User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Should our patients really go home for the holidays?
As an East Coast transplant residing in Texas, I look forward to the annual sojourn home to celebrate the holidays with family and friends – as do many of our patients and their families. But this is 2020. SARS-CoV-2, the causative agent of COVID-19, is still circulating. To make matters worse, cases are rising in 45 states and internationally. The day of this writing 102,831 new cases were reported in the United States. 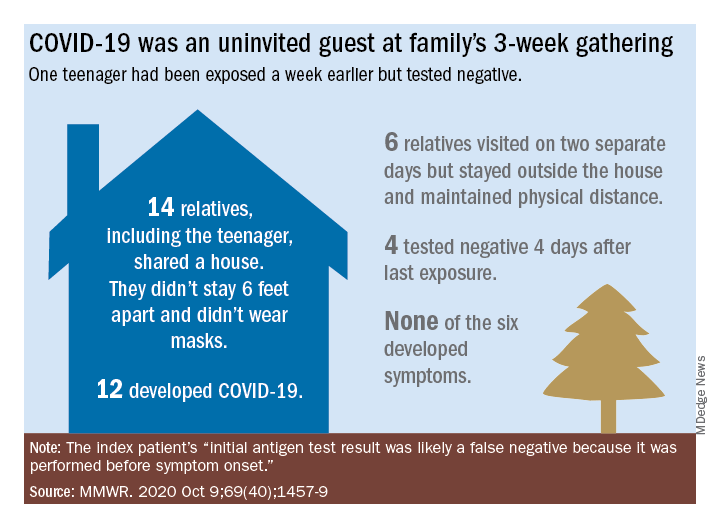
Social distancing, wearing masks, and hand washing have been strategies recommended to help mitigate the spread of the virus. We know adherence is not always 100%. The reality is that several families will consider traveling and gathering with others over the holidays. Their actions may lead to increased infections, hospitalizations, and even deaths. It behooves us to at least remind them of the potential consequences of the activity, and if travel and/or holiday gatherings are inevitable, to provide some guidance to help them look at both the risks and benefits and offer strategies to minimize infection and spread.
What should be considered prior to travel?
Here is a list of points to ponder:
- Is your patient is in a high-risk group for developing severe disease or visiting someone who is in a high-risk group?
- What is their mode of transportation?
- What is their destination?
- How prevalent is the disease at their destination, compared with their community?
- What will be their accommodations?
- How will attendees prepare for the gathering, if at all?
- Will multiple families congregate after quarantining for 2 weeks or simply arrive?
- At the destination, will people wear masks and socially distance?
- Is an outdoor venue an option?
All of these questions should be considered by patients.
Review high-risk groups
In terms of high-risk groups, we usually focus on underlying medical conditions or extremes of age, but Black and LatinX children and their families have been diagnosed with COVID-19 and hospitalized more frequently than other racial/ ethnic groups in the United States. Of 277,285 school-aged children infected between March 1 and Sept. 19, 2020, 42% were LatinX, 32% White, and 17% Black, yet they comprise 18%, 60%, and 11% of the U.S. population, respectively. Of those hospitalized, 45% were LatinX, 22% White, and 24% Black. LatinX and Black children also have disproportionately higher mortality rates.
Think about transmission and how to mitigate it
Many patients erroneously think combining multiple households for small group gatherings is inconsequential. These types of gatherings serve as a continued source of SARS-CoV-2 spread. For example, a person in Illinois with mild upper respiratory infection symptoms attended a funeral; he reported embracing the family members after the funeral. He dined with two people the evening prior to the funeral, sharing the meal using common serving dishes. Four days later, he attended a birthday party with nine family members. Some of the family members with symptoms subsequently attended church, infecting another church attendee. A cluster of 16 cases of COVID-19 was subsequently identified, including three deaths likely resulting from this one introduction of COVID-19 at these two family gatherings.
In Tennessee and Wisconsin, household transmission of SARS-CoV-2 was studied prospectively. A total of 101 index cases and 191 asymptomatic household contacts were enrolled between April and Sept. 2020; 102 of 191 (53%) had SARS-CoV-2 detected during the 14-day follow-up. Most infections (75%) were identified within 5 days and occurred whether the index case was an adult or child.
Lastly, one adolescent was identified as the source for an outbreak at a family gathering where 15 persons from five households and four states shared a house between 8 and 25 days in July 2020. Six additional members visited the house. The index case had an exposure to COVID-19 and had a negative antigen test 4 days after exposure. She was asymptomatic when tested. She developed nasal congestion 2 days later, the same day she and her family departed for the gathering. A total of 11 household contacts developed confirmed, suspected, or probable COVID-19, and the teen developed symptoms. This report illustrates how easily SARS-CoV-2 is transmitted, and how when implemented, mitigation strategies work because none of the six who only visited the house was infected. It also serves as a reminder that antigen testing is indicated only for use within the first 5-12 days of onset of symptoms. In this case, the adolescent was asymptomatic when tested and had a false-negative test result.
Ponder modes of transportation
How will your patient arrive to their holiday destination? Nonstop travel by car with household members is probably the safest way. However, for many families, buses and trains are the only options, and social distancing may be challenging. Air travel is a must for others. Acquisition of COVID-19 during air travel appears to be low, but not absent based on how air enters and leaves the cabin. The challenge is socially distancing throughout the check in and boarding processes, as well as minimizing contact with common surfaces. There also is loss of social distancing once on board. Ideally, masks should be worn during the flight. Additionally, for those with international destinations, most countries now require a negative polymerase chain reaction COVID-19 test within a specified time frame for entry.
Essentially the safest place for your patients during the holidays is celebrating at home with their household contacts. The risk for disease acquisition increases with travel. You will not have the opportunity to discuss holiday plans with most parents. However, you can encourage them to consider the pros and cons of travel with reminders via telephone, e-mail, and /or social messaging directly from your practices similar to those sent for other medically necessary interventions. As for me, I will be celebrating virtually this year. There is a first time for everything.
For additional information that also is patient friendly, the Centers for Disease Control and Prevention offers information about travel within the United States and international travel.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at [email protected].
As an East Coast transplant residing in Texas, I look forward to the annual sojourn home to celebrate the holidays with family and friends – as do many of our patients and their families. But this is 2020. SARS-CoV-2, the causative agent of COVID-19, is still circulating. To make matters worse, cases are rising in 45 states and internationally. The day of this writing 102,831 new cases were reported in the United States. 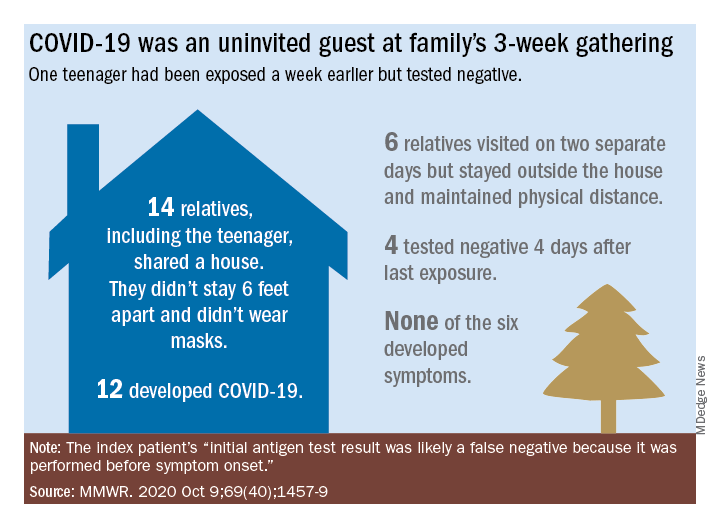
Social distancing, wearing masks, and hand washing have been strategies recommended to help mitigate the spread of the virus. We know adherence is not always 100%. The reality is that several families will consider traveling and gathering with others over the holidays. Their actions may lead to increased infections, hospitalizations, and even deaths. It behooves us to at least remind them of the potential consequences of the activity, and if travel and/or holiday gatherings are inevitable, to provide some guidance to help them look at both the risks and benefits and offer strategies to minimize infection and spread.
What should be considered prior to travel?
Here is a list of points to ponder:
- Is your patient is in a high-risk group for developing severe disease or visiting someone who is in a high-risk group?
- What is their mode of transportation?
- What is their destination?
- How prevalent is the disease at their destination, compared with their community?
- What will be their accommodations?
- How will attendees prepare for the gathering, if at all?
- Will multiple families congregate after quarantining for 2 weeks or simply arrive?
- At the destination, will people wear masks and socially distance?
- Is an outdoor venue an option?
All of these questions should be considered by patients.
Review high-risk groups
In terms of high-risk groups, we usually focus on underlying medical conditions or extremes of age, but Black and LatinX children and their families have been diagnosed with COVID-19 and hospitalized more frequently than other racial/ ethnic groups in the United States. Of 277,285 school-aged children infected between March 1 and Sept. 19, 2020, 42% were LatinX, 32% White, and 17% Black, yet they comprise 18%, 60%, and 11% of the U.S. population, respectively. Of those hospitalized, 45% were LatinX, 22% White, and 24% Black. LatinX and Black children also have disproportionately higher mortality rates.
Think about transmission and how to mitigate it
Many patients erroneously think combining multiple households for small group gatherings is inconsequential. These types of gatherings serve as a continued source of SARS-CoV-2 spread. For example, a person in Illinois with mild upper respiratory infection symptoms attended a funeral; he reported embracing the family members after the funeral. He dined with two people the evening prior to the funeral, sharing the meal using common serving dishes. Four days later, he attended a birthday party with nine family members. Some of the family members with symptoms subsequently attended church, infecting another church attendee. A cluster of 16 cases of COVID-19 was subsequently identified, including three deaths likely resulting from this one introduction of COVID-19 at these two family gatherings.
In Tennessee and Wisconsin, household transmission of SARS-CoV-2 was studied prospectively. A total of 101 index cases and 191 asymptomatic household contacts were enrolled between April and Sept. 2020; 102 of 191 (53%) had SARS-CoV-2 detected during the 14-day follow-up. Most infections (75%) were identified within 5 days and occurred whether the index case was an adult or child.
Lastly, one adolescent was identified as the source for an outbreak at a family gathering where 15 persons from five households and four states shared a house between 8 and 25 days in July 2020. Six additional members visited the house. The index case had an exposure to COVID-19 and had a negative antigen test 4 days after exposure. She was asymptomatic when tested. She developed nasal congestion 2 days later, the same day she and her family departed for the gathering. A total of 11 household contacts developed confirmed, suspected, or probable COVID-19, and the teen developed symptoms. This report illustrates how easily SARS-CoV-2 is transmitted, and how when implemented, mitigation strategies work because none of the six who only visited the house was infected. It also serves as a reminder that antigen testing is indicated only for use within the first 5-12 days of onset of symptoms. In this case, the adolescent was asymptomatic when tested and had a false-negative test result.
Ponder modes of transportation
How will your patient arrive to their holiday destination? Nonstop travel by car with household members is probably the safest way. However, for many families, buses and trains are the only options, and social distancing may be challenging. Air travel is a must for others. Acquisition of COVID-19 during air travel appears to be low, but not absent based on how air enters and leaves the cabin. The challenge is socially distancing throughout the check in and boarding processes, as well as minimizing contact with common surfaces. There also is loss of social distancing once on board. Ideally, masks should be worn during the flight. Additionally, for those with international destinations, most countries now require a negative polymerase chain reaction COVID-19 test within a specified time frame for entry.
Essentially the safest place for your patients during the holidays is celebrating at home with their household contacts. The risk for disease acquisition increases with travel. You will not have the opportunity to discuss holiday plans with most parents. However, you can encourage them to consider the pros and cons of travel with reminders via telephone, e-mail, and /or social messaging directly from your practices similar to those sent for other medically necessary interventions. As for me, I will be celebrating virtually this year. There is a first time for everything.
For additional information that also is patient friendly, the Centers for Disease Control and Prevention offers information about travel within the United States and international travel.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at [email protected].
As an East Coast transplant residing in Texas, I look forward to the annual sojourn home to celebrate the holidays with family and friends – as do many of our patients and their families. But this is 2020. SARS-CoV-2, the causative agent of COVID-19, is still circulating. To make matters worse, cases are rising in 45 states and internationally. The day of this writing 102,831 new cases were reported in the United States. 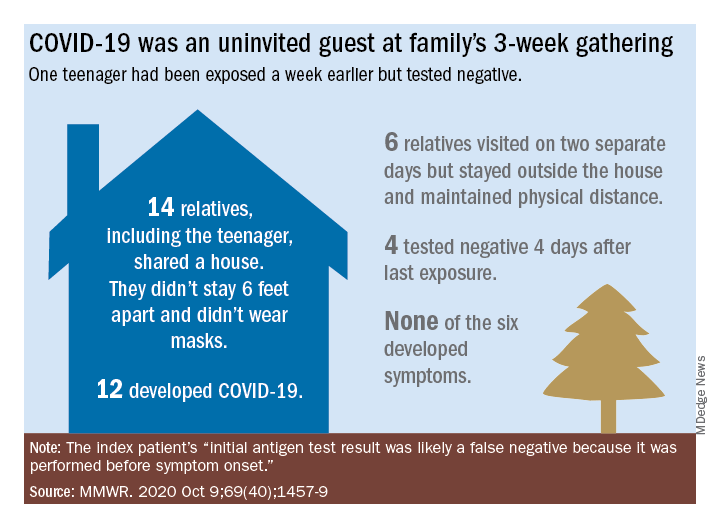
Social distancing, wearing masks, and hand washing have been strategies recommended to help mitigate the spread of the virus. We know adherence is not always 100%. The reality is that several families will consider traveling and gathering with others over the holidays. Their actions may lead to increased infections, hospitalizations, and even deaths. It behooves us to at least remind them of the potential consequences of the activity, and if travel and/or holiday gatherings are inevitable, to provide some guidance to help them look at both the risks and benefits and offer strategies to minimize infection and spread.
What should be considered prior to travel?
Here is a list of points to ponder:
- Is your patient is in a high-risk group for developing severe disease or visiting someone who is in a high-risk group?
- What is their mode of transportation?
- What is their destination?
- How prevalent is the disease at their destination, compared with their community?
- What will be their accommodations?
- How will attendees prepare for the gathering, if at all?
- Will multiple families congregate after quarantining for 2 weeks or simply arrive?
- At the destination, will people wear masks and socially distance?
- Is an outdoor venue an option?
All of these questions should be considered by patients.
Review high-risk groups
In terms of high-risk groups, we usually focus on underlying medical conditions or extremes of age, but Black and LatinX children and their families have been diagnosed with COVID-19 and hospitalized more frequently than other racial/ ethnic groups in the United States. Of 277,285 school-aged children infected between March 1 and Sept. 19, 2020, 42% were LatinX, 32% White, and 17% Black, yet they comprise 18%, 60%, and 11% of the U.S. population, respectively. Of those hospitalized, 45% were LatinX, 22% White, and 24% Black. LatinX and Black children also have disproportionately higher mortality rates.
Think about transmission and how to mitigate it
Many patients erroneously think combining multiple households for small group gatherings is inconsequential. These types of gatherings serve as a continued source of SARS-CoV-2 spread. For example, a person in Illinois with mild upper respiratory infection symptoms attended a funeral; he reported embracing the family members after the funeral. He dined with two people the evening prior to the funeral, sharing the meal using common serving dishes. Four days later, he attended a birthday party with nine family members. Some of the family members with symptoms subsequently attended church, infecting another church attendee. A cluster of 16 cases of COVID-19 was subsequently identified, including three deaths likely resulting from this one introduction of COVID-19 at these two family gatherings.
In Tennessee and Wisconsin, household transmission of SARS-CoV-2 was studied prospectively. A total of 101 index cases and 191 asymptomatic household contacts were enrolled between April and Sept. 2020; 102 of 191 (53%) had SARS-CoV-2 detected during the 14-day follow-up. Most infections (75%) were identified within 5 days and occurred whether the index case was an adult or child.
Lastly, one adolescent was identified as the source for an outbreak at a family gathering where 15 persons from five households and four states shared a house between 8 and 25 days in July 2020. Six additional members visited the house. The index case had an exposure to COVID-19 and had a negative antigen test 4 days after exposure. She was asymptomatic when tested. She developed nasal congestion 2 days later, the same day she and her family departed for the gathering. A total of 11 household contacts developed confirmed, suspected, or probable COVID-19, and the teen developed symptoms. This report illustrates how easily SARS-CoV-2 is transmitted, and how when implemented, mitigation strategies work because none of the six who only visited the house was infected. It also serves as a reminder that antigen testing is indicated only for use within the first 5-12 days of onset of symptoms. In this case, the adolescent was asymptomatic when tested and had a false-negative test result.
Ponder modes of transportation
How will your patient arrive to their holiday destination? Nonstop travel by car with household members is probably the safest way. However, for many families, buses and trains are the only options, and social distancing may be challenging. Air travel is a must for others. Acquisition of COVID-19 during air travel appears to be low, but not absent based on how air enters and leaves the cabin. The challenge is socially distancing throughout the check in and boarding processes, as well as minimizing contact with common surfaces. There also is loss of social distancing once on board. Ideally, masks should be worn during the flight. Additionally, for those with international destinations, most countries now require a negative polymerase chain reaction COVID-19 test within a specified time frame for entry.
Essentially the safest place for your patients during the holidays is celebrating at home with their household contacts. The risk for disease acquisition increases with travel. You will not have the opportunity to discuss holiday plans with most parents. However, you can encourage them to consider the pros and cons of travel with reminders via telephone, e-mail, and /or social messaging directly from your practices similar to those sent for other medically necessary interventions. As for me, I will be celebrating virtually this year. There is a first time for everything.
For additional information that also is patient friendly, the Centers for Disease Control and Prevention offers information about travel within the United States and international travel.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures. Email her at [email protected].
Virtual AHA 2020 may influence template for postpandemic scientific sessions
Cardiologists are already old hands at virtual meetings this year and are fast becoming experts on Zoom and other teleconferencing platforms, if not on how to unmute their microphones.
With expectations perhaps elevated and the new communications genre’s novelty on the wane, the American Heart Association (AHA) Scientific Sessions 2020 has a chance to both innovate with familiar formats and captivate with the field’s latest research findings.
Although the virtual AHA 2020 might not satisfy longings for face-to-face networking, shop talk, or kidding around over coffee, it will feature many traditional elements of the live conferences adapted for ear buds and small screens. They include late-breaking science (LBS) presentations and panel discussions, poster and live oral abstract presentations, meet-the-trialist talks, fireside-chat discussion forums, early career events, and satellite symposia.
The event may well hold lessons for future iterations of AHA Scientific Sessions in the postpandemic world, which some foresee as, potentially, an amalgam of the time-honored live format and a robust, complementary online presence.
“I can’t commit to exactly what AHA sessions will look like next November; I think that’s still being looked at,” the organization’s president-elect Donald M. Lloyd-Jones, MD, ScM, chair of the AHA Committee on Scientific Sessions Programming, told theheart.org | Medscape Cardiology.
There’s no debating that a live conference is valuable “for career networking and other opportunities, so I don’t think we can do without it. That has to be an important part of it,” he said. “When we can safely, of course.”
Still, “the virtual platform democratizes, right? I mean, it just allows greater access for a broader audience, and I think that’s important, too,” said Lloyd-Jones, MD, Northwestern University Feinberg School of Medicine, Chicago.
“I don’t think we’ll ever go completely back to it being all in-person,” he said. “I think the world has changed, and we’ll have to adapt our platforms to recognize that.”
Online, at least, meeting registrants will get a better look at Anthony Fauci, MD, than one might from the middle rows of a vast ballroom-turned-auditorium. Fauci is scheduled to speak on “Public Health and Scientific Challenges” during the Main Event Session “Latest Insights on COVID 19 and Cardiovascular Disease,” slated for the meeting’s final day.
Fauci has directed the National Institute of Allergy and Infectious Diseases (NIAID) since 1984, and has been celebrated for his leadership roles in the battles against AIDS and Ebola virus. Today, his name is close to a household word for his service as a prominent though embattled member of the White House Coronavirus Task Force.
The virtual AHA sessions will feature a core collection of LBS presentations from often high-profile clinical trials and other studies the organization deems worthy of special attention. There are nine such presentations arrayed across the meeting’s five days — from Friday, November 13 to Tuesday, November 17 — at times listed in this story and throughout the AHA Scientific Session program synched with the Central Standard Time (CST) zone of the AHA’s home office in Dallas.
Late-Breaking Science 1. Friday, November 13, 10:30 AM - 11:30 AM CST
The LBS sessions launch with the GALACTIC-HF trial, which — the world recently learned — may expand the burgeoning list of meds shown to improve clinical outcomes in chronic heart failure (HF) with reduced ejection fraction (HFrEF).
In cursory top-line results announced last month, those in the trial of more than 8000 patients who were randomly assigned to receive omecamtiv mecarbil (Amgen/Cytokinetics/Servier) showed a slight but significant benefit for the primary end point of cardiovascular (CV) death or HF events. The hazard ratio (HR), compared with standard care, was 0.92 (95% CI, 0.86 - 0.99; P = .025), noted a press release from Amgen.
Among the announcement’s few other details was a short take on safety outcomes: no difference in risk for “adverse events, including major ischemic cardiac events,” between the active and control groups. The presentation is sure to provide further insights and caveats, if any, along with other information crucial to the study’s interpretation.
Next on the schedule is the closely watched AFFIRM-AHF, billed as the first major outcomes trial of iron administration to iron-deficient patients with acute HF. It randomly assigned more than 1000 such patients to receive IV ferric carboxymaltose or a placebo. The first dose was given in-hospital and subsequent doses at home for 24 weeks or until patients were no longer iron deficient. They were followed to 1 year for the primary end point of recurrent HF hospitalizations or CV death.
The session wraps with the VITAL Rhythm trial, a substudy of the doubly randomized VITAL trial that explored the effects of vitamin D and omega-3 fatty acid supplementation on CV and cancer risk in more than 25,000 patients in the community. The substudy explored the effects of two active therapies, a preparation of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) (Omacor, Reliant Pharmaceuticals) or vitamin D3 supplements, on new-onset atrial fibrillation (AF) as the primary end point; it also looked at risk for sudden death.
Late-Breaking Science 2. Friday, November 13, 12:00 PM - 1:00 PM CST
Dominating the session in two presentations, the (TIPS)-3 trial explored a polypill primary-prevention strategy and daily aspirin with vitamin D supplementation in three separate placebo-controlled comparisons in more than 5700 “intermediate risk” participants 55 years and older, mostly in developing countries.
The daily polypill in this trial is a combination of hydrochlorothiazide 25 mg, atenolol 100 mg, ramipril 10 mg, and simvastatin 40 mg; aspirin was given at 75 mg daily and vitamin D at 60,000 IU monthly.
The participants are followed for a primary end point composed of major CV disease, HF, resuscitated cardiac arrest, or ischemia-driven revascularization for the polypill comparison; CV events or cancer for the aspirin comparison; and fracture risk for the vitamin D component of the trial.
In the Swedish Cardiopulmonary Bioimage Study (SCAPIS), presented third in the session, a random sample of adults from throughout Sweden, projected at about 30,000, underwent a 2-day evaluation for metabolic risk factors plus ultrasound and coronary and lung CT scans. The group has been followed for risks for myocardial infarction (MI), sudden death, and other cardiac diseases; and chronic obstructive pulmonary disease (COPD) and other lung disorders.
Late-Breaking Science 3. Saturday, November 14, 12:00 PM - 1:00 PM CST
The field may learn more mechanistically about MI associated with nonobstructed coronary arteries (MINOCA) than ever before from the Heart Attack Research Program-Imaging Study (HARP). The observational study is enrolling a projected 450 patients with suspected MI and ischemic symptoms who were referred for cardiac catheterization.
Their evaluation includes coronary optical coherence tomographic (OCT) scanning and cardiac magnetic resonance (CMR) imaging for evidence of coronary plaque disruption as the primary end point. The patients are to be followed for 10 years for a composite of death, unstable angina, stroke, recurrent MI, diagnostic or interventional catheterization, and cardiac hospitalization.
The major direct oral anticoagulant (DOAC) comparisons with warfarin in atrial fibrillation (AF) didn’t include many patients with prosthetic valve implants. In contrast, the RIVER trial enrolled 1005 adults with either persistent or paroxysmal AF and bioprosthetic mitral valves and assigned them to rivaroxaban 20 mg or the vitamin K antagonist.
The presentation will include the noninferiority primary outcome of major clinical events, which is stroke, transient ischemic attack (TIA), major bleeding, death from any cause, valve thrombosis, other systemic embolism, or HF hospitalization over 12 months.
This session also includes ALPHEUS, a trial pitting ticagrelor (Brilinta/Brilique, AstraZeneca) against mainstay clopidogrel in a setting that is mostly uncharted for such comparisons, elective percutaneous coronary intervention (PCI).
