User login
AAP ‘silencing debate’ on gender dysphoria, says doctor group
The American Academy of Pediatrics (AAP) is at the center of a row with an international group of doctors who question whether hormone treatment is the most appropriate way to treat adolescents with gender dysphoria.
After initially accepting the application and payment from the Society for Evidence-Based Gender Medicine (SEGM) for the organization to have an information booth at the AAP annual meeting in October, the AAP did a U-turn earlier this month and canceled the registration, with no explanation as to why.
“Just days earlier,” says SEGM in a statement on its website, “over 80% of AAP members” had indicated they wanted more discussion on the topic of “addressing alternatives to the use of hormone therapies for gender dysphoric youth.”
“This rejection sends a strong signal that the AAP does not want to see any debate on what constitutes evidence-based care for gender-diverse youth,” they add.
Asked for an explanation as to why it accepted but later rescinded SEGM’s application for a booth, the AAP has given no response to date.
A Wall Street Journal article on the furor, published last week, has clocked up 785 comments to date.
There has been an exponential increase in the number of adolescents who identify as transgender – reporting discomfort with their birth sex – in Western countries, and the debate has been covered in detail, having intensified worldwide in the last 12 months, regarding how best to treat youth with gender dysphoria.
Although “affirmative” medical care, defined as treatment with puberty blockers and cross-sex hormones to transition to the opposite sex, is supported by the AAP and other medical organizations, there is growing concern among many doctors and other health care professionals as to whether this is, in fact, the best way to proceed, given that there are a number of irreversible changes associated with treatment. There is also a growing number of “detransitioners” – mostly young people who transitioned and then changed their minds, and “detransitioned” back to their birth sex.
“Because of the low quality of the available evidence and the marked change in the presentation of gender dysphoria in youth in the last several years (many more adolescents with recently emerging transgender identities and significant mental health comorbidities are presenting for care), what constitutes good health care for this patient group is far from clear,” notes SEGM.
“Quelling the debate will not help America’s pediatricians guide patients and their families based on best available evidence. The politicization of the field of gender medicine must end, if we care about gender-variant youth and their long-term health,” they conclude.
A version of this article first appeared on Medscape.com.
The American Academy of Pediatrics (AAP) is at the center of a row with an international group of doctors who question whether hormone treatment is the most appropriate way to treat adolescents with gender dysphoria.
After initially accepting the application and payment from the Society for Evidence-Based Gender Medicine (SEGM) for the organization to have an information booth at the AAP annual meeting in October, the AAP did a U-turn earlier this month and canceled the registration, with no explanation as to why.
“Just days earlier,” says SEGM in a statement on its website, “over 80% of AAP members” had indicated they wanted more discussion on the topic of “addressing alternatives to the use of hormone therapies for gender dysphoric youth.”
“This rejection sends a strong signal that the AAP does not want to see any debate on what constitutes evidence-based care for gender-diverse youth,” they add.
Asked for an explanation as to why it accepted but later rescinded SEGM’s application for a booth, the AAP has given no response to date.
A Wall Street Journal article on the furor, published last week, has clocked up 785 comments to date.
There has been an exponential increase in the number of adolescents who identify as transgender – reporting discomfort with their birth sex – in Western countries, and the debate has been covered in detail, having intensified worldwide in the last 12 months, regarding how best to treat youth with gender dysphoria.
Although “affirmative” medical care, defined as treatment with puberty blockers and cross-sex hormones to transition to the opposite sex, is supported by the AAP and other medical organizations, there is growing concern among many doctors and other health care professionals as to whether this is, in fact, the best way to proceed, given that there are a number of irreversible changes associated with treatment. There is also a growing number of “detransitioners” – mostly young people who transitioned and then changed their minds, and “detransitioned” back to their birth sex.
“Because of the low quality of the available evidence and the marked change in the presentation of gender dysphoria in youth in the last several years (many more adolescents with recently emerging transgender identities and significant mental health comorbidities are presenting for care), what constitutes good health care for this patient group is far from clear,” notes SEGM.
“Quelling the debate will not help America’s pediatricians guide patients and their families based on best available evidence. The politicization of the field of gender medicine must end, if we care about gender-variant youth and their long-term health,” they conclude.
A version of this article first appeared on Medscape.com.
The American Academy of Pediatrics (AAP) is at the center of a row with an international group of doctors who question whether hormone treatment is the most appropriate way to treat adolescents with gender dysphoria.
After initially accepting the application and payment from the Society for Evidence-Based Gender Medicine (SEGM) for the organization to have an information booth at the AAP annual meeting in October, the AAP did a U-turn earlier this month and canceled the registration, with no explanation as to why.
“Just days earlier,” says SEGM in a statement on its website, “over 80% of AAP members” had indicated they wanted more discussion on the topic of “addressing alternatives to the use of hormone therapies for gender dysphoric youth.”
“This rejection sends a strong signal that the AAP does not want to see any debate on what constitutes evidence-based care for gender-diverse youth,” they add.
Asked for an explanation as to why it accepted but later rescinded SEGM’s application for a booth, the AAP has given no response to date.
A Wall Street Journal article on the furor, published last week, has clocked up 785 comments to date.
There has been an exponential increase in the number of adolescents who identify as transgender – reporting discomfort with their birth sex – in Western countries, and the debate has been covered in detail, having intensified worldwide in the last 12 months, regarding how best to treat youth with gender dysphoria.
Although “affirmative” medical care, defined as treatment with puberty blockers and cross-sex hormones to transition to the opposite sex, is supported by the AAP and other medical organizations, there is growing concern among many doctors and other health care professionals as to whether this is, in fact, the best way to proceed, given that there are a number of irreversible changes associated with treatment. There is also a growing number of “detransitioners” – mostly young people who transitioned and then changed their minds, and “detransitioned” back to their birth sex.
“Because of the low quality of the available evidence and the marked change in the presentation of gender dysphoria in youth in the last several years (many more adolescents with recently emerging transgender identities and significant mental health comorbidities are presenting for care), what constitutes good health care for this patient group is far from clear,” notes SEGM.
“Quelling the debate will not help America’s pediatricians guide patients and their families based on best available evidence. The politicization of the field of gender medicine must end, if we care about gender-variant youth and their long-term health,” they conclude.
A version of this article first appeared on Medscape.com.
WTC early responders have higher prevalence of liver disease
Emergency responders to the World Trade Center (WTC) attack in 2001 paid a significant physical cost for their service in the form of exposure to chemicals, dust, and airborne particulates causally linked to hepatotoxicity. As we near the 20th anniversary of these attacks, researchers have determined that those responders who arrived at the WTC site earlier have a significantly higher prevalence of hepatic steatosis compared with those who arrived in the days that followed.
“This research is some of the first to suggest that there may be a link between the amount of exposure experienced by responders to the WTC site and the higher likelihood of excessive accumulation of fat in their livers,” study author Artit Jirapatnakul, PhD, of Icahn School of Medicine at Mount Sinai, New York, said in an interview. These findings were published in the American Journal of Industrial Medicine.
The excessive accumulation of liver fat is an indicator of liver injury, which can also predict subsequent future disease, such as cirrhosis, liver failure, and liver cancer.
Dr. Jirapatnakul said that arrival time to the WTC disaster may prove an important factor for predicting the risk of liver disease in this population and directing treatment to them accordingly.
“By identifying individuals with markers of liver injury, such as excess fat, we can offer referral to liver specialists and thereby open the door to early treatment,” he said.
“Our most important message is that many liver diseases can be treated if caught early,” Dr. Jirapatnakul added. “Early detection requires proactive monitoring because most liver diseases have few, if any, symptoms during the early stages.”
More than 20,000 men and women who responded to the WTC site on Sept. 11, 2001, were exposed to particulate matter and chemicals known to cause liver damage and increase the risk of toxicant‐associated fatty liver disease. These responders have been offered screening and treatment of different conditions associated with the attack, including CT lung cancer screening for those meeting age and smoking status criteria.
Measuring the impact of response time on the liver
To investigate the dose-response association between WTC site exposure intensity and the risk of hepatic steatosis, Dr. Jirapatnakul and colleagues reviewed low-dose CT chest scans of all participants in the WTC General Responders Cohort (GRC) who had available laboratory data within a 12-month period from their first scan following the Sept. 11, 2001, attack. Only CT chest scans performed between Sept. 11, 2001, and Dec. 31, 2018, were collected and reviewed in the study.
A total of 1,788 WTC responders were included (83.7% were male; mean age at time of attack, 42.5 years). Up to 56% of WTC responders in the study were White, and 20.4% of responders were current smokers. The mean body mass index of the group was 30.1 kg/m2.
The investigators stratified dust exposure into five groups according to when the responders arrived at the WTC site: Sept. 11, 2001, in the dust cloud; Sept. 11, no dust cloud (same-day arrival); Sept. 12 or 13 (second‐ and third‐day arrival); Sept. 14 to the end of September (fourth‐day arrival); and October and beyond.
The median duration between Sept. 11, 2001, and the earliest available CT scan was 11.3 years. Liver density was measured via Statistics‐based Liver Density Estimation from Imaging, a previously validated algorithm, with a slice thickness of 1.25 mm or below. On their earliest CT, approximately 14.4% (n = 258) of responders had liver attenuation < 40 Hounsfield units (HU). The prevalence of liver attenuation < 40 HU was 17% for responders who arrived on the day of the attack, 16% for responders who arrived at the site on Sept. 12 or 13, 10.9% for responders who arrived Sept. 14 through 30, and 9% for responders who arrived at the WTC site on Oct. 1, 2001, or later (P =.0015).
There was a statistically significant trend of increasing liver steatosis with earlier times of arrival (P <.0001). The WTC arrival time retained its status as a significant independent factor for decreased liver attenuation in an analysis adjusted for sex, age, race, smoking status, alcohol use, body mass index, diabetes, gastroesophageal reflux disease, and forced expiratory volume in 1 second.
Dr. Jirapatnakul said that the next step will be to determine whether WTC responders with excessive liver fat also have increased liver scarring. In addition, he and his colleagues are working to establish a registry to collect information on the impact of liver disease as it relates to quality of life in members of the WTC GRC.
Importance of disease severity
Another direction of future research will be to differentiate between those with only hepatic steatosis, those with inflammation from hepatic steatosis (steatohepatitis), and those with hepatic fibrosis which is the most concerning outcome from fatty liver diseases, according to Albert Do, MD, clinical director of the fatty liver disease program at Yale University, New Haven, Conn.
“It is the latter group of patients which we are most concerned about, given this is the group at highest risk for harm from liver disease,” added Dr. Do, who wasn’t involved in the research study. “The degree of steatosis is not closely linked with subsequent inflammation nor hepatic fibrosis, and so linkage of disease severity to specific occupational exposures and timing is needed to determine the allocation of support for patients who had suffered harm from fatty liver disease.”
Dr. Do noted that additional research will also need to identify the specific exposure that may be causing hepatic steatosis in early WTC responders. “Currently, only a small number of medications are known to cause this,” he explained, “and thus such knowledge will help us further understand occupational exposures and their associated risks.”
The researchers received study funding from the National Institute for Occupational Safety and Health. They disclosed conflicts of interest with Genentech, AstraZeneca, Pfizer, Bayer Healthcare, Gilead Sciences, and Boehringer Ingelheim. Dr. Do had no conflicts to declare.
Emergency responders to the World Trade Center (WTC) attack in 2001 paid a significant physical cost for their service in the form of exposure to chemicals, dust, and airborne particulates causally linked to hepatotoxicity. As we near the 20th anniversary of these attacks, researchers have determined that those responders who arrived at the WTC site earlier have a significantly higher prevalence of hepatic steatosis compared with those who arrived in the days that followed.
“This research is some of the first to suggest that there may be a link between the amount of exposure experienced by responders to the WTC site and the higher likelihood of excessive accumulation of fat in their livers,” study author Artit Jirapatnakul, PhD, of Icahn School of Medicine at Mount Sinai, New York, said in an interview. These findings were published in the American Journal of Industrial Medicine.
The excessive accumulation of liver fat is an indicator of liver injury, which can also predict subsequent future disease, such as cirrhosis, liver failure, and liver cancer.
Dr. Jirapatnakul said that arrival time to the WTC disaster may prove an important factor for predicting the risk of liver disease in this population and directing treatment to them accordingly.
“By identifying individuals with markers of liver injury, such as excess fat, we can offer referral to liver specialists and thereby open the door to early treatment,” he said.
“Our most important message is that many liver diseases can be treated if caught early,” Dr. Jirapatnakul added. “Early detection requires proactive monitoring because most liver diseases have few, if any, symptoms during the early stages.”
More than 20,000 men and women who responded to the WTC site on Sept. 11, 2001, were exposed to particulate matter and chemicals known to cause liver damage and increase the risk of toxicant‐associated fatty liver disease. These responders have been offered screening and treatment of different conditions associated with the attack, including CT lung cancer screening for those meeting age and smoking status criteria.
Measuring the impact of response time on the liver
To investigate the dose-response association between WTC site exposure intensity and the risk of hepatic steatosis, Dr. Jirapatnakul and colleagues reviewed low-dose CT chest scans of all participants in the WTC General Responders Cohort (GRC) who had available laboratory data within a 12-month period from their first scan following the Sept. 11, 2001, attack. Only CT chest scans performed between Sept. 11, 2001, and Dec. 31, 2018, were collected and reviewed in the study.
