seasonal viruses typically return as winter approaches. We could conceivably still be mopping up from this outbreak when the virus – if it is seasonal – comes roaring back in October or November. Will we be ready? Or will it catch us with our pants amidships yet again?
I can envision two possibilities: Assuming we luck into a seasonal reprieve in the next few weeks, infection rates should drop, which could allow our private practices to return toward some semblance of normal – if health workers and patients alike can be convinced that our offices and clinics are safe. This might be accomplished as part of our overall preparation for a potential winter recurrence, by checking every patient’s temperature at the waiting room door. Similarly, all students should get a daily temperature check at school, as should all commuters, airline passengers, and individuals at any sizable gathering. Every fever should trigger a COVID-19 test, and every positive test should launch aggressive contact tracing and quarantines. Meanwhile, treatments and vaccines should get fast-tracked.
That’s what should happen. If it doesn’t, and COVID-19 recurs next winter, worse than before, it is anybody’s guess whether most private medical practices will be able to weather a second onslaught. Further government funding is not assured. We won’t have a vaccine by November. Chloroquine, hydroxychloroquine, and azithromycin might turn out to be helpful, but we can’t count on them.
Even if we do get lucky with seasonality, the question remains of how long it will take to restore public confidence and reboot the economy. Economies generally do not function like light switches that can be turned off for a while then simply turned back on, but act more like campfires. If you pour a bucket of water on one, it takes some time to get it cranked up again. After the “Great Recession” of 2008, it took nearly 10 years.
So now, with great reluctance, I must trot out a hoary old cliché: Hope for the best, but plan for the worst. Everyone’s situation will be different, of course, but I can make a few general suggestions. Perform a difficult mental exercise: What will you do if SARS-CoV-2 outlasts emergency funds from the Paycheck Protection and Economic Injury Disaster programs? Do the math – how long can you keep your practice afloat without floating further loans or dipping into personal savings? If you don’t know how many patients you need to see per day to break even, figure it out – now. On what day will you run out of money? When will you start putting your future at risk?
None of us thought we would ever have to face questions like these, of course – and how ironic is it that a medical emergency has forced them upon us? I sincerely hope that none of us will need to actually confront this Hobson’s choice in the coming months, but far better to address the hypothetical now than the reality later. As always, consult with your own attorney, accountant, and other business advisors before making any life-altering decisions.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected]. He has no disclosures.
Treating rectal cancer in the COVID-19 era: Expert guidance
As the COVID-19 pandemic continues, minimizing risks of infection to patients with cancer while maintaining good outcomes remains a priority. An international panel of experts has now issued recommendations for treating patients with rectal cancer, which includes using a short pre-operative course of radiotherapy (SCRT) and then delaying surgery.
Using SCRT translates to fewer hospital appointments, which will keep patients safer and allow them to maintain social distancing. The panel also found that surgery can be safely delayed by up to 12 weeks, and thus will allow procedures to be rescheduled after the pandemic peaks.
“The COVID-19 pandemic is a global emergency and we needed to work very quickly to identify changes that would benefit patients,” said David Sebag-Montefiore, MD, a professor of clinical oncology at the University of Leeds and honorary clinical oncologist with the Leeds Teaching Hospitals NHS Trust, who led the 15 member panel. “Our recommendations were published 20 days after our first meeting.”
“This process normally takes many months, if not years,” he said in a statement.
The recommendations were published online April 2 in Radiotherapy and Oncology.
The panel used the European Society for Medical Oncology (ESMO) rectal cancer guidelines as a framework to describe these new recommendations.
Recommendations by Stage
The recommendations were categorized into four subgroups based on cancer stage.
Early stage
- The ESMO guidelines recommend total mesorectal excision (TME) surgery without pre-operative radiotherapy for most cases.
- Panel recommendation also strongly supports the use of TME without pre-operative radiotherapy.
Intermediate stage
- The ESMO guidelines recommend TME alone or combined with SCRT or conventional radiotherapy (CRT) if there is uncertainty that a good quality mesorectal excision can be achieved.
- The panel strongly recommends TME alone in regions where high quality surgery is performed. The use of radiotherapy in this subgroup requires careful discussion, as the benefits of preoperative radiotherapy are likely to be small. If radiotherapy is used, then the preferred option should be SCRT.
Locally advanced
- The ESMO guideline recommends either pre-operative SCRT or CRT.
- The panel strongly recommends the use of SCRT and notes two phase 3 trials have compared SCRT and CRT and showed comparable outcomes for local recurrence, disease-free survival, overall survival, and late toxicity. In the COVID-19 setting, the panel points out that SCRT has many advantages over CRT, namely that there is less acute toxicity, fewer treatments which translate to less travel and contact with other patients and staff, and a significantly reduced risk of COVID-19 infection during treatment.
Timing of surgery after SCRT
- The ESMO guideline does not have any recommendations as they were issued before the Stockholm III trial (Lancet Oncol. 2017;18:336-46).
- The panel notes that the use of SCRT and delaying surgery has advantages that can be beneficial in both routine clinical practice and the COVID-19 setting. Several clinical trials have recommended that surgery should be performed within 3-7 days of completing radiotherapy, but the Stockholm III trial reported no difference in outcomes when surgery was delayed. It compared surgery performed within 1 week versus 4-8 weeks following SCRT and there was no difference in any survival endpoints. In addition, a longer delay to surgery was associated with a reduction in post-operative and surgical morbidity although no differences in severe complications or re-operations.
Advanced subgroup
- The ESMO guidelines recommend the use of pre-operative CRT or SCRT followed by neoadjuvant chemotherapy. CRT should be given as a fluoropyrimidine (usually capecitabine) combined with radiotherapy of 45-50.4 Gy over 5-5.5 weeks. Adjuvant chemotherapy should be considered but there is wide international variation in its use.
- The panel recommends that two options be considered based on the current evidence. The first is pre-op CRT, which is the most established standard of care, with the duration of concurrent capecitabine chemotherapy limited to 5-5.5 weeks. The second option is SCRT with or without neoadjuvant chemotherapy. In this case, the duration of radiotherapy is substantially less and has advantages versus CRT. “We consider both options to be acceptable but note the advantages of using SCRT in the COVID-19 setting,” the authors write. “The decision to use neoadjuvant chemotherapy in option 2 will reflect the attitudes to neoadjuvant and adjuvant chemotherapy in each country, the assessment of the risk-benefit ratio, considering the risk factors for COVID-19 increased mortality, and the capacity and prioritization of chemotherapy delivery.”
Organ Preservation
Organ preservation is being increasingly considered when a complete clinical response is achieved after CRT or SCRT, the panel points out. “An organ preservation approach may be considered during the COVID-19 period providing that resources for an adequate surveillance including imaging and endoscopy are available to detect local failures that require salvage surgery,” they write.
This article first appeared on Medscape.com.
As the COVID-19 pandemic continues, minimizing risks of infection to patients with cancer while maintaining good outcomes remains a priority. An international panel of experts has now issued recommendations for treating patients with rectal cancer, which includes using a short pre-operative course of radiotherapy (SCRT) and then delaying surgery.
Using SCRT translates to fewer hospital appointments, which will keep patients safer and allow them to maintain social distancing. The panel also found that surgery can be safely delayed by up to 12 weeks, and thus will allow procedures to be rescheduled after the pandemic peaks.
“The COVID-19 pandemic is a global emergency and we needed to work very quickly to identify changes that would benefit patients,” said David Sebag-Montefiore, MD, a professor of clinical oncology at the University of Leeds and honorary clinical oncologist with the Leeds Teaching Hospitals NHS Trust, who led the 15 member panel. “Our recommendations were published 20 days after our first meeting.”
“This process normally takes many months, if not years,” he said in a statement.
The recommendations were published online April 2 in Radiotherapy and Oncology.
The panel used the European Society for Medical Oncology (ESMO) rectal cancer guidelines as a framework to describe these new recommendations.
Recommendations by Stage
The recommendations were categorized into four subgroups based on cancer stage.
Early stage
- The ESMO guidelines recommend total mesorectal excision (TME) surgery without pre-operative radiotherapy for most cases.
- Panel recommendation also strongly supports the use of TME without pre-operative radiotherapy.
Intermediate stage
- The ESMO guidelines recommend TME alone or combined with SCRT or conventional radiotherapy (CRT) if there is uncertainty that a good quality mesorectal excision can be achieved.
- The panel strongly recommends TME alone in regions where high quality surgery is performed. The use of radiotherapy in this subgroup requires careful discussion, as the benefits of preoperative radiotherapy are likely to be small. If radiotherapy is used, then the preferred option should be SCRT.
Locally advanced
- The ESMO guideline recommends either pre-operative SCRT or CRT.
- The panel strongly recommends the use of SCRT and notes two phase 3 trials have compared SCRT and CRT and showed comparable outcomes for local recurrence, disease-free survival, overall survival, and late toxicity. In the COVID-19 setting, the panel points out that SCRT has many advantages over CRT, namely that there is less acute toxicity, fewer treatments which translate to less travel and contact with other patients and staff, and a significantly reduced risk of COVID-19 infection during treatment.
Timing of surgery after SCRT
- The ESMO guideline does not have any recommendations as they were issued before the Stockholm III trial (Lancet Oncol. 2017;18:336-46).
- The panel notes that the use of SCRT and delaying surgery has advantages that can be beneficial in both routine clinical practice and the COVID-19 setting. Several clinical trials have recommended that surgery should be performed within 3-7 days of completing radiotherapy, but the Stockholm III trial reported no difference in outcomes when surgery was delayed. It compared surgery performed within 1 week versus 4-8 weeks following SCRT and there was no difference in any survival endpoints. In addition, a longer delay to surgery was associated with a reduction in post-operative and surgical morbidity although no differences in severe complications or re-operations.
Advanced subgroup
- The ESMO guidelines recommend the use of pre-operative CRT or SCRT followed by neoadjuvant chemotherapy. CRT should be given as a fluoropyrimidine (usually capecitabine) combined with radiotherapy of 45-50.4 Gy over 5-5.5 weeks. Adjuvant chemotherapy should be considered but there is wide international variation in its use.
- The panel recommends that two options be considered based on the current evidence. The first is pre-op CRT, which is the most established standard of care, with the duration of concurrent capecitabine chemotherapy limited to 5-5.5 weeks. The second option is SCRT with or without neoadjuvant chemotherapy. In this case, the duration of radiotherapy is substantially less and has advantages versus CRT. “We consider both options to be acceptable but note the advantages of using SCRT in the COVID-19 setting,” the authors write. “The decision to use neoadjuvant chemotherapy in option 2 will reflect the attitudes to neoadjuvant and adjuvant chemotherapy in each country, the assessment of the risk-benefit ratio, considering the risk factors for COVID-19 increased mortality, and the capacity and prioritization of chemotherapy delivery.”
Organ Preservation
Organ preservation is being increasingly considered when a complete clinical response is achieved after CRT or SCRT, the panel points out. “An organ preservation approach may be considered during the COVID-19 period providing that resources for an adequate surveillance including imaging and endoscopy are available to detect local failures that require salvage surgery,” they write.
This article first appeared on Medscape.com.
As the COVID-19 pandemic continues, minimizing risks of infection to patients with cancer while maintaining good outcomes remains a priority. An international panel of experts has now issued recommendations for treating patients with rectal cancer, which includes using a short pre-operative course of radiotherapy (SCRT) and then delaying surgery.
Using SCRT translates to fewer hospital appointments, which will keep patients safer and allow them to maintain social distancing. The panel also found that surgery can be safely delayed by up to 12 weeks, and thus will allow procedures to be rescheduled after the pandemic peaks.
“The COVID-19 pandemic is a global emergency and we needed to work very quickly to identify changes that would benefit patients,” said David Sebag-Montefiore, MD, a professor of clinical oncology at the University of Leeds and honorary clinical oncologist with the Leeds Teaching Hospitals NHS Trust, who led the 15 member panel. “Our recommendations were published 20 days after our first meeting.”
“This process normally takes many months, if not years,” he said in a statement.
The recommendations were published online April 2 in Radiotherapy and Oncology.
The panel used the European Society for Medical Oncology (ESMO) rectal cancer guidelines as a framework to describe these new recommendations.
Recommendations by Stage
The recommendations were categorized into four subgroups based on cancer stage.
Early stage
- The ESMO guidelines recommend total mesorectal excision (TME) surgery without pre-operative radiotherapy for most cases.
- Panel recommendation also strongly supports the use of TME without pre-operative radiotherapy.
Intermediate stage
- The ESMO guidelines recommend TME alone or combined with SCRT or conventional radiotherapy (CRT) if there is uncertainty that a good quality mesorectal excision can be achieved.
- The panel strongly recommends TME alone in regions where high quality surgery is performed. The use of radiotherapy in this subgroup requires careful discussion, as the benefits of preoperative radiotherapy are likely to be small. If radiotherapy is used, then the preferred option should be SCRT.
Locally advanced
- The ESMO guideline recommends either pre-operative SCRT or CRT.
- The panel strongly recommends the use of SCRT and notes two phase 3 trials have compared SCRT and CRT and showed comparable outcomes for local recurrence, disease-free survival, overall survival, and late toxicity. In the COVID-19 setting, the panel points out that SCRT has many advantages over CRT, namely that there is less acute toxicity, fewer treatments which translate to less travel and contact with other patients and staff, and a significantly reduced risk of COVID-19 infection during treatment.
Timing of surgery after SCRT
- The ESMO guideline does not have any recommendations as they were issued before the Stockholm III trial (Lancet Oncol. 2017;18:336-46).
- The panel notes that the use of SCRT and delaying surgery has advantages that can be beneficial in both routine clinical practice and the COVID-19 setting. Several clinical trials have recommended that surgery should be performed within 3-7 days of completing radiotherapy, but the Stockholm III trial reported no difference in outcomes when surgery was delayed. It compared surgery performed within 1 week versus 4-8 weeks following SCRT and there was no difference in any survival endpoints. In addition, a longer delay to surgery was associated with a reduction in post-operative and surgical morbidity although no differences in severe complications or re-operations.
Advanced subgroup
- The ESMO guidelines recommend the use of pre-operative CRT or SCRT followed by neoadjuvant chemotherapy. CRT should be given as a fluoropyrimidine (usually capecitabine) combined with radiotherapy of 45-50.4 Gy over 5-5.5 weeks. Adjuvant chemotherapy should be considered but there is wide international variation in its use.
- The panel recommends that two options be considered based on the current evidence. The first is pre-op CRT, which is the most established standard of care, with the duration of concurrent capecitabine chemotherapy limited to 5-5.5 weeks. The second option is SCRT with or without neoadjuvant chemotherapy. In this case, the duration of radiotherapy is substantially less and has advantages versus CRT. “We consider both options to be acceptable but note the advantages of using SCRT in the COVID-19 setting,” the authors write. “The decision to use neoadjuvant chemotherapy in option 2 will reflect the attitudes to neoadjuvant and adjuvant chemotherapy in each country, the assessment of the risk-benefit ratio, considering the risk factors for COVID-19 increased mortality, and the capacity and prioritization of chemotherapy delivery.”
Organ Preservation
Organ preservation is being increasingly considered when a complete clinical response is achieved after CRT or SCRT, the panel points out. “An organ preservation approach may be considered during the COVID-19 period providing that resources for an adequate surveillance including imaging and endoscopy are available to detect local failures that require salvage surgery,” they write.
This article first appeared on Medscape.com.
Presymptomatic or asymptomatic? ID experts on shifting terminology
They also addressed racial disparities surrounding COVID-19, and announced new IDSA guidelines for diagnosis and treatment of the illness.
Regarding the shifting thinking on symptoms and transmission of the novel coronavirus, when it comes to presymptomatic or asymptomatic, “pre” is really the right terminology, Carlos del Rio, MD, professor of medicine, Division of Infectious Diseases, Emory University School of Medicine, Atlanta, Georgia, said during the briefing, because it’s not that people are asymptomatic but that they develop symptoms later and start transmitting the virus 24 to 48 hours before they develop symptoms.
“Clearly, this plays a role in transmission,” with some studies suggesting that 6% to 12% of transmissions occur during this presymptomatic stage, he explained.
Jeanne Marrazzo, MD, MPH, director of the Division of Infectious Diseases at University of Alabama at Birmingham, noted that early in the COVID-19 pandemic, the presymptomatic phase “could have been missed because we didn’t realize the wide ranging symptoms this disease has.”
This is turning out to be a “very interesting” virus with “fascinating” symptoms, she told reporters on the call.
The virus seems to have capacity to affect far more than just the respiratory tract. Initially, however, it was viewed “very much like a classic respiratory viral infection. As a result, a lot of people were refused testing because they were not showing the classic signs” of respiratory infection, Marrazzo noted.
It’s now clear that the range of symptoms is quite different, she said.
Notably, loss of smell seems to be “very characteristic and very specific to this infection. I can’t think of another common viral infection that causes loss of smell before you start to see other things,” Marrazzo said.
Data also suggest that gastrointestinal symptoms are common with COVID-19. Early data suggest that diarrhea probably occurs in about one third of patients. Some people have reported abdominal pain as the first sign, she said.
