User login
In Case You Missed It: COVID
Dermatology and Vaccines: We Must Do Better
Vaccines work. They are powerful tools that have saved millions of lives worldwide; however, a robust antivaccine movement has taken hold in the United States and worldwide despite overwhelming data in support of vaccination. In fact, vaccine hesitancy—the reluctance or refusal to vaccinate despite the availability of vaccines—was listed by the World Health Organization as one of the top 10 global health threats in 2019.1
Several vaccines have a role in dermatology, including the human papillomavirus (HPV) vaccine (Gardasil 9 [Merck Sharp & Dohme Corp]), the herpes zoster vaccines (Zostavax [Merck Sharp & Dohme Corp] and Shingrix [GlaxoSmithKline Biologicals]), and the measles-mumps-rubella vaccine, among others. These vaccinations are necessary for children and many adults alike, and they play a critical role in protecting both healthy and immunosuppressed patients.
Vaccine hesitancy is a growing threat to individual and public health that requires a response from all physicians. In our experience, dermatologists have been somewhat passive in advocating for vaccinations, possibly due to knowledge barriers or time constraints; however, this stance must change. Dermatologists must join the front lines in advocating for vaccinations, which are a proven and effective modality in promoting public health.
Dermatologists can employ the following practical tips to improve vaccination compliance among patients:
• Familiarize yourself with the Centers for Disease Control and Prevention immunization schedules and vaccination information sheets (https://www.cdc.gov/vaccines/hcp/vis/current-vis.html). Printed copies of informational handouts should be readily available to provide to patients in the office. The Centers for Disease Control and Prevention also offers tip sheets to guide conversations with patients (https://www.cdc.gov/vaccines/hcp/conversations/index.html).
• Prior to starting an immunosuppressive medication, confirm the patient’s immunization status. You should know which vaccines are live (containing an attenuated pathogen) and which are inactivated. Live vaccines typically are not administered to immunosuppressed patients.
• Use electronic medical records to help provide reminders to prompt administration of any necessary vaccines.
• Know the facts, especially regarding purported vaccine controversies, and be able to cite data on vaccine safety and efficacy. For example, when having a conversation with a patient you could state that vaccination against HPV, which can cause genital warts and certain cancers, has decreased the number of HPV infections by more than 70% in young women and 80% in teenaged girls.2 Cervical precancers were reduced by 40% in women vaccinated against HPV. Twelve years of monitoring data validates the safety and efficacy of the HPV vaccine—it is safe and effective, with benefits that outweigh any potential risks.2
• Tailor counseling based on the patient’s age and focus on benefits that directly impact the patient. For example, consider showing young adults photographs of genital warts while educating them that the HPV vaccine can help prevent this kind of infection in the future.
• Emphasize that vaccines are a routine part of comprehensive patient care and support this point by providing data and specific reasons for recommending vaccines.3 Avoid phrases such as, “Do you want the vaccine?” or “You could consider receiving the vaccine today,” which can imply that the vaccine is not necessary.
• Offer vaccines in your office or provide clear printed informational sheets directing patients to nearby primary care clinics, infectious disease clinics, or pharmacies where vaccinations are offered.
• Consider using social media to promote the benefits of vaccination among patients.
The recent coronavirus disease 2019 pandemic has brought the topic of vaccination into the limelight while highlighting that rampant misinformation can lead to distrust of health care workers. Dermatologists, along with all physicians, should be trusted advisors and advocates for public health. In addition to being knowledgeable, dermatologists must remain open-minded in having conversations with skeptical patients. Physicians must take the time and effort to promote vaccinations—the health of patients and the general public depends on it.
- Akbar R. Ten threats to global health in 2019. World Health Organization website. https://www.who.int/emergencies/ten-threats-to-global-health-in-2019. Published March 21, 2019. Accessed November 11, 2020.
- HPV vaccination is safe and effective. Centers for Disease Control and Prevention website. https://www.cdc.gov/hpv/parents/vaccinesafety.html. Updated April 29, 2019. Accessed November 11, 2020.
- How to give a strong recommendation to adult patients who require vaccination. Medscape website. https://www.medscape.com/viewarticle/842874. Published April 16, 2015. Accessed November 11, 2020.
Vaccines work. They are powerful tools that have saved millions of lives worldwide; however, a robust antivaccine movement has taken hold in the United States and worldwide despite overwhelming data in support of vaccination. In fact, vaccine hesitancy—the reluctance or refusal to vaccinate despite the availability of vaccines—was listed by the World Health Organization as one of the top 10 global health threats in 2019.1
Several vaccines have a role in dermatology, including the human papillomavirus (HPV) vaccine (Gardasil 9 [Merck Sharp & Dohme Corp]), the herpes zoster vaccines (Zostavax [Merck Sharp & Dohme Corp] and Shingrix [GlaxoSmithKline Biologicals]), and the measles-mumps-rubella vaccine, among others. These vaccinations are necessary for children and many adults alike, and they play a critical role in protecting both healthy and immunosuppressed patients.
Vaccine hesitancy is a growing threat to individual and public health that requires a response from all physicians. In our experience, dermatologists have been somewhat passive in advocating for vaccinations, possibly due to knowledge barriers or time constraints; however, this stance must change. Dermatologists must join the front lines in advocating for vaccinations, which are a proven and effective modality in promoting public health.
Dermatologists can employ the following practical tips to improve vaccination compliance among patients:
• Familiarize yourself with the Centers for Disease Control and Prevention immunization schedules and vaccination information sheets (https://www.cdc.gov/vaccines/hcp/vis/current-vis.html). Printed copies of informational handouts should be readily available to provide to patients in the office. The Centers for Disease Control and Prevention also offers tip sheets to guide conversations with patients (https://www.cdc.gov/vaccines/hcp/conversations/index.html).
• Prior to starting an immunosuppressive medication, confirm the patient’s immunization status. You should know which vaccines are live (containing an attenuated pathogen) and which are inactivated. Live vaccines typically are not administered to immunosuppressed patients.
• Use electronic medical records to help provide reminders to prompt administration of any necessary vaccines.
• Know the facts, especially regarding purported vaccine controversies, and be able to cite data on vaccine safety and efficacy. For example, when having a conversation with a patient you could state that vaccination against HPV, which can cause genital warts and certain cancers, has decreased the number of HPV infections by more than 70% in young women and 80% in teenaged girls.2 Cervical precancers were reduced by 40% in women vaccinated against HPV. Twelve years of monitoring data validates the safety and efficacy of the HPV vaccine—it is safe and effective, with benefits that outweigh any potential risks.2
• Tailor counseling based on the patient’s age and focus on benefits that directly impact the patient. For example, consider showing young adults photographs of genital warts while educating them that the HPV vaccine can help prevent this kind of infection in the future.
• Emphasize that vaccines are a routine part of comprehensive patient care and support this point by providing data and specific reasons for recommending vaccines.3 Avoid phrases such as, “Do you want the vaccine?” or “You could consider receiving the vaccine today,” which can imply that the vaccine is not necessary.
• Offer vaccines in your office or provide clear printed informational sheets directing patients to nearby primary care clinics, infectious disease clinics, or pharmacies where vaccinations are offered.
• Consider using social media to promote the benefits of vaccination among patients.
The recent coronavirus disease 2019 pandemic has brought the topic of vaccination into the limelight while highlighting that rampant misinformation can lead to distrust of health care workers. Dermatologists, along with all physicians, should be trusted advisors and advocates for public health. In addition to being knowledgeable, dermatologists must remain open-minded in having conversations with skeptical patients. Physicians must take the time and effort to promote vaccinations—the health of patients and the general public depends on it.
Vaccines work. They are powerful tools that have saved millions of lives worldwide; however, a robust antivaccine movement has taken hold in the United States and worldwide despite overwhelming data in support of vaccination. In fact, vaccine hesitancy—the reluctance or refusal to vaccinate despite the availability of vaccines—was listed by the World Health Organization as one of the top 10 global health threats in 2019.1
Several vaccines have a role in dermatology, including the human papillomavirus (HPV) vaccine (Gardasil 9 [Merck Sharp & Dohme Corp]), the herpes zoster vaccines (Zostavax [Merck Sharp & Dohme Corp] and Shingrix [GlaxoSmithKline Biologicals]), and the measles-mumps-rubella vaccine, among others. These vaccinations are necessary for children and many adults alike, and they play a critical role in protecting both healthy and immunosuppressed patients.
Vaccine hesitancy is a growing threat to individual and public health that requires a response from all physicians. In our experience, dermatologists have been somewhat passive in advocating for vaccinations, possibly due to knowledge barriers or time constraints; however, this stance must change. Dermatologists must join the front lines in advocating for vaccinations, which are a proven and effective modality in promoting public health.
Dermatologists can employ the following practical tips to improve vaccination compliance among patients:
• Familiarize yourself with the Centers for Disease Control and Prevention immunization schedules and vaccination information sheets (https://www.cdc.gov/vaccines/hcp/vis/current-vis.html). Printed copies of informational handouts should be readily available to provide to patients in the office. The Centers for Disease Control and Prevention also offers tip sheets to guide conversations with patients (https://www.cdc.gov/vaccines/hcp/conversations/index.html).
• Prior to starting an immunosuppressive medication, confirm the patient’s immunization status. You should know which vaccines are live (containing an attenuated pathogen) and which are inactivated. Live vaccines typically are not administered to immunosuppressed patients.
• Use electronic medical records to help provide reminders to prompt administration of any necessary vaccines.
• Know the facts, especially regarding purported vaccine controversies, and be able to cite data on vaccine safety and efficacy. For example, when having a conversation with a patient you could state that vaccination against HPV, which can cause genital warts and certain cancers, has decreased the number of HPV infections by more than 70% in young women and 80% in teenaged girls.2 Cervical precancers were reduced by 40% in women vaccinated against HPV. Twelve years of monitoring data validates the safety and efficacy of the HPV vaccine—it is safe and effective, with benefits that outweigh any potential risks.2
• Tailor counseling based on the patient’s age and focus on benefits that directly impact the patient. For example, consider showing young adults photographs of genital warts while educating them that the HPV vaccine can help prevent this kind of infection in the future.
• Emphasize that vaccines are a routine part of comprehensive patient care and support this point by providing data and specific reasons for recommending vaccines.3 Avoid phrases such as, “Do you want the vaccine?” or “You could consider receiving the vaccine today,” which can imply that the vaccine is not necessary.
• Offer vaccines in your office or provide clear printed informational sheets directing patients to nearby primary care clinics, infectious disease clinics, or pharmacies where vaccinations are offered.
• Consider using social media to promote the benefits of vaccination among patients.
The recent coronavirus disease 2019 pandemic has brought the topic of vaccination into the limelight while highlighting that rampant misinformation can lead to distrust of health care workers. Dermatologists, along with all physicians, should be trusted advisors and advocates for public health. In addition to being knowledgeable, dermatologists must remain open-minded in having conversations with skeptical patients. Physicians must take the time and effort to promote vaccinations—the health of patients and the general public depends on it.
- Akbar R. Ten threats to global health in 2019. World Health Organization website. https://www.who.int/emergencies/ten-threats-to-global-health-in-2019. Published March 21, 2019. Accessed November 11, 2020.
- HPV vaccination is safe and effective. Centers for Disease Control and Prevention website. https://www.cdc.gov/hpv/parents/vaccinesafety.html. Updated April 29, 2019. Accessed November 11, 2020.
- How to give a strong recommendation to adult patients who require vaccination. Medscape website. https://www.medscape.com/viewarticle/842874. Published April 16, 2015. Accessed November 11, 2020.
- Akbar R. Ten threats to global health in 2019. World Health Organization website. https://www.who.int/emergencies/ten-threats-to-global-health-in-2019. Published March 21, 2019. Accessed November 11, 2020.
- HPV vaccination is safe and effective. Centers for Disease Control and Prevention website. https://www.cdc.gov/hpv/parents/vaccinesafety.html. Updated April 29, 2019. Accessed November 11, 2020.
- How to give a strong recommendation to adult patients who require vaccination. Medscape website. https://www.medscape.com/viewarticle/842874. Published April 16, 2015. Accessed November 11, 2020.
COVID-19–related outcomes poor for patients with hematologic disease in ASH registry
Patients with hematologic disease who develop COVID-19 may experience substantial morbidity and mortality related to SARS-CoV-2 infection, according to recent registry data reported at the all-virtual annual meeting of the American Society of Hematology.
Overall mortality was 28% for the first 250 patients entered into the ASH Research Collaborative COVID-19 Registry for Hematology, researchers reported in an abstract of their study findings.
However, the burden of death and moderate-to-severe COVID-19 outcomes was highest in patients with poorer prognosis and those with relapsed/refractory hematological disease, they added.
The most commonly represented malignancies were acute leukemia, non-Hodgkin lymphoma, and myeloma or amyloidosis, according to the report.
Taken together, the findings do support an “emerging consensus” that COVID-19 related morbidity and mortality is significant in these patients, authors said – however, the current findings may not be reason enough to support a change in treatment course for the underlying disease.
“We see no reason, based on our data, to withhold intensive therapies from patients with underlying hematologic malignancies and favorable prognoses, if aggressive supportive care is consistent with patient preferences,” wrote the researchers.
ASH President Stephanie Lee, MD, MPH, said these registry findings are important to better understand how SARS-CoV-2 is affecting not only patients with hematologic diseases, but also individuals who experience COVID-19-related hematologic complications.
However, the findings are limited due to the heterogeneity of diseases, symptoms, and treatments represented in the registry, said Dr. Lee, associate director of the clinical research division at Fred Hutchinson Cancer Center in Seattle.
“More data will be coming in, but I think this is an example of trying to harness real-world information to try to learn things until we get more controlled studies,” Dr. Lee said in a media briefing held in advance of the ASH meeting.
Comorbidities and more
Patients with blood cancers are often older and may have comorbidities such as diabetes or hypertension that have been linked to poor COVID-19 outcomes, according to the authors of the report, led by William A. Wood, MD, MPH, associate professor of medicine with the UNC Lineberger Comprehensive Cancer Center in Chapel Hill, N.C.
Moreover, these patients may have underlying immune dysfunction and may receive chemotherapy or immunotherapy that is “profoundly immunosuppressive,” Dr. Wood and coauthors said in their report.
To date, however, risks of morbidity and mortality related to SARS-CoV-2 infection have not been well defined in this patient population, authors said.
More data is emerging now from the ASH Research Collaborative COVID-19 Registry for Hematology, which includes data on patients positive for COVID-19 who have a past or present hematologic condition or have experienced a hematologic complication related to COVID-19.
All data from the registry is being made available through a dashboard on the ASH Research Collaborative website, which as of Dec. 1, 2020, included 693 complete cases.
The data cut in the ASH abstract includes the first 250 patients enrolled at 74 sites around the world, the authors said. The most common malignancies included acute leukemia in 33%, non-Hodgkin lymphoma in 27%, and myeloma or amyloidosis in 16%.
The most frequently reported symptoms included fever in 73%, cough in 67%, dyspnea in 50%, and fatigue in 40%, according to that report.
At the time of this data snapshot, treatment with COVID-19-directed therapies including hydroxychloroquine or azithromycin were common, reported in 76 and 59 patients, respectively, in the cohort.
Batch submissions from sites with high incidence of COVID-19 infection are ongoing. The registry has been expanded to include nonmalignant hematologic diseases, and the registry will continue to accumulate data as a resource for the hematology community.
Overall mortality was 28% at the time, according to the abstract, with nearly all of the deaths occurring in patients classified as having COVID-19 that was moderate (i.e., requiring hospitalization) or severe (i.e., requiring ICU admission).
“In some instances, death occurred after a decision was made to forgo ICU admission in favor of a palliative approach,” said Dr. Wood and coauthors in their report.
Dr. Wood reported research funding from Pfizer, consultancy with Teladoc/Best Doctors, and honoraria from the ASH Research Collaborative. Coauthors provided disclosures related to Celgene, Madrigal Pharmaceuticals, Pharmacyclics, and Amgen, among others.
SOURCE: Wood WA et al. ASH 2020, Abstract 215.
Patients with hematologic disease who develop COVID-19 may experience substantial morbidity and mortality related to SARS-CoV-2 infection, according to recent registry data reported at the all-virtual annual meeting of the American Society of Hematology.
Overall mortality was 28% for the first 250 patients entered into the ASH Research Collaborative COVID-19 Registry for Hematology, researchers reported in an abstract of their study findings.
However, the burden of death and moderate-to-severe COVID-19 outcomes was highest in patients with poorer prognosis and those with relapsed/refractory hematological disease, they added.
The most commonly represented malignancies were acute leukemia, non-Hodgkin lymphoma, and myeloma or amyloidosis, according to the report.
Taken together, the findings do support an “emerging consensus” that COVID-19 related morbidity and mortality is significant in these patients, authors said – however, the current findings may not be reason enough to support a change in treatment course for the underlying disease.
“We see no reason, based on our data, to withhold intensive therapies from patients with underlying hematologic malignancies and favorable prognoses, if aggressive supportive care is consistent with patient preferences,” wrote the researchers.
ASH President Stephanie Lee, MD, MPH, said these registry findings are important to better understand how SARS-CoV-2 is affecting not only patients with hematologic diseases, but also individuals who experience COVID-19-related hematologic complications.
However, the findings are limited due to the heterogeneity of diseases, symptoms, and treatments represented in the registry, said Dr. Lee, associate director of the clinical research division at Fred Hutchinson Cancer Center in Seattle.
“More data will be coming in, but I think this is an example of trying to harness real-world information to try to learn things until we get more controlled studies,” Dr. Lee said in a media briefing held in advance of the ASH meeting.
Comorbidities and more
Patients with blood cancers are often older and may have comorbidities such as diabetes or hypertension that have been linked to poor COVID-19 outcomes, according to the authors of the report, led by William A. Wood, MD, MPH, associate professor of medicine with the UNC Lineberger Comprehensive Cancer Center in Chapel Hill, N.C.
Moreover, these patients may have underlying immune dysfunction and may receive chemotherapy or immunotherapy that is “profoundly immunosuppressive,” Dr. Wood and coauthors said in their report.
To date, however, risks of morbidity and mortality related to SARS-CoV-2 infection have not been well defined in this patient population, authors said.
More data is emerging now from the ASH Research Collaborative COVID-19 Registry for Hematology, which includes data on patients positive for COVID-19 who have a past or present hematologic condition or have experienced a hematologic complication related to COVID-19.
All data from the registry is being made available through a dashboard on the ASH Research Collaborative website, which as of Dec. 1, 2020, included 693 complete cases.
The data cut in the ASH abstract includes the first 250 patients enrolled at 74 sites around the world, the authors said. The most common malignancies included acute leukemia in 33%, non-Hodgkin lymphoma in 27%, and myeloma or amyloidosis in 16%.
The most frequently reported symptoms included fever in 73%, cough in 67%, dyspnea in 50%, and fatigue in 40%, according to that report.
