User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Cardiogenic shock teams again tied to lower mortality
A large multicenter study provides further evidence supporting the rationale for multidisciplinary teams for cardiogenic shock, one of the most lethal diseases in cardiovascular medicine.
The analysis of 24 critical care ICUs in the Critical Care Cardiology Trials Network showed that the presence of a shock team was independently associated with a 28% lower risk for CICU mortality (23% vs. 29%; odds ratio, 0.72; P = .016).
Patients treated by a shock team also had significantly shorter CICU stays and less need for mechanical ventilation or renal replacement therapy, as reported in the Journal of the American College of Cardiology.
“It’s observational, but the association that we’re seeing here, just because of our sample size, is the strongest that’s been published yet,” lead author Alexander Papolos, MD, MedStar Washington Hospital Center, said in an interview.
Although a causal relationship cannot be drawn, the authors suggest several factors that could explain the findings, including a shock team’s ability to rapidly diagnose and treat cardiogenic shock before multiorgan dysfunction occurs.
Centers with shock teams also used significantly more pulmonary artery catheters (60% vs. 49%; adjusted OR, 1.86; P < .001) and placed them earlier (0.3 vs. 0.66 days; P = .019).
Pulmonary artery catheter (PAC) use has declined after earlier trials like ESCAPE showed little or no benefit in other acutely ill patient groups, but positive results have been reported recently in cardiogenic shock, where a PAC is needed to determine the severity of the lesion and the phenotype, Dr. Papolos observed.
A 2018 study showed PAC use was tied to increased survival among patients with acute myocardial infarction cardiogenic shock (AMI-CS) supported with the Impella (Abiomed) device. Additionally, a 2021 study by the Cardiogenic Shock Working Group demonstrated a dose-dependent survival response based on the completeness of hemodynamic assessment by PAC prior to initiating mechanical circulatory support (MCS).
A third factor might be that a structured, team-based evaluation can facilitate timely and optimal MCS device selection, deployment, and management, suggested Dr. Papolos.
Centers with shock teams used more advanced types of MCS – defined as Impella, TandemHeart (LivaNova), extracorporeal membrane oxygenation, and temporary or durable surgical ventricular assist devices – than those without a shock team (53% vs. 43%; adjusted OR, 1.73; P = .005) and did so more often as the initial device (42% vs. 28%; P = .002).
Overall MCS use was lower at shock team centers (35% vs. 43%), driven by less frequent use of intra-aortic balloon pumps (58% vs. 72%).
“The standard, basic MCS has always been the balloon pump because it’s something that’s easy to put in at the cath lab or at the bedside,” Dr. Papolos said. “So, if you take away having all of the information and having the right people at the table to discuss what the best level of support is, then you’re going to end up with balloon pumps, and that’s what we saw here.”
The study involved 6,872 consecutive medical admissions at 24 level 1 CICU centers during an annual 2-month period from 2017 to 2019. Of these, 1,242 admissions were for cardiogenic shock and 546 (44%) were treated at one of 10 centers with a shock team.
Shock team centers had higher-acuity patients than centers without a shock team (Sequential Organ Failure Assessment score, 4 vs. 3) but a similar proportion of patients with AMI-CS (27% vs. 28%).
Among all admissions, CICU mortality was not significantly different between centers with and without a shock team.
For cardiogenic shock patients treated at centers with and without a shock team, the median CICU stay was 4.0 and 5.1 days, respectively, mechanical ventilation was used in 41% and 52%, respectively, and new renal replacement therapy in 11% and 19%, respectively (P < .001 for all).
Shock team centers used significantly more PACs for AMI-CS and non–AMI-CS admissions; advanced MCS therapy was also greater in the AMI-CS subgroup.
Lower CICU mortality at shock team centers persisted among patients with non-AMI-CS (adjusted OR, 0.67; P = .017) and AMI-CS (adjusted OR, 0.79; P = .344).
“This analysis supports that all AHA level 1 cardiac ICUs should strongly consider having a shock team,” Dr. Papolos said.
Evidence from single centers and the National Cardiogenic Shock Initiative has shown improved survival with a cardiogenic shock algorithm, but this is the first report specifically comparing no shock teams with shock teams, Perwaiz Meraj, MD, Northwell Health, Manhansett, N.Y., told this news organization.
“People may say that it’s just another paper that’s saying, ‘shock teams, shock teams, rah, rah, rah,’ but it’s important for all of us to really take a close look under the covers and see how are we best managing these patients, what teams are we putting together, and to create systems of care, where if you’re at a center that really doesn’t have the capabilities of doing this, then you should partner up with a center that does,” he said.
Notably, the 10 shock teams were present only in medium or large urban, academic medical centers with more than 500 beds. Although they followed individual protocols, survey results show service-line representation, structure, and operations were similar across centers.
They all had a centralized way to activate the shock team, the service was 24/7, and members came from areas such as critical care cardiology (100%), cardiac surgery (100%), interventional cardiology (90%), advanced heart failure (80%), and extracorporeal membrane oxygenation service (70%).
Limitations of the study include the possibility of residual confounding, the fact that the registry did not capture patients with cardiogenic shock managed outside the CICU or the time of onset of cardiogenic shock, and data were limited on inotropic strategies, sedation practices, and ventilator management, the authors wrote.
“Although many critics will continue to discuss the lack of randomized controlled trials in cardiogenic shock, this paper supports the process previously outlined of a multidisciplinary team-based approach improving survival,” Dr. Meraj and William W. O’Neill, MD, director of the Center for Structural Heart Disease and Henry Ford Health System, Detroit, and the force behind the National Cardiogenic Shock Initiative, wrote in an accompanying editorial.
They point out that the report doesn’t address the escalation of care based on invasive hemodynamics in the CICU and the protocols to prevent acute vascular/limb complications (ALI) that can arise from the use of MCS.
“Many procedural techniques and novel CICU models exist to mitigate the risk of ALI in CS patients with MCS,” they wrote. “Finally, escalation of care and support is vital to the continued success of any shock team and center.”
One coauthor has served as a consultant to Abbott. Another has served as a consultant to the Abiomed critical care advisory board. All other authors reported having no relevant financial relationships. Dr. Meraj has received research and grant funding from Abiomed, Medtronic, CSI, and Boston Scientific. Dr. O’Neill has received consulting/speaker honoraria from Abiomed, Boston Scientific, and Abbott.
A version of this article first appeared on Medscape.com.
A large multicenter study provides further evidence supporting the rationale for multidisciplinary teams for cardiogenic shock, one of the most lethal diseases in cardiovascular medicine.
The analysis of 24 critical care ICUs in the Critical Care Cardiology Trials Network showed that the presence of a shock team was independently associated with a 28% lower risk for CICU mortality (23% vs. 29%; odds ratio, 0.72; P = .016).
Patients treated by a shock team also had significantly shorter CICU stays and less need for mechanical ventilation or renal replacement therapy, as reported in the Journal of the American College of Cardiology.
“It’s observational, but the association that we’re seeing here, just because of our sample size, is the strongest that’s been published yet,” lead author Alexander Papolos, MD, MedStar Washington Hospital Center, said in an interview.
Although a causal relationship cannot be drawn, the authors suggest several factors that could explain the findings, including a shock team’s ability to rapidly diagnose and treat cardiogenic shock before multiorgan dysfunction occurs.
Centers with shock teams also used significantly more pulmonary artery catheters (60% vs. 49%; adjusted OR, 1.86; P < .001) and placed them earlier (0.3 vs. 0.66 days; P = .019).
Pulmonary artery catheter (PAC) use has declined after earlier trials like ESCAPE showed little or no benefit in other acutely ill patient groups, but positive results have been reported recently in cardiogenic shock, where a PAC is needed to determine the severity of the lesion and the phenotype, Dr. Papolos observed.
A 2018 study showed PAC use was tied to increased survival among patients with acute myocardial infarction cardiogenic shock (AMI-CS) supported with the Impella (Abiomed) device. Additionally, a 2021 study by the Cardiogenic Shock Working Group demonstrated a dose-dependent survival response based on the completeness of hemodynamic assessment by PAC prior to initiating mechanical circulatory support (MCS).
A third factor might be that a structured, team-based evaluation can facilitate timely and optimal MCS device selection, deployment, and management, suggested Dr. Papolos.
Centers with shock teams used more advanced types of MCS – defined as Impella, TandemHeart (LivaNova), extracorporeal membrane oxygenation, and temporary or durable surgical ventricular assist devices – than those without a shock team (53% vs. 43%; adjusted OR, 1.73; P = .005) and did so more often as the initial device (42% vs. 28%; P = .002).
Overall MCS use was lower at shock team centers (35% vs. 43%), driven by less frequent use of intra-aortic balloon pumps (58% vs. 72%).
“The standard, basic MCS has always been the balloon pump because it’s something that’s easy to put in at the cath lab or at the bedside,” Dr. Papolos said. “So, if you take away having all of the information and having the right people at the table to discuss what the best level of support is, then you’re going to end up with balloon pumps, and that’s what we saw here.”
The study involved 6,872 consecutive medical admissions at 24 level 1 CICU centers during an annual 2-month period from 2017 to 2019. Of these, 1,242 admissions were for cardiogenic shock and 546 (44%) were treated at one of 10 centers with a shock team.
Shock team centers had higher-acuity patients than centers without a shock team (Sequential Organ Failure Assessment score, 4 vs. 3) but a similar proportion of patients with AMI-CS (27% vs. 28%).
Among all admissions, CICU mortality was not significantly different between centers with and without a shock team.
For cardiogenic shock patients treated at centers with and without a shock team, the median CICU stay was 4.0 and 5.1 days, respectively, mechanical ventilation was used in 41% and 52%, respectively, and new renal replacement therapy in 11% and 19%, respectively (P < .001 for all).
Shock team centers used significantly more PACs for AMI-CS and non–AMI-CS admissions; advanced MCS therapy was also greater in the AMI-CS subgroup.
Lower CICU mortality at shock team centers persisted among patients with non-AMI-CS (adjusted OR, 0.67; P = .017) and AMI-CS (adjusted OR, 0.79; P = .344).
“This analysis supports that all AHA level 1 cardiac ICUs should strongly consider having a shock team,” Dr. Papolos said.
Evidence from single centers and the National Cardiogenic Shock Initiative has shown improved survival with a cardiogenic shock algorithm, but this is the first report specifically comparing no shock teams with shock teams, Perwaiz Meraj, MD, Northwell Health, Manhansett, N.Y., told this news organization.
“People may say that it’s just another paper that’s saying, ‘shock teams, shock teams, rah, rah, rah,’ but it’s important for all of us to really take a close look under the covers and see how are we best managing these patients, what teams are we putting together, and to create systems of care, where if you’re at a center that really doesn’t have the capabilities of doing this, then you should partner up with a center that does,” he said.
Notably, the 10 shock teams were present only in medium or large urban, academic medical centers with more than 500 beds. Although they followed individual protocols, survey results show service-line representation, structure, and operations were similar across centers.
They all had a centralized way to activate the shock team, the service was 24/7, and members came from areas such as critical care cardiology (100%), cardiac surgery (100%), interventional cardiology (90%), advanced heart failure (80%), and extracorporeal membrane oxygenation service (70%).
Limitations of the study include the possibility of residual confounding, the fact that the registry did not capture patients with cardiogenic shock managed outside the CICU or the time of onset of cardiogenic shock, and data were limited on inotropic strategies, sedation practices, and ventilator management, the authors wrote.
“Although many critics will continue to discuss the lack of randomized controlled trials in cardiogenic shock, this paper supports the process previously outlined of a multidisciplinary team-based approach improving survival,” Dr. Meraj and William W. O’Neill, MD, director of the Center for Structural Heart Disease and Henry Ford Health System, Detroit, and the force behind the National Cardiogenic Shock Initiative, wrote in an accompanying editorial.
They point out that the report doesn’t address the escalation of care based on invasive hemodynamics in the CICU and the protocols to prevent acute vascular/limb complications (ALI) that can arise from the use of MCS.
“Many procedural techniques and novel CICU models exist to mitigate the risk of ALI in CS patients with MCS,” they wrote. “Finally, escalation of care and support is vital to the continued success of any shock team and center.”
One coauthor has served as a consultant to Abbott. Another has served as a consultant to the Abiomed critical care advisory board. All other authors reported having no relevant financial relationships. Dr. Meraj has received research and grant funding from Abiomed, Medtronic, CSI, and Boston Scientific. Dr. O’Neill has received consulting/speaker honoraria from Abiomed, Boston Scientific, and Abbott.
A version of this article first appeared on Medscape.com.
A large multicenter study provides further evidence supporting the rationale for multidisciplinary teams for cardiogenic shock, one of the most lethal diseases in cardiovascular medicine.
The analysis of 24 critical care ICUs in the Critical Care Cardiology Trials Network showed that the presence of a shock team was independently associated with a 28% lower risk for CICU mortality (23% vs. 29%; odds ratio, 0.72; P = .016).
Patients treated by a shock team also had significantly shorter CICU stays and less need for mechanical ventilation or renal replacement therapy, as reported in the Journal of the American College of Cardiology.
“It’s observational, but the association that we’re seeing here, just because of our sample size, is the strongest that’s been published yet,” lead author Alexander Papolos, MD, MedStar Washington Hospital Center, said in an interview.
Although a causal relationship cannot be drawn, the authors suggest several factors that could explain the findings, including a shock team’s ability to rapidly diagnose and treat cardiogenic shock before multiorgan dysfunction occurs.
Centers with shock teams also used significantly more pulmonary artery catheters (60% vs. 49%; adjusted OR, 1.86; P < .001) and placed them earlier (0.3 vs. 0.66 days; P = .019).
Pulmonary artery catheter (PAC) use has declined after earlier trials like ESCAPE showed little or no benefit in other acutely ill patient groups, but positive results have been reported recently in cardiogenic shock, where a PAC is needed to determine the severity of the lesion and the phenotype, Dr. Papolos observed.
A 2018 study showed PAC use was tied to increased survival among patients with acute myocardial infarction cardiogenic shock (AMI-CS) supported with the Impella (Abiomed) device. Additionally, a 2021 study by the Cardiogenic Shock Working Group demonstrated a dose-dependent survival response based on the completeness of hemodynamic assessment by PAC prior to initiating mechanical circulatory support (MCS).
A third factor might be that a structured, team-based evaluation can facilitate timely and optimal MCS device selection, deployment, and management, suggested Dr. Papolos.
Centers with shock teams used more advanced types of MCS – defined as Impella, TandemHeart (LivaNova), extracorporeal membrane oxygenation, and temporary or durable surgical ventricular assist devices – than those without a shock team (53% vs. 43%; adjusted OR, 1.73; P = .005) and did so more often as the initial device (42% vs. 28%; P = .002).
Overall MCS use was lower at shock team centers (35% vs. 43%), driven by less frequent use of intra-aortic balloon pumps (58% vs. 72%).
“The standard, basic MCS has always been the balloon pump because it’s something that’s easy to put in at the cath lab or at the bedside,” Dr. Papolos said. “So, if you take away having all of the information and having the right people at the table to discuss what the best level of support is, then you’re going to end up with balloon pumps, and that’s what we saw here.”
The study involved 6,872 consecutive medical admissions at 24 level 1 CICU centers during an annual 2-month period from 2017 to 2019. Of these, 1,242 admissions were for cardiogenic shock and 546 (44%) were treated at one of 10 centers with a shock team.
Shock team centers had higher-acuity patients than centers without a shock team (Sequential Organ Failure Assessment score, 4 vs. 3) but a similar proportion of patients with AMI-CS (27% vs. 28%).
Among all admissions, CICU mortality was not significantly different between centers with and without a shock team.
For cardiogenic shock patients treated at centers with and without a shock team, the median CICU stay was 4.0 and 5.1 days, respectively, mechanical ventilation was used in 41% and 52%, respectively, and new renal replacement therapy in 11% and 19%, respectively (P < .001 for all).
Shock team centers used significantly more PACs for AMI-CS and non–AMI-CS admissions; advanced MCS therapy was also greater in the AMI-CS subgroup.
Lower CICU mortality at shock team centers persisted among patients with non-AMI-CS (adjusted OR, 0.67; P = .017) and AMI-CS (adjusted OR, 0.79; P = .344).
“This analysis supports that all AHA level 1 cardiac ICUs should strongly consider having a shock team,” Dr. Papolos said.
Evidence from single centers and the National Cardiogenic Shock Initiative has shown improved survival with a cardiogenic shock algorithm, but this is the first report specifically comparing no shock teams with shock teams, Perwaiz Meraj, MD, Northwell Health, Manhansett, N.Y., told this news organization.
“People may say that it’s just another paper that’s saying, ‘shock teams, shock teams, rah, rah, rah,’ but it’s important for all of us to really take a close look under the covers and see how are we best managing these patients, what teams are we putting together, and to create systems of care, where if you’re at a center that really doesn’t have the capabilities of doing this, then you should partner up with a center that does,” he said.
Notably, the 10 shock teams were present only in medium or large urban, academic medical centers with more than 500 beds. Although they followed individual protocols, survey results show service-line representation, structure, and operations were similar across centers.
They all had a centralized way to activate the shock team, the service was 24/7, and members came from areas such as critical care cardiology (100%), cardiac surgery (100%), interventional cardiology (90%), advanced heart failure (80%), and extracorporeal membrane oxygenation service (70%).
Limitations of the study include the possibility of residual confounding, the fact that the registry did not capture patients with cardiogenic shock managed outside the CICU or the time of onset of cardiogenic shock, and data were limited on inotropic strategies, sedation practices, and ventilator management, the authors wrote.
“Although many critics will continue to discuss the lack of randomized controlled trials in cardiogenic shock, this paper supports the process previously outlined of a multidisciplinary team-based approach improving survival,” Dr. Meraj and William W. O’Neill, MD, director of the Center for Structural Heart Disease and Henry Ford Health System, Detroit, and the force behind the National Cardiogenic Shock Initiative, wrote in an accompanying editorial.
They point out that the report doesn’t address the escalation of care based on invasive hemodynamics in the CICU and the protocols to prevent acute vascular/limb complications (ALI) that can arise from the use of MCS.
“Many procedural techniques and novel CICU models exist to mitigate the risk of ALI in CS patients with MCS,” they wrote. “Finally, escalation of care and support is vital to the continued success of any shock team and center.”
One coauthor has served as a consultant to Abbott. Another has served as a consultant to the Abiomed critical care advisory board. All other authors reported having no relevant financial relationships. Dr. Meraj has received research and grant funding from Abiomed, Medtronic, CSI, and Boston Scientific. Dr. O’Neill has received consulting/speaker honoraria from Abiomed, Boston Scientific, and Abbott.
A version of this article first appeared on Medscape.com.
FDA OKs Pfizer COVID booster for 65 and over, those at high risk
The agency’s move comes as a Centers for Disease Control and Prevention (CDC) panel ended the first day of a 2-day meeting. That panel, the Advisory Committee on Immunization Practices (ACIP), is expected to vote Sept. 23 to instruct doctors on how to administer the boosters.
The FDA officially authorized the vaccine not only for individuals 65 and older, but also for people 18 through 64 years of age who are at high risk for severe illness from the coronavirus, including essential workers whose jobs increase their risk for infection.
“After considering the totality of the available scientific evidence and the deliberations of our advisory committee of independent, external experts, the FDA amended the EUA for the Pfizer-BioNTech COVID-19 vaccine to allow for a booster dose in certain populations such as health care workers, teachers and daycare staff, grocery workers and those in homeless shelters or prisons, among others,” Acting FDA Commissioner Janet Woodcock, MD, said in a news release.
The recommendations align with those from an FDA advisory panel Sept. 17.
The agency determined that the benefits of a booster dose outweigh the risks for people now authorized to receive it, according to the news release.
Other questions remain
So, how will this work? That was the main question weighing on the minds of the CDC’s ACIP during their first day of a 2-day meeting where they are expected to make recommendations on booster doses for Americans.
The panel discussed situations the FDA will still need to consider, such as what should be done for Americans who were originally vaccinated with a Moderna or Johnson and Johnson vaccine, but are not covered under the revised EUA, which is only for those people who received Pfizer’s two-dose vaccine regimen.
“That’s going to leave half of the people immunized in this age group having received the vaccine and being told that they’re at risk now for waning immunity and hospitalization unable to get a booster dose,” said committee member Sarah S. Long, MD, a professor of pediatrics at Drexel University College of Medicine in Philadelphia. “So that’s a big public health panic that we would like to avoid.”
Johnson and Johnson recently reported that second doses of its vaccine boosted its efficacy to almost 94% against COVID-19. A new study, published ahead of peer review, suggests that the efficacy of the single-dose Johnson and Johnson shot has fallen to about 78% against symptomatic infection during the Delta surge.
Moderna has applied for permission to market third doses of its vaccine in the United States, but the FDA has given no timeline on when it might make a decision.
Doran Fink, MD, PhD, deputy director of the FDA’s Division of Vaccines and Related Products Applications, a representative advising the committee Sept. 22, said the agency was working as rapidly as possible on Moderna’s submission.
Regarding the question of whether it was OK to mix vaccines, rather than match them, Dr. Fink said there are currently not enough data available to inform that decision.
Those answers are coming, though. John Beigel, MD, associate director of clinical research at the National Institute of Allergy and Infectious Diseases, revealed that the federal government has a study underway to see what happens when the vaccines are mixed with each other.
He said that data from the study would be available later this fall, and would certainly help physicians and other healthcare providers know whether it’s effective or safe to use them interchangeably.
Correlates of immunity
The ACIP left much of its schedule open Sept. 23 to discuss extra Pfizer doses and vote on how they should be used.
Pfizer had originally applied to the FDA for an amendment to its FDA approval, which would have given doctors a freer hand to prescribe third doses as they saw fit, in patients as young as 16.
But the FDA’s Vaccines and Related Biological Products Advisory Committee voted Sept. 17 against granting the amendment. The committee was particularly concerned about the lack of data in teens ages 16 and 17, who have the highest risk for a rare side effect that causes heart inflammation that requires hospital care.
Instead, they recommended — and the FDA agreed per their decision Sept. 22 — that third doses should be given to people at higher risk for severe breakthrough infections because of advanced age or because they work in an occupation that puts them at high risk for exposure.
The CDC panel heard important presentations on new science that is helping to identify the correlates of immunity.
The correlates of immunity are biomarkers that can be measured in blood that help doctors understand how protected a person may be against COVID-19. These markers of immunity are not yet known for the COVID-19 vaccines.
Emerging evidence shows that booster doses of the Pfizer vaccine cause front-line immune defenders — called binding antibodies — to roughly triple soon after a person gets the third shot.
Neutralizing antibodies also jump soon after two vaccine doses, but they fall over time, which is natural. The body doesn’t need these foot soldiers to be on guard all the time, so they go away.
The body retains its memory of how to make them, however, so they can quickly be marshaled again, if needed.
Early studies suggest that antibodies account for about two thirds of a person’s protection against COVID, while the longer-lasting T-cells and B-cells account for about one third.
After the antibody levels fall, it may take a few days to recreate this army. In the meantime, the virus can try to break in. This can cause symptoms, which can make a person feel terrible, but for the most part, vaccinated individuals don’t need hospital care and are nearly always protected from dying — even against the Delta variant.
Those most likely to be at risk for a breakthrough infection are older, because immune function wanes with age.
Essential workers
Essential workers, such as those who work in healthcare, may also benefit from high antibody levels, which can minimize symptoms and help them get back to work more quickly.
Helen Talbot, MD, MPH, an associate professor of medicine at Vanderbilt University Medical Center in Nashville, said that in her area staffing levels are critical right now.
“I’m actually sitting in one of the deepest red [states] with high rates of COVID. We don’t have enough health care workers currently to take care of the unvaccinated,” she said.
“When we have beds, we are often missing staff, and so the idea of vaccinating health care workers is to be a little bit different than our idea of using vaccines in the general population,” Dr. Talbot said.
Oliver Brooks, MD, chief medical officer of the Watts Healthcare Corporation in Los Angeles, said he was in favor of making a public statement about the temporary nature of the potential recommendations Sept. 23, because they probably won’t cover all who might need a third shot.
“We may want to go on record stating what it is that would allow us to broaden our recommendation or restrict our recommendation,” Dr. Brooks said.
The considerations of who should get an extra dose are not always straightforward.
New modeling by the Harvard TH Chan School of Public Health and the CDC to assist the government’s decisions on boosters had a surprise finding: in nursing homes, it’s more effective to vaccinate healthcare workers than it is to give booster doses to these residents. Nursing homes are at the mercy of community transmission.
In regions with high transmission, it’s easy for a caregiver to bring the virus into a facility — so the models found that the transmission from these workers is a more effective strategy than giving third doses to the already highly vaccinated group of seniors who live in them.
A version of this article first appeared on Medscape.com.
The agency’s move comes as a Centers for Disease Control and Prevention (CDC) panel ended the first day of a 2-day meeting. That panel, the Advisory Committee on Immunization Practices (ACIP), is expected to vote Sept. 23 to instruct doctors on how to administer the boosters.
The FDA officially authorized the vaccine not only for individuals 65 and older, but also for people 18 through 64 years of age who are at high risk for severe illness from the coronavirus, including essential workers whose jobs increase their risk for infection.
“After considering the totality of the available scientific evidence and the deliberations of our advisory committee of independent, external experts, the FDA amended the EUA for the Pfizer-BioNTech COVID-19 vaccine to allow for a booster dose in certain populations such as health care workers, teachers and daycare staff, grocery workers and those in homeless shelters or prisons, among others,” Acting FDA Commissioner Janet Woodcock, MD, said in a news release.