“Now that we know about the more wide range of symptoms associated [with COVID-19], we are being much more open to considering people perhaps having this infection. There is a lower index of suspicion and much lower threshold for diagnostic testing,” Marrazzo said, adding that there are still many barriers to testing and getting test results.
Stark Racial Disparities Need Greater Understanding
The second major topic of discussion at the briefing was the growing realization of racial disparities in COVID-19.
“Racial disparities in our country are not new but racial disparities in this disease are pretty stark,” del Rio said. “We live in a country where disparities have really colored a lot of what our diseases are, from HIV to diabetes to hypertension, and it’s not surprising that we are seeing this now with COVID-19.”
Marrazzo noted that, in Alabama, around 20% of the population is African American, yet almost 40% of COVID-19 deaths are occurring in this population. “The most stark statistics are coming out of Illinois and Michigan, where less than around 15% of the population is African American and yet 70% of the deaths are occurring in that group,” she said.
Both del Rio and Marrazzo agreed that understanding the racial differences in COVID-19 deaths is going to require a lot of analysis in the coming months.
Part of it likely reflects the challenge of social distancing in urban areas, Marrazzo said. “Social distancing is a luxury afforded by having a really big space, and space is money.”
The other long-standing challenge of unequal access to healthcare also likely plays a role, she said. This includes missing out on preventive health appointments and screenings, which can translate into more comorbidities, particularly hypertension.
The evolving evidence about the virus, and the stark conditions that frontline clinicians face, make this an especially challenging public health crisis, del Rio said.
“Taking care of these patients is incredibly taxing and my hat is off to physicians, residents, nurses, everybody working on this in the hospitals because they are really doing a yeoman’s work,” he said.
“These are not easy patients to take care of. Not only are [the frontline clinicians] providing care, they are caring for the patient and providing a comfort and someone to listen to when family can’t be present,” del Rio emphasized.
New Guidelines
The IDSA just released new guidelines for diagnosis and treatment of COVID-19.
“We are learning new things every day about this virus. Things are rapidly changing, and as we learn new things we have to adapt and make changes,” del Rio said.
del Rio noted that the guildelines “will evolve and change as more information comes out.”
This article first appeared on Medscape.com.
They also addressed racial disparities surrounding COVID-19, and announced new IDSA guidelines for diagnosis and treatment of the illness.
Regarding the shifting thinking on symptoms and transmission of the novel coronavirus, when it comes to presymptomatic or asymptomatic, “pre” is really the right terminology, Carlos del Rio, MD, professor of medicine, Division of Infectious Diseases, Emory University School of Medicine, Atlanta, Georgia, said during the briefing, because it’s not that people are asymptomatic but that they develop symptoms later and start transmitting the virus 24 to 48 hours before they develop symptoms.
“Clearly, this plays a role in transmission,” with some studies suggesting that 6% to 12% of transmissions occur during this presymptomatic stage, he explained.
Jeanne Marrazzo, MD, MPH, director of the Division of Infectious Diseases at University of Alabama at Birmingham, noted that early in the COVID-19 pandemic, the presymptomatic phase “could have been missed because we didn’t realize the wide ranging symptoms this disease has.”
This is turning out to be a “very interesting” virus with “fascinating” symptoms, she told reporters on the call.
The virus seems to have capacity to affect far more than just the respiratory tract. Initially, however, it was viewed “very much like a classic respiratory viral infection. As a result, a lot of people were refused testing because they were not showing the classic signs” of respiratory infection, Marrazzo noted.
It’s now clear that the range of symptoms is quite different, she said.
Notably, loss of smell seems to be “very characteristic and very specific to this infection. I can’t think of another common viral infection that causes loss of smell before you start to see other things,” Marrazzo said.
Data also suggest that gastrointestinal symptoms are common with COVID-19. Early data suggest that diarrhea probably occurs in about one third of patients. Some people have reported abdominal pain as the first sign, she said.
“Now that we know about the more wide range of symptoms associated [with COVID-19], we are being much more open to considering people perhaps having this infection. There is a lower index of suspicion and much lower threshold for diagnostic testing,” Marrazzo said, adding that there are still many barriers to testing and getting test results.
Stark Racial Disparities Need Greater Understanding
The second major topic of discussion at the briefing was the growing realization of racial disparities in COVID-19.
“Racial disparities in our country are not new but racial disparities in this disease are pretty stark,” del Rio said. “We live in a country where disparities have really colored a lot of what our diseases are, from HIV to diabetes to hypertension, and it’s not surprising that we are seeing this now with COVID-19.”
Marrazzo noted that, in Alabama, around 20% of the population is African American, yet almost 40% of COVID-19 deaths are occurring in this population. “The most stark statistics are coming out of Illinois and Michigan, where less than around 15% of the population is African American and yet 70% of the deaths are occurring in that group,” she said.
Both del Rio and Marrazzo agreed that understanding the racial differences in COVID-19 deaths is going to require a lot of analysis in the coming months.
Part of it likely reflects the challenge of social distancing in urban areas, Marrazzo said. “Social distancing is a luxury afforded by having a really big space, and space is money.”
The other long-standing challenge of unequal access to healthcare also likely plays a role, she said. This includes missing out on preventive health appointments and screenings, which can translate into more comorbidities, particularly hypertension.
The evolving evidence about the virus, and the stark conditions that frontline clinicians face, make this an especially challenging public health crisis, del Rio said.
“Taking care of these patients is incredibly taxing and my hat is off to physicians, residents, nurses, everybody working on this in the hospitals because they are really doing a yeoman’s work,” he said.
“These are not easy patients to take care of. Not only are [the frontline clinicians] providing care, they are caring for the patient and providing a comfort and someone to listen to when family can’t be present,” del Rio emphasized.
New Guidelines
The IDSA just released new guidelines for diagnosis and treatment of COVID-19.
“We are learning new things every day about this virus. Things are rapidly changing, and as we learn new things we have to adapt and make changes,” del Rio said.
del Rio noted that the guildelines “will evolve and change as more information comes out.”
This article first appeared on Medscape.com.
They also addressed racial disparities surrounding COVID-19, and announced new IDSA guidelines for diagnosis and treatment of the illness.
Regarding the shifting thinking on symptoms and transmission of the novel coronavirus, when it comes to presymptomatic or asymptomatic, “pre” is really the right terminology, Carlos del Rio, MD, professor of medicine, Division of Infectious Diseases, Emory University School of Medicine, Atlanta, Georgia, said during the briefing, because it’s not that people are asymptomatic but that they develop symptoms later and start transmitting the virus 24 to 48 hours before they develop symptoms.
“Clearly, this plays a role in transmission,” with some studies suggesting that 6% to 12% of transmissions occur during this presymptomatic stage, he explained.
Jeanne Marrazzo, MD, MPH, director of the Division of Infectious Diseases at University of Alabama at Birmingham, noted that early in the COVID-19 pandemic, the presymptomatic phase “could have been missed because we didn’t realize the wide ranging symptoms this disease has.”
This is turning out to be a “very interesting” virus with “fascinating” symptoms, she told reporters on the call.
The virus seems to have capacity to affect far more than just the respiratory tract. Initially, however, it was viewed “very much like a classic respiratory viral infection. As a result, a lot of people were refused testing because they were not showing the classic signs” of respiratory infection, Marrazzo noted.
It’s now clear that the range of symptoms is quite different, she said.
Notably, loss of smell seems to be “very characteristic and very specific to this infection. I can’t think of another common viral infection that causes loss of smell before you start to see other things,” Marrazzo said.
Data also suggest that gastrointestinal symptoms are common with COVID-19. Early data suggest that diarrhea probably occurs in about one third of patients. Some people have reported abdominal pain as the first sign, she said.
“Now that we know about the more wide range of symptoms associated [with COVID-19], we are being much more open to considering people perhaps having this infection. There is a lower index of suspicion and much lower threshold for diagnostic testing,” Marrazzo said, adding that there are still many barriers to testing and getting test results.
Stark Racial Disparities Need Greater Understanding
The second major topic of discussion at the briefing was the growing realization of racial disparities in COVID-19.
“Racial disparities in our country are not new but racial disparities in this disease are pretty stark,” del Rio said. “We live in a country where disparities have really colored a lot of what our diseases are, from HIV to diabetes to hypertension, and it’s not surprising that we are seeing this now with COVID-19.”
Marrazzo noted that, in Alabama, around 20% of the population is African American, yet almost 40% of COVID-19 deaths are occurring in this population. “The most stark statistics are coming out of Illinois and Michigan, where less than around 15% of the population is African American and yet 70% of the deaths are occurring in that group,” she said.
Both del Rio and Marrazzo agreed that understanding the racial differences in COVID-19 deaths is going to require a lot of analysis in the coming months.
Part of it likely reflects the challenge of social distancing in urban areas, Marrazzo said. “Social distancing is a luxury afforded by having a really big space, and space is money.”
The other long-standing challenge of unequal access to healthcare also likely plays a role, she said. This includes missing out on preventive health appointments and screenings, which can translate into more comorbidities, particularly hypertension.
The evolving evidence about the virus, and the stark conditions that frontline clinicians face, make this an especially challenging public health crisis, del Rio said.
“Taking care of these patients is incredibly taxing and my hat is off to physicians, residents, nurses, everybody working on this in the hospitals because they are really doing a yeoman’s work,” he said.
“These are not easy patients to take care of. Not only are [the frontline clinicians] providing care, they are caring for the patient and providing a comfort and someone to listen to when family can’t be present,” del Rio emphasized.
New Guidelines
The IDSA just released new guidelines for diagnosis and treatment of COVID-19.
“We are learning new things every day about this virus. Things are rapidly changing, and as we learn new things we have to adapt and make changes,” del Rio said.
del Rio noted that the guildelines “will evolve and change as more information comes out.”
This article first appeared on Medscape.com.
CAR T-cell therapy effective for r/r B-cell lymphoma of the GI tract
The use of anti-CD22/CD19 CAR-T sequential infusion was shown to have promising efficacy and safety for relapsed/refractory aggressive B-cell lymphoma with GI involvement, according to the results of a small study reported in Cytotherapy.
The open-label, single-center study enrolled 14 patients with relapsed/refractory aggressive B-cell lymphoma involving the GI tract between November 2017 and January 2019. The researchers examined treatment with sequential infusion of anti-CD22 and anti-CD19 CAR T cells in terms of safety and effectiveness.
An objective response was seen in 10 patients, with 7 of these having a complete response. However, 6 of the patients with partial response or stable disease went on to develop progressive disease. In terms of safety, cytokine-release syndrome and GI adverse events were generally mild and manageable, according to the authors. The most serious events were infections: Two of the patients developed bacterial infections in the GI tract, and one of these died of sepsis early after CAR T-cell infusion.
“The [CD22/CD19 CAR T sequential infusion] regimen was generally safe; however, special attention should be paid to the risk of infection in patients with lymphoma involving the GI tract,” the researchers concluded.
The study was funded by the National Science Foundation of China. The authors reported they had no conflicts of interest.
SOURCE: Zheng C et al. Cytotherapy. 2020;22:166-71.
The use of anti-CD22/CD19 CAR-T sequential infusion was shown to have promising efficacy and safety for relapsed/refractory aggressive B-cell lymphoma with GI involvement, according to the results of a small study reported in Cytotherapy.
The open-label, single-center study enrolled 14 patients with relapsed/refractory aggressive B-cell lymphoma involving the GI tract between November 2017 and January 2019. The researchers examined treatment with sequential infusion of anti-CD22 and anti-CD19 CAR T cells in terms of safety and effectiveness.
An objective response was seen in 10 patients, with 7 of these having a complete response. However, 6 of the patients with partial response or stable disease went on to develop progressive disease. In terms of safety, cytokine-release syndrome and GI adverse events were generally mild and manageable, according to the authors. The most serious events were infections: Two of the patients developed bacterial infections in the GI tract, and one of these died of sepsis early after CAR T-cell infusion.
“The [CD22/CD19 CAR T sequential infusion] regimen was generally safe; however, special attention should be paid to the risk of infection in patients with lymphoma involving the GI tract,” the researchers concluded.
The study was funded by the National Science Foundation of China. The authors reported they had no conflicts of interest.
SOURCE: Zheng C et al. Cytotherapy. 2020;22:166-71.
The use of anti-CD22/CD19 CAR-T sequential infusion was shown to have promising efficacy and safety for relapsed/refractory aggressive B-cell lymphoma with GI involvement, according to the results of a small study reported in Cytotherapy.
The open-label, single-center study enrolled 14 patients with relapsed/refractory aggressive B-cell lymphoma involving the GI tract between November 2017 and January 2019. The researchers examined treatment with sequential infusion of anti-CD22 and anti-CD19 CAR T cells in terms of safety and effectiveness.
An objective response was seen in 10 patients, with 7 of these having a complete response. However, 6 of the patients with partial response or stable disease went on to develop progressive disease. In terms of safety, cytokine-release syndrome and GI adverse events were generally mild and manageable, according to the authors. The most serious events were infections: Two of the patients developed bacterial infections in the GI tract, and one of these died of sepsis early after CAR T-cell infusion.
“The [CD22/CD19 CAR T sequential infusion] regimen was generally safe; however, special attention should be paid to the risk of infection in patients with lymphoma involving the GI tract,” the researchers concluded.
The study was funded by the National Science Foundation of China. The authors reported they had no conflicts of interest.
SOURCE: Zheng C et al. Cytotherapy. 2020;22:166-71.
FROM CYTOTHERAPY
History of smoking gives higher risk for ANCA-associated vasculitis
according to data from a large case-control study.
Although smokers have shown an increased risk for ANCA-associated vasculitis (AAV), compared with nonsmokers, previous studies of the association between smoking and AAV risk have been small and the results have been inconsistent, Greg McDermott, MD, and colleagues at Massachusetts General Hospital, Boston, wrote in JAMA Internal Medicine.
The researchers reviewed data from 473 adults diagnosed with AAV between 2002 and 2017 and compared them with 1,419 matched controls without AAV who had completed a smoking history questionnaire.
Overall, the odds of having a diagnosis of AAV were significantly higher among former smokers or current smokers, compared with never smokers (odds ratios, 1.58 and 2.70, respectively). In addition, the researchers found a significant dose-response relationship between pack-years of exposure and risk of AAV. The average age of the cases and controls was 59 years, 59% were women, and 84% were white.
The association between AAV risk and former or current smoking was greater among the 147 former and 29 current smokers with AAV positive for myeloperoxidase (MPO) (OR, 1.73 and 3.54, respectively). “Proteinase 3-ANCA– and MPO-ANCA–positive AAV are increasingly recognized as distinct conditions characterized by differences in genetic risk, pathogenesis, disease manifestations, and response to treatment,” the researchers said. No stronger association was noted in patients with proteinase 3-ANCA–positive AAV, they said. However, the overall associations remained strong after adjustment for demographics and disease manifestations, they noted.
The study findings were limited by several factors including the observational design, homogeneous study population at a single center, and use of self-reports, the researchers wrote. However, the results were strengthened by the large sample size and number of patients who were MPO-ANCA positive, and the data associating smoking with AAV “expand the list of potential risk factors for AAV, including genetics and silica exposure,” they said. “Further studies to confirm these results and investigate a potential pathogenic mechanism are needed,” they concluded.
The study was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. The researchers had no financial conflicts to disclose.
SOURCE: McDermott G et al. JAMA Intern Med. 2020 Apr 13. doi: 10.1001/jamainternmed.2020.0675.
according to data from a large case-control study.
Although smokers have shown an increased risk for ANCA-associated vasculitis (AAV), compared with nonsmokers, previous studies of the association between smoking and AAV risk have been small and the results have been inconsistent, Greg McDermott, MD, and colleagues at Massachusetts General Hospital, Boston, wrote in JAMA Internal Medicine.
The researchers reviewed data from 473 adults diagnosed with AAV between 2002 and 2017 and compared them with 1,419 matched controls without AAV who had completed a smoking history questionnaire.
Overall, the odds of having a diagnosis of AAV were significantly higher among former smokers or current smokers, compared with never smokers (odds ratios, 1.58 and 2.70, respectively). In addition, the researchers found a significant dose-response relationship between pack-years of exposure and risk of AAV. The average age of the cases and controls was 59 years, 59% were women, and 84% were white.
The association between AAV risk and former or current smoking was greater among the 147 former and 29 current smokers with AAV positive for myeloperoxidase (MPO) (OR, 1.73 and 3.54, respectively). “Proteinase 3-ANCA– and MPO-ANCA–positive AAV are increasingly recognized as distinct conditions characterized by differences in genetic risk, pathogenesis, disease manifestations, and response to treatment,” the researchers said. No stronger association was noted in patients with proteinase 3-ANCA–positive AAV, they said. However, the overall associations remained strong after adjustment for demographics and disease manifestations, they noted.
The study findings were limited by several factors including the observational design, homogeneous study population at a single center, and use of self-reports, the researchers wrote. However, the results were strengthened by the large sample size and number of patients who were MPO-ANCA positive, and the data associating smoking with AAV “expand the list of potential risk factors for AAV, including genetics and silica exposure,” they said. “Further studies to confirm these results and investigate a potential pathogenic mechanism are needed,” they concluded.
The study was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. The researchers had no financial conflicts to disclose.
SOURCE: McDermott G et al. JAMA Intern Med. 2020 Apr 13. doi: 10.1001/jamainternmed.2020.0675.
according to data from a large case-control study.
