User login
Twenty Years of Breast Reduction Surgery at a Veterans Affairs Medical Center
Women make up an estimated 10% of the veteran population.1 The US Department of Veterans Affairs (VA) projected that there would be an increase of 18,000 female veterans per year for 10 years based on 2015 data. The number of women veterans enrolled in the VA health care increased from 397,024 to 729,989 (83.9%) between 2005 and 2015.2 This rise in the number of enrolled women veterans also increased the demand for female-specific health care services, such as breast reduction surgery, a reconstructive procedure provided at the Malcom Randall VA Medical Center (MRVAMC) federal teaching hospital in Gainesville, Florida.
Patients who experience symptomatic macromastia will report a history of neck and shoulder pain, shoulder grooving from bra straps, inframammary intertrigo, difficulty finding clothes that fit, and discomfort participating in sports. For the treatment of symptomatic macromastia, patients report a high satisfaction rate after breast reduction surgery.3-5 Unfortunately, the complications from the surgery can significantly disrupt a woman’s life due to previously unplanned hospital admissions, clinic appointments, wound care, time off work, and poor aesthetic outcome. Faculty awareness of a large number of complications for patients after breast reduction surgery prompted the MRVAMC Plastic Surgery Service to establish a stricter surgical screening protocol using body mass index (BMI) values and negative nicotine status to help patients be healthier and reduce the potential risk before offering surgery. A medical literature search did not find an existing study on veteran-specific breast reduction surgery.
Methods
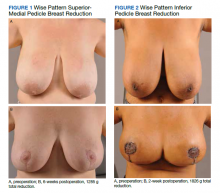
The University of Florida and North Florida/South Georgia Veterans Health System Institutional Review Board approved a retrospective chart review of all breast reduction surgeries performed at MRVAMC over a 20-year period (July 1, 2000-June 30, 2020). Electronic health records were queried for all primary bilateral breast reduction surgeries performed for symptomatic macromastia using Current Procedural Terminology code 19318. Potentially modifiable or predictable risk factors for wound complications were recorded: nicotine status, BMI, diabetes mellitus (DM) status, skin incision pattern, and pedicle location. Skin incision patterns were either vertical (periareolar plus a vertical scar from the areola to the inframammary fold) or traditional Wise pattern (also known as anchor pattern: periareolar scar, vertical scar to inframammary fold, plus a horizontal scar along the inframammary fold) as seen in Figures 1 and 2. The pedicle is the source of blood supply to the nipple, which was documented as either from the inferior aspect or the superior or superior/medial aspect.
For this study, the blood supply from the superior and superior/medial was logged in the same category. Records were reviewed 3 months after surgery for documentation of local wound complications, such as hematoma, infection, wound breakdown, skin necrosis, and nipple necrosis. Major complications were defined as requiring an unplanned hospital admission or urgent return to the operating room. A χ2 test using a P value of < .05 was used to determine statistical significance between the incidence of wound complications and the individually identifiable variables.
Results
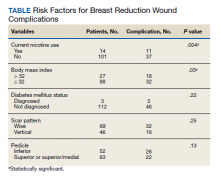
One hundred fifteen bilateral breast reduction surgeries were performed at MRVAMC over a 20-year period. Patient median age was 43 years. Median combined specimen weight was 1272 g. Forty-eight (41.7%) wound complications were documented, including 8 (7%) major complications. Most complications were identified in the first 7 years of the study before the new protocol and consult template became active. The new template resulted in the local complication rate dropping from 62% (July 2000-June 2007) to 26% (July 2007-June 2020). BMI > 32 (P = .03) and active nicotine use (P = .004) were found to be statistically significant independent risk factors for wound complications. Median BMI for all patients was 30. DM status (P = .22), skin incision pattern (P = .25), and pedicle location (P = .13) were not found to be predictors of wound complications (Table). There was no significant change in the incidence of major complications before and after the new protocols were enforced.
Discussion
Breast reduction surgery is an elective reconstructive option to treat symptomatic macromastia. There are several accepted ways to do the reduction surgical procedure where the blood supply (pedicle) to the nipple can vary and the visible scars can be in a horizontal, vertical, or Wise pattern. Technique is usually based on surgeon training, comfort, and preference. There are several known complications specific to this operation that include asymmetry, changes in nipple sensation, unattractive scars, diminished ability to breastfeed, and wound complications.5-7 Wound complications include seroma, hematoma, dehiscence, infection, wound breakdown, skin necrosis, and nipple necrosis.
This study focused on wound complications with the objective of identifying and modifying risk factors. Two known risk factors documented in the literature, nicotine use and obesity, already had been addressed by our service, and results were known anecdotally but had not been previously verified. This study also looked at other potential risk factors, including the pedicle location, skin incision, and DM status.
Residents or fellows participated in all the surgeries. An outcome analysis from The American College of Surgeons National Surgical Quality Improvement Program database from 2005 to 2011 found that resident participation was associated with morbidity, including wound complications.8 This study was performed at a federal hospital with a complexity level 1a rating, which is designated based on the highest level of patient volume, risk, teaching, research, intensive care unit beds, and specialty services.9 The hospital is closely affiliated with a level 1 trauma center and teaching hospital; therefore, resident and fellow participation is not a modifiable risk factor.
This study did not find an increased risk of wound complications in patients with DM, which has been found to be an independent risk factor in a prior study.10 DM status was indicated in only 3 histories, and they all had perioperative hemoglobin A1c levels < 8%. There is documentation of patients receiving perioperative antibiotics in 99 out of 116 of the surgical records; however, we did not include this in the analysis because the operative reports from the first year of the study were incomplete.
Smoking is a known risk factor for local wound complications in breast reduction surgery.10-15 The VA has a smoking cessation program through its mental health service that provides counseling and medication treatment options, including nicotine replacement, bupropion, and varenicline. We require patients to be at least 4 weeks nicotine free before surgery, which has been previously recommended in the literature.16
Existing studies that compare the traditional Wise pattern/inferior pedicle with vertical pattern/superior medial pedicle did not find an increased risk of wound complications.17-19 Our study separated the different incisions from the pedicle because the surgical technique among the different surgeons in the study varied, where sometimes the traditional Wise pattern was combined with the less traditional superior-medial pedicle. We did not find a statistical difference when comparing the incisions and pedicle location, which suggests that the incision type and source of blood supply to the nipple are not the determining factors for wound complications in the early postoperative period.
Obesity is a known risk factor for local wound complications.12,13,15,20-22 Studies have shown that patients who are obese benefit from breast reduction surgery; authors have argued against restricting surgery to these higher risk patients.4,23-25 Patients usually report decades of macromastia symptoms at consultation; so, we believe delaying the surgical procedure to get patients to a safer risk profile is in their best interest. We chose a cutoff BMI of 32 as a realistic value rather than 30, which is considered the definition of obesity. Patients at MRVAMC have access to MOVE!, a weight loss management program through primary care. We believe in being reasonable; so if a patient makes a significant improvement in her health but falls short of the required cutoff, we will still consider offering the surgical procedure after a full explanation of the surgical risks.
Wound complications, especially those that require admission or frequent appointments can seriously disrupt a patient’s life, creating unnecessary hardships and expense in time lost from work, travel, and child care. MRVAMC has a catchment area the size of North Carolina; so many of our patients travel hours for their appointments. The added scars and deformity from wound dehiscence and debridement can lead to asymmetry, widened scars, and future revision operations. Multiple clinic appointments for wound care not only impact that individual patient, but also has the effect of limiting access for all patients in a health care environment with high patient volume and limited providers, operating room time, and clinic appointments. As a result, minimizing predictable wound complications benefits the entire system.
Limitations and Strengths
This retrospective review comprised multiple different surgeons, including faculty and trainees, who were involved in the consultation, surgery, and postoperative care of the patients over a 20-year period; therefore, consistency in documentation is lacking. In addition, we were limited to only the information available on the charts. For example, wound size and laterality were not consistently documented. The MRVAMC complication rate was consistent with the current literature (range, 14-52%).12,18,20,24
The major strength of the study is that the veterans tend to stay within the VA, which makes complications easier to identify and follow. Patients who do not present initially to their surgeon due to travel limitations will typically contact their primary care provider or present to their local VA urgent care or emergency department provider, who will route the patient back to the surgical specialty service through the electronic health record.
Conclusions
Breast reduction surgery has a high wound complication rate, which can be predicted and improved on so that patients can receive their indicated surgical procedure with minimal inconvenience and downtime. This review confirms that preoperative weight loss and nicotine cessation were the appropriate focus of the MRVAMC plastic surgery service’s efforts to achieve a safer surgical experience. We will continue to enforce our protocol and encourage patients who are interested in breast reduction surgery and fall outside the requirements to work with their primary care provider on smoking cessation and weight loss through better nutrition and physical activity.
Acknowledgment
This manuscript is the result of work supported with resources and the use of facilities at the North Florida/South Georgia Veterans Health System in Gainesville, Florida.
1. US Department of Veterans Affairs. Statistics at a glance. Published February 2020. Accessed June 18, 2021. https://www.va.gov/vetdata/docs/Quickfacts/Homepage_slideshow_4_6_20.PDF
2. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Women veterans report: the past, present, and future of women veterans. Published February 2017. Accessed June 18, 2020. https://www.va.gov/vetdata/docs/specialreports/women_veterans_2015_final.pdf
3. Crittenden TA, Watson DI, Ratcliffe J, Griffin PA, Dean NR. Outcomes of breast reduction surgery using the breast-q: a prospective study and comparison with normative data. Plast Reconstr Surg. 2019;144(5):1034-1044. doi:10.1097/PRS.0000000000006114
4. Thoma A, Sprague S, Veltri K, Duku E, Furlong W. A prospective study of patients undergoing breast reduction surgery: health-related quality of life and clinical outcomes. Plast Reconstr Surg. 2007;120(1):13-26. doi:10.1097/01.prs.0000263370.94191.90
5. Nuzzi LC, Firriolo JM, Pike CM, DiVasta AD, Labow BI. Complications and quality of life following reduction mammaplasty in adolescents and young women.Plast Reconstr Surg. 2019;144(3):572-581. doi:10.1097/PRS.0000000000005907
6. Hall-Findlay EJ, Shestak KC. Breast reduction. Plast Reconstr Surg. 2015;136(4):531e-544e. doi:10.1097/PRS.0000000000001622
7. Kraut RY, Brown E, Korownyk C, et al. The impact of breast reduction surgery on breastfeeding: systematic review of observational studies. PLoS One. 2017;12(10):e0186591. doi:10.1371/journal.pone.0186591
8. Fischer JP, Wes AM, Kovach SJ. The impact of surgical resident participation in breast reduction surgery--outcome analysis from the 2005-2011 ACS-NSQIP datasets. J Plast Surg Hand Surg. 2014;48(5):315-321. doi:10.3109/2000656X.2014.882345
9. Site Facility Name and Complexity Summary of VHA Facility. Accessed June 18, 2021. https://www.vendorportal.ecms.va.gov/FBODocumentServer/DocumentServer.aspx?DocumentId=2793591&FileName=VA118-16-R-1059-A00002002.docx
10. Lewin R, Göransson M, Elander A, Thorarinsson A, Lundberg J, Lidén M. Risk factors for complications after breast reduction surgery. J Plast Surg Hand Surg. 2014;48(1):10-14. doi:10.3109/2000656X.2013.791625
11. Cunningham BL, Gear AJ, Kerrigan CL, Collins ED. Analysis of breast reduction complications derived from the BRAVO study. Plast Reconstr Surg. 2005;115(6):1597-1604. doi:10.1097/01.prs.0000160695.33457.db
12. Karamanos E, Wei B, Siddiqui A, Rubinfeld I. Tobacco use and body mass index as predictors of outcomes in patients undergoing breast reduction mammoplasty. Ann Plast Surg. 2015;75(4):383-387. doi:10.1097/SAP.0000000000000192
13. Manahan MA, Buretta KJ, Chang D, Mithani SK, Mallalieu J, Shermak MA. An outcomes analysis of 2142 breast reduction procedures. Ann Plast Surg. 2015;74(3):289-292. doi:10.1097/SAP.0b013e31829d2261
14. Hillam JS, Borsting EA, Chim JH, Thaller SR. Smoking as a risk factor for breast reduction: an analysis of 13,503 cases. J Plast Reconstr Aesthet Surg. 2017;70(6):734-740. doi:10.1016/j.bjps.2016.12.012
15. Zhang MX, Chen CY, Fang QQ, et al. Risk factors for complications after reduction mammoplasty: a meta-analysis. PLoS One. 2016;11(12):e0167746. doi:10.1371/journal.pone.0167746
16. Sørensen LT. Wound healing and infection in surgery: the pathophysiological impact of smoking, smoking cessation, and nicotine replacement therapy: a systematic review. Ann Surg. 2012;255(6):1069-1079.doi:10.1097/SLA.0b013e31824f632d
17. Antony AK, Yegiyants SS, Danielson KK, et al. A matched cohort study of superomedial pedicle vertical scar breast reduction (100 breasts) and traditional inferior pedicle Wise-pattern reduction (100 breasts): an outcomes study over 3 years. Plast Reconstr Surg. 2013;132(5):1068-1076. doi:10.1097/PRS.0b013e3182a48b2d
18. Hunter-Smith DJ, Smoll NR, Marne B, Maung H, Findlay MW. Comparing breast-reduction techniques: time-to-event analysis and recommendations. Aesthetic Plast Surg. 2012;36(3):600-606. doi:10.1007/s00266-011-9860-3
19. Ogunleye AA, Leroux O, Morrison N, Preminger AB. Complications after reduction mammaplasty: a comparison of wise pattern/inferior pedicle and vertical scar/superomedial pedicle. Ann Plast Surg. 2017;79(1):13-16. doi:10.1097/SAP.0000000000001059
20. Bauermeister AJ, Gill K, Zuriarrain A, Earle SA, Newman MI. Reduction mammaplasty with superomedial pedicle technique: a literature review and retrospective analysis of 938 consecutive breast reductions. J Plast Reconstr Aesthet Surg. 2019;72(3):410-418. doi:10.1016/j.bjps.2018.12.004
21. Nelson JA, Fischer JP, Chung CU, et al. Obesity and early complications following reduction mammaplasty: an analysis of 4545 patients from the 2005-2011 NSQIP datasets. J Plast Surg Hand Surg. 2014;48(5):334-339. doi:10.3109/2000656X.2014.886582
22. Kreithen J, Caffee H, Rosenberg J, et al. A comparison of the LeJour and Wise pattern methods of breast reduction. Ann Plast Surg. 2005;54(3):236-241. doi:10.3109/2000656X.2014.886582
23. Güemes A, Pérez E, Sousa R, et al. Quality of life and alleviation of symptoms after breast reduction for macromastia in obese patients: is surgery worth it? Aesthetic Plast Surg. 2016;40(1):62-70. doi:10.1007/s00266-015-0601-x
24. Setälä L, Papp A, Joukainen S, et al. Obesity and complications in breast reduction surgery: are restrictions justified? J Plast Reconstr Aesthet Surg. 2009;62(2):195-199. doi:10.1016/j.bjps.2007.10.043
25. Shah R, Al-Ajam Y, Stott D, Kang N. Obesity in mammaplasty: a study of complications following breast reduction. J Plast Reconstr Aesthet Surg. 2011;64(4):508-514. doi:10.1016/j.bjps.2007.10.043
Women make up an estimated 10% of the veteran population.1 The US Department of Veterans Affairs (VA) projected that there would be an increase of 18,000 female veterans per year for 10 years based on 2015 data. The number of women veterans enrolled in the VA health care increased from 397,024 to 729,989 (83.9%) between 2005 and 2015.2 This rise in the number of enrolled women veterans also increased the demand for female-specific health care services, such as breast reduction surgery, a reconstructive procedure provided at the Malcom Randall VA Medical Center (MRVAMC) federal teaching hospital in Gainesville, Florida.
Patients who experience symptomatic macromastia will report a history of neck and shoulder pain, shoulder grooving from bra straps, inframammary intertrigo, difficulty finding clothes that fit, and discomfort participating in sports. For the treatment of symptomatic macromastia, patients report a high satisfaction rate after breast reduction surgery.3-5 Unfortunately, the complications from the surgery can significantly disrupt a woman’s life due to previously unplanned hospital admissions, clinic appointments, wound care, time off work, and poor aesthetic outcome. Faculty awareness of a large number of complications for patients after breast reduction surgery prompted the MRVAMC Plastic Surgery Service to establish a stricter surgical screening protocol using body mass index (BMI) values and negative nicotine status to help patients be healthier and reduce the potential risk before offering surgery. A medical literature search did not find an existing study on veteran-specific breast reduction surgery.
Methods
The University of Florida and North Florida/South Georgia Veterans Health System Institutional Review Board approved a retrospective chart review of all breast reduction surgeries performed at MRVAMC over a 20-year period (July 1, 2000-June 30, 2020). Electronic health records were queried for all primary bilateral breast reduction surgeries performed for symptomatic macromastia using Current Procedural Terminology code 19318. Potentially modifiable or predictable risk factors for wound complications were recorded: nicotine status, BMI, diabetes mellitus (DM) status, skin incision pattern, and pedicle location. Skin incision patterns were either vertical (periareolar plus a vertical scar from the areola to the inframammary fold) or traditional Wise pattern (also known as anchor pattern: periareolar scar, vertical scar to inframammary fold, plus a horizontal scar along the inframammary fold) as seen in Figures 1 and 2. The pedicle is the source of blood supply to the nipple, which was documented as either from the inferior aspect or the superior or superior/medial aspect.
For this study, the blood supply from the superior and superior/medial was logged in the same category. Records were reviewed 3 months after surgery for documentation of local wound complications, such as hematoma, infection, wound breakdown, skin necrosis, and nipple necrosis. Major complications were defined as requiring an unplanned hospital admission or urgent return to the operating room. A χ2 test using a P value of < .05 was used to determine statistical significance between the incidence of wound complications and the individually identifiable variables.
Results
One hundred fifteen bilateral breast reduction surgeries were performed at MRVAMC over a 20-year period. Patient median age was 43 years. Median combined specimen weight was 1272 g. Forty-eight (41.7%) wound complications were documented, including 8 (7%) major complications. Most complications were identified in the first 7 years of the study before the new protocol and consult template became active. The new template resulted in the local complication rate dropping from 62% (July 2000-June 2007) to 26% (July 2007-June 2020). BMI > 32 (P = .03) and active nicotine use (P = .004) were found to be statistically significant independent risk factors for wound complications. Median BMI for all patients was 30. DM status (P = .22), skin incision pattern (P = .25), and pedicle location (P = .13) were not found to be predictors of wound complications (Table). There was no significant change in the incidence of major complications before and after the new protocols were enforced.
Discussion
Breast reduction surgery is an elective reconstructive option to treat symptomatic macromastia. There are several accepted ways to do the reduction surgical procedure where the blood supply (pedicle) to the nipple can vary and the visible scars can be in a horizontal, vertical, or Wise pattern. Technique is usually based on surgeon training, comfort, and preference. There are several known complications specific to this operation that include asymmetry, changes in nipple sensation, unattractive scars, diminished ability to breastfeed, and wound complications.5-7 Wound complications include seroma, hematoma, dehiscence, infection, wound breakdown, skin necrosis, and nipple necrosis.
This study focused on wound complications with the objective of identifying and modifying risk factors. Two known risk factors documented in the literature, nicotine use and obesity, already had been addressed by our service, and results were known anecdotally but had not been previously verified. This study also looked at other potential risk factors, including the pedicle location, skin incision, and DM status.
Residents or fellows participated in all the surgeries. An outcome analysis from The American College of Surgeons National Surgical Quality Improvement Program database from 2005 to 2011 found that resident participation was associated with morbidity, including wound complications.8 This study was performed at a federal hospital with a complexity level 1a rating, which is designated based on the highest level of patient volume, risk, teaching, research, intensive care unit beds, and specialty services.9 The hospital is closely affiliated with a level 1 trauma center and teaching hospital; therefore, resident and fellow participation is not a modifiable risk factor.
This study did not find an increased risk of wound complications in patients with DM, which has been found to be an independent risk factor in a prior study.10 DM status was indicated in only 3 histories, and they all had perioperative hemoglobin A1c levels < 8%. There is documentation of patients receiving perioperative antibiotics in 99 out of 116 of the surgical records; however, we did not include this in the analysis because the operative reports from the first year of the study were incomplete.
Smoking is a known risk factor for local wound complications in breast reduction surgery.10-15 The VA has a smoking cessation program through its mental health service that provides counseling and medication treatment options, including nicotine replacement, bupropion, and varenicline. We require patients to be at least 4 weeks nicotine free before surgery, which has been previously recommended in the literature.16
Existing studies that compare the traditional Wise pattern/inferior pedicle with vertical pattern/superior medial pedicle did not find an increased risk of wound complications.17-19 Our study separated the different incisions from the pedicle because the surgical technique among the different surgeons in the study varied, where sometimes the traditional Wise pattern was combined with the less traditional superior-medial pedicle. We did not find a statistical difference when comparing the incisions and pedicle location, which suggests that the incision type and source of blood supply to the nipple are not the determining factors for wound complications in the early postoperative period.
Obesity is a known risk factor for local wound complications.12,13,15,20-22 Studies have shown that patients who are obese benefit from breast reduction surgery; authors have argued against restricting surgery to these higher risk patients.4,23-25 Patients usually report decades of macromastia symptoms at consultation; so, we believe delaying the surgical procedure to get patients to a safer risk profile is in their best interest. We chose a cutoff BMI of 32 as a realistic value rather than 30, which is considered the definition of obesity. Patients at MRVAMC have access to MOVE!, a weight loss management program through primary care. We believe in being reasonable; so if a patient makes a significant improvement in her health but falls short of the required cutoff, we will still consider offering the surgical procedure after a full explanation of the surgical risks.
Wound complications, especially those that require admission or frequent appointments can seriously disrupt a patient’s life, creating unnecessary hardships and expense in time lost from work, travel, and child care. MRVAMC has a catchment area the size of North Carolina; so many of our patients travel hours for their appointments. The added scars and deformity from wound dehiscence and debridement can lead to asymmetry, widened scars, and future revision operations. Multiple clinic appointments for wound care not only impact that individual patient, but also has the effect of limiting access for all patients in a health care environment with high patient volume and limited providers, operating room time, and clinic appointments. As a result, minimizing predictable wound complications benefits the entire system.
Limitations and Strengths
This retrospective review comprised multiple different surgeons, including faculty and trainees, who were involved in the consultation, surgery, and postoperative care of the patients over a 20-year period; therefore, consistency in documentation is lacking. In addition, we were limited to only the information available on the charts. For example, wound size and laterality were not consistently documented. The MRVAMC complication rate was consistent with the current literature (range, 14-52%).12,18,20,24
The major strength of the study is that the veterans tend to stay within the VA, which makes complications easier to identify and follow. Patients who do not present initially to their surgeon due to travel limitations will typically contact their primary care provider or present to their local VA urgent care or emergency department provider, who will route the patient back to the surgical specialty service through the electronic health record.
Conclusions
Breast reduction surgery has a high wound complication rate, which can be predicted and improved on so that patients can receive their indicated surgical procedure with minimal inconvenience and downtime. This review confirms that preoperative weight loss and nicotine cessation were the appropriate focus of the MRVAMC plastic surgery service’s efforts to achieve a safer surgical experience. We will continue to enforce our protocol and encourage patients who are interested in breast reduction surgery and fall outside the requirements to work with their primary care provider on smoking cessation and weight loss through better nutrition and physical activity.
Acknowledgment
This manuscript is the result of work supported with resources and the use of facilities at the North Florida/South Georgia Veterans Health System in Gainesville, Florida.
Women make up an estimated 10% of the veteran population.1 The US Department of Veterans Affairs (VA) projected that there would be an increase of 18,000 female veterans per year for 10 years based on 2015 data. The number of women veterans enrolled in the VA health care increased from 397,024 to 729,989 (83.9%) between 2005 and 2015.2 This rise in the number of enrolled women veterans also increased the demand for female-specific health care services, such as breast reduction surgery, a reconstructive procedure provided at the Malcom Randall VA Medical Center (MRVAMC) federal teaching hospital in Gainesville, Florida.
Patients who experience symptomatic macromastia will report a history of neck and shoulder pain, shoulder grooving from bra straps, inframammary intertrigo, difficulty finding clothes that fit, and discomfort participating in sports. For the treatment of symptomatic macromastia, patients report a high satisfaction rate after breast reduction surgery.3-5 Unfortunately, the complications from the surgery can significantly disrupt a woman’s life due to previously unplanned hospital admissions, clinic appointments, wound care, time off work, and poor aesthetic outcome. Faculty awareness of a large number of complications for patients after breast reduction surgery prompted the MRVAMC Plastic Surgery Service to establish a stricter surgical screening protocol using body mass index (BMI) values and negative nicotine status to help patients be healthier and reduce the potential risk before offering surgery. A medical literature search did not find an existing study on veteran-specific breast reduction surgery.
Methods
The University of Florida and North Florida/South Georgia Veterans Health System Institutional Review Board approved a retrospective chart review of all breast reduction surgeries performed at MRVAMC over a 20-year period (July 1, 2000-June 30, 2020). Electronic health records were queried for all primary bilateral breast reduction surgeries performed for symptomatic macromastia using Current Procedural Terminology code 19318. Potentially modifiable or predictable risk factors for wound complications were recorded: nicotine status, BMI, diabetes mellitus (DM) status, skin incision pattern, and pedicle location. Skin incision patterns were either vertical (periareolar plus a vertical scar from the areola to the inframammary fold) or traditional Wise pattern (also known as anchor pattern: periareolar scar, vertical scar to inframammary fold, plus a horizontal scar along the inframammary fold) as seen in Figures 1 and 2. The pedicle is the source of blood supply to the nipple, which was documented as either from the inferior aspect or the superior or superior/medial aspect.
For this study, the blood supply from the superior and superior/medial was logged in the same category. Records were reviewed 3 months after surgery for documentation of local wound complications, such as hematoma, infection, wound breakdown, skin necrosis, and nipple necrosis. Major complications were defined as requiring an unplanned hospital admission or urgent return to the operating room. A χ2 test using a P value of < .05 was used to determine statistical significance between the incidence of wound complications and the individually identifiable variables.
Results
One hundred fifteen bilateral breast reduction surgeries were performed at MRVAMC over a 20-year period. Patient median age was 43 years. Median combined specimen weight was 1272 g. Forty-eight (41.7%) wound complications were documented, including 8 (7%) major complications. Most complications were identified in the first 7 years of the study before the new protocol and consult template became active. The new template resulted in the local complication rate dropping from 62% (July 2000-June 2007) to 26% (July 2007-June 2020). BMI > 32 (P = .03) and active nicotine use (P = .004) were found to be statistically significant independent risk factors for wound complications. Median BMI for all patients was 30. DM status (P = .22), skin incision pattern (P = .25), and pedicle location (P = .13) were not found to be predictors of wound complications (Table). There was no significant change in the incidence of major complications before and after the new protocols were enforced.
Discussion
Breast reduction surgery is an elective reconstructive option to treat symptomatic macromastia. There are several accepted ways to do the reduction surgical procedure where the blood supply (pedicle) to the nipple can vary and the visible scars can be in a horizontal, vertical, or Wise pattern. Technique is usually based on surgeon training, comfort, and preference. There are several known complications specific to this operation that include asymmetry, changes in nipple sensation, unattractive scars, diminished ability to breastfeed, and wound complications.5-7 Wound complications include seroma, hematoma, dehiscence, infection, wound breakdown, skin necrosis, and nipple necrosis.
