User login
ID Practitioner is an independent news source that provides infectious disease specialists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the infectious disease specialist’s practice. Specialty focus topics include antimicrobial resistance, emerging infections, global ID, hepatitis, HIV, hospital-acquired infections, immunizations and vaccines, influenza, mycoses, pediatric infections, and STIs. Infectious Diseases News is owned by Frontline Medical Communications.
sofosbuvir
ritonavir with dasabuvir
discount
support path
program
ritonavir
greedy
ledipasvir
assistance
viekira pak
vpak
advocacy
needy
protest
abbvie
paritaprevir
ombitasvir
direct-acting antivirals
dasabuvir
gilead
fake-ovir
support
v pak
oasis
harvoni
section[contains(@class, 'footer-nav-section-wrapper')]
div[contains(@class, 'pane-pub-article-idp')]
div[contains(@class, 'pane-medstat-latest-articles-articles-section')]
div[contains(@class, 'pane-pub-home-idp')]
div[contains(@class, 'pane-pub-topic-idp')]
The danger when doctors don’t get mental health help
As medical professionals, you’re continually exposed to overwork, burnout, stressful situations, and challenging ethical decisions. Yet seeking help for mental health care may be last on your to-do list – or completely off your radar.
That’s sad and dangerous, since the American College of Emergency Physicians said 300-400 physicians die by suicide each year, and the stigma keeps 69% of female physicians from seeking mental health care, according to a prepandemic study.
In the 2022 Medscape Physician Suicide Report, 11% of female doctors and 9% of male doctors said they have had thoughts of suicide, and 64% experienced colloquial depression (feeling down, sad, or blue).
What’s more, physicians are typically seen as strong and capable and are often put on a pedestal by loved ones, patients, and the public and thought of as superhuman. No wonder it isn’t easy when you need to take time away to decompress and treat your mental well-being.
“There is a real fear for physicians when it comes to getting mental health care,” said Emil Tsai, MD, PhD, MAS, professor at the department of psychiatry and behavioral sciences at the University of California, Los Angeles, and an internationally reputed scientist in neurosciences and brain disorders.
The fear, said Dr. Tsai, comes from the stigma of mental health issues, potential repercussions to employment, and conceivable medical board suspension or revocation of your medical license.
Dr. Tsai said in an interview that to combat anxiety about “punishment” that many physicians fear when seeking care for their mental health, we must allow physicians to take time away from their day-to-day patient care for respite and treatment without reprisal.
Since the medical profession is high stress and has a high depression and suicide rate, finding solutions is imperative. And physicians must feel supported enough to seek treatment when needed. So how can we normalize seeking mental health care among physicians?
Get honest about stress and burnout
The only way to normalize any behavior is to be open and candid, Dr. Tsai said in an interview. The mental health conversation must occur across the board, not just within the medical profession.
“The greatest thing we can do to try and lift the burden that we place on physicians is to be willing to talk and be honest about the stress that physicians deal with and the importance of everyone feeling free to seek treatment and rest to strengthen their mental health,” said Dr. Tsai.
The more we talk about mental health and its treatment, the more we lessen the stigma, said Dr. Tsai. That could be more employer-employee check-ins, counseling as part of physician wellness, and programs structured so as not to construe a penal system.
“Mental health in the medical profession is a big issue and one that has to be met with the same compassion and care as it should be for any patient. We have annual physical checkups. Why don’t we offer annual mental health checkups for all, physicians included?” asked Dr. Tsai.
Evaluate the workload
Elizabeth Lombardo, PhD, psychologist, coach, and global keynote speaker, thinks that health care employers should reexamine their physicians’ workloads to see if they’re contributing to mental health issues.
The conversation on mental health in the workplace shouldn’t be about whether a certain person can handle stressors that are “normal” for health care settings. Instead, workplace managers in health care institutions should redefine workloads to ensure that physicians aren’t too heavily burdened with responsibilities that can cause overwork, burnout, and mental health problems,” she said.
Lessen the stigma
Even when physicians want to seek help for their psychological struggles, they may be weary of how their colleagues would react if they knew.
Raffaello Antonino, MD, clinical director at Therapy Central in London, said several underlying fears may exist at a physician’s core that prevent them from seeking care – being seen as weak, being judged as unfit to practice medicine, and the notion that “something is wrong with them.”
Dr. Antonino said we need to understand that physicians face challenges of bereavement and trauma derived from losing patients and the inability to save someone’s life. “These issues can easily develop into an accumulation of difficult, unprocessed emotions, later arising in symptoms and signs of PTSD, anxiety, and depression.”
Education is the best way to end this stigma, just like with any form of prejudice and stereotypes. For instance, we know that health care professionals are at risk of developing burnout. So, educating physicians on the symptoms and management of burnout and its consequences and prevention strategies is a must.
“Imagine what could happen if there were regular opportunities to work through the day’s events before signing out from a shift. The idea that individual weekly therapy is the only way to relieve mental distress is false,” said Lori McIsaac Bewsher, MSW, RSW, a trauma therapist and owner of a trauma-focused mental health clinic in New Brunswick.
“There are ways of integrating individual care into our doctor’s offices and hospitals that can be brief, effective, and confidential. The best way to introduce these interventions is early and collectively; no one is immune to the potential impact of exposure to trauma. The earlier these interventions can be accessed, the better the outcomes for everyone,” she said.
Dr. Antonino suggests, perhaps in the future, organizations can have “burnout checks” or mental health wellness checks for physicians akin to how we also have quick examinations for various physical ailments. What if physicians regularly answered a 10-question mental health survey as part of a burnout or trauma prevention strategy?
“Theirs is a profession and an identity which is often linked with a sense of strength, leadership and [benevolent] power: adjectives, which on the surface one might see as incompatible with what instead, unfortunately, and wrongly, may be associated with mental health issues,” said Dr. Antonino.
Keep it private
When it comes to removing the stigma from mental health care and treatment for physicians, privacy is top of mind. There needs to be some form of privacy protection for physicians who seek professional help for mental health reasons. Dr. Lombardo said physicians need to have the choice to keep their mental health journeys private. “Ideally, normalization should mean openly conversing about mental health, but for physicians, it can be a matter of life or death for their career, so the choice to remain private is something that should be afforded to them.”
Along those lines, the American Medical Association is pushing for system changes in legislative and regulatory arenas to support the mental health of practicing physicians, residents, and medical students. The organization is also urging health systems and state medical licensing bodies to remove questions on their applications that ask about prior treatment for mental health conditions.
Among many programs across the country, the Foundation of the Pennsylvania Medical Society has also created a Physicians’ Health Program, which provides confidential assessment, counseling, and referral services for physicians with mental health concerns.
“All of these initiatives are important in helping to destigmatize mental health issues among physicians,” said Harold Hong, MD, a board-certified psychiatrist in Raleigh, N.C.
Hail the benefits of treatment
Dr. Hong said to continue to destigmatize mental health among physicians and normalize its treatment, we not only have to emphasize how attending to mental health has individual benefits but also how it helps us help our patients.
“One key aspect that perhaps underpins this issue is the still present separation between mental and physical health, between mind and body, Dr. Hong said in an interview. “Feeling sad or angry or anxious should become a fact of life, a characteristic of being human, just like catching a cold or breaking a leg.”
It’s a normalization that, perhaps more than anything else, can lead the way for improving physicians’ mental health outcomes while also improving them for the rest of society. When society can finally see the health and well-being of someone in both their psychological and physical status, some of the stigmas may dissipate, and perhaps more physicians’ lives can be saved.
A version of this article first appeared on Medscape.com.
As medical professionals, you’re continually exposed to overwork, burnout, stressful situations, and challenging ethical decisions. Yet seeking help for mental health care may be last on your to-do list – or completely off your radar.
That’s sad and dangerous, since the American College of Emergency Physicians said 300-400 physicians die by suicide each year, and the stigma keeps 69% of female physicians from seeking mental health care, according to a prepandemic study.
In the 2022 Medscape Physician Suicide Report, 11% of female doctors and 9% of male doctors said they have had thoughts of suicide, and 64% experienced colloquial depression (feeling down, sad, or blue).
What’s more, physicians are typically seen as strong and capable and are often put on a pedestal by loved ones, patients, and the public and thought of as superhuman. No wonder it isn’t easy when you need to take time away to decompress and treat your mental well-being.
“There is a real fear for physicians when it comes to getting mental health care,” said Emil Tsai, MD, PhD, MAS, professor at the department of psychiatry and behavioral sciences at the University of California, Los Angeles, and an internationally reputed scientist in neurosciences and brain disorders.
The fear, said Dr. Tsai, comes from the stigma of mental health issues, potential repercussions to employment, and conceivable medical board suspension or revocation of your medical license.
Dr. Tsai said in an interview that to combat anxiety about “punishment” that many physicians fear when seeking care for their mental health, we must allow physicians to take time away from their day-to-day patient care for respite and treatment without reprisal.
Since the medical profession is high stress and has a high depression and suicide rate, finding solutions is imperative. And physicians must feel supported enough to seek treatment when needed. So how can we normalize seeking mental health care among physicians?
Get honest about stress and burnout
The only way to normalize any behavior is to be open and candid, Dr. Tsai said in an interview. The mental health conversation must occur across the board, not just within the medical profession.
“The greatest thing we can do to try and lift the burden that we place on physicians is to be willing to talk and be honest about the stress that physicians deal with and the importance of everyone feeling free to seek treatment and rest to strengthen their mental health,” said Dr. Tsai.
The more we talk about mental health and its treatment, the more we lessen the stigma, said Dr. Tsai. That could be more employer-employee check-ins, counseling as part of physician wellness, and programs structured so as not to construe a penal system.
“Mental health in the medical profession is a big issue and one that has to be met with the same compassion and care as it should be for any patient. We have annual physical checkups. Why don’t we offer annual mental health checkups for all, physicians included?” asked Dr. Tsai.
Evaluate the workload
Elizabeth Lombardo, PhD, psychologist, coach, and global keynote speaker, thinks that health care employers should reexamine their physicians’ workloads to see if they’re contributing to mental health issues.
The conversation on mental health in the workplace shouldn’t be about whether a certain person can handle stressors that are “normal” for health care settings. Instead, workplace managers in health care institutions should redefine workloads to ensure that physicians aren’t too heavily burdened with responsibilities that can cause overwork, burnout, and mental health problems,” she said.
Lessen the stigma
Even when physicians want to seek help for their psychological struggles, they may be weary of how their colleagues would react if they knew.
Raffaello Antonino, MD, clinical director at Therapy Central in London, said several underlying fears may exist at a physician’s core that prevent them from seeking care – being seen as weak, being judged as unfit to practice medicine, and the notion that “something is wrong with them.”
Dr. Antonino said we need to understand that physicians face challenges of bereavement and trauma derived from losing patients and the inability to save someone’s life. “These issues can easily develop into an accumulation of difficult, unprocessed emotions, later arising in symptoms and signs of PTSD, anxiety, and depression.”
Education is the best way to end this stigma, just like with any form of prejudice and stereotypes. For instance, we know that health care professionals are at risk of developing burnout. So, educating physicians on the symptoms and management of burnout and its consequences and prevention strategies is a must.
“Imagine what could happen if there were regular opportunities to work through the day’s events before signing out from a shift. The idea that individual weekly therapy is the only way to relieve mental distress is false,” said Lori McIsaac Bewsher, MSW, RSW, a trauma therapist and owner of a trauma-focused mental health clinic in New Brunswick.
“There are ways of integrating individual care into our doctor’s offices and hospitals that can be brief, effective, and confidential. The best way to introduce these interventions is early and collectively; no one is immune to the potential impact of exposure to trauma. The earlier these interventions can be accessed, the better the outcomes for everyone,” she said.
Dr. Antonino suggests, perhaps in the future, organizations can have “burnout checks” or mental health wellness checks for physicians akin to how we also have quick examinations for various physical ailments. What if physicians regularly answered a 10-question mental health survey as part of a burnout or trauma prevention strategy?
“Theirs is a profession and an identity which is often linked with a sense of strength, leadership and [benevolent] power: adjectives, which on the surface one might see as incompatible with what instead, unfortunately, and wrongly, may be associated with mental health issues,” said Dr. Antonino.
Keep it private
When it comes to removing the stigma from mental health care and treatment for physicians, privacy is top of mind. There needs to be some form of privacy protection for physicians who seek professional help for mental health reasons. Dr. Lombardo said physicians need to have the choice to keep their mental health journeys private. “Ideally, normalization should mean openly conversing about mental health, but for physicians, it can be a matter of life or death for their career, so the choice to remain private is something that should be afforded to them.”
Along those lines, the American Medical Association is pushing for system changes in legislative and regulatory arenas to support the mental health of practicing physicians, residents, and medical students. The organization is also urging health systems and state medical licensing bodies to remove questions on their applications that ask about prior treatment for mental health conditions.
Among many programs across the country, the Foundation of the Pennsylvania Medical Society has also created a Physicians’ Health Program, which provides confidential assessment, counseling, and referral services for physicians with mental health concerns.
“All of these initiatives are important in helping to destigmatize mental health issues among physicians,” said Harold Hong, MD, a board-certified psychiatrist in Raleigh, N.C.
Hail the benefits of treatment
Dr. Hong said to continue to destigmatize mental health among physicians and normalize its treatment, we not only have to emphasize how attending to mental health has individual benefits but also how it helps us help our patients.
“One key aspect that perhaps underpins this issue is the still present separation between mental and physical health, between mind and body, Dr. Hong said in an interview. “Feeling sad or angry or anxious should become a fact of life, a characteristic of being human, just like catching a cold or breaking a leg.”
It’s a normalization that, perhaps more than anything else, can lead the way for improving physicians’ mental health outcomes while also improving them for the rest of society. When society can finally see the health and well-being of someone in both their psychological and physical status, some of the stigmas may dissipate, and perhaps more physicians’ lives can be saved.
A version of this article first appeared on Medscape.com.
As medical professionals, you’re continually exposed to overwork, burnout, stressful situations, and challenging ethical decisions. Yet seeking help for mental health care may be last on your to-do list – or completely off your radar.
