User login
The Journal of Clinical Outcomes Management® is an independent, peer-reviewed journal offering evidence-based, practical information for improving the quality, safety, and value of health care.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Three ‘synergistic’ problems when taking blood pressure
Insufficient blood pressure measurement during medical consultation, use of an inadequate technique for its determination, and lack of validated automatic sphygmomanometers are three problems that convergently complicate the diagnosis and control of arterial hypertension in the Americas, a silent disease that affects 180 million people in the region and is the main risk factor for cardiovascular diseases, said the Pan American Health Organization.
Jarbas Barbosa, MD, MPH, PhD, director of PAHO, said in an interview: “We don’t have specific data for each of these scenarios, but unfortunately, all three doubtless work together to make the situation worse.
“Often, the staff members at our primary care clinics are not prepared to diagnose and treat hypertension, because there aren’t national protocols to raise awareness and prepare them to provide this care to the correct standard. Also, they are often unqualified to take blood pressure readings properly,” he added.
This concern is reflected in the theme the organization chose for World Hypertension Day, which was observed on May 17: Measure your blood pressure accurately, control it, live longer! “We shouldn’t underestimate the importance of taking blood pressure,” warned Silvana Luciani, chief of PAHO’s noncommunicable diseases, violence, and injury prevention unit. But, the experts stressed, it must be done correctly.
Time no problem
It’s important to raise awareness of the value of blood pressure measurement for the general population. However, as multiple studies have shown, one barrier to detecting and controlling hypertension is that doctors and other health care professionals measure blood pressure less frequently in clinic than expected, or they use inappropriate techniques or obsolete or uncalibrated measurement devices.
“The importance of clinic blood pressure measurement has been recognized for many decades, but adherence to guidelines on proper, standardized blood pressure measurement remains uncommon in clinical practice,” concluded a consensus document signed by 25 experts from 13 institutions in the United States, Australia, Germany, the United Kingdom, Canada, Italy, Belgium, and Greece.
The first problem lies in the low quantity of measurements. A recent study in Argentina of nearly 3,000 visits to the doctor’s office at nine health care centers showed that doctors took blood pressure readings in only once in every seven encounters. Even cardiologists, the specialists with the best performance, did so only half of the time.
“Several factors can come into play: lack of awareness, medical inertia, or lack of appropriate equipment. But it is not for lack of time. How long does it take to take blood pressure three times within a 1-minute interval, with the patient seated and their back supported, as indicated? Four minutes. That’s not very much,” said Judith Zilberman, MD, PhD, said in an interview. Dr. Zilberman leads the department of hypertension and the women’s cardiovascular disease area at the Argerich Hospital in Buenos Aires, and is the former chair of the Argentinian Society of Hypertension.
Patricio López-Jaramillo, MD, PhD, said in an interview that the greatest obstacle is the lack of awareness among physicians and other health care staff about the importance of taking proper blood pressure measurements. Dr. López-Jaramillo is president and scientific director of the MASIRA Research Institute at the University of Santander in Bucaramanga, Colombia, and first author of the Manual Práctico de Diagnóstico y Manejo de la Hipertensión Arterial (Practice Guidelines for Diagnosing and Managing Hypertension), published by the Latin American Hypertension Society.
“Medical schools are also responsible for this. They go over this topic very superficially during undergraduate and, even worse, postgraduate training. The lack of time to take correct measurements, or the lack of appropriate instruments, is secondary to this lack of awareness among most health care staff members,” added Dr. López-Jaramillo, who is one of the researchers of the PURE epidemiologic study. Since 2002, it has followed a cohort of 225,000 participants from 27 high-, mid-, and low-income countries.
Dr. Zilberman added that it would be good practice for all primary care physicians to take blood pressure readings regardless of the reason for the visit and whether patients have been diagnosed with hypertension or not. “If a woman goes to her gynecologist because she wants to get pregnant, her blood pressure should also be taken! And any other specialist should interview the patient, ascertain her history, what medications she’s on, and then ask if her blood pressure has been taken recently,” she recommended.
Measure well
The second factor to consider is that a correct technique should be used to take blood pressure readings in the doctor’s office or clinic so as not to produce inaccurate results that could lead to underdiagnosis, overdiagnosis, or a poor assessment of the patient’s response to prescribed treatments. An observational study performed in Uruguay in 2017 showed that only 5% of 302 blood pressure measurements followed appropriate procedures.
A new fact sheet from the PAHO lists the following eight requirements for obtaining an accurate reading: don’t have a conversation, support the arm at heart level, put the cuff on a bare arm, use the correct cuff size, support the feet, keep the legs uncrossed, ensure the patient has an empty bladder, and support the back.
Though most guidelines recommend taking three readings, the “pragmatic” focus proposed in the international consensus accepts at least two readings separated by a minimum of 30 seconds. The two readings should then be averaged out. There is evidence that simplified protocols can be used, at least for population screening.
The authors of the new document also recommend preparing the patient before taking the measurement. The patient should be asked not to smoke, exercise, or consume alcohol or caffeine for at least 30 minutes beforehand. He or she should rest for a period of 3-5 minutes without speaking or being spoken to before the measurement is taken.
Lastly, clinically validated automated measurement devices should be used, as called for by the PAHO HEARTS initiative in the Americas. “The sphygmomanometer or classic aneroid tensiometer for the auscultatory method, which is still used way too often at doctor’s office visits in the region, has many weaknesses – not only the device itself but also the way it’s used (human error). This produces a rounded, approximate reading,” stressed Dr. Zilberman.
Automated devices also minimize interactions with the patient by reducing distractions during the preparation and measurement phases and freeing up time for the health care professional. “To [check for a] fever, we use the appropriate thermometer in the appropriate location. We should do the same for blood pressure,” she added.
The STRIDE-BP database, which is affiliated with the European Society of Hypertension, the International Society of Hypertension, and the World Hypertension League, contains an updated list of validated devices for measuring blood pressure.
The signers of the consensus likewise recognized that, beyond taking blood pressure measurements during office visits, the best measurements are those taken at home outside the context of medical care (doctor’s office or clinic) and that the same recommendations are directly applicable. “Few diseases can be detected so easily as with a simple at-home assessment performed by the individual himself or herself. If after three consecutive measurements, readings above 140/90 mm Hg are obtained, the individual should see the doctor to set up a comprehensive treatment program,” said Pablo Rodríguez, MD, secretary of the Argentinian Society of Hypertension. From now through September 14 (Day for Patients With Hypertension), the society is conducting a campaign to take blood pressure measurements at different locations across the country.
Dr. Zilberman and Dr. López-Jiménez disclosed no relevant financial relationships.
This article was translated from the Medscape Spanish Edition. A version appeared on Medscape.com.
Insufficient blood pressure measurement during medical consultation, use of an inadequate technique for its determination, and lack of validated automatic sphygmomanometers are three problems that convergently complicate the diagnosis and control of arterial hypertension in the Americas, a silent disease that affects 180 million people in the region and is the main risk factor for cardiovascular diseases, said the Pan American Health Organization.
Jarbas Barbosa, MD, MPH, PhD, director of PAHO, said in an interview: “We don’t have specific data for each of these scenarios, but unfortunately, all three doubtless work together to make the situation worse.
“Often, the staff members at our primary care clinics are not prepared to diagnose and treat hypertension, because there aren’t national protocols to raise awareness and prepare them to provide this care to the correct standard. Also, they are often unqualified to take blood pressure readings properly,” he added.
This concern is reflected in the theme the organization chose for World Hypertension Day, which was observed on May 17: Measure your blood pressure accurately, control it, live longer! “We shouldn’t underestimate the importance of taking blood pressure,” warned Silvana Luciani, chief of PAHO’s noncommunicable diseases, violence, and injury prevention unit. But, the experts stressed, it must be done correctly.
Time no problem
It’s important to raise awareness of the value of blood pressure measurement for the general population. However, as multiple studies have shown, one barrier to detecting and controlling hypertension is that doctors and other health care professionals measure blood pressure less frequently in clinic than expected, or they use inappropriate techniques or obsolete or uncalibrated measurement devices.
“The importance of clinic blood pressure measurement has been recognized for many decades, but adherence to guidelines on proper, standardized blood pressure measurement remains uncommon in clinical practice,” concluded a consensus document signed by 25 experts from 13 institutions in the United States, Australia, Germany, the United Kingdom, Canada, Italy, Belgium, and Greece.
The first problem lies in the low quantity of measurements. A recent study in Argentina of nearly 3,000 visits to the doctor’s office at nine health care centers showed that doctors took blood pressure readings in only once in every seven encounters. Even cardiologists, the specialists with the best performance, did so only half of the time.
“Several factors can come into play: lack of awareness, medical inertia, or lack of appropriate equipment. But it is not for lack of time. How long does it take to take blood pressure three times within a 1-minute interval, with the patient seated and their back supported, as indicated? Four minutes. That’s not very much,” said Judith Zilberman, MD, PhD, said in an interview. Dr. Zilberman leads the department of hypertension and the women’s cardiovascular disease area at the Argerich Hospital in Buenos Aires, and is the former chair of the Argentinian Society of Hypertension.
Patricio López-Jaramillo, MD, PhD, said in an interview that the greatest obstacle is the lack of awareness among physicians and other health care staff about the importance of taking proper blood pressure measurements. Dr. López-Jaramillo is president and scientific director of the MASIRA Research Institute at the University of Santander in Bucaramanga, Colombia, and first author of the Manual Práctico de Diagnóstico y Manejo de la Hipertensión Arterial (Practice Guidelines for Diagnosing and Managing Hypertension), published by the Latin American Hypertension Society.
“Medical schools are also responsible for this. They go over this topic very superficially during undergraduate and, even worse, postgraduate training. The lack of time to take correct measurements, or the lack of appropriate instruments, is secondary to this lack of awareness among most health care staff members,” added Dr. López-Jaramillo, who is one of the researchers of the PURE epidemiologic study. Since 2002, it has followed a cohort of 225,000 participants from 27 high-, mid-, and low-income countries.
Dr. Zilberman added that it would be good practice for all primary care physicians to take blood pressure readings regardless of the reason for the visit and whether patients have been diagnosed with hypertension or not. “If a woman goes to her gynecologist because she wants to get pregnant, her blood pressure should also be taken! And any other specialist should interview the patient, ascertain her history, what medications she’s on, and then ask if her blood pressure has been taken recently,” she recommended.
Measure well
The second factor to consider is that a correct technique should be used to take blood pressure readings in the doctor’s office or clinic so as not to produce inaccurate results that could lead to underdiagnosis, overdiagnosis, or a poor assessment of the patient’s response to prescribed treatments. An observational study performed in Uruguay in 2017 showed that only 5% of 302 blood pressure measurements followed appropriate procedures.
A new fact sheet from the PAHO lists the following eight requirements for obtaining an accurate reading: don’t have a conversation, support the arm at heart level, put the cuff on a bare arm, use the correct cuff size, support the feet, keep the legs uncrossed, ensure the patient has an empty bladder, and support the back.
Though most guidelines recommend taking three readings, the “pragmatic” focus proposed in the international consensus accepts at least two readings separated by a minimum of 30 seconds. The two readings should then be averaged out. There is evidence that simplified protocols can be used, at least for population screening.
The authors of the new document also recommend preparing the patient before taking the measurement. The patient should be asked not to smoke, exercise, or consume alcohol or caffeine for at least 30 minutes beforehand. He or she should rest for a period of 3-5 minutes without speaking or being spoken to before the measurement is taken.
Lastly, clinically validated automated measurement devices should be used, as called for by the PAHO HEARTS initiative in the Americas. “The sphygmomanometer or classic aneroid tensiometer for the auscultatory method, which is still used way too often at doctor’s office visits in the region, has many weaknesses – not only the device itself but also the way it’s used (human error). This produces a rounded, approximate reading,” stressed Dr. Zilberman.
Automated devices also minimize interactions with the patient by reducing distractions during the preparation and measurement phases and freeing up time for the health care professional. “To [check for a] fever, we use the appropriate thermometer in the appropriate location. We should do the same for blood pressure,” she added.
The STRIDE-BP database, which is affiliated with the European Society of Hypertension, the International Society of Hypertension, and the World Hypertension League, contains an updated list of validated devices for measuring blood pressure.
The signers of the consensus likewise recognized that, beyond taking blood pressure measurements during office visits, the best measurements are those taken at home outside the context of medical care (doctor’s office or clinic) and that the same recommendations are directly applicable. “Few diseases can be detected so easily as with a simple at-home assessment performed by the individual himself or herself. If after three consecutive measurements, readings above 140/90 mm Hg are obtained, the individual should see the doctor to set up a comprehensive treatment program,” said Pablo Rodríguez, MD, secretary of the Argentinian Society of Hypertension. From now through September 14 (Day for Patients With Hypertension), the society is conducting a campaign to take blood pressure measurements at different locations across the country.
Dr. Zilberman and Dr. López-Jiménez disclosed no relevant financial relationships.
This article was translated from the Medscape Spanish Edition. A version appeared on Medscape.com.
Insufficient blood pressure measurement during medical consultation, use of an inadequate technique for its determination, and lack of validated automatic sphygmomanometers are three problems that convergently complicate the diagnosis and control of arterial hypertension in the Americas, a silent disease that affects 180 million people in the region and is the main risk factor for cardiovascular diseases, said the Pan American Health Organization.
Jarbas Barbosa, MD, MPH, PhD, director of PAHO, said in an interview: “We don’t have specific data for each of these scenarios, but unfortunately, all three doubtless work together to make the situation worse.
“Often, the staff members at our primary care clinics are not prepared to diagnose and treat hypertension, because there aren’t national protocols to raise awareness and prepare them to provide this care to the correct standard. Also, they are often unqualified to take blood pressure readings properly,” he added.
This concern is reflected in the theme the organization chose for World Hypertension Day, which was observed on May 17: Measure your blood pressure accurately, control it, live longer! “We shouldn’t underestimate the importance of taking blood pressure,” warned Silvana Luciani, chief of PAHO’s noncommunicable diseases, violence, and injury prevention unit. But, the experts stressed, it must be done correctly.
Time no problem
It’s important to raise awareness of the value of blood pressure measurement for the general population. However, as multiple studies have shown, one barrier to detecting and controlling hypertension is that doctors and other health care professionals measure blood pressure less frequently in clinic than expected, or they use inappropriate techniques or obsolete or uncalibrated measurement devices.
“The importance of clinic blood pressure measurement has been recognized for many decades, but adherence to guidelines on proper, standardized blood pressure measurement remains uncommon in clinical practice,” concluded a consensus document signed by 25 experts from 13 institutions in the United States, Australia, Germany, the United Kingdom, Canada, Italy, Belgium, and Greece.
The first problem lies in the low quantity of measurements. A recent study in Argentina of nearly 3,000 visits to the doctor’s office at nine health care centers showed that doctors took blood pressure readings in only once in every seven encounters. Even cardiologists, the specialists with the best performance, did so only half of the time.
“Several factors can come into play: lack of awareness, medical inertia, or lack of appropriate equipment. But it is not for lack of time. How long does it take to take blood pressure three times within a 1-minute interval, with the patient seated and their back supported, as indicated? Four minutes. That’s not very much,” said Judith Zilberman, MD, PhD, said in an interview. Dr. Zilberman leads the department of hypertension and the women’s cardiovascular disease area at the Argerich Hospital in Buenos Aires, and is the former chair of the Argentinian Society of Hypertension.
Patricio López-Jaramillo, MD, PhD, said in an interview that the greatest obstacle is the lack of awareness among physicians and other health care staff about the importance of taking proper blood pressure measurements. Dr. López-Jaramillo is president and scientific director of the MASIRA Research Institute at the University of Santander in Bucaramanga, Colombia, and first author of the Manual Práctico de Diagnóstico y Manejo de la Hipertensión Arterial (Practice Guidelines for Diagnosing and Managing Hypertension), published by the Latin American Hypertension Society.
“Medical schools are also responsible for this. They go over this topic very superficially during undergraduate and, even worse, postgraduate training. The lack of time to take correct measurements, or the lack of appropriate instruments, is secondary to this lack of awareness among most health care staff members,” added Dr. López-Jaramillo, who is one of the researchers of the PURE epidemiologic study. Since 2002, it has followed a cohort of 225,000 participants from 27 high-, mid-, and low-income countries.
Dr. Zilberman added that it would be good practice for all primary care physicians to take blood pressure readings regardless of the reason for the visit and whether patients have been diagnosed with hypertension or not. “If a woman goes to her gynecologist because she wants to get pregnant, her blood pressure should also be taken! And any other specialist should interview the patient, ascertain her history, what medications she’s on, and then ask if her blood pressure has been taken recently,” she recommended.
Measure well
The second factor to consider is that a correct technique should be used to take blood pressure readings in the doctor’s office or clinic so as not to produce inaccurate results that could lead to underdiagnosis, overdiagnosis, or a poor assessment of the patient’s response to prescribed treatments. An observational study performed in Uruguay in 2017 showed that only 5% of 302 blood pressure measurements followed appropriate procedures.
A new fact sheet from the PAHO lists the following eight requirements for obtaining an accurate reading: don’t have a conversation, support the arm at heart level, put the cuff on a bare arm, use the correct cuff size, support the feet, keep the legs uncrossed, ensure the patient has an empty bladder, and support the back.
Though most guidelines recommend taking three readings, the “pragmatic” focus proposed in the international consensus accepts at least two readings separated by a minimum of 30 seconds. The two readings should then be averaged out. There is evidence that simplified protocols can be used, at least for population screening.
The authors of the new document also recommend preparing the patient before taking the measurement. The patient should be asked not to smoke, exercise, or consume alcohol or caffeine for at least 30 minutes beforehand. He or she should rest for a period of 3-5 minutes without speaking or being spoken to before the measurement is taken.
Lastly, clinically validated automated measurement devices should be used, as called for by the PAHO HEARTS initiative in the Americas. “The sphygmomanometer or classic aneroid tensiometer for the auscultatory method, which is still used way too often at doctor’s office visits in the region, has many weaknesses – not only the device itself but also the way it’s used (human error). This produces a rounded, approximate reading,” stressed Dr. Zilberman.
Automated devices also minimize interactions with the patient by reducing distractions during the preparation and measurement phases and freeing up time for the health care professional. “To [check for a] fever, we use the appropriate thermometer in the appropriate location. We should do the same for blood pressure,” she added.
The STRIDE-BP database, which is affiliated with the European Society of Hypertension, the International Society of Hypertension, and the World Hypertension League, contains an updated list of validated devices for measuring blood pressure.
The signers of the consensus likewise recognized that, beyond taking blood pressure measurements during office visits, the best measurements are those taken at home outside the context of medical care (doctor’s office or clinic) and that the same recommendations are directly applicable. “Few diseases can be detected so easily as with a simple at-home assessment performed by the individual himself or herself. If after three consecutive measurements, readings above 140/90 mm Hg are obtained, the individual should see the doctor to set up a comprehensive treatment program,” said Pablo Rodríguez, MD, secretary of the Argentinian Society of Hypertension. From now through September 14 (Day for Patients With Hypertension), the society is conducting a campaign to take blood pressure measurements at different locations across the country.
Dr. Zilberman and Dr. López-Jiménez disclosed no relevant financial relationships.
This article was translated from the Medscape Spanish Edition. A version appeared on Medscape.com.
When could you be sued for AI malpractice? You’re likely using it now
The ways in which artificial intelligence (AI) may transform the future of medicine is making headlines across the globe. But chances are, you’re already using AI in your practice every day – you may just not realize it.
And whether you recognize the presence of AI or not, the technology could be putting you in danger of a lawsuit, legal experts say.
“For physicians, AI has also not yet drastically changed or improved the way care is provided or consumed,” said Michael LeTang, chief nursing informatics officer and vice president of risk management and patient safety at Healthcare Risk Advisors, part of TDC Group. “Consequently, it may seem like AI is not present in their work streams, but in reality, it has been utilized in health care for several years. As AI technologies continue to develop and become more sophisticated, we can expect them to play an increasingly significant role in health care.”
Today, most AI applications in health care use narrow AI, which is designed to complete a single task without human assistance, as opposed to artificial general intelligence (AGI), which pertains to human-level reasoning and problem solving across a broad spectrum. Here are some ways doctors are using AI throughout the day – sometimes being aware of its assistance, and sometimes being unaware:
- Many doctors use electronic health records (EHRs) with integrated AI that include computerized clinical decision support tools designed to reduce the risk of diagnostic error and to integrate decision-making in the medication ordering function.
- Cardiologists, pathologists, and dermatologists use AI in the interpretation of vast amounts of images, tracings, and complex patterns.
- Surgeons are using AI-enhanced surgical robotics for orthopedic surgeries, such as joint replacement and spine surgery.
- A growing number of doctors are using ChatGPT to assist in drafting prior authorization letters for insurers. Experts say more doctors are also experimenting with ChatGPT to support medical decision-making.
- Within oncology, physicians use machine learning techniques in the form of computer-aided detection systems for early breast cancer detection.
- AI algorithms are often used by health systems for workflow, staffing optimization, population management, and care coordination.
- Some systems within EHRs use AI to indicate high-risk patients.
- Physicians are using AI applications for the early recognition of sepsis, including EHR-integrated decision tools, such as the Hospital Corporation of America Healthcare’s Sepsis Prediction and Optimization Therapy and the Sepsis Early Risk Assessment algorithm.
- About 30% of radiologists use AI in their practice to analyze x-rays and CT scans.
- Epic Systems recently announced a partnership with Microsoft to integrate ChatGPT into MyChart, Epic’s patient portal system. Pilot hospitals will utilize ChatGPT to automatically generate responses to patient-generated questions sent via the portal.
The growth of AI in health care has been enormous, and it’s only going to continue, said Ravi B. Parikh, MD, an assistant professor in the department of medical ethics and health policy and medicine at the University of Pennsylvania, Philadelphia.
“What’s really critical is that physicians, clinicians, and nurses using AI are provided with the tools to understand how artificial intelligence works and, most importantly, understand that they are still accountable for making the ultimate decision,” Mr. LeTang said, “The information is not always going to be the right thing to do or the most accurate thing to do. They’re still liable for making a bad decision, even if AI is driving that.”
What are the top AI legal dangers of today?
A pressing legal risk is becoming too reliant on the suggestions that AI-based systems provide, which can lead to poor care decisions, said Kenneth Rashbaum, a New York–based cybersecurity attorney with more than 25 years of experience in medical malpractice defense.
This can occur, for example, when using clinical support systems that leverage AI, machine learning, or statistical pattern recognition. Today, clinical support systems are commonly administered through EHRs and other computerized clinical workflows. In general, such systems match a patient’s characteristics to a computerized clinical knowledge base. An assessment or recommendation is then presented to the physician for a decision.
“If the clinician blindly accepts it without considering whether it’s appropriate for this patient at this time with this presentation, the clinician may bear some responsibility if there is an untoward result,” Mr. Rashbaum said.
