User login
Sarcoidosis Presenting as Telangiectatic Macules
To the Editor:
Sarcoidosis is a multisystem, noncaseating, granulomatous disorder thought to occur from a combination of immunologic, genetic, and environmental factors.1 Often referred to as the “great imitator,” the cutaneous manifestations of sarcoidosis encompass many morphologies, including papules, plaques, nodules, and scars.1 We report an unusual case of sarcoidosis presenting as telangiectatic macules on the lower extremities.
A woman in her early 30s presented with a burning, pruritic, erythematous, telangiectatic eruption on the lower extremities with concurrent ankle swelling of 4 weeks’ duration. The patient denied any fevers, chills, recent infections, or new medications. Evaluation by her primary care physician during the time of the eruption included unremarkable antinuclear antibodies, thyroid stimulating hormone level, complete blood cell count, comprehensive metabolic panel, urinalysis, chest radiography, and lower-extremity Doppler ultrasonography.
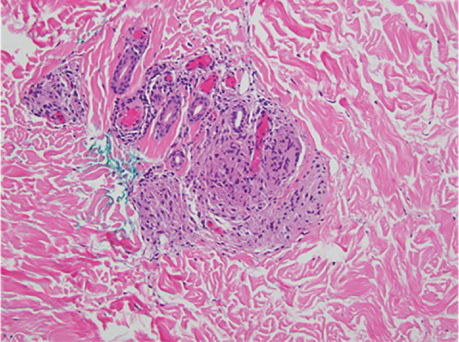
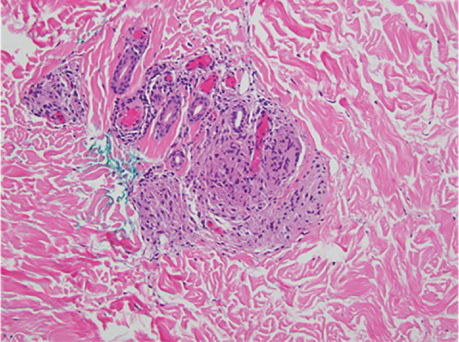
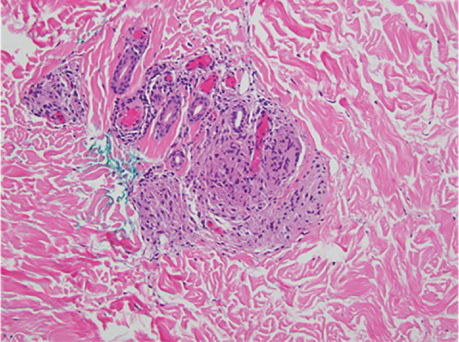
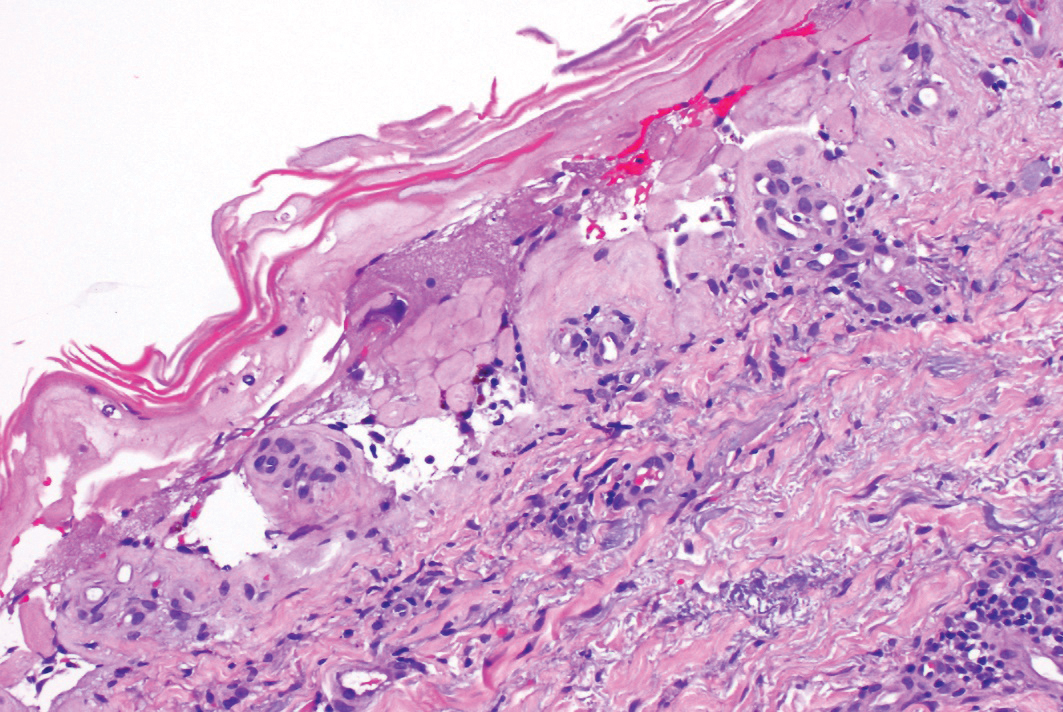
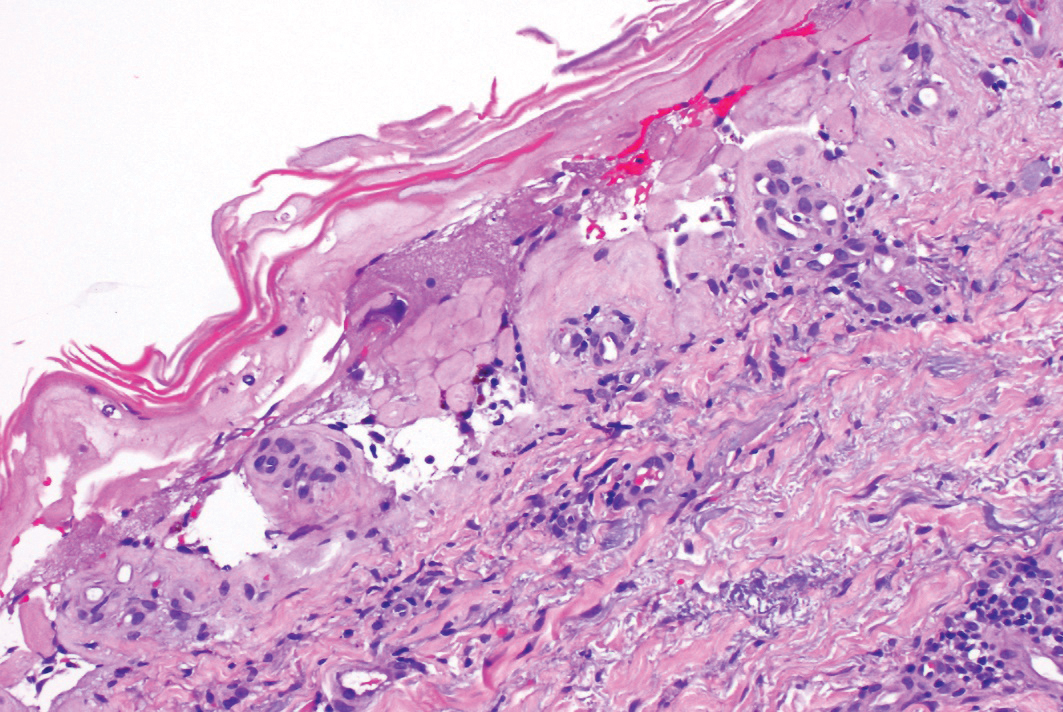
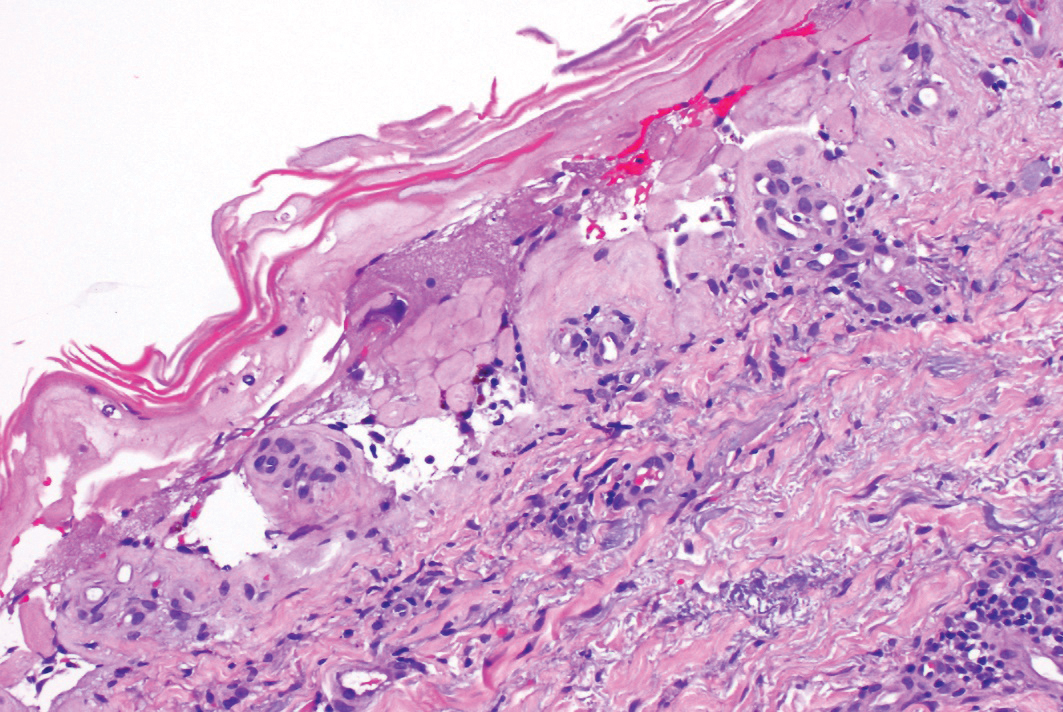
Physical examination at the current presentation revealed numerous scattered, faint, erythematous, blanchable macules on the lower extremities along with mild pitting edema (Figure 1). The patient’s current medications included cetirizine, which she had been taking for years, as well as an intrauterine device. A punch biopsy from the right lower leg revealed small, well-demarcated sarcoidal granulomatous inflammation surrounding vascular structures and skin appendages (Figure 2). No foreign bodies were observed with polarized light microscopy. Microscopic findings suggestive of an infection, including caseation necrosis and suppurative inflammation, also were absent. Angiotensin-converting enzyme levels were normal. Myeloperoxidase and proteinase 3 IgG antibody levels were evaluated due to potential vascular involvement but were negative. An infectious cause of the sarcoidal granulomas was unlikely given histopathologic findings and negative tuberculosis skin testing, which the patient underwent annually for her job, so a tissue culture was not performed. The patient was prescribed triamcinolone acetonide cream 0.1% for the itching and burning at the initial visit and was continued on this treatment after the diagnosis of sarcoidosis was made. At 2-month follow-up, the patient’s eruption had nearly resolved with topical therapy.

Cutaneous manifestation occurs in 20% to 35% of sarcoidosis cases and may develop in the presence or absence of systemic disease. Approximately 60% of individuals with cutaneous sarcoidosis are found to have systemic involvement; therefore, careful monitoring and diagnostic workup are important in the management of these patients.2 While most cases of cutaneous sarcoidosis are papular, it is important for clinicians to maintain a level of suspicion for sarcoidosis in any uncertain dermatologic presentation.1,2 Evidence of telangiectasias has been shown in rarer forms of sarcoidosis (eg, angiolupoid), but the lesions usually are confined to the face, ears, or neck.3 Granulomatous vasculitis has been reported in a small number of individuals with ulcerative sarcoidosis.4 In our case, no ulcerations were present, possibly indicating an early lesion or an entirely novel process. Lastly, although reticular dermal granulomas are found in drug-induced interstitial granulomatous dermatitis, these lesions often are dispersed interstitially amongst collagen bundles and are associated with necrobiosis of collagen and eosinophilic/neutrophilic infiltrates.5 The lack of these characteristic pathologic findings in our patient along with no known reported cases of cetirizine-induced granulomatous dermatitis led us to rule out reticular dermal granulomas as a diagnosis. We present our case as a reminder of the diversity of cutaneous sarcoidosis manifestations and the importance of early diagnosis of these lesions.
- Haimovic A, Sanchez M, Judson MA, et al. Sarcoidosis: a comprehensive review and update for the dermatologist: part I. cutaneous disease. J Am Acad Dermatol. 2012;66:699.E1-E18.
- Yanardag H, Tetikkurt C, Bilir M, et al. Diagnosis of cutaneous sarcoidosis; clinical and the prognostic significance of skin lesions. Multidiscip Respir Med. 2013;8:26.
- Arias-Santiago S, Fernández-Pugnaire MA, Aneiros- Fernández J, et al. Recurrent telangiectasias on the cheek: angiolupoid sarcoidosis. Am J Med. 2010;123:E7-E8.
- Wei C-H, Huang Y-H, Shih Y-C, et al. Sarcoidosis with cutaneous granulomatous vasculitis. Australas J Dermatol. 2010;51:198-201.
- Peroni A, Colato C, Schena D, et al. Interstitial granulomatous dermatitis: a distinct entity with characteristic histological and clinical pattern. Br J Dermatol. 2012;166:775-783.
To the Editor:
Sarcoidosis is a multisystem, noncaseating, granulomatous disorder thought to occur from a combination of immunologic, genetic, and environmental factors.1 Often referred to as the “great imitator,” the cutaneous manifestations of sarcoidosis encompass many morphologies, including papules, plaques, nodules, and scars.1 We report an unusual case of sarcoidosis presenting as telangiectatic macules on the lower extremities.
A woman in her early 30s presented with a burning, pruritic, erythematous, telangiectatic eruption on the lower extremities with concurrent ankle swelling of 4 weeks’ duration. The patient denied any fevers, chills, recent infections, or new medications. Evaluation by her primary care physician during the time of the eruption included unremarkable antinuclear antibodies, thyroid stimulating hormone level, complete blood cell count, comprehensive metabolic panel, urinalysis, chest radiography, and lower-extremity Doppler ultrasonography.
Physical examination at the current presentation revealed numerous scattered, faint, erythematous, blanchable macules on the lower extremities along with mild pitting edema (Figure 1). The patient’s current medications included cetirizine, which she had been taking for years, as well as an intrauterine device. A punch biopsy from the right lower leg revealed small, well-demarcated sarcoidal granulomatous inflammation surrounding vascular structures and skin appendages (Figure 2). No foreign bodies were observed with polarized light microscopy. Microscopic findings suggestive of an infection, including caseation necrosis and suppurative inflammation, also were absent. Angiotensin-converting enzyme levels were normal. Myeloperoxidase and proteinase 3 IgG antibody levels were evaluated due to potential vascular involvement but were negative. An infectious cause of the sarcoidal granulomas was unlikely given histopathologic findings and negative tuberculosis skin testing, which the patient underwent annually for her job, so a tissue culture was not performed. The patient was prescribed triamcinolone acetonide cream 0.1% for the itching and burning at the initial visit and was continued on this treatment after the diagnosis of sarcoidosis was made. At 2-month follow-up, the patient’s eruption had nearly resolved with topical therapy.

Cutaneous manifestation occurs in 20% to 35% of sarcoidosis cases and may develop in the presence or absence of systemic disease. Approximately 60% of individuals with cutaneous sarcoidosis are found to have systemic involvement; therefore, careful monitoring and diagnostic workup are important in the management of these patients.2 While most cases of cutaneous sarcoidosis are papular, it is important for clinicians to maintain a level of suspicion for sarcoidosis in any uncertain dermatologic presentation.1,2 Evidence of telangiectasias has been shown in rarer forms of sarcoidosis (eg, angiolupoid), but the lesions usually are confined to the face, ears, or neck.3 Granulomatous vasculitis has been reported in a small number of individuals with ulcerative sarcoidosis.4 In our case, no ulcerations were present, possibly indicating an early lesion or an entirely novel process. Lastly, although reticular dermal granulomas are found in drug-induced interstitial granulomatous dermatitis, these lesions often are dispersed interstitially amongst collagen bundles and are associated with necrobiosis of collagen and eosinophilic/neutrophilic infiltrates.5 The lack of these characteristic pathologic findings in our patient along with no known reported cases of cetirizine-induced granulomatous dermatitis led us to rule out reticular dermal granulomas as a diagnosis. We present our case as a reminder of the diversity of cutaneous sarcoidosis manifestations and the importance of early diagnosis of these lesions.
To the Editor:
Sarcoidosis is a multisystem, noncaseating, granulomatous disorder thought to occur from a combination of immunologic, genetic, and environmental factors.1 Often referred to as the “great imitator,” the cutaneous manifestations of sarcoidosis encompass many morphologies, including papules, plaques, nodules, and scars.1 We report an unusual case of sarcoidosis presenting as telangiectatic macules on the lower extremities.
A woman in her early 30s presented with a burning, pruritic, erythematous, telangiectatic eruption on the lower extremities with concurrent ankle swelling of 4 weeks’ duration. The patient denied any fevers, chills, recent infections, or new medications. Evaluation by her primary care physician during the time of the eruption included unremarkable antinuclear antibodies, thyroid stimulating hormone level, complete blood cell count, comprehensive metabolic panel, urinalysis, chest radiography, and lower-extremity Doppler ultrasonography.
Physical examination at the current presentation revealed numerous scattered, faint, erythematous, blanchable macules on the lower extremities along with mild pitting edema (Figure 1). The patient’s current medications included cetirizine, which she had been taking for years, as well as an intrauterine device. A punch biopsy from the right lower leg revealed small, well-demarcated sarcoidal granulomatous inflammation surrounding vascular structures and skin appendages (Figure 2). No foreign bodies were observed with polarized light microscopy. Microscopic findings suggestive of an infection, including caseation necrosis and suppurative inflammation, also were absent. Angiotensin-converting enzyme levels were normal. Myeloperoxidase and proteinase 3 IgG antibody levels were evaluated due to potential vascular involvement but were negative. An infectious cause of the sarcoidal granulomas was unlikely given histopathologic findings and negative tuberculosis skin testing, which the patient underwent annually for her job, so a tissue culture was not performed. The patient was prescribed triamcinolone acetonide cream 0.1% for the itching and burning at the initial visit and was continued on this treatment after the diagnosis of sarcoidosis was made. At 2-month follow-up, the patient’s eruption had nearly resolved with topical therapy.

