User login
Fertility doctors, IVF families, post Roe: ‘We’re anxious’
Married for nearly 5 years, Jessica King, 34, and her wife, Sarah, agreed on some things right from the start. “We always knew kids were in the equation,” Jessica says.
Now, Jessica is nearly 20 weeks pregnant, thanks to in vitro fertilization, or IVF. They did “reciprocal” IVF, with Sarah’s egg mixed with donor sperm and the embryo transferred into Jessica. “We’re excited – and terrified,” Jessica says.
But that terror goes beyond the typical concerns of excess weight gain and long labors. They live in Missouri, one of 13 states with so-called trigger laws that went into effect after the Supreme Court overturned Roe v. Wade and the constitutional right to abortion, giving states the power to regulate it. States with trigger laws either banned abortion immediately or within a specified time frame after the ruling. In all, 26 states are expected to have abortion restrictions.
Missouri now allows abortion only for medical emergencies. If her upcoming ultrasound shows serious issues, Jessica says they could easily travel to another state and pay for an abortion. She realizes not everyone can.
However, the concern about trigger laws goes well beyond abortion. Many experts worry about the “spill-over” effects the abortion laws – both the existing ones and future proposals – may have on fertility care and treatments.
‘Personhood’ laws drive the concern
“The current trigger laws on the books are not impacting people’s access to IVF,” says Barbara Collura, president and CEO of RESOLVE, an advocacy group for those with fertility issues. “What we are concerned about is they will come back and make them stronger.”
The chief concern for reproductive rights advocates is so-called “personhood” legislation. According to the Guttmacher Institute, at least six bills about personhood have been introduced in five states, including Iowa, Oklahoma, South Carolina, Vermont, and West Virginia. One of the two Oklahoma bills has gone the farthest, passed by one chamber.
Since the Guttmacher report, Ohio introduced its own personhood legislation July 11, recognizing the personhood of an unborn person from conception.
Personhood legislation defines a fertilized egg or embryo as a legal human entity, says Sean Tipton, chief policy and advocacy officer for the Washington-based American Society of Reproductive Medicine, a nonprofit advocacy group.
“If the legal status of fertilized eggs or early embryos is codified, in vitro fertilization procedures may become legally risky for patients, physicians and staff,” Mr. Tipton wrote in late June in Contemporary OB/GYN Journal. The American Society for Reproductive Medicine has posted a report on state abortion trigger laws and their potential implications for reproductive medicine. Of the 13 with trigger laws in effect, the report found concern about the potential effect on IVF only with Utah’s.
‘Safe’ states?
Even in states without trigger laws or personhood bills, IVF patients say they are anxious about how the Supreme Court ruling may ultimately affect care. Thanks to IVF, Shelly Battista and her husband Robert are expecting twins in December, little sisters to their daughter Emilia, who is 2½.
They live in Illinois, where abortion is legal. “Even though we are safe now, I think the overturning of Roe has made it clear to all of us that none of our freedoms are safe, especially reproductive rights,” Ms. Shelly says.
About one in eight U.S. couples are infertile, according to RESOLVE, In 2019, 2% of all babies born in the United States, or about 78,000 infants, were conceived with the use of assisted reproductive technologies, according to the Centers for Disease Control and Prevention. The most common assisted reproductive technology is IVF, in which the sperm fertilizes the egg outside the body and an embryo is then transferred. The standard of practice is to transfer a single embryo, freezing others for future use.
Trigger state doctors weigh in
Some fertility doctors in those “trigger” states are keeping a close eye on proposed legislation and talking to legislators for interpretation of current and proposed laws.
Eli Reshef, MD, a reproductive endocrinologist and fertility specialist at Bennett Fertility Institute in Oklahoma City, notes that his state has “the strictest abortion law in the land.” The law prohibits all abortions with few exceptions, such as the removal of an ectopic pregnancy (when a fertilized egg implants outside the uterus, such as in the fallopian tubes).
While IVF will not be affected for now, he worries that the Oklahoma law allows a private citizen to sue a health care provider that they feel is performing abortion. The Oklahoma law leaves interpretation of abortion up to the general public, who may be unfamiliar with the language of the law, House Bill 4327.
Dean Moutos, MD, a reproductive endocrinologist and medical director of Arkansas Fertility and Gynecology in Little Rock, says his state’s current trigger law should not affect IVF. “When you read the bill, it says abortion means to terminate the pregnancy of a woman.” Still, he says, “we are concerned about what might happen in the future” and the possibility that some legislators may interpret that differently.
A minority approach
John David Gordon, MD, a reproductive endocrinologist and medical director of Southeastern Fertility Center for Fertility and Reproductive Surgery in Knoxville, Tenn., is also in a trigger state. However, it’s not likely any personhood laws would affect his practice.
That’s because his center, which he acknowledges is clearly in the minority, only performs natural-cycle IVF, which usually results in a single egg, or “mini-stim IVF,” which usually results in three to eight eggs in order to limit the number that may be potentially fertilized. Often, he says, patients choose to freeze unfertilized eggs (alone) to avoid creating an excessive number of embryos. He has a “no discard” program, with any viable embryos frozen or transferred. Abandoned embryos are donated to others.
“This may work for young women,” says Marcelle Cedars, MD, director of reproductive endocrinology at the University of California, San Francisco, and president of the American Society of Reproductive Medicine. However, she says, it will be very inefficient for older patients, since they have a higher percentage of abnormal eggs.
Overall, that approach will also drive up costs, especially for older women, Dr. Cedars says. An average cycle of IVF costs $12,400, and most Americans’ insurance plans don’t cover IVF, according to Mr. Tipton.
Top concerns for IVF
“Personhood” legislation has the potential to upend many common IVF practices, experts say.
Of greatest concern to fertility practices are potential restrictions on the freezing or discarding of embryos, Dr. Cedars says. “This could have a critical impact on practicing the safest, most evidence-based medicine,” she says.
Most children born in the United States as a result of IVF procedures are born from frozen embryos, according to the Society for Assisted Reproductive Technology, an organization for reproductive specialists.
“The practice of IVF really requires that we generate more embryos than will be used in a given [IVF] cycle,” agrees Kara Goldman, MD, associate professor of obstetrics and gynecology and medical director of the fertility preservation program at Northwestern University, Chicago. She performed the embryo transfer for the Battistas.
In nature, she says, it’s known that only a small number of eggs will be competent to generate a baby. “We see the same thing in IVF.” In a single cycle, 20 eggs may be retrieved, but many fewer typically reach successful fertilization and are able to be implanted.
When patients have completed their family, unused embryos are donated to research, donated for adoption, or destroyed. If embryo destruction is outlawed, Dr. Goldman says, it will have serious ramifications for the practice of IVF.
And if personhood legislation prohibits destroying any embryos, others wonder: Would a lab technician who accidentally dropped and destroyed an embryo be subject to charges? If laws prohibit destruction of embryos, others wonder if will families be forced to pay the embryo storage fees, generally $500-$1,000 a year, in perpetuity.
If an embryo is declared a person, it could also affect a practice called preimplantation genetic testing, or PGT. In PGT, cells are retrieved from an embryo and checked for genetic disorders such as sickle cell anemia and cystic fibrosis, with some parents choosing to discard embryos that are found to be affected.
Some potential parents choose this testing because they know they are carriers for genetic diseases that are serious and even incompatible with life, says Art Caplan, PhD, head of the division of medical ethics at New York University. They may choose to discard embryos that show evidence of the diseases.
Also under fire could be “selective reduction,” reducing multiple fetuses to a single or twin, to reduce risks to babies and mother.
Dr. Caplan predicts if states have many restrictions, some providers will adopt the attitude that “if no one reports, it did not happen.” And those prospective parents with the means, he says, will go to court and fight restrictions. “When they do it, they are saying, ‘You say you are pro-life; I’m trying to have a child. What are you doing getting in my way?’”
IVF families: Tough decisions, emotional times
The Battistas, of Illinois, have had an especially rough road. Shelly was diagnosed with a fast-growing breast cancer in 2020, when Emilia was just an infant. Warned that the chemotherapy she needed would suppress her ovaries, Shelly underwent egg retrieval before starting the cancer treatment.
She opted to have a double mastectomy and her ovaries removed after learning she carried the BRCA1 genetic mutation, boosting the risk of both breast and ovarian cancer.
Once she was cancer-free, she was cleared to start IVF. The first two embryo transfers failed. The third transfer, of a single embryo, was successful. But it split, a rare occurrence, producing two embryos. “It was a big shock, but in the best way,” she says about learning they were having twins. “Now we are over the moon.”
Five frozen embryos remain. At the start, the Battistas decided to discard unused embryos. She and Robert are discussing what to do next. If they decide they are done building their family after the twins’ birth, she wonders, “do we need to discard our [other] embryos before that becomes something that isn’t eligible [possible] for us any longer?” She doesn’t want to be rushed into that decision, however, especially with her medical history.
Jessica King and Sarah have 20 more embryos.
The couple had decided to donate unused embryos for research, when the time comes, and for different reasons. Her wife’s decision is based on her belief in science, while Jessica cites her faith. “As a Jew, it is part of our faith, that we should be doing everything we can to advance humanity,” she says.
In the midst of all the uncertainty, Jessica says, only half-jokingly, that she is tempted to claim the frozen embryos as dependents. “If you are truly going to claim these are precious human lives, you should be giving me all the benefits from having children,” she says.
Shelly knows that having one daughter, with two more on the way, affects her thinking about the court’s ruling. “My overall wish would be that Roe v. Wade is reinstated, and my daughters have the same rights and options that I have … or I did have until my current 36 years of life.”
A version of this article first appeared on WebMD.com.
Married for nearly 5 years, Jessica King, 34, and her wife, Sarah, agreed on some things right from the start. “We always knew kids were in the equation,” Jessica says.
Now, Jessica is nearly 20 weeks pregnant, thanks to in vitro fertilization, or IVF. They did “reciprocal” IVF, with Sarah’s egg mixed with donor sperm and the embryo transferred into Jessica. “We’re excited – and terrified,” Jessica says.
But that terror goes beyond the typical concerns of excess weight gain and long labors. They live in Missouri, one of 13 states with so-called trigger laws that went into effect after the Supreme Court overturned Roe v. Wade and the constitutional right to abortion, giving states the power to regulate it. States with trigger laws either banned abortion immediately or within a specified time frame after the ruling. In all, 26 states are expected to have abortion restrictions.
Missouri now allows abortion only for medical emergencies. If her upcoming ultrasound shows serious issues, Jessica says they could easily travel to another state and pay for an abortion. She realizes not everyone can.
However, the concern about trigger laws goes well beyond abortion. Many experts worry about the “spill-over” effects the abortion laws – both the existing ones and future proposals – may have on fertility care and treatments.
‘Personhood’ laws drive the concern
“The current trigger laws on the books are not impacting people’s access to IVF,” says Barbara Collura, president and CEO of RESOLVE, an advocacy group for those with fertility issues. “What we are concerned about is they will come back and make them stronger.”
The chief concern for reproductive rights advocates is so-called “personhood” legislation. According to the Guttmacher Institute, at least six bills about personhood have been introduced in five states, including Iowa, Oklahoma, South Carolina, Vermont, and West Virginia. One of the two Oklahoma bills has gone the farthest, passed by one chamber.
Since the Guttmacher report, Ohio introduced its own personhood legislation July 11, recognizing the personhood of an unborn person from conception.
Personhood legislation defines a fertilized egg or embryo as a legal human entity, says Sean Tipton, chief policy and advocacy officer for the Washington-based American Society of Reproductive Medicine, a nonprofit advocacy group.
“If the legal status of fertilized eggs or early embryos is codified, in vitro fertilization procedures may become legally risky for patients, physicians and staff,” Mr. Tipton wrote in late June in Contemporary OB/GYN Journal. The American Society for Reproductive Medicine has posted a report on state abortion trigger laws and their potential implications for reproductive medicine. Of the 13 with trigger laws in effect, the report found concern about the potential effect on IVF only with Utah’s.
‘Safe’ states?
Even in states without trigger laws or personhood bills, IVF patients say they are anxious about how the Supreme Court ruling may ultimately affect care. Thanks to IVF, Shelly Battista and her husband Robert are expecting twins in December, little sisters to their daughter Emilia, who is 2½.
They live in Illinois, where abortion is legal. “Even though we are safe now, I think the overturning of Roe has made it clear to all of us that none of our freedoms are safe, especially reproductive rights,” Ms. Shelly says.
About one in eight U.S. couples are infertile, according to RESOLVE, In 2019, 2% of all babies born in the United States, or about 78,000 infants, were conceived with the use of assisted reproductive technologies, according to the Centers for Disease Control and Prevention. The most common assisted reproductive technology is IVF, in which the sperm fertilizes the egg outside the body and an embryo is then transferred. The standard of practice is to transfer a single embryo, freezing others for future use.
Trigger state doctors weigh in
Some fertility doctors in those “trigger” states are keeping a close eye on proposed legislation and talking to legislators for interpretation of current and proposed laws.
Eli Reshef, MD, a reproductive endocrinologist and fertility specialist at Bennett Fertility Institute in Oklahoma City, notes that his state has “the strictest abortion law in the land.” The law prohibits all abortions with few exceptions, such as the removal of an ectopic pregnancy (when a fertilized egg implants outside the uterus, such as in the fallopian tubes).
While IVF will not be affected for now, he worries that the Oklahoma law allows a private citizen to sue a health care provider that they feel is performing abortion. The Oklahoma law leaves interpretation of abortion up to the general public, who may be unfamiliar with the language of the law, House Bill 4327.
Dean Moutos, MD, a reproductive endocrinologist and medical director of Arkansas Fertility and Gynecology in Little Rock, says his state’s current trigger law should not affect IVF. “When you read the bill, it says abortion means to terminate the pregnancy of a woman.” Still, he says, “we are concerned about what might happen in the future” and the possibility that some legislators may interpret that differently.
A minority approach
John David Gordon, MD, a reproductive endocrinologist and medical director of Southeastern Fertility Center for Fertility and Reproductive Surgery in Knoxville, Tenn., is also in a trigger state. However, it’s not likely any personhood laws would affect his practice.
That’s because his center, which he acknowledges is clearly in the minority, only performs natural-cycle IVF, which usually results in a single egg, or “mini-stim IVF,” which usually results in three to eight eggs in order to limit the number that may be potentially fertilized. Often, he says, patients choose to freeze unfertilized eggs (alone) to avoid creating an excessive number of embryos. He has a “no discard” program, with any viable embryos frozen or transferred. Abandoned embryos are donated to others.
“This may work for young women,” says Marcelle Cedars, MD, director of reproductive endocrinology at the University of California, San Francisco, and president of the American Society of Reproductive Medicine. However, she says, it will be very inefficient for older patients, since they have a higher percentage of abnormal eggs.
Overall, that approach will also drive up costs, especially for older women, Dr. Cedars says. An average cycle of IVF costs $12,400, and most Americans’ insurance plans don’t cover IVF, according to Mr. Tipton.
Top concerns for IVF
“Personhood” legislation has the potential to upend many common IVF practices, experts say.
Of greatest concern to fertility practices are potential restrictions on the freezing or discarding of embryos, Dr. Cedars says. “This could have a critical impact on practicing the safest, most evidence-based medicine,” she says.
Most children born in the United States as a result of IVF procedures are born from frozen embryos, according to the Society for Assisted Reproductive Technology, an organization for reproductive specialists.
“The practice of IVF really requires that we generate more embryos than will be used in a given [IVF] cycle,” agrees Kara Goldman, MD, associate professor of obstetrics and gynecology and medical director of the fertility preservation program at Northwestern University, Chicago. She performed the embryo transfer for the Battistas.
In nature, she says, it’s known that only a small number of eggs will be competent to generate a baby. “We see the same thing in IVF.” In a single cycle, 20 eggs may be retrieved, but many fewer typically reach successful fertilization and are able to be implanted.
When patients have completed their family, unused embryos are donated to research, donated for adoption, or destroyed. If embryo destruction is outlawed, Dr. Goldman says, it will have serious ramifications for the practice of IVF.
And if personhood legislation prohibits destroying any embryos, others wonder: Would a lab technician who accidentally dropped and destroyed an embryo be subject to charges? If laws prohibit destruction of embryos, others wonder if will families be forced to pay the embryo storage fees, generally $500-$1,000 a year, in perpetuity.
If an embryo is declared a person, it could also affect a practice called preimplantation genetic testing, or PGT. In PGT, cells are retrieved from an embryo and checked for genetic disorders such as sickle cell anemia and cystic fibrosis, with some parents choosing to discard embryos that are found to be affected.
Some potential parents choose this testing because they know they are carriers for genetic diseases that are serious and even incompatible with life, says Art Caplan, PhD, head of the division of medical ethics at New York University. They may choose to discard embryos that show evidence of the diseases.
Also under fire could be “selective reduction,” reducing multiple fetuses to a single or twin, to reduce risks to babies and mother.
Dr. Caplan predicts if states have many restrictions, some providers will adopt the attitude that “if no one reports, it did not happen.” And those prospective parents with the means, he says, will go to court and fight restrictions. “When they do it, they are saying, ‘You say you are pro-life; I’m trying to have a child. What are you doing getting in my way?’”
IVF families: Tough decisions, emotional times
The Battistas, of Illinois, have had an especially rough road. Shelly was diagnosed with a fast-growing breast cancer in 2020, when Emilia was just an infant. Warned that the chemotherapy she needed would suppress her ovaries, Shelly underwent egg retrieval before starting the cancer treatment.
She opted to have a double mastectomy and her ovaries removed after learning she carried the BRCA1 genetic mutation, boosting the risk of both breast and ovarian cancer.
Once she was cancer-free, she was cleared to start IVF. The first two embryo transfers failed. The third transfer, of a single embryo, was successful. But it split, a rare occurrence, producing two embryos. “It was a big shock, but in the best way,” she says about learning they were having twins. “Now we are over the moon.”
Five frozen embryos remain. At the start, the Battistas decided to discard unused embryos. She and Robert are discussing what to do next. If they decide they are done building their family after the twins’ birth, she wonders, “do we need to discard our [other] embryos before that becomes something that isn’t eligible [possible] for us any longer?” She doesn’t want to be rushed into that decision, however, especially with her medical history.
Jessica King and Sarah have 20 more embryos.
The couple had decided to donate unused embryos for research, when the time comes, and for different reasons. Her wife’s decision is based on her belief in science, while Jessica cites her faith. “As a Jew, it is part of our faith, that we should be doing everything we can to advance humanity,” she says.
In the midst of all the uncertainty, Jessica says, only half-jokingly, that she is tempted to claim the frozen embryos as dependents. “If you are truly going to claim these are precious human lives, you should be giving me all the benefits from having children,” she says.
Shelly knows that having one daughter, with two more on the way, affects her thinking about the court’s ruling. “My overall wish would be that Roe v. Wade is reinstated, and my daughters have the same rights and options that I have … or I did have until my current 36 years of life.”
A version of this article first appeared on WebMD.com.
Married for nearly 5 years, Jessica King, 34, and her wife, Sarah, agreed on some things right from the start. “We always knew kids were in the equation,” Jessica says.
Now, Jessica is nearly 20 weeks pregnant, thanks to in vitro fertilization, or IVF. They did “reciprocal” IVF, with Sarah’s egg mixed with donor sperm and the embryo transferred into Jessica. “We’re excited – and terrified,” Jessica says.
But that terror goes beyond the typical concerns of excess weight gain and long labors. They live in Missouri, one of 13 states with so-called trigger laws that went into effect after the Supreme Court overturned Roe v. Wade and the constitutional right to abortion, giving states the power to regulate it. States with trigger laws either banned abortion immediately or within a specified time frame after the ruling. In all, 26 states are expected to have abortion restrictions.
Missouri now allows abortion only for medical emergencies. If her upcoming ultrasound shows serious issues, Jessica says they could easily travel to another state and pay for an abortion. She realizes not everyone can.
However, the concern about trigger laws goes well beyond abortion. Many experts worry about the “spill-over” effects the abortion laws – both the existing ones and future proposals – may have on fertility care and treatments.
‘Personhood’ laws drive the concern
“The current trigger laws on the books are not impacting people’s access to IVF,” says Barbara Collura, president and CEO of RESOLVE, an advocacy group for those with fertility issues. “What we are concerned about is they will come back and make them stronger.”
The chief concern for reproductive rights advocates is so-called “personhood” legislation. According to the Guttmacher Institute, at least six bills about personhood have been introduced in five states, including Iowa, Oklahoma, South Carolina, Vermont, and West Virginia. One of the two Oklahoma bills has gone the farthest, passed by one chamber.
Since the Guttmacher report, Ohio introduced its own personhood legislation July 11, recognizing the personhood of an unborn person from conception.
Personhood legislation defines a fertilized egg or embryo as a legal human entity, says Sean Tipton, chief policy and advocacy officer for the Washington-based American Society of Reproductive Medicine, a nonprofit advocacy group.
“If the legal status of fertilized eggs or early embryos is codified, in vitro fertilization procedures may become legally risky for patients, physicians and staff,” Mr. Tipton wrote in late June in Contemporary OB/GYN Journal. The American Society for Reproductive Medicine has posted a report on state abortion trigger laws and their potential implications for reproductive medicine. Of the 13 with trigger laws in effect, the report found concern about the potential effect on IVF only with Utah’s.
‘Safe’ states?
Even in states without trigger laws or personhood bills, IVF patients say they are anxious about how the Supreme Court ruling may ultimately affect care. Thanks to IVF, Shelly Battista and her husband Robert are expecting twins in December, little sisters to their daughter Emilia, who is 2½.
They live in Illinois, where abortion is legal. “Even though we are safe now, I think the overturning of Roe has made it clear to all of us that none of our freedoms are safe, especially reproductive rights,” Ms. Shelly says.
About one in eight U.S. couples are infertile, according to RESOLVE, In 2019, 2% of all babies born in the United States, or about 78,000 infants, were conceived with the use of assisted reproductive technologies, according to the Centers for Disease Control and Prevention. The most common assisted reproductive technology is IVF, in which the sperm fertilizes the egg outside the body and an embryo is then transferred. The standard of practice is to transfer a single embryo, freezing others for future use.
Trigger state doctors weigh in
Some fertility doctors in those “trigger” states are keeping a close eye on proposed legislation and talking to legislators for interpretation of current and proposed laws.
Eli Reshef, MD, a reproductive endocrinologist and fertility specialist at Bennett Fertility Institute in Oklahoma City, notes that his state has “the strictest abortion law in the land.” The law prohibits all abortions with few exceptions, such as the removal of an ectopic pregnancy (when a fertilized egg implants outside the uterus, such as in the fallopian tubes).
While IVF will not be affected for now, he worries that the Oklahoma law allows a private citizen to sue a health care provider that they feel is performing abortion. The Oklahoma law leaves interpretation of abortion up to the general public, who may be unfamiliar with the language of the law, House Bill 4327.
Dean Moutos, MD, a reproductive endocrinologist and medical director of Arkansas Fertility and Gynecology in Little Rock, says his state’s current trigger law should not affect IVF. “When you read the bill, it says abortion means to terminate the pregnancy of a woman.” Still, he says, “we are concerned about what might happen in the future” and the possibility that some legislators may interpret that differently.
A minority approach
John David Gordon, MD, a reproductive endocrinologist and medical director of Southeastern Fertility Center for Fertility and Reproductive Surgery in Knoxville, Tenn., is also in a trigger state. However, it’s not likely any personhood laws would affect his practice.
That’s because his center, which he acknowledges is clearly in the minority, only performs natural-cycle IVF, which usually results in a single egg, or “mini-stim IVF,” which usually results in three to eight eggs in order to limit the number that may be potentially fertilized. Often, he says, patients choose to freeze unfertilized eggs (alone) to avoid creating an excessive number of embryos. He has a “no discard” program, with any viable embryos frozen or transferred. Abandoned embryos are donated to others.
“This may work for young women,” says Marcelle Cedars, MD, director of reproductive endocrinology at the University of California, San Francisco, and president of the American Society of Reproductive Medicine. However, she says, it will be very inefficient for older patients, since they have a higher percentage of abnormal eggs.
Overall, that approach will also drive up costs, especially for older women, Dr. Cedars says. An average cycle of IVF costs $12,400, and most Americans’ insurance plans don’t cover IVF, according to Mr. Tipton.
Top concerns for IVF
“Personhood” legislation has the potential to upend many common IVF practices, experts say.
Of greatest concern to fertility practices are potential restrictions on the freezing or discarding of embryos, Dr. Cedars says. “This could have a critical impact on practicing the safest, most evidence-based medicine,” she says.
Most children born in the United States as a result of IVF procedures are born from frozen embryos, according to the Society for Assisted Reproductive Technology, an organization for reproductive specialists.
“The practice of IVF really requires that we generate more embryos than will be used in a given [IVF] cycle,” agrees Kara Goldman, MD, associate professor of obstetrics and gynecology and medical director of the fertility preservation program at Northwestern University, Chicago. She performed the embryo transfer for the Battistas.
In nature, she says, it’s known that only a small number of eggs will be competent to generate a baby. “We see the same thing in IVF.” In a single cycle, 20 eggs may be retrieved, but many fewer typically reach successful fertilization and are able to be implanted.
When patients have completed their family, unused embryos are donated to research, donated for adoption, or destroyed. If embryo destruction is outlawed, Dr. Goldman says, it will have serious ramifications for the practice of IVF.
