User login
European Scientists Assess Avian Flu Pandemic Risk
As avian influenza continues to spread among wild bird populations in the European Union (EU), scientists have described a wide range of factors that could drive the virus to spread efficiently among humans, thereby increasing its pandemic potential.
Although transmission of avian influenza A(H5N1) from infected birds to humans is rare, “new strains carrying potential mutations for mammalian adaptation” could occur, according to a report issued on April 3 by the European Centre for Disease Prevention and Control and the European Food Safety Authority. The analysis identified a threat of strains currently circulating outside Europe that could enter the EU and the wider European Economic Area (EEA).
“If avian A(H5N1) influenza viruses acquire the ability to spread efficiently among humans, large-scale transmission could occur due to the lack of immune defenses against H5 viruses in humans,” the report warned.
Evolution of Avian Influenza Remains Hard to Predict
However, despite many occurrences of human exposure to avian influenza since 2020, “no symptomatic or productive infection in a human has been identified in the EU/EEA,” the scientists stated. Furthermore, after almost three decades of human exposure to the A(H5N1) virus of the Gs/GD lineage, the virus has not yet acquired the mutations required for airborne transmissibility between humans. However, it remains “difficult to predict the evolutionary direction the virus will take in the future,” the scientists assessed.
“Clearly, humans are being exposed in the current USA cattle outbreak,” Professor James Wood, infectious disease epidemiologist at the University of Cambridge, United Kingdom, told this news organization. “But, arguably, what is more significant is how few cases there have been with this virus lineage and its close relatives, despite massive global exposures over the last 3 years. All diagnosed human cases seem to have been singletons, with no evidence of human-to-human transmission.”
Ian Jones, professor of virology at the University of Reading, United Kingdom, sees no evidence of an imminent spillover of avian influenza from birds. But he told this news organization: “The trouble is, the clock resets every minute. Every time the virus has come out of a bird and gone somewhere, the clock is reset. So you can never say that just because it hasn’t happened since whenever, it’s never going to happen.”
Preventive Measures Recommended
The European report recommended a range of cautionary measures that included enhanced surveillance, access to rapid diagnostics, and sharing of genetic sequence data. It urged EU authorities to work together, adopting a One Health perspective, to limit the exposure of mammals, including humans, to avian influenza viruses.
Sarah Pitt, a microbiologist at the University of Brighton, United Kingdom, said the emphasis on authorities taking a One Health approach was sound. “You’re looking at humans, animals, plants, and the environment and how they’re all closely interacted,” she told this news organization. “Putting all those things together is actually going to be good for human health. So they’ve mentioned One Health a lot and I’m sure that’s on purpose because it’s the latest buzzword, and presumably it’s a way of getting governments to take it seriously.”
Overall, Dr. Pitt believes the document is designed to move zoonotic infectious diseases a bit higher up the agenda. “They should have been higher up the agenda before COVID,” she said.
The report also called for consideration of preventative measures, such as vaccination of poultry flocks.
Overall, Dr. Jones assesses the European report as “a reworking of what’s been pretty well covered over the years.” Despite extensive work by scientists in the field, he said: “I’m not sure we’re any better at predicting an emerging virus than we’ve ever been. I would point out that we didn’t spot SARS-CoV-2 coming, even though we had SARS-CoV-1 a few years earlier. Nobody spotted the 2009 pandemic from influenza, even though there was a lot of surveillance around at the time.”
A version of this article appeared on Medscape.com.
As avian influenza continues to spread among wild bird populations in the European Union (EU), scientists have described a wide range of factors that could drive the virus to spread efficiently among humans, thereby increasing its pandemic potential.
Although transmission of avian influenza A(H5N1) from infected birds to humans is rare, “new strains carrying potential mutations for mammalian adaptation” could occur, according to a report issued on April 3 by the European Centre for Disease Prevention and Control and the European Food Safety Authority. The analysis identified a threat of strains currently circulating outside Europe that could enter the EU and the wider European Economic Area (EEA).
“If avian A(H5N1) influenza viruses acquire the ability to spread efficiently among humans, large-scale transmission could occur due to the lack of immune defenses against H5 viruses in humans,” the report warned.
Evolution of Avian Influenza Remains Hard to Predict
However, despite many occurrences of human exposure to avian influenza since 2020, “no symptomatic or productive infection in a human has been identified in the EU/EEA,” the scientists stated. Furthermore, after almost three decades of human exposure to the A(H5N1) virus of the Gs/GD lineage, the virus has not yet acquired the mutations required for airborne transmissibility between humans. However, it remains “difficult to predict the evolutionary direction the virus will take in the future,” the scientists assessed.
“Clearly, humans are being exposed in the current USA cattle outbreak,” Professor James Wood, infectious disease epidemiologist at the University of Cambridge, United Kingdom, told this news organization. “But, arguably, what is more significant is how few cases there have been with this virus lineage and its close relatives, despite massive global exposures over the last 3 years. All diagnosed human cases seem to have been singletons, with no evidence of human-to-human transmission.”
Ian Jones, professor of virology at the University of Reading, United Kingdom, sees no evidence of an imminent spillover of avian influenza from birds. But he told this news organization: “The trouble is, the clock resets every minute. Every time the virus has come out of a bird and gone somewhere, the clock is reset. So you can never say that just because it hasn’t happened since whenever, it’s never going to happen.”
Preventive Measures Recommended
The European report recommended a range of cautionary measures that included enhanced surveillance, access to rapid diagnostics, and sharing of genetic sequence data. It urged EU authorities to work together, adopting a One Health perspective, to limit the exposure of mammals, including humans, to avian influenza viruses.
Sarah Pitt, a microbiologist at the University of Brighton, United Kingdom, said the emphasis on authorities taking a One Health approach was sound. “You’re looking at humans, animals, plants, and the environment and how they’re all closely interacted,” she told this news organization. “Putting all those things together is actually going to be good for human health. So they’ve mentioned One Health a lot and I’m sure that’s on purpose because it’s the latest buzzword, and presumably it’s a way of getting governments to take it seriously.”
Overall, Dr. Pitt believes the document is designed to move zoonotic infectious diseases a bit higher up the agenda. “They should have been higher up the agenda before COVID,” she said.
The report also called for consideration of preventative measures, such as vaccination of poultry flocks.
Overall, Dr. Jones assesses the European report as “a reworking of what’s been pretty well covered over the years.” Despite extensive work by scientists in the field, he said: “I’m not sure we’re any better at predicting an emerging virus than we’ve ever been. I would point out that we didn’t spot SARS-CoV-2 coming, even though we had SARS-CoV-1 a few years earlier. Nobody spotted the 2009 pandemic from influenza, even though there was a lot of surveillance around at the time.”
A version of this article appeared on Medscape.com.
As avian influenza continues to spread among wild bird populations in the European Union (EU), scientists have described a wide range of factors that could drive the virus to spread efficiently among humans, thereby increasing its pandemic potential.
Although transmission of avian influenza A(H5N1) from infected birds to humans is rare, “new strains carrying potential mutations for mammalian adaptation” could occur, according to a report issued on April 3 by the European Centre for Disease Prevention and Control and the European Food Safety Authority. The analysis identified a threat of strains currently circulating outside Europe that could enter the EU and the wider European Economic Area (EEA).
“If avian A(H5N1) influenza viruses acquire the ability to spread efficiently among humans, large-scale transmission could occur due to the lack of immune defenses against H5 viruses in humans,” the report warned.
Evolution of Avian Influenza Remains Hard to Predict
However, despite many occurrences of human exposure to avian influenza since 2020, “no symptomatic or productive infection in a human has been identified in the EU/EEA,” the scientists stated. Furthermore, after almost three decades of human exposure to the A(H5N1) virus of the Gs/GD lineage, the virus has not yet acquired the mutations required for airborne transmissibility between humans. However, it remains “difficult to predict the evolutionary direction the virus will take in the future,” the scientists assessed.
“Clearly, humans are being exposed in the current USA cattle outbreak,” Professor James Wood, infectious disease epidemiologist at the University of Cambridge, United Kingdom, told this news organization. “But, arguably, what is more significant is how few cases there have been with this virus lineage and its close relatives, despite massive global exposures over the last 3 years. All diagnosed human cases seem to have been singletons, with no evidence of human-to-human transmission.”
Ian Jones, professor of virology at the University of Reading, United Kingdom, sees no evidence of an imminent spillover of avian influenza from birds. But he told this news organization: “The trouble is, the clock resets every minute. Every time the virus has come out of a bird and gone somewhere, the clock is reset. So you can never say that just because it hasn’t happened since whenever, it’s never going to happen.”
Preventive Measures Recommended
The European report recommended a range of cautionary measures that included enhanced surveillance, access to rapid diagnostics, and sharing of genetic sequence data. It urged EU authorities to work together, adopting a One Health perspective, to limit the exposure of mammals, including humans, to avian influenza viruses.
Sarah Pitt, a microbiologist at the University of Brighton, United Kingdom, said the emphasis on authorities taking a One Health approach was sound. “You’re looking at humans, animals, plants, and the environment and how they’re all closely interacted,” she told this news organization. “Putting all those things together is actually going to be good for human health. So they’ve mentioned One Health a lot and I’m sure that’s on purpose because it’s the latest buzzword, and presumably it’s a way of getting governments to take it seriously.”
Overall, Dr. Pitt believes the document is designed to move zoonotic infectious diseases a bit higher up the agenda. “They should have been higher up the agenda before COVID,” she said.
The report also called for consideration of preventative measures, such as vaccination of poultry flocks.
Overall, Dr. Jones assesses the European report as “a reworking of what’s been pretty well covered over the years.” Despite extensive work by scientists in the field, he said: “I’m not sure we’re any better at predicting an emerging virus than we’ve ever been. I would point out that we didn’t spot SARS-CoV-2 coming, even though we had SARS-CoV-1 a few years earlier. Nobody spotted the 2009 pandemic from influenza, even though there was a lot of surveillance around at the time.”
A version of this article appeared on Medscape.com.
Hepatitis E Vaccine Shows Long-Term Efficacy
The hepatitis E virus (HEV) is among the leading global causes of acute viral hepatitis. Molecular studies of HEV strains have identified four main genotypes. Genotypes 1 and 2 are limited to humans and are transmitted through contaminated water in resource-limited countries, mainly in Asia. Genotypes 3 and 4 are zoonotic, causing sporadic indigenous hepatitis E in nearly all countries.
Each year, approximately 20 million HEV infections occur worldwide, resulting in around 3.3 million symptomatic infections and 70,000 deaths. Despite this toll, HEV infection remains underestimated, and Western countries are likely not immune to the virus. To date, two recombinant vaccines against hepatitis E, based on genotype 1, have been developed and approved in China, but further studies are needed to determine the duration of vaccination protection.
Ten-Year Results
This study is an extension of a randomized, double-blind, placebo-controlled phase 3 clinical trial of the Hecolin hepatitis E vaccine that was conducted in Dongtai County, Jiangsu, China. In the initial trial, healthy adults aged 16-65 years were recruited, stratified by age and sex, and randomly assigned in a 1:1 ratio to receive three doses of intramuscular hepatitis E vaccine or placebo at months 0, 1, and 6.
A hepatitis E surveillance system, including 205 clinical sentinels covering the entire study region, was established before the study began and maintained for 10 years after vaccination to identify individuals with suspected hepatitis. In addition, an external control cohort was formed to assess vaccine efficacy. The primary endpoint was the vaccine’s efficacy in preventing confirmed hepatitis E occurring at least 30 days after the administration of the third vaccine dose.
Follow-up occurred every 3 months. Participants with hepatitis symptoms for 3 days or more underwent alanine aminotransferase (ALT) concentration measurement. Patients with ALT concentrations ≥ 2.5 times the upper limit of normal were considered to have acute hepatitis. A diagnosis of HEV-confirmed infection was made for patients with acute hepatitis presenting with at least two of the following markers: Presence of HEV RNA, presence of positive anti-HEV immunoglobulin (Ig) M antibodies, and at least fourfold increase in anti-HEV IgG concentrations.
For the efficacy analysis, a Poisson regression model was used to estimate the relative risk and its 95% CI of incidence between groups. Incidence was reported as the number of patients with hepatitis E per 10,000 person-years.
Immunogenicity persistence was assessed by measuring anti-HEV IgG in participants. Serum samples were collected at months 0, 7, 13, 19, 31, 43, 55, 79, and 103 for Qingdao district participants and at months 0, 7, 19, 31, 43, 67, and 91 for Anfeng district participants.
Efficacy and Duration
The follow-up period extended from 2007 to 2017. In total, 97,356 participants completed the three-dose regimen and were included in the per-protocol population (48,693 in the vaccine group and 48,663 in the placebo group), and 178,236 residents from the study region participated in the external control cohort. During the study period, 90 cases of hepatitis E were identified, with 13 in the vaccine group (0.2 per 10,000 person-years) and 77 in the placebo group (1.4 per 10,000 person-years). This indicated a vaccine efficacy of 86.6% in the per-protocol analysis.
In the subgroups evaluated for immunogenicity persistence, among those who were initially seronegative and received three doses of hepatitis E vaccine, 254 out of 291 vaccinated participants (87.3%) in Qingdao after 8.5 years and 1270 (73.0%) out of 1740 vaccinated participants in Anfeng after 7.5 years maintained detectable antibody concentrations.
The identification of infections despite vaccination is notable, especially with eight cases occurring beyond the fourth year following the last dose. This information is crucial for understanding potential immunity decline over time and highlights the importance of exploring various vaccination strategies to optimize protection.
An ongoing phase 4 clinical trial in Bangladesh, exploring different administration schedules and target populations, could help optimize vaccination strategies. The remarkable efficacy (100%) observed over a 30-month period for the two-dose schedule (doses are administered 1 month apart) is promising.
The observation of higher IgG antibody avidity in participants with infections despite vaccination underscores the importance of robust antibody responses to mitigate disease severity and duration. Several study limitations, such as lack of data on deaths and emigrations, a single-center study design, predominance of genotype 4 infections, and the risk for bias in the external control cohort, should be acknowledged.
In conclusion, this study provides compelling evidence of sustained protection of the hepatitis E vaccine over a decade. The observed persistence of induced antibodies for at least 8.5 years supports the long-term efficacy of the vaccine. Diverse global trials, further investigation into the impact of natural infections on vaccine-induced antibodies, and confirmation of inter-genotypic protection are needed.
This story was translated from JIM, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
The hepatitis E virus (HEV) is among the leading global causes of acute viral hepatitis. Molecular studies of HEV strains have identified four main genotypes. Genotypes 1 and 2 are limited to humans and are transmitted through contaminated water in resource-limited countries, mainly in Asia. Genotypes 3 and 4 are zoonotic, causing sporadic indigenous hepatitis E in nearly all countries.
Each year, approximately 20 million HEV infections occur worldwide, resulting in around 3.3 million symptomatic infections and 70,000 deaths. Despite this toll, HEV infection remains underestimated, and Western countries are likely not immune to the virus. To date, two recombinant vaccines against hepatitis E, based on genotype 1, have been developed and approved in China, but further studies are needed to determine the duration of vaccination protection.
Ten-Year Results
This study is an extension of a randomized, double-blind, placebo-controlled phase 3 clinical trial of the Hecolin hepatitis E vaccine that was conducted in Dongtai County, Jiangsu, China. In the initial trial, healthy adults aged 16-65 years were recruited, stratified by age and sex, and randomly assigned in a 1:1 ratio to receive three doses of intramuscular hepatitis E vaccine or placebo at months 0, 1, and 6.
A hepatitis E surveillance system, including 205 clinical sentinels covering the entire study region, was established before the study began and maintained for 10 years after vaccination to identify individuals with suspected hepatitis. In addition, an external control cohort was formed to assess vaccine efficacy. The primary endpoint was the vaccine’s efficacy in preventing confirmed hepatitis E occurring at least 30 days after the administration of the third vaccine dose.