Cutaneous manifestation occurs in 20% to 35% of sarcoidosis cases and may develop in the presence or absence of systemic disease. Approximately 60% of individuals with cutaneous sarcoidosis are found to have systemic involvement; therefore, careful monitoring and diagnostic workup are important in the management of these patients.2 While most cases of cutaneous sarcoidosis are papular, it is important for clinicians to maintain a level of suspicion for sarcoidosis in any uncertain dermatologic presentation.1,2 Evidence of telangiectasias has been shown in rarer forms of sarcoidosis (eg, angiolupoid), but the lesions usually are confined to the face, ears, or neck.3 Granulomatous vasculitis has been reported in a small number of individuals with ulcerative sarcoidosis.4 In our case, no ulcerations were present, possibly indicating an early lesion or an entirely novel process. Lastly, although reticular dermal granulomas are found in drug-induced interstitial granulomatous dermatitis, these lesions often are dispersed interstitially amongst collagen bundles and are associated with necrobiosis of collagen and eosinophilic/neutrophilic infiltrates.5 The lack of these characteristic pathologic findings in our patient along with no known reported cases of cetirizine-induced granulomatous dermatitis led us to rule out reticular dermal granulomas as a diagnosis. We present our case as a reminder of the diversity of cutaneous sarcoidosis manifestations and the importance of early diagnosis of these lesions.
- Haimovic A, Sanchez M, Judson MA, et al. Sarcoidosis: a comprehensive review and update for the dermatologist: part I. cutaneous disease. J Am Acad Dermatol. 2012;66:699.E1-E18.
- Yanardag H, Tetikkurt C, Bilir M, et al. Diagnosis of cutaneous sarcoidosis; clinical and the prognostic significance of skin lesions. Multidiscip Respir Med. 2013;8:26.
- Arias-Santiago S, Fernández-Pugnaire MA, Aneiros- Fernández J, et al. Recurrent telangiectasias on the cheek: angiolupoid sarcoidosis. Am J Med. 2010;123:E7-E8.
- Wei C-H, Huang Y-H, Shih Y-C, et al. Sarcoidosis with cutaneous granulomatous vasculitis. Australas J Dermatol. 2010;51:198-201.
- Peroni A, Colato C, Schena D, et al. Interstitial granulomatous dermatitis: a distinct entity with characteristic histological and clinical pattern. Br J Dermatol. 2012;166:775-783.
- Haimovic A, Sanchez M, Judson MA, et al. Sarcoidosis: a comprehensive review and update for the dermatologist: part I. cutaneous disease. J Am Acad Dermatol. 2012;66:699.E1-E18.
- Yanardag H, Tetikkurt C, Bilir M, et al. Diagnosis of cutaneous sarcoidosis; clinical and the prognostic significance of skin lesions. Multidiscip Respir Med. 2013;8:26.
- Arias-Santiago S, Fernández-Pugnaire MA, Aneiros- Fernández J, et al. Recurrent telangiectasias on the cheek: angiolupoid sarcoidosis. Am J Med. 2010;123:E7-E8.
- Wei C-H, Huang Y-H, Shih Y-C, et al. Sarcoidosis with cutaneous granulomatous vasculitis. Australas J Dermatol. 2010;51:198-201.
- Peroni A, Colato C, Schena D, et al. Interstitial granulomatous dermatitis: a distinct entity with characteristic histological and clinical pattern. Br J Dermatol. 2012;166:775-783.
Practice Points
- Cutaneous manifestations of sarcoidosis can encompass numerous morphologies. A high degree of suspicion should be maintained for any uncertain dermatologic presentation.
- Although papular eruptions are the most common cutaneous findings in sarcoidosis, this case report illustrates a less common vascular-appearing presentation.
- A systemic workup is indicated in any presentation of sarcoidosis.
Graft-vs-host Disease and Toxic Epidermal Necrolysis Following Hematopoietic Stem Cell Transplantation
To the Editor:
Acute graft-vs-host disease (GVHD) remains a limitation to hematopoietic stem cell transplantation (HSCT) in 20% to 50% of patients after transplant. Furthermore, failed treatment with corticosteroids is frequent and portends a poor prognosis.1 Toxic epidermal necrolysis (TEN) is an epidermolytic skin disorder thought to represent an adverse drug reaction, though its pathogenesis remains unclear. Severe forms of acute GVHD can mimic TEN clinically and histologically. Both can present with widespread cutaneous and mucosal bullae, erosions, and desquamation. Toxic epidermal necrolysis in the context of allogeneic hematopoietic stem cell transplantation is extremely rare, with almost 100% mortality in adult patients. Features that favor acute GVHD over TEN include diarrhea, elevation in bilirubin level, and chimerism.2 However, these features might be absent, posing a therapeutic dilemma, as current treatment preferences for each of these entities differ.
Growing evidence supports the use of anti–tumor necrosis factor (TNF) α drugs for the treatment of TEN. Success has been reported with both anti–TNF-α monoclonal antibodies as well as the soluble fusion protein etanercept.3,4 The use of TNF-α inhibitors in acute GVHD remains anecdotal.

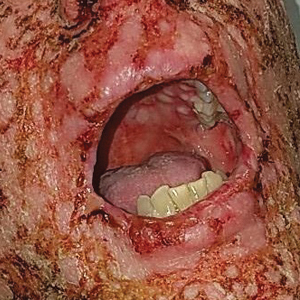
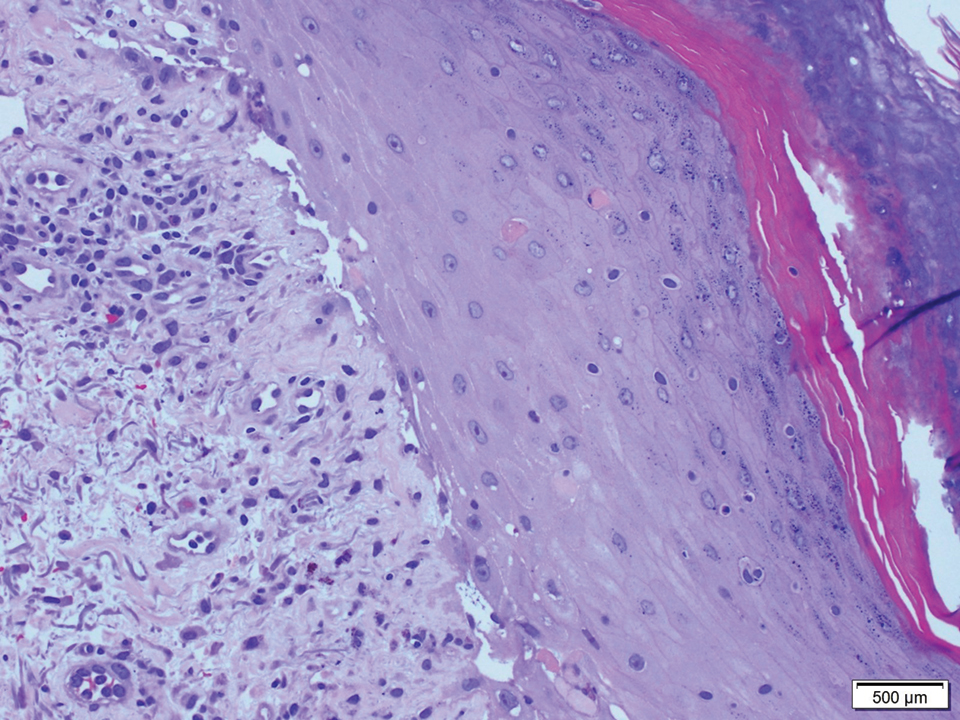
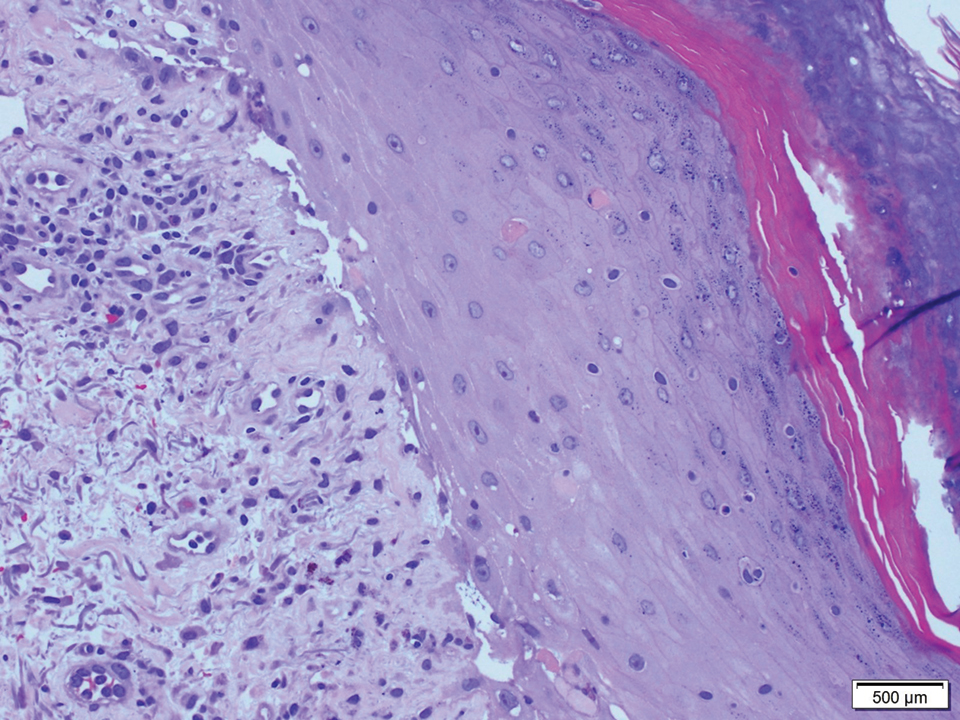
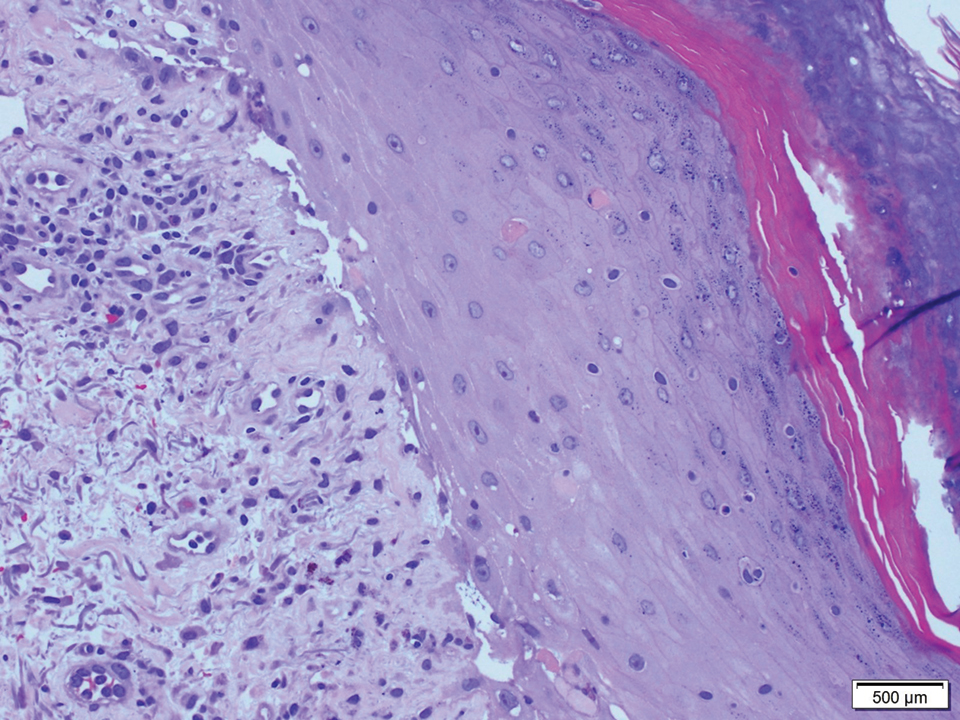
A 58-year-old man (patient 1) with a history of acute myelogenous leukemia presented with a pruritic morbilliform eruption 28 days after HSCT. There was no desquamation or mucosal involvement and the biopsy obtained was histologically suggestive of grade 2 acute GVHD. His immunosuppressive regimen included sirolimus and cyclophosphamide. He was receiving trimethoprim-sulfamethoxazole (TMP-SMX), voriconazole, and acyclovir for infectious prophylaxis. At the time of presentation, he was treated with high-dose systemic steroids (prednisone 2 mg/kg/d) for acute GVHD with partial improvement. Upon tapering of the steroids 3 weeks after initiating TMP-SMX and 1 week after initiating voriconazole, he developed painful desquamation and erosions involving 95% of the body surface area (BSA), necessitating admission to the local burn unit (Figure 1). Biopsies demonstrated full-thickness epidermal necrosis with subepidermal blistering and interface dermatitis (Figure 2). No gastrointestinal tract involvement of acute GVHD was noted. The patient was a 100% donor chimera, supporting the diagnosis of acute GVHD; however, the patient and donor carried the HLA-C*06:02 allele, which previously has been described in association with TMP-SMX–related Stevens-Johnson syndrome/TEN.5 In addition, causality assessment using the algorithm of drug causality for epidermal necrolysis indicated TMP-SMX as a probable cause and voriconazole as a possible cause. The diagnosis of TEN with a SCORe of Toxic Epidermal Necrosis (SCORTEN) of 4 in the setting of acute GVHD was favored, though grade 4 acute GVHD could not be excluded. Trimethoprim-sulfamethoxazole was discontinued, and voriconazole was changed to posaconazole. He received supportive care along with 1 dose of 25-mg subcutaneous etanercept and 3 days of intravenous immunoglobulin (IVIG). Skin re-epithelialization was complete by 3 weeks. At 4 weeks, the patient developed a new asymptomatic erythematous eruption. Biopsies demonstrated changes of acute and chronic GVHD (Figure 3) that resolved with up-titration of sirolimus. The patient remained hospitalized for 96 days and continued to follow up with his transplant team as well as ophthalmology and dermatology. He died 2 years after HSCT.
A 67-year-old woman (patient 2) with high-grade myelodysplastic syndrome presented with an erythematous morbilliform eruption on the torso on day 20 after a matched unrelated HSCT that histologically was consistent with grade 2 GVHD (Figure 4). She had been receiving sirolimus and tacrolimus for GVHD prophylaxis. Infectious prophylaxis included acyclovir, pentamidine, micafungin, and TMP-SMX. Despite high-dose systemic steroids, the rash progressed and ultimately involved 80% BSA. A positive Nikolsky sign was noted involving 21% BSA (Figure 5), in addition to oral and genital mucosal ulcers. She denied nausea, vomiting, fever, or diarrhea. Chimerism studies were negative. Trimethoprim-sulfamethoxazole was discontinued, and she was transferred to a burn unit. Biopsies showed full-thickness epidermal necrosis. A diagnosis of TEN with a SCORTEN of 4 in the setting of acute GVHD was favored; grade 4 acute GVHD could not be excluded. Steroids were discontinued. Because laboratory studies indicated IgA deficiency, IVIG was not considered as a systemic option for therapy. The patient received 1 dose of infliximab (5 mg/kg). Cyclophosphamide 1600 mg weekly was added for GVHD therapy. The wounds progressively healed, and 2 weeks into her admission she was noted to have only 3% BSA with denuded skin. The patient was transferred to the cancer treatment center for further management of the malignancy. Unfortunately, after 2 months she died due to ischemic colitis that was confirmed on autopsy.
Graft-vs-host disease and TEN are rare, life-threatening complications seen in patients with allogeneic HSCT.2 Graft-vs-host disease and TEN share clinicopathologic characteristics and effector immune mechanisms, largely the substantial role of T-cell activation and tissue destruction, which occur through mediators such as TNF-α.6-8

Given the sparse lymphocytic infiltrate, keratinocyte death in TEN is thought to result from soluble molecules, including TNF-α and TNF-related apoptosis-inducing ligand.9 Tumor necrosis factor α has been identified in blister fluid, biopsy specimens, and serum of patients with TEN. Tumor necrosis factor α increases the expression of keratinocyte-inducible nitric oxide synthase, which upregulates keratinocyte Fas ligand expression and subsequent Fas- and caspase-8–mediated keratinocyte cell death.10

Acute GVHD results from donor lymphocyte activation after infusion into damaged recipient tissues that previously have been radiated or chemoablated. Mismatches in histocompatibility complexes between donor cells and recipient tissue antigens serve as the initial trigger for immune activation. Activation of antigen-presenting cells followed by activation, proliferation, differentiation, and migration of donor T cells ultimately results in destruction of the target tissue.11 Immune mediators, such as TNF-α and lymphotoxin α (another member of the TNF superfamily), play a nonredundant role in the pathogenesis of GVHD.12
Current treatment strategies for severe acute GVHD and TEN differ. In North America, high-dose IVIG frequently is used as first-line systemic therapy, while high-dose systemic corticosteroids rarely are used.13 Studies have demonstrated successful use of anti–TNF-α drugs for the treatment of TEN.3,4 Moreover, etanercept has shown to effectively inhibit lymphotoxin α.14 Similarly, TNF inhibition in the management of steroid-refractory acute GVHD has been successful.1 These studies coupled with the underlying immune mechanisms that both diseases share encouraged initiating a trial of anti–TNF-α therapy in our patients.
Patient 1 merits further discussion because he was both a 100% donor chimera as well as a carrier of an human leukocyte antigen susceptibility candidate allele to TMP-SMX. Historical features of his presentation are consistent with either steroid-refractory GVHD or TEN superimposed on acute GVHD. His initial presentation of the more typical macular exanthem of cutaneous acute GVHD was both biopsy proven and supported by clinical improvement with steroid therapy, which was later followed by a robust blistering mucocutaneous presentation approximately 3 weeks after the administration of TMP-SMX and 1 week after initiating voriconazole that improved with IVIG and etanercept.
It is difficult to determine if TEN represents a continuum or result of the underlying drivers of acute GVHD vs a drug reaction. Although there is insufficient evidence to establish a clear-cut diagnosis of TEN, these cases illustrate the need for better diagnostic techniques to allow differentiation between TEN and grade 4 acute GVHD, and in the context of uncertainty, TNF-α inhibition poses a viable therapeutic strategy for these 2 often lethal conditions. Our cases do unequivocally indicate the benefit of this therapeutic modality, add to the current body of literature supporting the use of TNF-α inhibitors in patients such as ours without an official TEN diagnosis, and may guide future investigative efforts.
- Couriel DR, Saliba R, de Lima M, et al. A phase III study of infliximab and corticosteroids for the initial treatment of acute graft-versus-host disease. Biol Blood Marrow Transplant. 2009;15:1555-1562.
- Jeanmonod P, Hubbuch M, Grünhage F, et al. Graft-versus-host disease or toxic epidermal necrolysis: diagnostic dilemma after liver transplantation. Transpl Infect Dis. 2012;14:422-426.
- Paradisi A, Abeni D, Bergamo F, et al. Etanercept therapy for toxic epidermal necrolysis. J Am Acad Dermatol. 2014;71:278-283.
- Scott-Lang V, Tidman M, McKay D. Toxic epidermal necrolysis in a child successfully treated with infliximab. Pediatr Dermatol. 2014;31:532-534.
- Kingpin T, Mahasirimongkol S, Konyoung P, et al. Candidate HLA genes for prediction of co-trimoxazole-induced severe cutaneous reactions. Pharmacogenet Genomics. 2015;25:402-411.
- Correia O, Delgado L, Barbosa IL, et al. Increased interleukin 10, tumor necrosis factor alpha, and interleukin 6 levels in blister fluid of toxic epidermal necrolysis. J Am Acad Dermatol. 2002;47:58-62.
- French LE, Tschopp J. Fas-mediated cell death in toxic epidermal necrolysis and graft-versus-host disease: potential for therapeutic inhibition. Schweiz Med Wochenschr. 2000;130:1656-1661.
- Downey A, Jackson C, Harun N, et al. Toxic epidermal necrolysis: review of pathogenesis and management. J Am Acad Dermatol. 2012;66:995-1003.
- de Araujo E, Dessirier V, Laprée G, et al. Death ligand TRAIL, secreted by CD1a+ and CD14+ cells in blister fluids, is involved in killing keratinocytes in toxic epidermal necrolysis. Exp Dermatol. 2011;20:107-112.
- Viard-Leveugle I, Gaide O, Jankovic D, et al. TNF-α and IFN-γ are potential inducers of Fas-mediated keratinocyte apoptosis through activation of inducible nitric oxide synthase in toxic epidermal necrolysis. J Invest Dermatol. 2013;133:489-498.
- Choi SW, Levine JE, Ferrara JL. Pathogenesis and management of graft-versus-host disease. Immunol Allergy Clin North Am. 2010;30:75-101.
- Markey KA, Burman AC, Banovic T, et al. Soluble lymphotoxin is an important effector molecule in GVHD and GVL. Blood. 2010;115:122-132.
- Dodiuk-Gad RP, Olteanu C, Jeschke MG, et al. Treatment of toxic epidermal necrolysis in North America. J Am Acad Dermatol. 2015;73:876-877.
- Tracey D, Klareskog L, Sasso EH, et al. Tumor necrosis factor antagonist mechanisms of action: a comprehensive review. Pharmacol Ther. 2008;117:244-279.
To the Editor:
Acute graft-vs-host disease (GVHD) remains a limitation to hematopoietic stem cell transplantation (HSCT) in 20% to 50% of patients after transplant. Furthermore, failed treatment with corticosteroids is frequent and portends a poor prognosis.1 Toxic epidermal necrolysis (TEN) is an epidermolytic skin disorder thought to represent an adverse drug reaction, though its pathogenesis remains unclear. Severe forms of acute GVHD can mimic TEN clinically and histologically. Both can present with widespread cutaneous and mucosal bullae, erosions, and desquamation. Toxic epidermal necrolysis in the context of allogeneic hematopoietic stem cell transplantation is extremely rare, with almost 100% mortality in adult patients. Features that favor acute GVHD over TEN include diarrhea, elevation in bilirubin level, and chimerism.2 However, these features might be absent, posing a therapeutic dilemma, as current treatment preferences for each of these entities differ.
Growing evidence supports the use of anti–tumor necrosis factor (TNF) α drugs for the treatment of TEN. Success has been reported with both anti–TNF-α monoclonal antibodies as well as the soluble fusion protein etanercept.3,4 The use of TNF-α inhibitors in acute GVHD remains anecdotal.