The recommendations align with those from an FDA advisory panel Sept. 17.
The agency determined that the benefits of a booster dose outweigh the risks for people now authorized to receive it, according to the news release.
Other questions remain
So, how will this work? That was the main question weighing on the minds of the CDC’s ACIP during their first day of a 2-day meeting where they are expected to make recommendations on booster doses for Americans.
The panel discussed situations the FDA will still need to consider, such as what should be done for Americans who were originally vaccinated with a Moderna or Johnson and Johnson vaccine, but are not covered under the revised EUA, which is only for those people who received Pfizer’s two-dose vaccine regimen.
“That’s going to leave half of the people immunized in this age group having received the vaccine and being told that they’re at risk now for waning immunity and hospitalization unable to get a booster dose,” said committee member Sarah S. Long, MD, a professor of pediatrics at Drexel University College of Medicine in Philadelphia. “So that’s a big public health panic that we would like to avoid.”
Johnson and Johnson recently reported that second doses of its vaccine boosted its efficacy to almost 94% against COVID-19. A new study, published ahead of peer review, suggests that the efficacy of the single-dose Johnson and Johnson shot has fallen to about 78% against symptomatic infection during the Delta surge.
Moderna has applied for permission to market third doses of its vaccine in the United States, but the FDA has given no timeline on when it might make a decision.
Doran Fink, MD, PhD, deputy director of the FDA’s Division of Vaccines and Related Products Applications, a representative advising the committee Sept. 22, said the agency was working as rapidly as possible on Moderna’s submission.
Regarding the question of whether it was OK to mix vaccines, rather than match them, Dr. Fink said there are currently not enough data available to inform that decision.
Those answers are coming, though. John Beigel, MD, associate director of clinical research at the National Institute of Allergy and Infectious Diseases, revealed that the federal government has a study underway to see what happens when the vaccines are mixed with each other.
He said that data from the study would be available later this fall, and would certainly help physicians and other healthcare providers know whether it’s effective or safe to use them interchangeably.
Correlates of immunity
The ACIP left much of its schedule open Sept. 23 to discuss extra Pfizer doses and vote on how they should be used.
Pfizer had originally applied to the FDA for an amendment to its FDA approval, which would have given doctors a freer hand to prescribe third doses as they saw fit, in patients as young as 16.
But the FDA’s Vaccines and Related Biological Products Advisory Committee voted Sept. 17 against granting the amendment. The committee was particularly concerned about the lack of data in teens ages 16 and 17, who have the highest risk for a rare side effect that causes heart inflammation that requires hospital care.
Instead, they recommended — and the FDA agreed per their decision Sept. 22 — that third doses should be given to people at higher risk for severe breakthrough infections because of advanced age or because they work in an occupation that puts them at high risk for exposure.
The CDC panel heard important presentations on new science that is helping to identify the correlates of immunity.
The correlates of immunity are biomarkers that can be measured in blood that help doctors understand how protected a person may be against COVID-19. These markers of immunity are not yet known for the COVID-19 vaccines.
Emerging evidence shows that booster doses of the Pfizer vaccine cause front-line immune defenders — called binding antibodies — to roughly triple soon after a person gets the third shot.
Neutralizing antibodies also jump soon after two vaccine doses, but they fall over time, which is natural. The body doesn’t need these foot soldiers to be on guard all the time, so they go away.
The body retains its memory of how to make them, however, so they can quickly be marshaled again, if needed.
Early studies suggest that antibodies account for about two thirds of a person’s protection against COVID, while the longer-lasting T-cells and B-cells account for about one third.
After the antibody levels fall, it may take a few days to recreate this army. In the meantime, the virus can try to break in. This can cause symptoms, which can make a person feel terrible, but for the most part, vaccinated individuals don’t need hospital care and are nearly always protected from dying — even against the Delta variant.
Those most likely to be at risk for a breakthrough infection are older, because immune function wanes with age.
Essential workers
Essential workers, such as those who work in healthcare, may also benefit from high antibody levels, which can minimize symptoms and help them get back to work more quickly.
Helen Talbot, MD, MPH, an associate professor of medicine at Vanderbilt University Medical Center in Nashville, said that in her area staffing levels are critical right now.
“I’m actually sitting in one of the deepest red [states] with high rates of COVID. We don’t have enough health care workers currently to take care of the unvaccinated,” she said.
“When we have beds, we are often missing staff, and so the idea of vaccinating health care workers is to be a little bit different than our idea of using vaccines in the general population,” Dr. Talbot said.
Oliver Brooks, MD, chief medical officer of the Watts Healthcare Corporation in Los Angeles, said he was in favor of making a public statement about the temporary nature of the potential recommendations Sept. 23, because they probably won’t cover all who might need a third shot.
“We may want to go on record stating what it is that would allow us to broaden our recommendation or restrict our recommendation,” Dr. Brooks said.
The considerations of who should get an extra dose are not always straightforward.
New modeling by the Harvard TH Chan School of Public Health and the CDC to assist the government’s decisions on boosters had a surprise finding: in nursing homes, it’s more effective to vaccinate healthcare workers than it is to give booster doses to these residents. Nursing homes are at the mercy of community transmission.
In regions with high transmission, it’s easy for a caregiver to bring the virus into a facility — so the models found that the transmission from these workers is a more effective strategy than giving third doses to the already highly vaccinated group of seniors who live in them.
A version of this article first appeared on Medscape.com.
The agency’s move comes as a Centers for Disease Control and Prevention (CDC) panel ended the first day of a 2-day meeting. That panel, the Advisory Committee on Immunization Practices (ACIP), is expected to vote Sept. 23 to instruct doctors on how to administer the boosters.
The FDA officially authorized the vaccine not only for individuals 65 and older, but also for people 18 through 64 years of age who are at high risk for severe illness from the coronavirus, including essential workers whose jobs increase their risk for infection.
“After considering the totality of the available scientific evidence and the deliberations of our advisory committee of independent, external experts, the FDA amended the EUA for the Pfizer-BioNTech COVID-19 vaccine to allow for a booster dose in certain populations such as health care workers, teachers and daycare staff, grocery workers and those in homeless shelters or prisons, among others,” Acting FDA Commissioner Janet Woodcock, MD, said in a news release.
The recommendations align with those from an FDA advisory panel Sept. 17.
The agency determined that the benefits of a booster dose outweigh the risks for people now authorized to receive it, according to the news release.
Other questions remain
So, how will this work? That was the main question weighing on the minds of the CDC’s ACIP during their first day of a 2-day meeting where they are expected to make recommendations on booster doses for Americans.
The panel discussed situations the FDA will still need to consider, such as what should be done for Americans who were originally vaccinated with a Moderna or Johnson and Johnson vaccine, but are not covered under the revised EUA, which is only for those people who received Pfizer’s two-dose vaccine regimen.
“That’s going to leave half of the people immunized in this age group having received the vaccine and being told that they’re at risk now for waning immunity and hospitalization unable to get a booster dose,” said committee member Sarah S. Long, MD, a professor of pediatrics at Drexel University College of Medicine in Philadelphia. “So that’s a big public health panic that we would like to avoid.”
Johnson and Johnson recently reported that second doses of its vaccine boosted its efficacy to almost 94% against COVID-19. A new study, published ahead of peer review, suggests that the efficacy of the single-dose Johnson and Johnson shot has fallen to about 78% against symptomatic infection during the Delta surge.
Moderna has applied for permission to market third doses of its vaccine in the United States, but the FDA has given no timeline on when it might make a decision.
Doran Fink, MD, PhD, deputy director of the FDA’s Division of Vaccines and Related Products Applications, a representative advising the committee Sept. 22, said the agency was working as rapidly as possible on Moderna’s submission.
Regarding the question of whether it was OK to mix vaccines, rather than match them, Dr. Fink said there are currently not enough data available to inform that decision.
Those answers are coming, though. John Beigel, MD, associate director of clinical research at the National Institute of Allergy and Infectious Diseases, revealed that the federal government has a study underway to see what happens when the vaccines are mixed with each other.
He said that data from the study would be available later this fall, and would certainly help physicians and other healthcare providers know whether it’s effective or safe to use them interchangeably.
Correlates of immunity
The ACIP left much of its schedule open Sept. 23 to discuss extra Pfizer doses and vote on how they should be used.
Pfizer had originally applied to the FDA for an amendment to its FDA approval, which would have given doctors a freer hand to prescribe third doses as they saw fit, in patients as young as 16.
But the FDA’s Vaccines and Related Biological Products Advisory Committee voted Sept. 17 against granting the amendment. The committee was particularly concerned about the lack of data in teens ages 16 and 17, who have the highest risk for a rare side effect that causes heart inflammation that requires hospital care.
Instead, they recommended — and the FDA agreed per their decision Sept. 22 — that third doses should be given to people at higher risk for severe breakthrough infections because of advanced age or because they work in an occupation that puts them at high risk for exposure.
The CDC panel heard important presentations on new science that is helping to identify the correlates of immunity.
The correlates of immunity are biomarkers that can be measured in blood that help doctors understand how protected a person may be against COVID-19. These markers of immunity are not yet known for the COVID-19 vaccines.
Emerging evidence shows that booster doses of the Pfizer vaccine cause front-line immune defenders — called binding antibodies — to roughly triple soon after a person gets the third shot.
Neutralizing antibodies also jump soon after two vaccine doses, but they fall over time, which is natural. The body doesn’t need these foot soldiers to be on guard all the time, so they go away.
The body retains its memory of how to make them, however, so they can quickly be marshaled again, if needed.
Early studies suggest that antibodies account for about two thirds of a person’s protection against COVID, while the longer-lasting T-cells and B-cells account for about one third.
After the antibody levels fall, it may take a few days to recreate this army. In the meantime, the virus can try to break in. This can cause symptoms, which can make a person feel terrible, but for the most part, vaccinated individuals don’t need hospital care and are nearly always protected from dying — even against the Delta variant.
Those most likely to be at risk for a breakthrough infection are older, because immune function wanes with age.
Essential workers
Essential workers, such as those who work in healthcare, may also benefit from high antibody levels, which can minimize symptoms and help them get back to work more quickly.
Helen Talbot, MD, MPH, an associate professor of medicine at Vanderbilt University Medical Center in Nashville, said that in her area staffing levels are critical right now.
“I’m actually sitting in one of the deepest red [states] with high rates of COVID. We don’t have enough health care workers currently to take care of the unvaccinated,” she said.
“When we have beds, we are often missing staff, and so the idea of vaccinating health care workers is to be a little bit different than our idea of using vaccines in the general population,” Dr. Talbot said.
Oliver Brooks, MD, chief medical officer of the Watts Healthcare Corporation in Los Angeles, said he was in favor of making a public statement about the temporary nature of the potential recommendations Sept. 23, because they probably won’t cover all who might need a third shot.
“We may want to go on record stating what it is that would allow us to broaden our recommendation or restrict our recommendation,” Dr. Brooks said.
The considerations of who should get an extra dose are not always straightforward.
New modeling by the Harvard TH Chan School of Public Health and the CDC to assist the government’s decisions on boosters had a surprise finding: in nursing homes, it’s more effective to vaccinate healthcare workers than it is to give booster doses to these residents. Nursing homes are at the mercy of community transmission.
In regions with high transmission, it’s easy for a caregiver to bring the virus into a facility — so the models found that the transmission from these workers is a more effective strategy than giving third doses to the already highly vaccinated group of seniors who live in them.
A version of this article first appeared on Medscape.com.
Should hospitalists use albumin to treat non-SBP infections in patients with cirrhosis?
Caution is advised in patients at risk of pulmonary edema
Case
A 56 year-old male with hypertension, alcohol use disorder, stage II chronic kidney disease, and biopsy-proven cirrhosis presents with fever and chills, pyuria, flank pain, and an acute kidney injury concerning for pyelonephritis. Is there a benefit in treating with albumin in addition to guideline-based antibiotics?
Brief overview of the issue
Albumin is a negatively charged human protein produced by the liver. Albumin comprises 50% of plasma protein and over 75% of plasma oncotic pressure.1 It was first used at Walter Reed Hospital in 1940 and subsequently for burn injuries after the attack on Pearl Harbor in 1941.2
Albumin serves several important physiologic functions including maintaining oncotic pressure, endothelial support, antioxidation, nitrogen oxide scavenging, and buffering and transport of solutes and drugs, including antibiotics. In cirrhosis, albumin is diluted due to sodium and water retention. There is increased redistribution, decreased synthesis by the liver, and impaired albumin molecule binding.3
For patients with liver disease, per the European Association for the Study of the Liver (EASL) and the American Association for the Study of Liver Diseases (AASLD), albumin should be administered to prevent post paracentesis circulatory dysfunction after large volume paracentesis, to prevent renal failure and mortality in the setting of spontaneous bacterial peritonitis (SBP), and in the diagnosis and treatment of hepatorenal syndrome (HRS) type I to potentially improve mortality.4,5 Beyond these three guideline-based indications, other uses for albumin for patients with liver disease have been proposed, including treatment of hyponatremia, posttransplant fluid resuscitation, diuretic unresponsive ascites, and long-term management of cirrhosis. There has yet to be strong evidence supporting these additional indications. However, given the known benefits of albumin in patients with SBP, there has been recent research into treatment of non-SBP infections, including urinary tract infections.
Overview of the data
There have been three randomized controlled trials (RCTs) regarding albumin administration for the treatment of non-SBP infections for hospitalized patients with cirrhosis. All three trials randomized patients to a treatment arm of albumin and antibiotics versus a control group of antibiotics alone. The treatment protocol prescribed 20% albumin with 1.5 g/kg on day 1 and 1.0 g/kg on day 3. The most common infections studied were pneumonia and urinary tract infection. These RCTs found that albumin administration was associated with improved renal and/or circulatory function, but not with a reduction in mortality.

First, there was a single center RCT by Guevara et al. in 2012 of 110 patients with cirrhosis and infection based on SIRS criteria.6 The primary outcome was 90-day survival with secondary outcomes of renal failure development, renal function at days 3,7 and 14, and circulatory function measured by plasma renin, aldosterone, and norepinephrine. Renal function and circulatory function improved in the albumin group, but not mortality. In a multivariable regression analysis, albumin was statistically predictive of survival (hazard ratio of 0.294).
Second, there was a multicenter RCT by Thévenot et al. in 2015 of 193 patients.7 The primary outcome was 90-day renal failure and the secondary outcome was 90-day survival. Renal failure was chosen as the primary endpoint because of its association with survival in this patient population. The treatment group had delayed onset of renal failure, but no difference in the development of 90-day renal failure or 90-day mortality rate. Notably, eight patients (8.3%) in the albumin group developed pulmonary edema with two deaths. This led the oversight committee to prematurely terminate the study.
Third and most recently, there was a multicenter RCT by Fernández et al. in 2019 of 118 patients.8 The primary outcome was in-hospital mortality, with secondary outcomes of circulatory dysfunction measured by plasma renin concentration, systemic inflammation measured by plasma IL-6 and biomarkers, complications including acute-on-chronic liver failure (ACLF) and nosocomial bacterial infections, and 90-day mortality. Between the albumin and control group, there were no differences in in-hospital mortality (13.1% vs. 10.5%, P > .66), inflammation, circulatory dysfunction, or liver severity. However, a significantly higher proportion of patients in the albumin group had resolution of their ACLF (82.3% vs. 33.3%, P = .003) and a lower proportion developed nosocomial infections (6.6% vs. 24.6%, P = .007). A major weakness of this study was that patients in the albumin group had a higher combined rate of ACLF and kidney dysfunction (44.3% vs. 24.6%, P = .02).
Beyond these three randomized controlled trials, there was a study on the long-term administration of albumin for patients with cirrhosis and ascites. Patients who received twice weekly albumin infusions had a lower 2-year mortality rate and a reduction in the incidence of both SBP and non-SBP infections.9 Another long-term study of albumin administration found similar results with greater 18-month survival and fewer non-SBP infections.10 A trial looking at inflammation in patients without bacterial infections and in biobanked samples from cirrhotic patients with bacterial infections found that treatment with albumin reduced systemic inflammation.11
In summary, the three RCTs looked at comparable patients with cirrhosis and a non-SBP infection and all underwent similar treatment protocols with 20% albumin dosed at 1.5 g/kg on day 1 and 1.0 g/kg on day 3. All studies evaluated mortality in either the primary or secondary outcome, and none found significant differences in mortality between treatment and control groups. Each study also evaluated and found improvement in renal and/or circulatory function. Fernández et al. also found increased resolution of ACLF, fewer nosocomial infections, and reduction in some inflammatory markers. However, all studies had relatively small sample sizes that were underpowered to detect mortality differences. Furthermore, randomization did not lead to well-matched groups, with the treatment group patients in the Fernández study having higher rates of ACLF and kidney dysfunction.
The data suggest that albumin may be beneficial in improving renal and circulatory function. In select patients with ACLF and elevated serum creatinine, albumin treatment may be considered. There has been discussion about the use of albumin preferentially in patients with subdiaphragmatic bacterial infections, most related to increased risk of renal failure such as biliary and urinary tract infections.12 The authors of these studies also note that albumin may be more beneficial in patients with higher baseline creatinine. Caution is warranted for patients with impaired cardiac function or poor respiratory status given the possibility of pulmonary edema. Finally, the high cost of albumin in many medical centers is a major limitation of this treatment approach.
Application of data to our patient
Our patient has cirrhosis and is acutely presenting with pyelonephritis and acute kidney injury. He has no baseline pulmonary disease or oxygen requirement. His recent transthoracic echocardiogram is reviewed and he has no evidence of cardiac disease.
Because he has an elevated creatinine, an infectious process associated with progressive renal failure, and is not at an elevated baseline risk of developing pulmonary edema, albumin would be reasonable to administer at 1.5 g/kg on day 1 and 1.0 g/kg on day 3 of hospitalization.
Bottom line
In certain patients with cirrhosis and a non-SBP infection, the use of albumin to help improve renal and circulatory function is reasonable. There is no evidence that albumin will improve mortality and caution is warranted for patients at risk for pulmonary edema.
Dr. Rambachan is an academic hospital medicine fellow at the University of California, San Francisco.
References
1. Caironi P and Gattinoni L. The clinical use of albumin: the point of view of a specialist in intensive care. Blood Transfus. 2009;7(4):259-67. doi: 10.2450/2009.0002-09.
2. Paine CH et al. Albumin in cirrhosis: More than a colloid. Curr Treat Options Gastroenterol. 2019;17(2):231-43. doi: 10.1007/s11938-019-00227-4.
3. Walayat S et al. Role of albumin in cirrhosis: from a hospitalist’s perspective. J Community Hosp Intern Med Perspect. 2017;7(1):8-14. 2017 Mar 31. doi: 10.1080/20009666.2017.1302704.
4. Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline [for the] management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013 Apr;57(4):1651-3. doi: 10.1002/hep.26359.
5. European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis [published correction appears in J Hepatol. 2018 Nov;69(5):1207]. J Hepatol. 2018 Aug;69(2):406-60. doi: 10.1016/j.jhep.2018.03.024.
6. Guevara M et al. Albumin for bacterial infections other than spontaneous bacterial peritonitis in cirrhosis. A randomized, controlled study. J Hepatol. 2012 Oct;57(4):759-65. doi: 10.1016/j.jhep.2012.06.013.
7. Thévenot T et al. Effect of albumin in cirrhotic patients with infection other than spontaneous bacterial peritonitis. A randomized trial. J Hepatol. 2015 Apr;62(4):822-30. doi: 10.1016/j.jhep.2014.11.017.
8. Fernández J et al. Efficacy of albumin treatment for patients with cirrhosis and infections unrelated to spontaneous bacterial peritonitis. Clin Gastroenterol Hepatol. 2020 Apr;18(4):963-73.e14. doi: 10.1016/j.c gh.2019.07.055.
9. Di Pascoli M et al. Long-term administration of human albumin improves survival in patients with cirrhosis and refractory ascites. Liver Int. 2019 Jan;39(1):98-105. doi: 10.1111/liv.13968.
10. Caraceni P et al. Long-term albumin administration in decompensated cirrhosis (ANSWER): an open-label randomised trial [published correction appears in Lancet. 2018 Aug 4;392(10145):386]. Lancet. 2018 June;391(10138):2417-29. doi: 10.1016/S0140-6736(18)30840-7.
11. Fernández J et al. Effects of albumin treatment on systemic and portal hemodynamics and systemic inflammation in patients with decompensated cirrhosis. Gastroenterology. 2019 July;157(1):149-62. doi: 10.1053/j.gastro.2019.03.021.
12. Fasolato S et al. Renal failure and bacterial infections in patients with cirrhosis: Epidemiology and clinical features. Hepatology. 2007;45(1):223-9. doi: 10.1002/hep.21443.
Key points
- In patients with spontaneous bacterial peritonitis, hepatorenal syndrome, and for large volume paracentesis, albumin improves outcomes and is recommended by guidelines.
- In patients with cirrhosis and a non-SBP infection, there is some evidence that albumin may improve renal and circulatory function.
- Clinicians should be cautious about albumin use in patients at an elevated risk for development of pulmonary edema.
Quiz
Which of the following is not a guideline-recommended use of albumin for patients with cirrhosis?
A. Treatment of type 1 hepatorenal syndrome
B. Treatment of spontaneous bacterial peritonitis
C. To correct plasma albumin < 2.5 g/dL in nontransplant patients
D. Post large-volume paracentesis
The answer is C. Per the EASL and AASLD, A,B, and D are recommended. There is not strong evidence to support administering albumin to correct low plasma albumin.
Additional reading
- Bernardi M et al. Albumin in decompensated cirrhosis: new concepts and perspectives. Gut. 2020 June;69(6):1127-38. doi: 10.1136/gutjnl-2019-318843.
- Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline [for the] management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013 Apr;57(4):1651-3. doi: 10.1002/hep.26359.
- Paine CH et al. Albumin in cirrhosis: More than a colloid. Curr Treat Options Gastroenterol. 2019 June;17(2):231-43. doi: 10.1007/s11938-019-00227-4.
Caution is advised in patients at risk of pulmonary edema
Caution is advised in patients at risk of pulmonary edema
Case
A 56 year-old male with hypertension, alcohol use disorder, stage II chronic kidney disease, and biopsy-proven cirrhosis presents with fever and chills, pyuria, flank pain, and an acute kidney injury concerning for pyelonephritis. Is there a benefit in treating with albumin in addition to guideline-based antibiotics?
Brief overview of the issue
Albumin is a negatively charged human protein produced by the liver. Albumin comprises 50% of plasma protein and over 75% of plasma oncotic pressure.1 It was first used at Walter Reed Hospital in 1940 and subsequently for burn injuries after the attack on Pearl Harbor in 1941.2
Albumin serves several important physiologic functions including maintaining oncotic pressure, endothelial support, antioxidation, nitrogen oxide scavenging, and buffering and transport of solutes and drugs, including antibiotics. In cirrhosis, albumin is diluted due to sodium and water retention. There is increased redistribution, decreased synthesis by the liver, and impaired albumin molecule binding.3
For patients with liver disease, per the European Association for the Study of the Liver (EASL) and the American Association for the Study of Liver Diseases (AASLD), albumin should be administered to prevent post paracentesis circulatory dysfunction after large volume paracentesis, to prevent renal failure and mortality in the setting of spontaneous bacterial peritonitis (SBP), and in the diagnosis and treatment of hepatorenal syndrome (HRS) type I to potentially improve mortality.4,5 Beyond these three guideline-based indications, other uses for albumin for patients with liver disease have been proposed, including treatment of hyponatremia, posttransplant fluid resuscitation, diuretic unresponsive ascites, and long-term management of cirrhosis. There has yet to be strong evidence supporting these additional indications. However, given the known benefits of albumin in patients with SBP, there has been recent research into treatment of non-SBP infections, including urinary tract infections.
Overview of the data
There have been three randomized controlled trials (RCTs) regarding albumin administration for the treatment of non-SBP infections for hospitalized patients with cirrhosis. All three trials randomized patients to a treatment arm of albumin and antibiotics versus a control group of antibiotics alone. The treatment protocol prescribed 20% albumin with 1.5 g/kg on day 1 and 1.0 g/kg on day 3. The most common infections studied were pneumonia and urinary tract infection. These RCTs found that albumin administration was associated with improved renal and/or circulatory function, but not with a reduction in mortality.

First, there was a single center RCT by Guevara et al. in 2012 of 110 patients with cirrhosis and infection based on SIRS criteria.6 The primary outcome was 90-day survival with secondary outcomes of renal failure development, renal function at days 3,7 and 14, and circulatory function measured by plasma renin, aldosterone, and norepinephrine. Renal function and circulatory function improved in the albumin group, but not mortality. In a multivariable regression analysis, albumin was statistically predictive of survival (hazard ratio of 0.294).
Second, there was a multicenter RCT by Thévenot et al. in 2015 of 193 patients.7 The primary outcome was 90-day renal failure and the secondary outcome was 90-day survival. Renal failure was chosen as the primary endpoint because of its association with survival in this patient population. The treatment group had delayed onset of renal failure, but no difference in the development of 90-day renal failure or 90-day mortality rate. Notably, eight patients (8.3%) in the albumin group developed pulmonary edema with two deaths. This led the oversight committee to prematurely terminate the study.
