User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Three symptoms suggest higher risk for self-injury in cancer
, according to a Canadian study.
In a population-based, case-control study, each of these symptoms was associated with an increase of at least 60% in the risk for NFSI in the following 180 days, the investigators report.
“Clinicians should know that self-injury is a real problem after a cancer diagnosis,” lead investigator Julie Hallet, MD, an associate scientist at Sunnybrook Health Sciences Centre in Toronto, told this news organization.
Self-injury “does not necessarily represent an attempted suicide,” she added. “While our data do not allow us to know what the intent was, we know from other work that the repercussions of distress in patients with cancer are much broader than suicide. Self-injury can be a means to cope with psychological difficulties for some patients, without intent for suicide.”
The study was published online in JAMA Oncology.
Nine common symptoms
The study included adults who were diagnosed with cancer between Jan. 1, 2007, and March 31, 2019, and had completed the Edmonton Symptom Assessment System (ESAS) evaluation within 36 months of their index cancer diagnosis. ESAS evaluates nine common cancer-associated symptoms, including pain, tiredness, nausea, depression, anxiety, drowsiness, appetite, well-being, and shortness of breath, on a patient-reported scale of 0 (absence of symptom) to 10 (worst possible symptom).
The analysis included 406 patients who had visited an emergency department for an NFSI within 180 days of their ESAS evaluation, as well as 1,624 matched control patients with cancer who did not have an NFSI. Case patients and control patients were matched according to age at cancer diagnosis, sex, prior self-injury within 5 years of being diagnosed with cancer, and cancer type. Nonmatched covariates included psychiatric illness and therapy received before NFSI, comorbidity burden, material deprivation, and cancer stage.
Toward tailored intervention
A higher proportion of case patients than control patients reported moderate to severe scores for all nine ESAS symptoms. In an adjusted analysis, moderate to severe anxiety (odds ratio, 1.61), depression (OR, 1.66), and shortness of breath (OR, 1.65) were independently associated with higher odds of subsequent NFSI. Each 10-point increase in total ESAS score also was associated with increased risk (OR, 1.51).
“These findings are important to enhance the use of screening ESAS scores to better support patients,” say the authors. “Scores from ESAS assessments can be used to identify patients at higher risk of NFSI, indicating higher level of distress, and help direct tailored assessment and intervention.”
In prior work, Dr. Hallet’s group showed that NFSI occurs in 3 of every 1,000 patients with cancer. NFSI is more frequent among younger patients and those with a history of prior mental illness. “Identifying patients at risk in clinical practice requires you to inquire about a patient’s prior history, identify high symptom scores and ask about them, and trigger intervention pathways when risk is identified,” said Dr. Hallet.
“For example, a young patient with head and neck cancer and a prior history of mental illness who reports high scores for anxiety and drowsiness would be at high risk of self-injury,” she added. Such a patient should be referred to psycho-oncology, psychiatry, or social work. “To facilitate this, we are working on prognostic scores that can be integrated in clinical practice, such as an electronic medical record, to flag patients at risk,” said Dr. Hallet. “Future work will also need to identify the optimal care pathways for at-risk patients.”
Self-injury vs. suicidality
Commenting on the study for this news organization, Madeline Li, MD, PhD, a psychiatrist and clinician-scientist at Toronto’s Princess Margaret Cancer Centre, said that the findings are “underwhelming” because they tell us what is already known – that “NFSI is associated with distress, and cancer is a stressor.” It would have been more interesting to ask how to distinguish patients at risk for suicide from those at risk for self-harm without suicide, she added.
“The way these authors formulated NFSI included both self-harm intent and suicidal intent,” she explained. The researchers compared patients who were at risk for these two types of events with patients without NFSI. “When we see self-harm without suicidal intent in the emergency room, it’s mostly people making cries for help,” said Dr. Li. “These are people who cut their wrists or take small overdoses on purpose without the intent to die. It would have been more interesting to see if there are different risk factors for people who are just going to self-harm vs. those who are actually going to attempt suicide.”
The study’s identification of risk factors for NSFI is important because “it does tell us that when there’s anxiety, depression, and shortness of breath, we should pay attention to these patients and do something about it,” said Dr. Li. Still, research in cancer psychiatry needs to shift its focus from identifying and addressing existing risk factors to preventing them from developing, she added.
“We need to move earlier and provide emotional and mental health support to cancer patients to prevent them from becoming suicidal, rather than intervening when somebody already is,” Dr. Li concluded.
The study was funded by the Hanna Research Award from the division of surgical oncology at the Odette Cancer Centre–Sunnybrook Health Sciences Centre and by a Sunnybrook Health Sciences Centre Alternate Funding Plan Innovation grant. It was also supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. Dr. Hallet has received personal fees from Ipsen Biopharmaceuticals Canada and AAA outside the submitted work. Dr. Li reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to a Canadian study.
In a population-based, case-control study, each of these symptoms was associated with an increase of at least 60% in the risk for NFSI in the following 180 days, the investigators report.
“Clinicians should know that self-injury is a real problem after a cancer diagnosis,” lead investigator Julie Hallet, MD, an associate scientist at Sunnybrook Health Sciences Centre in Toronto, told this news organization.
Self-injury “does not necessarily represent an attempted suicide,” she added. “While our data do not allow us to know what the intent was, we know from other work that the repercussions of distress in patients with cancer are much broader than suicide. Self-injury can be a means to cope with psychological difficulties for some patients, without intent for suicide.”
The study was published online in JAMA Oncology.
Nine common symptoms
The study included adults who were diagnosed with cancer between Jan. 1, 2007, and March 31, 2019, and had completed the Edmonton Symptom Assessment System (ESAS) evaluation within 36 months of their index cancer diagnosis. ESAS evaluates nine common cancer-associated symptoms, including pain, tiredness, nausea, depression, anxiety, drowsiness, appetite, well-being, and shortness of breath, on a patient-reported scale of 0 (absence of symptom) to 10 (worst possible symptom).
The analysis included 406 patients who had visited an emergency department for an NFSI within 180 days of their ESAS evaluation, as well as 1,624 matched control patients with cancer who did not have an NFSI. Case patients and control patients were matched according to age at cancer diagnosis, sex, prior self-injury within 5 years of being diagnosed with cancer, and cancer type. Nonmatched covariates included psychiatric illness and therapy received before NFSI, comorbidity burden, material deprivation, and cancer stage.
Toward tailored intervention
A higher proportion of case patients than control patients reported moderate to severe scores for all nine ESAS symptoms. In an adjusted analysis, moderate to severe anxiety (odds ratio, 1.61), depression (OR, 1.66), and shortness of breath (OR, 1.65) were independently associated with higher odds of subsequent NFSI. Each 10-point increase in total ESAS score also was associated with increased risk (OR, 1.51).
“These findings are important to enhance the use of screening ESAS scores to better support patients,” say the authors. “Scores from ESAS assessments can be used to identify patients at higher risk of NFSI, indicating higher level of distress, and help direct tailored assessment and intervention.”
In prior work, Dr. Hallet’s group showed that NFSI occurs in 3 of every 1,000 patients with cancer. NFSI is more frequent among younger patients and those with a history of prior mental illness. “Identifying patients at risk in clinical practice requires you to inquire about a patient’s prior history, identify high symptom scores and ask about them, and trigger intervention pathways when risk is identified,” said Dr. Hallet.
“For example, a young patient with head and neck cancer and a prior history of mental illness who reports high scores for anxiety and drowsiness would be at high risk of self-injury,” she added. Such a patient should be referred to psycho-oncology, psychiatry, or social work. “To facilitate this, we are working on prognostic scores that can be integrated in clinical practice, such as an electronic medical record, to flag patients at risk,” said Dr. Hallet. “Future work will also need to identify the optimal care pathways for at-risk patients.”
Self-injury vs. suicidality
Commenting on the study for this news organization, Madeline Li, MD, PhD, a psychiatrist and clinician-scientist at Toronto’s Princess Margaret Cancer Centre, said that the findings are “underwhelming” because they tell us what is already known – that “NFSI is associated with distress, and cancer is a stressor.” It would have been more interesting to ask how to distinguish patients at risk for suicide from those at risk for self-harm without suicide, she added.
“The way these authors formulated NFSI included both self-harm intent and suicidal intent,” she explained. The researchers compared patients who were at risk for these two types of events with patients without NFSI. “When we see self-harm without suicidal intent in the emergency room, it’s mostly people making cries for help,” said Dr. Li. “These are people who cut their wrists or take small overdoses on purpose without the intent to die. It would have been more interesting to see if there are different risk factors for people who are just going to self-harm vs. those who are actually going to attempt suicide.”
The study’s identification of risk factors for NSFI is important because “it does tell us that when there’s anxiety, depression, and shortness of breath, we should pay attention to these patients and do something about it,” said Dr. Li. Still, research in cancer psychiatry needs to shift its focus from identifying and addressing existing risk factors to preventing them from developing, she added.
“We need to move earlier and provide emotional and mental health support to cancer patients to prevent them from becoming suicidal, rather than intervening when somebody already is,” Dr. Li concluded.
The study was funded by the Hanna Research Award from the division of surgical oncology at the Odette Cancer Centre–Sunnybrook Health Sciences Centre and by a Sunnybrook Health Sciences Centre Alternate Funding Plan Innovation grant. It was also supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. Dr. Hallet has received personal fees from Ipsen Biopharmaceuticals Canada and AAA outside the submitted work. Dr. Li reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to a Canadian study.
In a population-based, case-control study, each of these symptoms was associated with an increase of at least 60% in the risk for NFSI in the following 180 days, the investigators report.
“Clinicians should know that self-injury is a real problem after a cancer diagnosis,” lead investigator Julie Hallet, MD, an associate scientist at Sunnybrook Health Sciences Centre in Toronto, told this news organization.
Self-injury “does not necessarily represent an attempted suicide,” she added. “While our data do not allow us to know what the intent was, we know from other work that the repercussions of distress in patients with cancer are much broader than suicide. Self-injury can be a means to cope with psychological difficulties for some patients, without intent for suicide.”
The study was published online in JAMA Oncology.
Nine common symptoms
The study included adults who were diagnosed with cancer between Jan. 1, 2007, and March 31, 2019, and had completed the Edmonton Symptom Assessment System (ESAS) evaluation within 36 months of their index cancer diagnosis. ESAS evaluates nine common cancer-associated symptoms, including pain, tiredness, nausea, depression, anxiety, drowsiness, appetite, well-being, and shortness of breath, on a patient-reported scale of 0 (absence of symptom) to 10 (worst possible symptom).
The analysis included 406 patients who had visited an emergency department for an NFSI within 180 days of their ESAS evaluation, as well as 1,624 matched control patients with cancer who did not have an NFSI. Case patients and control patients were matched according to age at cancer diagnosis, sex, prior self-injury within 5 years of being diagnosed with cancer, and cancer type. Nonmatched covariates included psychiatric illness and therapy received before NFSI, comorbidity burden, material deprivation, and cancer stage.
Toward tailored intervention
A higher proportion of case patients than control patients reported moderate to severe scores for all nine ESAS symptoms. In an adjusted analysis, moderate to severe anxiety (odds ratio, 1.61), depression (OR, 1.66), and shortness of breath (OR, 1.65) were independently associated with higher odds of subsequent NFSI. Each 10-point increase in total ESAS score also was associated with increased risk (OR, 1.51).
“These findings are important to enhance the use of screening ESAS scores to better support patients,” say the authors. “Scores from ESAS assessments can be used to identify patients at higher risk of NFSI, indicating higher level of distress, and help direct tailored assessment and intervention.”
In prior work, Dr. Hallet’s group showed that NFSI occurs in 3 of every 1,000 patients with cancer. NFSI is more frequent among younger patients and those with a history of prior mental illness. “Identifying patients at risk in clinical practice requires you to inquire about a patient’s prior history, identify high symptom scores and ask about them, and trigger intervention pathways when risk is identified,” said Dr. Hallet.
“For example, a young patient with head and neck cancer and a prior history of mental illness who reports high scores for anxiety and drowsiness would be at high risk of self-injury,” she added. Such a patient should be referred to psycho-oncology, psychiatry, or social work. “To facilitate this, we are working on prognostic scores that can be integrated in clinical practice, such as an electronic medical record, to flag patients at risk,” said Dr. Hallet. “Future work will also need to identify the optimal care pathways for at-risk patients.”
Self-injury vs. suicidality
Commenting on the study for this news organization, Madeline Li, MD, PhD, a psychiatrist and clinician-scientist at Toronto’s Princess Margaret Cancer Centre, said that the findings are “underwhelming” because they tell us what is already known – that “NFSI is associated with distress, and cancer is a stressor.” It would have been more interesting to ask how to distinguish patients at risk for suicide from those at risk for self-harm without suicide, she added.
“The way these authors formulated NFSI included both self-harm intent and suicidal intent,” she explained. The researchers compared patients who were at risk for these two types of events with patients without NFSI. “When we see self-harm without suicidal intent in the emergency room, it’s mostly people making cries for help,” said Dr. Li. “These are people who cut their wrists or take small overdoses on purpose without the intent to die. It would have been more interesting to see if there are different risk factors for people who are just going to self-harm vs. those who are actually going to attempt suicide.”
The study’s identification of risk factors for NSFI is important because “it does tell us that when there’s anxiety, depression, and shortness of breath, we should pay attention to these patients and do something about it,” said Dr. Li. Still, research in cancer psychiatry needs to shift its focus from identifying and addressing existing risk factors to preventing them from developing, she added.
“We need to move earlier and provide emotional and mental health support to cancer patients to prevent them from becoming suicidal, rather than intervening when somebody already is,” Dr. Li concluded.
The study was funded by the Hanna Research Award from the division of surgical oncology at the Odette Cancer Centre–Sunnybrook Health Sciences Centre and by a Sunnybrook Health Sciences Centre Alternate Funding Plan Innovation grant. It was also supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. Dr. Hallet has received personal fees from Ipsen Biopharmaceuticals Canada and AAA outside the submitted work. Dr. Li reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA ONCOLOGY
How to address social determinants of health, according to expert panel
This patient is on prednisone for her RA because she can’t afford better drugs, and she has been occasionally skipping her insulin, Dr. Candler said during her presentation, at the annual meeting of the American College of Physicians
Plus, her first language is Turkish, and she’s missed many doctor appointments because she lives too far from the center-city clinics, said Dr. Candler, who is the care team medical director at Iora Primary Care in Houston.
How are this woman’s needs supposed to be met in a fee-for-service system that allows medical staff 15 to 30 minutes to help solve her problems?
Potential regulatory fixes
A panel of experts talked about potential policies and regulatory fixes that take into account the impact of “social determinants of health.” Some of these are gaining traction, but there is still a huge gap between how medicine in practiced in the United States and the health needs of people in the community, the panelists said.
The ACO REACH (Realizing Equity, Access and Community Health) model is a recent step forward, said Josh Liao, MD, MSc, associate chair for health systems at the University of Washington, Seattle. The accountable care organization model pays doctors more for caring for Medicare patients in underserved communities.
“To me, it represents that at least we’re moving in the direction where we’re acknowledging directly that social environment matters,” he said.
The American College of Physicians’ Medical Practice and Quality Committee helped improve payment for telehealth, an important step for equity to the underserved, said William Fox, MD, at Fox and Brantley Internal Medicine in Charlottesville, Va., and chair of the committee for ACP’s Virginia chapter. But many policies require much more work, he said.
One aim is getting to universal health coverage – 31 million people in the United States still don’t have health insurance, a number that is greatly improved since the Affordable Care Act but has plateaued recently.
Another is to invest more in primary care – which accounts for about 5% of spending even though 35% of patient visits are to primary care.
Dr. Fox said the U.S. system also needs to evolve beyond fee-for-service, invest in information technology to bridge the gap between the access for the rich and poor, continue to expand telehealth, and reform payment programs to recognize social factors.
“The current finance system and the quality payment program are focused on downstream impacts of poor health,” Dr. Fox said.
Primary care needs to shed the expectation that it must show that it reduces costs in order to be valued, he continued. Care sometimes is necessary but doesn’t reduce cost. Also, cost reduction is often seen in the long run, but studied only in the short term, and therefore the evidence for cost reduction can be elusive.
What can internists do to help?
Dr. Candler said internal medicine physicians can do their part by collecting data on patients and staff and measuring outcomes to identify disparities. Additionally, they could run their practices with community and cultural needs in mind, she said.
“Some of that might mean hiring differently. Think about it – if you’re in a position to start building new practices, go where they need you,” Dr. Candler explained. “It might mean a little bit more of a commute for you. But your patients are already doing that with their untreated cataracts, so who’s safer on the roads?”
George Abraham, MD, MPH – president of ACP and professor of medicine at the University of Massachusetts , Boston, who did not present in the session – suggested physicians should be looking at their own practice style, location, and the way their practice runs, and see where there are opportunities to be more in touch.
“I’m sure we all have practices where we have a diverse patient population,” he said. What doctors can do is to specifically focus on their minority population and ask: ‘What do they experience that others don’t experience as my patient coming into my office?’ he said.
Dr. Abraham, who received his medical degree in India and is ACP’s first president who is an international medical graduate, pointed to ACP’s emphasis on diversifying the internal medicine workforce to reflect the communities.
Recent measures have included the creation of an ACP international medical graduate task force and establishing an antiharassment policy and reporting process.
“The conversation has started a lot more,” he said.
Dr. Candler reports financial relationships with Abbott, AbbVie, Johnson & Johnson, Merck, Medtronic, Pfizer, and other companies. She is also a member of the editorial advisory board of Internal Medicine News. Dr. Fox reports financial relationships with Obagi Cosmeceuticals. Dr. Liao reports financial relationships with Eli Lilly, Gilead, Johnson & Johnson, Novavax, and other companies. Dr. Abraham reports no relevant financial relationships.
This patient is on prednisone for her RA because she can’t afford better drugs, and she has been occasionally skipping her insulin, Dr. Candler said during her presentation, at the annual meeting of the American College of Physicians
Plus, her first language is Turkish, and she’s missed many doctor appointments because she lives too far from the center-city clinics, said Dr. Candler, who is the care team medical director at Iora Primary Care in Houston.
How are this woman’s needs supposed to be met in a fee-for-service system that allows medical staff 15 to 30 minutes to help solve her problems?
Potential regulatory fixes
A panel of experts talked about potential policies and regulatory fixes that take into account the impact of “social determinants of health.” Some of these are gaining traction, but there is still a huge gap between how medicine in practiced in the United States and the health needs of people in the community, the panelists said.
The ACO REACH (Realizing Equity, Access and Community Health) model is a recent step forward, said Josh Liao, MD, MSc, associate chair for health systems at the University of Washington, Seattle. The accountable care organization model pays doctors more for caring for Medicare patients in underserved communities.
“To me, it represents that at least we’re moving in the direction where we’re acknowledging directly that social environment matters,” he said.