And if personhood legislation prohibits destroying any embryos, others wonder: Would a lab technician who accidentally dropped and destroyed an embryo be subject to charges? If laws prohibit destruction of embryos, others wonder if will families be forced to pay the embryo storage fees, generally $500-$1,000 a year, in perpetuity.
If an embryo is declared a person, it could also affect a practice called preimplantation genetic testing, or PGT. In PGT, cells are retrieved from an embryo and checked for genetic disorders such as sickle cell anemia and cystic fibrosis, with some parents choosing to discard embryos that are found to be affected.
Some potential parents choose this testing because they know they are carriers for genetic diseases that are serious and even incompatible with life, says Art Caplan, PhD, head of the division of medical ethics at New York University. They may choose to discard embryos that show evidence of the diseases.
Also under fire could be “selective reduction,” reducing multiple fetuses to a single or twin, to reduce risks to babies and mother.
Dr. Caplan predicts if states have many restrictions, some providers will adopt the attitude that “if no one reports, it did not happen.” And those prospective parents with the means, he says, will go to court and fight restrictions. “When they do it, they are saying, ‘You say you are pro-life; I’m trying to have a child. What are you doing getting in my way?’”
IVF families: Tough decisions, emotional times
The Battistas, of Illinois, have had an especially rough road. Shelly was diagnosed with a fast-growing breast cancer in 2020, when Emilia was just an infant. Warned that the chemotherapy she needed would suppress her ovaries, Shelly underwent egg retrieval before starting the cancer treatment.
She opted to have a double mastectomy and her ovaries removed after learning she carried the BRCA1 genetic mutation, boosting the risk of both breast and ovarian cancer.
Once she was cancer-free, she was cleared to start IVF. The first two embryo transfers failed. The third transfer, of a single embryo, was successful. But it split, a rare occurrence, producing two embryos. “It was a big shock, but in the best way,” she says about learning they were having twins. “Now we are over the moon.”
Five frozen embryos remain. At the start, the Battistas decided to discard unused embryos. She and Robert are discussing what to do next. If they decide they are done building their family after the twins’ birth, she wonders, “do we need to discard our [other] embryos before that becomes something that isn’t eligible [possible] for us any longer?” She doesn’t want to be rushed into that decision, however, especially with her medical history.
Jessica King and Sarah have 20 more embryos.
The couple had decided to donate unused embryos for research, when the time comes, and for different reasons. Her wife’s decision is based on her belief in science, while Jessica cites her faith. “As a Jew, it is part of our faith, that we should be doing everything we can to advance humanity,” she says.
In the midst of all the uncertainty, Jessica says, only half-jokingly, that she is tempted to claim the frozen embryos as dependents. “If you are truly going to claim these are precious human lives, you should be giving me all the benefits from having children,” she says.
Shelly knows that having one daughter, with two more on the way, affects her thinking about the court’s ruling. “My overall wish would be that Roe v. Wade is reinstated, and my daughters have the same rights and options that I have … or I did have until my current 36 years of life.”
A version of this article first appeared on WebMD.com.
LGBTQ+ Youth Consult: Let’s talk about PrEP!
As pediatricians, almost all of our clinic visits include some anticipatory guidance and recommendations on ways to promote well-being and prevent illness and injury for our patients. Because of minority stress, discrimination, and increased exposure to adverse childhood experiences, LGBTQ+ patients are disproportionately affected by certain health conditions including depression, anxiety, substance use, homelessness, as well as HIV and other sexually transmitted infections (STIs).1 While LGBTQ+ youth could benefit from additional guidance, counseling, and interventions related to these health disparities and have expressed interest in talking about these topics with their providers, sexual and gender minority youth also stress that they want to be treated as any other youth.2 Extending counseling for preventive care measures such as preexposure prophylaxis (PrEP) for HIV to all sexually active youth could help to destigmatize LGBTQ+ youth as being “different” from other youth and also help to increase overall access to HIV prevention services.3
Described by some as the “birth control” for HIV infection, PrEP is taken on an ongoing basis by those who are HIV negative before potential exposures to HIV in order to prevent new HIV infections. PrEP was first approved as a daily pill for adults in 2015 by the Food and Drug Administration with extension in 2018 to all individuals at risk for HIV weighing at least 35 kg after safety and efficacy data showed it could be used routinely for adolescents.4 When taken daily, oral PrEP can decrease the risk of HIV from sexual contact by more than 90% and from injection drug use by around 70%. As PrEP is highly effective with low risk for side effects, the U.S. Preventive Services Task Force (USPSTF) gave PrEP a “Grade A” recommendation for use in those at high risk for HIV infection in 2019.5 Since efficacy is closely tied to adherence, the first injectable PrEP (given at 0, 1, and 2 months with dosing then every 2 months) was also recently FDA approved in late 2021.6
Since HIV infection disproportionately affects LBGTQ+ individuals, and particularly LBGTQ+ youth of color, counseling related to PrEP has been largely targeted to these groups.7 Insurance and financial barriers to PrEP have been greatly reduced over the past several years through changes in insurance coverage (strengthened by the USPSTF recommendation), supplemental insurance programs, and pharmaceutical copay programs. Many states (but not all) also include HIV in the definition of STIs and allow minors to consent to PrEP services without a parent or guardian. Unfortunately, despite the high efficacy of PrEP and efforts to decrease barriers, rates of PrEP use continue to be extremely low, especially in youth, with only 15.6% of those aged 16-24 who are at risk for HIV in the United States actually taking PrEP in 2019.8 Many barriers to PrEP continue to exist including lack of awareness of PrEP, stigma surrounding HIV and PrEP, and lack of PrEP providers.
In order to address these low rates of PrEP uptake, the Centers for Disease Control and Prevention now recommends that medical providers discuss PrEP with all sexually active patients.6 PrEP should not be seen or discussed as something only relevant to LBGTQ+ populations, but rather as another tool in everyone’s “sexual health toolbox” that can allow us to experience human connection and pleasure through sexual activity while also having more control over what happens to our bodies. Not only will this allow more patients to access PrEP directly, it will also decrease the stigma of talking about HIV and PrEP and strengthen youths’ sense of autonomy and control over their own sexual health.
Since PrEP is a relatively new medical service, many providers will need to learn more about PrEP to at least have initial discussions with patients and to feel comfortable prescribing this themselves (See Resources). Below are also some suggestions to incorporate into your practice in order to advocate for the health and well-being of all your patients, including LGBTQ+ youth.
- Once your patients are 13 years and older, spend time with them alone to confidentially discuss more sensitive topics such as sexual health, mental health, and substance use.
- For all patients who are sexually active or considering sexual activity in the near future, discuss topics to help them control what happens to their bodies including consent, condoms, birth control, PrEP, and routine STI screening.
- Recommend PrEP to anyone who is sexually active and may be at increased risk for HIV infection or who is interested in taking PrEP for HIV prevention.
- Learn more about PrEP and start prescribing it to your own patients or become familiar with providers in your area to whom you could refer patients who are interested. While no certification is needed to prescribe PrEP, programs exist to help providers become more familiar with how to prescribe PrEP.
Dr. Warus is an adolescent medicine physician who specializes in care for transgender and gender-nonconforming youth, HIV prevention for adolescents and young adults, and LGBTQ health for youth at Children’s Hospital of Los Angeles. He is an assistant professor of clinical pediatrics and a University of Southern California faculty member.
Resources
CDC PrEP resources for clinicians: www.cdc.gov/hiv/clinicians/prevention/prep.html.Health HIV’s HIV Prevention Certified Provider Certification Program: https://healthhiv.org/programs/hpcp/.PrEP providers in the United States: https://preplocator.org/.Adolescent Health Working Group’s Sexual and Reproductive Health Toolkit for Adolescent Providers: https://ahwg.org/download/sexual-and-reproductive-health-toolkit-for-adolescent-providers/.
References
1. Lund EM and Burgess CM. Prim Care Clin Office Pract. 2021:48:179-89.
2. Hoffman ND et al. J Adolesc Health. 2009;45:222-9.
3. Mayer KH et al. Adv Ther. 2020;37:1778-811.
4. Hosek SG et al. JAMA Pediatr. 2017;171(11):1063-71.
5. U.S. Preventive Services Task Force; Owens DK et al. JAMA. 2019;321(22):2203-13.
6. Centers for Disease Control and Prevention: U.S. Public Health Service: Preexposure Prophylaxis for the Prevention of HIV Infection in the United States – 2021 Update: A Clinical Practice Guideline. Published 2021. Accessed July 10, 2022.
7. Centers for Disease Control and Prevention. Estimated HIV Incidence and Prevalence in the United States, 2015-2019. HIV Surveillance Supplemental Report. 2021;26(1). Published May 2021. Accessed July 10, 2022.
8. Centers for Disease Control and Prevention. Monitoring Selected National HIV Prevention and Care Objectives by Using HIV Surveillance Data–United States and 6 Dependent Areas, 2020. HIV Surveillance Supplemental Report. 2022;27(3).
As pediatricians, almost all of our clinic visits include some anticipatory guidance and recommendations on ways to promote well-being and prevent illness and injury for our patients. Because of minority stress, discrimination, and increased exposure to adverse childhood experiences, LGBTQ+ patients are disproportionately affected by certain health conditions including depression, anxiety, substance use, homelessness, as well as HIV and other sexually transmitted infections (STIs).1 While LGBTQ+ youth could benefit from additional guidance, counseling, and interventions related to these health disparities and have expressed interest in talking about these topics with their providers, sexual and gender minority youth also stress that they want to be treated as any other youth.2 Extending counseling for preventive care measures such as preexposure prophylaxis (PrEP) for HIV to all sexually active youth could help to destigmatize LGBTQ+ youth as being “different” from other youth and also help to increase overall access to HIV prevention services.3
Described by some as the “birth control” for HIV infection, PrEP is taken on an ongoing basis by those who are HIV negative before potential exposures to HIV in order to prevent new HIV infections. PrEP was first approved as a daily pill for adults in 2015 by the Food and Drug Administration with extension in 2018 to all individuals at risk for HIV weighing at least 35 kg after safety and efficacy data showed it could be used routinely for adolescents.4 When taken daily, oral PrEP can decrease the risk of HIV from sexual contact by more than 90% and from injection drug use by around 70%. As PrEP is highly effective with low risk for side effects, the U.S. Preventive Services Task Force (USPSTF) gave PrEP a “Grade A” recommendation for use in those at high risk for HIV infection in 2019.5 Since efficacy is closely tied to adherence, the first injectable PrEP (given at 0, 1, and 2 months with dosing then every 2 months) was also recently FDA approved in late 2021.6
Since HIV infection disproportionately affects LBGTQ+ individuals, and particularly LBGTQ+ youth of color, counseling related to PrEP has been largely targeted to these groups.7 Insurance and financial barriers to PrEP have been greatly reduced over the past several years through changes in insurance coverage (strengthened by the USPSTF recommendation), supplemental insurance programs, and pharmaceutical copay programs. Many states (but not all) also include HIV in the definition of STIs and allow minors to consent to PrEP services without a parent or guardian. Unfortunately, despite the high efficacy of PrEP and efforts to decrease barriers, rates of PrEP use continue to be extremely low, especially in youth, with only 15.6% of those aged 16-24 who are at risk for HIV in the United States actually taking PrEP in 2019.8 Many barriers to PrEP continue to exist including lack of awareness of PrEP, stigma surrounding HIV and PrEP, and lack of PrEP providers.
In order to address these low rates of PrEP uptake, the Centers for Disease Control and Prevention now recommends that medical providers discuss PrEP with all sexually active patients.6 PrEP should not be seen or discussed as something only relevant to LBGTQ+ populations, but rather as another tool in everyone’s “sexual health toolbox” that can allow us to experience human connection and pleasure through sexual activity while also having more control over what happens to our bodies. Not only will this allow more patients to access PrEP directly, it will also decrease the stigma of talking about HIV and PrEP and strengthen youths’ sense of autonomy and control over their own sexual health.
Since PrEP is a relatively new medical service, many providers will need to learn more about PrEP to at least have initial discussions with patients and to feel comfortable prescribing this themselves (See Resources). Below are also some suggestions to incorporate into your practice in order to advocate for the health and well-being of all your patients, including LGBTQ+ youth.
- Once your patients are 13 years and older, spend time with them alone to confidentially discuss more sensitive topics such as sexual health, mental health, and substance use.
- For all patients who are sexually active or considering sexual activity in the near future, discuss topics to help them control what happens to their bodies including consent, condoms, birth control, PrEP, and routine STI screening.
- Recommend PrEP to anyone who is sexually active and may be at increased risk for HIV infection or who is interested in taking PrEP for HIV prevention.
- Learn more about PrEP and start prescribing it to your own patients or become familiar with providers in your area to whom you could refer patients who are interested. While no certification is needed to prescribe PrEP, programs exist to help providers become more familiar with how to prescribe PrEP.
Dr. Warus is an adolescent medicine physician who specializes in care for transgender and gender-nonconforming youth, HIV prevention for adolescents and young adults, and LGBTQ health for youth at Children’s Hospital of Los Angeles. He is an assistant professor of clinical pediatrics and a University of Southern California faculty member.
Resources
CDC PrEP resources for clinicians: www.cdc.gov/hiv/clinicians/prevention/prep.html.Health HIV’s HIV Prevention Certified Provider Certification Program: https://healthhiv.org/programs/hpcp/.PrEP providers in the United States: https://preplocator.org/.Adolescent Health Working Group’s Sexual and Reproductive Health Toolkit for Adolescent Providers: https://ahwg.org/download/sexual-and-reproductive-health-toolkit-for-adolescent-providers/.
References
1. Lund EM and Burgess CM. Prim Care Clin Office Pract. 2021:48:179-89.
2. Hoffman ND et al. J Adolesc Health. 2009;45:222-9.
3. Mayer KH et al. Adv Ther. 2020;37:1778-811.
4. Hosek SG et al. JAMA Pediatr. 2017;171(11):1063-71.
5. U.S. Preventive Services Task Force; Owens DK et al. JAMA. 2019;321(22):2203-13.
6. Centers for Disease Control and Prevention: U.S. Public Health Service: Preexposure Prophylaxis for the Prevention of HIV Infection in the United States – 2021 Update: A Clinical Practice Guideline. Published 2021. Accessed July 10, 2022.
7. Centers for Disease Control and Prevention. Estimated HIV Incidence and Prevalence in the United States, 2015-2019. HIV Surveillance Supplemental Report. 2021;26(1). Published May 2021. Accessed July 10, 2022.
8. Centers for Disease Control and Prevention. Monitoring Selected National HIV Prevention and Care Objectives by Using HIV Surveillance Data–United States and 6 Dependent Areas, 2020. HIV Surveillance Supplemental Report. 2022;27(3).
As pediatricians, almost all of our clinic visits include some anticipatory guidance and recommendations on ways to promote well-being and prevent illness and injury for our patients. Because of minority stress, discrimination, and increased exposure to adverse childhood experiences, LGBTQ+ patients are disproportionately affected by certain health conditions including depression, anxiety, substance use, homelessness, as well as HIV and other sexually transmitted infections (STIs).1 While LGBTQ+ youth could benefit from additional guidance, counseling, and interventions related to these health disparities and have expressed interest in talking about these topics with their providers, sexual and gender minority youth also stress that they want to be treated as any other youth.2 Extending counseling for preventive care measures such as preexposure prophylaxis (PrEP) for HIV to all sexually active youth could help to destigmatize LGBTQ+ youth as being “different” from other youth and also help to increase overall access to HIV prevention services.3
Described by some as the “birth control” for HIV infection, PrEP is taken on an ongoing basis by those who are HIV negative before potential exposures to HIV in order to prevent new HIV infections. PrEP was first approved as a daily pill for adults in 2015 by the Food and Drug Administration with extension in 2018 to all individuals at risk for HIV weighing at least 35 kg after safety and efficacy data showed it could be used routinely for adolescents.4 When taken daily, oral PrEP can decrease the risk of HIV from sexual contact by more than 90% and from injection drug use by around 70%. As PrEP is highly effective with low risk for side effects, the U.S. Preventive Services Task Force (USPSTF) gave PrEP a “Grade A” recommendation for use in those at high risk for HIV infection in 2019.5 Since efficacy is closely tied to adherence, the first injectable PrEP (given at 0, 1, and 2 months with dosing then every 2 months) was also recently FDA approved in late 2021.6
Since HIV infection disproportionately affects LBGTQ+ individuals, and particularly LBGTQ+ youth of color, counseling related to PrEP has been largely targeted to these groups.7 Insurance and financial barriers to PrEP have been greatly reduced over the past several years through changes in insurance coverage (strengthened by the USPSTF recommendation), supplemental insurance programs, and pharmaceutical copay programs. Many states (but not all) also include HIV in the definition of STIs and allow minors to consent to PrEP services without a parent or guardian. Unfortunately, despite the high efficacy of PrEP and efforts to decrease barriers, rates of PrEP use continue to be extremely low, especially in youth, with only 15.6% of those aged 16-24 who are at risk for HIV in the United States actually taking PrEP in 2019.8 Many barriers to PrEP continue to exist including lack of awareness of PrEP, stigma surrounding HIV and PrEP, and lack of PrEP providers.
In order to address these low rates of PrEP uptake, the Centers for Disease Control and Prevention now recommends that medical providers discuss PrEP with all sexually active patients.6 PrEP should not be seen or discussed as something only relevant to LBGTQ+ populations, but rather as another tool in everyone’s “sexual health toolbox” that can allow us to experience human connection and pleasure through sexual activity while also having more control over what happens to our bodies. Not only will this allow more patients to access PrEP directly, it will also decrease the stigma of talking about HIV and PrEP and strengthen youths’ sense of autonomy and control over their own sexual health.
Since PrEP is a relatively new medical service, many providers will need to learn more about PrEP to at least have initial discussions with patients and to feel comfortable prescribing this themselves (See Resources). Below are also some suggestions to incorporate into your practice in order to advocate for the health and well-being of all your patients, including LGBTQ+ youth.
- Once your patients are 13 years and older, spend time with them alone to confidentially discuss more sensitive topics such as sexual health, mental health, and substance use.
- For all patients who are sexually active or considering sexual activity in the near future, discuss topics to help them control what happens to their bodies including consent, condoms, birth control, PrEP, and routine STI screening.
- Recommend PrEP to anyone who is sexually active and may be at increased risk for HIV infection or who is interested in taking PrEP for HIV prevention.
- Learn more about PrEP and start prescribing it to your own patients or become familiar with providers in your area to whom you could refer patients who are interested. While no certification is needed to prescribe PrEP, programs exist to help providers become more familiar with how to prescribe PrEP.
Dr. Warus is an adolescent medicine physician who specializes in care for transgender and gender-nonconforming youth, HIV prevention for adolescents and young adults, and LGBTQ health for youth at Children’s Hospital of Los Angeles. He is an assistant professor of clinical pediatrics and a University of Southern California faculty member.
Resources
CDC PrEP resources for clinicians: www.cdc.gov/hiv/clinicians/prevention/prep.html.Health HIV’s HIV Prevention Certified Provider Certification Program: https://healthhiv.org/programs/hpcp/.PrEP providers in the United States: https://preplocator.org/.Adolescent Health Working Group’s Sexual and Reproductive Health Toolkit for Adolescent Providers: https://ahwg.org/download/sexual-and-reproductive-health-toolkit-for-adolescent-providers/.
References
1. Lund EM and Burgess CM. Prim Care Clin Office Pract. 2021:48:179-89.
2. Hoffman ND et al. J Adolesc Health. 2009;45:222-9.
3. Mayer KH et al. Adv Ther. 2020;37:1778-811.
4. Hosek SG et al. JAMA Pediatr. 2017;171(11):1063-71.
5. U.S. Preventive Services Task Force; Owens DK et al. JAMA. 2019;321(22):2203-13.
6. Centers for Disease Control and Prevention: U.S. Public Health Service: Preexposure Prophylaxis for the Prevention of HIV Infection in the United States – 2021 Update: A Clinical Practice Guideline. Published 2021. Accessed July 10, 2022.
7. Centers for Disease Control and Prevention. Estimated HIV Incidence and Prevalence in the United States, 2015-2019. HIV Surveillance Supplemental Report. 2021;26(1). Published May 2021. Accessed July 10, 2022.
8. Centers for Disease Control and Prevention. Monitoring Selected National HIV Prevention and Care Objectives by Using HIV Surveillance Data–United States and 6 Dependent Areas, 2020. HIV Surveillance Supplemental Report. 2022;27(3).
Surgical Treatment of Nonmelanoma Skin Cancer in Older Adult Veterans
Skin cancer is the most diagnosed cancer in the United States. Nonmelanoma skin cancers (NMSC), which include basal cell carcinoma and squamous cell carcinoma, are usually cured with removal.1 The incidence of NMSC increases with age and is commonly found in nursing homes and geriatric units. These cancers are not usually metastatic or fatal but can cause local destruction and disfigurement if neglected.2 The current standard of care is to treat diagnosed NMSC; however, the dermatology and geriatric care literature have questioned the logic of treating asymptomatic skin cancers that will not affect a patient’s life expectancy.2-4
Forty-seven percent of the current living veteran population is aged ≥ 65 years.5 Older adult patients are frequently referred to the US Department of Veterans Affairs (VA) surgical service for the treatment of NMSC. The veteran population includes a higher percentage of individuals at an elevated risk of skin cancers (older, White, and male) compared with the general population.6 World War II veterans deployed in regions closer to the equator have been found to have an elevated risk of melanoma and nonmelanoma skin carcinomas.7 A retrospective study of Vietnam veterans exposed to Agent Orange (2,3,7,8-tetrachlorodibenzodioxin) found a significantly higher risk of invasive NMSC in Fitzpatrick skin types I-IV compared with an age-matched subset of the general population.8 Younger veterans who were deployed in Afghanistan and Iraq for Operation Enduring Freedom/Operation Iraqi Freedom worked at more equatorial latitudes than the rest of the US population and may be at increased risk of NMSC. Inadequate sunscreen access, immediate safety concerns, outdoor recreational activities, harsh weather, and insufficient emphasis on sun protection have created a multifactorial challenge for the military population. Riemenschneider and colleagues recommended targeted screening for at-risk veteran patients and prioritizing annual skin cancer screenings during medical mission physical examinations for active military.7
The plastic surgery service regularly receives consults from dermatology, general surgery, and primary care to remove skin cancers on the face, scalp, hands, and forearms. Skin cancer treatment can create serious hardships for older adult patients and their families with multiple appointments for the consult, procedure, and follow-up. Patients are often told to hold their anticoagulant medications when the surgery will be performed on a highly vascular region, such as the scalp or face. This can create wide swings in their laboratory test values and result in life-threatening complications from either bleeding or clotting. The appropriateness of offering surgery to patients with serious comorbidities and a limited life expectancy has been questioned.2-4 The purpose of this study was to measure the morbidity and unrelated 5-year mortality for patients with skin cancer referred to the plastic surgery service to help patients and families make a more informed treatment decision, particularly when the patients are aged > 80 years and have significant life-threatening comorbidities.
Methods
The University of Florida and Malcom Randall VA Medical Center Institutional review board in Gainesville, approved a retrospective review of all consults completed by the plastic surgery service for the treatment of NMSC performed from July 1, 2011 to June 30, 2015. Data collected included age and common life-limiting comorbidities at the time of referral. Morbidities were found on the electronic health record, including coronary artery disease (CAD), congestive heart failure (CHF), cerebral vascular disease (CVD), peripheral vascular disease, dementia, chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), tobacco use, diabetes mellitus (DM), liver disease, alcohol use, and obstructive sleep apnea.
Treatment, complications, and 5-year mortality were recorded. A χ2 analysis with P value < .05 was used to determine statistical significance between individual risk factors and 5-year mortality. The relative risk of 5-year mortality was calculated by combining advanced age (aged > 80 years) with the individual comorbidities.
Results
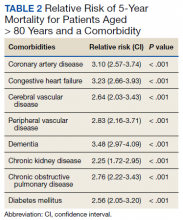
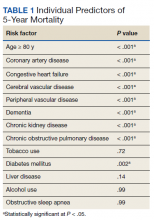
Over 4 years, 800 consults for NMSC were completed by the plastic surgery service. Treatment decisions included 210 excisions (with or without reconstruction) in the operating room, 402 excisions (with or without reconstruction) under local anesthesia in clinic, 55 Mohs surgical dermatology referrals, 21 other service or hospital referrals, and 112 patient who were observed, declined intervention, or died prior to intervention. Five-year mortality was 28.6%. No patients died of NMSC. The median age at consult submission for patients deceased 5 years later was 78 years. Complication rate was 5% and included wound infection, dehiscence, bleeding, or graft loss. Two patients, both deceased within 5 years, had unplanned admissions due to bleeding from either a skin graft donor site or recipient bleeding. Aged ≥ 80 years, CAD, CHF, CVD, peripheral vascular disease, dementia, CKD, COPD, and DM were all found individually to be statistically significant predictors of 5-year mortality (Table 1). Combining aged ≥ 80 years plus CAD, CHF, or dementia all increased the 5-year mortality by a relative risk of > 3 (Table 2).