That’s sad and dangerous, since the American College of Emergency Physicians said 300-400 physicians die by suicide each year, and the stigma keeps 69% of female physicians from seeking mental health care, according to a prepandemic study.
In the 2022 Medscape Physician Suicide Report, 11% of female doctors and 9% of male doctors said they have had thoughts of suicide, and 64% experienced colloquial depression (feeling down, sad, or blue).
What’s more, physicians are typically seen as strong and capable and are often put on a pedestal by loved ones, patients, and the public and thought of as superhuman. No wonder it isn’t easy when you need to take time away to decompress and treat your mental well-being.
“There is a real fear for physicians when it comes to getting mental health care,” said Emil Tsai, MD, PhD, MAS, professor at the department of psychiatry and behavioral sciences at the University of California, Los Angeles, and an internationally reputed scientist in neurosciences and brain disorders.
The fear, said Dr. Tsai, comes from the stigma of mental health issues, potential repercussions to employment, and conceivable medical board suspension or revocation of your medical license.
Dr. Tsai said in an interview that to combat anxiety about “punishment” that many physicians fear when seeking care for their mental health, we must allow physicians to take time away from their day-to-day patient care for respite and treatment without reprisal.
Since the medical profession is high stress and has a high depression and suicide rate, finding solutions is imperative. And physicians must feel supported enough to seek treatment when needed. So how can we normalize seeking mental health care among physicians?
Get honest about stress and burnout
The only way to normalize any behavior is to be open and candid, Dr. Tsai said in an interview. The mental health conversation must occur across the board, not just within the medical profession.
“The greatest thing we can do to try and lift the burden that we place on physicians is to be willing to talk and be honest about the stress that physicians deal with and the importance of everyone feeling free to seek treatment and rest to strengthen their mental health,” said Dr. Tsai.
The more we talk about mental health and its treatment, the more we lessen the stigma, said Dr. Tsai. That could be more employer-employee check-ins, counseling as part of physician wellness, and programs structured so as not to construe a penal system.
“Mental health in the medical profession is a big issue and one that has to be met with the same compassion and care as it should be for any patient. We have annual physical checkups. Why don’t we offer annual mental health checkups for all, physicians included?” asked Dr. Tsai.
Evaluate the workload
Elizabeth Lombardo, PhD, psychologist, coach, and global keynote speaker, thinks that health care employers should reexamine their physicians’ workloads to see if they’re contributing to mental health issues.
The conversation on mental health in the workplace shouldn’t be about whether a certain person can handle stressors that are “normal” for health care settings. Instead, workplace managers in health care institutions should redefine workloads to ensure that physicians aren’t too heavily burdened with responsibilities that can cause overwork, burnout, and mental health problems,” she said.
Lessen the stigma
Even when physicians want to seek help for their psychological struggles, they may be weary of how their colleagues would react if they knew.
Raffaello Antonino, MD, clinical director at Therapy Central in London, said several underlying fears may exist at a physician’s core that prevent them from seeking care – being seen as weak, being judged as unfit to practice medicine, and the notion that “something is wrong with them.”
Dr. Antonino said we need to understand that physicians face challenges of bereavement and trauma derived from losing patients and the inability to save someone’s life. “These issues can easily develop into an accumulation of difficult, unprocessed emotions, later arising in symptoms and signs of PTSD, anxiety, and depression.”
Education is the best way to end this stigma, just like with any form of prejudice and stereotypes. For instance, we know that health care professionals are at risk of developing burnout. So, educating physicians on the symptoms and management of burnout and its consequences and prevention strategies is a must.
“Imagine what could happen if there were regular opportunities to work through the day’s events before signing out from a shift. The idea that individual weekly therapy is the only way to relieve mental distress is false,” said Lori McIsaac Bewsher, MSW, RSW, a trauma therapist and owner of a trauma-focused mental health clinic in New Brunswick.
“There are ways of integrating individual care into our doctor’s offices and hospitals that can be brief, effective, and confidential. The best way to introduce these interventions is early and collectively; no one is immune to the potential impact of exposure to trauma. The earlier these interventions can be accessed, the better the outcomes for everyone,” she said.
Dr. Antonino suggests, perhaps in the future, organizations can have “burnout checks” or mental health wellness checks for physicians akin to how we also have quick examinations for various physical ailments. What if physicians regularly answered a 10-question mental health survey as part of a burnout or trauma prevention strategy?
“Theirs is a profession and an identity which is often linked with a sense of strength, leadership and [benevolent] power: adjectives, which on the surface one might see as incompatible with what instead, unfortunately, and wrongly, may be associated with mental health issues,” said Dr. Antonino.
Keep it private
When it comes to removing the stigma from mental health care and treatment for physicians, privacy is top of mind. There needs to be some form of privacy protection for physicians who seek professional help for mental health reasons. Dr. Lombardo said physicians need to have the choice to keep their mental health journeys private. “Ideally, normalization should mean openly conversing about mental health, but for physicians, it can be a matter of life or death for their career, so the choice to remain private is something that should be afforded to them.”
Along those lines, the American Medical Association is pushing for system changes in legislative and regulatory arenas to support the mental health of practicing physicians, residents, and medical students. The organization is also urging health systems and state medical licensing bodies to remove questions on their applications that ask about prior treatment for mental health conditions.
Among many programs across the country, the Foundation of the Pennsylvania Medical Society has also created a Physicians’ Health Program, which provides confidential assessment, counseling, and referral services for physicians with mental health concerns.
“All of these initiatives are important in helping to destigmatize mental health issues among physicians,” said Harold Hong, MD, a board-certified psychiatrist in Raleigh, N.C.
Hail the benefits of treatment
Dr. Hong said to continue to destigmatize mental health among physicians and normalize its treatment, we not only have to emphasize how attending to mental health has individual benefits but also how it helps us help our patients.
“One key aspect that perhaps underpins this issue is the still present separation between mental and physical health, between mind and body, Dr. Hong said in an interview. “Feeling sad or angry or anxious should become a fact of life, a characteristic of being human, just like catching a cold or breaking a leg.”
It’s a normalization that, perhaps more than anything else, can lead the way for improving physicians’ mental health outcomes while also improving them for the rest of society. When society can finally see the health and well-being of someone in both their psychological and physical status, some of the stigmas may dissipate, and perhaps more physicians’ lives can be saved.
A version of this article first appeared on Medscape.com.
Med students dismayed that residency match process won’t change
– mostly medical students, residents, and fellows – who supported the change.
The program’s decision comes after nearly 3 months of feedback from the public, medical students, and education community. Although about 60% of public respondents believed the change could reduce stress and allow students more time for momentous career decisions, the program’s board of directors decided the disadvantages were “of greater consequence,” according to a Oct. 28 statement.
Those disadvantages included introducing application or interview behaviors that could increase students’ stress; potentially identifying partially matched or unmatched applicants, which could lead to bias; and extending the match process time for those applicants.
In addition, members of 12 medical education and student organizations raised other concerns, such as the proposed change not addressing high application numbers, according to the statement. NRMP has reported record numbers of applicants over the past few years, typically with more applicants than available program slots.
“While the testimony gave nod to the positive aspects of the proposal ... there was substantially more concern voiced about the potential negative consequences identified in the public comments,” NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN, told this news organization. Some of those issues could not be addressed without further study, so the board decided not to proceed with the proposal, she explained.
The proposal would have separated the Main Residency Match into two phases and replaced the Supplemental Offer and Acceptance Program (SOAP), in which unmatched or partially matched applicants apply for unfilled residency positions. Under the proposed change, each phase would have operated the same way, from rank order lists and using a matching algorithm to a pair of Match Days instead of a single day.
The two-phase process would have given students who didn’t match more time to carefully weigh residency programs – they can apply to up to 45 placements as part of SOAP – that will guide their career path for the next few years, PGY-1 intern Asim A., who asked not to be identified further, told this news organization. The alternative is a hasty decision once students learn which residency spots are available, he added. “Applicants would have breathing room to make a more informed decision.”
Asim, who is Canadian, said he is participating in a transitional year in internal medicine in the hopes of being matched into internal medicine or psychiatry. He said Canada’s two-phase match is a “lot less stressful” than the U.S. system.
Meanwhile, students on Reddit’s medical school community also questioned NRMP’s decision.
“A significant majority of those surveyed thought it would be beneficial. But NRMP decides to not go through with it,” one Reddit user wrote. Another posted, “The one thing that could have improved the match and they chose not to do it.”
Others supported the decision to retain a 1-day match.
“I think this was the right call,” Bryan Carmody, MD, an outspoken medical education blogger, tweeted after learning of NRMP’s decision. Dr. Carmody, a pediatric nephrologist, previously expressed to this news organization misgivings about whether the two-phase match would make it difficult for programs to thoroughly review candidates and vice versa. He was concerned that it would compress the interview season and pressure programs to rapidly review applicants and conduct interviews.
More than 8,000 people responded to the public survey that began in August and ran for a month. Nearly two-thirds of the respondents (60%) were students, residents, or fellows. About 25% included faculty, program directors, and staff. Among the survey findings, respondents were equally divided between whether the two-phase match would be modestly advantageous (30%) or significantly advantageous (30%) compared to 20% who viewed it as modestly or significantly disadvantageous.
The NRMP said it would continue engaging with the community through focus groups and other means to improve the match experience and transition to residency.
“It is important to remember that a proposal is just that,” Dr. Lamb told this news orgnization, “an opportunity to discuss the pros and cons of an idea or framework ... and to mitigate unwanted consequences determined to be detrimental to learners and programs.”
The NRMP will involve the community in future discussions “to continue to give learners a voice,” she said.
A version of this article first appeared on Medscape.com.
– mostly medical students, residents, and fellows – who supported the change.
The program’s decision comes after nearly 3 months of feedback from the public, medical students, and education community. Although about 60% of public respondents believed the change could reduce stress and allow students more time for momentous career decisions, the program’s board of directors decided the disadvantages were “of greater consequence,” according to a Oct. 28 statement.
Those disadvantages included introducing application or interview behaviors that could increase students’ stress; potentially identifying partially matched or unmatched applicants, which could lead to bias; and extending the match process time for those applicants.
In addition, members of 12 medical education and student organizations raised other concerns, such as the proposed change not addressing high application numbers, according to the statement. NRMP has reported record numbers of applicants over the past few years, typically with more applicants than available program slots.
“While the testimony gave nod to the positive aspects of the proposal ... there was substantially more concern voiced about the potential negative consequences identified in the public comments,” NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN, told this news organization. Some of those issues could not be addressed without further study, so the board decided not to proceed with the proposal, she explained.
The proposal would have separated the Main Residency Match into two phases and replaced the Supplemental Offer and Acceptance Program (SOAP), in which unmatched or partially matched applicants apply for unfilled residency positions. Under the proposed change, each phase would have operated the same way, from rank order lists and using a matching algorithm to a pair of Match Days instead of a single day.
The two-phase process would have given students who didn’t match more time to carefully weigh residency programs – they can apply to up to 45 placements as part of SOAP – that will guide their career path for the next few years, PGY-1 intern Asim A., who asked not to be identified further, told this news organization. The alternative is a hasty decision once students learn which residency spots are available, he added. “Applicants would have breathing room to make a more informed decision.”
Asim, who is Canadian, said he is participating in a transitional year in internal medicine in the hopes of being matched into internal medicine or psychiatry. He said Canada’s two-phase match is a “lot less stressful” than the U.S. system.
Meanwhile, students on Reddit’s medical school community also questioned NRMP’s decision.
“A significant majority of those surveyed thought it would be beneficial. But NRMP decides to not go through with it,” one Reddit user wrote. Another posted, “The one thing that could have improved the match and they chose not to do it.”
Others supported the decision to retain a 1-day match.
“I think this was the right call,” Bryan Carmody, MD, an outspoken medical education blogger, tweeted after learning of NRMP’s decision. Dr. Carmody, a pediatric nephrologist, previously expressed to this news organization misgivings about whether the two-phase match would make it difficult for programs to thoroughly review candidates and vice versa. He was concerned that it would compress the interview season and pressure programs to rapidly review applicants and conduct interviews.
More than 8,000 people responded to the public survey that began in August and ran for a month. Nearly two-thirds of the respondents (60%) were students, residents, or fellows. About 25% included faculty, program directors, and staff. Among the survey findings, respondents were equally divided between whether the two-phase match would be modestly advantageous (30%) or significantly advantageous (30%) compared to 20% who viewed it as modestly or significantly disadvantageous.
The NRMP said it would continue engaging with the community through focus groups and other means to improve the match experience and transition to residency.
“It is important to remember that a proposal is just that,” Dr. Lamb told this news orgnization, “an opportunity to discuss the pros and cons of an idea or framework ... and to mitigate unwanted consequences determined to be detrimental to learners and programs.”
The NRMP will involve the community in future discussions “to continue to give learners a voice,” she said.
A version of this article first appeared on Medscape.com.
– mostly medical students, residents, and fellows – who supported the change.
The program’s decision comes after nearly 3 months of feedback from the public, medical students, and education community. Although about 60% of public respondents believed the change could reduce stress and allow students more time for momentous career decisions, the program’s board of directors decided the disadvantages were “of greater consequence,” according to a Oct. 28 statement.
Those disadvantages included introducing application or interview behaviors that could increase students’ stress; potentially identifying partially matched or unmatched applicants, which could lead to bias; and extending the match process time for those applicants.
In addition, members of 12 medical education and student organizations raised other concerns, such as the proposed change not addressing high application numbers, according to the statement. NRMP has reported record numbers of applicants over the past few years, typically with more applicants than available program slots.
“While the testimony gave nod to the positive aspects of the proposal ... there was substantially more concern voiced about the potential negative consequences identified in the public comments,” NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN, told this news organization. Some of those issues could not be addressed without further study, so the board decided not to proceed with the proposal, she explained.
The proposal would have separated the Main Residency Match into two phases and replaced the Supplemental Offer and Acceptance Program (SOAP), in which unmatched or partially matched applicants apply for unfilled residency positions. Under the proposed change, each phase would have operated the same way, from rank order lists and using a matching algorithm to a pair of Match Days instead of a single day.