The American College of Physicians’ Medical Practice and Quality Committee helped improve payment for telehealth, an important step for equity to the underserved, said William Fox, MD, at Fox and Brantley Internal Medicine in Charlottesville, Va., and chair of the committee for ACP’s Virginia chapter. But many policies require much more work, he said.
One aim is getting to universal health coverage – 31 million people in the United States still don’t have health insurance, a number that is greatly improved since the Affordable Care Act but has plateaued recently.
Another is to invest more in primary care – which accounts for about 5% of spending even though 35% of patient visits are to primary care.
Dr. Fox said the U.S. system also needs to evolve beyond fee-for-service, invest in information technology to bridge the gap between the access for the rich and poor, continue to expand telehealth, and reform payment programs to recognize social factors.
“The current finance system and the quality payment program are focused on downstream impacts of poor health,” Dr. Fox said.
Primary care needs to shed the expectation that it must show that it reduces costs in order to be valued, he continued. Care sometimes is necessary but doesn’t reduce cost. Also, cost reduction is often seen in the long run, but studied only in the short term, and therefore the evidence for cost reduction can be elusive.
What can internists do to help?
Dr. Candler said internal medicine physicians can do their part by collecting data on patients and staff and measuring outcomes to identify disparities. Additionally, they could run their practices with community and cultural needs in mind, she said.
“Some of that might mean hiring differently. Think about it – if you’re in a position to start building new practices, go where they need you,” Dr. Candler explained. “It might mean a little bit more of a commute for you. But your patients are already doing that with their untreated cataracts, so who’s safer on the roads?”
George Abraham, MD, MPH – president of ACP and professor of medicine at the University of Massachusetts , Boston, who did not present in the session – suggested physicians should be looking at their own practice style, location, and the way their practice runs, and see where there are opportunities to be more in touch.
“I’m sure we all have practices where we have a diverse patient population,” he said. What doctors can do is to specifically focus on their minority population and ask: ‘What do they experience that others don’t experience as my patient coming into my office?’ he said.
Dr. Abraham, who received his medical degree in India and is ACP’s first president who is an international medical graduate, pointed to ACP’s emphasis on diversifying the internal medicine workforce to reflect the communities.
Recent measures have included the creation of an ACP international medical graduate task force and establishing an antiharassment policy and reporting process.
“The conversation has started a lot more,” he said.
Dr. Candler reports financial relationships with Abbott, AbbVie, Johnson & Johnson, Merck, Medtronic, Pfizer, and other companies. She is also a member of the editorial advisory board of Internal Medicine News. Dr. Fox reports financial relationships with Obagi Cosmeceuticals. Dr. Liao reports financial relationships with Eli Lilly, Gilead, Johnson & Johnson, Novavax, and other companies. Dr. Abraham reports no relevant financial relationships.
This patient is on prednisone for her RA because she can’t afford better drugs, and she has been occasionally skipping her insulin, Dr. Candler said during her presentation, at the annual meeting of the American College of Physicians
Plus, her first language is Turkish, and she’s missed many doctor appointments because she lives too far from the center-city clinics, said Dr. Candler, who is the care team medical director at Iora Primary Care in Houston.
How are this woman’s needs supposed to be met in a fee-for-service system that allows medical staff 15 to 30 minutes to help solve her problems?
Potential regulatory fixes
A panel of experts talked about potential policies and regulatory fixes that take into account the impact of “social determinants of health.” Some of these are gaining traction, but there is still a huge gap between how medicine in practiced in the United States and the health needs of people in the community, the panelists said.
The ACO REACH (Realizing Equity, Access and Community Health) model is a recent step forward, said Josh Liao, MD, MSc, associate chair for health systems at the University of Washington, Seattle. The accountable care organization model pays doctors more for caring for Medicare patients in underserved communities.
“To me, it represents that at least we’re moving in the direction where we’re acknowledging directly that social environment matters,” he said.
The American College of Physicians’ Medical Practice and Quality Committee helped improve payment for telehealth, an important step for equity to the underserved, said William Fox, MD, at Fox and Brantley Internal Medicine in Charlottesville, Va., and chair of the committee for ACP’s Virginia chapter. But many policies require much more work, he said.
One aim is getting to universal health coverage – 31 million people in the United States still don’t have health insurance, a number that is greatly improved since the Affordable Care Act but has plateaued recently.
Another is to invest more in primary care – which accounts for about 5% of spending even though 35% of patient visits are to primary care.
Dr. Fox said the U.S. system also needs to evolve beyond fee-for-service, invest in information technology to bridge the gap between the access for the rich and poor, continue to expand telehealth, and reform payment programs to recognize social factors.
“The current finance system and the quality payment program are focused on downstream impacts of poor health,” Dr. Fox said.
Primary care needs to shed the expectation that it must show that it reduces costs in order to be valued, he continued. Care sometimes is necessary but doesn’t reduce cost. Also, cost reduction is often seen in the long run, but studied only in the short term, and therefore the evidence for cost reduction can be elusive.
What can internists do to help?
Dr. Candler said internal medicine physicians can do their part by collecting data on patients and staff and measuring outcomes to identify disparities. Additionally, they could run their practices with community and cultural needs in mind, she said.
“Some of that might mean hiring differently. Think about it – if you’re in a position to start building new practices, go where they need you,” Dr. Candler explained. “It might mean a little bit more of a commute for you. But your patients are already doing that with their untreated cataracts, so who’s safer on the roads?”
George Abraham, MD, MPH – president of ACP and professor of medicine at the University of Massachusetts , Boston, who did not present in the session – suggested physicians should be looking at their own practice style, location, and the way their practice runs, and see where there are opportunities to be more in touch.
“I’m sure we all have practices where we have a diverse patient population,” he said. What doctors can do is to specifically focus on their minority population and ask: ‘What do they experience that others don’t experience as my patient coming into my office?’ he said.
Dr. Abraham, who received his medical degree in India and is ACP’s first president who is an international medical graduate, pointed to ACP’s emphasis on diversifying the internal medicine workforce to reflect the communities.
Recent measures have included the creation of an ACP international medical graduate task force and establishing an antiharassment policy and reporting process.
“The conversation has started a lot more,” he said.
Dr. Candler reports financial relationships with Abbott, AbbVie, Johnson & Johnson, Merck, Medtronic, Pfizer, and other companies. She is also a member of the editorial advisory board of Internal Medicine News. Dr. Fox reports financial relationships with Obagi Cosmeceuticals. Dr. Liao reports financial relationships with Eli Lilly, Gilead, Johnson & Johnson, Novavax, and other companies. Dr. Abraham reports no relevant financial relationships.
AT INTERNAL MEDICINE 2022
Long-COVID symptoms a serious challenge for older patients, physicians
Even mundane tasks such as making a meal can be exhausting for Louise Salant.
“I’m totally wiped out,” said the 71-year-old former private music instructor with asthma who lives in New York City and has been coping with debilitating symptoms of fatigue, shortness of breath, and gastrointestinal symptoms since recovering from a severe bout of COVID-19 2 years ago. “I just don’t have the energy.”
Ms. Salant is not alone. Many older people who contract COVID-19 experience prolonged symptoms of the disease. An analysis of Medicare Advantage claims data published in the BMJ found that about one-third of roughly 87,000 adults aged 65 in the database with a COVID-19 diagnosis sought care for persistent or new symptoms 21 or more days later.
That figure is about twice the rate of persistent COVID-19 related symptoms seen in a cohort of adults younger than age 65 with commercial insurance analyzed by the same group of researchers in a separate BMJ study. Compared with a 2020 comparator group of patients in this age cohort, these patients had a greater likelihood of respiratory failure, fatigue, hypertension, memory problems, kidney injury, mental health conditions, hypercoagulability, and cardiac rhythm disorders. When they compared post–COVID-19 symptoms to lasting symptoms of another serious viral disease – influenza – the researchers found that only respiratory failure, dementia, and post-viral fatigue were more common in the COVID-19 group.
“It became clear early in the pandemic that there is going to be a second pandemic related to all of the complications that we’ve seen related to COVID-19 infections,” said Ken Cohen, MD, executive director of translational research and national senior medical director for Optum Labs in Minnetonka, Minn., who coauthored the BMJ studies.
The results are among a growing body of evidence suggesting that older adults are at high risk of persistent post-COVID-19 symptoms.
Researchers in Rome, for example, found that 83% of 165 patients aged 65 or older who had been hospitalized for COVID-19 reported at least one lasting symptom – problems like fatigue, shortness of breath, joint pain, and coughing – in the months after hospitalization. One-third of those had two symptoms, and 46% had three or more.
A similar study in Norway found that two-thirds of patients aged 60 or older reported reduced health-related quality of life during follow-up visits 6 months after hospitalization for COVID-19. The most-reported impairments among those patients were the inability to perform the tasks of daily life, reduced mobility, and increased pain and discomfort.
Cognitive concerns
Mounting evidence indicates that COVID-19 may contribute to chronic cognitive impairment in older adults. A multisite U.S. study found that 28% of 817 adults presenting to emergency departments with COVID-19 had delirium and poorer outcomes. A Chinese case-control study that enrolled 1,438 individuals hospitalized in Wuhan for COVID-19, along with 438 of their uninfected spouses, found that 12% of COVID-19 survivors experienced cognitive impairment a year after discharge. Matteo Tosato, MD, PhD, head of the outpatient clinic for patients with long COVID symptoms at Gemelli Hospital in Rome, called those findings “very concerning.”
Jin Ho Han, MD, associate professor of emergency medicine at Vanderbilt University, Nashville, Tenn., said cognitive impairment is common after an acute illness, particularly in frail or vulnerable patients.
“Hospitalization and the acute illness itself accelerate cognitive decline,” said Dr. Han, and previous evidence links delirium with worsening cognition. He and his colleagues are studying the potential role of delirium in longer-term cognitive decline in older patients after COVID-19.
Dr. Han emphasized the importance of preventing COVID-19-related delirium through vaccines and other strategies to reduce exposure of older patients to the virus. “Once you have cognitive decline, there are no interventions to reverse it,” he said.
Alarm bells for long-term care
Experts expressed concern that the situation might be even worse for people living in long-term care facilities. Many already need assistance with tasks of daily living and could be particularly vulnerable to lasting effects of COVID-19, said Karl Steinberg, MD, president of the Society for Post-Acute and Long-Term Care Medicine. He estimated that roughly half of his patients who have had COVID-19, regardless of the severity of their symptoms, have endured some degree of functional decline.
“It’s common for long-term care facility residents to experience functional and cognitive decline, even after seemingly minor things, like a cold or a trip to the hospital,” Dr. Steinberg, who has been a medical director of long-term care facilities in San Diego County for more than 2 decades, told this news organization. “It makes it a little harder to determine whether the declines we’ve been seeing post COVID in these residents are attributable to post COVID versus just an accelerated step in their overall expected decline.”
The pandemic may have contributed to worse outcomes for people in long-term care facilities in several ways: the disease itself, its effects on health care delivery, and necessary preventive measures to protect long-term care residents from exposure to the virus.
“During the many months where family visits were prohibited, we saw people – whether they had COVID-19 or not – suffer major clinical, functional, cognitive declines or severe psychological symptoms,” Dr. Steinberg said.
He emphasized the importance of preventive measures such as vaccines and boosters in patients in long-term care facilities. He said the benefit of preventing lasting symptoms is often a strong motivator for family caregivers of people with dementia to get them vaccinated or boosted.
“It’s clear that vaccination and booster reduce the incidence of post-COVID symptoms,” he said. Almost all studies have been in younger cohorts, but he expects the benefits would also apply to older patients.
Easing symptoms and offering support
As with long COVID generally, many questions remain about the causes of lasting symptoms of COVID-19 in older patients, and how best to treat them. Dr. Tosato, who led the study of long-COVID patients in Rome, is focusing on inflammation as a critical factor in the condition. He and colleagues across Europe hope to answer some of them by launching a multicenter study of lasting COVID-19 symptoms.
In the meantime, Dr. Steinberg and Dr. Tosato said they are doing their best to evaluate and treat patients empirically.
“We pull from our armamentarium to treat system-specific symptoms,” Dr. Steinberg said. “We want to improve the quality of life and help each day be the best it can.”
Physicians in long-term care facilities might use medications such as antidepressants or nonpharmacologic approaches for patients experiencing depression symptoms. Families are also crucial in helping patients by bringing in home-cooked meals and encouraging loved ones who may be experiencing loss of taste or smell to eat, Dr. Steinberg said.
“We’ve seen with the return of families and loved ones visiting to some extent has alleviated some people’s symptoms, especially psychological ones,” he said.
Dr. Tosato said he and his colleagues start with an individualized, multidisciplinary assessment to determine what types of care may help. He noted that physicians might recommend medications or rehabilitative therapies depending on the patient’s needs.
“A personalized approach is key,” Dr. Tosato said. His study also found that the proportion of older patients experiencing symptoms declined over time – a glimmer of hope that many will recover.
Dr. Cohen emphasized the need for a multimodal rehabilitation, an evidence-based approach used to care for patients who survived hospitalization with severe COVID-19 – a group that has substantially higher rates of persistent symptoms. This approach includes cognitive rehabilitation, physical therapy, occupational therapy, and a graded exercise program.
Dr. Han and colleagues are studying potential therapies such as cognitive rehabilitation in adults who’ve experienced delirium. But until evidence-based treatments are available, they stress the role of support for patients with cognitive decline and their families.
“A lot of the work we do is teach patients and their families to compensate for newly acquired cognitive deficits from any illness, including COVID-19,” Dr. Han said.
Ms. Salant said she has experienced some improvement in her energy since her pulmonologist recommended a new inhaler based on her symptoms. Her sense of smell and taste, lost to the infection, returned after she received her first dose of a vaccine against COVID-19. She takes comfort in participating in Survivor Corps, a group of more than 170,000 COVID-19 survivors and their families who advocate for more scientific research on the disease.
She also expressed gratitude for the support she receives from her primary care physician, who she said has taken the time to learn more about the symptoms of long COVID, listens to her, and respects what she has to say.
“I have hope that I will keep getting better by baby steps,” Ms. Salant said.
Dr. Tosato, Dr. Steinberg, and Dr. Han have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Even mundane tasks such as making a meal can be exhausting for Louise Salant.
“I’m totally wiped out,” said the 71-year-old former private music instructor with asthma who lives in New York City and has been coping with debilitating symptoms of fatigue, shortness of breath, and gastrointestinal symptoms since recovering from a severe bout of COVID-19 2 years ago. “I just don’t have the energy.”
Ms. Salant is not alone. Many older people who contract COVID-19 experience prolonged symptoms of the disease. An analysis of Medicare Advantage claims data published in the BMJ found that about one-third of roughly 87,000 adults aged 65 in the database with a COVID-19 diagnosis sought care for persistent or new symptoms 21 or more days later.
That figure is about twice the rate of persistent COVID-19 related symptoms seen in a cohort of adults younger than age 65 with commercial insurance analyzed by the same group of researchers in a separate BMJ study. Compared with a 2020 comparator group of patients in this age cohort, these patients had a greater likelihood of respiratory failure, fatigue, hypertension, memory problems, kidney injury, mental health conditions, hypercoagulability, and cardiac rhythm disorders. When they compared post–COVID-19 symptoms to lasting symptoms of another serious viral disease – influenza – the researchers found that only respiratory failure, dementia, and post-viral fatigue were more common in the COVID-19 group.
“It became clear early in the pandemic that there is going to be a second pandemic related to all of the complications that we’ve seen related to COVID-19 infections,” said Ken Cohen, MD, executive director of translational research and national senior medical director for Optum Labs in Minnetonka, Minn., who coauthored the BMJ studies.
The results are among a growing body of evidence suggesting that older adults are at high risk of persistent post-COVID-19 symptoms.
Researchers in Rome, for example, found that 83% of 165 patients aged 65 or older who had been hospitalized for COVID-19 reported at least one lasting symptom – problems like fatigue, shortness of breath, joint pain, and coughing – in the months after hospitalization. One-third of those had two symptoms, and 46% had three or more.
A similar study in Norway found that two-thirds of patients aged 60 or older reported reduced health-related quality of life during follow-up visits 6 months after hospitalization for COVID-19. The most-reported impairments among those patients were the inability to perform the tasks of daily life, reduced mobility, and increased pain and discomfort.
Cognitive concerns
Mounting evidence indicates that COVID-19 may contribute to chronic cognitive impairment in older adults. A multisite U.S. study found that 28% of 817 adults presenting to emergency departments with COVID-19 had delirium and poorer outcomes. A Chinese case-control study that enrolled 1,438 individuals hospitalized in Wuhan for COVID-19, along with 438 of their uninfected spouses, found that 12% of COVID-19 survivors experienced cognitive impairment a year after discharge. Matteo Tosato, MD, PhD, head of the outpatient clinic for patients with long COVID symptoms at Gemelli Hospital in Rome, called those findings “very concerning.”
Jin Ho Han, MD, associate professor of emergency medicine at Vanderbilt University, Nashville, Tenn., said cognitive impairment is common after an acute illness, particularly in frail or vulnerable patients.
“Hospitalization and the acute illness itself accelerate cognitive decline,” said Dr. Han, and previous evidence links delirium with worsening cognition. He and his colleagues are studying the potential role of delirium in longer-term cognitive decline in older patients after COVID-19.
Dr. Han emphasized the importance of preventing COVID-19-related delirium through vaccines and other strategies to reduce exposure of older patients to the virus. “Once you have cognitive decline, there are no interventions to reverse it,” he said.
Alarm bells for long-term care
Experts expressed concern that the situation might be even worse for people living in long-term care facilities. Many already need assistance with tasks of daily living and could be particularly vulnerable to lasting effects of COVID-19, said Karl Steinberg, MD, president of the Society for Post-Acute and Long-Term Care Medicine. He estimated that roughly half of his patients who have had COVID-19, regardless of the severity of their symptoms, have endured some degree of functional decline.
“It’s common for long-term care facility residents to experience functional and cognitive decline, even after seemingly minor things, like a cold or a trip to the hospital,” Dr. Steinberg, who has been a medical director of long-term care facilities in San Diego County for more than 2 decades, told this news organization. “It makes it a little harder to determine whether the declines we’ve been seeing post COVID in these residents are attributable to post COVID versus just an accelerated step in their overall expected decline.”
The pandemic may have contributed to worse outcomes for people in long-term care facilities in several ways: the disease itself, its effects on health care delivery, and necessary preventive measures to protect long-term care residents from exposure to the virus.
“During the many months where family visits were prohibited, we saw people – whether they had COVID-19 or not – suffer major clinical, functional, cognitive declines or severe psychological symptoms,” Dr. Steinberg said.
He emphasized the importance of preventive measures such as vaccines and boosters in patients in long-term care facilities. He said the benefit of preventing lasting symptoms is often a strong motivator for family caregivers of people with dementia to get them vaccinated or boosted.
“It’s clear that vaccination and booster reduce the incidence of post-COVID symptoms,” he said. Almost all studies have been in younger cohorts, but he expects the benefits would also apply to older patients.
