User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
COVID subvariants could cause ‘substantial’ summer cases
As the coronavirus continues to evolve, Omicron subvariants such as BA.4 and BA.5 are expected to lead to many COVID-19 cases in the coming months.
Researchers recently reported that the subvariants have mutated for better “immune escape,” or the ability to avoid antibodies from vaccination or previous infection.
“That has changed our view for what will happen this summer,” Ali Mokdad, PhD, an epidemiologist who has developed COVID-19 forecasts for the University of Washington’s Institute for Health Metrics and Evaluation in Seattle, told The Boston Globe.
Until recently, Dr. Mokdad expected the United States to have a “very good summer” in terms of cases, hospitalizations, and deaths through September. The U.S. is reporting about 100,000 new cases per day, according to the data tracker by The New York Times, which has remained flat throughout June. Cases will likely decrease this summer, Dr. Mokdad said, though the decline will be slower and smaller than first thought.
As of June 18, BA.4 and BA.5 accounted for about 35% of cases in the United States, according to the latest CDC data, with BA.5 making up 23.5% and BA.4 making up 11.4%. The two subvariants will likely take over BA.2.12.1 as top subvariants in coming weeks.
“I expect that BA.5 will likely become the dominant virus in the United States this summer,” Dan Barouch, MD, director of the Center for Virology and Vaccine Research at Beth Israel Deaconess Medical Center in Boston, told the Globe.
Dr. Barouch said the Omicron subvariants will likely create a summer of “substantial infections” but low rates of hospitalization and death. He published a recent study in the New England Journal of Medicine that found BA.4 and BA.5 are better at escaping antibodies than other coronavirus strains – about three times better than the Omicron variants BA.1 and BA.2 and 20 times better than the first coronavirus strain.
“What we’re seeing with each subsequent variant is iteratively higher levels of transmissibility and higher levels of antibody immune escape,” he said. “We’re seeing high levels of infection in populations that are highly vaccinated, as well as populations that have a high level of natural immunity to the prior variants.”
At the same time, current antibodies still appear to protect people against the worst outcomes, Dr. Barouch said.
“If people have vaccine immunity or natural immunity, then they have substantial protection against severe disease,” he said.
So far, researchers have found that Omicron subvariants tend to cause less severe disease than other variants, such as Delta. Dr. Mokdad estimated that 80% of Omicron infections don’t show symptoms.
He said there is a “remote possibility” of another wave during the summer, but he expects cases to rise significantly around the beginning of October, when the seasons change, and most people’s immunity will wane. Other things could play into the predictions this summer, he noted, such as coronavirus mutations and new variants.
“Anybody that models this more than a couple of weeks out is basically just using pixie dust,” Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, Minneapolis, told the newspaper.
“There is no pattern whatsoever developing from a seasonality standpoint. It’s all being driven by the variants,” he said. “We just have to be humble and acknowledge that we don’t know.”
A version of this article first appeared on WebMD.com.
As the coronavirus continues to evolve, Omicron subvariants such as BA.4 and BA.5 are expected to lead to many COVID-19 cases in the coming months.
Researchers recently reported that the subvariants have mutated for better “immune escape,” or the ability to avoid antibodies from vaccination or previous infection.
“That has changed our view for what will happen this summer,” Ali Mokdad, PhD, an epidemiologist who has developed COVID-19 forecasts for the University of Washington’s Institute for Health Metrics and Evaluation in Seattle, told The Boston Globe.
Until recently, Dr. Mokdad expected the United States to have a “very good summer” in terms of cases, hospitalizations, and deaths through September. The U.S. is reporting about 100,000 new cases per day, according to the data tracker by The New York Times, which has remained flat throughout June. Cases will likely decrease this summer, Dr. Mokdad said, though the decline will be slower and smaller than first thought.
As of June 18, BA.4 and BA.5 accounted for about 35% of cases in the United States, according to the latest CDC data, with BA.5 making up 23.5% and BA.4 making up 11.4%. The two subvariants will likely take over BA.2.12.1 as top subvariants in coming weeks.
“I expect that BA.5 will likely become the dominant virus in the United States this summer,” Dan Barouch, MD, director of the Center for Virology and Vaccine Research at Beth Israel Deaconess Medical Center in Boston, told the Globe.
Dr. Barouch said the Omicron subvariants will likely create a summer of “substantial infections” but low rates of hospitalization and death. He published a recent study in the New England Journal of Medicine that found BA.4 and BA.5 are better at escaping antibodies than other coronavirus strains – about three times better than the Omicron variants BA.1 and BA.2 and 20 times better than the first coronavirus strain.
“What we’re seeing with each subsequent variant is iteratively higher levels of transmissibility and higher levels of antibody immune escape,” he said. “We’re seeing high levels of infection in populations that are highly vaccinated, as well as populations that have a high level of natural immunity to the prior variants.”
At the same time, current antibodies still appear to protect people against the worst outcomes, Dr. Barouch said.
“If people have vaccine immunity or natural immunity, then they have substantial protection against severe disease,” he said.
So far, researchers have found that Omicron subvariants tend to cause less severe disease than other variants, such as Delta. Dr. Mokdad estimated that 80% of Omicron infections don’t show symptoms.
He said there is a “remote possibility” of another wave during the summer, but he expects cases to rise significantly around the beginning of October, when the seasons change, and most people’s immunity will wane. Other things could play into the predictions this summer, he noted, such as coronavirus mutations and new variants.
“Anybody that models this more than a couple of weeks out is basically just using pixie dust,” Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, Minneapolis, told the newspaper.
“There is no pattern whatsoever developing from a seasonality standpoint. It’s all being driven by the variants,” he said. “We just have to be humble and acknowledge that we don’t know.”
A version of this article first appeared on WebMD.com.
As the coronavirus continues to evolve, Omicron subvariants such as BA.4 and BA.5 are expected to lead to many COVID-19 cases in the coming months.
Researchers recently reported that the subvariants have mutated for better “immune escape,” or the ability to avoid antibodies from vaccination or previous infection.
“That has changed our view for what will happen this summer,” Ali Mokdad, PhD, an epidemiologist who has developed COVID-19 forecasts for the University of Washington’s Institute for Health Metrics and Evaluation in Seattle, told The Boston Globe.
Until recently, Dr. Mokdad expected the United States to have a “very good summer” in terms of cases, hospitalizations, and deaths through September. The U.S. is reporting about 100,000 new cases per day, according to the data tracker by The New York Times, which has remained flat throughout June. Cases will likely decrease this summer, Dr. Mokdad said, though the decline will be slower and smaller than first thought.
As of June 18, BA.4 and BA.5 accounted for about 35% of cases in the United States, according to the latest CDC data, with BA.5 making up 23.5% and BA.4 making up 11.4%. The two subvariants will likely take over BA.2.12.1 as top subvariants in coming weeks.
“I expect that BA.5 will likely become the dominant virus in the United States this summer,” Dan Barouch, MD, director of the Center for Virology and Vaccine Research at Beth Israel Deaconess Medical Center in Boston, told the Globe.
Dr. Barouch said the Omicron subvariants will likely create a summer of “substantial infections” but low rates of hospitalization and death. He published a recent study in the New England Journal of Medicine that found BA.4 and BA.5 are better at escaping antibodies than other coronavirus strains – about three times better than the Omicron variants BA.1 and BA.2 and 20 times better than the first coronavirus strain.
“What we’re seeing with each subsequent variant is iteratively higher levels of transmissibility and higher levels of antibody immune escape,” he said. “We’re seeing high levels of infection in populations that are highly vaccinated, as well as populations that have a high level of natural immunity to the prior variants.”
At the same time, current antibodies still appear to protect people against the worst outcomes, Dr. Barouch said.
“If people have vaccine immunity or natural immunity, then they have substantial protection against severe disease,” he said.
So far, researchers have found that Omicron subvariants tend to cause less severe disease than other variants, such as Delta. Dr. Mokdad estimated that 80% of Omicron infections don’t show symptoms.
He said there is a “remote possibility” of another wave during the summer, but he expects cases to rise significantly around the beginning of October, when the seasons change, and most people’s immunity will wane. Other things could play into the predictions this summer, he noted, such as coronavirus mutations and new variants.
“Anybody that models this more than a couple of weeks out is basically just using pixie dust,” Michael Osterholm, PhD, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, Minneapolis, told the newspaper.
“There is no pattern whatsoever developing from a seasonality standpoint. It’s all being driven by the variants,” he said. “We just have to be humble and acknowledge that we don’t know.”
A version of this article first appeared on WebMD.com.
Race drives disparities in life expectancy across states
“Life expectancy is an important measure of the health of the entire population,” corresponding author Gregory Roth, MD, a cardiologist at the University of Washington, Seattle, said in an interview. “We know race, ethnicity and where you live all affect health, but we wanted to look at the long arc over many decades to understand where subpopulations have been, and where they are headed. Also, it is important to understand how race and place interact, so we looked at race/ethnicity groups within each state to see where disparities exist that need to be addressed.”
In the study, published in Annals of Internal Medicine, researchers led by Catherine O. Johnson, PhD, of the University of Washington, Seattle, reviewed data from 23 states, using regression models based on Census data and deidentified death records. They examined life expectancy for subgroups of individuals reporting Hispanic, non-Hispanic Black, or non-Hispanic White race or ethnicity.
Overall, most states showed an improvement in life expectancy between 1990 and 2019. For women, the mean life expectancy across states increased from 79.3 years in 1990 to 81.3 years in 2019. For men, the mean life expectancy across states increased from 72.6 years in 1990 to 76.3 years in 2019.
However, the researchers found significant disparities across the three racial subgroups between and within states when life expectancy was examined by race/ethnicity, independent of the average life expectancy for an entire state overall. They defined disparity as the difference in life expectancy between states for those in different racial/ethnic groups.
Without considering race/ethnicity, disparities in life expectancy across states decreased from 8.0 years and 12.2 years in 1990 to 7.9 and 7.8 years in 2019, for females and males, respectively.
When race/ethnicity was taken into account, disparities in life expectancy decreased, but the differences across states were greater than when race was not considered; 20.7 years for females and 24.5 years for males in 1990, decreasing to 18.5 years for females and 23.7 years for males in 2019.
Despite the overall improvements, disparities in life expectancy persisted across all states within each race/ethnicity group.
Among females, for example, non-Hispanic Black females had the lowest mean life expectancy across states in 1990 (74.2 years) but had the greatest improvement on average (6.9% increase) by 2019. However, the mean LE for non-Hispanic Black females remained lower than it did for non-Hispanic White and Hispanic females.
Among males, the researchers found differences in life expectancies across states between the people of the three different ethnicities they studied. The greatest difference in life expectancies in 1990 was 24.5 years. This occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Georgia. The life expectancy for these non-Hispanic Black males was 59.4 years, versus 83.8 years for these Hispanic males that year.
This reduced life expectancy for non-Hispanic Black males persisted, although it improved slightly by 2019. That year, the largest race-based disparity – which was approximately 24 years – occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Virginia. For the Hispanic males in Virgina, the LE was 90.7 years versus 66.9 years for non-Hispanic Black males in the District of Columbia.
The findings were limited by several factors including the review of data from only 23 states, the focus on life expectancy from birth versus other ages, and the challenges of defining Hispanic ethnicity, the researchers noted. However, the results support that the potential use of state-level analysis that includes race/ethnicity could be a valuable tool for measuring health inequity as part of national average trends, they said.
Health has truly stagnated for some in certain states
“Subpopulations in some states have much longer life expectancy now than 30 years ago. But in some states, we were struck by how health has truly stagnated for some,” Dr. Roth said in an interview. “We were surprised by the scale of the overall gap; a difference of about 8 years between states is more than twice that if you drill down to race/ethnicity groups in each state.”
A key message from the study is the need for all clinicians to advocate for improved access to primary care, “which is increasingly hard to obtain for many people,” said Dr. Roth. “So much of health is determined by key risk factors such as high blood pressure, high cholesterol, obesity, diabetes, alcohol use, tobacco use. But many of the determinants of health are not in the healthcare system, and include efforts to improve education, interrupt cycles of poverty, and teach healthy behaviors at a very young age. “Racism remains a underdiscussed part of these disparities, and we need better ways to measure the impact of social policies that end up impacting health down the road,” he said.
Looking ahead: “There is a lot to be learned from the states that have improved life expectancy the most. We need researchers to work together to identify and communicate what are those best practices, and what state governments can do to play their part.”
State-level differences reveal variations in health care
“The findings add to our growing knowledge of large and persistent racial/ethnic health disparities and changes in disparities during recent stagnation in U.S. life expectancy,” wrote Hedwig Lee, PhD, of Washington University in St. Louis, and Kathleen M. Harris, PhD, of the University of North Carolina at Chapel Hill, in an accompanying editorial.
The focus on state-level differences provides a unique window into the huge variation in life expectancy by race/ethnicity across the United States. The data suggest that “a person’s life expectancy in the United States may depend more on where you live than it has in the past,” they noted. For example, the editorialists highlighted that life expectancy for non-Hispanic Black men in 2019 averaged 81.1 years in Rhode Island, but 66.9 years in the District of Columbia.
They also noted the study’s lack of data for many states with high mortality rates and high proportions of non-Hispanic Black persons, Hispanic persons, and those with low socioeconomic states. Including data from these areas may have yielded even greater disparities in life expectancy.
“Despite substantial declines in mortality among Black persons during the study period, a non-Hispanic Black person’s life expectancy remained persistently lower than that of non-Hispanic White and Hispanic persons, both within and across states,” the editorialists wrote. “Future research needs to unpack the complex web of factors driving health and well-being by enabling better understanding of the places where we see persistent health disadvantage and advantage and the state-based explanations for these increasingly important differences determining population risk and resilience. We should be outraged by disparities in longevity and called to act to eliminate them.”
Identifying the problem is the first step
“In order to address or fix a problem we should first identify and quantify the problem,” Noel Deep, MD, an internal medicine physician in private practice in Antigo, Wisc., said in an interview.
“This study provides us with the information regarding the trends in life expectancy within states and the disparities in life expectancy when race/ ethnicity and gender are factored into the equation,” said Dr. Deep, who was not involved in the study. “Based on previously available data, we are aware of the increase in life expectancy in the United States over the last few decades, as well as differences in life expectancy for the different ethnicities/races and genders, but these data provide averages, not state or geographical differences. By having this knowledge at a state level, we can use that data to make health policies that address those health inequities and allocate appropriate resources at a state or local level.”
Several studies have identified disparities in health care and life expectancy based on the zip codes, such as the U.S. Small-Area Life Expectancy Estimates Project in 2018. The current study “provides further information for health care professionals and policy makers about the disparities in health outcomes and life expectancy based on race as well as gender, and it is quite detailed,” he said.
“As clinicians, we should strive to ensure that we are addressing these health inequities through our provision of clinical care and through our advocacy on behalf of our patients so that our nation’s health will improve overall,” he said.
“I would like to see future studies look at the socioeconomic status (income), urban versus rural residence, and place of birth (especially for immigrants),” said Dr. Deep. He also emphasized a need for studies to include the demographics for Hispanic populations; given the possible selection error “because of only healthy individuals immigrating to the United States or the older sicker Hispanics who might be migrating back to their homelands and not being included in the data and falsely increasing the life expectancy for this race/ ethnic groups.
“I would also like to see some research into the cultural and social factors that might explain why Hispanic populations might have a higher life expectancy even if their socioeconomic status is poor,” he said.
The study was supported by the National Heart, Lung, and Blood Institute. The researchers had no financial conflicts to disclose. The editorialists had no financial conflicts to disclose. Dr. Deep had no financial conflicts to disclose, but serves on the editorial advisory board of Internal Medicine News and as chair of the AMA’s Council on Science and Public Health.
“Life expectancy is an important measure of the health of the entire population,” corresponding author Gregory Roth, MD, a cardiologist at the University of Washington, Seattle, said in an interview. “We know race, ethnicity and where you live all affect health, but we wanted to look at the long arc over many decades to understand where subpopulations have been, and where they are headed. Also, it is important to understand how race and place interact, so we looked at race/ethnicity groups within each state to see where disparities exist that need to be addressed.”
In the study, published in Annals of Internal Medicine, researchers led by Catherine O. Johnson, PhD, of the University of Washington, Seattle, reviewed data from 23 states, using regression models based on Census data and deidentified death records. They examined life expectancy for subgroups of individuals reporting Hispanic, non-Hispanic Black, or non-Hispanic White race or ethnicity.
Overall, most states showed an improvement in life expectancy between 1990 and 2019. For women, the mean life expectancy across states increased from 79.3 years in 1990 to 81.3 years in 2019. For men, the mean life expectancy across states increased from 72.6 years in 1990 to 76.3 years in 2019.
However, the researchers found significant disparities across the three racial subgroups between and within states when life expectancy was examined by race/ethnicity, independent of the average life expectancy for an entire state overall. They defined disparity as the difference in life expectancy between states for those in different racial/ethnic groups.
Without considering race/ethnicity, disparities in life expectancy across states decreased from 8.0 years and 12.2 years in 1990 to 7.9 and 7.8 years in 2019, for females and males, respectively.
When race/ethnicity was taken into account, disparities in life expectancy decreased, but the differences across states were greater than when race was not considered; 20.7 years for females and 24.5 years for males in 1990, decreasing to 18.5 years for females and 23.7 years for males in 2019.
Despite the overall improvements, disparities in life expectancy persisted across all states within each race/ethnicity group.
Among females, for example, non-Hispanic Black females had the lowest mean life expectancy across states in 1990 (74.2 years) but had the greatest improvement on average (6.9% increase) by 2019. However, the mean LE for non-Hispanic Black females remained lower than it did for non-Hispanic White and Hispanic females.
Among males, the researchers found differences in life expectancies across states between the people of the three different ethnicities they studied. The greatest difference in life expectancies in 1990 was 24.5 years. This occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Georgia. The life expectancy for these non-Hispanic Black males was 59.4 years, versus 83.8 years for these Hispanic males that year.
This reduced life expectancy for non-Hispanic Black males persisted, although it improved slightly by 2019. That year, the largest race-based disparity – which was approximately 24 years – occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Virginia. For the Hispanic males in Virgina, the LE was 90.7 years versus 66.9 years for non-Hispanic Black males in the District of Columbia.
The findings were limited by several factors including the review of data from only 23 states, the focus on life expectancy from birth versus other ages, and the challenges of defining Hispanic ethnicity, the researchers noted. However, the results support that the potential use of state-level analysis that includes race/ethnicity could be a valuable tool for measuring health inequity as part of national average trends, they said.
Health has truly stagnated for some in certain states
“Subpopulations in some states have much longer life expectancy now than 30 years ago. But in some states, we were struck by how health has truly stagnated for some,” Dr. Roth said in an interview. “We were surprised by the scale of the overall gap; a difference of about 8 years between states is more than twice that if you drill down to race/ethnicity groups in each state.”
A key message from the study is the need for all clinicians to advocate for improved access to primary care, “which is increasingly hard to obtain for many people,” said Dr. Roth. “So much of health is determined by key risk factors such as high blood pressure, high cholesterol, obesity, diabetes, alcohol use, tobacco use. But many of the determinants of health are not in the healthcare system, and include efforts to improve education, interrupt cycles of poverty, and teach healthy behaviors at a very young age. “Racism remains a underdiscussed part of these disparities, and we need better ways to measure the impact of social policies that end up impacting health down the road,” he said.
Looking ahead: “There is a lot to be learned from the states that have improved life expectancy the most. We need researchers to work together to identify and communicate what are those best practices, and what state governments can do to play their part.”
State-level differences reveal variations in health care
“The findings add to our growing knowledge of large and persistent racial/ethnic health disparities and changes in disparities during recent stagnation in U.S. life expectancy,” wrote Hedwig Lee, PhD, of Washington University in St. Louis, and Kathleen M. Harris, PhD, of the University of North Carolina at Chapel Hill, in an accompanying editorial.