This study focused on wound complications with the objective of identifying and modifying risk factors. Two known risk factors documented in the literature, nicotine use and obesity, already had been addressed by our service, and results were known anecdotally but had not been previously verified. This study also looked at other potential risk factors, including the pedicle location, skin incision, and DM status.
Residents or fellows participated in all the surgeries. An outcome analysis from The American College of Surgeons National Surgical Quality Improvement Program database from 2005 to 2011 found that resident participation was associated with morbidity, including wound complications.8 This study was performed at a federal hospital with a complexity level 1a rating, which is designated based on the highest level of patient volume, risk, teaching, research, intensive care unit beds, and specialty services.9 The hospital is closely affiliated with a level 1 trauma center and teaching hospital; therefore, resident and fellow participation is not a modifiable risk factor.
This study did not find an increased risk of wound complications in patients with DM, which has been found to be an independent risk factor in a prior study.10 DM status was indicated in only 3 histories, and they all had perioperative hemoglobin A1c levels < 8%. There is documentation of patients receiving perioperative antibiotics in 99 out of 116 of the surgical records; however, we did not include this in the analysis because the operative reports from the first year of the study were incomplete.
Smoking is a known risk factor for local wound complications in breast reduction surgery.10-15 The VA has a smoking cessation program through its mental health service that provides counseling and medication treatment options, including nicotine replacement, bupropion, and varenicline. We require patients to be at least 4 weeks nicotine free before surgery, which has been previously recommended in the literature.16
Existing studies that compare the traditional Wise pattern/inferior pedicle with vertical pattern/superior medial pedicle did not find an increased risk of wound complications.17-19 Our study separated the different incisions from the pedicle because the surgical technique among the different surgeons in the study varied, where sometimes the traditional Wise pattern was combined with the less traditional superior-medial pedicle. We did not find a statistical difference when comparing the incisions and pedicle location, which suggests that the incision type and source of blood supply to the nipple are not the determining factors for wound complications in the early postoperative period.
Obesity is a known risk factor for local wound complications.12,13,15,20-22 Studies have shown that patients who are obese benefit from breast reduction surgery; authors have argued against restricting surgery to these higher risk patients.4,23-25 Patients usually report decades of macromastia symptoms at consultation; so, we believe delaying the surgical procedure to get patients to a safer risk profile is in their best interest. We chose a cutoff BMI of 32 as a realistic value rather than 30, which is considered the definition of obesity. Patients at MRVAMC have access to MOVE!, a weight loss management program through primary care. We believe in being reasonable; so if a patient makes a significant improvement in her health but falls short of the required cutoff, we will still consider offering the surgical procedure after a full explanation of the surgical risks.
Wound complications, especially those that require admission or frequent appointments can seriously disrupt a patient’s life, creating unnecessary hardships and expense in time lost from work, travel, and child care. MRVAMC has a catchment area the size of North Carolina; so many of our patients travel hours for their appointments. The added scars and deformity from wound dehiscence and debridement can lead to asymmetry, widened scars, and future revision operations. Multiple clinic appointments for wound care not only impact that individual patient, but also has the effect of limiting access for all patients in a health care environment with high patient volume and limited providers, operating room time, and clinic appointments. As a result, minimizing predictable wound complications benefits the entire system.
Limitations and Strengths
This retrospective review comprised multiple different surgeons, including faculty and trainees, who were involved in the consultation, surgery, and postoperative care of the patients over a 20-year period; therefore, consistency in documentation is lacking. In addition, we were limited to only the information available on the charts. For example, wound size and laterality were not consistently documented. The MRVAMC complication rate was consistent with the current literature (range, 14-52%).12,18,20,24
The major strength of the study is that the veterans tend to stay within the VA, which makes complications easier to identify and follow. Patients who do not present initially to their surgeon due to travel limitations will typically contact their primary care provider or present to their local VA urgent care or emergency department provider, who will route the patient back to the surgical specialty service through the electronic health record.
Conclusions
Breast reduction surgery has a high wound complication rate, which can be predicted and improved on so that patients can receive their indicated surgical procedure with minimal inconvenience and downtime. This review confirms that preoperative weight loss and nicotine cessation were the appropriate focus of the MRVAMC plastic surgery service’s efforts to achieve a safer surgical experience. We will continue to enforce our protocol and encourage patients who are interested in breast reduction surgery and fall outside the requirements to work with their primary care provider on smoking cessation and weight loss through better nutrition and physical activity.
Acknowledgment
This manuscript is the result of work supported with resources and the use of facilities at the North Florida/South Georgia Veterans Health System in Gainesville, Florida.
1. US Department of Veterans Affairs. Statistics at a glance. Published February 2020. Accessed June 18, 2021. https://www.va.gov/vetdata/docs/Quickfacts/Homepage_slideshow_4_6_20.PDF
2. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Women veterans report: the past, present, and future of women veterans. Published February 2017. Accessed June 18, 2020. https://www.va.gov/vetdata/docs/specialreports/women_veterans_2015_final.pdf
3. Crittenden TA, Watson DI, Ratcliffe J, Griffin PA, Dean NR. Outcomes of breast reduction surgery using the breast-q: a prospective study and comparison with normative data. Plast Reconstr Surg. 2019;144(5):1034-1044. doi:10.1097/PRS.0000000000006114
4. Thoma A, Sprague S, Veltri K, Duku E, Furlong W. A prospective study of patients undergoing breast reduction surgery: health-related quality of life and clinical outcomes. Plast Reconstr Surg. 2007;120(1):13-26. doi:10.1097/01.prs.0000263370.94191.90
5. Nuzzi LC, Firriolo JM, Pike CM, DiVasta AD, Labow BI. Complications and quality of life following reduction mammaplasty in adolescents and young women.Plast Reconstr Surg. 2019;144(3):572-581. doi:10.1097/PRS.0000000000005907
6. Hall-Findlay EJ, Shestak KC. Breast reduction. Plast Reconstr Surg. 2015;136(4):531e-544e. doi:10.1097/PRS.0000000000001622
7. Kraut RY, Brown E, Korownyk C, et al. The impact of breast reduction surgery on breastfeeding: systematic review of observational studies. PLoS One. 2017;12(10):e0186591. doi:10.1371/journal.pone.0186591
8. Fischer JP, Wes AM, Kovach SJ. The impact of surgical resident participation in breast reduction surgery--outcome analysis from the 2005-2011 ACS-NSQIP datasets. J Plast Surg Hand Surg. 2014;48(5):315-321. doi:10.3109/2000656X.2014.882345
9. Site Facility Name and Complexity Summary of VHA Facility. Accessed June 18, 2021. https://www.vendorportal.ecms.va.gov/FBODocumentServer/DocumentServer.aspx?DocumentId=2793591&FileName=VA118-16-R-1059-A00002002.docx
10. Lewin R, Göransson M, Elander A, Thorarinsson A, Lundberg J, Lidén M. Risk factors for complications after breast reduction surgery. J Plast Surg Hand Surg. 2014;48(1):10-14. doi:10.3109/2000656X.2013.791625
11. Cunningham BL, Gear AJ, Kerrigan CL, Collins ED. Analysis of breast reduction complications derived from the BRAVO study. Plast Reconstr Surg. 2005;115(6):1597-1604. doi:10.1097/01.prs.0000160695.33457.db
12. Karamanos E, Wei B, Siddiqui A, Rubinfeld I. Tobacco use and body mass index as predictors of outcomes in patients undergoing breast reduction mammoplasty. Ann Plast Surg. 2015;75(4):383-387. doi:10.1097/SAP.0000000000000192
13. Manahan MA, Buretta KJ, Chang D, Mithani SK, Mallalieu J, Shermak MA. An outcomes analysis of 2142 breast reduction procedures. Ann Plast Surg. 2015;74(3):289-292. doi:10.1097/SAP.0b013e31829d2261
14. Hillam JS, Borsting EA, Chim JH, Thaller SR. Smoking as a risk factor for breast reduction: an analysis of 13,503 cases. J Plast Reconstr Aesthet Surg. 2017;70(6):734-740. doi:10.1016/j.bjps.2016.12.012
15. Zhang MX, Chen CY, Fang QQ, et al. Risk factors for complications after reduction mammoplasty: a meta-analysis. PLoS One. 2016;11(12):e0167746. doi:10.1371/journal.pone.0167746
16. Sørensen LT. Wound healing and infection in surgery: the pathophysiological impact of smoking, smoking cessation, and nicotine replacement therapy: a systematic review. Ann Surg. 2012;255(6):1069-1079.doi:10.1097/SLA.0b013e31824f632d
17. Antony AK, Yegiyants SS, Danielson KK, et al. A matched cohort study of superomedial pedicle vertical scar breast reduction (100 breasts) and traditional inferior pedicle Wise-pattern reduction (100 breasts): an outcomes study over 3 years. Plast Reconstr Surg. 2013;132(5):1068-1076. doi:10.1097/PRS.0b013e3182a48b2d
18. Hunter-Smith DJ, Smoll NR, Marne B, Maung H, Findlay MW. Comparing breast-reduction techniques: time-to-event analysis and recommendations. Aesthetic Plast Surg. 2012;36(3):600-606. doi:10.1007/s00266-011-9860-3
19. Ogunleye AA, Leroux O, Morrison N, Preminger AB. Complications after reduction mammaplasty: a comparison of wise pattern/inferior pedicle and vertical scar/superomedial pedicle. Ann Plast Surg. 2017;79(1):13-16. doi:10.1097/SAP.0000000000001059
20. Bauermeister AJ, Gill K, Zuriarrain A, Earle SA, Newman MI. Reduction mammaplasty with superomedial pedicle technique: a literature review and retrospective analysis of 938 consecutive breast reductions. J Plast Reconstr Aesthet Surg. 2019;72(3):410-418. doi:10.1016/j.bjps.2018.12.004
21. Nelson JA, Fischer JP, Chung CU, et al. Obesity and early complications following reduction mammaplasty: an analysis of 4545 patients from the 2005-2011 NSQIP datasets. J Plast Surg Hand Surg. 2014;48(5):334-339. doi:10.3109/2000656X.2014.886582
22. Kreithen J, Caffee H, Rosenberg J, et al. A comparison of the LeJour and Wise pattern methods of breast reduction. Ann Plast Surg. 2005;54(3):236-241. doi:10.3109/2000656X.2014.886582
23. Güemes A, Pérez E, Sousa R, et al. Quality of life and alleviation of symptoms after breast reduction for macromastia in obese patients: is surgery worth it? Aesthetic Plast Surg. 2016;40(1):62-70. doi:10.1007/s00266-015-0601-x
24. Setälä L, Papp A, Joukainen S, et al. Obesity and complications in breast reduction surgery: are restrictions justified? J Plast Reconstr Aesthet Surg. 2009;62(2):195-199. doi:10.1016/j.bjps.2007.10.043
25. Shah R, Al-Ajam Y, Stott D, Kang N. Obesity in mammaplasty: a study of complications following breast reduction. J Plast Reconstr Aesthet Surg. 2011;64(4):508-514. doi:10.1016/j.bjps.2007.10.043
1. US Department of Veterans Affairs. Statistics at a glance. Published February 2020. Accessed June 18, 2021. https://www.va.gov/vetdata/docs/Quickfacts/Homepage_slideshow_4_6_20.PDF
2. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Women veterans report: the past, present, and future of women veterans. Published February 2017. Accessed June 18, 2020. https://www.va.gov/vetdata/docs/specialreports/women_veterans_2015_final.pdf
3. Crittenden TA, Watson DI, Ratcliffe J, Griffin PA, Dean NR. Outcomes of breast reduction surgery using the breast-q: a prospective study and comparison with normative data. Plast Reconstr Surg. 2019;144(5):1034-1044. doi:10.1097/PRS.0000000000006114
4. Thoma A, Sprague S, Veltri K, Duku E, Furlong W. A prospective study of patients undergoing breast reduction surgery: health-related quality of life and clinical outcomes. Plast Reconstr Surg. 2007;120(1):13-26. doi:10.1097/01.prs.0000263370.94191.90
5. Nuzzi LC, Firriolo JM, Pike CM, DiVasta AD, Labow BI. Complications and quality of life following reduction mammaplasty in adolescents and young women.Plast Reconstr Surg. 2019;144(3):572-581. doi:10.1097/PRS.0000000000005907
6. Hall-Findlay EJ, Shestak KC. Breast reduction. Plast Reconstr Surg. 2015;136(4):531e-544e. doi:10.1097/PRS.0000000000001622
7. Kraut RY, Brown E, Korownyk C, et al. The impact of breast reduction surgery on breastfeeding: systematic review of observational studies. PLoS One. 2017;12(10):e0186591. doi:10.1371/journal.pone.0186591
8. Fischer JP, Wes AM, Kovach SJ. The impact of surgical resident participation in breast reduction surgery--outcome analysis from the 2005-2011 ACS-NSQIP datasets. J Plast Surg Hand Surg. 2014;48(5):315-321. doi:10.3109/2000656X.2014.882345
9. Site Facility Name and Complexity Summary of VHA Facility. Accessed June 18, 2021. https://www.vendorportal.ecms.va.gov/FBODocumentServer/DocumentServer.aspx?DocumentId=2793591&FileName=VA118-16-R-1059-A00002002.docx
10. Lewin R, Göransson M, Elander A, Thorarinsson A, Lundberg J, Lidén M. Risk factors for complications after breast reduction surgery. J Plast Surg Hand Surg. 2014;48(1):10-14. doi:10.3109/2000656X.2013.791625
11. Cunningham BL, Gear AJ, Kerrigan CL, Collins ED. Analysis of breast reduction complications derived from the BRAVO study. Plast Reconstr Surg. 2005;115(6):1597-1604. doi:10.1097/01.prs.0000160695.33457.db
12. Karamanos E, Wei B, Siddiqui A, Rubinfeld I. Tobacco use and body mass index as predictors of outcomes in patients undergoing breast reduction mammoplasty. Ann Plast Surg. 2015;75(4):383-387. doi:10.1097/SAP.0000000000000192
13. Manahan MA, Buretta KJ, Chang D, Mithani SK, Mallalieu J, Shermak MA. An outcomes analysis of 2142 breast reduction procedures. Ann Plast Surg. 2015;74(3):289-292. doi:10.1097/SAP.0b013e31829d2261
14. Hillam JS, Borsting EA, Chim JH, Thaller SR. Smoking as a risk factor for breast reduction: an analysis of 13,503 cases. J Plast Reconstr Aesthet Surg. 2017;70(6):734-740. doi:10.1016/j.bjps.2016.12.012
15. Zhang MX, Chen CY, Fang QQ, et al. Risk factors for complications after reduction mammoplasty: a meta-analysis. PLoS One. 2016;11(12):e0167746. doi:10.1371/journal.pone.0167746
16. Sørensen LT. Wound healing and infection in surgery: the pathophysiological impact of smoking, smoking cessation, and nicotine replacement therapy: a systematic review. Ann Surg. 2012;255(6):1069-1079.doi:10.1097/SLA.0b013e31824f632d
17. Antony AK, Yegiyants SS, Danielson KK, et al. A matched cohort study of superomedial pedicle vertical scar breast reduction (100 breasts) and traditional inferior pedicle Wise-pattern reduction (100 breasts): an outcomes study over 3 years. Plast Reconstr Surg. 2013;132(5):1068-1076. doi:10.1097/PRS.0b013e3182a48b2d
18. Hunter-Smith DJ, Smoll NR, Marne B, Maung H, Findlay MW. Comparing breast-reduction techniques: time-to-event analysis and recommendations. Aesthetic Plast Surg. 2012;36(3):600-606. doi:10.1007/s00266-011-9860-3
19. Ogunleye AA, Leroux O, Morrison N, Preminger AB. Complications after reduction mammaplasty: a comparison of wise pattern/inferior pedicle and vertical scar/superomedial pedicle. Ann Plast Surg. 2017;79(1):13-16. doi:10.1097/SAP.0000000000001059
20. Bauermeister AJ, Gill K, Zuriarrain A, Earle SA, Newman MI. Reduction mammaplasty with superomedial pedicle technique: a literature review and retrospective analysis of 938 consecutive breast reductions. J Plast Reconstr Aesthet Surg. 2019;72(3):410-418. doi:10.1016/j.bjps.2018.12.004
21. Nelson JA, Fischer JP, Chung CU, et al. Obesity and early complications following reduction mammaplasty: an analysis of 4545 patients from the 2005-2011 NSQIP datasets. J Plast Surg Hand Surg. 2014;48(5):334-339. doi:10.3109/2000656X.2014.886582
22. Kreithen J, Caffee H, Rosenberg J, et al. A comparison of the LeJour and Wise pattern methods of breast reduction. Ann Plast Surg. 2005;54(3):236-241. doi:10.3109/2000656X.2014.886582
23. Güemes A, Pérez E, Sousa R, et al. Quality of life and alleviation of symptoms after breast reduction for macromastia in obese patients: is surgery worth it? Aesthetic Plast Surg. 2016;40(1):62-70. doi:10.1007/s00266-015-0601-x
24. Setälä L, Papp A, Joukainen S, et al. Obesity and complications in breast reduction surgery: are restrictions justified? J Plast Reconstr Aesthet Surg. 2009;62(2):195-199. doi:10.1016/j.bjps.2007.10.043
25. Shah R, Al-Ajam Y, Stott D, Kang N. Obesity in mammaplasty: a study of complications following breast reduction. J Plast Reconstr Aesthet Surg. 2011;64(4):508-514. doi:10.1016/j.bjps.2007.10.043
A Pilot With Electrical Pain in the Face
An intracranial epidermoid cyst is an unusual but treatable cause of trigeminal neuralgia.
A 25-year-old male student pilot presented to his flight surgeon in Corpus Christi, Texas, with a 1-year history of episodic left-sided facial pain. He described the pain as electric-like with subsequent tingling sensation. These symptoms were always located on the left side of his tongue and lower lip. They were provoked by chewing, touching, or brushing his teeth. The most recent episode had lasted for 3 days before resolving. He noted 2 similar episodes a few months earlier that he related to periods of high stress.
On physical examination, the student pilot was well appearing with unremarkable vital signs. There were no skin lesions of the head or neck region. His tongue was midline without cutaneous lesions or atrophy. There was no facial numbness or weakness of the mastication muscles. There were no oropharyngeal mucosal or anatomic abnormalities. He had no lymphadenopathy. The remainder of the physical examination was unremarkable. He was seen by both dental medicine and oral surgery providers who did not identify an underlying cause for his symptoms.
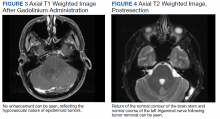
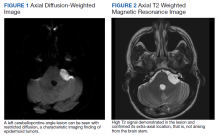
When symptoms recurred a fourth time, the student was referred for a magnetic resonance imaging (MRI) of the brain with and without contrast. The MRI demonstrated a left-sided extra-axial mass, involving the cerebellopontine angle (CPA), with imaging features most consistent with an epidermoid cyst (Figures 1, 2, and 3). An audiogram performed at the time of diagnosis revealed no sensorineural hearing loss.
Discussion
Epidermoid cysts are extra-axial tumors that are benign and slow growing. They constitute about 1% of all intracranial tumors.1 They most commonly occur at the CPA but can also arise in the fourth ventricle and suprasellar regions.2 Epidermoid cysts constitute about 5 to 7% of all CPA tumors.3,4 The 2 most common presenting symptoms of these tumors are headache and cranial nerve dysfunction.1 Other presenting symptoms may include ataxia, hemiparesis, and tinnitus.
On computed tomography (CT), epidermoid cysts can be identical in density to cerebrospinal fluid, making early detection difficult. On MRI, the lesion is easily seen on diffusion-weighted imaging, due to hyperintensity and restricted diffusion. The cysts rarely enhance, unlike the more common tumors in this region, vestibular schwannomas and meningiomas.5
Total neurosurgical resection of the epidermoid cyst is the optimal treatment and is possible in most cases.6 Management of these cysts may prove difficult because of their close proximity to the cranial nerves and brain stem. A near-total excision may be necessary for those tumors that have strong adhesions to neurovascular structures.7 Literature reports that recurrence after surgery is rare in cases of subtotal removal.8,9 Reported postoperative complications may include aseptic meningitis and cranial nerve dysfunction.10
Management
The patient was informed of the presumed diagnosis of brain epidermoid cyst and sent for neurosurgery evaluation. Surgery was indicated and via a retrosigmoid craniotomy, the tumor was removed in total with no complications. On 3-month postoperative follow-up, MRI showed no evidence of residual epidermoid (Figure 4). On physical examination at the follow-up, he was alert and oriented. His surgical incision was well healed. He was neurologically intact with a normal gait. He was released without restrictions from neurosurgical care.
The patient wished to continue flying after successful resection of his cyst. The neurosurgical procedure for removal of the epidermoid cyst medically disqualified him for military aviation.11 As the patient had no neurologic deficits, a waiver was submitted on his behalf to the Naval Aerospace Medical Institute. The waiver was granted for flying duties, and the patient returned to training. He has had no return of symptoms to date.
Conclusions
An intracranial epidermoid cyst is an unusual but treatable cause of trigeminal neuralgia. Gross total removal, without cranial nerve or cerebellar deficits, resulted in the patient’s complete return to health and training as a pilot.
1. Farhoud A, Khedr W, Aboul-Enein H. Surgical resection of cerebellopontine epidermoid cysts: limitations and outcome. J Neurol Surg B Skull Base. 2018;79(2):167‐172. doi:10.1055/s-0037-1606220
2. Hung LC, Wu CS, Lin CC, Fang WK, Hsu YC. Epidermoid cyst presenting as isolated trigeminal neuralgia - two case reports. Acta Neurol Taiwan. 2013;22(3):133‐137.
3. Feng R, Gu X, Hu J, et al. Surgical treatment and radiotherapy of epidermoid cyst with malignant transformation in cerebellopontine angle. Int J Clin Exp Med. 2014;7(1):312‐315.
4. Friedmann DR, Grobelny B, Golfinos JG, Roland JT. Nonschwannoma tumors of the cerebellopontine angle. Otolaryngol Clin North Am. 2015;48(3):461-475. doi:10.1016/j.ote.2015.02.006
5. CPA-IAC In: Harnsberger HR, Glastonbury CM, Michel MA, Koch BL Branstetter BF IV. Diagnostic Imaging: Head and Neck, 2nd ed. Amirsys, Inc; 2011:VI(8):6-9 6. Hasegawa M, Nouri M, Nagahisa S, et al. Cerebellopontine angle epidermoid cysts: clinical presentations and surgical outcome. Neurosurg Rev. 2016;39(2):259‐267. doi:10.1007/s10143-015-0684-5
7. Safavi-Abbasi S, Di Rocco F, Bambakidis N, et al. Has management of epidermoid tumors of the cerebellopontine angle improved? A surgical synopsis of the past and present. Skull Base. 2008;18(2):85‐98. doi:10.1055/s-2007-991108
8. Son DW, Choi CH, Cha SH. Epidermoid tumors in the cerebellopontine angle presenting with trigeminal neuralgia. J Korean Neurosurg Soc. 2010;47(4):271‐277. doi:10.3340/jkns.2010.47.4.271
9. Schiefer TK, Link MJ. Epidermoids of the cerebellopontine angle: a 20-year experience. Surg Neurol. 2008;70(6):584-590; discussion 590. doi:10.1016/j.surneu.2007.12.021
10. Meng L, Yuguang L, Feng L, Wandong S, Shugan Z, Chengyuan W. Cerebellopontine angle epidermoids presenting with trigeminal neuralgia. J Clin Neurosci. 2005;12(7):784‐786. doi:10.1016/j.jocn.2004.09.023
11. Naval Aerospace Medical Institute. US Navy Aeromedical reference and waiver guide. Updated March 31, 2021. Accessed June 17, 2021. https://www.med.navy.mil/sites/nmotc/nami/arwg/Documents/WaiverGuide/Complete_Waiver_Guide.pdf
An intracranial epidermoid cyst is an unusual but treatable cause of trigeminal neuralgia.
An intracranial epidermoid cyst is an unusual but treatable cause of trigeminal neuralgia.
A 25-year-old male student pilot presented to his flight surgeon in Corpus Christi, Texas, with a 1-year history of episodic left-sided facial pain. He described the pain as electric-like with subsequent tingling sensation. These symptoms were always located on the left side of his tongue and lower lip. They were provoked by chewing, touching, or brushing his teeth. The most recent episode had lasted for 3 days before resolving. He noted 2 similar episodes a few months earlier that he related to periods of high stress.
On physical examination, the student pilot was well appearing with unremarkable vital signs. There were no skin lesions of the head or neck region. His tongue was midline without cutaneous lesions or atrophy. There was no facial numbness or weakness of the mastication muscles. There were no oropharyngeal mucosal or anatomic abnormalities. He had no lymphadenopathy. The remainder of the physical examination was unremarkable. He was seen by both dental medicine and oral surgery providers who did not identify an underlying cause for his symptoms.
When symptoms recurred a fourth time, the student was referred for a magnetic resonance imaging (MRI) of the brain with and without contrast. The MRI demonstrated a left-sided extra-axial mass, involving the cerebellopontine angle (CPA), with imaging features most consistent with an epidermoid cyst (Figures 1, 2, and 3). An audiogram performed at the time of diagnosis revealed no sensorineural hearing loss.
Discussion
Epidermoid cysts are extra-axial tumors that are benign and slow growing. They constitute about 1% of all intracranial tumors.1 They most commonly occur at the CPA but can also arise in the fourth ventricle and suprasellar regions.2 Epidermoid cysts constitute about 5 to 7% of all CPA tumors.3,4 The 2 most common presenting symptoms of these tumors are headache and cranial nerve dysfunction.1 Other presenting symptoms may include ataxia, hemiparesis, and tinnitus.
On computed tomography (CT), epidermoid cysts can be identical in density to cerebrospinal fluid, making early detection difficult. On MRI, the lesion is easily seen on diffusion-weighted imaging, due to hyperintensity and restricted diffusion. The cysts rarely enhance, unlike the more common tumors in this region, vestibular schwannomas and meningiomas.5
Total neurosurgical resection of the epidermoid cyst is the optimal treatment and is possible in most cases.6 Management of these cysts may prove difficult because of their close proximity to the cranial nerves and brain stem. A near-total excision may be necessary for those tumors that have strong adhesions to neurovascular structures.7 Literature reports that recurrence after surgery is rare in cases of subtotal removal.8,9 Reported postoperative complications may include aseptic meningitis and cranial nerve dysfunction.10
Management
The patient was informed of the presumed diagnosis of brain epidermoid cyst and sent for neurosurgery evaluation. Surgery was indicated and via a retrosigmoid craniotomy, the tumor was removed in total with no complications. On 3-month postoperative follow-up, MRI showed no evidence of residual epidermoid (Figure 4). On physical examination at the follow-up, he was alert and oriented. His surgical incision was well healed. He was neurologically intact with a normal gait. He was released without restrictions from neurosurgical care.
The patient wished to continue flying after successful resection of his cyst. The neurosurgical procedure for removal of the epidermoid cyst medically disqualified him for military aviation.11 As the patient had no neurologic deficits, a waiver was submitted on his behalf to the Naval Aerospace Medical Institute. The waiver was granted for flying duties, and the patient returned to training. He has had no return of symptoms to date.
Conclusions
An intracranial epidermoid cyst is an unusual but treatable cause of trigeminal neuralgia. Gross total removal, without cranial nerve or cerebellar deficits, resulted in the patient’s complete return to health and training as a pilot.
A 25-year-old male student pilot presented to his flight surgeon in Corpus Christi, Texas, with a 1-year history of episodic left-sided facial pain. He described the pain as electric-like with subsequent tingling sensation. These symptoms were always located on the left side of his tongue and lower lip. They were provoked by chewing, touching, or brushing his teeth. The most recent episode had lasted for 3 days before resolving. He noted 2 similar episodes a few months earlier that he related to periods of high stress.