A 58-year-old man (patient 1) with a history of acute myelogenous leukemia presented with a pruritic morbilliform eruption 28 days after HSCT. There was no desquamation or mucosal involvement and the biopsy obtained was histologically suggestive of grade 2 acute GVHD. His immunosuppressive regimen included sirolimus and cyclophosphamide. He was receiving trimethoprim-sulfamethoxazole (TMP-SMX), voriconazole, and acyclovir for infectious prophylaxis. At the time of presentation, he was treated with high-dose systemic steroids (prednisone 2 mg/kg/d) for acute GVHD with partial improvement. Upon tapering of the steroids 3 weeks after initiating TMP-SMX and 1 week after initiating voriconazole, he developed painful desquamation and erosions involving 95% of the body surface area (BSA), necessitating admission to the local burn unit (Figure 1). Biopsies demonstrated full-thickness epidermal necrosis with subepidermal blistering and interface dermatitis (Figure 2). No gastrointestinal tract involvement of acute GVHD was noted. The patient was a 100% donor chimera, supporting the diagnosis of acute GVHD; however, the patient and donor carried the HLA-C*06:02 allele, which previously has been described in association with TMP-SMX–related Stevens-Johnson syndrome/TEN.5 In addition, causality assessment using the algorithm of drug causality for epidermal necrolysis indicated TMP-SMX as a probable cause and voriconazole as a possible cause. The diagnosis of TEN with a SCORe of Toxic Epidermal Necrosis (SCORTEN) of 4 in the setting of acute GVHD was favored, though grade 4 acute GVHD could not be excluded. Trimethoprim-sulfamethoxazole was discontinued, and voriconazole was changed to posaconazole. He received supportive care along with 1 dose of 25-mg subcutaneous etanercept and 3 days of intravenous immunoglobulin (IVIG). Skin re-epithelialization was complete by 3 weeks. At 4 weeks, the patient developed a new asymptomatic erythematous eruption. Biopsies demonstrated changes of acute and chronic GVHD (Figure 3) that resolved with up-titration of sirolimus. The patient remained hospitalized for 96 days and continued to follow up with his transplant team as well as ophthalmology and dermatology. He died 2 years after HSCT.
A 67-year-old woman (patient 2) with high-grade myelodysplastic syndrome presented with an erythematous morbilliform eruption on the torso on day 20 after a matched unrelated HSCT that histologically was consistent with grade 2 GVHD (Figure 4). She had been receiving sirolimus and tacrolimus for GVHD prophylaxis. Infectious prophylaxis included acyclovir, pentamidine, micafungin, and TMP-SMX. Despite high-dose systemic steroids, the rash progressed and ultimately involved 80% BSA. A positive Nikolsky sign was noted involving 21% BSA (Figure 5), in addition to oral and genital mucosal ulcers. She denied nausea, vomiting, fever, or diarrhea. Chimerism studies were negative. Trimethoprim-sulfamethoxazole was discontinued, and she was transferred to a burn unit. Biopsies showed full-thickness epidermal necrosis. A diagnosis of TEN with a SCORTEN of 4 in the setting of acute GVHD was favored; grade 4 acute GVHD could not be excluded. Steroids were discontinued. Because laboratory studies indicated IgA deficiency, IVIG was not considered as a systemic option for therapy. The patient received 1 dose of infliximab (5 mg/kg). Cyclophosphamide 1600 mg weekly was added for GVHD therapy. The wounds progressively healed, and 2 weeks into her admission she was noted to have only 3% BSA with denuded skin. The patient was transferred to the cancer treatment center for further management of the malignancy. Unfortunately, after 2 months she died due to ischemic colitis that was confirmed on autopsy.
Graft-vs-host disease and TEN are rare, life-threatening complications seen in patients with allogeneic HSCT.2 Graft-vs-host disease and TEN share clinicopathologic characteristics and effector immune mechanisms, largely the substantial role of T-cell activation and tissue destruction, which occur through mediators such as TNF-α.6-8

Given the sparse lymphocytic infiltrate, keratinocyte death in TEN is thought to result from soluble molecules, including TNF-α and TNF-related apoptosis-inducing ligand.9 Tumor necrosis factor α has been identified in blister fluid, biopsy specimens, and serum of patients with TEN. Tumor necrosis factor α increases the expression of keratinocyte-inducible nitric oxide synthase, which upregulates keratinocyte Fas ligand expression and subsequent Fas- and caspase-8–mediated keratinocyte cell death.10

Acute GVHD results from donor lymphocyte activation after infusion into damaged recipient tissues that previously have been radiated or chemoablated. Mismatches in histocompatibility complexes between donor cells and recipient tissue antigens serve as the initial trigger for immune activation. Activation of antigen-presenting cells followed by activation, proliferation, differentiation, and migration of donor T cells ultimately results in destruction of the target tissue.11 Immune mediators, such as TNF-α and lymphotoxin α (another member of the TNF superfamily), play a nonredundant role in the pathogenesis of GVHD.12
Current treatment strategies for severe acute GVHD and TEN differ. In North America, high-dose IVIG frequently is used as first-line systemic therapy, while high-dose systemic corticosteroids rarely are used.13 Studies have demonstrated successful use of anti–TNF-α drugs for the treatment of TEN.3,4 Moreover, etanercept has shown to effectively inhibit lymphotoxin α.14 Similarly, TNF inhibition in the management of steroid-refractory acute GVHD has been successful.1 These studies coupled with the underlying immune mechanisms that both diseases share encouraged initiating a trial of anti–TNF-α therapy in our patients.
Patient 1 merits further discussion because he was both a 100% donor chimera as well as a carrier of an human leukocyte antigen susceptibility candidate allele to TMP-SMX. Historical features of his presentation are consistent with either steroid-refractory GVHD or TEN superimposed on acute GVHD. His initial presentation of the more typical macular exanthem of cutaneous acute GVHD was both biopsy proven and supported by clinical improvement with steroid therapy, which was later followed by a robust blistering mucocutaneous presentation approximately 3 weeks after the administration of TMP-SMX and 1 week after initiating voriconazole that improved with IVIG and etanercept.
It is difficult to determine if TEN represents a continuum or result of the underlying drivers of acute GVHD vs a drug reaction. Although there is insufficient evidence to establish a clear-cut diagnosis of TEN, these cases illustrate the need for better diagnostic techniques to allow differentiation between TEN and grade 4 acute GVHD, and in the context of uncertainty, TNF-α inhibition poses a viable therapeutic strategy for these 2 often lethal conditions. Our cases do unequivocally indicate the benefit of this therapeutic modality, add to the current body of literature supporting the use of TNF-α inhibitors in patients such as ours without an official TEN diagnosis, and may guide future investigative efforts.
To the Editor:
Acute graft-vs-host disease (GVHD) remains a limitation to hematopoietic stem cell transplantation (HSCT) in 20% to 50% of patients after transplant. Furthermore, failed treatment with corticosteroids is frequent and portends a poor prognosis.1 Toxic epidermal necrolysis (TEN) is an epidermolytic skin disorder thought to represent an adverse drug reaction, though its pathogenesis remains unclear. Severe forms of acute GVHD can mimic TEN clinically and histologically. Both can present with widespread cutaneous and mucosal bullae, erosions, and desquamation. Toxic epidermal necrolysis in the context of allogeneic hematopoietic stem cell transplantation is extremely rare, with almost 100% mortality in adult patients. Features that favor acute GVHD over TEN include diarrhea, elevation in bilirubin level, and chimerism.2 However, these features might be absent, posing a therapeutic dilemma, as current treatment preferences for each of these entities differ.
Growing evidence supports the use of anti–tumor necrosis factor (TNF) α drugs for the treatment of TEN. Success has been reported with both anti–TNF-α monoclonal antibodies as well as the soluble fusion protein etanercept.3,4 The use of TNF-α inhibitors in acute GVHD remains anecdotal.

A 58-year-old man (patient 1) with a history of acute myelogenous leukemia presented with a pruritic morbilliform eruption 28 days after HSCT. There was no desquamation or mucosal involvement and the biopsy obtained was histologically suggestive of grade 2 acute GVHD. His immunosuppressive regimen included sirolimus and cyclophosphamide. He was receiving trimethoprim-sulfamethoxazole (TMP-SMX), voriconazole, and acyclovir for infectious prophylaxis. At the time of presentation, he was treated with high-dose systemic steroids (prednisone 2 mg/kg/d) for acute GVHD with partial improvement. Upon tapering of the steroids 3 weeks after initiating TMP-SMX and 1 week after initiating voriconazole, he developed painful desquamation and erosions involving 95% of the body surface area (BSA), necessitating admission to the local burn unit (Figure 1). Biopsies demonstrated full-thickness epidermal necrosis with subepidermal blistering and interface dermatitis (Figure 2). No gastrointestinal tract involvement of acute GVHD was noted. The patient was a 100% donor chimera, supporting the diagnosis of acute GVHD; however, the patient and donor carried the HLA-C*06:02 allele, which previously has been described in association with TMP-SMX–related Stevens-Johnson syndrome/TEN.5 In addition, causality assessment using the algorithm of drug causality for epidermal necrolysis indicated TMP-SMX as a probable cause and voriconazole as a possible cause. The diagnosis of TEN with a SCORe of Toxic Epidermal Necrosis (SCORTEN) of 4 in the setting of acute GVHD was favored, though grade 4 acute GVHD could not be excluded. Trimethoprim-sulfamethoxazole was discontinued, and voriconazole was changed to posaconazole. He received supportive care along with 1 dose of 25-mg subcutaneous etanercept and 3 days of intravenous immunoglobulin (IVIG). Skin re-epithelialization was complete by 3 weeks. At 4 weeks, the patient developed a new asymptomatic erythematous eruption. Biopsies demonstrated changes of acute and chronic GVHD (Figure 3) that resolved with up-titration of sirolimus. The patient remained hospitalized for 96 days and continued to follow up with his transplant team as well as ophthalmology and dermatology. He died 2 years after HSCT.
A 67-year-old woman (patient 2) with high-grade myelodysplastic syndrome presented with an erythematous morbilliform eruption on the torso on day 20 after a matched unrelated HSCT that histologically was consistent with grade 2 GVHD (Figure 4). She had been receiving sirolimus and tacrolimus for GVHD prophylaxis. Infectious prophylaxis included acyclovir, pentamidine, micafungin, and TMP-SMX. Despite high-dose systemic steroids, the rash progressed and ultimately involved 80% BSA. A positive Nikolsky sign was noted involving 21% BSA (Figure 5), in addition to oral and genital mucosal ulcers. She denied nausea, vomiting, fever, or diarrhea. Chimerism studies were negative. Trimethoprim-sulfamethoxazole was discontinued, and she was transferred to a burn unit. Biopsies showed full-thickness epidermal necrosis. A diagnosis of TEN with a SCORTEN of 4 in the setting of acute GVHD was favored; grade 4 acute GVHD could not be excluded. Steroids were discontinued. Because laboratory studies indicated IgA deficiency, IVIG was not considered as a systemic option for therapy. The patient received 1 dose of infliximab (5 mg/kg). Cyclophosphamide 1600 mg weekly was added for GVHD therapy. The wounds progressively healed, and 2 weeks into her admission she was noted to have only 3% BSA with denuded skin. The patient was transferred to the cancer treatment center for further management of the malignancy. Unfortunately, after 2 months she died due to ischemic colitis that was confirmed on autopsy.
Graft-vs-host disease and TEN are rare, life-threatening complications seen in patients with allogeneic HSCT.2 Graft-vs-host disease and TEN share clinicopathologic characteristics and effector immune mechanisms, largely the substantial role of T-cell activation and tissue destruction, which occur through mediators such as TNF-α.6-8

Given the sparse lymphocytic infiltrate, keratinocyte death in TEN is thought to result from soluble molecules, including TNF-α and TNF-related apoptosis-inducing ligand.9 Tumor necrosis factor α has been identified in blister fluid, biopsy specimens, and serum of patients with TEN. Tumor necrosis factor α increases the expression of keratinocyte-inducible nitric oxide synthase, which upregulates keratinocyte Fas ligand expression and subsequent Fas- and caspase-8–mediated keratinocyte cell death.10

Acute GVHD results from donor lymphocyte activation after infusion into damaged recipient tissues that previously have been radiated or chemoablated. Mismatches in histocompatibility complexes between donor cells and recipient tissue antigens serve as the initial trigger for immune activation. Activation of antigen-presenting cells followed by activation, proliferation, differentiation, and migration of donor T cells ultimately results in destruction of the target tissue.11 Immune mediators, such as TNF-α and lymphotoxin α (another member of the TNF superfamily), play a nonredundant role in the pathogenesis of GVHD.12
Current treatment strategies for severe acute GVHD and TEN differ. In North America, high-dose IVIG frequently is used as first-line systemic therapy, while high-dose systemic corticosteroids rarely are used.13 Studies have demonstrated successful use of anti–TNF-α drugs for the treatment of TEN.3,4 Moreover, etanercept has shown to effectively inhibit lymphotoxin α.14 Similarly, TNF inhibition in the management of steroid-refractory acute GVHD has been successful.1 These studies coupled with the underlying immune mechanisms that both diseases share encouraged initiating a trial of anti–TNF-α therapy in our patients.
Patient 1 merits further discussion because he was both a 100% donor chimera as well as a carrier of an human leukocyte antigen susceptibility candidate allele to TMP-SMX. Historical features of his presentation are consistent with either steroid-refractory GVHD or TEN superimposed on acute GVHD. His initial presentation of the more typical macular exanthem of cutaneous acute GVHD was both biopsy proven and supported by clinical improvement with steroid therapy, which was later followed by a robust blistering mucocutaneous presentation approximately 3 weeks after the administration of TMP-SMX and 1 week after initiating voriconazole that improved with IVIG and etanercept.
It is difficult to determine if TEN represents a continuum or result of the underlying drivers of acute GVHD vs a drug reaction. Although there is insufficient evidence to establish a clear-cut diagnosis of TEN, these cases illustrate the need for better diagnostic techniques to allow differentiation between TEN and grade 4 acute GVHD, and in the context of uncertainty, TNF-α inhibition poses a viable therapeutic strategy for these 2 often lethal conditions. Our cases do unequivocally indicate the benefit of this therapeutic modality, add to the current body of literature supporting the use of TNF-α inhibitors in patients such as ours without an official TEN diagnosis, and may guide future investigative efforts.
- Couriel DR, Saliba R, de Lima M, et al. A phase III study of infliximab and corticosteroids for the initial treatment of acute graft-versus-host disease. Biol Blood Marrow Transplant. 2009;15:1555-1562.
- Jeanmonod P, Hubbuch M, Grünhage F, et al. Graft-versus-host disease or toxic epidermal necrolysis: diagnostic dilemma after liver transplantation. Transpl Infect Dis. 2012;14:422-426.
- Paradisi A, Abeni D, Bergamo F, et al. Etanercept therapy for toxic epidermal necrolysis. J Am Acad Dermatol. 2014;71:278-283.
- Scott-Lang V, Tidman M, McKay D. Toxic epidermal necrolysis in a child successfully treated with infliximab. Pediatr Dermatol. 2014;31:532-534.
- Kingpin T, Mahasirimongkol S, Konyoung P, et al. Candidate HLA genes for prediction of co-trimoxazole-induced severe cutaneous reactions. Pharmacogenet Genomics. 2015;25:402-411.
- Correia O, Delgado L, Barbosa IL, et al. Increased interleukin 10, tumor necrosis factor alpha, and interleukin 6 levels in blister fluid of toxic epidermal necrolysis. J Am Acad Dermatol. 2002;47:58-62.
- French LE, Tschopp J. Fas-mediated cell death in toxic epidermal necrolysis and graft-versus-host disease: potential for therapeutic inhibition. Schweiz Med Wochenschr. 2000;130:1656-1661.
- Downey A, Jackson C, Harun N, et al. Toxic epidermal necrolysis: review of pathogenesis and management. J Am Acad Dermatol. 2012;66:995-1003.
- de Araujo E, Dessirier V, Laprée G, et al. Death ligand TRAIL, secreted by CD1a+ and CD14+ cells in blister fluids, is involved in killing keratinocytes in toxic epidermal necrolysis. Exp Dermatol. 2011;20:107-112.
- Viard-Leveugle I, Gaide O, Jankovic D, et al. TNF-α and IFN-γ are potential inducers of Fas-mediated keratinocyte apoptosis through activation of inducible nitric oxide synthase in toxic epidermal necrolysis. J Invest Dermatol. 2013;133:489-498.
- Choi SW, Levine JE, Ferrara JL. Pathogenesis and management of graft-versus-host disease. Immunol Allergy Clin North Am. 2010;30:75-101.
- Markey KA, Burman AC, Banovic T, et al. Soluble lymphotoxin is an important effector molecule in GVHD and GVL. Blood. 2010;115:122-132.
- Dodiuk-Gad RP, Olteanu C, Jeschke MG, et al. Treatment of toxic epidermal necrolysis in North America. J Am Acad Dermatol. 2015;73:876-877.
- Tracey D, Klareskog L, Sasso EH, et al. Tumor necrosis factor antagonist mechanisms of action: a comprehensive review. Pharmacol Ther. 2008;117:244-279.
- Couriel DR, Saliba R, de Lima M, et al. A phase III study of infliximab and corticosteroids for the initial treatment of acute graft-versus-host disease. Biol Blood Marrow Transplant. 2009;15:1555-1562.
- Jeanmonod P, Hubbuch M, Grünhage F, et al. Graft-versus-host disease or toxic epidermal necrolysis: diagnostic dilemma after liver transplantation. Transpl Infect Dis. 2012;14:422-426.
- Paradisi A, Abeni D, Bergamo F, et al. Etanercept therapy for toxic epidermal necrolysis. J Am Acad Dermatol. 2014;71:278-283.
- Scott-Lang V, Tidman M, McKay D. Toxic epidermal necrolysis in a child successfully treated with infliximab. Pediatr Dermatol. 2014;31:532-534.
- Kingpin T, Mahasirimongkol S, Konyoung P, et al. Candidate HLA genes for prediction of co-trimoxazole-induced severe cutaneous reactions. Pharmacogenet Genomics. 2015;25:402-411.
- Correia O, Delgado L, Barbosa IL, et al. Increased interleukin 10, tumor necrosis factor alpha, and interleukin 6 levels in blister fluid of toxic epidermal necrolysis. J Am Acad Dermatol. 2002;47:58-62.
- French LE, Tschopp J. Fas-mediated cell death in toxic epidermal necrolysis and graft-versus-host disease: potential for therapeutic inhibition. Schweiz Med Wochenschr. 2000;130:1656-1661.
- Downey A, Jackson C, Harun N, et al. Toxic epidermal necrolysis: review of pathogenesis and management. J Am Acad Dermatol. 2012;66:995-1003.
- de Araujo E, Dessirier V, Laprée G, et al. Death ligand TRAIL, secreted by CD1a+ and CD14+ cells in blister fluids, is involved in killing keratinocytes in toxic epidermal necrolysis. Exp Dermatol. 2011;20:107-112.
- Viard-Leveugle I, Gaide O, Jankovic D, et al. TNF-α and IFN-γ are potential inducers of Fas-mediated keratinocyte apoptosis through activation of inducible nitric oxide synthase in toxic epidermal necrolysis. J Invest Dermatol. 2013;133:489-498.
- Choi SW, Levine JE, Ferrara JL. Pathogenesis and management of graft-versus-host disease. Immunol Allergy Clin North Am. 2010;30:75-101.
- Markey KA, Burman AC, Banovic T, et al. Soluble lymphotoxin is an important effector molecule in GVHD and GVL. Blood. 2010;115:122-132.
- Dodiuk-Gad RP, Olteanu C, Jeschke MG, et al. Treatment of toxic epidermal necrolysis in North America. J Am Acad Dermatol. 2015;73:876-877.
- Tracey D, Klareskog L, Sasso EH, et al. Tumor necrosis factor antagonist mechanisms of action: a comprehensive review. Pharmacol Ther. 2008;117:244-279.
Practice Points
- Graft-vs-host disease (GVHD) and toxic epidermal necrolysis (TEN) are rare life-threatening complications seen in patients with allogeneic hematopoietic stem cell transplantation.
- Although mild acute GVHD easily is distinguished from TEN, severe acute GVHD and TEN share overlapping features and present a diagnostic challenge.
- Therapeutic decisions and associated outcomes hinge on accurate diagnosis, as high-dose systemic corticosteroids have been associated with higher mortality rates in TEN.
Phototoxic Contact Dermatitis From Over-the-counter 8-Methoxypsoralen
To the Editor:
A 71-year-old Hispanic man with a history of vitiligo presented with an acute-onset blistering rash on the face, arms, and hands. Physical examination demonstrated photodistributed erythematous plaques with overlying vesicles and erosions with hemorrhagic crust on the face, neck, dorsal aspects of the hands, and wrists (Figure). Further history revealed that the patient applied a new cream that was recommended to treat vitiligo the night before the rash onset; he obtained the cream from a Central American market without a prescription. He had gone running in the park without any form of sun protection and then developed the rash within several hours. He denied taking any other medications or supplements. The involvement of sun-protected areas (ie, upper eyelids, nasolabial folds, submental area) was explained when the patient further elaborated that he had performed supine exercises during his outdoor recreation. He brought his new cream into the clinic, which was found to contain prescription-strength methoxsalen (8-methoxypsoralen), confirming the diagnosis of acute phototoxic contact dermatitis. The acute reaction had subsided, and the patient already had discontinued the causative agent. He was counseled on further avoidance of the cream and sun-protective measures.