The focus on state-level differences provides a unique window into the huge variation in life expectancy by race/ethnicity across the United States. The data suggest that “a person’s life expectancy in the United States may depend more on where you live than it has in the past,” they noted. For example, the editorialists highlighted that life expectancy for non-Hispanic Black men in 2019 averaged 81.1 years in Rhode Island, but 66.9 years in the District of Columbia.
They also noted the study’s lack of data for many states with high mortality rates and high proportions of non-Hispanic Black persons, Hispanic persons, and those with low socioeconomic states. Including data from these areas may have yielded even greater disparities in life expectancy.
“Despite substantial declines in mortality among Black persons during the study period, a non-Hispanic Black person’s life expectancy remained persistently lower than that of non-Hispanic White and Hispanic persons, both within and across states,” the editorialists wrote. “Future research needs to unpack the complex web of factors driving health and well-being by enabling better understanding of the places where we see persistent health disadvantage and advantage and the state-based explanations for these increasingly important differences determining population risk and resilience. We should be outraged by disparities in longevity and called to act to eliminate them.”
Identifying the problem is the first step
“In order to address or fix a problem we should first identify and quantify the problem,” Noel Deep, MD, an internal medicine physician in private practice in Antigo, Wisc., said in an interview.
“This study provides us with the information regarding the trends in life expectancy within states and the disparities in life expectancy when race/ ethnicity and gender are factored into the equation,” said Dr. Deep, who was not involved in the study. “Based on previously available data, we are aware of the increase in life expectancy in the United States over the last few decades, as well as differences in life expectancy for the different ethnicities/races and genders, but these data provide averages, not state or geographical differences. By having this knowledge at a state level, we can use that data to make health policies that address those health inequities and allocate appropriate resources at a state or local level.”
Several studies have identified disparities in health care and life expectancy based on the zip codes, such as the U.S. Small-Area Life Expectancy Estimates Project in 2018. The current study “provides further information for health care professionals and policy makers about the disparities in health outcomes and life expectancy based on race as well as gender, and it is quite detailed,” he said.
“As clinicians, we should strive to ensure that we are addressing these health inequities through our provision of clinical care and through our advocacy on behalf of our patients so that our nation’s health will improve overall,” he said.
“I would like to see future studies look at the socioeconomic status (income), urban versus rural residence, and place of birth (especially for immigrants),” said Dr. Deep. He also emphasized a need for studies to include the demographics for Hispanic populations; given the possible selection error “because of only healthy individuals immigrating to the United States or the older sicker Hispanics who might be migrating back to their homelands and not being included in the data and falsely increasing the life expectancy for this race/ ethnic groups.
“I would also like to see some research into the cultural and social factors that might explain why Hispanic populations might have a higher life expectancy even if their socioeconomic status is poor,” he said.
The study was supported by the National Heart, Lung, and Blood Institute. The researchers had no financial conflicts to disclose. The editorialists had no financial conflicts to disclose. Dr. Deep had no financial conflicts to disclose, but serves on the editorial advisory board of Internal Medicine News and as chair of the AMA’s Council on Science and Public Health.
“Life expectancy is an important measure of the health of the entire population,” corresponding author Gregory Roth, MD, a cardiologist at the University of Washington, Seattle, said in an interview. “We know race, ethnicity and where you live all affect health, but we wanted to look at the long arc over many decades to understand where subpopulations have been, and where they are headed. Also, it is important to understand how race and place interact, so we looked at race/ethnicity groups within each state to see where disparities exist that need to be addressed.”
In the study, published in Annals of Internal Medicine, researchers led by Catherine O. Johnson, PhD, of the University of Washington, Seattle, reviewed data from 23 states, using regression models based on Census data and deidentified death records. They examined life expectancy for subgroups of individuals reporting Hispanic, non-Hispanic Black, or non-Hispanic White race or ethnicity.
Overall, most states showed an improvement in life expectancy between 1990 and 2019. For women, the mean life expectancy across states increased from 79.3 years in 1990 to 81.3 years in 2019. For men, the mean life expectancy across states increased from 72.6 years in 1990 to 76.3 years in 2019.
However, the researchers found significant disparities across the three racial subgroups between and within states when life expectancy was examined by race/ethnicity, independent of the average life expectancy for an entire state overall. They defined disparity as the difference in life expectancy between states for those in different racial/ethnic groups.
Without considering race/ethnicity, disparities in life expectancy across states decreased from 8.0 years and 12.2 years in 1990 to 7.9 and 7.8 years in 2019, for females and males, respectively.
When race/ethnicity was taken into account, disparities in life expectancy decreased, but the differences across states were greater than when race was not considered; 20.7 years for females and 24.5 years for males in 1990, decreasing to 18.5 years for females and 23.7 years for males in 2019.
Despite the overall improvements, disparities in life expectancy persisted across all states within each race/ethnicity group.
Among females, for example, non-Hispanic Black females had the lowest mean life expectancy across states in 1990 (74.2 years) but had the greatest improvement on average (6.9% increase) by 2019. However, the mean LE for non-Hispanic Black females remained lower than it did for non-Hispanic White and Hispanic females.
Among males, the researchers found differences in life expectancies across states between the people of the three different ethnicities they studied. The greatest difference in life expectancies in 1990 was 24.5 years. This occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Georgia. The life expectancy for these non-Hispanic Black males was 59.4 years, versus 83.8 years for these Hispanic males that year.
This reduced life expectancy for non-Hispanic Black males persisted, although it improved slightly by 2019. That year, the largest race-based disparity – which was approximately 24 years – occurred between non-Hispanic Black males in the District of Columbia and Hispanic males in Virginia. For the Hispanic males in Virgina, the LE was 90.7 years versus 66.9 years for non-Hispanic Black males in the District of Columbia.
The findings were limited by several factors including the review of data from only 23 states, the focus on life expectancy from birth versus other ages, and the challenges of defining Hispanic ethnicity, the researchers noted. However, the results support that the potential use of state-level analysis that includes race/ethnicity could be a valuable tool for measuring health inequity as part of national average trends, they said.
Health has truly stagnated for some in certain states
“Subpopulations in some states have much longer life expectancy now than 30 years ago. But in some states, we were struck by how health has truly stagnated for some,” Dr. Roth said in an interview. “We were surprised by the scale of the overall gap; a difference of about 8 years between states is more than twice that if you drill down to race/ethnicity groups in each state.”
A key message from the study is the need for all clinicians to advocate for improved access to primary care, “which is increasingly hard to obtain for many people,” said Dr. Roth. “So much of health is determined by key risk factors such as high blood pressure, high cholesterol, obesity, diabetes, alcohol use, tobacco use. But many of the determinants of health are not in the healthcare system, and include efforts to improve education, interrupt cycles of poverty, and teach healthy behaviors at a very young age. “Racism remains a underdiscussed part of these disparities, and we need better ways to measure the impact of social policies that end up impacting health down the road,” he said.
Looking ahead: “There is a lot to be learned from the states that have improved life expectancy the most. We need researchers to work together to identify and communicate what are those best practices, and what state governments can do to play their part.”
State-level differences reveal variations in health care
“The findings add to our growing knowledge of large and persistent racial/ethnic health disparities and changes in disparities during recent stagnation in U.S. life expectancy,” wrote Hedwig Lee, PhD, of Washington University in St. Louis, and Kathleen M. Harris, PhD, of the University of North Carolina at Chapel Hill, in an accompanying editorial.
The focus on state-level differences provides a unique window into the huge variation in life expectancy by race/ethnicity across the United States. The data suggest that “a person’s life expectancy in the United States may depend more on where you live than it has in the past,” they noted. For example, the editorialists highlighted that life expectancy for non-Hispanic Black men in 2019 averaged 81.1 years in Rhode Island, but 66.9 years in the District of Columbia.
They also noted the study’s lack of data for many states with high mortality rates and high proportions of non-Hispanic Black persons, Hispanic persons, and those with low socioeconomic states. Including data from these areas may have yielded even greater disparities in life expectancy.
“Despite substantial declines in mortality among Black persons during the study period, a non-Hispanic Black person’s life expectancy remained persistently lower than that of non-Hispanic White and Hispanic persons, both within and across states,” the editorialists wrote. “Future research needs to unpack the complex web of factors driving health and well-being by enabling better understanding of the places where we see persistent health disadvantage and advantage and the state-based explanations for these increasingly important differences determining population risk and resilience. We should be outraged by disparities in longevity and called to act to eliminate them.”
Identifying the problem is the first step
“In order to address or fix a problem we should first identify and quantify the problem,” Noel Deep, MD, an internal medicine physician in private practice in Antigo, Wisc., said in an interview.
“This study provides us with the information regarding the trends in life expectancy within states and the disparities in life expectancy when race/ ethnicity and gender are factored into the equation,” said Dr. Deep, who was not involved in the study. “Based on previously available data, we are aware of the increase in life expectancy in the United States over the last few decades, as well as differences in life expectancy for the different ethnicities/races and genders, but these data provide averages, not state or geographical differences. By having this knowledge at a state level, we can use that data to make health policies that address those health inequities and allocate appropriate resources at a state or local level.”
Several studies have identified disparities in health care and life expectancy based on the zip codes, such as the U.S. Small-Area Life Expectancy Estimates Project in 2018. The current study “provides further information for health care professionals and policy makers about the disparities in health outcomes and life expectancy based on race as well as gender, and it is quite detailed,” he said.
“As clinicians, we should strive to ensure that we are addressing these health inequities through our provision of clinical care and through our advocacy on behalf of our patients so that our nation’s health will improve overall,” he said.
“I would like to see future studies look at the socioeconomic status (income), urban versus rural residence, and place of birth (especially for immigrants),” said Dr. Deep. He also emphasized a need for studies to include the demographics for Hispanic populations; given the possible selection error “because of only healthy individuals immigrating to the United States or the older sicker Hispanics who might be migrating back to their homelands and not being included in the data and falsely increasing the life expectancy for this race/ ethnic groups.
“I would also like to see some research into the cultural and social factors that might explain why Hispanic populations might have a higher life expectancy even if their socioeconomic status is poor,” he said.
The study was supported by the National Heart, Lung, and Blood Institute. The researchers had no financial conflicts to disclose. The editorialists had no financial conflicts to disclose. Dr. Deep had no financial conflicts to disclose, but serves on the editorial advisory board of Internal Medicine News and as chair of the AMA’s Council on Science and Public Health.
FROM ANNALS OF INTERNAL MEDICINE
Cardiologists concerned for patient safety after abortion ruling
Pregnancy termination for medical reasons had been part of the fabric of everyday health care in the United States since the Supreme Court’s 1973 Roe v. Wade decision, which the current high court overturned in a ruling announced on June 24.
That means many clinicians across specialties are entering uncharted territory with the country’s new patchwork of abortion legality. Some specialties, cardiology among them, may feel the impact more than others.
“We know that the rising maternal mortality rate is predominantly driven by cardiovascular disease, women having children at older ages, and ... risk factors like hypertension, diabetes, and obesity,” Jennifer H. Haythe, MD, told this news organization.
So the high court’s decision in Dobbs v. Jackson Women’s Health Organization, which overturned Roe v. Wade and leaves the legality of abortion up to the 50 separate state legislatures, “is very relevant to cardiologists specifically,” said Dr. Haythe, who is director of cardiology in the cardio-obstetrics program at New York-Presbyterian/Columbia University Irving Medical Center, New York.
The ruling “is going to have a huge effect on women who may not be able to tolerate pregnancy,” she said. Whether to terminate a pregnancy “is a relatively common discussion I have with women with bad heart failure about their risk of further decompensation, death, or needing a heart transplant or heart pump after delivery, or the risk of death in women with pulmonary hypertension.”
The high court’s decision “is a direct attack on the practice of medicine and really the sanctity of the patient-clinician relationship,” Rachel M. Bond, MD, director of Women’s Heart Health Systems Dignity Health of Arizona, told this news organization.
Physicians take an oath “that we should do no harm to our patients, and once the law or governance impacts that, it places us in a very vulnerable situation,” Dr. Bond said. “As a cardiologist who focuses a lot on high-risk pregnancies, I am worried and hesitant to give guidance to many of these patients in the states that may not have access to something that is a medical right, which at times is an abortion.”
She has colleagues in obstetrics in states where abortion is newly illegal who “don’t know what to do,” Dr. Bond said. Many have sought guidance from their legal teams, she said, “and many of them are now trying to figure out what is the best path.”
Pregnancy is “a very significant cardiovascular stress test, and women who may tolerate certain conditions reasonably well outside of the setting of pregnancy may have severe issues, not just for the mother, but for the baby as well,” Ki Park, MD, University of Florida Health, Gainesville, said in an interview.
“As clinicians, none of us like recommending a medically indicated abortion. But it is health care, just like any other medication or treatment that we advise to our patients in cases where the risk of the mother is excessively high and mortality risk is elevated,” said Dr. Park, who is cochair of the American College of Cardiology Cardio-Obstetrics Work Group.
Some conditions, such as pulmonary hypertension and severe aortic valve stenosis, during pregnancy are well recognized as very high risk, and there are various scoring systems to help clinicians with risk stratification, she observed. “But there are also a lot of gray areas where patients don’t necessarily fit into these risk scores that we use.”
So physician-patient discussions in high-risk pregnancies “are already complicated,” Dr. Park said. “Patients want to have options, and they look to us as physicians for guidance with regard to their risks. And if abortion is not available as an option, then part of our toolbox is no longer available to help us care for the mother.”
In the new legal climate, clinicians in states where abortion is illegal may well want to put more emphasis on preconception counseling, so more of their patients with high-risk conditions are aware of the new barriers to pregnancy termination.
“Unfortunately,” Dr. Haythe said, “many of the states that are going to make or have made abortion illegal are not providing that kind of preconception counseling or good prenatal care to women.”
Cardiologists can provide such counseling to their female patients of childbearing age who have high-risk cardiac conditions, “but not everybody knows that they have a heart problem when they get pregnant, and not everybody is getting screened for heart problems when they’re of childbearing age,” Dr. Haythe said.
“Sometimes it’s not clear whether the problems could have been picked up until a woman is pregnant and has started to have symptoms.” For example, “a lot of women with poor access to health care have rheumatic heart disease. They may have no idea that they have severe aortic stenosis, and it’s not until their second trimester that they start to feel really short of breath.” Often that can be treated in the cath lab, “but again, that’s putting the woman and the baby at risk.”
Cardiologists in states where abortion is illegal will still present the option to their patients with high-risk pregnancies, noted Dr. Haythe. But the conversation may sound something like, “you are at very high risk, termination of the pregnancy takes that risk away, but you’ll have to find a state where it’s legal to do that.”
Dr. Park said such a situation, when abortion is recommended but locally unavailable, is much like any other in cardiology for which the patient may want a second opinion. If a center “doesn’t have the capability or the technology to offer a certain treatment, the patient can opt to seek another opinion at another center,” she said. “Patients will often travel out of state to get the care they need.”
A requirement for out-of-state travel to obtain abortions is likely to worsen socioeconomic disparities in health care, Dr. Bond observed, “because we know that those who are low-income won’t be able to afford that travel.”
Dr. Bond is cosignatory on a statement from the Association of Black Cardiologists (ABC) responding to the high court’s ruling in Dobbs v. Jackson. “This decision will isolate the poor, socioeconomically disadvantaged, and minority populations specifically, widening the already large gaps in health care for our most vulnerable communities,” it states.
“The loss of broad protections supporting the medical and often lifesaving procedure of abortions is likely to have a real impact on the maternal mortality rate, especially in those with congenital and/or acquired cardiovascular conditions where evidence-based guidelines advise at times on termination of such high-risk pregnancies.”
The ABC, it states, “believes that every woman, and every person, should be afforded the right to safe, accessible, legal, timely, patient-centered, equitable, and affordable health care.”
The American College of Cardiology (ACC) released a statement on the matter June 24, signed by its president, Edward T.A. Fry, MD, along with five former ACC presidents. “While the ACC has no official policy on abortion, clinical practice guidelines and other clinical guidance tools address the dangers of pregnancy in certain patient populations at higher risk of death or serious cardiac events.”
The college, it states, is “deeply concerned about the potential implications of the Supreme Court decision regarding Roe vs. Wade on the ability of patients and clinicians to engage in important shared discussions about maternal health, or to remove previously available health care options.”
Dr. Bond proposed that a “vocal stance” from medical societies involved in women’s health, “perhaps even a collective stance from our cardiovascular societies and our obstetrics societies,” would also perhaps reach “the masses of doctors in private practice who are dealing with these patients.”
A version of this article first appeared on Medscape.com.
Pregnancy termination for medical reasons had been part of the fabric of everyday health care in the United States since the Supreme Court’s 1973 Roe v. Wade decision, which the current high court overturned in a ruling announced on June 24.
That means many clinicians across specialties are entering uncharted territory with the country’s new patchwork of abortion legality. Some specialties, cardiology among them, may feel the impact more than others.
“We know that the rising maternal mortality rate is predominantly driven by cardiovascular disease, women having children at older ages, and ... risk factors like hypertension, diabetes, and obesity,” Jennifer H. Haythe, MD, told this news organization.
So the high court’s decision in Dobbs v. Jackson Women’s Health Organization, which overturned Roe v. Wade and leaves the legality of abortion up to the 50 separate state legislatures, “is very relevant to cardiologists specifically,” said Dr. Haythe, who is director of cardiology in the cardio-obstetrics program at New York-Presbyterian/Columbia University Irving Medical Center, New York.
The ruling “is going to have a huge effect on women who may not be able to tolerate pregnancy,” she said. Whether to terminate a pregnancy “is a relatively common discussion I have with women with bad heart failure about their risk of further decompensation, death, or needing a heart transplant or heart pump after delivery, or the risk of death in women with pulmonary hypertension.”
The high court’s decision “is a direct attack on the practice of medicine and really the sanctity of the patient-clinician relationship,” Rachel M. Bond, MD, director of Women’s Heart Health Systems Dignity Health of Arizona, told this news organization.
Physicians take an oath “that we should do no harm to our patients, and once the law or governance impacts that, it places us in a very vulnerable situation,” Dr. Bond said. “As a cardiologist who focuses a lot on high-risk pregnancies, I am worried and hesitant to give guidance to many of these patients in the states that may not have access to something that is a medical right, which at times is an abortion.”
She has colleagues in obstetrics in states where abortion is newly illegal who “don’t know what to do,” Dr. Bond said. Many have sought guidance from their legal teams, she said, “and many of them are now trying to figure out what is the best path.”
Pregnancy is “a very significant cardiovascular stress test, and women who may tolerate certain conditions reasonably well outside of the setting of pregnancy may have severe issues, not just for the mother, but for the baby as well,” Ki Park, MD, University of Florida Health, Gainesville, said in an interview.
“As clinicians, none of us like recommending a medically indicated abortion. But it is health care, just like any other medication or treatment that we advise to our patients in cases where the risk of the mother is excessively high and mortality risk is elevated,” said Dr. Park, who is cochair of the American College of Cardiology Cardio-Obstetrics Work Group.
Some conditions, such as pulmonary hypertension and severe aortic valve stenosis, during pregnancy are well recognized as very high risk, and there are various scoring systems to help clinicians with risk stratification, she observed. “But there are also a lot of gray areas where patients don’t necessarily fit into these risk scores that we use.”
So physician-patient discussions in high-risk pregnancies “are already complicated,” Dr. Park said. “Patients want to have options, and they look to us as physicians for guidance with regard to their risks. And if abortion is not available as an option, then part of our toolbox is no longer available to help us care for the mother.”
In the new legal climate, clinicians in states where abortion is illegal may well want to put more emphasis on preconception counseling, so more of their patients with high-risk conditions are aware of the new barriers to pregnancy termination.
“Unfortunately,” Dr. Haythe said, “many of the states that are going to make or have made abortion illegal are not providing that kind of preconception counseling or good prenatal care to women.”
Cardiologists can provide such counseling to their female patients of childbearing age who have high-risk cardiac conditions, “but not everybody knows that they have a heart problem when they get pregnant, and not everybody is getting screened for heart problems when they’re of childbearing age,” Dr. Haythe said.
