User login
The Journal of Clinical Outcomes Management® is an independent, peer-reviewed journal offering evidence-based, practical information for improving the quality, safety, and value of health care.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Mishap ruins millions of J&J COVID vaccine doses
About 15 million doses of the Johnson & Johnson COVID-19 vaccine were ruined after workers at a manufacturing plant mixed up ingredients, The New York Times reported.
The Baltimore plant is operated by a company called Emergent BioSolutions, the Times said. The company works with both Johnson & Johnson and AstraZeneca.
The mistake has stopped shipments of the vaccine until the FDA investigates, the paper said. The mishap, however, does not affect doses of the J&J one-shot vaccine already delivered and being used.
The problem is that tens of millions of doses were supposed to come from the Baltimore plant.
The Associated Press reported that Emergent has had numerous problems with the FDA, with the agency citing the company for poorly trained employees, cracked vials and mold.
The records cover inspections at Emergent facilities, including Bayview, since 2017. Following a December 2017 inspection at an Emergent plant in Canton, Massachusetts, the FDA said the company hadn’t corrected “continued low level mold and yeast isolates” found in the facility. Nearly a year later, agency investigators questioned why Emergent had “an unwritten policy of not conducting routine compliance audits” at a separate plant in Baltimore, known as Camden, where an anthrax vaccine is filled into vials.
Meanwhile, in a statement, Johnson & Johnson said its own quality control process identified the problem in one batch of ingredients. The company said the Emergent plant in Baltimore is “not yet authorized to manufacture drug substance for our COVID-19 vaccine. This batch was never advanced to the filling and finishing stages of our manufacturing process.”
The company said it plans to still seek emergency use authorization for a different Emergent facility and will provide more experts on site at Emergent.
The Times reports that President Joe Biden’s team still believes the administration can meet its commitment to have enough vaccine doses to immunize every adult by the end of May.
Johnson & Johnson said it still plans to deliver an additional 24 million doses through April.
A version of this article first appeared on WebMD.com.
This article was updated 4/1/21.
About 15 million doses of the Johnson & Johnson COVID-19 vaccine were ruined after workers at a manufacturing plant mixed up ingredients, The New York Times reported.
The Baltimore plant is operated by a company called Emergent BioSolutions, the Times said. The company works with both Johnson & Johnson and AstraZeneca.
The mistake has stopped shipments of the vaccine until the FDA investigates, the paper said. The mishap, however, does not affect doses of the J&J one-shot vaccine already delivered and being used.
The problem is that tens of millions of doses were supposed to come from the Baltimore plant.
The Associated Press reported that Emergent has had numerous problems with the FDA, with the agency citing the company for poorly trained employees, cracked vials and mold.
The records cover inspections at Emergent facilities, including Bayview, since 2017. Following a December 2017 inspection at an Emergent plant in Canton, Massachusetts, the FDA said the company hadn’t corrected “continued low level mold and yeast isolates” found in the facility. Nearly a year later, agency investigators questioned why Emergent had “an unwritten policy of not conducting routine compliance audits” at a separate plant in Baltimore, known as Camden, where an anthrax vaccine is filled into vials.
Meanwhile, in a statement, Johnson & Johnson said its own quality control process identified the problem in one batch of ingredients. The company said the Emergent plant in Baltimore is “not yet authorized to manufacture drug substance for our COVID-19 vaccine. This batch was never advanced to the filling and finishing stages of our manufacturing process.”
The company said it plans to still seek emergency use authorization for a different Emergent facility and will provide more experts on site at Emergent.
The Times reports that President Joe Biden’s team still believes the administration can meet its commitment to have enough vaccine doses to immunize every adult by the end of May.
Johnson & Johnson said it still plans to deliver an additional 24 million doses through April.
A version of this article first appeared on WebMD.com.
This article was updated 4/1/21.
About 15 million doses of the Johnson & Johnson COVID-19 vaccine were ruined after workers at a manufacturing plant mixed up ingredients, The New York Times reported.
The Baltimore plant is operated by a company called Emergent BioSolutions, the Times said. The company works with both Johnson & Johnson and AstraZeneca.
The mistake has stopped shipments of the vaccine until the FDA investigates, the paper said. The mishap, however, does not affect doses of the J&J one-shot vaccine already delivered and being used.
The problem is that tens of millions of doses were supposed to come from the Baltimore plant.
The Associated Press reported that Emergent has had numerous problems with the FDA, with the agency citing the company for poorly trained employees, cracked vials and mold.
The records cover inspections at Emergent facilities, including Bayview, since 2017. Following a December 2017 inspection at an Emergent plant in Canton, Massachusetts, the FDA said the company hadn’t corrected “continued low level mold and yeast isolates” found in the facility. Nearly a year later, agency investigators questioned why Emergent had “an unwritten policy of not conducting routine compliance audits” at a separate plant in Baltimore, known as Camden, where an anthrax vaccine is filled into vials.
Meanwhile, in a statement, Johnson & Johnson said its own quality control process identified the problem in one batch of ingredients. The company said the Emergent plant in Baltimore is “not yet authorized to manufacture drug substance for our COVID-19 vaccine. This batch was never advanced to the filling and finishing stages of our manufacturing process.”
The company said it plans to still seek emergency use authorization for a different Emergent facility and will provide more experts on site at Emergent.
The Times reports that President Joe Biden’s team still believes the administration can meet its commitment to have enough vaccine doses to immunize every adult by the end of May.
Johnson & Johnson said it still plans to deliver an additional 24 million doses through April.
A version of this article first appeared on WebMD.com.
This article was updated 4/1/21.
Children could become eligible for a COVID-19 vaccine by fall, expert predicts
If everything goes as planned,
According to Yvonne Maldonado, MD, Pfizer has fully enrolled adolescent trials and Moderna is currently enrolling 3,000 adolescents in a safety and reactogenicity trial known as TeenCOVE, in which participants will receive an intramuscular injection of 100 mcg mRNA-1273 on day 1 and on day 29. Meanwhile, Johnson & Johnson and AstraZeneca will be starting to enroll older children and adolescents into studies within the next several weeks.
The companies are also planning to enroll younger children, Dr. Maldonado, the Taube professor of global health and infectious diseases at Stanford (Calif.) University, said during the Society for Pediatric Dermatology pre-AAD meeting. “At least two of the vaccine companies have indicated that they would like to start enrolling children as young as 2-5 years of age and eventually getting down to infants and toddlers if the vaccines prove to be safe and effective in the older children. Eventually, we hope to get to the level where we can have several vaccine candidates for all children 6 months of age and older.”
In the future, she said, infectious disease experts hope to see antiviral, immunomodulatory, anti-inflammatory, and monoclonal therapies for all populations including children, although trials in this population have not begun. “Clinical trials must be flexible and adaptive to deal with children and adolescents,” added Dr. Maldonado, who is also senior associate dean for faculty development and diversity at Stanford.
“We would ideally like to have new correlates of protection, as well as biomarkers to follow for evidence of effectiveness. We also would love to see vaccines in the pediatric population as soon as possible, because herd immunity is the ultimate goal for protection against this disease and prevention of additional transmission over time.” However, she said, the degree and durability of immunity has yet to be determined, and vaccine-associated immune effects are unknown. In the meantime, infectious disease researchers expect nonpharmacologic interventions, such as wearing face masks and social distancing to continue for an undefined period.
(Less than 2 weeks after Dr. Maldonado spoke at the SPD meeting, Pfizer announced in a press release that, in phase 3 clinical trials, the company’s coronavirus vaccine was 100% effective in protecting children aged 12-15 years from infection, with a “robust” antibody responses and side effects similar to those experienced by those aged 16-25 years. The company also announced that it plans to seek Food and Drug Administration EUA for this age group. Asked to comment on this update, Dr. Maldonado said the results released by Pfizer “suggest that their COVID-19 vaccine is very safe and highly effective in preventing COVID-19 among children 12-15 years of age.” She added that additional data from the Pfizer trials as well as from Moderna and Johnson & Johnson vaccine trials “will hopefully lead to FDA EUA review in the coming weeks,” and that COVID-19 vaccinations for children “may be possible by this summer.”)
Children with underlying diseases or on immune suppressants
At the SPD meeting, an attendee asked if there were any pediatric patients for whom she would not recommend receiving a COVID-19 vaccine because of an underlying disease or concurrent therapy with immune suppressants. “We don’t have those data yet,” Dr. Maldonado said. “Based on what we’re seeing with adults, it does appear that those with underlying conditions are at somewhat higher risk of developing severe infection and may therefore most likely to need vaccination. Most of those risks are cardiovascular, obesity, and other factors, but not necessarily immunocompromising conditions. More likely what we’re seeing is that people with underlying immunocompromising conditions may not mount a good response to the vaccines at this time. It doesn’t mean we shouldn’t give the vaccines, but we need to learn more about that.”
Dr. Maldonado went on to note that, as vaccine manufacturers commence pediatric trials, healthy children will be tested first, followed in due time with children who have immunocompromised conditions. “The question will be whether or not we should give monoclonal antibodies to those particular children to help boost their immunity to SARS-CoV-2, because they might not have a good response to the vaccines,” she said. “Those things need to be sorted out, but there’s no safety signal or concerns at this point for vaccine to be given to immunocompromised individuals.”
Another meeting attendee asked Dr. Maldonado if she thinks there is a practical role for assessing markers of T-cell immunity when evaluating suspected COVID-19 patients who may test negative on serology, Dr. Maldonado said that she and her colleagues are seeking pediatric patients who were treated for COVID-19 at Stanford, in an effort to sort this out.
They are checking peripheral blood mononuclear cells in these patients “to try and tease out what the immune response is in kids who have serious disease, versus those who came in with acute disease, versus those who are asymptomatic,” and comparing them with children who don’t have infection, she explained. “The question is, what is the role of T cells and how much do they contribute? One of the biggest questions we have is, do we have an immune correlate? Can we detect a particular level of neutralizing antibody that seems to be protective? If so, how long is it protective, and can we look for T- and B-cell memory cells and effector vector cells and see how long those effector vector cells can be active in protection? Those are studies that are ongoing now.”
Dr. Maldonado disclosed that she is a member of the data safety monitoring board for a non–COVID-19 vaccine being developed by Pfizer.
If everything goes as planned,
According to Yvonne Maldonado, MD, Pfizer has fully enrolled adolescent trials and Moderna is currently enrolling 3,000 adolescents in a safety and reactogenicity trial known as TeenCOVE, in which participants will receive an intramuscular injection of 100 mcg mRNA-1273 on day 1 and on day 29. Meanwhile, Johnson & Johnson and AstraZeneca will be starting to enroll older children and adolescents into studies within the next several weeks.
The companies are also planning to enroll younger children, Dr. Maldonado, the Taube professor of global health and infectious diseases at Stanford (Calif.) University, said during the Society for Pediatric Dermatology pre-AAD meeting. “At least two of the vaccine companies have indicated that they would like to start enrolling children as young as 2-5 years of age and eventually getting down to infants and toddlers if the vaccines prove to be safe and effective in the older children. Eventually, we hope to get to the level where we can have several vaccine candidates for all children 6 months of age and older.”
In the future, she said, infectious disease experts hope to see antiviral, immunomodulatory, anti-inflammatory, and monoclonal therapies for all populations including children, although trials in this population have not begun. “Clinical trials must be flexible and adaptive to deal with children and adolescents,” added Dr. Maldonado, who is also senior associate dean for faculty development and diversity at Stanford.
“We would ideally like to have new correlates of protection, as well as biomarkers to follow for evidence of effectiveness. We also would love to see vaccines in the pediatric population as soon as possible, because herd immunity is the ultimate goal for protection against this disease and prevention of additional transmission over time.” However, she said, the degree and durability of immunity has yet to be determined, and vaccine-associated immune effects are unknown. In the meantime, infectious disease researchers expect nonpharmacologic interventions, such as wearing face masks and social distancing to continue for an undefined period.
(Less than 2 weeks after Dr. Maldonado spoke at the SPD meeting, Pfizer announced in a press release that, in phase 3 clinical trials, the company’s coronavirus vaccine was 100% effective in protecting children aged 12-15 years from infection, with a “robust” antibody responses and side effects similar to those experienced by those aged 16-25 years. The company also announced that it plans to seek Food and Drug Administration EUA for this age group. Asked to comment on this update, Dr. Maldonado said the results released by Pfizer “suggest that their COVID-19 vaccine is very safe and highly effective in preventing COVID-19 among children 12-15 years of age.” She added that additional data from the Pfizer trials as well as from Moderna and Johnson & Johnson vaccine trials “will hopefully lead to FDA EUA review in the coming weeks,” and that COVID-19 vaccinations for children “may be possible by this summer.”)
Children with underlying diseases or on immune suppressants
At the SPD meeting, an attendee asked if there were any pediatric patients for whom she would not recommend receiving a COVID-19 vaccine because of an underlying disease or concurrent therapy with immune suppressants. “We don’t have those data yet,” Dr. Maldonado said. “Based on what we’re seeing with adults, it does appear that those with underlying conditions are at somewhat higher risk of developing severe infection and may therefore most likely to need vaccination. Most of those risks are cardiovascular, obesity, and other factors, but not necessarily immunocompromising conditions. More likely what we’re seeing is that people with underlying immunocompromising conditions may not mount a good response to the vaccines at this time. It doesn’t mean we shouldn’t give the vaccines, but we need to learn more about that.”