The photosensitizing properties of certain compounds have been harnessed for therapeutic purposes. For example, psoralen plus UVA therapy has been used for psoriasis and vitiligo and photodynamic therapy for actinic keratoses and superficial nonmelanoma skin cancers.1 However, these agents can induce severe phototoxicity if UV light exposure is not carefully monitored, as seen in our patient. This case is a classic example of phototoxic contact dermatitis and highlights the importance of obtaining a detailed patient history to allow for proper diagnosis and identification of the causative agent. Importantly, because prescription-strength topical medications are readily available over-the-counter, particularly in stores specializing in international goods, patients should be questioned about the use of all topical and systemic medications, both prescription and nonprescription.2
- Richard EG. The science and (lost) art of psoralen plus UVA phototherapy. Dermatol Clin. 2020;38:11-23. doi:10.1016/j.det.2019.08.002
- Kimyon RS, Schlarbaum JP, Liou YL, et al. Prescription-strengthtopical corticosteroids available over the counter: cross-sectional study of 80 stores in 13 United States cities. J Am Acad Dermatol. 2020;82:524-525. doi:10.1016/j.jaad.2019.10.035
To the Editor:
A 71-year-old Hispanic man with a history of vitiligo presented with an acute-onset blistering rash on the face, arms, and hands. Physical examination demonstrated photodistributed erythematous plaques with overlying vesicles and erosions with hemorrhagic crust on the face, neck, dorsal aspects of the hands, and wrists (Figure). Further history revealed that the patient applied a new cream that was recommended to treat vitiligo the night before the rash onset; he obtained the cream from a Central American market without a prescription. He had gone running in the park without any form of sun protection and then developed the rash within several hours. He denied taking any other medications or supplements. The involvement of sun-protected areas (ie, upper eyelids, nasolabial folds, submental area) was explained when the patient further elaborated that he had performed supine exercises during his outdoor recreation. He brought his new cream into the clinic, which was found to contain prescription-strength methoxsalen (8-methoxypsoralen), confirming the diagnosis of acute phototoxic contact dermatitis. The acute reaction had subsided, and the patient already had discontinued the causative agent. He was counseled on further avoidance of the cream and sun-protective measures.

The photosensitizing properties of certain compounds have been harnessed for therapeutic purposes. For example, psoralen plus UVA therapy has been used for psoriasis and vitiligo and photodynamic therapy for actinic keratoses and superficial nonmelanoma skin cancers.1 However, these agents can induce severe phototoxicity if UV light exposure is not carefully monitored, as seen in our patient. This case is a classic example of phototoxic contact dermatitis and highlights the importance of obtaining a detailed patient history to allow for proper diagnosis and identification of the causative agent. Importantly, because prescription-strength topical medications are readily available over-the-counter, particularly in stores specializing in international goods, patients should be questioned about the use of all topical and systemic medications, both prescription and nonprescription.2
To the Editor:
A 71-year-old Hispanic man with a history of vitiligo presented with an acute-onset blistering rash on the face, arms, and hands. Physical examination demonstrated photodistributed erythematous plaques with overlying vesicles and erosions with hemorrhagic crust on the face, neck, dorsal aspects of the hands, and wrists (Figure). Further history revealed that the patient applied a new cream that was recommended to treat vitiligo the night before the rash onset; he obtained the cream from a Central American market without a prescription. He had gone running in the park without any form of sun protection and then developed the rash within several hours. He denied taking any other medications or supplements. The involvement of sun-protected areas (ie, upper eyelids, nasolabial folds, submental area) was explained when the patient further elaborated that he had performed supine exercises during his outdoor recreation. He brought his new cream into the clinic, which was found to contain prescription-strength methoxsalen (8-methoxypsoralen), confirming the diagnosis of acute phototoxic contact dermatitis. The acute reaction had subsided, and the patient already had discontinued the causative agent. He was counseled on further avoidance of the cream and sun-protective measures.