At the time of this data snapshot, treatment with COVID-19-directed therapies including hydroxychloroquine or azithromycin were common, reported in 76 and 59 patients, respectively, in the cohort.
Batch submissions from sites with high incidence of COVID-19 infection are ongoing. The registry has been expanded to include nonmalignant hematologic diseases, and the registry will continue to accumulate data as a resource for the hematology community.
Overall mortality was 28% at the time, according to the abstract, with nearly all of the deaths occurring in patients classified as having COVID-19 that was moderate (i.e., requiring hospitalization) or severe (i.e., requiring ICU admission).
“In some instances, death occurred after a decision was made to forgo ICU admission in favor of a palliative approach,” said Dr. Wood and coauthors in their report.
Dr. Wood reported research funding from Pfizer, consultancy with Teladoc/Best Doctors, and honoraria from the ASH Research Collaborative. Coauthors provided disclosures related to Celgene, Madrigal Pharmaceuticals, Pharmacyclics, and Amgen, among others.
SOURCE: Wood WA et al. ASH 2020, Abstract 215.
Patients with hematologic disease who develop COVID-19 may experience substantial morbidity and mortality related to SARS-CoV-2 infection, according to recent registry data reported at the all-virtual annual meeting of the American Society of Hematology.
Overall mortality was 28% for the first 250 patients entered into the ASH Research Collaborative COVID-19 Registry for Hematology, researchers reported in an abstract of their study findings.
However, the burden of death and moderate-to-severe COVID-19 outcomes was highest in patients with poorer prognosis and those with relapsed/refractory hematological disease, they added.
The most commonly represented malignancies were acute leukemia, non-Hodgkin lymphoma, and myeloma or amyloidosis, according to the report.
Taken together, the findings do support an “emerging consensus” that COVID-19 related morbidity and mortality is significant in these patients, authors said – however, the current findings may not be reason enough to support a change in treatment course for the underlying disease.
“We see no reason, based on our data, to withhold intensive therapies from patients with underlying hematologic malignancies and favorable prognoses, if aggressive supportive care is consistent with patient preferences,” wrote the researchers.
ASH President Stephanie Lee, MD, MPH, said these registry findings are important to better understand how SARS-CoV-2 is affecting not only patients with hematologic diseases, but also individuals who experience COVID-19-related hematologic complications.
However, the findings are limited due to the heterogeneity of diseases, symptoms, and treatments represented in the registry, said Dr. Lee, associate director of the clinical research division at Fred Hutchinson Cancer Center in Seattle.
“More data will be coming in, but I think this is an example of trying to harness real-world information to try to learn things until we get more controlled studies,” Dr. Lee said in a media briefing held in advance of the ASH meeting.
Comorbidities and more
Patients with blood cancers are often older and may have comorbidities such as diabetes or hypertension that have been linked to poor COVID-19 outcomes, according to the authors of the report, led by William A. Wood, MD, MPH, associate professor of medicine with the UNC Lineberger Comprehensive Cancer Center in Chapel Hill, N.C.
Moreover, these patients may have underlying immune dysfunction and may receive chemotherapy or immunotherapy that is “profoundly immunosuppressive,” Dr. Wood and coauthors said in their report.
To date, however, risks of morbidity and mortality related to SARS-CoV-2 infection have not been well defined in this patient population, authors said.
More data is emerging now from the ASH Research Collaborative COVID-19 Registry for Hematology, which includes data on patients positive for COVID-19 who have a past or present hematologic condition or have experienced a hematologic complication related to COVID-19.
All data from the registry is being made available through a dashboard on the ASH Research Collaborative website, which as of Dec. 1, 2020, included 693 complete cases.
The data cut in the ASH abstract includes the first 250 patients enrolled at 74 sites around the world, the authors said. The most common malignancies included acute leukemia in 33%, non-Hodgkin lymphoma in 27%, and myeloma or amyloidosis in 16%.
The most frequently reported symptoms included fever in 73%, cough in 67%, dyspnea in 50%, and fatigue in 40%, according to that report.
At the time of this data snapshot, treatment with COVID-19-directed therapies including hydroxychloroquine or azithromycin were common, reported in 76 and 59 patients, respectively, in the cohort.
Batch submissions from sites with high incidence of COVID-19 infection are ongoing. The registry has been expanded to include nonmalignant hematologic diseases, and the registry will continue to accumulate data as a resource for the hematology community.
Overall mortality was 28% at the time, according to the abstract, with nearly all of the deaths occurring in patients classified as having COVID-19 that was moderate (i.e., requiring hospitalization) or severe (i.e., requiring ICU admission).
“In some instances, death occurred after a decision was made to forgo ICU admission in favor of a palliative approach,” said Dr. Wood and coauthors in their report.
Dr. Wood reported research funding from Pfizer, consultancy with Teladoc/Best Doctors, and honoraria from the ASH Research Collaborative. Coauthors provided disclosures related to Celgene, Madrigal Pharmaceuticals, Pharmacyclics, and Amgen, among others.
SOURCE: Wood WA et al. ASH 2020, Abstract 215.
FROM ASH 2020
Infant’s COVID-19–related myocardial injury reversed
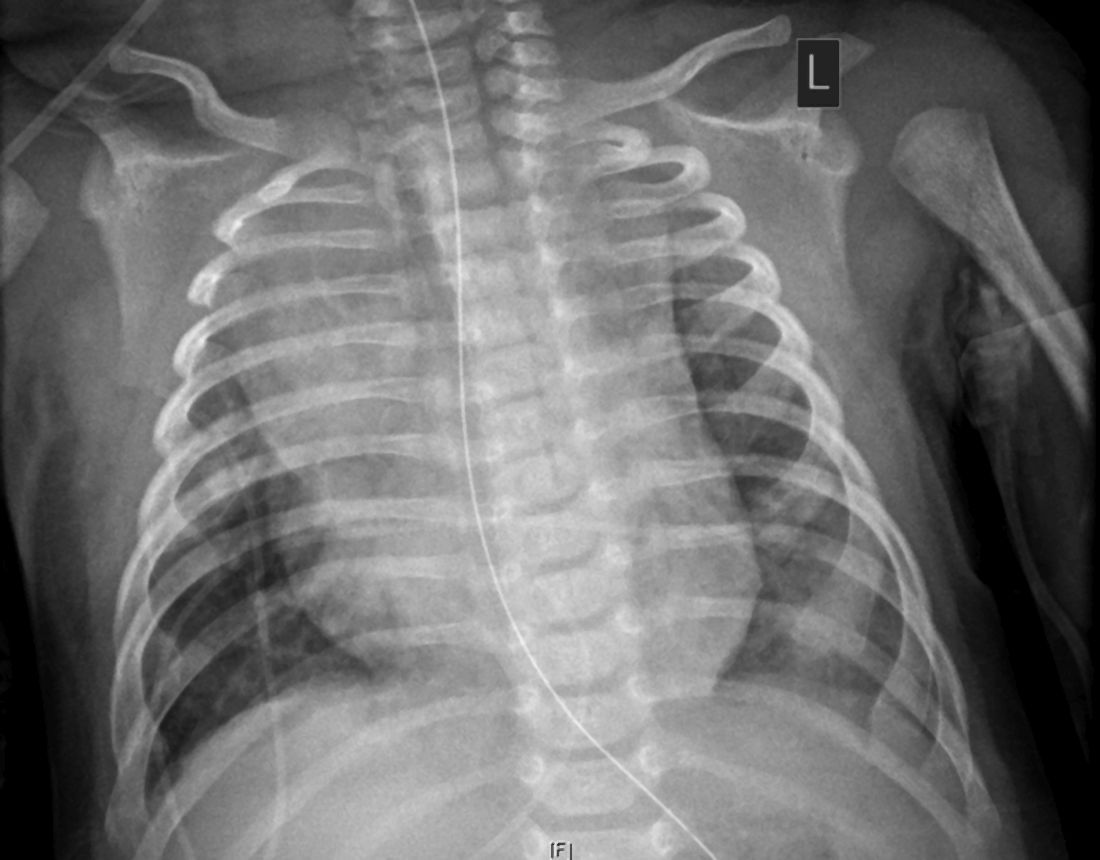
Reports of signs of heart failure in adults with COVID-19 have been rare – just four such cases have been published since the outbreak started in China – and now a team of pediatric cardiologists in New York have reported a case of acute but reversible myocardial injury in an infant with COVID-19.
and right upper lobe atelectasis.
The 2-month-old infant went home after more than 2 weeks in the hospital with no apparent lingering cardiac effects of the illness and not needing any oral heart failure medications, Madhu Sharma, MD, of the Children’s Hospital and Montefiore in New York and colleagues reported in JACC Case Reports. With close follow-up, the child’s left ventricle size and systolic function have remained normal and mitral regurgitation resolved. The case report didn’t mention the infant’s gender.
But before the straightforward postdischarge course emerged, the infant was in a precarious state, and Dr. Sharma and her team were challenged to diagnose the underlying causes.
The child, who was born about 7 weeks premature, first came to the hospital having turned blue after choking on food. Nonrebreather mask ventilation was initiated in the ED, and an examination detected a holosystolic murmur. A test for COVID-19 was negative, but a later test was positive, and a chest x-ray exhibited cardiomegaly and signs of fluid and inflammation in the lungs.
An electrocardiogram detected sinus tachycardia, ST-segment depression and other anomalies in cardiac function. Further investigation with a transthoracic ECG showed severely depressed left ventricle systolic function with an ejection fraction of 30%, severe mitral regurgitation, and normal right ventricular systolic function.
Treatment included remdesivir and intravenous antibiotics. Through the hospital course, the patient was extubated to noninvasive ventilation, reintubated, put on intravenous steroid (methylprednisolone) and low-molecular-weight heparin, extubated, and tested throughout for cardiac function.
By day 14, left ventricle size and function normalized, and while the mitral regurgitation remained severe, it improved later without HF therapies. Left ventricle ejection fraction had recovered to 60%, and key cardiac biomarkers had normalized. On day 16, milrinone was discontinued, and the care team determined the patient no longer needed oral heart failure therapies.
“Most children with COVID-19 are either asymptomatic or have mild symptoms, but our case shows the potential for reversible myocardial injury in infants with COVID-19,” said Dr. Sharma. “Testing for COVID-19 in children presenting with signs and symptoms of heart failure is very important as we learn more about the impact of this virus.”
Dr. Sharma and coauthors have no relevant financial relationships to disclose.
SOURCE: Sharma M et al. JACC Case Rep. 2020. doi: 10.1016/j.jaccas.2020.09.031.
Reports of signs of heart failure in adults with COVID-19 have been rare – just four such cases have been published since the outbreak started in China – and now a team of pediatric cardiologists in New York have reported a case of acute but reversible myocardial injury in an infant with COVID-19.
and right upper lobe atelectasis.
The 2-month-old infant went home after more than 2 weeks in the hospital with no apparent lingering cardiac effects of the illness and not needing any oral heart failure medications, Madhu Sharma, MD, of the Children’s Hospital and Montefiore in New York and colleagues reported in JACC Case Reports. With close follow-up, the child’s left ventricle size and systolic function have remained normal and mitral regurgitation resolved. The case report didn’t mention the infant’s gender.
But before the straightforward postdischarge course emerged, the infant was in a precarious state, and Dr. Sharma and her team were challenged to diagnose the underlying causes.
The child, who was born about 7 weeks premature, first came to the hospital having turned blue after choking on food. Nonrebreather mask ventilation was initiated in the ED, and an examination detected a holosystolic murmur. A test for COVID-19 was negative, but a later test was positive, and a chest x-ray exhibited cardiomegaly and signs of fluid and inflammation in the lungs.
An electrocardiogram detected sinus tachycardia, ST-segment depression and other anomalies in cardiac function. Further investigation with a transthoracic ECG showed severely depressed left ventricle systolic function with an ejection fraction of 30%, severe mitral regurgitation, and normal right ventricular systolic function.
Treatment included remdesivir and intravenous antibiotics. Through the hospital course, the patient was extubated to noninvasive ventilation, reintubated, put on intravenous steroid (methylprednisolone) and low-molecular-weight heparin, extubated, and tested throughout for cardiac function.
By day 14, left ventricle size and function normalized, and while the mitral regurgitation remained severe, it improved later without HF therapies. Left ventricle ejection fraction had recovered to 60%, and key cardiac biomarkers had normalized. On day 16, milrinone was discontinued, and the care team determined the patient no longer needed oral heart failure therapies.
“Most children with COVID-19 are either asymptomatic or have mild symptoms, but our case shows the potential for reversible myocardial injury in infants with COVID-19,” said Dr. Sharma. “Testing for COVID-19 in children presenting with signs and symptoms of heart failure is very important as we learn more about the impact of this virus.”
Dr. Sharma and coauthors have no relevant financial relationships to disclose.
SOURCE: Sharma M et al. JACC Case Rep. 2020. doi: 10.1016/j.jaccas.2020.09.031.
Reports of signs of heart failure in adults with COVID-19 have been rare – just four such cases have been published since the outbreak started in China – and now a team of pediatric cardiologists in New York have reported a case of acute but reversible myocardial injury in an infant with COVID-19.
and right upper lobe atelectasis.
The 2-month-old infant went home after more than 2 weeks in the hospital with no apparent lingering cardiac effects of the illness and not needing any oral heart failure medications, Madhu Sharma, MD, of the Children’s Hospital and Montefiore in New York and colleagues reported in JACC Case Reports. With close follow-up, the child’s left ventricle size and systolic function have remained normal and mitral regurgitation resolved. The case report didn’t mention the infant’s gender.
But before the straightforward postdischarge course emerged, the infant was in a precarious state, and Dr. Sharma and her team were challenged to diagnose the underlying causes.
The child, who was born about 7 weeks premature, first came to the hospital having turned blue after choking on food. Nonrebreather mask ventilation was initiated in the ED, and an examination detected a holosystolic murmur. A test for COVID-19 was negative, but a later test was positive, and a chest x-ray exhibited cardiomegaly and signs of fluid and inflammation in the lungs.
An electrocardiogram detected sinus tachycardia, ST-segment depression and other anomalies in cardiac function. Further investigation with a transthoracic ECG showed severely depressed left ventricle systolic function with an ejection fraction of 30%, severe mitral regurgitation, and normal right ventricular systolic function.
Treatment included remdesivir and intravenous antibiotics. Through the hospital course, the patient was extubated to noninvasive ventilation, reintubated, put on intravenous steroid (methylprednisolone) and low-molecular-weight heparin, extubated, and tested throughout for cardiac function.
By day 14, left ventricle size and function normalized, and while the mitral regurgitation remained severe, it improved later without HF therapies. Left ventricle ejection fraction had recovered to 60%, and key cardiac biomarkers had normalized. On day 16, milrinone was discontinued, and the care team determined the patient no longer needed oral heart failure therapies.
“Most children with COVID-19 are either asymptomatic or have mild symptoms, but our case shows the potential for reversible myocardial injury in infants with COVID-19,” said Dr. Sharma. “Testing for COVID-19 in children presenting with signs and symptoms of heart failure is very important as we learn more about the impact of this virus.”
Dr. Sharma and coauthors have no relevant financial relationships to disclose.
SOURCE: Sharma M et al. JACC Case Rep. 2020. doi: 10.1016/j.jaccas.2020.09.031.
FROM JACC CASE REPORTS
Key clinical point: Children presenting with COVID-19 should be tested for heart failure.
Major finding: A 2-month-old infant with COVID-19 had acute but reversible myocardial injury.
Study details: Single case report.
Disclosures: Dr. Sharma, MD, has no relevant financial relationships to disclose.
Source: Sharma M et al. JACC Case Rep. 2020. doi: 10.1016/j.jaccas.2020.09.031.
Obesity, hypoxia predict severity in children with COVID-19
based on data from 281 patients at 8 locations.
Manifestations of COVID-19 in children include respiratory disease similar to that seen in adults, but the full spectrum of disease in children has been studied mainly in single settings or with a focus on one clinical manifestation, wrote Danielle M. Fernandes, MD, of Albert Einstein College of Medicine, New York, and colleagues.
In a study published in the Journal of Pediatrics, the researchers identified 281 children hospitalized with COVID-19 and/or multisystem inflammatory syndrome in children (MIS-C) at 8 sites in Connecticut, New Jersey, and New York. A total of 143 (51%) had respiratory disease, 69 (25%) had MIS-C, and 69 (25%) had other manifestations of illness including 32 patients with gastrointestinal problems, 21 infants with fever, 6 cases of neurologic disease, 6 cases of diabetic ketoacidosis, and 4 patients with other indications. The median age of the patients was 10 years, 60% were male, 51% were Hispanic, and 23% were non-Hispanic Black. The most common comorbidities were obesity (34%) and asthma (14%).
Independent predictors of disease severity in children found
After controlling for multiple variables, obesity and hypoxia at hospital admission were significant independent predictors of severe respiratory disease, with odds ratios of 3.39 and 4.01, respectively. In addition, lower absolute lymphocyte count (OR, 8.33 per unit decrease in 109 cells/L) and higher C-reactive protein (OR, 1.06 per unit increase in mg/dL) were significantly predictive of severe MIS-C (P = .001 and P = .017, respectively).
“The association between weight and severe respiratory COVID-19 is consistent with the adult literature; however, the mechanisms of this association require further study,” Dr. Fernandes and associates noted.
Overall, children with MIS-C were significantly more likely to be non-Hispanic Black, compared with children with respiratory disease, an 18% difference. However, neither race/ethnicity nor socioeconomic status were significant predictors of disease severity, the researchers wrote.
During the study period, 7 patients (2%) died and 114 (41%) were admitted to the ICU.
“We found a wide array of clinical manifestations in children and youth hospitalized with SARS-CoV-2,” Dr. Fernandes and associates wrote. Notably, gastrointestinal symptoms, ocular symptoms, and dermatologic symptoms have rarely been noted in adults with COVID-19, but occurred in more than 30% of the pediatric patients.
“We also found that SARS-CoV-2 can be an incidental finding in a substantial number of hospitalized pediatric patients,” the researchers said.
The findings were limited by several factors including a population of patients only from Connecticut, New Jersey, and New York, and the possibility that decisions on hospital and ICU admission may have varied by location, the researchers said. In addition, approaches may have varied in the absence of data on the optimal treatment of MIS-C.
“This study builds on the growing body of evidence showing that mortality in hospitalized pediatric patients is low, compared with adults,” Dr. Fernandes and associates said. “However, it highlights that the young population is not universally spared from morbidity, and that even previously healthy children and youth can develop severe disease requiring supportive therapy.”
Findings confirm other clinical experience
The study was important to show that, “although most children are spared severe illness from COVID-19, some children are hospitalized both with acute COVID-19 respiratory disease, with MIS-C and with a range of other complications,” Adrienne Randolph, MD, of Boston Children’s Hospital and Harvard Medical School, Boston, said in an interview.