On physical examination, the student pilot was well appearing with unremarkable vital signs. There were no skin lesions of the head or neck region. His tongue was midline without cutaneous lesions or atrophy. There was no facial numbness or weakness of the mastication muscles. There were no oropharyngeal mucosal or anatomic abnormalities. He had no lymphadenopathy. The remainder of the physical examination was unremarkable. He was seen by both dental medicine and oral surgery providers who did not identify an underlying cause for his symptoms.
When symptoms recurred a fourth time, the student was referred for a magnetic resonance imaging (MRI) of the brain with and without contrast. The MRI demonstrated a left-sided extra-axial mass, involving the cerebellopontine angle (CPA), with imaging features most consistent with an epidermoid cyst (Figures 1, 2, and 3). An audiogram performed at the time of diagnosis revealed no sensorineural hearing loss.
Discussion
Epidermoid cysts are extra-axial tumors that are benign and slow growing. They constitute about 1% of all intracranial tumors.1 They most commonly occur at the CPA but can also arise in the fourth ventricle and suprasellar regions.2 Epidermoid cysts constitute about 5 to 7% of all CPA tumors.3,4 The 2 most common presenting symptoms of these tumors are headache and cranial nerve dysfunction.1 Other presenting symptoms may include ataxia, hemiparesis, and tinnitus.
On computed tomography (CT), epidermoid cysts can be identical in density to cerebrospinal fluid, making early detection difficult. On MRI, the lesion is easily seen on diffusion-weighted imaging, due to hyperintensity and restricted diffusion. The cysts rarely enhance, unlike the more common tumors in this region, vestibular schwannomas and meningiomas.5
Total neurosurgical resection of the epidermoid cyst is the optimal treatment and is possible in most cases.6 Management of these cysts may prove difficult because of their close proximity to the cranial nerves and brain stem. A near-total excision may be necessary for those tumors that have strong adhesions to neurovascular structures.7 Literature reports that recurrence after surgery is rare in cases of subtotal removal.8,9 Reported postoperative complications may include aseptic meningitis and cranial nerve dysfunction.10
Management
The patient was informed of the presumed diagnosis of brain epidermoid cyst and sent for neurosurgery evaluation. Surgery was indicated and via a retrosigmoid craniotomy, the tumor was removed in total with no complications. On 3-month postoperative follow-up, MRI showed no evidence of residual epidermoid (Figure 4). On physical examination at the follow-up, he was alert and oriented. His surgical incision was well healed. He was neurologically intact with a normal gait. He was released without restrictions from neurosurgical care.
The patient wished to continue flying after successful resection of his cyst. The neurosurgical procedure for removal of the epidermoid cyst medically disqualified him for military aviation.11 As the patient had no neurologic deficits, a waiver was submitted on his behalf to the Naval Aerospace Medical Institute. The waiver was granted for flying duties, and the patient returned to training. He has had no return of symptoms to date.
Conclusions
An intracranial epidermoid cyst is an unusual but treatable cause of trigeminal neuralgia. Gross total removal, without cranial nerve or cerebellar deficits, resulted in the patient’s complete return to health and training as a pilot.
1. Farhoud A, Khedr W, Aboul-Enein H. Surgical resection of cerebellopontine epidermoid cysts: limitations and outcome. J Neurol Surg B Skull Base. 2018;79(2):167‐172. doi:10.1055/s-0037-1606220
2. Hung LC, Wu CS, Lin CC, Fang WK, Hsu YC. Epidermoid cyst presenting as isolated trigeminal neuralgia - two case reports. Acta Neurol Taiwan. 2013;22(3):133‐137.
3. Feng R, Gu X, Hu J, et al. Surgical treatment and radiotherapy of epidermoid cyst with malignant transformation in cerebellopontine angle. Int J Clin Exp Med. 2014;7(1):312‐315.
4. Friedmann DR, Grobelny B, Golfinos JG, Roland JT. Nonschwannoma tumors of the cerebellopontine angle. Otolaryngol Clin North Am. 2015;48(3):461-475. doi:10.1016/j.ote.2015.02.006
5. CPA-IAC In: Harnsberger HR, Glastonbury CM, Michel MA, Koch BL Branstetter BF IV. Diagnostic Imaging: Head and Neck, 2nd ed. Amirsys, Inc; 2011:VI(8):6-9 6. Hasegawa M, Nouri M, Nagahisa S, et al. Cerebellopontine angle epidermoid cysts: clinical presentations and surgical outcome. Neurosurg Rev. 2016;39(2):259‐267. doi:10.1007/s10143-015-0684-5
7. Safavi-Abbasi S, Di Rocco F, Bambakidis N, et al. Has management of epidermoid tumors of the cerebellopontine angle improved? A surgical synopsis of the past and present. Skull Base. 2008;18(2):85‐98. doi:10.1055/s-2007-991108
8. Son DW, Choi CH, Cha SH. Epidermoid tumors in the cerebellopontine angle presenting with trigeminal neuralgia. J Korean Neurosurg Soc. 2010;47(4):271‐277. doi:10.3340/jkns.2010.47.4.271
9. Schiefer TK, Link MJ. Epidermoids of the cerebellopontine angle: a 20-year experience. Surg Neurol. 2008;70(6):584-590; discussion 590. doi:10.1016/j.surneu.2007.12.021
10. Meng L, Yuguang L, Feng L, Wandong S, Shugan Z, Chengyuan W. Cerebellopontine angle epidermoids presenting with trigeminal neuralgia. J Clin Neurosci. 2005;12(7):784‐786. doi:10.1016/j.jocn.2004.09.023
11. Naval Aerospace Medical Institute. US Navy Aeromedical reference and waiver guide. Updated March 31, 2021. Accessed June 17, 2021. https://www.med.navy.mil/sites/nmotc/nami/arwg/Documents/WaiverGuide/Complete_Waiver_Guide.pdf
1. Farhoud A, Khedr W, Aboul-Enein H. Surgical resection of cerebellopontine epidermoid cysts: limitations and outcome. J Neurol Surg B Skull Base. 2018;79(2):167‐172. doi:10.1055/s-0037-1606220
2. Hung LC, Wu CS, Lin CC, Fang WK, Hsu YC. Epidermoid cyst presenting as isolated trigeminal neuralgia - two case reports. Acta Neurol Taiwan. 2013;22(3):133‐137.
3. Feng R, Gu X, Hu J, et al. Surgical treatment and radiotherapy of epidermoid cyst with malignant transformation in cerebellopontine angle. Int J Clin Exp Med. 2014;7(1):312‐315.
4. Friedmann DR, Grobelny B, Golfinos JG, Roland JT. Nonschwannoma tumors of the cerebellopontine angle. Otolaryngol Clin North Am. 2015;48(3):461-475. doi:10.1016/j.ote.2015.02.006
5. CPA-IAC In: Harnsberger HR, Glastonbury CM, Michel MA, Koch BL Branstetter BF IV. Diagnostic Imaging: Head and Neck, 2nd ed. Amirsys, Inc; 2011:VI(8):6-9 6. Hasegawa M, Nouri M, Nagahisa S, et al. Cerebellopontine angle epidermoid cysts: clinical presentations and surgical outcome. Neurosurg Rev. 2016;39(2):259‐267. doi:10.1007/s10143-015-0684-5
7. Safavi-Abbasi S, Di Rocco F, Bambakidis N, et al. Has management of epidermoid tumors of the cerebellopontine angle improved? A surgical synopsis of the past and present. Skull Base. 2008;18(2):85‐98. doi:10.1055/s-2007-991108
8. Son DW, Choi CH, Cha SH. Epidermoid tumors in the cerebellopontine angle presenting with trigeminal neuralgia. J Korean Neurosurg Soc. 2010;47(4):271‐277. doi:10.3340/jkns.2010.47.4.271
9. Schiefer TK, Link MJ. Epidermoids of the cerebellopontine angle: a 20-year experience. Surg Neurol. 2008;70(6):584-590; discussion 590. doi:10.1016/j.surneu.2007.12.021
10. Meng L, Yuguang L, Feng L, Wandong S, Shugan Z, Chengyuan W. Cerebellopontine angle epidermoids presenting with trigeminal neuralgia. J Clin Neurosci. 2005;12(7):784‐786. doi:10.1016/j.jocn.2004.09.023
11. Naval Aerospace Medical Institute. US Navy Aeromedical reference and waiver guide. Updated March 31, 2021. Accessed June 17, 2021. https://www.med.navy.mil/sites/nmotc/nami/arwg/Documents/WaiverGuide/Complete_Waiver_Guide.pdf
Patient Education After Inadequate Bowel Preparation: Improving Care and Outcomes
Colorectal cancer is the second most common cause of death in the United States. 1 A colonoscopy is the current gold standard for prevention and early detection of colorectal cancers. During a colonoscopy procedure, polyps and lesions are biopsied and removed. The most effective method of colon cleansing for the procedure is achieved by using one of several commercially available colon lavage preparations. Before the colonoscopy, patients are prescribed and instructed to take one of these bowel preparations.
Background
Adequate bowel preparation is defined as sufficient for identification of polyps > 5 mm.2 The impact of inadequate bowel preparation extends beyond the need for additional or repeat procedure(s) and includes potentially missed polyps and cancers. Inferior bowel preparation quality is associated with a significant decrease in the detection of flat or sessile serrated polyps.3 Missed polyps increase the risk of interval colorectal cancers. A high-quality bowel preparation together with the individual skill and experience of the endoscopist are crucial for adequate polyp detection. In addition, other risks of inadequate bowel preparation and repeated colonoscopies reduce adenoma detection rates, undetected carcinomas, and increase the risk of complications, possibly resulting in lawsuits.3
A major difficulty facing the Veterans Health Administration (VHA) medical center gastroenterologists is what to do when a patient is not properly prepared after standard prescreening education and the bowel preparation regimen. Traditionally, the patient is given additional medication and asked to return the next day for a repeat colonoscopy. Alternatively, the patient is given a 2-day bowel preparation to be used prior to a new appointment.
The choice of bowel preparation has been standardized within the US Department of Veterans Affairs (VA) Connecticut Healthcare System in West Haven (
For patients who fail the standard 1-day preparation, the same trained RNs inquire about any difficulties in consuming the preparation and provide the standard 2-day bowel preparation instructions. Multiple factors impact the adherence with preparation directions. Several patient-specific factors, comorbidities, and medications can contribute to inadequate bowel preparation.4 These factors include failing to fast before the procedure; namely, consuming solid foods, not consuming the entire preparation, not taking the preparation as directed, and not consuming adequate amounts of clear liquids or calories. Other reasons for failing the preparation are nausea and vomiting, poor understanding of instructions (including illiteracy), chronic constipation, use of narcotics and psychotropic drugs, and lack of awareness of the consequences of inadequate bowel preparation.
A study by Hautefeuille and colleagues noted that approximately 20% of patients having colonoscopy failure were not adherent to bowel preparation instructions.5 Only 55% of patients were aware of these consequences; whereas 96% of physicians were convinced they had given appropriate and sufficient information.5 As noted earlier, approximately half of patients do not fully comprehend the need to follow all the instructions. Therefore, clear and concise cleansing instructions and patient adherence are key factors that contribute to efficiency and quality of colonoscopy. The preparation failure rate creates a large volume of repeat patients and contributes to reduced efficiency of outpatient endoscopic practice.
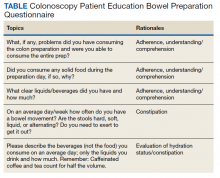
A meta-analysis conducted by Chang and colleagues demonstrated that a brief counseling session with patients before colonoscopy ensured better bowel preparation.6 The focus of this article is on using the Colonoscopy Patient Education Bowel Preparation Questionnaire to improve the outcomes of patient education (Table).
As this was part of ongoing care and medication education; the research did not require reviews by a research committee or need institutional review board approval.
Questionnaire
A gastroenterology (GI) advance practice registered nurse (APRN) developed a patient questionnaire after reviewing patient records from 2016 through 2018 and noting information gaps in patient re-education. The information was not clearly and completely documented relating to frequency of bowel movements, constipation, and daily hydration/fluid intake. Several questions were consistently asked of patients who had previously failed 2 bowel preparations to determine the issues preventing a successful bowel cleansing. Notes from the GI and nutrition clinics and the primary care provider (PCP) were reviewed for information on constipation, frequency and quality of bowel movements, average beverage consumption, and hydration status.
The GI APRN conducted the review and used notes from the past year as well as the notes for prior colon preparations documenting bowel preparations and their resulting quality. A review was conducted on each patient who failed the standard 2-day bowel preparation before the GI APRN bowel preparation education session. The review revealed that no single note provided all necessary information. All colonoscopy prescreening education notes contained information from the standard prescreening preparation education class presentation, and any individual patient issues related to preparation consumption. GI and PCP notes included constipation information; however, frequency of bowel movements was seldom mentioned; and no fluid consumption information was provided except for alcohol related to abuse/addiction issues. Of the patients that had been seen by the Nutrition Department staff, their notes included caloric intake, appropriate food/dietary choices, and soda consumption; alcohol use was documented but related only to caloric intake; again, no other fluid intake amounts were documented.
Design
The questionnaire consists of 5 closed-ended, patient-centered questions aimed at accomplishing patient education in a time-efficient manner. It also is a tool to achieve consistency among staff in determining barriers and issues, improve documentation, and then assist the patient in achieving a good-to-excellent quality bowel preparation. The questions elicit information that allow an RN or PCP determine the factors that contributed to bowel preparation failure and allow for a tailored patient-education session. With a clear picture of the patient’s issues and obstacles, the patient-centered prescreening preparation education could focus on solutions to specific barriers, increase patient comprehension and adherence to the instructions, and identify complicating behavioral factors of the prior bowel preparation. For example, question 1 was designed to discover whether the patient failed to consume the preparation and why, such as volume, timing, or taste; question 4 was designed to assist in figuring out whether constipation for any reason may be present, whether currently diagnosed or not; and question 5 determined the risk of dehydration with or without constipation as a key cleansing issue.
The answers to these few questions determined whether the inadequate bowel preparation quality was due to issues of poor understanding, poor following of the directions, or to other complicating factors.
The prescreening bowel preparation education classes are delivered in groups classes, telehealth group classes, and by phone.
Discussion
Following implementation of the questionnaire from 2018 to 2019, a clinical chart review was conducted in 2019 of the first 100 patients who failed the standardized 2-day preparation from 2018 to 2019. These patients were selected by the GI attending physicians based on their multiple prior research studies and the total number of veterans served within VACHS to reflect an adequate test of change. Twenty patients canceled their appointments or refused to obtain an additional colonoscopy. Of the remaining 80 patients, 68 (85%) improved on the bowel preparation screening to an adequate rating.
Within the VACHS, the result of inadequate colon preparation leads to either an aborted colonoscopy or a longer examination duration due to time spent washing the colon mucosa and then suctioning the liquified stool. Using newchoicehealth.com 2021 national data, the colonoscopy average price range was $1800 to $12,500; the national average amount paid is $2750.7 The average screening or diagnostic colonoscopy cost was $4469.8
Using the Colonoscopy Patient-Education Bowel Prep Questionnaire resulted in increased patient satisfaction, better use of current patient appointment slots, increased unique encounters, and direct and indirect fiscal savings. Patient satisfaction resulted from no additional repeat colonoscopies per patient’s statements. The other findings resulted from the reduction in repeat appointments: The appointment slots that would have been taken by repeat colonoscopies were available for new patients, resulting in an increase in unique encounters.
Fiscal savings resulted from avoiding the need for additional bowel preparations for those patients or using the GI staff time (nurses and clerks) to reschedule and educate patients. Prior to the use of the questionnaire, patients who failed preparations would be re-educated, given a new preparation prescription or mailed a new preparation, scheduled, and then mailed the appropriate paperwork, thus, increasing the workload for nurses and clerks.
Conclusions
Use of the questionnaire resulted in increased high-quality bowel preparation, an increase in the number of unique patients served, and improved efficiency. In addition, recovered appointment slots and modest reductions in additional purchases of preparation kits resulted in a potential cost savings for VACHS. Proper cleansing instructions as well as identifying and overcoming barriers to achieving adequate preparation for colonoscopy resulted in improved patient satisfaction, quality care, and cost savings.
Regardless of the type of colon preparation, addressing patient barriers to bowel preparation is translatable to other endoscopy facilities and practices that provide patient education within the VA.
1. American Cancer Society. Key statistics for colorectal cancer. Revised January 12, 2021. Accessed May 19, 2021. https://www.cancer.org/cancer/colon-rectal-cancer/about/key-statistics.html. 2020.
2. Clark BT, Protiva P, Nagar A, et al. Quantification of adequate bowel preparation for screening or surveillance colonoscopy in men. Gastroenterology. 2016;150(2):396-405; quiz e14-e15. doi:10.1053/j.gastro.2015.09.041
3. Clark BT, Laine L. High-quality bowel preparation is required for detection of sessile serrated polyps. Clin Gastroenterol Hepatol. 2016;14(8):1155-1162. doi:10.1016/j.cgh.2016.03.044
4. D’Souza SM, Parekh PJ, Johnson DA. The dirty side of colonoscopy: predictors of poor bowel preparation and novel approaches to overcome the shortcomings. Br J Gastroenterology. 2019:1:1.
5. Hautefeuille G, Lapuelle J, Chaussade S, et al. Factors related to bowel cleansing failure before colonoscopy: results of the PACOME study. J United European Gastroenterol J. 2014; 2(1):22-29. doi:10.1177/2050640613518200
6. Chang CW, Shih SC, Wang HY, et al. Meta-analysis: the effect of patient education on bowel preparation for colonoscopy. Endosc Int Open. 2015;3(6):E646-E652. doi:10.1055/s-0034-1392365
7. New Choice Health. How much does a colonoscopy cost? Accessed May 19, 2021. https://www.newchoicehealth.com/colonoscopy/cost
8. MDsave.com. Colonoscopy. Accessed May 19, 2021. https://www.mdsave.com/f/procedure/colonoscopy/06516?q=colonoscopy&type=procedure
Colorectal cancer is the second most common cause of death in the United States. 1 A colonoscopy is the current gold standard for prevention and early detection of colorectal cancers. During a colonoscopy procedure, polyps and lesions are biopsied and removed. The most effective method of colon cleansing for the procedure is achieved by using one of several commercially available colon lavage preparations. Before the colonoscopy, patients are prescribed and instructed to take one of these bowel preparations.
Background
Adequate bowel preparation is defined as sufficient for identification of polyps > 5 mm.2 The impact of inadequate bowel preparation extends beyond the need for additional or repeat procedure(s) and includes potentially missed polyps and cancers. Inferior bowel preparation quality is associated with a significant decrease in the detection of flat or sessile serrated polyps.3 Missed polyps increase the risk of interval colorectal cancers. A high-quality bowel preparation together with the individual skill and experience of the endoscopist are crucial for adequate polyp detection. In addition, other risks of inadequate bowel preparation and repeated colonoscopies reduce adenoma detection rates, undetected carcinomas, and increase the risk of complications, possibly resulting in lawsuits.3
A major difficulty facing the Veterans Health Administration (VHA) medical center gastroenterologists is what to do when a patient is not properly prepared after standard prescreening education and the bowel preparation regimen. Traditionally, the patient is given additional medication and asked to return the next day for a repeat colonoscopy. Alternatively, the patient is given a 2-day bowel preparation to be used prior to a new appointment.
The choice of bowel preparation has been standardized within the US Department of Veterans Affairs (VA) Connecticut Healthcare System in West Haven (
For patients who fail the standard 1-day preparation, the same trained RNs inquire about any difficulties in consuming the preparation and provide the standard 2-day bowel preparation instructions. Multiple factors impact the adherence with preparation directions. Several patient-specific factors, comorbidities, and medications can contribute to inadequate bowel preparation.4 These factors include failing to fast before the procedure; namely, consuming solid foods, not consuming the entire preparation, not taking the preparation as directed, and not consuming adequate amounts of clear liquids or calories. Other reasons for failing the preparation are nausea and vomiting, poor understanding of instructions (including illiteracy), chronic constipation, use of narcotics and psychotropic drugs, and lack of awareness of the consequences of inadequate bowel preparation.
A study by Hautefeuille and colleagues noted that approximately 20% of patients having colonoscopy failure were not adherent to bowel preparation instructions.5 Only 55% of patients were aware of these consequences; whereas 96% of physicians were convinced they had given appropriate and sufficient information.5 As noted earlier, approximately half of patients do not fully comprehend the need to follow all the instructions. Therefore, clear and concise cleansing instructions and patient adherence are key factors that contribute to efficiency and quality of colonoscopy. The preparation failure rate creates a large volume of repeat patients and contributes to reduced efficiency of outpatient endoscopic practice.
A meta-analysis conducted by Chang and colleagues demonstrated that a brief counseling session with patients before colonoscopy ensured better bowel preparation.6 The focus of this article is on using the Colonoscopy Patient Education Bowel Preparation Questionnaire to improve the outcomes of patient education (Table).
As this was part of ongoing care and medication education; the research did not require reviews by a research committee or need institutional review board approval.
Questionnaire
A gastroenterology (GI) advance practice registered nurse (APRN) developed a patient questionnaire after reviewing patient records from 2016 through 2018 and noting information gaps in patient re-education. The information was not clearly and completely documented relating to frequency of bowel movements, constipation, and daily hydration/fluid intake. Several questions were consistently asked of patients who had previously failed 2 bowel preparations to determine the issues preventing a successful bowel cleansing. Notes from the GI and nutrition clinics and the primary care provider (PCP) were reviewed for information on constipation, frequency and quality of bowel movements, average beverage consumption, and hydration status.
The GI APRN conducted the review and used notes from the past year as well as the notes for prior colon preparations documenting bowel preparations and their resulting quality. A review was conducted on each patient who failed the standard 2-day bowel preparation before the GI APRN bowel preparation education session. The review revealed that no single note provided all necessary information. All colonoscopy prescreening education notes contained information from the standard prescreening preparation education class presentation, and any individual patient issues related to preparation consumption. GI and PCP notes included constipation information; however, frequency of bowel movements was seldom mentioned; and no fluid consumption information was provided except for alcohol related to abuse/addiction issues. Of the patients that had been seen by the Nutrition Department staff, their notes included caloric intake, appropriate food/dietary choices, and soda consumption; alcohol use was documented but related only to caloric intake; again, no other fluid intake amounts were documented.
Design
The questionnaire consists of 5 closed-ended, patient-centered questions aimed at accomplishing patient education in a time-efficient manner. It also is a tool to achieve consistency among staff in determining barriers and issues, improve documentation, and then assist the patient in achieving a good-to-excellent quality bowel preparation. The questions elicit information that allow an RN or PCP determine the factors that contributed to bowel preparation failure and allow for a tailored patient-education session. With a clear picture of the patient’s issues and obstacles, the patient-centered prescreening preparation education could focus on solutions to specific barriers, increase patient comprehension and adherence to the instructions, and identify complicating behavioral factors of the prior bowel preparation. For example, question 1 was designed to discover whether the patient failed to consume the preparation and why, such as volume, timing, or taste; question 4 was designed to assist in figuring out whether constipation for any reason may be present, whether currently diagnosed or not; and question 5 determined the risk of dehydration with or without constipation as a key cleansing issue.
The answers to these few questions determined whether the inadequate bowel preparation quality was due to issues of poor understanding, poor following of the directions, or to other complicating factors.
The prescreening bowel preparation education classes are delivered in groups classes, telehealth group classes, and by phone.
Discussion
Following implementation of the questionnaire from 2018 to 2019, a clinical chart review was conducted in 2019 of the first 100 patients who failed the standardized 2-day preparation from 2018 to 2019. These patients were selected by the GI attending physicians based on their multiple prior research studies and the total number of veterans served within VACHS to reflect an adequate test of change. Twenty patients canceled their appointments or refused to obtain an additional colonoscopy. Of the remaining 80 patients, 68 (85%) improved on the bowel preparation screening to an adequate rating.
Within the VACHS, the result of inadequate colon preparation leads to either an aborted colonoscopy or a longer examination duration due to time spent washing the colon mucosa and then suctioning the liquified stool. Using newchoicehealth.com 2021 national data, the colonoscopy average price range was $1800 to $12,500; the national average amount paid is $2750.7 The average screening or diagnostic colonoscopy cost was $4469.8
Using the Colonoscopy Patient-Education Bowel Prep Questionnaire resulted in increased patient satisfaction, better use of current patient appointment slots, increased unique encounters, and direct and indirect fiscal savings. Patient satisfaction resulted from no additional repeat colonoscopies per patient’s statements. The other findings resulted from the reduction in repeat appointments: The appointment slots that would have been taken by repeat colonoscopies were available for new patients, resulting in an increase in unique encounters.
Fiscal savings resulted from avoiding the need for additional bowel preparations for those patients or using the GI staff time (nurses and clerks) to reschedule and educate patients. Prior to the use of the questionnaire, patients who failed preparations would be re-educated, given a new preparation prescription or mailed a new preparation, scheduled, and then mailed the appropriate paperwork, thus, increasing the workload for nurses and clerks.
Conclusions
Use of the questionnaire resulted in increased high-quality bowel preparation, an increase in the number of unique patients served, and improved efficiency. In addition, recovered appointment slots and modest reductions in additional purchases of preparation kits resulted in a potential cost savings for VACHS. Proper cleansing instructions as well as identifying and overcoming barriers to achieving adequate preparation for colonoscopy resulted in improved patient satisfaction, quality care, and cost savings.
Regardless of the type of colon preparation, addressing patient barriers to bowel preparation is translatable to other endoscopy facilities and practices that provide patient education within the VA.
Colorectal cancer is the second most common cause of death in the United States. 1 A colonoscopy is the current gold standard for prevention and early detection of colorectal cancers. During a colonoscopy procedure, polyps and lesions are biopsied and removed. The most effective method of colon cleansing for the procedure is achieved by using one of several commercially available colon lavage preparations. Before the colonoscopy, patients are prescribed and instructed to take one of these bowel preparations.
Background
Adequate bowel preparation is defined as sufficient for identification of polyps > 5 mm.2 The impact of inadequate bowel preparation extends beyond the need for additional or repeat procedure(s) and includes potentially missed polyps and cancers. Inferior bowel preparation quality is associated with a significant decrease in the detection of flat or sessile serrated polyps.3 Missed polyps increase the risk of interval colorectal cancers. A high-quality bowel preparation together with the individual skill and experience of the endoscopist are crucial for adequate polyp detection. In addition, other risks of inadequate bowel preparation and repeated colonoscopies reduce adenoma detection rates, undetected carcinomas, and increase the risk of complications, possibly resulting in lawsuits.3
A major difficulty facing the Veterans Health Administration (VHA) medical center gastroenterologists is what to do when a patient is not properly prepared after standard prescreening education and the bowel preparation regimen. Traditionally, the patient is given additional medication and asked to return the next day for a repeat colonoscopy. Alternatively, the patient is given a 2-day bowel preparation to be used prior to a new appointment.
The choice of bowel preparation has been standardized within the US Department of Veterans Affairs (VA) Connecticut Healthcare System in West Haven (
For patients who fail the standard 1-day preparation, the same trained RNs inquire about any difficulties in consuming the preparation and provide the standard 2-day bowel preparation instructions. Multiple factors impact the adherence with preparation directions. Several patient-specific factors, comorbidities, and medications can contribute to inadequate bowel preparation.4 These factors include failing to fast before the procedure; namely, consuming solid foods, not consuming the entire preparation, not taking the preparation as directed, and not consuming adequate amounts of clear liquids or calories. Other reasons for failing the preparation are nausea and vomiting, poor understanding of instructions (including illiteracy), chronic constipation, use of narcotics and psychotropic drugs, and lack of awareness of the consequences of inadequate bowel preparation.