A total of 1,788 WTC responders were included (83.7% were male; mean age at time of attack, 42.5 years). Up to 56% of WTC responders in the study were White, and 20.4% of responders were current smokers. The mean body mass index of the group was 30.1 kg/m2.
The investigators stratified dust exposure into five groups according to when the responders arrived at the WTC site: Sept. 11, 2001, in the dust cloud; Sept. 11, no dust cloud (same-day arrival); Sept. 12 or 13 (second‐ and third‐day arrival); Sept. 14 to the end of September (fourth‐day arrival); and October and beyond.
The median duration between Sept. 11, 2001, and the earliest available CT scan was 11.3 years. Liver density was measured via Statistics‐based Liver Density Estimation from Imaging, a previously validated algorithm, with a slice thickness of 1.25 mm or below. On their earliest CT, approximately 14.4% (n = 258) of responders had liver attenuation < 40 Hounsfield units (HU). The prevalence of liver attenuation < 40 HU was 17% for responders who arrived on the day of the attack, 16% for responders who arrived at the site on Sept. 12 or 13, 10.9% for responders who arrived Sept. 14 through 30, and 9% for responders who arrived at the WTC site on Oct. 1, 2001, or later (P =.0015).
There was a statistically significant trend of increasing liver steatosis with earlier times of arrival (P <.0001). The WTC arrival time retained its status as a significant independent factor for decreased liver attenuation in an analysis adjusted for sex, age, race, smoking status, alcohol use, body mass index, diabetes, gastroesophageal reflux disease, and forced expiratory volume in 1 second.
Dr. Jirapatnakul said that the next step will be to determine whether WTC responders with excessive liver fat also have increased liver scarring. In addition, he and his colleagues are working to establish a registry to collect information on the impact of liver disease as it relates to quality of life in members of the WTC GRC.
Importance of disease severity
Another direction of future research will be to differentiate between those with only hepatic steatosis, those with inflammation from hepatic steatosis (steatohepatitis), and those with hepatic fibrosis which is the most concerning outcome from fatty liver diseases, according to Albert Do, MD, clinical director of the fatty liver disease program at Yale University, New Haven, Conn.
“It is the latter group of patients which we are most concerned about, given this is the group at highest risk for harm from liver disease,” added Dr. Do, who wasn’t involved in the research study. “The degree of steatosis is not closely linked with subsequent inflammation nor hepatic fibrosis, and so linkage of disease severity to specific occupational exposures and timing is needed to determine the allocation of support for patients who had suffered harm from fatty liver disease.”
Dr. Do noted that additional research will also need to identify the specific exposure that may be causing hepatic steatosis in early WTC responders. “Currently, only a small number of medications are known to cause this,” he explained, “and thus such knowledge will help us further understand occupational exposures and their associated risks.”
The researchers received study funding from the National Institute for Occupational Safety and Health. They disclosed conflicts of interest with Genentech, AstraZeneca, Pfizer, Bayer Healthcare, Gilead Sciences, and Boehringer Ingelheim. Dr. Do had no conflicts to declare.
Emergency responders to the World Trade Center (WTC) attack in 2001 paid a significant physical cost for their service in the form of exposure to chemicals, dust, and airborne particulates causally linked to hepatotoxicity. As we near the 20th anniversary of these attacks, researchers have determined that those responders who arrived at the WTC site earlier have a significantly higher prevalence of hepatic steatosis compared with those who arrived in the days that followed.
“This research is some of the first to suggest that there may be a link between the amount of exposure experienced by responders to the WTC site and the higher likelihood of excessive accumulation of fat in their livers,” study author Artit Jirapatnakul, PhD, of Icahn School of Medicine at Mount Sinai, New York, said in an interview. These findings were published in the American Journal of Industrial Medicine.
The excessive accumulation of liver fat is an indicator of liver injury, which can also predict subsequent future disease, such as cirrhosis, liver failure, and liver cancer.
Dr. Jirapatnakul said that arrival time to the WTC disaster may prove an important factor for predicting the risk of liver disease in this population and directing treatment to them accordingly.
“By identifying individuals with markers of liver injury, such as excess fat, we can offer referral to liver specialists and thereby open the door to early treatment,” he said.
“Our most important message is that many liver diseases can be treated if caught early,” Dr. Jirapatnakul added. “Early detection requires proactive monitoring because most liver diseases have few, if any, symptoms during the early stages.”
More than 20,000 men and women who responded to the WTC site on Sept. 11, 2001, were exposed to particulate matter and chemicals known to cause liver damage and increase the risk of toxicant‐associated fatty liver disease. These responders have been offered screening and treatment of different conditions associated with the attack, including CT lung cancer screening for those meeting age and smoking status criteria.
Measuring the impact of response time on the liver
To investigate the dose-response association between WTC site exposure intensity and the risk of hepatic steatosis, Dr. Jirapatnakul and colleagues reviewed low-dose CT chest scans of all participants in the WTC General Responders Cohort (GRC) who had available laboratory data within a 12-month period from their first scan following the Sept. 11, 2001, attack. Only CT chest scans performed between Sept. 11, 2001, and Dec. 31, 2018, were collected and reviewed in the study.
A total of 1,788 WTC responders were included (83.7% were male; mean age at time of attack, 42.5 years). Up to 56% of WTC responders in the study were White, and 20.4% of responders were current smokers. The mean body mass index of the group was 30.1 kg/m2.
The investigators stratified dust exposure into five groups according to when the responders arrived at the WTC site: Sept. 11, 2001, in the dust cloud; Sept. 11, no dust cloud (same-day arrival); Sept. 12 or 13 (second‐ and third‐day arrival); Sept. 14 to the end of September (fourth‐day arrival); and October and beyond.
The median duration between Sept. 11, 2001, and the earliest available CT scan was 11.3 years. Liver density was measured via Statistics‐based Liver Density Estimation from Imaging, a previously validated algorithm, with a slice thickness of 1.25 mm or below. On their earliest CT, approximately 14.4% (n = 258) of responders had liver attenuation < 40 Hounsfield units (HU). The prevalence of liver attenuation < 40 HU was 17% for responders who arrived on the day of the attack, 16% for responders who arrived at the site on Sept. 12 or 13, 10.9% for responders who arrived Sept. 14 through 30, and 9% for responders who arrived at the WTC site on Oct. 1, 2001, or later (P =.0015).
There was a statistically significant trend of increasing liver steatosis with earlier times of arrival (P <.0001). The WTC arrival time retained its status as a significant independent factor for decreased liver attenuation in an analysis adjusted for sex, age, race, smoking status, alcohol use, body mass index, diabetes, gastroesophageal reflux disease, and forced expiratory volume in 1 second.
Dr. Jirapatnakul said that the next step will be to determine whether WTC responders with excessive liver fat also have increased liver scarring. In addition, he and his colleagues are working to establish a registry to collect information on the impact of liver disease as it relates to quality of life in members of the WTC GRC.
Importance of disease severity
Another direction of future research will be to differentiate between those with only hepatic steatosis, those with inflammation from hepatic steatosis (steatohepatitis), and those with hepatic fibrosis which is the most concerning outcome from fatty liver diseases, according to Albert Do, MD, clinical director of the fatty liver disease program at Yale University, New Haven, Conn.
“It is the latter group of patients which we are most concerned about, given this is the group at highest risk for harm from liver disease,” added Dr. Do, who wasn’t involved in the research study. “The degree of steatosis is not closely linked with subsequent inflammation nor hepatic fibrosis, and so linkage of disease severity to specific occupational exposures and timing is needed to determine the allocation of support for patients who had suffered harm from fatty liver disease.”
Dr. Do noted that additional research will also need to identify the specific exposure that may be causing hepatic steatosis in early WTC responders. “Currently, only a small number of medications are known to cause this,” he explained, “and thus such knowledge will help us further understand occupational exposures and their associated risks.”
The researchers received study funding from the National Institute for Occupational Safety and Health. They disclosed conflicts of interest with Genentech, AstraZeneca, Pfizer, Bayer Healthcare, Gilead Sciences, and Boehringer Ingelheim. Dr. Do had no conflicts to declare.
FROM THE AMERICAN JOURNAL OF INDUSTRIAL MEDICINE
Psychiatrists’ income, wealth gain ground despite COVID-19 challenges
Although many physicians endured pandemic-related income struggles in 2020, psychiatrists are doing fairly well with building their nest egg and paying down debt, according to the Medscape Psychiatrist Wealth and Debt Report 2021.
Surprisingly, despite COVID-19, psychiatrists’ income improved somewhat this year – from $268,000 in 2020 to $275,000 in 2021.
However, that still puts psychiatrists among the lower-paid specialists.
The highest-paying specialty is plastic surgery ($526,000), followed by orthopedics and orthopedic surgery ($511,000) and cardiology ($459,000), according to the overall Medscape Physician Wealth and Debt Report 2021. The report is based on responses from nearly 18,000 physicians in 29 specialties. All were surveyed between Oct. 6, 2020, and Feb. 11, 2021.
Psychiatrists’ overall wealth gained some ground over the past year, with 40% reporting a net worth of $1 million to $5 million this year – up from 38% last year. Just 6% of psychiatrists have a net worth north of $5 million, up slightly from 5% last year.
Keeping up with bills
based in St. Louis Park, Minn. He noted that the rise in the stock market also played a role, with the S&P 500 finishing the year up over 18%.
“I’ve seen clients accumulate cash, which has added to their net worth. They cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on,” Dr. Greenwald said.
The percentage of psychiatrists with a net worth under $500,000 decreased from 37% last year to 32% this year. Psychiatry is still among the specialties reporting a high percentage of members with net worth below $500,000.
But gender matters. Earnings overall are higher for male than female psychiatrists, and that is reflected in net worth. Fewer female than male psychiatrists are worth more than $5 million (4% vs. 7%), and more female psychiatrists have a net worth of less than $500,000 (41% vs. 26%).
As in prior years, most psychiatrists are paying down a home mortgage on their primary residence (66%). Psychiatrists’ mortgage payments span a wide range, from less than $100,000 (23%) to more than $500,000 (15%). However, 27% report having no mortgage.
Mortgage aside, other top expenses or debts for psychiatrists are car loan payments (36%), paying off college and medical school debt (26%), credit card debt (25%), and medical expenses for self or loved ones (19%).
Other expenses include college tuition for children (16%), car lease payments (14%), mortgage on a second home (13%), private-school tuition for a child (12%), and child care (12%).
Despite some financially challenging months, the vast majority of psychiatrists (94%) kept up with paying their bills.
That’s better than what much of America experienced. According to a U.S. Census Bureau survey conducted last July, roughly 25% of adults missed a mortgage or rent payment because of COVID-related difficulties.
About half of psychiatrists pool their income to pay for bills. One-quarter do not have joint accounts with a spouse or partner.
Spender or saver?
About three-quarters of psychiatrists continued to spend as usual in 2020. About one-quarter took significant steps to lower their expenses, such as refinancing their home or moving to a less costly home.
In line with prior Medscape surveys, about half of psychiatrists have a general idea of how much they spend and on what, but they do not track or formalize it.
According to a recent survey by Intuit, only 35% of Americans say they know how much they spent last month. Viewed by age, 27% of millennials, 34% of Gen Xers, and 46% of baby boomers knew how much they spent.
Many psychiatrists have a higher-than-average number of credit cards; 42% have at least five. By comparison, the average American has four.
Savings was mixed for psychiatrists this past year; 61% put in the same amount or more each month into their 401(k) plans, but 33% put in less money, compared with last year.
For taxable savings accounts, half of psychiatrists put the same amount or more into after-tax accounts – but 22% put in less money, compared with last year. Another one-quarter did not use these savings accounts at all.
The percentage of psychiatrists who experienced losses because of practice problems rose from 6% to 9% in the past year. Much of that was likely because of COVID. However, about the same percentage reported no financial losses this year (76%), compared with last year (75%).
The vast majority of psychiatrists report living within or below their means; only 5% live above their means.
“There are certainly folks who believe that, as long as they pay off their credit card each month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” Dr. Greenwald said.
However, “living within one’s means is having a 3-6 months’ emergency fund; saving at least 20% of gross income toward retirement; adequately funding 529 college accounts; and, for younger docs, paying down high-interest-rate debt at a good clip,” he added.
A version of this article first appeared on Medscape.com.
Although many physicians endured pandemic-related income struggles in 2020, psychiatrists are doing fairly well with building their nest egg and paying down debt, according to the Medscape Psychiatrist Wealth and Debt Report 2021.
Surprisingly, despite COVID-19, psychiatrists’ income improved somewhat this year – from $268,000 in 2020 to $275,000 in 2021.
However, that still puts psychiatrists among the lower-paid specialists.
The highest-paying specialty is plastic surgery ($526,000), followed by orthopedics and orthopedic surgery ($511,000) and cardiology ($459,000), according to the overall Medscape Physician Wealth and Debt Report 2021. The report is based on responses from nearly 18,000 physicians in 29 specialties. All were surveyed between Oct. 6, 2020, and Feb. 11, 2021.
Psychiatrists’ overall wealth gained some ground over the past year, with 40% reporting a net worth of $1 million to $5 million this year – up from 38% last year. Just 6% of psychiatrists have a net worth north of $5 million, up slightly from 5% last year.
Keeping up with bills
based in St. Louis Park, Minn. He noted that the rise in the stock market also played a role, with the S&P 500 finishing the year up over 18%.
“I’ve seen clients accumulate cash, which has added to their net worth. They cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on,” Dr. Greenwald said.
