User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Saddled with med school debt, yet left out of loan forgiveness plans
In a recently obtained plan by Politico, the Biden administration is zeroing in on a broad student loan forgiveness plan to be released imminently. The plan would broadly forgive $10,000 in federal student loans, including graduate and PLUS loans. However, there’s a rub: The plan restricts the forgiveness to those with incomes below $150,000.
This would unfairly exclude many in health care from receiving this forgiveness, an egregious oversight given how much health care providers have sacrificed during the pandemic.
What was proposed?
Previously, it was reported that the Biden administration was considering this same amount of forgiveness, but with plans to exclude borrowers by either career or income. Student loan payments have been on an extended CARES Act forbearance since March 2020, with payment resumption planned for Aug. 31. The administration has said that they would deliver a plan for further extensions before this date and have repeatedly teased including forgiveness.
Forgiveness for some ...
Forgiving $10,000 of federal student loans would relieve some 15 million borrowers of student debt, roughly one-third of the 45 million borrowers with debt.
This would provide a massive boost to these borrowers (who disproportionately are female, low-income, and non-White), many of whom were targeted by predatory institutions whose education didn’t offer any actual tangible benefit to their earnings. While this is a group that absolutely ought to have their loans forgiven, drawing an income line inappropriately restricts those in health care from receiving any forgiveness.
... But not for others
Someone making an annual gross income of $150,000 is in the 80th percentile of earners in the United States (for comparison, the top 1% took home more than $505,000 in 2021). What student loan borrowers make up the remaining 20%? Overwhelmingly, health care providers occupy that tier: physicians, dentists, veterinarians, and advanced-practice nurses.
These schools leave their graduates with some of the highest student loan burdens, with veterinarians, dentists, and physicians having the highest debt-to-income ratios of any professional careers.
Flat forgiveness is regressive
Forgiving any student debt is the right direction. Too may have fallen victim to an industry without quality control, appropriate regulation, or price control. Quite the opposite, the blank-check model of student loan financing has led to an arms race as it comes to capital improvements in university spending.

The price of medical schools has risen more than four times as fast as inflation over the past 30 years, with dental and veterinary schools and nursing education showing similarly exaggerated price increases. Trainees in these fields are more likely to have taken on six-figure debt, with average debt loads at graduation in the table below. While $10,000 will move the proverbial needle less for these borrowers, does that mean they should be excluded?
Health care workers’ income declines during the pandemic
Now, over 2½ years since the start of the COVID pandemic, multiple reports have demonstrated that health care workers have suffered a loss in income. This loss in income was never compensated for, as the Paycheck Protection Program and the individual economic stimuli typically excluded doctors and high earners.
COVID and the hazard tax
As a provider during the COVID-19 pandemic, I didn’t ask for hazard pay. I supported those who did but recognized their requests were more ceremonial than they were likely to be successful.
However, I flatly reject the idea that my fellow health care practitioners are not deserving of student loan forgiveness simply based on an arbitrary income threshold. Health care providers are saddled with high debt burden, have suffered lost income, and have given of themselves during a devastating pandemic, where more than 1 million perished in the United States.
Bottom line
Health care workers should not be excluded from student loan forgiveness. Sadly, the Biden administration has signaled that they are dropping career-based exclusions in favor of more broadly harmful income-based forgiveness restrictions. This will disproportionately harm physicians and other health care workers.
These practitioners have suffered financially as a result of working through the COVID pandemic; should they also be forced to shoulder another financial injury by being excluded from student loan forgiveness?
Dr. Palmer is the chief operating officer and cofounder of Panacea Financial. He is also a practicing pediatric hospitalist at Boston Children’s Hospital and is on faculty at Harvard Medical School, also in Boston.
A version of this article first appeared on Medscape.com.
In a recently obtained plan by Politico, the Biden administration is zeroing in on a broad student loan forgiveness plan to be released imminently. The plan would broadly forgive $10,000 in federal student loans, including graduate and PLUS loans. However, there’s a rub: The plan restricts the forgiveness to those with incomes below $150,000.
This would unfairly exclude many in health care from receiving this forgiveness, an egregious oversight given how much health care providers have sacrificed during the pandemic.
What was proposed?
Previously, it was reported that the Biden administration was considering this same amount of forgiveness, but with plans to exclude borrowers by either career or income. Student loan payments have been on an extended CARES Act forbearance since March 2020, with payment resumption planned for Aug. 31. The administration has said that they would deliver a plan for further extensions before this date and have repeatedly teased including forgiveness.
Forgiveness for some ...
Forgiving $10,000 of federal student loans would relieve some 15 million borrowers of student debt, roughly one-third of the 45 million borrowers with debt.
This would provide a massive boost to these borrowers (who disproportionately are female, low-income, and non-White), many of whom were targeted by predatory institutions whose education didn’t offer any actual tangible benefit to their earnings. While this is a group that absolutely ought to have their loans forgiven, drawing an income line inappropriately restricts those in health care from receiving any forgiveness.
... But not for others
Someone making an annual gross income of $150,000 is in the 80th percentile of earners in the United States (for comparison, the top 1% took home more than $505,000 in 2021). What student loan borrowers make up the remaining 20%? Overwhelmingly, health care providers occupy that tier: physicians, dentists, veterinarians, and advanced-practice nurses.
These schools leave their graduates with some of the highest student loan burdens, with veterinarians, dentists, and physicians having the highest debt-to-income ratios of any professional careers.
Flat forgiveness is regressive
Forgiving any student debt is the right direction. Too may have fallen victim to an industry without quality control, appropriate regulation, or price control. Quite the opposite, the blank-check model of student loan financing has led to an arms race as it comes to capital improvements in university spending.

The price of medical schools has risen more than four times as fast as inflation over the past 30 years, with dental and veterinary schools and nursing education showing similarly exaggerated price increases. Trainees in these fields are more likely to have taken on six-figure debt, with average debt loads at graduation in the table below. While $10,000 will move the proverbial needle less for these borrowers, does that mean they should be excluded?
Health care workers’ income declines during the pandemic
Now, over 2½ years since the start of the COVID pandemic, multiple reports have demonstrated that health care workers have suffered a loss in income. This loss in income was never compensated for, as the Paycheck Protection Program and the individual economic stimuli typically excluded doctors and high earners.
COVID and the hazard tax
As a provider during the COVID-19 pandemic, I didn’t ask for hazard pay. I supported those who did but recognized their requests were more ceremonial than they were likely to be successful.
However, I flatly reject the idea that my fellow health care practitioners are not deserving of student loan forgiveness simply based on an arbitrary income threshold. Health care providers are saddled with high debt burden, have suffered lost income, and have given of themselves during a devastating pandemic, where more than 1 million perished in the United States.
Bottom line
Health care workers should not be excluded from student loan forgiveness. Sadly, the Biden administration has signaled that they are dropping career-based exclusions in favor of more broadly harmful income-based forgiveness restrictions. This will disproportionately harm physicians and other health care workers.
These practitioners have suffered financially as a result of working through the COVID pandemic; should they also be forced to shoulder another financial injury by being excluded from student loan forgiveness?
Dr. Palmer is the chief operating officer and cofounder of Panacea Financial. He is also a practicing pediatric hospitalist at Boston Children’s Hospital and is on faculty at Harvard Medical School, also in Boston.
A version of this article first appeared on Medscape.com.
In a recently obtained plan by Politico, the Biden administration is zeroing in on a broad student loan forgiveness plan to be released imminently. The plan would broadly forgive $10,000 in federal student loans, including graduate and PLUS loans. However, there’s a rub: The plan restricts the forgiveness to those with incomes below $150,000.
This would unfairly exclude many in health care from receiving this forgiveness, an egregious oversight given how much health care providers have sacrificed during the pandemic.
What was proposed?
Previously, it was reported that the Biden administration was considering this same amount of forgiveness, but with plans to exclude borrowers by either career or income. Student loan payments have been on an extended CARES Act forbearance since March 2020, with payment resumption planned for Aug. 31. The administration has said that they would deliver a plan for further extensions before this date and have repeatedly teased including forgiveness.
Forgiveness for some ...
Forgiving $10,000 of federal student loans would relieve some 15 million borrowers of student debt, roughly one-third of the 45 million borrowers with debt.
This would provide a massive boost to these borrowers (who disproportionately are female, low-income, and non-White), many of whom were targeted by predatory institutions whose education didn’t offer any actual tangible benefit to their earnings. While this is a group that absolutely ought to have their loans forgiven, drawing an income line inappropriately restricts those in health care from receiving any forgiveness.
... But not for others
Someone making an annual gross income of $150,000 is in the 80th percentile of earners in the United States (for comparison, the top 1% took home more than $505,000 in 2021). What student loan borrowers make up the remaining 20%? Overwhelmingly, health care providers occupy that tier: physicians, dentists, veterinarians, and advanced-practice nurses.
These schools leave their graduates with some of the highest student loan burdens, with veterinarians, dentists, and physicians having the highest debt-to-income ratios of any professional careers.
Flat forgiveness is regressive
Forgiving any student debt is the right direction. Too may have fallen victim to an industry without quality control, appropriate regulation, or price control. Quite the opposite, the blank-check model of student loan financing has led to an arms race as it comes to capital improvements in university spending.

The price of medical schools has risen more than four times as fast as inflation over the past 30 years, with dental and veterinary schools and nursing education showing similarly exaggerated price increases. Trainees in these fields are more likely to have taken on six-figure debt, with average debt loads at graduation in the table below. While $10,000 will move the proverbial needle less for these borrowers, does that mean they should be excluded?
Health care workers’ income declines during the pandemic
Now, over 2½ years since the start of the COVID pandemic, multiple reports have demonstrated that health care workers have suffered a loss in income. This loss in income was never compensated for, as the Paycheck Protection Program and the individual economic stimuli typically excluded doctors and high earners.
COVID and the hazard tax
As a provider during the COVID-19 pandemic, I didn’t ask for hazard pay. I supported those who did but recognized their requests were more ceremonial than they were likely to be successful.
However, I flatly reject the idea that my fellow health care practitioners are not deserving of student loan forgiveness simply based on an arbitrary income threshold. Health care providers are saddled with high debt burden, have suffered lost income, and have given of themselves during a devastating pandemic, where more than 1 million perished in the United States.
Bottom line
Health care workers should not be excluded from student loan forgiveness. Sadly, the Biden administration has signaled that they are dropping career-based exclusions in favor of more broadly harmful income-based forgiveness restrictions. This will disproportionately harm physicians and other health care workers.
These practitioners have suffered financially as a result of working through the COVID pandemic; should they also be forced to shoulder another financial injury by being excluded from student loan forgiveness?
Dr. Palmer is the chief operating officer and cofounder of Panacea Financial. He is also a practicing pediatric hospitalist at Boston Children’s Hospital and is on faculty at Harvard Medical School, also in Boston.
A version of this article first appeared on Medscape.com.
Weight-loss surgery has a big effect on marriage
Kristal was only in her mid-30s when she decided to have surgery. Her doctor said it was too early. But the Oregon mom of three had found herself in the hospital twice for obesity-related lung complications before her 35th birthday. So she got the gastric sleeve.
And at first it seemed like the best decision for her and her family. She was losing weight – 100 pounds in 16 months – and so was her husband. The whole family was more active and seemed to have more energy. But then her husband’s weight began to creep back up.
While she joined a running group and signed up for half-marathons, her husband’s depression and drinking worsened. The healthier lifestyle they’d shared was now an unspoken wedge between them.
And the added attention Kristal was getting from men and women because of her thinner size only added to the tension. After 30 years together and 22 years of marriage, the high school sweethearts divorced in June 2021. Kristal’s weight loss wasn’t the only problem, but she and her ex-husband believe it was the beginning of the end.
An unexpected outcome?
New research from the University of Pittsburgh found that Kristal’s experience is a common one. The study looked at data from 1,441 bariatric surgery patients and found that never-married patients were over 50% more likely to get married, and married patients were more than twice as likely to get divorced, compared to the general U.S. population.
This U.S. data follows two Scandinavian studies from 2018 and 2020 that found similar relationship changes after bariatric surgery. But the postsurgery divorce rate in the United States was only about half that found in the Danish and Swedish studies, according to the new study published in Annals of Surgery.
It’s important to note that even with an increase in the divorce rate, most marriages in the study were unchanged, said epidemiologist and lead author Wendy King, PhD. In fact, 81% of couples were still married 5 years after surgery. But where the U.S. population has a divorce rate of 3.5%, bariatric patients in the study had an 8% divorce rate. Likewise, those who’d never been married before the surgery had a marriage rate of 18%, compared to 7% in the U.S. population.
Surgery certainly isn’t a death sentence for a patient’s love life. But the uptick in marriage and divorce suggests bariatric surgery significantly impacts how people engage in relationships.
“It makes sense,” said clinical psychologist Rachel Goldman, PhD, who specializes in health and wellness issues and bariatric surgery cases in New York City. “People are changing their lifestyle.” And those changes don’t start or stop the day of surgery, they begin as soon as someone decides to have surgery and continue as a lifelong process, she said.
For some patients, these healthy habits may offer a “new lease on life,” said Dr. King. According to the study, patients who had better physical health after surgery were more likely to get married.
But the continual lifestyle changes can dramatically impact the rituals of existing relationships, said Dr. Goldman. Maybe a couple loved to go out and enjoy an extravagant meal before surgery, or they had ice cream and watched a movie every Friday. The habit changes that come with bariatric surgery can require one partner to focus less on those rituals.
These sorts of changes may leave one or both people feeling like their partner is turning away from them, said Don Cole, DMin, a relationship therapist and clinical director at the Gottman Institute in Seattle, a think tank focused on the science of relationships. The person who had surgery may feel unsupported in the new journey if the partner keeps advocating for unhealthy habits, he said. And the person who didn’t have surgery may feel cast aside by the partner’s new health priorities.
Changes, even those that are positive and healthy, create a kind of crisis for relationships, Dr. Cole said. It’s not just bariatric surgery. Bringing a baby into the home, infertility treatments, and substance abuse recovery are all considered positive changes that are also predictors of relationship dissatisfaction and divorce, he said.
A couple could have a range of emotions after one partner gets bariatric surgery, Dr. Cole said. Unfortunately, “my experience as a therapist says they aren’t that good [at talking about it],” he said.
But bariatric surgery isn’t the only thing at play in these relationship changes, according to the study. Married patients had a much lower chance of separation or divorce (13%) than patients who were unmarried but living together (44%) by 5 years after surgery. Similarly, most people who were already separated either got divorced or resumed being married. It’s as if the surgery and lifestyle changes served as a catalyst for people who already had one foot out of (or in) the door, Dr. Goldman said.
A high sexual desire after surgery was also a predictor of divorce. In fact, there were more things before surgery that impacted divorce than surgery-related changes. It’s possible that many of these patients are “on the path toward change already,” Dr. King said. “Who knows how much the surgery had to do with it.”
Dr. Goldman recalled a patient who, before surgery, had very low self-worth. She wasn’t satisfied with her relationship but admitted to staying because she didn’t believe she could do any better than her current partner. After surgery, her perspective radically changed. She started to get healthier, invested in her education, and changed jobs. And when her partner refused to join her in making changes, she left. Maybe some of these patients “were already thinking about leaving but just didn’t have the confidence,” Dr. Goldman said.
Still, it’s critical that patients receive more counseling on how choosing to have bariatric surgery can impact their relationship before and after their weight loss procedure, Dr. King said. It should be the standard of care.
Currently, relationship-specific counseling isn’t required, Dr. Goldman said. Most programs do require a psychosocial evaluation before surgery, “but they are quite varied.” And even in programs where relationships are mentioned, there often isn’t a psychologist or licensed mental health professional on the team.
Since Dr. King’s previous research on substance abuse after bariatric surgery changed common practice in the field, Dr. Goldman said she hopes the new data will have a similar influence and relationship counseling will become the norm.
Dr. Cole actually had bariatric surgery. He recalled potential relationship issues were briefly mentioned. Someone at the clinic said if his marriage felt challenged, he should seek help from a professional, and that was it.
For Dr. Cole, there were unexpected negative feelings of shame and disappointment after surgery. He felt the extreme weight loss was all his colleagues could talk about and was very disappointed when there was no change in his chronic pain, a primary reason he had the procedure.
Fortunately, he could talk to his wife – also is a relationship therapist at Gottman – about the range of emotions. “One of the things that we know that creates a deep sense of trust is [when] I know my partner is there for me when I’m not well,” Dr. Cole said.
But these negative emotions can be the very things that feel most difficult to talk about or hear from a partner. It’s hard to share our own negative feelings and to hear someone else’s, Dr. Cole said.
He advises creating a new “ritual of connection: moments in time when you plan to turn toward one another.”
That could be a daily walk, where you intentionally talk about the surgery-related changes that both of you have had. Dr. Cole said to ask yourself, “Are we intentional about turning toward one another in those [challenging] moments?”
A version of this article first appeared on WebMD.com.
Kristal was only in her mid-30s when she decided to have surgery. Her doctor said it was too early. But the Oregon mom of three had found herself in the hospital twice for obesity-related lung complications before her 35th birthday. So she got the gastric sleeve.
And at first it seemed like the best decision for her and her family. She was losing weight – 100 pounds in 16 months – and so was her husband. The whole family was more active and seemed to have more energy. But then her husband’s weight began to creep back up.
While she joined a running group and signed up for half-marathons, her husband’s depression and drinking worsened. The healthier lifestyle they’d shared was now an unspoken wedge between them.
And the added attention Kristal was getting from men and women because of her thinner size only added to the tension. After 30 years together and 22 years of marriage, the high school sweethearts divorced in June 2021. Kristal’s weight loss wasn’t the only problem, but she and her ex-husband believe it was the beginning of the end.
An unexpected outcome?
New research from the University of Pittsburgh found that Kristal’s experience is a common one. The study looked at data from 1,441 bariatric surgery patients and found that never-married patients were over 50% more likely to get married, and married patients were more than twice as likely to get divorced, compared to the general U.S. population.
This U.S. data follows two Scandinavian studies from 2018 and 2020 that found similar relationship changes after bariatric surgery. But the postsurgery divorce rate in the United States was only about half that found in the Danish and Swedish studies, according to the new study published in Annals of Surgery.
It’s important to note that even with an increase in the divorce rate, most marriages in the study were unchanged, said epidemiologist and lead author Wendy King, PhD. In fact, 81% of couples were still married 5 years after surgery. But where the U.S. population has a divorce rate of 3.5%, bariatric patients in the study had an 8% divorce rate. Likewise, those who’d never been married before the surgery had a marriage rate of 18%, compared to 7% in the U.S. population.
Surgery certainly isn’t a death sentence for a patient’s love life. But the uptick in marriage and divorce suggests bariatric surgery significantly impacts how people engage in relationships.
“It makes sense,” said clinical psychologist Rachel Goldman, PhD, who specializes in health and wellness issues and bariatric surgery cases in New York City. “People are changing their lifestyle.” And those changes don’t start or stop the day of surgery, they begin as soon as someone decides to have surgery and continue as a lifelong process, she said.
For some patients, these healthy habits may offer a “new lease on life,” said Dr. King. According to the study, patients who had better physical health after surgery were more likely to get married.
But the continual lifestyle changes can dramatically impact the rituals of existing relationships, said Dr. Goldman. Maybe a couple loved to go out and enjoy an extravagant meal before surgery, or they had ice cream and watched a movie every Friday. The habit changes that come with bariatric surgery can require one partner to focus less on those rituals.