Dr. Maldonado went on to note that, as vaccine manufacturers commence pediatric trials, healthy children will be tested first, followed in due time with children who have immunocompromised conditions. “The question will be whether or not we should give monoclonal antibodies to those particular children to help boost their immunity to SARS-CoV-2, because they might not have a good response to the vaccines,” she said. “Those things need to be sorted out, but there’s no safety signal or concerns at this point for vaccine to be given to immunocompromised individuals.”
Another meeting attendee asked Dr. Maldonado if she thinks there is a practical role for assessing markers of T-cell immunity when evaluating suspected COVID-19 patients who may test negative on serology, Dr. Maldonado said that she and her colleagues are seeking pediatric patients who were treated for COVID-19 at Stanford, in an effort to sort this out.
They are checking peripheral blood mononuclear cells in these patients “to try and tease out what the immune response is in kids who have serious disease, versus those who came in with acute disease, versus those who are asymptomatic,” and comparing them with children who don’t have infection, she explained. “The question is, what is the role of T cells and how much do they contribute? One of the biggest questions we have is, do we have an immune correlate? Can we detect a particular level of neutralizing antibody that seems to be protective? If so, how long is it protective, and can we look for T- and B-cell memory cells and effector vector cells and see how long those effector vector cells can be active in protection? Those are studies that are ongoing now.”
Dr. Maldonado disclosed that she is a member of the data safety monitoring board for a non–COVID-19 vaccine being developed by Pfizer.
If everything goes as planned,
According to Yvonne Maldonado, MD, Pfizer has fully enrolled adolescent trials and Moderna is currently enrolling 3,000 adolescents in a safety and reactogenicity trial known as TeenCOVE, in which participants will receive an intramuscular injection of 100 mcg mRNA-1273 on day 1 and on day 29. Meanwhile, Johnson & Johnson and AstraZeneca will be starting to enroll older children and adolescents into studies within the next several weeks.
The companies are also planning to enroll younger children, Dr. Maldonado, the Taube professor of global health and infectious diseases at Stanford (Calif.) University, said during the Society for Pediatric Dermatology pre-AAD meeting. “At least two of the vaccine companies have indicated that they would like to start enrolling children as young as 2-5 years of age and eventually getting down to infants and toddlers if the vaccines prove to be safe and effective in the older children. Eventually, we hope to get to the level where we can have several vaccine candidates for all children 6 months of age and older.”
In the future, she said, infectious disease experts hope to see antiviral, immunomodulatory, anti-inflammatory, and monoclonal therapies for all populations including children, although trials in this population have not begun. “Clinical trials must be flexible and adaptive to deal with children and adolescents,” added Dr. Maldonado, who is also senior associate dean for faculty development and diversity at Stanford.
“We would ideally like to have new correlates of protection, as well as biomarkers to follow for evidence of effectiveness. We also would love to see vaccines in the pediatric population as soon as possible, because herd immunity is the ultimate goal for protection against this disease and prevention of additional transmission over time.” However, she said, the degree and durability of immunity has yet to be determined, and vaccine-associated immune effects are unknown. In the meantime, infectious disease researchers expect nonpharmacologic interventions, such as wearing face masks and social distancing to continue for an undefined period.
(Less than 2 weeks after Dr. Maldonado spoke at the SPD meeting, Pfizer announced in a press release that, in phase 3 clinical trials, the company’s coronavirus vaccine was 100% effective in protecting children aged 12-15 years from infection, with a “robust” antibody responses and side effects similar to those experienced by those aged 16-25 years. The company also announced that it plans to seek Food and Drug Administration EUA for this age group. Asked to comment on this update, Dr. Maldonado said the results released by Pfizer “suggest that their COVID-19 vaccine is very safe and highly effective in preventing COVID-19 among children 12-15 years of age.” She added that additional data from the Pfizer trials as well as from Moderna and Johnson & Johnson vaccine trials “will hopefully lead to FDA EUA review in the coming weeks,” and that COVID-19 vaccinations for children “may be possible by this summer.”)
Children with underlying diseases or on immune suppressants
At the SPD meeting, an attendee asked if there were any pediatric patients for whom she would not recommend receiving a COVID-19 vaccine because of an underlying disease or concurrent therapy with immune suppressants. “We don’t have those data yet,” Dr. Maldonado said. “Based on what we’re seeing with adults, it does appear that those with underlying conditions are at somewhat higher risk of developing severe infection and may therefore most likely to need vaccination. Most of those risks are cardiovascular, obesity, and other factors, but not necessarily immunocompromising conditions. More likely what we’re seeing is that people with underlying immunocompromising conditions may not mount a good response to the vaccines at this time. It doesn’t mean we shouldn’t give the vaccines, but we need to learn more about that.”
Dr. Maldonado went on to note that, as vaccine manufacturers commence pediatric trials, healthy children will be tested first, followed in due time with children who have immunocompromised conditions. “The question will be whether or not we should give monoclonal antibodies to those particular children to help boost their immunity to SARS-CoV-2, because they might not have a good response to the vaccines,” she said. “Those things need to be sorted out, but there’s no safety signal or concerns at this point for vaccine to be given to immunocompromised individuals.”
Another meeting attendee asked Dr. Maldonado if she thinks there is a practical role for assessing markers of T-cell immunity when evaluating suspected COVID-19 patients who may test negative on serology, Dr. Maldonado said that she and her colleagues are seeking pediatric patients who were treated for COVID-19 at Stanford, in an effort to sort this out.
They are checking peripheral blood mononuclear cells in these patients “to try and tease out what the immune response is in kids who have serious disease, versus those who came in with acute disease, versus those who are asymptomatic,” and comparing them with children who don’t have infection, she explained. “The question is, what is the role of T cells and how much do they contribute? One of the biggest questions we have is, do we have an immune correlate? Can we detect a particular level of neutralizing antibody that seems to be protective? If so, how long is it protective, and can we look for T- and B-cell memory cells and effector vector cells and see how long those effector vector cells can be active in protection? Those are studies that are ongoing now.”
Dr. Maldonado disclosed that she is a member of the data safety monitoring board for a non–COVID-19 vaccine being developed by Pfizer.
FROM THE SPD PRE-AAD MEETING
Detroit cardiologists prevail in retaliation suit against Tenet
After losing at arbitration, as well as in federal court and partially on appeal, Tenet Healthcare is refusing to comment on whether it will continue to battle two Detroit-area cardiologists whom the hospital corporation fired from leadership positions in 2018.
The cardiologists were awarded $10.6 million from an arbitrator, who found that Detroit Medical Center (DMC) and its parent, Tenet, retaliated against Amir Kaki, MD, and Mahir Elder, MD, when the doctors repeatedly reported concerns about patient safety and potential fraud.
The award was made public when it was upheld in federal court in February 2021 and was partially upheld on appeal days later by the Sixth Circuit Court of Appeals.
The Sixth Circuit Court of Appeals denied Tenet’s motion to bar Dr. Kaki and Dr. Elder from returning to work with full privileges but said it would continue to consider the overall appeal. Tenet argued that it needed to keep the cardiologists out of DMC because of “behavioral issues.”
Those allegations are “complete nonsense,” said the cardiologists’ attorney, Deborah Gordon, of Bloomfield Hills, Mich. The alleged problems regarding Dr. Kaki and Dr. Elder were examined by an arbitrator, who “found that all of those complaints were unsubstantiated,” Ms. Gordon said in an interview.
In her final ruling, arbitrator Mary Beth Kelly wrote, “Both Kaki and Elder testified credibly regarding the humiliation, the emotional distress and the reputational damage they have suffered to their national reputations.”
A spokesperson for Tenet and DMC said the organizations had no further comment.
Ms. Gordon said she believes it’s unlikely Tenet will prevail in the Sixth Circuit Court of Appeals, noting that the court already had examined the merits of the case to determine whether Dr. Kaki and Dr. Elder could go back to work. In the court’s opinion, shared in an interview, nothing substantive in Tenet’s appeal prevented the doctors from returning to the hospital, she said.
As of now, both cardiologists have 1 year of privileges at the DMC-affiliated hospitals. Only Dr. Kaki has returned to work, said Ms. Gordon. Neither is speaking to the media, she said.
From respected to reviled
Both Dr. Kaki and Dr. Elder were respected at DMC, according to court filings.
Dr. Kaki was recruited from Weill Cornell Medical College by a Detroit mayor because of his expertise in interventional cardiology. He had staff privileges at DMC beginning in 2012 and was a clinical associate professor and assistant program director of the interventional cardiology fellowship program at Wayne State University in Detroit. He became director of the cardiac catheterization services unit at the new DMC Heart Hospital at Harper-Hutzel Hospital in Detroit in 2014, and 4 years later was appointed director of the facility’s anticoagulation clinic. Dr. Kaki was nominated for and completed Tenet’s Leadership Academy.
Dr. Elder was a clinical professor and assistant fellowship director at Wayne State and was a clinical professor of medicine at Michigan State University. Beginning in 2008, he held directorships at DMC’s cardiac care unit, ambulatory services program, cardiac CT angiogram program, PERT program, and carotid stenting program. Dr. Elder was voted Teacher of the Year for 10 consecutive years by DMC cardiology fellows.
The two doctors aimed high when it came to quality of care and ethics, according to legal filings. Over the years, Dr. Kaki and Dr. Elder repeatedly reported what they considered to be egregious violations of patient safety and of Medicare and Medicaid fraud laws. The clinicians complained about unsterile surgical instruments and the removal of a stat laboratory from the cardiac catheterization unit, noting that the removal would cause delays that would endanger lives.
At peer review meetings, as well as with administrators, they flagged colleagues who they said were performing unnecessary or dangerous procedures solely to generate revenue. At least one doctor falsified records of such a procedure after a patient died, alleged Dr. Kaki and Dr. Elder.
Tenet hired outside attorneys in the fall of 2018, telling Dr. Kaki and Dr. Elder that the legal team would investigate their complaints. However, the investigation was a sham: Filings allege that the investigation was used instead to build a case against Dr. Kaki and Dr. Elder and that Tenet leadership used the inquiry to pressure the cardiologists to resign.
They refused, and in October 2018, they were fired from their leadership positions. DMC and Tenet then held a press conference in which they said that Dr. Kaki and Dr. Elder had been dismissed for “violations” of the “Tenet Standards of Conduct.”
Cardiologists push back
Dr. Kaki and Dr. Elder, however, were not willing to just walk away. They sought reinstatement through an internal DMC appeals panel of their peers. The clinicians who participated on that panel ruled that neither firing was justified.
But DMC’s governing board voted in April 2020 to deny privileges to both cardiologists.
Tenet continued a campaign of retaliation, according to legal filings, by not paying the clinicians for being on call, by removing them from peer review committees, and by prohibiting them from teaching or giving lectures. DMC refused to give Dr. Kaki his personnel record, stating that he was never an employee when he was in the leadership position. Dr. Kaki sued, and a Wayne County Circuit Court judge granted his motion to get his file. DMC and Tenet appealed that ruling but lost.
Eventually, Ms. Gordon sued DMC and Tenet in federal court, alleging the hospital retaliated against the cardiologists, interfered with their ability to earn a living by disparaging them, refused to renew their privileges in 2019, and committed violations under multiple federal and state statutes, including the False Claims Act and the Fair Labor Standards Act.
Tenet successfully argued that the case should go to arbitration.
Arbitrator Mary Beth Kelly, though, ruled in December 2020 that the vast majority of the complaints compiled against the two physicians in the external investigation were not verified or supported and that Tenet and DMC had retaliated against Dr. Kaki and Dr. Elder.
For that harm, Ms. Kelly awarded each clinician $1 million, according to the final ruling shared in an interview.
In addition, she awarded Dr. Kaki $2.3 million in back pay and 2 years of front pay (slightly more than $1 million). She awarded Dr. Elder $2.3 million in back pay and $2.1 million in front pay for 4 years, noting that “his strong association with DMC may make it more difficult for him to successfully transition into the situation he enjoyed prior to termination and nonrenewal.”
The clinicians also were awarded legal fees of $623,816 and court costs of $110,673.
“Wholesale retrial”
To secure the award, Ms. Gordon had to seek a ruling from the U.S. District Court for Eastern Michigan. Tenet asked that court to overturn the arbitrator’s award and to keep it sealed from public view.
In his February ruling, Judge Arthur J. Tarnow wrote that Tenet and DMC “not only attempt to relitigate the legal issues, but also endeavor to introduce a factual counternarrative unmoored from the findings of the Arbitrator and including evidence which the Arbitrator specifically found inadmissible.
“By seeking a wholesale retrial of their case after forcing plaintiffs to arbitrate in the first place,” Tenet and DMC basically ignored the goal of arbitration, which is to relieve judicial congestion and provide a faster and cheaper alternative to litigation, he wrote.
Judge Tarnow also warned Tenet and DMC against taking too long to reinstate privileges for Dr. Kaki and Dr. Elder. If they “continue to delay the restoration of plaintiffs’ privileges in the hopes of a different result on appeal, they will be in violation of this Order,” said the judge.
Tenet, however, tried one more avenue to block the cardiologists from getting privileges, appealing to the Sixth Circuit, which again ordered the company to grant the 1-year privileges.
A version of this article first appeared on Medscape.com.
After losing at arbitration, as well as in federal court and partially on appeal, Tenet Healthcare is refusing to comment on whether it will continue to battle two Detroit-area cardiologists whom the hospital corporation fired from leadership positions in 2018.
The cardiologists were awarded $10.6 million from an arbitrator, who found that Detroit Medical Center (DMC) and its parent, Tenet, retaliated against Amir Kaki, MD, and Mahir Elder, MD, when the doctors repeatedly reported concerns about patient safety and potential fraud.