Easing symptoms and offering support
As with long COVID generally, many questions remain about the causes of lasting symptoms of COVID-19 in older patients, and how best to treat them. Dr. Tosato, who led the study of long-COVID patients in Rome, is focusing on inflammation as a critical factor in the condition. He and colleagues across Europe hope to answer some of them by launching a multicenter study of lasting COVID-19 symptoms.
In the meantime, Dr. Steinberg and Dr. Tosato said they are doing their best to evaluate and treat patients empirically.
“We pull from our armamentarium to treat system-specific symptoms,” Dr. Steinberg said. “We want to improve the quality of life and help each day be the best it can.”
Physicians in long-term care facilities might use medications such as antidepressants or nonpharmacologic approaches for patients experiencing depression symptoms. Families are also crucial in helping patients by bringing in home-cooked meals and encouraging loved ones who may be experiencing loss of taste or smell to eat, Dr. Steinberg said.
“We’ve seen with the return of families and loved ones visiting to some extent has alleviated some people’s symptoms, especially psychological ones,” he said.
Dr. Tosato said he and his colleagues start with an individualized, multidisciplinary assessment to determine what types of care may help. He noted that physicians might recommend medications or rehabilitative therapies depending on the patient’s needs.
“A personalized approach is key,” Dr. Tosato said. His study also found that the proportion of older patients experiencing symptoms declined over time – a glimmer of hope that many will recover.
Dr. Cohen emphasized the need for a multimodal rehabilitation, an evidence-based approach used to care for patients who survived hospitalization with severe COVID-19 – a group that has substantially higher rates of persistent symptoms. This approach includes cognitive rehabilitation, physical therapy, occupational therapy, and a graded exercise program.
Dr. Han and colleagues are studying potential therapies such as cognitive rehabilitation in adults who’ve experienced delirium. But until evidence-based treatments are available, they stress the role of support for patients with cognitive decline and their families.
“A lot of the work we do is teach patients and their families to compensate for newly acquired cognitive deficits from any illness, including COVID-19,” Dr. Han said.
Ms. Salant said she has experienced some improvement in her energy since her pulmonologist recommended a new inhaler based on her symptoms. Her sense of smell and taste, lost to the infection, returned after she received her first dose of a vaccine against COVID-19. She takes comfort in participating in Survivor Corps, a group of more than 170,000 COVID-19 survivors and their families who advocate for more scientific research on the disease.
She also expressed gratitude for the support she receives from her primary care physician, who she said has taken the time to learn more about the symptoms of long COVID, listens to her, and respects what she has to say.
“I have hope that I will keep getting better by baby steps,” Ms. Salant said.
Dr. Tosato, Dr. Steinberg, and Dr. Han have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Even mundane tasks such as making a meal can be exhausting for Louise Salant.
“I’m totally wiped out,” said the 71-year-old former private music instructor with asthma who lives in New York City and has been coping with debilitating symptoms of fatigue, shortness of breath, and gastrointestinal symptoms since recovering from a severe bout of COVID-19 2 years ago. “I just don’t have the energy.”
Ms. Salant is not alone. Many older people who contract COVID-19 experience prolonged symptoms of the disease. An analysis of Medicare Advantage claims data published in the BMJ found that about one-third of roughly 87,000 adults aged 65 in the database with a COVID-19 diagnosis sought care for persistent or new symptoms 21 or more days later.
That figure is about twice the rate of persistent COVID-19 related symptoms seen in a cohort of adults younger than age 65 with commercial insurance analyzed by the same group of researchers in a separate BMJ study. Compared with a 2020 comparator group of patients in this age cohort, these patients had a greater likelihood of respiratory failure, fatigue, hypertension, memory problems, kidney injury, mental health conditions, hypercoagulability, and cardiac rhythm disorders. When they compared post–COVID-19 symptoms to lasting symptoms of another serious viral disease – influenza – the researchers found that only respiratory failure, dementia, and post-viral fatigue were more common in the COVID-19 group.
“It became clear early in the pandemic that there is going to be a second pandemic related to all of the complications that we’ve seen related to COVID-19 infections,” said Ken Cohen, MD, executive director of translational research and national senior medical director for Optum Labs in Minnetonka, Minn., who coauthored the BMJ studies.
The results are among a growing body of evidence suggesting that older adults are at high risk of persistent post-COVID-19 symptoms.
Researchers in Rome, for example, found that 83% of 165 patients aged 65 or older who had been hospitalized for COVID-19 reported at least one lasting symptom – problems like fatigue, shortness of breath, joint pain, and coughing – in the months after hospitalization. One-third of those had two symptoms, and 46% had three or more.
A similar study in Norway found that two-thirds of patients aged 60 or older reported reduced health-related quality of life during follow-up visits 6 months after hospitalization for COVID-19. The most-reported impairments among those patients were the inability to perform the tasks of daily life, reduced mobility, and increased pain and discomfort.
Cognitive concerns
Mounting evidence indicates that COVID-19 may contribute to chronic cognitive impairment in older adults. A multisite U.S. study found that 28% of 817 adults presenting to emergency departments with COVID-19 had delirium and poorer outcomes. A Chinese case-control study that enrolled 1,438 individuals hospitalized in Wuhan for COVID-19, along with 438 of their uninfected spouses, found that 12% of COVID-19 survivors experienced cognitive impairment a year after discharge. Matteo Tosato, MD, PhD, head of the outpatient clinic for patients with long COVID symptoms at Gemelli Hospital in Rome, called those findings “very concerning.”
Jin Ho Han, MD, associate professor of emergency medicine at Vanderbilt University, Nashville, Tenn., said cognitive impairment is common after an acute illness, particularly in frail or vulnerable patients.
“Hospitalization and the acute illness itself accelerate cognitive decline,” said Dr. Han, and previous evidence links delirium with worsening cognition. He and his colleagues are studying the potential role of delirium in longer-term cognitive decline in older patients after COVID-19.
Dr. Han emphasized the importance of preventing COVID-19-related delirium through vaccines and other strategies to reduce exposure of older patients to the virus. “Once you have cognitive decline, there are no interventions to reverse it,” he said.
Alarm bells for long-term care
Experts expressed concern that the situation might be even worse for people living in long-term care facilities. Many already need assistance with tasks of daily living and could be particularly vulnerable to lasting effects of COVID-19, said Karl Steinberg, MD, president of the Society for Post-Acute and Long-Term Care Medicine. He estimated that roughly half of his patients who have had COVID-19, regardless of the severity of their symptoms, have endured some degree of functional decline.
“It’s common for long-term care facility residents to experience functional and cognitive decline, even after seemingly minor things, like a cold or a trip to the hospital,” Dr. Steinberg, who has been a medical director of long-term care facilities in San Diego County for more than 2 decades, told this news organization. “It makes it a little harder to determine whether the declines we’ve been seeing post COVID in these residents are attributable to post COVID versus just an accelerated step in their overall expected decline.”
The pandemic may have contributed to worse outcomes for people in long-term care facilities in several ways: the disease itself, its effects on health care delivery, and necessary preventive measures to protect long-term care residents from exposure to the virus.
“During the many months where family visits were prohibited, we saw people – whether they had COVID-19 or not – suffer major clinical, functional, cognitive declines or severe psychological symptoms,” Dr. Steinberg said.
He emphasized the importance of preventive measures such as vaccines and boosters in patients in long-term care facilities. He said the benefit of preventing lasting symptoms is often a strong motivator for family caregivers of people with dementia to get them vaccinated or boosted.
“It’s clear that vaccination and booster reduce the incidence of post-COVID symptoms,” he said. Almost all studies have been in younger cohorts, but he expects the benefits would also apply to older patients.
Easing symptoms and offering support
As with long COVID generally, many questions remain about the causes of lasting symptoms of COVID-19 in older patients, and how best to treat them. Dr. Tosato, who led the study of long-COVID patients in Rome, is focusing on inflammation as a critical factor in the condition. He and colleagues across Europe hope to answer some of them by launching a multicenter study of lasting COVID-19 symptoms.
In the meantime, Dr. Steinberg and Dr. Tosato said they are doing their best to evaluate and treat patients empirically.
“We pull from our armamentarium to treat system-specific symptoms,” Dr. Steinberg said. “We want to improve the quality of life and help each day be the best it can.”
Physicians in long-term care facilities might use medications such as antidepressants or nonpharmacologic approaches for patients experiencing depression symptoms. Families are also crucial in helping patients by bringing in home-cooked meals and encouraging loved ones who may be experiencing loss of taste or smell to eat, Dr. Steinberg said.
“We’ve seen with the return of families and loved ones visiting to some extent has alleviated some people’s symptoms, especially psychological ones,” he said.
Dr. Tosato said he and his colleagues start with an individualized, multidisciplinary assessment to determine what types of care may help. He noted that physicians might recommend medications or rehabilitative therapies depending on the patient’s needs.
“A personalized approach is key,” Dr. Tosato said. His study also found that the proportion of older patients experiencing symptoms declined over time – a glimmer of hope that many will recover.
Dr. Cohen emphasized the need for a multimodal rehabilitation, an evidence-based approach used to care for patients who survived hospitalization with severe COVID-19 – a group that has substantially higher rates of persistent symptoms. This approach includes cognitive rehabilitation, physical therapy, occupational therapy, and a graded exercise program.
Dr. Han and colleagues are studying potential therapies such as cognitive rehabilitation in adults who’ve experienced delirium. But until evidence-based treatments are available, they stress the role of support for patients with cognitive decline and their families.
“A lot of the work we do is teach patients and their families to compensate for newly acquired cognitive deficits from any illness, including COVID-19,” Dr. Han said.
Ms. Salant said she has experienced some improvement in her energy since her pulmonologist recommended a new inhaler based on her symptoms. Her sense of smell and taste, lost to the infection, returned after she received her first dose of a vaccine against COVID-19. She takes comfort in participating in Survivor Corps, a group of more than 170,000 COVID-19 survivors and their families who advocate for more scientific research on the disease.
She also expressed gratitude for the support she receives from her primary care physician, who she said has taken the time to learn more about the symptoms of long COVID, listens to her, and respects what she has to say.
“I have hope that I will keep getting better by baby steps,” Ms. Salant said.
Dr. Tosato, Dr. Steinberg, and Dr. Han have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
How old is too old to work as a doctor?
Air traffic controllers face mandatory retirement at age 56, with exceptions up to 61. Commercial airline pilots must bow out at 65; same for foreign service employees. Physicians, however, have no age limit, regardless of specialty.
As the profession rapidly ages – some 30% of the physician workforce is currently a senior, according to the American Medical Association – the topic of whether or not there should be a standard measure or age for retirement is front and center. The AMA’s Council on Medical Education formed a workgroup to look into the issue in 2015 and 2018, and in 2021, delegates adopted a set of guidelines for screening and assessing physicians, but stopped short of a mandate.
Mark Katlic, MD, chair of surgery at Lifebridge Health System, Baltimore, has devoted a decade to studying this topic. “I’m a bit of an outlier looking into this,” he says. “The public is unaware and seemingly unconcerned about the issue. Even among the medical profession, there’s been a series of fits and starts to develop a cohesive approach.”
One of the reasons guidelines – mandatory or otherwise – have been tough to come by is that aging brings with it a huge degree of variability. “If you look at a group of 80-year-olds, there will be much more variability than within a group of 40-year-olds,” Dr. Katlic pointed out.
Indeed, some 80-year-olds can easily continue to teach college courses, keep up in 10K running races, or perform delicate surgeries. Yet others in their peer group might struggle to properly button a shirt, walk a flight of stairs, or remember yesterday’s meals. Functional age is not the same as chronological age.
Frank Stockdale, MD, PhD, an 86-year-old practicing oncologist at Stanford (Calif.) University Health, counts himself in the camp opposed to age-based assessments. “It’s age discrimination,” he says. “Physicians receive assessments throughout their careers as part of the accreditation process – there’s no need to change that as doctors reach a certain age.”
Dr. Stockdale suggests that in many cases, malpractice suits are filed against mid-career doctors, not those of advanced age. “If you’re using the argument that there is an accumulation of deficits with age, the fact is that those deficits begin well before your 70s,” he said. “It’s better to have a uniform screening policy and begin at a much younger age.”
At Stanford, in fact, there was a former assessment policy that included cognitive testing, but physicians were successful in seeing that portion of testing eliminated. “It is a physical examination, by a physician of choice, certifying that for the privileges requested there is no physical or mental reason the candidate cannot safely perform them,” Dr. Stockdale explained.
In some cases, medical staffs have filed lawsuits to fight age-related testing. In New Haven, Conn., for instance, the U.S. Equal Employment Opportunity Commission (EEOC) filed a suit in 2020 on behalf of the Yale New Haven Hospital staff, alleging a discriminatory “late career practitioner policy.”
A similar case in Minnesota reached a settlement in 2021, providing monetary relief to staff impacted by out-of-pocket costs for the assessment, in addition to requiring that the hospital in question report to the EEOC any complaints related to age discrimination.
James Ellison, MD, MPH, chair in Memory Care and Geriatrics with ChristianaCare in Wilmington, Del., points out that aging can bring benefits for practicing physicians. “Age is very individualized and there are good and bad consequences,” he said. “Experience can build knowledge and confidence and expertise, and it does improve diagnostic accuracy.”
On the flip side, however, age-related brain changes include loss of volume and lower levels of some neurotransmitters, resulting in cognitive changes. “Functional changes occur too,” Dr. Ellison said.
“Just as some aging athletes may lose a degree of speed, strength, and flexibility, and some aging scientists may lose a part of their former cognitive speed, flexibility, and mental strength, aging health care providers can lose some of the physical coordination, strength, and visual acuity necessary to perform demanding surgical operations. They can also lose some of the processing speed, working memory, and executive function that allows them to excel in cognitive professional tasks.”
An estimated 5.8 million Americans age 65 and older have Alzheimer’s dementia, according to the Alzheimer’s Association.
Picking an arbitrary age for mandatory retirement isn’t the right approach for physicians, said Dr. Katlic. Rather, he said, the answer is to establish late-practitioner screening programs. “Very few hospitals have them, however,” he pointed out. “We do [at Lifebridge Health], and so do a few dozen others, but that’s out of hundreds.”
Instead, what typically plays out is that hospital staff might begin to notice a decline in a colleague. Things like a disheveled appearance or lack of hygiene, or trouble with memory, such as getting lost en route back to his or her office. Even dangerous behaviors such as nodding off during a procedure are not unheard of.
There are many examples of physician decline that fly under the radar. “Unfortunately, it’s unusual for cognitively impaired health care providers to recognize and report their own difficulties,” said Dr. Ellison. “Although peers are expected to report cognitively impaired colleagues, they often fail to do so. In some other countries, age-based assessment is an accepted policy. In the U.S., this is not a uniform policy.”
Sometimes physicians can remain on the job in spite of decline thanks to certain “props,” according to Dr. Ellison. “Good procedures, efficient supports, and various workarounds compensate,” he said, “but often are not sufficient to maintain high-quality practice.”
Most often, these situations play out slowly, until the problem becomes glaringly obvious and potentially dangerous, and someone in a position of power must step in.
“Often, it’s hearsay from a nurse or another staff member, and then a hospital president or chief of staff must make a career-affecting decision for the doctor in question,” said Dr. Katlic.
Because there is little self- or colleague policing – and barring official or binding guidelines on the aging physician issue – both Dr. Katlic and Dr. Ellison are proponents of late-career screening.
How screening can help
As it stands, Dr. Katlic maintains that the profession isn’t doing enough to ensure public safety. “We have peer review and recertification processes, but when you get down to it, we don’t police ourselves well,” he said. “All physicians are assessed throughout their careers as part of the hospital accreditation process, which is fair and adequate.”
Dr. Katlic said that there are three main benchmarks that physicians should be able to meet at an agreed upon age: a physical exam, a neurocognitive screening, and an eye exam. “At some reasonable age, I personally believe these exams should take place,” he said. “We can allow doctors to pick their own practitioners for the eye and physical exams, but the neurocognitive exam should be completed by a PhD neuropsychologist.”
At Lifebridge, for instance, these screenings begin at age 75 and take place every 2 years, during the recredentialing process. It applies to all specialties, not just surgeons. “Surgery is a little different in that it requires fine motor skills in addition to the others we test, but you want any physician to be cognitively intact,” Dr. Katlic pointed out. “All doctors need the ability to make decisions quickly, often under noisy, distracting conditions.”
Dr. Ellison supports applying the screenings to all specialties. “Let’s not forget that all physicians must be alert to the many ways in which their patients reveal what needs attention, evaluation, and treatment,” he said. “Some health care tasks could be performed without visual input; for example, perhaps psychotherapy could be provided competently by a clinician who lacks visual acuity. Auditory input might not be necessary for reading x-rays – but the information a health care provider gets from their eyes and ears is important, not just for surgeons.”
University of California San Diego has established what it calls its Physician Assessment and Clinical Education (PACE) program. One of the nation’s oldest and largest such programs, the hospital founded PACE in 1996. Most physicians taking part arrive as a requirement of disciplinary action from the state medical board, but a small percentage self-refers.
PACE involves two phases. The first is a 2-day set of tests and measures core competency knowledge. Phase 2 is more comprehensive and lasts 5 days. Here, within their specialty, physicians participate in the activities of the corresponding residency program. Faculty evaluates the physician, and a multidisciplinary team meets to review all the findings of the combined phases.
Depending on the results, doctors may face remediation steps that range from programs to address performance deficiencies to residency-level clinical experiences. According to a paper on the program published by the institution, “most physicians referred to the PACE program are found to have mild to moderate performance dyscompetence.”
In the case of the 2021 guidelines adopted by AMA delegates, there are nine principles for assessment. They should be evidence-based, ethical, relevant, accountable, fair and equitable, transparent, supportive, and nonburdensome, and should afford physicians due process protections.
Looking ahead
Even Dr. Katlic worries about the possibility of Congress intervening to establish federal-level, mandatory retirement age. “This just doesn’t make sense for our profession given the great variability we see,” he said. “My biggest hope is that more individual hospitals will institute these screenings.”
As the physician population ages – and the influx of new doctors shrinks – the slope becomes even more slippery. The AMA is predicting a physician shortage of nearly 40,000 by the year 2034. This strengthens arguments to keep existing physicians practicing for as long as possible and might make institutions less likely to screen.
It’s all a delicate balancing act and a continuing work in progress, said Dr. Ellison. “Ultimately, I believe we need to find a way to understand and address the possible implications for public safety, while at the same time protecting the privacy and dignity of our valued older physicians and other health care providers.”
A version of this article first appeared on Medscape.com.
Air traffic controllers face mandatory retirement at age 56, with exceptions up to 61. Commercial airline pilots must bow out at 65; same for foreign service employees. Physicians, however, have no age limit, regardless of specialty.
