User login
The Journal of Clinical Outcomes Management® is an independent, peer-reviewed journal offering evidence-based, practical information for improving the quality, safety, and value of health care.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
ZUMA-5: Axi-cel yields high response rate in indolent NHL
, according to phase 2 study results presented at the annual meeting of the American Society of Hematology, held virtually this year.
The overall response rate exceeded 90% in the ZUMA-5 study, which included patients with multiply relapsed follicular lymphoma (FL) or marginal zone lymphoma (MZL) who were treated with this anti-CD19 chimeric antigen receptor (CAR) T cell therapy.
“Although longer follow-up is needed, these responses appear to be durable,” said investigator Caron Jacobson, MD, of Dana-Farber Cancer Institute in Boston.
Complete responses (CRs) after axi-cel treatment were seen in about three-quarters of patients, and most of those patients were still in response with a median follow-up that approached 1.5 years as of this report at the ASH meeting.
In her presentation, Dr. Jacobson said the safety profile of axi-cel in ZUMA-5 was manageable and “at least similar” to what was previously seen in aggressive relapsed lymphomas, referring to the ZUMA-1 study that led to 2017 approval by the Food and Drug Administration of the treatment for relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy.
The FL patient cohort in ZUMA-5 appeared to have lower rates of cytokine release syndrome (CRS) and high-grade neurotoxicity, compared with the MZL cohort in the study, she added.
Catherine Bollard, MD, of Children’s National Research Institute in Washington, said these results suggest axi-cel may be a “viable treatment option” for some patients with indolent lymphomas who have not responded to other therapies.
“What the field does need is long-term follow-up in the real-world setting to see what the true progression-free and disease-free survival is for these patients,” said Dr. Bollard, who moderated a media briefing that included the ZUMA-5 study.
“It’s really exciting to see this data in the [indolent] lymphoma setting, and I actually would like to see it moved further up in the treatment of patients, earlier in their disease process, if that’s going to be possible,” she added.
Promising results
The report on ZUMA-5, presented by Dr. Jacobson, involved 146 patients with relapsed/refractory indolent NHL: 124 patients with FL and an exploratory cohort of 22 patients with MZL. All patients had received at least two prior lines of therapy.
Following a fludarabine/cyclophosphamide conditioning regimen, patients received axi-cel at the FDA-approved dose of 2 x 106 CAR-positive T cells per kg of body weight. The primary endpoint of the study was overall response rate (ORR).
For 104 patients evaluable for efficacy, the ORR was 92% (96 patients), including CR in 76% (79 patients), data show. Among 84 FL patients evaluable for efficacy, ORR and CR were 94% (79 patients) and 80% (67 patients), respectively, while among 20 evaluable patients in the exploratory MZL cohort, ORR and CR were 60% (12 patients) and 25% (5 patients), respectively.
Sixty-four percent of patients with FL had an ongoing response at a median follow-up of 17.5 months, according to Dr. Jacobson, who added that median duration of response (DOR) had not been reached, while the 12-month DOR rate approached 72%.
The 12-month progression-free survival and overall survival rates were 73.7% and 92.9%, respectively, with medians not yet reached for either survival outcome, according to reported data.
Adverse effects
The incidence of grade 3 or greater neurologic events was lower in FL patients (15%), compared with MZL patients (41%), according to Dr. Jacobson.
While CRS occurred in 82% of patients, rates of grade 3 or greater CRS occurred in just 6% of FL patients and 9% of MZL patients, the investigator said.
There were no grade 5 neurologic events, and one grade 5 CRS was observed, she noted in her presentation.
The median time to onset of CRS was 4 days, compared with 2 days in the ZUMA-1 trial. “This may have implications for the possibility of outpatient therapy,” she said.
A study is planned to look at outpatient administration of axi-cel in patients with indolent NHL, she added.
Dr. Jacobson said she had no conflicts of interest to declare. Coauthors reported disclosures related to Kite, a Gilead Company; Genentech; Epizyme; Verastem; Novartis; and Pfizer, among others.
Correction, 12/7/20: An earlier version of this article misattributed some aspects of the ZUMA-5 trial to ZUMA-1.
SOURCE: Jacobson CA et al. ASH 2020, Abstract 700.
, according to phase 2 study results presented at the annual meeting of the American Society of Hematology, held virtually this year.
The overall response rate exceeded 90% in the ZUMA-5 study, which included patients with multiply relapsed follicular lymphoma (FL) or marginal zone lymphoma (MZL) who were treated with this anti-CD19 chimeric antigen receptor (CAR) T cell therapy.
“Although longer follow-up is needed, these responses appear to be durable,” said investigator Caron Jacobson, MD, of Dana-Farber Cancer Institute in Boston.
Complete responses (CRs) after axi-cel treatment were seen in about three-quarters of patients, and most of those patients were still in response with a median follow-up that approached 1.5 years as of this report at the ASH meeting.
In her presentation, Dr. Jacobson said the safety profile of axi-cel in ZUMA-5 was manageable and “at least similar” to what was previously seen in aggressive relapsed lymphomas, referring to the ZUMA-1 study that led to 2017 approval by the Food and Drug Administration of the treatment for relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy.
The FL patient cohort in ZUMA-5 appeared to have lower rates of cytokine release syndrome (CRS) and high-grade neurotoxicity, compared with the MZL cohort in the study, she added.
Catherine Bollard, MD, of Children’s National Research Institute in Washington, said these results suggest axi-cel may be a “viable treatment option” for some patients with indolent lymphomas who have not responded to other therapies.
“What the field does need is long-term follow-up in the real-world setting to see what the true progression-free and disease-free survival is for these patients,” said Dr. Bollard, who moderated a media briefing that included the ZUMA-5 study.
“It’s really exciting to see this data in the [indolent] lymphoma setting, and I actually would like to see it moved further up in the treatment of patients, earlier in their disease process, if that’s going to be possible,” she added.
Promising results
The report on ZUMA-5, presented by Dr. Jacobson, involved 146 patients with relapsed/refractory indolent NHL: 124 patients with FL and an exploratory cohort of 22 patients with MZL. All patients had received at least two prior lines of therapy.
Following a fludarabine/cyclophosphamide conditioning regimen, patients received axi-cel at the FDA-approved dose of 2 x 106 CAR-positive T cells per kg of body weight. The primary endpoint of the study was overall response rate (ORR).
For 104 patients evaluable for efficacy, the ORR was 92% (96 patients), including CR in 76% (79 patients), data show. Among 84 FL patients evaluable for efficacy, ORR and CR were 94% (79 patients) and 80% (67 patients), respectively, while among 20 evaluable patients in the exploratory MZL cohort, ORR and CR were 60% (12 patients) and 25% (5 patients), respectively.
Sixty-four percent of patients with FL had an ongoing response at a median follow-up of 17.5 months, according to Dr. Jacobson, who added that median duration of response (DOR) had not been reached, while the 12-month DOR rate approached 72%.
The 12-month progression-free survival and overall survival rates were 73.7% and 92.9%, respectively, with medians not yet reached for either survival outcome, according to reported data.
Adverse effects
The incidence of grade 3 or greater neurologic events was lower in FL patients (15%), compared with MZL patients (41%), according to Dr. Jacobson.
While CRS occurred in 82% of patients, rates of grade 3 or greater CRS occurred in just 6% of FL patients and 9% of MZL patients, the investigator said.
There were no grade 5 neurologic events, and one grade 5 CRS was observed, she noted in her presentation.
The median time to onset of CRS was 4 days, compared with 2 days in the ZUMA-1 trial. “This may have implications for the possibility of outpatient therapy,” she said.
A study is planned to look at outpatient administration of axi-cel in patients with indolent NHL, she added.
Dr. Jacobson said she had no conflicts of interest to declare. Coauthors reported disclosures related to Kite, a Gilead Company; Genentech; Epizyme; Verastem; Novartis; and Pfizer, among others.
Correction, 12/7/20: An earlier version of this article misattributed some aspects of the ZUMA-5 trial to ZUMA-1.
SOURCE: Jacobson CA et al. ASH 2020, Abstract 700.
, according to phase 2 study results presented at the annual meeting of the American Society of Hematology, held virtually this year.
The overall response rate exceeded 90% in the ZUMA-5 study, which included patients with multiply relapsed follicular lymphoma (FL) or marginal zone lymphoma (MZL) who were treated with this anti-CD19 chimeric antigen receptor (CAR) T cell therapy.
“Although longer follow-up is needed, these responses appear to be durable,” said investigator Caron Jacobson, MD, of Dana-Farber Cancer Institute in Boston.
Complete responses (CRs) after axi-cel treatment were seen in about three-quarters of patients, and most of those patients were still in response with a median follow-up that approached 1.5 years as of this report at the ASH meeting.
In her presentation, Dr. Jacobson said the safety profile of axi-cel in ZUMA-5 was manageable and “at least similar” to what was previously seen in aggressive relapsed lymphomas, referring to the ZUMA-1 study that led to 2017 approval by the Food and Drug Administration of the treatment for relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy.
The FL patient cohort in ZUMA-5 appeared to have lower rates of cytokine release syndrome (CRS) and high-grade neurotoxicity, compared with the MZL cohort in the study, she added.
Catherine Bollard, MD, of Children’s National Research Institute in Washington, said these results suggest axi-cel may be a “viable treatment option” for some patients with indolent lymphomas who have not responded to other therapies.
“What the field does need is long-term follow-up in the real-world setting to see what the true progression-free and disease-free survival is for these patients,” said Dr. Bollard, who moderated a media briefing that included the ZUMA-5 study.
“It’s really exciting to see this data in the [indolent] lymphoma setting, and I actually would like to see it moved further up in the treatment of patients, earlier in their disease process, if that’s going to be possible,” she added.
Promising results
The report on ZUMA-5, presented by Dr. Jacobson, involved 146 patients with relapsed/refractory indolent NHL: 124 patients with FL and an exploratory cohort of 22 patients with MZL. All patients had received at least two prior lines of therapy.
Following a fludarabine/cyclophosphamide conditioning regimen, patients received axi-cel at the FDA-approved dose of 2 x 106 CAR-positive T cells per kg of body weight. The primary endpoint of the study was overall response rate (ORR).
For 104 patients evaluable for efficacy, the ORR was 92% (96 patients), including CR in 76% (79 patients), data show. Among 84 FL patients evaluable for efficacy, ORR and CR were 94% (79 patients) and 80% (67 patients), respectively, while among 20 evaluable patients in the exploratory MZL cohort, ORR and CR were 60% (12 patients) and 25% (5 patients), respectively.
Sixty-four percent of patients with FL had an ongoing response at a median follow-up of 17.5 months, according to Dr. Jacobson, who added that median duration of response (DOR) had not been reached, while the 12-month DOR rate approached 72%.
The 12-month progression-free survival and overall survival rates were 73.7% and 92.9%, respectively, with medians not yet reached for either survival outcome, according to reported data.
Adverse effects
The incidence of grade 3 or greater neurologic events was lower in FL patients (15%), compared with MZL patients (41%), according to Dr. Jacobson.
While CRS occurred in 82% of patients, rates of grade 3 or greater CRS occurred in just 6% of FL patients and 9% of MZL patients, the investigator said.
There were no grade 5 neurologic events, and one grade 5 CRS was observed, she noted in her presentation.
The median time to onset of CRS was 4 days, compared with 2 days in the ZUMA-1 trial. “This may have implications for the possibility of outpatient therapy,” she said.
A study is planned to look at outpatient administration of axi-cel in patients with indolent NHL, she added.
Dr. Jacobson said she had no conflicts of interest to declare. Coauthors reported disclosures related to Kite, a Gilead Company; Genentech; Epizyme; Verastem; Novartis; and Pfizer, among others.
Correction, 12/7/20: An earlier version of this article misattributed some aspects of the ZUMA-5 trial to ZUMA-1.
SOURCE: Jacobson CA et al. ASH 2020, Abstract 700.
FROM ASH 2020
COVID-19–related outcomes poor for patients with hematologic disease in ASH registry
Patients with hematologic disease who develop COVID-19 may experience substantial morbidity and mortality related to SARS-CoV-2 infection, according to recent registry data reported at the all-virtual annual meeting of the American Society of Hematology.
Overall mortality was 28% for the first 250 patients entered into the ASH Research Collaborative COVID-19 Registry for Hematology, researchers reported in an abstract of their study findings.
However, the burden of death and moderate-to-severe COVID-19 outcomes was highest in patients with poorer prognosis and those with relapsed/refractory hematological disease, they added.
The most commonly represented malignancies were acute leukemia, non-Hodgkin lymphoma, and myeloma or amyloidosis, according to the report.
Taken together, the findings do support an “emerging consensus” that COVID-19 related morbidity and mortality is significant in these patients, authors said – however, the current findings may not be reason enough to support a change in treatment course for the underlying disease.
“We see no reason, based on our data, to withhold intensive therapies from patients with underlying hematologic malignancies and favorable prognoses, if aggressive supportive care is consistent with patient preferences,” wrote the researchers.
ASH President Stephanie Lee, MD, MPH, said these registry findings are important to better understand how SARS-CoV-2 is affecting not only patients with hematologic diseases, but also individuals who experience COVID-19-related hematologic complications.
However, the findings are limited due to the heterogeneity of diseases, symptoms, and treatments represented in the registry, said Dr. Lee, associate director of the clinical research division at Fred Hutchinson Cancer Center in Seattle.
“More data will be coming in, but I think this is an example of trying to harness real-world information to try to learn things until we get more controlled studies,” Dr. Lee said in a media briefing held in advance of the ASH meeting.
Comorbidities and more
Patients with blood cancers are often older and may have comorbidities such as diabetes or hypertension that have been linked to poor COVID-19 outcomes, according to the authors of the report, led by William A. Wood, MD, MPH, associate professor of medicine with the UNC Lineberger Comprehensive Cancer Center in Chapel Hill, N.C.
Moreover, these patients may have underlying immune dysfunction and may receive chemotherapy or immunotherapy that is “profoundly immunosuppressive,” Dr. Wood and coauthors said in their report.
To date, however, risks of morbidity and mortality related to SARS-CoV-2 infection have not been well defined in this patient population, authors said.
More data is emerging now from the ASH Research Collaborative COVID-19 Registry for Hematology, which includes data on patients positive for COVID-19 who have a past or present hematologic condition or have experienced a hematologic complication related to COVID-19.
All data from the registry is being made available through a dashboard on the ASH Research Collaborative website, which as of Dec. 1, 2020, included 693 complete cases.
The data cut in the ASH abstract includes the first 250 patients enrolled at 74 sites around the world, the authors said. The most common malignancies included acute leukemia in 33%, non-Hodgkin lymphoma in 27%, and myeloma or amyloidosis in 16%.
The most frequently reported symptoms included fever in 73%, cough in 67%, dyspnea in 50%, and fatigue in 40%, according to that report.
At the time of this data snapshot, treatment with COVID-19-directed therapies including hydroxychloroquine or azithromycin were common, reported in 76 and 59 patients, respectively, in the cohort.
Batch submissions from sites with high incidence of COVID-19 infection are ongoing. The registry has been expanded to include nonmalignant hematologic diseases, and the registry will continue to accumulate data as a resource for the hematology community.
Overall mortality was 28% at the time, according to the abstract, with nearly all of the deaths occurring in patients classified as having COVID-19 that was moderate (i.e., requiring hospitalization) or severe (i.e., requiring ICU admission).
“In some instances, death occurred after a decision was made to forgo ICU admission in favor of a palliative approach,” said Dr. Wood and coauthors in their report.
Dr. Wood reported research funding from Pfizer, consultancy with Teladoc/Best Doctors, and honoraria from the ASH Research Collaborative. Coauthors provided disclosures related to Celgene, Madrigal Pharmaceuticals, Pharmacyclics, and Amgen, among others.
SOURCE: Wood WA et al. ASH 2020, Abstract 215.
Patients with hematologic disease who develop COVID-19 may experience substantial morbidity and mortality related to SARS-CoV-2 infection, according to recent registry data reported at the all-virtual annual meeting of the American Society of Hematology.
Overall mortality was 28% for the first 250 patients entered into the ASH Research Collaborative COVID-19 Registry for Hematology, researchers reported in an abstract of their study findings.
However, the burden of death and moderate-to-severe COVID-19 outcomes was highest in patients with poorer prognosis and those with relapsed/refractory hematological disease, they added.
The most commonly represented malignancies were acute leukemia, non-Hodgkin lymphoma, and myeloma or amyloidosis, according to the report.
Taken together, the findings do support an “emerging consensus” that COVID-19 related morbidity and mortality is significant in these patients, authors said – however, the current findings may not be reason enough to support a change in treatment course for the underlying disease.
“We see no reason, based on our data, to withhold intensive therapies from patients with underlying hematologic malignancies and favorable prognoses, if aggressive supportive care is consistent with patient preferences,” wrote the researchers.
ASH President Stephanie Lee, MD, MPH, said these registry findings are important to better understand how SARS-CoV-2 is affecting not only patients with hematologic diseases, but also individuals who experience COVID-19-related hematologic complications.
However, the findings are limited due to the heterogeneity of diseases, symptoms, and treatments represented in the registry, said Dr. Lee, associate director of the clinical research division at Fred Hutchinson Cancer Center in Seattle.
“More data will be coming in, but I think this is an example of trying to harness real-world information to try to learn things until we get more controlled studies,” Dr. Lee said in a media briefing held in advance of the ASH meeting.
Comorbidities and more
Patients with blood cancers are often older and may have comorbidities such as diabetes or hypertension that have been linked to poor COVID-19 outcomes, according to the authors of the report, led by William A. Wood, MD, MPH, associate professor of medicine with the UNC Lineberger Comprehensive Cancer Center in Chapel Hill, N.C.
Moreover, these patients may have underlying immune dysfunction and may receive chemotherapy or immunotherapy that is “profoundly immunosuppressive,” Dr. Wood and coauthors said in their report.
To date, however, risks of morbidity and mortality related to SARS-CoV-2 infection have not been well defined in this patient population, authors said.
More data is emerging now from the ASH Research Collaborative COVID-19 Registry for Hematology, which includes data on patients positive for COVID-19 who have a past or present hematologic condition or have experienced a hematologic complication related to COVID-19.
All data from the registry is being made available through a dashboard on the ASH Research Collaborative website, which as of Dec. 1, 2020, included 693 complete cases.
The data cut in the ASH abstract includes the first 250 patients enrolled at 74 sites around the world, the authors said. The most common malignancies included acute leukemia in 33%, non-Hodgkin lymphoma in 27%, and myeloma or amyloidosis in 16%.
The most frequently reported symptoms included fever in 73%, cough in 67%, dyspnea in 50%, and fatigue in 40%, according to that report.
At the time of this data snapshot, treatment with COVID-19-directed therapies including hydroxychloroquine or azithromycin were common, reported in 76 and 59 patients, respectively, in the cohort.
Batch submissions from sites with high incidence of COVID-19 infection are ongoing. The registry has been expanded to include nonmalignant hematologic diseases, and the registry will continue to accumulate data as a resource for the hematology community.
Overall mortality was 28% at the time, according to the abstract, with nearly all of the deaths occurring in patients classified as having COVID-19 that was moderate (i.e., requiring hospitalization) or severe (i.e., requiring ICU admission).
“In some instances, death occurred after a decision was made to forgo ICU admission in favor of a palliative approach,” said Dr. Wood and coauthors in their report.
Dr. Wood reported research funding from Pfizer, consultancy with Teladoc/Best Doctors, and honoraria from the ASH Research Collaborative. Coauthors provided disclosures related to Celgene, Madrigal Pharmaceuticals, Pharmacyclics, and Amgen, among others.
SOURCE: Wood WA et al. ASH 2020, Abstract 215.
Patients with hematologic disease who develop COVID-19 may experience substantial morbidity and mortality related to SARS-CoV-2 infection, according to recent registry data reported at the all-virtual annual meeting of the American Society of Hematology.
Overall mortality was 28% for the first 250 patients entered into the ASH Research Collaborative COVID-19 Registry for Hematology, researchers reported in an abstract of their study findings.
However, the burden of death and moderate-to-severe COVID-19 outcomes was highest in patients with poorer prognosis and those with relapsed/refractory hematological disease, they added.
The most commonly represented malignancies were acute leukemia, non-Hodgkin lymphoma, and myeloma or amyloidosis, according to the report.
Taken together, the findings do support an “emerging consensus” that COVID-19 related morbidity and mortality is significant in these patients, authors said – however, the current findings may not be reason enough to support a change in treatment course for the underlying disease.
“We see no reason, based on our data, to withhold intensive therapies from patients with underlying hematologic malignancies and favorable prognoses, if aggressive supportive care is consistent with patient preferences,” wrote the researchers.
ASH President Stephanie Lee, MD, MPH, said these registry findings are important to better understand how SARS-CoV-2 is affecting not only patients with hematologic diseases, but also individuals who experience COVID-19-related hematologic complications.
However, the findings are limited due to the heterogeneity of diseases, symptoms, and treatments represented in the registry, said Dr. Lee, associate director of the clinical research division at Fred Hutchinson Cancer Center in Seattle.
“More data will be coming in, but I think this is an example of trying to harness real-world information to try to learn things until we get more controlled studies,” Dr. Lee said in a media briefing held in advance of the ASH meeting.
Comorbidities and more
Patients with blood cancers are often older and may have comorbidities such as diabetes or hypertension that have been linked to poor COVID-19 outcomes, according to the authors of the report, led by William A. Wood, MD, MPH, associate professor of medicine with the UNC Lineberger Comprehensive Cancer Center in Chapel Hill, N.C.
Moreover, these patients may have underlying immune dysfunction and may receive chemotherapy or immunotherapy that is “profoundly immunosuppressive,” Dr. Wood and coauthors said in their report.
To date, however, risks of morbidity and mortality related to SARS-CoV-2 infection have not been well defined in this patient population, authors said.
More data is emerging now from the ASH Research Collaborative COVID-19 Registry for Hematology, which includes data on patients positive for COVID-19 who have a past or present hematologic condition or have experienced a hematologic complication related to COVID-19.
All data from the registry is being made available through a dashboard on the ASH Research Collaborative website, which as of Dec. 1, 2020, included 693 complete cases.
The data cut in the ASH abstract includes the first 250 patients enrolled at 74 sites around the world, the authors said. The most common malignancies included acute leukemia in 33%, non-Hodgkin lymphoma in 27%, and myeloma or amyloidosis in 16%.
The most frequently reported symptoms included fever in 73%, cough in 67%, dyspnea in 50%, and fatigue in 40%, according to that report.
At the time of this data snapshot, treatment with COVID-19-directed therapies including hydroxychloroquine or azithromycin were common, reported in 76 and 59 patients, respectively, in the cohort.
Batch submissions from sites with high incidence of COVID-19 infection are ongoing. The registry has been expanded to include nonmalignant hematologic diseases, and the registry will continue to accumulate data as a resource for the hematology community.
Overall mortality was 28% at the time, according to the abstract, with nearly all of the deaths occurring in patients classified as having COVID-19 that was moderate (i.e., requiring hospitalization) or severe (i.e., requiring ICU admission).
“In some instances, death occurred after a decision was made to forgo ICU admission in favor of a palliative approach,” said Dr. Wood and coauthors in their report.
Dr. Wood reported research funding from Pfizer, consultancy with Teladoc/Best Doctors, and honoraria from the ASH Research Collaborative. Coauthors provided disclosures related to Celgene, Madrigal Pharmaceuticals, Pharmacyclics, and Amgen, among others.
SOURCE: Wood WA et al. ASH 2020, Abstract 215.
FROM ASH 2020
Infant’s COVID-19–related myocardial injury reversed
Reports of signs of heart failure in adults with COVID-19 have been rare – just four such cases have been published since the outbreak started in China – and now a team of pediatric cardiologists in New York have reported a case of acute but reversible myocardial injury in an infant with COVID-19.
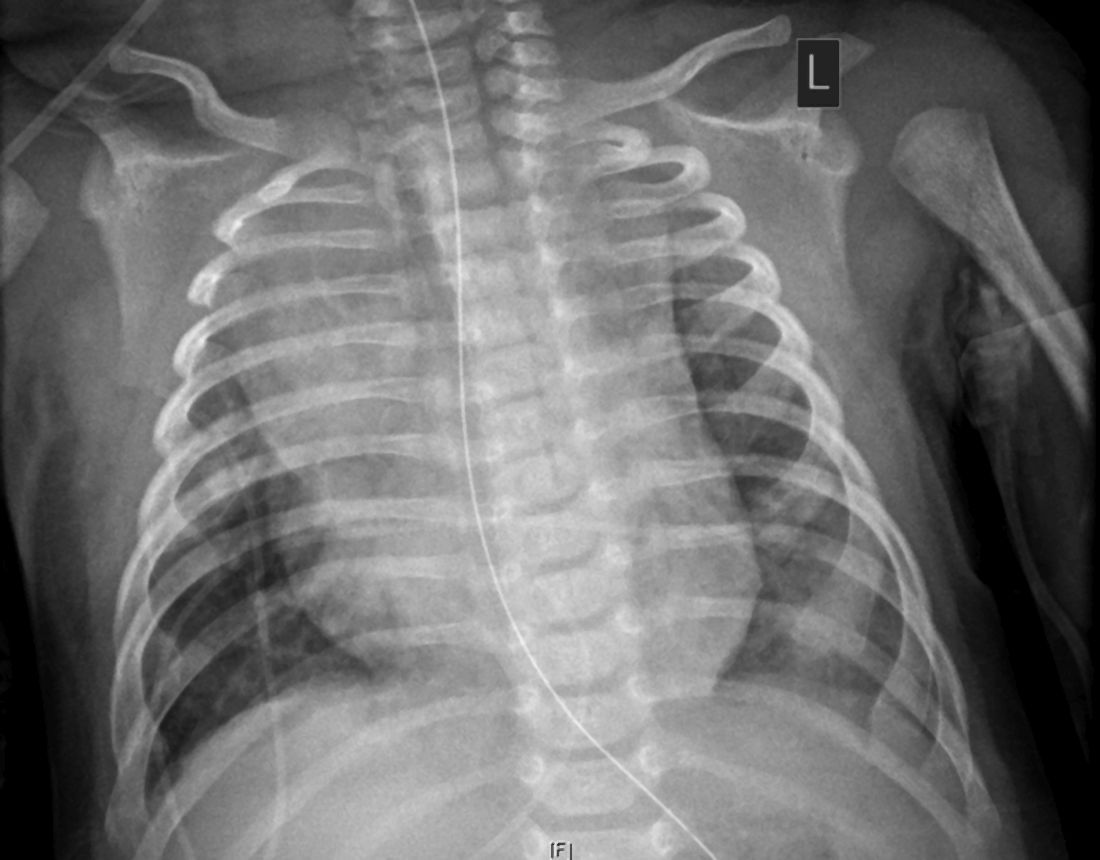
and right upper lobe atelectasis.
The 2-month-old infant went home after more than 2 weeks in the hospital with no apparent lingering cardiac effects of the illness and not needing any oral heart failure medications, Madhu Sharma, MD, of the Children’s Hospital and Montefiore in New York and colleagues reported in JACC Case Reports. With close follow-up, the child’s left ventricle size and systolic function have remained normal and mitral regurgitation resolved. The case report didn’t mention the infant’s gender.
But before the straightforward postdischarge course emerged, the infant was in a precarious state, and Dr. Sharma and her team were challenged to diagnose the underlying causes.
The child, who was born about 7 weeks premature, first came to the hospital having turned blue after choking on food. Nonrebreather mask ventilation was initiated in the ED, and an examination detected a holosystolic murmur. A test for COVID-19 was negative, but a later test was positive, and a chest x-ray exhibited cardiomegaly and signs of fluid and inflammation in the lungs.