About 1900 patients with stable coronary disease were randomly assigned to a month of treatment with either agent on top of continuous aspirin. The primary end point is PCI-related MI or myocardial injury within 48 hours of the procedure.
Late-Breaking Science 4. Sunday, November 15, 9:00 AM - 10:00 AM CST
The Self-Assessment Method for Statin Side-effects Or Nocebo (SAMSON) trial may be one of the AHA 2020 frontrunners for early buzz and anticipation. So it’s with some irony that it’s also among the smallest of the LBS studies, at 60 patients, which was nonetheless considered sufficient due to its unusual design.
SAMSON is the latest and perhaps most rigorous attempt to clarify whether symptoms, especially muscle pain or discomfort, attributed to statins by many patients are pharmacologic in origin or, rather, a nocebo effect from negative expectations about statin side effects.
The study patients, all of whom had previously halted statins because of side effects, were assigned to follow three separate regimens, each for month, in a randomized order; they did that four times, for a total of 12 months. The regimens consisted of atorvastatin 20 mg daily, a placebo, or neither.
Patients kept daily logs of any perceived side effects. Parity between side effects experienced on the statin and the placebo would point to a nocebo effect, whereas a significant excess on atorvastatin would suggest they are direct drug effects.
The session also features two randomized trials each on a unique omega-3 fatty acid preparation for either secondary prevention or high-risk primary prevention, in both cases compared with a corn-oil placebo.
The Omega-3 Fatty Acids in Elderly Patients with Myocardial Infarction (OMEMI) trial randomly assigned more than 1000 elderly post-MI patients to take Pikasol (Orkla Care) at 1.8 g EPA and DHA per day or the placebo. It looked for all-cause mortality, nonfatal MI, stroke, revascularization, or hospitalization for new or worsened HF over 24 months.
The STRENGTH trial, with a planned enrollment of about 13,000 high-vascular-risk patients, looked primarily at the effect of daily treatment with Epanova (AstraZeneca), which also contains DHA and EPA, on the composite of CV death, nonfatal MI or stroke, coronary revascularization, and hospitalization for unstable angina. The trial was halted early for low likelihood of benefit, AstraZeneca announced in January of this year.
Late-Breaking Science 5. Sunday, November 15, 7:15 PM - 8:30 PM CST
Slated for the session is the primary analysis of the PIONEER 3 trial, conducted in the United States, Europe, and Japan. It compared the BuMA Supreme biodegradable drug-coated stent (SinoMed) with the durable Xience (Abbott Vascular) and Promus (Boston Scientific) drug-eluting stents. The trial followed more than 1600 patients treated for chronic stable angina or acute coronary syndrome (ACS) for the 1-year composite of cardiac death, target-vessel-related MI, and clinically driven target-lesion revascularization.
Late-Breaking Science 6. Monday, November 16, 9:00 AM - 10:00 AM CST
The EARLY-AF trial enrolled 303 patients with symptomatic paroxysmal or persistent AF suitable for catheter ablation, assigning them to pulmonary vein isolation (PVI) by cryoablation using the Arctic Front (Medtronic) system or antiarrhythmic drug therapy for rhythm control. The primary end point is time to recurrence of AF, atrial flutter, or atrial tachycardia, whether symptomatic or asymptomatic, as determined by implantable loop recorder. Patients will also be followed for symptoms and arrhythmia burden.
Also in the session, the SEARCH-AF study randomized almost 400 patients undergoing cardiac surgery who were engaged subacutely with one of two commercial portable cardiac rhythm monitoring devices (CardioSTAT, Icentia; or SEEQ, Medtronic) or, alternatively, to receive usual postoperative care
The patients, considered to be at high risk for stroke with no history of AF, were followed for the primary end point of cumulative burden of AF or atrial flutter exceeding 6 minutes or documentation of either arrhythmia by 12-lead ECG within 30 days.
Two other studies in the session look at different approaches to AF screening, one using a handheld ECG monitor in the primary care setting and the other wearable monitors in the form of a patch or wristband. The VITAL-AF presentation is titled “Screening for Atrial Fibrillation in Older Adults at Primary Care Visits Using Single Lead Electrocardiograms.” The other presentation, on the study mSToPS, is called “Three-Year Clinical Outcomes in a Nationwide, Randomized, Pragmatic Clinical Trial of Atrial Fibrillation Screening — Mhealth Screening to Prevent Strokes.”
Late-Breaking Science 7. Monday, November 16, 7:00 PM - 8:30 PM CST
In the randomized FIDELIO-DKD trial with more than 5700 patients with type 2 diabetes and associated kidney disease, those assigned to the novel mineralocorticoid receptor antagonist (MRA) finerenone (Bayer) showed an 18% drop in risk for adverse renal events, including death from renal causes (P = .001), over a median of 2.6 years. That primary outcome was previously presented in detail at a nephrology meeting and published in the New England Journal of Medicine in October.
Patients on the MRA showed a similar reduction in a composite CV-event end point, it was also reported at that time. A follow-up presentation at the AHA sessions promises to dive deeper into the trial’s CV outcomes.
In the RAPID-CTCA study, slated next for the session, 1749 patients with suspected or confirmed intermediate-risk ACS were randomly assigned to undergo computed tomographic coronary angiography (CTCA) for guiding treatment decisions or a standard-of-care strategy. It followed patients for the primary end point of death or nonfatal MI over 1 year.
Rilonacept (Arcalyst, Kiniksa/Regeneron) is an interleukin-1α and -1β inhibitor used in several autoinflammatory diseases that went unsuccessfully before regulators for the treatment of gout. The RHAPSODY trial has now explored its use against recurrent pericarditis in a randomized trial that entered 86 patients 12 years and older who had previously experienced at least three episodes.
In top-line results reported to investors in June, patients assigned to receive the drug instead of placebo in weekly injections showed a 96% drop in risk for pericarditis recurrence and “no or minimal pain” on more than 90% of days in the trial. A full presentation is expected during this LBS session.
Also on the schedule is the THALES study, which led the US Food and Drug Administration (FDA) to expand indications for ticagrelor to include stroke prevention in patients with a history of acute ischemic stroke or high-risk TIA based on the trial’s primary results published in July.
In THALES, more than 11,000 patients with mild to moderate acute noncardiogenic ischemic stroke or TIA were randomly assigned within 24 hours to start on daily aspirin with or without ticagrelor given as a 180 mg loading dose followed by 90 mg twice daily for 30 days.
At the end of a month, it was reported, those on dual antiplatelet therapy showed a 17% risk reduction (P = .02) for the primary end point of stroke or death, at the cost of a slight but significant increase in “severe” bleeding (0.5% vs 0.1%; P = .001).
The session is to conclude with two related studies that fell victim in part to the COVID-19 pandemic, both of which explored sotagliflozin (Zynquista, Sanofi/Lexicon), an inhibitor of both sodium-glucose cotransporters 1 and 2 (SGLT1 and SGLT2, respectively) in patients with type 2 diabetes.
SOLOIST-WHF had entered 1222 such patients hospitalized with urgent or worsening HF at 466 centers and randomly assigned them to receive sotagliflozin or placebo; they were followed for the composite of CV death or HF events. SCORED reached an enrollment of 10,584 patients with diabetes and chronic kidney disease at 754 hospitals, following them for the same primary end point.
Lexicon announced in March that the trials would be “closed out early” because of the unavailability of funding “together with uncertainties relating to the COVID-19 pandemic on the trials.” The LBS presentation is expected to include analyses of available data; SOLOIST-WHF launched in summer 2018 and SCORED began in November 2017.
Late-Breaking Science 8. Tuesday, November 17, 9:00 AM - 10:00 AM CST
Most of this LBS session is devoted to the AHA COVID-19 Cardiovascular Disease registry, which is looking at the hospital journey, clinical course, and outcomes of patients hospitalized with SARS-CoV-2 infections at centers participating in the organization’s Get With The Guidelines (GWTG) quality-improvement program. As of September, the registry included data from more than 15,000 patients.
Scheduled presentations include a summary of the registry’s design and initial results; an analysis of racial and ethnic variation in therapy and clinical outcomes; an exploration of how body mass index influenced outcomes, including death, use of mechanical ventilation, and cardiovascular end points, in patients with COVID-19; and a deep dive into the relation between CV disease and clinical outcomes in the cohort.
The last of this LBS block’s five talks will cover the randomized Influenza Vaccine to Effectively Stop Cardio Thoracic Events and Decompensated Heart Failure (INVESTED) trial, which compared vaccination with high-dose trivalent influenza vaccine or a standard-dose quadrivalent vaccine in 5388 adults with a history of hospitalization for either MI or HF. Patients were required to have at least one other CV risk factor, such as older age, reduced left ventricular ejection fraction, or diabetes.
INVESTED tracked the patients at 190 centers across an initial pilot flu season and three subsequent flu seasons for the primary end point of death from any cause or cardiopulmonary hospitalization.
The trial is one of at least three that have been looking at the effect of flu vaccination on cardiovascular outcomes; results from the other two — IAMI, with more than 2500 participants, and RCT-IVVE, with an enrollment of 4871 — are planned for presentation in 2021, theheart.org | Medscape Cardiology recently reported.
Late-Breaking Science 9. Tuesday, November 17, 12:00 PM - 1:00 PM CST
The conference’s concluding LBS session features three studies that relied on technologic strategies for modifying patient compliance and other care behaviors and one that used human-centered design principles to develop a group-care model aimed improving the management of diabetes, hypertension, and other noncommunicable diseases in economically disadvantaged regions of Kenya.
The EPIC-HF trial tested a strategy for improving HFrEF medication-plan engagement by use of a video and documents delivered to patients several times by email or text prior to their follow-up clinic appointments. The strategy was compared with usual care for its effect on HF-medication optimization over 1 month and 1 year in a total of 306 patients.
Following EPIC-HF on the schedule is the MYROAD trial, looking at the efficacy of discharge instructions provided to patients with acute HF as an audio recording that they and their physicians could replay on demand, the idea being to increase adherence to the instructions. The trial’s 1073 patients were assigned to the novel strategy or usual care and followed for HF rehospitalization within 30 days.
MYROAD is to be followed by a presentation entitled “Digital Care Transformation: One-Year Report of >5,000 Patients Enrolled in a Remote Algorithm-Based CV Risk Management Program to Achieve Optimal Lipid and Hypertension Control.”
Rounding out the LBS session: the Bridging Income Generation With Group Integrated Care (BIGPIC) program, a pilot study that developed and executed “a healthcare delivery model targeting health behaviors, medication adherence, and financial barriers to accessing healthcare” in four rural counties in Kenya.
The model features locally developed plans, tailored for regional needs, that are said to “combine the benefits of microfinance with the peer support available through group medical care to enhance management of hypertension and diabetes.” The microfinance component is aimed at improving household economies to alleviate the financial burden of care and clinic attendance, and for the health effects of improved quality of life.
The study randomized 2890 adults with diabetes or prediabetes to one of four groups: usual care plus microfinance group support, group medical visits only or combined with microfinance group support, or usual care only. They were followed for changes in systolic blood pressure and CV-risk score over 12 months.
Lloyd-Jones and Fauci declared no conflicts.
This article first appeared on Medscape.com.
Cardiologists are already old hands at virtual meetings this year and are fast becoming experts on Zoom and other teleconferencing platforms, if not on how to unmute their microphones.
With expectations perhaps elevated and the new communications genre’s novelty on the wane, the American Heart Association (AHA) Scientific Sessions 2020 has a chance to both innovate with familiar formats and captivate with the field’s latest research findings.
Although the virtual AHA 2020 might not satisfy longings for face-to-face networking, shop talk, or kidding around over coffee, it will feature many traditional elements of the live conferences adapted for ear buds and small screens. They include late-breaking science (LBS) presentations and panel discussions, poster and live oral abstract presentations, meet-the-trialist talks, fireside-chat discussion forums, early career events, and satellite symposia.
The event may well hold lessons for future iterations of AHA Scientific Sessions in the postpandemic world, which some foresee as, potentially, an amalgam of the time-honored live format and a robust, complementary online presence.
“I can’t commit to exactly what AHA sessions will look like next November; I think that’s still being looked at,” the organization’s president-elect Donald M. Lloyd-Jones, MD, ScM, chair of the AHA Committee on Scientific Sessions Programming, told theheart.org | Medscape Cardiology.
There’s no debating that a live conference is valuable “for career networking and other opportunities, so I don’t think we can do without it. That has to be an important part of it,” he said. “When we can safely, of course.”
Still, “the virtual platform democratizes, right? I mean, it just allows greater access for a broader audience, and I think that’s important, too,” said Lloyd-Jones, MD, Northwestern University Feinberg School of Medicine, Chicago.
“I don’t think we’ll ever go completely back to it being all in-person,” he said. “I think the world has changed, and we’ll have to adapt our platforms to recognize that.”
Online, at least, meeting registrants will get a better look at Anthony Fauci, MD, than one might from the middle rows of a vast ballroom-turned-auditorium. Fauci is scheduled to speak on “Public Health and Scientific Challenges” during the Main Event Session “Latest Insights on COVID 19 and Cardiovascular Disease,” slated for the meeting’s final day.
Fauci has directed the National Institute of Allergy and Infectious Diseases (NIAID) since 1984, and has been celebrated for his leadership roles in the battles against AIDS and Ebola virus. Today, his name is close to a household word for his service as a prominent though embattled member of the White House Coronavirus Task Force.
The virtual AHA sessions will feature a core collection of LBS presentations from often high-profile clinical trials and other studies the organization deems worthy of special attention. There are nine such presentations arrayed across the meeting’s five days — from Friday, November 13 to Tuesday, November 17 — at times listed in this story and throughout the AHA Scientific Session program synched with the Central Standard Time (CST) zone of the AHA’s home office in Dallas.
Late-Breaking Science 1. Friday, November 13, 10:30 AM - 11:30 AM CST
The LBS sessions launch with the GALACTIC-HF trial, which — the world recently learned — may expand the burgeoning list of meds shown to improve clinical outcomes in chronic heart failure (HF) with reduced ejection fraction (HFrEF).
In cursory top-line results announced last month, those in the trial of more than 8000 patients who were randomly assigned to receive omecamtiv mecarbil (Amgen/Cytokinetics/Servier) showed a slight but significant benefit for the primary end point of cardiovascular (CV) death or HF events. The hazard ratio (HR), compared with standard care, was 0.92 (95% CI, 0.86 - 0.99; P = .025), noted a press release from Amgen.
Among the announcement’s few other details was a short take on safety outcomes: no difference in risk for “adverse events, including major ischemic cardiac events,” between the active and control groups. The presentation is sure to provide further insights and caveats, if any, along with other information crucial to the study’s interpretation.
Next on the schedule is the closely watched AFFIRM-AHF, billed as the first major outcomes trial of iron administration to iron-deficient patients with acute HF. It randomly assigned more than 1000 such patients to receive IV ferric carboxymaltose or a placebo. The first dose was given in-hospital and subsequent doses at home for 24 weeks or until patients were no longer iron deficient. They were followed to 1 year for the primary end point of recurrent HF hospitalizations or CV death.
The session wraps with the VITAL Rhythm trial, a substudy of the doubly randomized VITAL trial that explored the effects of vitamin D and omega-3 fatty acid supplementation on CV and cancer risk in more than 25,000 patients in the community. The substudy explored the effects of two active therapies, a preparation of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) (Omacor, Reliant Pharmaceuticals) or vitamin D3 supplements, on new-onset atrial fibrillation (AF) as the primary end point; it also looked at risk for sudden death.
Late-Breaking Science 2. Friday, November 13, 12:00 PM - 1:00 PM CST
Dominating the session in two presentations, the (TIPS)-3 trial explored a polypill primary-prevention strategy and daily aspirin with vitamin D supplementation in three separate placebo-controlled comparisons in more than 5700 “intermediate risk” participants 55 years and older, mostly in developing countries.
The daily polypill in this trial is a combination of hydrochlorothiazide 25 mg, atenolol 100 mg, ramipril 10 mg, and simvastatin 40 mg; aspirin was given at 75 mg daily and vitamin D at 60,000 IU monthly.
The participants are followed for a primary end point composed of major CV disease, HF, resuscitated cardiac arrest, or ischemia-driven revascularization for the polypill comparison; CV events or cancer for the aspirin comparison; and fracture risk for the vitamin D component of the trial.
In the Swedish Cardiopulmonary Bioimage Study (SCAPIS), presented third in the session, a random sample of adults from throughout Sweden, projected at about 30,000, underwent a 2-day evaluation for metabolic risk factors plus ultrasound and coronary and lung CT scans. The group has been followed for risks for myocardial infarction (MI), sudden death, and other cardiac diseases; and chronic obstructive pulmonary disease (COPD) and other lung disorders.
Late-Breaking Science 3. Saturday, November 14, 12:00 PM - 1:00 PM CST
The field may learn more mechanistically about MI associated with nonobstructed coronary arteries (MINOCA) than ever before from the Heart Attack Research Program-Imaging Study (HARP). The observational study is enrolling a projected 450 patients with suspected MI and ischemic symptoms who were referred for cardiac catheterization.
Their evaluation includes coronary optical coherence tomographic (OCT) scanning and cardiac magnetic resonance (CMR) imaging for evidence of coronary plaque disruption as the primary end point. The patients are to be followed for 10 years for a composite of death, unstable angina, stroke, recurrent MI, diagnostic or interventional catheterization, and cardiac hospitalization.
The major direct oral anticoagulant (DOAC) comparisons with warfarin in atrial fibrillation (AF) didn’t include many patients with prosthetic valve implants. In contrast, the RIVER trial enrolled 1005 adults with either persistent or paroxysmal AF and bioprosthetic mitral valves and assigned them to rivaroxaban 20 mg or the vitamin K antagonist.
The presentation will include the noninferiority primary outcome of major clinical events, which is stroke, transient ischemic attack (TIA), major bleeding, death from any cause, valve thrombosis, other systemic embolism, or HF hospitalization over 12 months.
This session also includes ALPHEUS, a trial pitting ticagrelor (Brilinta/Brilique, AstraZeneca) against mainstay clopidogrel in a setting that is mostly uncharted for such comparisons, elective percutaneous coronary intervention (PCI).
About 1900 patients with stable coronary disease were randomly assigned to a month of treatment with either agent on top of continuous aspirin. The primary end point is PCI-related MI or myocardial injury within 48 hours of the procedure.
Late-Breaking Science 4. Sunday, November 15, 9:00 AM - 10:00 AM CST
The Self-Assessment Method for Statin Side-effects Or Nocebo (SAMSON) trial may be one of the AHA 2020 frontrunners for early buzz and anticipation. So it’s with some irony that it’s also among the smallest of the LBS studies, at 60 patients, which was nonetheless considered sufficient due to its unusual design.
SAMSON is the latest and perhaps most rigorous attempt to clarify whether symptoms, especially muscle pain or discomfort, attributed to statins by many patients are pharmacologic in origin or, rather, a nocebo effect from negative expectations about statin side effects.
The study patients, all of whom had previously halted statins because of side effects, were assigned to follow three separate regimens, each for month, in a randomized order; they did that four times, for a total of 12 months. The regimens consisted of atorvastatin 20 mg daily, a placebo, or neither.
Patients kept daily logs of any perceived side effects. Parity between side effects experienced on the statin and the placebo would point to a nocebo effect, whereas a significant excess on atorvastatin would suggest they are direct drug effects.
The session also features two randomized trials each on a unique omega-3 fatty acid preparation for either secondary prevention or high-risk primary prevention, in both cases compared with a corn-oil placebo.
The Omega-3 Fatty Acids in Elderly Patients with Myocardial Infarction (OMEMI) trial randomly assigned more than 1000 elderly post-MI patients to take Pikasol (Orkla Care) at 1.8 g EPA and DHA per day or the placebo. It looked for all-cause mortality, nonfatal MI, stroke, revascularization, or hospitalization for new or worsened HF over 24 months.
The STRENGTH trial, with a planned enrollment of about 13,000 high-vascular-risk patients, looked primarily at the effect of daily treatment with Epanova (AstraZeneca), which also contains DHA and EPA, on the composite of CV death, nonfatal MI or stroke, coronary revascularization, and hospitalization for unstable angina. The trial was halted early for low likelihood of benefit, AstraZeneca announced in January of this year.
Late-Breaking Science 5. Sunday, November 15, 7:15 PM - 8:30 PM CST
Slated for the session is the primary analysis of the PIONEER 3 trial, conducted in the United States, Europe, and Japan. It compared the BuMA Supreme biodegradable drug-coated stent (SinoMed) with the durable Xience (Abbott Vascular) and Promus (Boston Scientific) drug-eluting stents. The trial followed more than 1600 patients treated for chronic stable angina or acute coronary syndrome (ACS) for the 1-year composite of cardiac death, target-vessel-related MI, and clinically driven target-lesion revascularization.
Late-Breaking Science 6. Monday, November 16, 9:00 AM - 10:00 AM CST
The EARLY-AF trial enrolled 303 patients with symptomatic paroxysmal or persistent AF suitable for catheter ablation, assigning them to pulmonary vein isolation (PVI) by cryoablation using the Arctic Front (Medtronic) system or antiarrhythmic drug therapy for rhythm control. The primary end point is time to recurrence of AF, atrial flutter, or atrial tachycardia, whether symptomatic or asymptomatic, as determined by implantable loop recorder. Patients will also be followed for symptoms and arrhythmia burden.
Also in the session, the SEARCH-AF study randomized almost 400 patients undergoing cardiac surgery who were engaged subacutely with one of two commercial portable cardiac rhythm monitoring devices (CardioSTAT, Icentia; or SEEQ, Medtronic) or, alternatively, to receive usual postoperative care
The patients, considered to be at high risk for stroke with no history of AF, were followed for the primary end point of cumulative burden of AF or atrial flutter exceeding 6 minutes or documentation of either arrhythmia by 12-lead ECG within 30 days.
Two other studies in the session look at different approaches to AF screening, one using a handheld ECG monitor in the primary care setting and the other wearable monitors in the form of a patch or wristband. The VITAL-AF presentation is titled “Screening for Atrial Fibrillation in Older Adults at Primary Care Visits Using Single Lead Electrocardiograms.” The other presentation, on the study mSToPS, is called “Three-Year Clinical Outcomes in a Nationwide, Randomized, Pragmatic Clinical Trial of Atrial Fibrillation Screening — Mhealth Screening to Prevent Strokes.”
Late-Breaking Science 7. Monday, November 16, 7:00 PM - 8:30 PM CST
In the randomized FIDELIO-DKD trial with more than 5700 patients with type 2 diabetes and associated kidney disease, those assigned to the novel mineralocorticoid receptor antagonist (MRA) finerenone (Bayer) showed an 18% drop in risk for adverse renal events, including death from renal causes (P = .001), over a median of 2.6 years. That primary outcome was previously presented in detail at a nephrology meeting and published in the New England Journal of Medicine in October.
Patients on the MRA showed a similar reduction in a composite CV-event end point, it was also reported at that time. A follow-up presentation at the AHA sessions promises to dive deeper into the trial’s CV outcomes.
In the RAPID-CTCA study, slated next for the session, 1749 patients with suspected or confirmed intermediate-risk ACS were randomly assigned to undergo computed tomographic coronary angiography (CTCA) for guiding treatment decisions or a standard-of-care strategy. It followed patients for the primary end point of death or nonfatal MI over 1 year.
Rilonacept (Arcalyst, Kiniksa/Regeneron) is an interleukin-1α and -1β inhibitor used in several autoinflammatory diseases that went unsuccessfully before regulators for the treatment of gout. The RHAPSODY trial has now explored its use against recurrent pericarditis in a randomized trial that entered 86 patients 12 years and older who had previously experienced at least three episodes.
In top-line results reported to investors in June, patients assigned to receive the drug instead of placebo in weekly injections showed a 96% drop in risk for pericarditis recurrence and “no or minimal pain” on more than 90% of days in the trial. A full presentation is expected during this LBS session.
Also on the schedule is the THALES study, which led the US Food and Drug Administration (FDA) to expand indications for ticagrelor to include stroke prevention in patients with a history of acute ischemic stroke or high-risk TIA based on the trial’s primary results published in July.
In THALES, more than 11,000 patients with mild to moderate acute noncardiogenic ischemic stroke or TIA were randomly assigned within 24 hours to start on daily aspirin with or without ticagrelor given as a 180 mg loading dose followed by 90 mg twice daily for 30 days.
At the end of a month, it was reported, those on dual antiplatelet therapy showed a 17% risk reduction (P = .02) for the primary end point of stroke or death, at the cost of a slight but significant increase in “severe” bleeding (0.5% vs 0.1%; P = .001).