As the profession rapidly ages – some 30% of the physician workforce is currently a senior, according to the American Medical Association – the topic of whether or not there should be a standard measure or age for retirement is front and center. The AMA’s Council on Medical Education formed a workgroup to look into the issue in 2015 and 2018, and in 2021, delegates adopted a set of guidelines for screening and assessing physicians, but stopped short of a mandate.
Mark Katlic, MD, chair of surgery at Lifebridge Health System, Baltimore, has devoted a decade to studying this topic. “I’m a bit of an outlier looking into this,” he says. “The public is unaware and seemingly unconcerned about the issue. Even among the medical profession, there’s been a series of fits and starts to develop a cohesive approach.”
One of the reasons guidelines – mandatory or otherwise – have been tough to come by is that aging brings with it a huge degree of variability. “If you look at a group of 80-year-olds, there will be much more variability than within a group of 40-year-olds,” Dr. Katlic pointed out.
Indeed, some 80-year-olds can easily continue to teach college courses, keep up in 10K running races, or perform delicate surgeries. Yet others in their peer group might struggle to properly button a shirt, walk a flight of stairs, or remember yesterday’s meals. Functional age is not the same as chronological age.
Frank Stockdale, MD, PhD, an 86-year-old practicing oncologist at Stanford (Calif.) University Health, counts himself in the camp opposed to age-based assessments. “It’s age discrimination,” he says. “Physicians receive assessments throughout their careers as part of the accreditation process – there’s no need to change that as doctors reach a certain age.”
Dr. Stockdale suggests that in many cases, malpractice suits are filed against mid-career doctors, not those of advanced age. “If you’re using the argument that there is an accumulation of deficits with age, the fact is that those deficits begin well before your 70s,” he said. “It’s better to have a uniform screening policy and begin at a much younger age.”
At Stanford, in fact, there was a former assessment policy that included cognitive testing, but physicians were successful in seeing that portion of testing eliminated. “It is a physical examination, by a physician of choice, certifying that for the privileges requested there is no physical or mental reason the candidate cannot safely perform them,” Dr. Stockdale explained.
In some cases, medical staffs have filed lawsuits to fight age-related testing. In New Haven, Conn., for instance, the U.S. Equal Employment Opportunity Commission (EEOC) filed a suit in 2020 on behalf of the Yale New Haven Hospital staff, alleging a discriminatory “late career practitioner policy.”
A similar case in Minnesota reached a settlement in 2021, providing monetary relief to staff impacted by out-of-pocket costs for the assessment, in addition to requiring that the hospital in question report to the EEOC any complaints related to age discrimination.
James Ellison, MD, MPH, chair in Memory Care and Geriatrics with ChristianaCare in Wilmington, Del., points out that aging can bring benefits for practicing physicians. “Age is very individualized and there are good and bad consequences,” he said. “Experience can build knowledge and confidence and expertise, and it does improve diagnostic accuracy.”
On the flip side, however, age-related brain changes include loss of volume and lower levels of some neurotransmitters, resulting in cognitive changes. “Functional changes occur too,” Dr. Ellison said.
“Just as some aging athletes may lose a degree of speed, strength, and flexibility, and some aging scientists may lose a part of their former cognitive speed, flexibility, and mental strength, aging health care providers can lose some of the physical coordination, strength, and visual acuity necessary to perform demanding surgical operations. They can also lose some of the processing speed, working memory, and executive function that allows them to excel in cognitive professional tasks.”
An estimated 5.8 million Americans age 65 and older have Alzheimer’s dementia, according to the Alzheimer’s Association.
Picking an arbitrary age for mandatory retirement isn’t the right approach for physicians, said Dr. Katlic. Rather, he said, the answer is to establish late-practitioner screening programs. “Very few hospitals have them, however,” he pointed out. “We do [at Lifebridge Health], and so do a few dozen others, but that’s out of hundreds.”
Instead, what typically plays out is that hospital staff might begin to notice a decline in a colleague. Things like a disheveled appearance or lack of hygiene, or trouble with memory, such as getting lost en route back to his or her office. Even dangerous behaviors such as nodding off during a procedure are not unheard of.
There are many examples of physician decline that fly under the radar. “Unfortunately, it’s unusual for cognitively impaired health care providers to recognize and report their own difficulties,” said Dr. Ellison. “Although peers are expected to report cognitively impaired colleagues, they often fail to do so. In some other countries, age-based assessment is an accepted policy. In the U.S., this is not a uniform policy.”
Sometimes physicians can remain on the job in spite of decline thanks to certain “props,” according to Dr. Ellison. “Good procedures, efficient supports, and various workarounds compensate,” he said, “but often are not sufficient to maintain high-quality practice.”
Most often, these situations play out slowly, until the problem becomes glaringly obvious and potentially dangerous, and someone in a position of power must step in.
“Often, it’s hearsay from a nurse or another staff member, and then a hospital president or chief of staff must make a career-affecting decision for the doctor in question,” said Dr. Katlic.
Because there is little self- or colleague policing – and barring official or binding guidelines on the aging physician issue – both Dr. Katlic and Dr. Ellison are proponents of late-career screening.
How screening can help
As it stands, Dr. Katlic maintains that the profession isn’t doing enough to ensure public safety. “We have peer review and recertification processes, but when you get down to it, we don’t police ourselves well,” he said. “All physicians are assessed throughout their careers as part of the hospital accreditation process, which is fair and adequate.”
Dr. Katlic said that there are three main benchmarks that physicians should be able to meet at an agreed upon age: a physical exam, a neurocognitive screening, and an eye exam. “At some reasonable age, I personally believe these exams should take place,” he said. “We can allow doctors to pick their own practitioners for the eye and physical exams, but the neurocognitive exam should be completed by a PhD neuropsychologist.”
At Lifebridge, for instance, these screenings begin at age 75 and take place every 2 years, during the recredentialing process. It applies to all specialties, not just surgeons. “Surgery is a little different in that it requires fine motor skills in addition to the others we test, but you want any physician to be cognitively intact,” Dr. Katlic pointed out. “All doctors need the ability to make decisions quickly, often under noisy, distracting conditions.”
Dr. Ellison supports applying the screenings to all specialties. “Let’s not forget that all physicians must be alert to the many ways in which their patients reveal what needs attention, evaluation, and treatment,” he said. “Some health care tasks could be performed without visual input; for example, perhaps psychotherapy could be provided competently by a clinician who lacks visual acuity. Auditory input might not be necessary for reading x-rays – but the information a health care provider gets from their eyes and ears is important, not just for surgeons.”
University of California San Diego has established what it calls its Physician Assessment and Clinical Education (PACE) program. One of the nation’s oldest and largest such programs, the hospital founded PACE in 1996. Most physicians taking part arrive as a requirement of disciplinary action from the state medical board, but a small percentage self-refers.
PACE involves two phases. The first is a 2-day set of tests and measures core competency knowledge. Phase 2 is more comprehensive and lasts 5 days. Here, within their specialty, physicians participate in the activities of the corresponding residency program. Faculty evaluates the physician, and a multidisciplinary team meets to review all the findings of the combined phases.
Depending on the results, doctors may face remediation steps that range from programs to address performance deficiencies to residency-level clinical experiences. According to a paper on the program published by the institution, “most physicians referred to the PACE program are found to have mild to moderate performance dyscompetence.”
In the case of the 2021 guidelines adopted by AMA delegates, there are nine principles for assessment. They should be evidence-based, ethical, relevant, accountable, fair and equitable, transparent, supportive, and nonburdensome, and should afford physicians due process protections.
Looking ahead
Even Dr. Katlic worries about the possibility of Congress intervening to establish federal-level, mandatory retirement age. “This just doesn’t make sense for our profession given the great variability we see,” he said. “My biggest hope is that more individual hospitals will institute these screenings.”
As the physician population ages – and the influx of new doctors shrinks – the slope becomes even more slippery. The AMA is predicting a physician shortage of nearly 40,000 by the year 2034. This strengthens arguments to keep existing physicians practicing for as long as possible and might make institutions less likely to screen.
It’s all a delicate balancing act and a continuing work in progress, said Dr. Ellison. “Ultimately, I believe we need to find a way to understand and address the possible implications for public safety, while at the same time protecting the privacy and dignity of our valued older physicians and other health care providers.”
A version of this article first appeared on Medscape.com.
Air traffic controllers face mandatory retirement at age 56, with exceptions up to 61. Commercial airline pilots must bow out at 65; same for foreign service employees. Physicians, however, have no age limit, regardless of specialty.
As the profession rapidly ages – some 30% of the physician workforce is currently a senior, according to the American Medical Association – the topic of whether or not there should be a standard measure or age for retirement is front and center. The AMA’s Council on Medical Education formed a workgroup to look into the issue in 2015 and 2018, and in 2021, delegates adopted a set of guidelines for screening and assessing physicians, but stopped short of a mandate.
Mark Katlic, MD, chair of surgery at Lifebridge Health System, Baltimore, has devoted a decade to studying this topic. “I’m a bit of an outlier looking into this,” he says. “The public is unaware and seemingly unconcerned about the issue. Even among the medical profession, there’s been a series of fits and starts to develop a cohesive approach.”
One of the reasons guidelines – mandatory or otherwise – have been tough to come by is that aging brings with it a huge degree of variability. “If you look at a group of 80-year-olds, there will be much more variability than within a group of 40-year-olds,” Dr. Katlic pointed out.
Indeed, some 80-year-olds can easily continue to teach college courses, keep up in 10K running races, or perform delicate surgeries. Yet others in their peer group might struggle to properly button a shirt, walk a flight of stairs, or remember yesterday’s meals. Functional age is not the same as chronological age.
Frank Stockdale, MD, PhD, an 86-year-old practicing oncologist at Stanford (Calif.) University Health, counts himself in the camp opposed to age-based assessments. “It’s age discrimination,” he says. “Physicians receive assessments throughout their careers as part of the accreditation process – there’s no need to change that as doctors reach a certain age.”
Dr. Stockdale suggests that in many cases, malpractice suits are filed against mid-career doctors, not those of advanced age. “If you’re using the argument that there is an accumulation of deficits with age, the fact is that those deficits begin well before your 70s,” he said. “It’s better to have a uniform screening policy and begin at a much younger age.”
At Stanford, in fact, there was a former assessment policy that included cognitive testing, but physicians were successful in seeing that portion of testing eliminated. “It is a physical examination, by a physician of choice, certifying that for the privileges requested there is no physical or mental reason the candidate cannot safely perform them,” Dr. Stockdale explained.
In some cases, medical staffs have filed lawsuits to fight age-related testing. In New Haven, Conn., for instance, the U.S. Equal Employment Opportunity Commission (EEOC) filed a suit in 2020 on behalf of the Yale New Haven Hospital staff, alleging a discriminatory “late career practitioner policy.”
A similar case in Minnesota reached a settlement in 2021, providing monetary relief to staff impacted by out-of-pocket costs for the assessment, in addition to requiring that the hospital in question report to the EEOC any complaints related to age discrimination.
James Ellison, MD, MPH, chair in Memory Care and Geriatrics with ChristianaCare in Wilmington, Del., points out that aging can bring benefits for practicing physicians. “Age is very individualized and there are good and bad consequences,” he said. “Experience can build knowledge and confidence and expertise, and it does improve diagnostic accuracy.”
On the flip side, however, age-related brain changes include loss of volume and lower levels of some neurotransmitters, resulting in cognitive changes. “Functional changes occur too,” Dr. Ellison said.
“Just as some aging athletes may lose a degree of speed, strength, and flexibility, and some aging scientists may lose a part of their former cognitive speed, flexibility, and mental strength, aging health care providers can lose some of the physical coordination, strength, and visual acuity necessary to perform demanding surgical operations. They can also lose some of the processing speed, working memory, and executive function that allows them to excel in cognitive professional tasks.”
An estimated 5.8 million Americans age 65 and older have Alzheimer’s dementia, according to the Alzheimer’s Association.
Picking an arbitrary age for mandatory retirement isn’t the right approach for physicians, said Dr. Katlic. Rather, he said, the answer is to establish late-practitioner screening programs. “Very few hospitals have them, however,” he pointed out. “We do [at Lifebridge Health], and so do a few dozen others, but that’s out of hundreds.”
Instead, what typically plays out is that hospital staff might begin to notice a decline in a colleague. Things like a disheveled appearance or lack of hygiene, or trouble with memory, such as getting lost en route back to his or her office. Even dangerous behaviors such as nodding off during a procedure are not unheard of.
There are many examples of physician decline that fly under the radar. “Unfortunately, it’s unusual for cognitively impaired health care providers to recognize and report their own difficulties,” said Dr. Ellison. “Although peers are expected to report cognitively impaired colleagues, they often fail to do so. In some other countries, age-based assessment is an accepted policy. In the U.S., this is not a uniform policy.”
Sometimes physicians can remain on the job in spite of decline thanks to certain “props,” according to Dr. Ellison. “Good procedures, efficient supports, and various workarounds compensate,” he said, “but often are not sufficient to maintain high-quality practice.”
Most often, these situations play out slowly, until the problem becomes glaringly obvious and potentially dangerous, and someone in a position of power must step in.
“Often, it’s hearsay from a nurse or another staff member, and then a hospital president or chief of staff must make a career-affecting decision for the doctor in question,” said Dr. Katlic.
Because there is little self- or colleague policing – and barring official or binding guidelines on the aging physician issue – both Dr. Katlic and Dr. Ellison are proponents of late-career screening.
How screening can help
As it stands, Dr. Katlic maintains that the profession isn’t doing enough to ensure public safety. “We have peer review and recertification processes, but when you get down to it, we don’t police ourselves well,” he said. “All physicians are assessed throughout their careers as part of the hospital accreditation process, which is fair and adequate.”
Dr. Katlic said that there are three main benchmarks that physicians should be able to meet at an agreed upon age: a physical exam, a neurocognitive screening, and an eye exam. “At some reasonable age, I personally believe these exams should take place,” he said. “We can allow doctors to pick their own practitioners for the eye and physical exams, but the neurocognitive exam should be completed by a PhD neuropsychologist.”
At Lifebridge, for instance, these screenings begin at age 75 and take place every 2 years, during the recredentialing process. It applies to all specialties, not just surgeons. “Surgery is a little different in that it requires fine motor skills in addition to the others we test, but you want any physician to be cognitively intact,” Dr. Katlic pointed out. “All doctors need the ability to make decisions quickly, often under noisy, distracting conditions.”
Dr. Ellison supports applying the screenings to all specialties. “Let’s not forget that all physicians must be alert to the many ways in which their patients reveal what needs attention, evaluation, and treatment,” he said. “Some health care tasks could be performed without visual input; for example, perhaps psychotherapy could be provided competently by a clinician who lacks visual acuity. Auditory input might not be necessary for reading x-rays – but the information a health care provider gets from their eyes and ears is important, not just for surgeons.”
University of California San Diego has established what it calls its Physician Assessment and Clinical Education (PACE) program. One of the nation’s oldest and largest such programs, the hospital founded PACE in 1996. Most physicians taking part arrive as a requirement of disciplinary action from the state medical board, but a small percentage self-refers.
PACE involves two phases. The first is a 2-day set of tests and measures core competency knowledge. Phase 2 is more comprehensive and lasts 5 days. Here, within their specialty, physicians participate in the activities of the corresponding residency program. Faculty evaluates the physician, and a multidisciplinary team meets to review all the findings of the combined phases.
Depending on the results, doctors may face remediation steps that range from programs to address performance deficiencies to residency-level clinical experiences. According to a paper on the program published by the institution, “most physicians referred to the PACE program are found to have mild to moderate performance dyscompetence.”
In the case of the 2021 guidelines adopted by AMA delegates, there are nine principles for assessment. They should be evidence-based, ethical, relevant, accountable, fair and equitable, transparent, supportive, and nonburdensome, and should afford physicians due process protections.
Looking ahead
Even Dr. Katlic worries about the possibility of Congress intervening to establish federal-level, mandatory retirement age. “This just doesn’t make sense for our profession given the great variability we see,” he said. “My biggest hope is that more individual hospitals will institute these screenings.”
As the physician population ages – and the influx of new doctors shrinks – the slope becomes even more slippery. The AMA is predicting a physician shortage of nearly 40,000 by the year 2034. This strengthens arguments to keep existing physicians practicing for as long as possible and might make institutions less likely to screen.
It’s all a delicate balancing act and a continuing work in progress, said Dr. Ellison. “Ultimately, I believe we need to find a way to understand and address the possible implications for public safety, while at the same time protecting the privacy and dignity of our valued older physicians and other health care providers.”
A version of this article first appeared on Medscape.com.
Hospital readmission remains common for teens with nonfatal drug overdose
Approximately 1 in 5 adolescents hospitalized for nonfatal drug overdoses were readmitted within 6 months, based on data from more than 12,000 individuals.
Previous studies suggest that many adolescents fail to receive timely treatment for addiction after a nonfatal overdose, but the rates of hospital readmission in this population have not been examined, according to Julie Gaither, PhD, of Yale University, New Haven, Conn.
In a study presented at the annual meeting of the Pediatric Academic Societies, Dr. Gaither and her colleague, John M. Leventhal, MD, also of Yale University, used data from the 2016 Nationwide Readmissions Database to examine incidence and recurrent hospitalizations for nonfatal drug overdoses in adolescents. The study population included 12,952 patients aged 11-21 years who were admitted to a hospital after a nonfatal drug overdose in 2016. Of these, 15% were younger than 15 years, and 52.1% were females.
Overall, 76.2% of the overdoses involved opioids; 77.9% involved a prescription opioid, 15.3% involved heroin, and 7.9% involved fentanyl.
Across all drug overdoses, the majority (86.5%) were attributed to accidental intent and 11.8% were attributed to self-harm. Notably, females were nearly four times more likely than males to attempt suicide (odds ratio, 3.57). After the initial hospitalization, 79.3% of the patients were discharged home, and 11.5% went to a short-term care facility.
The 6-month hospital readmission rate was 21.4%. Of the patients readmitted for any cause, 18.2% of readmissions were for recurrent overdoses, and 92.1% of these were attributed to opioids.
The median cost of the initial hospital admission was $23,705 (ranging from $11,902 to $54,682) and the median cost of the first readmission was $25,416 (ranging from $13,905 to $48,810). In 42.1% of all hospitalizations, Medicaid was the primary payer.
The study findings were limited by the relatively high number of Medicaid patients, which may limit generalizability, but is strengthened by the large sample size.
The findings highlight not only the need for prevention efforts to limit opioid use among adolescents, but also “speak to the need for timely evidenced-based addiction treatment and appropriate follow-up care for teens following hospitalization for a nonfatal drug overdose,” the researchers wrote in their abstract.
Potential for postpandemic surge in drug use
Interestingly, some recent research has shown a decline in teens’ substance use during the pandemic, Kelly Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, said in an interview.
“However, as the world begins ‘opening up’ again, I suspect rates of drug use will rise – especially with the significant burden of mental health issues adolescents have struggled with during the last few years,” said Dr. Curran, who was not involved with the current study.