These sorts of changes may leave one or both people feeling like their partner is turning away from them, said Don Cole, DMin, a relationship therapist and clinical director at the Gottman Institute in Seattle, a think tank focused on the science of relationships. The person who had surgery may feel unsupported in the new journey if the partner keeps advocating for unhealthy habits, he said. And the person who didn’t have surgery may feel cast aside by the partner’s new health priorities.
Changes, even those that are positive and healthy, create a kind of crisis for relationships, Dr. Cole said. It’s not just bariatric surgery. Bringing a baby into the home, infertility treatments, and substance abuse recovery are all considered positive changes that are also predictors of relationship dissatisfaction and divorce, he said.
A couple could have a range of emotions after one partner gets bariatric surgery, Dr. Cole said. Unfortunately, “my experience as a therapist says they aren’t that good [at talking about it],” he said.
But bariatric surgery isn’t the only thing at play in these relationship changes, according to the study. Married patients had a much lower chance of separation or divorce (13%) than patients who were unmarried but living together (44%) by 5 years after surgery. Similarly, most people who were already separated either got divorced or resumed being married. It’s as if the surgery and lifestyle changes served as a catalyst for people who already had one foot out of (or in) the door, Dr. Goldman said.
A high sexual desire after surgery was also a predictor of divorce. In fact, there were more things before surgery that impacted divorce than surgery-related changes. It’s possible that many of these patients are “on the path toward change already,” Dr. King said. “Who knows how much the surgery had to do with it.”
Dr. Goldman recalled a patient who, before surgery, had very low self-worth. She wasn’t satisfied with her relationship but admitted to staying because she didn’t believe she could do any better than her current partner. After surgery, her perspective radically changed. She started to get healthier, invested in her education, and changed jobs. And when her partner refused to join her in making changes, she left. Maybe some of these patients “were already thinking about leaving but just didn’t have the confidence,” Dr. Goldman said.
Still, it’s critical that patients receive more counseling on how choosing to have bariatric surgery can impact their relationship before and after their weight loss procedure, Dr. King said. It should be the standard of care.
Currently, relationship-specific counseling isn’t required, Dr. Goldman said. Most programs do require a psychosocial evaluation before surgery, “but they are quite varied.” And even in programs where relationships are mentioned, there often isn’t a psychologist or licensed mental health professional on the team.
Since Dr. King’s previous research on substance abuse after bariatric surgery changed common practice in the field, Dr. Goldman said she hopes the new data will have a similar influence and relationship counseling will become the norm.
Dr. Cole actually had bariatric surgery. He recalled potential relationship issues were briefly mentioned. Someone at the clinic said if his marriage felt challenged, he should seek help from a professional, and that was it.
For Dr. Cole, there were unexpected negative feelings of shame and disappointment after surgery. He felt the extreme weight loss was all his colleagues could talk about and was very disappointed when there was no change in his chronic pain, a primary reason he had the procedure.
Fortunately, he could talk to his wife – also is a relationship therapist at Gottman – about the range of emotions. “One of the things that we know that creates a deep sense of trust is [when] I know my partner is there for me when I’m not well,” Dr. Cole said.
But these negative emotions can be the very things that feel most difficult to talk about or hear from a partner. It’s hard to share our own negative feelings and to hear someone else’s, Dr. Cole said.
He advises creating a new “ritual of connection: moments in time when you plan to turn toward one another.”
That could be a daily walk, where you intentionally talk about the surgery-related changes that both of you have had. Dr. Cole said to ask yourself, “Are we intentional about turning toward one another in those [challenging] moments?”
A version of this article first appeared on WebMD.com.
Kristal was only in her mid-30s when she decided to have surgery. Her doctor said it was too early. But the Oregon mom of three had found herself in the hospital twice for obesity-related lung complications before her 35th birthday. So she got the gastric sleeve.
And at first it seemed like the best decision for her and her family. She was losing weight – 100 pounds in 16 months – and so was her husband. The whole family was more active and seemed to have more energy. But then her husband’s weight began to creep back up.
While she joined a running group and signed up for half-marathons, her husband’s depression and drinking worsened. The healthier lifestyle they’d shared was now an unspoken wedge between them.
And the added attention Kristal was getting from men and women because of her thinner size only added to the tension. After 30 years together and 22 years of marriage, the high school sweethearts divorced in June 2021. Kristal’s weight loss wasn’t the only problem, but she and her ex-husband believe it was the beginning of the end.
An unexpected outcome?
New research from the University of Pittsburgh found that Kristal’s experience is a common one. The study looked at data from 1,441 bariatric surgery patients and found that never-married patients were over 50% more likely to get married, and married patients were more than twice as likely to get divorced, compared to the general U.S. population.
This U.S. data follows two Scandinavian studies from 2018 and 2020 that found similar relationship changes after bariatric surgery. But the postsurgery divorce rate in the United States was only about half that found in the Danish and Swedish studies, according to the new study published in Annals of Surgery.
It’s important to note that even with an increase in the divorce rate, most marriages in the study were unchanged, said epidemiologist and lead author Wendy King, PhD. In fact, 81% of couples were still married 5 years after surgery. But where the U.S. population has a divorce rate of 3.5%, bariatric patients in the study had an 8% divorce rate. Likewise, those who’d never been married before the surgery had a marriage rate of 18%, compared to 7% in the U.S. population.
Surgery certainly isn’t a death sentence for a patient’s love life. But the uptick in marriage and divorce suggests bariatric surgery significantly impacts how people engage in relationships.
“It makes sense,” said clinical psychologist Rachel Goldman, PhD, who specializes in health and wellness issues and bariatric surgery cases in New York City. “People are changing their lifestyle.” And those changes don’t start or stop the day of surgery, they begin as soon as someone decides to have surgery and continue as a lifelong process, she said.
For some patients, these healthy habits may offer a “new lease on life,” said Dr. King. According to the study, patients who had better physical health after surgery were more likely to get married.
But the continual lifestyle changes can dramatically impact the rituals of existing relationships, said Dr. Goldman. Maybe a couple loved to go out and enjoy an extravagant meal before surgery, or they had ice cream and watched a movie every Friday. The habit changes that come with bariatric surgery can require one partner to focus less on those rituals.
These sorts of changes may leave one or both people feeling like their partner is turning away from them, said Don Cole, DMin, a relationship therapist and clinical director at the Gottman Institute in Seattle, a think tank focused on the science of relationships. The person who had surgery may feel unsupported in the new journey if the partner keeps advocating for unhealthy habits, he said. And the person who didn’t have surgery may feel cast aside by the partner’s new health priorities.
Changes, even those that are positive and healthy, create a kind of crisis for relationships, Dr. Cole said. It’s not just bariatric surgery. Bringing a baby into the home, infertility treatments, and substance abuse recovery are all considered positive changes that are also predictors of relationship dissatisfaction and divorce, he said.
A couple could have a range of emotions after one partner gets bariatric surgery, Dr. Cole said. Unfortunately, “my experience as a therapist says they aren’t that good [at talking about it],” he said.
But bariatric surgery isn’t the only thing at play in these relationship changes, according to the study. Married patients had a much lower chance of separation or divorce (13%) than patients who were unmarried but living together (44%) by 5 years after surgery. Similarly, most people who were already separated either got divorced or resumed being married. It’s as if the surgery and lifestyle changes served as a catalyst for people who already had one foot out of (or in) the door, Dr. Goldman said.
A high sexual desire after surgery was also a predictor of divorce. In fact, there were more things before surgery that impacted divorce than surgery-related changes. It’s possible that many of these patients are “on the path toward change already,” Dr. King said. “Who knows how much the surgery had to do with it.”
Dr. Goldman recalled a patient who, before surgery, had very low self-worth. She wasn’t satisfied with her relationship but admitted to staying because she didn’t believe she could do any better than her current partner. After surgery, her perspective radically changed. She started to get healthier, invested in her education, and changed jobs. And when her partner refused to join her in making changes, she left. Maybe some of these patients “were already thinking about leaving but just didn’t have the confidence,” Dr. Goldman said.
Still, it’s critical that patients receive more counseling on how choosing to have bariatric surgery can impact their relationship before and after their weight loss procedure, Dr. King said. It should be the standard of care.
Currently, relationship-specific counseling isn’t required, Dr. Goldman said. Most programs do require a psychosocial evaluation before surgery, “but they are quite varied.” And even in programs where relationships are mentioned, there often isn’t a psychologist or licensed mental health professional on the team.
Since Dr. King’s previous research on substance abuse after bariatric surgery changed common practice in the field, Dr. Goldman said she hopes the new data will have a similar influence and relationship counseling will become the norm.
Dr. Cole actually had bariatric surgery. He recalled potential relationship issues were briefly mentioned. Someone at the clinic said if his marriage felt challenged, he should seek help from a professional, and that was it.
For Dr. Cole, there were unexpected negative feelings of shame and disappointment after surgery. He felt the extreme weight loss was all his colleagues could talk about and was very disappointed when there was no change in his chronic pain, a primary reason he had the procedure.
Fortunately, he could talk to his wife – also is a relationship therapist at Gottman – about the range of emotions. “One of the things that we know that creates a deep sense of trust is [when] I know my partner is there for me when I’m not well,” Dr. Cole said.
But these negative emotions can be the very things that feel most difficult to talk about or hear from a partner. It’s hard to share our own negative feelings and to hear someone else’s, Dr. Cole said.
He advises creating a new “ritual of connection: moments in time when you plan to turn toward one another.”
That could be a daily walk, where you intentionally talk about the surgery-related changes that both of you have had. Dr. Cole said to ask yourself, “Are we intentional about turning toward one another in those [challenging] moments?”
A version of this article first appeared on WebMD.com.
FROM ANNALS OF SURGERY
Stressed about weight gain? Well, stress causes weight gain
Stress, meet weight gain. Weight gain, meet stress
You’re not eating differently and you’re keeping active, but your waistline is expanding. How is that happening? Since eating healthy and exercising shouldn’t make you gain weight, there may be a hidden factor getting in your way. Stress. The one thing that can have a grip on your circadian rhythm stronger than any bodybuilder.
Investigators at Weill Cornell Medicine published two mouse studies that suggest stress and other factors that throw the body’s circadian clocks out of rhythm may contribute to weight gain.
In the first study, the researchers imitated disruptive condition effects like high cortisol exposure and chronic stress by implanting pellets under the skin that released glucocorticoid at a constant rate for 21 days. Mice that received the pellets had twice as much white and brown fat, as well as much higher insulin levels, regardless of their unchanged and still-healthy diet.
In the second study, they used tagged proteins as markers to monitor the daily fluctuations of a protein that regulates fat cell production and circadian gene expression in mouse fat cell precursors. The results showed “that fat cell precursors commit to becoming fat cells only during the circadian cycle phase corresponding to evening in humans,” they said in a written statement.
“Every cell in our body has an intrinsic cell clock, just like the fat cells, and we have a master clock in our brain, which controls hormone secretion,” said senior author Mary Teruel of Cornell University. “A lot of forces are working against a healthy metabolism when we are out of circadian rhythm. The more we understand, the more likely we will be able to do something about it.”
So if you’re stressing out that the scale is or isn’t moving in the direction you want, you could be standing in your own way. Take a chill pill.
Who can smell cancer? The locust nose
If you need to smell some gas, there’s nothing better than a nose. Just ask a scientist: “Noses are still state of the art,” said Debajit Saha, PhD, of Michigan State University. “There’s really nothing like them when it comes to gas sensing.”
And when it comes to noses, dogs are best, right? After all, there’s a reason we don’t have bomb-sniffing wombats and drug-sniffing ostriches. Dogs are better. Better, but not perfect. And if they’re not perfect, then human technology can do better.
Enter the electronic nose. Which is better than dogs … except that it isn’t. “People have been working on ‘electronic noses’ for more than 15 years, but they’re still not close to achieving what biology can do seamlessly,” Dr. Saha explained in a statement from the university.
Which brings us back to dogs. If you want to detect early-stage cancer using smell, you go to the dogs, right? Nope.
Here’s Christopher Contag, PhD, also of Michigan State, who recruited Dr. Saha to the university: “I told him, ‘When you come here, we’ll detect cancer. I’m sure your locusts can do it.’ ”
Yes, locusts. Dr. Contag and his research team were looking at mouth cancers and noticed that different cell lines had different appearances. Then they discovered that those different-looking cell lines produced different metabolites, some of which were volatile.
Enter Dr. Saha’s locusts. They were able to tell the difference between normal cells and cancer cells and could even distinguish between the different cell lines. And how they were able to share this information? Not voluntarily, that’s for sure. The researchers attached electrodes to the insects’ brains and recorded their responses to gas samples from both healthy and cancer cells. Those brain signals were then used to create chemical profiles of the different cells. Piece of cake.
The whole getting-electrodes-attached-to-their-brains thing seemed at least a bit ethically ambiguous, so we contacted the locusts’ PR office, which offered some positive spin: “Humans get their early cancer detection and we get that whole swarms-that-devour-entire-countrysides thing off our backs. Win win.”
Bad news for vampires everywhere
Pop culture has been extraordinarily kind to the vampire. A few hundred years ago, vampires were demon-possessed, often-inhuman monsters. Now? They’re suave, sophisticated, beautiful, and oh-so dramatic and angst-filled about their “curse.” Drink a little human blood, live and look young forever. Such monsters they are.
It does make sense in a morbid sort of way. An old person receiving the blood of the young does seem like a good idea for rejuvenation, right? A team of Ukrainian researchers sought to find out, conducting a study in which older mice were linked with young mice via heterochronic parabiosis. For 3 months, old-young mice pairs were surgically connected and shared blood. After 3 months, the mice were disconnected from each other and the effects of the blood link were studied.
For all the vampire enthusiasts out there, we have bad news and worse news. The bad news first: The older mice received absolutely no benefit from heterochronic parabiosis. No youthfulness, no increased lifespan, nothing. The worse news is that the younger mice were adversely affected by the older blood. They aged more and experienced a shortened lifespan, even after the connection was severed. The old blood, according to the investigators, contains factors capable of inducing aging in younger mice, but the opposite is not true. Further research into aging, they added, should focus on suppressing the aging factors in older blood.
Of note, the paper was written by doctors who are currently refugees, fleeing the war in Ukraine. We don’t want to speculate on the true cause of the war, but we’re onto you, Putin. We know you wanted the vampire research for yourself, but it won’t work. Your dream of becoming Vlad “Dracula” Putin will never come to pass.
Hearing is not always believing
Have you ever heard yourself on a voice mail, or from a recording you did at work? No matter how good you sound, you still might feel like the recording sounds nothing like you. It may even cause low self-esteem for those who don’t like how their voice sounds or don’t recognize it when it’s played back to them.
Since one possible symptom of schizophrenia is not recognizing one’s own speech and having a false sense of control over actions, and those with schizophrenia may hallucinate or hear voices, not being able to recognize their own voices may be alarming.
A recent study on the sense of agency, or sense of control, involved having volunteers speak with different pitches in their voices and then having it played back to them to gauge their reactions.
“Our results demonstrate that hearing one’s own voice is a critical factor to increased self-agency over speech. In other words, we do not strongly feel that ‘I’ am generating the speech if we hear someone else’s voice as an outcome of the speech. Our study provides empirical evidence of the tight link between the sense of agency and self-voice identity,” lead author Ryu Ohata, PhD, of the University of Tokyo, said in a written statement.
As social interaction becomes more digital through platforms such as FaceTime, Zoom, and voicemail, especially since the pandemic has promoted social distancing, it makes sense that people may be more aware and more surprised by how they sound on recordings.
So, if you ever promised someone something that you don’t want to do, and they play it back to you from the recording you made, maybe you can just say you don’t recognize the voice. And if it’s not you, then you don’t have to do it.
Stress, meet weight gain. Weight gain, meet stress
You’re not eating differently and you’re keeping active, but your waistline is expanding. How is that happening? Since eating healthy and exercising shouldn’t make you gain weight, there may be a hidden factor getting in your way. Stress. The one thing that can have a grip on your circadian rhythm stronger than any bodybuilder.
Investigators at Weill Cornell Medicine published two mouse studies that suggest stress and other factors that throw the body’s circadian clocks out of rhythm may contribute to weight gain.
In the first study, the researchers imitated disruptive condition effects like high cortisol exposure and chronic stress by implanting pellets under the skin that released glucocorticoid at a constant rate for 21 days. Mice that received the pellets had twice as much white and brown fat, as well as much higher insulin levels, regardless of their unchanged and still-healthy diet.
In the second study, they used tagged proteins as markers to monitor the daily fluctuations of a protein that regulates fat cell production and circadian gene expression in mouse fat cell precursors. The results showed “that fat cell precursors commit to becoming fat cells only during the circadian cycle phase corresponding to evening in humans,” they said in a written statement.
“Every cell in our body has an intrinsic cell clock, just like the fat cells, and we have a master clock in our brain, which controls hormone secretion,” said senior author Mary Teruel of Cornell University. “A lot of forces are working against a healthy metabolism when we are out of circadian rhythm. The more we understand, the more likely we will be able to do something about it.”
So if you’re stressing out that the scale is or isn’t moving in the direction you want, you could be standing in your own way. Take a chill pill.
Who can smell cancer? The locust nose
If you need to smell some gas, there’s nothing better than a nose. Just ask a scientist: “Noses are still state of the art,” said Debajit Saha, PhD, of Michigan State University. “There’s really nothing like them when it comes to gas sensing.”
And when it comes to noses, dogs are best, right? After all, there’s a reason we don’t have bomb-sniffing wombats and drug-sniffing ostriches. Dogs are better. Better, but not perfect. And if they’re not perfect, then human technology can do better.
Enter the electronic nose. Which is better than dogs … except that it isn’t. “People have been working on ‘electronic noses’ for more than 15 years, but they’re still not close to achieving what biology can do seamlessly,” Dr. Saha explained in a statement from the university.
Which brings us back to dogs. If you want to detect early-stage cancer using smell, you go to the dogs, right? Nope.
Here’s Christopher Contag, PhD, also of Michigan State, who recruited Dr. Saha to the university: “I told him, ‘When you come here, we’ll detect cancer. I’m sure your locusts can do it.’ ”
Yes, locusts. Dr. Contag and his research team were looking at mouth cancers and noticed that different cell lines had different appearances. Then they discovered that those different-looking cell lines produced different metabolites, some of which were volatile.
Enter Dr. Saha’s locusts. They were able to tell the difference between normal cells and cancer cells and could even distinguish between the different cell lines. And how they were able to share this information? Not voluntarily, that’s for sure. The researchers attached electrodes to the insects’ brains and recorded their responses to gas samples from both healthy and cancer cells. Those brain signals were then used to create chemical profiles of the different cells. Piece of cake.
The whole getting-electrodes-attached-to-their-brains thing seemed at least a bit ethically ambiguous, so we contacted the locusts’ PR office, which offered some positive spin: “Humans get their early cancer detection and we get that whole swarms-that-devour-entire-countrysides thing off our backs. Win win.”
Bad news for vampires everywhere
Pop culture has been extraordinarily kind to the vampire. A few hundred years ago, vampires were demon-possessed, often-inhuman monsters. Now? They’re suave, sophisticated, beautiful, and oh-so dramatic and angst-filled about their “curse.” Drink a little human blood, live and look young forever. Such monsters they are.
It does make sense in a morbid sort of way. An old person receiving the blood of the young does seem like a good idea for rejuvenation, right? A team of Ukrainian researchers sought to find out, conducting a study in which older mice were linked with young mice via heterochronic parabiosis. For 3 months, old-young mice pairs were surgically connected and shared blood. After 3 months, the mice were disconnected from each other and the effects of the blood link were studied.