Although smokers have shown an increased risk for ANCA-associated vasculitis (AAV), compared with nonsmokers, previous studies of the association between smoking and AAV risk have been small and the results have been inconsistent, Greg McDermott, MD, and colleagues at Massachusetts General Hospital, Boston, wrote in JAMA Internal Medicine.
The researchers reviewed data from 473 adults diagnosed with AAV between 2002 and 2017 and compared them with 1,419 matched controls without AAV who had completed a smoking history questionnaire.
Overall, the odds of having a diagnosis of AAV were significantly higher among former smokers or current smokers, compared with never smokers (odds ratios, 1.58 and 2.70, respectively). In addition, the researchers found a significant dose-response relationship between pack-years of exposure and risk of AAV. The average age of the cases and controls was 59 years, 59% were women, and 84% were white.
The association between AAV risk and former or current smoking was greater among the 147 former and 29 current smokers with AAV positive for myeloperoxidase (MPO) (OR, 1.73 and 3.54, respectively). “Proteinase 3-ANCA– and MPO-ANCA–positive AAV are increasingly recognized as distinct conditions characterized by differences in genetic risk, pathogenesis, disease manifestations, and response to treatment,” the researchers said. No stronger association was noted in patients with proteinase 3-ANCA–positive AAV, they said. However, the overall associations remained strong after adjustment for demographics and disease manifestations, they noted.
The study findings were limited by several factors including the observational design, homogeneous study population at a single center, and use of self-reports, the researchers wrote. However, the results were strengthened by the large sample size and number of patients who were MPO-ANCA positive, and the data associating smoking with AAV “expand the list of potential risk factors for AAV, including genetics and silica exposure,” they said. “Further studies to confirm these results and investigate a potential pathogenic mechanism are needed,” they concluded.
The study was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. The researchers had no financial conflicts to disclose.
SOURCE: McDermott G et al. JAMA Intern Med. 2020 Apr 13. doi: 10.1001/jamainternmed.2020.0675.
FROM JAMA INTERNAL MEDICINE
FDA approves Koselugo for pediatric neurofibromatosis treatment
The Food and Drug Administration has approved selumetinib (Koselugo) for the treatment of pediatric patients aged 2 years and older with type 1 neurofibromatosis (NF1) with symptomatic, inoperable plexiform neurofibromas.
FDA approval was based on results from the phase 2 SPRINT Stratum 1 trial, in which 50 patients with NF1 received selumetinib as twice-daily oral monotherapy. Of this group, 33 (66%) patients had a partial response of at least a 20% reduction in tumor volume. There were no complete responses, according to a press release.
The most common adverse events were vomiting, rash, abdominal pain, diarrhea, nausea, dry skin, fatigue, musculoskeletal pain, pyrexia, rash acneiform, stomatitis, headache, paronychia, and pruritus. Dose interruptions, dose reductions, and permanent drug discontinuation occurred in 80%, 24%, and 12% of patients, respectively.
Serious adverse reactions included cardiomyopathy, ocular toxicity, gastrointestinal toxicity, increased creatinine phosphokinase, and increased vitamin E levels and risk of bleeding, according to the press release.
“Previously, there were no medicines approved for this disease. This approval has the potential to change how symptomatic, inoperable NF1 plexiform neurofibromas are treated and provides new hope to these patients,” Roy Baynes, MD, PhD, senior vice president, head of global clinical development, and chief medical officer of Merck Research Laboratories, said in the press release.
The Food and Drug Administration has approved selumetinib (Koselugo) for the treatment of pediatric patients aged 2 years and older with type 1 neurofibromatosis (NF1) with symptomatic, inoperable plexiform neurofibromas.
FDA approval was based on results from the phase 2 SPRINT Stratum 1 trial, in which 50 patients with NF1 received selumetinib as twice-daily oral monotherapy. Of this group, 33 (66%) patients had a partial response of at least a 20% reduction in tumor volume. There were no complete responses, according to a press release.
The most common adverse events were vomiting, rash, abdominal pain, diarrhea, nausea, dry skin, fatigue, musculoskeletal pain, pyrexia, rash acneiform, stomatitis, headache, paronychia, and pruritus. Dose interruptions, dose reductions, and permanent drug discontinuation occurred in 80%, 24%, and 12% of patients, respectively.
Serious adverse reactions included cardiomyopathy, ocular toxicity, gastrointestinal toxicity, increased creatinine phosphokinase, and increased vitamin E levels and risk of bleeding, according to the press release.
“Previously, there were no medicines approved for this disease. This approval has the potential to change how symptomatic, inoperable NF1 plexiform neurofibromas are treated and provides new hope to these patients,” Roy Baynes, MD, PhD, senior vice president, head of global clinical development, and chief medical officer of Merck Research Laboratories, said in the press release.
The Food and Drug Administration has approved selumetinib (Koselugo) for the treatment of pediatric patients aged 2 years and older with type 1 neurofibromatosis (NF1) with symptomatic, inoperable plexiform neurofibromas.
FDA approval was based on results from the phase 2 SPRINT Stratum 1 trial, in which 50 patients with NF1 received selumetinib as twice-daily oral monotherapy. Of this group, 33 (66%) patients had a partial response of at least a 20% reduction in tumor volume. There were no complete responses, according to a press release.
The most common adverse events were vomiting, rash, abdominal pain, diarrhea, nausea, dry skin, fatigue, musculoskeletal pain, pyrexia, rash acneiform, stomatitis, headache, paronychia, and pruritus. Dose interruptions, dose reductions, and permanent drug discontinuation occurred in 80%, 24%, and 12% of patients, respectively.
Serious adverse reactions included cardiomyopathy, ocular toxicity, gastrointestinal toxicity, increased creatinine phosphokinase, and increased vitamin E levels and risk of bleeding, according to the press release.
“Previously, there were no medicines approved for this disease. This approval has the potential to change how symptomatic, inoperable NF1 plexiform neurofibromas are treated and provides new hope to these patients,” Roy Baynes, MD, PhD, senior vice president, head of global clinical development, and chief medical officer of Merck Research Laboratories, said in the press release.
Lymphocyte, monocyte data can predict treatment response in follicular lymphoma
Absolute lymphocyte cell (ALC) and absolute monocyte cell (AMC) counts, as well as their ratio (LMR) proved to be prognostic factors for treatment results, as shown by a database analysis of follicular lymphoma (FL) patients.
Progressive disease and stable disease after first-line therapy, as well as the mortality rate, were significantly associated with lower ALC, higher AMC, and higher LMR, according to the report published online.
Researchers analyzed the data of 100 FL variant patients admitted and treated between January 2009 and June 2018 at a single center.
Area under the curve analysis for discriminating between survival times showed 0.57 x 109 cells/L was the most discriminative ALC cutoff value, 1.24 x 109/L was the most discriminative AMC cutoff value, and 1.63 x 109/L was the most discriminative LMR cutoff value.
Shorter overall survival (OS) was significantly associated with lower ALC, compared with those having higher ALC. Shorter OS and progression-free survival (PFS) were significantly associated with higher AMC, compared with those having lower AMC. Shorter OS and PFS were also significantly associated with lower LMR, compared with those having higher LMR.
Overall, a high-risk score in the Follicular Lymphoma International Prognostic Index (FLIPI) and having a low LMR were considered risk factors for prediction of OS in all the studied FL patients in univariate analysis and multivariate analysis, according to the researchers.
“Our results prove the effect of lymphocyte and monocyte in the tumor immune response, which gives opportunity to several therapeutic strategies that target myeloid-derived suppressor cells (MDSCs), including monocytes and their progeny and improves the T-cell function in eradication strategies,” the researchers concluded.
No study funding or disclosure details were provided.
SOURCE: Mohsen A et al. Clin Lymphoma Myeloma Leuk. 2020 Mar 20. doi: 10.1016/j.clml.2020.03.007.
Absolute lymphocyte cell (ALC) and absolute monocyte cell (AMC) counts, as well as their ratio (LMR) proved to be prognostic factors for treatment results, as shown by a database analysis of follicular lymphoma (FL) patients.
Progressive disease and stable disease after first-line therapy, as well as the mortality rate, were significantly associated with lower ALC, higher AMC, and higher LMR, according to the report published online.
Researchers analyzed the data of 100 FL variant patients admitted and treated between January 2009 and June 2018 at a single center.
Area under the curve analysis for discriminating between survival times showed 0.57 x 109 cells/L was the most discriminative ALC cutoff value, 1.24 x 109/L was the most discriminative AMC cutoff value, and 1.63 x 109/L was the most discriminative LMR cutoff value.
Shorter overall survival (OS) was significantly associated with lower ALC, compared with those having higher ALC. Shorter OS and progression-free survival (PFS) were significantly associated with higher AMC, compared with those having lower AMC. Shorter OS and PFS were also significantly associated with lower LMR, compared with those having higher LMR.
Overall, a high-risk score in the Follicular Lymphoma International Prognostic Index (FLIPI) and having a low LMR were considered risk factors for prediction of OS in all the studied FL patients in univariate analysis and multivariate analysis, according to the researchers.
“Our results prove the effect of lymphocyte and monocyte in the tumor immune response, which gives opportunity to several therapeutic strategies that target myeloid-derived suppressor cells (MDSCs), including monocytes and their progeny and improves the T-cell function in eradication strategies,” the researchers concluded.
No study funding or disclosure details were provided.
SOURCE: Mohsen A et al. Clin Lymphoma Myeloma Leuk. 2020 Mar 20. doi: 10.1016/j.clml.2020.03.007.
Absolute lymphocyte cell (ALC) and absolute monocyte cell (AMC) counts, as well as their ratio (LMR) proved to be prognostic factors for treatment results, as shown by a database analysis of follicular lymphoma (FL) patients.
Progressive disease and stable disease after first-line therapy, as well as the mortality rate, were significantly associated with lower ALC, higher AMC, and higher LMR, according to the report published online.
Researchers analyzed the data of 100 FL variant patients admitted and treated between January 2009 and June 2018 at a single center.
Area under the curve analysis for discriminating between survival times showed 0.57 x 109 cells/L was the most discriminative ALC cutoff value, 1.24 x 109/L was the most discriminative AMC cutoff value, and 1.63 x 109/L was the most discriminative LMR cutoff value.
Shorter overall survival (OS) was significantly associated with lower ALC, compared with those having higher ALC. Shorter OS and progression-free survival (PFS) were significantly associated with higher AMC, compared with those having lower AMC. Shorter OS and PFS were also significantly associated with lower LMR, compared with those having higher LMR.
Overall, a high-risk score in the Follicular Lymphoma International Prognostic Index (FLIPI) and having a low LMR were considered risk factors for prediction of OS in all the studied FL patients in univariate analysis and multivariate analysis, according to the researchers.
“Our results prove the effect of lymphocyte and monocyte in the tumor immune response, which gives opportunity to several therapeutic strategies that target myeloid-derived suppressor cells (MDSCs), including monocytes and their progeny and improves the T-cell function in eradication strategies,” the researchers concluded.
No study funding or disclosure details were provided.
SOURCE: Mohsen A et al. Clin Lymphoma Myeloma Leuk. 2020 Mar 20. doi: 10.1016/j.clml.2020.03.007.
FROM CLINICAL LYMPHOMA, MYELOMA AND LEUKEMIA
Edema Affecting the Penis and Scrotum
The Diagnosis: Cutaneous Crohn Disease
Crohn disease (CD) is an inflammatory bowel disease that can involve any region of the gastrointestinal (GI) tract from the mouth to the anus but most commonly presents in the terminal ileum, colon, or small bowel with transmural inflammation, fistula formation, and knife-cut fissures among the frequently described findings. Extraintestinal manifestations may be found in the liver, eyes, and joints, with cutaneous extraintestinal manifestations occurring in up to one-third of patients.1
Crohn disease can be associated with multiple cutaneous findings, including erythema nodosum, pyoderma gangrenosum, aphthous ulcers, pyodermatitis-pyostomatitis vegetans, necrotizing vasculitis, and metastatic Crohn disease (MCD).2 Typical histopathologic findings seen in MCD such as noncaseating granulomatous inflammation in the papillary and reticular dermis, possibly extending to the subcutaneous fat, are not specific to MCD. Associated genital edema is thought to be a consequence of granulomatous inflammation of lymphatics. In one study reviewing specimens from 10 cases of CD, a mean of 46% of all granulomas identified on the slides (264 granulomas in total) were located proximal to lymphatic vessels, suggesting a common pathway for development of intestinal disease and genital edema.3 The differential diagnosis for penile and scrotal swelling is broad, and the diagnosis may be missed if attention is not given to the clinical history of the patient in addition to histopathologic findings.2
Skin changes in CD also can be separated into perianal disease and true metastatic disease--the former recognized when anal lesions appear associated with segmental involvement of the GI tract and the latter as ulceration of the skin separated from the GI tract by normal tissue.1 The term sarcoidal reaction often is used to describe histopathologic findings in cutaneous CD, as it refers to the noncaseating granulomas found in approximately 60% of all cases.4 Ultimately, the location of noncaseating granulomas within the dermis of our patient's biopsy, taken in conjunction with the clinical history and the lack of defining features for other potential etiologies (eg, polarizable material, organisms on special stains), led to the diagnosis of cutaneous CD.