Third and most recently, there was a multicenter RCT by Fernández et al. in 2019 of 118 patients.8 The primary outcome was in-hospital mortality, with secondary outcomes of circulatory dysfunction measured by plasma renin concentration, systemic inflammation measured by plasma IL-6 and biomarkers, complications including acute-on-chronic liver failure (ACLF) and nosocomial bacterial infections, and 90-day mortality. Between the albumin and control group, there were no differences in in-hospital mortality (13.1% vs. 10.5%, P > .66), inflammation, circulatory dysfunction, or liver severity. However, a significantly higher proportion of patients in the albumin group had resolution of their ACLF (82.3% vs. 33.3%, P = .003) and a lower proportion developed nosocomial infections (6.6% vs. 24.6%, P = .007). A major weakness of this study was that patients in the albumin group had a higher combined rate of ACLF and kidney dysfunction (44.3% vs. 24.6%, P = .02).
Beyond these three randomized controlled trials, there was a study on the long-term administration of albumin for patients with cirrhosis and ascites. Patients who received twice weekly albumin infusions had a lower 2-year mortality rate and a reduction in the incidence of both SBP and non-SBP infections.9 Another long-term study of albumin administration found similar results with greater 18-month survival and fewer non-SBP infections.10 A trial looking at inflammation in patients without bacterial infections and in biobanked samples from cirrhotic patients with bacterial infections found that treatment with albumin reduced systemic inflammation.11
In summary, the three RCTs looked at comparable patients with cirrhosis and a non-SBP infection and all underwent similar treatment protocols with 20% albumin dosed at 1.5 g/kg on day 1 and 1.0 g/kg on day 3. All studies evaluated mortality in either the primary or secondary outcome, and none found significant differences in mortality between treatment and control groups. Each study also evaluated and found improvement in renal and/or circulatory function. Fernández et al. also found increased resolution of ACLF, fewer nosocomial infections, and reduction in some inflammatory markers. However, all studies had relatively small sample sizes that were underpowered to detect mortality differences. Furthermore, randomization did not lead to well-matched groups, with the treatment group patients in the Fernández study having higher rates of ACLF and kidney dysfunction.
The data suggest that albumin may be beneficial in improving renal and circulatory function. In select patients with ACLF and elevated serum creatinine, albumin treatment may be considered. There has been discussion about the use of albumin preferentially in patients with subdiaphragmatic bacterial infections, most related to increased risk of renal failure such as biliary and urinary tract infections.12 The authors of these studies also note that albumin may be more beneficial in patients with higher baseline creatinine. Caution is warranted for patients with impaired cardiac function or poor respiratory status given the possibility of pulmonary edema. Finally, the high cost of albumin in many medical centers is a major limitation of this treatment approach.
Application of data to our patient
Our patient has cirrhosis and is acutely presenting with pyelonephritis and acute kidney injury. He has no baseline pulmonary disease or oxygen requirement. His recent transthoracic echocardiogram is reviewed and he has no evidence of cardiac disease.
Because he has an elevated creatinine, an infectious process associated with progressive renal failure, and is not at an elevated baseline risk of developing pulmonary edema, albumin would be reasonable to administer at 1.5 g/kg on day 1 and 1.0 g/kg on day 3 of hospitalization.
Bottom line
In certain patients with cirrhosis and a non-SBP infection, the use of albumin to help improve renal and circulatory function is reasonable. There is no evidence that albumin will improve mortality and caution is warranted for patients at risk for pulmonary edema.
Dr. Rambachan is an academic hospital medicine fellow at the University of California, San Francisco.
References
1. Caironi P and Gattinoni L. The clinical use of albumin: the point of view of a specialist in intensive care. Blood Transfus. 2009;7(4):259-67. doi: 10.2450/2009.0002-09.
2. Paine CH et al. Albumin in cirrhosis: More than a colloid. Curr Treat Options Gastroenterol. 2019;17(2):231-43. doi: 10.1007/s11938-019-00227-4.
3. Walayat S et al. Role of albumin in cirrhosis: from a hospitalist’s perspective. J Community Hosp Intern Med Perspect. 2017;7(1):8-14. 2017 Mar 31. doi: 10.1080/20009666.2017.1302704.
4. Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline [for the] management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013 Apr;57(4):1651-3. doi: 10.1002/hep.26359.
5. European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis [published correction appears in J Hepatol. 2018 Nov;69(5):1207]. J Hepatol. 2018 Aug;69(2):406-60. doi: 10.1016/j.jhep.2018.03.024.
6. Guevara M et al. Albumin for bacterial infections other than spontaneous bacterial peritonitis in cirrhosis. A randomized, controlled study. J Hepatol. 2012 Oct;57(4):759-65. doi: 10.1016/j.jhep.2012.06.013.
7. Thévenot T et al. Effect of albumin in cirrhotic patients with infection other than spontaneous bacterial peritonitis. A randomized trial. J Hepatol. 2015 Apr;62(4):822-30. doi: 10.1016/j.jhep.2014.11.017.
8. Fernández J et al. Efficacy of albumin treatment for patients with cirrhosis and infections unrelated to spontaneous bacterial peritonitis. Clin Gastroenterol Hepatol. 2020 Apr;18(4):963-73.e14. doi: 10.1016/j.c gh.2019.07.055.
9. Di Pascoli M et al. Long-term administration of human albumin improves survival in patients with cirrhosis and refractory ascites. Liver Int. 2019 Jan;39(1):98-105. doi: 10.1111/liv.13968.
10. Caraceni P et al. Long-term albumin administration in decompensated cirrhosis (ANSWER): an open-label randomised trial [published correction appears in Lancet. 2018 Aug 4;392(10145):386]. Lancet. 2018 June;391(10138):2417-29. doi: 10.1016/S0140-6736(18)30840-7.
11. Fernández J et al. Effects of albumin treatment on systemic and portal hemodynamics and systemic inflammation in patients with decompensated cirrhosis. Gastroenterology. 2019 July;157(1):149-62. doi: 10.1053/j.gastro.2019.03.021.
12. Fasolato S et al. Renal failure and bacterial infections in patients with cirrhosis: Epidemiology and clinical features. Hepatology. 2007;45(1):223-9. doi: 10.1002/hep.21443.
Key points
- In patients with spontaneous bacterial peritonitis, hepatorenal syndrome, and for large volume paracentesis, albumin improves outcomes and is recommended by guidelines.
- In patients with cirrhosis and a non-SBP infection, there is some evidence that albumin may improve renal and circulatory function.
- Clinicians should be cautious about albumin use in patients at an elevated risk for development of pulmonary edema.
Quiz
Which of the following is not a guideline-recommended use of albumin for patients with cirrhosis?
A. Treatment of type 1 hepatorenal syndrome
B. Treatment of spontaneous bacterial peritonitis
C. To correct plasma albumin < 2.5 g/dL in nontransplant patients
D. Post large-volume paracentesis
The answer is C. Per the EASL and AASLD, A,B, and D are recommended. There is not strong evidence to support administering albumin to correct low plasma albumin.
Additional reading
- Bernardi M et al. Albumin in decompensated cirrhosis: new concepts and perspectives. Gut. 2020 June;69(6):1127-38. doi: 10.1136/gutjnl-2019-318843.
- Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline [for the] management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013 Apr;57(4):1651-3. doi: 10.1002/hep.26359.
- Paine CH et al. Albumin in cirrhosis: More than a colloid. Curr Treat Options Gastroenterol. 2019 June;17(2):231-43. doi: 10.1007/s11938-019-00227-4.
Case
A 56 year-old male with hypertension, alcohol use disorder, stage II chronic kidney disease, and biopsy-proven cirrhosis presents with fever and chills, pyuria, flank pain, and an acute kidney injury concerning for pyelonephritis. Is there a benefit in treating with albumin in addition to guideline-based antibiotics?
Brief overview of the issue
Albumin is a negatively charged human protein produced by the liver. Albumin comprises 50% of plasma protein and over 75% of plasma oncotic pressure.1 It was first used at Walter Reed Hospital in 1940 and subsequently for burn injuries after the attack on Pearl Harbor in 1941.2
Albumin serves several important physiologic functions including maintaining oncotic pressure, endothelial support, antioxidation, nitrogen oxide scavenging, and buffering and transport of solutes and drugs, including antibiotics. In cirrhosis, albumin is diluted due to sodium and water retention. There is increased redistribution, decreased synthesis by the liver, and impaired albumin molecule binding.3
For patients with liver disease, per the European Association for the Study of the Liver (EASL) and the American Association for the Study of Liver Diseases (AASLD), albumin should be administered to prevent post paracentesis circulatory dysfunction after large volume paracentesis, to prevent renal failure and mortality in the setting of spontaneous bacterial peritonitis (SBP), and in the diagnosis and treatment of hepatorenal syndrome (HRS) type I to potentially improve mortality.4,5 Beyond these three guideline-based indications, other uses for albumin for patients with liver disease have been proposed, including treatment of hyponatremia, posttransplant fluid resuscitation, diuretic unresponsive ascites, and long-term management of cirrhosis. There has yet to be strong evidence supporting these additional indications. However, given the known benefits of albumin in patients with SBP, there has been recent research into treatment of non-SBP infections, including urinary tract infections.
Overview of the data
There have been three randomized controlled trials (RCTs) regarding albumin administration for the treatment of non-SBP infections for hospitalized patients with cirrhosis. All three trials randomized patients to a treatment arm of albumin and antibiotics versus a control group of antibiotics alone. The treatment protocol prescribed 20% albumin with 1.5 g/kg on day 1 and 1.0 g/kg on day 3. The most common infections studied were pneumonia and urinary tract infection. These RCTs found that albumin administration was associated with improved renal and/or circulatory function, but not with a reduction in mortality.

First, there was a single center RCT by Guevara et al. in 2012 of 110 patients with cirrhosis and infection based on SIRS criteria.6 The primary outcome was 90-day survival with secondary outcomes of renal failure development, renal function at days 3,7 and 14, and circulatory function measured by plasma renin, aldosterone, and norepinephrine. Renal function and circulatory function improved in the albumin group, but not mortality. In a multivariable regression analysis, albumin was statistically predictive of survival (hazard ratio of 0.294).
Second, there was a multicenter RCT by Thévenot et al. in 2015 of 193 patients.7 The primary outcome was 90-day renal failure and the secondary outcome was 90-day survival. Renal failure was chosen as the primary endpoint because of its association with survival in this patient population. The treatment group had delayed onset of renal failure, but no difference in the development of 90-day renal failure or 90-day mortality rate. Notably, eight patients (8.3%) in the albumin group developed pulmonary edema with two deaths. This led the oversight committee to prematurely terminate the study.
Third and most recently, there was a multicenter RCT by Fernández et al. in 2019 of 118 patients.8 The primary outcome was in-hospital mortality, with secondary outcomes of circulatory dysfunction measured by plasma renin concentration, systemic inflammation measured by plasma IL-6 and biomarkers, complications including acute-on-chronic liver failure (ACLF) and nosocomial bacterial infections, and 90-day mortality. Between the albumin and control group, there were no differences in in-hospital mortality (13.1% vs. 10.5%, P > .66), inflammation, circulatory dysfunction, or liver severity. However, a significantly higher proportion of patients in the albumin group had resolution of their ACLF (82.3% vs. 33.3%, P = .003) and a lower proportion developed nosocomial infections (6.6% vs. 24.6%, P = .007). A major weakness of this study was that patients in the albumin group had a higher combined rate of ACLF and kidney dysfunction (44.3% vs. 24.6%, P = .02).
Beyond these three randomized controlled trials, there was a study on the long-term administration of albumin for patients with cirrhosis and ascites. Patients who received twice weekly albumin infusions had a lower 2-year mortality rate and a reduction in the incidence of both SBP and non-SBP infections.9 Another long-term study of albumin administration found similar results with greater 18-month survival and fewer non-SBP infections.10 A trial looking at inflammation in patients without bacterial infections and in biobanked samples from cirrhotic patients with bacterial infections found that treatment with albumin reduced systemic inflammation.11
In summary, the three RCTs looked at comparable patients with cirrhosis and a non-SBP infection and all underwent similar treatment protocols with 20% albumin dosed at 1.5 g/kg on day 1 and 1.0 g/kg on day 3. All studies evaluated mortality in either the primary or secondary outcome, and none found significant differences in mortality between treatment and control groups. Each study also evaluated and found improvement in renal and/or circulatory function. Fernández et al. also found increased resolution of ACLF, fewer nosocomial infections, and reduction in some inflammatory markers. However, all studies had relatively small sample sizes that were underpowered to detect mortality differences. Furthermore, randomization did not lead to well-matched groups, with the treatment group patients in the Fernández study having higher rates of ACLF and kidney dysfunction.
The data suggest that albumin may be beneficial in improving renal and circulatory function. In select patients with ACLF and elevated serum creatinine, albumin treatment may be considered. There has been discussion about the use of albumin preferentially in patients with subdiaphragmatic bacterial infections, most related to increased risk of renal failure such as biliary and urinary tract infections.12 The authors of these studies also note that albumin may be more beneficial in patients with higher baseline creatinine. Caution is warranted for patients with impaired cardiac function or poor respiratory status given the possibility of pulmonary edema. Finally, the high cost of albumin in many medical centers is a major limitation of this treatment approach.
Application of data to our patient
Our patient has cirrhosis and is acutely presenting with pyelonephritis and acute kidney injury. He has no baseline pulmonary disease or oxygen requirement. His recent transthoracic echocardiogram is reviewed and he has no evidence of cardiac disease.
Because he has an elevated creatinine, an infectious process associated with progressive renal failure, and is not at an elevated baseline risk of developing pulmonary edema, albumin would be reasonable to administer at 1.5 g/kg on day 1 and 1.0 g/kg on day 3 of hospitalization.
Bottom line
In certain patients with cirrhosis and a non-SBP infection, the use of albumin to help improve renal and circulatory function is reasonable. There is no evidence that albumin will improve mortality and caution is warranted for patients at risk for pulmonary edema.
Dr. Rambachan is an academic hospital medicine fellow at the University of California, San Francisco.
References
1. Caironi P and Gattinoni L. The clinical use of albumin: the point of view of a specialist in intensive care. Blood Transfus. 2009;7(4):259-67. doi: 10.2450/2009.0002-09.
2. Paine CH et al. Albumin in cirrhosis: More than a colloid. Curr Treat Options Gastroenterol. 2019;17(2):231-43. doi: 10.1007/s11938-019-00227-4.
3. Walayat S et al. Role of albumin in cirrhosis: from a hospitalist’s perspective. J Community Hosp Intern Med Perspect. 2017;7(1):8-14. 2017 Mar 31. doi: 10.1080/20009666.2017.1302704.
4. Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline [for the] management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013 Apr;57(4):1651-3. doi: 10.1002/hep.26359.
5. European Association for the Study of the Liver. EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis [published correction appears in J Hepatol. 2018 Nov;69(5):1207]. J Hepatol. 2018 Aug;69(2):406-60. doi: 10.1016/j.jhep.2018.03.024.
6. Guevara M et al. Albumin for bacterial infections other than spontaneous bacterial peritonitis in cirrhosis. A randomized, controlled study. J Hepatol. 2012 Oct;57(4):759-65. doi: 10.1016/j.jhep.2012.06.013.
7. Thévenot T et al. Effect of albumin in cirrhotic patients with infection other than spontaneous bacterial peritonitis. A randomized trial. J Hepatol. 2015 Apr;62(4):822-30. doi: 10.1016/j.jhep.2014.11.017.
8. Fernández J et al. Efficacy of albumin treatment for patients with cirrhosis and infections unrelated to spontaneous bacterial peritonitis. Clin Gastroenterol Hepatol. 2020 Apr;18(4):963-73.e14. doi: 10.1016/j.c gh.2019.07.055.
9. Di Pascoli M et al. Long-term administration of human albumin improves survival in patients with cirrhosis and refractory ascites. Liver Int. 2019 Jan;39(1):98-105. doi: 10.1111/liv.13968.
10. Caraceni P et al. Long-term albumin administration in decompensated cirrhosis (ANSWER): an open-label randomised trial [published correction appears in Lancet. 2018 Aug 4;392(10145):386]. Lancet. 2018 June;391(10138):2417-29. doi: 10.1016/S0140-6736(18)30840-7.
11. Fernández J et al. Effects of albumin treatment on systemic and portal hemodynamics and systemic inflammation in patients with decompensated cirrhosis. Gastroenterology. 2019 July;157(1):149-62. doi: 10.1053/j.gastro.2019.03.021.
12. Fasolato S et al. Renal failure and bacterial infections in patients with cirrhosis: Epidemiology and clinical features. Hepatology. 2007;45(1):223-9. doi: 10.1002/hep.21443.
Key points
- In patients with spontaneous bacterial peritonitis, hepatorenal syndrome, and for large volume paracentesis, albumin improves outcomes and is recommended by guidelines.
- In patients with cirrhosis and a non-SBP infection, there is some evidence that albumin may improve renal and circulatory function.
- Clinicians should be cautious about albumin use in patients at an elevated risk for development of pulmonary edema.
Quiz
Which of the following is not a guideline-recommended use of albumin for patients with cirrhosis?
A. Treatment of type 1 hepatorenal syndrome
B. Treatment of spontaneous bacterial peritonitis
C. To correct plasma albumin < 2.5 g/dL in nontransplant patients
D. Post large-volume paracentesis
The answer is C. Per the EASL and AASLD, A,B, and D are recommended. There is not strong evidence to support administering albumin to correct low plasma albumin.
Additional reading
- Bernardi M et al. Albumin in decompensated cirrhosis: new concepts and perspectives. Gut. 2020 June;69(6):1127-38. doi: 10.1136/gutjnl-2019-318843.
- Runyon BA; AASLD. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline [for the] management of adult patients with ascites due to cirrhosis 2012. Hepatology. 2013 Apr;57(4):1651-3. doi: 10.1002/hep.26359.
- Paine CH et al. Albumin in cirrhosis: More than a colloid. Curr Treat Options Gastroenterol. 2019 June;17(2):231-43. doi: 10.1007/s11938-019-00227-4.
Nurses ‘at the breaking point,’ consider quitting due to COVID issues: Survey
In the best of times, critical care nurses have one of the most difficult and stressful jobs in health care. The COVID-19 pandemic has made that immeasurably worse. As hospitals have been flooded with critically ill patients, nurses have been overwhelmed.
“What we’re hearing from our nurses is really shocking,” Amanda Bettencourt, PhD, APRN, CCRN-K, president-elect of the American Association of Critical-Care Nurses (AACN), told this news organization. “They’re saying they’re at the breaking point.”
Between August 26 and August 30, the AACN surveyed more than 6,000 critical care nurses, zeroing in on four key questions regarding the pandemic and its impact on nursing. The results were alarming – not only with regard to individual nurses but also for the nursing profession and the future of health care. A full 66% of those surveyed said their experiences during the pandemic have caused them to consider leaving nursing. The respondents’ take on their colleagues was even more concerning. Ninety-two percent agreed with the following two statements: “I believe the pandemic has depleted nurses at my hospital. Their careers will be shorter than they intended.”
“This puts the entire health care system at risk,” says Dr. Bettencourt, who is assistant professor in the department of family and community health at the University of Pennsylvania School of Nursing, Philadelphia. Intensive care unit (ICU) nurses are highly trained and are skilled in caring for critically ill patients with complex medical needs. “It’s not easy to replace a critical care nurse when one leaves,” she says.
And when nurses leave, patients suffer, says Beth Wathen, MSN, RN, CCRN-K, president of the ACCN and frontline nurse at Children’s Hospital Colorado, Aurora. “Hospitals can have all the beds and all the rooms and all the equipment they want, but without nurses and others at the front lines to provide that essential care, none of it really matters, whether we’re talking about caring for COVID patients or caring for patients with other health ailments.”
Heartbreak of the unvaccinated
The problem is not just overwork because of the flood of COVID-19 patients. The emotional strain is enormous as well. “What’s demoralizing for us is not that patients are sick and that it’s physically exhausting to take care of sick patients. We’re used to that,” says Dr. Bettencourt.
But few nurses have experienced the sheer magnitude of patients caused by this pandemic. “The past 18 months have been grueling,” says Ms. Wathen. “The burden on frontline caregivers and our nurses at the front line has been immense.”
The situation is made worse by how unnecessary much of the suffering is at this point. Seventy-six percent of the survey’s respondents agreed with the following statement: “People who hold out on getting vaccinated undermine nurses’ physical and mental well-being.” That comment doesn’t convey the nature or extent of the effect on caregivers’ well-being. “That 9 out of 10 of the people we’re seeing in ICU right now are unvaccinated just adds to the sense of heartbreak and frustration,” says Ms. Wathen. “These deaths don’t have to be happening right now. And that’s hard to bear witness to.”
The politicization of public health has also taken a toll. “That’s been the hard part of this entire pandemic,” says Ms. Wathen. “This really isn’t at all about politics. This is about your health; this is about my health. This is about our collective health as a community and as a country.”
Like the rest of the world, nurses are also concerned about their own loved ones. The survey statement, “I fear taking care of patients with COVID puts my family’s health at risk,” garnered 67% agreement. Ms. Wathen points out that nurses take the appropriate precautions but still worry about taking infection home to their families. “This disease is a tricky one,” she says. She points out that until this pandemic is over, in addition to being vaccinated, nurses and the public still need to be vigilant about wearing masks, social distancing, and taking other precautions to ensure the safety of us all. “Our individual decisions don’t just affect ourselves. They affect our family, the people in our circle, and the people in our community,” she says.
Avoiding a professional exodus
It’s too early yet to have reliable national data on how many nurses have already left their jobs because of COVID-19, but it is clear that there are too few nurses of all kinds. Earlier this month, the American Nurses Association sent a letter to the U.S. Secretary of Health and Human Services urging the agency to declare the nursing shortage a crisis and to take immediate steps to find solutions.
The nursing shortage predates the pandemic, and COVID-19 has brought a simmering problem to a boil. Nurses are calling on the public and the health care system for help. From inside the industry, the needs are pretty much what they were before the pandemic. Dr. Bettencourt and Ms. Wathen point to the need for supportive leadership, healthy work environments, sufficient staffing to meet patients’ needs, and a voice in decisions, such as decisions about staffing, that affect nurses and their patients. Nurses want to be heard and appreciated. “It’s not that these are new things,” says Dr. Bettencourt. “We just need them even more now because we’re stressed even more than we were before.”
Critical care nurses have a different request of the public. They’re asking – pleading, actually – with the public to get vaccinated, wear masks in public, practice social distancing, and bring this pandemic to an end.
“COVID kills, and it’s a really difficult, tragic, and lonely death,” says Ms. Wathen. “We’ve witnessed hundreds of thousands of those deaths. But now we have a way to stop it. If many more people get vaccinated, we can stop this pandemic. And hopefully that will stop this current trend of nurses leaving.”
A version of this article first appeared on Medscape.com.
In the best of times, critical care nurses have one of the most difficult and stressful jobs in health care. The COVID-19 pandemic has made that immeasurably worse. As hospitals have been flooded with critically ill patients, nurses have been overwhelmed.
“What we’re hearing from our nurses is really shocking,” Amanda Bettencourt, PhD, APRN, CCRN-K, president-elect of the American Association of Critical-Care Nurses (AACN), told this news organization. “They’re saying they’re at the breaking point.”
Between August 26 and August 30, the AACN surveyed more than 6,000 critical care nurses, zeroing in on four key questions regarding the pandemic and its impact on nursing. The results were alarming – not only with regard to individual nurses but also for the nursing profession and the future of health care. A full 66% of those surveyed said their experiences during the pandemic have caused them to consider leaving nursing. The respondents’ take on their colleagues was even more concerning. Ninety-two percent agreed with the following two statements: “I believe the pandemic has depleted nurses at my hospital. Their careers will be shorter than they intended.”
“This puts the entire health care system at risk,” says Dr. Bettencourt, who is assistant professor in the department of family and community health at the University of Pennsylvania School of Nursing, Philadelphia. Intensive care unit (ICU) nurses are highly trained and are skilled in caring for critically ill patients with complex medical needs. “It’s not easy to replace a critical care nurse when one leaves,” she says.
And when nurses leave, patients suffer, says Beth Wathen, MSN, RN, CCRN-K, president of the ACCN and frontline nurse at Children’s Hospital Colorado, Aurora. “Hospitals can have all the beds and all the rooms and all the equipment they want, but without nurses and others at the front lines to provide that essential care, none of it really matters, whether we’re talking about caring for COVID patients or caring for patients with other health ailments.”
Heartbreak of the unvaccinated
The problem is not just overwork because of the flood of COVID-19 patients. The emotional strain is enormous as well. “What’s demoralizing for us is not that patients are sick and that it’s physically exhausting to take care of sick patients. We’re used to that,” says Dr. Bettencourt.
But few nurses have experienced the sheer magnitude of patients caused by this pandemic. “The past 18 months have been grueling,” says Ms. Wathen. “The burden on frontline caregivers and our nurses at the front line has been immense.”
The situation is made worse by how unnecessary much of the suffering is at this point. Seventy-six percent of the survey’s respondents agreed with the following statement: “People who hold out on getting vaccinated undermine nurses’ physical and mental well-being.” That comment doesn’t convey the nature or extent of the effect on caregivers’ well-being. “That 9 out of 10 of the people we’re seeing in ICU right now are unvaccinated just adds to the sense of heartbreak and frustration,” says Ms. Wathen. “These deaths don’t have to be happening right now. And that’s hard to bear witness to.”