A study by Hautefeuille and colleagues noted that approximately 20% of patients having colonoscopy failure were not adherent to bowel preparation instructions.5 Only 55% of patients were aware of these consequences; whereas 96% of physicians were convinced they had given appropriate and sufficient information.5 As noted earlier, approximately half of patients do not fully comprehend the need to follow all the instructions. Therefore, clear and concise cleansing instructions and patient adherence are key factors that contribute to efficiency and quality of colonoscopy. The preparation failure rate creates a large volume of repeat patients and contributes to reduced efficiency of outpatient endoscopic practice.
A meta-analysis conducted by Chang and colleagues demonstrated that a brief counseling session with patients before colonoscopy ensured better bowel preparation.6 The focus of this article is on using the Colonoscopy Patient Education Bowel Preparation Questionnaire to improve the outcomes of patient education (Table).
As this was part of ongoing care and medication education; the research did not require reviews by a research committee or need institutional review board approval.
Questionnaire
A gastroenterology (GI) advance practice registered nurse (APRN) developed a patient questionnaire after reviewing patient records from 2016 through 2018 and noting information gaps in patient re-education. The information was not clearly and completely documented relating to frequency of bowel movements, constipation, and daily hydration/fluid intake. Several questions were consistently asked of patients who had previously failed 2 bowel preparations to determine the issues preventing a successful bowel cleansing. Notes from the GI and nutrition clinics and the primary care provider (PCP) were reviewed for information on constipation, frequency and quality of bowel movements, average beverage consumption, and hydration status.
The GI APRN conducted the review and used notes from the past year as well as the notes for prior colon preparations documenting bowel preparations and their resulting quality. A review was conducted on each patient who failed the standard 2-day bowel preparation before the GI APRN bowel preparation education session. The review revealed that no single note provided all necessary information. All colonoscopy prescreening education notes contained information from the standard prescreening preparation education class presentation, and any individual patient issues related to preparation consumption. GI and PCP notes included constipation information; however, frequency of bowel movements was seldom mentioned; and no fluid consumption information was provided except for alcohol related to abuse/addiction issues. Of the patients that had been seen by the Nutrition Department staff, their notes included caloric intake, appropriate food/dietary choices, and soda consumption; alcohol use was documented but related only to caloric intake; again, no other fluid intake amounts were documented.
Design
The questionnaire consists of 5 closed-ended, patient-centered questions aimed at accomplishing patient education in a time-efficient manner. It also is a tool to achieve consistency among staff in determining barriers and issues, improve documentation, and then assist the patient in achieving a good-to-excellent quality bowel preparation. The questions elicit information that allow an RN or PCP determine the factors that contributed to bowel preparation failure and allow for a tailored patient-education session. With a clear picture of the patient’s issues and obstacles, the patient-centered prescreening preparation education could focus on solutions to specific barriers, increase patient comprehension and adherence to the instructions, and identify complicating behavioral factors of the prior bowel preparation. For example, question 1 was designed to discover whether the patient failed to consume the preparation and why, such as volume, timing, or taste; question 4 was designed to assist in figuring out whether constipation for any reason may be present, whether currently diagnosed or not; and question 5 determined the risk of dehydration with or without constipation as a key cleansing issue.
The answers to these few questions determined whether the inadequate bowel preparation quality was due to issues of poor understanding, poor following of the directions, or to other complicating factors.
The prescreening bowel preparation education classes are delivered in groups classes, telehealth group classes, and by phone.
Discussion
Following implementation of the questionnaire from 2018 to 2019, a clinical chart review was conducted in 2019 of the first 100 patients who failed the standardized 2-day preparation from 2018 to 2019. These patients were selected by the GI attending physicians based on their multiple prior research studies and the total number of veterans served within VACHS to reflect an adequate test of change. Twenty patients canceled their appointments or refused to obtain an additional colonoscopy. Of the remaining 80 patients, 68 (85%) improved on the bowel preparation screening to an adequate rating.
Within the VACHS, the result of inadequate colon preparation leads to either an aborted colonoscopy or a longer examination duration due to time spent washing the colon mucosa and then suctioning the liquified stool. Using newchoicehealth.com 2021 national data, the colonoscopy average price range was $1800 to $12,500; the national average amount paid is $2750.7 The average screening or diagnostic colonoscopy cost was $4469.8
Using the Colonoscopy Patient-Education Bowel Prep Questionnaire resulted in increased patient satisfaction, better use of current patient appointment slots, increased unique encounters, and direct and indirect fiscal savings. Patient satisfaction resulted from no additional repeat colonoscopies per patient’s statements. The other findings resulted from the reduction in repeat appointments: The appointment slots that would have been taken by repeat colonoscopies were available for new patients, resulting in an increase in unique encounters.
Fiscal savings resulted from avoiding the need for additional bowel preparations for those patients or using the GI staff time (nurses and clerks) to reschedule and educate patients. Prior to the use of the questionnaire, patients who failed preparations would be re-educated, given a new preparation prescription or mailed a new preparation, scheduled, and then mailed the appropriate paperwork, thus, increasing the workload for nurses and clerks.
Conclusions
Use of the questionnaire resulted in increased high-quality bowel preparation, an increase in the number of unique patients served, and improved efficiency. In addition, recovered appointment slots and modest reductions in additional purchases of preparation kits resulted in a potential cost savings for VACHS. Proper cleansing instructions as well as identifying and overcoming barriers to achieving adequate preparation for colonoscopy resulted in improved patient satisfaction, quality care, and cost savings.
Regardless of the type of colon preparation, addressing patient barriers to bowel preparation is translatable to other endoscopy facilities and practices that provide patient education within the VA.
1. American Cancer Society. Key statistics for colorectal cancer. Revised January 12, 2021. Accessed May 19, 2021. https://www.cancer.org/cancer/colon-rectal-cancer/about/key-statistics.html. 2020.
2. Clark BT, Protiva P, Nagar A, et al. Quantification of adequate bowel preparation for screening or surveillance colonoscopy in men. Gastroenterology. 2016;150(2):396-405; quiz e14-e15. doi:10.1053/j.gastro.2015.09.041
3. Clark BT, Laine L. High-quality bowel preparation is required for detection of sessile serrated polyps. Clin Gastroenterol Hepatol. 2016;14(8):1155-1162. doi:10.1016/j.cgh.2016.03.044
4. D’Souza SM, Parekh PJ, Johnson DA. The dirty side of colonoscopy: predictors of poor bowel preparation and novel approaches to overcome the shortcomings. Br J Gastroenterology. 2019:1:1.
5. Hautefeuille G, Lapuelle J, Chaussade S, et al. Factors related to bowel cleansing failure before colonoscopy: results of the PACOME study. J United European Gastroenterol J. 2014; 2(1):22-29. doi:10.1177/2050640613518200
6. Chang CW, Shih SC, Wang HY, et al. Meta-analysis: the effect of patient education on bowel preparation for colonoscopy. Endosc Int Open. 2015;3(6):E646-E652. doi:10.1055/s-0034-1392365
7. New Choice Health. How much does a colonoscopy cost? Accessed May 19, 2021. https://www.newchoicehealth.com/colonoscopy/cost
8. MDsave.com. Colonoscopy. Accessed May 19, 2021. https://www.mdsave.com/f/procedure/colonoscopy/06516?q=colonoscopy&type=procedure
1. American Cancer Society. Key statistics for colorectal cancer. Revised January 12, 2021. Accessed May 19, 2021. https://www.cancer.org/cancer/colon-rectal-cancer/about/key-statistics.html. 2020.
2. Clark BT, Protiva P, Nagar A, et al. Quantification of adequate bowel preparation for screening or surveillance colonoscopy in men. Gastroenterology. 2016;150(2):396-405; quiz e14-e15. doi:10.1053/j.gastro.2015.09.041
3. Clark BT, Laine L. High-quality bowel preparation is required for detection of sessile serrated polyps. Clin Gastroenterol Hepatol. 2016;14(8):1155-1162. doi:10.1016/j.cgh.2016.03.044
4. D’Souza SM, Parekh PJ, Johnson DA. The dirty side of colonoscopy: predictors of poor bowel preparation and novel approaches to overcome the shortcomings. Br J Gastroenterology. 2019:1:1.
5. Hautefeuille G, Lapuelle J, Chaussade S, et al. Factors related to bowel cleansing failure before colonoscopy: results of the PACOME study. J United European Gastroenterol J. 2014; 2(1):22-29. doi:10.1177/2050640613518200
6. Chang CW, Shih SC, Wang HY, et al. Meta-analysis: the effect of patient education on bowel preparation for colonoscopy. Endosc Int Open. 2015;3(6):E646-E652. doi:10.1055/s-0034-1392365
7. New Choice Health. How much does a colonoscopy cost? Accessed May 19, 2021. https://www.newchoicehealth.com/colonoscopy/cost
8. MDsave.com. Colonoscopy. Accessed May 19, 2021. https://www.mdsave.com/f/procedure/colonoscopy/06516?q=colonoscopy&type=procedure
Assessment of a Medication Deprescribing Tool on Polypharmacy and Cost Avoidance
According to the Centers for Disease Control and Prevention National Center for Health Statistics (NCHS), the use of prescription drugs has increased in the past half century. Although prescription drugs have played an important role in preventing, controlling, and delaying onset or progression of disease, their growth in use also has posed many risks.1 One ramification of this growth is the occurrence of polypharmacy, which does not have a universal, clear definition. In general, it can be described as the concurrent use of multiple medications by a single patient to treat one or more medical ailments. Five or more medications taken simultaneously is the most common definition to date, but this is just one of many acceptable definitions and that varies from one health care facility to another.1,2
Regardless of the cutoffs established to indicate polypharmacy, its incidence can result in poor and potentially harmful health outcomes. Polypharmacy increases the risk of experiencing adverse drug events (ADEs), drug-drug interactions (DDIs), geriatric-related syndromes, falls, hospitalization, and mortality. Issues with adherence may begin to unfold secondary to increased pill burden. Both the patient and the health care system may encounter financial strain, as polypharmacy can lead to unnecessary and essentially preventable costs of care. When evaluating the likelihood of polypharmacy based on age group, NCHS found that 47.5% of patients taking ≥ 5 medications were aged ≥ 65 years.1-5 This indicates that polypharmacy is of great concern in the geriatric population, which also represents a large proportion of individuals accessing Veterans Health Administration (VHA) care.
Deprescibing
Deprescribing is the act of withdrawing or discontinuing potentially inappropriate medications (PIM), or medications used by older patients harboring ADEs that generally outweigh the clinical benefits of the drug. Deprescribing is an effective tool for managing or reducing polypharmacy. A variety of tools have been created whose sole purpose is to simplify deprescribing. Some tools explicitly identify PIM and are widely familiar in medical practice. Examples are the Beers Criteria developed in 1991 or Screening Tool to Alert Right Treatment/Screening Tool of Older Persons Prescriptions (START/STOPP) criteria created in 2003. Other tools that are less commonplace but equally as resourceful are MedStopper and Deprescribing.org. The former was launched in 2015 and is a Canadian online system that provides risk assessments for medications with guidance for tapering or stopping medications if continuation of the drug presents higher risk than benefit.5-7 The latter is a full-fledged website developed by a physician, a pharmacist, and their research teams that serves as an exchange hub for deprescribing information.
In 2016, the VIONE (Vital, Important, Optional, Not indicated/treatment complete, and Every medication has an indication) deprescribing tool was developed by Saraswathy Battar, MD, at Central Arkansas Veterans Healthcare System (CAVHS) in Little Rock, as a system that could go beyond medication reconciliation (Table 1). Health care providers (HCPs) and pharmacists evaluate each medication that a patient has been prescribed and places each medication in a VIONE category. Prescribers may then take the opportunity to deprescribe or discontinue medications if deemed appropriate based on their clinical assessments and shared decision making.8 Traditionally, medication reconciliation involves the process of obtaining a complete and accurate list of medications as reported by a patient or caregiver to a HCP. VIONE encourages HCPs and pharmacists not only to ensure medication lists are accurate, but also that each medication reported is appropriate for continued use. In other words, VIONE is meant to help implement deprescribing at opportune times. More than 14,000 medications have been deprescribed using the VIONE method, resulting in more than $2,000,000 of annualized cost avoidance after just 1 year of implementation at CAVHS.9
VIONE consists of 2 major components in the Computerized Patient Record System (CPRS): a template and a dropdown discontinuation menu. The template captured patient allergies, pertinent laboratory data, the patient’s active problem list and applicable diagnoses, and active medication list. Patient aligned care team (PACT) pharmacists used the information captured in the template to conduct medication reconciliations and polypharmacy reviews. Each medication is categorized in VIONE using data collected during reviews. A menu delineates reasons for discontinuation: optional, dose decrease, no diagnosis, not indicated/treatment complete, discontinue alternate medication prescribed, and patient reported no longer taking. The discontinuation menu allowed PACT pharmacists and physicians to choose 1 VIONE option per medication to clarify the reason for discontinuation. VIONE-based discontinuations are recorded in CPRS and identified as deprescribed.
At the time of this project, > 30 US Department of Veterans Affairs (VA) facilities had adopted VIONE. Use of VIONE at VA Southern Nevada Healthcare System (VASNHS) in North Las Vegas has been incorporated in the everyday practices of home-based primary care pharmacists and physicians but has yet to be implemented in other areas of the facility. The purpose of this project was to determine the impact of the VIONE tool on polypharmacy and cost avoidance at VASNHS when used by primary care physicians (PCPs) and PACT primary care clinics.
Methods
Veterans receiving care at VASNHS aged ≥ 65 years with ≥ 10 active medications noted in CPRS were included in this project. PACT pharmacists and physicians were educated on the proper use of the VIONE tool prior to its implementation. Education included a 15-minute slide presentation followed by dissemination of a 1-page VIONE tool handout during a PACT all-staff clinic meeting.
Data were collected for 3 months before and after the intervention. Data were made available for assessment by the Automated Data Processing Application Coordinator (ADPAC) at VASNHS. The ADPAC created and generated an Excel spreadsheet report, which listed all medications deprescribed using the VIONE method. The primary endpoint was the total number of medications discontinued using the VIONE template and/or discontinuation menu. For the purpose of this project, appropriate discontinuation was considered any prescription deprescribed, excluding medical supplies, by pharmacists and PCPs who received VIONE education.
The secondary endpoint was the estimated annualized cost avoidance for the facility (Figure). The calculation does not include medications discontinued due to the prescription of an alternative medication or dose decreases since these VIONE selections imply that a new prescription or order was placed and the original prescription was not deprescribed. Annualized cost avoidance was determined with use of the VIONE dashboard, a database that retrospectively gathers information regarding patients at risk of polypharmacy, polypharmacy-related ADEs, and cost. Manual adjustments were made to various parameters on the Veterans Integrated Service Network 15 VIONE dashboard by the author in order to obtain data specific to this project. These parameters allowed selection of service sections, specific staff members or the option to include or exclude chronic or nonchronic medications. The annualized cost avoidance figure was then compared to raw data pulled by a VIONE dashboard correspondent to ensure the manual calculation was accurate. Finally, the 5 most common classes of medications deprescribed were identified for information purposes and to provide a better postulation on the types of medications being discontinued using the VIONE method.
Results
A total of 2,442 veterans met inclusion criteria, and the VIONE method was applied to 598 between late October 2018 and January 2019. The 13 PACT pharmacists contacted at least 10 veterans each, thus at least 130 were randomly selected for telephone calls to perform polypharmacy reviews using the VIONE note template. The discontinuation menu was used if a medication qualified to be deprescribed. After 3 months, 1986 prescriptions were deprescribed using VIONE; however, 1060 prescriptions were considered appropriately deprescribed (Table 2). The 13 PACT pharmacists deprescribed 361 medications, and the 29 PACT physicians deprescribed 699 medications. These prescriptions were then separated into medication categories to determine the most common discontinued classes. Vitamins and supplements were the medication class most frequently deprescribed (19.4%), followed by pain medications (15.5%), antimicrobial agents (9.6%), antihypertensive medications (9.2%), and diabetes medications (6.4%) (Table 3). The top 5 medication categories accounted for 60% of all medications appropriately deprescribed.
The estimated annualized cost avoidance for all medications deprescribed in the 3-month project period was $84,030.46. To provide the most appropriate and accurate calculation, medication classes excluded from this figure were acute or short-term prescriptions and antimicrobial agents. Medications prescribed short-term typically are not suitable to continue for an extended period, and antimicrobial agents were excluded since they are normally associated with higher costs, and may overestimate the cost avoidance calculation for the facility.
Discussion
The outcomes for the primary and secondary endpoints of this project illustrate that using VIONE in PACT primary care clinics had a notable impact on polypharmacy and cost avoidance over a short period. This outcome can be attributed to 2 significant effects of using the deprescribing tool. VIONE’s simplicity in application allowed clinicians to incorporate daily use of the tool with minimal effort. Education was all that was required to fully enable clinicians to work together successfully and exercise collaborative practice to promote deprescribing. VIONE also elicited a cascade of favorable effects that improve patient safety and health outcomes. The tool aided in identification of PIM, which helped reduce polypharmacy and medication burden. The risk for DDIs and ADEs may decrease; therefore, the incidence of falls, need for emergency department visits or inpatient care related to polypharmacy may decline. Less complex medication regimens may alleviate issues with adherence and avoid the various consequences of polypharmacy in theory. Simplified regimens can potentially improve disease management and quality of life for patients. Further studies are needed to substantiate deprescribing and its true effect on patient adherence and better health outcomes at this time.10
Reducing polypharmacy can lead to cost savings. Based on the results of this 3-month study, we expect that VASNHS would save more than $84,000 by reducing polypharmacy among its patients. Those savings can be funneled back into the health care system, and allotted to necessary patient care, prescriptions, and health care facility needs.
Limitations
There are some important limitations to this study. Definitions of polypharmacy may vary from one health care facility to another. The cutoffs for polypharmacy may differ, causing the prevalence of polypharmacy and potential costs savings to vary. Use of VIONE may be inconsistent among users if not previously educated or properly trained. For instance, VIONE selections are listed in the same menu as the standard CPRS discontinuation options, which may lead to discontinuation of medical supplies or laboratory orders instead of prescriptions.
The method of data analysis and project design used in this study may have been subject to error. For example, the list of PCPs may have been inaccurate or outdated, which would result in an over- or underrepresentation of those who contributed to data collection. Furthermore, there is some volatility in calculating the total cost avoidance. For example, medications for chronic conditions that were only taken on an as needed basis may have overestimated savings. Either under- or overestimations could occur when parameters are adjusted on the VIONE discontinuation dashboard without appropriate guidance. With the ability to manually adjust the dashboard parameters, dissimilarities in calculations may follow.
Conclusions
The VIONE tool may be useful in improving patient safety through deprescribing and discontinuing PIM. Decreasing the number of medications being taken concomitantly by a patient and continuing only those that are imperative in their medical treatment is the first step to reducing the incidence of polypharmacy. Consequently, chances of ADEs or DDIs are lessened, especially among older individuals who are considered high risk for experiencing the detrimental effects that may ensue. These effects include geriatric-related syndromes, increased risk of fall, hospital visits or admissions, or death. Use of VIONE easily promotes collaboration among clinicians to evaluate medications eligible for discontinuation more regularly. If this deprescribing tool is continuously used, costs avoided can likely be maximized within VA health care systems.
The results of this project should serve as an incentive to push for better prescribing practices and increase deprescribing efforts. It should provoke the need for change in regimens and the subsequent discontinuation of prescriptions that are not considered vital to continue. Finally, the result of this project should substantiate the positive impact a deprescribing tool can possess to avert the issues commonly associated with polypharmacy.
1. Centers for Disease Control and Prevention, National Center for Health Statistics. Health, United States, 2013: with special feature on prescription drugs. Published May 2014. Accessed May 13, 2021. https://www.cdc.gov/nchs/data/hus/hus13.pdf
2. Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1):230. Published 2017 Oct 10. doi:10.1186/s12877-017-0621-2
3. Parulekar MS, Rogers CK. Polypharmacy and mobility. In: Cifu DX, Lew HL, Oh-Park M., eds Geriatric Rehabilitation. Elsevier; 2018. doi:10.1016/B978-0-323-54454-2.12001-1
4. Rieckert A, Trampisch US, Klaaßen-Mielke R, et al. Polypharmacy in older patients with chronic diseases: a cross-sectional analysis of factors associated with excessive polypharmacy. BMC Fam Pract. 2018;19(1):113. Published 2018 Jul 18. doi:10.1186/s12875-018-0795-5
5. Thompson CA. New medication review method cuts veterans’ Rx load, saves millions. Am J Health Syst Pharm. 2018;75(8):502-503. doi:10.2146/news180023
6. Reeve E. Deprescribing tools: a review of the types of tools available to aid deprescribing in clinical practice. J Pharm Pract Res. 2020;50(1):98-107. doi:10.1002/jppr.1626
7. Fried TR, Niehoff KM, Street RL, et al. Effect of the Tool to Reduce Inappropriate Medications on Medication Communication and Deprescribing. J Am Geriatr Soc. 2017;65(10):2265-2271. doi:10.1111/jgs.15042
8. Battar S, Dickerson KR, Sedgwick C, et al. Understanding principles of high reliability organizations through the eyes of VIONE, a clinical program to improve patient safety by deprescribing potentially inappropriate medications and reducing polypharmacy. Fed Pract. 2019;36(12):564-568.
9. Battar S, Cmelik T, Dickerson K, Scott, M. Experience better health with VIONE a safe medication deprescribing tool [Nonpublic source, not verified]
10. Ulley J, Harrop D, Ali A, et al. Desprescribing interventions and their impact on medication adherence in community-dwelling older adults with polypharmacy: a systematic review. BMC Geriatr. 2019;19(15):1-13.
According to the Centers for Disease Control and Prevention National Center for Health Statistics (NCHS), the use of prescription drugs has increased in the past half century. Although prescription drugs have played an important role in preventing, controlling, and delaying onset or progression of disease, their growth in use also has posed many risks.1 One ramification of this growth is the occurrence of polypharmacy, which does not have a universal, clear definition. In general, it can be described as the concurrent use of multiple medications by a single patient to treat one or more medical ailments. Five or more medications taken simultaneously is the most common definition to date, but this is just one of many acceptable definitions and that varies from one health care facility to another.1,2
Regardless of the cutoffs established to indicate polypharmacy, its incidence can result in poor and potentially harmful health outcomes. Polypharmacy increases the risk of experiencing adverse drug events (ADEs), drug-drug interactions (DDIs), geriatric-related syndromes, falls, hospitalization, and mortality. Issues with adherence may begin to unfold secondary to increased pill burden. Both the patient and the health care system may encounter financial strain, as polypharmacy can lead to unnecessary and essentially preventable costs of care. When evaluating the likelihood of polypharmacy based on age group, NCHS found that 47.5% of patients taking ≥ 5 medications were aged ≥ 65 years.1-5 This indicates that polypharmacy is of great concern in the geriatric population, which also represents a large proportion of individuals accessing Veterans Health Administration (VHA) care.
Deprescibing
Deprescribing is the act of withdrawing or discontinuing potentially inappropriate medications (PIM), or medications used by older patients harboring ADEs that generally outweigh the clinical benefits of the drug. Deprescribing is an effective tool for managing or reducing polypharmacy. A variety of tools have been created whose sole purpose is to simplify deprescribing. Some tools explicitly identify PIM and are widely familiar in medical practice. Examples are the Beers Criteria developed in 1991 or Screening Tool to Alert Right Treatment/Screening Tool of Older Persons Prescriptions (START/STOPP) criteria created in 2003. Other tools that are less commonplace but equally as resourceful are MedStopper and Deprescribing.org. The former was launched in 2015 and is a Canadian online system that provides risk assessments for medications with guidance for tapering or stopping medications if continuation of the drug presents higher risk than benefit.5-7 The latter is a full-fledged website developed by a physician, a pharmacist, and their research teams that serves as an exchange hub for deprescribing information.
In 2016, the VIONE (Vital, Important, Optional, Not indicated/treatment complete, and Every medication has an indication) deprescribing tool was developed by Saraswathy Battar, MD, at Central Arkansas Veterans Healthcare System (CAVHS) in Little Rock, as a system that could go beyond medication reconciliation (Table 1). Health care providers (HCPs) and pharmacists evaluate each medication that a patient has been prescribed and places each medication in a VIONE category. Prescribers may then take the opportunity to deprescribe or discontinue medications if deemed appropriate based on their clinical assessments and shared decision making.8 Traditionally, medication reconciliation involves the process of obtaining a complete and accurate list of medications as reported by a patient or caregiver to a HCP. VIONE encourages HCPs and pharmacists not only to ensure medication lists are accurate, but also that each medication reported is appropriate for continued use. In other words, VIONE is meant to help implement deprescribing at opportune times. More than 14,000 medications have been deprescribed using the VIONE method, resulting in more than $2,000,000 of annualized cost avoidance after just 1 year of implementation at CAVHS.9
VIONE consists of 2 major components in the Computerized Patient Record System (CPRS): a template and a dropdown discontinuation menu. The template captured patient allergies, pertinent laboratory data, the patient’s active problem list and applicable diagnoses, and active medication list. Patient aligned care team (PACT) pharmacists used the information captured in the template to conduct medication reconciliations and polypharmacy reviews. Each medication is categorized in VIONE using data collected during reviews. A menu delineates reasons for discontinuation: optional, dose decrease, no diagnosis, not indicated/treatment complete, discontinue alternate medication prescribed, and patient reported no longer taking. The discontinuation menu allowed PACT pharmacists and physicians to choose 1 VIONE option per medication to clarify the reason for discontinuation. VIONE-based discontinuations are recorded in CPRS and identified as deprescribed.
At the time of this project, > 30 US Department of Veterans Affairs (VA) facilities had adopted VIONE. Use of VIONE at VA Southern Nevada Healthcare System (VASNHS) in North Las Vegas has been incorporated in the everyday practices of home-based primary care pharmacists and physicians but has yet to be implemented in other areas of the facility. The purpose of this project was to determine the impact of the VIONE tool on polypharmacy and cost avoidance at VASNHS when used by primary care physicians (PCPs) and PACT primary care clinics.
Methods
Veterans receiving care at VASNHS aged ≥ 65 years with ≥ 10 active medications noted in CPRS were included in this project. PACT pharmacists and physicians were educated on the proper use of the VIONE tool prior to its implementation. Education included a 15-minute slide presentation followed by dissemination of a 1-page VIONE tool handout during a PACT all-staff clinic meeting.
Data were collected for 3 months before and after the intervention. Data were made available for assessment by the Automated Data Processing Application Coordinator (ADPAC) at VASNHS. The ADPAC created and generated an Excel spreadsheet report, which listed all medications deprescribed using the VIONE method. The primary endpoint was the total number of medications discontinued using the VIONE template and/or discontinuation menu. For the purpose of this project, appropriate discontinuation was considered any prescription deprescribed, excluding medical supplies, by pharmacists and PCPs who received VIONE education.
The secondary endpoint was the estimated annualized cost avoidance for the facility (Figure). The calculation does not include medications discontinued due to the prescription of an alternative medication or dose decreases since these VIONE selections imply that a new prescription or order was placed and the original prescription was not deprescribed. Annualized cost avoidance was determined with use of the VIONE dashboard, a database that retrospectively gathers information regarding patients at risk of polypharmacy, polypharmacy-related ADEs, and cost. Manual adjustments were made to various parameters on the Veterans Integrated Service Network 15 VIONE dashboard by the author in order to obtain data specific to this project. These parameters allowed selection of service sections, specific staff members or the option to include or exclude chronic or nonchronic medications. The annualized cost avoidance figure was then compared to raw data pulled by a VIONE dashboard correspondent to ensure the manual calculation was accurate. Finally, the 5 most common classes of medications deprescribed were identified for information purposes and to provide a better postulation on the types of medications being discontinued using the VIONE method.
