User login
Commentary: Babies die as congenital syphilis continues a decade-long surge across the U.S.
The data are shocking: Almost 35,000 U.S. syphilis cases by mid-July 2022 with the highest rates per/100,000 population in Nevada (n = 21), California (n = 19), and Mississippi (n = 16). Excluding Nevada, California, and Oklahoma, rates over 12/100,000 were concentrated in the southernmost U.S. states. Overall, the 2,268 congenital syphilis cases in U.S. children born in 2021 was a 6% increase over 2020, and a 680% increase over 2012. (Note: All 2021 data are not yet available because of public health STI resources being diverted to COVID-19 control.) A telling number is the 166 congenital syphilis deaths in babies born in 2021 – a 1,000% increase over 2012. Another concern is that 50% of U.S. counties reported at least one congenital syphilis case in 2019 – the last time frame from which county-specific data are available.
Syphilis afflicts the underserved and underprivileged more than other demographic groups, particularly when public health budgets are not adequate (funding for public health STI prevention/treatment efforts has lagged for more than a decade), and/or when public health emergencies such as the pandemic divert public health resources away from STI prevention/treatment efforts.
As pediatric care providers, we can help by heightening our vigilance and appropriately testing for and treating syphilis, particularly in newborns/infants, regardless of where we work. And we can advocate for increased public health STI funding allocation whenever possible. It is a smart economic move because it costs nearly 1,000 times more to manage congenital syphilis and its sequelae than to prevent or treat it.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
The data are shocking: Almost 35,000 U.S. syphilis cases by mid-July 2022 with the highest rates per/100,000 population in Nevada (n = 21), California (n = 19), and Mississippi (n = 16). Excluding Nevada, California, and Oklahoma, rates over 12/100,000 were concentrated in the southernmost U.S. states. Overall, the 2,268 congenital syphilis cases in U.S. children born in 2021 was a 6% increase over 2020, and a 680% increase over 2012. (Note: All 2021 data are not yet available because of public health STI resources being diverted to COVID-19 control.) A telling number is the 166 congenital syphilis deaths in babies born in 2021 – a 1,000% increase over 2012. Another concern is that 50% of U.S. counties reported at least one congenital syphilis case in 2019 – the last time frame from which county-specific data are available.
Syphilis afflicts the underserved and underprivileged more than other demographic groups, particularly when public health budgets are not adequate (funding for public health STI prevention/treatment efforts has lagged for more than a decade), and/or when public health emergencies such as the pandemic divert public health resources away from STI prevention/treatment efforts.
As pediatric care providers, we can help by heightening our vigilance and appropriately testing for and treating syphilis, particularly in newborns/infants, regardless of where we work. And we can advocate for increased public health STI funding allocation whenever possible. It is a smart economic move because it costs nearly 1,000 times more to manage congenital syphilis and its sequelae than to prevent or treat it.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
The data are shocking: Almost 35,000 U.S. syphilis cases by mid-July 2022 with the highest rates per/100,000 population in Nevada (n = 21), California (n = 19), and Mississippi (n = 16). Excluding Nevada, California, and Oklahoma, rates over 12/100,000 were concentrated in the southernmost U.S. states. Overall, the 2,268 congenital syphilis cases in U.S. children born in 2021 was a 6% increase over 2020, and a 680% increase over 2012. (Note: All 2021 data are not yet available because of public health STI resources being diverted to COVID-19 control.) A telling number is the 166 congenital syphilis deaths in babies born in 2021 – a 1,000% increase over 2012. Another concern is that 50% of U.S. counties reported at least one congenital syphilis case in 2019 – the last time frame from which county-specific data are available.
Syphilis afflicts the underserved and underprivileged more than other demographic groups, particularly when public health budgets are not adequate (funding for public health STI prevention/treatment efforts has lagged for more than a decade), and/or when public health emergencies such as the pandemic divert public health resources away from STI prevention/treatment efforts.
As pediatric care providers, we can help by heightening our vigilance and appropriately testing for and treating syphilis, particularly in newborns/infants, regardless of where we work. And we can advocate for increased public health STI funding allocation whenever possible. It is a smart economic move because it costs nearly 1,000 times more to manage congenital syphilis and its sequelae than to prevent or treat it.
Christopher J. Harrison, MD, is professor, University of Missouri Kansas City School of Medicine, department of medicine, infectious diseases section, Kansas City. He has no financial conflicts of interest.
The Enigma of MS Etiology: Find an Answer, Ask More Questions
Dr. Obeidat is an Assistant Professor in the Department of Neurology,
Neuroimmunology and Multiple Sclerosis and is the Founding Director of the Neuroimmunology and MS Fellowship Program at The Medical College of Wisconsin in Milwaukee, WI.
Dr. Obeidat reports having consulted with/spoken for/conducted clinical trials for AbbVie, Alexion, Atara Biotherapeutics, Biogen, Bristol-Myers Squibb, Central, Celgene, EMD Serono, GW Pharmaceuticals, Genentech, Horizon, Jazz Pharma, Novartis, Sanofi/Genzyme, TG Therapeutics, and Viela Bio. Dr. Obeidat serves on the editorial board of the International Journal of MS Care, the advisory board of Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS®), and the Board of Governors of the Consortium of Multiple Sclerosis Centers.
“Could multiple sclerosis be the direct result of a yet-to-be identified infection?” asked John Kurtzke, MD, of his audience during his Grand Rounds entitled “Epidemiology and the Cause of Multiple Sclerosis” at the National Institute of Health (NIH) in 2015.1 As a pioneer of neuroepidemiology, Dr Kurtzke had long considered that infection was a key step in the development of multiple sclerosis (MS), the most disabling nontraumatic neurologic disease in young adults. He and others, from the 1970s onwards, described disease outbreaks and patterns of disease distribution in various countries during periods of immigration and even wartime.1,2
A half century later and Dr Kurtzke’s question has a possible answer: The Epstein-Barr virus (EBV), a gamma herpes virus responsible for mononucleosis that has been long suspected as a link to the development of MS,3 is now more than a virus of interest. A longitudinal study pinpointed the virus’ almost universal presence in patients with MS.4 Not everyone who develops mononucleosis from EBV develops MS, but most people become infected with EBV at some point in their lives. EBV is highly prevalent in the general population, with some studies suggesting that more than 90% of people worldwide are infected with EBV.5 While the discovery raises many questions about MS etiology and disease progression, it also allows discussion on more therapeutic possibilities.
MS Numbers
With nearly 1 million people in the United States living with MS, and over 2.5 million people worldwide, MS has been the subject of numerous investigations.2 Its complexity and heterogeneity have gained significant interest from the scientific community, including from Dr. Kurtzke, who passed away the same year as his NIH presentation.1
Several investigators over the years have attempted to link viral infections to MS,3 especially EBV. In February 2022, a longitudinal study spanning 20 years shed additional light on this longstanding, controversial, heavily researched potential association.4 The collaborative group of investigators used a database of serial blood samples from more than 10 million active US military personnel to investigate the association between EBV and MS and to learn whether EBV infection preceded the development of MS.
Out of 801 persons with a documented diagnosis of MS in this study, only 1 case occurred in a person who tested negative for EBV infection.4 At baseline, 35 people with MS tested negative for EBV infection, but after receiving their MS diagnosis, they tested positive for the virus, suggesting a causal relationship between EBV and MS. The study also showed that the levels of serum neurofilament light (sNfL), a nonspecific biomarker indicative of neuroaxonal injury or degeneration, increased post-EBV infection in the sera of initially EBV-negative patients with MS.4 This raises the question again: Why do only a small subset of people with EBV develop MS?
Facts and Questions
MS is a complex, heterogeneous disease whose development would require more than a human gamma herpesvirus to directly trigger its life-long, unrelenting immune dysregulation in select people. The complexity, which has been reviewed in detail, 6 suggests a role for interaction between host genetics, vitamin D levels, vitamin D receptors, and a specific protein of EBV, called Epstein-Barr nuclear antigen 1 (EBNA1).6 A recent publication described the potential for molecular mimicry (also known as cross-reactivity) between (EBNA1)6 and a specific cell adhesion molecule expressed in glial cells of the central nervous system (GlialCAM).7
But this molecular mimicry is not sufficient to explain the EBV/MS relationship. Even in monozygotic twins, the concordance rate is around 25%, leaving three-fourths of the risk of MS to the environment and genetics-environment interaction.8 The chances for monozygotic twins to both be infected with EBV are estimated at much more than 25%, given the epidemiology of EBV. Thus, EBV infection combined with specific genetic susceptibility remains insufficient to explain the observed epidemiology of MS.
More Factors
Several investigators have reported on the association between low vitamin D levels and MS. Low vitamin D is thought to affect both disease development and inflammatory activity.9 So, does MS result from the interaction between EBV, genetics, and low vitamin D? This interaction is plausible and is supported by several lines of evidence.6 However, even the interaction between these 3 factors remains insufficient to explain the complexity of MS pathogenesis.
An Unknown Mechanism
The triggering mechanism from EBV into MS remains an open question, and further research is needed. Nevertheless, if infection by EBV is a necessary, yet insufficient, step for MS to occur, can we prevent MS simply by preventing the primary EBV infection via vaccination? If so, what considerations must we make? For example, if EBV infection triggers MS via the transformation of infected memory B cells, thereby triggering an autoreactive immune response, then a vaccine capable of preventing the primary EBV infection could reduce the number of new MS cases, or ambitiously eradicate the disease itself. On the other hand, if molecular mimicry is the leading mechanism by which EBV infection triggers MS, then an EBV vaccine may have detrimental effects and theoretically trigger MS in susceptible individuals. Thus, it is of utmost importance to clearly understand how EBV infection contributes to MS pathogenesis to evaluate potential EBV vaccine candidates.
Treatment Possibilities
What are some possible clinical implications for the EBV-MS story for people living with MS? An important consideration is whether latent EBV infection contributes to the disease process over time, or if the infection is just an initial step that triggers numerous events that then operate independently from the virus. Suppose latent EBV infection contributes to the ongoing inflammatory and neurodegenerative changes in MS. In that case, some may consider using antiviral therapies as possible therapeutics for MS (possibly as an add-on, in combination with existing or future classes of disease-modifying therapies). Other interventions targeted at infected, transformed, or autoreactive B cells may bring us closer to precision medicine in MS. On the other hand, if the role of EBV is mainly to kick off MS, then further interventions targeted at the virus may not prove to be clinically effective.
Finally, the recent evidence of possible molecular mimicry to support causality between EBV infection and MS needs further investigation to elucidate how a common, ubiquitous infection kicks off MS in selected individuals. Additionally, the complex interactions between EBV, the human immune system, and genetics, as well as with other factors such as emotional stress,10 low sun exposure,11 and other, yet-to-be-identified environmental factors, may add more pieces to the complex etiology puzzle of MS and perhaps allow for effective interventions to help reduce the incidence of MS and even modulate disease progression.
References
1. Obeidat AZ. John F. Kurtzke, MD (1926-2015). Neuroepidemiology. 2016;46(2):118-119.
2. Nathanson N, Miller A. Epidemiology of multiple sclerosis: critique of the evidence for a viral etiology. Am J Epidemiol. 1978;107(6):451-461.
3. Donati D. Viral infections and multiple sclerosis. Drug Discov Today Dis Models. 2020;32:27-33.
4. Bjornevik K, Cortese M, Healy BC, et al. Longitudinal analysis reveals high prevalence of Epstein-Barr virus associated with multiple sclerosis. Science. 2022;375(6578):296-301.
5. Smatti MK, Al-Sadeq DW, Ali NH, Pintus G, Abou-Saleh H, Nasrallah GK. Epstein-Barr virus epidemiology, serology, and genetic variability of LMP-1 oncogene among healthy population: an update. Front Oncol. 2018;8:211.
6. Marcucci SB, Obeidat AZ. EBNA1, EBNA2, and EBNA3 link Epstein-Barr virus and hypovitaminosis D in multiple sclerosis pathogenesis. J Neuroimmunol. 2020;339:577116.
7. Lanz, TV, Brewer RC, Ho PP, et al. Clonally expanded B cells in multiple sclerosis bind EBV EBNA1 and GlialCAM. Nature. 2022;603(7900):321-327.
8. Mumford CJ, Wood NW, Kellar-Wood H, Thorpe JW, Miller DH, Compston DA. The British Isles survey of multiple sclerosis in twins. Neurology. 1994;44(1):11-15.
9. Fitzgerald KC, Munger KL, Köchert K, et al. Association of vitamin D levels with multiple sclerosis activity and progression in patients receiving interferon beta-1b. JAMA Neurol. 2015;72(12):1458-1465.
10. Mohr DC, Hart SL, Julian L, Cox D, Pelletier D. Association between stressful life events and exacerbation in multiple sclerosis: a meta-analysis. BMJ. 2004;328(7442):731.
11. Hedström AK, Huang J, Brenner N, et al. Low sun exposure acts synergistically with high Epstein-Barr nuclear antigen 1 (EBNA-1) antibody levels in multiple sclerosis etiology. Eur J Neurol. 2021;28(12):4146-4152.
Dr. Obeidat is an Assistant Professor in the Department of Neurology,
Neuroimmunology and Multiple Sclerosis and is the Founding Director of the Neuroimmunology and MS Fellowship Program at The Medical College of Wisconsin in Milwaukee, WI.
Dr. Obeidat reports having consulted with/spoken for/conducted clinical trials for AbbVie, Alexion, Atara Biotherapeutics, Biogen, Bristol-Myers Squibb, Central, Celgene, EMD Serono, GW Pharmaceuticals, Genentech, Horizon, Jazz Pharma, Novartis, Sanofi/Genzyme, TG Therapeutics, and Viela Bio. Dr. Obeidat serves on the editorial board of the International Journal of MS Care, the advisory board of Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS®), and the Board of Governors of the Consortium of Multiple Sclerosis Centers.
“Could multiple sclerosis be the direct result of a yet-to-be identified infection?” asked John Kurtzke, MD, of his audience during his Grand Rounds entitled “Epidemiology and the Cause of Multiple Sclerosis” at the National Institute of Health (NIH) in 2015.1 As a pioneer of neuroepidemiology, Dr Kurtzke had long considered that infection was a key step in the development of multiple sclerosis (MS), the most disabling nontraumatic neurologic disease in young adults. He and others, from the 1970s onwards, described disease outbreaks and patterns of disease distribution in various countries during periods of immigration and even wartime.1,2
A half century later and Dr Kurtzke’s question has a possible answer: The Epstein-Barr virus (EBV), a gamma herpes virus responsible for mononucleosis that has been long suspected as a link to the development of MS,3 is now more than a virus of interest. A longitudinal study pinpointed the virus’ almost universal presence in patients with MS.4 Not everyone who develops mononucleosis from EBV develops MS, but most people become infected with EBV at some point in their lives. EBV is highly prevalent in the general population, with some studies suggesting that more than 90% of people worldwide are infected with EBV.5 While the discovery raises many questions about MS etiology and disease progression, it also allows discussion on more therapeutic possibilities.
MS Numbers
With nearly 1 million people in the United States living with MS, and over 2.5 million people worldwide, MS has been the subject of numerous investigations.2 Its complexity and heterogeneity have gained significant interest from the scientific community, including from Dr. Kurtzke, who passed away the same year as his NIH presentation.1
Several investigators over the years have attempted to link viral infections to MS,3 especially EBV. In February 2022, a longitudinal study spanning 20 years shed additional light on this longstanding, controversial, heavily researched potential association.4 The collaborative group of investigators used a database of serial blood samples from more than 10 million active US military personnel to investigate the association between EBV and MS and to learn whether EBV infection preceded the development of MS.
Out of 801 persons with a documented diagnosis of MS in this study, only 1 case occurred in a person who tested negative for EBV infection.4 At baseline, 35 people with MS tested negative for EBV infection, but after receiving their MS diagnosis, they tested positive for the virus, suggesting a causal relationship between EBV and MS. The study also showed that the levels of serum neurofilament light (sNfL), a nonspecific biomarker indicative of neuroaxonal injury or degeneration, increased post-EBV infection in the sera of initially EBV-negative patients with MS.4 This raises the question again: Why do only a small subset of people with EBV develop MS?
Facts and Questions
MS is a complex, heterogeneous disease whose development would require more than a human gamma herpesvirus to directly trigger its life-long, unrelenting immune dysregulation in select people. The complexity, which has been reviewed in detail, 6 suggests a role for interaction between host genetics, vitamin D levels, vitamin D receptors, and a specific protein of EBV, called Epstein-Barr nuclear antigen 1 (EBNA1).6 A recent publication described the potential for molecular mimicry (also known as cross-reactivity) between (EBNA1)6 and a specific cell adhesion molecule expressed in glial cells of the central nervous system (GlialCAM).7
But this molecular mimicry is not sufficient to explain the EBV/MS relationship. Even in monozygotic twins, the concordance rate is around 25%, leaving three-fourths of the risk of MS to the environment and genetics-environment interaction.8 The chances for monozygotic twins to both be infected with EBV are estimated at much more than 25%, given the epidemiology of EBV. Thus, EBV infection combined with specific genetic susceptibility remains insufficient to explain the observed epidemiology of MS.
More Factors
Several investigators have reported on the association between low vitamin D levels and MS. Low vitamin D is thought to affect both disease development and inflammatory activity.9 So, does MS result from the interaction between EBV, genetics, and low vitamin D? This interaction is plausible and is supported by several lines of evidence.6 However, even the interaction between these 3 factors remains insufficient to explain the complexity of MS pathogenesis.
An Unknown Mechanism
The triggering mechanism from EBV into MS remains an open question, and further research is needed. Nevertheless, if infection by EBV is a necessary, yet insufficient, step for MS to occur, can we prevent MS simply by preventing the primary EBV infection via vaccination? If so, what considerations must we make? For example, if EBV infection triggers MS via the transformation of infected memory B cells, thereby triggering an autoreactive immune response, then a vaccine capable of preventing the primary EBV infection could reduce the number of new MS cases, or ambitiously eradicate the disease itself. On the other hand, if molecular mimicry is the leading mechanism by which EBV infection triggers MS, then an EBV vaccine may have detrimental effects and theoretically trigger MS in susceptible individuals. Thus, it is of utmost importance to clearly understand how EBV infection contributes to MS pathogenesis to evaluate potential EBV vaccine candidates.
Treatment Possibilities
What are some possible clinical implications for the EBV-MS story for people living with MS? An important consideration is whether latent EBV infection contributes to the disease process over time, or if the infection is just an initial step that triggers numerous events that then operate independently from the virus. Suppose latent EBV infection contributes to the ongoing inflammatory and neurodegenerative changes in MS. In that case, some may consider using antiviral therapies as possible therapeutics for MS (possibly as an add-on, in combination with existing or future classes of disease-modifying therapies). Other interventions targeted at infected, transformed, or autoreactive B cells may bring us closer to precision medicine in MS. On the other hand, if the role of EBV is mainly to kick off MS, then further interventions targeted at the virus may not prove to be clinically effective.
Finally, the recent evidence of possible molecular mimicry to support causality between EBV infection and MS needs further investigation to elucidate how a common, ubiquitous infection kicks off MS in selected individuals. Additionally, the complex interactions between EBV, the human immune system, and genetics, as well as with other factors such as emotional stress,10 low sun exposure,11 and other, yet-to-be-identified environmental factors, may add more pieces to the complex etiology puzzle of MS and perhaps allow for effective interventions to help reduce the incidence of MS and even modulate disease progression.
Dr. Obeidat is an Assistant Professor in the Department of Neurology,
Neuroimmunology and Multiple Sclerosis and is the Founding Director of the Neuroimmunology and MS Fellowship Program at The Medical College of Wisconsin in Milwaukee, WI.
Dr. Obeidat reports having consulted with/spoken for/conducted clinical trials for AbbVie, Alexion, Atara Biotherapeutics, Biogen, Bristol-Myers Squibb, Central, Celgene, EMD Serono, GW Pharmaceuticals, Genentech, Horizon, Jazz Pharma, Novartis, Sanofi/Genzyme, TG Therapeutics, and Viela Bio. Dr. Obeidat serves on the editorial board of the International Journal of MS Care, the advisory board of Americas Committee for Treatment and Research in Multiple Sclerosis (ACTRIMS®), and the Board of Governors of the Consortium of Multiple Sclerosis Centers.
“Could multiple sclerosis be the direct result of a yet-to-be identified infection?” asked John Kurtzke, MD, of his audience during his Grand Rounds entitled “Epidemiology and the Cause of Multiple Sclerosis” at the National Institute of Health (NIH) in 2015.1 As a pioneer of neuroepidemiology, Dr Kurtzke had long considered that infection was a key step in the development of multiple sclerosis (MS), the most disabling nontraumatic neurologic disease in young adults. He and others, from the 1970s onwards, described disease outbreaks and patterns of disease distribution in various countries during periods of immigration and even wartime.1,2
A half century later and Dr Kurtzke’s question has a possible answer: The Epstein-Barr virus (EBV), a gamma herpes virus responsible for mononucleosis that has been long suspected as a link to the development of MS,3 is now more than a virus of interest. A longitudinal study pinpointed the virus’ almost universal presence in patients with MS.4 Not everyone who develops mononucleosis from EBV develops MS, but most people become infected with EBV at some point in their lives. EBV is highly prevalent in the general population, with some studies suggesting that more than 90% of people worldwide are infected with EBV.5 While the discovery raises many questions about MS etiology and disease progression, it also allows discussion on more therapeutic possibilities.
MS Numbers
With nearly 1 million people in the United States living with MS, and over 2.5 million people worldwide, MS has been the subject of numerous investigations.2 Its complexity and heterogeneity have gained significant interest from the scientific community, including from Dr. Kurtzke, who passed away the same year as his NIH presentation.1
Several investigators over the years have attempted to link viral infections to MS,3 especially EBV. In February 2022, a longitudinal study spanning 20 years shed additional light on this longstanding, controversial, heavily researched potential association.4 The collaborative group of investigators used a database of serial blood samples from more than 10 million active US military personnel to investigate the association between EBV and MS and to learn whether EBV infection preceded the development of MS.