The politicization of public health has also taken a toll. “That’s been the hard part of this entire pandemic,” says Ms. Wathen. “This really isn’t at all about politics. This is about your health; this is about my health. This is about our collective health as a community and as a country.”
Like the rest of the world, nurses are also concerned about their own loved ones. The survey statement, “I fear taking care of patients with COVID puts my family’s health at risk,” garnered 67% agreement. Ms. Wathen points out that nurses take the appropriate precautions but still worry about taking infection home to their families. “This disease is a tricky one,” she says. She points out that until this pandemic is over, in addition to being vaccinated, nurses and the public still need to be vigilant about wearing masks, social distancing, and taking other precautions to ensure the safety of us all. “Our individual decisions don’t just affect ourselves. They affect our family, the people in our circle, and the people in our community,” she says.
Avoiding a professional exodus
It’s too early yet to have reliable national data on how many nurses have already left their jobs because of COVID-19, but it is clear that there are too few nurses of all kinds. Earlier this month, the American Nurses Association sent a letter to the U.S. Secretary of Health and Human Services urging the agency to declare the nursing shortage a crisis and to take immediate steps to find solutions.
The nursing shortage predates the pandemic, and COVID-19 has brought a simmering problem to a boil. Nurses are calling on the public and the health care system for help. From inside the industry, the needs are pretty much what they were before the pandemic. Dr. Bettencourt and Ms. Wathen point to the need for supportive leadership, healthy work environments, sufficient staffing to meet patients’ needs, and a voice in decisions, such as decisions about staffing, that affect nurses and their patients. Nurses want to be heard and appreciated. “It’s not that these are new things,” says Dr. Bettencourt. “We just need them even more now because we’re stressed even more than we were before.”
Critical care nurses have a different request of the public. They’re asking – pleading, actually – with the public to get vaccinated, wear masks in public, practice social distancing, and bring this pandemic to an end.
“COVID kills, and it’s a really difficult, tragic, and lonely death,” says Ms. Wathen. “We’ve witnessed hundreds of thousands of those deaths. But now we have a way to stop it. If many more people get vaccinated, we can stop this pandemic. And hopefully that will stop this current trend of nurses leaving.”
A version of this article first appeared on Medscape.com.
In the best of times, critical care nurses have one of the most difficult and stressful jobs in health care. The COVID-19 pandemic has made that immeasurably worse. As hospitals have been flooded with critically ill patients, nurses have been overwhelmed.
“What we’re hearing from our nurses is really shocking,” Amanda Bettencourt, PhD, APRN, CCRN-K, president-elect of the American Association of Critical-Care Nurses (AACN), told this news organization. “They’re saying they’re at the breaking point.”
Between August 26 and August 30, the AACN surveyed more than 6,000 critical care nurses, zeroing in on four key questions regarding the pandemic and its impact on nursing. The results were alarming – not only with regard to individual nurses but also for the nursing profession and the future of health care. A full 66% of those surveyed said their experiences during the pandemic have caused them to consider leaving nursing. The respondents’ take on their colleagues was even more concerning. Ninety-two percent agreed with the following two statements: “I believe the pandemic has depleted nurses at my hospital. Their careers will be shorter than they intended.”
“This puts the entire health care system at risk,” says Dr. Bettencourt, who is assistant professor in the department of family and community health at the University of Pennsylvania School of Nursing, Philadelphia. Intensive care unit (ICU) nurses are highly trained and are skilled in caring for critically ill patients with complex medical needs. “It’s not easy to replace a critical care nurse when one leaves,” she says.
And when nurses leave, patients suffer, says Beth Wathen, MSN, RN, CCRN-K, president of the ACCN and frontline nurse at Children’s Hospital Colorado, Aurora. “Hospitals can have all the beds and all the rooms and all the equipment they want, but without nurses and others at the front lines to provide that essential care, none of it really matters, whether we’re talking about caring for COVID patients or caring for patients with other health ailments.”
Heartbreak of the unvaccinated
The problem is not just overwork because of the flood of COVID-19 patients. The emotional strain is enormous as well. “What’s demoralizing for us is not that patients are sick and that it’s physically exhausting to take care of sick patients. We’re used to that,” says Dr. Bettencourt.
But few nurses have experienced the sheer magnitude of patients caused by this pandemic. “The past 18 months have been grueling,” says Ms. Wathen. “The burden on frontline caregivers and our nurses at the front line has been immense.”
The situation is made worse by how unnecessary much of the suffering is at this point. Seventy-six percent of the survey’s respondents agreed with the following statement: “People who hold out on getting vaccinated undermine nurses’ physical and mental well-being.” That comment doesn’t convey the nature or extent of the effect on caregivers’ well-being. “That 9 out of 10 of the people we’re seeing in ICU right now are unvaccinated just adds to the sense of heartbreak and frustration,” says Ms. Wathen. “These deaths don’t have to be happening right now. And that’s hard to bear witness to.”
The politicization of public health has also taken a toll. “That’s been the hard part of this entire pandemic,” says Ms. Wathen. “This really isn’t at all about politics. This is about your health; this is about my health. This is about our collective health as a community and as a country.”
Like the rest of the world, nurses are also concerned about their own loved ones. The survey statement, “I fear taking care of patients with COVID puts my family’s health at risk,” garnered 67% agreement. Ms. Wathen points out that nurses take the appropriate precautions but still worry about taking infection home to their families. “This disease is a tricky one,” she says. She points out that until this pandemic is over, in addition to being vaccinated, nurses and the public still need to be vigilant about wearing masks, social distancing, and taking other precautions to ensure the safety of us all. “Our individual decisions don’t just affect ourselves. They affect our family, the people in our circle, and the people in our community,” she says.
Avoiding a professional exodus
It’s too early yet to have reliable national data on how many nurses have already left their jobs because of COVID-19, but it is clear that there are too few nurses of all kinds. Earlier this month, the American Nurses Association sent a letter to the U.S. Secretary of Health and Human Services urging the agency to declare the nursing shortage a crisis and to take immediate steps to find solutions.
The nursing shortage predates the pandemic, and COVID-19 has brought a simmering problem to a boil. Nurses are calling on the public and the health care system for help. From inside the industry, the needs are pretty much what they were before the pandemic. Dr. Bettencourt and Ms. Wathen point to the need for supportive leadership, healthy work environments, sufficient staffing to meet patients’ needs, and a voice in decisions, such as decisions about staffing, that affect nurses and their patients. Nurses want to be heard and appreciated. “It’s not that these are new things,” says Dr. Bettencourt. “We just need them even more now because we’re stressed even more than we were before.”
Critical care nurses have a different request of the public. They’re asking – pleading, actually – with the public to get vaccinated, wear masks in public, practice social distancing, and bring this pandemic to an end.
“COVID kills, and it’s a really difficult, tragic, and lonely death,” says Ms. Wathen. “We’ve witnessed hundreds of thousands of those deaths. But now we have a way to stop it. If many more people get vaccinated, we can stop this pandemic. And hopefully that will stop this current trend of nurses leaving.”
A version of this article first appeared on Medscape.com.
Decline in child COVID may signal end of latest surge
A second consecutive week of falling COVID-19 cases in children, along with continued declines in new admissions, may indicate that the latest surge has peaked.
Children made up over 25% of all new cases each week over that 3-week period covering the end of August and the first half of September, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.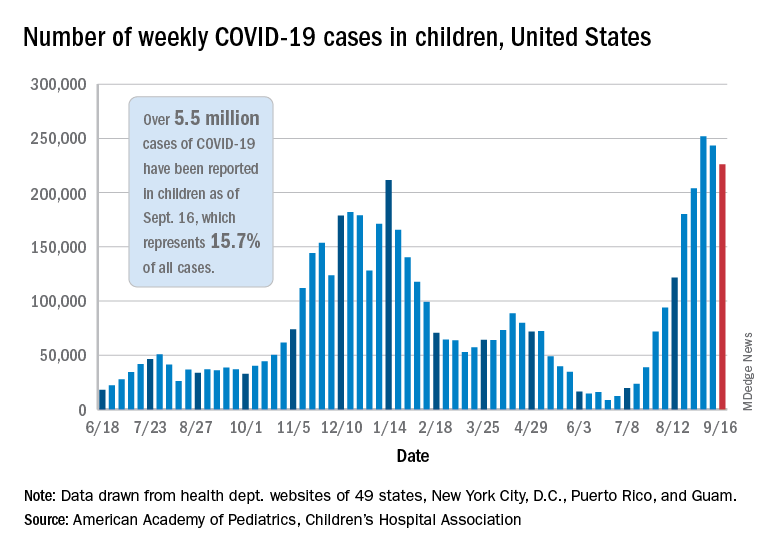
New hospitalizations in children aged 0-17 years peaked on Sept. 4 – when the rate reached 0.51 per 100,000 population – and were down to 0.47 as of Sept. 11, the latest date for which data should be considered reliable, the Centers for Disease Control and Prevention said.
The CDC’s data largely agree with the AAP/CHA report, showing that cases peaked during the week of Aug. 22-28. Cases per 100,000 for children that week looked like this: 154.7 (age 0-4 years), 276.6 (5-11 years), 320.0 (12-15), and 334.1 (16-17). The highest rates that week among adults were 288.6 per 100,000 in 30- to 39-year-olds and 286.5 for those aged 18-29, the CDC said on its COVID Data Tracker.
By the week of Sept. 5-11 – reporting delays can affect more recent data – the rates in children were down more than 20% in each of the four age groups, according to the CDC.
Vaccinations among children, unfortunately, continue to decline. Vaccine initiations for 12- to 15-year-olds slipped from 199,000 (Sept. 7-13) to 179,000 during the week of Sept. 14-20, while the 16- to 17-year-olds went from almost 83,000 down to 75,000. Initiations have dropped for 6 straight weeks in both age groups, based on the CDC data.
Despite those declines, however, the 16- and 17-year-olds just passed a couple of vaccination milestones. More than 60% – 60.9%, to be exact – have now received at least one dose of COVID vaccine, and 50.3% can be considered fully vaccinated. For those aged 12-15, the corresponding figures are 53.1% and 42.0%, the CDC reported.
When children under age 12 years are included – through clinical trial involvement or incorrect birth dates – the CDC data put the total count of Americans under age 18 who have received at least one dose of vaccine at almost 12.8 million, with vaccination complete in 10.3 million.
Total cases, as calculated by the APA and CHA, are now over 5.5 million, although that figure includes cases in individuals as old as 20 years, since many states differ from the CDC on the age range for a child. The CDC’s COVID Data Tracker put the total for children aged 0-17 at nearly 4.6 million.
The total number of COVID-related deaths in children is 480 as of Sept. 16, the AAP and CHA said, based on data from 45 states, New York, City, Puerto Rico, and Guam, but the CDC provides a higher number, 548, since the pandemic began. Children aged 0-4 years represent the largest share (32.3%) of those 548 deaths, followed by the 12- to 15-year-olds (26.5%), based on the CDC data.
A second consecutive week of falling COVID-19 cases in children, along with continued declines in new admissions, may indicate that the latest surge has peaked.
Children made up over 25% of all new cases each week over that 3-week period covering the end of August and the first half of September, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.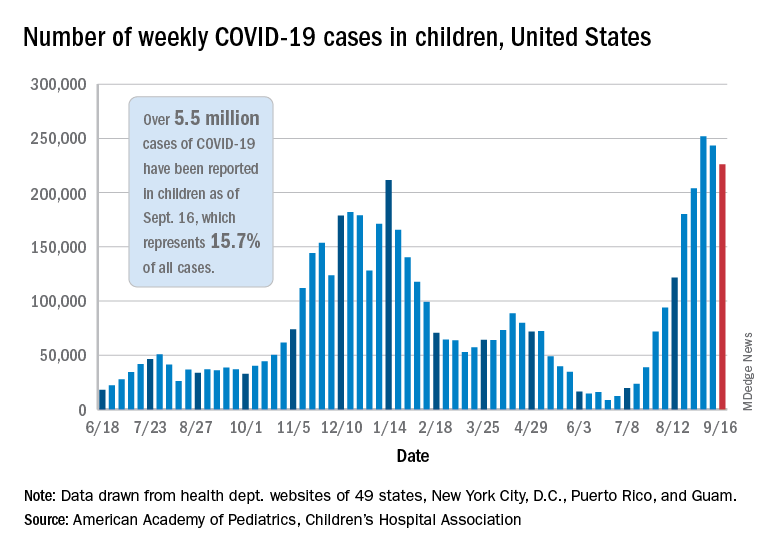
New hospitalizations in children aged 0-17 years peaked on Sept. 4 – when the rate reached 0.51 per 100,000 population – and were down to 0.47 as of Sept. 11, the latest date for which data should be considered reliable, the Centers for Disease Control and Prevention said.
The CDC’s data largely agree with the AAP/CHA report, showing that cases peaked during the week of Aug. 22-28. Cases per 100,000 for children that week looked like this: 154.7 (age 0-4 years), 276.6 (5-11 years), 320.0 (12-15), and 334.1 (16-17). The highest rates that week among adults were 288.6 per 100,000 in 30- to 39-year-olds and 286.5 for those aged 18-29, the CDC said on its COVID Data Tracker.
By the week of Sept. 5-11 – reporting delays can affect more recent data – the rates in children were down more than 20% in each of the four age groups, according to the CDC.
Vaccinations among children, unfortunately, continue to decline. Vaccine initiations for 12- to 15-year-olds slipped from 199,000 (Sept. 7-13) to 179,000 during the week of Sept. 14-20, while the 16- to 17-year-olds went from almost 83,000 down to 75,000. Initiations have dropped for 6 straight weeks in both age groups, based on the CDC data.
Despite those declines, however, the 16- and 17-year-olds just passed a couple of vaccination milestones. More than 60% – 60.9%, to be exact – have now received at least one dose of COVID vaccine, and 50.3% can be considered fully vaccinated. For those aged 12-15, the corresponding figures are 53.1% and 42.0%, the CDC reported.
When children under age 12 years are included – through clinical trial involvement or incorrect birth dates – the CDC data put the total count of Americans under age 18 who have received at least one dose of vaccine at almost 12.8 million, with vaccination complete in 10.3 million.
Total cases, as calculated by the APA and CHA, are now over 5.5 million, although that figure includes cases in individuals as old as 20 years, since many states differ from the CDC on the age range for a child. The CDC’s COVID Data Tracker put the total for children aged 0-17 at nearly 4.6 million.
The total number of COVID-related deaths in children is 480 as of Sept. 16, the AAP and CHA said, based on data from 45 states, New York, City, Puerto Rico, and Guam, but the CDC provides a higher number, 548, since the pandemic began. Children aged 0-4 years represent the largest share (32.3%) of those 548 deaths, followed by the 12- to 15-year-olds (26.5%), based on the CDC data.
A second consecutive week of falling COVID-19 cases in children, along with continued declines in new admissions, may indicate that the latest surge has peaked.
Children made up over 25% of all new cases each week over that 3-week period covering the end of August and the first half of September, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.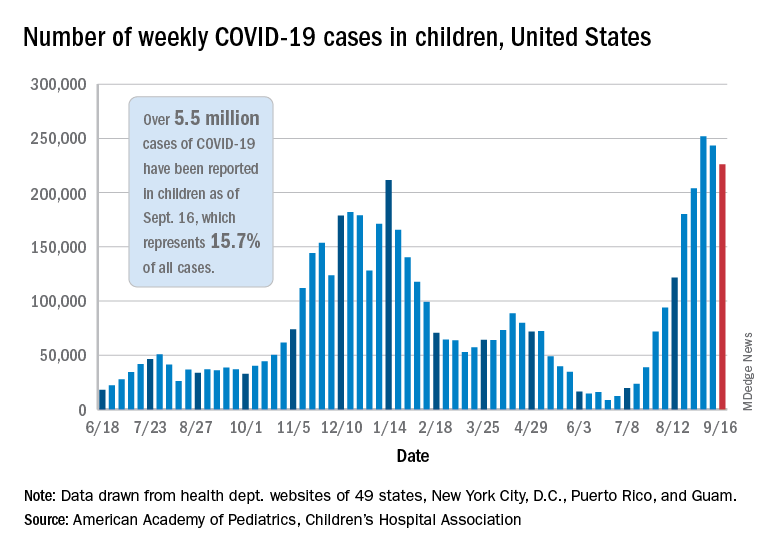
New hospitalizations in children aged 0-17 years peaked on Sept. 4 – when the rate reached 0.51 per 100,000 population – and were down to 0.47 as of Sept. 11, the latest date for which data should be considered reliable, the Centers for Disease Control and Prevention said.
The CDC’s data largely agree with the AAP/CHA report, showing that cases peaked during the week of Aug. 22-28. Cases per 100,000 for children that week looked like this: 154.7 (age 0-4 years), 276.6 (5-11 years), 320.0 (12-15), and 334.1 (16-17). The highest rates that week among adults were 288.6 per 100,000 in 30- to 39-year-olds and 286.5 for those aged 18-29, the CDC said on its COVID Data Tracker.
By the week of Sept. 5-11 – reporting delays can affect more recent data – the rates in children were down more than 20% in each of the four age groups, according to the CDC.
Vaccinations among children, unfortunately, continue to decline. Vaccine initiations for 12- to 15-year-olds slipped from 199,000 (Sept. 7-13) to 179,000 during the week of Sept. 14-20, while the 16- to 17-year-olds went from almost 83,000 down to 75,000. Initiations have dropped for 6 straight weeks in both age groups, based on the CDC data.
Despite those declines, however, the 16- and 17-year-olds just passed a couple of vaccination milestones. More than 60% – 60.9%, to be exact – have now received at least one dose of COVID vaccine, and 50.3% can be considered fully vaccinated. For those aged 12-15, the corresponding figures are 53.1% and 42.0%, the CDC reported.
When children under age 12 years are included – through clinical trial involvement or incorrect birth dates – the CDC data put the total count of Americans under age 18 who have received at least one dose of vaccine at almost 12.8 million, with vaccination complete in 10.3 million.
Total cases, as calculated by the APA and CHA, are now over 5.5 million, although that figure includes cases in individuals as old as 20 years, since many states differ from the CDC on the age range for a child. The CDC’s COVID Data Tracker put the total for children aged 0-17 at nearly 4.6 million.
The total number of COVID-related deaths in children is 480 as of Sept. 16, the AAP and CHA said, based on data from 45 states, New York, City, Puerto Rico, and Guam, but the CDC provides a higher number, 548, since the pandemic began. Children aged 0-4 years represent the largest share (32.3%) of those 548 deaths, followed by the 12- to 15-year-olds (26.5%), based on the CDC data.
Nurses ‘at the breaking point,’ consider quitting due to COVID issues: Survey
As hospitals have been flooded with critically ill patients, nurses have been overwhelmed.
“What we’re hearing from our nurses is really shocking,” Amanda Bettencourt, PhD, APRN, CCRN-K, president-elect of the American Association of Critical-Care Nurses (AACN), said in an interview. “They’re saying they’re at the breaking point.”
Between Aug. 26 and Aug. 30, the AACN surveyed more than 6,000 critical care nurses, zeroing in on four key questions regarding the pandemic and its impact on nursing. The results were alarming – not only with regard to individual nurses but also for the nursing profession and the future of health care. A full 66% of those surveyed said their experiences during the pandemic have caused them to consider leaving nursing. The respondents’ take on their colleagues was even more concerning. Ninety-two percent agreed with the following two statements: “I believe the pandemic has depleted nurses at my hospital. Their careers will be shorter than they intended.”
“This puts the entire health care system at risk,” says Dr. Bettencourt, assistant professor in the department of family and community health at the University of Pennsylvania School of Nursing, Philadelphia. Intensive care unit (ICU) nurses are highly trained and are skilled in caring for critically ill patients with complex medical needs. “It’s not easy to replace a critical care nurse when one leaves,” she said.
And when nurses leave, patients suffer, said Beth Wathen, MSN, RN, CCRN-K, president of the ACCN and frontline nurse at Children’s Hospital Colorado, in Aurora. “Hospitals can have all the beds and all the rooms and all the equipment they want, but without nurses and others at the front lines to provide that essential care, none of it really matters, whether we’re talking about caring for COVID patients or caring for patients with other health ailments.”
Heartbreak of the unvaccinated
The problem is not just overwork because of the flood of COVID-19 patients. The emotional strain is enormous as well. “What’s demoralizing for us is not that patients are sick and that it’s physically exhausting to take care of sick patients. We’re used to that,” said Dr. Bettencourt.
But few nurses have experienced the sheer magnitude of patients caused by this pandemic. “The past 18 months have been grueling,” says Ms. Wathen. “The burden on frontline caregivers and our nurses at the front line has been immense.”
The situation is made worse by how unnecessary much of the suffering is at this point. Seventy-six percent of the survey’s respondents agreed with the following statement: “People who hold out on getting vaccinated undermine nurses’ physical and mental well-being.” That comment doesn’t convey the nature or extent of the effect on caregivers’ well-being. “That 9 out of 10 of the people we’re seeing in ICU right now are unvaccinated just adds to the sense of heartbreak and frustration,” says Ms. Wathen. “These deaths don’t have to be happening right now. And that’s hard to bear witness to.”
The politicization of public health has also taken a toll. “That’s been the hard part of this entire pandemic,” says Ms. Wathen. “This really isn’t at all about politics. This is about your health; this is about my health. This is about our collective health as a community and as a country.”
Like the rest of the world, nurses are also concerned about their own loved ones. The survey statement, “I fear taking care of patients with COVID puts my family’s health at risk,” garnered 67% agreement. Ms. Wathen points out that nurses take the appropriate precautions but still worry about taking infection home to their families. “This disease is a tricky one,” she says. She points out that until this pandemic is over, in addition to being vaccinated, nurses and the public still need to be vigilant about wearing masks, social distancing, and taking other precautions to ensure the safety of us all. “Our individual decisions don’t just affect ourselves. They affect our family, the people in our circle, and the people in our community,” she said.
Avoiding a professional exodus
It’s too early yet to have reliable national data on how many nurses have already left their jobs because of COVID-19, but it is clear that there are too few nurses of all kinds. The American Nurses Association sent a letter to the U.S. Secretary of Health and Human Services urging the agency to declare the nursing shortage a crisis and to take immediate steps to find solutions.
The nursing shortage predates the pandemic, and COVID-19 has brought a simmering problem to the boil. Nurses are calling on the public and the health care system for help. From inside the industry, the needs are pretty much what they were before the pandemic. Dr. Bettencourt and Ms. Wathen point to the need for supportive leadership, healthy work environments, sufficient staffing to meet patients’ needs, and a voice in decisions, such as decisions about staffing, that affect nurses and their patients. Nurses want to be heard and appreciated. “It’s not that these are new things,” said Dr. Bettencourt. “We just need them even more now because we’re stressed even more than we were before.”
Critical care nurses have a different request of the public. They’re asking – pleading, actually – with the public to get vaccinated, wear masks in public, practice social distancing, and bring this pandemic to an end.
“COVID kills, and it’s a really difficult, tragic, and lonely death,” said Ms. Wathen. “We’ve witnessed hundreds of thousands of those deaths. But now we have a way to stop it. If many more people get vaccinated, we can stop this pandemic. And hopefully that will stop this current trend of nurses leaving.”
A version of this article first appeared on Medscape.com.
As hospitals have been flooded with critically ill patients, nurses have been overwhelmed.
“What we’re hearing from our nurses is really shocking,” Amanda Bettencourt, PhD, APRN, CCRN-K, president-elect of the American Association of Critical-Care Nurses (AACN), said in an interview. “They’re saying they’re at the breaking point.”
Between Aug. 26 and Aug. 30, the AACN surveyed more than 6,000 critical care nurses, zeroing in on four key questions regarding the pandemic and its impact on nursing. The results were alarming – not only with regard to individual nurses but also for the nursing profession and the future of health care. A full 66% of those surveyed said their experiences during the pandemic have caused them to consider leaving nursing. The respondents’ take on their colleagues was even more concerning. Ninety-two percent agreed with the following two statements: “I believe the pandemic has depleted nurses at my hospital. Their careers will be shorter than they intended.”
“This puts the entire health care system at risk,” says Dr. Bettencourt, assistant professor in the department of family and community health at the University of Pennsylvania School of Nursing, Philadelphia. Intensive care unit (ICU) nurses are highly trained and are skilled in caring for critically ill patients with complex medical needs. “It’s not easy to replace a critical care nurse when one leaves,” she said.
And when nurses leave, patients suffer, said Beth Wathen, MSN, RN, CCRN-K, president of the ACCN and frontline nurse at Children’s Hospital Colorado, in Aurora. “Hospitals can have all the beds and all the rooms and all the equipment they want, but without nurses and others at the front lines to provide that essential care, none of it really matters, whether we’re talking about caring for COVID patients or caring for patients with other health ailments.”
Heartbreak of the unvaccinated
The problem is not just overwork because of the flood of COVID-19 patients. The emotional strain is enormous as well. “What’s demoralizing for us is not that patients are sick and that it’s physically exhausting to take care of sick patients. We’re used to that,” said Dr. Bettencourt.
But few nurses have experienced the sheer magnitude of patients caused by this pandemic. “The past 18 months have been grueling,” says Ms. Wathen. “The burden on frontline caregivers and our nurses at the front line has been immense.”