The session is to conclude with two related studies that fell victim in part to the COVID-19 pandemic, both of which explored sotagliflozin (Zynquista, Sanofi/Lexicon), an inhibitor of both sodium-glucose cotransporters 1 and 2 (SGLT1 and SGLT2, respectively) in patients with type 2 diabetes.
SOLOIST-WHF had entered 1222 such patients hospitalized with urgent or worsening HF at 466 centers and randomly assigned them to receive sotagliflozin or placebo; they were followed for the composite of CV death or HF events. SCORED reached an enrollment of 10,584 patients with diabetes and chronic kidney disease at 754 hospitals, following them for the same primary end point.
Lexicon announced in March that the trials would be “closed out early” because of the unavailability of funding “together with uncertainties relating to the COVID-19 pandemic on the trials.” The LBS presentation is expected to include analyses of available data; SOLOIST-WHF launched in summer 2018 and SCORED began in November 2017.
Late-Breaking Science 8. Tuesday, November 17, 9:00 AM - 10:00 AM CST
Most of this LBS session is devoted to the AHA COVID-19 Cardiovascular Disease registry, which is looking at the hospital journey, clinical course, and outcomes of patients hospitalized with SARS-CoV-2 infections at centers participating in the organization’s Get With The Guidelines (GWTG) quality-improvement program. As of September, the registry included data from more than 15,000 patients.
Scheduled presentations include a summary of the registry’s design and initial results; an analysis of racial and ethnic variation in therapy and clinical outcomes; an exploration of how body mass index influenced outcomes, including death, use of mechanical ventilation, and cardiovascular end points, in patients with COVID-19; and a deep dive into the relation between CV disease and clinical outcomes in the cohort.
The last of this LBS block’s five talks will cover the randomized Influenza Vaccine to Effectively Stop Cardio Thoracic Events and Decompensated Heart Failure (INVESTED) trial, which compared vaccination with high-dose trivalent influenza vaccine or a standard-dose quadrivalent vaccine in 5388 adults with a history of hospitalization for either MI or HF. Patients were required to have at least one other CV risk factor, such as older age, reduced left ventricular ejection fraction, or diabetes.
INVESTED tracked the patients at 190 centers across an initial pilot flu season and three subsequent flu seasons for the primary end point of death from any cause or cardiopulmonary hospitalization.
The trial is one of at least three that have been looking at the effect of flu vaccination on cardiovascular outcomes; results from the other two — IAMI, with more than 2500 participants, and RCT-IVVE, with an enrollment of 4871 — are planned for presentation in 2021, theheart.org | Medscape Cardiology recently reported.
Late-Breaking Science 9. Tuesday, November 17, 12:00 PM - 1:00 PM CST
The conference’s concluding LBS session features three studies that relied on technologic strategies for modifying patient compliance and other care behaviors and one that used human-centered design principles to develop a group-care model aimed improving the management of diabetes, hypertension, and other noncommunicable diseases in economically disadvantaged regions of Kenya.
The EPIC-HF trial tested a strategy for improving HFrEF medication-plan engagement by use of a video and documents delivered to patients several times by email or text prior to their follow-up clinic appointments. The strategy was compared with usual care for its effect on HF-medication optimization over 1 month and 1 year in a total of 306 patients.
Following EPIC-HF on the schedule is the MYROAD trial, looking at the efficacy of discharge instructions provided to patients with acute HF as an audio recording that they and their physicians could replay on demand, the idea being to increase adherence to the instructions. The trial’s 1073 patients were assigned to the novel strategy or usual care and followed for HF rehospitalization within 30 days.
MYROAD is to be followed by a presentation entitled “Digital Care Transformation: One-Year Report of >5,000 Patients Enrolled in a Remote Algorithm-Based CV Risk Management Program to Achieve Optimal Lipid and Hypertension Control.”
Rounding out the LBS session: the Bridging Income Generation With Group Integrated Care (BIGPIC) program, a pilot study that developed and executed “a healthcare delivery model targeting health behaviors, medication adherence, and financial barriers to accessing healthcare” in four rural counties in Kenya.
The model features locally developed plans, tailored for regional needs, that are said to “combine the benefits of microfinance with the peer support available through group medical care to enhance management of hypertension and diabetes.” The microfinance component is aimed at improving household economies to alleviate the financial burden of care and clinic attendance, and for the health effects of improved quality of life.
The study randomized 2890 adults with diabetes or prediabetes to one of four groups: usual care plus microfinance group support, group medical visits only or combined with microfinance group support, or usual care only. They were followed for changes in systolic blood pressure and CV-risk score over 12 months.
Lloyd-Jones and Fauci declared no conflicts.
This article first appeared on Medscape.com.
Cardiologists are already old hands at virtual meetings this year and are fast becoming experts on Zoom and other teleconferencing platforms, if not on how to unmute their microphones.
With expectations perhaps elevated and the new communications genre’s novelty on the wane, the American Heart Association (AHA) Scientific Sessions 2020 has a chance to both innovate with familiar formats and captivate with the field’s latest research findings.
Although the virtual AHA 2020 might not satisfy longings for face-to-face networking, shop talk, or kidding around over coffee, it will feature many traditional elements of the live conferences adapted for ear buds and small screens. They include late-breaking science (LBS) presentations and panel discussions, poster and live oral abstract presentations, meet-the-trialist talks, fireside-chat discussion forums, early career events, and satellite symposia.
The event may well hold lessons for future iterations of AHA Scientific Sessions in the postpandemic world, which some foresee as, potentially, an amalgam of the time-honored live format and a robust, complementary online presence.
“I can’t commit to exactly what AHA sessions will look like next November; I think that’s still being looked at,” the organization’s president-elect Donald M. Lloyd-Jones, MD, ScM, chair of the AHA Committee on Scientific Sessions Programming, told theheart.org | Medscape Cardiology.
There’s no debating that a live conference is valuable “for career networking and other opportunities, so I don’t think we can do without it. That has to be an important part of it,” he said. “When we can safely, of course.”
Still, “the virtual platform democratizes, right? I mean, it just allows greater access for a broader audience, and I think that’s important, too,” said Lloyd-Jones, MD, Northwestern University Feinberg School of Medicine, Chicago.
“I don’t think we’ll ever go completely back to it being all in-person,” he said. “I think the world has changed, and we’ll have to adapt our platforms to recognize that.”
Online, at least, meeting registrants will get a better look at Anthony Fauci, MD, than one might from the middle rows of a vast ballroom-turned-auditorium. Fauci is scheduled to speak on “Public Health and Scientific Challenges” during the Main Event Session “Latest Insights on COVID 19 and Cardiovascular Disease,” slated for the meeting’s final day.
Fauci has directed the National Institute of Allergy and Infectious Diseases (NIAID) since 1984, and has been celebrated for his leadership roles in the battles against AIDS and Ebola virus. Today, his name is close to a household word for his service as a prominent though embattled member of the White House Coronavirus Task Force.
The virtual AHA sessions will feature a core collection of LBS presentations from often high-profile clinical trials and other studies the organization deems worthy of special attention. There are nine such presentations arrayed across the meeting’s five days — from Friday, November 13 to Tuesday, November 17 — at times listed in this story and throughout the AHA Scientific Session program synched with the Central Standard Time (CST) zone of the AHA’s home office in Dallas.
Late-Breaking Science 1. Friday, November 13, 10:30 AM - 11:30 AM CST
The LBS sessions launch with the GALACTIC-HF trial, which — the world recently learned — may expand the burgeoning list of meds shown to improve clinical outcomes in chronic heart failure (HF) with reduced ejection fraction (HFrEF).
In cursory top-line results announced last month, those in the trial of more than 8000 patients who were randomly assigned to receive omecamtiv mecarbil (Amgen/Cytokinetics/Servier) showed a slight but significant benefit for the primary end point of cardiovascular (CV) death or HF events. The hazard ratio (HR), compared with standard care, was 0.92 (95% CI, 0.86 - 0.99; P = .025), noted a press release from Amgen.
Among the announcement’s few other details was a short take on safety outcomes: no difference in risk for “adverse events, including major ischemic cardiac events,” between the active and control groups. The presentation is sure to provide further insights and caveats, if any, along with other information crucial to the study’s interpretation.
Next on the schedule is the closely watched AFFIRM-AHF, billed as the first major outcomes trial of iron administration to iron-deficient patients with acute HF. It randomly assigned more than 1000 such patients to receive IV ferric carboxymaltose or a placebo. The first dose was given in-hospital and subsequent doses at home for 24 weeks or until patients were no longer iron deficient. They were followed to 1 year for the primary end point of recurrent HF hospitalizations or CV death.
The session wraps with the VITAL Rhythm trial, a substudy of the doubly randomized VITAL trial that explored the effects of vitamin D and omega-3 fatty acid supplementation on CV and cancer risk in more than 25,000 patients in the community. The substudy explored the effects of two active therapies, a preparation of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) (Omacor, Reliant Pharmaceuticals) or vitamin D3 supplements, on new-onset atrial fibrillation (AF) as the primary end point; it also looked at risk for sudden death.
Late-Breaking Science 2. Friday, November 13, 12:00 PM - 1:00 PM CST
Dominating the session in two presentations, the (TIPS)-3 trial explored a polypill primary-prevention strategy and daily aspirin with vitamin D supplementation in three separate placebo-controlled comparisons in more than 5700 “intermediate risk” participants 55 years and older, mostly in developing countries.
The daily polypill in this trial is a combination of hydrochlorothiazide 25 mg, atenolol 100 mg, ramipril 10 mg, and simvastatin 40 mg; aspirin was given at 75 mg daily and vitamin D at 60,000 IU monthly.
The participants are followed for a primary end point composed of major CV disease, HF, resuscitated cardiac arrest, or ischemia-driven revascularization for the polypill comparison; CV events or cancer for the aspirin comparison; and fracture risk for the vitamin D component of the trial.
In the Swedish Cardiopulmonary Bioimage Study (SCAPIS), presented third in the session, a random sample of adults from throughout Sweden, projected at about 30,000, underwent a 2-day evaluation for metabolic risk factors plus ultrasound and coronary and lung CT scans. The group has been followed for risks for myocardial infarction (MI), sudden death, and other cardiac diseases; and chronic obstructive pulmonary disease (COPD) and other lung disorders.
Late-Breaking Science 3. Saturday, November 14, 12:00 PM - 1:00 PM CST
The field may learn more mechanistically about MI associated with nonobstructed coronary arteries (MINOCA) than ever before from the Heart Attack Research Program-Imaging Study (HARP). The observational study is enrolling a projected 450 patients with suspected MI and ischemic symptoms who were referred for cardiac catheterization.
Their evaluation includes coronary optical coherence tomographic (OCT) scanning and cardiac magnetic resonance (CMR) imaging for evidence of coronary plaque disruption as the primary end point. The patients are to be followed for 10 years for a composite of death, unstable angina, stroke, recurrent MI, diagnostic or interventional catheterization, and cardiac hospitalization.
The major direct oral anticoagulant (DOAC) comparisons with warfarin in atrial fibrillation (AF) didn’t include many patients with prosthetic valve implants. In contrast, the RIVER trial enrolled 1005 adults with either persistent or paroxysmal AF and bioprosthetic mitral valves and assigned them to rivaroxaban 20 mg or the vitamin K antagonist.
The presentation will include the noninferiority primary outcome of major clinical events, which is stroke, transient ischemic attack (TIA), major bleeding, death from any cause, valve thrombosis, other systemic embolism, or HF hospitalization over 12 months.
This session also includes ALPHEUS, a trial pitting ticagrelor (Brilinta/Brilique, AstraZeneca) against mainstay clopidogrel in a setting that is mostly uncharted for such comparisons, elective percutaneous coronary intervention (PCI).
About 1900 patients with stable coronary disease were randomly assigned to a month of treatment with either agent on top of continuous aspirin. The primary end point is PCI-related MI or myocardial injury within 48 hours of the procedure.
Late-Breaking Science 4. Sunday, November 15, 9:00 AM - 10:00 AM CST
The Self-Assessment Method for Statin Side-effects Or Nocebo (SAMSON) trial may be one of the AHA 2020 frontrunners for early buzz and anticipation. So it’s with some irony that it’s also among the smallest of the LBS studies, at 60 patients, which was nonetheless considered sufficient due to its unusual design.
SAMSON is the latest and perhaps most rigorous attempt to clarify whether symptoms, especially muscle pain or discomfort, attributed to statins by many patients are pharmacologic in origin or, rather, a nocebo effect from negative expectations about statin side effects.
The study patients, all of whom had previously halted statins because of side effects, were assigned to follow three separate regimens, each for month, in a randomized order; they did that four times, for a total of 12 months. The regimens consisted of atorvastatin 20 mg daily, a placebo, or neither.
Patients kept daily logs of any perceived side effects. Parity between side effects experienced on the statin and the placebo would point to a nocebo effect, whereas a significant excess on atorvastatin would suggest they are direct drug effects.
The session also features two randomized trials each on a unique omega-3 fatty acid preparation for either secondary prevention or high-risk primary prevention, in both cases compared with a corn-oil placebo.
The Omega-3 Fatty Acids in Elderly Patients with Myocardial Infarction (OMEMI) trial randomly assigned more than 1000 elderly post-MI patients to take Pikasol (Orkla Care) at 1.8 g EPA and DHA per day or the placebo. It looked for all-cause mortality, nonfatal MI, stroke, revascularization, or hospitalization for new or worsened HF over 24 months.
The STRENGTH trial, with a planned enrollment of about 13,000 high-vascular-risk patients, looked primarily at the effect of daily treatment with Epanova (AstraZeneca), which also contains DHA and EPA, on the composite of CV death, nonfatal MI or stroke, coronary revascularization, and hospitalization for unstable angina. The trial was halted early for low likelihood of benefit, AstraZeneca announced in January of this year.
Late-Breaking Science 5. Sunday, November 15, 7:15 PM - 8:30 PM CST
Slated for the session is the primary analysis of the PIONEER 3 trial, conducted in the United States, Europe, and Japan. It compared the BuMA Supreme biodegradable drug-coated stent (SinoMed) with the durable Xience (Abbott Vascular) and Promus (Boston Scientific) drug-eluting stents. The trial followed more than 1600 patients treated for chronic stable angina or acute coronary syndrome (ACS) for the 1-year composite of cardiac death, target-vessel-related MI, and clinically driven target-lesion revascularization.
Late-Breaking Science 6. Monday, November 16, 9:00 AM - 10:00 AM CST
The EARLY-AF trial enrolled 303 patients with symptomatic paroxysmal or persistent AF suitable for catheter ablation, assigning them to pulmonary vein isolation (PVI) by cryoablation using the Arctic Front (Medtronic) system or antiarrhythmic drug therapy for rhythm control. The primary end point is time to recurrence of AF, atrial flutter, or atrial tachycardia, whether symptomatic or asymptomatic, as determined by implantable loop recorder. Patients will also be followed for symptoms and arrhythmia burden.
Also in the session, the SEARCH-AF study randomized almost 400 patients undergoing cardiac surgery who were engaged subacutely with one of two commercial portable cardiac rhythm monitoring devices (CardioSTAT, Icentia; or SEEQ, Medtronic) or, alternatively, to receive usual postoperative care
The patients, considered to be at high risk for stroke with no history of AF, were followed for the primary end point of cumulative burden of AF or atrial flutter exceeding 6 minutes or documentation of either arrhythmia by 12-lead ECG within 30 days.
Two other studies in the session look at different approaches to AF screening, one using a handheld ECG monitor in the primary care setting and the other wearable monitors in the form of a patch or wristband. The VITAL-AF presentation is titled “Screening for Atrial Fibrillation in Older Adults at Primary Care Visits Using Single Lead Electrocardiograms.” The other presentation, on the study mSToPS, is called “Three-Year Clinical Outcomes in a Nationwide, Randomized, Pragmatic Clinical Trial of Atrial Fibrillation Screening — Mhealth Screening to Prevent Strokes.”
Late-Breaking Science 7. Monday, November 16, 7:00 PM - 8:30 PM CST
In the randomized FIDELIO-DKD trial with more than 5700 patients with type 2 diabetes and associated kidney disease, those assigned to the novel mineralocorticoid receptor antagonist (MRA) finerenone (Bayer) showed an 18% drop in risk for adverse renal events, including death from renal causes (P = .001), over a median of 2.6 years. That primary outcome was previously presented in detail at a nephrology meeting and published in the New England Journal of Medicine in October.
Patients on the MRA showed a similar reduction in a composite CV-event end point, it was also reported at that time. A follow-up presentation at the AHA sessions promises to dive deeper into the trial’s CV outcomes.
In the RAPID-CTCA study, slated next for the session, 1749 patients with suspected or confirmed intermediate-risk ACS were randomly assigned to undergo computed tomographic coronary angiography (CTCA) for guiding treatment decisions or a standard-of-care strategy. It followed patients for the primary end point of death or nonfatal MI over 1 year.
Rilonacept (Arcalyst, Kiniksa/Regeneron) is an interleukin-1α and -1β inhibitor used in several autoinflammatory diseases that went unsuccessfully before regulators for the treatment of gout. The RHAPSODY trial has now explored its use against recurrent pericarditis in a randomized trial that entered 86 patients 12 years and older who had previously experienced at least three episodes.
In top-line results reported to investors in June, patients assigned to receive the drug instead of placebo in weekly injections showed a 96% drop in risk for pericarditis recurrence and “no or minimal pain” on more than 90% of days in the trial. A full presentation is expected during this LBS session.
Also on the schedule is the THALES study, which led the US Food and Drug Administration (FDA) to expand indications for ticagrelor to include stroke prevention in patients with a history of acute ischemic stroke or high-risk TIA based on the trial’s primary results published in July.
In THALES, more than 11,000 patients with mild to moderate acute noncardiogenic ischemic stroke or TIA were randomly assigned within 24 hours to start on daily aspirin with or without ticagrelor given as a 180 mg loading dose followed by 90 mg twice daily for 30 days.
At the end of a month, it was reported, those on dual antiplatelet therapy showed a 17% risk reduction (P = .02) for the primary end point of stroke or death, at the cost of a slight but significant increase in “severe” bleeding (0.5% vs 0.1%; P = .001).
The session is to conclude with two related studies that fell victim in part to the COVID-19 pandemic, both of which explored sotagliflozin (Zynquista, Sanofi/Lexicon), an inhibitor of both sodium-glucose cotransporters 1 and 2 (SGLT1 and SGLT2, respectively) in patients with type 2 diabetes.
SOLOIST-WHF had entered 1222 such patients hospitalized with urgent or worsening HF at 466 centers and randomly assigned them to receive sotagliflozin or placebo; they were followed for the composite of CV death or HF events. SCORED reached an enrollment of 10,584 patients with diabetes and chronic kidney disease at 754 hospitals, following them for the same primary end point.
Lexicon announced in March that the trials would be “closed out early” because of the unavailability of funding “together with uncertainties relating to the COVID-19 pandemic on the trials.” The LBS presentation is expected to include analyses of available data; SOLOIST-WHF launched in summer 2018 and SCORED began in November 2017.
Late-Breaking Science 8. Tuesday, November 17, 9:00 AM - 10:00 AM CST
Most of this LBS session is devoted to the AHA COVID-19 Cardiovascular Disease registry, which is looking at the hospital journey, clinical course, and outcomes of patients hospitalized with SARS-CoV-2 infections at centers participating in the organization’s Get With The Guidelines (GWTG) quality-improvement program. As of September, the registry included data from more than 15,000 patients.
Scheduled presentations include a summary of the registry’s design and initial results; an analysis of racial and ethnic variation in therapy and clinical outcomes; an exploration of how body mass index influenced outcomes, including death, use of mechanical ventilation, and cardiovascular end points, in patients with COVID-19; and a deep dive into the relation between CV disease and clinical outcomes in the cohort.
The last of this LBS block’s five talks will cover the randomized Influenza Vaccine to Effectively Stop Cardio Thoracic Events and Decompensated Heart Failure (INVESTED) trial, which compared vaccination with high-dose trivalent influenza vaccine or a standard-dose quadrivalent vaccine in 5388 adults with a history of hospitalization for either MI or HF. Patients were required to have at least one other CV risk factor, such as older age, reduced left ventricular ejection fraction, or diabetes.
INVESTED tracked the patients at 190 centers across an initial pilot flu season and three subsequent flu seasons for the primary end point of death from any cause or cardiopulmonary hospitalization.
The trial is one of at least three that have been looking at the effect of flu vaccination on cardiovascular outcomes; results from the other two — IAMI, with more than 2500 participants, and RCT-IVVE, with an enrollment of 4871 — are planned for presentation in 2021, theheart.org | Medscape Cardiology recently reported.
Late-Breaking Science 9. Tuesday, November 17, 12:00 PM - 1:00 PM CST
The conference’s concluding LBS session features three studies that relied on technologic strategies for modifying patient compliance and other care behaviors and one that used human-centered design principles to develop a group-care model aimed improving the management of diabetes, hypertension, and other noncommunicable diseases in economically disadvantaged regions of Kenya.
The EPIC-HF trial tested a strategy for improving HFrEF medication-plan engagement by use of a video and documents delivered to patients several times by email or text prior to their follow-up clinic appointments. The strategy was compared with usual care for its effect on HF-medication optimization over 1 month and 1 year in a total of 306 patients.
Following EPIC-HF on the schedule is the MYROAD trial, looking at the efficacy of discharge instructions provided to patients with acute HF as an audio recording that they and their physicians could replay on demand, the idea being to increase adherence to the instructions. The trial’s 1073 patients were assigned to the novel strategy or usual care and followed for HF rehospitalization within 30 days.
MYROAD is to be followed by a presentation entitled “Digital Care Transformation: One-Year Report of >5,000 Patients Enrolled in a Remote Algorithm-Based CV Risk Management Program to Achieve Optimal Lipid and Hypertension Control.”
Rounding out the LBS session: the Bridging Income Generation With Group Integrated Care (BIGPIC) program, a pilot study that developed and executed “a healthcare delivery model targeting health behaviors, medication adherence, and financial barriers to accessing healthcare” in four rural counties in Kenya.
The model features locally developed plans, tailored for regional needs, that are said to “combine the benefits of microfinance with the peer support available through group medical care to enhance management of hypertension and diabetes.” The microfinance component is aimed at improving household economies to alleviate the financial burden of care and clinic attendance, and for the health effects of improved quality of life.
The study randomized 2890 adults with diabetes or prediabetes to one of four groups: usual care plus microfinance group support, group medical visits only or combined with microfinance group support, or usual care only. They were followed for changes in systolic blood pressure and CV-risk score over 12 months.
Lloyd-Jones and Fauci declared no conflicts.
This article first appeared on Medscape.com.
Biden plan to lower Medicare eligibility age to 60 faces hostility from hospitals
Of his many plans to expand insurance coverage, President-elect Joe Biden’s simplest strategy is lowering the eligibility age for Medicare from 65 to 60.
But the plan is sure to face long odds, even if the Democrats can snag control of the Senate in January by winning two runoff elections in Georgia.
Republicans, who fought the creation of Medicare in the 1960s and typically oppose expanding government entitlement programs, are not the biggest obstacle. Instead, the nation’s hospitals, a powerful political force, are poised to derail any effort.
“Hospitals certainly are not going to be happy with it,” said Jonathan Oberlander, professor of health policy and management at the University of North Carolina at Chapel Hill.
Medicare reimbursement rates for patients admitted to hospitals average half what commercial or employer-sponsored insurance plans pay.
“It will be a huge lift [in Congress] as the realities of lower Medicare reimbursement rates will activate some powerful interests against this,” said Josh Archambault, a senior fellow with the conservative Foundation for Government Accountability.
Biden, who turns 78 this month, said his plan will help Americans who retire early and those who are unemployed or can’t find jobs with health benefits.
“It reflects the reality that, even after the current crisis ends, older Americans are likely to find it difficult to secure jobs,” Biden wrote in April.
Lowering the Medicare eligibility age is popular. About 85% of Democrats and 69% of Republicans favor allowing those as young as 50 to buy into Medicare, according to a KFF tracking poll from January 2019. (KHN is an editorially independent program of KFF.)
Although opposition from the hospital industry is expected to be fierce, that is not the only obstacle to Biden’s plan.
Critics, especially Republicans on Capitol Hill, will point to the nation’s $3 trillion budget deficit as well as the dim outlook for the Medicare Hospital Insurance Trust Fund. That fund is on track to reach insolvency in 2024. That means there won’t be enough money to fully pay hospitals and nursing homes for inpatient care for Medicare beneficiaries.
Moreover, it’s unclear whether expanding Medicare will fit on the Democrats’ crowded health agenda, which also includes dealing with the COVID-19 pandemic, possibly rescuing the Affordable Care Act if the Supreme Court strikes down part or all of the law in a current case, expanding Obamacare subsidies and lowering drug costs.