The two-phase process would have given students who didn’t match more time to carefully weigh residency programs – they can apply to up to 45 placements as part of SOAP – that will guide their career path for the next few years, PGY-1 intern Asim A., who asked not to be identified further, told this news organization. The alternative is a hasty decision once students learn which residency spots are available, he added. “Applicants would have breathing room to make a more informed decision.”
Asim, who is Canadian, said he is participating in a transitional year in internal medicine in the hopes of being matched into internal medicine or psychiatry. He said Canada’s two-phase match is a “lot less stressful” than the U.S. system.
Meanwhile, students on Reddit’s medical school community also questioned NRMP’s decision.
“A significant majority of those surveyed thought it would be beneficial. But NRMP decides to not go through with it,” one Reddit user wrote. Another posted, “The one thing that could have improved the match and they chose not to do it.”
Others supported the decision to retain a 1-day match.
“I think this was the right call,” Bryan Carmody, MD, an outspoken medical education blogger, tweeted after learning of NRMP’s decision. Dr. Carmody, a pediatric nephrologist, previously expressed to this news organization misgivings about whether the two-phase match would make it difficult for programs to thoroughly review candidates and vice versa. He was concerned that it would compress the interview season and pressure programs to rapidly review applicants and conduct interviews.
More than 8,000 people responded to the public survey that began in August and ran for a month. Nearly two-thirds of the respondents (60%) were students, residents, or fellows. About 25% included faculty, program directors, and staff. Among the survey findings, respondents were equally divided between whether the two-phase match would be modestly advantageous (30%) or significantly advantageous (30%) compared to 20% who viewed it as modestly or significantly disadvantageous.
The NRMP said it would continue engaging with the community through focus groups and other means to improve the match experience and transition to residency.
“It is important to remember that a proposal is just that,” Dr. Lamb told this news orgnization, “an opportunity to discuss the pros and cons of an idea or framework ... and to mitigate unwanted consequences determined to be detrimental to learners and programs.”
The NRMP will involve the community in future discussions “to continue to give learners a voice,” she said.
A version of this article first appeared on Medscape.com.
Children and COVID: New cases increase for second straight week
New COVID-19 cases rose among U.S. children for the second consecutive week, while hospitals saw signs of renewed activity on the part of SARS-CoV-2.
, when the count fell to its lowest level in more than a year, the American Academy of Pediatrics and the Children’s Hospital Association said in their joint report.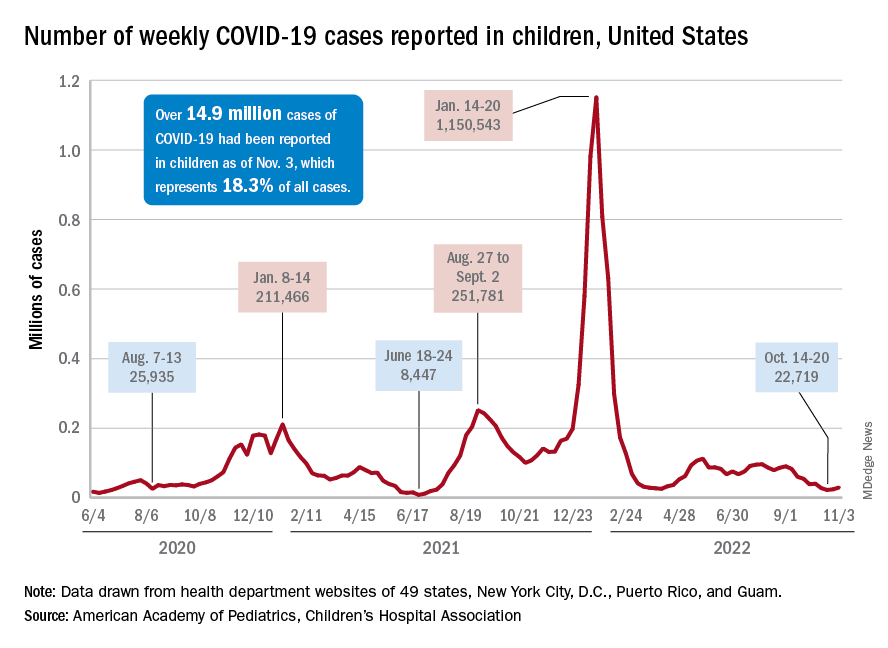
The 7-day average for ED visits with diagnosed COVID was down to just 0.6% of all ED visits for 12- to 15-year-olds as late as Oct. 23 but has moved up to 0.7% since then. Among those aged 16-17 years, the 7-day average was also down to 0.6% for just one day, Oct. 19, but was up to 0.8% as of Nov. 4. So far, though, a similar increase has not yet occurred for ED visits among children aged 0-11 years, the CDC said on its COVID Data Tracker.
The trend is discernible, however, when looking at hospitalizations of children with confirmed COVID. The rate of new admissions of children aged 0-17 years was 0.16 per 100,000 population as late as Oct. 23 but ticked up a notch after that and has been 0.17 per 100,000 since, according to the CDC. As with the ED rate, hospitalizations had been steadily declining since late August.
Vaccine initiation continues to slow
During the week of Oct. 27 to Nov. 2, about 30,000 children under 5 years of age received their initial COVID vaccination. A month earlier (Sept. 29 to Oct. 5), that number was about 40,000. A month before that, about 53,000 children aged 0-5 years received their initial dose, the AAP said in a separate vaccination report based on CDC data.
All of that reduced interest adds up to 7.4% of the age group having received at least one dose and just 3.2% being fully vaccinated as of Nov. 2. Among children aged 5-11 years, the corresponding vaccination rates are 38.9% and 31.8%, while those aged 12-17 years are at 71.3% and 61.1%, the CDC said.
Looking at just the first 20 weeks of the vaccination experience for each age group shows that 1.6 million children under 5 years of age had received at least an initial dose, compared with 8.1 million children aged 5-11 years and 8.1 million children aged 12-15, the AAP said.
New COVID-19 cases rose among U.S. children for the second consecutive week, while hospitals saw signs of renewed activity on the part of SARS-CoV-2.
, when the count fell to its lowest level in more than a year, the American Academy of Pediatrics and the Children’s Hospital Association said in their joint report.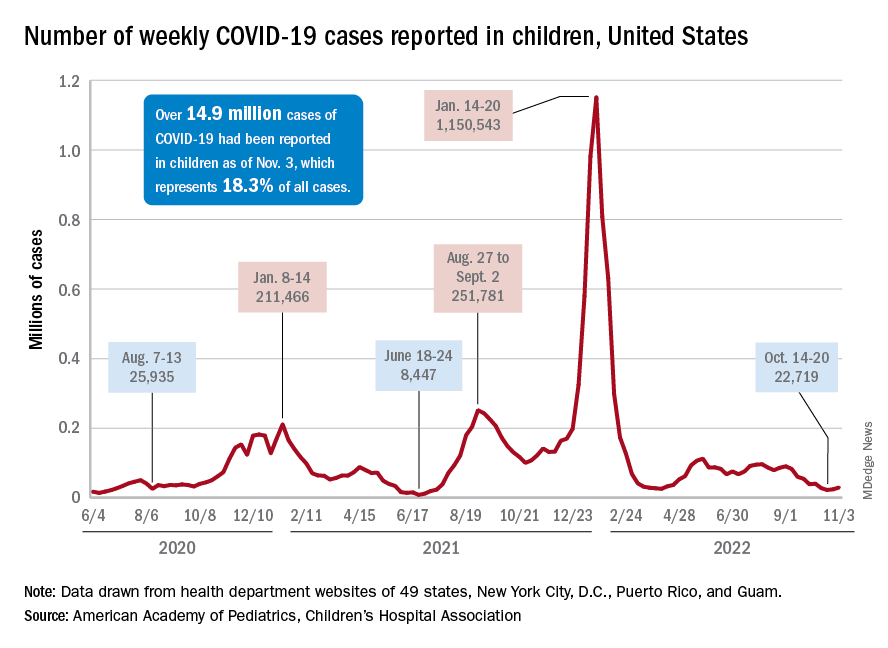
The 7-day average for ED visits with diagnosed COVID was down to just 0.6% of all ED visits for 12- to 15-year-olds as late as Oct. 23 but has moved up to 0.7% since then. Among those aged 16-17 years, the 7-day average was also down to 0.6% for just one day, Oct. 19, but was up to 0.8% as of Nov. 4. So far, though, a similar increase has not yet occurred for ED visits among children aged 0-11 years, the CDC said on its COVID Data Tracker.
The trend is discernible, however, when looking at hospitalizations of children with confirmed COVID. The rate of new admissions of children aged 0-17 years was 0.16 per 100,000 population as late as Oct. 23 but ticked up a notch after that and has been 0.17 per 100,000 since, according to the CDC. As with the ED rate, hospitalizations had been steadily declining since late August.
Vaccine initiation continues to slow
During the week of Oct. 27 to Nov. 2, about 30,000 children under 5 years of age received their initial COVID vaccination. A month earlier (Sept. 29 to Oct. 5), that number was about 40,000. A month before that, about 53,000 children aged 0-5 years received their initial dose, the AAP said in a separate vaccination report based on CDC data.
All of that reduced interest adds up to 7.4% of the age group having received at least one dose and just 3.2% being fully vaccinated as of Nov. 2. Among children aged 5-11 years, the corresponding vaccination rates are 38.9% and 31.8%, while those aged 12-17 years are at 71.3% and 61.1%, the CDC said.
Looking at just the first 20 weeks of the vaccination experience for each age group shows that 1.6 million children under 5 years of age had received at least an initial dose, compared with 8.1 million children aged 5-11 years and 8.1 million children aged 12-15, the AAP said.
New COVID-19 cases rose among U.S. children for the second consecutive week, while hospitals saw signs of renewed activity on the part of SARS-CoV-2.
, when the count fell to its lowest level in more than a year, the American Academy of Pediatrics and the Children’s Hospital Association said in their joint report.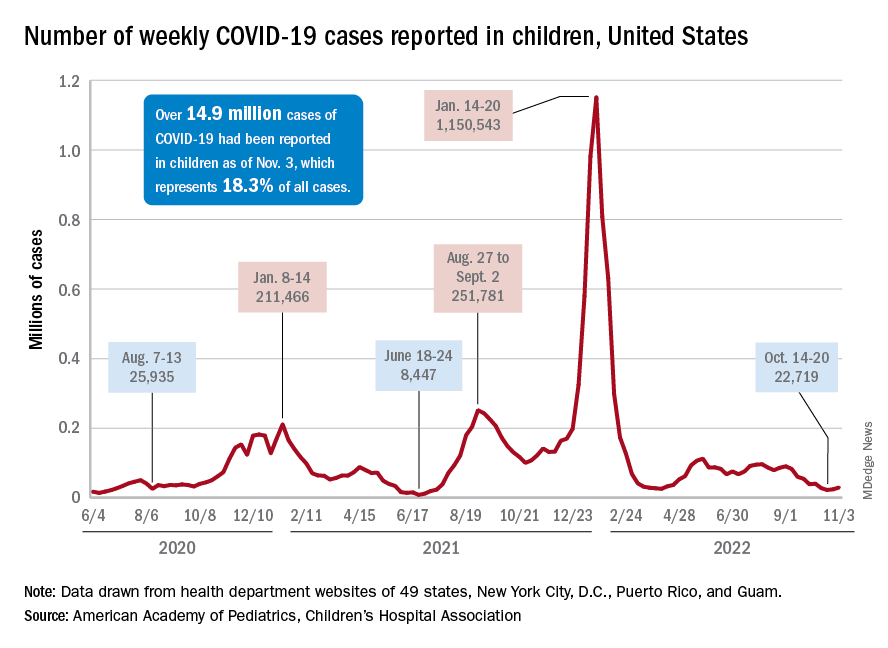
The 7-day average for ED visits with diagnosed COVID was down to just 0.6% of all ED visits for 12- to 15-year-olds as late as Oct. 23 but has moved up to 0.7% since then. Among those aged 16-17 years, the 7-day average was also down to 0.6% for just one day, Oct. 19, but was up to 0.8% as of Nov. 4. So far, though, a similar increase has not yet occurred for ED visits among children aged 0-11 years, the CDC said on its COVID Data Tracker.
The trend is discernible, however, when looking at hospitalizations of children with confirmed COVID. The rate of new admissions of children aged 0-17 years was 0.16 per 100,000 population as late as Oct. 23 but ticked up a notch after that and has been 0.17 per 100,000 since, according to the CDC. As with the ED rate, hospitalizations had been steadily declining since late August.
Vaccine initiation continues to slow
During the week of Oct. 27 to Nov. 2, about 30,000 children under 5 years of age received their initial COVID vaccination. A month earlier (Sept. 29 to Oct. 5), that number was about 40,000. A month before that, about 53,000 children aged 0-5 years received their initial dose, the AAP said in a separate vaccination report based on CDC data.
All of that reduced interest adds up to 7.4% of the age group having received at least one dose and just 3.2% being fully vaccinated as of Nov. 2. Among children aged 5-11 years, the corresponding vaccination rates are 38.9% and 31.8%, while those aged 12-17 years are at 71.3% and 61.1%, the CDC said.
Looking at just the first 20 weeks of the vaccination experience for each age group shows that 1.6 million children under 5 years of age had received at least an initial dose, compared with 8.1 million children aged 5-11 years and 8.1 million children aged 12-15, the AAP said.
World falls short on HBV, HCV elimination targets
Vaccination campaigns in more than 80 nations have successfully reduced the prevalence of hepatitis B virus (HBV) surface antigen. That’s the good news.
Less good is the news that reported Sarah Blach, MHS, associate director of the Center for Disease Analysis Foundation, based in Lafayette, Colo.
“As countries progress toward eliminating hepatitis B and C, we really need to do more to expand political will and financing of national elimination programs. It’s great to see that it’s happening in some of these countries, but we really need that to expand,” she said at the annual meeting of the American Association for the Study of Liver Diseases.
Ms. Blach presented data from the foundation’s Polaris Observatory, an initiative that provides epidemiological data, modeling tools, training, and decision analytics to support eliminating HBV and HCV globally by 2030.