The photosensitizing properties of certain compounds have been harnessed for therapeutic purposes. For example, psoralen plus UVA therapy has been used for psoriasis and vitiligo and photodynamic therapy for actinic keratoses and superficial nonmelanoma skin cancers.1 However, these agents can induce severe phototoxicity if UV light exposure is not carefully monitored, as seen in our patient. This case is a classic example of phototoxic contact dermatitis and highlights the importance of obtaining a detailed patient history to allow for proper diagnosis and identification of the causative agent. Importantly, because prescription-strength topical medications are readily available over-the-counter, particularly in stores specializing in international goods, patients should be questioned about the use of all topical and systemic medications, both prescription and nonprescription.2
- Richard EG. The science and (lost) art of psoralen plus UVA phototherapy. Dermatol Clin. 2020;38:11-23. doi:10.1016/j.det.2019.08.002
- Kimyon RS, Schlarbaum JP, Liou YL, et al. Prescription-strengthtopical corticosteroids available over the counter: cross-sectional study of 80 stores in 13 United States cities. J Am Acad Dermatol. 2020;82:524-525. doi:10.1016/j.jaad.2019.10.035
- Richard EG. The science and (lost) art of psoralen plus UVA phototherapy. Dermatol Clin. 2020;38:11-23. doi:10.1016/j.det.2019.08.002
- Kimyon RS, Schlarbaum JP, Liou YL, et al. Prescription-strengthtopical corticosteroids available over the counter: cross-sectional study of 80 stores in 13 United States cities. J Am Acad Dermatol. 2020;82:524-525. doi:10.1016/j.jaad.2019.10.035
Practice Points
- Phototoxic contact dermatitis is an irritant reaction resembling an exaggerated sunburn that occurs with the use of a photosensitizing agent and UV light exposure.
- A range of topical and systemic medications, plants, and natural products can elicit phototoxic reactions.
- With the wide availability of prescription-strength over-the-counter medications, a detailed history often is necessary to identify the causative agents of phototoxic contact dermatitis and ensure future avoidance.
Strep infection and tics in children: new data
Group A streptococcus (GAS) infection is not associated with new-onset tic disorders in at-risk children, findings from a large prospective study show.
The results mean that if preteens present with a new-onset tic condition, “they’re unlikely to have it as a result of a group A streptococcal throat infection,” study author Anette Eleonore Schrag, MD, PhD, professor, department of clinical neuroscience, Institute of Neurology, University College London, told this news organization.
Therefore, clinicians should not automatically prescribe antibiotics for children with tics, which sometimes occurs, said Dr. Schrag.
The study was published online Feb. 2 in Neurology.
Ongoing controversy
Research shows that genetic and environmental factors contribute to chronic tic disorders (CTDs) and Tourette syndrome (TS). Prenatal exposure to maternal smoking and central nervous system (CNS) stimulants, as well as psychosocial stress, may play a role.
There has been an ongoing controversy regarding the possible role of GAS in tics, with some studies showing an association and others not showing a link. However, previous studies have been retrospective, registry based, or had limited sample size.
This new prospective study is the first in children without a tic disorder but who were at relatively high risk of developing one. The children were followed to assess development of streptococcal infections and tics, said Dr. Schrag.
The study included 259 children aged 3-10 years (mean baseline age, 6.8 years; over half female) who had a first-degree relative such as a parent or sibling with TS or CTD.
The average age at TS onset is 7 years, peaking in prevalence and severity at about 9-12 years. GAS throat infections are common in this age group.
Although study participants did not have tics themselves, they represented “an enriched group,” said Dr. Schrag. “Because they had family history, we knew they were at increased risk for developing tics.”
Participants were evaluated every 2 months, alternating between scheduled hospital visits and telephone interviews. Parents kept a weekly diary and were instructed to bring their child in for assessment if they showed any signs of tics.
The average follow-up period was 1.6 years, but some of the children were followed for up to 48 months. During the study, there were a total of 1,944 assessments, including 939 telephone interviews and 1,005 clinical visits.
More common in boys
Investigators defined tic onset as the first occurrence of any sudden, rapid, recurrent, nonrhythmic involuntary movement and/or vocalization on at least three separate days within a period of 3 weeks.
The investigators assessed GAS exposure using parameters from throat swabs, serum anti-streptolysin O titers, and anti-DNAse B titers.
They used multiple definitions and combinations of GAS exposures “to make sure we weren’t missing any association because we didn’t use the right definition,” said Dr. Schrag. She explained a definitive strep infection is not always clear-cut.
At baseline, 17.0% participants tested positive for GAS, and 78.8% tested negative. No throat swab was available from 4.2% of participants.
During follow-up, the number of confirmed positive GAS exposures was 59, 102, 125, and 138, depending on the definition.
Researchers identified 61 tic cases during the study period. There was no evidence of an association of tic onset with GAS exposure after adjusting for age, sex, and parental education level.
However, there was a strong association between tic onset and sex, with girls being 60% less likely to develop tics than boys (hazard ratio, 0.4; 95% CI, 0.2-0.7; P < .01).
This result wasn’t particularly surprising, as it’s known that more boys develop tics than girls. “We just confirmed that in a prospective way,” said Dr. Schrag.
Results from sensitivity analyses confirmed the results. This was also the case with analyses that excluded visits with missing data on GAS exposure and that further adjusted for clinical site and psychotropic medication use.
Other pathogens?
Although the results showed no association between strep and tics in this population, it does not “close the door completely” on a potential relationship, said Dr. Schrag.
“By and large, the development of tics in children is not associated with group A strep, but differences in small subgroups can never be excluded by a study like this.”
Participants in this study were part of the European Multicentre Tics in Children Studies (EMTICS), a prospective cohort study exploring the role of environmental and genetic factors in pediatric CTD. That project is also looking at immune system factors, “which might play a role in the development of chronic tic disorder and associated conditions,” said Dr. Schrag.
It’s still possible, she added, that other pathogens could play a role in tic development. “That’s going to be the subject of further analysis and future studies,” she said.
Tamara Pringsheim, MD, professor of clinical neurosciences, psychiatry, pediatrics, and community health sciences, University of Calgary (Alta.), praised the research.
“This was a well-designed study, with a large sample of 260 children followed for up to 4 years, using a standardized protocol to assess for group A streptococcal infection and new onset of tics.”
The study, which did not uncover an association between GAS exposure and tic onset, “provides high level evidence that group A streptococcal exposure is not an important risk factor for the new onset of tics in children with a family history of tic disorders.”
The study received funding from the European Union Seventh Framework Program for research technological development and demonstration. Dr. Schrag reports receiving consultancy or advisory board honoraria from Biogen, Abbvie, Bial, and Neurotechnology; research support from the National Institute of Health Research, Parkinsons UK, and the Economic and Social Research Council and the European Commission; and Royalties from Oxford University Press. Dr. Pringsheim reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Group A streptococcus (GAS) infection is not associated with new-onset tic disorders in at-risk children, findings from a large prospective study show.
The results mean that if preteens present with a new-onset tic condition, “they’re unlikely to have it as a result of a group A streptococcal throat infection,” study author Anette Eleonore Schrag, MD, PhD, professor, department of clinical neuroscience, Institute of Neurology, University College London, told this news organization.
Therefore, clinicians should not automatically prescribe antibiotics for children with tics, which sometimes occurs, said Dr. Schrag.
The study was published online Feb. 2 in Neurology.
Ongoing controversy
Research shows that genetic and environmental factors contribute to chronic tic disorders (CTDs) and Tourette syndrome (TS). Prenatal exposure to maternal smoking and central nervous system (CNS) stimulants, as well as psychosocial stress, may play a role.
There has been an ongoing controversy regarding the possible role of GAS in tics, with some studies showing an association and others not showing a link. However, previous studies have been retrospective, registry based, or had limited sample size.
This new prospective study is the first in children without a tic disorder but who were at relatively high risk of developing one. The children were followed to assess development of streptococcal infections and tics, said Dr. Schrag.
The study included 259 children aged 3-10 years (mean baseline age, 6.8 years; over half female) who had a first-degree relative such as a parent or sibling with TS or CTD.
The average age at TS onset is 7 years, peaking in prevalence and severity at about 9-12 years. GAS throat infections are common in this age group.
Although study participants did not have tics themselves, they represented “an enriched group,” said Dr. Schrag. “Because they had family history, we knew they were at increased risk for developing tics.”
Participants were evaluated every 2 months, alternating between scheduled hospital visits and telephone interviews. Parents kept a weekly diary and were instructed to bring their child in for assessment if they showed any signs of tics.
The average follow-up period was 1.6 years, but some of the children were followed for up to 48 months. During the study, there were a total of 1,944 assessments, including 939 telephone interviews and 1,005 clinical visits.
More common in boys
Investigators defined tic onset as the first occurrence of any sudden, rapid, recurrent, nonrhythmic involuntary movement and/or vocalization on at least three separate days within a period of 3 weeks.
The investigators assessed GAS exposure using parameters from throat swabs, serum anti-streptolysin O titers, and anti-DNAse B titers.
They used multiple definitions and combinations of GAS exposures “to make sure we weren’t missing any association because we didn’t use the right definition,” said Dr. Schrag. She explained a definitive strep infection is not always clear-cut.
At baseline, 17.0% participants tested positive for GAS, and 78.8% tested negative. No throat swab was available from 4.2% of participants.
During follow-up, the number of confirmed positive GAS exposures was 59, 102, 125, and 138, depending on the definition.
Researchers identified 61 tic cases during the study period. There was no evidence of an association of tic onset with GAS exposure after adjusting for age, sex, and parental education level.
However, there was a strong association between tic onset and sex, with girls being 60% less likely to develop tics than boys (hazard ratio, 0.4; 95% CI, 0.2-0.7; P < .01).
This result wasn’t particularly surprising, as it’s known that more boys develop tics than girls. “We just confirmed that in a prospective way,” said Dr. Schrag.
Results from sensitivity analyses confirmed the results. This was also the case with analyses that excluded visits with missing data on GAS exposure and that further adjusted for clinical site and psychotropic medication use.
Other pathogens?
Although the results showed no association between strep and tics in this population, it does not “close the door completely” on a potential relationship, said Dr. Schrag.
“By and large, the development of tics in children is not associated with group A strep, but differences in small subgroups can never be excluded by a study like this.”
Participants in this study were part of the European Multicentre Tics in Children Studies (EMTICS), a prospective cohort study exploring the role of environmental and genetic factors in pediatric CTD. That project is also looking at immune system factors, “which might play a role in the development of chronic tic disorder and associated conditions,” said Dr. Schrag.
It’s still possible, she added, that other pathogens could play a role in tic development. “That’s going to be the subject of further analysis and future studies,” she said.
Tamara Pringsheim, MD, professor of clinical neurosciences, psychiatry, pediatrics, and community health sciences, University of Calgary (Alta.), praised the research.
“This was a well-designed study, with a large sample of 260 children followed for up to 4 years, using a standardized protocol to assess for group A streptococcal infection and new onset of tics.”
The study, which did not uncover an association between GAS exposure and tic onset, “provides high level evidence that group A streptococcal exposure is not an important risk factor for the new onset of tics in children with a family history of tic disorders.”
The study received funding from the European Union Seventh Framework Program for research technological development and demonstration. Dr. Schrag reports receiving consultancy or advisory board honoraria from Biogen, Abbvie, Bial, and Neurotechnology; research support from the National Institute of Health Research, Parkinsons UK, and the Economic and Social Research Council and the European Commission; and Royalties from Oxford University Press. Dr. Pringsheim reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Group A streptococcus (GAS) infection is not associated with new-onset tic disorders in at-risk children, findings from a large prospective study show.
The results mean that if preteens present with a new-onset tic condition, “they’re unlikely to have it as a result of a group A streptococcal throat infection,” study author Anette Eleonore Schrag, MD, PhD, professor, department of clinical neuroscience, Institute of Neurology, University College London, told this news organization.
Therefore, clinicians should not automatically prescribe antibiotics for children with tics, which sometimes occurs, said Dr. Schrag.
The study was published online Feb. 2 in Neurology.
Ongoing controversy
Research shows that genetic and environmental factors contribute to chronic tic disorders (CTDs) and Tourette syndrome (TS). Prenatal exposure to maternal smoking and central nervous system (CNS) stimulants, as well as psychosocial stress, may play a role.
There has been an ongoing controversy regarding the possible role of GAS in tics, with some studies showing an association and others not showing a link. However, previous studies have been retrospective, registry based, or had limited sample size.
This new prospective study is the first in children without a tic disorder but who were at relatively high risk of developing one. The children were followed to assess development of streptococcal infections and tics, said Dr. Schrag.
The study included 259 children aged 3-10 years (mean baseline age, 6.8 years; over half female) who had a first-degree relative such as a parent or sibling with TS or CTD.
The average age at TS onset is 7 years, peaking in prevalence and severity at about 9-12 years. GAS throat infections are common in this age group.
Although study participants did not have tics themselves, they represented “an enriched group,” said Dr. Schrag. “Because they had family history, we knew they were at increased risk for developing tics.”
Participants were evaluated every 2 months, alternating between scheduled hospital visits and telephone interviews. Parents kept a weekly diary and were instructed to bring their child in for assessment if they showed any signs of tics.
The average follow-up period was 1.6 years, but some of the children were followed for up to 48 months. During the study, there were a total of 1,944 assessments, including 939 telephone interviews and 1,005 clinical visits.
More common in boys
Investigators defined tic onset as the first occurrence of any sudden, rapid, recurrent, nonrhythmic involuntary movement and/or vocalization on at least three separate days within a period of 3 weeks.
The investigators assessed GAS exposure using parameters from throat swabs, serum anti-streptolysin O titers, and anti-DNAse B titers.
They used multiple definitions and combinations of GAS exposures “to make sure we weren’t missing any association because we didn’t use the right definition,” said Dr. Schrag. She explained a definitive strep infection is not always clear-cut.
At baseline, 17.0% participants tested positive for GAS, and 78.8% tested negative. No throat swab was available from 4.2% of participants.
During follow-up, the number of confirmed positive GAS exposures was 59, 102, 125, and 138, depending on the definition.
Researchers identified 61 tic cases during the study period. There was no evidence of an association of tic onset with GAS exposure after adjusting for age, sex, and parental education level.
However, there was a strong association between tic onset and sex, with girls being 60% less likely to develop tics than boys (hazard ratio, 0.4; 95% CI, 0.2-0.7; P < .01).
This result wasn’t particularly surprising, as it’s known that more boys develop tics than girls. “We just confirmed that in a prospective way,” said Dr. Schrag.
Results from sensitivity analyses confirmed the results. This was also the case with analyses that excluded visits with missing data on GAS exposure and that further adjusted for clinical site and psychotropic medication use.
Other pathogens?
Although the results showed no association between strep and tics in this population, it does not “close the door completely” on a potential relationship, said Dr. Schrag.
“By and large, the development of tics in children is not associated with group A strep, but differences in small subgroups can never be excluded by a study like this.”
Participants in this study were part of the European Multicentre Tics in Children Studies (EMTICS), a prospective cohort study exploring the role of environmental and genetic factors in pediatric CTD. That project is also looking at immune system factors, “which might play a role in the development of chronic tic disorder and associated conditions,” said Dr. Schrag.
It’s still possible, she added, that other pathogens could play a role in tic development. “That’s going to be the subject of further analysis and future studies,” she said.
Tamara Pringsheim, MD, professor of clinical neurosciences, psychiatry, pediatrics, and community health sciences, University of Calgary (Alta.), praised the research.
“This was a well-designed study, with a large sample of 260 children followed for up to 4 years, using a standardized protocol to assess for group A streptococcal infection and new onset of tics.”
The study, which did not uncover an association between GAS exposure and tic onset, “provides high level evidence that group A streptococcal exposure is not an important risk factor for the new onset of tics in children with a family history of tic disorders.”
The study received funding from the European Union Seventh Framework Program for research technological development and demonstration. Dr. Schrag reports receiving consultancy or advisory board honoraria from Biogen, Abbvie, Bial, and Neurotechnology; research support from the National Institute of Health Research, Parkinsons UK, and the Economic and Social Research Council and the European Commission; and Royalties from Oxford University Press. Dr. Pringsheim reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
COVID vaccines open rifts between parents, children
The picture of rebellious teenagers sneaking “shots” has widened beyond breaking into Mom and Dad’s liquor cabinet. For some teens now, it means getting a COVID-19 vaccination without their parents’ consent – and, unlike the cabinet raids for the booze, they have adults willing to endorse the practice.
Since the U.S. Food and Drug Administration first granted emergency use authorization to Pfizer’s COVID-19 vaccine for teenagers in mid-2021, health officials have had to deal with a small subset of vaccine hesitancy where minors want the shot over the objections of their reluctant parents. The split has buoyed groups that were formed initially to convince teenagers to get vaccinated against other diseases.
When 14-year-old Arin Parsa of San Jose, California founded Teens for Vaccines in 2019 after a measles outbreak among unvaccinated children, “hardly anyone was interested,” he said. “Many teens were into climate change and other causes. Then, when the pandemic hit, so many were suddenly aware.”
Heavy toll on teens
Mr. Parsa’s parents fully supported Teens for Vaccines, he said, but he quickly found out how “politicized” COVID shots had become.
“We find people who are sad, angry, and frustrated at this stage of the pandemic,” he told this news organization. “The anti-vax lobby is riding the coat-tails of other movements. It has a very severe effect on their mental health. They can’t go out with their friends and socialize.”
In the pandemic’s initial stages, children were less likely to fall sick with COVID, but the Omicron variant led to a dramatic increase in illnesses among young people. The American Academy of Pediatrics has found that 3.5 million of the 11.4 million pediatric cases of the virus in the United States were reported in January 2022 alone. Meanwhile, vaccination rates for children aged 12-17, which were only 34% in June 2021 and lagged through the fall, are now at about 61% thanks to a sharp uptick during the Omicron surge, according to polling by the Kaiser Family Foundation.
No statistics are available on how many minors have received a COVID vaccine against their parents’ wishes.
“It’s not like there’s a big movement,” said Arthur Caplan, PhD, who heads the Division of Medical Ethics at the NYU Grossman School of Medicine. He said he noticed a divide around the HPV and hepatitis B vaccines. “They were tied up with sexual behavior,” he said, but “there were also some kids whose parents were really antivaxxers.”
Mr. Parsa said his and similar teen-oriented groups, such as VaxTeen, seek to educate their teen cohort, convince family members of the vaccines’ benefits, and to connect them with resources to get a shot. They also strive to change laws to make it easier for teenagers to receive the vaccine.
Consent laws vary from state to state (and within states), and proposed changes are afoot – some to loosen the laws and some to tighten them. Currently a 14-year-old in Alabama may get a COVID shot without parental permission, according to VaxTeen. In California, minors may receive the HPV shot without parental consent but not a COVID vaccine, although groups like Teens for Vaccines are pushing to change that. A bill now before the state legislature, the Teens Choose Vaccines Act (Senate Bill 866), would allow adolescents aged 12 and older to be able receive any FDA-approved vaccine – including COVID vaccines – without parental consent.
A second bill in California, the Keep Schools Open and Safe Act, would add the COVID-19 vaccines to the required list of immunizations needed to attend school in the state as well as eliminate the “personal belief” exemption against immunization.
California Sen. Richard Pan, MD (D-6th District), cowrote both bills with fellow Democrat Sen. Scott Wiener (D-11th District) and teen advocates from Teens for Vaccines and Generation Up, who helped draft the language in consultation with the lawmakers.
“As a pediatrician, I have seen all manner of situations where the requirement for a signed form has prevented teens from being able to get a vaccine that otherwise they and their guardians approved of them getting,” Dr. Pan told this news organization. “As a father, I don’t want to see my kids or any teen that wishes to protect themselves from deadly diseases unable to do so, particularly as we continue to fight off the dangers of the COVID-19 pandemic. I always encourage parents or teens that have questions about vaccines to speak directly with their pediatrician.”
Lawmakers in Philadelphia passed a provision last year to allow anyone age 11 or over to get the COVID vaccine without parental permission, keeping it in line with other vaccinations like hepatitis or HPV. “People from surrounding counties have come into the city, but it hasn’t been a huge rush,” says James Garrow, MPH, a spokesman for the city’s Department of Health.
Strive for collaboration, but listen to the children
Experts say the best solution is to for a doctor to meet with minors and their reluctant parents to get them on board for a COVID shot.
“Physicians are still the trusted messengers,” said Emma Olivera, MD, a pediatrician in suburban Chicago who advises groups that combat COVID misinformation.
Dr. Olivera said she often finds that internet-savvy teenagers have access to more information than older people, including their parents.
Thanks to COVID policies, office meetings are “difficult to do,” NYU’s Dr. Caplan added. In such a meeting, Dr. Caplan said he would try to convince the parents that the shots are needed for their children to stay in school or play sports. In the end, he said minors should get the shot but would also notify the parents before that happens: “My duty is to them.”
If parents take opposite stances, the pro-vaccine side is likely to prevail, even in California, said Patrick Baghdaserians, JD, a family law attorney in Pasadena. Mr. Baghdaserians said he is now representing a father who wants his teenager to get vaccinated but the mother doesn’t. “The court will fall on our side,” he predicted.
A version of this article first appeared on Medscape.com.
The picture of rebellious teenagers sneaking “shots” has widened beyond breaking into Mom and Dad’s liquor cabinet. For some teens now, it means getting a COVID-19 vaccination without their parents’ consent – and, unlike the cabinet raids for the booze, they have adults willing to endorse the practice.
Since the U.S. Food and Drug Administration first granted emergency use authorization to Pfizer’s COVID-19 vaccine for teenagers in mid-2021, health officials have had to deal with a small subset of vaccine hesitancy where minors want the shot over the objections of their reluctant parents. The split has buoyed groups that were formed initially to convince teenagers to get vaccinated against other diseases.