Biden’s proposal is a nod to the liberal wing of the Democratic Party, which has advocated for Sen. Bernie Sanders’ (I-Vt.) government-run “Medicare for All” health system that would provide universal coverage. Biden opposed that effort, saying the nation could not afford it. He wanted to retain the private health insurance system, which covers 180 million people.
To expand coverage, Biden has proposed two major initiatives. In addition to the Medicare eligibility change, he wants Congress to approve a government-run health plan that people could buy into instead of purchasing coverage from insurance companies on their own or through the Obamacare marketplaces. Insurers helped beat back this “public option” initiative in 2009 during the congressional debate over the ACA.
The appeal of lowering Medicare eligibility to help those without insurance lies with leveraging a popular government program that has low administrative costs.
“It is hard to find a reform idea that is more popular than opening up Medicare” to people as young as 60, Oberlander said. He said early retirees would like the concept, as would employers, who could save on their health costs as workers gravitate to Medicare.
The eligibility age has been set at 65 since Medicare was created in 1965 as part of President Lyndon Johnson’s Great Society reform package. It was designed to coincide with the age when people at that time qualified for Social Security. Today, people generally qualify for early, reduced Social Security benefits at age 62, though they have to wait until age 66 for full benefits.
While people can qualify on the basis of other criteria, such as having a disability or end-stage renal disease, 85% of the 57 million Medicare enrollees are in the program simply because they’re old enough.
Lowering the age to 60 could add as many as 23 million people to Medicare, according to an analysis by the consulting firm Avalere Health. It’s unclear, however, if everyone who would be eligible would sign up or if Biden would limit the expansion to the 1.7 million people in that age range who are uninsured and the 3.2 million who buy coverage on their own.
Avalere says 3.2 million people in that age group buy coverage on the individual market.
While the 60-to-65 group has the lowest uninsured rate (8%) among adults, it has the highest health costs and pays the highest rates for individual coverage, said Cristina Boccuti, director of health policy at West Health, a nonpartisan research group.
About 13 million of those between 60 and 65 have coverage through their employer, according to Avalere. While they would not have to drop coverage to join Medicare, they could possibly opt to also pay to join the federal program and use it as a wraparound for their existing coverage. Medicare might then pick up costs for some services that the consumers would have to shoulder out-of-pocket.
Some 4 million people between 60 and 65 are enrolled in Medicaid, the state-federal health insurance program for low-income people. Shifting them to Medicare would make that their primary health insurer, a move that would save states money since they split Medicaid costs with the federal government.
Chris Pope, a senior fellow with the conservative Manhattan Institute, said getting health industry support, particularly from hospitals, will be vital for any health coverage expansion. “Hospitals are very aware about generous commercial rates being replaced by lower Medicare rates,” he said.
“Members of Congress, a lot of them are close to their hospitals and do not want to see them with a revenue hole,” he said.
President Barack Obama made a deal with the industry on the way to passing the ACA. In exchange for gaining millions of paying customers and lowering their uncompensated care by billions of dollars, the hospital industry agreed to give up future Medicare funds designed to help them cope with the uninsured. Showing the industry’s prowess on Capitol Hill, Congress has delayed those funding cuts for more than six years.
Jacob Hacker, a Yale University political scientist, noted that expanding Medicare would reduce the number of Americans who rely on employer-sponsored coverage. The pitfalls of the employer system were highlighted in 2020 as millions lost their jobs and workplace health coverage.
Even if they can win the two Georgia seats and take control of the Senate with the vice president breaking any ties, Democrats would be unlikely to pass major legislation without GOP support — unless they are willing to jettison the long-standing filibuster rule so they can pass most legislation with a simple 51-vote majority instead of 60 votes.
Hacker said that slim margin would make it difficult for Democrats to deal with many health issues all at once.
“Congress is not good at parallel processing,” Hacker said, referring to handling multiple priorities at the same time. “And the window is relatively short.”
KHN (Kaiser Health News) is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Of his many plans to expand insurance coverage, President-elect Joe Biden’s simplest strategy is lowering the eligibility age for Medicare from 65 to 60.
But the plan is sure to face long odds, even if the Democrats can snag control of the Senate in January by winning two runoff elections in Georgia.
Republicans, who fought the creation of Medicare in the 1960s and typically oppose expanding government entitlement programs, are not the biggest obstacle. Instead, the nation’s hospitals, a powerful political force, are poised to derail any effort.
“Hospitals certainly are not going to be happy with it,” said Jonathan Oberlander, professor of health policy and management at the University of North Carolina at Chapel Hill.
Medicare reimbursement rates for patients admitted to hospitals average half what commercial or employer-sponsored insurance plans pay.
“It will be a huge lift [in Congress] as the realities of lower Medicare reimbursement rates will activate some powerful interests against this,” said Josh Archambault, a senior fellow with the conservative Foundation for Government Accountability.
Biden, who turns 78 this month, said his plan will help Americans who retire early and those who are unemployed or can’t find jobs with health benefits.
“It reflects the reality that, even after the current crisis ends, older Americans are likely to find it difficult to secure jobs,” Biden wrote in April.
Lowering the Medicare eligibility age is popular. About 85% of Democrats and 69% of Republicans favor allowing those as young as 50 to buy into Medicare, according to a KFF tracking poll from January 2019. (KHN is an editorially independent program of KFF.)
Although opposition from the hospital industry is expected to be fierce, that is not the only obstacle to Biden’s plan.
Critics, especially Republicans on Capitol Hill, will point to the nation’s $3 trillion budget deficit as well as the dim outlook for the Medicare Hospital Insurance Trust Fund. That fund is on track to reach insolvency in 2024. That means there won’t be enough money to fully pay hospitals and nursing homes for inpatient care for Medicare beneficiaries.
Moreover, it’s unclear whether expanding Medicare will fit on the Democrats’ crowded health agenda, which also includes dealing with the COVID-19 pandemic, possibly rescuing the Affordable Care Act if the Supreme Court strikes down part or all of the law in a current case, expanding Obamacare subsidies and lowering drug costs.
Biden’s proposal is a nod to the liberal wing of the Democratic Party, which has advocated for Sen. Bernie Sanders’ (I-Vt.) government-run “Medicare for All” health system that would provide universal coverage. Biden opposed that effort, saying the nation could not afford it. He wanted to retain the private health insurance system, which covers 180 million people.
To expand coverage, Biden has proposed two major initiatives. In addition to the Medicare eligibility change, he wants Congress to approve a government-run health plan that people could buy into instead of purchasing coverage from insurance companies on their own or through the Obamacare marketplaces. Insurers helped beat back this “public option” initiative in 2009 during the congressional debate over the ACA.
The appeal of lowering Medicare eligibility to help those without insurance lies with leveraging a popular government program that has low administrative costs.
“It is hard to find a reform idea that is more popular than opening up Medicare” to people as young as 60, Oberlander said. He said early retirees would like the concept, as would employers, who could save on their health costs as workers gravitate to Medicare.
The eligibility age has been set at 65 since Medicare was created in 1965 as part of President Lyndon Johnson’s Great Society reform package. It was designed to coincide with the age when people at that time qualified for Social Security. Today, people generally qualify for early, reduced Social Security benefits at age 62, though they have to wait until age 66 for full benefits.
While people can qualify on the basis of other criteria, such as having a disability or end-stage renal disease, 85% of the 57 million Medicare enrollees are in the program simply because they’re old enough.
Lowering the age to 60 could add as many as 23 million people to Medicare, according to an analysis by the consulting firm Avalere Health. It’s unclear, however, if everyone who would be eligible would sign up or if Biden would limit the expansion to the 1.7 million people in that age range who are uninsured and the 3.2 million who buy coverage on their own.
Avalere says 3.2 million people in that age group buy coverage on the individual market.
While the 60-to-65 group has the lowest uninsured rate (8%) among adults, it has the highest health costs and pays the highest rates for individual coverage, said Cristina Boccuti, director of health policy at West Health, a nonpartisan research group.
About 13 million of those between 60 and 65 have coverage through their employer, according to Avalere. While they would not have to drop coverage to join Medicare, they could possibly opt to also pay to join the federal program and use it as a wraparound for their existing coverage. Medicare might then pick up costs for some services that the consumers would have to shoulder out-of-pocket.
Some 4 million people between 60 and 65 are enrolled in Medicaid, the state-federal health insurance program for low-income people. Shifting them to Medicare would make that their primary health insurer, a move that would save states money since they split Medicaid costs with the federal government.
Chris Pope, a senior fellow with the conservative Manhattan Institute, said getting health industry support, particularly from hospitals, will be vital for any health coverage expansion. “Hospitals are very aware about generous commercial rates being replaced by lower Medicare rates,” he said.
“Members of Congress, a lot of them are close to their hospitals and do not want to see them with a revenue hole,” he said.
President Barack Obama made a deal with the industry on the way to passing the ACA. In exchange for gaining millions of paying customers and lowering their uncompensated care by billions of dollars, the hospital industry agreed to give up future Medicare funds designed to help them cope with the uninsured. Showing the industry’s prowess on Capitol Hill, Congress has delayed those funding cuts for more than six years.
Jacob Hacker, a Yale University political scientist, noted that expanding Medicare would reduce the number of Americans who rely on employer-sponsored coverage. The pitfalls of the employer system were highlighted in 2020 as millions lost their jobs and workplace health coverage.
Even if they can win the two Georgia seats and take control of the Senate with the vice president breaking any ties, Democrats would be unlikely to pass major legislation without GOP support — unless they are willing to jettison the long-standing filibuster rule so they can pass most legislation with a simple 51-vote majority instead of 60 votes.
Hacker said that slim margin would make it difficult for Democrats to deal with many health issues all at once.
“Congress is not good at parallel processing,” Hacker said, referring to handling multiple priorities at the same time. “And the window is relatively short.”
KHN (Kaiser Health News) is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Of his many plans to expand insurance coverage, President-elect Joe Biden’s simplest strategy is lowering the eligibility age for Medicare from 65 to 60.
But the plan is sure to face long odds, even if the Democrats can snag control of the Senate in January by winning two runoff elections in Georgia.
Republicans, who fought the creation of Medicare in the 1960s and typically oppose expanding government entitlement programs, are not the biggest obstacle. Instead, the nation’s hospitals, a powerful political force, are poised to derail any effort.
“Hospitals certainly are not going to be happy with it,” said Jonathan Oberlander, professor of health policy and management at the University of North Carolina at Chapel Hill.
Medicare reimbursement rates for patients admitted to hospitals average half what commercial or employer-sponsored insurance plans pay.
“It will be a huge lift [in Congress] as the realities of lower Medicare reimbursement rates will activate some powerful interests against this,” said Josh Archambault, a senior fellow with the conservative Foundation for Government Accountability.
Biden, who turns 78 this month, said his plan will help Americans who retire early and those who are unemployed or can’t find jobs with health benefits.
“It reflects the reality that, even after the current crisis ends, older Americans are likely to find it difficult to secure jobs,” Biden wrote in April.
Lowering the Medicare eligibility age is popular. About 85% of Democrats and 69% of Republicans favor allowing those as young as 50 to buy into Medicare, according to a KFF tracking poll from January 2019. (KHN is an editorially independent program of KFF.)
Although opposition from the hospital industry is expected to be fierce, that is not the only obstacle to Biden’s plan.
Critics, especially Republicans on Capitol Hill, will point to the nation’s $3 trillion budget deficit as well as the dim outlook for the Medicare Hospital Insurance Trust Fund. That fund is on track to reach insolvency in 2024. That means there won’t be enough money to fully pay hospitals and nursing homes for inpatient care for Medicare beneficiaries.
Moreover, it’s unclear whether expanding Medicare will fit on the Democrats’ crowded health agenda, which also includes dealing with the COVID-19 pandemic, possibly rescuing the Affordable Care Act if the Supreme Court strikes down part or all of the law in a current case, expanding Obamacare subsidies and lowering drug costs.
Biden’s proposal is a nod to the liberal wing of the Democratic Party, which has advocated for Sen. Bernie Sanders’ (I-Vt.) government-run “Medicare for All” health system that would provide universal coverage. Biden opposed that effort, saying the nation could not afford it. He wanted to retain the private health insurance system, which covers 180 million people.
To expand coverage, Biden has proposed two major initiatives. In addition to the Medicare eligibility change, he wants Congress to approve a government-run health plan that people could buy into instead of purchasing coverage from insurance companies on their own or through the Obamacare marketplaces. Insurers helped beat back this “public option” initiative in 2009 during the congressional debate over the ACA.
The appeal of lowering Medicare eligibility to help those without insurance lies with leveraging a popular government program that has low administrative costs.
“It is hard to find a reform idea that is more popular than opening up Medicare” to people as young as 60, Oberlander said. He said early retirees would like the concept, as would employers, who could save on their health costs as workers gravitate to Medicare.
The eligibility age has been set at 65 since Medicare was created in 1965 as part of President Lyndon Johnson’s Great Society reform package. It was designed to coincide with the age when people at that time qualified for Social Security. Today, people generally qualify for early, reduced Social Security benefits at age 62, though they have to wait until age 66 for full benefits.
While people can qualify on the basis of other criteria, such as having a disability or end-stage renal disease, 85% of the 57 million Medicare enrollees are in the program simply because they’re old enough.
Lowering the age to 60 could add as many as 23 million people to Medicare, according to an analysis by the consulting firm Avalere Health. It’s unclear, however, if everyone who would be eligible would sign up or if Biden would limit the expansion to the 1.7 million people in that age range who are uninsured and the 3.2 million who buy coverage on their own.
Avalere says 3.2 million people in that age group buy coverage on the individual market.
While the 60-to-65 group has the lowest uninsured rate (8%) among adults, it has the highest health costs and pays the highest rates for individual coverage, said Cristina Boccuti, director of health policy at West Health, a nonpartisan research group.
About 13 million of those between 60 and 65 have coverage through their employer, according to Avalere. While they would not have to drop coverage to join Medicare, they could possibly opt to also pay to join the federal program and use it as a wraparound for their existing coverage. Medicare might then pick up costs for some services that the consumers would have to shoulder out-of-pocket.
Some 4 million people between 60 and 65 are enrolled in Medicaid, the state-federal health insurance program for low-income people. Shifting them to Medicare would make that their primary health insurer, a move that would save states money since they split Medicaid costs with the federal government.
Chris Pope, a senior fellow with the conservative Manhattan Institute, said getting health industry support, particularly from hospitals, will be vital for any health coverage expansion. “Hospitals are very aware about generous commercial rates being replaced by lower Medicare rates,” he said.
“Members of Congress, a lot of them are close to their hospitals and do not want to see them with a revenue hole,” he said.
President Barack Obama made a deal with the industry on the way to passing the ACA. In exchange for gaining millions of paying customers and lowering their uncompensated care by billions of dollars, the hospital industry agreed to give up future Medicare funds designed to help them cope with the uninsured. Showing the industry’s prowess on Capitol Hill, Congress has delayed those funding cuts for more than six years.
Jacob Hacker, a Yale University political scientist, noted that expanding Medicare would reduce the number of Americans who rely on employer-sponsored coverage. The pitfalls of the employer system were highlighted in 2020 as millions lost their jobs and workplace health coverage.
Even if they can win the two Georgia seats and take control of the Senate with the vice president breaking any ties, Democrats would be unlikely to pass major legislation without GOP support — unless they are willing to jettison the long-standing filibuster rule so they can pass most legislation with a simple 51-vote majority instead of 60 votes.
Hacker said that slim margin would make it difficult for Democrats to deal with many health issues all at once.
“Congress is not good at parallel processing,” Hacker said, referring to handling multiple priorities at the same time. “And the window is relatively short.”
KHN (Kaiser Health News) is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
What happened to melanoma care during COVID-19 sequestration
Initial evidence suggests that the , Rebecca I. Hartman, MD, MPH, said at a virtual forum on cutaneous malignancies jointly presented by Postgraduate Institute for Medicine and Global Academy for Medication Education.
This is not what National Comprehensive Cancer Network officials expected when they issued short-term recommendations on how to manage cutaneous melanoma during the first wave of the COVID-19 pandemic. Those recommendations for restriction of care, which Dr. Hartman characterized as “pretty significant changes from how we typically practice melanoma care in the U.S.,” came at a time when there was justifiable concern that the first COVID-19 surge would strain the U.S. health care system beyond the breaking point.
The rationale given for the NCCN recommendations was that most time-to-treat studies have shown no adverse patient outcomes for 90-day delays in treatment, even for thicker melanomas. But those studies, all retrospective, have been called into question. And the first real-world data on the impact of care restrictions during the lockdown, reported by Italian dermatologists, highlights adverse effects with potentially far-reaching consequences, noted Dr. Hartman, director of melanoma epidemiology at Brigham and Women’s Hospital and a dermatologist, Harvard University, Boston.
Analysis of the impact of lockdown-induced delays in melanoma care is not merely an academic exercise, she added. While everyone hopes that the spring 2020 COVID-19 shelter-in-place was a once-in-a-lifetime event, there’s no guarantee that will be the case. Moreover, the lockdown provides a natural experiment addressing the possible consequences of melanoma care delays on patient outcomes, a topic that for ethical reasons could never be addressed in a randomized trial.
The short-term NCCN recommendations included the use of excisional biopsies for melanoma diagnosis whenever possible; and delay of up to 3 months for wide local excision of in situ melanoma, any invasive melanoma with negative margins, and even T1 melanomas with positive margins provided the bulk of the lesion had been excised. The guidance also suggested delaying sentinel lymph node biopsy (SLNB), along with increased use of neoadjuvant therapy in patients with clinically palpable regional lymph nodes in order to delay surgery for up to 8 weeks. Single-agent systemic therapy at the least-frequent dosing was advised in order to minimize toxicity and reduce the need for additional health care resources: for example, nivolumab (Opdivo) at 480 mg every 4 weeks instead of every 2 weeks, and pembrolizumab (Keytruda) at 400 mg every 6 weeks, rather than every 3 weeks.
So, that’s what the NCCN recommended. Here’s what actually happened during shelter-in-place as captured in Dr. Hartman’s survey of 18 U.S. members of the Melanoma Prevention Working Group, all practicing dermatology in centers particularly hard-hit in the first wave of the pandemic: In-person new melanoma patient visits plunged from an average of 4.83 per week per provider to 0.83 per week. Telemedicine visits with new melanoma patients went from zero prepandemic to 0.67 visits per week per provider, which doesn’t come close to making up for the drop in in-person visits. Interestingly, two respondents reported turning to gene-expression profile testing for patient prognostication because of delays in SLNB.
Wide local excision was delayed by an average of 6 weeks in roughly one-third of melanoma patients with early tumor stage disease, regardless of margin status. For patients with stage T1b disease, wide local excision was typically performed on time during shelter-in-place; however, SLNB was delayed by an average of 5 weeks in 22% of patients with positive margins and 28% of those with negative margins. In contrast, 80% of patients with more advanced T2-T4 melanoma underwent on-schedule definitive management with wide local excision and SLNB, Dr. Hartman reported.
Critics have taken issue with the NCCN’s conclusion that most time-to-treatment studies show no harm arising from 90-day treatment delays. A review of the relevant published literature by Dr. Hartman’s Harvard colleagues, published in July, found that the evidence is mixed. “There is insufficient evidence to definitively conclude that delayed wide resection after gross removal of the primary melanoma is without harm,” they concluded in the review.
Spanish dermatologists performed a modeling study in order to estimate the potential impact of COVID-19 lockdowns on 5- and 10-year survival of melanoma patients. Using the growth rate of a random sample of 1,000 melanomas to model estimates of tumor thickness after various delays, coupled with American Joint Committee on Cancer survival data for different T stages, they estimated that 5-year survival would be reduced from 94.2% to 92.3% with a 90-day delay in diagnosis, and that 10-year survival would drop from 90.0% to 87.6%.
But that’s merely modeling. Francesco Ricci, MD, PhD, and colleagues from the melanoma unit at the Istituto Dermopatico dell’Immacolata, Rome, have provided a first look at the real-world impact of the lockdown. In the prelockdown period of January through March 9th, 2020, the referral center averaged 2.3 new melanoma diagnoses per day. During the Rome lockdown, from March 10th through May 3rd, this figure dropped to a mean of 0.6 melanoma diagnoses per day. Postlockdown, from May 4th to June 6th, the average climbed to 1.3 per day. The rate of newly diagnosed nodular melanoma was 5.5-fold greater postlockdown, compared with prelockdown; the rate of ulcerated melanoma was 4.9-fold greater.
“We can hypothesize that this may have been due to delays in diagnosis and care,” Dr. Hartman commented. “This is important because we know that nodular melanoma as well as ulceration tend to have a worse prognosis in terms of mortality.”
The mean Breslow thickness of newly diagnosed melanomas was 0.88 mm prelockdown, 0.66 mm during lockdown, and 1.96 mm postlockdown. The investigators speculated that the reduced Breslow thickness of melanomas diagnosed during lockdown might be explained by a greater willingness of more health-conscious people to defy the shelter-in-place instructions because of their concern about a suspicious skin lesion. “Though it is way too early to gauge the consequences of such diagnostic delay, should this issue be neglected, dermatologists and their patients may pay a higher price later with increased morbidity, mortality, and financial burden,” according to the investigators.
Dr. Hartman observed that it will be important to learn whether similar experiences occurred elsewhere during lockdown.
Another speaker, John M. Kirkwood, MD, said he has seen several melanoma patients referred from outside centers who had delays of up to 3 months in sentinel lymph node management of T2 and T3 tumors during lockdown who now have widespread metastatic disease.
“Now, is that anecdotal? I don’t know, it’s just worrisome to me,” commented Dr. Kirkwood, professor of medicine, dermatology, and translational science at the University of Pittsburgh.
Merrick Ross, MD, professor of surgical oncology at M.D. Anderson Cancer Center, Houston, recalled, “There was a period of time [during the lockdown] when we weren’t allowed to do certain elective procedures, if you want to call cancer surgery elective.”
“It’s too soon to talk about outcomes because a lot of patients are still in the process of being treated after what I would consider a significant delay in diagnosis,” the surgeon added.
An audience member asked if there will be an opportunity to see data on the damage done by delaying melanoma management as compared to lives saved through the lockdown for COVID-19. Dr. Ross replied that M.D. Anderson is in the midst of an institution-wide study analyzing the delay in diagnosis of a range of cancers.
“In our melanoma center it is absolutely clear, although we’re still collecting data, that the median tumor thickness is much higher since the lockdown,” Dr. Ross commented.
Dr. Hartman said she and her coinvestigators in the Melanoma Prevention Working Group are attempting to tally up the damage done via the lockdown by delaying melanoma diagnosis and treatment. But she agreed with the questioner that the most important thing is overall net lives saved through shelter-in-place.
“I’m sure that, separately, nondermatologists – perhaps infectious disease doctors and internists – are looking at how many lives were saved by the lockdown policy. So I do think all that data will come out,” Dr. Hartman predicted.
She reported having no financial conflicts regarding her presentation.
Global Academy for Medical Education and this news organization are owned by the same company.
SOURCE: Hartman, R. Cutaneous malignancies forum.
Initial evidence suggests that the , Rebecca I. Hartman, MD, MPH, said at a virtual forum on cutaneous malignancies jointly presented by Postgraduate Institute for Medicine and Global Academy for Medication Education.
This is not what National Comprehensive Cancer Network officials expected when they issued short-term recommendations on how to manage cutaneous melanoma during the first wave of the COVID-19 pandemic. Those recommendations for restriction of care, which Dr. Hartman characterized as “pretty significant changes from how we typically practice melanoma care in the U.S.,” came at a time when there was justifiable concern that the first COVID-19 surge would strain the U.S. health care system beyond the breaking point.
The rationale given for the NCCN recommendations was that most time-to-treat studies have shown no adverse patient outcomes for 90-day delays in treatment, even for thicker melanomas. But those studies, all retrospective, have been called into question. And the first real-world data on the impact of care restrictions during the lockdown, reported by Italian dermatologists, highlights adverse effects with potentially far-reaching consequences, noted Dr. Hartman, director of melanoma epidemiology at Brigham and Women’s Hospital and a dermatologist, Harvard University, Boston.
Analysis of the impact of lockdown-induced delays in melanoma care is not merely an academic exercise, she added. While everyone hopes that the spring 2020 COVID-19 shelter-in-place was a once-in-a-lifetime event, there’s no guarantee that will be the case. Moreover, the lockdown provides a natural experiment addressing the possible consequences of melanoma care delays on patient outcomes, a topic that for ethical reasons could never be addressed in a randomized trial.