“A common claim even in the days before the EMR [electronic medical record] and AI, was that the clinician did not take all available information into account in rendering treatment, including history of past and present condition, as reflected in the records, communication with past and other present treating clinicians, lab and radiology results, discussions with the patient, and physical examination findings,” he said. “So, if the clinician relied upon the support prompt to the exclusion of these other sources of information, that could be a very strong argument for the plaintiff.”
Chatbots, such OpenAI’s ChatGPT, are another form of AI raising legal red flags. ChatGPT, trained on a massive set of text data, can carry out conversations, write code, draft emails, and answer any question posed. The chatbot has gained considerable credibility for accurately diagnosing rare conditions in seconds, and it recently passed the U.S. Medical Licensing Examination.
It’s unclear how many doctors are signing onto the ChatGPT website daily, but physicians are actively using the chatbot, particularly for assistance with prior authorization letters and to support decision-making processes in their practices, said Mr. LeTang.
When physicians ask ChatGPT a question, however, they should be mindful that ChatGPT could “hallucinate,” a term that refers to a generated response that sounds plausible but is factually incorrect or is unrelated to the context, explains Harvey Castro, MD, an emergency physician, ChatGPT health care expert, and author of the 2023 book “ChatGPT and Healthcare: Unlocking the Potential of Patient Empowerment.”
Acting on ChatGPT’s response without vetting the information places doctors at serious risk of a lawsuit, he said.
“Sometimes, the response is half true and half false,” he said. “Say, I go outside my specialty of emergency medicine and ask it about a pediatric surgical procedure. It could give me a response that sounds medically correct, but then I ask a pediatric cardiologist, and he says, ‘We don’t even do this. This doesn’t even exist!’ Physicians really have to make sure they are vetting the information provided.”
In response to ChatGPT’s growing usage by health care professionals, hospitals and practices are quickly implementing guidelines, policies, and restrictions that caution physicians about the accuracy of ChatGPT-generated information, adds Mr. LeTang.
Emerging best practices include avoiding the input of patient health information, personally identifiable information, or any data that could be commercially valuable or considered the intellectual property of a hospital or health system, he said.
“Another crucial guideline is not to rely solely on ChatGPT as a definitive source for clinical decision-making; physicians must exercise their professional judgment,” he said. “If best practices are not adhered to, the associated risks are present today. However, these risks may become more significant as AI technologies continue to evolve and become increasingly integrated into health care.”
The potential for misdiagnosis by AI systems and the risk of unnecessary procedures if physicians do not thoroughly evaluate and validate AI predictions are other dangers.
As an example, Mr. LeTang described a case in which a physician documents in the EHR that a patient has presented to the emergency department with chest pains and other signs of a heart attack, and an AI algorithm predicts that the patient is experiencing an active myocardial infarction. If the physician then sends the patient for stenting or an angioplasty without other concrete evidence or tests to confirm the diagnosis, the doctor could later face a misdiagnosis complaint if the costly procedures were unnecessary.
“That’s one of the risks of using artificial intelligence,” he said. “A large percentage of malpractice claims is failure to diagnose, delayed diagnosis, or inaccurate diagnosis. What falls in the category of failure to diagnose is sending a patient for an unnecessary procedure or having an adverse event or bad outcome because of the failure to diagnose.”
So far, no AI lawsuits have been filed, but they may make an appearance soon, said Sue Boisvert, senior patient safety risk manager at The Doctors Company, a national medical liability insurer.
“There are hundreds of AI programs currently in use in health care,” she said. “At some point, a provider will make a decision that is contrary to what the AI recommended. The AI may be wrong, or the provider may be wrong. Either way, the provider will neglect to document their clinical reasoning, a patient will be harmed, and we will have the first AI claim.”
Upcoming AI legal risks to watch for
Lawsuits that allege biased patient care by physicians on the basis of algorithmic bias may also be forthcoming, analysts warn.
Much has been written about algorithmic bias that compounds and worsens inequities in socioeconomic status, ethnicity, sexual orientation, and gender in health systems. In 2019, a groundbreaking article in Science shed light on commonly used algorithms that are considered racially biased and how health care professionals often use such information to make medical decisions.
No claims involving AI bias have come down the pipeline yet, but it’s an area to watch, said Ms. Boisvert. She noted a website that highlights complaints and accusations of AI bias, including in health care.
“We need to be sure the training of the AI is appropriate, current, and broad enough so that there is no bias in the AI when it’s participating in the decision-making,” said Ms. Boisvert. “Imagine if the AI is diagnosing based on a dataset that is not local. It doesn’t represent the population at that particular hospital, and it’s providing inaccurate information to the physicians who are then making decisions about treatment.”
In pain management, for example, there are known differences in how patients experience pain, Ms. Boisvert said. If AI was being used to develop an algorithm for how a particular patient’s postoperative pain should be managed, and the algorithm did not include the differences, the pain control for a certain patient could be inappropriate. A poor outcome resulting from the treatment could lead to a claim against the physician or hospital that used the biased AI system, she said.
In the future, as AI becomes more integrated and accepted in medicine, there may be a risk of legal complaints against doctors for not using AI, said Saurabh Jha, MD, an associate professor of radiology at the University of Pennsylvania, Philadelphia, and a scholar of AI in radiology.
“Ultimately, we might get to a place where AI starts helping physicians detect more or reduce the miss of certain conditions, and it becomes the standard of care,” Dr. Jha said. “For example, if it became part of the standard of care for pulmonary embolism [PE] detection, and you didn’t use it for PE detection, and there was a miss. That could put you at legal risk. We’re not at that stage yet, but that is one future possibility.”
Dr. Parikh envisions an even cloudier liability landscape as the potential grows for AI to control patient care decisions. In such a scenario, rather than just issuing an alert or prediction to a physician, the AI system could trigger an action.
For instance, if an algorithm is trained to predict sepsis and, once triggered, the AI could initiate a nurse-led rapid response or a change in patient care outside the clinician’s control, said Dr. Parikh, who coauthored a recent article on AI and medical liability in The Milbank Quarterly.
“That’s still very much the minority of how AI is being used, but as evidence is growing that AI-based diagnostic tools perform equivalent or even superior to physicians, these autonomous workflows are being considered,” Dr. Parikh said. “When the ultimate action upon the patient is more determined by the AI than what the clinician does, then I think the liability picture gets murkier, and we should be thinking about how we can respond to that from a liability framework.”
How you can prevent AI-related lawsuits
The first step to preventing an AI-related claim is being aware of when and how you are using AI.
Ensure you’re informed about how the AI was trained, Ms. Boisvert stresses.
“Ask questions!” she said. “Is the AI safe? Are the recommendations accurate? Does the AI perform better than current systems? In what way? What databases were used, and did the programmers consider bias? Do I understand how to use the results?”
Never blindly trust the AI but rather view it as a data point in a medical decision, said Dr. Parikh. Ensure that other sources of medical information are properly accessed and that best practices for your specialty are still being followed.
When using any form of AI, document your usage, adds Mr. Rashbaum. A record that clearly outlines how the physician incorporated the AI is critical if a claim later arises in which the doctor is accused of AI-related malpractice, he said.
“Indicating how the AI tool was used, why it was used, and that it was used in conjunction with available clinical information and the clinician’s best judgment could reduce the risk of being found responsible as a result of AI use in a particular case,” he said.
Use chatbots, such as ChatGPT, the way they were intended, as support tools, rather than definitive diagnostic instruments, adds Dr. Castro.
“Doctors should also be well-trained in interpreting and understanding the suggestions provided by ChatGPT and should use their clinical judgment and experience alongside the AI tool for more accurate decision-making,” he said.
In addition, because no AI insurance product exists on the market, physicians and organizations using AI – particularly for direct health care – should evaluate their current insurance or insurance-like products to determine where a claim involving AI might fall and whether the policy would respond, said Ms. Boisvert. The AI vendor/manufacturer will likely have indemnified themselves in the purchase and sale agreement or contract, she said.
It will also become increasingly important for medical practices, hospitals, and health systems to put in place strong data governance strategies, Mr. LeTang said.
“AI relies on good data,” he said. “A data governance strategy is a key component to making sure we understand where the data is coming from, what is represents, how accurate it is, if it’s reproducible, what controls are in place to ensure the right people have the right access, and that if we’re starting to use it to build algorithms, that it’s deidentified.”
While no malpractice claims associated with the use of AI have yet surfaced, this may change as legal courts catch up on the backlog of malpractice claims that were delayed because of COVID-19, and even more so as AI becomes more prevalent in health care, Mr. LeTang said.
“Similar to the attention that autonomous driving systems, like Tesla, receive when the system fails and accidents occur, we can be assured that media outlets will widely publicize AI-related medical adverse events,” he said. “It is crucial for health care professionals, AI developers, and regulatory authorities to work together to ensure the responsible use of AI in health care, with patient safety as the top priority. By doing so, they can mitigate the risks associated with AI implementation and minimize the potential for legal disputes arising from AI-related medical errors.”
A version of this article first appeared on Medscape.com.
The ways in which artificial intelligence (AI) may transform the future of medicine is making headlines across the globe. But chances are, you’re already using AI in your practice every day – you may just not realize it.
And whether you recognize the presence of AI or not, the technology could be putting you in danger of a lawsuit, legal experts say.
“For physicians, AI has also not yet drastically changed or improved the way care is provided or consumed,” said Michael LeTang, chief nursing informatics officer and vice president of risk management and patient safety at Healthcare Risk Advisors, part of TDC Group. “Consequently, it may seem like AI is not present in their work streams, but in reality, it has been utilized in health care for several years. As AI technologies continue to develop and become more sophisticated, we can expect them to play an increasingly significant role in health care.”
Today, most AI applications in health care use narrow AI, which is designed to complete a single task without human assistance, as opposed to artificial general intelligence (AGI), which pertains to human-level reasoning and problem solving across a broad spectrum. Here are some ways doctors are using AI throughout the day – sometimes being aware of its assistance, and sometimes being unaware:
- Many doctors use electronic health records (EHRs) with integrated AI that include computerized clinical decision support tools designed to reduce the risk of diagnostic error and to integrate decision-making in the medication ordering function.
- Cardiologists, pathologists, and dermatologists use AI in the interpretation of vast amounts of images, tracings, and complex patterns.
- Surgeons are using AI-enhanced surgical robotics for orthopedic surgeries, such as joint replacement and spine surgery.
- A growing number of doctors are using ChatGPT to assist in drafting prior authorization letters for insurers. Experts say more doctors are also experimenting with ChatGPT to support medical decision-making.
- Within oncology, physicians use machine learning techniques in the form of computer-aided detection systems for early breast cancer detection.
- AI algorithms are often used by health systems for workflow, staffing optimization, population management, and care coordination.
- Some systems within EHRs use AI to indicate high-risk patients.
- Physicians are using AI applications for the early recognition of sepsis, including EHR-integrated decision tools, such as the Hospital Corporation of America Healthcare’s Sepsis Prediction and Optimization Therapy and the Sepsis Early Risk Assessment algorithm.
- About 30% of radiologists use AI in their practice to analyze x-rays and CT scans.
- Epic Systems recently announced a partnership with Microsoft to integrate ChatGPT into MyChart, Epic’s patient portal system. Pilot hospitals will utilize ChatGPT to automatically generate responses to patient-generated questions sent via the portal.
The growth of AI in health care has been enormous, and it’s only going to continue, said Ravi B. Parikh, MD, an assistant professor in the department of medical ethics and health policy and medicine at the University of Pennsylvania, Philadelphia.
“What’s really critical is that physicians, clinicians, and nurses using AI are provided with the tools to understand how artificial intelligence works and, most importantly, understand that they are still accountable for making the ultimate decision,” Mr. LeTang said, “The information is not always going to be the right thing to do or the most accurate thing to do. They’re still liable for making a bad decision, even if AI is driving that.”
What are the top AI legal dangers of today?
A pressing legal risk is becoming too reliant on the suggestions that AI-based systems provide, which can lead to poor care decisions, said Kenneth Rashbaum, a New York–based cybersecurity attorney with more than 25 years of experience in medical malpractice defense.
This can occur, for example, when using clinical support systems that leverage AI, machine learning, or statistical pattern recognition. Today, clinical support systems are commonly administered through EHRs and other computerized clinical workflows. In general, such systems match a patient’s characteristics to a computerized clinical knowledge base. An assessment or recommendation is then presented to the physician for a decision.
“If the clinician blindly accepts it without considering whether it’s appropriate for this patient at this time with this presentation, the clinician may bear some responsibility if there is an untoward result,” Mr. Rashbaum said.
“A common claim even in the days before the EMR [electronic medical record] and AI, was that the clinician did not take all available information into account in rendering treatment, including history of past and present condition, as reflected in the records, communication with past and other present treating clinicians, lab and radiology results, discussions with the patient, and physical examination findings,” he said. “So, if the clinician relied upon the support prompt to the exclusion of these other sources of information, that could be a very strong argument for the plaintiff.”
Chatbots, such OpenAI’s ChatGPT, are another form of AI raising legal red flags. ChatGPT, trained on a massive set of text data, can carry out conversations, write code, draft emails, and answer any question posed. The chatbot has gained considerable credibility for accurately diagnosing rare conditions in seconds, and it recently passed the U.S. Medical Licensing Examination.
It’s unclear how many doctors are signing onto the ChatGPT website daily, but physicians are actively using the chatbot, particularly for assistance with prior authorization letters and to support decision-making processes in their practices, said Mr. LeTang.
When physicians ask ChatGPT a question, however, they should be mindful that ChatGPT could “hallucinate,” a term that refers to a generated response that sounds plausible but is factually incorrect or is unrelated to the context, explains Harvey Castro, MD, an emergency physician, ChatGPT health care expert, and author of the 2023 book “ChatGPT and Healthcare: Unlocking the Potential of Patient Empowerment.”
Acting on ChatGPT’s response without vetting the information places doctors at serious risk of a lawsuit, he said.
“Sometimes, the response is half true and half false,” he said. “Say, I go outside my specialty of emergency medicine and ask it about a pediatric surgical procedure. It could give me a response that sounds medically correct, but then I ask a pediatric cardiologist, and he says, ‘We don’t even do this. This doesn’t even exist!’ Physicians really have to make sure they are vetting the information provided.”
In response to ChatGPT’s growing usage by health care professionals, hospitals and practices are quickly implementing guidelines, policies, and restrictions that caution physicians about the accuracy of ChatGPT-generated information, adds Mr. LeTang.
Emerging best practices include avoiding the input of patient health information, personally identifiable information, or any data that could be commercially valuable or considered the intellectual property of a hospital or health system, he said.
“Another crucial guideline is not to rely solely on ChatGPT as a definitive source for clinical decision-making; physicians must exercise their professional judgment,” he said. “If best practices are not adhered to, the associated risks are present today. However, these risks may become more significant as AI technologies continue to evolve and become increasingly integrated into health care.”
The potential for misdiagnosis by AI systems and the risk of unnecessary procedures if physicians do not thoroughly evaluate and validate AI predictions are other dangers.
As an example, Mr. LeTang described a case in which a physician documents in the EHR that a patient has presented to the emergency department with chest pains and other signs of a heart attack, and an AI algorithm predicts that the patient is experiencing an active myocardial infarction. If the physician then sends the patient for stenting or an angioplasty without other concrete evidence or tests to confirm the diagnosis, the doctor could later face a misdiagnosis complaint if the costly procedures were unnecessary.
“That’s one of the risks of using artificial intelligence,” he said. “A large percentage of malpractice claims is failure to diagnose, delayed diagnosis, or inaccurate diagnosis. What falls in the category of failure to diagnose is sending a patient for an unnecessary procedure or having an adverse event or bad outcome because of the failure to diagnose.”
So far, no AI lawsuits have been filed, but they may make an appearance soon, said Sue Boisvert, senior patient safety risk manager at The Doctors Company, a national medical liability insurer.
“There are hundreds of AI programs currently in use in health care,” she said. “At some point, a provider will make a decision that is contrary to what the AI recommended. The AI may be wrong, or the provider may be wrong. Either way, the provider will neglect to document their clinical reasoning, a patient will be harmed, and we will have the first AI claim.”
Upcoming AI legal risks to watch for
Lawsuits that allege biased patient care by physicians on the basis of algorithmic bias may also be forthcoming, analysts warn.
Much has been written about algorithmic bias that compounds and worsens inequities in socioeconomic status, ethnicity, sexual orientation, and gender in health systems. In 2019, a groundbreaking article in Science shed light on commonly used algorithms that are considered racially biased and how health care professionals often use such information to make medical decisions.
No claims involving AI bias have come down the pipeline yet, but it’s an area to watch, said Ms. Boisvert. She noted a website that highlights complaints and accusations of AI bias, including in health care.
“We need to be sure the training of the AI is appropriate, current, and broad enough so that there is no bias in the AI when it’s participating in the decision-making,” said Ms. Boisvert. “Imagine if the AI is diagnosing based on a dataset that is not local. It doesn’t represent the population at that particular hospital, and it’s providing inaccurate information to the physicians who are then making decisions about treatment.”
In pain management, for example, there are known differences in how patients experience pain, Ms. Boisvert said. If AI was being used to develop an algorithm for how a particular patient’s postoperative pain should be managed, and the algorithm did not include the differences, the pain control for a certain patient could be inappropriate. A poor outcome resulting from the treatment could lead to a claim against the physician or hospital that used the biased AI system, she said.
In the future, as AI becomes more integrated and accepted in medicine, there may be a risk of legal complaints against doctors for not using AI, said Saurabh Jha, MD, an associate professor of radiology at the University of Pennsylvania, Philadelphia, and a scholar of AI in radiology.
“Ultimately, we might get to a place where AI starts helping physicians detect more or reduce the miss of certain conditions, and it becomes the standard of care,” Dr. Jha said. “For example, if it became part of the standard of care for pulmonary embolism [PE] detection, and you didn’t use it for PE detection, and there was a miss. That could put you at legal risk. We’re not at that stage yet, but that is one future possibility.”
Dr. Parikh envisions an even cloudier liability landscape as the potential grows for AI to control patient care decisions. In such a scenario, rather than just issuing an alert or prediction to a physician, the AI system could trigger an action.
For instance, if an algorithm is trained to predict sepsis and, once triggered, the AI could initiate a nurse-led rapid response or a change in patient care outside the clinician’s control, said Dr. Parikh, who coauthored a recent article on AI and medical liability in The Milbank Quarterly.
“That’s still very much the minority of how AI is being used, but as evidence is growing that AI-based diagnostic tools perform equivalent or even superior to physicians, these autonomous workflows are being considered,” Dr. Parikh said. “When the ultimate action upon the patient is more determined by the AI than what the clinician does, then I think the liability picture gets murkier, and we should be thinking about how we can respond to that from a liability framework.”
How you can prevent AI-related lawsuits
The first step to preventing an AI-related claim is being aware of when and how you are using AI.
Ensure you’re informed about how the AI was trained, Ms. Boisvert stresses.
“Ask questions!” she said. “Is the AI safe? Are the recommendations accurate? Does the AI perform better than current systems? In what way? What databases were used, and did the programmers consider bias? Do I understand how to use the results?”
Never blindly trust the AI but rather view it as a data point in a medical decision, said Dr. Parikh. Ensure that other sources of medical information are properly accessed and that best practices for your specialty are still being followed.
When using any form of AI, document your usage, adds Mr. Rashbaum. A record that clearly outlines how the physician incorporated the AI is critical if a claim later arises in which the doctor is accused of AI-related malpractice, he said.
“Indicating how the AI tool was used, why it was used, and that it was used in conjunction with available clinical information and the clinician’s best judgment could reduce the risk of being found responsible as a result of AI use in a particular case,” he said.
Use chatbots, such as ChatGPT, the way they were intended, as support tools, rather than definitive diagnostic instruments, adds Dr. Castro.
“Doctors should also be well-trained in interpreting and understanding the suggestions provided by ChatGPT and should use their clinical judgment and experience alongside the AI tool for more accurate decision-making,” he said.
In addition, because no AI insurance product exists on the market, physicians and organizations using AI – particularly for direct health care – should evaluate their current insurance or insurance-like products to determine where a claim involving AI might fall and whether the policy would respond, said Ms. Boisvert. The AI vendor/manufacturer will likely have indemnified themselves in the purchase and sale agreement or contract, she said.
It will also become increasingly important for medical practices, hospitals, and health systems to put in place strong data governance strategies, Mr. LeTang said.
“AI relies on good data,” he said. “A data governance strategy is a key component to making sure we understand where the data is coming from, what is represents, how accurate it is, if it’s reproducible, what controls are in place to ensure the right people have the right access, and that if we’re starting to use it to build algorithms, that it’s deidentified.”
While no malpractice claims associated with the use of AI have yet surfaced, this may change as legal courts catch up on the backlog of malpractice claims that were delayed because of COVID-19, and even more so as AI becomes more prevalent in health care, Mr. LeTang said.
“Similar to the attention that autonomous driving systems, like Tesla, receive when the system fails and accidents occur, we can be assured that media outlets will widely publicize AI-related medical adverse events,” he said. “It is crucial for health care professionals, AI developers, and regulatory authorities to work together to ensure the responsible use of AI in health care, with patient safety as the top priority. By doing so, they can mitigate the risks associated with AI implementation and minimize the potential for legal disputes arising from AI-related medical errors.”
A version of this article first appeared on Medscape.com.
The ways in which artificial intelligence (AI) may transform the future of medicine is making headlines across the globe. But chances are, you’re already using AI in your practice every day – you may just not realize it.
And whether you recognize the presence of AI or not, the technology could be putting you in danger of a lawsuit, legal experts say.
“For physicians, AI has also not yet drastically changed or improved the way care is provided or consumed,” said Michael LeTang, chief nursing informatics officer and vice president of risk management and patient safety at Healthcare Risk Advisors, part of TDC Group. “Consequently, it may seem like AI is not present in their work streams, but in reality, it has been utilized in health care for several years. As AI technologies continue to develop and become more sophisticated, we can expect them to play an increasingly significant role in health care.”
Today, most AI applications in health care use narrow AI, which is designed to complete a single task without human assistance, as opposed to artificial general intelligence (AGI), which pertains to human-level reasoning and problem solving across a broad spectrum. Here are some ways doctors are using AI throughout the day – sometimes being aware of its assistance, and sometimes being unaware:
- Many doctors use electronic health records (EHRs) with integrated AI that include computerized clinical decision support tools designed to reduce the risk of diagnostic error and to integrate decision-making in the medication ordering function.
- Cardiologists, pathologists, and dermatologists use AI in the interpretation of vast amounts of images, tracings, and complex patterns.
- Surgeons are using AI-enhanced surgical robotics for orthopedic surgeries, such as joint replacement and spine surgery.
- A growing number of doctors are using ChatGPT to assist in drafting prior authorization letters for insurers. Experts say more doctors are also experimenting with ChatGPT to support medical decision-making.
- Within oncology, physicians use machine learning techniques in the form of computer-aided detection systems for early breast cancer detection.