The investigators used mathematical disease burden models for HBV and HCV to assess worldwide trends toward viral elimination. They also evaluated HBV and HCV elimination policies as reported by authorities in various countries.
They forecast the year in which each country or territory would meet each of the World Health Organization’s four elimination targets from 110 HCV models and 166 HBV models. The targets are 90% diagnosed, 80% of the eligible population treated, 65% reduction in mortality, and 80% incidence reduction for HCV and either 95% incidence reduction or prevalence of 0.1% or less in children aged 5 years and younger for HBV.
Investigators summarized the results across countries by disease area and time period of elimination; that is, elimination before 2030, between 2031 and 2050, or after 2050.
Results for HCV and HBV targets
The 11 nations on track to achieve all absolute or relative (programmatic) targets for HCV by 2030 are Australia, Canada, Denmark, Egypt, Finland, France, Georgia, Japan, Norway, Spain, and the United Kingdom.
An additional 24 countries are on track to meet their goals for HCV between 2031 and 2050.
But the rest, including the United States, much of sub-Saharan Africa, China, and South Asia, are not on track to meet their goals for HCV by 2050.
No countries are on track to achieve the absolute or relative (programmatic) targets for elimination of HBV, Ms. Blach said.
However, 83 countries or territories, including the United States, are on track for achieving the HBV surface antigen prevalence target of less than 0.1% in children aged 5 years and younger by 2030.
Ms. Blach and colleagues also looked at results of quantitative policy surveys submitted by 61 countries. The respondents were asked to report on linkage to care, awareness and screening, monitoring and evaluation, ability to expand capacity, harm-reduction programs, financing of national programs, and political will to achieve targets.
The investigators scored countries on a scale of 1-10, with 10 being the highest score, in each category. For HCV, 25 countries (42%) had high scores, defined as 9 or 10, for political will, and 33 countries (54%) had high scores for national funding. For HBV, 17 countries (30%) received the high scores for political will, and 30 (51%) received the high scores for financing the national program.
The big picture
Most countries have not expanded HBV or HCV treatment beyond specialists, and HBV policies appear to lag behind policies directed toward HCV elimination, Ms. Blach noted.
“We do need to expand screening and treatment for hepatitis B moving forward,” she said.
The United States and the rest of the world need to do better, especially regarding HBV elimination, but the United States does appear to be making progress, said Richard Sterling, MD, MSc, from Virginia Commonwealth University, Richmond, who comoderated the session where Ms. Blach reported the data.
“My impression is that we’re doing a pretty good job with [HBV] vaccinations in the United States,” Dr. Sterling, who was not involved in the study, said in an interview.
One way to make progress, he said, may be to expand eligibility for HBV vaccines beyond the current upper age limit of 59 years.
Implementing simpler dosing regimens – the currently available vaccine is split into three doses – could improve vaccine compliance and lower costs, Dr. Sterling added.
During the session, Brian Conway, MD, medical director of the Vancouver Infectious Disease Centre, said it seems hard to use a composite set of data to determine a yes/no answer about whether a country is on track to reach targets.
“When you take my country of Canada, we have absolutely no national program, no hope of a national program, very little funding, and yet we make the cut. So how do you balance all these different variables to arrive at a yes/no answer and is there a way of putting a bit more subtlety into it?” Dr. Conway asked Ms. Blach.
Ms. Blach replied that the data are fluid, and countries can move closer or farther from reaching targets over time as conditions change.
Some countries seem to be improving efforts and “just need a bit more” work, Ms. Blach said.
“But we also saw some countries who we thought were going to be a shoo-in, and as time progressed the number of treatments just dropped in shocking ways. The reality is that a lot of countries are struggling to treat patients,” she said.
Canada “has a really great health system. It’s not a fragmented health system, and so even if you don’t have some of that push for elimination from the government level, having access to treatment, having access to those services, means that at least patients can come in and get what they need,” Ms. Blach said.
The study data are available for free on the Center for Disease Analysis Foundation’s Polaris website.
The study was funded by grants from the John C. Martin Foundation, ZeShan Foundation, EndHep2030, Gilead Sciences, and AbbVie. Ms. Blach is employed by the Center for Disease Analysis Foundation, which receives research grants from Gilead and AbbVie. Dr. Sterling and Dr. Conway reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Vaccination campaigns in more than 80 nations have successfully reduced the prevalence of hepatitis B virus (HBV) surface antigen. That’s the good news.
Less good is the news that reported Sarah Blach, MHS, associate director of the Center for Disease Analysis Foundation, based in Lafayette, Colo.
“As countries progress toward eliminating hepatitis B and C, we really need to do more to expand political will and financing of national elimination programs. It’s great to see that it’s happening in some of these countries, but we really need that to expand,” she said at the annual meeting of the American Association for the Study of Liver Diseases.
Ms. Blach presented data from the foundation’s Polaris Observatory, an initiative that provides epidemiological data, modeling tools, training, and decision analytics to support eliminating HBV and HCV globally by 2030.
The investigators used mathematical disease burden models for HBV and HCV to assess worldwide trends toward viral elimination. They also evaluated HBV and HCV elimination policies as reported by authorities in various countries.
They forecast the year in which each country or territory would meet each of the World Health Organization’s four elimination targets from 110 HCV models and 166 HBV models. The targets are 90% diagnosed, 80% of the eligible population treated, 65% reduction in mortality, and 80% incidence reduction for HCV and either 95% incidence reduction or prevalence of 0.1% or less in children aged 5 years and younger for HBV.
Investigators summarized the results across countries by disease area and time period of elimination; that is, elimination before 2030, between 2031 and 2050, or after 2050.
Results for HCV and HBV targets
The 11 nations on track to achieve all absolute or relative (programmatic) targets for HCV by 2030 are Australia, Canada, Denmark, Egypt, Finland, France, Georgia, Japan, Norway, Spain, and the United Kingdom.
An additional 24 countries are on track to meet their goals for HCV between 2031 and 2050.
But the rest, including the United States, much of sub-Saharan Africa, China, and South Asia, are not on track to meet their goals for HCV by 2050.
No countries are on track to achieve the absolute or relative (programmatic) targets for elimination of HBV, Ms. Blach said.
However, 83 countries or territories, including the United States, are on track for achieving the HBV surface antigen prevalence target of less than 0.1% in children aged 5 years and younger by 2030.
Ms. Blach and colleagues also looked at results of quantitative policy surveys submitted by 61 countries. The respondents were asked to report on linkage to care, awareness and screening, monitoring and evaluation, ability to expand capacity, harm-reduction programs, financing of national programs, and political will to achieve targets.
The investigators scored countries on a scale of 1-10, with 10 being the highest score, in each category. For HCV, 25 countries (42%) had high scores, defined as 9 or 10, for political will, and 33 countries (54%) had high scores for national funding. For HBV, 17 countries (30%) received the high scores for political will, and 30 (51%) received the high scores for financing the national program.
The big picture
Most countries have not expanded HBV or HCV treatment beyond specialists, and HBV policies appear to lag behind policies directed toward HCV elimination, Ms. Blach noted.
“We do need to expand screening and treatment for hepatitis B moving forward,” she said.
The United States and the rest of the world need to do better, especially regarding HBV elimination, but the United States does appear to be making progress, said Richard Sterling, MD, MSc, from Virginia Commonwealth University, Richmond, who comoderated the session where Ms. Blach reported the data.
“My impression is that we’re doing a pretty good job with [HBV] vaccinations in the United States,” Dr. Sterling, who was not involved in the study, said in an interview.
One way to make progress, he said, may be to expand eligibility for HBV vaccines beyond the current upper age limit of 59 years.
Implementing simpler dosing regimens – the currently available vaccine is split into three doses – could improve vaccine compliance and lower costs, Dr. Sterling added.
During the session, Brian Conway, MD, medical director of the Vancouver Infectious Disease Centre, said it seems hard to use a composite set of data to determine a yes/no answer about whether a country is on track to reach targets.
“When you take my country of Canada, we have absolutely no national program, no hope of a national program, very little funding, and yet we make the cut. So how do you balance all these different variables to arrive at a yes/no answer and is there a way of putting a bit more subtlety into it?” Dr. Conway asked Ms. Blach.
Ms. Blach replied that the data are fluid, and countries can move closer or farther from reaching targets over time as conditions change.
Some countries seem to be improving efforts and “just need a bit more” work, Ms. Blach said.
“But we also saw some countries who we thought were going to be a shoo-in, and as time progressed the number of treatments just dropped in shocking ways. The reality is that a lot of countries are struggling to treat patients,” she said.
Canada “has a really great health system. It’s not a fragmented health system, and so even if you don’t have some of that push for elimination from the government level, having access to treatment, having access to those services, means that at least patients can come in and get what they need,” Ms. Blach said.
The study data are available for free on the Center for Disease Analysis Foundation’s Polaris website.
The study was funded by grants from the John C. Martin Foundation, ZeShan Foundation, EndHep2030, Gilead Sciences, and AbbVie. Ms. Blach is employed by the Center for Disease Analysis Foundation, which receives research grants from Gilead and AbbVie. Dr. Sterling and Dr. Conway reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Vaccination campaigns in more than 80 nations have successfully reduced the prevalence of hepatitis B virus (HBV) surface antigen. That’s the good news.
Less good is the news that reported Sarah Blach, MHS, associate director of the Center for Disease Analysis Foundation, based in Lafayette, Colo.
“As countries progress toward eliminating hepatitis B and C, we really need to do more to expand political will and financing of national elimination programs. It’s great to see that it’s happening in some of these countries, but we really need that to expand,” she said at the annual meeting of the American Association for the Study of Liver Diseases.
Ms. Blach presented data from the foundation’s Polaris Observatory, an initiative that provides epidemiological data, modeling tools, training, and decision analytics to support eliminating HBV and HCV globally by 2030.
The investigators used mathematical disease burden models for HBV and HCV to assess worldwide trends toward viral elimination. They also evaluated HBV and HCV elimination policies as reported by authorities in various countries.
They forecast the year in which each country or territory would meet each of the World Health Organization’s four elimination targets from 110 HCV models and 166 HBV models. The targets are 90% diagnosed, 80% of the eligible population treated, 65% reduction in mortality, and 80% incidence reduction for HCV and either 95% incidence reduction or prevalence of 0.1% or less in children aged 5 years and younger for HBV.
Investigators summarized the results across countries by disease area and time period of elimination; that is, elimination before 2030, between 2031 and 2050, or after 2050.
Results for HCV and HBV targets
The 11 nations on track to achieve all absolute or relative (programmatic) targets for HCV by 2030 are Australia, Canada, Denmark, Egypt, Finland, France, Georgia, Japan, Norway, Spain, and the United Kingdom.
An additional 24 countries are on track to meet their goals for HCV between 2031 and 2050.
But the rest, including the United States, much of sub-Saharan Africa, China, and South Asia, are not on track to meet their goals for HCV by 2050.
No countries are on track to achieve the absolute or relative (programmatic) targets for elimination of HBV, Ms. Blach said.
However, 83 countries or territories, including the United States, are on track for achieving the HBV surface antigen prevalence target of less than 0.1% in children aged 5 years and younger by 2030.
Ms. Blach and colleagues also looked at results of quantitative policy surveys submitted by 61 countries. The respondents were asked to report on linkage to care, awareness and screening, monitoring and evaluation, ability to expand capacity, harm-reduction programs, financing of national programs, and political will to achieve targets.
The investigators scored countries on a scale of 1-10, with 10 being the highest score, in each category. For HCV, 25 countries (42%) had high scores, defined as 9 or 10, for political will, and 33 countries (54%) had high scores for national funding. For HBV, 17 countries (30%) received the high scores for political will, and 30 (51%) received the high scores for financing the national program.
The big picture
Most countries have not expanded HBV or HCV treatment beyond specialists, and HBV policies appear to lag behind policies directed toward HCV elimination, Ms. Blach noted.
“We do need to expand screening and treatment for hepatitis B moving forward,” she said.
The United States and the rest of the world need to do better, especially regarding HBV elimination, but the United States does appear to be making progress, said Richard Sterling, MD, MSc, from Virginia Commonwealth University, Richmond, who comoderated the session where Ms. Blach reported the data.
“My impression is that we’re doing a pretty good job with [HBV] vaccinations in the United States,” Dr. Sterling, who was not involved in the study, said in an interview.
One way to make progress, he said, may be to expand eligibility for HBV vaccines beyond the current upper age limit of 59 years.
Implementing simpler dosing regimens – the currently available vaccine is split into three doses – could improve vaccine compliance and lower costs, Dr. Sterling added.
During the session, Brian Conway, MD, medical director of the Vancouver Infectious Disease Centre, said it seems hard to use a composite set of data to determine a yes/no answer about whether a country is on track to reach targets.
“When you take my country of Canada, we have absolutely no national program, no hope of a national program, very little funding, and yet we make the cut. So how do you balance all these different variables to arrive at a yes/no answer and is there a way of putting a bit more subtlety into it?” Dr. Conway asked Ms. Blach.
Ms. Blach replied that the data are fluid, and countries can move closer or farther from reaching targets over time as conditions change.
Some countries seem to be improving efforts and “just need a bit more” work, Ms. Blach said.
“But we also saw some countries who we thought were going to be a shoo-in, and as time progressed the number of treatments just dropped in shocking ways. The reality is that a lot of countries are struggling to treat patients,” she said.
Canada “has a really great health system. It’s not a fragmented health system, and so even if you don’t have some of that push for elimination from the government level, having access to treatment, having access to those services, means that at least patients can come in and get what they need,” Ms. Blach said.
The study data are available for free on the Center for Disease Analysis Foundation’s Polaris website.
The study was funded by grants from the John C. Martin Foundation, ZeShan Foundation, EndHep2030, Gilead Sciences, and AbbVie. Ms. Blach is employed by the Center for Disease Analysis Foundation, which receives research grants from Gilead and AbbVie. Dr. Sterling and Dr. Conway reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM THE LIVER MEETING
Red blood cells made to deliver antibiotics to bacteria
Over several years, “we developed experimental and computational techniques to study how proteins and drugs interact with membranes,” Hannah Krivić, a graduate student, and Maikel C. Rheinstädter, PhD, a professor of physics, both at McMaster University in Hamilton, Ont., told this news organization.