An electrocardiogram detected sinus tachycardia, ST-segment depression and other anomalies in cardiac function. Further investigation with a transthoracic ECG showed severely depressed left ventricle systolic function with an ejection fraction of 30%, severe mitral regurgitation, and normal right ventricular systolic function.
Treatment included remdesivir and intravenous antibiotics. Through the hospital course, the patient was extubated to noninvasive ventilation, reintubated, put on intravenous steroid (methylprednisolone) and low-molecular-weight heparin, extubated, and tested throughout for cardiac function.
By day 14, left ventricle size and function normalized, and while the mitral regurgitation remained severe, it improved later without HF therapies. Left ventricle ejection fraction had recovered to 60%, and key cardiac biomarkers had normalized. On day 16, milrinone was discontinued, and the care team determined the patient no longer needed oral heart failure therapies.
“Most children with COVID-19 are either asymptomatic or have mild symptoms, but our case shows the potential for reversible myocardial injury in infants with COVID-19,” said Dr. Sharma. “Testing for COVID-19 in children presenting with signs and symptoms of heart failure is very important as we learn more about the impact of this virus.”
Dr. Sharma and coauthors have no relevant financial relationships to disclose.
SOURCE: Sharma M et al. JACC Case Rep. 2020. doi: 10.1016/j.jaccas.2020.09.031.
Reports of signs of heart failure in adults with COVID-19 have been rare – just four such cases have been published since the outbreak started in China – and now a team of pediatric cardiologists in New York have reported a case of acute but reversible myocardial injury in an infant with COVID-19.
and right upper lobe atelectasis.
The 2-month-old infant went home after more than 2 weeks in the hospital with no apparent lingering cardiac effects of the illness and not needing any oral heart failure medications, Madhu Sharma, MD, of the Children’s Hospital and Montefiore in New York and colleagues reported in JACC Case Reports. With close follow-up, the child’s left ventricle size and systolic function have remained normal and mitral regurgitation resolved. The case report didn’t mention the infant’s gender.
But before the straightforward postdischarge course emerged, the infant was in a precarious state, and Dr. Sharma and her team were challenged to diagnose the underlying causes.
The child, who was born about 7 weeks premature, first came to the hospital having turned blue after choking on food. Nonrebreather mask ventilation was initiated in the ED, and an examination detected a holosystolic murmur. A test for COVID-19 was negative, but a later test was positive, and a chest x-ray exhibited cardiomegaly and signs of fluid and inflammation in the lungs.
An electrocardiogram detected sinus tachycardia, ST-segment depression and other anomalies in cardiac function. Further investigation with a transthoracic ECG showed severely depressed left ventricle systolic function with an ejection fraction of 30%, severe mitral regurgitation, and normal right ventricular systolic function.
Treatment included remdesivir and intravenous antibiotics. Through the hospital course, the patient was extubated to noninvasive ventilation, reintubated, put on intravenous steroid (methylprednisolone) and low-molecular-weight heparin, extubated, and tested throughout for cardiac function.
By day 14, left ventricle size and function normalized, and while the mitral regurgitation remained severe, it improved later without HF therapies. Left ventricle ejection fraction had recovered to 60%, and key cardiac biomarkers had normalized. On day 16, milrinone was discontinued, and the care team determined the patient no longer needed oral heart failure therapies.
“Most children with COVID-19 are either asymptomatic or have mild symptoms, but our case shows the potential for reversible myocardial injury in infants with COVID-19,” said Dr. Sharma. “Testing for COVID-19 in children presenting with signs and symptoms of heart failure is very important as we learn more about the impact of this virus.”
Dr. Sharma and coauthors have no relevant financial relationships to disclose.
SOURCE: Sharma M et al. JACC Case Rep. 2020. doi: 10.1016/j.jaccas.2020.09.031.
Reports of signs of heart failure in adults with COVID-19 have been rare – just four such cases have been published since the outbreak started in China – and now a team of pediatric cardiologists in New York have reported a case of acute but reversible myocardial injury in an infant with COVID-19.
and right upper lobe atelectasis.
The 2-month-old infant went home after more than 2 weeks in the hospital with no apparent lingering cardiac effects of the illness and not needing any oral heart failure medications, Madhu Sharma, MD, of the Children’s Hospital and Montefiore in New York and colleagues reported in JACC Case Reports. With close follow-up, the child’s left ventricle size and systolic function have remained normal and mitral regurgitation resolved. The case report didn’t mention the infant’s gender.
But before the straightforward postdischarge course emerged, the infant was in a precarious state, and Dr. Sharma and her team were challenged to diagnose the underlying causes.
The child, who was born about 7 weeks premature, first came to the hospital having turned blue after choking on food. Nonrebreather mask ventilation was initiated in the ED, and an examination detected a holosystolic murmur. A test for COVID-19 was negative, but a later test was positive, and a chest x-ray exhibited cardiomegaly and signs of fluid and inflammation in the lungs.
An electrocardiogram detected sinus tachycardia, ST-segment depression and other anomalies in cardiac function. Further investigation with a transthoracic ECG showed severely depressed left ventricle systolic function with an ejection fraction of 30%, severe mitral regurgitation, and normal right ventricular systolic function.
Treatment included remdesivir and intravenous antibiotics. Through the hospital course, the patient was extubated to noninvasive ventilation, reintubated, put on intravenous steroid (methylprednisolone) and low-molecular-weight heparin, extubated, and tested throughout for cardiac function.
By day 14, left ventricle size and function normalized, and while the mitral regurgitation remained severe, it improved later without HF therapies. Left ventricle ejection fraction had recovered to 60%, and key cardiac biomarkers had normalized. On day 16, milrinone was discontinued, and the care team determined the patient no longer needed oral heart failure therapies.
“Most children with COVID-19 are either asymptomatic or have mild symptoms, but our case shows the potential for reversible myocardial injury in infants with COVID-19,” said Dr. Sharma. “Testing for COVID-19 in children presenting with signs and symptoms of heart failure is very important as we learn more about the impact of this virus.”
Dr. Sharma and coauthors have no relevant financial relationships to disclose.
SOURCE: Sharma M et al. JACC Case Rep. 2020. doi: 10.1016/j.jaccas.2020.09.031.
FROM JACC CASE REPORTS
Key clinical point: Children presenting with COVID-19 should be tested for heart failure.
Major finding: A 2-month-old infant with COVID-19 had acute but reversible myocardial injury.
Study details: Single case report.
Disclosures: Dr. Sharma, MD, has no relevant financial relationships to disclose.
Source: Sharma M et al. JACC Case Rep. 2020. doi: 10.1016/j.jaccas.2020.09.031.
Cancer rates on the rise in adolescents and young adults
Rates of cancer increased by 30% from 1973 to 2015 in adolescents and young adults (AYAs) aged 15–39 years in the United States, according to a review of almost a half million cases in the National Institutes of Health’s Surveillance, Epidemiology, and End Results database.
There was an annual increase of 0.537 new cases per 100,000 people, from 57.2 cases per 100,000 in 1973 to 74.2 in 2015.
Kidney carcinoma led with the highest rate increase. There were also marked increases in thyroid and colorectal carcinoma, germ cell and trophoblastic neoplasms, and melanoma, among others.
The report was published online December 1 in JAMA Network Open.
“Clinicians should be on the lookout for these cancers in their adolescent and young adult patients,” said senior investigator Nicholas Zaorsky, MD, an assistant professor of radiation oncology and public health sciences at the Penn State Cancer Institute, Hershey, Pennsylvania.
“Now that there is a better understanding of the types of cancer that are prevalent and rising in this age group, prevention, screening, diagnosis and treatment protocols specifically targeted to this population should be developed,” he said in a press release.
The reasons for the increases are unclear, but environmental and dietary factors, increasing obesity, and changing screening practices are likely in play, the authors comment. In addition, “cancer screening and overdiagnosis are thought to account for much of the increasing rates of thyroid and kidney carcinoma, among others,” they add.
The American Cancer Society (ACS) recently found similar increases in thyroid, kidney, and colorectal cancer among AYAs, as well as an increase in uterine cancer.
It’s important to note, however, that “this phenomenon is largely driven by trends for thyroid cancer, which is thought to be a result of overdiagnosis,” said ACS surveillance researcher Kimberly Miller, MPH, when asked to comment on the new study.
“As such, it is extremely important to also consider trends in cancer mortality rates among this age group, which are declining overall but are increasing for colorectal and uterine cancers. The fact that both incidence and mortality rates are increasing for these two cancers suggests a true increase in disease burden and certainly requires further attention and research,” she said.
Historically, management of cancer in AYAs has fallen somewhere between pediatric and adult oncology, neither of which capture the distinct biological, social, and economic needs of AYAs. Research has also focused on childhood and adult cancers, leaving cancer in AYAs inadequately studied.
The new findings are “valuable to guide more targeted research and interventions specifically to AYAs,” Zaorsky and colleagues say in their report.
Among female patients ― 59.1% of the study population ― incidence increased for 15 cancers, including kidney carcinoma (annual percent change [APC], 3.632), thyroid carcinoma (APC, 3.456), and myeloma, mast cell, and miscellaneous lymphoreticular neoplasms not otherwise specified (APC, 2.805). Rates of five cancers declined, led by astrocytoma not otherwise specified (APC, –3.369) and carcinoma of the gonads (APC, –1.743).
Among male patients, incidence increased for 14 cancers, including kidney carcinoma (APC, 3.572), unspecified soft tissue sarcoma (APC 2.543), and thyroid carcinoma (APC, 2.273). Incidence fell for seven, led by astrocytoma not otherwise specified (APC, –3.759) and carcinoma of the trachea, bronchus, and lung (APC, –2.635).
Increased testicular cancer rates (APC, 1.246) could be related to greater prenatal exposure to estrogen and progesterone or through dairy consumption; increasing survival of premature infants; and greater exposure to cannabis, among other possibilities, the investigators say.
Increases in colorectal cancer might be related to fewer vegetables and more fat and processed meat in the diet; lack of exercise; and increasing obesity. Human papillomavirus infection has also been implicated.
Higher rates of melanoma could be related to tanning bed use.
Declines in some cancers could be related to greater use of oral contraceptives; laws reducing exposure to benzene and other chemicals; and fewer people smoking.
Although kidney carcinoma has increased at the greatest rate, it’s uncommon. Colorectal and thyroid carcinoma, melanoma, non-Hodgkin lymphoma, and germ cell and trophoblastic neoplasms of the gonads contribute more to the overall increase in cancers among AYAs, the investigators note.
Almost 80% of the patients were White; 10.3% were Black.
The study was funded by the National Center for Advancing Translational Sciences. The investigators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Rates of cancer increased by 30% from 1973 to 2015 in adolescents and young adults (AYAs) aged 15–39 years in the United States, according to a review of almost a half million cases in the National Institutes of Health’s Surveillance, Epidemiology, and End Results database.
There was an annual increase of 0.537 new cases per 100,000 people, from 57.2 cases per 100,000 in 1973 to 74.2 in 2015.
Kidney carcinoma led with the highest rate increase. There were also marked increases in thyroid and colorectal carcinoma, germ cell and trophoblastic neoplasms, and melanoma, among others.
The report was published online December 1 in JAMA Network Open.
“Clinicians should be on the lookout for these cancers in their adolescent and young adult patients,” said senior investigator Nicholas Zaorsky, MD, an assistant professor of radiation oncology and public health sciences at the Penn State Cancer Institute, Hershey, Pennsylvania.
“Now that there is a better understanding of the types of cancer that are prevalent and rising in this age group, prevention, screening, diagnosis and treatment protocols specifically targeted to this population should be developed,” he said in a press release.
The reasons for the increases are unclear, but environmental and dietary factors, increasing obesity, and changing screening practices are likely in play, the authors comment. In addition, “cancer screening and overdiagnosis are thought to account for much of the increasing rates of thyroid and kidney carcinoma, among others,” they add.
The American Cancer Society (ACS) recently found similar increases in thyroid, kidney, and colorectal cancer among AYAs, as well as an increase in uterine cancer.
It’s important to note, however, that “this phenomenon is largely driven by trends for thyroid cancer, which is thought to be a result of overdiagnosis,” said ACS surveillance researcher Kimberly Miller, MPH, when asked to comment on the new study.
“As such, it is extremely important to also consider trends in cancer mortality rates among this age group, which are declining overall but are increasing for colorectal and uterine cancers. The fact that both incidence and mortality rates are increasing for these two cancers suggests a true increase in disease burden and certainly requires further attention and research,” she said.
Historically, management of cancer in AYAs has fallen somewhere between pediatric and adult oncology, neither of which capture the distinct biological, social, and economic needs of AYAs. Research has also focused on childhood and adult cancers, leaving cancer in AYAs inadequately studied.
The new findings are “valuable to guide more targeted research and interventions specifically to AYAs,” Zaorsky and colleagues say in their report.
Among female patients ― 59.1% of the study population ― incidence increased for 15 cancers, including kidney carcinoma (annual percent change [APC], 3.632), thyroid carcinoma (APC, 3.456), and myeloma, mast cell, and miscellaneous lymphoreticular neoplasms not otherwise specified (APC, 2.805). Rates of five cancers declined, led by astrocytoma not otherwise specified (APC, –3.369) and carcinoma of the gonads (APC, –1.743).
Among male patients, incidence increased for 14 cancers, including kidney carcinoma (APC, 3.572), unspecified soft tissue sarcoma (APC 2.543), and thyroid carcinoma (APC, 2.273). Incidence fell for seven, led by astrocytoma not otherwise specified (APC, –3.759) and carcinoma of the trachea, bronchus, and lung (APC, –2.635).
Increased testicular cancer rates (APC, 1.246) could be related to greater prenatal exposure to estrogen and progesterone or through dairy consumption; increasing survival of premature infants; and greater exposure to cannabis, among other possibilities, the investigators say.
Increases in colorectal cancer might be related to fewer vegetables and more fat and processed meat in the diet; lack of exercise; and increasing obesity. Human papillomavirus infection has also been implicated.
Higher rates of melanoma could be related to tanning bed use.
Declines in some cancers could be related to greater use of oral contraceptives; laws reducing exposure to benzene and other chemicals; and fewer people smoking.
Although kidney carcinoma has increased at the greatest rate, it’s uncommon. Colorectal and thyroid carcinoma, melanoma, non-Hodgkin lymphoma, and germ cell and trophoblastic neoplasms of the gonads contribute more to the overall increase in cancers among AYAs, the investigators note.
Almost 80% of the patients were White; 10.3% were Black.
The study was funded by the National Center for Advancing Translational Sciences. The investigators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Rates of cancer increased by 30% from 1973 to 2015 in adolescents and young adults (AYAs) aged 15–39 years in the United States, according to a review of almost a half million cases in the National Institutes of Health’s Surveillance, Epidemiology, and End Results database.
There was an annual increase of 0.537 new cases per 100,000 people, from 57.2 cases per 100,000 in 1973 to 74.2 in 2015.
Kidney carcinoma led with the highest rate increase. There were also marked increases in thyroid and colorectal carcinoma, germ cell and trophoblastic neoplasms, and melanoma, among others.
The report was published online December 1 in JAMA Network Open.
“Clinicians should be on the lookout for these cancers in their adolescent and young adult patients,” said senior investigator Nicholas Zaorsky, MD, an assistant professor of radiation oncology and public health sciences at the Penn State Cancer Institute, Hershey, Pennsylvania.
“Now that there is a better understanding of the types of cancer that are prevalent and rising in this age group, prevention, screening, diagnosis and treatment protocols specifically targeted to this population should be developed,” he said in a press release.
The reasons for the increases are unclear, but environmental and dietary factors, increasing obesity, and changing screening practices are likely in play, the authors comment. In addition, “cancer screening and overdiagnosis are thought to account for much of the increasing rates of thyroid and kidney carcinoma, among others,” they add.
The American Cancer Society (ACS) recently found similar increases in thyroid, kidney, and colorectal cancer among AYAs, as well as an increase in uterine cancer.
It’s important to note, however, that “this phenomenon is largely driven by trends for thyroid cancer, which is thought to be a result of overdiagnosis,” said ACS surveillance researcher Kimberly Miller, MPH, when asked to comment on the new study.
“As such, it is extremely important to also consider trends in cancer mortality rates among this age group, which are declining overall but are increasing for colorectal and uterine cancers. The fact that both incidence and mortality rates are increasing for these two cancers suggests a true increase in disease burden and certainly requires further attention and research,” she said.
Historically, management of cancer in AYAs has fallen somewhere between pediatric and adult oncology, neither of which capture the distinct biological, social, and economic needs of AYAs. Research has also focused on childhood and adult cancers, leaving cancer in AYAs inadequately studied.
The new findings are “valuable to guide more targeted research and interventions specifically to AYAs,” Zaorsky and colleagues say in their report.
Among female patients ― 59.1% of the study population ― incidence increased for 15 cancers, including kidney carcinoma (annual percent change [APC], 3.632), thyroid carcinoma (APC, 3.456), and myeloma, mast cell, and miscellaneous lymphoreticular neoplasms not otherwise specified (APC, 2.805). Rates of five cancers declined, led by astrocytoma not otherwise specified (APC, –3.369) and carcinoma of the gonads (APC, –1.743).
Among male patients, incidence increased for 14 cancers, including kidney carcinoma (APC, 3.572), unspecified soft tissue sarcoma (APC 2.543), and thyroid carcinoma (APC, 2.273). Incidence fell for seven, led by astrocytoma not otherwise specified (APC, –3.759) and carcinoma of the trachea, bronchus, and lung (APC, –2.635).
Increased testicular cancer rates (APC, 1.246) could be related to greater prenatal exposure to estrogen and progesterone or through dairy consumption; increasing survival of premature infants; and greater exposure to cannabis, among other possibilities, the investigators say.
Increases in colorectal cancer might be related to fewer vegetables and more fat and processed meat in the diet; lack of exercise; and increasing obesity. Human papillomavirus infection has also been implicated.
Higher rates of melanoma could be related to tanning bed use.
Declines in some cancers could be related to greater use of oral contraceptives; laws reducing exposure to benzene and other chemicals; and fewer people smoking.
Although kidney carcinoma has increased at the greatest rate, it’s uncommon. Colorectal and thyroid carcinoma, melanoma, non-Hodgkin lymphoma, and germ cell and trophoblastic neoplasms of the gonads contribute more to the overall increase in cancers among AYAs, the investigators note.
Almost 80% of the patients were White; 10.3% were Black.
The study was funded by the National Center for Advancing Translational Sciences. The investigators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
FDA clears first drug for rare genetic causes of severe obesity
The Food and Drug Administration has approved setmelanotide (Imcivree, Rhythm Pharmaceuticals) for weight management in adults and children as young as 6 years with obesity because of proopiomelanocortin (POMC), proprotein convertase subtilisin/kexin type 1 (PCSK1), or leptin receptor (LEPR) deficiency confirmed by genetic testing.
Individuals with these rare genetic causes of severe obesity have a normal weight at birth but develop persistent severe obesity within months because of insatiable hunger (hyperphagia).
Setmelanotide, a melanocortin-4 receptor (MC4R) agonist, is the first FDA-approved therapy for these disorders.
“Many patients and families who live with these diseases face an often-burdensome stigma associated with severe obesity. To manage this obesity and control disruptive food-seeking behavior, caregivers often lock cabinets and refrigerators and significantly limit social activities,” said Jennifer Miller, MD, a pediatric endocrinologist at University of Florida Health, Gainesville, in a press release issued by the company.
“This FDA approval marks an important turning point, providing a much needed therapy and supporting the use of genetic testing to identify and properly diagnose patients with these rare genetic diseases of obesity,” she noted.
David Meeker, MD, chair, president, and CEO of Rhythm Pharmaceuticals, added: “We are advancing a first-in-class, precision medicine that is designed to directly address the underlying cause of obesities driven by genetic deficits in the MC4R pathway.”
Setmelanotide was evaluated in two phase 3 clinical trials. In one trial, 80% of patients with obesity caused by POMC or PCSK1 deficiency achieved greater than 10% weight loss after 1 year of treatment.
In the other trial, 45.5% of patients with obesity caused by LEPR deficiency achieved greater than 10% weight loss with 1 year of treatment.
Results for the two trials were recently published in The Lancet Diabetes & Endocrinology and discussed at the ObesityWeek Interactive 2020 meeting.
Setmelanotide was generally well tolerated in both trials. The most common adverse events were injection-site reactions, skin hyperpigmentation, and nausea.
The drug label notes that disturbances in sexual arousal, depression, and suicidal ideation; skin pigmentation; and darkening of preexisting nevi may occur with setmelanotide treatment.
The drug label also notes a risk for serious adverse reactions because of benzyl alcohol preservative in neonates and low-birth-weight infants. Setmelanotide is not approved for use in neonates or infants.
The company expects the drug to be commercially available in the United States in the first quarter of 2021.
Setmelanotide for the treatment of obesity associated with rare genetic defects had FDA breakthrough therapy designation as well as orphan drug designation.
The company is also evaluating setmelanotide for reduction in hunger and body weight in a pivotal phase 3 trial in people living with Bardet-Biedl or Alström syndrome, and top-line data are due soon.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration has approved setmelanotide (Imcivree, Rhythm Pharmaceuticals) for weight management in adults and children as young as 6 years with obesity because of proopiomelanocortin (POMC), proprotein convertase subtilisin/kexin type 1 (PCSK1), or leptin receptor (LEPR) deficiency confirmed by genetic testing.
Individuals with these rare genetic causes of severe obesity have a normal weight at birth but develop persistent severe obesity within months because of insatiable hunger (hyperphagia).
Setmelanotide, a melanocortin-4 receptor (MC4R) agonist, is the first FDA-approved therapy for these disorders.
“Many patients and families who live with these diseases face an often-burdensome stigma associated with severe obesity. To manage this obesity and control disruptive food-seeking behavior, caregivers often lock cabinets and refrigerators and significantly limit social activities,” said Jennifer Miller, MD, a pediatric endocrinologist at University of Florida Health, Gainesville, in a press release issued by the company.
“This FDA approval marks an important turning point, providing a much needed therapy and supporting the use of genetic testing to identify and properly diagnose patients with these rare genetic diseases of obesity,” she noted.
David Meeker, MD, chair, president, and CEO of Rhythm Pharmaceuticals, added: “We are advancing a first-in-class, precision medicine that is designed to directly address the underlying cause of obesities driven by genetic deficits in the MC4R pathway.”
Setmelanotide was evaluated in two phase 3 clinical trials. In one trial, 80% of patients with obesity caused by POMC or PCSK1 deficiency achieved greater than 10% weight loss after 1 year of treatment.
In the other trial, 45.5% of patients with obesity caused by LEPR deficiency achieved greater than 10% weight loss with 1 year of treatment.
Results for the two trials were recently published in The Lancet Diabetes & Endocrinology and discussed at the ObesityWeek Interactive 2020 meeting.
Setmelanotide was generally well tolerated in both trials. The most common adverse events were injection-site reactions, skin hyperpigmentation, and nausea.
The drug label notes that disturbances in sexual arousal, depression, and suicidal ideation; skin pigmentation; and darkening of preexisting nevi may occur with setmelanotide treatment.
The drug label also notes a risk for serious adverse reactions because of benzyl alcohol preservative in neonates and low-birth-weight infants. Setmelanotide is not approved for use in neonates or infants.
The company expects the drug to be commercially available in the United States in the first quarter of 2021.
Setmelanotide for the treatment of obesity associated with rare genetic defects had FDA breakthrough therapy designation as well as orphan drug designation.
The company is also evaluating setmelanotide for reduction in hunger and body weight in a pivotal phase 3 trial in people living with Bardet-Biedl or Alström syndrome, and top-line data are due soon.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration has approved setmelanotide (Imcivree, Rhythm Pharmaceuticals) for weight management in adults and children as young as 6 years with obesity because of proopiomelanocortin (POMC), proprotein convertase subtilisin/kexin type 1 (PCSK1), or leptin receptor (LEPR) deficiency confirmed by genetic testing.
Individuals with these rare genetic causes of severe obesity have a normal weight at birth but develop persistent severe obesity within months because of insatiable hunger (hyperphagia).
Setmelanotide, a melanocortin-4 receptor (MC4R) agonist, is the first FDA-approved therapy for these disorders.
“Many patients and families who live with these diseases face an often-burdensome stigma associated with severe obesity. To manage this obesity and control disruptive food-seeking behavior, caregivers often lock cabinets and refrigerators and significantly limit social activities,” said Jennifer Miller, MD, a pediatric endocrinologist at University of Florida Health, Gainesville, in a press release issued by the company.
“This FDA approval marks an important turning point, providing a much needed therapy and supporting the use of genetic testing to identify and properly diagnose patients with these rare genetic diseases of obesity,” she noted.
David Meeker, MD, chair, president, and CEO of Rhythm Pharmaceuticals, added: “We are advancing a first-in-class, precision medicine that is designed to directly address the underlying cause of obesities driven by genetic deficits in the MC4R pathway.”
Setmelanotide was evaluated in two phase 3 clinical trials. In one trial, 80% of patients with obesity caused by POMC or PCSK1 deficiency achieved greater than 10% weight loss after 1 year of treatment.
In the other trial, 45.5% of patients with obesity caused by LEPR deficiency achieved greater than 10% weight loss with 1 year of treatment.
Results for the two trials were recently published in The Lancet Diabetes & Endocrinology and discussed at the ObesityWeek Interactive 2020 meeting.
Setmelanotide was generally well tolerated in both trials. The most common adverse events were injection-site reactions, skin hyperpigmentation, and nausea.
The drug label notes that disturbances in sexual arousal, depression, and suicidal ideation; skin pigmentation; and darkening of preexisting nevi may occur with setmelanotide treatment.
The drug label also notes a risk for serious adverse reactions because of benzyl alcohol preservative in neonates and low-birth-weight infants. Setmelanotide is not approved for use in neonates or infants.
The company expects the drug to be commercially available in the United States in the first quarter of 2021.
Setmelanotide for the treatment of obesity associated with rare genetic defects had FDA breakthrough therapy designation as well as orphan drug designation.
The company is also evaluating setmelanotide for reduction in hunger and body weight in a pivotal phase 3 trial in people living with Bardet-Biedl or Alström syndrome, and top-line data are due soon.
A version of this article originally appeared on Medscape.com.
VTE prophylaxis is feasible, effective in some high-risk cancer patients
Primary thromboprophylaxis is feasible and worth considering for high-risk ambulatory patients with cancer who are initiating systemic chemotherapy, according to Marc Carrier, MD.
Risk scores can identify patients at high risk for venous thromboembolism (VTE), and treatments that are effective and associated with low bleeding risk are available, Dr. Carrier explained at the biennial summit of the Thrombosis & Hemostasis Societies of North America.
However, caution is advised in patients with certain types of cancer, including some gastrointestinal and genitourinary cancers, because of the possibility of increased major and clinically relevant nonmajor bleeding risk, he said.
VTE and cancer
VTE is relatively rare in the general population, occurring in about 1 or 2 per 1,000 people annually. The risk increases 4.1-fold in patients with cancer, and 6.5-fold in patients with cancer receiving chemotherapy.
“So just putting these numbers together, we’re no longer talking about 1 in 1,000, but 1 in 200, so [this is] something that is very common among cancer patients,” said Dr. Carrier, a professor at the University of Ottawa and chief of the division of hematology at The Ottawa Hospital.
The mortality rate associated with cancer-associated thrombosis is about 9%, comparable to that associated with infection in the cancer outpatient setting, which underscores the importance of educating patients about the signs and symptoms of VTE so they can seek medical treatment quickly if necessary, he added.