Discussion
The standard of care is to treat NMSC. Most NMSCs are treated surgically without consideration of patient age or life expectancy.2,4,9,10 A prospective cohort study involving a university-based private practice and a VA medical center in San Francisco found a 22.6% overall 5-year mortality and a 43.3% mortality in the group defined as limited life expectancy (LLE) based on age (≥ 85 years) and medical comorbidities. None died due to the NMSC. Leading cause of death was cardiac, cerebrovascular, and respiratory disease, lung and prostate cancer, and Alzheimer disease. The authors suggested the LLE group may be exposed to wound complications without benefiting from the treatment.4
Another study of 440 patients receiving excision for biopsy-proven facial NMSC at the Roudebush VA Medical Center in Indianapolis, Indiana, found no residual carcinoma in 35.3% of excisions, and in patients aged > 90 years, more than half of the excisions had no residual carcinoma. More than half of the patients aged > 90 years died within 1 year, not as a result of the NMSC. The authors argued for watchful waiting in select patients to maximize comfort and outcomes.10
NMSCs are often asymptomatic and not immediately life threatening. Although NMSCs tend to have a favorable prognosis, studies have found that NMSC may be a marker for other poor health outcomes. A significant increased risk for all-cause mortality was found for patients with a history of SCC, which may be attributed to immune status.11 The aging veteran population has more complex health care needs to be considered when developing surgical treatment plans. These medical problems may limit their life expectancy much sooner than the skin cancer will become symptomatic. We found that individuals aged ≥ 80 years who had CAD, CHF, or dementia had a relative risk of 3 or higher for 5-year mortality. The leading cause of death in the United States in years 2011 to 2015 was heart disease. Alzheimer disease was the sixth leading cause of death in those same years.12-14
Skin cancer excisions do not typically require general anesthesia, deep sedation, or large fluid shifts; however, studies have found that when frail patients undergo low-risk procedures, they tend to have a higher mortality rate than their healthier counterparts.15 Frailty is a concept that identifies patients who are at increased risk of dying in 6 to 60 months due to a decline in their physical reserve. Frail patients have increased rates of perioperative mortality and complications. Various tools have been used to assess the components of physical performance, speed, mobility, nutrition status, mental health, and cognition.16 Frailty screening has been initiated in several VA hospitals, including our own in Gainesville, Florida, with the goal of decreasing postoperative morbidity and mortality in older adult patients.17 The patients are given a 1-page screening assessment that asks about their living situation, medical conditions, nutrition status, cognition, and activities of daily living. The results can trigger the clinician to rethink the surgical plan and mobilize more resources to optimize the patient’s health. This study period precedes the initiative at our institution.
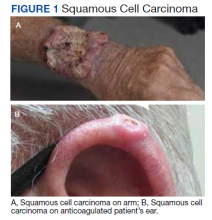
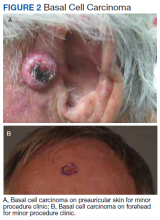
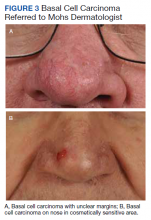
The plastic surgery service’s routine practice is to excise skin cancers in the operating room if sedation or general anesthesia will be needed (Figure 1A), for optimal control of bleeding (Figure 1B) in a patient who cannot safely stop blood thinners, or for excision of a highly vascularized area such as the scalp. Surgery is offered in an office-based setting if the area can be closed primarily, left open to close secondarily, or closed with a small skin graft under local anesthesia only (Figure 2). We prefer treating frail patients in the minor procedure clinic, when possible, to avoid the risks of sedation and the additional preoperative visits and transportation requirements. NMSC with unclear margins (Figure 3A) or in cosmetically sensitive areas where tissue needs to be preserved (Figure 3B) are referred to the Mohs dermatologist. The skin cancers in this study were most frequently found on the face, scalp, hands, and forearms based on referral patterns.
Other treatment options for NMSC include curettage and electrodessication, cryotherapy, and radiation; however, ours is a surgical service and patients are typically referred to us by primary care or dermatology when those are not reasonable or desirable options.18 Published complication rates of patients having skin cancer surgery without age restriction have a rate of 3% to 6%, which is consistent with our study of 5%.19-21 Two bleeding complications that needed to be admitted did not require more than a bedside procedure and neither required transfusions. One patient had been instructed to continue taking coumadin during the perioperative office-based procedure due to a recent carotid stent placement in the setting of a rapidly growing basal cell on an easily accessible location.
The most noted comorbidity in patients with wound complications was found to be DM; however, this was not found to be a statistically significant risk factor for wound complications (P = .10). We do not have a set rule for advising for or against NMSC surgery. We do counsel frail patients and their families that not all cancer is immediately life threatening and will work with them to do whatever makes the most sense to achieve their goals, occasionally accepting positive margins in order to debulk a symptomatic growth. The objective of this paper is to contribute to the discussion of performing invasive procedures on older adult veterans with life-limiting comorbidities. Patients and their families will have different thresholds for what they feel needs intervention, especially if other medical problems are consuming much of their time. We also have the community care referral option for patients whose treatment decisions are being dictated by travel hardships.
Strengths and Limitations
A strength of this study is that the data were obtained from a closed system. Patients tend to stay long-term within the VA and their health record is accessible throughout the country as long as they are seen at a VA facility. Complications, therefore, return to the treating service or primary care, who would route the patient back to the surgeon.
One limitation of the study is that this is a retrospective review from 2011. The authors are limited to data that are recorded in the patient record. Multiple health care professionals saw the patients and notes lack consistency in detail. Size of the lesions were not consistently recorded and did not get logged into our database for that reason.
Conclusions
Treatment of NMSC in older adult patients has a low morbidity but needs to be balanced against a patient and family’s goals when the patient presents with life-limiting comorbidities. An elevated 5-year mortality in patients aged > 80 years with serious unrelated medical conditions is intuitive, but this study may help put treatment plans into perspective for families and health care professionals who want to provide an indicated service while maximizing patient quality of life.
Acknowledgments
This manuscript is the result of work supported with resources and the use of facilities at the North Florida/South Georgia Veterans Health System, Gainesville, Florida.
1. American Cancer Society. Cancer Facts & Figures 2021. Accessed May 26, 2022. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2021/cancer-facts-and-figures-2021.pdf
2. Albert A, Knoll MA, Conti JA, Zbar RIS. Non-melanoma skin cancers in the older patient. Curr Oncol Rep. 2019;21(9):79. Published 2019 Jul 29. doi:10.1007/s11912-019-0828-9
3. Linos E, Chren MM, Stijacic Cenzer I, Covinsky KE. Skin cancer in U.S. elderly adults: does life expectancy play a role in treatment decisions? J Am Geriatr Soc. 2016;64(8):1610-1615. doi:10.1111/jgs.14202
4. Linos E, Parvataneni R, Stuart SE, Boscardin WJ, Landefeld CS, Chren MM. Treatment of nonfatal conditions at the end of life: nonmelanoma skin cancer. JAMA Intern Med. 2013;173(11):1006-1012. doi:10.1001/jamainternmed.2013.639
5. O’Malley KA, Vinson L, Kaiser AP, Sager Z, Hinrichs K. Mental health and aging veterans: how the Veterans Health Administration meets the needs of aging veterans. Public Policy Aging Rep. 2020;30(1):19-23. doi:10.1093/ppar/prz027
6. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Profile of veterans: 2017. Accessed May 26, 2022. https://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Veterans_2017.pdf 7. Riemenschneider K, Liu J, Powers JG. Skin cancer in the military: a systematic review of melanoma and nonmelanoma skin cancer incidence, prevention, and screening among active duty and veteran personnel. J Am Acad Dermatol. 2018;78(6):1185-1192. doi:10.1016/j.jaad.2017.11.062
8. Clemens MW, Kochuba AL, Carter ME, Han K, Liu J, Evans K. Association between Agent Orange exposure and nonmelanotic invasive skin cancer: a pilot study. Plast Reconstr Surg. 2014;133(2):432-437. doi:10.1097/01.prs.0000436859.40151.cf
9. Cameron MC, Lee E, Hibler BP, et al. Basal cell carcinoma: epidemiology; pathophysiology; clinical and histological subtypes; and disease associations. J Am Acad Dermatol. 2019;80(2):303-317. doi:10.1016/j.jaad.2018.03.060
10. Chauhan R, Munger BN, Chu MW, et al. Age at diagnosis as a relative contraindication for intervention in facial nonmelanoma skin cancer. JAMA Surg. 2018;153(4):390-392. doi:10.1001/jamasurg.2017.5073
11. Barton V, Armeson K, Hampras S, et al. Nonmelanoma skin cancer and risk of all-cause and cancer-related mortality: a systematic review. Arch Dermatol Res. 2017;309(4):243-251. doi:10.1007/s00403-017-1724-5
12. Kochanek KD, Murphy SL, Xu JQ, Arias E. Mortality in the United States, 2013. NCHS Data Brief 178. Accessed May 26, 2022. https://www.cdc.gov/nchs/products/databriefs/db178.htm
13. Xu JQ, Kochanek KD, Murphy SL, Arias E. Mortality in the United States, 2012. NCHS Data Brief 168. Accessed May 26, 2022. https://www.cdc.gov/nchs/products/databriefs/db168.htm
14. Xu JQ, Murphy SL, Kochanek KD, Arias E. Mortality in the United States, 2015. NCHS Data Brief 267. Accessed May 26, 2022. https://www.cdc.gov/nchs/products/databriefs/db267.htm
15. Varley PR , Borrebach JD, Arya S, et al. Clinical utility of the risk analysis index as a prospective frailty screening tool within a multi-practice, multi-hospital integrated healthcare system. Ann Surg. 2021;274(6):e1230-e1237. doi:10.1097/SLA.0000000000003808
16. Hall DE, Arya S , Schmid KK, et al. Development and initial validation of the risk analysis index for measuring frailty in surgical populations. JAMA Surg. 2017;152(2):175-182. doi:10.1001/jamasurg.2016.4202
17. US Department of Veterans Affairs, Health Services Research & Development. Improving healthcare for aging veterans. Updated August 30, 2017. Accessed May 26, 2022. https://www.hsrd.research.va.gov/news/feature/aging0917.cfm
18. Leus AJG, Frie M, Haisma MS, et al. Treatment of keratinocyte carcinoma in elderly patients – a review of the current literature. J Eur Acad Dermatol Venereol. 2020;34(9):1932-1943. doi:10.1111/jdv.16268
19. Amici JM, Rogues AM, Lasheras A, et al. A prospective study of the incidence of complications associated with dermatological surgery. Br J Dermatol. 2005;153(5):967-971. doi:10.1111/j.1365-2133.2005.06861.x
20. Arguello-Guerra L, Vargas-Chandomid E, Díaz-González JM, Méndez-Flores S, Ruelas-Villavicencio A, Domínguez-Cherit J. Incidence of complications in dermatological surgery of melanoma and non-melanoma skin cancer in patients with multiple comorbidity and/or antiplatelet-anticoagulants. Five-year experience in our hospital. Cir Cir. 2019;86(1):15-23. doi:10.24875/CIRUE.M18000003
21. Keith DJ, de Berker DA, Bray AP, Cheung ST, Brain A, Mohd Mustapa MF. British Association of Dermatologists’ national audit on nonmelanoma skin cancer excision, 2014. Clin Exp Dermatol. 2017;42(1):46-53. doi:10.1111/ced.12990
Skin cancer is the most diagnosed cancer in the United States. Nonmelanoma skin cancers (NMSC), which include basal cell carcinoma and squamous cell carcinoma, are usually cured with removal.1 The incidence of NMSC increases with age and is commonly found in nursing homes and geriatric units. These cancers are not usually metastatic or fatal but can cause local destruction and disfigurement if neglected.2 The current standard of care is to treat diagnosed NMSC; however, the dermatology and geriatric care literature have questioned the logic of treating asymptomatic skin cancers that will not affect a patient’s life expectancy.2-4
Forty-seven percent of the current living veteran population is aged ≥ 65 years.5 Older adult patients are frequently referred to the US Department of Veterans Affairs (VA) surgical service for the treatment of NMSC. The veteran population includes a higher percentage of individuals at an elevated risk of skin cancers (older, White, and male) compared with the general population.6 World War II veterans deployed in regions closer to the equator have been found to have an elevated risk of melanoma and nonmelanoma skin carcinomas.7 A retrospective study of Vietnam veterans exposed to Agent Orange (2,3,7,8-tetrachlorodibenzodioxin) found a significantly higher risk of invasive NMSC in Fitzpatrick skin types I-IV compared with an age-matched subset of the general population.8 Younger veterans who were deployed in Afghanistan and Iraq for Operation Enduring Freedom/Operation Iraqi Freedom worked at more equatorial latitudes than the rest of the US population and may be at increased risk of NMSC. Inadequate sunscreen access, immediate safety concerns, outdoor recreational activities, harsh weather, and insufficient emphasis on sun protection have created a multifactorial challenge for the military population. Riemenschneider and colleagues recommended targeted screening for at-risk veteran patients and prioritizing annual skin cancer screenings during medical mission physical examinations for active military.7
The plastic surgery service regularly receives consults from dermatology, general surgery, and primary care to remove skin cancers on the face, scalp, hands, and forearms. Skin cancer treatment can create serious hardships for older adult patients and their families with multiple appointments for the consult, procedure, and follow-up. Patients are often told to hold their anticoagulant medications when the surgery will be performed on a highly vascular region, such as the scalp or face. This can create wide swings in their laboratory test values and result in life-threatening complications from either bleeding or clotting. The appropriateness of offering surgery to patients with serious comorbidities and a limited life expectancy has been questioned.2-4 The purpose of this study was to measure the morbidity and unrelated 5-year mortality for patients with skin cancer referred to the plastic surgery service to help patients and families make a more informed treatment decision, particularly when the patients are aged > 80 years and have significant life-threatening comorbidities.
Methods
The University of Florida and Malcom Randall VA Medical Center Institutional review board in Gainesville, approved a retrospective review of all consults completed by the plastic surgery service for the treatment of NMSC performed from July 1, 2011 to June 30, 2015. Data collected included age and common life-limiting comorbidities at the time of referral. Morbidities were found on the electronic health record, including coronary artery disease (CAD), congestive heart failure (CHF), cerebral vascular disease (CVD), peripheral vascular disease, dementia, chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), tobacco use, diabetes mellitus (DM), liver disease, alcohol use, and obstructive sleep apnea.
Treatment, complications, and 5-year mortality were recorded. A χ2 analysis with P value < .05 was used to determine statistical significance between individual risk factors and 5-year mortality. The relative risk of 5-year mortality was calculated by combining advanced age (aged > 80 years) with the individual comorbidities.
Results
Over 4 years, 800 consults for NMSC were completed by the plastic surgery service. Treatment decisions included 210 excisions (with or without reconstruction) in the operating room, 402 excisions (with or without reconstruction) under local anesthesia in clinic, 55 Mohs surgical dermatology referrals, 21 other service or hospital referrals, and 112 patient who were observed, declined intervention, or died prior to intervention. Five-year mortality was 28.6%. No patients died of NMSC. The median age at consult submission for patients deceased 5 years later was 78 years. Complication rate was 5% and included wound infection, dehiscence, bleeding, or graft loss. Two patients, both deceased within 5 years, had unplanned admissions due to bleeding from either a skin graft donor site or recipient bleeding. Aged ≥ 80 years, CAD, CHF, CVD, peripheral vascular disease, dementia, CKD, COPD, and DM were all found individually to be statistically significant predictors of 5-year mortality (Table 1). Combining aged ≥ 80 years plus CAD, CHF, or dementia all increased the 5-year mortality by a relative risk of > 3 (Table 2).
Discussion
The standard of care is to treat NMSC. Most NMSCs are treated surgically without consideration of patient age or life expectancy.2,4,9,10 A prospective cohort study involving a university-based private practice and a VA medical center in San Francisco found a 22.6% overall 5-year mortality and a 43.3% mortality in the group defined as limited life expectancy (LLE) based on age (≥ 85 years) and medical comorbidities. None died due to the NMSC. Leading cause of death was cardiac, cerebrovascular, and respiratory disease, lung and prostate cancer, and Alzheimer disease. The authors suggested the LLE group may be exposed to wound complications without benefiting from the treatment.4
Another study of 440 patients receiving excision for biopsy-proven facial NMSC at the Roudebush VA Medical Center in Indianapolis, Indiana, found no residual carcinoma in 35.3% of excisions, and in patients aged > 90 years, more than half of the excisions had no residual carcinoma. More than half of the patients aged > 90 years died within 1 year, not as a result of the NMSC. The authors argued for watchful waiting in select patients to maximize comfort and outcomes.10
NMSCs are often asymptomatic and not immediately life threatening. Although NMSCs tend to have a favorable prognosis, studies have found that NMSC may be a marker for other poor health outcomes. A significant increased risk for all-cause mortality was found for patients with a history of SCC, which may be attributed to immune status.11 The aging veteran population has more complex health care needs to be considered when developing surgical treatment plans. These medical problems may limit their life expectancy much sooner than the skin cancer will become symptomatic. We found that individuals aged ≥ 80 years who had CAD, CHF, or dementia had a relative risk of 3 or higher for 5-year mortality. The leading cause of death in the United States in years 2011 to 2015 was heart disease. Alzheimer disease was the sixth leading cause of death in those same years.12-14
Skin cancer excisions do not typically require general anesthesia, deep sedation, or large fluid shifts; however, studies have found that when frail patients undergo low-risk procedures, they tend to have a higher mortality rate than their healthier counterparts.15 Frailty is a concept that identifies patients who are at increased risk of dying in 6 to 60 months due to a decline in their physical reserve. Frail patients have increased rates of perioperative mortality and complications. Various tools have been used to assess the components of physical performance, speed, mobility, nutrition status, mental health, and cognition.16 Frailty screening has been initiated in several VA hospitals, including our own in Gainesville, Florida, with the goal of decreasing postoperative morbidity and mortality in older adult patients.17 The patients are given a 1-page screening assessment that asks about their living situation, medical conditions, nutrition status, cognition, and activities of daily living. The results can trigger the clinician to rethink the surgical plan and mobilize more resources to optimize the patient’s health. This study period precedes the initiative at our institution.
The plastic surgery service’s routine practice is to excise skin cancers in the operating room if sedation or general anesthesia will be needed (Figure 1A), for optimal control of bleeding (Figure 1B) in a patient who cannot safely stop blood thinners, or for excision of a highly vascularized area such as the scalp. Surgery is offered in an office-based setting if the area can be closed primarily, left open to close secondarily, or closed with a small skin graft under local anesthesia only (Figure 2). We prefer treating frail patients in the minor procedure clinic, when possible, to avoid the risks of sedation and the additional preoperative visits and transportation requirements. NMSC with unclear margins (Figure 3A) or in cosmetically sensitive areas where tissue needs to be preserved (Figure 3B) are referred to the Mohs dermatologist. The skin cancers in this study were most frequently found on the face, scalp, hands, and forearms based on referral patterns.
Other treatment options for NMSC include curettage and electrodessication, cryotherapy, and radiation; however, ours is a surgical service and patients are typically referred to us by primary care or dermatology when those are not reasonable or desirable options.18 Published complication rates of patients having skin cancer surgery without age restriction have a rate of 3% to 6%, which is consistent with our study of 5%.19-21 Two bleeding complications that needed to be admitted did not require more than a bedside procedure and neither required transfusions. One patient had been instructed to continue taking coumadin during the perioperative office-based procedure due to a recent carotid stent placement in the setting of a rapidly growing basal cell on an easily accessible location.
The most noted comorbidity in patients with wound complications was found to be DM; however, this was not found to be a statistically significant risk factor for wound complications (P = .10). We do not have a set rule for advising for or against NMSC surgery. We do counsel frail patients and their families that not all cancer is immediately life threatening and will work with them to do whatever makes the most sense to achieve their goals, occasionally accepting positive margins in order to debulk a symptomatic growth. The objective of this paper is to contribute to the discussion of performing invasive procedures on older adult veterans with life-limiting comorbidities. Patients and their families will have different thresholds for what they feel needs intervention, especially if other medical problems are consuming much of their time. We also have the community care referral option for patients whose treatment decisions are being dictated by travel hardships.
Strengths and Limitations
A strength of this study is that the data were obtained from a closed system. Patients tend to stay long-term within the VA and their health record is accessible throughout the country as long as they are seen at a VA facility. Complications, therefore, return to the treating service or primary care, who would route the patient back to the surgeon.
One limitation of the study is that this is a retrospective review from 2011. The authors are limited to data that are recorded in the patient record. Multiple health care professionals saw the patients and notes lack consistency in detail. Size of the lesions were not consistently recorded and did not get logged into our database for that reason.
Conclusions
Treatment of NMSC in older adult patients has a low morbidity but needs to be balanced against a patient and family’s goals when the patient presents with life-limiting comorbidities. An elevated 5-year mortality in patients aged > 80 years with serious unrelated medical conditions is intuitive, but this study may help put treatment plans into perspective for families and health care professionals who want to provide an indicated service while maximizing patient quality of life.
Acknowledgments
This manuscript is the result of work supported with resources and the use of facilities at the North Florida/South Georgia Veterans Health System, Gainesville, Florida.
Skin cancer is the most diagnosed cancer in the United States. Nonmelanoma skin cancers (NMSC), which include basal cell carcinoma and squamous cell carcinoma, are usually cured with removal.1 The incidence of NMSC increases with age and is commonly found in nursing homes and geriatric units. These cancers are not usually metastatic or fatal but can cause local destruction and disfigurement if neglected.2 The current standard of care is to treat diagnosed NMSC; however, the dermatology and geriatric care literature have questioned the logic of treating asymptomatic skin cancers that will not affect a patient’s life expectancy.2-4
Forty-seven percent of the current living veteran population is aged ≥ 65 years.5 Older adult patients are frequently referred to the US Department of Veterans Affairs (VA) surgical service for the treatment of NMSC. The veteran population includes a higher percentage of individuals at an elevated risk of skin cancers (older, White, and male) compared with the general population.6 World War II veterans deployed in regions closer to the equator have been found to have an elevated risk of melanoma and nonmelanoma skin carcinomas.7 A retrospective study of Vietnam veterans exposed to Agent Orange (2,3,7,8-tetrachlorodibenzodioxin) found a significantly higher risk of invasive NMSC in Fitzpatrick skin types I-IV compared with an age-matched subset of the general population.8 Younger veterans who were deployed in Afghanistan and Iraq for Operation Enduring Freedom/Operation Iraqi Freedom worked at more equatorial latitudes than the rest of the US population and may be at increased risk of NMSC. Inadequate sunscreen access, immediate safety concerns, outdoor recreational activities, harsh weather, and insufficient emphasis on sun protection have created a multifactorial challenge for the military population. Riemenschneider and colleagues recommended targeted screening for at-risk veteran patients and prioritizing annual skin cancer screenings during medical mission physical examinations for active military.7
The plastic surgery service regularly receives consults from dermatology, general surgery, and primary care to remove skin cancers on the face, scalp, hands, and forearms. Skin cancer treatment can create serious hardships for older adult patients and their families with multiple appointments for the consult, procedure, and follow-up. Patients are often told to hold their anticoagulant medications when the surgery will be performed on a highly vascular region, such as the scalp or face. This can create wide swings in their laboratory test values and result in life-threatening complications from either bleeding or clotting. The appropriateness of offering surgery to patients with serious comorbidities and a limited life expectancy has been questioned.2-4 The purpose of this study was to measure the morbidity and unrelated 5-year mortality for patients with skin cancer referred to the plastic surgery service to help patients and families make a more informed treatment decision, particularly when the patients are aged > 80 years and have significant life-threatening comorbidities.
Methods
The University of Florida and Malcom Randall VA Medical Center Institutional review board in Gainesville, approved a retrospective review of all consults completed by the plastic surgery service for the treatment of NMSC performed from July 1, 2011 to June 30, 2015. Data collected included age and common life-limiting comorbidities at the time of referral. Morbidities were found on the electronic health record, including coronary artery disease (CAD), congestive heart failure (CHF), cerebral vascular disease (CVD), peripheral vascular disease, dementia, chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), tobacco use, diabetes mellitus (DM), liver disease, alcohol use, and obstructive sleep apnea.
Treatment, complications, and 5-year mortality were recorded. A χ2 analysis with P value < .05 was used to determine statistical significance between individual risk factors and 5-year mortality. The relative risk of 5-year mortality was calculated by combining advanced age (aged > 80 years) with the individual comorbidities.
Results
Over 4 years, 800 consults for NMSC were completed by the plastic surgery service. Treatment decisions included 210 excisions (with or without reconstruction) in the operating room, 402 excisions (with or without reconstruction) under local anesthesia in clinic, 55 Mohs surgical dermatology referrals, 21 other service or hospital referrals, and 112 patient who were observed, declined intervention, or died prior to intervention. Five-year mortality was 28.6%. No patients died of NMSC. The median age at consult submission for patients deceased 5 years later was 78 years. Complication rate was 5% and included wound infection, dehiscence, bleeding, or graft loss. Two patients, both deceased within 5 years, had unplanned admissions due to bleeding from either a skin graft donor site or recipient bleeding. Aged ≥ 80 years, CAD, CHF, CVD, peripheral vascular disease, dementia, CKD, COPD, and DM were all found individually to be statistically significant predictors of 5-year mortality (Table 1). Combining aged ≥ 80 years plus CAD, CHF, or dementia all increased the 5-year mortality by a relative risk of > 3 (Table 2).