Follow-up occurred every 3 months. Participants with hepatitis symptoms for 3 days or more underwent alanine aminotransferase (ALT) concentration measurement. Patients with ALT concentrations ≥ 2.5 times the upper limit of normal were considered to have acute hepatitis. A diagnosis of HEV-confirmed infection was made for patients with acute hepatitis presenting with at least two of the following markers: Presence of HEV RNA, presence of positive anti-HEV immunoglobulin (Ig) M antibodies, and at least fourfold increase in anti-HEV IgG concentrations.
For the efficacy analysis, a Poisson regression model was used to estimate the relative risk and its 95% CI of incidence between groups. Incidence was reported as the number of patients with hepatitis E per 10,000 person-years.
Immunogenicity persistence was assessed by measuring anti-HEV IgG in participants. Serum samples were collected at months 0, 7, 13, 19, 31, 43, 55, 79, and 103 for Qingdao district participants and at months 0, 7, 19, 31, 43, 67, and 91 for Anfeng district participants.
Efficacy and Duration
The follow-up period extended from 2007 to 2017. In total, 97,356 participants completed the three-dose regimen and were included in the per-protocol population (48,693 in the vaccine group and 48,663 in the placebo group), and 178,236 residents from the study region participated in the external control cohort. During the study period, 90 cases of hepatitis E were identified, with 13 in the vaccine group (0.2 per 10,000 person-years) and 77 in the placebo group (1.4 per 10,000 person-years). This indicated a vaccine efficacy of 86.6% in the per-protocol analysis.
In the subgroups evaluated for immunogenicity persistence, among those who were initially seronegative and received three doses of hepatitis E vaccine, 254 out of 291 vaccinated participants (87.3%) in Qingdao after 8.5 years and 1270 (73.0%) out of 1740 vaccinated participants in Anfeng after 7.5 years maintained detectable antibody concentrations.
The identification of infections despite vaccination is notable, especially with eight cases occurring beyond the fourth year following the last dose. This information is crucial for understanding potential immunity decline over time and highlights the importance of exploring various vaccination strategies to optimize protection.
An ongoing phase 4 clinical trial in Bangladesh, exploring different administration schedules and target populations, could help optimize vaccination strategies. The remarkable efficacy (100%) observed over a 30-month period for the two-dose schedule (doses are administered 1 month apart) is promising.
The observation of higher IgG antibody avidity in participants with infections despite vaccination underscores the importance of robust antibody responses to mitigate disease severity and duration. Several study limitations, such as lack of data on deaths and emigrations, a single-center study design, predominance of genotype 4 infections, and the risk for bias in the external control cohort, should be acknowledged.
In conclusion, this study provides compelling evidence of sustained protection of the hepatitis E vaccine over a decade. The observed persistence of induced antibodies for at least 8.5 years supports the long-term efficacy of the vaccine. Diverse global trials, further investigation into the impact of natural infections on vaccine-induced antibodies, and confirmation of inter-genotypic protection are needed.
This story was translated from JIM, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
The hepatitis E virus (HEV) is among the leading global causes of acute viral hepatitis. Molecular studies of HEV strains have identified four main genotypes. Genotypes 1 and 2 are limited to humans and are transmitted through contaminated water in resource-limited countries, mainly in Asia. Genotypes 3 and 4 are zoonotic, causing sporadic indigenous hepatitis E in nearly all countries.
Each year, approximately 20 million HEV infections occur worldwide, resulting in around 3.3 million symptomatic infections and 70,000 deaths. Despite this toll, HEV infection remains underestimated, and Western countries are likely not immune to the virus. To date, two recombinant vaccines against hepatitis E, based on genotype 1, have been developed and approved in China, but further studies are needed to determine the duration of vaccination protection.
Ten-Year Results
This study is an extension of a randomized, double-blind, placebo-controlled phase 3 clinical trial of the Hecolin hepatitis E vaccine that was conducted in Dongtai County, Jiangsu, China. In the initial trial, healthy adults aged 16-65 years were recruited, stratified by age and sex, and randomly assigned in a 1:1 ratio to receive three doses of intramuscular hepatitis E vaccine or placebo at months 0, 1, and 6.
A hepatitis E surveillance system, including 205 clinical sentinels covering the entire study region, was established before the study began and maintained for 10 years after vaccination to identify individuals with suspected hepatitis. In addition, an external control cohort was formed to assess vaccine efficacy. The primary endpoint was the vaccine’s efficacy in preventing confirmed hepatitis E occurring at least 30 days after the administration of the third vaccine dose.
Follow-up occurred every 3 months. Participants with hepatitis symptoms for 3 days or more underwent alanine aminotransferase (ALT) concentration measurement. Patients with ALT concentrations ≥ 2.5 times the upper limit of normal were considered to have acute hepatitis. A diagnosis of HEV-confirmed infection was made for patients with acute hepatitis presenting with at least two of the following markers: Presence of HEV RNA, presence of positive anti-HEV immunoglobulin (Ig) M antibodies, and at least fourfold increase in anti-HEV IgG concentrations.
For the efficacy analysis, a Poisson regression model was used to estimate the relative risk and its 95% CI of incidence between groups. Incidence was reported as the number of patients with hepatitis E per 10,000 person-years.
Immunogenicity persistence was assessed by measuring anti-HEV IgG in participants. Serum samples were collected at months 0, 7, 13, 19, 31, 43, 55, 79, and 103 for Qingdao district participants and at months 0, 7, 19, 31, 43, 67, and 91 for Anfeng district participants.
Efficacy and Duration
The follow-up period extended from 2007 to 2017. In total, 97,356 participants completed the three-dose regimen and were included in the per-protocol population (48,693 in the vaccine group and 48,663 in the placebo group), and 178,236 residents from the study region participated in the external control cohort. During the study period, 90 cases of hepatitis E were identified, with 13 in the vaccine group (0.2 per 10,000 person-years) and 77 in the placebo group (1.4 per 10,000 person-years). This indicated a vaccine efficacy of 86.6% in the per-protocol analysis.
In the subgroups evaluated for immunogenicity persistence, among those who were initially seronegative and received three doses of hepatitis E vaccine, 254 out of 291 vaccinated participants (87.3%) in Qingdao after 8.5 years and 1270 (73.0%) out of 1740 vaccinated participants in Anfeng after 7.5 years maintained detectable antibody concentrations.
The identification of infections despite vaccination is notable, especially with eight cases occurring beyond the fourth year following the last dose. This information is crucial for understanding potential immunity decline over time and highlights the importance of exploring various vaccination strategies to optimize protection.
An ongoing phase 4 clinical trial in Bangladesh, exploring different administration schedules and target populations, could help optimize vaccination strategies. The remarkable efficacy (100%) observed over a 30-month period for the two-dose schedule (doses are administered 1 month apart) is promising.
The observation of higher IgG antibody avidity in participants with infections despite vaccination underscores the importance of robust antibody responses to mitigate disease severity and duration. Several study limitations, such as lack of data on deaths and emigrations, a single-center study design, predominance of genotype 4 infections, and the risk for bias in the external control cohort, should be acknowledged.
In conclusion, this study provides compelling evidence of sustained protection of the hepatitis E vaccine over a decade. The observed persistence of induced antibodies for at least 8.5 years supports the long-term efficacy of the vaccine. Diverse global trials, further investigation into the impact of natural infections on vaccine-induced antibodies, and confirmation of inter-genotypic protection are needed.
This story was translated from JIM, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
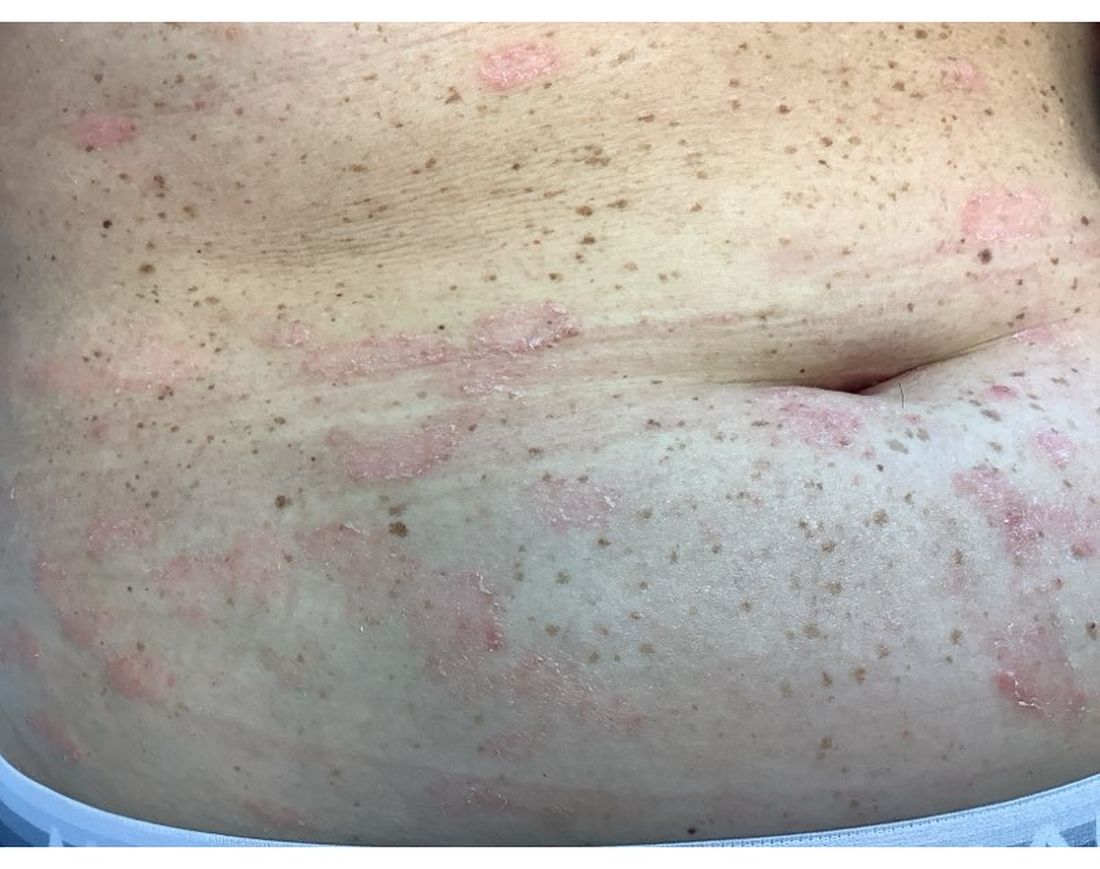
Consider Skin Cancer, Infection Risks in Solid Organ Transplant Recipients
SAN DIEGO — because of their suppressed immune systems.
“There are over 450,000 people with a solid organ transplant living in the United States. If you do the math, that works out to about 40 organ transplant recipients for every dermatologist, so there’s a lot of them out there for us to take care of,” Sean Christensen, MD, PhD, associate professor of dermatology, Yale University, New Haven, Connecticut, said at the annual meeting of the American Academy of Dermatology (AAD). “If we expand that umbrella to include all types of immunosuppression, that’s over 4 million adults in the US.”
Dr. Christensen encouraged dermatologists to be aware of the varying risks for immunosuppressive drugs and best screening practices for these patients, and to take advantage of a validated skin cancer risk assessment tool for transplant patients.
During his presentation, he highlighted five classes of immunosuppressive drugs and their associated skin cancer risks:
- Calcineurin inhibitors (tacrolimus or cyclosporine), which cause severe immune suppression and pose a severe skin cancer risk. They may also cause gingival hyperplasia and sebaceous hyperplasia.
- Antimetabolites (mycophenolate mofetil or azathioprine), which cause moderate to severe immune suppression and pose a severe skin cancer risk.
- Mammalian target of rapamycin inhibitors (sirolimus or everolimus), which cause severe immune suppression and pose a moderate skin cancer risk. They also impair wound healing.
- Corticosteroids (prednisone), which cause mild to severe immune suppression and pose a minimal skin cancer risk.
- A decoy receptor protein (belatacept), which causes severe immune suppression and poses a mild skin cancer risk.
“Most of our solid-organ transplant recipients will be on both a calcineurin inhibitor and an antimetabolite,” Dr. Christensen said. “In addition to the skin cancer risk associated with immunosuppression, there is an additive risk” that is a direct effect of these medications on the skin. “That means our transplant recipients have a severely and disproportionate increase in skin cancer,” he noted.
Up to half of solid-organ transplant recipients will develop skin cancer, Dr. Christensen said. These patients have a sixfold to 10-fold increased risk for basal cell carcinoma (BCC), a 35- to 65-fold increased risk for squamous cell carcinoma (SCC), a twofold to sevenfold increased risk for melanoma, and a 16- to 100-fold increased risk for Merkel cell carcinoma.
Transplant recipients with SCC, he said, have a twofold to threefold higher risk for metastasis (4%-8% nodal metastasis) and twofold to fivefold higher risk for death (2%-7% mortality) from SCC.
As for other kinds of immunosuppression, HIV positivity, treatment with 6-mercaptopurine or azathioprine (for inflammatory bowel disease and rheumatoid arthritis), and antitumor necrosis factor agents (for psoriasis, inflammatory bowel disease, and rheumatoid arthritis) have been linked in studies to a higher risk for nonmelanoma skin cancer.
Dr. Christensen also highlighted graft-versus-host disease (GVHD). “It does look like there is a disproportionate and increased risk of SCC of the oropharynx and of the skin in patients who have chronic GVHD. This is probably due to a combination of both the immunosuppressive medications that are required but also from chronic and ongoing inflammation in the skin.”
Chronic GVHD has been linked to a 5.3-fold increase in the risk for SCC and a twofold increase in the risk for BCC, he added.
Moreover, new medications for treating GVHD have been linked to an increased risk for SCC, including a 3.2-fold increased risk for SCC associated with ruxolitinib, a Janus kinase (JAK) 1 and JAK2 inhibitor, in a study of patients with polycythemia vera and myelofibrosis; and a case report of SCC in a patient treated with belumosudil, a rho-associated coiled-coil-containing protein kinase-2 kinase inhibitor, for chronic GVHD. Risk for SCC appears to increase based on duration of use with voriconazole, an antifungal, which, he said, is a potent photosynthesizer.
Dr. Christensen also noted the higher risk for infections in immunocompromised patients and added that these patients can develop inflammatory disease despite immunosuppression:
Staphylococcus, Streptococcus, and Dermatophytes are the most common skin pathogens in these patients. There’s a significantly increased risk for reactivation of herpes simplex, varicella-zoster viruses, and cytomegalovirus. Opportunistic and disseminated fungal infections, such as mycobacteria, Candida, histoplasma, cryptococcus, aspergillus, and mucormycosis, can also appear.
More than 80% of transplant recipients develop molluscum and verruca vulgaris/human papillomavirus infection. They may also develop noninfectious inflammatory dermatoses.
Risk Calculator
What can dermatologists do to help transplant patients? Dr. Christensen highlighted the Skin and UV Neoplasia Transplant Risk Assessment Calculator, which predicts skin cancer risk based on points given for race, gender, skin cancer history, age at transplant, and site of transplant.
The tool, validated in a 2023 study of transplant recipients in Europe, is available online and as an app. It makes recommendations to users about when patients should have initial skin screening exams. Those with the most risk — 45% at 5 years — should be screened within 6 months. “We can use [the tool] to triage these cases when we first meet them and get them plugged into the appropriate care,” Dr. Christensen said.
He recommended seeing high-risk patients at least annually. Patients with a prior SCC and a heavy burden of actinic keratosis should be followed more frequently, he said.
In regard to SCC, he highlighted a 2024 study of solid organ transplant recipients that found the risk for a second SCC after a first SCC was 74%, the risk for a third SCC after a second SCC was 83%, and the risk for another SCC after five SCCs was 92%.
Dr. Christensen disclosed relationships with Canfield Scientific Inc. (consulting), Inhibitor Therapeutics (advisory board), and Sol-Gel Technologies Ltd. (grants/research funding).
A version of this article first appeared on Medscape.com.
SAN DIEGO — because of their suppressed immune systems.