For all the vampire enthusiasts out there, we have bad news and worse news. The bad news first: The older mice received absolutely no benefit from heterochronic parabiosis. No youthfulness, no increased lifespan, nothing. The worse news is that the younger mice were adversely affected by the older blood. They aged more and experienced a shortened lifespan, even after the connection was severed. The old blood, according to the investigators, contains factors capable of inducing aging in younger mice, but the opposite is not true. Further research into aging, they added, should focus on suppressing the aging factors in older blood.
Of note, the paper was written by doctors who are currently refugees, fleeing the war in Ukraine. We don’t want to speculate on the true cause of the war, but we’re onto you, Putin. We know you wanted the vampire research for yourself, but it won’t work. Your dream of becoming Vlad “Dracula” Putin will never come to pass.
Hearing is not always believing
Have you ever heard yourself on a voice mail, or from a recording you did at work? No matter how good you sound, you still might feel like the recording sounds nothing like you. It may even cause low self-esteem for those who don’t like how their voice sounds or don’t recognize it when it’s played back to them.
Since one possible symptom of schizophrenia is not recognizing one’s own speech and having a false sense of control over actions, and those with schizophrenia may hallucinate or hear voices, not being able to recognize their own voices may be alarming.
A recent study on the sense of agency, or sense of control, involved having volunteers speak with different pitches in their voices and then having it played back to them to gauge their reactions.
“Our results demonstrate that hearing one’s own voice is a critical factor to increased self-agency over speech. In other words, we do not strongly feel that ‘I’ am generating the speech if we hear someone else’s voice as an outcome of the speech. Our study provides empirical evidence of the tight link between the sense of agency and self-voice identity,” lead author Ryu Ohata, PhD, of the University of Tokyo, said in a written statement.
As social interaction becomes more digital through platforms such as FaceTime, Zoom, and voicemail, especially since the pandemic has promoted social distancing, it makes sense that people may be more aware and more surprised by how they sound on recordings.
So, if you ever promised someone something that you don’t want to do, and they play it back to you from the recording you made, maybe you can just say you don’t recognize the voice. And if it’s not you, then you don’t have to do it.
Stress, meet weight gain. Weight gain, meet stress
You’re not eating differently and you’re keeping active, but your waistline is expanding. How is that happening? Since eating healthy and exercising shouldn’t make you gain weight, there may be a hidden factor getting in your way. Stress. The one thing that can have a grip on your circadian rhythm stronger than any bodybuilder.
Investigators at Weill Cornell Medicine published two mouse studies that suggest stress and other factors that throw the body’s circadian clocks out of rhythm may contribute to weight gain.
In the first study, the researchers imitated disruptive condition effects like high cortisol exposure and chronic stress by implanting pellets under the skin that released glucocorticoid at a constant rate for 21 days. Mice that received the pellets had twice as much white and brown fat, as well as much higher insulin levels, regardless of their unchanged and still-healthy diet.
In the second study, they used tagged proteins as markers to monitor the daily fluctuations of a protein that regulates fat cell production and circadian gene expression in mouse fat cell precursors. The results showed “that fat cell precursors commit to becoming fat cells only during the circadian cycle phase corresponding to evening in humans,” they said in a written statement.
“Every cell in our body has an intrinsic cell clock, just like the fat cells, and we have a master clock in our brain, which controls hormone secretion,” said senior author Mary Teruel of Cornell University. “A lot of forces are working against a healthy metabolism when we are out of circadian rhythm. The more we understand, the more likely we will be able to do something about it.”
So if you’re stressing out that the scale is or isn’t moving in the direction you want, you could be standing in your own way. Take a chill pill.
Who can smell cancer? The locust nose
If you need to smell some gas, there’s nothing better than a nose. Just ask a scientist: “Noses are still state of the art,” said Debajit Saha, PhD, of Michigan State University. “There’s really nothing like them when it comes to gas sensing.”
And when it comes to noses, dogs are best, right? After all, there’s a reason we don’t have bomb-sniffing wombats and drug-sniffing ostriches. Dogs are better. Better, but not perfect. And if they’re not perfect, then human technology can do better.
Enter the electronic nose. Which is better than dogs … except that it isn’t. “People have been working on ‘electronic noses’ for more than 15 years, but they’re still not close to achieving what biology can do seamlessly,” Dr. Saha explained in a statement from the university.
Which brings us back to dogs. If you want to detect early-stage cancer using smell, you go to the dogs, right? Nope.
Here’s Christopher Contag, PhD, also of Michigan State, who recruited Dr. Saha to the university: “I told him, ‘When you come here, we’ll detect cancer. I’m sure your locusts can do it.’ ”
Yes, locusts. Dr. Contag and his research team were looking at mouth cancers and noticed that different cell lines had different appearances. Then they discovered that those different-looking cell lines produced different metabolites, some of which were volatile.
Enter Dr. Saha’s locusts. They were able to tell the difference between normal cells and cancer cells and could even distinguish between the different cell lines. And how they were able to share this information? Not voluntarily, that’s for sure. The researchers attached electrodes to the insects’ brains and recorded their responses to gas samples from both healthy and cancer cells. Those brain signals were then used to create chemical profiles of the different cells. Piece of cake.
The whole getting-electrodes-attached-to-their-brains thing seemed at least a bit ethically ambiguous, so we contacted the locusts’ PR office, which offered some positive spin: “Humans get their early cancer detection and we get that whole swarms-that-devour-entire-countrysides thing off our backs. Win win.”
Bad news for vampires everywhere
Pop culture has been extraordinarily kind to the vampire. A few hundred years ago, vampires were demon-possessed, often-inhuman monsters. Now? They’re suave, sophisticated, beautiful, and oh-so dramatic and angst-filled about their “curse.” Drink a little human blood, live and look young forever. Such monsters they are.
It does make sense in a morbid sort of way. An old person receiving the blood of the young does seem like a good idea for rejuvenation, right? A team of Ukrainian researchers sought to find out, conducting a study in which older mice were linked with young mice via heterochronic parabiosis. For 3 months, old-young mice pairs were surgically connected and shared blood. After 3 months, the mice were disconnected from each other and the effects of the blood link were studied.
For all the vampire enthusiasts out there, we have bad news and worse news. The bad news first: The older mice received absolutely no benefit from heterochronic parabiosis. No youthfulness, no increased lifespan, nothing. The worse news is that the younger mice were adversely affected by the older blood. They aged more and experienced a shortened lifespan, even after the connection was severed. The old blood, according to the investigators, contains factors capable of inducing aging in younger mice, but the opposite is not true. Further research into aging, they added, should focus on suppressing the aging factors in older blood.
Of note, the paper was written by doctors who are currently refugees, fleeing the war in Ukraine. We don’t want to speculate on the true cause of the war, but we’re onto you, Putin. We know you wanted the vampire research for yourself, but it won’t work. Your dream of becoming Vlad “Dracula” Putin will never come to pass.
Hearing is not always believing
Have you ever heard yourself on a voice mail, or from a recording you did at work? No matter how good you sound, you still might feel like the recording sounds nothing like you. It may even cause low self-esteem for those who don’t like how their voice sounds or don’t recognize it when it’s played back to them.
Since one possible symptom of schizophrenia is not recognizing one’s own speech and having a false sense of control over actions, and those with schizophrenia may hallucinate or hear voices, not being able to recognize their own voices may be alarming.
A recent study on the sense of agency, or sense of control, involved having volunteers speak with different pitches in their voices and then having it played back to them to gauge their reactions.
“Our results demonstrate that hearing one’s own voice is a critical factor to increased self-agency over speech. In other words, we do not strongly feel that ‘I’ am generating the speech if we hear someone else’s voice as an outcome of the speech. Our study provides empirical evidence of the tight link between the sense of agency and self-voice identity,” lead author Ryu Ohata, PhD, of the University of Tokyo, said in a written statement.
As social interaction becomes more digital through platforms such as FaceTime, Zoom, and voicemail, especially since the pandemic has promoted social distancing, it makes sense that people may be more aware and more surprised by how they sound on recordings.
So, if you ever promised someone something that you don’t want to do, and they play it back to you from the recording you made, maybe you can just say you don’t recognize the voice. And if it’s not you, then you don’t have to do it.
Power-morcellation hysterectomies declined and most performed with no containment bag
The use of laparoscopic power morcellators for minimally invasive hysterectomy has significantly decreased, and while the use of containment bags increased after the U.S. Food and Drug Administration’s 2014 safety warning about power morcellators, most procedures employing them are still performed without bags, according to a large database study in Obstetrics & Gynecology.
Containment bags are thought to limit the dissemination of potentially pathologic tissue, including unsuspected cancerous cells.
Rates of uterine cancer in women having morcellation were similar before and after the 2014 FDA guidance, and containment bags were used in only a small proportion of women with uterine cancer, according to findings from a research group led by Jason D. Wright, MD, of the division of gynecologic oncology at Columbia University, New York.
“Despite warnings from professional societies and regulatory agencies, as well as intense public scrutiny after the FDA warnings, the majority of morcellated uterine cancers occurred with uncontained laparoscopic power morcellation,” Dr. Wright and associates wrote, adding that the findings have important policy implications. First, efforts are needed to ensure morcellation is avoided in women with pathologic abnormalities. Second, despite regulatory approval, the safety and efficacy of containment bags remain uncertain, and the use and outcomes of these devices should be monitored closely.
The authors noted that laparoscopic power morcellation with a containment bag actually carries a small but significant increase in the risk of complications, compared with uncontained morcellation.
The study
Drawing on the Premier Healthcare Database, the researchers looked at deidentified patients aged 18 years or older who underwent laparoscopic supracervical hysterectomy from 2010 to 2018. The largest age group having the procedure consisted of women aged 40-49.
Patients were stratified based on use of laparoscopic power morcellators.
The cohort was further stratified as either pre–FDA guidance (2010 quarter 1 to 2014 quarter 1) or post–FDA guidance (2014 quarter 2 to 2018 quarter 2).
In the final cohort of 67,115 patients, laparoscopic power morcellator use decreased from 66.7% in 2013 quarter 4 to 13.3% by 2018 quarter 2. The likelihood of using this device decreased by 9.5% for each quarter elapsed in the post–FDA warning period (risk ratio, 0.91; 95% confidence interval, 0.90-0.91).
In other findings, containment bag use rose from 5.2% in 2013 quarter 4 to 15.2% by 2018 quarter 2. The likelihood of containment bag use rose by 3% for each quarter elapsed in the post–FDA warning period (RR, 1.03; 95% CI, 1.02-1.05).
Among women who underwent surgery with laparoscopic power morcellator use, uterine cancers or sarcomas were identified in 54 (0.17%) before the FDA guidance, compared with 7 (0.12%) after the guidance (P = .45).
Containment bags were used in 11.1% of women with uterine cancers or sarcomas before the FDA guidance, compared with 14.3% after the guidance (P = .12). The perioperative complication rate was 3.3% among women who had laparoscopic power morcellator use without a containment bag, compared with 4.5% (P = .001) in those with a containment bag (adjusted RR, 1.35; 95% CI, 1.12-1.64).
A related editorial argued that the backlash against power morcellation was unwarranted and an example of “reactionary medicine.”
Ben A. Abdu, MD, and Cameron Lowry, MD, of the department of obstetrics and gynecology at the University of Tennessee Health Science Center in Memphis, noted that with the known advantages of laparoscopy over laparotomy – decreased blood loss, decreased pain, and fewer wound complications and infections – it is of paramount importance to continue to offer minimally invasive surgery whenever possible. After the FDA raised safety concerns, there was a rise in the rate of open abdominal hysterectomy, which was accompanied by an increase in surgical morbidity. “Perhaps for now we should avoid throwing the baby out with the bath water,” they wrote.
The editorialists pointed out that any surgery may entail unintended complications. “It is also important to remember that there is a risk of dissemination of malignant tissue whether or not power morcellation is used, and it has even been observed in laparotomy,” they stated, noting that bag rupture and tissue spillage can occur even when the containment bag remains intact.
The downward trend in the use of power morcellators observed by Dr. Wright’s group is of serious concern, the commentators added, especially because the FDA communication was made in response to a rare occurrence and possibly resting on an overestimation of risk. “Based on their review of the medical literature at the time, the FDA cited prevalence estimates of 1 in 352 for any uterine sarcoma and 1 in 498 for leiomyosarcoma,” they wrote. “Many authors have expressed concern that the FDA data review was overestimated.” For example, they cite a meta-analysis using prospective data in which the prevalence of occult leiomyosarcoma was estimated at 1 in 8,300. Despite this extremely low prevalence, there has been an almost total nationwide hospital moratorium on the use of power morcellation, which will likely continue. Some manufacturers have ceased or limited production, distribution, and sales of these devices, they noted.
According to Dr. Michael L. Nimaroff, MD, however, chief of minimally invasive gynecologic surgery at Northwell Health in New Hyde Park, N.Y., the general post–FDA-guidance backlash did not have much effect on expert practitioners in this surgical field. “Those of us who specialize in minimally invasive gynecologic surgery, which has many benefits for the patients, never pivoted,” he told this news organization. “We continued to perform it but more conscientiously and with more concern for safety.”
As for morcellator use, added Dr. Nimaroff, specialists were so accustomed to doing these surgeries before the containment systems were made available that they don’t miss the power morcellator. “We actually retrieve tissue manually, and most of our morcellations, if they’re not contained manually, are retrieved vaginally or through a slightly bigger incision. So patients still benefit from minimally invasive surgery, and in some cases these techniques actually shorten the operation.”
This study received no external funding. Dr. Wright is editor in chief of Obstetrics & Gynecology. He reported royalties from UpToDate and has received research support from Merck. Coauthor Dr. Hou has served as a consultant for Foundation Medicine and Natera. Dr. Abdu and Dr. Lowry disclosed no competing interests, as did Dr. Nimaroff.
The use of laparoscopic power morcellators for minimally invasive hysterectomy has significantly decreased, and while the use of containment bags increased after the U.S. Food and Drug Administration’s 2014 safety warning about power morcellators, most procedures employing them are still performed without bags, according to a large database study in Obstetrics & Gynecology.
Containment bags are thought to limit the dissemination of potentially pathologic tissue, including unsuspected cancerous cells.
Rates of uterine cancer in women having morcellation were similar before and after the 2014 FDA guidance, and containment bags were used in only a small proportion of women with uterine cancer, according to findings from a research group led by Jason D. Wright, MD, of the division of gynecologic oncology at Columbia University, New York.
“Despite warnings from professional societies and regulatory agencies, as well as intense public scrutiny after the FDA warnings, the majority of morcellated uterine cancers occurred with uncontained laparoscopic power morcellation,” Dr. Wright and associates wrote, adding that the findings have important policy implications. First, efforts are needed to ensure morcellation is avoided in women with pathologic abnormalities. Second, despite regulatory approval, the safety and efficacy of containment bags remain uncertain, and the use and outcomes of these devices should be monitored closely.
The authors noted that laparoscopic power morcellation with a containment bag actually carries a small but significant increase in the risk of complications, compared with uncontained morcellation.
The study
Drawing on the Premier Healthcare Database, the researchers looked at deidentified patients aged 18 years or older who underwent laparoscopic supracervical hysterectomy from 2010 to 2018. The largest age group having the procedure consisted of women aged 40-49.
Patients were stratified based on use of laparoscopic power morcellators.
The cohort was further stratified as either pre–FDA guidance (2010 quarter 1 to 2014 quarter 1) or post–FDA guidance (2014 quarter 2 to 2018 quarter 2).
In the final cohort of 67,115 patients, laparoscopic power morcellator use decreased from 66.7% in 2013 quarter 4 to 13.3% by 2018 quarter 2. The likelihood of using this device decreased by 9.5% for each quarter elapsed in the post–FDA warning period (risk ratio, 0.91; 95% confidence interval, 0.90-0.91).
In other findings, containment bag use rose from 5.2% in 2013 quarter 4 to 15.2% by 2018 quarter 2. The likelihood of containment bag use rose by 3% for each quarter elapsed in the post–FDA warning period (RR, 1.03; 95% CI, 1.02-1.05).
Among women who underwent surgery with laparoscopic power morcellator use, uterine cancers or sarcomas were identified in 54 (0.17%) before the FDA guidance, compared with 7 (0.12%) after the guidance (P = .45).
Containment bags were used in 11.1% of women with uterine cancers or sarcomas before the FDA guidance, compared with 14.3% after the guidance (P = .12). The perioperative complication rate was 3.3% among women who had laparoscopic power morcellator use without a containment bag, compared with 4.5% (P = .001) in those with a containment bag (adjusted RR, 1.35; 95% CI, 1.12-1.64).
A related editorial argued that the backlash against power morcellation was unwarranted and an example of “reactionary medicine.”
Ben A. Abdu, MD, and Cameron Lowry, MD, of the department of obstetrics and gynecology at the University of Tennessee Health Science Center in Memphis, noted that with the known advantages of laparoscopy over laparotomy – decreased blood loss, decreased pain, and fewer wound complications and infections – it is of paramount importance to continue to offer minimally invasive surgery whenever possible. After the FDA raised safety concerns, there was a rise in the rate of open abdominal hysterectomy, which was accompanied by an increase in surgical morbidity. “Perhaps for now we should avoid throwing the baby out with the bath water,” they wrote.
The editorialists pointed out that any surgery may entail unintended complications. “It is also important to remember that there is a risk of dissemination of malignant tissue whether or not power morcellation is used, and it has even been observed in laparotomy,” they stated, noting that bag rupture and tissue spillage can occur even when the containment bag remains intact.
The downward trend in the use of power morcellators observed by Dr. Wright’s group is of serious concern, the commentators added, especially because the FDA communication was made in response to a rare occurrence and possibly resting on an overestimation of risk. “Based on their review of the medical literature at the time, the FDA cited prevalence estimates of 1 in 352 for any uterine sarcoma and 1 in 498 for leiomyosarcoma,” they wrote. “Many authors have expressed concern that the FDA data review was overestimated.” For example, they cite a meta-analysis using prospective data in which the prevalence of occult leiomyosarcoma was estimated at 1 in 8,300. Despite this extremely low prevalence, there has been an almost total nationwide hospital moratorium on the use of power morcellation, which will likely continue. Some manufacturers have ceased or limited production, distribution, and sales of these devices, they noted.
According to Dr. Michael L. Nimaroff, MD, however, chief of minimally invasive gynecologic surgery at Northwell Health in New Hyde Park, N.Y., the general post–FDA-guidance backlash did not have much effect on expert practitioners in this surgical field. “Those of us who specialize in minimally invasive gynecologic surgery, which has many benefits for the patients, never pivoted,” he told this news organization. “We continued to perform it but more conscientiously and with more concern for safety.”
As for morcellator use, added Dr. Nimaroff, specialists were so accustomed to doing these surgeries before the containment systems were made available that they don’t miss the power morcellator. “We actually retrieve tissue manually, and most of our morcellations, if they’re not contained manually, are retrieved vaginally or through a slightly bigger incision. So patients still benefit from minimally invasive surgery, and in some cases these techniques actually shorten the operation.”
This study received no external funding. Dr. Wright is editor in chief of Obstetrics & Gynecology. He reported royalties from UpToDate and has received research support from Merck. Coauthor Dr. Hou has served as a consultant for Foundation Medicine and Natera. Dr. Abdu and Dr. Lowry disclosed no competing interests, as did Dr. Nimaroff.