The short-term NCCN recommendations included the use of excisional biopsies for melanoma diagnosis whenever possible; and delay of up to 3 months for wide local excision of in situ melanoma, any invasive melanoma with negative margins, and even T1 melanomas with positive margins provided the bulk of the lesion had been excised. The guidance also suggested delaying sentinel lymph node biopsy (SLNB), along with increased use of neoadjuvant therapy in patients with clinically palpable regional lymph nodes in order to delay surgery for up to 8 weeks. Single-agent systemic therapy at the least-frequent dosing was advised in order to minimize toxicity and reduce the need for additional health care resources: for example, nivolumab (Opdivo) at 480 mg every 4 weeks instead of every 2 weeks, and pembrolizumab (Keytruda) at 400 mg every 6 weeks, rather than every 3 weeks.
So, that’s what the NCCN recommended. Here’s what actually happened during shelter-in-place as captured in Dr. Hartman’s survey of 18 U.S. members of the Melanoma Prevention Working Group, all practicing dermatology in centers particularly hard-hit in the first wave of the pandemic: In-person new melanoma patient visits plunged from an average of 4.83 per week per provider to 0.83 per week. Telemedicine visits with new melanoma patients went from zero prepandemic to 0.67 visits per week per provider, which doesn’t come close to making up for the drop in in-person visits. Interestingly, two respondents reported turning to gene-expression profile testing for patient prognostication because of delays in SLNB.
Wide local excision was delayed by an average of 6 weeks in roughly one-third of melanoma patients with early tumor stage disease, regardless of margin status. For patients with stage T1b disease, wide local excision was typically performed on time during shelter-in-place; however, SLNB was delayed by an average of 5 weeks in 22% of patients with positive margins and 28% of those with negative margins. In contrast, 80% of patients with more advanced T2-T4 melanoma underwent on-schedule definitive management with wide local excision and SLNB, Dr. Hartman reported.
Critics have taken issue with the NCCN’s conclusion that most time-to-treatment studies show no harm arising from 90-day treatment delays. A review of the relevant published literature by Dr. Hartman’s Harvard colleagues, published in July, found that the evidence is mixed. “There is insufficient evidence to definitively conclude that delayed wide resection after gross removal of the primary melanoma is without harm,” they concluded in the review.
Spanish dermatologists performed a modeling study in order to estimate the potential impact of COVID-19 lockdowns on 5- and 10-year survival of melanoma patients. Using the growth rate of a random sample of 1,000 melanomas to model estimates of tumor thickness after various delays, coupled with American Joint Committee on Cancer survival data for different T stages, they estimated that 5-year survival would be reduced from 94.2% to 92.3% with a 90-day delay in diagnosis, and that 10-year survival would drop from 90.0% to 87.6%.
But that’s merely modeling. Francesco Ricci, MD, PhD, and colleagues from the melanoma unit at the Istituto Dermopatico dell’Immacolata, Rome, have provided a first look at the real-world impact of the lockdown. In the prelockdown period of January through March 9th, 2020, the referral center averaged 2.3 new melanoma diagnoses per day. During the Rome lockdown, from March 10th through May 3rd, this figure dropped to a mean of 0.6 melanoma diagnoses per day. Postlockdown, from May 4th to June 6th, the average climbed to 1.3 per day. The rate of newly diagnosed nodular melanoma was 5.5-fold greater postlockdown, compared with prelockdown; the rate of ulcerated melanoma was 4.9-fold greater.
“We can hypothesize that this may have been due to delays in diagnosis and care,” Dr. Hartman commented. “This is important because we know that nodular melanoma as well as ulceration tend to have a worse prognosis in terms of mortality.”
The mean Breslow thickness of newly diagnosed melanomas was 0.88 mm prelockdown, 0.66 mm during lockdown, and 1.96 mm postlockdown. The investigators speculated that the reduced Breslow thickness of melanomas diagnosed during lockdown might be explained by a greater willingness of more health-conscious people to defy the shelter-in-place instructions because of their concern about a suspicious skin lesion. “Though it is way too early to gauge the consequences of such diagnostic delay, should this issue be neglected, dermatologists and their patients may pay a higher price later with increased morbidity, mortality, and financial burden,” according to the investigators.
Dr. Hartman observed that it will be important to learn whether similar experiences occurred elsewhere during lockdown.
Another speaker, John M. Kirkwood, MD, said he has seen several melanoma patients referred from outside centers who had delays of up to 3 months in sentinel lymph node management of T2 and T3 tumors during lockdown who now have widespread metastatic disease.
“Now, is that anecdotal? I don’t know, it’s just worrisome to me,” commented Dr. Kirkwood, professor of medicine, dermatology, and translational science at the University of Pittsburgh.
Merrick Ross, MD, professor of surgical oncology at M.D. Anderson Cancer Center, Houston, recalled, “There was a period of time [during the lockdown] when we weren’t allowed to do certain elective procedures, if you want to call cancer surgery elective.”
“It’s too soon to talk about outcomes because a lot of patients are still in the process of being treated after what I would consider a significant delay in diagnosis,” the surgeon added.
An audience member asked if there will be an opportunity to see data on the damage done by delaying melanoma management as compared to lives saved through the lockdown for COVID-19. Dr. Ross replied that M.D. Anderson is in the midst of an institution-wide study analyzing the delay in diagnosis of a range of cancers.
“In our melanoma center it is absolutely clear, although we’re still collecting data, that the median tumor thickness is much higher since the lockdown,” Dr. Ross commented.
Dr. Hartman said she and her coinvestigators in the Melanoma Prevention Working Group are attempting to tally up the damage done via the lockdown by delaying melanoma diagnosis and treatment. But she agreed with the questioner that the most important thing is overall net lives saved through shelter-in-place.
“I’m sure that, separately, nondermatologists – perhaps infectious disease doctors and internists – are looking at how many lives were saved by the lockdown policy. So I do think all that data will come out,” Dr. Hartman predicted.
She reported having no financial conflicts regarding her presentation.
Global Academy for Medical Education and this news organization are owned by the same company.
SOURCE: Hartman, R. Cutaneous malignancies forum.
Initial evidence suggests that the , Rebecca I. Hartman, MD, MPH, said at a virtual forum on cutaneous malignancies jointly presented by Postgraduate Institute for Medicine and Global Academy for Medication Education.
This is not what National Comprehensive Cancer Network officials expected when they issued short-term recommendations on how to manage cutaneous melanoma during the first wave of the COVID-19 pandemic. Those recommendations for restriction of care, which Dr. Hartman characterized as “pretty significant changes from how we typically practice melanoma care in the U.S.,” came at a time when there was justifiable concern that the first COVID-19 surge would strain the U.S. health care system beyond the breaking point.
The rationale given for the NCCN recommendations was that most time-to-treat studies have shown no adverse patient outcomes for 90-day delays in treatment, even for thicker melanomas. But those studies, all retrospective, have been called into question. And the first real-world data on the impact of care restrictions during the lockdown, reported by Italian dermatologists, highlights adverse effects with potentially far-reaching consequences, noted Dr. Hartman, director of melanoma epidemiology at Brigham and Women’s Hospital and a dermatologist, Harvard University, Boston.
Analysis of the impact of lockdown-induced delays in melanoma care is not merely an academic exercise, she added. While everyone hopes that the spring 2020 COVID-19 shelter-in-place was a once-in-a-lifetime event, there’s no guarantee that will be the case. Moreover, the lockdown provides a natural experiment addressing the possible consequences of melanoma care delays on patient outcomes, a topic that for ethical reasons could never be addressed in a randomized trial.
The short-term NCCN recommendations included the use of excisional biopsies for melanoma diagnosis whenever possible; and delay of up to 3 months for wide local excision of in situ melanoma, any invasive melanoma with negative margins, and even T1 melanomas with positive margins provided the bulk of the lesion had been excised. The guidance also suggested delaying sentinel lymph node biopsy (SLNB), along with increased use of neoadjuvant therapy in patients with clinically palpable regional lymph nodes in order to delay surgery for up to 8 weeks. Single-agent systemic therapy at the least-frequent dosing was advised in order to minimize toxicity and reduce the need for additional health care resources: for example, nivolumab (Opdivo) at 480 mg every 4 weeks instead of every 2 weeks, and pembrolizumab (Keytruda) at 400 mg every 6 weeks, rather than every 3 weeks.
So, that’s what the NCCN recommended. Here’s what actually happened during shelter-in-place as captured in Dr. Hartman’s survey of 18 U.S. members of the Melanoma Prevention Working Group, all practicing dermatology in centers particularly hard-hit in the first wave of the pandemic: In-person new melanoma patient visits plunged from an average of 4.83 per week per provider to 0.83 per week. Telemedicine visits with new melanoma patients went from zero prepandemic to 0.67 visits per week per provider, which doesn’t come close to making up for the drop in in-person visits. Interestingly, two respondents reported turning to gene-expression profile testing for patient prognostication because of delays in SLNB.
Wide local excision was delayed by an average of 6 weeks in roughly one-third of melanoma patients with early tumor stage disease, regardless of margin status. For patients with stage T1b disease, wide local excision was typically performed on time during shelter-in-place; however, SLNB was delayed by an average of 5 weeks in 22% of patients with positive margins and 28% of those with negative margins. In contrast, 80% of patients with more advanced T2-T4 melanoma underwent on-schedule definitive management with wide local excision and SLNB, Dr. Hartman reported.
Critics have taken issue with the NCCN’s conclusion that most time-to-treatment studies show no harm arising from 90-day treatment delays. A review of the relevant published literature by Dr. Hartman’s Harvard colleagues, published in July, found that the evidence is mixed. “There is insufficient evidence to definitively conclude that delayed wide resection after gross removal of the primary melanoma is without harm,” they concluded in the review.
Spanish dermatologists performed a modeling study in order to estimate the potential impact of COVID-19 lockdowns on 5- and 10-year survival of melanoma patients. Using the growth rate of a random sample of 1,000 melanomas to model estimates of tumor thickness after various delays, coupled with American Joint Committee on Cancer survival data for different T stages, they estimated that 5-year survival would be reduced from 94.2% to 92.3% with a 90-day delay in diagnosis, and that 10-year survival would drop from 90.0% to 87.6%.
But that’s merely modeling. Francesco Ricci, MD, PhD, and colleagues from the melanoma unit at the Istituto Dermopatico dell’Immacolata, Rome, have provided a first look at the real-world impact of the lockdown. In the prelockdown period of January through March 9th, 2020, the referral center averaged 2.3 new melanoma diagnoses per day. During the Rome lockdown, from March 10th through May 3rd, this figure dropped to a mean of 0.6 melanoma diagnoses per day. Postlockdown, from May 4th to June 6th, the average climbed to 1.3 per day. The rate of newly diagnosed nodular melanoma was 5.5-fold greater postlockdown, compared with prelockdown; the rate of ulcerated melanoma was 4.9-fold greater.
“We can hypothesize that this may have been due to delays in diagnosis and care,” Dr. Hartman commented. “This is important because we know that nodular melanoma as well as ulceration tend to have a worse prognosis in terms of mortality.”
The mean Breslow thickness of newly diagnosed melanomas was 0.88 mm prelockdown, 0.66 mm during lockdown, and 1.96 mm postlockdown. The investigators speculated that the reduced Breslow thickness of melanomas diagnosed during lockdown might be explained by a greater willingness of more health-conscious people to defy the shelter-in-place instructions because of their concern about a suspicious skin lesion. “Though it is way too early to gauge the consequences of such diagnostic delay, should this issue be neglected, dermatologists and their patients may pay a higher price later with increased morbidity, mortality, and financial burden,” according to the investigators.
Dr. Hartman observed that it will be important to learn whether similar experiences occurred elsewhere during lockdown.
Another speaker, John M. Kirkwood, MD, said he has seen several melanoma patients referred from outside centers who had delays of up to 3 months in sentinel lymph node management of T2 and T3 tumors during lockdown who now have widespread metastatic disease.
“Now, is that anecdotal? I don’t know, it’s just worrisome to me,” commented Dr. Kirkwood, professor of medicine, dermatology, and translational science at the University of Pittsburgh.
Merrick Ross, MD, professor of surgical oncology at M.D. Anderson Cancer Center, Houston, recalled, “There was a period of time [during the lockdown] when we weren’t allowed to do certain elective procedures, if you want to call cancer surgery elective.”
“It’s too soon to talk about outcomes because a lot of patients are still in the process of being treated after what I would consider a significant delay in diagnosis,” the surgeon added.
An audience member asked if there will be an opportunity to see data on the damage done by delaying melanoma management as compared to lives saved through the lockdown for COVID-19. Dr. Ross replied that M.D. Anderson is in the midst of an institution-wide study analyzing the delay in diagnosis of a range of cancers.
“In our melanoma center it is absolutely clear, although we’re still collecting data, that the median tumor thickness is much higher since the lockdown,” Dr. Ross commented.
Dr. Hartman said she and her coinvestigators in the Melanoma Prevention Working Group are attempting to tally up the damage done via the lockdown by delaying melanoma diagnosis and treatment. But she agreed with the questioner that the most important thing is overall net lives saved through shelter-in-place.
“I’m sure that, separately, nondermatologists – perhaps infectious disease doctors and internists – are looking at how many lives were saved by the lockdown policy. So I do think all that data will come out,” Dr. Hartman predicted.
She reported having no financial conflicts regarding her presentation.
Global Academy for Medical Education and this news organization are owned by the same company.
SOURCE: Hartman, R. Cutaneous malignancies forum.
REPORTING FROM THE CUTANEOUS MALIGNANCIES FORUM
Trump could clean house at health agencies
Others may soon depart voluntarily. Politico reported in late October that more than two dozen political appointees had already left the U.S. Department Health and Human Services (HHS) since the start of the COVID-19 pandemic in February and that potentially dozens of the more than 100 in the department would leave if Trump was not reelected.
Trump hasn’t conceded, he is challenging the election results, and he has already fired his Defense Secretary, Mark Esper.
Among those possibly in Trump’s sights: HHS Secretary Alex Azar, US Food and Drug Administration (FDA) Commissioner Stephen Hahn, MD, Centers for Disease Control and Prevention (CDC) Director Robert Redfield, MD, and White House Coronavirus Task Force member Anthony Fauci, MD, who is also the director of the National Institutes of Allergy and Infectious Diseases.
Seema Verma, the administrator of the Centers for Medicare & Medicaid Services (CMS), is likely safe. According to Politico, Verma is expected to leave on her own terms.
Azar has had a long run as a Trump appointee. He took office in January 2018 and has been a staunch loyalist. But he’s frequently been the butt of grousing by Trump for not doing enough to help lower drug prices and for his handling of the coronavirus pandemic. Azar was initially in charge of the Trump virus effort but was quickly replaced by Vice President Mike Pence.
It was widely reported in late April that Trump was considering firing Azar, but the president called that “fake news” in a tweet.
Azar has complained about Hahn, who was confirmed in December 2019. According to Politico, Azar was looking into how to remove Hahn as commissioner because of the FDA’s battle with the White House over standards for emergency use authorization of a coronavirus vaccine.
In addition, Trump was infuriated by the agency’s insistence that it stick to the highest bar for an emergency approval. “The deep state, or whoever, over at the FDA is making it very difficult for drug companies to get people in order to test the vaccines and therapeutics. Obviously, they are hoping to delay the answer until after November 3rd,” Trump tweeted at Hahn.
Fauci on the firing line?
Most of the president’s ire has been directed at Fauci. As far back as April, Trump retweeted a call for Fauci’s firing. Twitter removed the original tweet but kept Trump’s comments on the original tweet.
The president has frequently questioned Fauci’s advice, sidelined him from task force meetings, and infrequently met with him. Trump called Fauci a “disaster” during a call with supporters in October, and then, at a campaign rally in November, intimated that he would fire the scientist after the election, according to The Washington Post.
But such a firing cannot be easily done. Some have speculated that Trump could pressure Fauci’s boss, Francis Collins, MD, PhD — the director of the National Institutes of Health (NIH), who is a political appointee — to get rid of him. But Collins would have to come up with a reason to fire Fauci. Because he is not a political appointee, Fauci is afforded a raft of protections given to civil service employees of the federal government.
To demote or fire Fauci, Collins would have to give him 30 days’ notice unless there’s a belief that he committed a crime. Fauci would have at least a week to offer evidence and affidavits in support of his service.
He’d also be entitled to legal representation, a written decision, and the specific reasons for the action being taken quickly. He could also request a hearing, and he’d be able to appeal any action to the Merit Systems Protection Board. The process could take months, if not years.
In late October, Trump issued an executive order that would reclassify certain federal employees so that they wouldn’t have such protections. But agencies have until mid-January to come up with lists of such workers, according to Government Executive.
Collins has been with NIH since 1993, when he headed the Human Genome Project and the National Human Genome Research Institute. Politico has speculated that Collins, 70, might retire if Trump was reelected. It’s unclear what he’ll do now.
Redfield, who has taken heat for his leadership from many in public health — and was asked in October to stand up to Trump by former CDC Director William H. Foege, MD — has been openly contradicted by the president on more than one occasion, according to The New York Times.
In September, The Hill reported that Trump told reporters that he’d chastised Redfield by phone soon after Redfield had told a Senate committee that a coronavirus vaccine would not be available until mid-2021.
This article first appeared on Medscape.com.
Others may soon depart voluntarily. Politico reported in late October that more than two dozen political appointees had already left the U.S. Department Health and Human Services (HHS) since the start of the COVID-19 pandemic in February and that potentially dozens of the more than 100 in the department would leave if Trump was not reelected.
Trump hasn’t conceded, he is challenging the election results, and he has already fired his Defense Secretary, Mark Esper.
Among those possibly in Trump’s sights: HHS Secretary Alex Azar, US Food and Drug Administration (FDA) Commissioner Stephen Hahn, MD, Centers for Disease Control and Prevention (CDC) Director Robert Redfield, MD, and White House Coronavirus Task Force member Anthony Fauci, MD, who is also the director of the National Institutes of Allergy and Infectious Diseases.
Seema Verma, the administrator of the Centers for Medicare & Medicaid Services (CMS), is likely safe. According to Politico, Verma is expected to leave on her own terms.
Azar has had a long run as a Trump appointee. He took office in January 2018 and has been a staunch loyalist. But he’s frequently been the butt of grousing by Trump for not doing enough to help lower drug prices and for his handling of the coronavirus pandemic. Azar was initially in charge of the Trump virus effort but was quickly replaced by Vice President Mike Pence.
It was widely reported in late April that Trump was considering firing Azar, but the president called that “fake news” in a tweet.
Azar has complained about Hahn, who was confirmed in December 2019. According to Politico, Azar was looking into how to remove Hahn as commissioner because of the FDA’s battle with the White House over standards for emergency use authorization of a coronavirus vaccine.
In addition, Trump was infuriated by the agency’s insistence that it stick to the highest bar for an emergency approval. “The deep state, or whoever, over at the FDA is making it very difficult for drug companies to get people in order to test the vaccines and therapeutics. Obviously, they are hoping to delay the answer until after November 3rd,” Trump tweeted at Hahn.
Fauci on the firing line?
Most of the president’s ire has been directed at Fauci. As far back as April, Trump retweeted a call for Fauci’s firing. Twitter removed the original tweet but kept Trump’s comments on the original tweet.
The president has frequently questioned Fauci’s advice, sidelined him from task force meetings, and infrequently met with him. Trump called Fauci a “disaster” during a call with supporters in October, and then, at a campaign rally in November, intimated that he would fire the scientist after the election, according to The Washington Post.
But such a firing cannot be easily done. Some have speculated that Trump could pressure Fauci’s boss, Francis Collins, MD, PhD — the director of the National Institutes of Health (NIH), who is a political appointee — to get rid of him. But Collins would have to come up with a reason to fire Fauci. Because he is not a political appointee, Fauci is afforded a raft of protections given to civil service employees of the federal government.
To demote or fire Fauci, Collins would have to give him 30 days’ notice unless there’s a belief that he committed a crime. Fauci would have at least a week to offer evidence and affidavits in support of his service.
He’d also be entitled to legal representation, a written decision, and the specific reasons for the action being taken quickly. He could also request a hearing, and he’d be able to appeal any action to the Merit Systems Protection Board. The process could take months, if not years.
In late October, Trump issued an executive order that would reclassify certain federal employees so that they wouldn’t have such protections. But agencies have until mid-January to come up with lists of such workers, according to Government Executive.
Collins has been with NIH since 1993, when he headed the Human Genome Project and the National Human Genome Research Institute. Politico has speculated that Collins, 70, might retire if Trump was reelected. It’s unclear what he’ll do now.
Redfield, who has taken heat for his leadership from many in public health — and was asked in October to stand up to Trump by former CDC Director William H. Foege, MD — has been openly contradicted by the president on more than one occasion, according to The New York Times.
In September, The Hill reported that Trump told reporters that he’d chastised Redfield by phone soon after Redfield had told a Senate committee that a coronavirus vaccine would not be available until mid-2021.
This article first appeared on Medscape.com.
Others may soon depart voluntarily. Politico reported in late October that more than two dozen political appointees had already left the U.S. Department Health and Human Services (HHS) since the start of the COVID-19 pandemic in February and that potentially dozens of the more than 100 in the department would leave if Trump was not reelected.
Trump hasn’t conceded, he is challenging the election results, and he has already fired his Defense Secretary, Mark Esper.
Among those possibly in Trump’s sights: HHS Secretary Alex Azar, US Food and Drug Administration (FDA) Commissioner Stephen Hahn, MD, Centers for Disease Control and Prevention (CDC) Director Robert Redfield, MD, and White House Coronavirus Task Force member Anthony Fauci, MD, who is also the director of the National Institutes of Allergy and Infectious Diseases.
Seema Verma, the administrator of the Centers for Medicare & Medicaid Services (CMS), is likely safe. According to Politico, Verma is expected to leave on her own terms.
Azar has had a long run as a Trump appointee. He took office in January 2018 and has been a staunch loyalist. But he’s frequently been the butt of grousing by Trump for not doing enough to help lower drug prices and for his handling of the coronavirus pandemic. Azar was initially in charge of the Trump virus effort but was quickly replaced by Vice President Mike Pence.
It was widely reported in late April that Trump was considering firing Azar, but the president called that “fake news” in a tweet.
Azar has complained about Hahn, who was confirmed in December 2019. According to Politico, Azar was looking into how to remove Hahn as commissioner because of the FDA’s battle with the White House over standards for emergency use authorization of a coronavirus vaccine.
In addition, Trump was infuriated by the agency’s insistence that it stick to the highest bar for an emergency approval. “The deep state, or whoever, over at the FDA is making it very difficult for drug companies to get people in order to test the vaccines and therapeutics. Obviously, they are hoping to delay the answer until after November 3rd,” Trump tweeted at Hahn.
Fauci on the firing line?
Most of the president’s ire has been directed at Fauci. As far back as April, Trump retweeted a call for Fauci’s firing. Twitter removed the original tweet but kept Trump’s comments on the original tweet.
The president has frequently questioned Fauci’s advice, sidelined him from task force meetings, and infrequently met with him. Trump called Fauci a “disaster” during a call with supporters in October, and then, at a campaign rally in November, intimated that he would fire the scientist after the election, according to The Washington Post.
But such a firing cannot be easily done. Some have speculated that Trump could pressure Fauci’s boss, Francis Collins, MD, PhD — the director of the National Institutes of Health (NIH), who is a political appointee — to get rid of him. But Collins would have to come up with a reason to fire Fauci. Because he is not a political appointee, Fauci is afforded a raft of protections given to civil service employees of the federal government.
To demote or fire Fauci, Collins would have to give him 30 days’ notice unless there’s a belief that he committed a crime. Fauci would have at least a week to offer evidence and affidavits in support of his service.
He’d also be entitled to legal representation, a written decision, and the specific reasons for the action being taken quickly. He could also request a hearing, and he’d be able to appeal any action to the Merit Systems Protection Board. The process could take months, if not years.
In late October, Trump issued an executive order that would reclassify certain federal employees so that they wouldn’t have such protections. But agencies have until mid-January to come up with lists of such workers, according to Government Executive.
Collins has been with NIH since 1993, when he headed the Human Genome Project and the National Human Genome Research Institute. Politico has speculated that Collins, 70, might retire if Trump was reelected. It’s unclear what he’ll do now.
Redfield, who has taken heat for his leadership from many in public health — and was asked in October to stand up to Trump by former CDC Director William H. Foege, MD — has been openly contradicted by the president on more than one occasion, according to The New York Times.
In September, The Hill reported that Trump told reporters that he’d chastised Redfield by phone soon after Redfield had told a Senate committee that a coronavirus vaccine would not be available until mid-2021.
This article first appeared on Medscape.com.
Supreme Court Justices seem skeptical of case to overturn ACA
The Justices conducted arguments by telephone in the case, California v Texas (previously California v US), which was brought by 18 Republican state officials and two individual plaintiffs. The Trump administration joined the plaintiffs in June, arguing that the entire law should be overturned. The ACA is being defended by Democratic state officials from 16 states and Washington, D.C.