Dr. Randolph said she was not surprised by the study findings, “as we are also seeing these types of complications at Boston Children’s Hospital where I work.”
Additional research is needed on the outcomes of these patients, “especially the longer-term sequelae of having COVID-19 or MIS-C early in life,” she emphasized.
The take-home message to clinicians from the findings at this time is to be aware that children and adolescents can become severely ill from COVID-19–related complications, said Dr. Randolph. “Some of the laboratory values on presentation appear to be associated with disease severity.”
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Randolph disclosed funding from the Centers for Disease Control and Prevention to lead the Overcoming COVID-19 Study in U.S. Children and Adults.
SOURCE: Fernandes DM et al. J Pediatr. 2020 Nov 13. doi: 10.1016/j.jpeds.2020.11.016.
based on data from 281 patients at 8 locations.
Manifestations of COVID-19 in children include respiratory disease similar to that seen in adults, but the full spectrum of disease in children has been studied mainly in single settings or with a focus on one clinical manifestation, wrote Danielle M. Fernandes, MD, of Albert Einstein College of Medicine, New York, and colleagues.
In a study published in the Journal of Pediatrics, the researchers identified 281 children hospitalized with COVID-19 and/or multisystem inflammatory syndrome in children (MIS-C) at 8 sites in Connecticut, New Jersey, and New York. A total of 143 (51%) had respiratory disease, 69 (25%) had MIS-C, and 69 (25%) had other manifestations of illness including 32 patients with gastrointestinal problems, 21 infants with fever, 6 cases of neurologic disease, 6 cases of diabetic ketoacidosis, and 4 patients with other indications. The median age of the patients was 10 years, 60% were male, 51% were Hispanic, and 23% were non-Hispanic Black. The most common comorbidities were obesity (34%) and asthma (14%).
Independent predictors of disease severity in children found
After controlling for multiple variables, obesity and hypoxia at hospital admission were significant independent predictors of severe respiratory disease, with odds ratios of 3.39 and 4.01, respectively. In addition, lower absolute lymphocyte count (OR, 8.33 per unit decrease in 109 cells/L) and higher C-reactive protein (OR, 1.06 per unit increase in mg/dL) were significantly predictive of severe MIS-C (P = .001 and P = .017, respectively).
“The association between weight and severe respiratory COVID-19 is consistent with the adult literature; however, the mechanisms of this association require further study,” Dr. Fernandes and associates noted.
Overall, children with MIS-C were significantly more likely to be non-Hispanic Black, compared with children with respiratory disease, an 18% difference. However, neither race/ethnicity nor socioeconomic status were significant predictors of disease severity, the researchers wrote.
During the study period, 7 patients (2%) died and 114 (41%) were admitted to the ICU.
“We found a wide array of clinical manifestations in children and youth hospitalized with SARS-CoV-2,” Dr. Fernandes and associates wrote. Notably, gastrointestinal symptoms, ocular symptoms, and dermatologic symptoms have rarely been noted in adults with COVID-19, but occurred in more than 30% of the pediatric patients.
“We also found that SARS-CoV-2 can be an incidental finding in a substantial number of hospitalized pediatric patients,” the researchers said.
The findings were limited by several factors including a population of patients only from Connecticut, New Jersey, and New York, and the possibility that decisions on hospital and ICU admission may have varied by location, the researchers said. In addition, approaches may have varied in the absence of data on the optimal treatment of MIS-C.
“This study builds on the growing body of evidence showing that mortality in hospitalized pediatric patients is low, compared with adults,” Dr. Fernandes and associates said. “However, it highlights that the young population is not universally spared from morbidity, and that even previously healthy children and youth can develop severe disease requiring supportive therapy.”
Findings confirm other clinical experience
The study was important to show that, “although most children are spared severe illness from COVID-19, some children are hospitalized both with acute COVID-19 respiratory disease, with MIS-C and with a range of other complications,” Adrienne Randolph, MD, of Boston Children’s Hospital and Harvard Medical School, Boston, said in an interview.
Dr. Randolph said she was not surprised by the study findings, “as we are also seeing these types of complications at Boston Children’s Hospital where I work.”
Additional research is needed on the outcomes of these patients, “especially the longer-term sequelae of having COVID-19 or MIS-C early in life,” she emphasized.
The take-home message to clinicians from the findings at this time is to be aware that children and adolescents can become severely ill from COVID-19–related complications, said Dr. Randolph. “Some of the laboratory values on presentation appear to be associated with disease severity.”
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Randolph disclosed funding from the Centers for Disease Control and Prevention to lead the Overcoming COVID-19 Study in U.S. Children and Adults.
SOURCE: Fernandes DM et al. J Pediatr. 2020 Nov 13. doi: 10.1016/j.jpeds.2020.11.016.
based on data from 281 patients at 8 locations.
Manifestations of COVID-19 in children include respiratory disease similar to that seen in adults, but the full spectrum of disease in children has been studied mainly in single settings or with a focus on one clinical manifestation, wrote Danielle M. Fernandes, MD, of Albert Einstein College of Medicine, New York, and colleagues.
In a study published in the Journal of Pediatrics, the researchers identified 281 children hospitalized with COVID-19 and/or multisystem inflammatory syndrome in children (MIS-C) at 8 sites in Connecticut, New Jersey, and New York. A total of 143 (51%) had respiratory disease, 69 (25%) had MIS-C, and 69 (25%) had other manifestations of illness including 32 patients with gastrointestinal problems, 21 infants with fever, 6 cases of neurologic disease, 6 cases of diabetic ketoacidosis, and 4 patients with other indications. The median age of the patients was 10 years, 60% were male, 51% were Hispanic, and 23% were non-Hispanic Black. The most common comorbidities were obesity (34%) and asthma (14%).
Independent predictors of disease severity in children found
After controlling for multiple variables, obesity and hypoxia at hospital admission were significant independent predictors of severe respiratory disease, with odds ratios of 3.39 and 4.01, respectively. In addition, lower absolute lymphocyte count (OR, 8.33 per unit decrease in 109 cells/L) and higher C-reactive protein (OR, 1.06 per unit increase in mg/dL) were significantly predictive of severe MIS-C (P = .001 and P = .017, respectively).
“The association between weight and severe respiratory COVID-19 is consistent with the adult literature; however, the mechanisms of this association require further study,” Dr. Fernandes and associates noted.
Overall, children with MIS-C were significantly more likely to be non-Hispanic Black, compared with children with respiratory disease, an 18% difference. However, neither race/ethnicity nor socioeconomic status were significant predictors of disease severity, the researchers wrote.
During the study period, 7 patients (2%) died and 114 (41%) were admitted to the ICU.
“We found a wide array of clinical manifestations in children and youth hospitalized with SARS-CoV-2,” Dr. Fernandes and associates wrote. Notably, gastrointestinal symptoms, ocular symptoms, and dermatologic symptoms have rarely been noted in adults with COVID-19, but occurred in more than 30% of the pediatric patients.
“We also found that SARS-CoV-2 can be an incidental finding in a substantial number of hospitalized pediatric patients,” the researchers said.
The findings were limited by several factors including a population of patients only from Connecticut, New Jersey, and New York, and the possibility that decisions on hospital and ICU admission may have varied by location, the researchers said. In addition, approaches may have varied in the absence of data on the optimal treatment of MIS-C.
“This study builds on the growing body of evidence showing that mortality in hospitalized pediatric patients is low, compared with adults,” Dr. Fernandes and associates said. “However, it highlights that the young population is not universally spared from morbidity, and that even previously healthy children and youth can develop severe disease requiring supportive therapy.”
Findings confirm other clinical experience
The study was important to show that, “although most children are spared severe illness from COVID-19, some children are hospitalized both with acute COVID-19 respiratory disease, with MIS-C and with a range of other complications,” Adrienne Randolph, MD, of Boston Children’s Hospital and Harvard Medical School, Boston, said in an interview.
Dr. Randolph said she was not surprised by the study findings, “as we are also seeing these types of complications at Boston Children’s Hospital where I work.”
Additional research is needed on the outcomes of these patients, “especially the longer-term sequelae of having COVID-19 or MIS-C early in life,” she emphasized.
The take-home message to clinicians from the findings at this time is to be aware that children and adolescents can become severely ill from COVID-19–related complications, said Dr. Randolph. “Some of the laboratory values on presentation appear to be associated with disease severity.”
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Randolph disclosed funding from the Centers for Disease Control and Prevention to lead the Overcoming COVID-19 Study in U.S. Children and Adults.
SOURCE: Fernandes DM et al. J Pediatr. 2020 Nov 13. doi: 10.1016/j.jpeds.2020.11.016.
FROM THE JOURNAL OF PEDIATRICS
Leading hospitalists during a pandemic
As I write this, we are entering the third surge of the COVID-19 pandemic, with new cases, hospitalizations, and deaths from COVID-19 skyrocketing around the country. Worst of all, this surge has been most severely affecting areas of the nation least prepared to handle it (rural) and populations already marginalized by the health care system (Latinx and Black). Despite the onslaught of COVID-19, “pandemic fatigue” has begun to set in amongst colleagues, friends, and family, leading to challenges in adhering to social distancing and other infection-control measures, both at work and home.
In the face of the pandemic’s onslaught, hospitalists – who have faced the brunt of caring for patients with COVID-19, despite the absence of reporting about the subspecialty’s role – are faced with mustering the grit to respond with resolve, coordinated action, and empathy. Luckily, hospitalists are equipped with the very characteristics needed to lead teams, groups, and hospitals through the crisis of this pandemic. Ask yourself, why did you become a hospitalist? If you wanted steady predictability and control, there were many office-based specialties you could have chosen. You chose to become a hospitalist because you seek the challenges of clinical variety, problem-solving, systems improvement, and you are a natural team leader, whether you have been designated as such or not. In the words of John Quincy Adams, “if your actions inspire others to dream more, learn more, do more, and become more, you are a leader.”
As a leader, how can you lead your team through the series of trials and tribulations that this year has thrown at you? From COVID-19 to racism directed against Black and Latinx people to the behavioral health crisis, 2020 has likely made you feel as if you’re stuck in a ghoulish carnival fun house without an exit.
Yet this is where some leaders hit their stride, in what Bennis and Thomas describe as the “crucible of leadership.”1 There are many types of “crucibles of leadership,” according to Bennis and Thomas, and this year has thrown most of these at us: prejudice/bias, physical fatigue and illness, sudden elevation of responsibility to lead new processes, not to mention family stressors. Leaders who succeed in guiding their colleagues through these challenges have manifested critical skills: engaging others in shared meaning, having a distinctive and compelling voice, displaying integrity, and having adaptive capacity.
What exactly is adaptive capacity, the most important of these, in my opinion? Adaptive capacity requires understanding the new context of a crisis and how it has shifted team members’ needs and perceptions. It also requires what Bennis and Thomas call hardiness and what I call grit – the ability to face adversity, get knocked down, get up, and do it again.
There is probably no better example of a crisis leader with extraordinary adaptive capacity than Anglo-Irish explorer Sir Ernest Shackleton. Bitten by the bug of exploration, Shackleton failed at reaching the South Pole (1908-1909) but subsequently attempted to cross the Antarctic, departing South Georgia Island on Dec. 5, 1914. Depressingly for Shackleton, his ship, the Endurance, became stuck in sea ice on Jan. 19, 1915 before even reaching the continent. Drifting with the ice floe, his crew had set up a winter station hoping to be released from the ice later, but the Endurance was crushed by the pressure of sea ice and sank on Nov. 21, 1915. From there, Shackleton hoped to drift north to Paulet Island, 250 miles away, but eventually was forced to take his crew on lifeboats to the nearest land, Elephant Island, 346 miles from where the Endurance sank. He then took five of his men on an open boat, 828-mile journey to South Georgia Island. Encountering hurricane-force winds, the team landed on South Georgia Island 15 days later, only to face a climb of 32 miles over mountainous terrain to reach a whaling station. Shackleton eventually organized his men’s rescue on Elephant Island, reaching them on Aug. 30, 1916, 4½ months after he had set out for South Georgia Island. His entire crew survived, only to have two of them killed later in World War I.
You might consider Shackleton a failure for not even coming close to his original goal, but his success in saving his crew is regarded as the epitome of crisis leadership. As Harvard Business School professor Nancy F. Koehn, PhD, whose case study of Shackleton is one of the most popular at HBS, stated, “He thought he was going to be an entrepreneur of exploration, but he became an entrepreneur of survival.”2 Upon realizing the futility of his original mission, he pivoted immediately to the survival of his crew. “A man must shape himself to a new mark directly the old one goes to ground,” wrote Shackleton in his diary.3
Realizing that preserving his crew’s morale was critical, he maintained the crew’s everyday activities, despite the prospect of dying on the ice. He realized that he needed to keep up his own courage and confidence as well as that of his crew. Despite his ability to share the strategic focus of getting to safety with his men, he didn’t lose sight of day-to-day needs, such as keeping the crew entertained. When he encountered crew members who seemed problematic to his mission goals, he assigned them to his own tent.
Despite the extreme cold, his decision-making did not freeze – he acted decisively. He took risks when he thought appropriate, twice needing to abandon his efforts to drag a lifeboat full of supplies with his men toward the sea. “You can’t be afraid to make smart mistakes,” says Dr. Koehn. “That’s something we have no training in.”4 Most importantly, Shackleton took ultimate responsibility for his men’s survival, never resting until they had all been rescued. And he modeled a culture of shared responsibility for one another5 – he had once offered his only biscuit of the day on a prior expedition to his fellow explorer Frank Wild.
As winter arrives in 2020 and deepens into 2021, we will all be faced with leading our teams across the ice and to the safety of spring, and hopefully a vaccine. Whether we can get there with our entire crew depends on effective crisis leadership. But we can draw on the lessons provided by Shackleton and other crisis leaders in the past to guide us in the present.
Author disclosure: I studied the HBS case study “Leadership in Crisis: Ernest Shackleton and the Epic Voyage of the Endurance” as part of a 12-month certificate course in Safety, Quality, Informatics, and Leadership (SQIL) offered by Harvard Medical School.
Dr. Chang is chief of pediatric hospital medicine at Baystate Children’s Hospital in Springfield, Mass., and associate professor of pediatrics at the University of Massachusetts, also in Springfield.
References
1. HBR’s 10 must reads on leadership. Boston: Harvard Business Review Press, 2011.
2. Lagace M. Shackleton: An entrepreneur of survival. Harvard Business School. Working Knowledge website. Published 2003. Accessed 2020 Nov 19.
3. Koehn N. Leadership lessons from the Shackleton Expedition. The New York Times. 2011 Dec 25.
4. Potier B. Shackleton in business school. Harvard Public Affairs and Communications. The Harvard Gazette website. Published 2004. Accessed 2020 Nov 19.
5. Perkins D. 4 Lessons in crisis leadership from Shackleton’s expedition. In Leadership Essentials by HarpersCollins Leadership. Vol 2020. New York: HarpersCollins, 2020.
As I write this, we are entering the third surge of the COVID-19 pandemic, with new cases, hospitalizations, and deaths from COVID-19 skyrocketing around the country. Worst of all, this surge has been most severely affecting areas of the nation least prepared to handle it (rural) and populations already marginalized by the health care system (Latinx and Black). Despite the onslaught of COVID-19, “pandemic fatigue” has begun to set in amongst colleagues, friends, and family, leading to challenges in adhering to social distancing and other infection-control measures, both at work and home.
In the face of the pandemic’s onslaught, hospitalists – who have faced the brunt of caring for patients with COVID-19, despite the absence of reporting about the subspecialty’s role – are faced with mustering the grit to respond with resolve, coordinated action, and empathy. Luckily, hospitalists are equipped with the very characteristics needed to lead teams, groups, and hospitals through the crisis of this pandemic. Ask yourself, why did you become a hospitalist? If you wanted steady predictability and control, there were many office-based specialties you could have chosen. You chose to become a hospitalist because you seek the challenges of clinical variety, problem-solving, systems improvement, and you are a natural team leader, whether you have been designated as such or not. In the words of John Quincy Adams, “if your actions inspire others to dream more, learn more, do more, and become more, you are a leader.”
As a leader, how can you lead your team through the series of trials and tribulations that this year has thrown at you? From COVID-19 to racism directed against Black and Latinx people to the behavioral health crisis, 2020 has likely made you feel as if you’re stuck in a ghoulish carnival fun house without an exit.
Yet this is where some leaders hit their stride, in what Bennis and Thomas describe as the “crucible of leadership.”1 There are many types of “crucibles of leadership,” according to Bennis and Thomas, and this year has thrown most of these at us: prejudice/bias, physical fatigue and illness, sudden elevation of responsibility to lead new processes, not to mention family stressors. Leaders who succeed in guiding their colleagues through these challenges have manifested critical skills: engaging others in shared meaning, having a distinctive and compelling voice, displaying integrity, and having adaptive capacity.
What exactly is adaptive capacity, the most important of these, in my opinion? Adaptive capacity requires understanding the new context of a crisis and how it has shifted team members’ needs and perceptions. It also requires what Bennis and Thomas call hardiness and what I call grit – the ability to face adversity, get knocked down, get up, and do it again.
There is probably no better example of a crisis leader with extraordinary adaptive capacity than Anglo-Irish explorer Sir Ernest Shackleton. Bitten by the bug of exploration, Shackleton failed at reaching the South Pole (1908-1909) but subsequently attempted to cross the Antarctic, departing South Georgia Island on Dec. 5, 1914. Depressingly for Shackleton, his ship, the Endurance, became stuck in sea ice on Jan. 19, 1915 before even reaching the continent. Drifting with the ice floe, his crew had set up a winter station hoping to be released from the ice later, but the Endurance was crushed by the pressure of sea ice and sank on Nov. 21, 1915. From there, Shackleton hoped to drift north to Paulet Island, 250 miles away, but eventually was forced to take his crew on lifeboats to the nearest land, Elephant Island, 346 miles from where the Endurance sank. He then took five of his men on an open boat, 828-mile journey to South Georgia Island. Encountering hurricane-force winds, the team landed on South Georgia Island 15 days later, only to face a climb of 32 miles over mountainous terrain to reach a whaling station. Shackleton eventually organized his men’s rescue on Elephant Island, reaching them on Aug. 30, 1916, 4½ months after he had set out for South Georgia Island. His entire crew survived, only to have two of them killed later in World War I.
You might consider Shackleton a failure for not even coming close to his original goal, but his success in saving his crew is regarded as the epitome of crisis leadership. As Harvard Business School professor Nancy F. Koehn, PhD, whose case study of Shackleton is one of the most popular at HBS, stated, “He thought he was going to be an entrepreneur of exploration, but he became an entrepreneur of survival.”2 Upon realizing the futility of his original mission, he pivoted immediately to the survival of his crew. “A man must shape himself to a new mark directly the old one goes to ground,” wrote Shackleton in his diary.3
Realizing that preserving his crew’s morale was critical, he maintained the crew’s everyday activities, despite the prospect of dying on the ice. He realized that he needed to keep up his own courage and confidence as well as that of his crew. Despite his ability to share the strategic focus of getting to safety with his men, he didn’t lose sight of day-to-day needs, such as keeping the crew entertained. When he encountered crew members who seemed problematic to his mission goals, he assigned them to his own tent.