It may also be useful to discuss prophylaxis or other ways to prevent venous thromboembolic complications with certain patients, he said, noting that in an observational cohort study of nearly 600 patients at the University of Ottawa, 25% of those initiating chemotherapy were identified as intermediate or high risk using the validated Khorana risk score, and thus would likely benefit from thromboprophylaxis.
Risk assessment
The Khorana risk score assesses VTE risk based on cancer site, blood counts, and body mass index. It is simple to use and has been validated in more than 20,000 people in multiple countries, Dr. Carrier said.
In a well-known validation study, Ay et al. showed a VTE complication rate of 10% in patients with a Khorana risk score of 2 or higher who were followed up to 6 months.
“This is huge,” Dr. Carrier stressed. “This is much higher than what we tolerate for all sorts of different populations for which we would recommend anticoagulation or thromboprophylaxis.”
The question is whether the risk score can be helpful in a real-world clinic setting, he said, adding: “I’d like to think the answer to that is yes.”
In the University of Ottawa cohort study, 11% of high-risk patients experienced a VTE complication, compared with 4% of those with lower risk, suggesting that the validation data for the Khorana risk score is not only accurate, it is “actually applicable in real-world practice, and you can use it in your own center,” he said.
Further, recent studies have demonstrated that treatment based on Khorana risk score assessment reduces VTE complications.
Prophylaxis options
Low-molecular-weight heparin (LMWH) has been shown in several studies to be associated with a significant relative VTE risk reduction in patients with cancer initiating chemotherapy – with only a slight, nonsignificant increase in the risk of major bleeding.
However, the absolute benefit was small, and LMWH is “parenteral, relatively costly, and, based on that, although we showed relatively good risk-benefit ratio, it never really got translated to clinical practice,” Dr. Carrier said.
In fact, a 2015 American Society of Clinical Oncology guidelines update recommended against routine thromboprophylaxis in this setting, but stated that it could be considered in select high-risk patients identified using a validated risk-assessment tool.
The guidelines noted that “individual risk factors such as biomarkers and cancer site don’t reliably identify high-risk patients.”
More recent data provide additional support for risk assessment and treatment based on Khorana risk score of 2 or higher.
The AVERT trial, for which Dr. Carrier was the first author, showed that the direct-acting oral anticoagulant (DOAC) apixaban reduced VTE incidence, compared with placebo, in patients with Khorana score of 2 or higher (4.2% vs. 10.2%; hazard ratio, 0.41 overall, and 1.0 vs. 7.3; HR, 0.14 on treatment), and the CASSINI trial showed that another DOAC, rivaroxaban, reduced VTE incidence, compared with placebo, in those with Khorana score of 2 or higher (5.9 vs. 6.7; HR, 0.6 overall, and 2.6 vs. 6.4; HR, 0.40 on treatment). The differences in the on-treatment populations were statistically significant.
The two trials, which included a variety of tumor types, showed similar rates of major bleeding, with an absolute difference of about 1% between treatment and placebo, which was not statistically significant in the on-treatment analyses (HR, 1.89 in AVERT and HR, 1.96 in CASSINI).
A systematic review of these trials showed an overall significant decrease in VTE complication risk with treatment in high-risk patients, and a nonstatistically significant major bleeding risk increase.
Based on these findings, ASCO guidelines were updated in 2020 to state that “routine thromboprophylaxis should not be offered to all patients with cancer. ... However, high-risk outpatients with cancer may be offered thromboprophylaxis with apixaban, rivaroxaban or LMWH, providing there are no significant risk factors for bleeding or drug-drug interactions, and after having a full discussion with patients ... to make sure they understand the risk-benefit ratio and the rationale for that particular recommendation,” he said.
Real-world implementation
Implementing this approach in the clinic setting requires a practical model, such as the Venous Thromboembolism Prevention in the Ambulatory Cancer Clinic (VTEPACC) program, a prospective quality improvement research initiative developed in collaboration with the Jeffords Institute for Quality at the University of Vermont Medical Center and described in a recent report, Dr. Carrier said.
The “Vermont model” is “really a comprehensive model that includes identifying patients with the electronic medical records, gathering the formal education and insight from other health care providers like pharmacists and nurses in order to really come up with personalized care for your patients,” he explained.
In 918 outpatients with cancer who were included in the program, VTE awareness increased from less than 5% before VTEPACC to nearly 82% during the implementation phase and 94.7% after 2 years, with nearly 94% of high-risk patients receiving VTE prophylaxis at that time.
“So we can certainly do that in our own center.” he said. “It’s a matter of coming up with the model and making sure that the patients are seen at the right time.”
Given the high frequency of VTE in patients with cancer initiating chemotherapy, the usefulness of risk scores such as the Khorana risk score for identifying those at high risk, and the availability of safe and effective interventions for reducing risk, “we should probably use the data and incorporate them into clinical practice by implementation of programs for primary prevention,” he said.
A word of caution
Caution is warranted, however, when it comes to using DOACs in patients with higher-risk or potentially higher-risk tumor types, he added.
“It’s an important question we are facing as clinicians on a daily basis,” he said, responding to an attendee’s query, as shared by session moderator James Douketis, MD, professor of medicine at McMaster University, Hamilton, Ont., regarding possible bleeding risks in certain genitourinary cancers.
A recent meta-analysis published in Nature, for example, noted that, in the SELECT-D trial, rivaroxaban was associated with significantly higher incidence of clinically relevant nonmajor bleeding, most often in bladder and colorectal cancers, and most often at genitourinary and gastrointestinal sites.
Both Dr. Carrier and fellow panelist Michael Streiff, MD, professor of medicine at Johns Hopkins University and medical director at the Johns Hopkins Hospital Special Coagulation Laboratory, Baltimore, said they approach DOAC use cautiously, but don’t rule it out entirely, in patients with unresected genitourinary tumors that could pose a risk of bleeding.
“It’s worth mentioning and being cautious. In my own personal practice, I’m very careful with unresected urothelial-type tumors or, for example, bladder cancer, for the same reason as [with] unresected luminal GI tumors,” Dr. Carrier said, adding that he’s also mindful that patients with nephropathy were excluded from U.S. DOAC trials because of bleeding risk.
He said he sometimes tries a LMWH challenge first in higher-risk patients, and then might try a DOAC if no bleeding occurs.
“But it certainly is controversial,” he noted.
Dr. Streiff added that he also worries less with genitourinary cancers than with upper GI lesions because “the signals weren’t as big as in GI” cancers, but he noted that “the drugs are going out through the kidneys ... so I’m cautious in those populations.”
“So caution, but not complete exclusion, is the operative management,” Dr. Douketis said, summarizing the panelists’ consensus.
Dr. Carrier reported clinical trial or advisory board participation for Bayer, Pfizer, Servier, Leo Pharma, and/or BMS.
Primary thromboprophylaxis is feasible and worth considering for high-risk ambulatory patients with cancer who are initiating systemic chemotherapy, according to Marc Carrier, MD.
Risk scores can identify patients at high risk for venous thromboembolism (VTE), and treatments that are effective and associated with low bleeding risk are available, Dr. Carrier explained at the biennial summit of the Thrombosis & Hemostasis Societies of North America.
However, caution is advised in patients with certain types of cancer, including some gastrointestinal and genitourinary cancers, because of the possibility of increased major and clinically relevant nonmajor bleeding risk, he said.
VTE and cancer
VTE is relatively rare in the general population, occurring in about 1 or 2 per 1,000 people annually. The risk increases 4.1-fold in patients with cancer, and 6.5-fold in patients with cancer receiving chemotherapy.
“So just putting these numbers together, we’re no longer talking about 1 in 1,000, but 1 in 200, so [this is] something that is very common among cancer patients,” said Dr. Carrier, a professor at the University of Ottawa and chief of the division of hematology at The Ottawa Hospital.
The mortality rate associated with cancer-associated thrombosis is about 9%, comparable to that associated with infection in the cancer outpatient setting, which underscores the importance of educating patients about the signs and symptoms of VTE so they can seek medical treatment quickly if necessary, he added.
It may also be useful to discuss prophylaxis or other ways to prevent venous thromboembolic complications with certain patients, he said, noting that in an observational cohort study of nearly 600 patients at the University of Ottawa, 25% of those initiating chemotherapy were identified as intermediate or high risk using the validated Khorana risk score, and thus would likely benefit from thromboprophylaxis.
Risk assessment
The Khorana risk score assesses VTE risk based on cancer site, blood counts, and body mass index. It is simple to use and has been validated in more than 20,000 people in multiple countries, Dr. Carrier said.
In a well-known validation study, Ay et al. showed a VTE complication rate of 10% in patients with a Khorana risk score of 2 or higher who were followed up to 6 months.
“This is huge,” Dr. Carrier stressed. “This is much higher than what we tolerate for all sorts of different populations for which we would recommend anticoagulation or thromboprophylaxis.”
The question is whether the risk score can be helpful in a real-world clinic setting, he said, adding: “I’d like to think the answer to that is yes.”
In the University of Ottawa cohort study, 11% of high-risk patients experienced a VTE complication, compared with 4% of those with lower risk, suggesting that the validation data for the Khorana risk score is not only accurate, it is “actually applicable in real-world practice, and you can use it in your own center,” he said.
Further, recent studies have demonstrated that treatment based on Khorana risk score assessment reduces VTE complications.
Prophylaxis options
Low-molecular-weight heparin (LMWH) has been shown in several studies to be associated with a significant relative VTE risk reduction in patients with cancer initiating chemotherapy – with only a slight, nonsignificant increase in the risk of major bleeding.
However, the absolute benefit was small, and LMWH is “parenteral, relatively costly, and, based on that, although we showed relatively good risk-benefit ratio, it never really got translated to clinical practice,” Dr. Carrier said.
In fact, a 2015 American Society of Clinical Oncology guidelines update recommended against routine thromboprophylaxis in this setting, but stated that it could be considered in select high-risk patients identified using a validated risk-assessment tool.
The guidelines noted that “individual risk factors such as biomarkers and cancer site don’t reliably identify high-risk patients.”
More recent data provide additional support for risk assessment and treatment based on Khorana risk score of 2 or higher.
The AVERT trial, for which Dr. Carrier was the first author, showed that the direct-acting oral anticoagulant (DOAC) apixaban reduced VTE incidence, compared with placebo, in patients with Khorana score of 2 or higher (4.2% vs. 10.2%; hazard ratio, 0.41 overall, and 1.0 vs. 7.3; HR, 0.14 on treatment), and the CASSINI trial showed that another DOAC, rivaroxaban, reduced VTE incidence, compared with placebo, in those with Khorana score of 2 or higher (5.9 vs. 6.7; HR, 0.6 overall, and 2.6 vs. 6.4; HR, 0.40 on treatment). The differences in the on-treatment populations were statistically significant.
The two trials, which included a variety of tumor types, showed similar rates of major bleeding, with an absolute difference of about 1% between treatment and placebo, which was not statistically significant in the on-treatment analyses (HR, 1.89 in AVERT and HR, 1.96 in CASSINI).
A systematic review of these trials showed an overall significant decrease in VTE complication risk with treatment in high-risk patients, and a nonstatistically significant major bleeding risk increase.
Based on these findings, ASCO guidelines were updated in 2020 to state that “routine thromboprophylaxis should not be offered to all patients with cancer. ... However, high-risk outpatients with cancer may be offered thromboprophylaxis with apixaban, rivaroxaban or LMWH, providing there are no significant risk factors for bleeding or drug-drug interactions, and after having a full discussion with patients ... to make sure they understand the risk-benefit ratio and the rationale for that particular recommendation,” he said.
Real-world implementation
Implementing this approach in the clinic setting requires a practical model, such as the Venous Thromboembolism Prevention in the Ambulatory Cancer Clinic (VTEPACC) program, a prospective quality improvement research initiative developed in collaboration with the Jeffords Institute for Quality at the University of Vermont Medical Center and described in a recent report, Dr. Carrier said.
The “Vermont model” is “really a comprehensive model that includes identifying patients with the electronic medical records, gathering the formal education and insight from other health care providers like pharmacists and nurses in order to really come up with personalized care for your patients,” he explained.
In 918 outpatients with cancer who were included in the program, VTE awareness increased from less than 5% before VTEPACC to nearly 82% during the implementation phase and 94.7% after 2 years, with nearly 94% of high-risk patients receiving VTE prophylaxis at that time.
“So we can certainly do that in our own center.” he said. “It’s a matter of coming up with the model and making sure that the patients are seen at the right time.”
Given the high frequency of VTE in patients with cancer initiating chemotherapy, the usefulness of risk scores such as the Khorana risk score for identifying those at high risk, and the availability of safe and effective interventions for reducing risk, “we should probably use the data and incorporate them into clinical practice by implementation of programs for primary prevention,” he said.
A word of caution
Caution is warranted, however, when it comes to using DOACs in patients with higher-risk or potentially higher-risk tumor types, he added.
“It’s an important question we are facing as clinicians on a daily basis,” he said, responding to an attendee’s query, as shared by session moderator James Douketis, MD, professor of medicine at McMaster University, Hamilton, Ont., regarding possible bleeding risks in certain genitourinary cancers.
A recent meta-analysis published in Nature, for example, noted that, in the SELECT-D trial, rivaroxaban was associated with significantly higher incidence of clinically relevant nonmajor bleeding, most often in bladder and colorectal cancers, and most often at genitourinary and gastrointestinal sites.
Both Dr. Carrier and fellow panelist Michael Streiff, MD, professor of medicine at Johns Hopkins University and medical director at the Johns Hopkins Hospital Special Coagulation Laboratory, Baltimore, said they approach DOAC use cautiously, but don’t rule it out entirely, in patients with unresected genitourinary tumors that could pose a risk of bleeding.
“It’s worth mentioning and being cautious. In my own personal practice, I’m very careful with unresected urothelial-type tumors or, for example, bladder cancer, for the same reason as [with] unresected luminal GI tumors,” Dr. Carrier said, adding that he’s also mindful that patients with nephropathy were excluded from U.S. DOAC trials because of bleeding risk.
He said he sometimes tries a LMWH challenge first in higher-risk patients, and then might try a DOAC if no bleeding occurs.
“But it certainly is controversial,” he noted.
Dr. Streiff added that he also worries less with genitourinary cancers than with upper GI lesions because “the signals weren’t as big as in GI” cancers, but he noted that “the drugs are going out through the kidneys ... so I’m cautious in those populations.”
“So caution, but not complete exclusion, is the operative management,” Dr. Douketis said, summarizing the panelists’ consensus.
Dr. Carrier reported clinical trial or advisory board participation for Bayer, Pfizer, Servier, Leo Pharma, and/or BMS.
Primary thromboprophylaxis is feasible and worth considering for high-risk ambulatory patients with cancer who are initiating systemic chemotherapy, according to Marc Carrier, MD.
Risk scores can identify patients at high risk for venous thromboembolism (VTE), and treatments that are effective and associated with low bleeding risk are available, Dr. Carrier explained at the biennial summit of the Thrombosis & Hemostasis Societies of North America.
However, caution is advised in patients with certain types of cancer, including some gastrointestinal and genitourinary cancers, because of the possibility of increased major and clinically relevant nonmajor bleeding risk, he said.
VTE and cancer
VTE is relatively rare in the general population, occurring in about 1 or 2 per 1,000 people annually. The risk increases 4.1-fold in patients with cancer, and 6.5-fold in patients with cancer receiving chemotherapy.
“So just putting these numbers together, we’re no longer talking about 1 in 1,000, but 1 in 200, so [this is] something that is very common among cancer patients,” said Dr. Carrier, a professor at the University of Ottawa and chief of the division of hematology at The Ottawa Hospital.
The mortality rate associated with cancer-associated thrombosis is about 9%, comparable to that associated with infection in the cancer outpatient setting, which underscores the importance of educating patients about the signs and symptoms of VTE so they can seek medical treatment quickly if necessary, he added.
It may also be useful to discuss prophylaxis or other ways to prevent venous thromboembolic complications with certain patients, he said, noting that in an observational cohort study of nearly 600 patients at the University of Ottawa, 25% of those initiating chemotherapy were identified as intermediate or high risk using the validated Khorana risk score, and thus would likely benefit from thromboprophylaxis.
Risk assessment
The Khorana risk score assesses VTE risk based on cancer site, blood counts, and body mass index. It is simple to use and has been validated in more than 20,000 people in multiple countries, Dr. Carrier said.
In a well-known validation study, Ay et al. showed a VTE complication rate of 10% in patients with a Khorana risk score of 2 or higher who were followed up to 6 months.
“This is huge,” Dr. Carrier stressed. “This is much higher than what we tolerate for all sorts of different populations for which we would recommend anticoagulation or thromboprophylaxis.”
The question is whether the risk score can be helpful in a real-world clinic setting, he said, adding: “I’d like to think the answer to that is yes.”
In the University of Ottawa cohort study, 11% of high-risk patients experienced a VTE complication, compared with 4% of those with lower risk, suggesting that the validation data for the Khorana risk score is not only accurate, it is “actually applicable in real-world practice, and you can use it in your own center,” he said.
Further, recent studies have demonstrated that treatment based on Khorana risk score assessment reduces VTE complications.
Prophylaxis options
Low-molecular-weight heparin (LMWH) has been shown in several studies to be associated with a significant relative VTE risk reduction in patients with cancer initiating chemotherapy – with only a slight, nonsignificant increase in the risk of major bleeding.
However, the absolute benefit was small, and LMWH is “parenteral, relatively costly, and, based on that, although we showed relatively good risk-benefit ratio, it never really got translated to clinical practice,” Dr. Carrier said.
In fact, a 2015 American Society of Clinical Oncology guidelines update recommended against routine thromboprophylaxis in this setting, but stated that it could be considered in select high-risk patients identified using a validated risk-assessment tool.
The guidelines noted that “individual risk factors such as biomarkers and cancer site don’t reliably identify high-risk patients.”
More recent data provide additional support for risk assessment and treatment based on Khorana risk score of 2 or higher.
The AVERT trial, for which Dr. Carrier was the first author, showed that the direct-acting oral anticoagulant (DOAC) apixaban reduced VTE incidence, compared with placebo, in patients with Khorana score of 2 or higher (4.2% vs. 10.2%; hazard ratio, 0.41 overall, and 1.0 vs. 7.3; HR, 0.14 on treatment), and the CASSINI trial showed that another DOAC, rivaroxaban, reduced VTE incidence, compared with placebo, in those with Khorana score of 2 or higher (5.9 vs. 6.7; HR, 0.6 overall, and 2.6 vs. 6.4; HR, 0.40 on treatment). The differences in the on-treatment populations were statistically significant.
The two trials, which included a variety of tumor types, showed similar rates of major bleeding, with an absolute difference of about 1% between treatment and placebo, which was not statistically significant in the on-treatment analyses (HR, 1.89 in AVERT and HR, 1.96 in CASSINI).
A systematic review of these trials showed an overall significant decrease in VTE complication risk with treatment in high-risk patients, and a nonstatistically significant major bleeding risk increase.
Based on these findings, ASCO guidelines were updated in 2020 to state that “routine thromboprophylaxis should not be offered to all patients with cancer. ... However, high-risk outpatients with cancer may be offered thromboprophylaxis with apixaban, rivaroxaban or LMWH, providing there are no significant risk factors for bleeding or drug-drug interactions, and after having a full discussion with patients ... to make sure they understand the risk-benefit ratio and the rationale for that particular recommendation,” he said.
Real-world implementation
Implementing this approach in the clinic setting requires a practical model, such as the Venous Thromboembolism Prevention in the Ambulatory Cancer Clinic (VTEPACC) program, a prospective quality improvement research initiative developed in collaboration with the Jeffords Institute for Quality at the University of Vermont Medical Center and described in a recent report, Dr. Carrier said.
The “Vermont model” is “really a comprehensive model that includes identifying patients with the electronic medical records, gathering the formal education and insight from other health care providers like pharmacists and nurses in order to really come up with personalized care for your patients,” he explained.
In 918 outpatients with cancer who were included in the program, VTE awareness increased from less than 5% before VTEPACC to nearly 82% during the implementation phase and 94.7% after 2 years, with nearly 94% of high-risk patients receiving VTE prophylaxis at that time.
“So we can certainly do that in our own center.” he said. “It’s a matter of coming up with the model and making sure that the patients are seen at the right time.”
Given the high frequency of VTE in patients with cancer initiating chemotherapy, the usefulness of risk scores such as the Khorana risk score for identifying those at high risk, and the availability of safe and effective interventions for reducing risk, “we should probably use the data and incorporate them into clinical practice by implementation of programs for primary prevention,” he said.
A word of caution
Caution is warranted, however, when it comes to using DOACs in patients with higher-risk or potentially higher-risk tumor types, he added.
“It’s an important question we are facing as clinicians on a daily basis,” he said, responding to an attendee’s query, as shared by session moderator James Douketis, MD, professor of medicine at McMaster University, Hamilton, Ont., regarding possible bleeding risks in certain genitourinary cancers.
A recent meta-analysis published in Nature, for example, noted that, in the SELECT-D trial, rivaroxaban was associated with significantly higher incidence of clinically relevant nonmajor bleeding, most often in bladder and colorectal cancers, and most often at genitourinary and gastrointestinal sites.
Both Dr. Carrier and fellow panelist Michael Streiff, MD, professor of medicine at Johns Hopkins University and medical director at the Johns Hopkins Hospital Special Coagulation Laboratory, Baltimore, said they approach DOAC use cautiously, but don’t rule it out entirely, in patients with unresected genitourinary tumors that could pose a risk of bleeding.
“It’s worth mentioning and being cautious. In my own personal practice, I’m very careful with unresected urothelial-type tumors or, for example, bladder cancer, for the same reason as [with] unresected luminal GI tumors,” Dr. Carrier said, adding that he’s also mindful that patients with nephropathy were excluded from U.S. DOAC trials because of bleeding risk.
He said he sometimes tries a LMWH challenge first in higher-risk patients, and then might try a DOAC if no bleeding occurs.
“But it certainly is controversial,” he noted.
Dr. Streiff added that he also worries less with genitourinary cancers than with upper GI lesions because “the signals weren’t as big as in GI” cancers, but he noted that “the drugs are going out through the kidneys ... so I’m cautious in those populations.”
“So caution, but not complete exclusion, is the operative management,” Dr. Douketis said, summarizing the panelists’ consensus.
Dr. Carrier reported clinical trial or advisory board participation for Bayer, Pfizer, Servier, Leo Pharma, and/or BMS.
FROM THE THSNA BIENNIAL SUMMIT
Understanding and addressing suicide risk in LGBTQ+ youth
Even as dozens of state legislature bills attempt to limit the rights of sexual-diverse and gender-diverse youth, researchers are learning more and more that can help pediatricians better support this population in their practices, according to David Inwards-Breland, MD, MPH, a professor of clinical pediatrics at the University of California, San Diego.
Dr. Inwards-Breland highlighted two key studies in recent years during the LGBTQ+ section at the annual meeting of the American Academy of Pediatrics, held virtually in 2020.
High suicide rates among sexual minority youth
Past research has found that adolescents who identify as sexual minorities have nearly five times the rate of suicide attempts, compared with their heterosexual peers, Dr. Inwards-Breland said as he introduced a recent study on disparities in adolescent suicide.
“This may be from a disproportionate burden of poor mental health that has been linked to stigma,” he said, adding that an estimated 125 state bills have been introduced in the United States that would restrict the rights of sexual minorities.
The study, published in Pediatrics in March 2020, compiled data from 110,243 adolescents in six states on sexual orientation identity; 25,994 adolescents in four states on same-sex sexual contact and sexual assault; and 20,655 adolescents in three states on sexual orientation identity, the sex of sexual contacts, and sexual assault.
The authors found that heterosexual identity dropped from 93% to 86% between 2009 and 2017, but sexual minority youth accounted for an increasing share of suicide attempts over the same period. A quarter of adolescents who attempted suicide in 2009 were sexual minorities, which increased to 36% in 2017. Similarly, among sexually active teens who attempted suicide, the proportion of those who had same-sex contact nearly doubled, from 16% to 30%.
The good news, Dr. Inwards-Breland said, was that overall suicide attempts declined among sexual minorities, but they remain three times as likely to attempt suicide, compared with their heterosexual counterparts.
“As the number of adolescents increase in our country, there will be increasing numbers of adolescents identifying as sexual minorities or who have had same-sex sexual contact,” Dr. Inwards-Breland said. “Therefore, providing confidential services is even more important to allow youth to feel comfortable with their health care provider.” He also emphasized the importance of consistent universal depression screening and advocacy to eliminate and prevent policies that harm these youth.
Using youths’ chosen names
Transgender and nonbinary youth – those who do not identify as male or female – have a higher risk of poor mental health and higher levels of suicidal ideation and behaviors, compared with their “cis” peers, those who identify with the gender they were assigned at birth, Dr. Inwards-Breland said. However, using the chosen, or assertive, name of transgender and nonbinary youth predicted fewer depressive symptoms and less suicidal ideation and behavior in a study published in the Journal of Adolescent Health in October 2018.
“Choosing a name is an important part of social transition of transgender individuals, yet they’re unable to use their name because of interpersonal or institutional barriers,” he said. In addition, using a name other than their legally given name can subject them to discrimination and victimization.
The study, drawing from a larger cohort of LGBTQ youth, involved 129 transgender and nonbinary adolescents, aged 15-21, of whom 74 had a chosen name. No other differences in personal characteristics were associated with depressive symptoms or suicidal ideation besides increased use of their assertive name in different life contexts.
An increase in one context where chosen name could be used predicted a 5.37-unit decrease in depressive symptoms, a 29% decrease in suicidal ideation, and a 56% decrease in suicidal behavior, the study found. All three outcomes were at their lowest levels when chosen names were used in all four contexts explored in the study.
“The chosen name affirms their gender identity,” Dr. Inwards-Breland said, but “the legal name change process is very onerous.” He highlighted the need for institutions to adjust regulations and information systems, for policies that promote the transition process, and for youths’ names to be affirmed in multiple contexts.
“We as pediatricians, specialists, and primary care doctors can support families as they adjust the transition process by helping them with assertive names and pronouns and giving them resources,” Dr. Inwards-Breland said. He also called for school policies and teacher/staff training that promote the use of assertive names and pronouns, and ensuring that the assertive name and pronouns are in the medical record and used by office staff and other medical professionals.
‘A light in the dark’ for LGBTQ+ youth
Clair Kronk of the University of Cincinnati and Cincinnati Children’s Hospital and Medical Center attended the LGBTQ+ section at the AAP meeting because of concerns about she and her transgender siblings have been treated by the medical community.
“It has always been important to be ‘on the pulse’ of what is happening in the medical community, especially with new, more discriminatory policies being passed seemingly willy-nilly these days, both in the medical realm and outside of it,” Ms. Kronk said in an interview. “I was overjoyed to see how many people seemed to care so much about the transgender community and LGBTQIA+ people generally.”
As an ontologist and bioinformatician, she did not recall many big clinical takeaways for her particular work, but she appreciated how many areas the session covered, especially given the dearth of instruction about LGBTQ+ care in medical training.
“This session was a bit of a light in the dark given the state of LGBTQIA+ health care rights,” she said. “There is a lot at stake in the next year or so, and providers’ and LGBTQIA+ persons’ voices need to be heard right now more than ever.”
Sonia Khan, MD, a pediatrician and the medical director of the substance use disorder counseling program in the department of health and human services in Fremont, Calif., also attended the session and came away feeling invigorated.
“These data make me feel more optimistic than I have been in ages in terms of increasing the safety of young people being able to come out,” Dr. Khan said in the comments during the session. “These last 4 years felt so regressive. [It’s] good to get the big picture.”
The presenters and commentators had no disclosures.