Results
A total of 2,442 veterans met inclusion criteria, and the VIONE method was applied to 598 between late October 2018 and January 2019. The 13 PACT pharmacists contacted at least 10 veterans each, thus at least 130 were randomly selected for telephone calls to perform polypharmacy reviews using the VIONE note template. The discontinuation menu was used if a medication qualified to be deprescribed. After 3 months, 1986 prescriptions were deprescribed using VIONE; however, 1060 prescriptions were considered appropriately deprescribed (Table 2). The 13 PACT pharmacists deprescribed 361 medications, and the 29 PACT physicians deprescribed 699 medications. These prescriptions were then separated into medication categories to determine the most common discontinued classes. Vitamins and supplements were the medication class most frequently deprescribed (19.4%), followed by pain medications (15.5%), antimicrobial agents (9.6%), antihypertensive medications (9.2%), and diabetes medications (6.4%) (Table 3). The top 5 medication categories accounted for 60% of all medications appropriately deprescribed.
The estimated annualized cost avoidance for all medications deprescribed in the 3-month project period was $84,030.46. To provide the most appropriate and accurate calculation, medication classes excluded from this figure were acute or short-term prescriptions and antimicrobial agents. Medications prescribed short-term typically are not suitable to continue for an extended period, and antimicrobial agents were excluded since they are normally associated with higher costs, and may overestimate the cost avoidance calculation for the facility.
Discussion
The outcomes for the primary and secondary endpoints of this project illustrate that using VIONE in PACT primary care clinics had a notable impact on polypharmacy and cost avoidance over a short period. This outcome can be attributed to 2 significant effects of using the deprescribing tool. VIONE’s simplicity in application allowed clinicians to incorporate daily use of the tool with minimal effort. Education was all that was required to fully enable clinicians to work together successfully and exercise collaborative practice to promote deprescribing. VIONE also elicited a cascade of favorable effects that improve patient safety and health outcomes. The tool aided in identification of PIM, which helped reduce polypharmacy and medication burden. The risk for DDIs and ADEs may decrease; therefore, the incidence of falls, need for emergency department visits or inpatient care related to polypharmacy may decline. Less complex medication regimens may alleviate issues with adherence and avoid the various consequences of polypharmacy in theory. Simplified regimens can potentially improve disease management and quality of life for patients. Further studies are needed to substantiate deprescribing and its true effect on patient adherence and better health outcomes at this time.10
Reducing polypharmacy can lead to cost savings. Based on the results of this 3-month study, we expect that VASNHS would save more than $84,000 by reducing polypharmacy among its patients. Those savings can be funneled back into the health care system, and allotted to necessary patient care, prescriptions, and health care facility needs.
Limitations
There are some important limitations to this study. Definitions of polypharmacy may vary from one health care facility to another. The cutoffs for polypharmacy may differ, causing the prevalence of polypharmacy and potential costs savings to vary. Use of VIONE may be inconsistent among users if not previously educated or properly trained. For instance, VIONE selections are listed in the same menu as the standard CPRS discontinuation options, which may lead to discontinuation of medical supplies or laboratory orders instead of prescriptions.
The method of data analysis and project design used in this study may have been subject to error. For example, the list of PCPs may have been inaccurate or outdated, which would result in an over- or underrepresentation of those who contributed to data collection. Furthermore, there is some volatility in calculating the total cost avoidance. For example, medications for chronic conditions that were only taken on an as needed basis may have overestimated savings. Either under- or overestimations could occur when parameters are adjusted on the VIONE discontinuation dashboard without appropriate guidance. With the ability to manually adjust the dashboard parameters, dissimilarities in calculations may follow.
Conclusions
The VIONE tool may be useful in improving patient safety through deprescribing and discontinuing PIM. Decreasing the number of medications being taken concomitantly by a patient and continuing only those that are imperative in their medical treatment is the first step to reducing the incidence of polypharmacy. Consequently, chances of ADEs or DDIs are lessened, especially among older individuals who are considered high risk for experiencing the detrimental effects that may ensue. These effects include geriatric-related syndromes, increased risk of fall, hospital visits or admissions, or death. Use of VIONE easily promotes collaboration among clinicians to evaluate medications eligible for discontinuation more regularly. If this deprescribing tool is continuously used, costs avoided can likely be maximized within VA health care systems.
The results of this project should serve as an incentive to push for better prescribing practices and increase deprescribing efforts. It should provoke the need for change in regimens and the subsequent discontinuation of prescriptions that are not considered vital to continue. Finally, the result of this project should substantiate the positive impact a deprescribing tool can possess to avert the issues commonly associated with polypharmacy.
According to the Centers for Disease Control and Prevention National Center for Health Statistics (NCHS), the use of prescription drugs has increased in the past half century. Although prescription drugs have played an important role in preventing, controlling, and delaying onset or progression of disease, their growth in use also has posed many risks.1 One ramification of this growth is the occurrence of polypharmacy, which does not have a universal, clear definition. In general, it can be described as the concurrent use of multiple medications by a single patient to treat one or more medical ailments. Five or more medications taken simultaneously is the most common definition to date, but this is just one of many acceptable definitions and that varies from one health care facility to another.1,2
Regardless of the cutoffs established to indicate polypharmacy, its incidence can result in poor and potentially harmful health outcomes. Polypharmacy increases the risk of experiencing adverse drug events (ADEs), drug-drug interactions (DDIs), geriatric-related syndromes, falls, hospitalization, and mortality. Issues with adherence may begin to unfold secondary to increased pill burden. Both the patient and the health care system may encounter financial strain, as polypharmacy can lead to unnecessary and essentially preventable costs of care. When evaluating the likelihood of polypharmacy based on age group, NCHS found that 47.5% of patients taking ≥ 5 medications were aged ≥ 65 years.1-5 This indicates that polypharmacy is of great concern in the geriatric population, which also represents a large proportion of individuals accessing Veterans Health Administration (VHA) care.
Deprescibing
Deprescribing is the act of withdrawing or discontinuing potentially inappropriate medications (PIM), or medications used by older patients harboring ADEs that generally outweigh the clinical benefits of the drug. Deprescribing is an effective tool for managing or reducing polypharmacy. A variety of tools have been created whose sole purpose is to simplify deprescribing. Some tools explicitly identify PIM and are widely familiar in medical practice. Examples are the Beers Criteria developed in 1991 or Screening Tool to Alert Right Treatment/Screening Tool of Older Persons Prescriptions (START/STOPP) criteria created in 2003. Other tools that are less commonplace but equally as resourceful are MedStopper and Deprescribing.org. The former was launched in 2015 and is a Canadian online system that provides risk assessments for medications with guidance for tapering or stopping medications if continuation of the drug presents higher risk than benefit.5-7 The latter is a full-fledged website developed by a physician, a pharmacist, and their research teams that serves as an exchange hub for deprescribing information.
In 2016, the VIONE (Vital, Important, Optional, Not indicated/treatment complete, and Every medication has an indication) deprescribing tool was developed by Saraswathy Battar, MD, at Central Arkansas Veterans Healthcare System (CAVHS) in Little Rock, as a system that could go beyond medication reconciliation (Table 1). Health care providers (HCPs) and pharmacists evaluate each medication that a patient has been prescribed and places each medication in a VIONE category. Prescribers may then take the opportunity to deprescribe or discontinue medications if deemed appropriate based on their clinical assessments and shared decision making.8 Traditionally, medication reconciliation involves the process of obtaining a complete and accurate list of medications as reported by a patient or caregiver to a HCP. VIONE encourages HCPs and pharmacists not only to ensure medication lists are accurate, but also that each medication reported is appropriate for continued use. In other words, VIONE is meant to help implement deprescribing at opportune times. More than 14,000 medications have been deprescribed using the VIONE method, resulting in more than $2,000,000 of annualized cost avoidance after just 1 year of implementation at CAVHS.9
VIONE consists of 2 major components in the Computerized Patient Record System (CPRS): a template and a dropdown discontinuation menu. The template captured patient allergies, pertinent laboratory data, the patient’s active problem list and applicable diagnoses, and active medication list. Patient aligned care team (PACT) pharmacists used the information captured in the template to conduct medication reconciliations and polypharmacy reviews. Each medication is categorized in VIONE using data collected during reviews. A menu delineates reasons for discontinuation: optional, dose decrease, no diagnosis, not indicated/treatment complete, discontinue alternate medication prescribed, and patient reported no longer taking. The discontinuation menu allowed PACT pharmacists and physicians to choose 1 VIONE option per medication to clarify the reason for discontinuation. VIONE-based discontinuations are recorded in CPRS and identified as deprescribed.
At the time of this project, > 30 US Department of Veterans Affairs (VA) facilities had adopted VIONE. Use of VIONE at VA Southern Nevada Healthcare System (VASNHS) in North Las Vegas has been incorporated in the everyday practices of home-based primary care pharmacists and physicians but has yet to be implemented in other areas of the facility. The purpose of this project was to determine the impact of the VIONE tool on polypharmacy and cost avoidance at VASNHS when used by primary care physicians (PCPs) and PACT primary care clinics.
Methods
Veterans receiving care at VASNHS aged ≥ 65 years with ≥ 10 active medications noted in CPRS were included in this project. PACT pharmacists and physicians were educated on the proper use of the VIONE tool prior to its implementation. Education included a 15-minute slide presentation followed by dissemination of a 1-page VIONE tool handout during a PACT all-staff clinic meeting.
Data were collected for 3 months before and after the intervention. Data were made available for assessment by the Automated Data Processing Application Coordinator (ADPAC) at VASNHS. The ADPAC created and generated an Excel spreadsheet report, which listed all medications deprescribed using the VIONE method. The primary endpoint was the total number of medications discontinued using the VIONE template and/or discontinuation menu. For the purpose of this project, appropriate discontinuation was considered any prescription deprescribed, excluding medical supplies, by pharmacists and PCPs who received VIONE education.
The secondary endpoint was the estimated annualized cost avoidance for the facility (Figure). The calculation does not include medications discontinued due to the prescription of an alternative medication or dose decreases since these VIONE selections imply that a new prescription or order was placed and the original prescription was not deprescribed. Annualized cost avoidance was determined with use of the VIONE dashboard, a database that retrospectively gathers information regarding patients at risk of polypharmacy, polypharmacy-related ADEs, and cost. Manual adjustments were made to various parameters on the Veterans Integrated Service Network 15 VIONE dashboard by the author in order to obtain data specific to this project. These parameters allowed selection of service sections, specific staff members or the option to include or exclude chronic or nonchronic medications. The annualized cost avoidance figure was then compared to raw data pulled by a VIONE dashboard correspondent to ensure the manual calculation was accurate. Finally, the 5 most common classes of medications deprescribed were identified for information purposes and to provide a better postulation on the types of medications being discontinued using the VIONE method.
Results
A total of 2,442 veterans met inclusion criteria, and the VIONE method was applied to 598 between late October 2018 and January 2019. The 13 PACT pharmacists contacted at least 10 veterans each, thus at least 130 were randomly selected for telephone calls to perform polypharmacy reviews using the VIONE note template. The discontinuation menu was used if a medication qualified to be deprescribed. After 3 months, 1986 prescriptions were deprescribed using VIONE; however, 1060 prescriptions were considered appropriately deprescribed (Table 2). The 13 PACT pharmacists deprescribed 361 medications, and the 29 PACT physicians deprescribed 699 medications. These prescriptions were then separated into medication categories to determine the most common discontinued classes. Vitamins and supplements were the medication class most frequently deprescribed (19.4%), followed by pain medications (15.5%), antimicrobial agents (9.6%), antihypertensive medications (9.2%), and diabetes medications (6.4%) (Table 3). The top 5 medication categories accounted for 60% of all medications appropriately deprescribed.
The estimated annualized cost avoidance for all medications deprescribed in the 3-month project period was $84,030.46. To provide the most appropriate and accurate calculation, medication classes excluded from this figure were acute or short-term prescriptions and antimicrobial agents. Medications prescribed short-term typically are not suitable to continue for an extended period, and antimicrobial agents were excluded since they are normally associated with higher costs, and may overestimate the cost avoidance calculation for the facility.
Discussion
The outcomes for the primary and secondary endpoints of this project illustrate that using VIONE in PACT primary care clinics had a notable impact on polypharmacy and cost avoidance over a short period. This outcome can be attributed to 2 significant effects of using the deprescribing tool. VIONE’s simplicity in application allowed clinicians to incorporate daily use of the tool with minimal effort. Education was all that was required to fully enable clinicians to work together successfully and exercise collaborative practice to promote deprescribing. VIONE also elicited a cascade of favorable effects that improve patient safety and health outcomes. The tool aided in identification of PIM, which helped reduce polypharmacy and medication burden. The risk for DDIs and ADEs may decrease; therefore, the incidence of falls, need for emergency department visits or inpatient care related to polypharmacy may decline. Less complex medication regimens may alleviate issues with adherence and avoid the various consequences of polypharmacy in theory. Simplified regimens can potentially improve disease management and quality of life for patients. Further studies are needed to substantiate deprescribing and its true effect on patient adherence and better health outcomes at this time.10
Reducing polypharmacy can lead to cost savings. Based on the results of this 3-month study, we expect that VASNHS would save more than $84,000 by reducing polypharmacy among its patients. Those savings can be funneled back into the health care system, and allotted to necessary patient care, prescriptions, and health care facility needs.
Limitations
There are some important limitations to this study. Definitions of polypharmacy may vary from one health care facility to another. The cutoffs for polypharmacy may differ, causing the prevalence of polypharmacy and potential costs savings to vary. Use of VIONE may be inconsistent among users if not previously educated or properly trained. For instance, VIONE selections are listed in the same menu as the standard CPRS discontinuation options, which may lead to discontinuation of medical supplies or laboratory orders instead of prescriptions.
The method of data analysis and project design used in this study may have been subject to error. For example, the list of PCPs may have been inaccurate or outdated, which would result in an over- or underrepresentation of those who contributed to data collection. Furthermore, there is some volatility in calculating the total cost avoidance. For example, medications for chronic conditions that were only taken on an as needed basis may have overestimated savings. Either under- or overestimations could occur when parameters are adjusted on the VIONE discontinuation dashboard without appropriate guidance. With the ability to manually adjust the dashboard parameters, dissimilarities in calculations may follow.
Conclusions
The VIONE tool may be useful in improving patient safety through deprescribing and discontinuing PIM. Decreasing the number of medications being taken concomitantly by a patient and continuing only those that are imperative in their medical treatment is the first step to reducing the incidence of polypharmacy. Consequently, chances of ADEs or DDIs are lessened, especially among older individuals who are considered high risk for experiencing the detrimental effects that may ensue. These effects include geriatric-related syndromes, increased risk of fall, hospital visits or admissions, or death. Use of VIONE easily promotes collaboration among clinicians to evaluate medications eligible for discontinuation more regularly. If this deprescribing tool is continuously used, costs avoided can likely be maximized within VA health care systems.
The results of this project should serve as an incentive to push for better prescribing practices and increase deprescribing efforts. It should provoke the need for change in regimens and the subsequent discontinuation of prescriptions that are not considered vital to continue. Finally, the result of this project should substantiate the positive impact a deprescribing tool can possess to avert the issues commonly associated with polypharmacy.
1. Centers for Disease Control and Prevention, National Center for Health Statistics. Health, United States, 2013: with special feature on prescription drugs. Published May 2014. Accessed May 13, 2021. https://www.cdc.gov/nchs/data/hus/hus13.pdf
2. Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1):230. Published 2017 Oct 10. doi:10.1186/s12877-017-0621-2
3. Parulekar MS, Rogers CK. Polypharmacy and mobility. In: Cifu DX, Lew HL, Oh-Park M., eds Geriatric Rehabilitation. Elsevier; 2018. doi:10.1016/B978-0-323-54454-2.12001-1
4. Rieckert A, Trampisch US, Klaaßen-Mielke R, et al. Polypharmacy in older patients with chronic diseases: a cross-sectional analysis of factors associated with excessive polypharmacy. BMC Fam Pract. 2018;19(1):113. Published 2018 Jul 18. doi:10.1186/s12875-018-0795-5
5. Thompson CA. New medication review method cuts veterans’ Rx load, saves millions. Am J Health Syst Pharm. 2018;75(8):502-503. doi:10.2146/news180023
6. Reeve E. Deprescribing tools: a review of the types of tools available to aid deprescribing in clinical practice. J Pharm Pract Res. 2020;50(1):98-107. doi:10.1002/jppr.1626
7. Fried TR, Niehoff KM, Street RL, et al. Effect of the Tool to Reduce Inappropriate Medications on Medication Communication and Deprescribing. J Am Geriatr Soc. 2017;65(10):2265-2271. doi:10.1111/jgs.15042
8. Battar S, Dickerson KR, Sedgwick C, et al. Understanding principles of high reliability organizations through the eyes of VIONE, a clinical program to improve patient safety by deprescribing potentially inappropriate medications and reducing polypharmacy. Fed Pract. 2019;36(12):564-568.
9. Battar S, Cmelik T, Dickerson K, Scott, M. Experience better health with VIONE a safe medication deprescribing tool [Nonpublic source, not verified]
10. Ulley J, Harrop D, Ali A, et al. Desprescribing interventions and their impact on medication adherence in community-dwelling older adults with polypharmacy: a systematic review. BMC Geriatr. 2019;19(15):1-13.
1. Centers for Disease Control and Prevention, National Center for Health Statistics. Health, United States, 2013: with special feature on prescription drugs. Published May 2014. Accessed May 13, 2021. https://www.cdc.gov/nchs/data/hus/hus13.pdf
2. Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1):230. Published 2017 Oct 10. doi:10.1186/s12877-017-0621-2
3. Parulekar MS, Rogers CK. Polypharmacy and mobility. In: Cifu DX, Lew HL, Oh-Park M., eds Geriatric Rehabilitation. Elsevier; 2018. doi:10.1016/B978-0-323-54454-2.12001-1
4. Rieckert A, Trampisch US, Klaaßen-Mielke R, et al. Polypharmacy in older patients with chronic diseases: a cross-sectional analysis of factors associated with excessive polypharmacy. BMC Fam Pract. 2018;19(1):113. Published 2018 Jul 18. doi:10.1186/s12875-018-0795-5
5. Thompson CA. New medication review method cuts veterans’ Rx load, saves millions. Am J Health Syst Pharm. 2018;75(8):502-503. doi:10.2146/news180023
6. Reeve E. Deprescribing tools: a review of the types of tools available to aid deprescribing in clinical practice. J Pharm Pract Res. 2020;50(1):98-107. doi:10.1002/jppr.1626
7. Fried TR, Niehoff KM, Street RL, et al. Effect of the Tool to Reduce Inappropriate Medications on Medication Communication and Deprescribing. J Am Geriatr Soc. 2017;65(10):2265-2271. doi:10.1111/jgs.15042
8. Battar S, Dickerson KR, Sedgwick C, et al. Understanding principles of high reliability organizations through the eyes of VIONE, a clinical program to improve patient safety by deprescribing potentially inappropriate medications and reducing polypharmacy. Fed Pract. 2019;36(12):564-568.
9. Battar S, Cmelik T, Dickerson K, Scott, M. Experience better health with VIONE a safe medication deprescribing tool [Nonpublic source, not verified]
10. Ulley J, Harrop D, Ali A, et al. Desprescribing interventions and their impact on medication adherence in community-dwelling older adults with polypharmacy: a systematic review. BMC Geriatr. 2019;19(15):1-13.
Can overweight docs really give credible weight loss advice?
Kevin Gendreau, MD, a weight loss doctor at Southcoast Health in Fall River, Maine, lets patients know that he was once obese. He says this knowledge inspires and motivates them to lose weight.

After dropping 125 pounds over 18 months, “I can relate to their binges, hardships, and plateaus on a very personal level,” he says.
Peminda Cabandugama, MD, an endocrinologist and obesity medicine specialist at Truman Medical Center at the University of Missouri-Kansas City, has weighed between 180 and 240 pounds in the past decade. He now weighs 225 pounds and has a healthy lifestyle.
“I have had patients come to me saying, ‘I used to see a different weight loss doctor who was not heavy. But how can he understand what I’m going through?’” he says.
Dr. Cabandugama shares his weight loss struggles with patients “to dispel this myth that weight management is as simple as just eating too much and not exercising. It involves a smorgasbord of emotions and hormones, some within and outside of our control. I hope that sharing this allows me to connect more with my patients so that they know that even their health care professional goes through the same challenges that they do.”
“Patients are more likely to make behavior changes when doctors are supportive and have had similar experiences and talk about their stories,” says Wendy Bennett, MD, an obesity researcher and associate professor of medicine at Johns Hopkins University in Baltimore.
Do patients respect overweight doctors?
While Dr. Gendreau and Dr. Cabandugama have lost weight,
Doctors sometimes have biased attitudes toward overweight patients, but few studies have looked at whether patients have biases towards overweight doctors. The results vary and may depend on whether or not the patients are overweight.
A random online survey of 358 participants suggested that regardless of their own weight, people had biases about doctor weight gain. They viewed the overweight or obese doctors as less trustworthy and credible, which could lead the participants to reject their medical advice and change doctors.
“Patients expect doctors who are providing health care to be doing everything they can to take care of their own health and well-being,” says Pamela Peeke, MD, an assistant clinical professor of medicine at the University of Maryland in Baltimore.
“I am a physician who believes you have to walk the talk — that the best teachers are those who live it,” she says.
Still, “I don’t think based on this one experimental study that we can conclude that overweight physicians are harming patients’ efforts to change their behavior,” notes Dr. Bennett, who was not involved in the study.
“I think that patients do often want to connect with their physicians on more personal levels, but without the story behind where the advice is coming from, patients may struggle to trust a provider who seems to be contradicting the messages,” she says.
A study that Dr. Bennett helped lead suggests that patients are not biased against overweight doctors if they themselves need to lose weight. A national survey of 600 overweight patients showed that 87% trusted diet advice from overweight primary care doctors, compared to 77% who trusted diet advice from doctors who had a healthy weight.
“This shows that patients were more trusting of physicians who are more like them, which can lead to better relationships. We know from the studies on race that patients are often more trusting of physicians from the same race as them,” says Dr. Bennett.
Dr. Gendreau says that when he was severely obese, some patients questioned whether to trust his weight loss advice.
“It was very awkward when they turned to me and said, ‘What about you?’ I would respond that it’s my job to inform them about the risks to their health,” he says.
Nearly half (48%) of doctors said they are trying to lose weight, according to the 2021 Medscape Physician Lifestyle and Happiness Report. As a result, many doctors may end up in the position of seemingly advising to “do what I say, not what I do.”
Nearly three in five Americans are trying to lose weight, according to Gelesis poll results released in December 2020.
Should doctors pay more attention to wellness?
Doctors have an ethical duty to maintain their own health and wellness so they can provide safe and effective medical care. If they don’t have a healthy lifestyle, they need to make adjustments, the American Medical Association Code of Ethics advises.
Dr. Peeke agrees with the AMA. “We signed on to do this — we have to go out of our way to carve out time, even if it’s just 15 minutes where we hide away and eat that healthy lunch that we brought with us,” she says.
Dr. Gendreau suggests busy doctors do what he did.
“I started by bringing healthy snacks — small Ziploc bags filled with mixed nuts and berries — and expanded from there. This way, if I got hungry or stressed between patients, I would have easy access to something nutritious,” he says.
He and Dr. Peeke also suggest making protein shakes or berry smoothies that are low in sugar.
“These can keep you full for hours as you sip them between patients,” says Dr. Gendreau.
Convincing busy doctors to make lifestyle changes may be challenging. Sixty-five percent of those who responded to the Physician Lifestyle and Happiness Report say that they sometimes, rarely, or never focus on their health and wellness. Only 45% said they are eating healthy, and 65% said they exercise.
“Self-care isn’t a priority for most physicians because we are taught to take care of others and to put them first,” says Dr. Gendreau. “Like many doctors, I had so many other priorities — family, friends, career. Also, my last year of medical school was so difficult that my priority was finishing. I pushed my health to the side and told myself that I could fix this later.”
Only about one in five medical schools require students to take a nutrition course, according to David Eisenberg, MD, an adjunct associate professor of nutrition at the Harvard T.H. Chan School of Public Health, Boston.
“I didn’t get one ounce of nutrition training, which is the reason I became a Pew Foundation scholar in nutrition and metabolism. I had to go outside of my traditional training,” says Dr. Peeke.
“Physicians are not adequately trained to do the behavioral counseling and motivational interviewing that is needed,” says Dr. Bennett. “We do a good job of diagnosing obesity based on body mass index and understanding the relationship with future health conditions. But most doctors struggle with both a lack of time and the skill set to make significant behavior changes.”
“Medical school curriculum is focused so heavily on the pathology and pathophysiology of obesity, rather than how to prevent it with the appropriate diet and exercise regimen,” Dr. Gendreau says. “My physician patients often tell me that their own education in the field of nutrition is lacking, which can affect their weight loss journey and what they teach their patients.”
Dr. Gendreau, crediting his own weight loss journey as well as his obesity medicine fellowship, says his confidence in discussing weight loss with patients has soared.
Reframing obesity as a chronic disease
Rather than criticizing overweight people, including doctors, for their personal health choices, a better approach is to think of weight or obesity as a chronic illness, says Dr. Bennett.
“If we understand that obesity is a chronic health condition that people are struggling with, we can empathize with them,” she says, recommending that more providers share their weight loss journeys with patients they give lifestyle advice to, which may help address and repair potential biases.
A version of this article first appeared on WebMD.com.
Kevin Gendreau, MD, a weight loss doctor at Southcoast Health in Fall River, Maine, lets patients know that he was once obese. He says this knowledge inspires and motivates them to lose weight.

After dropping 125 pounds over 18 months, “I can relate to their binges, hardships, and plateaus on a very personal level,” he says.
Peminda Cabandugama, MD, an endocrinologist and obesity medicine specialist at Truman Medical Center at the University of Missouri-Kansas City, has weighed between 180 and 240 pounds in the past decade. He now weighs 225 pounds and has a healthy lifestyle.
“I have had patients come to me saying, ‘I used to see a different weight loss doctor who was not heavy. But how can he understand what I’m going through?’” he says.
Dr. Cabandugama shares his weight loss struggles with patients “to dispel this myth that weight management is as simple as just eating too much and not exercising. It involves a smorgasbord of emotions and hormones, some within and outside of our control. I hope that sharing this allows me to connect more with my patients so that they know that even their health care professional goes through the same challenges that they do.”
“Patients are more likely to make behavior changes when doctors are supportive and have had similar experiences and talk about their stories,” says Wendy Bennett, MD, an obesity researcher and associate professor of medicine at Johns Hopkins University in Baltimore.
Do patients respect overweight doctors?
While Dr. Gendreau and Dr. Cabandugama have lost weight,
Doctors sometimes have biased attitudes toward overweight patients, but few studies have looked at whether patients have biases towards overweight doctors. The results vary and may depend on whether or not the patients are overweight.
A random online survey of 358 participants suggested that regardless of their own weight, people had biases about doctor weight gain. They viewed the overweight or obese doctors as less trustworthy and credible, which could lead the participants to reject their medical advice and change doctors.
“Patients expect doctors who are providing health care to be doing everything they can to take care of their own health and well-being,” says Pamela Peeke, MD, an assistant clinical professor of medicine at the University of Maryland in Baltimore.