“There are over 450,000 people with a solid organ transplant living in the United States. If you do the math, that works out to about 40 organ transplant recipients for every dermatologist, so there’s a lot of them out there for us to take care of,” Sean Christensen, MD, PhD, associate professor of dermatology, Yale University, New Haven, Connecticut, said at the annual meeting of the American Academy of Dermatology (AAD). “If we expand that umbrella to include all types of immunosuppression, that’s over 4 million adults in the US.”
Dr. Christensen encouraged dermatologists to be aware of the varying risks for immunosuppressive drugs and best screening practices for these patients, and to take advantage of a validated skin cancer risk assessment tool for transplant patients.
During his presentation, he highlighted five classes of immunosuppressive drugs and their associated skin cancer risks:
- Calcineurin inhibitors (tacrolimus or cyclosporine), which cause severe immune suppression and pose a severe skin cancer risk. They may also cause gingival hyperplasia and sebaceous hyperplasia.
- Antimetabolites (mycophenolate mofetil or azathioprine), which cause moderate to severe immune suppression and pose a severe skin cancer risk.
- Mammalian target of rapamycin inhibitors (sirolimus or everolimus), which cause severe immune suppression and pose a moderate skin cancer risk. They also impair wound healing.
- Corticosteroids (prednisone), which cause mild to severe immune suppression and pose a minimal skin cancer risk.
- A decoy receptor protein (belatacept), which causes severe immune suppression and poses a mild skin cancer risk.
“Most of our solid-organ transplant recipients will be on both a calcineurin inhibitor and an antimetabolite,” Dr. Christensen said. “In addition to the skin cancer risk associated with immunosuppression, there is an additive risk” that is a direct effect of these medications on the skin. “That means our transplant recipients have a severely and disproportionate increase in skin cancer,” he noted.
Up to half of solid-organ transplant recipients will develop skin cancer, Dr. Christensen said. These patients have a sixfold to 10-fold increased risk for basal cell carcinoma (BCC), a 35- to 65-fold increased risk for squamous cell carcinoma (SCC), a twofold to sevenfold increased risk for melanoma, and a 16- to 100-fold increased risk for Merkel cell carcinoma.
Transplant recipients with SCC, he said, have a twofold to threefold higher risk for metastasis (4%-8% nodal metastasis) and twofold to fivefold higher risk for death (2%-7% mortality) from SCC.
As for other kinds of immunosuppression, HIV positivity, treatment with 6-mercaptopurine or azathioprine (for inflammatory bowel disease and rheumatoid arthritis), and antitumor necrosis factor agents (for psoriasis, inflammatory bowel disease, and rheumatoid arthritis) have been linked in studies to a higher risk for nonmelanoma skin cancer.
Dr. Christensen also highlighted graft-versus-host disease (GVHD). “It does look like there is a disproportionate and increased risk of SCC of the oropharynx and of the skin in patients who have chronic GVHD. This is probably due to a combination of both the immunosuppressive medications that are required but also from chronic and ongoing inflammation in the skin.”
Chronic GVHD has been linked to a 5.3-fold increase in the risk for SCC and a twofold increase in the risk for BCC, he added.
Moreover, new medications for treating GVHD have been linked to an increased risk for SCC, including a 3.2-fold increased risk for SCC associated with ruxolitinib, a Janus kinase (JAK) 1 and JAK2 inhibitor, in a study of patients with polycythemia vera and myelofibrosis; and a case report of SCC in a patient treated with belumosudil, a rho-associated coiled-coil-containing protein kinase-2 kinase inhibitor, for chronic GVHD. Risk for SCC appears to increase based on duration of use with voriconazole, an antifungal, which, he said, is a potent photosynthesizer.
Dr. Christensen also noted the higher risk for infections in immunocompromised patients and added that these patients can develop inflammatory disease despite immunosuppression:
Staphylococcus, Streptococcus, and Dermatophytes are the most common skin pathogens in these patients. There’s a significantly increased risk for reactivation of herpes simplex, varicella-zoster viruses, and cytomegalovirus. Opportunistic and disseminated fungal infections, such as mycobacteria, Candida, histoplasma, cryptococcus, aspergillus, and mucormycosis, can also appear.
More than 80% of transplant recipients develop molluscum and verruca vulgaris/human papillomavirus infection. They may also develop noninfectious inflammatory dermatoses.
Risk Calculator
What can dermatologists do to help transplant patients? Dr. Christensen highlighted the Skin and UV Neoplasia Transplant Risk Assessment Calculator, which predicts skin cancer risk based on points given for race, gender, skin cancer history, age at transplant, and site of transplant.
The tool, validated in a 2023 study of transplant recipients in Europe, is available online and as an app. It makes recommendations to users about when patients should have initial skin screening exams. Those with the most risk — 45% at 5 years — should be screened within 6 months. “We can use [the tool] to triage these cases when we first meet them and get them plugged into the appropriate care,” Dr. Christensen said.
He recommended seeing high-risk patients at least annually. Patients with a prior SCC and a heavy burden of actinic keratosis should be followed more frequently, he said.
In regard to SCC, he highlighted a 2024 study of solid organ transplant recipients that found the risk for a second SCC after a first SCC was 74%, the risk for a third SCC after a second SCC was 83%, and the risk for another SCC after five SCCs was 92%.
Dr. Christensen disclosed relationships with Canfield Scientific Inc. (consulting), Inhibitor Therapeutics (advisory board), and Sol-Gel Technologies Ltd. (grants/research funding).
A version of this article first appeared on Medscape.com.
SAN DIEGO — because of their suppressed immune systems.
“There are over 450,000 people with a solid organ transplant living in the United States. If you do the math, that works out to about 40 organ transplant recipients for every dermatologist, so there’s a lot of them out there for us to take care of,” Sean Christensen, MD, PhD, associate professor of dermatology, Yale University, New Haven, Connecticut, said at the annual meeting of the American Academy of Dermatology (AAD). “If we expand that umbrella to include all types of immunosuppression, that’s over 4 million adults in the US.”
Dr. Christensen encouraged dermatologists to be aware of the varying risks for immunosuppressive drugs and best screening practices for these patients, and to take advantage of a validated skin cancer risk assessment tool for transplant patients.
During his presentation, he highlighted five classes of immunosuppressive drugs and their associated skin cancer risks:
- Calcineurin inhibitors (tacrolimus or cyclosporine), which cause severe immune suppression and pose a severe skin cancer risk. They may also cause gingival hyperplasia and sebaceous hyperplasia.
- Antimetabolites (mycophenolate mofetil or azathioprine), which cause moderate to severe immune suppression and pose a severe skin cancer risk.
- Mammalian target of rapamycin inhibitors (sirolimus or everolimus), which cause severe immune suppression and pose a moderate skin cancer risk. They also impair wound healing.
- Corticosteroids (prednisone), which cause mild to severe immune suppression and pose a minimal skin cancer risk.
- A decoy receptor protein (belatacept), which causes severe immune suppression and poses a mild skin cancer risk.
“Most of our solid-organ transplant recipients will be on both a calcineurin inhibitor and an antimetabolite,” Dr. Christensen said. “In addition to the skin cancer risk associated with immunosuppression, there is an additive risk” that is a direct effect of these medications on the skin. “That means our transplant recipients have a severely and disproportionate increase in skin cancer,” he noted.
Up to half of solid-organ transplant recipients will develop skin cancer, Dr. Christensen said. These patients have a sixfold to 10-fold increased risk for basal cell carcinoma (BCC), a 35- to 65-fold increased risk for squamous cell carcinoma (SCC), a twofold to sevenfold increased risk for melanoma, and a 16- to 100-fold increased risk for Merkel cell carcinoma.
Transplant recipients with SCC, he said, have a twofold to threefold higher risk for metastasis (4%-8% nodal metastasis) and twofold to fivefold higher risk for death (2%-7% mortality) from SCC.
As for other kinds of immunosuppression, HIV positivity, treatment with 6-mercaptopurine or azathioprine (for inflammatory bowel disease and rheumatoid arthritis), and antitumor necrosis factor agents (for psoriasis, inflammatory bowel disease, and rheumatoid arthritis) have been linked in studies to a higher risk for nonmelanoma skin cancer.
Dr. Christensen also highlighted graft-versus-host disease (GVHD). “It does look like there is a disproportionate and increased risk of SCC of the oropharynx and of the skin in patients who have chronic GVHD. This is probably due to a combination of both the immunosuppressive medications that are required but also from chronic and ongoing inflammation in the skin.”
Chronic GVHD has been linked to a 5.3-fold increase in the risk for SCC and a twofold increase in the risk for BCC, he added.
Moreover, new medications for treating GVHD have been linked to an increased risk for SCC, including a 3.2-fold increased risk for SCC associated with ruxolitinib, a Janus kinase (JAK) 1 and JAK2 inhibitor, in a study of patients with polycythemia vera and myelofibrosis; and a case report of SCC in a patient treated with belumosudil, a rho-associated coiled-coil-containing protein kinase-2 kinase inhibitor, for chronic GVHD. Risk for SCC appears to increase based on duration of use with voriconazole, an antifungal, which, he said, is a potent photosynthesizer.
Dr. Christensen also noted the higher risk for infections in immunocompromised patients and added that these patients can develop inflammatory disease despite immunosuppression:
Staphylococcus, Streptococcus, and Dermatophytes are the most common skin pathogens in these patients. There’s a significantly increased risk for reactivation of herpes simplex, varicella-zoster viruses, and cytomegalovirus. Opportunistic and disseminated fungal infections, such as mycobacteria, Candida, histoplasma, cryptococcus, aspergillus, and mucormycosis, can also appear.
More than 80% of transplant recipients develop molluscum and verruca vulgaris/human papillomavirus infection. They may also develop noninfectious inflammatory dermatoses.
Risk Calculator
What can dermatologists do to help transplant patients? Dr. Christensen highlighted the Skin and UV Neoplasia Transplant Risk Assessment Calculator, which predicts skin cancer risk based on points given for race, gender, skin cancer history, age at transplant, and site of transplant.
The tool, validated in a 2023 study of transplant recipients in Europe, is available online and as an app. It makes recommendations to users about when patients should have initial skin screening exams. Those with the most risk — 45% at 5 years — should be screened within 6 months. “We can use [the tool] to triage these cases when we first meet them and get them plugged into the appropriate care,” Dr. Christensen said.
He recommended seeing high-risk patients at least annually. Patients with a prior SCC and a heavy burden of actinic keratosis should be followed more frequently, he said.
In regard to SCC, he highlighted a 2024 study of solid organ transplant recipients that found the risk for a second SCC after a first SCC was 74%, the risk for a third SCC after a second SCC was 83%, and the risk for another SCC after five SCCs was 92%.
Dr. Christensen disclosed relationships with Canfield Scientific Inc. (consulting), Inhibitor Therapeutics (advisory board), and Sol-Gel Technologies Ltd. (grants/research funding).
A version of this article first appeared on Medscape.com.
FROM AAD 2024
Metabolite in Red Meat Increases Kidney Disease Risk
TOPLINE:
Trimethylamine N-oxide (TMAO) is a gut microbiota-derived metabolite generated by metabolism of dietary L-carnitine, primarily from red meat, and choline, from a variety of animal source foods. TMAO has been shown to cause kidney injury and tubulointerstitial fibrosis in experimental models.
In this study, TMAO was independently associated with higher risks for incident chronic kidney disease (CKD) and faster kidney function decline in humans.
METHODOLOGY:
- Study population was 10,564 participants from two community-based, prospective cohorts without baseline CKD (estimated glomerular filtration rate [eGFR] ≥ 60 mL/min/1.73 m2).
- Incident CKD was defined as eGFR decline ≥ 30% from baseline, resulting in eGFR < 60 mL/min/1.73 m2.
TAKEAWAY:
- During a median 9.4 years, 979 incident CKD events occurred.
- Correlation between baseline TMAO and total meat intake was small but statistically significant (P = .08).
- After adjustments for sociodemographic, lifestyle, diet, and cardiovascular risk factors, higher plasma TMAO was associated with more than doubled CKD incidence (hazard ratio, 2.24 for top vs bottom quintile).
- Higher TMAO levels were also associated with greater annual eGFR decline (top vs bottom quintile eGFR change = −0.43 mL/min/1.73 m2 per year.
- Compared with other major CKD risk factors, the association for the top vs bottom TMAO quintile (−0.43 mL/min/1.73 m2 per year) was similar to that seen per 10 years of older age (−0.43) and presence of diabetes (−0.51), and larger than that seen comparing Black vs non-Black race (−0.28) and per 10 mm Hg systolic blood pressure (−0.16).
IN PRACTICE:
“TMAO levels are highly modifiable by both lifestyle-like diet and pharmacologic interventions. Besides using novel drugs to lower TMAO in patients, using dietary interventions to lower TMAO in the general population could be a cost-efficient and low-risk preventive strategy for chronic kidney disease development. ... These findings support future studies to investigate whether lifestyle and pharmacologic interventions to lower TMAO may prevent CKD development and progression.”
SOURCE:
The study was conducted by Meng Wang, PhD, of Tufts University, Boston, and colleagues and published online in the Journal of the American Society of Nephrology.
LIMITATIONS:
Observational design, can’t exclude residual confounding.
Inter-assay variability.
Use of International Classification of Diseases codes for hospitalization-based CKD, subject to reporting errors.
DISCLOSURES:
The study was supported by grants from the National Institutes of Health and an American Heart Association Postdoctoral Fellowship. Dr. Wang had no disclosures but several coauthors have patents on various diagnostics and/or industry disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
Trimethylamine N-oxide (TMAO) is a gut microbiota-derived metabolite generated by metabolism of dietary L-carnitine, primarily from red meat, and choline, from a variety of animal source foods. TMAO has been shown to cause kidney injury and tubulointerstitial fibrosis in experimental models.
In this study, TMAO was independently associated with higher risks for incident chronic kidney disease (CKD) and faster kidney function decline in humans.
METHODOLOGY:
- Study population was 10,564 participants from two community-based, prospective cohorts without baseline CKD (estimated glomerular filtration rate [eGFR] ≥ 60 mL/min/1.73 m2).
- Incident CKD was defined as eGFR decline ≥ 30% from baseline, resulting in eGFR < 60 mL/min/1.73 m2.
TAKEAWAY:
- During a median 9.4 years, 979 incident CKD events occurred.
- Correlation between baseline TMAO and total meat intake was small but statistically significant (P = .08).
- After adjustments for sociodemographic, lifestyle, diet, and cardiovascular risk factors, higher plasma TMAO was associated with more than doubled CKD incidence (hazard ratio, 2.24 for top vs bottom quintile).
- Higher TMAO levels were also associated with greater annual eGFR decline (top vs bottom quintile eGFR change = −0.43 mL/min/1.73 m2 per year.
- Compared with other major CKD risk factors, the association for the top vs bottom TMAO quintile (−0.43 mL/min/1.73 m2 per year) was similar to that seen per 10 years of older age (−0.43) and presence of diabetes (−0.51), and larger than that seen comparing Black vs non-Black race (−0.28) and per 10 mm Hg systolic blood pressure (−0.16).
IN PRACTICE:
“TMAO levels are highly modifiable by both lifestyle-like diet and pharmacologic interventions. Besides using novel drugs to lower TMAO in patients, using dietary interventions to lower TMAO in the general population could be a cost-efficient and low-risk preventive strategy for chronic kidney disease development. ... These findings support future studies to investigate whether lifestyle and pharmacologic interventions to lower TMAO may prevent CKD development and progression.”
SOURCE:
The study was conducted by Meng Wang, PhD, of Tufts University, Boston, and colleagues and published online in the Journal of the American Society of Nephrology.
LIMITATIONS:
Observational design, can’t exclude residual confounding.
Inter-assay variability.
Use of International Classification of Diseases codes for hospitalization-based CKD, subject to reporting errors.
DISCLOSURES:
The study was supported by grants from the National Institutes of Health and an American Heart Association Postdoctoral Fellowship. Dr. Wang had no disclosures but several coauthors have patents on various diagnostics and/or industry disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
Trimethylamine N-oxide (TMAO) is a gut microbiota-derived metabolite generated by metabolism of dietary L-carnitine, primarily from red meat, and choline, from a variety of animal source foods. TMAO has been shown to cause kidney injury and tubulointerstitial fibrosis in experimental models.