Discussion
The standard of care is to treat NMSC. Most NMSCs are treated surgically without consideration of patient age or life expectancy.2,4,9,10 A prospective cohort study involving a university-based private practice and a VA medical center in San Francisco found a 22.6% overall 5-year mortality and a 43.3% mortality in the group defined as limited life expectancy (LLE) based on age (≥ 85 years) and medical comorbidities. None died due to the NMSC. Leading cause of death was cardiac, cerebrovascular, and respiratory disease, lung and prostate cancer, and Alzheimer disease. The authors suggested the LLE group may be exposed to wound complications without benefiting from the treatment.4
Another study of 440 patients receiving excision for biopsy-proven facial NMSC at the Roudebush VA Medical Center in Indianapolis, Indiana, found no residual carcinoma in 35.3% of excisions, and in patients aged > 90 years, more than half of the excisions had no residual carcinoma. More than half of the patients aged > 90 years died within 1 year, not as a result of the NMSC. The authors argued for watchful waiting in select patients to maximize comfort and outcomes.10
NMSCs are often asymptomatic and not immediately life threatening. Although NMSCs tend to have a favorable prognosis, studies have found that NMSC may be a marker for other poor health outcomes. A significant increased risk for all-cause mortality was found for patients with a history of SCC, which may be attributed to immune status.11 The aging veteran population has more complex health care needs to be considered when developing surgical treatment plans. These medical problems may limit their life expectancy much sooner than the skin cancer will become symptomatic. We found that individuals aged ≥ 80 years who had CAD, CHF, or dementia had a relative risk of 3 or higher for 5-year mortality. The leading cause of death in the United States in years 2011 to 2015 was heart disease. Alzheimer disease was the sixth leading cause of death in those same years.12-14
Skin cancer excisions do not typically require general anesthesia, deep sedation, or large fluid shifts; however, studies have found that when frail patients undergo low-risk procedures, they tend to have a higher mortality rate than their healthier counterparts.15 Frailty is a concept that identifies patients who are at increased risk of dying in 6 to 60 months due to a decline in their physical reserve. Frail patients have increased rates of perioperative mortality and complications. Various tools have been used to assess the components of physical performance, speed, mobility, nutrition status, mental health, and cognition.16 Frailty screening has been initiated in several VA hospitals, including our own in Gainesville, Florida, with the goal of decreasing postoperative morbidity and mortality in older adult patients.17 The patients are given a 1-page screening assessment that asks about their living situation, medical conditions, nutrition status, cognition, and activities of daily living. The results can trigger the clinician to rethink the surgical plan and mobilize more resources to optimize the patient’s health. This study period precedes the initiative at our institution.
The plastic surgery service’s routine practice is to excise skin cancers in the operating room if sedation or general anesthesia will be needed (Figure 1A), for optimal control of bleeding (Figure 1B) in a patient who cannot safely stop blood thinners, or for excision of a highly vascularized area such as the scalp. Surgery is offered in an office-based setting if the area can be closed primarily, left open to close secondarily, or closed with a small skin graft under local anesthesia only (Figure 2). We prefer treating frail patients in the minor procedure clinic, when possible, to avoid the risks of sedation and the additional preoperative visits and transportation requirements. NMSC with unclear margins (Figure 3A) or in cosmetically sensitive areas where tissue needs to be preserved (Figure 3B) are referred to the Mohs dermatologist. The skin cancers in this study were most frequently found on the face, scalp, hands, and forearms based on referral patterns.
Other treatment options for NMSC include curettage and electrodessication, cryotherapy, and radiation; however, ours is a surgical service and patients are typically referred to us by primary care or dermatology when those are not reasonable or desirable options.18 Published complication rates of patients having skin cancer surgery without age restriction have a rate of 3% to 6%, which is consistent with our study of 5%.19-21 Two bleeding complications that needed to be admitted did not require more than a bedside procedure and neither required transfusions. One patient had been instructed to continue taking coumadin during the perioperative office-based procedure due to a recent carotid stent placement in the setting of a rapidly growing basal cell on an easily accessible location.
The most noted comorbidity in patients with wound complications was found to be DM; however, this was not found to be a statistically significant risk factor for wound complications (P = .10). We do not have a set rule for advising for or against NMSC surgery. We do counsel frail patients and their families that not all cancer is immediately life threatening and will work with them to do whatever makes the most sense to achieve their goals, occasionally accepting positive margins in order to debulk a symptomatic growth. The objective of this paper is to contribute to the discussion of performing invasive procedures on older adult veterans with life-limiting comorbidities. Patients and their families will have different thresholds for what they feel needs intervention, especially if other medical problems are consuming much of their time. We also have the community care referral option for patients whose treatment decisions are being dictated by travel hardships.
Strengths and Limitations
A strength of this study is that the data were obtained from a closed system. Patients tend to stay long-term within the VA and their health record is accessible throughout the country as long as they are seen at a VA facility. Complications, therefore, return to the treating service or primary care, who would route the patient back to the surgeon.
One limitation of the study is that this is a retrospective review from 2011. The authors are limited to data that are recorded in the patient record. Multiple health care professionals saw the patients and notes lack consistency in detail. Size of the lesions were not consistently recorded and did not get logged into our database for that reason.
Conclusions
Treatment of NMSC in older adult patients has a low morbidity but needs to be balanced against a patient and family’s goals when the patient presents with life-limiting comorbidities. An elevated 5-year mortality in patients aged > 80 years with serious unrelated medical conditions is intuitive, but this study may help put treatment plans into perspective for families and health care professionals who want to provide an indicated service while maximizing patient quality of life.
Acknowledgments
This manuscript is the result of work supported with resources and the use of facilities at the North Florida/South Georgia Veterans Health System, Gainesville, Florida.
1. American Cancer Society. Cancer Facts & Figures 2021. Accessed May 26, 2022. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2021/cancer-facts-and-figures-2021.pdf
2. Albert A, Knoll MA, Conti JA, Zbar RIS. Non-melanoma skin cancers in the older patient. Curr Oncol Rep. 2019;21(9):79. Published 2019 Jul 29. doi:10.1007/s11912-019-0828-9
3. Linos E, Chren MM, Stijacic Cenzer I, Covinsky KE. Skin cancer in U.S. elderly adults: does life expectancy play a role in treatment decisions? J Am Geriatr Soc. 2016;64(8):1610-1615. doi:10.1111/jgs.14202
4. Linos E, Parvataneni R, Stuart SE, Boscardin WJ, Landefeld CS, Chren MM. Treatment of nonfatal conditions at the end of life: nonmelanoma skin cancer. JAMA Intern Med. 2013;173(11):1006-1012. doi:10.1001/jamainternmed.2013.639
5. O’Malley KA, Vinson L, Kaiser AP, Sager Z, Hinrichs K. Mental health and aging veterans: how the Veterans Health Administration meets the needs of aging veterans. Public Policy Aging Rep. 2020;30(1):19-23. doi:10.1093/ppar/prz027
6. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Profile of veterans: 2017. Accessed May 26, 2022. https://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Veterans_2017.pdf 7. Riemenschneider K, Liu J, Powers JG. Skin cancer in the military: a systematic review of melanoma and nonmelanoma skin cancer incidence, prevention, and screening among active duty and veteran personnel. J Am Acad Dermatol. 2018;78(6):1185-1192. doi:10.1016/j.jaad.2017.11.062
8. Clemens MW, Kochuba AL, Carter ME, Han K, Liu J, Evans K. Association between Agent Orange exposure and nonmelanotic invasive skin cancer: a pilot study. Plast Reconstr Surg. 2014;133(2):432-437. doi:10.1097/01.prs.0000436859.40151.cf
9. Cameron MC, Lee E, Hibler BP, et al. Basal cell carcinoma: epidemiology; pathophysiology; clinical and histological subtypes; and disease associations. J Am Acad Dermatol. 2019;80(2):303-317. doi:10.1016/j.jaad.2018.03.060
10. Chauhan R, Munger BN, Chu MW, et al. Age at diagnosis as a relative contraindication for intervention in facial nonmelanoma skin cancer. JAMA Surg. 2018;153(4):390-392. doi:10.1001/jamasurg.2017.5073
11. Barton V, Armeson K, Hampras S, et al. Nonmelanoma skin cancer and risk of all-cause and cancer-related mortality: a systematic review. Arch Dermatol Res. 2017;309(4):243-251. doi:10.1007/s00403-017-1724-5
12. Kochanek KD, Murphy SL, Xu JQ, Arias E. Mortality in the United States, 2013. NCHS Data Brief 178. Accessed May 26, 2022. https://www.cdc.gov/nchs/products/databriefs/db178.htm
13. Xu JQ, Kochanek KD, Murphy SL, Arias E. Mortality in the United States, 2012. NCHS Data Brief 168. Accessed May 26, 2022. https://www.cdc.gov/nchs/products/databriefs/db168.htm
14. Xu JQ, Murphy SL, Kochanek KD, Arias E. Mortality in the United States, 2015. NCHS Data Brief 267. Accessed May 26, 2022. https://www.cdc.gov/nchs/products/databriefs/db267.htm
15. Varley PR , Borrebach JD, Arya S, et al. Clinical utility of the risk analysis index as a prospective frailty screening tool within a multi-practice, multi-hospital integrated healthcare system. Ann Surg. 2021;274(6):e1230-e1237. doi:10.1097/SLA.0000000000003808
16. Hall DE, Arya S , Schmid KK, et al. Development and initial validation of the risk analysis index for measuring frailty in surgical populations. JAMA Surg. 2017;152(2):175-182. doi:10.1001/jamasurg.2016.4202
17. US Department of Veterans Affairs, Health Services Research & Development. Improving healthcare for aging veterans. Updated August 30, 2017. Accessed May 26, 2022. https://www.hsrd.research.va.gov/news/feature/aging0917.cfm
18. Leus AJG, Frie M, Haisma MS, et al. Treatment of keratinocyte carcinoma in elderly patients – a review of the current literature. J Eur Acad Dermatol Venereol. 2020;34(9):1932-1943. doi:10.1111/jdv.16268
19. Amici JM, Rogues AM, Lasheras A, et al. A prospective study of the incidence of complications associated with dermatological surgery. Br J Dermatol. 2005;153(5):967-971. doi:10.1111/j.1365-2133.2005.06861.x
20. Arguello-Guerra L, Vargas-Chandomid E, Díaz-González JM, Méndez-Flores S, Ruelas-Villavicencio A, Domínguez-Cherit J. Incidence of complications in dermatological surgery of melanoma and non-melanoma skin cancer in patients with multiple comorbidity and/or antiplatelet-anticoagulants. Five-year experience in our hospital. Cir Cir. 2019;86(1):15-23. doi:10.24875/CIRUE.M18000003
21. Keith DJ, de Berker DA, Bray AP, Cheung ST, Brain A, Mohd Mustapa MF. British Association of Dermatologists’ national audit on nonmelanoma skin cancer excision, 2014. Clin Exp Dermatol. 2017;42(1):46-53. doi:10.1111/ced.12990
1. American Cancer Society. Cancer Facts & Figures 2021. Accessed May 26, 2022. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2021/cancer-facts-and-figures-2021.pdf
2. Albert A, Knoll MA, Conti JA, Zbar RIS. Non-melanoma skin cancers in the older patient. Curr Oncol Rep. 2019;21(9):79. Published 2019 Jul 29. doi:10.1007/s11912-019-0828-9
3. Linos E, Chren MM, Stijacic Cenzer I, Covinsky KE. Skin cancer in U.S. elderly adults: does life expectancy play a role in treatment decisions? J Am Geriatr Soc. 2016;64(8):1610-1615. doi:10.1111/jgs.14202
4. Linos E, Parvataneni R, Stuart SE, Boscardin WJ, Landefeld CS, Chren MM. Treatment of nonfatal conditions at the end of life: nonmelanoma skin cancer. JAMA Intern Med. 2013;173(11):1006-1012. doi:10.1001/jamainternmed.2013.639
5. O’Malley KA, Vinson L, Kaiser AP, Sager Z, Hinrichs K. Mental health and aging veterans: how the Veterans Health Administration meets the needs of aging veterans. Public Policy Aging Rep. 2020;30(1):19-23. doi:10.1093/ppar/prz027
6. US Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Profile of veterans: 2017. Accessed May 26, 2022. https://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Veterans_2017.pdf 7. Riemenschneider K, Liu J, Powers JG. Skin cancer in the military: a systematic review of melanoma and nonmelanoma skin cancer incidence, prevention, and screening among active duty and veteran personnel. J Am Acad Dermatol. 2018;78(6):1185-1192. doi:10.1016/j.jaad.2017.11.062
8. Clemens MW, Kochuba AL, Carter ME, Han K, Liu J, Evans K. Association between Agent Orange exposure and nonmelanotic invasive skin cancer: a pilot study. Plast Reconstr Surg. 2014;133(2):432-437. doi:10.1097/01.prs.0000436859.40151.cf
9. Cameron MC, Lee E, Hibler BP, et al. Basal cell carcinoma: epidemiology; pathophysiology; clinical and histological subtypes; and disease associations. J Am Acad Dermatol. 2019;80(2):303-317. doi:10.1016/j.jaad.2018.03.060
10. Chauhan R, Munger BN, Chu MW, et al. Age at diagnosis as a relative contraindication for intervention in facial nonmelanoma skin cancer. JAMA Surg. 2018;153(4):390-392. doi:10.1001/jamasurg.2017.5073
11. Barton V, Armeson K, Hampras S, et al. Nonmelanoma skin cancer and risk of all-cause and cancer-related mortality: a systematic review. Arch Dermatol Res. 2017;309(4):243-251. doi:10.1007/s00403-017-1724-5
12. Kochanek KD, Murphy SL, Xu JQ, Arias E. Mortality in the United States, 2013. NCHS Data Brief 178. Accessed May 26, 2022. https://www.cdc.gov/nchs/products/databriefs/db178.htm
13. Xu JQ, Kochanek KD, Murphy SL, Arias E. Mortality in the United States, 2012. NCHS Data Brief 168. Accessed May 26, 2022. https://www.cdc.gov/nchs/products/databriefs/db168.htm
14. Xu JQ, Murphy SL, Kochanek KD, Arias E. Mortality in the United States, 2015. NCHS Data Brief 267. Accessed May 26, 2022. https://www.cdc.gov/nchs/products/databriefs/db267.htm
15. Varley PR , Borrebach JD, Arya S, et al. Clinical utility of the risk analysis index as a prospective frailty screening tool within a multi-practice, multi-hospital integrated healthcare system. Ann Surg. 2021;274(6):e1230-e1237. doi:10.1097/SLA.0000000000003808
16. Hall DE, Arya S , Schmid KK, et al. Development and initial validation of the risk analysis index for measuring frailty in surgical populations. JAMA Surg. 2017;152(2):175-182. doi:10.1001/jamasurg.2016.4202
17. US Department of Veterans Affairs, Health Services Research & Development. Improving healthcare for aging veterans. Updated August 30, 2017. Accessed May 26, 2022. https://www.hsrd.research.va.gov/news/feature/aging0917.cfm
18. Leus AJG, Frie M, Haisma MS, et al. Treatment of keratinocyte carcinoma in elderly patients – a review of the current literature. J Eur Acad Dermatol Venereol. 2020;34(9):1932-1943. doi:10.1111/jdv.16268
19. Amici JM, Rogues AM, Lasheras A, et al. A prospective study of the incidence of complications associated with dermatological surgery. Br J Dermatol. 2005;153(5):967-971. doi:10.1111/j.1365-2133.2005.06861.x
20. Arguello-Guerra L, Vargas-Chandomid E, Díaz-González JM, Méndez-Flores S, Ruelas-Villavicencio A, Domínguez-Cherit J. Incidence of complications in dermatological surgery of melanoma and non-melanoma skin cancer in patients with multiple comorbidity and/or antiplatelet-anticoagulants. Five-year experience in our hospital. Cir Cir. 2019;86(1):15-23. doi:10.24875/CIRUE.M18000003
21. Keith DJ, de Berker DA, Bray AP, Cheung ST, Brain A, Mohd Mustapa MF. British Association of Dermatologists’ national audit on nonmelanoma skin cancer excision, 2014. Clin Exp Dermatol. 2017;42(1):46-53. doi:10.1111/ced.12990
SARS-CoV-2: A Novel Precipitant of Ischemic Priapism
Priapism is a disorder that occurs when the penis maintains a prolonged erection in the absence of appropriate stimulation. The disorder is typically divided into subgroups based on arterial flow: low flow (ischemic) and high flow (nonischemic). Ischemic priapism is the most common form and results from venous congestion due to obstructed outflow and inability of cavernous smooth muscle to contract, resulting in compartment syndrome, tissue hypoxia, hypercapnia, and acidosis.1 Conditions that result in hypercoagulable states and hyperviscosity are associated with ischemic priapism. COVID-19 is well known to cause an acute respiratory illness and systemic inflammatory response and has been increasingly associated with coagulopathy. Studies have shown that 20% to 55% of patients admitted to the hospital for COVID-19 show objective laboratory evidence of a hypercoagulable state.2
To date, there are 6 reported cases of priapism occurring in the setting of COVID-19 with all cases demonstrating the ischemic subtype. The onset of priapism from the beginning of infectious symptoms ranged from 2 days to more than a month. Five of the cases occurred in patients with critical COVID-19 and 1 in the setting of mild disease.3-8 Two critically ill patients did not receive treatment for their ischemic priapism as they were transitioned to expectant management and/or comfort measures.Most were treated with cavernosal blood aspiration and intracavernosal injections of phenylephrine or ethylephrine. Some patients were managed with prophylactic doses of anticoagulation after the identification of priapism; others were transitioned to therapeutic doses. Two patients were followed postdischarge; one patient reported normal nighttime erections with sexual desire 2 weeks postdischarge, and another patient, who underwent a bilateral T-shunt procedure after unsuccessful phenylephrine injections, reported complete erectile dysfunction at 3 months postdischarge.4,7 There was a potentially confounding variable in 2 cases in which propofol infusions were used for sedation management in the setting of mechanical ventilation.6,8 Propofol has been linked to priapism through its blockade of sympathetic activation resulting in persistent relaxation of cavernosal smooth muscle.9 We present a unique case of COVID-19–associated ischemic priapism as our patient had moderate rather than critical COVID-19.
Case Presentation
A 67-year-old male patient presented to the emergency department for a painful erection of 34-hour duration. The patient had been exposed to COVID-19 roughly 2 months prior. Since the exposure, he had experienced headache, nonproductive cough, sore throat, and decreased appetite with weight loss. His medical history included hypertension, thoracic aortic aneurysm, B-cell type chronic lymphocytic leukemia (CLL), and obstructive sleep apnea. Daily outpatient medications included atenolol 100 mg, hydrochlorothiazide 25 mg, and omeprazole 20 mg. The patient stopped tobacco use about 30 years previously. He reported no alcohol consumption or illicit drug use and had no previous episodes of prolonged erection.
The patient was afebrile, hemodynamically stable, and had an oxygen saturation of 92% on room air. Physical examination revealed clear breath sounds and an erect circumcised penis without any lesions, discoloration, or skin necrosis. Laboratory data were remarkable for the following values: 125,660 cells/μL white blood cells (WBCs), 13.82 × 103/ μL neutrophils, 110.58 × 103/μL lymphocytes, 1.26 × 103/μL monocytes, no blasts, 9.4 gm/dL hemoglobin, 100.3 fl mean corpuscular volume, 417,000 cells/μL platelets, 23,671 ng/mL D-dimer, 29.6 seconds activated partial thromboplastin time (aPTT), 16.3 seconds prothrombin time, 743 mg/dL fibrinogen, 474 U/L lactate dehydrogenase, and 202.1 mg/dL haptoglobin. A nasopharyngeal reverse transcription polymerase chain reaction test resulted positive for the SARS-CoV-2 virus, and subsequent chest X-ray revealed bilateral, hazy opacities predominantly in a peripheral distribution. Computed tomography (CT) angiogram of the chest did not reveal pulmonary emboli, pneumothorax, effusions, or lobar consolidation. However, it displayed bilateral ground-glass opacities with interstitial consolidation worst in the upper lobes. Corporal aspiration and blood gas analysis revealed a pH of 7.05, P
Differential Diagnosis
The first consideration in the differential diagnosis of priapism is to differentiate between ischemic and nonischemic. Based on the abnormal blood gas results above, this case clearly falls within the ischemic spectrum. Ischemic priapism secondary to CLL-induced hyperleukocytosis was considered. It has been noted that up to 20% of priapism cases in adults are related to hematologic disorders.10 While it is not uncommon to see hyperleukocytosis (total WBC count > 100 × 109/L) in CLL, leukostasis is rare with most reports demonstrating WBC counts > 1000 × 109/L.11 Hematology, vascular surgery, and urology services were consulted and agreed that ischemic priapism was due to microthrombi or pelvic vein thrombosis secondary to COVID-19–associated coagulopathy (CAC) was the most likely etiology.
Treatment
After corporal aspiration, intracorporal phenylephrine was administered. Diluted phenylephrine (100 ug/mL) was injected every 5 to 10 minutes while intermittently aspirating and irrigating multiple sites along the lateral length of the penile shaft. This initial procedure reduced the erection from 100% to 30% rigidity, with repeat blood gas analysis revealing minimal improvement. CT of the abdomen and pelvis with IV contrast revealed no evidence of pelvic thrombi. A second round of phenylephrine injections were administered, resulting in detumescence. The patient was treated with 2 to 3 L/min of oxygen supplementation via nasal cannula, a 5-day course of remdesivir and low-intensity heparin drip. Following the initial low-intensity heparin drip, the patient transitioned to therapeutic enoxaparin and subsequently was discharged on apixaban for a 3-month course. Since discharge, the patient followed up with hematology. He tolerated and completed the anticoagulation regimen without any recurrences of priapism or residual deficits.
Discussion
Recent studies have overwhelmingly analyzed the incidence and presentation of thrombotic complications in critically ill patients with COVID-19. CAC has been postulated to result from endotheliopathy along with immune cell activation and propagation of coagulation. While COVID-19 has been noted to create lung injury through binding angiotensin-converting enzyme 2 receptors expressed on alveolar pneumocytes, it increasingly has been found to affect endothelial cells throughout the body. Recent postmortem analyses have demonstrated direct viral infection of endothelial cells with consequent diffuse endothelial inflammation, as evidenced by viral inclusions, sequestered immune cells, and endothelial apoptosis.12,13 Manifestations of this endotheliopathy have been delineated through various studies.
An early retrospective study in Wuhan, China, illustrated that 36% of the first 99 patients hospitalized with COVID-19 demonstrated an elevated D-dimer, 6% an elevated aPTT, and 5% an elevated prothrombin time.14 Another retrospective study conducted in Wuhan found a 25% incidence of venous thromboembolic complications in critically ill patients with severe COVID-19.15 In the Netherlands, a study reported the incidence of arterial and venous thrombotic complications to be 31% in 184 critically ill patients with COVID-19, with 81% of these cases involving pulmonary emboli.16
To our knowledge, our patient is the seventh reported case of ischemic priapism occurring in the setting of a COVID-19 infection, and the first to have occurred in its moderate form. Ischemic priapism is often a consequence of penile venous outflow obstruction and resultant stasis of hypoxic blood.7 The prothrombotic state induced by CAC has been proposed to cause the obstruction of small emissary veins in the subtunical space and in turn lead to venous stasis, which propagates the formation of ischemic priapism.8 Furthermore, 4 of the previously reported cases shared laboratory data on their patients, and all demonstrated elevated D-dimer and fibrinogen levels, which strengthens this hypothesis.3,5,7,8 CLL presents a potential confounding variable in this case; however, as we have reviewed earlier, the risk of leukostasis at WBC counts < 1000 × 109/L is very low.11 It is also probable that the patient had some level of immune dysregulation secondary to CLL, leading to his prolonged course and slow clearance of the virus.
Conclusions
Although only a handful of CAC cases leading to ischemic priapism have been reported, the true incidence may be much higher. While our case highlights the importance of considering COVID-19 infection in the differential diagnosis of ischemic priapism, more research is needed to understand incidence and definitively establish a causative relationship.