“Sometimes it’s not clear whether the problems could have been picked up until a woman is pregnant and has started to have symptoms.” For example, “a lot of women with poor access to health care have rheumatic heart disease. They may have no idea that they have severe aortic stenosis, and it’s not until their second trimester that they start to feel really short of breath.” Often that can be treated in the cath lab, “but again, that’s putting the woman and the baby at risk.”
Cardiologists in states where abortion is illegal will still present the option to their patients with high-risk pregnancies, noted Dr. Haythe. But the conversation may sound something like, “you are at very high risk, termination of the pregnancy takes that risk away, but you’ll have to find a state where it’s legal to do that.”
Dr. Park said such a situation, when abortion is recommended but locally unavailable, is much like any other in cardiology for which the patient may want a second opinion. If a center “doesn’t have the capability or the technology to offer a certain treatment, the patient can opt to seek another opinion at another center,” she said. “Patients will often travel out of state to get the care they need.”
A requirement for out-of-state travel to obtain abortions is likely to worsen socioeconomic disparities in health care, Dr. Bond observed, “because we know that those who are low-income won’t be able to afford that travel.”
Dr. Bond is cosignatory on a statement from the Association of Black Cardiologists (ABC) responding to the high court’s ruling in Dobbs v. Jackson. “This decision will isolate the poor, socioeconomically disadvantaged, and minority populations specifically, widening the already large gaps in health care for our most vulnerable communities,” it states.
“The loss of broad protections supporting the medical and often lifesaving procedure of abortions is likely to have a real impact on the maternal mortality rate, especially in those with congenital and/or acquired cardiovascular conditions where evidence-based guidelines advise at times on termination of such high-risk pregnancies.”
The ABC, it states, “believes that every woman, and every person, should be afforded the right to safe, accessible, legal, timely, patient-centered, equitable, and affordable health care.”
The American College of Cardiology (ACC) released a statement on the matter June 24, signed by its president, Edward T.A. Fry, MD, along with five former ACC presidents. “While the ACC has no official policy on abortion, clinical practice guidelines and other clinical guidance tools address the dangers of pregnancy in certain patient populations at higher risk of death or serious cardiac events.”
The college, it states, is “deeply concerned about the potential implications of the Supreme Court decision regarding Roe vs. Wade on the ability of patients and clinicians to engage in important shared discussions about maternal health, or to remove previously available health care options.”
Dr. Bond proposed that a “vocal stance” from medical societies involved in women’s health, “perhaps even a collective stance from our cardiovascular societies and our obstetrics societies,” would also perhaps reach “the masses of doctors in private practice who are dealing with these patients.”
A version of this article first appeared on Medscape.com.
Pregnancy termination for medical reasons had been part of the fabric of everyday health care in the United States since the Supreme Court’s 1973 Roe v. Wade decision, which the current high court overturned in a ruling announced on June 24.
That means many clinicians across specialties are entering uncharted territory with the country’s new patchwork of abortion legality. Some specialties, cardiology among them, may feel the impact more than others.
“We know that the rising maternal mortality rate is predominantly driven by cardiovascular disease, women having children at older ages, and ... risk factors like hypertension, diabetes, and obesity,” Jennifer H. Haythe, MD, told this news organization.
So the high court’s decision in Dobbs v. Jackson Women’s Health Organization, which overturned Roe v. Wade and leaves the legality of abortion up to the 50 separate state legislatures, “is very relevant to cardiologists specifically,” said Dr. Haythe, who is director of cardiology in the cardio-obstetrics program at New York-Presbyterian/Columbia University Irving Medical Center, New York.
The ruling “is going to have a huge effect on women who may not be able to tolerate pregnancy,” she said. Whether to terminate a pregnancy “is a relatively common discussion I have with women with bad heart failure about their risk of further decompensation, death, or needing a heart transplant or heart pump after delivery, or the risk of death in women with pulmonary hypertension.”
The high court’s decision “is a direct attack on the practice of medicine and really the sanctity of the patient-clinician relationship,” Rachel M. Bond, MD, director of Women’s Heart Health Systems Dignity Health of Arizona, told this news organization.
Physicians take an oath “that we should do no harm to our patients, and once the law or governance impacts that, it places us in a very vulnerable situation,” Dr. Bond said. “As a cardiologist who focuses a lot on high-risk pregnancies, I am worried and hesitant to give guidance to many of these patients in the states that may not have access to something that is a medical right, which at times is an abortion.”
She has colleagues in obstetrics in states where abortion is newly illegal who “don’t know what to do,” Dr. Bond said. Many have sought guidance from their legal teams, she said, “and many of them are now trying to figure out what is the best path.”
Pregnancy is “a very significant cardiovascular stress test, and women who may tolerate certain conditions reasonably well outside of the setting of pregnancy may have severe issues, not just for the mother, but for the baby as well,” Ki Park, MD, University of Florida Health, Gainesville, said in an interview.
“As clinicians, none of us like recommending a medically indicated abortion. But it is health care, just like any other medication or treatment that we advise to our patients in cases where the risk of the mother is excessively high and mortality risk is elevated,” said Dr. Park, who is cochair of the American College of Cardiology Cardio-Obstetrics Work Group.
Some conditions, such as pulmonary hypertension and severe aortic valve stenosis, during pregnancy are well recognized as very high risk, and there are various scoring systems to help clinicians with risk stratification, she observed. “But there are also a lot of gray areas where patients don’t necessarily fit into these risk scores that we use.”
So physician-patient discussions in high-risk pregnancies “are already complicated,” Dr. Park said. “Patients want to have options, and they look to us as physicians for guidance with regard to their risks. And if abortion is not available as an option, then part of our toolbox is no longer available to help us care for the mother.”
In the new legal climate, clinicians in states where abortion is illegal may well want to put more emphasis on preconception counseling, so more of their patients with high-risk conditions are aware of the new barriers to pregnancy termination.
“Unfortunately,” Dr. Haythe said, “many of the states that are going to make or have made abortion illegal are not providing that kind of preconception counseling or good prenatal care to women.”
Cardiologists can provide such counseling to their female patients of childbearing age who have high-risk cardiac conditions, “but not everybody knows that they have a heart problem when they get pregnant, and not everybody is getting screened for heart problems when they’re of childbearing age,” Dr. Haythe said.
“Sometimes it’s not clear whether the problems could have been picked up until a woman is pregnant and has started to have symptoms.” For example, “a lot of women with poor access to health care have rheumatic heart disease. They may have no idea that they have severe aortic stenosis, and it’s not until their second trimester that they start to feel really short of breath.” Often that can be treated in the cath lab, “but again, that’s putting the woman and the baby at risk.”
Cardiologists in states where abortion is illegal will still present the option to their patients with high-risk pregnancies, noted Dr. Haythe. But the conversation may sound something like, “you are at very high risk, termination of the pregnancy takes that risk away, but you’ll have to find a state where it’s legal to do that.”
Dr. Park said such a situation, when abortion is recommended but locally unavailable, is much like any other in cardiology for which the patient may want a second opinion. If a center “doesn’t have the capability or the technology to offer a certain treatment, the patient can opt to seek another opinion at another center,” she said. “Patients will often travel out of state to get the care they need.”
A requirement for out-of-state travel to obtain abortions is likely to worsen socioeconomic disparities in health care, Dr. Bond observed, “because we know that those who are low-income won’t be able to afford that travel.”
Dr. Bond is cosignatory on a statement from the Association of Black Cardiologists (ABC) responding to the high court’s ruling in Dobbs v. Jackson. “This decision will isolate the poor, socioeconomically disadvantaged, and minority populations specifically, widening the already large gaps in health care for our most vulnerable communities,” it states.
“The loss of broad protections supporting the medical and often lifesaving procedure of abortions is likely to have a real impact on the maternal mortality rate, especially in those with congenital and/or acquired cardiovascular conditions where evidence-based guidelines advise at times on termination of such high-risk pregnancies.”
The ABC, it states, “believes that every woman, and every person, should be afforded the right to safe, accessible, legal, timely, patient-centered, equitable, and affordable health care.”
The American College of Cardiology (ACC) released a statement on the matter June 24, signed by its president, Edward T.A. Fry, MD, along with five former ACC presidents. “While the ACC has no official policy on abortion, clinical practice guidelines and other clinical guidance tools address the dangers of pregnancy in certain patient populations at higher risk of death or serious cardiac events.”
The college, it states, is “deeply concerned about the potential implications of the Supreme Court decision regarding Roe vs. Wade on the ability of patients and clinicians to engage in important shared discussions about maternal health, or to remove previously available health care options.”
Dr. Bond proposed that a “vocal stance” from medical societies involved in women’s health, “perhaps even a collective stance from our cardiovascular societies and our obstetrics societies,” would also perhaps reach “the masses of doctors in private practice who are dealing with these patients.”
A version of this article first appeared on Medscape.com.
Children and COVID: Vaccination off to slow start for the newly eligible
New cases of COVID-19 continue to drop among children, but the vaccination effort in those under age 5 years began with something less than a bang.
In the first 2 days after their respective approvals, almost 99,000 children aged 5-11 years and over 675,000 children aged 12-15 were vaccinated, according to data from the Centers for Disease Control and Prevention. Children aged 0-4 years represent almost 6% of the overall population, compared with 8.7% for the 5- to 11-year-olds and 5.1% for those aged 12-15.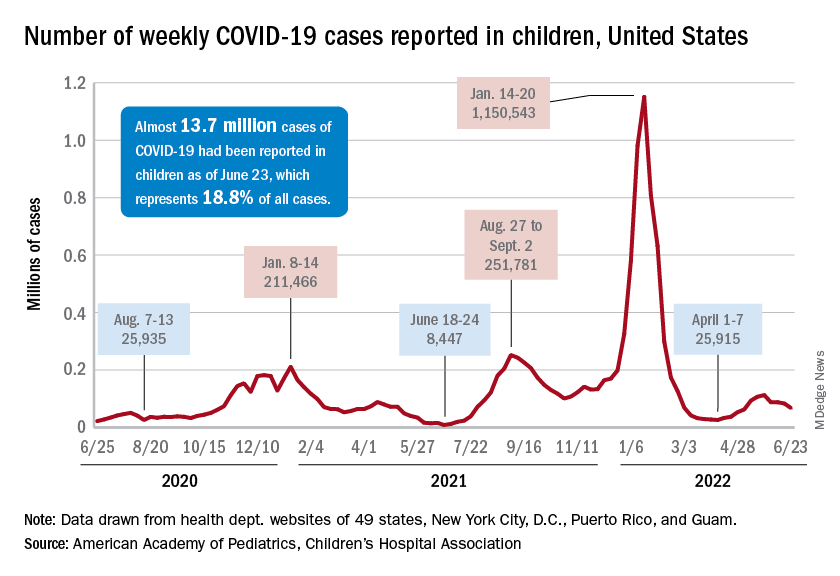
The recent decline in new cases over the past 4 weeks and the substantial decline since the Omicron surge could be a factor in the lack of response, but it is worth noting that the almost 68,000 new child cases reported in the past week, June 17-23, are “far higher than 1 year ago, June 24, 2021, when 8,400 child cases were reported,” the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID report.
That total for June 17-23 was 19% lower than the previous week and down by 40% since new cases hit a spring peak of 112,000 in late May. Regionally, new cases were down in the Midwest, the South, and the West, the AAP/CHA report showed, but the Northeast saw a small increase, which could be a signal of things to come for the summer.
The decline in new cases, however, has not been accompanied by decreases in hospitalizations or emergency department visits. New admissions of children aged 0-17 with confirmed COVID were at 0.31 per 100,000 population on June 24 after reaching that level on June 15, so no drop-off has occurred yet but there are signs of leveling off, based on CDC data.
The ED visit rates have been fairly steady through June, although COVID-related visits were up to 3.4% of all ED visits on June 22 for children aged 0-11 years, after being below 3% for the first 2 weeks of the month. The rate for children aged 12-15 has been between 1.6% and 1.9% for the past 3 weeks and the rate for 16- and 17-year-olds has been hovering between 1.7% and 2.2% for most of June, after going as high as 2.7% in late May, the CDC said on its COVID Data Tracker.
New cases of COVID-19 continue to drop among children, but the vaccination effort in those under age 5 years began with something less than a bang.
In the first 2 days after their respective approvals, almost 99,000 children aged 5-11 years and over 675,000 children aged 12-15 were vaccinated, according to data from the Centers for Disease Control and Prevention. Children aged 0-4 years represent almost 6% of the overall population, compared with 8.7% for the 5- to 11-year-olds and 5.1% for those aged 12-15.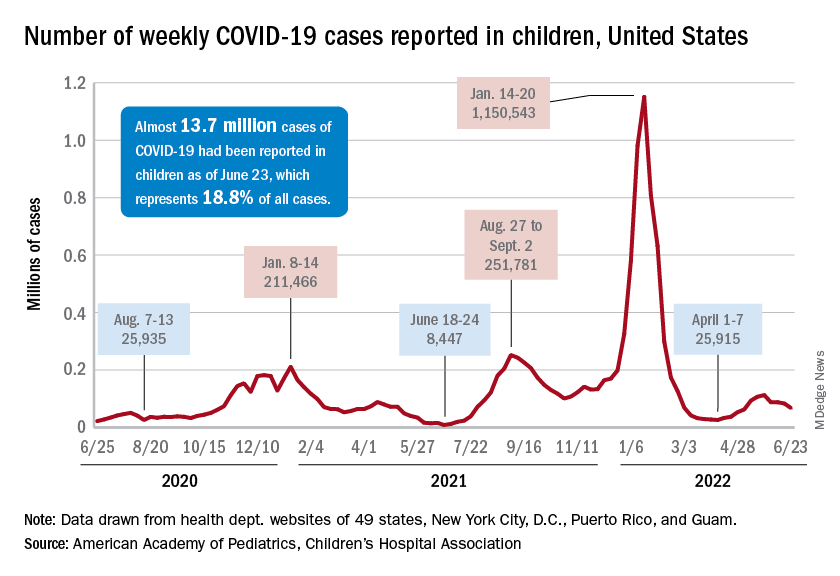
The recent decline in new cases over the past 4 weeks and the substantial decline since the Omicron surge could be a factor in the lack of response, but it is worth noting that the almost 68,000 new child cases reported in the past week, June 17-23, are “far higher than 1 year ago, June 24, 2021, when 8,400 child cases were reported,” the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID report.
That total for June 17-23 was 19% lower than the previous week and down by 40% since new cases hit a spring peak of 112,000 in late May. Regionally, new cases were down in the Midwest, the South, and the West, the AAP/CHA report showed, but the Northeast saw a small increase, which could be a signal of things to come for the summer.
The decline in new cases, however, has not been accompanied by decreases in hospitalizations or emergency department visits. New admissions of children aged 0-17 with confirmed COVID were at 0.31 per 100,000 population on June 24 after reaching that level on June 15, so no drop-off has occurred yet but there are signs of leveling off, based on CDC data.
The ED visit rates have been fairly steady through June, although COVID-related visits were up to 3.4% of all ED visits on June 22 for children aged 0-11 years, after being below 3% for the first 2 weeks of the month. The rate for children aged 12-15 has been between 1.6% and 1.9% for the past 3 weeks and the rate for 16- and 17-year-olds has been hovering between 1.7% and 2.2% for most of June, after going as high as 2.7% in late May, the CDC said on its COVID Data Tracker.
New cases of COVID-19 continue to drop among children, but the vaccination effort in those under age 5 years began with something less than a bang.
In the first 2 days after their respective approvals, almost 99,000 children aged 5-11 years and over 675,000 children aged 12-15 were vaccinated, according to data from the Centers for Disease Control and Prevention. Children aged 0-4 years represent almost 6% of the overall population, compared with 8.7% for the 5- to 11-year-olds and 5.1% for those aged 12-15.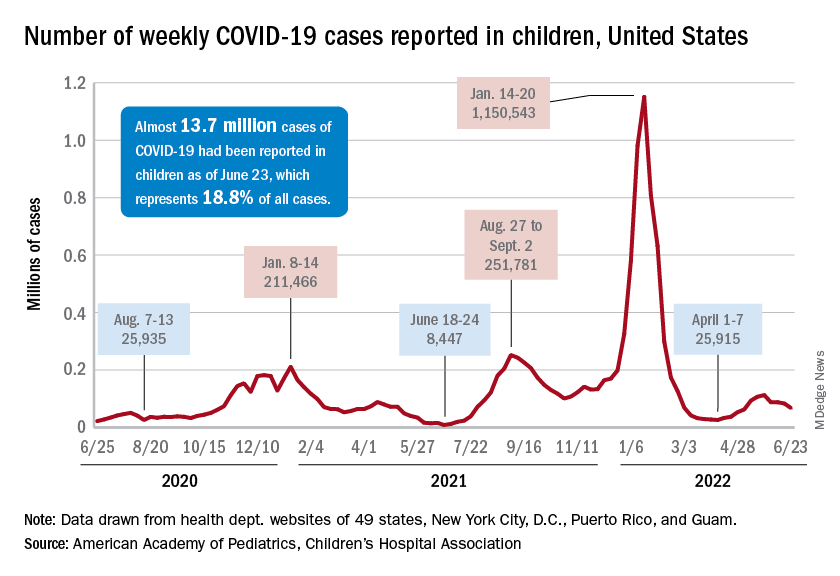
The recent decline in new cases over the past 4 weeks and the substantial decline since the Omicron surge could be a factor in the lack of response, but it is worth noting that the almost 68,000 new child cases reported in the past week, June 17-23, are “far higher than 1 year ago, June 24, 2021, when 8,400 child cases were reported,” the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID report.
That total for June 17-23 was 19% lower than the previous week and down by 40% since new cases hit a spring peak of 112,000 in late May. Regionally, new cases were down in the Midwest, the South, and the West, the AAP/CHA report showed, but the Northeast saw a small increase, which could be a signal of things to come for the summer.
The decline in new cases, however, has not been accompanied by decreases in hospitalizations or emergency department visits. New admissions of children aged 0-17 with confirmed COVID were at 0.31 per 100,000 population on June 24 after reaching that level on June 15, so no drop-off has occurred yet but there are signs of leveling off, based on CDC data.
The ED visit rates have been fairly steady through June, although COVID-related visits were up to 3.4% of all ED visits on June 22 for children aged 0-11 years, after being below 3% for the first 2 weeks of the month. The rate for children aged 12-15 has been between 1.6% and 1.9% for the past 3 weeks and the rate for 16- and 17-year-olds has been hovering between 1.7% and 2.2% for most of June, after going as high as 2.7% in late May, the CDC said on its COVID Data Tracker.
Hydroxychloroquine risk found in some older patients with RA
Hydroxychloroquine should be initiated with caution in older patients with rheumatoid arthritis who also have heart failure or are at risk for it, say the authors of a study suggesting that the drug could increase their risk for major adverse cardiovascular events (MACE), compared with methotrexate.
A cohort study published online in the Journal of the American College of Cardiology looked at outcomes in 54,462 patients with RA aged 65 years or older and not previously treated with disease-modifying antirheumatic drugs. Half were initiated on methotrexate and half on hydroxychloroquine, making 27,231 propensity-matched pairs.
Across the entire cohort, hydroxychloroquine was not associated with a higher risk for sudden cardiac arrest, ventricular arrhythmia, or MACE, compared with methotrexate. When broken down into individual cardiovascular events, the data suggested a statistically significant 17% increase in the risk for cardiovascular mortality and 10% increase in all-cause mortality with hydroxychloroquine, although there were no differences in the risks for myocardial infarction or stroke.
However, a subgroup analysis revealed a significant 30% increase in the risk for MACE among patients starting hydroxychloroquine who also had a history of heart failure, compared with patients taking methotrexate. The researchers found no difference between the two drugs in patients without a history of heart failure. The study also suggested an overall 41% increase in the risk for hospitalization with heart failure with hydroxychloroquine, regardless of heart failure history.