In this study, TMAO was independently associated with higher risks for incident chronic kidney disease (CKD) and faster kidney function decline in humans.
METHODOLOGY:
- Study population was 10,564 participants from two community-based, prospective cohorts without baseline CKD (estimated glomerular filtration rate [eGFR] ≥ 60 mL/min/1.73 m2).
- Incident CKD was defined as eGFR decline ≥ 30% from baseline, resulting in eGFR < 60 mL/min/1.73 m2.
TAKEAWAY:
- During a median 9.4 years, 979 incident CKD events occurred.
- Correlation between baseline TMAO and total meat intake was small but statistically significant (P = .08).
- After adjustments for sociodemographic, lifestyle, diet, and cardiovascular risk factors, higher plasma TMAO was associated with more than doubled CKD incidence (hazard ratio, 2.24 for top vs bottom quintile).
- Higher TMAO levels were also associated with greater annual eGFR decline (top vs bottom quintile eGFR change = −0.43 mL/min/1.73 m2 per year.
- Compared with other major CKD risk factors, the association for the top vs bottom TMAO quintile (−0.43 mL/min/1.73 m2 per year) was similar to that seen per 10 years of older age (−0.43) and presence of diabetes (−0.51), and larger than that seen comparing Black vs non-Black race (−0.28) and per 10 mm Hg systolic blood pressure (−0.16).
IN PRACTICE:
“TMAO levels are highly modifiable by both lifestyle-like diet and pharmacologic interventions. Besides using novel drugs to lower TMAO in patients, using dietary interventions to lower TMAO in the general population could be a cost-efficient and low-risk preventive strategy for chronic kidney disease development. ... These findings support future studies to investigate whether lifestyle and pharmacologic interventions to lower TMAO may prevent CKD development and progression.”
SOURCE:
The study was conducted by Meng Wang, PhD, of Tufts University, Boston, and colleagues and published online in the Journal of the American Society of Nephrology.
LIMITATIONS:
Observational design, can’t exclude residual confounding.
Inter-assay variability.
Use of International Classification of Diseases codes for hospitalization-based CKD, subject to reporting errors.
DISCLOSURES:
The study was supported by grants from the National Institutes of Health and an American Heart Association Postdoctoral Fellowship. Dr. Wang had no disclosures but several coauthors have patents on various diagnostics and/or industry disclosures.
A version of this article appeared on Medscape.com.
Hormone Therapy After 65 a Good Option for Most Women
Hormone Therapy (HT) is a good option for most women over age 65, despite entrenched fears about HT safety, according to findings from a new study published in Menopause.
The study, led by Seo H. Baik, PhD, of Lister Hill National Center for Biomedical Communications, National Library of Medicine, in Bethesda, Maryland, and colleagues is based on the health records of 10 million senior women on Medicare from 2007 to 2020. It concludes there are important health benefits with HT beyond age 65 and the effects of using HT after age 65 vary by type of therapy, route of administration, and dose.
Controversial Since Women’s Health Initiative
Use of HT after age 65 has been controversial in light of the findings of the Women’s Health Initiative (WHI) study in 2002. Since that study, many women have decided against HT, especially after age 65, because of fears of increased risks for cancers and heart disease.
Baik et al. concluded that, compared with never using or stopping use of HT before the age of 65 years, the use of estrogen alone beyond age 65 years was associated with the following significant risk reductions: mortality (19%); breast cancer (16%); lung cancer (13%); colorectal cancer (12%); congestive heart failure (5%); venous thromboembolism (5%); atrial fibrillation (4%); acute myocardial infarction (11%); and dementia (2%).
The authors further found that estrogen plus progestin was associated with significant risk reductions in endometrial cancer (45%); ovarian cancer (21%); ischemic heart disease (5%); congestive heart failure (5%); and venous thromboembolism (5%).
Estrogen plus progesterone, however, was linked with risk reduction only in congestive heart failure (4%).
Reassuring Results
“These results should provide additional reassurance to women about hormone therapy,” said Lisa C, Larkin, MD, president of The Menopause Society. “This data is largely consistent with the WHI data as we understand it today — that for the majority of women with symptoms transitioning through menopause, hormone therapy is the most effective treatment and has benefits that outweigh risks.”
There may be some exceptions, she noted, particularly in older women with high risk for cardiovascular disease and stroke. Among those women, she explained, the risks of HT may outweigh the benefits and it may be appropriate to stop hormone therapy.
“In these older women with specific risk factors, the discussion of continuing or stopping HT is nuanced and complex and must involve shared decision-making,” she said.
Elevated Breast Cancer Risk Can be Mitigated
With a therapy combining estrogen and progestogen, both estrogen plus progestin and estrogen plus progesterone were associated with a 10%-19% increased risk of breast cancer, but the authors say that risk can be mitigated using low doses of transdermal or vaginal estrogen plus progestin.
“In general, risk reductions appear to be greater with low rather than medium or high doses, vaginal or transdermal rather than oral preparations, and with E2 (estradiol) rather than conjugated estrogen,” the authors write.
The authors report that over 14 years of follow-up (from 2007 to 2020), the proportion of senior women taking any HT-containing estrogen dropped by half, from 11.4% to 5.5%. E2 has largely replaced conjugated estrogen (CEE); and vaginal administration largely replaced oral.
Controversy Remains
Even with these results, hormone use will remain controversial, Dr. Larkin said, without enormous efforts to educate. Menopausal HT therapy in young 50-year-old women having symptoms is still controversial — despite the large body of evidence supporting safety and benefit in the majority of women, she said.
“For the last 25 years we have completely neglected education of clinicians about menopause and the data on hormone therapy,” she said. “As a result, most of the clinicians practicing do not understand the data and remain very negative about hormones even in younger women. The decades of lack of education of clinicians about menopause is one of the major reasons far too many young, healthy, 50-year-old women with symptoms are not getting the care they need [hormone therapy] at menopause.” Instead, she says, women are told to take supplements because some providers think hormone therapy is too dangerous.
Lauren Streicher, MD, a clinical professor of obstetrics and gynecology at Northwestern University’s Feinberg School of Medicine, and founding director of the Northwestern Medical Center for Sexual Medicine and Menopause, both in Chicago, says, “In the WHI, 70% of the women were over the age of 65 when they initiated therapy, which partially accounts for the negative outcomes. In addition, in WHI, everyone was taking oral [HT]. This (current) data is very reassuring — and validating — for women who would like to continue taking HT.”
Dr. Streicher says women who would like to start HT after 65 should be counseled on individual risks and after cardiac health is evaluated. But, she notes, this study did not address that.
‘Best Time to Stop HT is When You Die’
She says in her practice she will counsel women who are on HT and would like to continue after age 65 the way she always has: “If someone is taking HT and has no specific reason to stop, there is no reason to stop at some arbitrary age or time and that if they do, they will lose many of the benefits,” particularly bone, cognitive, cardiovascular, and vulvovaginal benefits, she explained. “The best time to stop HT is when you die,” Dr. Streicher said, “And, given the reduction in mortality in women who take HT, that will be at a much older age than women who don’t take HT.”
So will these new data be convincing?
“It will convince the already convinced — menopause experts who follow the data. It is the rare menopause expert that tells women to stop HT,” Dr. Streicher said.
However, she said, “The overwhelming majority of clinicians in the US currently do not prescribe HT. Sadly, I don’t think this will change much.”
The authors report no relevant financial relationships. Dr. Larkin consults for several women’s health companies including Mayne Pharma, Astellas, Johnson & Johnson, Grail, Pfizer, and Solv Wellness. Dr. Streicher reports no relevant financial relationships.
Hormone Therapy (HT) is a good option for most women over age 65, despite entrenched fears about HT safety, according to findings from a new study published in Menopause.
The study, led by Seo H. Baik, PhD, of Lister Hill National Center for Biomedical Communications, National Library of Medicine, in Bethesda, Maryland, and colleagues is based on the health records of 10 million senior women on Medicare from 2007 to 2020. It concludes there are important health benefits with HT beyond age 65 and the effects of using HT after age 65 vary by type of therapy, route of administration, and dose.
Controversial Since Women’s Health Initiative
Use of HT after age 65 has been controversial in light of the findings of the Women’s Health Initiative (WHI) study in 2002. Since that study, many women have decided against HT, especially after age 65, because of fears of increased risks for cancers and heart disease.
Baik et al. concluded that, compared with never using or stopping use of HT before the age of 65 years, the use of estrogen alone beyond age 65 years was associated with the following significant risk reductions: mortality (19%); breast cancer (16%); lung cancer (13%); colorectal cancer (12%); congestive heart failure (5%); venous thromboembolism (5%); atrial fibrillation (4%); acute myocardial infarction (11%); and dementia (2%).
The authors further found that estrogen plus progestin was associated with significant risk reductions in endometrial cancer (45%); ovarian cancer (21%); ischemic heart disease (5%); congestive heart failure (5%); and venous thromboembolism (5%).
Estrogen plus progesterone, however, was linked with risk reduction only in congestive heart failure (4%).
Reassuring Results
“These results should provide additional reassurance to women about hormone therapy,” said Lisa C, Larkin, MD, president of The Menopause Society. “This data is largely consistent with the WHI data as we understand it today — that for the majority of women with symptoms transitioning through menopause, hormone therapy is the most effective treatment and has benefits that outweigh risks.”
There may be some exceptions, she noted, particularly in older women with high risk for cardiovascular disease and stroke. Among those women, she explained, the risks of HT may outweigh the benefits and it may be appropriate to stop hormone therapy.
“In these older women with specific risk factors, the discussion of continuing or stopping HT is nuanced and complex and must involve shared decision-making,” she said.
Elevated Breast Cancer Risk Can be Mitigated
With a therapy combining estrogen and progestogen, both estrogen plus progestin and estrogen plus progesterone were associated with a 10%-19% increased risk of breast cancer, but the authors say that risk can be mitigated using low doses of transdermal or vaginal estrogen plus progestin.
“In general, risk reductions appear to be greater with low rather than medium or high doses, vaginal or transdermal rather than oral preparations, and with E2 (estradiol) rather than conjugated estrogen,” the authors write.
The authors report that over 14 years of follow-up (from 2007 to 2020), the proportion of senior women taking any HT-containing estrogen dropped by half, from 11.4% to 5.5%. E2 has largely replaced conjugated estrogen (CEE); and vaginal administration largely replaced oral.
Controversy Remains
Even with these results, hormone use will remain controversial, Dr. Larkin said, without enormous efforts to educate. Menopausal HT therapy in young 50-year-old women having symptoms is still controversial — despite the large body of evidence supporting safety and benefit in the majority of women, she said.
“For the last 25 years we have completely neglected education of clinicians about menopause and the data on hormone therapy,” she said. “As a result, most of the clinicians practicing do not understand the data and remain very negative about hormones even in younger women. The decades of lack of education of clinicians about menopause is one of the major reasons far too many young, healthy, 50-year-old women with symptoms are not getting the care they need [hormone therapy] at menopause.” Instead, she says, women are told to take supplements because some providers think hormone therapy is too dangerous.
Lauren Streicher, MD, a clinical professor of obstetrics and gynecology at Northwestern University’s Feinberg School of Medicine, and founding director of the Northwestern Medical Center for Sexual Medicine and Menopause, both in Chicago, says, “In the WHI, 70% of the women were over the age of 65 when they initiated therapy, which partially accounts for the negative outcomes. In addition, in WHI, everyone was taking oral [HT]. This (current) data is very reassuring — and validating — for women who would like to continue taking HT.”
Dr. Streicher says women who would like to start HT after 65 should be counseled on individual risks and after cardiac health is evaluated. But, she notes, this study did not address that.
‘Best Time to Stop HT is When You Die’
She says in her practice she will counsel women who are on HT and would like to continue after age 65 the way she always has: “If someone is taking HT and has no specific reason to stop, there is no reason to stop at some arbitrary age or time and that if they do, they will lose many of the benefits,” particularly bone, cognitive, cardiovascular, and vulvovaginal benefits, she explained. “The best time to stop HT is when you die,” Dr. Streicher said, “And, given the reduction in mortality in women who take HT, that will be at a much older age than women who don’t take HT.”
So will these new data be convincing?
“It will convince the already convinced — menopause experts who follow the data. It is the rare menopause expert that tells women to stop HT,” Dr. Streicher said.
However, she said, “The overwhelming majority of clinicians in the US currently do not prescribe HT. Sadly, I don’t think this will change much.”
The authors report no relevant financial relationships. Dr. Larkin consults for several women’s health companies including Mayne Pharma, Astellas, Johnson & Johnson, Grail, Pfizer, and Solv Wellness. Dr. Streicher reports no relevant financial relationships.
Hormone Therapy (HT) is a good option for most women over age 65, despite entrenched fears about HT safety, according to findings from a new study published in Menopause.
The study, led by Seo H. Baik, PhD, of Lister Hill National Center for Biomedical Communications, National Library of Medicine, in Bethesda, Maryland, and colleagues is based on the health records of 10 million senior women on Medicare from 2007 to 2020. It concludes there are important health benefits with HT beyond age 65 and the effects of using HT after age 65 vary by type of therapy, route of administration, and dose.
Controversial Since Women’s Health Initiative
Use of HT after age 65 has been controversial in light of the findings of the Women’s Health Initiative (WHI) study in 2002. Since that study, many women have decided against HT, especially after age 65, because of fears of increased risks for cancers and heart disease.
Baik et al. concluded that, compared with never using or stopping use of HT before the age of 65 years, the use of estrogen alone beyond age 65 years was associated with the following significant risk reductions: mortality (19%); breast cancer (16%); lung cancer (13%); colorectal cancer (12%); congestive heart failure (5%); venous thromboembolism (5%); atrial fibrillation (4%); acute myocardial infarction (11%); and dementia (2%).
The authors further found that estrogen plus progestin was associated with significant risk reductions in endometrial cancer (45%); ovarian cancer (21%); ischemic heart disease (5%); congestive heart failure (5%); and venous thromboembolism (5%).
Estrogen plus progesterone, however, was linked with risk reduction only in congestive heart failure (4%).
Reassuring Results
“These results should provide additional reassurance to women about hormone therapy,” said Lisa C, Larkin, MD, president of The Menopause Society. “This data is largely consistent with the WHI data as we understand it today — that for the majority of women with symptoms transitioning through menopause, hormone therapy is the most effective treatment and has benefits that outweigh risks.”
There may be some exceptions, she noted, particularly in older women with high risk for cardiovascular disease and stroke. Among those women, she explained, the risks of HT may outweigh the benefits and it may be appropriate to stop hormone therapy.
“In these older women with specific risk factors, the discussion of continuing or stopping HT is nuanced and complex and must involve shared decision-making,” she said.
Elevated Breast Cancer Risk Can be Mitigated
With a therapy combining estrogen and progestogen, both estrogen plus progestin and estrogen plus progesterone were associated with a 10%-19% increased risk of breast cancer, but the authors say that risk can be mitigated using low doses of transdermal or vaginal estrogen plus progestin.
“In general, risk reductions appear to be greater with low rather than medium or high doses, vaginal or transdermal rather than oral preparations, and with E2 (estradiol) rather than conjugated estrogen,” the authors write.
The authors report that over 14 years of follow-up (from 2007 to 2020), the proportion of senior women taking any HT-containing estrogen dropped by half, from 11.4% to 5.5%. E2 has largely replaced conjugated estrogen (CEE); and vaginal administration largely replaced oral.
Controversy Remains
Even with these results, hormone use will remain controversial, Dr. Larkin said, without enormous efforts to educate. Menopausal HT therapy in young 50-year-old women having symptoms is still controversial — despite the large body of evidence supporting safety and benefit in the majority of women, she said.
“For the last 25 years we have completely neglected education of clinicians about menopause and the data on hormone therapy,” she said. “As a result, most of the clinicians practicing do not understand the data and remain very negative about hormones even in younger women. The decades of lack of education of clinicians about menopause is one of the major reasons far too many young, healthy, 50-year-old women with symptoms are not getting the care they need [hormone therapy] at menopause.” Instead, she says, women are told to take supplements because some providers think hormone therapy is too dangerous.