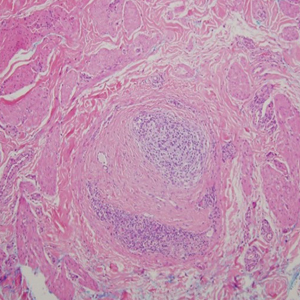
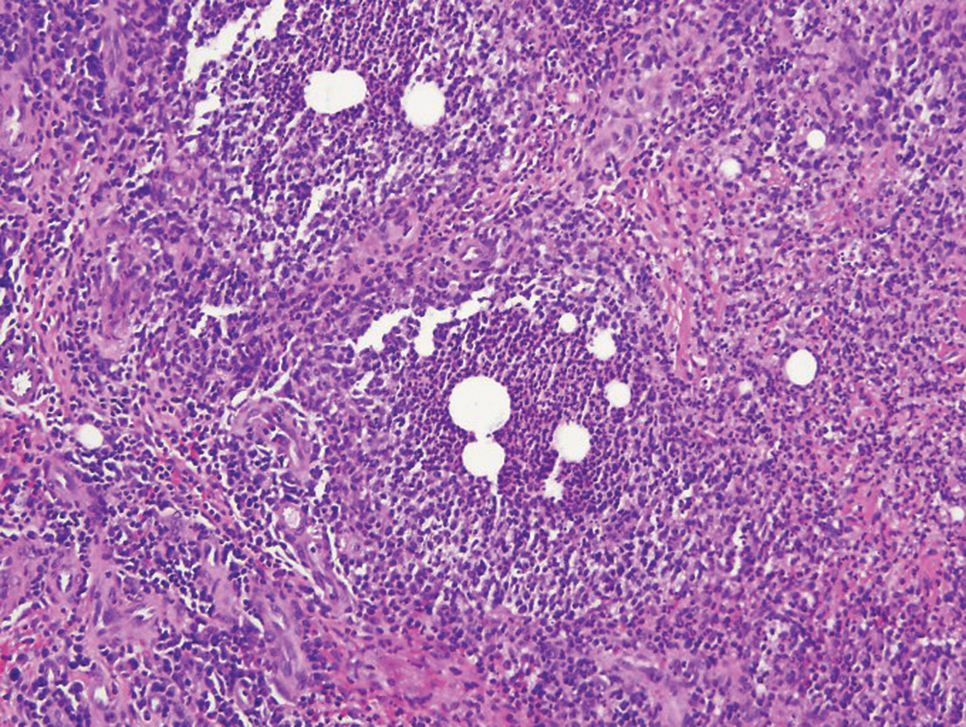
Cutaneous manifestations of sarcoidosis most commonly occur as papules, plaques, and subcutaneous nodules predominantly on the face, upper back, arms, and legs. Although the histologic features of sarcoidosis are characterized by lymphocyte-poor noncaseating granulomas (Figure 1), these findings also can be seen as a consequence of multiple granulomatous causes.5,6 In a review of 48 cutaneous specimens from patients with sarcoidosis, the granulomas were found most frequently in the deep dermis (34/48 [70.8%]), with superficial dermis (21/48) and subcutaneous fat granulomas (20/48) each present in less than 50% of biopsies.5 Although less typical, cutaneous sarcoidosis also has been noted in the literature to present in the perianal and gluteal region, demonstrating dermal noncaseating granulomas on biopsy.7 One distinction in particular to be noted between sarcoid and CD is that sarcoid lesions in the skin rarely ulcerate, while the lesions of cutaneous CD often are ulcerated.4,6
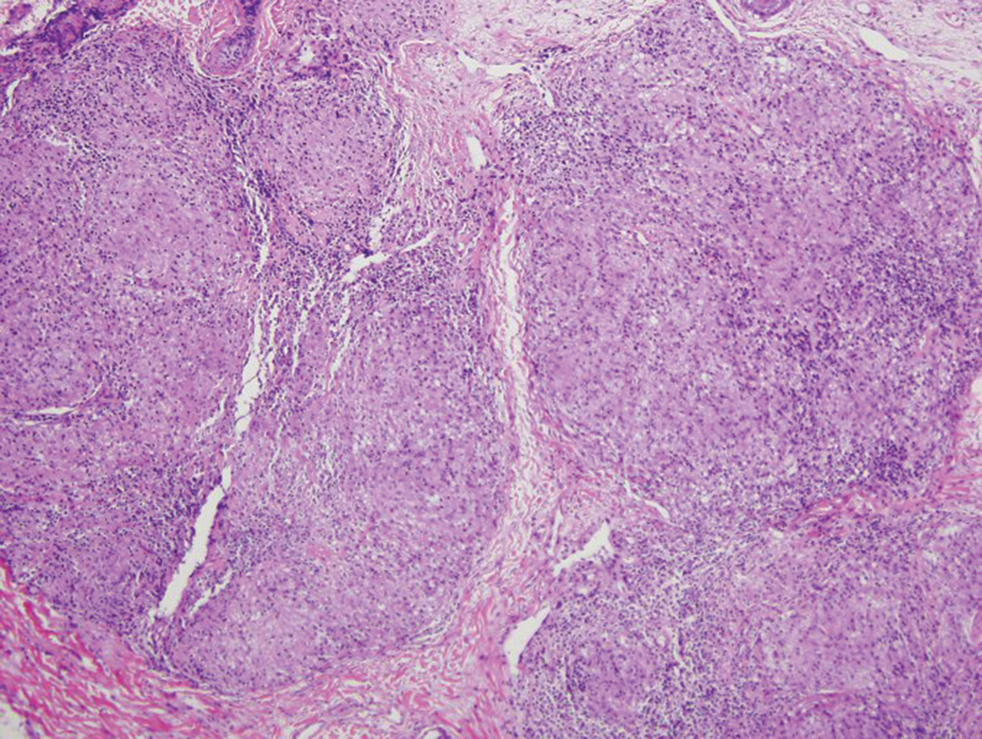
Lesions including abscesses in the groin may raise concern for hidradenitis suppurativa (HS), a disease of the apocrine gland-bearing skin. Typical lesions are tender subcutaneous erythematous nodules, cysts, and comedones that develop rapidly and may rupture to drain suppurative bloody discharge, subsequently healing with an atrophic scar.8 More persistent inflammation and rupture of nodules into the dermis may lead to formation of dermal tunnels with palpable cords and sinus tracts.8 Typical areas of disease involvement are in the axillae, inframammary folds, groin, or perigenital or perineal regions, with the diagnosis made on a combination of lesion morphology, location, and progression/recurrence frequency.9 Histologic examination of HS specimens can demonstrate a perifollicular lymphocytic infiltrate, with more advanced disease characterized by increased inflammatory cells, predominantly neutrophils, monocytes, and mast cells (Figure 2). The presence of granulomas in HS most often is of the foreign body type.9 Epithelioid granulomas noted in an area separate from inflammation in a patient with HS serve as a clue to be alert for systemic granulomatous disease.10
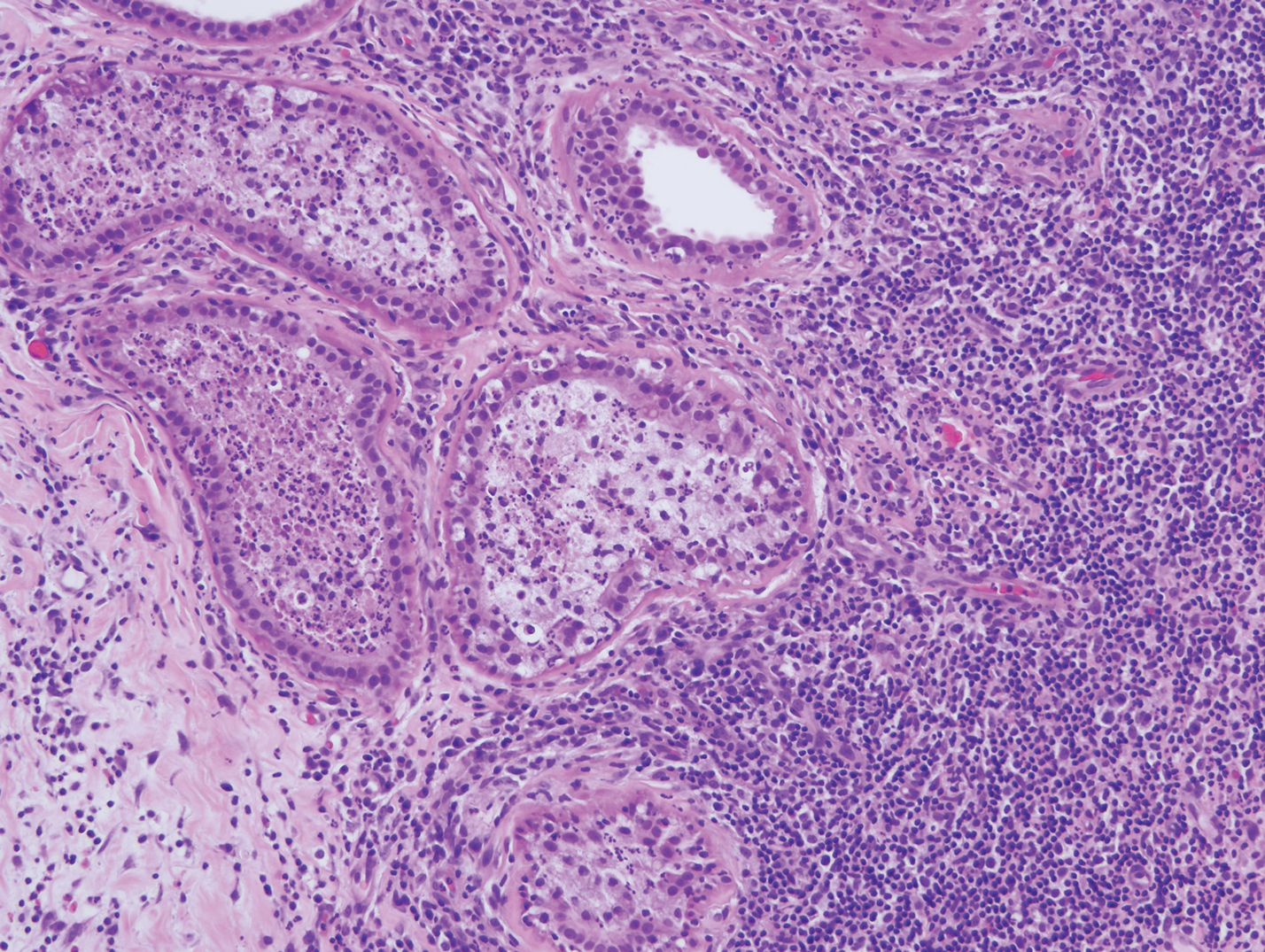
Mycosis fungoides is the most common primary cutaneous lymphoma to show a granulomatous infiltrate; the granuloma generally is sarcoidal, though other forms are described (Figure 3).11 Beyond these granulomatous foci, the key histopathologic feature of granulomatous mycosis fungoides (GMF) is diffuse dermal infiltration by atypical lymphoid cells. Epidermotropism and sparing of dermal nerves is the most critical finding in the diagnosis of GMF, especially in geographic regions where leprosy is endemic and high on the differential, as the conditions have histopathologic similarities.11,12 At the same time, lack of epidermotropism does not exclude the diagnosis of GMF.13 Clinically, GMF presentation is variable, but common findings include erythematous and hyperpigmented patches and plaques. Given the lack of clear clinical criteria, the diagnosis relies primarily on histopathologic features.11
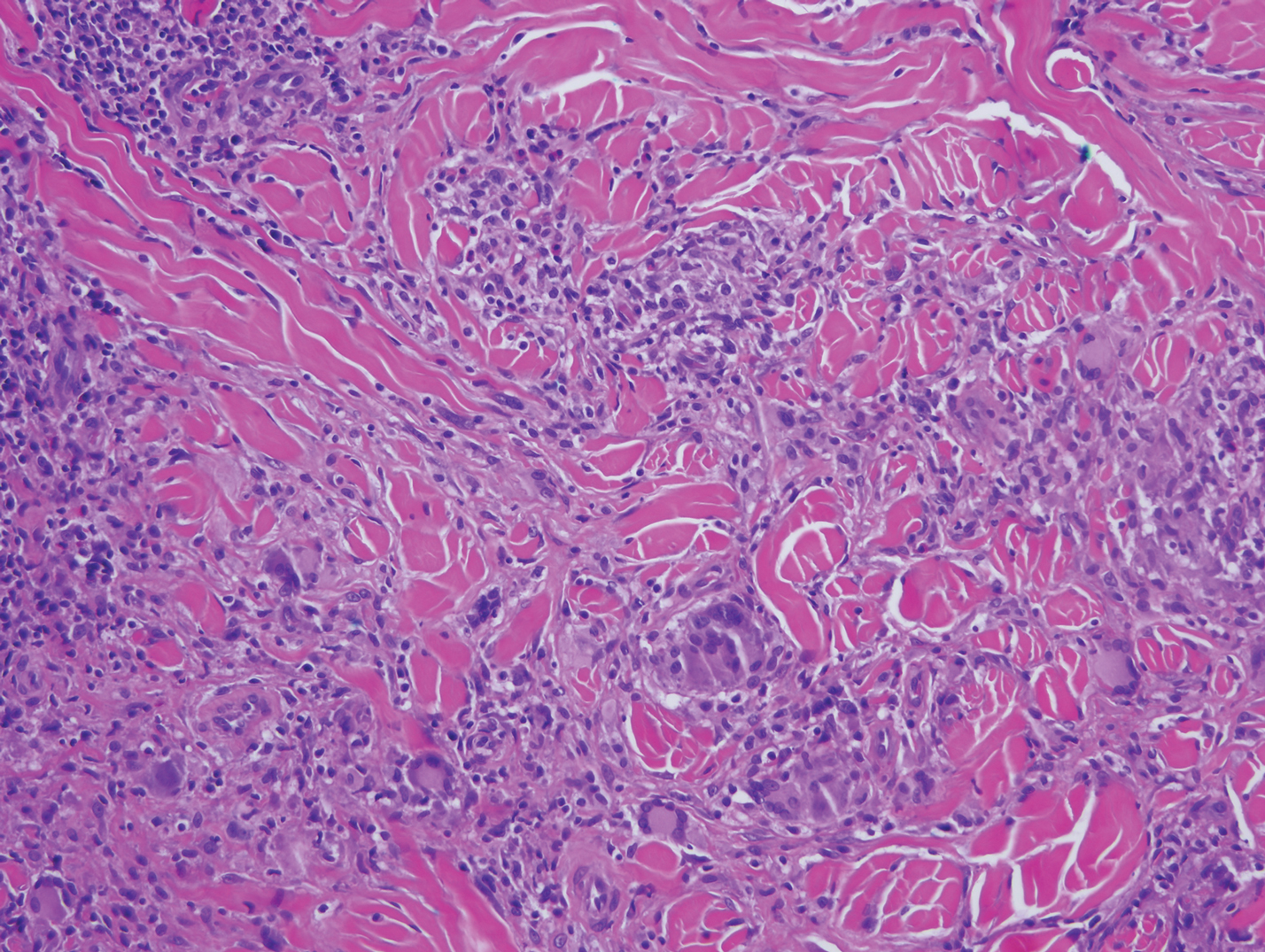
Mycobacterial skin and soft tissue infections may be attributed to both tuberculous and nontuberculous strains (atypical species).14 Clinical features range from small papules to large deformative plaques and ulcers.15 Histologic features also distinguish cutaneous tuberculosis (TB) from nontuberculous mycobacterial causes. Cutaneous TB shows caseous granulomas in the upper and mid dermis, while nontuberculous mycobacterial infections have more prominent neutrophil infiltration and interstitial granulomas (Figure 4).16
In cutaneous TB specifically, extrapulmonary manifestations may involve the skin in 1% to 1.5% of all TB cases, and although rare, ulcerative skin TB has been noted in one report as a nonhealing perianal ulcer that showed necrotizing granulomas on biopsy.17 Ultimately, diagnosis of cutaneous mycobacterial infection is confirmed with detection of acid-fast bacilli in the biopsy specimen.16
Diagnosis of cutaneous CD requires clinicopathologic correlation, as the clinical and histopathologic differential diagnoses of genital edema and noncaseating granulomas, respectively, are broad. Even though the clinical context was appropriate for cutaneous CD in this case, correct diagnosis required confirmatory histologic findings. Furthermore, taking multiple biopsies is prudent. In our patient, diagnostic findings only were present in the biopsy from the scrotum.
- Hagen JW, Swoger JM, Grandinetti LM. Cutaneous manifestations of Crohn disease. Dermatol Clin. 2015;33:417-431.
- Barrick BJ, Tollefson MM, Schoch JJ, et al. Penile and scrotal swelling: an underrecognized presentation of Crohn's disease. Pediatr Dermatol. 2016;33:172-177.
- Mooney EE, Walker J, Hourihane DO. Relation of granulomas to lymphatic vessels in Crohn's disease. J Clin Pathol. 1995;48:335-338.
- Parks AG, Morson BC, Pegum JS. Crohn's disease with cutaneous involvement. Proc R Soc Med. 1965;58:241-242.
- García-Colmenero L, Sánchez-Schmidt JM, Barranco C, et al. The natural history of cutaneous sarcoidosis: clinical spectrum and histological analysis of 40 cases [published online October 18, 2018]. Int J Dermatol. 2019;58:178-184.
- Yoo SS, Mimouni D, Nikolskaia OV, et al. Clinicopathologic features of ulcerative-atrophic sarcoidosis. Int J Dermatol. 2004;43:108-112.
- Cohen GF, Wolfe CM. Recalcitrant diffuse cutaneous sarcoidosis with perianal involvement responding to adalimumab. J Drugs Dermatol. 2017;16:1305-1306.
- Hoffman LK, Ghias MH, Lowes MA. Pathophysiology of hidradenitis suppurativa. Semin Cutan Med Surg. 2017;36:47-54.
- Saunte DML, Jemec GBE. Hidradenitis suppurativa: advances in diagnosis and treatment. JAMA. 2017;318:2019-2032.
- Attanoos RL, Appleton MA, Hughes LE, et al. Granulomatous hidradenitis suppurativa and cutaneous Crohn's disease. Histopathology. 1993;23:111-115.
- Gutte R, Kharkar V, Mahajan S, et al. Granulomatous mycosis fungoides with hypohydrosis mimicking lepromatous leprosy. Indian J Dermatol Venerol Leprol. 2010;76:686-690.
- Pousa CM, Nery NS, Mann D, et al. Granulomatous mycosis fungoides--a diagnostic challenge. An Bras Dermatol. 2015;90:554-556.
- Kempf W, Ostheeren-Michaelis S, Paulli M, et al. Granulomatous mycosis fungoides and granulomatous slack skin: a multicenter study of the Cutaneous Lymphoma Histopathology Task Force Group of the European Organization for Research and Treatment of Cancer (EORTC). Arch Dermatol. 2008;144:1609-1617.
- van Mechelen M, van der Hilst J, Gyssens IC, et al. Mycobacterial skin and soft tissue infections: TB or not TB? Neth J Med. 2018;76:269-274.
- van Zyl L, du Plessis J, Viljoen J. Cutaneous tuberculosis overview and current treatment regimens. Tuberculosis (Edinb). 2015;95:629-638.
- De Maio F, Trecarichi EM, Visconti E, et al. Understanding cutaneous tuberculosis: two clinical cases. JMM Case Rep. 2016;3:E005070.
- Wu S, Wang W, Chen H, et al. Perianal ulcerative skin tuberculosis: a case report. Medicine (Baltimore). 2018;97:E10836.
The Diagnosis: Cutaneous Crohn Disease
Crohn disease (CD) is an inflammatory bowel disease that can involve any region of the gastrointestinal (GI) tract from the mouth to the anus but most commonly presents in the terminal ileum, colon, or small bowel with transmural inflammation, fistula formation, and knife-cut fissures among the frequently described findings. Extraintestinal manifestations may be found in the liver, eyes, and joints, with cutaneous extraintestinal manifestations occurring in up to one-third of patients.1
Crohn disease can be associated with multiple cutaneous findings, including erythema nodosum, pyoderma gangrenosum, aphthous ulcers, pyodermatitis-pyostomatitis vegetans, necrotizing vasculitis, and metastatic Crohn disease (MCD).2 Typical histopathologic findings seen in MCD such as noncaseating granulomatous inflammation in the papillary and reticular dermis, possibly extending to the subcutaneous fat, are not specific to MCD. Associated genital edema is thought to be a consequence of granulomatous inflammation of lymphatics. In one study reviewing specimens from 10 cases of CD, a mean of 46% of all granulomas identified on the slides (264 granulomas in total) were located proximal to lymphatic vessels, suggesting a common pathway for development of intestinal disease and genital edema.3 The differential diagnosis for penile and scrotal swelling is broad, and the diagnosis may be missed if attention is not given to the clinical history of the patient in addition to histopathologic findings.2
Skin changes in CD also can be separated into perianal disease and true metastatic disease--the former recognized when anal lesions appear associated with segmental involvement of the GI tract and the latter as ulceration of the skin separated from the GI tract by normal tissue.1 The term sarcoidal reaction often is used to describe histopathologic findings in cutaneous CD, as it refers to the noncaseating granulomas found in approximately 60% of all cases.4 Ultimately, the location of noncaseating granulomas within the dermis of our patient's biopsy, taken in conjunction with the clinical history and the lack of defining features for other potential etiologies (eg, polarizable material, organisms on special stains), led to the diagnosis of cutaneous CD.