Hydroxychloroquine was also associated with a 34% increase in the risk for cardiovascular mortality, a 22% increase in the risk for all-cause mortality, and a 74% increase in the risk for MI.
The lead author of the study, Elvira D’Andrea, MD, PhD, of Brigham and Women’s Hospital and Harvard Medical School in Boston, said that hydroxychloroquine is used as a first-line treatment for RA, but there was limited evidence on its cardiovascular risks. The pandemic in particular shined a spotlight on these concerns and prompted the researchers to extend their original prepandemic study to encompass additional cardiovascular outcomes.
“The emerging concerns on its cardiovascular safety in early 2020 has led the rheumatological community, and patients regularly taking hydroxychloroquine for rheumatoid arthritis, to confusion,” Dr. D’Andrea said in an interview.
She advised that clinicians be cautious when initiating hydroxychloroquine in older patients with existing heart failure or who have risk factors for it. “Although heart failure is a known concern for hydroxychloroquine use, these findings helped to clarify the relationship between the use of hydroxychloroquine or methotrexate and heart failure. Clinicians should pay careful attention to clinical manifestations of cardiomyopathy or heart failure in older patients with rheumatoid arthritis treated with hydroxychloroquine.”
Hydroxychloroquine is associated with cardiotoxicity, particularly cardiomyopathy, which may help precipitate MACE or heart failure exacerbations in patients who already have deterioration of their cardiac tissue, the authors suggested.
Short follow-up period leaves risk attribution under question
In an accompanying editorial, Elizabeth Blair Solow, MD, and Bonnie L. Bermas, MD, of the University of Texas Southwestern Medical Center, Dallas, commented that the lack of an increased risk for arrhythmic events or MACE in the overall cohort taking hydroxychloroquine was reassuring. They also suggested the subgroup analysis findings among patients with preexisting heart failure were still “exploratory and hypothesis-generating” and should be interpreted with caution.
They noted that the follow-up time of the study was relatively short – a median of 209 days – given that hydroxychloroquine does not reach a steady-state level for 6 months.
“Evidence to date suggests cardiomyopathy from HCQ [hydroxychloroquine] takes years to develop, many months beyond the exposures described here, bringing into question as to whether HCQ itself increased HF hospitalizations,” the editorialists wrote.
The editorial also raised the question of whether the association observed in the study was related to a possible cardioprotective effect of methotrexate, given that previous studies have suggested this effect in older patients with RA.
The study authors did an exploratory analysis comparing hydroxychloroquine with sulfasalazine, which appeared to support their main findings of a possible cardiovascular effect of hydroxychloroquine. However, they qualified this by pointing out that the analysis involved small numbers of patients.
Senior investigator Seoyoung C. Kim, MD, ScD, of Brigham and Women’s Hospital and Harvard Medical School, both in Boston, also noted that the study only looked at outcomes in patients aged 65 years and older.
“It would be clinically important to further examine the cardiovascular safety of hydroxychloroquine versus methotrexate in a younger population with rheumatic conditions,” she said.
The study was supported by the National Institutes of Health, Brigham and Women’s Hospital, and Harvard Medical School. Four authors declared unrelated research grants from the pharmaceutical sector, with one also declaring stock options and consulting work with the pharmaceutical sector. No other conflicts of interest were declared.
A version of this article first appeared on Medscape.com.
Hydroxychloroquine should be initiated with caution in older patients with rheumatoid arthritis who also have heart failure or are at risk for it, say the authors of a study suggesting that the drug could increase their risk for major adverse cardiovascular events (MACE), compared with methotrexate.
A cohort study published online in the Journal of the American College of Cardiology looked at outcomes in 54,462 patients with RA aged 65 years or older and not previously treated with disease-modifying antirheumatic drugs. Half were initiated on methotrexate and half on hydroxychloroquine, making 27,231 propensity-matched pairs.
Across the entire cohort, hydroxychloroquine was not associated with a higher risk for sudden cardiac arrest, ventricular arrhythmia, or MACE, compared with methotrexate. When broken down into individual cardiovascular events, the data suggested a statistically significant 17% increase in the risk for cardiovascular mortality and 10% increase in all-cause mortality with hydroxychloroquine, although there were no differences in the risks for myocardial infarction or stroke.
However, a subgroup analysis revealed a significant 30% increase in the risk for MACE among patients starting hydroxychloroquine who also had a history of heart failure, compared with patients taking methotrexate. The researchers found no difference between the two drugs in patients without a history of heart failure. The study also suggested an overall 41% increase in the risk for hospitalization with heart failure with hydroxychloroquine, regardless of heart failure history.
Hydroxychloroquine was also associated with a 34% increase in the risk for cardiovascular mortality, a 22% increase in the risk for all-cause mortality, and a 74% increase in the risk for MI.
The lead author of the study, Elvira D’Andrea, MD, PhD, of Brigham and Women’s Hospital and Harvard Medical School in Boston, said that hydroxychloroquine is used as a first-line treatment for RA, but there was limited evidence on its cardiovascular risks. The pandemic in particular shined a spotlight on these concerns and prompted the researchers to extend their original prepandemic study to encompass additional cardiovascular outcomes.
“The emerging concerns on its cardiovascular safety in early 2020 has led the rheumatological community, and patients regularly taking hydroxychloroquine for rheumatoid arthritis, to confusion,” Dr. D’Andrea said in an interview.
She advised that clinicians be cautious when initiating hydroxychloroquine in older patients with existing heart failure or who have risk factors for it. “Although heart failure is a known concern for hydroxychloroquine use, these findings helped to clarify the relationship between the use of hydroxychloroquine or methotrexate and heart failure. Clinicians should pay careful attention to clinical manifestations of cardiomyopathy or heart failure in older patients with rheumatoid arthritis treated with hydroxychloroquine.”
Hydroxychloroquine is associated with cardiotoxicity, particularly cardiomyopathy, which may help precipitate MACE or heart failure exacerbations in patients who already have deterioration of their cardiac tissue, the authors suggested.
Short follow-up period leaves risk attribution under question
In an accompanying editorial, Elizabeth Blair Solow, MD, and Bonnie L. Bermas, MD, of the University of Texas Southwestern Medical Center, Dallas, commented that the lack of an increased risk for arrhythmic events or MACE in the overall cohort taking hydroxychloroquine was reassuring. They also suggested the subgroup analysis findings among patients with preexisting heart failure were still “exploratory and hypothesis-generating” and should be interpreted with caution.
They noted that the follow-up time of the study was relatively short – a median of 209 days – given that hydroxychloroquine does not reach a steady-state level for 6 months.
“Evidence to date suggests cardiomyopathy from HCQ [hydroxychloroquine] takes years to develop, many months beyond the exposures described here, bringing into question as to whether HCQ itself increased HF hospitalizations,” the editorialists wrote.
The editorial also raised the question of whether the association observed in the study was related to a possible cardioprotective effect of methotrexate, given that previous studies have suggested this effect in older patients with RA.
The study authors did an exploratory analysis comparing hydroxychloroquine with sulfasalazine, which appeared to support their main findings of a possible cardiovascular effect of hydroxychloroquine. However, they qualified this by pointing out that the analysis involved small numbers of patients.
Senior investigator Seoyoung C. Kim, MD, ScD, of Brigham and Women’s Hospital and Harvard Medical School, both in Boston, also noted that the study only looked at outcomes in patients aged 65 years and older.
“It would be clinically important to further examine the cardiovascular safety of hydroxychloroquine versus methotrexate in a younger population with rheumatic conditions,” she said.
The study was supported by the National Institutes of Health, Brigham and Women’s Hospital, and Harvard Medical School. Four authors declared unrelated research grants from the pharmaceutical sector, with one also declaring stock options and consulting work with the pharmaceutical sector. No other conflicts of interest were declared.
A version of this article first appeared on Medscape.com.
Hydroxychloroquine should be initiated with caution in older patients with rheumatoid arthritis who also have heart failure or are at risk for it, say the authors of a study suggesting that the drug could increase their risk for major adverse cardiovascular events (MACE), compared with methotrexate.
A cohort study published online in the Journal of the American College of Cardiology looked at outcomes in 54,462 patients with RA aged 65 years or older and not previously treated with disease-modifying antirheumatic drugs. Half were initiated on methotrexate and half on hydroxychloroquine, making 27,231 propensity-matched pairs.
Across the entire cohort, hydroxychloroquine was not associated with a higher risk for sudden cardiac arrest, ventricular arrhythmia, or MACE, compared with methotrexate. When broken down into individual cardiovascular events, the data suggested a statistically significant 17% increase in the risk for cardiovascular mortality and 10% increase in all-cause mortality with hydroxychloroquine, although there were no differences in the risks for myocardial infarction or stroke.
However, a subgroup analysis revealed a significant 30% increase in the risk for MACE among patients starting hydroxychloroquine who also had a history of heart failure, compared with patients taking methotrexate. The researchers found no difference between the two drugs in patients without a history of heart failure. The study also suggested an overall 41% increase in the risk for hospitalization with heart failure with hydroxychloroquine, regardless of heart failure history.
Hydroxychloroquine was also associated with a 34% increase in the risk for cardiovascular mortality, a 22% increase in the risk for all-cause mortality, and a 74% increase in the risk for MI.
The lead author of the study, Elvira D’Andrea, MD, PhD, of Brigham and Women’s Hospital and Harvard Medical School in Boston, said that hydroxychloroquine is used as a first-line treatment for RA, but there was limited evidence on its cardiovascular risks. The pandemic in particular shined a spotlight on these concerns and prompted the researchers to extend their original prepandemic study to encompass additional cardiovascular outcomes.
“The emerging concerns on its cardiovascular safety in early 2020 has led the rheumatological community, and patients regularly taking hydroxychloroquine for rheumatoid arthritis, to confusion,” Dr. D’Andrea said in an interview.
She advised that clinicians be cautious when initiating hydroxychloroquine in older patients with existing heart failure or who have risk factors for it. “Although heart failure is a known concern for hydroxychloroquine use, these findings helped to clarify the relationship between the use of hydroxychloroquine or methotrexate and heart failure. Clinicians should pay careful attention to clinical manifestations of cardiomyopathy or heart failure in older patients with rheumatoid arthritis treated with hydroxychloroquine.”
Hydroxychloroquine is associated with cardiotoxicity, particularly cardiomyopathy, which may help precipitate MACE or heart failure exacerbations in patients who already have deterioration of their cardiac tissue, the authors suggested.
Short follow-up period leaves risk attribution under question
In an accompanying editorial, Elizabeth Blair Solow, MD, and Bonnie L. Bermas, MD, of the University of Texas Southwestern Medical Center, Dallas, commented that the lack of an increased risk for arrhythmic events or MACE in the overall cohort taking hydroxychloroquine was reassuring. They also suggested the subgroup analysis findings among patients with preexisting heart failure were still “exploratory and hypothesis-generating” and should be interpreted with caution.
They noted that the follow-up time of the study was relatively short – a median of 209 days – given that hydroxychloroquine does not reach a steady-state level for 6 months.
“Evidence to date suggests cardiomyopathy from HCQ [hydroxychloroquine] takes years to develop, many months beyond the exposures described here, bringing into question as to whether HCQ itself increased HF hospitalizations,” the editorialists wrote.
The editorial also raised the question of whether the association observed in the study was related to a possible cardioprotective effect of methotrexate, given that previous studies have suggested this effect in older patients with RA.
The study authors did an exploratory analysis comparing hydroxychloroquine with sulfasalazine, which appeared to support their main findings of a possible cardiovascular effect of hydroxychloroquine. However, they qualified this by pointing out that the analysis involved small numbers of patients.
Senior investigator Seoyoung C. Kim, MD, ScD, of Brigham and Women’s Hospital and Harvard Medical School, both in Boston, also noted that the study only looked at outcomes in patients aged 65 years and older.
“It would be clinically important to further examine the cardiovascular safety of hydroxychloroquine versus methotrexate in a younger population with rheumatic conditions,” she said.
The study was supported by the National Institutes of Health, Brigham and Women’s Hospital, and Harvard Medical School. Four authors declared unrelated research grants from the pharmaceutical sector, with one also declaring stock options and consulting work with the pharmaceutical sector. No other conflicts of interest were declared.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
LGBTQ students would get new protections under Biden plan
On the 50th anniversary of Title IX’s inception, the Biden administration has proposed changes to the law that would protect transgender students and assault survivors on college and university campuses.
With these changes, the protections provided by Title IX – a civil rights law that prohibits sex-based discrimination in schools that receive federal funding – would now be extended to students who identify as trans. The update would ensure that government-funded schools make proper accommodations for a trans student population, such as allowing students to use bathrooms and other facilities that align with their gender identity, and enforcing the use of students’ correct pronouns.
The revisions also seek to undo amendments made to the law by Betsy DeVos, who was secretary of education during the Trump presidency, which strengthened due process protections for students accused of sexual assault and narrowed the definition of sexual harassment. These rules “weakened protections for survivors of sexual assault and diminished the promise of an education free from discrimination,” the Biden administration said.
“Our proposed changes will allow us to continue that progress and ensure all our nation’s students – no matter where they live, who they are, or whom they love – can learn, grow, and thrive in school,” Education Secretary Miguel Cardona, PhD, said in a news release. “We welcome public comment on these critical regulations so we can further the Biden-Harris Administration’s mission of creating educational environments free from sex discrimination and sexual violence.”
The revisions will go through a long period of public comment before they are set into law. Still, the proposed changes mark a way forward for trans students who are not explicitly protected under Title IX, and they offer solace to assault survivors who may have felt discouraged to come forward and report under Ms. DeVos’s rules.
“The proposed regulations reflect the [Education] Department’s commitment to give full effect to Title IX, ensuring that no person experiences sex discrimination in education, and that school procedures for addressing complaints of sex discrimination, including sexual violence and other forms of sex-based harassment, are clear, effective, and fair to all involved,” said Catherine Lhamon, JD, assistant secretary for the Education Department’s Office Of Civil Rights.
More specific rules about transgender students’ participation in school sports are still to come.
A version of this article first appeared on WebMD.com.
On the 50th anniversary of Title IX’s inception, the Biden administration has proposed changes to the law that would protect transgender students and assault survivors on college and university campuses.
With these changes, the protections provided by Title IX – a civil rights law that prohibits sex-based discrimination in schools that receive federal funding – would now be extended to students who identify as trans. The update would ensure that government-funded schools make proper accommodations for a trans student population, such as allowing students to use bathrooms and other facilities that align with their gender identity, and enforcing the use of students’ correct pronouns.
The revisions also seek to undo amendments made to the law by Betsy DeVos, who was secretary of education during the Trump presidency, which strengthened due process protections for students accused of sexual assault and narrowed the definition of sexual harassment. These rules “weakened protections for survivors of sexual assault and diminished the promise of an education free from discrimination,” the Biden administration said.
“Our proposed changes will allow us to continue that progress and ensure all our nation’s students – no matter where they live, who they are, or whom they love – can learn, grow, and thrive in school,” Education Secretary Miguel Cardona, PhD, said in a news release. “We welcome public comment on these critical regulations so we can further the Biden-Harris Administration’s mission of creating educational environments free from sex discrimination and sexual violence.”
The revisions will go through a long period of public comment before they are set into law. Still, the proposed changes mark a way forward for trans students who are not explicitly protected under Title IX, and they offer solace to assault survivors who may have felt discouraged to come forward and report under Ms. DeVos’s rules.
“The proposed regulations reflect the [Education] Department’s commitment to give full effect to Title IX, ensuring that no person experiences sex discrimination in education, and that school procedures for addressing complaints of sex discrimination, including sexual violence and other forms of sex-based harassment, are clear, effective, and fair to all involved,” said Catherine Lhamon, JD, assistant secretary for the Education Department’s Office Of Civil Rights.
More specific rules about transgender students’ participation in school sports are still to come.
A version of this article first appeared on WebMD.com.
On the 50th anniversary of Title IX’s inception, the Biden administration has proposed changes to the law that would protect transgender students and assault survivors on college and university campuses.
With these changes, the protections provided by Title IX – a civil rights law that prohibits sex-based discrimination in schools that receive federal funding – would now be extended to students who identify as trans. The update would ensure that government-funded schools make proper accommodations for a trans student population, such as allowing students to use bathrooms and other facilities that align with their gender identity, and enforcing the use of students’ correct pronouns.
The revisions also seek to undo amendments made to the law by Betsy DeVos, who was secretary of education during the Trump presidency, which strengthened due process protections for students accused of sexual assault and narrowed the definition of sexual harassment. These rules “weakened protections for survivors of sexual assault and diminished the promise of an education free from discrimination,” the Biden administration said.
“Our proposed changes will allow us to continue that progress and ensure all our nation’s students – no matter where they live, who they are, or whom they love – can learn, grow, and thrive in school,” Education Secretary Miguel Cardona, PhD, said in a news release. “We welcome public comment on these critical regulations so we can further the Biden-Harris Administration’s mission of creating educational environments free from sex discrimination and sexual violence.”
The revisions will go through a long period of public comment before they are set into law. Still, the proposed changes mark a way forward for trans students who are not explicitly protected under Title IX, and they offer solace to assault survivors who may have felt discouraged to come forward and report under Ms. DeVos’s rules.
“The proposed regulations reflect the [Education] Department’s commitment to give full effect to Title IX, ensuring that no person experiences sex discrimination in education, and that school procedures for addressing complaints of sex discrimination, including sexual violence and other forms of sex-based harassment, are clear, effective, and fair to all involved,” said Catherine Lhamon, JD, assistant secretary for the Education Department’s Office Of Civil Rights.
More specific rules about transgender students’ participation in school sports are still to come.
A version of this article first appeared on WebMD.com.
Roe v. Wade: Medical groups react to Supreme Court decision
The country’s top medical organizations condemned the overturning of Roe v. Wade, saying the removal of federal protections for women to access abortion services marks a “dark day.”
“It is unfathomable. It is unfair. It is wrong,” said the President of the American College of Obstetricians and Gynecologists (ACOG) Iffath Abbasi Hoskins, MD.
“Today is a very dark day in health care. It is a dark day, indeed, for the tens of millions of patients who have suddenly and unfairly lost access to safe legal and evidence-based abortion care,” Dr. Hoskins said at a press conference June 24 sponsored by ACOG.
“It is dark for the thousands of clinicians who now, instead of focusing on providing health care to their patients, have to live with the threats of legal, civil, and even professional penalties,” Dr. Hoskins added.
ACOG has 62,000 members and is the leading group of doctors that provides obstetric and gynecologic care.
Dilemma for some doctors?
“I’d like to take a moment to talk about the future of the medical profession,” said ACOG Chief Executive Officer Maureen G. Phipps, MD, MPH. “[The] decision is, as Dr. Hoskins clearly said, a tragic one for our patients in states across the country, but the harm does not end there.”
Dr. Phipps described overturning Roe v. Wade as “the boldest act of legislative interference that we have seen in this country. It will allow state legislators to tell physicians what care they can and cannot provide to their patients.”
“It will leave physicians looking over our shoulders, wondering if a patient is in enough of a crisis to permit an exception to a law,” Dr. Phipps added. “This is an affront to all that drew my colleagues and me into medicine.”
Although the impact on doctor training remains to be seen, she said 44% of ob.gyn. residents are trained in states now empowered to ban abortions.
The effect of the Supreme Court decision on miscarriage management is another unknown.
“It’s going to be very difficult for us, the clinicians, to manage miscarriage,” Dr. Hoskins said. “Many miscarriages could be what we call ‘incomplete’ in the beginning,” where there is still a heartbeat and the patient is cramping and/or bleeding.
In that instance, Dr. Hoskins said, clinicians may be thinking that they have to wait.
“They may be needing to get additional opinions, whether it’s a legal opinion ... or another medical opinion.”
“It’s going to have a devastating effect on every aspect of a woman’s health care, including if she is spontaneously miscarrying,” Dr. Hoskins predicted.
Physician protect thyself?
To what extent doctors can shield themselves from potential prosecution “is a hard question to answer,” Molly Meegan, JD, ACOG’s chief legal officer and general counsel, said.