Lauren Streicher, MD, a clinical professor of obstetrics and gynecology at Northwestern University’s Feinberg School of Medicine, and founding director of the Northwestern Medical Center for Sexual Medicine and Menopause, both in Chicago, says, “In the WHI, 70% of the women were over the age of 65 when they initiated therapy, which partially accounts for the negative outcomes. In addition, in WHI, everyone was taking oral [HT]. This (current) data is very reassuring — and validating — for women who would like to continue taking HT.”
Dr. Streicher says women who would like to start HT after 65 should be counseled on individual risks and after cardiac health is evaluated. But, she notes, this study did not address that.
‘Best Time to Stop HT is When You Die’
She says in her practice she will counsel women who are on HT and would like to continue after age 65 the way she always has: “If someone is taking HT and has no specific reason to stop, there is no reason to stop at some arbitrary age or time and that if they do, they will lose many of the benefits,” particularly bone, cognitive, cardiovascular, and vulvovaginal benefits, she explained. “The best time to stop HT is when you die,” Dr. Streicher said, “And, given the reduction in mortality in women who take HT, that will be at a much older age than women who don’t take HT.”
So will these new data be convincing?
“It will convince the already convinced — menopause experts who follow the data. It is the rare menopause expert that tells women to stop HT,” Dr. Streicher said.
However, she said, “The overwhelming majority of clinicians in the US currently do not prescribe HT. Sadly, I don’t think this will change much.”
The authors report no relevant financial relationships. Dr. Larkin consults for several women’s health companies including Mayne Pharma, Astellas, Johnson & Johnson, Grail, Pfizer, and Solv Wellness. Dr. Streicher reports no relevant financial relationships.
FROM MENOPAUSE
FDA OKs Benralizumab for Asthma in Children as Young as 6 Years
Benralizumab is now approved by the US Food and Drug Administration (FDA) for the treatment of asthma in children older than 6 years.
Marketed as Fasenra, the medication first was approved in 2017 for patients aged 12 years or older.
AstraZeneca, which markets the drug, announced the approval for younger patients on April 11.
The expanded indication was supported by a study that showed that the drug functions in the same way with younger children and their adolescent peers. The safety and tolerability were also consistent with the known profile of the medicine, the company said.
For children who weigh ≥ 35 kg, the recommended dose is 30 mg. For patients aged 6-11 years who weigh < 35 kg, a new 10-mg dose will be available, according to the announcement.
The drug, a monoclonal antibody that depletes eosinophils by binding to interleukin 5 receptor alpha on eosinophils, is administered by subcutaneous injection every 4 weeks for the first three doses and then every 8 weeks.
Benralizumab should not be used to treat acute asthma symptoms. Hypersensitivity reasons have occurred after administration of the drug. The most common adverse reactions include headache and pharyngitis.
A version of this article appeared on Medscape.com.
Benralizumab is now approved by the US Food and Drug Administration (FDA) for the treatment of asthma in children older than 6 years.
Marketed as Fasenra, the medication first was approved in 2017 for patients aged 12 years or older.
AstraZeneca, which markets the drug, announced the approval for younger patients on April 11.
The expanded indication was supported by a study that showed that the drug functions in the same way with younger children and their adolescent peers. The safety and tolerability were also consistent with the known profile of the medicine, the company said.
For children who weigh ≥ 35 kg, the recommended dose is 30 mg. For patients aged 6-11 years who weigh < 35 kg, a new 10-mg dose will be available, according to the announcement.
The drug, a monoclonal antibody that depletes eosinophils by binding to interleukin 5 receptor alpha on eosinophils, is administered by subcutaneous injection every 4 weeks for the first three doses and then every 8 weeks.
Benralizumab should not be used to treat acute asthma symptoms. Hypersensitivity reasons have occurred after administration of the drug. The most common adverse reactions include headache and pharyngitis.
A version of this article appeared on Medscape.com.
Benralizumab is now approved by the US Food and Drug Administration (FDA) for the treatment of asthma in children older than 6 years.
Marketed as Fasenra, the medication first was approved in 2017 for patients aged 12 years or older.
AstraZeneca, which markets the drug, announced the approval for younger patients on April 11.
The expanded indication was supported by a study that showed that the drug functions in the same way with younger children and their adolescent peers. The safety and tolerability were also consistent with the known profile of the medicine, the company said.
For children who weigh ≥ 35 kg, the recommended dose is 30 mg. For patients aged 6-11 years who weigh < 35 kg, a new 10-mg dose will be available, according to the announcement.
The drug, a monoclonal antibody that depletes eosinophils by binding to interleukin 5 receptor alpha on eosinophils, is administered by subcutaneous injection every 4 weeks for the first three doses and then every 8 weeks.
Benralizumab should not be used to treat acute asthma symptoms. Hypersensitivity reasons have occurred after administration of the drug. The most common adverse reactions include headache and pharyngitis.
A version of this article appeared on Medscape.com.
Alopecia Areata: Late Responses Complicate Definition of JAK Inhibitor Failure
SAN DIEGO — , according to late breaker data presented at the annual meeting of the American Academy of Dermatology.
Although the majority respond within months, response curves have so far climbed for as long as patients are followed, allowing many with disappointing early results to catch up, according to Rodney D. Sinclair, MD, professor of dermatology at the University of Melbourne, Australia.
His remarks were derived specifically from new long-term follow-up with baricitinib, the first JAK inhibitor approved for AA, but the pattern appears to be similar with ritlecitinib, the only other JAK inhibitor approved for AA, and for several if not all JAK inhibitors in phase 3 AA trials.
“We have had patients on baricitinib where not much was happening at 18 months, but now, at 4 years, they have a SALT score of zero,” Dr. Sinclair reported
A Severity of Alopecia Tool (SALT) score of 0 signifies complete hair regrowth. On a scale with a maximum score of 100 (complete hair loss), a SALT score of 20 or less, signaling clinical success, has been a primary endpoint in many JAK inhibitor trials, including those conducted with baricitinib.
Providing the most recent analysis in patients with severe AA participating in the phase 3 BRAVE-AA1 and BRAVE-AA2 trials of baricitinib, which were published together in 2022, Dr. Sinclair broke the data down into responders, mixed responders, and nonresponders at 52 weeks. The proportion of patients who responded with even longer follow-up were then tallied.
In the as-observed responses over time, the trajectory of response continued to climb through 76 weeks of follow-up in all three groups.
Relative to the 44.5% rate of overall response (SALT ≤ 20 ) at 52 weeks, there was some further growth in every group maintained on JAK inhibitor therapy over longer follow-up. In Dr. Sinclair’s late breaking analysis, this did not include nonresponders, who stopped therapy by week 52, but 78.4% of the combined responders and mixed responders who remained on treatment had reached treatment success at 76 weeks.
Response Curves Climb More Slowly With Severe Alopecia
While improvement in SALT scores was even seen in nonresponders over time as long as they remained on therapy, Dr. Sinclair reported that response curves tended to climb more slowly in those with more severe alopecia at baseline. Yet, they still climbed. For example, 28.1% of those with a baseline SALT score of 95 to 100 had reached treatment success at week 52, but the proportion had climbed to 35.4% by week 76.
The response curves climbed more quickly among those with a SALT score between 50 and 95 at baseline than among those with more severe alopecia, but the differences in SALT scores at 52 weeks and 76 weeks among patients in this range of baseline SALT scores were small.
Basically, “those with a SALT score of 94 did just as well as those with a SALT score of 51 when followed long-term,” he said, noting that this was among several findings that confounded expectations.
Duration of AA was found to be an important prognostic factor, with 4 years emerging as a general threshold separating those with a diminished likelihood of benefit relative to those with a shorter AA duration.
“When the duration of AA is more than 4 years, the response to any JAK inhibitor seems to fall off a cliff,” Dr. Sinclair said.
To clarify this observation, Dr. Sinclair made an analogy between acute and chronic urticaria. Chronicity appears to change the pathophysiology of both urticaria and AA, making durable remissions more difficult to achieve if the inflammatory response was persistently upregulated, he said.
The delayed responses in some patients “suggests that it is not enough to control inflammation for the hair to regrow. You actually have to activate the hair to grow as well as treat the inflammation,” Dr. Sinclair said.
This heterogeneity that has been observed in the speed of AA response to JAK inhibitors might be explained at least in part by the individual differences in hair growth activation. For ritlecitinib, the only other JAK inhibitor approved for AA to date, 62% were categorized as responders in the registration ALLEGRO trials, but only 44% were early responders, meaning SALT scores of ≤ 20 by week 24, according to a summary published last year. Of the remaining 16%, 11% were middle responders, meaning a SALT score of ≤ 20 reached at week 48, and 6% were late responders, meaning a SALT score of ≤ 20 reached at week 96.
In the context of late breaking 68-week data with deuruxolitinib, an oral JAK inhibitor currently under FDA review for treating moderate to severe AA, presented in the same AAD session as Dr. Sinclair’s baricitinib data, Brett King, MD, PhD, associate professor of dermatology, Yale University, New Haven, Connecticut, described similar long-term response curves. At 24 weeks, the SALT ≤ 20 response was achieved in 34.9% of patients, but climbed to 62.8% with continuous therapy over 68 weeks.
The difference between AA and most other inflammatory conditions treated with a JAK inhibitor is that “it takes time to treat,” Dr. King said.
Time Factor Is Important for Response
“What we are learning is that patients keep getting better over time,” Dr. Sinclair said. Asked specifically how long he would treat a patient before giving up, he acknowledged that he used to consider 6 months adequate, but that he has now changed his mind.
“It might be that even 2 years is too short,” he said, although he conceded that a trial of therapy for this long “might be an issue for third-part payers.”
Asked to comment, Melissa Piliang, MD, chair of the department of dermatology at the Cleveland Clinic, agreed with the principle that early responses are not necessarily predictive of complete response.
“In my clinical experience, 6 months is not long enough to assess response,” she told this news organization. “Some patients have hair growth after 18 months to 2 years” of treatment. Additional studies to identify the characteristics and predictors of late response, she said, “would be very helpful, as would trials allowing multiple therapies to simulate real-world practice.”
Like Dr. Sinclair, Dr. Piliang is interested in the possibility of combining a JAK inhibitor with another therapy aimed specially at promoting hair regrowth.
“Using a secondary therapy to stimulate regrowth as an addition to an anti-inflammatory medicine like a JAK inhibitor might speed up response in some patients,” she speculated. Dr. Sinclair reports financial relationships with more than 30 pharmaceutical companies, including Eli Lilly, the manufacturer of baricitinib. Dr. King reports financial relationships with multiple companies, including Concert Pharmaceuticals (consultant and investigator), the manufacturer of deuruxolitinib. Dr. Piliang reports financial relationships with Eli Lilly, Pfizer, and Proctor & Gamble.
SAN DIEGO — , according to late breaker data presented at the annual meeting of the American Academy of Dermatology.
Although the majority respond within months, response curves have so far climbed for as long as patients are followed, allowing many with disappointing early results to catch up, according to Rodney D. Sinclair, MD, professor of dermatology at the University of Melbourne, Australia.
His remarks were derived specifically from new long-term follow-up with baricitinib, the first JAK inhibitor approved for AA, but the pattern appears to be similar with ritlecitinib, the only other JAK inhibitor approved for AA, and for several if not all JAK inhibitors in phase 3 AA trials.
“We have had patients on baricitinib where not much was happening at 18 months, but now, at 4 years, they have a SALT score of zero,” Dr. Sinclair reported
A Severity of Alopecia Tool (SALT) score of 0 signifies complete hair regrowth. On a scale with a maximum score of 100 (complete hair loss), a SALT score of 20 or less, signaling clinical success, has been a primary endpoint in many JAK inhibitor trials, including those conducted with baricitinib.
Providing the most recent analysis in patients with severe AA participating in the phase 3 BRAVE-AA1 and BRAVE-AA2 trials of baricitinib, which were published together in 2022, Dr. Sinclair broke the data down into responders, mixed responders, and nonresponders at 52 weeks. The proportion of patients who responded with even longer follow-up were then tallied.
In the as-observed responses over time, the trajectory of response continued to climb through 76 weeks of follow-up in all three groups.
Relative to the 44.5% rate of overall response (SALT ≤ 20 ) at 52 weeks, there was some further growth in every group maintained on JAK inhibitor therapy over longer follow-up. In Dr. Sinclair’s late breaking analysis, this did not include nonresponders, who stopped therapy by week 52, but 78.4% of the combined responders and mixed responders who remained on treatment had reached treatment success at 76 weeks.
Response Curves Climb More Slowly With Severe Alopecia
While improvement in SALT scores was even seen in nonresponders over time as long as they remained on therapy, Dr. Sinclair reported that response curves tended to climb more slowly in those with more severe alopecia at baseline. Yet, they still climbed. For example, 28.1% of those with a baseline SALT score of 95 to 100 had reached treatment success at week 52, but the proportion had climbed to 35.4% by week 76.
The response curves climbed more quickly among those with a SALT score between 50 and 95 at baseline than among those with more severe alopecia, but the differences in SALT scores at 52 weeks and 76 weeks among patients in this range of baseline SALT scores were small.
Basically, “those with a SALT score of 94 did just as well as those with a SALT score of 51 when followed long-term,” he said, noting that this was among several findings that confounded expectations.
Duration of AA was found to be an important prognostic factor, with 4 years emerging as a general threshold separating those with a diminished likelihood of benefit relative to those with a shorter AA duration.
“When the duration of AA is more than 4 years, the response to any JAK inhibitor seems to fall off a cliff,” Dr. Sinclair said.
To clarify this observation, Dr. Sinclair made an analogy between acute and chronic urticaria. Chronicity appears to change the pathophysiology of both urticaria and AA, making durable remissions more difficult to achieve if the inflammatory response was persistently upregulated, he said.
The delayed responses in some patients “suggests that it is not enough to control inflammation for the hair to regrow. You actually have to activate the hair to grow as well as treat the inflammation,” Dr. Sinclair said.
This heterogeneity that has been observed in the speed of AA response to JAK inhibitors might be explained at least in part by the individual differences in hair growth activation. For ritlecitinib, the only other JAK inhibitor approved for AA to date, 62% were categorized as responders in the registration ALLEGRO trials, but only 44% were early responders, meaning SALT scores of ≤ 20 by week 24, according to a summary published last year. Of the remaining 16%, 11% were middle responders, meaning a SALT score of ≤ 20 reached at week 48, and 6% were late responders, meaning a SALT score of ≤ 20 reached at week 96.
In the context of late breaking 68-week data with deuruxolitinib, an oral JAK inhibitor currently under FDA review for treating moderate to severe AA, presented in the same AAD session as Dr. Sinclair’s baricitinib data, Brett King, MD, PhD, associate professor of dermatology, Yale University, New Haven, Connecticut, described similar long-term response curves. At 24 weeks, the SALT ≤ 20 response was achieved in 34.9% of patients, but climbed to 62.8% with continuous therapy over 68 weeks.
The difference between AA and most other inflammatory conditions treated with a JAK inhibitor is that “it takes time to treat,” Dr. King said.
Time Factor Is Important for Response
“What we are learning is that patients keep getting better over time,” Dr. Sinclair said. Asked specifically how long he would treat a patient before giving up, he acknowledged that he used to consider 6 months adequate, but that he has now changed his mind.
“It might be that even 2 years is too short,” he said, although he conceded that a trial of therapy for this long “might be an issue for third-part payers.”
Asked to comment, Melissa Piliang, MD, chair of the department of dermatology at the Cleveland Clinic, agreed with the principle that early responses are not necessarily predictive of complete response.
“In my clinical experience, 6 months is not long enough to assess response,” she told this news organization. “Some patients have hair growth after 18 months to 2 years” of treatment. Additional studies to identify the characteristics and predictors of late response, she said, “would be very helpful, as would trials allowing multiple therapies to simulate real-world practice.”
Like Dr. Sinclair, Dr. Piliang is interested in the possibility of combining a JAK inhibitor with another therapy aimed specially at promoting hair regrowth.