Cutaneous manifestations of sarcoidosis most commonly occur as papules, plaques, and subcutaneous nodules predominantly on the face, upper back, arms, and legs. Although the histologic features of sarcoidosis are characterized by lymphocyte-poor noncaseating granulomas (Figure 1), these findings also can be seen as a consequence of multiple granulomatous causes.5,6 In a review of 48 cutaneous specimens from patients with sarcoidosis, the granulomas were found most frequently in the deep dermis (34/48 [70.8%]), with superficial dermis (21/48) and subcutaneous fat granulomas (20/48) each present in less than 50% of biopsies.5 Although less typical, cutaneous sarcoidosis also has been noted in the literature to present in the perianal and gluteal region, demonstrating dermal noncaseating granulomas on biopsy.7 One distinction in particular to be noted between sarcoid and CD is that sarcoid lesions in the skin rarely ulcerate, while the lesions of cutaneous CD often are ulcerated.4,6
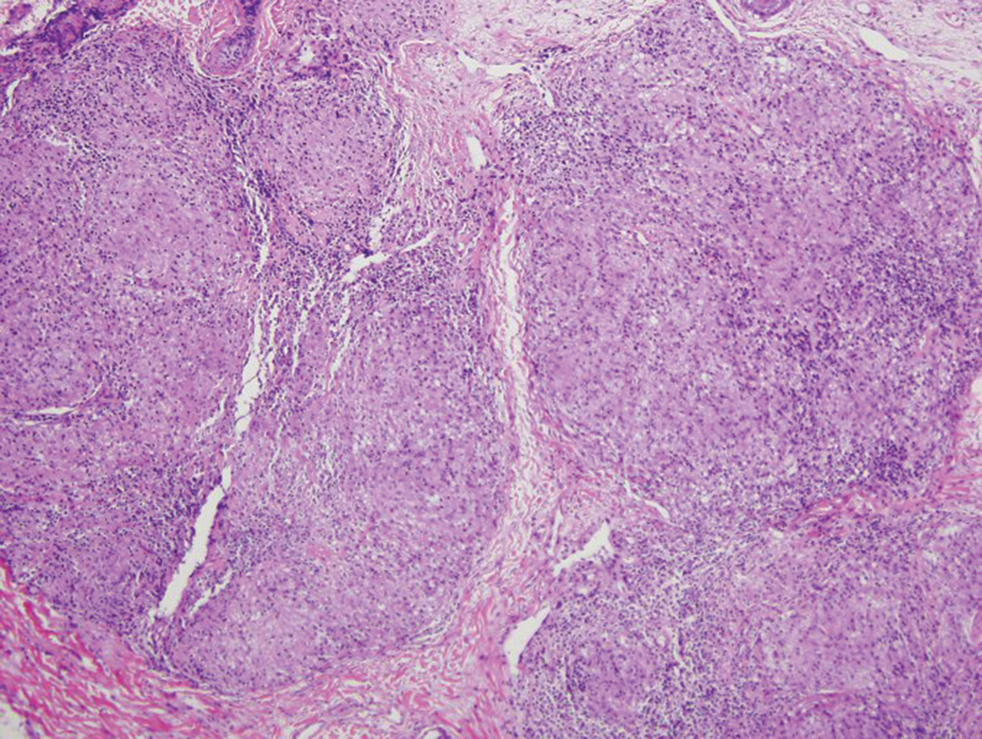
Lesions including abscesses in the groin may raise concern for hidradenitis suppurativa (HS), a disease of the apocrine gland-bearing skin. Typical lesions are tender subcutaneous erythematous nodules, cysts, and comedones that develop rapidly and may rupture to drain suppurative bloody discharge, subsequently healing with an atrophic scar.8 More persistent inflammation and rupture of nodules into the dermis may lead to formation of dermal tunnels with palpable cords and sinus tracts.8 Typical areas of disease involvement are in the axillae, inframammary folds, groin, or perigenital or perineal regions, with the diagnosis made on a combination of lesion morphology, location, and progression/recurrence frequency.9 Histologic examination of HS specimens can demonstrate a perifollicular lymphocytic infiltrate, with more advanced disease characterized by increased inflammatory cells, predominantly neutrophils, monocytes, and mast cells (Figure 2). The presence of granulomas in HS most often is of the foreign body type.9 Epithelioid granulomas noted in an area separate from inflammation in a patient with HS serve as a clue to be alert for systemic granulomatous disease.10
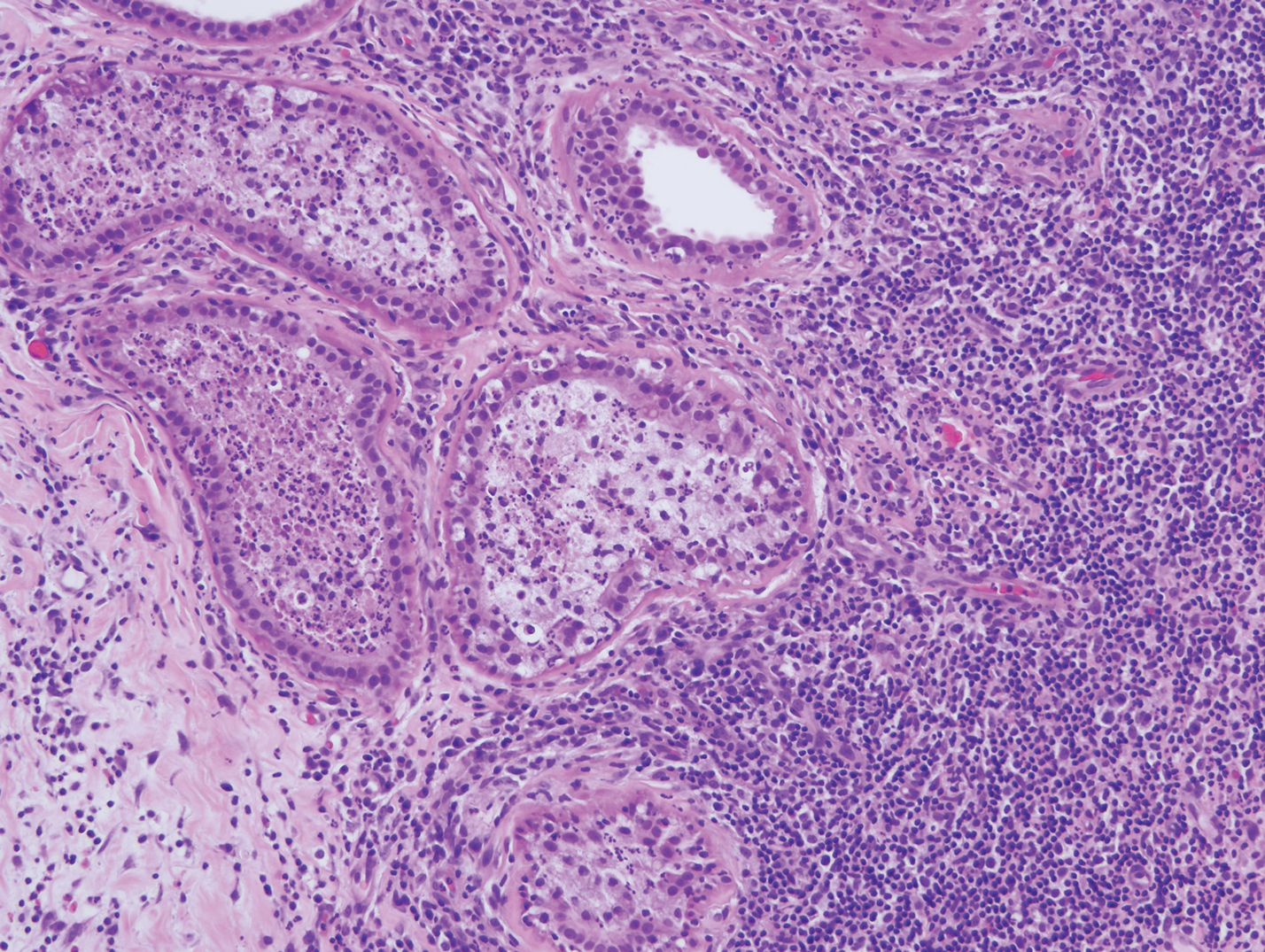
Mycosis fungoides is the most common primary cutaneous lymphoma to show a granulomatous infiltrate; the granuloma generally is sarcoidal, though other forms are described (Figure 3).11 Beyond these granulomatous foci, the key histopathologic feature of granulomatous mycosis fungoides (GMF) is diffuse dermal infiltration by atypical lymphoid cells. Epidermotropism and sparing of dermal nerves is the most critical finding in the diagnosis of GMF, especially in geographic regions where leprosy is endemic and high on the differential, as the conditions have histopathologic similarities.11,12 At the same time, lack of epidermotropism does not exclude the diagnosis of GMF.13 Clinically, GMF presentation is variable, but common findings include erythematous and hyperpigmented patches and plaques. Given the lack of clear clinical criteria, the diagnosis relies primarily on histopathologic features.11
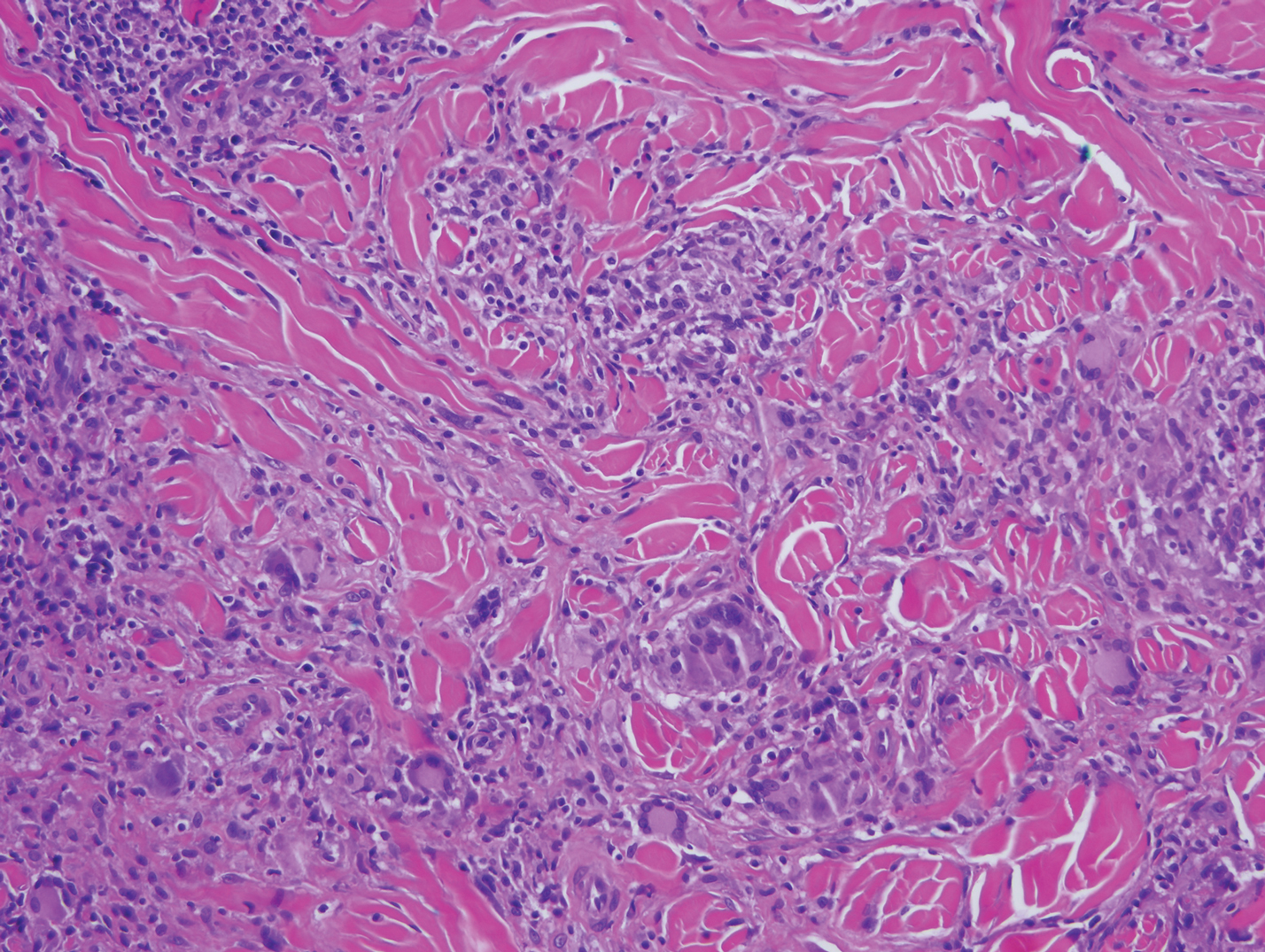
Mycobacterial skin and soft tissue infections may be attributed to both tuberculous and nontuberculous strains (atypical species).14 Clinical features range from small papules to large deformative plaques and ulcers.15 Histologic features also distinguish cutaneous tuberculosis (TB) from nontuberculous mycobacterial causes. Cutaneous TB shows caseous granulomas in the upper and mid dermis, while nontuberculous mycobacterial infections have more prominent neutrophil infiltration and interstitial granulomas (Figure 4).16
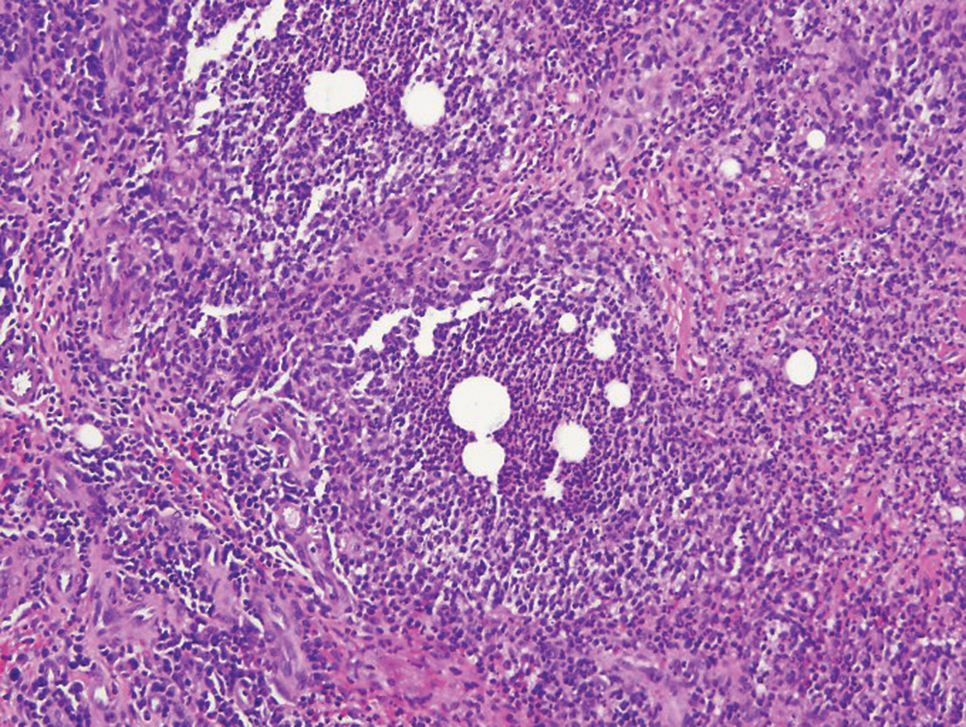
In cutaneous TB specifically, extrapulmonary manifestations may involve the skin in 1% to 1.5% of all TB cases, and although rare, ulcerative skin TB has been noted in one report as a nonhealing perianal ulcer that showed necrotizing granulomas on biopsy.17 Ultimately, diagnosis of cutaneous mycobacterial infection is confirmed with detection of acid-fast bacilli in the biopsy specimen.16
Diagnosis of cutaneous CD requires clinicopathologic correlation, as the clinical and histopathologic differential diagnoses of genital edema and noncaseating granulomas, respectively, are broad. Even though the clinical context was appropriate for cutaneous CD in this case, correct diagnosis required confirmatory histologic findings. Furthermore, taking multiple biopsies is prudent. In our patient, diagnostic findings only were present in the biopsy from the scrotum.