Despite the extreme cold, his decision-making did not freeze – he acted decisively. He took risks when he thought appropriate, twice needing to abandon his efforts to drag a lifeboat full of supplies with his men toward the sea. “You can’t be afraid to make smart mistakes,” says Dr. Koehn. “That’s something we have no training in.”4 Most importantly, Shackleton took ultimate responsibility for his men’s survival, never resting until they had all been rescued. And he modeled a culture of shared responsibility for one another5 – he had once offered his only biscuit of the day on a prior expedition to his fellow explorer Frank Wild.
As winter arrives in 2020 and deepens into 2021, we will all be faced with leading our teams across the ice and to the safety of spring, and hopefully a vaccine. Whether we can get there with our entire crew depends on effective crisis leadership. But we can draw on the lessons provided by Shackleton and other crisis leaders in the past to guide us in the present.
Author disclosure: I studied the HBS case study “Leadership in Crisis: Ernest Shackleton and the Epic Voyage of the Endurance” as part of a 12-month certificate course in Safety, Quality, Informatics, and Leadership (SQIL) offered by Harvard Medical School.
Dr. Chang is chief of pediatric hospital medicine at Baystate Children’s Hospital in Springfield, Mass., and associate professor of pediatrics at the University of Massachusetts, also in Springfield.
References
1. HBR’s 10 must reads on leadership. Boston: Harvard Business Review Press, 2011.
2. Lagace M. Shackleton: An entrepreneur of survival. Harvard Business School. Working Knowledge website. Published 2003. Accessed 2020 Nov 19.
3. Koehn N. Leadership lessons from the Shackleton Expedition. The New York Times. 2011 Dec 25.
4. Potier B. Shackleton in business school. Harvard Public Affairs and Communications. The Harvard Gazette website. Published 2004. Accessed 2020 Nov 19.
5. Perkins D. 4 Lessons in crisis leadership from Shackleton’s expedition. In Leadership Essentials by HarpersCollins Leadership. Vol 2020. New York: HarpersCollins, 2020.
As I write this, we are entering the third surge of the COVID-19 pandemic, with new cases, hospitalizations, and deaths from COVID-19 skyrocketing around the country. Worst of all, this surge has been most severely affecting areas of the nation least prepared to handle it (rural) and populations already marginalized by the health care system (Latinx and Black). Despite the onslaught of COVID-19, “pandemic fatigue” has begun to set in amongst colleagues, friends, and family, leading to challenges in adhering to social distancing and other infection-control measures, both at work and home.
In the face of the pandemic’s onslaught, hospitalists – who have faced the brunt of caring for patients with COVID-19, despite the absence of reporting about the subspecialty’s role – are faced with mustering the grit to respond with resolve, coordinated action, and empathy. Luckily, hospitalists are equipped with the very characteristics needed to lead teams, groups, and hospitals through the crisis of this pandemic. Ask yourself, why did you become a hospitalist? If you wanted steady predictability and control, there were many office-based specialties you could have chosen. You chose to become a hospitalist because you seek the challenges of clinical variety, problem-solving, systems improvement, and you are a natural team leader, whether you have been designated as such or not. In the words of John Quincy Adams, “if your actions inspire others to dream more, learn more, do more, and become more, you are a leader.”
As a leader, how can you lead your team through the series of trials and tribulations that this year has thrown at you? From COVID-19 to racism directed against Black and Latinx people to the behavioral health crisis, 2020 has likely made you feel as if you’re stuck in a ghoulish carnival fun house without an exit.
Yet this is where some leaders hit their stride, in what Bennis and Thomas describe as the “crucible of leadership.”1 There are many types of “crucibles of leadership,” according to Bennis and Thomas, and this year has thrown most of these at us: prejudice/bias, physical fatigue and illness, sudden elevation of responsibility to lead new processes, not to mention family stressors. Leaders who succeed in guiding their colleagues through these challenges have manifested critical skills: engaging others in shared meaning, having a distinctive and compelling voice, displaying integrity, and having adaptive capacity.
What exactly is adaptive capacity, the most important of these, in my opinion? Adaptive capacity requires understanding the new context of a crisis and how it has shifted team members’ needs and perceptions. It also requires what Bennis and Thomas call hardiness and what I call grit – the ability to face adversity, get knocked down, get up, and do it again.
There is probably no better example of a crisis leader with extraordinary adaptive capacity than Anglo-Irish explorer Sir Ernest Shackleton. Bitten by the bug of exploration, Shackleton failed at reaching the South Pole (1908-1909) but subsequently attempted to cross the Antarctic, departing South Georgia Island on Dec. 5, 1914. Depressingly for Shackleton, his ship, the Endurance, became stuck in sea ice on Jan. 19, 1915 before even reaching the continent. Drifting with the ice floe, his crew had set up a winter station hoping to be released from the ice later, but the Endurance was crushed by the pressure of sea ice and sank on Nov. 21, 1915. From there, Shackleton hoped to drift north to Paulet Island, 250 miles away, but eventually was forced to take his crew on lifeboats to the nearest land, Elephant Island, 346 miles from where the Endurance sank. He then took five of his men on an open boat, 828-mile journey to South Georgia Island. Encountering hurricane-force winds, the team landed on South Georgia Island 15 days later, only to face a climb of 32 miles over mountainous terrain to reach a whaling station. Shackleton eventually organized his men’s rescue on Elephant Island, reaching them on Aug. 30, 1916, 4½ months after he had set out for South Georgia Island. His entire crew survived, only to have two of them killed later in World War I.
You might consider Shackleton a failure for not even coming close to his original goal, but his success in saving his crew is regarded as the epitome of crisis leadership. As Harvard Business School professor Nancy F. Koehn, PhD, whose case study of Shackleton is one of the most popular at HBS, stated, “He thought he was going to be an entrepreneur of exploration, but he became an entrepreneur of survival.”2 Upon realizing the futility of his original mission, he pivoted immediately to the survival of his crew. “A man must shape himself to a new mark directly the old one goes to ground,” wrote Shackleton in his diary.3
Realizing that preserving his crew’s morale was critical, he maintained the crew’s everyday activities, despite the prospect of dying on the ice. He realized that he needed to keep up his own courage and confidence as well as that of his crew. Despite his ability to share the strategic focus of getting to safety with his men, he didn’t lose sight of day-to-day needs, such as keeping the crew entertained. When he encountered crew members who seemed problematic to his mission goals, he assigned them to his own tent.
Despite the extreme cold, his decision-making did not freeze – he acted decisively. He took risks when he thought appropriate, twice needing to abandon his efforts to drag a lifeboat full of supplies with his men toward the sea. “You can’t be afraid to make smart mistakes,” says Dr. Koehn. “That’s something we have no training in.”4 Most importantly, Shackleton took ultimate responsibility for his men’s survival, never resting until they had all been rescued. And he modeled a culture of shared responsibility for one another5 – he had once offered his only biscuit of the day on a prior expedition to his fellow explorer Frank Wild.
As winter arrives in 2020 and deepens into 2021, we will all be faced with leading our teams across the ice and to the safety of spring, and hopefully a vaccine. Whether we can get there with our entire crew depends on effective crisis leadership. But we can draw on the lessons provided by Shackleton and other crisis leaders in the past to guide us in the present.
Author disclosure: I studied the HBS case study “Leadership in Crisis: Ernest Shackleton and the Epic Voyage of the Endurance” as part of a 12-month certificate course in Safety, Quality, Informatics, and Leadership (SQIL) offered by Harvard Medical School.
Dr. Chang is chief of pediatric hospital medicine at Baystate Children’s Hospital in Springfield, Mass., and associate professor of pediatrics at the University of Massachusetts, also in Springfield.
References
1. HBR’s 10 must reads on leadership. Boston: Harvard Business Review Press, 2011.
2. Lagace M. Shackleton: An entrepreneur of survival. Harvard Business School. Working Knowledge website. Published 2003. Accessed 2020 Nov 19.
3. Koehn N. Leadership lessons from the Shackleton Expedition. The New York Times. 2011 Dec 25.
4. Potier B. Shackleton in business school. Harvard Public Affairs and Communications. The Harvard Gazette website. Published 2004. Accessed 2020 Nov 19.
5. Perkins D. 4 Lessons in crisis leadership from Shackleton’s expedition. In Leadership Essentials by HarpersCollins Leadership. Vol 2020. New York: HarpersCollins, 2020.
Several strategies can prevent pandemic-related weight gain
If you have been faithfully following the COVID-19 stay-at-home restrictive orders, you may have become a victim of “COVID-15,” the additional, unexpected, unwanted 10- to 15-pound weight gain that is making your clothes not fit so well any more.
A change in routine; being home in comfy, stretchable clothing in front of the TV; and having unhealthy, processed foods ready to grab have set us up to lose the battle with COVID-15. We are set up to gain the weight because of excessive or unhealthful eating, taking an extra daily shot of alcohol, and being inactive, bored, depressed, anxious, and isolated from coworkers and family. Beware – weight gain can be “catching”; we tend to adopt the same poor eating habits and eat the same junk foods as those around us.
Since psychiatry can be a sedentary profession, I’ve (R.W.C.) kept myself very active and physically fit. Prior to the pandemic, I played tennis and ran every day. I was obese only once in my life. I had not realized that I had gained a lot of weight.
Thankfully, a physician called me “obese.” Initially, I was angry at the doctor, however, I realized that he did me the biggest favor of my life. I changed my diet and eating habits, and for the past 20 years, kept my weight between 135-140 pounds and my BMI at 23 consistently – until the pandemic stress caused me to fall into the same bad eating habits that have caused many others to gain the COVID-15.
I was surprised to see that when I weighed myself, and I had gained 12 pounds! I immediately modified my diet and increased my physical activity. I have now lost the extra 12 pounds and will offer suggestions that may help you and your patients exceed your prepandemic physical condition.
Possible solutions
1. Keep a food journal. Write down what you eat, the amount of food you eat, the time you are eating, and your mood at that moment. Keeping a small notebook to record what and when you eat is important because upon review, it will make you face reality and be accountable for what you put in your mouth. Until you review your journal, you may have underestimated the amount, as well as the kinds, of food and drinks you actually consume. A food journal can show your areas of struggle and unhealthy eating habits and help you make necessary changes in your habits and diet to eventually lose weight. You will be less likely to eat junk food or have an extra serving of food. If you do not want to use paper and pencil, you can download an app on your phone, such as myplate tracker to keep track of your food and calorie intake. Do your journaling immediately after you eat and include snacks; do not wait until night time to record your food and journal. Include your mood or how you felt during your meal or snack (for example, were you bored, sad, or anxious) since this information will indicate why you may be overeating.
2. Develop healthful eating habits. Eat a maximum of three meals and three snacks per day but eat only when you are hungry (that is, when your stomach growls or you feel light headed). Limiting yourself to eating only when you are hungry will help eliminate emotional eating to fill a loss in your life or to deal with feelings of stress, anxiety, sadness, or isolation, which have been exacerbated by the pandemic. Buy eat only healthful foods and not items with empty calories, such as chips, cake, and items with sugar. When you are eating, devote yourself to that activity only, eat slowly, and savor each bite. Do not watch television during your meal time.
3. Record the amount and type of exercise you engage in each day and determine the number of calories burned. Walk, run, or bicycle outside, or exercise inside with stretching, weights, or an exercycle. You may use a website, such as diet tool on WebMD.com to calculate daily calories burned. To lose weight, calories burned during a day must exceed caloric intake. You may want to invest in a Fitbit or an Apple Watch and use the health section to determine your caloric intake versus output. Analyzing your caloric data will provide a concrete measure of your progress.
4. Do not overconsume calories or underconsume protein. Protein plays a key role in the creation and maintenance of every cell of your body, and because the body does not store protein, it is important to consume it every day. To meet basic protein requirements, the DRI (Dietary Reference Intake) recommends 0.36 grams of protein per pound (0.8 grams per kg) of body weight. This amounts to: 56 grams per day for the average sedentary man, and 46 grams per day for the average sedentary woman. There is also an app entitled the Protein Tracker that can simplify your calculations.
5. Drink water. It is important to be hydrated to regulate body temperature, keep joints lubricated, prevent infections, deliver nutrients to cells, and keep organs functioning properly. Being well hydrated also improves sleep, cognition, and mood. Your daily water intake by ounce should be equal to your weight in pounds multiplied by two-thirds (or 67%) to determine the amount of water to drink daily. For example, if you weigh 175 pounds, you would multiply 175 by two-thirds and learn that you should be drinking about 117 ounces of water every day. You can also meet some of your daily water requirements by consuming fruits and vegetables, such as tomatoes, watermelon, lettuce, etc.
Also, drink 2 cups (16 oz.) of water before every meal: Often when you feel hungry, it is because your body simply needs water. Science has proven that drinking 2 cups of water before every meal helps you to eat less during meal time and lose weight. If you do this three times daily – at breakfast, lunch, and dinner – you have already consumed 48 ounces of water.
6. Keep track of your progress. In addition to keeping and analyzing your food journal, weigh yourself once or twice a week. Do not weigh yourself every day; you will not see any results on a day-to-day basis, but once a week gives your body time to regulate and show progress. Always calibrate/zero your scale before each use, and weigh yourself at the same time of the day (preferably after you first wake up in the morning) while wearing the same type of clothing. Keep a record of your weight in your journal to track your progress. Do not panic if the scale indicates you gained 1, 2, or 3 pounds, your weight can fluctuate because of glycogen storage, sodium retention, human bias, reporting or recall errors, and home scales can have a plus or minus 3 pound margin of error. Look at your weight trend over time. You may prefer buying a scale that indicates both weight and body mass index.
7. Celebrate and reward yourself with nonfood items. A healthful fitness and diet regime requires energy and dedication, so if you are able to follow a healthful routine, reward yourself with nonfood rewards for your good choices and new habits as an incentive to maintain your healthful behavior.
8. Don’t buy it if you can’t stop eating it. The biggest decision you make is when you decide what you are going to buy. Don’t lie to yourself in the store that you will only eat one at a time. Only buy what you can afford to binge eat if you can’t stop yourself from eating any particular type of food.
9. Have someone hide the food you can’t resist. You can’t eat what you can’t find. If you can’t avoid having irresistible food around, ask another adult to hide the food from you.
10. Learn what harm foods can cause in your body. Read about the effects of high blood sugar and high blood pressure can cause in your body. Find out which foods boost your immune system. Demonize the bad foods in your mind. Make up your mind before you go into the store that you are going to read food labels and find the best quality food with the lowest amount of sugar or saturated fat. Appreciate the flavor of vegetables and fruit.
11. Treat sugar as if it were an addictive drug. You can’t have just one. If you reduce your craving for sugar by slowly reducing your intake of sugar, you will find that you don’t crave sugar any more. This won’t be easy, but once it is done, you will be preventing many of the ravages that sugar takes on your body over time. But you can’t have one piece of pie because the craving will come back. At some point, it may be more likely that you find that piece of pie too sweet.
Here are a few other ideas: Buy a gift for yourself or new clothes, makeup, a plant or flowers, running shoes, exercise clothes, fitness tracker, water bottle, book, movie or network subscription. Improve your home décor. Or treat yourself to online lessons for painting, music, and so on. Or you might adopt a dog, donate food to a shelter or food bank; or organize and declutter your home since staying busy will give you a reason not to eat. In nice weather, enjoy the outdoors by going for a walk, run, bikeride or by gardening.
We are all worried about getting COVID-19. Preventing COVID-15 will go a long way toward boosting our immune systems to help protect us from the coronavirus.
Dr. Cohen is board-certified in psychiatry and has had a private practice in Philadelphia for more than 35 years. His areas of specialty include sports psychiatry, agoraphobia, depression, and substance abuse. In addition, Dr. Cohen is a former professor of psychiatry, family medicine, and otolaryngology at Thomas Jefferson University in Philadelphia. He has no conflicts of interest. Ms. Cohen holds an MBA from Temple University in Philadelphia with a focus on health care administration. Previously, Ms. Cohen was an associate administrator at Hahnemann University Hospital and an executive at the Health Services Council, both in Philadelphia. She currently writes biographical summaries of notable 18th- and 19th-century women. Ms. Cohen has no conflicts of interest.
If you have been faithfully following the COVID-19 stay-at-home restrictive orders, you may have become a victim of “COVID-15,” the additional, unexpected, unwanted 10- to 15-pound weight gain that is making your clothes not fit so well any more.
A change in routine; being home in comfy, stretchable clothing in front of the TV; and having unhealthy, processed foods ready to grab have set us up to lose the battle with COVID-15. We are set up to gain the weight because of excessive or unhealthful eating, taking an extra daily shot of alcohol, and being inactive, bored, depressed, anxious, and isolated from coworkers and family. Beware – weight gain can be “catching”; we tend to adopt the same poor eating habits and eat the same junk foods as those around us.
Since psychiatry can be a sedentary profession, I’ve (R.W.C.) kept myself very active and physically fit. Prior to the pandemic, I played tennis and ran every day. I was obese only once in my life. I had not realized that I had gained a lot of weight.
Thankfully, a physician called me “obese.” Initially, I was angry at the doctor, however, I realized that he did me the biggest favor of my life. I changed my diet and eating habits, and for the past 20 years, kept my weight between 135-140 pounds and my BMI at 23 consistently – until the pandemic stress caused me to fall into the same bad eating habits that have caused many others to gain the COVID-15.
I was surprised to see that when I weighed myself, and I had gained 12 pounds! I immediately modified my diet and increased my physical activity. I have now lost the extra 12 pounds and will offer suggestions that may help you and your patients exceed your prepandemic physical condition.
Possible solutions
1. Keep a food journal. Write down what you eat, the amount of food you eat, the time you are eating, and your mood at that moment. Keeping a small notebook to record what and when you eat is important because upon review, it will make you face reality and be accountable for what you put in your mouth. Until you review your journal, you may have underestimated the amount, as well as the kinds, of food and drinks you actually consume. A food journal can show your areas of struggle and unhealthy eating habits and help you make necessary changes in your habits and diet to eventually lose weight. You will be less likely to eat junk food or have an extra serving of food. If you do not want to use paper and pencil, you can download an app on your phone, such as myplate tracker to keep track of your food and calorie intake. Do your journaling immediately after you eat and include snacks; do not wait until night time to record your food and journal. Include your mood or how you felt during your meal or snack (for example, were you bored, sad, or anxious) since this information will indicate why you may be overeating.