The Republican plaintiffs have essentially argued that the ACA cannot stand without the individual mandate requirement – that it is not possible to “sever” it from the rest of the Act. In 2017, Congress set the tax penalty to $0 if an individual did not buy insurance. The mandate to buy insurance was left in place, but there were no longer any consequences. The plaintiffs said that congressional act was equivalent to severing the mandate.
But many Justices appeared to take a dim view of that argument.
“It’s a very straightforward case for severability under our precedents,” said Justice Brett Kavanaugh. “Meaning that we would excise the mandate and leave the rest of the Act in play. Congress knows how to write an inseverability clause and that is not the language that they chose here,” he said.
Justice Elena Kagan also questioned how it would jibe with legal precedent to allow the severing of one part of a law when there was no clear instruction from Congress on the issue. She also raised the concern that it would open the door to all sorts of challenges.
“It would seem a big deal to say that, if you can point to injury with respect to one provision and you can concoct some kind of inseverability argument, that allows you to challenge anything else in the statute,” she said.
“Isn’t that something that really cuts against all of our doctrine?” asked Kagan.
“I think it’s hard for you to argue that Congress intended the entire Act to fall if the mandate was struck down when the same Congress that lowered the penalty to zero did not even try to repeal the rest of the act,” said Chief Justice John Roberts.
“I think, frankly, that they wanted the Court to do that but that’s not our job,” he added.
Proof of harm?
To have the standing to sue, the plaintiffs have to prove they have been harmed by the ACA. Texas Solicitor General Kyle Hawkins said that individuals feel compelled to buy insurance – even without a penalty hanging over their heads.
Justice Stephen Breyer argued that many laws include what he called “precatory” language – that is, they seek to compel citizens to do something. But most don’t penalize those who fail to act – just like the ACA currently.
If, as the Texas plaintiffs argued, it’s still unconstitutional to make such a request, “I think there will be an awful lot of language in an awful lot of statutes that will suddenly be the subject of court constitutional challenge,” he said.
Hawkins disagreed. He said the ACA’s mandate “is not some suggestion, not some hortatory statement. It is the law of the United States of America today that you have to purchase health insurance and not just any health insurance, but health insurance that the federal government has decided would be best for you.”
Hawkins said that, if just one additional person signed up for Medicaid, the state of Texas and the other plaintiff states would be harmed. He said people were continuing to enroll in the program because they believed the law required them to get health insurance.
Justice Sonia Sotomayor said that defied common sense. “The problem is that your theory assumes people that people are going to pay a tax and break the law by not buying insurance, but they wouldn’t do it when the tax is zero.”
What’s at stake
It’s unlikely the justices will issue a decision immediately. They have until the end of the term in June to rule.
Katie Keith, JD, MPH, a principal at Keith Policy Solutions, LLC, outlined the potential outcomes in Health Affairs .
“The most likely scenario is that the Court maintains the status quo,” she wrote. They could get there by deciding Texas et al. did not have standing to bring the case. Or they could decide that either the mandate is constitutional or that it is unconstitutional but can be severed from the rest of the ACA.
The Court could alternatively find that some or all of the law’s insurance provisions – such as protections for people with pre-existing conditions – can’t be severed from the mandate. Or the justices could strike down all of the insurance consumer protections, the health insurance marketplaces, premium tax credits, and other provisions, which would force states to come up with the money to help people buy insurance. And states are unlikely to be able to do so, especially with the pandemic stretching their budgets.
Finally, the Court could find that the mandate can’t be separated, which would essentially overturn the law.
If that happens, some 15 million people could lose Medicaid coverage, 11 million who buy on health insurance exchanges could lose coverage, and 2.3 million young adults would no longer be able to stay on parents’ policies, according to the Kaiser Family Foundation. Kaiser also estimates that 54 million people under age 65 who have pre-existing conditions would no longer be guaranteed coverage.
The Urban Institute estimates that 21 million people could lose insurance – 15 million through Medicaid and the Children’s Health Insurance Program (CHIP) and 7.6 million through private nongroup coverage.
Medical societies weigh in
Multiple physicians’ groups, patient advocates, and hospital organizations have filed briefs with the Court in favor of keeping the law intact.
Twenty patient groups representing millions with pre-existing conditions – including the American Cancer Society, American Diabetes Association, American Heart Association, National Alliance on Mental Illness, National Organization for Rare Disorders, and the Kennedy Forum – filed a court brief in May arguing that the law has expanded access to insurance and improved patient outcomes.
“The coronavirus pandemic has only served to underscore the necessity of meaningful coverage – especially for those who are at high risk of being severely affected by the virus – including countless Americans who have pre-existing, acute or chronic conditions like heart disease, cancer, diabetes, lung diseases and multiple sclerosis,” they said in a statement.
Jacqueline W. Fincher, MD, MACP, president of the American College of Physicians, which joined a court brief in support of the law with 19 other medical organizations, said the law has worked.
“The coverage, protections and benefits provided by the ACA are critical to the well-being of millions of Americans,” she said in a statement.
“If the ACA were to be thrown out at the same time that we face the pandemic, it would cause chaos for physicians and our patients, and for the entire health care system,” said Fincher, adding that millions of Americans who have been infected could lose insurance if protections for pre-existing conditions disappeared.
“The ACA has revolutionized access to care for tens of millions of women by helping them obtain meaningful health coverage, ensuring that essential care is covered by insurers, and protecting patients from unfair insurance practices,” said Maureen G. Phipps, MD, MPH, CEO of the American College of Obstetricians and Gynecologists (ACOG), in a statement.
Overturning the ACA “would be one of the most singularly disruptive acts to be committed during this public health crisis,” she said.
American Psychiatric Association President Jeffrey Geller, MD, MPH, also warned of disruptions to care, especially for those with mental health and substance use disorders. “We urge the Supreme Court to preserve the entire Act, including the individual mandate,” he said, in a statement.
“In the midst of COVID is no time to let down the millions who we serve as our patients,” said Chip Kahn, Federation of American Health Systems president and CEO, in a statement.
“As caregivers, the goal of hospitals for our patients is to see increased access to affordable coverage for all Americans – not new obstacles,” he said, adding that the ACA “can accomplish this goal. We hope the Supreme Court will see its way clear to allow it to go forward.”
For the defense
Many legal analysts on social media who listened in to today’s hearing agreed that the tenor of the proceedings seemed to lean toward survival of the ACA.
“At this point I would say it is *extremely* likely that the ACA will be upheld, but the mandate struck down and severed out,” tweeted Raffi Melkonian, an appellate lawyer in Houston, Texas. “A decision on standing (throwing out the case entirely) is also possible. The chance that the ACA is struck down v. low.”
“Both Kavanaugh and Roberts have suggested this morning that they may view the individual mandate as severable from the rest of the law. If those two justices join the court’s three liberals in finding that the mandate is severable, that would be five votes to save the ACA,” tweeted the analysts at SCOTUS Blog.
Sean Marotta, a lawyer with Hogan Lovells’ Supreme Court group, agreed. “Oral argument is always an imperfect measure, but the Act’s defenders should feel good today,” he tweeted.
This article first appeared on Medscape.com.
The Justices conducted arguments by telephone in the case, California v Texas (previously California v US), which was brought by 18 Republican state officials and two individual plaintiffs. The Trump administration joined the plaintiffs in June, arguing that the entire law should be overturned. The ACA is being defended by Democratic state officials from 16 states and Washington, D.C.
The Republican plaintiffs have essentially argued that the ACA cannot stand without the individual mandate requirement – that it is not possible to “sever” it from the rest of the Act. In 2017, Congress set the tax penalty to $0 if an individual did not buy insurance. The mandate to buy insurance was left in place, but there were no longer any consequences. The plaintiffs said that congressional act was equivalent to severing the mandate.
But many Justices appeared to take a dim view of that argument.
“It’s a very straightforward case for severability under our precedents,” said Justice Brett Kavanaugh. “Meaning that we would excise the mandate and leave the rest of the Act in play. Congress knows how to write an inseverability clause and that is not the language that they chose here,” he said.
Justice Elena Kagan also questioned how it would jibe with legal precedent to allow the severing of one part of a law when there was no clear instruction from Congress on the issue. She also raised the concern that it would open the door to all sorts of challenges.
“It would seem a big deal to say that, if you can point to injury with respect to one provision and you can concoct some kind of inseverability argument, that allows you to challenge anything else in the statute,” she said.
“Isn’t that something that really cuts against all of our doctrine?” asked Kagan.
“I think it’s hard for you to argue that Congress intended the entire Act to fall if the mandate was struck down when the same Congress that lowered the penalty to zero did not even try to repeal the rest of the act,” said Chief Justice John Roberts.
“I think, frankly, that they wanted the Court to do that but that’s not our job,” he added.
Proof of harm?
To have the standing to sue, the plaintiffs have to prove they have been harmed by the ACA. Texas Solicitor General Kyle Hawkins said that individuals feel compelled to buy insurance – even without a penalty hanging over their heads.
Justice Stephen Breyer argued that many laws include what he called “precatory” language – that is, they seek to compel citizens to do something. But most don’t penalize those who fail to act – just like the ACA currently.
If, as the Texas plaintiffs argued, it’s still unconstitutional to make such a request, “I think there will be an awful lot of language in an awful lot of statutes that will suddenly be the subject of court constitutional challenge,” he said.
Hawkins disagreed. He said the ACA’s mandate “is not some suggestion, not some hortatory statement. It is the law of the United States of America today that you have to purchase health insurance and not just any health insurance, but health insurance that the federal government has decided would be best for you.”
Hawkins said that, if just one additional person signed up for Medicaid, the state of Texas and the other plaintiff states would be harmed. He said people were continuing to enroll in the program because they believed the law required them to get health insurance.
Justice Sonia Sotomayor said that defied common sense. “The problem is that your theory assumes people that people are going to pay a tax and break the law by not buying insurance, but they wouldn’t do it when the tax is zero.”
What’s at stake
It’s unlikely the justices will issue a decision immediately. They have until the end of the term in June to rule.
Katie Keith, JD, MPH, a principal at Keith Policy Solutions, LLC, outlined the potential outcomes in Health Affairs .
“The most likely scenario is that the Court maintains the status quo,” she wrote. They could get there by deciding Texas et al. did not have standing to bring the case. Or they could decide that either the mandate is constitutional or that it is unconstitutional but can be severed from the rest of the ACA.
The Court could alternatively find that some or all of the law’s insurance provisions – such as protections for people with pre-existing conditions – can’t be severed from the mandate. Or the justices could strike down all of the insurance consumer protections, the health insurance marketplaces, premium tax credits, and other provisions, which would force states to come up with the money to help people buy insurance. And states are unlikely to be able to do so, especially with the pandemic stretching their budgets.
Finally, the Court could find that the mandate can’t be separated, which would essentially overturn the law.
If that happens, some 15 million people could lose Medicaid coverage, 11 million who buy on health insurance exchanges could lose coverage, and 2.3 million young adults would no longer be able to stay on parents’ policies, according to the Kaiser Family Foundation. Kaiser also estimates that 54 million people under age 65 who have pre-existing conditions would no longer be guaranteed coverage.
The Urban Institute estimates that 21 million people could lose insurance – 15 million through Medicaid and the Children’s Health Insurance Program (CHIP) and 7.6 million through private nongroup coverage.
Medical societies weigh in
Multiple physicians’ groups, patient advocates, and hospital organizations have filed briefs with the Court in favor of keeping the law intact.
Twenty patient groups representing millions with pre-existing conditions – including the American Cancer Society, American Diabetes Association, American Heart Association, National Alliance on Mental Illness, National Organization for Rare Disorders, and the Kennedy Forum – filed a court brief in May arguing that the law has expanded access to insurance and improved patient outcomes.
“The coronavirus pandemic has only served to underscore the necessity of meaningful coverage – especially for those who are at high risk of being severely affected by the virus – including countless Americans who have pre-existing, acute or chronic conditions like heart disease, cancer, diabetes, lung diseases and multiple sclerosis,” they said in a statement.
Jacqueline W. Fincher, MD, MACP, president of the American College of Physicians, which joined a court brief in support of the law with 19 other medical organizations, said the law has worked.
“The coverage, protections and benefits provided by the ACA are critical to the well-being of millions of Americans,” she said in a statement.
“If the ACA were to be thrown out at the same time that we face the pandemic, it would cause chaos for physicians and our patients, and for the entire health care system,” said Fincher, adding that millions of Americans who have been infected could lose insurance if protections for pre-existing conditions disappeared.
“The ACA has revolutionized access to care for tens of millions of women by helping them obtain meaningful health coverage, ensuring that essential care is covered by insurers, and protecting patients from unfair insurance practices,” said Maureen G. Phipps, MD, MPH, CEO of the American College of Obstetricians and Gynecologists (ACOG), in a statement.
Overturning the ACA “would be one of the most singularly disruptive acts to be committed during this public health crisis,” she said.
American Psychiatric Association President Jeffrey Geller, MD, MPH, also warned of disruptions to care, especially for those with mental health and substance use disorders. “We urge the Supreme Court to preserve the entire Act, including the individual mandate,” he said, in a statement.
“In the midst of COVID is no time to let down the millions who we serve as our patients,” said Chip Kahn, Federation of American Health Systems president and CEO, in a statement.
“As caregivers, the goal of hospitals for our patients is to see increased access to affordable coverage for all Americans – not new obstacles,” he said, adding that the ACA “can accomplish this goal. We hope the Supreme Court will see its way clear to allow it to go forward.”
For the defense
Many legal analysts on social media who listened in to today’s hearing agreed that the tenor of the proceedings seemed to lean toward survival of the ACA.
“At this point I would say it is *extremely* likely that the ACA will be upheld, but the mandate struck down and severed out,” tweeted Raffi Melkonian, an appellate lawyer in Houston, Texas. “A decision on standing (throwing out the case entirely) is also possible. The chance that the ACA is struck down v. low.”
“Both Kavanaugh and Roberts have suggested this morning that they may view the individual mandate as severable from the rest of the law. If those two justices join the court’s three liberals in finding that the mandate is severable, that would be five votes to save the ACA,” tweeted the analysts at SCOTUS Blog.
Sean Marotta, a lawyer with Hogan Lovells’ Supreme Court group, agreed. “Oral argument is always an imperfect measure, but the Act’s defenders should feel good today,” he tweeted.
This article first appeared on Medscape.com.
The Justices conducted arguments by telephone in the case, California v Texas (previously California v US), which was brought by 18 Republican state officials and two individual plaintiffs. The Trump administration joined the plaintiffs in June, arguing that the entire law should be overturned. The ACA is being defended by Democratic state officials from 16 states and Washington, D.C.
The Republican plaintiffs have essentially argued that the ACA cannot stand without the individual mandate requirement – that it is not possible to “sever” it from the rest of the Act. In 2017, Congress set the tax penalty to $0 if an individual did not buy insurance. The mandate to buy insurance was left in place, but there were no longer any consequences. The plaintiffs said that congressional act was equivalent to severing the mandate.
But many Justices appeared to take a dim view of that argument.
“It’s a very straightforward case for severability under our precedents,” said Justice Brett Kavanaugh. “Meaning that we would excise the mandate and leave the rest of the Act in play. Congress knows how to write an inseverability clause and that is not the language that they chose here,” he said.
Justice Elena Kagan also questioned how it would jibe with legal precedent to allow the severing of one part of a law when there was no clear instruction from Congress on the issue. She also raised the concern that it would open the door to all sorts of challenges.
“It would seem a big deal to say that, if you can point to injury with respect to one provision and you can concoct some kind of inseverability argument, that allows you to challenge anything else in the statute,” she said.
“Isn’t that something that really cuts against all of our doctrine?” asked Kagan.
“I think it’s hard for you to argue that Congress intended the entire Act to fall if the mandate was struck down when the same Congress that lowered the penalty to zero did not even try to repeal the rest of the act,” said Chief Justice John Roberts.
“I think, frankly, that they wanted the Court to do that but that’s not our job,” he added.
Proof of harm?
To have the standing to sue, the plaintiffs have to prove they have been harmed by the ACA. Texas Solicitor General Kyle Hawkins said that individuals feel compelled to buy insurance – even without a penalty hanging over their heads.
Justice Stephen Breyer argued that many laws include what he called “precatory” language – that is, they seek to compel citizens to do something. But most don’t penalize those who fail to act – just like the ACA currently.
If, as the Texas plaintiffs argued, it’s still unconstitutional to make such a request, “I think there will be an awful lot of language in an awful lot of statutes that will suddenly be the subject of court constitutional challenge,” he said.
Hawkins disagreed. He said the ACA’s mandate “is not some suggestion, not some hortatory statement. It is the law of the United States of America today that you have to purchase health insurance and not just any health insurance, but health insurance that the federal government has decided would be best for you.”
Hawkins said that, if just one additional person signed up for Medicaid, the state of Texas and the other plaintiff states would be harmed. He said people were continuing to enroll in the program because they believed the law required them to get health insurance.
Justice Sonia Sotomayor said that defied common sense. “The problem is that your theory assumes people that people are going to pay a tax and break the law by not buying insurance, but they wouldn’t do it when the tax is zero.”
What’s at stake
It’s unlikely the justices will issue a decision immediately. They have until the end of the term in June to rule.
Katie Keith, JD, MPH, a principal at Keith Policy Solutions, LLC, outlined the potential outcomes in Health Affairs .
“The most likely scenario is that the Court maintains the status quo,” she wrote. They could get there by deciding Texas et al. did not have standing to bring the case. Or they could decide that either the mandate is constitutional or that it is unconstitutional but can be severed from the rest of the ACA.
The Court could alternatively find that some or all of the law’s insurance provisions – such as protections for people with pre-existing conditions – can’t be severed from the mandate. Or the justices could strike down all of the insurance consumer protections, the health insurance marketplaces, premium tax credits, and other provisions, which would force states to come up with the money to help people buy insurance. And states are unlikely to be able to do so, especially with the pandemic stretching their budgets.
Finally, the Court could find that the mandate can’t be separated, which would essentially overturn the law.
If that happens, some 15 million people could lose Medicaid coverage, 11 million who buy on health insurance exchanges could lose coverage, and 2.3 million young adults would no longer be able to stay on parents’ policies, according to the Kaiser Family Foundation. Kaiser also estimates that 54 million people under age 65 who have pre-existing conditions would no longer be guaranteed coverage.
The Urban Institute estimates that 21 million people could lose insurance – 15 million through Medicaid and the Children’s Health Insurance Program (CHIP) and 7.6 million through private nongroup coverage.
Medical societies weigh in
Multiple physicians’ groups, patient advocates, and hospital organizations have filed briefs with the Court in favor of keeping the law intact.
Twenty patient groups representing millions with pre-existing conditions – including the American Cancer Society, American Diabetes Association, American Heart Association, National Alliance on Mental Illness, National Organization for Rare Disorders, and the Kennedy Forum – filed a court brief in May arguing that the law has expanded access to insurance and improved patient outcomes.
“The coronavirus pandemic has only served to underscore the necessity of meaningful coverage – especially for those who are at high risk of being severely affected by the virus – including countless Americans who have pre-existing, acute or chronic conditions like heart disease, cancer, diabetes, lung diseases and multiple sclerosis,” they said in a statement.
Jacqueline W. Fincher, MD, MACP, president of the American College of Physicians, which joined a court brief in support of the law with 19 other medical organizations, said the law has worked.
“The coverage, protections and benefits provided by the ACA are critical to the well-being of millions of Americans,” she said in a statement.
“If the ACA were to be thrown out at the same time that we face the pandemic, it would cause chaos for physicians and our patients, and for the entire health care system,” said Fincher, adding that millions of Americans who have been infected could lose insurance if protections for pre-existing conditions disappeared.
“The ACA has revolutionized access to care for tens of millions of women by helping them obtain meaningful health coverage, ensuring that essential care is covered by insurers, and protecting patients from unfair insurance practices,” said Maureen G. Phipps, MD, MPH, CEO of the American College of Obstetricians and Gynecologists (ACOG), in a statement.
Overturning the ACA “would be one of the most singularly disruptive acts to be committed during this public health crisis,” she said.
American Psychiatric Association President Jeffrey Geller, MD, MPH, also warned of disruptions to care, especially for those with mental health and substance use disorders. “We urge the Supreme Court to preserve the entire Act, including the individual mandate,” he said, in a statement.
“In the midst of COVID is no time to let down the millions who we serve as our patients,” said Chip Kahn, Federation of American Health Systems president and CEO, in a statement.
“As caregivers, the goal of hospitals for our patients is to see increased access to affordable coverage for all Americans – not new obstacles,” he said, adding that the ACA “can accomplish this goal. We hope the Supreme Court will see its way clear to allow it to go forward.”
For the defense
Many legal analysts on social media who listened in to today’s hearing agreed that the tenor of the proceedings seemed to lean toward survival of the ACA.
“At this point I would say it is *extremely* likely that the ACA will be upheld, but the mandate struck down and severed out,” tweeted Raffi Melkonian, an appellate lawyer in Houston, Texas. “A decision on standing (throwing out the case entirely) is also possible. The chance that the ACA is struck down v. low.”
“Both Kavanaugh and Roberts have suggested this morning that they may view the individual mandate as severable from the rest of the law. If those two justices join the court’s three liberals in finding that the mandate is severable, that would be five votes to save the ACA,” tweeted the analysts at SCOTUS Blog.
Sean Marotta, a lawyer with Hogan Lovells’ Supreme Court group, agreed. “Oral argument is always an imperfect measure, but the Act’s defenders should feel good today,” he tweeted.
This article first appeared on Medscape.com.
FDA grants emergency use authorization to Lilly’s antibody COVID-19 therapy
The monoclonal antibody therapy has emergency authorization for treating patients who have tested positive for SARS-CoV-2 infection and who are considered to be at high risk for progression to severe COVID-19 or hospitalization. To be eligible for treatment with bamlanivimab, patients must be at least 12 years of age and weigh at least 40 kg (approximately 88 lb). The agency notes that this includes patients aged 65 years and older or people with certain chronic conditions.
Bamlanivimab is not authorized for use in patients who are hospitalized or who require oxygen therapy because of COVID-19. The FDA’s action comes less than 2 weeks after Eli Lilly halted the ACTIV-3 study of the therapy for severe, hospitalized COVID-19 patients after evidence showed that adding the antibody therapy to standard care did not improve outcomes over standard care alone for patients with advanced COVID-19.
The government contract with Eli Lilly involves the purchase of 300,000 doses through December, with the option to procure another 650,000 doses through June 2021.
Because of Operation Warp Speed, “we have supplies to distribute now. Product distribution will begin this week,” US Health & Human Services (HHS) Secretary Alex Azar said at a news conference today.
“We talked about building the bridge to safe and effective vaccines” for COVID-19, Azar added. “With this therapeutic, the bridge is taking shape.”
Bamlanivimab 700 mg will be administered as a 1-hour infusion followed by a 1-hour observation period for detecting any infusion-related side effects. The authorized dose is 700 mg, which was on the lower end of the dose range evaluated in studies.
During the press conference, a reporter asked whether the lower dose was chosen in order that more doses of the antibody could be made available. “The lower dose is a rational choice in this situation because we don’t want to give more of a drug than you need,” said Janet Woodcock, MD, the therapeutics lead for Operation Warp Speed. “I think we could probably go lower.”
Bamlanivimab works by attaching to the virus and blocking its entry into the cells and possibly by helping the patients’ immune system clear the virus, said Woodcock, who is also director of the FDA’s Center for Drug Evaluation and Research.
“The goal is to treat high-risk people as soon as possible after they show symptoms and are diagnosed,” she added.
Infusions an initial challenge?
There could be some logistic challenges at first because the antibody is administered via infusion. “We expect there will initially be a challenge in administering ... these infusions and setting up infusion centers,” Woodcock said.
Outpatient intravenous infusions are normally performed at infusion centers for patients with cancer and immune disorders, she noted. “You really don’t want them mixing with people who have COVID-19 disease, so we will need to set up separate sites.”
Bamlanivimab will be provided free of cost to patients, Azar said. Patients should be aware that coinsurance may be required for the infusion.
“Fair and equitable” distribution planned
During phase 1 of distribution, the agent will first be allocated to hospitals and hospital-affiliated locations only, John Redd, MD, MPH, chief medical officer, Office of the Assistant Secretary for Preparedness and Response at HHS, said at the press conference.
During phase 2, “there will be expanded distribution to outpatient sites,” he said. In an effort to keep the process transparent, a new website features the latest updates on the distribution of bamlanivimab.
Allocation will be based on two factors: the number of new cases reported in a state or territory in the prior 7 days, and rates of COVID-19 hospitalization during the same period.