Even as dozens of state legislature bills attempt to limit the rights of sexual-diverse and gender-diverse youth, researchers are learning more and more that can help pediatricians better support this population in their practices, according to David Inwards-Breland, MD, MPH, a professor of clinical pediatrics at the University of California, San Diego.
Dr. Inwards-Breland highlighted two key studies in recent years during the LGBTQ+ section at the annual meeting of the American Academy of Pediatrics, held virtually in 2020.
High suicide rates among sexual minority youth
Past research has found that adolescents who identify as sexual minorities have nearly five times the rate of suicide attempts, compared with their heterosexual peers, Dr. Inwards-Breland said as he introduced a recent study on disparities in adolescent suicide.
“This may be from a disproportionate burden of poor mental health that has been linked to stigma,” he said, adding that an estimated 125 state bills have been introduced in the United States that would restrict the rights of sexual minorities.
The study, published in Pediatrics in March 2020, compiled data from 110,243 adolescents in six states on sexual orientation identity; 25,994 adolescents in four states on same-sex sexual contact and sexual assault; and 20,655 adolescents in three states on sexual orientation identity, the sex of sexual contacts, and sexual assault.
The authors found that heterosexual identity dropped from 93% to 86% between 2009 and 2017, but sexual minority youth accounted for an increasing share of suicide attempts over the same period. A quarter of adolescents who attempted suicide in 2009 were sexual minorities, which increased to 36% in 2017. Similarly, among sexually active teens who attempted suicide, the proportion of those who had same-sex contact nearly doubled, from 16% to 30%.
The good news, Dr. Inwards-Breland said, was that overall suicide attempts declined among sexual minorities, but they remain three times as likely to attempt suicide, compared with their heterosexual counterparts.
“As the number of adolescents increase in our country, there will be increasing numbers of adolescents identifying as sexual minorities or who have had same-sex sexual contact,” Dr. Inwards-Breland said. “Therefore, providing confidential services is even more important to allow youth to feel comfortable with their health care provider.” He also emphasized the importance of consistent universal depression screening and advocacy to eliminate and prevent policies that harm these youth.
Using youths’ chosen names
Transgender and nonbinary youth – those who do not identify as male or female – have a higher risk of poor mental health and higher levels of suicidal ideation and behaviors, compared with their “cis” peers, those who identify with the gender they were assigned at birth, Dr. Inwards-Breland said. However, using the chosen, or assertive, name of transgender and nonbinary youth predicted fewer depressive symptoms and less suicidal ideation and behavior in a study published in the Journal of Adolescent Health in October 2018.
“Choosing a name is an important part of social transition of transgender individuals, yet they’re unable to use their name because of interpersonal or institutional barriers,” he said. In addition, using a name other than their legally given name can subject them to discrimination and victimization.
The study, drawing from a larger cohort of LGBTQ youth, involved 129 transgender and nonbinary adolescents, aged 15-21, of whom 74 had a chosen name. No other differences in personal characteristics were associated with depressive symptoms or suicidal ideation besides increased use of their assertive name in different life contexts.
An increase in one context where chosen name could be used predicted a 5.37-unit decrease in depressive symptoms, a 29% decrease in suicidal ideation, and a 56% decrease in suicidal behavior, the study found. All three outcomes were at their lowest levels when chosen names were used in all four contexts explored in the study.
“The chosen name affirms their gender identity,” Dr. Inwards-Breland said, but “the legal name change process is very onerous.” He highlighted the need for institutions to adjust regulations and information systems, for policies that promote the transition process, and for youths’ names to be affirmed in multiple contexts.
“We as pediatricians, specialists, and primary care doctors can support families as they adjust the transition process by helping them with assertive names and pronouns and giving them resources,” Dr. Inwards-Breland said. He also called for school policies and teacher/staff training that promote the use of assertive names and pronouns, and ensuring that the assertive name and pronouns are in the medical record and used by office staff and other medical professionals.
‘A light in the dark’ for LGBTQ+ youth
Clair Kronk of the University of Cincinnati and Cincinnati Children’s Hospital and Medical Center attended the LGBTQ+ section at the AAP meeting because of concerns about she and her transgender siblings have been treated by the medical community.
“It has always been important to be ‘on the pulse’ of what is happening in the medical community, especially with new, more discriminatory policies being passed seemingly willy-nilly these days, both in the medical realm and outside of it,” Ms. Kronk said in an interview. “I was overjoyed to see how many people seemed to care so much about the transgender community and LGBTQIA+ people generally.”
As an ontologist and bioinformatician, she did not recall many big clinical takeaways for her particular work, but she appreciated how many areas the session covered, especially given the dearth of instruction about LGBTQ+ care in medical training.
“This session was a bit of a light in the dark given the state of LGBTQIA+ health care rights,” she said. “There is a lot at stake in the next year or so, and providers’ and LGBTQIA+ persons’ voices need to be heard right now more than ever.”
Sonia Khan, MD, a pediatrician and the medical director of the substance use disorder counseling program in the department of health and human services in Fremont, Calif., also attended the session and came away feeling invigorated.
“These data make me feel more optimistic than I have been in ages in terms of increasing the safety of young people being able to come out,” Dr. Khan said in the comments during the session. “These last 4 years felt so regressive. [It’s] good to get the big picture.”
The presenters and commentators had no disclosures.
Even as dozens of state legislature bills attempt to limit the rights of sexual-diverse and gender-diverse youth, researchers are learning more and more that can help pediatricians better support this population in their practices, according to David Inwards-Breland, MD, MPH, a professor of clinical pediatrics at the University of California, San Diego.
Dr. Inwards-Breland highlighted two key studies in recent years during the LGBTQ+ section at the annual meeting of the American Academy of Pediatrics, held virtually in 2020.
High suicide rates among sexual minority youth
Past research has found that adolescents who identify as sexual minorities have nearly five times the rate of suicide attempts, compared with their heterosexual peers, Dr. Inwards-Breland said as he introduced a recent study on disparities in adolescent suicide.
“This may be from a disproportionate burden of poor mental health that has been linked to stigma,” he said, adding that an estimated 125 state bills have been introduced in the United States that would restrict the rights of sexual minorities.
The study, published in Pediatrics in March 2020, compiled data from 110,243 adolescents in six states on sexual orientation identity; 25,994 adolescents in four states on same-sex sexual contact and sexual assault; and 20,655 adolescents in three states on sexual orientation identity, the sex of sexual contacts, and sexual assault.
The authors found that heterosexual identity dropped from 93% to 86% between 2009 and 2017, but sexual minority youth accounted for an increasing share of suicide attempts over the same period. A quarter of adolescents who attempted suicide in 2009 were sexual minorities, which increased to 36% in 2017. Similarly, among sexually active teens who attempted suicide, the proportion of those who had same-sex contact nearly doubled, from 16% to 30%.
The good news, Dr. Inwards-Breland said, was that overall suicide attempts declined among sexual minorities, but they remain three times as likely to attempt suicide, compared with their heterosexual counterparts.
“As the number of adolescents increase in our country, there will be increasing numbers of adolescents identifying as sexual minorities or who have had same-sex sexual contact,” Dr. Inwards-Breland said. “Therefore, providing confidential services is even more important to allow youth to feel comfortable with their health care provider.” He also emphasized the importance of consistent universal depression screening and advocacy to eliminate and prevent policies that harm these youth.
Using youths’ chosen names
Transgender and nonbinary youth – those who do not identify as male or female – have a higher risk of poor mental health and higher levels of suicidal ideation and behaviors, compared with their “cis” peers, those who identify with the gender they were assigned at birth, Dr. Inwards-Breland said. However, using the chosen, or assertive, name of transgender and nonbinary youth predicted fewer depressive symptoms and less suicidal ideation and behavior in a study published in the Journal of Adolescent Health in October 2018.
“Choosing a name is an important part of social transition of transgender individuals, yet they’re unable to use their name because of interpersonal or institutional barriers,” he said. In addition, using a name other than their legally given name can subject them to discrimination and victimization.
The study, drawing from a larger cohort of LGBTQ youth, involved 129 transgender and nonbinary adolescents, aged 15-21, of whom 74 had a chosen name. No other differences in personal characteristics were associated with depressive symptoms or suicidal ideation besides increased use of their assertive name in different life contexts.
An increase in one context where chosen name could be used predicted a 5.37-unit decrease in depressive symptoms, a 29% decrease in suicidal ideation, and a 56% decrease in suicidal behavior, the study found. All three outcomes were at their lowest levels when chosen names were used in all four contexts explored in the study.
“The chosen name affirms their gender identity,” Dr. Inwards-Breland said, but “the legal name change process is very onerous.” He highlighted the need for institutions to adjust regulations and information systems, for policies that promote the transition process, and for youths’ names to be affirmed in multiple contexts.
“We as pediatricians, specialists, and primary care doctors can support families as they adjust the transition process by helping them with assertive names and pronouns and giving them resources,” Dr. Inwards-Breland said. He also called for school policies and teacher/staff training that promote the use of assertive names and pronouns, and ensuring that the assertive name and pronouns are in the medical record and used by office staff and other medical professionals.
‘A light in the dark’ for LGBTQ+ youth
Clair Kronk of the University of Cincinnati and Cincinnati Children’s Hospital and Medical Center attended the LGBTQ+ section at the AAP meeting because of concerns about she and her transgender siblings have been treated by the medical community.
“It has always been important to be ‘on the pulse’ of what is happening in the medical community, especially with new, more discriminatory policies being passed seemingly willy-nilly these days, both in the medical realm and outside of it,” Ms. Kronk said in an interview. “I was overjoyed to see how many people seemed to care so much about the transgender community and LGBTQIA+ people generally.”
As an ontologist and bioinformatician, she did not recall many big clinical takeaways for her particular work, but she appreciated how many areas the session covered, especially given the dearth of instruction about LGBTQ+ care in medical training.
“This session was a bit of a light in the dark given the state of LGBTQIA+ health care rights,” she said. “There is a lot at stake in the next year or so, and providers’ and LGBTQIA+ persons’ voices need to be heard right now more than ever.”
Sonia Khan, MD, a pediatrician and the medical director of the substance use disorder counseling program in the department of health and human services in Fremont, Calif., also attended the session and came away feeling invigorated.
“These data make me feel more optimistic than I have been in ages in terms of increasing the safety of young people being able to come out,” Dr. Khan said in the comments during the session. “These last 4 years felt so regressive. [It’s] good to get the big picture.”
The presenters and commentators had no disclosures.
FROM AAP 2020
An alternative path to recertification
Recertification will include physicians who were initially board certified with UCNS in the subspecialties of autonomic disorders, behavioral neurology and neuropsychiatry, clinical neuromuscular pathology, geriatric neurology, headache medicine, neurocritical care, neuroimaging, and neuro-oncology.
In 2020, UCNS transitioned to a new continuous-certification (C-cert) model that requires its diplomates to pay an annual fee of $175 and complete a 25-question online quiz based on preselected journal articles with an 80% passing grade. In a press release outlining the details of the new C-cert program, UCNS said that diplomates began the transition last year by “attesting they have participated in subspecialty-specific continuing medical education (CME) requirements from the time their most recent certificate was issued through 2019.” Diplomates have a 2-year window, which began in 2019, to meet these transitional CME requirements and complete an attestation statement before their certification lapses. “Diplomates with a status of ‘meeting requirements’ will be issued a replacement certificate that shows their original certification date and will reflect there is no expiration date after they pay the first annual C-cert fee in 2020,” UCNS said in the press release.
“It is unfortunate that despite requests from diplomates and other stakeholders, UCNS has decided to impose new requirements and additional fees on diplomates who have unexpired certificates based on passing an examination that granted a 10-year certification,” Paul G. Mathew, MD, assistant professor of neurology at Harvard Medical School in Boston and Director of Legislative Affairs at NBPAS, said in an interview. “A one-size-fits-all approach for learning with preselected articles is not ideal, and physicians should be able to choose CME and other learning activities that best suit their individual interests and practice.”
The added requirements and fees have caused some UCNS diplomates to consider letting their certification lapse, Dr. Mathew said, but the NBPAS decision offers them a new path to recertification. “Many physicians who would have otherwise let their certification lapse and would no longer be considered board certified in headache medicine and other UCNS subspecialties will now have the option to recertify with NBPAS,” he said.
NBPAS was formed in 2014 in response to controversial American Board of Medical Specialties Maintenance of Certification (MOC) programs. NBPAS recertifies diplomates of all specialties and subspecialties offered by the ABMS and its member boards, including board certification in neurology and neurologic subspecialties offered by the American Board of Psychiatry and Neurology.
Board recertification with NBPAS requires an unrestricted license to practice medicine in the United States, an initial certification with ABPN, the American Osteopathic Association, and/or UCNS, a medical staff appointment/membership in good standing, active hospital privileges based on specialty, and 50 hours of relevant CME credits every 2 years.
“Although MOC compliance is not required for licensure, the vast majority of insurance carriers in the United States require to some extent that their physicians be MOC compliant. As such, the ABMS has a monopoly in that a physician cannot practice medicine without complying with MOC,” Dr. Mathew said. “That’s very gradually changing.”
So far, 13 states have passed legislation limiting ABMS MOC compliance as a requirement for credentialing or licensure, and 136 healthcare institutions have recognized NBPAS as a pathway for physician credentialing, according to an NBPAS press release.
Changing the rules
Alan Rapoport, MD, was asked to comment on the recertification situtaion. Dr. Rapoport is clinical professor of neurology at UCLA and the Editor in Chief of Neurology Reviews. “As Dr. Mathew aptly states, it is unfortunate that despite requests from diplomates and other stakeholders, UCNS has decided to impose new requirements and additional fees on diplomates who have unexpired certificates based on passing an examination that granted a 10-year certification,”
For context, Dr. Rapoport explained what has happened to him and about 200 neurologists and a few other specialists who took the first UCNS certifying exam in Headache Medicine. “I sat for the first exam in a testing center in 2006, after paying a large fee. I passed and was granted a certificate for a 10-year certification in Headache Medicine. Prior to the expiration of that certificate, I was told I had to pay about $1,800 and take a similar examination to certify for another 10 years. I was not sure I needed to do that, but I did so anyway and passed and was granted a new, dated certificate for another 10 years of certification in Headache Medicine. Shortly after that I began to get notices from UCNS saying that they were changing their certification process and I would soon have to read their designated articles, take an examination on that literature, pay $175 for this privilege of C-Cert yearly, all in spite of the fact that I had a valid certificate for 10 years of certification.”
After complaints from Dr. Rapoport and many others, “UCNS said we would only have to do this when we had 5 years left on our certification. When they advertised this new C-Cert plan on the AAN Headache Listserv, even though advertising was against the rules of the Listserv, I complained about it saying we had paid for a 10-year certification. Their response was to abruptly take me off the Listserv. Then they temporarily shut it down when others agreed with what I had written.”
Dr. Rapoport has the certificate that proves that he has 6 years left on his certification, but UCNS will not recognize this, he said. “I believe that to be unfair, unethical, and probably illegal, as do many senior Headache specialists in the country who have the same issue. The attorney for the UCNS, who is also the attorney for the AAN, has disregarded our objections to this move.”
Now the NBPAS will be recertifying Headache Medicine doctors and those of other specialties who are in a similar situation and do not want to pay for the privilege of taking exams yearly when they have already been certified. “I expect many specialists will switch to this new way of certifying,” Dr. Rapoport said.
“I believe the UCNS has cheapened the value of their certifications by not honoring them,” Dr. Rapoort said.
Dr. Mathew reports that he collects no salary for his role with NBPAS, but receives reimbursement for travel expenses, and occasionally receives honoraria for speaking on behalf of NBPAS.
Recertification will include physicians who were initially board certified with UCNS in the subspecialties of autonomic disorders, behavioral neurology and neuropsychiatry, clinical neuromuscular pathology, geriatric neurology, headache medicine, neurocritical care, neuroimaging, and neuro-oncology.
In 2020, UCNS transitioned to a new continuous-certification (C-cert) model that requires its diplomates to pay an annual fee of $175 and complete a 25-question online quiz based on preselected journal articles with an 80% passing grade. In a press release outlining the details of the new C-cert program, UCNS said that diplomates began the transition last year by “attesting they have participated in subspecialty-specific continuing medical education (CME) requirements from the time their most recent certificate was issued through 2019.” Diplomates have a 2-year window, which began in 2019, to meet these transitional CME requirements and complete an attestation statement before their certification lapses. “Diplomates with a status of ‘meeting requirements’ will be issued a replacement certificate that shows their original certification date and will reflect there is no expiration date after they pay the first annual C-cert fee in 2020,” UCNS said in the press release.
“It is unfortunate that despite requests from diplomates and other stakeholders, UCNS has decided to impose new requirements and additional fees on diplomates who have unexpired certificates based on passing an examination that granted a 10-year certification,” Paul G. Mathew, MD, assistant professor of neurology at Harvard Medical School in Boston and Director of Legislative Affairs at NBPAS, said in an interview. “A one-size-fits-all approach for learning with preselected articles is not ideal, and physicians should be able to choose CME and other learning activities that best suit their individual interests and practice.”
The added requirements and fees have caused some UCNS diplomates to consider letting their certification lapse, Dr. Mathew said, but the NBPAS decision offers them a new path to recertification. “Many physicians who would have otherwise let their certification lapse and would no longer be considered board certified in headache medicine and other UCNS subspecialties will now have the option to recertify with NBPAS,” he said.
NBPAS was formed in 2014 in response to controversial American Board of Medical Specialties Maintenance of Certification (MOC) programs. NBPAS recertifies diplomates of all specialties and subspecialties offered by the ABMS and its member boards, including board certification in neurology and neurologic subspecialties offered by the American Board of Psychiatry and Neurology.
Board recertification with NBPAS requires an unrestricted license to practice medicine in the United States, an initial certification with ABPN, the American Osteopathic Association, and/or UCNS, a medical staff appointment/membership in good standing, active hospital privileges based on specialty, and 50 hours of relevant CME credits every 2 years.
“Although MOC compliance is not required for licensure, the vast majority of insurance carriers in the United States require to some extent that their physicians be MOC compliant. As such, the ABMS has a monopoly in that a physician cannot practice medicine without complying with MOC,” Dr. Mathew said. “That’s very gradually changing.”
So far, 13 states have passed legislation limiting ABMS MOC compliance as a requirement for credentialing or licensure, and 136 healthcare institutions have recognized NBPAS as a pathway for physician credentialing, according to an NBPAS press release.
Changing the rules
Alan Rapoport, MD, was asked to comment on the recertification situtaion. Dr. Rapoport is clinical professor of neurology at UCLA and the Editor in Chief of Neurology Reviews. “As Dr. Mathew aptly states, it is unfortunate that despite requests from diplomates and other stakeholders, UCNS has decided to impose new requirements and additional fees on diplomates who have unexpired certificates based on passing an examination that granted a 10-year certification,”
For context, Dr. Rapoport explained what has happened to him and about 200 neurologists and a few other specialists who took the first UCNS certifying exam in Headache Medicine. “I sat for the first exam in a testing center in 2006, after paying a large fee. I passed and was granted a certificate for a 10-year certification in Headache Medicine. Prior to the expiration of that certificate, I was told I had to pay about $1,800 and take a similar examination to certify for another 10 years. I was not sure I needed to do that, but I did so anyway and passed and was granted a new, dated certificate for another 10 years of certification in Headache Medicine. Shortly after that I began to get notices from UCNS saying that they were changing their certification process and I would soon have to read their designated articles, take an examination on that literature, pay $175 for this privilege of C-Cert yearly, all in spite of the fact that I had a valid certificate for 10 years of certification.”
After complaints from Dr. Rapoport and many others, “UCNS said we would only have to do this when we had 5 years left on our certification. When they advertised this new C-Cert plan on the AAN Headache Listserv, even though advertising was against the rules of the Listserv, I complained about it saying we had paid for a 10-year certification. Their response was to abruptly take me off the Listserv. Then they temporarily shut it down when others agreed with what I had written.”
Dr. Rapoport has the certificate that proves that he has 6 years left on his certification, but UCNS will not recognize this, he said. “I believe that to be unfair, unethical, and probably illegal, as do many senior Headache specialists in the country who have the same issue. The attorney for the UCNS, who is also the attorney for the AAN, has disregarded our objections to this move.”
Now the NBPAS will be recertifying Headache Medicine doctors and those of other specialties who are in a similar situation and do not want to pay for the privilege of taking exams yearly when they have already been certified. “I expect many specialists will switch to this new way of certifying,” Dr. Rapoport said.
“I believe the UCNS has cheapened the value of their certifications by not honoring them,” Dr. Rapoort said.
Dr. Mathew reports that he collects no salary for his role with NBPAS, but receives reimbursement for travel expenses, and occasionally receives honoraria for speaking on behalf of NBPAS.
Recertification will include physicians who were initially board certified with UCNS in the subspecialties of autonomic disorders, behavioral neurology and neuropsychiatry, clinical neuromuscular pathology, geriatric neurology, headache medicine, neurocritical care, neuroimaging, and neuro-oncology.
In 2020, UCNS transitioned to a new continuous-certification (C-cert) model that requires its diplomates to pay an annual fee of $175 and complete a 25-question online quiz based on preselected journal articles with an 80% passing grade. In a press release outlining the details of the new C-cert program, UCNS said that diplomates began the transition last year by “attesting they have participated in subspecialty-specific continuing medical education (CME) requirements from the time their most recent certificate was issued through 2019.” Diplomates have a 2-year window, which began in 2019, to meet these transitional CME requirements and complete an attestation statement before their certification lapses. “Diplomates with a status of ‘meeting requirements’ will be issued a replacement certificate that shows their original certification date and will reflect there is no expiration date after they pay the first annual C-cert fee in 2020,” UCNS said in the press release.
“It is unfortunate that despite requests from diplomates and other stakeholders, UCNS has decided to impose new requirements and additional fees on diplomates who have unexpired certificates based on passing an examination that granted a 10-year certification,” Paul G. Mathew, MD, assistant professor of neurology at Harvard Medical School in Boston and Director of Legislative Affairs at NBPAS, said in an interview. “A one-size-fits-all approach for learning with preselected articles is not ideal, and physicians should be able to choose CME and other learning activities that best suit their individual interests and practice.”
The added requirements and fees have caused some UCNS diplomates to consider letting their certification lapse, Dr. Mathew said, but the NBPAS decision offers them a new path to recertification. “Many physicians who would have otherwise let their certification lapse and would no longer be considered board certified in headache medicine and other UCNS subspecialties will now have the option to recertify with NBPAS,” he said.
NBPAS was formed in 2014 in response to controversial American Board of Medical Specialties Maintenance of Certification (MOC) programs. NBPAS recertifies diplomates of all specialties and subspecialties offered by the ABMS and its member boards, including board certification in neurology and neurologic subspecialties offered by the American Board of Psychiatry and Neurology.
Board recertification with NBPAS requires an unrestricted license to practice medicine in the United States, an initial certification with ABPN, the American Osteopathic Association, and/or UCNS, a medical staff appointment/membership in good standing, active hospital privileges based on specialty, and 50 hours of relevant CME credits every 2 years.
“Although MOC compliance is not required for licensure, the vast majority of insurance carriers in the United States require to some extent that their physicians be MOC compliant. As such, the ABMS has a monopoly in that a physician cannot practice medicine without complying with MOC,” Dr. Mathew said. “That’s very gradually changing.”
So far, 13 states have passed legislation limiting ABMS MOC compliance as a requirement for credentialing or licensure, and 136 healthcare institutions have recognized NBPAS as a pathway for physician credentialing, according to an NBPAS press release.
Changing the rules
Alan Rapoport, MD, was asked to comment on the recertification situtaion. Dr. Rapoport is clinical professor of neurology at UCLA and the Editor in Chief of Neurology Reviews. “As Dr. Mathew aptly states, it is unfortunate that despite requests from diplomates and other stakeholders, UCNS has decided to impose new requirements and additional fees on diplomates who have unexpired certificates based on passing an examination that granted a 10-year certification,”
For context, Dr. Rapoport explained what has happened to him and about 200 neurologists and a few other specialists who took the first UCNS certifying exam in Headache Medicine. “I sat for the first exam in a testing center in 2006, after paying a large fee. I passed and was granted a certificate for a 10-year certification in Headache Medicine. Prior to the expiration of that certificate, I was told I had to pay about $1,800 and take a similar examination to certify for another 10 years. I was not sure I needed to do that, but I did so anyway and passed and was granted a new, dated certificate for another 10 years of certification in Headache Medicine. Shortly after that I began to get notices from UCNS saying that they were changing their certification process and I would soon have to read their designated articles, take an examination on that literature, pay $175 for this privilege of C-Cert yearly, all in spite of the fact that I had a valid certificate for 10 years of certification.”
After complaints from Dr. Rapoport and many others, “UCNS said we would only have to do this when we had 5 years left on our certification. When they advertised this new C-Cert plan on the AAN Headache Listserv, even though advertising was against the rules of the Listserv, I complained about it saying we had paid for a 10-year certification. Their response was to abruptly take me off the Listserv. Then they temporarily shut it down when others agreed with what I had written.”
Dr. Rapoport has the certificate that proves that he has 6 years left on his certification, but UCNS will not recognize this, he said. “I believe that to be unfair, unethical, and probably illegal, as do many senior Headache specialists in the country who have the same issue. The attorney for the UCNS, who is also the attorney for the AAN, has disregarded our objections to this move.”
Now the NBPAS will be recertifying Headache Medicine doctors and those of other specialties who are in a similar situation and do not want to pay for the privilege of taking exams yearly when they have already been certified. “I expect many specialists will switch to this new way of certifying,” Dr. Rapoport said.
“I believe the UCNS has cheapened the value of their certifications by not honoring them,” Dr. Rapoort said.
Dr. Mathew reports that he collects no salary for his role with NBPAS, but receives reimbursement for travel expenses, and occasionally receives honoraria for speaking on behalf of NBPAS.
Challenges in the Management of Peptic Ulcer Disease
From the University of Alabama at Birmingham, Birmingham, AL.
Abstract
Objective: To review current challenges in the management of peptic ulcer disease.
Methods: Review of the literature.
Results: Peptic ulcer disease affects 5% to 10% of the population worldwide, with recent decreases in lifetime prevalence in high-income countries. Helicobacter pylori infection and nonsteroidal anti-inflammatory drug (NSAID) use are the most important drivers of peptic ulcer disease. Current management strategies for peptic ulcer disease focus on ulcer healing; management of complications such as bleeding, perforation, and obstruction; and prevention of ulcer recurrence. Proton pump inhibitors (PPIs) are the cornerstone of medical therapy for peptic ulcers, and complement testing for and treatment of H. pylori infection as well as elimination of NSAID use. Although advances have been made in the medical and endoscopic treatment of peptic ulcer disease and the management of ulcer complications, such as bleeding and obstruction, challenges remain.
Conclusion: Peptic ulcer disease is a common health problem globally, with persistent challenges related to refractory ulcers, antiplatelet and anticoagulant use, and continued bleeding in the face of endoscopic therapy. These challenges should be met with PPI therapy of adequate frequency and duration, vigilant attention to and treatment of ulcer etiology, evidence-based handling of antiplatelet and anticoagulant medications, and utilization of novel endoscopic tools to obtain improved clinical outcomes.
Keywords: H. pylori; nonsteroidal anti-inflammatory drugs; NSAIDs; proton pump inhibitor; PPI; bleeding; perforation; obstruction; refractory ulcer; salvage endoscopic therapy; transcatheter angiographic embolization.