2. Develop healthful eating habits. Eat a maximum of three meals and three snacks per day but eat only when you are hungry (that is, when your stomach growls or you feel light headed). Limiting yourself to eating only when you are hungry will help eliminate emotional eating to fill a loss in your life or to deal with feelings of stress, anxiety, sadness, or isolation, which have been exacerbated by the pandemic. Buy eat only healthful foods and not items with empty calories, such as chips, cake, and items with sugar. When you are eating, devote yourself to that activity only, eat slowly, and savor each bite. Do not watch television during your meal time.
3. Record the amount and type of exercise you engage in each day and determine the number of calories burned. Walk, run, or bicycle outside, or exercise inside with stretching, weights, or an exercycle. You may use a website, such as diet tool on WebMD.com to calculate daily calories burned. To lose weight, calories burned during a day must exceed caloric intake. You may want to invest in a Fitbit or an Apple Watch and use the health section to determine your caloric intake versus output. Analyzing your caloric data will provide a concrete measure of your progress.
4. Do not overconsume calories or underconsume protein. Protein plays a key role in the creation and maintenance of every cell of your body, and because the body does not store protein, it is important to consume it every day. To meet basic protein requirements, the DRI (Dietary Reference Intake) recommends 0.36 grams of protein per pound (0.8 grams per kg) of body weight. This amounts to: 56 grams per day for the average sedentary man, and 46 grams per day for the average sedentary woman. There is also an app entitled the Protein Tracker that can simplify your calculations.
5. Drink water. It is important to be hydrated to regulate body temperature, keep joints lubricated, prevent infections, deliver nutrients to cells, and keep organs functioning properly. Being well hydrated also improves sleep, cognition, and mood. Your daily water intake by ounce should be equal to your weight in pounds multiplied by two-thirds (or 67%) to determine the amount of water to drink daily. For example, if you weigh 175 pounds, you would multiply 175 by two-thirds and learn that you should be drinking about 117 ounces of water every day. You can also meet some of your daily water requirements by consuming fruits and vegetables, such as tomatoes, watermelon, lettuce, etc.
Also, drink 2 cups (16 oz.) of water before every meal: Often when you feel hungry, it is because your body simply needs water. Science has proven that drinking 2 cups of water before every meal helps you to eat less during meal time and lose weight. If you do this three times daily – at breakfast, lunch, and dinner – you have already consumed 48 ounces of water.
6. Keep track of your progress. In addition to keeping and analyzing your food journal, weigh yourself once or twice a week. Do not weigh yourself every day; you will not see any results on a day-to-day basis, but once a week gives your body time to regulate and show progress. Always calibrate/zero your scale before each use, and weigh yourself at the same time of the day (preferably after you first wake up in the morning) while wearing the same type of clothing. Keep a record of your weight in your journal to track your progress. Do not panic if the scale indicates you gained 1, 2, or 3 pounds, your weight can fluctuate because of glycogen storage, sodium retention, human bias, reporting or recall errors, and home scales can have a plus or minus 3 pound margin of error. Look at your weight trend over time. You may prefer buying a scale that indicates both weight and body mass index.
7. Celebrate and reward yourself with nonfood items. A healthful fitness and diet regime requires energy and dedication, so if you are able to follow a healthful routine, reward yourself with nonfood rewards for your good choices and new habits as an incentive to maintain your healthful behavior.
8. Don’t buy it if you can’t stop eating it. The biggest decision you make is when you decide what you are going to buy. Don’t lie to yourself in the store that you will only eat one at a time. Only buy what you can afford to binge eat if you can’t stop yourself from eating any particular type of food.
9. Have someone hide the food you can’t resist. You can’t eat what you can’t find. If you can’t avoid having irresistible food around, ask another adult to hide the food from you.
10. Learn what harm foods can cause in your body. Read about the effects of high blood sugar and high blood pressure can cause in your body. Find out which foods boost your immune system. Demonize the bad foods in your mind. Make up your mind before you go into the store that you are going to read food labels and find the best quality food with the lowest amount of sugar or saturated fat. Appreciate the flavor of vegetables and fruit.
11. Treat sugar as if it were an addictive drug. You can’t have just one. If you reduce your craving for sugar by slowly reducing your intake of sugar, you will find that you don’t crave sugar any more. This won’t be easy, but once it is done, you will be preventing many of the ravages that sugar takes on your body over time. But you can’t have one piece of pie because the craving will come back. At some point, it may be more likely that you find that piece of pie too sweet.
Here are a few other ideas: Buy a gift for yourself or new clothes, makeup, a plant or flowers, running shoes, exercise clothes, fitness tracker, water bottle, book, movie or network subscription. Improve your home décor. Or treat yourself to online lessons for painting, music, and so on. Or you might adopt a dog, donate food to a shelter or food bank; or organize and declutter your home since staying busy will give you a reason not to eat. In nice weather, enjoy the outdoors by going for a walk, run, bikeride or by gardening.
We are all worried about getting COVID-19. Preventing COVID-15 will go a long way toward boosting our immune systems to help protect us from the coronavirus.
Dr. Cohen is board-certified in psychiatry and has had a private practice in Philadelphia for more than 35 years. His areas of specialty include sports psychiatry, agoraphobia, depression, and substance abuse. In addition, Dr. Cohen is a former professor of psychiatry, family medicine, and otolaryngology at Thomas Jefferson University in Philadelphia. He has no conflicts of interest. Ms. Cohen holds an MBA from Temple University in Philadelphia with a focus on health care administration. Previously, Ms. Cohen was an associate administrator at Hahnemann University Hospital and an executive at the Health Services Council, both in Philadelphia. She currently writes biographical summaries of notable 18th- and 19th-century women. Ms. Cohen has no conflicts of interest.
If you have been faithfully following the COVID-19 stay-at-home restrictive orders, you may have become a victim of “COVID-15,” the additional, unexpected, unwanted 10- to 15-pound weight gain that is making your clothes not fit so well any more.
A change in routine; being home in comfy, stretchable clothing in front of the TV; and having unhealthy, processed foods ready to grab have set us up to lose the battle with COVID-15. We are set up to gain the weight because of excessive or unhealthful eating, taking an extra daily shot of alcohol, and being inactive, bored, depressed, anxious, and isolated from coworkers and family. Beware – weight gain can be “catching”; we tend to adopt the same poor eating habits and eat the same junk foods as those around us.
Since psychiatry can be a sedentary profession, I’ve (R.W.C.) kept myself very active and physically fit. Prior to the pandemic, I played tennis and ran every day. I was obese only once in my life. I had not realized that I had gained a lot of weight.
Thankfully, a physician called me “obese.” Initially, I was angry at the doctor, however, I realized that he did me the biggest favor of my life. I changed my diet and eating habits, and for the past 20 years, kept my weight between 135-140 pounds and my BMI at 23 consistently – until the pandemic stress caused me to fall into the same bad eating habits that have caused many others to gain the COVID-15.
I was surprised to see that when I weighed myself, and I had gained 12 pounds! I immediately modified my diet and increased my physical activity. I have now lost the extra 12 pounds and will offer suggestions that may help you and your patients exceed your prepandemic physical condition.
Possible solutions
1. Keep a food journal. Write down what you eat, the amount of food you eat, the time you are eating, and your mood at that moment. Keeping a small notebook to record what and when you eat is important because upon review, it will make you face reality and be accountable for what you put in your mouth. Until you review your journal, you may have underestimated the amount, as well as the kinds, of food and drinks you actually consume. A food journal can show your areas of struggle and unhealthy eating habits and help you make necessary changes in your habits and diet to eventually lose weight. You will be less likely to eat junk food or have an extra serving of food. If you do not want to use paper and pencil, you can download an app on your phone, such as myplate tracker to keep track of your food and calorie intake. Do your journaling immediately after you eat and include snacks; do not wait until night time to record your food and journal. Include your mood or how you felt during your meal or snack (for example, were you bored, sad, or anxious) since this information will indicate why you may be overeating.
2. Develop healthful eating habits. Eat a maximum of three meals and three snacks per day but eat only when you are hungry (that is, when your stomach growls or you feel light headed). Limiting yourself to eating only when you are hungry will help eliminate emotional eating to fill a loss in your life or to deal with feelings of stress, anxiety, sadness, or isolation, which have been exacerbated by the pandemic. Buy eat only healthful foods and not items with empty calories, such as chips, cake, and items with sugar. When you are eating, devote yourself to that activity only, eat slowly, and savor each bite. Do not watch television during your meal time.
3. Record the amount and type of exercise you engage in each day and determine the number of calories burned. Walk, run, or bicycle outside, or exercise inside with stretching, weights, or an exercycle. You may use a website, such as diet tool on WebMD.com to calculate daily calories burned. To lose weight, calories burned during a day must exceed caloric intake. You may want to invest in a Fitbit or an Apple Watch and use the health section to determine your caloric intake versus output. Analyzing your caloric data will provide a concrete measure of your progress.
4. Do not overconsume calories or underconsume protein. Protein plays a key role in the creation and maintenance of every cell of your body, and because the body does not store protein, it is important to consume it every day. To meet basic protein requirements, the DRI (Dietary Reference Intake) recommends 0.36 grams of protein per pound (0.8 grams per kg) of body weight. This amounts to: 56 grams per day for the average sedentary man, and 46 grams per day for the average sedentary woman. There is also an app entitled the Protein Tracker that can simplify your calculations.
5. Drink water. It is important to be hydrated to regulate body temperature, keep joints lubricated, prevent infections, deliver nutrients to cells, and keep organs functioning properly. Being well hydrated also improves sleep, cognition, and mood. Your daily water intake by ounce should be equal to your weight in pounds multiplied by two-thirds (or 67%) to determine the amount of water to drink daily. For example, if you weigh 175 pounds, you would multiply 175 by two-thirds and learn that you should be drinking about 117 ounces of water every day. You can also meet some of your daily water requirements by consuming fruits and vegetables, such as tomatoes, watermelon, lettuce, etc.
Also, drink 2 cups (16 oz.) of water before every meal: Often when you feel hungry, it is because your body simply needs water. Science has proven that drinking 2 cups of water before every meal helps you to eat less during meal time and lose weight. If you do this three times daily – at breakfast, lunch, and dinner – you have already consumed 48 ounces of water.
6. Keep track of your progress. In addition to keeping and analyzing your food journal, weigh yourself once or twice a week. Do not weigh yourself every day; you will not see any results on a day-to-day basis, but once a week gives your body time to regulate and show progress. Always calibrate/zero your scale before each use, and weigh yourself at the same time of the day (preferably after you first wake up in the morning) while wearing the same type of clothing. Keep a record of your weight in your journal to track your progress. Do not panic if the scale indicates you gained 1, 2, or 3 pounds, your weight can fluctuate because of glycogen storage, sodium retention, human bias, reporting or recall errors, and home scales can have a plus or minus 3 pound margin of error. Look at your weight trend over time. You may prefer buying a scale that indicates both weight and body mass index.
7. Celebrate and reward yourself with nonfood items. A healthful fitness and diet regime requires energy and dedication, so if you are able to follow a healthful routine, reward yourself with nonfood rewards for your good choices and new habits as an incentive to maintain your healthful behavior.
8. Don’t buy it if you can’t stop eating it. The biggest decision you make is when you decide what you are going to buy. Don’t lie to yourself in the store that you will only eat one at a time. Only buy what you can afford to binge eat if you can’t stop yourself from eating any particular type of food.
9. Have someone hide the food you can’t resist. You can’t eat what you can’t find. If you can’t avoid having irresistible food around, ask another adult to hide the food from you.
10. Learn what harm foods can cause in your body. Read about the effects of high blood sugar and high blood pressure can cause in your body. Find out which foods boost your immune system. Demonize the bad foods in your mind. Make up your mind before you go into the store that you are going to read food labels and find the best quality food with the lowest amount of sugar or saturated fat. Appreciate the flavor of vegetables and fruit.
11. Treat sugar as if it were an addictive drug. You can’t have just one. If you reduce your craving for sugar by slowly reducing your intake of sugar, you will find that you don’t crave sugar any more. This won’t be easy, but once it is done, you will be preventing many of the ravages that sugar takes on your body over time. But you can’t have one piece of pie because the craving will come back. At some point, it may be more likely that you find that piece of pie too sweet.
Here are a few other ideas: Buy a gift for yourself or new clothes, makeup, a plant or flowers, running shoes, exercise clothes, fitness tracker, water bottle, book, movie or network subscription. Improve your home décor. Or treat yourself to online lessons for painting, music, and so on. Or you might adopt a dog, donate food to a shelter or food bank; or organize and declutter your home since staying busy will give you a reason not to eat. In nice weather, enjoy the outdoors by going for a walk, run, bikeride or by gardening.
We are all worried about getting COVID-19. Preventing COVID-15 will go a long way toward boosting our immune systems to help protect us from the coronavirus.
Dr. Cohen is board-certified in psychiatry and has had a private practice in Philadelphia for more than 35 years. His areas of specialty include sports psychiatry, agoraphobia, depression, and substance abuse. In addition, Dr. Cohen is a former professor of psychiatry, family medicine, and otolaryngology at Thomas Jefferson University in Philadelphia. He has no conflicts of interest. Ms. Cohen holds an MBA from Temple University in Philadelphia with a focus on health care administration. Previously, Ms. Cohen was an associate administrator at Hahnemann University Hospital and an executive at the Health Services Council, both in Philadelphia. She currently writes biographical summaries of notable 18th- and 19th-century women. Ms. Cohen has no conflicts of interest.
Diabetic retinopathy may predict greater risk of COVID-19 severity
Risk of intubation for COVID-19 in very sick hospitalized patients was increased over fivefold in those with diabetic retinopathy, compared with those without, in a small single-center study from the United Kingdom.
Importantly, the risk of intubation was independent of conventional risk factors for poor COVID-19 outcomes.
“People with preexisting diabetes-related vascular damage, such as retinopathy, might be predisposed to a more severe form of COVID-19 requiring ventilation in the intensive therapy unit,” said lead investigator Janaka Karalliedde, MBBS, PhD.
Dr. Karalliedde and colleagues note that this is “the first description of diabetic retinopathy as a potential risk factor for poor COVID-19 outcomes.”
“For this reason, looking for the presence or history of retinopathy or other vascular complications of diabetes may help health care professionals identify patients at high risk of severe COVID-19,” added Dr. Karalliedde, of Guy’s and St Thomas’ NHS Foundation Trust, London.
The study was published online in Diabetes Research and Clinical Practice.
Preexisting diabetic retinopathy and COVID-19 outcomes
The prevalence of diabetic retinopathy is thought to be around 55% in people with type 1 diabetes and 30% in people with type 2 diabetes, on average.
Dr. Karalliedde is part of a research group at King’s College London that has been focused on how vascular disease may predispose to more severe COVID-19.
“COVID-19 affects the blood vessels all over the body,” he said, so they wondered whether having preexisting retinopathy “would predispose to a severe manifestation of COVID-19.”
The observational study included 187 patients with diabetes (179 patients with type 2 diabetes and 8 patients with type 1 diabetes) hospitalized with COVID-19 at Guy’s and St Thomas’ NHS Foundation Trust between March 12 and April 7 (the peak of the first wave of the pandemic in the United Kingdom).
“It was an ethnically diverse population who were very sick and provides a clinical observation of real life,” Dr. Karalliedde said.
Nearly half of patients were African Caribbean (44%), 39% were White, and 17% were of other ethnicities, including 8% who were Asian. The mean age of the cohort was 68 years (range, 22-97 years), and 60% were men.
Diabetic retinopathy was reported in 67 (36%) patients, of whom 80% had background retinopathy and 20% had more advanced retinopathy.
They then looked at whether the presence of retinopathy was associated with a more severe manifestation of COVID-19 as defined by the need for tracheal intubation.
Of the 187 patients, 26% were intubated and 45% of these patients had diabetic retinopathy.
The analysis showed those with diabetic retinopathy had an over-fivefold increased risk for intubation (odds ratio, 5.81; 95% confidence interval, 1.37-24.66).
Of the entire cohort, 32% of patients died, although no association was observed between retinopathy and mortality.
“A greater number of diabetes patients with COVID-19 ended up on the intensive therapy unit. Upon multivariate analysis, we found retinopathy was independently associated with ending up on the intensive therapy unit,” stressed Dr. Karalliedde.
However, they noted that, “due to the cross-sectional design of our study, we cannot prove causality [between retinopathy and intubation]. Further studies are required to understand the mechanisms that explain the associations between retinopathy and other indices of microangiopathy with severe COVID-19.”
A version of this article originally appeared on Medscape.com.
Risk of intubation for COVID-19 in very sick hospitalized patients was increased over fivefold in those with diabetic retinopathy, compared with those without, in a small single-center study from the United Kingdom.
Importantly, the risk of intubation was independent of conventional risk factors for poor COVID-19 outcomes.
“People with preexisting diabetes-related vascular damage, such as retinopathy, might be predisposed to a more severe form of COVID-19 requiring ventilation in the intensive therapy unit,” said lead investigator Janaka Karalliedde, MBBS, PhD.
Dr. Karalliedde and colleagues note that this is “the first description of diabetic retinopathy as a potential risk factor for poor COVID-19 outcomes.”
“For this reason, looking for the presence or history of retinopathy or other vascular complications of diabetes may help health care professionals identify patients at high risk of severe COVID-19,” added Dr. Karalliedde, of Guy’s and St Thomas’ NHS Foundation Trust, London.
The study was published online in Diabetes Research and Clinical Practice.
Preexisting diabetic retinopathy and COVID-19 outcomes
The prevalence of diabetic retinopathy is thought to be around 55% in people with type 1 diabetes and 30% in people with type 2 diabetes, on average.
Dr. Karalliedde is part of a research group at King’s College London that has been focused on how vascular disease may predispose to more severe COVID-19.
“COVID-19 affects the blood vessels all over the body,” he said, so they wondered whether having preexisting retinopathy “would predispose to a severe manifestation of COVID-19.”
The observational study included 187 patients with diabetes (179 patients with type 2 diabetes and 8 patients with type 1 diabetes) hospitalized with COVID-19 at Guy’s and St Thomas’ NHS Foundation Trust between March 12 and April 7 (the peak of the first wave of the pandemic in the United Kingdom).
“It was an ethnically diverse population who were very sick and provides a clinical observation of real life,” Dr. Karalliedde said.
Nearly half of patients were African Caribbean (44%), 39% were White, and 17% were of other ethnicities, including 8% who were Asian. The mean age of the cohort was 68 years (range, 22-97 years), and 60% were men.
Diabetic retinopathy was reported in 67 (36%) patients, of whom 80% had background retinopathy and 20% had more advanced retinopathy.
They then looked at whether the presence of retinopathy was associated with a more severe manifestation of COVID-19 as defined by the need for tracheal intubation.
Of the 187 patients, 26% were intubated and 45% of these patients had diabetic retinopathy.
The analysis showed those with diabetic retinopathy had an over-fivefold increased risk for intubation (odds ratio, 5.81; 95% confidence interval, 1.37-24.66).