Asked why the government would determine distribution of the antibody on the basis of the number of hospitalized patients when the indication includes prevention of admission, Woodcock replied that hospitalization is a surrogate measure that can reflect risk factors in a particular state population, such as obesity, diabetes, or the proportion of older people.
Furthermore, the confirmed cases are a “leading indicator,” she said, that can help identify a steep rise in COVID-19 cases that could indicate more hospitalizations are likely soon. “We don’t want to miss that.”
Data underlying the EUA decision
A decrease in hospitalizations or emergency department visits within 28 days of treatment in preclinical studies was “the most important evidence that bamlanivimab may be effective,” the agency noted in the press release announcing the EUA. Among patients at high risk for progression, 3% required such interventions, compared with 10% of placebo-treated patients.
Potential side effects of bamlanivimab include anaphylaxis, infusion-related reactions, nausea, diarrhea, dizziness, headache, itching, and vomiting.
“As illustrated by today’s action, the FDA remains committed to expediting the development and availability of potential COVID-19 treatments and providing sick patients timely access to new therapies where appropriate,” FDA Commissioner Stephen M. Hahn, MD, said in the news release.
Healthcare providers can download a detailed FDA fact sheet on the EUA for bamlanivimab, which includes dosing instructions.
This article first appeared on Medscape.com.
The monoclonal antibody therapy has emergency authorization for treating patients who have tested positive for SARS-CoV-2 infection and who are considered to be at high risk for progression to severe COVID-19 or hospitalization. To be eligible for treatment with bamlanivimab, patients must be at least 12 years of age and weigh at least 40 kg (approximately 88 lb). The agency notes that this includes patients aged 65 years and older or people with certain chronic conditions.
Bamlanivimab is not authorized for use in patients who are hospitalized or who require oxygen therapy because of COVID-19. The FDA’s action comes less than 2 weeks after Eli Lilly halted the ACTIV-3 study of the therapy for severe, hospitalized COVID-19 patients after evidence showed that adding the antibody therapy to standard care did not improve outcomes over standard care alone for patients with advanced COVID-19.
The government contract with Eli Lilly involves the purchase of 300,000 doses through December, with the option to procure another 650,000 doses through June 2021.
Because of Operation Warp Speed, “we have supplies to distribute now. Product distribution will begin this week,” US Health & Human Services (HHS) Secretary Alex Azar said at a news conference today.
“We talked about building the bridge to safe and effective vaccines” for COVID-19, Azar added. “With this therapeutic, the bridge is taking shape.”
Bamlanivimab 700 mg will be administered as a 1-hour infusion followed by a 1-hour observation period for detecting any infusion-related side effects. The authorized dose is 700 mg, which was on the lower end of the dose range evaluated in studies.
During the press conference, a reporter asked whether the lower dose was chosen in order that more doses of the antibody could be made available. “The lower dose is a rational choice in this situation because we don’t want to give more of a drug than you need,” said Janet Woodcock, MD, the therapeutics lead for Operation Warp Speed. “I think we could probably go lower.”
Bamlanivimab works by attaching to the virus and blocking its entry into the cells and possibly by helping the patients’ immune system clear the virus, said Woodcock, who is also director of the FDA’s Center for Drug Evaluation and Research.
“The goal is to treat high-risk people as soon as possible after they show symptoms and are diagnosed,” she added.
Infusions an initial challenge?
There could be some logistic challenges at first because the antibody is administered via infusion. “We expect there will initially be a challenge in administering ... these infusions and setting up infusion centers,” Woodcock said.
Outpatient intravenous infusions are normally performed at infusion centers for patients with cancer and immune disorders, she noted. “You really don’t want them mixing with people who have COVID-19 disease, so we will need to set up separate sites.”
Bamlanivimab will be provided free of cost to patients, Azar said. Patients should be aware that coinsurance may be required for the infusion.
“Fair and equitable” distribution planned
During phase 1 of distribution, the agent will first be allocated to hospitals and hospital-affiliated locations only, John Redd, MD, MPH, chief medical officer, Office of the Assistant Secretary for Preparedness and Response at HHS, said at the press conference.
During phase 2, “there will be expanded distribution to outpatient sites,” he said. In an effort to keep the process transparent, a new website features the latest updates on the distribution of bamlanivimab.
Allocation will be based on two factors: the number of new cases reported in a state or territory in the prior 7 days, and rates of COVID-19 hospitalization during the same period.
Asked why the government would determine distribution of the antibody on the basis of the number of hospitalized patients when the indication includes prevention of admission, Woodcock replied that hospitalization is a surrogate measure that can reflect risk factors in a particular state population, such as obesity, diabetes, or the proportion of older people.
Furthermore, the confirmed cases are a “leading indicator,” she said, that can help identify a steep rise in COVID-19 cases that could indicate more hospitalizations are likely soon. “We don’t want to miss that.”
Data underlying the EUA decision
A decrease in hospitalizations or emergency department visits within 28 days of treatment in preclinical studies was “the most important evidence that bamlanivimab may be effective,” the agency noted in the press release announcing the EUA. Among patients at high risk for progression, 3% required such interventions, compared with 10% of placebo-treated patients.
Potential side effects of bamlanivimab include anaphylaxis, infusion-related reactions, nausea, diarrhea, dizziness, headache, itching, and vomiting.
“As illustrated by today’s action, the FDA remains committed to expediting the development and availability of potential COVID-19 treatments and providing sick patients timely access to new therapies where appropriate,” FDA Commissioner Stephen M. Hahn, MD, said in the news release.
Healthcare providers can download a detailed FDA fact sheet on the EUA for bamlanivimab, which includes dosing instructions.
This article first appeared on Medscape.com.
The monoclonal antibody therapy has emergency authorization for treating patients who have tested positive for SARS-CoV-2 infection and who are considered to be at high risk for progression to severe COVID-19 or hospitalization. To be eligible for treatment with bamlanivimab, patients must be at least 12 years of age and weigh at least 40 kg (approximately 88 lb). The agency notes that this includes patients aged 65 years and older or people with certain chronic conditions.
Bamlanivimab is not authorized for use in patients who are hospitalized or who require oxygen therapy because of COVID-19. The FDA’s action comes less than 2 weeks after Eli Lilly halted the ACTIV-3 study of the therapy for severe, hospitalized COVID-19 patients after evidence showed that adding the antibody therapy to standard care did not improve outcomes over standard care alone for patients with advanced COVID-19.
The government contract with Eli Lilly involves the purchase of 300,000 doses through December, with the option to procure another 650,000 doses through June 2021.
Because of Operation Warp Speed, “we have supplies to distribute now. Product distribution will begin this week,” US Health & Human Services (HHS) Secretary Alex Azar said at a news conference today.
“We talked about building the bridge to safe and effective vaccines” for COVID-19, Azar added. “With this therapeutic, the bridge is taking shape.”
Bamlanivimab 700 mg will be administered as a 1-hour infusion followed by a 1-hour observation period for detecting any infusion-related side effects. The authorized dose is 700 mg, which was on the lower end of the dose range evaluated in studies.
During the press conference, a reporter asked whether the lower dose was chosen in order that more doses of the antibody could be made available. “The lower dose is a rational choice in this situation because we don’t want to give more of a drug than you need,” said Janet Woodcock, MD, the therapeutics lead for Operation Warp Speed. “I think we could probably go lower.”
Bamlanivimab works by attaching to the virus and blocking its entry into the cells and possibly by helping the patients’ immune system clear the virus, said Woodcock, who is also director of the FDA’s Center for Drug Evaluation and Research.
“The goal is to treat high-risk people as soon as possible after they show symptoms and are diagnosed,” she added.
Infusions an initial challenge?
There could be some logistic challenges at first because the antibody is administered via infusion. “We expect there will initially be a challenge in administering ... these infusions and setting up infusion centers,” Woodcock said.
Outpatient intravenous infusions are normally performed at infusion centers for patients with cancer and immune disorders, she noted. “You really don’t want them mixing with people who have COVID-19 disease, so we will need to set up separate sites.”
Bamlanivimab will be provided free of cost to patients, Azar said. Patients should be aware that coinsurance may be required for the infusion.
“Fair and equitable” distribution planned
During phase 1 of distribution, the agent will first be allocated to hospitals and hospital-affiliated locations only, John Redd, MD, MPH, chief medical officer, Office of the Assistant Secretary for Preparedness and Response at HHS, said at the press conference.
During phase 2, “there will be expanded distribution to outpatient sites,” he said. In an effort to keep the process transparent, a new website features the latest updates on the distribution of bamlanivimab.
Allocation will be based on two factors: the number of new cases reported in a state or territory in the prior 7 days, and rates of COVID-19 hospitalization during the same period.
Asked why the government would determine distribution of the antibody on the basis of the number of hospitalized patients when the indication includes prevention of admission, Woodcock replied that hospitalization is a surrogate measure that can reflect risk factors in a particular state population, such as obesity, diabetes, or the proportion of older people.
Furthermore, the confirmed cases are a “leading indicator,” she said, that can help identify a steep rise in COVID-19 cases that could indicate more hospitalizations are likely soon. “We don’t want to miss that.”
Data underlying the EUA decision
A decrease in hospitalizations or emergency department visits within 28 days of treatment in preclinical studies was “the most important evidence that bamlanivimab may be effective,” the agency noted in the press release announcing the EUA. Among patients at high risk for progression, 3% required such interventions, compared with 10% of placebo-treated patients.
Potential side effects of bamlanivimab include anaphylaxis, infusion-related reactions, nausea, diarrhea, dizziness, headache, itching, and vomiting.
“As illustrated by today’s action, the FDA remains committed to expediting the development and availability of potential COVID-19 treatments and providing sick patients timely access to new therapies where appropriate,” FDA Commissioner Stephen M. Hahn, MD, said in the news release.
Healthcare providers can download a detailed FDA fact sheet on the EUA for bamlanivimab, which includes dosing instructions.
This article first appeared on Medscape.com.
FAST trial clears febuxostat of increased mortality in gout
Febuxostat (Uloric) emerged as noninferior to allopurinol regarding risk of cardiovascular death among people 60 years and older with gout and at least one additional cardiovascular risk factor, results of the Febuxostat versus Allopurinol Streamlined Trial (FAST) suggest.
This primary outcome of the FAST trial stands in contrast to results of the CARES trial in 2018. The CARES researchers previously reported a 4.3% increased risk of cardiovascular death associated with febuxostat, compared with a 3.2% rate with allopurinol, a statistically significant 34% increase in the relative risk.
“In contrast to previous studies, there was no evidence of increased mortality with febuxostat, and we believe the regulators should review febuxostat licensing restrictions,” senior author Thomas MacDonald, MD, of the University of Dundee (Scotland), said during a late-breaking abstract session at the virtual annual meeting of the American College of Rheumatology.
The results of the FAST trial were simultaneously published online in The Lancet.
Both febuxostat and allopurinol treat gout by lowering urate levels. Concerns about the cardiovascular safety of febuxostat led to two post-licensing studies: the Cardiovascular Safety of Febuxostat and Allopurinol in Participants with Gout and Cardiovascular Comorbidities (CARES) study, mandated by the U.S. Food and Drug Administration, and FAST, requested by the European Medicines Agency. In February 2019, the FDA added a warning about elevated cardiovascular death and death risk associated with febuxostat.
“When CARES was published, it was somewhat of a threat to our study,” Dr. MacDonald said. “After hearing from our data-monitoring committee, we were told we could continue the trial.”
Some switched from allopurinol to febuxostat
So Dr. MacDonald, lead author Isla Mackenzie, MBChB, and their colleagues enrolled 6,128 people with gout in the United Kingdom, Sweden, and Denmark between December 2011 and January 2018. They followed patients for a median of 4 years. Participants had a mean age of 71 years, 85% were men, and 33% had a history of cardiovascular disease. The investigators excluded anyone with a stroke or myocardial infarction in the previous 6 months.
All participants were being treated with allopurinol. The investigators titrated those not at target up to an ideal dose that achieved a serum urate concentration of less than 0.357 mmol/L (< 6 mg/dL). Next, they randomly assigned 3,065 people to continue allopurinol and another 3,063 to switch to 80-120 mg of febuxostat.
The primary outcome of the multicenter, prospective, randomized, open-label FAST trial was a composite of hospitalization for nonfatal MI or biomarker positive for acute coronary syndrome, nonfatal stroke, or cardiovascular death.
Key findings
“There was definitely a noninferior primary outcome,” Dr. MacDonald said. In the on-treatment analysis, 172 patients in the febuxostat group reached the composite endpoint versus 241 patients in the allopurinol group. There were 1.72 events per 100 patient-years in the febuxostat group versus 2.05 events in the allopurinol group (adjusted hazard ratio, 0.85; 95% confidence interval, 0.70-1.03). An intent-to-treat analysis also found that febuxostat was noninferior to allopurinol on this measure.
Urate levels were approximately 80 micromoles lower in the febuxostat group versus the allopurinol group each year of the study, Dr. MacDonald said.
At least one gout flare was experienced by 1,017 patients in the febuxostat group and by 1,044 participants in the allopurinol group. “However, there was no placebo group, so we don’t know the effectiveness of either of these agents at preventing flares” based on this research, he said.
Both the on-treatment and intention-to-treat (ITT) secondary analyses demonstrated the noninferiority of febuxostat, compared with allopurinol, for all-cause death, each individual component of the composite primary outcome – cardiovascular death, hospitalization for heart failure, and hospitalization for new, unstable, or worsening angina.
In contrast, the ITT analysis revealed a “nominally significant increase” in hospitalization for arrhythmia with no evidence of ischemia in the febuxostat group. The 0.583 events per 100 patient-years in this group versus 0.385 events in the allopurinol cohort generated an adjusted HR of 1.51 (95% CI, 1.05-2.17).
In terms of all-cause mortality, 222 participants (7.2%) in the febuxostat group died, compared with 263 people (8.6%) in the allopurinol group.
Adverse events and withdrawals
A total 1,720 participants (57.3%) in the febuxostat group experienced at least one serious adverse event, as did 1,812 participants (59.4%) in the allopurinol group. Less than 1% of serious adverse events in each group were considered treatment-related.
Dr. MacDonald said that 6.2% of the febuxostat patients and 5.5% of the allopurinol group withdrew from the study. “We had pretty good follow-up [94%],” Dr. MacDonald said. “I don’t want to criticize CARES, but 47% did drop out of that study, and they could not follow them anymore.”
Limitations of FAST include its open-label design and lack of a placebo group, although Dr. MacDonald pointed out that a placebo group would have been unethical. Strengths included its large randomized trial design and good external validity, he added. “This is what will happen in clinical practice if you switch people from allopurinol to febuxostat.”
When asked how he would treat people with gout now given the FAST findings, Dr. MacDonald said, “I’m not a rheumatologist, I’m a cardiovascular physician. But I would say from the evidence from the FAST trial, it appears to be safe to give patients febuxostat whether or not they have cardiovascular risk factors or prior cardiovascular disease.”
“The FAST study indicates that febuxostat is similar to allopurinol in terms of cardiovascular events during the treatment period. The strengths of this study are its large sample size, excellent follow-up rate, and the relatively long follow-up time,” session moderator Shervin Assassi, MD, said when asked for comment. Dr. Assassi, director of the division of rheumatology at the University of Texas Health Science Center at Houston, was not involved in the research.
Menarini, Ipsen, and Teijin Pharma funded the study. The University of Dundee receives research funds from Menarini. Dr. MacDonald disclosed that he received speaker or consultant fees from Menarini. Dr. Assassi had no relevant disclosures.
SOURCE: MacDonald T et al. Arthritis Rheumatol. 2020;72(suppl 10). ACR 2020, Abstract L08.
Febuxostat (Uloric) emerged as noninferior to allopurinol regarding risk of cardiovascular death among people 60 years and older with gout and at least one additional cardiovascular risk factor, results of the Febuxostat versus Allopurinol Streamlined Trial (FAST) suggest.
This primary outcome of the FAST trial stands in contrast to results of the CARES trial in 2018. The CARES researchers previously reported a 4.3% increased risk of cardiovascular death associated with febuxostat, compared with a 3.2% rate with allopurinol, a statistically significant 34% increase in the relative risk.
“In contrast to previous studies, there was no evidence of increased mortality with febuxostat, and we believe the regulators should review febuxostat licensing restrictions,” senior author Thomas MacDonald, MD, of the University of Dundee (Scotland), said during a late-breaking abstract session at the virtual annual meeting of the American College of Rheumatology.
The results of the FAST trial were simultaneously published online in The Lancet.
Both febuxostat and allopurinol treat gout by lowering urate levels. Concerns about the cardiovascular safety of febuxostat led to two post-licensing studies: the Cardiovascular Safety of Febuxostat and Allopurinol in Participants with Gout and Cardiovascular Comorbidities (CARES) study, mandated by the U.S. Food and Drug Administration, and FAST, requested by the European Medicines Agency. In February 2019, the FDA added a warning about elevated cardiovascular death and death risk associated with febuxostat.
“When CARES was published, it was somewhat of a threat to our study,” Dr. MacDonald said. “After hearing from our data-monitoring committee, we were told we could continue the trial.”
Some switched from allopurinol to febuxostat
So Dr. MacDonald, lead author Isla Mackenzie, MBChB, and their colleagues enrolled 6,128 people with gout in the United Kingdom, Sweden, and Denmark between December 2011 and January 2018. They followed patients for a median of 4 years. Participants had a mean age of 71 years, 85% were men, and 33% had a history of cardiovascular disease. The investigators excluded anyone with a stroke or myocardial infarction in the previous 6 months.
All participants were being treated with allopurinol. The investigators titrated those not at target up to an ideal dose that achieved a serum urate concentration of less than 0.357 mmol/L (< 6 mg/dL). Next, they randomly assigned 3,065 people to continue allopurinol and another 3,063 to switch to 80-120 mg of febuxostat.
The primary outcome of the multicenter, prospective, randomized, open-label FAST trial was a composite of hospitalization for nonfatal MI or biomarker positive for acute coronary syndrome, nonfatal stroke, or cardiovascular death.
Key findings
“There was definitely a noninferior primary outcome,” Dr. MacDonald said. In the on-treatment analysis, 172 patients in the febuxostat group reached the composite endpoint versus 241 patients in the allopurinol group. There were 1.72 events per 100 patient-years in the febuxostat group versus 2.05 events in the allopurinol group (adjusted hazard ratio, 0.85; 95% confidence interval, 0.70-1.03). An intent-to-treat analysis also found that febuxostat was noninferior to allopurinol on this measure.
Urate levels were approximately 80 micromoles lower in the febuxostat group versus the allopurinol group each year of the study, Dr. MacDonald said.
At least one gout flare was experienced by 1,017 patients in the febuxostat group and by 1,044 participants in the allopurinol group. “However, there was no placebo group, so we don’t know the effectiveness of either of these agents at preventing flares” based on this research, he said.
Both the on-treatment and intention-to-treat (ITT) secondary analyses demonstrated the noninferiority of febuxostat, compared with allopurinol, for all-cause death, each individual component of the composite primary outcome – cardiovascular death, hospitalization for heart failure, and hospitalization for new, unstable, or worsening angina.
In contrast, the ITT analysis revealed a “nominally significant increase” in hospitalization for arrhythmia with no evidence of ischemia in the febuxostat group. The 0.583 events per 100 patient-years in this group versus 0.385 events in the allopurinol cohort generated an adjusted HR of 1.51 (95% CI, 1.05-2.17).
In terms of all-cause mortality, 222 participants (7.2%) in the febuxostat group died, compared with 263 people (8.6%) in the allopurinol group.
Adverse events and withdrawals
A total 1,720 participants (57.3%) in the febuxostat group experienced at least one serious adverse event, as did 1,812 participants (59.4%) in the allopurinol group. Less than 1% of serious adverse events in each group were considered treatment-related.
Dr. MacDonald said that 6.2% of the febuxostat patients and 5.5% of the allopurinol group withdrew from the study. “We had pretty good follow-up [94%],” Dr. MacDonald said. “I don’t want to criticize CARES, but 47% did drop out of that study, and they could not follow them anymore.”
Limitations of FAST include its open-label design and lack of a placebo group, although Dr. MacDonald pointed out that a placebo group would have been unethical. Strengths included its large randomized trial design and good external validity, he added. “This is what will happen in clinical practice if you switch people from allopurinol to febuxostat.”
When asked how he would treat people with gout now given the FAST findings, Dr. MacDonald said, “I’m not a rheumatologist, I’m a cardiovascular physician. But I would say from the evidence from the FAST trial, it appears to be safe to give patients febuxostat whether or not they have cardiovascular risk factors or prior cardiovascular disease.”
“The FAST study indicates that febuxostat is similar to allopurinol in terms of cardiovascular events during the treatment period. The strengths of this study are its large sample size, excellent follow-up rate, and the relatively long follow-up time,” session moderator Shervin Assassi, MD, said when asked for comment. Dr. Assassi, director of the division of rheumatology at the University of Texas Health Science Center at Houston, was not involved in the research.
Menarini, Ipsen, and Teijin Pharma funded the study. The University of Dundee receives research funds from Menarini. Dr. MacDonald disclosed that he received speaker or consultant fees from Menarini. Dr. Assassi had no relevant disclosures.
SOURCE: MacDonald T et al. Arthritis Rheumatol. 2020;72(suppl 10). ACR 2020, Abstract L08.
Febuxostat (Uloric) emerged as noninferior to allopurinol regarding risk of cardiovascular death among people 60 years and older with gout and at least one additional cardiovascular risk factor, results of the Febuxostat versus Allopurinol Streamlined Trial (FAST) suggest.
This primary outcome of the FAST trial stands in contrast to results of the CARES trial in 2018. The CARES researchers previously reported a 4.3% increased risk of cardiovascular death associated with febuxostat, compared with a 3.2% rate with allopurinol, a statistically significant 34% increase in the relative risk.
“In contrast to previous studies, there was no evidence of increased mortality with febuxostat, and we believe the regulators should review febuxostat licensing restrictions,” senior author Thomas MacDonald, MD, of the University of Dundee (Scotland), said during a late-breaking abstract session at the virtual annual meeting of the American College of Rheumatology.
The results of the FAST trial were simultaneously published online in The Lancet.
Both febuxostat and allopurinol treat gout by lowering urate levels. Concerns about the cardiovascular safety of febuxostat led to two post-licensing studies: the Cardiovascular Safety of Febuxostat and Allopurinol in Participants with Gout and Cardiovascular Comorbidities (CARES) study, mandated by the U.S. Food and Drug Administration, and FAST, requested by the European Medicines Agency. In February 2019, the FDA added a warning about elevated cardiovascular death and death risk associated with febuxostat.
“When CARES was published, it was somewhat of a threat to our study,” Dr. MacDonald said. “After hearing from our data-monitoring committee, we were told we could continue the trial.”
Some switched from allopurinol to febuxostat
So Dr. MacDonald, lead author Isla Mackenzie, MBChB, and their colleagues enrolled 6,128 people with gout in the United Kingdom, Sweden, and Denmark between December 2011 and January 2018. They followed patients for a median of 4 years. Participants had a mean age of 71 years, 85% were men, and 33% had a history of cardiovascular disease. The investigators excluded anyone with a stroke or myocardial infarction in the previous 6 months.
All participants were being treated with allopurinol. The investigators titrated those not at target up to an ideal dose that achieved a serum urate concentration of less than 0.357 mmol/L (< 6 mg/dL). Next, they randomly assigned 3,065 people to continue allopurinol and another 3,063 to switch to 80-120 mg of febuxostat.
The primary outcome of the multicenter, prospective, randomized, open-label FAST trial was a composite of hospitalization for nonfatal MI or biomarker positive for acute coronary syndrome, nonfatal stroke, or cardiovascular death.
Key findings
“There was definitely a noninferior primary outcome,” Dr. MacDonald said. In the on-treatment analysis, 172 patients in the febuxostat group reached the composite endpoint versus 241 patients in the allopurinol group. There were 1.72 events per 100 patient-years in the febuxostat group versus 2.05 events in the allopurinol group (adjusted hazard ratio, 0.85; 95% confidence interval, 0.70-1.03). An intent-to-treat analysis also found that febuxostat was noninferior to allopurinol on this measure.
Urate levels were approximately 80 micromoles lower in the febuxostat group versus the allopurinol group each year of the study, Dr. MacDonald said.
At least one gout flare was experienced by 1,017 patients in the febuxostat group and by 1,044 participants in the allopurinol group. “However, there was no placebo group, so we don’t know the effectiveness of either of these agents at preventing flares” based on this research, he said.
Both the on-treatment and intention-to-treat (ITT) secondary analyses demonstrated the noninferiority of febuxostat, compared with allopurinol, for all-cause death, each individual component of the composite primary outcome – cardiovascular death, hospitalization for heart failure, and hospitalization for new, unstable, or worsening angina.