The award was made public when it was upheld in federal court in February 2021 and was partially upheld on appeal days later by the Sixth Circuit Court of Appeals.
The Sixth Circuit Court of Appeals denied Tenet’s motion to bar Dr. Kaki and Dr. Elder from returning to work with full privileges but said it would continue to consider the overall appeal. Tenet argued that it needed to keep the cardiologists out of DMC because of “behavioral issues.”
Those allegations are “complete nonsense,” said the cardiologists’ attorney, Deborah Gordon, of Bloomfield Hills, Mich. The alleged problems regarding Dr. Kaki and Dr. Elder were examined by an arbitrator, who “found that all of those complaints were unsubstantiated,” Ms. Gordon said in an interview.
In her final ruling, arbitrator Mary Beth Kelly wrote, “Both Kaki and Elder testified credibly regarding the humiliation, the emotional distress and the reputational damage they have suffered to their national reputations.”
A spokesperson for Tenet and DMC said the organizations had no further comment.
Ms. Gordon said she believes it’s unlikely Tenet will prevail in the Sixth Circuit Court of Appeals, noting that the court already had examined the merits of the case to determine whether Dr. Kaki and Dr. Elder could go back to work. In the court’s opinion, shared in an interview, nothing substantive in Tenet’s appeal prevented the doctors from returning to the hospital, she said.
As of now, both cardiologists have 1 year of privileges at the DMC-affiliated hospitals. Only Dr. Kaki has returned to work, said Ms. Gordon. Neither is speaking to the media, she said.
From respected to reviled
Both Dr. Kaki and Dr. Elder were respected at DMC, according to court filings.
Dr. Kaki was recruited from Weill Cornell Medical College by a Detroit mayor because of his expertise in interventional cardiology. He had staff privileges at DMC beginning in 2012 and was a clinical associate professor and assistant program director of the interventional cardiology fellowship program at Wayne State University in Detroit. He became director of the cardiac catheterization services unit at the new DMC Heart Hospital at Harper-Hutzel Hospital in Detroit in 2014, and 4 years later was appointed director of the facility’s anticoagulation clinic. Dr. Kaki was nominated for and completed Tenet’s Leadership Academy.
Dr. Elder was a clinical professor and assistant fellowship director at Wayne State and was a clinical professor of medicine at Michigan State University. Beginning in 2008, he held directorships at DMC’s cardiac care unit, ambulatory services program, cardiac CT angiogram program, PERT program, and carotid stenting program. Dr. Elder was voted Teacher of the Year for 10 consecutive years by DMC cardiology fellows.
The two doctors aimed high when it came to quality of care and ethics, according to legal filings. Over the years, Dr. Kaki and Dr. Elder repeatedly reported what they considered to be egregious violations of patient safety and of Medicare and Medicaid fraud laws. The clinicians complained about unsterile surgical instruments and the removal of a stat laboratory from the cardiac catheterization unit, noting that the removal would cause delays that would endanger lives.
At peer review meetings, as well as with administrators, they flagged colleagues who they said were performing unnecessary or dangerous procedures solely to generate revenue. At least one doctor falsified records of such a procedure after a patient died, alleged Dr. Kaki and Dr. Elder.
Tenet hired outside attorneys in the fall of 2018, telling Dr. Kaki and Dr. Elder that the legal team would investigate their complaints. However, the investigation was a sham: Filings allege that the investigation was used instead to build a case against Dr. Kaki and Dr. Elder and that Tenet leadership used the inquiry to pressure the cardiologists to resign.
They refused, and in October 2018, they were fired from their leadership positions. DMC and Tenet then held a press conference in which they said that Dr. Kaki and Dr. Elder had been dismissed for “violations” of the “Tenet Standards of Conduct.”
Cardiologists push back
Dr. Kaki and Dr. Elder, however, were not willing to just walk away. They sought reinstatement through an internal DMC appeals panel of their peers. The clinicians who participated on that panel ruled that neither firing was justified.
But DMC’s governing board voted in April 2020 to deny privileges to both cardiologists.
Tenet continued a campaign of retaliation, according to legal filings, by not paying the clinicians for being on call, by removing them from peer review committees, and by prohibiting them from teaching or giving lectures. DMC refused to give Dr. Kaki his personnel record, stating that he was never an employee when he was in the leadership position. Dr. Kaki sued, and a Wayne County Circuit Court judge granted his motion to get his file. DMC and Tenet appealed that ruling but lost.
Eventually, Ms. Gordon sued DMC and Tenet in federal court, alleging the hospital retaliated against the cardiologists, interfered with their ability to earn a living by disparaging them, refused to renew their privileges in 2019, and committed violations under multiple federal and state statutes, including the False Claims Act and the Fair Labor Standards Act.
Tenet successfully argued that the case should go to arbitration.
Arbitrator Mary Beth Kelly, though, ruled in December 2020 that the vast majority of the complaints compiled against the two physicians in the external investigation were not verified or supported and that Tenet and DMC had retaliated against Dr. Kaki and Dr. Elder.
For that harm, Ms. Kelly awarded each clinician $1 million, according to the final ruling shared in an interview.
In addition, she awarded Dr. Kaki $2.3 million in back pay and 2 years of front pay (slightly more than $1 million). She awarded Dr. Elder $2.3 million in back pay and $2.1 million in front pay for 4 years, noting that “his strong association with DMC may make it more difficult for him to successfully transition into the situation he enjoyed prior to termination and nonrenewal.”
The clinicians also were awarded legal fees of $623,816 and court costs of $110,673.
“Wholesale retrial”
To secure the award, Ms. Gordon had to seek a ruling from the U.S. District Court for Eastern Michigan. Tenet asked that court to overturn the arbitrator’s award and to keep it sealed from public view.
In his February ruling, Judge Arthur J. Tarnow wrote that Tenet and DMC “not only attempt to relitigate the legal issues, but also endeavor to introduce a factual counternarrative unmoored from the findings of the Arbitrator and including evidence which the Arbitrator specifically found inadmissible.
“By seeking a wholesale retrial of their case after forcing plaintiffs to arbitrate in the first place,” Tenet and DMC basically ignored the goal of arbitration, which is to relieve judicial congestion and provide a faster and cheaper alternative to litigation, he wrote.
Judge Tarnow also warned Tenet and DMC against taking too long to reinstate privileges for Dr. Kaki and Dr. Elder. If they “continue to delay the restoration of plaintiffs’ privileges in the hopes of a different result on appeal, they will be in violation of this Order,” said the judge.
Tenet, however, tried one more avenue to block the cardiologists from getting privileges, appealing to the Sixth Circuit, which again ordered the company to grant the 1-year privileges.
A version of this article first appeared on Medscape.com.
After losing at arbitration, as well as in federal court and partially on appeal, Tenet Healthcare is refusing to comment on whether it will continue to battle two Detroit-area cardiologists whom the hospital corporation fired from leadership positions in 2018.
The cardiologists were awarded $10.6 million from an arbitrator, who found that Detroit Medical Center (DMC) and its parent, Tenet, retaliated against Amir Kaki, MD, and Mahir Elder, MD, when the doctors repeatedly reported concerns about patient safety and potential fraud.
The award was made public when it was upheld in federal court in February 2021 and was partially upheld on appeal days later by the Sixth Circuit Court of Appeals.
The Sixth Circuit Court of Appeals denied Tenet’s motion to bar Dr. Kaki and Dr. Elder from returning to work with full privileges but said it would continue to consider the overall appeal. Tenet argued that it needed to keep the cardiologists out of DMC because of “behavioral issues.”
Those allegations are “complete nonsense,” said the cardiologists’ attorney, Deborah Gordon, of Bloomfield Hills, Mich. The alleged problems regarding Dr. Kaki and Dr. Elder were examined by an arbitrator, who “found that all of those complaints were unsubstantiated,” Ms. Gordon said in an interview.
In her final ruling, arbitrator Mary Beth Kelly wrote, “Both Kaki and Elder testified credibly regarding the humiliation, the emotional distress and the reputational damage they have suffered to their national reputations.”
A spokesperson for Tenet and DMC said the organizations had no further comment.
Ms. Gordon said she believes it’s unlikely Tenet will prevail in the Sixth Circuit Court of Appeals, noting that the court already had examined the merits of the case to determine whether Dr. Kaki and Dr. Elder could go back to work. In the court’s opinion, shared in an interview, nothing substantive in Tenet’s appeal prevented the doctors from returning to the hospital, she said.
As of now, both cardiologists have 1 year of privileges at the DMC-affiliated hospitals. Only Dr. Kaki has returned to work, said Ms. Gordon. Neither is speaking to the media, she said.
From respected to reviled
Both Dr. Kaki and Dr. Elder were respected at DMC, according to court filings.
Dr. Kaki was recruited from Weill Cornell Medical College by a Detroit mayor because of his expertise in interventional cardiology. He had staff privileges at DMC beginning in 2012 and was a clinical associate professor and assistant program director of the interventional cardiology fellowship program at Wayne State University in Detroit. He became director of the cardiac catheterization services unit at the new DMC Heart Hospital at Harper-Hutzel Hospital in Detroit in 2014, and 4 years later was appointed director of the facility’s anticoagulation clinic. Dr. Kaki was nominated for and completed Tenet’s Leadership Academy.
Dr. Elder was a clinical professor and assistant fellowship director at Wayne State and was a clinical professor of medicine at Michigan State University. Beginning in 2008, he held directorships at DMC’s cardiac care unit, ambulatory services program, cardiac CT angiogram program, PERT program, and carotid stenting program. Dr. Elder was voted Teacher of the Year for 10 consecutive years by DMC cardiology fellows.
The two doctors aimed high when it came to quality of care and ethics, according to legal filings. Over the years, Dr. Kaki and Dr. Elder repeatedly reported what they considered to be egregious violations of patient safety and of Medicare and Medicaid fraud laws. The clinicians complained about unsterile surgical instruments and the removal of a stat laboratory from the cardiac catheterization unit, noting that the removal would cause delays that would endanger lives.
At peer review meetings, as well as with administrators, they flagged colleagues who they said were performing unnecessary or dangerous procedures solely to generate revenue. At least one doctor falsified records of such a procedure after a patient died, alleged Dr. Kaki and Dr. Elder.
Tenet hired outside attorneys in the fall of 2018, telling Dr. Kaki and Dr. Elder that the legal team would investigate their complaints. However, the investigation was a sham: Filings allege that the investigation was used instead to build a case against Dr. Kaki and Dr. Elder and that Tenet leadership used the inquiry to pressure the cardiologists to resign.
They refused, and in October 2018, they were fired from their leadership positions. DMC and Tenet then held a press conference in which they said that Dr. Kaki and Dr. Elder had been dismissed for “violations” of the “Tenet Standards of Conduct.”
Cardiologists push back
Dr. Kaki and Dr. Elder, however, were not willing to just walk away. They sought reinstatement through an internal DMC appeals panel of their peers. The clinicians who participated on that panel ruled that neither firing was justified.
But DMC’s governing board voted in April 2020 to deny privileges to both cardiologists.
Tenet continued a campaign of retaliation, according to legal filings, by not paying the clinicians for being on call, by removing them from peer review committees, and by prohibiting them from teaching or giving lectures. DMC refused to give Dr. Kaki his personnel record, stating that he was never an employee when he was in the leadership position. Dr. Kaki sued, and a Wayne County Circuit Court judge granted his motion to get his file. DMC and Tenet appealed that ruling but lost.
Eventually, Ms. Gordon sued DMC and Tenet in federal court, alleging the hospital retaliated against the cardiologists, interfered with their ability to earn a living by disparaging them, refused to renew their privileges in 2019, and committed violations under multiple federal and state statutes, including the False Claims Act and the Fair Labor Standards Act.
Tenet successfully argued that the case should go to arbitration.
Arbitrator Mary Beth Kelly, though, ruled in December 2020 that the vast majority of the complaints compiled against the two physicians in the external investigation were not verified or supported and that Tenet and DMC had retaliated against Dr. Kaki and Dr. Elder.
For that harm, Ms. Kelly awarded each clinician $1 million, according to the final ruling shared in an interview.
In addition, she awarded Dr. Kaki $2.3 million in back pay and 2 years of front pay (slightly more than $1 million). She awarded Dr. Elder $2.3 million in back pay and $2.1 million in front pay for 4 years, noting that “his strong association with DMC may make it more difficult for him to successfully transition into the situation he enjoyed prior to termination and nonrenewal.”
The clinicians also were awarded legal fees of $623,816 and court costs of $110,673.
“Wholesale retrial”
To secure the award, Ms. Gordon had to seek a ruling from the U.S. District Court for Eastern Michigan. Tenet asked that court to overturn the arbitrator’s award and to keep it sealed from public view.
In his February ruling, Judge Arthur J. Tarnow wrote that Tenet and DMC “not only attempt to relitigate the legal issues, but also endeavor to introduce a factual counternarrative unmoored from the findings of the Arbitrator and including evidence which the Arbitrator specifically found inadmissible.
“By seeking a wholesale retrial of their case after forcing plaintiffs to arbitrate in the first place,” Tenet and DMC basically ignored the goal of arbitration, which is to relieve judicial congestion and provide a faster and cheaper alternative to litigation, he wrote.
Judge Tarnow also warned Tenet and DMC against taking too long to reinstate privileges for Dr. Kaki and Dr. Elder. If they “continue to delay the restoration of plaintiffs’ privileges in the hopes of a different result on appeal, they will be in violation of this Order,” said the judge.