In earlier work, these researchers investigated how antibiotics target bacterial membranes and how those membranes enable the development of antibiotic resistance. Then, they said, “we started to ... manipulate membranes by tuning their properties [with] synthetic lipid molecules to create ‘hybrid’ membranes – that is, functionalized biological membranes with optimized properties.
“We are now using this approach to functionalize red blood cells by using them as drug carriers. We optimize these cells to carry certain loads, such as drug molecules, and anchor proteins in their membranes that target receptors in bacteria to selectively and efficiently deliver that load.”
The strategy, they said, “has become a universal red blood cell–based delivery platform that we call ‘smart blood’ ... that can safely and selectively deliver antibiotics to certain bacterial targets.”
The platform currently is being tested in vitro, and in vivo testing is slated to begin in early 2023. Their study was published online in ACS Infectious Diseases.
Optimizing dosing
Polymyxin B (PmB) is one of a few potent antibiotics with promising efficacy against drug-resistant bacteria such as E. coli. PmB, however, is widely considered a treatment of last resort because of its toxic side effects (which include nephrotoxicity, neurotoxicity, and neuromuscular blockade) particularly at higher doses.
The researchers hypothesized that targeted delivery of PmB might lead to optimized dosing and potentially reduce the need for higher or repeated doses. In the current study, they tested the ability of the smart blood platform to deliver PmB to E. coli.
Creating “erythro-PmBs” involves removing the inner components of red blood cells, loading the cells with PmB, and coating the cell membranes (liposomes) with antibacterial (in this case, anti–E. coli) antibodies.
The in vitro experiments showed that the cells could be loaded with PmB and retain and selectively deliver the drug to E. coli, with no apparent hemolytic activity or nephrotoxicity. Specifically, the erythro-PmBs had a loading efficiency of approximately 90% and delivered PmB to E. coli with values for the minimum inhibitory concentration that were comparable with those of free PmB.
“In contrast to drug-delivery systems based on synthetic carriers, our erythrocytes have a high biocompatibility and can stay in circulation in the body for several weeks to provide a sustained and targeted release of the drug,” said Ms. Krivić and Dr. Rheinstädter. “This [profile] can make existing drugs safer by, for instance, increasing their efficacy while at the same time lowering the required dosage, thereby reducing side effects.”
The researchers are now exploring the ability of the smart blood platform to deliver neurotrophic factors across the blood-brain barrier to potentially treat neurodegenerative diseases. Their approach is identical to that used in the current study, they said, except in this case, the red blood cell membranes are designed to deliver neurotrophic factors specifically to the blood-brain barrier.
‘Certainly promising’
David W. Deamer, PhD, research professor of biomolecular engineering at the University of California, Santa Cruz, said in a comment: “This is certainly promising. The erythro-PmBs have a greater loading capacity and longer circulation time than ordinary liposomes used for drug delivery. They can also be prepared with specific antibodies so that the antibiotic is delivered more directly when they bind to bacterial pathogens.”
The effect on bacterial growth, however, was tested in a model system, not in an actual infection, he said, adding that an important next step will be to perform animal testing. “One of the simplest tests is induced sepsis in mice, which mimics a burst appendix. If the erythro-PmBs can treat sepsis effectively, it will be an encouraging sign that they have potential therapeutic value. It will also be interesting to see whether the antigens responsible for ABO blood groups are retained on the surfaces of the erythro-PmBs. If they are, it might be necessary to match donor blood to that of the recipient.
“Getting a product ready for clinical use will require partnership with a major pharmaceutical firm, several years of animal testing, and then several more years carrying out phase 1, 2, and 3 clinical trials in human patients,” Dr. Deamer concluded.
No commercial funding was disclosed. Ms. Krivić, Dr. Rheinstädter, and Dr. Deamer reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Over several years, “we developed experimental and computational techniques to study how proteins and drugs interact with membranes,” Hannah Krivić, a graduate student, and Maikel C. Rheinstädter, PhD, a professor of physics, both at McMaster University in Hamilton, Ont., told this news organization.
In earlier work, these researchers investigated how antibiotics target bacterial membranes and how those membranes enable the development of antibiotic resistance. Then, they said, “we started to ... manipulate membranes by tuning their properties [with] synthetic lipid molecules to create ‘hybrid’ membranes – that is, functionalized biological membranes with optimized properties.
“We are now using this approach to functionalize red blood cells by using them as drug carriers. We optimize these cells to carry certain loads, such as drug molecules, and anchor proteins in their membranes that target receptors in bacteria to selectively and efficiently deliver that load.”
The strategy, they said, “has become a universal red blood cell–based delivery platform that we call ‘smart blood’ ... that can safely and selectively deliver antibiotics to certain bacterial targets.”
The platform currently is being tested in vitro, and in vivo testing is slated to begin in early 2023. Their study was published online in ACS Infectious Diseases.
Optimizing dosing
Polymyxin B (PmB) is one of a few potent antibiotics with promising efficacy against drug-resistant bacteria such as E. coli. PmB, however, is widely considered a treatment of last resort because of its toxic side effects (which include nephrotoxicity, neurotoxicity, and neuromuscular blockade) particularly at higher doses.
The researchers hypothesized that targeted delivery of PmB might lead to optimized dosing and potentially reduce the need for higher or repeated doses. In the current study, they tested the ability of the smart blood platform to deliver PmB to E. coli.
Creating “erythro-PmBs” involves removing the inner components of red blood cells, loading the cells with PmB, and coating the cell membranes (liposomes) with antibacterial (in this case, anti–E. coli) antibodies.
The in vitro experiments showed that the cells could be loaded with PmB and retain and selectively deliver the drug to E. coli, with no apparent hemolytic activity or nephrotoxicity. Specifically, the erythro-PmBs had a loading efficiency of approximately 90% and delivered PmB to E. coli with values for the minimum inhibitory concentration that were comparable with those of free PmB.
“In contrast to drug-delivery systems based on synthetic carriers, our erythrocytes have a high biocompatibility and can stay in circulation in the body for several weeks to provide a sustained and targeted release of the drug,” said Ms. Krivić and Dr. Rheinstädter. “This [profile] can make existing drugs safer by, for instance, increasing their efficacy while at the same time lowering the required dosage, thereby reducing side effects.”
The researchers are now exploring the ability of the smart blood platform to deliver neurotrophic factors across the blood-brain barrier to potentially treat neurodegenerative diseases. Their approach is identical to that used in the current study, they said, except in this case, the red blood cell membranes are designed to deliver neurotrophic factors specifically to the blood-brain barrier.
‘Certainly promising’
David W. Deamer, PhD, research professor of biomolecular engineering at the University of California, Santa Cruz, said in a comment: “This is certainly promising. The erythro-PmBs have a greater loading capacity and longer circulation time than ordinary liposomes used for drug delivery. They can also be prepared with specific antibodies so that the antibiotic is delivered more directly when they bind to bacterial pathogens.”
The effect on bacterial growth, however, was tested in a model system, not in an actual infection, he said, adding that an important next step will be to perform animal testing. “One of the simplest tests is induced sepsis in mice, which mimics a burst appendix. If the erythro-PmBs can treat sepsis effectively, it will be an encouraging sign that they have potential therapeutic value. It will also be interesting to see whether the antigens responsible for ABO blood groups are retained on the surfaces of the erythro-PmBs. If they are, it might be necessary to match donor blood to that of the recipient.
“Getting a product ready for clinical use will require partnership with a major pharmaceutical firm, several years of animal testing, and then several more years carrying out phase 1, 2, and 3 clinical trials in human patients,” Dr. Deamer concluded.
No commercial funding was disclosed. Ms. Krivić, Dr. Rheinstädter, and Dr. Deamer reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Over several years, “we developed experimental and computational techniques to study how proteins and drugs interact with membranes,” Hannah Krivić, a graduate student, and Maikel C. Rheinstädter, PhD, a professor of physics, both at McMaster University in Hamilton, Ont., told this news organization.
In earlier work, these researchers investigated how antibiotics target bacterial membranes and how those membranes enable the development of antibiotic resistance. Then, they said, “we started to ... manipulate membranes by tuning their properties [with] synthetic lipid molecules to create ‘hybrid’ membranes – that is, functionalized biological membranes with optimized properties.
“We are now using this approach to functionalize red blood cells by using them as drug carriers. We optimize these cells to carry certain loads, such as drug molecules, and anchor proteins in their membranes that target receptors in bacteria to selectively and efficiently deliver that load.”
The strategy, they said, “has become a universal red blood cell–based delivery platform that we call ‘smart blood’ ... that can safely and selectively deliver antibiotics to certain bacterial targets.”
The platform currently is being tested in vitro, and in vivo testing is slated to begin in early 2023. Their study was published online in ACS Infectious Diseases.
Optimizing dosing
Polymyxin B (PmB) is one of a few potent antibiotics with promising efficacy against drug-resistant bacteria such as E. coli. PmB, however, is widely considered a treatment of last resort because of its toxic side effects (which include nephrotoxicity, neurotoxicity, and neuromuscular blockade) particularly at higher doses.
The researchers hypothesized that targeted delivery of PmB might lead to optimized dosing and potentially reduce the need for higher or repeated doses. In the current study, they tested the ability of the smart blood platform to deliver PmB to E. coli.
Creating “erythro-PmBs” involves removing the inner components of red blood cells, loading the cells with PmB, and coating the cell membranes (liposomes) with antibacterial (in this case, anti–E. coli) antibodies.
The in vitro experiments showed that the cells could be loaded with PmB and retain and selectively deliver the drug to E. coli, with no apparent hemolytic activity or nephrotoxicity. Specifically, the erythro-PmBs had a loading efficiency of approximately 90% and delivered PmB to E. coli with values for the minimum inhibitory concentration that were comparable with those of free PmB.
“In contrast to drug-delivery systems based on synthetic carriers, our erythrocytes have a high biocompatibility and can stay in circulation in the body for several weeks to provide a sustained and targeted release of the drug,” said Ms. Krivić and Dr. Rheinstädter. “This [profile] can make existing drugs safer by, for instance, increasing their efficacy while at the same time lowering the required dosage, thereby reducing side effects.”
The researchers are now exploring the ability of the smart blood platform to deliver neurotrophic factors across the blood-brain barrier to potentially treat neurodegenerative diseases. Their approach is identical to that used in the current study, they said, except in this case, the red blood cell membranes are designed to deliver neurotrophic factors specifically to the blood-brain barrier.
‘Certainly promising’
David W. Deamer, PhD, research professor of biomolecular engineering at the University of California, Santa Cruz, said in a comment: “This is certainly promising. The erythro-PmBs have a greater loading capacity and longer circulation time than ordinary liposomes used for drug delivery. They can also be prepared with specific antibodies so that the antibiotic is delivered more directly when they bind to bacterial pathogens.”
The effect on bacterial growth, however, was tested in a model system, not in an actual infection, he said, adding that an important next step will be to perform animal testing. “One of the simplest tests is induced sepsis in mice, which mimics a burst appendix. If the erythro-PmBs can treat sepsis effectively, it will be an encouraging sign that they have potential therapeutic value. It will also be interesting to see whether the antigens responsible for ABO blood groups are retained on the surfaces of the erythro-PmBs. If they are, it might be necessary to match donor blood to that of the recipient.
“Getting a product ready for clinical use will require partnership with a major pharmaceutical firm, several years of animal testing, and then several more years carrying out phase 1, 2, and 3 clinical trials in human patients,” Dr. Deamer concluded.
No commercial funding was disclosed. Ms. Krivić, Dr. Rheinstädter, and Dr. Deamer reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM ACS INFECTIOUS DISEASES
Promising new antibiotic emerges for treating UTIs
A new antibiotic for urinary tract infections is heading toward government approval.
It would be the first new treatment in 20 years for UTIs, which affect more than half of women at least sometime in their lives, according to data compiled by the Department of Health and Human Services.
Called Gepotidacin, the antibiotic’s trial has halted enrollment early due to excellent effectiveness and safety results thus far, drugmaker GSK announced in a press release Nov. 3. GSK will seek approval and peer-reviewed publication early next year.
There is a need for new antibiotics such as this because of increasing antibiotic resistance. Antibiotic resistance to bacteria has become so prevalent that the World Health Organization recently began publishing a list of bacteria that pose the greatest public health threats.
“It’s definitely a big deal,” Cindy Liu, MD, MPH, PhD, of the Antibiotic Resistance Action Center at George Washington University, told CNN.
However, antibiotics are not a particularly profitable type of drug, The Wall Street Journal reported. The newspaper noted that they need to be used sparingly to limit resistance, and the cheapest option is usually prescribed. Some small companies that make antibiotics have even gone bankrupt recently, the Journal noted.
The U.S. government has invested in GSK’s development of Gepotidacin. The company predicts the drug could be a “blockbuster” and earn more than $1 billion due to UTI resistance to other drugs, the Journal reported.
“I think it will be really interesting and important to the field to see both how the drug companies sort of market this product and sort of how it does,” Dr. Liu said.
A version of this article first appeared on Medscape.com.
A new antibiotic for urinary tract infections is heading toward government approval.
It would be the first new treatment in 20 years for UTIs, which affect more than half of women at least sometime in their lives, according to data compiled by the Department of Health and Human Services.
Called Gepotidacin, the antibiotic’s trial has halted enrollment early due to excellent effectiveness and safety results thus far, drugmaker GSK announced in a press release Nov. 3. GSK will seek approval and peer-reviewed publication early next year.
There is a need for new antibiotics such as this because of increasing antibiotic resistance. Antibiotic resistance to bacteria has become so prevalent that the World Health Organization recently began publishing a list of bacteria that pose the greatest public health threats.
“It’s definitely a big deal,” Cindy Liu, MD, MPH, PhD, of the Antibiotic Resistance Action Center at George Washington University, told CNN.
However, antibiotics are not a particularly profitable type of drug, The Wall Street Journal reported. The newspaper noted that they need to be used sparingly to limit resistance, and the cheapest option is usually prescribed. Some small companies that make antibiotics have even gone bankrupt recently, the Journal noted.