Out of 801 persons with a documented diagnosis of MS in this study, only 1 case occurred in a person who tested negative for EBV infection.4 At baseline, 35 people with MS tested negative for EBV infection, but after receiving their MS diagnosis, they tested positive for the virus, suggesting a causal relationship between EBV and MS. The study also showed that the levels of serum neurofilament light (sNfL), a nonspecific biomarker indicative of neuroaxonal injury or degeneration, increased post-EBV infection in the sera of initially EBV-negative patients with MS.4 This raises the question again: Why do only a small subset of people with EBV develop MS?
Facts and Questions
MS is a complex, heterogeneous disease whose development would require more than a human gamma herpesvirus to directly trigger its life-long, unrelenting immune dysregulation in select people. The complexity, which has been reviewed in detail, 6 suggests a role for interaction between host genetics, vitamin D levels, vitamin D receptors, and a specific protein of EBV, called Epstein-Barr nuclear antigen 1 (EBNA1).6 A recent publication described the potential for molecular mimicry (also known as cross-reactivity) between (EBNA1)6 and a specific cell adhesion molecule expressed in glial cells of the central nervous system (GlialCAM).7
But this molecular mimicry is not sufficient to explain the EBV/MS relationship. Even in monozygotic twins, the concordance rate is around 25%, leaving three-fourths of the risk of MS to the environment and genetics-environment interaction.8 The chances for monozygotic twins to both be infected with EBV are estimated at much more than 25%, given the epidemiology of EBV. Thus, EBV infection combined with specific genetic susceptibility remains insufficient to explain the observed epidemiology of MS.
More Factors
Several investigators have reported on the association between low vitamin D levels and MS. Low vitamin D is thought to affect both disease development and inflammatory activity.9 So, does MS result from the interaction between EBV, genetics, and low vitamin D? This interaction is plausible and is supported by several lines of evidence.6 However, even the interaction between these 3 factors remains insufficient to explain the complexity of MS pathogenesis.
An Unknown Mechanism
The triggering mechanism from EBV into MS remains an open question, and further research is needed. Nevertheless, if infection by EBV is a necessary, yet insufficient, step for MS to occur, can we prevent MS simply by preventing the primary EBV infection via vaccination? If so, what considerations must we make? For example, if EBV infection triggers MS via the transformation of infected memory B cells, thereby triggering an autoreactive immune response, then a vaccine capable of preventing the primary EBV infection could reduce the number of new MS cases, or ambitiously eradicate the disease itself. On the other hand, if molecular mimicry is the leading mechanism by which EBV infection triggers MS, then an EBV vaccine may have detrimental effects and theoretically trigger MS in susceptible individuals. Thus, it is of utmost importance to clearly understand how EBV infection contributes to MS pathogenesis to evaluate potential EBV vaccine candidates.
Treatment Possibilities
What are some possible clinical implications for the EBV-MS story for people living with MS? An important consideration is whether latent EBV infection contributes to the disease process over time, or if the infection is just an initial step that triggers numerous events that then operate independently from the virus. Suppose latent EBV infection contributes to the ongoing inflammatory and neurodegenerative changes in MS. In that case, some may consider using antiviral therapies as possible therapeutics for MS (possibly as an add-on, in combination with existing or future classes of disease-modifying therapies). Other interventions targeted at infected, transformed, or autoreactive B cells may bring us closer to precision medicine in MS. On the other hand, if the role of EBV is mainly to kick off MS, then further interventions targeted at the virus may not prove to be clinically effective.
Finally, the recent evidence of possible molecular mimicry to support causality between EBV infection and MS needs further investigation to elucidate how a common, ubiquitous infection kicks off MS in selected individuals. Additionally, the complex interactions between EBV, the human immune system, and genetics, as well as with other factors such as emotional stress,10 low sun exposure,11 and other, yet-to-be-identified environmental factors, may add more pieces to the complex etiology puzzle of MS and perhaps allow for effective interventions to help reduce the incidence of MS and even modulate disease progression.
References
1. Obeidat AZ. John F. Kurtzke, MD (1926-2015). Neuroepidemiology. 2016;46(2):118-119.
2. Nathanson N, Miller A. Epidemiology of multiple sclerosis: critique of the evidence for a viral etiology. Am J Epidemiol. 1978;107(6):451-461.
3. Donati D. Viral infections and multiple sclerosis. Drug Discov Today Dis Models. 2020;32:27-33.
4. Bjornevik K, Cortese M, Healy BC, et al. Longitudinal analysis reveals high prevalence of Epstein-Barr virus associated with multiple sclerosis. Science. 2022;375(6578):296-301.
5. Smatti MK, Al-Sadeq DW, Ali NH, Pintus G, Abou-Saleh H, Nasrallah GK. Epstein-Barr virus epidemiology, serology, and genetic variability of LMP-1 oncogene among healthy population: an update. Front Oncol. 2018;8:211.
6. Marcucci SB, Obeidat AZ. EBNA1, EBNA2, and EBNA3 link Epstein-Barr virus and hypovitaminosis D in multiple sclerosis pathogenesis. J Neuroimmunol. 2020;339:577116.
7. Lanz, TV, Brewer RC, Ho PP, et al. Clonally expanded B cells in multiple sclerosis bind EBV EBNA1 and GlialCAM. Nature. 2022;603(7900):321-327.
8. Mumford CJ, Wood NW, Kellar-Wood H, Thorpe JW, Miller DH, Compston DA. The British Isles survey of multiple sclerosis in twins. Neurology. 1994;44(1):11-15.
9. Fitzgerald KC, Munger KL, Köchert K, et al. Association of vitamin D levels with multiple sclerosis activity and progression in patients receiving interferon beta-1b. JAMA Neurol. 2015;72(12):1458-1465.
10. Mohr DC, Hart SL, Julian L, Cox D, Pelletier D. Association between stressful life events and exacerbation in multiple sclerosis: a meta-analysis. BMJ. 2004;328(7442):731.
11. Hedström AK, Huang J, Brenner N, et al. Low sun exposure acts synergistically with high Epstein-Barr nuclear antigen 1 (EBNA-1) antibody levels in multiple sclerosis etiology. Eur J Neurol. 2021;28(12):4146-4152.
References
1. Obeidat AZ. John F. Kurtzke, MD (1926-2015). Neuroepidemiology. 2016;46(2):118-119.
2. Nathanson N, Miller A. Epidemiology of multiple sclerosis: critique of the evidence for a viral etiology. Am J Epidemiol. 1978;107(6):451-461.
3. Donati D. Viral infections and multiple sclerosis. Drug Discov Today Dis Models. 2020;32:27-33.
4. Bjornevik K, Cortese M, Healy BC, et al. Longitudinal analysis reveals high prevalence of Epstein-Barr virus associated with multiple sclerosis. Science. 2022;375(6578):296-301.
5. Smatti MK, Al-Sadeq DW, Ali NH, Pintus G, Abou-Saleh H, Nasrallah GK. Epstein-Barr virus epidemiology, serology, and genetic variability of LMP-1 oncogene among healthy population: an update. Front Oncol. 2018;8:211.
6. Marcucci SB, Obeidat AZ. EBNA1, EBNA2, and EBNA3 link Epstein-Barr virus and hypovitaminosis D in multiple sclerosis pathogenesis. J Neuroimmunol. 2020;339:577116.
7. Lanz, TV, Brewer RC, Ho PP, et al. Clonally expanded B cells in multiple sclerosis bind EBV EBNA1 and GlialCAM. Nature. 2022;603(7900):321-327.
8. Mumford CJ, Wood NW, Kellar-Wood H, Thorpe JW, Miller DH, Compston DA. The British Isles survey of multiple sclerosis in twins. Neurology. 1994;44(1):11-15.
9. Fitzgerald KC, Munger KL, Köchert K, et al. Association of vitamin D levels with multiple sclerosis activity and progression in patients receiving interferon beta-1b. JAMA Neurol. 2015;72(12):1458-1465.
10. Mohr DC, Hart SL, Julian L, Cox D, Pelletier D. Association between stressful life events and exacerbation in multiple sclerosis: a meta-analysis. BMJ. 2004;328(7442):731.
11. Hedström AK, Huang J, Brenner N, et al. Low sun exposure acts synergistically with high Epstein-Barr nuclear antigen 1 (EBNA-1) antibody levels in multiple sclerosis etiology. Eur J Neurol. 2021;28(12):4146-4152.
Global incidence, deaths from CRC doubled over past 3 decades
, according to a new analysis of 204 countries.
However, trends in CRC incidence and deaths varied by age, region, and sex. Investigators expressed particular concern over the rising incidence rates among people younger than 50 and those living in low and middle sociodemographic index countries in Asia and Africa.
“These results provide comprehensive and comparable estimates that can inform efforts for equitable colorectal cancer control worldwide,” the authors write. However, “further research is required to understand the causes of the colorectal cancer burden in younger adults (aged less than 50 years) and the main risk factors, including obesity, physical inactivity, alcohol consumption, smoking, and an altered gut microbiome, that might have led to the rise in the colorectal cancer burden.”
The study was published online in the Lancet Gastroenterology and Hepatology.
CRC is the third leading cause of cancer deaths worldwide, but data on incidence and mortality by location, age, and sex remain less clear.
In the current Global Burden of Diseases, Injuries and Risk Factors Study, researchers evaluated age, sex, and geography-level estimates of CRC incidence, deaths, and disability-adjusted life-years (DALYs) from 204 countries between 1990 and 2019.
The authors found that cases of CRC increased by almost 2.6-fold over the 30-year study period, from 842,098 to 2.17 million. Deaths from CRC increased at a similar but slightly lower rate – rising 2.1-fold over the same period, from 518,126 to 1.09 million. DALYs also nearly doubled, going from 12.4 million in 1990 to 24.3 million in 2019.
In addition, the global age-standardized incidence rate increased from 22.2 to 26.7 per 100,000.
Overall, the age-standardized mortality rate decreased slightly, from 14.3 to 13.7 per 100,000; however, only high-middle and high sociodemographic index regions experienced a decrease; low and middle sociodemographic index regions experienced an increase. The age-standardized DALY rate also declined overall, from 308.5 per 100,000 in 1900 to 295.5 per 100,000 in 2019.
The authors further broke down CRC incidence and deaths by age, region, and sex.
Over the study period, males demonstrated greater increases in CRC incidence, deaths, and DALYs, compared with females. In 2019, the age-standardized CRC incidence rate was 1.5 times higher in males (33.1 vs 21.2 per 100,000), as was the age-standardized mortality rate (16.6 vs. 11.2 per 100,000). The age-standardized DALY rate showed a similar trend by sex – 360 versus 238 per 100,000 in males versus females.
Trends varied by age as well. CRC incidence rates increased the most in people aged 85 and older, followed by those between 20 and 49 years, while rates decreased for those between 50 and 80 years in high sociodemographic index countries.
Geography mattered too. China, the United States, and Japan demonstrated the highest number of new CRC cases across all ages and for both sexes in 2019 – 607,900 in China, 227,242 in the United States, and 160,211 in Japan.
In terms of mortality, China, the United States, and India had the highest CRC death counts: 261,777 in China, 84,026 in the United States, and 79,098 in India.
When it comes to age-standardized incidence rates, Taiwan, Monaco, and Andorra were at the top: Taiwan with 62 per 100,000 cases, Monaco with 60.7 per 100,000, and Andorra with 56.6 per 100,000.
On the other hand, Somalia, Niger, and Bangladesh had the lowest age-standardized incidence rates, 5 per 100,000 in Somalia and 5.6 per 100,000 in Niger and Bangladesh.
The highest age-standardized mortality rates occurred in Greenland, Brunei, and Hungary: 31.4 per 100,000 in Greenland, 30.3 per 100,000 in Brunei, and 28.6 per 100,000 in Hungary.
The relative contribution of different risk factors also varied by region. For example, in sub-Saharan Africa and lower-income countries in Asia, diets low in calcium and milk were the main CRC risk factors. In contrast, smoking and alcohol consumption were the main risk factors driving CRC in high-income regions.
Still, the reasons underlying some of these trends – such as the increasing incidence of CRC in patients under the age of 50 – remain uncertain. One possible explanation for this trend, the researchers point out, is the birth cohort effect, which suggests that those born in the second half of the 20th century are increasingly exposed to potentially modifiable risk factors, such as an unhealthy diet, obesity, and sedentary lifestyles.
Overall, the authors note that the data generated in this study provide an important resource for both patients and oncologists about current trends in incidence and mortality and where gaps in preventive measures may exist.
In particular, the authors conclude that “public health interventions for colorectal cancer awareness, screening, and prevention through containment of modifiable risk factors such as alcohol, smoking, unhealthy diet ... and obesity are key to stemming the tide of colorectal cancer worldwide.”
The study was funded by the Bill & Melinda Gates Foundation. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to a new analysis of 204 countries.
However, trends in CRC incidence and deaths varied by age, region, and sex. Investigators expressed particular concern over the rising incidence rates among people younger than 50 and those living in low and middle sociodemographic index countries in Asia and Africa.
“These results provide comprehensive and comparable estimates that can inform efforts for equitable colorectal cancer control worldwide,” the authors write. However, “further research is required to understand the causes of the colorectal cancer burden in younger adults (aged less than 50 years) and the main risk factors, including obesity, physical inactivity, alcohol consumption, smoking, and an altered gut microbiome, that might have led to the rise in the colorectal cancer burden.”
The study was published online in the Lancet Gastroenterology and Hepatology.
CRC is the third leading cause of cancer deaths worldwide, but data on incidence and mortality by location, age, and sex remain less clear.
In the current Global Burden of Diseases, Injuries and Risk Factors Study, researchers evaluated age, sex, and geography-level estimates of CRC incidence, deaths, and disability-adjusted life-years (DALYs) from 204 countries between 1990 and 2019.
The authors found that cases of CRC increased by almost 2.6-fold over the 30-year study period, from 842,098 to 2.17 million. Deaths from CRC increased at a similar but slightly lower rate – rising 2.1-fold over the same period, from 518,126 to 1.09 million. DALYs also nearly doubled, going from 12.4 million in 1990 to 24.3 million in 2019.
In addition, the global age-standardized incidence rate increased from 22.2 to 26.7 per 100,000.
Overall, the age-standardized mortality rate decreased slightly, from 14.3 to 13.7 per 100,000; however, only high-middle and high sociodemographic index regions experienced a decrease; low and middle sociodemographic index regions experienced an increase. The age-standardized DALY rate also declined overall, from 308.5 per 100,000 in 1900 to 295.5 per 100,000 in 2019.
The authors further broke down CRC incidence and deaths by age, region, and sex.
Over the study period, males demonstrated greater increases in CRC incidence, deaths, and DALYs, compared with females. In 2019, the age-standardized CRC incidence rate was 1.5 times higher in males (33.1 vs 21.2 per 100,000), as was the age-standardized mortality rate (16.6 vs. 11.2 per 100,000). The age-standardized DALY rate showed a similar trend by sex – 360 versus 238 per 100,000 in males versus females.
Trends varied by age as well. CRC incidence rates increased the most in people aged 85 and older, followed by those between 20 and 49 years, while rates decreased for those between 50 and 80 years in high sociodemographic index countries.
Geography mattered too. China, the United States, and Japan demonstrated the highest number of new CRC cases across all ages and for both sexes in 2019 – 607,900 in China, 227,242 in the United States, and 160,211 in Japan.
In terms of mortality, China, the United States, and India had the highest CRC death counts: 261,777 in China, 84,026 in the United States, and 79,098 in India.
When it comes to age-standardized incidence rates, Taiwan, Monaco, and Andorra were at the top: Taiwan with 62 per 100,000 cases, Monaco with 60.7 per 100,000, and Andorra with 56.6 per 100,000.
On the other hand, Somalia, Niger, and Bangladesh had the lowest age-standardized incidence rates, 5 per 100,000 in Somalia and 5.6 per 100,000 in Niger and Bangladesh.
The highest age-standardized mortality rates occurred in Greenland, Brunei, and Hungary: 31.4 per 100,000 in Greenland, 30.3 per 100,000 in Brunei, and 28.6 per 100,000 in Hungary.
The relative contribution of different risk factors also varied by region. For example, in sub-Saharan Africa and lower-income countries in Asia, diets low in calcium and milk were the main CRC risk factors. In contrast, smoking and alcohol consumption were the main risk factors driving CRC in high-income regions.
Still, the reasons underlying some of these trends – such as the increasing incidence of CRC in patients under the age of 50 – remain uncertain. One possible explanation for this trend, the researchers point out, is the birth cohort effect, which suggests that those born in the second half of the 20th century are increasingly exposed to potentially modifiable risk factors, such as an unhealthy diet, obesity, and sedentary lifestyles.
Overall, the authors note that the data generated in this study provide an important resource for both patients and oncologists about current trends in incidence and mortality and where gaps in preventive measures may exist.
In particular, the authors conclude that “public health interventions for colorectal cancer awareness, screening, and prevention through containment of modifiable risk factors such as alcohol, smoking, unhealthy diet ... and obesity are key to stemming the tide of colorectal cancer worldwide.”
The study was funded by the Bill & Melinda Gates Foundation. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to a new analysis of 204 countries.
However, trends in CRC incidence and deaths varied by age, region, and sex. Investigators expressed particular concern over the rising incidence rates among people younger than 50 and those living in low and middle sociodemographic index countries in Asia and Africa.
“These results provide comprehensive and comparable estimates that can inform efforts for equitable colorectal cancer control worldwide,” the authors write. However, “further research is required to understand the causes of the colorectal cancer burden in younger adults (aged less than 50 years) and the main risk factors, including obesity, physical inactivity, alcohol consumption, smoking, and an altered gut microbiome, that might have led to the rise in the colorectal cancer burden.”
The study was published online in the Lancet Gastroenterology and Hepatology.
CRC is the third leading cause of cancer deaths worldwide, but data on incidence and mortality by location, age, and sex remain less clear.
In the current Global Burden of Diseases, Injuries and Risk Factors Study, researchers evaluated age, sex, and geography-level estimates of CRC incidence, deaths, and disability-adjusted life-years (DALYs) from 204 countries between 1990 and 2019.
The authors found that cases of CRC increased by almost 2.6-fold over the 30-year study period, from 842,098 to 2.17 million. Deaths from CRC increased at a similar but slightly lower rate – rising 2.1-fold over the same period, from 518,126 to 1.09 million. DALYs also nearly doubled, going from 12.4 million in 1990 to 24.3 million in 2019.
In addition, the global age-standardized incidence rate increased from 22.2 to 26.7 per 100,000.
Overall, the age-standardized mortality rate decreased slightly, from 14.3 to 13.7 per 100,000; however, only high-middle and high sociodemographic index regions experienced a decrease; low and middle sociodemographic index regions experienced an increase. The age-standardized DALY rate also declined overall, from 308.5 per 100,000 in 1900 to 295.5 per 100,000 in 2019.
The authors further broke down CRC incidence and deaths by age, region, and sex.
Over the study period, males demonstrated greater increases in CRC incidence, deaths, and DALYs, compared with females. In 2019, the age-standardized CRC incidence rate was 1.5 times higher in males (33.1 vs 21.2 per 100,000), as was the age-standardized mortality rate (16.6 vs. 11.2 per 100,000). The age-standardized DALY rate showed a similar trend by sex – 360 versus 238 per 100,000 in males versus females.
Trends varied by age as well. CRC incidence rates increased the most in people aged 85 and older, followed by those between 20 and 49 years, while rates decreased for those between 50 and 80 years in high sociodemographic index countries.
Geography mattered too. China, the United States, and Japan demonstrated the highest number of new CRC cases across all ages and for both sexes in 2019 – 607,900 in China, 227,242 in the United States, and 160,211 in Japan.
In terms of mortality, China, the United States, and India had the highest CRC death counts: 261,777 in China, 84,026 in the United States, and 79,098 in India.
When it comes to age-standardized incidence rates, Taiwan, Monaco, and Andorra were at the top: Taiwan with 62 per 100,000 cases, Monaco with 60.7 per 100,000, and Andorra with 56.6 per 100,000.
On the other hand, Somalia, Niger, and Bangladesh had the lowest age-standardized incidence rates, 5 per 100,000 in Somalia and 5.6 per 100,000 in Niger and Bangladesh.
The highest age-standardized mortality rates occurred in Greenland, Brunei, and Hungary: 31.4 per 100,000 in Greenland, 30.3 per 100,000 in Brunei, and 28.6 per 100,000 in Hungary.
The relative contribution of different risk factors also varied by region. For example, in sub-Saharan Africa and lower-income countries in Asia, diets low in calcium and milk were the main CRC risk factors. In contrast, smoking and alcohol consumption were the main risk factors driving CRC in high-income regions.
Still, the reasons underlying some of these trends – such as the increasing incidence of CRC in patients under the age of 50 – remain uncertain. One possible explanation for this trend, the researchers point out, is the birth cohort effect, which suggests that those born in the second half of the 20th century are increasingly exposed to potentially modifiable risk factors, such as an unhealthy diet, obesity, and sedentary lifestyles.
Overall, the authors note that the data generated in this study provide an important resource for both patients and oncologists about current trends in incidence and mortality and where gaps in preventive measures may exist.
In particular, the authors conclude that “public health interventions for colorectal cancer awareness, screening, and prevention through containment of modifiable risk factors such as alcohol, smoking, unhealthy diet ... and obesity are key to stemming the tide of colorectal cancer worldwide.”
The study was funded by the Bill & Melinda Gates Foundation. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE LANCET GASTROENTEROLOGY AND HEPATOLOGY
USPSTF recommends for the first time that kids 8 and older get screened for anxiety
The U.S. Preventive Services Task Force on Apr. 12 posted draft recommendations on screening for depression and anxiety in children and adolescents.
For the first time, the USPSTF is recommending screening children ages 8 and older for anxiety.
It also recommended screening children ages 12 and older for depression, which was consistent with the USPSTF’s prior recommendations on the topic.