A peptic ulcer is a fibrin-covered break in the mucosa of the digestive tract extending to the submucosa that is caused by acid injury (Figure 1). Most peptic ulcers occur in the stomach or proximal duodenum, though they may also occur in the esophagus or, less frequently, in a Meckel’s diverticulum.1,2 The estimated worldwide prevalence of peptic ulcer disease is 5% to 10%, with an annual incidence of 0.1% to 0.3%1; both rates are declining.3 The annual incidence of peptic ulcer disease requiring medical or surgical treatment is also declining, and currently is estimated to be 0.1% to 0.2%.4 The lifetime prevalence of peptic ulcers has been decreasing in high-income countries since the mid-20th century due to both the widespread use of medications that suppress gastric acid secretion and the declining prevalence of Helicobacter pylori infection.1,3
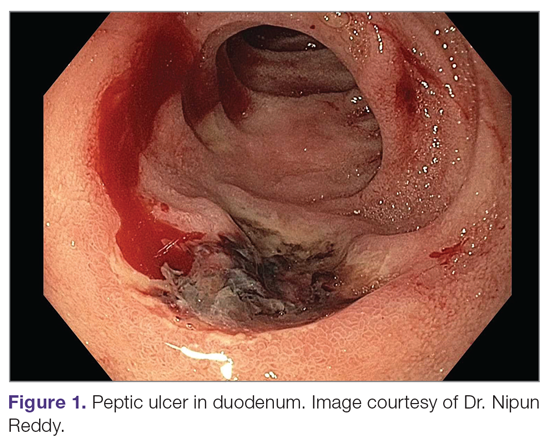
Peptic ulcer disease in most individuals results from H. pylori infection, chronic use of nonsteroidal anti-inflammatory drugs (NSAIDs), including aspirin, or both. A combination of H. pylori factors and host factors lead to mucosal disruption in infected individuals who develop peptic ulcers. H. pylori–specific factors include the expression of virulence factors such as CagA and VacA, which interact with the host inflammatory response to cause mucosal injury. The mucosal inflammatory response is at least partially determined by polymorphisms in the host’s cytokine genes.1,4 NSAIDs inhibit the production of cyclooxygenase-1-derived prostaglandins, with subsequent decreases in epithelial mucous formation, bicarbonate secretion, cell proliferation, and mucosal blood flow, all of which are key elements in the maintenance of mucosal integrity.1,5 Less common causes of peptic ulcers include gastrinoma, adenocarcinoma, idiopathic ulcers, use of sympathomimetic drugs (eg, cocaine or methamphetamine), certain anticancer agents, and bariatric surgery.4,6
This article provides an overview of current management principles for peptic ulcer disease and discusses current challenges in peptic ulcer management, including proton pump inhibitor (PPI) therapy, refractory ulcers, handling of antiplatelet and anticoagulants during and after peptic ulcer bleeding, and ulcer bleeding that continues despite salvage endoscopic therapy.
Methods
We searched MEDLINE using the term peptic ulcer disease in combination with the terms current challenges, epidemiology, bleeding, anticoagulant, antiplatelet, PPI potency, etiology, treatment, management, and refractory. We selected publications from the past 35 years that we judged to be relevant.
Current Management
The goals of peptic ulcer disease management are ulcer healing and prevention of recurrence. The primary interventions used in the management of peptic ulcer disease are medical therapy and implementation of measures that address the underlying etiology of the disease.
Medical Therapy
Introduced in the late 1980s, PPIs are the cornerstone of medical therapy for peptic ulcer disease.6 These agents irreversibly inhibit the H+/K+-ATPase pump in the gastric mucosa and thereby inhibit gastric acid secretion, promoting ulcer healing. PPIs improve rates of ulcer healing compared to H2-receptor antagonists.4,7
Underlying Causes
The underlying cause of peptic ulcer disease should be addressed, in addition to initiating medical therapy. A detailed history of NSAID use should be obtained, and patients with peptic ulcers caused by NSAIDs should be counseled to avoid them, if possible. Patients with peptic ulcer disease who require long-term use of NSAIDs should be placed on long-term PPI therapy.6 Any patient with peptic ulcer disease, regardless of any history of H. pylori infection or treatment, should be tested for infection. Tests that identify active infection, such as urea breath test, stool antigen assay, or mucosal biopsy–based testing, are preferred to IgG antibody testing, although the latter is acceptable in the context of peptic ulcer disease with a high pretest probability of infection.8 Any evidence of active infection warrants appropriate treatment to allow ulcer healing and prevent recurrence.1H. pylori infection is most often treated with clarithromycin triple therapy or bismuth quadruple therapy for 14 days, with regimens selected based on the presence or absence of penicillin allergy, prior antibiotic exposure, and local clarithromycin resistance rates, when known.4,8
Managing Complications
An additional aspect of care in peptic ulcer disease is managing the complications of bleeding, perforation, and gastric outlet obstruction. Acute upper gastrointestinal bleeding (GIB) is the most common complication of peptic ulcer disease, which accounts for 40% to 60% of nonvariceal acute upper GIB.1,6 The first step in the management of acute GIB from a peptic ulcer is fluid resuscitation to ensure hemodynamic stability. If there is associated anemia with a hemoglobin level < 8 g/dL, blood transfusion should be undertaken to target a hemoglobin level > 8 g/dL. In patients with peptic ulcer disease–related acute upper GIB and comorbid cardiovascular disease, the transfusion threshold is higher, with the specific cutoff depending on clinical status, type and severity of cardiovascular disease, and degree of bleeding. Endoscopic management should generally be undertaken within 24 hours of presentation and should not be delayed in patients taking anticoagulants.9 Combination endoscopic treatment with through-the-scope clips plus thermocoagulation or sclerosant injection is recommended for acutely bleeding peptic ulcers with high-risk stigmata.
Pharmacologic management of patients with bleeding peptic ulcers with high-risk stigmata includes PPI therapy, with an 80 mg intravenous (IV) loading dose followed by continuous infusion of 8 mg/hr for 72 hours to reduce rebleeding and mortality. Following completion of IV therapy, oral PPI therapy should be continued twice daily for 14 days, followed by once-daily dosing thereafter.9Patients with peptic ulcer perforation present with sudden-onset epigastric abdominal pain and have tenderness to palpation, guarding, and rigidity on examination, often along with tachycardia and hypotension.1,4 Computed tomography (CT) of the abdomen is 98% sensitive for identifying and localizing a perforation. Most perforations occur in the duodenum or antrum.
Management of a peptic ulcer perforation requires consultation with a surgeon to determine whether a nonoperative approach may be employed (eg, a stable patient with a contained perforation), or if surgery is indicated. The surgical approach to peptic ulcer perforation has been impacted by the clinical success of gastric acid suppression with PPIs and H. pylori eradication, but a range of surgical approaches are still used to repair perforations, from omental patch repair with peritoneal drain placement, to more extensive surgeries such as wedge resection or partial gastrectomy.4 Perforation carries a high mortality risk, up to 20% to 30%, and is the leading cause of death in patients with peptic ulcer disease.1,4
Gastric outlet obstruction, a rare complication of peptic ulcer disease, results from recurrent ulcer formation and scarring. Obstruction often presents with hypovolemia and metabolic alkalosis from prolonged vomiting. CT imaging with oral contrast is often the first diagnostic test employed to demonstrate obstruction. Upper endoscopy should be performed to evaluate the appearance and degree of obstruction as well as to obtain biopsies to evaluate for a malignant etiology of the ulcer disease. Endoscopic balloon dilation has become the cornerstone of initial therapy for obstruction from peptic ulcer disease, especially in the case of ulcers due to reversible causes. Surgery is now typically reserved for cases of refractory obstruction, after repeated endoscopic balloon dilation has failed to remove the obstruction. However, because nearly all patients with gastric outlet obstruction present with malnutrition, nutritional deficiencies should be addressed prior to the patient undergoing surgical intervention. Surgical options include pyloroplasty, antrectomy, and gastrojejunostomy.4
Current Challenges
Rapid Metabolism of PPIs
High-dose PPI therapy is a key component of therapy for peptic ulcer healing. PPIs are metabolized by the cytochrome P450 system, which is comprised of multiple isoenzymes. CYP2C19, an isoenzyme involved in PPI metabolism, has 21 polymorphisms, which have variable effects leading to ultra-rapid, extensive, intermediate, or poor metabolism of PPIs.10 With rapid metabolism of PPIs, standard dosing can result in inadequate suppression of acid secretion. Despite this knowledge, routine testing of CYP2C19 phenotype is not recommended due to the cost of testing. Instead, inadequate ulcer healing should prompt consideration of increased PPI dosing to 80 mg orally twice daily, which may be sufficient to overcome rapid PPI metabolism.11
Relative Potency of PPIs
In addition to variation in PPI metabolism, the relative potency of various PPIs has been questioned. A review of all available clinical studies of the effects of PPIs on mean 24-hour intragastric pH reported a quantitative difference in the potency of 5 PPIs, with omeprazole as the reference standard. Potencies ranged from 0.23 omeprazole equivalents for pantoprazole to 1.82 omeprazole equivalents for rabeprazole.12 An additional study of data from 56 randomized clinical trials confirmed that PPIs vary in potency, which was measured as time that gastric pH is less than 4. A linear increase in intragastric pH time less than 4 was observed from 9 to 64 mg omeprazole equivalents; higher doses yielded no additional benefit. An increase in PPI dosing from once daily to twice daily also increased the duration of intragastric pH time less than 4 from 15 to 21 hours.13 Earlier modeling of the relationship between duodenal ulcer healing and antisecretory therapy showed a strong correlation of ulcer healing with the duration of acid suppression, length of therapy, and the degree of acid suppression. Additional benefit was not observed after intragastric pH rose above 3.14 Thus, as the frequency and duration of acid suppression therapy are more important than PPI potency, PPIs can be used interchangeably.13,14
Addressing Underlying Causes
Continued NSAID Use. Refractory peptic ulcers are defined as those that do not heal despite adherence to 8 to 12 weeks of standard acid-suppression therapy. A cause of refractory peptic ulcer disease that must be considered is continued NSAID use.1,15 In a study of patients with refractory peptic ulcers, 27% of patients continued NSAID use, as determined by eventual disclosure by the patients or platelet cyclooxygenase activity assay, despite extensive counseling to avoid NSAIDs at the time of the diagnosis of their refractory ulcer and at subsequent visits.16 Pain may make NSAID cessation difficult for some patients, while others do not realize that over-the-counter preparations they take contain NSAIDs.15
Another group of patients with continued NSAID exposure are those who require long-term NSAID therapy for control of arthritis or the management of cardiovascular conditions. If NSAID therapy cannot be discontinued, the risk of NSAID-related gastrointestinal injury can be assessed based on the presence of multiple risk factors, including age > 65 years, high-dose NSAID therapy, a history of peptic ulcer, and concurrent use of aspirin, corticosteroids, or anticoagulants. Individuals with 3 or more of the preceding risk factors or a history of a peptic ulcer with a complication, especially if recent, are considered to be at high risk of developing an NSAID-related ulcer and possible subsequent complications.17 In these individuals, NSAID therapy should be continued with agents that have the lowest risk for gastrointestinal toxicity and at the lowest possible dose. A meta-analysis comparing nonselective NSAIDs to placebo demonstrated naproxen to have the highest risk of gastrointestinal complications, including GIB, perforation, and obstruction (adjusted rate ratio, 4.2), while diclofenac demonstrated the lowest risk (adjusted rate ratio, 1.89). High-dose NSAID therapy demonstrated a 2-fold increase in risk of peptic ulcer formation as compared to low-dose therapy.18
In addition to selecting the NSAID with the least gastrointestinal toxicity at the lowest possible dose, additional strategies to prevent peptic ulcer disease and its complications in chronic NSAID users include co-administration of a PPI and substitution of a COX-2 selective NSAID for nonselective NSAIDs.1,9 Prior double-blind, placebo-controlled, randomized, multicenter trials with patients requiring daily NSAIDs demonstrated an up to 15% absolute reduction in the risk of developing peptic ulcers over 6 months while taking esomeprazole.19
Persistent Infection. Persistent H. pylori infection, due either to initial false-negative testing or ongoing infection despite first-line therapy, is another cause of refractory peptic ulcer disease.1,15 Because antibiotics and PPIs can reduce the number of H. pylori bacteria, use of these medications concurrent with H. pylori testing can lead to false-negative results with several testing modalities. When suspicion for H. pylori is high, 2 or more diagnostic tests may be needed to effectively rule out infection.15
When H. pylori is detected, successful eradication is becoming more difficult due to an increasing prevalence of antibiotic resistance, leading to persistent infection in many cases and maintained risk of peptic ulcer disease, despite appropriate first-line therapy.8 Options for salvage therapy for persistent H. pylori, as well as information on the role and best timing of susceptibility testing, are beyond the scope of this review, but are reviewed by Lanas and Chan1 and in the American College of Gastroenterology guideline on the treatment of H. pylori infection.8
Other Causes. In a meta-analysis of rigorously designed studies from North America, 20% of patients experienced ulcer recurrence at 6 months, despite successful H. pylori eradication and no NSAID use.20 In addition, as H. pylori prevalence is decreasing, idiopathic ulcers are increasingly being diagnosed, and such ulcers may be associated with high rates of GIB and mortality.1 In this subset of patients with non-H. pylori, non-NSAID ulcers, increased effort is required to further evaluate the differential diagnosis for rarer causes of upper GI tract ulcer disease (Table). Certain malignancies, including adenocarcinoma and lymphoma, can cause ulcer formation and should be considered in refractory cases. Repeat biopsy at follow-up endoscopy for persistent ulcers should always be obtained to further evaluate for malignancy.1,15 Infectious diseases other than H. pylori infection, such as tuberculosis, syphilis, cytomegalovirus, and herpes simplex virus, are also reported as etiologies of refractory ulcers, and require specific antimicrobial treatment over and above PPI monotherapy. Special attention in biopsy sampling and sample processing is often required when infectious etiologies are being considered, as specific histologic stains and cultures may be needed for identification.15
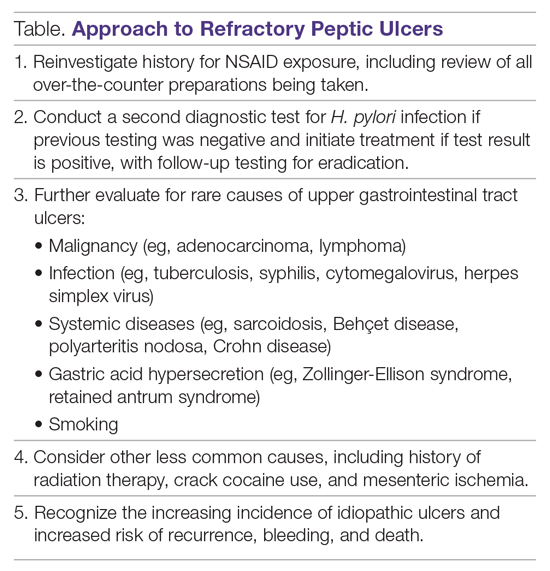
Systemic conditions, including sarcoidosis,21 Behçet disease,22 and polyarteritis nodosa,15,23 can also cause refractory ulcers. Approximately 15% of patients with Crohn disease have gastroduodenal involvement, which may include ulcers of variable sizes.1,15,24 The increased gastric acid production seen in Zollinger-Ellison syndrome commonly presents as refractory peptic ulcers in the duodenum beyond the bulb that do not heal with standard doses of PPIs.1,15 More rare causes of acid hypersecretion leading to refractory ulcers include idiopathic gastric acid hypersecretion and retained gastric antrum syndrome after partial gastrectomy with Billroth II anastomosis.15 Smoking is a known risk factor for impaired tissue healing throughout the body, and can contribute to impaired healing of peptic ulcers through decreased prostaglandin synthesis25 and reduced gastric mucosal blood flow.26 Smoking should always be addressed in patients with refractory peptic ulcers, and cessation should be strongly encouraged. Other less common causes of refractory upper GI tract ulcers include radiation therapy, crack cocaine use, and mesenteric ischemia.15
Managing Antiplatelet and Anticoagulant Medications
Use of antiplatelets and anticoagulants, alone or in combination, increases the risk of peptic ulcer bleeding. In patients who continue to take aspirin after a peptic ulcer bleed, recurrent bleeding occurs in up to 300 cases per 1000 person-years. The rate of GIB associated with aspirin use ranges from 1.1% to 2.5%, depending on the dose. Prior peptic ulcer disease, age greater than 70 years, and concurrent NSAID, steroid, anticoagulant, or dual antiplatelet therapy (DAPT) use increase the risk of bleeding while on aspirin. The rate of GIB while taking a thienopyridine alone is slightly less than that when taking aspirin, ranging from 0.5% to 1.6%. Studies to date have yielded mixed estimates of the effect of DAPT on the risk of GIB. Estimates of the risk of GIB with DAPT range from an odds ratio for serious GIB of 7.4 to an absolute risk increase of only 1.3% when compared to clopidogrel alone.27
Many patients are also on warfarin or a direct oral anticoagulant (DOAC). In a study from the United Kingdom, the adjusted rate ratio of GIB with warfarin alone was 1.94, and this increased to 6.48 when warfarin was used with aspirin.28 The use of warfarin and DAPT, often called triple therapy, further increases the risk of GIB, with a hazard ratio of 5.0 compared to DAPT alone, and 5.38 when compared to warfarin alone. DOACs are increasingly prescribed for the treatment and prevention of thromboembolism, and by 2014 were prescribed as often as warfarin for stroke prevention in atrial fibrillation in the United States. A meta-analysis showed the risk of major GIB did not differ between DOACs and warfarin or low-molecular-weight heparin, but among DOACs factor Xa inhibitors showed a reduced risk of GIB compared with dabigatran, a direct thrombin inhibitor.29
The use of antiplatelets and anticoagulants in the context of peptic ulcer bleeding is a current management challenge. Data to guide decision-making in patients on antiplatelet and/or anticoagulant therapy who experience peptic ulcer bleeding are scarce. Decision-making in this group of patients requires balancing the severity and risk of bleeding with the risk of thromboembolism.1,27 In patients on antiplatelet therapy for primary prophylaxis of atherothrombosis who develop bleeding from a peptic ulcer, the antiplatelet should generally be held and the indication for the medication reassessed. In patients on antiplatelet therapy for secondary prevention, the agent may be immediately resumed after endoscopy if bleeding is found to be due to an ulcer with low-risk stigmata. With bleeding resulting from an ulcer with high-risk stigmata, antiplatelet agents employed for secondary prevention may be held initially, with consideration given to early reintroduction, as early as day 3 after endoscopy.1 In patients at high risk for atherothrombotic events, including those on aspirin for secondary prophylaxis, withholding aspirin leads to a 3-fold increase in the risk of a major adverse cardiac event, with events occurring as early as 5 days after aspirin cessation in some cases.27 A randomized controlled trial of continuing low-dose aspirin versus withholding it for 8 weeks in patients on aspirin for secondary prophylaxis of cardiovascular events who experienced peptic ulcer bleeding that required endoscopic therapy demonstrated lower all-cause mortality (1.3% vs 12.9%), including death from cardiovascular or cerebrovascular events, among those who continued aspirin therapy, with a small increased risk of recurrent ulcer bleeding (10.3% vs 5.4%).30 Thus, it is recommended that antiplatelet therapy, when held, be resumed as early as possible when the risk of a cardiovascular or cerebrovascular event is considered to be higher than the risk of bleeding.27
When patients are on DAPT for a history of drug-eluting stent placement, withholding both antiplatelet medications should be avoided, even for a brief period of time, given the risk of in-stent thrombosis. When DAPT is employed for other reasons, it should be continued, if indicated, after bleeding that is found to be due to peptic ulcers with low-risk stigmata. If bleeding is due to a peptic ulcer with high-risk stigmata at endoscopy, then aspirin monotherapy should be continued and consultation should be obtained with a cardiologist to determine optimal timing to resume the second antiplatelet agent.1 In patients on anticoagulants, anticoagulation should be resumed once hemostasis is achieved when the risk of withholding anticoagulation is thought to be greater than the risk of rebleeding. For example, anticoagulation should be resumed early in a patient with a mechanical heart valve to prevent thrombosis.1,27 Following upper GIB from peptic ulcer disease, patients who will require long-term aspirin, DAPT, or anticoagulation with either warfarin or DOACs should be maintained on long-term PPI therapy to reduce the risk of recurrent bleeding.9,27
Failure of Endoscopic Therapy to Control Peptic Ulcer Bleeding
Bleeding recurs in as many as 10% to 20% of patients after initial endoscopic control of peptic ulcer bleeding.4,31 In this context, repeat upper endoscopy for hemostasis is preferred to surgery, as it leads to less morbidity while providing long-term control of bleeding in more than 70% of cases.31,32 Two potential endoscopic rescue therapies that may be employed are over-the-scope clips (OTSCs) and hemostatic powder.32,33
While through-the-scope (TTS) hemostatic clips are often used during endoscopy to control active peptic ulcer bleeding, their use may be limited in large or fibrotic ulcers due to the smaller size of the clips and method of application. OTSCs have several advantages over TTS clips; notably, their larger size allows the endoscopist to achieve deeper mucosal or submucosal clip attachment via suction of the targeted tissue into the endoscopic cap (Figure 2). In a systematic review of OTSCs, successful hemostasis was achieved in 84% of 761 lesions, including 75% of lesions due to peptic ulcer disease.34 Some have argued that OTSCs may be preferred as first-line therapy over epinephrine with TTS clips for hemostasis in bleeding from high-risk peptic ulcers (ie, those with visualized arterial bleeding or a visible vessel) given observed decreases in rebleeding events.35
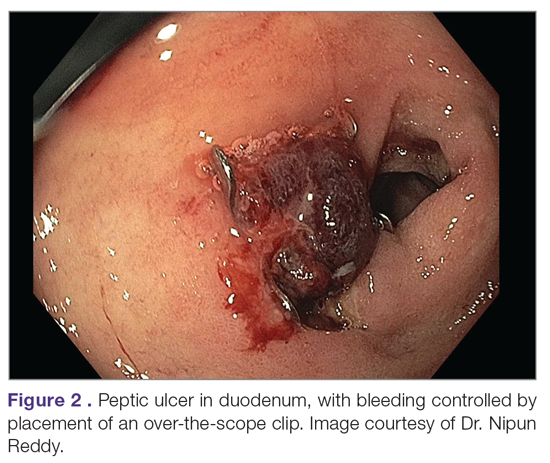
Despite the advantages of OTSCs, endoscopists should be mindful of the potential complications of OTSC use, including luminal obstruction, particularly in the duodenum, and perforation, which occurs in 0.3% to 2% of cases. Additionally, retrieval of misplaced OTSCs presents a significant challenge. Careful decision-making with consideration of the location, size, and depth of lesions is required when deciding on OTSC placement.34,36
A newer endoscopic tool developed for refractory bleeding from peptic ulcers and other causes is hemostatic powder. Hemostatic powders accelerate the coagulation cascade, leading to shortened coagulation times and enhanced clot formation.37 A recent meta-analysis showed that immediate hemostasis could be achieved in 95% of cases of bleeding, including in 96% of cases of bleeding from peptic ulcer disease.38 The primary limitation of hemostatic powders is the temporary nature of hemostasis, which requires the underlying etiology of bleeding to be addressed in order to provide long-term hemostasis. In the above meta-analysis, rebleeding occurred in 17% of cases after 30 days.38
Hypotension and ulcer diameter ≥ 2 cm are independent predictors of failure of endoscopic salvage therapy.31 When severe bleeding is not controlled with initial endoscopic therapy or bleeding recurs despite salvage endoscopic therapy, transcatheter angiographic embolization (TAE) is the treatment of choice.4 Systematic reviews and meta-analyses of studies that compared TAE to surgery have shown that the rate of rebleeding may be higher with TAE, but with less morbidity and either decreased or equivalent rates of mortality, with no increased need for additional interventions.4,32 In a case series examining 5 years of experience at a single medical center in China, massive GIB from duodenal ulcers was successfully treated with TAE in 27 of 29 cases (93% clinical success rate), with no mucosal ischemic necrosis observed.39
If repeated endoscopic therapy has not led to hemostasis of a bleeding peptic ulcer and TAE is not available, then surgery is the next best option. Bleeding gastric ulcers may be excised, wedge resected, or oversewn after an anterior gastrostomy. Bleeding duodenal ulcers may require use of a Kocher maneuver and linear incision of the anterior duodenum followed by ligation of the gastroduodenal artery. Fortunately, such surgical management is rarely necessary given the availability of TAE at most centers.4
Conclusion
Peptic ulcer disease is a common health problem globally, with persistent challenges related to refractory ulcers, antiplatelet and anticoagulant use, and continued bleeding in the face of endoscopic therapy. These challenges should be met with adequate frequency and duration of PPI therapy, vigilant attention to and treatment of ulcer etiology, evidence-based handling of antiplatelet and anticoagulant medications, and utilization of novel endoscopic tools to obtain improved clinical outcomes.
Acknowledgment: We thank Dr. Nipun Reddy from our institution for providing the endoscopic images used in this article.
Corresponding author: Adam L. Edwards, MD, MS; [email protected].
Financial disclosures: None.
1. Lanas A, Chan FKL. Peptic ulcer disease. Lancet. 2017;390:613-624.
2. Malfertheiner P, Chan FK, McColl KE. Peptic ulcer disease. Lancet. 2009;374:1449-1461.
3. Roberts-Thomson IC. Rise and fall of peptic ulceration: A disease of civilization? J Gastroenterol Hepatol. 2018;33:1321-1326.
4. Kempenich JW, Sirinek KR. Acid peptic disease. Surg Clin North Am. 2018;98:933-944.
5. Cryer B, Feldman M. Effects of very low dose daily, long-term aspirin therapy on gastric, duodenal, and rectal prostaglandin levels and on mucosal injury in healthy humans. Gastroenterology. 1999;117:17-25.
6. Kavitt RT, Lipowska AM, Anyane-Yeboa A, Gralnek IM. Diagnosis and treatment of peptic ulcer disease. Am J Med. 2019;132:447-456.
7. Walan A, Bader JP, Classen M, et al. Effect of omeprazole and ranitidine on ulcer healing and relapse rates in patients with benign gastric ulcer. New Engl J Med. 1989;320:69-75.
8. Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG Clinical Guideline: Treatment of Helicobacter pylori Infection. Am J Gastroenterol. 2017;112:212-239.
9. Barkun AN, Almadi M, Kuipers EJ, et al. Management of nonvariceal upper gastrointestinal bleeding: Guideline recommendations from the International Consensus Group. Ann Intern Med. 2019;171:805-822.
10. Arevalo Galvis A, Trespalacios Rangel AA, Otero Regino W. Personalized therapy for Helicobacter pylori: CYP2C19 genotype effect on first-line triple therapy. Helicobacter. 2019;24:e12574.
11. Furuta T, Ohashi K, Kamata T, et al. Effect of genetic differences in omeprazole metabolism on cure rates for Helicobacter pylori infection and peptic ulcer. Ann Intern Med. 1998;129:1027-1030.
12. Kirchheiner J, Glatt S, Fuhr U, et al. Relative potency of proton-pump inhibitors-comparison of effects on intragastric pH. Eur J Clin Pharmacol. 2009;65:19-31.
13. Graham DY, Tansel A. Interchangeable use of proton pump inhibitors based on relative potency. Clin Gastroenterol Hepatol. 2018;16:800-808.e7.
14. Burget DW, Chiverton SG, Hunt RH. Is there an optimal degree of acid suppression for healing of duodenal ulcers? A model of the relationship between ulcer healing and acid suppression. Gastroenterology. 1990;99:345-351.
15. Kim HU. Diagnostic and treatment approaches for refractory peptic ulcers. Clin Endosc. 2015;48:285-290.
16. Lanas AI, Remacha B, Esteva F, Sainz R. Risk factors associated with refractory peptic ulcers. Gastroenterology. 1995;109:124-133.