Of the entire cohort, 32% of patients died, although no association was observed between retinopathy and mortality.
“A greater number of diabetes patients with COVID-19 ended up on the intensive therapy unit. Upon multivariate analysis, we found retinopathy was independently associated with ending up on the intensive therapy unit,” stressed Dr. Karalliedde.
However, they noted that, “due to the cross-sectional design of our study, we cannot prove causality [between retinopathy and intubation]. Further studies are required to understand the mechanisms that explain the associations between retinopathy and other indices of microangiopathy with severe COVID-19.”
A version of this article originally appeared on Medscape.com.
Risk of intubation for COVID-19 in very sick hospitalized patients was increased over fivefold in those with diabetic retinopathy, compared with those without, in a small single-center study from the United Kingdom.
Importantly, the risk of intubation was independent of conventional risk factors for poor COVID-19 outcomes.
“People with preexisting diabetes-related vascular damage, such as retinopathy, might be predisposed to a more severe form of COVID-19 requiring ventilation in the intensive therapy unit,” said lead investigator Janaka Karalliedde, MBBS, PhD.
Dr. Karalliedde and colleagues note that this is “the first description of diabetic retinopathy as a potential risk factor for poor COVID-19 outcomes.”
“For this reason, looking for the presence or history of retinopathy or other vascular complications of diabetes may help health care professionals identify patients at high risk of severe COVID-19,” added Dr. Karalliedde, of Guy’s and St Thomas’ NHS Foundation Trust, London.
The study was published online in Diabetes Research and Clinical Practice.
Preexisting diabetic retinopathy and COVID-19 outcomes
The prevalence of diabetic retinopathy is thought to be around 55% in people with type 1 diabetes and 30% in people with type 2 diabetes, on average.
Dr. Karalliedde is part of a research group at King’s College London that has been focused on how vascular disease may predispose to more severe COVID-19.
“COVID-19 affects the blood vessels all over the body,” he said, so they wondered whether having preexisting retinopathy “would predispose to a severe manifestation of COVID-19.”
The observational study included 187 patients with diabetes (179 patients with type 2 diabetes and 8 patients with type 1 diabetes) hospitalized with COVID-19 at Guy’s and St Thomas’ NHS Foundation Trust between March 12 and April 7 (the peak of the first wave of the pandemic in the United Kingdom).
“It was an ethnically diverse population who were very sick and provides a clinical observation of real life,” Dr. Karalliedde said.
Nearly half of patients were African Caribbean (44%), 39% were White, and 17% were of other ethnicities, including 8% who were Asian. The mean age of the cohort was 68 years (range, 22-97 years), and 60% were men.
Diabetic retinopathy was reported in 67 (36%) patients, of whom 80% had background retinopathy and 20% had more advanced retinopathy.
They then looked at whether the presence of retinopathy was associated with a more severe manifestation of COVID-19 as defined by the need for tracheal intubation.
Of the 187 patients, 26% were intubated and 45% of these patients had diabetic retinopathy.
The analysis showed those with diabetic retinopathy had an over-fivefold increased risk for intubation (odds ratio, 5.81; 95% confidence interval, 1.37-24.66).
Of the entire cohort, 32% of patients died, although no association was observed between retinopathy and mortality.
“A greater number of diabetes patients with COVID-19 ended up on the intensive therapy unit. Upon multivariate analysis, we found retinopathy was independently associated with ending up on the intensive therapy unit,” stressed Dr. Karalliedde.
However, they noted that, “due to the cross-sectional design of our study, we cannot prove causality [between retinopathy and intubation]. Further studies are required to understand the mechanisms that explain the associations between retinopathy and other indices of microangiopathy with severe COVID-19.”
A version of this article originally appeared on Medscape.com.
COVID redefines curriculum for hospitalists-in-training
Pandemic brings ‘clarity and urgency’
The coronavirus pandemic has impacted all facets of the education and training of this country’s future hospitalists, including their medical school coursework, elective rotations, clerkships, and residency training – although with variations between settings and localities.
The COVID-19 crisis demanded immediate changes in traditional approaches to medical education. Training programs responded quickly to institute those changes. As hospitals geared up for potential surges in COVID cases starting in mid-March, many onsite training activities for medical students were shut down in order to reserve personal protective equipment for essential personnel and not put learners at risk of catching the virus. A variety of events related to their education were canceled. Didactic presentations and meetings were converted to virtual gatherings on internet platforms such as Zoom. Many of these changes were adopted even in settings with few actual COVID cases.
Medical students on clinical rotations were provided with virtual didactics when in-person clinical experiences were put on hold. In some cases, academic years ended early and fourth-year students graduated early so they might potentially join the hospital work force. Residents’ assignments were also changed, perhaps seeing patients on non–COVID-19 units only or taking different shifts, assignments, or rotations. Public health or research projects replaced elective placements. New electives were created, along with journal clubs, online care conferences, and technology-facilitated, self-directed learning.
But every advancing medical student needs to rotate through an experience of taking care of real patients, said Amy Guiot, MD, MEd, a hospitalist and associate director of medical student education in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. “The Liaison Committee of Medical Education, jointly sponsored by the Association of American Medical Colleges and the American Medical Association, will not let you graduate a medical student without actual hands-on encounters with patients,” she explained.
For future doctors, especially those pursuing internal medicine – many of whom will practice as hospitalists – their training can’t duplicate “in the hospital” experiences except in the hospital, said Dr. Guiot, who is involved in pediatric training for medical students from the University of Cincinnati and residents.
For third- and fourth-year medical students, getting that personal contact with patients has been the hardest part, she added. But from March to May 2020, that experience was completely shut down at CCHMC, as at many medical schools, because of precautions aimed at preventing exposure to the novel coronavirus for both students and patients. That meant hospitals had to get creative, reshuffling schedules and the order of learning experiences; converting everything possible to virtual encounters on platforms such as Zoom; and reducing the length of rotations, the total number of in-person encounters, and the number of learners participating in an activity.
“We needed to use shift work for medical students, which hadn’t been done before,” Dr. Guiot said. Having students on different shifts, including nights, created more opportunities to fit clinical experiences into the schedule. The use of standardized patients – actors following a script who are examined by a student as part of learning how to do a physical exam – was also put on hold.
“Now we’re starting to get it back, but maybe not as often,” she said. “The actor wears a mask. The student wears a mask and shield. But it’s been harder for us to find actors – who tend to be older adults who may fear coming to the medical center – to perform their role, teaching medical students the art of examining a patient.”
Back to basics
The COVID-19 pandemic forced medical schools to get back to basics, figuring out the key competencies students needed to learn, said Alison Whelan, MD, AAMC’s chief medical education officer. Both medical schools and residency programs needed to respond quickly and in new ways, including with course content that would teach students about the virus and its management and treatment.
Schools have faced crises before, responding in real time to SARS (severe acute respiratory syndrome), Ebola, HIV, and natural disasters, Dr. Whelan said. “But there was a nimbleness and rapidity of adapting to COVID – with a lot of sharing of curriculums among medical colleges.” Back in late March, AAMC put out guidelines that recommended removing students from direct patient contact – not just for the student’s protection but for the community’s. A subsequent guidance, released Aug. 14, emphasized the need for medical schools to continue medical education – with appropriate attention to safety and local conditions while working closely with clinical partners.
Dr. Guiot, with her colleague Leslie Farrell, MD, and four very creative medical students, developed an online fourth-year elective course for University of Cincinnati medical students, offered asynchronously. It aimed to transmit a comprehensive understanding of COVID-19, its virology, transmission, clinical prevention, diagnosis and treatment, as well as examining national and international responses to the pandemic and their consequences and related issues of race, ethnicity, socioeconomic status, and health disparities. “We used several articles from the Journal of Hospital Medicine for students to read and discuss,” Dr. Guiot said.
Christopher Sankey, MD, SFHM, associate program director of the traditional internal medicine residency program and associate professor of medicine at Yale University, New Haven, Conn., oversees the inpatient educational experience for internal medicine residents at Yale. “As with most programs, there was a lot of trepidation as we made the transition from in-person to virtual education,” he said.
The two principal, non–ward-based educational opportunities for the Yale residents are morning report, which involves a case-based discussion of various medical issues, usually led by a chief resident, and noon conference, which is more didactic and content based. Both made the transition to virtual meetings for residents.
“We wondered, could these still be well-attended, well-liked, and successful learning experiences if offered virtually? What I found when I surveyed our residents was that the virtual conferences were not only well received, but actually preferred,” Dr. Sankey said. “We have a large campus with lots of internal medicine services, so it’s hard to assemble everyone for meetings. There were also situations in which there were so many residents that they couldn’t all fit into the same room.” Zoom, the virtual platform of choice, has actually increased attendance.
Marc Miller, MD, a pediatric hospitalist at the Cleveland Clinic, helped his team develop a virtual curriculum in pediatrics presented to third-year medical students during the month of May, when medical students were being taken off the wards. “Some third-year students still needed to get their pediatric clerkships done. We had to balance clinical exposure with a lot of other things,” he explained.
The curriculum included a focus on interprofessional aspects of interdisciplinary, family-centered bedside rounds; a COVID literature review; and a lot of case-based scenarios. “Most challenging was how to remake family rounds. We tried to incorporate students into table rounds, but that didn’t feel as valuable,” Dr. Miller said. “Because pediatrics is so family centered, talking to patients and families at the bedside is highly valued. So we had virtual sessions talking about how to do that, with videos to illustrate it put out by Cincinnati Children’s Hospital.”
The most interactive sessions got the best feedback, but all the sessions went over very well, Dr. Miller said. “Larger lessons from COVID include things we already knew, but now with extra importance, such as the need to encourage interactivity to get students to buy in and take part in these conversations – whatever the structure.”
Vineet Arora, MD, MHM, an academic hospitalist and chief medical officer for the clinical learning environment at the University of Chicago, said that the changes wrought by COVID have also produced unexpected gains for medical education. “We’ve also had to think differently and more creatively about how to get the same information across in this new environment,” she explained. “In some cases, we saw that it was easier for learners to attend conferences and meetings online, with increased attendance for our events.” That includes participation on quality improvement committees, and attending online medical conferences presented locally and regionally.
“Another question: How do we teach interdisciplinary rounds and how to work with other members of the team without having face-to-face interactions?” Dr. Arora said. “Our old interdisciplinary rounding model had to change. It forced us to rethink how to create that kind of learning. We can’t have as many people in the patient’s room at one time. Can there be a physically distanced ‘touch-base’ with the nurse outside the patient’s room after a doctor has gone in to meet the patient?”
Transformational change
In a recent JAMA Viewpoint column, Catherine R. Lucey, MD, and S. Claiborne Johnston, MD, PhD,1 called the impact of COVID-19 “transformational,” in line with changes in medical curriculums recommended by the 2010 Global Independent Commission on Education of Health Professionals for the 21st Century,2 which asserted that the purpose of professional education is to improve the health of communities.
The authors stated that COVID-19 brought clarity and urgency to this purpose, and will someday be viewed as a catalyst for the needed transformation of medical education as medical schools embarked on curriculum redesign to embrace new competencies for current health challenges.
They suggested that medical students not only continued to learn during the COVID crisis “but in many circumstances, accelerated their attainment of the types of competencies that 21st century physicians must master.” Emerging competencies identified by Dr. Lucey and Dr. Johnston include:
- Being able to address population and public health issues
- Designing and continuously improving of the health care system
- Incorporating data and technology in service to patient care, research, and education
- Eliminating health care disparities and discrimination in medicine
- Adapting the curriculum to current issues in real-time
- Engaging in crisis communication and active change leadership
How is the curriculum changing? It’s still a work in progress. “After the disruptions of the spring and summer, schools are now trying to figure which of the changes should stay,” said Dr. Whelan. “The virus has also highlighted other crises, with social determinants of health and racial disparities becoming more front and center. In terms of content, medical educators are rethinking a lot of things – in a good way.”
Another important trend cast in sharper relief by the pandemic is a gradual evolution toward competency-based education and how to assess when someone is ready to be a doctor, Dr. Whelan said. “There’s been an accelerated consideration of how to be sure each student is competent to practice medicine.”3
Many practicing physicians and students were redeployed in the crisis, she said. Pediatric physicians were asked to take care of adult patients, and internists were drafted to work in the ICU. Hospitals quickly developed refresher courses and competency-based assessments to facilitate these redeployments. What can be learned from such on-the-fly assessments? What was needed to make a pediatrician, under the supervision of an internist, able to take good care of adult patients?
And does competency-based assessment point toward some kind of time-variable graduate medical education of the future – with graduation when the competencies are achieved, rather than just tethered to time- and case volume–based requirements? It seems Canada is moving in this direction, and COVID might catalyze a similar transformation in the United States.3
Changing the curriculum
Does the content of the curriculum for preparing future hospitalists need to change significantly? “My honest answer is yes and no,” Dr. Sankey said. “One thing we found in our training program is that it’s possible to become consumed by this pandemic. We need to educate residents about it, but future doctors still need to learn a lot of other things. Heart failure has not gone away.
“It’s okay to stick to the general curriculum, but with a wider variety of learning opportunities. Adding content sessions on population health, social determinants of health, race and bias, and equity is a start, but it’s by no means sufficient to give these topics the importance they deserve. We need to interpolate these subjects into sessions we’re already doing,” he said. “It is not enough to do a couple of lectures on diversity. We need to weave these concepts into the education we provide for residents every day.
“I think the pandemic has posed an opportunity to critically consider what’s the ideal teaching and learning environment. How can we make it better? Societal events around race have demonstrated essential areas for curricular development, and the pandemic had us primed and already thinking about how we educate future doctors – both in terms of medium and content,” he said.
Some medical schools started their new academic year in July; others put it off until September. Patient care at CCHMC is nearly back to where it used to be before COVID-19 began, Dr. Guiot said in a September interview, “but in masks and goggles.” As a result, hospitals are having to get creative all over again to accommodate medical students.
“I am amazed at the camaraderie of hospitals and medical schools, trying to support our learners in the midst of the pandemic,” she said. “I learned that we can be more adaptive than I ever imagined. We were all nervous about the risks, but we learned how to support each other and still provide excellent care in the midst of the pandemic. We’re forever changed. We also learned how to present didactics on Zoom, but that was the easy part.”
References
1. Lucey CR, Johnston SC. The transformational effects of COVID-19 on medical education. JAMA. 2020;324(11):1033-4.
2. Bhutta ZA et al. Education of health professionals for the 21st century: A global independent Commission. Lancet. 2010 Apr 3;375(9721):1137-8.
3. Goldhamer MEJ et al. Can COVID catalyze an educational transformation? Competency-based advancement in a crisis. N Engl J Med. 2020;383:1003-5.
Pandemic brings ‘clarity and urgency’
Pandemic brings ‘clarity and urgency’
The coronavirus pandemic has impacted all facets of the education and training of this country’s future hospitalists, including their medical school coursework, elective rotations, clerkships, and residency training – although with variations between settings and localities.
The COVID-19 crisis demanded immediate changes in traditional approaches to medical education. Training programs responded quickly to institute those changes. As hospitals geared up for potential surges in COVID cases starting in mid-March, many onsite training activities for medical students were shut down in order to reserve personal protective equipment for essential personnel and not put learners at risk of catching the virus. A variety of events related to their education were canceled. Didactic presentations and meetings were converted to virtual gatherings on internet platforms such as Zoom. Many of these changes were adopted even in settings with few actual COVID cases.
Medical students on clinical rotations were provided with virtual didactics when in-person clinical experiences were put on hold. In some cases, academic years ended early and fourth-year students graduated early so they might potentially join the hospital work force. Residents’ assignments were also changed, perhaps seeing patients on non–COVID-19 units only or taking different shifts, assignments, or rotations. Public health or research projects replaced elective placements. New electives were created, along with journal clubs, online care conferences, and technology-facilitated, self-directed learning.
But every advancing medical student needs to rotate through an experience of taking care of real patients, said Amy Guiot, MD, MEd, a hospitalist and associate director of medical student education in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. “The Liaison Committee of Medical Education, jointly sponsored by the Association of American Medical Colleges and the American Medical Association, will not let you graduate a medical student without actual hands-on encounters with patients,” she explained.
For future doctors, especially those pursuing internal medicine – many of whom will practice as hospitalists – their training can’t duplicate “in the hospital” experiences except in the hospital, said Dr. Guiot, who is involved in pediatric training for medical students from the University of Cincinnati and residents.
For third- and fourth-year medical students, getting that personal contact with patients has been the hardest part, she added. But from March to May 2020, that experience was completely shut down at CCHMC, as at many medical schools, because of precautions aimed at preventing exposure to the novel coronavirus for both students and patients. That meant hospitals had to get creative, reshuffling schedules and the order of learning experiences; converting everything possible to virtual encounters on platforms such as Zoom; and reducing the length of rotations, the total number of in-person encounters, and the number of learners participating in an activity.
“We needed to use shift work for medical students, which hadn’t been done before,” Dr. Guiot said. Having students on different shifts, including nights, created more opportunities to fit clinical experiences into the schedule. The use of standardized patients – actors following a script who are examined by a student as part of learning how to do a physical exam – was also put on hold.
“Now we’re starting to get it back, but maybe not as often,” she said. “The actor wears a mask. The student wears a mask and shield. But it’s been harder for us to find actors – who tend to be older adults who may fear coming to the medical center – to perform their role, teaching medical students the art of examining a patient.”
Back to basics
The COVID-19 pandemic forced medical schools to get back to basics, figuring out the key competencies students needed to learn, said Alison Whelan, MD, AAMC’s chief medical education officer. Both medical schools and residency programs needed to respond quickly and in new ways, including with course content that would teach students about the virus and its management and treatment.
Schools have faced crises before, responding in real time to SARS (severe acute respiratory syndrome), Ebola, HIV, and natural disasters, Dr. Whelan said. “But there was a nimbleness and rapidity of adapting to COVID – with a lot of sharing of curriculums among medical colleges.” Back in late March, AAMC put out guidelines that recommended removing students from direct patient contact – not just for the student’s protection but for the community’s. A subsequent guidance, released Aug. 14, emphasized the need for medical schools to continue medical education – with appropriate attention to safety and local conditions while working closely with clinical partners.
Dr. Guiot, with her colleague Leslie Farrell, MD, and four very creative medical students, developed an online fourth-year elective course for University of Cincinnati medical students, offered asynchronously. It aimed to transmit a comprehensive understanding of COVID-19, its virology, transmission, clinical prevention, diagnosis and treatment, as well as examining national and international responses to the pandemic and their consequences and related issues of race, ethnicity, socioeconomic status, and health disparities. “We used several articles from the Journal of Hospital Medicine for students to read and discuss,” Dr. Guiot said.
Christopher Sankey, MD, SFHM, associate program director of the traditional internal medicine residency program and associate professor of medicine at Yale University, New Haven, Conn., oversees the inpatient educational experience for internal medicine residents at Yale. “As with most programs, there was a lot of trepidation as we made the transition from in-person to virtual education,” he said.