The situation is made worse by how unnecessary much of the suffering is at this point. Seventy-six percent of the survey’s respondents agreed with the following statement: “People who hold out on getting vaccinated undermine nurses’ physical and mental well-being.” That comment doesn’t convey the nature or extent of the effect on caregivers’ well-being. “That 9 out of 10 of the people we’re seeing in ICU right now are unvaccinated just adds to the sense of heartbreak and frustration,” says Ms. Wathen. “These deaths don’t have to be happening right now. And that’s hard to bear witness to.”
The politicization of public health has also taken a toll. “That’s been the hard part of this entire pandemic,” says Ms. Wathen. “This really isn’t at all about politics. This is about your health; this is about my health. This is about our collective health as a community and as a country.”
Like the rest of the world, nurses are also concerned about their own loved ones. The survey statement, “I fear taking care of patients with COVID puts my family’s health at risk,” garnered 67% agreement. Ms. Wathen points out that nurses take the appropriate precautions but still worry about taking infection home to their families. “This disease is a tricky one,” she says. She points out that until this pandemic is over, in addition to being vaccinated, nurses and the public still need to be vigilant about wearing masks, social distancing, and taking other precautions to ensure the safety of us all. “Our individual decisions don’t just affect ourselves. They affect our family, the people in our circle, and the people in our community,” she said.
Avoiding a professional exodus
It’s too early yet to have reliable national data on how many nurses have already left their jobs because of COVID-19, but it is clear that there are too few nurses of all kinds. The American Nurses Association sent a letter to the U.S. Secretary of Health and Human Services urging the agency to declare the nursing shortage a crisis and to take immediate steps to find solutions.
The nursing shortage predates the pandemic, and COVID-19 has brought a simmering problem to the boil. Nurses are calling on the public and the health care system for help. From inside the industry, the needs are pretty much what they were before the pandemic. Dr. Bettencourt and Ms. Wathen point to the need for supportive leadership, healthy work environments, sufficient staffing to meet patients’ needs, and a voice in decisions, such as decisions about staffing, that affect nurses and their patients. Nurses want to be heard and appreciated. “It’s not that these are new things,” said Dr. Bettencourt. “We just need them even more now because we’re stressed even more than we were before.”
Critical care nurses have a different request of the public. They’re asking – pleading, actually – with the public to get vaccinated, wear masks in public, practice social distancing, and bring this pandemic to an end.
“COVID kills, and it’s a really difficult, tragic, and lonely death,” said Ms. Wathen. “We’ve witnessed hundreds of thousands of those deaths. But now we have a way to stop it. If many more people get vaccinated, we can stop this pandemic. And hopefully that will stop this current trend of nurses leaving.”
A version of this article first appeared on Medscape.com.
As hospitals have been flooded with critically ill patients, nurses have been overwhelmed.
“What we’re hearing from our nurses is really shocking,” Amanda Bettencourt, PhD, APRN, CCRN-K, president-elect of the American Association of Critical-Care Nurses (AACN), said in an interview. “They’re saying they’re at the breaking point.”
Between Aug. 26 and Aug. 30, the AACN surveyed more than 6,000 critical care nurses, zeroing in on four key questions regarding the pandemic and its impact on nursing. The results were alarming – not only with regard to individual nurses but also for the nursing profession and the future of health care. A full 66% of those surveyed said their experiences during the pandemic have caused them to consider leaving nursing. The respondents’ take on their colleagues was even more concerning. Ninety-two percent agreed with the following two statements: “I believe the pandemic has depleted nurses at my hospital. Their careers will be shorter than they intended.”
“This puts the entire health care system at risk,” says Dr. Bettencourt, assistant professor in the department of family and community health at the University of Pennsylvania School of Nursing, Philadelphia. Intensive care unit (ICU) nurses are highly trained and are skilled in caring for critically ill patients with complex medical needs. “It’s not easy to replace a critical care nurse when one leaves,” she said.
And when nurses leave, patients suffer, said Beth Wathen, MSN, RN, CCRN-K, president of the ACCN and frontline nurse at Children’s Hospital Colorado, in Aurora. “Hospitals can have all the beds and all the rooms and all the equipment they want, but without nurses and others at the front lines to provide that essential care, none of it really matters, whether we’re talking about caring for COVID patients or caring for patients with other health ailments.”
Heartbreak of the unvaccinated
The problem is not just overwork because of the flood of COVID-19 patients. The emotional strain is enormous as well. “What’s demoralizing for us is not that patients are sick and that it’s physically exhausting to take care of sick patients. We’re used to that,” said Dr. Bettencourt.
But few nurses have experienced the sheer magnitude of patients caused by this pandemic. “The past 18 months have been grueling,” says Ms. Wathen. “The burden on frontline caregivers and our nurses at the front line has been immense.”
The situation is made worse by how unnecessary much of the suffering is at this point. Seventy-six percent of the survey’s respondents agreed with the following statement: “People who hold out on getting vaccinated undermine nurses’ physical and mental well-being.” That comment doesn’t convey the nature or extent of the effect on caregivers’ well-being. “That 9 out of 10 of the people we’re seeing in ICU right now are unvaccinated just adds to the sense of heartbreak and frustration,” says Ms. Wathen. “These deaths don’t have to be happening right now. And that’s hard to bear witness to.”
The politicization of public health has also taken a toll. “That’s been the hard part of this entire pandemic,” says Ms. Wathen. “This really isn’t at all about politics. This is about your health; this is about my health. This is about our collective health as a community and as a country.”
Like the rest of the world, nurses are also concerned about their own loved ones. The survey statement, “I fear taking care of patients with COVID puts my family’s health at risk,” garnered 67% agreement. Ms. Wathen points out that nurses take the appropriate precautions but still worry about taking infection home to their families. “This disease is a tricky one,” she says. She points out that until this pandemic is over, in addition to being vaccinated, nurses and the public still need to be vigilant about wearing masks, social distancing, and taking other precautions to ensure the safety of us all. “Our individual decisions don’t just affect ourselves. They affect our family, the people in our circle, and the people in our community,” she said.
Avoiding a professional exodus
It’s too early yet to have reliable national data on how many nurses have already left their jobs because of COVID-19, but it is clear that there are too few nurses of all kinds. The American Nurses Association sent a letter to the U.S. Secretary of Health and Human Services urging the agency to declare the nursing shortage a crisis and to take immediate steps to find solutions.
The nursing shortage predates the pandemic, and COVID-19 has brought a simmering problem to the boil. Nurses are calling on the public and the health care system for help. From inside the industry, the needs are pretty much what they were before the pandemic. Dr. Bettencourt and Ms. Wathen point to the need for supportive leadership, healthy work environments, sufficient staffing to meet patients’ needs, and a voice in decisions, such as decisions about staffing, that affect nurses and their patients. Nurses want to be heard and appreciated. “It’s not that these are new things,” said Dr. Bettencourt. “We just need them even more now because we’re stressed even more than we were before.”
Critical care nurses have a different request of the public. They’re asking – pleading, actually – with the public to get vaccinated, wear masks in public, practice social distancing, and bring this pandemic to an end.
“COVID kills, and it’s a really difficult, tragic, and lonely death,” said Ms. Wathen. “We’ve witnessed hundreds of thousands of those deaths. But now we have a way to stop it. If many more people get vaccinated, we can stop this pandemic. And hopefully that will stop this current trend of nurses leaving.”
A version of this article first appeared on Medscape.com.
Embedding diversity, equity, inclusion, and justice in hospital medicine
A road map for success
The language of equality in America’s founding was never truly embraced, resulting in a painful legacy of slavery, racial injustice, and gender inequality inherited by all generations. However, for as long as America has fallen short of this unfulfilled promise, individuals have dedicated their lives to the tireless work of correcting injustice. Although the process has been painstakingly slow, our nation has incrementally inched toward the promised vision of equality, and these efforts continue today. With increased attention to social justice movements such as #MeToo and Black Lives Matter, our collective social consciousness may be finally waking up to the systemic injustices embedded into our fundamental institutions.
Medicine is not immune to these injustices. Persistent underrepresentation of women and minorities remains in medical school faculty and the broader physician workforce, and the same inequities exist in hospital medicine.1-6 The report by the Association of American Medical Colleges (AAMC) on diversity in medicine highlights the impact widespread implicit and explicit bias has on creating exclusionary environments, exemplified by research demonstrating lower promotion rates in non-White faculty.7-8 The report calls us, as physicians, to a broader mission: “Focusing solely on increasing compositional diversity along the academic continuum is insufficient. To effectively enact institutional change at academic medical centers ... leaders must focus their efforts on developing inclusive, equity-minded environments.”7
We have a clear moral imperative to correct these shortcomings for our profession and our patients. It is incumbent on our institutions and hospital medicine groups (HMGs) to embark on the necessary process of systemic institutional change to address inequality and justice within our field.
A road map for DEI and justice in hospital medicine
The policies and biases allowing these inequities to persist have existed for decades, and superficial efforts will not bring sufficient change. Our institutions require new building blocks from which the foundation of a wholly inclusive and equal system of practice can be constructed. Encouragingly, some institutions and HMGs have taken steps to modernize their practices. We offer examples and suggestions of concrete practices to begin this journey, organizing these efforts into three broad categories:
1. Recruitment and retention
2. Scholarship, mentorship, and sponsorship
3. Community engagement and partnership.
Recruitment and retention
Improving equity and inclusion begins with recruitment. Search and hiring committees should be assembled intentionally, with gender balance, and ideally with diversity or equity experts invited to join. All members should receive unconscious bias training. For example, the University of Colorado utilizes a toolkit to ensure appropriate steps are followed in the recruitment process, including predetermined candidate selection criteria that are ranked in advance.
Job descriptions should be reviewed by a diversity expert, ensuring unbiased and ungendered language within written text. Advertisements should be wide-reaching, and the committee should consider asking applicants for a diversity statement. Interviews should include a variety of interviewers and interview types (e.g., 1:1, group, etc.). Letters of recommendation deserve special scrutiny; letters for women and minorities may be at risk of being shorter and less record focused, and may be subject to less professional respect, such as use of first names over honorifics or titles.
Once candidates are hired, institutions and HMGs should prioritize developing strategies to improve retention of a diverse workforce. This includes special attention to workplace culture, and thoughtfully striving for cultural intelligence within the group. Some examples may include developing affinity groups, such as underrepresented in medicine (UIM), women in medicine (WIM), or LGBTQ+ groups. Affinity groups provide a safe space for members and allies to support and uplift each other. Institutional and HMG leaders must educate themselves and their members on the importance of language (see table), and the more insidious forms of bias and discrimination that adversely affect workplace culture. Microinsults and microinvalidations, for example, can hurt and result in failure to recruit or turnover. 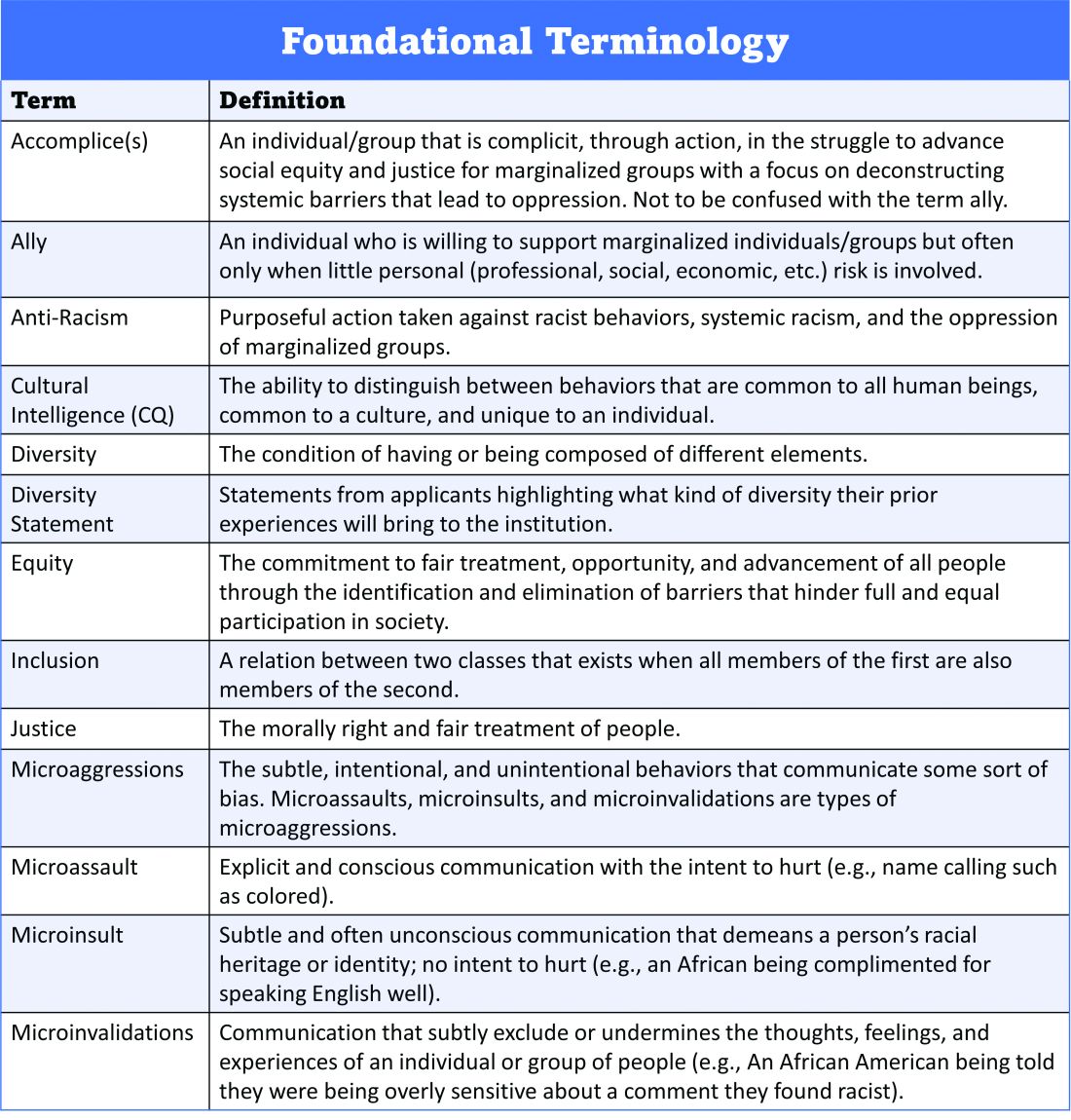
Conducting exit interviews when any hospitalist leaves is important to learn how to improve, but holding ‘stay’ interviews is mission critical. Stay interviews are an opportunity for HMG leaders to proactively understand why hospitalists stay, and what can be done to create more inclusive and equitable environments to retain them. This process creates psychological safety that brings challenges to the fore to be addressed, and spotlights best practices to be maintained and scaled.
Scholarship, mentorship, and sponsorship
Women and minorities are known to be over-mentored and under-sponsored. Sponsorship is defined by Ayyala et al. as “active support by someone appropriately placed in the organization who has significant influence on decision making processes or structures and who is advocating for the career advancement of an individual and recommends them for leadership roles, awards, or high-profile speaking opportunities.”9 While the goal of mentorship is professional development, sponsorship emphasizes professional advancement. Deliberate steps to both mentor and then sponsor diverse hospitalists and future hospitalists (including trainees) are important to ensure equity.
More inclusive HMGs can be bolstered by prioritizing peer education on the professional imperative that we have a diverse workforce and equitable, just workplaces. Academic institutions may use existing structures such as grand rounds to provide education on these crucial topics, and all HMGs can host journal clubs and professional development sessions on leadership competencies that foster inclusion and equity. Sessions coordinated by women and minorities are also a form of justice, by helping overcome barriers to career advancement. Diverse faculty presenting in educational venues will result in content that is relevant to more audience members and will exemplify that leaders and experts are of all races, ethnicities, genders, ages, and abilities.
Groups should prioritize mentoring trainees and early-career hospitalists on scholarly projects that examine equity in opportunities of care, which signals that this science is valued as much as basic research. When used to demonstrate areas needing improvement, these projects can drive meaningful change. Even projects as straightforward as studying diversity in conference presenters, disparities in adherence to guidelines, or QI projects on how race is portrayed in the medical record can be powerful tools in advancing equity.
A key part of mentoring is training hospitalists and future hospitalists in how to be an upstander, as in how to intervene when a peer or patient is affected by bias, harassment, or discrimination. Receiving such training can prepare hospitalists for these nearly inevitable experiences and receiving training during usual work hours communicates that this is a valuable and necessary professional competency.
Community engagement and partnership
Institutions and HMGs should deliberately work to promote community engagement and partnership within their groups. Beyond promoting health equity, community engagement also fosters inclusivity by allowing community members to share their ideas and give recommendations to the institutions that serve them.
There is a growing body of literature that demonstrates how disadvantages by individual and neighborhood-level socioeconomic status (SES) contribute to disparities in specific disease conditions.10-11 Strategies to narrow the gap in SES disadvantages may help reduce race-related health disparities. Institutions that engage the community and develop programs to promote health equity can do so through bidirectional exchange of knowledge and mutual benefit.
An institution-specific example is Medicine for the Greater Good at Johns Hopkins. The founders of this program wrote, “health is not synonymous with medicine. To truly care for our patients and their communities, health care professionals must understand how to deliver equitable health care that meets the needs of the diverse populations we care for. The mission of Medicine for the Greater Good is to promote health and wellness beyond the confines of the hospital through an interactive and engaging partnership with the community ...” Community engagement also provides an opportunity for growing the cultural intelligence of institutions and HMGs.
Tools for advancing comprehensive change – Repurposing PDSA cycles
Whether institutions and HMGs are at the beginning of their journey or further along in the work of reducing disparities, having a systematic approach for implementing and refining policies and procedures can cultivate more inclusive and equitable environments. Thankfully, hospitalists are already equipped with the fundamental tools needed to advance change across their institutions – QI processes in the form of Plan-Do-Study-Act (PDSA) cycles.
They allow a continuous cycle of successful incremental change based on direct evidence and experience. Any efforts to deconstruct systematic bias within our organizations must also be a continual process. Our female colleagues and colleagues of color need our institutions to engage unceasingly to bring about the equality they deserve. To that end, PDSA cycles are an apt tool to utilize in this work as they can naturally function in a never-ending process of improvement.
With PDSA as a model, we envision a cycle with steps that are intentionally purposed to fit the needs of equitable institutional change: Target-Engage-Assess-Modify. As highlighted (see graphic), these modifications ensure that stakeholders (i.e., those that unequal practices and policies affect the most) are engaged early and remain involved throughout the cycle. 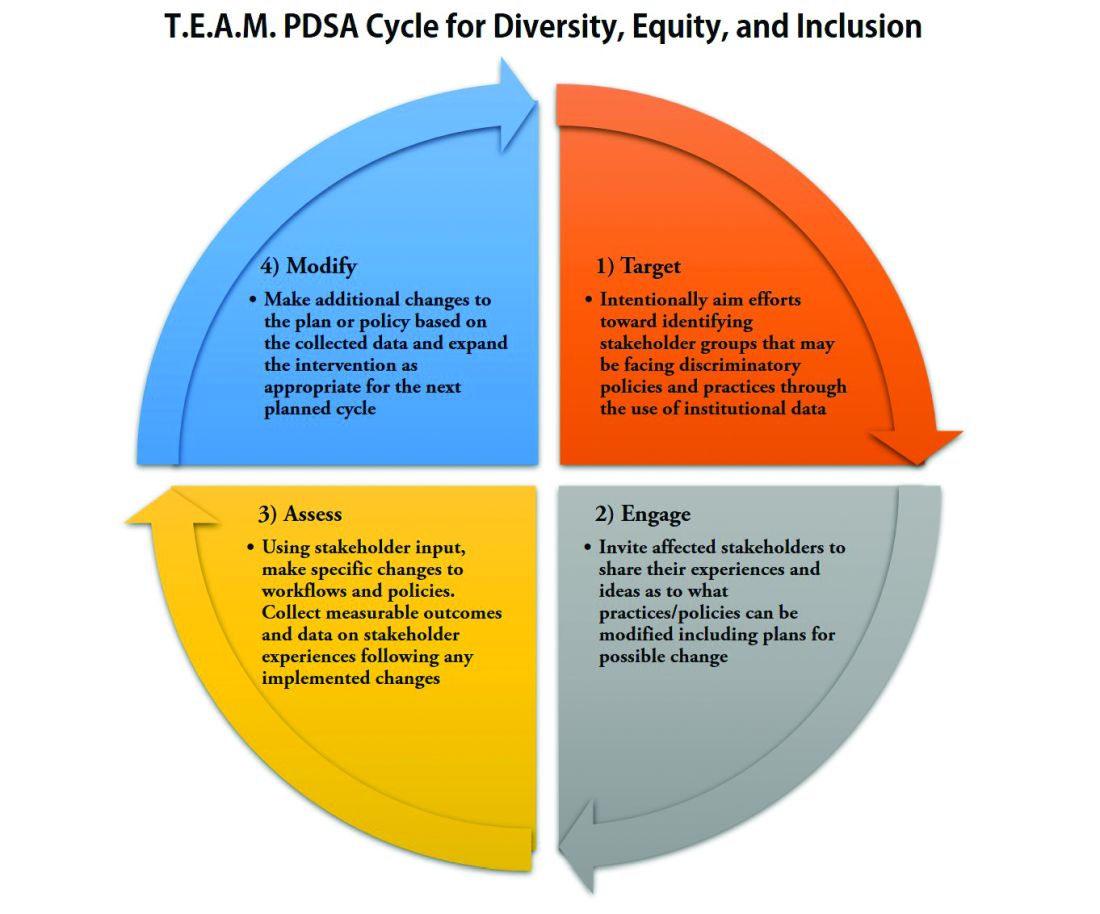
As hospitalists, we have significant work ahead to ensure that we develop and maintain a diverse, equitable and inclusive workforce. This work to bring change will not be easy and will require a considerable investment of time and resources. However, with the strategies and tools that we have outlined, our institutions and HMGs can start the change needed in our profession for our patients and the workforce. In doing so, we can all be accomplices in the fight to achieve racial and gender equity, and social justice.
Dr. Delapenha and Dr. Kisuule are based in the department of internal medicine, division of hospital medicine, at the Johns Hopkins University, Baltimore. Dr. Martin is based in the department of medicine, section of hospital medicine at the University of Chicago. Dr. Barrett is a hospitalist in the department of internal medicine, University of New Mexico, Albuquerque.
References
1. Diversity in Medicine: Facts and Figures 2019: Figure 19. Percentage of physicians by sex, 2018. AAMC website.
2. Diversity in Medicine: Facts and Figures 2019. Figure 16. Percentage of full-time U.S. medical school faculty by sex and race/ethnicity, 2018. AAMC website.
3. Diversity in Medicine: Facts and Figures 2019. Figure 15. Percentage of full-time U.S. medical school faculty by race/ethnicity, 2018. AAMC website.
4. Diversity in Medicine: Facts and Figures 2019. Figure 6. Percentage of acceptees to U.S. medical schools by race/ethnicity (alone), academic year 2018-2019. AAMC website.
5. Diversity in Medicine: Facts and Figures 2019 Figure 18. Percentage of all active physicians by race/ethnicity, 2018. AAMC website.
6. Herzke C et al. Gender issues in academic hospital medicine: A national survey of hospitalist leaders. J Gen Intern Med. 2020;35(6):1641-6.
7. Diversity in Medicine: Facts and Figures 2019. Fostering diversity and inclusion. AAMC website.
8. Diversity in Medicine: Facts and Figures 2019. Executive summary. AAMC website.
9. Ayyala MS et al. Mentorship is not enough: Exploring sponsorship and its role in career advancement in academic medicine. Acad Med. 2019;94(1):94-100.
10. Ejike OC et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. 2021 Apr 15;203(8):987-97.
11. Galiatsatos P et al. The effect of community socioeconomic status on sepsis-attributable mortality. J Crit Care. 2018 Aug;46:129-33.
A road map for success
A road map for success
The language of equality in America’s founding was never truly embraced, resulting in a painful legacy of slavery, racial injustice, and gender inequality inherited by all generations. However, for as long as America has fallen short of this unfulfilled promise, individuals have dedicated their lives to the tireless work of correcting injustice. Although the process has been painstakingly slow, our nation has incrementally inched toward the promised vision of equality, and these efforts continue today. With increased attention to social justice movements such as #MeToo and Black Lives Matter, our collective social consciousness may be finally waking up to the systemic injustices embedded into our fundamental institutions.
Medicine is not immune to these injustices. Persistent underrepresentation of women and minorities remains in medical school faculty and the broader physician workforce, and the same inequities exist in hospital medicine.1-6 The report by the Association of American Medical Colleges (AAMC) on diversity in medicine highlights the impact widespread implicit and explicit bias has on creating exclusionary environments, exemplified by research demonstrating lower promotion rates in non-White faculty.7-8 The report calls us, as physicians, to a broader mission: “Focusing solely on increasing compositional diversity along the academic continuum is insufficient. To effectively enact institutional change at academic medical centers ... leaders must focus their efforts on developing inclusive, equity-minded environments.”7
We have a clear moral imperative to correct these shortcomings for our profession and our patients. It is incumbent on our institutions and hospital medicine groups (HMGs) to embark on the necessary process of systemic institutional change to address inequality and justice within our field.