1. Pryor J, Akkus E, Alter G, et al. Priapism. J Sex Med. 2004;1(1):116-120. doi:10.1111/j.1743-6109.2004.10117.x
2. Lee SG, Fralick M, Sholzberg M. Coagulopathy associated with COVID-19. CMAJ. 2020;192(21):E583. doi:10.1503/cmaj.200685
3. Lam G, McCarthy R, Haider R. A peculiar case of priapism: the hypercoagulable state in patients with severe COVID-19 infection. Eur J Case Rep Intern Med. 2020;7(8):001779. doi:10.12890/2020_001779
4. Addar A, Al Fraidi O, Nazer A, Althonayan N, Ghazwani Y. Priapism for 10 days in a patient with SARS-CoV-2 pneumonia: a case report. J Surg Case Rep. 2021;2021(4):rjab020. doi:10.1093/jscr/rjab020
5. Lamamri M, Chebbi A, Mamane J, et al. Priapism in a patient with coronavirus disease 2019 (COVID-19). Am J Emerg Med. 2021;39:251.e5-251.e7. doi:10.1016/j.ajem.2020.06.027
6. Silverman ML, VanDerVeer SJ, Donnelly TJ. Priapism in COVID-19: a thromboembolic complication. Am J Emerg Med. 2021;45:686.e5-686.e6. doi:10.1016/j.ajem.2020.12.072
7. Giuliano AFM, Vulpi M, Passerini F, et al. SARS-CoV-2 infection as a determining factor to the precipitation of ischemic priapism in a young patient with asymptomatic COVID-19. Case Rep Urol. 2021;2021:9936891. doi:10.1155/2021/9936891
8. Carreno BD, Perez CP, Vasquez D, Oyola JA, Suarez O, Bedoya C. Veno-occlusive priapism in COVID-19 disease. Urol Int. 2021;105(9-10):916-919. doi:10.1159/000514421
9. Senthilkumaran S, Shah S, Ganapathysubramanian, Balamurgan N, Thirumalaikolundusubramanian P. Propofol and priapism. Indian J Pharmacol. 2010;42(4):238-239. doi:10.4103/0253-7613.68430
10. Qu M, Lu X, Wang L, Liu Z, Sun Y, Gao X. Priapism secondary to chronic myeloid leukemia treated by a surgical cavernosa-corpus spongiosum shunt: case report. Asian J Urol. 2019;6(4):373-376. doi:10.1016/j.ajur.2018.12.004
11. Singh N, Singh Lubana S, Dabrowski L, Sidhu G. Leukostasis in chronic lymphocytic leukemia. Am J Case Rep. 2020;21:e924798. doi:10.12659/AJCR.924798
12. Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417-1418. doi:10.1016/S0140-6736(20)30937-5
13. Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135(23):2033-2040. doi:10.1182/blood.2020006000
14. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507-513. doi:10.1016/S0140-6736(20)30211-7
15. Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. 2020;18(6):1421-1424. doi:10.1111/jth.14830
16. Klok FA, Kruip M, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145-147. doi:10.1016/j.thromres.2020.04.013
Priapism is a disorder that occurs when the penis maintains a prolonged erection in the absence of appropriate stimulation. The disorder is typically divided into subgroups based on arterial flow: low flow (ischemic) and high flow (nonischemic). Ischemic priapism is the most common form and results from venous congestion due to obstructed outflow and inability of cavernous smooth muscle to contract, resulting in compartment syndrome, tissue hypoxia, hypercapnia, and acidosis.1 Conditions that result in hypercoagulable states and hyperviscosity are associated with ischemic priapism. COVID-19 is well known to cause an acute respiratory illness and systemic inflammatory response and has been increasingly associated with coagulopathy. Studies have shown that 20% to 55% of patients admitted to the hospital for COVID-19 show objective laboratory evidence of a hypercoagulable state.2
To date, there are 6 reported cases of priapism occurring in the setting of COVID-19 with all cases demonstrating the ischemic subtype. The onset of priapism from the beginning of infectious symptoms ranged from 2 days to more than a month. Five of the cases occurred in patients with critical COVID-19 and 1 in the setting of mild disease.3-8 Two critically ill patients did not receive treatment for their ischemic priapism as they were transitioned to expectant management and/or comfort measures.Most were treated with cavernosal blood aspiration and intracavernosal injections of phenylephrine or ethylephrine. Some patients were managed with prophylactic doses of anticoagulation after the identification of priapism; others were transitioned to therapeutic doses. Two patients were followed postdischarge; one patient reported normal nighttime erections with sexual desire 2 weeks postdischarge, and another patient, who underwent a bilateral T-shunt procedure after unsuccessful phenylephrine injections, reported complete erectile dysfunction at 3 months postdischarge.4,7 There was a potentially confounding variable in 2 cases in which propofol infusions were used for sedation management in the setting of mechanical ventilation.6,8 Propofol has been linked to priapism through its blockade of sympathetic activation resulting in persistent relaxation of cavernosal smooth muscle.9 We present a unique case of COVID-19–associated ischemic priapism as our patient had moderate rather than critical COVID-19.
Case Presentation
A 67-year-old male patient presented to the emergency department for a painful erection of 34-hour duration. The patient had been exposed to COVID-19 roughly 2 months prior. Since the exposure, he had experienced headache, nonproductive cough, sore throat, and decreased appetite with weight loss. His medical history included hypertension, thoracic aortic aneurysm, B-cell type chronic lymphocytic leukemia (CLL), and obstructive sleep apnea. Daily outpatient medications included atenolol 100 mg, hydrochlorothiazide 25 mg, and omeprazole 20 mg. The patient stopped tobacco use about 30 years previously. He reported no alcohol consumption or illicit drug use and had no previous episodes of prolonged erection.
The patient was afebrile, hemodynamically stable, and had an oxygen saturation of 92% on room air. Physical examination revealed clear breath sounds and an erect circumcised penis without any lesions, discoloration, or skin necrosis. Laboratory data were remarkable for the following values: 125,660 cells/μL white blood cells (WBCs), 13.82 × 103/ μL neutrophils, 110.58 × 103/μL lymphocytes, 1.26 × 103/μL monocytes, no blasts, 9.4 gm/dL hemoglobin, 100.3 fl mean corpuscular volume, 417,000 cells/μL platelets, 23,671 ng/mL D-dimer, 29.6 seconds activated partial thromboplastin time (aPTT), 16.3 seconds prothrombin time, 743 mg/dL fibrinogen, 474 U/L lactate dehydrogenase, and 202.1 mg/dL haptoglobin. A nasopharyngeal reverse transcription polymerase chain reaction test resulted positive for the SARS-CoV-2 virus, and subsequent chest X-ray revealed bilateral, hazy opacities predominantly in a peripheral distribution. Computed tomography (CT) angiogram of the chest did not reveal pulmonary emboli, pneumothorax, effusions, or lobar consolidation. However, it displayed bilateral ground-glass opacities with interstitial consolidation worst in the upper lobes. Corporal aspiration and blood gas analysis revealed a pH of 7.05, P
Differential Diagnosis
The first consideration in the differential diagnosis of priapism is to differentiate between ischemic and nonischemic. Based on the abnormal blood gas results above, this case clearly falls within the ischemic spectrum. Ischemic priapism secondary to CLL-induced hyperleukocytosis was considered. It has been noted that up to 20% of priapism cases in adults are related to hematologic disorders.10 While it is not uncommon to see hyperleukocytosis (total WBC count > 100 × 109/L) in CLL, leukostasis is rare with most reports demonstrating WBC counts > 1000 × 109/L.11 Hematology, vascular surgery, and urology services were consulted and agreed that ischemic priapism was due to microthrombi or pelvic vein thrombosis secondary to COVID-19–associated coagulopathy (CAC) was the most likely etiology.
Treatment
After corporal aspiration, intracorporal phenylephrine was administered. Diluted phenylephrine (100 ug/mL) was injected every 5 to 10 minutes while intermittently aspirating and irrigating multiple sites along the lateral length of the penile shaft. This initial procedure reduced the erection from 100% to 30% rigidity, with repeat blood gas analysis revealing minimal improvement. CT of the abdomen and pelvis with IV contrast revealed no evidence of pelvic thrombi. A second round of phenylephrine injections were administered, resulting in detumescence. The patient was treated with 2 to 3 L/min of oxygen supplementation via nasal cannula, a 5-day course of remdesivir and low-intensity heparin drip. Following the initial low-intensity heparin drip, the patient transitioned to therapeutic enoxaparin and subsequently was discharged on apixaban for a 3-month course. Since discharge, the patient followed up with hematology. He tolerated and completed the anticoagulation regimen without any recurrences of priapism or residual deficits.
Discussion
Recent studies have overwhelmingly analyzed the incidence and presentation of thrombotic complications in critically ill patients with COVID-19. CAC has been postulated to result from endotheliopathy along with immune cell activation and propagation of coagulation. While COVID-19 has been noted to create lung injury through binding angiotensin-converting enzyme 2 receptors expressed on alveolar pneumocytes, it increasingly has been found to affect endothelial cells throughout the body. Recent postmortem analyses have demonstrated direct viral infection of endothelial cells with consequent diffuse endothelial inflammation, as evidenced by viral inclusions, sequestered immune cells, and endothelial apoptosis.12,13 Manifestations of this endotheliopathy have been delineated through various studies.
An early retrospective study in Wuhan, China, illustrated that 36% of the first 99 patients hospitalized with COVID-19 demonstrated an elevated D-dimer, 6% an elevated aPTT, and 5% an elevated prothrombin time.14 Another retrospective study conducted in Wuhan found a 25% incidence of venous thromboembolic complications in critically ill patients with severe COVID-19.15 In the Netherlands, a study reported the incidence of arterial and venous thrombotic complications to be 31% in 184 critically ill patients with COVID-19, with 81% of these cases involving pulmonary emboli.16
To our knowledge, our patient is the seventh reported case of ischemic priapism occurring in the setting of a COVID-19 infection, and the first to have occurred in its moderate form. Ischemic priapism is often a consequence of penile venous outflow obstruction and resultant stasis of hypoxic blood.7 The prothrombotic state induced by CAC has been proposed to cause the obstruction of small emissary veins in the subtunical space and in turn lead to venous stasis, which propagates the formation of ischemic priapism.8 Furthermore, 4 of the previously reported cases shared laboratory data on their patients, and all demonstrated elevated D-dimer and fibrinogen levels, which strengthens this hypothesis.3,5,7,8 CLL presents a potential confounding variable in this case; however, as we have reviewed earlier, the risk of leukostasis at WBC counts < 1000 × 109/L is very low.11 It is also probable that the patient had some level of immune dysregulation secondary to CLL, leading to his prolonged course and slow clearance of the virus.
Conclusions
Although only a handful of CAC cases leading to ischemic priapism have been reported, the true incidence may be much higher. While our case highlights the importance of considering COVID-19 infection in the differential diagnosis of ischemic priapism, more research is needed to understand incidence and definitively establish a causative relationship.
Priapism is a disorder that occurs when the penis maintains a prolonged erection in the absence of appropriate stimulation. The disorder is typically divided into subgroups based on arterial flow: low flow (ischemic) and high flow (nonischemic). Ischemic priapism is the most common form and results from venous congestion due to obstructed outflow and inability of cavernous smooth muscle to contract, resulting in compartment syndrome, tissue hypoxia, hypercapnia, and acidosis.1 Conditions that result in hypercoagulable states and hyperviscosity are associated with ischemic priapism. COVID-19 is well known to cause an acute respiratory illness and systemic inflammatory response and has been increasingly associated with coagulopathy. Studies have shown that 20% to 55% of patients admitted to the hospital for COVID-19 show objective laboratory evidence of a hypercoagulable state.2
To date, there are 6 reported cases of priapism occurring in the setting of COVID-19 with all cases demonstrating the ischemic subtype. The onset of priapism from the beginning of infectious symptoms ranged from 2 days to more than a month. Five of the cases occurred in patients with critical COVID-19 and 1 in the setting of mild disease.3-8 Two critically ill patients did not receive treatment for their ischemic priapism as they were transitioned to expectant management and/or comfort measures.Most were treated with cavernosal blood aspiration and intracavernosal injections of phenylephrine or ethylephrine. Some patients were managed with prophylactic doses of anticoagulation after the identification of priapism; others were transitioned to therapeutic doses. Two patients were followed postdischarge; one patient reported normal nighttime erections with sexual desire 2 weeks postdischarge, and another patient, who underwent a bilateral T-shunt procedure after unsuccessful phenylephrine injections, reported complete erectile dysfunction at 3 months postdischarge.4,7 There was a potentially confounding variable in 2 cases in which propofol infusions were used for sedation management in the setting of mechanical ventilation.6,8 Propofol has been linked to priapism through its blockade of sympathetic activation resulting in persistent relaxation of cavernosal smooth muscle.9 We present a unique case of COVID-19–associated ischemic priapism as our patient had moderate rather than critical COVID-19.
Case Presentation
A 67-year-old male patient presented to the emergency department for a painful erection of 34-hour duration. The patient had been exposed to COVID-19 roughly 2 months prior. Since the exposure, he had experienced headache, nonproductive cough, sore throat, and decreased appetite with weight loss. His medical history included hypertension, thoracic aortic aneurysm, B-cell type chronic lymphocytic leukemia (CLL), and obstructive sleep apnea. Daily outpatient medications included atenolol 100 mg, hydrochlorothiazide 25 mg, and omeprazole 20 mg. The patient stopped tobacco use about 30 years previously. He reported no alcohol consumption or illicit drug use and had no previous episodes of prolonged erection.
The patient was afebrile, hemodynamically stable, and had an oxygen saturation of 92% on room air. Physical examination revealed clear breath sounds and an erect circumcised penis without any lesions, discoloration, or skin necrosis. Laboratory data were remarkable for the following values: 125,660 cells/μL white blood cells (WBCs), 13.82 × 103/ μL neutrophils, 110.58 × 103/μL lymphocytes, 1.26 × 103/μL monocytes, no blasts, 9.4 gm/dL hemoglobin, 100.3 fl mean corpuscular volume, 417,000 cells/μL platelets, 23,671 ng/mL D-dimer, 29.6 seconds activated partial thromboplastin time (aPTT), 16.3 seconds prothrombin time, 743 mg/dL fibrinogen, 474 U/L lactate dehydrogenase, and 202.1 mg/dL haptoglobin. A nasopharyngeal reverse transcription polymerase chain reaction test resulted positive for the SARS-CoV-2 virus, and subsequent chest X-ray revealed bilateral, hazy opacities predominantly in a peripheral distribution. Computed tomography (CT) angiogram of the chest did not reveal pulmonary emboli, pneumothorax, effusions, or lobar consolidation. However, it displayed bilateral ground-glass opacities with interstitial consolidation worst in the upper lobes. Corporal aspiration and blood gas analysis revealed a pH of 7.05, P
Differential Diagnosis
The first consideration in the differential diagnosis of priapism is to differentiate between ischemic and nonischemic. Based on the abnormal blood gas results above, this case clearly falls within the ischemic spectrum. Ischemic priapism secondary to CLL-induced hyperleukocytosis was considered. It has been noted that up to 20% of priapism cases in adults are related to hematologic disorders.10 While it is not uncommon to see hyperleukocytosis (total WBC count > 100 × 109/L) in CLL, leukostasis is rare with most reports demonstrating WBC counts > 1000 × 109/L.11 Hematology, vascular surgery, and urology services were consulted and agreed that ischemic priapism was due to microthrombi or pelvic vein thrombosis secondary to COVID-19–associated coagulopathy (CAC) was the most likely etiology.
Treatment
After corporal aspiration, intracorporal phenylephrine was administered. Diluted phenylephrine (100 ug/mL) was injected every 5 to 10 minutes while intermittently aspirating and irrigating multiple sites along the lateral length of the penile shaft. This initial procedure reduced the erection from 100% to 30% rigidity, with repeat blood gas analysis revealing minimal improvement. CT of the abdomen and pelvis with IV contrast revealed no evidence of pelvic thrombi. A second round of phenylephrine injections were administered, resulting in detumescence. The patient was treated with 2 to 3 L/min of oxygen supplementation via nasal cannula, a 5-day course of remdesivir and low-intensity heparin drip. Following the initial low-intensity heparin drip, the patient transitioned to therapeutic enoxaparin and subsequently was discharged on apixaban for a 3-month course. Since discharge, the patient followed up with hematology. He tolerated and completed the anticoagulation regimen without any recurrences of priapism or residual deficits.
Discussion
Recent studies have overwhelmingly analyzed the incidence and presentation of thrombotic complications in critically ill patients with COVID-19. CAC has been postulated to result from endotheliopathy along with immune cell activation and propagation of coagulation. While COVID-19 has been noted to create lung injury through binding angiotensin-converting enzyme 2 receptors expressed on alveolar pneumocytes, it increasingly has been found to affect endothelial cells throughout the body. Recent postmortem analyses have demonstrated direct viral infection of endothelial cells with consequent diffuse endothelial inflammation, as evidenced by viral inclusions, sequestered immune cells, and endothelial apoptosis.12,13 Manifestations of this endotheliopathy have been delineated through various studies.
An early retrospective study in Wuhan, China, illustrated that 36% of the first 99 patients hospitalized with COVID-19 demonstrated an elevated D-dimer, 6% an elevated aPTT, and 5% an elevated prothrombin time.14 Another retrospective study conducted in Wuhan found a 25% incidence of venous thromboembolic complications in critically ill patients with severe COVID-19.15 In the Netherlands, a study reported the incidence of arterial and venous thrombotic complications to be 31% in 184 critically ill patients with COVID-19, with 81% of these cases involving pulmonary emboli.16
To our knowledge, our patient is the seventh reported case of ischemic priapism occurring in the setting of a COVID-19 infection, and the first to have occurred in its moderate form. Ischemic priapism is often a consequence of penile venous outflow obstruction and resultant stasis of hypoxic blood.7 The prothrombotic state induced by CAC has been proposed to cause the obstruction of small emissary veins in the subtunical space and in turn lead to venous stasis, which propagates the formation of ischemic priapism.8 Furthermore, 4 of the previously reported cases shared laboratory data on their patients, and all demonstrated elevated D-dimer and fibrinogen levels, which strengthens this hypothesis.3,5,7,8 CLL presents a potential confounding variable in this case; however, as we have reviewed earlier, the risk of leukostasis at WBC counts < 1000 × 109/L is very low.11 It is also probable that the patient had some level of immune dysregulation secondary to CLL, leading to his prolonged course and slow clearance of the virus.
Conclusions
Although only a handful of CAC cases leading to ischemic priapism have been reported, the true incidence may be much higher. While our case highlights the importance of considering COVID-19 infection in the differential diagnosis of ischemic priapism, more research is needed to understand incidence and definitively establish a causative relationship.
1. Pryor J, Akkus E, Alter G, et al. Priapism. J Sex Med. 2004;1(1):116-120. doi:10.1111/j.1743-6109.2004.10117.x
2. Lee SG, Fralick M, Sholzberg M. Coagulopathy associated with COVID-19. CMAJ. 2020;192(21):E583. doi:10.1503/cmaj.200685
3. Lam G, McCarthy R, Haider R. A peculiar case of priapism: the hypercoagulable state in patients with severe COVID-19 infection. Eur J Case Rep Intern Med. 2020;7(8):001779. doi:10.12890/2020_001779
4. Addar A, Al Fraidi O, Nazer A, Althonayan N, Ghazwani Y. Priapism for 10 days in a patient with SARS-CoV-2 pneumonia: a case report. J Surg Case Rep. 2021;2021(4):rjab020. doi:10.1093/jscr/rjab020
5. Lamamri M, Chebbi A, Mamane J, et al. Priapism in a patient with coronavirus disease 2019 (COVID-19). Am J Emerg Med. 2021;39:251.e5-251.e7. doi:10.1016/j.ajem.2020.06.027
6. Silverman ML, VanDerVeer SJ, Donnelly TJ. Priapism in COVID-19: a thromboembolic complication. Am J Emerg Med. 2021;45:686.e5-686.e6. doi:10.1016/j.ajem.2020.12.072
7. Giuliano AFM, Vulpi M, Passerini F, et al. SARS-CoV-2 infection as a determining factor to the precipitation of ischemic priapism in a young patient with asymptomatic COVID-19. Case Rep Urol. 2021;2021:9936891. doi:10.1155/2021/9936891
8. Carreno BD, Perez CP, Vasquez D, Oyola JA, Suarez O, Bedoya C. Veno-occlusive priapism in COVID-19 disease. Urol Int. 2021;105(9-10):916-919. doi:10.1159/000514421
9. Senthilkumaran S, Shah S, Ganapathysubramanian, Balamurgan N, Thirumalaikolundusubramanian P. Propofol and priapism. Indian J Pharmacol. 2010;42(4):238-239. doi:10.4103/0253-7613.68430
10. Qu M, Lu X, Wang L, Liu Z, Sun Y, Gao X. Priapism secondary to chronic myeloid leukemia treated by a surgical cavernosa-corpus spongiosum shunt: case report. Asian J Urol. 2019;6(4):373-376. doi:10.1016/j.ajur.2018.12.004
11. Singh N, Singh Lubana S, Dabrowski L, Sidhu G. Leukostasis in chronic lymphocytic leukemia. Am J Case Rep. 2020;21:e924798. doi:10.12659/AJCR.924798
12. Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417-1418. doi:10.1016/S0140-6736(20)30937-5
13. Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135(23):2033-2040. doi:10.1182/blood.2020006000
14. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507-513. doi:10.1016/S0140-6736(20)30211-7
15. Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. 2020;18(6):1421-1424. doi:10.1111/jth.14830
16. Klok FA, Kruip M, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145-147. doi:10.1016/j.thromres.2020.04.013
1. Pryor J, Akkus E, Alter G, et al. Priapism. J Sex Med. 2004;1(1):116-120. doi:10.1111/j.1743-6109.2004.10117.x
2. Lee SG, Fralick M, Sholzberg M. Coagulopathy associated with COVID-19. CMAJ. 2020;192(21):E583. doi:10.1503/cmaj.200685
3. Lam G, McCarthy R, Haider R. A peculiar case of priapism: the hypercoagulable state in patients with severe COVID-19 infection. Eur J Case Rep Intern Med. 2020;7(8):001779. doi:10.12890/2020_001779
4. Addar A, Al Fraidi O, Nazer A, Althonayan N, Ghazwani Y. Priapism for 10 days in a patient with SARS-CoV-2 pneumonia: a case report. J Surg Case Rep. 2021;2021(4):rjab020. doi:10.1093/jscr/rjab020
5. Lamamri M, Chebbi A, Mamane J, et al. Priapism in a patient with coronavirus disease 2019 (COVID-19). Am J Emerg Med. 2021;39:251.e5-251.e7. doi:10.1016/j.ajem.2020.06.027
6. Silverman ML, VanDerVeer SJ, Donnelly TJ. Priapism in COVID-19: a thromboembolic complication. Am J Emerg Med. 2021;45:686.e5-686.e6. doi:10.1016/j.ajem.2020.12.072
7. Giuliano AFM, Vulpi M, Passerini F, et al. SARS-CoV-2 infection as a determining factor to the precipitation of ischemic priapism in a young patient with asymptomatic COVID-19. Case Rep Urol. 2021;2021:9936891. doi:10.1155/2021/9936891
8. Carreno BD, Perez CP, Vasquez D, Oyola JA, Suarez O, Bedoya C. Veno-occlusive priapism in COVID-19 disease. Urol Int. 2021;105(9-10):916-919. doi:10.1159/000514421
9. Senthilkumaran S, Shah S, Ganapathysubramanian, Balamurgan N, Thirumalaikolundusubramanian P. Propofol and priapism. Indian J Pharmacol. 2010;42(4):238-239. doi:10.4103/0253-7613.68430
10. Qu M, Lu X, Wang L, Liu Z, Sun Y, Gao X. Priapism secondary to chronic myeloid leukemia treated by a surgical cavernosa-corpus spongiosum shunt: case report. Asian J Urol. 2019;6(4):373-376. doi:10.1016/j.ajur.2018.12.004
11. Singh N, Singh Lubana S, Dabrowski L, Sidhu G. Leukostasis in chronic lymphocytic leukemia. Am J Case Rep. 2020;21:e924798. doi:10.12659/AJCR.924798
12. Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417-1418. doi:10.1016/S0140-6736(20)30937-5
13. Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135(23):2033-2040. doi:10.1182/blood.2020006000
14. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507-513. doi:10.1016/S0140-6736(20)30211-7
15. Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. 2020;18(6):1421-1424. doi:10.1111/jth.14830
16. Klok FA, Kruip M, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145-147. doi:10.1016/j.thromres.2020.04.013
Nodular Sclerosing Hodgkin Lymphoma With Paraneoplastic Cerebellar Degeneration
Paraneoplastic syndrome is a rare disorder involving manifestations of immune dysregulation triggered by malignancy. The immune system develops antibodies to the malignancy, which can cause cross reactivation with various tissues in the body, resulting in an autoimmune response. Paraneoplastic cerebellar degeneration (PCD) is a rare condition caused by immune-mediated damage to the Purkinje cells of the cerebellar tract. Symptoms may include gait instability, double vision, decreased fine motor skills, and ataxia, with progression to brainstem-associated symptoms, such as nystagmus, dysarthria, and dysphagia. Early detection and treatment of the underlying malignancy is critical to halt the progression of autoimmune-mediated destruction. We present a case of a young adult female patient with PCD caused by Purkinje cell cytoplasmic–Tr (PCA-Tr) antibody with Hodgkin lymphoma.
Case Presentation
A 20-year-old previously healthy active-duty female patient presented to the emergency department with acute worsening of chronic intermittent, recurrent episodes of lightheadedness and vertigo. Symptoms persisted for 9 months until acutely worsening over the 2 weeks prior to presentation. She reported left eye double vision but did not report seeing spots, photophobia, tinnitus, or headache. She felt off-balance, leaning on nearby objects to remain standing. Symptoms primarily occurred during ambulation; however, occasionally they happened at rest. Episodes lasted up to several minutes and occurred up to 15 times a day. The patient reported no fever, night sweats, unexplained weight loss, muscle aches, weakness, numbness or tingling, loss of bowel or bladder function, or rash. She had no recent illnesses, changes to medications, or recent travel. Oral intake to include food and water was adequate and unchanged. The patient had a remote history of mild concussions without loss of consciousness while playing sports 4 years previously. She reported no recent trauma. Nine months before, she received treatment for benign paroxysmal positional vertigo (BPPV) with the Epley maneuver with full resolution of symptoms lasting several days. She reported no prescription or over-the-counter medications, herbal remedies, or supplements. She reported no other medical or surgical history and no pertinent social or family history.