- AI algorithms are often used by health systems for workflow, staffing optimization, population management, and care coordination.
- Some systems within EHRs use AI to indicate high-risk patients.
- Physicians are using AI applications for the early recognition of sepsis, including EHR-integrated decision tools, such as the Hospital Corporation of America Healthcare’s Sepsis Prediction and Optimization Therapy and the Sepsis Early Risk Assessment algorithm.
- About 30% of radiologists use AI in their practice to analyze x-rays and CT scans.
- Epic Systems recently announced a partnership with Microsoft to integrate ChatGPT into MyChart, Epic’s patient portal system. Pilot hospitals will utilize ChatGPT to automatically generate responses to patient-generated questions sent via the portal.
The growth of AI in health care has been enormous, and it’s only going to continue, said Ravi B. Parikh, MD, an assistant professor in the department of medical ethics and health policy and medicine at the University of Pennsylvania, Philadelphia.
“What’s really critical is that physicians, clinicians, and nurses using AI are provided with the tools to understand how artificial intelligence works and, most importantly, understand that they are still accountable for making the ultimate decision,” Mr. LeTang said, “The information is not always going to be the right thing to do or the most accurate thing to do. They’re still liable for making a bad decision, even if AI is driving that.”
What are the top AI legal dangers of today?
A pressing legal risk is becoming too reliant on the suggestions that AI-based systems provide, which can lead to poor care decisions, said Kenneth Rashbaum, a New York–based cybersecurity attorney with more than 25 years of experience in medical malpractice defense.
This can occur, for example, when using clinical support systems that leverage AI, machine learning, or statistical pattern recognition. Today, clinical support systems are commonly administered through EHRs and other computerized clinical workflows. In general, such systems match a patient’s characteristics to a computerized clinical knowledge base. An assessment or recommendation is then presented to the physician for a decision.
“If the clinician blindly accepts it without considering whether it’s appropriate for this patient at this time with this presentation, the clinician may bear some responsibility if there is an untoward result,” Mr. Rashbaum said.
“A common claim even in the days before the EMR [electronic medical record] and AI, was that the clinician did not take all available information into account in rendering treatment, including history of past and present condition, as reflected in the records, communication with past and other present treating clinicians, lab and radiology results, discussions with the patient, and physical examination findings,” he said. “So, if the clinician relied upon the support prompt to the exclusion of these other sources of information, that could be a very strong argument for the plaintiff.”
Chatbots, such OpenAI’s ChatGPT, are another form of AI raising legal red flags. ChatGPT, trained on a massive set of text data, can carry out conversations, write code, draft emails, and answer any question posed. The chatbot has gained considerable credibility for accurately diagnosing rare conditions in seconds, and it recently passed the U.S. Medical Licensing Examination.
It’s unclear how many doctors are signing onto the ChatGPT website daily, but physicians are actively using the chatbot, particularly for assistance with prior authorization letters and to support decision-making processes in their practices, said Mr. LeTang.
When physicians ask ChatGPT a question, however, they should be mindful that ChatGPT could “hallucinate,” a term that refers to a generated response that sounds plausible but is factually incorrect or is unrelated to the context, explains Harvey Castro, MD, an emergency physician, ChatGPT health care expert, and author of the 2023 book “ChatGPT and Healthcare: Unlocking the Potential of Patient Empowerment.”
Acting on ChatGPT’s response without vetting the information places doctors at serious risk of a lawsuit, he said.
“Sometimes, the response is half true and half false,” he said. “Say, I go outside my specialty of emergency medicine and ask it about a pediatric surgical procedure. It could give me a response that sounds medically correct, but then I ask a pediatric cardiologist, and he says, ‘We don’t even do this. This doesn’t even exist!’ Physicians really have to make sure they are vetting the information provided.”
In response to ChatGPT’s growing usage by health care professionals, hospitals and practices are quickly implementing guidelines, policies, and restrictions that caution physicians about the accuracy of ChatGPT-generated information, adds Mr. LeTang.
Emerging best practices include avoiding the input of patient health information, personally identifiable information, or any data that could be commercially valuable or considered the intellectual property of a hospital or health system, he said.
“Another crucial guideline is not to rely solely on ChatGPT as a definitive source for clinical decision-making; physicians must exercise their professional judgment,” he said. “If best practices are not adhered to, the associated risks are present today. However, these risks may become more significant as AI technologies continue to evolve and become increasingly integrated into health care.”
The potential for misdiagnosis by AI systems and the risk of unnecessary procedures if physicians do not thoroughly evaluate and validate AI predictions are other dangers.
As an example, Mr. LeTang described a case in which a physician documents in the EHR that a patient has presented to the emergency department with chest pains and other signs of a heart attack, and an AI algorithm predicts that the patient is experiencing an active myocardial infarction. If the physician then sends the patient for stenting or an angioplasty without other concrete evidence or tests to confirm the diagnosis, the doctor could later face a misdiagnosis complaint if the costly procedures were unnecessary.
“That’s one of the risks of using artificial intelligence,” he said. “A large percentage of malpractice claims is failure to diagnose, delayed diagnosis, or inaccurate diagnosis. What falls in the category of failure to diagnose is sending a patient for an unnecessary procedure or having an adverse event or bad outcome because of the failure to diagnose.”
So far, no AI lawsuits have been filed, but they may make an appearance soon, said Sue Boisvert, senior patient safety risk manager at The Doctors Company, a national medical liability insurer.
“There are hundreds of AI programs currently in use in health care,” she said. “At some point, a provider will make a decision that is contrary to what the AI recommended. The AI may be wrong, or the provider may be wrong. Either way, the provider will neglect to document their clinical reasoning, a patient will be harmed, and we will have the first AI claim.”
Upcoming AI legal risks to watch for
Lawsuits that allege biased patient care by physicians on the basis of algorithmic bias may also be forthcoming, analysts warn.
Much has been written about algorithmic bias that compounds and worsens inequities in socioeconomic status, ethnicity, sexual orientation, and gender in health systems. In 2019, a groundbreaking article in Science shed light on commonly used algorithms that are considered racially biased and how health care professionals often use such information to make medical decisions.
No claims involving AI bias have come down the pipeline yet, but it’s an area to watch, said Ms. Boisvert. She noted a website that highlights complaints and accusations of AI bias, including in health care.
“We need to be sure the training of the AI is appropriate, current, and broad enough so that there is no bias in the AI when it’s participating in the decision-making,” said Ms. Boisvert. “Imagine if the AI is diagnosing based on a dataset that is not local. It doesn’t represent the population at that particular hospital, and it’s providing inaccurate information to the physicians who are then making decisions about treatment.”
In pain management, for example, there are known differences in how patients experience pain, Ms. Boisvert said. If AI was being used to develop an algorithm for how a particular patient’s postoperative pain should be managed, and the algorithm did not include the differences, the pain control for a certain patient could be inappropriate. A poor outcome resulting from the treatment could lead to a claim against the physician or hospital that used the biased AI system, she said.
In the future, as AI becomes more integrated and accepted in medicine, there may be a risk of legal complaints against doctors for not using AI, said Saurabh Jha, MD, an associate professor of radiology at the University of Pennsylvania, Philadelphia, and a scholar of AI in radiology.
“Ultimately, we might get to a place where AI starts helping physicians detect more or reduce the miss of certain conditions, and it becomes the standard of care,” Dr. Jha said. “For example, if it became part of the standard of care for pulmonary embolism [PE] detection, and you didn’t use it for PE detection, and there was a miss. That could put you at legal risk. We’re not at that stage yet, but that is one future possibility.”
Dr. Parikh envisions an even cloudier liability landscape as the potential grows for AI to control patient care decisions. In such a scenario, rather than just issuing an alert or prediction to a physician, the AI system could trigger an action.
For instance, if an algorithm is trained to predict sepsis and, once triggered, the AI could initiate a nurse-led rapid response or a change in patient care outside the clinician’s control, said Dr. Parikh, who coauthored a recent article on AI and medical liability in The Milbank Quarterly.
“That’s still very much the minority of how AI is being used, but as evidence is growing that AI-based diagnostic tools perform equivalent or even superior to physicians, these autonomous workflows are being considered,” Dr. Parikh said. “When the ultimate action upon the patient is more determined by the AI than what the clinician does, then I think the liability picture gets murkier, and we should be thinking about how we can respond to that from a liability framework.”
How you can prevent AI-related lawsuits
The first step to preventing an AI-related claim is being aware of when and how you are using AI.
Ensure you’re informed about how the AI was trained, Ms. Boisvert stresses.
“Ask questions!” she said. “Is the AI safe? Are the recommendations accurate? Does the AI perform better than current systems? In what way? What databases were used, and did the programmers consider bias? Do I understand how to use the results?”
Never blindly trust the AI but rather view it as a data point in a medical decision, said Dr. Parikh. Ensure that other sources of medical information are properly accessed and that best practices for your specialty are still being followed.
When using any form of AI, document your usage, adds Mr. Rashbaum. A record that clearly outlines how the physician incorporated the AI is critical if a claim later arises in which the doctor is accused of AI-related malpractice, he said.
“Indicating how the AI tool was used, why it was used, and that it was used in conjunction with available clinical information and the clinician’s best judgment could reduce the risk of being found responsible as a result of AI use in a particular case,” he said.
Use chatbots, such as ChatGPT, the way they were intended, as support tools, rather than definitive diagnostic instruments, adds Dr. Castro.
“Doctors should also be well-trained in interpreting and understanding the suggestions provided by ChatGPT and should use their clinical judgment and experience alongside the AI tool for more accurate decision-making,” he said.
In addition, because no AI insurance product exists on the market, physicians and organizations using AI – particularly for direct health care – should evaluate their current insurance or insurance-like products to determine where a claim involving AI might fall and whether the policy would respond, said Ms. Boisvert. The AI vendor/manufacturer will likely have indemnified themselves in the purchase and sale agreement or contract, she said.
It will also become increasingly important for medical practices, hospitals, and health systems to put in place strong data governance strategies, Mr. LeTang said.
“AI relies on good data,” he said. “A data governance strategy is a key component to making sure we understand where the data is coming from, what is represents, how accurate it is, if it’s reproducible, what controls are in place to ensure the right people have the right access, and that if we’re starting to use it to build algorithms, that it’s deidentified.”
While no malpractice claims associated with the use of AI have yet surfaced, this may change as legal courts catch up on the backlog of malpractice claims that were delayed because of COVID-19, and even more so as AI becomes more prevalent in health care, Mr. LeTang said.
“Similar to the attention that autonomous driving systems, like Tesla, receive when the system fails and accidents occur, we can be assured that media outlets will widely publicize AI-related medical adverse events,” he said. “It is crucial for health care professionals, AI developers, and regulatory authorities to work together to ensure the responsible use of AI in health care, with patient safety as the top priority. By doing so, they can mitigate the risks associated with AI implementation and minimize the potential for legal disputes arising from AI-related medical errors.”
A version of this article first appeared on Medscape.com.
Antibiotics for acute exacerbation of COPD: It’s still controversial
In late 2021, the Rome Proposal for diagnosing acute exacerbations of chronic obstructive pulmonary disease (AECOPD) and grading their severity was published. The 2023 Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease (GOLD) Report has adopted the Rome Proposal criteria. Given that an endorsement by GOLD is tantamount to acceptance by clinicians, researchers, and policymakers alike, I guess we’re all using them now.
Anyone who’s ever cared for patients with COPD knows that treatment and reduction of exacerbations is how we improve outcomes. AECOPD are associated with considerable morbidity, greater health care utilization and costs, and a long-term decline in lung function. While we hope our pharmacotherapies improve symptoms, we know they reduce AECOPD. If our pharmacotherapies have any impact on mortality, it’s probably via AECOPD prevention.
Since antibiotic indications are tied to severity, using the Rome Proposal criteria may affect management in unpredictable ways. As such, it’s worth reviewing the data on antibiotics for AECOPD.
What do the data reveal?
To start, it’s important to note that GOLD doesn’t equate having an AECOPD with needing an antibiotic. I myself have conflated the diagnosis with the indication and thereby overprescribed. The bar for diagnosis is quite low. In previous GOLD summaries, any “change in respiratory symptoms” would warrant the AECOPD label. Although the Rome Proposal definition is more specific, it leaves room for liberal interpretation. It’s likely to have a greater effect on research than on clinical practice. My guess is that AECOPD prevalence doesn’t change.
The antibiotic hurdle is slightly higher than that for diagnosis but is equally open to interpretation. In part, that’s related to the inherent subjectivity of judging symptoms, sputum production, and changes in color, but it’s also because the data are so poor. The meta-analyses that have been used to establish the indications include fewer than 1000 patients spread across 10 to 11 trials. Thus, the individual trials are small, and the sample size remains nominal even after adding them together. The addition of antibiotics – and it doesn’t seem to matter which class, type, or duration – will decrease mortality and hospital length of stay. One study says these effects are limited to inpatients while the other does not. After reading GOLD 2013, GOLD 2023, and both the meta-analyses they used to support their recommendations, I’m still not sure who benefits. Do you have to be hospitalized? Is some sort of ventilatory support required? Does C-reactive protein help or not?
In accordance with the classic Anthonisen criteria, GOLD relies on sputum volume and color as evidence of a bacterial infection. Soon after GOLD 2023 was published, a meta-analysis found that sputum color isn’t particularly accurate for detecting bacterial infection. Because it doesn’t seem to matter which antibiotic class is used, I always thought we were using antibiotics for their magical, pleiotropic anti-inflammatory effects anyway. I didn’t think the presence of an actual bacterial infection was important. If I saw an infiltrate on chest x-ray, I’d change my diagnosis from AECOPD to community-acquired pneumonia (CAP) and switch to CAP coverage. I’ve been doing this so long that I swear it’s in a guideline somewhere, though admittedly I couldn’t find said guideline while reading for this piece.
Key takeaways
In summary, I believe that the guidance reflects the data, which is muddy. The Rome Proposal should be seen as just that – a framework for moving forward with AECOPD classification and antibiotic indications that will need to be refined over time as better data become available. In fact, they allow for a more objective, point-of-care assessment of severity that can be validated and tied to antibiotic benefits. The Rome criteria aren’t evidence-based; they’re a necessary first step toward creating the evidence.
In the meantime, if your AECOPD patients are hospitalized, they probably warrant an antibiotic. If they’re not, sputum changes may be a reasonable surrogate for a bacterial infection. Considerable uncertainty remains.
Aaron B. Holley, MD, is a professor of medicine at Uniformed Services University in Bethesda, Md., and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington. He reported conflicts of interest with Metapharm, CHEST College, and WebMD.
A version of this article first appeared on Medscape.com.
In late 2021, the Rome Proposal for diagnosing acute exacerbations of chronic obstructive pulmonary disease (AECOPD) and grading their severity was published. The 2023 Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease (GOLD) Report has adopted the Rome Proposal criteria. Given that an endorsement by GOLD is tantamount to acceptance by clinicians, researchers, and policymakers alike, I guess we’re all using them now.
Anyone who’s ever cared for patients with COPD knows that treatment and reduction of exacerbations is how we improve outcomes. AECOPD are associated with considerable morbidity, greater health care utilization and costs, and a long-term decline in lung function. While we hope our pharmacotherapies improve symptoms, we know they reduce AECOPD. If our pharmacotherapies have any impact on mortality, it’s probably via AECOPD prevention.
Since antibiotic indications are tied to severity, using the Rome Proposal criteria may affect management in unpredictable ways. As such, it’s worth reviewing the data on antibiotics for AECOPD.
What do the data reveal?
To start, it’s important to note that GOLD doesn’t equate having an AECOPD with needing an antibiotic. I myself have conflated the diagnosis with the indication and thereby overprescribed. The bar for diagnosis is quite low. In previous GOLD summaries, any “change in respiratory symptoms” would warrant the AECOPD label. Although the Rome Proposal definition is more specific, it leaves room for liberal interpretation. It’s likely to have a greater effect on research than on clinical practice. My guess is that AECOPD prevalence doesn’t change.
The antibiotic hurdle is slightly higher than that for diagnosis but is equally open to interpretation. In part, that’s related to the inherent subjectivity of judging symptoms, sputum production, and changes in color, but it’s also because the data are so poor. The meta-analyses that have been used to establish the indications include fewer than 1000 patients spread across 10 to 11 trials. Thus, the individual trials are small, and the sample size remains nominal even after adding them together. The addition of antibiotics – and it doesn’t seem to matter which class, type, or duration – will decrease mortality and hospital length of stay. One study says these effects are limited to inpatients while the other does not. After reading GOLD 2013, GOLD 2023, and both the meta-analyses they used to support their recommendations, I’m still not sure who benefits. Do you have to be hospitalized? Is some sort of ventilatory support required? Does C-reactive protein help or not?
In accordance with the classic Anthonisen criteria, GOLD relies on sputum volume and color as evidence of a bacterial infection. Soon after GOLD 2023 was published, a meta-analysis found that sputum color isn’t particularly accurate for detecting bacterial infection. Because it doesn’t seem to matter which antibiotic class is used, I always thought we were using antibiotics for their magical, pleiotropic anti-inflammatory effects anyway. I didn’t think the presence of an actual bacterial infection was important. If I saw an infiltrate on chest x-ray, I’d change my diagnosis from AECOPD to community-acquired pneumonia (CAP) and switch to CAP coverage. I’ve been doing this so long that I swear it’s in a guideline somewhere, though admittedly I couldn’t find said guideline while reading for this piece.
Key takeaways
In summary, I believe that the guidance reflects the data, which is muddy. The Rome Proposal should be seen as just that – a framework for moving forward with AECOPD classification and antibiotic indications that will need to be refined over time as better data become available. In fact, they allow for a more objective, point-of-care assessment of severity that can be validated and tied to antibiotic benefits. The Rome criteria aren’t evidence-based; they’re a necessary first step toward creating the evidence.
In the meantime, if your AECOPD patients are hospitalized, they probably warrant an antibiotic. If they’re not, sputum changes may be a reasonable surrogate for a bacterial infection. Considerable uncertainty remains.
Aaron B. Holley, MD, is a professor of medicine at Uniformed Services University in Bethesda, Md., and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington. He reported conflicts of interest with Metapharm, CHEST College, and WebMD.
A version of this article first appeared on Medscape.com.
In late 2021, the Rome Proposal for diagnosing acute exacerbations of chronic obstructive pulmonary disease (AECOPD) and grading their severity was published. The 2023 Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease (GOLD) Report has adopted the Rome Proposal criteria. Given that an endorsement by GOLD is tantamount to acceptance by clinicians, researchers, and policymakers alike, I guess we’re all using them now.
Anyone who’s ever cared for patients with COPD knows that treatment and reduction of exacerbations is how we improve outcomes. AECOPD are associated with considerable morbidity, greater health care utilization and costs, and a long-term decline in lung function. While we hope our pharmacotherapies improve symptoms, we know they reduce AECOPD. If our pharmacotherapies have any impact on mortality, it’s probably via AECOPD prevention.
Since antibiotic indications are tied to severity, using the Rome Proposal criteria may affect management in unpredictable ways. As such, it’s worth reviewing the data on antibiotics for AECOPD.
What do the data reveal?
To start, it’s important to note that GOLD doesn’t equate having an AECOPD with needing an antibiotic. I myself have conflated the diagnosis with the indication and thereby overprescribed. The bar for diagnosis is quite low. In previous GOLD summaries, any “change in respiratory symptoms” would warrant the AECOPD label. Although the Rome Proposal definition is more specific, it leaves room for liberal interpretation. It’s likely to have a greater effect on research than on clinical practice. My guess is that AECOPD prevalence doesn’t change.
The antibiotic hurdle is slightly higher than that for diagnosis but is equally open to interpretation. In part, that’s related to the inherent subjectivity of judging symptoms, sputum production, and changes in color, but it’s also because the data are so poor. The meta-analyses that have been used to establish the indications include fewer than 1000 patients spread across 10 to 11 trials. Thus, the individual trials are small, and the sample size remains nominal even after adding them together. The addition of antibiotics – and it doesn’t seem to matter which class, type, or duration – will decrease mortality and hospital length of stay. One study says these effects are limited to inpatients while the other does not. After reading GOLD 2013, GOLD 2023, and both the meta-analyses they used to support their recommendations, I’m still not sure who benefits. Do you have to be hospitalized? Is some sort of ventilatory support required? Does C-reactive protein help or not?
In accordance with the classic Anthonisen criteria, GOLD relies on sputum volume and color as evidence of a bacterial infection. Soon after GOLD 2023 was published, a meta-analysis found that sputum color isn’t particularly accurate for detecting bacterial infection. Because it doesn’t seem to matter which antibiotic class is used, I always thought we were using antibiotics for their magical, pleiotropic anti-inflammatory effects anyway. I didn’t think the presence of an actual bacterial infection was important. If I saw an infiltrate on chest x-ray, I’d change my diagnosis from AECOPD to community-acquired pneumonia (CAP) and switch to CAP coverage. I’ve been doing this so long that I swear it’s in a guideline somewhere, though admittedly I couldn’t find said guideline while reading for this piece.
Key takeaways
In summary, I believe that the guidance reflects the data, which is muddy. The Rome Proposal should be seen as just that – a framework for moving forward with AECOPD classification and antibiotic indications that will need to be refined over time as better data become available. In fact, they allow for a more objective, point-of-care assessment of severity that can be validated and tied to antibiotic benefits. The Rome criteria aren’t evidence-based; they’re a necessary first step toward creating the evidence.
In the meantime, if your AECOPD patients are hospitalized, they probably warrant an antibiotic. If they’re not, sputum changes may be a reasonable surrogate for a bacterial infection. Considerable uncertainty remains.
Aaron B. Holley, MD, is a professor of medicine at Uniformed Services University in Bethesda, Md., and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington. He reported conflicts of interest with Metapharm, CHEST College, and WebMD.
A version of this article first appeared on Medscape.com.
Blood biomarker may help predict who will develop Alzheimer’s
A blood biomarker that measures astrocyte reactivity may help determine who, among cognitively unimpaired older adults with amyloid-beta, will go on to develop Alzheimer’s disease (AD), new research suggests.
Investigators tested the blood of 1,000 cognitively healthy individuals with and without amyloid-beta pathology and found that only those with a combination of amyloid-beta burden and abnormal astrocyte activation subsequently progressed to AD.
“Our study argues that testing for the presence of brain amyloid along with blood biomarkers of astrocyte reactivity is the optimal screening to identify patients who are most at risk for progressing to Alzheimer’s disease,” senior investigator Tharick A. Pascoal, MD, PhD, associate professor of psychiatry and neurology, University of Pittsburgh, said in a release.
At this point, the biomarker is a research tool, but its application in clinical practice “is not very far away,” Dr. Pascoal told this news organization.
The study was published online in Nature Medicine.
Multicenter study
In AD, accumulation of amyloid-beta in the brain precedes tau pathology, but not everyone with amyloid-beta develops tau, and, consequently, clinical symptoms. Approximately 30% of older adults have brain amyloid but many never progress to AD, said Dr. Pascoal.