The Diagnosis: Cutaneous Crohn Disease
Crohn disease (CD) is an inflammatory bowel disease that can involve any region of the gastrointestinal (GI) tract from the mouth to the anus but most commonly presents in the terminal ileum, colon, or small bowel with transmural inflammation, fistula formation, and knife-cut fissures among the frequently described findings. Extraintestinal manifestations may be found in the liver, eyes, and joints, with cutaneous extraintestinal manifestations occurring in up to one-third of patients.1
Crohn disease can be associated with multiple cutaneous findings, including erythema nodosum, pyoderma gangrenosum, aphthous ulcers, pyodermatitis-pyostomatitis vegetans, necrotizing vasculitis, and metastatic Crohn disease (MCD).2 Typical histopathologic findings seen in MCD such as noncaseating granulomatous inflammation in the papillary and reticular dermis, possibly extending to the subcutaneous fat, are not specific to MCD. Associated genital edema is thought to be a consequence of granulomatous inflammation of lymphatics. In one study reviewing specimens from 10 cases of CD, a mean of 46% of all granulomas identified on the slides (264 granulomas in total) were located proximal to lymphatic vessels, suggesting a common pathway for development of intestinal disease and genital edema.3 The differential diagnosis for penile and scrotal swelling is broad, and the diagnosis may be missed if attention is not given to the clinical history of the patient in addition to histopathologic findings.2
Skin changes in CD also can be separated into perianal disease and true metastatic disease--the former recognized when anal lesions appear associated with segmental involvement of the GI tract and the latter as ulceration of the skin separated from the GI tract by normal tissue.1 The term sarcoidal reaction often is used to describe histopathologic findings in cutaneous CD, as it refers to the noncaseating granulomas found in approximately 60% of all cases.4 Ultimately, the location of noncaseating granulomas within the dermis of our patient's biopsy, taken in conjunction with the clinical history and the lack of defining features for other potential etiologies (eg, polarizable material, organisms on special stains), led to the diagnosis of cutaneous CD.
Cutaneous manifestations of sarcoidosis most commonly occur as papules, plaques, and subcutaneous nodules predominantly on the face, upper back, arms, and legs. Although the histologic features of sarcoidosis are characterized by lymphocyte-poor noncaseating granulomas (Figure 1), these findings also can be seen as a consequence of multiple granulomatous causes.5,6 In a review of 48 cutaneous specimens from patients with sarcoidosis, the granulomas were found most frequently in the deep dermis (34/48 [70.8%]), with superficial dermis (21/48) and subcutaneous fat granulomas (20/48) each present in less than 50% of biopsies.5 Although less typical, cutaneous sarcoidosis also has been noted in the literature to present in the perianal and gluteal region, demonstrating dermal noncaseating granulomas on biopsy.7 One distinction in particular to be noted between sarcoid and CD is that sarcoid lesions in the skin rarely ulcerate, while the lesions of cutaneous CD often are ulcerated.4,6
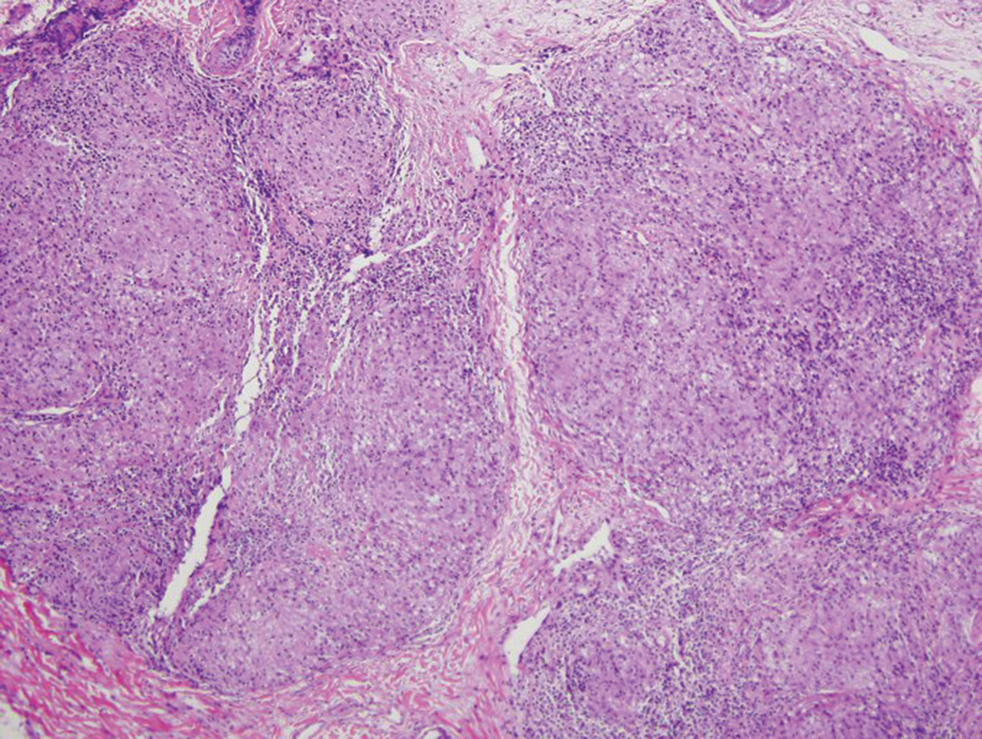
Lesions including abscesses in the groin may raise concern for hidradenitis suppurativa (HS), a disease of the apocrine gland-bearing skin. Typical lesions are tender subcutaneous erythematous nodules, cysts, and comedones that develop rapidly and may rupture to drain suppurative bloody discharge, subsequently healing with an atrophic scar.8 More persistent inflammation and rupture of nodules into the dermis may lead to formation of dermal tunnels with palpable cords and sinus tracts.8 Typical areas of disease involvement are in the axillae, inframammary folds, groin, or perigenital or perineal regions, with the diagnosis made on a combination of lesion morphology, location, and progression/recurrence frequency.9 Histologic examination of HS specimens can demonstrate a perifollicular lymphocytic infiltrate, with more advanced disease characterized by increased inflammatory cells, predominantly neutrophils, monocytes, and mast cells (Figure 2). The presence of granulomas in HS most often is of the foreign body type.9 Epithelioid granulomas noted in an area separate from inflammation in a patient with HS serve as a clue to be alert for systemic granulomatous disease.10
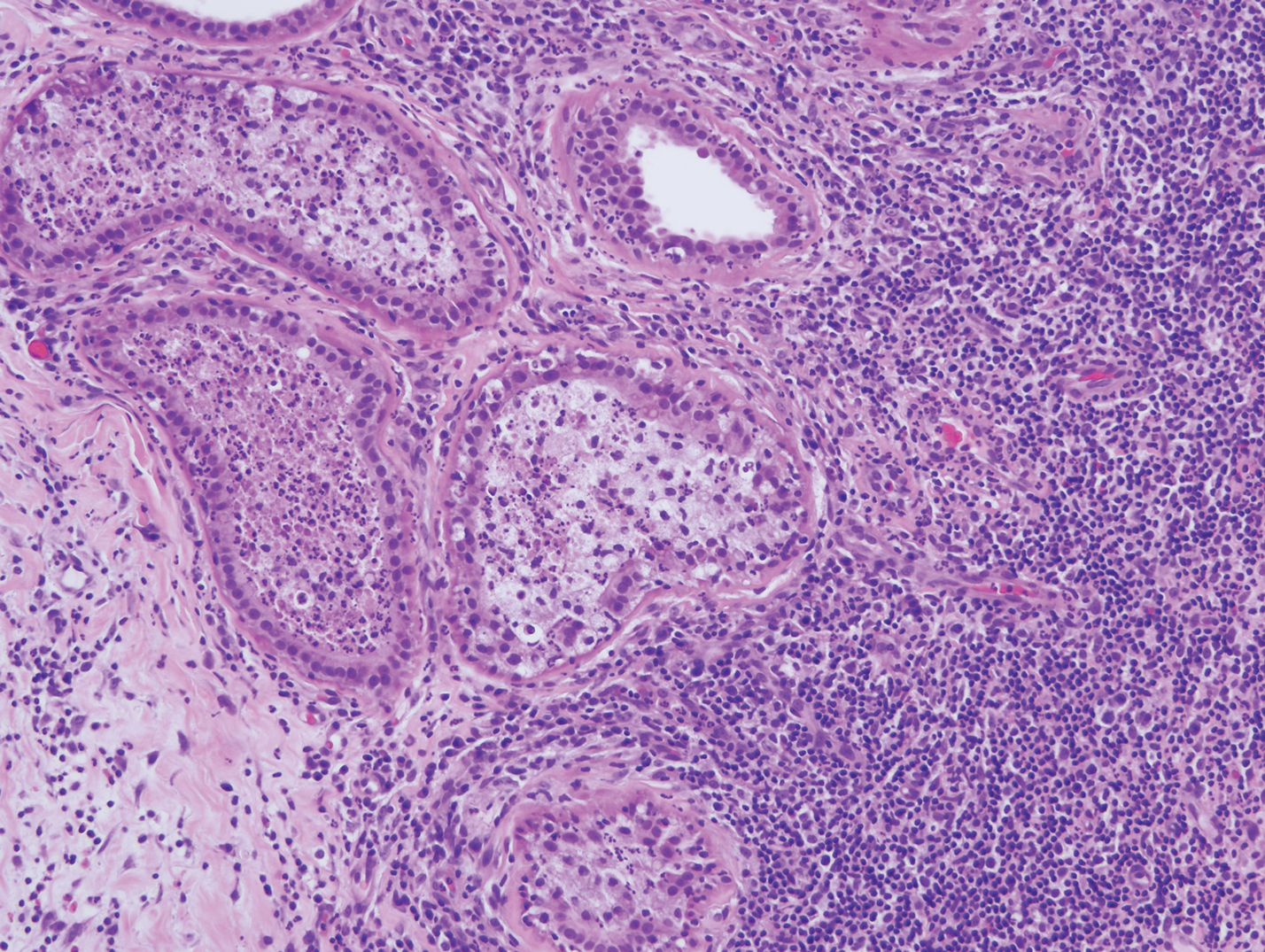
Mycosis fungoides is the most common primary cutaneous lymphoma to show a granulomatous infiltrate; the granuloma generally is sarcoidal, though other forms are described (Figure 3).11 Beyond these granulomatous foci, the key histopathologic feature of granulomatous mycosis fungoides (GMF) is diffuse dermal infiltration by atypical lymphoid cells. Epidermotropism and sparing of dermal nerves is the most critical finding in the diagnosis of GMF, especially in geographic regions where leprosy is endemic and high on the differential, as the conditions have histopathologic similarities.11,12 At the same time, lack of epidermotropism does not exclude the diagnosis of GMF.13 Clinically, GMF presentation is variable, but common findings include erythematous and hyperpigmented patches and plaques. Given the lack of clear clinical criteria, the diagnosis relies primarily on histopathologic features.11
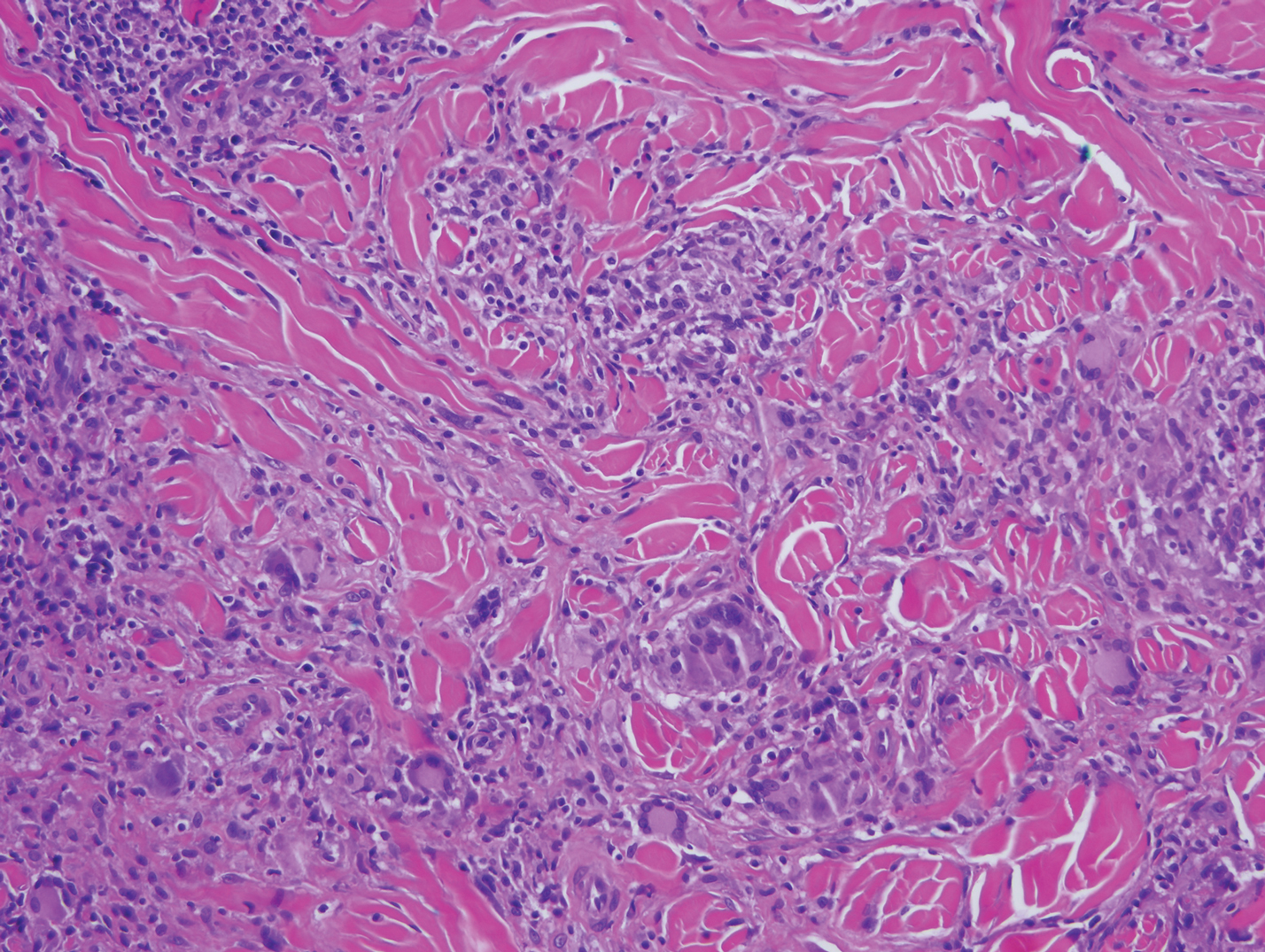
Mycobacterial skin and soft tissue infections may be attributed to both tuberculous and nontuberculous strains (atypical species).14 Clinical features range from small papules to large deformative plaques and ulcers.15 Histologic features also distinguish cutaneous tuberculosis (TB) from nontuberculous mycobacterial causes. Cutaneous TB shows caseous granulomas in the upper and mid dermis, while nontuberculous mycobacterial infections have more prominent neutrophil infiltration and interstitial granulomas (Figure 4).16
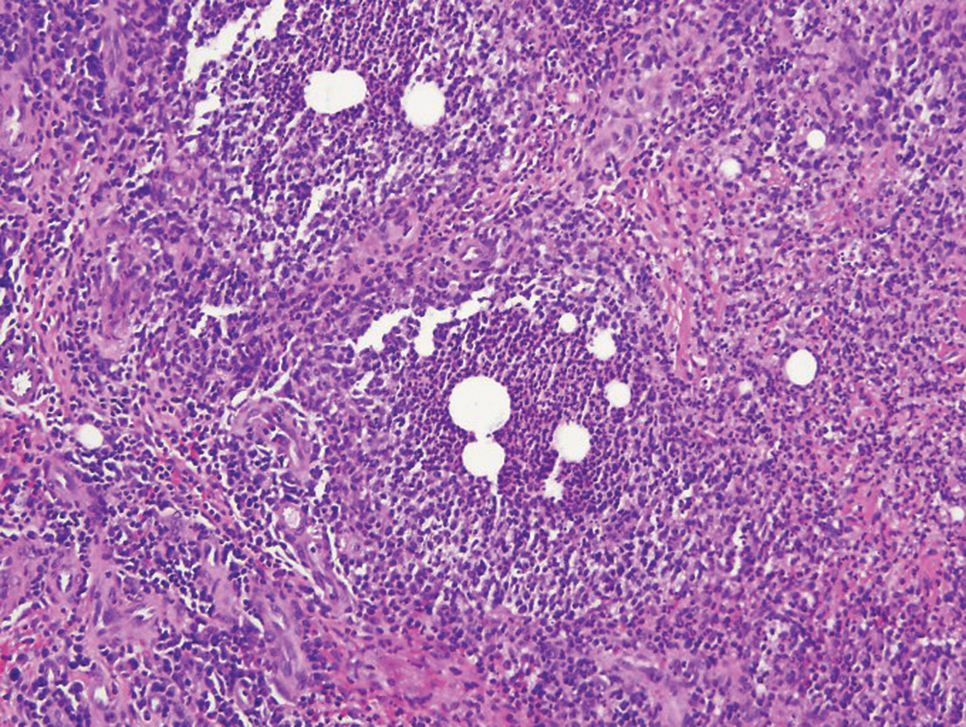
In cutaneous TB specifically, extrapulmonary manifestations may involve the skin in 1% to 1.5% of all TB cases, and although rare, ulcerative skin TB has been noted in one report as a nonhealing perianal ulcer that showed necrotizing granulomas on biopsy.17 Ultimately, diagnosis of cutaneous mycobacterial infection is confirmed with detection of acid-fast bacilli in the biopsy specimen.16
Diagnosis of cutaneous CD requires clinicopathologic correlation, as the clinical and histopathologic differential diagnoses of genital edema and noncaseating granulomas, respectively, are broad. Even though the clinical context was appropriate for cutaneous CD in this case, correct diagnosis required confirmatory histologic findings. Furthermore, taking multiple biopsies is prudent. In our patient, diagnostic findings only were present in the biopsy from the scrotum.