Physical examination revealed a nontoxic-appearing female patient with intermittent conversational dysarthria, saccadic pursuits, horizontal nystagmus with lateral gaze, and vertical nystagmus with vertical gaze. The patient exhibited dysdiadochokinesia, or impaired ability to perform rapid alternating hand movements with repetition. Finger-to-nose testing was impaired and heel-to-shin motion remained intact. A Romberg test was positive, and the patient had tandem gait instability. Strength testing, sensation, reflexes, and cranial nerves were otherwise intact. Initial laboratory testing was unremarkable except for mild normocytic anemia. Her infectious workup, including testing for venereal disease, HIV, COVID-19, and Coccidioidies was negative. Heavy metals analysis and urine drug screen were negative. Ophthalmology was consulted and workup revealed small amplitude downbeat nystagmus in primary gaze, sustained gaze evoked lateral beating jerk nystagmus with rebound nystagmus R>L gaze, but there was no evidence of afferent package defect and optic nerve function remained intact. Magnetic resonance imaging of the brain demonstrated cerebellar vermis hypoplasia with prominence of the superior cerebellar folia. Due to concerns for autoimmune encephalitis, a lumbar puncture was performed. Antibody testing revealed PCA-Tr antibodies, which is commonly associated with Hodgkin lymphoma, prompting further evaluation for malignancy.
Computed tomography (CT) of the chest with contrast demonstrated multiple mediastinal masses with a conglomeration of lymph nodes along the right paratracheal region. Further evaluation was performed with a positron emission tomography (PET)–CT, revealing a large conglomeration of hypermetabolic pretracheal, mediastinal, and right supraclavicular lymph that were suggestive of lymphoma. Mediastinoscopy with excisional lymph node biopsy was performed with immunohistochemical staining confirming diagnosis of a nodular sclerosing variant of Hodgkin lymphoma. The patient was treated with IV immunoglobulin at 0.4g/kg daily for 5 days. A central venous catheter was placed into the patient’s right internal jugular vein and a chemotherapy regimen of doxorubicin 46 mg, vinblastine 11 mg, bleomycin 19 units, and dacarbazine 700 mg was initiated. The patient’s symptoms improved with resolution of dysarthria; however, her visual impairment and gait instability persisted. Repeat PET-CT imaging 2 months later revealed interval improvement with decreased intensity and extent of the hypermetabolic lymph nodes and no new hypermetabolic foci.
Discussion
PCA-Tr antibodies affect the delta/notchlike epidermal growth factor–related receptor, expressed on the dendrites of cerebellar Purkinje cells.1 These fibers are the only output neurons of the cerebellar cortex and are critical to the coordination of motor movements, accounting for the ataxia experienced by patients with this subtype of PCD.2 The link between Hodgkin lymphoma and PCA-Tr antibodies has been established; however, most reports involve men with a median age of 61 years with lymphoma-associated symptoms (such as lymphadenopathy) or systemic symptoms (fever, night sweats, or weight loss) preceding neurologic manifestations in 80% of cases.3
Our patient was a young, previously healthy adult female who initially presented with vertigo, a common concern with frequently benign origins. Although there was temporary resolution of symptoms after Epley maneuvers, symptoms recurred and progressed over several months to include brainstem manifestations of nystagmus, diplopia, and dysarthria. Previous reports indicate that after remission of the Hodgkin lymphoma, PCA-Tr antibodies disappear and symptoms can improve or resolve.4,5 Treatment has just begun for our patient and although there has been initial clinical improvement, given the chronicity of symptoms, it is unclear if complete resolution will be achieved.
Conclusions
PCD can result in debilitating neurologic dysfunction and may be associated with malignancy such as Hodgkin lymphoma. This case offers unique insight due to the patient’s demographics and presentation, which involved brainstem pathology typically associated with late-onset disease and preceded by constitutional symptoms. Clinical suspicion of this rare disorder should be considered in all ages, especially if symptoms are progressive or neurologic manifestations arise, as early detection and treatment of the underlying malignancy are paramount to the prevention of significant disability.
1. de Graaff E, Maat P, Hulsenboom E, et al. Identification of delta/notch-like epidermal growth factor-related receptor as the Tr antigen in paraneoplastic cerebellar degeneration. Ann Neurol. 2012;71(6):815-824. doi:10.1002/ana.23550
2. MacKenzie-Graham A, Tiwari-Woodruff SK, Sharma G, et al. Purkinje cell loss in experimental autoimmune encephalomyelitis. Neuroimage. 2009;48(4):637-651. doi:10.1016/j.neuroimage.2009.06.073
3. Bernal F, Shams’ili S, Rojas I, et al. Anti-Tr antibodies as markers of paraneoplastic cerebellar degeneration and Hodgkin’s disease. Neurology. 2003;60(2):230-234. doi:10.1212/01.wnl.0000041495.87539.98
4. Graus F, Ariño H, Dalmau J. Paraneoplastic neurological syndromes in Hodgkin and non-Hodgkin lymphomas. Blood. 2014;123(21):3230-3238. doi:10.1182/blood-2014-03-537506
5. Aly R, Emmady PD. Paraneoplastic cerebellar degeneration. Updated May 8, 2022. Accessed March 30, 2022. https://www.ncbi.nlm.nih.gov/books/NBK560638
Paraneoplastic syndrome is a rare disorder involving manifestations of immune dysregulation triggered by malignancy. The immune system develops antibodies to the malignancy, which can cause cross reactivation with various tissues in the body, resulting in an autoimmune response. Paraneoplastic cerebellar degeneration (PCD) is a rare condition caused by immune-mediated damage to the Purkinje cells of the cerebellar tract. Symptoms may include gait instability, double vision, decreased fine motor skills, and ataxia, with progression to brainstem-associated symptoms, such as nystagmus, dysarthria, and dysphagia. Early detection and treatment of the underlying malignancy is critical to halt the progression of autoimmune-mediated destruction. We present a case of a young adult female patient with PCD caused by Purkinje cell cytoplasmic–Tr (PCA-Tr) antibody with Hodgkin lymphoma.
Case Presentation
A 20-year-old previously healthy active-duty female patient presented to the emergency department with acute worsening of chronic intermittent, recurrent episodes of lightheadedness and vertigo. Symptoms persisted for 9 months until acutely worsening over the 2 weeks prior to presentation. She reported left eye double vision but did not report seeing spots, photophobia, tinnitus, or headache. She felt off-balance, leaning on nearby objects to remain standing. Symptoms primarily occurred during ambulation; however, occasionally they happened at rest. Episodes lasted up to several minutes and occurred up to 15 times a day. The patient reported no fever, night sweats, unexplained weight loss, muscle aches, weakness, numbness or tingling, loss of bowel or bladder function, or rash. She had no recent illnesses, changes to medications, or recent travel. Oral intake to include food and water was adequate and unchanged. The patient had a remote history of mild concussions without loss of consciousness while playing sports 4 years previously. She reported no recent trauma. Nine months before, she received treatment for benign paroxysmal positional vertigo (BPPV) with the Epley maneuver with full resolution of symptoms lasting several days. She reported no prescription or over-the-counter medications, herbal remedies, or supplements. She reported no other medical or surgical history and no pertinent social or family history.
Physical examination revealed a nontoxic-appearing female patient with intermittent conversational dysarthria, saccadic pursuits, horizontal nystagmus with lateral gaze, and vertical nystagmus with vertical gaze. The patient exhibited dysdiadochokinesia, or impaired ability to perform rapid alternating hand movements with repetition. Finger-to-nose testing was impaired and heel-to-shin motion remained intact. A Romberg test was positive, and the patient had tandem gait instability. Strength testing, sensation, reflexes, and cranial nerves were otherwise intact. Initial laboratory testing was unremarkable except for mild normocytic anemia. Her infectious workup, including testing for venereal disease, HIV, COVID-19, and Coccidioidies was negative. Heavy metals analysis and urine drug screen were negative. Ophthalmology was consulted and workup revealed small amplitude downbeat nystagmus in primary gaze, sustained gaze evoked lateral beating jerk nystagmus with rebound nystagmus R>L gaze, but there was no evidence of afferent package defect and optic nerve function remained intact. Magnetic resonance imaging of the brain demonstrated cerebellar vermis hypoplasia with prominence of the superior cerebellar folia. Due to concerns for autoimmune encephalitis, a lumbar puncture was performed. Antibody testing revealed PCA-Tr antibodies, which is commonly associated with Hodgkin lymphoma, prompting further evaluation for malignancy.
Computed tomography (CT) of the chest with contrast demonstrated multiple mediastinal masses with a conglomeration of lymph nodes along the right paratracheal region. Further evaluation was performed with a positron emission tomography (PET)–CT, revealing a large conglomeration of hypermetabolic pretracheal, mediastinal, and right supraclavicular lymph that were suggestive of lymphoma. Mediastinoscopy with excisional lymph node biopsy was performed with immunohistochemical staining confirming diagnosis of a nodular sclerosing variant of Hodgkin lymphoma. The patient was treated with IV immunoglobulin at 0.4g/kg daily for 5 days. A central venous catheter was placed into the patient’s right internal jugular vein and a chemotherapy regimen of doxorubicin 46 mg, vinblastine 11 mg, bleomycin 19 units, and dacarbazine 700 mg was initiated. The patient’s symptoms improved with resolution of dysarthria; however, her visual impairment and gait instability persisted. Repeat PET-CT imaging 2 months later revealed interval improvement with decreased intensity and extent of the hypermetabolic lymph nodes and no new hypermetabolic foci.
Discussion
PCA-Tr antibodies affect the delta/notchlike epidermal growth factor–related receptor, expressed on the dendrites of cerebellar Purkinje cells.1 These fibers are the only output neurons of the cerebellar cortex and are critical to the coordination of motor movements, accounting for the ataxia experienced by patients with this subtype of PCD.2 The link between Hodgkin lymphoma and PCA-Tr antibodies has been established; however, most reports involve men with a median age of 61 years with lymphoma-associated symptoms (such as lymphadenopathy) or systemic symptoms (fever, night sweats, or weight loss) preceding neurologic manifestations in 80% of cases.3
Our patient was a young, previously healthy adult female who initially presented with vertigo, a common concern with frequently benign origins. Although there was temporary resolution of symptoms after Epley maneuvers, symptoms recurred and progressed over several months to include brainstem manifestations of nystagmus, diplopia, and dysarthria. Previous reports indicate that after remission of the Hodgkin lymphoma, PCA-Tr antibodies disappear and symptoms can improve or resolve.4,5 Treatment has just begun for our patient and although there has been initial clinical improvement, given the chronicity of symptoms, it is unclear if complete resolution will be achieved.
Conclusions
PCD can result in debilitating neurologic dysfunction and may be associated with malignancy such as Hodgkin lymphoma. This case offers unique insight due to the patient’s demographics and presentation, which involved brainstem pathology typically associated with late-onset disease and preceded by constitutional symptoms. Clinical suspicion of this rare disorder should be considered in all ages, especially if symptoms are progressive or neurologic manifestations arise, as early detection and treatment of the underlying malignancy are paramount to the prevention of significant disability.
Paraneoplastic syndrome is a rare disorder involving manifestations of immune dysregulation triggered by malignancy. The immune system develops antibodies to the malignancy, which can cause cross reactivation with various tissues in the body, resulting in an autoimmune response. Paraneoplastic cerebellar degeneration (PCD) is a rare condition caused by immune-mediated damage to the Purkinje cells of the cerebellar tract. Symptoms may include gait instability, double vision, decreased fine motor skills, and ataxia, with progression to brainstem-associated symptoms, such as nystagmus, dysarthria, and dysphagia. Early detection and treatment of the underlying malignancy is critical to halt the progression of autoimmune-mediated destruction. We present a case of a young adult female patient with PCD caused by Purkinje cell cytoplasmic–Tr (PCA-Tr) antibody with Hodgkin lymphoma.
Case Presentation
A 20-year-old previously healthy active-duty female patient presented to the emergency department with acute worsening of chronic intermittent, recurrent episodes of lightheadedness and vertigo. Symptoms persisted for 9 months until acutely worsening over the 2 weeks prior to presentation. She reported left eye double vision but did not report seeing spots, photophobia, tinnitus, or headache. She felt off-balance, leaning on nearby objects to remain standing. Symptoms primarily occurred during ambulation; however, occasionally they happened at rest. Episodes lasted up to several minutes and occurred up to 15 times a day. The patient reported no fever, night sweats, unexplained weight loss, muscle aches, weakness, numbness or tingling, loss of bowel or bladder function, or rash. She had no recent illnesses, changes to medications, or recent travel. Oral intake to include food and water was adequate and unchanged. The patient had a remote history of mild concussions without loss of consciousness while playing sports 4 years previously. She reported no recent trauma. Nine months before, she received treatment for benign paroxysmal positional vertigo (BPPV) with the Epley maneuver with full resolution of symptoms lasting several days. She reported no prescription or over-the-counter medications, herbal remedies, or supplements. She reported no other medical or surgical history and no pertinent social or family history.
Physical examination revealed a nontoxic-appearing female patient with intermittent conversational dysarthria, saccadic pursuits, horizontal nystagmus with lateral gaze, and vertical nystagmus with vertical gaze. The patient exhibited dysdiadochokinesia, or impaired ability to perform rapid alternating hand movements with repetition. Finger-to-nose testing was impaired and heel-to-shin motion remained intact. A Romberg test was positive, and the patient had tandem gait instability. Strength testing, sensation, reflexes, and cranial nerves were otherwise intact. Initial laboratory testing was unremarkable except for mild normocytic anemia. Her infectious workup, including testing for venereal disease, HIV, COVID-19, and Coccidioidies was negative. Heavy metals analysis and urine drug screen were negative. Ophthalmology was consulted and workup revealed small amplitude downbeat nystagmus in primary gaze, sustained gaze evoked lateral beating jerk nystagmus with rebound nystagmus R>L gaze, but there was no evidence of afferent package defect and optic nerve function remained intact. Magnetic resonance imaging of the brain demonstrated cerebellar vermis hypoplasia with prominence of the superior cerebellar folia. Due to concerns for autoimmune encephalitis, a lumbar puncture was performed. Antibody testing revealed PCA-Tr antibodies, which is commonly associated with Hodgkin lymphoma, prompting further evaluation for malignancy.
Computed tomography (CT) of the chest with contrast demonstrated multiple mediastinal masses with a conglomeration of lymph nodes along the right paratracheal region. Further evaluation was performed with a positron emission tomography (PET)–CT, revealing a large conglomeration of hypermetabolic pretracheal, mediastinal, and right supraclavicular lymph that were suggestive of lymphoma. Mediastinoscopy with excisional lymph node biopsy was performed with immunohistochemical staining confirming diagnosis of a nodular sclerosing variant of Hodgkin lymphoma. The patient was treated with IV immunoglobulin at 0.4g/kg daily for 5 days. A central venous catheter was placed into the patient’s right internal jugular vein and a chemotherapy regimen of doxorubicin 46 mg, vinblastine 11 mg, bleomycin 19 units, and dacarbazine 700 mg was initiated. The patient’s symptoms improved with resolution of dysarthria; however, her visual impairment and gait instability persisted. Repeat PET-CT imaging 2 months later revealed interval improvement with decreased intensity and extent of the hypermetabolic lymph nodes and no new hypermetabolic foci.
Discussion
PCA-Tr antibodies affect the delta/notchlike epidermal growth factor–related receptor, expressed on the dendrites of cerebellar Purkinje cells.1 These fibers are the only output neurons of the cerebellar cortex and are critical to the coordination of motor movements, accounting for the ataxia experienced by patients with this subtype of PCD.2 The link between Hodgkin lymphoma and PCA-Tr antibodies has been established; however, most reports involve men with a median age of 61 years with lymphoma-associated symptoms (such as lymphadenopathy) or systemic symptoms (fever, night sweats, or weight loss) preceding neurologic manifestations in 80% of cases.3
Our patient was a young, previously healthy adult female who initially presented with vertigo, a common concern with frequently benign origins. Although there was temporary resolution of symptoms after Epley maneuvers, symptoms recurred and progressed over several months to include brainstem manifestations of nystagmus, diplopia, and dysarthria. Previous reports indicate that after remission of the Hodgkin lymphoma, PCA-Tr antibodies disappear and symptoms can improve or resolve.4,5 Treatment has just begun for our patient and although there has been initial clinical improvement, given the chronicity of symptoms, it is unclear if complete resolution will be achieved.
Conclusions
PCD can result in debilitating neurologic dysfunction and may be associated with malignancy such as Hodgkin lymphoma. This case offers unique insight due to the patient’s demographics and presentation, which involved brainstem pathology typically associated with late-onset disease and preceded by constitutional symptoms. Clinical suspicion of this rare disorder should be considered in all ages, especially if symptoms are progressive or neurologic manifestations arise, as early detection and treatment of the underlying malignancy are paramount to the prevention of significant disability.
1. de Graaff E, Maat P, Hulsenboom E, et al. Identification of delta/notch-like epidermal growth factor-related receptor as the Tr antigen in paraneoplastic cerebellar degeneration. Ann Neurol. 2012;71(6):815-824. doi:10.1002/ana.23550
2. MacKenzie-Graham A, Tiwari-Woodruff SK, Sharma G, et al. Purkinje cell loss in experimental autoimmune encephalomyelitis. Neuroimage. 2009;48(4):637-651. doi:10.1016/j.neuroimage.2009.06.073
3. Bernal F, Shams’ili S, Rojas I, et al. Anti-Tr antibodies as markers of paraneoplastic cerebellar degeneration and Hodgkin’s disease. Neurology. 2003;60(2):230-234. doi:10.1212/01.wnl.0000041495.87539.98
4. Graus F, Ariño H, Dalmau J. Paraneoplastic neurological syndromes in Hodgkin and non-Hodgkin lymphomas. Blood. 2014;123(21):3230-3238. doi:10.1182/blood-2014-03-537506
5. Aly R, Emmady PD. Paraneoplastic cerebellar degeneration. Updated May 8, 2022. Accessed March 30, 2022. https://www.ncbi.nlm.nih.gov/books/NBK560638
1. de Graaff E, Maat P, Hulsenboom E, et al. Identification of delta/notch-like epidermal growth factor-related receptor as the Tr antigen in paraneoplastic cerebellar degeneration. Ann Neurol. 2012;71(6):815-824. doi:10.1002/ana.23550
2. MacKenzie-Graham A, Tiwari-Woodruff SK, Sharma G, et al. Purkinje cell loss in experimental autoimmune encephalomyelitis. Neuroimage. 2009;48(4):637-651. doi:10.1016/j.neuroimage.2009.06.073
3. Bernal F, Shams’ili S, Rojas I, et al. Anti-Tr antibodies as markers of paraneoplastic cerebellar degeneration and Hodgkin’s disease. Neurology. 2003;60(2):230-234. doi:10.1212/01.wnl.0000041495.87539.98
4. Graus F, Ariño H, Dalmau J. Paraneoplastic neurological syndromes in Hodgkin and non-Hodgkin lymphomas. Blood. 2014;123(21):3230-3238. doi:10.1182/blood-2014-03-537506
5. Aly R, Emmady PD. Paraneoplastic cerebellar degeneration. Updated May 8, 2022. Accessed March 30, 2022. https://www.ncbi.nlm.nih.gov/books/NBK560638
Two congressmen targeting ‘gender transition’ physicians
Two GOP congressmen have introduced legislation aimed at holding doctors who perform gender transition procedures on minors liable for their actions, says a story reported on KATV.com, among other news sites.
The two GOP lawmakers – Rep. Jim Banks (IN) and Sen. Tom Cotton (AR) – introduced the Protecting Minors from Medical Malpractice Act in their respective chambers.
If passed, the House and Senate bills would make doctors liable for any gender transition surgery on a minor that results in injury, whether physical, psychological, emotional, or physiological. Minors who believe they’ve been harmed would have up to 30 years from when they turn 18 to file a claim.
The House proposal would also strip federal funding from states that require health care professionals to provide gender transition procedures, including puberty blockers, cross-sex hormones, and gender reassignment surgeries.
A companion House bill, also sponsored by Banks, targets another issue related to gender transitioning for minors: parental consent.
If passed, the Empower Parents to Protect Their Kids Act of 2022 would deny federal funding to any elementary and secondary schools that initiate a minor’s gender transition without first securing parental consent. (Last October, Sen. Cotton released a similar bill in the Senate.)
The content contained in this article is for informational purposes only and does not constitute legal advice. Reliance on any information provided in this article is solely at your own risk.
A version of this article first appeared on Medscape.com.
Two GOP congressmen have introduced legislation aimed at holding doctors who perform gender transition procedures on minors liable for their actions, says a story reported on KATV.com, among other news sites.
The two GOP lawmakers – Rep. Jim Banks (IN) and Sen. Tom Cotton (AR) – introduced the Protecting Minors from Medical Malpractice Act in their respective chambers.
If passed, the House and Senate bills would make doctors liable for any gender transition surgery on a minor that results in injury, whether physical, psychological, emotional, or physiological. Minors who believe they’ve been harmed would have up to 30 years from when they turn 18 to file a claim.
The House proposal would also strip federal funding from states that require health care professionals to provide gender transition procedures, including puberty blockers, cross-sex hormones, and gender reassignment surgeries.
A companion House bill, also sponsored by Banks, targets another issue related to gender transitioning for minors: parental consent.
If passed, the Empower Parents to Protect Their Kids Act of 2022 would deny federal funding to any elementary and secondary schools that initiate a minor’s gender transition without first securing parental consent. (Last October, Sen. Cotton released a similar bill in the Senate.)
The content contained in this article is for informational purposes only and does not constitute legal advice. Reliance on any information provided in this article is solely at your own risk.
A version of this article first appeared on Medscape.com.
Two GOP congressmen have introduced legislation aimed at holding doctors who perform gender transition procedures on minors liable for their actions, says a story reported on KATV.com, among other news sites.
The two GOP lawmakers – Rep. Jim Banks (IN) and Sen. Tom Cotton (AR) – introduced the Protecting Minors from Medical Malpractice Act in their respective chambers.
If passed, the House and Senate bills would make doctors liable for any gender transition surgery on a minor that results in injury, whether physical, psychological, emotional, or physiological. Minors who believe they’ve been harmed would have up to 30 years from when they turn 18 to file a claim.
The House proposal would also strip federal funding from states that require health care professionals to provide gender transition procedures, including puberty blockers, cross-sex hormones, and gender reassignment surgeries.
A companion House bill, also sponsored by Banks, targets another issue related to gender transitioning for minors: parental consent.
If passed, the Empower Parents to Protect Their Kids Act of 2022 would deny federal funding to any elementary and secondary schools that initiate a minor’s gender transition without first securing parental consent. (Last October, Sen. Cotton released a similar bill in the Senate.)
The content contained in this article is for informational purposes only and does not constitute legal advice. Reliance on any information provided in this article is solely at your own risk.
A version of this article first appeared on Medscape.com.
Link between pediatric hepatitis and adenovirus 41 still unclear
While two new studies reiterate a possible relationship between adenovirus 41 and acute hepatitis of unknown cause in children, whether these infections are significant or merely bystanders remains unclear.
In both studies – one conducted in Alabama and the other conducted in the United Kingdom – researchers found that 90% of children with acute hepatitis of unknown cause tested positive for adenovirus 41. The virus subtype is not an uncommon infection, but it usually causes gastroenteritis in children.
“Across the world, adenovirus continues to be a common signal” in these pediatric hepatitis cases, said Helena Gutierrez, MD, the medical director of the Pediatric Liver Transplant Program at the University of Alabama at Birmingham, in an interview. She led one of the studies. More data are necessary to understand what role this virus may play in these cases, she said.
In November, the Alabama Department of Public Health and the U.S. Centers for Disease Control and Prevention began investigating a cluster of severe pediatric hepatitis cases at the Children’s of Alabama hospital in Birmingham. These children also tested positive for adenovirus. In April, the United Kingdom announced they were investigating similar cases, and the CDC expanded their search nationally. As of July 8, 1,010 cases in 35 countries have been reported to the World Health Organization. There are 263 confirmed cases in the United Kingdom and 332 cases under investigation by the CDC in the United States, according to the most recent counts.
The two studies, both published in the New England Journal of Medicine, provide additional clinical data on a number of these mysterious hepatitis cases. Dr. Gutierrez’s study looked at nine children admitted for hepatitis of unknown origin between October 1 and February 28. Patients had a median age of 2 years 11 months and two required liver transplants, and there were no deaths.
Eight out of nine patients (89%) tested positive for adenovirus, and all five of the samples that were of sufficient quality for gene sequencing tested positive for adenovirus 41. None of the six liver biopsies performed found signs of adenovirus infection, but the liver tissue samples of three patients tested positive for adenovirus via PCR.
The second study involved 44 children referred to a liver transplantation center in the United Kingdom between January 1 and April 11, 2022. The median age for patients was 4 years. Six children required liver transplants, and there were no deaths. Of the 30 patients who underwent molecular adenovirus testing, 27 (90%) were positive for adenovirus 41. Liver samples of nine children (3 from biopsies and 6 from explanted livers) all tested negative for adenovirus antibodies.
In both studies, however, the median adenovirus viral load of patients needing a transplant was much higher than the viral loads in children who did not require liver transplants.
Although most of the clinical features and test results of these cases suggest that adenovirus may be involved, the negative results in histology are “intriguing,” Chayarani Kelgeri, MD, a consultant pediatric hepatologist at the Birmingham Women’s and Children’s Hospital, U.K., said in an email. She is the lead author of the U.K. study. “Whether this is because the liver injury we see is an aftermath of the viral infection, the mechanism of injury is immune mediated, and if other cofactors are involved is being explored,” she added. “Further investigations being undertaken by UK Health Security Agency will add to our understanding of this illness.”
Although there is a high adenovirus positivity rate amongst these cases, there is not enough evidence yet to say adenovirus 41 is a new cause of pediatric hepatitis in previously healthy children, said Saul Karpen, MD, PhD, the division chief of pediatric gastroenterology, hepatology, and nutrition at Emory University School of Medicine, Atlanta. He wrote an editorial accompanying the two NEJM studies.