These B-grade draft recommendations are for children and teens who are not showing signs or symptoms of these conditions. The task force emphasized that anyone who has concerns about or shows signs of these conditions should be connected to care.
Task force member Martha Kubik, PhD, RN, a professor with George Mason University, Fairfax, Va, said in a statement: “Fortunately, we found that screening older children for anxiety and depression is effective in identifying these conditions so children and teens can be connected to the support they need.”
The group cited in its recommendation on anxiety the 2018-2019 National Survey of Children’s Health, which found that 7.8% of children and adolescents ages 3-17 years had a current anxiety disorder. It also noted that the National Survey on LGBTQ Youth Mental Health found that 72% of LGBTQ youth and 77% of transgender and nonbinary youth described general anxiety disorder symptoms.
“Anxiety disorders in childhood and adolescence are associated with an increased likelihood of a future anxiety disorder or depression,” the task force authors wrote.
They highlighted that “the prevalence of anxiety in Black youth may be evolving.” Previously, studies had suggested that young Black people may have had lower rates of mental health disorders, compared with their White counterparts.
“However, recent cohorts of Black children or adolescents have reported a higher prevalence of anxiety disorders than in the past,” the authors wrote.
Joanna Quigley, MD, clinical associate professor and associate medical director for child & adolescent services at the University of Michigan, Ann Arbor, said in an interview she was not surprised the USPSTF recommended screening for anxiety starting at age 8.
That’s when parents and providers see anxiety disorders begin to present or become more problematic, she said.
“It’s also acknowledging the importance of prevention,” she said. “The sooner we can identify these challenges for kids, the sooner we can intervene and have better outcomes for that child across their lifespan.”
Screening gets providers and families in the habit of thinking about these concerns when a child or adolescent comes in for another kind of visit, Dr. Quigley said. Chest pains in a well-child check, for example, may trigger thoughts to consider anxiety later if the child is brought in for a cardiac check for chest pains.
“It creates a culture of awareness that is important as well,” Dr. Quigley said. “I think part of what the task force is trying to do is saying that identifying anxiety can be a precursor to what could turn out to be related to depression or related to ADHD and factors we think about when we think about suicide risk as well.
“We’re seeing an increase in suicide in the younger age group as well, which is a huge concern, “ she noted.
Dr. Quigley said, if these recommendations are adopted after the comment period, pediatricians and family practice providers will likely be doing most of the screening for anxiety, but there may also be a role for the screening in pediatric subspecialty care, such as those treating children with chronic illness and in specialized mental health care.
She added: “This builds on the national conversation going on about the mental health crisis, declared a national emergency in the fall. This deserves attention in continuing the momentum.”
Factors that may signal higher risk for depression
While the USPSTF recommends screening for major depressive disorder in all adolescents aged 12 years and older, the USPSTF notes that several risk factors might help identify those at higher risk.
Markers for higher risk include a combination of factors such as a family history of depression, prior episode of depression, and other mental health or behavioral problems.
“Other psychosocial risk factors include childhood abuse or neglect, exposure to traumatic events, bullying (either as perpetrators or as victims), adverse life events, early exposure to stress, maltreatment, and an insecure parental relationship,” the task force authors wrote.
There was limited evidence, however, on the benefits and harms of screening children younger than 8 for anxiety and screening kids younger than 12 for depression.
Not enough evidence for suicide risk screening
The authors of the recommendations acknowledged that, while suicide is a leading cause of death for older children and teens, evidence is still too sparse to make recommendations regarding screening for suicide risk in those without signs or symptoms at any age.
They also explained that evidence is lacking and inconsistent on the effectiveness of treatment (psychotherapy, pharmacotherapy, or collaborative care) for suicide risk in improving outcomes in children and adolescents.
Comments on the USPSTF recommendations may be submitted until May 9, 2022. The USPSTF topic leads review all comments, revise the draft recommendations, put them to a vote by the full task force, and then post the final versions to the website.
The task force authors and Dr. Quigley reported no financial disclosures.
The U.S. Preventive Services Task Force on Apr. 12 posted draft recommendations on screening for depression and anxiety in children and adolescents.
For the first time, the USPSTF is recommending screening children ages 8 and older for anxiety.
It also recommended screening children ages 12 and older for depression, which was consistent with the USPSTF’s prior recommendations on the topic.
These B-grade draft recommendations are for children and teens who are not showing signs or symptoms of these conditions. The task force emphasized that anyone who has concerns about or shows signs of these conditions should be connected to care.
Task force member Martha Kubik, PhD, RN, a professor with George Mason University, Fairfax, Va, said in a statement: “Fortunately, we found that screening older children for anxiety and depression is effective in identifying these conditions so children and teens can be connected to the support they need.”
The group cited in its recommendation on anxiety the 2018-2019 National Survey of Children’s Health, which found that 7.8% of children and adolescents ages 3-17 years had a current anxiety disorder. It also noted that the National Survey on LGBTQ Youth Mental Health found that 72% of LGBTQ youth and 77% of transgender and nonbinary youth described general anxiety disorder symptoms.
“Anxiety disorders in childhood and adolescence are associated with an increased likelihood of a future anxiety disorder or depression,” the task force authors wrote.
They highlighted that “the prevalence of anxiety in Black youth may be evolving.” Previously, studies had suggested that young Black people may have had lower rates of mental health disorders, compared with their White counterparts.
“However, recent cohorts of Black children or adolescents have reported a higher prevalence of anxiety disorders than in the past,” the authors wrote.
Joanna Quigley, MD, clinical associate professor and associate medical director for child & adolescent services at the University of Michigan, Ann Arbor, said in an interview she was not surprised the USPSTF recommended screening for anxiety starting at age 8.
That’s when parents and providers see anxiety disorders begin to present or become more problematic, she said.
“It’s also acknowledging the importance of prevention,” she said. “The sooner we can identify these challenges for kids, the sooner we can intervene and have better outcomes for that child across their lifespan.”
Screening gets providers and families in the habit of thinking about these concerns when a child or adolescent comes in for another kind of visit, Dr. Quigley said. Chest pains in a well-child check, for example, may trigger thoughts to consider anxiety later if the child is brought in for a cardiac check for chest pains.
“It creates a culture of awareness that is important as well,” Dr. Quigley said. “I think part of what the task force is trying to do is saying that identifying anxiety can be a precursor to what could turn out to be related to depression or related to ADHD and factors we think about when we think about suicide risk as well.
“We’re seeing an increase in suicide in the younger age group as well, which is a huge concern, “ she noted.
Dr. Quigley said, if these recommendations are adopted after the comment period, pediatricians and family practice providers will likely be doing most of the screening for anxiety, but there may also be a role for the screening in pediatric subspecialty care, such as those treating children with chronic illness and in specialized mental health care.
She added: “This builds on the national conversation going on about the mental health crisis, declared a national emergency in the fall. This deserves attention in continuing the momentum.”
Factors that may signal higher risk for depression
While the USPSTF recommends screening for major depressive disorder in all adolescents aged 12 years and older, the USPSTF notes that several risk factors might help identify those at higher risk.
Markers for higher risk include a combination of factors such as a family history of depression, prior episode of depression, and other mental health or behavioral problems.
“Other psychosocial risk factors include childhood abuse or neglect, exposure to traumatic events, bullying (either as perpetrators or as victims), adverse life events, early exposure to stress, maltreatment, and an insecure parental relationship,” the task force authors wrote.
There was limited evidence, however, on the benefits and harms of screening children younger than 8 for anxiety and screening kids younger than 12 for depression.
Not enough evidence for suicide risk screening
The authors of the recommendations acknowledged that, while suicide is a leading cause of death for older children and teens, evidence is still too sparse to make recommendations regarding screening for suicide risk in those without signs or symptoms at any age.
They also explained that evidence is lacking and inconsistent on the effectiveness of treatment (psychotherapy, pharmacotherapy, or collaborative care) for suicide risk in improving outcomes in children and adolescents.
Comments on the USPSTF recommendations may be submitted until May 9, 2022. The USPSTF topic leads review all comments, revise the draft recommendations, put them to a vote by the full task force, and then post the final versions to the website.
The task force authors and Dr. Quigley reported no financial disclosures.
The U.S. Preventive Services Task Force on Apr. 12 posted draft recommendations on screening for depression and anxiety in children and adolescents.
For the first time, the USPSTF is recommending screening children ages 8 and older for anxiety.
It also recommended screening children ages 12 and older for depression, which was consistent with the USPSTF’s prior recommendations on the topic.
These B-grade draft recommendations are for children and teens who are not showing signs or symptoms of these conditions. The task force emphasized that anyone who has concerns about or shows signs of these conditions should be connected to care.
Task force member Martha Kubik, PhD, RN, a professor with George Mason University, Fairfax, Va, said in a statement: “Fortunately, we found that screening older children for anxiety and depression is effective in identifying these conditions so children and teens can be connected to the support they need.”
The group cited in its recommendation on anxiety the 2018-2019 National Survey of Children’s Health, which found that 7.8% of children and adolescents ages 3-17 years had a current anxiety disorder. It also noted that the National Survey on LGBTQ Youth Mental Health found that 72% of LGBTQ youth and 77% of transgender and nonbinary youth described general anxiety disorder symptoms.
“Anxiety disorders in childhood and adolescence are associated with an increased likelihood of a future anxiety disorder or depression,” the task force authors wrote.
They highlighted that “the prevalence of anxiety in Black youth may be evolving.” Previously, studies had suggested that young Black people may have had lower rates of mental health disorders, compared with their White counterparts.
“However, recent cohorts of Black children or adolescents have reported a higher prevalence of anxiety disorders than in the past,” the authors wrote.
Joanna Quigley, MD, clinical associate professor and associate medical director for child & adolescent services at the University of Michigan, Ann Arbor, said in an interview she was not surprised the USPSTF recommended screening for anxiety starting at age 8.
That’s when parents and providers see anxiety disorders begin to present or become more problematic, she said.
“It’s also acknowledging the importance of prevention,” she said. “The sooner we can identify these challenges for kids, the sooner we can intervene and have better outcomes for that child across their lifespan.”
Screening gets providers and families in the habit of thinking about these concerns when a child or adolescent comes in for another kind of visit, Dr. Quigley said. Chest pains in a well-child check, for example, may trigger thoughts to consider anxiety later if the child is brought in for a cardiac check for chest pains.
“It creates a culture of awareness that is important as well,” Dr. Quigley said. “I think part of what the task force is trying to do is saying that identifying anxiety can be a precursor to what could turn out to be related to depression or related to ADHD and factors we think about when we think about suicide risk as well.
“We’re seeing an increase in suicide in the younger age group as well, which is a huge concern, “ she noted.
Dr. Quigley said, if these recommendations are adopted after the comment period, pediatricians and family practice providers will likely be doing most of the screening for anxiety, but there may also be a role for the screening in pediatric subspecialty care, such as those treating children with chronic illness and in specialized mental health care.
She added: “This builds on the national conversation going on about the mental health crisis, declared a national emergency in the fall. This deserves attention in continuing the momentum.”
Factors that may signal higher risk for depression
While the USPSTF recommends screening for major depressive disorder in all adolescents aged 12 years and older, the USPSTF notes that several risk factors might help identify those at higher risk.
Markers for higher risk include a combination of factors such as a family history of depression, prior episode of depression, and other mental health or behavioral problems.
“Other psychosocial risk factors include childhood abuse or neglect, exposure to traumatic events, bullying (either as perpetrators or as victims), adverse life events, early exposure to stress, maltreatment, and an insecure parental relationship,” the task force authors wrote.
There was limited evidence, however, on the benefits and harms of screening children younger than 8 for anxiety and screening kids younger than 12 for depression.
Not enough evidence for suicide risk screening
The authors of the recommendations acknowledged that, while suicide is a leading cause of death for older children and teens, evidence is still too sparse to make recommendations regarding screening for suicide risk in those without signs or symptoms at any age.
They also explained that evidence is lacking and inconsistent on the effectiveness of treatment (psychotherapy, pharmacotherapy, or collaborative care) for suicide risk in improving outcomes in children and adolescents.
Comments on the USPSTF recommendations may be submitted until May 9, 2022. The USPSTF topic leads review all comments, revise the draft recommendations, put them to a vote by the full task force, and then post the final versions to the website.
The task force authors and Dr. Quigley reported no financial disclosures.
A new target in schizophrenia treatment: Brain gamma oscillations
In a randomized, double-blind study that included two dozen men with schizophrenia, AUT00206, compared with placebo, increased the power of gamma oscillations, which were in turn associated with positive symptom scores.
The investigators note that targeting a potassium channel linked to brain gamma oscillations may offer a novel way to treat schizophrenia.
In addition, lead author Charles Large, PhD, chief executive officer, Autifony Therapeutics, Stevenage, United Kingdom, told this news organization that it may be “important” to study patients relatively early in their disease course. Participants in the current study were diagnosed less than 5 years previously.
Many previous trials in this area have failed, “and some of the questions were maybe the patients were sort of beyond the point in which you can actually make a difference,” Dr. Large said.
The findings were presented at the Congress of the Schizophrenia International Research Society (SIRS) 2022.
‘Opportunity to intervene’
Dr. Large noted that patients with chronic, long-term symptoms of schizophrenia have been treated with antipsychotics for decades, “and the pathology of that stage is then different.”
For the current study, the investigators hypothesized that the brain may be more “plastic” earlier on in the disease course, and so “maybe there’s an opportunity to intervene and make a change,” said Dr. Large.
In addition, patients with schizophrenia have abnormalities in both their resting state and induced and evolved gamma oscillations, which can include increased resting state power – and reduced power and “phase locking” to cyclical stimuli – the researchers note.
Previous studies have suggested such abnormalities are associated with dysfunction in parvalbumin-expressing interneurons (PVINs) found in cortical and subcortical circuits.
Moreover, Kv3.1 potassium channels expressed on PVINs are integral to establishing and maintaining fast-firing activity and to network synchronization across the brain. They may, therefore, offer a “potential therapeutic approach” for countering PVIN dysfunction, the investigators write.
To examine the impact of AUT00206, a novel Kv3.1/Kv3.2 positive neuromodulator, on resting state and induced gamma oscillations, they conducted a randomized, double-blind study in 24 men with schizophrenia who were aged 18-50 years.
Participants had been diagnosed less than 5 years previously and were stable on a maximum of two antipsychotic medications. They were randomly assigned 2:1 to a loading 2,000-mg dose of AUT00206 on day 1 and then 800 mg twice daily for 27 days or to placebo.
At baseline/day 1, and on a further 3 days over the treatment period, the men underwent resting-state electroencephalography, 40-Hz auditory steady-state response stimulation, and deviant and standard stimulation in an auditory oddball paradigm to assess resting state, induced, and evoked oscillations, respectively.
Positive associations
Results showed that early auditory gamma responses were increased at day 28 in patients who received AUT00206 but not in those who received placebo. The active drug was also associated with increases in the power of gamma oscillations from Day 5 in response to stimuli but not in phase locking.
There was also a significant positive association between frontal resting gamma power and baseline Positive and Negative Syndrome Scale (PANSS) positive symptom severity scores (r = 0.675; P < .001).
Moreover, changes in PANSS positive scores were significantly correlated with a decrease in frontal resting gamma power in patients treated with AUT00206 (r = 0.532; P = .05).
While a similar correlation was not found with placebo, the investigators note this “may be in part due to the low number” of individuals in the group.
They add that a larger study is now needed to confirm their findings and to “explore efficacy versus clinical symptoms.”
However, Dr. Large noted that participants in their next study will have fragile X syndrome.
He added the reason for this is “not because we’ve given up on schizophrenia – we feel that schizophrenia is a massive opportunity.”
Patients with schizophrenia are heterogeneous, both in terms of their clinical course and prior treatment. So it is “impossible” for a company of their size to take all of that into account in a single study, Dr. Large said.
In contrast, fragile X is “genetically homogenous,” and so it is possible to focus on the deficit and then translate the findings out into a “broader population.”
Preliminary but worth pursuing?
Commenting on the study, James M. McNally, PhD, assistant professor of psychiatry, Harvard Medical School, Boston, said the findings are “quite preliminary” and that the investigators provided “limited information as to how their findings were derived.”
Nevertheless, it is “nice to see that they observed a significant correlation between resting gamma and positive symptom severity at baseline [and] that the observed change in gamma correlates with change in PANSS scores,” said Dr. McNally, who was not involved with the research.
He added that the “idea of targeting Kv3.1 function to restore PV neuron/gamma activity is very interesting and worth pursuing.”
The study was funded by Autifony Therapeutics, of which Dr. Large is an employee.
A version of this article first appeared on Medscape.com.
In a randomized, double-blind study that included two dozen men with schizophrenia, AUT00206, compared with placebo, increased the power of gamma oscillations, which were in turn associated with positive symptom scores.
The investigators note that targeting a potassium channel linked to brain gamma oscillations may offer a novel way to treat schizophrenia.
In addition, lead author Charles Large, PhD, chief executive officer, Autifony Therapeutics, Stevenage, United Kingdom, told this news organization that it may be “important” to study patients relatively early in their disease course. Participants in the current study were diagnosed less than 5 years previously.
Many previous trials in this area have failed, “and some of the questions were maybe the patients were sort of beyond the point in which you can actually make a difference,” Dr. Large said.
The findings were presented at the Congress of the Schizophrenia International Research Society (SIRS) 2022.
‘Opportunity to intervene’
Dr. Large noted that patients with chronic, long-term symptoms of schizophrenia have been treated with antipsychotics for decades, “and the pathology of that stage is then different.”
For the current study, the investigators hypothesized that the brain may be more “plastic” earlier on in the disease course, and so “maybe there’s an opportunity to intervene and make a change,” said Dr. Large.
In addition, patients with schizophrenia have abnormalities in both their resting state and induced and evolved gamma oscillations, which can include increased resting state power – and reduced power and “phase locking” to cyclical stimuli – the researchers note.
Previous studies have suggested such abnormalities are associated with dysfunction in parvalbumin-expressing interneurons (PVINs) found in cortical and subcortical circuits.
Moreover, Kv3.1 potassium channels expressed on PVINs are integral to establishing and maintaining fast-firing activity and to network synchronization across the brain. They may, therefore, offer a “potential therapeutic approach” for countering PVIN dysfunction, the investigators write.
To examine the impact of AUT00206, a novel Kv3.1/Kv3.2 positive neuromodulator, on resting state and induced gamma oscillations, they conducted a randomized, double-blind study in 24 men with schizophrenia who were aged 18-50 years.
Participants had been diagnosed less than 5 years previously and were stable on a maximum of two antipsychotic medications. They were randomly assigned 2:1 to a loading 2,000-mg dose of AUT00206 on day 1 and then 800 mg twice daily for 27 days or to placebo.
At baseline/day 1, and on a further 3 days over the treatment period, the men underwent resting-state electroencephalography, 40-Hz auditory steady-state response stimulation, and deviant and standard stimulation in an auditory oddball paradigm to assess resting state, induced, and evoked oscillations, respectively.
Positive associations
Results showed that early auditory gamma responses were increased at day 28 in patients who received AUT00206 but not in those who received placebo. The active drug was also associated with increases in the power of gamma oscillations from Day 5 in response to stimuli but not in phase locking.
There was also a significant positive association between frontal resting gamma power and baseline Positive and Negative Syndrome Scale (PANSS) positive symptom severity scores (r = 0.675; P < .001).
Moreover, changes in PANSS positive scores were significantly correlated with a decrease in frontal resting gamma power in patients treated with AUT00206 (r = 0.532; P = .05).
While a similar correlation was not found with placebo, the investigators note this “may be in part due to the low number” of individuals in the group.
They add that a larger study is now needed to confirm their findings and to “explore efficacy versus clinical symptoms.”
However, Dr. Large noted that participants in their next study will have fragile X syndrome.
He added the reason for this is “not because we’ve given up on schizophrenia – we feel that schizophrenia is a massive opportunity.”
Patients with schizophrenia are heterogeneous, both in terms of their clinical course and prior treatment. So it is “impossible” for a company of their size to take all of that into account in a single study, Dr. Large said.
In contrast, fragile X is “genetically homogenous,” and so it is possible to focus on the deficit and then translate the findings out into a “broader population.”
Preliminary but worth pursuing?
Commenting on the study, James M. McNally, PhD, assistant professor of psychiatry, Harvard Medical School, Boston, said the findings are “quite preliminary” and that the investigators provided “limited information as to how their findings were derived.”
Nevertheless, it is “nice to see that they observed a significant correlation between resting gamma and positive symptom severity at baseline [and] that the observed change in gamma correlates with change in PANSS scores,” said Dr. McNally, who was not involved with the research.
He added that the “idea of targeting Kv3.1 function to restore PV neuron/gamma activity is very interesting and worth pursuing.”
The study was funded by Autifony Therapeutics, of which Dr. Large is an employee.
A version of this article first appeared on Medscape.com.
In a randomized, double-blind study that included two dozen men with schizophrenia, AUT00206, compared with placebo, increased the power of gamma oscillations, which were in turn associated with positive symptom scores.
The investigators note that targeting a potassium channel linked to brain gamma oscillations may offer a novel way to treat schizophrenia.
In addition, lead author Charles Large, PhD, chief executive officer, Autifony Therapeutics, Stevenage, United Kingdom, told this news organization that it may be “important” to study patients relatively early in their disease course. Participants in the current study were diagnosed less than 5 years previously.
Many previous trials in this area have failed, “and some of the questions were maybe the patients were sort of beyond the point in which you can actually make a difference,” Dr. Large said.
The findings were presented at the Congress of the Schizophrenia International Research Society (SIRS) 2022.
‘Opportunity to intervene’
Dr. Large noted that patients with chronic, long-term symptoms of schizophrenia have been treated with antipsychotics for decades, “and the pathology of that stage is then different.”
For the current study, the investigators hypothesized that the brain may be more “plastic” earlier on in the disease course, and so “maybe there’s an opportunity to intervene and make a change,” said Dr. Large.