The U.S. government has invested in GSK’s development of Gepotidacin. The company predicts the drug could be a “blockbuster” and earn more than $1 billion due to UTI resistance to other drugs, the Journal reported.
“I think it will be really interesting and important to the field to see both how the drug companies sort of market this product and sort of how it does,” Dr. Liu said.
A version of this article first appeared on Medscape.com.
A new antibiotic for urinary tract infections is heading toward government approval.
It would be the first new treatment in 20 years for UTIs, which affect more than half of women at least sometime in their lives, according to data compiled by the Department of Health and Human Services.
Called Gepotidacin, the antibiotic’s trial has halted enrollment early due to excellent effectiveness and safety results thus far, drugmaker GSK announced in a press release Nov. 3. GSK will seek approval and peer-reviewed publication early next year.
There is a need for new antibiotics such as this because of increasing antibiotic resistance. Antibiotic resistance to bacteria has become so prevalent that the World Health Organization recently began publishing a list of bacteria that pose the greatest public health threats.
“It’s definitely a big deal,” Cindy Liu, MD, MPH, PhD, of the Antibiotic Resistance Action Center at George Washington University, told CNN.
However, antibiotics are not a particularly profitable type of drug, The Wall Street Journal reported. The newspaper noted that they need to be used sparingly to limit resistance, and the cheapest option is usually prescribed. Some small companies that make antibiotics have even gone bankrupt recently, the Journal noted.
The U.S. government has invested in GSK’s development of Gepotidacin. The company predicts the drug could be a “blockbuster” and earn more than $1 billion due to UTI resistance to other drugs, the Journal reported.
“I think it will be really interesting and important to the field to see both how the drug companies sort of market this product and sort of how it does,” Dr. Liu said.
A version of this article first appeared on Medscape.com.
HPV vaccine effectiveness dependent on age at receipt
The effectiveness of the human papillomavirus (HPV) vaccine against HPV types 16 and 18 is highly dependent on the age at which it is given. Prevalence rates have been shown to be significantly lower among girls who are vaccinated at the recommended ages of 9-12 years, compared with those who are vaccinated after their sexual debut, data from the National Health and Nutrition Examination Survey (NHANES) indicate.
“HPV vaccination does not have any therapeutic effect on HPV infections already acquired, which is more likely to explain the difference in prevalence between predebut versus postdebut recipients than a lower immune response [among older recipients],” lead study author Didem Egemen, PhD, National Cancer Institute, Rockville, Md., told this news organization in an email.
“Still, among older females, the immune response of the vaccine is likely to still be quite strong, and we would encourage vaccination [of female patients] if unvaccinated, as our paper showed that vaccination post debut will still reduce HPV 16/18 prevalence by half,” she added.
The research letter was published online in JAMA Network Open.
National sample evaluated
Using data from NHANES, a biennial, cross-sectional sample (cycles 2011 through 2018), the researchers identified female persons who were aged 26 years or younger in 2006, when HPV vaccination was introduced, and who were eligible for routine vaccination or “catch-up” vaccination (given between the ages of 13 and 26 years), as per recommendations from the Advisory Committee on Immunization Practices. The investigators then compared the prevalence of HPV types 16 and 18 among unvaccinated female patients, female patients who had been vaccinated prior to their sexual debut (predebut group), and those who had been vaccinated after their sexual debut (postdebut group).
They also estimated vaccine uptake among those who were eligible for routine vaccination, as well as the proportion of vaccinated female patients with respect to racial and ethnic subgroups.
In the overall cohort, the prevalence of HPV types 16 and 18 decreased by 6% (95% confidence interval, 4%-7%) in the unvaccinated group to 3% (95% CI, 1%-6%) in the postdebut group and to less than 1% (95% CI, <1%-1%) in the predebut group, Dr. Egemen and colleagues report.
In real percentages, the prevalence of HPV 16 and 18 was 89% lower in the predebut group (P < .001) but only 41% lower in the postdebut group (P = .29) compared with unvaccinated female patients. And compared with female patients who were vaccinated after their sexual debut, the prevalence of HPV 16 and 18 was reduced by 82% among those who had received the vaccine at the recommended ages of 9-12 years (P = .08).
In the current study, Dr. Egeman acknowledged that only 38% of ever-eligible female patients received the vaccine, although the prevalence increased to 56% when only female patients who were eligible for routine vaccination were taken into account. On the other hand, only 21% (95% CI, 14%-28%) of female patients eligible for routine vaccination received their first dose by age 12 years.
Indeed, the mean age on receipt of the first vaccination dose was 14.5 years (95% CI, 14.1-14.8 years), the authors note, and only 59% of girls received their first dose prior to their sexual debut. Additionally, among routine vaccination–eligible girls aged 12 years or younger in 2006, 33% were vaccinated before and 23% after their sexual debut, and the rest were not vaccinated.
Interestingly, differences in the age at which the HPV vaccine was received by race and ethnicity were negligible, the investigators point out.
Vaccination rates increasing
Asked to comment on the findings, Rebecca Perkins, MD, professor of obstetrics and gynecology at Boston University, Boston Medical Center, pointed out that the investigators evaluated data from 2011 to 2018. “We know that HPV vaccination rates have increased over that period and continue to increase,” she emphasized in an email to this news organization.
Physicians also know that more persons are being vaccinated between the ages of 9 and 12 than was the case at the beginning of this study. “This is good news,” she said, “as it means that more adolescents now in 2022 are benefiting fully from vaccination than they were in 2011,” she added.
At the same time, Dr. Perkins acknowledged that many persons are still missing out on the chance to receive the vaccine on time – which means they are missing out on the chance to prevent cancer.
“Making sure that all adolescents receive vaccination between the ages of 9 to 12 has the potential to prevent up to 40,000 cancers every year in the U.S., [including] the most common HPV-related cancers, such as cervical cancer in women and tongue and tonsillar cancer in men,” Dr. Perkins noted.
“Thus, it’s critical that doctors and parents get the message that you can’t vaccinate too early, only too late,” she emphasized.
Dr. Edgman and Dr. Perkins report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The effectiveness of the human papillomavirus (HPV) vaccine against HPV types 16 and 18 is highly dependent on the age at which it is given. Prevalence rates have been shown to be significantly lower among girls who are vaccinated at the recommended ages of 9-12 years, compared with those who are vaccinated after their sexual debut, data from the National Health and Nutrition Examination Survey (NHANES) indicate.
“HPV vaccination does not have any therapeutic effect on HPV infections already acquired, which is more likely to explain the difference in prevalence between predebut versus postdebut recipients than a lower immune response [among older recipients],” lead study author Didem Egemen, PhD, National Cancer Institute, Rockville, Md., told this news organization in an email.
“Still, among older females, the immune response of the vaccine is likely to still be quite strong, and we would encourage vaccination [of female patients] if unvaccinated, as our paper showed that vaccination post debut will still reduce HPV 16/18 prevalence by half,” she added.
The research letter was published online in JAMA Network Open.
National sample evaluated
Using data from NHANES, a biennial, cross-sectional sample (cycles 2011 through 2018), the researchers identified female persons who were aged 26 years or younger in 2006, when HPV vaccination was introduced, and who were eligible for routine vaccination or “catch-up” vaccination (given between the ages of 13 and 26 years), as per recommendations from the Advisory Committee on Immunization Practices. The investigators then compared the prevalence of HPV types 16 and 18 among unvaccinated female patients, female patients who had been vaccinated prior to their sexual debut (predebut group), and those who had been vaccinated after their sexual debut (postdebut group).
They also estimated vaccine uptake among those who were eligible for routine vaccination, as well as the proportion of vaccinated female patients with respect to racial and ethnic subgroups.
In the overall cohort, the prevalence of HPV types 16 and 18 decreased by 6% (95% confidence interval, 4%-7%) in the unvaccinated group to 3% (95% CI, 1%-6%) in the postdebut group and to less than 1% (95% CI, <1%-1%) in the predebut group, Dr. Egemen and colleagues report.
In real percentages, the prevalence of HPV 16 and 18 was 89% lower in the predebut group (P < .001) but only 41% lower in the postdebut group (P = .29) compared with unvaccinated female patients. And compared with female patients who were vaccinated after their sexual debut, the prevalence of HPV 16 and 18 was reduced by 82% among those who had received the vaccine at the recommended ages of 9-12 years (P = .08).
In the current study, Dr. Egeman acknowledged that only 38% of ever-eligible female patients received the vaccine, although the prevalence increased to 56% when only female patients who were eligible for routine vaccination were taken into account. On the other hand, only 21% (95% CI, 14%-28%) of female patients eligible for routine vaccination received their first dose by age 12 years.
Indeed, the mean age on receipt of the first vaccination dose was 14.5 years (95% CI, 14.1-14.8 years), the authors note, and only 59% of girls received their first dose prior to their sexual debut. Additionally, among routine vaccination–eligible girls aged 12 years or younger in 2006, 33% were vaccinated before and 23% after their sexual debut, and the rest were not vaccinated.
Interestingly, differences in the age at which the HPV vaccine was received by race and ethnicity were negligible, the investigators point out.
Vaccination rates increasing
Asked to comment on the findings, Rebecca Perkins, MD, professor of obstetrics and gynecology at Boston University, Boston Medical Center, pointed out that the investigators evaluated data from 2011 to 2018. “We know that HPV vaccination rates have increased over that period and continue to increase,” she emphasized in an email to this news organization.
Physicians also know that more persons are being vaccinated between the ages of 9 and 12 than was the case at the beginning of this study. “This is good news,” she said, “as it means that more adolescents now in 2022 are benefiting fully from vaccination than they were in 2011,” she added.
At the same time, Dr. Perkins acknowledged that many persons are still missing out on the chance to receive the vaccine on time – which means they are missing out on the chance to prevent cancer.
“Making sure that all adolescents receive vaccination between the ages of 9 to 12 has the potential to prevent up to 40,000 cancers every year in the U.S., [including] the most common HPV-related cancers, such as cervical cancer in women and tongue and tonsillar cancer in men,” Dr. Perkins noted.
“Thus, it’s critical that doctors and parents get the message that you can’t vaccinate too early, only too late,” she emphasized.
Dr. Edgman and Dr. Perkins report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The effectiveness of the human papillomavirus (HPV) vaccine against HPV types 16 and 18 is highly dependent on the age at which it is given. Prevalence rates have been shown to be significantly lower among girls who are vaccinated at the recommended ages of 9-12 years, compared with those who are vaccinated after their sexual debut, data from the National Health and Nutrition Examination Survey (NHANES) indicate.
“HPV vaccination does not have any therapeutic effect on HPV infections already acquired, which is more likely to explain the difference in prevalence between predebut versus postdebut recipients than a lower immune response [among older recipients],” lead study author Didem Egemen, PhD, National Cancer Institute, Rockville, Md., told this news organization in an email.
“Still, among older females, the immune response of the vaccine is likely to still be quite strong, and we would encourage vaccination [of female patients] if unvaccinated, as our paper showed that vaccination post debut will still reduce HPV 16/18 prevalence by half,” she added.
The research letter was published online in JAMA Network Open.
National sample evaluated
Using data from NHANES, a biennial, cross-sectional sample (cycles 2011 through 2018), the researchers identified female persons who were aged 26 years or younger in 2006, when HPV vaccination was introduced, and who were eligible for routine vaccination or “catch-up” vaccination (given between the ages of 13 and 26 years), as per recommendations from the Advisory Committee on Immunization Practices. The investigators then compared the prevalence of HPV types 16 and 18 among unvaccinated female patients, female patients who had been vaccinated prior to their sexual debut (predebut group), and those who had been vaccinated after their sexual debut (postdebut group).
They also estimated vaccine uptake among those who were eligible for routine vaccination, as well as the proportion of vaccinated female patients with respect to racial and ethnic subgroups.
In the overall cohort, the prevalence of HPV types 16 and 18 decreased by 6% (95% confidence interval, 4%-7%) in the unvaccinated group to 3% (95% CI, 1%-6%) in the postdebut group and to less than 1% (95% CI, <1%-1%) in the predebut group, Dr. Egemen and colleagues report.
In real percentages, the prevalence of HPV 16 and 18 was 89% lower in the predebut group (P < .001) but only 41% lower in the postdebut group (P = .29) compared with unvaccinated female patients. And compared with female patients who were vaccinated after their sexual debut, the prevalence of HPV 16 and 18 was reduced by 82% among those who had received the vaccine at the recommended ages of 9-12 years (P = .08).
In the current study, Dr. Egeman acknowledged that only 38% of ever-eligible female patients received the vaccine, although the prevalence increased to 56% when only female patients who were eligible for routine vaccination were taken into account. On the other hand, only 21% (95% CI, 14%-28%) of female patients eligible for routine vaccination received their first dose by age 12 years.
Indeed, the mean age on receipt of the first vaccination dose was 14.5 years (95% CI, 14.1-14.8 years), the authors note, and only 59% of girls received their first dose prior to their sexual debut. Additionally, among routine vaccination–eligible girls aged 12 years or younger in 2006, 33% were vaccinated before and 23% after their sexual debut, and the rest were not vaccinated.
Interestingly, differences in the age at which the HPV vaccine was received by race and ethnicity were negligible, the investigators point out.
Vaccination rates increasing
Asked to comment on the findings, Rebecca Perkins, MD, professor of obstetrics and gynecology at Boston University, Boston Medical Center, pointed out that the investigators evaluated data from 2011 to 2018. “We know that HPV vaccination rates have increased over that period and continue to increase,” she emphasized in an email to this news organization.
Physicians also know that more persons are being vaccinated between the ages of 9 and 12 than was the case at the beginning of this study. “This is good news,” she said, “as it means that more adolescents now in 2022 are benefiting fully from vaccination than they were in 2011,” she added.
At the same time, Dr. Perkins acknowledged that many persons are still missing out on the chance to receive the vaccine on time – which means they are missing out on the chance to prevent cancer.
“Making sure that all adolescents receive vaccination between the ages of 9 to 12 has the potential to prevent up to 40,000 cancers every year in the U.S., [including] the most common HPV-related cancers, such as cervical cancer in women and tongue and tonsillar cancer in men,” Dr. Perkins noted.
“Thus, it’s critical that doctors and parents get the message that you can’t vaccinate too early, only too late,” she emphasized.