17. Lanza FL, Chan FK, Quigley EM. Guidelines for prevention of NSAID-related ulcer complications. Am J Gastroenterol. 2009;104:728-738.
18. Richy F, Bruyere O, Ethgen O, et al. Time dependent risk of gastrointestinal complications induced by non-steroidal anti-inflammatory drug use: a consensus statement using a meta-analytic approach. Ann Rheum Dis. 2004;63:759-766.
19. Scheiman JM, Yeomans ND, Talley NJ, et al. Prevention of ulcers by esomeprazole in at-risk patients using non-selective NSAIDs and COX-2 inhibitors. Am J Gastroenterol. 2006;101:701-710.
20. Laine L, Hopkins RJ, Girardi LS. Has the impact of Helicobacter pylori therapy on ulcer recurrence in the United States been overstated? A meta-analysis of rigorously designed trials. Am J Gastroenterol. 1998;93:1409-1415.
21. Akiyama T, Endo H, Inamori M, et al. Symptomatic gastric sarcoidosis with multiple antral ulcers. Endoscopy. 2009;41 Suppl 2:E159.
22. Sonoda A, Ogawa R, Mizukami K, et al. Marked improvement in gastric involvement in Behcet’s disease with adalimumab treatment. Turk J Gastroenterol. 2017;28:405-407.
23. Saikia N, Talukdar R, Mazumder S, et al. Polyarteritis nodosa presenting as massive upper gastrointestinal hemorrhage. Gastrointest Endosc. 2006;63:868-870.
24. Annunziata ML, Caviglia R, Papparella LG, Cicala M. Upper gastrointestinal involvement of Crohn’s disease: a prospective study on the role of upper endoscopy in the diagnostic work-up. Dig Dis Sci. 2012;57:1618-1623.
25. Quimby GF, Bonnice CA, Burstein SH, Eastwood GL. Active smoking depresses prostaglandin synthesis in human gastric mucosa. Ann Intern Med. 1986;104:616-619.
26. Iwao T, Toyonaga A, Ikegami M, et al. Gastric mucosal blood flow after smoking in healthy human beings assessed by laser Doppler flowmetry. Gastrointest Endosc. 1993;39:400-403.
27. Almadi MA, Barkun A, Brophy J. Antiplatelet and anticoagulant therapy in patients with gastrointestinal bleeding: an 86-year-old woman with peptic ulcer disease. JAMA. 2011;306:2367-2374.
28. Delaney JA, Opatrny L, Brophy JM, Suissa S. Drug drug interactions between antithrombotic medications and the risk of gastrointestinal bleeding. CMAJ. 2007;177:347-351.
29. Burr N, Lummis K, Sood R, et al. Risk of gastrointestinal bleeding with direct oral anticoagulants: a systematic review and network meta-analysis. Lancet Gastroenterol Hepatol. 2017;2:85-93.
30. Sung JJ, Lau JY, Ching JY, et al. Continuation of low-dose aspirin therapy in peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2010;152:1-9.
31. Lau JY, Sung JJ, Lam YH, et al. Endoscopic retreatment compared with surgery in patients with recurrent bleeding after initial endoscopic control of bleeding ulcers. N Engl J Med. 1999;340:751-756.
32. Gralnek IM, Dumonceau JM, Kuipers EJ, et al. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47:a1-46.
33. Skinner M, Gutierrez JP, Neumann H, et al. Over-the-scope clip placement is effective rescue therapy for severe acute upper gastrointestinal bleeding. Endosc Int Open. 2014;2:E37-40.
34. Zhong C, Tan S, Ren Y, et al. Clinical outcomes of over-the-scope-clip system for the treatment of acute upper non-variceal gastrointestinal bleeding: a systematic review and meta-analysis. BMC Gastroenterol. 2019;19:225.
35. Mangiafico S, Pigo F, Bertani H, et al. Over-the-scope clip vs epinephrine with clip for first-line hemostasis in non-variceal upper gastrointestinal bleeding: a propensity score match analysis. Endosc Int Open. 2020;8:E50-e8.
36. Wedi E, Gonzalez S, Menke D, et al. One hundred and one over-the-scope-clip applications for severe gastrointestinal bleeding, leaks and fistulas. World J Gastroenterol. 2016;22:1844-1853.
37. Holster IL, van Beusekom HM, Kuipers EJ, et al. Effects of a hemostatic powder hemospray on coagulation and clot formation. Endoscopy. 2015;47:638-645.
38. Facciorusso A, Straus Takahashi M, et al. Efficacy of hemostatic powders in upper gastrointestinal bleeding: A systematic review and meta-analysis. Dig Liver Dis. 2019;51:1633-1640.
39. Wang YL, Cheng YS, et al. Emergency transcatheter arterial embolization for patients with acute massive duodenal ulcer hemorrhage. World J Gastroenterol. 2012;18:4765-4770.
From the University of Alabama at Birmingham, Birmingham, AL.
Abstract
Objective: To review current challenges in the management of peptic ulcer disease.
Methods: Review of the literature.
Results: Peptic ulcer disease affects 5% to 10% of the population worldwide, with recent decreases in lifetime prevalence in high-income countries. Helicobacter pylori infection and nonsteroidal anti-inflammatory drug (NSAID) use are the most important drivers of peptic ulcer disease. Current management strategies for peptic ulcer disease focus on ulcer healing; management of complications such as bleeding, perforation, and obstruction; and prevention of ulcer recurrence. Proton pump inhibitors (PPIs) are the cornerstone of medical therapy for peptic ulcers, and complement testing for and treatment of H. pylori infection as well as elimination of NSAID use. Although advances have been made in the medical and endoscopic treatment of peptic ulcer disease and the management of ulcer complications, such as bleeding and obstruction, challenges remain.
Conclusion: Peptic ulcer disease is a common health problem globally, with persistent challenges related to refractory ulcers, antiplatelet and anticoagulant use, and continued bleeding in the face of endoscopic therapy. These challenges should be met with PPI therapy of adequate frequency and duration, vigilant attention to and treatment of ulcer etiology, evidence-based handling of antiplatelet and anticoagulant medications, and utilization of novel endoscopic tools to obtain improved clinical outcomes.
Keywords: H. pylori; nonsteroidal anti-inflammatory drugs; NSAIDs; proton pump inhibitor; PPI; bleeding; perforation; obstruction; refractory ulcer; salvage endoscopic therapy; transcatheter angiographic embolization.
A peptic ulcer is a fibrin-covered break in the mucosa of the digestive tract extending to the submucosa that is caused by acid injury (Figure 1). Most peptic ulcers occur in the stomach or proximal duodenum, though they may also occur in the esophagus or, less frequently, in a Meckel’s diverticulum.1,2 The estimated worldwide prevalence of peptic ulcer disease is 5% to 10%, with an annual incidence of 0.1% to 0.3%1; both rates are declining.3 The annual incidence of peptic ulcer disease requiring medical or surgical treatment is also declining, and currently is estimated to be 0.1% to 0.2%.4 The lifetime prevalence of peptic ulcers has been decreasing in high-income countries since the mid-20th century due to both the widespread use of medications that suppress gastric acid secretion and the declining prevalence of Helicobacter pylori infection.1,3
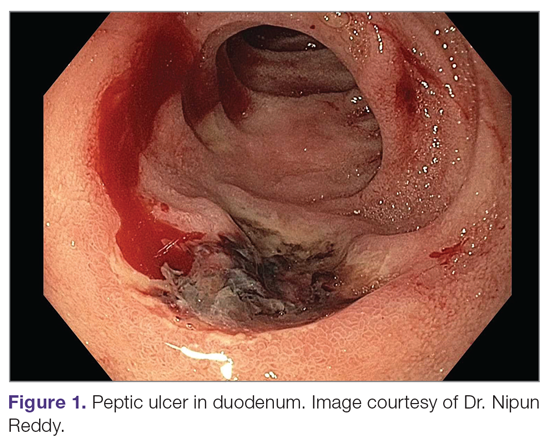
Peptic ulcer disease in most individuals results from H. pylori infection, chronic use of nonsteroidal anti-inflammatory drugs (NSAIDs), including aspirin, or both. A combination of H. pylori factors and host factors lead to mucosal disruption in infected individuals who develop peptic ulcers. H. pylori–specific factors include the expression of virulence factors such as CagA and VacA, which interact with the host inflammatory response to cause mucosal injury. The mucosal inflammatory response is at least partially determined by polymorphisms in the host’s cytokine genes.1,4 NSAIDs inhibit the production of cyclooxygenase-1-derived prostaglandins, with subsequent decreases in epithelial mucous formation, bicarbonate secretion, cell proliferation, and mucosal blood flow, all of which are key elements in the maintenance of mucosal integrity.1,5 Less common causes of peptic ulcers include gastrinoma, adenocarcinoma, idiopathic ulcers, use of sympathomimetic drugs (eg, cocaine or methamphetamine), certain anticancer agents, and bariatric surgery.4,6
This article provides an overview of current management principles for peptic ulcer disease and discusses current challenges in peptic ulcer management, including proton pump inhibitor (PPI) therapy, refractory ulcers, handling of antiplatelet and anticoagulants during and after peptic ulcer bleeding, and ulcer bleeding that continues despite salvage endoscopic therapy.
Methods
We searched MEDLINE using the term peptic ulcer disease in combination with the terms current challenges, epidemiology, bleeding, anticoagulant, antiplatelet, PPI potency, etiology, treatment, management, and refractory. We selected publications from the past 35 years that we judged to be relevant.
Current Management
The goals of peptic ulcer disease management are ulcer healing and prevention of recurrence. The primary interventions used in the management of peptic ulcer disease are medical therapy and implementation of measures that address the underlying etiology of the disease.
Medical Therapy
Introduced in the late 1980s, PPIs are the cornerstone of medical therapy for peptic ulcer disease.6 These agents irreversibly inhibit the H+/K+-ATPase pump in the gastric mucosa and thereby inhibit gastric acid secretion, promoting ulcer healing. PPIs improve rates of ulcer healing compared to H2-receptor antagonists.4,7
Underlying Causes
The underlying cause of peptic ulcer disease should be addressed, in addition to initiating medical therapy. A detailed history of NSAID use should be obtained, and patients with peptic ulcers caused by NSAIDs should be counseled to avoid them, if possible. Patients with peptic ulcer disease who require long-term use of NSAIDs should be placed on long-term PPI therapy.6 Any patient with peptic ulcer disease, regardless of any history of H. pylori infection or treatment, should be tested for infection. Tests that identify active infection, such as urea breath test, stool antigen assay, or mucosal biopsy–based testing, are preferred to IgG antibody testing, although the latter is acceptable in the context of peptic ulcer disease with a high pretest probability of infection.8 Any evidence of active infection warrants appropriate treatment to allow ulcer healing and prevent recurrence.1H. pylori infection is most often treated with clarithromycin triple therapy or bismuth quadruple therapy for 14 days, with regimens selected based on the presence or absence of penicillin allergy, prior antibiotic exposure, and local clarithromycin resistance rates, when known.4,8
Managing Complications
An additional aspect of care in peptic ulcer disease is managing the complications of bleeding, perforation, and gastric outlet obstruction. Acute upper gastrointestinal bleeding (GIB) is the most common complication of peptic ulcer disease, which accounts for 40% to 60% of nonvariceal acute upper GIB.1,6 The first step in the management of acute GIB from a peptic ulcer is fluid resuscitation to ensure hemodynamic stability. If there is associated anemia with a hemoglobin level < 8 g/dL, blood transfusion should be undertaken to target a hemoglobin level > 8 g/dL. In patients with peptic ulcer disease–related acute upper GIB and comorbid cardiovascular disease, the transfusion threshold is higher, with the specific cutoff depending on clinical status, type and severity of cardiovascular disease, and degree of bleeding. Endoscopic management should generally be undertaken within 24 hours of presentation and should not be delayed in patients taking anticoagulants.9 Combination endoscopic treatment with through-the-scope clips plus thermocoagulation or sclerosant injection is recommended for acutely bleeding peptic ulcers with high-risk stigmata.
Pharmacologic management of patients with bleeding peptic ulcers with high-risk stigmata includes PPI therapy, with an 80 mg intravenous (IV) loading dose followed by continuous infusion of 8 mg/hr for 72 hours to reduce rebleeding and mortality. Following completion of IV therapy, oral PPI therapy should be continued twice daily for 14 days, followed by once-daily dosing thereafter.9Patients with peptic ulcer perforation present with sudden-onset epigastric abdominal pain and have tenderness to palpation, guarding, and rigidity on examination, often along with tachycardia and hypotension.1,4 Computed tomography (CT) of the abdomen is 98% sensitive for identifying and localizing a perforation. Most perforations occur in the duodenum or antrum.
Management of a peptic ulcer perforation requires consultation with a surgeon to determine whether a nonoperative approach may be employed (eg, a stable patient with a contained perforation), or if surgery is indicated. The surgical approach to peptic ulcer perforation has been impacted by the clinical success of gastric acid suppression with PPIs and H. pylori eradication, but a range of surgical approaches are still used to repair perforations, from omental patch repair with peritoneal drain placement, to more extensive surgeries such as wedge resection or partial gastrectomy.4 Perforation carries a high mortality risk, up to 20% to 30%, and is the leading cause of death in patients with peptic ulcer disease.1,4
Gastric outlet obstruction, a rare complication of peptic ulcer disease, results from recurrent ulcer formation and scarring. Obstruction often presents with hypovolemia and metabolic alkalosis from prolonged vomiting. CT imaging with oral contrast is often the first diagnostic test employed to demonstrate obstruction. Upper endoscopy should be performed to evaluate the appearance and degree of obstruction as well as to obtain biopsies to evaluate for a malignant etiology of the ulcer disease. Endoscopic balloon dilation has become the cornerstone of initial therapy for obstruction from peptic ulcer disease, especially in the case of ulcers due to reversible causes. Surgery is now typically reserved for cases of refractory obstruction, after repeated endoscopic balloon dilation has failed to remove the obstruction. However, because nearly all patients with gastric outlet obstruction present with malnutrition, nutritional deficiencies should be addressed prior to the patient undergoing surgical intervention. Surgical options include pyloroplasty, antrectomy, and gastrojejunostomy.4
Current Challenges
Rapid Metabolism of PPIs
High-dose PPI therapy is a key component of therapy for peptic ulcer healing. PPIs are metabolized by the cytochrome P450 system, which is comprised of multiple isoenzymes. CYP2C19, an isoenzyme involved in PPI metabolism, has 21 polymorphisms, which have variable effects leading to ultra-rapid, extensive, intermediate, or poor metabolism of PPIs.10 With rapid metabolism of PPIs, standard dosing can result in inadequate suppression of acid secretion. Despite this knowledge, routine testing of CYP2C19 phenotype is not recommended due to the cost of testing. Instead, inadequate ulcer healing should prompt consideration of increased PPI dosing to 80 mg orally twice daily, which may be sufficient to overcome rapid PPI metabolism.11
Relative Potency of PPIs
In addition to variation in PPI metabolism, the relative potency of various PPIs has been questioned. A review of all available clinical studies of the effects of PPIs on mean 24-hour intragastric pH reported a quantitative difference in the potency of 5 PPIs, with omeprazole as the reference standard. Potencies ranged from 0.23 omeprazole equivalents for pantoprazole to 1.82 omeprazole equivalents for rabeprazole.12 An additional study of data from 56 randomized clinical trials confirmed that PPIs vary in potency, which was measured as time that gastric pH is less than 4. A linear increase in intragastric pH time less than 4 was observed from 9 to 64 mg omeprazole equivalents; higher doses yielded no additional benefit. An increase in PPI dosing from once daily to twice daily also increased the duration of intragastric pH time less than 4 from 15 to 21 hours.13 Earlier modeling of the relationship between duodenal ulcer healing and antisecretory therapy showed a strong correlation of ulcer healing with the duration of acid suppression, length of therapy, and the degree of acid suppression. Additional benefit was not observed after intragastric pH rose above 3.14 Thus, as the frequency and duration of acid suppression therapy are more important than PPI potency, PPIs can be used interchangeably.13,14
Addressing Underlying Causes
Continued NSAID Use. Refractory peptic ulcers are defined as those that do not heal despite adherence to 8 to 12 weeks of standard acid-suppression therapy. A cause of refractory peptic ulcer disease that must be considered is continued NSAID use.1,15 In a study of patients with refractory peptic ulcers, 27% of patients continued NSAID use, as determined by eventual disclosure by the patients or platelet cyclooxygenase activity assay, despite extensive counseling to avoid NSAIDs at the time of the diagnosis of their refractory ulcer and at subsequent visits.16 Pain may make NSAID cessation difficult for some patients, while others do not realize that over-the-counter preparations they take contain NSAIDs.15
Another group of patients with continued NSAID exposure are those who require long-term NSAID therapy for control of arthritis or the management of cardiovascular conditions. If NSAID therapy cannot be discontinued, the risk of NSAID-related gastrointestinal injury can be assessed based on the presence of multiple risk factors, including age > 65 years, high-dose NSAID therapy, a history of peptic ulcer, and concurrent use of aspirin, corticosteroids, or anticoagulants. Individuals with 3 or more of the preceding risk factors or a history of a peptic ulcer with a complication, especially if recent, are considered to be at high risk of developing an NSAID-related ulcer and possible subsequent complications.17 In these individuals, NSAID therapy should be continued with agents that have the lowest risk for gastrointestinal toxicity and at the lowest possible dose. A meta-analysis comparing nonselective NSAIDs to placebo demonstrated naproxen to have the highest risk of gastrointestinal complications, including GIB, perforation, and obstruction (adjusted rate ratio, 4.2), while diclofenac demonstrated the lowest risk (adjusted rate ratio, 1.89). High-dose NSAID therapy demonstrated a 2-fold increase in risk of peptic ulcer formation as compared to low-dose therapy.18
In addition to selecting the NSAID with the least gastrointestinal toxicity at the lowest possible dose, additional strategies to prevent peptic ulcer disease and its complications in chronic NSAID users include co-administration of a PPI and substitution of a COX-2 selective NSAID for nonselective NSAIDs.1,9 Prior double-blind, placebo-controlled, randomized, multicenter trials with patients requiring daily NSAIDs demonstrated an up to 15% absolute reduction in the risk of developing peptic ulcers over 6 months while taking esomeprazole.19
Persistent Infection. Persistent H. pylori infection, due either to initial false-negative testing or ongoing infection despite first-line therapy, is another cause of refractory peptic ulcer disease.1,15 Because antibiotics and PPIs can reduce the number of H. pylori bacteria, use of these medications concurrent with H. pylori testing can lead to false-negative results with several testing modalities. When suspicion for H. pylori is high, 2 or more diagnostic tests may be needed to effectively rule out infection.15
When H. pylori is detected, successful eradication is becoming more difficult due to an increasing prevalence of antibiotic resistance, leading to persistent infection in many cases and maintained risk of peptic ulcer disease, despite appropriate first-line therapy.8 Options for salvage therapy for persistent H. pylori, as well as information on the role and best timing of susceptibility testing, are beyond the scope of this review, but are reviewed by Lanas and Chan1 and in the American College of Gastroenterology guideline on the treatment of H. pylori infection.8
Other Causes. In a meta-analysis of rigorously designed studies from North America, 20% of patients experienced ulcer recurrence at 6 months, despite successful H. pylori eradication and no NSAID use.20 In addition, as H. pylori prevalence is decreasing, idiopathic ulcers are increasingly being diagnosed, and such ulcers may be associated with high rates of GIB and mortality.1 In this subset of patients with non-H. pylori, non-NSAID ulcers, increased effort is required to further evaluate the differential diagnosis for rarer causes of upper GI tract ulcer disease (Table). Certain malignancies, including adenocarcinoma and lymphoma, can cause ulcer formation and should be considered in refractory cases. Repeat biopsy at follow-up endoscopy for persistent ulcers should always be obtained to further evaluate for malignancy.1,15 Infectious diseases other than H. pylori infection, such as tuberculosis, syphilis, cytomegalovirus, and herpes simplex virus, are also reported as etiologies of refractory ulcers, and require specific antimicrobial treatment over and above PPI monotherapy. Special attention in biopsy sampling and sample processing is often required when infectious etiologies are being considered, as specific histologic stains and cultures may be needed for identification.15
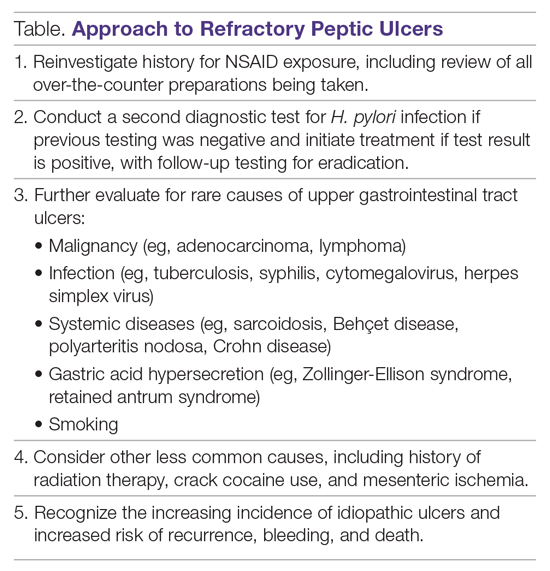
Systemic conditions, including sarcoidosis,21 Behçet disease,22 and polyarteritis nodosa,15,23 can also cause refractory ulcers. Approximately 15% of patients with Crohn disease have gastroduodenal involvement, which may include ulcers of variable sizes.1,15,24 The increased gastric acid production seen in Zollinger-Ellison syndrome commonly presents as refractory peptic ulcers in the duodenum beyond the bulb that do not heal with standard doses of PPIs.1,15 More rare causes of acid hypersecretion leading to refractory ulcers include idiopathic gastric acid hypersecretion and retained gastric antrum syndrome after partial gastrectomy with Billroth II anastomosis.15 Smoking is a known risk factor for impaired tissue healing throughout the body, and can contribute to impaired healing of peptic ulcers through decreased prostaglandin synthesis25 and reduced gastric mucosal blood flow.26 Smoking should always be addressed in patients with refractory peptic ulcers, and cessation should be strongly encouraged. Other less common causes of refractory upper GI tract ulcers include radiation therapy, crack cocaine use, and mesenteric ischemia.15
Managing Antiplatelet and Anticoagulant Medications
Use of antiplatelets and anticoagulants, alone or in combination, increases the risk of peptic ulcer bleeding. In patients who continue to take aspirin after a peptic ulcer bleed, recurrent bleeding occurs in up to 300 cases per 1000 person-years. The rate of GIB associated with aspirin use ranges from 1.1% to 2.5%, depending on the dose. Prior peptic ulcer disease, age greater than 70 years, and concurrent NSAID, steroid, anticoagulant, or dual antiplatelet therapy (DAPT) use increase the risk of bleeding while on aspirin. The rate of GIB while taking a thienopyridine alone is slightly less than that when taking aspirin, ranging from 0.5% to 1.6%. Studies to date have yielded mixed estimates of the effect of DAPT on the risk of GIB. Estimates of the risk of GIB with DAPT range from an odds ratio for serious GIB of 7.4 to an absolute risk increase of only 1.3% when compared to clopidogrel alone.27
Many patients are also on warfarin or a direct oral anticoagulant (DOAC). In a study from the United Kingdom, the adjusted rate ratio of GIB with warfarin alone was 1.94, and this increased to 6.48 when warfarin was used with aspirin.28 The use of warfarin and DAPT, often called triple therapy, further increases the risk of GIB, with a hazard ratio of 5.0 compared to DAPT alone, and 5.38 when compared to warfarin alone. DOACs are increasingly prescribed for the treatment and prevention of thromboembolism, and by 2014 were prescribed as often as warfarin for stroke prevention in atrial fibrillation in the United States. A meta-analysis showed the risk of major GIB did not differ between DOACs and warfarin or low-molecular-weight heparin, but among DOACs factor Xa inhibitors showed a reduced risk of GIB compared with dabigatran, a direct thrombin inhibitor.29
The use of antiplatelets and anticoagulants in the context of peptic ulcer bleeding is a current management challenge. Data to guide decision-making in patients on antiplatelet and/or anticoagulant therapy who experience peptic ulcer bleeding are scarce. Decision-making in this group of patients requires balancing the severity and risk of bleeding with the risk of thromboembolism.1,27 In patients on antiplatelet therapy for primary prophylaxis of atherothrombosis who develop bleeding from a peptic ulcer, the antiplatelet should generally be held and the indication for the medication reassessed. In patients on antiplatelet therapy for secondary prevention, the agent may be immediately resumed after endoscopy if bleeding is found to be due to an ulcer with low-risk stigmata. With bleeding resulting from an ulcer with high-risk stigmata, antiplatelet agents employed for secondary prevention may be held initially, with consideration given to early reintroduction, as early as day 3 after endoscopy.1 In patients at high risk for atherothrombotic events, including those on aspirin for secondary prophylaxis, withholding aspirin leads to a 3-fold increase in the risk of a major adverse cardiac event, with events occurring as early as 5 days after aspirin cessation in some cases.27 A randomized controlled trial of continuing low-dose aspirin versus withholding it for 8 weeks in patients on aspirin for secondary prophylaxis of cardiovascular events who experienced peptic ulcer bleeding that required endoscopic therapy demonstrated lower all-cause mortality (1.3% vs 12.9%), including death from cardiovascular or cerebrovascular events, among those who continued aspirin therapy, with a small increased risk of recurrent ulcer bleeding (10.3% vs 5.4%).30 Thus, it is recommended that antiplatelet therapy, when held, be resumed as early as possible when the risk of a cardiovascular or cerebrovascular event is considered to be higher than the risk of bleeding.27
When patients are on DAPT for a history of drug-eluting stent placement, withholding both antiplatelet medications should be avoided, even for a brief period of time, given the risk of in-stent thrombosis. When DAPT is employed for other reasons, it should be continued, if indicated, after bleeding that is found to be due to peptic ulcers with low-risk stigmata. If bleeding is due to a peptic ulcer with high-risk stigmata at endoscopy, then aspirin monotherapy should be continued and consultation should be obtained with a cardiologist to determine optimal timing to resume the second antiplatelet agent.1 In patients on anticoagulants, anticoagulation should be resumed once hemostasis is achieved when the risk of withholding anticoagulation is thought to be greater than the risk of rebleeding. For example, anticoagulation should be resumed early in a patient with a mechanical heart valve to prevent thrombosis.1,27 Following upper GIB from peptic ulcer disease, patients who will require long-term aspirin, DAPT, or anticoagulation with either warfarin or DOACs should be maintained on long-term PPI therapy to reduce the risk of recurrent bleeding.9,27
Failure of Endoscopic Therapy to Control Peptic Ulcer Bleeding
Bleeding recurs in as many as 10% to 20% of patients after initial endoscopic control of peptic ulcer bleeding.4,31 In this context, repeat upper endoscopy for hemostasis is preferred to surgery, as it leads to less morbidity while providing long-term control of bleeding in more than 70% of cases.31,32 Two potential endoscopic rescue therapies that may be employed are over-the-scope clips (OTSCs) and hemostatic powder.32,33
While through-the-scope (TTS) hemostatic clips are often used during endoscopy to control active peptic ulcer bleeding, their use may be limited in large or fibrotic ulcers due to the smaller size of the clips and method of application. OTSCs have several advantages over TTS clips; notably, their larger size allows the endoscopist to achieve deeper mucosal or submucosal clip attachment via suction of the targeted tissue into the endoscopic cap (Figure 2). In a systematic review of OTSCs, successful hemostasis was achieved in 84% of 761 lesions, including 75% of lesions due to peptic ulcer disease.34 Some have argued that OTSCs may be preferred as first-line therapy over epinephrine with TTS clips for hemostasis in bleeding from high-risk peptic ulcers (ie, those with visualized arterial bleeding or a visible vessel) given observed decreases in rebleeding events.35
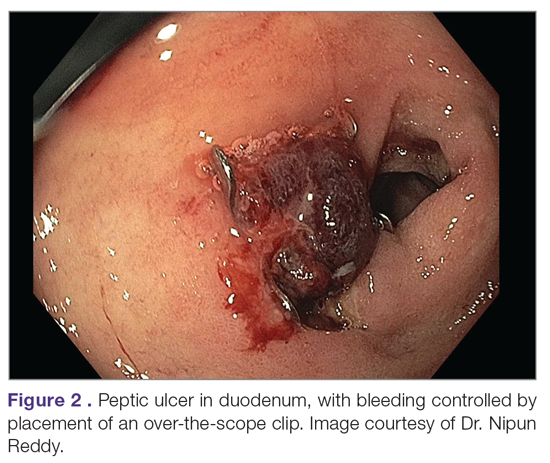
Despite the advantages of OTSCs, endoscopists should be mindful of the potential complications of OTSC use, including luminal obstruction, particularly in the duodenum, and perforation, which occurs in 0.3% to 2% of cases. Additionally, retrieval of misplaced OTSCs presents a significant challenge. Careful decision-making with consideration of the location, size, and depth of lesions is required when deciding on OTSC placement.34,36
A newer endoscopic tool developed for refractory bleeding from peptic ulcers and other causes is hemostatic powder. Hemostatic powders accelerate the coagulation cascade, leading to shortened coagulation times and enhanced clot formation.37 A recent meta-analysis showed that immediate hemostasis could be achieved in 95% of cases of bleeding, including in 96% of cases of bleeding from peptic ulcer disease.38 The primary limitation of hemostatic powders is the temporary nature of hemostasis, which requires the underlying etiology of bleeding to be addressed in order to provide long-term hemostasis. In the above meta-analysis, rebleeding occurred in 17% of cases after 30 days.38
Hypotension and ulcer diameter ≥ 2 cm are independent predictors of failure of endoscopic salvage therapy.31 When severe bleeding is not controlled with initial endoscopic therapy or bleeding recurs despite salvage endoscopic therapy, transcatheter angiographic embolization (TAE) is the treatment of choice.4 Systematic reviews and meta-analyses of studies that compared TAE to surgery have shown that the rate of rebleeding may be higher with TAE, but with less morbidity and either decreased or equivalent rates of mortality, with no increased need for additional interventions.4,32 In a case series examining 5 years of experience at a single medical center in China, massive GIB from duodenal ulcers was successfully treated with TAE in 27 of 29 cases (93% clinical success rate), with no mucosal ischemic necrosis observed.39
If repeated endoscopic therapy has not led to hemostasis of a bleeding peptic ulcer and TAE is not available, then surgery is the next best option. Bleeding gastric ulcers may be excised, wedge resected, or oversewn after an anterior gastrostomy. Bleeding duodenal ulcers may require use of a Kocher maneuver and linear incision of the anterior duodenum followed by ligation of the gastroduodenal artery. Fortunately, such surgical management is rarely necessary given the availability of TAE at most centers.4
Conclusion
Peptic ulcer disease is a common health problem globally, with persistent challenges related to refractory ulcers, antiplatelet and anticoagulant use, and continued bleeding in the face of endoscopic therapy. These challenges should be met with adequate frequency and duration of PPI therapy, vigilant attention to and treatment of ulcer etiology, evidence-based handling of antiplatelet and anticoagulant medications, and utilization of novel endoscopic tools to obtain improved clinical outcomes.