In addition, patients with schizophrenia have abnormalities in both their resting state and induced and evolved gamma oscillations, which can include increased resting state power – and reduced power and “phase locking” to cyclical stimuli – the researchers note.
Previous studies have suggested such abnormalities are associated with dysfunction in parvalbumin-expressing interneurons (PVINs) found in cortical and subcortical circuits.
Moreover, Kv3.1 potassium channels expressed on PVINs are integral to establishing and maintaining fast-firing activity and to network synchronization across the brain. They may, therefore, offer a “potential therapeutic approach” for countering PVIN dysfunction, the investigators write.
To examine the impact of AUT00206, a novel Kv3.1/Kv3.2 positive neuromodulator, on resting state and induced gamma oscillations, they conducted a randomized, double-blind study in 24 men with schizophrenia who were aged 18-50 years.
Participants had been diagnosed less than 5 years previously and were stable on a maximum of two antipsychotic medications. They were randomly assigned 2:1 to a loading 2,000-mg dose of AUT00206 on day 1 and then 800 mg twice daily for 27 days or to placebo.
At baseline/day 1, and on a further 3 days over the treatment period, the men underwent resting-state electroencephalography, 40-Hz auditory steady-state response stimulation, and deviant and standard stimulation in an auditory oddball paradigm to assess resting state, induced, and evoked oscillations, respectively.
Positive associations
Results showed that early auditory gamma responses were increased at day 28 in patients who received AUT00206 but not in those who received placebo. The active drug was also associated with increases in the power of gamma oscillations from Day 5 in response to stimuli but not in phase locking.
There was also a significant positive association between frontal resting gamma power and baseline Positive and Negative Syndrome Scale (PANSS) positive symptom severity scores (r = 0.675; P < .001).
Moreover, changes in PANSS positive scores were significantly correlated with a decrease in frontal resting gamma power in patients treated with AUT00206 (r = 0.532; P = .05).
While a similar correlation was not found with placebo, the investigators note this “may be in part due to the low number” of individuals in the group.
They add that a larger study is now needed to confirm their findings and to “explore efficacy versus clinical symptoms.”
However, Dr. Large noted that participants in their next study will have fragile X syndrome.
He added the reason for this is “not because we’ve given up on schizophrenia – we feel that schizophrenia is a massive opportunity.”
Patients with schizophrenia are heterogeneous, both in terms of their clinical course and prior treatment. So it is “impossible” for a company of their size to take all of that into account in a single study, Dr. Large said.
In contrast, fragile X is “genetically homogenous,” and so it is possible to focus on the deficit and then translate the findings out into a “broader population.”
Preliminary but worth pursuing?
Commenting on the study, James M. McNally, PhD, assistant professor of psychiatry, Harvard Medical School, Boston, said the findings are “quite preliminary” and that the investigators provided “limited information as to how their findings were derived.”
Nevertheless, it is “nice to see that they observed a significant correlation between resting gamma and positive symptom severity at baseline [and] that the observed change in gamma correlates with change in PANSS scores,” said Dr. McNally, who was not involved with the research.
He added that the “idea of targeting Kv3.1 function to restore PV neuron/gamma activity is very interesting and worth pursuing.”
The study was funded by Autifony Therapeutics, of which Dr. Large is an employee.
A version of this article first appeared on Medscape.com.
FROM SIRS 2022
COVID-19 cardiovascular complications in children: AHA statement
Cardiovascular complications are uncommon for children and young adults after COVID-19 disease or SARS-CoV-2 infection, according to a new scientific statement from the American Heart Association.
However, the infection can cause some children and young people to experience arrhythmias, myocarditis, pericarditis, or multisystem inflammatory syndrome (MIS-C), a new condition identified during the pandemic, it notes.
The statement details what has been learned about how to treat, manage, and prevent cardiovascular complications associated with COVID-19 in children and young adults and calls for more research, including studies following the short- and long-term cardiovascular effects.
It also reports that COVID-19 vaccines have been found to prevent severe COVID-19 disease and decrease the risk of developing MIS-C by 91% among children ages 12-18 years.
On returning to sports, it says data suggest it is safe for young people with mild or asymptomatic COVID-19 to resume exercise after recovery from symptoms. For those with more serious infections, it recommends additional tests, including cardiac enzyme levels, electrocardiogram, and echocardiogram, before returning to sports or strenuous physical exercise.
The scientific statement was published online on in Circulation.
“Two years into the pandemic and with vast amounts of research conducted in children with COVID-19, this statement summarizes what we know so far related to COVID-19 in children,” said chair of the statement writing group Pei-Ni Jone, MD, from the Children’s Hospital Colorado, Aurora.
Analysis of the latest research indicates children generally have mild symptoms from SARS-CoV-2 infection. In the U.S., as of Feb. 24, 2022, children under 18 years of age have accounted for 17.6% of total COVID-19 cases and about 0.1% of deaths from the virus, the report states.
In addition, young adults, ages 18-29 years, have accounted for 21.3% of cases and 0.8% of deaths from COVID-19.
Like adults, children with underlying medical conditions such as chronic lung disease or obesity and those who are immunocompromised are more likely to be hospitalized, to be admitted to an intensive care unit, and to die of COVID-19, the statement notes. There are conflicting reports on the risk of severe COVID-19 in children and young adults with congenital heart disease, with some reports suggesting a slightly increased risk of severe COVID-19.
In terms of cardiovascular complications of COVID-19 in children, arrhythmias have included ventricular tachycardia and atrial tachycardia, as well as first-degree atrioventricular block. Although arrhythmias generally self-resolve without the need for treatment, prophylactic antiarrhythmics have been administered in some cases, and death caused by recurrent ventricular tachycardia in an adolescent with hypertrophic cardiomyopathy has been described.
Elevations of troponin, electrocardiographic abnormalities, including ST-segment changes, and delayed gadolinium enhancement on cardiac magnetic resonance imaging have been seen in those with myocardial involvement. Although death is rare, both sudden cardiac death and death after intensive medical and supportive therapies have occurred in children with severe myocardial involvement.
In a large retrospective pediatric case series of SARS-CoV-2–associated deaths in individuals under 21 years of age, the median age at death was 17 years, 63% were male, 28% were Black, and 46% were Hispanic. Of those who died, 86% had a comorbid condition, with obesity (42%) and asthma (29%) being the most common.
But the report concludes that: “Although children with comorbidities are at increased risk for symptomatic SARS-CoV-2 infection, compared with healthy children, cardiovascular complications, severe illness, and death are uncommon.”
MIS-C: Rare but severe
The authors of the statement explain that children and some young adults may develop MIS-C, a relatively rare but severe inflammatory syndrome generally occurring 2-6 weeks after infection with SARS-CoV-2 that can affect the heart and multiple organ systems.
In the first year of the pandemic, more than 2,600 cases of MIS-C were reported to the Centers for Disease Control and Prevention, at an estimated rate of 1 case per 3,164 cases of SARS-CoV-2 infection in children, with MIS-C disproportionately affecting Hispanic and Black children.
As many as 50% of children with MIS-C have myocardial involvement, including decreased left ventricular function, coronary artery dilation or aneurysms, myocarditis, elevated troponin and BNP or NT-proBNP, or pericardial effusion. Acute-phase reactants, including C-reactive protein, D-dimer, ferritin, and fibrinogen, can be significantly elevated in MIS-C, neutrophil/lymphocyte ratio may be higher, and platelet counts lower than those with non–MIS-C febrile illnesses.
Fortunately, the outcome of MIS-C is generally very good, with resolution of inflammation and cardiovascular abnormalities within 1-4 weeks of diagnosis, the report says.
However, there have been reports of progression of coronary artery aneurysms after discharge, highlighting the potential for long-term complications. Death resulting from MIS-C is rare, with a mortality rate of 1.4%-1.9%.
Compared with children and young adults who died of acute SARS-CoV-2 infection, most of the fatalities from MIS-C were in previously healthy individuals without comorbidities.
The authors recommend structured follow-up of patients with MIS-C because of concern about progression of cardiac complications and an unclear long-term prognosis.
The statement notes that the first-line treatment for MIS-C is typically intravenous immunoglobulin (IVIG) and patients with poor ventricular function may need to have IVIG in divided doses to tolerate the fluid load.
Supportive treatment for heart failure and vasoplegic shock often requires aggressive management in an ICU for administration of inotropes and vasoactive medications. Antiplatelet therapy with low-dose aspirin is considered in patients with coronary artery involvement, and anticoagulation is added, depending on the degree of coronary artery dilation.
COVID-19 vaccination
The statement notes that vaccines can prevent patients from getting COVID-19 and decrease the risk of MIS-C by 91% among children 12-18 years of age.
On vaccine-associated myocarditis, it concludes the benefits of getting the vaccines outweigh the risks.
For example, for every 1 million doses of the mRNA COVID-19 vaccines in males ages 12-29 years (the highest risk group for vaccine-associated myocarditis), it is estimated that 11,000 COVID-19 cases, 560 hospitalizations, and six deaths would be prevented, whereas 39-47 cases of myocarditis would be expected.
But it adds that the CDC is continuing to follow myocarditis in children and young adults closely, particularly a possible connection to the mRNA COVID-19 vaccines.
The statement says that more research is needed to better understand the mechanisms and optimal treatment approaches for SARS-CoV-2 infection, vaccine-associated myocarditis, the long-term outcomes of both COVID-19 and MIS-C, and the impact of these various conditions on the heart in children and young adults. In addition, any new antiviral therapies need to be tested in clinical trials focused on children.
“Although much has been learned about how the virus impacts children’s and young adult’s hearts, how to best treat cardiovascular complications, and prevent severe illness, continued clinical research trials are needed to better understand the long-term cardiovascular impacts,” Dr. Jone said. “It is also important to address health disparities that have become more apparent during the pandemic. We must work to ensure all children receive equal access to vaccination and high-quality care.”
A version of this article first appeared on Medscape.com.
Cardiovascular complications are uncommon for children and young adults after COVID-19 disease or SARS-CoV-2 infection, according to a new scientific statement from the American Heart Association.
However, the infection can cause some children and young people to experience arrhythmias, myocarditis, pericarditis, or multisystem inflammatory syndrome (MIS-C), a new condition identified during the pandemic, it notes.
The statement details what has been learned about how to treat, manage, and prevent cardiovascular complications associated with COVID-19 in children and young adults and calls for more research, including studies following the short- and long-term cardiovascular effects.
It also reports that COVID-19 vaccines have been found to prevent severe COVID-19 disease and decrease the risk of developing MIS-C by 91% among children ages 12-18 years.
On returning to sports, it says data suggest it is safe for young people with mild or asymptomatic COVID-19 to resume exercise after recovery from symptoms. For those with more serious infections, it recommends additional tests, including cardiac enzyme levels, electrocardiogram, and echocardiogram, before returning to sports or strenuous physical exercise.
The scientific statement was published online on in Circulation.
“Two years into the pandemic and with vast amounts of research conducted in children with COVID-19, this statement summarizes what we know so far related to COVID-19 in children,” said chair of the statement writing group Pei-Ni Jone, MD, from the Children’s Hospital Colorado, Aurora.
Analysis of the latest research indicates children generally have mild symptoms from SARS-CoV-2 infection. In the U.S., as of Feb. 24, 2022, children under 18 years of age have accounted for 17.6% of total COVID-19 cases and about 0.1% of deaths from the virus, the report states.
In addition, young adults, ages 18-29 years, have accounted for 21.3% of cases and 0.8% of deaths from COVID-19.
Like adults, children with underlying medical conditions such as chronic lung disease or obesity and those who are immunocompromised are more likely to be hospitalized, to be admitted to an intensive care unit, and to die of COVID-19, the statement notes. There are conflicting reports on the risk of severe COVID-19 in children and young adults with congenital heart disease, with some reports suggesting a slightly increased risk of severe COVID-19.
In terms of cardiovascular complications of COVID-19 in children, arrhythmias have included ventricular tachycardia and atrial tachycardia, as well as first-degree atrioventricular block. Although arrhythmias generally self-resolve without the need for treatment, prophylactic antiarrhythmics have been administered in some cases, and death caused by recurrent ventricular tachycardia in an adolescent with hypertrophic cardiomyopathy has been described.
Elevations of troponin, electrocardiographic abnormalities, including ST-segment changes, and delayed gadolinium enhancement on cardiac magnetic resonance imaging have been seen in those with myocardial involvement. Although death is rare, both sudden cardiac death and death after intensive medical and supportive therapies have occurred in children with severe myocardial involvement.
In a large retrospective pediatric case series of SARS-CoV-2–associated deaths in individuals under 21 years of age, the median age at death was 17 years, 63% were male, 28% were Black, and 46% were Hispanic. Of those who died, 86% had a comorbid condition, with obesity (42%) and asthma (29%) being the most common.
But the report concludes that: “Although children with comorbidities are at increased risk for symptomatic SARS-CoV-2 infection, compared with healthy children, cardiovascular complications, severe illness, and death are uncommon.”
MIS-C: Rare but severe
The authors of the statement explain that children and some young adults may develop MIS-C, a relatively rare but severe inflammatory syndrome generally occurring 2-6 weeks after infection with SARS-CoV-2 that can affect the heart and multiple organ systems.
In the first year of the pandemic, more than 2,600 cases of MIS-C were reported to the Centers for Disease Control and Prevention, at an estimated rate of 1 case per 3,164 cases of SARS-CoV-2 infection in children, with MIS-C disproportionately affecting Hispanic and Black children.
As many as 50% of children with MIS-C have myocardial involvement, including decreased left ventricular function, coronary artery dilation or aneurysms, myocarditis, elevated troponin and BNP or NT-proBNP, or pericardial effusion. Acute-phase reactants, including C-reactive protein, D-dimer, ferritin, and fibrinogen, can be significantly elevated in MIS-C, neutrophil/lymphocyte ratio may be higher, and platelet counts lower than those with non–MIS-C febrile illnesses.
Fortunately, the outcome of MIS-C is generally very good, with resolution of inflammation and cardiovascular abnormalities within 1-4 weeks of diagnosis, the report says.
However, there have been reports of progression of coronary artery aneurysms after discharge, highlighting the potential for long-term complications. Death resulting from MIS-C is rare, with a mortality rate of 1.4%-1.9%.
Compared with children and young adults who died of acute SARS-CoV-2 infection, most of the fatalities from MIS-C were in previously healthy individuals without comorbidities.
The authors recommend structured follow-up of patients with MIS-C because of concern about progression of cardiac complications and an unclear long-term prognosis.
The statement notes that the first-line treatment for MIS-C is typically intravenous immunoglobulin (IVIG) and patients with poor ventricular function may need to have IVIG in divided doses to tolerate the fluid load.
Supportive treatment for heart failure and vasoplegic shock often requires aggressive management in an ICU for administration of inotropes and vasoactive medications. Antiplatelet therapy with low-dose aspirin is considered in patients with coronary artery involvement, and anticoagulation is added, depending on the degree of coronary artery dilation.
COVID-19 vaccination
The statement notes that vaccines can prevent patients from getting COVID-19 and decrease the risk of MIS-C by 91% among children 12-18 years of age.
On vaccine-associated myocarditis, it concludes the benefits of getting the vaccines outweigh the risks.
For example, for every 1 million doses of the mRNA COVID-19 vaccines in males ages 12-29 years (the highest risk group for vaccine-associated myocarditis), it is estimated that 11,000 COVID-19 cases, 560 hospitalizations, and six deaths would be prevented, whereas 39-47 cases of myocarditis would be expected.
But it adds that the CDC is continuing to follow myocarditis in children and young adults closely, particularly a possible connection to the mRNA COVID-19 vaccines.
The statement says that more research is needed to better understand the mechanisms and optimal treatment approaches for SARS-CoV-2 infection, vaccine-associated myocarditis, the long-term outcomes of both COVID-19 and MIS-C, and the impact of these various conditions on the heart in children and young adults. In addition, any new antiviral therapies need to be tested in clinical trials focused on children.
“Although much has been learned about how the virus impacts children’s and young adult’s hearts, how to best treat cardiovascular complications, and prevent severe illness, continued clinical research trials are needed to better understand the long-term cardiovascular impacts,” Dr. Jone said. “It is also important to address health disparities that have become more apparent during the pandemic. We must work to ensure all children receive equal access to vaccination and high-quality care.”
A version of this article first appeared on Medscape.com.
Cardiovascular complications are uncommon for children and young adults after COVID-19 disease or SARS-CoV-2 infection, according to a new scientific statement from the American Heart Association.
However, the infection can cause some children and young people to experience arrhythmias, myocarditis, pericarditis, or multisystem inflammatory syndrome (MIS-C), a new condition identified during the pandemic, it notes.
The statement details what has been learned about how to treat, manage, and prevent cardiovascular complications associated with COVID-19 in children and young adults and calls for more research, including studies following the short- and long-term cardiovascular effects.
It also reports that COVID-19 vaccines have been found to prevent severe COVID-19 disease and decrease the risk of developing MIS-C by 91% among children ages 12-18 years.
On returning to sports, it says data suggest it is safe for young people with mild or asymptomatic COVID-19 to resume exercise after recovery from symptoms. For those with more serious infections, it recommends additional tests, including cardiac enzyme levels, electrocardiogram, and echocardiogram, before returning to sports or strenuous physical exercise.
The scientific statement was published online on in Circulation.
“Two years into the pandemic and with vast amounts of research conducted in children with COVID-19, this statement summarizes what we know so far related to COVID-19 in children,” said chair of the statement writing group Pei-Ni Jone, MD, from the Children’s Hospital Colorado, Aurora.
Analysis of the latest research indicates children generally have mild symptoms from SARS-CoV-2 infection. In the U.S., as of Feb. 24, 2022, children under 18 years of age have accounted for 17.6% of total COVID-19 cases and about 0.1% of deaths from the virus, the report states.
In addition, young adults, ages 18-29 years, have accounted for 21.3% of cases and 0.8% of deaths from COVID-19.
Like adults, children with underlying medical conditions such as chronic lung disease or obesity and those who are immunocompromised are more likely to be hospitalized, to be admitted to an intensive care unit, and to die of COVID-19, the statement notes. There are conflicting reports on the risk of severe COVID-19 in children and young adults with congenital heart disease, with some reports suggesting a slightly increased risk of severe COVID-19.
In terms of cardiovascular complications of COVID-19 in children, arrhythmias have included ventricular tachycardia and atrial tachycardia, as well as first-degree atrioventricular block. Although arrhythmias generally self-resolve without the need for treatment, prophylactic antiarrhythmics have been administered in some cases, and death caused by recurrent ventricular tachycardia in an adolescent with hypertrophic cardiomyopathy has been described.
Elevations of troponin, electrocardiographic abnormalities, including ST-segment changes, and delayed gadolinium enhancement on cardiac magnetic resonance imaging have been seen in those with myocardial involvement. Although death is rare, both sudden cardiac death and death after intensive medical and supportive therapies have occurred in children with severe myocardial involvement.
In a large retrospective pediatric case series of SARS-CoV-2–associated deaths in individuals under 21 years of age, the median age at death was 17 years, 63% were male, 28% were Black, and 46% were Hispanic. Of those who died, 86% had a comorbid condition, with obesity (42%) and asthma (29%) being the most common.
But the report concludes that: “Although children with comorbidities are at increased risk for symptomatic SARS-CoV-2 infection, compared with healthy children, cardiovascular complications, severe illness, and death are uncommon.”
MIS-C: Rare but severe
The authors of the statement explain that children and some young adults may develop MIS-C, a relatively rare but severe inflammatory syndrome generally occurring 2-6 weeks after infection with SARS-CoV-2 that can affect the heart and multiple organ systems.
In the first year of the pandemic, more than 2,600 cases of MIS-C were reported to the Centers for Disease Control and Prevention, at an estimated rate of 1 case per 3,164 cases of SARS-CoV-2 infection in children, with MIS-C disproportionately affecting Hispanic and Black children.
As many as 50% of children with MIS-C have myocardial involvement, including decreased left ventricular function, coronary artery dilation or aneurysms, myocarditis, elevated troponin and BNP or NT-proBNP, or pericardial effusion. Acute-phase reactants, including C-reactive protein, D-dimer, ferritin, and fibrinogen, can be significantly elevated in MIS-C, neutrophil/lymphocyte ratio may be higher, and platelet counts lower than those with non–MIS-C febrile illnesses.
Fortunately, the outcome of MIS-C is generally very good, with resolution of inflammation and cardiovascular abnormalities within 1-4 weeks of diagnosis, the report says.
However, there have been reports of progression of coronary artery aneurysms after discharge, highlighting the potential for long-term complications. Death resulting from MIS-C is rare, with a mortality rate of 1.4%-1.9%.
Compared with children and young adults who died of acute SARS-CoV-2 infection, most of the fatalities from MIS-C were in previously healthy individuals without comorbidities.
The authors recommend structured follow-up of patients with MIS-C because of concern about progression of cardiac complications and an unclear long-term prognosis.
The statement notes that the first-line treatment for MIS-C is typically intravenous immunoglobulin (IVIG) and patients with poor ventricular function may need to have IVIG in divided doses to tolerate the fluid load.
Supportive treatment for heart failure and vasoplegic shock often requires aggressive management in an ICU for administration of inotropes and vasoactive medications. Antiplatelet therapy with low-dose aspirin is considered in patients with coronary artery involvement, and anticoagulation is added, depending on the degree of coronary artery dilation.
COVID-19 vaccination
The statement notes that vaccines can prevent patients from getting COVID-19 and decrease the risk of MIS-C by 91% among children 12-18 years of age.
On vaccine-associated myocarditis, it concludes the benefits of getting the vaccines outweigh the risks.
For example, for every 1 million doses of the mRNA COVID-19 vaccines in males ages 12-29 years (the highest risk group for vaccine-associated myocarditis), it is estimated that 11,000 COVID-19 cases, 560 hospitalizations, and six deaths would be prevented, whereas 39-47 cases of myocarditis would be expected.
But it adds that the CDC is continuing to follow myocarditis in children and young adults closely, particularly a possible connection to the mRNA COVID-19 vaccines.