Dr. Edgman and Dr. Perkins report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
CDC warns of early uptick in respiratory disease
The Centers for Disease Control and Prevention is warning of an early surge in respiratory disease caused by multiple viruses. As influenza viruses, respiratory syncytial virus (RSV), SARS-CoV-2, and rhinovirus/enterovirus simultaneously circulate, the agency cautioned that this confluence of viral activity could strain the health care system, according to a CDC Health Network Alert advisory issued Nov. 4.
“This early increase in disease incidence highlights the importance of optimizing respiratory virus prevention and treatment measures, including prompt vaccination and antiviral treatment,” the alert stated.
The CDC reports that RSV activity is increasing nationally, but in some areas – such as the South and Mountain West – cases appear to be trending downward.
Influenza cases continue to climb, with the virus activity being the highest in the South, Mid-Atlantic, and the south-central West Coast, according to CDC data. “In fact, we’re seeing the highest influenza hospitalization rates going back a decade,” said José Romero, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases, during a press briefing. The agency estimates that there have been 1.6 million illnesses, 13,000 hospitalizations, and 730 deaths from the flu so far this season. As of Nov. 4, there have been two pediatric deaths.
COVID-19 cases appear to have plateaued in the past three weeks, Dr. Romero said; however, the CDC expects that there will be “high-level circulation of SARS-CoV-2 this fall and winter,” the health alert stated.
The CDC advised that all eligible individuals aged 6-months or older should be vaccinated against COVID-19 and influenza. To protect against RSV-hospitalization, high-risk children should receive the monoclonal antibody drug palivizumab (Synagis). High-risk children include infants born before 29 weeks, children younger than age 2 with chronic lung disease or hemodynamically significant congenital heart disease, and children with suppressed immune systems or neuromuscular disorders.
Any patient with confirmed or suspected flu who is hospitalized, at higher risk for influenza complications, or who has a severe or progressive illness should be treated as early as possible with antivirals, such as oral oseltamivir (Tamiflu).
Patients with confirmed SARS-CoV-2 infection with increased risk of complications should also be treated with antivirals, such as nirmatrelvir and ritonavir (Paxlovid) or remdesivir (Veklury).
Patients should also be reminded to wash their hands frequently, cover coughs and sneezes, stay home when sick, and avoid close contact with people who are sick, the CDC advised.
“There’s no doubt that we will face some challenges this winter,” said Dawn O’Connell, HHS Assistant Secretary for Preparedness and Response, “but it’s important to remember that RSV and flu are not new, and we have safe and effective vaccines for COVID-19 and the flu.”
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention is warning of an early surge in respiratory disease caused by multiple viruses. As influenza viruses, respiratory syncytial virus (RSV), SARS-CoV-2, and rhinovirus/enterovirus simultaneously circulate, the agency cautioned that this confluence of viral activity could strain the health care system, according to a CDC Health Network Alert advisory issued Nov. 4.
“This early increase in disease incidence highlights the importance of optimizing respiratory virus prevention and treatment measures, including prompt vaccination and antiviral treatment,” the alert stated.
The CDC reports that RSV activity is increasing nationally, but in some areas – such as the South and Mountain West – cases appear to be trending downward.
Influenza cases continue to climb, with the virus activity being the highest in the South, Mid-Atlantic, and the south-central West Coast, according to CDC data. “In fact, we’re seeing the highest influenza hospitalization rates going back a decade,” said José Romero, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases, during a press briefing. The agency estimates that there have been 1.6 million illnesses, 13,000 hospitalizations, and 730 deaths from the flu so far this season. As of Nov. 4, there have been two pediatric deaths.
COVID-19 cases appear to have plateaued in the past three weeks, Dr. Romero said; however, the CDC expects that there will be “high-level circulation of SARS-CoV-2 this fall and winter,” the health alert stated.
The CDC advised that all eligible individuals aged 6-months or older should be vaccinated against COVID-19 and influenza. To protect against RSV-hospitalization, high-risk children should receive the monoclonal antibody drug palivizumab (Synagis). High-risk children include infants born before 29 weeks, children younger than age 2 with chronic lung disease or hemodynamically significant congenital heart disease, and children with suppressed immune systems or neuromuscular disorders.
Any patient with confirmed or suspected flu who is hospitalized, at higher risk for influenza complications, or who has a severe or progressive illness should be treated as early as possible with antivirals, such as oral oseltamivir (Tamiflu).
Patients with confirmed SARS-CoV-2 infection with increased risk of complications should also be treated with antivirals, such as nirmatrelvir and ritonavir (Paxlovid) or remdesivir (Veklury).
Patients should also be reminded to wash their hands frequently, cover coughs and sneezes, stay home when sick, and avoid close contact with people who are sick, the CDC advised.
“There’s no doubt that we will face some challenges this winter,” said Dawn O’Connell, HHS Assistant Secretary for Preparedness and Response, “but it’s important to remember that RSV and flu are not new, and we have safe and effective vaccines for COVID-19 and the flu.”
A version of this article first appeared on Medscape.com.
The Centers for Disease Control and Prevention is warning of an early surge in respiratory disease caused by multiple viruses. As influenza viruses, respiratory syncytial virus (RSV), SARS-CoV-2, and rhinovirus/enterovirus simultaneously circulate, the agency cautioned that this confluence of viral activity could strain the health care system, according to a CDC Health Network Alert advisory issued Nov. 4.
“This early increase in disease incidence highlights the importance of optimizing respiratory virus prevention and treatment measures, including prompt vaccination and antiviral treatment,” the alert stated.
The CDC reports that RSV activity is increasing nationally, but in some areas – such as the South and Mountain West – cases appear to be trending downward.
Influenza cases continue to climb, with the virus activity being the highest in the South, Mid-Atlantic, and the south-central West Coast, according to CDC data. “In fact, we’re seeing the highest influenza hospitalization rates going back a decade,” said José Romero, MD, director of the CDC’s National Center for Immunization and Respiratory Diseases, during a press briefing. The agency estimates that there have been 1.6 million illnesses, 13,000 hospitalizations, and 730 deaths from the flu so far this season. As of Nov. 4, there have been two pediatric deaths.
COVID-19 cases appear to have plateaued in the past three weeks, Dr. Romero said; however, the CDC expects that there will be “high-level circulation of SARS-CoV-2 this fall and winter,” the health alert stated.
The CDC advised that all eligible individuals aged 6-months or older should be vaccinated against COVID-19 and influenza. To protect against RSV-hospitalization, high-risk children should receive the monoclonal antibody drug palivizumab (Synagis). High-risk children include infants born before 29 weeks, children younger than age 2 with chronic lung disease or hemodynamically significant congenital heart disease, and children with suppressed immune systems or neuromuscular disorders.
Any patient with confirmed or suspected flu who is hospitalized, at higher risk for influenza complications, or who has a severe or progressive illness should be treated as early as possible with antivirals, such as oral oseltamivir (Tamiflu).
Patients with confirmed SARS-CoV-2 infection with increased risk of complications should also be treated with antivirals, such as nirmatrelvir and ritonavir (Paxlovid) or remdesivir (Veklury).
Patients should also be reminded to wash their hands frequently, cover coughs and sneezes, stay home when sick, and avoid close contact with people who are sick, the CDC advised.
“There’s no doubt that we will face some challenges this winter,” said Dawn O’Connell, HHS Assistant Secretary for Preparedness and Response, “but it’s important to remember that RSV and flu are not new, and we have safe and effective vaccines for COVID-19 and the flu.”
A version of this article first appeared on Medscape.com.
New Medicare physician fee schedule leaves docs fuming over pay cuts
The rule also seeks to ease financial and administrative burdens on accountable care organizations (ACOs).
But physician groups’ initial reactions centered on what the American Medical Association describes as a “damaging across-the-board reduction” of 4.4% in a base calculation, known as a conversion factor.
The reduction is only one of the current threats to physician’s finances, Jack Resneck Jr, MD, AMA’s president, said in a statement. Medicare payment rates also fail to account for inflation in practice costs and COVID-related challenges. Physician’s Medicare payments could be cut by nearly 8.5% in 2023, factoring in other budget cuts, Dr. Resneck said in the statement.
That “would severely impede patient access to care due to the forced closure of physician practices and put further strain on those that remained open during the pandemic,” he said.
A key driver of these cuts is a law that was intended to resolve budget battles between Congress and physicians, while also transitioning Medicare away from fee-for-service payments and pegging reimbursement to judgments about value of care provided. The Centers for Medicare & Medicaid Services thus had little choice about cuts mandated by the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015.
For AMA and other physician groups, the finalization of the Medicare rule served as a rallying point to build support for pending legislation intended to stave off at least some payment cuts.
Federal officials should act soon to block the expected cuts before this season of Congress ends in January, said Anders Gilberg, senior vice president for government affairs at the Medical Group Management Association, in a statement.
“This cannot wait until next Congress – there are claims-processing implications for retroactively applying these policies,” Mr. Gilberg said.
He said MGMA would work with Congress and CMS “to mitigate these cuts and develop sustainable payment policies to allow physician practices to focus on treating patients instead of scrambling to keep their doors open.”
Chronic budget battles
Once seen as a promising resolution to chronic annual budget battles between physicians and Medicare, MACRA has proven a near-universal disappointment. A federal advisory commission in 2018 recommended that Congress scrap MACRA’s Merit-based Incentive Payment System (MIPS) and replace it with a new approach for attempting to tie reimbursement to judgments about the quality of medical care.
MACRA replaced an earlier budgeting approach on Medicare physician pay, known as the sustainable growth rate (SGR). Physician groups successfully lobbied Congress for many years to block threatened Medicare payment cuts. Between 2003 and April 2014, Congress passed 17 laws overriding the cuts to physician pay that the lawmakers earlier mandated through the SGR.
A similar pattern has emerged as Congress now acts on short-term fixes to stave off MACRA-mandated cuts. A law passed last December postponed cuts in physician pay from MACRA and federal budget laws.
And more than 70 members of the House support a bill (HR 8800) intended to block a slated 4.4% MACRA-related cut in physician pay for 2023. Two physicians, Rep. Ami Bera, MD, (D-CA) and Rep. Larry Bucshon (R-IN) sponsored the bill.
Among the groups backing the bill are the AMA, American Academy of Family Physicians, and American College of Physicians. The lawmakers may try to attach this bill to a large spending measure, known as an omnibus, that Congress will try to clear in December to avoid a partial government shutdown.
In a statement, Tochi Iroku-Malize, MD, MPH, MBA, the president of AAFP, urged Congress to factor in inflation in setting physician reimbursement and to reconsider Medicare’s approach to paying physicians.
“It’s past time to end the untenable physician payment cuts – which have now become an annual threat to the stability of physician practices – caused by Medicare budget neutrality requirements and the ongoing freeze in annual payment updates,” Dr. Iroku-Malize said.
Congress also needs to retool its approach to alternative payment models (APMs) intended to improve the quality of patient care, Dr. Iroku-Malize said.
“Physicians in APMs are better equipped to address unmet social needs and provide other enhanced services that are not supported by fee-for-service payment rates,” Dr. Iroku-Malize said. “However, insufficient Medicare fee-for-service payment rates, inadequate support, and burdensome timelines are undermining the move to value-based care and exacerbating our nation’s underinvestment in primary care.”
Policy changes
But the new rule did have some good news for family physicians, Dr. Iroku-Malize told this news organization in an email.
CMS said it will pay psychologists and social workers to help manage behavioral health needs as part of the primary care team, in addition to their own services. This change will give primary care practices more flexibility to coordinate with behavioral health professionals, Dr. Iroku-Malize noted.
“We know that primary care physicians are the first point of contact for many patients, and behavioral health integration increases critical access to mental health care, decreases stigma for patients, and can prevent more severe medical and behavioral health events,” she wrote.
CMS also eased a supervision requirement for nonphysicians providing behavioral health services.
It intends to allow certain health professionals to provide this care without requiring that a supervising physician or nurse practitioner be physically on site. This shift from direct supervision to what’s called general supervision applies to marriage and family therapists, licensed professional counselors, addiction counselors, certified peer recovery specialists, and behavioral health specialists, CMS said.
Other major policy changes include:
Medicare will pay for telehealth opioid treatment programs allowing patients to initiate treatment with buprenorphine. CMS also clarified that certain programs can bill for opioid use disorder treatment services provided through mobile units, such as vans.
Medicare enrollees may see audiologists for nonacute hearing conditions without an order from a physician or nurse practitioner. The policy is meant to allow audiologists to examine patients to prescribe, fit, or change hearing aids, or to provide hearing tests unrelated to disequilibrium.
CMS created new reimbursement codes for chronic pain management and treatment services to encourage clinicians to see patients with this condition. The codes also are meant to encourage practitioners already treating Medicare patients with chronic pain to spend more time helping them manage their condition “within a trusting, supportive, and ongoing care partnership,” CMS said.
CMS also made changes to the Medicare Shared Savings Program (MSSP) intended to reduce administrative burdens and offer more financial support to practices involved in ACOs. These steps include expanding opportunities for certain low-revenue ACOs to share in savings even if they do not meet a target rate.
A version of this article first appeared on Medscape.com.
The rule also seeks to ease financial and administrative burdens on accountable care organizations (ACOs).
But physician groups’ initial reactions centered on what the American Medical Association describes as a “damaging across-the-board reduction” of 4.4% in a base calculation, known as a conversion factor.
The reduction is only one of the current threats to physician’s finances, Jack Resneck Jr, MD, AMA’s president, said in a statement. Medicare payment rates also fail to account for inflation in practice costs and COVID-related challenges. Physician’s Medicare payments could be cut by nearly 8.5% in 2023, factoring in other budget cuts, Dr. Resneck said in the statement.
That “would severely impede patient access to care due to the forced closure of physician practices and put further strain on those that remained open during the pandemic,” he said.
A key driver of these cuts is a law that was intended to resolve budget battles between Congress and physicians, while also transitioning Medicare away from fee-for-service payments and pegging reimbursement to judgments about value of care provided. The Centers for Medicare & Medicaid Services thus had little choice about cuts mandated by the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015.