In contrast, the ITT analysis revealed a “nominally significant increase” in hospitalization for arrhythmia with no evidence of ischemia in the febuxostat group. The 0.583 events per 100 patient-years in this group versus 0.385 events in the allopurinol cohort generated an adjusted HR of 1.51 (95% CI, 1.05-2.17).
In terms of all-cause mortality, 222 participants (7.2%) in the febuxostat group died, compared with 263 people (8.6%) in the allopurinol group.
Adverse events and withdrawals
A total 1,720 participants (57.3%) in the febuxostat group experienced at least one serious adverse event, as did 1,812 participants (59.4%) in the allopurinol group. Less than 1% of serious adverse events in each group were considered treatment-related.
Dr. MacDonald said that 6.2% of the febuxostat patients and 5.5% of the allopurinol group withdrew from the study. “We had pretty good follow-up [94%],” Dr. MacDonald said. “I don’t want to criticize CARES, but 47% did drop out of that study, and they could not follow them anymore.”
Limitations of FAST include its open-label design and lack of a placebo group, although Dr. MacDonald pointed out that a placebo group would have been unethical. Strengths included its large randomized trial design and good external validity, he added. “This is what will happen in clinical practice if you switch people from allopurinol to febuxostat.”
When asked how he would treat people with gout now given the FAST findings, Dr. MacDonald said, “I’m not a rheumatologist, I’m a cardiovascular physician. But I would say from the evidence from the FAST trial, it appears to be safe to give patients febuxostat whether or not they have cardiovascular risk factors or prior cardiovascular disease.”
“The FAST study indicates that febuxostat is similar to allopurinol in terms of cardiovascular events during the treatment period. The strengths of this study are its large sample size, excellent follow-up rate, and the relatively long follow-up time,” session moderator Shervin Assassi, MD, said when asked for comment. Dr. Assassi, director of the division of rheumatology at the University of Texas Health Science Center at Houston, was not involved in the research.
Menarini, Ipsen, and Teijin Pharma funded the study. The University of Dundee receives research funds from Menarini. Dr. MacDonald disclosed that he received speaker or consultant fees from Menarini. Dr. Assassi had no relevant disclosures.
SOURCE: MacDonald T et al. Arthritis Rheumatol. 2020;72(suppl 10). ACR 2020, Abstract L08.
FROM ACR 2020
Study explores reasons for link between gastroparesis symptoms, constipation
Severe constipation affected 34% of adults with gastroparesis symptoms and showed a significant positive correlation with symptom severity in a multicenter prospective study.
Henry P. Parkman, MD, of Temple University in Philadelphia and his associates used a modified GI symptoms questionnaire, gastric-emptying scintigraphy, and wireless motility capsule studies of 338 participants in the National Institutes of Health Gastroparesis Registry, which enrolls individuals with gastroparesis symptoms (whether or not they have delayed gastric emptying). In the multivariable analysis, severe constipation (a score of 4 or 5 on a 5-point scale) correlated significantly with a higher score on the Gastroparesis Cardinal Symptoms Index (GCSI), with an odds ratio of 1.85 (95% confidence interval, 1.30-2.67). In addition, patients with gastroparesis symptoms were significantly more likely to report pain in the lower abdomen (OR, 1.34; 95% CI, 1.06-1.69) and to use medications to manage constipation (OR, 5.09; 95% CI, 2.75-9.41). The findings were published online in Clinical Gastroenterology and Hepatology.
Constipation was not significantly linked with the use of individual drug classes, including opiates, tricyclic antidepressants, 5HT3 receptor antagonists, or cannabinoids. However, many patients were taking combinations of medications, and it is unclear if these induced constipation or if patients had primary disorders, such as abnormal colonic motility or anorectal dysfunction, said Adil E. Bharucha, MBBS, MD, a professor of medicine in the gastroenterology and hepatology division and a medical director in the office of clinical trials at Mayo Clinic, Rochester, Minn., who was not involved in the study. For patients with gastroparesis and constipation, clinicians should consider withdrawing constipating medications, performing anorectal testing, and referring patients for pelvic floor biofeedback therapy if anorectal tests are positive, he said while acknowledging the need for more data on these approaches. For patients without evidence of anorectal disorders, he recommended “simple laxatives or, if necessary, prescription medications, some of which may also benefit upper gastrointestinal symptoms.”
In this study, constipation also did not correlate with gastric emptying, which suggests that “motility disturbances in the foregut are separable from those in the hindgut,” said David Levinthal, MD, PhD, director of the neurogastroenterology and motility center at the University of Pittsburgh Medical Center, who also was not involved in the work. Constipation was only marginally linked with colonic transit time (OR, 1.04; 95% CI, 1.00-1.07), and delayed gastric emptying did not predict the severity of dyspepsia, he noted. “These observations highlight that sensory mechanisms are very important factors that are not interrogated by physiological motility tests, but that nonetheless may have an outsized impact on how patients feel.”
Despite “fairly good phenotyping of patients [based on] physiological measures, medication use, and detailed symptom questionnaires,” the study’s method of grouping patients based on continuous variables could mask relevant clinical nuances, Dr. Levinthal said. He emphasized that individual physiological tests do not reliably predict the presence or severity of GI symptoms: “What would you make of a 50-hour colonic transit time [CTT]? Or a 60-hour CTT? One could have either no constipation or severe constipation with those values. In clinical practice, it is less certain how useful it is to know a specific CTT result [when] formulating a treatment plan.”
Therefore, future studies of patients with gastroparesis and constipation should forgo grouping patients based on GI motor patterns and instead validate patient-reported symptom measures by using novel sensory tests with stimuli such as eating, drinking, and balloon distension, Dr. Levinthal said. He also recommended studying cognitive and emotional functioning in this patients, given that conditions such as depression and anxiety are known to affect GI sensation.
The National Institute of Diabetes and Digestive and Kidney Diseases provided funding. The investigators reported having no conflicts of interest. Dr. Bharucha reported having filed patents for anorectal devices jointly with Minnesota Medical Technologies, Medspira, and Medtronic and receiving royalties from Medspira. Dr. Levinthal reported having served on advisory boards for Takeda Pharmaceuticals and Alexza Pharmaceuticals.
SOURCE: Parkman HP et al. Clin Gastroenterol Hepatol. 2020 Oct 28. doi: 10.1016/j.cgh.2020.10.045.
Severe constipation affected 34% of adults with gastroparesis symptoms and showed a significant positive correlation with symptom severity in a multicenter prospective study.
Henry P. Parkman, MD, of Temple University in Philadelphia and his associates used a modified GI symptoms questionnaire, gastric-emptying scintigraphy, and wireless motility capsule studies of 338 participants in the National Institutes of Health Gastroparesis Registry, which enrolls individuals with gastroparesis symptoms (whether or not they have delayed gastric emptying). In the multivariable analysis, severe constipation (a score of 4 or 5 on a 5-point scale) correlated significantly with a higher score on the Gastroparesis Cardinal Symptoms Index (GCSI), with an odds ratio of 1.85 (95% confidence interval, 1.30-2.67). In addition, patients with gastroparesis symptoms were significantly more likely to report pain in the lower abdomen (OR, 1.34; 95% CI, 1.06-1.69) and to use medications to manage constipation (OR, 5.09; 95% CI, 2.75-9.41). The findings were published online in Clinical Gastroenterology and Hepatology.
Constipation was not significantly linked with the use of individual drug classes, including opiates, tricyclic antidepressants, 5HT3 receptor antagonists, or cannabinoids. However, many patients were taking combinations of medications, and it is unclear if these induced constipation or if patients had primary disorders, such as abnormal colonic motility or anorectal dysfunction, said Adil E. Bharucha, MBBS, MD, a professor of medicine in the gastroenterology and hepatology division and a medical director in the office of clinical trials at Mayo Clinic, Rochester, Minn., who was not involved in the study. For patients with gastroparesis and constipation, clinicians should consider withdrawing constipating medications, performing anorectal testing, and referring patients for pelvic floor biofeedback therapy if anorectal tests are positive, he said while acknowledging the need for more data on these approaches. For patients without evidence of anorectal disorders, he recommended “simple laxatives or, if necessary, prescription medications, some of which may also benefit upper gastrointestinal symptoms.”
In this study, constipation also did not correlate with gastric emptying, which suggests that “motility disturbances in the foregut are separable from those in the hindgut,” said David Levinthal, MD, PhD, director of the neurogastroenterology and motility center at the University of Pittsburgh Medical Center, who also was not involved in the work. Constipation was only marginally linked with colonic transit time (OR, 1.04; 95% CI, 1.00-1.07), and delayed gastric emptying did not predict the severity of dyspepsia, he noted. “These observations highlight that sensory mechanisms are very important factors that are not interrogated by physiological motility tests, but that nonetheless may have an outsized impact on how patients feel.”
Despite “fairly good phenotyping of patients [based on] physiological measures, medication use, and detailed symptom questionnaires,” the study’s method of grouping patients based on continuous variables could mask relevant clinical nuances, Dr. Levinthal said. He emphasized that individual physiological tests do not reliably predict the presence or severity of GI symptoms: “What would you make of a 50-hour colonic transit time [CTT]? Or a 60-hour CTT? One could have either no constipation or severe constipation with those values. In clinical practice, it is less certain how useful it is to know a specific CTT result [when] formulating a treatment plan.”
Therefore, future studies of patients with gastroparesis and constipation should forgo grouping patients based on GI motor patterns and instead validate patient-reported symptom measures by using novel sensory tests with stimuli such as eating, drinking, and balloon distension, Dr. Levinthal said. He also recommended studying cognitive and emotional functioning in this patients, given that conditions such as depression and anxiety are known to affect GI sensation.
The National Institute of Diabetes and Digestive and Kidney Diseases provided funding. The investigators reported having no conflicts of interest. Dr. Bharucha reported having filed patents for anorectal devices jointly with Minnesota Medical Technologies, Medspira, and Medtronic and receiving royalties from Medspira. Dr. Levinthal reported having served on advisory boards for Takeda Pharmaceuticals and Alexza Pharmaceuticals.
SOURCE: Parkman HP et al. Clin Gastroenterol Hepatol. 2020 Oct 28. doi: 10.1016/j.cgh.2020.10.045.
Severe constipation affected 34% of adults with gastroparesis symptoms and showed a significant positive correlation with symptom severity in a multicenter prospective study.
Henry P. Parkman, MD, of Temple University in Philadelphia and his associates used a modified GI symptoms questionnaire, gastric-emptying scintigraphy, and wireless motility capsule studies of 338 participants in the National Institutes of Health Gastroparesis Registry, which enrolls individuals with gastroparesis symptoms (whether or not they have delayed gastric emptying). In the multivariable analysis, severe constipation (a score of 4 or 5 on a 5-point scale) correlated significantly with a higher score on the Gastroparesis Cardinal Symptoms Index (GCSI), with an odds ratio of 1.85 (95% confidence interval, 1.30-2.67). In addition, patients with gastroparesis symptoms were significantly more likely to report pain in the lower abdomen (OR, 1.34; 95% CI, 1.06-1.69) and to use medications to manage constipation (OR, 5.09; 95% CI, 2.75-9.41). The findings were published online in Clinical Gastroenterology and Hepatology.
Constipation was not significantly linked with the use of individual drug classes, including opiates, tricyclic antidepressants, 5HT3 receptor antagonists, or cannabinoids. However, many patients were taking combinations of medications, and it is unclear if these induced constipation or if patients had primary disorders, such as abnormal colonic motility or anorectal dysfunction, said Adil E. Bharucha, MBBS, MD, a professor of medicine in the gastroenterology and hepatology division and a medical director in the office of clinical trials at Mayo Clinic, Rochester, Minn., who was not involved in the study. For patients with gastroparesis and constipation, clinicians should consider withdrawing constipating medications, performing anorectal testing, and referring patients for pelvic floor biofeedback therapy if anorectal tests are positive, he said while acknowledging the need for more data on these approaches. For patients without evidence of anorectal disorders, he recommended “simple laxatives or, if necessary, prescription medications, some of which may also benefit upper gastrointestinal symptoms.”
In this study, constipation also did not correlate with gastric emptying, which suggests that “motility disturbances in the foregut are separable from those in the hindgut,” said David Levinthal, MD, PhD, director of the neurogastroenterology and motility center at the University of Pittsburgh Medical Center, who also was not involved in the work. Constipation was only marginally linked with colonic transit time (OR, 1.04; 95% CI, 1.00-1.07), and delayed gastric emptying did not predict the severity of dyspepsia, he noted. “These observations highlight that sensory mechanisms are very important factors that are not interrogated by physiological motility tests, but that nonetheless may have an outsized impact on how patients feel.”
Despite “fairly good phenotyping of patients [based on] physiological measures, medication use, and detailed symptom questionnaires,” the study’s method of grouping patients based on continuous variables could mask relevant clinical nuances, Dr. Levinthal said. He emphasized that individual physiological tests do not reliably predict the presence or severity of GI symptoms: “What would you make of a 50-hour colonic transit time [CTT]? Or a 60-hour CTT? One could have either no constipation or severe constipation with those values. In clinical practice, it is less certain how useful it is to know a specific CTT result [when] formulating a treatment plan.”
Therefore, future studies of patients with gastroparesis and constipation should forgo grouping patients based on GI motor patterns and instead validate patient-reported symptom measures by using novel sensory tests with stimuli such as eating, drinking, and balloon distension, Dr. Levinthal said. He also recommended studying cognitive and emotional functioning in this patients, given that conditions such as depression and anxiety are known to affect GI sensation.
The National Institute of Diabetes and Digestive and Kidney Diseases provided funding. The investigators reported having no conflicts of interest. Dr. Bharucha reported having filed patents for anorectal devices jointly with Minnesota Medical Technologies, Medspira, and Medtronic and receiving royalties from Medspira. Dr. Levinthal reported having served on advisory boards for Takeda Pharmaceuticals and Alexza Pharmaceuticals.
SOURCE: Parkman HP et al. Clin Gastroenterol Hepatol. 2020 Oct 28. doi: 10.1016/j.cgh.2020.10.045.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Triple combination therapy for cystic fibrosis linked to plunging hospitalizations
.
The triple combination therapy elexacaftor/tezacaftor/ivacaftor was associated with a near elimination of hospital stays in one hospital in Oregon, according to a new report. The hospital savings still weren’t nearly enough to pay for the cost of therapy, but the study underscores what many institutions have observed and adds a new layer to the view of quality of life improvements that the new therapy brings.
“After we started prescribing it, we noticed pretty quickly that hospitalizations appeared to be declining after patients started triple combination therapy, and we were hearing [similar reports] from other centers as well. We wanted to quantify this,” Eric C. Walter, MD, a pulmonologist at the Kaiser Permanente Cystic Fibrosis Clinic in Portland, Ore., said during a presentation of the results at the virtual North American Cystic Fibrosis Conference.
“We’re seeing that across the board in real practice, the number of cystic fibrosis patients that have to be hospitalized since starting this triple combination has gone down,” Robert Giusti, MD, said in an interview. “When they’ve had pulmonary exacerbations in the past, it was frequently because they failed outpatient antibiotics, but I think with triple combination therapy, if they do get sick, the likelihood is they will respond to oral antibiotics, so they may not need that prolonged IV course in the hospital.” Dr. Giusti is clinical professor of pediatrics at New York University and director of the Pediatric Cystic Fibrosis Center. He was not involved in the study.
The therapy gained Food and Drug Administration approval in 2019 for the treatment of individuals with CF who are aged 12 years and older, and who have at least one copy of the F508del mutation. Its cost is about $317,000 per year within the Kaiser Permanente system, according to Dr. Walter. His group compared hospitalization days for CF-related diagnoses from Jan. 1 through Aug. 31, 2020, before and after initiation of triple combination therapy.
Of 47 eligible patients, 32 initiated therapy during the study period; 38% had severe lung disease, defined by forced expiratory volume in 1 second (FEV1) value less than 40%. In 2020, before initiation of therapy, there were an average of 27 hospital days per month, all among patients with severe lung disease.
Among the therapy group, there were no hospitalizations after initiation of therapy through Aug. 31. Dr. Walter noted that the first hospitalization of a patient on triple combination therapy didn’t occur until early October.
At an average daily cost of $6,700, the researchers calculated that triple combination therapy saved about $189,000 per month in this group of patients. Comparing numbers to previous years, in which some patients with FEV1 greater than 40% were hospitalized, the researchers calculated that the therapy saved about $151,000 per month among individuals with severe lung disease: Patients with severe lung disease contributed about 80% to total hospital costs.
The drug itself for the whole group cost $845,000, dwarfing the $189,000 savings overall. But among patients with severe disease, hospitalization savings were about $151,000 per month, while the drug cost in this group was $316,800 per month.
Cost savings are important, but the improvement in quality of life for a patient – avoiding hospitalization, fewer impacts on work and education – should not be overlooked, according to Ryan Perkins, MD, a pediatric and adult pulmonary fellow at Boston Children’s Hospital and Brigham and Women’s Hospital, who moderated the session. “Some of these aren’t things people typically quantify and assign a price tag to,” Dr. Perkins said in an interview.
A big limitation of the work is that it was conducted during the COVID-19 pandemic, which may have reduced hospitalizations. “We did have patients that called in, told us they were sick, that they needed to be treated for an exacerbation but didn’t want to go to the hospital,” said Dr. Walter. To help adjust for this, Dr. Walter’s team plans to compare intravenous antibiotic exposure before and after triple combination therapy, reasoning that it could help clarify the pandemic’s impact on hospitalizations.
Dr. Walter, Dr. Giusti, and Dr. Perkins have no relevant financial disclosures.
SOURCE: Walter E et al. NACFC 2020. Abstract 795.
.
The triple combination therapy elexacaftor/tezacaftor/ivacaftor was associated with a near elimination of hospital stays in one hospital in Oregon, according to a new report. The hospital savings still weren’t nearly enough to pay for the cost of therapy, but the study underscores what many institutions have observed and adds a new layer to the view of quality of life improvements that the new therapy brings.
“After we started prescribing it, we noticed pretty quickly that hospitalizations appeared to be declining after patients started triple combination therapy, and we were hearing [similar reports] from other centers as well. We wanted to quantify this,” Eric C. Walter, MD, a pulmonologist at the Kaiser Permanente Cystic Fibrosis Clinic in Portland, Ore., said during a presentation of the results at the virtual North American Cystic Fibrosis Conference.
“We’re seeing that across the board in real practice, the number of cystic fibrosis patients that have to be hospitalized since starting this triple combination has gone down,” Robert Giusti, MD, said in an interview. “When they’ve had pulmonary exacerbations in the past, it was frequently because they failed outpatient antibiotics, but I think with triple combination therapy, if they do get sick, the likelihood is they will respond to oral antibiotics, so they may not need that prolonged IV course in the hospital.” Dr. Giusti is clinical professor of pediatrics at New York University and director of the Pediatric Cystic Fibrosis Center. He was not involved in the study.
The therapy gained Food and Drug Administration approval in 2019 for the treatment of individuals with CF who are aged 12 years and older, and who have at least one copy of the F508del mutation. Its cost is about $317,000 per year within the Kaiser Permanente system, according to Dr. Walter. His group compared hospitalization days for CF-related diagnoses from Jan. 1 through Aug. 31, 2020, before and after initiation of triple combination therapy.
Of 47 eligible patients, 32 initiated therapy during the study period; 38% had severe lung disease, defined by forced expiratory volume in 1 second (FEV1) value less than 40%. In 2020, before initiation of therapy, there were an average of 27 hospital days per month, all among patients with severe lung disease.
Among the therapy group, there were no hospitalizations after initiation of therapy through Aug. 31. Dr. Walter noted that the first hospitalization of a patient on triple combination therapy didn’t occur until early October.
At an average daily cost of $6,700, the researchers calculated that triple combination therapy saved about $189,000 per month in this group of patients. Comparing numbers to previous years, in which some patients with FEV1 greater than 40% were hospitalized, the researchers calculated that the therapy saved about $151,000 per month among individuals with severe lung disease: Patients with severe lung disease contributed about 80% to total hospital costs.
The drug itself for the whole group cost $845,000, dwarfing the $189,000 savings overall. But among patients with severe disease, hospitalization savings were about $151,000 per month, while the drug cost in this group was $316,800 per month.
Cost savings are important, but the improvement in quality of life for a patient – avoiding hospitalization, fewer impacts on work and education – should not be overlooked, according to Ryan Perkins, MD, a pediatric and adult pulmonary fellow at Boston Children’s Hospital and Brigham and Women’s Hospital, who moderated the session. “Some of these aren’t things people typically quantify and assign a price tag to,” Dr. Perkins said in an interview.
A big limitation of the work is that it was conducted during the COVID-19 pandemic, which may have reduced hospitalizations. “We did have patients that called in, told us they were sick, that they needed to be treated for an exacerbation but didn’t want to go to the hospital,” said Dr. Walter. To help adjust for this, Dr. Walter’s team plans to compare intravenous antibiotic exposure before and after triple combination therapy, reasoning that it could help clarify the pandemic’s impact on hospitalizations.
Dr. Walter, Dr. Giusti, and Dr. Perkins have no relevant financial disclosures.
SOURCE: Walter E et al. NACFC 2020. Abstract 795.
.
The triple combination therapy elexacaftor/tezacaftor/ivacaftor was associated with a near elimination of hospital stays in one hospital in Oregon, according to a new report. The hospital savings still weren’t nearly enough to pay for the cost of therapy, but the study underscores what many institutions have observed and adds a new layer to the view of quality of life improvements that the new therapy brings.
“After we started prescribing it, we noticed pretty quickly that hospitalizations appeared to be declining after patients started triple combination therapy, and we were hearing [similar reports] from other centers as well. We wanted to quantify this,” Eric C. Walter, MD, a pulmonologist at the Kaiser Permanente Cystic Fibrosis Clinic in Portland, Ore., said during a presentation of the results at the virtual North American Cystic Fibrosis Conference.
“We’re seeing that across the board in real practice, the number of cystic fibrosis patients that have to be hospitalized since starting this triple combination has gone down,” Robert Giusti, MD, said in an interview. “When they’ve had pulmonary exacerbations in the past, it was frequently because they failed outpatient antibiotics, but I think with triple combination therapy, if they do get sick, the likelihood is they will respond to oral antibiotics, so they may not need that prolonged IV course in the hospital.” Dr. Giusti is clinical professor of pediatrics at New York University and director of the Pediatric Cystic Fibrosis Center. He was not involved in the study.
The therapy gained Food and Drug Administration approval in 2019 for the treatment of individuals with CF who are aged 12 years and older, and who have at least one copy of the F508del mutation. Its cost is about $317,000 per year within the Kaiser Permanente system, according to Dr. Walter. His group compared hospitalization days for CF-related diagnoses from Jan. 1 through Aug. 31, 2020, before and after initiation of triple combination therapy.
Of 47 eligible patients, 32 initiated therapy during the study period; 38% had severe lung disease, defined by forced expiratory volume in 1 second (FEV1) value less than 40%. In 2020, before initiation of therapy, there were an average of 27 hospital days per month, all among patients with severe lung disease.
Among the therapy group, there were no hospitalizations after initiation of therapy through Aug. 31. Dr. Walter noted that the first hospitalization of a patient on triple combination therapy didn’t occur until early October.
At an average daily cost of $6,700, the researchers calculated that triple combination therapy saved about $189,000 per month in this group of patients. Comparing numbers to previous years, in which some patients with FEV1 greater than 40% were hospitalized, the researchers calculated that the therapy saved about $151,000 per month among individuals with severe lung disease: Patients with severe lung disease contributed about 80% to total hospital costs.
The drug itself for the whole group cost $845,000, dwarfing the $189,000 savings overall. But among patients with severe disease, hospitalization savings were about $151,000 per month, while the drug cost in this group was $316,800 per month.
Cost savings are important, but the improvement in quality of life for a patient – avoiding hospitalization, fewer impacts on work and education – should not be overlooked, according to Ryan Perkins, MD, a pediatric and adult pulmonary fellow at Boston Children’s Hospital and Brigham and Women’s Hospital, who moderated the session. “Some of these aren’t things people typically quantify and assign a price tag to,” Dr. Perkins said in an interview.
A big limitation of the work is that it was conducted during the COVID-19 pandemic, which may have reduced hospitalizations. “We did have patients that called in, told us they were sick, that they needed to be treated for an exacerbation but didn’t want to go to the hospital,” said Dr. Walter. To help adjust for this, Dr. Walter’s team plans to compare intravenous antibiotic exposure before and after triple combination therapy, reasoning that it could help clarify the pandemic’s impact on hospitalizations.
Dr. Walter, Dr. Giusti, and Dr. Perkins have no relevant financial disclosures.
SOURCE: Walter E et al. NACFC 2020. Abstract 795.
FROM NACFC 2020