This suggests other biological processes may trigger the deleterious effects of amyloid-beta in the early stages of AD.
Finding predictive markers of early amyloid-beta–related tau pathology would help identify cognitively normal individuals who are more likely to develop AD.
Post-mortem studies show astrocyte reactivity – changes in glial cells in the brain and spinal cord because of an insult in the brain – is an early AD abnormality. Other research suggests a close link between amyloid-beta, astrocyte reactivity, and tau.
In addition, evidence suggests plasma measures of glial fibrillary acidic protein (GFAP) could be a strong proxy of astrocyte reactivity in the brain. Dr. Pascoal explained that when astrocytes are changed or become bigger, more GFAP is released.
The study included 1,016 cognitively normal individuals from three centers; some had amyloid pathology, some did not. Participants’ mean age was 69.6 years, and all were deemed negative or positive for astrocyte reactivity based on plasma GFAP levels.
Results showed amyloid-beta is associated with increased plasma phosphorylated tau only in individuals positive for astrocyte reactivity. In addition, analyses using PET scans showed an AD-like pattern of tau tangle accumulation as a function of amyloid-beta exclusively in those same individuals.
Early upstream event
The findings suggest abnormalities in astrocyte reactivity is an early upstream event that likely occurs prior to tau pathology, which is closely related to the development of neurodegeneration and cognitive decline.
It’s likely many types of insults or processes can lead to astrocyte reactivity, possibly including COVID, but more research in this area is needed, said Dr. Pascoal.
“Our study only looked at the consequence of having both amyloid and astrocyte reactivity; it did not elucidate what is causing either of them,” he said.
Although “we were able to have very good results” in the current study, additional studies are needed to better establish the cut-off for GFAP levels that signal progression, said Dr. Pascoal.
The effect of astrocyte reactivity on the association between amyloid-beta and tau phosphorylation was greater in men than women. Dr. Pascoal noted anti-amyloid therapies, which might be modifying the amyloid-beta-astrocyte-tau pathway, tend to have a much larger effect in men than women.
Further studies that measure amyloid-beta, tau, and GFAP biomarkers at multiple timepoints, and with long follow-up, are needed, the investigators note.
The results may have implications for clinical trials, which have increasingly focused on individuals in the earliest preclinical phases of AD. Future studies should include cognitively normal patients who are positive for both amyloid pathology and astrocyte reactivity but have no overt p-tau abnormality, said Dr. Pascoal.
This may provide a time window for interventions very early in the disease process in those at increased risk for AD-related progression.
The study did not determine whether participants with both amyloid and astrocyte reactivity will inevitably develop AD, and to do so would require a longer follow up. “Our outcome was correlation to tau in the brain, which is something we know will lead to AD.”
Although the cohort represents significant socioeconomic diversity, a main limitation of the study was that subjects were mainly White, which limits the generalizability of the findings to a more diverse population.
The study received support from the National Institute of Aging; National Heart Lung and Blood Institute; Alzheimer’s Association; Fonds de Recherche du Québec-Santé; Canadian Consortium of Neurodegeneration in Aging; Weston Brain Institute; Colin Adair Charitable Foundation; Swedish Research Council; Wallenberg Scholar; BrightFocus Foundation; Swedish Alzheimer Foundation; Swedish Brain Foundation; Agneta Prytz-Folkes & Gösta Folkes Foundation; European Union; Swedish State Support for Clinical Research; Alzheimer Drug Discovery Foundation; Bluefield Project, the Olav Thon Foundation, the Erling-Persson Family Foundation, Stiftelsen för Gamla Tjänarinnor, Hjärnfonden, Sweden; the UK Dementia Research Institute at UCL; National Academy of Neuropsychology; Fundação de Amparo a pesquisa do Rio Grande do Sul; Instituto Serrapilheira; and Hjärnfonden.
Dr. Pascoal reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A blood biomarker that measures astrocyte reactivity may help determine who, among cognitively unimpaired older adults with amyloid-beta, will go on to develop Alzheimer’s disease (AD), new research suggests.
Investigators tested the blood of 1,000 cognitively healthy individuals with and without amyloid-beta pathology and found that only those with a combination of amyloid-beta burden and abnormal astrocyte activation subsequently progressed to AD.
“Our study argues that testing for the presence of brain amyloid along with blood biomarkers of astrocyte reactivity is the optimal screening to identify patients who are most at risk for progressing to Alzheimer’s disease,” senior investigator Tharick A. Pascoal, MD, PhD, associate professor of psychiatry and neurology, University of Pittsburgh, said in a release.
At this point, the biomarker is a research tool, but its application in clinical practice “is not very far away,” Dr. Pascoal told this news organization.
The study was published online in Nature Medicine.
Multicenter study
In AD, accumulation of amyloid-beta in the brain precedes tau pathology, but not everyone with amyloid-beta develops tau, and, consequently, clinical symptoms. Approximately 30% of older adults have brain amyloid but many never progress to AD, said Dr. Pascoal.
This suggests other biological processes may trigger the deleterious effects of amyloid-beta in the early stages of AD.
Finding predictive markers of early amyloid-beta–related tau pathology would help identify cognitively normal individuals who are more likely to develop AD.
Post-mortem studies show astrocyte reactivity – changes in glial cells in the brain and spinal cord because of an insult in the brain – is an early AD abnormality. Other research suggests a close link between amyloid-beta, astrocyte reactivity, and tau.
In addition, evidence suggests plasma measures of glial fibrillary acidic protein (GFAP) could be a strong proxy of astrocyte reactivity in the brain. Dr. Pascoal explained that when astrocytes are changed or become bigger, more GFAP is released.
The study included 1,016 cognitively normal individuals from three centers; some had amyloid pathology, some did not. Participants’ mean age was 69.6 years, and all were deemed negative or positive for astrocyte reactivity based on plasma GFAP levels.
Results showed amyloid-beta is associated with increased plasma phosphorylated tau only in individuals positive for astrocyte reactivity. In addition, analyses using PET scans showed an AD-like pattern of tau tangle accumulation as a function of amyloid-beta exclusively in those same individuals.
Early upstream event
The findings suggest abnormalities in astrocyte reactivity is an early upstream event that likely occurs prior to tau pathology, which is closely related to the development of neurodegeneration and cognitive decline.
It’s likely many types of insults or processes can lead to astrocyte reactivity, possibly including COVID, but more research in this area is needed, said Dr. Pascoal.
“Our study only looked at the consequence of having both amyloid and astrocyte reactivity; it did not elucidate what is causing either of them,” he said.
Although “we were able to have very good results” in the current study, additional studies are needed to better establish the cut-off for GFAP levels that signal progression, said Dr. Pascoal.
The effect of astrocyte reactivity on the association between amyloid-beta and tau phosphorylation was greater in men than women. Dr. Pascoal noted anti-amyloid therapies, which might be modifying the amyloid-beta-astrocyte-tau pathway, tend to have a much larger effect in men than women.
Further studies that measure amyloid-beta, tau, and GFAP biomarkers at multiple timepoints, and with long follow-up, are needed, the investigators note.
The results may have implications for clinical trials, which have increasingly focused on individuals in the earliest preclinical phases of AD. Future studies should include cognitively normal patients who are positive for both amyloid pathology and astrocyte reactivity but have no overt p-tau abnormality, said Dr. Pascoal.
This may provide a time window for interventions very early in the disease process in those at increased risk for AD-related progression.
The study did not determine whether participants with both amyloid and astrocyte reactivity will inevitably develop AD, and to do so would require a longer follow up. “Our outcome was correlation to tau in the brain, which is something we know will lead to AD.”
Although the cohort represents significant socioeconomic diversity, a main limitation of the study was that subjects were mainly White, which limits the generalizability of the findings to a more diverse population.
The study received support from the National Institute of Aging; National Heart Lung and Blood Institute; Alzheimer’s Association; Fonds de Recherche du Québec-Santé; Canadian Consortium of Neurodegeneration in Aging; Weston Brain Institute; Colin Adair Charitable Foundation; Swedish Research Council; Wallenberg Scholar; BrightFocus Foundation; Swedish Alzheimer Foundation; Swedish Brain Foundation; Agneta Prytz-Folkes & Gösta Folkes Foundation; European Union; Swedish State Support for Clinical Research; Alzheimer Drug Discovery Foundation; Bluefield Project, the Olav Thon Foundation, the Erling-Persson Family Foundation, Stiftelsen för Gamla Tjänarinnor, Hjärnfonden, Sweden; the UK Dementia Research Institute at UCL; National Academy of Neuropsychology; Fundação de Amparo a pesquisa do Rio Grande do Sul; Instituto Serrapilheira; and Hjärnfonden.
Dr. Pascoal reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A blood biomarker that measures astrocyte reactivity may help determine who, among cognitively unimpaired older adults with amyloid-beta, will go on to develop Alzheimer’s disease (AD), new research suggests.
Investigators tested the blood of 1,000 cognitively healthy individuals with and without amyloid-beta pathology and found that only those with a combination of amyloid-beta burden and abnormal astrocyte activation subsequently progressed to AD.
“Our study argues that testing for the presence of brain amyloid along with blood biomarkers of astrocyte reactivity is the optimal screening to identify patients who are most at risk for progressing to Alzheimer’s disease,” senior investigator Tharick A. Pascoal, MD, PhD, associate professor of psychiatry and neurology, University of Pittsburgh, said in a release.
At this point, the biomarker is a research tool, but its application in clinical practice “is not very far away,” Dr. Pascoal told this news organization.
The study was published online in Nature Medicine.
Multicenter study
In AD, accumulation of amyloid-beta in the brain precedes tau pathology, but not everyone with amyloid-beta develops tau, and, consequently, clinical symptoms. Approximately 30% of older adults have brain amyloid but many never progress to AD, said Dr. Pascoal.
This suggests other biological processes may trigger the deleterious effects of amyloid-beta in the early stages of AD.
Finding predictive markers of early amyloid-beta–related tau pathology would help identify cognitively normal individuals who are more likely to develop AD.
Post-mortem studies show astrocyte reactivity – changes in glial cells in the brain and spinal cord because of an insult in the brain – is an early AD abnormality. Other research suggests a close link between amyloid-beta, astrocyte reactivity, and tau.
In addition, evidence suggests plasma measures of glial fibrillary acidic protein (GFAP) could be a strong proxy of astrocyte reactivity in the brain. Dr. Pascoal explained that when astrocytes are changed or become bigger, more GFAP is released.
The study included 1,016 cognitively normal individuals from three centers; some had amyloid pathology, some did not. Participants’ mean age was 69.6 years, and all were deemed negative or positive for astrocyte reactivity based on plasma GFAP levels.
Results showed amyloid-beta is associated with increased plasma phosphorylated tau only in individuals positive for astrocyte reactivity. In addition, analyses using PET scans showed an AD-like pattern of tau tangle accumulation as a function of amyloid-beta exclusively in those same individuals.
Early upstream event
The findings suggest abnormalities in astrocyte reactivity is an early upstream event that likely occurs prior to tau pathology, which is closely related to the development of neurodegeneration and cognitive decline.
It’s likely many types of insults or processes can lead to astrocyte reactivity, possibly including COVID, but more research in this area is needed, said Dr. Pascoal.
“Our study only looked at the consequence of having both amyloid and astrocyte reactivity; it did not elucidate what is causing either of them,” he said.
Although “we were able to have very good results” in the current study, additional studies are needed to better establish the cut-off for GFAP levels that signal progression, said Dr. Pascoal.
The effect of astrocyte reactivity on the association between amyloid-beta and tau phosphorylation was greater in men than women. Dr. Pascoal noted anti-amyloid therapies, which might be modifying the amyloid-beta-astrocyte-tau pathway, tend to have a much larger effect in men than women.
Further studies that measure amyloid-beta, tau, and GFAP biomarkers at multiple timepoints, and with long follow-up, are needed, the investigators note.
The results may have implications for clinical trials, which have increasingly focused on individuals in the earliest preclinical phases of AD. Future studies should include cognitively normal patients who are positive for both amyloid pathology and astrocyte reactivity but have no overt p-tau abnormality, said Dr. Pascoal.
This may provide a time window for interventions very early in the disease process in those at increased risk for AD-related progression.
The study did not determine whether participants with both amyloid and astrocyte reactivity will inevitably develop AD, and to do so would require a longer follow up. “Our outcome was correlation to tau in the brain, which is something we know will lead to AD.”
Although the cohort represents significant socioeconomic diversity, a main limitation of the study was that subjects were mainly White, which limits the generalizability of the findings to a more diverse population.
The study received support from the National Institute of Aging; National Heart Lung and Blood Institute; Alzheimer’s Association; Fonds de Recherche du Québec-Santé; Canadian Consortium of Neurodegeneration in Aging; Weston Brain Institute; Colin Adair Charitable Foundation; Swedish Research Council; Wallenberg Scholar; BrightFocus Foundation; Swedish Alzheimer Foundation; Swedish Brain Foundation; Agneta Prytz-Folkes & Gösta Folkes Foundation; European Union; Swedish State Support for Clinical Research; Alzheimer Drug Discovery Foundation; Bluefield Project, the Olav Thon Foundation, the Erling-Persson Family Foundation, Stiftelsen för Gamla Tjänarinnor, Hjärnfonden, Sweden; the UK Dementia Research Institute at UCL; National Academy of Neuropsychology; Fundação de Amparo a pesquisa do Rio Grande do Sul; Instituto Serrapilheira; and Hjärnfonden.
Dr. Pascoal reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
How can we make medical training less ‘toxic’?
This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Joining me to discuss ways to address and reform the toxic culture associated with medical training is Dr. Amy Faith Ho, senior vice president of clinical informatics and analytics at Integrative Emergency Services in Dallas. Also joining us is Dr. Júlia Loyola Ferreira, a pediatric surgeon originally from Brazil, now practicing at Montreal Children’s and focused on advocacy for gender equity and patient-centered care.
Welcome to both of you. Thanks so much for joining me.
Amy Faith Ho, MD, MPH: Thanks so much for having us, Rob.
Dr. Glatter: Amy, I noticed a tweet recently where you talked about how your career choice was affected by the toxic environment in medical school, affecting your choice of residency. Can you elaborate on that?
Dr. Ho: In this instance, what we’re talking about is gender, but it can be directed toward any number of other groups as well.
What you’re alluding to is a tweet by Stanford Surgery Group showing the next residency class, and what was really stunning about this residency class was that it was almost all females. And this was something that took off on social media.
When I saw this, I was really brought back to one of my personal experiences that I chose to share, which was basically that, as a medical student, I really wanted to be a surgeon. I’m an emergency medicine doctor now, so you know that didn’t happen.
The story that I was sharing was that when I was a third-year medical student rotating on surgery, we had a male attending who was very well known at that school at the time who basically would take the female medical students, and instead of clinic, he would round us up. He would have us sit around him in the workplace room while everyone else was seeing patients, and he would have you look at news clippings of himself. He would tell you stories about himself, like he was holding court for the ladies.
It was this very weird culture where my takeaway as a med student was like, “Wow, this is kind of abusive patriarchy that is supported,” because everyone knew about it and was complicit. Even though I really liked surgery, this was just one instance and one example of where you see this culture that really resonates into the rest of life that I didn’t really want to be a part of.
I went into emergency medicine and loved it. It’s also highly procedural, and I was very happy with where I was. What was really interesting about this tweet to me, though, is that it really took off and garnered hundreds of thousands of views on a very niche topic, because what was most revealing is that everyone has a story like this.
It is not just surgery. It is definitely not just one specialty and it is not just one school. It is an endemic problem in medicine. Not only does it change the lives of young women, but it also says so much about the complicity and the culture that we have in medicine that many people were upset about just the same way I was.
Medical training experience in other countries vs. the United States
Dr. Glatter: Júlia, I want to hear about your experience in medical school, surgery, and then fellowship training and up to the present, if possible.
Júlia Loyola Ferreira, MD: In Brazil, as in many countries now, women have made up the majority of the medical students since 2010. It’s a more female-friendly environment when you’re going through medical school, and I was lucky enough to do rotations in areas of surgery where people were friendly to women.
I lived in this tiny bubble that also gave me the privilege of not facing some things that I can imagine that people in Brazil in different areas and smaller towns face. In Brazil, people try to not talk about this gender agenda. This is something that’s being talked about outside Brazil. But in Brazil, we are years back. People are not really engaging on this conversation. I thought it was going to be hard for me as a woman, because Brazil has around 20% female surgeons.
I knew it was going to be challenging, but I had no idea how bad it was. When I started and things started happening, the list was big. I have an example of everything that is written about – microaggression, implicit bias, discrimination, harassment.
Every time I would try to speak about it and talk to someone, I would be strongly gaslighted. It was the whole training, the whole 5 years. People would say, “Oh, I don’t think it was like that. I think you were overreacting.” People would come with all these different answers for what I was experiencing, and that was frustrating. That was even harder because I had to cope with everything that was happening and I had no one to turn to. I had no mentors.
When I looked up to women who were in surgery, they would be tougher on us young surgeons than the men and they would tell us that we should not complain because in their time it was even harder. Now, it’s getting better and we are supposed to accept whatever comes.
That was at least a little bit of what I experienced in my training. It was only after I finished and started to do research about it that I really encountered a field of people who would echo what I was trying to say to many people in different hospitals that I attended to.
That was the key for me to get out of that situation of being gaslighted and of not being able to really talk about it. Suddenly, I started to publish things about Brazil that nobody was even writing or studying. That gave me a large amount of responsibility, but also motivation to keep going and to see the change.
Valuing women in medicine
Dr. Glatter: This is a very important point that you’re raising about the environment of women being hard on other women. We know that men can be very difficult on and also judgmental toward their trainees.
Amy, how would you respond to that? Was your experience similar in emergency medicine training?
Dr. Ho: I actually don’t feel like it was. I think what Júlia is alluding to is this “mean girls” idea, of “I went through it and thus you have to go through it.” I think you do see this in many specialties. One of the classic ones we hear about, and I don’t want to speak to it too much because it’s not my specialty, is ob.gyn., where it is a very female-dominant surgery group. There’s almost a hazing level that you hear about in some of the more malignant workplaces.
I think that you speak to two really important things. Number one is the numbers game. As you were saying, Brazil actually has many women. That’s awesome. That’s actually different from the United States, especially for the historic, existing workplace and less so for the medical students and for residents. I think step one is having minorities like women just present and there.
Step two is actually including and valuing them. While I think it’s really easy to move away from the women discussion, because there are women when you look around in medicine, it doesn’t mean that women are actually being heard, that they’re actually being accepted, or that their viewpoints are being listened to. A big part of it is normalizing not only seeing women in medicine but also normalizing the narrative of women in medicine.
It’s not just about motherhood; it’s about things like normalizing talking about advancement, academic promotions, pay, culture, being called things like “too reactive,” “anxious,” or “too assertive.” These are all classic things that we hear about when we talk about women.
That’s why we’re looking to not only conversations like this, but also structured ways for women to discuss being women in medicine. There are many women in medicine groups in emergency medicine, including: Females Working in Emergency Medicine (FemInEM); the American College of Emergency Physicians (ACEP) and Society for Academic Emergency Medicine (SAEM) women’s groups, which are American Association of Women Emergency Physicians (AAWEP) and Academy for Women in Academic Emergency Medicine (AWAEM), respectively; and the American Medical Women’s Association (AMWA), which is the American Medical Association’s offshoot.
All of these groups are geared toward normalizing women in medicine, normalizing the narrative of women in medicine, and then working on mentoring and educating so that we can advance our initiatives.
Gender balance is not gender equity
Dr. Glatter: Amy, you bring up a very critical point that mentoring is sort of the antidote to gender-based discrimination. Júlia had written a paper back in November of 2022 that was published in the Journal of Surgical Research talking exactly about this and how important it is to develop mentoring. Part of her research showed that about 20% of medical students who took the survey, about 1,000 people, had mentors, which was very disturbing.
Dr. Loyola Ferreira: Mentorship is one of the ways of changing the reality about gender-based discrimination. Amy’s comment was very strong and we need to really keep saying it, which is that gender balance is not gender equity.
The idea of having more women is not the same as women being recognized as equals, as able as men, and as valued as men. To change this very long culture of male domination, we need support, and this support comes from mentorship.
Although I didn’t have one, I feel that since I started being a mentor for some students, it changed not only them but myself. It gave me strength to keep going, studying, publishing, and going further with this discussion. I feel like the relationship was as good for them as it is for me. That’s how things change.
Diversity, equity, and inclusion training
Dr. Glatter: We’re talking about the reality of gender equity in terms of the ability to have equal respect, recognition, opportunities, and access. That’s really an important point to realize, and for our audience, to understand that gender equity is not gender balance.
Amy, I want to talk about medical school curriculums. Are there advances that you’re aware of being made at certain schools, programs, even in residencies, to enforce these things and make it a priority?
Dr. Ho: We’re really lucky that, as a culture in the United States, medical training is certainly very geared toward diversity. Some of that is certainly unofficial. Some of that just means when they’re looking at a medical school class or looking at rank lists for residency, that they’re cognizant of the different backgrounds that people have. That’s still a step. That is a step, that we’re at least acknowledging it.
There are multiple medical schools and residencies that have more formal unconscious-bias training or diversity, equity, and inclusion (DEI) training, both of which are excellent not only for us in the workplace but also for our patients. Almost all of us will see patients of highly diverse backgrounds. I think the biggest push is looking toward the criteria that we use for selecting trainees and students into our programs. Historically, it’s been MCAT, GPA, and so on.
We’ve really started to ask the question of, are these sorts of “objective criteria” actually biased in institutional ways? They talk about this all the time where GPAs will bias against students from underrepresented minorities (URM). I think all medical students and residencies have really acknowledged that. Although there are still test cutoffs, we are putting an inquisitive eye to what those mean, why they exist, and what are the other things that we should consider. This is all very heartening from what I’m seeing in medical training.
Dr. Glatter: There’s no formal rating system for DEI curriculums right now, like ranking of this school, or this program has more advanced recognition in terms of DEI?
Dr. Ho: No, but on the flip side, the U.S. News & World Report was classically one of the major rankings for medical schools. What we saw fairly recently was that very high-tier schools like Harvard and University of Chicago pulled out of that ranking because that ranking did not acknowledge the value of diversity. That was an incredible stance for medical schools to take, to say, “Hey, you are not evaluating an important criterion of ours.”
Dr. Glatter: That’s a great point. Júlia, where are we now in Brazil in terms of awareness of DEI and curriculum in schools and training programs?
Dr. Loyola Ferreira: Our reality is not as good as in the U.S., unfortunately. I don’t see much discussion on residency programs or medical schools at the moment. I see many students bringing it out and trying to make their schools engage in that discussion. This is something that is coming from the bottom up and not from the top down. I think it can lead to change as well. It is a step and it’s a beginning. Institutions should take the responsibility of doing this from the beginning. This is something where Brazil is still years behind you guys.