For AMA and other physician groups, the finalization of the Medicare rule served as a rallying point to build support for pending legislation intended to stave off at least some payment cuts.
Federal officials should act soon to block the expected cuts before this season of Congress ends in January, said Anders Gilberg, senior vice president for government affairs at the Medical Group Management Association, in a statement.
“This cannot wait until next Congress – there are claims-processing implications for retroactively applying these policies,” Mr. Gilberg said.
He said MGMA would work with Congress and CMS “to mitigate these cuts and develop sustainable payment policies to allow physician practices to focus on treating patients instead of scrambling to keep their doors open.”
Chronic budget battles
Once seen as a promising resolution to chronic annual budget battles between physicians and Medicare, MACRA has proven a near-universal disappointment. A federal advisory commission in 2018 recommended that Congress scrap MACRA’s Merit-based Incentive Payment System (MIPS) and replace it with a new approach for attempting to tie reimbursement to judgments about the quality of medical care.
MACRA replaced an earlier budgeting approach on Medicare physician pay, known as the sustainable growth rate (SGR). Physician groups successfully lobbied Congress for many years to block threatened Medicare payment cuts. Between 2003 and April 2014, Congress passed 17 laws overriding the cuts to physician pay that the lawmakers earlier mandated through the SGR.
A similar pattern has emerged as Congress now acts on short-term fixes to stave off MACRA-mandated cuts. A law passed last December postponed cuts in physician pay from MACRA and federal budget laws.
And more than 70 members of the House support a bill (HR 8800) intended to block a slated 4.4% MACRA-related cut in physician pay for 2023. Two physicians, Rep. Ami Bera, MD, (D-CA) and Rep. Larry Bucshon (R-IN) sponsored the bill.
Among the groups backing the bill are the AMA, American Academy of Family Physicians, and American College of Physicians. The lawmakers may try to attach this bill to a large spending measure, known as an omnibus, that Congress will try to clear in December to avoid a partial government shutdown.
In a statement, Tochi Iroku-Malize, MD, MPH, MBA, the president of AAFP, urged Congress to factor in inflation in setting physician reimbursement and to reconsider Medicare’s approach to paying physicians.
“It’s past time to end the untenable physician payment cuts – which have now become an annual threat to the stability of physician practices – caused by Medicare budget neutrality requirements and the ongoing freeze in annual payment updates,” Dr. Iroku-Malize said.
Congress also needs to retool its approach to alternative payment models (APMs) intended to improve the quality of patient care, Dr. Iroku-Malize said.
“Physicians in APMs are better equipped to address unmet social needs and provide other enhanced services that are not supported by fee-for-service payment rates,” Dr. Iroku-Malize said. “However, insufficient Medicare fee-for-service payment rates, inadequate support, and burdensome timelines are undermining the move to value-based care and exacerbating our nation’s underinvestment in primary care.”
Policy changes
But the new rule did have some good news for family physicians, Dr. Iroku-Malize told this news organization in an email.
CMS said it will pay psychologists and social workers to help manage behavioral health needs as part of the primary care team, in addition to their own services. This change will give primary care practices more flexibility to coordinate with behavioral health professionals, Dr. Iroku-Malize noted.
“We know that primary care physicians are the first point of contact for many patients, and behavioral health integration increases critical access to mental health care, decreases stigma for patients, and can prevent more severe medical and behavioral health events,” she wrote.
CMS also eased a supervision requirement for nonphysicians providing behavioral health services.
It intends to allow certain health professionals to provide this care without requiring that a supervising physician or nurse practitioner be physically on site. This shift from direct supervision to what’s called general supervision applies to marriage and family therapists, licensed professional counselors, addiction counselors, certified peer recovery specialists, and behavioral health specialists, CMS said.
Other major policy changes include:
Medicare will pay for telehealth opioid treatment programs allowing patients to initiate treatment with buprenorphine. CMS also clarified that certain programs can bill for opioid use disorder treatment services provided through mobile units, such as vans.
Medicare enrollees may see audiologists for nonacute hearing conditions without an order from a physician or nurse practitioner. The policy is meant to allow audiologists to examine patients to prescribe, fit, or change hearing aids, or to provide hearing tests unrelated to disequilibrium.
CMS created new reimbursement codes for chronic pain management and treatment services to encourage clinicians to see patients with this condition. The codes also are meant to encourage practitioners already treating Medicare patients with chronic pain to spend more time helping them manage their condition “within a trusting, supportive, and ongoing care partnership,” CMS said.
CMS also made changes to the Medicare Shared Savings Program (MSSP) intended to reduce administrative burdens and offer more financial support to practices involved in ACOs. These steps include expanding opportunities for certain low-revenue ACOs to share in savings even if they do not meet a target rate.
A version of this article first appeared on Medscape.com.
The rule also seeks to ease financial and administrative burdens on accountable care organizations (ACOs).
But physician groups’ initial reactions centered on what the American Medical Association describes as a “damaging across-the-board reduction” of 4.4% in a base calculation, known as a conversion factor.
The reduction is only one of the current threats to physician’s finances, Jack Resneck Jr, MD, AMA’s president, said in a statement. Medicare payment rates also fail to account for inflation in practice costs and COVID-related challenges. Physician’s Medicare payments could be cut by nearly 8.5% in 2023, factoring in other budget cuts, Dr. Resneck said in the statement.
That “would severely impede patient access to care due to the forced closure of physician practices and put further strain on those that remained open during the pandemic,” he said.
A key driver of these cuts is a law that was intended to resolve budget battles between Congress and physicians, while also transitioning Medicare away from fee-for-service payments and pegging reimbursement to judgments about value of care provided. The Centers for Medicare & Medicaid Services thus had little choice about cuts mandated by the Medicare Access and CHIP Reauthorization Act (MACRA) of 2015.
For AMA and other physician groups, the finalization of the Medicare rule served as a rallying point to build support for pending legislation intended to stave off at least some payment cuts.
Federal officials should act soon to block the expected cuts before this season of Congress ends in January, said Anders Gilberg, senior vice president for government affairs at the Medical Group Management Association, in a statement.
“This cannot wait until next Congress – there are claims-processing implications for retroactively applying these policies,” Mr. Gilberg said.
He said MGMA would work with Congress and CMS “to mitigate these cuts and develop sustainable payment policies to allow physician practices to focus on treating patients instead of scrambling to keep their doors open.”
Chronic budget battles
Once seen as a promising resolution to chronic annual budget battles between physicians and Medicare, MACRA has proven a near-universal disappointment. A federal advisory commission in 2018 recommended that Congress scrap MACRA’s Merit-based Incentive Payment System (MIPS) and replace it with a new approach for attempting to tie reimbursement to judgments about the quality of medical care.
MACRA replaced an earlier budgeting approach on Medicare physician pay, known as the sustainable growth rate (SGR). Physician groups successfully lobbied Congress for many years to block threatened Medicare payment cuts. Between 2003 and April 2014, Congress passed 17 laws overriding the cuts to physician pay that the lawmakers earlier mandated through the SGR.
A similar pattern has emerged as Congress now acts on short-term fixes to stave off MACRA-mandated cuts. A law passed last December postponed cuts in physician pay from MACRA and federal budget laws.
And more than 70 members of the House support a bill (HR 8800) intended to block a slated 4.4% MACRA-related cut in physician pay for 2023. Two physicians, Rep. Ami Bera, MD, (D-CA) and Rep. Larry Bucshon (R-IN) sponsored the bill.
Among the groups backing the bill are the AMA, American Academy of Family Physicians, and American College of Physicians. The lawmakers may try to attach this bill to a large spending measure, known as an omnibus, that Congress will try to clear in December to avoid a partial government shutdown.
In a statement, Tochi Iroku-Malize, MD, MPH, MBA, the president of AAFP, urged Congress to factor in inflation in setting physician reimbursement and to reconsider Medicare’s approach to paying physicians.
“It’s past time to end the untenable physician payment cuts – which have now become an annual threat to the stability of physician practices – caused by Medicare budget neutrality requirements and the ongoing freeze in annual payment updates,” Dr. Iroku-Malize said.
Congress also needs to retool its approach to alternative payment models (APMs) intended to improve the quality of patient care, Dr. Iroku-Malize said.
“Physicians in APMs are better equipped to address unmet social needs and provide other enhanced services that are not supported by fee-for-service payment rates,” Dr. Iroku-Malize said. “However, insufficient Medicare fee-for-service payment rates, inadequate support, and burdensome timelines are undermining the move to value-based care and exacerbating our nation’s underinvestment in primary care.”
Policy changes
But the new rule did have some good news for family physicians, Dr. Iroku-Malize told this news organization in an email.
CMS said it will pay psychologists and social workers to help manage behavioral health needs as part of the primary care team, in addition to their own services. This change will give primary care practices more flexibility to coordinate with behavioral health professionals, Dr. Iroku-Malize noted.
“We know that primary care physicians are the first point of contact for many patients, and behavioral health integration increases critical access to mental health care, decreases stigma for patients, and can prevent more severe medical and behavioral health events,” she wrote.
CMS also eased a supervision requirement for nonphysicians providing behavioral health services.
It intends to allow certain health professionals to provide this care without requiring that a supervising physician or nurse practitioner be physically on site. This shift from direct supervision to what’s called general supervision applies to marriage and family therapists, licensed professional counselors, addiction counselors, certified peer recovery specialists, and behavioral health specialists, CMS said.
Other major policy changes include:
Medicare will pay for telehealth opioid treatment programs allowing patients to initiate treatment with buprenorphine. CMS also clarified that certain programs can bill for opioid use disorder treatment services provided through mobile units, such as vans.
Medicare enrollees may see audiologists for nonacute hearing conditions without an order from a physician or nurse practitioner. The policy is meant to allow audiologists to examine patients to prescribe, fit, or change hearing aids, or to provide hearing tests unrelated to disequilibrium.
CMS created new reimbursement codes for chronic pain management and treatment services to encourage clinicians to see patients with this condition. The codes also are meant to encourage practitioners already treating Medicare patients with chronic pain to spend more time helping them manage their condition “within a trusting, supportive, and ongoing care partnership,” CMS said.
CMS also made changes to the Medicare Shared Savings Program (MSSP) intended to reduce administrative burdens and offer more financial support to practices involved in ACOs. These steps include expanding opportunities for certain low-revenue ACOs to share in savings even if they do not meet a target rate.
A version of this article first appeared on Medscape.com.
Man with COVID finally tests negative after 411 days
according to experts in the United Kingdom.
The man was treated with a mixture of neutralizing monoclonal antibodies, King’s College London said in a news release.
The man, 59, tested positive in December 2020 and tested negative in January 2022. He had a weakened immune system because of a previous kidney transplant. He received three doses of vaccine and his symptoms lessened, but he kept testing positive for COVID.
To find out if the man had a persistent infection or had been infected several times, doctors did a genetic analysis of the virus.
“This revealed that the patient’s infection was a persistent infection with an early COVID variant – a variation of the original Wuhan variant that was dominant in the United Kingdom in the later months of 2020. Analysis found the patient’s virus had multiple mutations since he was first infected,” King’s College said.
The doctors treated him with a Regeneron treatment that is no longer widely used because it’s not effective against newer COVID variants.
“Some new variants of the virus are resistant to all the antibody treatments available in the United Kingdom and Europe. Some people with weakened immune systems are still at risk of severe illness and becoming persistently infected. We are still working to understand the best way to protect and treat them,” Luke Snell, MD, from the King’s College School of Immunology & Microbial Sciences, said in the news release.
This is one of the longest known cases of COVID infection. Another man in England was infected with COVID for 505 days before his death, which King’s College said was the longest known COVID infection.
A version of this article first appeared on WebMD.com.
according to experts in the United Kingdom.
The man was treated with a mixture of neutralizing monoclonal antibodies, King’s College London said in a news release.
The man, 59, tested positive in December 2020 and tested negative in January 2022. He had a weakened immune system because of a previous kidney transplant. He received three doses of vaccine and his symptoms lessened, but he kept testing positive for COVID.
To find out if the man had a persistent infection or had been infected several times, doctors did a genetic analysis of the virus.
“This revealed that the patient’s infection was a persistent infection with an early COVID variant – a variation of the original Wuhan variant that was dominant in the United Kingdom in the later months of 2020. Analysis found the patient’s virus had multiple mutations since he was first infected,” King’s College said.
The doctors treated him with a Regeneron treatment that is no longer widely used because it’s not effective against newer COVID variants.
“Some new variants of the virus are resistant to all the antibody treatments available in the United Kingdom and Europe. Some people with weakened immune systems are still at risk of severe illness and becoming persistently infected. We are still working to understand the best way to protect and treat them,” Luke Snell, MD, from the King’s College School of Immunology & Microbial Sciences, said in the news release.
This is one of the longest known cases of COVID infection. Another man in England was infected with COVID for 505 days before his death, which King’s College said was the longest known COVID infection.
A version of this article first appeared on WebMD.com.
according to experts in the United Kingdom.
The man was treated with a mixture of neutralizing monoclonal antibodies, King’s College London said in a news release.
The man, 59, tested positive in December 2020 and tested negative in January 2022. He had a weakened immune system because of a previous kidney transplant. He received three doses of vaccine and his symptoms lessened, but he kept testing positive for COVID.
To find out if the man had a persistent infection or had been infected several times, doctors did a genetic analysis of the virus.
“This revealed that the patient’s infection was a persistent infection with an early COVID variant – a variation of the original Wuhan variant that was dominant in the United Kingdom in the later months of 2020. Analysis found the patient’s virus had multiple mutations since he was first infected,” King’s College said.
The doctors treated him with a Regeneron treatment that is no longer widely used because it’s not effective against newer COVID variants.
“Some new variants of the virus are resistant to all the antibody treatments available in the United Kingdom and Europe. Some people with weakened immune systems are still at risk of severe illness and becoming persistently infected. We are still working to understand the best way to protect and treat them,” Luke Snell, MD, from the King’s College School of Immunology & Microbial Sciences, said in the news release.
This is one of the longest known cases of COVID infection. Another man in England was infected with COVID for 505 days before his death, which King’s College said was the longest known COVID infection.
A version of this article first appeared on WebMD.com.