Acknowledgment: We thank Dr. Nipun Reddy from our institution for providing the endoscopic images used in this article.
Corresponding author: Adam L. Edwards, MD, MS; [email protected].
Financial disclosures: None.
From the University of Alabama at Birmingham, Birmingham, AL.
Abstract
Objective: To review current challenges in the management of peptic ulcer disease.
Methods: Review of the literature.
Results: Peptic ulcer disease affects 5% to 10% of the population worldwide, with recent decreases in lifetime prevalence in high-income countries. Helicobacter pylori infection and nonsteroidal anti-inflammatory drug (NSAID) use are the most important drivers of peptic ulcer disease. Current management strategies for peptic ulcer disease focus on ulcer healing; management of complications such as bleeding, perforation, and obstruction; and prevention of ulcer recurrence. Proton pump inhibitors (PPIs) are the cornerstone of medical therapy for peptic ulcers, and complement testing for and treatment of H. pylori infection as well as elimination of NSAID use. Although advances have been made in the medical and endoscopic treatment of peptic ulcer disease and the management of ulcer complications, such as bleeding and obstruction, challenges remain.
Conclusion: Peptic ulcer disease is a common health problem globally, with persistent challenges related to refractory ulcers, antiplatelet and anticoagulant use, and continued bleeding in the face of endoscopic therapy. These challenges should be met with PPI therapy of adequate frequency and duration, vigilant attention to and treatment of ulcer etiology, evidence-based handling of antiplatelet and anticoagulant medications, and utilization of novel endoscopic tools to obtain improved clinical outcomes.
Keywords: H. pylori; nonsteroidal anti-inflammatory drugs; NSAIDs; proton pump inhibitor; PPI; bleeding; perforation; obstruction; refractory ulcer; salvage endoscopic therapy; transcatheter angiographic embolization.
A peptic ulcer is a fibrin-covered break in the mucosa of the digestive tract extending to the submucosa that is caused by acid injury (Figure 1). Most peptic ulcers occur in the stomach or proximal duodenum, though they may also occur in the esophagus or, less frequently, in a Meckel’s diverticulum.1,2 The estimated worldwide prevalence of peptic ulcer disease is 5% to 10%, with an annual incidence of 0.1% to 0.3%1; both rates are declining.3 The annual incidence of peptic ulcer disease requiring medical or surgical treatment is also declining, and currently is estimated to be 0.1% to 0.2%.4 The lifetime prevalence of peptic ulcers has been decreasing in high-income countries since the mid-20th century due to both the widespread use of medications that suppress gastric acid secretion and the declining prevalence of Helicobacter pylori infection.1,3
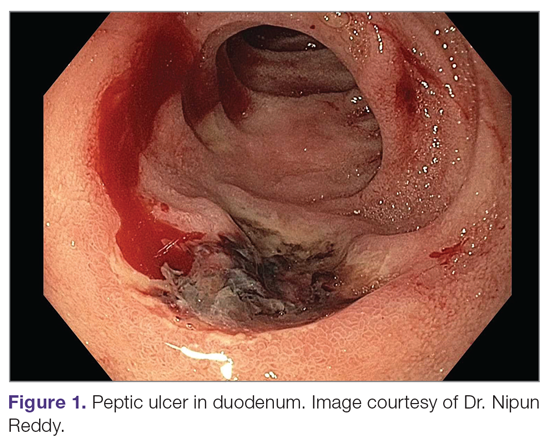
Peptic ulcer disease in most individuals results from H. pylori infection, chronic use of nonsteroidal anti-inflammatory drugs (NSAIDs), including aspirin, or both. A combination of H. pylori factors and host factors lead to mucosal disruption in infected individuals who develop peptic ulcers. H. pylori–specific factors include the expression of virulence factors such as CagA and VacA, which interact with the host inflammatory response to cause mucosal injury. The mucosal inflammatory response is at least partially determined by polymorphisms in the host’s cytokine genes.1,4 NSAIDs inhibit the production of cyclooxygenase-1-derived prostaglandins, with subsequent decreases in epithelial mucous formation, bicarbonate secretion, cell proliferation, and mucosal blood flow, all of which are key elements in the maintenance of mucosal integrity.1,5 Less common causes of peptic ulcers include gastrinoma, adenocarcinoma, idiopathic ulcers, use of sympathomimetic drugs (eg, cocaine or methamphetamine), certain anticancer agents, and bariatric surgery.4,6
This article provides an overview of current management principles for peptic ulcer disease and discusses current challenges in peptic ulcer management, including proton pump inhibitor (PPI) therapy, refractory ulcers, handling of antiplatelet and anticoagulants during and after peptic ulcer bleeding, and ulcer bleeding that continues despite salvage endoscopic therapy.
Methods
We searched MEDLINE using the term peptic ulcer disease in combination with the terms current challenges, epidemiology, bleeding, anticoagulant, antiplatelet, PPI potency, etiology, treatment, management, and refractory. We selected publications from the past 35 years that we judged to be relevant.
Current Management
The goals of peptic ulcer disease management are ulcer healing and prevention of recurrence. The primary interventions used in the management of peptic ulcer disease are medical therapy and implementation of measures that address the underlying etiology of the disease.
Medical Therapy
Introduced in the late 1980s, PPIs are the cornerstone of medical therapy for peptic ulcer disease.6 These agents irreversibly inhibit the H+/K+-ATPase pump in the gastric mucosa and thereby inhibit gastric acid secretion, promoting ulcer healing. PPIs improve rates of ulcer healing compared to H2-receptor antagonists.4,7
Underlying Causes
The underlying cause of peptic ulcer disease should be addressed, in addition to initiating medical therapy. A detailed history of NSAID use should be obtained, and patients with peptic ulcers caused by NSAIDs should be counseled to avoid them, if possible. Patients with peptic ulcer disease who require long-term use of NSAIDs should be placed on long-term PPI therapy.6 Any patient with peptic ulcer disease, regardless of any history of H. pylori infection or treatment, should be tested for infection. Tests that identify active infection, such as urea breath test, stool antigen assay, or mucosal biopsy–based testing, are preferred to IgG antibody testing, although the latter is acceptable in the context of peptic ulcer disease with a high pretest probability of infection.8 Any evidence of active infection warrants appropriate treatment to allow ulcer healing and prevent recurrence.1H. pylori infection is most often treated with clarithromycin triple therapy or bismuth quadruple therapy for 14 days, with regimens selected based on the presence or absence of penicillin allergy, prior antibiotic exposure, and local clarithromycin resistance rates, when known.4,8
Managing Complications
An additional aspect of care in peptic ulcer disease is managing the complications of bleeding, perforation, and gastric outlet obstruction. Acute upper gastrointestinal bleeding (GIB) is the most common complication of peptic ulcer disease, which accounts for 40% to 60% of nonvariceal acute upper GIB.1,6 The first step in the management of acute GIB from a peptic ulcer is fluid resuscitation to ensure hemodynamic stability. If there is associated anemia with a hemoglobin level < 8 g/dL, blood transfusion should be undertaken to target a hemoglobin level > 8 g/dL. In patients with peptic ulcer disease–related acute upper GIB and comorbid cardiovascular disease, the transfusion threshold is higher, with the specific cutoff depending on clinical status, type and severity of cardiovascular disease, and degree of bleeding. Endoscopic management should generally be undertaken within 24 hours of presentation and should not be delayed in patients taking anticoagulants.9 Combination endoscopic treatment with through-the-scope clips plus thermocoagulation or sclerosant injection is recommended for acutely bleeding peptic ulcers with high-risk stigmata.
Pharmacologic management of patients with bleeding peptic ulcers with high-risk stigmata includes PPI therapy, with an 80 mg intravenous (IV) loading dose followed by continuous infusion of 8 mg/hr for 72 hours to reduce rebleeding and mortality. Following completion of IV therapy, oral PPI therapy should be continued twice daily for 14 days, followed by once-daily dosing thereafter.9Patients with peptic ulcer perforation present with sudden-onset epigastric abdominal pain and have tenderness to palpation, guarding, and rigidity on examination, often along with tachycardia and hypotension.1,4 Computed tomography (CT) of the abdomen is 98% sensitive for identifying and localizing a perforation. Most perforations occur in the duodenum or antrum.
Management of a peptic ulcer perforation requires consultation with a surgeon to determine whether a nonoperative approach may be employed (eg, a stable patient with a contained perforation), or if surgery is indicated. The surgical approach to peptic ulcer perforation has been impacted by the clinical success of gastric acid suppression with PPIs and H. pylori eradication, but a range of surgical approaches are still used to repair perforations, from omental patch repair with peritoneal drain placement, to more extensive surgeries such as wedge resection or partial gastrectomy.4 Perforation carries a high mortality risk, up to 20% to 30%, and is the leading cause of death in patients with peptic ulcer disease.1,4
Gastric outlet obstruction, a rare complication of peptic ulcer disease, results from recurrent ulcer formation and scarring. Obstruction often presents with hypovolemia and metabolic alkalosis from prolonged vomiting. CT imaging with oral contrast is often the first diagnostic test employed to demonstrate obstruction. Upper endoscopy should be performed to evaluate the appearance and degree of obstruction as well as to obtain biopsies to evaluate for a malignant etiology of the ulcer disease. Endoscopic balloon dilation has become the cornerstone of initial therapy for obstruction from peptic ulcer disease, especially in the case of ulcers due to reversible causes. Surgery is now typically reserved for cases of refractory obstruction, after repeated endoscopic balloon dilation has failed to remove the obstruction. However, because nearly all patients with gastric outlet obstruction present with malnutrition, nutritional deficiencies should be addressed prior to the patient undergoing surgical intervention. Surgical options include pyloroplasty, antrectomy, and gastrojejunostomy.4
Current Challenges
Rapid Metabolism of PPIs
High-dose PPI therapy is a key component of therapy for peptic ulcer healing. PPIs are metabolized by the cytochrome P450 system, which is comprised of multiple isoenzymes. CYP2C19, an isoenzyme involved in PPI metabolism, has 21 polymorphisms, which have variable effects leading to ultra-rapid, extensive, intermediate, or poor metabolism of PPIs.10 With rapid metabolism of PPIs, standard dosing can result in inadequate suppression of acid secretion. Despite this knowledge, routine testing of CYP2C19 phenotype is not recommended due to the cost of testing. Instead, inadequate ulcer healing should prompt consideration of increased PPI dosing to 80 mg orally twice daily, which may be sufficient to overcome rapid PPI metabolism.11
Relative Potency of PPIs
In addition to variation in PPI metabolism, the relative potency of various PPIs has been questioned. A review of all available clinical studies of the effects of PPIs on mean 24-hour intragastric pH reported a quantitative difference in the potency of 5 PPIs, with omeprazole as the reference standard. Potencies ranged from 0.23 omeprazole equivalents for pantoprazole to 1.82 omeprazole equivalents for rabeprazole.12 An additional study of data from 56 randomized clinical trials confirmed that PPIs vary in potency, which was measured as time that gastric pH is less than 4. A linear increase in intragastric pH time less than 4 was observed from 9 to 64 mg omeprazole equivalents; higher doses yielded no additional benefit. An increase in PPI dosing from once daily to twice daily also increased the duration of intragastric pH time less than 4 from 15 to 21 hours.13 Earlier modeling of the relationship between duodenal ulcer healing and antisecretory therapy showed a strong correlation of ulcer healing with the duration of acid suppression, length of therapy, and the degree of acid suppression. Additional benefit was not observed after intragastric pH rose above 3.14 Thus, as the frequency and duration of acid suppression therapy are more important than PPI potency, PPIs can be used interchangeably.13,14
Addressing Underlying Causes
Continued NSAID Use. Refractory peptic ulcers are defined as those that do not heal despite adherence to 8 to 12 weeks of standard acid-suppression therapy. A cause of refractory peptic ulcer disease that must be considered is continued NSAID use.1,15 In a study of patients with refractory peptic ulcers, 27% of patients continued NSAID use, as determined by eventual disclosure by the patients or platelet cyclooxygenase activity assay, despite extensive counseling to avoid NSAIDs at the time of the diagnosis of their refractory ulcer and at subsequent visits.16 Pain may make NSAID cessation difficult for some patients, while others do not realize that over-the-counter preparations they take contain NSAIDs.15
Another group of patients with continued NSAID exposure are those who require long-term NSAID therapy for control of arthritis or the management of cardiovascular conditions. If NSAID therapy cannot be discontinued, the risk of NSAID-related gastrointestinal injury can be assessed based on the presence of multiple risk factors, including age > 65 years, high-dose NSAID therapy, a history of peptic ulcer, and concurrent use of aspirin, corticosteroids, or anticoagulants. Individuals with 3 or more of the preceding risk factors or a history of a peptic ulcer with a complication, especially if recent, are considered to be at high risk of developing an NSAID-related ulcer and possible subsequent complications.17 In these individuals, NSAID therapy should be continued with agents that have the lowest risk for gastrointestinal toxicity and at the lowest possible dose. A meta-analysis comparing nonselective NSAIDs to placebo demonstrated naproxen to have the highest risk of gastrointestinal complications, including GIB, perforation, and obstruction (adjusted rate ratio, 4.2), while diclofenac demonstrated the lowest risk (adjusted rate ratio, 1.89). High-dose NSAID therapy demonstrated a 2-fold increase in risk of peptic ulcer formation as compared to low-dose therapy.18
In addition to selecting the NSAID with the least gastrointestinal toxicity at the lowest possible dose, additional strategies to prevent peptic ulcer disease and its complications in chronic NSAID users include co-administration of a PPI and substitution of a COX-2 selective NSAID for nonselective NSAIDs.1,9 Prior double-blind, placebo-controlled, randomized, multicenter trials with patients requiring daily NSAIDs demonstrated an up to 15% absolute reduction in the risk of developing peptic ulcers over 6 months while taking esomeprazole.19
Persistent Infection. Persistent H. pylori infection, due either to initial false-negative testing or ongoing infection despite first-line therapy, is another cause of refractory peptic ulcer disease.1,15 Because antibiotics and PPIs can reduce the number of H. pylori bacteria, use of these medications concurrent with H. pylori testing can lead to false-negative results with several testing modalities. When suspicion for H. pylori is high, 2 or more diagnostic tests may be needed to effectively rule out infection.15
When H. pylori is detected, successful eradication is becoming more difficult due to an increasing prevalence of antibiotic resistance, leading to persistent infection in many cases and maintained risk of peptic ulcer disease, despite appropriate first-line therapy.8 Options for salvage therapy for persistent H. pylori, as well as information on the role and best timing of susceptibility testing, are beyond the scope of this review, but are reviewed by Lanas and Chan1 and in the American College of Gastroenterology guideline on the treatment of H. pylori infection.8
Other Causes. In a meta-analysis of rigorously designed studies from North America, 20% of patients experienced ulcer recurrence at 6 months, despite successful H. pylori eradication and no NSAID use.20 In addition, as H. pylori prevalence is decreasing, idiopathic ulcers are increasingly being diagnosed, and such ulcers may be associated with high rates of GIB and mortality.1 In this subset of patients with non-H. pylori, non-NSAID ulcers, increased effort is required to further evaluate the differential diagnosis for rarer causes of upper GI tract ulcer disease (Table). Certain malignancies, including adenocarcinoma and lymphoma, can cause ulcer formation and should be considered in refractory cases. Repeat biopsy at follow-up endoscopy for persistent ulcers should always be obtained to further evaluate for malignancy.1,15 Infectious diseases other than H. pylori infection, such as tuberculosis, syphilis, cytomegalovirus, and herpes simplex virus, are also reported as etiologies of refractory ulcers, and require specific antimicrobial treatment over and above PPI monotherapy. Special attention in biopsy sampling and sample processing is often required when infectious etiologies are being considered, as specific histologic stains and cultures may be needed for identification.15
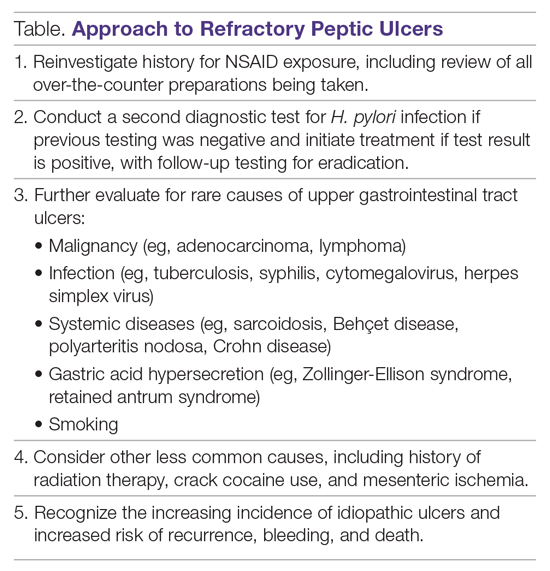
Systemic conditions, including sarcoidosis,21 Behçet disease,22 and polyarteritis nodosa,15,23 can also cause refractory ulcers. Approximately 15% of patients with Crohn disease have gastroduodenal involvement, which may include ulcers of variable sizes.1,15,24 The increased gastric acid production seen in Zollinger-Ellison syndrome commonly presents as refractory peptic ulcers in the duodenum beyond the bulb that do not heal with standard doses of PPIs.1,15 More rare causes of acid hypersecretion leading to refractory ulcers include idiopathic gastric acid hypersecretion and retained gastric antrum syndrome after partial gastrectomy with Billroth II anastomosis.15 Smoking is a known risk factor for impaired tissue healing throughout the body, and can contribute to impaired healing of peptic ulcers through decreased prostaglandin synthesis25 and reduced gastric mucosal blood flow.26 Smoking should always be addressed in patients with refractory peptic ulcers, and cessation should be strongly encouraged. Other less common causes of refractory upper GI tract ulcers include radiation therapy, crack cocaine use, and mesenteric ischemia.15
Managing Antiplatelet and Anticoagulant Medications
Use of antiplatelets and anticoagulants, alone or in combination, increases the risk of peptic ulcer bleeding. In patients who continue to take aspirin after a peptic ulcer bleed, recurrent bleeding occurs in up to 300 cases per 1000 person-years. The rate of GIB associated with aspirin use ranges from 1.1% to 2.5%, depending on the dose. Prior peptic ulcer disease, age greater than 70 years, and concurrent NSAID, steroid, anticoagulant, or dual antiplatelet therapy (DAPT) use increase the risk of bleeding while on aspirin. The rate of GIB while taking a thienopyridine alone is slightly less than that when taking aspirin, ranging from 0.5% to 1.6%. Studies to date have yielded mixed estimates of the effect of DAPT on the risk of GIB. Estimates of the risk of GIB with DAPT range from an odds ratio for serious GIB of 7.4 to an absolute risk increase of only 1.3% when compared to clopidogrel alone.27
Many patients are also on warfarin or a direct oral anticoagulant (DOAC). In a study from the United Kingdom, the adjusted rate ratio of GIB with warfarin alone was 1.94, and this increased to 6.48 when warfarin was used with aspirin.28 The use of warfarin and DAPT, often called triple therapy, further increases the risk of GIB, with a hazard ratio of 5.0 compared to DAPT alone, and 5.38 when compared to warfarin alone. DOACs are increasingly prescribed for the treatment and prevention of thromboembolism, and by 2014 were prescribed as often as warfarin for stroke prevention in atrial fibrillation in the United States. A meta-analysis showed the risk of major GIB did not differ between DOACs and warfarin or low-molecular-weight heparin, but among DOACs factor Xa inhibitors showed a reduced risk of GIB compared with dabigatran, a direct thrombin inhibitor.29
The use of antiplatelets and anticoagulants in the context of peptic ulcer bleeding is a current management challenge. Data to guide decision-making in patients on antiplatelet and/or anticoagulant therapy who experience peptic ulcer bleeding are scarce. Decision-making in this group of patients requires balancing the severity and risk of bleeding with the risk of thromboembolism.1,27 In patients on antiplatelet therapy for primary prophylaxis of atherothrombosis who develop bleeding from a peptic ulcer, the antiplatelet should generally be held and the indication for the medication reassessed. In patients on antiplatelet therapy for secondary prevention, the agent may be immediately resumed after endoscopy if bleeding is found to be due to an ulcer with low-risk stigmata. With bleeding resulting from an ulcer with high-risk stigmata, antiplatelet agents employed for secondary prevention may be held initially, with consideration given to early reintroduction, as early as day 3 after endoscopy.1 In patients at high risk for atherothrombotic events, including those on aspirin for secondary prophylaxis, withholding aspirin leads to a 3-fold increase in the risk of a major adverse cardiac event, with events occurring as early as 5 days after aspirin cessation in some cases.27 A randomized controlled trial of continuing low-dose aspirin versus withholding it for 8 weeks in patients on aspirin for secondary prophylaxis of cardiovascular events who experienced peptic ulcer bleeding that required endoscopic therapy demonstrated lower all-cause mortality (1.3% vs 12.9%), including death from cardiovascular or cerebrovascular events, among those who continued aspirin therapy, with a small increased risk of recurrent ulcer bleeding (10.3% vs 5.4%).30 Thus, it is recommended that antiplatelet therapy, when held, be resumed as early as possible when the risk of a cardiovascular or cerebrovascular event is considered to be higher than the risk of bleeding.27
When patients are on DAPT for a history of drug-eluting stent placement, withholding both antiplatelet medications should be avoided, even for a brief period of time, given the risk of in-stent thrombosis. When DAPT is employed for other reasons, it should be continued, if indicated, after bleeding that is found to be due to peptic ulcers with low-risk stigmata. If bleeding is due to a peptic ulcer with high-risk stigmata at endoscopy, then aspirin monotherapy should be continued and consultation should be obtained with a cardiologist to determine optimal timing to resume the second antiplatelet agent.1 In patients on anticoagulants, anticoagulation should be resumed once hemostasis is achieved when the risk of withholding anticoagulation is thought to be greater than the risk of rebleeding. For example, anticoagulation should be resumed early in a patient with a mechanical heart valve to prevent thrombosis.1,27 Following upper GIB from peptic ulcer disease, patients who will require long-term aspirin, DAPT, or anticoagulation with either warfarin or DOACs should be maintained on long-term PPI therapy to reduce the risk of recurrent bleeding.9,27
Failure of Endoscopic Therapy to Control Peptic Ulcer Bleeding
Bleeding recurs in as many as 10% to 20% of patients after initial endoscopic control of peptic ulcer bleeding.4,31 In this context, repeat upper endoscopy for hemostasis is preferred to surgery, as it leads to less morbidity while providing long-term control of bleeding in more than 70% of cases.31,32 Two potential endoscopic rescue therapies that may be employed are over-the-scope clips (OTSCs) and hemostatic powder.32,33
While through-the-scope (TTS) hemostatic clips are often used during endoscopy to control active peptic ulcer bleeding, their use may be limited in large or fibrotic ulcers due to the smaller size of the clips and method of application. OTSCs have several advantages over TTS clips; notably, their larger size allows the endoscopist to achieve deeper mucosal or submucosal clip attachment via suction of the targeted tissue into the endoscopic cap (Figure 2). In a systematic review of OTSCs, successful hemostasis was achieved in 84% of 761 lesions, including 75% of lesions due to peptic ulcer disease.34 Some have argued that OTSCs may be preferred as first-line therapy over epinephrine with TTS clips for hemostasis in bleeding from high-risk peptic ulcers (ie, those with visualized arterial bleeding or a visible vessel) given observed decreases in rebleeding events.35
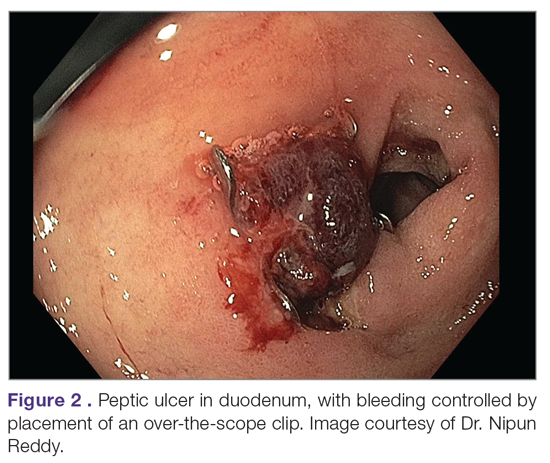
Despite the advantages of OTSCs, endoscopists should be mindful of the potential complications of OTSC use, including luminal obstruction, particularly in the duodenum, and perforation, which occurs in 0.3% to 2% of cases. Additionally, retrieval of misplaced OTSCs presents a significant challenge. Careful decision-making with consideration of the location, size, and depth of lesions is required when deciding on OTSC placement.34,36
A newer endoscopic tool developed for refractory bleeding from peptic ulcers and other causes is hemostatic powder. Hemostatic powders accelerate the coagulation cascade, leading to shortened coagulation times and enhanced clot formation.37 A recent meta-analysis showed that immediate hemostasis could be achieved in 95% of cases of bleeding, including in 96% of cases of bleeding from peptic ulcer disease.38 The primary limitation of hemostatic powders is the temporary nature of hemostasis, which requires the underlying etiology of bleeding to be addressed in order to provide long-term hemostasis. In the above meta-analysis, rebleeding occurred in 17% of cases after 30 days.38
Hypotension and ulcer diameter ≥ 2 cm are independent predictors of failure of endoscopic salvage therapy.31 When severe bleeding is not controlled with initial endoscopic therapy or bleeding recurs despite salvage endoscopic therapy, transcatheter angiographic embolization (TAE) is the treatment of choice.4 Systematic reviews and meta-analyses of studies that compared TAE to surgery have shown that the rate of rebleeding may be higher with TAE, but with less morbidity and either decreased or equivalent rates of mortality, with no increased need for additional interventions.4,32 In a case series examining 5 years of experience at a single medical center in China, massive GIB from duodenal ulcers was successfully treated with TAE in 27 of 29 cases (93% clinical success rate), with no mucosal ischemic necrosis observed.39
If repeated endoscopic therapy has not led to hemostasis of a bleeding peptic ulcer and TAE is not available, then surgery is the next best option. Bleeding gastric ulcers may be excised, wedge resected, or oversewn after an anterior gastrostomy. Bleeding duodenal ulcers may require use of a Kocher maneuver and linear incision of the anterior duodenum followed by ligation of the gastroduodenal artery. Fortunately, such surgical management is rarely necessary given the availability of TAE at most centers.4
Conclusion
Peptic ulcer disease is a common health problem globally, with persistent challenges related to refractory ulcers, antiplatelet and anticoagulant use, and continued bleeding in the face of endoscopic therapy. These challenges should be met with adequate frequency and duration of PPI therapy, vigilant attention to and treatment of ulcer etiology, evidence-based handling of antiplatelet and anticoagulant medications, and utilization of novel endoscopic tools to obtain improved clinical outcomes.