“Sadly, I am not surprised by this study’s findings. Too often, teens with substance abuse issues are not connected to effective, evidenced-based treatment, and for those who are, the wait list can be long,” she said.
“Teens who are misusing drugs – either to get high or to attempt suicide – who are admitted for nonfatal overdose have a high rate of readmission for recurrent drug overdose,” Dr. Curran said. “This high rate of readmission has serious social and financial implications,” she added. “This study is part of a growing body of literature that supports the importance of getting adolescents into effective, evidence-based substance abuse treatment, such as medication-assisted treatment in opioid abuse. However, we also should be advocating for improved funding for and access to these treatments for all individuals.”
The study received no outside funding. Dr. Gaither had no financial conflicts to disclose. Dr. Curran had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
Approximately 1 in 5 adolescents hospitalized for nonfatal drug overdoses were readmitted within 6 months, based on data from more than 12,000 individuals.
Previous studies suggest that many adolescents fail to receive timely treatment for addiction after a nonfatal overdose, but the rates of hospital readmission in this population have not been examined, according to Julie Gaither, PhD, of Yale University, New Haven, Conn.
In a study presented at the annual meeting of the Pediatric Academic Societies, Dr. Gaither and her colleague, John M. Leventhal, MD, also of Yale University, used data from the 2016 Nationwide Readmissions Database to examine incidence and recurrent hospitalizations for nonfatal drug overdoses in adolescents. The study population included 12,952 patients aged 11-21 years who were admitted to a hospital after a nonfatal drug overdose in 2016. Of these, 15% were younger than 15 years, and 52.1% were females.
Overall, 76.2% of the overdoses involved opioids; 77.9% involved a prescription opioid, 15.3% involved heroin, and 7.9% involved fentanyl.
Across all drug overdoses, the majority (86.5%) were attributed to accidental intent and 11.8% were attributed to self-harm. Notably, females were nearly four times more likely than males to attempt suicide (odds ratio, 3.57). After the initial hospitalization, 79.3% of the patients were discharged home, and 11.5% went to a short-term care facility.
The 6-month hospital readmission rate was 21.4%. Of the patients readmitted for any cause, 18.2% of readmissions were for recurrent overdoses, and 92.1% of these were attributed to opioids.
The median cost of the initial hospital admission was $23,705 (ranging from $11,902 to $54,682) and the median cost of the first readmission was $25,416 (ranging from $13,905 to $48,810). In 42.1% of all hospitalizations, Medicaid was the primary payer.
The study findings were limited by the relatively high number of Medicaid patients, which may limit generalizability, but is strengthened by the large sample size.
The findings highlight not only the need for prevention efforts to limit opioid use among adolescents, but also “speak to the need for timely evidenced-based addiction treatment and appropriate follow-up care for teens following hospitalization for a nonfatal drug overdose,” the researchers wrote in their abstract.
Potential for postpandemic surge in drug use
Interestingly, some recent research has shown a decline in teens’ substance use during the pandemic, Kelly Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, said in an interview.
“However, as the world begins ‘opening up’ again, I suspect rates of drug use will rise – especially with the significant burden of mental health issues adolescents have struggled with during the last few years,” said Dr. Curran, who was not involved with the current study.
“Sadly, I am not surprised by this study’s findings. Too often, teens with substance abuse issues are not connected to effective, evidenced-based treatment, and for those who are, the wait list can be long,” she said.
“Teens who are misusing drugs – either to get high or to attempt suicide – who are admitted for nonfatal overdose have a high rate of readmission for recurrent drug overdose,” Dr. Curran said. “This high rate of readmission has serious social and financial implications,” she added. “This study is part of a growing body of literature that supports the importance of getting adolescents into effective, evidence-based substance abuse treatment, such as medication-assisted treatment in opioid abuse. However, we also should be advocating for improved funding for and access to these treatments for all individuals.”
The study received no outside funding. Dr. Gaither had no financial conflicts to disclose. Dr. Curran had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
Approximately 1 in 5 adolescents hospitalized for nonfatal drug overdoses were readmitted within 6 months, based on data from more than 12,000 individuals.
Previous studies suggest that many adolescents fail to receive timely treatment for addiction after a nonfatal overdose, but the rates of hospital readmission in this population have not been examined, according to Julie Gaither, PhD, of Yale University, New Haven, Conn.
In a study presented at the annual meeting of the Pediatric Academic Societies, Dr. Gaither and her colleague, John M. Leventhal, MD, also of Yale University, used data from the 2016 Nationwide Readmissions Database to examine incidence and recurrent hospitalizations for nonfatal drug overdoses in adolescents. The study population included 12,952 patients aged 11-21 years who were admitted to a hospital after a nonfatal drug overdose in 2016. Of these, 15% were younger than 15 years, and 52.1% were females.
Overall, 76.2% of the overdoses involved opioids; 77.9% involved a prescription opioid, 15.3% involved heroin, and 7.9% involved fentanyl.
Across all drug overdoses, the majority (86.5%) were attributed to accidental intent and 11.8% were attributed to self-harm. Notably, females were nearly four times more likely than males to attempt suicide (odds ratio, 3.57). After the initial hospitalization, 79.3% of the patients were discharged home, and 11.5% went to a short-term care facility.
The 6-month hospital readmission rate was 21.4%. Of the patients readmitted for any cause, 18.2% of readmissions were for recurrent overdoses, and 92.1% of these were attributed to opioids.
The median cost of the initial hospital admission was $23,705 (ranging from $11,902 to $54,682) and the median cost of the first readmission was $25,416 (ranging from $13,905 to $48,810). In 42.1% of all hospitalizations, Medicaid was the primary payer.
The study findings were limited by the relatively high number of Medicaid patients, which may limit generalizability, but is strengthened by the large sample size.
The findings highlight not only the need for prevention efforts to limit opioid use among adolescents, but also “speak to the need for timely evidenced-based addiction treatment and appropriate follow-up care for teens following hospitalization for a nonfatal drug overdose,” the researchers wrote in their abstract.
Potential for postpandemic surge in drug use
Interestingly, some recent research has shown a decline in teens’ substance use during the pandemic, Kelly Curran, MD, of the University of Oklahoma Health Sciences Center, Oklahoma City, said in an interview.
“However, as the world begins ‘opening up’ again, I suspect rates of drug use will rise – especially with the significant burden of mental health issues adolescents have struggled with during the last few years,” said Dr. Curran, who was not involved with the current study.
“Sadly, I am not surprised by this study’s findings. Too often, teens with substance abuse issues are not connected to effective, evidenced-based treatment, and for those who are, the wait list can be long,” she said.
“Teens who are misusing drugs – either to get high or to attempt suicide – who are admitted for nonfatal overdose have a high rate of readmission for recurrent drug overdose,” Dr. Curran said. “This high rate of readmission has serious social and financial implications,” she added. “This study is part of a growing body of literature that supports the importance of getting adolescents into effective, evidence-based substance abuse treatment, such as medication-assisted treatment in opioid abuse. However, we also should be advocating for improved funding for and access to these treatments for all individuals.”
The study received no outside funding. Dr. Gaither had no financial conflicts to disclose. Dr. Curran had no financial conflicts to disclose and serves on the editorial advisory board of Pediatric News.
FROM PAS 2022
Nap length linked to cognitive changes
No wonder we feel worse after naps
Some of us have hectic schedules that may make a nap feel more necessary. It’s common knowledge that naps shouldn’t be too long – maybe 20 minutes or so – but if you frequently take 3-hour naps and wake up thinking you’re late for school even though you’re 47 and have your PhD, this LOTME is for you.
Studies have shown that there is a link between napping during the day and Alzheimer’s/cognitive decline, but now we’ve got a double whammy for you: Longer and more frequent napping is linked to worse cognition after a year, and in turn, those with cognitive decline and Alzheimer’s are known to nap longer and more frequently during the day.
“We now know that the pathology related to cognitive decline can cause other changes in function,” he said. “It’s really a multisystem disorder, also including difficulty sleeping, changes in movement, changes in body composition, depression symptoms, behavioral changes, etc.,” coauthor Aron Buchman, MD, said in a statement from Rush University Medical Center.
The investigators monitored 1,400 patients over the course of 14 years with wrist bracelets that recorded when a person was not active during the day and considered that a nap.
At the beginning of the study, 75% of the study subjects had no cognitive impairment, 19.5% had some cognitive impairment, and approximately 4% had Alzheimer’s. Napping during the day only increased about 11 minutes a year for those with no signs of cognitive impairment, but those who showed significantly more signs of cognitive decline doubled their nap time and those actually diagnosed with Alzheimer’s tripled theirs.
The investigators did not imply that napping causes Alzheimer’s, but they noted that people who are older and nap more than an hour a day are 40% more likely to be at risk. It is something to consider and monitor.
Sometimes, after all, a nap seems like the best idea ever, but more often than not we wake up feeling 10 times worse. Our bodies may be giving us a heads up.
Pokemon Go away depression
The summer of 2016 was a great time if you happened to be a fan of Pokemon. Which is quite a lot of people. For almost 20 years millions have enjoyed the games and animated series, but Pokemon Go brought the thrill of catching Pokemon to life in a whole new way. For the first time, you could go out into the world and pretend you were a real Pokemon trainer, and everywhere you went, there would be others like you.
The ability to chase after Pikachu and Charizard in real life (well, augmented reality, but close enough) seemed to bring people a lot of joy, but seemed is never good enough for science. Can’t have anecdotes, we need data! So researchers at the London School of Economics and Political Science conducted a study into how Pokemon Go affected local Internet search rates of depression as the game was released slowly around the world.
Through analyzing Google Trend data of words like “depression,” “anxiety,” and “stress,” the researchers found that the release of Pokemon Go was significantly associated with a noticeable, though short-term, drop in depression-related Internet searches. Location-based augmented reality games may alleviate symptoms of mild depression, the researchers said, as they encourage physical activity, face-to-face socialization, and exposure to nature, though they added that simply going outside is likely not enough to combat clinical cases of severe depression.
Still, augmented reality games represent a viable target for public health investment, since they’re easy to use and inexpensive to make. That said, we’re not sure we want the FDA or CDC making a new Pokemon Go game. They’d probably end up filling the streets with Mr. Mime. And no one would leave their house for that.
And now a word from our sponsor
How many times has this happened to you? You need to repair a jet engine, inspect a nuclear reactor cooling system, AND perform bowel surgery, but you can’t carry around all the heavy, old-fashioned tools needed for those jobs.
Well, we’ve got one tool that can do it all! And that tool is a snake. No, it’s a robot.
It’s both! It’s the COntinuum roBot for Remote Applications. COBRA is the robot that looks like a snake! A snake that’s 5 meters long but only as thick as a pencil (about 9 mm in diameter). A robot with “extraordinary manoeuvrability and responsiveness due to … a compliant-joint structure and multiple continuous sections that enable it to bend at around 90 degrees,” according to the team at the University of Nottingham (England) that developed it.
COBRA comes equipped with a stereovision camera and a miniature cutting tool to perform complex industrial repair, but other devices can be interchanged for possible medical use.
COBRA and its joystick-like controller were designed to be easy to use. Dr. Oladejo Olaleye, the ear, nose, and throat and robotic surgeon at University Hospitals of Leicester who is directing its surgical development, was able to use COBRA on a dummy after just 5 minutes of training. He called it “the future of diagnostic endoscopy and therapeutic surgery.”
Don’t be the last aircraft engineer/nuclear technician/surgeon on your block to have this ultraslender, ultramaneuverable reptilian repair robot. Get your COBRA now! Operators are standing by.
Disclaimer: Robot is still under development and not yet on sale.
Rule, (worm) Britannia!
As long as there have been people, there have been parasitic worms living in their guts. Helminth infection is a continuing and largely ignored crisis in poor, tropical nations, though worm-based diseases have been basically eliminated from wealthier countries.
This wasn’t always the case, however, as a study published in PLOS Neglected Tropical Diseases (now there’s a specific topic) has found. The researchers detail the glorious history of helminth infestation in the United Kingdom from the Victorian era all the way back to prehistory, scouring hundreds of skeletons found in 17 sites across the country for eggs, which can remain intact for thousands of years.
The researchers found that two eras in particular had very high rates of infection. Unsurprisingly, the late medieval era was one of them, but the other is less obvious. The Romans were famous for their hygiene, their baths, and their plumbing, but maybe they also should be famous for the abundance of worms in their bellies. That doesn’t make sense at first: Shouldn’t good hygiene lower infection? The benefits of a good sewer system, however, are lessened when the waste containing said infectious organisms is used to fertilize crops. Recycling is generally a good thing, but less so when you’re recycling parasitic worms.
Curiously, of the three sites from the industrial age, only the one in London had high levels of worm infestation. Considering how dirty and cramped 19th-century British cities were, one might expect disease to run rampant (tuberculosis certainly did), but the sites in Oxford and Birmingham were almost devoid of worms. The researchers theorized that this was because of access to clean well water. Or maybe worms just have a thing for London. [Editor’s note: It’s probably not that.]
No wonder we feel worse after naps
Some of us have hectic schedules that may make a nap feel more necessary. It’s common knowledge that naps shouldn’t be too long – maybe 20 minutes or so – but if you frequently take 3-hour naps and wake up thinking you’re late for school even though you’re 47 and have your PhD, this LOTME is for you.
Studies have shown that there is a link between napping during the day and Alzheimer’s/cognitive decline, but now we’ve got a double whammy for you: Longer and more frequent napping is linked to worse cognition after a year, and in turn, those with cognitive decline and Alzheimer’s are known to nap longer and more frequently during the day.
“We now know that the pathology related to cognitive decline can cause other changes in function,” he said. “It’s really a multisystem disorder, also including difficulty sleeping, changes in movement, changes in body composition, depression symptoms, behavioral changes, etc.,” coauthor Aron Buchman, MD, said in a statement from Rush University Medical Center.
The investigators monitored 1,400 patients over the course of 14 years with wrist bracelets that recorded when a person was not active during the day and considered that a nap.
At the beginning of the study, 75% of the study subjects had no cognitive impairment, 19.5% had some cognitive impairment, and approximately 4% had Alzheimer’s. Napping during the day only increased about 11 minutes a year for those with no signs of cognitive impairment, but those who showed significantly more signs of cognitive decline doubled their nap time and those actually diagnosed with Alzheimer’s tripled theirs.
The investigators did not imply that napping causes Alzheimer’s, but they noted that people who are older and nap more than an hour a day are 40% more likely to be at risk. It is something to consider and monitor.
Sometimes, after all, a nap seems like the best idea ever, but more often than not we wake up feeling 10 times worse. Our bodies may be giving us a heads up.
Pokemon Go away depression
The summer of 2016 was a great time if you happened to be a fan of Pokemon. Which is quite a lot of people. For almost 20 years millions have enjoyed the games and animated series, but Pokemon Go brought the thrill of catching Pokemon to life in a whole new way. For the first time, you could go out into the world and pretend you were a real Pokemon trainer, and everywhere you went, there would be others like you.
The ability to chase after Pikachu and Charizard in real life (well, augmented reality, but close enough) seemed to bring people a lot of joy, but seemed is never good enough for science. Can’t have anecdotes, we need data! So researchers at the London School of Economics and Political Science conducted a study into how Pokemon Go affected local Internet search rates of depression as the game was released slowly around the world.
Through analyzing Google Trend data of words like “depression,” “anxiety,” and “stress,” the researchers found that the release of Pokemon Go was significantly associated with a noticeable, though short-term, drop in depression-related Internet searches. Location-based augmented reality games may alleviate symptoms of mild depression, the researchers said, as they encourage physical activity, face-to-face socialization, and exposure to nature, though they added that simply going outside is likely not enough to combat clinical cases of severe depression.
Still, augmented reality games represent a viable target for public health investment, since they’re easy to use and inexpensive to make. That said, we’re not sure we want the FDA or CDC making a new Pokemon Go game. They’d probably end up filling the streets with Mr. Mime. And no one would leave their house for that.
And now a word from our sponsor
How many times has this happened to you? You need to repair a jet engine, inspect a nuclear reactor cooling system, AND perform bowel surgery, but you can’t carry around all the heavy, old-fashioned tools needed for those jobs.
Well, we’ve got one tool that can do it all! And that tool is a snake. No, it’s a robot.
It’s both! It’s the COntinuum roBot for Remote Applications. COBRA is the robot that looks like a snake! A snake that’s 5 meters long but only as thick as a pencil (about 9 mm in diameter). A robot with “extraordinary manoeuvrability and responsiveness due to … a compliant-joint structure and multiple continuous sections that enable it to bend at around 90 degrees,” according to the team at the University of Nottingham (England) that developed it.
COBRA comes equipped with a stereovision camera and a miniature cutting tool to perform complex industrial repair, but other devices can be interchanged for possible medical use.
COBRA and its joystick-like controller were designed to be easy to use. Dr. Oladejo Olaleye, the ear, nose, and throat and robotic surgeon at University Hospitals of Leicester who is directing its surgical development, was able to use COBRA on a dummy after just 5 minutes of training. He called it “the future of diagnostic endoscopy and therapeutic surgery.”
Don’t be the last aircraft engineer/nuclear technician/surgeon on your block to have this ultraslender, ultramaneuverable reptilian repair robot. Get your COBRA now! Operators are standing by.
Disclaimer: Robot is still under development and not yet on sale.
Rule, (worm) Britannia!
As long as there have been people, there have been parasitic worms living in their guts. Helminth infection is a continuing and largely ignored crisis in poor, tropical nations, though worm-based diseases have been basically eliminated from wealthier countries.
This wasn’t always the case, however, as a study published in PLOS Neglected Tropical Diseases (now there’s a specific topic) has found. The researchers detail the glorious history of helminth infestation in the United Kingdom from the Victorian era all the way back to prehistory, scouring hundreds of skeletons found in 17 sites across the country for eggs, which can remain intact for thousands of years.
The researchers found that two eras in particular had very high rates of infection. Unsurprisingly, the late medieval era was one of them, but the other is less obvious. The Romans were famous for their hygiene, their baths, and their plumbing, but maybe they also should be famous for the abundance of worms in their bellies. That doesn’t make sense at first: Shouldn’t good hygiene lower infection? The benefits of a good sewer system, however, are lessened when the waste containing said infectious organisms is used to fertilize crops. Recycling is generally a good thing, but less so when you’re recycling parasitic worms.
Curiously, of the three sites from the industrial age, only the one in London had high levels of worm infestation. Considering how dirty and cramped 19th-century British cities were, one might expect disease to run rampant (tuberculosis certainly did), but the sites in Oxford and Birmingham were almost devoid of worms. The researchers theorized that this was because of access to clean well water. Or maybe worms just have a thing for London. [Editor’s note: It’s probably not that.]
No wonder we feel worse after naps
Some of us have hectic schedules that may make a nap feel more necessary. It’s common knowledge that naps shouldn’t be too long – maybe 20 minutes or so – but if you frequently take 3-hour naps and wake up thinking you’re late for school even though you’re 47 and have your PhD, this LOTME is for you.