Tenet, however, tried one more avenue to block the cardiologists from getting privileges, appealing to the Sixth Circuit, which again ordered the company to grant the 1-year privileges.
A version of this article first appeared on Medscape.com.
Pfizer: Vaccine shown 100% effective in children aged 12-15
The study enrolled 2,260 adolescents aged 12-15. No infections were reported in the group given the vaccine produced by Pfizer and its European partner, BioNTech, the release said. The placebo group reported 18 cases of COVID-19.
The vaccinated children showed a strong antibody response with no serious side effects.
Albert Bourla, PhD, chairman and CEO of Pfizer, said the company plans to seek Food and Drug Administration emergency use authorization, which could allow this age group to be vaccinated before the start of the next school year. Pfizer will also seek authorization from the European Medicines Agency.
“We share the urgency to expand the authorization of our vaccine to use in younger populations and are encouraged by the clinical trial data from adolescents between the ages of 12 and 15,” Dr. Bourla said in the release.
The clinical trials showed a stronger response in children aged 12-15 than the 95% effectiveness reported in clinical trials in adults. The Pfizer vaccine is now authorized to be given to people aged 16 and up in the United States.
Health experts said the clinical trials – while not peer-reviewed – amounted to very good news.
“The sooner that we can get vaccines into as many people as possible, regardless of their age, the sooner we will be able to really feel like we’re ending this pandemic for good,” Angela Rasmussen, PhD, a virologist affiliated with Georgetown University in Washington, told The New York Times.
Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, recently said that getting children vaccinated is an important step toward achieving herd immunity.
“We don’t really know what that magical point of herd immunity is, but we do know that if we get the overwhelming population vaccinated, we’re going to be in good shape,” he said earlier in March during a hearing of the Senate Health, Education, Labor, and Pensions Committee. “We ultimately would like to get and have to get children into that mix.”
Pfizer said it started clinical trials during the week of March 23 with children aged 5-11 and will next start trials with children aged 2-5, followed by children aged 6 months to 2 years. Vaccine makers Moderna and AstraZeneca also have started clinical trials in younger children.
A version of this article first appeared on WebMD.com.
The study enrolled 2,260 adolescents aged 12-15. No infections were reported in the group given the vaccine produced by Pfizer and its European partner, BioNTech, the release said. The placebo group reported 18 cases of COVID-19.
The vaccinated children showed a strong antibody response with no serious side effects.
Albert Bourla, PhD, chairman and CEO of Pfizer, said the company plans to seek Food and Drug Administration emergency use authorization, which could allow this age group to be vaccinated before the start of the next school year. Pfizer will also seek authorization from the European Medicines Agency.
“We share the urgency to expand the authorization of our vaccine to use in younger populations and are encouraged by the clinical trial data from adolescents between the ages of 12 and 15,” Dr. Bourla said in the release.
The clinical trials showed a stronger response in children aged 12-15 than the 95% effectiveness reported in clinical trials in adults. The Pfizer vaccine is now authorized to be given to people aged 16 and up in the United States.
Health experts said the clinical trials – while not peer-reviewed – amounted to very good news.
“The sooner that we can get vaccines into as many people as possible, regardless of their age, the sooner we will be able to really feel like we’re ending this pandemic for good,” Angela Rasmussen, PhD, a virologist affiliated with Georgetown University in Washington, told The New York Times.
Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, recently said that getting children vaccinated is an important step toward achieving herd immunity.
“We don’t really know what that magical point of herd immunity is, but we do know that if we get the overwhelming population vaccinated, we’re going to be in good shape,” he said earlier in March during a hearing of the Senate Health, Education, Labor, and Pensions Committee. “We ultimately would like to get and have to get children into that mix.”
Pfizer said it started clinical trials during the week of March 23 with children aged 5-11 and will next start trials with children aged 2-5, followed by children aged 6 months to 2 years. Vaccine makers Moderna and AstraZeneca also have started clinical trials in younger children.
A version of this article first appeared on WebMD.com.
The study enrolled 2,260 adolescents aged 12-15. No infections were reported in the group given the vaccine produced by Pfizer and its European partner, BioNTech, the release said. The placebo group reported 18 cases of COVID-19.
The vaccinated children showed a strong antibody response with no serious side effects.
Albert Bourla, PhD, chairman and CEO of Pfizer, said the company plans to seek Food and Drug Administration emergency use authorization, which could allow this age group to be vaccinated before the start of the next school year. Pfizer will also seek authorization from the European Medicines Agency.
“We share the urgency to expand the authorization of our vaccine to use in younger populations and are encouraged by the clinical trial data from adolescents between the ages of 12 and 15,” Dr. Bourla said in the release.
The clinical trials showed a stronger response in children aged 12-15 than the 95% effectiveness reported in clinical trials in adults. The Pfizer vaccine is now authorized to be given to people aged 16 and up in the United States.
Health experts said the clinical trials – while not peer-reviewed – amounted to very good news.
“The sooner that we can get vaccines into as many people as possible, regardless of their age, the sooner we will be able to really feel like we’re ending this pandemic for good,” Angela Rasmussen, PhD, a virologist affiliated with Georgetown University in Washington, told The New York Times.
Anthony Fauci, MD, director of the National Institute of Allergy and Infectious Diseases, recently said that getting children vaccinated is an important step toward achieving herd immunity.
“We don’t really know what that magical point of herd immunity is, but we do know that if we get the overwhelming population vaccinated, we’re going to be in good shape,” he said earlier in March during a hearing of the Senate Health, Education, Labor, and Pensions Committee. “We ultimately would like to get and have to get children into that mix.”
Pfizer said it started clinical trials during the week of March 23 with children aged 5-11 and will next start trials with children aged 2-5, followed by children aged 6 months to 2 years. Vaccine makers Moderna and AstraZeneca also have started clinical trials in younger children.
A version of this article first appeared on WebMD.com.
CDC adds new medical conditions to COVID-19 high-risk list
The Centers for Disease Control and Prevention has added several new medical conditions to its list of those that predispose adults to more severe COVID-19 illness.
Conditions that had previously been categorized as “might be” placing individuals at increased risk – but now are listed as high risk – include type 1 diabetes (in addition to type 2), moderate-to-severe asthma, liver disease, dementia or other neurologic conditions, stroke/cerebrovascular disease, HIV infection, cystic fibrosis, and overweight (in addition to obesity).
Substance use disorders, which hadn’t been previously listed, are now also considered high risk.
The new list groups together certain categories, such as chronic lung diseases (chronic obstructive pulmonary disease, asthma, cystic fibrosis, etc) and heart conditions (heart failure, coronary artery disease, hypertension, etc).
Both diabetes types are now grouped under “diabetes.”
The added medical conditions were posted on the CDC website’s COVID-19 page on March 29.
Type 1 diabetes and other conditions now priority for vaccination
The CDC refers to the medical conditions list as phase 1c in regard to COVID-19 vaccine prioritization, which means that anyone with any of these conditions can now be prioritized for vaccination, following those in groups 1a (frontline essential workers and those in long-term care facilities) and 1b (people aged 65-74 years; other essential workers; and people aged 16-64 years with underlying conditions that increase the risk of serious, life-threatening complications from COVID-19).
But in many cases, multiple states have already either fully opened up vaccine eligibility to all adults or have created their own lists of underlying high-risk medical conditions, CDC spokeswoman Kristen Nordlund told this news organization.
No conditions have been removed from the list.
In January, the American Diabetes Association and 18 other organizations sent a letter to the CDC requesting that type 1 diabetes be prioritized along with type 2, based on data from studies showing people with both types to be at high risk for severe COVID-19 illness.
Now, ADA says, “this updated guidance will help to address the fact that in many states, millions of people with type 1 diabetes have not been prioritized equally, slowing their access to critical vaccines.”
While awaiting this latest CDC move, ADA had been urging state governors to prioritize type 1 and type 2 diabetes equally. As of now, 38 states and the District of Columbia had either done so or announced that they would.
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention has added several new medical conditions to its list of those that predispose adults to more severe COVID-19 illness.
Conditions that had previously been categorized as “might be” placing individuals at increased risk – but now are listed as high risk – include type 1 diabetes (in addition to type 2), moderate-to-severe asthma, liver disease, dementia or other neurologic conditions, stroke/cerebrovascular disease, HIV infection, cystic fibrosis, and overweight (in addition to obesity).
Substance use disorders, which hadn’t been previously listed, are now also considered high risk.
The new list groups together certain categories, such as chronic lung diseases (chronic obstructive pulmonary disease, asthma, cystic fibrosis, etc) and heart conditions (heart failure, coronary artery disease, hypertension, etc).
Both diabetes types are now grouped under “diabetes.”
The added medical conditions were posted on the CDC website’s COVID-19 page on March 29.
Type 1 diabetes and other conditions now priority for vaccination
The CDC refers to the medical conditions list as phase 1c in regard to COVID-19 vaccine prioritization, which means that anyone with any of these conditions can now be prioritized for vaccination, following those in groups 1a (frontline essential workers and those in long-term care facilities) and 1b (people aged 65-74 years; other essential workers; and people aged 16-64 years with underlying conditions that increase the risk of serious, life-threatening complications from COVID-19).
But in many cases, multiple states have already either fully opened up vaccine eligibility to all adults or have created their own lists of underlying high-risk medical conditions, CDC spokeswoman Kristen Nordlund told this news organization.
No conditions have been removed from the list.
In January, the American Diabetes Association and 18 other organizations sent a letter to the CDC requesting that type 1 diabetes be prioritized along with type 2, based on data from studies showing people with both types to be at high risk for severe COVID-19 illness.
Now, ADA says, “this updated guidance will help to address the fact that in many states, millions of people with type 1 diabetes have not been prioritized equally, slowing their access to critical vaccines.”
While awaiting this latest CDC move, ADA had been urging state governors to prioritize type 1 and type 2 diabetes equally. As of now, 38 states and the District of Columbia had either done so or announced that they would.
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention has added several new medical conditions to its list of those that predispose adults to more severe COVID-19 illness.
Conditions that had previously been categorized as “might be” placing individuals at increased risk – but now are listed as high risk – include type 1 diabetes (in addition to type 2), moderate-to-severe asthma, liver disease, dementia or other neurologic conditions, stroke/cerebrovascular disease, HIV infection, cystic fibrosis, and overweight (in addition to obesity).
Substance use disorders, which hadn’t been previously listed, are now also considered high risk.
The new list groups together certain categories, such as chronic lung diseases (chronic obstructive pulmonary disease, asthma, cystic fibrosis, etc) and heart conditions (heart failure, coronary artery disease, hypertension, etc).
Both diabetes types are now grouped under “diabetes.”
The added medical conditions were posted on the CDC website’s COVID-19 page on March 29.
Type 1 diabetes and other conditions now priority for vaccination
The CDC refers to the medical conditions list as phase 1c in regard to COVID-19 vaccine prioritization, which means that anyone with any of these conditions can now be prioritized for vaccination, following those in groups 1a (frontline essential workers and those in long-term care facilities) and 1b (people aged 65-74 years; other essential workers; and people aged 16-64 years with underlying conditions that increase the risk of serious, life-threatening complications from COVID-19).
But in many cases, multiple states have already either fully opened up vaccine eligibility to all adults or have created their own lists of underlying high-risk medical conditions, CDC spokeswoman Kristen Nordlund told this news organization.
No conditions have been removed from the list.
In January, the American Diabetes Association and 18 other organizations sent a letter to the CDC requesting that type 1 diabetes be prioritized along with type 2, based on data from studies showing people with both types to be at high risk for severe COVID-19 illness.
Now, ADA says, “this updated guidance will help to address the fact that in many states, millions of people with type 1 diabetes have not been prioritized equally, slowing their access to critical vaccines.”
While awaiting this latest CDC move, ADA had been urging state governors to prioritize type 1 and type 2 diabetes equally. As of now, 38 states and the District of Columbia had either done so or announced that they would.
A version of this article first appeared on Medscape.com.
Vaccine mismatch: What to do after dose 1 when plans change
Ideally, Americans receiving their Pfizer/BioNTech or Moderna COVID-19 vaccines will get both doses from the same manufacturer, said Gregory Poland, MD, a vaccinologist at the Mayo Clinic in Rochester, Minn.
After all, that’s how they were tested for efficacy and safety, and it was results from those studies that led to emergency use authorization (EUA) being granted by the Food and Drug Administration.
But states and countries have struggled to keep up with the demand for vaccine, and more flexible vaccination schedules could help.
So researchers are exploring whether it is safe and effective to get the first and second doses from different manufacturers. And they are even wondering whether mixing doses from different manufacturers could increase effectiveness, particularly in light of emerging variants.
It’s called the “interchangeability issue,” said Dr. Poland, who has gotten a steady stream of questions about it.
For example, a patient recently asked about options for his father, who had gotten his first dose of the AstraZeneca vaccine in Ecuador, but had since moved to the United States, where that product has not been approved for use.
Dr. Poland said in an interview that he prefaces each answer with: “I’ve got no science for what I’m about to tell you.”
In this particular case, he recommended that the man’s father talk with his doctor about his level of COVID-19 risk and consider whether he should gamble on the AstraZeneca vaccine getting approved in the United States soon, or whether he should ask for a second dose from one of the three vaccines currently approved.
On March 22, 2021, AstraZeneca released positive results from its phase 3 trial, which will likely speed its path toward use in the United States.
Although clinical trials have started to test combinations and boosters, there’s currently no definitive evidence from human trials on mixing COVID vaccines, Dr. Poland pointed out.