The statement says that more research is needed to better understand the mechanisms and optimal treatment approaches for SARS-CoV-2 infection, vaccine-associated myocarditis, the long-term outcomes of both COVID-19 and MIS-C, and the impact of these various conditions on the heart in children and young adults. In addition, any new antiviral therapies need to be tested in clinical trials focused on children.
“Although much has been learned about how the virus impacts children’s and young adult’s hearts, how to best treat cardiovascular complications, and prevent severe illness, continued clinical research trials are needed to better understand the long-term cardiovascular impacts,” Dr. Jone said. “It is also important to address health disparities that have become more apparent during the pandemic. We must work to ensure all children receive equal access to vaccination and high-quality care.”
A version of this article first appeared on Medscape.com.
FROM CIRCULATION
Central centrifugal cicatricial alopecia
THE PRESENTATION
A Early central centrifugal cicatricial alopecia with a small central patch of hair loss in a 45-year-old Black woman.
B Late central centrifugal cicatricial alopecia with a large central patch of hair loss in a 43-year-old Black woman.
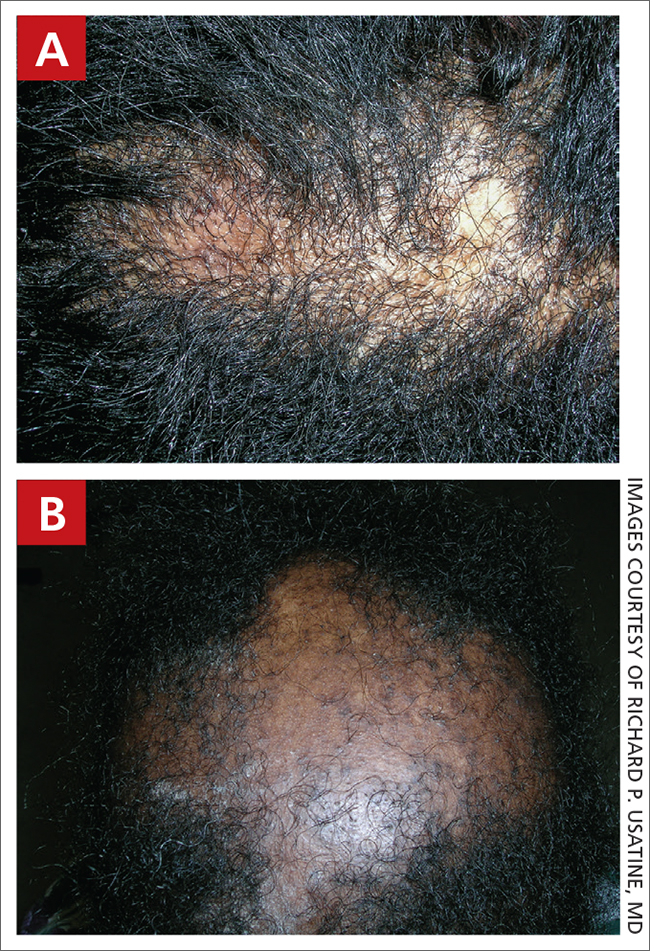
Scarring alopecia is a collection of hair loss disorders including chronic cutaneous lupus erythematosus (discoid lupus), lichen planopilaris, dissecting cellulitis, acne keloidalis, and central centrifugal cicatricial alopecia.1 CCCA (formerly hot comb alopecia or follicular degeneration syndrome) is a progressive, scarring, inflammatory alopecia and represents the most common form of scarring alopecia in women of African descent. It results in permanent destruction of hair follicles.
Epidemiology
CCCA predominantly affects women of African descent but also may affect men. The prevalence of CCCA in those of African descent has varied in the literature. Khumalo2 reported a prevalence of 1.2% for women younger than 50 years and 6.7% in women older than 50 years. CCCA has been reported in other ethnic groups, such as those of Asian descent.3
Historically, hair care practices that are more common in those of African descent, such as high-tension hairstyles as well as heat and chemical hair relaxers, were implicated in the development of CCCA. However, the causes of CCCA are most likely multifactorial, including family history, genetic mutations, and hair care practices.4-7 PADI3 mutations likely predispose some women to CCCA. Mutations in PADI3, which encodes peptidyl arginine deiminase 3 (an enzyme that modifies proteins crucial for the formation of hair shafts), were found in some patients with CCCA.8 Moreover, other genetic defects also likely play a role.7
Key clinical features
Early recognition is key for patients with CCCA.
- CCCA begins in the central scalp (crown area, vertex) and spreads centrifugally.
- Scalp symptoms such as tenderness, pain, a tingling or crawling sensation, and itching may occur.9 Some patients may not have any symptoms at all, and hair loss may progress painlessly.
- Central hair breakage—forme fruste CCCA—may be a presenting sign of CCCA.9
- Loss of follicular ostia and mottled hypopigmented and hyperpigmented macules are common findings.6
- CCCA can be diagnosed clinically and by histopathology.
Worth noting
Patients may experience hair loss and scalp symptoms for years before seeking medical evaluation. In some cultures, hair breakage or itching on the top of the scalp may be viewed as a normal occurrence in life.
It is important to set patient expectations that CCCA is a scarring alopecia, and the initial goal often is to maintain the patient's existing hair. However, hair and areas responding to treatment should still be treated. Without any intervention, the resulting scarring from CCCA may permanently scar follicles on the entire scalp.
Continue to: Due to the inflammatory...
Due to the inflammatory nature of CCCA, potent topical corticosteroids (eg, clobetasol propionate), intralesional corticosteroids (eg, triamcinolone acetonide), and oral antiinflammatory agents (eg, doxycycline) are utilized in the treatment of CCCA. Minoxidil is another treatment option. Adjuvant therapies such as topical metformin also have been tried.10 Importantly, treatment of CCCA may halt further permanent destruction of hair follicles, but scalp symptoms may reappear periodically and require re-treatment with anti-inflammatory agents.
Health care highlight
Thorough scalp examination and awareness of clinical features of CCCA may prompt earlier diagnosis and prevent future severe permanent alopecia. Clinicians should encourage patients with suggestive signs or symptoms of CCCA to seek care from a dermatologist.
1. Sperling LC. Scarring alopecia and the dermatopathologist. J Cutan Pathol. 2001;28:333-342. doi:10.1034/ j.1600-0560.2001.280701.x
2. Khumalo NP. Prevalence of central centrifugal cicatricial alopecia. Arch Dermatol. 2011;147:1453-1454. doi:10.1001/ archderm.147.12.1453
3. Su HJ, Cheng AY, Liu CH, et al. Primary scarring alopecia: a retrospective study of 89 patients in Taiwan [published online January 16, 2018]. J Dermatol. 2018;45:450-455. doi:10.1111/ 1346-8138.14217
4. Sperling LC, Cowper SE. The histopathology of primary cicatricial alopecia. Semin Cutan Med Surg. 2006;25:41-50
5. Dlova NC, Forder M. Central centrifugal cicatricial alopecia: possible familial aetiology in two African families from South Africa. Int J Dermatol. 2012;51(supp 1):17-20, 20-23.
6. Ogunleye TA, Quinn CR, McMichael A. Alopecia. In: Taylor SC, Kelly AP, Lim HW, et al, eds. Dermatology for Skin of Color. McGraw Hill; 2016:253-264.
7. Uitto J. Genetic susceptibility to alopecia [published online February 13, 2019]. N Engl J Med. 2019;380:873-876. doi:10.1056/ NEJMe1900042
8. Malki L, Sarig O, Romano MT, et al. Variant PADI3 in central centrifugal cicatricial alopecia. N Engl J Med. 2019;380:833-841.
9. Callender VD, Wright DR, Davis EC, et al. Hair breakage as a presenting sign of early or occult central centrifugal cicatricial alopecia: clinicopathologic findings in 9 patients. Arch Dermatol. 2012;148:1047-1052.
10. Araoye EF, Thomas JAL, Aguh CU. Hair regrowth in 2 patients with recalcitrant central centrifugal cicatricial alopecia after use of topical metformin. JAAD Case Rep. 2020;6:106-108. doi:10.1016/ j.jdcr.2019.12.008.
THE PRESENTATION
A Early central centrifugal cicatricial alopecia with a small central patch of hair loss in a 45-year-old Black woman.
B Late central centrifugal cicatricial alopecia with a large central patch of hair loss in a 43-year-old Black woman.
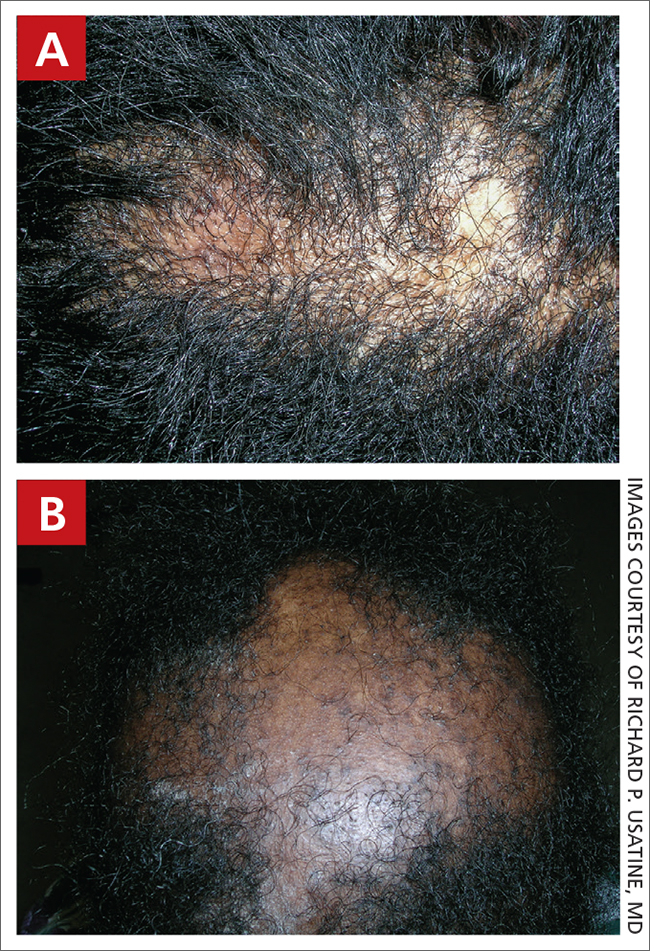
Scarring alopecia is a collection of hair loss disorders including chronic cutaneous lupus erythematosus (discoid lupus), lichen planopilaris, dissecting cellulitis, acne keloidalis, and central centrifugal cicatricial alopecia.1 CCCA (formerly hot comb alopecia or follicular degeneration syndrome) is a progressive, scarring, inflammatory alopecia and represents the most common form of scarring alopecia in women of African descent. It results in permanent destruction of hair follicles.
Epidemiology
CCCA predominantly affects women of African descent but also may affect men. The prevalence of CCCA in those of African descent has varied in the literature. Khumalo2 reported a prevalence of 1.2% for women younger than 50 years and 6.7% in women older than 50 years. CCCA has been reported in other ethnic groups, such as those of Asian descent.3
Historically, hair care practices that are more common in those of African descent, such as high-tension hairstyles as well as heat and chemical hair relaxers, were implicated in the development of CCCA. However, the causes of CCCA are most likely multifactorial, including family history, genetic mutations, and hair care practices.4-7 PADI3 mutations likely predispose some women to CCCA. Mutations in PADI3, which encodes peptidyl arginine deiminase 3 (an enzyme that modifies proteins crucial for the formation of hair shafts), were found in some patients with CCCA.8 Moreover, other genetic defects also likely play a role.7
Key clinical features
Early recognition is key for patients with CCCA.
- CCCA begins in the central scalp (crown area, vertex) and spreads centrifugally.
- Scalp symptoms such as tenderness, pain, a tingling or crawling sensation, and itching may occur.9 Some patients may not have any symptoms at all, and hair loss may progress painlessly.
- Central hair breakage—forme fruste CCCA—may be a presenting sign of CCCA.9
- Loss of follicular ostia and mottled hypopigmented and hyperpigmented macules are common findings.6
- CCCA can be diagnosed clinically and by histopathology.
Worth noting
Patients may experience hair loss and scalp symptoms for years before seeking medical evaluation. In some cultures, hair breakage or itching on the top of the scalp may be viewed as a normal occurrence in life.
It is important to set patient expectations that CCCA is a scarring alopecia, and the initial goal often is to maintain the patient's existing hair. However, hair and areas responding to treatment should still be treated. Without any intervention, the resulting scarring from CCCA may permanently scar follicles on the entire scalp.
Continue to: Due to the inflammatory...
Due to the inflammatory nature of CCCA, potent topical corticosteroids (eg, clobetasol propionate), intralesional corticosteroids (eg, triamcinolone acetonide), and oral antiinflammatory agents (eg, doxycycline) are utilized in the treatment of CCCA. Minoxidil is another treatment option. Adjuvant therapies such as topical metformin also have been tried.10 Importantly, treatment of CCCA may halt further permanent destruction of hair follicles, but scalp symptoms may reappear periodically and require re-treatment with anti-inflammatory agents.
Health care highlight
Thorough scalp examination and awareness of clinical features of CCCA may prompt earlier diagnosis and prevent future severe permanent alopecia. Clinicians should encourage patients with suggestive signs or symptoms of CCCA to seek care from a dermatologist.
THE PRESENTATION
A Early central centrifugal cicatricial alopecia with a small central patch of hair loss in a 45-year-old Black woman.
B Late central centrifugal cicatricial alopecia with a large central patch of hair loss in a 43-year-old Black woman.
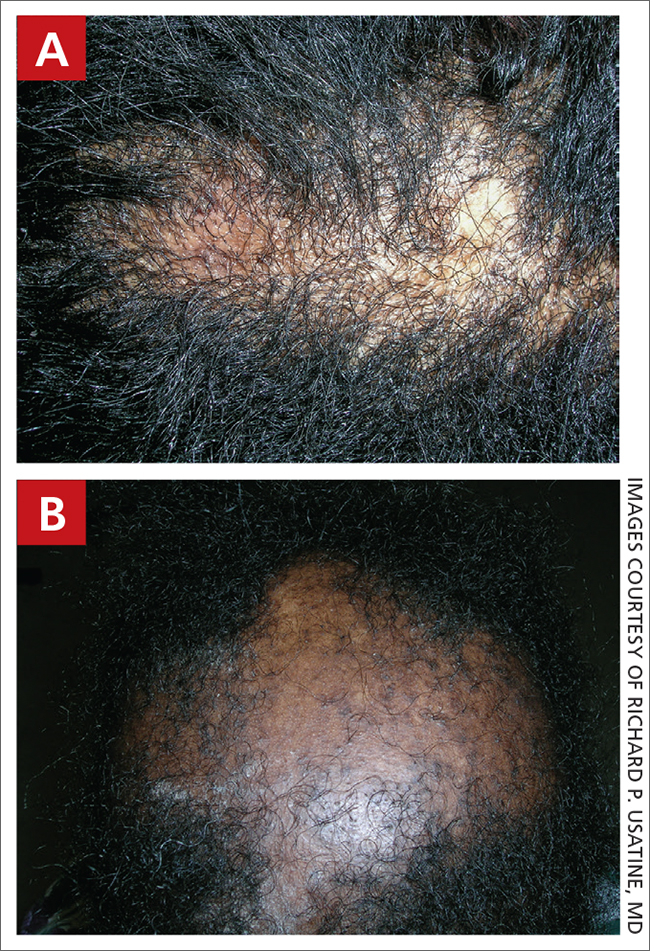
Scarring alopecia is a collection of hair loss disorders including chronic cutaneous lupus erythematosus (discoid lupus), lichen planopilaris, dissecting cellulitis, acne keloidalis, and central centrifugal cicatricial alopecia.1 CCCA (formerly hot comb alopecia or follicular degeneration syndrome) is a progressive, scarring, inflammatory alopecia and represents the most common form of scarring alopecia in women of African descent. It results in permanent destruction of hair follicles.
Epidemiology
CCCA predominantly affects women of African descent but also may affect men. The prevalence of CCCA in those of African descent has varied in the literature. Khumalo2 reported a prevalence of 1.2% for women younger than 50 years and 6.7% in women older than 50 years. CCCA has been reported in other ethnic groups, such as those of Asian descent.3
Historically, hair care practices that are more common in those of African descent, such as high-tension hairstyles as well as heat and chemical hair relaxers, were implicated in the development of CCCA. However, the causes of CCCA are most likely multifactorial, including family history, genetic mutations, and hair care practices.4-7 PADI3 mutations likely predispose some women to CCCA. Mutations in PADI3, which encodes peptidyl arginine deiminase 3 (an enzyme that modifies proteins crucial for the formation of hair shafts), were found in some patients with CCCA.8 Moreover, other genetic defects also likely play a role.7
Key clinical features
Early recognition is key for patients with CCCA.
- CCCA begins in the central scalp (crown area, vertex) and spreads centrifugally.
- Scalp symptoms such as tenderness, pain, a tingling or crawling sensation, and itching may occur.9 Some patients may not have any symptoms at all, and hair loss may progress painlessly.
- Central hair breakage—forme fruste CCCA—may be a presenting sign of CCCA.9
- Loss of follicular ostia and mottled hypopigmented and hyperpigmented macules are common findings.6
- CCCA can be diagnosed clinically and by histopathology.
Worth noting
Patients may experience hair loss and scalp symptoms for years before seeking medical evaluation. In some cultures, hair breakage or itching on the top of the scalp may be viewed as a normal occurrence in life.
It is important to set patient expectations that CCCA is a scarring alopecia, and the initial goal often is to maintain the patient's existing hair. However, hair and areas responding to treatment should still be treated. Without any intervention, the resulting scarring from CCCA may permanently scar follicles on the entire scalp.
Continue to: Due to the inflammatory...
Due to the inflammatory nature of CCCA, potent topical corticosteroids (eg, clobetasol propionate), intralesional corticosteroids (eg, triamcinolone acetonide), and oral antiinflammatory agents (eg, doxycycline) are utilized in the treatment of CCCA. Minoxidil is another treatment option. Adjuvant therapies such as topical metformin also have been tried.10 Importantly, treatment of CCCA may halt further permanent destruction of hair follicles, but scalp symptoms may reappear periodically and require re-treatment with anti-inflammatory agents.
Health care highlight
Thorough scalp examination and awareness of clinical features of CCCA may prompt earlier diagnosis and prevent future severe permanent alopecia. Clinicians should encourage patients with suggestive signs or symptoms of CCCA to seek care from a dermatologist.
1. Sperling LC. Scarring alopecia and the dermatopathologist. J Cutan Pathol. 2001;28:333-342. doi:10.1034/ j.1600-0560.2001.280701.x
2. Khumalo NP. Prevalence of central centrifugal cicatricial alopecia. Arch Dermatol. 2011;147:1453-1454. doi:10.1001/ archderm.147.12.1453
3. Su HJ, Cheng AY, Liu CH, et al. Primary scarring alopecia: a retrospective study of 89 patients in Taiwan [published online January 16, 2018]. J Dermatol. 2018;45:450-455. doi:10.1111/ 1346-8138.14217
4. Sperling LC, Cowper SE. The histopathology of primary cicatricial alopecia. Semin Cutan Med Surg. 2006;25:41-50
5. Dlova NC, Forder M. Central centrifugal cicatricial alopecia: possible familial aetiology in two African families from South Africa. Int J Dermatol. 2012;51(supp 1):17-20, 20-23.
6. Ogunleye TA, Quinn CR, McMichael A. Alopecia. In: Taylor SC, Kelly AP, Lim HW, et al, eds. Dermatology for Skin of Color. McGraw Hill; 2016:253-264.
7. Uitto J. Genetic susceptibility to alopecia [published online February 13, 2019]. N Engl J Med. 2019;380:873-876. doi:10.1056/ NEJMe1900042
8. Malki L, Sarig O, Romano MT, et al. Variant PADI3 in central centrifugal cicatricial alopecia. N Engl J Med. 2019;380:833-841.
9. Callender VD, Wright DR, Davis EC, et al. Hair breakage as a presenting sign of early or occult central centrifugal cicatricial alopecia: clinicopathologic findings in 9 patients. Arch Dermatol. 2012;148:1047-1052.
10. Araoye EF, Thomas JAL, Aguh CU. Hair regrowth in 2 patients with recalcitrant central centrifugal cicatricial alopecia after use of topical metformin. JAAD Case Rep. 2020;6:106-108. doi:10.1016/ j.jdcr.2019.12.008.
1. Sperling LC. Scarring alopecia and the dermatopathologist. J Cutan Pathol. 2001;28:333-342. doi:10.1034/ j.1600-0560.2001.280701.x
2. Khumalo NP. Prevalence of central centrifugal cicatricial alopecia. Arch Dermatol. 2011;147:1453-1454. doi:10.1001/ archderm.147.12.1453
3. Su HJ, Cheng AY, Liu CH, et al. Primary scarring alopecia: a retrospective study of 89 patients in Taiwan [published online January 16, 2018]. J Dermatol. 2018;45:450-455. doi:10.1111/ 1346-8138.14217
4. Sperling LC, Cowper SE. The histopathology of primary cicatricial alopecia. Semin Cutan Med Surg. 2006;25:41-50
5. Dlova NC, Forder M. Central centrifugal cicatricial alopecia: possible familial aetiology in two African families from South Africa. Int J Dermatol. 2012;51(supp 1):17-20, 20-23.
6. Ogunleye TA, Quinn CR, McMichael A. Alopecia. In: Taylor SC, Kelly AP, Lim HW, et al, eds. Dermatology for Skin of Color. McGraw Hill; 2016:253-264.
7. Uitto J. Genetic susceptibility to alopecia [published online February 13, 2019]. N Engl J Med. 2019;380:873-876. doi:10.1056/ NEJMe1900042
8. Malki L, Sarig O, Romano MT, et al. Variant PADI3 in central centrifugal cicatricial alopecia. N Engl J Med. 2019;380:833-841.