- Hagen JW, Swoger JM, Grandinetti LM. Cutaneous manifestations of Crohn disease. Dermatol Clin. 2015;33:417-431.
- Barrick BJ, Tollefson MM, Schoch JJ, et al. Penile and scrotal swelling: an underrecognized presentation of Crohn's disease. Pediatr Dermatol. 2016;33:172-177.
- Mooney EE, Walker J, Hourihane DO. Relation of granulomas to lymphatic vessels in Crohn's disease. J Clin Pathol. 1995;48:335-338.
- Parks AG, Morson BC, Pegum JS. Crohn's disease with cutaneous involvement. Proc R Soc Med. 1965;58:241-242.
- García-Colmenero L, Sánchez-Schmidt JM, Barranco C, et al. The natural history of cutaneous sarcoidosis: clinical spectrum and histological analysis of 40 cases [published online October 18, 2018]. Int J Dermatol. 2019;58:178-184.
- Yoo SS, Mimouni D, Nikolskaia OV, et al. Clinicopathologic features of ulcerative-atrophic sarcoidosis. Int J Dermatol. 2004;43:108-112.
- Cohen GF, Wolfe CM. Recalcitrant diffuse cutaneous sarcoidosis with perianal involvement responding to adalimumab. J Drugs Dermatol. 2017;16:1305-1306.
- Hoffman LK, Ghias MH, Lowes MA. Pathophysiology of hidradenitis suppurativa. Semin Cutan Med Surg. 2017;36:47-54.
- Saunte DML, Jemec GBE. Hidradenitis suppurativa: advances in diagnosis and treatment. JAMA. 2017;318:2019-2032.
- Attanoos RL, Appleton MA, Hughes LE, et al. Granulomatous hidradenitis suppurativa and cutaneous Crohn's disease. Histopathology. 1993;23:111-115.
- Gutte R, Kharkar V, Mahajan S, et al. Granulomatous mycosis fungoides with hypohydrosis mimicking lepromatous leprosy. Indian J Dermatol Venerol Leprol. 2010;76:686-690.
- Pousa CM, Nery NS, Mann D, et al. Granulomatous mycosis fungoides--a diagnostic challenge. An Bras Dermatol. 2015;90:554-556.
- Kempf W, Ostheeren-Michaelis S, Paulli M, et al. Granulomatous mycosis fungoides and granulomatous slack skin: a multicenter study of the Cutaneous Lymphoma Histopathology Task Force Group of the European Organization for Research and Treatment of Cancer (EORTC). Arch Dermatol. 2008;144:1609-1617.
- van Mechelen M, van der Hilst J, Gyssens IC, et al. Mycobacterial skin and soft tissue infections: TB or not TB? Neth J Med. 2018;76:269-274.
- van Zyl L, du Plessis J, Viljoen J. Cutaneous tuberculosis overview and current treatment regimens. Tuberculosis (Edinb). 2015;95:629-638.
- De Maio F, Trecarichi EM, Visconti E, et al. Understanding cutaneous tuberculosis: two clinical cases. JMM Case Rep. 2016;3:E005070.
- Wu S, Wang W, Chen H, et al. Perianal ulcerative skin tuberculosis: a case report. Medicine (Baltimore). 2018;97:E10836.
- Hagen JW, Swoger JM, Grandinetti LM. Cutaneous manifestations of Crohn disease. Dermatol Clin. 2015;33:417-431.
- Barrick BJ, Tollefson MM, Schoch JJ, et al. Penile and scrotal swelling: an underrecognized presentation of Crohn's disease. Pediatr Dermatol. 2016;33:172-177.
- Mooney EE, Walker J, Hourihane DO. Relation of granulomas to lymphatic vessels in Crohn's disease. J Clin Pathol. 1995;48:335-338.
- Parks AG, Morson BC, Pegum JS. Crohn's disease with cutaneous involvement. Proc R Soc Med. 1965;58:241-242.
- García-Colmenero L, Sánchez-Schmidt JM, Barranco C, et al. The natural history of cutaneous sarcoidosis: clinical spectrum and histological analysis of 40 cases [published online October 18, 2018]. Int J Dermatol. 2019;58:178-184.
- Yoo SS, Mimouni D, Nikolskaia OV, et al. Clinicopathologic features of ulcerative-atrophic sarcoidosis. Int J Dermatol. 2004;43:108-112.
- Cohen GF, Wolfe CM. Recalcitrant diffuse cutaneous sarcoidosis with perianal involvement responding to adalimumab. J Drugs Dermatol. 2017;16:1305-1306.
- Hoffman LK, Ghias MH, Lowes MA. Pathophysiology of hidradenitis suppurativa. Semin Cutan Med Surg. 2017;36:47-54.
- Saunte DML, Jemec GBE. Hidradenitis suppurativa: advances in diagnosis and treatment. JAMA. 2017;318:2019-2032.
- Attanoos RL, Appleton MA, Hughes LE, et al. Granulomatous hidradenitis suppurativa and cutaneous Crohn's disease. Histopathology. 1993;23:111-115.
- Gutte R, Kharkar V, Mahajan S, et al. Granulomatous mycosis fungoides with hypohydrosis mimicking lepromatous leprosy. Indian J Dermatol Venerol Leprol. 2010;76:686-690.
- Pousa CM, Nery NS, Mann D, et al. Granulomatous mycosis fungoides--a diagnostic challenge. An Bras Dermatol. 2015;90:554-556.
- Kempf W, Ostheeren-Michaelis S, Paulli M, et al. Granulomatous mycosis fungoides and granulomatous slack skin: a multicenter study of the Cutaneous Lymphoma Histopathology Task Force Group of the European Organization for Research and Treatment of Cancer (EORTC). Arch Dermatol. 2008;144:1609-1617.
- van Mechelen M, van der Hilst J, Gyssens IC, et al. Mycobacterial skin and soft tissue infections: TB or not TB? Neth J Med. 2018;76:269-274.
- van Zyl L, du Plessis J, Viljoen J. Cutaneous tuberculosis overview and current treatment regimens. Tuberculosis (Edinb). 2015;95:629-638.
- De Maio F, Trecarichi EM, Visconti E, et al. Understanding cutaneous tuberculosis: two clinical cases. JMM Case Rep. 2016;3:E005070.
- Wu S, Wang W, Chen H, et al. Perianal ulcerative skin tuberculosis: a case report. Medicine (Baltimore). 2018;97:E10836.

A 44-year-old man presented for evaluation of self-described "skin ripping" on the penis with penile and scrotal edema of 1 year's duration. He had a history of bowel symptoms and anorectal fistula of 3 years' duration. Purulent penile drainage and inguinal lymphadenopathy were noted on physical examination. Excisional biopsies of the scrotum and penis were performed. Special stains for organisms were negative.
COVID-19 hits physician couple: Dramatically different responses
A physician couple who both had COVID-19 had very different responses — one ending up in intensive care, the other asymptomatic.
Their story, one of two people living together but with such different responses to the infection, illustrates how much is still to be learned about COVID-19, says Noopur Raje, MD, professor of medicine at Harvard Medical School and director of the Center for Multiple Myeloma at Massachusetts General Hospital (MGH) in Boston.
“After experiencing #Covid_19 from the patient/caregiver end despite both of us being physicians at a major academic medical center, this has been a challenge like no other I have experienced,” Raje (@NoopurRajeMD) wrote on Twitter.
She outlined their experiences in a Twitter thread and elaborated in an interview with Medscape Medical News.
Raje says that she wants clinicians to know how symptoms can evolve both quickly and suddenly.
She recalls how for 10 days, she cared for her COVID-19–positive husband at home, separated from him by a floor in their Boston townhouse and wearing a surgical mask and gloves to bring him food and fluids, as he was too weak to help himself.
Despite the high fevers, chills, extreme fatigue, and dramatic weight loss, Raje says she felt reasonably confident that her husband was getting better. His temperature had dropped from around 103 to 101, his heart rate was in the 80s, and his blood pressure was “OK,” she recalls.
But then Jag Singh, MD, an otherwise healthy 55-year-old Harvard professor and cardiologist, started to cough — and everything suddenly changed.
The cough sounded chesty, and he was weak and unwell. They decided that he needed medical help.
“I was planning on driving him to the hospital, but I ended up having to call 911, although we literally live across the street,” she said.
“We have stairs here and I wasn’t sure that he would be able to make it coming down with me trying to help him, so the safest thing was for me to call for help.”
Singh was admitted straight to the medical intensive care unit (MICU) while his wife waited at home.
“I was blown away when I saw Jag’s x-ray and CT scan and the bilateral pneumonia he had developed,” she commented. “I would not have believed it, the way he was clinically — and seeing that x-ray.
“Honestly, when I took him in to hospital, I thought he’d be there a couple of days — over the weekend — and I’d get him back Monday. But it didn’t turn out that way. He was there for about 9 days.”
That first night in the hospital, Singh consented to intubation — should he need it. “He called me then,” said Raje. “I said we’ve got to do what we’ve got to do, it’s OK — it is what it is, and we’ll do whatever it takes.”
He remained in the MICU overnight and through the next day, still breathing on his own, but with the looming prospect of mechanical ventilation.
“The good news is he maintained his oxygen saturations throughout,” said Raje. “I was able to see his vitals with EPIC [remote monitoring] ... It was crazy,” she recalls. “Seeing a respiratory rate of 26 was difficult. When you see that, you worry about somebody tiring with the breathing. His inflammatory markers kept climbing, his fevers persisted.”
Thankfully, he never needed the ventilator.
But by this time Raje had another worry: She, too, had tested positive and was now alone at home.
“I was unable to talk to my extended family as they all looked to us as physicians for support,” she tweeted. Both children came to Boston to see her, but she saw them only through a window.
Alone, she waited for the same symptoms that had slammed her husband; but they never came — something she wants caregivers to know.
“The fear and anxiety of taking care of somebody who’s COVID positive ... I am hoping that can be alleviated a little bit at least,” she said. “If you’ve been taking care of someone, chances are you’re probably positive already and if you’re not sick, the chances of you getting sick are really low, so don’t be afraid to take care of that person.”
Singh is recovering well at home now, almost a month into his illness. During the interview, conducted via Zoom, he could be heard coughing in the background.
While in the MICU, Singh was treated with azithromycin and hydroxychloroquine — standard at MGH for critically ill COVID-19 patients — and he was also enrolled into a double-blind, randomized, placebo-controlled trial of the investigational agent remdesivir (Gilead).
Raje is not sure what, if anything, helped him turn the corner.
“I saw his inflammatory markers get worse actually — I don’t think we can know if the drugs made a difference,” she says. “His first dose of hydroxychloroquine was Friday night when he was admitted, and the markers continued to climb until the next Thursday.”
In particular, his C-reactive protein (CRP) kept rising, reaching the 260 to 270 mg/dL range, “which to me was scary,” she said. “I do think he had a cytokine storm going, but I didn’t see those results.”
“Understanding the immune compartment is going to be so, so critically important and what it is that we can do to boost folks’ immune systems,” she said.
“If you have a very high viral load and your immune system is not 100% even though you’re otherwise healthy, you might be the person who ends up with that more serious response to this virus. Trying to study this in a focused way, looking at the immune compartment, looking at the antibody status, looking at the viral load — there’s so much more we need to look at. Until we get the vaccine, which is probably a year-and-a-half away, we need to look at how can we develop that herd immunity so we don’t have folks getting as critically ill as they do.”
Despite feeling perfectly healthy, Raje is still at home. Three weeks after her first test, she is still testing positive for COVID-19, waiting for two consecutive negative results 72 hours apart before she is allowed back to work at the hospital.
When she gets the green light, she plans to go work on the COVID-19 floor, if needed. “It’s people like us [who have had COVID-19] who have to get back in the trenches and do the work now,” she says.
“My biggest concern is that it’s a very isolating experience for the COVID-positive patient. We are doing complete-barrier nursing — they are completely alone. The only person who ever walks into the room is the nurse — and the physician goes in once a day. It’s so important that we don’t lose sight of compassion,” she says.
“That’s why, in terms of alleviating anxiety, it is so important we do antibody testing so that people can actually go in and take care of these folks.”
‘Look for red flag’
Raje wants physicians to warn their self-isolating patients and caregivers to look for red flags. “There are primary care physicians who reached out to me [after my tweets] and said ‘when someone calls me and says it’s been 5-7 days and I am still not feeling well, I am going to look at that more seriously.’
“Part of me wanting to share this experience was basically to dispel the notion that 2 weeks into this you’re going to be fine,” she said, because it is not widely appreciated, she feels that “in week 2, you could become pretty sick.”
This article first appeared on Medscape.com.
A physician couple who both had COVID-19 had very different responses — one ending up in intensive care, the other asymptomatic.
Their story, one of two people living together but with such different responses to the infection, illustrates how much is still to be learned about COVID-19, says Noopur Raje, MD, professor of medicine at Harvard Medical School and director of the Center for Multiple Myeloma at Massachusetts General Hospital (MGH) in Boston.
“After experiencing #Covid_19 from the patient/caregiver end despite both of us being physicians at a major academic medical center, this has been a challenge like no other I have experienced,” Raje (@NoopurRajeMD) wrote on Twitter.
She outlined their experiences in a Twitter thread and elaborated in an interview with Medscape Medical News.
Raje says that she wants clinicians to know how symptoms can evolve both quickly and suddenly.
She recalls how for 10 days, she cared for her COVID-19–positive husband at home, separated from him by a floor in their Boston townhouse and wearing a surgical mask and gloves to bring him food and fluids, as he was too weak to help himself.
Despite the high fevers, chills, extreme fatigue, and dramatic weight loss, Raje says she felt reasonably confident that her husband was getting better. His temperature had dropped from around 103 to 101, his heart rate was in the 80s, and his blood pressure was “OK,” she recalls.
But then Jag Singh, MD, an otherwise healthy 55-year-old Harvard professor and cardiologist, started to cough — and everything suddenly changed.
The cough sounded chesty, and he was weak and unwell. They decided that he needed medical help.
“I was planning on driving him to the hospital, but I ended up having to call 911, although we literally live across the street,” she said.
“We have stairs here and I wasn’t sure that he would be able to make it coming down with me trying to help him, so the safest thing was for me to call for help.”
Singh was admitted straight to the medical intensive care unit (MICU) while his wife waited at home.
“I was blown away when I saw Jag’s x-ray and CT scan and the bilateral pneumonia he had developed,” she commented. “I would not have believed it, the way he was clinically — and seeing that x-ray.
“Honestly, when I took him in to hospital, I thought he’d be there a couple of days — over the weekend — and I’d get him back Monday. But it didn’t turn out that way. He was there for about 9 days.”
That first night in the hospital, Singh consented to intubation — should he need it. “He called me then,” said Raje. “I said we’ve got to do what we’ve got to do, it’s OK — it is what it is, and we’ll do whatever it takes.”
He remained in the MICU overnight and through the next day, still breathing on his own, but with the looming prospect of mechanical ventilation.
“The good news is he maintained his oxygen saturations throughout,” said Raje. “I was able to see his vitals with EPIC [remote monitoring] ... It was crazy,” she recalls. “Seeing a respiratory rate of 26 was difficult. When you see that, you worry about somebody tiring with the breathing. His inflammatory markers kept climbing, his fevers persisted.”
Thankfully, he never needed the ventilator.
But by this time Raje had another worry: She, too, had tested positive and was now alone at home.
“I was unable to talk to my extended family as they all looked to us as physicians for support,” she tweeted. Both children came to Boston to see her, but she saw them only through a window.
Alone, she waited for the same symptoms that had slammed her husband; but they never came — something she wants caregivers to know.
“The fear and anxiety of taking care of somebody who’s COVID positive ... I am hoping that can be alleviated a little bit at least,” she said. “If you’ve been taking care of someone, chances are you’re probably positive already and if you’re not sick, the chances of you getting sick are really low, so don’t be afraid to take care of that person.”
Singh is recovering well at home now, almost a month into his illness. During the interview, conducted via Zoom, he could be heard coughing in the background.
While in the MICU, Singh was treated with azithromycin and hydroxychloroquine — standard at MGH for critically ill COVID-19 patients — and he was also enrolled into a double-blind, randomized, placebo-controlled trial of the investigational agent remdesivir (Gilead).
Raje is not sure what, if anything, helped him turn the corner.
“I saw his inflammatory markers get worse actually — I don’t think we can know if the drugs made a difference,” she says. “His first dose of hydroxychloroquine was Friday night when he was admitted, and the markers continued to climb until the next Thursday.”
In particular, his C-reactive protein (CRP) kept rising, reaching the 260 to 270 mg/dL range, “which to me was scary,” she said. “I do think he had a cytokine storm going, but I didn’t see those results.”
“Understanding the immune compartment is going to be so, so critically important and what it is that we can do to boost folks’ immune systems,” she said.