But a study of a mixed-vaccine regimen is currently underway in the United Kingdom.
Participants in that 13-month trial will be given the Oxford/AstraZeneca and Pfizer/BioNTech vaccines in different combinations and at different intervals. The first results from that trial are expected this summer.
And interim results from a trial combining Russia’s Sputnik V and the AstraZeneca vaccines are expected in 2 months, according to a Reuters report.
Mix only in ‘exceptional situations’
The Centers for Disease Control and Prevention has been hesitant to open the door to mixing Pfizer and Moderna vaccinations, noting that the two “are not interchangeable.” But CDC guidance has changed slightly. Now, instead of saying the two vaccines should not be mixed, CDC guidance says they can be mixed in “exceptional situations,” and that the second dose can be administered up to 6 weeks after the first dose.
It is reasonable to assume that mixing COVID-19 vaccines that use the same platform – such as the mRNA platform used by both the Pfizer and Moderna vaccines – will be acceptable, Dr. Poland said, although human trials have not proven that.
However, it is unclear whether vaccines that use different platforms can be mixed. Can the first dose of an mRNA vaccine be followed by an adenovirus-based vaccine, like the Johnson & Johnson product or Novavax, if that vaccine is granted an EUA?
Ross Kedl, PhD, a vaccine researcher and professor of immunology at the University of Colorado at Denver, Aurora, said matching vaccine platforms might not be the preferred vaccination strategy.
He disagreed that there’s a lack of science surrounding the issue, and said all signs point to mixing as not only a good option, but probably a better one.
Researcher says science backs mixing
A mix of two different vaccine platforms likely enhances immunity, Dr. Kedl said. The heterologous prime-boost strategy has been used in animal studies for decades, “and it is well known that this promotes a much better immune response than when immunizing with the same vaccine twice.
“If you think about it in a Venn diagram sort of way, it makes sense,” he said in an interview. “Each vaccine has a number of components in it that influence immunity in various ways, but between the two of them, they only have one component that is similar. In the case of the coronavirus vaccines, the one thing both have in common is the spike protein from SARS-CoV-2. In essence, this gives you two shots at generating immunity against the one thing in each vaccine you care most about, but only one shot for the other vaccine components in each platform, resulting in an amplified response against the common target.”
In fact, the heterologous prime-boost vaccination strategy has proven to be effective in humans in early studies.
For example, an Ebola regimen that consisted of an adenovirus vector, similar to the AstraZeneca COVID vaccine, and a modified vaccinia virus vector showed promise in a phase 1 study. And an HIV regimen that consisted of the combination of a DNA vaccine, similar to the Pfizer and Moderna mRNA vaccines, and another viral vector showed encouraging results in a proof-of-concept study.
In both these cases, the heterologous prime-boost strategy was far better than single-vaccine prime-boost regimens, Dr. Kedl pointed out. And neither study reported any safety issues with the combinations.
For now, it’s best to stick with the same manufacturer for both shots, as the CDC guidance suggests, he said, agreeing with Dr. Poland.
But “I would be very surprised if we didn’t move to a mixing of vaccine platforms for the population,” Dr. Kedl said.
A version of this article first appeared on Medscape.com.
Ideally, Americans receiving their Pfizer/BioNTech or Moderna COVID-19 vaccines will get both doses from the same manufacturer, said Gregory Poland, MD, a vaccinologist at the Mayo Clinic in Rochester, Minn.
After all, that’s how they were tested for efficacy and safety, and it was results from those studies that led to emergency use authorization (EUA) being granted by the Food and Drug Administration.
But states and countries have struggled to keep up with the demand for vaccine, and more flexible vaccination schedules could help.
So researchers are exploring whether it is safe and effective to get the first and second doses from different manufacturers. And they are even wondering whether mixing doses from different manufacturers could increase effectiveness, particularly in light of emerging variants.
It’s called the “interchangeability issue,” said Dr. Poland, who has gotten a steady stream of questions about it.
For example, a patient recently asked about options for his father, who had gotten his first dose of the AstraZeneca vaccine in Ecuador, but had since moved to the United States, where that product has not been approved for use.
Dr. Poland said in an interview that he prefaces each answer with: “I’ve got no science for what I’m about to tell you.”
In this particular case, he recommended that the man’s father talk with his doctor about his level of COVID-19 risk and consider whether he should gamble on the AstraZeneca vaccine getting approved in the United States soon, or whether he should ask for a second dose from one of the three vaccines currently approved.
On March 22, 2021, AstraZeneca released positive results from its phase 3 trial, which will likely speed its path toward use in the United States.
Although clinical trials have started to test combinations and boosters, there’s currently no definitive evidence from human trials on mixing COVID vaccines, Dr. Poland pointed out.
But a study of a mixed-vaccine regimen is currently underway in the United Kingdom.
Participants in that 13-month trial will be given the Oxford/AstraZeneca and Pfizer/BioNTech vaccines in different combinations and at different intervals. The first results from that trial are expected this summer.
And interim results from a trial combining Russia’s Sputnik V and the AstraZeneca vaccines are expected in 2 months, according to a Reuters report.
Mix only in ‘exceptional situations’
The Centers for Disease Control and Prevention has been hesitant to open the door to mixing Pfizer and Moderna vaccinations, noting that the two “are not interchangeable.” But CDC guidance has changed slightly. Now, instead of saying the two vaccines should not be mixed, CDC guidance says they can be mixed in “exceptional situations,” and that the second dose can be administered up to 6 weeks after the first dose.
It is reasonable to assume that mixing COVID-19 vaccines that use the same platform – such as the mRNA platform used by both the Pfizer and Moderna vaccines – will be acceptable, Dr. Poland said, although human trials have not proven that.
However, it is unclear whether vaccines that use different platforms can be mixed. Can the first dose of an mRNA vaccine be followed by an adenovirus-based vaccine, like the Johnson & Johnson product or Novavax, if that vaccine is granted an EUA?
Ross Kedl, PhD, a vaccine researcher and professor of immunology at the University of Colorado at Denver, Aurora, said matching vaccine platforms might not be the preferred vaccination strategy.
He disagreed that there’s a lack of science surrounding the issue, and said all signs point to mixing as not only a good option, but probably a better one.
Researcher says science backs mixing
A mix of two different vaccine platforms likely enhances immunity, Dr. Kedl said. The heterologous prime-boost strategy has been used in animal studies for decades, “and it is well known that this promotes a much better immune response than when immunizing with the same vaccine twice.
“If you think about it in a Venn diagram sort of way, it makes sense,” he said in an interview. “Each vaccine has a number of components in it that influence immunity in various ways, but between the two of them, they only have one component that is similar. In the case of the coronavirus vaccines, the one thing both have in common is the spike protein from SARS-CoV-2. In essence, this gives you two shots at generating immunity against the one thing in each vaccine you care most about, but only one shot for the other vaccine components in each platform, resulting in an amplified response against the common target.”
In fact, the heterologous prime-boost vaccination strategy has proven to be effective in humans in early studies.
For example, an Ebola regimen that consisted of an adenovirus vector, similar to the AstraZeneca COVID vaccine, and a modified vaccinia virus vector showed promise in a phase 1 study. And an HIV regimen that consisted of the combination of a DNA vaccine, similar to the Pfizer and Moderna mRNA vaccines, and another viral vector showed encouraging results in a proof-of-concept study.
In both these cases, the heterologous prime-boost strategy was far better than single-vaccine prime-boost regimens, Dr. Kedl pointed out. And neither study reported any safety issues with the combinations.
For now, it’s best to stick with the same manufacturer for both shots, as the CDC guidance suggests, he said, agreeing with Dr. Poland.
But “I would be very surprised if we didn’t move to a mixing of vaccine platforms for the population,” Dr. Kedl said.
A version of this article first appeared on Medscape.com.
Ideally, Americans receiving their Pfizer/BioNTech or Moderna COVID-19 vaccines will get both doses from the same manufacturer, said Gregory Poland, MD, a vaccinologist at the Mayo Clinic in Rochester, Minn.
After all, that’s how they were tested for efficacy and safety, and it was results from those studies that led to emergency use authorization (EUA) being granted by the Food and Drug Administration.
But states and countries have struggled to keep up with the demand for vaccine, and more flexible vaccination schedules could help.
So researchers are exploring whether it is safe and effective to get the first and second doses from different manufacturers. And they are even wondering whether mixing doses from different manufacturers could increase effectiveness, particularly in light of emerging variants.
It’s called the “interchangeability issue,” said Dr. Poland, who has gotten a steady stream of questions about it.
For example, a patient recently asked about options for his father, who had gotten his first dose of the AstraZeneca vaccine in Ecuador, but had since moved to the United States, where that product has not been approved for use.
Dr. Poland said in an interview that he prefaces each answer with: “I’ve got no science for what I’m about to tell you.”
In this particular case, he recommended that the man’s father talk with his doctor about his level of COVID-19 risk and consider whether he should gamble on the AstraZeneca vaccine getting approved in the United States soon, or whether he should ask for a second dose from one of the three vaccines currently approved.
On March 22, 2021, AstraZeneca released positive results from its phase 3 trial, which will likely speed its path toward use in the United States.
Although clinical trials have started to test combinations and boosters, there’s currently no definitive evidence from human trials on mixing COVID vaccines, Dr. Poland pointed out.
But a study of a mixed-vaccine regimen is currently underway in the United Kingdom.
Participants in that 13-month trial will be given the Oxford/AstraZeneca and Pfizer/BioNTech vaccines in different combinations and at different intervals. The first results from that trial are expected this summer.
And interim results from a trial combining Russia’s Sputnik V and the AstraZeneca vaccines are expected in 2 months, according to a Reuters report.
Mix only in ‘exceptional situations’
The Centers for Disease Control and Prevention has been hesitant to open the door to mixing Pfizer and Moderna vaccinations, noting that the two “are not interchangeable.” But CDC guidance has changed slightly. Now, instead of saying the two vaccines should not be mixed, CDC guidance says they can be mixed in “exceptional situations,” and that the second dose can be administered up to 6 weeks after the first dose.
It is reasonable to assume that mixing COVID-19 vaccines that use the same platform – such as the mRNA platform used by both the Pfizer and Moderna vaccines – will be acceptable, Dr. Poland said, although human trials have not proven that.
However, it is unclear whether vaccines that use different platforms can be mixed. Can the first dose of an mRNA vaccine be followed by an adenovirus-based vaccine, like the Johnson & Johnson product or Novavax, if that vaccine is granted an EUA?
Ross Kedl, PhD, a vaccine researcher and professor of immunology at the University of Colorado at Denver, Aurora, said matching vaccine platforms might not be the preferred vaccination strategy.
He disagreed that there’s a lack of science surrounding the issue, and said all signs point to mixing as not only a good option, but probably a better one.
Researcher says science backs mixing
A mix of two different vaccine platforms likely enhances immunity, Dr. Kedl said. The heterologous prime-boost strategy has been used in animal studies for decades, “and it is well known that this promotes a much better immune response than when immunizing with the same vaccine twice.
“If you think about it in a Venn diagram sort of way, it makes sense,” he said in an interview. “Each vaccine has a number of components in it that influence immunity in various ways, but between the two of them, they only have one component that is similar. In the case of the coronavirus vaccines, the one thing both have in common is the spike protein from SARS-CoV-2. In essence, this gives you two shots at generating immunity against the one thing in each vaccine you care most about, but only one shot for the other vaccine components in each platform, resulting in an amplified response against the common target.”
In fact, the heterologous prime-boost vaccination strategy has proven to be effective in humans in early studies.
For example, an Ebola regimen that consisted of an adenovirus vector, similar to the AstraZeneca COVID vaccine, and a modified vaccinia virus vector showed promise in a phase 1 study. And an HIV regimen that consisted of the combination of a DNA vaccine, similar to the Pfizer and Moderna mRNA vaccines, and another viral vector showed encouraging results in a proof-of-concept study.
In both these cases, the heterologous prime-boost strategy was far better than single-vaccine prime-boost regimens, Dr. Kedl pointed out. And neither study reported any safety issues with the combinations.
For now, it’s best to stick with the same manufacturer for both shots, as the CDC guidance suggests, he said, agreeing with Dr. Poland.
But “I would be very surprised if we didn’t move to a mixing of vaccine platforms for the population,” Dr. Kedl said.
A version of this article first appeared on Medscape.com.
COVID vaccines could lose their punch within a year, experts say
In a survey of 77 epidemiologists from 28 countries by the People’s Vaccine Alliance, 66.2% predicted that the world has a year or less before variants make current vaccines ineffective. The People’s Vaccine Alliance is a coalition of more than 50 organizations, including the African Alliance, Oxfam, Public Citizen, and UNAIDS (the Joint United Nations Programme on HIV/AIDS).
Almost a third (32.5%) of those surveyed said ineffectiveness would happen in 9 months or less; 18.2% said 6 months or less.
Paul A. Offit, MD, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, said in an interview that, while it’s hard to say whether vaccines could become ineffective in that time frame, “It’s perfectly reasonable to think it could happen.”
The good news, said Dr. Offit, who was not involved with the survey, is that SARS-CoV-2 mutates slowly, compared with other viruses such as influenza.
“To date,” he said, “the mutations that have occurred are not far enough away from the immunity induced by your natural infection or immunization such that one isn’t protected at least against severe and critical disease.”
That’s the goal of vaccines, he noted: “to keep people from suffering mightily.”
A line may be crossed
“And so far that’s happening, even with the variants,” Dr. Offit said. “That line has not been crossed. But I think we should assume that it might be.”