The percentage of psychiatrists with a net worth under $500,000 decreased from 37% last year to 32% this year. Psychiatry is still among the specialties reporting a high percentage of members with net worth below $500,000.
But gender matters. Earnings overall are higher for male than female psychiatrists, and that is reflected in net worth. Fewer female than male psychiatrists are worth more than $5 million (4% vs. 7%), and more female psychiatrists have a net worth of less than $500,000 (41% vs. 26%).
As in prior years, most psychiatrists are paying down a home mortgage on their primary residence (66%). Psychiatrists’ mortgage payments span a wide range, from less than $100,000 (23%) to more than $500,000 (15%). However, 27% report having no mortgage.
Mortgage aside, other top expenses or debts for psychiatrists are car loan payments (36%), paying off college and medical school debt (26%), credit card debt (25%), and medical expenses for self or loved ones (19%).
Other expenses include college tuition for children (16%), car lease payments (14%), mortgage on a second home (13%), private-school tuition for a child (12%), and child care (12%).
Despite some financially challenging months, the vast majority of psychiatrists (94%) kept up with paying their bills.
That’s better than what much of America experienced. According to a U.S. Census Bureau survey conducted last July, roughly 25% of adults missed a mortgage or rent payment because of COVID-related difficulties.
About half of psychiatrists pool their income to pay for bills. One-quarter do not have joint accounts with a spouse or partner.
Spender or saver?
About three-quarters of psychiatrists continued to spend as usual in 2020. About one-quarter took significant steps to lower their expenses, such as refinancing their home or moving to a less costly home.
In line with prior Medscape surveys, about half of psychiatrists have a general idea of how much they spend and on what, but they do not track or formalize it.
According to a recent survey by Intuit, only 35% of Americans say they know how much they spent last month. Viewed by age, 27% of millennials, 34% of Gen Xers, and 46% of baby boomers knew how much they spent.
Many psychiatrists have a higher-than-average number of credit cards; 42% have at least five. By comparison, the average American has four.
Savings was mixed for psychiatrists this past year; 61% put in the same amount or more each month into their 401(k) plans, but 33% put in less money, compared with last year.
For taxable savings accounts, half of psychiatrists put the same amount or more into after-tax accounts – but 22% put in less money, compared with last year. Another one-quarter did not use these savings accounts at all.
The percentage of psychiatrists who experienced losses because of practice problems rose from 6% to 9% in the past year. Much of that was likely because of COVID. However, about the same percentage reported no financial losses this year (76%), compared with last year (75%).
The vast majority of psychiatrists report living within or below their means; only 5% live above their means.
“There are certainly folks who believe that, as long as they pay off their credit card each month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” Dr. Greenwald said.
However, “living within one’s means is having a 3-6 months’ emergency fund; saving at least 20% of gross income toward retirement; adequately funding 529 college accounts; and, for younger docs, paying down high-interest-rate debt at a good clip,” he added.
A version of this article first appeared on Medscape.com.
Although many physicians endured pandemic-related income struggles in 2020, psychiatrists are doing fairly well with building their nest egg and paying down debt, according to the Medscape Psychiatrist Wealth and Debt Report 2021.
Surprisingly, despite COVID-19, psychiatrists’ income improved somewhat this year – from $268,000 in 2020 to $275,000 in 2021.
However, that still puts psychiatrists among the lower-paid specialists.
The highest-paying specialty is plastic surgery ($526,000), followed by orthopedics and orthopedic surgery ($511,000) and cardiology ($459,000), according to the overall Medscape Physician Wealth and Debt Report 2021. The report is based on responses from nearly 18,000 physicians in 29 specialties. All were surveyed between Oct. 6, 2020, and Feb. 11, 2021.
Psychiatrists’ overall wealth gained some ground over the past year, with 40% reporting a net worth of $1 million to $5 million this year – up from 38% last year. Just 6% of psychiatrists have a net worth north of $5 million, up slightly from 5% last year.
Keeping up with bills
based in St. Louis Park, Minn. He noted that the rise in the stock market also played a role, with the S&P 500 finishing the year up over 18%.
“I’ve seen clients accumulate cash, which has added to their net worth. They cut back on spending because they were worried about big declines in income and also because there was simply less to spend money on,” Dr. Greenwald said.
The percentage of psychiatrists with a net worth under $500,000 decreased from 37% last year to 32% this year. Psychiatry is still among the specialties reporting a high percentage of members with net worth below $500,000.
But gender matters. Earnings overall are higher for male than female psychiatrists, and that is reflected in net worth. Fewer female than male psychiatrists are worth more than $5 million (4% vs. 7%), and more female psychiatrists have a net worth of less than $500,000 (41% vs. 26%).
As in prior years, most psychiatrists are paying down a home mortgage on their primary residence (66%). Psychiatrists’ mortgage payments span a wide range, from less than $100,000 (23%) to more than $500,000 (15%). However, 27% report having no mortgage.
Mortgage aside, other top expenses or debts for psychiatrists are car loan payments (36%), paying off college and medical school debt (26%), credit card debt (25%), and medical expenses for self or loved ones (19%).
Other expenses include college tuition for children (16%), car lease payments (14%), mortgage on a second home (13%), private-school tuition for a child (12%), and child care (12%).
Despite some financially challenging months, the vast majority of psychiatrists (94%) kept up with paying their bills.
That’s better than what much of America experienced. According to a U.S. Census Bureau survey conducted last July, roughly 25% of adults missed a mortgage or rent payment because of COVID-related difficulties.
About half of psychiatrists pool their income to pay for bills. One-quarter do not have joint accounts with a spouse or partner.
Spender or saver?
About three-quarters of psychiatrists continued to spend as usual in 2020. About one-quarter took significant steps to lower their expenses, such as refinancing their home or moving to a less costly home.
In line with prior Medscape surveys, about half of psychiatrists have a general idea of how much they spend and on what, but they do not track or formalize it.
According to a recent survey by Intuit, only 35% of Americans say they know how much they spent last month. Viewed by age, 27% of millennials, 34% of Gen Xers, and 46% of baby boomers knew how much they spent.
Many psychiatrists have a higher-than-average number of credit cards; 42% have at least five. By comparison, the average American has four.
Savings was mixed for psychiatrists this past year; 61% put in the same amount or more each month into their 401(k) plans, but 33% put in less money, compared with last year.
For taxable savings accounts, half of psychiatrists put the same amount or more into after-tax accounts – but 22% put in less money, compared with last year. Another one-quarter did not use these savings accounts at all.
The percentage of psychiatrists who experienced losses because of practice problems rose from 6% to 9% in the past year. Much of that was likely because of COVID. However, about the same percentage reported no financial losses this year (76%), compared with last year (75%).
The vast majority of psychiatrists report living within or below their means; only 5% live above their means.
“There are certainly folks who believe that, as long as they pay off their credit card each month and contribute to their 401(k) enough to get their employer match, they’re doing okay,” Dr. Greenwald said.
However, “living within one’s means is having a 3-6 months’ emergency fund; saving at least 20% of gross income toward retirement; adequately funding 529 college accounts; and, for younger docs, paying down high-interest-rate debt at a good clip,” he added.
A version of this article first appeared on Medscape.com.
What’s under my toenail?
After the teledermatology consultation, an x-ray was recommended. The x-ray showed an elongated irregular radiopaque mass projecting from the anterior medial aspect of the midshaft of the distal phalanx of the great toe (Picture 3). With these findings, subungual exostosis was suspected, and she was referred to orthopedic surgery for excision of the lesion. Histopathology showed a stack of trabecular bone with a fibrocartilaginous cap, confirming the diagnosis of subungual exostosis.
Subungual exostosis is a benign osteocartilaginous tumor, first described by Dupuytren in 1874. These lesions are rare and are seen mainly in children and young adults. Females appear to be affected more often than males.1 In a systematic review by DaCambra and colleagues, 55% of the cases occur in patients aged younger than 18 years, and the hallux was the most commonly affected digit, though any finger or toe can be affected.2 There are reported case of congenital multiple exostosis delineated to translocation t(X;6)(q22;q13-14).3
The exact cause of these lesions is unknown, but there are multiple theories, which include a reactive process secondary to trauma, infection, or genetic causes. Pathologic examination of the lesions shows an osseous center covered by a fibrocartilaginous cap. There is proliferation of spindle cells that generate cartilage, which later forms trabecular bone.4
On physical examination, subungual exostosis appear like a firm, fixed nodule with a hyperkeratotic smooth surface at the distal end of the nail bed, that slowly grows and can distort and lift up the nail. Dermoscopy features of these lesions include vascular ectasia, hyperkeratosis, onycholysis, and ulceration.
The differential diagnosis of subungual growths includes osteochondromas, which can present in a similar way but are rarer. Pathologic examination is usually required to differentiate between both lesions.5 In exostoses, bone is formed directly from fibrous tissue, whereas in osteochondromas they derive from enchondral ossification.6 The cartilaginous cap of this lesion is what helps to differentiate it in histopathology. In subungual exostosis, the cap is composed of fibrocartilage, while in osteochondromas it is made of hyaline cartilage similar to what is seen in normal growing epiphysis.5 Subungual exostosis can be confused with pyogenic granulomas and verruca, and often are treated as such, which delays appropriate surgical management.
Firm, slow-growing tumors in the fingers or toes of children should raise suspicion for underlying bony lesions like subungual exostosis and osteochondromas. X-rays of the lesion should be performed in order to clarify the diagnosis. Referral to orthopedic surgery is needed for definitive surgical management.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
1. Zhang W et al. JAAD Case Rep. 2020 Jun 1;6(8):725-6.
2. DaCambra MP et al. Clin Orthop Relat Res. 2014 Apr;472(4):1251-9.
3. Torlazzi C et al. Int J Cancer. 2006;118:1972-6.
4. Calonje E et al. McKee’s pathology of the skin: With clinical correlations. (4th ed.) Philadelphia: Elsevier/Saunders, 2012.
5. Lee SK et al. Foot Ankle Int. 2007 May;28(5):595-601.
6. Mavrogenis A et al. Orthopedics. 2008 Oct;31(10).
After the teledermatology consultation, an x-ray was recommended. The x-ray showed an elongated irregular radiopaque mass projecting from the anterior medial aspect of the midshaft of the distal phalanx of the great toe (Picture 3). With these findings, subungual exostosis was suspected, and she was referred to orthopedic surgery for excision of the lesion. Histopathology showed a stack of trabecular bone with a fibrocartilaginous cap, confirming the diagnosis of subungual exostosis.
Subungual exostosis is a benign osteocartilaginous tumor, first described by Dupuytren in 1874. These lesions are rare and are seen mainly in children and young adults. Females appear to be affected more often than males.1 In a systematic review by DaCambra and colleagues, 55% of the cases occur in patients aged younger than 18 years, and the hallux was the most commonly affected digit, though any finger or toe can be affected.2 There are reported case of congenital multiple exostosis delineated to translocation t(X;6)(q22;q13-14).3
The exact cause of these lesions is unknown, but there are multiple theories, which include a reactive process secondary to trauma, infection, or genetic causes. Pathologic examination of the lesions shows an osseous center covered by a fibrocartilaginous cap. There is proliferation of spindle cells that generate cartilage, which later forms trabecular bone.4
On physical examination, subungual exostosis appear like a firm, fixed nodule with a hyperkeratotic smooth surface at the distal end of the nail bed, that slowly grows and can distort and lift up the nail. Dermoscopy features of these lesions include vascular ectasia, hyperkeratosis, onycholysis, and ulceration.
The differential diagnosis of subungual growths includes osteochondromas, which can present in a similar way but are rarer. Pathologic examination is usually required to differentiate between both lesions.5 In exostoses, bone is formed directly from fibrous tissue, whereas in osteochondromas they derive from enchondral ossification.6 The cartilaginous cap of this lesion is what helps to differentiate it in histopathology. In subungual exostosis, the cap is composed of fibrocartilage, while in osteochondromas it is made of hyaline cartilage similar to what is seen in normal growing epiphysis.5 Subungual exostosis can be confused with pyogenic granulomas and verruca, and often are treated as such, which delays appropriate surgical management.
Firm, slow-growing tumors in the fingers or toes of children should raise suspicion for underlying bony lesions like subungual exostosis and osteochondromas. X-rays of the lesion should be performed in order to clarify the diagnosis. Referral to orthopedic surgery is needed for definitive surgical management.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
1. Zhang W et al. JAAD Case Rep. 2020 Jun 1;6(8):725-6.
2. DaCambra MP et al. Clin Orthop Relat Res. 2014 Apr;472(4):1251-9.
3. Torlazzi C et al. Int J Cancer. 2006;118:1972-6.
4. Calonje E et al. McKee’s pathology of the skin: With clinical correlations. (4th ed.) Philadelphia: Elsevier/Saunders, 2012.
5. Lee SK et al. Foot Ankle Int. 2007 May;28(5):595-601.
6. Mavrogenis A et al. Orthopedics. 2008 Oct;31(10).
After the teledermatology consultation, an x-ray was recommended. The x-ray showed an elongated irregular radiopaque mass projecting from the anterior medial aspect of the midshaft of the distal phalanx of the great toe (Picture 3). With these findings, subungual exostosis was suspected, and she was referred to orthopedic surgery for excision of the lesion. Histopathology showed a stack of trabecular bone with a fibrocartilaginous cap, confirming the diagnosis of subungual exostosis.