A road map for DEI and justice in hospital medicine
The policies and biases allowing these inequities to persist have existed for decades, and superficial efforts will not bring sufficient change. Our institutions require new building blocks from which the foundation of a wholly inclusive and equal system of practice can be constructed. Encouragingly, some institutions and HMGs have taken steps to modernize their practices. We offer examples and suggestions of concrete practices to begin this journey, organizing these efforts into three broad categories:
1. Recruitment and retention
2. Scholarship, mentorship, and sponsorship
3. Community engagement and partnership.
Recruitment and retention
Improving equity and inclusion begins with recruitment. Search and hiring committees should be assembled intentionally, with gender balance, and ideally with diversity or equity experts invited to join. All members should receive unconscious bias training. For example, the University of Colorado utilizes a toolkit to ensure appropriate steps are followed in the recruitment process, including predetermined candidate selection criteria that are ranked in advance.
Job descriptions should be reviewed by a diversity expert, ensuring unbiased and ungendered language within written text. Advertisements should be wide-reaching, and the committee should consider asking applicants for a diversity statement. Interviews should include a variety of interviewers and interview types (e.g., 1:1, group, etc.). Letters of recommendation deserve special scrutiny; letters for women and minorities may be at risk of being shorter and less record focused, and may be subject to less professional respect, such as use of first names over honorifics or titles.
Once candidates are hired, institutions and HMGs should prioritize developing strategies to improve retention of a diverse workforce. This includes special attention to workplace culture, and thoughtfully striving for cultural intelligence within the group. Some examples may include developing affinity groups, such as underrepresented in medicine (UIM), women in medicine (WIM), or LGBTQ+ groups. Affinity groups provide a safe space for members and allies to support and uplift each other. Institutional and HMG leaders must educate themselves and their members on the importance of language (see table), and the more insidious forms of bias and discrimination that adversely affect workplace culture. Microinsults and microinvalidations, for example, can hurt and result in failure to recruit or turnover. 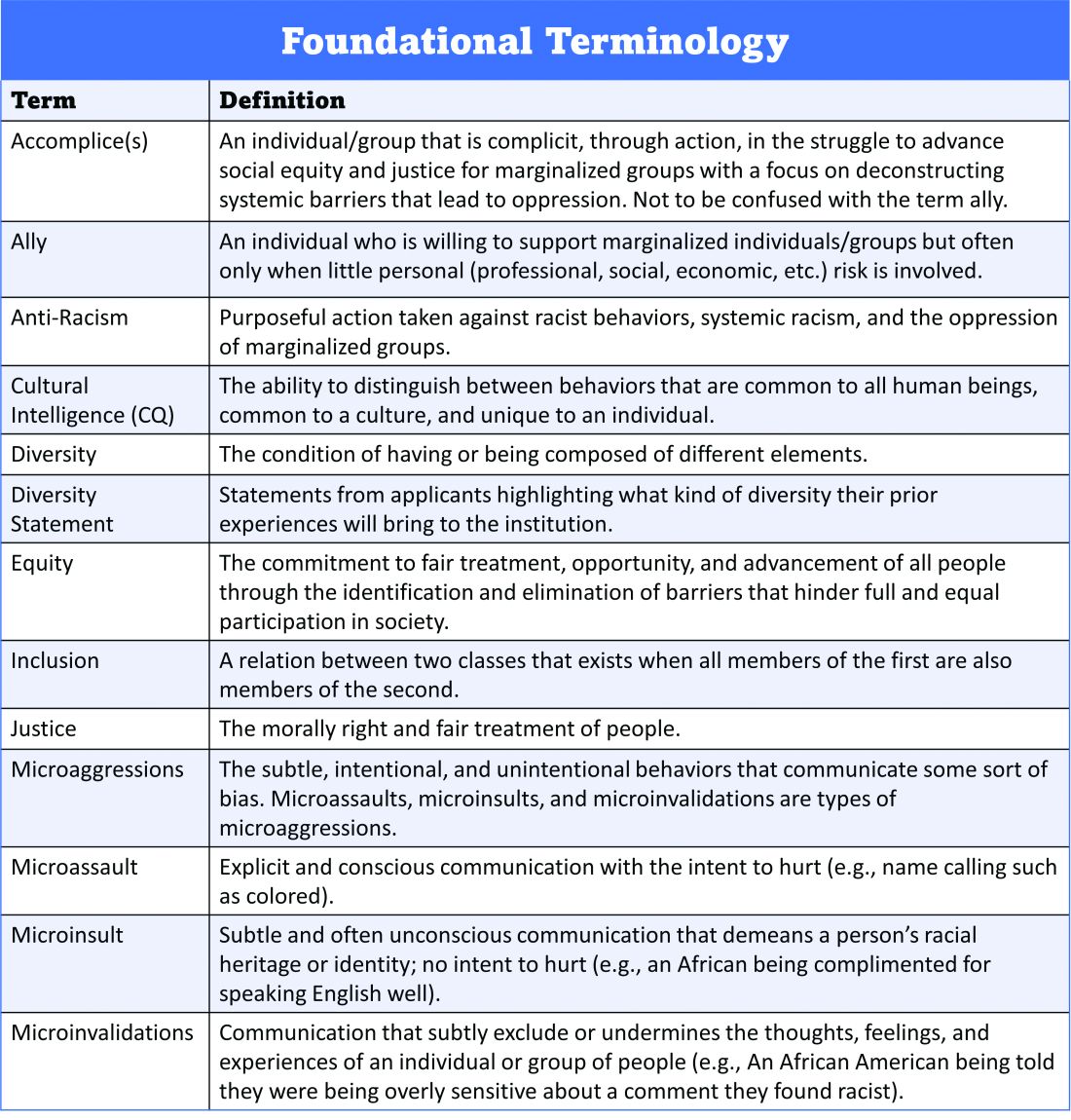
Conducting exit interviews when any hospitalist leaves is important to learn how to improve, but holding ‘stay’ interviews is mission critical. Stay interviews are an opportunity for HMG leaders to proactively understand why hospitalists stay, and what can be done to create more inclusive and equitable environments to retain them. This process creates psychological safety that brings challenges to the fore to be addressed, and spotlights best practices to be maintained and scaled.
Scholarship, mentorship, and sponsorship
Women and minorities are known to be over-mentored and under-sponsored. Sponsorship is defined by Ayyala et al. as “active support by someone appropriately placed in the organization who has significant influence on decision making processes or structures and who is advocating for the career advancement of an individual and recommends them for leadership roles, awards, or high-profile speaking opportunities.”9 While the goal of mentorship is professional development, sponsorship emphasizes professional advancement. Deliberate steps to both mentor and then sponsor diverse hospitalists and future hospitalists (including trainees) are important to ensure equity.
More inclusive HMGs can be bolstered by prioritizing peer education on the professional imperative that we have a diverse workforce and equitable, just workplaces. Academic institutions may use existing structures such as grand rounds to provide education on these crucial topics, and all HMGs can host journal clubs and professional development sessions on leadership competencies that foster inclusion and equity. Sessions coordinated by women and minorities are also a form of justice, by helping overcome barriers to career advancement. Diverse faculty presenting in educational venues will result in content that is relevant to more audience members and will exemplify that leaders and experts are of all races, ethnicities, genders, ages, and abilities.
Groups should prioritize mentoring trainees and early-career hospitalists on scholarly projects that examine equity in opportunities of care, which signals that this science is valued as much as basic research. When used to demonstrate areas needing improvement, these projects can drive meaningful change. Even projects as straightforward as studying diversity in conference presenters, disparities in adherence to guidelines, or QI projects on how race is portrayed in the medical record can be powerful tools in advancing equity.
A key part of mentoring is training hospitalists and future hospitalists in how to be an upstander, as in how to intervene when a peer or patient is affected by bias, harassment, or discrimination. Receiving such training can prepare hospitalists for these nearly inevitable experiences and receiving training during usual work hours communicates that this is a valuable and necessary professional competency.
Community engagement and partnership
Institutions and HMGs should deliberately work to promote community engagement and partnership within their groups. Beyond promoting health equity, community engagement also fosters inclusivity by allowing community members to share their ideas and give recommendations to the institutions that serve them.
There is a growing body of literature that demonstrates how disadvantages by individual and neighborhood-level socioeconomic status (SES) contribute to disparities in specific disease conditions.10-11 Strategies to narrow the gap in SES disadvantages may help reduce race-related health disparities. Institutions that engage the community and develop programs to promote health equity can do so through bidirectional exchange of knowledge and mutual benefit.
An institution-specific example is Medicine for the Greater Good at Johns Hopkins. The founders of this program wrote, “health is not synonymous with medicine. To truly care for our patients and their communities, health care professionals must understand how to deliver equitable health care that meets the needs of the diverse populations we care for. The mission of Medicine for the Greater Good is to promote health and wellness beyond the confines of the hospital through an interactive and engaging partnership with the community ...” Community engagement also provides an opportunity for growing the cultural intelligence of institutions and HMGs.
Tools for advancing comprehensive change – Repurposing PDSA cycles
Whether institutions and HMGs are at the beginning of their journey or further along in the work of reducing disparities, having a systematic approach for implementing and refining policies and procedures can cultivate more inclusive and equitable environments. Thankfully, hospitalists are already equipped with the fundamental tools needed to advance change across their institutions – QI processes in the form of Plan-Do-Study-Act (PDSA) cycles.
They allow a continuous cycle of successful incremental change based on direct evidence and experience. Any efforts to deconstruct systematic bias within our organizations must also be a continual process. Our female colleagues and colleagues of color need our institutions to engage unceasingly to bring about the equality they deserve. To that end, PDSA cycles are an apt tool to utilize in this work as they can naturally function in a never-ending process of improvement.
With PDSA as a model, we envision a cycle with steps that are intentionally purposed to fit the needs of equitable institutional change: Target-Engage-Assess-Modify. As highlighted (see graphic), these modifications ensure that stakeholders (i.e., those that unequal practices and policies affect the most) are engaged early and remain involved throughout the cycle. 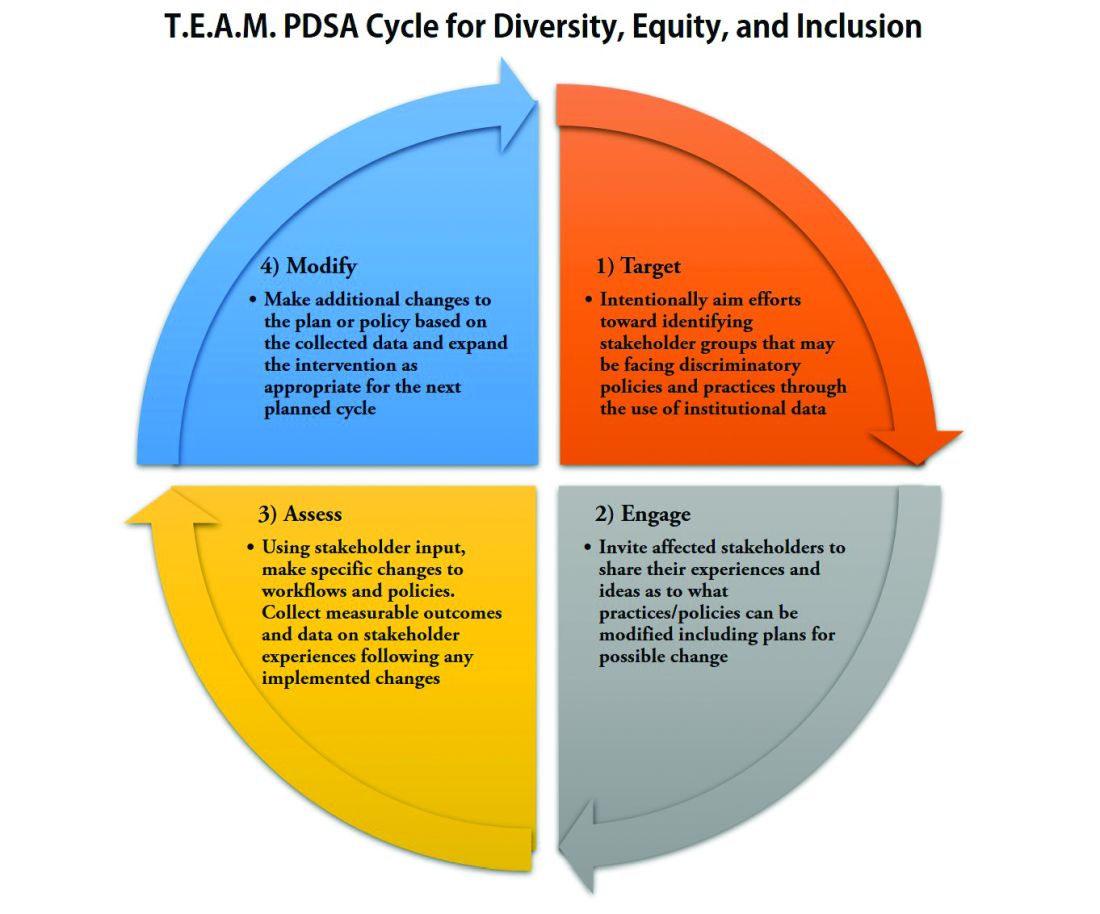
As hospitalists, we have significant work ahead to ensure that we develop and maintain a diverse, equitable and inclusive workforce. This work to bring change will not be easy and will require a considerable investment of time and resources. However, with the strategies and tools that we have outlined, our institutions and HMGs can start the change needed in our profession for our patients and the workforce. In doing so, we can all be accomplices in the fight to achieve racial and gender equity, and social justice.
Dr. Delapenha and Dr. Kisuule are based in the department of internal medicine, division of hospital medicine, at the Johns Hopkins University, Baltimore. Dr. Martin is based in the department of medicine, section of hospital medicine at the University of Chicago. Dr. Barrett is a hospitalist in the department of internal medicine, University of New Mexico, Albuquerque.
References
1. Diversity in Medicine: Facts and Figures 2019: Figure 19. Percentage of physicians by sex, 2018. AAMC website.
2. Diversity in Medicine: Facts and Figures 2019. Figure 16. Percentage of full-time U.S. medical school faculty by sex and race/ethnicity, 2018. AAMC website.
3. Diversity in Medicine: Facts and Figures 2019. Figure 15. Percentage of full-time U.S. medical school faculty by race/ethnicity, 2018. AAMC website.
4. Diversity in Medicine: Facts and Figures 2019. Figure 6. Percentage of acceptees to U.S. medical schools by race/ethnicity (alone), academic year 2018-2019. AAMC website.
5. Diversity in Medicine: Facts and Figures 2019 Figure 18. Percentage of all active physicians by race/ethnicity, 2018. AAMC website.
6. Herzke C et al. Gender issues in academic hospital medicine: A national survey of hospitalist leaders. J Gen Intern Med. 2020;35(6):1641-6.
7. Diversity in Medicine: Facts and Figures 2019. Fostering diversity and inclusion. AAMC website.
8. Diversity in Medicine: Facts and Figures 2019. Executive summary. AAMC website.
9. Ayyala MS et al. Mentorship is not enough: Exploring sponsorship and its role in career advancement in academic medicine. Acad Med. 2019;94(1):94-100.
10. Ejike OC et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. 2021 Apr 15;203(8):987-97.
11. Galiatsatos P et al. The effect of community socioeconomic status on sepsis-attributable mortality. J Crit Care. 2018 Aug;46:129-33.
The language of equality in America’s founding was never truly embraced, resulting in a painful legacy of slavery, racial injustice, and gender inequality inherited by all generations. However, for as long as America has fallen short of this unfulfilled promise, individuals have dedicated their lives to the tireless work of correcting injustice. Although the process has been painstakingly slow, our nation has incrementally inched toward the promised vision of equality, and these efforts continue today. With increased attention to social justice movements such as #MeToo and Black Lives Matter, our collective social consciousness may be finally waking up to the systemic injustices embedded into our fundamental institutions.
Medicine is not immune to these injustices. Persistent underrepresentation of women and minorities remains in medical school faculty and the broader physician workforce, and the same inequities exist in hospital medicine.1-6 The report by the Association of American Medical Colleges (AAMC) on diversity in medicine highlights the impact widespread implicit and explicit bias has on creating exclusionary environments, exemplified by research demonstrating lower promotion rates in non-White faculty.7-8 The report calls us, as physicians, to a broader mission: “Focusing solely on increasing compositional diversity along the academic continuum is insufficient. To effectively enact institutional change at academic medical centers ... leaders must focus their efforts on developing inclusive, equity-minded environments.”7
We have a clear moral imperative to correct these shortcomings for our profession and our patients. It is incumbent on our institutions and hospital medicine groups (HMGs) to embark on the necessary process of systemic institutional change to address inequality and justice within our field.
A road map for DEI and justice in hospital medicine
The policies and biases allowing these inequities to persist have existed for decades, and superficial efforts will not bring sufficient change. Our institutions require new building blocks from which the foundation of a wholly inclusive and equal system of practice can be constructed. Encouragingly, some institutions and HMGs have taken steps to modernize their practices. We offer examples and suggestions of concrete practices to begin this journey, organizing these efforts into three broad categories:
1. Recruitment and retention
2. Scholarship, mentorship, and sponsorship
3. Community engagement and partnership.
Recruitment and retention
Improving equity and inclusion begins with recruitment. Search and hiring committees should be assembled intentionally, with gender balance, and ideally with diversity or equity experts invited to join. All members should receive unconscious bias training. For example, the University of Colorado utilizes a toolkit to ensure appropriate steps are followed in the recruitment process, including predetermined candidate selection criteria that are ranked in advance.
Job descriptions should be reviewed by a diversity expert, ensuring unbiased and ungendered language within written text. Advertisements should be wide-reaching, and the committee should consider asking applicants for a diversity statement. Interviews should include a variety of interviewers and interview types (e.g., 1:1, group, etc.). Letters of recommendation deserve special scrutiny; letters for women and minorities may be at risk of being shorter and less record focused, and may be subject to less professional respect, such as use of first names over honorifics or titles.
Once candidates are hired, institutions and HMGs should prioritize developing strategies to improve retention of a diverse workforce. This includes special attention to workplace culture, and thoughtfully striving for cultural intelligence within the group. Some examples may include developing affinity groups, such as underrepresented in medicine (UIM), women in medicine (WIM), or LGBTQ+ groups. Affinity groups provide a safe space for members and allies to support and uplift each other. Institutional and HMG leaders must educate themselves and their members on the importance of language (see table), and the more insidious forms of bias and discrimination that adversely affect workplace culture. Microinsults and microinvalidations, for example, can hurt and result in failure to recruit or turnover. 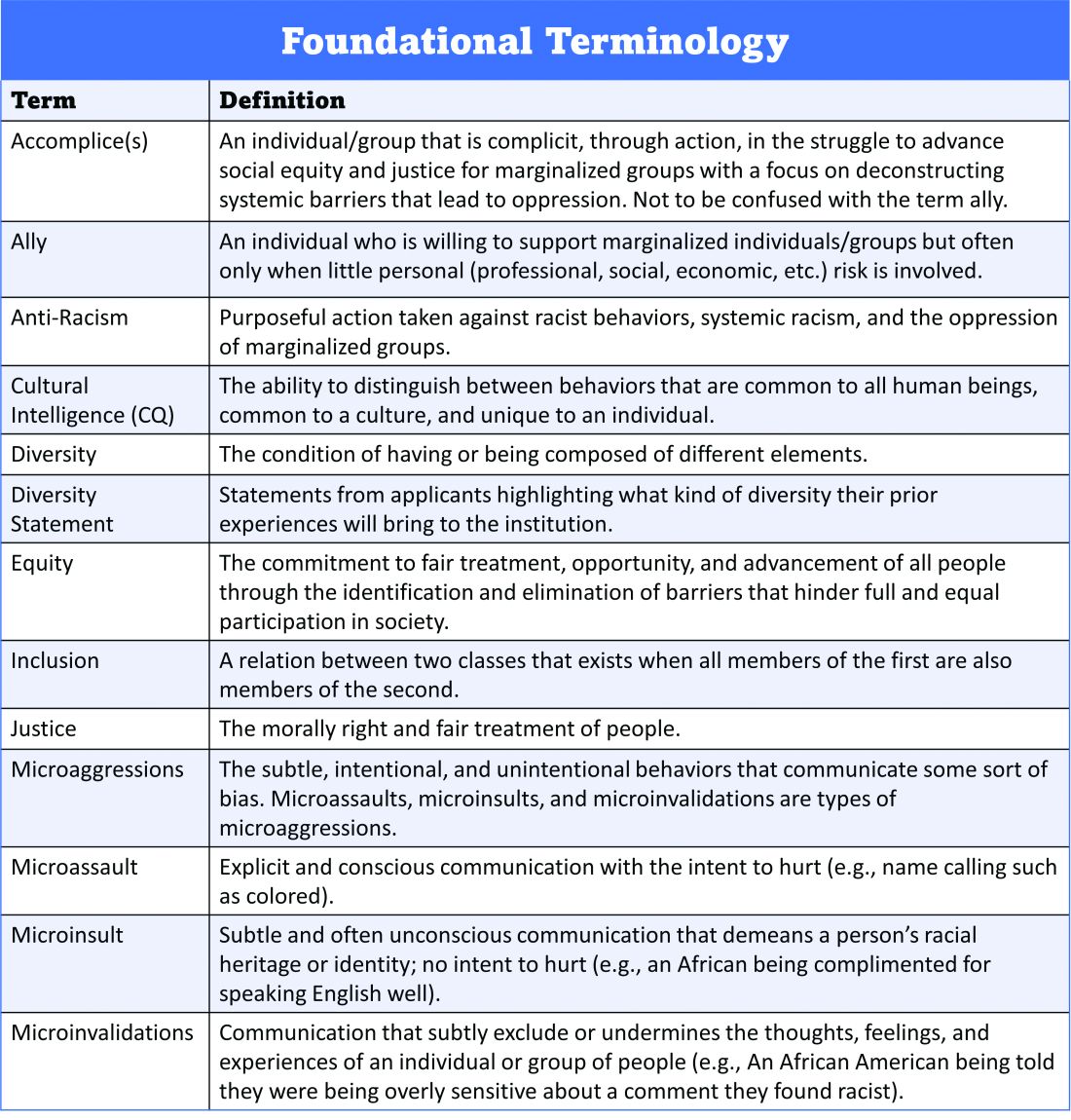
Conducting exit interviews when any hospitalist leaves is important to learn how to improve, but holding ‘stay’ interviews is mission critical. Stay interviews are an opportunity for HMG leaders to proactively understand why hospitalists stay, and what can be done to create more inclusive and equitable environments to retain them. This process creates psychological safety that brings challenges to the fore to be addressed, and spotlights best practices to be maintained and scaled.
Scholarship, mentorship, and sponsorship
Women and minorities are known to be over-mentored and under-sponsored. Sponsorship is defined by Ayyala et al. as “active support by someone appropriately placed in the organization who has significant influence on decision making processes or structures and who is advocating for the career advancement of an individual and recommends them for leadership roles, awards, or high-profile speaking opportunities.”9 While the goal of mentorship is professional development, sponsorship emphasizes professional advancement. Deliberate steps to both mentor and then sponsor diverse hospitalists and future hospitalists (including trainees) are important to ensure equity.
More inclusive HMGs can be bolstered by prioritizing peer education on the professional imperative that we have a diverse workforce and equitable, just workplaces. Academic institutions may use existing structures such as grand rounds to provide education on these crucial topics, and all HMGs can host journal clubs and professional development sessions on leadership competencies that foster inclusion and equity. Sessions coordinated by women and minorities are also a form of justice, by helping overcome barriers to career advancement. Diverse faculty presenting in educational venues will result in content that is relevant to more audience members and will exemplify that leaders and experts are of all races, ethnicities, genders, ages, and abilities.
Groups should prioritize mentoring trainees and early-career hospitalists on scholarly projects that examine equity in opportunities of care, which signals that this science is valued as much as basic research. When used to demonstrate areas needing improvement, these projects can drive meaningful change. Even projects as straightforward as studying diversity in conference presenters, disparities in adherence to guidelines, or QI projects on how race is portrayed in the medical record can be powerful tools in advancing equity.
A key part of mentoring is training hospitalists and future hospitalists in how to be an upstander, as in how to intervene when a peer or patient is affected by bias, harassment, or discrimination. Receiving such training can prepare hospitalists for these nearly inevitable experiences and receiving training during usual work hours communicates that this is a valuable and necessary professional competency.
Community engagement and partnership
Institutions and HMGs should deliberately work to promote community engagement and partnership within their groups. Beyond promoting health equity, community engagement also fosters inclusivity by allowing community members to share their ideas and give recommendations to the institutions that serve them.
There is a growing body of literature that demonstrates how disadvantages by individual and neighborhood-level socioeconomic status (SES) contribute to disparities in specific disease conditions.10-11 Strategies to narrow the gap in SES disadvantages may help reduce race-related health disparities. Institutions that engage the community and develop programs to promote health equity can do so through bidirectional exchange of knowledge and mutual benefit.
An institution-specific example is Medicine for the Greater Good at Johns Hopkins. The founders of this program wrote, “health is not synonymous with medicine. To truly care for our patients and their communities, health care professionals must understand how to deliver equitable health care that meets the needs of the diverse populations we care for. The mission of Medicine for the Greater Good is to promote health and wellness beyond the confines of the hospital through an interactive and engaging partnership with the community ...” Community engagement also provides an opportunity for growing the cultural intelligence of institutions and HMGs.
Tools for advancing comprehensive change – Repurposing PDSA cycles
Whether institutions and HMGs are at the beginning of their journey or further along in the work of reducing disparities, having a systematic approach for implementing and refining policies and procedures can cultivate more inclusive and equitable environments. Thankfully, hospitalists are already equipped with the fundamental tools needed to advance change across their institutions – QI processes in the form of Plan-Do-Study-Act (PDSA) cycles.