The use of laparoscopic power morcellators for minimally invasive hysterectomy has significantly decreased, and while the use of containment bags increased after the U.S. Food and Drug Administration’s 2014 safety warning about power morcellators, most procedures employing them are still performed without bags, according to a large database study in Obstetrics & Gynecology.
Containment bags are thought to limit the dissemination of potentially pathologic tissue, including unsuspected cancerous cells.
Rates of uterine cancer in women having morcellation were similar before and after the 2014 FDA guidance, and containment bags were used in only a small proportion of women with uterine cancer, according to findings from a research group led by Jason D. Wright, MD, of the division of gynecologic oncology at Columbia University, New York.
“Despite warnings from professional societies and regulatory agencies, as well as intense public scrutiny after the FDA warnings, the majority of morcellated uterine cancers occurred with uncontained laparoscopic power morcellation,” Dr. Wright and associates wrote, adding that the findings have important policy implications. First, efforts are needed to ensure morcellation is avoided in women with pathologic abnormalities. Second, despite regulatory approval, the safety and efficacy of containment bags remain uncertain, and the use and outcomes of these devices should be monitored closely.
The authors noted that laparoscopic power morcellation with a containment bag actually carries a small but significant increase in the risk of complications, compared with uncontained morcellation.
The study
Drawing on the Premier Healthcare Database, the researchers looked at deidentified patients aged 18 years or older who underwent laparoscopic supracervical hysterectomy from 2010 to 2018. The largest age group having the procedure consisted of women aged 40-49.
Patients were stratified based on use of laparoscopic power morcellators.
The cohort was further stratified as either pre–FDA guidance (2010 quarter 1 to 2014 quarter 1) or post–FDA guidance (2014 quarter 2 to 2018 quarter 2).
In the final cohort of 67,115 patients, laparoscopic power morcellator use decreased from 66.7% in 2013 quarter 4 to 13.3% by 2018 quarter 2. The likelihood of using this device decreased by 9.5% for each quarter elapsed in the post–FDA warning period (risk ratio, 0.91; 95% confidence interval, 0.90-0.91).
In other findings, containment bag use rose from 5.2% in 2013 quarter 4 to 15.2% by 2018 quarter 2. The likelihood of containment bag use rose by 3% for each quarter elapsed in the post–FDA warning period (RR, 1.03; 95% CI, 1.02-1.05).
Among women who underwent surgery with laparoscopic power morcellator use, uterine cancers or sarcomas were identified in 54 (0.17%) before the FDA guidance, compared with 7 (0.12%) after the guidance (P = .45).
Containment bags were used in 11.1% of women with uterine cancers or sarcomas before the FDA guidance, compared with 14.3% after the guidance (P = .12). The perioperative complication rate was 3.3% among women who had laparoscopic power morcellator use without a containment bag, compared with 4.5% (P = .001) in those with a containment bag (adjusted RR, 1.35; 95% CI, 1.12-1.64).
A related editorial argued that the backlash against power morcellation was unwarranted and an example of “reactionary medicine.”
Ben A. Abdu, MD, and Cameron Lowry, MD, of the department of obstetrics and gynecology at the University of Tennessee Health Science Center in Memphis, noted that with the known advantages of laparoscopy over laparotomy – decreased blood loss, decreased pain, and fewer wound complications and infections – it is of paramount importance to continue to offer minimally invasive surgery whenever possible. After the FDA raised safety concerns, there was a rise in the rate of open abdominal hysterectomy, which was accompanied by an increase in surgical morbidity. “Perhaps for now we should avoid throwing the baby out with the bath water,” they wrote.
The editorialists pointed out that any surgery may entail unintended complications. “It is also important to remember that there is a risk of dissemination of malignant tissue whether or not power morcellation is used, and it has even been observed in laparotomy,” they stated, noting that bag rupture and tissue spillage can occur even when the containment bag remains intact.
The downward trend in the use of power morcellators observed by Dr. Wright’s group is of serious concern, the commentators added, especially because the FDA communication was made in response to a rare occurrence and possibly resting on an overestimation of risk. “Based on their review of the medical literature at the time, the FDA cited prevalence estimates of 1 in 352 for any uterine sarcoma and 1 in 498 for leiomyosarcoma,” they wrote. “Many authors have expressed concern that the FDA data review was overestimated.” For example, they cite a meta-analysis using prospective data in which the prevalence of occult leiomyosarcoma was estimated at 1 in 8,300. Despite this extremely low prevalence, there has been an almost total nationwide hospital moratorium on the use of power morcellation, which will likely continue. Some manufacturers have ceased or limited production, distribution, and sales of these devices, they noted.
According to Dr. Michael L. Nimaroff, MD, however, chief of minimally invasive gynecologic surgery at Northwell Health in New Hyde Park, N.Y., the general post–FDA-guidance backlash did not have much effect on expert practitioners in this surgical field. “Those of us who specialize in minimally invasive gynecologic surgery, which has many benefits for the patients, never pivoted,” he told this news organization. “We continued to perform it but more conscientiously and with more concern for safety.”
As for morcellator use, added Dr. Nimaroff, specialists were so accustomed to doing these surgeries before the containment systems were made available that they don’t miss the power morcellator. “We actually retrieve tissue manually, and most of our morcellations, if they’re not contained manually, are retrieved vaginally or through a slightly bigger incision. So patients still benefit from minimally invasive surgery, and in some cases these techniques actually shorten the operation.”
This study received no external funding. Dr. Wright is editor in chief of Obstetrics & Gynecology. He reported royalties from UpToDate and has received research support from Merck. Coauthor Dr. Hou has served as a consultant for Foundation Medicine and Natera. Dr. Abdu and Dr. Lowry disclosed no competing interests, as did Dr. Nimaroff.
FROM OBSTETRICS & GYNECOLOGY
10 new ways docs could face legal troubles post Roe
Doctors in states where abortion is legal are likely to be the next target for antiabortion activists who want to deter residents from seeking abortions across state lines, say legal experts.
Antiabortion legislators in several states are mounting efforts to clamp down on out-of-state abortions, which they view as a legal loophole.
Nineteen states have already banned the use of telemedicine to prescribe medication abortion by requiring the clinician to be physically present when the medication is administered. These states include Arizona, Louisiana, Tennessee, and Texas, which also recently criminalized sending abortion pills through the mail.
Some state legislators plan to introduce legislation based on a Texas abortion ban enacted last year in which private citizens can sue anyone who assists state residents in obtaining an out-of-state abortion.
Meanwhile, legislators in states including New York where abortion is legal have introduced bills to shield doctors involved in reproductive care from possible negative actions by medical malpractice companies and professional misconduct charges.
This news organization asked legal experts for advice on how doctors can protect themselves and still provide appropriate medical care in this rapidly changing legal landscape. Here’s what they had to say.
1. What if patients from states where abortion is banned want to come to my practice in a legal state? What should I be aware of?
“Doctors should do what they think is medically necessary, but they should be aware of potential criminal and/or civil consequences in a patient’s home state, especially if those states have staked out more extreme positions on abortion such as Texas, Oklahoma, and Louisiana,” says Katherine Florey, JD, a professor at the University of California, Davis, School of Law.
The patient’s home state would need to have criminal laws in place that would explicitly ban residents from obtaining out-of-state abortions. “Probably the greater risk on the criminal front is that many states have existing laws that don’t specify their geographical reach but that could be construed to allow for criminal jurisdiction over out-of-state providers who help residents in obtaining an abortion,” she says.
However, criminal laws would be harder to enforce because of constitutional obstacles that would require the U.S. Supreme Court to resolve in a court case. Another barrier is that criminal law typically requires that a significant element of the offense take place in the prosecuting state, says Ms. Florey.
2. Am I likely to be sued by a patient from a state with an abortion ban?
“It’s more likely that states with abortion bans will pursue civil liability cases, particularly in states such as Texas and Oklahoma that allow private individuals to pursue lawsuits against individuals providing or assisting with abortions.”
Such liability is particularly appealing to antiabortion states because it allows them to target abortion care providers rather than the women seeking abortions, an approach that might be both more politically palatable and more effective in achieving abortion-restriction goals, says Ms. Florey.
“It’s not just the threat of jail time that can deter physicians from providing abortions. They can face significant career consequences from civil liability, including being reported to their medical licensing boards and having their malpractice insurance premiums increase,” says Ms. Florey.
3. What if I provide ‘abortion pill’ prescriptions by telemedicine to a patient in another state?
Doctors need to know what the rules are in the patient’s home state because states generally regard where the patient is located as where telemedicine is legally conducted, says Ms. Florey. “It’s more problematic to conduct telemedicine in states where it’s illegal. It could be viewed legally as if the doctor were prescribing a medication abortion in the patient’s state.”
Ms. Florey also advises doctors to find out whether the patient’s home state bans medication abortions. “The courts or states could decide that the physician is practicing in the jurisdiction where the patient is located even if care is provided remotely. In that case, the doctor would have to comply with all the laws of that state.”
She recommends that doctors counsel patients seeking medication abortions to come to the state where abortion is legal and get on their computers there.
“It’s not a perfect solution, but it provides more legal protection than providing medication abortion across state lines,” says Ms. Florey.
4. Can doctors be sued by patients for not informing them of the full range of treatment options, including abortion, when their health is at risk?
If the doctor is in a state that has banned abortion and the procedure is illegal, they can’t recommend something that the law doesn’t allow, says Ms. Florey.
It’s a tough call for doctors in states where abortion is illegal because they could get into legal trouble if they counsel a woman to get an abortion and the court later deems it was not medically necessary, says Ms. Florey.
But doctors could also get into legal trouble if they don’t counsel a woman to get an abortion if her life is in danger and she meets the exception in the abortion ban.
“Ultimately, I think doctors have to follow their conscience and best medical judgment but recognize the legal hazards that exist. If a physician is seeing a lot of out-of-state patients from a single jurisdiction (such as a neighboring state), it would be best to consult with an attorney from that state,” advises Ms. Florey.
5. If a patient from another state comes to me (in a legal state) for abortion care, am I required to provide them with any warnings, information, and so on?
Doctors may be required by some antiabortion states to mention certain risks, especially to the mother’s mental health, that could arise from abortions even if they are not well-supported by evidence, says Ms. Florey.
If a warning is required in a patient’s home state and there were complications from the procedure or the patient became depressed, it could be grounds for a civil lawsuit, says Ms. Florey.
“There is a Montana case, for example, where the plaintiff sued for malpractice after having an abortion. She alleged that she was given medically inaccurate information about the fetus’s HIV status, but she also claimed that she wasn’t informed that she might become depressed as a result of the abortion,” says Ms. Florey. (The case was ultimately decided on a different ground.)
6. What about complications from abortion care that I provided to a patient from another state? What are my responsibilities and risks? Can I be sued for malpractice when the patient returns to her home state?
If physicians can’t monitor the patients after their visit and something goes wrong, the doctors are at greater risk of negligence and being sued for malpractice in the patient’s home state, says Ms. Florey.
She recommends that doctors ask patients to stay for monitoring after the procedure. “I realize that may not be possible for all patients, but it’s a much safer alternative,” says Ms. Florey.
Otherwise, if the doctor communicates with the patient about the complications in her antiabortion state, the state’s courts could view the doctor as having ties to the state and claim they have jurisdiction in the case and apply the state’s laws, says Ms. Florey.
“Criminal jurisdiction would be more of stretch because the central conduct happened out of state, but states could still try to prosecute a case,” she says.
7. If a patient comes to me from another state, are there any residency requirements, or does the person need to find residence in my state for a period of time? Am I responsible for knowing their arrangements?
Generally, as a constitutional principle, a person can go to another state and have the services that a resident is entitled to, says Ms. Florey.
“States can’t normally discriminate against patients from out of state, so it’s not a residency requirement unless a state imposes one. If a state did that, it would probably be unconstitutional,” she says.
It would be less risky legally, though, if a patient remains in the state where she received abortion care for a significant period of time, says Ms. Florey.
8. How can I protect the privacy of patients’ medical records if they received an abortion or other reproductive care in the state?
To some extent, HIPAA accommodates state laws that mandate reporting of patient information, says Lisa C. Ikemoto, JD, also a professor at the UC Davis School of Law.
The Privacy Rule doesn’t require doctors to disclose protected health information about a patient when state laws require reporting. But the rule allows them to disclose private health information when there’s a court order such as a warrant or subpoena, says Ms. Ikemoto.
“Providers should make sure that patient information remains in records that are HIPAA protected. Some states, including California, have enacted privacy laws that are more protective of patient information,” she says.
The Department of Health & Human Services issued new guidance in June for health care professionals to clarify what the Privacy Rule requires them to report in light of the restrictive abortion laws.
9. I practice in a state where abortion is legal. Can I be extradited to another state if I’m prosecuted for crimes relating to reproductive health services?
Yes, generally, if your state allows it, says Ms. Florey. States have a constitutional obligation to extradite citizens of a different state if that person’s home state asks for that, but states do not have to extradite their own citizens.
However, traditionally, states have cooperated with extradition requests and most states have laws in place providing for extradition in those circumstances, which they could change to exempt abortion providers.
A handful of states – Connecticut, New York, Delaware, and New Jersey – have passed laws specifically shielding medical providers from being prosecuted under abortion restrictions passed in other states.
Governors in Massachusetts, Minnesota, New Mexico, and Nevada have issued executive orders saying they will not extradite abortion providers to states that have banned abortion provision, and that state employees will generally not comply with those out-of-state investigations.
10. Should I increase my malpractice insurance in anticipation of more potential legal problems from patients coming to me from antiabortion states?
Yes, I would recommend that doctors increase their malpractice coverage because of the increased legal risks they could face.
“It’s possible that a state might file a lawsuit against out-of-state abortion providers. Criminal prosecution is also a possibility, but the obstacles to prosecuting a case against an out-of-state provider would be considerable, especially if their home state has passed laws shielding abortion providers,” says Ms. Florey.
Individual malpractice claims or some sort of private enforcement action in a state that has established one would be more likely, she adds.
Ms. Florey advises doctors to monitor this rapidly evolving area of law. “Everything I am saying today could change with a single Supreme Court case. There will also be this kind of push/pull as antiabortion states try to crack down on out-of-state residents who provide or assist in abortion and physicians’ home states that try to protect them from legal consequences.”
A version of this article first appeared on Medscape.com.
Doctors in states where abortion is legal are likely to be the next target for antiabortion activists who want to deter residents from seeking abortions across state lines, say legal experts.
Antiabortion legislators in several states are mounting efforts to clamp down on out-of-state abortions, which they view as a legal loophole.
Nineteen states have already banned the use of telemedicine to prescribe medication abortion by requiring the clinician to be physically present when the medication is administered. These states include Arizona, Louisiana, Tennessee, and Texas, which also recently criminalized sending abortion pills through the mail.
Some state legislators plan to introduce legislation based on a Texas abortion ban enacted last year in which private citizens can sue anyone who assists state residents in obtaining an out-of-state abortion.
Meanwhile, legislators in states including New York where abortion is legal have introduced bills to shield doctors involved in reproductive care from possible negative actions by medical malpractice companies and professional misconduct charges.
This news organization asked legal experts for advice on how doctors can protect themselves and still provide appropriate medical care in this rapidly changing legal landscape. Here’s what they had to say.
1. What if patients from states where abortion is banned want to come to my practice in a legal state? What should I be aware of?
“Doctors should do what they think is medically necessary, but they should be aware of potential criminal and/or civil consequences in a patient’s home state, especially if those states have staked out more extreme positions on abortion such as Texas, Oklahoma, and Louisiana,” says Katherine Florey, JD, a professor at the University of California, Davis, School of Law.
The patient’s home state would need to have criminal laws in place that would explicitly ban residents from obtaining out-of-state abortions. “Probably the greater risk on the criminal front is that many states have existing laws that don’t specify their geographical reach but that could be construed to allow for criminal jurisdiction over out-of-state providers who help residents in obtaining an abortion,” she says.
However, criminal laws would be harder to enforce because of constitutional obstacles that would require the U.S. Supreme Court to resolve in a court case. Another barrier is that criminal law typically requires that a significant element of the offense take place in the prosecuting state, says Ms. Florey.
2. Am I likely to be sued by a patient from a state with an abortion ban?
“It’s more likely that states with abortion bans will pursue civil liability cases, particularly in states such as Texas and Oklahoma that allow private individuals to pursue lawsuits against individuals providing or assisting with abortions.”
Such liability is particularly appealing to antiabortion states because it allows them to target abortion care providers rather than the women seeking abortions, an approach that might be both more politically palatable and more effective in achieving abortion-restriction goals, says Ms. Florey.
“It’s not just the threat of jail time that can deter physicians from providing abortions. They can face significant career consequences from civil liability, including being reported to their medical licensing boards and having their malpractice insurance premiums increase,” says Ms. Florey.
3. What if I provide ‘abortion pill’ prescriptions by telemedicine to a patient in another state?
Doctors need to know what the rules are in the patient’s home state because states generally regard where the patient is located as where telemedicine is legally conducted, says Ms. Florey. “It’s more problematic to conduct telemedicine in states where it’s illegal. It could be viewed legally as if the doctor were prescribing a medication abortion in the patient’s state.”
Ms. Florey also advises doctors to find out whether the patient’s home state bans medication abortions. “The courts or states could decide that the physician is practicing in the jurisdiction where the patient is located even if care is provided remotely. In that case, the doctor would have to comply with all the laws of that state.”
She recommends that doctors counsel patients seeking medication abortions to come to the state where abortion is legal and get on their computers there.
“It’s not a perfect solution, but it provides more legal protection than providing medication abortion across state lines,” says Ms. Florey.
4. Can doctors be sued by patients for not informing them of the full range of treatment options, including abortion, when their health is at risk?
If the doctor is in a state that has banned abortion and the procedure is illegal, they can’t recommend something that the law doesn’t allow, says Ms. Florey.
It’s a tough call for doctors in states where abortion is illegal because they could get into legal trouble if they counsel a woman to get an abortion and the court later deems it was not medically necessary, says Ms. Florey.
But doctors could also get into legal trouble if they don’t counsel a woman to get an abortion if her life is in danger and she meets the exception in the abortion ban.
“Ultimately, I think doctors have to follow their conscience and best medical judgment but recognize the legal hazards that exist. If a physician is seeing a lot of out-of-state patients from a single jurisdiction (such as a neighboring state), it would be best to consult with an attorney from that state,” advises Ms. Florey.
5. If a patient from another state comes to me (in a legal state) for abortion care, am I required to provide them with any warnings, information, and so on?
Doctors may be required by some antiabortion states to mention certain risks, especially to the mother’s mental health, that could arise from abortions even if they are not well-supported by evidence, says Ms. Florey.
If a warning is required in a patient’s home state and there were complications from the procedure or the patient became depressed, it could be grounds for a civil lawsuit, says Ms. Florey.
“There is a Montana case, for example, where the plaintiff sued for malpractice after having an abortion. She alleged that she was given medically inaccurate information about the fetus’s HIV status, but she also claimed that she wasn’t informed that she might become depressed as a result of the abortion,” says Ms. Florey. (The case was ultimately decided on a different ground.)
6. What about complications from abortion care that I provided to a patient from another state? What are my responsibilities and risks? Can I be sued for malpractice when the patient returns to her home state?
If physicians can’t monitor the patients after their visit and something goes wrong, the doctors are at greater risk of negligence and being sued for malpractice in the patient’s home state, says Ms. Florey.
She recommends that doctors ask patients to stay for monitoring after the procedure. “I realize that may not be possible for all patients, but it’s a much safer alternative,” says Ms. Florey.