Dr. Offit said it will be critical to monitor anyone who gets hospitalized who is known to have been infected or fully vaccinated. Then countries need to get really good at sequencing those viruses.
The great majority of those surveyed (88%) said that persistently low vaccine coverage in many countries would make it more likely that vaccine-resistant mutations will appear.
Coverage comparisons between countries are stark.
Many countries haven’t given a single vaccine dose
While rich countries are giving COVID-19 vaccinations at the rate of a person a second, many of the poorest countries have given hardly any vaccines, the People’s Vaccine Alliance says.
Additionally, according to researchers at the Global Health Innovation Center at Duke University, Durham, N.C., high- and upper-middle–income countries, which represent one-fifth of the world’s population, have bought about 6 billion doses. But low- and lower-middle–income countries, which make up four-fifths of the population, have bought only about 2.6 billion, an article in Nature reports.
“You’re only as strong as your weakest country,” Dr. Offit said. “If we haven’t learned that what happens in other countries can [affect the global population], we haven’t been paying attention.”
Gregg Gonsalves, PhD, associate professor of epidemiology at Yale University, New Haven, Conn., one of the academic centers surveyed, didn’t specify a timeline for when vaccines would become ineffective, but said in a press release that the urgency for widespread global vaccination is real.
“Unless we vaccinate the world,” he said, “we leave the playing field open to more and more mutations, which could churn out variants that could evade our current vaccines and require booster shots to deal with them.”
“Dire, but not surprising”
Panagis Galiatsatos, MD, MHS, a pulmonologist at John Hopkins University, Baltimore, whose research focuses on health care disparities, said the survey findings were “dire, but not surprising.”
Johns Hopkins was another of the centers surveyed, but Dr. Galiatsatos wasn’t personally involved with the survey.
COVID-19, Dr. Galiatsatos pointed out, has laid bare disparities, both in who gets the vaccine and who’s involved in trials to develop the vaccines.
“It’s morally concerning and an ethical reckoning,” he said in an interview.
Recognition of the borderless swath of destruction the virus is exacting is critical, he said.
The United States “has to realize this can’t be a U.S.-centric issue,” he said. “We’re going to be back to the beginning if we don’t make sure that every country is doing well. We haven’t seen that level of uniform approach.”
He noted that scientists have always known that viruses mutate, but now the race is on to find the parts of SARS-CoV-2 that don’t mutate as much.
“My suspicion is we’ll probably need boosters instead of a whole different vaccine,” Dr. Galiatsatos said.
Among the strategies sought by the People’s Vaccine Alliance is for all pharmaceutical companies working on COVID-19 vaccines to openly share technology and intellectual property through the World Health Organization COVID-19 Technology Access Pool, to speed production and rollout of vaccines to all countries.
In the survey, 74% said that open sharing of technology and intellectual property could boost global vaccine coverage; 23% said maybe and 3% said it wouldn’t help.
The survey was carried out between Feb. 17 and March 25, 2021. Respondents included epidemiologists, virologists, and infection disease specialists from the following countries: Algeria, Argentina, Australia, Belgium, Bolivia, Canada, Denmark, Ethiopia, France, Guatemala, India, Italy, Kenya, Lebanon, Norway, Philippines, Senegal, Somalia, South Africa, South Sudan, Spain, United Arab Emirates, Uganda, United Kingdom, United States, Vietnam, Zambia, and Zimbabwe.
Dr. Offit and Dr. Galiatsatos reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a survey of 77 epidemiologists from 28 countries by the People’s Vaccine Alliance, 66.2% predicted that the world has a year or less before variants make current vaccines ineffective. The People’s Vaccine Alliance is a coalition of more than 50 organizations, including the African Alliance, Oxfam, Public Citizen, and UNAIDS (the Joint United Nations Programme on HIV/AIDS).
Almost a third (32.5%) of those surveyed said ineffectiveness would happen in 9 months or less; 18.2% said 6 months or less.
Paul A. Offit, MD, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, said in an interview that, while it’s hard to say whether vaccines could become ineffective in that time frame, “It’s perfectly reasonable to think it could happen.”
The good news, said Dr. Offit, who was not involved with the survey, is that SARS-CoV-2 mutates slowly, compared with other viruses such as influenza.
“To date,” he said, “the mutations that have occurred are not far enough away from the immunity induced by your natural infection or immunization such that one isn’t protected at least against severe and critical disease.”
That’s the goal of vaccines, he noted: “to keep people from suffering mightily.”
A line may be crossed
“And so far that’s happening, even with the variants,” Dr. Offit said. “That line has not been crossed. But I think we should assume that it might be.”
Dr. Offit said it will be critical to monitor anyone who gets hospitalized who is known to have been infected or fully vaccinated. Then countries need to get really good at sequencing those viruses.
The great majority of those surveyed (88%) said that persistently low vaccine coverage in many countries would make it more likely that vaccine-resistant mutations will appear.
Coverage comparisons between countries are stark.
Many countries haven’t given a single vaccine dose
While rich countries are giving COVID-19 vaccinations at the rate of a person a second, many of the poorest countries have given hardly any vaccines, the People’s Vaccine Alliance says.
Additionally, according to researchers at the Global Health Innovation Center at Duke University, Durham, N.C., high- and upper-middle–income countries, which represent one-fifth of the world’s population, have bought about 6 billion doses. But low- and lower-middle–income countries, which make up four-fifths of the population, have bought only about 2.6 billion, an article in Nature reports.
“You’re only as strong as your weakest country,” Dr. Offit said. “If we haven’t learned that what happens in other countries can [affect the global population], we haven’t been paying attention.”
Gregg Gonsalves, PhD, associate professor of epidemiology at Yale University, New Haven, Conn., one of the academic centers surveyed, didn’t specify a timeline for when vaccines would become ineffective, but said in a press release that the urgency for widespread global vaccination is real.
“Unless we vaccinate the world,” he said, “we leave the playing field open to more and more mutations, which could churn out variants that could evade our current vaccines and require booster shots to deal with them.”
“Dire, but not surprising”
Panagis Galiatsatos, MD, MHS, a pulmonologist at John Hopkins University, Baltimore, whose research focuses on health care disparities, said the survey findings were “dire, but not surprising.”
Johns Hopkins was another of the centers surveyed, but Dr. Galiatsatos wasn’t personally involved with the survey.
COVID-19, Dr. Galiatsatos pointed out, has laid bare disparities, both in who gets the vaccine and who’s involved in trials to develop the vaccines.
“It’s morally concerning and an ethical reckoning,” he said in an interview.
Recognition of the borderless swath of destruction the virus is exacting is critical, he said.
The United States “has to realize this can’t be a U.S.-centric issue,” he said. “We’re going to be back to the beginning if we don’t make sure that every country is doing well. We haven’t seen that level of uniform approach.”
He noted that scientists have always known that viruses mutate, but now the race is on to find the parts of SARS-CoV-2 that don’t mutate as much.
“My suspicion is we’ll probably need boosters instead of a whole different vaccine,” Dr. Galiatsatos said.
Among the strategies sought by the People’s Vaccine Alliance is for all pharmaceutical companies working on COVID-19 vaccines to openly share technology and intellectual property through the World Health Organization COVID-19 Technology Access Pool, to speed production and rollout of vaccines to all countries.
In the survey, 74% said that open sharing of technology and intellectual property could boost global vaccine coverage; 23% said maybe and 3% said it wouldn’t help.
The survey was carried out between Feb. 17 and March 25, 2021. Respondents included epidemiologists, virologists, and infection disease specialists from the following countries: Algeria, Argentina, Australia, Belgium, Bolivia, Canada, Denmark, Ethiopia, France, Guatemala, India, Italy, Kenya, Lebanon, Norway, Philippines, Senegal, Somalia, South Africa, South Sudan, Spain, United Arab Emirates, Uganda, United Kingdom, United States, Vietnam, Zambia, and Zimbabwe.
Dr. Offit and Dr. Galiatsatos reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a survey of 77 epidemiologists from 28 countries by the People’s Vaccine Alliance, 66.2% predicted that the world has a year or less before variants make current vaccines ineffective. The People’s Vaccine Alliance is a coalition of more than 50 organizations, including the African Alliance, Oxfam, Public Citizen, and UNAIDS (the Joint United Nations Programme on HIV/AIDS).
Almost a third (32.5%) of those surveyed said ineffectiveness would happen in 9 months or less; 18.2% said 6 months or less.
Paul A. Offit, MD, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, said in an interview that, while it’s hard to say whether vaccines could become ineffective in that time frame, “It’s perfectly reasonable to think it could happen.”
The good news, said Dr. Offit, who was not involved with the survey, is that SARS-CoV-2 mutates slowly, compared with other viruses such as influenza.
“To date,” he said, “the mutations that have occurred are not far enough away from the immunity induced by your natural infection or immunization such that one isn’t protected at least against severe and critical disease.”
That’s the goal of vaccines, he noted: “to keep people from suffering mightily.”
A line may be crossed
“And so far that’s happening, even with the variants,” Dr. Offit said. “That line has not been crossed. But I think we should assume that it might be.”
Dr. Offit said it will be critical to monitor anyone who gets hospitalized who is known to have been infected or fully vaccinated. Then countries need to get really good at sequencing those viruses.
The great majority of those surveyed (88%) said that persistently low vaccine coverage in many countries would make it more likely that vaccine-resistant mutations will appear.
Coverage comparisons between countries are stark.
Many countries haven’t given a single vaccine dose
While rich countries are giving COVID-19 vaccinations at the rate of a person a second, many of the poorest countries have given hardly any vaccines, the People’s Vaccine Alliance says.
Additionally, according to researchers at the Global Health Innovation Center at Duke University, Durham, N.C., high- and upper-middle–income countries, which represent one-fifth of the world’s population, have bought about 6 billion doses. But low- and lower-middle–income countries, which make up four-fifths of the population, have bought only about 2.6 billion, an article in Nature reports.
“You’re only as strong as your weakest country,” Dr. Offit said. “If we haven’t learned that what happens in other countries can [affect the global population], we haven’t been paying attention.”
Gregg Gonsalves, PhD, associate professor of epidemiology at Yale University, New Haven, Conn., one of the academic centers surveyed, didn’t specify a timeline for when vaccines would become ineffective, but said in a press release that the urgency for widespread global vaccination is real.
“Unless we vaccinate the world,” he said, “we leave the playing field open to more and more mutations, which could churn out variants that could evade our current vaccines and require booster shots to deal with them.”
“Dire, but not surprising”
Panagis Galiatsatos, MD, MHS, a pulmonologist at John Hopkins University, Baltimore, whose research focuses on health care disparities, said the survey findings were “dire, but not surprising.”
Johns Hopkins was another of the centers surveyed, but Dr. Galiatsatos wasn’t personally involved with the survey.
COVID-19, Dr. Galiatsatos pointed out, has laid bare disparities, both in who gets the vaccine and who’s involved in trials to develop the vaccines.
“It’s morally concerning and an ethical reckoning,” he said in an interview.
Recognition of the borderless swath of destruction the virus is exacting is critical, he said.
The United States “has to realize this can’t be a U.S.-centric issue,” he said. “We’re going to be back to the beginning if we don’t make sure that every country is doing well. We haven’t seen that level of uniform approach.”
He noted that scientists have always known that viruses mutate, but now the race is on to find the parts of SARS-CoV-2 that don’t mutate as much.
“My suspicion is we’ll probably need boosters instead of a whole different vaccine,” Dr. Galiatsatos said.
Among the strategies sought by the People’s Vaccine Alliance is for all pharmaceutical companies working on COVID-19 vaccines to openly share technology and intellectual property through the World Health Organization COVID-19 Technology Access Pool, to speed production and rollout of vaccines to all countries.
In the survey, 74% said that open sharing of technology and intellectual property could boost global vaccine coverage; 23% said maybe and 3% said it wouldn’t help.
The survey was carried out between Feb. 17 and March 25, 2021. Respondents included epidemiologists, virologists, and infection disease specialists from the following countries: Algeria, Argentina, Australia, Belgium, Bolivia, Canada, Denmark, Ethiopia, France, Guatemala, India, Italy, Kenya, Lebanon, Norway, Philippines, Senegal, Somalia, South Africa, South Sudan, Spain, United Arab Emirates, Uganda, United Kingdom, United States, Vietnam, Zambia, and Zimbabwe.
Dr. Offit and Dr. Galiatsatos reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
National Psoriasis Foundation recommends some stop methotrexate for 2 weeks after J&J vaccine
The , Joel M. Gelfand, MD, said at Innovations in Dermatology: Virtual Spring Conference 2021.
The new guidance states: “Patients 60 or older who have at least one comorbidity associated with an increased risk for poor COVID-19 outcomes, and who are taking methotrexate with well-controlled psoriatic disease, may, in consultation with their prescriber, consider holding it for 2 weeks after receiving the Ad26.COV2.S [Johnson & Johnson] vaccine in order to potentially improve vaccine response.”
The key word here is “potentially.” There is no hard evidence that a 2-week hold on methotrexate after receiving the killed adenovirus vaccine will actually provide a clinically meaningful benefit. But it’s a hypothetical possibility. The rationale stems from a small randomized trial conducted in South Korea several years ago in which patients with rheumatoid arthritis were assigned to hold or continue their methotrexate for the first 2 weeks after receiving an inactivated-virus influenza vaccine. The antibody response to the vaccine was better in those who temporarily halted their methotrexate, explained Dr. Gelfand, cochair of the NPF COVID-19 Task Force and professor of dermatology and of epidemiology at the University of Pennsylvania, Philadelphia.