When 14-year-old Arin Parsa of San Jose, California founded Teens for Vaccines in 2019 after a measles outbreak among unvaccinated children, “hardly anyone was interested,” he said. “Many teens were into climate change and other causes. Then, when the pandemic hit, so many were suddenly aware.”
Heavy toll on teens
Mr. Parsa’s parents fully supported Teens for Vaccines, he said, but he quickly found out how “politicized” COVID shots had become.
“We find people who are sad, angry, and frustrated at this stage of the pandemic,” he told this news organization. “The anti-vax lobby is riding the coat-tails of other movements. It has a very severe effect on their mental health. They can’t go out with their friends and socialize.”
In the pandemic’s initial stages, children were less likely to fall sick with COVID, but the Omicron variant led to a dramatic increase in illnesses among young people. The American Academy of Pediatrics has found that 3.5 million of the 11.4 million pediatric cases of the virus in the United States were reported in January 2022 alone. Meanwhile, vaccination rates for children aged 12-17, which were only 34% in June 2021 and lagged through the fall, are now at about 61% thanks to a sharp uptick during the Omicron surge, according to polling by the Kaiser Family Foundation.
No statistics are available on how many minors have received a COVID vaccine against their parents’ wishes.
“It’s not like there’s a big movement,” said Arthur Caplan, PhD, who heads the Division of Medical Ethics at the NYU Grossman School of Medicine. He said he noticed a divide around the HPV and hepatitis B vaccines. “They were tied up with sexual behavior,” he said, but “there were also some kids whose parents were really antivaxxers.”
Mr. Parsa said his and similar teen-oriented groups, such as VaxTeen, seek to educate their teen cohort, convince family members of the vaccines’ benefits, and to connect them with resources to get a shot. They also strive to change laws to make it easier for teenagers to receive the vaccine.
Consent laws vary from state to state (and within states), and proposed changes are afoot – some to loosen the laws and some to tighten them. Currently a 14-year-old in Alabama may get a COVID shot without parental permission, according to VaxTeen. In California, minors may receive the HPV shot without parental consent but not a COVID vaccine, although groups like Teens for Vaccines are pushing to change that. A bill now before the state legislature, the Teens Choose Vaccines Act (Senate Bill 866), would allow adolescents aged 12 and older to be able receive any FDA-approved vaccine – including COVID vaccines – without parental consent.
A second bill in California, the Keep Schools Open and Safe Act, would add the COVID-19 vaccines to the required list of immunizations needed to attend school in the state as well as eliminate the “personal belief” exemption against immunization.
California Sen. Richard Pan, MD (D-6th District), cowrote both bills with fellow Democrat Sen. Scott Wiener (D-11th District) and teen advocates from Teens for Vaccines and Generation Up, who helped draft the language in consultation with the lawmakers.
“As a pediatrician, I have seen all manner of situations where the requirement for a signed form has prevented teens from being able to get a vaccine that otherwise they and their guardians approved of them getting,” Dr. Pan told this news organization. “As a father, I don’t want to see my kids or any teen that wishes to protect themselves from deadly diseases unable to do so, particularly as we continue to fight off the dangers of the COVID-19 pandemic. I always encourage parents or teens that have questions about vaccines to speak directly with their pediatrician.”
Lawmakers in Philadelphia passed a provision last year to allow anyone age 11 or over to get the COVID vaccine without parental permission, keeping it in line with other vaccinations like hepatitis or HPV. “People from surrounding counties have come into the city, but it hasn’t been a huge rush,” says James Garrow, MPH, a spokesman for the city’s Department of Health.
Strive for collaboration, but listen to the children
Experts say the best solution is to for a doctor to meet with minors and their reluctant parents to get them on board for a COVID shot.
“Physicians are still the trusted messengers,” said Emma Olivera, MD, a pediatrician in suburban Chicago who advises groups that combat COVID misinformation.
Dr. Olivera said she often finds that internet-savvy teenagers have access to more information than older people, including their parents.
Thanks to COVID policies, office meetings are “difficult to do,” NYU’s Dr. Caplan added. In such a meeting, Dr. Caplan said he would try to convince the parents that the shots are needed for their children to stay in school or play sports. In the end, he said minors should get the shot but would also notify the parents before that happens: “My duty is to them.”
If parents take opposite stances, the pro-vaccine side is likely to prevail, even in California, said Patrick Baghdaserians, JD, a family law attorney in Pasadena. Mr. Baghdaserians said he is now representing a father who wants his teenager to get vaccinated but the mother doesn’t. “The court will fall on our side,” he predicted.
A version of this article first appeared on Medscape.com.
The picture of rebellious teenagers sneaking “shots” has widened beyond breaking into Mom and Dad’s liquor cabinet. For some teens now, it means getting a COVID-19 vaccination without their parents’ consent – and, unlike the cabinet raids for the booze, they have adults willing to endorse the practice.
Since the U.S. Food and Drug Administration first granted emergency use authorization to Pfizer’s COVID-19 vaccine for teenagers in mid-2021, health officials have had to deal with a small subset of vaccine hesitancy where minors want the shot over the objections of their reluctant parents. The split has buoyed groups that were formed initially to convince teenagers to get vaccinated against other diseases.
When 14-year-old Arin Parsa of San Jose, California founded Teens for Vaccines in 2019 after a measles outbreak among unvaccinated children, “hardly anyone was interested,” he said. “Many teens were into climate change and other causes. Then, when the pandemic hit, so many were suddenly aware.”
Heavy toll on teens
Mr. Parsa’s parents fully supported Teens for Vaccines, he said, but he quickly found out how “politicized” COVID shots had become.
“We find people who are sad, angry, and frustrated at this stage of the pandemic,” he told this news organization. “The anti-vax lobby is riding the coat-tails of other movements. It has a very severe effect on their mental health. They can’t go out with their friends and socialize.”
In the pandemic’s initial stages, children were less likely to fall sick with COVID, but the Omicron variant led to a dramatic increase in illnesses among young people. The American Academy of Pediatrics has found that 3.5 million of the 11.4 million pediatric cases of the virus in the United States were reported in January 2022 alone. Meanwhile, vaccination rates for children aged 12-17, which were only 34% in June 2021 and lagged through the fall, are now at about 61% thanks to a sharp uptick during the Omicron surge, according to polling by the Kaiser Family Foundation.
No statistics are available on how many minors have received a COVID vaccine against their parents’ wishes.
“It’s not like there’s a big movement,” said Arthur Caplan, PhD, who heads the Division of Medical Ethics at the NYU Grossman School of Medicine. He said he noticed a divide around the HPV and hepatitis B vaccines. “They were tied up with sexual behavior,” he said, but “there were also some kids whose parents were really antivaxxers.”
Mr. Parsa said his and similar teen-oriented groups, such as VaxTeen, seek to educate their teen cohort, convince family members of the vaccines’ benefits, and to connect them with resources to get a shot. They also strive to change laws to make it easier for teenagers to receive the vaccine.
Consent laws vary from state to state (and within states), and proposed changes are afoot – some to loosen the laws and some to tighten them. Currently a 14-year-old in Alabama may get a COVID shot without parental permission, according to VaxTeen. In California, minors may receive the HPV shot without parental consent but not a COVID vaccine, although groups like Teens for Vaccines are pushing to change that. A bill now before the state legislature, the Teens Choose Vaccines Act (Senate Bill 866), would allow adolescents aged 12 and older to be able receive any FDA-approved vaccine – including COVID vaccines – without parental consent.
A second bill in California, the Keep Schools Open and Safe Act, would add the COVID-19 vaccines to the required list of immunizations needed to attend school in the state as well as eliminate the “personal belief” exemption against immunization.
California Sen. Richard Pan, MD (D-6th District), cowrote both bills with fellow Democrat Sen. Scott Wiener (D-11th District) and teen advocates from Teens for Vaccines and Generation Up, who helped draft the language in consultation with the lawmakers.
“As a pediatrician, I have seen all manner of situations where the requirement for a signed form has prevented teens from being able to get a vaccine that otherwise they and their guardians approved of them getting,” Dr. Pan told this news organization. “As a father, I don’t want to see my kids or any teen that wishes to protect themselves from deadly diseases unable to do so, particularly as we continue to fight off the dangers of the COVID-19 pandemic. I always encourage parents or teens that have questions about vaccines to speak directly with their pediatrician.”
Lawmakers in Philadelphia passed a provision last year to allow anyone age 11 or over to get the COVID vaccine without parental permission, keeping it in line with other vaccinations like hepatitis or HPV. “People from surrounding counties have come into the city, but it hasn’t been a huge rush,” says James Garrow, MPH, a spokesman for the city’s Department of Health.
Strive for collaboration, but listen to the children
Experts say the best solution is to for a doctor to meet with minors and their reluctant parents to get them on board for a COVID shot.
“Physicians are still the trusted messengers,” said Emma Olivera, MD, a pediatrician in suburban Chicago who advises groups that combat COVID misinformation.
Dr. Olivera said she often finds that internet-savvy teenagers have access to more information than older people, including their parents.
Thanks to COVID policies, office meetings are “difficult to do,” NYU’s Dr. Caplan added. In such a meeting, Dr. Caplan said he would try to convince the parents that the shots are needed for their children to stay in school or play sports. In the end, he said minors should get the shot but would also notify the parents before that happens: “My duty is to them.”
If parents take opposite stances, the pro-vaccine side is likely to prevail, even in California, said Patrick Baghdaserians, JD, a family law attorney in Pasadena. Mr. Baghdaserians said he is now representing a father who wants his teenager to get vaccinated but the mother doesn’t. “The court will fall on our side,” he predicted.
A version of this article first appeared on Medscape.com.
Caring for suicidal youth: An approach for pediatricians
This month’s column is driven by the recent increase of youth in crisis, and COVID-19–related limitations of higher-level services. Suicide is the second leading cause of death among youth1 and populations who face discrimination are at increased risk.2,3
A pediatrician colleague recently asked me about how to support patients who may be at risk. With inpatient units and emergency departments over capacity, properly allocating resources to patients with the most acute needs is crucial. When appropriate, providing preventive suicide care in primary care similarly saves lives.
Case summary
Cassandra is a 16-year-old Black girl who told a friend on Snapchat that she did not want to be alive. The friend told her parents and Cassandra’s parents brought their daughter to an urgent primary care appointment. Cassandra has had a history of difficulty with large transitions like a family move when she was 13. She spent more time in her room for several months before joining the volleyball team and making new friends. She has always done well academically in school but struggled with insomnia and classwork when her high school shifted to remote learning for the 2020-2021 school year because of the pandemic. This year she attends school in person but is unable to play volleyball because of COVID-19 restrictions. Her parents report that she is again spending more time online in her room. She is passing her classes and doing well in math, but overall, her grades have fallen since the pandemic began. She reports recent difficulties with friends and notes feeling hopeless about a changing climate and race relations in the United States.
Discussion
This case example illustrates some factors pediatricians can consider in determining how to proceed in similar circumstances. What are Cassandra’s immediate risk and treatment needs? In cases like Cassandra’s, the American Academy of Pediatrics recommends the ABCD (Assess, Build hope, Connect, Develop a safety plan) approach.4 Preparing practices to deliver this best possible preventive suicide care is essential.
1. Is this patient at imminent risk of harming herself?
Assess: Screen for suicide risk and assess risk level. Several standardized screening tools exist for gauging a patient’s risk. The Ask Suicide Screening Questionnaire (asQ) is a straightforward screening tool (not to be confused with the ASQ Ages and Stages developmental screening). These questionnaires take only a few minutes and next steps are suggested depending on the score (low, moderate, or high risk) and clinical judgment. What matters most is using a standardized screener to directly ask questions about suicide and then follow up appropriately based on risk.
2. What can be done during the visit to promote a good outcome?
Build hope/reasons for living. Validate that people sometimes feel suicidal when things are difficult, but that the feelings come and go and people go on to live meaningful lives. Tell the patients that you care about keeping them safe when the feelings come up. Motivational interviewing can be helpful to reflect back patient-identified reasons for living. Genuinely tell the patients how much you care about their wellbeing.
3. What can be done outside the visit to promote a good outcome?
Connect: Strengthen connections with protective adults. Make a plan to have the patient connect regularly with parents/trusted adults. She could engage in social action, or connect one-on-one. With more structured social opportunities, she will spend less time online. Medical practices can reach out with postcards and phone calls to show that they care about the patient, an intervention called “Caring Contacts” that has been shown to decrease suicide.
4. Once suicide risk is identified, what are specific tools to use during the visit to keep her safe?
Develop a plan for staying safe: Restrict access to lethal means, develop a safety plan and healthy ways of coping. There is a free 2-hour CALM (Counseling on Access to Lethal Means) training to help providers feel competent in restricting access to lethal means prior to increased risk. This resource provides safety plan templates that help identify triggers, specific ways to stay safe, people to talk to, and suicide prevention resources including lifelines (988) and chat options (text 2 letter state to 741741).
Enacting suicide prevention requires practice readiness and workflow changes. Providers should assess mental health supports in and out of the office, and then rehearse workflow around suicide prevention care. Increasingly, there are embedded case managers or behavioral health providers available. Sometimes local mental health crisis services are the best option. A practice introductory letter to community mental health practitioners can improve later coordination efforts when caring for suicidal youth. Having practice-level support for provider well-being can improve outcomes.
Case follow-up
After interviewing the girl separately, and performing a PHQ-A and an asQ, followed by the Brief Suicide Safety Assessment to screen for acuity, the pediatrician felt confident that Cassandra was suffering from moderate depression and had moderate but not imminent risk of suicide. Options to treat her depression were discussed with Cassandra and her parents, and a referral to therapy was made.
The provider knew that depression care is complementary but not sufficient as standalone suicide prevention. The provider used the asQ pathway to determine next steps. He made a safety plan, and referred her to an outpatient mental health clinician with whom the practice had an established relationship for an urgent mental health evaluation. A follow-up primary care appointment was scheduled within 72 hours to re-check safety and ensure that she had an appointment scheduled to start therapy. A nurse contacted the patient and her family regularly to check on her wellbeing. Her parents made a plan with her volleyball coach to organize outdoor off-season conditioning to help with exercise and socializing. The family removed screens prior to bedtime and sleep improved. At a 3-month follow-up, Cassandra had only mild depressive symptoms and the frequency and intensity of her suicidal ideation had decreased.
Dr. Spottswood is a child psychiatrist practicing in an integrated care clinic at the Community Health Centers of Burlington, Vermont, a Federally Qualified Health Center. She is the medical director of the Vermont Child Psychiatry Access Program and a clinical assistant professor in the department of psychiatry at the University of Vermont.
References
1. National Institute of Mental Health: Suicide.
2. Hottes TS et al. Am J Public Health. 2016 May;106(5):e1-12.
3. Bridge JA et al. JAMA Pediatr. 2018;172(7):697-9.
4. Asarnow JR. SAMHSA Center for Adolescent Suicide and Self-Harm..
This month’s column is driven by the recent increase of youth in crisis, and COVID-19–related limitations of higher-level services. Suicide is the second leading cause of death among youth1 and populations who face discrimination are at increased risk.2,3
A pediatrician colleague recently asked me about how to support patients who may be at risk. With inpatient units and emergency departments over capacity, properly allocating resources to patients with the most acute needs is crucial. When appropriate, providing preventive suicide care in primary care similarly saves lives.
Case summary
Cassandra is a 16-year-old Black girl who told a friend on Snapchat that she did not want to be alive. The friend told her parents and Cassandra’s parents brought their daughter to an urgent primary care appointment. Cassandra has had a history of difficulty with large transitions like a family move when she was 13. She spent more time in her room for several months before joining the volleyball team and making new friends. She has always done well academically in school but struggled with insomnia and classwork when her high school shifted to remote learning for the 2020-2021 school year because of the pandemic. This year she attends school in person but is unable to play volleyball because of COVID-19 restrictions. Her parents report that she is again spending more time online in her room. She is passing her classes and doing well in math, but overall, her grades have fallen since the pandemic began. She reports recent difficulties with friends and notes feeling hopeless about a changing climate and race relations in the United States.
Discussion
This case example illustrates some factors pediatricians can consider in determining how to proceed in similar circumstances. What are Cassandra’s immediate risk and treatment needs? In cases like Cassandra’s, the American Academy of Pediatrics recommends the ABCD (Assess, Build hope, Connect, Develop a safety plan) approach.4 Preparing practices to deliver this best possible preventive suicide care is essential.
1. Is this patient at imminent risk of harming herself?
Assess: Screen for suicide risk and assess risk level. Several standardized screening tools exist for gauging a patient’s risk. The Ask Suicide Screening Questionnaire (asQ) is a straightforward screening tool (not to be confused with the ASQ Ages and Stages developmental screening). These questionnaires take only a few minutes and next steps are suggested depending on the score (low, moderate, or high risk) and clinical judgment. What matters most is using a standardized screener to directly ask questions about suicide and then follow up appropriately based on risk.
2. What can be done during the visit to promote a good outcome?
Build hope/reasons for living. Validate that people sometimes feel suicidal when things are difficult, but that the feelings come and go and people go on to live meaningful lives. Tell the patients that you care about keeping them safe when the feelings come up. Motivational interviewing can be helpful to reflect back patient-identified reasons for living. Genuinely tell the patients how much you care about their wellbeing.
3. What can be done outside the visit to promote a good outcome?
Connect: Strengthen connections with protective adults. Make a plan to have the patient connect regularly with parents/trusted adults. She could engage in social action, or connect one-on-one. With more structured social opportunities, she will spend less time online. Medical practices can reach out with postcards and phone calls to show that they care about the patient, an intervention called “Caring Contacts” that has been shown to decrease suicide.
4. Once suicide risk is identified, what are specific tools to use during the visit to keep her safe?
Develop a plan for staying safe: Restrict access to lethal means, develop a safety plan and healthy ways of coping. There is a free 2-hour CALM (Counseling on Access to Lethal Means) training to help providers feel competent in restricting access to lethal means prior to increased risk. This resource provides safety plan templates that help identify triggers, specific ways to stay safe, people to talk to, and suicide prevention resources including lifelines (988) and chat options (text 2 letter state to 741741).
Enacting suicide prevention requires practice readiness and workflow changes. Providers should assess mental health supports in and out of the office, and then rehearse workflow around suicide prevention care. Increasingly, there are embedded case managers or behavioral health providers available. Sometimes local mental health crisis services are the best option. A practice introductory letter to community mental health practitioners can improve later coordination efforts when caring for suicidal youth. Having practice-level support for provider well-being can improve outcomes.
Case follow-up
After interviewing the girl separately, and performing a PHQ-A and an asQ, followed by the Brief Suicide Safety Assessment to screen for acuity, the pediatrician felt confident that Cassandra was suffering from moderate depression and had moderate but not imminent risk of suicide. Options to treat her depression were discussed with Cassandra and her parents, and a referral to therapy was made.
The provider knew that depression care is complementary but not sufficient as standalone suicide prevention. The provider used the asQ pathway to determine next steps. He made a safety plan, and referred her to an outpatient mental health clinician with whom the practice had an established relationship for an urgent mental health evaluation. A follow-up primary care appointment was scheduled within 72 hours to re-check safety and ensure that she had an appointment scheduled to start therapy. A nurse contacted the patient and her family regularly to check on her wellbeing. Her parents made a plan with her volleyball coach to organize outdoor off-season conditioning to help with exercise and socializing. The family removed screens prior to bedtime and sleep improved. At a 3-month follow-up, Cassandra had only mild depressive symptoms and the frequency and intensity of her suicidal ideation had decreased.
Dr. Spottswood is a child psychiatrist practicing in an integrated care clinic at the Community Health Centers of Burlington, Vermont, a Federally Qualified Health Center. She is the medical director of the Vermont Child Psychiatry Access Program and a clinical assistant professor in the department of psychiatry at the University of Vermont.
References
1. National Institute of Mental Health: Suicide.
2. Hottes TS et al. Am J Public Health. 2016 May;106(5):e1-12.
3. Bridge JA et al. JAMA Pediatr. 2018;172(7):697-9.
4. Asarnow JR. SAMHSA Center for Adolescent Suicide and Self-Harm..
This month’s column is driven by the recent increase of youth in crisis, and COVID-19–related limitations of higher-level services. Suicide is the second leading cause of death among youth1 and populations who face discrimination are at increased risk.2,3
A pediatrician colleague recently asked me about how to support patients who may be at risk. With inpatient units and emergency departments over capacity, properly allocating resources to patients with the most acute needs is crucial. When appropriate, providing preventive suicide care in primary care similarly saves lives.
Case summary
Cassandra is a 16-year-old Black girl who told a friend on Snapchat that she did not want to be alive. The friend told her parents and Cassandra’s parents brought their daughter to an urgent primary care appointment. Cassandra has had a history of difficulty with large transitions like a family move when she was 13. She spent more time in her room for several months before joining the volleyball team and making new friends. She has always done well academically in school but struggled with insomnia and classwork when her high school shifted to remote learning for the 2020-2021 school year because of the pandemic. This year she attends school in person but is unable to play volleyball because of COVID-19 restrictions. Her parents report that she is again spending more time online in her room. She is passing her classes and doing well in math, but overall, her grades have fallen since the pandemic began. She reports recent difficulties with friends and notes feeling hopeless about a changing climate and race relations in the United States.
Discussion
This case example illustrates some factors pediatricians can consider in determining how to proceed in similar circumstances. What are Cassandra’s immediate risk and treatment needs? In cases like Cassandra’s, the American Academy of Pediatrics recommends the ABCD (Assess, Build hope, Connect, Develop a safety plan) approach.4 Preparing practices to deliver this best possible preventive suicide care is essential.
1. Is this patient at imminent risk of harming herself?