Subungual exostosis is a benign osteocartilaginous tumor, first described by Dupuytren in 1874. These lesions are rare and are seen mainly in children and young adults. Females appear to be affected more often than males.1 In a systematic review by DaCambra and colleagues, 55% of the cases occur in patients aged younger than 18 years, and the hallux was the most commonly affected digit, though any finger or toe can be affected.2 There are reported case of congenital multiple exostosis delineated to translocation t(X;6)(q22;q13-14).3
The exact cause of these lesions is unknown, but there are multiple theories, which include a reactive process secondary to trauma, infection, or genetic causes. Pathologic examination of the lesions shows an osseous center covered by a fibrocartilaginous cap. There is proliferation of spindle cells that generate cartilage, which later forms trabecular bone.4
On physical examination, subungual exostosis appear like a firm, fixed nodule with a hyperkeratotic smooth surface at the distal end of the nail bed, that slowly grows and can distort and lift up the nail. Dermoscopy features of these lesions include vascular ectasia, hyperkeratosis, onycholysis, and ulceration.
The differential diagnosis of subungual growths includes osteochondromas, which can present in a similar way but are rarer. Pathologic examination is usually required to differentiate between both lesions.5 In exostoses, bone is formed directly from fibrous tissue, whereas in osteochondromas they derive from enchondral ossification.6 The cartilaginous cap of this lesion is what helps to differentiate it in histopathology. In subungual exostosis, the cap is composed of fibrocartilage, while in osteochondromas it is made of hyaline cartilage similar to what is seen in normal growing epiphysis.5 Subungual exostosis can be confused with pyogenic granulomas and verruca, and often are treated as such, which delays appropriate surgical management.
Firm, slow-growing tumors in the fingers or toes of children should raise suspicion for underlying bony lesions like subungual exostosis and osteochondromas. X-rays of the lesion should be performed in order to clarify the diagnosis. Referral to orthopedic surgery is needed for definitive surgical management.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
1. Zhang W et al. JAAD Case Rep. 2020 Jun 1;6(8):725-6.
2. DaCambra MP et al. Clin Orthop Relat Res. 2014 Apr;472(4):1251-9.
3. Torlazzi C et al. Int J Cancer. 2006;118:1972-6.
4. Calonje E et al. McKee’s pathology of the skin: With clinical correlations. (4th ed.) Philadelphia: Elsevier/Saunders, 2012.
5. Lee SK et al. Foot Ankle Int. 2007 May;28(5):595-601.
6. Mavrogenis A et al. Orthopedics. 2008 Oct;31(10).
A 13-year-old female was seen by her pediatrician for a lesion that had been on her right toe for about 6 months. She is unaware of any trauma to the area. The lesion has been growing slowly and recently it started lifting up the nail, became tender, and was bleeding, which is the reason why she sought care.
At the pediatrician's office, he noted a pink crusted papule under the nail. The nail was lifting up and was tender to the touch. She is a healthy girl who is not taking any medications and has no allergies. There is no family history of similar lesions.
The pediatrician took a picture of the lesion and he send it to our pediatric teledermatology service for consultation.
FDA approves Abbott’s Amplatzer Amulet for AFib
The Food and Drug Administration has approved the Amplatzer Amulet left atrial appendage occluder (Abbott) to treat people with nonvalvular atrial fibrillation who are at increased risk for stroke and systemic embolism.
The Amulet and its competitor, Boston Scientific’s Watchman, are minimally invasive devices used to close off the left atrial appendage (LAA), an area where blood clots tend to form in people with atrial fibrillation.
Amulet uses dual-seal technology to completely and immediately seal the LAA, the company says, whereas the other minimally invasive solution uses a single component to seal the LAA that requires blood-thinning drugs to heal and additional patient monitoring. The Amulet also has the widest range of occluder sizes on the market and is recapturable and repositionable to ensure optimal placement.
“As the world’s population continues to age, we’re seeing a surge in atrial fibrillation cases, and with that comes increased risk of stroke. The approval of Abbott’s Amulet device provides physicians with a treatment option that reduces the risk of stroke and eliminates the need for blood-thinning medication immediately after the procedure, which is incredibly valuable given the bleeding risks associated with these medicines,” Dhanunjaya Lakkireddy, MD, Kansas City Heart Rhythm Institute at HCA Midwest Health, Overland Park, Kan., and principal investigator for the study that led to FDA approval, said in a news release from Abbott.
The FDA approval is supported by findings from the global Amulet IDE trial, a head-to-head comparison of the Amulet and Watchman devices in 1,878 participants with nonvalvular atrial fibrillation. The results will be presented virtually on Aug. 30 at the 2021 annual congress of the European Society of Cardiology.
The Amplatzer Amulet received CE Mark designation in 2013 and is approved for use in more than 80 countries, including in Australia, Canada, and European countries.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved the Amplatzer Amulet left atrial appendage occluder (Abbott) to treat people with nonvalvular atrial fibrillation who are at increased risk for stroke and systemic embolism.
The Amulet and its competitor, Boston Scientific’s Watchman, are minimally invasive devices used to close off the left atrial appendage (LAA), an area where blood clots tend to form in people with atrial fibrillation.
Amulet uses dual-seal technology to completely and immediately seal the LAA, the company says, whereas the other minimally invasive solution uses a single component to seal the LAA that requires blood-thinning drugs to heal and additional patient monitoring. The Amulet also has the widest range of occluder sizes on the market and is recapturable and repositionable to ensure optimal placement.
“As the world’s population continues to age, we’re seeing a surge in atrial fibrillation cases, and with that comes increased risk of stroke. The approval of Abbott’s Amulet device provides physicians with a treatment option that reduces the risk of stroke and eliminates the need for blood-thinning medication immediately after the procedure, which is incredibly valuable given the bleeding risks associated with these medicines,” Dhanunjaya Lakkireddy, MD, Kansas City Heart Rhythm Institute at HCA Midwest Health, Overland Park, Kan., and principal investigator for the study that led to FDA approval, said in a news release from Abbott.
The FDA approval is supported by findings from the global Amulet IDE trial, a head-to-head comparison of the Amulet and Watchman devices in 1,878 participants with nonvalvular atrial fibrillation. The results will be presented virtually on Aug. 30 at the 2021 annual congress of the European Society of Cardiology.
The Amplatzer Amulet received CE Mark designation in 2013 and is approved for use in more than 80 countries, including in Australia, Canada, and European countries.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved the Amplatzer Amulet left atrial appendage occluder (Abbott) to treat people with nonvalvular atrial fibrillation who are at increased risk for stroke and systemic embolism.
The Amulet and its competitor, Boston Scientific’s Watchman, are minimally invasive devices used to close off the left atrial appendage (LAA), an area where blood clots tend to form in people with atrial fibrillation.
Amulet uses dual-seal technology to completely and immediately seal the LAA, the company says, whereas the other minimally invasive solution uses a single component to seal the LAA that requires blood-thinning drugs to heal and additional patient monitoring. The Amulet also has the widest range of occluder sizes on the market and is recapturable and repositionable to ensure optimal placement.
“As the world’s population continues to age, we’re seeing a surge in atrial fibrillation cases, and with that comes increased risk of stroke. The approval of Abbott’s Amulet device provides physicians with a treatment option that reduces the risk of stroke and eliminates the need for blood-thinning medication immediately after the procedure, which is incredibly valuable given the bleeding risks associated with these medicines,” Dhanunjaya Lakkireddy, MD, Kansas City Heart Rhythm Institute at HCA Midwest Health, Overland Park, Kan., and principal investigator for the study that led to FDA approval, said in a news release from Abbott.
The FDA approval is supported by findings from the global Amulet IDE trial, a head-to-head comparison of the Amulet and Watchman devices in 1,878 participants with nonvalvular atrial fibrillation. The results will be presented virtually on Aug. 30 at the 2021 annual congress of the European Society of Cardiology.
The Amplatzer Amulet received CE Mark designation in 2013 and is approved for use in more than 80 countries, including in Australia, Canada, and European countries.
A version of this article first appeared on Medscape.com.
Children and COVID: New cases rise to winter levels
Weekly cases of COVID-19 in children topped 100,000 for the first time since early February, according to the American Academy of Pediatrics and the Children’s Hospital Association.
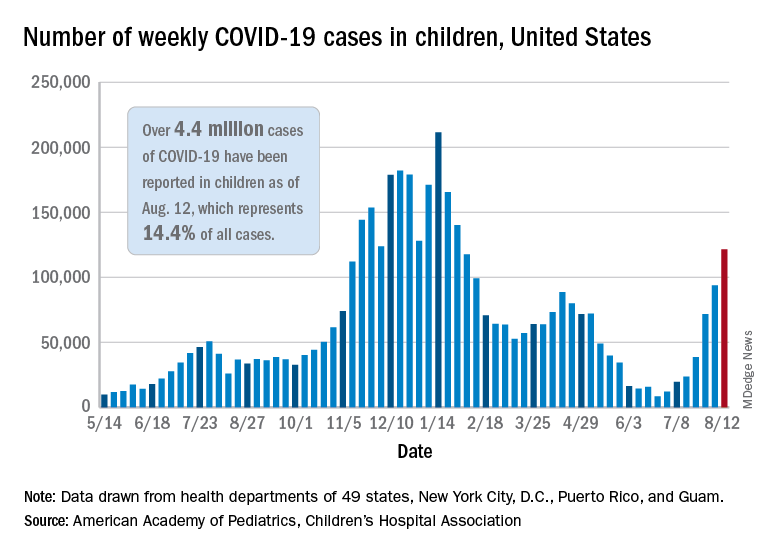
the AAP and CHA said in their weekly COVD-19 report. The recent surge in child COVID has also brought a record high in hospitalizations and shortages of pediatric ICU beds in some areas.
The 121,000 new cases represent an increase of almost 1,400% since June 18-24, when the weekly tally was just 8,447 and at its lowest point in over a year, the AAP/CHA data show.
On the vaccination front in the last week (Aug. 10-16), vaccine initiation for 12- to 17-year-olds was fairly robust but still down slightly, compared with the previous week. Just over 402,000 children aged 12-15 years received a first vaccination, which was down slightly from 411,000 the week before but still higher than any of the 6 weeks from June 22 to Aug. 2, based on data from the Centers for Disease Control and Prevention. Vaccinations were down by a similar margin for 15- to-17-year-olds.
Over 10.9 million children aged 12-17 have had at least one dose of COVID-19 vaccine administered, of whom 8.1 million are fully vaccinated. Among those aged 12-15 years, 44.5% have gotten at least one dose and 31.8% are fully vaccinated, with corresponding figures of 53.9% and 42.5% for 16- and 17-year-olds, according to the CDC’s COVID Data Tracker.
The number of COVID-19 cases reported in children since the start of the pandemic is up to 4.4 million, which makes up 14.4% of all cases in the United States, the AAP and CHA said. Other cumulative figures through Aug. 12 include almost 18,000 hospitalizations – reported by 23 states and New York City – and 378 deaths – reported by 43 states, New York City, Puerto Rico, and Guam.
In the latest edition of their ongoing report, compiled using state data since the summer of 2020, the two groups noted that, “in the summer of 2021, some states have revised cases counts previously reported, begun reporting less frequently, or dropped metrics previously reported.” Among those states are Nebraska, which shut down its online COVID dashboard in late June, and Alabama, which stopped reporting cumulative cases and deaths after July 29.
Weekly cases of COVID-19 in children topped 100,000 for the first time since early February, according to the American Academy of Pediatrics and the Children’s Hospital Association.
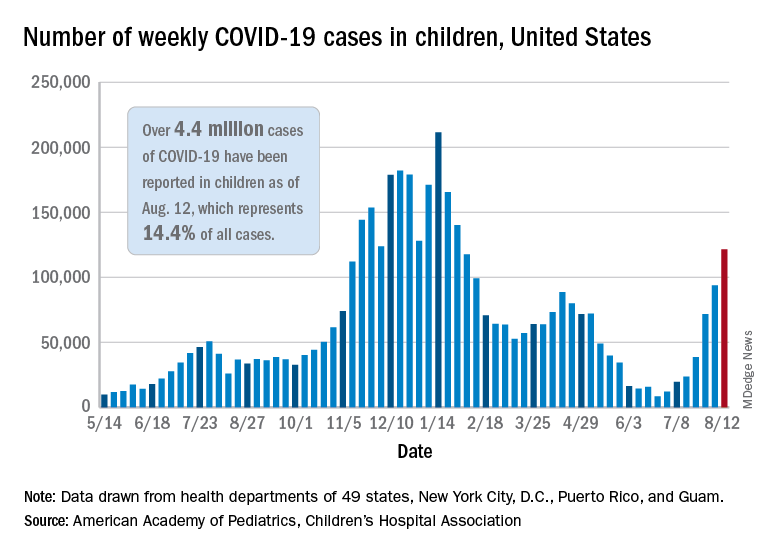
the AAP and CHA said in their weekly COVD-19 report. The recent surge in child COVID has also brought a record high in hospitalizations and shortages of pediatric ICU beds in some areas.
The 121,000 new cases represent an increase of almost 1,400% since June 18-24, when the weekly tally was just 8,447 and at its lowest point in over a year, the AAP/CHA data show.
On the vaccination front in the last week (Aug. 10-16), vaccine initiation for 12- to 17-year-olds was fairly robust but still down slightly, compared with the previous week. Just over 402,000 children aged 12-15 years received a first vaccination, which was down slightly from 411,000 the week before but still higher than any of the 6 weeks from June 22 to Aug. 2, based on data from the Centers for Disease Control and Prevention. Vaccinations were down by a similar margin for 15- to-17-year-olds.