Ms. Meegan recommended members speak to the risk managers at their individual institutions for guidance.
“It is a real patchwork [of laws] out there, she said. “And that patchwork itself is a danger to people as they seek essential reproductive health care.”
Also, she added, “If a doctor can’t tell what the law is at the time they’re trying to provide the care, it has a terribly chilling effect on medical care.”
Another potential threat to doctors in states that still allow abortion services is action from a neighboring state.
“We are going to be advocating very strongly that states do not have extra-territorial jurisdiction to reach beyond the edges of their state.”
The worry is if a doctor in New Mexico, where abortion is legal, performs an abortion for a person from Texas, where it will soon be illegal, is then prosecuted by Texas, for example.
Medication abortion
Asked about any potential effects on medication abortions, ACOG’s Jen Villavicencio, MD, said it remains to be seen.
“Certainly many of the laws that we have seen, including trigger ban laws, encompass medication abortion,” she said. Several states have these so-called trigger laws, which put into effect laws passed to ban abortion in case Roe was overturned.
This means, she said, that any abortion option, whether it’s procedural or medication, could be and will be banned in some of these states.
Ms. Meegan added that ACOG will continue to support access to medication abortion and that it should be decided by the U.S. Food and Drug Administration and not individual states.
Maternal mortality may rise
“Maternal mortality in and of itself is a very difficult topic,” Dr. Hoskins said, but [the] decision amplifies the implications. “I think of the patients who will have to manage severe complications and mental health challenges while they are carrying a pregnancy that they are forced to carry.”
“I also think of the patients who need to end their pregnancies in order to save their own lives,” Dr. Hoskins added.
Dr. Hoskins said the United States already has a high maternal mortality rate. This new law, she added, could force women into higher-risk situations if they experience high blood pressure, preeclampsia, or bleeding after the birth of the baby.
Growing inequality possible?
“The grievous inequities that exist in this country will grow and expand unchecked without safe access to legal abortion,” Dr. Phipps said.
She noted that women, based on location, will continue “to have protected access to safe evidence-based abortion. Others will have the means and resources and opportunities to secure the care.”
But the same may not be true for women in underserved or disadvantaged communities, Dr. Phipps added.
American Medical Association
ACOG was not the only group to react. “The American Medical Association is deeply disturbed by the U.S. Supreme Court’s decision to overturn nearly a half century of precedent protecting patients’ right to critical reproductive health care,” President Jack Resneck Jr., MD, said in a statement.
The decision represents “an egregious allowance of government intrusion into the medical examination room, a direct attack on the practice of medicine and the patient-physician relationship, and a brazen violation of patients’ rights to evidence-based reproductive health services.”
American Academy of Family Physicians
“The American Academy of Family Physicians is disappointed and disheartened by the Supreme Court’s decision to strike down longstanding protections afforded by Roe v. Wade and Planned Parenthood v. Casey,” President Sterling N. Ransone Jr., MD, said in a statement.
The organization has 127,600 physician and medical student members.
“This decision negatively impacts our practices and our patients by undermining the patient-physician relationship and potentially criminalizing evidence-based medical care,” added Dr. Ransone.
American College of Physicians
“A patient’s decision about whether to continue a pregnancy should be a private decision made in consultation with a physician or other health care professional, without interference from the government,” President Ryan D. Mire, MD, said in a statement. “We strongly oppose medically unnecessary government restrictions on any health care services,” added Dr. Mire on behalf of the group’s 161,000 members.
American Academy of Pediatrics
“This decision carries grave consequences for our adolescent patients, who already face many more barriers than adults in accessing comprehensive reproductive health care services and abortion care,” President Moira Szilagyi, MD, PhD, said in a statement.
“In the wake of this ruling, the American Academy of Pediatrics will continue to support our chapters as states consider policies affecting access to abortion care, and pediatricians will continue to support our patients,” Dr. Szilagyi added.
American Public Health Association
The court’s decision “is a catastrophic judicial failure that will reverberate differently in each state and portends to jeopardize the health and lives of all Americans,” Executive Director Georges C. Benjamin, MD, said in a statement.
American Urogynecologic Society
“The American Urogynecologic Society opposes any ruling that restricts a person’s access to health care and criminalizes the practice of medicine,” the group said in a statement. “This ruling ultimately poses a serious threat to the patient-provider relationship and subsequent decisionmaking necessary to ensure optimal outcomes for patients. As practitioners, we should be free to provide what is in the best interest of our patients.”
A version of this article first appeared on Medscape.com.
The country’s top medical organizations condemned the overturning of Roe v. Wade, saying the removal of federal protections for women to access abortion services marks a “dark day.”
“It is unfathomable. It is unfair. It is wrong,” said the President of the American College of Obstetricians and Gynecologists (ACOG) Iffath Abbasi Hoskins, MD.
“Today is a very dark day in health care. It is a dark day, indeed, for the tens of millions of patients who have suddenly and unfairly lost access to safe legal and evidence-based abortion care,” Dr. Hoskins said at a press conference June 24 sponsored by ACOG.
“It is dark for the thousands of clinicians who now, instead of focusing on providing health care to their patients, have to live with the threats of legal, civil, and even professional penalties,” Dr. Hoskins added.
ACOG has 62,000 members and is the leading group of doctors that provides obstetric and gynecologic care.
Dilemma for some doctors?
“I’d like to take a moment to talk about the future of the medical profession,” said ACOG Chief Executive Officer Maureen G. Phipps, MD, MPH. “[The] decision is, as Dr. Hoskins clearly said, a tragic one for our patients in states across the country, but the harm does not end there.”
Dr. Phipps described overturning Roe v. Wade as “the boldest act of legislative interference that we have seen in this country. It will allow state legislators to tell physicians what care they can and cannot provide to their patients.”
“It will leave physicians looking over our shoulders, wondering if a patient is in enough of a crisis to permit an exception to a law,” Dr. Phipps added. “This is an affront to all that drew my colleagues and me into medicine.”
Although the impact on doctor training remains to be seen, she said 44% of ob.gyn. residents are trained in states now empowered to ban abortions.
The effect of the Supreme Court decision on miscarriage management is another unknown.
“It’s going to be very difficult for us, the clinicians, to manage miscarriage,” Dr. Hoskins said. “Many miscarriages could be what we call ‘incomplete’ in the beginning,” where there is still a heartbeat and the patient is cramping and/or bleeding.
In that instance, Dr. Hoskins said, clinicians may be thinking that they have to wait.
“They may be needing to get additional opinions, whether it’s a legal opinion ... or another medical opinion.”
“It’s going to have a devastating effect on every aspect of a woman’s health care, including if she is spontaneously miscarrying,” Dr. Hoskins predicted.
Physician protect thyself?
To what extent doctors can shield themselves from potential prosecution “is a hard question to answer,” Molly Meegan, JD, ACOG’s chief legal officer and general counsel, said.
Ms. Meegan recommended members speak to the risk managers at their individual institutions for guidance.
“It is a real patchwork [of laws] out there, she said. “And that patchwork itself is a danger to people as they seek essential reproductive health care.”
Also, she added, “If a doctor can’t tell what the law is at the time they’re trying to provide the care, it has a terribly chilling effect on medical care.”
Another potential threat to doctors in states that still allow abortion services is action from a neighboring state.
“We are going to be advocating very strongly that states do not have extra-territorial jurisdiction to reach beyond the edges of their state.”
The worry is if a doctor in New Mexico, where abortion is legal, performs an abortion for a person from Texas, where it will soon be illegal, is then prosecuted by Texas, for example.
Medication abortion
Asked about any potential effects on medication abortions, ACOG’s Jen Villavicencio, MD, said it remains to be seen.
“Certainly many of the laws that we have seen, including trigger ban laws, encompass medication abortion,” she said. Several states have these so-called trigger laws, which put into effect laws passed to ban abortion in case Roe was overturned.
This means, she said, that any abortion option, whether it’s procedural or medication, could be and will be banned in some of these states.
Ms. Meegan added that ACOG will continue to support access to medication abortion and that it should be decided by the U.S. Food and Drug Administration and not individual states.
Maternal mortality may rise
“Maternal mortality in and of itself is a very difficult topic,” Dr. Hoskins said, but [the] decision amplifies the implications. “I think of the patients who will have to manage severe complications and mental health challenges while they are carrying a pregnancy that they are forced to carry.”
“I also think of the patients who need to end their pregnancies in order to save their own lives,” Dr. Hoskins added.
Dr. Hoskins said the United States already has a high maternal mortality rate. This new law, she added, could force women into higher-risk situations if they experience high blood pressure, preeclampsia, or bleeding after the birth of the baby.
Growing inequality possible?
“The grievous inequities that exist in this country will grow and expand unchecked without safe access to legal abortion,” Dr. Phipps said.
She noted that women, based on location, will continue “to have protected access to safe evidence-based abortion. Others will have the means and resources and opportunities to secure the care.”
But the same may not be true for women in underserved or disadvantaged communities, Dr. Phipps added.
American Medical Association
ACOG was not the only group to react. “The American Medical Association is deeply disturbed by the U.S. Supreme Court’s decision to overturn nearly a half century of precedent protecting patients’ right to critical reproductive health care,” President Jack Resneck Jr., MD, said in a statement.
The decision represents “an egregious allowance of government intrusion into the medical examination room, a direct attack on the practice of medicine and the patient-physician relationship, and a brazen violation of patients’ rights to evidence-based reproductive health services.”
American Academy of Family Physicians
“The American Academy of Family Physicians is disappointed and disheartened by the Supreme Court’s decision to strike down longstanding protections afforded by Roe v. Wade and Planned Parenthood v. Casey,” President Sterling N. Ransone Jr., MD, said in a statement.
The organization has 127,600 physician and medical student members.
“This decision negatively impacts our practices and our patients by undermining the patient-physician relationship and potentially criminalizing evidence-based medical care,” added Dr. Ransone.
American College of Physicians
“A patient’s decision about whether to continue a pregnancy should be a private decision made in consultation with a physician or other health care professional, without interference from the government,” President Ryan D. Mire, MD, said in a statement. “We strongly oppose medically unnecessary government restrictions on any health care services,” added Dr. Mire on behalf of the group’s 161,000 members.
American Academy of Pediatrics
“This decision carries grave consequences for our adolescent patients, who already face many more barriers than adults in accessing comprehensive reproductive health care services and abortion care,” President Moira Szilagyi, MD, PhD, said in a statement.
“In the wake of this ruling, the American Academy of Pediatrics will continue to support our chapters as states consider policies affecting access to abortion care, and pediatricians will continue to support our patients,” Dr. Szilagyi added.
American Public Health Association
The court’s decision “is a catastrophic judicial failure that will reverberate differently in each state and portends to jeopardize the health and lives of all Americans,” Executive Director Georges C. Benjamin, MD, said in a statement.
American Urogynecologic Society
“The American Urogynecologic Society opposes any ruling that restricts a person’s access to health care and criminalizes the practice of medicine,” the group said in a statement. “This ruling ultimately poses a serious threat to the patient-provider relationship and subsequent decisionmaking necessary to ensure optimal outcomes for patients. As practitioners, we should be free to provide what is in the best interest of our patients.”
A version of this article first appeared on Medscape.com.
The country’s top medical organizations condemned the overturning of Roe v. Wade, saying the removal of federal protections for women to access abortion services marks a “dark day.”
“It is unfathomable. It is unfair. It is wrong,” said the President of the American College of Obstetricians and Gynecologists (ACOG) Iffath Abbasi Hoskins, MD.
“Today is a very dark day in health care. It is a dark day, indeed, for the tens of millions of patients who have suddenly and unfairly lost access to safe legal and evidence-based abortion care,” Dr. Hoskins said at a press conference June 24 sponsored by ACOG.
“It is dark for the thousands of clinicians who now, instead of focusing on providing health care to their patients, have to live with the threats of legal, civil, and even professional penalties,” Dr. Hoskins added.
ACOG has 62,000 members and is the leading group of doctors that provides obstetric and gynecologic care.
Dilemma for some doctors?
“I’d like to take a moment to talk about the future of the medical profession,” said ACOG Chief Executive Officer Maureen G. Phipps, MD, MPH. “[The] decision is, as Dr. Hoskins clearly said, a tragic one for our patients in states across the country, but the harm does not end there.”
Dr. Phipps described overturning Roe v. Wade as “the boldest act of legislative interference that we have seen in this country. It will allow state legislators to tell physicians what care they can and cannot provide to their patients.”
“It will leave physicians looking over our shoulders, wondering if a patient is in enough of a crisis to permit an exception to a law,” Dr. Phipps added. “This is an affront to all that drew my colleagues and me into medicine.”
Although the impact on doctor training remains to be seen, she said 44% of ob.gyn. residents are trained in states now empowered to ban abortions.
The effect of the Supreme Court decision on miscarriage management is another unknown.
“It’s going to be very difficult for us, the clinicians, to manage miscarriage,” Dr. Hoskins said. “Many miscarriages could be what we call ‘incomplete’ in the beginning,” where there is still a heartbeat and the patient is cramping and/or bleeding.
In that instance, Dr. Hoskins said, clinicians may be thinking that they have to wait.
“They may be needing to get additional opinions, whether it’s a legal opinion ... or another medical opinion.”
“It’s going to have a devastating effect on every aspect of a woman’s health care, including if she is spontaneously miscarrying,” Dr. Hoskins predicted.
Physician protect thyself?
To what extent doctors can shield themselves from potential prosecution “is a hard question to answer,” Molly Meegan, JD, ACOG’s chief legal officer and general counsel, said.
Ms. Meegan recommended members speak to the risk managers at their individual institutions for guidance.
“It is a real patchwork [of laws] out there, she said. “And that patchwork itself is a danger to people as they seek essential reproductive health care.”
Also, she added, “If a doctor can’t tell what the law is at the time they’re trying to provide the care, it has a terribly chilling effect on medical care.”
Another potential threat to doctors in states that still allow abortion services is action from a neighboring state.
“We are going to be advocating very strongly that states do not have extra-territorial jurisdiction to reach beyond the edges of their state.”
The worry is if a doctor in New Mexico, where abortion is legal, performs an abortion for a person from Texas, where it will soon be illegal, is then prosecuted by Texas, for example.
Medication abortion
Asked about any potential effects on medication abortions, ACOG’s Jen Villavicencio, MD, said it remains to be seen.
“Certainly many of the laws that we have seen, including trigger ban laws, encompass medication abortion,” she said. Several states have these so-called trigger laws, which put into effect laws passed to ban abortion in case Roe was overturned.
This means, she said, that any abortion option, whether it’s procedural or medication, could be and will be banned in some of these states.
Ms. Meegan added that ACOG will continue to support access to medication abortion and that it should be decided by the U.S. Food and Drug Administration and not individual states.
Maternal mortality may rise
“Maternal mortality in and of itself is a very difficult topic,” Dr. Hoskins said, but [the] decision amplifies the implications. “I think of the patients who will have to manage severe complications and mental health challenges while they are carrying a pregnancy that they are forced to carry.”
“I also think of the patients who need to end their pregnancies in order to save their own lives,” Dr. Hoskins added.
Dr. Hoskins said the United States already has a high maternal mortality rate. This new law, she added, could force women into higher-risk situations if they experience high blood pressure, preeclampsia, or bleeding after the birth of the baby.
Growing inequality possible?
“The grievous inequities that exist in this country will grow and expand unchecked without safe access to legal abortion,” Dr. Phipps said.
She noted that women, based on location, will continue “to have protected access to safe evidence-based abortion. Others will have the means and resources and opportunities to secure the care.”
But the same may not be true for women in underserved or disadvantaged communities, Dr. Phipps added.
American Medical Association
ACOG was not the only group to react. “The American Medical Association is deeply disturbed by the U.S. Supreme Court’s decision to overturn nearly a half century of precedent protecting patients’ right to critical reproductive health care,” President Jack Resneck Jr., MD, said in a statement.
The decision represents “an egregious allowance of government intrusion into the medical examination room, a direct attack on the practice of medicine and the patient-physician relationship, and a brazen violation of patients’ rights to evidence-based reproductive health services.”
American Academy of Family Physicians
“The American Academy of Family Physicians is disappointed and disheartened by the Supreme Court’s decision to strike down longstanding protections afforded by Roe v. Wade and Planned Parenthood v. Casey,” President Sterling N. Ransone Jr., MD, said in a statement.
The organization has 127,600 physician and medical student members.
“This decision negatively impacts our practices and our patients by undermining the patient-physician relationship and potentially criminalizing evidence-based medical care,” added Dr. Ransone.
American College of Physicians
“A patient’s decision about whether to continue a pregnancy should be a private decision made in consultation with a physician or other health care professional, without interference from the government,” President Ryan D. Mire, MD, said in a statement. “We strongly oppose medically unnecessary government restrictions on any health care services,” added Dr. Mire on behalf of the group’s 161,000 members.
American Academy of Pediatrics
“This decision carries grave consequences for our adolescent patients, who already face many more barriers than adults in accessing comprehensive reproductive health care services and abortion care,” President Moira Szilagyi, MD, PhD, said in a statement.
“In the wake of this ruling, the American Academy of Pediatrics will continue to support our chapters as states consider policies affecting access to abortion care, and pediatricians will continue to support our patients,” Dr. Szilagyi added.
American Public Health Association
The court’s decision “is a catastrophic judicial failure that will reverberate differently in each state and portends to jeopardize the health and lives of all Americans,” Executive Director Georges C. Benjamin, MD, said in a statement.
American Urogynecologic Society
“The American Urogynecologic Society opposes any ruling that restricts a person’s access to health care and criminalizes the practice of medicine,” the group said in a statement. “This ruling ultimately poses a serious threat to the patient-provider relationship and subsequent decisionmaking necessary to ensure optimal outcomes for patients. As practitioners, we should be free to provide what is in the best interest of our patients.”
A version of this article first appeared on Medscape.com.
Typhoid fever bacteria becoming more resistant to antibiotics
Bacteria that cause typhoid fever are becoming increasingly resistant to common antibiotics worldwide, a new analysis indicates.
Resistant strains of Salmonella enterica serovar typhi – almost all originating in South Asia – have spread across borders nearly 200 times since 1990.
Until now, analysis has been limited by small samples. This genome analysis is the largest to date and included 3,489 newly sequenced isolates (collected between 2014 and 2019) from prospective surveillance studies in four of the countries with the highest typhoid burden: Bangladesh, Nepal, Pakistan, and India.
Findings of the study, led by Kesia Esther da Silva, PhD, with the division of infectious diseases and geographic medicine at Stanford (Calif.) University, were published online in The Lancet Microbe.
Global deaths: 100,000 annually
Typhoid fever remains a global public health threat, causing 11 million infections and more than 100,000 deaths each year. Most cases (70%) are in South Asia, but typhoid also has significant presence in sub-Saharan Africa, Southeast Asia, and Oceania.
The findings are further evidence of the need for a global response, the authors write.
Jason Andrews, MD, a coauthor and associate professor in the division of infectious diseases and geographic medicine at Stanford University, said in an interview that the research helps pinpoint where the highest burden is and where the biggest need is for the two highly effective typhoid vaccines.
“We’re seeing higher levels of resistance than we’ve ever seen before against our latest and greatest antibiotics,” he said.
He said so far, strategies for tackling typhoid have involved country-level decisions and local funding and that needs to be shifted to a global priority. “Given contemporary travel migration patterns, what we see is that when antimicrobial resistance develops in one country, it quickly spreads to other countries.”
Dr. Andrews said the United States sees about 300-500 typhoid cases a year. “About 80% of those cases involve people traveling from South Asia,” he said.
Infections also come from people from the United States visiting high-burden countries, especially to see family. Often they don’t perceive the risk and skip vaccination, he said. U.S. clinicians can help with educating patients traveling to typhoid-endemic regions on pretravel vaccination.
Physician awareness is also important when patients have recently returned from such regions. Data from this study show a need to carefully consider which antibiotics will be effective with the growing resistance.
Only one oral option left in Pakistan
“We are running low on treatment options for typhoid,” Dr. Andrews said. The resistance pattern in Pakistan, for example, has left only one oral option, azithromycin, and resistance is building to that.