“If you have a patient on methotrexate who’s 60 or older and whose psoriasis is completely controlled and quiescent and the patient is concerned about how well the vaccine is going to work, this is a reasonable thing to consider in someone who’s at higher risk for poor outcomes if they get infected,” he said.
If the informed patient wants to continue on methotrexate without interruption, that’s fine, too, in light of the lack of compelling evidence on this issue, the dermatologist added at the conference, sponsored by MedscapeLIVE! and the producers of the Hawaii Dermatology Seminar and Caribbean Dermatology Symposium.
The NPF task force does not extend the recommendation to consider holding methotrexate in recipients of the mRNA-based Moderna and Pfizer vaccines because of their very different mechanisms of action. Nor is it recommended to hold biologic agents after receiving any of the available COVID-19 vaccines. Studies have shown no altered immunologic response to influenza or pneumococcal vaccines in patients who continued on tumor necrosis factor inhibitors or interleukin-17 inhibitors. The interleukin-23 inhibitors haven’t been studied in this regard.
The task force recommends that most psoriasis patients should continue on treatment throughout the pandemic, and newly diagnosed patients should commence appropriate therapy as if there was no pandemic.
“We’ve learned that many patients who stopped their treatment for psoriatic disease early in the pandemic came to regret that decision because their psoriasis flared and got worse and required reinstitution of therapy,” Dr. Gelfand said. “The current data is largely reassuring that if there is an effect of our therapies on the risk of COVID, it must be rather small and therefore unlikely to be clinically meaningful for our patients.”
Dr. Gelfand reported serving as a consultant to and recipient of institutional research grants from Pfizer and numerous other pharmaceutical companies.
MedscapeLIVE and this news organization are owned by the same parent company.
The , Joel M. Gelfand, MD, said at Innovations in Dermatology: Virtual Spring Conference 2021.
The new guidance states: “Patients 60 or older who have at least one comorbidity associated with an increased risk for poor COVID-19 outcomes, and who are taking methotrexate with well-controlled psoriatic disease, may, in consultation with their prescriber, consider holding it for 2 weeks after receiving the Ad26.COV2.S [Johnson & Johnson] vaccine in order to potentially improve vaccine response.”
The key word here is “potentially.” There is no hard evidence that a 2-week hold on methotrexate after receiving the killed adenovirus vaccine will actually provide a clinically meaningful benefit. But it’s a hypothetical possibility. The rationale stems from a small randomized trial conducted in South Korea several years ago in which patients with rheumatoid arthritis were assigned to hold or continue their methotrexate for the first 2 weeks after receiving an inactivated-virus influenza vaccine. The antibody response to the vaccine was better in those who temporarily halted their methotrexate, explained Dr. Gelfand, cochair of the NPF COVID-19 Task Force and professor of dermatology and of epidemiology at the University of Pennsylvania, Philadelphia.
“If you have a patient on methotrexate who’s 60 or older and whose psoriasis is completely controlled and quiescent and the patient is concerned about how well the vaccine is going to work, this is a reasonable thing to consider in someone who’s at higher risk for poor outcomes if they get infected,” he said.
If the informed patient wants to continue on methotrexate without interruption, that’s fine, too, in light of the lack of compelling evidence on this issue, the dermatologist added at the conference, sponsored by MedscapeLIVE! and the producers of the Hawaii Dermatology Seminar and Caribbean Dermatology Symposium.
The NPF task force does not extend the recommendation to consider holding methotrexate in recipients of the mRNA-based Moderna and Pfizer vaccines because of their very different mechanisms of action. Nor is it recommended to hold biologic agents after receiving any of the available COVID-19 vaccines. Studies have shown no altered immunologic response to influenza or pneumococcal vaccines in patients who continued on tumor necrosis factor inhibitors or interleukin-17 inhibitors. The interleukin-23 inhibitors haven’t been studied in this regard.
The task force recommends that most psoriasis patients should continue on treatment throughout the pandemic, and newly diagnosed patients should commence appropriate therapy as if there was no pandemic.
“We’ve learned that many patients who stopped their treatment for psoriatic disease early in the pandemic came to regret that decision because their psoriasis flared and got worse and required reinstitution of therapy,” Dr. Gelfand said. “The current data is largely reassuring that if there is an effect of our therapies on the risk of COVID, it must be rather small and therefore unlikely to be clinically meaningful for our patients.”
Dr. Gelfand reported serving as a consultant to and recipient of institutional research grants from Pfizer and numerous other pharmaceutical companies.
MedscapeLIVE and this news organization are owned by the same parent company.
The , Joel M. Gelfand, MD, said at Innovations in Dermatology: Virtual Spring Conference 2021.
The new guidance states: “Patients 60 or older who have at least one comorbidity associated with an increased risk for poor COVID-19 outcomes, and who are taking methotrexate with well-controlled psoriatic disease, may, in consultation with their prescriber, consider holding it for 2 weeks after receiving the Ad26.COV2.S [Johnson & Johnson] vaccine in order to potentially improve vaccine response.”
The key word here is “potentially.” There is no hard evidence that a 2-week hold on methotrexate after receiving the killed adenovirus vaccine will actually provide a clinically meaningful benefit. But it’s a hypothetical possibility. The rationale stems from a small randomized trial conducted in South Korea several years ago in which patients with rheumatoid arthritis were assigned to hold or continue their methotrexate for the first 2 weeks after receiving an inactivated-virus influenza vaccine. The antibody response to the vaccine was better in those who temporarily halted their methotrexate, explained Dr. Gelfand, cochair of the NPF COVID-19 Task Force and professor of dermatology and of epidemiology at the University of Pennsylvania, Philadelphia.
“If you have a patient on methotrexate who’s 60 or older and whose psoriasis is completely controlled and quiescent and the patient is concerned about how well the vaccine is going to work, this is a reasonable thing to consider in someone who’s at higher risk for poor outcomes if they get infected,” he said.
If the informed patient wants to continue on methotrexate without interruption, that’s fine, too, in light of the lack of compelling evidence on this issue, the dermatologist added at the conference, sponsored by MedscapeLIVE! and the producers of the Hawaii Dermatology Seminar and Caribbean Dermatology Symposium.
The NPF task force does not extend the recommendation to consider holding methotrexate in recipients of the mRNA-based Moderna and Pfizer vaccines because of their very different mechanisms of action. Nor is it recommended to hold biologic agents after receiving any of the available COVID-19 vaccines. Studies have shown no altered immunologic response to influenza or pneumococcal vaccines in patients who continued on tumor necrosis factor inhibitors or interleukin-17 inhibitors. The interleukin-23 inhibitors haven’t been studied in this regard.
The task force recommends that most psoriasis patients should continue on treatment throughout the pandemic, and newly diagnosed patients should commence appropriate therapy as if there was no pandemic.
“We’ve learned that many patients who stopped their treatment for psoriatic disease early in the pandemic came to regret that decision because their psoriasis flared and got worse and required reinstitution of therapy,” Dr. Gelfand said. “The current data is largely reassuring that if there is an effect of our therapies on the risk of COVID, it must be rather small and therefore unlikely to be clinically meaningful for our patients.”
Dr. Gelfand reported serving as a consultant to and recipient of institutional research grants from Pfizer and numerous other pharmaceutical companies.
MedscapeLIVE and this news organization are owned by the same parent company.
FROM INNOVATIONS IN DERMATOLOGY
Use of complimentary and alternative medicine common in diabetes patients
An updated worldwide estimate of complementary and alternative medicine (CAM) use among individuals with diabetes found widespread use, though it varied greatly by region and is sometimes hard to define.
The report is the first literature review of the subject since 2007. The researchers looked at CAM use by region, as well as by patient categories such as those with advanced diabetes and by length of time since diagnosis. The most commonly reported CAMs in use were herbal medicine, acupuncture, homeopathy, and spiritual healing.
Only about one-third of patients disclosed their CAM use to their physician or health care provider. “We suggest that health care professionals should carefully anticipate the likelihood of their [patients’] diabetic CAM use in order to enhance treatment optimization and promote medication adherence, as well as to provide a fully informed consultation,” said first author Abdulaziz S. Alzahrani, a PhD student at the University of Birmingham (England). The study was published March 8, 2021, in the European Journal of Clinical Pharmacology.
Patients also have a responsibility, said Gregory Rhee, PhD, assistant professor of public health sciences at the University of Connecticut, Farmington. He was the lead author of a 2018 survey of CAM use in adults aged 65 years and older with diabetes in the United States using data from the 2012 National Health Interview Survey, and found that 25% had used CAM in some form in the prior year. “They need to be more up front, more proactive talking about CAM use with their doctors, and the second part is the physician. They also should be better educated in terms of CAM use. Traditionally, the physician in Western societies have pretty much ignored CAM use. But they are getting aware of CAM use and also we know that people are coming from multiple cultural backgrounds. The physicians and other health care providers should be better informed about CAM, and they should be better educated about it to provide patients better practice,” said Dr. Rhee.
He also distinguished between approaches like yoga or Tai Chi, which are physically oriented and not particularly controversial, and herbal medicines or dietary supplements. “Those can be controversial because we do not have strong scientific evidence to support those modalities for effectiveness on diabetes management,” Dr. Rhee added.
Mr. Alzahrani and colleagues conducted a meta-analysis of 38 studies, which included data from 25 countries. The included studies varied in their approach. For example, 16 studies focused exclusively on herbal and nutritional supplements. The most commonly mentioned CAMs were acupuncture and mind-body therapies (each named in six studies), religious and spiritual healing (five studies), and homeopathy (four studies). Among 31 studies focusing on herbal and nutritional supplements, the most common herbs mentioned were cinnamon and fenugreek (mentioned in 18 studies), garlic (17 studies), aloe vera (14 studies), and black seed (12 studies).
Prevalence of CAM use varied widely, ranging from 17% in Jordan to 89% in India and in a separate study in Jordan. The pooled prevalence of CAM use was 51% (95% confidence interval, 43%-59%). Subgroup analyses found the highest rate of CAM use in Europe (76%) and Africa (55%), and the lowest in North America (45%).
When the researchers examined patient characteristics, they found no significant relationship between CAM use and established ethnicity groups, or between type 1 and type 2 diabetes. The prevalence ratio was lower among men (PR, 0.86; 95% CI, 0.81-0.91). PRs for CAM use were lower among those with diabetic complications (PR, 0.81; 95% CI, 0.66-0.99). Individuals with diabetes of at least 5 years’ duration were more likely to use CAM than those with shorter duration of illness (PR, 1.71; 95% CI, 1.04-1.32).
Most (78%) CAM users employed it as an addition to their treatment regimen (95% CI, 56-94%), while 21% used it as an alternative to prescribed medicine (95% CI, 12-31%). More than two-thirds (67%) of individuals did not disclose CAM use to health care professionals (95% CI, 58-76%).
Although CAM use can be a source of friction between patients and physicians, Dr. Rhee also sees it as an opportunity. Patients from diverse backgrounds may be using CAM, often as a result of different cultural backgrounds. He cited the belief in some Asian countries that the balance of Yin and Yang is key to health, which many patients believe can be addressed through CAM. “If we want to promote cultural diversity, if we really care about patient diversity, I think CAM is one of the potential sources where the doctors should know [more about] the issue,” said Dr. Rhee.
The study was funded by the University of Birmingham. Dr. Rhee and Mr. Alzahrani have no relevant financial disclosures.
An updated worldwide estimate of complementary and alternative medicine (CAM) use among individuals with diabetes found widespread use, though it varied greatly by region and is sometimes hard to define.
The report is the first literature review of the subject since 2007. The researchers looked at CAM use by region, as well as by patient categories such as those with advanced diabetes and by length of time since diagnosis. The most commonly reported CAMs in use were herbal medicine, acupuncture, homeopathy, and spiritual healing.
Only about one-third of patients disclosed their CAM use to their physician or health care provider. “We suggest that health care professionals should carefully anticipate the likelihood of their [patients’] diabetic CAM use in order to enhance treatment optimization and promote medication adherence, as well as to provide a fully informed consultation,” said first author Abdulaziz S. Alzahrani, a PhD student at the University of Birmingham (England). The study was published March 8, 2021, in the European Journal of Clinical Pharmacology.
Patients also have a responsibility, said Gregory Rhee, PhD, assistant professor of public health sciences at the University of Connecticut, Farmington. He was the lead author of a 2018 survey of CAM use in adults aged 65 years and older with diabetes in the United States using data from the 2012 National Health Interview Survey, and found that 25% had used CAM in some form in the prior year. “They need to be more up front, more proactive talking about CAM use with their doctors, and the second part is the physician. They also should be better educated in terms of CAM use. Traditionally, the physician in Western societies have pretty much ignored CAM use. But they are getting aware of CAM use and also we know that people are coming from multiple cultural backgrounds. The physicians and other health care providers should be better informed about CAM, and they should be better educated about it to provide patients better practice,” said Dr. Rhee.
He also distinguished between approaches like yoga or Tai Chi, which are physically oriented and not particularly controversial, and herbal medicines or dietary supplements. “Those can be controversial because we do not have strong scientific evidence to support those modalities for effectiveness on diabetes management,” Dr. Rhee added.
Mr. Alzahrani and colleagues conducted a meta-analysis of 38 studies, which included data from 25 countries. The included studies varied in their approach. For example, 16 studies focused exclusively on herbal and nutritional supplements. The most commonly mentioned CAMs were acupuncture and mind-body therapies (each named in six studies), religious and spiritual healing (five studies), and homeopathy (four studies). Among 31 studies focusing on herbal and nutritional supplements, the most common herbs mentioned were cinnamon and fenugreek (mentioned in 18 studies), garlic (17 studies), aloe vera (14 studies), and black seed (12 studies).