Over 10.9 million children aged 12-17 have had at least one dose of COVID-19 vaccine administered, of whom 8.1 million are fully vaccinated. Among those aged 12-15 years, 44.5% have gotten at least one dose and 31.8% are fully vaccinated, with corresponding figures of 53.9% and 42.5% for 16- and 17-year-olds, according to the CDC’s COVID Data Tracker.
The number of COVID-19 cases reported in children since the start of the pandemic is up to 4.4 million, which makes up 14.4% of all cases in the United States, the AAP and CHA said. Other cumulative figures through Aug. 12 include almost 18,000 hospitalizations – reported by 23 states and New York City – and 378 deaths – reported by 43 states, New York City, Puerto Rico, and Guam.
In the latest edition of their ongoing report, compiled using state data since the summer of 2020, the two groups noted that, “in the summer of 2021, some states have revised cases counts previously reported, begun reporting less frequently, or dropped metrics previously reported.” Among those states are Nebraska, which shut down its online COVID dashboard in late June, and Alabama, which stopped reporting cumulative cases and deaths after July 29.
Weekly cases of COVID-19 in children topped 100,000 for the first time since early February, according to the American Academy of Pediatrics and the Children’s Hospital Association.
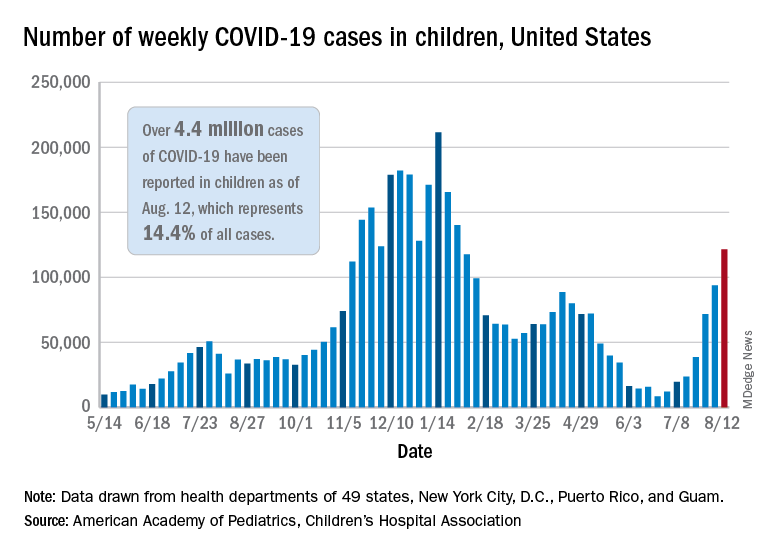
the AAP and CHA said in their weekly COVD-19 report. The recent surge in child COVID has also brought a record high in hospitalizations and shortages of pediatric ICU beds in some areas.
The 121,000 new cases represent an increase of almost 1,400% since June 18-24, when the weekly tally was just 8,447 and at its lowest point in over a year, the AAP/CHA data show.
On the vaccination front in the last week (Aug. 10-16), vaccine initiation for 12- to 17-year-olds was fairly robust but still down slightly, compared with the previous week. Just over 402,000 children aged 12-15 years received a first vaccination, which was down slightly from 411,000 the week before but still higher than any of the 6 weeks from June 22 to Aug. 2, based on data from the Centers for Disease Control and Prevention. Vaccinations were down by a similar margin for 15- to-17-year-olds.
Over 10.9 million children aged 12-17 have had at least one dose of COVID-19 vaccine administered, of whom 8.1 million are fully vaccinated. Among those aged 12-15 years, 44.5% have gotten at least one dose and 31.8% are fully vaccinated, with corresponding figures of 53.9% and 42.5% for 16- and 17-year-olds, according to the CDC’s COVID Data Tracker.
The number of COVID-19 cases reported in children since the start of the pandemic is up to 4.4 million, which makes up 14.4% of all cases in the United States, the AAP and CHA said. Other cumulative figures through Aug. 12 include almost 18,000 hospitalizations – reported by 23 states and New York City – and 378 deaths – reported by 43 states, New York City, Puerto Rico, and Guam.
In the latest edition of their ongoing report, compiled using state data since the summer of 2020, the two groups noted that, “in the summer of 2021, some states have revised cases counts previously reported, begun reporting less frequently, or dropped metrics previously reported.” Among those states are Nebraska, which shut down its online COVID dashboard in late June, and Alabama, which stopped reporting cumulative cases and deaths after July 29.
COVID-19 hospitalizations for 30- to 39-year-olds hit record high
Hospitals are reporting record numbers of COVID-19 patients in their 30s, largely because of the contagious Delta variant, according to The Wall Street Journal.
The rate of new hospitalizations for ages 30-39 reached 2.5 per 100,000 people last week, according to the latest CDC data, which is up from the previous peak of 2 per 100,000 people in January.
What’s more, new hospital admissions for patients in their 30s reached an average of 1,113 a day during the last week, which was up from 908 the week before.
“It means Delta is really bad,” James Lawler, MD, an infectious disease doctor and codirector of the Global Center for Health Security at the University of Nebraska Medical Center, told the newspaper.
People in the age group mostly avoided hospitalization throughout the pandemic because of their relatively good health and young age, the newspaper reported. But in recent weeks, those between ages 30 and 39 are contracting the coronavirus because of their active lifestyle – for many in their 30s, these are prime years for working, parenting, and socializing.
Hospitalizations are mostly among unvaccinated adults, according to the Wall Street Journal. Nationally, less than half of those ages 25-39 are fully vaccinated, compared with 61% of all adults, according to CDC data updated Sunday.
“It loves social mobility,” James Fiorica, MD, chief medical officer of Sarasota Memorial Health Care System in Florida, told the newspaper.
“An unvaccinated 30-year-old can be a perfect carrier,” he said.
On top of that, COVID-19 patients in their 30s are arriving at hospitals with more severe disease than in earlier waves, the Journal reported. At the University of Arkansas for Medical Sciences hospital, for instance, doctors are now monitoring younger patients daily with a scoring system for possible organ failure. That wasn’t necessary earlier in the pandemic for people in their 30s.
“This age group pretty much went unscathed,” Nikhil Meena, MD, director of the hospital’s Medical Intensive Care Unit, told the newspaper.
Now, he said, “they’re all out there doing their thing and getting infected and getting sick enough to be in this hospital.”
A version of this article first appeared on WebMD.com.
Hospitals are reporting record numbers of COVID-19 patients in their 30s, largely because of the contagious Delta variant, according to The Wall Street Journal.
The rate of new hospitalizations for ages 30-39 reached 2.5 per 100,000 people last week, according to the latest CDC data, which is up from the previous peak of 2 per 100,000 people in January.
What’s more, new hospital admissions for patients in their 30s reached an average of 1,113 a day during the last week, which was up from 908 the week before.
“It means Delta is really bad,” James Lawler, MD, an infectious disease doctor and codirector of the Global Center for Health Security at the University of Nebraska Medical Center, told the newspaper.
People in the age group mostly avoided hospitalization throughout the pandemic because of their relatively good health and young age, the newspaper reported. But in recent weeks, those between ages 30 and 39 are contracting the coronavirus because of their active lifestyle – for many in their 30s, these are prime years for working, parenting, and socializing.
Hospitalizations are mostly among unvaccinated adults, according to the Wall Street Journal. Nationally, less than half of those ages 25-39 are fully vaccinated, compared with 61% of all adults, according to CDC data updated Sunday.
“It loves social mobility,” James Fiorica, MD, chief medical officer of Sarasota Memorial Health Care System in Florida, told the newspaper.
“An unvaccinated 30-year-old can be a perfect carrier,” he said.
On top of that, COVID-19 patients in their 30s are arriving at hospitals with more severe disease than in earlier waves, the Journal reported. At the University of Arkansas for Medical Sciences hospital, for instance, doctors are now monitoring younger patients daily with a scoring system for possible organ failure. That wasn’t necessary earlier in the pandemic for people in their 30s.
“This age group pretty much went unscathed,” Nikhil Meena, MD, director of the hospital’s Medical Intensive Care Unit, told the newspaper.
Now, he said, “they’re all out there doing their thing and getting infected and getting sick enough to be in this hospital.”
A version of this article first appeared on WebMD.com.
Hospitals are reporting record numbers of COVID-19 patients in their 30s, largely because of the contagious Delta variant, according to The Wall Street Journal.
The rate of new hospitalizations for ages 30-39 reached 2.5 per 100,000 people last week, according to the latest CDC data, which is up from the previous peak of 2 per 100,000 people in January.
What’s more, new hospital admissions for patients in their 30s reached an average of 1,113 a day during the last week, which was up from 908 the week before.
“It means Delta is really bad,” James Lawler, MD, an infectious disease doctor and codirector of the Global Center for Health Security at the University of Nebraska Medical Center, told the newspaper.
People in the age group mostly avoided hospitalization throughout the pandemic because of their relatively good health and young age, the newspaper reported. But in recent weeks, those between ages 30 and 39 are contracting the coronavirus because of their active lifestyle – for many in their 30s, these are prime years for working, parenting, and socializing.
Hospitalizations are mostly among unvaccinated adults, according to the Wall Street Journal. Nationally, less than half of those ages 25-39 are fully vaccinated, compared with 61% of all adults, according to CDC data updated Sunday.
“It loves social mobility,” James Fiorica, MD, chief medical officer of Sarasota Memorial Health Care System in Florida, told the newspaper.
“An unvaccinated 30-year-old can be a perfect carrier,” he said.
On top of that, COVID-19 patients in their 30s are arriving at hospitals with more severe disease than in earlier waves, the Journal reported. At the University of Arkansas for Medical Sciences hospital, for instance, doctors are now monitoring younger patients daily with a scoring system for possible organ failure. That wasn’t necessary earlier in the pandemic for people in their 30s.
“This age group pretty much went unscathed,” Nikhil Meena, MD, director of the hospital’s Medical Intensive Care Unit, told the newspaper.
Now, he said, “they’re all out there doing their thing and getting infected and getting sick enough to be in this hospital.”
A version of this article first appeared on WebMD.com.
Trial finds that intranasal DHE is well tolerated and may reduce migraine symptoms
, a new study suggests.
A phase 3, open-label trial of INP104, or Trudhesa – Impel NeuroPharma’s proprietary Precision Olfactory Delivery of DHE – found that most patients experienced symptom relief within 2 hours and reported that the medication was easy to use and preferable to their current therapy.
Another treatment option?
Of about 18 million diagnosed migraine patients in the United States, 4 million receive prescription treatment. Nearly 80% of migraine therapies involve triptans, but 30%-40% of patients don’t find adequate relief with triptans. Moreover, the majority of patients who do respond to triptans report that they’d like to try a different therapy.
“INP104 has the potential to deliver rapid symptom relief, without injection, that is well tolerated and suitable for outpatient us,” lead author Timothy Smith, MD, of StudyMetrix Research, St. Louis, and colleagues wrote in the paper.
The results were published online Aug. 7 in Headache.
A total of 360 patients aged 18-65 years with a diagnosis of migraine with or without aura with at least two attacks per month over the course of the previous 6 months were enrolled in the 24-week safety study, which had a 28-week extension period. Participants used their “best usual care” to treat their migraines during the initial 28-day screening period. Afterward, they were given 1.45-mg doses of INP04 to self-administer into the upper nasal space to treat self-recognized attacks. No more than two doses per 24 hours and three doses per 7 days were allowed. The Full Safety Set analysis comprised 354 patients who dosed at least once. The Primary Safety Set involved 185 patients who administered an average of two or more doses per 28-day period during the 24-week treatment period. A total of 4,515 self-recognized migraines were treated during the 24-week period; 6,332 doses of INP04 were analyzed.
Nearly 37% (130/354) of patients reported treatment-emergent adverse events (TEAEs); 6.8% (24/354) discontinued treatment because of the TEAEs over the 24 weeks. The most common TEAE was nasal congestion (15%, 53/354), followed by nausea (6.8%, 24/354).
Within an hour of INP104 administration, 47.6% of patients reported pain relief. After 2 hours of INP104 administration, 38% reported pain freedom and 66.3% reported pain relief. Headache recurrence was observed in 7.1% and 14.3% of patients at 24 and 48 hours, respectively.
In a questionnaire, 84% of patients agreed or strongly agreed that INP04 was easy to use. Most reported that INP104 slowed the recurrence of their migraines and was more rapidly and consistently effective than their previous best usual care treatment.
Intranasal delivery of DHE was developed in response to the challenges of traditional IV administration.
“While intravenous (IV) dihydroergotamine (DHE) mesylate has a long, established history as an effective migraine therapy, its use as an acute treatment can be limited by the high rate of nausea and vomiting reported by patients, which often requires pretreatment with antiemetics,” Dr. Smith and colleagues wrote. “Furthermore, IV DHE mesylate needs to be administered in emergency room settings or by headache specialists, limiting convenience.”
A novel delivery system
“There’s already a nasal spray on the market right now which doesn’t seem to work that well in a large number of people. This device [INP04] was designed to get the same substances to a part of the nose that’s higher and farther back, where there may be better absorption,” said Alan Rapoport, MD, clinical professor of neurology at the University of California, Los Angeles, said in an interview. Dr. Rapoport was not involved with the study.
The proprietary Precision Olfactory Delivery (POD) is meant to improve on current nasal delivery methods such as sprays, droppers, and pumps, which may deliver “less than 5% of the active drug to the upper nasal space,” according to a press release from Impel NeuroPharma.