9. Callender VD, Wright DR, Davis EC, et al. Hair breakage as a presenting sign of early or occult central centrifugal cicatricial alopecia: clinicopathologic findings in 9 patients. Arch Dermatol. 2012;148:1047-1052.
10. Araoye EF, Thomas JAL, Aguh CU. Hair regrowth in 2 patients with recalcitrant central centrifugal cicatricial alopecia after use of topical metformin. JAAD Case Rep. 2020;6:106-108. doi:10.1016/ j.jdcr.2019.12.008.
High comorbidity rate seen before osteoarthritis diagnosis
presented at the OARSI 2022 World Congress.
“Some of the associations that we have found are previously known, such as of course, obesity, which is a known risk factor, but also other musculoskeletal conditions, depression, and reflux disease,” said Anne Kamps, an MD and PhD student at Erasmus University Medical Centre in Rotterdam, the Netherlands.
“But there are also some remarkable associations that we have found that are less well known, such as liver cirrhosis, thromboembolic disease, sinusitis, allergy, and migraine,” said Dr. Kamps during her presentation at the conference, sponsored by the Osteoarthritis Research Society International.
The results are “very interesting starting points for future research, because of course, this was an explorative study,” she added. Indeed, is still not known whether the comorbidities found share the same risk factors as OA, or if they have a causal effect and add to development of osteoarthritis.
Comorbidity and OA
One of the issues in managing osteoarthritis so far is that it’s often addressed as one disease, commented Andrea Dell’isola, PT, PhD, a postdoctoral researcher from Lund University who was not involved in the study.
“All of the treatments that have been developed and the treatment process are tailored to take care of one single disease,” he explained. However, “when we look at the characteristics of people with osteoarthritis, we see that roughly 70% of them have other conditions on top of their joint disease.” This high comorbidity rate is significantly higher than in “healthy” people of the same age and sex, he added.
“So, this means that either there is something linked to osteoarthritis that makes people frailer and more likely to develop other diseases, or there may be links between these other diseases, that we often call comorbidities, and osteoarthritis,” Dr. Dell’isola observed.
While the work Dr. Kamps presented looked at the rate of comorbidities that existed before the diagnosis of OA, some of Dr. Dell’isola’s recent research has considered the rate of developing comorbid disease in the years following an OA diagnosis. Associations were found between having hip or knee OA and an increased risk for coexisting depression, cardiovascular diseases, back pain, osteoporosis, and, in the case of knee OA only, diabetes. “It’s interesting to see that certain diseases seem to have a bidirectional association. This means that they can both precede and follow osteoarthritis,” said Dr. Dell’isola. These are just associations, not causation, he stressed, but they might help identify people visiting a doctor for other reasons who may be at risk for developing OA.
“One of the biggest challenges is that once a person develops osteoarthritis, there is not any treatment that can really change their disease,” he added.
Perhaps, “if we can target certain conditions that increase the risk of developing osteoarthritis, and maybe convince people to exercise earlier, or undergo some lifestyle changes early on, we can maybe prevent or delay the onset of the disease,” he suggested.
Results and perspective
Dr. Kamps and associates performed a nested case-control study using data from a large Dutch general practice database. All new cases of OA – which included hip, knee, and other peripheral OA – that were logged between the start of 2006 and the end of 2019 were considered and matched to one to four control subjects of a similar age, sex, and type of general practice. In all, there were just under 80,000 people with newly diagnosed OA who were matched to just over 318,000 controls; the mean age in both groups was 64 years.
Of 58 comorbidities that were assessed, 42 showed a positive association with OA and had odds ratios of 1 or more. The highest associations were found for fibromyalgia (OR, 1.9), obesity (1.8), polymyalgia rheumatica (1.5), spinal disc herniation (1.4), and gout (1.4). A further 13 comorbidities had an OR of about 1, and 3 (all neuropsychiatric conditions – dementia, schizophrenia, and multiple sclerosis) had an OR of below 1.
Dr. Kamps conceded that this type of research has its limitations, the two most important being the coding behavior of the GP and the consulting behavior of patients.
“It’s known that the prevalence of osteoarthritis is underestimated if you only use the diagnostic codes, because some GPs will write the diagnosis in free text or use symptom ICPC codes,” she said.
“We have matched on general practice, so the cases and controls were from the same general practice and therefore we hope that this potential underestimation is balanced and did not affect our odds ratios.”
One of the important outcomes for this research is that it will hopefully be used to inform future clinical practice guidelines, said Dr. Dell’isola.
“Guidelines in osteoarthritis report that is important to screen for comorbidities, but they give no indication on how to deal with the presence of multimorbidity,” he added. Looking at which comorbidities may be associated with OA diagnosis could potentially help to give a bit more of a prescriptive guide on what to look out for.
“Maybe people with a certain disease profile should be screened a bit more often by their doctor. For example, if someone has their blood pressure and diabetes under control, maybe there should be also a bit more attention to their joint health and encouragement to do exercise, not only for being active per se, but maybe also to reinforce their lower limbs,” he explained.
The study was funded by the Foundation for Research in Rheumatology (FOREUM). Dr. Kamps and Dr. Dell’isola, had no conflicts of interest to disclose.
presented at the OARSI 2022 World Congress.
“Some of the associations that we have found are previously known, such as of course, obesity, which is a known risk factor, but also other musculoskeletal conditions, depression, and reflux disease,” said Anne Kamps, an MD and PhD student at Erasmus University Medical Centre in Rotterdam, the Netherlands.
“But there are also some remarkable associations that we have found that are less well known, such as liver cirrhosis, thromboembolic disease, sinusitis, allergy, and migraine,” said Dr. Kamps during her presentation at the conference, sponsored by the Osteoarthritis Research Society International.
The results are “very interesting starting points for future research, because of course, this was an explorative study,” she added. Indeed, is still not known whether the comorbidities found share the same risk factors as OA, or if they have a causal effect and add to development of osteoarthritis.
Comorbidity and OA
One of the issues in managing osteoarthritis so far is that it’s often addressed as one disease, commented Andrea Dell’isola, PT, PhD, a postdoctoral researcher from Lund University who was not involved in the study.
“All of the treatments that have been developed and the treatment process are tailored to take care of one single disease,” he explained. However, “when we look at the characteristics of people with osteoarthritis, we see that roughly 70% of them have other conditions on top of their joint disease.” This high comorbidity rate is significantly higher than in “healthy” people of the same age and sex, he added.
“So, this means that either there is something linked to osteoarthritis that makes people frailer and more likely to develop other diseases, or there may be links between these other diseases, that we often call comorbidities, and osteoarthritis,” Dr. Dell’isola observed.
While the work Dr. Kamps presented looked at the rate of comorbidities that existed before the diagnosis of OA, some of Dr. Dell’isola’s recent research has considered the rate of developing comorbid disease in the years following an OA diagnosis. Associations were found between having hip or knee OA and an increased risk for coexisting depression, cardiovascular diseases, back pain, osteoporosis, and, in the case of knee OA only, diabetes. “It’s interesting to see that certain diseases seem to have a bidirectional association. This means that they can both precede and follow osteoarthritis,” said Dr. Dell’isola. These are just associations, not causation, he stressed, but they might help identify people visiting a doctor for other reasons who may be at risk for developing OA.
“One of the biggest challenges is that once a person develops osteoarthritis, there is not any treatment that can really change their disease,” he added.
Perhaps, “if we can target certain conditions that increase the risk of developing osteoarthritis, and maybe convince people to exercise earlier, or undergo some lifestyle changes early on, we can maybe prevent or delay the onset of the disease,” he suggested.
Results and perspective
Dr. Kamps and associates performed a nested case-control study using data from a large Dutch general practice database. All new cases of OA – which included hip, knee, and other peripheral OA – that were logged between the start of 2006 and the end of 2019 were considered and matched to one to four control subjects of a similar age, sex, and type of general practice. In all, there were just under 80,000 people with newly diagnosed OA who were matched to just over 318,000 controls; the mean age in both groups was 64 years.
Of 58 comorbidities that were assessed, 42 showed a positive association with OA and had odds ratios of 1 or more. The highest associations were found for fibromyalgia (OR, 1.9), obesity (1.8), polymyalgia rheumatica (1.5), spinal disc herniation (1.4), and gout (1.4). A further 13 comorbidities had an OR of about 1, and 3 (all neuropsychiatric conditions – dementia, schizophrenia, and multiple sclerosis) had an OR of below 1.
Dr. Kamps conceded that this type of research has its limitations, the two most important being the coding behavior of the GP and the consulting behavior of patients.
“It’s known that the prevalence of osteoarthritis is underestimated if you only use the diagnostic codes, because some GPs will write the diagnosis in free text or use symptom ICPC codes,” she said.
“We have matched on general practice, so the cases and controls were from the same general practice and therefore we hope that this potential underestimation is balanced and did not affect our odds ratios.”
One of the important outcomes for this research is that it will hopefully be used to inform future clinical practice guidelines, said Dr. Dell’isola.
“Guidelines in osteoarthritis report that is important to screen for comorbidities, but they give no indication on how to deal with the presence of multimorbidity,” he added. Looking at which comorbidities may be associated with OA diagnosis could potentially help to give a bit more of a prescriptive guide on what to look out for.
“Maybe people with a certain disease profile should be screened a bit more often by their doctor. For example, if someone has their blood pressure and diabetes under control, maybe there should be also a bit more attention to their joint health and encouragement to do exercise, not only for being active per se, but maybe also to reinforce their lower limbs,” he explained.
The study was funded by the Foundation for Research in Rheumatology (FOREUM). Dr. Kamps and Dr. Dell’isola, had no conflicts of interest to disclose.
presented at the OARSI 2022 World Congress.
“Some of the associations that we have found are previously known, such as of course, obesity, which is a known risk factor, but also other musculoskeletal conditions, depression, and reflux disease,” said Anne Kamps, an MD and PhD student at Erasmus University Medical Centre in Rotterdam, the Netherlands.
“But there are also some remarkable associations that we have found that are less well known, such as liver cirrhosis, thromboembolic disease, sinusitis, allergy, and migraine,” said Dr. Kamps during her presentation at the conference, sponsored by the Osteoarthritis Research Society International.
The results are “very interesting starting points for future research, because of course, this was an explorative study,” she added. Indeed, is still not known whether the comorbidities found share the same risk factors as OA, or if they have a causal effect and add to development of osteoarthritis.
Comorbidity and OA
One of the issues in managing osteoarthritis so far is that it’s often addressed as one disease, commented Andrea Dell’isola, PT, PhD, a postdoctoral researcher from Lund University who was not involved in the study.
“All of the treatments that have been developed and the treatment process are tailored to take care of one single disease,” he explained. However, “when we look at the characteristics of people with osteoarthritis, we see that roughly 70% of them have other conditions on top of their joint disease.” This high comorbidity rate is significantly higher than in “healthy” people of the same age and sex, he added.
“So, this means that either there is something linked to osteoarthritis that makes people frailer and more likely to develop other diseases, or there may be links between these other diseases, that we often call comorbidities, and osteoarthritis,” Dr. Dell’isola observed.
While the work Dr. Kamps presented looked at the rate of comorbidities that existed before the diagnosis of OA, some of Dr. Dell’isola’s recent research has considered the rate of developing comorbid disease in the years following an OA diagnosis. Associations were found between having hip or knee OA and an increased risk for coexisting depression, cardiovascular diseases, back pain, osteoporosis, and, in the case of knee OA only, diabetes. “It’s interesting to see that certain diseases seem to have a bidirectional association. This means that they can both precede and follow osteoarthritis,” said Dr. Dell’isola. These are just associations, not causation, he stressed, but they might help identify people visiting a doctor for other reasons who may be at risk for developing OA.
“One of the biggest challenges is that once a person develops osteoarthritis, there is not any treatment that can really change their disease,” he added.
Perhaps, “if we can target certain conditions that increase the risk of developing osteoarthritis, and maybe convince people to exercise earlier, or undergo some lifestyle changes early on, we can maybe prevent or delay the onset of the disease,” he suggested.
Results and perspective
Dr. Kamps and associates performed a nested case-control study using data from a large Dutch general practice database. All new cases of OA – which included hip, knee, and other peripheral OA – that were logged between the start of 2006 and the end of 2019 were considered and matched to one to four control subjects of a similar age, sex, and type of general practice. In all, there were just under 80,000 people with newly diagnosed OA who were matched to just over 318,000 controls; the mean age in both groups was 64 years.
Of 58 comorbidities that were assessed, 42 showed a positive association with OA and had odds ratios of 1 or more. The highest associations were found for fibromyalgia (OR, 1.9), obesity (1.8), polymyalgia rheumatica (1.5), spinal disc herniation (1.4), and gout (1.4). A further 13 comorbidities had an OR of about 1, and 3 (all neuropsychiatric conditions – dementia, schizophrenia, and multiple sclerosis) had an OR of below 1.
Dr. Kamps conceded that this type of research has its limitations, the two most important being the coding behavior of the GP and the consulting behavior of patients.
“It’s known that the prevalence of osteoarthritis is underestimated if you only use the diagnostic codes, because some GPs will write the diagnosis in free text or use symptom ICPC codes,” she said.
“We have matched on general practice, so the cases and controls were from the same general practice and therefore we hope that this potential underestimation is balanced and did not affect our odds ratios.”
One of the important outcomes for this research is that it will hopefully be used to inform future clinical practice guidelines, said Dr. Dell’isola.
“Guidelines in osteoarthritis report that is important to screen for comorbidities, but they give no indication on how to deal with the presence of multimorbidity,” he added. Looking at which comorbidities may be associated with OA diagnosis could potentially help to give a bit more of a prescriptive guide on what to look out for.
“Maybe people with a certain disease profile should be screened a bit more often by their doctor. For example, if someone has their blood pressure and diabetes under control, maybe there should be also a bit more attention to their joint health and encouragement to do exercise, not only for being active per se, but maybe also to reinforce their lower limbs,” he explained.
The study was funded by the Foundation for Research in Rheumatology (FOREUM). Dr. Kamps and Dr. Dell’isola, had no conflicts of interest to disclose.
FROM OARSI 2022
Empagliflozin rapidly improves acute heart failure symptoms in hospitalized patients
WASHINGTON – Treatment of patients acutely hospitalized for heart failure with the SGLT2 inhibitor empagliflozin led to a rapid incremental increase in patient well-being, compared with control patients who received placebo, that appeared after 2 weeks on treatment in a secondary analysis from 530 randomized patients in the EMPULSE trial.
To Mikhail N. Kosiborod, MD, a coinvestigator for EMPULSE who presented new analysis at the annual scientific sessions of the American College of Cardiology, the message from the quick response of acutely hospitalized patients to empagliflozin was clear: “Use these medications, SGLT2 [sodium-glucose cotransporter 2] inhibitors, as early as possible. We’ve seen with other medications that if they are not prescribed during hospitalization it’s unlikely to happen post discharge,” said Dr. Kosiborod, a cardiologist and codirector of the Haverty Cardiometabolic Center of Excellence at Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
“To our knowledge, the very early improvement in the Kansas City Cardiomyopathy Questionnaire [KCCQ] score – a well-known predictor of cardiovascular death and heart failure readmissions – that we observed with empagliflozin at 15 days is the first such observation, and if corroborated by future studies would suggest that initiation of SGLT2 inhibitors during hospitalization for acute heart failure may be a tool for improving the quality of hospital-to-home transitions,” wrote Dr. Kosiborod and his associates in the published version of their report that appeared concurrently with his report at the meeting.
“These data really support initiation [of empagliflozin or another SGLT2 inhibitor] in hospital, presuming that the patient has no contraindications,” commented Deepak L. Bhatt, MD, professor of medicine at Harvard Medical School in Boston and designated discussant for the report.
“The fact that the benefit kicks in so early is really important, because there is a bit of a penalty to wait” to start treatment with an agent from the SGLT2-inhibitor class, added Dr. Bhatt, who is also executive director of interventional cardiovascular programs at Brigham and Women’s Health, in Boston.
In hospital creates a teachable moment
Starting treatment when a patient is hospitalized is also important as “a teachable moment,” added Dr. Bhatt in an interview. “A physician can say to a patient ‘take this drug, and it will prevent you from returning to the hospital,’ at a time when it’s more likely to be impactful, compared with when a patient is out of the hospital and feeling okay and adherence will likely be much lower.”
The results Dr. Kosiborod reported on quality-of-life parameters measured with the KCCQ expanded on what he and his coinvestigators first reported in 2021 with the primary results from EMPULSE, which enrolled 530 patients at 118 centers in 15 countries during June 2020–February 2021. The trial randomized patients hospitalized for acute heart failure after a brief period of stabilization regardless of their left ventricular ejection fraction or presence of diabetes to receive a single, daily dose of 10 mg of empagliflozin (Jardiance) or placebo starting a median of 3 days after admission. Enrolled patients averaged about 71 years of age, about two-thirds were men, 45% had diabetes, 32% had left ventricular ejection fraction greater than 40%, and about two-thirds had decompensated chronic heart failure, while a third had acute de novo heart failure.
The primary outcome for EMPULSE was a combined endpoint of “total clinical endpoints” that included all-cause mortality, heart failure events (heart failure hospitalizations, urgent heart failure visits, and unplanned outpatient heart failure visits) or at least a 5-point change from baseline in the KCCQ score. Using a “win ratio” method for analyzing the composite endpoint, the primary analysis showed that treatment with empagliflozin for 90 days boosted the win ratio by a significant 36% relative to placebo (Nature Med. 2022 Mar;28[3]: 568-74).
Benefit independent of baseline symptomatic impairment
Among the new secondary analyses that Dr. Kosiborod reported was a post-hoc calculation that divided the study cohort into tertiles of baseline KCCQ score. The results showed that the degree of improvement for the primary, 90-day outcome of “total clinical benefit” compared with placebo was consistent across all three KCCQ-score tertiles, showing that empagliflozin’s benefit was “independent of symptomatic impairment at baseline,” he said.
The degree of improvement was also similar across all the tested domains of the KCCQ, including the overall summary, clinical summary, the physical limitations, and quality-of-life scores. Average improvement in KCCQ total symptom score 15 days after treatment onset was 5.35 points, compared with control patients. On an individual-patient basis, a change in KCCQ score of 5 points or more was previously shown to represent a clinically meaningful change.
“Treatment of patients with heart failure is geared to making patients live longer and stay out of the hospital. Enabling patients to feel better is an equally important goal of management, but not all treatments for heart failure can do that. These data from EMPULSE show that, in addition to other clinical benefits, patients also feel better on an SGLT2 inhibitor after just 2 weeks,” Dr. Kosiborod said in an interview.
EMPULSE builds on SOLOIST-WHF
EMPULSE is the second trial to show that an SGLT2 inhibitor can safely and effectively treat patients hospitalized for acute heart failure. Previously, results from the SOLOIST-WHF pivotal trial, which enrolled 1,222 patients with type 2 diabetes recently hospitalized for worsening heart failure, showed that treatment with an investigational, combined SGLT2 and SGLT1 inhibitor, sotagliflozin, resulted in a significant, 33% relative reduction in the primary outcome compared with placebo after a median 9 months of treatment.
“It’s reassuring to see two different drugs and research groups get essentially the same result, showing that starting an SGLT2 inhibitor is safe and effective in selected patients with no contraindications,” said Dr. Bhatt, who was lead investigator for SOLOIST-WHF.
The accumulating evidence for the safety and value of starting an SGLT2 inhibitor when patients are hospitalized for acute heart failure is making this approach increasingly routine for patients who present with heart failure with reduced ejection fraction at Saint Luke’s-Mid America Heart Institute, said Dr. Kosiborod, who is also a professor of medicine at the University of Missouri, Kansas City.
“I think we’ll also gradually start using [an SGLT2 inhibitor] in patients hospitalized with heart failure with preserved ejection fraction [HFpEF],” he added, based on the findings from SOLOIST-WHF and EMPULSE, and also recent evidence showing safety and efficacy of empagliflozin in patients with chronic HFpEF in the EMPEROR-Preserved trial, and for dapagliflozin (Farxiga) in the PRESERVED-HF trial.
Empagliflozin recently received from the U.S. Food and Drug Administration an expanded label indication for treating patients with heart failure with no specification for a level of left ventricular ejection fraction. An outcome trial of dapagliflozin in more than 6,000 patients with HFpEF, DELIVER, is currently ongoing but is expected to report results soon.
“The evidence is already compelling that the benefits outweigh the risk. Results from both SOLOIST-WHF and EMPULSE show that there are no significant safety concerns” when these agents are used in patients with acute heart failure,” Dr. Kosiborod declared.
EMPULSE was sponsored by Boehringer Ingelheim and Eli Lilly, the companies that jointly market empagliflozin (Jardiance). SOLOIST-WHF was sponsored by Sanofi and Lexicon, the companies that have been developing sotagliflozin. Dr. Kosiborod has been a consultant to and received research funding from Boehringer Ingelheim and Eli Lilly, and he has been a consultant or adviser to or led trials on behalf of numerous other companies. Dr. Bhatt has been an adviser to Boehringer Ingelheim and numerous other companies, and he has received research funding from Sanofi, Lexicon, Boehringer Ingelheim, Eli Lilly, and numerous other companies.
WASHINGTON – Treatment of patients acutely hospitalized for heart failure with the SGLT2 inhibitor empagliflozin led to a rapid incremental increase in patient well-being, compared with control patients who received placebo, that appeared after 2 weeks on treatment in a secondary analysis from 530 randomized patients in the EMPULSE trial.
To Mikhail N. Kosiborod, MD, a coinvestigator for EMPULSE who presented new analysis at the annual scientific sessions of the American College of Cardiology, the message from the quick response of acutely hospitalized patients to empagliflozin was clear: “Use these medications, SGLT2 [sodium-glucose cotransporter 2] inhibitors, as early as possible. We’ve seen with other medications that if they are not prescribed during hospitalization it’s unlikely to happen post discharge,” said Dr. Kosiborod, a cardiologist and codirector of the Haverty Cardiometabolic Center of Excellence at Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
“To our knowledge, the very early improvement in the Kansas City Cardiomyopathy Questionnaire [KCCQ] score – a well-known predictor of cardiovascular death and heart failure readmissions – that we observed with empagliflozin at 15 days is the first such observation, and if corroborated by future studies would suggest that initiation of SGLT2 inhibitors during hospitalization for acute heart failure may be a tool for improving the quality of hospital-to-home transitions,” wrote Dr. Kosiborod and his associates in the published version of their report that appeared concurrently with his report at the meeting.