“I am a physician who believes you have to walk the talk — that the best teachers are those who live it,” she says.
Still, “I don’t think based on this one experimental study that we can conclude that overweight physicians are harming patients’ efforts to change their behavior,” notes Dr. Bennett, who was not involved in the study.
“I think that patients do often want to connect with their physicians on more personal levels, but without the story behind where the advice is coming from, patients may struggle to trust a provider who seems to be contradicting the messages,” she says.
A study that Dr. Bennett helped lead suggests that patients are not biased against overweight doctors if they themselves need to lose weight. A national survey of 600 overweight patients showed that 87% trusted diet advice from overweight primary care doctors, compared to 77% who trusted diet advice from doctors who had a healthy weight.
“This shows that patients were more trusting of physicians who are more like them, which can lead to better relationships. We know from the studies on race that patients are often more trusting of physicians from the same race as them,” says Dr. Bennett.
Dr. Gendreau says that when he was severely obese, some patients questioned whether to trust his weight loss advice.
“It was very awkward when they turned to me and said, ‘What about you?’ I would respond that it’s my job to inform them about the risks to their health,” he says.
Nearly half (48%) of doctors said they are trying to lose weight, according to the 2021 Medscape Physician Lifestyle and Happiness Report. As a result, many doctors may end up in the position of seemingly advising to “do what I say, not what I do.”
Nearly three in five Americans are trying to lose weight, according to Gelesis poll results released in December 2020.
Should doctors pay more attention to wellness?
Doctors have an ethical duty to maintain their own health and wellness so they can provide safe and effective medical care. If they don’t have a healthy lifestyle, they need to make adjustments, the American Medical Association Code of Ethics advises.
Dr. Peeke agrees with the AMA. “We signed on to do this — we have to go out of our way to carve out time, even if it’s just 15 minutes where we hide away and eat that healthy lunch that we brought with us,” she says.
Dr. Gendreau suggests busy doctors do what he did.
“I started by bringing healthy snacks — small Ziploc bags filled with mixed nuts and berries — and expanded from there. This way, if I got hungry or stressed between patients, I would have easy access to something nutritious,” he says.
He and Dr. Peeke also suggest making protein shakes or berry smoothies that are low in sugar.
“These can keep you full for hours as you sip them between patients,” says Dr. Gendreau.
Convincing busy doctors to make lifestyle changes may be challenging. Sixty-five percent of those who responded to the Physician Lifestyle and Happiness Report say that they sometimes, rarely, or never focus on their health and wellness. Only 45% said they are eating healthy, and 65% said they exercise.
“Self-care isn’t a priority for most physicians because we are taught to take care of others and to put them first,” says Dr. Gendreau. “Like many doctors, I had so many other priorities — family, friends, career. Also, my last year of medical school was so difficult that my priority was finishing. I pushed my health to the side and told myself that I could fix this later.”
Only about one in five medical schools require students to take a nutrition course, according to David Eisenberg, MD, an adjunct associate professor of nutrition at the Harvard T.H. Chan School of Public Health, Boston.
“I didn’t get one ounce of nutrition training, which is the reason I became a Pew Foundation scholar in nutrition and metabolism. I had to go outside of my traditional training,” says Dr. Peeke.
“Physicians are not adequately trained to do the behavioral counseling and motivational interviewing that is needed,” says Dr. Bennett. “We do a good job of diagnosing obesity based on body mass index and understanding the relationship with future health conditions. But most doctors struggle with both a lack of time and the skill set to make significant behavior changes.”
“Medical school curriculum is focused so heavily on the pathology and pathophysiology of obesity, rather than how to prevent it with the appropriate diet and exercise regimen,” Dr. Gendreau says. “My physician patients often tell me that their own education in the field of nutrition is lacking, which can affect their weight loss journey and what they teach their patients.”
Dr. Gendreau, crediting his own weight loss journey as well as his obesity medicine fellowship, says his confidence in discussing weight loss with patients has soared.
Reframing obesity as a chronic disease
Rather than criticizing overweight people, including doctors, for their personal health choices, a better approach is to think of weight or obesity as a chronic illness, says Dr. Bennett.
“If we understand that obesity is a chronic health condition that people are struggling with, we can empathize with them,” she says, recommending that more providers share their weight loss journeys with patients they give lifestyle advice to, which may help address and repair potential biases.
A version of this article first appeared on WebMD.com.
Kevin Gendreau, MD, a weight loss doctor at Southcoast Health in Fall River, Maine, lets patients know that he was once obese. He says this knowledge inspires and motivates them to lose weight.

After dropping 125 pounds over 18 months, “I can relate to their binges, hardships, and plateaus on a very personal level,” he says.
Peminda Cabandugama, MD, an endocrinologist and obesity medicine specialist at Truman Medical Center at the University of Missouri-Kansas City, has weighed between 180 and 240 pounds in the past decade. He now weighs 225 pounds and has a healthy lifestyle.
“I have had patients come to me saying, ‘I used to see a different weight loss doctor who was not heavy. But how can he understand what I’m going through?’” he says.
Dr. Cabandugama shares his weight loss struggles with patients “to dispel this myth that weight management is as simple as just eating too much and not exercising. It involves a smorgasbord of emotions and hormones, some within and outside of our control. I hope that sharing this allows me to connect more with my patients so that they know that even their health care professional goes through the same challenges that they do.”
“Patients are more likely to make behavior changes when doctors are supportive and have had similar experiences and talk about their stories,” says Wendy Bennett, MD, an obesity researcher and associate professor of medicine at Johns Hopkins University in Baltimore.
Do patients respect overweight doctors?
While Dr. Gendreau and Dr. Cabandugama have lost weight,
Doctors sometimes have biased attitudes toward overweight patients, but few studies have looked at whether patients have biases towards overweight doctors. The results vary and may depend on whether or not the patients are overweight.
A random online survey of 358 participants suggested that regardless of their own weight, people had biases about doctor weight gain. They viewed the overweight or obese doctors as less trustworthy and credible, which could lead the participants to reject their medical advice and change doctors.
“Patients expect doctors who are providing health care to be doing everything they can to take care of their own health and well-being,” says Pamela Peeke, MD, an assistant clinical professor of medicine at the University of Maryland in Baltimore.
“I am a physician who believes you have to walk the talk — that the best teachers are those who live it,” she says.
Still, “I don’t think based on this one experimental study that we can conclude that overweight physicians are harming patients’ efforts to change their behavior,” notes Dr. Bennett, who was not involved in the study.
“I think that patients do often want to connect with their physicians on more personal levels, but without the story behind where the advice is coming from, patients may struggle to trust a provider who seems to be contradicting the messages,” she says.
A study that Dr. Bennett helped lead suggests that patients are not biased against overweight doctors if they themselves need to lose weight. A national survey of 600 overweight patients showed that 87% trusted diet advice from overweight primary care doctors, compared to 77% who trusted diet advice from doctors who had a healthy weight.
“This shows that patients were more trusting of physicians who are more like them, which can lead to better relationships. We know from the studies on race that patients are often more trusting of physicians from the same race as them,” says Dr. Bennett.
Dr. Gendreau says that when he was severely obese, some patients questioned whether to trust his weight loss advice.
“It was very awkward when they turned to me and said, ‘What about you?’ I would respond that it’s my job to inform them about the risks to their health,” he says.
Nearly half (48%) of doctors said they are trying to lose weight, according to the 2021 Medscape Physician Lifestyle and Happiness Report. As a result, many doctors may end up in the position of seemingly advising to “do what I say, not what I do.”
Nearly three in five Americans are trying to lose weight, according to Gelesis poll results released in December 2020.
Should doctors pay more attention to wellness?
Doctors have an ethical duty to maintain their own health and wellness so they can provide safe and effective medical care. If they don’t have a healthy lifestyle, they need to make adjustments, the American Medical Association Code of Ethics advises.
Dr. Peeke agrees with the AMA. “We signed on to do this — we have to go out of our way to carve out time, even if it’s just 15 minutes where we hide away and eat that healthy lunch that we brought with us,” she says.
Dr. Gendreau suggests busy doctors do what he did.
“I started by bringing healthy snacks — small Ziploc bags filled with mixed nuts and berries — and expanded from there. This way, if I got hungry or stressed between patients, I would have easy access to something nutritious,” he says.
He and Dr. Peeke also suggest making protein shakes or berry smoothies that are low in sugar.
“These can keep you full for hours as you sip them between patients,” says Dr. Gendreau.
Convincing busy doctors to make lifestyle changes may be challenging. Sixty-five percent of those who responded to the Physician Lifestyle and Happiness Report say that they sometimes, rarely, or never focus on their health and wellness. Only 45% said they are eating healthy, and 65% said they exercise.
“Self-care isn’t a priority for most physicians because we are taught to take care of others and to put them first,” says Dr. Gendreau. “Like many doctors, I had so many other priorities — family, friends, career. Also, my last year of medical school was so difficult that my priority was finishing. I pushed my health to the side and told myself that I could fix this later.”
Only about one in five medical schools require students to take a nutrition course, according to David Eisenberg, MD, an adjunct associate professor of nutrition at the Harvard T.H. Chan School of Public Health, Boston.
“I didn’t get one ounce of nutrition training, which is the reason I became a Pew Foundation scholar in nutrition and metabolism. I had to go outside of my traditional training,” says Dr. Peeke.
“Physicians are not adequately trained to do the behavioral counseling and motivational interviewing that is needed,” says Dr. Bennett. “We do a good job of diagnosing obesity based on body mass index and understanding the relationship with future health conditions. But most doctors struggle with both a lack of time and the skill set to make significant behavior changes.”
“Medical school curriculum is focused so heavily on the pathology and pathophysiology of obesity, rather than how to prevent it with the appropriate diet and exercise regimen,” Dr. Gendreau says. “My physician patients often tell me that their own education in the field of nutrition is lacking, which can affect their weight loss journey and what they teach their patients.”
Dr. Gendreau, crediting his own weight loss journey as well as his obesity medicine fellowship, says his confidence in discussing weight loss with patients has soared.
Reframing obesity as a chronic disease
Rather than criticizing overweight people, including doctors, for their personal health choices, a better approach is to think of weight or obesity as a chronic illness, says Dr. Bennett.
“If we understand that obesity is a chronic health condition that people are struggling with, we can empathize with them,” she says, recommending that more providers share their weight loss journeys with patients they give lifestyle advice to, which may help address and repair potential biases.
A version of this article first appeared on WebMD.com.
FDA head calls for investigation into agency’s approval of aducanumab (Aduhelm)
After several weeks of outcry and heated debate over the Food and Drug Administration’s controversial approval of the Alzheimer’s drug aducanumab (Aduhelm), the head of the agency is now calling for a federal investigation into its own approval proceedings.
Janet Woodcock, MD, the FDA’s acting commissioner, sent a letter to the Office of the Inspector General on July 9, she announced in a tweet.
Dr. Woodcock is asking for an investigation into questionable meetings and other interactions between Biogen and FDA staff members prior to the drug’s approval that “may have occurred outside of the formal correspondence process.”
The letter explains that concerns around these issues “could undermine the public’s confidence in the FDA’s decision.” Therefore, an independent investigation is needed to determine whether anything occurred that was “inconsistent with FDA policies and procedures.”
Dr. Woodcock noted that she has “tremendous confidence in the integrity of the staff and leadership of the Center for Drug Evaluation and Research” involved in the review process.
However, “FDA is dedicated to scientific integrity, to reviewing data without bias, and to basing its regulatory decisions on data,” she wrote. “You have my personal commitment that the Agency will fully cooperate should your office undertake a review.”
Dr. Woodcock concluded by urging that a review be conducted as soon as possible, noting that “should such a review result in actionable items, you also have my commitment to addressing these issues.”
A version of this article first appeared on Medscape.com.
After several weeks of outcry and heated debate over the Food and Drug Administration’s controversial approval of the Alzheimer’s drug aducanumab (Aduhelm), the head of the agency is now calling for a federal investigation into its own approval proceedings.
Janet Woodcock, MD, the FDA’s acting commissioner, sent a letter to the Office of the Inspector General on July 9, she announced in a tweet.
Dr. Woodcock is asking for an investigation into questionable meetings and other interactions between Biogen and FDA staff members prior to the drug’s approval that “may have occurred outside of the formal correspondence process.”
The letter explains that concerns around these issues “could undermine the public’s confidence in the FDA’s decision.” Therefore, an independent investigation is needed to determine whether anything occurred that was “inconsistent with FDA policies and procedures.”
Dr. Woodcock noted that she has “tremendous confidence in the integrity of the staff and leadership of the Center for Drug Evaluation and Research” involved in the review process.
However, “FDA is dedicated to scientific integrity, to reviewing data without bias, and to basing its regulatory decisions on data,” she wrote. “You have my personal commitment that the Agency will fully cooperate should your office undertake a review.”
Dr. Woodcock concluded by urging that a review be conducted as soon as possible, noting that “should such a review result in actionable items, you also have my commitment to addressing these issues.”
A version of this article first appeared on Medscape.com.
After several weeks of outcry and heated debate over the Food and Drug Administration’s controversial approval of the Alzheimer’s drug aducanumab (Aduhelm), the head of the agency is now calling for a federal investigation into its own approval proceedings.
Janet Woodcock, MD, the FDA’s acting commissioner, sent a letter to the Office of the Inspector General on July 9, she announced in a tweet.
Dr. Woodcock is asking for an investigation into questionable meetings and other interactions between Biogen and FDA staff members prior to the drug’s approval that “may have occurred outside of the formal correspondence process.”
The letter explains that concerns around these issues “could undermine the public’s confidence in the FDA’s decision.” Therefore, an independent investigation is needed to determine whether anything occurred that was “inconsistent with FDA policies and procedures.”
Dr. Woodcock noted that she has “tremendous confidence in the integrity of the staff and leadership of the Center for Drug Evaluation and Research” involved in the review process.
However, “FDA is dedicated to scientific integrity, to reviewing data without bias, and to basing its regulatory decisions on data,” she wrote. “You have my personal commitment that the Agency will fully cooperate should your office undertake a review.”
Dr. Woodcock concluded by urging that a review be conducted as soon as possible, noting that “should such a review result in actionable items, you also have my commitment to addressing these issues.”
A version of this article first appeared on Medscape.com.
Respiratory infection– and asthma-prone children
Some children are more susceptible to viral and bacterial respiratory infections in the first few years of life than others. However, the factors contributing to this susceptibility are incompletely understood. The pathogenesis, development, severity, and clinical outcomes of respiratory infections are largely dependent on the resident composition of the nasopharyngeal microbiome and immune defense.1
Respiratory infections caused by bacteria and/or viruses are a leading cause of death in children in the United States and worldwide. The well-recognized, predominant causative bacteria are Streptococcus pneumoniae (pneumococcus), nontypeable Haemophilus influenzae (Hflu), and Moraxella catarrhalis (Mcat). Respiratory infections caused by these pathogens result in considerable morbidity, mortality, and account for high health care costs. The clinical and laboratory group that I lead in Rochester, N.Y., has been studying acute otitis media (AOM) etiology, epidemiology, pathogenesis, prevention, and treatment for over 3 decades. Our research findings are likely applicable and generalizable to understanding the pathogenesis and immune response to other infectious diseases induced by pneumococcus, Hflu, and Mcat since they are also key pathogens causing sinusitis and lung infections.
Previous immunologic analysis of children with AOM by our group provided clarity in differences between infection-prone children manifest as otitis prone (OP; often referred to in our publications as stringently defined OP because of the stringent diagnostic requirement of tympanocentesis-proven etiology of infection) and non-OP children. We showed that about 90% of OP children have deficient immune responses following nasopharyngeal colonization and AOM, demonstrated by inadequate innate responses and adaptive immune responses.2 Many of these children also showed an increased propensity to viral upper respiratory infection and 30% fail to produce protective antibody responses after injection of routine pediatric vaccines.3,4
In this column, I want to share new information regarding differences in the nasopharyngeal microbiome of children who are respiratory infection prone versus those who are non–respiratory infection prone and children with asthma versus those who do not exhibit that clinical phenotype. We performed a retrospective analysis of clinical samples collected from 358 children, aged 6 months to 5 years, from our prospectively enrolled cohort in Rochester, N.Y., to determine associations between AOM and other childhood respiratory illnesses and nasopharyngeal microbiota. In order to define subgroups of children within the cohort, we used a statistical method called unsupervised clustering analysis to see if relatively unique groups of children could be discerned. The overall cohort successfully clustered into two groups, showing marked differences in the prevalence of respiratory infections and asthma.5 We termed the two clinical phenotypes infection and asthma prone (n = 99, 28% of the children) and non–infection and asthma prone (n = 259, 72% of the children). Infection- and asthma-prone children were significantly more likely to experience recurrent AOM, influenza, sinusitis, pneumonia, asthma, and allergic rhinitis, compared with non–infection- and asthma-prone children (Figure).
The two groups did not experience significantly different rates of eczema, food allergy, skin infections, urinary tract infections, or acute gastroenteritis, suggesting a common thread involving the respiratory tract that did not cross over to the gastrointestinal, skin, or urinary tract. We found that age at first nasopharyngeal colonization with any of the three bacterial respiratory pathogens (pneumococcus, Hflu, or Mcat) was significantly associated with the respiratory infection– and asthma-prone clinical phenotype. Specifically, respiratory infection– and asthma-prone children experienced colonization at a significantly earlier age than nonprone children did for all three bacteria. In an analysis of individual conditions, early Mcat colonization significantly associated with pneumonia, sinusitis, and asthma susceptibility; Hflu with pneumonia, sinusitis, influenza, and allergic rhinitis; and pneumococcus with sinusitis.
Since early colonization with the three bacterial respiratory pathogens was strongly associated with respiratory illnesses and asthma, nasopharyngeal microbiome analysis was performed on an available subset of samples. Bacterial diversity trended lower in infection- and asthma-prone children, consistent with dysbiosis in the respiratory infection– and asthma-prone clinical phenotype. Nine different bacteria genera were found to be differentially abundant when comparing respiratory infection– and asthma-prone and nonprone children, pointing the way to possible interventions to make the respiratory infection– and asthma-prone child nasopharyngeal microbiome more like the nonprone child.
As I have written previously in this column, recent accumulating data have shed light on the importance of the human microbiome in modulating immune homeostasis and disease susceptibility.6 My group is working toward generating new knowledge for the long-term goal of identifying new therapeutic strategies to facilitate a protective, diverse nasopharyngeal microbiome (with appropriately tuned intranasal probiotics) to prevent respiratory pathogen colonization and/or subsequent progression to respiratory infection and asthma. Also, vaccines directed against colonization-enhancing members of the microbiome may provide a means to indirectly control respiratory pathogen nasopharyngeal colonization.
Dr. Pichichero is a specialist in pediatric infectious diseases and director of the Research Institute at Rochester (N.Y.) General Hospital. He has no conflicts to declare. Contact him at [email protected]
References
1. Man WH et al. Nat Rev Microbiol. 2017;15(5):259-70.
2. Pichichero ME. J Infect. 2020;80(6):614-22.
3. Ren D et al. Clin Infect Dis. 2019;68(9):1566-74.
4. Pichichero ME et al. Pediatr Infect Dis J. 2013;32(11):1163-8.
5. Chapman T et al. PLoS One. 2020 Dec 11;15(12).
6. Blaser MJ. The microbiome revolution. J Clin Invest. 2014;124:4162-5.
Some children are more susceptible to viral and bacterial respiratory infections in the first few years of life than others. However, the factors contributing to this susceptibility are incompletely understood. The pathogenesis, development, severity, and clinical outcomes of respiratory infections are largely dependent on the resident composition of the nasopharyngeal microbiome and immune defense.1
Respiratory infections caused by bacteria and/or viruses are a leading cause of death in children in the United States and worldwide. The well-recognized, predominant causative bacteria are Streptococcus pneumoniae (pneumococcus), nontypeable Haemophilus influenzae (Hflu), and Moraxella catarrhalis (Mcat). Respiratory infections caused by these pathogens result in considerable morbidity, mortality, and account for high health care costs. The clinical and laboratory group that I lead in Rochester, N.Y., has been studying acute otitis media (AOM) etiology, epidemiology, pathogenesis, prevention, and treatment for over 3 decades. Our research findings are likely applicable and generalizable to understanding the pathogenesis and immune response to other infectious diseases induced by pneumococcus, Hflu, and Mcat since they are also key pathogens causing sinusitis and lung infections.
Previous immunologic analysis of children with AOM by our group provided clarity in differences between infection-prone children manifest as otitis prone (OP; often referred to in our publications as stringently defined OP because of the stringent diagnostic requirement of tympanocentesis-proven etiology of infection) and non-OP children. We showed that about 90% of OP children have deficient immune responses following nasopharyngeal colonization and AOM, demonstrated by inadequate innate responses and adaptive immune responses.2 Many of these children also showed an increased propensity to viral upper respiratory infection and 30% fail to produce protective antibody responses after injection of routine pediatric vaccines.3,4
In this column, I want to share new information regarding differences in the nasopharyngeal microbiome of children who are respiratory infection prone versus those who are non–respiratory infection prone and children with asthma versus those who do not exhibit that clinical phenotype. We performed a retrospective analysis of clinical samples collected from 358 children, aged 6 months to 5 years, from our prospectively enrolled cohort in Rochester, N.Y., to determine associations between AOM and other childhood respiratory illnesses and nasopharyngeal microbiota. In order to define subgroups of children within the cohort, we used a statistical method called unsupervised clustering analysis to see if relatively unique groups of children could be discerned. The overall cohort successfully clustered into two groups, showing marked differences in the prevalence of respiratory infections and asthma.5 We termed the two clinical phenotypes infection and asthma prone (n = 99, 28% of the children) and non–infection and asthma prone (n = 259, 72% of the children). Infection- and asthma-prone children were significantly more likely to experience recurrent AOM, influenza, sinusitis, pneumonia, asthma, and allergic rhinitis, compared with non–infection- and asthma-prone children (Figure).
The two groups did not experience significantly different rates of eczema, food allergy, skin infections, urinary tract infections, or acute gastroenteritis, suggesting a common thread involving the respiratory tract that did not cross over to the gastrointestinal, skin, or urinary tract. We found that age at first nasopharyngeal colonization with any of the three bacterial respiratory pathogens (pneumococcus, Hflu, or Mcat) was significantly associated with the respiratory infection– and asthma-prone clinical phenotype. Specifically, respiratory infection– and asthma-prone children experienced colonization at a significantly earlier age than nonprone children did for all three bacteria. In an analysis of individual conditions, early Mcat colonization significantly associated with pneumonia, sinusitis, and asthma susceptibility; Hflu with pneumonia, sinusitis, influenza, and allergic rhinitis; and pneumococcus with sinusitis.
Since early colonization with the three bacterial respiratory pathogens was strongly associated with respiratory illnesses and asthma, nasopharyngeal microbiome analysis was performed on an available subset of samples. Bacterial diversity trended lower in infection- and asthma-prone children, consistent with dysbiosis in the respiratory infection– and asthma-prone clinical phenotype. Nine different bacteria genera were found to be differentially abundant when comparing respiratory infection– and asthma-prone and nonprone children, pointing the way to possible interventions to make the respiratory infection– and asthma-prone child nasopharyngeal microbiome more like the nonprone child.
As I have written previously in this column, recent accumulating data have shed light on the importance of the human microbiome in modulating immune homeostasis and disease susceptibility.6 My group is working toward generating new knowledge for the long-term goal of identifying new therapeutic strategies to facilitate a protective, diverse nasopharyngeal microbiome (with appropriately tuned intranasal probiotics) to prevent respiratory pathogen colonization and/or subsequent progression to respiratory infection and asthma. Also, vaccines directed against colonization-enhancing members of the microbiome may provide a means to indirectly control respiratory pathogen nasopharyngeal colonization.
Dr. Pichichero is a specialist in pediatric infectious diseases and director of the Research Institute at Rochester (N.Y.) General Hospital. He has no conflicts to declare. Contact him at [email protected]
References
1. Man WH et al. Nat Rev Microbiol. 2017;15(5):259-70.
2. Pichichero ME. J Infect. 2020;80(6):614-22.
3. Ren D et al. Clin Infect Dis. 2019;68(9):1566-74.
4. Pichichero ME et al. Pediatr Infect Dis J. 2013;32(11):1163-8.
5. Chapman T et al. PLoS One. 2020 Dec 11;15(12).
6. Blaser MJ. The microbiome revolution. J Clin Invest. 2014;124:4162-5.
Some children are more susceptible to viral and bacterial respiratory infections in the first few years of life than others. However, the factors contributing to this susceptibility are incompletely understood. The pathogenesis, development, severity, and clinical outcomes of respiratory infections are largely dependent on the resident composition of the nasopharyngeal microbiome and immune defense.1
Respiratory infections caused by bacteria and/or viruses are a leading cause of death in children in the United States and worldwide. The well-recognized, predominant causative bacteria are Streptococcus pneumoniae (pneumococcus), nontypeable Haemophilus influenzae (Hflu), and Moraxella catarrhalis (Mcat). Respiratory infections caused by these pathogens result in considerable morbidity, mortality, and account for high health care costs. The clinical and laboratory group that I lead in Rochester, N.Y., has been studying acute otitis media (AOM) etiology, epidemiology, pathogenesis, prevention, and treatment for over 3 decades. Our research findings are likely applicable and generalizable to understanding the pathogenesis and immune response to other infectious diseases induced by pneumococcus, Hflu, and Mcat since they are also key pathogens causing sinusitis and lung infections.
Previous immunologic analysis of children with AOM by our group provided clarity in differences between infection-prone children manifest as otitis prone (OP; often referred to in our publications as stringently defined OP because of the stringent diagnostic requirement of tympanocentesis-proven etiology of infection) and non-OP children. We showed that about 90% of OP children have deficient immune responses following nasopharyngeal colonization and AOM, demonstrated by inadequate innate responses and adaptive immune responses.2 Many of these children also showed an increased propensity to viral upper respiratory infection and 30% fail to produce protective antibody responses after injection of routine pediatric vaccines.3,4
In this column, I want to share new information regarding differences in the nasopharyngeal microbiome of children who are respiratory infection prone versus those who are non–respiratory infection prone and children with asthma versus those who do not exhibit that clinical phenotype. We performed a retrospective analysis of clinical samples collected from 358 children, aged 6 months to 5 years, from our prospectively enrolled cohort in Rochester, N.Y., to determine associations between AOM and other childhood respiratory illnesses and nasopharyngeal microbiota. In order to define subgroups of children within the cohort, we used a statistical method called unsupervised clustering analysis to see if relatively unique groups of children could be discerned. The overall cohort successfully clustered into two groups, showing marked differences in the prevalence of respiratory infections and asthma.5 We termed the two clinical phenotypes infection and asthma prone (n = 99, 28% of the children) and non–infection and asthma prone (n = 259, 72% of the children). Infection- and asthma-prone children were significantly more likely to experience recurrent AOM, influenza, sinusitis, pneumonia, asthma, and allergic rhinitis, compared with non–infection- and asthma-prone children (Figure).
The two groups did not experience significantly different rates of eczema, food allergy, skin infections, urinary tract infections, or acute gastroenteritis, suggesting a common thread involving the respiratory tract that did not cross over to the gastrointestinal, skin, or urinary tract. We found that age at first nasopharyngeal colonization with any of the three bacterial respiratory pathogens (pneumococcus, Hflu, or Mcat) was significantly associated with the respiratory infection– and asthma-prone clinical phenotype. Specifically, respiratory infection– and asthma-prone children experienced colonization at a significantly earlier age than nonprone children did for all three bacteria. In an analysis of individual conditions, early Mcat colonization significantly associated with pneumonia, sinusitis, and asthma susceptibility; Hflu with pneumonia, sinusitis, influenza, and allergic rhinitis; and pneumococcus with sinusitis.