They allow a continuous cycle of successful incremental change based on direct evidence and experience. Any efforts to deconstruct systematic bias within our organizations must also be a continual process. Our female colleagues and colleagues of color need our institutions to engage unceasingly to bring about the equality they deserve. To that end, PDSA cycles are an apt tool to utilize in this work as they can naturally function in a never-ending process of improvement.
With PDSA as a model, we envision a cycle with steps that are intentionally purposed to fit the needs of equitable institutional change: Target-Engage-Assess-Modify. As highlighted (see graphic), these modifications ensure that stakeholders (i.e., those that unequal practices and policies affect the most) are engaged early and remain involved throughout the cycle. 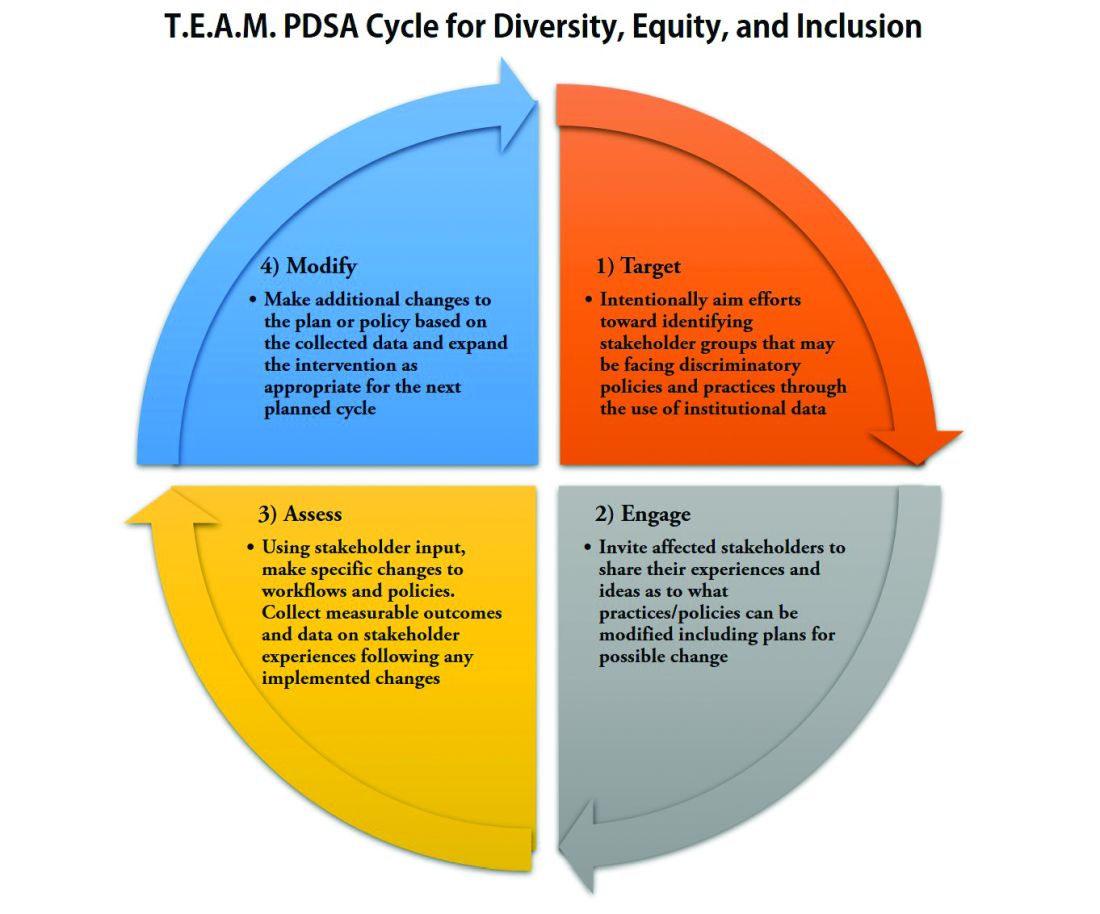
As hospitalists, we have significant work ahead to ensure that we develop and maintain a diverse, equitable and inclusive workforce. This work to bring change will not be easy and will require a considerable investment of time and resources. However, with the strategies and tools that we have outlined, our institutions and HMGs can start the change needed in our profession for our patients and the workforce. In doing so, we can all be accomplices in the fight to achieve racial and gender equity, and social justice.
Dr. Delapenha and Dr. Kisuule are based in the department of internal medicine, division of hospital medicine, at the Johns Hopkins University, Baltimore. Dr. Martin is based in the department of medicine, section of hospital medicine at the University of Chicago. Dr. Barrett is a hospitalist in the department of internal medicine, University of New Mexico, Albuquerque.
References
1. Diversity in Medicine: Facts and Figures 2019: Figure 19. Percentage of physicians by sex, 2018. AAMC website.
2. Diversity in Medicine: Facts and Figures 2019. Figure 16. Percentage of full-time U.S. medical school faculty by sex and race/ethnicity, 2018. AAMC website.
3. Diversity in Medicine: Facts and Figures 2019. Figure 15. Percentage of full-time U.S. medical school faculty by race/ethnicity, 2018. AAMC website.
4. Diversity in Medicine: Facts and Figures 2019. Figure 6. Percentage of acceptees to U.S. medical schools by race/ethnicity (alone), academic year 2018-2019. AAMC website.
5. Diversity in Medicine: Facts and Figures 2019 Figure 18. Percentage of all active physicians by race/ethnicity, 2018. AAMC website.
6. Herzke C et al. Gender issues in academic hospital medicine: A national survey of hospitalist leaders. J Gen Intern Med. 2020;35(6):1641-6.
7. Diversity in Medicine: Facts and Figures 2019. Fostering diversity and inclusion. AAMC website.
8. Diversity in Medicine: Facts and Figures 2019. Executive summary. AAMC website.
9. Ayyala MS et al. Mentorship is not enough: Exploring sponsorship and its role in career advancement in academic medicine. Acad Med. 2019;94(1):94-100.
10. Ejike OC et al. Contribution of individual and neighborhood factors to racial disparities in respiratory outcomes. Am J Respir Crit Care Med. 2021 Apr 15;203(8):987-97.
11. Galiatsatos P et al. The effect of community socioeconomic status on sepsis-attributable mortality. J Crit Care. 2018 Aug;46:129-33.
Refined heart rate cutoffs may improve prognostic value of acute PE scoring systems
In patients with acute pulmonary embolism, using cutoff values other than 110 beats per minute might improve the prognostic value of heart rate at admission, a recent observational study suggests.
For identifying low-risk patients, a cutoff of 80 bpm increased the sensitivity of the simplified Pulmonary Embolism Severity Index (sPESI) from about 94% to nearly 99% among nonhypotensive patients with acute symptomatic pulmonary embolism (PE), according to results of the large, registry-based study.
Similarly, using a 140-bpm cutoff increased the specificity of the Bova score for identifying intermediate-high–risk patients from about 93% to 98% in the study, which was recently published in the journal CHEST.
“Although standard dichotomization of HR [i.e., HR less than 110 vs. greater than 110 bpm] may be useful for guideline recommendations, our results will allow for more accuracy regarding clinical decision-making,” wrote lead author Ana Jaureguízar, MD, of the University of Alcalá in Madrid, on behalf of the RIETE (Registro Informatizado de la Enfermedad TromboEmbólica) investigators.
Intuitive findings inform future research
These observational findings are intuitive and do at least have the potential to inform the design of future randomized clinical trials, according to Albert J. Polito, MD, chief of the division of pulmonary medicine and medical director for the lung center at Mercy Medical Center in Baltimore.
“In medicine, there is a spectrum of risk,” Dr. Polito said in an interview. “While we love our cutoffs, which in this case has traditionally always been that 110 beats per minute for heart rate, it makes sense that there would be some range of risks of bad outcomes.”
Building on the observations of the present study, subsequent prospective randomized studies could potentially aim to determine, for example, when thrombolytic therapy should be considered in nonhypotensive patients with acute PE and higher heart rates.
“It would not be easy to design, but it’s a straightforward question to ask whether patients with the highest heart rates are the ones who potentially might benefit the most from thrombolytic therapy,” Dr. Polito said.
Value of alternative HR cutoffs
Heart rate is a simple and easily available vital sign that is clearly linked to prognosis in patients with pulmonary embolism, authors of the RIETE registry study say in their report. Accordingly, a heart rate threshold of 110 bpm has made its way into scoring systems that seek to identify low-risk patients, such as the sPESI, and those focused on identifying higher-risk patients, such as the Bova score.
However, it has not been clear whether alternative HR cutoffs would improve upon the 110-bpm threshold, they added. At the low-risk end, more accurate scoring systems could optimize the selection of patients for home treatment, while at the intermediate-high–risk end, they could better select patients for close monitoring or advanced PE treatments.
Better granularity on heart rate risks?
To better define the prognostic value of different heart rate thresholds, investigators analyzed data from RIETE, a large, ongoing, multinational prospective registry including patients with objectively confirmed acute venous thromboembolism.
For 44,331 consecutive nonhypotensive symptomatic PEs, the overall rate of 30-day all-cause mortality was 5.1%, and the 30-day PE-related mortality was 1.9%, the authors report.
Significantly poorer outcomes were seen in patients with higher heart rates as compared to patients in the 80-99 bpm range, they also found. As compared to that reference range, odds ratios for 30-day all-cause death ranged from 1.5 for heart rates of 100-109, up to 2.4 for those with heart rates of 140 bpm or greater.
Likewise, patients with higher heart rates had a 1.7- to 2.4-fold greater risk of 30-day PE-related death as compared to the 80- to 99-bpm reference range, while patients with lower heart rates had lesser risk, the data published in CHEST show.
Toward refinement of prognostic scoring
Next, investigators sought to refine the prognostic scoring systems for low-risk PE (sPESI) and intermediate-high–risk PE (Bova).
For sPESI, they found that dropping the cutoff value from 110 to 100 bpm increased the sensitivity of the score from 93.4% to 95.3%. Going down even further to 80 bpm increased sensitivity to 98.8%, according to the report.
By going down from 110 to 80 bpm, the proportion of patients defined as low-risk dropped from 35% to 12%, according to the investigators.
For the Bova score, increasing the cutoff value from 110 to 120 bpm likewise increased specificity from 93.2% to 95%, while going up even further to 140 bpm increased specificity to 98.0%, the report shows.
In sensitivity analyses, the findings were not impacted by excluding younger patients, those who received reperfusion therapies, or those with atrial fibrillation, according to the study findings.
Potential implications for clinical practice
Taken together, these findings could serve as a resource to inform discussions regarding PE management that include whether home therapy or use of thrombolytic therapy is appropriate, investigators said in their report.
“For instance, among low-risk sPESI patients, those with borderline tachycardia [i.e., a heart rate between 100-109 bpm] might benefit from initial hospital observation for trending,” they wrote.
Dr. Jaureguízar reported no disclosures. One coinvestigator reported funding support from the Institute of Health Carlos III (ISCIII) and the European Development Regional Fund (ERDF). One coinvestigator reported consulting in litigation involving two models of inferior vena cava filters.
Dr. Polito reported no disclosures.
In patients with acute pulmonary embolism, using cutoff values other than 110 beats per minute might improve the prognostic value of heart rate at admission, a recent observational study suggests.
For identifying low-risk patients, a cutoff of 80 bpm increased the sensitivity of the simplified Pulmonary Embolism Severity Index (sPESI) from about 94% to nearly 99% among nonhypotensive patients with acute symptomatic pulmonary embolism (PE), according to results of the large, registry-based study.
Similarly, using a 140-bpm cutoff increased the specificity of the Bova score for identifying intermediate-high–risk patients from about 93% to 98% in the study, which was recently published in the journal CHEST.
“Although standard dichotomization of HR [i.e., HR less than 110 vs. greater than 110 bpm] may be useful for guideline recommendations, our results will allow for more accuracy regarding clinical decision-making,” wrote lead author Ana Jaureguízar, MD, of the University of Alcalá in Madrid, on behalf of the RIETE (Registro Informatizado de la Enfermedad TromboEmbólica) investigators.
Intuitive findings inform future research
These observational findings are intuitive and do at least have the potential to inform the design of future randomized clinical trials, according to Albert J. Polito, MD, chief of the division of pulmonary medicine and medical director for the lung center at Mercy Medical Center in Baltimore.
“In medicine, there is a spectrum of risk,” Dr. Polito said in an interview. “While we love our cutoffs, which in this case has traditionally always been that 110 beats per minute for heart rate, it makes sense that there would be some range of risks of bad outcomes.”
Building on the observations of the present study, subsequent prospective randomized studies could potentially aim to determine, for example, when thrombolytic therapy should be considered in nonhypotensive patients with acute PE and higher heart rates.
“It would not be easy to design, but it’s a straightforward question to ask whether patients with the highest heart rates are the ones who potentially might benefit the most from thrombolytic therapy,” Dr. Polito said.
Value of alternative HR cutoffs
Heart rate is a simple and easily available vital sign that is clearly linked to prognosis in patients with pulmonary embolism, authors of the RIETE registry study say in their report. Accordingly, a heart rate threshold of 110 bpm has made its way into scoring systems that seek to identify low-risk patients, such as the sPESI, and those focused on identifying higher-risk patients, such as the Bova score.
However, it has not been clear whether alternative HR cutoffs would improve upon the 110-bpm threshold, they added. At the low-risk end, more accurate scoring systems could optimize the selection of patients for home treatment, while at the intermediate-high–risk end, they could better select patients for close monitoring or advanced PE treatments.
Better granularity on heart rate risks?
To better define the prognostic value of different heart rate thresholds, investigators analyzed data from RIETE, a large, ongoing, multinational prospective registry including patients with objectively confirmed acute venous thromboembolism.
For 44,331 consecutive nonhypotensive symptomatic PEs, the overall rate of 30-day all-cause mortality was 5.1%, and the 30-day PE-related mortality was 1.9%, the authors report.
Significantly poorer outcomes were seen in patients with higher heart rates as compared to patients in the 80-99 bpm range, they also found. As compared to that reference range, odds ratios for 30-day all-cause death ranged from 1.5 for heart rates of 100-109, up to 2.4 for those with heart rates of 140 bpm or greater.
Likewise, patients with higher heart rates had a 1.7- to 2.4-fold greater risk of 30-day PE-related death as compared to the 80- to 99-bpm reference range, while patients with lower heart rates had lesser risk, the data published in CHEST show.
Toward refinement of prognostic scoring
Next, investigators sought to refine the prognostic scoring systems for low-risk PE (sPESI) and intermediate-high–risk PE (Bova).
For sPESI, they found that dropping the cutoff value from 110 to 100 bpm increased the sensitivity of the score from 93.4% to 95.3%. Going down even further to 80 bpm increased sensitivity to 98.8%, according to the report.
By going down from 110 to 80 bpm, the proportion of patients defined as low-risk dropped from 35% to 12%, according to the investigators.
For the Bova score, increasing the cutoff value from 110 to 120 bpm likewise increased specificity from 93.2% to 95%, while going up even further to 140 bpm increased specificity to 98.0%, the report shows.
In sensitivity analyses, the findings were not impacted by excluding younger patients, those who received reperfusion therapies, or those with atrial fibrillation, according to the study findings.
Potential implications for clinical practice
Taken together, these findings could serve as a resource to inform discussions regarding PE management that include whether home therapy or use of thrombolytic therapy is appropriate, investigators said in their report.
“For instance, among low-risk sPESI patients, those with borderline tachycardia [i.e., a heart rate between 100-109 bpm] might benefit from initial hospital observation for trending,” they wrote.
Dr. Jaureguízar reported no disclosures. One coinvestigator reported funding support from the Institute of Health Carlos III (ISCIII) and the European Development Regional Fund (ERDF). One coinvestigator reported consulting in litigation involving two models of inferior vena cava filters.
Dr. Polito reported no disclosures.
In patients with acute pulmonary embolism, using cutoff values other than 110 beats per minute might improve the prognostic value of heart rate at admission, a recent observational study suggests.
For identifying low-risk patients, a cutoff of 80 bpm increased the sensitivity of the simplified Pulmonary Embolism Severity Index (sPESI) from about 94% to nearly 99% among nonhypotensive patients with acute symptomatic pulmonary embolism (PE), according to results of the large, registry-based study.
Similarly, using a 140-bpm cutoff increased the specificity of the Bova score for identifying intermediate-high–risk patients from about 93% to 98% in the study, which was recently published in the journal CHEST.
“Although standard dichotomization of HR [i.e., HR less than 110 vs. greater than 110 bpm] may be useful for guideline recommendations, our results will allow for more accuracy regarding clinical decision-making,” wrote lead author Ana Jaureguízar, MD, of the University of Alcalá in Madrid, on behalf of the RIETE (Registro Informatizado de la Enfermedad TromboEmbólica) investigators.
Intuitive findings inform future research
These observational findings are intuitive and do at least have the potential to inform the design of future randomized clinical trials, according to Albert J. Polito, MD, chief of the division of pulmonary medicine and medical director for the lung center at Mercy Medical Center in Baltimore.
“In medicine, there is a spectrum of risk,” Dr. Polito said in an interview. “While we love our cutoffs, which in this case has traditionally always been that 110 beats per minute for heart rate, it makes sense that there would be some range of risks of bad outcomes.”
Building on the observations of the present study, subsequent prospective randomized studies could potentially aim to determine, for example, when thrombolytic therapy should be considered in nonhypotensive patients with acute PE and higher heart rates.
“It would not be easy to design, but it’s a straightforward question to ask whether patients with the highest heart rates are the ones who potentially might benefit the most from thrombolytic therapy,” Dr. Polito said.
Value of alternative HR cutoffs
Heart rate is a simple and easily available vital sign that is clearly linked to prognosis in patients with pulmonary embolism, authors of the RIETE registry study say in their report. Accordingly, a heart rate threshold of 110 bpm has made its way into scoring systems that seek to identify low-risk patients, such as the sPESI, and those focused on identifying higher-risk patients, such as the Bova score.
However, it has not been clear whether alternative HR cutoffs would improve upon the 110-bpm threshold, they added. At the low-risk end, more accurate scoring systems could optimize the selection of patients for home treatment, while at the intermediate-high–risk end, they could better select patients for close monitoring or advanced PE treatments.
Better granularity on heart rate risks?
To better define the prognostic value of different heart rate thresholds, investigators analyzed data from RIETE, a large, ongoing, multinational prospective registry including patients with objectively confirmed acute venous thromboembolism.
For 44,331 consecutive nonhypotensive symptomatic PEs, the overall rate of 30-day all-cause mortality was 5.1%, and the 30-day PE-related mortality was 1.9%, the authors report.
Significantly poorer outcomes were seen in patients with higher heart rates as compared to patients in the 80-99 bpm range, they also found. As compared to that reference range, odds ratios for 30-day all-cause death ranged from 1.5 for heart rates of 100-109, up to 2.4 for those with heart rates of 140 bpm or greater.
Likewise, patients with higher heart rates had a 1.7- to 2.4-fold greater risk of 30-day PE-related death as compared to the 80- to 99-bpm reference range, while patients with lower heart rates had lesser risk, the data published in CHEST show.
Toward refinement of prognostic scoring
Next, investigators sought to refine the prognostic scoring systems for low-risk PE (sPESI) and intermediate-high–risk PE (Bova).
For sPESI, they found that dropping the cutoff value from 110 to 100 bpm increased the sensitivity of the score from 93.4% to 95.3%. Going down even further to 80 bpm increased sensitivity to 98.8%, according to the report.
By going down from 110 to 80 bpm, the proportion of patients defined as low-risk dropped from 35% to 12%, according to the investigators.
For the Bova score, increasing the cutoff value from 110 to 120 bpm likewise increased specificity from 93.2% to 95%, while going up even further to 140 bpm increased specificity to 98.0%, the report shows.
In sensitivity analyses, the findings were not impacted by excluding younger patients, those who received reperfusion therapies, or those with atrial fibrillation, according to the study findings.
Potential implications for clinical practice
Taken together, these findings could serve as a resource to inform discussions regarding PE management that include whether home therapy or use of thrombolytic therapy is appropriate, investigators said in their report.
“For instance, among low-risk sPESI patients, those with borderline tachycardia [i.e., a heart rate between 100-109 bpm] might benefit from initial hospital observation for trending,” they wrote.
Dr. Jaureguízar reported no disclosures. One coinvestigator reported funding support from the Institute of Health Carlos III (ISCIII) and the European Development Regional Fund (ERDF). One coinvestigator reported consulting in litigation involving two models of inferior vena cava filters.
Dr. Polito reported no disclosures.
FROM CHEST
COVID-19 claims more than 675,000 U.S. lives, surpassing the 1918 flu
, according to data collected by Johns Hopkins University.
Although the raw numbers match, epidemiologists point out that 675,000 deaths in 1918 was a much greater proportion of the population. In 1918, the U.S. population was 105 million, less than one third of what it is today.
The AIDS pandemic of the 1980s remains the deadliest of the 20th Century, claiming the lives of 700,000 Americans. But at our current pace of 2,000 COVID deaths a day, we could quickly eclipse that death toll, too.
Even though the 1918 epidemic is often called the “Spanish Flu,” there is no universal consensus regarding where the virus originated, according to the Centers for Disease Control and Prevention.
Still, the almost incomprehensible loss harkens back to a time when medicine and technology were far less advanced than they are today.
In 1918, the United States didn’t have access to a vaccine, or near real-time tools to trace the spread and communicate the threat.
In some ways, the United States has failed to learn from the mistakes of the past.
There are many similarities between the two pandemics. In the spring of 1918, when the first wave of influenza hit, the United States and its allies were nearing victory in Europe in World War I. Just this summer the United States has ended its longest war, the conflict in Afghanistan, as COVID cases surge.
In both pandemics, hospitals and funeral homes were overrun and makeshift clinics were opened where space was available. Mask mandates were installed; schools, churches, and theaters closed; and social distancing was encouraged.
As is the case today, different jurisdictions took different steps to fight the pandemic and some were more successful than others.
According to History.com, in 1918, Philadelphia’s mayor said a popular annual parade could be held, and an estimated 200,000 people attended. In less than 2 weeks, more than 1,000 local residents were dead. But in St. Louis, public gatherings were banned, schools and theaters closed, and the death toll there was one eighth of Philadelphia’s.
Just as in 1918, America has at times continued to fan the flames of the epidemic by relaxing restrictions too quickly and relying on unproven treatments. Poor communication allowed younger people to feel that they wouldn’t necessarily face the worst consequences of the virus, contributing to a false sense of security in the age group that was fueling the spread.
“A lot of the mistakes that we definitely fell into in 1918, we hoped we wouldn’t fall into in 2020,” epidemiologist Stephen Kissler, PhD, of the Harvard T.H. Chan School of Public Health, told CNN. “We did.”
A version of this article first appeared on Medscape.com.
, according to data collected by Johns Hopkins University.
Although the raw numbers match, epidemiologists point out that 675,000 deaths in 1918 was a much greater proportion of the population. In 1918, the U.S. population was 105 million, less than one third of what it is today.
The AIDS pandemic of the 1980s remains the deadliest of the 20th Century, claiming the lives of 700,000 Americans. But at our current pace of 2,000 COVID deaths a day, we could quickly eclipse that death toll, too.
Even though the 1918 epidemic is often called the “Spanish Flu,” there is no universal consensus regarding where the virus originated, according to the Centers for Disease Control and Prevention.
Still, the almost incomprehensible loss harkens back to a time when medicine and technology were far less advanced than they are today.
In 1918, the United States didn’t have access to a vaccine, or near real-time tools to trace the spread and communicate the threat.
In some ways, the United States has failed to learn from the mistakes of the past.
There are many similarities between the two pandemics. In the spring of 1918, when the first wave of influenza hit, the United States and its allies were nearing victory in Europe in World War I. Just this summer the United States has ended its longest war, the conflict in Afghanistan, as COVID cases surge.
In both pandemics, hospitals and funeral homes were overrun and makeshift clinics were opened where space was available. Mask mandates were installed; schools, churches, and theaters closed; and social distancing was encouraged.
As is the case today, different jurisdictions took different steps to fight the pandemic and some were more successful than others.
According to History.com, in 1918, Philadelphia’s mayor said a popular annual parade could be held, and an estimated 200,000 people attended. In less than 2 weeks, more than 1,000 local residents were dead. But in St. Louis, public gatherings were banned, schools and theaters closed, and the death toll there was one eighth of Philadelphia’s.
Just as in 1918, America has at times continued to fan the flames of the epidemic by relaxing restrictions too quickly and relying on unproven treatments. Poor communication allowed younger people to feel that they wouldn’t necessarily face the worst consequences of the virus, contributing to a false sense of security in the age group that was fueling the spread.
“A lot of the mistakes that we definitely fell into in 1918, we hoped we wouldn’t fall into in 2020,” epidemiologist Stephen Kissler, PhD, of the Harvard T.H. Chan School of Public Health, told CNN. “We did.”
A version of this article first appeared on Medscape.com.
, according to data collected by Johns Hopkins University.
Although the raw numbers match, epidemiologists point out that 675,000 deaths in 1918 was a much greater proportion of the population. In 1918, the U.S. population was 105 million, less than one third of what it is today.
The AIDS pandemic of the 1980s remains the deadliest of the 20th Century, claiming the lives of 700,000 Americans. But at our current pace of 2,000 COVID deaths a day, we could quickly eclipse that death toll, too.