Studies have shown that there is a link between napping during the day and Alzheimer’s/cognitive decline, but now we’ve got a double whammy for you: Longer and more frequent napping is linked to worse cognition after a year, and in turn, those with cognitive decline and Alzheimer’s are known to nap longer and more frequently during the day.
“We now know that the pathology related to cognitive decline can cause other changes in function,” he said. “It’s really a multisystem disorder, also including difficulty sleeping, changes in movement, changes in body composition, depression symptoms, behavioral changes, etc.,” coauthor Aron Buchman, MD, said in a statement from Rush University Medical Center.
The investigators monitored 1,400 patients over the course of 14 years with wrist bracelets that recorded when a person was not active during the day and considered that a nap.
At the beginning of the study, 75% of the study subjects had no cognitive impairment, 19.5% had some cognitive impairment, and approximately 4% had Alzheimer’s. Napping during the day only increased about 11 minutes a year for those with no signs of cognitive impairment, but those who showed significantly more signs of cognitive decline doubled their nap time and those actually diagnosed with Alzheimer’s tripled theirs.
The investigators did not imply that napping causes Alzheimer’s, but they noted that people who are older and nap more than an hour a day are 40% more likely to be at risk. It is something to consider and monitor.
Sometimes, after all, a nap seems like the best idea ever, but more often than not we wake up feeling 10 times worse. Our bodies may be giving us a heads up.
Pokemon Go away depression
The summer of 2016 was a great time if you happened to be a fan of Pokemon. Which is quite a lot of people. For almost 20 years millions have enjoyed the games and animated series, but Pokemon Go brought the thrill of catching Pokemon to life in a whole new way. For the first time, you could go out into the world and pretend you were a real Pokemon trainer, and everywhere you went, there would be others like you.
The ability to chase after Pikachu and Charizard in real life (well, augmented reality, but close enough) seemed to bring people a lot of joy, but seemed is never good enough for science. Can’t have anecdotes, we need data! So researchers at the London School of Economics and Political Science conducted a study into how Pokemon Go affected local Internet search rates of depression as the game was released slowly around the world.
Through analyzing Google Trend data of words like “depression,” “anxiety,” and “stress,” the researchers found that the release of Pokemon Go was significantly associated with a noticeable, though short-term, drop in depression-related Internet searches. Location-based augmented reality games may alleviate symptoms of mild depression, the researchers said, as they encourage physical activity, face-to-face socialization, and exposure to nature, though they added that simply going outside is likely not enough to combat clinical cases of severe depression.
Still, augmented reality games represent a viable target for public health investment, since they’re easy to use and inexpensive to make. That said, we’re not sure we want the FDA or CDC making a new Pokemon Go game. They’d probably end up filling the streets with Mr. Mime. And no one would leave their house for that.
And now a word from our sponsor
How many times has this happened to you? You need to repair a jet engine, inspect a nuclear reactor cooling system, AND perform bowel surgery, but you can’t carry around all the heavy, old-fashioned tools needed for those jobs.
Well, we’ve got one tool that can do it all! And that tool is a snake. No, it’s a robot.
It’s both! It’s the COntinuum roBot for Remote Applications. COBRA is the robot that looks like a snake! A snake that’s 5 meters long but only as thick as a pencil (about 9 mm in diameter). A robot with “extraordinary manoeuvrability and responsiveness due to … a compliant-joint structure and multiple continuous sections that enable it to bend at around 90 degrees,” according to the team at the University of Nottingham (England) that developed it.
COBRA comes equipped with a stereovision camera and a miniature cutting tool to perform complex industrial repair, but other devices can be interchanged for possible medical use.
COBRA and its joystick-like controller were designed to be easy to use. Dr. Oladejo Olaleye, the ear, nose, and throat and robotic surgeon at University Hospitals of Leicester who is directing its surgical development, was able to use COBRA on a dummy after just 5 minutes of training. He called it “the future of diagnostic endoscopy and therapeutic surgery.”
Don’t be the last aircraft engineer/nuclear technician/surgeon on your block to have this ultraslender, ultramaneuverable reptilian repair robot. Get your COBRA now! Operators are standing by.
Disclaimer: Robot is still under development and not yet on sale.
Rule, (worm) Britannia!
As long as there have been people, there have been parasitic worms living in their guts. Helminth infection is a continuing and largely ignored crisis in poor, tropical nations, though worm-based diseases have been basically eliminated from wealthier countries.
This wasn’t always the case, however, as a study published in PLOS Neglected Tropical Diseases (now there’s a specific topic) has found. The researchers detail the glorious history of helminth infestation in the United Kingdom from the Victorian era all the way back to prehistory, scouring hundreds of skeletons found in 17 sites across the country for eggs, which can remain intact for thousands of years.
The researchers found that two eras in particular had very high rates of infection. Unsurprisingly, the late medieval era was one of them, but the other is less obvious. The Romans were famous for their hygiene, their baths, and their plumbing, but maybe they also should be famous for the abundance of worms in their bellies. That doesn’t make sense at first: Shouldn’t good hygiene lower infection? The benefits of a good sewer system, however, are lessened when the waste containing said infectious organisms is used to fertilize crops. Recycling is generally a good thing, but less so when you’re recycling parasitic worms.
Curiously, of the three sites from the industrial age, only the one in London had high levels of worm infestation. Considering how dirty and cramped 19th-century British cities were, one might expect disease to run rampant (tuberculosis certainly did), but the sites in Oxford and Birmingham were almost devoid of worms. The researchers theorized that this was because of access to clean well water. Or maybe worms just have a thing for London. [Editor’s note: It’s probably not that.]
Almost 60% of U.S. population has been infected by COVID-19: CDC
The percentage of Americans who have been infected with COVID-19 jumped from 34% in December 2021 to 58% in February 2022, a new study from the Centers for Disease Control and Prevention reveals.
This is the first time the seroprevalence of prior infection is more than 50% in the American population.
“I definitely expected that we were going to see an increase continue ... but I didn’t expect it to increase quite this much. But we follow the data ... and this is what the evidence is showing us,” lead study researcher Kristie E. N. Clarke, MD, said during a CDC media briefing April 26.
Researchers found that presence of antinucleocapsid (anti-N) antibodies from prior infection varied by age. The rate varied from as high as 75% in children and teenagers 17 years and younger to 33% in those 65 and older, for example.
The study showed that the anti-N antibodies were more common in age groups with the lowest vaccination numbers.
Combined with up-to-date CDC data on deaths, hospitalizations, and cases, the study provides a clearer picture of where we are now and where we might be headed in terms of the pandemic.
Vaccination still valuable
The fact that nearly 60% of Americans have antibodies from prior infection is not a reason to think people with a history of COVID-19 should skip vaccination, said CDC director Rochelle P. Walensky, MD.
“I can’t underscore enough that those with detectable antibodies from previous infection, we encourage them to still get vaccinated,” Dr. Walensky said.
“We do know that reinfections happen,” she said, “so that’s important in terms of thinking forward.”
The CDC continues to encourage all Americans to stay up to date with their COVID-19 vaccinations, said Dr. Clarke, colead for the CDC’s COVID-19 Epidemiology and Surveillance Taskforce Seroprevalence Team. “Having infection-induced antibodies does not necessarily mean you are protected against future infections.”
The study, published in the CDC’s Morbidity and Mortality Weekly Report (MMWR), did not evaluate antibody protection from COVID-19 vaccination.
It should also be noted that the study looked at presence or absence of anti-N antibodies, and not whether certain levels were linked to less or more protection.
Where are we now?
Dr. Walensky used the media briefing as an opportunity to share current COVID-19 numbers.
“Overall, we can continue to have some mixed trends. Deaths, fortunately, are continuing to trend downward with a 7-day average of about 300 per day, which represents an estimated 18% decline from the prior week,” she said.
Hospital admissions also remain low, at about 1,500 per day. “But we should note that for the second week in a row, they are slowly trending upwards,” Dr. Walensky said. There was an increase of about 9% at press time compared with the prior week.
Cases remain “comparatively low” to even where we were a month ago, at 44,000 per day,” Dr. Walensky said. “Although this too represents an increase of about 25% in the past week.”
Dr. Walensky noted that positive test numbers are not as reliable a metric as they were before the growth in use of rapid home tests. But it’s not the only measure. “We continue to believe that our PCR testing data, especially when we corroborate it with information from our other surveillance systems – like wastewater surveillance and emergency department surveillance – provide us a reliable picture of the trajectory of COVID-19 across our country.”
She recommended that people continue to consult the CDC’s COVID-19 county tracker to monitor local levels of COVID-19.
Dr. Walensky also shared recent findings from genomic sequencing that continue to show the predominance of the Omicron variant. “Essentially a hundred percent of what we’re finding now is Omicron,” she said. In terms of individual variants, the Omicron BA.1 variant is about 3% of circulating virus, the BA.2 variant is about 68%, and BA.2.12.1 makes up about 35%.
“We’re just starting to learn about the impact of BA2.121,” Dr. Walensky said. “It appears it might have a transmission advantage of about 25% over the BA2 subvariant.”
A version of this article first appeared on Medscape.com.
The percentage of Americans who have been infected with COVID-19 jumped from 34% in December 2021 to 58% in February 2022, a new study from the Centers for Disease Control and Prevention reveals.
This is the first time the seroprevalence of prior infection is more than 50% in the American population.
“I definitely expected that we were going to see an increase continue ... but I didn’t expect it to increase quite this much. But we follow the data ... and this is what the evidence is showing us,” lead study researcher Kristie E. N. Clarke, MD, said during a CDC media briefing April 26.
Researchers found that presence of antinucleocapsid (anti-N) antibodies from prior infection varied by age. The rate varied from as high as 75% in children and teenagers 17 years and younger to 33% in those 65 and older, for example.
The study showed that the anti-N antibodies were more common in age groups with the lowest vaccination numbers.
Combined with up-to-date CDC data on deaths, hospitalizations, and cases, the study provides a clearer picture of where we are now and where we might be headed in terms of the pandemic.
Vaccination still valuable
The fact that nearly 60% of Americans have antibodies from prior infection is not a reason to think people with a history of COVID-19 should skip vaccination, said CDC director Rochelle P. Walensky, MD.
“I can’t underscore enough that those with detectable antibodies from previous infection, we encourage them to still get vaccinated,” Dr. Walensky said.
“We do know that reinfections happen,” she said, “so that’s important in terms of thinking forward.”
The CDC continues to encourage all Americans to stay up to date with their COVID-19 vaccinations, said Dr. Clarke, colead for the CDC’s COVID-19 Epidemiology and Surveillance Taskforce Seroprevalence Team. “Having infection-induced antibodies does not necessarily mean you are protected against future infections.”
The study, published in the CDC’s Morbidity and Mortality Weekly Report (MMWR), did not evaluate antibody protection from COVID-19 vaccination.
It should also be noted that the study looked at presence or absence of anti-N antibodies, and not whether certain levels were linked to less or more protection.
Where are we now?
Dr. Walensky used the media briefing as an opportunity to share current COVID-19 numbers.
“Overall, we can continue to have some mixed trends. Deaths, fortunately, are continuing to trend downward with a 7-day average of about 300 per day, which represents an estimated 18% decline from the prior week,” she said.
Hospital admissions also remain low, at about 1,500 per day. “But we should note that for the second week in a row, they are slowly trending upwards,” Dr. Walensky said. There was an increase of about 9% at press time compared with the prior week.
Cases remain “comparatively low” to even where we were a month ago, at 44,000 per day,” Dr. Walensky said. “Although this too represents an increase of about 25% in the past week.”
Dr. Walensky noted that positive test numbers are not as reliable a metric as they were before the growth in use of rapid home tests. But it’s not the only measure. “We continue to believe that our PCR testing data, especially when we corroborate it with information from our other surveillance systems – like wastewater surveillance and emergency department surveillance – provide us a reliable picture of the trajectory of COVID-19 across our country.”
She recommended that people continue to consult the CDC’s COVID-19 county tracker to monitor local levels of COVID-19.
Dr. Walensky also shared recent findings from genomic sequencing that continue to show the predominance of the Omicron variant. “Essentially a hundred percent of what we’re finding now is Omicron,” she said. In terms of individual variants, the Omicron BA.1 variant is about 3% of circulating virus, the BA.2 variant is about 68%, and BA.2.12.1 makes up about 35%.
“We’re just starting to learn about the impact of BA2.121,” Dr. Walensky said. “It appears it might have a transmission advantage of about 25% over the BA2 subvariant.”
A version of this article first appeared on Medscape.com.
The percentage of Americans who have been infected with COVID-19 jumped from 34% in December 2021 to 58% in February 2022, a new study from the Centers for Disease Control and Prevention reveals.
This is the first time the seroprevalence of prior infection is more than 50% in the American population.
“I definitely expected that we were going to see an increase continue ... but I didn’t expect it to increase quite this much. But we follow the data ... and this is what the evidence is showing us,” lead study researcher Kristie E. N. Clarke, MD, said during a CDC media briefing April 26.
Researchers found that presence of antinucleocapsid (anti-N) antibodies from prior infection varied by age. The rate varied from as high as 75% in children and teenagers 17 years and younger to 33% in those 65 and older, for example.
The study showed that the anti-N antibodies were more common in age groups with the lowest vaccination numbers.
Combined with up-to-date CDC data on deaths, hospitalizations, and cases, the study provides a clearer picture of where we are now and where we might be headed in terms of the pandemic.
Vaccination still valuable
The fact that nearly 60% of Americans have antibodies from prior infection is not a reason to think people with a history of COVID-19 should skip vaccination, said CDC director Rochelle P. Walensky, MD.
“I can’t underscore enough that those with detectable antibodies from previous infection, we encourage them to still get vaccinated,” Dr. Walensky said.
“We do know that reinfections happen,” she said, “so that’s important in terms of thinking forward.”
The CDC continues to encourage all Americans to stay up to date with their COVID-19 vaccinations, said Dr. Clarke, colead for the CDC’s COVID-19 Epidemiology and Surveillance Taskforce Seroprevalence Team. “Having infection-induced antibodies does not necessarily mean you are protected against future infections.”
The study, published in the CDC’s Morbidity and Mortality Weekly Report (MMWR), did not evaluate antibody protection from COVID-19 vaccination.
It should also be noted that the study looked at presence or absence of anti-N antibodies, and not whether certain levels were linked to less or more protection.
Where are we now?
Dr. Walensky used the media briefing as an opportunity to share current COVID-19 numbers.
“Overall, we can continue to have some mixed trends. Deaths, fortunately, are continuing to trend downward with a 7-day average of about 300 per day, which represents an estimated 18% decline from the prior week,” she said.
Hospital admissions also remain low, at about 1,500 per day. “But we should note that for the second week in a row, they are slowly trending upwards,” Dr. Walensky said. There was an increase of about 9% at press time compared with the prior week.
Cases remain “comparatively low” to even where we were a month ago, at 44,000 per day,” Dr. Walensky said. “Although this too represents an increase of about 25% in the past week.”
Dr. Walensky noted that positive test numbers are not as reliable a metric as they were before the growth in use of rapid home tests. But it’s not the only measure. “We continue to believe that our PCR testing data, especially when we corroborate it with information from our other surveillance systems – like wastewater surveillance and emergency department surveillance – provide us a reliable picture of the trajectory of COVID-19 across our country.”
She recommended that people continue to consult the CDC’s COVID-19 county tracker to monitor local levels of COVID-19.
Dr. Walensky also shared recent findings from genomic sequencing that continue to show the predominance of the Omicron variant. “Essentially a hundred percent of what we’re finding now is Omicron,” she said. In terms of individual variants, the Omicron BA.1 variant is about 3% of circulating virus, the BA.2 variant is about 68%, and BA.2.12.1 makes up about 35%.
“We’re just starting to learn about the impact of BA2.121,” Dr. Walensky said. “It appears it might have a transmission advantage of about 25% over the BA2 subvariant.”
A version of this article first appeared on Medscape.com.
FROM MMWR
Pfizer recalls more quinapril because of potential carcinogen
, the company announced.
The Accupril recall comes one month after Pfizer recalled six lots of Accuretic (Quinapril HCI/hydrochlorathiazide) tablets for the same problem.
Accupril is indicated for the treatment of hypertension and management of heart failure when added to conventional therapy, including diuretics and/or digitalis.
To date, Pfizer is not aware of any reports of adverse events related to the Accupril recall, and the company believes the benefit/risk profile remains positive based on currently available data.
“Although long-term ingestion of N-nitroso-quinapril may be associated with a potential increased cancer risk in humans, there is no immediate risk to patients taking this medication,” the company said April 22 in a news release.
Patients currently taking the recalled products are asked to consult with their doctor about alternative treatment options.
The recalled Accupril tablets were sold in 90-count bottles distributed nationwide to wholesalers and distributors in the United States and Puerto Rico from December 2019 to April 2022.
National drug codes (NDC), lot numbers, and expiration dates are listed in the company announcement posted on the Food and Drug Administration’s website.
Patients who are taking this product should consult with their health care provider or pharmacy to determine if they have the affected product. Those with the affected tablets should contact claims management firm Sedgwick by phone at 888-345-0481 Monday through Friday from 8 AM to 5 PM ET for instructions on how to return the product and obtain reimbursement.
Healthcare providers with questions regarding the recall can contact Pfizer by telephone at 800-438-1985, option 3, Monday through Friday from 8 AM to 9 PM ET.
Adverse reactions or quality problems related to this recall should be reported to the FDA’s MedWatch program.
A version of this article first appeared on Medscape.com.
, the company announced.
The Accupril recall comes one month after Pfizer recalled six lots of Accuretic (Quinapril HCI/hydrochlorathiazide) tablets for the same problem.
Accupril is indicated for the treatment of hypertension and management of heart failure when added to conventional therapy, including diuretics and/or digitalis.
To date, Pfizer is not aware of any reports of adverse events related to the Accupril recall, and the company believes the benefit/risk profile remains positive based on currently available data.
“Although long-term ingestion of N-nitroso-quinapril may be associated with a potential increased cancer risk in humans, there is no immediate risk to patients taking this medication,” the company said April 22 in a news release.
Patients currently taking the recalled products are asked to consult with their doctor about alternative treatment options.
The recalled Accupril tablets were sold in 90-count bottles distributed nationwide to wholesalers and distributors in the United States and Puerto Rico from December 2019 to April 2022.
National drug codes (NDC), lot numbers, and expiration dates are listed in the company announcement posted on the Food and Drug Administration’s website.
Patients who are taking this product should consult with their health care provider or pharmacy to determine if they have the affected product. Those with the affected tablets should contact claims management firm Sedgwick by phone at 888-345-0481 Monday through Friday from 8 AM to 5 PM ET for instructions on how to return the product and obtain reimbursement.
Healthcare providers with questions regarding the recall can contact Pfizer by telephone at 800-438-1985, option 3, Monday through Friday from 8 AM to 9 PM ET.