Dr. Glatter: It’s unfortunate, but certainly it’s important to hear that. What about in Canada and certainly your institution, McGill, where you just completed a master’s degree?
Dr. Loyola Ferreira: Canada is very much like the U.S. This is something that is really happening and it’s happening fast. I see, at least at McGill, a large amount of DEI inclusion and everything on this discussion. They have institutional courses for us to do as students, and we are all obliged to do many courses, which I think is really educating, especially for people with different cultures and backgrounds.
Dr. Glatter: Amy, where do you think we are in emergency medicine to look at the other side of it? Comparing surgery with emergency medicine, do you think we’re well advanced in terms of DEI, inclusion criteria, respect, and dignity, or are we really far off?
Dr. Ho: I may be biased, but I think emergency medicine is one of the best in terms of this, and I think there are a couple of reasons for it. One is that we are an inherently team-based organization. The attending, the residents, and the students all work in line with one another. There’s less of a hierarchy.
The same is true for our nurses, pharmacists, techs, and EMS. We all work together as a team. Because of that fairly flat structure, it’s really easy for us to value one another as individuals with our diverse backgrounds. In a way, that’s harder for specialties that are more hierarchical, and I think surgery is certainly one of the most hierarchical.
The second reason why emergency medicine is fairly well off in this is that we’re, by nature, a safety-net specialty. We see patients of all-comers, all walks, all backgrounds. I think we both recognize the value of physician-patient concordance. When we share characteristics with our patients, we recognize that value immediately at the bedside.
It exposes us to so much diversity. I see a refugee one day and the next patient is someone who is incarcerated. The next patient after that is an important businessman in society. That diversity and whiplash in the type of patients that we see back-to-back helps us see the playing field in a really flat, diverse way. Because of that, I think our culture is much better, as is our understanding of the value and importance of diversity not only for our programs, but also for our patients.
Do female doctors have better patient outcomes?
Dr. Glatter: Specialties working together in the emergency department is so important. Building that team and that togetherness is so critical. Júlia, would you agree?
Dr. Loyola Ferreira: Definitely. Something Amy said that is beautiful is that you recognize yourself in these patients. In surgery, we are taught to try to be away from the patients and not to put ourselves in the same position. We are taught to be less engaging, and this is not good. The good thing is when we really have patient-centered care, when we listen to them, and when we are involved with them.
I saw a publication showing that female and male surgeons treating similar patients had the same surgical outcomes. Women are as good as men technically to do surgery and have the same surgical outcomes. However, there is research showing that surgical teams with greater representation of women have improved surgical outcomes because of patient-centered care and the way women conduct bedside attention to patients. And they have better patient experience measures afterward. That is not only from the women who are treating the patients, but the whole environment. Women end up bringing men [into the conversation] and this better improves patient-centered care, and that makes the whole team a better team attending patients. Definitely, we are in the moment of patient experience and satisfaction, and increasing women is a way of achieving better patient satisfaction and experience.
Dr. Ho: There’s much to be said about having female clinicians available for patients. It doesn’t have to be just for female patients, although again, concordance between physicians and patients is certainly beneficial. Besides outcomes benefit, there’s even just a communication benefit. The way that women and men communicate is inherently different. The way women and men experience certain things is also inherently different.
A classic example of this is women who are experiencing a heart attack may not actually have chest pain but present with nausea. As a female who’s sensitive to this, when I see a woman throwing up, I am very attuned to something actually being wrong, knowing that they may not present with classic pain for a syndrome, but actually may be presenting with nausea instead. It doesn’t have to be a woman who takes that knowledge and turns it into something at the bedside. It certainly doesn’t have to, but it is just a natural, easy thing to step into as a female.
While I’m really careful to not step into this “women are better than men” or “men are better than women” argument, there’s something to be said about how the availability of female clinicians for all patients, not just female patients, can have benefit. Again, it’s shown in studies with cardiovascular outcomes and cardiologists, it’s certainly shown in ob.gyn., particularly for underrepresented minorities as well for maternal outcomes of Black mothers. It’s certainly shown again in patient satisfaction, which is concordance.
There is a profound level of research already on this that goes beyond just the idea of stacking the bench and putting more women in there. That’s not the value. We’re not just here to check off the box. We’re here to actually lend some value to our patients and, again, to one another as well.
Dr. Glatter: Absolutely. These are excellent points. The point you make about patient presentation is so vital. The fact that women have nausea sometimes in ACS presentations, the research never was really attentive to this. It was biased. The symptoms that women may have that are not “typical” for ACS weren’t included in patient presentations. Educating everyone about, overall, the types of presentations that we can recognize is vital and important.
Dr. Ho: Yes. It’s worth saying that, when you look at how medicine and research developed, classically, who were the research participants? They were often White men. They were college students who, historically, because women were not allowed to go to college, were men.
I say that not to fault the institution, because that was the culture of our history, but to just say it is okay to question things. It is okay to realize that someone’s presenting outside of the box and that maybe we actually need to reframe what even created the walls of the box in the first place.
Dr. Glatter: Thank you again for joining us. I truly appreciate your insight and expertise.
Dr. Glatter is assistant professor of emergency medicine, department of emergency medicine, Hofstra/Northwell, New York. Dr. Ho is senior vice president of clinical informatics & analytics, department of emergency medicine, Integrative Emergency Services, Dallas. Dr. Loyola Ferreira is a master of science candidate, department of experimental surgery, McGill University, Montreal. They reported that they had no conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Joining me to discuss ways to address and reform the toxic culture associated with medical training is Dr. Amy Faith Ho, senior vice president of clinical informatics and analytics at Integrative Emergency Services in Dallas. Also joining us is Dr. Júlia Loyola Ferreira, a pediatric surgeon originally from Brazil, now practicing at Montreal Children’s and focused on advocacy for gender equity and patient-centered care.
Welcome to both of you. Thanks so much for joining me.
Amy Faith Ho, MD, MPH: Thanks so much for having us, Rob.
Dr. Glatter: Amy, I noticed a tweet recently where you talked about how your career choice was affected by the toxic environment in medical school, affecting your choice of residency. Can you elaborate on that?
Dr. Ho: In this instance, what we’re talking about is gender, but it can be directed toward any number of other groups as well.
What you’re alluding to is a tweet by Stanford Surgery Group showing the next residency class, and what was really stunning about this residency class was that it was almost all females. And this was something that took off on social media.
When I saw this, I was really brought back to one of my personal experiences that I chose to share, which was basically that, as a medical student, I really wanted to be a surgeon. I’m an emergency medicine doctor now, so you know that didn’t happen.
The story that I was sharing was that when I was a third-year medical student rotating on surgery, we had a male attending who was very well known at that school at the time who basically would take the female medical students, and instead of clinic, he would round us up. He would have us sit around him in the workplace room while everyone else was seeing patients, and he would have you look at news clippings of himself. He would tell you stories about himself, like he was holding court for the ladies.
It was this very weird culture where my takeaway as a med student was like, “Wow, this is kind of abusive patriarchy that is supported,” because everyone knew about it and was complicit. Even though I really liked surgery, this was just one instance and one example of where you see this culture that really resonates into the rest of life that I didn’t really want to be a part of.
I went into emergency medicine and loved it. It’s also highly procedural, and I was very happy with where I was. What was really interesting about this tweet to me, though, is that it really took off and garnered hundreds of thousands of views on a very niche topic, because what was most revealing is that everyone has a story like this.
It is not just surgery. It is definitely not just one specialty and it is not just one school. It is an endemic problem in medicine. Not only does it change the lives of young women, but it also says so much about the complicity and the culture that we have in medicine that many people were upset about just the same way I was.
Medical training experience in other countries vs. the United States
Dr. Glatter: Júlia, I want to hear about your experience in medical school, surgery, and then fellowship training and up to the present, if possible.
Júlia Loyola Ferreira, MD: In Brazil, as in many countries now, women have made up the majority of the medical students since 2010. It’s a more female-friendly environment when you’re going through medical school, and I was lucky enough to do rotations in areas of surgery where people were friendly to women.
I lived in this tiny bubble that also gave me the privilege of not facing some things that I can imagine that people in Brazil in different areas and smaller towns face. In Brazil, people try to not talk about this gender agenda. This is something that’s being talked about outside Brazil. But in Brazil, we are years back. People are not really engaging on this conversation. I thought it was going to be hard for me as a woman, because Brazil has around 20% female surgeons.
I knew it was going to be challenging, but I had no idea how bad it was. When I started and things started happening, the list was big. I have an example of everything that is written about – microaggression, implicit bias, discrimination, harassment.
Every time I would try to speak about it and talk to someone, I would be strongly gaslighted. It was the whole training, the whole 5 years. People would say, “Oh, I don’t think it was like that. I think you were overreacting.” People would come with all these different answers for what I was experiencing, and that was frustrating. That was even harder because I had to cope with everything that was happening and I had no one to turn to. I had no mentors.
When I looked up to women who were in surgery, they would be tougher on us young surgeons than the men and they would tell us that we should not complain because in their time it was even harder. Now, it’s getting better and we are supposed to accept whatever comes.
That was at least a little bit of what I experienced in my training. It was only after I finished and started to do research about it that I really encountered a field of people who would echo what I was trying to say to many people in different hospitals that I attended to.
That was the key for me to get out of that situation of being gaslighted and of not being able to really talk about it. Suddenly, I started to publish things about Brazil that nobody was even writing or studying. That gave me a large amount of responsibility, but also motivation to keep going and to see the change.
Valuing women in medicine
Dr. Glatter: This is a very important point that you’re raising about the environment of women being hard on other women. We know that men can be very difficult on and also judgmental toward their trainees.
Amy, how would you respond to that? Was your experience similar in emergency medicine training?
Dr. Ho: I actually don’t feel like it was. I think what Júlia is alluding to is this “mean girls” idea, of “I went through it and thus you have to go through it.” I think you do see this in many specialties. One of the classic ones we hear about, and I don’t want to speak to it too much because it’s not my specialty, is ob.gyn., where it is a very female-dominant surgery group. There’s almost a hazing level that you hear about in some of the more malignant workplaces.
I think that you speak to two really important things. Number one is the numbers game. As you were saying, Brazil actually has many women. That’s awesome. That’s actually different from the United States, especially for the historic, existing workplace and less so for the medical students and for residents. I think step one is having minorities like women just present and there.
Step two is actually including and valuing them. While I think it’s really easy to move away from the women discussion, because there are women when you look around in medicine, it doesn’t mean that women are actually being heard, that they’re actually being accepted, or that their viewpoints are being listened to. A big part of it is normalizing not only seeing women in medicine but also normalizing the narrative of women in medicine.
It’s not just about motherhood; it’s about things like normalizing talking about advancement, academic promotions, pay, culture, being called things like “too reactive,” “anxious,” or “too assertive.” These are all classic things that we hear about when we talk about women.
That’s why we’re looking to not only conversations like this, but also structured ways for women to discuss being women in medicine. There are many women in medicine groups in emergency medicine, including: Females Working in Emergency Medicine (FemInEM); the American College of Emergency Physicians (ACEP) and Society for Academic Emergency Medicine (SAEM) women’s groups, which are American Association of Women Emergency Physicians (AAWEP) and Academy for Women in Academic Emergency Medicine (AWAEM), respectively; and the American Medical Women’s Association (AMWA), which is the American Medical Association’s offshoot.
All of these groups are geared toward normalizing women in medicine, normalizing the narrative of women in medicine, and then working on mentoring and educating so that we can advance our initiatives.
Gender balance is not gender equity
Dr. Glatter: Amy, you bring up a very critical point that mentoring is sort of the antidote to gender-based discrimination. Júlia had written a paper back in November of 2022 that was published in the Journal of Surgical Research talking exactly about this and how important it is to develop mentoring. Part of her research showed that about 20% of medical students who took the survey, about 1,000 people, had mentors, which was very disturbing.
Dr. Loyola Ferreira: Mentorship is one of the ways of changing the reality about gender-based discrimination. Amy’s comment was very strong and we need to really keep saying it, which is that gender balance is not gender equity.
The idea of having more women is not the same as women being recognized as equals, as able as men, and as valued as men. To change this very long culture of male domination, we need support, and this support comes from mentorship.
Although I didn’t have one, I feel that since I started being a mentor for some students, it changed not only them but myself. It gave me strength to keep going, studying, publishing, and going further with this discussion. I feel like the relationship was as good for them as it is for me. That’s how things change.
Diversity, equity, and inclusion training
Dr. Glatter: We’re talking about the reality of gender equity in terms of the ability to have equal respect, recognition, opportunities, and access. That’s really an important point to realize, and for our audience, to understand that gender equity is not gender balance.
Amy, I want to talk about medical school curriculums. Are there advances that you’re aware of being made at certain schools, programs, even in residencies, to enforce these things and make it a priority?
Dr. Ho: We’re really lucky that, as a culture in the United States, medical training is certainly very geared toward diversity. Some of that is certainly unofficial. Some of that just means when they’re looking at a medical school class or looking at rank lists for residency, that they’re cognizant of the different backgrounds that people have. That’s still a step. That is a step, that we’re at least acknowledging it.
There are multiple medical schools and residencies that have more formal unconscious-bias training or diversity, equity, and inclusion (DEI) training, both of which are excellent not only for us in the workplace but also for our patients. Almost all of us will see patients of highly diverse backgrounds. I think the biggest push is looking toward the criteria that we use for selecting trainees and students into our programs. Historically, it’s been MCAT, GPA, and so on.
We’ve really started to ask the question of, are these sorts of “objective criteria” actually biased in institutional ways? They talk about this all the time where GPAs will bias against students from underrepresented minorities (URM). I think all medical students and residencies have really acknowledged that. Although there are still test cutoffs, we are putting an inquisitive eye to what those mean, why they exist, and what are the other things that we should consider. This is all very heartening from what I’m seeing in medical training.
Dr. Glatter: There’s no formal rating system for DEI curriculums right now, like ranking of this school, or this program has more advanced recognition in terms of DEI?
Dr. Ho: No, but on the flip side, the U.S. News & World Report was classically one of the major rankings for medical schools. What we saw fairly recently was that very high-tier schools like Harvard and University of Chicago pulled out of that ranking because that ranking did not acknowledge the value of diversity. That was an incredible stance for medical schools to take, to say, “Hey, you are not evaluating an important criterion of ours.”
Dr. Glatter: That’s a great point. Júlia, where are we now in Brazil in terms of awareness of DEI and curriculum in schools and training programs?
Dr. Loyola Ferreira: Our reality is not as good as in the U.S., unfortunately. I don’t see much discussion on residency programs or medical schools at the moment. I see many students bringing it out and trying to make their schools engage in that discussion. This is something that is coming from the bottom up and not from the top down. I think it can lead to change as well. It is a step and it’s a beginning. Institutions should take the responsibility of doing this from the beginning. This is something where Brazil is still years behind you guys.
Dr. Glatter: It’s unfortunate, but certainly it’s important to hear that. What about in Canada and certainly your institution, McGill, where you just completed a master’s degree?
Dr. Loyola Ferreira: Canada is very much like the U.S. This is something that is really happening and it’s happening fast. I see, at least at McGill, a large amount of DEI inclusion and everything on this discussion. They have institutional courses for us to do as students, and we are all obliged to do many courses, which I think is really educating, especially for people with different cultures and backgrounds.
Dr. Glatter: Amy, where do you think we are in emergency medicine to look at the other side of it? Comparing surgery with emergency medicine, do you think we’re well advanced in terms of DEI, inclusion criteria, respect, and dignity, or are we really far off?
Dr. Ho: I may be biased, but I think emergency medicine is one of the best in terms of this, and I think there are a couple of reasons for it. One is that we are an inherently team-based organization. The attending, the residents, and the students all work in line with one another. There’s less of a hierarchy.
The same is true for our nurses, pharmacists, techs, and EMS. We all work together as a team. Because of that fairly flat structure, it’s really easy for us to value one another as individuals with our diverse backgrounds. In a way, that’s harder for specialties that are more hierarchical, and I think surgery is certainly one of the most hierarchical.
The second reason why emergency medicine is fairly well off in this is that we’re, by nature, a safety-net specialty. We see patients of all-comers, all walks, all backgrounds. I think we both recognize the value of physician-patient concordance. When we share characteristics with our patients, we recognize that value immediately at the bedside.
It exposes us to so much diversity. I see a refugee one day and the next patient is someone who is incarcerated. The next patient after that is an important businessman in society. That diversity and whiplash in the type of patients that we see back-to-back helps us see the playing field in a really flat, diverse way. Because of that, I think our culture is much better, as is our understanding of the value and importance of diversity not only for our programs, but also for our patients.
Do female doctors have better patient outcomes?
Dr. Glatter: Specialties working together in the emergency department is so important. Building that team and that togetherness is so critical. Júlia, would you agree?
Dr. Loyola Ferreira: Definitely. Something Amy said that is beautiful is that you recognize yourself in these patients. In surgery, we are taught to try to be away from the patients and not to put ourselves in the same position. We are taught to be less engaging, and this is not good. The good thing is when we really have patient-centered care, when we listen to them, and when we are involved with them.
I saw a publication showing that female and male surgeons treating similar patients had the same surgical outcomes. Women are as good as men technically to do surgery and have the same surgical outcomes. However, there is research showing that surgical teams with greater representation of women have improved surgical outcomes because of patient-centered care and the way women conduct bedside attention to patients. And they have better patient experience measures afterward. That is not only from the women who are treating the patients, but the whole environment. Women end up bringing men [into the conversation] and this better improves patient-centered care, and that makes the whole team a better team attending patients. Definitely, we are in the moment of patient experience and satisfaction, and increasing women is a way of achieving better patient satisfaction and experience.
Dr. Ho: There’s much to be said about having female clinicians available for patients. It doesn’t have to be just for female patients, although again, concordance between physicians and patients is certainly beneficial. Besides outcomes benefit, there’s even just a communication benefit. The way that women and men communicate is inherently different. The way women and men experience certain things is also inherently different.
A classic example of this is women who are experiencing a heart attack may not actually have chest pain but present with nausea. As a female who’s sensitive to this, when I see a woman throwing up, I am very attuned to something actually being wrong, knowing that they may not present with classic pain for a syndrome, but actually may be presenting with nausea instead. It doesn’t have to be a woman who takes that knowledge and turns it into something at the bedside. It certainly doesn’t have to, but it is just a natural, easy thing to step into as a female.
While I’m really careful to not step into this “women are better than men” or “men are better than women” argument, there’s something to be said about how the availability of female clinicians for all patients, not just female patients, can have benefit. Again, it’s shown in studies with cardiovascular outcomes and cardiologists, it’s certainly shown in ob.gyn., particularly for underrepresented minorities as well for maternal outcomes of Black mothers. It’s certainly shown again in patient satisfaction, which is concordance.
There is a profound level of research already on this that goes beyond just the idea of stacking the bench and putting more women in there. That’s not the value. We’re not just here to check off the box. We’re here to actually lend some value to our patients and, again, to one another as well.
Dr. Glatter: Absolutely. These are excellent points. The point you make about patient presentation is so vital. The fact that women have nausea sometimes in ACS presentations, the research never was really attentive to this. It was biased. The symptoms that women may have that are not “typical” for ACS weren’t included in patient presentations. Educating everyone about, overall, the types of presentations that we can recognize is vital and important.
Dr. Ho: Yes. It’s worth saying that, when you look at how medicine and research developed, classically, who were the research participants? They were often White men. They were college students who, historically, because women were not allowed to go to college, were men.
I say that not to fault the institution, because that was the culture of our history, but to just say it is okay to question things. It is okay to realize that someone’s presenting outside of the box and that maybe we actually need to reframe what even created the walls of the box in the first place.
Dr. Glatter: Thank you again for joining us. I truly appreciate your insight and expertise.
Dr. Glatter is assistant professor of emergency medicine, department of emergency medicine, Hofstra/Northwell, New York. Dr. Ho is senior vice president of clinical informatics & analytics, department of emergency medicine, Integrative Emergency Services, Dallas. Dr. Loyola Ferreira is a master of science candidate, department of experimental surgery, McGill University, Montreal. They reported that they had no conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Robert D. Glatter, MD: Welcome. I’m Dr. Robert Glatter, medical adviser for Medscape Emergency Medicine. Joining me to discuss ways to address and reform the toxic culture associated with medical training is Dr. Amy Faith Ho, senior vice president of clinical informatics and analytics at Integrative Emergency Services in Dallas. Also joining us is Dr. Júlia Loyola Ferreira, a pediatric surgeon originally from Brazil, now practicing at Montreal Children’s and focused on advocacy for gender equity and patient-centered care.
Welcome to both of you. Thanks so much for joining me.
Amy Faith Ho, MD, MPH: Thanks so much for having us, Rob.
Dr. Glatter: Amy, I noticed a tweet recently where you talked about how your career choice was affected by the toxic environment in medical school, affecting your choice of residency. Can you elaborate on that?
Dr. Ho: In this instance, what we’re talking about is gender, but it can be directed toward any number of other groups as well.
What you’re alluding to is a tweet by Stanford Surgery Group showing the next residency class, and what was really stunning about this residency class was that it was almost all females. And this was something that took off on social media.
When I saw this, I was really brought back to one of my personal experiences that I chose to share, which was basically that, as a medical student, I really wanted to be a surgeon. I’m an emergency medicine doctor now, so you know that didn’t happen.
The story that I was sharing was that when I was a third-year medical student rotating on surgery, we had a male attending who was very well known at that school at the time who basically would take the female medical students, and instead of clinic, he would round us up. He would have us sit around him in the workplace room while everyone else was seeing patients, and he would have you look at news clippings of himself. He would tell you stories about himself, like he was holding court for the ladies.
It was this very weird culture where my takeaway as a med student was like, “Wow, this is kind of abusive patriarchy that is supported,” because everyone knew about it and was complicit. Even though I really liked surgery, this was just one instance and one example of where you see this culture that really resonates into the rest of life that I didn’t really want to be a part of.
I went into emergency medicine and loved it. It’s also highly procedural, and I was very happy with where I was. What was really interesting about this tweet to me, though, is that it really took off and garnered hundreds of thousands of views on a very niche topic, because what was most revealing is that everyone has a story like this.
It is not just surgery. It is definitely not just one specialty and it is not just one school. It is an endemic problem in medicine. Not only does it change the lives of young women, but it also says so much about the complicity and the culture that we have in medicine that many people were upset about just the same way I was.
Medical training experience in other countries vs. the United States
Dr. Glatter: Júlia, I want to hear about your experience in medical school, surgery, and then fellowship training and up to the present, if possible.
Júlia Loyola Ferreira, MD: In Brazil, as in many countries now, women have made up the majority of the medical students since 2010. It’s a more female-friendly environment when you’re going through medical school, and I was lucky enough to do rotations in areas of surgery where people were friendly to women.