Assess: Screen for suicide risk and assess risk level. Several standardized screening tools exist for gauging a patient’s risk. The Ask Suicide Screening Questionnaire (asQ) is a straightforward screening tool (not to be confused with the ASQ Ages and Stages developmental screening). These questionnaires take only a few minutes and next steps are suggested depending on the score (low, moderate, or high risk) and clinical judgment. What matters most is using a standardized screener to directly ask questions about suicide and then follow up appropriately based on risk.
2. What can be done during the visit to promote a good outcome?
Build hope/reasons for living. Validate that people sometimes feel suicidal when things are difficult, but that the feelings come and go and people go on to live meaningful lives. Tell the patients that you care about keeping them safe when the feelings come up. Motivational interviewing can be helpful to reflect back patient-identified reasons for living. Genuinely tell the patients how much you care about their wellbeing.
3. What can be done outside the visit to promote a good outcome?
Connect: Strengthen connections with protective adults. Make a plan to have the patient connect regularly with parents/trusted adults. She could engage in social action, or connect one-on-one. With more structured social opportunities, she will spend less time online. Medical practices can reach out with postcards and phone calls to show that they care about the patient, an intervention called “Caring Contacts” that has been shown to decrease suicide.
4. Once suicide risk is identified, what are specific tools to use during the visit to keep her safe?
Develop a plan for staying safe: Restrict access to lethal means, develop a safety plan and healthy ways of coping. There is a free 2-hour CALM (Counseling on Access to Lethal Means) training to help providers feel competent in restricting access to lethal means prior to increased risk. This resource provides safety plan templates that help identify triggers, specific ways to stay safe, people to talk to, and suicide prevention resources including lifelines (988) and chat options (text 2 letter state to 741741).
Enacting suicide prevention requires practice readiness and workflow changes. Providers should assess mental health supports in and out of the office, and then rehearse workflow around suicide prevention care. Increasingly, there are embedded case managers or behavioral health providers available. Sometimes local mental health crisis services are the best option. A practice introductory letter to community mental health practitioners can improve later coordination efforts when caring for suicidal youth. Having practice-level support for provider well-being can improve outcomes.
Case follow-up
After interviewing the girl separately, and performing a PHQ-A and an asQ, followed by the Brief Suicide Safety Assessment to screen for acuity, the pediatrician felt confident that Cassandra was suffering from moderate depression and had moderate but not imminent risk of suicide. Options to treat her depression were discussed with Cassandra and her parents, and a referral to therapy was made.
The provider knew that depression care is complementary but not sufficient as standalone suicide prevention. The provider used the asQ pathway to determine next steps. He made a safety plan, and referred her to an outpatient mental health clinician with whom the practice had an established relationship for an urgent mental health evaluation. A follow-up primary care appointment was scheduled within 72 hours to re-check safety and ensure that she had an appointment scheduled to start therapy. A nurse contacted the patient and her family regularly to check on her wellbeing. Her parents made a plan with her volleyball coach to organize outdoor off-season conditioning to help with exercise and socializing. The family removed screens prior to bedtime and sleep improved. At a 3-month follow-up, Cassandra had only mild depressive symptoms and the frequency and intensity of her suicidal ideation had decreased.
Dr. Spottswood is a child psychiatrist practicing in an integrated care clinic at the Community Health Centers of Burlington, Vermont, a Federally Qualified Health Center. She is the medical director of the Vermont Child Psychiatry Access Program and a clinical assistant professor in the department of psychiatry at the University of Vermont.
References
1. National Institute of Mental Health: Suicide.
2. Hottes TS et al. Am J Public Health. 2016 May;106(5):e1-12.
3. Bridge JA et al. JAMA Pediatr. 2018;172(7):697-9.
4. Asarnow JR. SAMHSA Center for Adolescent Suicide and Self-Harm..
Medicaid expansion benefits some colorectal patients, others not so lucky
Two new studies suggest the expansion of Medicaid under the Patient Protection and Affordable Care Act in 2010 may be leading to more frequent diagnosis of colorectal cancer (CRC) among Hispanics.
The studies, presented at the 2022 Gastrointestinal Cancers Symposium, suggest that Medicaid expansion may have a diverse impact on various ethnic groups.
“The take-home message for both physicians and policy makers is that health policy has the capacity to shift health care delivery, yet we need to consider the effects of health policy might influence subgroups of patients differently. This is useful information for providers caring for a diverse group of patients. For policy makers, this study emphasizes the importance of evaluating the impact of health policy among different racial and ethnic subgroups to fully understand the impact of [policy] change,” said study lead author James D. Murphy, MD, MS, assistant vice chair of radiation medicine at the University of California San Diego.
Dr. Murphy and associates cautioned that other factors, not just Medicaid expansion, could be responsible for the uptick in colon cancer diagnoses.
“Our observations could potentially be influenced by other risk factors. Medicaid expansion was not a ‘randomized experiment,’ and states which opted to expand Medicaid might have fundamental differences which could impact colorectal cancer incidence,” he said.
His group’s analysis of the Surveillance, Epidemiology, and End Results database included 21 states where Medicaid was expanded and 16 states where expansion did not occur. Between 2010-2013 and 2014-2018, among patients under 65, overall colorectal cancer incidence rates did not differ by Medicaid expansion status. In nonexpansion states, there was a greater increase in CRC rates among Hispanics (5.4 vs. 1.6 increase per 100,000; P = .002) and Asian/Pacific Islanders (4.3 vs. 0.4 per 100,000; P = .02), but there was no difference among Black or non-Hispanic White individuals.
Early-onset colorectal cancer diagnoses increase under Medicaid expansion
In another study presented at the meeting, researchers examined early-onset CRC data from the National Cancer Database. Among Hispanics, the rate of change of incidence of newly diagnosed cases among patients age 40-49 in Medicaid expansion states increased from 4.3% per year between 2010 and 2014 and 9.8% between 2014 and 2017. That compares with the general background increase in incidence of about 2%. In nonexpansion states, the rate of change decreased from 6.4% to 1% (P = .03). There were no statistically significant differences in the change of incidence among Blacks or Whites between expansion and nonexpansion states.
The reduced rate of change among Hispanics in nonexpansion states was a surprise, and the researchers haven’t determined the reason, according to Sanjay Goel, MD, an oncologist with Montefiore Medical Center, New York, and lead author on the National Cancer Database study. Dr. Goel speculated that some people may have migrated from nonexpansion states to states that expanded Medicaid in order to gain health care coverage.
The apparent benefit seen in Hispanics, but not Black patients, may be caused by greater susceptibility to early-onset CRC among Hispanics, leading to a stronger effect on that population when Medicaid was expanded, Dr. Goel said.
“At this point, with our available data, we do not have the ability to understand the underlying sources of these disparities, though these are questions which deserve additional research,” Dr. Murphy said.
Regardless of the reason, the message is clear, Dr. Goel said. “The bottom we want to state is that politics aside, providing health care coverage to as many people as possible, ideally to everyone, is the right way of going forward.”
The implications of the findings extend beyond policy. “The general advice I give is that, especially if you treat a Hispanic person, regardless of age, with any symptom or sign that could be suggestive of a malignancy, do not take it lightly. Follow the patient closely. I’m not advocating that you refer everybody with lower abdominal pain or bleeding for a colonoscopy, but do factor it in mind. Call them back in a week or 2, or have them make a follow-up appointment in a month so that they don’t get neglected by the system.”
Dr. Murphy and Dr. Goel have no relevant financial disclosures. The Gastrointestinal Cancers Symposium is sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Two new studies suggest the expansion of Medicaid under the Patient Protection and Affordable Care Act in 2010 may be leading to more frequent diagnosis of colorectal cancer (CRC) among Hispanics.
The studies, presented at the 2022 Gastrointestinal Cancers Symposium, suggest that Medicaid expansion may have a diverse impact on various ethnic groups.
“The take-home message for both physicians and policy makers is that health policy has the capacity to shift health care delivery, yet we need to consider the effects of health policy might influence subgroups of patients differently. This is useful information for providers caring for a diverse group of patients. For policy makers, this study emphasizes the importance of evaluating the impact of health policy among different racial and ethnic subgroups to fully understand the impact of [policy] change,” said study lead author James D. Murphy, MD, MS, assistant vice chair of radiation medicine at the University of California San Diego.
Dr. Murphy and associates cautioned that other factors, not just Medicaid expansion, could be responsible for the uptick in colon cancer diagnoses.
“Our observations could potentially be influenced by other risk factors. Medicaid expansion was not a ‘randomized experiment,’ and states which opted to expand Medicaid might have fundamental differences which could impact colorectal cancer incidence,” he said.
His group’s analysis of the Surveillance, Epidemiology, and End Results database included 21 states where Medicaid was expanded and 16 states where expansion did not occur. Between 2010-2013 and 2014-2018, among patients under 65, overall colorectal cancer incidence rates did not differ by Medicaid expansion status. In nonexpansion states, there was a greater increase in CRC rates among Hispanics (5.4 vs. 1.6 increase per 100,000; P = .002) and Asian/Pacific Islanders (4.3 vs. 0.4 per 100,000; P = .02), but there was no difference among Black or non-Hispanic White individuals.
Early-onset colorectal cancer diagnoses increase under Medicaid expansion
In another study presented at the meeting, researchers examined early-onset CRC data from the National Cancer Database. Among Hispanics, the rate of change of incidence of newly diagnosed cases among patients age 40-49 in Medicaid expansion states increased from 4.3% per year between 2010 and 2014 and 9.8% between 2014 and 2017. That compares with the general background increase in incidence of about 2%. In nonexpansion states, the rate of change decreased from 6.4% to 1% (P = .03). There were no statistically significant differences in the change of incidence among Blacks or Whites between expansion and nonexpansion states.
The reduced rate of change among Hispanics in nonexpansion states was a surprise, and the researchers haven’t determined the reason, according to Sanjay Goel, MD, an oncologist with Montefiore Medical Center, New York, and lead author on the National Cancer Database study. Dr. Goel speculated that some people may have migrated from nonexpansion states to states that expanded Medicaid in order to gain health care coverage.
The apparent benefit seen in Hispanics, but not Black patients, may be caused by greater susceptibility to early-onset CRC among Hispanics, leading to a stronger effect on that population when Medicaid was expanded, Dr. Goel said.
“At this point, with our available data, we do not have the ability to understand the underlying sources of these disparities, though these are questions which deserve additional research,” Dr. Murphy said.
Regardless of the reason, the message is clear, Dr. Goel said. “The bottom we want to state is that politics aside, providing health care coverage to as many people as possible, ideally to everyone, is the right way of going forward.”
The implications of the findings extend beyond policy. “The general advice I give is that, especially if you treat a Hispanic person, regardless of age, with any symptom or sign that could be suggestive of a malignancy, do not take it lightly. Follow the patient closely. I’m not advocating that you refer everybody with lower abdominal pain or bleeding for a colonoscopy, but do factor it in mind. Call them back in a week or 2, or have them make a follow-up appointment in a month so that they don’t get neglected by the system.”
Dr. Murphy and Dr. Goel have no relevant financial disclosures. The Gastrointestinal Cancers Symposium is sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
Two new studies suggest the expansion of Medicaid under the Patient Protection and Affordable Care Act in 2010 may be leading to more frequent diagnosis of colorectal cancer (CRC) among Hispanics.
The studies, presented at the 2022 Gastrointestinal Cancers Symposium, suggest that Medicaid expansion may have a diverse impact on various ethnic groups.
“The take-home message for both physicians and policy makers is that health policy has the capacity to shift health care delivery, yet we need to consider the effects of health policy might influence subgroups of patients differently. This is useful information for providers caring for a diverse group of patients. For policy makers, this study emphasizes the importance of evaluating the impact of health policy among different racial and ethnic subgroups to fully understand the impact of [policy] change,” said study lead author James D. Murphy, MD, MS, assistant vice chair of radiation medicine at the University of California San Diego.
Dr. Murphy and associates cautioned that other factors, not just Medicaid expansion, could be responsible for the uptick in colon cancer diagnoses.
“Our observations could potentially be influenced by other risk factors. Medicaid expansion was not a ‘randomized experiment,’ and states which opted to expand Medicaid might have fundamental differences which could impact colorectal cancer incidence,” he said.
His group’s analysis of the Surveillance, Epidemiology, and End Results database included 21 states where Medicaid was expanded and 16 states where expansion did not occur. Between 2010-2013 and 2014-2018, among patients under 65, overall colorectal cancer incidence rates did not differ by Medicaid expansion status. In nonexpansion states, there was a greater increase in CRC rates among Hispanics (5.4 vs. 1.6 increase per 100,000; P = .002) and Asian/Pacific Islanders (4.3 vs. 0.4 per 100,000; P = .02), but there was no difference among Black or non-Hispanic White individuals.
Early-onset colorectal cancer diagnoses increase under Medicaid expansion
In another study presented at the meeting, researchers examined early-onset CRC data from the National Cancer Database. Among Hispanics, the rate of change of incidence of newly diagnosed cases among patients age 40-49 in Medicaid expansion states increased from 4.3% per year between 2010 and 2014 and 9.8% between 2014 and 2017. That compares with the general background increase in incidence of about 2%. In nonexpansion states, the rate of change decreased from 6.4% to 1% (P = .03). There were no statistically significant differences in the change of incidence among Blacks or Whites between expansion and nonexpansion states.
The reduced rate of change among Hispanics in nonexpansion states was a surprise, and the researchers haven’t determined the reason, according to Sanjay Goel, MD, an oncologist with Montefiore Medical Center, New York, and lead author on the National Cancer Database study. Dr. Goel speculated that some people may have migrated from nonexpansion states to states that expanded Medicaid in order to gain health care coverage.
The apparent benefit seen in Hispanics, but not Black patients, may be caused by greater susceptibility to early-onset CRC among Hispanics, leading to a stronger effect on that population when Medicaid was expanded, Dr. Goel said.
“At this point, with our available data, we do not have the ability to understand the underlying sources of these disparities, though these are questions which deserve additional research,” Dr. Murphy said.
Regardless of the reason, the message is clear, Dr. Goel said. “The bottom we want to state is that politics aside, providing health care coverage to as many people as possible, ideally to everyone, is the right way of going forward.”
The implications of the findings extend beyond policy. “The general advice I give is that, especially if you treat a Hispanic person, regardless of age, with any symptom or sign that could be suggestive of a malignancy, do not take it lightly. Follow the patient closely. I’m not advocating that you refer everybody with lower abdominal pain or bleeding for a colonoscopy, but do factor it in mind. Call them back in a week or 2, or have them make a follow-up appointment in a month so that they don’t get neglected by the system.”
Dr. Murphy and Dr. Goel have no relevant financial disclosures. The Gastrointestinal Cancers Symposium is sponsored by the American Gastroenterological Association, the American Society for Clinical Oncology, the American Society for Radiation Oncology, and the Society of Surgical Oncology.
FROM THE GI CANCERS SYMPOSIUM 2022
Restless legs syndrome surged early during pandemic
according to data from 500 participants in the National Restless Legs Syndrome Opioid Registry.
Sufferers of restless legs syndrome (RLS) experience not only sleep disturbance, but also daytime sleepiness, and high levels of depression, anxiety, and panic, wrote Benjamin Wipper of Harvard Medical School, Boston, and colleagues.
“Considering the link between RLS and psychiatric illness, it has been speculated that there may have been increases in RLS symptom severity alongside the recent rise in depression and anxiety,” but this association has not been explored, they said.
In a study published in Sleep Medicine , the researchers reviewed data from 500 adult participants in the National RLS Opioid Registry, a longitudinal observational study. Participants reported RLS symptom severity before and during the COVID-19 pandemic at 6-month intervals. Survey responses were collected from the early phase of the pandemic in the United States in January/February 2020, then in April/May 2020, and then 6 months later, from September 2020 through February 2021, and also 1 year later, in March 2021 through June 2021.
Participants completed a baseline phone interview and online survey, with symptoms assessed via the International Restless Legs Syndrome Study Group severity scale (IRLS), the Insomnia Severity Index (ISI), the General Anxiety Disorder-7 scale (GAD-7), and the Patient Health Questionnaire (PHQ-9).
In all, 153 participants completed surveys during January and February 2020, and 155 completed surveys during April and May 2020. Baseline characteristics were similar for all participants.
In a between-subjects analysis for these time periods, symptom scores on the IRLS were significantly higher in January/February 2020; participants were approximately twice as likely to have IRLS scores of 20 or higher compared to April/May 2020 (37.7% vs. 20.9%).
The researchers also compared responses by the same participants at baseline and 6 months later, from September 2020 through February 2021, and 1 year later, from March 2021 through June 2021. In this within-subjects analysis, 51.3% of the participants had increased IRLS scores in spring 2020. Participants were significantly more likely to have IRLS scores of 20 or above in the early COVID-19 period in April and May 2020 compared with baseline (37.7% vs. 26.6%). Both PHQ-9 and GAD-7 scores were higher during early COVID-19 in April and May 2020 than at baseline.
“Changes in IRLS were also significantly correlated with changes in both PHQ-9 and GAD-7 scores, providing further support for the associations of RLS to both depression and anxiety,” the researchers wrote. “Notably, individuals who completed surveys in January and February 2020 did not see increases in RLS severity or other mental health questionnaire values on subsequent six-month surveys completed during the pandemic or on the following iteration of surveys 1 year later. We suspect that these findings may be at least partially related to the timing of the surveys,” the researchers said. Six-month survey data for most patients were collected during a decline in cases and hospitalizations, and 1-year data in early 2021 may have reflected optimism with the availability of vaccines, they said.
The study findings were limited by several factors including the observational design, which prevented conclusions about causality, and the lack of data on the effect of COVID-19 infection on RLS symptoms, which should be investigated in future studies, the researchers said.
However, the results are the first evidence of increased RLS symptom severity during the COVID-19 pandemic, and elevated scores were associated with sleep disturbance, depression, and anxiety, they wrote. “These data suggest that clinicians should attend to RLS symptoms during the current pandemic and in future instances of socioeconomic and/or political uncertainty. Future studies need to confirm these findings in other populations of patients with RLS,” they concluded.
The National RLS Opioid Registry has received research funding from the RLS Foundation, the Baszucki Brain Research Fund, Florence Petrlik Family Foundation, Diane and Richard Brainerd, Steven Silin, and Jerry Blakeley. The researchers had no financial conflicts to disclose.
according to data from 500 participants in the National Restless Legs Syndrome Opioid Registry.
Sufferers of restless legs syndrome (RLS) experience not only sleep disturbance, but also daytime sleepiness, and high levels of depression, anxiety, and panic, wrote Benjamin Wipper of Harvard Medical School, Boston, and colleagues.
“Considering the link between RLS and psychiatric illness, it has been speculated that there may have been increases in RLS symptom severity alongside the recent rise in depression and anxiety,” but this association has not been explored, they said.
In a study published in Sleep Medicine , the researchers reviewed data from 500 adult participants in the National RLS Opioid Registry, a longitudinal observational study. Participants reported RLS symptom severity before and during the COVID-19 pandemic at 6-month intervals. Survey responses were collected from the early phase of the pandemic in the United States in January/February 2020, then in April/May 2020, and then 6 months later, from September 2020 through February 2021, and also 1 year later, in March 2021 through June 2021.
Participants completed a baseline phone interview and online survey, with symptoms assessed via the International Restless Legs Syndrome Study Group severity scale (IRLS), the Insomnia Severity Index (ISI), the General Anxiety Disorder-7 scale (GAD-7), and the Patient Health Questionnaire (PHQ-9).
In all, 153 participants completed surveys during January and February 2020, and 155 completed surveys during April and May 2020. Baseline characteristics were similar for all participants.
In a between-subjects analysis for these time periods, symptom scores on the IRLS were significantly higher in January/February 2020; participants were approximately twice as likely to have IRLS scores of 20 or higher compared to April/May 2020 (37.7% vs. 20.9%).
The researchers also compared responses by the same participants at baseline and 6 months later, from September 2020 through February 2021, and 1 year later, from March 2021 through June 2021. In this within-subjects analysis, 51.3% of the participants had increased IRLS scores in spring 2020. Participants were significantly more likely to have IRLS scores of 20 or above in the early COVID-19 period in April and May 2020 compared with baseline (37.7% vs. 26.6%). Both PHQ-9 and GAD-7 scores were higher during early COVID-19 in April and May 2020 than at baseline.
“Changes in IRLS were also significantly correlated with changes in both PHQ-9 and GAD-7 scores, providing further support for the associations of RLS to both depression and anxiety,” the researchers wrote. “Notably, individuals who completed surveys in January and February 2020 did not see increases in RLS severity or other mental health questionnaire values on subsequent six-month surveys completed during the pandemic or on the following iteration of surveys 1 year later. We suspect that these findings may be at least partially related to the timing of the surveys,” the researchers said. Six-month survey data for most patients were collected during a decline in cases and hospitalizations, and 1-year data in early 2021 may have reflected optimism with the availability of vaccines, they said.
The study findings were limited by several factors including the observational design, which prevented conclusions about causality, and the lack of data on the effect of COVID-19 infection on RLS symptoms, which should be investigated in future studies, the researchers said.
However, the results are the first evidence of increased RLS symptom severity during the COVID-19 pandemic, and elevated scores were associated with sleep disturbance, depression, and anxiety, they wrote. “These data suggest that clinicians should attend to RLS symptoms during the current pandemic and in future instances of socioeconomic and/or political uncertainty. Future studies need to confirm these findings in other populations of patients with RLS,” they concluded.
The National RLS Opioid Registry has received research funding from the RLS Foundation, the Baszucki Brain Research Fund, Florence Petrlik Family Foundation, Diane and Richard Brainerd, Steven Silin, and Jerry Blakeley. The researchers had no financial conflicts to disclose.
according to data from 500 participants in the National Restless Legs Syndrome Opioid Registry.
Sufferers of restless legs syndrome (RLS) experience not only sleep disturbance, but also daytime sleepiness, and high levels of depression, anxiety, and panic, wrote Benjamin Wipper of Harvard Medical School, Boston, and colleagues.