“Using a secondary therapy to stimulate regrowth as an addition to an anti-inflammatory medicine like a JAK inhibitor might speed up response in some patients,” she speculated. Dr. Sinclair reports financial relationships with more than 30 pharmaceutical companies, including Eli Lilly, the manufacturer of baricitinib. Dr. King reports financial relationships with multiple companies, including Concert Pharmaceuticals (consultant and investigator), the manufacturer of deuruxolitinib. Dr. Piliang reports financial relationships with Eli Lilly, Pfizer, and Proctor & Gamble.
SAN DIEGO — , according to late breaker data presented at the annual meeting of the American Academy of Dermatology.
Although the majority respond within months, response curves have so far climbed for as long as patients are followed, allowing many with disappointing early results to catch up, according to Rodney D. Sinclair, MD, professor of dermatology at the University of Melbourne, Australia.
His remarks were derived specifically from new long-term follow-up with baricitinib, the first JAK inhibitor approved for AA, but the pattern appears to be similar with ritlecitinib, the only other JAK inhibitor approved for AA, and for several if not all JAK inhibitors in phase 3 AA trials.
“We have had patients on baricitinib where not much was happening at 18 months, but now, at 4 years, they have a SALT score of zero,” Dr. Sinclair reported
A Severity of Alopecia Tool (SALT) score of 0 signifies complete hair regrowth. On a scale with a maximum score of 100 (complete hair loss), a SALT score of 20 or less, signaling clinical success, has been a primary endpoint in many JAK inhibitor trials, including those conducted with baricitinib.
Providing the most recent analysis in patients with severe AA participating in the phase 3 BRAVE-AA1 and BRAVE-AA2 trials of baricitinib, which were published together in 2022, Dr. Sinclair broke the data down into responders, mixed responders, and nonresponders at 52 weeks. The proportion of patients who responded with even longer follow-up were then tallied.
In the as-observed responses over time, the trajectory of response continued to climb through 76 weeks of follow-up in all three groups.
Relative to the 44.5% rate of overall response (SALT ≤ 20 ) at 52 weeks, there was some further growth in every group maintained on JAK inhibitor therapy over longer follow-up. In Dr. Sinclair’s late breaking analysis, this did not include nonresponders, who stopped therapy by week 52, but 78.4% of the combined responders and mixed responders who remained on treatment had reached treatment success at 76 weeks.
Response Curves Climb More Slowly With Severe Alopecia
While improvement in SALT scores was even seen in nonresponders over time as long as they remained on therapy, Dr. Sinclair reported that response curves tended to climb more slowly in those with more severe alopecia at baseline. Yet, they still climbed. For example, 28.1% of those with a baseline SALT score of 95 to 100 had reached treatment success at week 52, but the proportion had climbed to 35.4% by week 76.
The response curves climbed more quickly among those with a SALT score between 50 and 95 at baseline than among those with more severe alopecia, but the differences in SALT scores at 52 weeks and 76 weeks among patients in this range of baseline SALT scores were small.
Basically, “those with a SALT score of 94 did just as well as those with a SALT score of 51 when followed long-term,” he said, noting that this was among several findings that confounded expectations.
Duration of AA was found to be an important prognostic factor, with 4 years emerging as a general threshold separating those with a diminished likelihood of benefit relative to those with a shorter AA duration.
“When the duration of AA is more than 4 years, the response to any JAK inhibitor seems to fall off a cliff,” Dr. Sinclair said.
To clarify this observation, Dr. Sinclair made an analogy between acute and chronic urticaria. Chronicity appears to change the pathophysiology of both urticaria and AA, making durable remissions more difficult to achieve if the inflammatory response was persistently upregulated, he said.
The delayed responses in some patients “suggests that it is not enough to control inflammation for the hair to regrow. You actually have to activate the hair to grow as well as treat the inflammation,” Dr. Sinclair said.
This heterogeneity that has been observed in the speed of AA response to JAK inhibitors might be explained at least in part by the individual differences in hair growth activation. For ritlecitinib, the only other JAK inhibitor approved for AA to date, 62% were categorized as responders in the registration ALLEGRO trials, but only 44% were early responders, meaning SALT scores of ≤ 20 by week 24, according to a summary published last year. Of the remaining 16%, 11% were middle responders, meaning a SALT score of ≤ 20 reached at week 48, and 6% were late responders, meaning a SALT score of ≤ 20 reached at week 96.
In the context of late breaking 68-week data with deuruxolitinib, an oral JAK inhibitor currently under FDA review for treating moderate to severe AA, presented in the same AAD session as Dr. Sinclair’s baricitinib data, Brett King, MD, PhD, associate professor of dermatology, Yale University, New Haven, Connecticut, described similar long-term response curves. At 24 weeks, the SALT ≤ 20 response was achieved in 34.9% of patients, but climbed to 62.8% with continuous therapy over 68 weeks.
The difference between AA and most other inflammatory conditions treated with a JAK inhibitor is that “it takes time to treat,” Dr. King said.
Time Factor Is Important for Response
“What we are learning is that patients keep getting better over time,” Dr. Sinclair said. Asked specifically how long he would treat a patient before giving up, he acknowledged that he used to consider 6 months adequate, but that he has now changed his mind.
“It might be that even 2 years is too short,” he said, although he conceded that a trial of therapy for this long “might be an issue for third-part payers.”
Asked to comment, Melissa Piliang, MD, chair of the department of dermatology at the Cleveland Clinic, agreed with the principle that early responses are not necessarily predictive of complete response.
“In my clinical experience, 6 months is not long enough to assess response,” she told this news organization. “Some patients have hair growth after 18 months to 2 years” of treatment. Additional studies to identify the characteristics and predictors of late response, she said, “would be very helpful, as would trials allowing multiple therapies to simulate real-world practice.”
Like Dr. Sinclair, Dr. Piliang is interested in the possibility of combining a JAK inhibitor with another therapy aimed specially at promoting hair regrowth.
“Using a secondary therapy to stimulate regrowth as an addition to an anti-inflammatory medicine like a JAK inhibitor might speed up response in some patients,” she speculated. Dr. Sinclair reports financial relationships with more than 30 pharmaceutical companies, including Eli Lilly, the manufacturer of baricitinib. Dr. King reports financial relationships with multiple companies, including Concert Pharmaceuticals (consultant and investigator), the manufacturer of deuruxolitinib. Dr. Piliang reports financial relationships with Eli Lilly, Pfizer, and Proctor & Gamble.
FROM AAD 2024
A 16-Year-Old Female Presents With Multiple Areas of Hair Loss on the Scalp
KOH analysis of the scales from the scalp areas revealed no fungal elements. Given the observed erythema and scaling, a punch biopsy was conducted. Histopathological examination of the biopsy sample displayed interface inflammation affecting both the infundibular and lower portions of hair follicles. The presence of folliculosebaceous units transitioning from intermediate to terminal size follicles was noted. A perifollicular, peri eccrine, superficial, and deep perivascular lymphoplasmacytic infiltrate was identified, alongside increased dermal mucin, findings consistent with a diagnosis of discoid lupus erythematosus.
Subsequent laboratory investigations were largely unremarkable, except for an elevated ANA titer (1:320, with a speckled pattern). The patient was initiated on a treatment regimen comprising intralesional triamcinolone and oral hydroxychloroquine (Plaquenil).
Discussion
It predominantly affects adults, yet pediatric cases account for 5%-7% of DLE diagnoses, with a significant predominance in females. Pediatric scalp DLE is particularly concerning due to its potential for causing scarring and permanent hair loss, which can significantly impact the psychological wellbeing of affected children.
The pathogenesis of DLE is multifactorial, involving genetic predispositions, environmental factors like UV light exposure, and immunological mechanisms leading to skin damage.
In children, DLE typically presents as well-demarcated, erythematous plaques with scale and follicular plugging, primarily affecting the scalp. Lesions may also exhibit changes in pigmentation, atrophy, and telangiectasia. The scalp involvement often leads to scarring alopecia, which can be distressing for pediatric patients. Unlike systemic lupus erythematosus (SLE), DLE is usually limited to the skin without systemic involvement. The progression of DLE to systemic lupus erythematosus in children has been previously described to be 22.2%. In a recent report of 201 pediatric cases of DLE, 12% of the cases progressed to systemic lupus erythematosus (SLE) and 14.5% had concurrent SLE. The onset of symptoms before the age of 10 years was the only statistically significant predictor for progression to SLE. Pruritus is a common symptom and may be correlated with disease activity.
The differential diagnosis for this patient encompassed a variety of conditions, including tinea capitis, alopecia areata, trichotillomania, and lichen planopilaris, each considered based on clinical presentation but ultimately excluded through clinical, microscopic, and biopsy findings.
Management strategies for pediatric scalp DLE aim at preventing disease progression, minimizing scarring, and addressing aesthetic concerns. These include the use of topical and intralesional corticosteroids, calcineurin inhibitors, and antimalarial agents like hydroxychloroquine, alongside stringent photoprotection to mitigate UV-triggered exacerbations.
Conclusion
The prognosis for pediatric scalp DLE can be favorable with timely and appropriate management, underscoring the importance of early diagnosis and intervention to prevent scarring and hair loss. However, ongoing surveillance is crucial for monitoring potential progression to systemic lupus erythematosus, albeit a low-risk transformation.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
1. George PM and Tunnessen WW. Childhood discoid lupus erythematosus. Arch Dermatol. 1993;129(5):613-617.
2. Hawat T et al. Pediatric discoid lupus erythematosus: Short report. Dermatol Ther. 2022 Jan;35(1):e15170. doi: 10.1111/dth.15170.
3. Arkin LM et al. Practice-based differences in paediatric discoid lupus erythematosus. Br J Dermatol. 2019 Oct;181(4):805-810. doi: 10.1111/bjd.17780.
KOH analysis of the scales from the scalp areas revealed no fungal elements. Given the observed erythema and scaling, a punch biopsy was conducted. Histopathological examination of the biopsy sample displayed interface inflammation affecting both the infundibular and lower portions of hair follicles. The presence of folliculosebaceous units transitioning from intermediate to terminal size follicles was noted. A perifollicular, peri eccrine, superficial, and deep perivascular lymphoplasmacytic infiltrate was identified, alongside increased dermal mucin, findings consistent with a diagnosis of discoid lupus erythematosus.
Subsequent laboratory investigations were largely unremarkable, except for an elevated ANA titer (1:320, with a speckled pattern). The patient was initiated on a treatment regimen comprising intralesional triamcinolone and oral hydroxychloroquine (Plaquenil).
Discussion
It predominantly affects adults, yet pediatric cases account for 5%-7% of DLE diagnoses, with a significant predominance in females. Pediatric scalp DLE is particularly concerning due to its potential for causing scarring and permanent hair loss, which can significantly impact the psychological wellbeing of affected children.
The pathogenesis of DLE is multifactorial, involving genetic predispositions, environmental factors like UV light exposure, and immunological mechanisms leading to skin damage.
In children, DLE typically presents as well-demarcated, erythematous plaques with scale and follicular plugging, primarily affecting the scalp. Lesions may also exhibit changes in pigmentation, atrophy, and telangiectasia. The scalp involvement often leads to scarring alopecia, which can be distressing for pediatric patients. Unlike systemic lupus erythematosus (SLE), DLE is usually limited to the skin without systemic involvement. The progression of DLE to systemic lupus erythematosus in children has been previously described to be 22.2%. In a recent report of 201 pediatric cases of DLE, 12% of the cases progressed to systemic lupus erythematosus (SLE) and 14.5% had concurrent SLE. The onset of symptoms before the age of 10 years was the only statistically significant predictor for progression to SLE. Pruritus is a common symptom and may be correlated with disease activity.
The differential diagnosis for this patient encompassed a variety of conditions, including tinea capitis, alopecia areata, trichotillomania, and lichen planopilaris, each considered based on clinical presentation but ultimately excluded through clinical, microscopic, and biopsy findings.
Management strategies for pediatric scalp DLE aim at preventing disease progression, minimizing scarring, and addressing aesthetic concerns. These include the use of topical and intralesional corticosteroids, calcineurin inhibitors, and antimalarial agents like hydroxychloroquine, alongside stringent photoprotection to mitigate UV-triggered exacerbations.
Conclusion
The prognosis for pediatric scalp DLE can be favorable with timely and appropriate management, underscoring the importance of early diagnosis and intervention to prevent scarring and hair loss. However, ongoing surveillance is crucial for monitoring potential progression to systemic lupus erythematosus, albeit a low-risk transformation.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
1. George PM and Tunnessen WW. Childhood discoid lupus erythematosus. Arch Dermatol. 1993;129(5):613-617.
2. Hawat T et al. Pediatric discoid lupus erythematosus: Short report. Dermatol Ther. 2022 Jan;35(1):e15170. doi: 10.1111/dth.15170.
3. Arkin LM et al. Practice-based differences in paediatric discoid lupus erythematosus. Br J Dermatol. 2019 Oct;181(4):805-810. doi: 10.1111/bjd.17780.
KOH analysis of the scales from the scalp areas revealed no fungal elements. Given the observed erythema and scaling, a punch biopsy was conducted. Histopathological examination of the biopsy sample displayed interface inflammation affecting both the infundibular and lower portions of hair follicles. The presence of folliculosebaceous units transitioning from intermediate to terminal size follicles was noted. A perifollicular, peri eccrine, superficial, and deep perivascular lymphoplasmacytic infiltrate was identified, alongside increased dermal mucin, findings consistent with a diagnosis of discoid lupus erythematosus.
Subsequent laboratory investigations were largely unremarkable, except for an elevated ANA titer (1:320, with a speckled pattern). The patient was initiated on a treatment regimen comprising intralesional triamcinolone and oral hydroxychloroquine (Plaquenil).
Discussion
It predominantly affects adults, yet pediatric cases account for 5%-7% of DLE diagnoses, with a significant predominance in females. Pediatric scalp DLE is particularly concerning due to its potential for causing scarring and permanent hair loss, which can significantly impact the psychological wellbeing of affected children.
The pathogenesis of DLE is multifactorial, involving genetic predispositions, environmental factors like UV light exposure, and immunological mechanisms leading to skin damage.
In children, DLE typically presents as well-demarcated, erythematous plaques with scale and follicular plugging, primarily affecting the scalp. Lesions may also exhibit changes in pigmentation, atrophy, and telangiectasia. The scalp involvement often leads to scarring alopecia, which can be distressing for pediatric patients. Unlike systemic lupus erythematosus (SLE), DLE is usually limited to the skin without systemic involvement. The progression of DLE to systemic lupus erythematosus in children has been previously described to be 22.2%. In a recent report of 201 pediatric cases of DLE, 12% of the cases progressed to systemic lupus erythematosus (SLE) and 14.5% had concurrent SLE. The onset of symptoms before the age of 10 years was the only statistically significant predictor for progression to SLE. Pruritus is a common symptom and may be correlated with disease activity.
The differential diagnosis for this patient encompassed a variety of conditions, including tinea capitis, alopecia areata, trichotillomania, and lichen planopilaris, each considered based on clinical presentation but ultimately excluded through clinical, microscopic, and biopsy findings.
Management strategies for pediatric scalp DLE aim at preventing disease progression, minimizing scarring, and addressing aesthetic concerns. These include the use of topical and intralesional corticosteroids, calcineurin inhibitors, and antimalarial agents like hydroxychloroquine, alongside stringent photoprotection to mitigate UV-triggered exacerbations.
Conclusion
The prognosis for pediatric scalp DLE can be favorable with timely and appropriate management, underscoring the importance of early diagnosis and intervention to prevent scarring and hair loss. However, ongoing surveillance is crucial for monitoring potential progression to systemic lupus erythematosus, albeit a low-risk transformation.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
1. George PM and Tunnessen WW. Childhood discoid lupus erythematosus. Arch Dermatol. 1993;129(5):613-617.
2. Hawat T et al. Pediatric discoid lupus erythematosus: Short report. Dermatol Ther. 2022 Jan;35(1):e15170. doi: 10.1111/dth.15170.
3. Arkin LM et al. Practice-based differences in paediatric discoid lupus erythematosus. Br J Dermatol. 2019 Oct;181(4):805-810. doi: 10.1111/bjd.17780.