I lived in this tiny bubble that also gave me the privilege of not facing some things that I can imagine that people in Brazil in different areas and smaller towns face. In Brazil, people try to not talk about this gender agenda. This is something that’s being talked about outside Brazil. But in Brazil, we are years back. People are not really engaging on this conversation. I thought it was going to be hard for me as a woman, because Brazil has around 20% female surgeons.
I knew it was going to be challenging, but I had no idea how bad it was. When I started and things started happening, the list was big. I have an example of everything that is written about – microaggression, implicit bias, discrimination, harassment.
Every time I would try to speak about it and talk to someone, I would be strongly gaslighted. It was the whole training, the whole 5 years. People would say, “Oh, I don’t think it was like that. I think you were overreacting.” People would come with all these different answers for what I was experiencing, and that was frustrating. That was even harder because I had to cope with everything that was happening and I had no one to turn to. I had no mentors.
When I looked up to women who were in surgery, they would be tougher on us young surgeons than the men and they would tell us that we should not complain because in their time it was even harder. Now, it’s getting better and we are supposed to accept whatever comes.
That was at least a little bit of what I experienced in my training. It was only after I finished and started to do research about it that I really encountered a field of people who would echo what I was trying to say to many people in different hospitals that I attended to.
That was the key for me to get out of that situation of being gaslighted and of not being able to really talk about it. Suddenly, I started to publish things about Brazil that nobody was even writing or studying. That gave me a large amount of responsibility, but also motivation to keep going and to see the change.
Valuing women in medicine
Dr. Glatter: This is a very important point that you’re raising about the environment of women being hard on other women. We know that men can be very difficult on and also judgmental toward their trainees.
Amy, how would you respond to that? Was your experience similar in emergency medicine training?
Dr. Ho: I actually don’t feel like it was. I think what Júlia is alluding to is this “mean girls” idea, of “I went through it and thus you have to go through it.” I think you do see this in many specialties. One of the classic ones we hear about, and I don’t want to speak to it too much because it’s not my specialty, is ob.gyn., where it is a very female-dominant surgery group. There’s almost a hazing level that you hear about in some of the more malignant workplaces.
I think that you speak to two really important things. Number one is the numbers game. As you were saying, Brazil actually has many women. That’s awesome. That’s actually different from the United States, especially for the historic, existing workplace and less so for the medical students and for residents. I think step one is having minorities like women just present and there.
Step two is actually including and valuing them. While I think it’s really easy to move away from the women discussion, because there are women when you look around in medicine, it doesn’t mean that women are actually being heard, that they’re actually being accepted, or that their viewpoints are being listened to. A big part of it is normalizing not only seeing women in medicine but also normalizing the narrative of women in medicine.
It’s not just about motherhood; it’s about things like normalizing talking about advancement, academic promotions, pay, culture, being called things like “too reactive,” “anxious,” or “too assertive.” These are all classic things that we hear about when we talk about women.
That’s why we’re looking to not only conversations like this, but also structured ways for women to discuss being women in medicine. There are many women in medicine groups in emergency medicine, including: Females Working in Emergency Medicine (FemInEM); the American College of Emergency Physicians (ACEP) and Society for Academic Emergency Medicine (SAEM) women’s groups, which are American Association of Women Emergency Physicians (AAWEP) and Academy for Women in Academic Emergency Medicine (AWAEM), respectively; and the American Medical Women’s Association (AMWA), which is the American Medical Association’s offshoot.
All of these groups are geared toward normalizing women in medicine, normalizing the narrative of women in medicine, and then working on mentoring and educating so that we can advance our initiatives.
Gender balance is not gender equity
Dr. Glatter: Amy, you bring up a very critical point that mentoring is sort of the antidote to gender-based discrimination. Júlia had written a paper back in November of 2022 that was published in the Journal of Surgical Research talking exactly about this and how important it is to develop mentoring. Part of her research showed that about 20% of medical students who took the survey, about 1,000 people, had mentors, which was very disturbing.
Dr. Loyola Ferreira: Mentorship is one of the ways of changing the reality about gender-based discrimination. Amy’s comment was very strong and we need to really keep saying it, which is that gender balance is not gender equity.
The idea of having more women is not the same as women being recognized as equals, as able as men, and as valued as men. To change this very long culture of male domination, we need support, and this support comes from mentorship.
Although I didn’t have one, I feel that since I started being a mentor for some students, it changed not only them but myself. It gave me strength to keep going, studying, publishing, and going further with this discussion. I feel like the relationship was as good for them as it is for me. That’s how things change.
Diversity, equity, and inclusion training
Dr. Glatter: We’re talking about the reality of gender equity in terms of the ability to have equal respect, recognition, opportunities, and access. That’s really an important point to realize, and for our audience, to understand that gender equity is not gender balance.
Amy, I want to talk about medical school curriculums. Are there advances that you’re aware of being made at certain schools, programs, even in residencies, to enforce these things and make it a priority?
Dr. Ho: We’re really lucky that, as a culture in the United States, medical training is certainly very geared toward diversity. Some of that is certainly unofficial. Some of that just means when they’re looking at a medical school class or looking at rank lists for residency, that they’re cognizant of the different backgrounds that people have. That’s still a step. That is a step, that we’re at least acknowledging it.
There are multiple medical schools and residencies that have more formal unconscious-bias training or diversity, equity, and inclusion (DEI) training, both of which are excellent not only for us in the workplace but also for our patients. Almost all of us will see patients of highly diverse backgrounds. I think the biggest push is looking toward the criteria that we use for selecting trainees and students into our programs. Historically, it’s been MCAT, GPA, and so on.
We’ve really started to ask the question of, are these sorts of “objective criteria” actually biased in institutional ways? They talk about this all the time where GPAs will bias against students from underrepresented minorities (URM). I think all medical students and residencies have really acknowledged that. Although there are still test cutoffs, we are putting an inquisitive eye to what those mean, why they exist, and what are the other things that we should consider. This is all very heartening from what I’m seeing in medical training.
Dr. Glatter: There’s no formal rating system for DEI curriculums right now, like ranking of this school, or this program has more advanced recognition in terms of DEI?
Dr. Ho: No, but on the flip side, the U.S. News & World Report was classically one of the major rankings for medical schools. What we saw fairly recently was that very high-tier schools like Harvard and University of Chicago pulled out of that ranking because that ranking did not acknowledge the value of diversity. That was an incredible stance for medical schools to take, to say, “Hey, you are not evaluating an important criterion of ours.”
Dr. Glatter: That’s a great point. Júlia, where are we now in Brazil in terms of awareness of DEI and curriculum in schools and training programs?
Dr. Loyola Ferreira: Our reality is not as good as in the U.S., unfortunately. I don’t see much discussion on residency programs or medical schools at the moment. I see many students bringing it out and trying to make their schools engage in that discussion. This is something that is coming from the bottom up and not from the top down. I think it can lead to change as well. It is a step and it’s a beginning. Institutions should take the responsibility of doing this from the beginning. This is something where Brazil is still years behind you guys.
Dr. Glatter: It’s unfortunate, but certainly it’s important to hear that. What about in Canada and certainly your institution, McGill, where you just completed a master’s degree?
Dr. Loyola Ferreira: Canada is very much like the U.S. This is something that is really happening and it’s happening fast. I see, at least at McGill, a large amount of DEI inclusion and everything on this discussion. They have institutional courses for us to do as students, and we are all obliged to do many courses, which I think is really educating, especially for people with different cultures and backgrounds.
Dr. Glatter: Amy, where do you think we are in emergency medicine to look at the other side of it? Comparing surgery with emergency medicine, do you think we’re well advanced in terms of DEI, inclusion criteria, respect, and dignity, or are we really far off?
Dr. Ho: I may be biased, but I think emergency medicine is one of the best in terms of this, and I think there are a couple of reasons for it. One is that we are an inherently team-based organization. The attending, the residents, and the students all work in line with one another. There’s less of a hierarchy.
The same is true for our nurses, pharmacists, techs, and EMS. We all work together as a team. Because of that fairly flat structure, it’s really easy for us to value one another as individuals with our diverse backgrounds. In a way, that’s harder for specialties that are more hierarchical, and I think surgery is certainly one of the most hierarchical.
The second reason why emergency medicine is fairly well off in this is that we’re, by nature, a safety-net specialty. We see patients of all-comers, all walks, all backgrounds. I think we both recognize the value of physician-patient concordance. When we share characteristics with our patients, we recognize that value immediately at the bedside.
It exposes us to so much diversity. I see a refugee one day and the next patient is someone who is incarcerated. The next patient after that is an important businessman in society. That diversity and whiplash in the type of patients that we see back-to-back helps us see the playing field in a really flat, diverse way. Because of that, I think our culture is much better, as is our understanding of the value and importance of diversity not only for our programs, but also for our patients.
Do female doctors have better patient outcomes?
Dr. Glatter: Specialties working together in the emergency department is so important. Building that team and that togetherness is so critical. Júlia, would you agree?
Dr. Loyola Ferreira: Definitely. Something Amy said that is beautiful is that you recognize yourself in these patients. In surgery, we are taught to try to be away from the patients and not to put ourselves in the same position. We are taught to be less engaging, and this is not good. The good thing is when we really have patient-centered care, when we listen to them, and when we are involved with them.
I saw a publication showing that female and male surgeons treating similar patients had the same surgical outcomes. Women are as good as men technically to do surgery and have the same surgical outcomes. However, there is research showing that surgical teams with greater representation of women have improved surgical outcomes because of patient-centered care and the way women conduct bedside attention to patients. And they have better patient experience measures afterward. That is not only from the women who are treating the patients, but the whole environment. Women end up bringing men [into the conversation] and this better improves patient-centered care, and that makes the whole team a better team attending patients. Definitely, we are in the moment of patient experience and satisfaction, and increasing women is a way of achieving better patient satisfaction and experience.
Dr. Ho: There’s much to be said about having female clinicians available for patients. It doesn’t have to be just for female patients, although again, concordance between physicians and patients is certainly beneficial. Besides outcomes benefit, there’s even just a communication benefit. The way that women and men communicate is inherently different. The way women and men experience certain things is also inherently different.
A classic example of this is women who are experiencing a heart attack may not actually have chest pain but present with nausea. As a female who’s sensitive to this, when I see a woman throwing up, I am very attuned to something actually being wrong, knowing that they may not present with classic pain for a syndrome, but actually may be presenting with nausea instead. It doesn’t have to be a woman who takes that knowledge and turns it into something at the bedside. It certainly doesn’t have to, but it is just a natural, easy thing to step into as a female.
While I’m really careful to not step into this “women are better than men” or “men are better than women” argument, there’s something to be said about how the availability of female clinicians for all patients, not just female patients, can have benefit. Again, it’s shown in studies with cardiovascular outcomes and cardiologists, it’s certainly shown in ob.gyn., particularly for underrepresented minorities as well for maternal outcomes of Black mothers. It’s certainly shown again in patient satisfaction, which is concordance.
There is a profound level of research already on this that goes beyond just the idea of stacking the bench and putting more women in there. That’s not the value. We’re not just here to check off the box. We’re here to actually lend some value to our patients and, again, to one another as well.
Dr. Glatter: Absolutely. These are excellent points. The point you make about patient presentation is so vital. The fact that women have nausea sometimes in ACS presentations, the research never was really attentive to this. It was biased. The symptoms that women may have that are not “typical” for ACS weren’t included in patient presentations. Educating everyone about, overall, the types of presentations that we can recognize is vital and important.
Dr. Ho: Yes. It’s worth saying that, when you look at how medicine and research developed, classically, who were the research participants? They were often White men. They were college students who, historically, because women were not allowed to go to college, were men.
I say that not to fault the institution, because that was the culture of our history, but to just say it is okay to question things. It is okay to realize that someone’s presenting outside of the box and that maybe we actually need to reframe what even created the walls of the box in the first place.
Dr. Glatter: Thank you again for joining us. I truly appreciate your insight and expertise.
Dr. Glatter is assistant professor of emergency medicine, department of emergency medicine, Hofstra/Northwell, New York. Dr. Ho is senior vice president of clinical informatics & analytics, department of emergency medicine, Integrative Emergency Services, Dallas. Dr. Loyola Ferreira is a master of science candidate, department of experimental surgery, McGill University, Montreal. They reported that they had no conflicts of interest.
A version of this article first appeared on Medscape.com.
Acute diffuse rash on trunk
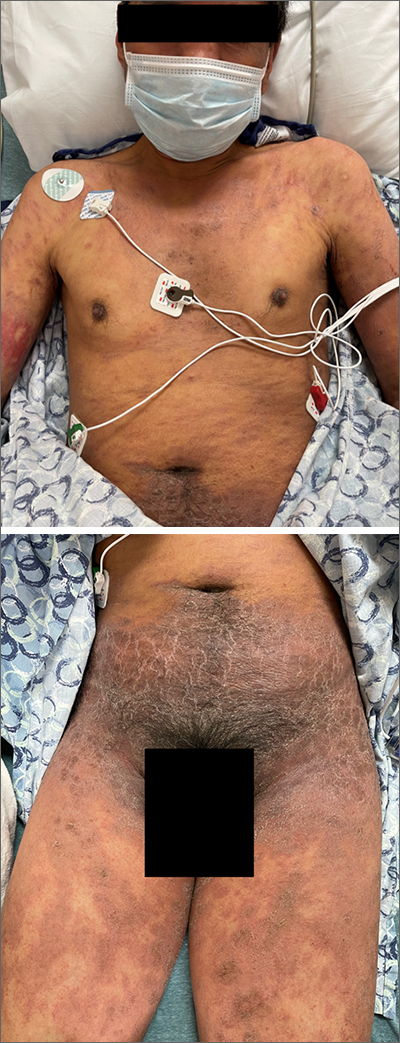
This patient’s diffusely erythematous and scaly rash, in association with recent antibiotic use, was a classic presentation of a drug eruption. Drug eruptions are adverse cutaneous reactions to various medications; they frequently involve antibiotics and anti-epileptics. They can manifest in a multitude of ways with different morphologies. Medication history and timing to onset of symptoms are paramount in making the diagnosis.
Classic reactions include those that are morbilliform (erythematous macules and papules), lichenoid (violaceous and hyperpigmented papules), exfoliative/erythrodermic, and/or urticarial.1 Petechiae and palpable purpura may also manifest.1 Severe reactions, while less common, must always be considered, given their significant morbidity and mortality. These include2:
- Stevens-Johnson syndrome/toxic epidermal necrolysis with diffuse erythema and areas of denuded, necrotic epidermis,
- Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome, and
- Acute, generalized, exanthematous pustulosis (AGEP) consisting of confluent, nonfollicular pustules.
A general principle in the management of drug eruptions is the discontinuation of the offending drug (if known) as soon as possible. If the agent is not known, it is important to discontinue all drugs that are not deemed as essential, particularly medications that are often associated with reactions, such as antibiotics and anti-epileptics. Additionally, evaluation of the oral mucosa, eyes, and genitourinary tract is helpful to diagnose Stevens-Johnson syndrome, if indicated by symptoms or history.
Wound care with cleansing and covering of denuded skin with emollients and wet dressings should be performed. Infections are common complications in these patients due to the increased inflammation, fissuring, and excoriations that accompany the rash, with sepsis from staphylococcal bacteria being the most concerning complication of infection. Additionally, the compromised skin barrier may lead to heat loss and hypothermia, a compensatory hypermetabolism with hyperthermia, and electrolyte imbalances from insensible water losses.2
Most mild eruptions can be treated with topical corticosteroids and antihistamines. However, in severe eruptions, systemic corticosteroids, or referral for immunosuppressive and anticytokine therapies, also should be considered.1
This patient was treated with both a short course of systemic corticosteroids (prednisone 40 mg/d for 5 days, then tapered over 15 days) and topical steroids (triamcinolone 0.1% ointment bid) for symptomatic care. He also was started on an antihistamine (cetirizine 10 mg bid) for itching. Doxycycline and Augmentin were added to his allergy list. At a 1-week follow up, the patient had near resolution of his rash.
Images courtesy of Jose L. Cortez, MD. Text courtesy of Jose L. Cortez, MD, Department of Dermatology, University of New Mexico School of Medicine, and Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, Western Michigan University Homer Stryker, MD School of Medicine, Kalamazoo.
1. Riedl MA, Casillas AM. Adverse drug reactions: types and treatment options. Am Fam Physician. 2003;68:1781-1790.
2. Zhang J, Lei Z, Xu C, et al. Current perspectives on severe drug eruption. Clin Rev Allergy Immunol. 2021;61:282-298. doi: 10.1007/s12016-021-08859-0
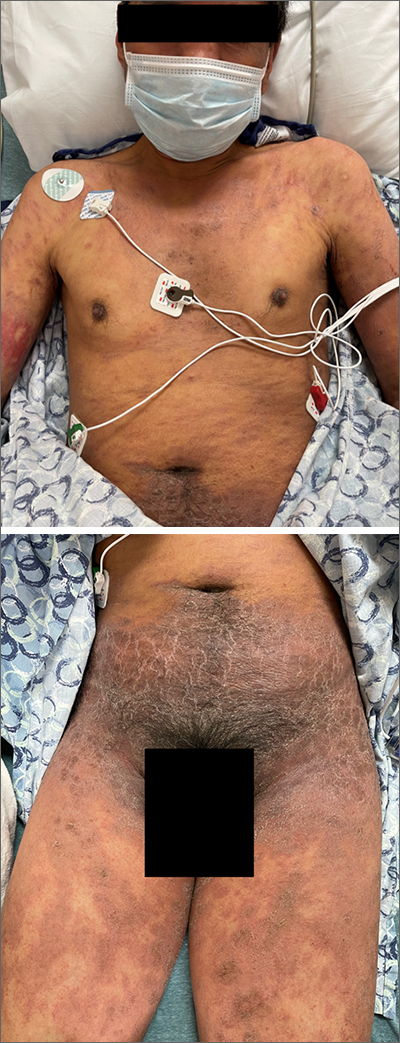
This patient’s diffusely erythematous and scaly rash, in association with recent antibiotic use, was a classic presentation of a drug eruption. Drug eruptions are adverse cutaneous reactions to various medications; they frequently involve antibiotics and anti-epileptics. They can manifest in a multitude of ways with different morphologies. Medication history and timing to onset of symptoms are paramount in making the diagnosis.
Classic reactions include those that are morbilliform (erythematous macules and papules), lichenoid (violaceous and hyperpigmented papules), exfoliative/erythrodermic, and/or urticarial.1 Petechiae and palpable purpura may also manifest.1 Severe reactions, while less common, must always be considered, given their significant morbidity and mortality. These include2:
- Stevens-Johnson syndrome/toxic epidermal necrolysis with diffuse erythema and areas of denuded, necrotic epidermis,
- Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome, and
- Acute, generalized, exanthematous pustulosis (AGEP) consisting of confluent, nonfollicular pustules.
A general principle in the management of drug eruptions is the discontinuation of the offending drug (if known) as soon as possible. If the agent is not known, it is important to discontinue all drugs that are not deemed as essential, particularly medications that are often associated with reactions, such as antibiotics and anti-epileptics. Additionally, evaluation of the oral mucosa, eyes, and genitourinary tract is helpful to diagnose Stevens-Johnson syndrome, if indicated by symptoms or history.
Wound care with cleansing and covering of denuded skin with emollients and wet dressings should be performed. Infections are common complications in these patients due to the increased inflammation, fissuring, and excoriations that accompany the rash, with sepsis from staphylococcal bacteria being the most concerning complication of infection. Additionally, the compromised skin barrier may lead to heat loss and hypothermia, a compensatory hypermetabolism with hyperthermia, and electrolyte imbalances from insensible water losses.2
Most mild eruptions can be treated with topical corticosteroids and antihistamines. However, in severe eruptions, systemic corticosteroids, or referral for immunosuppressive and anticytokine therapies, also should be considered.1
This patient was treated with both a short course of systemic corticosteroids (prednisone 40 mg/d for 5 days, then tapered over 15 days) and topical steroids (triamcinolone 0.1% ointment bid) for symptomatic care. He also was started on an antihistamine (cetirizine 10 mg bid) for itching. Doxycycline and Augmentin were added to his allergy list. At a 1-week follow up, the patient had near resolution of his rash.
Images courtesy of Jose L. Cortez, MD. Text courtesy of Jose L. Cortez, MD, Department of Dermatology, University of New Mexico School of Medicine, and Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, Western Michigan University Homer Stryker, MD School of Medicine, Kalamazoo.
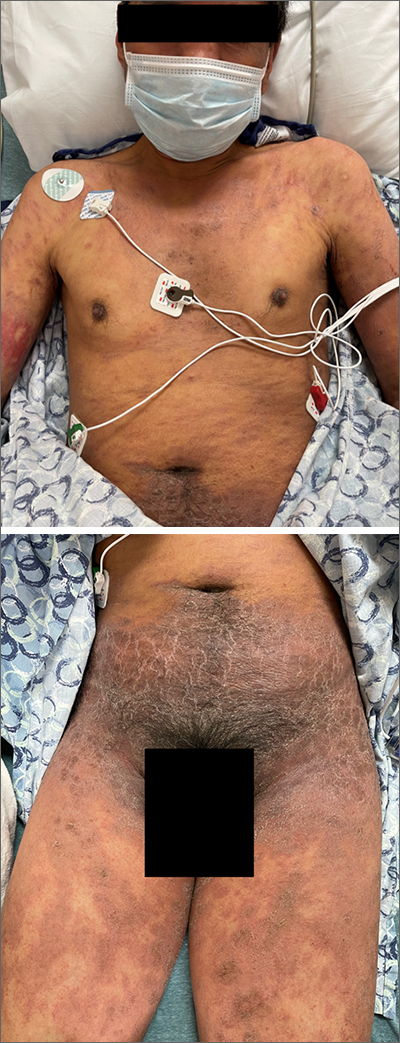
This patient’s diffusely erythematous and scaly rash, in association with recent antibiotic use, was a classic presentation of a drug eruption. Drug eruptions are adverse cutaneous reactions to various medications; they frequently involve antibiotics and anti-epileptics. They can manifest in a multitude of ways with different morphologies. Medication history and timing to onset of symptoms are paramount in making the diagnosis.
Classic reactions include those that are morbilliform (erythematous macules and papules), lichenoid (violaceous and hyperpigmented papules), exfoliative/erythrodermic, and/or urticarial.1 Petechiae and palpable purpura may also manifest.1 Severe reactions, while less common, must always be considered, given their significant morbidity and mortality. These include2:
- Stevens-Johnson syndrome/toxic epidermal necrolysis with diffuse erythema and areas of denuded, necrotic epidermis,
- Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome, and
- Acute, generalized, exanthematous pustulosis (AGEP) consisting of confluent, nonfollicular pustules.
A general principle in the management of drug eruptions is the discontinuation of the offending drug (if known) as soon as possible. If the agent is not known, it is important to discontinue all drugs that are not deemed as essential, particularly medications that are often associated with reactions, such as antibiotics and anti-epileptics. Additionally, evaluation of the oral mucosa, eyes, and genitourinary tract is helpful to diagnose Stevens-Johnson syndrome, if indicated by symptoms or history.