Nasal delivery also may have advantages over oral medications. People with migraines may be more likely to have gastroparesis – delayed stomach emptying – which may affect their ability to absorb oral medications and delay symptom relief. However, patients may hesitate to agree to a medication that involves nasal delivery, Dr. Rapoport said.
“I will say it’s a little more difficult getting your patients to take a nasal spray,” Dr. Rapoport said. “Patients are used to taking tablets for their headaches,” he said. “But if the doctor spends a little more time with the patient and says, ‘Look, this could work faster for your migraine as a nasal spray. Why don’t you try it a couple of times and see if you like it or not?’ patients are usually willing to give it a try.”
The study’s limitations include the lack of a control group given that it was an open-label trial. It was carried out at 38 sites in one geographical area, which may affect the generalizability of the results. The study did not assess patients with new-onset migraine or chronic migraine.
The Food and Drug Administration approved Trudhesa on Sept. 2, 2021.
The study was funded by Impel NeuroPharma. Dr. Smith has received funding from a number of pharmaceutical companies. Dr. Rapoport disclosed no relevant financial relationships.
, a new study suggests.
A phase 3, open-label trial of INP104, or Trudhesa – Impel NeuroPharma’s proprietary Precision Olfactory Delivery of DHE – found that most patients experienced symptom relief within 2 hours and reported that the medication was easy to use and preferable to their current therapy.
Another treatment option?
Of about 18 million diagnosed migraine patients in the United States, 4 million receive prescription treatment. Nearly 80% of migraine therapies involve triptans, but 30%-40% of patients don’t find adequate relief with triptans. Moreover, the majority of patients who do respond to triptans report that they’d like to try a different therapy.
“INP104 has the potential to deliver rapid symptom relief, without injection, that is well tolerated and suitable for outpatient us,” lead author Timothy Smith, MD, of StudyMetrix Research, St. Louis, and colleagues wrote in the paper.
The results were published online Aug. 7 in Headache.
A total of 360 patients aged 18-65 years with a diagnosis of migraine with or without aura with at least two attacks per month over the course of the previous 6 months were enrolled in the 24-week safety study, which had a 28-week extension period. Participants used their “best usual care” to treat their migraines during the initial 28-day screening period. Afterward, they were given 1.45-mg doses of INP04 to self-administer into the upper nasal space to treat self-recognized attacks. No more than two doses per 24 hours and three doses per 7 days were allowed. The Full Safety Set analysis comprised 354 patients who dosed at least once. The Primary Safety Set involved 185 patients who administered an average of two or more doses per 28-day period during the 24-week treatment period. A total of 4,515 self-recognized migraines were treated during the 24-week period; 6,332 doses of INP04 were analyzed.
Nearly 37% (130/354) of patients reported treatment-emergent adverse events (TEAEs); 6.8% (24/354) discontinued treatment because of the TEAEs over the 24 weeks. The most common TEAE was nasal congestion (15%, 53/354), followed by nausea (6.8%, 24/354).
Within an hour of INP104 administration, 47.6% of patients reported pain relief. After 2 hours of INP104 administration, 38% reported pain freedom and 66.3% reported pain relief. Headache recurrence was observed in 7.1% and 14.3% of patients at 24 and 48 hours, respectively.
In a questionnaire, 84% of patients agreed or strongly agreed that INP04 was easy to use. Most reported that INP104 slowed the recurrence of their migraines and was more rapidly and consistently effective than their previous best usual care treatment.
Intranasal delivery of DHE was developed in response to the challenges of traditional IV administration.
“While intravenous (IV) dihydroergotamine (DHE) mesylate has a long, established history as an effective migraine therapy, its use as an acute treatment can be limited by the high rate of nausea and vomiting reported by patients, which often requires pretreatment with antiemetics,” Dr. Smith and colleagues wrote. “Furthermore, IV DHE mesylate needs to be administered in emergency room settings or by headache specialists, limiting convenience.”
A novel delivery system
“There’s already a nasal spray on the market right now which doesn’t seem to work that well in a large number of people. This device [INP04] was designed to get the same substances to a part of the nose that’s higher and farther back, where there may be better absorption,” said Alan Rapoport, MD, clinical professor of neurology at the University of California, Los Angeles, said in an interview. Dr. Rapoport was not involved with the study.
The proprietary Precision Olfactory Delivery (POD) is meant to improve on current nasal delivery methods such as sprays, droppers, and pumps, which may deliver “less than 5% of the active drug to the upper nasal space,” according to a press release from Impel NeuroPharma.
Nasal delivery also may have advantages over oral medications. People with migraines may be more likely to have gastroparesis – delayed stomach emptying – which may affect their ability to absorb oral medications and delay symptom relief. However, patients may hesitate to agree to a medication that involves nasal delivery, Dr. Rapoport said.
“I will say it’s a little more difficult getting your patients to take a nasal spray,” Dr. Rapoport said. “Patients are used to taking tablets for their headaches,” he said. “But if the doctor spends a little more time with the patient and says, ‘Look, this could work faster for your migraine as a nasal spray. Why don’t you try it a couple of times and see if you like it or not?’ patients are usually willing to give it a try.”
The study’s limitations include the lack of a control group given that it was an open-label trial. It was carried out at 38 sites in one geographical area, which may affect the generalizability of the results. The study did not assess patients with new-onset migraine or chronic migraine.
The Food and Drug Administration approved Trudhesa on Sept. 2, 2021.
The study was funded by Impel NeuroPharma. Dr. Smith has received funding from a number of pharmaceutical companies. Dr. Rapoport disclosed no relevant financial relationships.
, a new study suggests.
A phase 3, open-label trial of INP104, or Trudhesa – Impel NeuroPharma’s proprietary Precision Olfactory Delivery of DHE – found that most patients experienced symptom relief within 2 hours and reported that the medication was easy to use and preferable to their current therapy.
Another treatment option?
Of about 18 million diagnosed migraine patients in the United States, 4 million receive prescription treatment. Nearly 80% of migraine therapies involve triptans, but 30%-40% of patients don’t find adequate relief with triptans. Moreover, the majority of patients who do respond to triptans report that they’d like to try a different therapy.
“INP104 has the potential to deliver rapid symptom relief, without injection, that is well tolerated and suitable for outpatient us,” lead author Timothy Smith, MD, of StudyMetrix Research, St. Louis, and colleagues wrote in the paper.
The results were published online Aug. 7 in Headache.
A total of 360 patients aged 18-65 years with a diagnosis of migraine with or without aura with at least two attacks per month over the course of the previous 6 months were enrolled in the 24-week safety study, which had a 28-week extension period. Participants used their “best usual care” to treat their migraines during the initial 28-day screening period. Afterward, they were given 1.45-mg doses of INP04 to self-administer into the upper nasal space to treat self-recognized attacks. No more than two doses per 24 hours and three doses per 7 days were allowed. The Full Safety Set analysis comprised 354 patients who dosed at least once. The Primary Safety Set involved 185 patients who administered an average of two or more doses per 28-day period during the 24-week treatment period. A total of 4,515 self-recognized migraines were treated during the 24-week period; 6,332 doses of INP04 were analyzed.
Nearly 37% (130/354) of patients reported treatment-emergent adverse events (TEAEs); 6.8% (24/354) discontinued treatment because of the TEAEs over the 24 weeks. The most common TEAE was nasal congestion (15%, 53/354), followed by nausea (6.8%, 24/354).
Within an hour of INP104 administration, 47.6% of patients reported pain relief. After 2 hours of INP104 administration, 38% reported pain freedom and 66.3% reported pain relief. Headache recurrence was observed in 7.1% and 14.3% of patients at 24 and 48 hours, respectively.
In a questionnaire, 84% of patients agreed or strongly agreed that INP04 was easy to use. Most reported that INP104 slowed the recurrence of their migraines and was more rapidly and consistently effective than their previous best usual care treatment.
Intranasal delivery of DHE was developed in response to the challenges of traditional IV administration.
“While intravenous (IV) dihydroergotamine (DHE) mesylate has a long, established history as an effective migraine therapy, its use as an acute treatment can be limited by the high rate of nausea and vomiting reported by patients, which often requires pretreatment with antiemetics,” Dr. Smith and colleagues wrote. “Furthermore, IV DHE mesylate needs to be administered in emergency room settings or by headache specialists, limiting convenience.”
A novel delivery system
“There’s already a nasal spray on the market right now which doesn’t seem to work that well in a large number of people. This device [INP04] was designed to get the same substances to a part of the nose that’s higher and farther back, where there may be better absorption,” said Alan Rapoport, MD, clinical professor of neurology at the University of California, Los Angeles, said in an interview. Dr. Rapoport was not involved with the study.
The proprietary Precision Olfactory Delivery (POD) is meant to improve on current nasal delivery methods such as sprays, droppers, and pumps, which may deliver “less than 5% of the active drug to the upper nasal space,” according to a press release from Impel NeuroPharma.
Nasal delivery also may have advantages over oral medications. People with migraines may be more likely to have gastroparesis – delayed stomach emptying – which may affect their ability to absorb oral medications and delay symptom relief. However, patients may hesitate to agree to a medication that involves nasal delivery, Dr. Rapoport said.
“I will say it’s a little more difficult getting your patients to take a nasal spray,” Dr. Rapoport said. “Patients are used to taking tablets for their headaches,” he said. “But if the doctor spends a little more time with the patient and says, ‘Look, this could work faster for your migraine as a nasal spray. Why don’t you try it a couple of times and see if you like it or not?’ patients are usually willing to give it a try.”
The study’s limitations include the lack of a control group given that it was an open-label trial. It was carried out at 38 sites in one geographical area, which may affect the generalizability of the results. The study did not assess patients with new-onset migraine or chronic migraine.
The Food and Drug Administration approved Trudhesa on Sept. 2, 2021.
The study was funded by Impel NeuroPharma. Dr. Smith has received funding from a number of pharmaceutical companies. Dr. Rapoport disclosed no relevant financial relationships.
From Headache
U.S. pediatric hospitals in peril as Delta hits children
Over the course of the pandemic, COVID-19 has been a less serious illness for children than it has been for adults, and that continues to be true. But with the arrival of Delta, the risk for kids is rising, and that’s creating a perilous situation for hospitals across the United States that treat them.
Roughly 1,800 kids were hospitalized with COVID-19 in the United States last week, a 500% increase in the rate of COVID-19 hospitalizations for children since early July, according to data from the Centers for Disease Control and Prevention.
Emerging data from a large study in Canada suggest that children who test positive for COVID-19 during the Delta wave may be more than twice as likely to be hospitalized as they were when previous variants were dominating transmission. The new data support what many pediatric infectious disease experts say they’ve been seeing: Younger kids with more serious symptoms.
That may sound concerning, but keep in mind that the overall risk of hospitalization for kids who have COVID-19 is still very low – about one child for every hundred who test positive for the virus will end up needing hospital care for their symptoms, according to current statistics maintained by the American Academy of Pediatrics.
‘This is different’
At Le Bonheur Children’s Hospital in Memphis, they saw Delta coming.
Since last year, every kid that comes to the emergency department at the hospital gets a screening test for COVID-19.
In past waves, doctors usually found kids who were infected by accident – they tested positive after coming in for some other problem, a broken leg or appendicitis, said Nick Hysmith, MD, medical director of infection prevention at the hospital. But within the last few weeks, kids with fevers, sore throats, coughs, and runny noses started testing positive for COVID-19.
“We have seen our positive numbers go from, you know, close to about 8%-10% jump up to 20%, and then in recent weeks, we can get as high as 26% or 30%,” Dr. Hysmith said. “Then we started seeing kids sick enough to be admitted.”
“Over the last week, we’ve really seen an increase,” he said. As of August 16, the hospital had 24 children with COVID-19 admitted. Seven of the children were in the PICU, and two were on ventilators.
Arkansas Children’s Hospital had 23 young COVID-19 patients, 10 in intensive care, and five on ventilators, as of Friday, according to the Washington Post. At Children’s of Mississippi, the only hospital for kids in that state, 22 youth were hospitalized as of Monday, with three in intensive care as of August 16, according to the hospital. The nonprofit relief organization Samaritan’s Purse is setting up a second field hospital in the basement of Children’s to expand the hospital’s capacity.
“This is different,” Dr. Hysmith said. “What we’re seeing now is previously healthy kids coming in with symptomatic infection.”
This increased virulence is happening at a bad time. Schools around the United States are reopening for in-person classes, some for the first time in more than a year. Eight states have blocked districts from requiring masks, while many more have made them optional.
Children under 12 still have no access to a vaccine, so they are facing increased exposure to a germ that’s become more dangerous with little protection, especially in schools that have eschewed masks.
More than just COVID-19
Then there are the latent effects of the virus to contend with.
“We’re not only seeing more children now with acute SARS-CoV-2 in the hospital, we’re starting also to see an uptick of MISC – or Multisystem Inflammatory Syndrome in Children,” said Charlotte Hobbs, MD, a pediatric infectious disease specialist at Mississippi Children’s Hospital. “We are just beginning to [see] those cases, and we anticipate that’s going to get worse.”
Adding to COVID-19’s misery, another virus is also capitalizing on this increased mixing of kids back into the community. Respiratory syncytial virus (RSV) hospitalizes about 58,000 children under age 5 in the United States each year. The typical RSV season starts in the fall and peaks in February, along with influenza. This year, the RSV season is early, and it is ferocious.