Acknowledgment: We thank Dr. Nipun Reddy from our institution for providing the endoscopic images used in this article.
Corresponding author: Adam L. Edwards, MD, MS; [email protected].
Financial disclosures: None.
1. Lanas A, Chan FKL. Peptic ulcer disease. Lancet. 2017;390:613-624.
2. Malfertheiner P, Chan FK, McColl KE. Peptic ulcer disease. Lancet. 2009;374:1449-1461.
3. Roberts-Thomson IC. Rise and fall of peptic ulceration: A disease of civilization? J Gastroenterol Hepatol. 2018;33:1321-1326.
4. Kempenich JW, Sirinek KR. Acid peptic disease. Surg Clin North Am. 2018;98:933-944.
5. Cryer B, Feldman M. Effects of very low dose daily, long-term aspirin therapy on gastric, duodenal, and rectal prostaglandin levels and on mucosal injury in healthy humans. Gastroenterology. 1999;117:17-25.
6. Kavitt RT, Lipowska AM, Anyane-Yeboa A, Gralnek IM. Diagnosis and treatment of peptic ulcer disease. Am J Med. 2019;132:447-456.
7. Walan A, Bader JP, Classen M, et al. Effect of omeprazole and ranitidine on ulcer healing and relapse rates in patients with benign gastric ulcer. New Engl J Med. 1989;320:69-75.
8. Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG Clinical Guideline: Treatment of Helicobacter pylori Infection. Am J Gastroenterol. 2017;112:212-239.
9. Barkun AN, Almadi M, Kuipers EJ, et al. Management of nonvariceal upper gastrointestinal bleeding: Guideline recommendations from the International Consensus Group. Ann Intern Med. 2019;171:805-822.
10. Arevalo Galvis A, Trespalacios Rangel AA, Otero Regino W. Personalized therapy for Helicobacter pylori: CYP2C19 genotype effect on first-line triple therapy. Helicobacter. 2019;24:e12574.
11. Furuta T, Ohashi K, Kamata T, et al. Effect of genetic differences in omeprazole metabolism on cure rates for Helicobacter pylori infection and peptic ulcer. Ann Intern Med. 1998;129:1027-1030.
12. Kirchheiner J, Glatt S, Fuhr U, et al. Relative potency of proton-pump inhibitors-comparison of effects on intragastric pH. Eur J Clin Pharmacol. 2009;65:19-31.
13. Graham DY, Tansel A. Interchangeable use of proton pump inhibitors based on relative potency. Clin Gastroenterol Hepatol. 2018;16:800-808.e7.
14. Burget DW, Chiverton SG, Hunt RH. Is there an optimal degree of acid suppression for healing of duodenal ulcers? A model of the relationship between ulcer healing and acid suppression. Gastroenterology. 1990;99:345-351.
15. Kim HU. Diagnostic and treatment approaches for refractory peptic ulcers. Clin Endosc. 2015;48:285-290.
16. Lanas AI, Remacha B, Esteva F, Sainz R. Risk factors associated with refractory peptic ulcers. Gastroenterology. 1995;109:124-133.
17. Lanza FL, Chan FK, Quigley EM. Guidelines for prevention of NSAID-related ulcer complications. Am J Gastroenterol. 2009;104:728-738.
18. Richy F, Bruyere O, Ethgen O, et al. Time dependent risk of gastrointestinal complications induced by non-steroidal anti-inflammatory drug use: a consensus statement using a meta-analytic approach. Ann Rheum Dis. 2004;63:759-766.
19. Scheiman JM, Yeomans ND, Talley NJ, et al. Prevention of ulcers by esomeprazole in at-risk patients using non-selective NSAIDs and COX-2 inhibitors. Am J Gastroenterol. 2006;101:701-710.
20. Laine L, Hopkins RJ, Girardi LS. Has the impact of Helicobacter pylori therapy on ulcer recurrence in the United States been overstated? A meta-analysis of rigorously designed trials. Am J Gastroenterol. 1998;93:1409-1415.
21. Akiyama T, Endo H, Inamori M, et al. Symptomatic gastric sarcoidosis with multiple antral ulcers. Endoscopy. 2009;41 Suppl 2:E159.
22. Sonoda A, Ogawa R, Mizukami K, et al. Marked improvement in gastric involvement in Behcet’s disease with adalimumab treatment. Turk J Gastroenterol. 2017;28:405-407.
23. Saikia N, Talukdar R, Mazumder S, et al. Polyarteritis nodosa presenting as massive upper gastrointestinal hemorrhage. Gastrointest Endosc. 2006;63:868-870.
24. Annunziata ML, Caviglia R, Papparella LG, Cicala M. Upper gastrointestinal involvement of Crohn’s disease: a prospective study on the role of upper endoscopy in the diagnostic work-up. Dig Dis Sci. 2012;57:1618-1623.
25. Quimby GF, Bonnice CA, Burstein SH, Eastwood GL. Active smoking depresses prostaglandin synthesis in human gastric mucosa. Ann Intern Med. 1986;104:616-619.
26. Iwao T, Toyonaga A, Ikegami M, et al. Gastric mucosal blood flow after smoking in healthy human beings assessed by laser Doppler flowmetry. Gastrointest Endosc. 1993;39:400-403.
27. Almadi MA, Barkun A, Brophy J. Antiplatelet and anticoagulant therapy in patients with gastrointestinal bleeding: an 86-year-old woman with peptic ulcer disease. JAMA. 2011;306:2367-2374.
28. Delaney JA, Opatrny L, Brophy JM, Suissa S. Drug drug interactions between antithrombotic medications and the risk of gastrointestinal bleeding. CMAJ. 2007;177:347-351.
29. Burr N, Lummis K, Sood R, et al. Risk of gastrointestinal bleeding with direct oral anticoagulants: a systematic review and network meta-analysis. Lancet Gastroenterol Hepatol. 2017;2:85-93.
30. Sung JJ, Lau JY, Ching JY, et al. Continuation of low-dose aspirin therapy in peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2010;152:1-9.
31. Lau JY, Sung JJ, Lam YH, et al. Endoscopic retreatment compared with surgery in patients with recurrent bleeding after initial endoscopic control of bleeding ulcers. N Engl J Med. 1999;340:751-756.
32. Gralnek IM, Dumonceau JM, Kuipers EJ, et al. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47:a1-46.
33. Skinner M, Gutierrez JP, Neumann H, et al. Over-the-scope clip placement is effective rescue therapy for severe acute upper gastrointestinal bleeding. Endosc Int Open. 2014;2:E37-40.
34. Zhong C, Tan S, Ren Y, et al. Clinical outcomes of over-the-scope-clip system for the treatment of acute upper non-variceal gastrointestinal bleeding: a systematic review and meta-analysis. BMC Gastroenterol. 2019;19:225.
35. Mangiafico S, Pigo F, Bertani H, et al. Over-the-scope clip vs epinephrine with clip for first-line hemostasis in non-variceal upper gastrointestinal bleeding: a propensity score match analysis. Endosc Int Open. 2020;8:E50-e8.
36. Wedi E, Gonzalez S, Menke D, et al. One hundred and one over-the-scope-clip applications for severe gastrointestinal bleeding, leaks and fistulas. World J Gastroenterol. 2016;22:1844-1853.
37. Holster IL, van Beusekom HM, Kuipers EJ, et al. Effects of a hemostatic powder hemospray on coagulation and clot formation. Endoscopy. 2015;47:638-645.
38. Facciorusso A, Straus Takahashi M, et al. Efficacy of hemostatic powders in upper gastrointestinal bleeding: A systematic review and meta-analysis. Dig Liver Dis. 2019;51:1633-1640.
39. Wang YL, Cheng YS, et al. Emergency transcatheter arterial embolization for patients with acute massive duodenal ulcer hemorrhage. World J Gastroenterol. 2012;18:4765-4770.
1. Lanas A, Chan FKL. Peptic ulcer disease. Lancet. 2017;390:613-624.
2. Malfertheiner P, Chan FK, McColl KE. Peptic ulcer disease. Lancet. 2009;374:1449-1461.
3. Roberts-Thomson IC. Rise and fall of peptic ulceration: A disease of civilization? J Gastroenterol Hepatol. 2018;33:1321-1326.
4. Kempenich JW, Sirinek KR. Acid peptic disease. Surg Clin North Am. 2018;98:933-944.
5. Cryer B, Feldman M. Effects of very low dose daily, long-term aspirin therapy on gastric, duodenal, and rectal prostaglandin levels and on mucosal injury in healthy humans. Gastroenterology. 1999;117:17-25.
6. Kavitt RT, Lipowska AM, Anyane-Yeboa A, Gralnek IM. Diagnosis and treatment of peptic ulcer disease. Am J Med. 2019;132:447-456.
7. Walan A, Bader JP, Classen M, et al. Effect of omeprazole and ranitidine on ulcer healing and relapse rates in patients with benign gastric ulcer. New Engl J Med. 1989;320:69-75.
8. Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG Clinical Guideline: Treatment of Helicobacter pylori Infection. Am J Gastroenterol. 2017;112:212-239.
9. Barkun AN, Almadi M, Kuipers EJ, et al. Management of nonvariceal upper gastrointestinal bleeding: Guideline recommendations from the International Consensus Group. Ann Intern Med. 2019;171:805-822.
10. Arevalo Galvis A, Trespalacios Rangel AA, Otero Regino W. Personalized therapy for Helicobacter pylori: CYP2C19 genotype effect on first-line triple therapy. Helicobacter. 2019;24:e12574.
11. Furuta T, Ohashi K, Kamata T, et al. Effect of genetic differences in omeprazole metabolism on cure rates for Helicobacter pylori infection and peptic ulcer. Ann Intern Med. 1998;129:1027-1030.
12. Kirchheiner J, Glatt S, Fuhr U, et al. Relative potency of proton-pump inhibitors-comparison of effects on intragastric pH. Eur J Clin Pharmacol. 2009;65:19-31.
13. Graham DY, Tansel A. Interchangeable use of proton pump inhibitors based on relative potency. Clin Gastroenterol Hepatol. 2018;16:800-808.e7.
14. Burget DW, Chiverton SG, Hunt RH. Is there an optimal degree of acid suppression for healing of duodenal ulcers? A model of the relationship between ulcer healing and acid suppression. Gastroenterology. 1990;99:345-351.
15. Kim HU. Diagnostic and treatment approaches for refractory peptic ulcers. Clin Endosc. 2015;48:285-290.
16. Lanas AI, Remacha B, Esteva F, Sainz R. Risk factors associated with refractory peptic ulcers. Gastroenterology. 1995;109:124-133.
17. Lanza FL, Chan FK, Quigley EM. Guidelines for prevention of NSAID-related ulcer complications. Am J Gastroenterol. 2009;104:728-738.
18. Richy F, Bruyere O, Ethgen O, et al. Time dependent risk of gastrointestinal complications induced by non-steroidal anti-inflammatory drug use: a consensus statement using a meta-analytic approach. Ann Rheum Dis. 2004;63:759-766.
19. Scheiman JM, Yeomans ND, Talley NJ, et al. Prevention of ulcers by esomeprazole in at-risk patients using non-selective NSAIDs and COX-2 inhibitors. Am J Gastroenterol. 2006;101:701-710.
20. Laine L, Hopkins RJ, Girardi LS. Has the impact of Helicobacter pylori therapy on ulcer recurrence in the United States been overstated? A meta-analysis of rigorously designed trials. Am J Gastroenterol. 1998;93:1409-1415.
21. Akiyama T, Endo H, Inamori M, et al. Symptomatic gastric sarcoidosis with multiple antral ulcers. Endoscopy. 2009;41 Suppl 2:E159.
22. Sonoda A, Ogawa R, Mizukami K, et al. Marked improvement in gastric involvement in Behcet’s disease with adalimumab treatment. Turk J Gastroenterol. 2017;28:405-407.
23. Saikia N, Talukdar R, Mazumder S, et al. Polyarteritis nodosa presenting as massive upper gastrointestinal hemorrhage. Gastrointest Endosc. 2006;63:868-870.
24. Annunziata ML, Caviglia R, Papparella LG, Cicala M. Upper gastrointestinal involvement of Crohn’s disease: a prospective study on the role of upper endoscopy in the diagnostic work-up. Dig Dis Sci. 2012;57:1618-1623.
25. Quimby GF, Bonnice CA, Burstein SH, Eastwood GL. Active smoking depresses prostaglandin synthesis in human gastric mucosa. Ann Intern Med. 1986;104:616-619.
26. Iwao T, Toyonaga A, Ikegami M, et al. Gastric mucosal blood flow after smoking in healthy human beings assessed by laser Doppler flowmetry. Gastrointest Endosc. 1993;39:400-403.
27. Almadi MA, Barkun A, Brophy J. Antiplatelet and anticoagulant therapy in patients with gastrointestinal bleeding: an 86-year-old woman with peptic ulcer disease. JAMA. 2011;306:2367-2374.
28. Delaney JA, Opatrny L, Brophy JM, Suissa S. Drug drug interactions between antithrombotic medications and the risk of gastrointestinal bleeding. CMAJ. 2007;177:347-351.
29. Burr N, Lummis K, Sood R, et al. Risk of gastrointestinal bleeding with direct oral anticoagulants: a systematic review and network meta-analysis. Lancet Gastroenterol Hepatol. 2017;2:85-93.
30. Sung JJ, Lau JY, Ching JY, et al. Continuation of low-dose aspirin therapy in peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2010;152:1-9.
31. Lau JY, Sung JJ, Lam YH, et al. Endoscopic retreatment compared with surgery in patients with recurrent bleeding after initial endoscopic control of bleeding ulcers. N Engl J Med. 1999;340:751-756.
32. Gralnek IM, Dumonceau JM, Kuipers EJ, et al. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47:a1-46.
33. Skinner M, Gutierrez JP, Neumann H, et al. Over-the-scope clip placement is effective rescue therapy for severe acute upper gastrointestinal bleeding. Endosc Int Open. 2014;2:E37-40.
34. Zhong C, Tan S, Ren Y, et al. Clinical outcomes of over-the-scope-clip system for the treatment of acute upper non-variceal gastrointestinal bleeding: a systematic review and meta-analysis. BMC Gastroenterol. 2019;19:225.
35. Mangiafico S, Pigo F, Bertani H, et al. Over-the-scope clip vs epinephrine with clip for first-line hemostasis in non-variceal upper gastrointestinal bleeding: a propensity score match analysis. Endosc Int Open. 2020;8:E50-e8.
36. Wedi E, Gonzalez S, Menke D, et al. One hundred and one over-the-scope-clip applications for severe gastrointestinal bleeding, leaks and fistulas. World J Gastroenterol. 2016;22:1844-1853.
37. Holster IL, van Beusekom HM, Kuipers EJ, et al. Effects of a hemostatic powder hemospray on coagulation and clot formation. Endoscopy. 2015;47:638-645.
38. Facciorusso A, Straus Takahashi M, et al. Efficacy of hemostatic powders in upper gastrointestinal bleeding: A systematic review and meta-analysis. Dig Liver Dis. 2019;51:1633-1640.
39. Wang YL, Cheng YS, et al. Emergency transcatheter arterial embolization for patients with acute massive duodenal ulcer hemorrhage. World J Gastroenterol. 2012;18:4765-4770.
Blood vessels in the eye may diagnose Parkinson’s disease
new research shows. Using an advanced machine-learning algorithm and fundus eye images, which depict the small blood vessels and more at the back of the eye, investigators are able to classify patients with Parkinson’s disease compared against a control group. “We discovered that micro blood vessels decreased in both size and number in patients with Parkinson’s disease,” said Maximillian Diaz, a PhD student at the University of Florida, Gainesville.
The simple eye examination may offer a way to diagnose Parkinson’s early in the disease progression.
Mr. Diaz said the test could be incorporated to a patient’s annual physical examination not only to look for Parkinson’s disease but also for other neurological diseases. Researchers at the University of Florida are also looking at whether the same technique can diagnose Alzheimer’s disease.
The beauty of this is that “the technique is simple,” he said. “What surprised us is that we can do this with fundus images, which can be taken in a clinical setting with a lens that attaches to your smartphone. It’s affordable and portable and it takes less than a minute.”
Machine learning on fundus eye images
Researchers, under the direction of Ruogu Fang, PhD, director of the J. Crayton Pruitt Department of Biomedical Engineering’s Smart Medical Informatics Learning and Evaluation Lab (SMILE) at the University of Florida, Gainesville, collected fundus eye images from 476 age- and gender-matched individuals, 238 diagnosed with Parkinson’s disease and 238 control group images. Another set of 100 images were collected from the University of Florida database using green color channels (UKB-Green and UF-UKB Green) and used to improve vessel segmentation. Of these, 28 were controls and 72 from patients with Parkinson’s disease. Researchers added 44 more control images from the U.K. Biobank to complete the second age- and gender-matched dataset.
“We used 80% of the images to develop the machine-learning network,” Mr. Diaz said. The other 20% of images, which were new to the algorithm, were used to test it, to determine true or false, Parkinson’s disease or control?
“We were able to achieve an accuracy of 85%,” Mr. Diaz said. Currently, there are no biomarkers to diagnose Parkinson’s disease. The disease is only recognizable once 80% of dopaminergic cells have already decayed. “Clinically, there’s no way to tell how long someone has had it,” Mr. Diaz said. He hopes that by doing additional research and testing earlier – with a longitudinal study of images – a pattern may be detected to better predict disease.
Eye vasculature reveals disease
“This concept [studying eye vasculature] is getting a lot of interest right now,” said Anant Madabhushi, PhD, Case Western Reserve University, Cleveland. “The eye is the proverbial window to the soul, and in this case, shows what’s happening in rest of the body.”
Dr. Madabhushi, who was not involved in the Parkinson’s research, has also been working with a team in Cleveland to look at how vessels in the eye predict response to drug therapies in diabetic macular edema, including treatment durability. “What we’ve found is the more twisted the vessels, the more constricted, and the less likely the person would respond to therapy,” he said, adding that studying the pathology of the eye makes a lot of sense. “The arrangement of vessels in the eye are likely to have implications in all kinds of diseases.”
Since Parkinson’s disease does not have any biomarkers, this technology could be very useful in diagnosis. “With specific quantitative measurements, we could have computational imaging biomarkers to predict the risk of onset of Parkinson’s, and the prognosis of disease. That’s the true utility of this approach,” he said.
Mr. Diaz disclosed no relevant financial relationships. Dr. Madabhushi has consulted for Aiforia and has had research sponsored by AstraZeneca, Bristol-Myers Squibb, and Boehringer Ingelheim.
A version of this article originally appeared on Medscape.com.
new research shows. Using an advanced machine-learning algorithm and fundus eye images, which depict the small blood vessels and more at the back of the eye, investigators are able to classify patients with Parkinson’s disease compared against a control group. “We discovered that micro blood vessels decreased in both size and number in patients with Parkinson’s disease,” said Maximillian Diaz, a PhD student at the University of Florida, Gainesville.
The simple eye examination may offer a way to diagnose Parkinson’s early in the disease progression.
Mr. Diaz said the test could be incorporated to a patient’s annual physical examination not only to look for Parkinson’s disease but also for other neurological diseases. Researchers at the University of Florida are also looking at whether the same technique can diagnose Alzheimer’s disease.
The beauty of this is that “the technique is simple,” he said. “What surprised us is that we can do this with fundus images, which can be taken in a clinical setting with a lens that attaches to your smartphone. It’s affordable and portable and it takes less than a minute.”
Machine learning on fundus eye images
Researchers, under the direction of Ruogu Fang, PhD, director of the J. Crayton Pruitt Department of Biomedical Engineering’s Smart Medical Informatics Learning and Evaluation Lab (SMILE) at the University of Florida, Gainesville, collected fundus eye images from 476 age- and gender-matched individuals, 238 diagnosed with Parkinson’s disease and 238 control group images. Another set of 100 images were collected from the University of Florida database using green color channels (UKB-Green and UF-UKB Green) and used to improve vessel segmentation. Of these, 28 were controls and 72 from patients with Parkinson’s disease. Researchers added 44 more control images from the U.K. Biobank to complete the second age- and gender-matched dataset.
“We used 80% of the images to develop the machine-learning network,” Mr. Diaz said. The other 20% of images, which were new to the algorithm, were used to test it, to determine true or false, Parkinson’s disease or control?
“We were able to achieve an accuracy of 85%,” Mr. Diaz said. Currently, there are no biomarkers to diagnose Parkinson’s disease. The disease is only recognizable once 80% of dopaminergic cells have already decayed. “Clinically, there’s no way to tell how long someone has had it,” Mr. Diaz said. He hopes that by doing additional research and testing earlier – with a longitudinal study of images – a pattern may be detected to better predict disease.
Eye vasculature reveals disease
“This concept [studying eye vasculature] is getting a lot of interest right now,” said Anant Madabhushi, PhD, Case Western Reserve University, Cleveland. “The eye is the proverbial window to the soul, and in this case, shows what’s happening in rest of the body.”
Dr. Madabhushi, who was not involved in the Parkinson’s research, has also been working with a team in Cleveland to look at how vessels in the eye predict response to drug therapies in diabetic macular edema, including treatment durability. “What we’ve found is the more twisted the vessels, the more constricted, and the less likely the person would respond to therapy,” he said, adding that studying the pathology of the eye makes a lot of sense. “The arrangement of vessels in the eye are likely to have implications in all kinds of diseases.”
Since Parkinson’s disease does not have any biomarkers, this technology could be very useful in diagnosis. “With specific quantitative measurements, we could have computational imaging biomarkers to predict the risk of onset of Parkinson’s, and the prognosis of disease. That’s the true utility of this approach,” he said.
Mr. Diaz disclosed no relevant financial relationships. Dr. Madabhushi has consulted for Aiforia and has had research sponsored by AstraZeneca, Bristol-Myers Squibb, and Boehringer Ingelheim.
A version of this article originally appeared on Medscape.com.
new research shows. Using an advanced machine-learning algorithm and fundus eye images, which depict the small blood vessels and more at the back of the eye, investigators are able to classify patients with Parkinson’s disease compared against a control group. “We discovered that micro blood vessels decreased in both size and number in patients with Parkinson’s disease,” said Maximillian Diaz, a PhD student at the University of Florida, Gainesville.
The simple eye examination may offer a way to diagnose Parkinson’s early in the disease progression.
Mr. Diaz said the test could be incorporated to a patient’s annual physical examination not only to look for Parkinson’s disease but also for other neurological diseases. Researchers at the University of Florida are also looking at whether the same technique can diagnose Alzheimer’s disease.
The beauty of this is that “the technique is simple,” he said. “What surprised us is that we can do this with fundus images, which can be taken in a clinical setting with a lens that attaches to your smartphone. It’s affordable and portable and it takes less than a minute.”
Machine learning on fundus eye images
Researchers, under the direction of Ruogu Fang, PhD, director of the J. Crayton Pruitt Department of Biomedical Engineering’s Smart Medical Informatics Learning and Evaluation Lab (SMILE) at the University of Florida, Gainesville, collected fundus eye images from 476 age- and gender-matched individuals, 238 diagnosed with Parkinson’s disease and 238 control group images. Another set of 100 images were collected from the University of Florida database using green color channels (UKB-Green and UF-UKB Green) and used to improve vessel segmentation. Of these, 28 were controls and 72 from patients with Parkinson’s disease. Researchers added 44 more control images from the U.K. Biobank to complete the second age- and gender-matched dataset.
“We used 80% of the images to develop the machine-learning network,” Mr. Diaz said. The other 20% of images, which were new to the algorithm, were used to test it, to determine true or false, Parkinson’s disease or control?
“We were able to achieve an accuracy of 85%,” Mr. Diaz said. Currently, there are no biomarkers to diagnose Parkinson’s disease. The disease is only recognizable once 80% of dopaminergic cells have already decayed. “Clinically, there’s no way to tell how long someone has had it,” Mr. Diaz said. He hopes that by doing additional research and testing earlier – with a longitudinal study of images – a pattern may be detected to better predict disease.
Eye vasculature reveals disease
“This concept [studying eye vasculature] is getting a lot of interest right now,” said Anant Madabhushi, PhD, Case Western Reserve University, Cleveland. “The eye is the proverbial window to the soul, and in this case, shows what’s happening in rest of the body.”
Dr. Madabhushi, who was not involved in the Parkinson’s research, has also been working with a team in Cleveland to look at how vessels in the eye predict response to drug therapies in diabetic macular edema, including treatment durability. “What we’ve found is the more twisted the vessels, the more constricted, and the less likely the person would respond to therapy,” he said, adding that studying the pathology of the eye makes a lot of sense. “The arrangement of vessels in the eye are likely to have implications in all kinds of diseases.”
Since Parkinson’s disease does not have any biomarkers, this technology could be very useful in diagnosis. “With specific quantitative measurements, we could have computational imaging biomarkers to predict the risk of onset of Parkinson’s, and the prognosis of disease. That’s the true utility of this approach,” he said.
Mr. Diaz disclosed no relevant financial relationships. Dr. Madabhushi has consulted for Aiforia and has had research sponsored by AstraZeneca, Bristol-Myers Squibb, and Boehringer Ingelheim.
A version of this article originally appeared on Medscape.com.