The CDC has not yet found an increase in pediatric hepatitis cases, according to a recent analysis, though the United Kingdom has found an uptick in cases this year, he told this news organization. Also, the cases highlighted in both articles showed no histological evidence of adenovirus in liver biopsies. “That’s completely opposite of what we generally see in adenoviral hepatitis that can be quite severe,” he said, adding that in general, there are detectable viral particles and antigens in affected livers.
“These two important reports indicate to those inside and outside the field of pediatric hepatology that registries and clinical studies of acute hepatitis in children are sorely needed,” Dr. Karpen writes in the editorial; “It is likely that with greater attention to collecting data on cases and biospecimens from children with acute hepatitis, we will be able to determine whether this one virus, human adenovirus 41, is of relevance to this important and serious condition in children.”
Dr. Gutierrez, Dr. Kelgeri, and Dr. Karpen report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
While two new studies reiterate a possible relationship between adenovirus 41 and acute hepatitis of unknown cause in children, whether these infections are significant or merely bystanders remains unclear.
In both studies – one conducted in Alabama and the other conducted in the United Kingdom – researchers found that 90% of children with acute hepatitis of unknown cause tested positive for adenovirus 41. The virus subtype is not an uncommon infection, but it usually causes gastroenteritis in children.
“Across the world, adenovirus continues to be a common signal” in these pediatric hepatitis cases, said Helena Gutierrez, MD, the medical director of the Pediatric Liver Transplant Program at the University of Alabama at Birmingham, in an interview. She led one of the studies. More data are necessary to understand what role this virus may play in these cases, she said.
In November, the Alabama Department of Public Health and the U.S. Centers for Disease Control and Prevention began investigating a cluster of severe pediatric hepatitis cases at the Children’s of Alabama hospital in Birmingham. These children also tested positive for adenovirus. In April, the United Kingdom announced they were investigating similar cases, and the CDC expanded their search nationally. As of July 8, 1,010 cases in 35 countries have been reported to the World Health Organization. There are 263 confirmed cases in the United Kingdom and 332 cases under investigation by the CDC in the United States, according to the most recent counts.
The two studies, both published in the New England Journal of Medicine, provide additional clinical data on a number of these mysterious hepatitis cases. Dr. Gutierrez’s study looked at nine children admitted for hepatitis of unknown origin between October 1 and February 28. Patients had a median age of 2 years 11 months and two required liver transplants, and there were no deaths.
Eight out of nine patients (89%) tested positive for adenovirus, and all five of the samples that were of sufficient quality for gene sequencing tested positive for adenovirus 41. None of the six liver biopsies performed found signs of adenovirus infection, but the liver tissue samples of three patients tested positive for adenovirus via PCR.
The second study involved 44 children referred to a liver transplantation center in the United Kingdom between January 1 and April 11, 2022. The median age for patients was 4 years. Six children required liver transplants, and there were no deaths. Of the 30 patients who underwent molecular adenovirus testing, 27 (90%) were positive for adenovirus 41. Liver samples of nine children (3 from biopsies and 6 from explanted livers) all tested negative for adenovirus antibodies.
In both studies, however, the median adenovirus viral load of patients needing a transplant was much higher than the viral loads in children who did not require liver transplants.
Although most of the clinical features and test results of these cases suggest that adenovirus may be involved, the negative results in histology are “intriguing,” Chayarani Kelgeri, MD, a consultant pediatric hepatologist at the Birmingham Women’s and Children’s Hospital, U.K., said in an email. She is the lead author of the U.K. study. “Whether this is because the liver injury we see is an aftermath of the viral infection, the mechanism of injury is immune mediated, and if other cofactors are involved is being explored,” she added. “Further investigations being undertaken by UK Health Security Agency will add to our understanding of this illness.”
Although there is a high adenovirus positivity rate amongst these cases, there is not enough evidence yet to say adenovirus 41 is a new cause of pediatric hepatitis in previously healthy children, said Saul Karpen, MD, PhD, the division chief of pediatric gastroenterology, hepatology, and nutrition at Emory University School of Medicine, Atlanta. He wrote an editorial accompanying the two NEJM studies.
The CDC has not yet found an increase in pediatric hepatitis cases, according to a recent analysis, though the United Kingdom has found an uptick in cases this year, he told this news organization. Also, the cases highlighted in both articles showed no histological evidence of adenovirus in liver biopsies. “That’s completely opposite of what we generally see in adenoviral hepatitis that can be quite severe,” he said, adding that in general, there are detectable viral particles and antigens in affected livers.
“These two important reports indicate to those inside and outside the field of pediatric hepatology that registries and clinical studies of acute hepatitis in children are sorely needed,” Dr. Karpen writes in the editorial; “It is likely that with greater attention to collecting data on cases and biospecimens from children with acute hepatitis, we will be able to determine whether this one virus, human adenovirus 41, is of relevance to this important and serious condition in children.”
Dr. Gutierrez, Dr. Kelgeri, and Dr. Karpen report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
While two new studies reiterate a possible relationship between adenovirus 41 and acute hepatitis of unknown cause in children, whether these infections are significant or merely bystanders remains unclear.
In both studies – one conducted in Alabama and the other conducted in the United Kingdom – researchers found that 90% of children with acute hepatitis of unknown cause tested positive for adenovirus 41. The virus subtype is not an uncommon infection, but it usually causes gastroenteritis in children.
“Across the world, adenovirus continues to be a common signal” in these pediatric hepatitis cases, said Helena Gutierrez, MD, the medical director of the Pediatric Liver Transplant Program at the University of Alabama at Birmingham, in an interview. She led one of the studies. More data are necessary to understand what role this virus may play in these cases, she said.
In November, the Alabama Department of Public Health and the U.S. Centers for Disease Control and Prevention began investigating a cluster of severe pediatric hepatitis cases at the Children’s of Alabama hospital in Birmingham. These children also tested positive for adenovirus. In April, the United Kingdom announced they were investigating similar cases, and the CDC expanded their search nationally. As of July 8, 1,010 cases in 35 countries have been reported to the World Health Organization. There are 263 confirmed cases in the United Kingdom and 332 cases under investigation by the CDC in the United States, according to the most recent counts.
The two studies, both published in the New England Journal of Medicine, provide additional clinical data on a number of these mysterious hepatitis cases. Dr. Gutierrez’s study looked at nine children admitted for hepatitis of unknown origin between October 1 and February 28. Patients had a median age of 2 years 11 months and two required liver transplants, and there were no deaths.
Eight out of nine patients (89%) tested positive for adenovirus, and all five of the samples that were of sufficient quality for gene sequencing tested positive for adenovirus 41. None of the six liver biopsies performed found signs of adenovirus infection, but the liver tissue samples of three patients tested positive for adenovirus via PCR.
The second study involved 44 children referred to a liver transplantation center in the United Kingdom between January 1 and April 11, 2022. The median age for patients was 4 years. Six children required liver transplants, and there were no deaths. Of the 30 patients who underwent molecular adenovirus testing, 27 (90%) were positive for adenovirus 41. Liver samples of nine children (3 from biopsies and 6 from explanted livers) all tested negative for adenovirus antibodies.
In both studies, however, the median adenovirus viral load of patients needing a transplant was much higher than the viral loads in children who did not require liver transplants.
Although most of the clinical features and test results of these cases suggest that adenovirus may be involved, the negative results in histology are “intriguing,” Chayarani Kelgeri, MD, a consultant pediatric hepatologist at the Birmingham Women’s and Children’s Hospital, U.K., said in an email. She is the lead author of the U.K. study. “Whether this is because the liver injury we see is an aftermath of the viral infection, the mechanism of injury is immune mediated, and if other cofactors are involved is being explored,” she added. “Further investigations being undertaken by UK Health Security Agency will add to our understanding of this illness.”
Although there is a high adenovirus positivity rate amongst these cases, there is not enough evidence yet to say adenovirus 41 is a new cause of pediatric hepatitis in previously healthy children, said Saul Karpen, MD, PhD, the division chief of pediatric gastroenterology, hepatology, and nutrition at Emory University School of Medicine, Atlanta. He wrote an editorial accompanying the two NEJM studies.
The CDC has not yet found an increase in pediatric hepatitis cases, according to a recent analysis, though the United Kingdom has found an uptick in cases this year, he told this news organization. Also, the cases highlighted in both articles showed no histological evidence of adenovirus in liver biopsies. “That’s completely opposite of what we generally see in adenoviral hepatitis that can be quite severe,” he said, adding that in general, there are detectable viral particles and antigens in affected livers.
“These two important reports indicate to those inside and outside the field of pediatric hepatology that registries and clinical studies of acute hepatitis in children are sorely needed,” Dr. Karpen writes in the editorial; “It is likely that with greater attention to collecting data on cases and biospecimens from children with acute hepatitis, we will be able to determine whether this one virus, human adenovirus 41, is of relevance to this important and serious condition in children.”
Dr. Gutierrez, Dr. Kelgeri, and Dr. Karpen report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Recommendations on breastfeeding: A case of too much information
The American Academy of Pediatrics is built on good intentions. It wants the best for children in the world, and it hopes to support its members in their efforts to achieve this goal. But from time to time, the academy loses sight of reality and makes recommendations that are counterproductive to its stated goals.
The recent release of its new policy “Breastfeeding and the Use of Human Milk” is another unfortunate example of poorly aimed recommendations. A careful reading of the document reveals it to be a well-researched treatise on breastfeeding and the value of human milk, including a discussion of the numerous impediments to the universal adoption of breastfeeding in our society. However, when a document of this breadth and complexity is released to the public it is never surprising that the messages deserving the most attention are lost in the press coverage. Most of the headlines I saw mentioned pediatricians supporting breastfeeding for a year or 2.
Who was the target audience? If it was pediatricians, most of us don’t need a longer list of the health benefits of breastfeeding. We already believe it is the best nutritional source for human babies and realize that the institutional framework in this country continues to be unfriendly to women who intend to breastfeed.
If the audience is politicians and public health decision-makers, the new policy contains a wealth of supportive evidence. However, most pediatricians I know are too busy or lack the skills and enthusiasm to become political activists. For the rest of population, including parents, the recommendations represent a collection of TMI (too much information).
If the audience is women who are considering breastfeeding I suspect nearly 100% already know pediatricians think it is the preferred way to feed their babies. And, likewise, a longer list won’t convince them to try nursing. Additional evidence may simply make them feel more guilty when they aren’t successful.
Many pregnant women have already been told that breastfeeding can be a challenge and given their situation breast milk alone for the first 6 months may sound like an unreasonable goal. The new recommendation that breastfeeding for a year or 2 is good is not a message they want to hear.
On the other hand, if the target audience is women who will be comforted to hear an official statement that normalizes breastfeeding longer than a year, the new policy statement has hit the nail on the head.
Of course the new policy document is sprinkled with caveats that vaguely hint at the possibility that pediatricians are sensitive human beings who under certain circumstances may be able to compromise when it comes to the duration of breastfeeding and the introduction of formula. But this whiff of reality is certainly not the dominant odor in these new recommendations.
Don’t get me wrong: I think the academy was overdue for a policy revision on breastfeeding. However, it should have been one that was reality based. It should acknowledge that there are institutional and societal biases against breastfeeding, and it should remind pediatricians that they can effect change by discussing these realities honestly with parents, while making it clear that we are there for them and their children regardless of how they feed their baby. Pediatricians believe that breastfeeding is the best but not the only way to feed a baby. We have (or will provide) the skills to assist parents succeed in whatever method they choose and strive to minimize the impediments that are within our power to change.
If the academy had chosen to release a separate statement simply supporting mothers who chose to nurse longer than a year, then that would have been a good idea. However, when presented as part of the larger document, that message dominated in the media and only served to fuel the guilt that many new mothers must endure.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
The American Academy of Pediatrics is built on good intentions. It wants the best for children in the world, and it hopes to support its members in their efforts to achieve this goal. But from time to time, the academy loses sight of reality and makes recommendations that are counterproductive to its stated goals.
The recent release of its new policy “Breastfeeding and the Use of Human Milk” is another unfortunate example of poorly aimed recommendations. A careful reading of the document reveals it to be a well-researched treatise on breastfeeding and the value of human milk, including a discussion of the numerous impediments to the universal adoption of breastfeeding in our society. However, when a document of this breadth and complexity is released to the public it is never surprising that the messages deserving the most attention are lost in the press coverage. Most of the headlines I saw mentioned pediatricians supporting breastfeeding for a year or 2.
Who was the target audience? If it was pediatricians, most of us don’t need a longer list of the health benefits of breastfeeding. We already believe it is the best nutritional source for human babies and realize that the institutional framework in this country continues to be unfriendly to women who intend to breastfeed.
If the audience is politicians and public health decision-makers, the new policy contains a wealth of supportive evidence. However, most pediatricians I know are too busy or lack the skills and enthusiasm to become political activists. For the rest of population, including parents, the recommendations represent a collection of TMI (too much information).
If the audience is women who are considering breastfeeding I suspect nearly 100% already know pediatricians think it is the preferred way to feed their babies. And, likewise, a longer list won’t convince them to try nursing. Additional evidence may simply make them feel more guilty when they aren’t successful.
Many pregnant women have already been told that breastfeeding can be a challenge and given their situation breast milk alone for the first 6 months may sound like an unreasonable goal. The new recommendation that breastfeeding for a year or 2 is good is not a message they want to hear.
On the other hand, if the target audience is women who will be comforted to hear an official statement that normalizes breastfeeding longer than a year, the new policy statement has hit the nail on the head.
Of course the new policy document is sprinkled with caveats that vaguely hint at the possibility that pediatricians are sensitive human beings who under certain circumstances may be able to compromise when it comes to the duration of breastfeeding and the introduction of formula. But this whiff of reality is certainly not the dominant odor in these new recommendations.
Don’t get me wrong: I think the academy was overdue for a policy revision on breastfeeding. However, it should have been one that was reality based. It should acknowledge that there are institutional and societal biases against breastfeeding, and it should remind pediatricians that they can effect change by discussing these realities honestly with parents, while making it clear that we are there for them and their children regardless of how they feed their baby. Pediatricians believe that breastfeeding is the best but not the only way to feed a baby. We have (or will provide) the skills to assist parents succeed in whatever method they choose and strive to minimize the impediments that are within our power to change.
If the academy had chosen to release a separate statement simply supporting mothers who chose to nurse longer than a year, then that would have been a good idea. However, when presented as part of the larger document, that message dominated in the media and only served to fuel the guilt that many new mothers must endure.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
The American Academy of Pediatrics is built on good intentions. It wants the best for children in the world, and it hopes to support its members in their efforts to achieve this goal. But from time to time, the academy loses sight of reality and makes recommendations that are counterproductive to its stated goals.
The recent release of its new policy “Breastfeeding and the Use of Human Milk” is another unfortunate example of poorly aimed recommendations. A careful reading of the document reveals it to be a well-researched treatise on breastfeeding and the value of human milk, including a discussion of the numerous impediments to the universal adoption of breastfeeding in our society. However, when a document of this breadth and complexity is released to the public it is never surprising that the messages deserving the most attention are lost in the press coverage. Most of the headlines I saw mentioned pediatricians supporting breastfeeding for a year or 2.
Who was the target audience? If it was pediatricians, most of us don’t need a longer list of the health benefits of breastfeeding. We already believe it is the best nutritional source for human babies and realize that the institutional framework in this country continues to be unfriendly to women who intend to breastfeed.
If the audience is politicians and public health decision-makers, the new policy contains a wealth of supportive evidence. However, most pediatricians I know are too busy or lack the skills and enthusiasm to become political activists. For the rest of population, including parents, the recommendations represent a collection of TMI (too much information).
If the audience is women who are considering breastfeeding I suspect nearly 100% already know pediatricians think it is the preferred way to feed their babies. And, likewise, a longer list won’t convince them to try nursing. Additional evidence may simply make them feel more guilty when they aren’t successful.
Many pregnant women have already been told that breastfeeding can be a challenge and given their situation breast milk alone for the first 6 months may sound like an unreasonable goal. The new recommendation that breastfeeding for a year or 2 is good is not a message they want to hear.
On the other hand, if the target audience is women who will be comforted to hear an official statement that normalizes breastfeeding longer than a year, the new policy statement has hit the nail on the head.
Of course the new policy document is sprinkled with caveats that vaguely hint at the possibility that pediatricians are sensitive human beings who under certain circumstances may be able to compromise when it comes to the duration of breastfeeding and the introduction of formula. But this whiff of reality is certainly not the dominant odor in these new recommendations.
Don’t get me wrong: I think the academy was overdue for a policy revision on breastfeeding. However, it should have been one that was reality based. It should acknowledge that there are institutional and societal biases against breastfeeding, and it should remind pediatricians that they can effect change by discussing these realities honestly with parents, while making it clear that we are there for them and their children regardless of how they feed their baby. Pediatricians believe that breastfeeding is the best but not the only way to feed a baby. We have (or will provide) the skills to assist parents succeed in whatever method they choose and strive to minimize the impediments that are within our power to change.
If the academy had chosen to release a separate statement simply supporting mothers who chose to nurse longer than a year, then that would have been a good idea. However, when presented as part of the larger document, that message dominated in the media and only served to fuel the guilt that many new mothers must endure.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Don’t wait for a cyberattack; know what coverage you have now
Barbara L. McAneny, MD, CEO of New Mexico Oncology Hematology Consultants, experienced a data breach about 10 years ago, when a laptop was stolen from her large practice.
She and the other physicians were upset and worried that the individual would attempt to log in to the computer system and hack their patients’ private health information.
Dr. McAneny was also worried that the practice would have to pay a hefty fine to the government for having unsecured private health information on a laptop. She could have paid from $50,000 to more than $1.9 million for lost and stolen devices (although that didn’t happen).
Dr. McAneny had a standard cyber liability benefit in her med-mal policy that covered up to $50,000 of the data breach costs. That covered the legal advice The Doctors Company provided about state and federal reporting requirements when a data breach occurs and the costs the practice incurred from mailing letters to all of its patients notifying them of the data breach, says Dr. McAneny.
“The data breach taught me a lot. Our practice spent a lot of money on increasing our internal controls, cybersecurity, and monitoring. Our IT department started testing our computer firewalls periodically, and that’s how we discovered that cybercriminals were attempting to break into our computer system at least 100 times daily,” says Dr. McAneny.
That discovery changed how she thought about insurance. “I decided the med-mal benefit wasn’t enough. I bought the best cybersecurity policy we could afford to protect against future breaches, especially malware or ransomware attacks.”
Her practice also had to make its electronic health records (EHRs) more secure to comply with the Department of Health & Human Services Office of Civil Rights standards for protected health information. The cost of increased security wasn’t covered by her cyber benefit.
Cyberattacks increasing in health care
Despite having comprehensive coverage, Dr. McAneny worries that the cybercriminals are a step ahead of the cybersecurity experts and her practice will eventually have another data breach.
“The policy only covers things that we know about today. As we upgrade our defenses, criminals are finding new ways to breach firewalls and work around our defenses,” she says.
So far this year, nearly 200 medical groups have reported cyberattacks involving 500 or more of their patients’ medical records to the federal government.
EHRs are valuable targets to cybercriminals because of the protected health information they contain. Cybercriminals grab information such as Social Security numbers, dates of birth, medical procedures and results, and in some cases billing and financial information and sell it on the dark web.
They typically bundle the information and sell it to other criminals who later use it for various kinds of fraud and extortion such as banking and credit fraud, health care fraud, identity theft, and ransom extortion.
What do most doctors have?
The vast majority (82%) of doctors polled by the Medical Group Management Association last year said they had cyber insurance, compared with 54% in 2018.
For those who answered “yes,” many said they have coverage through their malpractice insurance carrier.
David Zetter, president of Zetter HealthCare Management Consultants, recommends that physicians speak with their malpractice carrier to determine what coverage they have, if any, within their malpractice policy.
A typical cybersecurity benefit is limited to what is needed to fix and resolve the hacking incident, says Raj Shah, senior regulatory attorney and policyholder advisor at MagMutual, which insures medical practices for malpractice and cyber liability.
That usually covers investigating the cause of the breach and the extent of the damage, legal advice about federal and state reporting requirements, whether to pay a ransom, and a public relations professional to handle patient communication, says Mr. Shah.
The benefit doesn’t cover lost patient revenue when practices have to shut down their operations, the cost of replacing damaged computers, or the ransom payment, he says.
Mr. Zetter advises doctors to consider buying cybersecurity coverage. “I recommend that they speak with an insurance broker who is experienced with cybersecurity policies sold to health care professionals to determine what type of coverage and how much coverage they may need. Their malpractice carrier may also be able to provide some answers,” says Mr. Zetter.
The physician will need to be able to answer questions about their network and how many staff they have and may need to involve their IT vendor too, he adds.
How does comprehensive coverage compare?
Ransomware attacks continue to be one of the most frequent types of attacks, and the amount criminals are demanding has risen significantly. The median ransom payment was $5,000 in the fourth quarter of 2018, compared with over $300,000 during the fourth quarter of 2021.
Cybercriminals now engage in “double extortion” – demanding a ransom payment to hand over the code that will unlock their encrypted data – and then another ransom payment to not post patients’ sensitive medical information they copied onto the dark web.
Comprehensive cybersecurity insurance will cover “double extortion” payments, legal costs that may arise from defending against patient lawsuits, and the costs of meeting federal and state privacy requirements, including notifying patients of the data breach and regulatory investigations, says Michael Carr, head of risk engineering for North America for Coalition, a cyber insurance firm.
Cyber insurers also contract with vendors who sell bitcoin, which is the currency cybercriminals typically demand for ransom payments, and work with ransom negotiators.
For example, once Coalition decided to pay the ransom on behalf of a health care client, it negotiated the ransom demand down by nearly 75% from $750,000 to $200,000, and proceeded to help the company restore all of its data.
The costs to respond to the incident, to recover lost data, and to pay the extortion, together with the lost business income resulting from the incident, were covered by Coalition’s cyber insurance policy.
Other clients have had their funds retrieved before a fraudulent wire transfer was completed. “Medical practices have vendors they pay regularly. A cybercriminal may compromise your email or take over a bank account and then impersonate a vendor asking to be paid for services they didn’t provide,” says Mr. Carr.
How much coverage do you need? Cost?
Dr. McAneny has increased her cybersecurity coverage every year. “It’s expensive, but I think it’s worth it. But you can never buy enough protection due to the coverage limits.”
She worries that the costs could exceed the limits if a ransomware attack disrupts her practice for days, weeks, or longer, or if the Office for Civil Rights fines her practice $10,000 per patient chart – the practice has 100,000 health records. “That can run several millions of dollars and ruin a practice,” she says.
Health systems and hospitals need massive amounts of coverage, which often runs from $20 million to $30 million, says Mr. Shah. However, practices insured through MagMutual have lower coverage limits that range from $1 million to $5 million, he says.
“A large practice does not necessarily need more than $1,000,000 in coverage if they have limited loss in this area and strong internal processes and controls. Most large practices also have a dedicated information security director, which reduces their risk, so they may be comfortable with $1,000,000 in coverage,” says Mr. Shah.
Premiums are based on the number of patient health records per practice, which translates into higher premiums for larger practices.
Other factors that come into play include the underlying coverage, risk controls the practice has implemented, and its claims history, says Mr. Shah.
However, the cost for cyber liability insurance has increased, and practices can expect to pay higher premiums and deductibles. For example, a practice that paid $10,000 in premiums for a new policy last year will have to pay $20,000 this year, says Dan Hanson, senior vice president of management liability and client experience at Marsh & McLennon Agency, a risk management firm that sells cyber insurance policies.
“We saw 71% of our self-insured clients experience higher deductibles over last year due to increased claim activity and the lack of capacity in the market. The carriers are saying they will set limits, but you are going to pay a lot more, and you are going to participate more in losses through the higher deductibles,” says Mr. Hanson.
Are you eligible?
Cyber insurance companies have a vested interest in avoiding claims. With increasing cyberattacks and larger payouts, many insurers are requiring practices to implement some defensive measures before they insure them. Some insurers, such as Coalition, say they may still insure small practices for comprehensive coverage, but it may impact the pricing or what’s covered, says Mr. Carr.
Here are some of the security measures that cyber insurers are looking for:
- Multifactorial authentication (MFA) requires an extra layer of security to access the system. For example, when logging into your organization’s EHR platform, instead of just using a username and password to access the platform, MFA would require you to input an additional unique login credential before you can access the EHR. A secondary login credential may include security questions, a one-time PIN, or biometrics.
- Removing a terminated employee’s login credentials quickly from the computer system. “One of the most damaging and expensive types of attacks are by disgruntled employees who still have their login credentials and take revenge by logging back into the system and planting malware,” says Mr. Shah.
- Automatic system updates (patches). “Phishing email compromises usually result from a failure to fix vulnerabilities. When a system needs to restart, it should be set to automatically update any potential security loopholes within programs or products,” says Mr. Carr. The firewall settings should also be updated.
- Prior hacking incidents: Are the attackers out of your system? Once criminals hack into the system, your practice is vulnerable to repeat attacks. “If a cyberattack is not completely addressed, threat actors will maintain access to or a presence on the compromised network. In general, we will work with the insured to ensure that the initial point of compromise has been addressed and that any threat actor presence in the network has been removed,” says Mr. Carr.