The two principal, non–ward-based educational opportunities for the Yale residents are morning report, which involves a case-based discussion of various medical issues, usually led by a chief resident, and noon conference, which is more didactic and content based. Both made the transition to virtual meetings for residents.
“We wondered, could these still be well-attended, well-liked, and successful learning experiences if offered virtually? What I found when I surveyed our residents was that the virtual conferences were not only well received, but actually preferred,” Dr. Sankey said. “We have a large campus with lots of internal medicine services, so it’s hard to assemble everyone for meetings. There were also situations in which there were so many residents that they couldn’t all fit into the same room.” Zoom, the virtual platform of choice, has actually increased attendance.
Marc Miller, MD, a pediatric hospitalist at the Cleveland Clinic, helped his team develop a virtual curriculum in pediatrics presented to third-year medical students during the month of May, when medical students were being taken off the wards. “Some third-year students still needed to get their pediatric clerkships done. We had to balance clinical exposure with a lot of other things,” he explained.
The curriculum included a focus on interprofessional aspects of interdisciplinary, family-centered bedside rounds; a COVID literature review; and a lot of case-based scenarios. “Most challenging was how to remake family rounds. We tried to incorporate students into table rounds, but that didn’t feel as valuable,” Dr. Miller said. “Because pediatrics is so family centered, talking to patients and families at the bedside is highly valued. So we had virtual sessions talking about how to do that, with videos to illustrate it put out by Cincinnati Children’s Hospital.”
The most interactive sessions got the best feedback, but all the sessions went over very well, Dr. Miller said. “Larger lessons from COVID include things we already knew, but now with extra importance, such as the need to encourage interactivity to get students to buy in and take part in these conversations – whatever the structure.”
Vineet Arora, MD, MHM, an academic hospitalist and chief medical officer for the clinical learning environment at the University of Chicago, said that the changes wrought by COVID have also produced unexpected gains for medical education. “We’ve also had to think differently and more creatively about how to get the same information across in this new environment,” she explained. “In some cases, we saw that it was easier for learners to attend conferences and meetings online, with increased attendance for our events.” That includes participation on quality improvement committees, and attending online medical conferences presented locally and regionally.
“Another question: How do we teach interdisciplinary rounds and how to work with other members of the team without having face-to-face interactions?” Dr. Arora said. “Our old interdisciplinary rounding model had to change. It forced us to rethink how to create that kind of learning. We can’t have as many people in the patient’s room at one time. Can there be a physically distanced ‘touch-base’ with the nurse outside the patient’s room after a doctor has gone in to meet the patient?”
Transformational change
In a recent JAMA Viewpoint column, Catherine R. Lucey, MD, and S. Claiborne Johnston, MD, PhD,1 called the impact of COVID-19 “transformational,” in line with changes in medical curriculums recommended by the 2010 Global Independent Commission on Education of Health Professionals for the 21st Century,2 which asserted that the purpose of professional education is to improve the health of communities.
The authors stated that COVID-19 brought clarity and urgency to this purpose, and will someday be viewed as a catalyst for the needed transformation of medical education as medical schools embarked on curriculum redesign to embrace new competencies for current health challenges.
They suggested that medical students not only continued to learn during the COVID crisis “but in many circumstances, accelerated their attainment of the types of competencies that 21st century physicians must master.” Emerging competencies identified by Dr. Lucey and Dr. Johnston include:
- Being able to address population and public health issues
- Designing and continuously improving of the health care system
- Incorporating data and technology in service to patient care, research, and education
- Eliminating health care disparities and discrimination in medicine
- Adapting the curriculum to current issues in real-time
- Engaging in crisis communication and active change leadership
How is the curriculum changing? It’s still a work in progress. “After the disruptions of the spring and summer, schools are now trying to figure which of the changes should stay,” said Dr. Whelan. “The virus has also highlighted other crises, with social determinants of health and racial disparities becoming more front and center. In terms of content, medical educators are rethinking a lot of things – in a good way.”
Another important trend cast in sharper relief by the pandemic is a gradual evolution toward competency-based education and how to assess when someone is ready to be a doctor, Dr. Whelan said. “There’s been an accelerated consideration of how to be sure each student is competent to practice medicine.”3
Many practicing physicians and students were redeployed in the crisis, she said. Pediatric physicians were asked to take care of adult patients, and internists were drafted to work in the ICU. Hospitals quickly developed refresher courses and competency-based assessments to facilitate these redeployments. What can be learned from such on-the-fly assessments? What was needed to make a pediatrician, under the supervision of an internist, able to take good care of adult patients?
And does competency-based assessment point toward some kind of time-variable graduate medical education of the future – with graduation when the competencies are achieved, rather than just tethered to time- and case volume–based requirements? It seems Canada is moving in this direction, and COVID might catalyze a similar transformation in the United States.3
Changing the curriculum
Does the content of the curriculum for preparing future hospitalists need to change significantly? “My honest answer is yes and no,” Dr. Sankey said. “One thing we found in our training program is that it’s possible to become consumed by this pandemic. We need to educate residents about it, but future doctors still need to learn a lot of other things. Heart failure has not gone away.
“It’s okay to stick to the general curriculum, but with a wider variety of learning opportunities. Adding content sessions on population health, social determinants of health, race and bias, and equity is a start, but it’s by no means sufficient to give these topics the importance they deserve. We need to interpolate these subjects into sessions we’re already doing,” he said. “It is not enough to do a couple of lectures on diversity. We need to weave these concepts into the education we provide for residents every day.
“I think the pandemic has posed an opportunity to critically consider what’s the ideal teaching and learning environment. How can we make it better? Societal events around race have demonstrated essential areas for curricular development, and the pandemic had us primed and already thinking about how we educate future doctors – both in terms of medium and content,” he said.
Some medical schools started their new academic year in July; others put it off until September. Patient care at CCHMC is nearly back to where it used to be before COVID-19 began, Dr. Guiot said in a September interview, “but in masks and goggles.” As a result, hospitals are having to get creative all over again to accommodate medical students.
“I am amazed at the camaraderie of hospitals and medical schools, trying to support our learners in the midst of the pandemic,” she said. “I learned that we can be more adaptive than I ever imagined. We were all nervous about the risks, but we learned how to support each other and still provide excellent care in the midst of the pandemic. We’re forever changed. We also learned how to present didactics on Zoom, but that was the easy part.”
References
1. Lucey CR, Johnston SC. The transformational effects of COVID-19 on medical education. JAMA. 2020;324(11):1033-4.
2. Bhutta ZA et al. Education of health professionals for the 21st century: A global independent Commission. Lancet. 2010 Apr 3;375(9721):1137-8.
3. Goldhamer MEJ et al. Can COVID catalyze an educational transformation? Competency-based advancement in a crisis. N Engl J Med. 2020;383:1003-5.
The coronavirus pandemic has impacted all facets of the education and training of this country’s future hospitalists, including their medical school coursework, elective rotations, clerkships, and residency training – although with variations between settings and localities.
The COVID-19 crisis demanded immediate changes in traditional approaches to medical education. Training programs responded quickly to institute those changes. As hospitals geared up for potential surges in COVID cases starting in mid-March, many onsite training activities for medical students were shut down in order to reserve personal protective equipment for essential personnel and not put learners at risk of catching the virus. A variety of events related to their education were canceled. Didactic presentations and meetings were converted to virtual gatherings on internet platforms such as Zoom. Many of these changes were adopted even in settings with few actual COVID cases.
Medical students on clinical rotations were provided with virtual didactics when in-person clinical experiences were put on hold. In some cases, academic years ended early and fourth-year students graduated early so they might potentially join the hospital work force. Residents’ assignments were also changed, perhaps seeing patients on non–COVID-19 units only or taking different shifts, assignments, or rotations. Public health or research projects replaced elective placements. New electives were created, along with journal clubs, online care conferences, and technology-facilitated, self-directed learning.
But every advancing medical student needs to rotate through an experience of taking care of real patients, said Amy Guiot, MD, MEd, a hospitalist and associate director of medical student education in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. “The Liaison Committee of Medical Education, jointly sponsored by the Association of American Medical Colleges and the American Medical Association, will not let you graduate a medical student without actual hands-on encounters with patients,” she explained.
For future doctors, especially those pursuing internal medicine – many of whom will practice as hospitalists – their training can’t duplicate “in the hospital” experiences except in the hospital, said Dr. Guiot, who is involved in pediatric training for medical students from the University of Cincinnati and residents.
For third- and fourth-year medical students, getting that personal contact with patients has been the hardest part, she added. But from March to May 2020, that experience was completely shut down at CCHMC, as at many medical schools, because of precautions aimed at preventing exposure to the novel coronavirus for both students and patients. That meant hospitals had to get creative, reshuffling schedules and the order of learning experiences; converting everything possible to virtual encounters on platforms such as Zoom; and reducing the length of rotations, the total number of in-person encounters, and the number of learners participating in an activity.
“We needed to use shift work for medical students, which hadn’t been done before,” Dr. Guiot said. Having students on different shifts, including nights, created more opportunities to fit clinical experiences into the schedule. The use of standardized patients – actors following a script who are examined by a student as part of learning how to do a physical exam – was also put on hold.
“Now we’re starting to get it back, but maybe not as often,” she said. “The actor wears a mask. The student wears a mask and shield. But it’s been harder for us to find actors – who tend to be older adults who may fear coming to the medical center – to perform their role, teaching medical students the art of examining a patient.”
Back to basics
The COVID-19 pandemic forced medical schools to get back to basics, figuring out the key competencies students needed to learn, said Alison Whelan, MD, AAMC’s chief medical education officer. Both medical schools and residency programs needed to respond quickly and in new ways, including with course content that would teach students about the virus and its management and treatment.
Schools have faced crises before, responding in real time to SARS (severe acute respiratory syndrome), Ebola, HIV, and natural disasters, Dr. Whelan said. “But there was a nimbleness and rapidity of adapting to COVID – with a lot of sharing of curriculums among medical colleges.” Back in late March, AAMC put out guidelines that recommended removing students from direct patient contact – not just for the student’s protection but for the community’s. A subsequent guidance, released Aug. 14, emphasized the need for medical schools to continue medical education – with appropriate attention to safety and local conditions while working closely with clinical partners.
Dr. Guiot, with her colleague Leslie Farrell, MD, and four very creative medical students, developed an online fourth-year elective course for University of Cincinnati medical students, offered asynchronously. It aimed to transmit a comprehensive understanding of COVID-19, its virology, transmission, clinical prevention, diagnosis and treatment, as well as examining national and international responses to the pandemic and their consequences and related issues of race, ethnicity, socioeconomic status, and health disparities. “We used several articles from the Journal of Hospital Medicine for students to read and discuss,” Dr. Guiot said.
Christopher Sankey, MD, SFHM, associate program director of the traditional internal medicine residency program and associate professor of medicine at Yale University, New Haven, Conn., oversees the inpatient educational experience for internal medicine residents at Yale. “As with most programs, there was a lot of trepidation as we made the transition from in-person to virtual education,” he said.
The two principal, non–ward-based educational opportunities for the Yale residents are morning report, which involves a case-based discussion of various medical issues, usually led by a chief resident, and noon conference, which is more didactic and content based. Both made the transition to virtual meetings for residents.
“We wondered, could these still be well-attended, well-liked, and successful learning experiences if offered virtually? What I found when I surveyed our residents was that the virtual conferences were not only well received, but actually preferred,” Dr. Sankey said. “We have a large campus with lots of internal medicine services, so it’s hard to assemble everyone for meetings. There were also situations in which there were so many residents that they couldn’t all fit into the same room.” Zoom, the virtual platform of choice, has actually increased attendance.
Marc Miller, MD, a pediatric hospitalist at the Cleveland Clinic, helped his team develop a virtual curriculum in pediatrics presented to third-year medical students during the month of May, when medical students were being taken off the wards. “Some third-year students still needed to get their pediatric clerkships done. We had to balance clinical exposure with a lot of other things,” he explained.
The curriculum included a focus on interprofessional aspects of interdisciplinary, family-centered bedside rounds; a COVID literature review; and a lot of case-based scenarios. “Most challenging was how to remake family rounds. We tried to incorporate students into table rounds, but that didn’t feel as valuable,” Dr. Miller said. “Because pediatrics is so family centered, talking to patients and families at the bedside is highly valued. So we had virtual sessions talking about how to do that, with videos to illustrate it put out by Cincinnati Children’s Hospital.”
The most interactive sessions got the best feedback, but all the sessions went over very well, Dr. Miller said. “Larger lessons from COVID include things we already knew, but now with extra importance, such as the need to encourage interactivity to get students to buy in and take part in these conversations – whatever the structure.”
Vineet Arora, MD, MHM, an academic hospitalist and chief medical officer for the clinical learning environment at the University of Chicago, said that the changes wrought by COVID have also produced unexpected gains for medical education. “We’ve also had to think differently and more creatively about how to get the same information across in this new environment,” she explained. “In some cases, we saw that it was easier for learners to attend conferences and meetings online, with increased attendance for our events.” That includes participation on quality improvement committees, and attending online medical conferences presented locally and regionally.
“Another question: How do we teach interdisciplinary rounds and how to work with other members of the team without having face-to-face interactions?” Dr. Arora said. “Our old interdisciplinary rounding model had to change. It forced us to rethink how to create that kind of learning. We can’t have as many people in the patient’s room at one time. Can there be a physically distanced ‘touch-base’ with the nurse outside the patient’s room after a doctor has gone in to meet the patient?”
Transformational change
In a recent JAMA Viewpoint column, Catherine R. Lucey, MD, and S. Claiborne Johnston, MD, PhD,1 called the impact of COVID-19 “transformational,” in line with changes in medical curriculums recommended by the 2010 Global Independent Commission on Education of Health Professionals for the 21st Century,2 which asserted that the purpose of professional education is to improve the health of communities.
The authors stated that COVID-19 brought clarity and urgency to this purpose, and will someday be viewed as a catalyst for the needed transformation of medical education as medical schools embarked on curriculum redesign to embrace new competencies for current health challenges.
They suggested that medical students not only continued to learn during the COVID crisis “but in many circumstances, accelerated their attainment of the types of competencies that 21st century physicians must master.” Emerging competencies identified by Dr. Lucey and Dr. Johnston include:
- Being able to address population and public health issues
- Designing and continuously improving of the health care system
- Incorporating data and technology in service to patient care, research, and education
- Eliminating health care disparities and discrimination in medicine
- Adapting the curriculum to current issues in real-time
- Engaging in crisis communication and active change leadership
How is the curriculum changing? It’s still a work in progress. “After the disruptions of the spring and summer, schools are now trying to figure which of the changes should stay,” said Dr. Whelan. “The virus has also highlighted other crises, with social determinants of health and racial disparities becoming more front and center. In terms of content, medical educators are rethinking a lot of things – in a good way.”
Another important trend cast in sharper relief by the pandemic is a gradual evolution toward competency-based education and how to assess when someone is ready to be a doctor, Dr. Whelan said. “There’s been an accelerated consideration of how to be sure each student is competent to practice medicine.”3
Many practicing physicians and students were redeployed in the crisis, she said. Pediatric physicians were asked to take care of adult patients, and internists were drafted to work in the ICU. Hospitals quickly developed refresher courses and competency-based assessments to facilitate these redeployments. What can be learned from such on-the-fly assessments? What was needed to make a pediatrician, under the supervision of an internist, able to take good care of adult patients?
And does competency-based assessment point toward some kind of time-variable graduate medical education of the future – with graduation when the competencies are achieved, rather than just tethered to time- and case volume–based requirements? It seems Canada is moving in this direction, and COVID might catalyze a similar transformation in the United States.3
Changing the curriculum
Does the content of the curriculum for preparing future hospitalists need to change significantly? “My honest answer is yes and no,” Dr. Sankey said. “One thing we found in our training program is that it’s possible to become consumed by this pandemic. We need to educate residents about it, but future doctors still need to learn a lot of other things. Heart failure has not gone away.
“It’s okay to stick to the general curriculum, but with a wider variety of learning opportunities. Adding content sessions on population health, social determinants of health, race and bias, and equity is a start, but it’s by no means sufficient to give these topics the importance they deserve. We need to interpolate these subjects into sessions we’re already doing,” he said. “It is not enough to do a couple of lectures on diversity. We need to weave these concepts into the education we provide for residents every day.
“I think the pandemic has posed an opportunity to critically consider what’s the ideal teaching and learning environment. How can we make it better? Societal events around race have demonstrated essential areas for curricular development, and the pandemic had us primed and already thinking about how we educate future doctors – both in terms of medium and content,” he said.
Some medical schools started their new academic year in July; others put it off until September. Patient care at CCHMC is nearly back to where it used to be before COVID-19 began, Dr. Guiot said in a September interview, “but in masks and goggles.” As a result, hospitals are having to get creative all over again to accommodate medical students.
“I am amazed at the camaraderie of hospitals and medical schools, trying to support our learners in the midst of the pandemic,” she said. “I learned that we can be more adaptive than I ever imagined. We were all nervous about the risks, but we learned how to support each other and still provide excellent care in the midst of the pandemic. We’re forever changed. We also learned how to present didactics on Zoom, but that was the easy part.”
References
1. Lucey CR, Johnston SC. The transformational effects of COVID-19 on medical education. JAMA. 2020;324(11):1033-4.
2. Bhutta ZA et al. Education of health professionals for the 21st century: A global independent Commission. Lancet. 2010 Apr 3;375(9721):1137-8.
3. Goldhamer MEJ et al. Can COVID catalyze an educational transformation? Competency-based advancement in a crisis. N Engl J Med. 2020;383:1003-5.
COVID-19 vaccine distribution could start in 2 weeks, Pence says
Initial doses of a coronavirus vaccine could be sent out as early as mid-December, Vice President Mike Pence told governors during a call on Monday.
The distribution process could start during the week of Dec. 14, according to audio of a White House Coronavirus Task Force call obtained by CBS News. The call focused on the timeline of vaccine approval and distribution.
“With this morning’s news that Moderna is joining Pfizer in submitting an emergency-use authorization [to the Food and Drug Administration], we continue to be on pace,” Pence said.
The FDA is scheduled to make a decision about Pfizer’s emergency use authorization after an advisory panel meets on Dec. 10 to review the company’s application. FDA Commissioner Stephen Hahn, MD, didn’t commit to the Dec. 14 date, CBS News reported.
“We do all the number crunching ourselves,” Dr. Hahn said. “We look line by line by line on all the data, on all the patients and manufacturing. We do statistical analyses and we come to our own conclusions to support a decision of either thumbs-up or thumbs-down.”
According to a meeting agenda, Pfizer vaccine deliveries should start on Dec. 15, followed by the Moderna vaccine on Dec. 22, CBS News reported.