Since early colonization with the three bacterial respiratory pathogens was strongly associated with respiratory illnesses and asthma, nasopharyngeal microbiome analysis was performed on an available subset of samples. Bacterial diversity trended lower in infection- and asthma-prone children, consistent with dysbiosis in the respiratory infection– and asthma-prone clinical phenotype. Nine different bacteria genera were found to be differentially abundant when comparing respiratory infection– and asthma-prone and nonprone children, pointing the way to possible interventions to make the respiratory infection– and asthma-prone child nasopharyngeal microbiome more like the nonprone child.
As I have written previously in this column, recent accumulating data have shed light on the importance of the human microbiome in modulating immune homeostasis and disease susceptibility.6 My group is working toward generating new knowledge for the long-term goal of identifying new therapeutic strategies to facilitate a protective, diverse nasopharyngeal microbiome (with appropriately tuned intranasal probiotics) to prevent respiratory pathogen colonization and/or subsequent progression to respiratory infection and asthma. Also, vaccines directed against colonization-enhancing members of the microbiome may provide a means to indirectly control respiratory pathogen nasopharyngeal colonization.
Dr. Pichichero is a specialist in pediatric infectious diseases and director of the Research Institute at Rochester (N.Y.) General Hospital. He has no conflicts to declare. Contact him at [email protected]
References
1. Man WH et al. Nat Rev Microbiol. 2017;15(5):259-70.
2. Pichichero ME. J Infect. 2020;80(6):614-22.
3. Ren D et al. Clin Infect Dis. 2019;68(9):1566-74.
4. Pichichero ME et al. Pediatr Infect Dis J. 2013;32(11):1163-8.
5. Chapman T et al. PLoS One. 2020 Dec 11;15(12).
6. Blaser MJ. The microbiome revolution. J Clin Invest. 2014;124:4162-5.
‘Long haul’ COVID recovery worse than cancer rehab for some: CDC
People experiencing ongoing or “long-haul” symptoms after COVID-19 illness were more likely to report pain, challenges with physical activities, and “substantially worse health,” compared with people needing rehabilitation because of cancer, lead author Jessica Rogers-Brown, PhD, and colleagues report.
The study was published online July 9 in Morbidity and Mortality Weekly Report (MMWR).
The CDC investigators compared the self-reported physical and mental health symptoms, physical endurance, and use of health services of 1,295 outpatients recovering from COVID-19 and a control group of another 2,395 outpatients rehabilitating from a previous or current cancer diagnosis who had not experienced COVID-19.
Researchers used electronic health record data from January 2020 to March 2021 in the Select Medical network of outpatient clinics. The study included patients from 36 states and the District of Columbia.
Compared with people referred for cancer rehabilitation, those with COVID-19 symptoms lasting beyond 4 weeks were 2.3 times more likely to report pain, 1.8 times more likely to report worse physical health, and 1.6 times more likely to report difficulty with physical activities, an adjusted odds ratio analysis reveals.
The COVID-19 rehabilitation group also performed significantly worse on a 6-minute walk test, suggesting less physical endurance than people recovering from cancer (P < .001). They also used more rehabilitation services overall than the control group.
The researchers suggest services tailored to the unique physical and mental health rehabilitation needs of the post–COVID-19 patient population could be warranted.
The study does not suggest all people recovering with COVID-19 will fare worse than people recovering from cancer, the authors caution. They note that “these results should not be interpreted to mean that post–COVID-19 patients overall had poorer physical and mental health than patients with cancer.”
“Instead, results indicate that post–COVID-19 patients specifically referred to a large physical rehabilitation network had poorer health measures than those referred for cancer, which indicates that some patients recovering from COVID-19 had substantial rehabilitation needs.”
A version of this article first appeared on Medscape.com.
People experiencing ongoing or “long-haul” symptoms after COVID-19 illness were more likely to report pain, challenges with physical activities, and “substantially worse health,” compared with people needing rehabilitation because of cancer, lead author Jessica Rogers-Brown, PhD, and colleagues report.
The study was published online July 9 in Morbidity and Mortality Weekly Report (MMWR).
The CDC investigators compared the self-reported physical and mental health symptoms, physical endurance, and use of health services of 1,295 outpatients recovering from COVID-19 and a control group of another 2,395 outpatients rehabilitating from a previous or current cancer diagnosis who had not experienced COVID-19.
Researchers used electronic health record data from January 2020 to March 2021 in the Select Medical network of outpatient clinics. The study included patients from 36 states and the District of Columbia.
Compared with people referred for cancer rehabilitation, those with COVID-19 symptoms lasting beyond 4 weeks were 2.3 times more likely to report pain, 1.8 times more likely to report worse physical health, and 1.6 times more likely to report difficulty with physical activities, an adjusted odds ratio analysis reveals.
The COVID-19 rehabilitation group also performed significantly worse on a 6-minute walk test, suggesting less physical endurance than people recovering from cancer (P < .001). They also used more rehabilitation services overall than the control group.
The researchers suggest services tailored to the unique physical and mental health rehabilitation needs of the post–COVID-19 patient population could be warranted.
The study does not suggest all people recovering with COVID-19 will fare worse than people recovering from cancer, the authors caution. They note that “these results should not be interpreted to mean that post–COVID-19 patients overall had poorer physical and mental health than patients with cancer.”
“Instead, results indicate that post–COVID-19 patients specifically referred to a large physical rehabilitation network had poorer health measures than those referred for cancer, which indicates that some patients recovering from COVID-19 had substantial rehabilitation needs.”
A version of this article first appeared on Medscape.com.
People experiencing ongoing or “long-haul” symptoms after COVID-19 illness were more likely to report pain, challenges with physical activities, and “substantially worse health,” compared with people needing rehabilitation because of cancer, lead author Jessica Rogers-Brown, PhD, and colleagues report.
The study was published online July 9 in Morbidity and Mortality Weekly Report (MMWR).
The CDC investigators compared the self-reported physical and mental health symptoms, physical endurance, and use of health services of 1,295 outpatients recovering from COVID-19 and a control group of another 2,395 outpatients rehabilitating from a previous or current cancer diagnosis who had not experienced COVID-19.
Researchers used electronic health record data from January 2020 to March 2021 in the Select Medical network of outpatient clinics. The study included patients from 36 states and the District of Columbia.
Compared with people referred for cancer rehabilitation, those with COVID-19 symptoms lasting beyond 4 weeks were 2.3 times more likely to report pain, 1.8 times more likely to report worse physical health, and 1.6 times more likely to report difficulty with physical activities, an adjusted odds ratio analysis reveals.
The COVID-19 rehabilitation group also performed significantly worse on a 6-minute walk test, suggesting less physical endurance than people recovering from cancer (P < .001). They also used more rehabilitation services overall than the control group.
The researchers suggest services tailored to the unique physical and mental health rehabilitation needs of the post–COVID-19 patient population could be warranted.
The study does not suggest all people recovering with COVID-19 will fare worse than people recovering from cancer, the authors caution. They note that “these results should not be interpreted to mean that post–COVID-19 patients overall had poorer physical and mental health than patients with cancer.”
“Instead, results indicate that post–COVID-19 patients specifically referred to a large physical rehabilitation network had poorer health measures than those referred for cancer, which indicates that some patients recovering from COVID-19 had substantial rehabilitation needs.”
A version of this article first appeared on Medscape.com.
South Asian ancestry associated with twice the risk of heart disease
according to the results of a new study.
These findings confirm previous reports and practice guidelines that identify South Asian ancestry as a risk enhancer for atherosclerotic cardiovascular disease (ASCVD), suggesting that earlier heart disease screening and prevention is warranted in this patient population, lead author Aniruddh P. Patel, MD, research fellow at the Center for Genomic Medicine, Massachusetts General Hospital, Boston, and colleagues said.
“Previous studies in multiple countries have estimated a 1.7- to 4-fold higher risk of ASCVD among South Asian individuals, compared with other ancestries, but have important potential limitations,” Dr. Patel and colleagues wrote in the paper on their prospective cohort study, published in Circulation.
The INTERHEART case-control study, for example, which assessed risk factors for acute myocardial infarction among more than 15,000 cases from 52 countries, is now 2 decades old, and “may not reflect recent advances in cardiovascular disease prevention,” the investigators wrote.
Most studies in the area have been small and retrospective, they added, and have not adequately assessed emerging risk factors, such as prediabetes, which appear to play a relatively greater role in the development of heart disease among South Asians.
Methods and results
To address this knowledge gap, Dr. Patel and colleagues analyzed data from the UK Biobank prospective cohort study, including 449,349 middle-aged participants of European ancestry and 8,124 similarly aged participants of South Asian descent who did not have heart disease upon enrollment. Respective rates of incident ASCVD (i.e., MI, ischemic stroke, or coronary revascularization) were analyzed in the context of a variety of lifestyle, anthropometric, and clinical factors.
After a median follow-up of 11.1 years, individuals of South Asian descent had an incident ASCVD rate of 6.8%, compared with 4.4% for individuals of European descent, representing twice the relative risk (adjusted hazard ratio, 2.03; 95% CI, 1.86-2.22; P < .001). Even after accounting for all covariates, risk of ASCVD remained 45% higher for South Asian individuals (aHR, 1.45; 95% CI, 1.28-1.65; P < .001). This elevation in risk was not captured by existing risk calculators, including the American College of Cardiology/American Heart Association Pooled Cohort Equations, or the QRISK3 equations.
The findings were “largely consistent across a range of age, sex, and clinical subgroups,” and “confirm and extend previous reports that hypertension, diabetes, and central adiposity are the leading associations in this observed disparity,” the investigators wrote.
Two diabetes subtypes are more prevalent in South Asians
Hypertension, diabetes, and central adiposity do not fully explain South Asians’ higher risk for ASCVD, wrote Namratha R. Kandula, MD, of Northwestern University Medical Center, Chicago, and Alka M. Kanaya, MD, of the University of California, San Francisco, in an accompanying editorial published in Circulation.
Some of the undetected risk may stem from unique diabetes disease factors, Dr. Kandula and Dr. Kanaya added.
“Newer data have demonstrated distinct subtypes of type 2 diabetes, with South Asians having a higher prevalence of both a severe insulin resistant with obesity subtype and a less recognized severe insulin deficient subtype,” they wrote. “Importantly, both of these more prevalent diabetes subtypes in South Asians were associated with a higher incidence of coronary artery calcium, a marker of subclinical atherosclerosis and strong predictor of future ASCVD, compared to other diabetes subtypes.”
Diabetes rate is higher for South Asians in the U.S.
Although the present study was conducted in the United Kingdom, the findings likely apply to individuals of South Asian ancestry living in the United States, according to principal author Amit V. Khera, MD, associate director of the precision medicine unit at the Center for Genomic Medicine, Massachusetts General Hospital.
“There are already more than 5 million individuals of South Asian ancestry in the U.S. and this represents one of the fastest-growing ethnic subgroups,” Dr. Khera said in an interview. “As in our study of individuals in the U.K., South Asians in the U.S. suffer from diabetes at much higher rates – 23% versus 12% – and this often occurs even in the absence of obesity.”
Dr. Khera noted that the 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease identify South Asian ancestry as a risk-enhancing factor, calling this a “stopgap measure.” More work is needed, he said, in the research arena and in the clinic.
Zero South Asians included in studies used to develop risk estimator
“I think the first step is to simply acknowledge that the risk estimators we use in clinical practice have important limitations when it comes to diverse patient populations,” Dr. Khera said in an interview. “We saw this in our study, where – despite a more than doubling of risk – the predicted risk based on the equations used in primary care showed no difference. This risk estimator was developed based on legacy cohort studies, in [which] zero South Asians were included. Despite important differences across race/ethnicity, the current state-of-the-art in the U.S. is to use one equation for Black individuals and another for all other ethnicities.”
Experts suggest steps for reducing heart disease risk
While risk modeling remains suboptimal, Dr. Khera suggested that clinicians can take immediate steps to reduce the risk of heart disease among individuals with South Asian ancestry.
“Despite all of the uncertainty – we still don’t have a complete understanding of why the risk is so high – there are still several things primary care doctors can do for their patients,” Dr. Khera said.
Foremost, he recommended lifestyle and dietary counseling.
“Dietary counseling is particularly effective if put in the context of cultural norms,” Dr. Khera said. “Many South Asians consider fruit juices or white rice to be healthy, when they lead to rapid spikes in blood sugar.”
Dr. Khera also advised earlier heart disease screening, such as coronary calcium scanning “sometime between age 40-50 years,” noting that positive test results may motivate patients to start or adhere to medications, such as cholesterol-lowering therapies. If necessary, clinicians can also refer to heart centers for South Asian patients, which are becoming increasingly common.
According to Cheryl A.M. Anderson, PhD, chair of the AHA’s Council on Epidemiology and Prevention, and professor and dean of the Herbert Wertheim School of Public Health and Human Longevity Science at the University of California, San Diego, the current study suggests that heart disease management strategies for South Asian patients may be lacking.
“We have had a tradition of preventing or trying to treat heart disease in a fashion that doesn’t yet account for the increased risk that might be prevalent in those of South Asian ancestry,” Dr. Anderson said in an interview.
She suggested that improving associated risk-analysis tools could be beneficial, although the tools themselves, in the context of race or ethnicity, may present their own risks.
“We want to be mindful of potential adverse implications from having everything linked to one’s ancestry, which I think this tool doesn’t do,” Dr. Anderson said, referring to the AHA/ACC Pooled Cohort Equations. “But in sort of the bigger picture of things, we always want to expand and refine our toolkit.”
According to Rajesh Dash, MD, PhD, associate professor, cardiologist, and director of the South Asian Translational Heart Initiative (SSATHI) Prevention Clinic and CardioClick Telemedicine Clinic at Stanford (Calif.) HealthCare, the science supports more active risk mitigation strategies for South Asian patients, and the AHA and the ACC “are the two entities that need to lead the way.”
“Certainly the American Heart Association and the American College of Cardiology should be taking a more active leadership role in this,” Dr. Dash said in an interview.
In 2018, the AHA issued a scientific statement about the elevated risk of ASCVD among South Asian individuals, “but it did not rise to the level of specific recommendations, and did not necessarily go as far as to incorporate new screening parameters for that population,” Dr. Dash said. He also noted that the most recent AHA/ACC guideline identifies South Asian ancestry as a risk-enhancing feature, a statement similarly lacking in actionable value.
“That does not definitively lead someone like a primary care physician to a decision to start a statin, or to be more aggressive with a diagnostic workup, like a stress test, for instance, for a patient who they otherwise would not have done one in had they not been South Asian,” Dr. Dash said.
The steps taken by the AHA and the ACC are “a healthy step forward,” he noted, “but not nearly the degree of attention or vigilance that is required, as well as the level of action that is required to change the narrative for the population.”
At the SSATHI Prevention Clinic, Dr. Dash and colleagues aren’t waiting for the narrative to change, and are already taking a more aggressive approach.
The clinic has an average patient age of 41 years, “easily 15 years younger than the average age in most cardiology clinics,” Dr. Dash said, based on the fact that approximately two-thirds of heart attacks in South Asian individuals occur under the age of 55. “We have to look earlier.”
The SSATHI Prevention Clinic screens for both traditional and emerging risk factors, and Dr. Dash suggested that primary care doctors should do the same.
“If you have a South Asian patient as a primary care physician, you should be aggressively looking for risk factors, traditional ones to start, like elevated cholesterol, hypertension, diabetes, or – and I would argue strongly – prediabetes or insulin resistance.”
Dr. Dash also recommended looking into family history, and considering screening for inflammatory biomarkers, the latter of which are commonly elevated at an earlier age among South Asian individuals, and may have a relatively greater prognostic impact.
To encourage broader implementation of this kind of approach, Dr. Dash called for more large-scale studies. Ideally, these would be randomized clinical trials, but, realistically, real-world datasets may be the answer.
The study was supported by the National Heart, Lung, and Blood Institute; the Broad Institute at MIT and Harvard; the National Human Genome Research Institute; and others. The investigators disclosed relationships with IBM Research, Sanofi, Amgen, and others. Dr. Dash disclosed relationships with HealthPals and AstraZeneca. Dr. Anderson reported no relevant conflicts of interest.
according to the results of a new study.
These findings confirm previous reports and practice guidelines that identify South Asian ancestry as a risk enhancer for atherosclerotic cardiovascular disease (ASCVD), suggesting that earlier heart disease screening and prevention is warranted in this patient population, lead author Aniruddh P. Patel, MD, research fellow at the Center for Genomic Medicine, Massachusetts General Hospital, Boston, and colleagues said.
“Previous studies in multiple countries have estimated a 1.7- to 4-fold higher risk of ASCVD among South Asian individuals, compared with other ancestries, but have important potential limitations,” Dr. Patel and colleagues wrote in the paper on their prospective cohort study, published in Circulation.
The INTERHEART case-control study, for example, which assessed risk factors for acute myocardial infarction among more than 15,000 cases from 52 countries, is now 2 decades old, and “may not reflect recent advances in cardiovascular disease prevention,” the investigators wrote.
Most studies in the area have been small and retrospective, they added, and have not adequately assessed emerging risk factors, such as prediabetes, which appear to play a relatively greater role in the development of heart disease among South Asians.
Methods and results
To address this knowledge gap, Dr. Patel and colleagues analyzed data from the UK Biobank prospective cohort study, including 449,349 middle-aged participants of European ancestry and 8,124 similarly aged participants of South Asian descent who did not have heart disease upon enrollment. Respective rates of incident ASCVD (i.e., MI, ischemic stroke, or coronary revascularization) were analyzed in the context of a variety of lifestyle, anthropometric, and clinical factors.
After a median follow-up of 11.1 years, individuals of South Asian descent had an incident ASCVD rate of 6.8%, compared with 4.4% for individuals of European descent, representing twice the relative risk (adjusted hazard ratio, 2.03; 95% CI, 1.86-2.22; P < .001). Even after accounting for all covariates, risk of ASCVD remained 45% higher for South Asian individuals (aHR, 1.45; 95% CI, 1.28-1.65; P < .001). This elevation in risk was not captured by existing risk calculators, including the American College of Cardiology/American Heart Association Pooled Cohort Equations, or the QRISK3 equations.
The findings were “largely consistent across a range of age, sex, and clinical subgroups,” and “confirm and extend previous reports that hypertension, diabetes, and central adiposity are the leading associations in this observed disparity,” the investigators wrote.
Two diabetes subtypes are more prevalent in South Asians
Hypertension, diabetes, and central adiposity do not fully explain South Asians’ higher risk for ASCVD, wrote Namratha R. Kandula, MD, of Northwestern University Medical Center, Chicago, and Alka M. Kanaya, MD, of the University of California, San Francisco, in an accompanying editorial published in Circulation.
Some of the undetected risk may stem from unique diabetes disease factors, Dr. Kandula and Dr. Kanaya added.
“Newer data have demonstrated distinct subtypes of type 2 diabetes, with South Asians having a higher prevalence of both a severe insulin resistant with obesity subtype and a less recognized severe insulin deficient subtype,” they wrote. “Importantly, both of these more prevalent diabetes subtypes in South Asians were associated with a higher incidence of coronary artery calcium, a marker of subclinical atherosclerosis and strong predictor of future ASCVD, compared to other diabetes subtypes.”
Diabetes rate is higher for South Asians in the U.S.
Although the present study was conducted in the United Kingdom, the findings likely apply to individuals of South Asian ancestry living in the United States, according to principal author Amit V. Khera, MD, associate director of the precision medicine unit at the Center for Genomic Medicine, Massachusetts General Hospital.
“There are already more than 5 million individuals of South Asian ancestry in the U.S. and this represents one of the fastest-growing ethnic subgroups,” Dr. Khera said in an interview. “As in our study of individuals in the U.K., South Asians in the U.S. suffer from diabetes at much higher rates – 23% versus 12% – and this often occurs even in the absence of obesity.”
Dr. Khera noted that the 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease identify South Asian ancestry as a risk-enhancing factor, calling this a “stopgap measure.” More work is needed, he said, in the research arena and in the clinic.
Zero South Asians included in studies used to develop risk estimator
“I think the first step is to simply acknowledge that the risk estimators we use in clinical practice have important limitations when it comes to diverse patient populations,” Dr. Khera said in an interview. “We saw this in our study, where – despite a more than doubling of risk – the predicted risk based on the equations used in primary care showed no difference. This risk estimator was developed based on legacy cohort studies, in [which] zero South Asians were included. Despite important differences across race/ethnicity, the current state-of-the-art in the U.S. is to use one equation for Black individuals and another for all other ethnicities.”
Experts suggest steps for reducing heart disease risk
While risk modeling remains suboptimal, Dr. Khera suggested that clinicians can take immediate steps to reduce the risk of heart disease among individuals with South Asian ancestry.
“Despite all of the uncertainty – we still don’t have a complete understanding of why the risk is so high – there are still several things primary care doctors can do for their patients,” Dr. Khera said.
Foremost, he recommended lifestyle and dietary counseling.
“Dietary counseling is particularly effective if put in the context of cultural norms,” Dr. Khera said. “Many South Asians consider fruit juices or white rice to be healthy, when they lead to rapid spikes in blood sugar.”
Dr. Khera also advised earlier heart disease screening, such as coronary calcium scanning “sometime between age 40-50 years,” noting that positive test results may motivate patients to start or adhere to medications, such as cholesterol-lowering therapies. If necessary, clinicians can also refer to heart centers for South Asian patients, which are becoming increasingly common.
According to Cheryl A.M. Anderson, PhD, chair of the AHA’s Council on Epidemiology and Prevention, and professor and dean of the Herbert Wertheim School of Public Health and Human Longevity Science at the University of California, San Diego, the current study suggests that heart disease management strategies for South Asian patients may be lacking.
“We have had a tradition of preventing or trying to treat heart disease in a fashion that doesn’t yet account for the increased risk that might be prevalent in those of South Asian ancestry,” Dr. Anderson said in an interview.
She suggested that improving associated risk-analysis tools could be beneficial, although the tools themselves, in the context of race or ethnicity, may present their own risks.
“We want to be mindful of potential adverse implications from having everything linked to one’s ancestry, which I think this tool doesn’t do,” Dr. Anderson said, referring to the AHA/ACC Pooled Cohort Equations. “But in sort of the bigger picture of things, we always want to expand and refine our toolkit.”
According to Rajesh Dash, MD, PhD, associate professor, cardiologist, and director of the South Asian Translational Heart Initiative (SSATHI) Prevention Clinic and CardioClick Telemedicine Clinic at Stanford (Calif.) HealthCare, the science supports more active risk mitigation strategies for South Asian patients, and the AHA and the ACC “are the two entities that need to lead the way.”
“Certainly the American Heart Association and the American College of Cardiology should be taking a more active leadership role in this,” Dr. Dash said in an interview.
In 2018, the AHA issued a scientific statement about the elevated risk of ASCVD among South Asian individuals, “but it did not rise to the level of specific recommendations, and did not necessarily go as far as to incorporate new screening parameters for that population,” Dr. Dash said. He also noted that the most recent AHA/ACC guideline identifies South Asian ancestry as a risk-enhancing feature, a statement similarly lacking in actionable value.
“That does not definitively lead someone like a primary care physician to a decision to start a statin, or to be more aggressive with a diagnostic workup, like a stress test, for instance, for a patient who they otherwise would not have done one in had they not been South Asian,” Dr. Dash said.
The steps taken by the AHA and the ACC are “a healthy step forward,” he noted, “but not nearly the degree of attention or vigilance that is required, as well as the level of action that is required to change the narrative for the population.”
At the SSATHI Prevention Clinic, Dr. Dash and colleagues aren’t waiting for the narrative to change, and are already taking a more aggressive approach.
The clinic has an average patient age of 41 years, “easily 15 years younger than the average age in most cardiology clinics,” Dr. Dash said, based on the fact that approximately two-thirds of heart attacks in South Asian individuals occur under the age of 55. “We have to look earlier.”
The SSATHI Prevention Clinic screens for both traditional and emerging risk factors, and Dr. Dash suggested that primary care doctors should do the same.
“If you have a South Asian patient as a primary care physician, you should be aggressively looking for risk factors, traditional ones to start, like elevated cholesterol, hypertension, diabetes, or – and I would argue strongly – prediabetes or insulin resistance.”
Dr. Dash also recommended looking into family history, and considering screening for inflammatory biomarkers, the latter of which are commonly elevated at an earlier age among South Asian individuals, and may have a relatively greater prognostic impact.
To encourage broader implementation of this kind of approach, Dr. Dash called for more large-scale studies. Ideally, these would be randomized clinical trials, but, realistically, real-world datasets may be the answer.
The study was supported by the National Heart, Lung, and Blood Institute; the Broad Institute at MIT and Harvard; the National Human Genome Research Institute; and others. The investigators disclosed relationships with IBM Research, Sanofi, Amgen, and others. Dr. Dash disclosed relationships with HealthPals and AstraZeneca. Dr. Anderson reported no relevant conflicts of interest.
according to the results of a new study.
These findings confirm previous reports and practice guidelines that identify South Asian ancestry as a risk enhancer for atherosclerotic cardiovascular disease (ASCVD), suggesting that earlier heart disease screening and prevention is warranted in this patient population, lead author Aniruddh P. Patel, MD, research fellow at the Center for Genomic Medicine, Massachusetts General Hospital, Boston, and colleagues said.
“Previous studies in multiple countries have estimated a 1.7- to 4-fold higher risk of ASCVD among South Asian individuals, compared with other ancestries, but have important potential limitations,” Dr. Patel and colleagues wrote in the paper on their prospective cohort study, published in Circulation.
The INTERHEART case-control study, for example, which assessed risk factors for acute myocardial infarction among more than 15,000 cases from 52 countries, is now 2 decades old, and “may not reflect recent advances in cardiovascular disease prevention,” the investigators wrote.
Most studies in the area have been small and retrospective, they added, and have not adequately assessed emerging risk factors, such as prediabetes, which appear to play a relatively greater role in the development of heart disease among South Asians.
Methods and results
To address this knowledge gap, Dr. Patel and colleagues analyzed data from the UK Biobank prospective cohort study, including 449,349 middle-aged participants of European ancestry and 8,124 similarly aged participants of South Asian descent who did not have heart disease upon enrollment. Respective rates of incident ASCVD (i.e., MI, ischemic stroke, or coronary revascularization) were analyzed in the context of a variety of lifestyle, anthropometric, and clinical factors.
After a median follow-up of 11.1 years, individuals of South Asian descent had an incident ASCVD rate of 6.8%, compared with 4.4% for individuals of European descent, representing twice the relative risk (adjusted hazard ratio, 2.03; 95% CI, 1.86-2.22; P < .001). Even after accounting for all covariates, risk of ASCVD remained 45% higher for South Asian individuals (aHR, 1.45; 95% CI, 1.28-1.65; P < .001). This elevation in risk was not captured by existing risk calculators, including the American College of Cardiology/American Heart Association Pooled Cohort Equations, or the QRISK3 equations.
The findings were “largely consistent across a range of age, sex, and clinical subgroups,” and “confirm and extend previous reports that hypertension, diabetes, and central adiposity are the leading associations in this observed disparity,” the investigators wrote.
Two diabetes subtypes are more prevalent in South Asians
Hypertension, diabetes, and central adiposity do not fully explain South Asians’ higher risk for ASCVD, wrote Namratha R. Kandula, MD, of Northwestern University Medical Center, Chicago, and Alka M. Kanaya, MD, of the University of California, San Francisco, in an accompanying editorial published in Circulation.
Some of the undetected risk may stem from unique diabetes disease factors, Dr. Kandula and Dr. Kanaya added.