Even though the 1918 epidemic is often called the “Spanish Flu,” there is no universal consensus regarding where the virus originated, according to the Centers for Disease Control and Prevention.
Still, the almost incomprehensible loss harkens back to a time when medicine and technology were far less advanced than they are today.
In 1918, the United States didn’t have access to a vaccine, or near real-time tools to trace the spread and communicate the threat.
In some ways, the United States has failed to learn from the mistakes of the past.
There are many similarities between the two pandemics. In the spring of 1918, when the first wave of influenza hit, the United States and its allies were nearing victory in Europe in World War I. Just this summer the United States has ended its longest war, the conflict in Afghanistan, as COVID cases surge.
In both pandemics, hospitals and funeral homes were overrun and makeshift clinics were opened where space was available. Mask mandates were installed; schools, churches, and theaters closed; and social distancing was encouraged.
As is the case today, different jurisdictions took different steps to fight the pandemic and some were more successful than others.
According to History.com, in 1918, Philadelphia’s mayor said a popular annual parade could be held, and an estimated 200,000 people attended. In less than 2 weeks, more than 1,000 local residents were dead. But in St. Louis, public gatherings were banned, schools and theaters closed, and the death toll there was one eighth of Philadelphia’s.
Just as in 1918, America has at times continued to fan the flames of the epidemic by relaxing restrictions too quickly and relying on unproven treatments. Poor communication allowed younger people to feel that they wouldn’t necessarily face the worst consequences of the virus, contributing to a false sense of security in the age group that was fueling the spread.
“A lot of the mistakes that we definitely fell into in 1918, we hoped we wouldn’t fall into in 2020,” epidemiologist Stephen Kissler, PhD, of the Harvard T.H. Chan School of Public Health, told CNN. “We did.”
A version of this article first appeared on Medscape.com.
EMPEROR-Preserved: Empagliflozin’s HFpEF efficacy catalyzes a heart failure redefinition
Groundbreaking results from the EMPEROR-Preserved trial did more than establish for the first time that a drug, empagliflozin, has clearly proven efficacy for treating patients with heart failure with preserved ejection fraction (HFpEF). The results also helped catalyze a paradigm shift in how heart failure thought leaders think about the role of ejection fraction for making important distinctions among patients with heart failure.
EMPEROR-Preserved may also be the final nail in the coffin for defining patients with heart failure as having HFpEF or heart failure with reduced ejection fraction (HFrEF).
This new consensus essentially throws out left ventricular ejection fraction (EF) as the key metric for matching patients to heart failure treatments. Experts have instead begun suggesting a more unified treatment approach for all heart failure patients regardless of their EF.
‘Forget about ejection fraction’
“We encourage you to forget about ejection fraction,” declared Milton Packer, MD, during discussion at a session of the annual scientific meeting of the Heart Failure Society of America. “We certainly encourage you to forget about an ejection fraction of less than 40%” as having special significance,” added Dr. Packer, a lead investigator for both the EMPEROR-Reduced and EMPEROR-Preserved trials (which researchers combined in a unified analysis with a total of 9,718 patients with heart failure called EMPEROR-Pooled), and a heart failure researcher at Baylor University Medical Center in Dallas.
“The 40% ejection fraction divide is artificial. It was created in 2003 as part of a trial design, but it has no physiological significance,” Dr. Packer explained. A much better way to distinguish systolic and diastolic heart failure is by strain assessment rather than by ejection fraction. “Strain is a measure of myocardial shortening, a measure of what the heart does. Ejection fraction is a measure of volume,” said Dr. Packer. “Sign me up to get rid of ejection fraction,” he added.
“Ejection fraction is not as valuable as we thought for distinguishing the therapeutic benefit” of heart failure drugs, agreed Marvin A. Konstam, MD, professor of medicine at Tufts University and chief physician executive of the CardioVascular Center of Tufts Medical Center, both in Boston, who spoke during a different session at the meeting.
“It would easier if we didn’t spend time parsing this number,” ejection fraction, commented Clyde W. Yancy, MD, professor of medicine and chief of cardiology at Northwestern Medicine in Chicago. “Wouldn’t it be easier if we said that every patient with heart failure needs to receive one agent from each of the four [pillar] drug classes, and put them in a polypill” at reduced dosages, he proposed, envisioning one potential consequence of jettisoning ejection fraction.
The four pillar drug classes, recently identified as essential for patients with HFrEF but until now not endorsed for patients with HFpEF, are the sodium-glucose cotransporter 2 (SGLT2) inhibitors, such as empagliflozin (Jardiance); an angiotensin receptor blocker neprilysin inhibitor compound such as sacubitril/valsartan (Entresto); beta-blockers; and mineralocorticoid receptor antagonists such as spironolactone and eplerenone.
An opportunity for ‘simpler and easier’ treatments
“This is an opportunity to disrupt the way we’ve been doing things and think about something that is simpler and easier,” said Dr. Yancy, who chaired some of the panels serially formed by the American Heart Association and American College of Cardiology to write guidelines for treating heart failure. “An approach that would be easier to implement without worrying about staggering the start of each drug class and an incessant focus on titrating individual elements and taking 6 months to get to a certain place.”
Results from EMPEROR-Preserved and the combined EMPEROR-Pooled analysis triggered these paradigm-shifting sentiments by showing clear evidence that treatment with empagliflozin exerts consistent benefit – and is consistently safe – for patients with heart failure across a spectrum of EFs, from less than 25% to 64%, though its performance in patients with HFpEF and EFs of 65% or greater in the EMPEROR-Preserved trial remains unclear.
The consequence is that clinicians should feel comfortable prescribing empagliflozin to most patients with heart failure without regard to EF, even patients with EF values in the mid-60% range.
The EMPEROR-Preserved results showed a clear signal of attenuated benefit among patients with an EF of 65% or greater “on a population basis,” stressed Dr. Packer. “But on an individual basis, ejection fraction is not that reproducible, so measuring ejection fraction will not help you determine whom to treat or not treat. “
“There is significant variability” measuring EF using the most common modality, echocardiography, noted Javed Butler, MD, an EMPEROR coinvestigator who also spoke at the meeting session. A person with a measured EF of 65% could actually have a value that may be as low as 58% or as high as about 72%, noted Dr. Butler, who is professor and chair of medicine at the University of Mississippi, Jackson. The upshot is that any patient diagnosed with heart failure should receive an SGLT2 inhibitor “irrespective of their ejection fraction,” Dr. Butler advised.
“Ejection fraction is very crude, and probably not sufficient to identify a phenotype,” for treatment, said Dr. Yancy. “The real takeaway may be that we need to revisit what we call HFrEF, and then let that be the new standard for treatment.”
“Is [an EF of] 60% the new 40%?” asked Dr. Packer, implying that the answer was yes.
Results from several trials suggest redefining HFrEF
The idea that patients without traditionally defined HFrEF – an EF of 40% or less – could also benefit from other classes of heart failure drugs has been gestating for a while, and then rose to a new level with the August 2021 report of results from EMPEROR-Preserved. Two years ago, in September 2019, Dr. Butler, Dr. Packer, and a third colleague advanced the notion of redefining HFrEF by raising the ejection fraction ceiling in a published commentary.
They cited the experience with the angiotensin receptor blocker candesartan in a post hoc analysis of data collected in the CHARM-Preserved trial, which showed a strong signal of benefit in the subgroup of patients with EFs of 41%-49%, but not in those with an EF of 50% or higher. This finding prompted Dr. Konstam to express doubts about relying on EF to define heart failure subgroups in trials and guide management in a commentary published more than 3 years ago.
Another crack in the traditional EF framework came from analysis of results from the TOPCAT trial that tested spironolactone as a treatment for patients with HFpEF, according to the 2019 opinion published by Dr. Butler and Dr. Packer. Once again a post hoc analysis, this time using data from TOPCAT, suggested a benefit from the mineralocorticoid receptor antagonist spironolactone in patients with heart failure and an EF of 45%-49% (45% was the minimum EF for enrollment into the study).
Recently, data from a third trial that tested sacubitril/valsartan in patients with HFpEF, PARAGON-HF, showed benefit among patients with EFs below the study median of 57%. This finding led the Food and Drug Administration in February 2021 to amend its initial approval for sacubitril/valsartan by removing a specific EF ceiling from the drug’s indication and instead saying that patient’s receiving the drug should have a “below normal” EF.
Writing in a recent commentary, Dr. Yancy called the FDA’s action on sacubitril/valsartan “reasonable,” and that the subgroup assessment of data from the PARAGON-HF trial creates a “new, reasonably evidence-based therapy for HFpEF.” He also predicted that guideline-writing panels will “likely align with a permissive statement of indication” for sacubitril/valsartan in patients with HFpEF, especially those with EFs of less than 57%.
The idea of using an SGLT2 inhibitor like empagliflozin on all heart failure patients, and also adding agents like sacubitril/valsartan and spironolactone in patients with HFpEF and EFs in the mid-50% range or lower may take some time to catch on, but it already has one influential advocate.
“If a patient has HFpEF with an EF of less than 55%, use quadruple-class therapy,” summed up Dr. Butler during the HFSA session, while also suggesting prescribing an SGLT2 inhibitor to essentially all patients with heart failure regardless of their EF.
The EMPEROR-Preserved and EMPEROR-Reduced trials and the EMPEROR-Pooled analysis were sponsored by Boehringer Ingelheim and Lilly, the companies that jointly market empagliflozin (Jardiance). Dr. Packer has had financial relationships with BI and Lilly and numerous other companies. Dr. Konstam has served on data monitoring committees for trials funded by Boehringer Ingelheim and by Amgen, Luitpold, and Pfizer, and has been a consultant to Arena, LivaNova, Merck, SC Pharma, and Takeda. Dr. Yancy had no disclosures. Dr. Butler has had financial relationships with Boehringer Ingelheim and numerous other companies.
Groundbreaking results from the EMPEROR-Preserved trial did more than establish for the first time that a drug, empagliflozin, has clearly proven efficacy for treating patients with heart failure with preserved ejection fraction (HFpEF). The results also helped catalyze a paradigm shift in how heart failure thought leaders think about the role of ejection fraction for making important distinctions among patients with heart failure.
EMPEROR-Preserved may also be the final nail in the coffin for defining patients with heart failure as having HFpEF or heart failure with reduced ejection fraction (HFrEF).
This new consensus essentially throws out left ventricular ejection fraction (EF) as the key metric for matching patients to heart failure treatments. Experts have instead begun suggesting a more unified treatment approach for all heart failure patients regardless of their EF.
‘Forget about ejection fraction’
“We encourage you to forget about ejection fraction,” declared Milton Packer, MD, during discussion at a session of the annual scientific meeting of the Heart Failure Society of America. “We certainly encourage you to forget about an ejection fraction of less than 40%” as having special significance,” added Dr. Packer, a lead investigator for both the EMPEROR-Reduced and EMPEROR-Preserved trials (which researchers combined in a unified analysis with a total of 9,718 patients with heart failure called EMPEROR-Pooled), and a heart failure researcher at Baylor University Medical Center in Dallas.
“The 40% ejection fraction divide is artificial. It was created in 2003 as part of a trial design, but it has no physiological significance,” Dr. Packer explained. A much better way to distinguish systolic and diastolic heart failure is by strain assessment rather than by ejection fraction. “Strain is a measure of myocardial shortening, a measure of what the heart does. Ejection fraction is a measure of volume,” said Dr. Packer. “Sign me up to get rid of ejection fraction,” he added.
“Ejection fraction is not as valuable as we thought for distinguishing the therapeutic benefit” of heart failure drugs, agreed Marvin A. Konstam, MD, professor of medicine at Tufts University and chief physician executive of the CardioVascular Center of Tufts Medical Center, both in Boston, who spoke during a different session at the meeting.
“It would easier if we didn’t spend time parsing this number,” ejection fraction, commented Clyde W. Yancy, MD, professor of medicine and chief of cardiology at Northwestern Medicine in Chicago. “Wouldn’t it be easier if we said that every patient with heart failure needs to receive one agent from each of the four [pillar] drug classes, and put them in a polypill” at reduced dosages, he proposed, envisioning one potential consequence of jettisoning ejection fraction.
The four pillar drug classes, recently identified as essential for patients with HFrEF but until now not endorsed for patients with HFpEF, are the sodium-glucose cotransporter 2 (SGLT2) inhibitors, such as empagliflozin (Jardiance); an angiotensin receptor blocker neprilysin inhibitor compound such as sacubitril/valsartan (Entresto); beta-blockers; and mineralocorticoid receptor antagonists such as spironolactone and eplerenone.
An opportunity for ‘simpler and easier’ treatments
“This is an opportunity to disrupt the way we’ve been doing things and think about something that is simpler and easier,” said Dr. Yancy, who chaired some of the panels serially formed by the American Heart Association and American College of Cardiology to write guidelines for treating heart failure. “An approach that would be easier to implement without worrying about staggering the start of each drug class and an incessant focus on titrating individual elements and taking 6 months to get to a certain place.”
Results from EMPEROR-Preserved and the combined EMPEROR-Pooled analysis triggered these paradigm-shifting sentiments by showing clear evidence that treatment with empagliflozin exerts consistent benefit – and is consistently safe – for patients with heart failure across a spectrum of EFs, from less than 25% to 64%, though its performance in patients with HFpEF and EFs of 65% or greater in the EMPEROR-Preserved trial remains unclear.
The consequence is that clinicians should feel comfortable prescribing empagliflozin to most patients with heart failure without regard to EF, even patients with EF values in the mid-60% range.
The EMPEROR-Preserved results showed a clear signal of attenuated benefit among patients with an EF of 65% or greater “on a population basis,” stressed Dr. Packer. “But on an individual basis, ejection fraction is not that reproducible, so measuring ejection fraction will not help you determine whom to treat or not treat. “
“There is significant variability” measuring EF using the most common modality, echocardiography, noted Javed Butler, MD, an EMPEROR coinvestigator who also spoke at the meeting session. A person with a measured EF of 65% could actually have a value that may be as low as 58% or as high as about 72%, noted Dr. Butler, who is professor and chair of medicine at the University of Mississippi, Jackson. The upshot is that any patient diagnosed with heart failure should receive an SGLT2 inhibitor “irrespective of their ejection fraction,” Dr. Butler advised.
“Ejection fraction is very crude, and probably not sufficient to identify a phenotype,” for treatment, said Dr. Yancy. “The real takeaway may be that we need to revisit what we call HFrEF, and then let that be the new standard for treatment.”
“Is [an EF of] 60% the new 40%?” asked Dr. Packer, implying that the answer was yes.
Results from several trials suggest redefining HFrEF
The idea that patients without traditionally defined HFrEF – an EF of 40% or less – could also benefit from other classes of heart failure drugs has been gestating for a while, and then rose to a new level with the August 2021 report of results from EMPEROR-Preserved. Two years ago, in September 2019, Dr. Butler, Dr. Packer, and a third colleague advanced the notion of redefining HFrEF by raising the ejection fraction ceiling in a published commentary.
They cited the experience with the angiotensin receptor blocker candesartan in a post hoc analysis of data collected in the CHARM-Preserved trial, which showed a strong signal of benefit in the subgroup of patients with EFs of 41%-49%, but not in those with an EF of 50% or higher. This finding prompted Dr. Konstam to express doubts about relying on EF to define heart failure subgroups in trials and guide management in a commentary published more than 3 years ago.
Another crack in the traditional EF framework came from analysis of results from the TOPCAT trial that tested spironolactone as a treatment for patients with HFpEF, according to the 2019 opinion published by Dr. Butler and Dr. Packer. Once again a post hoc analysis, this time using data from TOPCAT, suggested a benefit from the mineralocorticoid receptor antagonist spironolactone in patients with heart failure and an EF of 45%-49% (45% was the minimum EF for enrollment into the study).
Recently, data from a third trial that tested sacubitril/valsartan in patients with HFpEF, PARAGON-HF, showed benefit among patients with EFs below the study median of 57%. This finding led the Food and Drug Administration in February 2021 to amend its initial approval for sacubitril/valsartan by removing a specific EF ceiling from the drug’s indication and instead saying that patient’s receiving the drug should have a “below normal” EF.
Writing in a recent commentary, Dr. Yancy called the FDA’s action on sacubitril/valsartan “reasonable,” and that the subgroup assessment of data from the PARAGON-HF trial creates a “new, reasonably evidence-based therapy for HFpEF.” He also predicted that guideline-writing panels will “likely align with a permissive statement of indication” for sacubitril/valsartan in patients with HFpEF, especially those with EFs of less than 57%.
The idea of using an SGLT2 inhibitor like empagliflozin on all heart failure patients, and also adding agents like sacubitril/valsartan and spironolactone in patients with HFpEF and EFs in the mid-50% range or lower may take some time to catch on, but it already has one influential advocate.
“If a patient has HFpEF with an EF of less than 55%, use quadruple-class therapy,” summed up Dr. Butler during the HFSA session, while also suggesting prescribing an SGLT2 inhibitor to essentially all patients with heart failure regardless of their EF.
The EMPEROR-Preserved and EMPEROR-Reduced trials and the EMPEROR-Pooled analysis were sponsored by Boehringer Ingelheim and Lilly, the companies that jointly market empagliflozin (Jardiance). Dr. Packer has had financial relationships with BI and Lilly and numerous other companies. Dr. Konstam has served on data monitoring committees for trials funded by Boehringer Ingelheim and by Amgen, Luitpold, and Pfizer, and has been a consultant to Arena, LivaNova, Merck, SC Pharma, and Takeda. Dr. Yancy had no disclosures. Dr. Butler has had financial relationships with Boehringer Ingelheim and numerous other companies.
Groundbreaking results from the EMPEROR-Preserved trial did more than establish for the first time that a drug, empagliflozin, has clearly proven efficacy for treating patients with heart failure with preserved ejection fraction (HFpEF). The results also helped catalyze a paradigm shift in how heart failure thought leaders think about the role of ejection fraction for making important distinctions among patients with heart failure.
EMPEROR-Preserved may also be the final nail in the coffin for defining patients with heart failure as having HFpEF or heart failure with reduced ejection fraction (HFrEF).
This new consensus essentially throws out left ventricular ejection fraction (EF) as the key metric for matching patients to heart failure treatments. Experts have instead begun suggesting a more unified treatment approach for all heart failure patients regardless of their EF.
‘Forget about ejection fraction’
“We encourage you to forget about ejection fraction,” declared Milton Packer, MD, during discussion at a session of the annual scientific meeting of the Heart Failure Society of America. “We certainly encourage you to forget about an ejection fraction of less than 40%” as having special significance,” added Dr. Packer, a lead investigator for both the EMPEROR-Reduced and EMPEROR-Preserved trials (which researchers combined in a unified analysis with a total of 9,718 patients with heart failure called EMPEROR-Pooled), and a heart failure researcher at Baylor University Medical Center in Dallas.
“The 40% ejection fraction divide is artificial. It was created in 2003 as part of a trial design, but it has no physiological significance,” Dr. Packer explained. A much better way to distinguish systolic and diastolic heart failure is by strain assessment rather than by ejection fraction. “Strain is a measure of myocardial shortening, a measure of what the heart does. Ejection fraction is a measure of volume,” said Dr. Packer. “Sign me up to get rid of ejection fraction,” he added.
“Ejection fraction is not as valuable as we thought for distinguishing the therapeutic benefit” of heart failure drugs, agreed Marvin A. Konstam, MD, professor of medicine at Tufts University and chief physician executive of the CardioVascular Center of Tufts Medical Center, both in Boston, who spoke during a different session at the meeting.
“It would easier if we didn’t spend time parsing this number,” ejection fraction, commented Clyde W. Yancy, MD, professor of medicine and chief of cardiology at Northwestern Medicine in Chicago. “Wouldn’t it be easier if we said that every patient with heart failure needs to receive one agent from each of the four [pillar] drug classes, and put them in a polypill” at reduced dosages, he proposed, envisioning one potential consequence of jettisoning ejection fraction.
The four pillar drug classes, recently identified as essential for patients with HFrEF but until now not endorsed for patients with HFpEF, are the sodium-glucose cotransporter 2 (SGLT2) inhibitors, such as empagliflozin (Jardiance); an angiotensin receptor blocker neprilysin inhibitor compound such as sacubitril/valsartan (Entresto); beta-blockers; and mineralocorticoid receptor antagonists such as spironolactone and eplerenone.
An opportunity for ‘simpler and easier’ treatments
“This is an opportunity to disrupt the way we’ve been doing things and think about something that is simpler and easier,” said Dr. Yancy, who chaired some of the panels serially formed by the American Heart Association and American College of Cardiology to write guidelines for treating heart failure. “An approach that would be easier to implement without worrying about staggering the start of each drug class and an incessant focus on titrating individual elements and taking 6 months to get to a certain place.”
Results from EMPEROR-Preserved and the combined EMPEROR-Pooled analysis triggered these paradigm-shifting sentiments by showing clear evidence that treatment with empagliflozin exerts consistent benefit – and is consistently safe – for patients with heart failure across a spectrum of EFs, from less than 25% to 64%, though its performance in patients with HFpEF and EFs of 65% or greater in the EMPEROR-Preserved trial remains unclear.
The consequence is that clinicians should feel comfortable prescribing empagliflozin to most patients with heart failure without regard to EF, even patients with EF values in the mid-60% range.
The EMPEROR-Preserved results showed a clear signal of attenuated benefit among patients with an EF of 65% or greater “on a population basis,” stressed Dr. Packer. “But on an individual basis, ejection fraction is not that reproducible, so measuring ejection fraction will not help you determine whom to treat or not treat. “
“There is significant variability” measuring EF using the most common modality, echocardiography, noted Javed Butler, MD, an EMPEROR coinvestigator who also spoke at the meeting session. A person with a measured EF of 65% could actually have a value that may be as low as 58% or as high as about 72%, noted Dr. Butler, who is professor and chair of medicine at the University of Mississippi, Jackson. The upshot is that any patient diagnosed with heart failure should receive an SGLT2 inhibitor “irrespective of their ejection fraction,” Dr. Butler advised.
“Ejection fraction is very crude, and probably not sufficient to identify a phenotype,” for treatment, said Dr. Yancy. “The real takeaway may be that we need to revisit what we call HFrEF, and then let that be the new standard for treatment.”
“Is [an EF of] 60% the new 40%?” asked Dr. Packer, implying that the answer was yes.
Results from several trials suggest redefining HFrEF
The idea that patients without traditionally defined HFrEF – an EF of 40% or less – could also benefit from other classes of heart failure drugs has been gestating for a while, and then rose to a new level with the August 2021 report of results from EMPEROR-Preserved. Two years ago, in September 2019, Dr. Butler, Dr. Packer, and a third colleague advanced the notion of redefining HFrEF by raising the ejection fraction ceiling in a published commentary.
They cited the experience with the angiotensin receptor blocker candesartan in a post hoc analysis of data collected in the CHARM-Preserved trial, which showed a strong signal of benefit in the subgroup of patients with EFs of 41%-49%, but not in those with an EF of 50% or higher. This finding prompted Dr. Konstam to express doubts about relying on EF to define heart failure subgroups in trials and guide management in a commentary published more than 3 years ago.
Another crack in the traditional EF framework came from analysis of results from the TOPCAT trial that tested spironolactone as a treatment for patients with HFpEF, according to the 2019 opinion published by Dr. Butler and Dr. Packer. Once again a post hoc analysis, this time using data from TOPCAT, suggested a benefit from the mineralocorticoid receptor antagonist spironolactone in patients with heart failure and an EF of 45%-49% (45% was the minimum EF for enrollment into the study).
Recently, data from a third trial that tested sacubitril/valsartan in patients with HFpEF, PARAGON-HF, showed benefit among patients with EFs below the study median of 57%. This finding led the Food and Drug Administration in February 2021 to amend its initial approval for sacubitril/valsartan by removing a specific EF ceiling from the drug’s indication and instead saying that patient’s receiving the drug should have a “below normal” EF.
Writing in a recent commentary, Dr. Yancy called the FDA’s action on sacubitril/valsartan “reasonable,” and that the subgroup assessment of data from the PARAGON-HF trial creates a “new, reasonably evidence-based therapy for HFpEF.” He also predicted that guideline-writing panels will “likely align with a permissive statement of indication” for sacubitril/valsartan in patients with HFpEF, especially those with EFs of less than 57%.
The idea of using an SGLT2 inhibitor like empagliflozin on all heart failure patients, and also adding agents like sacubitril/valsartan and spironolactone in patients with HFpEF and EFs in the mid-50% range or lower may take some time to catch on, but it already has one influential advocate.
“If a patient has HFpEF with an EF of less than 55%, use quadruple-class therapy,” summed up Dr. Butler during the HFSA session, while also suggesting prescribing an SGLT2 inhibitor to essentially all patients with heart failure regardless of their EF.
The EMPEROR-Preserved and EMPEROR-Reduced trials and the EMPEROR-Pooled analysis were sponsored by Boehringer Ingelheim and Lilly, the companies that jointly market empagliflozin (Jardiance). Dr. Packer has had financial relationships with BI and Lilly and numerous other companies. Dr. Konstam has served on data monitoring committees for trials funded by Boehringer Ingelheim and by Amgen, Luitpold, and Pfizer, and has been a consultant to Arena, LivaNova, Merck, SC Pharma, and Takeda. Dr. Yancy had no disclosures. Dr. Butler has had financial relationships with Boehringer Ingelheim and numerous other companies.
FROM HFSA 2021