Otherwise, if the doctor communicates with the patient about the complications in her antiabortion state, the state’s courts could view the doctor as having ties to the state and claim they have jurisdiction in the case and apply the state’s laws, says Ms. Florey.
“Criminal jurisdiction would be more of stretch because the central conduct happened out of state, but states could still try to prosecute a case,” she says.
7. If a patient comes to me from another state, are there any residency requirements, or does the person need to find residence in my state for a period of time? Am I responsible for knowing their arrangements?
Generally, as a constitutional principle, a person can go to another state and have the services that a resident is entitled to, says Ms. Florey.
“States can’t normally discriminate against patients from out of state, so it’s not a residency requirement unless a state imposes one. If a state did that, it would probably be unconstitutional,” she says.
It would be less risky legally, though, if a patient remains in the state where she received abortion care for a significant period of time, says Ms. Florey.
8. How can I protect the privacy of patients’ medical records if they received an abortion or other reproductive care in the state?
To some extent, HIPAA accommodates state laws that mandate reporting of patient information, says Lisa C. Ikemoto, JD, also a professor at the UC Davis School of Law.
The Privacy Rule doesn’t require doctors to disclose protected health information about a patient when state laws require reporting. But the rule allows them to disclose private health information when there’s a court order such as a warrant or subpoena, says Ms. Ikemoto.
“Providers should make sure that patient information remains in records that are HIPAA protected. Some states, including California, have enacted privacy laws that are more protective of patient information,” she says.
The Department of Health & Human Services issued new guidance in June for health care professionals to clarify what the Privacy Rule requires them to report in light of the restrictive abortion laws.
9. I practice in a state where abortion is legal. Can I be extradited to another state if I’m prosecuted for crimes relating to reproductive health services?
Yes, generally, if your state allows it, says Ms. Florey. States have a constitutional obligation to extradite citizens of a different state if that person’s home state asks for that, but states do not have to extradite their own citizens.
However, traditionally, states have cooperated with extradition requests and most states have laws in place providing for extradition in those circumstances, which they could change to exempt abortion providers.
A handful of states – Connecticut, New York, Delaware, and New Jersey – have passed laws specifically shielding medical providers from being prosecuted under abortion restrictions passed in other states.
Governors in Massachusetts, Minnesota, New Mexico, and Nevada have issued executive orders saying they will not extradite abortion providers to states that have banned abortion provision, and that state employees will generally not comply with those out-of-state investigations.
10. Should I increase my malpractice insurance in anticipation of more potential legal problems from patients coming to me from antiabortion states?
Yes, I would recommend that doctors increase their malpractice coverage because of the increased legal risks they could face.
“It’s possible that a state might file a lawsuit against out-of-state abortion providers. Criminal prosecution is also a possibility, but the obstacles to prosecuting a case against an out-of-state provider would be considerable, especially if their home state has passed laws shielding abortion providers,” says Ms. Florey.
Individual malpractice claims or some sort of private enforcement action in a state that has established one would be more likely, she adds.
Ms. Florey advises doctors to monitor this rapidly evolving area of law. “Everything I am saying today could change with a single Supreme Court case. There will also be this kind of push/pull as antiabortion states try to crack down on out-of-state residents who provide or assist in abortion and physicians’ home states that try to protect them from legal consequences.”
A version of this article first appeared on Medscape.com.
Doctors in states where abortion is legal are likely to be the next target for antiabortion activists who want to deter residents from seeking abortions across state lines, say legal experts.
Antiabortion legislators in several states are mounting efforts to clamp down on out-of-state abortions, which they view as a legal loophole.
Nineteen states have already banned the use of telemedicine to prescribe medication abortion by requiring the clinician to be physically present when the medication is administered. These states include Arizona, Louisiana, Tennessee, and Texas, which also recently criminalized sending abortion pills through the mail.
Some state legislators plan to introduce legislation based on a Texas abortion ban enacted last year in which private citizens can sue anyone who assists state residents in obtaining an out-of-state abortion.
Meanwhile, legislators in states including New York where abortion is legal have introduced bills to shield doctors involved in reproductive care from possible negative actions by medical malpractice companies and professional misconduct charges.
This news organization asked legal experts for advice on how doctors can protect themselves and still provide appropriate medical care in this rapidly changing legal landscape. Here’s what they had to say.
1. What if patients from states where abortion is banned want to come to my practice in a legal state? What should I be aware of?
“Doctors should do what they think is medically necessary, but they should be aware of potential criminal and/or civil consequences in a patient’s home state, especially if those states have staked out more extreme positions on abortion such as Texas, Oklahoma, and Louisiana,” says Katherine Florey, JD, a professor at the University of California, Davis, School of Law.
The patient’s home state would need to have criminal laws in place that would explicitly ban residents from obtaining out-of-state abortions. “Probably the greater risk on the criminal front is that many states have existing laws that don’t specify their geographical reach but that could be construed to allow for criminal jurisdiction over out-of-state providers who help residents in obtaining an abortion,” she says.
However, criminal laws would be harder to enforce because of constitutional obstacles that would require the U.S. Supreme Court to resolve in a court case. Another barrier is that criminal law typically requires that a significant element of the offense take place in the prosecuting state, says Ms. Florey.
2. Am I likely to be sued by a patient from a state with an abortion ban?
“It’s more likely that states with abortion bans will pursue civil liability cases, particularly in states such as Texas and Oklahoma that allow private individuals to pursue lawsuits against individuals providing or assisting with abortions.”
Such liability is particularly appealing to antiabortion states because it allows them to target abortion care providers rather than the women seeking abortions, an approach that might be both more politically palatable and more effective in achieving abortion-restriction goals, says Ms. Florey.
“It’s not just the threat of jail time that can deter physicians from providing abortions. They can face significant career consequences from civil liability, including being reported to their medical licensing boards and having their malpractice insurance premiums increase,” says Ms. Florey.
3. What if I provide ‘abortion pill’ prescriptions by telemedicine to a patient in another state?
Doctors need to know what the rules are in the patient’s home state because states generally regard where the patient is located as where telemedicine is legally conducted, says Ms. Florey. “It’s more problematic to conduct telemedicine in states where it’s illegal. It could be viewed legally as if the doctor were prescribing a medication abortion in the patient’s state.”
Ms. Florey also advises doctors to find out whether the patient’s home state bans medication abortions. “The courts or states could decide that the physician is practicing in the jurisdiction where the patient is located even if care is provided remotely. In that case, the doctor would have to comply with all the laws of that state.”
She recommends that doctors counsel patients seeking medication abortions to come to the state where abortion is legal and get on their computers there.
“It’s not a perfect solution, but it provides more legal protection than providing medication abortion across state lines,” says Ms. Florey.
4. Can doctors be sued by patients for not informing them of the full range of treatment options, including abortion, when their health is at risk?
If the doctor is in a state that has banned abortion and the procedure is illegal, they can’t recommend something that the law doesn’t allow, says Ms. Florey.
It’s a tough call for doctors in states where abortion is illegal because they could get into legal trouble if they counsel a woman to get an abortion and the court later deems it was not medically necessary, says Ms. Florey.
But doctors could also get into legal trouble if they don’t counsel a woman to get an abortion if her life is in danger and she meets the exception in the abortion ban.
“Ultimately, I think doctors have to follow their conscience and best medical judgment but recognize the legal hazards that exist. If a physician is seeing a lot of out-of-state patients from a single jurisdiction (such as a neighboring state), it would be best to consult with an attorney from that state,” advises Ms. Florey.
5. If a patient from another state comes to me (in a legal state) for abortion care, am I required to provide them with any warnings, information, and so on?
Doctors may be required by some antiabortion states to mention certain risks, especially to the mother’s mental health, that could arise from abortions even if they are not well-supported by evidence, says Ms. Florey.
If a warning is required in a patient’s home state and there were complications from the procedure or the patient became depressed, it could be grounds for a civil lawsuit, says Ms. Florey.
“There is a Montana case, for example, where the plaintiff sued for malpractice after having an abortion. She alleged that she was given medically inaccurate information about the fetus’s HIV status, but she also claimed that she wasn’t informed that she might become depressed as a result of the abortion,” says Ms. Florey. (The case was ultimately decided on a different ground.)
6. What about complications from abortion care that I provided to a patient from another state? What are my responsibilities and risks? Can I be sued for malpractice when the patient returns to her home state?
If physicians can’t monitor the patients after their visit and something goes wrong, the doctors are at greater risk of negligence and being sued for malpractice in the patient’s home state, says Ms. Florey.
She recommends that doctors ask patients to stay for monitoring after the procedure. “I realize that may not be possible for all patients, but it’s a much safer alternative,” says Ms. Florey.
Otherwise, if the doctor communicates with the patient about the complications in her antiabortion state, the state’s courts could view the doctor as having ties to the state and claim they have jurisdiction in the case and apply the state’s laws, says Ms. Florey.
“Criminal jurisdiction would be more of stretch because the central conduct happened out of state, but states could still try to prosecute a case,” she says.
7. If a patient comes to me from another state, are there any residency requirements, or does the person need to find residence in my state for a period of time? Am I responsible for knowing their arrangements?
Generally, as a constitutional principle, a person can go to another state and have the services that a resident is entitled to, says Ms. Florey.
“States can’t normally discriminate against patients from out of state, so it’s not a residency requirement unless a state imposes one. If a state did that, it would probably be unconstitutional,” she says.
It would be less risky legally, though, if a patient remains in the state where she received abortion care for a significant period of time, says Ms. Florey.
8. How can I protect the privacy of patients’ medical records if they received an abortion or other reproductive care in the state?
To some extent, HIPAA accommodates state laws that mandate reporting of patient information, says Lisa C. Ikemoto, JD, also a professor at the UC Davis School of Law.
The Privacy Rule doesn’t require doctors to disclose protected health information about a patient when state laws require reporting. But the rule allows them to disclose private health information when there’s a court order such as a warrant or subpoena, says Ms. Ikemoto.
“Providers should make sure that patient information remains in records that are HIPAA protected. Some states, including California, have enacted privacy laws that are more protective of patient information,” she says.
The Department of Health & Human Services issued new guidance in June for health care professionals to clarify what the Privacy Rule requires them to report in light of the restrictive abortion laws.
9. I practice in a state where abortion is legal. Can I be extradited to another state if I’m prosecuted for crimes relating to reproductive health services?
Yes, generally, if your state allows it, says Ms. Florey. States have a constitutional obligation to extradite citizens of a different state if that person’s home state asks for that, but states do not have to extradite their own citizens.
However, traditionally, states have cooperated with extradition requests and most states have laws in place providing for extradition in those circumstances, which they could change to exempt abortion providers.
A handful of states – Connecticut, New York, Delaware, and New Jersey – have passed laws specifically shielding medical providers from being prosecuted under abortion restrictions passed in other states.
Governors in Massachusetts, Minnesota, New Mexico, and Nevada have issued executive orders saying they will not extradite abortion providers to states that have banned abortion provision, and that state employees will generally not comply with those out-of-state investigations.
10. Should I increase my malpractice insurance in anticipation of more potential legal problems from patients coming to me from antiabortion states?
Yes, I would recommend that doctors increase their malpractice coverage because of the increased legal risks they could face.
“It’s possible that a state might file a lawsuit against out-of-state abortion providers. Criminal prosecution is also a possibility, but the obstacles to prosecuting a case against an out-of-state provider would be considerable, especially if their home state has passed laws shielding abortion providers,” says Ms. Florey.
Individual malpractice claims or some sort of private enforcement action in a state that has established one would be more likely, she adds.
Ms. Florey advises doctors to monitor this rapidly evolving area of law. “Everything I am saying today could change with a single Supreme Court case. There will also be this kind of push/pull as antiabortion states try to crack down on out-of-state residents who provide or assist in abortion and physicians’ home states that try to protect them from legal consequences.”
A version of this article first appeared on Medscape.com.
Should patients undergoing surgical treatment for cervical lesions also receive an HPV vaccination?
Human papillomavirus (HPV) vaccine given around the time women have surgery for precancerous cervical lesions might lead to a reduction in the risk of lesions returning, as well as other HPV-related diseases, but the effects of this remain unclear.
The authors of the new study, published in The BMJ, explained that women who have been treated for high-grade cervical intra-epithelial neoplasia (CIN) have a “lifelong residual high risk of cervical cancer and other malignancies related to HPV infection,” and some research suggests that giving a preventive HPV vaccine alongside treatment for CIN might help to “reduce the risk in these women.”
HPV vaccination is highly effective at preventing the development of precancerous cervical lesions, CIN, and in the U.K., HPV vaccination is offered to girls and boys around the age of 12 or 13.
Eluned Hughes, head of information and engagement at Jo’s Cervical Cancer Trust, said: “Recent evidence has found that cases of cervical cancer have fallen 87% since the introduction of the HPV vaccine program in U.K. schools in 2008.”
“However, women over the age of 27, for whom the vaccine was not available, remain at increased risk of cervical cancer,” she highlighted.
Significant risk of bias and scarcity of data
In the study, researchers set out to explore the efficacy of HPV vaccination on the risk of HPV infection and recurrent diseases related to HPV infection in individuals undergoing local surgical treatment of preinvasive genital disease.
The systematic review and meta-analysis, led by researchers at Imperial College London, screened data from PubMed (Medline), Scopus, Cochrane, Web of Science, and ClinicalTrials.gov from inception to March 31, 2021.
The researchers analyzed the results of 18 studies – two randomized controlled trials (RCTs), 12 observational studies, and four post-hoc analyses of RCTs.
The authors said that the two RCTs were classified as low risk of bias, while in the observational studies and post-hoc analyses, risk of bias was moderate for seven, serious for seven, and critical for two. Average length of follow-up was 36 months.
There was a reduction of 57% in the risk of recurrence of high-grade pre-invasive disease (CIN2+) in individuals who were vaccinated, compared with those who were not vaccinated. “The effect estimate was “even more pronounced” – a relative 74% reduction – when the risk of recurrence of CIN2+ was assessed for disease related to the two high-risk HPV types – HPV16 and HPV18,” explained the authors.
However, the researchers noted that these effects are unclear because of the “scarcity of data” and the “moderate to high overall risk of bias” of the available studies.
Quality of evidence inconclusive – more trials needed
With regards to CIN3, the risk of recurrence of was also reduced in patients who were vaccinated, but there was a high level of uncertainty about the quality of this evidence, cautioned the authors.
Evidence was also lacking on the benefit of HPV vaccination for recurrence of vulvar, vaginal, and anal lesions, as well as genital warts.
Analysis of the post-hoc studies from randomized controlled trial data with historic vaccination at randomization before the development of the disease reported inconsistent results, the authors said.
Several study limitations were acknowledged by the authors, including that most of the studies were observational, of low to moderate quality, and with relatively short follow-up times, which they pointed out prevented assessment of long-term effects. In addition, the average age of participants was not provided in most studies, and factors such as smoking – associated with a higher risk of recurrence – were not controlled for in many studies.
“HPV vaccination might reduce the risk of recurrence of CIN, in particular when related to HPV16 or HPV18, in women treated with local excision,” they concluded. However, they cautioned that “quality of evidence indicated that the data were inconclusive.”
“Large, appropriately powered, randomized controlled trials are required to establish the effectiveness of adjuvant HPV vaccination at the time of local surgical treatment of CIN,” they recommended.
“Given that the incidence of recurrence of high-grade disease is low in quality assured national screening programs, such as in the United Kingdom, absolute risks and a cost effectiveness analysis would be important in determining the implementation strategy of HPV vaccination after treatment,” the authors said.
Ms. Hughes said that the charity was pleased to see emerging research into the value of using the HPV vaccine to prevent the recurrence of cervical cell changes. She said that the charity looks forward to seeing “further large-scale studies into the effectiveness of this method.”
In the meantime, the charity encourages all women and other people with a cervix to attend their cervical screening and for young people to have the HPV vaccination when invited, as “these are the best tools we currently have to prevent cervical cancer,” she said.
A version of this article first appeared on Medscape UK.
Human papillomavirus (HPV) vaccine given around the time women have surgery for precancerous cervical lesions might lead to a reduction in the risk of lesions returning, as well as other HPV-related diseases, but the effects of this remain unclear.
The authors of the new study, published in The BMJ, explained that women who have been treated for high-grade cervical intra-epithelial neoplasia (CIN) have a “lifelong residual high risk of cervical cancer and other malignancies related to HPV infection,” and some research suggests that giving a preventive HPV vaccine alongside treatment for CIN might help to “reduce the risk in these women.”
HPV vaccination is highly effective at preventing the development of precancerous cervical lesions, CIN, and in the U.K., HPV vaccination is offered to girls and boys around the age of 12 or 13.
Eluned Hughes, head of information and engagement at Jo’s Cervical Cancer Trust, said: “Recent evidence has found that cases of cervical cancer have fallen 87% since the introduction of the HPV vaccine program in U.K. schools in 2008.”
“However, women over the age of 27, for whom the vaccine was not available, remain at increased risk of cervical cancer,” she highlighted.
Significant risk of bias and scarcity of data
In the study, researchers set out to explore the efficacy of HPV vaccination on the risk of HPV infection and recurrent diseases related to HPV infection in individuals undergoing local surgical treatment of preinvasive genital disease.
The systematic review and meta-analysis, led by researchers at Imperial College London, screened data from PubMed (Medline), Scopus, Cochrane, Web of Science, and ClinicalTrials.gov from inception to March 31, 2021.
The researchers analyzed the results of 18 studies – two randomized controlled trials (RCTs), 12 observational studies, and four post-hoc analyses of RCTs.
The authors said that the two RCTs were classified as low risk of bias, while in the observational studies and post-hoc analyses, risk of bias was moderate for seven, serious for seven, and critical for two. Average length of follow-up was 36 months.
There was a reduction of 57% in the risk of recurrence of high-grade pre-invasive disease (CIN2+) in individuals who were vaccinated, compared with those who were not vaccinated. “The effect estimate was “even more pronounced” – a relative 74% reduction – when the risk of recurrence of CIN2+ was assessed for disease related to the two high-risk HPV types – HPV16 and HPV18,” explained the authors.
However, the researchers noted that these effects are unclear because of the “scarcity of data” and the “moderate to high overall risk of bias” of the available studies.
Quality of evidence inconclusive – more trials needed
With regards to CIN3, the risk of recurrence of was also reduced in patients who were vaccinated, but there was a high level of uncertainty about the quality of this evidence, cautioned the authors.
Evidence was also lacking on the benefit of HPV vaccination for recurrence of vulvar, vaginal, and anal lesions, as well as genital warts.
Analysis of the post-hoc studies from randomized controlled trial data with historic vaccination at randomization before the development of the disease reported inconsistent results, the authors said.
Several study limitations were acknowledged by the authors, including that most of the studies were observational, of low to moderate quality, and with relatively short follow-up times, which they pointed out prevented assessment of long-term effects. In addition, the average age of participants was not provided in most studies, and factors such as smoking – associated with a higher risk of recurrence – were not controlled for in many studies.
“HPV vaccination might reduce the risk of recurrence of CIN, in particular when related to HPV16 or HPV18, in women treated with local excision,” they concluded. However, they cautioned that “quality of evidence indicated that the data were inconclusive.”
“Large, appropriately powered, randomized controlled trials are required to establish the effectiveness of adjuvant HPV vaccination at the time of local surgical treatment of CIN,” they recommended.
“Given that the incidence of recurrence of high-grade disease is low in quality assured national screening programs, such as in the United Kingdom, absolute risks and a cost effectiveness analysis would be important in determining the implementation strategy of HPV vaccination after treatment,” the authors said.