Without that option, “we’ll have to hospitalize patients and give intravenous antibiotics,” he said. “That’s concerning.”
Moreover, some resistant strains from Pakistan have been turning up in the United States.
“There are actually some cases that have not been tracked at all to travelers going to Pakistan and are thought to be from local transmission in the United States,” he said.
Valida Bajrovic, MD, assistant professor of medicine in infectious diseases at the Icahn School of Medicine at Mount Sinai, New York, said in an interview that, in addition to vaccinating travelers before they head to typhoid-endemic areas, physicians should educate patients on avoiding fecal transmission of typhoid with vigilant hand washing, drinking bottled water, and avoiding foods that may have been prepared in unsanitary conditions.
Dr. Bajrovic, who directs the antimicrobial stewardship efforts at the Mount Sinai Morningside and Mount Sinai West Hospitals, said stricter antimicrobial stewardship efforts are needed, particularly in Europe and South Asia, but also in the United States.
“Restriction of antibiotic use is the way to prevent antibiotic resistance,” she said, adding that such restrictions need to be part of a global effort.
Strains in the study were classified as multidrug resistant (MDR) if they contained genes resistant to ampicillin, chloramphenicol, and trimethoprim/sulfamethoxazole. The authors also traced the presence of genes demonstrating resistance to macrolides and quinolones.
At first, fluoroquinolones were effective against MDR S. typhi and in the 1990s became the primary therapy. By the 2010s, however, the majority of S. typhi in south Asia contained mutations in the quinolone resistance-determining regions.
The authors wrote: “We found evidence of frequent international (n = 138) and intercontinental transfers (n = 59) of antimicrobial-resistant S. typhi.”
According to the analysis, since 2000, MDR S. typhi has declined steadily in Bangladesh and India and remained at less than 5% of typhoid strains in Nepal, though it has increased slightly in Pakistan.
However, these are being replaced “with strains containing ceftriaxone resistance (extensively drug resistant), high-level fluoroquinolone resistance, or azithromycin resistance, which are reversing declines in the effective population size of S. typhi,” the authors wrote.
The analysis supports urgency for prevention measures, including use of typhoid conjugate vaccines in typhoid-endemic countries, the authors said.
But given the rise in international spread of increasingly resistant strains, they said, preventive measures should not be limited to those countries.
The study was funded by the Bill & Melinda Gates Foundation. Dr. Da Silva, Dr. Andrews, and Dr. Bajrovic have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Bacteria that cause typhoid fever are becoming increasingly resistant to common antibiotics worldwide, a new analysis indicates.
Resistant strains of Salmonella enterica serovar typhi – almost all originating in South Asia – have spread across borders nearly 200 times since 1990.
Until now, analysis has been limited by small samples. This genome analysis is the largest to date and included 3,489 newly sequenced isolates (collected between 2014 and 2019) from prospective surveillance studies in four of the countries with the highest typhoid burden: Bangladesh, Nepal, Pakistan, and India.
Findings of the study, led by Kesia Esther da Silva, PhD, with the division of infectious diseases and geographic medicine at Stanford (Calif.) University, were published online in The Lancet Microbe.
Global deaths: 100,000 annually
Typhoid fever remains a global public health threat, causing 11 million infections and more than 100,000 deaths each year. Most cases (70%) are in South Asia, but typhoid also has significant presence in sub-Saharan Africa, Southeast Asia, and Oceania.
The findings are further evidence of the need for a global response, the authors write.
Jason Andrews, MD, a coauthor and associate professor in the division of infectious diseases and geographic medicine at Stanford University, said in an interview that the research helps pinpoint where the highest burden is and where the biggest need is for the two highly effective typhoid vaccines.
“We’re seeing higher levels of resistance than we’ve ever seen before against our latest and greatest antibiotics,” he said.
He said so far, strategies for tackling typhoid have involved country-level decisions and local funding and that needs to be shifted to a global priority. “Given contemporary travel migration patterns, what we see is that when antimicrobial resistance develops in one country, it quickly spreads to other countries.”
Dr. Andrews said the United States sees about 300-500 typhoid cases a year. “About 80% of those cases involve people traveling from South Asia,” he said.
Infections also come from people from the United States visiting high-burden countries, especially to see family. Often they don’t perceive the risk and skip vaccination, he said. U.S. clinicians can help with educating patients traveling to typhoid-endemic regions on pretravel vaccination.
Physician awareness is also important when patients have recently returned from such regions. Data from this study show a need to carefully consider which antibiotics will be effective with the growing resistance.
Only one oral option left in Pakistan
“We are running low on treatment options for typhoid,” Dr. Andrews said. The resistance pattern in Pakistan, for example, has left only one oral option, azithromycin, and resistance is building to that.
Without that option, “we’ll have to hospitalize patients and give intravenous antibiotics,” he said. “That’s concerning.”
Moreover, some resistant strains from Pakistan have been turning up in the United States.
“There are actually some cases that have not been tracked at all to travelers going to Pakistan and are thought to be from local transmission in the United States,” he said.
Valida Bajrovic, MD, assistant professor of medicine in infectious diseases at the Icahn School of Medicine at Mount Sinai, New York, said in an interview that, in addition to vaccinating travelers before they head to typhoid-endemic areas, physicians should educate patients on avoiding fecal transmission of typhoid with vigilant hand washing, drinking bottled water, and avoiding foods that may have been prepared in unsanitary conditions.
Dr. Bajrovic, who directs the antimicrobial stewardship efforts at the Mount Sinai Morningside and Mount Sinai West Hospitals, said stricter antimicrobial stewardship efforts are needed, particularly in Europe and South Asia, but also in the United States.
“Restriction of antibiotic use is the way to prevent antibiotic resistance,” she said, adding that such restrictions need to be part of a global effort.
Strains in the study were classified as multidrug resistant (MDR) if they contained genes resistant to ampicillin, chloramphenicol, and trimethoprim/sulfamethoxazole. The authors also traced the presence of genes demonstrating resistance to macrolides and quinolones.
At first, fluoroquinolones were effective against MDR S. typhi and in the 1990s became the primary therapy. By the 2010s, however, the majority of S. typhi in south Asia contained mutations in the quinolone resistance-determining regions.
The authors wrote: “We found evidence of frequent international (n = 138) and intercontinental transfers (n = 59) of antimicrobial-resistant S. typhi.”
According to the analysis, since 2000, MDR S. typhi has declined steadily in Bangladesh and India and remained at less than 5% of typhoid strains in Nepal, though it has increased slightly in Pakistan.
However, these are being replaced “with strains containing ceftriaxone resistance (extensively drug resistant), high-level fluoroquinolone resistance, or azithromycin resistance, which are reversing declines in the effective population size of S. typhi,” the authors wrote.
The analysis supports urgency for prevention measures, including use of typhoid conjugate vaccines in typhoid-endemic countries, the authors said.
But given the rise in international spread of increasingly resistant strains, they said, preventive measures should not be limited to those countries.
The study was funded by the Bill & Melinda Gates Foundation. Dr. Da Silva, Dr. Andrews, and Dr. Bajrovic have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Bacteria that cause typhoid fever are becoming increasingly resistant to common antibiotics worldwide, a new analysis indicates.
Resistant strains of Salmonella enterica serovar typhi – almost all originating in South Asia – have spread across borders nearly 200 times since 1990.
Until now, analysis has been limited by small samples. This genome analysis is the largest to date and included 3,489 newly sequenced isolates (collected between 2014 and 2019) from prospective surveillance studies in four of the countries with the highest typhoid burden: Bangladesh, Nepal, Pakistan, and India.
Findings of the study, led by Kesia Esther da Silva, PhD, with the division of infectious diseases and geographic medicine at Stanford (Calif.) University, were published online in The Lancet Microbe.
Global deaths: 100,000 annually
Typhoid fever remains a global public health threat, causing 11 million infections and more than 100,000 deaths each year. Most cases (70%) are in South Asia, but typhoid also has significant presence in sub-Saharan Africa, Southeast Asia, and Oceania.
The findings are further evidence of the need for a global response, the authors write.
Jason Andrews, MD, a coauthor and associate professor in the division of infectious diseases and geographic medicine at Stanford University, said in an interview that the research helps pinpoint where the highest burden is and where the biggest need is for the two highly effective typhoid vaccines.
“We’re seeing higher levels of resistance than we’ve ever seen before against our latest and greatest antibiotics,” he said.
He said so far, strategies for tackling typhoid have involved country-level decisions and local funding and that needs to be shifted to a global priority. “Given contemporary travel migration patterns, what we see is that when antimicrobial resistance develops in one country, it quickly spreads to other countries.”
Dr. Andrews said the United States sees about 300-500 typhoid cases a year. “About 80% of those cases involve people traveling from South Asia,” he said.
Infections also come from people from the United States visiting high-burden countries, especially to see family. Often they don’t perceive the risk and skip vaccination, he said. U.S. clinicians can help with educating patients traveling to typhoid-endemic regions on pretravel vaccination.
Physician awareness is also important when patients have recently returned from such regions. Data from this study show a need to carefully consider which antibiotics will be effective with the growing resistance.
Only one oral option left in Pakistan
“We are running low on treatment options for typhoid,” Dr. Andrews said. The resistance pattern in Pakistan, for example, has left only one oral option, azithromycin, and resistance is building to that.
Without that option, “we’ll have to hospitalize patients and give intravenous antibiotics,” he said. “That’s concerning.”
Moreover, some resistant strains from Pakistan have been turning up in the United States.
“There are actually some cases that have not been tracked at all to travelers going to Pakistan and are thought to be from local transmission in the United States,” he said.
Valida Bajrovic, MD, assistant professor of medicine in infectious diseases at the Icahn School of Medicine at Mount Sinai, New York, said in an interview that, in addition to vaccinating travelers before they head to typhoid-endemic areas, physicians should educate patients on avoiding fecal transmission of typhoid with vigilant hand washing, drinking bottled water, and avoiding foods that may have been prepared in unsanitary conditions.
Dr. Bajrovic, who directs the antimicrobial stewardship efforts at the Mount Sinai Morningside and Mount Sinai West Hospitals, said stricter antimicrobial stewardship efforts are needed, particularly in Europe and South Asia, but also in the United States.
“Restriction of antibiotic use is the way to prevent antibiotic resistance,” she said, adding that such restrictions need to be part of a global effort.
Strains in the study were classified as multidrug resistant (MDR) if they contained genes resistant to ampicillin, chloramphenicol, and trimethoprim/sulfamethoxazole. The authors also traced the presence of genes demonstrating resistance to macrolides and quinolones.
At first, fluoroquinolones were effective against MDR S. typhi and in the 1990s became the primary therapy. By the 2010s, however, the majority of S. typhi in south Asia contained mutations in the quinolone resistance-determining regions.
The authors wrote: “We found evidence of frequent international (n = 138) and intercontinental transfers (n = 59) of antimicrobial-resistant S. typhi.”
According to the analysis, since 2000, MDR S. typhi has declined steadily in Bangladesh and India and remained at less than 5% of typhoid strains in Nepal, though it has increased slightly in Pakistan.
However, these are being replaced “with strains containing ceftriaxone resistance (extensively drug resistant), high-level fluoroquinolone resistance, or azithromycin resistance, which are reversing declines in the effective population size of S. typhi,” the authors wrote.
The analysis supports urgency for prevention measures, including use of typhoid conjugate vaccines in typhoid-endemic countries, the authors said.
But given the rise in international spread of increasingly resistant strains, they said, preventive measures should not be limited to those countries.
The study was funded by the Bill & Melinda Gates Foundation. Dr. Da Silva, Dr. Andrews, and Dr. Bajrovic have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Why it’s so hard to prevent physician suicide
Kip Wenger, DO, an emergency physician and systems medical director of Team Health, Knoxville, Tenn., was asked to see a patient in the emergency department. He was shocked when he realized who the patient was – a 33-year-old female physician friend and colleague.
She was bleeding from multiple self-inflicted injuries and ultimately died. “I was devastated and couldn’t wrap my head around what had just happened,” Dr. Wenger told this news organization.
It’s important for physicians to be aware of warning signs in their colleagues, such as showing up late, being irritable and short-tempered with staff, missing shifts, making mistakes, or receiving an increasing number of patient complaints, Dr. Wenger says.
Dr. Wenger had had dinner with her several weeks earlier and saw some subtle changes. He had known her as a “positive, upbeat person,” but her demeanor was different during dinner.
“There were no typical telltale signs – she was talking about her plans for the future, including buying a new bicycle – but she wasn’t herself and seemed to become tearful when I hugged her at the end of the evening,” he said. He later heard from another colleague that she had shared feeling “hopeless.”
The scope of the problem
According to the American Society for Suicide Prevention, roughly 300-400 physicians die by suicide annually. Although one study suggests a lower number, official reports likely underestimate suicides, study author Katherine Gold, MD, MSW, associate professor of family medicine, obstetrics, and gynecology, Michigan Medicine, University of Michigan, Ann Arbor, said in an interview.
Peter Yellowlees, MD, MBBS, professor of psychiatry, University of California, Davis, concurs, suggesting that some single-car accidents involving physicians might be suicides. Perry Lin, MD, assistant clinical professor, Heritage College of Osteopathic Medicine, Ohio University, Athens, and national co-chair of the Physician Suicide Awareness Committee of the American Association of Suicidology, says that some death certificates state that the deceased died of “accidental causes” because the physician who completes the certificate, possibly a colleague, is reluctant to list the actual cause of death to protect his colleague’s memory or the family’s feelings.
In general, and among physicians, White men older than 65 “represent the largest percentage of people who die from suicide nationwide,” says Dr. Lin.
But younger people are also susceptible, Dr. Lin adds. One of the most vulnerable periods for potential suicide is during the first few months of residency. This dovetails with the findings of Medscape’s 2022 report Suicide: A Tragedy of the Profession. In that report, a difference was found between frequency of suicidal thoughts in younger physicians, compared with older physicians (14% in those < 35 years vs. 8% for those ≥ 45 years).
Hurdles to preventing physician suicide
“The best thing that can happen in our profession is upstream intervention – if people seek help before they get to the point of suicidality, recognizing they’re under stress and duress and that they might be going down a bad pathway,” says Dr. Lin. But research suggests that many physicians don’t do so.
Gary Price, MD, attending surgeon and clinical assistant professor of surgery, Yale–New Haven Hospital, Connecticut, and president of the Physicians Foundation, says his organization has identified barriers that prevent physicians from seeking help.
Physicians feel they may put their licensure at risk if they admit to receiving help for mental issues. These concerns were expressed by respondents in Medscape’s above mentioned 2022 report, many of whom didn’t seek treatment for depression, burnout, or suicidal thoughts lest it affect their professional standing when renewing their license or seeking credentialing.
Although organizations and societies are advocating against these questions, a recent study found that almost 70% of U.S. states and territories continue to ask physicians about their mental health, and 28% ask for diagnoses (beyond current impairments) – a violation of the Americans With Disabilities Act.
“Mental health illness is different from mental health impairment,” Ryan Mire, MD, a Nashville, Tenn.–based internist, said in an interview. “As physicians, we’re comfortable with licensing boards asking whether the physician has any condition that might impair their care for patients, but not about a history of mental illness.”
The second barrier, says Dr. Price, is that hospital credentialing committees sometimes ask similar questions, as do commercial and malpractice insurers.
Another roadblock is that in some states, undergoing treatment for a mental health problem could be subject to discovery by a plaintiff’s attorney in a malpractice case, even if the physician’s mental health history had no effect on patient care. But that’s uncommon, says Daniel Shapiro, PhD, author of “Delivering Doctor Amelia,” a book about his treatment of a suicidal physician who underwent a malpractice lawsuit. “I’ve never seen that happen.”
A final barrier is that many employers require employees to receive treatment within their own institution or health system. “Physicians may be reluctant to get help where they work, with colleagues and friends knowing about their illness or being involved with their care,” says Dr. Price.
In 2022, the American College of Physicians (ACP) issued a toolkit to help members encourage licensing and credentialing boards to remove questions about mental health on applications and include language that supports receiving treatment, Dr. Mire says.
Layers of vulnerability
There are few data regarding relative risk among particular races or ethnicities, “but we know racism is a social stressor,” says Dr. Mire. “Obviously, people from historically disadvantaged populations tend to have societal stressors like discrimination and racism that add an extra layer of burden.”
Intersectionality – having multiple intersecting risk factors – may confer even higher risk. “For example, if you’re a female physician from a historically marginalized race and a resident dealing with the ‘hidden curriculum’ of trying to be resilient, you have multiple layers of vulnerability.”
There are also limited data regarding which specialties or work environments are associated with highest risk. “Obviously, challenges exist in every segment of medicine and at different ages, stages, and work environments, and they intersect with each individual physician’s personal risk factors,” says Dr. Mire, president of the ACP and assistant clinical professor of clinical medical education, University of Tennessee Health Science Center, Memphis.
Pamela Wible, MD, is an Oregon-based retired physician who herself went through a suicidal period about 11 years into her career that motivated her to embrace a new vision of clinical practice and change her practice model. After a series of physician suicides in her area, she began to speak and write openly about physician suicide, and since her retirement from clinical practice, she makes herself available on a full-time basis to distressed physicians. “When I address a conference of a particular medical specialty or a group in a particular geographical region, I focus on the specific vulnerabilities in that specialty or region,” she says.
What increases the chances of suicide?
“Many factors, both within and outside the professional setting, affect someone’s decision to die by suicide – after all, physicians have the same stressors as other people, like family, finances, and their own health,” Dr. Mire says. When it comes to non–work-related factors, marital stressors and comorbid psychiatric illness particularly raise the risk, says Dr. Lin.
But certain drivers are specific to the practice of medicine, with burnout and depression first in line.
Dr. Shapiro, who is vice dean for faculty and administrative affairs, Penn State University, Hershey, and the Garner James Cline Professor of Medical Humanism, conducts burnout evaluations throughout the country. “Simple depression screeners prior to the pandemic showed about a 10% major depression rate in physicians,” he told this news organization. “Now, we’re seeing a 30%-33% depression rate, even in those who weren’t frontline providers during the pandemic.”
Dr. Price agrees, noting that burnout in physicians has gone from 40% to 60% since the pandemic. But burnout doesn’t always lead to suicide. It’s when burnout progresses to depression, becomes more severe, and is untreated that the suicidal risk arises, he emphasizes.
Additionally, being a doctor isn’t “just a profession” but a “calling and identity,” says Dr. Gold. Job-related problems (for example, a malpractice suit, complaints to the medical board, loss of autonomy, changing work demands) can raise suicidal risk.
And job-related problems can inform the location of suicide, says Dr. Wible, who is the author of “Physicians Suicide Letters – Answered.”
“A work-related catalyst makes it more likely that the person will attempt or complete suicide in the work setting. Physicians have stepped off hospital rooftops, shot or stabbed themselves in hospital parking lots, or [hanged] themselves in hospital chapels. Perhaps it’s because they’re choosing to die in the place where they’ve been most wounded.”
You are not at fault
“If you’re feeling suicidal, you might feel utterly alone, but if there’s one message I can give you, it’s that you’re not alone, and there are many things you can do to mitigate your pain and despair,” Dr. Wible says. “And you’re not defective. It’s the health care system that’s defective. You have nothing to be ashamed of.”
Some institutions have a “buddy system” that pairs clinicians to provide mutual peer support. A partner who notices concerning signs can refer the other partner for help. Physicians can also be paired with a “buddy,” even without a formal institutional structure.
A “buddy” is a step in the right direction, but Dr. Shapiro cautions it might be necessary to consult a trained professional for serious depression or suicidality. Several states provide connection to local resources. Employee assistance programs (EAPs) might be helpful, although many physicians don’t trust their institution’s EAP. Or physicians can ask colleagues to recommend a “doctor’s doctor” who specializes in treating physicians, suggests Dr. Yellowlees, author of “Physician Suicide: Cases and Commentaries.”