“Considering the link between RLS and psychiatric illness, it has been speculated that there may have been increases in RLS symptom severity alongside the recent rise in depression and anxiety,” but this association has not been explored, they said.
In a study published in Sleep Medicine , the researchers reviewed data from 500 adult participants in the National RLS Opioid Registry, a longitudinal observational study. Participants reported RLS symptom severity before and during the COVID-19 pandemic at 6-month intervals. Survey responses were collected from the early phase of the pandemic in the United States in January/February 2020, then in April/May 2020, and then 6 months later, from September 2020 through February 2021, and also 1 year later, in March 2021 through June 2021.
Participants completed a baseline phone interview and online survey, with symptoms assessed via the International Restless Legs Syndrome Study Group severity scale (IRLS), the Insomnia Severity Index (ISI), the General Anxiety Disorder-7 scale (GAD-7), and the Patient Health Questionnaire (PHQ-9).
In all, 153 participants completed surveys during January and February 2020, and 155 completed surveys during April and May 2020. Baseline characteristics were similar for all participants.
In a between-subjects analysis for these time periods, symptom scores on the IRLS were significantly higher in January/February 2020; participants were approximately twice as likely to have IRLS scores of 20 or higher compared to April/May 2020 (37.7% vs. 20.9%).
The researchers also compared responses by the same participants at baseline and 6 months later, from September 2020 through February 2021, and 1 year later, from March 2021 through June 2021. In this within-subjects analysis, 51.3% of the participants had increased IRLS scores in spring 2020. Participants were significantly more likely to have IRLS scores of 20 or above in the early COVID-19 period in April and May 2020 compared with baseline (37.7% vs. 26.6%). Both PHQ-9 and GAD-7 scores were higher during early COVID-19 in April and May 2020 than at baseline.
“Changes in IRLS were also significantly correlated with changes in both PHQ-9 and GAD-7 scores, providing further support for the associations of RLS to both depression and anxiety,” the researchers wrote. “Notably, individuals who completed surveys in January and February 2020 did not see increases in RLS severity or other mental health questionnaire values on subsequent six-month surveys completed during the pandemic or on the following iteration of surveys 1 year later. We suspect that these findings may be at least partially related to the timing of the surveys,” the researchers said. Six-month survey data for most patients were collected during a decline in cases and hospitalizations, and 1-year data in early 2021 may have reflected optimism with the availability of vaccines, they said.
The study findings were limited by several factors including the observational design, which prevented conclusions about causality, and the lack of data on the effect of COVID-19 infection on RLS symptoms, which should be investigated in future studies, the researchers said.
However, the results are the first evidence of increased RLS symptom severity during the COVID-19 pandemic, and elevated scores were associated with sleep disturbance, depression, and anxiety, they wrote. “These data suggest that clinicians should attend to RLS symptoms during the current pandemic and in future instances of socioeconomic and/or political uncertainty. Future studies need to confirm these findings in other populations of patients with RLS,” they concluded.
The National RLS Opioid Registry has received research funding from the RLS Foundation, the Baszucki Brain Research Fund, Florence Petrlik Family Foundation, Diane and Richard Brainerd, Steven Silin, and Jerry Blakeley. The researchers had no financial conflicts to disclose.
FROM SLEEP MEDICINE
Shorter courses of chemo treatment taking hold in colon cancer
In the wake of the pivotal IDEA TRIAL, oncologists have shifted towards shorter adjuvant chemotherapy regimens for stage III colon cancer and a greater reliance on CAPOX (capecitabine plus oxaliplatin) instead of FOLFOX (oxaliplatin, 5-fluorouracil, and leucovorin), according to a review of 366 patients.
The international IDEA trial showed that, across almost 13,000 subjects, 3 months of treatment with either regimen was not inferior to 6 months, which was standard at the time for low-risk disease and often led to significantly less grade 2, but more neuropathy.
In high-risk patients (T4, N2), 3-year disease-free survival was almost identical between 3 months of CAPOX (64.1%) and 6 months (64.0%), but 3 months of FOLFOX was inferior to 6 months of FOLFOX (61.5% vs. 64.7%).
Oncologists paid attention, according to the new review, which was presented at the 2022 Gastrointestinal Cancers Symposium.
Overall, 16.3% of patients were prescribed CAPOX in June 2016, but before the study was published in the New England Journal of Medicine, the number rose to 66.8% by June 2020.
“We are using a lot more CAPOX in this country now, and it’s interesting we are doing that because the data aren’t quite there” yet for patients in the United States, said lead investigator Daniel Walden, MD, a hematology/oncology fellow at Mayo Clinic Arizona, Phoenix.
IDEA pulled data from six trials, but only one included U.S. patients and it did not permit CAPOX, only FOLFOX. As a result, the growing use of CAPOX in the United States is based on outcomes elsewhere, primarily Europe and Japan.
The problem, Dr. Walden said, is that U.S. patients don’t tolerate capecitabine as well as people in other countries because of the high intake of dietary folic acid, which is added to grains in the United States and interferes with capecitabine clearance.
He and his team are now looking into outcomes, particularly with CAPOX, in their U.S. cohort, which was pulled from Mayo Clinic campuses in Arizona, Minnesota, and Florida, with additional subjects from Emory and Vanderbilt Universities. “Hopefully,” data to support the shift to adjuvant CAPOX in the United States “will be here soon. I feel more confident prescribing 3 months of CAPOX for high-risk patients, seeing that more people do it than I would have thought,” Dr. Walden said. His study found a 25.9% adoption in June 2020, which was up from 1.3% in June 2016.
Among other findings, 78.3% of patients received 6 months of FOLFOX in June 2016, which fell to 17.3% 4 years later. There was a corresponding shift in 3-month courses of CAPOX, up from 7.4% to 67.5% over the same period.
By June 2020, low-risk patients were far more likely to receive 3 months of CAPOX (67.9%) than any other regimen.
Among high-risk patients, the number who received 6 months of FOLFOX fell from 86.6% to 47.8%, while the number who received 3 months of FOLFOX increased from 0.9% to 3.9%. Use of CAPOX for 6 months in high-risk patients climbed from 11.2% of patients to 22.4%.
There was no funding for the work, and Dr. Walden didn’t have any disclosures.
In the wake of the pivotal IDEA TRIAL, oncologists have shifted towards shorter adjuvant chemotherapy regimens for stage III colon cancer and a greater reliance on CAPOX (capecitabine plus oxaliplatin) instead of FOLFOX (oxaliplatin, 5-fluorouracil, and leucovorin), according to a review of 366 patients.
The international IDEA trial showed that, across almost 13,000 subjects, 3 months of treatment with either regimen was not inferior to 6 months, which was standard at the time for low-risk disease and often led to significantly less grade 2, but more neuropathy.
In high-risk patients (T4, N2), 3-year disease-free survival was almost identical between 3 months of CAPOX (64.1%) and 6 months (64.0%), but 3 months of FOLFOX was inferior to 6 months of FOLFOX (61.5% vs. 64.7%).
Oncologists paid attention, according to the new review, which was presented at the 2022 Gastrointestinal Cancers Symposium.
Overall, 16.3% of patients were prescribed CAPOX in June 2016, but before the study was published in the New England Journal of Medicine, the number rose to 66.8% by June 2020.
“We are using a lot more CAPOX in this country now, and it’s interesting we are doing that because the data aren’t quite there” yet for patients in the United States, said lead investigator Daniel Walden, MD, a hematology/oncology fellow at Mayo Clinic Arizona, Phoenix.
IDEA pulled data from six trials, but only one included U.S. patients and it did not permit CAPOX, only FOLFOX. As a result, the growing use of CAPOX in the United States is based on outcomes elsewhere, primarily Europe and Japan.
The problem, Dr. Walden said, is that U.S. patients don’t tolerate capecitabine as well as people in other countries because of the high intake of dietary folic acid, which is added to grains in the United States and interferes with capecitabine clearance.
He and his team are now looking into outcomes, particularly with CAPOX, in their U.S. cohort, which was pulled from Mayo Clinic campuses in Arizona, Minnesota, and Florida, with additional subjects from Emory and Vanderbilt Universities. “Hopefully,” data to support the shift to adjuvant CAPOX in the United States “will be here soon. I feel more confident prescribing 3 months of CAPOX for high-risk patients, seeing that more people do it than I would have thought,” Dr. Walden said. His study found a 25.9% adoption in June 2020, which was up from 1.3% in June 2016.
Among other findings, 78.3% of patients received 6 months of FOLFOX in June 2016, which fell to 17.3% 4 years later. There was a corresponding shift in 3-month courses of CAPOX, up from 7.4% to 67.5% over the same period.
By June 2020, low-risk patients were far more likely to receive 3 months of CAPOX (67.9%) than any other regimen.
Among high-risk patients, the number who received 6 months of FOLFOX fell from 86.6% to 47.8%, while the number who received 3 months of FOLFOX increased from 0.9% to 3.9%. Use of CAPOX for 6 months in high-risk patients climbed from 11.2% of patients to 22.4%.
There was no funding for the work, and Dr. Walden didn’t have any disclosures.
In the wake of the pivotal IDEA TRIAL, oncologists have shifted towards shorter adjuvant chemotherapy regimens for stage III colon cancer and a greater reliance on CAPOX (capecitabine plus oxaliplatin) instead of FOLFOX (oxaliplatin, 5-fluorouracil, and leucovorin), according to a review of 366 patients.
The international IDEA trial showed that, across almost 13,000 subjects, 3 months of treatment with either regimen was not inferior to 6 months, which was standard at the time for low-risk disease and often led to significantly less grade 2, but more neuropathy.
In high-risk patients (T4, N2), 3-year disease-free survival was almost identical between 3 months of CAPOX (64.1%) and 6 months (64.0%), but 3 months of FOLFOX was inferior to 6 months of FOLFOX (61.5% vs. 64.7%).
Oncologists paid attention, according to the new review, which was presented at the 2022 Gastrointestinal Cancers Symposium.
Overall, 16.3% of patients were prescribed CAPOX in June 2016, but before the study was published in the New England Journal of Medicine, the number rose to 66.8% by June 2020.
“We are using a lot more CAPOX in this country now, and it’s interesting we are doing that because the data aren’t quite there” yet for patients in the United States, said lead investigator Daniel Walden, MD, a hematology/oncology fellow at Mayo Clinic Arizona, Phoenix.
IDEA pulled data from six trials, but only one included U.S. patients and it did not permit CAPOX, only FOLFOX. As a result, the growing use of CAPOX in the United States is based on outcomes elsewhere, primarily Europe and Japan.
The problem, Dr. Walden said, is that U.S. patients don’t tolerate capecitabine as well as people in other countries because of the high intake of dietary folic acid, which is added to grains in the United States and interferes with capecitabine clearance.
He and his team are now looking into outcomes, particularly with CAPOX, in their U.S. cohort, which was pulled from Mayo Clinic campuses in Arizona, Minnesota, and Florida, with additional subjects from Emory and Vanderbilt Universities. “Hopefully,” data to support the shift to adjuvant CAPOX in the United States “will be here soon. I feel more confident prescribing 3 months of CAPOX for high-risk patients, seeing that more people do it than I would have thought,” Dr. Walden said. His study found a 25.9% adoption in June 2020, which was up from 1.3% in June 2016.
Among other findings, 78.3% of patients received 6 months of FOLFOX in June 2016, which fell to 17.3% 4 years later. There was a corresponding shift in 3-month courses of CAPOX, up from 7.4% to 67.5% over the same period.
By June 2020, low-risk patients were far more likely to receive 3 months of CAPOX (67.9%) than any other regimen.
Among high-risk patients, the number who received 6 months of FOLFOX fell from 86.6% to 47.8%, while the number who received 3 months of FOLFOX increased from 0.9% to 3.9%. Use of CAPOX for 6 months in high-risk patients climbed from 11.2% of patients to 22.4%.
There was no funding for the work, and Dr. Walden didn’t have any disclosures.
FROM THE ASCO GI CANCERS SYMPOSIUM 2022
Proposed insurance policy ignites debate over transgender health care
A new proposed insurance rule to limit discrimination in health plans has ignited a debate over transgender health care.
The policy, known as the Notice of Benefit and Payment Parameters, is part of the Biden administration’s proposal for 2023 for government health insurance exchanges. The rule would require health plans to ensure their benefit designs and implementation don’t discriminate based on sexual orientation, gender identity, age, sociodemographic factors, or other conditions.
The Obama administration first implemented the standard, but the Trump administration removed “sexual orientation” and “gender identity” from the antidiscrimination language in 2020. The Biden proposal would restore protections for those categories.
“We believe such amendments are warranted in light of the existing trends in health care discrimination and are necessary to better address barriers to health equity for LGBTQI+ individuals,” the Department of Health and Human Services wrote in the proposed rule.
The Biden administration, Democratic lawmakers, and advocacy groups have noted that the rule is vital for LGBTQ consumers to access care. But some private insurance companies have said the policy could drive up costs and that the language about what constitutes discrimination is too vague. Conservative groups have also argued that no clinical evidence supports covering care that affirms gender identity, such as hormone blockers or surgery.
Under the proposed rule, an insurer in the government health exchanges wouldn’t be classified as providing “essential health benefits” under federal law if discrimination was found, Roll Call reported. State regulators would be required to enforce the proposal.
The Department of Health and Human Services and the Centers for Medicare and Medicaid Services listed examples of presumptive discrimination that would be banned, such as limiting gender-affirmative care within a health plan. Several state health plains either don’t address coverage or limit coverage for specific services for transgender people, Roll Call reported.
Health benefit plans wouldn’t have to cover every possible health care service, Katie Keith, a researcher at Georgetown University’s Center on Health Insurance Reforms, wrote in an article for Health Affairs. However, an insurer can’t have a different policy or restricted plans for transgender people over patients whose gender identity and sexual orientation match their birth gender.
The proposed rule has sparked a flurry of reactions in recent weeks. America’s Health Insurance Plans, a trade association for health insurance companies, said the nondiscrimination framework is overly broad and limits insurers’ abilities to design plans with controlled costs.
The rule “could create a slippery slope of eliminating benefit limits that are based on clinical evidence, support value-based care, and ensure affordable premiums,” the group wrote in a response letter.
Some conservative groups have pushed back against the coverage requirements as well. The Family Research Council and the Heritage Foundation have questioned the benefits or validity of gender-affirmative care, according to Roll Call.
On the other hand, the HIV+ Hepatitis Policy Initiative said the new rule could help patients who have long faced coverage issues. For instance, some insurers put HIV drugs on the highest-cost plan tiers, which can lead to major expenses for patients.
“It’s not just HIV. It’s other [chronic disease] patients, too,” Carl Schmid, executive director of the patient advocacy group, told Roll Call.
Other insurers, such as the Alliance of Community Health Plans, have said that the updated rule doesn’t give insurers enough time to implement changes. Under the proposal, insurers would have 60 days from final publication to ensure that plans meet the nondiscrimination framework. The group has suggested an effective date of 2024 or later, rather than 2023.
At the same time, some insurance groups have said they’re ready for the change now. The Association for Community Affiliated Plans, which represents small nonprofit plans, said many of its member health plans have already committed resources to ensure all patients can access services, including gender-affirming services or gender identity support for LGBTQ patients.
“We find that their forward-thinking work is – and should be – increasingly the norm,” Margaret Murray, the association’s CEO, wrote in a response letter.
Comments on the proposed rule were due Jan. 27. Now the proposal will wind through the annual approval process.
A version of this article first appeared on WebMD.com.
A new proposed insurance rule to limit discrimination in health plans has ignited a debate over transgender health care.
The policy, known as the Notice of Benefit and Payment Parameters, is part of the Biden administration’s proposal for 2023 for government health insurance exchanges. The rule would require health plans to ensure their benefit designs and implementation don’t discriminate based on sexual orientation, gender identity, age, sociodemographic factors, or other conditions.
The Obama administration first implemented the standard, but the Trump administration removed “sexual orientation” and “gender identity” from the antidiscrimination language in 2020. The Biden proposal would restore protections for those categories.
“We believe such amendments are warranted in light of the existing trends in health care discrimination and are necessary to better address barriers to health equity for LGBTQI+ individuals,” the Department of Health and Human Services wrote in the proposed rule.
The Biden administration, Democratic lawmakers, and advocacy groups have noted that the rule is vital for LGBTQ consumers to access care. But some private insurance companies have said the policy could drive up costs and that the language about what constitutes discrimination is too vague. Conservative groups have also argued that no clinical evidence supports covering care that affirms gender identity, such as hormone blockers or surgery.
Under the proposed rule, an insurer in the government health exchanges wouldn’t be classified as providing “essential health benefits” under federal law if discrimination was found, Roll Call reported. State regulators would be required to enforce the proposal.
The Department of Health and Human Services and the Centers for Medicare and Medicaid Services listed examples of presumptive discrimination that would be banned, such as limiting gender-affirmative care within a health plan. Several state health plains either don’t address coverage or limit coverage for specific services for transgender people, Roll Call reported.
Health benefit plans wouldn’t have to cover every possible health care service, Katie Keith, a researcher at Georgetown University’s Center on Health Insurance Reforms, wrote in an article for Health Affairs. However, an insurer can’t have a different policy or restricted plans for transgender people over patients whose gender identity and sexual orientation match their birth gender.
The proposed rule has sparked a flurry of reactions in recent weeks. America’s Health Insurance Plans, a trade association for health insurance companies, said the nondiscrimination framework is overly broad and limits insurers’ abilities to design plans with controlled costs.
The rule “could create a slippery slope of eliminating benefit limits that are based on clinical evidence, support value-based care, and ensure affordable premiums,” the group wrote in a response letter.
Some conservative groups have pushed back against the coverage requirements as well. The Family Research Council and the Heritage Foundation have questioned the benefits or validity of gender-affirmative care, according to Roll Call.
On the other hand, the HIV+ Hepatitis Policy Initiative said the new rule could help patients who have long faced coverage issues. For instance, some insurers put HIV drugs on the highest-cost plan tiers, which can lead to major expenses for patients.
“It’s not just HIV. It’s other [chronic disease] patients, too,” Carl Schmid, executive director of the patient advocacy group, told Roll Call.
Other insurers, such as the Alliance of Community Health Plans, have said that the updated rule doesn’t give insurers enough time to implement changes. Under the proposal, insurers would have 60 days from final publication to ensure that plans meet the nondiscrimination framework. The group has suggested an effective date of 2024 or later, rather than 2023.
At the same time, some insurance groups have said they’re ready for the change now. The Association for Community Affiliated Plans, which represents small nonprofit plans, said many of its member health plans have already committed resources to ensure all patients can access services, including gender-affirming services or gender identity support for LGBTQ patients.
“We find that their forward-thinking work is – and should be – increasingly the norm,” Margaret Murray, the association’s CEO, wrote in a response letter.
Comments on the proposed rule were due Jan. 27. Now the proposal will wind through the annual approval process.
A version of this article first appeared on WebMD.com.
A new proposed insurance rule to limit discrimination in health plans has ignited a debate over transgender health care.
The policy, known as the Notice of Benefit and Payment Parameters, is part of the Biden administration’s proposal for 2023 for government health insurance exchanges. The rule would require health plans to ensure their benefit designs and implementation don’t discriminate based on sexual orientation, gender identity, age, sociodemographic factors, or other conditions.
The Obama administration first implemented the standard, but the Trump administration removed “sexual orientation” and “gender identity” from the antidiscrimination language in 2020. The Biden proposal would restore protections for those categories.
“We believe such amendments are warranted in light of the existing trends in health care discrimination and are necessary to better address barriers to health equity for LGBTQI+ individuals,” the Department of Health and Human Services wrote in the proposed rule.
The Biden administration, Democratic lawmakers, and advocacy groups have noted that the rule is vital for LGBTQ consumers to access care. But some private insurance companies have said the policy could drive up costs and that the language about what constitutes discrimination is too vague. Conservative groups have also argued that no clinical evidence supports covering care that affirms gender identity, such as hormone blockers or surgery.
Under the proposed rule, an insurer in the government health exchanges wouldn’t be classified as providing “essential health benefits” under federal law if discrimination was found, Roll Call reported. State regulators would be required to enforce the proposal.
The Department of Health and Human Services and the Centers for Medicare and Medicaid Services listed examples of presumptive discrimination that would be banned, such as limiting gender-affirmative care within a health plan. Several state health plains either don’t address coverage or limit coverage for specific services for transgender people, Roll Call reported.
Health benefit plans wouldn’t have to cover every possible health care service, Katie Keith, a researcher at Georgetown University’s Center on Health Insurance Reforms, wrote in an article for Health Affairs. However, an insurer can’t have a different policy or restricted plans for transgender people over patients whose gender identity and sexual orientation match their birth gender.
The proposed rule has sparked a flurry of reactions in recent weeks. America’s Health Insurance Plans, a trade association for health insurance companies, said the nondiscrimination framework is overly broad and limits insurers’ abilities to design plans with controlled costs.
The rule “could create a slippery slope of eliminating benefit limits that are based on clinical evidence, support value-based care, and ensure affordable premiums,” the group wrote in a response letter.
Some conservative groups have pushed back against the coverage requirements as well. The Family Research Council and the Heritage Foundation have questioned the benefits or validity of gender-affirmative care, according to Roll Call.
On the other hand, the HIV+ Hepatitis Policy Initiative said the new rule could help patients who have long faced coverage issues. For instance, some insurers put HIV drugs on the highest-cost plan tiers, which can lead to major expenses for patients.
“It’s not just HIV. It’s other [chronic disease] patients, too,” Carl Schmid, executive director of the patient advocacy group, told Roll Call.
Other insurers, such as the Alliance of Community Health Plans, have said that the updated rule doesn’t give insurers enough time to implement changes. Under the proposal, insurers would have 60 days from final publication to ensure that plans meet the nondiscrimination framework. The group has suggested an effective date of 2024 or later, rather than 2023.
At the same time, some insurance groups have said they’re ready for the change now. The Association for Community Affiliated Plans, which represents small nonprofit plans, said many of its member health plans have already committed resources to ensure all patients can access services, including gender-affirming services or gender identity support for LGBTQ patients.
“We find that their forward-thinking work is – and should be – increasingly the norm,” Margaret Murray, the association’s CEO, wrote in a response letter.
Comments on the proposed rule were due Jan. 27. Now the proposal will wind through the annual approval process.
A version of this article first appeared on WebMD.com.