Between Dec. 13-19, Pfizer is slated to deliver 6.4 million doses, which is enough to immunize about 3 million people with two shots. An “undetermined number” are reserved for backup doses, the news outlet reported.
During the next week, Pfizer and Moderna are scheduled to produce enough doses to vaccinate an additional 10 million people. By the end of the month, about 30 million people should receive doses.
As vaccines begin to roll out, Mr. Pence said “we have a ways to go” in reassuring the public about immunization. He urged governors to use their “bully pulpit” to educate their states and “develop public confidence” in the vaccines.
During the call, Anthony Fauci, MD, director of the National Institute for Allergy and Infectious Diseases, supported the safety and efficacy of the vaccines. Although the vaccine development and approval process was accelerated this year, he said, it “does not at all compromise safety, nor does it compromise scientific integrity.”
“Any misrepresentation that the vaccines had government interference or company interference is patently untrue,” he said.
This article first appeared on Medscape.com.
Initial doses of a coronavirus vaccine could be sent out as early as mid-December, Vice President Mike Pence told governors during a call on Monday.
The distribution process could start during the week of Dec. 14, according to audio of a White House Coronavirus Task Force call obtained by CBS News. The call focused on the timeline of vaccine approval and distribution.
“With this morning’s news that Moderna is joining Pfizer in submitting an emergency-use authorization [to the Food and Drug Administration], we continue to be on pace,” Pence said.
The FDA is scheduled to make a decision about Pfizer’s emergency use authorization after an advisory panel meets on Dec. 10 to review the company’s application. FDA Commissioner Stephen Hahn, MD, didn’t commit to the Dec. 14 date, CBS News reported.
“We do all the number crunching ourselves,” Dr. Hahn said. “We look line by line by line on all the data, on all the patients and manufacturing. We do statistical analyses and we come to our own conclusions to support a decision of either thumbs-up or thumbs-down.”
According to a meeting agenda, Pfizer vaccine deliveries should start on Dec. 15, followed by the Moderna vaccine on Dec. 22, CBS News reported.
Between Dec. 13-19, Pfizer is slated to deliver 6.4 million doses, which is enough to immunize about 3 million people with two shots. An “undetermined number” are reserved for backup doses, the news outlet reported.
During the next week, Pfizer and Moderna are scheduled to produce enough doses to vaccinate an additional 10 million people. By the end of the month, about 30 million people should receive doses.
As vaccines begin to roll out, Mr. Pence said “we have a ways to go” in reassuring the public about immunization. He urged governors to use their “bully pulpit” to educate their states and “develop public confidence” in the vaccines.
During the call, Anthony Fauci, MD, director of the National Institute for Allergy and Infectious Diseases, supported the safety and efficacy of the vaccines. Although the vaccine development and approval process was accelerated this year, he said, it “does not at all compromise safety, nor does it compromise scientific integrity.”
“Any misrepresentation that the vaccines had government interference or company interference is patently untrue,” he said.
This article first appeared on Medscape.com.
Initial doses of a coronavirus vaccine could be sent out as early as mid-December, Vice President Mike Pence told governors during a call on Monday.
The distribution process could start during the week of Dec. 14, according to audio of a White House Coronavirus Task Force call obtained by CBS News. The call focused on the timeline of vaccine approval and distribution.
“With this morning’s news that Moderna is joining Pfizer in submitting an emergency-use authorization [to the Food and Drug Administration], we continue to be on pace,” Pence said.
The FDA is scheduled to make a decision about Pfizer’s emergency use authorization after an advisory panel meets on Dec. 10 to review the company’s application. FDA Commissioner Stephen Hahn, MD, didn’t commit to the Dec. 14 date, CBS News reported.
“We do all the number crunching ourselves,” Dr. Hahn said. “We look line by line by line on all the data, on all the patients and manufacturing. We do statistical analyses and we come to our own conclusions to support a decision of either thumbs-up or thumbs-down.”
According to a meeting agenda, Pfizer vaccine deliveries should start on Dec. 15, followed by the Moderna vaccine on Dec. 22, CBS News reported.
Between Dec. 13-19, Pfizer is slated to deliver 6.4 million doses, which is enough to immunize about 3 million people with two shots. An “undetermined number” are reserved for backup doses, the news outlet reported.
During the next week, Pfizer and Moderna are scheduled to produce enough doses to vaccinate an additional 10 million people. By the end of the month, about 30 million people should receive doses.
As vaccines begin to roll out, Mr. Pence said “we have a ways to go” in reassuring the public about immunization. He urged governors to use their “bully pulpit” to educate their states and “develop public confidence” in the vaccines.
During the call, Anthony Fauci, MD, director of the National Institute for Allergy and Infectious Diseases, supported the safety and efficacy of the vaccines. Although the vaccine development and approval process was accelerated this year, he said, it “does not at all compromise safety, nor does it compromise scientific integrity.”
“Any misrepresentation that the vaccines had government interference or company interference is patently untrue,” he said.
This article first appeared on Medscape.com.
Colchicine a case study for what’s wrong with U.S. drug pricing
Public spending on colchicine has grown exponentially over the past decade despite generics suggesting an uphill slog for patients seeking access to long-term therapy for gout or cardiac conditions.
Medicaid spending on single-ingredient colchicine jumped 2,833%, from $1.1 million in 2008 to $32.2 million in 2017, new findings show. Medicaid expansion likely played a role in the increase, but 58% was due to price hikes alone.
The centuries-old drug sold for pennies in the United States before increasing 50-fold to about $5 per pill in 2009 after the first FDA-approved colchicine product, Colcrys, was granted 3 years’ market exclusivity for the treatment of acute gout based on a 1-week trial.
If prices had remained at pre-Colcrys levels, Medicaid spending in 2017 would have totaled just $2.1 million rather than $32.2 million according to the analysis, published online Nov. 30 in JAMA Internal Medicine (doi: 10.1001/jamainternmed.2020.5017).
The study was motivated by difficulties gout patients have in accessing colchicine, but also last year’s COLCOT trial, which reported fewer ischemic cardiovascular events in patients receiving colchicine after MI, observed Natalie McCormick, PhD, of Massachusetts General Hospital and Harvard Medical School, both in Boston.
“They were suggesting it could be a cost-effective way for secondary prevention and it is fairly inexpensive in most countries, but not the U.S.,” she said in an interview. “So there’s really a potential to increase public spending if more and more patients are then taking colchicine for prevention of cardiovascular events and the prices don’t change.”
The current pandemic could potentially further increase demand. Results initially slated for September are expected this month from the COLCORONA trial, which is testing whether the anti-inflammatory agent can prevent hospitalizations, lung complications, and death when given early in the course of COVID-19.
University of Oxford (England) researchers also announced last week that colchicine is being added to the massive RECOVERY trial, which is studying treatments for hospitalized COVID-19 patients.
Notably, the Canadian-based COLCOT trial did not use Colcrys, but rather a colchicine product that costs just $0.26 a pill in Canada, roughly the price of most generics available worldwide.
Authorized generics typically drive down drug prices when competing with independent generics, but this competition is missing in the United States, where Colcrys holds patents until 2029, Dr. McCormick and colleagues noted. More than a half-dozen independent generics have FDA approval to date, but only authorized generics with price points set by the brand-name companies are available to treat acute gout, pericarditis, and potentially millions with MI.
“One of the key takeaways is this difference between the brand names and the authorized generics and the independents,” she said. “The authorized [generics] have really not saved money. The list prices were just slightly lower and patients can also have more difficulty in getting those covered.”
For this analysis, the investigators used Medicaid and Medicare data to examine prices for all available forms of colchicine from 2008 to 2017, including unregulated/unapproved colchicine (2008-2010), generic combination probenecid-colchicine (2008-2017), Colcrys (2009-2017), brand-name single-ingredient colchicine Mitigare (approved in late 2014 but not marketed until 2015), and their authorized generics (2015-2017). Medicare trends from 2012 to 2017 were analyzed separately because pre-Colcrys Medicare data were not available.
Based on the results, combined spending on Medicare and Medicaid claims for single-ingredient colchicine exceeded $340 million in 2017.
Inflation- and rebate-adjusted Medicaid unit prices rose from $0.24 a pill in 2008, when unapproved formulations were still available, to $4.20 a pill in 2011 (Colcrys only), and peaked at $4.66 a pill in 2015 (Colcrys plus authorized generics).
Prescribing of lower-priced probenecid-colchicine ($0.66/pill in 2017) remained stable throughout. Medicaid rebate-adjusted prices in 2017 were $3.99/pill for all single-ingredient colchicine products, $5.13/pill for Colcrys, $4.49/pill for Mitigare, and $3.88/pill for authorized generics.
Medicare rebate-adjusted 2017 per-pill prices were $5.81 for all single-ingredient colchicine products, $6.78 for Colcrys, $5.68 for Mitigare, $5.16 for authorized generics, and $0.70 for probenecid-colchicine.
“Authorized generics have still driven high spending,” Dr. McCormick said. “We really need to encourage more competition in order to improve access.”
In an accompanying commentary, B. Joseph Guglielmo, PharmD, University of California, San Francisco, pointed out that the estimated median research and development cost to bring a drug to market is between $985 million and $1,335 million, which inevitably translates into a high selling price for the drug. Such investment and its resultant cost, however, should be associated with potential worth to society.
“Only a fraction of an investment was required for Colcrys, a product that has provided no increased value and an unnecessary, long-term cost burden to the health care system,” he wrote. “The current study findings illustrate that we can never allow such an egregious case to take place again.”
Dr. McCormick reported grants from Canadian Institutes of Health Research during the conduct of the study. Dr. Guglielmo reported having no relevant conflicts of interest.
This article first appeared on Medscape.com.
Public spending on colchicine has grown exponentially over the past decade despite generics suggesting an uphill slog for patients seeking access to long-term therapy for gout or cardiac conditions.
Medicaid spending on single-ingredient colchicine jumped 2,833%, from $1.1 million in 2008 to $32.2 million in 2017, new findings show. Medicaid expansion likely played a role in the increase, but 58% was due to price hikes alone.
The centuries-old drug sold for pennies in the United States before increasing 50-fold to about $5 per pill in 2009 after the first FDA-approved colchicine product, Colcrys, was granted 3 years’ market exclusivity for the treatment of acute gout based on a 1-week trial.
If prices had remained at pre-Colcrys levels, Medicaid spending in 2017 would have totaled just $2.1 million rather than $32.2 million according to the analysis, published online Nov. 30 in JAMA Internal Medicine (doi: 10.1001/jamainternmed.2020.5017).
The study was motivated by difficulties gout patients have in accessing colchicine, but also last year’s COLCOT trial, which reported fewer ischemic cardiovascular events in patients receiving colchicine after MI, observed Natalie McCormick, PhD, of Massachusetts General Hospital and Harvard Medical School, both in Boston.
“They were suggesting it could be a cost-effective way for secondary prevention and it is fairly inexpensive in most countries, but not the U.S.,” she said in an interview. “So there’s really a potential to increase public spending if more and more patients are then taking colchicine for prevention of cardiovascular events and the prices don’t change.”
The current pandemic could potentially further increase demand. Results initially slated for September are expected this month from the COLCORONA trial, which is testing whether the anti-inflammatory agent can prevent hospitalizations, lung complications, and death when given early in the course of COVID-19.
University of Oxford (England) researchers also announced last week that colchicine is being added to the massive RECOVERY trial, which is studying treatments for hospitalized COVID-19 patients.
Notably, the Canadian-based COLCOT trial did not use Colcrys, but rather a colchicine product that costs just $0.26 a pill in Canada, roughly the price of most generics available worldwide.
Authorized generics typically drive down drug prices when competing with independent generics, but this competition is missing in the United States, where Colcrys holds patents until 2029, Dr. McCormick and colleagues noted. More than a half-dozen independent generics have FDA approval to date, but only authorized generics with price points set by the brand-name companies are available to treat acute gout, pericarditis, and potentially millions with MI.
“One of the key takeaways is this difference between the brand names and the authorized generics and the independents,” she said. “The authorized [generics] have really not saved money. The list prices were just slightly lower and patients can also have more difficulty in getting those covered.”
For this analysis, the investigators used Medicaid and Medicare data to examine prices for all available forms of colchicine from 2008 to 2017, including unregulated/unapproved colchicine (2008-2010), generic combination probenecid-colchicine (2008-2017), Colcrys (2009-2017), brand-name single-ingredient colchicine Mitigare (approved in late 2014 but not marketed until 2015), and their authorized generics (2015-2017). Medicare trends from 2012 to 2017 were analyzed separately because pre-Colcrys Medicare data were not available.
Based on the results, combined spending on Medicare and Medicaid claims for single-ingredient colchicine exceeded $340 million in 2017.
Inflation- and rebate-adjusted Medicaid unit prices rose from $0.24 a pill in 2008, when unapproved formulations were still available, to $4.20 a pill in 2011 (Colcrys only), and peaked at $4.66 a pill in 2015 (Colcrys plus authorized generics).
Prescribing of lower-priced probenecid-colchicine ($0.66/pill in 2017) remained stable throughout. Medicaid rebate-adjusted prices in 2017 were $3.99/pill for all single-ingredient colchicine products, $5.13/pill for Colcrys, $4.49/pill for Mitigare, and $3.88/pill for authorized generics.
Medicare rebate-adjusted 2017 per-pill prices were $5.81 for all single-ingredient colchicine products, $6.78 for Colcrys, $5.68 for Mitigare, $5.16 for authorized generics, and $0.70 for probenecid-colchicine.
“Authorized generics have still driven high spending,” Dr. McCormick said. “We really need to encourage more competition in order to improve access.”
In an accompanying commentary, B. Joseph Guglielmo, PharmD, University of California, San Francisco, pointed out that the estimated median research and development cost to bring a drug to market is between $985 million and $1,335 million, which inevitably translates into a high selling price for the drug. Such investment and its resultant cost, however, should be associated with potential worth to society.
“Only a fraction of an investment was required for Colcrys, a product that has provided no increased value and an unnecessary, long-term cost burden to the health care system,” he wrote. “The current study findings illustrate that we can never allow such an egregious case to take place again.”
Dr. McCormick reported grants from Canadian Institutes of Health Research during the conduct of the study. Dr. Guglielmo reported having no relevant conflicts of interest.
This article first appeared on Medscape.com.
Public spending on colchicine has grown exponentially over the past decade despite generics suggesting an uphill slog for patients seeking access to long-term therapy for gout or cardiac conditions.
Medicaid spending on single-ingredient colchicine jumped 2,833%, from $1.1 million in 2008 to $32.2 million in 2017, new findings show. Medicaid expansion likely played a role in the increase, but 58% was due to price hikes alone.
The centuries-old drug sold for pennies in the United States before increasing 50-fold to about $5 per pill in 2009 after the first FDA-approved colchicine product, Colcrys, was granted 3 years’ market exclusivity for the treatment of acute gout based on a 1-week trial.
If prices had remained at pre-Colcrys levels, Medicaid spending in 2017 would have totaled just $2.1 million rather than $32.2 million according to the analysis, published online Nov. 30 in JAMA Internal Medicine (doi: 10.1001/jamainternmed.2020.5017).
The study was motivated by difficulties gout patients have in accessing colchicine, but also last year’s COLCOT trial, which reported fewer ischemic cardiovascular events in patients receiving colchicine after MI, observed Natalie McCormick, PhD, of Massachusetts General Hospital and Harvard Medical School, both in Boston.
“They were suggesting it could be a cost-effective way for secondary prevention and it is fairly inexpensive in most countries, but not the U.S.,” she said in an interview. “So there’s really a potential to increase public spending if more and more patients are then taking colchicine for prevention of cardiovascular events and the prices don’t change.”
The current pandemic could potentially further increase demand. Results initially slated for September are expected this month from the COLCORONA trial, which is testing whether the anti-inflammatory agent can prevent hospitalizations, lung complications, and death when given early in the course of COVID-19.
University of Oxford (England) researchers also announced last week that colchicine is being added to the massive RECOVERY trial, which is studying treatments for hospitalized COVID-19 patients.
Notably, the Canadian-based COLCOT trial did not use Colcrys, but rather a colchicine product that costs just $0.26 a pill in Canada, roughly the price of most generics available worldwide.
Authorized generics typically drive down drug prices when competing with independent generics, but this competition is missing in the United States, where Colcrys holds patents until 2029, Dr. McCormick and colleagues noted. More than a half-dozen independent generics have FDA approval to date, but only authorized generics with price points set by the brand-name companies are available to treat acute gout, pericarditis, and potentially millions with MI.
“One of the key takeaways is this difference between the brand names and the authorized generics and the independents,” she said. “The authorized [generics] have really not saved money. The list prices were just slightly lower and patients can also have more difficulty in getting those covered.”
For this analysis, the investigators used Medicaid and Medicare data to examine prices for all available forms of colchicine from 2008 to 2017, including unregulated/unapproved colchicine (2008-2010), generic combination probenecid-colchicine (2008-2017), Colcrys (2009-2017), brand-name single-ingredient colchicine Mitigare (approved in late 2014 but not marketed until 2015), and their authorized generics (2015-2017). Medicare trends from 2012 to 2017 were analyzed separately because pre-Colcrys Medicare data were not available.
Based on the results, combined spending on Medicare and Medicaid claims for single-ingredient colchicine exceeded $340 million in 2017.
Inflation- and rebate-adjusted Medicaid unit prices rose from $0.24 a pill in 2008, when unapproved formulations were still available, to $4.20 a pill in 2011 (Colcrys only), and peaked at $4.66 a pill in 2015 (Colcrys plus authorized generics).
Prescribing of lower-priced probenecid-colchicine ($0.66/pill in 2017) remained stable throughout. Medicaid rebate-adjusted prices in 2017 were $3.99/pill for all single-ingredient colchicine products, $5.13/pill for Colcrys, $4.49/pill for Mitigare, and $3.88/pill for authorized generics.
Medicare rebate-adjusted 2017 per-pill prices were $5.81 for all single-ingredient colchicine products, $6.78 for Colcrys, $5.68 for Mitigare, $5.16 for authorized generics, and $0.70 for probenecid-colchicine.
“Authorized generics have still driven high spending,” Dr. McCormick said. “We really need to encourage more competition in order to improve access.”
In an accompanying commentary, B. Joseph Guglielmo, PharmD, University of California, San Francisco, pointed out that the estimated median research and development cost to bring a drug to market is between $985 million and $1,335 million, which inevitably translates into a high selling price for the drug. Such investment and its resultant cost, however, should be associated with potential worth to society.
“Only a fraction of an investment was required for Colcrys, a product that has provided no increased value and an unnecessary, long-term cost burden to the health care system,” he wrote. “The current study findings illustrate that we can never allow such an egregious case to take place again.”
Dr. McCormick reported grants from Canadian Institutes of Health Research during the conduct of the study. Dr. Guglielmo reported having no relevant conflicts of interest.
This article first appeared on Medscape.com.