Adverse reactions or quality problems related to this recall should be reported to the FDA’s MedWatch program.
A version of this article first appeared on Medscape.com.
, the company announced.
The Accupril recall comes one month after Pfizer recalled six lots of Accuretic (Quinapril HCI/hydrochlorathiazide) tablets for the same problem.
Accupril is indicated for the treatment of hypertension and management of heart failure when added to conventional therapy, including diuretics and/or digitalis.
To date, Pfizer is not aware of any reports of adverse events related to the Accupril recall, and the company believes the benefit/risk profile remains positive based on currently available data.
“Although long-term ingestion of N-nitroso-quinapril may be associated with a potential increased cancer risk in humans, there is no immediate risk to patients taking this medication,” the company said April 22 in a news release.
Patients currently taking the recalled products are asked to consult with their doctor about alternative treatment options.
The recalled Accupril tablets were sold in 90-count bottles distributed nationwide to wholesalers and distributors in the United States and Puerto Rico from December 2019 to April 2022.
National drug codes (NDC), lot numbers, and expiration dates are listed in the company announcement posted on the Food and Drug Administration’s website.
Patients who are taking this product should consult with their health care provider or pharmacy to determine if they have the affected product. Those with the affected tablets should contact claims management firm Sedgwick by phone at 888-345-0481 Monday through Friday from 8 AM to 5 PM ET for instructions on how to return the product and obtain reimbursement.
Healthcare providers with questions regarding the recall can contact Pfizer by telephone at 800-438-1985, option 3, Monday through Friday from 8 AM to 9 PM ET.
Adverse reactions or quality problems related to this recall should be reported to the FDA’s MedWatch program.
A version of this article first appeared on Medscape.com.
Lowering BP according to newest guidance would cut CV events
Using the 2021 Kidney Disease: Improving Global Outcomes (KDIGO) guideline target of systolic blood pressure (BP) < 120 mm Hg, 66% of adults with chronic kidney disease (CKD) would be eligible for BP lowering, according to a study from Korea.
This represents an added > 10% of patients compared with two earlier guidelines, and these patients have a high risk of cardiovascular disease (CVD), Hyeok-Hee Lee, MD, Yonsei University College of Medicine, Seoul, South Korea, and colleagues reported.
The study was published online in the Journal of the American College of Cardiology.
“New candidates for BP-lowering treatment per the 2021 KDIGO guideline account for a substantial proportion of the total CKD population and bear significantly high CVD risk,” the researchers concluded.
“Undoubtedly, a multipronged approach will be required to address the swelling number of people needing more intense treatment, especially against a background of falling rates of BP control in the general community,” Alexander G. Logan, MD, of Mount Sinai Hospital, Toronto, and the University of Toronto, wrote in an accompanying editorial.
“Let’s not forget hypertension is the number one killer today,” Valentin Fuster, MD, of Icahn School of Medicine at Mount Sinai, New York, who is editor-in-chief of the Journal of the American College of Cardiology, stressed in a podcast that accompanied the article.
“Only 50% of individuals know of their blood pressure, and from this, less than half are properly treated,” he said.
“Today the details of knowing blood pressure levels appear to dominate over the huge ignorance of not knowing about blood pressure at all. Let’s think more and more about this reality,” he urged.
Three guidelines, two study objectives
The researchers compared three guidelines:
- The 2021 KDIGO guidelines, with a target systolic BP of < 120 mm Hg (largely based on the SPRINT trial).
- The 2012 KDIGO guidelines, with a target BP of ≤ 130/80 mm Hg for patients with albuminuria and ≤ 140/90 mm Hg for patients without albuminuria.
- The 2017 American College of Cardiology/American Heart Association (ACC/AHA) BP guideline target of < 130/80 mm Hg.
The study had two objectives:
- To examine the proportions of concordance and discordance between the three guidelines among adults with CKD based on cross-sectional data from the Korea National Health and Nutrition Examination Survey (KNHANES).
- To evaluate the association of each concordance/discordance group with cardiovascular outcomes of patients in the Korean National Health Insurance Service (NHIS) database.
For the first objective, the researchers identified 1,939 adults with CKD from the 2011-2014 survey cycles of KNHANES. Patients were a median age of 59 and 51% were men.
Comparison of the KDIGO 2021 versus 2012 BP targets showed that 50% of patients had BP above both targets; 16% had BP above the KDIGO 2021 target only; 4% had BP above the KDIGO 2012 target only; and 30% had BP control within both targets.
Comparison of the KDIGO 2021 versus 2017 ACC/AHA BP targets showed that 55% of patients had BP above both targets; 11% had BP above the KDIGO 2021 target only; 5% had BP above the 2017 ACC/AHA target only; and 29% had BP control within both targets.
For the second objective, using the NHIS database, researchers identified 412,167 adults with CKD who had routine health examinations during 2009 and 2010. The patients were a median age of 65 and 44% were men.
During a median follow-up of 10 years, the patients had 37,912 incident CVD events, defined as the first hospitalization for myocardial infarction, stroke, or heart failure, or death from CVD.
The adjusted risk of a composite CVD event was higher in patients with BP above the 2021 KDIGO target only (HR, 1.28) or above both the 2012 and 2021 KDIGO targets (HR, 1.52), compared to patients who had BP within both targets.
The adjusted risk of a composite CVD event was also higher in patients with BP above the 2021 KDIGO target only (HR, 1.18) or above both the 2021 KDIGO target and the 2017 ACC/AHA target (HR, 1.41), compared with patients who had BP within both targets.
Editorialist highlights three study aspects
Dr. Fuster noted three main points made by Dr. Logan.
First, the KDIGO 2021 guideline is based on office blood pressure, measured according to the procedure used in the 2017 ACC/AHA guideline. However, the SPRINT ambulatory BP ancillary study found that daytime ambulatory systolic BP was 6.8 mm Hg higher in the < 120 mm Hg group than clinic systolic BP that was measured with an automated BP device, mostly without study personnel.
Second, Dr. Logan noted that “not surprisingly, the investigators showed that the weighted proportion of adults with CKD eligible for BP lowering was highest (66.1%) according to 2021 KDIGO guideline,” compared with the two earlier guidelines.
The findings by Dr. Lee and colleagues align with those of a study that used data from the 2015-2018 U.S. NHANES to estimate the proportion of U.S. adults with CKD eligible for BP lowering according to the 2021 KDIGO guidelines, Dr. Logan added. The study found that 69% of U.S. adults (roughly 24.5 million) should correct their BP.
Third, the study in Korea showed a small percentage of patients (3%-5% of the total) had elevated diastolic BP but controlled systolic BP (< 120 mm Hg) with no increased risk of CVD compared to a reference group of patients with well-controlled BP.
“There is a paucity of evidence examining the relationship between diastolic hypertension and outcomes independently from systolic BP level in CKD patients,” Dr. Logan wrote. Similarly, Dr. Lee and colleagues identified this as an area for further research.
This work was supported by the Korea Health Technology R&D Project through the Korea Health Industry Development Institute funded by the Ministry of Health and Welfare, Republic of Korea. The authors and editorialist have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Using the 2021 Kidney Disease: Improving Global Outcomes (KDIGO) guideline target of systolic blood pressure (BP) < 120 mm Hg, 66% of adults with chronic kidney disease (CKD) would be eligible for BP lowering, according to a study from Korea.
This represents an added > 10% of patients compared with two earlier guidelines, and these patients have a high risk of cardiovascular disease (CVD), Hyeok-Hee Lee, MD, Yonsei University College of Medicine, Seoul, South Korea, and colleagues reported.
The study was published online in the Journal of the American College of Cardiology.
“New candidates for BP-lowering treatment per the 2021 KDIGO guideline account for a substantial proportion of the total CKD population and bear significantly high CVD risk,” the researchers concluded.
“Undoubtedly, a multipronged approach will be required to address the swelling number of people needing more intense treatment, especially against a background of falling rates of BP control in the general community,” Alexander G. Logan, MD, of Mount Sinai Hospital, Toronto, and the University of Toronto, wrote in an accompanying editorial.
“Let’s not forget hypertension is the number one killer today,” Valentin Fuster, MD, of Icahn School of Medicine at Mount Sinai, New York, who is editor-in-chief of the Journal of the American College of Cardiology, stressed in a podcast that accompanied the article.
“Only 50% of individuals know of their blood pressure, and from this, less than half are properly treated,” he said.
“Today the details of knowing blood pressure levels appear to dominate over the huge ignorance of not knowing about blood pressure at all. Let’s think more and more about this reality,” he urged.
Three guidelines, two study objectives
The researchers compared three guidelines:
- The 2021 KDIGO guidelines, with a target systolic BP of < 120 mm Hg (largely based on the SPRINT trial).
- The 2012 KDIGO guidelines, with a target BP of ≤ 130/80 mm Hg for patients with albuminuria and ≤ 140/90 mm Hg for patients without albuminuria.
- The 2017 American College of Cardiology/American Heart Association (ACC/AHA) BP guideline target of < 130/80 mm Hg.
The study had two objectives:
- To examine the proportions of concordance and discordance between the three guidelines among adults with CKD based on cross-sectional data from the Korea National Health and Nutrition Examination Survey (KNHANES).
- To evaluate the association of each concordance/discordance group with cardiovascular outcomes of patients in the Korean National Health Insurance Service (NHIS) database.
For the first objective, the researchers identified 1,939 adults with CKD from the 2011-2014 survey cycles of KNHANES. Patients were a median age of 59 and 51% were men.
Comparison of the KDIGO 2021 versus 2012 BP targets showed that 50% of patients had BP above both targets; 16% had BP above the KDIGO 2021 target only; 4% had BP above the KDIGO 2012 target only; and 30% had BP control within both targets.
Comparison of the KDIGO 2021 versus 2017 ACC/AHA BP targets showed that 55% of patients had BP above both targets; 11% had BP above the KDIGO 2021 target only; 5% had BP above the 2017 ACC/AHA target only; and 29% had BP control within both targets.
For the second objective, using the NHIS database, researchers identified 412,167 adults with CKD who had routine health examinations during 2009 and 2010. The patients were a median age of 65 and 44% were men.
During a median follow-up of 10 years, the patients had 37,912 incident CVD events, defined as the first hospitalization for myocardial infarction, stroke, or heart failure, or death from CVD.
The adjusted risk of a composite CVD event was higher in patients with BP above the 2021 KDIGO target only (HR, 1.28) or above both the 2012 and 2021 KDIGO targets (HR, 1.52), compared to patients who had BP within both targets.
The adjusted risk of a composite CVD event was also higher in patients with BP above the 2021 KDIGO target only (HR, 1.18) or above both the 2021 KDIGO target and the 2017 ACC/AHA target (HR, 1.41), compared with patients who had BP within both targets.
Editorialist highlights three study aspects
Dr. Fuster noted three main points made by Dr. Logan.
First, the KDIGO 2021 guideline is based on office blood pressure, measured according to the procedure used in the 2017 ACC/AHA guideline. However, the SPRINT ambulatory BP ancillary study found that daytime ambulatory systolic BP was 6.8 mm Hg higher in the < 120 mm Hg group than clinic systolic BP that was measured with an automated BP device, mostly without study personnel.
Second, Dr. Logan noted that “not surprisingly, the investigators showed that the weighted proportion of adults with CKD eligible for BP lowering was highest (66.1%) according to 2021 KDIGO guideline,” compared with the two earlier guidelines.
The findings by Dr. Lee and colleagues align with those of a study that used data from the 2015-2018 U.S. NHANES to estimate the proportion of U.S. adults with CKD eligible for BP lowering according to the 2021 KDIGO guidelines, Dr. Logan added. The study found that 69% of U.S. adults (roughly 24.5 million) should correct their BP.
Third, the study in Korea showed a small percentage of patients (3%-5% of the total) had elevated diastolic BP but controlled systolic BP (< 120 mm Hg) with no increased risk of CVD compared to a reference group of patients with well-controlled BP.
“There is a paucity of evidence examining the relationship between diastolic hypertension and outcomes independently from systolic BP level in CKD patients,” Dr. Logan wrote. Similarly, Dr. Lee and colleagues identified this as an area for further research.
This work was supported by the Korea Health Technology R&D Project through the Korea Health Industry Development Institute funded by the Ministry of Health and Welfare, Republic of Korea. The authors and editorialist have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Using the 2021 Kidney Disease: Improving Global Outcomes (KDIGO) guideline target of systolic blood pressure (BP) < 120 mm Hg, 66% of adults with chronic kidney disease (CKD) would be eligible for BP lowering, according to a study from Korea.
This represents an added > 10% of patients compared with two earlier guidelines, and these patients have a high risk of cardiovascular disease (CVD), Hyeok-Hee Lee, MD, Yonsei University College of Medicine, Seoul, South Korea, and colleagues reported.
The study was published online in the Journal of the American College of Cardiology.
“New candidates for BP-lowering treatment per the 2021 KDIGO guideline account for a substantial proportion of the total CKD population and bear significantly high CVD risk,” the researchers concluded.
“Undoubtedly, a multipronged approach will be required to address the swelling number of people needing more intense treatment, especially against a background of falling rates of BP control in the general community,” Alexander G. Logan, MD, of Mount Sinai Hospital, Toronto, and the University of Toronto, wrote in an accompanying editorial.
“Let’s not forget hypertension is the number one killer today,” Valentin Fuster, MD, of Icahn School of Medicine at Mount Sinai, New York, who is editor-in-chief of the Journal of the American College of Cardiology, stressed in a podcast that accompanied the article.
“Only 50% of individuals know of their blood pressure, and from this, less than half are properly treated,” he said.
“Today the details of knowing blood pressure levels appear to dominate over the huge ignorance of not knowing about blood pressure at all. Let’s think more and more about this reality,” he urged.
Three guidelines, two study objectives
The researchers compared three guidelines:
- The 2021 KDIGO guidelines, with a target systolic BP of < 120 mm Hg (largely based on the SPRINT trial).
- The 2012 KDIGO guidelines, with a target BP of ≤ 130/80 mm Hg for patients with albuminuria and ≤ 140/90 mm Hg for patients without albuminuria.
- The 2017 American College of Cardiology/American Heart Association (ACC/AHA) BP guideline target of < 130/80 mm Hg.
The study had two objectives:
- To examine the proportions of concordance and discordance between the three guidelines among adults with CKD based on cross-sectional data from the Korea National Health and Nutrition Examination Survey (KNHANES).
- To evaluate the association of each concordance/discordance group with cardiovascular outcomes of patients in the Korean National Health Insurance Service (NHIS) database.
For the first objective, the researchers identified 1,939 adults with CKD from the 2011-2014 survey cycles of KNHANES. Patients were a median age of 59 and 51% were men.
Comparison of the KDIGO 2021 versus 2012 BP targets showed that 50% of patients had BP above both targets; 16% had BP above the KDIGO 2021 target only; 4% had BP above the KDIGO 2012 target only; and 30% had BP control within both targets.
Comparison of the KDIGO 2021 versus 2017 ACC/AHA BP targets showed that 55% of patients had BP above both targets; 11% had BP above the KDIGO 2021 target only; 5% had BP above the 2017 ACC/AHA target only; and 29% had BP control within both targets.
For the second objective, using the NHIS database, researchers identified 412,167 adults with CKD who had routine health examinations during 2009 and 2010. The patients were a median age of 65 and 44% were men.
During a median follow-up of 10 years, the patients had 37,912 incident CVD events, defined as the first hospitalization for myocardial infarction, stroke, or heart failure, or death from CVD.
The adjusted risk of a composite CVD event was higher in patients with BP above the 2021 KDIGO target only (HR, 1.28) or above both the 2012 and 2021 KDIGO targets (HR, 1.52), compared to patients who had BP within both targets.
The adjusted risk of a composite CVD event was also higher in patients with BP above the 2021 KDIGO target only (HR, 1.18) or above both the 2021 KDIGO target and the 2017 ACC/AHA target (HR, 1.41), compared with patients who had BP within both targets.
Editorialist highlights three study aspects
Dr. Fuster noted three main points made by Dr. Logan.
First, the KDIGO 2021 guideline is based on office blood pressure, measured according to the procedure used in the 2017 ACC/AHA guideline. However, the SPRINT ambulatory BP ancillary study found that daytime ambulatory systolic BP was 6.8 mm Hg higher in the < 120 mm Hg group than clinic systolic BP that was measured with an automated BP device, mostly without study personnel.
Second, Dr. Logan noted that “not surprisingly, the investigators showed that the weighted proportion of adults with CKD eligible for BP lowering was highest (66.1%) according to 2021 KDIGO guideline,” compared with the two earlier guidelines.
The findings by Dr. Lee and colleagues align with those of a study that used data from the 2015-2018 U.S. NHANES to estimate the proportion of U.S. adults with CKD eligible for BP lowering according to the 2021 KDIGO guidelines, Dr. Logan added. The study found that 69% of U.S. adults (roughly 24.5 million) should correct their BP.
Third, the study in Korea showed a small percentage of patients (3%-5% of the total) had elevated diastolic BP but controlled systolic BP (< 120 mm Hg) with no increased risk of CVD compared to a reference group of patients with well-controlled BP.
“There is a paucity of evidence examining the relationship between diastolic hypertension and outcomes independently from systolic BP level in CKD patients,” Dr. Logan wrote. Similarly, Dr. Lee and colleagues identified this as an area for further research.
This work was supported by the Korea Health Technology R&D Project through the Korea Health Industry Development Institute funded by the Ministry of Health and Welfare, Republic of Korea. The authors and editorialist have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
How do we distinguish between viral and bacterial meningitis?
Bacteria and viruses are the leading causes of community-acquired meningitis. Bacterial meningitis is associated with high morbidity and mortality, and prompt treatment with appropriate antibiotics is essential to optimize outcomes. Early diagnosis is therefore crucial for selecting patients who need antibiotics. On the other hand, the course of viral meningitis is generally benign, and there is usually no specific antimicrobial treatment required. Distinguishing between viral and bacterial causes of meningitis can be challenging; therefore, many patients receive empiric antibiotic treatment.
Etiology
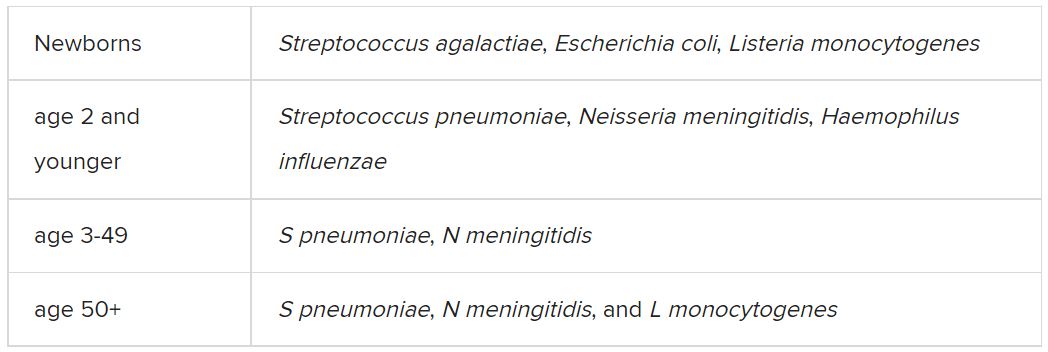
Among the etiologic agents of viral meningitis, the nonpolio enteroviruses (Echovirus 30, 11, 9, 6, 7, 18, 16, 71, 25; Coxsackie B2, A9, B1, B3, B4) are the most common, responsible for more than 85% of cases. Other viruses potentially responsible for meningitis include the herpes simplex virus (HSV), primarily type 2, and flavivirus (such as the Dengue virus).