In Medscape’s 2022 report, almost all respondents who reported having suicidal colleagues said they offered help, including emotional support, practical assistance, referrals, speaking to family members, or even personally taking the colleague to the ED or to a therapist.
To enhance physicians’ ability to help each other, Dr. Lin recommends “gatekeeper training,” which has been shown to reduce suicide. “This strategy utilizes a peer-to-peer model, but, rather than a single ‘peer buddy,’ everyone is a ‘gatekeeper’ trained in approaches, such as QPR – Question, Persuade, Refer. ‘Gatekeepers’ are taught how to recognize warning signs of suicide, question the potentially suicidal individual, persuade him/her to get help, and provide referrals.”
Other ways to prevent suicide
Dr. Lin advises physicians to “create a personalized safety plan and write down signs and clues that they may be going down the wrong path and what they can do – like breathing exercises, relaxation – and identifying people to talk to, places to go, or phone numbers to call, if those initial measures aren’t enough.” The plan is private and allows the physician to determine at what point help is needed and who should be consulted. “Sometimes, when a person is in acute stress, even looking up a phone number can seem insurmountable. But having it on paper lowers the barrier, making it more achievable.”
Resources should be posted in places where physicians gather so that those who don’t already have a safety plan have easy access to that information, he suggests.
In addition, consideration may be given to reaching out for support if a colleague has died by suicide, experts suggest. Whether offered by one’s institution, a peer arrangement, spiritual counseling, or psychotherapy, one may need help dealing with the trauma, guilt, and grief that often accompany this type of loss.
A version of this article first appeared on Medscape.com.
Kip Wenger, DO, an emergency physician and systems medical director of Team Health, Knoxville, Tenn., was asked to see a patient in the emergency department. He was shocked when he realized who the patient was – a 33-year-old female physician friend and colleague.
She was bleeding from multiple self-inflicted injuries and ultimately died. “I was devastated and couldn’t wrap my head around what had just happened,” Dr. Wenger told this news organization.
It’s important for physicians to be aware of warning signs in their colleagues, such as showing up late, being irritable and short-tempered with staff, missing shifts, making mistakes, or receiving an increasing number of patient complaints, Dr. Wenger says.
Dr. Wenger had had dinner with her several weeks earlier and saw some subtle changes. He had known her as a “positive, upbeat person,” but her demeanor was different during dinner.
“There were no typical telltale signs – she was talking about her plans for the future, including buying a new bicycle – but she wasn’t herself and seemed to become tearful when I hugged her at the end of the evening,” he said. He later heard from another colleague that she had shared feeling “hopeless.”
The scope of the problem
According to the American Society for Suicide Prevention, roughly 300-400 physicians die by suicide annually. Although one study suggests a lower number, official reports likely underestimate suicides, study author Katherine Gold, MD, MSW, associate professor of family medicine, obstetrics, and gynecology, Michigan Medicine, University of Michigan, Ann Arbor, said in an interview.
Peter Yellowlees, MD, MBBS, professor of psychiatry, University of California, Davis, concurs, suggesting that some single-car accidents involving physicians might be suicides. Perry Lin, MD, assistant clinical professor, Heritage College of Osteopathic Medicine, Ohio University, Athens, and national co-chair of the Physician Suicide Awareness Committee of the American Association of Suicidology, says that some death certificates state that the deceased died of “accidental causes” because the physician who completes the certificate, possibly a colleague, is reluctant to list the actual cause of death to protect his colleague’s memory or the family’s feelings.
In general, and among physicians, White men older than 65 “represent the largest percentage of people who die from suicide nationwide,” says Dr. Lin.
But younger people are also susceptible, Dr. Lin adds. One of the most vulnerable periods for potential suicide is during the first few months of residency. This dovetails with the findings of Medscape’s 2022 report Suicide: A Tragedy of the Profession. In that report, a difference was found between frequency of suicidal thoughts in younger physicians, compared with older physicians (14% in those < 35 years vs. 8% for those ≥ 45 years).
Hurdles to preventing physician suicide
“The best thing that can happen in our profession is upstream intervention – if people seek help before they get to the point of suicidality, recognizing they’re under stress and duress and that they might be going down a bad pathway,” says Dr. Lin. But research suggests that many physicians don’t do so.
Gary Price, MD, attending surgeon and clinical assistant professor of surgery, Yale–New Haven Hospital, Connecticut, and president of the Physicians Foundation, says his organization has identified barriers that prevent physicians from seeking help.
Physicians feel they may put their licensure at risk if they admit to receiving help for mental issues. These concerns were expressed by respondents in Medscape’s above mentioned 2022 report, many of whom didn’t seek treatment for depression, burnout, or suicidal thoughts lest it affect their professional standing when renewing their license or seeking credentialing.
Although organizations and societies are advocating against these questions, a recent study found that almost 70% of U.S. states and territories continue to ask physicians about their mental health, and 28% ask for diagnoses (beyond current impairments) – a violation of the Americans With Disabilities Act.
“Mental health illness is different from mental health impairment,” Ryan Mire, MD, a Nashville, Tenn.–based internist, said in an interview. “As physicians, we’re comfortable with licensing boards asking whether the physician has any condition that might impair their care for patients, but not about a history of mental illness.”
The second barrier, says Dr. Price, is that hospital credentialing committees sometimes ask similar questions, as do commercial and malpractice insurers.
Another roadblock is that in some states, undergoing treatment for a mental health problem could be subject to discovery by a plaintiff’s attorney in a malpractice case, even if the physician’s mental health history had no effect on patient care. But that’s uncommon, says Daniel Shapiro, PhD, author of “Delivering Doctor Amelia,” a book about his treatment of a suicidal physician who underwent a malpractice lawsuit. “I’ve never seen that happen.”
A final barrier is that many employers require employees to receive treatment within their own institution or health system. “Physicians may be reluctant to get help where they work, with colleagues and friends knowing about their illness or being involved with their care,” says Dr. Price.
In 2022, the American College of Physicians (ACP) issued a toolkit to help members encourage licensing and credentialing boards to remove questions about mental health on applications and include language that supports receiving treatment, Dr. Mire says.
Layers of vulnerability
There are few data regarding relative risk among particular races or ethnicities, “but we know racism is a social stressor,” says Dr. Mire. “Obviously, people from historically disadvantaged populations tend to have societal stressors like discrimination and racism that add an extra layer of burden.”
Intersectionality – having multiple intersecting risk factors – may confer even higher risk. “For example, if you’re a female physician from a historically marginalized race and a resident dealing with the ‘hidden curriculum’ of trying to be resilient, you have multiple layers of vulnerability.”
There are also limited data regarding which specialties or work environments are associated with highest risk. “Obviously, challenges exist in every segment of medicine and at different ages, stages, and work environments, and they intersect with each individual physician’s personal risk factors,” says Dr. Mire, president of the ACP and assistant clinical professor of clinical medical education, University of Tennessee Health Science Center, Memphis.
Pamela Wible, MD, is an Oregon-based retired physician who herself went through a suicidal period about 11 years into her career that motivated her to embrace a new vision of clinical practice and change her practice model. After a series of physician suicides in her area, she began to speak and write openly about physician suicide, and since her retirement from clinical practice, she makes herself available on a full-time basis to distressed physicians. “When I address a conference of a particular medical specialty or a group in a particular geographical region, I focus on the specific vulnerabilities in that specialty or region,” she says.
What increases the chances of suicide?
“Many factors, both within and outside the professional setting, affect someone’s decision to die by suicide – after all, physicians have the same stressors as other people, like family, finances, and their own health,” Dr. Mire says. When it comes to non–work-related factors, marital stressors and comorbid psychiatric illness particularly raise the risk, says Dr. Lin.
But certain drivers are specific to the practice of medicine, with burnout and depression first in line.
Dr. Shapiro, who is vice dean for faculty and administrative affairs, Penn State University, Hershey, and the Garner James Cline Professor of Medical Humanism, conducts burnout evaluations throughout the country. “Simple depression screeners prior to the pandemic showed about a 10% major depression rate in physicians,” he told this news organization. “Now, we’re seeing a 30%-33% depression rate, even in those who weren’t frontline providers during the pandemic.”
Dr. Price agrees, noting that burnout in physicians has gone from 40% to 60% since the pandemic. But burnout doesn’t always lead to suicide. It’s when burnout progresses to depression, becomes more severe, and is untreated that the suicidal risk arises, he emphasizes.
Additionally, being a doctor isn’t “just a profession” but a “calling and identity,” says Dr. Gold. Job-related problems (for example, a malpractice suit, complaints to the medical board, loss of autonomy, changing work demands) can raise suicidal risk.
And job-related problems can inform the location of suicide, says Dr. Wible, who is the author of “Physicians Suicide Letters – Answered.”
“A work-related catalyst makes it more likely that the person will attempt or complete suicide in the work setting. Physicians have stepped off hospital rooftops, shot or stabbed themselves in hospital parking lots, or [hanged] themselves in hospital chapels. Perhaps it’s because they’re choosing to die in the place where they’ve been most wounded.”
You are not at fault
“If you’re feeling suicidal, you might feel utterly alone, but if there’s one message I can give you, it’s that you’re not alone, and there are many things you can do to mitigate your pain and despair,” Dr. Wible says. “And you’re not defective. It’s the health care system that’s defective. You have nothing to be ashamed of.”
Some institutions have a “buddy system” that pairs clinicians to provide mutual peer support. A partner who notices concerning signs can refer the other partner for help. Physicians can also be paired with a “buddy,” even without a formal institutional structure.
A “buddy” is a step in the right direction, but Dr. Shapiro cautions it might be necessary to consult a trained professional for serious depression or suicidality. Several states provide connection to local resources. Employee assistance programs (EAPs) might be helpful, although many physicians don’t trust their institution’s EAP. Or physicians can ask colleagues to recommend a “doctor’s doctor” who specializes in treating physicians, suggests Dr. Yellowlees, author of “Physician Suicide: Cases and Commentaries.”
In Medscape’s 2022 report, almost all respondents who reported having suicidal colleagues said they offered help, including emotional support, practical assistance, referrals, speaking to family members, or even personally taking the colleague to the ED or to a therapist.
To enhance physicians’ ability to help each other, Dr. Lin recommends “gatekeeper training,” which has been shown to reduce suicide. “This strategy utilizes a peer-to-peer model, but, rather than a single ‘peer buddy,’ everyone is a ‘gatekeeper’ trained in approaches, such as QPR – Question, Persuade, Refer. ‘Gatekeepers’ are taught how to recognize warning signs of suicide, question the potentially suicidal individual, persuade him/her to get help, and provide referrals.”
Other ways to prevent suicide
Dr. Lin advises physicians to “create a personalized safety plan and write down signs and clues that they may be going down the wrong path and what they can do – like breathing exercises, relaxation – and identifying people to talk to, places to go, or phone numbers to call, if those initial measures aren’t enough.” The plan is private and allows the physician to determine at what point help is needed and who should be consulted. “Sometimes, when a person is in acute stress, even looking up a phone number can seem insurmountable. But having it on paper lowers the barrier, making it more achievable.”
Resources should be posted in places where physicians gather so that those who don’t already have a safety plan have easy access to that information, he suggests.
In addition, consideration may be given to reaching out for support if a colleague has died by suicide, experts suggest. Whether offered by one’s institution, a peer arrangement, spiritual counseling, or psychotherapy, one may need help dealing with the trauma, guilt, and grief that often accompany this type of loss.
A version of this article first appeared on Medscape.com.
Kip Wenger, DO, an emergency physician and systems medical director of Team Health, Knoxville, Tenn., was asked to see a patient in the emergency department. He was shocked when he realized who the patient was – a 33-year-old female physician friend and colleague.
She was bleeding from multiple self-inflicted injuries and ultimately died. “I was devastated and couldn’t wrap my head around what had just happened,” Dr. Wenger told this news organization.
It’s important for physicians to be aware of warning signs in their colleagues, such as showing up late, being irritable and short-tempered with staff, missing shifts, making mistakes, or receiving an increasing number of patient complaints, Dr. Wenger says.
Dr. Wenger had had dinner with her several weeks earlier and saw some subtle changes. He had known her as a “positive, upbeat person,” but her demeanor was different during dinner.
“There were no typical telltale signs – she was talking about her plans for the future, including buying a new bicycle – but she wasn’t herself and seemed to become tearful when I hugged her at the end of the evening,” he said. He later heard from another colleague that she had shared feeling “hopeless.”
The scope of the problem
According to the American Society for Suicide Prevention, roughly 300-400 physicians die by suicide annually. Although one study suggests a lower number, official reports likely underestimate suicides, study author Katherine Gold, MD, MSW, associate professor of family medicine, obstetrics, and gynecology, Michigan Medicine, University of Michigan, Ann Arbor, said in an interview.
Peter Yellowlees, MD, MBBS, professor of psychiatry, University of California, Davis, concurs, suggesting that some single-car accidents involving physicians might be suicides. Perry Lin, MD, assistant clinical professor, Heritage College of Osteopathic Medicine, Ohio University, Athens, and national co-chair of the Physician Suicide Awareness Committee of the American Association of Suicidology, says that some death certificates state that the deceased died of “accidental causes” because the physician who completes the certificate, possibly a colleague, is reluctant to list the actual cause of death to protect his colleague’s memory or the family’s feelings.
In general, and among physicians, White men older than 65 “represent the largest percentage of people who die from suicide nationwide,” says Dr. Lin.
But younger people are also susceptible, Dr. Lin adds. One of the most vulnerable periods for potential suicide is during the first few months of residency. This dovetails with the findings of Medscape’s 2022 report Suicide: A Tragedy of the Profession. In that report, a difference was found between frequency of suicidal thoughts in younger physicians, compared with older physicians (14% in those < 35 years vs. 8% for those ≥ 45 years).
Hurdles to preventing physician suicide
“The best thing that can happen in our profession is upstream intervention – if people seek help before they get to the point of suicidality, recognizing they’re under stress and duress and that they might be going down a bad pathway,” says Dr. Lin. But research suggests that many physicians don’t do so.
Gary Price, MD, attending surgeon and clinical assistant professor of surgery, Yale–New Haven Hospital, Connecticut, and president of the Physicians Foundation, says his organization has identified barriers that prevent physicians from seeking help.
Physicians feel they may put their licensure at risk if they admit to receiving help for mental issues. These concerns were expressed by respondents in Medscape’s above mentioned 2022 report, many of whom didn’t seek treatment for depression, burnout, or suicidal thoughts lest it affect their professional standing when renewing their license or seeking credentialing.
Although organizations and societies are advocating against these questions, a recent study found that almost 70% of U.S. states and territories continue to ask physicians about their mental health, and 28% ask for diagnoses (beyond current impairments) – a violation of the Americans With Disabilities Act.
“Mental health illness is different from mental health impairment,” Ryan Mire, MD, a Nashville, Tenn.–based internist, said in an interview. “As physicians, we’re comfortable with licensing boards asking whether the physician has any condition that might impair their care for patients, but not about a history of mental illness.”
The second barrier, says Dr. Price, is that hospital credentialing committees sometimes ask similar questions, as do commercial and malpractice insurers.
Another roadblock is that in some states, undergoing treatment for a mental health problem could be subject to discovery by a plaintiff’s attorney in a malpractice case, even if the physician’s mental health history had no effect on patient care. But that’s uncommon, says Daniel Shapiro, PhD, author of “Delivering Doctor Amelia,” a book about his treatment of a suicidal physician who underwent a malpractice lawsuit. “I’ve never seen that happen.”
A final barrier is that many employers require employees to receive treatment within their own institution or health system. “Physicians may be reluctant to get help where they work, with colleagues and friends knowing about their illness or being involved with their care,” says Dr. Price.
In 2022, the American College of Physicians (ACP) issued a toolkit to help members encourage licensing and credentialing boards to remove questions about mental health on applications and include language that supports receiving treatment, Dr. Mire says.
Layers of vulnerability
There are few data regarding relative risk among particular races or ethnicities, “but we know racism is a social stressor,” says Dr. Mire. “Obviously, people from historically disadvantaged populations tend to have societal stressors like discrimination and racism that add an extra layer of burden.”
Intersectionality – having multiple intersecting risk factors – may confer even higher risk. “For example, if you’re a female physician from a historically marginalized race and a resident dealing with the ‘hidden curriculum’ of trying to be resilient, you have multiple layers of vulnerability.”
There are also limited data regarding which specialties or work environments are associated with highest risk. “Obviously, challenges exist in every segment of medicine and at different ages, stages, and work environments, and they intersect with each individual physician’s personal risk factors,” says Dr. Mire, president of the ACP and assistant clinical professor of clinical medical education, University of Tennessee Health Science Center, Memphis.
Pamela Wible, MD, is an Oregon-based retired physician who herself went through a suicidal period about 11 years into her career that motivated her to embrace a new vision of clinical practice and change her practice model. After a series of physician suicides in her area, she began to speak and write openly about physician suicide, and since her retirement from clinical practice, she makes herself available on a full-time basis to distressed physicians. “When I address a conference of a particular medical specialty or a group in a particular geographical region, I focus on the specific vulnerabilities in that specialty or region,” she says.
What increases the chances of suicide?
“Many factors, both within and outside the professional setting, affect someone’s decision to die by suicide – after all, physicians have the same stressors as other people, like family, finances, and their own health,” Dr. Mire says. When it comes to non–work-related factors, marital stressors and comorbid psychiatric illness particularly raise the risk, says Dr. Lin.
But certain drivers are specific to the practice of medicine, with burnout and depression first in line.
Dr. Shapiro, who is vice dean for faculty and administrative affairs, Penn State University, Hershey, and the Garner James Cline Professor of Medical Humanism, conducts burnout evaluations throughout the country. “Simple depression screeners prior to the pandemic showed about a 10% major depression rate in physicians,” he told this news organization. “Now, we’re seeing a 30%-33% depression rate, even in those who weren’t frontline providers during the pandemic.”
Dr. Price agrees, noting that burnout in physicians has gone from 40% to 60% since the pandemic. But burnout doesn’t always lead to suicide. It’s when burnout progresses to depression, becomes more severe, and is untreated that the suicidal risk arises, he emphasizes.
Additionally, being a doctor isn’t “just a profession” but a “calling and identity,” says Dr. Gold. Job-related problems (for example, a malpractice suit, complaints to the medical board, loss of autonomy, changing work demands) can raise suicidal risk.
And job-related problems can inform the location of suicide, says Dr. Wible, who is the author of “Physicians Suicide Letters – Answered.”
“A work-related catalyst makes it more likely that the person will attempt or complete suicide in the work setting. Physicians have stepped off hospital rooftops, shot or stabbed themselves in hospital parking lots, or [hanged] themselves in hospital chapels. Perhaps it’s because they’re choosing to die in the place where they’ve been most wounded.”
You are not at fault
“If you’re feeling suicidal, you might feel utterly alone, but if there’s one message I can give you, it’s that you’re not alone, and there are many things you can do to mitigate your pain and despair,” Dr. Wible says. “And you’re not defective. It’s the health care system that’s defective. You have nothing to be ashamed of.”
Some institutions have a “buddy system” that pairs clinicians to provide mutual peer support. A partner who notices concerning signs can refer the other partner for help. Physicians can also be paired with a “buddy,” even without a formal institutional structure.
A “buddy” is a step in the right direction, but Dr. Shapiro cautions it might be necessary to consult a trained professional for serious depression or suicidality. Several states provide connection to local resources. Employee assistance programs (EAPs) might be helpful, although many physicians don’t trust their institution’s EAP. Or physicians can ask colleagues to recommend a “doctor’s doctor” who specializes in treating physicians, suggests Dr. Yellowlees, author of “Physician Suicide: Cases and Commentaries.”
In Medscape’s 2022 report, almost all respondents who reported having suicidal colleagues said they offered help, including emotional support, practical assistance, referrals, speaking to family members, or even personally taking the colleague to the ED or to a therapist.