Ms. Hughes said that the charity was pleased to see emerging research into the value of using the HPV vaccine to prevent the recurrence of cervical cell changes. She said that the charity looks forward to seeing “further large-scale studies into the effectiveness of this method.”
In the meantime, the charity encourages all women and other people with a cervix to attend their cervical screening and for young people to have the HPV vaccination when invited, as “these are the best tools we currently have to prevent cervical cancer,” she said.
A version of this article first appeared on Medscape UK.
Human papillomavirus (HPV) vaccine given around the time women have surgery for precancerous cervical lesions might lead to a reduction in the risk of lesions returning, as well as other HPV-related diseases, but the effects of this remain unclear.
The authors of the new study, published in The BMJ, explained that women who have been treated for high-grade cervical intra-epithelial neoplasia (CIN) have a “lifelong residual high risk of cervical cancer and other malignancies related to HPV infection,” and some research suggests that giving a preventive HPV vaccine alongside treatment for CIN might help to “reduce the risk in these women.”
HPV vaccination is highly effective at preventing the development of precancerous cervical lesions, CIN, and in the U.K., HPV vaccination is offered to girls and boys around the age of 12 or 13.
Eluned Hughes, head of information and engagement at Jo’s Cervical Cancer Trust, said: “Recent evidence has found that cases of cervical cancer have fallen 87% since the introduction of the HPV vaccine program in U.K. schools in 2008.”
“However, women over the age of 27, for whom the vaccine was not available, remain at increased risk of cervical cancer,” she highlighted.
Significant risk of bias and scarcity of data
In the study, researchers set out to explore the efficacy of HPV vaccination on the risk of HPV infection and recurrent diseases related to HPV infection in individuals undergoing local surgical treatment of preinvasive genital disease.
The systematic review and meta-analysis, led by researchers at Imperial College London, screened data from PubMed (Medline), Scopus, Cochrane, Web of Science, and ClinicalTrials.gov from inception to March 31, 2021.
The researchers analyzed the results of 18 studies – two randomized controlled trials (RCTs), 12 observational studies, and four post-hoc analyses of RCTs.
The authors said that the two RCTs were classified as low risk of bias, while in the observational studies and post-hoc analyses, risk of bias was moderate for seven, serious for seven, and critical for two. Average length of follow-up was 36 months.
There was a reduction of 57% in the risk of recurrence of high-grade pre-invasive disease (CIN2+) in individuals who were vaccinated, compared with those who were not vaccinated. “The effect estimate was “even more pronounced” – a relative 74% reduction – when the risk of recurrence of CIN2+ was assessed for disease related to the two high-risk HPV types – HPV16 and HPV18,” explained the authors.
However, the researchers noted that these effects are unclear because of the “scarcity of data” and the “moderate to high overall risk of bias” of the available studies.
Quality of evidence inconclusive – more trials needed
With regards to CIN3, the risk of recurrence of was also reduced in patients who were vaccinated, but there was a high level of uncertainty about the quality of this evidence, cautioned the authors.
Evidence was also lacking on the benefit of HPV vaccination for recurrence of vulvar, vaginal, and anal lesions, as well as genital warts.
Analysis of the post-hoc studies from randomized controlled trial data with historic vaccination at randomization before the development of the disease reported inconsistent results, the authors said.
Several study limitations were acknowledged by the authors, including that most of the studies were observational, of low to moderate quality, and with relatively short follow-up times, which they pointed out prevented assessment of long-term effects. In addition, the average age of participants was not provided in most studies, and factors such as smoking – associated with a higher risk of recurrence – were not controlled for in many studies.
“HPV vaccination might reduce the risk of recurrence of CIN, in particular when related to HPV16 or HPV18, in women treated with local excision,” they concluded. However, they cautioned that “quality of evidence indicated that the data were inconclusive.”
“Large, appropriately powered, randomized controlled trials are required to establish the effectiveness of adjuvant HPV vaccination at the time of local surgical treatment of CIN,” they recommended.
“Given that the incidence of recurrence of high-grade disease is low in quality assured national screening programs, such as in the United Kingdom, absolute risks and a cost effectiveness analysis would be important in determining the implementation strategy of HPV vaccination after treatment,” the authors said.
Ms. Hughes said that the charity was pleased to see emerging research into the value of using the HPV vaccine to prevent the recurrence of cervical cell changes. She said that the charity looks forward to seeing “further large-scale studies into the effectiveness of this method.”
In the meantime, the charity encourages all women and other people with a cervix to attend their cervical screening and for young people to have the HPV vaccination when invited, as “these are the best tools we currently have to prevent cervical cancer,” she said.
A version of this article first appeared on Medscape UK.
The gut microbes have spoken: All fiber is good fiber
Finding a fiber of good moral fiber
If you’ve ever wandered into the supplement aisle at your local grocery store, you’ve probably noticed an overabundance of fiber supplements that claim to do this for you and benefit that. Since there’s no Food and Drug Administration regulation on fiber supplements, manufacturers are free to (and do) make whatever wild claims they like. And much like choosing which of 500 shows to watch on Netflix, when you’re spoiled for choice, it can be difficult to pick.
Enter a team of molecular geneticists and microbiologists from Duke University. They can’t tell you what show to watch next, but they can tell you which fiber to choose, thanks to their new study. And the answer? Yes.
Well that’s not very helpful, but let us explain. For their study, a group of 28 received three of the main fiber supplements (inulin, dextrin, and galactooligosaccharides) for a week each, followed by a week off of fibers for their gut to return to baseline until they’d received all three. Those who consumed the least fiber at baseline saw the greatest benefit from fiber supplementation, with no appreciable difference between the three types. It was the same story for study participants who already consumed enough fiber; because their guts already hosted a more-optimal microbiome, the type of supplement didn’t matter. The benefits were the same across the board.
In an additional study, the Duke researchers found that gut microbiomes reacted to new fiber within a day, being primed to consume fiber on the first dose and digesting it more quickly on the second fiber dose.
The results, the researchers pointed out, make sense, since the average American only consumes 20%-40% of their daily recommended supply of fiber. Our digestive systems aren’t picky; they just want more, so go out there and choose whatever fiber you’d like. Do that, and then feel free to eat as many double bacon cheeseburgers as you’d like. That is the pinnacle of diet right there. Dietitians literally could not complain about it.
Jarlsberg vs. Camembert: This time it’s skeletal
Fiber is fabulous, of course, but the road to dietary health and wellness fulfillment takes us to many other, equally wondrous places. Hey, look! This next exit is covered with cheese.
All the cheeses are here, from Abbaye de Belloc to Zwitser, and there, right between the jalapeno cheddar and the Jermi tortes you’ll find Jarlsberg, a mild, semisoft, nutty-flavored cheese that comes from Jarlsberg in eastern Norway. A recent study also suggests that Jarlsberg may help to prevent osteopenia and osteoporosis.
A group of Norwegian investigators gathered together 66 healthy women and gave them a daily portion of either Jarlsberg or Camembert for 6 weeks, at which point the Camembert group was switched to Jarlsberg for another 6 weeks.
The research team choose Camembert because of its similarity to Jarlsberg in fat and protein content. Jarlsberg, however, also is rich in vitamin K2, which is important for bone health, and a substance known as DHNA, which “might combat bone thinning and increase bone tissue formation,” they said in a Eurekalert release.
After the first 6 weeks, blood levels of osteocalcin; vitamin K2; and PINP, a peptide involved in bone turnover, were significantly higher in the Jarlsberg group only. All those measures rose significantly after the switch from Camembert to Jarlsberg, while levels of total and LDL cholesterol “fell significantly in the Camembert group after they switched to Jarlsberg,” the team added.
But wait! There’s more! HbA1c fell significantly among those initially eating the Jarlsberg but rose sharply in those eating Camembert. Do you see where this is going? After the Camembert group made the switch to Jarlsberg, their HbA1c levels fell significantly as well.
So it’s not just a cheese thing: The effects are specific to Jarlsberg. Can you guess what we’re having for lunch? Double bacon and fiber Jarlsbergers. Mmm, Jarlsburgers.
Luck be a lady: The mother of twins
It’s widely believed that women who have twins must be more fertile, giving birth to more than one child at a time. Some studies have supported the idea, but more recent work is refuting that claim. In actuality, it might just be more statistics and luck than fertility after all.
Those earlier studies supporting fertility didn’t specify whether the chances of twin births were based on the ability to produce more than one egg at a time or on the number of births that women had overall. Looking at 100,000 preindustrial European births, before contraception was available, researchers from Norway, Germany, France, and the United Kingdom found that the number of total births, twins included, makes all the difference.
“When a woman gives birth several times, the chances increase that at least one of these births will be a twin birth,” investigator Gine Roll Skjærvø of the Norwegian University of Science and Technology said in a written statement.
Since twins occur in 1%-3% of all births, the more births that a woman has, the better her chances of giving birth to twins. The researchers compared it to playing the lottery. You buy enough tickets, eventually your numbers are going to come up. Despite that, however, they found that women who give birth to twins give birth less often than those who don’t have twins. Which raises the idea of sheer luck.
The researchers said that there’s still a lot to uncover in twin births, noting that “uncritically comparing groups of women with and without twins can trick us into believing the opposite of what is really true. These groupings may either hide the effects of twinning and fertility genes where they exist, or vice versa, create the illusion of these if they do not exist.”
For now, this new research claims that it’s basically a lottery. And women who give birth to twins hit the jackpot.
Those with low wages may be earning future memory loss
Not only are low wages detrimental to our souls, hopes, and dreams, but a new study shows that low wages also are linked to quicker memory decline later in life. Sustained low wages not only cause stress and food insecurity in the lives of many, but they also can cause diseases such as depression, obesity, and high blood pressure, which are risk factors for cognitive aging.
The study was conducted using records from the Health and Retirement Study for the years 1992-2016 and focused on 2,879 adults born between 1936 and 1941. The participants were divided into three groups: those who never earned low wages, those who sometimes did, and those who always did.
The investigators found that workers who earned sustained low wages – defined as an hourly wage lower than two-thirds of the federal median wage for the corresponding year – “experienced significantly faster memory decline in older age” than did those who never earned low wages.
There are signs of inflation everywhere we look these days, but many people are not earning higher wages to compensate for the extra expenses. “Increasing the federal minimum wage, for example to $15 per hour, remains a gridlock issue in Congress,” lead author Katrina Kezios of the Columbia University Mailman School of Public Health, said in a statement released by the university.
If only salaries would rise instead of prices for once.
Finding a fiber of good moral fiber
If you’ve ever wandered into the supplement aisle at your local grocery store, you’ve probably noticed an overabundance of fiber supplements that claim to do this for you and benefit that. Since there’s no Food and Drug Administration regulation on fiber supplements, manufacturers are free to (and do) make whatever wild claims they like. And much like choosing which of 500 shows to watch on Netflix, when you’re spoiled for choice, it can be difficult to pick.
Enter a team of molecular geneticists and microbiologists from Duke University. They can’t tell you what show to watch next, but they can tell you which fiber to choose, thanks to their new study. And the answer? Yes.
Well that’s not very helpful, but let us explain. For their study, a group of 28 received three of the main fiber supplements (inulin, dextrin, and galactooligosaccharides) for a week each, followed by a week off of fibers for their gut to return to baseline until they’d received all three. Those who consumed the least fiber at baseline saw the greatest benefit from fiber supplementation, with no appreciable difference between the three types. It was the same story for study participants who already consumed enough fiber; because their guts already hosted a more-optimal microbiome, the type of supplement didn’t matter. The benefits were the same across the board.
In an additional study, the Duke researchers found that gut microbiomes reacted to new fiber within a day, being primed to consume fiber on the first dose and digesting it more quickly on the second fiber dose.
The results, the researchers pointed out, make sense, since the average American only consumes 20%-40% of their daily recommended supply of fiber. Our digestive systems aren’t picky; they just want more, so go out there and choose whatever fiber you’d like. Do that, and then feel free to eat as many double bacon cheeseburgers as you’d like. That is the pinnacle of diet right there. Dietitians literally could not complain about it.
Jarlsberg vs. Camembert: This time it’s skeletal
Fiber is fabulous, of course, but the road to dietary health and wellness fulfillment takes us to many other, equally wondrous places. Hey, look! This next exit is covered with cheese.
All the cheeses are here, from Abbaye de Belloc to Zwitser, and there, right between the jalapeno cheddar and the Jermi tortes you’ll find Jarlsberg, a mild, semisoft, nutty-flavored cheese that comes from Jarlsberg in eastern Norway. A recent study also suggests that Jarlsberg may help to prevent osteopenia and osteoporosis.
A group of Norwegian investigators gathered together 66 healthy women and gave them a daily portion of either Jarlsberg or Camembert for 6 weeks, at which point the Camembert group was switched to Jarlsberg for another 6 weeks.
The research team choose Camembert because of its similarity to Jarlsberg in fat and protein content. Jarlsberg, however, also is rich in vitamin K2, which is important for bone health, and a substance known as DHNA, which “might combat bone thinning and increase bone tissue formation,” they said in a Eurekalert release.
After the first 6 weeks, blood levels of osteocalcin; vitamin K2; and PINP, a peptide involved in bone turnover, were significantly higher in the Jarlsberg group only. All those measures rose significantly after the switch from Camembert to Jarlsberg, while levels of total and LDL cholesterol “fell significantly in the Camembert group after they switched to Jarlsberg,” the team added.
But wait! There’s more! HbA1c fell significantly among those initially eating the Jarlsberg but rose sharply in those eating Camembert. Do you see where this is going? After the Camembert group made the switch to Jarlsberg, their HbA1c levels fell significantly as well.
So it’s not just a cheese thing: The effects are specific to Jarlsberg. Can you guess what we’re having for lunch? Double bacon and fiber Jarlsbergers. Mmm, Jarlsburgers.
Luck be a lady: The mother of twins
It’s widely believed that women who have twins must be more fertile, giving birth to more than one child at a time. Some studies have supported the idea, but more recent work is refuting that claim. In actuality, it might just be more statistics and luck than fertility after all.
Those earlier studies supporting fertility didn’t specify whether the chances of twin births were based on the ability to produce more than one egg at a time or on the number of births that women had overall. Looking at 100,000 preindustrial European births, before contraception was available, researchers from Norway, Germany, France, and the United Kingdom found that the number of total births, twins included, makes all the difference.
“When a woman gives birth several times, the chances increase that at least one of these births will be a twin birth,” investigator Gine Roll Skjærvø of the Norwegian University of Science and Technology said in a written statement.
Since twins occur in 1%-3% of all births, the more births that a woman has, the better her chances of giving birth to twins. The researchers compared it to playing the lottery. You buy enough tickets, eventually your numbers are going to come up. Despite that, however, they found that women who give birth to twins give birth less often than those who don’t have twins. Which raises the idea of sheer luck.
The researchers said that there’s still a lot to uncover in twin births, noting that “uncritically comparing groups of women with and without twins can trick us into believing the opposite of what is really true. These groupings may either hide the effects of twinning and fertility genes where they exist, or vice versa, create the illusion of these if they do not exist.”
For now, this new research claims that it’s basically a lottery. And women who give birth to twins hit the jackpot.
Those with low wages may be earning future memory loss
Not only are low wages detrimental to our souls, hopes, and dreams, but a new study shows that low wages also are linked to quicker memory decline later in life. Sustained low wages not only cause stress and food insecurity in the lives of many, but they also can cause diseases such as depression, obesity, and high blood pressure, which are risk factors for cognitive aging.
The study was conducted using records from the Health and Retirement Study for the years 1992-2016 and focused on 2,879 adults born between 1936 and 1941. The participants were divided into three groups: those who never earned low wages, those who sometimes did, and those who always did.
The investigators found that workers who earned sustained low wages – defined as an hourly wage lower than two-thirds of the federal median wage for the corresponding year – “experienced significantly faster memory decline in older age” than did those who never earned low wages.
There are signs of inflation everywhere we look these days, but many people are not earning higher wages to compensate for the extra expenses. “Increasing the federal minimum wage, for example to $15 per hour, remains a gridlock issue in Congress,” lead author Katrina Kezios of the Columbia University Mailman School of Public Health, said in a statement released by the university.
If only salaries would rise instead of prices for once.
Finding a fiber of good moral fiber
If you’ve ever wandered into the supplement aisle at your local grocery store, you’ve probably noticed an overabundance of fiber supplements that claim to do this for you and benefit that. Since there’s no Food and Drug Administration regulation on fiber supplements, manufacturers are free to (and do) make whatever wild claims they like. And much like choosing which of 500 shows to watch on Netflix, when you’re spoiled for choice, it can be difficult to pick.
Enter a team of molecular geneticists and microbiologists from Duke University. They can’t tell you what show to watch next, but they can tell you which fiber to choose, thanks to their new study. And the answer? Yes.
Well that’s not very helpful, but let us explain. For their study, a group of 28 received three of the main fiber supplements (inulin, dextrin, and galactooligosaccharides) for a week each, followed by a week off of fibers for their gut to return to baseline until they’d received all three. Those who consumed the least fiber at baseline saw the greatest benefit from fiber supplementation, with no appreciable difference between the three types. It was the same story for study participants who already consumed enough fiber; because their guts already hosted a more-optimal microbiome, the type of supplement didn’t matter. The benefits were the same across the board.
In an additional study, the Duke researchers found that gut microbiomes reacted to new fiber within a day, being primed to consume fiber on the first dose and digesting it more quickly on the second fiber dose.
The results, the researchers pointed out, make sense, since the average American only consumes 20%-40% of their daily recommended supply of fiber. Our digestive systems aren’t picky; they just want more, so go out there and choose whatever fiber you’d like. Do that, and then feel free to eat as many double bacon cheeseburgers as you’d like. That is the pinnacle of diet right there. Dietitians literally could not complain about it.
Jarlsberg vs. Camembert: This time it’s skeletal
Fiber is fabulous, of course, but the road to dietary health and wellness fulfillment takes us to many other, equally wondrous places. Hey, look! This next exit is covered with cheese.
All the cheeses are here, from Abbaye de Belloc to Zwitser, and there, right between the jalapeno cheddar and the Jermi tortes you’ll find Jarlsberg, a mild, semisoft, nutty-flavored cheese that comes from Jarlsberg in eastern Norway. A recent study also suggests that Jarlsberg may help to prevent osteopenia and osteoporosis.
A group of Norwegian investigators gathered together 66 healthy women and gave them a daily portion of either Jarlsberg or Camembert for 6 weeks, at which point the Camembert group was switched to Jarlsberg for another 6 weeks.
The research team choose Camembert because of its similarity to Jarlsberg in fat and protein content. Jarlsberg, however, also is rich in vitamin K2, which is important for bone health, and a substance known as DHNA, which “might combat bone thinning and increase bone tissue formation,” they said in a Eurekalert release.
After the first 6 weeks, blood levels of osteocalcin; vitamin K2; and PINP, a peptide involved in bone turnover, were significantly higher in the Jarlsberg group only. All those measures rose significantly after the switch from Camembert to Jarlsberg, while levels of total and LDL cholesterol “fell significantly in the Camembert group after they switched to Jarlsberg,” the team added.
But wait! There’s more! HbA1c fell significantly among those initially eating the Jarlsberg but rose sharply in those eating Camembert. Do you see where this is going? After the Camembert group made the switch to Jarlsberg, their HbA1c levels fell significantly as well.
So it’s not just a cheese thing: The effects are specific to Jarlsberg. Can you guess what we’re having for lunch? Double bacon and fiber Jarlsbergers. Mmm, Jarlsburgers.