“Newer data have demonstrated distinct subtypes of type 2 diabetes, with South Asians having a higher prevalence of both a severe insulin resistant with obesity subtype and a less recognized severe insulin deficient subtype,” they wrote. “Importantly, both of these more prevalent diabetes subtypes in South Asians were associated with a higher incidence of coronary artery calcium, a marker of subclinical atherosclerosis and strong predictor of future ASCVD, compared to other diabetes subtypes.”
Diabetes rate is higher for South Asians in the U.S.
Although the present study was conducted in the United Kingdom, the findings likely apply to individuals of South Asian ancestry living in the United States, according to principal author Amit V. Khera, MD, associate director of the precision medicine unit at the Center for Genomic Medicine, Massachusetts General Hospital.
“There are already more than 5 million individuals of South Asian ancestry in the U.S. and this represents one of the fastest-growing ethnic subgroups,” Dr. Khera said in an interview. “As in our study of individuals in the U.K., South Asians in the U.S. suffer from diabetes at much higher rates – 23% versus 12% – and this often occurs even in the absence of obesity.”
Dr. Khera noted that the 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease identify South Asian ancestry as a risk-enhancing factor, calling this a “stopgap measure.” More work is needed, he said, in the research arena and in the clinic.
Zero South Asians included in studies used to develop risk estimator
“I think the first step is to simply acknowledge that the risk estimators we use in clinical practice have important limitations when it comes to diverse patient populations,” Dr. Khera said in an interview. “We saw this in our study, where – despite a more than doubling of risk – the predicted risk based on the equations used in primary care showed no difference. This risk estimator was developed based on legacy cohort studies, in [which] zero South Asians were included. Despite important differences across race/ethnicity, the current state-of-the-art in the U.S. is to use one equation for Black individuals and another for all other ethnicities.”
Experts suggest steps for reducing heart disease risk
While risk modeling remains suboptimal, Dr. Khera suggested that clinicians can take immediate steps to reduce the risk of heart disease among individuals with South Asian ancestry.
“Despite all of the uncertainty – we still don’t have a complete understanding of why the risk is so high – there are still several things primary care doctors can do for their patients,” Dr. Khera said.
Foremost, he recommended lifestyle and dietary counseling.
“Dietary counseling is particularly effective if put in the context of cultural norms,” Dr. Khera said. “Many South Asians consider fruit juices or white rice to be healthy, when they lead to rapid spikes in blood sugar.”
Dr. Khera also advised earlier heart disease screening, such as coronary calcium scanning “sometime between age 40-50 years,” noting that positive test results may motivate patients to start or adhere to medications, such as cholesterol-lowering therapies. If necessary, clinicians can also refer to heart centers for South Asian patients, which are becoming increasingly common.
According to Cheryl A.M. Anderson, PhD, chair of the AHA’s Council on Epidemiology and Prevention, and professor and dean of the Herbert Wertheim School of Public Health and Human Longevity Science at the University of California, San Diego, the current study suggests that heart disease management strategies for South Asian patients may be lacking.
“We have had a tradition of preventing or trying to treat heart disease in a fashion that doesn’t yet account for the increased risk that might be prevalent in those of South Asian ancestry,” Dr. Anderson said in an interview.
She suggested that improving associated risk-analysis tools could be beneficial, although the tools themselves, in the context of race or ethnicity, may present their own risks.
“We want to be mindful of potential adverse implications from having everything linked to one’s ancestry, which I think this tool doesn’t do,” Dr. Anderson said, referring to the AHA/ACC Pooled Cohort Equations. “But in sort of the bigger picture of things, we always want to expand and refine our toolkit.”
According to Rajesh Dash, MD, PhD, associate professor, cardiologist, and director of the South Asian Translational Heart Initiative (SSATHI) Prevention Clinic and CardioClick Telemedicine Clinic at Stanford (Calif.) HealthCare, the science supports more active risk mitigation strategies for South Asian patients, and the AHA and the ACC “are the two entities that need to lead the way.”
“Certainly the American Heart Association and the American College of Cardiology should be taking a more active leadership role in this,” Dr. Dash said in an interview.
In 2018, the AHA issued a scientific statement about the elevated risk of ASCVD among South Asian individuals, “but it did not rise to the level of specific recommendations, and did not necessarily go as far as to incorporate new screening parameters for that population,” Dr. Dash said. He also noted that the most recent AHA/ACC guideline identifies South Asian ancestry as a risk-enhancing feature, a statement similarly lacking in actionable value.
“That does not definitively lead someone like a primary care physician to a decision to start a statin, or to be more aggressive with a diagnostic workup, like a stress test, for instance, for a patient who they otherwise would not have done one in had they not been South Asian,” Dr. Dash said.
The steps taken by the AHA and the ACC are “a healthy step forward,” he noted, “but not nearly the degree of attention or vigilance that is required, as well as the level of action that is required to change the narrative for the population.”
At the SSATHI Prevention Clinic, Dr. Dash and colleagues aren’t waiting for the narrative to change, and are already taking a more aggressive approach.
The clinic has an average patient age of 41 years, “easily 15 years younger than the average age in most cardiology clinics,” Dr. Dash said, based on the fact that approximately two-thirds of heart attacks in South Asian individuals occur under the age of 55. “We have to look earlier.”
The SSATHI Prevention Clinic screens for both traditional and emerging risk factors, and Dr. Dash suggested that primary care doctors should do the same.
“If you have a South Asian patient as a primary care physician, you should be aggressively looking for risk factors, traditional ones to start, like elevated cholesterol, hypertension, diabetes, or – and I would argue strongly – prediabetes or insulin resistance.”
Dr. Dash also recommended looking into family history, and considering screening for inflammatory biomarkers, the latter of which are commonly elevated at an earlier age among South Asian individuals, and may have a relatively greater prognostic impact.
To encourage broader implementation of this kind of approach, Dr. Dash called for more large-scale studies. Ideally, these would be randomized clinical trials, but, realistically, real-world datasets may be the answer.
The study was supported by the National Heart, Lung, and Blood Institute; the Broad Institute at MIT and Harvard; the National Human Genome Research Institute; and others. The investigators disclosed relationships with IBM Research, Sanofi, Amgen, and others. Dr. Dash disclosed relationships with HealthPals and AstraZeneca. Dr. Anderson reported no relevant conflicts of interest.
FROM CIRCULATION
Meta-analysis supports cardiovascular benefits of EPA
Support for a cardiovascular benefit of omega-3 fatty acids, particularly eicosapentaenoic acid (EPA), has come from a new systematic review and meta-analysis of randomized trials.
The meta-analysis of 38 randomized controlled trials found that omega-3 fatty acids improved cardiovascular outcomes, with a greater reduction in cardiovascular risk in studies of EPA alone rather than of combined eicosapentaenoic plus docosahexaenoic acid (DHA) supplements.
The paper was published online in EClinicalMedicine.
Senior author Deepak Bhatt, MD, Brigham and Women’s Hospital, Boston, was also lead investigator of the REDUCE-IT trial, which is included in the analysis and showed a 25% relative risk reduction in major cardiovascular events with a high-dose EPA product.
But the REDUCE-IT trial has been mired in controversy, with suggestions that the benefit seen might have been exaggerated because of the use of a harmful placebo. In addition, a second large trial of high-dose omega-3 fatty acids, STRENGTH (which tested a combination EPA/DHA product) showed no benefit on cardiovascular outcomes.
Dr. Bhatt said the new meta-analysis provides “a totality of evidence” that “supports a robust and consistent benefit of EPA.”
In the review, the authors concluded: “In this systematic review and meta-analysis, we noted moderate certainty of evidence favoring omega-3 fatty acids for reducing cardiovascular mortality and outcomes. ... The magnitude of relative reductions was robust in EPA trials versus those of EPA+DHA, suggesting differential effects of EPA and DHA in cardiovascular risk reduction.”
Controversy continues
But commenting on the publication for an interview, Steven Nissen, MD, Cleveland Clinic, who led the STRENGTH trial, pointed out that 85% of the EPA data in the new meta-analysis came from REDUCE-IT, so the results were a “foregone conclusion.”
“The purpose of a meta-analysis is to answer scientific questions when existing studies are too small to yield statistically robust results. That is not the case here,” Dr. Nissen stated.
He added: “There are only two major trials of EPA and both have important flaws. REDUCE-IT used a questionable placebo (mineral oil) and JELIS was an open-label trial that studied patients with baseline LDL [cholesterol] of 180 mg/dL that was not appropriately treated. A meta-analysis is only as good as the studies that it includes. The other EPA plus DHA studies were essentially neutral.”
Dr. Bhatt responded that, “to date, every randomized trial of EPA only has been positive. Some have been placebo controlled, some have been open label. This meta-analysis corroborates the results of each of those trials in a statistically robust way.”
He added: “Of course, REDUCE-IT is the most rigorous, contemporary trial of EPA. However, in our meta-analysis, even when excluding REDUCE-IT (or for that matter, JELIS), the EPA trials still significantly reduced cardiovascular events.”
Dr. Bhatt also pointed out that two randomized imaging studies, CHERRY and EVAPORATE, have shown benefits of EPA.
“Beyond the clinical trial data, there is a growing amount of evidence supporting the unique biological actions of different omega-3 fatty acids. EPA, in particular, appears to have the strongest basic science evidence supporting cardiovascular benefits. Overall, it is a remarkably consistent scientific story in support of EPA’s beneficial effects on cardiovascular health,” he stated.
38 trials included
For the current paper, Dr. Bhatt and coauthors performed a comprehensive literature search for randomized trials comparing omega-3 fatty acids with control (placebo, no supplementation, or lower dose of omega-3 fatty acids) in adults, with a follow-up of at least 12 months, and mortality and cardiovascular outcomes as endpoints.
Ultimately, 38 trials encompassing 149,051 patients were included. Of these, four trials compared EPA with control, 34 trials compared EPA+DHA with control, and 22 trials were in primary prevention. The dose of omega-3 fatty acids ranged from 0.4 g/day to 5.5 g/day.
A total of 25 trials with 143,514 individuals reported 5,550 events of cardiovascular mortality, and 24 trials with 140,983 individuals reported 10,795 events of all-cause mortality.
Omega-3 fatty acids were associated with reduced cardiovascular mortality (rate ratio, 0.93; P = .01), but not all-cause mortality (RR, 0.97; P = .27). The meta-analysis showed reduction in cardiovascular mortality with EPA monotherapy (RR, 0.82; P = .04) and EPA+DHA combination (RR, 0.94; P = .02).
A total of 20 trials with 125,611 individuals reported 2,989 nonfatal myocardial infarction events, and 29 trials with 144,384 individuals reported 9,153 coronary heart disease (CHD) events.
Omega-3 fatty acids were associated with reducing nonfatal MI (RR, 0.87; P = .0001) and CHD (RR, 0.91; P = .0002). The meta-analysis showed higher risk reductions in nonfatal MI with EPA monotherapy (RR, 0.72; P = .00002) than with EPA+DHA combination (RR, 0.92; P = .05), and also for CHD events with EPA monotherapy (RR, 0.73; P = .00004) than with EPA+DHA combination (RR, 0.94; P = .01).
A total of 17 trials (n = 135,019) reported 13,234 events of MACE, and 13 trials (n = 117,890) reported 7,416 events of revascularization.
Omega-3 fatty acids were associated with reducing MACE (RR, 0.95; P = .002) and revascularization (RR, 0.91; P = .0001). The meta-analysis showed higher risk reductions in MACE with EPA monotherapy (RR, 0.78; P = .00000001), whereas EPA+DHA combination did not reduce MACE (RR, 0.99; P = .48). This effect was consistent for revascularization.
A total of eight trials with 65,404 individuals reported 935 nonfatal strokes, and eight trials with 51,336 individuals reported 1,572 events of atrial fibrillation (AFib).
Omega-3 fatty acids did not significantly reduce nonfatal stroke (RR, 1.04; P = .55), but EPA monotherapy was associated with a reduction of nonfatal stroke, compared with control (RR: 0.71; P = .01).
Conversely, omega-3 fatty acids were associated with increased risk for AFib (RR, 1.26; P = .004), with a higher risk with EPA monotherapy than with control (RR, 1.35; P = .004).
Overall, omega-3 fatty acids did not prevent sudden cardiac death or increase gastrointestinal-related adverse events, total bleeding, or major or minor bleeding; however, the meta-analysis showed a higher risk of total bleeding with EPA monotherapy than with control (RR, 1.49; P = .006).
An influence analysis with stepwise exclusion of one trial at a time, including REDUCE-IT, did not alter the overall summary estimates. “Despite the exclusion of REDUCE-IT, EPA monotherapy reduced MACE by 23%, compared with the control,” the authors reported.
They said these new findings also have important implications for clinical practice and treatment guidelines.
“After REDUCE-IT, several national and international guidelines endorsed EPA in their therapeutic recommendations. However, the publication of two recent negative trials of EPA + DHA has created some confusion in the scientific community about the value of omega-3 FAs in preventing atherosclerotic cardiovascular disease [ASCVD],” they stated.
“This meta-analysis provides reassurance about the role of omega-3 fatty acids, specifically EPA, in the current treatment framework of ASCVD residual cardiovascular risk reduction and encourages investigators to explore further the cardiovascular effects of EPA across different clinical settings,” they added.
REDUCE-IT was sponsored by Amarin. Brigham and Women’s Hospital receives research funding from Amarin for the work Dr. Bhatt did as the trial chair and as the international principal investigator. The present analysis was unfunded.
A version of this article first appeared on Medscape.com.
Support for a cardiovascular benefit of omega-3 fatty acids, particularly eicosapentaenoic acid (EPA), has come from a new systematic review and meta-analysis of randomized trials.
The meta-analysis of 38 randomized controlled trials found that omega-3 fatty acids improved cardiovascular outcomes, with a greater reduction in cardiovascular risk in studies of EPA alone rather than of combined eicosapentaenoic plus docosahexaenoic acid (DHA) supplements.
The paper was published online in EClinicalMedicine.
Senior author Deepak Bhatt, MD, Brigham and Women’s Hospital, Boston, was also lead investigator of the REDUCE-IT trial, which is included in the analysis and showed a 25% relative risk reduction in major cardiovascular events with a high-dose EPA product.
But the REDUCE-IT trial has been mired in controversy, with suggestions that the benefit seen might have been exaggerated because of the use of a harmful placebo. In addition, a second large trial of high-dose omega-3 fatty acids, STRENGTH (which tested a combination EPA/DHA product) showed no benefit on cardiovascular outcomes.
Dr. Bhatt said the new meta-analysis provides “a totality of evidence” that “supports a robust and consistent benefit of EPA.”
In the review, the authors concluded: “In this systematic review and meta-analysis, we noted moderate certainty of evidence favoring omega-3 fatty acids for reducing cardiovascular mortality and outcomes. ... The magnitude of relative reductions was robust in EPA trials versus those of EPA+DHA, suggesting differential effects of EPA and DHA in cardiovascular risk reduction.”
Controversy continues
But commenting on the publication for an interview, Steven Nissen, MD, Cleveland Clinic, who led the STRENGTH trial, pointed out that 85% of the EPA data in the new meta-analysis came from REDUCE-IT, so the results were a “foregone conclusion.”
“The purpose of a meta-analysis is to answer scientific questions when existing studies are too small to yield statistically robust results. That is not the case here,” Dr. Nissen stated.
He added: “There are only two major trials of EPA and both have important flaws. REDUCE-IT used a questionable placebo (mineral oil) and JELIS was an open-label trial that studied patients with baseline LDL [cholesterol] of 180 mg/dL that was not appropriately treated. A meta-analysis is only as good as the studies that it includes. The other EPA plus DHA studies were essentially neutral.”
Dr. Bhatt responded that, “to date, every randomized trial of EPA only has been positive. Some have been placebo controlled, some have been open label. This meta-analysis corroborates the results of each of those trials in a statistically robust way.”
He added: “Of course, REDUCE-IT is the most rigorous, contemporary trial of EPA. However, in our meta-analysis, even when excluding REDUCE-IT (or for that matter, JELIS), the EPA trials still significantly reduced cardiovascular events.”
Dr. Bhatt also pointed out that two randomized imaging studies, CHERRY and EVAPORATE, have shown benefits of EPA.
“Beyond the clinical trial data, there is a growing amount of evidence supporting the unique biological actions of different omega-3 fatty acids. EPA, in particular, appears to have the strongest basic science evidence supporting cardiovascular benefits. Overall, it is a remarkably consistent scientific story in support of EPA’s beneficial effects on cardiovascular health,” he stated.
38 trials included
For the current paper, Dr. Bhatt and coauthors performed a comprehensive literature search for randomized trials comparing omega-3 fatty acids with control (placebo, no supplementation, or lower dose of omega-3 fatty acids) in adults, with a follow-up of at least 12 months, and mortality and cardiovascular outcomes as endpoints.
Ultimately, 38 trials encompassing 149,051 patients were included. Of these, four trials compared EPA with control, 34 trials compared EPA+DHA with control, and 22 trials were in primary prevention. The dose of omega-3 fatty acids ranged from 0.4 g/day to 5.5 g/day.
A total of 25 trials with 143,514 individuals reported 5,550 events of cardiovascular mortality, and 24 trials with 140,983 individuals reported 10,795 events of all-cause mortality.
Omega-3 fatty acids were associated with reduced cardiovascular mortality (rate ratio, 0.93; P = .01), but not all-cause mortality (RR, 0.97; P = .27). The meta-analysis showed reduction in cardiovascular mortality with EPA monotherapy (RR, 0.82; P = .04) and EPA+DHA combination (RR, 0.94; P = .02).
A total of 20 trials with 125,611 individuals reported 2,989 nonfatal myocardial infarction events, and 29 trials with 144,384 individuals reported 9,153 coronary heart disease (CHD) events.
Omega-3 fatty acids were associated with reducing nonfatal MI (RR, 0.87; P = .0001) and CHD (RR, 0.91; P = .0002). The meta-analysis showed higher risk reductions in nonfatal MI with EPA monotherapy (RR, 0.72; P = .00002) than with EPA+DHA combination (RR, 0.92; P = .05), and also for CHD events with EPA monotherapy (RR, 0.73; P = .00004) than with EPA+DHA combination (RR, 0.94; P = .01).
A total of 17 trials (n = 135,019) reported 13,234 events of MACE, and 13 trials (n = 117,890) reported 7,416 events of revascularization.
Omega-3 fatty acids were associated with reducing MACE (RR, 0.95; P = .002) and revascularization (RR, 0.91; P = .0001). The meta-analysis showed higher risk reductions in MACE with EPA monotherapy (RR, 0.78; P = .00000001), whereas EPA+DHA combination did not reduce MACE (RR, 0.99; P = .48). This effect was consistent for revascularization.
A total of eight trials with 65,404 individuals reported 935 nonfatal strokes, and eight trials with 51,336 individuals reported 1,572 events of atrial fibrillation (AFib).
Omega-3 fatty acids did not significantly reduce nonfatal stroke (RR, 1.04; P = .55), but EPA monotherapy was associated with a reduction of nonfatal stroke, compared with control (RR: 0.71; P = .01).
Conversely, omega-3 fatty acids were associated with increased risk for AFib (RR, 1.26; P = .004), with a higher risk with EPA monotherapy than with control (RR, 1.35; P = .004).
Overall, omega-3 fatty acids did not prevent sudden cardiac death or increase gastrointestinal-related adverse events, total bleeding, or major or minor bleeding; however, the meta-analysis showed a higher risk of total bleeding with EPA monotherapy than with control (RR, 1.49; P = .006).
An influence analysis with stepwise exclusion of one trial at a time, including REDUCE-IT, did not alter the overall summary estimates. “Despite the exclusion of REDUCE-IT, EPA monotherapy reduced MACE by 23%, compared with the control,” the authors reported.
They said these new findings also have important implications for clinical practice and treatment guidelines.
“After REDUCE-IT, several national and international guidelines endorsed EPA in their therapeutic recommendations. However, the publication of two recent negative trials of EPA + DHA has created some confusion in the scientific community about the value of omega-3 FAs in preventing atherosclerotic cardiovascular disease [ASCVD],” they stated.
“This meta-analysis provides reassurance about the role of omega-3 fatty acids, specifically EPA, in the current treatment framework of ASCVD residual cardiovascular risk reduction and encourages investigators to explore further the cardiovascular effects of EPA across different clinical settings,” they added.
REDUCE-IT was sponsored by Amarin. Brigham and Women’s Hospital receives research funding from Amarin for the work Dr. Bhatt did as the trial chair and as the international principal investigator. The present analysis was unfunded.
A version of this article first appeared on Medscape.com.
Support for a cardiovascular benefit of omega-3 fatty acids, particularly eicosapentaenoic acid (EPA), has come from a new systematic review and meta-analysis of randomized trials.
The meta-analysis of 38 randomized controlled trials found that omega-3 fatty acids improved cardiovascular outcomes, with a greater reduction in cardiovascular risk in studies of EPA alone rather than of combined eicosapentaenoic plus docosahexaenoic acid (DHA) supplements.
The paper was published online in EClinicalMedicine.
Senior author Deepak Bhatt, MD, Brigham and Women’s Hospital, Boston, was also lead investigator of the REDUCE-IT trial, which is included in the analysis and showed a 25% relative risk reduction in major cardiovascular events with a high-dose EPA product.
But the REDUCE-IT trial has been mired in controversy, with suggestions that the benefit seen might have been exaggerated because of the use of a harmful placebo. In addition, a second large trial of high-dose omega-3 fatty acids, STRENGTH (which tested a combination EPA/DHA product) showed no benefit on cardiovascular outcomes.
Dr. Bhatt said the new meta-analysis provides “a totality of evidence” that “supports a robust and consistent benefit of EPA.”
In the review, the authors concluded: “In this systematic review and meta-analysis, we noted moderate certainty of evidence favoring omega-3 fatty acids for reducing cardiovascular mortality and outcomes. ... The magnitude of relative reductions was robust in EPA trials versus those of EPA+DHA, suggesting differential effects of EPA and DHA in cardiovascular risk reduction.”
Controversy continues
But commenting on the publication for an interview, Steven Nissen, MD, Cleveland Clinic, who led the STRENGTH trial, pointed out that 85% of the EPA data in the new meta-analysis came from REDUCE-IT, so the results were a “foregone conclusion.”
“The purpose of a meta-analysis is to answer scientific questions when existing studies are too small to yield statistically robust results. That is not the case here,” Dr. Nissen stated.
He added: “There are only two major trials of EPA and both have important flaws. REDUCE-IT used a questionable placebo (mineral oil) and JELIS was an open-label trial that studied patients with baseline LDL [cholesterol] of 180 mg/dL that was not appropriately treated. A meta-analysis is only as good as the studies that it includes. The other EPA plus DHA studies were essentially neutral.”
Dr. Bhatt responded that, “to date, every randomized trial of EPA only has been positive. Some have been placebo controlled, some have been open label. This meta-analysis corroborates the results of each of those trials in a statistically robust way.”
He added: “Of course, REDUCE-IT is the most rigorous, contemporary trial of EPA. However, in our meta-analysis, even when excluding REDUCE-IT (or for that matter, JELIS), the EPA trials still significantly reduced cardiovascular events.”
Dr. Bhatt also pointed out that two randomized imaging studies, CHERRY and EVAPORATE, have shown benefits of EPA.
“Beyond the clinical trial data, there is a growing amount of evidence supporting the unique biological actions of different omega-3 fatty acids. EPA, in particular, appears to have the strongest basic science evidence supporting cardiovascular benefits. Overall, it is a remarkably consistent scientific story in support of EPA’s beneficial effects on cardiovascular health,” he stated.
38 trials included
For the current paper, Dr. Bhatt and coauthors performed a comprehensive literature search for randomized trials comparing omega-3 fatty acids with control (placebo, no supplementation, or lower dose of omega-3 fatty acids) in adults, with a follow-up of at least 12 months, and mortality and cardiovascular outcomes as endpoints.
Ultimately, 38 trials encompassing 149,051 patients were included. Of these, four trials compared EPA with control, 34 trials compared EPA+DHA with control, and 22 trials were in primary prevention. The dose of omega-3 fatty acids ranged from 0.4 g/day to 5.5 g/day.
A total of 25 trials with 143,514 individuals reported 5,550 events of cardiovascular mortality, and 24 trials with 140,983 individuals reported 10,795 events of all-cause mortality.
Omega-3 fatty acids were associated with reduced cardiovascular mortality (rate ratio, 0.93; P = .01), but not all-cause mortality (RR, 0.97; P = .27). The meta-analysis showed reduction in cardiovascular mortality with EPA monotherapy (RR, 0.82; P = .04) and EPA+DHA combination (RR, 0.94; P = .02).
A total of 20 trials with 125,611 individuals reported 2,989 nonfatal myocardial infarction events, and 29 trials with 144,384 individuals reported 9,153 coronary heart disease (CHD) events.
Omega-3 fatty acids were associated with reducing nonfatal MI (RR, 0.87; P = .0001) and CHD (RR, 0.91; P = .0002). The meta-analysis showed higher risk reductions in nonfatal MI with EPA monotherapy (RR, 0.72; P = .00002) than with EPA+DHA combination (RR, 0.92; P = .05), and also for CHD events with EPA monotherapy (RR, 0.73; P = .00004) than with EPA+DHA combination (RR, 0.94; P = .01).
A total of 17 trials (n = 135,019) reported 13,234 events of MACE, and 13 trials (n = 117,890) reported 7,416 events of revascularization.
Omega-3 fatty acids were associated with reducing MACE (RR, 0.95; P = .002) and revascularization (RR, 0.91; P = .0001). The meta-analysis showed higher risk reductions in MACE with EPA monotherapy (RR, 0.78; P = .00000001), whereas EPA+DHA combination did not reduce MACE (RR, 0.99; P = .48). This effect was consistent for revascularization.
A total of eight trials with 65,404 individuals reported 935 nonfatal strokes, and eight trials with 51,336 individuals reported 1,572 events of atrial fibrillation (AFib).
Omega-3 fatty acids did not significantly reduce nonfatal stroke (RR, 1.04; P = .55), but EPA monotherapy was associated with a reduction of nonfatal stroke, compared with control (RR: 0.71; P = .01).
Conversely, omega-3 fatty acids were associated with increased risk for AFib (RR, 1.26; P = .004), with a higher risk with EPA monotherapy than with control (RR, 1.35; P = .004).
Overall, omega-3 fatty acids did not prevent sudden cardiac death or increase gastrointestinal-related adverse events, total bleeding, or major or minor bleeding; however, the meta-analysis showed a higher risk of total bleeding with EPA monotherapy than with control (RR, 1.49; P = .006).
An influence analysis with stepwise exclusion of one trial at a time, including REDUCE-IT, did not alter the overall summary estimates. “Despite the exclusion of REDUCE-IT, EPA monotherapy reduced MACE by 23%, compared with the control,” the authors reported.
They said these new findings also have important implications for clinical practice and treatment guidelines.
“After REDUCE-IT, several national and international guidelines endorsed EPA in their therapeutic recommendations. However, the publication of two recent negative trials of EPA + DHA has created some confusion in the scientific community about the value of omega-3 FAs in preventing atherosclerotic cardiovascular disease [ASCVD],” they stated.
“This meta-analysis provides reassurance about the role of omega-3 fatty acids, specifically EPA, in the current treatment framework of ASCVD residual cardiovascular risk reduction and encourages investigators to explore further the cardiovascular effects of EPA across different clinical settings,” they added.
REDUCE-IT was sponsored by Amarin. Brigham and Women’s Hospital receives research funding from Amarin for the work Dr. Bhatt did as the trial chair and as the international principal investigator. The present analysis was unfunded.
A version of this article first appeared on Medscape.com.