Prevalence of CAM use varied widely, ranging from 17% in Jordan to 89% in India and in a separate study in Jordan. The pooled prevalence of CAM use was 51% (95% confidence interval, 43%-59%). Subgroup analyses found the highest rate of CAM use in Europe (76%) and Africa (55%), and the lowest in North America (45%).
When the researchers examined patient characteristics, they found no significant relationship between CAM use and established ethnicity groups, or between type 1 and type 2 diabetes. The prevalence ratio was lower among men (PR, 0.86; 95% CI, 0.81-0.91). PRs for CAM use were lower among those with diabetic complications (PR, 0.81; 95% CI, 0.66-0.99). Individuals with diabetes of at least 5 years’ duration were more likely to use CAM than those with shorter duration of illness (PR, 1.71; 95% CI, 1.04-1.32).
Most (78%) CAM users employed it as an addition to their treatment regimen (95% CI, 56-94%), while 21% used it as an alternative to prescribed medicine (95% CI, 12-31%). More than two-thirds (67%) of individuals did not disclose CAM use to health care professionals (95% CI, 58-76%).
Although CAM use can be a source of friction between patients and physicians, Dr. Rhee also sees it as an opportunity. Patients from diverse backgrounds may be using CAM, often as a result of different cultural backgrounds. He cited the belief in some Asian countries that the balance of Yin and Yang is key to health, which many patients believe can be addressed through CAM. “If we want to promote cultural diversity, if we really care about patient diversity, I think CAM is one of the potential sources where the doctors should know [more about] the issue,” said Dr. Rhee.
The study was funded by the University of Birmingham. Dr. Rhee and Mr. Alzahrani have no relevant financial disclosures.
An updated worldwide estimate of complementary and alternative medicine (CAM) use among individuals with diabetes found widespread use, though it varied greatly by region and is sometimes hard to define.
The report is the first literature review of the subject since 2007. The researchers looked at CAM use by region, as well as by patient categories such as those with advanced diabetes and by length of time since diagnosis. The most commonly reported CAMs in use were herbal medicine, acupuncture, homeopathy, and spiritual healing.
Only about one-third of patients disclosed their CAM use to their physician or health care provider. “We suggest that health care professionals should carefully anticipate the likelihood of their [patients’] diabetic CAM use in order to enhance treatment optimization and promote medication adherence, as well as to provide a fully informed consultation,” said first author Abdulaziz S. Alzahrani, a PhD student at the University of Birmingham (England). The study was published March 8, 2021, in the European Journal of Clinical Pharmacology.
Patients also have a responsibility, said Gregory Rhee, PhD, assistant professor of public health sciences at the University of Connecticut, Farmington. He was the lead author of a 2018 survey of CAM use in adults aged 65 years and older with diabetes in the United States using data from the 2012 National Health Interview Survey, and found that 25% had used CAM in some form in the prior year. “They need to be more up front, more proactive talking about CAM use with their doctors, and the second part is the physician. They also should be better educated in terms of CAM use. Traditionally, the physician in Western societies have pretty much ignored CAM use. But they are getting aware of CAM use and also we know that people are coming from multiple cultural backgrounds. The physicians and other health care providers should be better informed about CAM, and they should be better educated about it to provide patients better practice,” said Dr. Rhee.
He also distinguished between approaches like yoga or Tai Chi, which are physically oriented and not particularly controversial, and herbal medicines or dietary supplements. “Those can be controversial because we do not have strong scientific evidence to support those modalities for effectiveness on diabetes management,” Dr. Rhee added.
Mr. Alzahrani and colleagues conducted a meta-analysis of 38 studies, which included data from 25 countries. The included studies varied in their approach. For example, 16 studies focused exclusively on herbal and nutritional supplements. The most commonly mentioned CAMs were acupuncture and mind-body therapies (each named in six studies), religious and spiritual healing (five studies), and homeopathy (four studies). Among 31 studies focusing on herbal and nutritional supplements, the most common herbs mentioned were cinnamon and fenugreek (mentioned in 18 studies), garlic (17 studies), aloe vera (14 studies), and black seed (12 studies).
Prevalence of CAM use varied widely, ranging from 17% in Jordan to 89% in India and in a separate study in Jordan. The pooled prevalence of CAM use was 51% (95% confidence interval, 43%-59%). Subgroup analyses found the highest rate of CAM use in Europe (76%) and Africa (55%), and the lowest in North America (45%).
When the researchers examined patient characteristics, they found no significant relationship between CAM use and established ethnicity groups, or between type 1 and type 2 diabetes. The prevalence ratio was lower among men (PR, 0.86; 95% CI, 0.81-0.91). PRs for CAM use were lower among those with diabetic complications (PR, 0.81; 95% CI, 0.66-0.99). Individuals with diabetes of at least 5 years’ duration were more likely to use CAM than those with shorter duration of illness (PR, 1.71; 95% CI, 1.04-1.32).
Most (78%) CAM users employed it as an addition to their treatment regimen (95% CI, 56-94%), while 21% used it as an alternative to prescribed medicine (95% CI, 12-31%). More than two-thirds (67%) of individuals did not disclose CAM use to health care professionals (95% CI, 58-76%).
Although CAM use can be a source of friction between patients and physicians, Dr. Rhee also sees it as an opportunity. Patients from diverse backgrounds may be using CAM, often as a result of different cultural backgrounds. He cited the belief in some Asian countries that the balance of Yin and Yang is key to health, which many patients believe can be addressed through CAM. “If we want to promote cultural diversity, if we really care about patient diversity, I think CAM is one of the potential sources where the doctors should know [more about] the issue,” said Dr. Rhee.
The study was funded by the University of Birmingham. Dr. Rhee and Mr. Alzahrani have no relevant financial disclosures.
FROM THE EUROPEAN JOURNAL OF CLINICAL PHARMACOLOGY
New COVID-19 cases rise again in children
The number of new COVID-19 cases in children increased for the second consecutive week in the United States, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
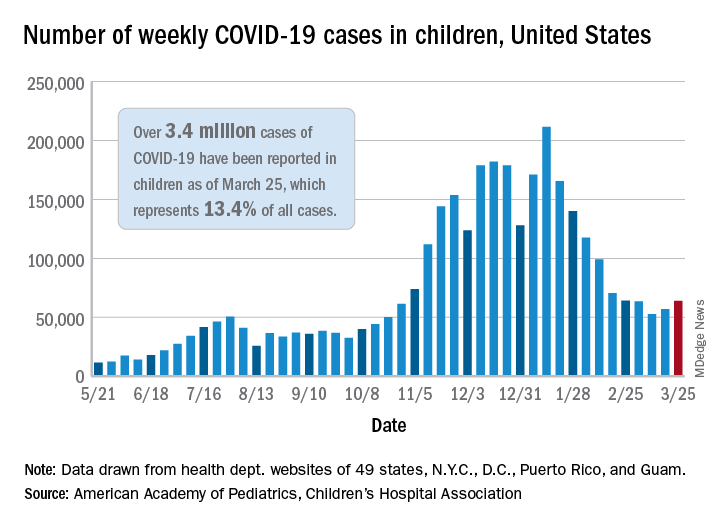
That brings the number of children infected with the coronavirus to over 3.4 million since the beginning of the pandemic, or 13.4% of all reported cases, the AAP and CHA said in their weekly COVID-19 report.
For just the week of March 19-25, however, the proportion of all cases occurring in children was quite a bit higher, 19.1%. That’s higher than at any other point during the pandemic, passing the previous high of 18.7% set just a week earlier, based on the data collected by AAP/CHA from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
The national infection rate was 4,525 cases per 100,000 children for the week of March 19-25, compared with 4,440 per 100,000 the previous week. States falling the farthest from that national mark were Hawaii at 1,101 per 100,000 and North Dakota at 8,848, the AAP and CHA said.
There was double-digit increase, 11, in the number of child deaths, as the total went from 268 to 279 despite Virginia’s revising its mortality data downward. The mortality rate for children remains 0.01%, and children represent only 0.06% of all COVID-19–related deaths in the 43 states, along with New York City, Puerto Rico, and Guam, that are reporting deaths by age, the report shows.
The state/local-level data show that Texas has the highest number of child deaths (48), followed by Arizona (26), New York City (22), California (16), and Illinois (16), while nine states and the District of Columbia have not yet reported a death, the AAP and CHA said.
The number of new COVID-19 cases in children increased for the second consecutive week in the United States, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
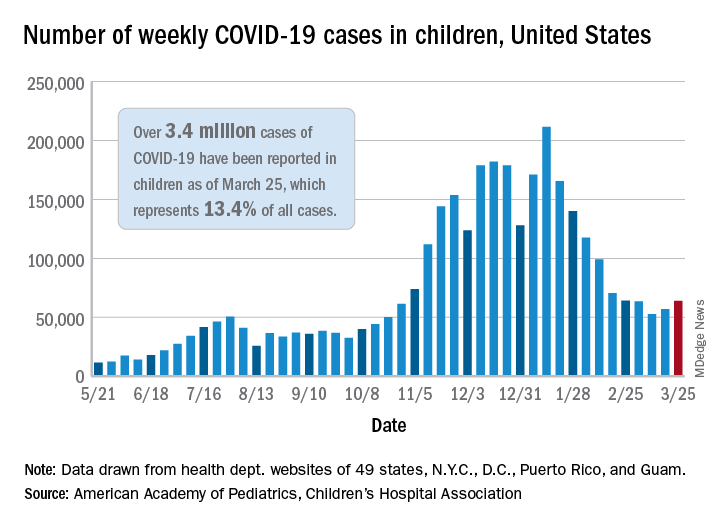
That brings the number of children infected with the coronavirus to over 3.4 million since the beginning of the pandemic, or 13.4% of all reported cases, the AAP and CHA said in their weekly COVID-19 report.
For just the week of March 19-25, however, the proportion of all cases occurring in children was quite a bit higher, 19.1%. That’s higher than at any other point during the pandemic, passing the previous high of 18.7% set just a week earlier, based on the data collected by AAP/CHA from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
The national infection rate was 4,525 cases per 100,000 children for the week of March 19-25, compared with 4,440 per 100,000 the previous week. States falling the farthest from that national mark were Hawaii at 1,101 per 100,000 and North Dakota at 8,848, the AAP and CHA said.
There was double-digit increase, 11, in the number of child deaths, as the total went from 268 to 279 despite Virginia’s revising its mortality data downward. The mortality rate for children remains 0.01%, and children represent only 0.06% of all COVID-19–related deaths in the 43 states, along with New York City, Puerto Rico, and Guam, that are reporting deaths by age, the report shows.
The state/local-level data show that Texas has the highest number of child deaths (48), followed by Arizona (26), New York City (22), California (16), and Illinois (16), while nine states and the District of Columbia have not yet reported a death, the AAP and CHA said.
The number of new COVID-19 cases in children increased for the second consecutive week in the United States, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
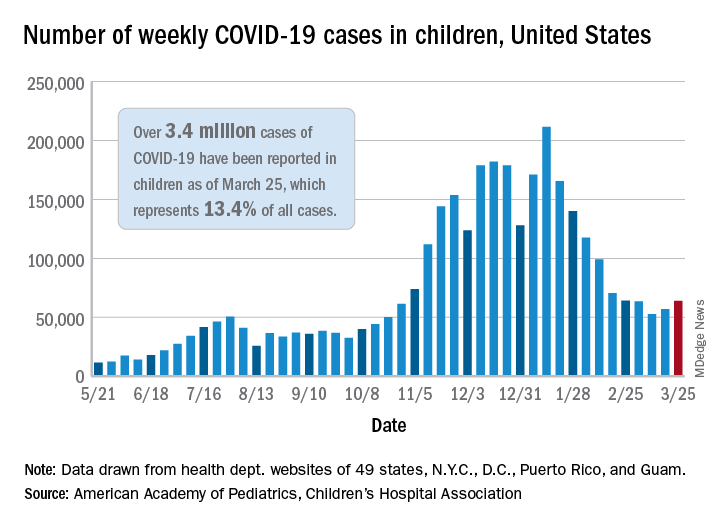
That brings the number of children infected with the coronavirus to over 3.4 million since the beginning of the pandemic, or 13.4% of all reported cases, the AAP and CHA said in their weekly COVID-19 report.
For just the week of March 19-25, however, the proportion of all cases occurring in children was quite a bit higher, 19.1%. That’s higher than at any other point during the pandemic, passing the previous high of 18.7% set just a week earlier, based on the data collected by AAP/CHA from 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.
The national infection rate was 4,525 cases per 100,000 children for the week of March 19-25, compared with 4,440 per 100,000 the previous week. States falling the farthest from that national mark were Hawaii at 1,101 per 100,000 and North Dakota at 8,848, the AAP and CHA said.
There was double-digit increase, 11, in the number of child deaths, as the total went from 268 to 279 despite Virginia’s revising its mortality data downward. The mortality rate for children remains 0.01%, and children represent only 0.06% of all COVID-19–related deaths in the 43 states, along with New York City, Puerto Rico, and Guam, that are reporting deaths by age, the report shows.
The state/local-level data show that Texas has the highest number of child deaths (48), followed by Arizona (26), New York City (22), California (16), and Illinois (16), while nine states and the District of Columbia have not yet reported a death, the AAP and CHA said.