When doctors compare cybersecurity policies, experts recommend avoiding companies that may offer lower prices but lack a proven track record of handling claims and do not offer resources that can detect a threat, such as ongoing network monitoring and employee training with simulated exercises.
“Practices tend to think, ‘It won’t happen to me.’ Every practice needs to take this seriously,” says Dr. McAneny.
A version of this article first appeared on Medscape.com.
Barbara L. McAneny, MD, CEO of New Mexico Oncology Hematology Consultants, experienced a data breach about 10 years ago, when a laptop was stolen from her large practice.
She and the other physicians were upset and worried that the individual would attempt to log in to the computer system and hack their patients’ private health information.
Dr. McAneny was also worried that the practice would have to pay a hefty fine to the government for having unsecured private health information on a laptop. She could have paid from $50,000 to more than $1.9 million for lost and stolen devices (although that didn’t happen).
Dr. McAneny had a standard cyber liability benefit in her med-mal policy that covered up to $50,000 of the data breach costs. That covered the legal advice The Doctors Company provided about state and federal reporting requirements when a data breach occurs and the costs the practice incurred from mailing letters to all of its patients notifying them of the data breach, says Dr. McAneny.
“The data breach taught me a lot. Our practice spent a lot of money on increasing our internal controls, cybersecurity, and monitoring. Our IT department started testing our computer firewalls periodically, and that’s how we discovered that cybercriminals were attempting to break into our computer system at least 100 times daily,” says Dr. McAneny.
That discovery changed how she thought about insurance. “I decided the med-mal benefit wasn’t enough. I bought the best cybersecurity policy we could afford to protect against future breaches, especially malware or ransomware attacks.”
Her practice also had to make its electronic health records (EHRs) more secure to comply with the Department of Health & Human Services Office of Civil Rights standards for protected health information. The cost of increased security wasn’t covered by her cyber benefit.
Cyberattacks increasing in health care
Despite having comprehensive coverage, Dr. McAneny worries that the cybercriminals are a step ahead of the cybersecurity experts and her practice will eventually have another data breach.
“The policy only covers things that we know about today. As we upgrade our defenses, criminals are finding new ways to breach firewalls and work around our defenses,” she says.
So far this year, nearly 200 medical groups have reported cyberattacks involving 500 or more of their patients’ medical records to the federal government.
EHRs are valuable targets to cybercriminals because of the protected health information they contain. Cybercriminals grab information such as Social Security numbers, dates of birth, medical procedures and results, and in some cases billing and financial information and sell it on the dark web.
They typically bundle the information and sell it to other criminals who later use it for various kinds of fraud and extortion such as banking and credit fraud, health care fraud, identity theft, and ransom extortion.
What do most doctors have?
The vast majority (82%) of doctors polled by the Medical Group Management Association last year said they had cyber insurance, compared with 54% in 2018.
For those who answered “yes,” many said they have coverage through their malpractice insurance carrier.
David Zetter, president of Zetter HealthCare Management Consultants, recommends that physicians speak with their malpractice carrier to determine what coverage they have, if any, within their malpractice policy.
A typical cybersecurity benefit is limited to what is needed to fix and resolve the hacking incident, says Raj Shah, senior regulatory attorney and policyholder advisor at MagMutual, which insures medical practices for malpractice and cyber liability.
That usually covers investigating the cause of the breach and the extent of the damage, legal advice about federal and state reporting requirements, whether to pay a ransom, and a public relations professional to handle patient communication, says Mr. Shah.
The benefit doesn’t cover lost patient revenue when practices have to shut down their operations, the cost of replacing damaged computers, or the ransom payment, he says.
Mr. Zetter advises doctors to consider buying cybersecurity coverage. “I recommend that they speak with an insurance broker who is experienced with cybersecurity policies sold to health care professionals to determine what type of coverage and how much coverage they may need. Their malpractice carrier may also be able to provide some answers,” says Mr. Zetter.
The physician will need to be able to answer questions about their network and how many staff they have and may need to involve their IT vendor too, he adds.
How does comprehensive coverage compare?
Ransomware attacks continue to be one of the most frequent types of attacks, and the amount criminals are demanding has risen significantly. The median ransom payment was $5,000 in the fourth quarter of 2018, compared with over $300,000 during the fourth quarter of 2021.
Cybercriminals now engage in “double extortion” – demanding a ransom payment to hand over the code that will unlock their encrypted data – and then another ransom payment to not post patients’ sensitive medical information they copied onto the dark web.
Comprehensive cybersecurity insurance will cover “double extortion” payments, legal costs that may arise from defending against patient lawsuits, and the costs of meeting federal and state privacy requirements, including notifying patients of the data breach and regulatory investigations, says Michael Carr, head of risk engineering for North America for Coalition, a cyber insurance firm.
Cyber insurers also contract with vendors who sell bitcoin, which is the currency cybercriminals typically demand for ransom payments, and work with ransom negotiators.
For example, once Coalition decided to pay the ransom on behalf of a health care client, it negotiated the ransom demand down by nearly 75% from $750,000 to $200,000, and proceeded to help the company restore all of its data.
The costs to respond to the incident, to recover lost data, and to pay the extortion, together with the lost business income resulting from the incident, were covered by Coalition’s cyber insurance policy.
Other clients have had their funds retrieved before a fraudulent wire transfer was completed. “Medical practices have vendors they pay regularly. A cybercriminal may compromise your email or take over a bank account and then impersonate a vendor asking to be paid for services they didn’t provide,” says Mr. Carr.
How much coverage do you need? Cost?
Dr. McAneny has increased her cybersecurity coverage every year. “It’s expensive, but I think it’s worth it. But you can never buy enough protection due to the coverage limits.”
She worries that the costs could exceed the limits if a ransomware attack disrupts her practice for days, weeks, or longer, or if the Office for Civil Rights fines her practice $10,000 per patient chart – the practice has 100,000 health records. “That can run several millions of dollars and ruin a practice,” she says.
Health systems and hospitals need massive amounts of coverage, which often runs from $20 million to $30 million, says Mr. Shah. However, practices insured through MagMutual have lower coverage limits that range from $1 million to $5 million, he says.
“A large practice does not necessarily need more than $1,000,000 in coverage if they have limited loss in this area and strong internal processes and controls. Most large practices also have a dedicated information security director, which reduces their risk, so they may be comfortable with $1,000,000 in coverage,” says Mr. Shah.
Premiums are based on the number of patient health records per practice, which translates into higher premiums for larger practices.
Other factors that come into play include the underlying coverage, risk controls the practice has implemented, and its claims history, says Mr. Shah.
However, the cost for cyber liability insurance has increased, and practices can expect to pay higher premiums and deductibles. For example, a practice that paid $10,000 in premiums for a new policy last year will have to pay $20,000 this year, says Dan Hanson, senior vice president of management liability and client experience at Marsh & McLennon Agency, a risk management firm that sells cyber insurance policies.
“We saw 71% of our self-insured clients experience higher deductibles over last year due to increased claim activity and the lack of capacity in the market. The carriers are saying they will set limits, but you are going to pay a lot more, and you are going to participate more in losses through the higher deductibles,” says Mr. Hanson.
Are you eligible?
Cyber insurance companies have a vested interest in avoiding claims. With increasing cyberattacks and larger payouts, many insurers are requiring practices to implement some defensive measures before they insure them. Some insurers, such as Coalition, say they may still insure small practices for comprehensive coverage, but it may impact the pricing or what’s covered, says Mr. Carr.
Here are some of the security measures that cyber insurers are looking for:
- Multifactorial authentication (MFA) requires an extra layer of security to access the system. For example, when logging into your organization’s EHR platform, instead of just using a username and password to access the platform, MFA would require you to input an additional unique login credential before you can access the EHR. A secondary login credential may include security questions, a one-time PIN, or biometrics.
- Removing a terminated employee’s login credentials quickly from the computer system. “One of the most damaging and expensive types of attacks are by disgruntled employees who still have their login credentials and take revenge by logging back into the system and planting malware,” says Mr. Shah.
- Automatic system updates (patches). “Phishing email compromises usually result from a failure to fix vulnerabilities. When a system needs to restart, it should be set to automatically update any potential security loopholes within programs or products,” says Mr. Carr. The firewall settings should also be updated.
- Prior hacking incidents: Are the attackers out of your system? Once criminals hack into the system, your practice is vulnerable to repeat attacks. “If a cyberattack is not completely addressed, threat actors will maintain access to or a presence on the compromised network. In general, we will work with the insured to ensure that the initial point of compromise has been addressed and that any threat actor presence in the network has been removed,” says Mr. Carr.
When doctors compare cybersecurity policies, experts recommend avoiding companies that may offer lower prices but lack a proven track record of handling claims and do not offer resources that can detect a threat, such as ongoing network monitoring and employee training with simulated exercises.
“Practices tend to think, ‘It won’t happen to me.’ Every practice needs to take this seriously,” says Dr. McAneny.
A version of this article first appeared on Medscape.com.
Barbara L. McAneny, MD, CEO of New Mexico Oncology Hematology Consultants, experienced a data breach about 10 years ago, when a laptop was stolen from her large practice.
She and the other physicians were upset and worried that the individual would attempt to log in to the computer system and hack their patients’ private health information.
Dr. McAneny was also worried that the practice would have to pay a hefty fine to the government for having unsecured private health information on a laptop. She could have paid from $50,000 to more than $1.9 million for lost and stolen devices (although that didn’t happen).
Dr. McAneny had a standard cyber liability benefit in her med-mal policy that covered up to $50,000 of the data breach costs. That covered the legal advice The Doctors Company provided about state and federal reporting requirements when a data breach occurs and the costs the practice incurred from mailing letters to all of its patients notifying them of the data breach, says Dr. McAneny.
“The data breach taught me a lot. Our practice spent a lot of money on increasing our internal controls, cybersecurity, and monitoring. Our IT department started testing our computer firewalls periodically, and that’s how we discovered that cybercriminals were attempting to break into our computer system at least 100 times daily,” says Dr. McAneny.
That discovery changed how she thought about insurance. “I decided the med-mal benefit wasn’t enough. I bought the best cybersecurity policy we could afford to protect against future breaches, especially malware or ransomware attacks.”
Her practice also had to make its electronic health records (EHRs) more secure to comply with the Department of Health & Human Services Office of Civil Rights standards for protected health information. The cost of increased security wasn’t covered by her cyber benefit.
Cyberattacks increasing in health care
Despite having comprehensive coverage, Dr. McAneny worries that the cybercriminals are a step ahead of the cybersecurity experts and her practice will eventually have another data breach.
“The policy only covers things that we know about today. As we upgrade our defenses, criminals are finding new ways to breach firewalls and work around our defenses,” she says.
So far this year, nearly 200 medical groups have reported cyberattacks involving 500 or more of their patients’ medical records to the federal government.
EHRs are valuable targets to cybercriminals because of the protected health information they contain. Cybercriminals grab information such as Social Security numbers, dates of birth, medical procedures and results, and in some cases billing and financial information and sell it on the dark web.
They typically bundle the information and sell it to other criminals who later use it for various kinds of fraud and extortion such as banking and credit fraud, health care fraud, identity theft, and ransom extortion.
What do most doctors have?
The vast majority (82%) of doctors polled by the Medical Group Management Association last year said they had cyber insurance, compared with 54% in 2018.
For those who answered “yes,” many said they have coverage through their malpractice insurance carrier.
David Zetter, president of Zetter HealthCare Management Consultants, recommends that physicians speak with their malpractice carrier to determine what coverage they have, if any, within their malpractice policy.
A typical cybersecurity benefit is limited to what is needed to fix and resolve the hacking incident, says Raj Shah, senior regulatory attorney and policyholder advisor at MagMutual, which insures medical practices for malpractice and cyber liability.
That usually covers investigating the cause of the breach and the extent of the damage, legal advice about federal and state reporting requirements, whether to pay a ransom, and a public relations professional to handle patient communication, says Mr. Shah.
The benefit doesn’t cover lost patient revenue when practices have to shut down their operations, the cost of replacing damaged computers, or the ransom payment, he says.
Mr. Zetter advises doctors to consider buying cybersecurity coverage. “I recommend that they speak with an insurance broker who is experienced with cybersecurity policies sold to health care professionals to determine what type of coverage and how much coverage they may need. Their malpractice carrier may also be able to provide some answers,” says Mr. Zetter.
The physician will need to be able to answer questions about their network and how many staff they have and may need to involve their IT vendor too, he adds.
How does comprehensive coverage compare?
Ransomware attacks continue to be one of the most frequent types of attacks, and the amount criminals are demanding has risen significantly. The median ransom payment was $5,000 in the fourth quarter of 2018, compared with over $300,000 during the fourth quarter of 2021.
Cybercriminals now engage in “double extortion” – demanding a ransom payment to hand over the code that will unlock their encrypted data – and then another ransom payment to not post patients’ sensitive medical information they copied onto the dark web.
Comprehensive cybersecurity insurance will cover “double extortion” payments, legal costs that may arise from defending against patient lawsuits, and the costs of meeting federal and state privacy requirements, including notifying patients of the data breach and regulatory investigations, says Michael Carr, head of risk engineering for North America for Coalition, a cyber insurance firm.
Cyber insurers also contract with vendors who sell bitcoin, which is the currency cybercriminals typically demand for ransom payments, and work with ransom negotiators.
For example, once Coalition decided to pay the ransom on behalf of a health care client, it negotiated the ransom demand down by nearly 75% from $750,000 to $200,000, and proceeded to help the company restore all of its data.
The costs to respond to the incident, to recover lost data, and to pay the extortion, together with the lost business income resulting from the incident, were covered by Coalition’s cyber insurance policy.
Other clients have had their funds retrieved before a fraudulent wire transfer was completed. “Medical practices have vendors they pay regularly. A cybercriminal may compromise your email or take over a bank account and then impersonate a vendor asking to be paid for services they didn’t provide,” says Mr. Carr.
How much coverage do you need? Cost?
Dr. McAneny has increased her cybersecurity coverage every year. “It’s expensive, but I think it’s worth it. But you can never buy enough protection due to the coverage limits.”
She worries that the costs could exceed the limits if a ransomware attack disrupts her practice for days, weeks, or longer, or if the Office for Civil Rights fines her practice $10,000 per patient chart – the practice has 100,000 health records. “That can run several millions of dollars and ruin a practice,” she says.
Health systems and hospitals need massive amounts of coverage, which often runs from $20 million to $30 million, says Mr. Shah. However, practices insured through MagMutual have lower coverage limits that range from $1 million to $5 million, he says.
“A large practice does not necessarily need more than $1,000,000 in coverage if they have limited loss in this area and strong internal processes and controls. Most large practices also have a dedicated information security director, which reduces their risk, so they may be comfortable with $1,000,000 in coverage,” says Mr. Shah.
Premiums are based on the number of patient health records per practice, which translates into higher premiums for larger practices.
Other factors that come into play include the underlying coverage, risk controls the practice has implemented, and its claims history, says Mr. Shah.
However, the cost for cyber liability insurance has increased, and practices can expect to pay higher premiums and deductibles. For example, a practice that paid $10,000 in premiums for a new policy last year will have to pay $20,000 this year, says Dan Hanson, senior vice president of management liability and client experience at Marsh & McLennon Agency, a risk management firm that sells cyber insurance policies.
“We saw 71% of our self-insured clients experience higher deductibles over last year due to increased claim activity and the lack of capacity in the market. The carriers are saying they will set limits, but you are going to pay a lot more, and you are going to participate more in losses through the higher deductibles,” says Mr. Hanson.
Are you eligible?
Cyber insurance companies have a vested interest in avoiding claims. With increasing cyberattacks and larger payouts, many insurers are requiring practices to implement some defensive measures before they insure them. Some insurers, such as Coalition, say they may still insure small practices for comprehensive coverage, but it may impact the pricing or what’s covered, says Mr. Carr.
Here are some of the security measures that cyber insurers are looking for:
- Multifactorial authentication (MFA) requires an extra layer of security to access the system. For example, when logging into your organization’s EHR platform, instead of just using a username and password to access the platform, MFA would require you to input an additional unique login credential before you can access the EHR. A secondary login credential may include security questions, a one-time PIN, or biometrics.
- Removing a terminated employee’s login credentials quickly from the computer system. “One of the most damaging and expensive types of attacks are by disgruntled employees who still have their login credentials and take revenge by logging back into the system and planting malware,” says Mr. Shah.
- Automatic system updates (patches). “Phishing email compromises usually result from a failure to fix vulnerabilities. When a system needs to restart, it should be set to automatically update any potential security loopholes within programs or products,” says Mr. Carr. The firewall settings should also be updated.
- Prior hacking incidents: Are the attackers out of your system? Once criminals hack into the system, your practice is vulnerable to repeat attacks. “If a cyberattack is not completely addressed, threat actors will maintain access to or a presence on the compromised network. In general, we will work with the insured to ensure that the initial point of compromise has been addressed and that any threat actor presence in the network has been removed,” says Mr. Carr.
When doctors compare cybersecurity policies, experts recommend avoiding companies that may offer lower prices but lack a proven track record of handling claims and do not offer resources that can detect a threat, such as ongoing network monitoring and employee training with simulated exercises.
“Practices tend to think, ‘It won’t happen to me.’ Every practice needs to take this seriously,” says Dr. McAneny.
A version of this article first appeared on Medscape.com.
Cancer drug significantly cuts risk for COVID-19 death
, an interim analysis of a phase 3 placebo-controlled trial found.
Sabizabulin treatment consistently and significantly reduced deaths across patient subgroups “regardless of standard of care treatment received, baseline World Health Organization scores, age, comorbidities, vaccination status, COVID-19 variant, or geography,” study investigator Mitchell Steiner, MD, chairman, president, and CEO of Veru, said in a news release.
The company has submitted an emergency use authorization request to the U.S. Food and Drug Administration to use sabizabulin to treat COVID-19.
The analysis was published online in NEJM Evidence.
Sabizabulin, originally developed to treat metastatic castration-resistant prostate cancer, is a novel, investigational, oral microtubule disruptor with dual antiviral and anti-inflammatory activities. Given the drug’s mechanism, researchers at Veru thought that sabizabulin could help treat lung inflammation in patients with COVID-19 as well.
Findings of the interim analysis are based on 150 adults hospitalized with moderate to severe COVID-19 at high risk for acute respiratory distress syndrome and death. The patients were randomly allocated to receive 9 mg oral sabizabulin (n = 98) or placebo (n = 52) once daily for up to 21 days.
Overall, the mortality rate was 20.2% in the sabizabulin group vs. 45.1% in the placebo group. Compared with placebo, treatment with sabizabulin led to a 24.9–percentage point absolute reduction and a 55.2% relative reduction in death (odds ratio, 3.23; P = .0042).
The key secondary endpoint of mortality through day 29 also favored sabizabulin over placebo, with a mortality rate of 17% vs. 35.3%. In this scenario, treatment with sabizabulin resulted in an absolute reduction in deaths of 18.3 percentage points and a relative reduction of 51.8%.
Sabizabulin led to a significant 43% relative reduction in ICU days, a 49% relative reduction in days on mechanical ventilation, and a 26% relative reduction in days in the hospital, compared with placebo.
Adverse and serious adverse events were also lower in the sabizabulin group (61.5%) than the placebo group (78.3%).
The data are “pretty impressive and in a group of patients that we really have limited things to offer,” Aaron Glatt, MD, a spokesperson for the Infectious Diseases Society of America and chief of infectious diseases and hospital epidemiologist at Mount Sinai South Nassau in Oceanside, N.Y., said in an interview. “This is an interim analysis and obviously we’d like to see more data, but it certainly is something that is novel and quite interesting.”
David Boulware, MD, MPH, an infectious disease expert at the University of Minnesota, Minneapolis, told the New York Times that the large number of deaths in the placebo group seemed “rather high” and that the final analysis might reveal a more modest benefit for sabizabulin.
“I would be skeptical” that the reduced risk for death remains 55%, he noted.
The study was funded by Veru Pharmaceuticals. Several authors are employed by the company or have financial relationships with the company.
A version of this article first appeared on Medscape.com.
, an interim analysis of a phase 3 placebo-controlled trial found.
Sabizabulin treatment consistently and significantly reduced deaths across patient subgroups “regardless of standard of care treatment received, baseline World Health Organization scores, age, comorbidities, vaccination status, COVID-19 variant, or geography,” study investigator Mitchell Steiner, MD, chairman, president, and CEO of Veru, said in a news release.
The company has submitted an emergency use authorization request to the U.S. Food and Drug Administration to use sabizabulin to treat COVID-19.
The analysis was published online in NEJM Evidence.
Sabizabulin, originally developed to treat metastatic castration-resistant prostate cancer, is a novel, investigational, oral microtubule disruptor with dual antiviral and anti-inflammatory activities. Given the drug’s mechanism, researchers at Veru thought that sabizabulin could help treat lung inflammation in patients with COVID-19 as well.
Findings of the interim analysis are based on 150 adults hospitalized with moderate to severe COVID-19 at high risk for acute respiratory distress syndrome and death. The patients were randomly allocated to receive 9 mg oral sabizabulin (n = 98) or placebo (n = 52) once daily for up to 21 days.
Overall, the mortality rate was 20.2% in the sabizabulin group vs. 45.1% in the placebo group. Compared with placebo, treatment with sabizabulin led to a 24.9–percentage point absolute reduction and a 55.2% relative reduction in death (odds ratio, 3.23; P = .0042).
The key secondary endpoint of mortality through day 29 also favored sabizabulin over placebo, with a mortality rate of 17% vs. 35.3%. In this scenario, treatment with sabizabulin resulted in an absolute reduction in deaths of 18.3 percentage points and a relative reduction of 51.8%.
Sabizabulin led to a significant 43% relative reduction in ICU days, a 49% relative reduction in days on mechanical ventilation, and a 26% relative reduction in days in the hospital, compared with placebo.
Adverse and serious adverse events were also lower in the sabizabulin group (61.5%) than the placebo group (78.3%).
The data are “pretty impressive and in a group of patients that we really have limited things to offer,” Aaron Glatt, MD, a spokesperson for the Infectious Diseases Society of America and chief of infectious diseases and hospital epidemiologist at Mount Sinai South Nassau in Oceanside, N.Y., said in an interview. “This is an interim analysis and obviously we’d like to see more data, but it certainly is something that is novel and quite interesting.”
David Boulware, MD, MPH, an infectious disease expert at the University of Minnesota, Minneapolis, told the New York Times that the large number of deaths in the placebo group seemed “rather high” and that the final analysis might reveal a more modest benefit for sabizabulin.
“I would be skeptical” that the reduced risk for death remains 55%, he noted.
The study was funded by Veru Pharmaceuticals. Several authors are employed by the company or have financial relationships with the company.
A version of this article first appeared on Medscape.com.
, an interim analysis of a phase 3 placebo-controlled trial found.
Sabizabulin treatment consistently and significantly reduced deaths across patient subgroups “regardless of standard of care treatment received, baseline World Health Organization scores, age, comorbidities, vaccination status, COVID-19 variant, or geography,” study investigator Mitchell Steiner, MD, chairman, president, and CEO of Veru, said in a news release.
The company has submitted an emergency use authorization request to the U.S. Food and Drug Administration to use sabizabulin to treat COVID-19.
The analysis was published online in NEJM Evidence.
Sabizabulin, originally developed to treat metastatic castration-resistant prostate cancer, is a novel, investigational, oral microtubule disruptor with dual antiviral and anti-inflammatory activities. Given the drug’s mechanism, researchers at Veru thought that sabizabulin could help treat lung inflammation in patients with COVID-19 as well.
Findings of the interim analysis are based on 150 adults hospitalized with moderate to severe COVID-19 at high risk for acute respiratory distress syndrome and death. The patients were randomly allocated to receive 9 mg oral sabizabulin (n = 98) or placebo (n = 52) once daily for up to 21 days.
Overall, the mortality rate was 20.2% in the sabizabulin group vs. 45.1% in the placebo group. Compared with placebo, treatment with sabizabulin led to a 24.9–percentage point absolute reduction and a 55.2% relative reduction in death (odds ratio, 3.23; P = .0042).
The key secondary endpoint of mortality through day 29 also favored sabizabulin over placebo, with a mortality rate of 17% vs. 35.3%. In this scenario, treatment with sabizabulin resulted in an absolute reduction in deaths of 18.3 percentage points and a relative reduction of 51.8%.
Sabizabulin led to a significant 43% relative reduction in ICU days, a 49% relative reduction in days on mechanical ventilation, and a 26% relative reduction in days in the hospital, compared with placebo.
Adverse and serious adverse events were also lower in the sabizabulin group (61.5%) than the placebo group (78.3%).
The data are “pretty impressive and in a group of patients that we really have limited things to offer,” Aaron Glatt, MD, a spokesperson for the Infectious Diseases Society of America and chief of infectious diseases and hospital epidemiologist at Mount Sinai South Nassau in Oceanside, N.Y., said in an interview. “This is an interim analysis and obviously we’d like to see more data, but it certainly is something that is novel and quite interesting.”
David Boulware, MD, MPH, an infectious disease expert at the University of Minnesota, Minneapolis, told the New York Times that the large number of deaths in the placebo group seemed “rather high” and that the final analysis might reveal a more modest benefit for sabizabulin.
“I would be skeptical” that the reduced risk for death remains 55%, he noted.
The study was funded by Veru Pharmaceuticals. Several authors are employed by the company or have financial relationships with the company.
A version of this article first appeared on Medscape.com.
FROM NEJM EVIDENCE