Wound care with cleansing and covering of denuded skin with emollients and wet dressings should be performed. Infections are common complications in these patients due to the increased inflammation, fissuring, and excoriations that accompany the rash, with sepsis from staphylococcal bacteria being the most concerning complication of infection. Additionally, the compromised skin barrier may lead to heat loss and hypothermia, a compensatory hypermetabolism with hyperthermia, and electrolyte imbalances from insensible water losses.2
Most mild eruptions can be treated with topical corticosteroids and antihistamines. However, in severe eruptions, systemic corticosteroids, or referral for immunosuppressive and anticytokine therapies, also should be considered.1
This patient was treated with both a short course of systemic corticosteroids (prednisone 40 mg/d for 5 days, then tapered over 15 days) and topical steroids (triamcinolone 0.1% ointment bid) for symptomatic care. He also was started on an antihistamine (cetirizine 10 mg bid) for itching. Doxycycline and Augmentin were added to his allergy list. At a 1-week follow up, the patient had near resolution of his rash.
Images courtesy of Jose L. Cortez, MD. Text courtesy of Jose L. Cortez, MD, Department of Dermatology, University of New Mexico School of Medicine, and Daniel Stulberg, MD, FAAFP, Department of Family and Community Medicine, Western Michigan University Homer Stryker, MD School of Medicine, Kalamazoo.
1. Riedl MA, Casillas AM. Adverse drug reactions: types and treatment options. Am Fam Physician. 2003;68:1781-1790.
2. Zhang J, Lei Z, Xu C, et al. Current perspectives on severe drug eruption. Clin Rev Allergy Immunol. 2021;61:282-298. doi: 10.1007/s12016-021-08859-0
1. Riedl MA, Casillas AM. Adverse drug reactions: types and treatment options. Am Fam Physician. 2003;68:1781-1790.
2. Zhang J, Lei Z, Xu C, et al. Current perspectives on severe drug eruption. Clin Rev Allergy Immunol. 2021;61:282-298. doi: 10.1007/s12016-021-08859-0
Menopause and long COVID: What women should know
British researchers have noted that women at midlife who have long COVID seem to get specific, and severe, symptoms, including brain fog, fatigue, new-onset dizziness, and difficulty sleeping through the night.
Doctors also think it’s possible that long COVID worsens the symptoms of perimenopause and menopause. Lower levels of estrogen and testosterone appear to be the reason.
“A long COVID theory is that there is a temporary disruption to physiological ovarian steroid hormone production, which could [worsen] symptoms of perimenopause and menopause,” said JoAnn V. Pinkerton, MD, professor of obstetrics at the University of Virginia, Charlottesville, and executive director of the North American Menopause Society.
Long COVID symptoms and menopause symptoms can also be very hard to tell apart.
Another U.K. study cautions that because of this kind of symptom overlap, women at midlife may be misdiagnosed. Research from the North American Menopause Society shows that many women may have trouble recovering from long COVID unless their hormone deficiency is treated.
What are the symptoms of long COVID?
There are over 200 symptoms that have been associated with long COVID, according to the American Medical Association. Some common symptoms are currently defined as the following: feeling extremely tired, feeling depleted after exertion, cognitive issues such as brain fog, heart beating over 100 times a minute, and a loss of sense of smell and taste.
Long COVID symptoms begin a few weeks to a few months after a COVID infection. They can last an indefinite amount of time, but “the hope is that long COVID will not be lifelong,” said Clare Flannery, MD, an endocrinologist and associate professor in the departments of obstetrics, gynecology and reproductive sciences and internal medicine at Yale University, New Haven, Conn.
What are the symptoms of menopause?
Some symptoms of menopause include vaginal infections, irregular bleeding, urinary problems, and sexual problems.
Women in their middle years have other symptoms that can be the same as perimenopause/menopause symptoms.
“Common symptoms of perimenopause and menopause which may also be symptoms ascribed to long COVID include hot flashes, night sweats, disrupted sleep, low mood, depression or anxiety, decreased concentration, memory problems, joint and muscle pains, and headaches,” Dr. Pinkerton said.
Can long COVID actually bring on menopause?
In short: Possibly.
A new study from the Massachusetts Institute of Technology/Patient-Led Research Collaborative/University of California, San Francisco, found that long COVID can cause disruptions to a woman’s menstrual cycle, ovaries, fertility, and menopause itself.
This could be caused by chronic inflammation caused by long COVID on hormones as well. This kind of inflammatory response could explain irregularities in a woman’s menstrual cycle, according to the Newson Health Research and Education study. For instance, “when the body has inflammation, ovulation can happen,” Dr. Flannery said.
The mechanism for how long COVID could spur menopause can also involve a woman’s ovaries.
“Since the theory is that COVID affects the ovary with declines in ovarian reserve and ovarian function, it makes sense that long COVID could bring on symptoms of perimenopause or menopause more acutely or more severely and lengthen the symptoms of the perimenopause and menopausal transition,” Dr. Pinkerton said.
How can hormone replacement therapy benefit women dealing with long COVID during menopause?
Estradiol, the strongest estrogen hormone in a woman’s body, has already been shown to have a positive effect against COVID.
“Estradiol therapy treats symptoms more aggressively in the setting of long COVID,” said Dr. Flannery.
Estradiol is also a form of hormone therapy for menopause symptoms.
“Estradiol has been shown to help hot flashes, night sweats, and sleep and improve mood during perimenopause,” said Dr. Pinkerton. “So it’s likely that perimenopausal or menopausal women with long COVID would see improvements both due to the action of estradiol on the ovary seen during COVID and the improvements in symptoms.”
Estrogen-based hormone therapy has been linked to an increased risk for endometrial, breast, and ovarian cancer, according to the American Cancer Society. This means you should carefully consider how comfortable you are with those additional risks before starting this kind of therapy.
“Which of your symptoms are the most difficult to manage? You may see if you can navigate one to three of them. What are you willing to do for your symptoms? If a woman is willing to favor her sleep for the next 6 months to a year, she may be willing to change how she perceives her risk for cancer,” Dr. Flannery said. “What risk is a woman willing to take? I think if someone has a very low concern about a risk of cancer, and she’s suffering a disrupted life, then taking estradiol in a 1- to 2-year trial period could be critical to help.”
What else can help ease long COVID during menopause?
Getting the COVID vaccine, as well as getting a booster, could help. Not only will this help prevent people from being reinfected with COVID, which can worsen symptoms, but a new Swedish study says there is no evidence that it will cause postmenopausal problems like irregular bleeding.
“Weak and inconsistent associations were observed between SARS-CoV-2 vaccination and healthcare contacts for bleeding in women who are postmenopausal, and even less evidence was recorded of an association for menstrual disturbance or bleeding in women who were premenopausal,” said study coauthor Rickard Ljung, MD, PhD, MPH, professor and acting head of the pharmacoepidemiology and analysis department in the division of use and information of the Swedish Medical Products Agency in Uppsala.
A version of this article first appeared on WebMD.com.
British researchers have noted that women at midlife who have long COVID seem to get specific, and severe, symptoms, including brain fog, fatigue, new-onset dizziness, and difficulty sleeping through the night.
Doctors also think it’s possible that long COVID worsens the symptoms of perimenopause and menopause. Lower levels of estrogen and testosterone appear to be the reason.
“A long COVID theory is that there is a temporary disruption to physiological ovarian steroid hormone production, which could [worsen] symptoms of perimenopause and menopause,” said JoAnn V. Pinkerton, MD, professor of obstetrics at the University of Virginia, Charlottesville, and executive director of the North American Menopause Society.
Long COVID symptoms and menopause symptoms can also be very hard to tell apart.
Another U.K. study cautions that because of this kind of symptom overlap, women at midlife may be misdiagnosed. Research from the North American Menopause Society shows that many women may have trouble recovering from long COVID unless their hormone deficiency is treated.
What are the symptoms of long COVID?
There are over 200 symptoms that have been associated with long COVID, according to the American Medical Association. Some common symptoms are currently defined as the following: feeling extremely tired, feeling depleted after exertion, cognitive issues such as brain fog, heart beating over 100 times a minute, and a loss of sense of smell and taste.
Long COVID symptoms begin a few weeks to a few months after a COVID infection. They can last an indefinite amount of time, but “the hope is that long COVID will not be lifelong,” said Clare Flannery, MD, an endocrinologist and associate professor in the departments of obstetrics, gynecology and reproductive sciences and internal medicine at Yale University, New Haven, Conn.
What are the symptoms of menopause?
Some symptoms of menopause include vaginal infections, irregular bleeding, urinary problems, and sexual problems.
Women in their middle years have other symptoms that can be the same as perimenopause/menopause symptoms.
“Common symptoms of perimenopause and menopause which may also be symptoms ascribed to long COVID include hot flashes, night sweats, disrupted sleep, low mood, depression or anxiety, decreased concentration, memory problems, joint and muscle pains, and headaches,” Dr. Pinkerton said.
Can long COVID actually bring on menopause?
In short: Possibly.
A new study from the Massachusetts Institute of Technology/Patient-Led Research Collaborative/University of California, San Francisco, found that long COVID can cause disruptions to a woman’s menstrual cycle, ovaries, fertility, and menopause itself.
This could be caused by chronic inflammation caused by long COVID on hormones as well. This kind of inflammatory response could explain irregularities in a woman’s menstrual cycle, according to the Newson Health Research and Education study. For instance, “when the body has inflammation, ovulation can happen,” Dr. Flannery said.
The mechanism for how long COVID could spur menopause can also involve a woman’s ovaries.
“Since the theory is that COVID affects the ovary with declines in ovarian reserve and ovarian function, it makes sense that long COVID could bring on symptoms of perimenopause or menopause more acutely or more severely and lengthen the symptoms of the perimenopause and menopausal transition,” Dr. Pinkerton said.
How can hormone replacement therapy benefit women dealing with long COVID during menopause?
Estradiol, the strongest estrogen hormone in a woman’s body, has already been shown to have a positive effect against COVID.
“Estradiol therapy treats symptoms more aggressively in the setting of long COVID,” said Dr. Flannery.
Estradiol is also a form of hormone therapy for menopause symptoms.
“Estradiol has been shown to help hot flashes, night sweats, and sleep and improve mood during perimenopause,” said Dr. Pinkerton. “So it’s likely that perimenopausal or menopausal women with long COVID would see improvements both due to the action of estradiol on the ovary seen during COVID and the improvements in symptoms.”
Estrogen-based hormone therapy has been linked to an increased risk for endometrial, breast, and ovarian cancer, according to the American Cancer Society. This means you should carefully consider how comfortable you are with those additional risks before starting this kind of therapy.
“Which of your symptoms are the most difficult to manage? You may see if you can navigate one to three of them. What are you willing to do for your symptoms? If a woman is willing to favor her sleep for the next 6 months to a year, she may be willing to change how she perceives her risk for cancer,” Dr. Flannery said. “What risk is a woman willing to take? I think if someone has a very low concern about a risk of cancer, and she’s suffering a disrupted life, then taking estradiol in a 1- to 2-year trial period could be critical to help.”
What else can help ease long COVID during menopause?
Getting the COVID vaccine, as well as getting a booster, could help. Not only will this help prevent people from being reinfected with COVID, which can worsen symptoms, but a new Swedish study says there is no evidence that it will cause postmenopausal problems like irregular bleeding.
“Weak and inconsistent associations were observed between SARS-CoV-2 vaccination and healthcare contacts for bleeding in women who are postmenopausal, and even less evidence was recorded of an association for menstrual disturbance or bleeding in women who were premenopausal,” said study coauthor Rickard Ljung, MD, PhD, MPH, professor and acting head of the pharmacoepidemiology and analysis department in the division of use and information of the Swedish Medical Products Agency in Uppsala.
A version of this article first appeared on WebMD.com.
British researchers have noted that women at midlife who have long COVID seem to get specific, and severe, symptoms, including brain fog, fatigue, new-onset dizziness, and difficulty sleeping through the night.
Doctors also think it’s possible that long COVID worsens the symptoms of perimenopause and menopause. Lower levels of estrogen and testosterone appear to be the reason.
“A long COVID theory is that there is a temporary disruption to physiological ovarian steroid hormone production, which could [worsen] symptoms of perimenopause and menopause,” said JoAnn V. Pinkerton, MD, professor of obstetrics at the University of Virginia, Charlottesville, and executive director of the North American Menopause Society.
Long COVID symptoms and menopause symptoms can also be very hard to tell apart.
Another U.K. study cautions that because of this kind of symptom overlap, women at midlife may be misdiagnosed. Research from the North American Menopause Society shows that many women may have trouble recovering from long COVID unless their hormone deficiency is treated.
What are the symptoms of long COVID?
There are over 200 symptoms that have been associated with long COVID, according to the American Medical Association. Some common symptoms are currently defined as the following: feeling extremely tired, feeling depleted after exertion, cognitive issues such as brain fog, heart beating over 100 times a minute, and a loss of sense of smell and taste.
Long COVID symptoms begin a few weeks to a few months after a COVID infection. They can last an indefinite amount of time, but “the hope is that long COVID will not be lifelong,” said Clare Flannery, MD, an endocrinologist and associate professor in the departments of obstetrics, gynecology and reproductive sciences and internal medicine at Yale University, New Haven, Conn.
What are the symptoms of menopause?
Some symptoms of menopause include vaginal infections, irregular bleeding, urinary problems, and sexual problems.
Women in their middle years have other symptoms that can be the same as perimenopause/menopause symptoms.
“Common symptoms of perimenopause and menopause which may also be symptoms ascribed to long COVID include hot flashes, night sweats, disrupted sleep, low mood, depression or anxiety, decreased concentration, memory problems, joint and muscle pains, and headaches,” Dr. Pinkerton said.
Can long COVID actually bring on menopause?
In short: Possibly.
A new study from the Massachusetts Institute of Technology/Patient-Led Research Collaborative/University of California, San Francisco, found that long COVID can cause disruptions to a woman’s menstrual cycle, ovaries, fertility, and menopause itself.
This could be caused by chronic inflammation caused by long COVID on hormones as well. This kind of inflammatory response could explain irregularities in a woman’s menstrual cycle, according to the Newson Health Research and Education study. For instance, “when the body has inflammation, ovulation can happen,” Dr. Flannery said.
The mechanism for how long COVID could spur menopause can also involve a woman’s ovaries.
“Since the theory is that COVID affects the ovary with declines in ovarian reserve and ovarian function, it makes sense that long COVID could bring on symptoms of perimenopause or menopause more acutely or more severely and lengthen the symptoms of the perimenopause and menopausal transition,” Dr. Pinkerton said.
How can hormone replacement therapy benefit women dealing with long COVID during menopause?
Estradiol, the strongest estrogen hormone in a woman’s body, has already been shown to have a positive effect against COVID.
“Estradiol therapy treats symptoms more aggressively in the setting of long COVID,” said Dr. Flannery.
Estradiol is also a form of hormone therapy for menopause symptoms.
“Estradiol has been shown to help hot flashes, night sweats, and sleep and improve mood during perimenopause,” said Dr. Pinkerton. “So it’s likely that perimenopausal or menopausal women with long COVID would see improvements both due to the action of estradiol on the ovary seen during COVID and the improvements in symptoms.”
Estrogen-based hormone therapy has been linked to an increased risk for endometrial, breast, and ovarian cancer, according to the American Cancer Society. This means you should carefully consider how comfortable you are with those additional risks before starting this kind of therapy.
“Which of your symptoms are the most difficult to manage? You may see if you can navigate one to three of them. What are you willing to do for your symptoms? If a woman is willing to favor her sleep for the next 6 months to a year, she may be willing to change how she perceives her risk for cancer,” Dr. Flannery said. “What risk is a woman willing to take? I think if someone has a very low concern about a risk of cancer, and she’s suffering a disrupted life, then taking estradiol in a 1- to 2-year trial period could be critical to help.”
What else can help ease long COVID during menopause?
Getting the COVID vaccine, as well as getting a booster, could help. Not only will this help prevent people from being reinfected with COVID, which can worsen symptoms, but a new Swedish study says there is no evidence that it will cause postmenopausal problems like irregular bleeding.
“Weak and inconsistent associations were observed between SARS-CoV-2 vaccination and healthcare contacts for bleeding in women who are postmenopausal, and even less evidence was recorded of an association for menstrual disturbance or bleeding in women who were premenopausal,” said study coauthor Rickard Ljung, MD, PhD, MPH, professor and acting head of the pharmacoepidemiology and analysis department in the division of use and information of the Swedish Medical Products Agency in Uppsala.
A version of this article first appeared on WebMD.com.
COVID vaccines safe for young children, study finds
TOPLINE:
COVID-19 vaccines from Moderna and Pfizer-BioNTech are safe for children under age 5 years, according to findings from a study funded by the Centers for Disease Control and Prevention.
METHODOLOGY:
- Data came from the Vaccine Safety Datalink, which gathers information from eight health systems in the United States.
- Analyzed data from 135,005 doses given to children age 4 and younger who received the Pfizer-BioNTech , and 112,006 doses given to children aged 5 and younger who received the Moderna version.
- Assessed for 23 safety outcomes, including myocarditis, pericarditis, and seizures.
TAKEAWAY:
- One case of hemorrhagic stroke and one case of pulmonary embolism occurred after vaccination but these were linked to preexisting congenital abnormalities.
IN PRACTICE:
“These results can provide reassurance to clinicians, parents, and policymakers alike.”
STUDY DETAILS:
The study was led by Kristin Goddard, MPH, a researcher at the Kaiser Permanente Vaccine Study Center in Oakland, Calif., and was funded by the Centers for Disease Control and Prevention.
LIMITATIONS:
The researchers reported low statistical power for early analysis, especially for rare outcomes. In addition, fewer than 25% of children in the database had received a vaccine at the time of analysis.
DISCLOSURES:
A coauthor reported receiving funding from Janssen Vaccines and Prevention for a study unrelated to COVID-19 vaccines. Another coauthor reported receiving grants from Pfizer in 2019 for clinical trials for coronavirus vaccines, and from Merck, GSK, and Sanofi Pasteur for unrelated research.
A version of this article first appeared on Medscape.com.
TOPLINE:
COVID-19 vaccines from Moderna and Pfizer-BioNTech are safe for children under age 5 years, according to findings from a study funded by the Centers for Disease Control and Prevention.
METHODOLOGY:
- Data came from the Vaccine Safety Datalink, which gathers information from eight health systems in the United States.
- Analyzed data from 135,005 doses given to children age 4 and younger who received the Pfizer-BioNTech , and 112,006 doses given to children aged 5 and younger who received the Moderna version.
- Assessed for 23 safety outcomes, including myocarditis, pericarditis, and seizures.
TAKEAWAY:
- One case of hemorrhagic stroke and one case of pulmonary embolism occurred after vaccination but these were linked to preexisting congenital abnormalities.
IN PRACTICE:
“These results can provide reassurance to clinicians, parents, and policymakers alike.”
STUDY DETAILS:
The study was led by Kristin Goddard, MPH, a researcher at the Kaiser Permanente Vaccine Study Center in Oakland, Calif., and was funded by the Centers for Disease Control and Prevention.
LIMITATIONS:
The researchers reported low statistical power for early analysis, especially for rare outcomes. In addition, fewer than 25% of children in the database had received a vaccine at the time of analysis.
DISCLOSURES:
A coauthor reported receiving funding from Janssen Vaccines and Prevention for a study unrelated to COVID-19 vaccines. Another coauthor reported receiving grants from Pfizer in 2019 for clinical trials for coronavirus vaccines, and from Merck, GSK, and Sanofi Pasteur for unrelated research.
A version of this article first appeared on Medscape.com.
TOPLINE:
COVID-19 vaccines from Moderna and Pfizer-BioNTech are safe for children under age 5 years, according to findings from a study funded by the Centers for Disease Control and Prevention.
METHODOLOGY:
- Data came from the Vaccine Safety Datalink, which gathers information from eight health systems in the United States.
- Analyzed data from 135,005 doses given to children age 4 and younger who received the Pfizer-BioNTech , and 112,006 doses given to children aged 5 and younger who received the Moderna version.
- Assessed for 23 safety outcomes, including myocarditis, pericarditis, and seizures.
TAKEAWAY:
- One case of hemorrhagic stroke and one case of pulmonary embolism occurred after vaccination but these were linked to preexisting congenital abnormalities.
IN PRACTICE:
“These results can provide reassurance to clinicians, parents, and policymakers alike.”
STUDY DETAILS:
The study was led by Kristin Goddard, MPH, a researcher at the Kaiser Permanente Vaccine Study Center in Oakland, Calif., and was funded by the Centers for Disease Control and Prevention.
LIMITATIONS:
The researchers reported low statistical power for early analysis, especially for rare outcomes. In addition, fewer than 25% of children in the database had received a vaccine at the time of analysis.
DISCLOSURES:
A coauthor reported receiving funding from Janssen Vaccines and Prevention for a study unrelated to COVID-19 vaccines. Another coauthor reported receiving grants from Pfizer in 2019 for clinical trials for coronavirus vaccines, and from Merck, GSK, and Sanofi Pasteur for unrelated research.
A version of this article first appeared on Medscape.com.
FROM PEDIATRICS
Medicaid patients with heart failure get poor follow-up after hospital discharge
Nearly 60% of Medicaid-covered adults with concurrent diabetes and heart failure did not receive guideline-concordant postdischarge care within 7-10 days of leaving the hospital, according to a large Alabama study. Moreover, affected Black and Hispanic/other Alabamians were less likely than were their White counterparts to receive recommended postdischarge care.
In comparison with White participants, Black and Hispanic adults were less likely to have any postdischarge ambulatory care visits after HF hospitalization or had a delayed visit, according to researchers led by Yulia Khodneva, MD, PhD, an internist at the University of Alabama at Birmingham. “This is likely a reflection of a structural racism and implicit bias against racial and ethnic minorities that persists in the U.S. health care system,” she and her colleagues wrote.
The findings point to the need for strategies to improve access to postdischarge care for lower-income HF patients.
Among U.S. states, Alabama is the sixth-poorest, the third in diabetes prevalence (14%), and has the highest rates of heart failure hospitalizations and cardiovascular mortality, the authors noted.
Study details
The cohort included 9,857 adults with diabetes and first hospitalizations for heart failure who were covered by Alabama Medicaid during 2010-2019. The investigators analyzed patients’ claims for ambulatory care (any, primary, cardiology, or endocrinology) within 60 days of discharge.
The mean age of participants was 53.7 years; 47.3% were Black; 41.8% non-Hispanic White; and 10.9% Hispanic/other, with other including those identifying as non-White Hispanic, American Indian, Pacific Islander, and Asian. About two-thirds (65.4%) of participants were women.
Analysis revealed low rates of follow-up care after hospital discharge; 26.7% had an ambulatory visit within 0-7 days, 15.2% within 8-14 days, 31.3% within 15-60 days, and 26.8% had no follow-up visit at all. Of those having a follow-up visit, 71% saw a primary care physician and 12% saw a cardiologist.