Luck be a lady: The mother of twins
It’s widely believed that women who have twins must be more fertile, giving birth to more than one child at a time. Some studies have supported the idea, but more recent work is refuting that claim. In actuality, it might just be more statistics and luck than fertility after all.
Those earlier studies supporting fertility didn’t specify whether the chances of twin births were based on the ability to produce more than one egg at a time or on the number of births that women had overall. Looking at 100,000 preindustrial European births, before contraception was available, researchers from Norway, Germany, France, and the United Kingdom found that the number of total births, twins included, makes all the difference.
“When a woman gives birth several times, the chances increase that at least one of these births will be a twin birth,” investigator Gine Roll Skjærvø of the Norwegian University of Science and Technology said in a written statement.
Since twins occur in 1%-3% of all births, the more births that a woman has, the better her chances of giving birth to twins. The researchers compared it to playing the lottery. You buy enough tickets, eventually your numbers are going to come up. Despite that, however, they found that women who give birth to twins give birth less often than those who don’t have twins. Which raises the idea of sheer luck.
The researchers said that there’s still a lot to uncover in twin births, noting that “uncritically comparing groups of women with and without twins can trick us into believing the opposite of what is really true. These groupings may either hide the effects of twinning and fertility genes where they exist, or vice versa, create the illusion of these if they do not exist.”
For now, this new research claims that it’s basically a lottery. And women who give birth to twins hit the jackpot.
Those with low wages may be earning future memory loss
Not only are low wages detrimental to our souls, hopes, and dreams, but a new study shows that low wages also are linked to quicker memory decline later in life. Sustained low wages not only cause stress and food insecurity in the lives of many, but they also can cause diseases such as depression, obesity, and high blood pressure, which are risk factors for cognitive aging.
The study was conducted using records from the Health and Retirement Study for the years 1992-2016 and focused on 2,879 adults born between 1936 and 1941. The participants were divided into three groups: those who never earned low wages, those who sometimes did, and those who always did.
The investigators found that workers who earned sustained low wages – defined as an hourly wage lower than two-thirds of the federal median wage for the corresponding year – “experienced significantly faster memory decline in older age” than did those who never earned low wages.
There are signs of inflation everywhere we look these days, but many people are not earning higher wages to compensate for the extra expenses. “Increasing the federal minimum wage, for example to $15 per hour, remains a gridlock issue in Congress,” lead author Katrina Kezios of the Columbia University Mailman School of Public Health, said in a statement released by the university.
If only salaries would rise instead of prices for once.
Burnout and stress of today: How do we cope?
Interestingly, the group that seems to be least impacted by this was health care administrators (with 12% of them planning on leaving their jobs).
I couldn’t stop thinking about these percentages.
I am reminded every day of the commitment and excellence of my colleagues in the health care field, and I do not want to lose them. I am hoping the following information and my thoughts on this topic will be helpful for those thinking about leaving health care.
Surgeon general’s burnout report
The surgeon general recently released a report on addressing health care worker burnout.2 It includes several very interesting and appropriate observations. I will summarize the most important ones here:
1. Our health depends on the well-being of our health workforce.
2. Direct harm to health care workers can lead to anxiety, depression, insomnia, and interpersonal and relationship struggles.
3. Health care workers experience exhaustion from providing overwhelming care and empathy.
4. Health care workers spend less time with patients and too much time with EHRs.
5. There are health workforce shortages.
The report is comprehensive, and everything in it is correct. The real issue is how does it go from being a report to true actionable items that we as health care professionals benefit from? I think in regards to exhaustion from overwhelming care responsibilities, and empathy fatigue, we need better boundaries.
Those who go into medicine, and especially those who go into primary care, always put the patients’ needs first. When operating in a broken system, it stays broken when individuals cover for the deficiencies in the system. Adding four extra patients every day because there is no one to refer them to with availability is injurious to the health care provider, and those providers who accept these additional patients will eventually be part of the 23% who want to leave their jobs. It feels awful to say no, but until the system stops accommodating there will not be substantial change.
The empathy drain
One of the unreported stresses of open access for patients through EHR communications is the empathy drain on physicians. When I see a patient in clinic with chronic symptoms or issues, I spend important time making sure we have a plan and an agreed upon time frame.
With the EHR, patients frequently send multiple messages for the same symptoms between visits. It is okay to redirect the patient and share that these issues will be discussed at length at appointments. My reasoning on this is that I think it is better for me to better care for myself and stay as the doctor for my patients, than always say yes to limitless needs and soon be looking for the off ramp.
The following statistic in the surgeon general’s report really hit home. For every hour of direct patient care, physicians currently spend 2 hours on the EHR system. Most practices allow 10%-20% of time for catch up, where with statistics like this it should be 50%. This concept is fully lost on administrators, or ignored.
It is only when we refuse to continue to accept and follow a broken system that it will change. A minority of internal medicine and family doctors (4.5% in 2018) practice in direct primary care models, where these issues are addressed. Unfortunately, this model as it is currently available is not an option for lower income patients.
A major theme in the surgeon general’s report was that administrative burdens need to be reduced by 75% by 2025. When I look at the report, I see the suggestions, I just don’t see how it will be achieved. Despite almost all clinics moving to the EHR, paperwork in the form of faxes and forms has increased.
A sweeping reform would be needed to eliminate daily faxes from PT offices, visiting nurse services, prior authorization, patients reminders from insurance companies, and disability forms from patients. I am glad that there is acknowledgment of the problem, but this change will take more than 3 years.
Takeaways
So what do we do?
Be good to yourself, and your colleagues. The pandemic has isolated us, which accelerates burnout.
Reach out to people you care about.
We are all feeling this. Set boundaries that allow you to care for yourself, and accept that you are doing your best, even if you can’t meet the needs of all your patients all the time.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Sinsky CA et al. Covid-related stress and work intentions in a sample of US health care workers. Mayo Clin Proc Innov Qual Outcomes. 2021 Dec;5(6):1165-73.
2. Addressing health worker burnout. The U.S. Surgeon General’s advisory on building a thriving health workforce.
Interestingly, the group that seems to be least impacted by this was health care administrators (with 12% of them planning on leaving their jobs).
I couldn’t stop thinking about these percentages.
I am reminded every day of the commitment and excellence of my colleagues in the health care field, and I do not want to lose them. I am hoping the following information and my thoughts on this topic will be helpful for those thinking about leaving health care.
Surgeon general’s burnout report
The surgeon general recently released a report on addressing health care worker burnout.2 It includes several very interesting and appropriate observations. I will summarize the most important ones here:
1. Our health depends on the well-being of our health workforce.
2. Direct harm to health care workers can lead to anxiety, depression, insomnia, and interpersonal and relationship struggles.
3. Health care workers experience exhaustion from providing overwhelming care and empathy.
4. Health care workers spend less time with patients and too much time with EHRs.
5. There are health workforce shortages.
The report is comprehensive, and everything in it is correct. The real issue is how does it go from being a report to true actionable items that we as health care professionals benefit from? I think in regards to exhaustion from overwhelming care responsibilities, and empathy fatigue, we need better boundaries.
Those who go into medicine, and especially those who go into primary care, always put the patients’ needs first. When operating in a broken system, it stays broken when individuals cover for the deficiencies in the system. Adding four extra patients every day because there is no one to refer them to with availability is injurious to the health care provider, and those providers who accept these additional patients will eventually be part of the 23% who want to leave their jobs. It feels awful to say no, but until the system stops accommodating there will not be substantial change.
The empathy drain
One of the unreported stresses of open access for patients through EHR communications is the empathy drain on physicians. When I see a patient in clinic with chronic symptoms or issues, I spend important time making sure we have a plan and an agreed upon time frame.
With the EHR, patients frequently send multiple messages for the same symptoms between visits. It is okay to redirect the patient and share that these issues will be discussed at length at appointments. My reasoning on this is that I think it is better for me to better care for myself and stay as the doctor for my patients, than always say yes to limitless needs and soon be looking for the off ramp.
The following statistic in the surgeon general’s report really hit home. For every hour of direct patient care, physicians currently spend 2 hours on the EHR system. Most practices allow 10%-20% of time for catch up, where with statistics like this it should be 50%. This concept is fully lost on administrators, or ignored.
It is only when we refuse to continue to accept and follow a broken system that it will change. A minority of internal medicine and family doctors (4.5% in 2018) practice in direct primary care models, where these issues are addressed. Unfortunately, this model as it is currently available is not an option for lower income patients.
A major theme in the surgeon general’s report was that administrative burdens need to be reduced by 75% by 2025. When I look at the report, I see the suggestions, I just don’t see how it will be achieved. Despite almost all clinics moving to the EHR, paperwork in the form of faxes and forms has increased.
A sweeping reform would be needed to eliminate daily faxes from PT offices, visiting nurse services, prior authorization, patients reminders from insurance companies, and disability forms from patients. I am glad that there is acknowledgment of the problem, but this change will take more than 3 years.
Takeaways
So what do we do?
Be good to yourself, and your colleagues. The pandemic has isolated us, which accelerates burnout.
Reach out to people you care about.
We are all feeling this. Set boundaries that allow you to care for yourself, and accept that you are doing your best, even if you can’t meet the needs of all your patients all the time.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Sinsky CA et al. Covid-related stress and work intentions in a sample of US health care workers. Mayo Clin Proc Innov Qual Outcomes. 2021 Dec;5(6):1165-73.
2. Addressing health worker burnout. The U.S. Surgeon General’s advisory on building a thriving health workforce.
Interestingly, the group that seems to be least impacted by this was health care administrators (with 12% of them planning on leaving their jobs).
I couldn’t stop thinking about these percentages.
I am reminded every day of the commitment and excellence of my colleagues in the health care field, and I do not want to lose them. I am hoping the following information and my thoughts on this topic will be helpful for those thinking about leaving health care.
Surgeon general’s burnout report
The surgeon general recently released a report on addressing health care worker burnout.2 It includes several very interesting and appropriate observations. I will summarize the most important ones here:
1. Our health depends on the well-being of our health workforce.
2. Direct harm to health care workers can lead to anxiety, depression, insomnia, and interpersonal and relationship struggles.
3. Health care workers experience exhaustion from providing overwhelming care and empathy.
4. Health care workers spend less time with patients and too much time with EHRs.
5. There are health workforce shortages.
The report is comprehensive, and everything in it is correct. The real issue is how does it go from being a report to true actionable items that we as health care professionals benefit from? I think in regards to exhaustion from overwhelming care responsibilities, and empathy fatigue, we need better boundaries.
Those who go into medicine, and especially those who go into primary care, always put the patients’ needs first. When operating in a broken system, it stays broken when individuals cover for the deficiencies in the system. Adding four extra patients every day because there is no one to refer them to with availability is injurious to the health care provider, and those providers who accept these additional patients will eventually be part of the 23% who want to leave their jobs. It feels awful to say no, but until the system stops accommodating there will not be substantial change.
The empathy drain
One of the unreported stresses of open access for patients through EHR communications is the empathy drain on physicians. When I see a patient in clinic with chronic symptoms or issues, I spend important time making sure we have a plan and an agreed upon time frame.
With the EHR, patients frequently send multiple messages for the same symptoms between visits. It is okay to redirect the patient and share that these issues will be discussed at length at appointments. My reasoning on this is that I think it is better for me to better care for myself and stay as the doctor for my patients, than always say yes to limitless needs and soon be looking for the off ramp.
The following statistic in the surgeon general’s report really hit home. For every hour of direct patient care, physicians currently spend 2 hours on the EHR system. Most practices allow 10%-20% of time for catch up, where with statistics like this it should be 50%. This concept is fully lost on administrators, or ignored.
It is only when we refuse to continue to accept and follow a broken system that it will change. A minority of internal medicine and family doctors (4.5% in 2018) practice in direct primary care models, where these issues are addressed. Unfortunately, this model as it is currently available is not an option for lower income patients.
A major theme in the surgeon general’s report was that administrative burdens need to be reduced by 75% by 2025. When I look at the report, I see the suggestions, I just don’t see how it will be achieved. Despite almost all clinics moving to the EHR, paperwork in the form of faxes and forms has increased.
A sweeping reform would be needed to eliminate daily faxes from PT offices, visiting nurse services, prior authorization, patients reminders from insurance companies, and disability forms from patients. I am glad that there is acknowledgment of the problem, but this change will take more than 3 years.
Takeaways
So what do we do?
Be good to yourself, and your colleagues. The pandemic has isolated us, which accelerates burnout.
Reach out to people you care about.
We are all feeling this. Set boundaries that allow you to care for yourself, and accept that you are doing your best, even if you can’t meet the needs of all your patients all the time.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Sinsky CA et al. Covid-related stress and work intentions in a sample of US health care workers. Mayo Clin Proc Innov Qual Outcomes. 2021 Dec;5(6):1165-73.
2. Addressing health worker burnout. The U.S. Surgeon General’s advisory on building a thriving health workforce.
Six specialties attracting the highest private equity acquisitions
While tracking the extent of physician practice acquisition by private equity firms may be difficult, new research highlights what specialties and U.S. regions are most affected by such purchases.
The study, supported by the National Institute for Health Care Management (NIHCM), examined 97,094 physicians practicing in six specialties, 4,738 of whom worked in private equity–acquired practices. Of these specialties, 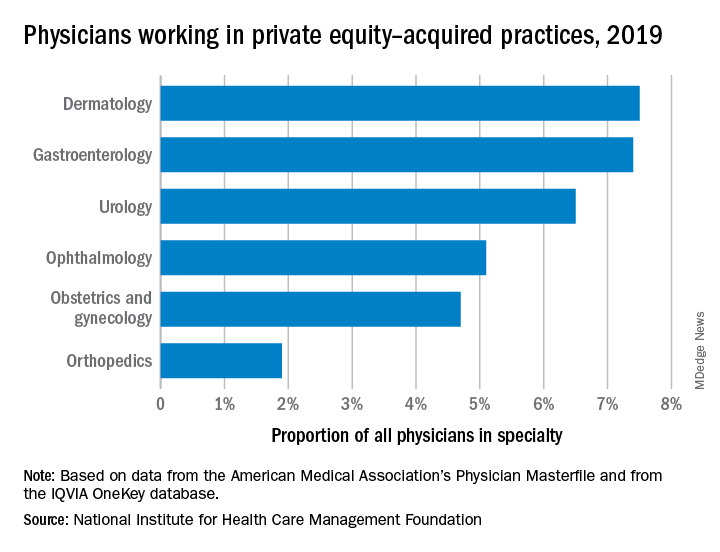
“These specialties offer private equity firms diverse revenue streams. You have a mix of commercially insured individuals with Medicare insurance and self-pay,” said Yashaswini Singh, MPA, a doctoral student at the Johns Hopkins Bloomberg School of Public Health, Baltimore, and coauthor of the study, which was published in JAMA Health Forum as a research letter.
“In dermatology, you have a mix of surgical procedures that are covered under insurance, but also a lot of cosmetic procedures that are most likely to be self-pay procedures. This offers private equity several mechanisms to which they can increase their revenues.”
Ms. Singh’s coauthors were part of a previous study looking at private practice penetration by private equity firms. That research found such deals surged from 59 deals in 2013 representing 843 physicians, to 136 private equity acquisition deals representing 1,882 physicians in 2016.
The most recent study notes limited data and use of nondisclosure agreements during early negotiations as part of the difficulty in truly pinpointing private equity’s presence in health care. Monitoring private equity activity has become necessary across all industries, noted the authors of the study. If continued at this rate, long-term private equity acquisition has a multitude of potential pros and cons.
Ms. Singh explained that such specialties are highly fragmented and they allow for economies of scale and scope. In particular, an aging population increases demand for dermatology, ophthalmology, and gastroenterology services such as skin biopsies, cataracts, and colonoscopies. This makes these specialties very attractive to private equity firms. The same can be said for obstetrics and gynecology, as fertility clinics have attracted many private equity investments.
“This is another area where understanding changes to physician practice patterns and patient outcomes is critical as women continue to delay motherhood,” said Ms. Singh.
Reducing competition, increasing focus on patient care
Researchers found significant geographical trends for private equity penetration, as it varies across the country. It is highest in the Northeast, Florida, and Arizona in hospital referral regions. Researchers are still analyzing the cause of this occurrence.
Geographic concentration of private equity penetration likely reflects strategic selection of investment opportunities by private equity funds as the decision to invest in a practice does not happen at random, Ms. Singh noted.
Ms. Singh said she hopes that by documenting a variation and geographic concentration that the NIHCM is providing the first foundational step to tackle questions related to incentives and regulations that facilitate investment.
“Understanding the regulatory and economic environments that facilitate private equity activity is an interesting and important question to explore further,” she said in an interview. “This can include supply-side factors that can shape the business environment, e.g., taxation environment, regulatory burden to complete acquisitions, as well as demand-side factors that facilitate growth.”
Researchers found that continued growth of private equity penetration may lead to consolidation among independent practices facing financial pressures, as well as reduced competition and increased prices within each local health care market.
“Localized consolidation in certain markets has the potential for competition to reduce, [and] reduced competition has been shown in a variety of settings to be associated with increases in prices and reduced access for patients,” said Ms. Singh.
Conversely, Ms. Singh addressed several benefits of growing private equity presence. Companies can exploit their full potential through the addition of private equity expertise and contacts. Specifically, health care development of technological infrastructure is likely, along with reduced patient wait times and the expansion of business hours. It could also be a way for practices to offload administrative responsibilities and for physicians to focus more on the care delivery process.
A version of this article first appeared on Medscape.com.
While tracking the extent of physician practice acquisition by private equity firms may be difficult, new research highlights what specialties and U.S. regions are most affected by such purchases.
The study, supported by the National Institute for Health Care Management (NIHCM), examined 97,094 physicians practicing in six specialties, 4,738 of whom worked in private equity–acquired practices. Of these specialties, 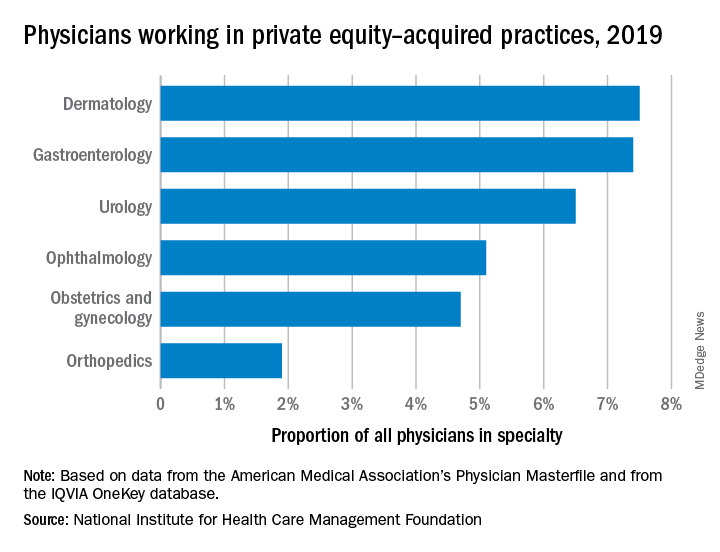
“These specialties offer private equity firms diverse revenue streams. You have a mix of commercially insured individuals with Medicare insurance and self-pay,” said Yashaswini Singh, MPA, a doctoral student at the Johns Hopkins Bloomberg School of Public Health, Baltimore, and coauthor of the study, which was published in JAMA Health Forum as a research letter.