Clinical presentation
The clinical presentation of bacterial meningitis is more severe than that of viral meningitis. The classic clinical triad of bacterial meningitis consists of fever, neck stiffness, and altered mental status. Only 41% of cases present with these three symptoms, however. Other clinical characteristics include severe headaches, decreased level of consciousness, nausea, vomiting, seizures, focal neurologic signs, and skin rash.
Viral meningitis is usually not associated with a decreased level of consciousness or significant decline in overall health status. The most frequently reported symptoms are unusual headaches, fever, nausea, vomiting, sensitivity to light, and neck stiffness. Patients may also present with skin changes and lymphadenopathy, and, depending on etiology, genital ulcers.
Diagnosis
The diagnosis of bacterial meningitis is based on clinical symptoms, blood panels (blood count, inflammation markers, cultures), and cerebrospinal fluid (CSF) cultures. Gram staining and latex agglutination may lead to false-negative results, and cultures may take a few days to provide a definitive result. Therefore, empiric antibiotic treatment is often started until the etiology can be determined.
A spinal tap must always be performed, preferably after a scan is taken, to rule out the risk of herniation. After CSF samples have been collected, they must undergo complete analysis, including cytological, biochemical, and microbiological evaluation, using conventional and molecular testing methods, when available.
Cytological and biochemical analyses of CSF may be helpful, as findings may indicate a higher probability of either bacterial or viral etiology.
CSF samples collected from patients with acute bacterial meningitis present characteristic neutrophilic pleocytosis (cell count usually ranging from hundreds to a few thousand, with >80% polymorphonuclear cells). In some cases of L. monocytogenes meningitis (from 25% to 30%), a lymphocytic predominance may occur. Normally, glucose is low (CSF glucose-to-blood-glucose ratio of ≤0.4 or <40 mg/dL), protein is very high (>200 mg/dL), and the CSF lactate level is high (≥31.53 mg/dL).
In viral meningitis, the white blood cell count is generally 10-300 cells/mm3. Although glucose levels are normal in most cases, they may be below normal limits in lymphocytic choriomeningitis virus (LCMV), HSV, mumps virus, and poliovirus meningitis. Protein levels tend to be slightly elevated, but they may still be within the reference range.
A recent study investigated which of the cytological or biochemical markers best correlate with the definite etiologic diagnosis. This study, in which CSF samples were collected and analyzed from 2013 to 2017, considered cases of bacterial or viral meningitis confirmed via microbiological evaluation or polymerase chain reaction (PCR). CSF lactate was the best single CSF parameter, and CSF lactate above 30 mg/dL virtually excludes the possibility of a viral etiology.
Etiologic determination
Despite the major contribution of globally analyzing CSF and secondary parameters, particularly CSF lactate, the precise etiologic definition is of great importance in cases of acute meningitis. Such precise definition is not simple, as identification of the causative microorganism is often difficult. Moreover, there are limits to conventional microbiological methods. Bacterioscopy is poorly sensitive, and although bacterial cultures are more sensitive, they can delay diagnosis because of the time it takes for the bacteria to grow in culture media.
Targeted molecular detection methods are usually more sensitive than conventional microbiological methods. Panel-based molecular tests identify multiple pathogens in a single test. In 2015, the U.S. Food and Drug Administration authorized the first commercial multiplex detection system for infectious causes of community-acquired meningitis and encephalitis. This test, the BioFire FilmArray system, detects 14 bacterial, viral, and fungal pathogens in a turnaround time of about 1 hour, including S. pneumoniae, N. meningitidis, H. influenzae, S. agalactiae (i.e., group B Streptococcus), E. coli (serotype K1), L. monocytogenes, HSV-1, HSV-2, varicella-zoster virus (VZV), cytomegalovirus (CMV), human herpesvirus 6 (HHV-6), human parechovirus (HPeV), and Cryptococcus neoformans/gattii.
A meta-analysis of eight precise diagnostic studies evaluating the BioFire FilmArray system showed a high sensitivity of 90% (95% confidence interval, 86%-93%) and specificity of 97% (95% CI, 94%-99%). The FilmArray ME panel can halve the time to microbiological result, allowing for earlier discontinuation of antimicrobial agents and hospital discharge in cases of viral meningitis.
Conclusion
Acute community-acquired meningitis is usually the result of viral or bacterial infections. Given the low specificity of clinical symptoms and, very often, of the general laboratory panel findings, many patients are empirically treated with antibiotics. High-sensitivity and -specificity molecular techniques allow for rapid identification of the bacterial etiology (which requires antibiotic therapy) or the viral etiology of meningitis. The latter can be managed only with symptom-specific medications and does not usually require extended hospitalization. Therefore, these new techniques can improve the quality of care for these patients with viral meningitis.
A version of this article first appeared on Medscape.com.
Bacteria and viruses are the leading causes of community-acquired meningitis. Bacterial meningitis is associated with high morbidity and mortality, and prompt treatment with appropriate antibiotics is essential to optimize outcomes. Early diagnosis is therefore crucial for selecting patients who need antibiotics. On the other hand, the course of viral meningitis is generally benign, and there is usually no specific antimicrobial treatment required. Distinguishing between viral and bacterial causes of meningitis can be challenging; therefore, many patients receive empiric antibiotic treatment.
Etiology
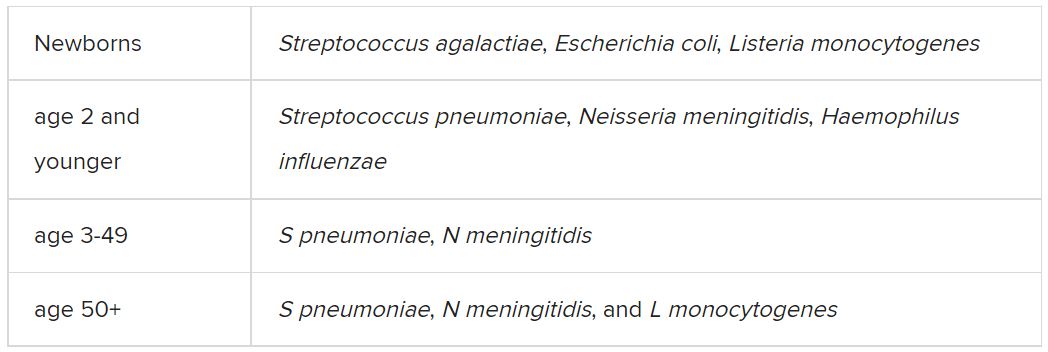
Among the etiologic agents of viral meningitis, the nonpolio enteroviruses (Echovirus 30, 11, 9, 6, 7, 18, 16, 71, 25; Coxsackie B2, A9, B1, B3, B4) are the most common, responsible for more than 85% of cases. Other viruses potentially responsible for meningitis include the herpes simplex virus (HSV), primarily type 2, and flavivirus (such as the Dengue virus).
Clinical presentation
The clinical presentation of bacterial meningitis is more severe than that of viral meningitis. The classic clinical triad of bacterial meningitis consists of fever, neck stiffness, and altered mental status. Only 41% of cases present with these three symptoms, however. Other clinical characteristics include severe headaches, decreased level of consciousness, nausea, vomiting, seizures, focal neurologic signs, and skin rash.
Viral meningitis is usually not associated with a decreased level of consciousness or significant decline in overall health status. The most frequently reported symptoms are unusual headaches, fever, nausea, vomiting, sensitivity to light, and neck stiffness. Patients may also present with skin changes and lymphadenopathy, and, depending on etiology, genital ulcers.
Diagnosis
The diagnosis of bacterial meningitis is based on clinical symptoms, blood panels (blood count, inflammation markers, cultures), and cerebrospinal fluid (CSF) cultures. Gram staining and latex agglutination may lead to false-negative results, and cultures may take a few days to provide a definitive result. Therefore, empiric antibiotic treatment is often started until the etiology can be determined.
A spinal tap must always be performed, preferably after a scan is taken, to rule out the risk of herniation. After CSF samples have been collected, they must undergo complete analysis, including cytological, biochemical, and microbiological evaluation, using conventional and molecular testing methods, when available.
Cytological and biochemical analyses of CSF may be helpful, as findings may indicate a higher probability of either bacterial or viral etiology.
CSF samples collected from patients with acute bacterial meningitis present characteristic neutrophilic pleocytosis (cell count usually ranging from hundreds to a few thousand, with >80% polymorphonuclear cells). In some cases of L. monocytogenes meningitis (from 25% to 30%), a lymphocytic predominance may occur. Normally, glucose is low (CSF glucose-to-blood-glucose ratio of ≤0.4 or <40 mg/dL), protein is very high (>200 mg/dL), and the CSF lactate level is high (≥31.53 mg/dL).
In viral meningitis, the white blood cell count is generally 10-300 cells/mm3. Although glucose levels are normal in most cases, they may be below normal limits in lymphocytic choriomeningitis virus (LCMV), HSV, mumps virus, and poliovirus meningitis. Protein levels tend to be slightly elevated, but they may still be within the reference range.
A recent study investigated which of the cytological or biochemical markers best correlate with the definite etiologic diagnosis. This study, in which CSF samples were collected and analyzed from 2013 to 2017, considered cases of bacterial or viral meningitis confirmed via microbiological evaluation or polymerase chain reaction (PCR). CSF lactate was the best single CSF parameter, and CSF lactate above 30 mg/dL virtually excludes the possibility of a viral etiology.
Etiologic determination
Despite the major contribution of globally analyzing CSF and secondary parameters, particularly CSF lactate, the precise etiologic definition is of great importance in cases of acute meningitis. Such precise definition is not simple, as identification of the causative microorganism is often difficult. Moreover, there are limits to conventional microbiological methods. Bacterioscopy is poorly sensitive, and although bacterial cultures are more sensitive, they can delay diagnosis because of the time it takes for the bacteria to grow in culture media.
Targeted molecular detection methods are usually more sensitive than conventional microbiological methods. Panel-based molecular tests identify multiple pathogens in a single test. In 2015, the U.S. Food and Drug Administration authorized the first commercial multiplex detection system for infectious causes of community-acquired meningitis and encephalitis. This test, the BioFire FilmArray system, detects 14 bacterial, viral, and fungal pathogens in a turnaround time of about 1 hour, including S. pneumoniae, N. meningitidis, H. influenzae, S. agalactiae (i.e., group B Streptococcus), E. coli (serotype K1), L. monocytogenes, HSV-1, HSV-2, varicella-zoster virus (VZV), cytomegalovirus (CMV), human herpesvirus 6 (HHV-6), human parechovirus (HPeV), and Cryptococcus neoformans/gattii.
A meta-analysis of eight precise diagnostic studies evaluating the BioFire FilmArray system showed a high sensitivity of 90% (95% confidence interval, 86%-93%) and specificity of 97% (95% CI, 94%-99%). The FilmArray ME panel can halve the time to microbiological result, allowing for earlier discontinuation of antimicrobial agents and hospital discharge in cases of viral meningitis.
Conclusion
Acute community-acquired meningitis is usually the result of viral or bacterial infections. Given the low specificity of clinical symptoms and, very often, of the general laboratory panel findings, many patients are empirically treated with antibiotics. High-sensitivity and -specificity molecular techniques allow for rapid identification of the bacterial etiology (which requires antibiotic therapy) or the viral etiology of meningitis. The latter can be managed only with symptom-specific medications and does not usually require extended hospitalization. Therefore, these new techniques can improve the quality of care for these patients with viral meningitis.
A version of this article first appeared on Medscape.com.
Bacteria and viruses are the leading causes of community-acquired meningitis. Bacterial meningitis is associated with high morbidity and mortality, and prompt treatment with appropriate antibiotics is essential to optimize outcomes. Early diagnosis is therefore crucial for selecting patients who need antibiotics. On the other hand, the course of viral meningitis is generally benign, and there is usually no specific antimicrobial treatment required. Distinguishing between viral and bacterial causes of meningitis can be challenging; therefore, many patients receive empiric antibiotic treatment.
Etiology
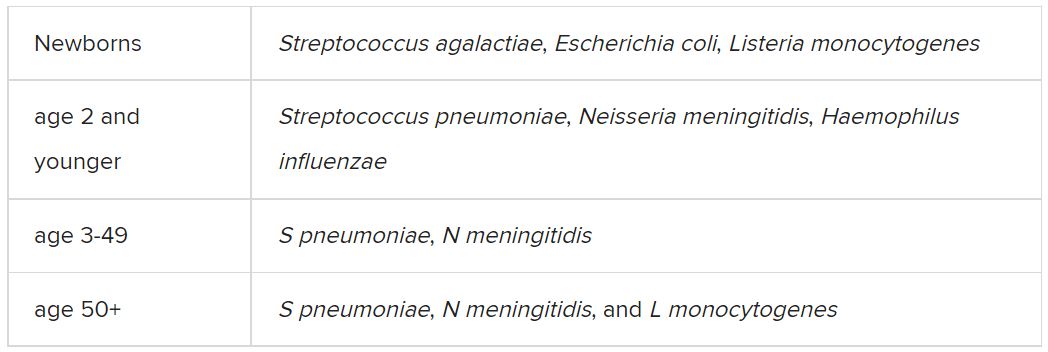
Among the etiologic agents of viral meningitis, the nonpolio enteroviruses (Echovirus 30, 11, 9, 6, 7, 18, 16, 71, 25; Coxsackie B2, A9, B1, B3, B4) are the most common, responsible for more than 85% of cases. Other viruses potentially responsible for meningitis include the herpes simplex virus (HSV), primarily type 2, and flavivirus (such as the Dengue virus).
Clinical presentation
The clinical presentation of bacterial meningitis is more severe than that of viral meningitis. The classic clinical triad of bacterial meningitis consists of fever, neck stiffness, and altered mental status. Only 41% of cases present with these three symptoms, however. Other clinical characteristics include severe headaches, decreased level of consciousness, nausea, vomiting, seizures, focal neurologic signs, and skin rash.
Viral meningitis is usually not associated with a decreased level of consciousness or significant decline in overall health status. The most frequently reported symptoms are unusual headaches, fever, nausea, vomiting, sensitivity to light, and neck stiffness. Patients may also present with skin changes and lymphadenopathy, and, depending on etiology, genital ulcers.
Diagnosis
The diagnosis of bacterial meningitis is based on clinical symptoms, blood panels (blood count, inflammation markers, cultures), and cerebrospinal fluid (CSF) cultures. Gram staining and latex agglutination may lead to false-negative results, and cultures may take a few days to provide a definitive result. Therefore, empiric antibiotic treatment is often started until the etiology can be determined.
A spinal tap must always be performed, preferably after a scan is taken, to rule out the risk of herniation. After CSF samples have been collected, they must undergo complete analysis, including cytological, biochemical, and microbiological evaluation, using conventional and molecular testing methods, when available.
Cytological and biochemical analyses of CSF may be helpful, as findings may indicate a higher probability of either bacterial or viral etiology.
CSF samples collected from patients with acute bacterial meningitis present characteristic neutrophilic pleocytosis (cell count usually ranging from hundreds to a few thousand, with >80% polymorphonuclear cells). In some cases of L. monocytogenes meningitis (from 25% to 30%), a lymphocytic predominance may occur. Normally, glucose is low (CSF glucose-to-blood-glucose ratio of ≤0.4 or <40 mg/dL), protein is very high (>200 mg/dL), and the CSF lactate level is high (≥31.53 mg/dL).
In viral meningitis, the white blood cell count is generally 10-300 cells/mm3. Although glucose levels are normal in most cases, they may be below normal limits in lymphocytic choriomeningitis virus (LCMV), HSV, mumps virus, and poliovirus meningitis. Protein levels tend to be slightly elevated, but they may still be within the reference range.
A recent study investigated which of the cytological or biochemical markers best correlate with the definite etiologic diagnosis. This study, in which CSF samples were collected and analyzed from 2013 to 2017, considered cases of bacterial or viral meningitis confirmed via microbiological evaluation or polymerase chain reaction (PCR). CSF lactate was the best single CSF parameter, and CSF lactate above 30 mg/dL virtually excludes the possibility of a viral etiology.
Etiologic determination
Despite the major contribution of globally analyzing CSF and secondary parameters, particularly CSF lactate, the precise etiologic definition is of great importance in cases of acute meningitis. Such precise definition is not simple, as identification of the causative microorganism is often difficult. Moreover, there are limits to conventional microbiological methods. Bacterioscopy is poorly sensitive, and although bacterial cultures are more sensitive, they can delay diagnosis because of the time it takes for the bacteria to grow in culture media.
Targeted molecular detection methods are usually more sensitive than conventional microbiological methods. Panel-based molecular tests identify multiple pathogens in a single test. In 2015, the U.S. Food and Drug Administration authorized the first commercial multiplex detection system for infectious causes of community-acquired meningitis and encephalitis. This test, the BioFire FilmArray system, detects 14 bacterial, viral, and fungal pathogens in a turnaround time of about 1 hour, including S. pneumoniae, N. meningitidis, H. influenzae, S. agalactiae (i.e., group B Streptococcus), E. coli (serotype K1), L. monocytogenes, HSV-1, HSV-2, varicella-zoster virus (VZV), cytomegalovirus (CMV), human herpesvirus 6 (HHV-6), human parechovirus (HPeV), and Cryptococcus neoformans/gattii.
A meta-analysis of eight precise diagnostic studies evaluating the BioFire FilmArray system showed a high sensitivity of 90% (95% confidence interval, 86%-93%) and specificity of 97% (95% CI, 94%-99%). The FilmArray ME panel can halve the time to microbiological result, allowing for earlier discontinuation of antimicrobial agents and hospital discharge in cases of viral meningitis.
Conclusion
Acute community-acquired meningitis is usually the result of viral or bacterial infections. Given the low specificity of clinical symptoms and, very often, of the general laboratory panel findings, many patients are empirically treated with antibiotics. High-sensitivity and -specificity molecular techniques allow for rapid identification of the bacterial etiology (which requires antibiotic therapy) or the viral etiology of meningitis. The latter can be managed only with symptom-specific medications and does not usually require extended hospitalization. Therefore, these new techniques can improve the quality of care for these patients with viral meningitis.
A version of this article first appeared on Medscape.com.