In contrast, a much higher proportion of heart failure patients in a Swedish registry – 63% – received ambulatory follow-up in cardiology.
Ethnic/gender/age disparities
Black and Hispanic/other adults were less likely to have any postdischarge ambulatory visit (P <.0001) or had the visit delayed by 1.8 days (P = .0006) and 2.8 days (P = .0016), respectively. They were less likely to see a primary care physician than were non-Hispanic White adults: adjusted incidence rate ratio, 0.96 (95% confidence interval [CI], 0.91-1.00) and 0.91 (95% CI, 0.89-0.98), respectively.
Men and those with longer-standing heart failure were less likely to be seen in primary care, while the presence of multiple comorbidities was associated with a higher likelihood of a postdischarge primary care visit. Men were more likely to be seen by a cardiologist, while older discharged patients were less likely to be seen by an endocrinologist within 60 days. There was a U-shaped relationship between the timing of the first postdischarge ambulatory visit and all-cause mortality among adults with diabetes and heart failure. Higher rates of 60-day all-cause mortality were observed both in those who had seen a provider within 0-7 days after discharge and in those who had not seen any provider during the 60-day study period compared with those having an ambulatory care visit within 7-14 or 15-60 days. “The group with early follow-up (0-7 days) likely represents a sicker population of patients with heart failure with more comorbidity burden and higher overall health care use, including readmissions, as was demonstrated in our analysis,” Dr. Khodneva and associates wrote. “Interventions that improve access to postdischarge ambulatory care for low-income patients with diabetes and heart failure and eliminate racial and ethnic disparities may be warranted,” they added.
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases and the University of Alabama at Birmingham Diabetes Research Center. Dr. Khodneva reported funding from the University of Alabama at Birmingham and the Forge Ahead Center as well as from the NIDDK, the National Institutes of Health, the Agency for Healthcare Research and Quality, and the Alabama Medicaid Agency. Coauthor Emily Levitan, ScD, reported research funding from Amgen and has served on Amgen advisory boards. She has also served as a scientific consultant for a research project funded by Novartis.
Nearly 60% of Medicaid-covered adults with concurrent diabetes and heart failure did not receive guideline-concordant postdischarge care within 7-10 days of leaving the hospital, according to a large Alabama study. Moreover, affected Black and Hispanic/other Alabamians were less likely than were their White counterparts to receive recommended postdischarge care.
In comparison with White participants, Black and Hispanic adults were less likely to have any postdischarge ambulatory care visits after HF hospitalization or had a delayed visit, according to researchers led by Yulia Khodneva, MD, PhD, an internist at the University of Alabama at Birmingham. “This is likely a reflection of a structural racism and implicit bias against racial and ethnic minorities that persists in the U.S. health care system,” she and her colleagues wrote.
The findings point to the need for strategies to improve access to postdischarge care for lower-income HF patients.
Among U.S. states, Alabama is the sixth-poorest, the third in diabetes prevalence (14%), and has the highest rates of heart failure hospitalizations and cardiovascular mortality, the authors noted.
Study details
The cohort included 9,857 adults with diabetes and first hospitalizations for heart failure who were covered by Alabama Medicaid during 2010-2019. The investigators analyzed patients’ claims for ambulatory care (any, primary, cardiology, or endocrinology) within 60 days of discharge.
The mean age of participants was 53.7 years; 47.3% were Black; 41.8% non-Hispanic White; and 10.9% Hispanic/other, with other including those identifying as non-White Hispanic, American Indian, Pacific Islander, and Asian. About two-thirds (65.4%) of participants were women.
Analysis revealed low rates of follow-up care after hospital discharge; 26.7% had an ambulatory visit within 0-7 days, 15.2% within 8-14 days, 31.3% within 15-60 days, and 26.8% had no follow-up visit at all. Of those having a follow-up visit, 71% saw a primary care physician and 12% saw a cardiologist.
In contrast, a much higher proportion of heart failure patients in a Swedish registry – 63% – received ambulatory follow-up in cardiology.
Ethnic/gender/age disparities
Black and Hispanic/other adults were less likely to have any postdischarge ambulatory visit (P <.0001) or had the visit delayed by 1.8 days (P = .0006) and 2.8 days (P = .0016), respectively. They were less likely to see a primary care physician than were non-Hispanic White adults: adjusted incidence rate ratio, 0.96 (95% confidence interval [CI], 0.91-1.00) and 0.91 (95% CI, 0.89-0.98), respectively.
Men and those with longer-standing heart failure were less likely to be seen in primary care, while the presence of multiple comorbidities was associated with a higher likelihood of a postdischarge primary care visit. Men were more likely to be seen by a cardiologist, while older discharged patients were less likely to be seen by an endocrinologist within 60 days. There was a U-shaped relationship between the timing of the first postdischarge ambulatory visit and all-cause mortality among adults with diabetes and heart failure. Higher rates of 60-day all-cause mortality were observed both in those who had seen a provider within 0-7 days after discharge and in those who had not seen any provider during the 60-day study period compared with those having an ambulatory care visit within 7-14 or 15-60 days. “The group with early follow-up (0-7 days) likely represents a sicker population of patients with heart failure with more comorbidity burden and higher overall health care use, including readmissions, as was demonstrated in our analysis,” Dr. Khodneva and associates wrote. “Interventions that improve access to postdischarge ambulatory care for low-income patients with diabetes and heart failure and eliminate racial and ethnic disparities may be warranted,” they added.
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases and the University of Alabama at Birmingham Diabetes Research Center. Dr. Khodneva reported funding from the University of Alabama at Birmingham and the Forge Ahead Center as well as from the NIDDK, the National Institutes of Health, the Agency for Healthcare Research and Quality, and the Alabama Medicaid Agency. Coauthor Emily Levitan, ScD, reported research funding from Amgen and has served on Amgen advisory boards. She has also served as a scientific consultant for a research project funded by Novartis.
Nearly 60% of Medicaid-covered adults with concurrent diabetes and heart failure did not receive guideline-concordant postdischarge care within 7-10 days of leaving the hospital, according to a large Alabama study. Moreover, affected Black and Hispanic/other Alabamians were less likely than were their White counterparts to receive recommended postdischarge care.
In comparison with White participants, Black and Hispanic adults were less likely to have any postdischarge ambulatory care visits after HF hospitalization or had a delayed visit, according to researchers led by Yulia Khodneva, MD, PhD, an internist at the University of Alabama at Birmingham. “This is likely a reflection of a structural racism and implicit bias against racial and ethnic minorities that persists in the U.S. health care system,” she and her colleagues wrote.
The findings point to the need for strategies to improve access to postdischarge care for lower-income HF patients.
Among U.S. states, Alabama is the sixth-poorest, the third in diabetes prevalence (14%), and has the highest rates of heart failure hospitalizations and cardiovascular mortality, the authors noted.
Study details
The cohort included 9,857 adults with diabetes and first hospitalizations for heart failure who were covered by Alabama Medicaid during 2010-2019. The investigators analyzed patients’ claims for ambulatory care (any, primary, cardiology, or endocrinology) within 60 days of discharge.
The mean age of participants was 53.7 years; 47.3% were Black; 41.8% non-Hispanic White; and 10.9% Hispanic/other, with other including those identifying as non-White Hispanic, American Indian, Pacific Islander, and Asian. About two-thirds (65.4%) of participants were women.
Analysis revealed low rates of follow-up care after hospital discharge; 26.7% had an ambulatory visit within 0-7 days, 15.2% within 8-14 days, 31.3% within 15-60 days, and 26.8% had no follow-up visit at all. Of those having a follow-up visit, 71% saw a primary care physician and 12% saw a cardiologist.
In contrast, a much higher proportion of heart failure patients in a Swedish registry – 63% – received ambulatory follow-up in cardiology.
Ethnic/gender/age disparities
Black and Hispanic/other adults were less likely to have any postdischarge ambulatory visit (P <.0001) or had the visit delayed by 1.8 days (P = .0006) and 2.8 days (P = .0016), respectively. They were less likely to see a primary care physician than were non-Hispanic White adults: adjusted incidence rate ratio, 0.96 (95% confidence interval [CI], 0.91-1.00) and 0.91 (95% CI, 0.89-0.98), respectively.
Men and those with longer-standing heart failure were less likely to be seen in primary care, while the presence of multiple comorbidities was associated with a higher likelihood of a postdischarge primary care visit. Men were more likely to be seen by a cardiologist, while older discharged patients were less likely to be seen by an endocrinologist within 60 days. There was a U-shaped relationship between the timing of the first postdischarge ambulatory visit and all-cause mortality among adults with diabetes and heart failure. Higher rates of 60-day all-cause mortality were observed both in those who had seen a provider within 0-7 days after discharge and in those who had not seen any provider during the 60-day study period compared with those having an ambulatory care visit within 7-14 or 15-60 days. “The group with early follow-up (0-7 days) likely represents a sicker population of patients with heart failure with more comorbidity burden and higher overall health care use, including readmissions, as was demonstrated in our analysis,” Dr. Khodneva and associates wrote. “Interventions that improve access to postdischarge ambulatory care for low-income patients with diabetes and heart failure and eliminate racial and ethnic disparities may be warranted,” they added.
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases and the University of Alabama at Birmingham Diabetes Research Center. Dr. Khodneva reported funding from the University of Alabama at Birmingham and the Forge Ahead Center as well as from the NIDDK, the National Institutes of Health, the Agency for Healthcare Research and Quality, and the Alabama Medicaid Agency. Coauthor Emily Levitan, ScD, reported research funding from Amgen and has served on Amgen advisory boards. She has also served as a scientific consultant for a research project funded by Novartis.
FROM JOURNAL OF THE AMERICAN HEART ASSOCIATION
EHR nudges a bust for boosting guideline-directed meds in acute HF: PROMPT-AHF
in a randomized trial conducted at several centers in the same health care system.
The results of the PROMPT-AHF trial, which assigned such patients to have or not have the GDMT-promoting physician nudges as part of their in-hospital management, were “not entirely surprising,” Tariq Ahmad, MD, MPH, of Yale University, New Haven, Conn., said in an interview.
“We have created an environment in the hospital that makes care quite fractured for patients with heart failure,” he said. “They are cared for by many different clinicians, which leads to well-known behaviors such as diffusion of responsibility.”
Moreover, many clinicians focus on stabilizing patients “rather than starting them on a comprehensive set of medications, which most think should be done after discharge,” Dr. Ahmad added.
“Importantly, there has been a logarithmic increase in alerts while patients are hospitalized that has caused clinician burnout and is leading to even very important alerts being ignored.”
Likely as a result, the trial saw no significant difference between the alert and no-alert groups in how often the number of GDMT prescriptions rose by at least one drug class, whether beta blockers, renin-angiotensin system inhibitors, mineralocorticoid receptor antagonists, or SGLT2 inhibitors. That happened for 34% of patients in both groups, reported Dr. Ahmad at the Heart Failure Association of the European Society of Cardiology (HFA-ESC) 2023 sessions
Nor was there a difference in the secondary endpoint of increased number of GDMT meds or escalated dosage of prescribed GDMT drugs.
GDMT ‘uncommon’ in AHF
In an earlier trial in outpatients with chronic HF, conducted by many of the same researchers, use of a targeted EHR-based alert system was associated with significantly higher rates of GDMT prescriptions 30 days after discharge, compared with usual care, Dr. Ahmad observed in his presentation.
Because GDMT is similarly “uncommon” among patients hospitalized with acute HF, the team designed the current trial, a test of the hypothesis that a similar system of nudges would lead to higher rates of prescriptions of the four core GDMT drug classes.
The study enrolled 920 adults with acute HF, an EF of 40% or lower (their median was 28%), and NT-proBNP levels higher than 500 pg/mL. The patients received IV diuretics for the first 24 in-hospital hours and were not taking medications from any of the four core HF drug classes. Their mean age was 74, 36% were women, and 25% were Black.
Physicians of patients who were randomly assigned to the intervention received the alerts as they entered information that involved ejection fraction, blood pressure, potassium levels, heart rate, glomerular filtration rate, and meds they were currently or should be taking, “along with an order set that made ordering those medications very easy,” Dr. Ahmad said.
“There was absolutely no evidence that the alert made any difference. There were zero patients on all four classes of GDMT at baseline, and at the time of discharge, only 11.2% of patients were on all four pillars – essentially, one in nine patients,” Dr. Ahmad said. Nor were there any subgroup differences in age, sex, race, ejection fraction, type of health insurance, or whether care was provided by a cardiologist or noncardiologist physician.
The study was limited by having been conducted within a single health care network using only the Epic EHR system. The alerts did not go exclusively to cardiologists, and patient preferences were not considered in the analysis. Also, the study’s alerts represented only some of the many that were received by the clinicians during the course of the trial.
Better incentives needed
“We believe this shows that refinement of the nudges is needed, as well as changes to clinician incentives to overcome barriers to implementation of GDMT during hospitalizations for AHF,” Dr. Ahmad said.
Responding to a postpresentation question on whether the postdischarge phase might be a more effective time to intervene with nudges, Dr. Ahmad observed that many clinicians who care for patients in the hospital assume that someone else will have the patient receive appropriate meds after discharge. “But we know that things that are started in the hospital tend to stick better.
“I do think that a lot of the clinicians were thinking, ‘I’m just going to get this patient out and someone in the outside will get them on GDMT,’ ” he said.
In the United States there are many incentives to reduce hospital length of stay and to expedite discharge so more beds are available for incoming patients, Dr. Ahmad observed. “I think it’s a combination of these kinds of perverse incentives that are not allowing us to get patients on appropriate GDMT during hospitalization.”
Furthermore, Dr. Ahmad told this news organization, “additions to the EHR should be evaluated in an evidence-based manner. However, the opposite has occurred, with an unregulated data tsunami crushing clinicians, which has been bad both for the clinicians and for patients.”
The study was funded by AstraZeneca. Dr. Ahmad discloses receiving research funding from and consulting for AstraZeneca; and receiving research funding from Boehringer Ingelheim, Cytokinetics, and Relypsa. Three other coauthors are employees of AstraZeneca.
A version of this article first appeared on Medscape.com.
in a randomized trial conducted at several centers in the same health care system.
The results of the PROMPT-AHF trial, which assigned such patients to have or not have the GDMT-promoting physician nudges as part of their in-hospital management, were “not entirely surprising,” Tariq Ahmad, MD, MPH, of Yale University, New Haven, Conn., said in an interview.
“We have created an environment in the hospital that makes care quite fractured for patients with heart failure,” he said. “They are cared for by many different clinicians, which leads to well-known behaviors such as diffusion of responsibility.”
Moreover, many clinicians focus on stabilizing patients “rather than starting them on a comprehensive set of medications, which most think should be done after discharge,” Dr. Ahmad added.
“Importantly, there has been a logarithmic increase in alerts while patients are hospitalized that has caused clinician burnout and is leading to even very important alerts being ignored.”
Likely as a result, the trial saw no significant difference between the alert and no-alert groups in how often the number of GDMT prescriptions rose by at least one drug class, whether beta blockers, renin-angiotensin system inhibitors, mineralocorticoid receptor antagonists, or SGLT2 inhibitors. That happened for 34% of patients in both groups, reported Dr. Ahmad at the Heart Failure Association of the European Society of Cardiology (HFA-ESC) 2023 sessions
Nor was there a difference in the secondary endpoint of increased number of GDMT meds or escalated dosage of prescribed GDMT drugs.
GDMT ‘uncommon’ in AHF
In an earlier trial in outpatients with chronic HF, conducted by many of the same researchers, use of a targeted EHR-based alert system was associated with significantly higher rates of GDMT prescriptions 30 days after discharge, compared with usual care, Dr. Ahmad observed in his presentation.
Because GDMT is similarly “uncommon” among patients hospitalized with acute HF, the team designed the current trial, a test of the hypothesis that a similar system of nudges would lead to higher rates of prescriptions of the four core GDMT drug classes.
The study enrolled 920 adults with acute HF, an EF of 40% or lower (their median was 28%), and NT-proBNP levels higher than 500 pg/mL. The patients received IV diuretics for the first 24 in-hospital hours and were not taking medications from any of the four core HF drug classes. Their mean age was 74, 36% were women, and 25% were Black.
Physicians of patients who were randomly assigned to the intervention received the alerts as they entered information that involved ejection fraction, blood pressure, potassium levels, heart rate, glomerular filtration rate, and meds they were currently or should be taking, “along with an order set that made ordering those medications very easy,” Dr. Ahmad said.
“There was absolutely no evidence that the alert made any difference. There were zero patients on all four classes of GDMT at baseline, and at the time of discharge, only 11.2% of patients were on all four pillars – essentially, one in nine patients,” Dr. Ahmad said. Nor were there any subgroup differences in age, sex, race, ejection fraction, type of health insurance, or whether care was provided by a cardiologist or noncardiologist physician.
The study was limited by having been conducted within a single health care network using only the Epic EHR system. The alerts did not go exclusively to cardiologists, and patient preferences were not considered in the analysis. Also, the study’s alerts represented only some of the many that were received by the clinicians during the course of the trial.
Better incentives needed
“We believe this shows that refinement of the nudges is needed, as well as changes to clinician incentives to overcome barriers to implementation of GDMT during hospitalizations for AHF,” Dr. Ahmad said.
Responding to a postpresentation question on whether the postdischarge phase might be a more effective time to intervene with nudges, Dr. Ahmad observed that many clinicians who care for patients in the hospital assume that someone else will have the patient receive appropriate meds after discharge. “But we know that things that are started in the hospital tend to stick better.
“I do think that a lot of the clinicians were thinking, ‘I’m just going to get this patient out and someone in the outside will get them on GDMT,’ ” he said.
In the United States there are many incentives to reduce hospital length of stay and to expedite discharge so more beds are available for incoming patients, Dr. Ahmad observed. “I think it’s a combination of these kinds of perverse incentives that are not allowing us to get patients on appropriate GDMT during hospitalization.”
Furthermore, Dr. Ahmad told this news organization, “additions to the EHR should be evaluated in an evidence-based manner. However, the opposite has occurred, with an unregulated data tsunami crushing clinicians, which has been bad both for the clinicians and for patients.”
The study was funded by AstraZeneca. Dr. Ahmad discloses receiving research funding from and consulting for AstraZeneca; and receiving research funding from Boehringer Ingelheim, Cytokinetics, and Relypsa. Three other coauthors are employees of AstraZeneca.
A version of this article first appeared on Medscape.com.
in a randomized trial conducted at several centers in the same health care system.
The results of the PROMPT-AHF trial, which assigned such patients to have or not have the GDMT-promoting physician nudges as part of their in-hospital management, were “not entirely surprising,” Tariq Ahmad, MD, MPH, of Yale University, New Haven, Conn., said in an interview.
“We have created an environment in the hospital that makes care quite fractured for patients with heart failure,” he said. “They are cared for by many different clinicians, which leads to well-known behaviors such as diffusion of responsibility.”
Moreover, many clinicians focus on stabilizing patients “rather than starting them on a comprehensive set of medications, which most think should be done after discharge,” Dr. Ahmad added.
“Importantly, there has been a logarithmic increase in alerts while patients are hospitalized that has caused clinician burnout and is leading to even very important alerts being ignored.”
Likely as a result, the trial saw no significant difference between the alert and no-alert groups in how often the number of GDMT prescriptions rose by at least one drug class, whether beta blockers, renin-angiotensin system inhibitors, mineralocorticoid receptor antagonists, or SGLT2 inhibitors. That happened for 34% of patients in both groups, reported Dr. Ahmad at the Heart Failure Association of the European Society of Cardiology (HFA-ESC) 2023 sessions
Nor was there a difference in the secondary endpoint of increased number of GDMT meds or escalated dosage of prescribed GDMT drugs.
GDMT ‘uncommon’ in AHF
In an earlier trial in outpatients with chronic HF, conducted by many of the same researchers, use of a targeted EHR-based alert system was associated with significantly higher rates of GDMT prescriptions 30 days after discharge, compared with usual care, Dr. Ahmad observed in his presentation.
Because GDMT is similarly “uncommon” among patients hospitalized with acute HF, the team designed the current trial, a test of the hypothesis that a similar system of nudges would lead to higher rates of prescriptions of the four core GDMT drug classes.
The study enrolled 920 adults with acute HF, an EF of 40% or lower (their median was 28%), and NT-proBNP levels higher than 500 pg/mL. The patients received IV diuretics for the first 24 in-hospital hours and were not taking medications from any of the four core HF drug classes. Their mean age was 74, 36% were women, and 25% were Black.
Physicians of patients who were randomly assigned to the intervention received the alerts as they entered information that involved ejection fraction, blood pressure, potassium levels, heart rate, glomerular filtration rate, and meds they were currently or should be taking, “along with an order set that made ordering those medications very easy,” Dr. Ahmad said.
“There was absolutely no evidence that the alert made any difference. There were zero patients on all four classes of GDMT at baseline, and at the time of discharge, only 11.2% of patients were on all four pillars – essentially, one in nine patients,” Dr. Ahmad said. Nor were there any subgroup differences in age, sex, race, ejection fraction, type of health insurance, or whether care was provided by a cardiologist or noncardiologist physician.
The study was limited by having been conducted within a single health care network using only the Epic EHR system. The alerts did not go exclusively to cardiologists, and patient preferences were not considered in the analysis. Also, the study’s alerts represented only some of the many that were received by the clinicians during the course of the trial.
Better incentives needed
“We believe this shows that refinement of the nudges is needed, as well as changes to clinician incentives to overcome barriers to implementation of GDMT during hospitalizations for AHF,” Dr. Ahmad said.
Responding to a postpresentation question on whether the postdischarge phase might be a more effective time to intervene with nudges, Dr. Ahmad observed that many clinicians who care for patients in the hospital assume that someone else will have the patient receive appropriate meds after discharge. “But we know that things that are started in the hospital tend to stick better.
“I do think that a lot of the clinicians were thinking, ‘I’m just going to get this patient out and someone in the outside will get them on GDMT,’ ” he said.
In the United States there are many incentives to reduce hospital length of stay and to expedite discharge so more beds are available for incoming patients, Dr. Ahmad observed. “I think it’s a combination of these kinds of perverse incentives that are not allowing us to get patients on appropriate GDMT during hospitalization.”
Furthermore, Dr. Ahmad told this news organization, “additions to the EHR should be evaluated in an evidence-based manner. However, the opposite has occurred, with an unregulated data tsunami crushing clinicians, which has been bad both for the clinicians and for patients.”
The study was funded by AstraZeneca. Dr. Ahmad discloses receiving research funding from and consulting for AstraZeneca; and receiving research funding from Boehringer Ingelheim, Cytokinetics, and Relypsa. Three other coauthors are employees of AstraZeneca.
A version of this article first appeared on Medscape.com.
FROM ESC Heart Failure 2023