The combination of the two infections is hitting children’s hospitals hard, and it’s layered on top of the indirect effects of the pandemic, such as the increased population of kids and teens who need mental health care in the wake of the crisis.
“It’s all these things happening at the same time,” said Mark Wietecha, CEO of the Children’s Hospital Association. “To have our hospitals this crowded in August is unusual.
And children’s hospitals are grappling with the same workforce shortages as hospitals that treat adults, while their pool of potential staff is much smaller.
“We can’t easily recruit physicians and nurses from adult hospitals in any practical way to staff a kids’ hospital,” Mr. Wietecha said.
Although pediatric doctors and nurses were trained to care for adults before they specialized, clinicians who primarily care for adults typically haven’t been taught how to care for kids.
Clinicians have fewer tools to fight COVID-19 infections in children than are available for adults.
“There have been many studies in terms of therapies and treatments for acute SARS-CoV-2 infection in adults. We have less data and information in children, and on top of that, some of these treatments aren’t even available under an EUA [emergency use authorization] to children: For example, the monoclonal antibodies,” Dr. Hobbs said.
Antibody treatments are being widely deployed to ease the pressure on hospitals that treat adults. But these therapies aren’t available for kids.
That means children’s hospitals could quickly become overwhelmed, especially in areas where community transmission is high, vaccination rates are low, and parents are screaming about masks.
“So we really have this constellation of events that really doesn’t favor children under the age of 12,” Dr. Hobbs said.
“Universal masking shouldn’t be a debate, because it’s the one thing, with adult vaccination, that can be done to protect this vulnerable population,” she said. “This isn’t a political issue. It’s a public health issue. Period.”
A version of this article first appeared on Medscape.com.
Over the course of the pandemic, COVID-19 has been a less serious illness for children than it has been for adults, and that continues to be true. But with the arrival of Delta, the risk for kids is rising, and that’s creating a perilous situation for hospitals across the United States that treat them.
Roughly 1,800 kids were hospitalized with COVID-19 in the United States last week, a 500% increase in the rate of COVID-19 hospitalizations for children since early July, according to data from the Centers for Disease Control and Prevention.
Emerging data from a large study in Canada suggest that children who test positive for COVID-19 during the Delta wave may be more than twice as likely to be hospitalized as they were when previous variants were dominating transmission. The new data support what many pediatric infectious disease experts say they’ve been seeing: Younger kids with more serious symptoms.
That may sound concerning, but keep in mind that the overall risk of hospitalization for kids who have COVID-19 is still very low – about one child for every hundred who test positive for the virus will end up needing hospital care for their symptoms, according to current statistics maintained by the American Academy of Pediatrics.
‘This is different’
At Le Bonheur Children’s Hospital in Memphis, they saw Delta coming.
Since last year, every kid that comes to the emergency department at the hospital gets a screening test for COVID-19.
In past waves, doctors usually found kids who were infected by accident – they tested positive after coming in for some other problem, a broken leg or appendicitis, said Nick Hysmith, MD, medical director of infection prevention at the hospital. But within the last few weeks, kids with fevers, sore throats, coughs, and runny noses started testing positive for COVID-19.
“We have seen our positive numbers go from, you know, close to about 8%-10% jump up to 20%, and then in recent weeks, we can get as high as 26% or 30%,” Dr. Hysmith said. “Then we started seeing kids sick enough to be admitted.”
“Over the last week, we’ve really seen an increase,” he said. As of August 16, the hospital had 24 children with COVID-19 admitted. Seven of the children were in the PICU, and two were on ventilators.
Arkansas Children’s Hospital had 23 young COVID-19 patients, 10 in intensive care, and five on ventilators, as of Friday, according to the Washington Post. At Children’s of Mississippi, the only hospital for kids in that state, 22 youth were hospitalized as of Monday, with three in intensive care as of August 16, according to the hospital. The nonprofit relief organization Samaritan’s Purse is setting up a second field hospital in the basement of Children’s to expand the hospital’s capacity.
“This is different,” Dr. Hysmith said. “What we’re seeing now is previously healthy kids coming in with symptomatic infection.”
This increased virulence is happening at a bad time. Schools around the United States are reopening for in-person classes, some for the first time in more than a year. Eight states have blocked districts from requiring masks, while many more have made them optional.
Children under 12 still have no access to a vaccine, so they are facing increased exposure to a germ that’s become more dangerous with little protection, especially in schools that have eschewed masks.
More than just COVID-19
Then there are the latent effects of the virus to contend with.
“We’re not only seeing more children now with acute SARS-CoV-2 in the hospital, we’re starting also to see an uptick of MISC – or Multisystem Inflammatory Syndrome in Children,” said Charlotte Hobbs, MD, a pediatric infectious disease specialist at Mississippi Children’s Hospital. “We are just beginning to [see] those cases, and we anticipate that’s going to get worse.”
Adding to COVID-19’s misery, another virus is also capitalizing on this increased mixing of kids back into the community. Respiratory syncytial virus (RSV) hospitalizes about 58,000 children under age 5 in the United States each year. The typical RSV season starts in the fall and peaks in February, along with influenza. This year, the RSV season is early, and it is ferocious.
The combination of the two infections is hitting children’s hospitals hard, and it’s layered on top of the indirect effects of the pandemic, such as the increased population of kids and teens who need mental health care in the wake of the crisis.
“It’s all these things happening at the same time,” said Mark Wietecha, CEO of the Children’s Hospital Association. “To have our hospitals this crowded in August is unusual.
And children’s hospitals are grappling with the same workforce shortages as hospitals that treat adults, while their pool of potential staff is much smaller.
“We can’t easily recruit physicians and nurses from adult hospitals in any practical way to staff a kids’ hospital,” Mr. Wietecha said.
Although pediatric doctors and nurses were trained to care for adults before they specialized, clinicians who primarily care for adults typically haven’t been taught how to care for kids.
Clinicians have fewer tools to fight COVID-19 infections in children than are available for adults.
“There have been many studies in terms of therapies and treatments for acute SARS-CoV-2 infection in adults. We have less data and information in children, and on top of that, some of these treatments aren’t even available under an EUA [emergency use authorization] to children: For example, the monoclonal antibodies,” Dr. Hobbs said.
Antibody treatments are being widely deployed to ease the pressure on hospitals that treat adults. But these therapies aren’t available for kids.
That means children’s hospitals could quickly become overwhelmed, especially in areas where community transmission is high, vaccination rates are low, and parents are screaming about masks.
“So we really have this constellation of events that really doesn’t favor children under the age of 12,” Dr. Hobbs said.
“Universal masking shouldn’t be a debate, because it’s the one thing, with adult vaccination, that can be done to protect this vulnerable population,” she said. “This isn’t a political issue. It’s a public health issue. Period.”
A version of this article first appeared on Medscape.com.
Over the course of the pandemic, COVID-19 has been a less serious illness for children than it has been for adults, and that continues to be true. But with the arrival of Delta, the risk for kids is rising, and that’s creating a perilous situation for hospitals across the United States that treat them.
Roughly 1,800 kids were hospitalized with COVID-19 in the United States last week, a 500% increase in the rate of COVID-19 hospitalizations for children since early July, according to data from the Centers for Disease Control and Prevention.
Emerging data from a large study in Canada suggest that children who test positive for COVID-19 during the Delta wave may be more than twice as likely to be hospitalized as they were when previous variants were dominating transmission. The new data support what many pediatric infectious disease experts say they’ve been seeing: Younger kids with more serious symptoms.
That may sound concerning, but keep in mind that the overall risk of hospitalization for kids who have COVID-19 is still very low – about one child for every hundred who test positive for the virus will end up needing hospital care for their symptoms, according to current statistics maintained by the American Academy of Pediatrics.
‘This is different’
At Le Bonheur Children’s Hospital in Memphis, they saw Delta coming.
Since last year, every kid that comes to the emergency department at the hospital gets a screening test for COVID-19.
In past waves, doctors usually found kids who were infected by accident – they tested positive after coming in for some other problem, a broken leg or appendicitis, said Nick Hysmith, MD, medical director of infection prevention at the hospital. But within the last few weeks, kids with fevers, sore throats, coughs, and runny noses started testing positive for COVID-19.
“We have seen our positive numbers go from, you know, close to about 8%-10% jump up to 20%, and then in recent weeks, we can get as high as 26% or 30%,” Dr. Hysmith said. “Then we started seeing kids sick enough to be admitted.”
“Over the last week, we’ve really seen an increase,” he said. As of August 16, the hospital had 24 children with COVID-19 admitted. Seven of the children were in the PICU, and two were on ventilators.
Arkansas Children’s Hospital had 23 young COVID-19 patients, 10 in intensive care, and five on ventilators, as of Friday, according to the Washington Post. At Children’s of Mississippi, the only hospital for kids in that state, 22 youth were hospitalized as of Monday, with three in intensive care as of August 16, according to the hospital. The nonprofit relief organization Samaritan’s Purse is setting up a second field hospital in the basement of Children’s to expand the hospital’s capacity.
“This is different,” Dr. Hysmith said. “What we’re seeing now is previously healthy kids coming in with symptomatic infection.”
This increased virulence is happening at a bad time. Schools around the United States are reopening for in-person classes, some for the first time in more than a year. Eight states have blocked districts from requiring masks, while many more have made them optional.
Children under 12 still have no access to a vaccine, so they are facing increased exposure to a germ that’s become more dangerous with little protection, especially in schools that have eschewed masks.
More than just COVID-19
Then there are the latent effects of the virus to contend with.
“We’re not only seeing more children now with acute SARS-CoV-2 in the hospital, we’re starting also to see an uptick of MISC – or Multisystem Inflammatory Syndrome in Children,” said Charlotte Hobbs, MD, a pediatric infectious disease specialist at Mississippi Children’s Hospital. “We are just beginning to [see] those cases, and we anticipate that’s going to get worse.”
Adding to COVID-19’s misery, another virus is also capitalizing on this increased mixing of kids back into the community. Respiratory syncytial virus (RSV) hospitalizes about 58,000 children under age 5 in the United States each year. The typical RSV season starts in the fall and peaks in February, along with influenza. This year, the RSV season is early, and it is ferocious.
The combination of the two infections is hitting children’s hospitals hard, and it’s layered on top of the indirect effects of the pandemic, such as the increased population of kids and teens who need mental health care in the wake of the crisis.
“It’s all these things happening at the same time,” said Mark Wietecha, CEO of the Children’s Hospital Association. “To have our hospitals this crowded in August is unusual.
And children’s hospitals are grappling with the same workforce shortages as hospitals that treat adults, while their pool of potential staff is much smaller.
“We can’t easily recruit physicians and nurses from adult hospitals in any practical way to staff a kids’ hospital,” Mr. Wietecha said.
Although pediatric doctors and nurses were trained to care for adults before they specialized, clinicians who primarily care for adults typically haven’t been taught how to care for kids.
Clinicians have fewer tools to fight COVID-19 infections in children than are available for adults.
“There have been many studies in terms of therapies and treatments for acute SARS-CoV-2 infection in adults. We have less data and information in children, and on top of that, some of these treatments aren’t even available under an EUA [emergency use authorization] to children: For example, the monoclonal antibodies,” Dr. Hobbs said.
Antibody treatments are being widely deployed to ease the pressure on hospitals that treat adults. But these therapies aren’t available for kids.
That means children’s hospitals could quickly become overwhelmed, especially in areas where community transmission is high, vaccination rates are low, and parents are screaming about masks.
“So we really have this constellation of events that really doesn’t favor children under the age of 12,” Dr. Hobbs said.
“Universal masking shouldn’t be a debate, because it’s the one thing, with adult vaccination, that can be done to protect this vulnerable population,” she said. “This isn’t a political issue. It’s a public health issue. Period.”
A version of this article first appeared on Medscape.com.
Youngest children more likely to spread SARS-CoV-2 to family: Study
Young children are more likely than are their older siblings to transmit SARS-CoV-2 in their households, according to an analysis of public health records in Ontario, Canada – a finding that upends the common belief that children play a minimal role in COVID-19 spread.
The study by researchers from Public Health Ontario, published online in JAMA Pediatrics, found that teenagers (14- to 17-year-olds) were more likely than were their younger siblings to bring the virus into the household, while infants and toddlers (up to age 3) were about 43% more likely than were the older teens to spread it to others in the home.
Children or teens were the source of SARS-CoV-2 in about 1 in 13 Ontario households between June and December 2020, the study shows. The researchers analyzed health records from 6,280 households with a pediatric COVID-19 case and a subset of 1,717 households in which a child up to age 17 was the source of transmission in a household.
When analyzing the data, the researchers controlled for gender differences, month of disease onset, testing delay, and mean family size.
The role of young children in transmission seemed logical to some experts who have been tracking the evolution of the pandemic. “I think what was more surprising was how long the narrative persisted that children weren’t transmitting SARS-CoV-2,” said Samuel Scarpino, PhD, managing director of pathogen surveillance at the Rockefeller Foundation.
Meanwhile, less mask-wearing, the return to school and activities, and the onslaught of the Delta variant have changed the dynamics of spread, said Andrew Pavia, MD, chief of the division of pediatric infectious diseases at the University of Utah.
“Adolescents and high-school-aged kids have had much, much higher rates of infection in the past,” he said. “Now when we look at the rates of school-aged kids, they are the same as high-school-aged kids, and we’re seeing more and more in the preschool age groups.”
Cases may be underestimated
If anything, the study may underestimate the role young children play in spreading COVID-19 in families, since it included only symptomatic cases as the initial source and young children are more likely to be asymptomatic, Dr. Pavia said.