Upon physical examination, the patient exhibited several patches of alopecia with accompanying perifollicular scaling, crusting, and erythema on the affected areas. Examination of her face revealed comedones and papules.
Circulating Tumor DNA Predicts Early Treatment Response in Patients With HER2-Positive Cancers
This was the main finding of new data presented by study author Razelle Kurzrock, MD, at the American Association for Cancer Research annual meeting.
“We found that on-treatment ctDNA can detect progression before standard-of-care response assessments. These data suggest that monitoring ctDNA can provide clinicians with important prognostic information that may guide treatment decisions,” Dr. Kurzrock, professor at the Medical College of Wisconsin, Milwaukee, said during her presentation.
Commenting on the clinical implications of these findings during an interview, she said the results suggest that ctDNA dynamics provide an early window into predicting response to targeted therapies in patients with HER2-altered cancers, confirming previous findings of the predictive value of ctDNA in other cancer types.
“Such monitoring may be useful in clinical trials and eventually in practice,” she added.
Need for new methods to predict early tumor response
Limitations of standard radiographic tumor assessments present challenges in determining clinical response, particularly for patients receiving targeted therapies.
During her talk, Dr. Kurzrock explained that although targeted therapies are effective for patients with specific molecular alterations, standard imaging assessments fail to uncover molecular-level changes within tumors, limiting the ability of clinicians to accurately assess a patient’s response to targeted therapies.
“In addition to limitations with imaging, patients and physicians want to know as soon as possible whether or not the agents are effective, especially if there are side effects,” Dr. Kurzrock during an interview. She added that monitoring early response may be especially important across tumor types, as HER2 therapies are increasingly being considered in the pan-cancer setting.
Commenting on the potential use of this method in other cancer types with HER2 alterations, Pashtoon Murtaza Kasi, MD, MS, noted that since the study relied on a tumor-informed assay, it would be applicable across diverse tumor types.
“It is less about tissue type but more about that particular patient’s tumor at that instant in time for which a unique barcode is created,” said Dr. Kasi, a medical oncologist at Weill Cornell Medicine, New York, who was not involved in the study.
In an interview, he added that the shedding and biology would affect the assay’s performance for some tissue types.
Design of patient-specific ctDNA assays
In this retrospective study, the researchers examined ctDNA dynamics in 58 patients with various HER2-positive tumor types, including breast, colorectal, and other solid malignancies harboring HER2 alterations. All the patients received combination HER2-targeted therapy with trastuzumab and pertuzumab in the phase 2 basket trial My Pathway (NCT02091141).
By leveraging comprehensive genomic profiling of each patient’s tumor, the researchers designed personalized ctDNA assays, tracking 2-16 tumor-specific genetic variants in the patients’ blood samples. FoundationOne Tracker was used to detect and quantify ctDNA at baseline and the third cycle of therapy (cycle 3 day 1, or C3D1).
During an interview, Dr. Kurzrock explained that FoundationOne Tracker is a personalized ctDNA monitoring assay that allows for the detection of ctDNA in plasma, enabling ongoing liquid-based monitoring and highly sensitive quantification of ctDNA levels as mean tumor molecules per milliliter of plasma.
Among the 52 patients for whom personalized ctDNA assays were successfully designed, 48 (92.3%) had ctDNA data available at baseline, with a median of 100.7 tumor molecules per milliliter of plasma. Most patients (89.6%) were deemed ctDNA-positive, with a median of 119.5 tumor molecules per milliliter of plasma.
Changes in ctDNA levels predict patient survival
The researchers found that patients who experienced a greater than 90% decline in ctDNA levels by the third treatment cycle had significantly longer overall survival (OS) than those with less than 90% ctDNA decline or any increase. According to data presented by Dr. Kurzrock, the median OS was not reached in the group with greater than 90% decline in on-treatment ctDNA levels, versus 9.4 months in the group with less than 90% decline or ctDNA increase (P = .007). These findings held true when the analysis was limited to the 14 patients with colorectal cancer, in which median OS was not reached in the group with greater than 90% decline in on-treatment ctDNA levels, versus 10.2 months in the group with less than 90% decline or ctDNA increase (P = 0.04).
Notably, the prognostic significance of ctDNA changes remained even among patients exhibiting radiographic stable disease, underscoring the limitations of relying solely on anatomic tumor measurements and highlighting the potential for ctDNA monitoring to complement standard clinical assessments. In the subset of patients with radiographic stable disease, those with a greater than 90% ctDNA decline had significantly longer OS than those with less ctDNA reduction (not reached versus 9.4 months; P = .01).
“When used as a complement to imaging, tissue-informed ctDNA monitoring with FoundationOne Tracker can provide more accuracy than imaging alone,” Dr. Kurzrock noted in an interview.
Dr. Kasi echoed Dr. Kurzrock’s enthusiasm regarding the clinical usefulness of these findings, saying, “Not only can you see very early on in whom the ctDNA is going down and clearing, but you can also tell apart within the group who has ‘stable disease’ as to who is deriving more benefit.”
The researchers also observed that increases in on-treatment ctDNA levels often preceded radiographic evidence of disease progression by a median of 1.3 months. These findings highlight the potential for ctDNA monitoring to complement standard clinical assessments, allowing us to detect treatment response and disease progression earlier than what is possible with imaging alone, Dr. Kurzrock explained during her talk. “This early warning signal could allow clinicians to intervene and modify treatment strategies before overt clinical deterioration,” she said.
In an interview, Dr. Kasi highlighted that this high sensitivity and specificity and the short half-life of the tumor-informed ctDNA assay make this liquid biopsy of great clinical value. “The short half-life of a few hours means that if you do an intervention to treat cancer with HER2-directed therapy, you can very quickly assess response to therapy way earlier than traditional radiographic methods.”
Dr. Kasi cautioned, however, that this assay would not capture whether new mutations or HER2 loss occurred at the time of resistance. “A repeat tissue biopsy or a next-generation sequencing-based plasma-only assay would be required for that,” he said.
Implementation of ctDNA monitoring in clinical trials
Dr. Kurzrock acknowledged that further research is needed to validate these results in larger, prospective cohorts before FoundationOne Tracker is adopted in the clinic. She noted, however, that this retrospective analysis, along with results from previous studies, provides a rationale for the use of ctDNA monitoring in clinical trials.
“In some centers like ours, ctDNA monitoring is already part of our standard of care since not only does it help from a physician standpoint to have a more accurate and early assessment of response, but patients also appreciate the information gained from ctDNA dynamics,” Dr. Kasi said in an interview. He explained that when radiographic findings are equivocal, ctDNA monitoring is an additional tool in their toolbox to help guide care.
He noted, however, that the cost is a challenge for implementing ctDNA monitoring as a complementary tool for real-time treatment response monitoring. “For serial monitoring, helping to reduce costs would be important in the long run,” he said in an interview. He added that obtaining sufficient tissue for testing using a tumor-informed assay can present a logistical challenge, at least for the first test. “You need sufficient tissue to make the barcode that you then follow along,” he explained.
“Developing guidelines through systematic studies about testing cadence would also be important. This would help establish whether ctDNA monitoring is helpful,” Dr. Kasi said in an interview. He explained that in some situations, biological variables affect the shedding and detection of ctDNA beyond the assay — in those cases, ctDNA monitoring may not be helpful. “Like any test, it is not meant for every patient or clinical question,” Dr. Kasi concluded.
Dr. Kurzrock and Dr. Kasi reported no relationships with entities whose primary business is producing, marketing, selling, reselling, or distributing healthcare products used by or on patients.
This was the main finding of new data presented by study author Razelle Kurzrock, MD, at the American Association for Cancer Research annual meeting.
“We found that on-treatment ctDNA can detect progression before standard-of-care response assessments. These data suggest that monitoring ctDNA can provide clinicians with important prognostic information that may guide treatment decisions,” Dr. Kurzrock, professor at the Medical College of Wisconsin, Milwaukee, said during her presentation.
Commenting on the clinical implications of these findings during an interview, she said the results suggest that ctDNA dynamics provide an early window into predicting response to targeted therapies in patients with HER2-altered cancers, confirming previous findings of the predictive value of ctDNA in other cancer types.
“Such monitoring may be useful in clinical trials and eventually in practice,” she added.
Need for new methods to predict early tumor response
Limitations of standard radiographic tumor assessments present challenges in determining clinical response, particularly for patients receiving targeted therapies.
During her talk, Dr. Kurzrock explained that although targeted therapies are effective for patients with specific molecular alterations, standard imaging assessments fail to uncover molecular-level changes within tumors, limiting the ability of clinicians to accurately assess a patient’s response to targeted therapies.
“In addition to limitations with imaging, patients and physicians want to know as soon as possible whether or not the agents are effective, especially if there are side effects,” Dr. Kurzrock during an interview. She added that monitoring early response may be especially important across tumor types, as HER2 therapies are increasingly being considered in the pan-cancer setting.
Commenting on the potential use of this method in other cancer types with HER2 alterations, Pashtoon Murtaza Kasi, MD, MS, noted that since the study relied on a tumor-informed assay, it would be applicable across diverse tumor types.
“It is less about tissue type but more about that particular patient’s tumor at that instant in time for which a unique barcode is created,” said Dr. Kasi, a medical oncologist at Weill Cornell Medicine, New York, who was not involved in the study.
In an interview, he added that the shedding and biology would affect the assay’s performance for some tissue types.
Design of patient-specific ctDNA assays
In this retrospective study, the researchers examined ctDNA dynamics in 58 patients with various HER2-positive tumor types, including breast, colorectal, and other solid malignancies harboring HER2 alterations. All the patients received combination HER2-targeted therapy with trastuzumab and pertuzumab in the phase 2 basket trial My Pathway (NCT02091141).
By leveraging comprehensive genomic profiling of each patient’s tumor, the researchers designed personalized ctDNA assays, tracking 2-16 tumor-specific genetic variants in the patients’ blood samples. FoundationOne Tracker was used to detect and quantify ctDNA at baseline and the third cycle of therapy (cycle 3 day 1, or C3D1).
During an interview, Dr. Kurzrock explained that FoundationOne Tracker is a personalized ctDNA monitoring assay that allows for the detection of ctDNA in plasma, enabling ongoing liquid-based monitoring and highly sensitive quantification of ctDNA levels as mean tumor molecules per milliliter of plasma.
Among the 52 patients for whom personalized ctDNA assays were successfully designed, 48 (92.3%) had ctDNA data available at baseline, with a median of 100.7 tumor molecules per milliliter of plasma. Most patients (89.6%) were deemed ctDNA-positive, with a median of 119.5 tumor molecules per milliliter of plasma.
Changes in ctDNA levels predict patient survival
The researchers found that patients who experienced a greater than 90% decline in ctDNA levels by the third treatment cycle had significantly longer overall survival (OS) than those with less than 90% ctDNA decline or any increase. According to data presented by Dr. Kurzrock, the median OS was not reached in the group with greater than 90% decline in on-treatment ctDNA levels, versus 9.4 months in the group with less than 90% decline or ctDNA increase (P = .007). These findings held true when the analysis was limited to the 14 patients with colorectal cancer, in which median OS was not reached in the group with greater than 90% decline in on-treatment ctDNA levels, versus 10.2 months in the group with less than 90% decline or ctDNA increase (P = 0.04).
Notably, the prognostic significance of ctDNA changes remained even among patients exhibiting radiographic stable disease, underscoring the limitations of relying solely on anatomic tumor measurements and highlighting the potential for ctDNA monitoring to complement standard clinical assessments. In the subset of patients with radiographic stable disease, those with a greater than 90% ctDNA decline had significantly longer OS than those with less ctDNA reduction (not reached versus 9.4 months; P = .01).
“When used as a complement to imaging, tissue-informed ctDNA monitoring with FoundationOne Tracker can provide more accuracy than imaging alone,” Dr. Kurzrock noted in an interview.
Dr. Kasi echoed Dr. Kurzrock’s enthusiasm regarding the clinical usefulness of these findings, saying, “Not only can you see very early on in whom the ctDNA is going down and clearing, but you can also tell apart within the group who has ‘stable disease’ as to who is deriving more benefit.”
The researchers also observed that increases in on-treatment ctDNA levels often preceded radiographic evidence of disease progression by a median of 1.3 months. These findings highlight the potential for ctDNA monitoring to complement standard clinical assessments, allowing us to detect treatment response and disease progression earlier than what is possible with imaging alone, Dr. Kurzrock explained during her talk. “This early warning signal could allow clinicians to intervene and modify treatment strategies before overt clinical deterioration,” she said.
In an interview, Dr. Kasi highlighted that this high sensitivity and specificity and the short half-life of the tumor-informed ctDNA assay make this liquid biopsy of great clinical value. “The short half-life of a few hours means that if you do an intervention to treat cancer with HER2-directed therapy, you can very quickly assess response to therapy way earlier than traditional radiographic methods.”
Dr. Kasi cautioned, however, that this assay would not capture whether new mutations or HER2 loss occurred at the time of resistance. “A repeat tissue biopsy or a next-generation sequencing-based plasma-only assay would be required for that,” he said.
Implementation of ctDNA monitoring in clinical trials
Dr. Kurzrock acknowledged that further research is needed to validate these results in larger, prospective cohorts before FoundationOne Tracker is adopted in the clinic. She noted, however, that this retrospective analysis, along with results from previous studies, provides a rationale for the use of ctDNA monitoring in clinical trials.
“In some centers like ours, ctDNA monitoring is already part of our standard of care since not only does it help from a physician standpoint to have a more accurate and early assessment of response, but patients also appreciate the information gained from ctDNA dynamics,” Dr. Kasi said in an interview. He explained that when radiographic findings are equivocal, ctDNA monitoring is an additional tool in their toolbox to help guide care.
He noted, however, that the cost is a challenge for implementing ctDNA monitoring as a complementary tool for real-time treatment response monitoring. “For serial monitoring, helping to reduce costs would be important in the long run,” he said in an interview. He added that obtaining sufficient tissue for testing using a tumor-informed assay can present a logistical challenge, at least for the first test. “You need sufficient tissue to make the barcode that you then follow along,” he explained.
“Developing guidelines through systematic studies about testing cadence would also be important. This would help establish whether ctDNA monitoring is helpful,” Dr. Kasi said in an interview. He explained that in some situations, biological variables affect the shedding and detection of ctDNA beyond the assay — in those cases, ctDNA monitoring may not be helpful. “Like any test, it is not meant for every patient or clinical question,” Dr. Kasi concluded.
Dr. Kurzrock and Dr. Kasi reported no relationships with entities whose primary business is producing, marketing, selling, reselling, or distributing healthcare products used by or on patients.
This was the main finding of new data presented by study author Razelle Kurzrock, MD, at the American Association for Cancer Research annual meeting.
“We found that on-treatment ctDNA can detect progression before standard-of-care response assessments. These data suggest that monitoring ctDNA can provide clinicians with important prognostic information that may guide treatment decisions,” Dr. Kurzrock, professor at the Medical College of Wisconsin, Milwaukee, said during her presentation.
Commenting on the clinical implications of these findings during an interview, she said the results suggest that ctDNA dynamics provide an early window into predicting response to targeted therapies in patients with HER2-altered cancers, confirming previous findings of the predictive value of ctDNA in other cancer types.
“Such monitoring may be useful in clinical trials and eventually in practice,” she added.
Need for new methods to predict early tumor response
Limitations of standard radiographic tumor assessments present challenges in determining clinical response, particularly for patients receiving targeted therapies.
During her talk, Dr. Kurzrock explained that although targeted therapies are effective for patients with specific molecular alterations, standard imaging assessments fail to uncover molecular-level changes within tumors, limiting the ability of clinicians to accurately assess a patient’s response to targeted therapies.
“In addition to limitations with imaging, patients and physicians want to know as soon as possible whether or not the agents are effective, especially if there are side effects,” Dr. Kurzrock during an interview. She added that monitoring early response may be especially important across tumor types, as HER2 therapies are increasingly being considered in the pan-cancer setting.