“If you have a very high viral load and your immune system is not 100% even though you’re otherwise healthy, you might be the person who ends up with that more serious response to this virus. Trying to study this in a focused way, looking at the immune compartment, looking at the antibody status, looking at the viral load — there’s so much more we need to look at. Until we get the vaccine, which is probably a year-and-a-half away, we need to look at how can we develop that herd immunity so we don’t have folks getting as critically ill as they do.”
Despite feeling perfectly healthy, Raje is still at home. Three weeks after her first test, she is still testing positive for COVID-19, waiting for two consecutive negative results 72 hours apart before she is allowed back to work at the hospital.
When she gets the green light, she plans to go work on the COVID-19 floor, if needed. “It’s people like us [who have had COVID-19] who have to get back in the trenches and do the work now,” she says.
“My biggest concern is that it’s a very isolating experience for the COVID-positive patient. We are doing complete-barrier nursing — they are completely alone. The only person who ever walks into the room is the nurse — and the physician goes in once a day. It’s so important that we don’t lose sight of compassion,” she says.
“That’s why, in terms of alleviating anxiety, it is so important we do antibody testing so that people can actually go in and take care of these folks.”
‘Look for red flag’
Raje wants physicians to warn their self-isolating patients and caregivers to look for red flags. “There are primary care physicians who reached out to me [after my tweets] and said ‘when someone calls me and says it’s been 5-7 days and I am still not feeling well, I am going to look at that more seriously.’
“Part of me wanting to share this experience was basically to dispel the notion that 2 weeks into this you’re going to be fine,” she said, because it is not widely appreciated, she feels that “in week 2, you could become pretty sick.”
This article first appeared on Medscape.com.
A physician couple who both had COVID-19 had very different responses — one ending up in intensive care, the other asymptomatic.
Their story, one of two people living together but with such different responses to the infection, illustrates how much is still to be learned about COVID-19, says Noopur Raje, MD, professor of medicine at Harvard Medical School and director of the Center for Multiple Myeloma at Massachusetts General Hospital (MGH) in Boston.
“After experiencing #Covid_19 from the patient/caregiver end despite both of us being physicians at a major academic medical center, this has been a challenge like no other I have experienced,” Raje (@NoopurRajeMD) wrote on Twitter.
She outlined their experiences in a Twitter thread and elaborated in an interview with Medscape Medical News.
Raje says that she wants clinicians to know how symptoms can evolve both quickly and suddenly.
She recalls how for 10 days, she cared for her COVID-19–positive husband at home, separated from him by a floor in their Boston townhouse and wearing a surgical mask and gloves to bring him food and fluids, as he was too weak to help himself.
Despite the high fevers, chills, extreme fatigue, and dramatic weight loss, Raje says she felt reasonably confident that her husband was getting better. His temperature had dropped from around 103 to 101, his heart rate was in the 80s, and his blood pressure was “OK,” she recalls.
But then Jag Singh, MD, an otherwise healthy 55-year-old Harvard professor and cardiologist, started to cough — and everything suddenly changed.
The cough sounded chesty, and he was weak and unwell. They decided that he needed medical help.
“I was planning on driving him to the hospital, but I ended up having to call 911, although we literally live across the street,” she said.
“We have stairs here and I wasn’t sure that he would be able to make it coming down with me trying to help him, so the safest thing was for me to call for help.”
Singh was admitted straight to the medical intensive care unit (MICU) while his wife waited at home.
“I was blown away when I saw Jag’s x-ray and CT scan and the bilateral pneumonia he had developed,” she commented. “I would not have believed it, the way he was clinically — and seeing that x-ray.
“Honestly, when I took him in to hospital, I thought he’d be there a couple of days — over the weekend — and I’d get him back Monday. But it didn’t turn out that way. He was there for about 9 days.”
That first night in the hospital, Singh consented to intubation — should he need it. “He called me then,” said Raje. “I said we’ve got to do what we’ve got to do, it’s OK — it is what it is, and we’ll do whatever it takes.”
He remained in the MICU overnight and through the next day, still breathing on his own, but with the looming prospect of mechanical ventilation.
“The good news is he maintained his oxygen saturations throughout,” said Raje. “I was able to see his vitals with EPIC [remote monitoring] ... It was crazy,” she recalls. “Seeing a respiratory rate of 26 was difficult. When you see that, you worry about somebody tiring with the breathing. His inflammatory markers kept climbing, his fevers persisted.”
Thankfully, he never needed the ventilator.
But by this time Raje had another worry: She, too, had tested positive and was now alone at home.
“I was unable to talk to my extended family as they all looked to us as physicians for support,” she tweeted. Both children came to Boston to see her, but she saw them only through a window.
Alone, she waited for the same symptoms that had slammed her husband; but they never came — something she wants caregivers to know.
“The fear and anxiety of taking care of somebody who’s COVID positive ... I am hoping that can be alleviated a little bit at least,” she said. “If you’ve been taking care of someone, chances are you’re probably positive already and if you’re not sick, the chances of you getting sick are really low, so don’t be afraid to take care of that person.”
Singh is recovering well at home now, almost a month into his illness. During the interview, conducted via Zoom, he could be heard coughing in the background.
While in the MICU, Singh was treated with azithromycin and hydroxychloroquine — standard at MGH for critically ill COVID-19 patients — and he was also enrolled into a double-blind, randomized, placebo-controlled trial of the investigational agent remdesivir (Gilead).
Raje is not sure what, if anything, helped him turn the corner.
“I saw his inflammatory markers get worse actually — I don’t think we can know if the drugs made a difference,” she says. “His first dose of hydroxychloroquine was Friday night when he was admitted, and the markers continued to climb until the next Thursday.”
In particular, his C-reactive protein (CRP) kept rising, reaching the 260 to 270 mg/dL range, “which to me was scary,” she said. “I do think he had a cytokine storm going, but I didn’t see those results.”
“Understanding the immune compartment is going to be so, so critically important and what it is that we can do to boost folks’ immune systems,” she said.
“If you have a very high viral load and your immune system is not 100% even though you’re otherwise healthy, you might be the person who ends up with that more serious response to this virus. Trying to study this in a focused way, looking at the immune compartment, looking at the antibody status, looking at the viral load — there’s so much more we need to look at. Until we get the vaccine, which is probably a year-and-a-half away, we need to look at how can we develop that herd immunity so we don’t have folks getting as critically ill as they do.”
Despite feeling perfectly healthy, Raje is still at home. Three weeks after her first test, she is still testing positive for COVID-19, waiting for two consecutive negative results 72 hours apart before she is allowed back to work at the hospital.
When she gets the green light, she plans to go work on the COVID-19 floor, if needed. “It’s people like us [who have had COVID-19] who have to get back in the trenches and do the work now,” she says.
“My biggest concern is that it’s a very isolating experience for the COVID-positive patient. We are doing complete-barrier nursing — they are completely alone. The only person who ever walks into the room is the nurse — and the physician goes in once a day. It’s so important that we don’t lose sight of compassion,” she says.
“That’s why, in terms of alleviating anxiety, it is so important we do antibody testing so that people can actually go in and take care of these folks.”
‘Look for red flag’
Raje wants physicians to warn their self-isolating patients and caregivers to look for red flags. “There are primary care physicians who reached out to me [after my tweets] and said ‘when someone calls me and says it’s been 5-7 days and I am still not feeling well, I am going to look at that more seriously.’
“Part of me wanting to share this experience was basically to dispel the notion that 2 weeks into this you’re going to be fine,” she said, because it is not widely appreciated, she feels that “in week 2, you could become pretty sick.”
This article first appeared on Medscape.com.
NYC hospitals require health care workers to report in person, even for phone and telehealth work
A social worker in New York City was home, caring for his sick son, when the hospital at which he works ordered him to report back to work. His son had COVID-19, yet his hospital told him he had to show up in person.
The social worker’s situation is just one of many NYC Health + Hospitals employees who could work remotely yet are required to report in person. His circumstances were described in a letter sent by Lichten & Bright, a law firm representing the New York City Health Services Employees Union, Local 768.
“Despite the fact that all or virtually all of the work social workers perform can be done remotely, only a handful…are being permitted to work from home,” said the letter, which was written on behalf of about 1000 social workers and 150 medical records specialists and addressed to NYC H+H CEO Mitchell Katz, MD.
Most social workers stopped seeing patients in person in early March. But many still face crowded conditions at several points during their work day. They take public transportation to work, come face-to-face with other health care workers and patients in elevators, and some attend daily meetings with up to 10 employees in conference rooms too small to stay six feet apart, the letter says.
“The social workers are scared to go to work,” said Daniel Bright, the letter’s author. “They’re baffled by the lack of any management response that would allow them to work from home. They are worried about getting exposed to the coronavirus while riding the subway or the bus to work or at work from a doctor or nurse or patient, and getting sick themselves or taking it home to their families.”
There is no good reason that the social workers should be compelled to be physically at work during the COVID-19 pandemic, Bright said. The handful of social workers at NYC H+H’s World Trade Center Environmental Health Center clinic at Bellevue who have been allowed to work from home on an ad hoc basis, he said, have done so successfully.
In response to Bright’s letter, the hospital system issued a statement that seemed to downplay workers’ assessment of the situation, and included the following: “NYC Health + Hospital social workers…play different roles in our system, from acting as front-line providers to navigating safe discharges and helping patients and families with important health care decisions. Depending on the facility, the department, and the role they play, decisions are made by our hospital leaders on whether their critical work could be done remotely.”
Recently, many medical associations have issued statements supporting the rights of health care workers to speak up without fear of repercussion. But NYC H+H social workers have been complying with the orders because they say they’re scared of retaliation: In daily video conference calls, an administrator at one of NYC H+H’s hospitals has shown exasperation when asked about working from home, multiple employees told Medscape Medical News. And other questions, they said, such as whether staff could receive hazard pay, were scoffed at. Instead, the administration mentioned disciplinary action for those who didn’t show up to work.
During Thursday’s call, a recording of which was obtained by Medscape, the CEO of one NYC H+H hospital chastised his employees for taking their concerns to the press.
“People are just taking things and you know, using things for their benefit to be able to create problems for us who are trying to do our jobs,” he said, adding that he refuses to be bullied or blackmailed and that he’ll continue to do what he needs to do as CEO — but he wanted people to know “some of the garbage I have to deal with.”
He also reminded employees of documentation people need to provide if they don’t come in to work for being sick or taking a personal leave so the hospital can verify that “you have a condition that warrants you being out.”
Christopher Miller, a spokesperson for the hospital system, said that “some employees in certain functions may be approved to telecommute.” But employees contacted by Medscape who see all of their clients remotely said their requests to telecommute have not been approved.
At this point, it’s no longer a theoretical problem. COVID-19 appears to have spread among a cluster of people reporting to work in one of the H+H hospitals, employees said. In some cases, employees’ family members also became ill.
This article first appeared on Medscape.com.
A social worker in New York City was home, caring for his sick son, when the hospital at which he works ordered him to report back to work. His son had COVID-19, yet his hospital told him he had to show up in person.
The social worker’s situation is just one of many NYC Health + Hospitals employees who could work remotely yet are required to report in person. His circumstances were described in a letter sent by Lichten & Bright, a law firm representing the New York City Health Services Employees Union, Local 768.
“Despite the fact that all or virtually all of the work social workers perform can be done remotely, only a handful…are being permitted to work from home,” said the letter, which was written on behalf of about 1000 social workers and 150 medical records specialists and addressed to NYC H+H CEO Mitchell Katz, MD.
Most social workers stopped seeing patients in person in early March. But many still face crowded conditions at several points during their work day. They take public transportation to work, come face-to-face with other health care workers and patients in elevators, and some attend daily meetings with up to 10 employees in conference rooms too small to stay six feet apart, the letter says.
“The social workers are scared to go to work,” said Daniel Bright, the letter’s author. “They’re baffled by the lack of any management response that would allow them to work from home. They are worried about getting exposed to the coronavirus while riding the subway or the bus to work or at work from a doctor or nurse or patient, and getting sick themselves or taking it home to their families.”
There is no good reason that the social workers should be compelled to be physically at work during the COVID-19 pandemic, Bright said. The handful of social workers at NYC H+H’s World Trade Center Environmental Health Center clinic at Bellevue who have been allowed to work from home on an ad hoc basis, he said, have done so successfully.
In response to Bright’s letter, the hospital system issued a statement that seemed to downplay workers’ assessment of the situation, and included the following: “NYC Health + Hospital social workers…play different roles in our system, from acting as front-line providers to navigating safe discharges and helping patients and families with important health care decisions. Depending on the facility, the department, and the role they play, decisions are made by our hospital leaders on whether their critical work could be done remotely.”
Recently, many medical associations have issued statements supporting the rights of health care workers to speak up without fear of repercussion. But NYC H+H social workers have been complying with the orders because they say they’re scared of retaliation: In daily video conference calls, an administrator at one of NYC H+H’s hospitals has shown exasperation when asked about working from home, multiple employees told Medscape Medical News. And other questions, they said, such as whether staff could receive hazard pay, were scoffed at. Instead, the administration mentioned disciplinary action for those who didn’t show up to work.
During Thursday’s call, a recording of which was obtained by Medscape, the CEO of one NYC H+H hospital chastised his employees for taking their concerns to the press.
“People are just taking things and you know, using things for their benefit to be able to create problems for us who are trying to do our jobs,” he said, adding that he refuses to be bullied or blackmailed and that he’ll continue to do what he needs to do as CEO — but he wanted people to know “some of the garbage I have to deal with.”
He also reminded employees of documentation people need to provide if they don’t come in to work for being sick or taking a personal leave so the hospital can verify that “you have a condition that warrants you being out.”
Christopher Miller, a spokesperson for the hospital system, said that “some employees in certain functions may be approved to telecommute.” But employees contacted by Medscape who see all of their clients remotely said their requests to telecommute have not been approved.
At this point, it’s no longer a theoretical problem. COVID-19 appears to have spread among a cluster of people reporting to work in one of the H+H hospitals, employees said. In some cases, employees’ family members also became ill.
This article first appeared on Medscape.com.
A social worker in New York City was home, caring for his sick son, when the hospital at which he works ordered him to report back to work. His son had COVID-19, yet his hospital told him he had to show up in person.
The social worker’s situation is just one of many NYC Health + Hospitals employees who could work remotely yet are required to report in person. His circumstances were described in a letter sent by Lichten & Bright, a law firm representing the New York City Health Services Employees Union, Local 768.
“Despite the fact that all or virtually all of the work social workers perform can be done remotely, only a handful…are being permitted to work from home,” said the letter, which was written on behalf of about 1000 social workers and 150 medical records specialists and addressed to NYC H+H CEO Mitchell Katz, MD.
Most social workers stopped seeing patients in person in early March. But many still face crowded conditions at several points during their work day. They take public transportation to work, come face-to-face with other health care workers and patients in elevators, and some attend daily meetings with up to 10 employees in conference rooms too small to stay six feet apart, the letter says.
“The social workers are scared to go to work,” said Daniel Bright, the letter’s author. “They’re baffled by the lack of any management response that would allow them to work from home. They are worried about getting exposed to the coronavirus while riding the subway or the bus to work or at work from a doctor or nurse or patient, and getting sick themselves or taking it home to their families.”
There is no good reason that the social workers should be compelled to be physically at work during the COVID-19 pandemic, Bright said. The handful of social workers at NYC H+H’s World Trade Center Environmental Health Center clinic at Bellevue who have been allowed to work from home on an ad hoc basis, he said, have done so successfully.
In response to Bright’s letter, the hospital system issued a statement that seemed to downplay workers’ assessment of the situation, and included the following: “NYC Health + Hospital social workers…play different roles in our system, from acting as front-line providers to navigating safe discharges and helping patients and families with important health care decisions. Depending on the facility, the department, and the role they play, decisions are made by our hospital leaders on whether their critical work could be done remotely.”
Recently, many medical associations have issued statements supporting the rights of health care workers to speak up without fear of repercussion. But NYC H+H social workers have been complying with the orders because they say they’re scared of retaliation: In daily video conference calls, an administrator at one of NYC H+H’s hospitals has shown exasperation when asked about working from home, multiple employees told Medscape Medical News. And other questions, they said, such as whether staff could receive hazard pay, were scoffed at. Instead, the administration mentioned disciplinary action for those who didn’t show up to work.
During Thursday’s call, a recording of which was obtained by Medscape, the CEO of one NYC H+H hospital chastised his employees for taking their concerns to the press.
“People are just taking things and you know, using things for their benefit to be able to create problems for us who are trying to do our jobs,” he said, adding that he refuses to be bullied or blackmailed and that he’ll continue to do what he needs to do as CEO — but he wanted people to know “some of the garbage I have to deal with.”
He also reminded employees of documentation people need to provide if they don’t come in to work for being sick or taking a personal leave so the hospital can verify that “you have a condition that warrants you being out.”
Christopher Miller, a spokesperson for the hospital system, said that “some employees in certain functions may be approved to telecommute.” But employees contacted by Medscape who see all of their clients remotely said their requests to telecommute have not been approved.
At this point, it’s no longer a theoretical problem. COVID-19 appears to have spread among a cluster of people reporting to work in one of the H+H hospitals, employees said. In some cases, employees’ family members also became ill.
This article first appeared on Medscape.com.