To enhance physicians’ ability to help each other, Dr. Lin recommends “gatekeeper training,” which has been shown to reduce suicide. “This strategy utilizes a peer-to-peer model, but, rather than a single ‘peer buddy,’ everyone is a ‘gatekeeper’ trained in approaches, such as QPR – Question, Persuade, Refer. ‘Gatekeepers’ are taught how to recognize warning signs of suicide, question the potentially suicidal individual, persuade him/her to get help, and provide referrals.”
Other ways to prevent suicide
Dr. Lin advises physicians to “create a personalized safety plan and write down signs and clues that they may be going down the wrong path and what they can do – like breathing exercises, relaxation – and identifying people to talk to, places to go, or phone numbers to call, if those initial measures aren’t enough.” The plan is private and allows the physician to determine at what point help is needed and who should be consulted. “Sometimes, when a person is in acute stress, even looking up a phone number can seem insurmountable. But having it on paper lowers the barrier, making it more achievable.”
Resources should be posted in places where physicians gather so that those who don’t already have a safety plan have easy access to that information, he suggests.
In addition, consideration may be given to reaching out for support if a colleague has died by suicide, experts suggest. Whether offered by one’s institution, a peer arrangement, spiritual counseling, or psychotherapy, one may need help dealing with the trauma, guilt, and grief that often accompany this type of loss.
A version of this article first appeared on Medscape.com.
Childhood melatonin poisonings skyrocket in the past 10 years
The number of children in the United States who unintentionally ingested melatonin supplements over the past 10 years has skyrocketed to the point where, as of 2021, melatonin ingestions by children accounted for almost 5% of all poisonings reported to poison control centers in the United States, data from the National Poison Data System (NPDS) indicate.
This compared with only 0.6% of melatonin ingestions reported to poison control centers in 2012, the authors added.
“Basically the number of pediatric melatonin ingestions increased 530% from 8,337 in 2012 to 52,563 in 2021 so it’s a 6.3-fold increase from the beginning of the study until the end,” Michael Toce, MD, one of the study authors and attending, pediatric emergency medicine/medical toxicology, Boston Children’s Hospital, said in an interview.
“And I think the biggest driver of this increase is simply that sales of melatonin have increased astronomically so there is just more melatonin at home and studies have shown there is a correlation between the amount of an individual medication in the home and the risk of pediatric exposure – so simply put: The more of a single substance in a home, the greater the chance that a child is going to get into it,” he underscored.
The study was published in the Morbidity and Mortality Weekly Report .
Melatonin ingestions
All cases of single substance melatonin ingestions involving children and adolescents between Jan. 1, 2012, and Dec. 31, 2021, were included in the analysis. During the 10-year study interval, 260,435 pediatric melatonin ingestions were reported to the NPDS. Over 94% of the reported ingestions were unintentional and 99% occurred in the home.
Over 88% of them were managed on-site; most involved young male children aged 5 years and under, and almost 83% of children who ingested melatonin supplements remained asymptomatic. On the other hand, 27,795 patients sought care at a health care facility and close to 15% of them were hospitalized. Among all melatonin ingestions, 1.6% resulted in more serious outcomes; more serious outcomes being defined as a moderate or major effects or death. Five children required mechanical ventilation in order to treat their symptoms and 2 patients died.
The largest number of patients who were hospitalized were adolescents who took melatonin intentionally but the largest increase in the rate of exposure was in young, unintentional patients, as Dr. Toce observed. Interestingly, the largest yearly increase in pediatric melatonin ingestions – almost 38% – coincided with the onset of the COVID-19 pandemic.
“This might be related to increased accessibility of melatonin during the pandemic, as children spent more time at home because of stay-at-home orders and school closures,” the authors speculate. Moreover, sleep disturbances were common during the pandemic, leading to a greater likelihood that parents were buying melatonin and thus exposing children to more melatonin at home.
Taken appropriately and at normal does, melatonin in itself is quite safe, as Dr. Toce stressed. However, “for any substance, the dose makes the poison, so taken in any significant quantity, anything is going to be dangerous.” Moreover, it’s important to appreciate that melatonin, at least in the United States, is regulated as a dietary supplement, not as a pharmaceutical.
“Thus, it doesn’t get the same rigorous testing that something like acetaminophen does by the FDA and that means two things,” Dr. Toce noted. First, if the product says that each gummy contains 3 mg of melatonin, no independent body is verifying whether or not that statement is true so there could be 3 mg of melatonin in each gummy or there could be 10 mg,.
Secondly, because there is no impartial oversight for dietary supplements, there may in fact be no melatonin at all in the product or something else may be added to it that might be harmful. “Just because something is sold over-the-counter does not necessarily mean that it’s safe,” Dr. Toce stressed. To keep children safe from pharmaceuticals and supplements, he recommended several generic poison prevention tips. This advice could be passed on to patients who are parents.
- Keep all pharmaceuticals and supplements preferably locked away so there is less risk of children and adolescents taking products either unintentionally or intentionally
- If parents have no place to lock their products up, put them out of reach, high-up so children cannot easily access them
- Keep the product in the original child-resistant packaging as opposed to taking the pills out of the packaging and putting it in a plastic bag bag. “Certainly we’ve seen that when medications are moved into a non–child-resistant container, ingestions go up,” Dr. Toce warned
- Don’t refer to any medicine or supplement a child might take as “candy.” “A lot of children have difficulty taking medications so some families will say: ‘It’s time for your candy,’ ” Dr. Toce explained. Then, if a child does discover the “candy” on a table where they have access to it, they will not recognize it as medication and they’re likely to pop it into their mouth, thinking it is candy.
Lastly, and most importantly, parents who are considering trying a melatonin supplement to help a child sleep better should first establish a stable sleep routine for their child. “They also need to limit caffeinated beverages before bed as well as screen time,” Dr. Toce added.
And they should talk with their primary care provider as to whether or not initiation of a melatonin supplement is appropriate for their child – “and not just jump right into giving them melatonin without first discussing whether it is appropriate to do so,” Dr. Toce stressed.
Remarkable rise
In a comment on his own experience with melatonin poisoning over recent years, toxicology expert Kevin Osterhoudt, MD, of the University of Pennsylvania, Philadelphia and the Children’s Hospital of Philadelphia, noted that it has been their experience that there has been a remarkable rise in poison center reports of children ingesting melatonin in the recent past. For example, the Poison Control Center at CHOP received nearly 4,000 calls involving melatonin ingestion by children 5 years old or younger in the 5 years between 2017 and 2021 with increasing numbers every year.
“The [current study] supports that our regional observation that this has been a national trend,” Dr. Osterhoudt said. Dr. Osterhoudt agreed with Dr. Toce that good sleep is healthy, and it is very important to develop good sleep habits and a regular bedtime routine in order to do so. “In some situations, melatonin may be useful as a short-term sleep aid and that’s a good discussion to have with your child’s health care provider.”
If parents do decide to give their child a melatonin supplement, they need to keep in mind that melatonin may alter how the body handles other drugs such as those used to treat epilepsy or blood clotting. They also need to know experts are still uncertain about how melatonin affects the body over the long term and whether it is safe for mothers to take during pregnancy.
Dr. Osterhoudt offered his own recommendations for safe melatonin use in the home:
- Discuss planned melatonin use with your health care provider.
- Buy only high-quality supplements by looking for the “USP Verified” mark.
- Insist that manufacturers sell products in child-resistant bottles.
- Periodically inspect the medications in your home and dispose of medications that are no longer being used.
- Program the phone number of your regional poison control center into your phone; poison center experts are available 24/7 to answer questions and concerns about ingestions of melatonin (in the United States the number is 1-800-222-1222).
The study authors and neither Dr. Toce nor Dr. Osterhoudt had any relevant conflicts of interest to declare.
The number of children in the United States who unintentionally ingested melatonin supplements over the past 10 years has skyrocketed to the point where, as of 2021, melatonin ingestions by children accounted for almost 5% of all poisonings reported to poison control centers in the United States, data from the National Poison Data System (NPDS) indicate.
This compared with only 0.6% of melatonin ingestions reported to poison control centers in 2012, the authors added.
“Basically the number of pediatric melatonin ingestions increased 530% from 8,337 in 2012 to 52,563 in 2021 so it’s a 6.3-fold increase from the beginning of the study until the end,” Michael Toce, MD, one of the study authors and attending, pediatric emergency medicine/medical toxicology, Boston Children’s Hospital, said in an interview.
“And I think the biggest driver of this increase is simply that sales of melatonin have increased astronomically so there is just more melatonin at home and studies have shown there is a correlation between the amount of an individual medication in the home and the risk of pediatric exposure – so simply put: The more of a single substance in a home, the greater the chance that a child is going to get into it,” he underscored.
The study was published in the Morbidity and Mortality Weekly Report .
Melatonin ingestions
All cases of single substance melatonin ingestions involving children and adolescents between Jan. 1, 2012, and Dec. 31, 2021, were included in the analysis. During the 10-year study interval, 260,435 pediatric melatonin ingestions were reported to the NPDS. Over 94% of the reported ingestions were unintentional and 99% occurred in the home.
Over 88% of them were managed on-site; most involved young male children aged 5 years and under, and almost 83% of children who ingested melatonin supplements remained asymptomatic. On the other hand, 27,795 patients sought care at a health care facility and close to 15% of them were hospitalized. Among all melatonin ingestions, 1.6% resulted in more serious outcomes; more serious outcomes being defined as a moderate or major effects or death. Five children required mechanical ventilation in order to treat their symptoms and 2 patients died.
The largest number of patients who were hospitalized were adolescents who took melatonin intentionally but the largest increase in the rate of exposure was in young, unintentional patients, as Dr. Toce observed. Interestingly, the largest yearly increase in pediatric melatonin ingestions – almost 38% – coincided with the onset of the COVID-19 pandemic.
“This might be related to increased accessibility of melatonin during the pandemic, as children spent more time at home because of stay-at-home orders and school closures,” the authors speculate. Moreover, sleep disturbances were common during the pandemic, leading to a greater likelihood that parents were buying melatonin and thus exposing children to more melatonin at home.
Taken appropriately and at normal does, melatonin in itself is quite safe, as Dr. Toce stressed. However, “for any substance, the dose makes the poison, so taken in any significant quantity, anything is going to be dangerous.” Moreover, it’s important to appreciate that melatonin, at least in the United States, is regulated as a dietary supplement, not as a pharmaceutical.
“Thus, it doesn’t get the same rigorous testing that something like acetaminophen does by the FDA and that means two things,” Dr. Toce noted. First, if the product says that each gummy contains 3 mg of melatonin, no independent body is verifying whether or not that statement is true so there could be 3 mg of melatonin in each gummy or there could be 10 mg,.
Secondly, because there is no impartial oversight for dietary supplements, there may in fact be no melatonin at all in the product or something else may be added to it that might be harmful. “Just because something is sold over-the-counter does not necessarily mean that it’s safe,” Dr. Toce stressed. To keep children safe from pharmaceuticals and supplements, he recommended several generic poison prevention tips. This advice could be passed on to patients who are parents.
- Keep all pharmaceuticals and supplements preferably locked away so there is less risk of children and adolescents taking products either unintentionally or intentionally
- If parents have no place to lock their products up, put them out of reach, high-up so children cannot easily access them
- Keep the product in the original child-resistant packaging as opposed to taking the pills out of the packaging and putting it in a plastic bag bag. “Certainly we’ve seen that when medications are moved into a non–child-resistant container, ingestions go up,” Dr. Toce warned
- Don’t refer to any medicine or supplement a child might take as “candy.” “A lot of children have difficulty taking medications so some families will say: ‘It’s time for your candy,’ ” Dr. Toce explained. Then, if a child does discover the “candy” on a table where they have access to it, they will not recognize it as medication and they’re likely to pop it into their mouth, thinking it is candy.
Lastly, and most importantly, parents who are considering trying a melatonin supplement to help a child sleep better should first establish a stable sleep routine for their child. “They also need to limit caffeinated beverages before bed as well as screen time,” Dr. Toce added.
And they should talk with their primary care provider as to whether or not initiation of a melatonin supplement is appropriate for their child – “and not just jump right into giving them melatonin without first discussing whether it is appropriate to do so,” Dr. Toce stressed.
Remarkable rise
In a comment on his own experience with melatonin poisoning over recent years, toxicology expert Kevin Osterhoudt, MD, of the University of Pennsylvania, Philadelphia and the Children’s Hospital of Philadelphia, noted that it has been their experience that there has been a remarkable rise in poison center reports of children ingesting melatonin in the recent past. For example, the Poison Control Center at CHOP received nearly 4,000 calls involving melatonin ingestion by children 5 years old or younger in the 5 years between 2017 and 2021 with increasing numbers every year.
“The [current study] supports that our regional observation that this has been a national trend,” Dr. Osterhoudt said. Dr. Osterhoudt agreed with Dr. Toce that good sleep is healthy, and it is very important to develop good sleep habits and a regular bedtime routine in order to do so. “In some situations, melatonin may be useful as a short-term sleep aid and that’s a good discussion to have with your child’s health care provider.”
If parents do decide to give their child a melatonin supplement, they need to keep in mind that melatonin may alter how the body handles other drugs such as those used to treat epilepsy or blood clotting. They also need to know experts are still uncertain about how melatonin affects the body over the long term and whether it is safe for mothers to take during pregnancy.
Dr. Osterhoudt offered his own recommendations for safe melatonin use in the home:
- Discuss planned melatonin use with your health care provider.
- Buy only high-quality supplements by looking for the “USP Verified” mark.
- Insist that manufacturers sell products in child-resistant bottles.
- Periodically inspect the medications in your home and dispose of medications that are no longer being used.
- Program the phone number of your regional poison control center into your phone; poison center experts are available 24/7 to answer questions and concerns about ingestions of melatonin (in the United States the number is 1-800-222-1222).
The study authors and neither Dr. Toce nor Dr. Osterhoudt had any relevant conflicts of interest to declare.
The number of children in the United States who unintentionally ingested melatonin supplements over the past 10 years has skyrocketed to the point where, as of 2021, melatonin ingestions by children accounted for almost 5% of all poisonings reported to poison control centers in the United States, data from the National Poison Data System (NPDS) indicate.
This compared with only 0.6% of melatonin ingestions reported to poison control centers in 2012, the authors added.
“Basically the number of pediatric melatonin ingestions increased 530% from 8,337 in 2012 to 52,563 in 2021 so it’s a 6.3-fold increase from the beginning of the study until the end,” Michael Toce, MD, one of the study authors and attending, pediatric emergency medicine/medical toxicology, Boston Children’s Hospital, said in an interview.
“And I think the biggest driver of this increase is simply that sales of melatonin have increased astronomically so there is just more melatonin at home and studies have shown there is a correlation between the amount of an individual medication in the home and the risk of pediatric exposure – so simply put: The more of a single substance in a home, the greater the chance that a child is going to get into it,” he underscored.
The study was published in the Morbidity and Mortality Weekly Report .
Melatonin ingestions
All cases of single substance melatonin ingestions involving children and adolescents between Jan. 1, 2012, and Dec. 31, 2021, were included in the analysis. During the 10-year study interval, 260,435 pediatric melatonin ingestions were reported to the NPDS. Over 94% of the reported ingestions were unintentional and 99% occurred in the home.
Over 88% of them were managed on-site; most involved young male children aged 5 years and under, and almost 83% of children who ingested melatonin supplements remained asymptomatic. On the other hand, 27,795 patients sought care at a health care facility and close to 15% of them were hospitalized. Among all melatonin ingestions, 1.6% resulted in more serious outcomes; more serious outcomes being defined as a moderate or major effects or death. Five children required mechanical ventilation in order to treat their symptoms and 2 patients died.
The largest number of patients who were hospitalized were adolescents who took melatonin intentionally but the largest increase in the rate of exposure was in young, unintentional patients, as Dr. Toce observed. Interestingly, the largest yearly increase in pediatric melatonin ingestions – almost 38% – coincided with the onset of the COVID-19 pandemic.
“This might be related to increased accessibility of melatonin during the pandemic, as children spent more time at home because of stay-at-home orders and school closures,” the authors speculate. Moreover, sleep disturbances were common during the pandemic, leading to a greater likelihood that parents were buying melatonin and thus exposing children to more melatonin at home.
Taken appropriately and at normal does, melatonin in itself is quite safe, as Dr. Toce stressed. However, “for any substance, the dose makes the poison, so taken in any significant quantity, anything is going to be dangerous.” Moreover, it’s important to appreciate that melatonin, at least in the United States, is regulated as a dietary supplement, not as a pharmaceutical.
“Thus, it doesn’t get the same rigorous testing that something like acetaminophen does by the FDA and that means two things,” Dr. Toce noted. First, if the product says that each gummy contains 3 mg of melatonin, no independent body is verifying whether or not that statement is true so there could be 3 mg of melatonin in each gummy or there could be 10 mg,.
Secondly, because there is no impartial oversight for dietary supplements, there may in fact be no melatonin at all in the product or something else may be added to it that might be harmful. “Just because something is sold over-the-counter does not necessarily mean that it’s safe,” Dr. Toce stressed. To keep children safe from pharmaceuticals and supplements, he recommended several generic poison prevention tips. This advice could be passed on to patients who are parents.
- Keep all pharmaceuticals and supplements preferably locked away so there is less risk of children and adolescents taking products either unintentionally or intentionally
- If parents have no place to lock their products up, put them out of reach, high-up so children cannot easily access them
- Keep the product in the original child-resistant packaging as opposed to taking the pills out of the packaging and putting it in a plastic bag bag. “Certainly we’ve seen that when medications are moved into a non–child-resistant container, ingestions go up,” Dr. Toce warned
- Don’t refer to any medicine or supplement a child might take as “candy.” “A lot of children have difficulty taking medications so some families will say: ‘It’s time for your candy,’ ” Dr. Toce explained. Then, if a child does discover the “candy” on a table where they have access to it, they will not recognize it as medication and they’re likely to pop it into their mouth, thinking it is candy.
Lastly, and most importantly, parents who are considering trying a melatonin supplement to help a child sleep better should first establish a stable sleep routine for their child. “They also need to limit caffeinated beverages before bed as well as screen time,” Dr. Toce added.
And they should talk with their primary care provider as to whether or not initiation of a melatonin supplement is appropriate for their child – “and not just jump right into giving them melatonin without first discussing whether it is appropriate to do so,” Dr. Toce stressed.
Remarkable rise
In a comment on his own experience with melatonin poisoning over recent years, toxicology expert Kevin Osterhoudt, MD, of the University of Pennsylvania, Philadelphia and the Children’s Hospital of Philadelphia, noted that it has been their experience that there has been a remarkable rise in poison center reports of children ingesting melatonin in the recent past. For example, the Poison Control Center at CHOP received nearly 4,000 calls involving melatonin ingestion by children 5 years old or younger in the 5 years between 2017 and 2021 with increasing numbers every year.
“The [current study] supports that our regional observation that this has been a national trend,” Dr. Osterhoudt said. Dr. Osterhoudt agreed with Dr. Toce that good sleep is healthy, and it is very important to develop good sleep habits and a regular bedtime routine in order to do so. “In some situations, melatonin may be useful as a short-term sleep aid and that’s a good discussion to have with your child’s health care provider.”
If parents do decide to give their child a melatonin supplement, they need to keep in mind that melatonin may alter how the body handles other drugs such as those used to treat epilepsy or blood clotting. They also need to know experts are still uncertain about how melatonin affects the body over the long term and whether it is safe for mothers to take during pregnancy.
Dr. Osterhoudt offered his own recommendations for safe melatonin use in the home:
- Discuss planned melatonin use with your health care provider.
- Buy only high-quality supplements by looking for the “USP Verified” mark.
- Insist that manufacturers sell products in child-resistant bottles.
- Periodically inspect the medications in your home and dispose of medications that are no longer being used.
- Program the phone number of your regional poison control center into your phone; poison center experts are available 24/7 to answer questions and concerns about ingestions of melatonin (in the United States the number is 1-800-222-1222).
The study authors and neither Dr. Toce nor Dr. Osterhoudt had any relevant conflicts of interest to declare.
FROM THE MMWR