Commenting on the potential use of this method in other cancer types with HER2 alterations, Pashtoon Murtaza Kasi, MD, MS, noted that since the study relied on a tumor-informed assay, it would be applicable across diverse tumor types.
“It is less about tissue type but more about that particular patient’s tumor at that instant in time for which a unique barcode is created,” said Dr. Kasi, a medical oncologist at Weill Cornell Medicine, New York, who was not involved in the study.
In an interview, he added that the shedding and biology would affect the assay’s performance for some tissue types.
Design of patient-specific ctDNA assays
In this retrospective study, the researchers examined ctDNA dynamics in 58 patients with various HER2-positive tumor types, including breast, colorectal, and other solid malignancies harboring HER2 alterations. All the patients received combination HER2-targeted therapy with trastuzumab and pertuzumab in the phase 2 basket trial My Pathway (NCT02091141).
By leveraging comprehensive genomic profiling of each patient’s tumor, the researchers designed personalized ctDNA assays, tracking 2-16 tumor-specific genetic variants in the patients’ blood samples. FoundationOne Tracker was used to detect and quantify ctDNA at baseline and the third cycle of therapy (cycle 3 day 1, or C3D1).
During an interview, Dr. Kurzrock explained that FoundationOne Tracker is a personalized ctDNA monitoring assay that allows for the detection of ctDNA in plasma, enabling ongoing liquid-based monitoring and highly sensitive quantification of ctDNA levels as mean tumor molecules per milliliter of plasma.
Among the 52 patients for whom personalized ctDNA assays were successfully designed, 48 (92.3%) had ctDNA data available at baseline, with a median of 100.7 tumor molecules per milliliter of plasma. Most patients (89.6%) were deemed ctDNA-positive, with a median of 119.5 tumor molecules per milliliter of plasma.
Changes in ctDNA levels predict patient survival
The researchers found that patients who experienced a greater than 90% decline in ctDNA levels by the third treatment cycle had significantly longer overall survival (OS) than those with less than 90% ctDNA decline or any increase. According to data presented by Dr. Kurzrock, the median OS was not reached in the group with greater than 90% decline in on-treatment ctDNA levels, versus 9.4 months in the group with less than 90% decline or ctDNA increase (P = .007). These findings held true when the analysis was limited to the 14 patients with colorectal cancer, in which median OS was not reached in the group with greater than 90% decline in on-treatment ctDNA levels, versus 10.2 months in the group with less than 90% decline or ctDNA increase (P = 0.04).
Notably, the prognostic significance of ctDNA changes remained even among patients exhibiting radiographic stable disease, underscoring the limitations of relying solely on anatomic tumor measurements and highlighting the potential for ctDNA monitoring to complement standard clinical assessments. In the subset of patients with radiographic stable disease, those with a greater than 90% ctDNA decline had significantly longer OS than those with less ctDNA reduction (not reached versus 9.4 months; P = .01).
“When used as a complement to imaging, tissue-informed ctDNA monitoring with FoundationOne Tracker can provide more accuracy than imaging alone,” Dr. Kurzrock noted in an interview.
Dr. Kasi echoed Dr. Kurzrock’s enthusiasm regarding the clinical usefulness of these findings, saying, “Not only can you see very early on in whom the ctDNA is going down and clearing, but you can also tell apart within the group who has ‘stable disease’ as to who is deriving more benefit.”
The researchers also observed that increases in on-treatment ctDNA levels often preceded radiographic evidence of disease progression by a median of 1.3 months. These findings highlight the potential for ctDNA monitoring to complement standard clinical assessments, allowing us to detect treatment response and disease progression earlier than what is possible with imaging alone, Dr. Kurzrock explained during her talk. “This early warning signal could allow clinicians to intervene and modify treatment strategies before overt clinical deterioration,” she said.
In an interview, Dr. Kasi highlighted that this high sensitivity and specificity and the short half-life of the tumor-informed ctDNA assay make this liquid biopsy of great clinical value. “The short half-life of a few hours means that if you do an intervention to treat cancer with HER2-directed therapy, you can very quickly assess response to therapy way earlier than traditional radiographic methods.”
Dr. Kasi cautioned, however, that this assay would not capture whether new mutations or HER2 loss occurred at the time of resistance. “A repeat tissue biopsy or a next-generation sequencing-based plasma-only assay would be required for that,” he said.
Implementation of ctDNA monitoring in clinical trials
Dr. Kurzrock acknowledged that further research is needed to validate these results in larger, prospective cohorts before FoundationOne Tracker is adopted in the clinic. She noted, however, that this retrospective analysis, along with results from previous studies, provides a rationale for the use of ctDNA monitoring in clinical trials.
“In some centers like ours, ctDNA monitoring is already part of our standard of care since not only does it help from a physician standpoint to have a more accurate and early assessment of response, but patients also appreciate the information gained from ctDNA dynamics,” Dr. Kasi said in an interview. He explained that when radiographic findings are equivocal, ctDNA monitoring is an additional tool in their toolbox to help guide care.
He noted, however, that the cost is a challenge for implementing ctDNA monitoring as a complementary tool for real-time treatment response monitoring. “For serial monitoring, helping to reduce costs would be important in the long run,” he said in an interview. He added that obtaining sufficient tissue for testing using a tumor-informed assay can present a logistical challenge, at least for the first test. “You need sufficient tissue to make the barcode that you then follow along,” he explained.
“Developing guidelines through systematic studies about testing cadence would also be important. This would help establish whether ctDNA monitoring is helpful,” Dr. Kasi said in an interview. He explained that in some situations, biological variables affect the shedding and detection of ctDNA beyond the assay — in those cases, ctDNA monitoring may not be helpful. “Like any test, it is not meant for every patient or clinical question,” Dr. Kasi concluded.
Dr. Kurzrock and Dr. Kasi reported no relationships with entities whose primary business is producing, marketing, selling, reselling, or distributing healthcare products used by or on patients.
FROM AACR 2024
A 30-Year-Old White Female Presented With a 4-Month History of Scaly, Erythematous Patches and Plaques on Her Trunk and Extremities
Tumor necrosis factor (TNF)-alpha inhibitors are used to treat a variety of autoimmune conditions including psoriasis, psoriatic arthritis, rheumatoid arthritis (RA), spondyloarthritis, and inflammatory bowel disease (IBD). Interestingly, they have also been observed to cause paradoxical psoriasis with an incidence between 0.6%-5.3%, most commonly occurring in patients with underlying Crohn’s disease and rheumatoid arthritis (RA). Infliximab is the most common TNF inhibitor associated with this condition (52.6%-62.6% of cases) followed by etanercept (12%-29%). .
Psoriasis is traditionally divided into two types. Patients with type I psoriasis have a family history, develop symptoms before the age of 40 and are often positive for HLA-Cw6. Type II psoriasis is not related to HLA-Cw6, lacks a family history, and typically manifests after age 40. Psoriatic lesions are well-defined, erythematous plaques with silvery scales most commonly appearing on extensor surfaces and the scalp. Variants include nail psoriasis, pustular psoriasis, inverse psoriasis, and guttate psoriasis.
Although psoriasis is typically a clinical diagnosis, histologic examination may be used to differentiate from other dermatoses if necessary. The lesions of TNF inhibitor-induced psoriasis characteristically display patterns similar to primary psoriasis, including parakeratosis, microabscesses, and rete ridges. Eosinophilic hypersensitivity reactions and features overlapping with eczematous hypersensitivity (psoriasiform dermatitis) may also be present.
The pathogenesis of this condition is not well understood, but theories include a variety of immune processes including interferon overproduction, interleukin and T-cell activation, and the presence of an infectious nidus. Classical psoriasis is related to type 1 interferon release, so theoretically, immunosuppression caused by TNF inhibitor treatment may permit uncontrolled production of interferons, resulting in psoriatic lesions. Another theory is that interleukin (IL)-23, a pro-inflammatory cytokine, promotes activation of T-helper 17 (Th17) cells. Th17 cells are part of the pathogenesis of primary psoriasis and other inflammatory conditions, such as RA and inflammatory bowel disease. Of note, individuals with gastrointestinal inflammatory diseases are already known to be at a greater risk for developing psoriasis. Immunosuppression caused by a TNF inhibitor may leave patients more susceptible to other infections, which may induce psoriatic plaques.
There are multiple approaches to treatment depending on the severity of the disease. If the psoriatic eruption is mild, the medication may be continued. This “treat-through” method is often considered when stopping the current immunotherapy would cause the patient significant issues. Moderate to severe cases of TNF inhibitor-induced psoriasis may warrant switching TNF inhibitor therapy or completely changing the drug class used in the treatment of the underlying autoimmune condition. Additional treatments include topical and oral steroids, UV therapy, methotrexate, cyclosporine, and acitretin.
This case and the photo were submitted by Lucas Shapiro, BS, of Nova Southeastern University College of Osteopathic Medicine, Fort Lauderdale, Florida, and Leon S. Maratchi, MD, Gastro Health, Hollywood, Florida. The column was edited by Donna Bilu Martin, MD.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
1. Li SJ et al. J Psoriasis Psoriatic Arthritis. 2019 Apr;4(2):70-80. doi: 10.1177/2475530318810851.
2. Lu J and Lu Y. J Transl Autoimmun. 2023 Sep 6:7:100211. doi: 10.1016/j.jtauto.2023.100211.
3. Nair PA and Badri T. Psoriasis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: www.ncbi.nlm.nih.gov/books/NBK448194/
Tumor necrosis factor (TNF)-alpha inhibitors are used to treat a variety of autoimmune conditions including psoriasis, psoriatic arthritis, rheumatoid arthritis (RA), spondyloarthritis, and inflammatory bowel disease (IBD). Interestingly, they have also been observed to cause paradoxical psoriasis with an incidence between 0.6%-5.3%, most commonly occurring in patients with underlying Crohn’s disease and rheumatoid arthritis (RA). Infliximab is the most common TNF inhibitor associated with this condition (52.6%-62.6% of cases) followed by etanercept (12%-29%). .
Psoriasis is traditionally divided into two types. Patients with type I psoriasis have a family history, develop symptoms before the age of 40 and are often positive for HLA-Cw6. Type II psoriasis is not related to HLA-Cw6, lacks a family history, and typically manifests after age 40. Psoriatic lesions are well-defined, erythematous plaques with silvery scales most commonly appearing on extensor surfaces and the scalp. Variants include nail psoriasis, pustular psoriasis, inverse psoriasis, and guttate psoriasis.
Although psoriasis is typically a clinical diagnosis, histologic examination may be used to differentiate from other dermatoses if necessary. The lesions of TNF inhibitor-induced psoriasis characteristically display patterns similar to primary psoriasis, including parakeratosis, microabscesses, and rete ridges. Eosinophilic hypersensitivity reactions and features overlapping with eczematous hypersensitivity (psoriasiform dermatitis) may also be present.
The pathogenesis of this condition is not well understood, but theories include a variety of immune processes including interferon overproduction, interleukin and T-cell activation, and the presence of an infectious nidus. Classical psoriasis is related to type 1 interferon release, so theoretically, immunosuppression caused by TNF inhibitor treatment may permit uncontrolled production of interferons, resulting in psoriatic lesions. Another theory is that interleukin (IL)-23, a pro-inflammatory cytokine, promotes activation of T-helper 17 (Th17) cells. Th17 cells are part of the pathogenesis of primary psoriasis and other inflammatory conditions, such as RA and inflammatory bowel disease. Of note, individuals with gastrointestinal inflammatory diseases are already known to be at a greater risk for developing psoriasis. Immunosuppression caused by a TNF inhibitor may leave patients more susceptible to other infections, which may induce psoriatic plaques.
There are multiple approaches to treatment depending on the severity of the disease. If the psoriatic eruption is mild, the medication may be continued. This “treat-through” method is often considered when stopping the current immunotherapy would cause the patient significant issues. Moderate to severe cases of TNF inhibitor-induced psoriasis may warrant switching TNF inhibitor therapy or completely changing the drug class used in the treatment of the underlying autoimmune condition. Additional treatments include topical and oral steroids, UV therapy, methotrexate, cyclosporine, and acitretin.
This case and the photo were submitted by Lucas Shapiro, BS, of Nova Southeastern University College of Osteopathic Medicine, Fort Lauderdale, Florida, and Leon S. Maratchi, MD, Gastro Health, Hollywood, Florida. The column was edited by Donna Bilu Martin, MD.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
1. Li SJ et al. J Psoriasis Psoriatic Arthritis. 2019 Apr;4(2):70-80. doi: 10.1177/2475530318810851.
2. Lu J and Lu Y. J Transl Autoimmun. 2023 Sep 6:7:100211. doi: 10.1016/j.jtauto.2023.100211.
3. Nair PA and Badri T. Psoriasis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: www.ncbi.nlm.nih.gov/books/NBK448194/
Tumor necrosis factor (TNF)-alpha inhibitors are used to treat a variety of autoimmune conditions including psoriasis, psoriatic arthritis, rheumatoid arthritis (RA), spondyloarthritis, and inflammatory bowel disease (IBD). Interestingly, they have also been observed to cause paradoxical psoriasis with an incidence between 0.6%-5.3%, most commonly occurring in patients with underlying Crohn’s disease and rheumatoid arthritis (RA). Infliximab is the most common TNF inhibitor associated with this condition (52.6%-62.6% of cases) followed by etanercept (12%-29%). .
Psoriasis is traditionally divided into two types. Patients with type I psoriasis have a family history, develop symptoms before the age of 40 and are often positive for HLA-Cw6. Type II psoriasis is not related to HLA-Cw6, lacks a family history, and typically manifests after age 40. Psoriatic lesions are well-defined, erythematous plaques with silvery scales most commonly appearing on extensor surfaces and the scalp. Variants include nail psoriasis, pustular psoriasis, inverse psoriasis, and guttate psoriasis.
Although psoriasis is typically a clinical diagnosis, histologic examination may be used to differentiate from other dermatoses if necessary. The lesions of TNF inhibitor-induced psoriasis characteristically display patterns similar to primary psoriasis, including parakeratosis, microabscesses, and rete ridges. Eosinophilic hypersensitivity reactions and features overlapping with eczematous hypersensitivity (psoriasiform dermatitis) may also be present.
The pathogenesis of this condition is not well understood, but theories include a variety of immune processes including interferon overproduction, interleukin and T-cell activation, and the presence of an infectious nidus. Classical psoriasis is related to type 1 interferon release, so theoretically, immunosuppression caused by TNF inhibitor treatment may permit uncontrolled production of interferons, resulting in psoriatic lesions. Another theory is that interleukin (IL)-23, a pro-inflammatory cytokine, promotes activation of T-helper 17 (Th17) cells. Th17 cells are part of the pathogenesis of primary psoriasis and other inflammatory conditions, such as RA and inflammatory bowel disease. Of note, individuals with gastrointestinal inflammatory diseases are already known to be at a greater risk for developing psoriasis. Immunosuppression caused by a TNF inhibitor may leave patients more susceptible to other infections, which may induce psoriatic plaques.
There are multiple approaches to treatment depending on the severity of the disease. If the psoriatic eruption is mild, the medication may be continued. This “treat-through” method is often considered when stopping the current immunotherapy would cause the patient significant issues. Moderate to severe cases of TNF inhibitor-induced psoriasis may warrant switching TNF inhibitor therapy or completely changing the drug class used in the treatment of the underlying autoimmune condition. Additional treatments include topical and oral steroids, UV therapy, methotrexate, cyclosporine, and acitretin.
This case and the photo were submitted by Lucas Shapiro, BS, of Nova Southeastern University College of Osteopathic Medicine, Fort Lauderdale, Florida, and Leon S. Maratchi, MD, Gastro Health, Hollywood, Florida. The column was edited by Donna Bilu Martin, MD.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
1. Li SJ et al. J Psoriasis Psoriatic Arthritis. 2019 Apr;4(2):70-80. doi: 10.1177/2475530318810851.
2. Lu J and Lu Y. J Transl Autoimmun. 2023 Sep 6:7:100211. doi: 10.1016/j.jtauto.2023.100211.
3. Nair PA and Badri T. Psoriasis. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: www.ncbi.nlm.nih.gov/books/NBK448194/