The Delta variant heightens the concern; it is more than twice as infectious as previous strains and has spurred a rise in pediatric cases, including some coinfection with other circulating respiratory diseases, such as respiratory syncytial virus (RSV).
The Ontario study covers a period before vaccination and the spread of the Delta variant. “As the number of pediatric cases increases worldwide, the role of children in household transmission will continue to grow,” the authors concluded.
Following recommended respiratory hygiene is clearly more difficult with very young children. For example, parents, caregivers, and older siblings aren’t going to stay 6 feet away from a sick baby or toddler, Susan Coffin, MD, MPH, a pediatric infectious disease physician, and David Rubin, MD, a pediatrician and director of PolicyLab at Children’s Hospital of Philadelphia, noted in an accompanying commentary.
“Cuddling and touching are part and parcel of taking care of a sick young child, and that will obviously come with an increased risk of transmission to parents as well as to older siblings who may be helping to care for their sick brother or sister,” they wrote.
While parents may wash their hands more frequently when caring for a sick child, they aren’t likely to wear a mask, said William Schaffner, MD, an infectious disease specialist at Vanderbilt University, Nashville, Tenn.
“I imagine some moms even take a sick child into bed with them,” he said. “It’s probably just the extensive contact one has with a sick, very small child that augments their capacity to transmit this infection.”
What can be done
What can be done, then, to reduce the household spread of COVID-19? “The obvious solution to protect a household with a sick young infant or toddler is to make sure that all eligible members of the household are vaccinated,” Dr. Coffin and Dr. Rubin stated in their commentary.
The American Academy of Pediatrics recently wrote to Janet Woodcock, MD, acting commissioner of the Food and Drug Administration, asking for the agency to authorize use of SARS-CoV-2 vaccines for children under age 12 “as soon as possible,” noting that “the Delta variant has created a new and pressing risk to children and adolescents across this country, as it has also done for unvaccinated adults.”
The FDA reportedly asked vaccine makers Pfizer and Moderna to expand the clinical trials of children, which may delay authorization for younger age groups. Pfizer has said it plans to submit a request for emergency use authorization of its vaccine for 5- to 11-year-olds in September or October.
As with adult vaccination, hesitancy is likely to be a barrier. Less than half of parents said they are very or somewhat likely to have their children get a COVID-19 vaccine, according to a national survey conducted by researchers at the University of California, Los Angeles.
The Ontario study provides valuable evidence to support taking steps to protect children from transmission in schools, including mask requirements, frequent testing, and improved ventilation, said Dr. Scarpino.
“We’re not going to be able to control COVID without vaccinating younger individuals,” he said.
Dr. Pavia has consulted for GlaxoSmithKline on non–COVID-19–related issues. Sarah Buchan, PhD, study author and scientist at Public Health Ontario, reported grants from the Canadian Institutes of Health Research for research on influenza, RSV, and COVID-19, and grants from the Canadian Immunity Task Force for COVID-19 outside the submitted work. Dr. Coffin reported grants as a Centers for Disease Control and Prevention coinvestigator at a Vaccine and Treatment Evaluation Unit site conducting COVID-19 vaccine trials in children. Dr. Scarpino holds unexercised options in ILiAD Biotechnologies, which is focused on the prevention and treatment of pertussis. Dr. Schaffner is a consultant for VBI Vaccines.
A version of this article first appeared on Medscape.com.
Young children are more likely than are their older siblings to transmit SARS-CoV-2 in their households, according to an analysis of public health records in Ontario, Canada – a finding that upends the common belief that children play a minimal role in COVID-19 spread.
The study by researchers from Public Health Ontario, published online in JAMA Pediatrics, found that teenagers (14- to 17-year-olds) were more likely than were their younger siblings to bring the virus into the household, while infants and toddlers (up to age 3) were about 43% more likely than were the older teens to spread it to others in the home.
Children or teens were the source of SARS-CoV-2 in about 1 in 13 Ontario households between June and December 2020, the study shows. The researchers analyzed health records from 6,280 households with a pediatric COVID-19 case and a subset of 1,717 households in which a child up to age 17 was the source of transmission in a household.
When analyzing the data, the researchers controlled for gender differences, month of disease onset, testing delay, and mean family size.
The role of young children in transmission seemed logical to some experts who have been tracking the evolution of the pandemic. “I think what was more surprising was how long the narrative persisted that children weren’t transmitting SARS-CoV-2,” said Samuel Scarpino, PhD, managing director of pathogen surveillance at the Rockefeller Foundation.
Meanwhile, less mask-wearing, the return to school and activities, and the onslaught of the Delta variant have changed the dynamics of spread, said Andrew Pavia, MD, chief of the division of pediatric infectious diseases at the University of Utah.
“Adolescents and high-school-aged kids have had much, much higher rates of infection in the past,” he said. “Now when we look at the rates of school-aged kids, they are the same as high-school-aged kids, and we’re seeing more and more in the preschool age groups.”
Cases may be underestimated
If anything, the study may underestimate the role young children play in spreading COVID-19 in families, since it included only symptomatic cases as the initial source and young children are more likely to be asymptomatic, Dr. Pavia said.
The Delta variant heightens the concern; it is more than twice as infectious as previous strains and has spurred a rise in pediatric cases, including some coinfection with other circulating respiratory diseases, such as respiratory syncytial virus (RSV).
The Ontario study covers a period before vaccination and the spread of the Delta variant. “As the number of pediatric cases increases worldwide, the role of children in household transmission will continue to grow,” the authors concluded.
Following recommended respiratory hygiene is clearly more difficult with very young children. For example, parents, caregivers, and older siblings aren’t going to stay 6 feet away from a sick baby or toddler, Susan Coffin, MD, MPH, a pediatric infectious disease physician, and David Rubin, MD, a pediatrician and director of PolicyLab at Children’s Hospital of Philadelphia, noted in an accompanying commentary.
“Cuddling and touching are part and parcel of taking care of a sick young child, and that will obviously come with an increased risk of transmission to parents as well as to older siblings who may be helping to care for their sick brother or sister,” they wrote.
While parents may wash their hands more frequently when caring for a sick child, they aren’t likely to wear a mask, said William Schaffner, MD, an infectious disease specialist at Vanderbilt University, Nashville, Tenn.
“I imagine some moms even take a sick child into bed with them,” he said. “It’s probably just the extensive contact one has with a sick, very small child that augments their capacity to transmit this infection.”
What can be done
What can be done, then, to reduce the household spread of COVID-19? “The obvious solution to protect a household with a sick young infant or toddler is to make sure that all eligible members of the household are vaccinated,” Dr. Coffin and Dr. Rubin stated in their commentary.
The American Academy of Pediatrics recently wrote to Janet Woodcock, MD, acting commissioner of the Food and Drug Administration, asking for the agency to authorize use of SARS-CoV-2 vaccines for children under age 12 “as soon as possible,” noting that “the Delta variant has created a new and pressing risk to children and adolescents across this country, as it has also done for unvaccinated adults.”
The FDA reportedly asked vaccine makers Pfizer and Moderna to expand the clinical trials of children, which may delay authorization for younger age groups. Pfizer has said it plans to submit a request for emergency use authorization of its vaccine for 5- to 11-year-olds in September or October.
As with adult vaccination, hesitancy is likely to be a barrier. Less than half of parents said they are very or somewhat likely to have their children get a COVID-19 vaccine, according to a national survey conducted by researchers at the University of California, Los Angeles.
The Ontario study provides valuable evidence to support taking steps to protect children from transmission in schools, including mask requirements, frequent testing, and improved ventilation, said Dr. Scarpino.
“We’re not going to be able to control COVID without vaccinating younger individuals,” he said.
Dr. Pavia has consulted for GlaxoSmithKline on non–COVID-19–related issues. Sarah Buchan, PhD, study author and scientist at Public Health Ontario, reported grants from the Canadian Institutes of Health Research for research on influenza, RSV, and COVID-19, and grants from the Canadian Immunity Task Force for COVID-19 outside the submitted work. Dr. Coffin reported grants as a Centers for Disease Control and Prevention coinvestigator at a Vaccine and Treatment Evaluation Unit site conducting COVID-19 vaccine trials in children. Dr. Scarpino holds unexercised options in ILiAD Biotechnologies, which is focused on the prevention and treatment of pertussis. Dr. Schaffner is a consultant for VBI Vaccines.
A version of this article first appeared on Medscape.com.
Young children are more likely than are their older siblings to transmit SARS-CoV-2 in their households, according to an analysis of public health records in Ontario, Canada – a finding that upends the common belief that children play a minimal role in COVID-19 spread.
The study by researchers from Public Health Ontario, published online in JAMA Pediatrics, found that teenagers (14- to 17-year-olds) were more likely than were their younger siblings to bring the virus into the household, while infants and toddlers (up to age 3) were about 43% more likely than were the older teens to spread it to others in the home.
Children or teens were the source of SARS-CoV-2 in about 1 in 13 Ontario households between June and December 2020, the study shows. The researchers analyzed health records from 6,280 households with a pediatric COVID-19 case and a subset of 1,717 households in which a child up to age 17 was the source of transmission in a household.
When analyzing the data, the researchers controlled for gender differences, month of disease onset, testing delay, and mean family size.
The role of young children in transmission seemed logical to some experts who have been tracking the evolution of the pandemic. “I think what was more surprising was how long the narrative persisted that children weren’t transmitting SARS-CoV-2,” said Samuel Scarpino, PhD, managing director of pathogen surveillance at the Rockefeller Foundation.
Meanwhile, less mask-wearing, the return to school and activities, and the onslaught of the Delta variant have changed the dynamics of spread, said Andrew Pavia, MD, chief of the division of pediatric infectious diseases at the University of Utah.
“Adolescents and high-school-aged kids have had much, much higher rates of infection in the past,” he said. “Now when we look at the rates of school-aged kids, they are the same as high-school-aged kids, and we’re seeing more and more in the preschool age groups.”
Cases may be underestimated
If anything, the study may underestimate the role young children play in spreading COVID-19 in families, since it included only symptomatic cases as the initial source and young children are more likely to be asymptomatic, Dr. Pavia said.
The Delta variant heightens the concern; it is more than twice as infectious as previous strains and has spurred a rise in pediatric cases, including some coinfection with other circulating respiratory diseases, such as respiratory syncytial virus (RSV).
The Ontario study covers a period before vaccination and the spread of the Delta variant. “As the number of pediatric cases increases worldwide, the role of children in household transmission will continue to grow,” the authors concluded.
Following recommended respiratory hygiene is clearly more difficult with very young children. For example, parents, caregivers, and older siblings aren’t going to stay 6 feet away from a sick baby or toddler, Susan Coffin, MD, MPH, a pediatric infectious disease physician, and David Rubin, MD, a pediatrician and director of PolicyLab at Children’s Hospital of Philadelphia, noted in an accompanying commentary.
“Cuddling and touching are part and parcel of taking care of a sick young child, and that will obviously come with an increased risk of transmission to parents as well as to older siblings who may be helping to care for their sick brother or sister,” they wrote.
While parents may wash their hands more frequently when caring for a sick child, they aren’t likely to wear a mask, said William Schaffner, MD, an infectious disease specialist at Vanderbilt University, Nashville, Tenn.
“I imagine some moms even take a sick child into bed with them,” he said. “It’s probably just the extensive contact one has with a sick, very small child that augments their capacity to transmit this infection.”
What can be done
What can be done, then, to reduce the household spread of COVID-19? “The obvious solution to protect a household with a sick young infant or toddler is to make sure that all eligible members of the household are vaccinated,” Dr. Coffin and Dr. Rubin stated in their commentary.
The American Academy of Pediatrics recently wrote to Janet Woodcock, MD, acting commissioner of the Food and Drug Administration, asking for the agency to authorize use of SARS-CoV-2 vaccines for children under age 12 “as soon as possible,” noting that “the Delta variant has created a new and pressing risk to children and adolescents across this country, as it has also done for unvaccinated adults.”
The FDA reportedly asked vaccine makers Pfizer and Moderna to expand the clinical trials of children, which may delay authorization for younger age groups. Pfizer has said it plans to submit a request for emergency use authorization of its vaccine for 5- to 11-year-olds in September or October.
As with adult vaccination, hesitancy is likely to be a barrier. Less than half of parents said they are very or somewhat likely to have their children get a COVID-19 vaccine, according to a national survey conducted by researchers at the University of California, Los Angeles.
The Ontario study provides valuable evidence to support taking steps to protect children from transmission in schools, including mask requirements, frequent testing, and improved ventilation, said Dr. Scarpino.
“We’re not going to be able to control COVID without vaccinating younger individuals,” he said.
Dr. Pavia has consulted for GlaxoSmithKline on non–COVID-19–related issues. Sarah Buchan, PhD, study author and scientist at Public Health Ontario, reported grants from the Canadian Institutes of Health Research for research on influenza, RSV, and COVID-19, and grants from the Canadian Immunity Task Force for COVID-19 outside the submitted work. Dr. Coffin reported grants as a Centers for Disease Control and Prevention coinvestigator at a Vaccine and Treatment Evaluation Unit site conducting COVID-19 vaccine trials in children. Dr. Scarpino holds unexercised options in ILiAD Biotechnologies, which is focused on the prevention and treatment of pertussis. Dr. Schaffner is a consultant for VBI Vaccines.
A version of this article first appeared on Medscape.com.