“These data really support initiation [of empagliflozin or another SGLT2 inhibitor] in hospital, presuming that the patient has no contraindications,” commented Deepak L. Bhatt, MD, professor of medicine at Harvard Medical School in Boston and designated discussant for the report.
“The fact that the benefit kicks in so early is really important, because there is a bit of a penalty to wait” to start treatment with an agent from the SGLT2-inhibitor class, added Dr. Bhatt, who is also executive director of interventional cardiovascular programs at Brigham and Women’s Health, in Boston.
In hospital creates a teachable moment
Starting treatment when a patient is hospitalized is also important as “a teachable moment,” added Dr. Bhatt in an interview. “A physician can say to a patient ‘take this drug, and it will prevent you from returning to the hospital,’ at a time when it’s more likely to be impactful, compared with when a patient is out of the hospital and feeling okay and adherence will likely be much lower.”
The results Dr. Kosiborod reported on quality-of-life parameters measured with the KCCQ expanded on what he and his coinvestigators first reported in 2021 with the primary results from EMPULSE, which enrolled 530 patients at 118 centers in 15 countries during June 2020–February 2021. The trial randomized patients hospitalized for acute heart failure after a brief period of stabilization regardless of their left ventricular ejection fraction or presence of diabetes to receive a single, daily dose of 10 mg of empagliflozin (Jardiance) or placebo starting a median of 3 days after admission. Enrolled patients averaged about 71 years of age, about two-thirds were men, 45% had diabetes, 32% had left ventricular ejection fraction greater than 40%, and about two-thirds had decompensated chronic heart failure, while a third had acute de novo heart failure.
The primary outcome for EMPULSE was a combined endpoint of “total clinical endpoints” that included all-cause mortality, heart failure events (heart failure hospitalizations, urgent heart failure visits, and unplanned outpatient heart failure visits) or at least a 5-point change from baseline in the KCCQ score. Using a “win ratio” method for analyzing the composite endpoint, the primary analysis showed that treatment with empagliflozin for 90 days boosted the win ratio by a significant 36% relative to placebo (Nature Med. 2022 Mar;28[3]: 568-74).
Benefit independent of baseline symptomatic impairment
Among the new secondary analyses that Dr. Kosiborod reported was a post-hoc calculation that divided the study cohort into tertiles of baseline KCCQ score. The results showed that the degree of improvement for the primary, 90-day outcome of “total clinical benefit” compared with placebo was consistent across all three KCCQ-score tertiles, showing that empagliflozin’s benefit was “independent of symptomatic impairment at baseline,” he said.
The degree of improvement was also similar across all the tested domains of the KCCQ, including the overall summary, clinical summary, the physical limitations, and quality-of-life scores. Average improvement in KCCQ total symptom score 15 days after treatment onset was 5.35 points, compared with control patients. On an individual-patient basis, a change in KCCQ score of 5 points or more was previously shown to represent a clinically meaningful change.
“Treatment of patients with heart failure is geared to making patients live longer and stay out of the hospital. Enabling patients to feel better is an equally important goal of management, but not all treatments for heart failure can do that. These data from EMPULSE show that, in addition to other clinical benefits, patients also feel better on an SGLT2 inhibitor after just 2 weeks,” Dr. Kosiborod said in an interview.
EMPULSE builds on SOLOIST-WHF
EMPULSE is the second trial to show that an SGLT2 inhibitor can safely and effectively treat patients hospitalized for acute heart failure. Previously, results from the SOLOIST-WHF pivotal trial, which enrolled 1,222 patients with type 2 diabetes recently hospitalized for worsening heart failure, showed that treatment with an investigational, combined SGLT2 and SGLT1 inhibitor, sotagliflozin, resulted in a significant, 33% relative reduction in the primary outcome compared with placebo after a median 9 months of treatment.
“It’s reassuring to see two different drugs and research groups get essentially the same result, showing that starting an SGLT2 inhibitor is safe and effective in selected patients with no contraindications,” said Dr. Bhatt, who was lead investigator for SOLOIST-WHF.
The accumulating evidence for the safety and value of starting an SGLT2 inhibitor when patients are hospitalized for acute heart failure is making this approach increasingly routine for patients who present with heart failure with reduced ejection fraction at Saint Luke’s-Mid America Heart Institute, said Dr. Kosiborod, who is also a professor of medicine at the University of Missouri, Kansas City.
“I think we’ll also gradually start using [an SGLT2 inhibitor] in patients hospitalized with heart failure with preserved ejection fraction [HFpEF],” he added, based on the findings from SOLOIST-WHF and EMPULSE, and also recent evidence showing safety and efficacy of empagliflozin in patients with chronic HFpEF in the EMPEROR-Preserved trial, and for dapagliflozin (Farxiga) in the PRESERVED-HF trial.
Empagliflozin recently received from the U.S. Food and Drug Administration an expanded label indication for treating patients with heart failure with no specification for a level of left ventricular ejection fraction. An outcome trial of dapagliflozin in more than 6,000 patients with HFpEF, DELIVER, is currently ongoing but is expected to report results soon.
“The evidence is already compelling that the benefits outweigh the risk. Results from both SOLOIST-WHF and EMPULSE show that there are no significant safety concerns” when these agents are used in patients with acute heart failure,” Dr. Kosiborod declared.
EMPULSE was sponsored by Boehringer Ingelheim and Eli Lilly, the companies that jointly market empagliflozin (Jardiance). SOLOIST-WHF was sponsored by Sanofi and Lexicon, the companies that have been developing sotagliflozin. Dr. Kosiborod has been a consultant to and received research funding from Boehringer Ingelheim and Eli Lilly, and he has been a consultant or adviser to or led trials on behalf of numerous other companies. Dr. Bhatt has been an adviser to Boehringer Ingelheim and numerous other companies, and he has received research funding from Sanofi, Lexicon, Boehringer Ingelheim, Eli Lilly, and numerous other companies.
WASHINGTON – Treatment of patients acutely hospitalized for heart failure with the SGLT2 inhibitor empagliflozin led to a rapid incremental increase in patient well-being, compared with control patients who received placebo, that appeared after 2 weeks on treatment in a secondary analysis from 530 randomized patients in the EMPULSE trial.
To Mikhail N. Kosiborod, MD, a coinvestigator for EMPULSE who presented new analysis at the annual scientific sessions of the American College of Cardiology, the message from the quick response of acutely hospitalized patients to empagliflozin was clear: “Use these medications, SGLT2 [sodium-glucose cotransporter 2] inhibitors, as early as possible. We’ve seen with other medications that if they are not prescribed during hospitalization it’s unlikely to happen post discharge,” said Dr. Kosiborod, a cardiologist and codirector of the Haverty Cardiometabolic Center of Excellence at Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
“To our knowledge, the very early improvement in the Kansas City Cardiomyopathy Questionnaire [KCCQ] score – a well-known predictor of cardiovascular death and heart failure readmissions – that we observed with empagliflozin at 15 days is the first such observation, and if corroborated by future studies would suggest that initiation of SGLT2 inhibitors during hospitalization for acute heart failure may be a tool for improving the quality of hospital-to-home transitions,” wrote Dr. Kosiborod and his associates in the published version of their report that appeared concurrently with his report at the meeting.
“These data really support initiation [of empagliflozin or another SGLT2 inhibitor] in hospital, presuming that the patient has no contraindications,” commented Deepak L. Bhatt, MD, professor of medicine at Harvard Medical School in Boston and designated discussant for the report.
“The fact that the benefit kicks in so early is really important, because there is a bit of a penalty to wait” to start treatment with an agent from the SGLT2-inhibitor class, added Dr. Bhatt, who is also executive director of interventional cardiovascular programs at Brigham and Women’s Health, in Boston.
In hospital creates a teachable moment
Starting treatment when a patient is hospitalized is also important as “a teachable moment,” added Dr. Bhatt in an interview. “A physician can say to a patient ‘take this drug, and it will prevent you from returning to the hospital,’ at a time when it’s more likely to be impactful, compared with when a patient is out of the hospital and feeling okay and adherence will likely be much lower.”
The results Dr. Kosiborod reported on quality-of-life parameters measured with the KCCQ expanded on what he and his coinvestigators first reported in 2021 with the primary results from EMPULSE, which enrolled 530 patients at 118 centers in 15 countries during June 2020–February 2021. The trial randomized patients hospitalized for acute heart failure after a brief period of stabilization regardless of their left ventricular ejection fraction or presence of diabetes to receive a single, daily dose of 10 mg of empagliflozin (Jardiance) or placebo starting a median of 3 days after admission. Enrolled patients averaged about 71 years of age, about two-thirds were men, 45% had diabetes, 32% had left ventricular ejection fraction greater than 40%, and about two-thirds had decompensated chronic heart failure, while a third had acute de novo heart failure.
The primary outcome for EMPULSE was a combined endpoint of “total clinical endpoints” that included all-cause mortality, heart failure events (heart failure hospitalizations, urgent heart failure visits, and unplanned outpatient heart failure visits) or at least a 5-point change from baseline in the KCCQ score. Using a “win ratio” method for analyzing the composite endpoint, the primary analysis showed that treatment with empagliflozin for 90 days boosted the win ratio by a significant 36% relative to placebo (Nature Med. 2022 Mar;28[3]: 568-74).
Benefit independent of baseline symptomatic impairment
Among the new secondary analyses that Dr. Kosiborod reported was a post-hoc calculation that divided the study cohort into tertiles of baseline KCCQ score. The results showed that the degree of improvement for the primary, 90-day outcome of “total clinical benefit” compared with placebo was consistent across all three KCCQ-score tertiles, showing that empagliflozin’s benefit was “independent of symptomatic impairment at baseline,” he said.
The degree of improvement was also similar across all the tested domains of the KCCQ, including the overall summary, clinical summary, the physical limitations, and quality-of-life scores. Average improvement in KCCQ total symptom score 15 days after treatment onset was 5.35 points, compared with control patients. On an individual-patient basis, a change in KCCQ score of 5 points or more was previously shown to represent a clinically meaningful change.
“Treatment of patients with heart failure is geared to making patients live longer and stay out of the hospital. Enabling patients to feel better is an equally important goal of management, but not all treatments for heart failure can do that. These data from EMPULSE show that, in addition to other clinical benefits, patients also feel better on an SGLT2 inhibitor after just 2 weeks,” Dr. Kosiborod said in an interview.
EMPULSE builds on SOLOIST-WHF
EMPULSE is the second trial to show that an SGLT2 inhibitor can safely and effectively treat patients hospitalized for acute heart failure. Previously, results from the SOLOIST-WHF pivotal trial, which enrolled 1,222 patients with type 2 diabetes recently hospitalized for worsening heart failure, showed that treatment with an investigational, combined SGLT2 and SGLT1 inhibitor, sotagliflozin, resulted in a significant, 33% relative reduction in the primary outcome compared with placebo after a median 9 months of treatment.
“It’s reassuring to see two different drugs and research groups get essentially the same result, showing that starting an SGLT2 inhibitor is safe and effective in selected patients with no contraindications,” said Dr. Bhatt, who was lead investigator for SOLOIST-WHF.
The accumulating evidence for the safety and value of starting an SGLT2 inhibitor when patients are hospitalized for acute heart failure is making this approach increasingly routine for patients who present with heart failure with reduced ejection fraction at Saint Luke’s-Mid America Heart Institute, said Dr. Kosiborod, who is also a professor of medicine at the University of Missouri, Kansas City.
“I think we’ll also gradually start using [an SGLT2 inhibitor] in patients hospitalized with heart failure with preserved ejection fraction [HFpEF],” he added, based on the findings from SOLOIST-WHF and EMPULSE, and also recent evidence showing safety and efficacy of empagliflozin in patients with chronic HFpEF in the EMPEROR-Preserved trial, and for dapagliflozin (Farxiga) in the PRESERVED-HF trial.
Empagliflozin recently received from the U.S. Food and Drug Administration an expanded label indication for treating patients with heart failure with no specification for a level of left ventricular ejection fraction. An outcome trial of dapagliflozin in more than 6,000 patients with HFpEF, DELIVER, is currently ongoing but is expected to report results soon.
“The evidence is already compelling that the benefits outweigh the risk. Results from both SOLOIST-WHF and EMPULSE show that there are no significant safety concerns” when these agents are used in patients with acute heart failure,” Dr. Kosiborod declared.
EMPULSE was sponsored by Boehringer Ingelheim and Eli Lilly, the companies that jointly market empagliflozin (Jardiance). SOLOIST-WHF was sponsored by Sanofi and Lexicon, the companies that have been developing sotagliflozin. Dr. Kosiborod has been a consultant to and received research funding from Boehringer Ingelheim and Eli Lilly, and he has been a consultant or adviser to or led trials on behalf of numerous other companies. Dr. Bhatt has been an adviser to Boehringer Ingelheim and numerous other companies, and he has received research funding from Sanofi, Lexicon, Boehringer Ingelheim, Eli Lilly, and numerous other companies.
AT ACC 2022
No Veteran Leaves Alone: Ensuring Veterans Receive a Hero’s Final Salute
It is a great honor and privilege to care for the men and women who have bravely served our country, and to give a hero’s Final Salute in recognition of the veteran’s service and sacrifices. US Department of Veterans Affairs (VA) and other non-VA health care facilities caring for veterans find meaning and take pride in providing a Final Salute to veterans who spend their last days of life at their facilities. The Final Salute aligns with the mission of the VA: To fulfill President Lincoln’s promise “To care for him who shall have borne the battle, and for his widow, and his orphan” by serving and honoring the people who are America’s veterans.1 As health care professionals, we feel and grieve the loss when a veteran dies within our facilities. While some VA and community health care facilities honor veterans at the time of death, others have yet to implement a Final Salute program.2 How can we ensure that veterans at the time of death receive a hero’s Final Salute?
There are 26 million veterans alive today, representing about 8% of the total US adult population.3 Yet more than 1800 veterans die every day, representing about a quarter of all US deaths.4,5 Most veterans die in the community; only 4% of veteran deaths occur in VA facilities.5,6 This article highlights the unique tradition that a few VA and community health care facilities have launched to honor veterans whose journeys end under their care. This article also is a call to action to raise awareness of the importance of instituting the Final Salute program that is part of the end-of-life protocol for veterans.
A Final Salute ceremony (also called Honors Escort or Honor Walk) takes place when a veteran who dies in the hospital or nursing home is transported on the gurney from the location of their passing to the funeral home vehicle or the morgue. Staff, family members, visitors, and other veterans silently line the hallways from the veteran’s room to the health care facility exit and pay their respects to the deceased veteran. A Final Salute is a quiet, yet profound and powerful way for care teams to ensure that the deceased veteran does not leave alone.
VA-Based Ceremonies
There are many acts of remembrance at the bedside from the time of death to the time when the veteran’s body approaches the funeral home vehicle or the doors of the morgue. Tonya Ross, social worker and Honors Escort program manager at the Robert J. Dole VA Medical Center (VAMC) in Wichita, Kansas, reported that following the death of a veteran, there is a bedside remembrance that begins with a flag ceremony. Afterward, the veteran’s gurney is draped with the American flag, and as the procession moves through the medical center, the veterans salute, and all others place their hands over their hearts
Chaplain Michael Halyard at the Ozarks VAMC in Fayetteville, Arkansas, reported that following the death of a veteran, the chaplain greets family members with condolences and allows them to grieve and reflect on their life with the deceased veteran. On arrival of the funeral home team, an announcement for an Honor Walk is made. Staff, visitors, and family are lined up on the first floor of the hospital waiting to pay their final respects to the veteran. A slow processional of the veteran covered by a handmade quilt is escorted by a VA police officer and the chaplain. The processional stops in the middle and the chaplain announces, “Let us pause for a moment of silence as we honor one of our own US Army veterans who has completed the journey of life.”
The Final Salute at the VA Wilkes-Barre Community Living Center (CLC) in Pennsylvania begins with a bedside flag ceremony. Afterward, the veteran’s gurney is draped with the flag, and as the procession moves through the CLC, all who are standing along the route offer their respects. Throughout the ceremony, a team member remains with the family of the deceased, providing comfort and support. Once the ceremony is completed, the team member remains with the family to ensure all issues are addressed and all questions or concerns are answered.
Residents of the Philadelphia VAMC CLC in Pennsylvania have found a way to say a last goodbye to fellow veterans in a unique and dignified manner. Bettyanne Corkery, nurse manager for the Heroes’ Crossing hospice and palliative care unit explains, “Our Honor Guard evolved from our residents’ requests. We used to drape a flag over the body of veterans leaving us for the last time, but our residents came to us and said they wanted to do more.” CLC residents wanted to form an Honor Guard and say goodbye with dignity and grace. Gerry Donlon, a US Army Vietnam veteran and president of the residents council and chief program coordinator, explained that Honor Guard members are called to the deceased’s room and stand guard until the hearse comes. Donlon adds, “We proceed forward, along with the family, and the speaker system for the hospital plays patriotic songs, including Taps. When we get to the lobby, we stop, and I say a prayer. We fold the flag military style and hand it over to the family members, we render a Final Salute, and then the veteran is taken to the hearse.”7
Community Cermeonies
Texas Health Arlington Memorial Hospital (THAM) has honored 531 veterans with Final Salutes since 2015. Before the official procession begins, designated employees drape the patient’s body with the flag. Physicians, nurses, and volunteers escort the body in a silent procession along with the family. On leaving, the veteran’s family receives the flag in honor of their loved one. A specially designed medallion has been placed in the lobby floor at the location where the Final Salute is rendered. Christi Evans, RN, BSN, ACM, manager for care
coordination at AnMed Health, Anderson, South Carolina, witnessed a Final Salute at THAM for a relative and took the idea to Mike Johnston, Director of Spiritual Care to establish the program at AnMed Health, which has provided 118 Final Salutes since 2018.
Central Maine Healthcare (CMH), which operates 3 hospitals, provides 2 ceremonies. The Final Salute occurs prior to the veteran’s passing and the Honor Walk gathers hospital personnel outside the patient’s room as they are moved. During the Final Salute, with the approval of a veteran’s family, a veteran employed by CMF presents the veteran with a folded flag and certificate and thanks them for their service and hospital employee salute. After the veteran dies, staff members gather in the hallway for the Honor Walk. Ascension Sacred Heart (ASH), Florida, where on average 260 veterans look for treatment every month, has taken the Final Salute to all 4 of their hospitals. Sabrina Granese, BSN, RN, Military Service Line Director at ASH explains, “Patients that are active duty or veterans are identified at the time of admission. When a veteran passes away, with the approval of a veteran’s family, ‘Code veteran’ will be heard over the hospital intercom. Staff members will have 5 minutes to make their way to the main hospital entrance for the Honor Walk.” Similarly, the skilled nursing facilities operated by Bethesda Health Group, St. Louis, Missouri, have implemented the Veteran Escort Ceremony. Employees, volunteers, family members, and residents line the hallways during the procession to salute and honor the passing of the veteran’s body.
Closure For Families
Simple yet magnificent, a Final Salute shows that a veteran is “gone but not forgotten” and also shows families they are not alone as they too made sacrifices to allow their loved ones to serve in the Armed Forces; it signals the hope of healing and closure.8 “The staff came to pay their respects,” recalled Cindy Roberts, a social worker at the VA Bay Pines, when her relative died at the Ozarks VAMC. She explained, I wasn’t expecting as much because it was 2 AM. I have never in my life had an experience like that. I wish there were words to describe it; I wish every VAMC in the country did that.”
Hope Danishanko, social worker at the VA Wilkes-Barre CLC, said veterans are appreciative of the program. “I have had many CLC residents tell me that the Honors Escort allows them to have closure. They also feel it provides respect to the veteran who has passed.”
Bettyanne Corkery noted that the Philadelphia CLC Honor Guard program is unique because it is veteran driven. “They have sessions in which they talk about what works and what doesn’t, and they recruit new volunteers themselves,” she said. “It has evolved into the most beautiful ceremony, and they are constantly tweaking it.” According to Gerry Donlon, “When you see all 8 members of the Honor Guard get a call at 2 AM, and everyone shows up, you know there’s personal satisfaction. I’d like to see every CLC [throughout VA] do this. I really would.”7
“Family members tell us they feel blessed and honored to be a part of the program. They are so grateful for the way we pay tribute to their veteran loved one,” says Leslie Schaeffer, support services manager and bereavement coordinator and coordinator of the Veteran Escort Ceremony at Bethesda Health Group communities.
Privileged and humbled—that is how staff and family members describe feeling after participating in a Final Salute. Its impact on the families has been amazing. Between the tears, there are thanks for the recognition of the sacrifices their loved ones made. When one family was informed of the ceremony by Reverend Tricia Lytle, Manager of Spiritual Care at AnMed Health, the “whole family responded by explaining how much that meant at such a difficult time. They began sharing stories about his service and how proud he was to be a veteran,” she reported. “As I [Rev. Lytle] leaned over to present the flag at the bedside, the wife reached up and took hold as she tearfully accepted it and embraced it close to her heart. The staff in the hallway looked on respectfully also in tears.”
Conclusions
The Final Salute is a brief ceremonial procession demonstrating that the mission to care for America’s veterans does not end at the bedside. It ensures that no veteran’s body is alone when led out of the health facility room to the exit. With these Final Salute practices, I hope that the rest of VA and community health facilities caring for veterans will implement a Final Salute program to better honor veterans who depart in their care.
Acknowledgments
The author would like to express gratitude to everyone who so openly shared their stories—your insight, advice, and encouragement are inspiring and invaluable. Thank you to all the facilities that consented to be featured in this article.