“In dermatology, you have a mix of surgical procedures that are covered under insurance, but also a lot of cosmetic procedures that are most likely to be self-pay procedures. This offers private equity several mechanisms to which they can increase their revenues.”
Ms. Singh’s coauthors were part of a previous study looking at private practice penetration by private equity firms. That research found such deals surged from 59 deals in 2013 representing 843 physicians, to 136 private equity acquisition deals representing 1,882 physicians in 2016.
The most recent study notes limited data and use of nondisclosure agreements during early negotiations as part of the difficulty in truly pinpointing private equity’s presence in health care. Monitoring private equity activity has become necessary across all industries, noted the authors of the study. If continued at this rate, long-term private equity acquisition has a multitude of potential pros and cons.
Ms. Singh explained that such specialties are highly fragmented and they allow for economies of scale and scope. In particular, an aging population increases demand for dermatology, ophthalmology, and gastroenterology services such as skin biopsies, cataracts, and colonoscopies. This makes these specialties very attractive to private equity firms. The same can be said for obstetrics and gynecology, as fertility clinics have attracted many private equity investments.
“This is another area where understanding changes to physician practice patterns and patient outcomes is critical as women continue to delay motherhood,” said Ms. Singh.
Reducing competition, increasing focus on patient care
Researchers found significant geographical trends for private equity penetration, as it varies across the country. It is highest in the Northeast, Florida, and Arizona in hospital referral regions. Researchers are still analyzing the cause of this occurrence.
Geographic concentration of private equity penetration likely reflects strategic selection of investment opportunities by private equity funds as the decision to invest in a practice does not happen at random, Ms. Singh noted.
Ms. Singh said she hopes that by documenting a variation and geographic concentration that the NIHCM is providing the first foundational step to tackle questions related to incentives and regulations that facilitate investment.
“Understanding the regulatory and economic environments that facilitate private equity activity is an interesting and important question to explore further,” she said in an interview. “This can include supply-side factors that can shape the business environment, e.g., taxation environment, regulatory burden to complete acquisitions, as well as demand-side factors that facilitate growth.”
Researchers found that continued growth of private equity penetration may lead to consolidation among independent practices facing financial pressures, as well as reduced competition and increased prices within each local health care market.
“Localized consolidation in certain markets has the potential for competition to reduce, [and] reduced competition has been shown in a variety of settings to be associated with increases in prices and reduced access for patients,” said Ms. Singh.
Conversely, Ms. Singh addressed several benefits of growing private equity presence. Companies can exploit their full potential through the addition of private equity expertise and contacts. Specifically, health care development of technological infrastructure is likely, along with reduced patient wait times and the expansion of business hours. It could also be a way for practices to offload administrative responsibilities and for physicians to focus more on the care delivery process.
A version of this article first appeared on Medscape.com.
While tracking the extent of physician practice acquisition by private equity firms may be difficult, new research highlights what specialties and U.S. regions are most affected by such purchases.
The study, supported by the National Institute for Health Care Management (NIHCM), examined 97,094 physicians practicing in six specialties, 4,738 of whom worked in private equity–acquired practices. Of these specialties, 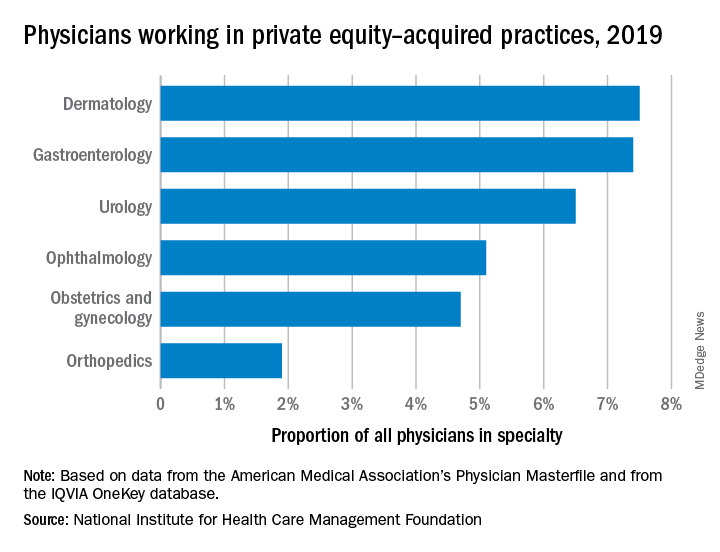
“These specialties offer private equity firms diverse revenue streams. You have a mix of commercially insured individuals with Medicare insurance and self-pay,” said Yashaswini Singh, MPA, a doctoral student at the Johns Hopkins Bloomberg School of Public Health, Baltimore, and coauthor of the study, which was published in JAMA Health Forum as a research letter.
“In dermatology, you have a mix of surgical procedures that are covered under insurance, but also a lot of cosmetic procedures that are most likely to be self-pay procedures. This offers private equity several mechanisms to which they can increase their revenues.”
Ms. Singh’s coauthors were part of a previous study looking at private practice penetration by private equity firms. That research found such deals surged from 59 deals in 2013 representing 843 physicians, to 136 private equity acquisition deals representing 1,882 physicians in 2016.
The most recent study notes limited data and use of nondisclosure agreements during early negotiations as part of the difficulty in truly pinpointing private equity’s presence in health care. Monitoring private equity activity has become necessary across all industries, noted the authors of the study. If continued at this rate, long-term private equity acquisition has a multitude of potential pros and cons.
Ms. Singh explained that such specialties are highly fragmented and they allow for economies of scale and scope. In particular, an aging population increases demand for dermatology, ophthalmology, and gastroenterology services such as skin biopsies, cataracts, and colonoscopies. This makes these specialties very attractive to private equity firms. The same can be said for obstetrics and gynecology, as fertility clinics have attracted many private equity investments.
“This is another area where understanding changes to physician practice patterns and patient outcomes is critical as women continue to delay motherhood,” said Ms. Singh.
Reducing competition, increasing focus on patient care
Researchers found significant geographical trends for private equity penetration, as it varies across the country. It is highest in the Northeast, Florida, and Arizona in hospital referral regions. Researchers are still analyzing the cause of this occurrence.
Geographic concentration of private equity penetration likely reflects strategic selection of investment opportunities by private equity funds as the decision to invest in a practice does not happen at random, Ms. Singh noted.
Ms. Singh said she hopes that by documenting a variation and geographic concentration that the NIHCM is providing the first foundational step to tackle questions related to incentives and regulations that facilitate investment.
“Understanding the regulatory and economic environments that facilitate private equity activity is an interesting and important question to explore further,” she said in an interview. “This can include supply-side factors that can shape the business environment, e.g., taxation environment, regulatory burden to complete acquisitions, as well as demand-side factors that facilitate growth.”
Researchers found that continued growth of private equity penetration may lead to consolidation among independent practices facing financial pressures, as well as reduced competition and increased prices within each local health care market.
“Localized consolidation in certain markets has the potential for competition to reduce, [and] reduced competition has been shown in a variety of settings to be associated with increases in prices and reduced access for patients,” said Ms. Singh.
Conversely, Ms. Singh addressed several benefits of growing private equity presence. Companies can exploit their full potential through the addition of private equity expertise and contacts. Specifically, health care development of technological infrastructure is likely, along with reduced patient wait times and the expansion of business hours. It could also be a way for practices to offload administrative responsibilities and for physicians to focus more on the care delivery process.
A version of this article first appeared on Medscape.com.
FROM JAMA HEALTH FORUM
Evusheld for COVID-19: Lifesaving and free, but still few takers
Evusheld (AstraZeneca), a medication used to prevent SARS-CoV-2 infection in patients at high risk, has problems: Namely, that supplies of the potentially lifesaving drug outweigh demand.
At least 7 million people who are immunocompromised could benefit from it, as could many others who are undergoing cancer treatment, have received a transplant, or who are allergic to the COVID-19 vaccines. The medication has laboratory-produced antibodies against SARS-CoV-2 and helps the body protect itself. It can slash the chances of becoming infected by 77%, according to the U.S. Food and Drug Administration.
And it’s free to eligible patients (although there may be an out-of-pocket administrative fee in some cases).
To meet demand, the Biden administration secured 1.7 million doses of the medicine, which was granted emergency use authorization by the FDA in December 2021. As of July 25, however, 793,348 doses have been ordered by the administration sites, and only 398,181 doses have been reported as used, a spokesperson for the Department of Health & Human Services tells this news organization.
Each week, a certain amount of doses from the 1.7 million dose stockpile is made available to state and territorial health departments. States have not been asking for their full allotment, the spokesperson said July 28.
Now, HHS and AstraZeneca have taken a number of steps to increase awareness of the medication and access to it.
- On July 27, HHS announced that individual providers and smaller sites of care that don’t currently receive Evusheld through the federal distribution process via the HHS Health Partner Order Portal can now order up to three patient courses of the medicine. These can be
- Health care providers can use the HHS’s COVID-19 Therapeutics Locator to find Evusheld in their area.
- AstraZeneca has launched a new website with educational materials and says it is working closely with patient and professional groups to inform patients and health care providers.
- A direct-to-consumer ad launched on June 22 and will run in the United States online and on TV (Yahoo, Fox, CBS Sports, MSN, ESPN) and be amplified on social and digital channels through year’s end, an AstraZeneca spokesperson said in an interview.
- AstraZeneca set up a toll-free number for providers: 1-833-EVUSHLD.
Evusheld includes two monoclonal antibodies, tixagevimab and cilgavimab. The medication is given as two consecutive intramuscular injections during a single visit to a doctor’s office, infusion center, or other health care facility. The antibodies bind to the SARS-CoV-2 spike protein and prevent the virus from getting into human cells and infecting them. It’s authorized for use in children and adults aged 12 years and older who weigh at least 88 pounds.
Studies have found that the medication decreases the risk of getting COVID-19 for up to 6 months after it is given. The FDA recommends repeat dosing every 6 months with the doses of 300 mg of each monoclonal antibody. In clinical trials, Evusheld reduced the incidence of COVID-19 symptomatic illness by 77%, compared with placebo.
Physicians monitor patients for an hour after administering Evusheld for allergic reactions. Other possible side effects include cardiac events, but they are not common.
Doctors and patients weigh in
Physicians – and patients – from the United States to the United Kingdom and beyond are questioning why the medication is underused while lauding the recent efforts to expand access and increase awareness.
The U.S. federal government may have underestimated the amount of communication needed to increase awareness of the medication and its applications, said infectious disease specialist William Schaffner, MD, professor of preventive medicine at Vanderbilt University School of Medicine, Nashville, Tenn.
“HHS hasn’t made a major educational effort to promote it,” he said in an interview.
Many physicians who need to know about it, such as transplant doctors and rheumatologists, are outside the typical public health communications loop, he said.
Eric Topol, MD, director of the Scripps Research Transational Institute and editor-in-chief of Medscape, has taken to social media to bemoan the lack of awareness.
Another infectious disease expert agrees. “In my experience, the awareness of Evusheld is low amongst many patients as well as many providers,” said Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, Baltimore.
“Initially, there were scarce supplies of the drug, and certain hospital systems tiered eligibility based on degrees of immunosuppression, and only the most immunosuppressed were proactively approached for treatment.”
“Also, many community hospitals never initially ordered Evusheld – they may have been crowded out by academic centers who treat many more immunosuppressed patients and may not currently see it as a priority,” Dr. Adalja said in an interview. “As such, many immunosuppressed patients would have to seek treatment at academic medical centers, where the drug is more likely to be available.”
A version of this article first appeared on Medscape.com.
Evusheld (AstraZeneca), a medication used to prevent SARS-CoV-2 infection in patients at high risk, has problems: Namely, that supplies of the potentially lifesaving drug outweigh demand.
At least 7 million people who are immunocompromised could benefit from it, as could many others who are undergoing cancer treatment, have received a transplant, or who are allergic to the COVID-19 vaccines. The medication has laboratory-produced antibodies against SARS-CoV-2 and helps the body protect itself. It can slash the chances of becoming infected by 77%, according to the U.S. Food and Drug Administration.
And it’s free to eligible patients (although there may be an out-of-pocket administrative fee in some cases).
To meet demand, the Biden administration secured 1.7 million doses of the medicine, which was granted emergency use authorization by the FDA in December 2021. As of July 25, however, 793,348 doses have been ordered by the administration sites, and only 398,181 doses have been reported as used, a spokesperson for the Department of Health & Human Services tells this news organization.
Each week, a certain amount of doses from the 1.7 million dose stockpile is made available to state and territorial health departments. States have not been asking for their full allotment, the spokesperson said July 28.
Now, HHS and AstraZeneca have taken a number of steps to increase awareness of the medication and access to it.
- On July 27, HHS announced that individual providers and smaller sites of care that don’t currently receive Evusheld through the federal distribution process via the HHS Health Partner Order Portal can now order up to three patient courses of the medicine. These can be
- Health care providers can use the HHS’s COVID-19 Therapeutics Locator to find Evusheld in their area.
- AstraZeneca has launched a new website with educational materials and says it is working closely with patient and professional groups to inform patients and health care providers.
- A direct-to-consumer ad launched on June 22 and will run in the United States online and on TV (Yahoo, Fox, CBS Sports, MSN, ESPN) and be amplified on social and digital channels through year’s end, an AstraZeneca spokesperson said in an interview.
- AstraZeneca set up a toll-free number for providers: 1-833-EVUSHLD.
Evusheld includes two monoclonal antibodies, tixagevimab and cilgavimab. The medication is given as two consecutive intramuscular injections during a single visit to a doctor’s office, infusion center, or other health care facility. The antibodies bind to the SARS-CoV-2 spike protein and prevent the virus from getting into human cells and infecting them. It’s authorized for use in children and adults aged 12 years and older who weigh at least 88 pounds.
Studies have found that the medication decreases the risk of getting COVID-19 for up to 6 months after it is given. The FDA recommends repeat dosing every 6 months with the doses of 300 mg of each monoclonal antibody. In clinical trials, Evusheld reduced the incidence of COVID-19 symptomatic illness by 77%, compared with placebo.
Physicians monitor patients for an hour after administering Evusheld for allergic reactions. Other possible side effects include cardiac events, but they are not common.
Doctors and patients weigh in
Physicians – and patients – from the United States to the United Kingdom and beyond are questioning why the medication is underused while lauding the recent efforts to expand access and increase awareness.
The U.S. federal government may have underestimated the amount of communication needed to increase awareness of the medication and its applications, said infectious disease specialist William Schaffner, MD, professor of preventive medicine at Vanderbilt University School of Medicine, Nashville, Tenn.
“HHS hasn’t made a major educational effort to promote it,” he said in an interview.
Many physicians who need to know about it, such as transplant doctors and rheumatologists, are outside the typical public health communications loop, he said.
Eric Topol, MD, director of the Scripps Research Transational Institute and editor-in-chief of Medscape, has taken to social media to bemoan the lack of awareness.
Another infectious disease expert agrees. “In my experience, the awareness of Evusheld is low amongst many patients as well as many providers,” said Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, Baltimore.
“Initially, there were scarce supplies of the drug, and certain hospital systems tiered eligibility based on degrees of immunosuppression, and only the most immunosuppressed were proactively approached for treatment.”
“Also, many community hospitals never initially ordered Evusheld – they may have been crowded out by academic centers who treat many more immunosuppressed patients and may not currently see it as a priority,” Dr. Adalja said in an interview. “As such, many immunosuppressed patients would have to seek treatment at academic medical centers, where the drug is more likely to be available.”
A version of this article first appeared on Medscape.com.
Evusheld (AstraZeneca), a medication used to prevent SARS-CoV-2 infection in patients at high risk, has problems: Namely, that supplies of the potentially lifesaving drug outweigh demand.
At least 7 million people who are immunocompromised could benefit from it, as could many others who are undergoing cancer treatment, have received a transplant, or who are allergic to the COVID-19 vaccines. The medication has laboratory-produced antibodies against SARS-CoV-2 and helps the body protect itself. It can slash the chances of becoming infected by 77%, according to the U.S. Food and Drug Administration.
And it’s free to eligible patients (although there may be an out-of-pocket administrative fee in some cases).
To meet demand, the Biden administration secured 1.7 million doses of the medicine, which was granted emergency use authorization by the FDA in December 2021. As of July 25, however, 793,348 doses have been ordered by the administration sites, and only 398,181 doses have been reported as used, a spokesperson for the Department of Health & Human Services tells this news organization.
Each week, a certain amount of doses from the 1.7 million dose stockpile is made available to state and territorial health departments. States have not been asking for their full allotment, the spokesperson said July 28.
Now, HHS and AstraZeneca have taken a number of steps to increase awareness of the medication and access to it.
- On July 27, HHS announced that individual providers and smaller sites of care that don’t currently receive Evusheld through the federal distribution process via the HHS Health Partner Order Portal can now order up to three patient courses of the medicine. These can be
- Health care providers can use the HHS’s COVID-19 Therapeutics Locator to find Evusheld in their area.
- AstraZeneca has launched a new website with educational materials and says it is working closely with patient and professional groups to inform patients and health care providers.
- A direct-to-consumer ad launched on June 22 and will run in the United States online and on TV (Yahoo, Fox, CBS Sports, MSN, ESPN) and be amplified on social and digital channels through year’s end, an AstraZeneca spokesperson said in an interview.
- AstraZeneca set up a toll-free number for providers: 1-833-EVUSHLD.
Evusheld includes two monoclonal antibodies, tixagevimab and cilgavimab. The medication is given as two consecutive intramuscular injections during a single visit to a doctor’s office, infusion center, or other health care facility. The antibodies bind to the SARS-CoV-2 spike protein and prevent the virus from getting into human cells and infecting them. It’s authorized for use in children and adults aged 12 years and older who weigh at least 88 pounds.
Studies have found that the medication decreases the risk of getting COVID-19 for up to 6 months after it is given. The FDA recommends repeat dosing every 6 months with the doses of 300 mg of each monoclonal antibody. In clinical trials, Evusheld reduced the incidence of COVID-19 symptomatic illness by 77%, compared with placebo.
Physicians monitor patients for an hour after administering Evusheld for allergic reactions. Other possible side effects include cardiac events, but they are not common.
Doctors and patients weigh in
Physicians – and patients – from the United States to the United Kingdom and beyond are questioning why the medication is underused while lauding the recent efforts to expand access and increase awareness.
The U.S. federal government may have underestimated the amount of communication needed to increase awareness of the medication and its applications, said infectious disease specialist William Schaffner, MD, professor of preventive medicine at Vanderbilt University School of Medicine, Nashville, Tenn.
“HHS hasn’t made a major educational effort to promote it,” he said in an interview.
Many physicians who need to know about it, such as transplant doctors and rheumatologists, are outside the typical public health communications loop, he said.
Eric Topol, MD, director of the Scripps Research Transational Institute and editor-in-chief of Medscape, has taken to social media to bemoan the lack of awareness.
Another infectious disease expert agrees. “In my experience, the awareness of Evusheld is low amongst many patients as well as many providers,” said Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, Baltimore.
“Initially, there were scarce supplies of the drug, and certain hospital systems tiered eligibility based on degrees of immunosuppression, and only the most immunosuppressed were proactively approached for treatment.”
“Also, many community hospitals never initially ordered Evusheld – they may have been crowded out by academic centers who treat many more immunosuppressed patients and may not currently see it as a priority,” Dr. Adalja said in an interview. “As such, many immunosuppressed patients would have to seek treatment at academic medical centers, where the drug is more likely to be available.”
A version of this article first appeared on Medscape.com.