1. US Department of Veteran Affairs. About VA: mission, vision, core values & goals. Updated September 30, 2021. Accessed September 30, 2021. https://www.va.gov /about_va/mission.asp
2. Kuznik R. Hospital program presentation, 2021 national convention. Accessed September 30, 2021. https:// vfwauxiliary.org/wp-content/uploads/2021.2022-National -Hospital-Ambassador-Presentation-Notes.pdf
3. US Department of Veteran Affairs, National Center for Veterans Analysis and Statistics. Veteran population projections 2017-2037. Published 2016. Accessed September 30, 2021. https://www.va.gov/vetdata/docs /Demographics/New_Vetpop_Model/Vetpop_Infographic _Final31.pdf
4. Calkins H. Psychologists, veterans and end-of-life care. Good Practice. Winter 2018. Accessed September 30, 2021. https://www.apaservices.org/practice/good -practice/veterans-end-of-life.pdf
5. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Accessed September 30, 2021. http://www.va.gov/vetdata
6. Grassman D. Veterans: an underserved population. Published 2007. Accessed September 30, 2021. https:// www.wehonorveterans.org/wp-content/uploads/2020/02 /WHVP_Toolkit.pdf
7. US Department of Veterans Affairs, VA Healthcare-VISN 4. An honorable procession: Philadelphia’s Honor Guard provides veterans a dignified farewell. 2015. Updated December 15, 2015. Accessed Semptember 30, 2021. https://www.visn4.va.gov/VISN4/news/vision/issue21 /honors-escort.asp
8. Nathan S, Dunn KM. Gone but not forgotten: how VA remembers. Federal Practitioner. 2019;36(6):254-256.
It is a great honor and privilege to care for the men and women who have bravely served our country, and to give a hero’s Final Salute in recognition of the veteran’s service and sacrifices. US Department of Veterans Affairs (VA) and other non-VA health care facilities caring for veterans find meaning and take pride in providing a Final Salute to veterans who spend their last days of life at their facilities. The Final Salute aligns with the mission of the VA: To fulfill President Lincoln’s promise “To care for him who shall have borne the battle, and for his widow, and his orphan” by serving and honoring the people who are America’s veterans.1 As health care professionals, we feel and grieve the loss when a veteran dies within our facilities. While some VA and community health care facilities honor veterans at the time of death, others have yet to implement a Final Salute program.2 How can we ensure that veterans at the time of death receive a hero’s Final Salute?
There are 26 million veterans alive today, representing about 8% of the total US adult population.3 Yet more than 1800 veterans die every day, representing about a quarter of all US deaths.4,5 Most veterans die in the community; only 4% of veteran deaths occur in VA facilities.5,6 This article highlights the unique tradition that a few VA and community health care facilities have launched to honor veterans whose journeys end under their care. This article also is a call to action to raise awareness of the importance of instituting the Final Salute program that is part of the end-of-life protocol for veterans.
A Final Salute ceremony (also called Honors Escort or Honor Walk) takes place when a veteran who dies in the hospital or nursing home is transported on the gurney from the location of their passing to the funeral home vehicle or the morgue. Staff, family members, visitors, and other veterans silently line the hallways from the veteran’s room to the health care facility exit and pay their respects to the deceased veteran. A Final Salute is a quiet, yet profound and powerful way for care teams to ensure that the deceased veteran does not leave alone.
VA-Based Ceremonies
There are many acts of remembrance at the bedside from the time of death to the time when the veteran’s body approaches the funeral home vehicle or the doors of the morgue. Tonya Ross, social worker and Honors Escort program manager at the Robert J. Dole VA Medical Center (VAMC) in Wichita, Kansas, reported that following the death of a veteran, there is a bedside remembrance that begins with a flag ceremony. Afterward, the veteran’s gurney is draped with the American flag, and as the procession moves through the medical center, the veterans salute, and all others place their hands over their hearts
Chaplain Michael Halyard at the Ozarks VAMC in Fayetteville, Arkansas, reported that following the death of a veteran, the chaplain greets family members with condolences and allows them to grieve and reflect on their life with the deceased veteran. On arrival of the funeral home team, an announcement for an Honor Walk is made. Staff, visitors, and family are lined up on the first floor of the hospital waiting to pay their final respects to the veteran. A slow processional of the veteran covered by a handmade quilt is escorted by a VA police officer and the chaplain. The processional stops in the middle and the chaplain announces, “Let us pause for a moment of silence as we honor one of our own US Army veterans who has completed the journey of life.”
The Final Salute at the VA Wilkes-Barre Community Living Center (CLC) in Pennsylvania begins with a bedside flag ceremony. Afterward, the veteran’s gurney is draped with the flag, and as the procession moves through the CLC, all who are standing along the route offer their respects. Throughout the ceremony, a team member remains with the family of the deceased, providing comfort and support. Once the ceremony is completed, the team member remains with the family to ensure all issues are addressed and all questions or concerns are answered.
Residents of the Philadelphia VAMC CLC in Pennsylvania have found a way to say a last goodbye to fellow veterans in a unique and dignified manner. Bettyanne Corkery, nurse manager for the Heroes’ Crossing hospice and palliative care unit explains, “Our Honor Guard evolved from our residents’ requests. We used to drape a flag over the body of veterans leaving us for the last time, but our residents came to us and said they wanted to do more.” CLC residents wanted to form an Honor Guard and say goodbye with dignity and grace. Gerry Donlon, a US Army Vietnam veteran and president of the residents council and chief program coordinator, explained that Honor Guard members are called to the deceased’s room and stand guard until the hearse comes. Donlon adds, “We proceed forward, along with the family, and the speaker system for the hospital plays patriotic songs, including Taps. When we get to the lobby, we stop, and I say a prayer. We fold the flag military style and hand it over to the family members, we render a Final Salute, and then the veteran is taken to the hearse.”7
Community Cermeonies
Texas Health Arlington Memorial Hospital (THAM) has honored 531 veterans with Final Salutes since 2015. Before the official procession begins, designated employees drape the patient’s body with the flag. Physicians, nurses, and volunteers escort the body in a silent procession along with the family. On leaving, the veteran’s family receives the flag in honor of their loved one. A specially designed medallion has been placed in the lobby floor at the location where the Final Salute is rendered. Christi Evans, RN, BSN, ACM, manager for care
coordination at AnMed Health, Anderson, South Carolina, witnessed a Final Salute at THAM for a relative and took the idea to Mike Johnston, Director of Spiritual Care to establish the program at AnMed Health, which has provided 118 Final Salutes since 2018.
Central Maine Healthcare (CMH), which operates 3 hospitals, provides 2 ceremonies. The Final Salute occurs prior to the veteran’s passing and the Honor Walk gathers hospital personnel outside the patient’s room as they are moved. During the Final Salute, with the approval of a veteran’s family, a veteran employed by CMF presents the veteran with a folded flag and certificate and thanks them for their service and hospital employee salute. After the veteran dies, staff members gather in the hallway for the Honor Walk. Ascension Sacred Heart (ASH), Florida, where on average 260 veterans look for treatment every month, has taken the Final Salute to all 4 of their hospitals. Sabrina Granese, BSN, RN, Military Service Line Director at ASH explains, “Patients that are active duty or veterans are identified at the time of admission. When a veteran passes away, with the approval of a veteran’s family, ‘Code veteran’ will be heard over the hospital intercom. Staff members will have 5 minutes to make their way to the main hospital entrance for the Honor Walk.” Similarly, the skilled nursing facilities operated by Bethesda Health Group, St. Louis, Missouri, have implemented the Veteran Escort Ceremony. Employees, volunteers, family members, and residents line the hallways during the procession to salute and honor the passing of the veteran’s body.
Closure For Families
Simple yet magnificent, a Final Salute shows that a veteran is “gone but not forgotten” and also shows families they are not alone as they too made sacrifices to allow their loved ones to serve in the Armed Forces; it signals the hope of healing and closure.8 “The staff came to pay their respects,” recalled Cindy Roberts, a social worker at the VA Bay Pines, when her relative died at the Ozarks VAMC. She explained, I wasn’t expecting as much because it was 2 AM. I have never in my life had an experience like that. I wish there were words to describe it; I wish every VAMC in the country did that.”
Hope Danishanko, social worker at the VA Wilkes-Barre CLC, said veterans are appreciative of the program. “I have had many CLC residents tell me that the Honors Escort allows them to have closure. They also feel it provides respect to the veteran who has passed.”
Bettyanne Corkery noted that the Philadelphia CLC Honor Guard program is unique because it is veteran driven. “They have sessions in which they talk about what works and what doesn’t, and they recruit new volunteers themselves,” she said. “It has evolved into the most beautiful ceremony, and they are constantly tweaking it.” According to Gerry Donlon, “When you see all 8 members of the Honor Guard get a call at 2 AM, and everyone shows up, you know there’s personal satisfaction. I’d like to see every CLC [throughout VA] do this. I really would.”7
“Family members tell us they feel blessed and honored to be a part of the program. They are so grateful for the way we pay tribute to their veteran loved one,” says Leslie Schaeffer, support services manager and bereavement coordinator and coordinator of the Veteran Escort Ceremony at Bethesda Health Group communities.
Privileged and humbled—that is how staff and family members describe feeling after participating in a Final Salute. Its impact on the families has been amazing. Between the tears, there are thanks for the recognition of the sacrifices their loved ones made. When one family was informed of the ceremony by Reverend Tricia Lytle, Manager of Spiritual Care at AnMed Health, the “whole family responded by explaining how much that meant at such a difficult time. They began sharing stories about his service and how proud he was to be a veteran,” she reported. “As I [Rev. Lytle] leaned over to present the flag at the bedside, the wife reached up and took hold as she tearfully accepted it and embraced it close to her heart. The staff in the hallway looked on respectfully also in tears.”
Conclusions
The Final Salute is a brief ceremonial procession demonstrating that the mission to care for America’s veterans does not end at the bedside. It ensures that no veteran’s body is alone when led out of the health facility room to the exit. With these Final Salute practices, I hope that the rest of VA and community health facilities caring for veterans will implement a Final Salute program to better honor veterans who depart in their care.
Acknowledgments
The author would like to express gratitude to everyone who so openly shared their stories—your insight, advice, and encouragement are inspiring and invaluable. Thank you to all the facilities that consented to be featured in this article.
It is a great honor and privilege to care for the men and women who have bravely served our country, and to give a hero’s Final Salute in recognition of the veteran’s service and sacrifices. US Department of Veterans Affairs (VA) and other non-VA health care facilities caring for veterans find meaning and take pride in providing a Final Salute to veterans who spend their last days of life at their facilities. The Final Salute aligns with the mission of the VA: To fulfill President Lincoln’s promise “To care for him who shall have borne the battle, and for his widow, and his orphan” by serving and honoring the people who are America’s veterans.1 As health care professionals, we feel and grieve the loss when a veteran dies within our facilities. While some VA and community health care facilities honor veterans at the time of death, others have yet to implement a Final Salute program.2 How can we ensure that veterans at the time of death receive a hero’s Final Salute?
There are 26 million veterans alive today, representing about 8% of the total US adult population.3 Yet more than 1800 veterans die every day, representing about a quarter of all US deaths.4,5 Most veterans die in the community; only 4% of veteran deaths occur in VA facilities.5,6 This article highlights the unique tradition that a few VA and community health care facilities have launched to honor veterans whose journeys end under their care. This article also is a call to action to raise awareness of the importance of instituting the Final Salute program that is part of the end-of-life protocol for veterans.
A Final Salute ceremony (also called Honors Escort or Honor Walk) takes place when a veteran who dies in the hospital or nursing home is transported on the gurney from the location of their passing to the funeral home vehicle or the morgue. Staff, family members, visitors, and other veterans silently line the hallways from the veteran’s room to the health care facility exit and pay their respects to the deceased veteran. A Final Salute is a quiet, yet profound and powerful way for care teams to ensure that the deceased veteran does not leave alone.
VA-Based Ceremonies
There are many acts of remembrance at the bedside from the time of death to the time when the veteran’s body approaches the funeral home vehicle or the doors of the morgue. Tonya Ross, social worker and Honors Escort program manager at the Robert J. Dole VA Medical Center (VAMC) in Wichita, Kansas, reported that following the death of a veteran, there is a bedside remembrance that begins with a flag ceremony. Afterward, the veteran’s gurney is draped with the American flag, and as the procession moves through the medical center, the veterans salute, and all others place their hands over their hearts
Chaplain Michael Halyard at the Ozarks VAMC in Fayetteville, Arkansas, reported that following the death of a veteran, the chaplain greets family members with condolences and allows them to grieve and reflect on their life with the deceased veteran. On arrival of the funeral home team, an announcement for an Honor Walk is made. Staff, visitors, and family are lined up on the first floor of the hospital waiting to pay their final respects to the veteran. A slow processional of the veteran covered by a handmade quilt is escorted by a VA police officer and the chaplain. The processional stops in the middle and the chaplain announces, “Let us pause for a moment of silence as we honor one of our own US Army veterans who has completed the journey of life.”
The Final Salute at the VA Wilkes-Barre Community Living Center (CLC) in Pennsylvania begins with a bedside flag ceremony. Afterward, the veteran’s gurney is draped with the flag, and as the procession moves through the CLC, all who are standing along the route offer their respects. Throughout the ceremony, a team member remains with the family of the deceased, providing comfort and support. Once the ceremony is completed, the team member remains with the family to ensure all issues are addressed and all questions or concerns are answered.
Residents of the Philadelphia VAMC CLC in Pennsylvania have found a way to say a last goodbye to fellow veterans in a unique and dignified manner. Bettyanne Corkery, nurse manager for the Heroes’ Crossing hospice and palliative care unit explains, “Our Honor Guard evolved from our residents’ requests. We used to drape a flag over the body of veterans leaving us for the last time, but our residents came to us and said they wanted to do more.” CLC residents wanted to form an Honor Guard and say goodbye with dignity and grace. Gerry Donlon, a US Army Vietnam veteran and president of the residents council and chief program coordinator, explained that Honor Guard members are called to the deceased’s room and stand guard until the hearse comes. Donlon adds, “We proceed forward, along with the family, and the speaker system for the hospital plays patriotic songs, including Taps. When we get to the lobby, we stop, and I say a prayer. We fold the flag military style and hand it over to the family members, we render a Final Salute, and then the veteran is taken to the hearse.”7
Community Cermeonies
Texas Health Arlington Memorial Hospital (THAM) has honored 531 veterans with Final Salutes since 2015. Before the official procession begins, designated employees drape the patient’s body with the flag. Physicians, nurses, and volunteers escort the body in a silent procession along with the family. On leaving, the veteran’s family receives the flag in honor of their loved one. A specially designed medallion has been placed in the lobby floor at the location where the Final Salute is rendered. Christi Evans, RN, BSN, ACM, manager for care
coordination at AnMed Health, Anderson, South Carolina, witnessed a Final Salute at THAM for a relative and took the idea to Mike Johnston, Director of Spiritual Care to establish the program at AnMed Health, which has provided 118 Final Salutes since 2018.
Central Maine Healthcare (CMH), which operates 3 hospitals, provides 2 ceremonies. The Final Salute occurs prior to the veteran’s passing and the Honor Walk gathers hospital personnel outside the patient’s room as they are moved. During the Final Salute, with the approval of a veteran’s family, a veteran employed by CMF presents the veteran with a folded flag and certificate and thanks them for their service and hospital employee salute. After the veteran dies, staff members gather in the hallway for the Honor Walk. Ascension Sacred Heart (ASH), Florida, where on average 260 veterans look for treatment every month, has taken the Final Salute to all 4 of their hospitals. Sabrina Granese, BSN, RN, Military Service Line Director at ASH explains, “Patients that are active duty or veterans are identified at the time of admission. When a veteran passes away, with the approval of a veteran’s family, ‘Code veteran’ will be heard over the hospital intercom. Staff members will have 5 minutes to make their way to the main hospital entrance for the Honor Walk.” Similarly, the skilled nursing facilities operated by Bethesda Health Group, St. Louis, Missouri, have implemented the Veteran Escort Ceremony. Employees, volunteers, family members, and residents line the hallways during the procession to salute and honor the passing of the veteran’s body.
Closure For Families
Simple yet magnificent, a Final Salute shows that a veteran is “gone but not forgotten” and also shows families they are not alone as they too made sacrifices to allow their loved ones to serve in the Armed Forces; it signals the hope of healing and closure.8 “The staff came to pay their respects,” recalled Cindy Roberts, a social worker at the VA Bay Pines, when her relative died at the Ozarks VAMC. She explained, I wasn’t expecting as much because it was 2 AM. I have never in my life had an experience like that. I wish there were words to describe it; I wish every VAMC in the country did that.”
Hope Danishanko, social worker at the VA Wilkes-Barre CLC, said veterans are appreciative of the program. “I have had many CLC residents tell me that the Honors Escort allows them to have closure. They also feel it provides respect to the veteran who has passed.”
Bettyanne Corkery noted that the Philadelphia CLC Honor Guard program is unique because it is veteran driven. “They have sessions in which they talk about what works and what doesn’t, and they recruit new volunteers themselves,” she said. “It has evolved into the most beautiful ceremony, and they are constantly tweaking it.” According to Gerry Donlon, “When you see all 8 members of the Honor Guard get a call at 2 AM, and everyone shows up, you know there’s personal satisfaction. I’d like to see every CLC [throughout VA] do this. I really would.”7
“Family members tell us they feel blessed and honored to be a part of the program. They are so grateful for the way we pay tribute to their veteran loved one,” says Leslie Schaeffer, support services manager and bereavement coordinator and coordinator of the Veteran Escort Ceremony at Bethesda Health Group communities.
Privileged and humbled—that is how staff and family members describe feeling after participating in a Final Salute. Its impact on the families has been amazing. Between the tears, there are thanks for the recognition of the sacrifices their loved ones made. When one family was informed of the ceremony by Reverend Tricia Lytle, Manager of Spiritual Care at AnMed Health, the “whole family responded by explaining how much that meant at such a difficult time. They began sharing stories about his service and how proud he was to be a veteran,” she reported. “As I [Rev. Lytle] leaned over to present the flag at the bedside, the wife reached up and took hold as she tearfully accepted it and embraced it close to her heart. The staff in the hallway looked on respectfully also in tears.”
Conclusions
The Final Salute is a brief ceremonial procession demonstrating that the mission to care for America’s veterans does not end at the bedside. It ensures that no veteran’s body is alone when led out of the health facility room to the exit. With these Final Salute practices, I hope that the rest of VA and community health facilities caring for veterans will implement a Final Salute program to better honor veterans who depart in their care.
Acknowledgments
The author would like to express gratitude to everyone who so openly shared their stories—your insight, advice, and encouragement are inspiring and invaluable. Thank you to all the facilities that consented to be featured in this article.
1. US Department of Veteran Affairs. About VA: mission, vision, core values & goals. Updated September 30, 2021. Accessed September 30, 2021. https://www.va.gov /about_va/mission.asp
2. Kuznik R. Hospital program presentation, 2021 national convention. Accessed September 30, 2021. https:// vfwauxiliary.org/wp-content/uploads/2021.2022-National -Hospital-Ambassador-Presentation-Notes.pdf
3. US Department of Veteran Affairs, National Center for Veterans Analysis and Statistics. Veteran population projections 2017-2037. Published 2016. Accessed September 30, 2021. https://www.va.gov/vetdata/docs /Demographics/New_Vetpop_Model/Vetpop_Infographic _Final31.pdf
4. Calkins H. Psychologists, veterans and end-of-life care. Good Practice. Winter 2018. Accessed September 30, 2021. https://www.apaservices.org/practice/good -practice/veterans-end-of-life.pdf
5. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Accessed September 30, 2021. http://www.va.gov/vetdata
6. Grassman D. Veterans: an underserved population. Published 2007. Accessed September 30, 2021. https:// www.wehonorveterans.org/wp-content/uploads/2020/02 /WHVP_Toolkit.pdf
7. US Department of Veterans Affairs, VA Healthcare-VISN 4. An honorable procession: Philadelphia’s Honor Guard provides veterans a dignified farewell. 2015. Updated December 15, 2015. Accessed Semptember 30, 2021. https://www.visn4.va.gov/VISN4/news/vision/issue21 /honors-escort.asp
8. Nathan S, Dunn KM. Gone but not forgotten: how VA remembers. Federal Practitioner. 2019;36(6):254-256.
1. US Department of Veteran Affairs. About VA: mission, vision, core values & goals. Updated September 30, 2021. Accessed September 30, 2021. https://www.va.gov /about_va/mission.asp
2. Kuznik R. Hospital program presentation, 2021 national convention. Accessed September 30, 2021. https:// vfwauxiliary.org/wp-content/uploads/2021.2022-National -Hospital-Ambassador-Presentation-Notes.pdf
3. US Department of Veteran Affairs, National Center for Veterans Analysis and Statistics. Veteran population projections 2017-2037. Published 2016. Accessed September 30, 2021. https://www.va.gov/vetdata/docs /Demographics/New_Vetpop_Model/Vetpop_Infographic _Final31.pdf
4. Calkins H. Psychologists, veterans and end-of-life care. Good Practice. Winter 2018. Accessed September 30, 2021. https://www.apaservices.org/practice/good -practice/veterans-end-of-life.pdf
5. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Accessed September 30, 2021. http://www.va.gov/vetdata
6. Grassman D. Veterans: an underserved population. Published 2007. Accessed September 30, 2021. https:// www.wehonorveterans.org/wp-content/uploads/2020/02 /WHVP_Toolkit.pdf
7. US Department of Veterans Affairs, VA Healthcare-VISN 4. An honorable procession: Philadelphia’s Honor Guard provides veterans a dignified farewell. 2015. Updated December 15, 2015. Accessed Semptember 30, 2021. https://www.visn4.va.gov/VISN4/news/vision/issue21 /honors-escort.asp
8. Nathan S, Dunn KM. Gone but not forgotten: how VA remembers. Federal Practitioner. 2019;36(6):254-256.




